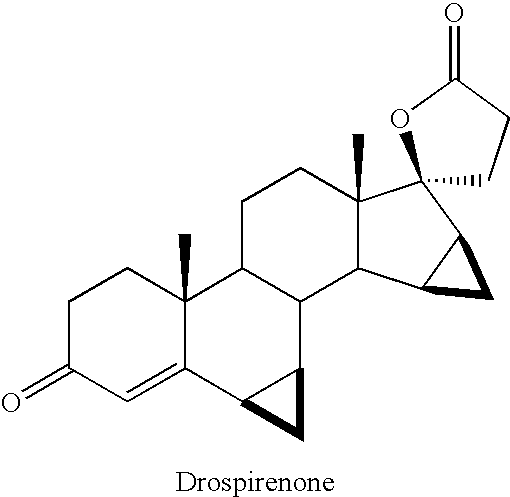
Drospirenone
FDA APPROVED 4/15/2021, To prevent pregnancy Nextstellis
New Drug Application (NDA): 214154
Company: MAYNE PHARMALabel (PDF)
Letter (PDF)
ReviewLabel (PDF)DrospirenoneCAS Registry Number: 67392-87-4
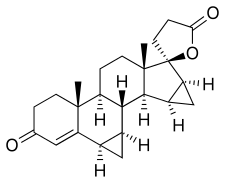
CAS Name: (2¢S,6R,7R,8R,9S,10R,13S,14S,15S,16S)-1,3¢,4¢,6,7,8,9,10,11,12,13,14,15,16,20,21-Hexadecahydro-10,13-dimethylspiro[17H-dicyclopropa[6,7:15,16]cyclopenta[a]phenanthrene-17,2¢(5¢H)-furan]-3,5¢(2H)-dione
Additional Names: 6b,7b,15b,16b-dimethylene-3-oxo-4-androstene-[17(b-1¢)-spiro-5¢]perhydrofuran-2¢-one; 6b,7b,15b,16b-dimethylen-3-oxo-17a-pregn-4-ene-21,17-carbolactone; dihydrospirorenone
Manufacturers’ Codes: ZK-30595
Molecular Formula: C24H30O3Molecular Weight: 366.49Percent Composition: C 78.65%, H 8.25%, O 13.10%
Literature References: Synthetic progestogen exhibiting antimineralocorticoid and antiandrogenic activity. Prepn: R. Wiechert et al.,DE2652761; eidem,US4129564 (both 1978 to Schering AG); D. Bittler et al.,Angew. Chem.94, 718 (1982). HPLC determn in human plasma: W. Krause, U. Jakobs, J. Chromatogr.230, 37 (1982). Pharmacological profile: P. Muhn et al.,Contraception51, 99 (1995). Review of synthesis: H. Laurent et al.,J. Steroid Biochem.19, 771-776 (1983); of pharmacology and clinical experience: W. Oelkers, Mol. Cell. Endocrinol.217, 255-261 (2004).
Properties: mp 201.3°. [a]D22 -182° (c = 0.5 in chloroform). uv (methanol): 265 nm (e 19000).
Melting point: mp 201.3°
Optical Rotation: [a]D22 -182° (c = 0.5 in chloroform)
Derivative Type: Mixture with ethinyl estradiolTrademarks: Angeliq (Schering AG); Yasmin (Schering AG)Literature References: Clinical trial as oral contraceptive: K. S. Parsey, A. Pong, Contraception61, 105 (2000); in treatment of menopausal symptoms: R. Schürmann et al., Climacteric7, 189 (2004).
Therap-Cat: Progestogen. In combination with estrogen as oral contaceptive and in treatment of menopausal symptoms.Keywords: Progestogen; Contraceptive (Oral).SYNhttps://www.sciencedirect.com/science/article/abs/pii/S0039128X15002135
Abstract
A general methodology for the synthesis of different steroidal 17-spirolactones is described. This method uses lithium acetylide of ethyl propiolate as the three carbon synthon and the method was successfully applied for the process development of drospirenone.
Graphical abstract

SYN
Steroid Hormones
Ruben Vardanyan, Victor Hruby, in Synthesis of Best-Seller Drugs, 2016
Drospirenone–Yaz
The synthesis of drospirenone (27.4.12) is believed to have been described for the first time in Wiechert et al [79], with a total yield of approximately 2 to 3% via the pathway presented in Scheme 27.4.

Each compound produced after each reaction step was purified by column chromatography.
Androsta-5,15-diene-3-ol-17-one was methylenated at the 15,16-position (27.4.13) and reacted with organometallic reagent (3,3-dimethoxypropyl)lithium prepared from 3-bromo-1,1-dimethoxypropane (27.4.14) and lithium in THF to produce the tertiary alcohol (27.4.15), which on short-term reflux with toluenesulfonic acid in acetone transformed to cyclic 21,17-hemiacetal (27.4.16). Oppenanuer oxidation with aluminium isopropoxide in excess of cyclohexanone in toluene was brought to mild oxidation of both secondary alcohol groups, and the simultaneous isomerization of the 5,6 double bond to the 4,5 position produced the compound (27.4.17). The last was oxidized with Jones reagent—chromic trioxide in diluted sulfuric acid—producing conjugated diene-one (27.4.18). Corey methylenation of the obtained product with dimethyloxosulfonium methylide in DMSO containing sodium hydride produced the final compound, the desired drospirenone (27.4.12).
The following patents and publications [80-83], which differ slightly from one another, disclose similar processes for preparing drospirenone and are presented in Scheme 27.5.

In Scheme 27.5, drospirenone (27.4.12) is prepared by converting the key starting compound (27.4.19) into the corresponding chloride (27.4.20) via reaction with triphenylphosphine and tetrachloromethane under mild conditions. Reductive dechlorination with Zn in acetic acid in THF tetrahydrofuran produced 5-hydroxy-15β,16β-methylene-3β-pivaloyloxy-5β-androst-6-en-17-one (27.4.21). The pivaloyl protecting group of the last was removed with the mixture of potassium hydroxide and sodium perchlorate in THF/methanol mixture to produce the diol (27.4.22). Simmons–Smith cyclopropanation reaction was applied to this compound. For that purpose, solution of (27.4.22) in dimethyl Cellosolve was stirred at 80°C with zinc-copper couple and methylene iodide, which produced the desired compound (27.4.23). The compound (27.4.23) underwent ethinylation with propargyl alcohol using potassium methylate in THF as a base to produce the 1,4-butindiol derivative (27.4.24). The triple bond of the 1,4-butindiol derivative (27.4.24) was hydrogenated in aTHF/methanol/pyridine mixture in the presence of palladium on carbon to produce the 1,4-butanediol derivative (27.4.25). The obtained compound underwent oxidation–lactonization at 50°C using a solution of CrO3 in water and pyridine to produce the desired drospirenone (27.4.12).
Several other synthetic routes for the production of drospirenone have been proposed [84-96], one of which [96] is presented in Scheme 27.6.

According to Scheme 27.6, a mixture of the key starting ketodiol (27.4.26), synthesis of which was described previously [84], with ethyl propiolate in THF was added to a solution of lithium hexamethyldisilylamide to produce, after quenching with acetic acid and saturated ammonium chloride solution, ethinyl alcohol (27.4.27). This product was hydrogenated on H2-Pd/C catalyst to produce ethyl 4-hydroxybutanoate (27.4.28). The 3-hydroxy group in the obtained product was oxidized to the keto group with (2,2,6,6-tetramethyl-piperidin-1-yl)oxyl, resulting in the compound (27.4.29). Treatment of the last with potassium hydroxide in a methanol–water mixture affects both hydrolysis of the ester group and dehydration of 5-hydroxy substituent. Acidification of the resulting intermediate results in drospirenone (27.4.12).
Drospirenone is a unique synthetic progestogen derived from 17α-spirolactone; it has a pharmacological profile very similar to that of endogenous progesterone. Drospirenone prevents ovulation and is used in contraceptive pills; it is also used as a postmenopausal hormone replacement. Drospirenone provides reliable and well-tolerated contraception and effective treatment of menopause. It has progestational, antialdosterone, and antiandrogenic properties, but is devoid of any estrogenic, androgenic, glucocorticoid, antiglucocorticoid, and mineralocorticoid activities. The affinity of drospirenone for the mineralocorticoid receptor makes it an antagonist of aldosterone, which is not only important in the renin–angiotensin–aldosterone system, but also means it acts directly on the cardiovascular system. It is progestin with antimineralocorticoid property that acts to suppress gonadotropins. It is thus able to prevent excessive sodium loss and regulate blood pressure. Drospirenone slightly decreases body weight and blood pressure and shares many pharmacodynamic properties with progesterone [97-110].
PATENT
https://patents.google.com/patent/US8334375B2/enDrospirenone is a synthetic steroid with progestin, anti-mineral corticoid and anti androgen activity. Drospirenone is currently being used as a synthetic progestin in oral contraceptive formulations. A regioselective synthesis for drospirenone has been described (see e.g., Angew. Chem. 94, 1982, 718) that uses the 17 keto derivative (1) as a key intermediate.

The synthesis of intermediate (1) and the transformation of intermediate (1) into drospirenone has been described in, for example, U.S. Published Patent Application Nos. 2009/0023914; 20080207575; 2008/0200668; 2008/0076915, 20070049747, and 20050192450; U.S. Pat. Nos. 6,933,395; 6,121,465, and 4,129,564, European Patent No. 0 075 189 and PCT Publication No. WO 2006/061309, all of which are incorporated herein by reference. Many of these routes introduce the required C3 side chain in the 17 position of intermediate (1). These conversions are usually carried out with carbanions, such as propargylalcohol, trimethylsulfoxonium iodide, or the use of the anion generated from a suitably protected derivative of 1-bromopropionaldehyde. After oxidation of the 3-hydroxy substituent to a 3-keto group, and the oxidative formation of the 17-spirolactone, the 3-keto-5-hydroxy-17-spirolactone is transformed via acid catalysis into drospireneone. If the oxidation is performed under acidic conditions at elevated temperatures, the oxidation and elimination can be run without isolation of the intermediate products.Most of these procedures rely on the acid-catalyzed elimination of the 5-hydroxy group in the last step of the synthesis. It has been documented that 15,16-methylene-17-spirolactones are prone to undergo rearrangement to generate the inverted 17-spirolactone under mild acidic conditions (see, for example, Tetrahedron Letters, Vol. 27, No 45, 5463-5466) in considerable amounts. This isomer has very similar physical chemical properties, and typically requires chromatographic separation or repeated fractional recrystallizations to purify the product. This isomerization can make these approaches less desirable from an economical point of view.FIG. 1Experimental Example

A solution of compound (1) (5 g; 15.2 mmol) and tert-butyldimethyl (2-propynyloxy)silane (2.83 g, 16.7 mmol) in 75 ml of dry THF was added dropwise through an addition funnel to a precooled slurry of potassium tert-butoxide (8.49 g, 75.7 mmol) at −10 C. A thick white precipitate is formed during the addition and the resulting mixture was stirred for an hour at 0 C. TLC analysis (70% EtOAc/Hexanes) showed completion of the reaction and showed a less polar product. The reaction was quenched by the addition of ice water (100 ml) and neutralized by adding acetic acid (4.3 ml). The THF layer was separated and the aqueous layer was extracted with EtOAc (2×50 ml). The combined organic layers were washed with water (2×100 ml), brine (100 ml) and dried over anhydrous sodium sulfate. The solvent was removed under vacuum to afford compound (2a) (7.5 g, 99.2%) as a solid which was used in the next step without any purification.NMR (CDCl3) δ 0.139 (s, 6H, S1—CH3), 0.385 (m, 1H), 0.628 (m, 1H), 0.857 (s, 18-Me), 0.896 (s, 19-Me), 0.918 (s, 3H, Si—CH3), 0.927 (s, 6H, Si—CH3), 4.05 (s, 1H), 4.428 (s, 2H, —O—CH2) FTIR (ATR): 3311, 3017, 2929, 2858, 2270, 1058 cm−1

Compound (2a) (5 g, 9.98 mmol) was dissolved in 100 ml of ethyl acetate in a Parr hydrogenation bottle and was mixed with 10% palladium on charcoal (1 g, 0.09 mmol). This mixture was hydrogenated on a Parr apparatus at a pressure of 20 psi for 90 minutes. The catalyst was filtered and washed with ethyl acetate. The solvent was removed in vacuo to afford compound (3a) as a colorless foam (5.01 g, 99%).NMR (CDCl3) δ 0.0758 (s, 6H, Si—CH3), 0.283 (m, 1H), 0.628 (m, 1H), 0.856 (s, 18-Me), 0.893 (s, 19-Me), 0.918 (s, 9H, Si—CH3), 3.69 (m, 2H), 4.05 (s, 1H). FTIR (ATR): 3374, 3017, 2929, 2858, 1259, 1091, 1049, 835 cm−1

Chromium trioxide (4.95 g, 49.5 mmol) was added to a solution of pyridine (7.83 g, 99.05 mmol) in anhydrous dichloromethane (100 ml). The resulting mixture was stirred for 15 minutes during which time the color changed to burgundy. A solution of compound (1a) (5 g, 9.90 mmol) in 50 ml of dichloromethane was added and the mixture was stirred at room temperature for 6 h. The excess oxidizing agent was quenched by adding isopropanol. The reaction mixture was diluted with MTBE (50 ml) and was passed through a short pad of Celite. The solid was washed again with 2:1 MTBE-CH2Cl2 (50 ml x2). The solvent was removed in vacuo to give a residue which was dissolved in 100 ml of EtOAc, was washed with water, and dried over anhydrous sodium sulfate. The solvent was removed in vacuo to afford compound (4a) as a pale yellow foam (4.5 g, 90.3%).NMR (CDCl3) δ 0.08 (s, 6H, Si—CH3), 0.31 (m, 1H), 0.914 (s, 9H, Si—CH3), 0.931 (s, 6H, 18-Me, 19-Me) 3.70 (m, 2H). FTIR (ATR): 3399, 3022, 2950, 2929, 2862, 1708, 1649, 1259, 1041 cm−1

A solution of compound (4a) (5 g, 9.94 mmol) in 50 ml of MeOH was refluxed with NaOH (397 mg, 9.94 mmol) for 3 h. When the reaction was over, as shown by TLC, the reaction mixture was cooled to room temperature and added to ice cold water (150 ml). The mixture was extracted with ethyl acetate (3×50 mL). The combined EtOAc layers were washed with water (100 ml) brine (50 ml) and dried over sodium sulfate. The solvent was removed in vacuo to afford compound (5) as a colorless amorphous solid (4.5 g, 92%).NMR (CDCl3) δ 0.05 (s, 6H, Si—CH3), 0.296 (m, 1H), 0.886 (s, 9H, Si—CH3), 0.908 (s, 3H, 18-Me), 1.07 (s, 3H, 19-Me), 3.68 (m, 2-H), 5.95 (s, 1H). FTIR (ATR): 3450, 3009, 2950, 2858, 1653, 1603, 1095 cm−1

A solution of compound (5a) (5 g, 9.94 mmol) in 30 ml of acetone was cooled to −15 C as a 2.7M solution of Jones reagent (3.68 ml, 9.94 mmol) was added drop wise. The reaction mixture was stirred at 0 C for 2 h, during this time TLC showed completion of the reaction. The reaction was quenched by adding isopropanol and diluted with water. The reaction mixture was extracted with EtOAc. The combined EtOAc layers were washed with water, sat. NaHCO3 and brine. The EtOAc layers were dried over sodium sulfate and solvent was removed by vacuum to afford crude drospirenone as a pale yellow foam (3 g, 82%) Recrystallization from acetone-hexane gave 1.5 g of pure drospirenone as white solid.NMR (CDCl3) δ 0.0548 (m, 1H), 0.88 (m, 1H), 1.008 (s, 3H, 18-Me), 1.11 (s, 3H, 18-Me), 6.03 (s, 1H). FTIR (ATR): 3025, 2971, 2942, 1763, 1654, 1590, 1186 cm−1FIG. 2Experimental Example

Lithium hexamethyldisilylamide (LiHMDS) 1.0 M/THF (75.7 mL, 75.7 mmol) was introduced into a 500 mL, 3-neck flask equipped with an addition funnel and a pierced septa for the introduction of a thermocouple probe. The mixture was diluted with THF (25 mL). The solution was stirred (Teflon paddle) and chilled to an internal temperature of −72° C. A THF (75 mL) solution of ketodiol (5 g, 15.13 mmol) containing ethyl propiolate (3.07 mL, 30.26 mmol) was added dropwise over 1 hour while not allowing the temperature to rise above −65° C. Upon completion of the addition the mixture was stirred for 3 hrs while allowing the temperature to warm slowly to −60° C. Finally, the mixture was warned to −40° C. over 1 hour.The mixture was quenched through the addition of acetic acid (4.25 mL)/water (5.0 mL) followed by the addition of saturated ammonium chloride solution (100 mL). The mixture was stirred for 3 min and then transferred to a separatory funnel. The layers were separated and the upper, THF layer was diluted with ethyl acetate (75 mL). The organic phase was washed with water (3×100 mL) and brine (1×100 mL). All the aqueous washes were extracted with ethyl acetate (2×30 mL). The combined organic extract was dried over sodium sulfate, filtered, and evaporated in vacuo (45° C.) to afford a thick oil. Dichloromethane (ca. 35 mL) was added and evaporated in vacuo. The flask was cooled slightly and dichloromethane (33 ml) was added to give a solid mass. The solid was broken up and stirred until a homogeneous slurry was obtained. Hexanes (35 mL) was added slowly to the stirred mixture and the mixture was stored at 2-4 C overnight. The solid was filtered, washed with 30% dichloromethane/hexanes, and dried in vacuo at ambient temperature for 4 hours to give (2b) 5.86 g (90.4%) of a white powder.
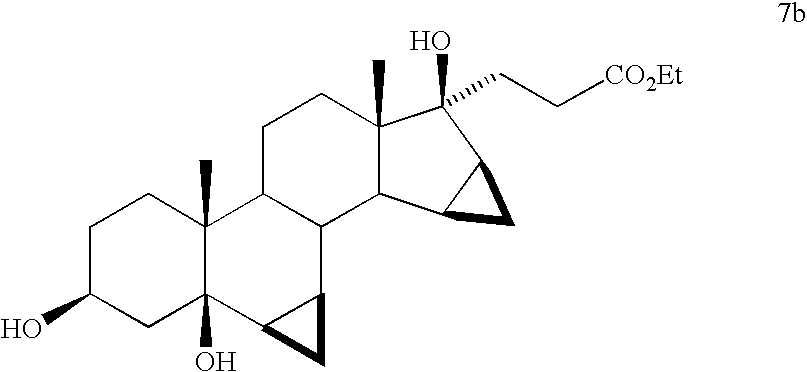
Compound (2b) (5.0 g, 11.67 mmol) was dissolved in THF (50 mL) and 5% Pd/C (622 mg, 0.29 mmol Pd) was added and the mixture was shaken at 15 psi H2 for 2 hours. The mixture was diluted with ethyl acetate (25 mL) and filtered through a pad of Celite. The filter pad was washed with ethyl acetate (3×25 mL) and the filtrate was evaporated to dryness to afford 5.0 g (99.1%) of triol (7b) as a stable foam.

Compound (7a) (5.0 g, 11.56 mmol) was dissolved in dichloromethane (50 mL) and the solution was stirred vigorously and chilled to −15° C. (NaCl/ice) and TEMPO (45.16 mg, 0.29 mmol, 2.5 mol %) was added. The mixture was treated dropwise over about 15-20 min. with a mixture of sodium hypochlorite (12.5%) (11.17 mL, 23.12 mmol) in water (8.0 mL) containing potassium bicarbonate (833 mg, 8.32 mmol). The mixture was allowed to warm to 0 C for 1.25 hrs. Analysis of the reaction by TLC (60% EtOAc/hex) shows the appearance of a slightly less polar product (ΔRf=0.8 cm). The mixture was chilled to −5 C and was quenched through the dropwise addition (ca 10-15 min) of a water (15.0 mL) solution of sodium phosphate (1.27 g, 7.75 mmol) and sodium metabisulfite (1.10 g, 5.78 mmol). The layers were separated and the dichloromethane solution was washed with water (2×) and brine. All aqueous washes were extracted with additional dichloromethane (2×15 mL). The combined dichloromethane extract was dried over sodium sulfate, filtered, and evaporated to give 4.88 g (98.08%) of ketone (8b) as a stable foam.

Compound (8b) was added to a methanol (10 mL) solution containing 8.0 M KOH solution (6.3 mL, 50.36 mmol) preheated to 60 C. The solution was heated at reflux for 2.5 hours. The mixture was chilled in an ice bath and treated with acetic acid (36 mL) and water (5.0 mL). The solution was stirred at 50-60 C for 15 hours. The volatiles were evaporated in vacuo and the acetic acid solution was poured into cold water (150 mL) to give a white precipitate. The aqueous mixture was extracted with ethyl acetate (2×100 mL). The ethyl acetate extracts were washed with water (2×), saturated sodium bicarbonate solution, and brine. The combined ethyl acetate extract was dried over sodium sulfate. Evaporation of the solvent gave a yellow foam. Trituration of the foam with acetone/hexane followed by evaporation gave 4.27 g (92.62%) of a light yellow solid. Recrystallization of the solid from acetone/hexanes gave 3.07 g of drospirenone with an HPLC purity of 99.66%. Evaporation of the mother liquor and recrystallization of the residue affords an additional 0.54 g of slightly impure drospirenone.FIG. 3Experimental Example

Lithium hexamethyldisilylamide (LiHMDS) 1.0 M/THF (75.7 mL, 75.7 mmol) was introduced into a 500 mL, 3-neck flask equipped with an addition funnel and a pierced septa for the introduction of a thermocouple probe. The mixture was diluted with THF (25 mL). The solution was stirred (Teflon paddle) and chilled to an internal temperature of −72° C. A THF (75 mL) solution of ketodiol (5 g, 15.13 mmol) containing ethyl propiolate (3.07 mL, 30.26 mmol) was added dropwise over 1 hour while not allowing the temperature to rise above −65° C. Upon completion of the addition the mixture was stirred for 3 hrs while allowing the temperature to warm slowly to −60° C. Finally, the mixture was warmed to −40° C. over 1 hour.The mixture was quenched through the addition of acetic acid (4.25 mL)/water (5.0 mL) followed by the addition of saturated ammonium chloride solution (100 mL). The mixture was stirred for 3 min and then transferred to a separatory funnel. The layers were separated and the upper, THF layer was diluted with ethyl acetate (75 mL). The organic phase was washed with water (3×100 mL) and brine (1×100 mL). All the aqueous washes were extracted with ethyl acetate (2×30 mL). The combined organic extract was dried over sodium sulfate, filtered, and evaporated in vacuo (45° C.) to afford a thick oil. Dichloromethane (ca. 35 mL) was added and evaporated in vacuo. The flask was cooled slightly and dichloromethane (33 ml) was added to give a solid mass. The solid was broken up and stirred until a homogeneous slurry was obtained. Hexanes (35 mL) was added slowly to the stirred mixture and the mixture was stored at 2-4 C overnight. The solid was filtered, washed with 30% dichloromethane/hexanes, and dried in vacuo at ambient temperature for 4 hours to give (2c) 5.86 g (90.4%) of a white powder.

Propiolate adduct (2c) (5.86 g, 13.67 mmol) was suspended in dichloromethane (60 mL). The mixture was stirred vigorously and chilled to −15° C. (NaCl/ice) and TEMPO (54 mg, 0.35 mmol, 2.5 mol %) was added. The mixture was treated dropwise over about 15-20 min. with a mixture of sodium hypochlorite (12.5%) (13.2 mL, 27.34 mmol) in water (8.0 mL) containing potassium bicarbonate (985 mg, 9.84 mmol). During the addition of the hypochlorite solution, a 5-8 C temperature rise was observed and the mixture became yellow. The mixture was allowed to warm to at 0 C for 2 hrs. Analysis of the reaction by TLC (60% EtOAc/hex) shows the appearance of a slightly less polar product (ΔRf=0.8 cm). The mixture was chilled to −5 C and was quenched through the dropwise addition (ca 10-15 min) of a water (150 mL) solution of sodium phosphate (1.50 g, 9.16 mmol) and sodium metabisulfite (1.30 g, 6.84 mmol). Once again, a temperature rise of 5-8 C was observed and the yellow color was quenched. The layers were separated and the dichloromethane solution was washed with water (2×) and brine. All aqueous washes were extracted with additional dichloromethane (2×15 mL). The combined dichloromethane extract was dried over sodium sulfate and the bulk of the solvent was evaporated in vacuo. Upon the observation of solids in the mixture during the evaporation, the evaporation was discontinued and the residue in the flask diluted with MTBE (35 mL). While stirring, the mixture was slowly diluted with hexanes (35 mL). The mixture was then chilled in an ice bath for 30 min. The solid was filtered, washed with 25% MTBE/hexane, and dried to give intermediate (9c) (4.98 g, 85.31%) as a white solid.NMR (CDCl3) δ 0.462 (q, 1H), 0.699 (m, 1H), 0.924 (s, 18-Me), 0.952 (s, 19-Me), 1.338 (t, J=7 Hz, OCH2CH 3), 2.517 (d, 1H), 3.021 (d, 1H), 4.269 (t, OCH 2CH3) ppm. FTIR (ATR): 3493, 3252, 2948, 2226, 1697, 1241 cm−1.
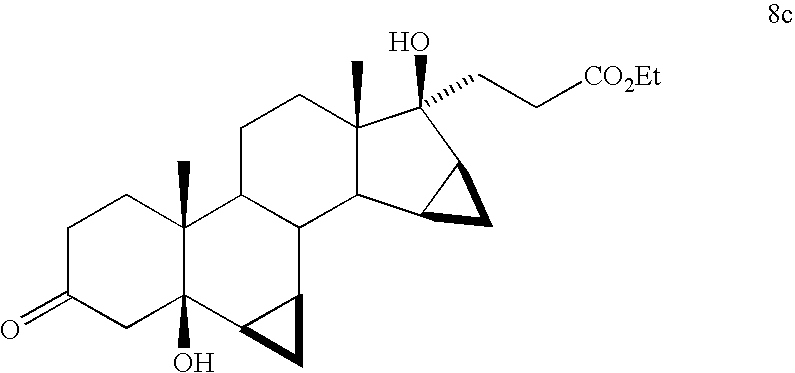
Alkynyl ketone (9c) (5.37 g, 12.59 mmol) was dissolved in THF (27 mL) in a 250 mL shaker bottle. 5% Pd/C (670 mg, 2.5 mol %) was added to the solution and the mixture was shaken under a hydrogen pressure of 15 psi. Over approximately 30 min, there was observed a rapid up take of hydrogen. The pressure was continually adjusted to 15 psi until the uptake of hydrogen ceased and was shaken for a total of 1.5 hrs. The mixture was diluted with a small amount of methanol and filtered through Celite. The filter pad was washed with methanol (ca. 3×25 mL).NMR (CDCl3) δ 0.353 (q, 1H), 0.704 (m, 2H), 0.930 (s, 18-Me), 0.933 (s, 19-Me), 1.279 (t, J=7 Hz, OCH2CH 3), 2.480 (d, 1H), 2.672 (m, 2H), 3.981 (d, 1H), 4.162 (t, OCH 2CH3) ppm. FTIR (ATR): 3465, 2946, 1712, cm−1.

The filtrate containing compound (8c) described above, was added in one portion to a methanol (10 mL) solution containing 8.0 M KOH solution (6.3 mL, 50.36 mmol) preheated to 60 C. The solution was heated at reflux for 2.5 hours. The mixture was chilled in an ice bath and treated with acetic acid (36 mL) and water (5.0 mL). The solution was stirred at 50-60 C for 15 hours. The volatiles were evaporated in vacuo and the acetic acid solution was poured into cold water (150 mL) to give a white precipitate. The aqueous mixture was extracted with ethyl acetate (2×100 mL). The ethyl acetate extracts were washed with water (2×), saturated sodium bicarbonate solution, and brine. The combined ethyl acetate extract was dried over sodium sulfate. Evaporation of the solvent gave a yellow foam. Trituration of the foam with acetone/hexane followed by evaporation gave 4.27 g (92.62%) of a light yellow solid. Recrystallization of the solid from acetone/hexanes gave 3.07 g of drospirenone with an HPLC purity of 99.66%. Evaporation of the mother liquor and recrystallization of the residue affords an additional 0.54 g of slightly impure drospirenone.FIG. 4Experimental Example

Lithium hexamethyldisilylamide (LiHMDS) 1.0 M/THF (75.7 mL, 75.7 mmol) was introduced into a 500 mL, 3-neck flask equipped with an addition funnel and a pierced septa for the introduction of a theiniocouple probe. The mixture was diluted with THF (25 mL). The solution was stirred (Teflon paddle) and chilled to an internal temperature of −72° C. A THF (75 mL) solution of ketodiol (5 g, 15.13 mmol) containing ethyl propiolate (3.07 mL, 30.26 mmol) was added dropwise over 1 hour while not allowing the temperature to rise above −65° C. Upon completion of the addition the mixture was stirred for 3 hrs while allowing the temperature to warm slowly to −60° C. Finally, the mixture was warmed to −40° C. over 1 hour.The mixture was quenched through the addition of acetic acid (4.25 mL)/water (5.0 mL) followed by the addition of saturated ammonium chloride solution (100 mL). The mixture was stirred for 3 min and then transferred to a separatory funnel. The layers were separated and the upper, THF layer was diluted with ethyl acetate (75 mL). The organic phase was washed with water (3×100 mL) and brine (1×100 mL). All the aqueous washes were extracted with ethyl acetate (2×30 mL). The combined organic extract was dried over sodium sulfate, filtered, and evaporated in vacuo (45° C.) to afford a thick oil. Dichloromethane (ca. 35 mL) was added and evaporated in vacuo. The flask was cooled slightly and dichloromethane (33 ml) was added to give a solid mass. The solid was broken up and stirred until a homogeneous slurry was obtained. Hexanes (35 mL) was added slowly to the stirred mixture and the mixture was stored at 2-4 C overnight. The solid was filtered, washed with 30% dichloromethane/hexanes, and dried in vacuo at ambient temperature for 4 hours to give (2d) 5.86 g (90.4%) of a white powder.

Propiolate adduct (2d) (5.86 g, 13.67 mmol) was suspended in dichloromethane (60 mL). The mixture was stirred vigorously and chilled to −15° C. (NaCl/ice) and TEMPO (54 mg, 0.35 mmol, 2.5 mol %) was added. The mixture was treated dropwise over about 15-20 min. with a mixture of sodium hypochlorite (12.5%) (13.2 mL, 27.34 mmol) in water (8.0 mL) containing potassium bicarbonate (985 mg, 9.84 mmol). During the addition of the hypochlorite solution, a 5-8 C temperature rise was observed and the mixture became yellow. The mixture was allowed to warm to at 0 C for 2 hrs. Analysis of the reaction by TLC (60% EtOAc/hex) shows the appearance of a slightly less polar product (ΔRf=0.8 cm). The mixture was chilled to −5 C and was quenched through the dropwise addition (ca 10-15 min) of a water (15.0 mL) solution of sodium phosphate (1.50 g, 9.16 mmol) and sodium metabisulfite (1.30 g, 6.84 mmol). Once again, a temperature rise of 5-8 C was observed and the yellow color was quenched. The layers were separated and the dichloromethane solution was washed with water (2×) and brine. All aqueous washes were extracted with additional dichloromethane (2×15 mL). The combined dichloromethane extract was dried over sodium sulfate and the bulk of the solvent was evaporated in vacuo. Upon the observation of solids in the mixture during the evaporation, the evaporation was discontinued and the residue in the flask diluted with MTBE (35 mL). While stirring, the mixture was slowly diluted with hexanes (35 mL). The mixture was then chilled in an ice bath for 30 min. The solid was filtered, washed with 25% MTBE/hexane, and dried to give intermediate (9d) (4.98 g, 85.31%) as a white solid.NMR (CDCl3) δ 0.462 (q, 1H), 0.699 (m, 1H), 0.924 (s, 18-Me), 0.952 (s, 19-Me), 1.338 (t, J=7 Hz, OCH2CH 3), 2.517 (d, 1H), 3.021 (d, 1H), 4.269 (t, OCH 2CH3) ppm. FTIR (ATR): 3493, 3252, 2948, 2226, 1697, 1241 cm−1.

Compound (9d) (5.0 g) was dissolved in methanol (50 mL) and treated with 1.0 N sulfuric acid (10 mL). The mixture was heated to reflux for 3 hours, cooled, and neutralized through the addition of saturated sodium bicarbonate solution. Most of the methanol was evaporated in vacuo at ambient temperature and diluted with water. The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water and brine, dried over sodium sulfate, filtered, and evaporated to give 4.95 g of unsaturated ketone (10d) as a stable foam.

Compound (10d) (5.0 g, 12.24 mmol) was dissolved in degassed benzene (50 mL) and treated with chlorotris(triphenylphosphine)rhodium (I) (283.1 mg, 0.31 mmol and the resulting mixture was stirred in a hydrogen atmosphere for 10 hours. The solution was evaporated, reconstituted in 50% ethyl acetate/hexanes, and passed through a short column of neutral alumina. Evaporation of the solvent gave 4.95 g of (11d) as a stable foam.

Compound (11d) (4.95 g, 12.01 mmol) was dissolved in 10% aqueous methanol (50 mL) and solid potassium carbonate (4.98 g, 36.04 mmol) was added. The mixture was stirred at room temperature for 30 min and the bicarbonate was neutralized through the addition of acetic acid (2.06 mL, 36.04 mmol). The methanol was evaporated in vacuo at ambient temperature and diluted with water. The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water and brine, dried over sodium sulfate, filtered, and evaporated to give 4.10 g (93%) of a semi solid. The material was dissolved in dichloromethane and evaporated in vacuo to give a stable foam. The foam was dissolved in ethyl acetate (5 mL) and allowed to stand overnight. The resulting solid was filtered, washed with cold ethyl acetate, and dried in vacuo to afford 2.86 g (66%) of pure drospirenone.FIG. 5Experimental Example 1

A dichloromethane (50 mL) solution of ketodiol (1) (5.0 g, 15.13 mmol) was treated with ethyl vinyl ether (7.24 mL, 75.65 mmol), followed by the addition of pyridinium tosylate (380 mg, 1.15 mmol). The solution was stirred at room temperature for 30 min. The dichloromethane solution was washed with water (2×), brine, and dried over sodium sulfate. Following filtration, evaporation of the solvent gave 6.14 g of the 3-protected compound (1e) as a stable foam.
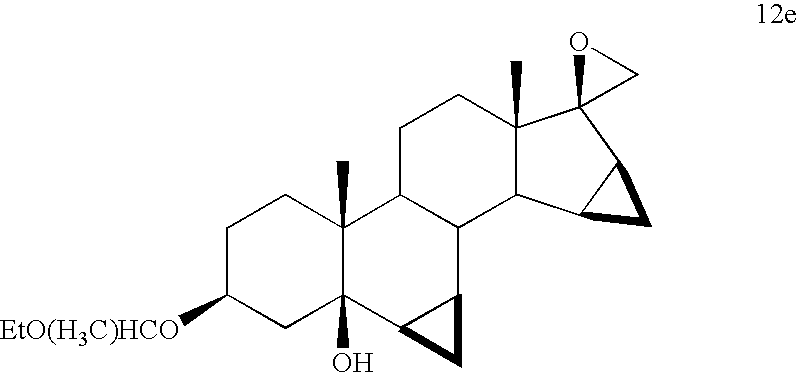
Compound (1e) (6.14 g, 15.13 mmol) was dissolved in DMSO/THF (15 mL/15 mL), treated with trimethylsulfonium iodide (4.63 g, 22.70 mmol) and the mixture was chilled to −15 C. The mixture was treated portion wise with potassium t-butoxide (3.23 g, 28.82 mmol). The mixture was stirred at −15 C for 45 min and then poured into ice/water (200 mL). The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (2×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 6.21 g (98.42%) of oxirane (12e) as a stable foam.

A THF (30 mL) solution of di-isopropyl amine (12.02 mL, 85.03 mmol) was chilled to −40 C and treated with butyl lithium (2.5 M/hexanes, 34.01 mL, 85.03 mmol) and the mixture was stirred for 15 min. A THF (5 mL) solution of acetonitrile (4.7 mL, 90.79 mmol) was added dropwise to the in situ generated lithium di-isopropylamide (LDA) solution to give a slurry of the acetonitrile anion. After stirring for 15 min at −40° C., compound (12e) (6.21 g, 14.91 mmol) as a THF (25 mL) solution was added dropwise over 10 min. The mixture was stirred for 30 min and then quenched through the addition of saturated ammonium chloride solution (210 mL). The mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (3×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 7.07 g of the addition product (13e) as a tacky foam.

Compound 13e (5.0 g, 10.93 mmol) was dissolved in acetone (25 mL) and chilled to 0 C. The stirred solution was treated dropwise with 2.7M chromic acid (Jones Reagent) (7.0 mL, 18.91 mmol). After 1.5 hrs, the excess Cr (VI) was quenched through the addition of 2-propanol until the green color of Cr (IV) was evident. Water (300 mL) was added and the mixture was stirred until all the chromium salts were dissolved. The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (2×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 3.83 g (96%) of ketone (14e) as a stable foam.

Compound (14e) (3.83 g, 10.48 mmol) was dissolved in methanol (38 mL) and treated with 8.0 M KOH solution (7.0 mL, 56 mmol) and the mixture was heated at reflux for 5 hours. The mixture was cooled to 0 C and treated with acetic acid (15 mL) and water (6 mL) and the mixture was stirred at 50 C for 6 hours. The solvents were evaporated in vacuo and the residue was diluted with water (200 mL). The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (2×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 3.76 g (94%) of crude drospirenone as a stable foam. The crude drospirenone was dissolved in 60% ethyl acetate/hexanes and passed through a short column of neutral alumina (10× w/w) and the column was eluted with the same solvent. Following evaporation of the solvent, 2.58 g (65%) of crystalline drospirenone was obtained. Recrystallization from acetone/hexanes afforded pure drospirenone.FIG. 5Experimental Example 2

Intermediate (1) (5 g, 15.13 mmol) was dissolved in DMSO/THF (50 mL/50 mL), treated with trimethylsulfonium iodide (4.63 g, 22.70 mmol), and the mixture was chilled to −15 C. The mixture was treated portion wise with potassium t-butoxide (5.03 g, 43.88 mmol). The mixture was stirred at −15 C for 45 min and then poured into ice/water (200 mL). The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (2×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 5.11 g (98%) of oxirane (12f) as a stable foam.

A THF (30 mL) solution of di-isopropyl amine (12.02 mL, 85.03 mmol) was chilled to −40 C and treated with butyl lithium (2.5 M/hexanes, 34.01 mL, 85.03 mmol) and the mixture was stirred for 15 min. A THF (5 mL) solution of acetonitrile (4.7 mL, 90.79 mmol) was added dropwise to the above lithium di-isopropylamide (LDA) solution to give a slurry of the acetonitrile anion. After stirring for 15 min at −40 C, compound (12f) (5.11 g, 14.83 mmol) as a THF (75 mL) solution was added dropwise over 10 min. The mixture was stirred for 30 min and then quenched through the addition of saturated ammonium chloride solution (300 mL). The mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (3×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 5.75 g of addition product (13f) as a tacky foam.

Compound 13f (5.75 g, 14.95 mmol) was dissolved in acetone (25 mL) and chilled to 0 C. The stirred solution was treated dropwise with 2.7M chromic acid (Jones Reagent) until the orange color of Cr (VI) persisted. After 1.5 hrs, the excess Cr (VI) was quenched through the addition of 2-propanol until the green color of Cr (IV) was evident. Water (300 mL) was added and the mixture was stirred until all the chromium salts were dissolved. The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (2×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 5.5 g (96%) of ketone (14f) as a stable foam.
Compound (14f) (5.5 g, 14.38 mmol) was dissolved in methanol (50 mL) and treated with 8.0 M KOH solution (9.35 mL, 74.77 mmol) and the mixture was heated at reflux for 5 hours. The mixture was cooled to 0 C and treated with acetic acid (25 mL) and water (10 mL) and the mixture was stirred at 50 C for 6 hours. The solvents were evaporated in vacuo and the residue was diluted with water (300 mL). The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (2×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 4.95 g (94%) of crude drospirenone as a stable foam. The crude drospirenone was dissolved in 60% ethyl acetate/hexanes and passed through a short column of neutral alumina (10× w/w) and the column was eluted with the same solvent. Following evaporation of the solvent, 3.43 g (65%) of crystalline drospirenone was obtained. Recrystallization from acetone/hexanes afforded pure drospirenone.
Drospirenone is a progestin medication which is used in birth control pills to prevent pregnancy and in menopausal hormone therapy, among other uses.[1][7] It is available both alone under the brand name Slynd and in combination with an estrogen under the brand name Yasmin among others.[7][2] The medication is taken by mouth.[2][1]
Common side effects include acne, headache, breast tenderness, weight increase, and menstrual changes.[2] Rare side effects may include high potassium levels and blood clots, among others.[2][8] Drospirenone is a progestin, or a synthetic progestogen, and hence is an agonist of the progesterone receptor, the biological target of progestogens like progesterone.[1] It has additional antimineralocorticoid and antiandrogenic activity and no other important hormonal activity.[1] Because of its antimineralocorticoid activity and lack of undesirable off-target activity, drospirenone is said to more closely resemble bioidentical progesterone than other progestins.[9][10]
Drospirenone was patented in 1976 and introduced for medical use in 2000.[11][12] It is available widely throughout the world.[7] The medication is sometimes referred to as a “fourth-generation” progestin.[13][14] It is available as a generic medication.[15] In 2018, a formulation of drospirenone with ethinylestradiol was the 167th most commonly prescribed medication in the United States, with more than 3 million prescriptions.[16][17]
Medical uses
Drospirenone (DRSP) is used by itself as a progestogen-only birth control pill, in combination with the estrogens ethinylestradiol (EE) or estetrol (E4), with or without supplemental folic acid (vitamin B9), as a combined birth control pill, and in combination with the estrogen estradiol (E2) for use in menopausal hormone therapy.[2] A birth control pill with low-dose ethinylestradiol is also indicated for the treatment of moderate acne, premenstrual syndrome (PMS), premenstrual dysphoric disorder (PMDD), and dysmenorrhea (painful menstruation).[18][19] For use in menopausal hormone therapy, E2/DRSP is specifically approved to treat moderate to severe vasomotor symptoms (hot flashes), vaginal atrophy, and postmenopausal osteoporosis.[20][21][22] The drospirenone component in this formulation is included specifically to prevent estrogen-induced endometrial hyperplasia.[23] Drospirenone has also been used in combination with an estrogen as a component of hormone therapy for transgender women.[24][25]
Studies have found that EE/DRSP is superior to placebo in reducing premenstrual emotional and physical symptoms while also improving quality of life.[26][27] E2/DRSP has been found to increase bone mineral density and to reduce the occurrence of bone fractures in postmenopausal women.[28][23][29][30] In addition, E2/DRSP has a favorable influence on cholesterol and triglyceride levels and decreases blood pressure in women with high blood pressure.[29][30] Due to its antimineralocorticoid activity, drospirenone opposes estrogen-induced salt and water retention and maintains or slightly reduces body weight.[31]
Available forms
Drospirenone is available in the following formulations, brand names, and indications:[32][33]
- Drospirenone 4 mg (Slynd) – progestogen-only birth control pill[2]
- Drospirenone 3 mg and estetrol 14.2 mg (Nextstellis (US)) – combined birth control pill[34][35][36]
- Ethinylestradiol 30 μg and drospirenone 3 mg (Ocella, Syeda, Yasmin, Zarah, Zumandimine) – combined birth control pill[37][38][39][40]
- Ethinylestradiol 20 μg and drospirenone 3 mg (Gianvi, Jasmiel, Loryna, Lo-Zumandimine, Nikki, Vestura, Yaz) – combined birth control pill, acne, PMS, PMDD, dysmenorrhea[18]
- Ethinylestradiol 30 μg, drospirenone 3 mg, and levomefolate calcium 0.451 mg (Beyaz, Tydemy) – combined birth control pill with vitamin B9 supplementation, acne, PMS[41][42]
- Estetrol 15 mg and drospirenone 3 mg (Nextstellis (CA)) – combined birth control pill[43][44]
- Estradiol 0.5 or 1 mg and drospirenone 0.25 or 0.5 mg (Angeliq) – menopausal hormone therapy (menopausal syndrome, postmenopausal osteoporosis)[20]
Contraindications
Contraindications of drospirenone include renal impairment or chronic kidney disease, adrenal insufficiency, presence or history of cervical cancer or other progestogen-sensitive cancers, benign or malignant liver tumors or hepatic impairment, undiagnosed abnormal uterine bleeding, and hyperkalemia (high potassium levels).[2][45][46] Renal impairment, hepatic impairment, and adrenal insufficiency are contraindicated because they increase exposure to drospirenone and/or increase the risk of hyperkalemia with drospirenone.[2]
Side effects
Adverse effects of drospirenone alone occurring in more than 1% of women may include unscheduled menstrual bleeding (breakthrough or intracyclic) (40.3–64.4%), acne (3.8%), metrorrhagia (2.8%), headache (2.7%), breast pain (2.2%), weight gain (1.9%), dysmenorrhea (1.9%), nausea (1.8%), vaginal hemorrhage (1.7%), decreased libido (1.3%), breast tenderness (1.2%), and irregular menstruation (1.2%).[2]
High potassium levels
Drospirenone is an antimineralocorticoid with potassium-sparing properties, though in most cases no increase of potassium levels is to be expected.[45] In women with mild or moderate chronic kidney disease, or in combination with chronic daily use of other potassium-sparing medications (ACE inhibitors, angiotensin II receptor antagonists, potassium-sparing diuretics, heparin, antimineralocorticoids, or nonsteroidal anti-inflammatory drugs), a potassium level should be checked after two weeks of use to test for hyperkalemia.[45][47] Persistent hyperkalemia that required discontinuation occurred in 2 out of around 1,000 women (0.2%) with 4 mg/day drospirenone alone in clinical trials.[2]
Blood clots
Birth control pills containing ethinylestradiol and a progestin are associated with an increased risk of venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE).[48] The incidence is about 4-fold higher on average than in women not taking a birth control pill.[48] The absolute risk of VTE with ethinylestradiol-containing birth control pills is small, in the area of 3 to 10 out of 10,000 women per year, relative to 1 to 5 out of 10,000 women per year not taking a birth control pill.[49][50] The risk of VTE during pregnancy is 5 to 20 in 10,000 women per year and during the postpartum period is 40 to 65 per 10,000 women per year.[50] The higher risk of VTE with combined birth control pills is thought to be due to the ethinylestradiol component, as ethinylestradiol has estrogenic effects on liver synthesis of coagulation factors which result in a procoagulatory state.[8] In contrast to ethinylestradiol-containing birth control pills, neither progestogen-only birth control nor the combination of transdermal estradiol and an oral progestin in menopausal hormone therapy is associated with an increased risk of VTE.[8][51]
Different progestins in ethinylestradiol-containing birth control pills have been associated with different risks of VTE.[8] Birth control pills containing progestins such as desogestrel, gestodene, drospirenone, and cyproterone acetate have been found to have 2- to 3-fold the risk of VTE of birth control pills containing levonorgestrel in retrospective cohort and nested case–control observational studies.[8][49] However, this area of research is controversial, and confounding factors may have been present in these studies.[8][49][52] Other observational studies, specifically prospective cohort and case control studies, have found no differences in risk between different progestins, including between birth control pills containing drospirenone and birth control pills containing levonorgestrel.[8][49][52][53] These kinds of observational studies have certain advantages over the aforementioned types of studies, like better ability to control for confounding factors.[53] Systematic reviews and meta-analyses of all of the data in the mid-to-late 2010s found that birth control pills containing cyproterone acetate, desogestrel, drospirenone, or gestodene overall were associated with a risk of VTE of about 1.3- to 2.0-fold compared to that of levonorgestrel-containing birth control pills.[54][55][49]
Androgenic progestins have been found to antagonize to some degree the effects of ethinylestradiol on coagulation.[56][57][58][59] As a result, more androgenic progestins, like levonorgestrel and norethisterone, may oppose the procoagulatory effects of ethinylestradiol and result in a lower increase in risk of VTE.[8][60] Conversely, this would be the case less or not at all with progestins that are less androgenic, like desogestrel and gestodene, as well as progestins that are antiandrogenic, like drospirenone and cyproterone acetate.[8][60]
In the early 2010s, the FDA updated the label for birth control pills containing drospirenone and other progestins to include warnings for stopping use prior to and after surgery, and to warn that such birth control pills may have a higher risk of blood clots.[46]
Breast cancer
Drospirenone has been found to stimulate the proliferation and migration of breast cancer cells in preclinical research, similarly to certain other progestins.[61][62] However, some evidence suggests that drospirenone may do this more weakly than certain other progestins, like medroxyprogesterone acetate.[61][62] The combination of estradiol and drospirenone has been found to increase breast density, an established risk factor for breast cancer, in postmenopausal women.[63][64][65]
Data on risk of breast cancer in women with newer progestins like drospirenone are lacking at present.[66] Progestogen-only birth control is not generally associated with a higher risk of breast cancer.[66] Conversely, combined birth control and menopausal hormone therapy with an estrogen and a progestogen are associated with higher risks of breast cancer.[67][66][68]
Overdose
These have been no reports of serious adverse effects with overdose of drospirenone.[2] Symptoms that may occur in the event of an overdose may include nausea, vomiting, and vaginal bleeding.[2] There is no antidote for overdose of drospirenone and treatment of overdose should be based on symptoms.[2] Since drospirenone has antimineralocorticoid activity, levels of potassium and sodium should be measured and signs of metabolic acidosis should be monitored.[2]
Interactions
Inhibitors and inducers of the cytochrome P450 enzyme CYP3A4 may influence the levels and efficacy of drospirenone.[2] Treatment for 10 days with 200 mg twice daily ketoconazole, a strong CYP3A4 inhibitor among other actions, has been found to result in a moderate 2.0- to 2.7-fold increase in exposure to drospirenone.[2] Drospirenone does not appear to influence the metabolism of omeprazole (metabolized via CYP2C19), simvastatin (metabolized via CYP3A4), or midazolam (metabolized via CYP3A4), and likely does not influence the metabolism of other medications that are metabolized via these pathways.[2] Drospirenone may interact with potassium-sparing medications such as ACE inhibitors, angiotensin II receptor antagonists, potassium-sparing diuretics, potassium supplements, heparin, antimineralocorticoids, and nonsteroidal anti-inflammatory drugs to further increase potassium levels.[2] This may increase the risk of hyperkalemia (high potassium levels).[2]
Pharmacology
Pharmacodynamics
Drospirenone binds with high affinity to the progesterone receptor (PR) and mineralocorticoid receptor (MR), with lower affinity to the androgen receptor (AR), and with very low affinity to the glucocorticoid receptor (GR).[1][69][70][4] It is an agonist of the PR and an antagonist of the MR and AR, and hence is a progestogen, antimineralocorticoid, and antiandrogen.[1][69][4][62] Drospirenone has no estrogenic activity and no appreciable glucocorticoid or antiglucocorticoid activity.[1][69][4][62]
Progestogenic activity
Drospirenone is an agonist of the PR, the biological target of progestogens like progesterone.[1][69] It has about 35% of the affinity of promegestone for the PR and about 19 to 70% of the affinity of progesterone for the PR.[1][3][62] Drospirenone has antigonadotropic and functional antiestrogenic effects as a result of PR activation.[1][69] The ovulation-inhibiting dosage of drospirenone is 2 to 3 mg/day.[72][73][1][74] Inhibition of ovulation occurred in about 90% of women at a dose of 0.5 to 2 mg/day and in 100% of women at a dose of 3 mg/day.[75] The total endometrial transformation dose of drospirenone is about 50 mg per cycle, whereas its daily dose is 2 mg for partial transformation and 4 to 6 mg for full transformation.[1][76][75] The medication acts as a contraceptive by activating the PR, which suppresses the secretion of luteinizing hormone, inhibits ovulation, and alters the cervical membrane and endometrium.[77][2]
Due to its antigonadotropic effects, drospirenone inhibits the secretion of the gonadotropins, luteinizing hormone (LH) and follicle-stimulating hormone (FSH), and suppresses gonadal sex hormone production, including of estradiol, progesterone, and testosterone.[1][78][3] Drospirenone alone at 4 mg/day has been found to suppress estradiol levels in premenopausal women to about 40 to 80 pg/mL depending on the time of the cycle.[78] No studies of the antigonadotropic effects of drospirenone or its influence on hormone levels appear to have been conducted in men.[79][80][81] In male cynomolgus monkeys however, 4 mg/kg/day oral drospirenone strongly suppressed testosterone levels.[69]
Antimineralocorticoid activity
Drospirenone is an antagonist of the MR, the biological target of mineralocorticoids like aldosterone, and hence is an antimineralocorticoid.[69] It has about 100 to 500% of the affinity of aldosterone for the MR and about 50 to 230% of the affinity of progesterone for the MR.[1][3][71][62] Drospirenone is about 5.5 to 11 times more potent as an antimineralocorticoid than spironolactone in animals.[69][75][82] Accordingly, 3 to 4 mg drospirenone is said to be equivalent to about 20 to 25 mg spironolactone in terms of antimineralocorticoid activity.[83][2] It has been said that the pharmacological profile of drospirenone more closely resembles that of progesterone than other progestins due to its antimineralocorticoid activity.[69] Drospirenone is the only clinically used progestogen with prominent antimineralocorticoid activity besides progesterone.[1] For comparison to progesterone, a 200 mg dose of oral progesterone is considered to be approximately equivalent in antimineralocorticoid effect to a 25 to 50 mg dose of spironolactone.[84] Both drospirenone and progesterone are actually weak partial agonists of the MR in the absence of mineralocorticoids.[4][3][62]
Due to its antimineralocorticoid activity, drospirenone increases natriuresis, decreases water retention and blood pressure, and produces compensatory increases in plasma renin activity as well as circulating levels and urinary excretion of aldosterone.[3][85][1] This has been shown to occur at doses of 2 to 4 mg/day.[3] Similar effects occur during the luteal phase of the menstrual cycle due to increased progesterone levels and the resulting antagonism of the MR.[3] Estrogens, particularly ethinylestradiol, activate liver production of angiotensinogen and increase levels of angiotensinogen and angiotensin II, thereby activating the renin–angiotensin–aldosterone system.[3][1] As a result, they can produce undesirable side effects including increased sodium excretion, water retention, weight gain, and increased blood pressure.[3] Progesterone and drospirenone counteract these undesirable effects via their antimineralocorticoid activity.[3] Accumulating research indicates that antimineralocorticoids like drospirenone and spironolactone may also have positive effects on adipose tissue and metabolic health.[86][87]
Antiandrogenic activity
Drospirenone is an antagonist of the AR, the biological target of androgens like testosterone and dihydrotestosterone (DHT).[1][3] It has about 1 to 65% of the affinity of the synthetic anabolic steroid metribolone for the AR.[1][3][4][62] The medication is more potent as an antiandrogen than spironolactone, but is less potent than cyproterone acetate, with about 30% of its antiandrogenic activity in animals.[1][88][69][75] Progesterone displays antiandrogenic activity in some assays similarly to drospirenone,[3] although this issue is controversial and many researchers regard progesterone as having no significant antiandrogenic activity.[89][1][4]
Drospirenone shows antiandrogenic effects on the serum lipid profile, including higher HDL cholesterol and triglyceride levels and lower LDL cholesterol levels, at a dose of 3 mg/day in women.[3] The medication does not inhibit the effects of ethinylestradiol on sex hormone-binding globulin (SHBG) and serum lipids, in contrast to androgenic progestins like levonorgestrel but similarly to other antiandrogenic progestins like cyproterone acetate.[3][1][74] SHBG levels are significantly higher with ethinylestradiol and cyproterone acetate than with ethinylestradiol and drospirenone, owing to the more potent antiandrogenic activity of cyproterone acetate relative to drospirenone.[90] Androgenic progestins like levonorgestrel have been found to inhibit the procoagulatory effects of estrogens like ethinylestradiol on hepatic synthesis of coagulation factors, whereas this may occur less or not at all with weakly androgenic progestins like desogestrel and antiandrogenic progestins like drospirenone.[8][60][56][57][58][59]
Other activity
Drospirenone stimulates the proliferation of MCF-7 breast cancer cells in vitro, an action that is independent of the classical PRs and is instead mediated via the progesterone receptor membrane component-1 (PGRMC1).[91] Certain other progestins act similarly in this assay, whereas progesterone acts neutrally.[91] It is unclear if these findings may explain the different risks of breast cancer observed with progesterone and progestins in clinical studies.[66]
Pharmacokinetics
Absorption
The oral bioavailability of drospirenone is between 66 and 85%.[1][3][4] Peak levels occur 1 to 6 hours after an oral dose.[1][3][2][82] Levels are about 27 ng/mL after a single 4 mg dose.[2] There is 1.5- to 2-fold accumulation in drospirenone levels with continuous administration, with steady-state levels of drospirenone achieved after 7 to 10 days of administration.[1][2][3] Peak levels of drospirenone at steady state with 4 mg/day drospirenone are about 41 ng/mL.[2] With the combination of 30 μg/day ethinylestradiol and 3 mg/day drospirenone, peak levels of drospirenone after a single dose are 35 ng/mL, and levels at steady state are 60 to 87 ng/mL at peak and 20 to 25 ng/mL at trough.[3][1] The pharmacokinetics of oral drospirenone are linear with a single dose across a dose range of 1 to 10 mg.[2][3] Intake of drospirenone with food does not influence the absorption of drospirenone.[2]
Distribution
The distribution half-life of drospirenone is about 1.6 to 2 hours.[3][1] The apparent volume of distribution of drospirenone is approximately 4 L/kg.[2] The plasma protein binding of drospirenone is 95 to 97%.[2][1] It is bound to albumin and 3 to 5% circulates freely or unbound.[2][1] Drospirenone has no affinity for sex hormone-binding globulin (SHBG) or corticosteroid-binding globulin (CBG), and hence is not bound by these plasma proteins in the circulation.[1]
Metabolism
The metabolism of drospirenone is extensive.[3] It is metabolized into the acid form of drospirenone by opening of its lactone ring.[1][2] The medication is also metabolized by reduction of its double bond between the C4 and C5 positions and subsequent sulfation.[1][2] The two major metabolites of drospirenone are drospirenone acid and 4,5-dihydrodrospirenone 3-sulfate, and are both formed independently of the cytochrome P450 system.[2][3] Neither of these metabolites are known to be pharmacologically active.[2] Drospirenone also undergoes oxidative metabolism by CYP3A4.[2][3][5][6]
Elimination
Drospirenone is excreted in urine and feces, with slightly more excreted in feces than in urine.[2] Only trace amounts of unchanged drospirenone can be found in urine and feces.[2] At least 20 different metabolites can be identified in urine and feces.[3] Drospirenone and its metabolites are excreted in urine about 38% as glucuronide conjugates, 47% as sulfate conjugates, and less than 10% in unconjugated form.[3] In feces, excretion is about 17% glucuronide conjugates, 20% sulfate conjugates, and 33% unconjugated.[3]
The elimination half-life of drospirenone is between 25 and 33 hours.[2][3][1] The half-life of drospirenone is unchanged with repeated administration.[2] Elimination of drospirenone is virtually complete 10 days after the last dose.[3][2]
Chemistry
See also: Spirolactone, List of progestogens § Spirolactone derivatives, and List of steroidal antiandrogens § Spirolactone derivatives
vteChemical structures of spirolactones ProgesteroneSpirolactoneCanrenoneSpironolactoneDrospirenoneSpirorenone ProgesteroneSpirolactoneCanrenoneSpironolactoneDrospirenoneSpirorenone |
Drospirenone, also known as 1,2-dihydrospirorenone or as 17β-hydroxy-6β,7β:15β,16β-dimethylene-3-oxo-17α-pregn-4-ene-21-carboxylic acid, γ-lactone, is a synthetic steroidal 17α-spirolactone, or more simply a spirolactone.[7][92] It is an analogue of other spirolactones like spironolactone, canrenone, and spirorenone.[7][92] Drospirenone differs structurally from spironolactone only in that the C7α acetylthio substitution of spironolactone has been removed and two methylene groups have been substituted in at the C6β–7β and C15β–16β positions.[93]
Spirolactones like drospirenone and spironolactone are derivatives of progesterone, which likewise has progestogenic and antimineralocorticoid activity.[94][95][96] The loss of the C7α acetylthio group of spironolactone, a compound with negligible progestogenic activity,[97][98] appears to be involved in the restoration of progestogenic activity in drospirenone, as SC-5233, the analogue of spironolactone without a C7α substitution, has potent progestogenic activity similarly to drospirenone.[99]
History
Drospirenone was patented in 1976 and introduced for medical use in 2000.[11][12] Schering AG of Germany has been granted several patents on the production of drospirenone, including WIPO and US patents, granted in 1998 and 2000, respectively.[100][101] It was introduced for medical use in combination with ethinylestradiol as a combined birth control pill in 2000.[11] Drospirenone is sometimes described as a “fourth-generation” progestin based on its time of introduction.[13][14] The medication was approved for use in menopausal hormone therapy in combination with estradiol in 2005.[20] Drospirenone was introduced for use as a progestogen-only birth control pill in 2019.[2] A combined birth control pill containing estetrol and drospirenone was approved in 2021.[102]
Society and culture
Generic names
Drospirenone is the generic name of the drug and its INN, USAN, BAN, and JAN, while drospirénone is its DCF.[7] Its name is a shortened form of the name 1,2-dihydrospirorenone or dihydrospirenone.[7][92] Drospirenone is also known by its developmental code names SH-470 and ZK-30595 (alone), BAY 86-5300, BAY 98-7071, and SH-T-00186D (in combination with ethinylestradiol), BAY 86-4891 (in combination with estradiol), and FSN-013 (in combination with estetrol).[7][92][103][104][105][106][102]
Brand names
Drospirenone is marketed in combination with an estrogen under a variety of brand names throughout the world.[7] Among others, it is marketed in combination with ethinylestradiol under the brand names Yasmin and Yaz, in combination with estetrol under the brand name Nextstellis, and in combination with estradiol under the brand name Angeliq.[7][102]
Availability
See also: List of progestogens available in the United States
Drospirenone is marketed widely throughout the world.[7]
Generation
Drospirenone has been categorized as a “fourth-generation” progestin.[62]
Litigation
Many lawsuits have been filed against Bayer, the manufacturer of drospirenone, due to the higher risk of venous thromboembolism (VTE) that has been observed with combined birth control pills containing drospirenone and certain other progestins relative to the risk with levonorgestrel-containing combined birth control pills.[52]
In July 2012, Bayer notified its stockholders that there were more than 12,000 such lawsuits against the company involving Yaz, Yasmin, and other birth control pills with drospirenone.[107] They also noted that the company by then had settled 1,977 cases for US$402.6 million, for an average of US$212,000 per case, while setting aside US$610.5 million to settle the others.[107]
As of July 17, 2015, there have been at least 4,000 lawsuits and claims still pending regarding VTE related to drospirenone.[108] This is in addition to around 10,000 claims that Bayer has already settled without admitting liability.[108] These claims of VTE have amounted to US$1.97 billion.[108] Bayer also reached a settlement for arterial thromboembolic events, including stroke and heart attacks, for US$56.9 million.[108]
Research
See also: Estetrol/drospirenone and Ethinylestradiol/drospirenone/prasterone
A combination of ethinylestradiol, drospirenone, and prasterone is under development by Pantarhei Bioscience as a combined birth control pill for prevention of pregnancy in women.[109] It includes prasterone (dehydroepiandrosterone; DHEA), an oral androgen prohormone, to replace testosterone and avoid testosterone deficiency caused by suppression of testosterone by ethinylestradiol and drospirenone.[109] As of August 2018, the formulation is in phase II/III clinical trials.[109]
Drospirenone has been suggested for potential use as a progestin in male hormonal contraception.[79]
Drospirenone has been studied in forms for parenteral administration.[110][111][112][113]
References
- ^ Jump up to:a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai ajak al Kuhl, H (2005). “Pharmacology of estrogens and progestogens: influence of different routes of administration”. Climacteric. 8 (sup1): 3–63. doi:10.1080/13697130500148875. ISSN 1369-7137. PMID 16112947. S2CID 24616324.
- ^ Jump up to:a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai ajak al am an ao ap aq ar as at au “Slynd- drospirenone tablet, film coated”. DailyMed. Retrieved 17 April 2021.
- ^ Jump up to:a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ahKrattenmacher, Rolf (2000). “Drospirenone: pharmacology and pharmacokinetics of a unique progestogen”. Contraception. 62 (1): 29–38. doi:10.1016/S0010-7824(00)00133-5. ISSN 0010-7824. PMID 11024226.
- ^ Jump up to:a b c d e f g h i Stanczyk FZ, Hapgood JP, Winer S, Mishell DR (April 2013). “Progestogens used in postmenopausal hormone therapy: differences in their pharmacological properties, intracellular actions, and clinical effects”. Endocr. Rev. 34 (2): 171–208. doi:10.1210/er.2012-1008. PMC 3610676. PMID 23238854.
- ^ Jump up to:a b Bachmann, Gloria (2009). “Drospirenone/ethinyl estradiol 3 mg/20 μg (24/4 day regimen): hormonal contraceptive choices – use of a fourth-generation progestin”. Patient Preference and Adherence. 3: 259–64. doi:10.2147/PPA.S3901. ISSN 1177-889X. PMC 2778416. PMID 19936169.
- ^ Jump up to:a b Wiesinger, Herbert; Berse, Matthias; Klein, Stefan; Gschwend, Simone; Höchel, Joachim; Zollmann, Frank S.; Schütt, Barbara (2015). “Pharmacokinetic interaction between the CYP3A4 inhibitor ketoconazole and the hormone drospirenone in combination with ethinylestradiol or estradiol”. British Journal of Clinical Pharmacology. 80 (6): 1399–1410. doi:10.1111/bcp.12745. ISSN 0306-5251. PMC 4693482. PMID 26271371.
- ^ Jump up to:a b c d e f g h i j k “Drospirenone”.
- ^ Jump up to:a b c d e f g h i j Han L, Jensen JT (December 2015). “Does the Progestogen Used in Combined Hormonal Contraception Affect Venous Thrombosis Risk?”. Obstet. Gynecol. Clin. North Am. 42(4): 683–98. doi:10.1016/j.ogc.2015.07.007. PMID 26598309.
- ^ Oelkers W (December 2000). “Drospirenone–a new progestogen with antimineralocorticoid activity, resembling natural progesterone”. Eur J Contracept Reprod Health Care. 5 Suppl 3: 17–24. PMID 11246598.
- ^ Oelkers W (December 2002). “Antimineralocorticoid activity of a novel oral contraceptive containing drospirenone, a unique progestogen resembling natural progesterone”. Eur J Contracept Reprod Health Care. 7 Suppl 3: 19–26, discussion 42–3. PMID 12659403.
- ^ Jump up to:a b c Enrique Ravina (11 January 2011). The Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs. John Wiley & Sons. pp. 193–. ISBN 978-3-527-32669-3.
- ^ Jump up to:a b Fischer, Jnos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 459. ISBN 9783527607495.
- ^ Jump up to:a b Robert Anthony Hatcher; Anita L. Nelson, M.D. (2007). Contraceptive Technology. Ardent Media. pp. 196–. ISBN 978-1-59708-001-9.
- ^ Jump up to:a b James Q. Del Rosso; Joshua A. Zeichner (20 April 2016). Advances in Acne Management, An Issue of Dermatologic Clinics, E-Book. Elsevier Health Sciences. pp. 160–. ISBN 978-0-323-41753-2.
- ^ “Generic Yasmin Availability”.
- ^ “The Top 300 of 2021”. ClinCalc. Retrieved 18 February 2021.
- ^ “Drospirenone; Ethinyl Estradiol – Drug Usage Statistics”. ClinCalc. Retrieved 18 February 2021.
- ^ Jump up to:a b “Yaz- drospirenone and ethinyl estradiol kit”. DailyMed. Retrieved 17 April 2021.
- ^ Cerner Multum, Inc. (June 11, 2012). “drospirenone and ethinyl estradiol”. Auckland, New Zealand: Drugs.com. Retrieved October 24, 2011.
- ^ Jump up to:a b c “Angeliq- drospirenone and estradiol tablet, film coated”. DailyMed. Retrieved 17 April 2021.
- ^ Maclennan, A. H.; Broadbent, J. L.; Lester, S.; Moore, V. (18 October 2004). “Oral oestrogen and combined oestrogen/progestogen therapy versus placebo for hot flushes”. The Cochrane Database of Systematic Reviews (4): CD002978. doi:10.1002/14651858.CD002978.pub2. ISSN 1469-493X. PMC 7004247. PMID 15495039.
- ^ Torgerson, D. J.; Bell-Syer, S. E. (13 June 2001). “Hormone replacement therapy and prevention of nonvertebral fractures: a meta-analysis of randomized trials”. JAMA. 285 (22): 2891–2897. doi:10.1001/jama.285.22.2891. ISSN 0098-7484. PMID 11401611. S2CID 25078579.
- ^ Jump up to:a b Whitehead M (March 2006). “Hormone replacement therapy with estradiol and drospirenone: an overview of the clinical data”. J Br Menopause Soc. 12 Suppl 1: 4–7. doi:10.1258/136218006775992185. PMID 16513012. S2CID 38095916.
- ^ Majumder A, Sanyal D (2017). “Outcome and preferences in male-to-female subjects with gender dysphoria: Experience from Eastern India”. Indian J Endocrinol Metab. 21 (1): 21–25. doi:10.4103/2230-8210.196000. PMC 5240066. PMID 28217493.
- ^ Majumder, Anirban; Chatterjee, Sudip; Maji, Debasis; Roychaudhuri, Soumyabrata; Ghosh, Sujoy; Selvan, Chitra; George, Belinda; Kalra, Pramila; Maisnam, Indira; Sanyal, Debmalya (2020). “IDEA group consensus statement on medical management of adult gender incongruent individuals seeking gender reaffirmation as female”. Indian Journal of Endocrinology and Metabolism. 24 (2): 128–135. doi:10.4103/ijem.IJEM_593_19. ISSN 2230-8210. PMC 7333765. PMID 32699777.
- ^ Lanza di Scalea, Teresa (June 2017). “Premenstrual Dysphoric Disorder”. Psychiatric Clinics of North America. 40 (2): 201–206. doi:10.1016/j.psc.2017.01.002. PMID 28477648.
- ^ Lopez LM, Kaptein AA, Helmerhorst FM (February 2012). “Oral contraceptives containing drospirenone for premenstrual syndrome”. Cochrane Database Syst Rev (2): CD006586. doi:10.1002/14651858.CD006586.pub4. PMID 22336820.
- ^ Christiansen C (October 2005). “Effects of drospirenone/estrogen combinations on bone metabolism”. Climacteric. 8 Suppl 3: 35–41. doi:10.1080/13697130500330283. PMID 16203654. S2CID 42803561.
- ^ Jump up to:a b Archer DF (February 2007). “Drospirenone and estradiol: a new option for the postmenopausal woman”. Climacteric. 10 Suppl 1: 3–10. doi:10.1080/13697130601114859. PMID 17364592. S2CID 9221524.
- ^ Jump up to:a b “Drospirenone in HRT?”. Drug Ther Bull. 47 (4): 41–4. April 2009. doi:10.1136/dtb.2009.03.0011. PMID 19357298. S2CID 1909717.
- ^ Foidart JM, Faustmann T (December 2007). “Advances in hormone replacement therapy: weight benefits of drospirenone, a 17alpha-spirolactone-derived progestogen”. Gynecol. Endocrinol. 23 (12): 692–9. doi:10.1080/09513590701582323. PMID 18075844. S2CID 12572825.
- ^ “Drugs@FDA: FDA Approved Drug Products”. United States Food and Drug Administration. Retrieved 23 December 2019.
- ^ Research, Center for Drug Evaluation and. “Drug Safety and Availability – FDA Drug Safety Communication: Updated information about the risk of blood clots in women taking birth control pills containing drospirenone”. http://www.fda.gov. Retrieved 2017-11-07.
- ^https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/214154s000lbl.pdf
- ^https://www.maynepharma.com/media/2507/mayne_pharma_drsp-e4_news_release_041421.pdf
- ^ https://www.maynepharma.com/media/2506/fda-approval-of-novel-oral-contraceptive-nextstellis.pdf
- ^ “Ocella- drospirenone and ethinyl estradiol kit”. DailyMed. Retrieved 17 April 2021.
- ^ “Syeda- drospirenone and ethinyl estradiol kit”. DailyMed. Retrieved 17 April 2021.
- ^ “Yasmin- drospirenone and ethinyl estradiol kit”. DailyMed. Retrieved 17 April 2021.
- ^ “Zarah- drospirenone and ethinyl estradiol kit”. DailyMed. Retrieved 17 April 2021.
- ^ “Beyaz- drospirenone/ethinyl estradiol/levomefolate calcium and levomefolate calcium kit”. DailyMed. Retrieved 17 April 2021.
- ^ “Tydemy- drospirenone, ethinyl estradiol and levomefolate calcium and levomefolate calcium kit”. DailyMed. Retrieved 17 April 2021.
- ^https://web.archive.org/web/20210413054728/https://pdf.hres.ca/dpd_pm/00060352.PDF
- ^ “Mithra and Searchlight Pharma Announce Nextstellis Approval in Canada”. Searchlight Pharma (Press release). 8 March 2021. Retrieved 17 April 2021.
- ^ Jump up to:a b c Bayer (March 25, 2013). “Summary of Product Characteristics (SPC): Yasmin”. London: electronic Medicines Compendium (eMC), Datapharm. Retrieved April 24, 2014.
4.3. Contraindications: • Severe chronic kidney disease or acute kidney failure. • Presence or history of severe hepatic disease as long as liver function values have not returned to normal.
- ^ Jump up to:a b Bayer (April 10, 2012). “Yasmin full prescribing information”(PDF). Silver Spring, Md.: Food and Drug Administration (FDA). Retrieved April 14, 2012.
4. Contraindications: • Renal impairment. • Adrenal insufficiency. • Liver disease.
- ^ Nelson, Anita L.; Cwiak, Carrie (2011). “Combined oral contraceptives (COCs)”. In Hatcher, Robert A.; Trussell, James; Nelson, Anita L.; Cates, Willard Jr.; Kowal, Deborah; Policar, Michael S. (eds.). Contraceptive Technology (20th revised ed.). New York: Ardent Media. pp. 249–341. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734.
- ^ Jump up to:a b Heit JA, Spencer FA, White RH (2016). “The epidemiology of venous thromboembolism”. J. Thromb. Thrombolysis. 41 (1): 3–14. doi:10.1007/s11239-015-1311-6. PMC 4715842. PMID 26780736.
- ^ Jump up to:a b c d e Bateson D, Butcher BE, Donovan C, Farrell L, Kovacs G, Mezzini T, Raynes-Greenow C, Pecoraro G, Read C, Baber R (2016). “Risk of venous thromboembolism in women taking the combined oral contraceptive: A systematic review and meta-analysis”. Aust Fam Physician. 45 (1): 59–64. PMID 27051991.
- ^ Jump up to:a b “FDA Drug Safety Communication: Updated information about the risk of blood clots in women taking birth control pills containing drospirenone”. April 27, 2019. Archived from the original on 2019-04-27.
- ^ Vinogradova Y, Coupland C, Hippisley-Cox J (January 2019). “Use of hormone replacement therapy and risk of venous thromboembolism: nested case-control studies using the QResearch and CPRD databases”. BMJ. 364: k4810. doi:10.1136/bmj.k4810. PMC 6326068. PMID 30626577.
- ^ Jump up to:a b c Batur P, Casey PM (February 2017). “Drospirenone Litigation: Does the Punishment Fit the Crime?”. J Womens Health (Larchmt). 26 (2): 99–102. doi:10.1089/jwh.2016.6092. PMID 27854556.
- ^ Jump up to:a b Sitruk-Ware R (November 2016). “Hormonal contraception and thrombosis”. Fertil. Steril. 106 (6): 1289–1294. doi:10.1016/j.fertnstert.2016.08.039. PMID 27678035.
- ^ Oedingen C, Scholz S, Razum O (May 2018). “Systematic review and meta-analysis of the association of combined oral contraceptives on the risk of venous thromboembolism: The role of the progestogen type and estrogen dose”. Thromb. Res. 165: 68–78. doi:10.1016/j.thromres.2018.03.005. PMID 29573722.
- ^ Dragoman MV, Tepper NK, Fu R, Curtis KM, Chou R, Gaffield ME (June 2018). “A systematic review and meta-analysis of venous thrombosis risk among users of combined oral contraception”. Int J Gynaecol Obstet. 141 (3): 287–294. doi:10.1002/ijgo.12455. PMC 5969307. PMID 29388678.
- ^ Jump up to:a b Wiegratz I, Kuhl H (September 2006). “Metabolic and clinical effects of progestogens”. Eur J Contracept Reprod Health Care. 11(3): 153–61. doi:10.1080/13625180600772741. PMID 17056444. S2CID 27088428.
- ^ Jump up to:a b Kuhl H (May 1996). “Effects of progestogens on haemostasis”. Maturitas. 24 (1–2): 1–19. doi:10.1016/0378-5122(96)00994-2. PMID 8794429.
- ^ Jump up to:a b Sitruk-Ware R, Nath A (February 2013). “Characteristics and metabolic effects of estrogen and progestins contained in oral contraceptive pills”. Best Pract. Res. Clin. Endocrinol. Metab. 27 (1): 13–24. doi:10.1016/j.beem.2012.09.004. PMID 23384742.
- ^ Jump up to:a b Nelson AL (2015). “An update on new orally administered contraceptives for women”. Expert Opin Pharmacother. 16 (18): 2759–72. doi:10.1517/14656566.2015.1100173. PMID 26512437. S2CID 207481206.
- ^ Jump up to:a b c Farris M, Bastianelli C, Rosato E, Brosens I, Benagiano G (October 2017). “Pharmacodynamics of combined estrogen-progestin oral contraceptives: 2. effects on hemostasis”. Expert Rev Clin Pharmacol. 10 (10): 1129–1144. doi:10.1080/17512433.2017.1356718. PMID 28712325. S2CID 205931204.
- ^ Jump up to:a b Simoncini T, Genazzani AR (February 2010). “A review of the cardiovascular and breast actions of drospirenone in preclinical studies”. Climacteric. 13 (1): 22–33. doi:10.3109/13697130903437375. PMID 19938948. S2CID 4306359.
- ^ Jump up to:a b c d e f g h i j Africander D, Verhoog N, Hapgood JP (June 2011). “Molecular mechanisms of steroid receptor-mediated actions by synthetic progestins used in HRT and contraception”. Steroids. 76 (7): 636–52. doi:10.1016/j.steroids.2011.03.001. PMID 21414337. S2CID 23630452.
- ^ Palacios S, Mejía A (November 2016). “Progestogen safety and tolerance in hormonal replacement therapy”. Expert Opin Drug Saf. 15 (11): 1515–1525. doi:10.1080/14740338.2016.1223041. PMID 27548404. S2CID 31497860.
- ^ Caglayan EK, Caglayan K, Alkis I, Arslan E, Okur A, Banli O, Engin-Ustün Y (August 2015). “Factors Associated with Mammographic Density in Postmenopausal Women”. J Menopausal Med. 21 (2): 82–8. doi:10.6118/jmm.2015.21.2.82. PMC 4561745. PMID 26357645.
- ^ Hirschberg AL, Tani E, Brismar K, Lundström E (August 2019). “Effects of drospirenone and norethisterone acetate combined with estradiol on mammographic density and proliferation of breast epithelial cells-A prospective randomized trial”. Maturitas. 126: 18–24. doi:10.1016/j.maturitas.2019.04.205. PMID 31239112.
- ^ Jump up to:a b c d Trabert B, Sherman ME, Kannan N, Stanczyk FZ (September 2019). “Progesterone and breast cancer”. Endocr. Rev. 41 (2): 320–344. doi:10.1210/endrev/bnz001. PMC 7156851. PMID 31512725.
- ^ Collaborative Group on Hormonal Factors in Breast Cancer (September 2019). “Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence”. Lancet. 394 (10204): 1159–1168. doi:10.1016/S0140-6736(19)31709-X. PMC 6891893. PMID 31474332.
- ^ Sturdee DW (2013). “Are progestins really necessary as part of a combined HRT regimen?”. Climacteric. 16 Suppl 1: 79–84. doi:10.3109/13697137.2013.803311. PMID 23651281. S2CID 21894200.
- ^ Jump up to:a b c d e f g h i j Muhn P, Fuhrmann U, Fritzemeier KH, Krattenmacher R, Schillinger E (1995). “Drospirenone: a novel progestogen with antimineralocorticoid and antiandrogenic activity”. Ann. N. Y. Acad. Sci. 761 (3): 311–35. Bibcode:1995NYASA.761..311M. doi:10.1111/j.1749-6632.1995.tb31386.x. PMID 7625729. S2CID 36861309.
- ^ Fuhrmann, Ulrike; Krattenmacher, Rolf; Slater, Emily P.; Fritzemeier, Karl-Heinrich (1996). “The novel progestin drospirenone and its natural counterpart progesterone: Biochemical profile and antiandrogenic potential”. Contraception. 54 (4): 243–251. doi:10.1016/S0010-7824(96)00195-3. ISSN 0010-7824. PMID 8922878.
- ^ Jump up to:a b Hapgood JP, Africander D, Louw R, Ray RM, Rohwer JM (July 2014). “Potency of progestogens used in hormonal therapy: toward understanding differential actions”. J. Steroid Biochem. Mol. Biol. 142: 39–47. doi:10.1016/j.jsbmb.2013.08.001. PMID 23954501. S2CID 12142015.
- ^ Bastianelli C, Farris M, Rosato E, Brosens I, Benagiano G (November 2018). “Pharmacodynamics of combined estrogen-progestin oral contraceptives 3. Inhibition of ovulation”. Expert Rev Clin Pharmacol. 11 (11): 1085–1098. doi:10.1080/17512433.2018.1536544. PMID 30325245. S2CID 53246678.
- ^ Endrikat J, Gerlinger C, Richard S, Rosenbaum P, Düsterberg B (December 2011). “Ovulation inhibition doses of progestins: a systematic review of the available literature and of marketed preparations worldwide”. Contraception. 84 (6): 549–57. doi:10.1016/j.contraception.2011.04.009. PMID 22078182.
- ^ Jump up to:a b Kuhl H (2011). “Pharmacology of Progestogens” (PDF). J Reproduktionsmed Endokrinol. 8 (1): 157–177.
- ^ Jump up to:a b c d Elger W, Beier S, Pollow K, Garfield R, Shi SQ, Hillisch A (November 2003). “Conception and pharmacodynamic profile of drospirenone”. Steroids. 68 (10–13): 891–905. doi:10.1016/j.steroids.2003.08.008. PMID 14667981. S2CID 41756726.
- ^ Schindler AE, Campagnoli C, Druckmann R, Huber J, Pasqualini JR, Schweppe KW, Thijssen JH (December 2003). “Classification and pharmacology of progestins”. Maturitas. 46 Suppl 1: S7–S16. doi:10.1016/j.maturitas.2003.09.014. PMID 14670641.
- ^ “Drospirenone”. pubchem.ncbi.nlm.nih.gov.
- ^ Jump up to:a b Hadji P, Colli E, Regidor PA (December 2019). “Bone health in estrogen-free contraception”. Osteoporos Int. 30 (12): 2391–2400. doi:10.1007/s00198-019-05103-6. PMC 7203087. PMID 31446440.
- ^ Jump up to:a b Cornia, Paul B; Anawalt, Bradley D (2005). “Male hormonal contraceptives: a potentially patentable and profitable product”. Expert Opinion on Therapeutic Patents. 15 (12): 1727–1737. doi:10.1517/13543776.15.12.1727. ISSN 1354-3776. S2CID 83941717.
- ^ Nieschlag E (2010). “Clinical trials in male hormonal contraception” (PDF). Contraception. 82 (5): 457–70. doi:10.1016/j.contraception.2010.03.020. PMID 20933120.
- ^ Nieschlag, Eberhard; Behre, Hermann M.; Nieschlag, Eberhard; Behre, Hermann M.; Nieschlag, Susan (2012). “The essential role of testosterone in hormonal male contraception”. In Nieschlag, Eberhard; Behre, Hermann M; Nieschlag, Susan (eds.). Testosterone. pp. 470–493. doi:10.1017/CBO9781139003353.023. ISBN 9781139003353.
- ^ Jump up to:a b Stanczyk, Frank Z. (2007). “Structure –Function Relationships, Pharmacokinetics, and Potency of Orally and Parenterally Administered Progestogens”. Treatment of the Postmenopausal Woman. pp. 779–798. doi:10.1016/B978-012369443-0/50067-3. ISBN 9780123694430.
- ^ Hermann P.G. Schneider; Frederick Naftolin (22 September 2004). Climacteric Medicine – Where Do We Go?: Proceedings of the 4th Workshop of the International Menopause Society. CRC Press. pp. 133–. ISBN 978-0-203-02496-6.
- ^ Simon JA (December 1995). “Micronized progesterone: vaginal and oral uses”. Clinical Obstetrics and Gynecology. 38 (4): 902–14. doi:10.1097/00003081-199538040-00024. PMID 8616985.
- ^ Genazzani, Andrea R.; Mannella, Paolo; Simoncini, Tommaso (February 2007). “Drospirenone and its antialdosterone properties”. Climacteric. 10 (Supplement 1): 11–18. doi:10.1080/13697130601114891. PMID 17364593. S2CID 24872884. Retrieved November 26, 2011.
- ^ Infante, Marco; Armani, Andrea; Marzolla, Vincenzo; Fabbri, Andrea; Caprio, Massimiliano (2019). “Adipocyte Mineralocorticoid Receptor”. Vitamins and Hormones. Elsevier. 109: 189–209. doi:10.1016/bs.vh.2018.10.005. ISBN 9780128177822. ISSN 0083-6729. PMID 30678856.
- ^ Giordano A, Frontini A, Cinti S (June 2016). “Convertible visceral fat as a therapeutic target to curb obesity”. Nat Rev Drug Discov. 15(6): 405–24. doi:10.1038/nrd.2016.31. PMID 26965204. S2CID 2632187.
- ^ Sitruk-Ware R, Husmann F, Thijssen JH, Skouby SO, Fruzzetti F, Hanker J, Huber J, Druckmann R (September 2004). “Role of progestins with partial antiandrogenic effects”. Climacteric. 7 (3): 238–54. doi:10.1080/13697130400001307. PMID 15669548. S2CID 23112620.
- ^ Yeh YT, Chang CW, Wei RJ, Wang SN (2013). “Progesterone and related compounds in hepatocellular carcinoma: basic and clinical aspects”. Biomed Res Int. 2013: 290575. doi:10.1155/2013/290575. PMC 3581253. PMID 23484104.
- ^ Schindler, Adolf E. (2015). “Hormonal Contraceptives: Progestogen and Thrombotic Risk”. Frontiers in Gynecological Endocrinology. ISGE Series. pp. 69–75. doi:10.1007/978-3-319-09662-9_8. ISBN 978-3-319-09661-2. ISSN 2197-8735.
- ^ Jump up to:a b Neubauer H, Ma Q, Zhou J, Yu Q, Ruan X, Seeger H, Fehm T, Mueck AO (October 2013). “Possible role of PGRMC1 in breast cancer development”. Climacteric. 16 (5): 509–13. doi:10.3109/13697137.2013.800038. PMID 23758160. S2CID 29808177.
- ^ Jump up to:a b c d Martin Negwer; Hans-Georg Scharnow (4 October 2001). Organic-chemical drugs and their synonyms: (an international survey). Wiley-VCH. p. 2539. ISBN 978-3-527-30247-5.
- ^ Howard J.A. Carp (9 April 2015). Progestogens in Obstetrics and Gynecology. Springer. pp. 115–. ISBN 978-3-319-14385-9.
- ^ Ménard J (2004). “The 45-year story of the development of an anti-aldosterone more specific than spironolactone”. Mol. Cell. Endocrinol. 217 (1–2): 45–52. doi:10.1016/j.mce.2003.10.008. PMID 15134800. S2CID 19701784.
[Spironolactone] was synthesized after the demonstration of the natriuretic effect of progesterone (Landau et al., 1955).
- ^ J. Larry Jameson; Leslie J. De Groot (18 May 2010). Endocrinology – E-Book: Adult and Pediatric. Elsevier Health Sciences. pp. 2401–. ISBN 978-1-4557-1126-0.
[Spironolactone] is a potent antimineralocorticoid which was developed as a progestational analog […]
- ^ Aldosterone. Elsevier Science. 23 January 2019. p. 46. ISBN 978-0-12-817783-9.
In addition to spironolactone, which is a derivative of progesterone […]
- ^ Hu X, Li S, McMahon EG, Lala DS, Rudolph AE (2005). “Molecular mechanisms of mineralocorticoid receptor antagonism by eplerenone”. Mini Rev Med Chem. 5 (8): 709–18. doi:10.2174/1389557054553811. PMID 16101407.
- ^ Nakajima ST, Brumsted JR, Riddick DH, Gibson M (1989). “Absence of progestational activity of oral spironolactone”. Fertil. Steril. 52 (1): 155–8. doi:10.1016/s0015-0282(16)60807-5. PMID 2744183.
- ^ Hertz R, Tullner WW (1958). “Progestational activity of certain steroid-17-spirolactones”. Proc. Soc. Exp. Biol. Med. 99 (2): 451–2. doi:10.3181/00379727-99-24380. PMID 13601900. S2CID 20150966.
- ^ WO patent 9806738, Mohr, Jörg-Thorsten & Klaus Nickisch, “PROCESS FOR PRODUCING DROSPIRENONE (6ss,7ss;15ss,16ss-DIMETHYLENE-3-OXO-17 alpha -PREGN-4-EN-21,17-CARBOLACTONE, DRSP), AS WELL AS 7 alpha -(3-HYDROXY-1-PROPYL)-6ss,7ss;15ss,16ss-DIMETHYLENE-5ss-ANDROSTANE-3ss,5,17ss-TRIOL (ZK 92836) AND 6ss,7ss;15ss,16ss-DIMETHYLENE-5ss HYDROXY-5-OXO-17 alpha -ANDROSTANE-21, 17-CARBOLACTONE”, issued 1998-02-19, assigned to Shering AG
- ^ US patent 6121465, Mohr, Joerg-Thorston & Klaus Nickisch, “Process for production drospirenone and intermediate products of the process”, issued 2000-09-19, assigned to Scheiring AG and Bayer Schering Pharma
- ^ Jump up to:a b c “Drospirenone/Estetrol – Mithra Pharmaceuticals – AdisInsight”.
- ^ “Ethinylestradiol/drospirenone – AdisInsight”.
- ^ “Ethinylestradiol/drospirenone/folic acid – AdisInsight”.
- ^ “Drospirenone/ethinylestradiol low-dose – Bayer HealthCare Pharmaceuticals – AdisInsight”.
- ^ “Estradiol/drospirenone – Bayer HealthCare Pharmaceuticals – AdisInsight”.
- ^ Jump up to:a b Feeley, Jef; Kresge, Naomi (July 31, 2012). “Bayer’s Yasmin lawsuit settlements rise to $402.6 million”. Bloomberg News. New York. Retrieved November 11, 2012.
- ^ Jump up to:a b c d AG, Bayer. “Quarterly Reports of Bayer”. http://www.bayer.com.
- ^ Jump up to:a b c “Drospirenone/estradiol/prasterone – ANI Pharmaceuticals/Pantarhei Bioscience – AdisInsight”. adisinsight.springer.com.
- ^ Nippe S, General S (September 2011). “Parenteral oil-based drospirenone microcrystal suspensions-evaluation of physicochemical stability and influence of stabilising agents”. Int J Pharm. 416 (1): 181–8. doi:10.1016/j.ijpharm.2011.06.036. PMID 21729745.
- ^ Nippe S, General S (November 2012). “Combination of injectable ethinyl estradiol and drospirenone drug-delivery systems and characterization of their in vitro release”. Eur J Pharm Sci. 47 (4): 790–800. doi:10.1016/j.ejps.2012.08.009. PMID 22940138.
- ^ Nippe S, Preuße C, General S (February 2013). “Evaluation of the in vitro release and pharmacokinetics of parenteral injectable formulations for steroids”. Eur J Pharm Biopharm. 83 (2): 253–65. doi:10.1016/j.ejpb.2012.09.006. PMID 23116659.
- ^ Nippe S, General S (April 2015). “Investigation of injectable drospirenone organogels with regard to their rheology and comparison to non-stabilized oil-based drospirenone suspensions”. Drug Dev Ind Pharm. 41 (4): 681–91. doi:10.3109/03639045.2014.895375. PMID 24621345. S2CID 42932558.
Further reading
- Archer DF (February 2007). “Drospirenone and estradiol: a new option for the postmenopausal woman”. Climacteric. 10 Suppl 1: 3–10. doi:10.1080/13697130601114859. PMID 17364592. S2CID 9221524.
- Archer DF (February 2007). “Drospirenone-containing hormone therapy for postmenopausal women. Perspective on current data”. J Reprod Med. 52 (2 Suppl): 159–64. PMID 17477110.
- Archer DF (2007). “Drospirenone, a progestin with added value for hypertensive postmenopausal women”. Menopause. 14 (3 Pt 1): 352–4. doi:10.1097/gme.0b013e31804d440b. PMID 17414576.
- Batur P, Casey PM (February 2017). “Drospirenone Litigation: Does the Punishment Fit the Crime?”. J Womens Health (Larchmt). 26 (2): 99–102. doi:10.1089/jwh.2016.6092. PMID 27854556.
- Bitzer J, Paoletti AM (2009). “Added benefits and user satisfaction with a low-dose oral contraceptive containing drospirenone: results of three multicentre trials”. Clin Drug Investig. 29 (2): 73–8. doi:10.2165/0044011-200929020-00001. PMID 19133702. S2CID 10356578.
- Carranza-Lira S (2009). “Safety, efficacy and patient acceptability of drospirenone and estradiol in the treatment of menopausal vasomotor symptoms: a review”. Clin Interv Aging. 4: 59–62. doi:10.2147/CIA.S4117. PMC 2685225. PMID 19503766.
- Christiansen C (October 2005). “Effects of drospirenone/estrogen combinations on bone metabolism”. Climacteric. 8 Suppl 3: 35–41. doi:10.1080/13697130500330283. PMID 16203654. S2CID 42803561.
- Dickerson V (November 2002). “Quality of life issues. Potential role for an oral contraceptive containing ethinyl estradiol and drospirenone”. J Reprod Med. 47 (11 Suppl): 985–93. PMID 12497673.
- Fenton C, Wellington K, Moen MD, Robinson DM (2007). “Drospirenone/ethinylestradiol 3mg/20microg (24/4 day regimen): a review of its use in contraception, premenstrual dysphoric disorder and moderate acne vulgaris”. Drugs. 67 (12): 1749–65. doi:10.2165/00003495-200767120-00007. PMID 17683173. S2CID 46976925.
- Foidart JM (October 2005). “Added benefits of drospirenone for compliance”. Climacteric. 8 Suppl 3: 28–34. doi:10.1080/13697130500330309. PMID 16203653. S2CID 31883491.
- Foidart JM, Faustmann T (December 2007). “Advances in hormone replacement therapy: weight benefits of drospirenone, a 17alpha-spirolactone-derived progestogen”. Gynecol. Endocrinol. 23 (12): 692–9. doi:10.1080/09513590701582323. PMID 18075844. S2CID 12572825.
- Genazzani AR, Mannella P, Simoncini T (February 2007). “Drospirenone and its antialdosterone properties”. Climacteric. 10 Suppl 1: 11–8. doi:10.1080/13697130601114891. PMID 17364593. S2CID 24872884.
- Han L, Jensen JT (October 2014). “Expert opinion on a flexible extended regimen of drospirenone/ethinyl estradiol contraceptive”. Expert Opin Pharmacother. 15 (14): 2071–9. doi:10.1517/14656566.2014.949237. PMID 25186109. S2CID 25338932.
- Heinemann LA, Dinger J (2004). “Safety of a new oral contraceptive containing drospirenone”. Drug Saf. 27 (13): 1001–18. doi:10.2165/00002018-200427130-00003. PMID 15471507. S2CID 1773936.
- Idota N, Kobayashi M, Miyamori D, Kakiuchi Y, Ikegaya H (March 2015). “Drospirenone detected in postmortem blood of a young woman with pulmonary thromboembolism: A case report and review of the literature”. Leg Med (Tokyo). 17 (2): 109–15. doi:10.1016/j.legalmed.2014.10.001. PMID 25454533.
- Keam SJ, Wagstaff AJ (2003). “Ethinylestradiol/drospirenone: a review of its use as an oral contraceptive”. Treat Endocrinol. 2 (1): 49–70. doi:10.2165/00024677-200302010-00005. PMID 15871554. S2CID 209144694.
- Krattenmacher R (July 2000). “Drospirenone: pharmacology and pharmacokinetics of a unique progestogen”. Contraception. 62 (1): 29–38. doi:10.1016/S0010-7824(00)00133-5. PMID 11024226.
- Larivée N, Suissa S, Khosrow-Khavar F, Tagalakis V, Filion KB (September 2017). “Drospirenone-containing oral contraceptive pills and the risk of venous thromboembolism: a systematic review of observational studies”. BJOG. 124 (10): 1490–1499. doi:10.1111/1471-0528.14623. PMID 28276140.
- Lete I, Chabbert-Buffet N, Jamin C, Lello S, Lobo P, Nappi RE, Pintiaux A (2015). “Haemostatic and metabolic impact of estradiol pills and drospirenone-containing ethinylestradiol pills vs. levonorgestrel-containing ethinylestradiol pills: A literature review”. Eur J Contracept Reprod Health Care. 20 (5): 329–43. doi:10.3109/13625187.2015.1050091. PMID 26007631. S2CID 41601833.
- Li J, Ren J, Sun W (March 2017). “A comparative systematic review of Yasmin (drospirenone pill) versus standard treatment options for symptoms of polycystic ovary syndrome”. Eur. J. Obstet. Gynecol. Reprod. Biol. 210: 13–21. doi:10.1016/j.ejogrb.2016.11.013. PMID 27923166.
- Lopez LM, Kaptein AA, Helmerhorst FM (February 2012). “Oral contraceptives containing drospirenone for premenstrual syndrome”. Cochrane Database Syst Rev (2): CD006586. doi:10.1002/14651858.CD006586.pub4. PMID 22336820.
- Machado RB, Pompei Lde M, Giribela AG, Giribela CG (January 2011). “Drospirenone/ethinylestradiol: a review on efficacy and noncontraceptive benefits”. Womens Health (Lond). 7 (1): 19–30. doi:10.2217/whe.10.84. PMID 21175386.
- Mallareddy M, Hanes V, White WB (2007). “Drospirenone, a new progestogen, for postmenopausal women with hypertension”. Drugs Aging. 24 (6): 453–66. doi:10.2165/00002512-200724060-00002. PMID 17571911. S2CID 39236155.
- Motivala A, Pitt B (2007). “Drospirenone for oral contraception and hormone replacement therapy: are its cardiovascular risks and benefits the same as other progestogens?”. Drugs. 67 (5): 647–55. doi:10.2165/00003495-200767050-00001. PMID 17385938. S2CID 22985078.
- Oelkers W (December 2002). “Antimineralocorticoid activity of a novel oral contraceptive containing drospirenone, a unique progestogen resembling natural progesterone”. Eur J Contracept Reprod Health Care. 7 Suppl 3: 19–26, discussion 42–3. PMID 12659403.
- Oelkers W (December 2000). “Drospirenone–a new progestogen with antimineralocorticoid activity, resembling natural progesterone”. Eur J Contracept Reprod Health Care. 5 Suppl 3: 17–24. PMID 11246598.
- Oelkers W (March 2004). “Drospirenone, a progestogen with antimineralocorticoid properties: a short review”. Mol. Cell. Endocrinol. 217 (1–2): 255–61. doi:10.1016/j.mce.2003.10.030. PMID 15134826. S2CID 19936032.
- Oelkers W (February 2002). “The renin-aldosterone system and drospirenone”. Gynecol. Endocrinol. 16 (1): 83–7. doi:10.1080/gye.16.1.83.87. PMID 11915587. S2CID 32410408.
- Oelkers WH (October 2005). “Drospirenone in combination with estrogens: for contraception and hormone replacement therapy”. Climacteric. 8 Suppl 3: 19–27. doi:10.1080/13697130500330341. PMID 16203652. S2CID 42837148.
- Palacios S, Foidart JM, Genazzani AR (November 2006). “Advances in hormone replacement therapy with drospirenone, a unique progestogen with aldosterone receptor antagonism” (PDF). Maturitas. 55 (4): 297–307. doi:10.1016/j.maturitas.2006.07.009. hdl:2268/9932. PMID 16949774.
- Pérez-López FR (June 2008). “Clinical experiences with drospirenone: from reproductive to postmenopausal years”. Maturitas. 60 (2): 78–91. doi:10.1016/j.maturitas.2008.03.009. PMID 18468818.
- Rapkin AJ, Sorger SN, Winer SA (February 2008). “Drospirenone/ethinyl estradiol”. Drugs Today. 44 (2): 133–45. doi:10.1358/dot.2008.44.2.1191057. PMID 18389090. S2CID 32413831.
- Rapkin AJ, Winer SA (May 2007). “Drospirenone: a novel progestin”. Expert Opin Pharmacother. 8 (7): 989–99. doi:10.1517/14656566.8.7.989. PMID 17472544. S2CID 6954183.
- Rapkin RB, Creinin MD (October 2011). “The combined oral contraceptive pill containing drospirenone and ethinyl estradiol plus levomefolate calcium”. Expert Opin Pharmacother. 12 (15): 2403–10. doi:10.1517/14656566.2011.610791. PMID 21877996. S2CID 40231903.
- Rübig A (October 2003). “Drospirenone: a new cardiovascular-active progestin with antialdosterone and antiandrogenic properties”. Climacteric. 6 Suppl 3: 49–54. PMID 15018248.
- Scheinfeld NS (2007). “Yaz (3 mg drospirenone/20 microg ethinyl estradiol)”. Skinmed. 6 (6): 289. doi:10.1111/j.1540-9740.2007.07338.x. PMID 17975349.
- Sehovic N, Smith KP (May 2010). “Risk of venous thromboembolism with drospirenone in combined oral contraceptive products”. Ann Pharmacother. 44 (5): 898–903. doi:10.1345/aph.1M649. PMID 20371756. S2CID 8248469.
- Shulman LP (June 2006). “A review of drospirenone for safety and tolerability and effects on endometrial safety and lipid parameters contrasted with medroxyprogesterone acetate, levonorgestrel, and micronized progesterone”. J Womens Health (Larchmt). 15 (5): 584–90. doi:10.1089/jwh.2006.15.584. PMID 16796485.
- Simoncini T, Genazzani AR (February 2010). “A review of the cardiovascular and breast actions of drospirenone in preclinical studies”. Climacteric. 13 (1): 22–33. doi:10.3109/13697130903437375. PMID 19938948. S2CID 4306359.
- Sitruk-Ware R (October 2005). “Pharmacology of different progestogens: the special case of drospirenone”. Climacteric. 8 Suppl 3: 4–12. doi:10.1080/13697130500330382. PMID 16203650. S2CID 24205704.
- Thorneycroft IH (November 2002). “Evolution of progestins. Focus on the novel progestin drospirenone”. J Reprod Med. 47 (11 Suppl): 975–80. PMID 12497671.
- Toni I, Neubert A, Botzenhardt S, Gratzki N, Rascher W (September 2013). “Venous thromboembolism in adolescents associated with drospirenone-containing oral contraceptives – two case reports”. Klin Padiatr. 225 (5): 266–7. doi:10.1055/s-0033-1353169. PMID 23975850.
- White WB (February 2007). “Drospirenone with 17beta-estradiol in the postmenopausal woman with hypertension”. Climacteric. 10 Suppl 1: 25–31. doi:10.1080/13697130601114933. PMID 17364595. S2CID 9451771.
- Whitehead M (March 2006). “Hormone replacement therapy with estradiol and drospirenone: an overview of the clinical data”. J Br Menopause Soc. 12 Suppl 1: 4–7. doi:10.1258/136218006775992185. PMID 16513012. S2CID 38095916.
- Wu CQ, Grandi SM, Filion KB, Abenhaim HA, Joseph L, Eisenberg MJ (June 2013). “Drospirenone-containing oral contraceptive pills and the risk of venous and arterial thrombosis: a systematic review”. BJOG. 120 (7): 801–10. doi:10.1111/1471-0528.12210. PMID 23530659. S2CID 206904730.
- Zhao X, Zhang XF, Zhao Y, Lin X, Li NY, Paudel G, Wang QY, Zhang XW, Li XL, Yu J (September 2016). “Effect of combined drospirenone with estradiol for hypertensive postmenopausal women: a systemic review and meta-analysis”. Gynecol. Endocrinol. 32 (9): 685–689. doi:10.1080/09513590.2016.1183629. PMID 27176003. S2CID 9116138.
- “Drospirenone in HRT?”. Drug Ther Bull. 47 (4): 41–4. April 2009. doi:10.1136/dtb.2009.03.0011 (inactive 2021-05-06). PMID 19357298. S2CID 1909717.
External links
- “Drospirenone”. Drug Information Portal. U.S. National Library of Medicine.
//////////drospirenone, Nextstellis, ZK 30595, FDA 2021, APPROVALS 2021

NEW DRUG APPROVALS
ONE TIME
$10.00

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....

Very creative posst
LikeLike