FDA approves treatment Cimzia (certolizumab pegol) for patients with a type of inflammatory arthritis
FDA approves treatment Cimzia (certolizumab pegol) for patients with a type of inflammatory arthritis
March 28, 2019
Release
The U.S. Food and Drug Administration today approved Cimzia (certolizumab pegol) injection for treatment of adults with a certain type of inflammatory arthritis called non-radiographic axial spondyloarthritis (nr-axSpA), with objective signs of inflammation. This is the first time that the FDA has approved a treatment for nr-axSpA.
“Today’s approval of Cimzia fulfills an unmet need for patients suffering from non-radiographic axial spondyloarthritis as there has been no FDA-approved treatments until now,” said Nikolay Nikolov, M.D., associate director for rheumatology of the Division of Pulmonary, Allergy, and Rheumatology Products in the FDA’s Center for Drug Evaluation and Research.
Nr-axSpA is a type of inflammatory arthritis that causes inflammation in the spine and other symptoms. There is no visible damage seen on x-rays, so it is referred to as non-radiographic.
The efficacy of Cimzia for the treatment of nr-axSpA was studied in a randomized clinical trial in 317 adult patients with nr-axSpA with objective signs of inflammation, indicated by elevated C-reactive protein (CRP) levels and/or sacroiliitis (inflammation of the sacroiliac joints) on MRI. The trial measured the improvement response on the Ankylosing Spondylitis Disease Activity Score, a composite scoring system that assesses disease activity including patient-reported outcomes and CRP levels. Responses were greater for patients treated with Cimzia compared to patients treated with placebo. The overall safety profile observed in the Cimzia treatment group was consistent with the known safety profile of Cimzia.
The prescribing information for Cimzia includes a Boxed Warning to advise health care professionals and patients about the increased risk of serious infections leading to hospitalization or death including tuberculosis (TB), bacterial sepsis (infection in the blood steam), invasive fungal infections (such as histoplasmosis, an infection that affects the lungs), and other infections. Cimzia should be discontinued if a patient develops a serious infection or sepsis. Health care providers are advised to perform testing for latent TB and, if positive, to start treatment for TB prior to starting Cimzia. All patients should be monitored for active TB during treatment, even if the initial latent TB test is negative. The Boxed Warning also advises that lymphoma (cancer in blood cells) and other malignancies, some fatal, have been reported in children and adolescent patients treated with tumor necrosis factor (TNF) blockers, of which Cimzia is a member. Cimzia is not indicated for use in pediatric patients. Cimzia must be dispensed with a patient Medication Guide that describes important information about the drug’s uses and risks.
Cimzia was originally approved in 2008 and is also indicated for adult patients with Crohn’s disease, moderate-to-severe rheumatoid arthritis, active ankylosing spondylitis (AS) and moderate-to-severe plaque psoriasis who are candidates for systemic therapy or phototherapy.
The FDA granted the approval of Cimzia to UCB.
///////////////FDA 2019, Cimzia, certolizumab pegol, inflammatory arthritis, UCB
FDA approves new oral treatment for multiple sclerosis, Mavenclad (cladribine)
March 29, 2019
Release
The U.S. Food and Drug Administration today approved Mavenclad (cladribine) tablets to treat relapsing forms of multiple sclerosis (MS) in adults, to include relapsing-remitting disease and active secondary progressive disease. Mavenclad is not recommended for MS patients with clinically isolated syndrome. Because of its safety profile, the use of Mavenclad is generally recommended for patients who have had an inadequate response to, or are unable to tolerate, an alternate drug indicated for the treatment of MS.
“We are committed to supporting the development of safe and effective treatments for patients with multiple sclerosis,” said Billy Dunn, M.D., director of the Division of Neurology Products in the FDA’s Center for Drug Evaluation and Research. “The approval of Mavenclad represents an additional option for patients who have tried another treatment without success.”
MS is a chronic, inflammatory, autoimmune disease of the central nervous system that disrupts communications between the brain and other parts of the body. Most people experience their first symptoms of MS between the ages of 20 and 40. MS is among the most common causes of neurological disability in young adults and occurs more frequently in women than in men.
For most people, MS starts with a relapsing-remitting course, in which episodes of worsening function (relapses) are followed by recovery periods (remissions). These remissions may not be complete and may leave patients with some degree of residual disability. Many, but not all, patients with MS experience some degree of persistent disability that gradually worsens over time. In some patients, disability may progress independent of relapses, a process termed secondary progressive multiple sclerosis (SPMS). In the first few years of this process, many patients continue to experience relapses, a phase of the disease described as active SPMS. Active SPMS is one of the relapsing forms of MS, and drugs approved for the treatment of relapsing forms of MS can be used to treat active SPMS.
The efficacy of Mavenclad was shown in a clinical trial in 1,326 patients with relapsing forms of MS who had least one relapse in the previous 12 months. Mavenclad significantly decreased the number of relapses experienced by these patients compared to placebo. Mavenclad also reduced the progression of disability compared to placebo.
Mavenclad must be dispensed with a patient Medication Guide that describes important information about the drug’s uses and risks. Mavenclad has a Boxed Warning for an increased risk of malignancy and fetal harm. Mavenclad is not to be used in patients with current malignancy. In patients with prior malignancy or with increased risk of malignancy, health care professionals should evaluate the benefits and risks of the use of Mavenclad on an individual patient basis. Health care professionals should follow standard cancer screening guidelines in patients treated with Mavenclad. The drug should not be used in pregnant women and in women and men of reproductive potential who do not plan to use effective contraception during treatment and for six months after the course of therapy because of the potential for fetal harm. Mavenclad should be stopped if the patient becomes pregnant.
Other warnings include the risk of decreased lymphocyte (white blood cell) counts; lymphocyte counts should be monitored before, during and after treatment. Mavenclad may increase the risk of infections; health care professionals should screen patients for infections and treatment with Mavenclad should be delayed if necessary. Mavenclad may cause hematologic toxicity and bone marrow suppression so health care professionals should measure a patient’s complete blood counts before, during and after therapy. The drug has been associated with graft-versus-host-disease following blood transfusions with non-irradiated blood. Mavenclad may cause liver injury and treatment should be interrupted or discontinued, as appropriate, if clinically significant liver injury is suspected.
The most common adverse reactions reported by patients receiving Mavenclad in the clinical trials include upper respiratory tract infections, headache and decreased lymphocyte counts.
The FDA granted approval of Mavenclad to EMD Serono, Inc.
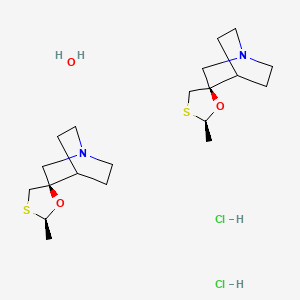
Cevimeline, セビメリン
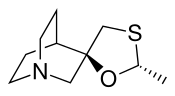
Cevimeline
セビメリン
- Molecular FormulaC10H17NOS
- Average mass199.313 Da
Cevimeline hydrochloride
-
- Synonyms:AF-102B, SNI-2011, SNK-508, Evoxac
- ATC:N07
- Use:cognition disorder, treatment of Sjogren’s syndrome, muscarinic M3-receptor agonist
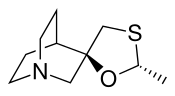
- Chemical name:(2′R,3R)-rel-2′-methylspiro[1-azabicyclo[2.2.2]octane-3,5′-[1,3]oxathiolane] hydrochloride hydrate (2:2:1)
- Formula:C10H17NOS • HCl • 1/2H2O
- MW:489.57 g/mol
- CAS-RN:153504-70-2
- InChI Key:SURWTGAXEIEOGY-GHXDPTCOSA-N
- InChI:InChI=1S/C10H17NOS.ClH/c1-8-12-10(7-13-8)6-11-4-2-9(10)3-5-11;/h8-9H,2-7H2,1H3;1H/t8-,10-;/m1./s1
Derivatives
base
- Formula:C10H17NOS
- MW:199.32 g/mol
- CAS-RN:107233-08-9
anhydrous hydrochloride
- Formula:C10H17NOS • HCl
- MW:235.78 g/mol
- CAS-RN:107220-28-0
Cevimeline is cis-2′-methylspiro {1-azabicyclo [2.2.2] octane-3, 5′ -[1,3] oxathiolane} hydro-chloride, hydrate (2:1). Its empirical formula is C10H17NOS•HCl•½ H2O, and its structural formula is:
 Cevimeline has a molecular weight of 244.79. It is a white to off white crystalline powder with a melting point range of 201 to 203°C. It is freely soluble in alcohol and chloroform, very soluble in water, and virtually insoluble in ether. The pH of a 1% solution ranges from 4.6 to 5.6. Inactive ingredients include lactose monohydrate, hydroxypropyl cellulose, and magnesium stearate.
Cevimeline has a molecular weight of 244.79. It is a white to off white crystalline powder with a melting point range of 201 to 203°C. It is freely soluble in alcohol and chloroform, very soluble in water, and virtually insoluble in ether. The pH of a 1% solution ranges from 4.6 to 5.6. Inactive ingredients include lactose monohydrate, hydroxypropyl cellulose, and magnesium stearate.
Cevimeline hydrochloride [USAN]
RN: 153504-70-2
(+-)-cis-2-Methylspiro(1,3-oxathiolane-5,3′-quinuclidine) hydrochloride, hemihydrate
Cevimeline (trade name Evoxac) is a parasympathomimetic and muscarinic agonist,[1] with particular effect on M1 and M3 receptors. It is used in the treatment of dry mouth and especially associated with Sjögren’s syndrome.
Mechanism of action
By activating the M3 receptors of the parasympathetic nervous system, cevimeline stimulates secretion by the salivary glands, thereby alleviating dry mouth.
Side effects
Known side effects include nausea, vomiting, diarrhea, excessive sweating, rash, headache, runny nose, cough, drowsiness, hot flashes, blurred vision, and difficulty sleeping.[2]
Contraindications include asthma and angle closure glaucoma.
Clip
https://www.sciencedirect.com/science/article/abs/pii/S0731708515302260



CLIP
https://www.sciencedirect.com/science/article/pii/S0040403913005042



CLIP
CLIP

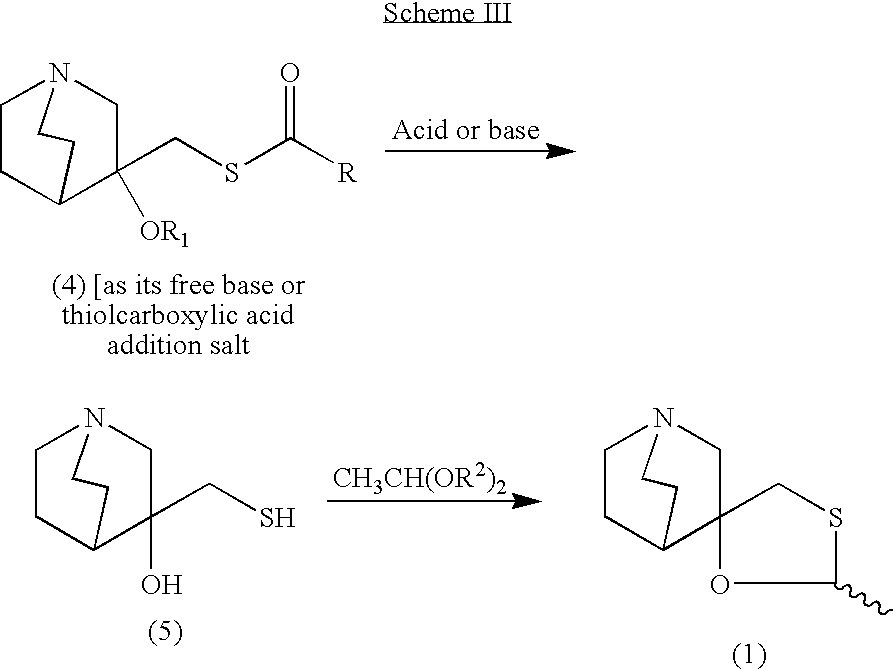
- Reaction of quinuclidin-3-one (I) with trimethylsulfoxonium iodide and NaH in DMSO gives epoxide (II), which is opened with SH2 in NaOH/water, yielding 3-hydroxy-3-(sulfanylmethyl)quinuclidine (III). The cyclization of compound (III) with acetaldehyde (IV) catalyzed by boron trifluoride ethearate or by SnCl4, POCl3, H3PO4 or p-toluenesulfonic acid affords a mixture of two diastereomeric spiroracemates, the (?-trans (V) and (?-cis (cevimeline). This mixture is separated by fractional recrystallization in acetone or by TLC chromatography, and treated with hydrochloric acid. The (?-trans-compound (V) can be isomerized to cevimeline by treatment with an acidic catalyst such as an organic sulfonic acid (trifluoromethanesulfonic acid, p-toluenesulfonic acid or methanesulfonic acid), a Lewis acid (SnCl4, FeCl3, BF3 or AlCl3) or sulfuric acid in refluxing toluene, hexane or CHCl3. Cevimeline hydrochloride hemihydrate is obtained from the above mentioned hydrochloride by a complex work-up using water, isopropanol and n-hexane.
- Synthesis of Cevimeline Hydrochloride (EN:134916): Reaction of quinuclidin-3-one (I) with trimethylsulfoxonium iodide and NaH in DMSO gives epoxide (II), which is opened with SH2 in NaOH/water, yielding 3-hydroxy-3-(sulfanylmethyl)quinuclidine (III) (1,2). The cyclization of compound (III) with acetaldehyde (IV) catalyzed by boron trifluoride ethearate (1) or by SnCl4, POCl3, H3PO4 or p-toluenesulfonic acid (2) affords a mixture of two diastereomeric spiro-racemates, the (?-trans (V) and (?-cis (cevimeline). This mixture is separated by fractional recrystallization in acetone or by TLC chromatography, and treated with hydrochloric acid (1,2). The (?-trans-compound (V) can be isomerized to cevimeline by treatment with an acidic catalyst such as an organic sulfonic acid (trifluoromethanesulfonic acid, p-toluenesulfonic acid or methanesulfonic acid), a Lewis acid (SnCl4, FeCl3, BF3 or AlCl3) or sulfuric acid in refluxing toluene, hexane or CHCl3 (2,3). Cevimeline hydrochloride hemihydrate is obtained from the above mentioned hydrochloride by a complex work-up using water, isopropanol and n-hexane (4).(Scheme 13491601a) Description M.p. 203 C (4). Sources Discovered by Israel Institute for Biological Research, Ness-Ziona (IL) and licensed to Snow Brand Milk Products Co. Ltd. (JP). In the U.S., comarketed by Snow Brand Milk Products and Daiichi Pharmaceutical Co., Ltd. In Japan, codeveloped with Nippon Kayaku Co. Ltd. Ishihara Sangyo Co., Ltd. (JP) is the bulk supplier. References 1. Fisher, A., Heldman, E., Grunfeld, Y., Karton, I., Levy, A. (Israel Institute for Biological Research); Derivs. of quinuclidine; EP 0205247, JP 1986280497, US 4855290. 2. Hayashi, K., Tokumoto, S., Yoshizawa, H., Isogai, T. (Ishihara Sangyo Kaisha, Ltd.); Method for producing 2-methylspiro(1,3-oxathiolan-5,3′)quinuclidine; EP 0683168, US 5571918. 3. Haga, T., Koyanagi, T., Hara, K., Maeda, M., Shigehara, I. (Ishihara Sangyo Kaisha, Ltd.); Method for isomerization of trans-form 2-methylspiro(1,3-oxathiolane-5,3′)quinuclidine or acid addition salts thereof; EP 0298491, US 4861886. 4. Saito, K., Ono, T., Honda, N. (Snow Brand Milk Products Co., Ltd.); Preparation method of cis-2-methylspiro(1,3-oxathiolane-5,3′)quinuclidine hydrochloride.1/2 hydrate capable of disgregating easily; JP 1992108792.
PATENT
https://patents.google.com/patent/US8080663B2/en
The present invention refers to a novel, industrially advantageous process for the preparation of an intermediate useful for the preparation of Cevimeline hydrochloride (1, cis-2-methylspiro(1,3-oxathiolane-5,3′)quiniclidine, Scheme 1). This pharmaceutical is useful for the treatment of diseases of the central nervous system due to disturbances of central cholinergic function and autoimmune system (Sjörgen’s syndrome) and is marketed as Evoxac®.
U.S. Pat. No. 4,855,290 describes a process for preparation of 2-methylspiro(1,3-oxathiolane-5,3′)quiniclidine (1). The process comprises the preparation of the epoxide of 3-methylenequiniclidine, which is subsequently reacted with hydrogen sulfide to produce 3-hydroxy-3-mercaptomethylquiniclidine and condensed with acetaldehyde in the presence of a Lewis acid (boron trifluoride etherate) to provide 2-methylspiro(1,3-oxathiolane-5,3′)quiniclidine. This process is depicted in Scheme I.
This process suffers from major disadvantages when transiting to industrial scale. These include the use of the highly hazardous and difficult to handle hydrogen sulfide gas. Also, boron trifluoride etherate is employed during the condensation step with acetaldehyde. The boron trifluoride etherate reagent is an air and moisture sensitive Lewis acid which has to be used under anhydrous conditions, thus creating a serious disadvantage in industrial settings. Another drawback of this process is the use of sodium hydride. U.S. Pat. Nos. 5,571,918 and 4,861,886 relate to the isomerization of the trans- to cis-form of 2-methylspiro(1,3-oxathiolane-5,3′)quiniclidine but do not describe methods for its preparation. Thus, an industrially acceptable and cost-effective method for the preparation of Cevimeline hydrochloride which overcomes the deficiencies of the prior art is required.
Further and other objects of the invention will be realized by those skilled in the art from the following Summary of the Invention and Detailed Description of Preferred Embodiments of the Invention thereof.
According to one aspect of the invention, a novel process is provided for the preparation of 2-methylspiro(1,3-oxathiolane-5,3′)quiniclidine (1). The process is industrially practical, efficient, safe and economical, as well as being environmentally friendly. The general method is shown in the Scheme II.
wherein R is selected from C1 to C6 alkyl and aryl groups, most preferably a methyl, ethyl or propyl group; R1 is hydrogen or a C2 to C7 alkyl or aryl carbonyl group; R2 is a C1 to C6 alkyl group, preferably methyl, ethyl, propyl, or butyl group.
EXAMPLE I Preparation of the Epoxide of 3-methylenequiniclidine (3)
A mixture of the hydrochloric salt of 3-quiniclidinone (2, 120 g, 795.7 mmol) and trimethylsulfoxonium iodide (219 g, 993.3 mmol) in dimethylsulfoxide (91.0 g, 0.63 mol) was cooled to 0-5° C. in an ice/water bath under nitrogen atmosphere. A solution of potassium tert-butoxide (201 g, 1789.1 mmol) in dimethylsulfoxide (500 mL) was added dropwise over 45 minutes. The mixture was warmed gradually to room temperature and stirred for an additional 16 hours at room temperature. After cooling to 0-5° C. (ice/water bath) the mixture was poured into an ice/water mixture (500 g) and then sodium chloride (300 g) was added. The mixture was stirred for 30 minutes and extracted with toluene (3×400 mL). The toluene phase was dried over sodium sulfate, filtered and evaporated to furnish the epoxide of 3-methylenequiniclidine (60 g, 431.7 mmol, 54% yield) as a yellow oil. The product could be used in the next step neat or as toluene solution after the extraction without further purification.
1H NMR (400 MHz, CDCl3): δ=3.10 (d, 1H, J=14.6 Hz); 2.98-2.77 (m, 5H); 2.74 (d, 1H, J=4.8 Hz); 2.70 (d, 1H, J=4.8 Hz); 1.96-1.89 (m, 1H); 1.79-1.62 (m, 2H); 1.60-1.54 (m, 1H); 1.38-1.36 (m,1H).
LRMS (ES+): 140.0 (100, M+H+).
EXAMPLE II Preparation of the Thiolacetic Acid Salt of 3-hydroxy-3-acetoxymercaptomethylquiniclidine (4)
A solution of the epoxide of 3-methylenequiniclidine (3, 54 g, 388.5 mmol) in toluene (200 mL) was cooled to 0-5° C. (ice/water bath). Thiolacetic acid was added dropwise over 10-15 minutes. The mixture was stirred at 0-5° C. for 30 minutes and then allowed to come to room temperature. After stirring at room temperature for 2 hours the formed precipitate was filtered and washed with toluene (2×100 mL) to give the 3-hydroxy-3-acetoxymercaptomethylquiniclidine thiolacetic acid salt (4 wherein R1 is H and R is methyl, 77 g, 264.6 mmol, 68%) as a light yellow solid. The product was used in the next step without any further purification.
1H NMR (400 MHz CD3OD): δ=3.47 (d, 1H, J=14.1 Hz); 3.37-3.18 (m, 7H); 2.40 (s, 3H); 2.38 (s, 3H); 2.36-2.27 (m, 1H), 2.14-2.05 (m, 2H); 2.03-1.93 (m, 1H); 1.81-1.78 (m, 1H).
LRMS (ES+): 216.1 (100, M−[SCOCH3]−+H+).
EXAMPLE III Preparation of 2-methylspiro(1,3-oxathiolane-5,3′)quiniclidine using p-toluenesulfonic acid (1)
To a solution of 3-hydroxy-3-acetoxymercaptomethylquiniclidine thiolacetic acid salt (4 wherein R1 is H and R is methyl, 3 g, 10.3 mmol) in iso-propanol (50 mL) was added p-toluenesulfonic acid monohydrate (5.9 g, 30.9 mmol) and the mixture was heated to reflux for 3.5 hours. The mixture was cooled to room temperature and acetaldehyde diethyl acetal (6.1 g, 51.5 mmol) was added. The mixture was heated to reflux and stirred for an additional 3 hours. The solvent was evaporated and the residue was dissolved in dichloromethane (50 mL). The mixture was cooled to 0-5° C. and a 25% aqueous solution of sodium hydroxide (80 mL) was added. The mixture was stirred for 10-15 minutes and the phases were separated. The aqueous phase was extracted with dichloromethane (3×50 mL). The organic phases were combined and extracted with 5% aqueous solution of sulfuric acid (3×50 mL). The acidic aqueous phases were combined and the pH was adjusted to 12 with a 25% aqueous solution of sodium hydroxide. The aqueous phase was extracted with heptane (3×50 mL) and the organic phases were combined, dried over sodium sulfate and the solvent was evaporated to give 2-methylspiro(1,3-oxathiolane-5,3′)quiniclidine (1.8 g, 9.2 mmol, 89% yield) as a 3:1 cis/trans ratio mixture of diastereomers (determined by 1H NMR).
LRMS (ES+): 200.1 (100, M+H+).
EXAMPLE IV Preparation of 2-methylspiro(1,3-oxathiolane-5,3′)quiniclidine (1) using racemic camphorsulfonic acid
In a similar experiment as Example III, racemic camphorsulfonic acid (7.2 g, 30.9 mmol) was added to a solution of 3-hydroxy-3-acetoxymercaptomethylquiniclidine thiolacetic acid salt (4 wherein R1 is H and R is methyl, 3 g, 10.3 mmol) in iso-propanol (50 mL). The mixture was refluxed for 5 h, cooled to room temperature and acetaldehyde diethyl acetal (6.1 g, 51.5 mmol) was added. The mixture was refluxed for an additional an 8 hours and processed according to Example III to give 2-methylspiro(1,3-oxathiolane-5,3′)quiniclidine (1.32 g, 6.63 mmol, 64% yield) in a 3.5:1 cis/trans ratio mixture of diastereomers (determined by 1H NMR).
EXAMPLE V Preparation of 2-methylspiro(1,3-oxathiolane-5,3′)quiniclidine (1) using phenyl sulfonic acid
In a similar experiment as Example III, to a solution of 3-hydroxy-3-acetoxymercaptomethylquiniclidine thiolacetic acid salt (4 wherein R1 is H and R is methyl, 3 g, 10.3 mmol) in iso-propanol (50 mL) was added phenyl sulfonic acid (4.9 g, 30.9 mmol) and the mixture was refluxed 5 h, cooled to room temperature and acetaldehyde diethyl acetal (6.1 g, 51.5 mmol) was added. The mixture was refluxed for an additional 8 hours and worked up in a manner similar to Example III to furnish 2-methylspiro(1,3-oxathiolane-5,3′)quiniclidine (1.6 g, 8.2 mmol, 80% yield) as a 2.5:1 cis/trans ratio mixture of diastereomers (determined by 1H NMR).
EXAMPLE VI Preparation of 2-methylspiro(1,3-oxathiolane-5,3′)quiniclidine (1) using p-toluenesulfonic acid in butanol
To a solution of 3-hydroxy-3-acetoxymercaptomethylquiniclidine thiolacetic acid salt (4 wherein R1 is H and R is methyl, 3 g, 10.3 mmol) in butanol (100 mL) was added of p-toluenesulfonic acid monohydrate (5.9 g, 30.9 mmol) and the mixture was refluxed for 3 hours with a Dean-Stark apparatus attached to the flask. The reaction mixture was cooled to room temperature and acetaldehyde diethyl acetal (6.1 g, 51.5 mmol) was added. The mixture was heated to 80° C. for an additional 8 h and worked up according to Example III to afford 2-methylspiro(1,3-oxathiolane-5,3′)quiniclidine (1.8 g, 9.2 mmol, 89% yield) as a 3:1 cis/trans ratio mixture of diastereomers (determined by 1H NMR).
References
- ^ Ono M, Takamura E, Shinozaki K, et al. (July 2004). “Therapeutic effect of cevimeline on dry eye in patients with Sjögren’s syndrome: a randomized, double-blind clinical study”. Am. J. Ophthalmol. 138 (1): 6–17. doi:10.1016/j.ajo.2004.02.010. PMID 15234277.
- ^ [1] MedicineNet: Cevimeline. Accessed 10/12/2007
-
- US 4 855 290 (Israel Institute for Biological Research; 8.8.1989; IL-prior. 10.5.1985).
- US 4 876 260 (Israel Institute for Biological Research; 24.10.1989; USA-prior. 28.10.1987).
- EP 683 168 (Ishihara Sangyo Kaisha; appl. 19.5.1995; J-prior. 19.5.1994).
-
Method for isomerization of trans-isomer:
- US 4 861 886 (Ishihara Sangyo Kaisha; 29.8.1989; J-prior. 10.7.1987).
-
Method of separation:
- IL 81 652 (Israel Institute for Biological Research; 12.5.1991; appl. 23.2.1987).
- JP 01 290 680 (Ishihara Sangyo Kaisha; 22.11.1989; J-prior. 18.5.1988).
-
Synthesis of enantiomerically pure (S)-3-hydroxy-3-mercaptomethylquinuclidine (S)-II:
- Bos, M.; Canesso, R.: Heterocycles (HTCYAM) 38 (8), 1889 (1994).
-
Synthesis of 3-quinuclidone:
- Sternbach, L.H.; Kaiser, S.: J. Am. Chem. Soc. (JACSAT) 74, 2215 (1952).
-
External links
 |
|
 |
|
| Clinical data | |
|---|---|
| Trade names | Evoxac |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a608025 |
| Pregnancy category |
|
| Routes of administration |
By mouth (capsules) |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Protein binding | <20% |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C10H17NOS |
| Molar mass | 199.31308 g/mol g·mol−1 |
| 3D model (JSmol) | |
/////////// Cevimeline, AF-102B, SNI-2011, SNK-508, Evoxac, セビメリン
FDA approves new oral testosterone capsule for treatment of men with certain forms of hypogonadism
FDA approves new oral testosterone capsule (testosterone undecanoate) for treatment of men with certain forms of hypogonadism
March 27, 2019
Release
The U.S. Food and Drug Administration today approved Jatenzo (testosterone undecanoate), an oral testosterone capsule to treat men with certain forms of hypogonadism. These men have low testosterone levels due to specific medical conditions, such as genetic disorders like Klinefelter syndrome or tumors that have damaged the pituitary gland. Jatenzo should not be used to treat men with “age-related hypogonadism,” in which testosterone levels decline due to aging, even if these men have symptoms that appear to be related to low testosterone. Jatenzo’s benefits do not outweigh its risks for that use.
“Jatenzo’s oral route of administration provides an important addition to current treatment options available for men with certain hypogonadal conditions who up until now have most commonly been treated with testosterone products that are applied to the skin or injected,” said Hylton V. Joffe, M.D, M.M.Sc., director of the Division of Bone, Reproductive and Urologic Products in the FDA’s Center for Drug Evaluation and Research. “But it’s important to emphasize that this drug should not, like other testosterone treatments, be used to treat older men with ‘age-related hypogonadism.’ The benefits of testosterone therapy, including Jatenzo, have not been established for this use, and Jatenzo’s effects on raising blood pressure can increase the risks of heart attack, stroke and cardiovascular death in this population.”
The efficacy of Jatenzo was demonstrated in a four-month clinical trial involving 166 men with hypogonadism. Study participants initially were given Jatenzo at a dose of 237 mg twice per day, and the dose was adjusted downward or upward to a maximum of 396 mg twice per day on the basis of testosterone levels. Eighty-seven percent of Jatenzo-treated men achieved an average testosterone level within the normal range, which was the primary study endpoint.
Jatenzo contains a boxed warning on its labeling stating that the drug can cause blood pressure to rise, increasing the risk of heart attack, stroke and cardiovascular death. Health care providers should consider a patient’s individual heart disease risks and ensure that blood pressure is adequately controlled before prescribing Jatenzo; they should also periodically monitor patient blood pressure during treatment. Jatenzo is currently one of two testosterone products that have this boxed warning. The FDA is requiring all testosterone product manufacturers to conduct blood pressure postmarketing trials to more clearly address whether these products increase blood pressure.
Common side effects, occurring in more than 2 percent of patients in the Jatenzo clinical trial, included headache, an increase in hematocrit (red blood cell count), a decrease in high-density lipoprotein cholesterol (“good” cholesterol), high blood pressure and nausea. An increase in prostate specific antigen (PSA) was also observed. Patients should have their hematocrit, cholesterol and PSA monitored regularly to check for changes. Those with benign prostate hyperplasia should be monitored for worsening of symptoms.
The FDA granted the approval of Jatenzo to Clarus Therapeutics.
//////////FDA 2019, Jatenzo, Clarus Therapeutics, (testosterone undecanoate,
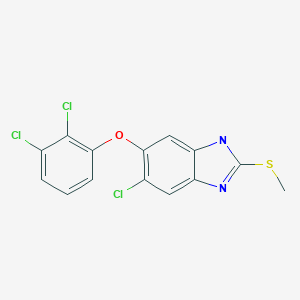
Batimastat, バチマスタット

| Formula |
C23H31N3O4S2
|
|---|---|
| cas |
130370-60-4
|
| Mol weight |
477.6399
|
Batimastat (INN/USAN, codenamed BB-94) is an anticancer drug that belongs to the family of drugs called angiogenesis inhibitors. It acts as a matrix metalloproteinase inhibitor (MMPI) by mimicking natural MMPI peptides.
Batimastat was the first MMPI that went into clinical trials. First results of a Phase I trial appeared in 1994. The drug reached Phase III but was never marketed; mainly because it couldn’t be administered orally (as opposed to the newer and chemically similar MMPI marimastat), and injection into the peritoneum caused peritonitis.[1]
SYN
U.S. Patent 5,453,438
U.S. Patent 5,240,958
U.S. Patent 5,530,161

SYN
US 5240958; US 5310763; WO 9005719
The treatment of D-leucine (I) with NaNO2, H2SO4 and NaBr gives 2(R)-bromo-5-methylpentanoic acid (II), which is esterified with isobutene and H2SO4 to the corresponding tert-butyl ester (III). The condensation of (III) with dibenzyl malonate (IV) by means of potassium tert-butoxide in DMF yields the malonyl derivative (V), which is treated with trifluoroacetic acid to hydrolyze the tert-butyl ester, and without isolation is condensed with L-phenylalanine methyl amide (VI) by means of hydroxybenzotriazole (HOBT) and dicyclohexylcarbodiimide (DCC), affording 4-benzyloxy-3-(benzyloxycarbonyl)-2(R)-isobutylsuccinyl-L-phenylalanine methylamide (VII). The elimination of the benzyl groups of (VII) by hydrogenolysis over Pd/C in ethanol gives the dicarboxylic acid (VIII), which by partial decarboxylation and reaction with aqueous formaldehyde and piperidine yields 4-hydroxy-2(R)-isobutyl-3-methylenesuccinyl-L-phenylalanine methylamide (IX). The addition of thiophene-2-thiol (X) to the double bond of (IX) affords 4-hydroxy-2(R)-isobutyl-3(S)-(2-thienylsulfanylmethyl)succinyl-L-phenylalanine methylamide (XI), which is finally treated with hydroxylamine and hydroxybenzotriazole in dichloromethane/DMF.
SPEC

HPLC

References
- ^ Rothenberg, M. L.; Nelson, A. R.; Hande, K. R. (1999). “New Drugs on the Horizon: Matrix Metalloproteinase Inhibitors”. Stem Cells. 17 (4): 237–240. doi:10.1002/stem.170237. PMID 10437989.
 |
|
| Clinical data | |
|---|---|
| Pregnancy category |
|
| Routes of administration |
Injection into pleural space or abdomen |
| ATC code |
|
| Legal status | |
| Legal status |
|
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| ECHA InfoCard | 100.222.897 |
| Chemical and physical data | |
| Formula | C23H31N3O4S2 |
| Molar mass | 477.64 g/mol g·mol−1 |
| 3D model (JSmol) | |
//////////Batimastat, BB-94, バチマスタット ,
[H][C@@](CC1=CC=CC=C1)(NC(=O)[C@]([H])(CC(C)C)[C@]([H])(CSC1=CC=CS1)C(=O)NO)C(=O)NC
Abikoviromycin
- Molecular FormulaC10H11NO
- Average mass161.200 Da
Journal of Antibiotics (2003), 56, (9), 801-804.
“ALL FOR DRUGS” CATERS TO EDUCATION GLOBALLY, No commercial exploits are done or advertisements added by me. This is a compilation for educational purposes only. P.S. : The views expressed are my personal and in no-way suggest the views of the professional body or the company that I represent
READ
 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO …..FOR BLOG HOME CLICK HERE
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO …..FOR BLOG HOME CLICK HERE amcrasto@gmail.com
amcrasto@gmail.com
Industry-Oriented Route Evaluation and Process Optimization for the Preparation of Brexpiprazole
Efforts toward route evaluation and process optimization for the preparation of brexpiprazole (1) are described. Starting from commercially available dihydroquinolinone 11, a three-step synthesis route composed of O-alkylation, oxidation, and N-alkylation was selected for industry-oriented process development aiming to reduce side reactions and achieve better impurity profiles. The reaction conditions of the three steps were investigated, and the control strategy for the process-related impurities was established. The optimized process was validated on the kilogram scale and now is viable for commercialization, with the results of not less than 99.90% purity of 1 (by HPLC) and not more than 0.05% of persistent impurities 15 and 16
Industry-Oriented Route Evaluation and Process Optimization for the Preparation of Brexpiprazole


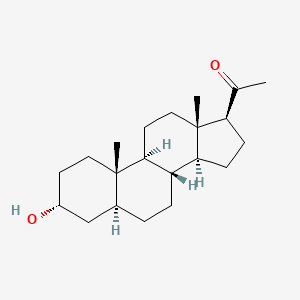
ブレキサノロン , Brexanolone, Allopregnanolone

Brexanolone
318.501 g/mol, C21H34O2
CAS: 516-54-1
ブレキサノロン
The U.S. Food and Drug Administration today approved Zulresso (brexanolone) injection for intravenous (IV) use for the treatment of postpartum depression (PPD) in adult women. This is the first drug approved by the FDA specifically for PPD.
March 19, 2019
Release
The U.S. Food and Drug Administration today approved Zulresso (brexanolone) injection for intravenous (IV) use for the treatment of postpartum depression (PPD) in adult women. This is the first drug approved by the FDA specifically for PPD.
“Postpartum depression is a serious condition that, when severe, can be life-threatening. Women may experience thoughts about harming themselves or harming their child. Postpartum depression can also interfere with the maternal-infant bond. This approval marks the first time a drug has been specifically approved to treat postpartum depression, providing an important new treatment option,” said Tiffany Farchione, M.D., acting director of the Division of Psychiatry Products in the FDA’s Center for Drug Evaluation and Research. “Because of concerns about serious risks, including excessive sedation or sudden loss of consciousness during administration, Zulresso has been approved with a Risk Evaluation and Mitigation Strategy (REMS) and is only available to patients through a restricted distribution program at certified health care facilities where the health care provider can carefully monitor the patient.”
PPD is a major depressive episode that occurs following childbirth, although symptoms can start during pregnancy. As with other forms of depression, it is characterized by sadness and/or loss of interest in activities that one used to enjoy and a decreased ability to feel pleasure (anhedonia) and may present with symptoms such as cognitive impairment, feelings of worthlessness or guilt, or suicidal ideation.
Zulresso will be available only through a restricted program called the Zulresso REMS Program that requires the drug be administered by a health care provider in a certified health care facility. The REMS requires that patients be enrolled in the program prior to administration of the drug. Zulresso is administered as a continuous IV infusion over a total of 60 hours (2.5 days). Because of the risk of serious harm due to the sudden loss of consciousness, patients must be monitored for excessive sedation and sudden loss of consciousness and have continuous pulse oximetry monitoring (monitors oxygen levels in the blood). While receiving the infusion, patients must be accompanied during interactions with their child(ren). The need for these steps is addressed in a Boxed Warning in the drug’s prescribing information. Patients will be counseled on the risks of Zulresso treatment and instructed that they must be monitored for these effects at a health care facility for the entire 60 hours of infusion. Patients should not drive, operate machinery, or do other dangerous activities until feelings of sleepiness from the treatment have completely gone away.
The efficacy of Zulresso was shown in two clinical studies in participants who received a 60-hour continuous intravenous infusion of Zulresso or placebo and were then followed for four weeks. One study included patients with severe PPD and the other included patients with moderate PPD. The primary measure in the study was the mean change from baseline in depressive symptoms as measured by a depression rating scale. In both placebo controlled studies, Zulresso demonstrated superiority to placebo in improvement of depressive symptoms at the end of the first infusion. The improvement in depression was also observed at the end of the 30-day follow-up period.
The most common adverse reactions reported by patients treated with Zulresso in clinical trials include sleepiness, dry mouth, loss of consciousness and flushing. Health care providers should consider changing the therapeutic regimen, including discontinuing Zulresso in patients whose PPD becomes worse or who experience emergent suicidal thoughts and behaviors.
The FDA granted this application Priority Review and Breakthrough Therapydesignation.
Approval of Zulresso was granted to Sage Therapeutics, Inc.
Allopregnanolone, also known as 5α-pregnan-3α-ol-20-one or 3α,5α-tetrahydroprogesterone (3α,5α-THP), as well as brexanolone (USAN),[1] is an endogenous inhibitory pregnane neurosteroid[2] which has been approved by the FDA as a treatment for post-partum depression. It is synthesized from progesterone, and is a potent positive allosteric modulator of the action of γ-aminobutyric acid (GABA) at GABAA receptor.[2] Allopregnanolone has effects similar to those of other positive allosteric modulators of the GABA action at GABAA receptor such as the benzodiazepines, including anxiolytic, sedative, and anticonvulsant activity.[2][3][4] Endogenously produced allopregnanolone exerts a pivotal neurophysiological role by fine-tuning of GABAA receptor and modulating the action of several positive allosteric modulators and agonists at GABAA receptor.[5] The 21-hydroxylated derivative of this compound, tetrahydrodeoxycorticosterone (THDOC), is an endogenous inhibitory neurosteroid with similar properties to those of allopregnanolone, and the 3β-methyl analogue of allopregnanolone, ganaxolone, is under development to treat epilepsy and other conditions, including post-traumatic stress disorder (PTSD).[2]
Biochemistry
Biosynthesis
The biosynthesis of allopregnanolone in the brain starts with the conversion of progesterone into 5α-dihydroprogesterone by 5α-reductase type I. After that, 3α-hydroxysteroid dehydrogenase converts this intermediate into allopregnanolone.[2] Allopregnanolone in the brain is produced by cortical and hippocampus pyramidal neurons and pyramidal-like neurons of the basolateral amygdala.[6]
Biological activity
Allopregnanolone acts as a highly potent positive allosteric modulator of the GABAA receptor.[2] While allopregnanolone, like other inhibitory neurosteroids such as THDOC, positively modulates all GABAA receptor isoforms, those isoforms containing δ subunitsexhibit the greatest potentiation.[7] Allopregnanolone has also been found to act as a positive allosteric modulator of the GABAA-ρ receptor, though the implications of this action are unclear.[8][9] In addition to its actions on GABA receptors, allopregnanolone, like progesterone, is known to be a negative allosteric modulator of nACh receptors,[10] and also appears to act as a negative allosteric modulator of the 5-HT3 receptor.[11] Along with the other inhibitory neurosteroids, allopregnanolone appears to have little or no action at other ligand-gated ion channels, including the NMDA, AMPA, kainate, and glycine receptors.[12]
Unlike progesterone, allopregnanolone is inactive at the nuclear progesterone receptor (nPR).[12] However, allopregnanolone can be intracellularly oxidized into 5α-dihydroprogesterone, which is an agonist of the nPR, and thus/in accordance, allopregnanolone does appear to have indirect nPR-mediated progestogenic effects.[13] In addition, allopregnanolone has recently been found to be an agonist of the newly discovered membrane progesterone receptors (mPR), including mPRδ, mPRα, and mPRβ, with its activity at these receptors about a magnitude more potent than at the GABAA receptor.[14][15] The action of allopregnanolone at these receptors may be related, in part, to its neuroprotective and antigonadotropic properties.[14][16] Also like progesterone, recent evidence has shown that allopregnanolone is an activator of the pregnane X receptor.[12][17]
Similarly to many other GABAA receptor positive allosteric modulators, allopregnanolone has been found to act as an inhibitor of L-type voltage-gated calcium channels (L-VGCCs),[18] including α1 subtypes Cav1.2 and Cav1.3.[19] However, the threshold concentration of allopregnanolone to inhibit L-VGCCs was determined to be 3 μM (3,000 nM), which is far greater than the concentration of 5 nM that has been estimated to be naturally produced in the human brain.[19] Thus, inhibition of L-VGCCs is unlikely of any actual significance in the effects of endogenous allopregnanolone.[19] Also, allopregnanolone, along with several other neurosteroids, has been found to activate the G protein-coupled bile acid receptor (GPBAR1, or TGR5).[20] However, it is only able to do so at micromolar concentrations, which, similarly to the case of the L-VGCCs, are far greater than the low nanomolar concentrations of allopregnanolone estimated to be present in the brain.[20]
Biological function
Allopregnanolone possesses a wide variety of effects, including, in no particular order, antidepressant, anxiolytic, stress-reducing, rewarding,[21] prosocial,[22] antiaggressive,[23]prosexual,[22] sedative, pro-sleep,[24] cognitive, memory-impairment, analgesic,[25] anesthetic, anticonvulsant, neuroprotective, and neurogenic effects.[2] Fluctuations in the levels of allopregnanolone and the other neurosteroids seem to play an important role in the pathophysiology of mood, anxiety, premenstrual syndrome, catamenial epilepsy, and various other neuropsychiatric conditions.[26][27][28]
Increased levels of allopregnanolone can produce paradoxical effects, including negative mood, anxiety, irritability, and aggression.[29][30][31] This appears to be because allopregnanolone possesses biphasic, U-shaped actions at the GABAA receptor – moderate level increases (in the range of 1.5–2 nM/L total allopregnanolone, which are approximately equivalent to luteal phase levels) inhibit the activity of the receptor, while lower and higher concentration increases stimulate it.[29][30] This seems to be a common effect of many GABAA receptor positive allosteric modulators.[26][31] In accordance, acute administration of low doses of micronized progesterone (which reliably elevates allopregnanolone levels) has been found to have negative effects on mood, while higher doses have a neutral effect.[32]
During pregnancy, allopregnanolone and pregnanolone are involved in sedation and anesthesia of the fetus.[33][34]
Chemistry
Allopregnanolone is a pregnane (C21) steroid and is also known as 5α-pregnan-3α-ol-20-one, 3α-hydroxy-5α-pregnan-20-one, or 3α,5α-tetrahydroprogesterone (3α,5α-THP). It is very closely related structurally to 5-pregnenolone (pregn-5-en-3β-ol-20-dione), progesterone (pregn-4-ene-3,20-dione), the isomers of pregnanedione (5-dihydroprogesterone; 5-pregnane-3,20-dione), the isomers of 4-pregnenolone (3-dihydroprogesterone; pregn-4-en-3-ol-20-one), and the isomers of pregnanediol (5-pregnane-3,20-diol). In addition, allopregnanolone is one of four isomers of pregnanolone (3,5-tetrahydroprogesterone), with the other three isomers being pregnanolone (5β-pregnan-3α-ol-20-one), isopregnanolone(5α-pregnan-3β-ol-20-one), and epipregnanolone (5β-pregnan-3β-ol-20-one).
Derivatives
A variety of synthetic derivatives and analogues of allopregnanolone with similar activity and effects exist, including alfadolone (3α,21-dihydroxy-5α-pregnane-11,20-dione), alfaxolone (3α-hydroxy-5α-pregnane-11,20-dione), ganaxolone (3α-hydroxy-3β-methyl-5α-pregnan-20-one), hydroxydione (21-hydroxy-5β-pregnane-3,20-dione), minaxolone (11α-(dimethylamino)-2β-ethoxy-3α-hydroxy-5α-pregnan-20-one), Org 20599 (21-chloro-3α-hydroxy-2β-morpholin-4-yl-5β-pregnan-20-one), Org 21465 (2β-(2,2-dimethyl-4-morpholinyl)-3α-hydroxy-11,20-dioxo-5α-pregnan-21-yl methanesulfonate), and renanolone (3α-hydroxy-5β-pregnan-11,20-dione).
Research
Allopregnanolone and the other endogenous inhibitory neurosteroids have short terminal half-lives and poor oral bioavailability, and for these reason, have not been pursued for clinical use as oral therapies, although development as a parenteral therapy for multiple indications has been carried out. However, synthetic analogs with improved pharmacokineticprofiles have been synthesized and are being investigated as potential oral therapeutic agents.
In other studies of compounds related to allopregnanolone, exogenous progesterone, such as oral micronized progesterone (OMP), elevates allopregnanolone levels in the body with good dose-to-serum level correlations.[35] Due to this, it has been suggested that OMP could be described as a prodrug of sorts for allopregnanolone.[35] As a result, there has been some interest in using OMP to treat catamenial epilepsy,[36] as well as other menstrual cycle-related and neurosteroid-associated conditions. In addition to OMP, oral pregnenolonehas also been found to act as a prodrug of allopregnanolone,[37][38][39] though also of pregnenolone sulfate.[40]
Allopregnanolone has been under development by Sage Therapeutics as an intravenously administered drug for the treatment of super-refractory status epilepticus, postpartum depression, and essential tremor.[41] As of 19 March 2019 the FDA has approved allopregnanolone for postpartum depression.
References
- ^ “ChemIDplus – 516-54-1 – AURFZBICLPNKBZ-SYBPFIFISA-N – Brexanolone [USAN] – Similar structures search, synonyms, formulas, resource links, and other chemical information”. NIH Toxnet. Retrieved 26 December 2017.
- ^ Jump up to:a b c d e f g Reddy DS (2010). Neurosteroids: endogenous role in the human brain and therapeutic potentials. Prog. Brain Res. Progress in Brain Research. 186. pp. 113–37. doi:10.1016/B978-0-444-53630-3.00008-7. ISBN 9780444536303. PMC 3139029. PMID 21094889.
- ^ Reddy DS, Rogawski MA (2012). “Neurosteroids — Endogenous Regulators of Seizure Susceptibility and Role in the Treatment of Epilepsy”. Jasper’s Basic Mechanisms of the Epilepsies, 4th Edition: 984–1002. doi:10.1093/med/9780199746545.003.0077. ISBN 9780199746545.
- ^ T. G. Kokate, B. E. Svensson & M. A. Rogawski (September 1994). “Anticonvulsant activity of neurosteroids: correlation with γ-aminobutyric acid-evoked chloride current potentiation”. The Journal of Pharmacology and Experimental Therapeutics. 270 (3): 1223–1229. PMID 7932175.
- ^ Pinna, G; Uzunova, V; Matsumoto, K; Puia, G; Mienville, J. -M; Costa, E; Guidotti, A (2000-03-01). “Brain allopregnanolone regulates the potency of the GABAA receptor agonist muscimol”. Neuropharmacology. 39 (3): 440–448. doi:10.1016/S0028-3908(99)00149-5. PMID 10698010.
- ^ Agís-Balboa, Roberto C.; Pinna, Graziano; Zhubi, Adrian; Maloku, Ekrem; Veldic, Marin; Costa, Erminio; Guidotti, Alessandro (2006-09-26). “Characterization of brain neurons that express enzymes mediating neurosteroid biosynthesis”. Proceedings of the National Academy of Sciences. 103 (39): 14602–14607. doi:10.1073/pnas.0606544103. ISSN 0027-8424. PMC 1600006. PMID 16984997.
- ^ Mousavi Nik A, Pressly B, Singh V, Antrobus S, Hulsizer S, Rogawski MA, Wulff H, Pessah IN (2017). “Rapid Throughput Analysis of GABAA Receptor Subtype Modulators and Blockers Using DiSBAC1(3) Membrane Potential Red Dye”. Mol. Pharmacol. 92 (1): 88–99. doi:10.1124/mol.117.108563. PMC 5452057. PMID 28428226.
- ^ Morris KD, Moorefield CN, Amin J (October 1999). “Differential modulation of the gamma-aminobutyric acid type C receptor by neuroactive steroids”. Mol. Pharmacol. 56 (4): 752–9. PMID 10496958.
- ^ Li W, Jin X, Covey DF, Steinbach JH (October 2007). “Neuroactive steroids and human recombinant rho1 GABAC receptors”. J. Pharmacol. Exp. Ther. 323 (1): 236–47. doi:10.1124/jpet.107.127365. PMC 3905684. PMID 17636008.
- ^ Bullock AE, Clark AL, Grady SR, et al. (June 1997). “Neurosteroids modulate nicotinic receptor function in mouse striatal and thalamic synaptosomes”. J. Neurochem. 68 (6): 2412–23. doi:10.1046/j.1471-4159.1997.68062412.x. PMID 9166735.
- ^ Wetzel CH, Hermann B, Behl C, et al. (September 1998). “Functional antagonism of gonadal steroids at the 5-hydroxytryptamine type 3 receptor”. Mol. Endocrinol. 12 (9): 1441–51. doi:10.1210/mend.12.9.0163. PMID 9731711.
- ^ Jump up to:a b c Mellon SH (October 2007). “Neurosteroid regulation of central nervous system development”. Pharmacol. Ther. 116 (1): 107–24. doi:10.1016/j.pharmthera.2007.04.011. PMC 2386997. PMID 17651807.
- ^ Rupprecht R, Reul JM, Trapp T, et al. (September 1993). “Progesterone receptor-mediated effects of neuroactive steroids”. Neuron. 11 (3): 523–30. doi:10.1016/0896-6273(93)90156-l. PMID 8398145.
- ^ Jump up to:a b Thomas P, Pang Y (2012). “Membrane progesterone receptors: evidence for neuroprotective, neurosteroid signaling and neuroendocrine functions in neuronal cells”. Neuroendocrinology. 96 (2): 162–71. doi:10.1159/000339822. PMC 3489003. PMID 22687885.
- ^ Pang Y, Dong J, Thomas P (January 2013). “Characterization, neurosteroid binding and brain distribution of human membrane progesterone receptors δ and {epsilon} (mPRδ and mPR{epsilon}) and mPRδ involvement in neurosteroid inhibition of apoptosis”. Endocrinology. 154 (1): 283–95. doi:10.1210/en.2012-1772. PMC 3529379. PMID 23161870.
- ^ Sleiter N, Pang Y, Park C, et al. (August 2009). “Progesterone receptor A (PRA) and PRB-independent effects of progesterone on gonadotropin-releasing hormone release”. Endocrinology. 150 (8): 3833–44. doi:10.1210/en.2008-0774. PMC 2717864. PMID 19423765.
- ^ Lamba V, Yasuda K, Lamba JK, et al. (September 2004). “PXR (NR1I2): splice variants in human tissues, including brain, and identification of neurosteroids and nicotine as PXR activators”. Toxicol. Appl. Pharmacol. 199 (3): 251–65. doi:10.1016/j.taap.2003.12.027. PMID 15364541.
- ^ Hu AQ, Wang ZM, Lan DM, et al. (July 2007). “Inhibition of evoked glutamate release by neurosteroid allopregnanolone via inhibition of L-type calcium channels in rat medial prefrontal cortex”. Neuropsychopharmacology. 32 (7): 1477–89. doi:10.1038/sj.npp.1301261. PMID 17151597.
- ^ Jump up to:a b c Earl DE, Tietz EI (April 2011). “Inhibition of recombinant L-type voltage-gated calcium channels by positive allosteric modulators of GABAA receptors”. J. Pharmacol. Exp. Ther. 337 (1): 301–11. doi:10.1124/jpet.110.178244. PMC 3063747. PMID 21262851.
- ^ Jump up to:a b Keitel V, Görg B, Bidmon HJ, et al. (November 2010). “The bile acid receptor TGR5 (Gpbar-1) acts as a neurosteroid receptor in brain”. Glia. 58 (15): 1794–805. doi:10.1002/glia.21049. PMID 20665558.
- ^ Rougé-Pont F, Mayo W, Marinelli M, Gingras M, Le Moal M, Piazza PV (July 2002). “The neurosteroid allopregnanolone increases dopamine release and dopaminergic response to morphine in the rat nucleus accumbens”. Eur. J. Neurosci. 16 (1): 169–73. doi:10.1046/j.1460-9568.2002.02084.x. PMID 12153544.
- ^ Jump up to:a b Frye CA (December 2009). “Neurosteroids’ effects and mechanisms for social, cognitive, emotional, and physical functions”. Psychoneuroendocrinology. 34 Suppl 1: S143–61. doi:10.1016/j.psyneuen.2009.07.005. PMC 2898141. PMID 19656632.
- ^ Pinna G, Costa E, Guidotti A (February 2005). “Changes in brain testosterone and allopregnanolone biosynthesis elicit aggressive behavior”. Proc. Natl. Acad. Sci. U.S.A. 102 (6): 2135–40. doi:10.1073/pnas.0409643102. PMC 548579. PMID 15677716.
- ^ Terán-Pérez G, Arana-Lechuga Y, Esqueda-León E, Santana-Miranda R, Rojas-Zamorano JÁ, Velázquez Moctezuma J (October 2012). “Steroid hormones and sleep regulation”. Mini Rev Med Chem. 12 (11): 1040–8. doi:10.2174/138955712802762167. PMID 23092405.
- ^ Patte-Mensah C, Meyer L, Taleb O, Mensah-Nyagan AG (February 2014). “Potential role of allopregnanolone for a safe and effective therapy of neuropathic pain”. Prog. Neurobiol. 113: 70–8. doi:10.1016/j.pneurobio.2013.07.004. PMID 23948490.
- ^ Jump up to:a b Bäckström T, Andersson A, Andreé L, et al. (December 2003). “Pathogenesis in menstrual cycle-linked CNS disorders”. Ann. N. Y. Acad. Sci. 1007: 42–53. doi:10.1196/annals.1286.005. PMID 14993039.
- ^ Guille C, Spencer S, Cavus I, Epperson CN (July 2008). “The role of sex steroids in catamenial epilepsy and premenstrual dysphoric disorder: implications for diagnosis and treatment”. Epilepsy Behav. 13 (1): 12–24. doi:10.1016/j.yebeh.2008.02.004. PMC 4112568. PMID 18346939.
- ^ Finocchi C, Ferrari M (May 2011). “Female reproductive steroids and neuronal excitability”. Neurol. Sci. 32 Suppl 1: S31–5. doi:10.1007/s10072-011-0532-5. PMID 21533709.
- ^ Jump up to:a b Bäckström T, Haage D, Löfgren M, et al. (September 2011). “Paradoxical effects of GABA-A modulators may explain sex steroid induced negative mood symptoms in some persons”. Neuroscience. 191: 46–54. doi:10.1016/j.neuroscience.2011.03.061. PMID 21600269.
- ^ Jump up to:a b Andréen L, Nyberg S, Turkmen S, van Wingen G, Fernández G, Bäckström T (September 2009). “Sex steroid induced negative mood may be explained by the paradoxical effect mediated by GABAA modulators”. Psychoneuroendocrinology. 34 (8): 1121–32. doi:10.1016/j.psyneuen.2009.02.003. PMID 19272715.
- ^ Jump up to:a b Bäckström T, Bixo M, Johansson M, et al. (February 2014). “Allopregnanolone and mood disorders”. Prog. Neurobiol. 113: 88–94. doi:10.1016/j.pneurobio.2013.07.005. PMID 23978486.
- ^ Andréen L, Sundström-Poromaa I, Bixo M, Nyberg S, Bäckström T (August 2006). “Allopregnanolone concentration and mood–a bimodal association in postmenopausal women treated with oral progesterone”. Psychopharmacology. 187 (2): 209–21. doi:10.1007/s00213-006-0417-0. PMID 16724185.
- ^ Mellor DJ, Diesch TJ, Gunn AJ, Bennet L (2005). “The importance of ‘awareness’ for understanding fetal pain”. Brain Res. Brain Res. Rev. 49 (3): 455–71. doi:10.1016/j.brainresrev.2005.01.006. PMID 16269314.
- ^ Lagercrantz H, Changeux JP (2009). “The emergence of human consciousness: from fetal to neonatal life”. Pediatr. Res. 65 (3): 255–60. doi:10.1203/PDR.0b013e3181973b0d. PMID 19092726.
[…] the fetus is sedated by the low oxygen tension of the fetal blood and the neurosteroid anesthetics pregnanolone and the sleep-inducing prostaglandin D2 provided by the placenta (36).
- ^ Jump up to:a b Andréen L, Spigset O, Andersson A, Nyberg S, Bäckström T (June 2006). “Pharmacokinetics of progesterone and its metabolites allopregnanolone and pregnanolone after oral administration of low-dose progesterone”. Maturitas. 54 (3): 238–44. doi:10.1016/j.maturitas.2005.11.005. PMID 16406399.
- ^ Orrin Devinsky; Steven Schachter; Steven Pacia (1 January 2005). Complementary and Alternative Therapies for Epilepsy. Demos Medical Publishing. pp. 378–. ISBN 978-1-934559-08-6.
- ^ Saudan C, Desmarchelier A, Sottas PE, Mangin P, Saugy M (2005). “Urinary marker of oral pregnenolone administration”. Steroids. 70 (3): 179–83. doi:10.1016/j.steroids.2004.12.007. PMID 15763596.
- ^ Piper T, Schlug C, Mareck U, Schänzer W (2011). “Investigations on changes in ¹³C/¹²C ratios of endogenous urinary steroids after pregnenolone administration”. Drug Test Anal. 3(5): 283–90. doi:10.1002/dta.281. PMID 21538944.
- ^ Sripada RK, Marx CE, King AP, Rampton JC, Ho SS, Liberzon I (2013). “Allopregnanolone elevations following pregnenolone administration are associated with enhanced activation of emotion regulation neurocircuits”. Biol. Psychiatry. 73 (11): 1045–53. doi:10.1016/j.biopsych.2012.12.008. PMC 3648625. PMID 23348009.
- ^ Ducharme N, Banks WA, Morley JE, Robinson SM, Niehoff ML, Mattern C, Farr SA (2010). “Brain distribution and behavioral effects of progesterone and pregnenolone after intranasal or intravenous administration”. Eur. J. Pharmacol. 641 (2–3): 128–34. doi:10.1016/j.ejphar.2010.05.033. PMC 3008321. PMID 20570588.
- ^ “Brexanolone – Sage Therapeutics”. AdisInsight.
Further reading
- Herd, MB; Belelli, D; Lambert, JJ (2007). “Neurosteroid modulation of synaptic and extrasynaptic GABA(A) receptors”. Pharmacology & Therapeutics. 116 (1): 20–34. doi:10.1016/j.pharmthera.2007.03.007. PMID 17531325.
 |
|
 |
|
| Names | |
|---|---|
| IUPAC name
1-(3-Hydroxy-10,13-dimethyl-2,3,4,5,6,7,8,9,11,12,14,15,16,17-tetradecahydro-1H-cyclopenta[a]phenanthren-17-yl)ethanone
|
|
| Other names
ALLO; Allo; ALLOP; AlloP; Brexanolone; 5α-Pregnan-3α-ol-20-one; 3α-Hydroxy-5α-pregnan-20-one; 3α,5α-Tetrahydroprogesterone; 3α,5α-THP; Zulresso
|
|
| Identifiers | |
|
3D model (JSmol)
|
|
| ChEMBL | |
| ChemSpider | |
|
PubChemCID
|
|
| UNII | |
| Properties | |
| C21H34O2 | |
| Molar mass | 318.501 g·mol−1 |
|
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
|
|
//////////Brexanolone, Priority Review, Breakthrough Therapy designation, Zulresso, Sage Therapeutics Inc, FDA 2019, ブレキサノロン , Brexanolone, Allopregnanolone
CC(=O)C1CCC2C1(CCC3C2CCC4C3(CCC(C4)O)C)C
Prabotulinumtoxin A, プラボツリナムトキシンA
>Botulinum Toxin Type A Sequence MPFVNKQFNYKDPVNGVDIAYIKIPNVGQMQPVKAFKIHNKIWVIPERDTFTNPEEGDLN PPPEAKQVPVSYYDSTYLSTDNEKDNYLKGVTKLFERIYSTDLGRMLLTSIVRGIPFWGG STIDTELKVIDTNCINVIQPDGSYRSEELNLVIIGPSADIIQFECKSFGHEVLNLTRNGY GSTQYIRFSPDFTFGFEESLEVDTNPLLGAGKFATDPAVTLAHELIHAGHRLYGIAINPN RVFKVNTNAYYEMSGLEVSFEELRTFGGHDAKFIDSLQENEFRLYYYNKFKDIASTLNKA KSIVGTTASLQYMKNVFKEKYLLSEDTSGKFSVDKLKFDKLYKMLTEIYTEDNFVKFFKV LNRKTYLNFDKAVFKINIVPKVNYTIYDGFNLRNTNLAANFNGQNTEINNMNFTKLKNFT GLFEFYKLLCVRGIITSKTKSLDKGYNKALNDLCIKVNNWDLFFSPSEDNFTNDLNKGEE ITSDTNIEAAEENISLDLIQQYYLTFNFDNEPENISIENLSSDIIGQLELMPNIERFPNG KKYELDKYTMFHYLRAQEFEHGKSRIALTNSVNEALLNPSRVYTFFSSDYVKKVNKATEA AMFLGWVEQLVYDFTDETSEVSTTDKIADITIIIPYIGPALNIGNMLYKDDFVGALIFSG AVILLEFIPEIAIPVLGTFALVSYIANKVLTVQTIDNALSKRNEKWDEVYKYIVTNWLAK VNTQIDLIRKKMKEALENQAEATKAIINYQYNQYTEEEKNNINFNIDDLSSKLNESINKA MININKFLNQCSVSYLMNSMIPYGVKRLEDFDASLKDALLKYIYDNRGTLIGQVDRLKDK VNNTLSTDIPFQLSKYVDNQRLLSTFTEYIKNIINTSILNLRYESNHLIDLSRYASKINI GSKVNFDPIDKNQIQLFNLESSKIEVILKNAIVYNSMYENFSTSFWIRIPKYFNSISLNN EYTIINCMENNSGWKVSLNYGEIIWTLQDTQEIKQRVVFKYSQMINISDYINRWIFVTIT NNRLNNSKIYINGRLIDQKPISNLGNIHASNNIMFKLDGCRDTHRYIWIKYFNLFDKELN EKEIKDLYDNQSNSGILKDFWGDYLQYDKPYYMLNLYDPNKYVDVNNVGIRGYMYLKGPR GSVMTTNIYLNSSLYRGTKFIIKKYASGNKDNIVRNNDRVYINVVVKNKEYRLATNASQA GVEKILSALEIPDVGNLSQVVVMKSKNDQGITNKCKMNLQDNNGNDIGFIGFHQFNNIAK LVASNWYNRQIERSSRTLGCSWEFIPVDDGWGERPL
Prabotulinumtoxin A
プラボツリナムトキシンA;

| Formula |
C6760H10447N1743O2010S32
|
|---|---|
| CAS |
93384-43-1
|
| Mol weight |
149320.8333
|
AGN 191622 / ANT-1207 / ANT-1401 / ANT-1403 / NT 201
-
-
-
- APPROVED , FDA 2019, Jeuveau, 2019/2/1
-
-

- Purified botulinum toxin from Clostridium botulinum, purified from culture via dialysis and acid precipitation.
- Originator Daewoong Pharmaceutical
- Developer Daewoong Pharmaceutical; Evolus
- Class Analgesics; Antidepressants; Antimigraines; Antispasmodics; Bacterial proteins; Bacterial toxins; Botulinum toxins; Eye disorder therapies; Muscle relaxants; Skin disorder therapies; Urologics
- Mechanism of Action Acetylcholine inhibitors; Glutamate antagonists; Membrane transport protein modulators; Neuromuscular blocking agents
- Marketed Glabellar lines
- Phase III Muscle spasticity
- Phase II/III Blepharospasm; Facial wrinkles
- 27 Feb 2019 Evolus plans to launch prabotulinumtoxin A for Glabellar lines in USA (IM)
- 01 Feb 2019 Registered for Glabellar lines in USA (IM)
- 26 Nov 2018 Daewoong Pharmaceutical expects to launch prabotulinumtoxin A for Glabellar lines in eight Middle Eastern countries, including UAE and Kuwait in 2018 (Parenteral)
- AbobotulinumtoxinA
- Botulinum A neurotoxin
- Botulinum toxin A
- Botulinum toxin type A
- BTX-A
- Evabotulinumtoxina
- IncobotulinumtoxinA
- OnabotulinumtoxinA
- Prabotulinumtoxin A
- Toxina botulínica A
- Toxine botulinique A
For the treatment of cervical dystonia in adults to decrease the severity of abnormal head position and neck pain associated with cervical dystonia. Also for the treatment of severe primary axillary hyperhidrosis that is inadequately managed with topical agents and for the treatment of strabismus and blepharospasm associated with dystonia, including benign essential blepharospasm or VII nerve disorders in patients 12 years of age and above. Also used cosmetically to temporarily improve the appearance of moderate-to-severe frown lines between the eyebrows (glabellar lines) as well as for the treatment of excessive underarm sweating.
Botulinum toxin (BTX) is a neurotoxic protein produced by the bacterium Clostridium botulinum and related species.[1] It prevents the release of the neurotransmitter acetylcholine from axon endings at the neuromuscular junction and thus causes flaccid paralysis.[2]Infection with the bacterium causes the disease botulism. The toxin is also used commercially in medicine, cosmetics and research.
Botulinum is the most acutely lethal toxin known, with an estimated human median lethal dose (LD50) of 1.3–2.1 ng/kg intravenously or intramuscularly and 10–13 ng/kg when inhaled.[3][clarification needed]
There are eight types of botulinum toxin, named type A–H. Types A and B are capable of causing disease in humans, and are also used commercially and medically.[4] Types C–G are less common; types E and F can cause disease in humans, while the other types cause disease in other animals.[5] Type H is considered the deadliest substance in the world – an injection of only 2 ng can cause death to an adult.[6] Botulinum toxin types A and B are used in medicine to treat various muscle spasms and diseases characterized by overactive muscle. Commercial forms are marketed under the brand names Botox and Dysport, among others.[7][8]
Medical uses
Botulinum toxin is used to treat a number of problems.
Muscle spasticity
Botulinum toxin is used to treat a number of disorders characterized by overactive muscle movement, including post-stroke spasticity, post-spinal cord injury spasticity, spasms of the head and neck,[9] eyelid,[10] vagina,[11] limbs, jaw, and vocal cords.[12] Similarly, botulinum toxin is used to relax clenching of muscles, including those of the oesophagus,[13] jaw,[14]lower urinary tract and bladder,[15] or clenching of the anus which can exacerbate anal fissure.[16] It may also be used for improper eye alignment.[17] Botulinum toxin appears to be effective for refractory overactive bladder.[18]
Other muscle disorders
Strabismus is caused by imbalances in the actions of muscles that rotate the eyes, and can sometimes be relieved by weakening a muscle that pulls too strongly, or pulls against one that has been weakened by disease or trauma. Muscles weakened by toxin injection recover from paralysis after several months, so it might seem that injection would then need to be repeated. However, muscles adapt to the lengths at which they are chronically held,[19] so that if a paralyzed muscle is stretched by its antagonist, it grows longer, while the antagonist shortens, yielding a permanent effect. If there is good binocular vision, the brain mechanism of motor fusion, which aligns the eyes on a target visible to both, can stabilize the corrected alignment.
In January 2014, botulinum toxin was approved by UK’s Medicines and Healthcare Products Regulatory Agency (MHRA) for treatment of restricted ankle motion due to lower limb spasticity associated with stroke in adults.[20]
On July 29, 2016, Food and Drug Administration (FDA), of the United States of America approved abobotulinumtoxinA for injection for the treatment of lower limb spasticity in pediatric patients two years of age and older.[21] AbobotulinumtoxinA is the first and only FDA-approved botulinum toxin for the treatment of pediatric lower limb spasticity. In the United States of America, the FDA approves the text of the labels of prescription medicines. The FDA approves which medical conditions the drug manufacturer may sell the drug for. However, those approved by the FDA to prescribe these drugs may freely prescribe them for any condition they wish, called off-label use. Botulinum toxins have been used off-label for several pediatric conditions, including infantile esotropia.[22]
Excessive Sweating
Khalaf Bushara and David Park were the first to demonstrate a nonmuscular use of BTX-A while treating patients with hemifacial spasm in England in 1993, showing that botulinum toxin injections inhibit sweating, and so are useful in treating hyperhidrosis (excessive sweating).[23] BTX-A has since been approved for the treatment of severe primary axillary hyperhidrosis (excessive underarm sweating of unknown cause), which cannot be managed by topical agents.[12][24]
Migraine
In 2010, the FDA approved intramuscular botulinum toxin injections for prophylactic treatment of chronic migraine headache.[25]
Cosmetics
In cosmetic applications, botulinum toxin is considered safe and effective for reduction of facial wrinkles, especially in the uppermost third of the face.[26] Injection of botulinum toxin into the muscles under facial wrinkles causes relaxation of those muscles, resulting in the smoothing of the overlying skin.[26] Smoothing of wrinkles is usually visible three days after treatment and is maximally visible two weeks following injection.[26] The treated muscles gradually regain function, and generally return to their former appearance three to four months after treatment.[26] Muscles can be treated repeatedly to maintain the smoothed appearance.[26]
Other
Botulinum toxin is also used to treat disorders of hyperactive nerves including excessive sweating,[24] neuropathic pain,[27] and some allergysymptoms.[12] In addition to these uses, botulinum toxin is being evaluated for use in treating chronic pain.[28]
Side effects
While botulinum toxin is generally considered safe in a clinical setting, there can be serious side effects from its use. Most commonly, botulinum toxin can be injected into the wrong muscle group or spread from the injection site, causing paralysis of unintended muscles.
Side effects from cosmetic use generally result from unintended paralysis of facial muscles. These include partial facial paralysis, muscle weakness, and trouble swallowing. Side effects are not limited to direct paralysis however, and can also include headaches, flu-like symptoms, and allergic reactions.[29] Just as cosmetic treatments only last a number of months, paralysis side-effects can have the same durations.[citation needed] At least in some cases, these effects are reported to dissipate in the weeks after treatment.[citation needed] Bruising at the site of injection is not a side effect of the toxin but rather of the mode of administration, and is reported as preventable if the clinician applies pressure to the injection site; when it occurs, it is reported in specific cases to last 7–11 days.[citation needed] When injecting the masseter muscle of the jaw, loss of muscle function can result in a loss or reduction of power to chew solid foods.[29]
Side effects from therapeutic use can be much more varied depending on the location of injection and the dose of toxin injected. In general, side effects from therapeutic use can be more serious than those that arise during cosmetic use. These can arise from paralysis of critical muscle groups and can include arrhythmia, heart attack, and in some cases seizures, respiratory arrest, and death.[29] Additionally, side effects which are common in cosmetic use are also common in therapeutic use, including trouble swallowing, muscle weakness, allergic reactions, and flu-like syndromes.[29]
In response to the occurrence of these side effects, in 2008 the U.S. Food and Drug Administration notified the public of the potential dangers of the botulinum toxin as a therapeutic. Namely, they warned that the toxin can spread to areas distant from the site of injection and paralyze unintended muscle groups, especially when used for treating muscle spasticity in children treated for cerebral palsy.[30] In 2009, the FDA announced that boxed warnings would be added to available botulinum toxin products, warning of their ability to spread from the injection site.[31] Additionally, the FDA announced name changes to several botulinum toxin products, meant to emphasize that the products are not interchangeable and require different doses for proper use. Botox and Botox Cosmetic were renamed onabotulinumtoxinA, Myobloc was renamed rimabotulinumtoxinB, and Dysport name renamed abobotulinumtoxinA.[31] In conjunction with this, the FDA issued a communication to health care professionals reiterating the new drug names and the approved uses for each.[32] A similar warning was issued by Health Canada in 2009, warning that botulinum toxin products can spread to other parts of the body.[33]
Role in disease
Botulinum toxin produced by Clostridium botulinum is the cause of botulism.[10] Humans most commonly ingest the toxin from eating improperly-canned foods in which C. botulinumhas grown. However, the toxin can also be introduced through an infected wound. In infants, the bacteria can sometimes grow in the intestines and produce botulinum toxin within the intestine and can cause a condition known as floppy baby syndrome.[34] In all cases, the toxin can then spread, blocking nerves and muscle function. In severe cases, the toxin can block nerves controlling the respiratory system or heart, resulting in death.[1] Botulism can be difficult to diagnose, as it may appear similar to diseases such as Guillain–Barré syndrome, myasthenia gravis, and stroke. Other tests, such as brain scan and spinal fluid examination, may help to rule out other causes. If the symptoms of botulism are diagnosed early, various treatments can be administered. In an effort to remove contaminated food which remains in the gut, enemas or induced vomiting may be used.[35] For wound infections, infected material may be removed surgically.[35] Botulinum antitoxin is available and may be used to prevent the worsening of symptoms, though it will not reverse existing nerve damage. In severe cases, mechanical respiration may be used to support patients suffering from respiratory failure.[35] The nerve damage heals over time, generally over weeks to months.[5] With proper treatment, the case fatality rate for botulinum poisoning can be greatly reduced.[35]
Two preparations of botulinum antitoxins are available for treatment of botulism. Trivalent (A,B,E) botulinum antitoxin is derived from equine sources using whole antibodies. The second antitoxin is Heptavalent (A,B,C,D,E,F,G) botulinum antitoxin, which is derived from equine antibodies which have been altered to make them less immunogenic. This antitoxin is effective against all known strains of botulism.
Mechanism of action
Target molecules of botulinum neurotoxin (abbreviated BoNT) and tetanus neurotoxin (TeNT), toxins acting inside the axon terminal.[36]
Botulinum toxin exerts its effect by cleaving key proteins required for nerve activation. First, the toxin binds specifically to nerves which use the neurotransmitter acetylcholine. Once bound to the nerve terminal, the neuron takes up the toxin into a vesicle by receptor-mediated endocytosis.[37] As the vesicle moves farther into the cell, it acidifies, activating a portion of the toxin which triggers it to push across the vesicle membrane and into the cell cytoplasm.[1] Once inside the cytoplasm, the toxin cleaves SNARE proteins, meaning that the acetylcholine vesicles can’t bind to the intracellular cell membrane,[37] preventing the cell from releasing vesicles of neurotransmitter. This stops nerve signaling, leading to paralysis.[1]
The toxin itself is released from the bacterium as a single chain, then becomes activated when cleaved by its own proteases.[12] The active form consists of a two-chain protein composed of a 100-kDa heavy chain polypeptide joined via disulfide bond to a 50-kDa light chain polypeptide.[38] The heavy chain contains domains with several functions: it has the domain responsible for binding specifically to presynaptic nerve terminals, as well as the domain responsible for mediating translocation of the light chain into the cell cytoplasm as the vacuole acidifies.[1][38] The light chain is a zinc metalloprotease and is the active part of the toxin. It is translocated into the host cell cytoplasm where it cleaves the host protein SNAP-25, a member of the SNARE protein family which is responsible for fusion. The cleaved SNAP-25 is unable to mediate fusion of vesicles with the host cell membrane, thus preventing the release of the neurotransmitteracetylcholine from axon endings.[1] This blockage is slowly reversed as the toxin loses activity and the SNARE proteins are slowly regenerated by the affected cell.[1]
The seven toxin types (A-G) have different tertiary structures and sequence differences.[38][39] While the different toxin types all target members of the SNARE family, different toxin types target different SNARE family members.[36] The A, B, and E serotypes cause human botulism, with the activities of types A and B enduring longest in vivo (from several weeks to months).[38]
History
In 1820, Justinus Kerner, a small-town German medical officer and romantic poet, gave the first complete description of clinical botulism based on extensive clinical observations of so-called “sausage poisoning”.[40] Following experiments on animals and on himself, he concluded that the toxin acts by interrupting signal transmission in the somatic and autonomic motor systems, without affecting sensory signals or mental functions. He observed that the toxin develops under anaerobic conditions, and can be lethal in minute doses.[41] His prescience in suggesting that the toxin might be used therapeutically earned him recognition as the pioneer of modern botulinum toxin therapy.[42]
In 1895 (seventy-five years later), Émile van Ermengem, professor of bacteriology and a student of Robert Koch, correctly described Clostridium botulinum as the bacterial source of the toxin. Thirty-four attendees at a funeral were poisoned by eating partially salted ham, an extract of which was found to cause botulism-like paralysis in laboratory animals. Van Ermengem isolated and grew the bacterium, and described its toxin,[43] which was later purified by P Tessmer Snipe and Hermann Sommer.[44]
Food canning
Over the next three decades, 1895-1925, as food canning was approaching a billion-dollar-a-year industry, botulism was becoming a public health hazard. Karl Friedrich Meyer, a prodigiously productive Swiss-American veterinary scientist created a center at the Hooper Foundation in San Francisco, where he developed techniques for growing the organism and extracting the toxin, and conversely, for preventing organism growth and toxin production, and inactivating the toxin by heating. The California canning industry was thereby preserved.
World War II
With the outbreak of World War II, weaponization of botulinum toxin was investigated at Fort Detrick in Maryland. Carl Lamanna and James Duff[45] developed the concentration and crystallization techniques that Edward J. Schantz used to create the first clinical product. When the Army’s Chemical Corps was disbanded, Schantz moved to the Food Research Institute in Wisconsin, where he manufactured toxin for experimental use and generously provided it to the academic community.
The mechanism of botulinum toxin action – blocking the release from nerve endings of the neurotransmitter acetylcholine – was elucidated in the mid-1900s,[46] and remains an important research topic. Nearly all toxin treatments are based on this effect in various body tissues.
Strabismus
Ophthalmologists specializing in eye muscle disorders (strabismus) had developed the method of EMG-guided injection (using the electromyogram, the electrical signal from an activated muscle, to guide injection) of local anesthetics as a diagnostic technique for evaluating an individual muscle’s contribution to an eye movement.[47] Because strabismus surgery frequently needed repeating, a search was undertaken for non-surgical, injection treatments using various anesthetics, alcohols, enzymes, enzyme blockers, and snake neurotoxins. Finally, inspired by Daniel Drachman’s work with chicks at Johns Hopkins,[48] Alan B. Scott and colleagues injected botulinum toxin into monkey extraocular muscles.[49]The result was remarkable: a few picograms induced paralysis that was confined to the target muscle, long in duration, and without side-effects.
After working out techniques for freeze-drying, buffering with albumin, and assuring sterility, potency, and safety, Scott applied to the FDA for investigational drug use, and began manufacturing botulinum type A neurotoxin in his San Francisco lab. He injected the first strabismus patients in 1977, reported its clinical utility in 1980,[50] and had soon trained hundreds of ophthalmologists in EMG-guided injection of the drug he named Oculinum (“eye aligner”).
In 1986, Oculinum Inc, Scott’s micromanufacturer and distributor of botulinum toxin, was unable to obtain product liability insurance, and could no longer supply the drug. As supplies became exhausted, patients who had come to rely on periodic injections became desperate. For 4 months, as liability issues were resolved, American blepharospasm patients traveled to Canadian eye centers for their injections.[51]
Based on data from thousands of patients collected by 240 investigators, Allergan received FDA approval in 1989 to market Oculinum for clinical use in the United States to treat adult strabismus and blepharospasm, using the trademark Botox.[52] This was under the 1983 US Orphan Drug Act.[53]
Cosmetics
Richard Clark, a plastic surgeon from Sacramento (CA), was the first to document a cosmetic use for botulinum toxin.[54] He treated forehead asymmetry caused by left sided forehead nerve paralysis that occurred during a cosmetic facelift. Since the injured nerve could possibly regenerate by 24 months, a two-year waiting period was necessary before definitive surgical treatment could be done. Clark realized that botulinum toxin, which had been previously used only for cross eyed babies and facial tics, could also be injected to smooth the wrinkles of the right forehead to match her paralyzed left. He received FDA approval for this cosmetic application of the toxin and successfully treated the person and published the case study in 1989.[54]
Marrying ophthalmology to dermatology, Jean and Alistair Carruthers observed that blepharospasm patients who received injections around the eyes and upper face also enjoyed diminished facial glabellar lines (“frown lines” between the eyebrows), thereby initiating the highly-popular cosmetic use of the toxin.[55] Brin, and a group at Columbia University under Monte Keen made similar reports.[56] In 2002, following clinical trials, the FDA approved Botox Cosmetic, botulinum A toxin to temporarily improve the appearance of moderate-to-severe glabellar lines.[57] The FDA approved a fully in vitro assay for use in the stability and potency testing of Botox in response to increasing public concern that LD50testing was required for each batch sold in the market.[58][59]
Chronic pain
William J. Binder reported in 2000 that patients who had cosmetic injections around the face reported relief from chronic headache.[60] This was initially thought to be an indirect effect of reduced muscle tension, but it is now known that the toxin inhibits release of peripheral nociceptive neurotransmitters, suppressing the central pain processing systems responsible for migraine headache.[61][62]
Society and culture
Economics
As of 2013, botulinum toxin injections are the most common cosmetic operation, with 6.3 million procedures in the United States, according to the American Society of Plastic Surgeons. Qualifications for Botox injectors vary by county, state and country. Botox cosmetic providers include dermatologists, plastic surgeons, aesthetic spa physicians, dentists, nurse practitioners, nurses and physician assistants.
The global market for botulinum toxin products, driven by their cosmetic applications, is forecast to reach $2.9 billion by 2018. The facial aesthetics market, of which they are a component, is forecast to reach $4.7 billion ($2 billion in the U.S.) in the same timeframe.[63]
Bioterrorism
Botulinum toxin has been recognized as a potential agent for use in bioterrorism.[64] It can be absorbed through the eyes, mucous membranes, respiratory tract, or non-intact skin.[65]
The effects of botulinum toxin are different from those of nerve agents involved insofar in that botulism symptoms develop relatively slowly (over several days), while nerve agent effects are generally much more rapid and can be instantaneous.[citation needed] Evidence suggests that nerve exposure (simulated by injection of atropine and pralidoxime) will increase mortality by enhancing botulinum toxin’s mechanism of toxicity.[citation needed]
With regard to detection, current protocols using NBC detection equipment (such as M-8 paper or the ICAM) will not indicate a “positive” when samples containing botulinum toxin are tested.[citation needed] To confirm a diagnosis of botulinum toxin poisoning, therapeutically or to provide evidence in death investigations, botulinum toxin may be quantitated by immunoassay of human biological fluids; serum levels of 12–24 mouse LD50 units per milliliter have been detected in poisoned patients.[66]
The Japanese doomsday cult Aum Shinrikyo produced botulinum toxin and spread it as an aerosol in downtown Tokyo during the 1990s, but the attacks caused no fatalities.[67]
During the early 1980s, the German and French newspapers reported that the police had raided a Baader-Meinhof gang safe house in Paris and had found a makeshift laboratory that contained flasks full of Clostridium botulinum, which makes botulinum toxin. Their reports were later found to be incorrect; no such lab was ever found.[68]
Brand names
Botulinum toxin A is marketed under the brand names Botox and Xeomin. Botulinum toxin B is marketed under the brand name Myobloc.
In the United States, botulinum toxin products are manufactured by a variety of companies, for both therapeutic and cosmetic use. A U.S. supplier reported in its company materials in 2011 that it could “supply the world’s requirements for 25 indications approved by Government agencies around the world” with less than one gram of raw botulinum toxin.[69]Myobloc or Neurobloc, a botulinum toxin type B product, is produced by Solstice Neurosciences, a subsidiary of US WorldMeds. AbobotulinumtoxinA), a therapeutic formulation of the type A toxin manufactured by Galderma in the United Kingdom, is licensed for the treatment of focal dystonias and certain cosmetic uses in the U.S. and other countries.[32]
Besides the three primary U.S. manufacturers, there are numerous other botulinum toxin producers. Xeomin, manufactured in Germany by Merz, is also available for both therapeutic and cosmetic use in the U.S.[70] Lanzhou Institute of Biological Products in China manufactures a BTX-A product; as of 2014 it was the only BTX-A approved in China.[70] BTX-A is also sold as Lantox and Prosigne on the global market.[71] Neuronox, a BTX-A product, was introduced by Medy-Tox Inc. of South Korea in 2009;[72]
Toxin production
Botulism toxins are produced by bacteria of the genus Clostridium, namely Clostridium botulinum, C. butyricum, C. baratii and C. argentinense,[73] which are widely distributed, including in soil and dust. As well, the bacteria can be found inside homes on floors, carpet, and countertops even after cleaning.[citation needed] Some food products such as honey can contain amounts of the bacteria.[citation needed]
Food-borne botulism results, indirectly, from ingestion of food contaminated with Clostridium spores, where exposure to an anaerobic environment allows the spores to germinate, after which the bacteria can multiply and produce toxin.[citation needed] Critically, it is ingestion of toxin rather than spores or vegetative bacteria that causes botulism.[citation needed]Botulism is nevertheless known to be transmitted through canned foods not cooked correctly before canning or after can opening, and so is preventable.[citation needed] Infant botulism cases arise chiefly as a result of environmental exposure and are therefore more difficult to prevent.[citation needed] Infant botulism arising from consumption of honey can be prevented by eliminating honey from diets of children less than 12 months old.[74]
Organism and toxin susceptibilities
Proper refrigeration at temperatures below 3 °C (38 °F) retards the growth of Clostridium botulinum. The organism is also susceptible to high salt, high oxygen, and low pH levels.[5]The toxin itself is rapidly destroyed by heat, such as in thorough cooking.[75] The spores that produce the toxin are heat-tolerant and will survive boiling water for an extended period of time.[76]
The botulinum toxin is denatured and thus deactivated at temperatures greater than 80 °C (176 °F).[77] As a zinc metalloprotease (see below), the toxin’s activity is also susceptible, post-exposure, to inhibition by protease inhibitors, e.g., zinc-coordinating hydroxamates.[38][78]
Research
Blepharospasm and strabismus
University-based ophthalmologists in the USA and Canada further refined the use of botulinum toxin as a therapeutic agent. By 1985, a scientific protocol of injection sites and dosage had been empirically determined for treatment of blepharospasm and strabismus.[79] Side effects in treatment of this condition were deemed to be rare, mild and treatable.[80]The beneficial effects of the injection lasted only 4–6 months. Thus, blepharospasm patients required re-injection two or three times a year.
In 1986, Scott’s micromanufacturer and distributor of Botox was no longer able to supply the drug because of an inability to obtain product liability insurance. Patients became desperate, as supplies of Botox were gradually consumed, forcing him to abandon patients who would have been due for their next injection. For a period of four months, American blepharospasm patients had to arrange to have their injections performed by participating doctors at Canadian eye centers until the liability issues could be resolved.[51]
In December 1989, Botox was approved by the US Food and Drug Administration (FDA) for the treatment of strabismus, blepharospasm, and hemifacial spasm in patients over 12 years old.[52]
Botox has not been approved for any pediatric use.[32] It has, however, been used off-label by physicians for several conditions. including spastic conditions in pediatric patients with cerebral palsy, a therapeutic course that has resulted in patient deaths.[32] In the case of treatment of infantile esotropia in patients younger than 12 years of age, several studies have yielded differing results.[22][better source needed]
Cosmetic
The cosmetic effect of BTX-A on wrinkles was originally documented by a plastic surgeon from Sacramento, California, Richard Clark, and published in the journal Plastic and Reconstructive Surgery in 1989.[54] Canadian husband and wife ophthalmologist and dermatologist physicians, JD and JA Carruthers, were the first to publish a study on BTX-A for the treatment of glabellar frown lines in 1992.[55] Similar effects had reportedly been observed by a number of independent groups (Brin, and the Columbia University group under Monte Keen.[56]) After formal trials, on April 12, 2002, the FDA announced regulatory approval of botulinum toxin type A (Botox Cosmetic) to temporarily improve the appearance of moderate-to-severe frown lines between the eyebrows (glabellar lines).[57] Subsequently, cosmetic use of botulinum toxin type A has become widespread.[81] The results of Botox Cosmetic can last up to four months and may vary with each patient.[82] The US Food and Drug Administration approved an alternative product-safety testing method in response to increasing public concern that LD50 testing was required for each batch sold in the market.[58][59]
BTX-A has also been used in the treatment of gummy smiles,[83][84] the material is injected into the hyperactive muscles of upper lip, which causes a reduction in the upward movement of lip thus resulting in a smile with a less exposure of gingiva.[85] Botox is usually injected in the three lip elevator muscles that converge on the lateral side of the ala of the nose; the levator labii superioris (LLS), the levator labii superioris alaeque nasi muscle (LLSAN), and the zygomaticus minor (ZMi).[86][87]
Upper motor neuron syndrome
BTX-A is now a common treatment for muscles affected by the upper motor neuron syndrome (UMNS), such as cerebral palsy, for muscles with an impaired ability to effectively lengthen. Muscles affected by UMNS frequently are limited by weakness, loss of reciprocal inhibition, decreased movement control and hypertonicity (including spasticity). In January 2014, Botulinum toxin was approved by UK’s Medicines and Healthcare Products Regulatory Agency (MHRA) for the treatment of ankle disability due to lower limb spasticity associated with stroke in adults.[20] Joint motion may be restricted by severe muscle imbalance related to the syndrome, when some muscles are markedly hypertonic, and lack effective active lengthening. Injecting an overactive muscle to decrease its level of contraction can allow improved reciprocal motion, so improved ability to move and exercise.
Sweating
Khalaf Bushara and David Park were the first to demonstrate a nonmuscular use of BTX-A while treating patients with hemifacial spasm in England in 1993, showing that botulinum toxin injections inhibit sweating, and so are useful in treating hyperhidrosis (excessive sweating).[23] BTX-A has since been approved for the treatment of severe primary axillary hyperhidrosis (excessive underarm sweating of unknown cause), which cannot be managed by topical agents.[12][24]
Cervical dystonia
BTX-A is commonly used to treat cervical dystonia, but it can become ineffective after a time. Botulinum toxin type B (BTX-B) received FDA approval for treatment of cervical dystonia on December 21, 2000. Trade names for BTX-B are Myobloc in the United States, and Neurobloc in the European Union.[70]
Chronic migraine
Onabotulinumtoxin A (trade name Botox) received FDA approval for treatment of chronic migraines on October 15, 2010. The toxin is injected into the head and neck to treat these chronic headaches. Approval followed evidence presented to the agency from two studies funded by Allergan showing a very slight improvement in incidence of chronic migraines for migraine sufferers undergoing the Botox treatment.[88][89]
Since then, several randomized control trials have shown botulinum toxin type A to improve headache symptoms and quality of life when used prophylactically for patients with chronic migraine[90] who exhibit headache characteristics consistent with: pressure perceived from outside source, shorter total duration of chronic migraines (<30 years), “detoxification” of patients with coexisting chronic daily headache due to medication overuse, and no current history of other preventive headache medications.[91]
Depression
A few small trials have found benefits in people with depression.[92][93]
Premature ejaculation
The drug is under development for the treatment of premature ejaculation.[93]
References
- ^ Jump up to:a b c d e f g Montecucco C, Molgó J (June 2005). “Botulinal neurotoxins: revival of an old killer”. Current Opinion in Pharmacology. 5 (3): 274–79. doi:10.1016/j.coph.2004.12.006. PMID 15907915.
- ^ Figgitt, David P.; Noble, Stuart (2002). “Botulinum Toxin B”. Drugs. 62 (4): 705–722. doi:10.2165/00003495-200262040-00011. PMID 11893235.
- ^ Arnon SS, Schechter R, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Hauer J, Layton M, Lillibridge S, Osterholm MT, O’Toole T, Parker G, Perl TM, Russell PK, Swerdlow DL, Tonat K (February 2001). “Botulinum toxin as a biological weapon: medical and public health management”. JAMA. 285 (8): 1059–70. doi:10.1001/jama.285.8.1059. PMID 11209178.
- ^ American Society of Health-System Pharmacists (October 27, 2011). “Botulinum Toxin Type A”. drugs.com. Retrieved 4 March 2015.
- ^ Jump up to:a b c “Fact Sheet: Botulism”. World Health Organization. Retrieved 4 October 2016.
- ^ Weller C (15 October 2013). “New Botulinum Toxin Deemed Deadliest Substance Ever: Sniffing 13-Billionths of a Gram Can Kill”. Medical Daily.
- ^ Egan M (17 November 2014). “Botox maker bought for $66 billion in biggest deal of 2014”. cnn.com.
- ^ “Actavis plc is now Allergan plc”. Allergan. 15 June 2015. Retrieved 16 June 2015.
- ^ “Cervical dystonia”. Mayo Clinic. 2014-01-28. Retrieved 2015-10-14.
- ^ Jump up to:a b Shukla HD, Sharma SK (2005). “Clostridium botulinum: a bug with beauty and weapon”. Critical Reviews in Microbiology. 31 (1): 11–18. doi:10.1080/10408410590912952. PMID 15839401.
- ^ Pacik PT (December 2009). “Botox treatment for vaginismus”. Plastic and Reconstructive Surgery. 124 (6): 455e–56e. doi:10.1097/PRS.0b013e3181bf7f11. PMID 19952618.
- ^ Jump up to:a b c d e Felber ES (October 2006). “Botulinum toxin in primary care medicine”. The Journal of the American Osteopathic Association. 106 (10): 609–14. PMID 17122031.
- ^ Stavropoulos SN, Friedel D, Modayil R, Iqbal S, Grendell JH (March 2013). “Endoscopic approaches to treatment of achalasia”. Therapeutic Advances in Gastroenterology. 6 (2): 115–35. doi:10.1177/1756283X12468039. PMC 3589133. PMID 23503707.
- ^ Long H, Liao Z, Wang Y, Liao L, Lai W (February 2012). “Efficacy of botulinum toxins on bruxism: an evidence-based review”. International Dental Journal. 62 (1): 1–5. doi:10.1111/j.1875-595X.2011.00085.x. PMID 22251031.
- ^ Mangera A, Andersson KE, Apostolidis A, Chapple C, Dasgupta P, Giannantoni A, Gravas S, Madersbacher S (October 2011). “Contemporary management of lower urinary tract disease with botulinum toxin A: a systematic review of botox (onabotulinumtoxinA) and dysport (abobotulinumtoxinA)”. European Urology. 60 (4): 784–95. doi:10.1016/j.eururo.2011.07.001. PMID 21782318.
- ^ Trzciński R, Dziki A, Tchórzewski M (2002). “Injections of botulinum A toxin for the treatment of anal fissures”. The European Journal of Surgery = Acta Chirurgica. 168 (12): 720–23. doi:10.1080/11024150201680030. PMID 15362583.
- ^ Kowal L, Wong E, Yahalom C (December 2007). “Botulinum toxin in the treatment of strabismus. A review of its use and effects”. Disability and Rehabilitation. 29 (23): 1823–31. doi:10.1080/09638280701568189. PMID 18033607.
- ^ Duthie JB, Vincent M, Herbison GP, Wilson DI, Wilson D (December 2011). “Botulinum toxin injections for adults with overactive bladder syndrome”. The Cochrane Database of Systematic Reviews (12): CD005493. doi:10.1002/14651858.CD005493.pub3. PMID 22161392.
- ^ Scott AB (1994). “Change of eye muscle sarcomeres according to eye position”. Journal of Pediatric Ophthalmology and Strabismus. 31 (2): 85–88. PMID 8014792.
- ^ Jump up to:a b UK Approves New Botox Use Archived 2014-02-22 at the Wayback Machine. dddmag.com. February 4, 2014
- ^ “FDA Approved Drug Products – Dysport”. http://www.accessdata.fda.gov. U.S. Food and Drug Administration. Retrieved 2016-11-07.
- ^ Jump up to:a b Ocampo VV, Foster CS (May 30, 2012). “Infantile Esotropia Treatment & Management”. Medscape. Retrieved April 6, 2014.
- ^ Jump up to:a b Bushara KO, Park DM (November 1994). “Botulinum toxin and sweating”. Journal of Neurology, Neurosurgery, and Psychiatry. 57 (11): 1437–38. doi:10.1136/jnnp.57.11.1437. PMC 1073208. PMID 7964832.
- ^ Jump up to:a b c Eisenach JH, Atkinson JL, Fealey RD (May 2005). “Hyperhidrosis: evolving therapies for a well-established phenomenon”. Mayo Clinic Proceedings. 80 (5): 657–66. doi:10.4065/80.5.657. PMID 15887434.
- ^ “FDA Approves Botox to Treat Chronic Migraines”. WebMD. Retrieved 12 May 2017.
- ^ Jump up to:a b c d e Small R (August 2014). “Botulinum toxin injection for facial wrinkles”. American Family Physician. 90 (3): 168–75. PMID 25077722.
- ^ Mittal SO, Safarpour D, Jabbari B (February 2016). “Botulinum Toxin Treatment of Neuropathic Pain”. Seminars in Neurology. 36 (1): 73–83. doi:10.1055/s-0036-1571953. PMID 26866499.
- ^ Charles PD (November 2004). “Botulinum neurotoxin serotype A: a clinical update on non-cosmetic uses”. American Journal of Health-System Pharmacy. 61 (22 Suppl 6): S11–23. doi:10.1093/ajhp/61.suppl_6.S11. PMID 15598005.
- ^ Jump up to:a b c d Coté TR, Mohan AK, Polder JA, Walton MK, Braun MM (September 2005). “Botulinum toxin type A injections: adverse events reported to the US Food and Drug Administration in therapeutic and cosmetic cases”. Journal of the American Academy of Dermatology. 53 (3): 407–15. doi:10.1016/j.jaad.2005.06.011. PMID 16112345.
- ^ “FDA Notifies Public of Adverse Reactions Linked to Botox Use”. Fda.gov. 8 February 2008. Retrieved May 6, 2012.
- ^ Jump up to:a b “FDA Gives Update on Botulinum Toxin Safety Warnings; Established Names of Drugs Changed”. FDA Press Announcement. August 3, 2009. Retrieved 21 September 2016.
- ^ Jump up to:a b c d “Information for Healthcare Professionals: OnabotulinumtoxinA (marketed as Botox/Botox Cosmetic), AbobotulinumtoxinA (marketed as Dysport) and RimabotulinumtoxinB (marketed as Myobloc)”. fda.gov. Food and Drug Administration. Retrieved 1 September 2015.
- ^ “Botox chemical may spread, Health Canada confirms”. CBC News. January 13, 2009. Archived from the original on 21 February 2009.
- ^ “Kinds of Botulism”. Centers for Disease Control and Prevention. Retrieved 4 October2016.
- ^ Jump up to:a b c d “Botulism – Diagnosis and Treatment”. Centers for Disease Control and Prevention. Retrieved 5 October 2016.
- ^ Jump up to:a b Barr JR, Moura H, Boyer AE, Woolfitt AR, Kalb SR, Pavlopoulos A, McWilliams LG, Schmidt JG, Martinez RA, Ashley DL (October 2005). “Botulinum neurotoxin detection and differentiation by mass spectrometry”. Emerging Infectious Diseases. 11 (10): 1578–83. doi:10.3201/eid1110.041279. PMC 3366733. PMID 16318699.
- ^ Jump up to:a b Dressler, D; Saberi, FA; Barbosa, ER (March 2005). “Botulinum toxin: mechanisms of action”. Arquivos de Neuro-Psiquiatria. 63 (1): 180–5. doi:10.1159/000083259. PMID 15830090.
- ^ Jump up to:a b c d e Li B, Peet NP, Butler MM, Burnett JC, Moir DT, Bowlin TL (December 2010). “Small molecule inhibitors as countermeasures for botulinum neurotoxin intoxication”. Molecules. 16 (1): 202–20. doi:10.3390/molecules16010202. PMC 6259422. PMID 21193845.
- ^ Hill KK, Smith TJ (2013). “Genetic Diversity Within Clostridium botulinum Serotypes, Botulinum Neurotoxin Gene Clusters and Toxin Subtypes”. In Rummel A, Binz T. Botulinum neurotoxins. Current Topics in Microbiology and Immunology. 364. Heidelberg: Springer. pp. 1–20. doi:10.1007/978-3-642-33570-9_1. ISBN 978-3-642-33569-3. PMID 23239346.
- ^ Kerner J (1820). Neue Beobachtungen über die in Württemberg so häufig vorfallenden tödlichen Vergiftungen durch den Genuss geräucherter Würste. Tübingen: Osiander.
- ^ Kerner J (1822). Das Fettgift oder die Fettsäure und ihre Wirkungen auf den thierischen Organismus, ein Beytrag zur Untersuchung des in verdorbenen Würsten giftig wirkenden Stoffes. Stuttgart, Tübingen: Cotta. pp. 681–87. OCLC 863571562.
- ^ Erbguth FJ, Naumann M (November 1999). “Historical aspects of botulinum toxin: Justinus Kerner (1786–1862) and the “sausage poison““. Neurology. 53 (8): 1850–53. doi:10.1212/wnl.53.8.1850. PMID 10563638.
- ^ van Ermengem E (1979). “Classics in infectious diseases. A new anaerobic bacillus and its relation to botulism. E. van Ermengem. Originally published as “Ueber einen neuen anaëroben Bacillus und seine Beziehungen zum Botulismus” in Zeitschrift für Hygiene und Infektionskrankheiten 26: 1–56, 1897″. Reviews of Infectious Diseases (in German). 1 (4): 701–19. PMID 399378. Original doi:10.1007/BF02220526
- ^ Snipe PT, Sommer H (August 1928). “Studies on Botulinus Toxin: 3. Acid Precipitation of Botulinus Toxin”. The Journal of Infectious Diseases. 43 (2): 152–60. doi:10.1093/infdis/43.2.152. JSTOR 30083772.
- ^ Lamanna C, McElroy OE, Eklund HW (May 1946). “The purification and crystallization of Clostridium botulinum type A toxin”. Science. 103 (2681): 613–14. Bibcode:1946Sci…103..613L. doi:10.1126/science.103.2681.613. PMID 21026141.
- ^ Burgen AS, Dickens F, Zatman LJ (August 1949). “The action of botulinum toxin on the neuro-muscular junction”. The Journal of Physiology. 109 (1–2): 10–24. doi:10.1113/jphysiol.1949.sp004364. PMC 1392572. PMID 15394302.
- ^ Magoon E, Cruciger M, Scott AB, Jampolsky A (May 1982). “Diagnostic injection of Xylocaine into extraocular muscles”. Ophthalmology. 89 (5): 489–91. doi:10.1016/s0161-6420(82)34764-8. PMID 7099568.
- ^ Drachman DB (August 1964). “Atrophy of skeletal muscle in chick embryos treated with botulinum toxin”. Science. 145 (3633): 719–21. Bibcode:1964Sci…145..719D. doi:10.1126/science.145.3633.719. PMID 14163805.
- ^ Scott AB, Rosenbaum A, Collins CC (December 1973). “Pharmacologic weakening of extraocular muscles”. Investigative Ophthalmology. 12 (12): 924–27. PMID 4203467.
- ^ Scott AB (October 1980). “Botulinum toxin injection into extraocular muscles as an alternative to strabismus surgery”. Ophthalmology. 87 (10): 1044–49. doi:10.1016/s0161-6420(80)35127-0. PMID 7243198.
- ^ Jump up to:a b Boffey, Philip M. (October 14, 1986). “Loss Of Drug Relegates Many To Blindness Again”. The New York Times. Retrieved July 14, 2010.
- ^ Jump up to:a b United States Department of Health and Human Services (April 30, 2009). “Re: Docket No. FDA-2008-P-0061” (PDF). Food and Drug Administration. Retrieved July 26, 2010.
- ^ Wellman-Labadie O, Zhou Y (May 2010). “The US Orphan Drug Act: rare disease research stimulator or commercial opportunity?”. Health Policy. 95 (2–3): 216–28. doi:10.1016/j.healthpol.2009.12.001. PMID 20036435.
- ^ Jump up to:a b c Clark RP, Berris CE (August 1989). “Botulinum toxin: a treatment for facial asymmetry caused by facial nerve paralysis”. Plastic and Reconstructive Surgery. 84 (2): 353–55. doi:10.1097/01.prs.0000205566.47797.8d. PMID 2748749.
- ^ Jump up to:a b Carruthers JD, Carruthers JA (January 1992). “Treatment of glabellar frown lines with C. botulinum-A exotoxin”. The Journal of Dermatologic Surgery and Oncology. 18 (1): 17–21. doi:10.1111/j.1524-4725.1992.tb03295.x. PMID 1740562.
- ^ Jump up to:a b Keen M, Kopelman JE, Aviv JE, Binder W, Brin M, Blitzer A (April 1994). “Botulinum toxin A: a novel method to remove periorbital wrinkles”. Facial Plastic Surgery. 10 (2): 141–46. doi:10.1055/s-2008-1064563. PMID 7995530.
- ^ Jump up to:a b “Botulinum Toxin Type A Product Approval Information – Licensing Action 4/12/02”. Food and Drug Administration. October 29, 2009. Retrieved July 26, 2010.
- ^ Jump up to:a b “Allergan Receives FDA Approval for First-of-Its-Kind, Fully in vitro, Cell-Based Assay for BOTOX and BOTOX Cosmetic (onabotulinumtoxinA)”. Allergan. June 24, 2011. Archived from the original on June 26, 2011. Retrieved June 26, 2011.
- ^ Jump up to:a b “In U.S., Few Alternatives To Testing On Animals”. Washington Post. April 12, 2008. Retrieved June 26, 2011.
- ^ Binder WJ, Brin MF, Blitzer A, Schoenrock LD, Pogoda JM (December 2000). “Botulinum toxin type A (BOTOX) for treatment of migraine headaches: an open-label study”. Otolaryngology–Head and Neck Surgery. 123 (6): 669–76. doi:10.1067/mhn.2000.110960. PMID 11112955.
- ^ Jackson JL, Kuriyama A, Hayashino Y (April 2012). “Botulinum toxin A for prophylactic treatment of migraine and tension headaches in adults: a meta-analysis”. JAMA. 307 (16): 1736–45. doi:10.1001/jama.2012.505. PMID 22535858.
- ^ Ramachandran R, Yaksh TL (September 2014). “Therapeutic use of botulinum toxin in migraine: mechanisms of action”. British Journal of Pharmacology. 171 (18): 4177–92. doi:10.1111/bph.12763. PMC 4241086. PMID 24819339.
- ^ Chapman, Paul (May 10, 2012). “The global botox market forecast to reach $2.9 billion by 2018”. Archived from the original on 2012-08-06. Retrieved October 5, 2012.
- ^ Koirala J, Basnet S (July 14, 2004). “Botulism, Botulinum Toxin, and Bioterrorism: Review and Update”. Medscape. Cliggott Publishing. Retrieved July 14, 2010.
- ^ Clostridium botulinum – Public Health Agency of Canada. Phac-aspc.gc.ca (April 19, 2011). Retrieved on May 6, 2012.
- ^ Baselt RC (2014). Disposition of toxic drugs and chemicals in man. Seal Beach, Ca.: Biomedical Publications. pp. 260–61. ISBN 978-0-9626523-9-4.
- ^ http://www.emsworld.com/article/10324792/botulinum-toxin-a-bioterrorism-weapon
- ^ McAdams D, Kornblet S (15 July 2011). “Baader-Meinhof Group (OR Baader-Meinhof Gang”. In Pilch RF, Zilinskas RA. Encyclopedia of Bioterrorism Defense. Wiley-Liss. doi:10.1002/0471686786.ebd0012.pub2. ISBN 978-0-471-68678-1.
- ^ “2011 Allergan Annual Report” (PDF). Allergan. Retrieved May 3, 2012. See PDF p. 7.
- ^ Jump up to:a b c Walker TJ, Dayan SH (February 2014). “Comparison and overview of currently available neurotoxins”. The Journal of Clinical and Aesthetic Dermatology. 7 (2): 31–39. PMC 3935649. PMID 24587850.
- ^ “Botulinum Toxin Type A”. Hugh Source (International) Limited. Retrieved July 14, 2010.
- ^ Petrou I (Spring 2009). “Medy-Tox Introduces Neuronox to the Botulinum Toxin Arena”(PDF). The European Aesthetic Guide. Archived from the original (PDF) on 2013-03-20. Retrieved 2009-12-09.
- ^ Schantz EJ, Johnson EA (March 1992). “Properties and use of botulinum toxin and other microbial neurotoxins in medicine”. Microbiological Reviews. 56 (1): 80–99. PMC 372855. PMID 1579114.
- ^ Botulism, General Information – NCZVED. Cdc.gov. Retrieved on May 6, 2012.
- ^ Licciardello JJ, Nickerson JT, Ribich CA, Goldblith SA (March 1967). “Thermal inactivation of type E botulinum toxin”. Applied Microbiology. 15 (2): 249–56. PMC 546888. PMID 5339838.
- ^ Setlow P (April 2007). “I will survive: DNA protection in bacterial spores”. Trends in Microbiology. 15 (4): 172–80. doi:10.1016/j.tim.2007.02.004. PMID 17336071.
- ^ Jay JM, Loessner MJ, Golden DA (2005). “Chapter 24: Food Poisoning Caused by Gram-Positive Sporeforming Bacteria”. Modern Food Microbiology: Seventh Edition. New York: Springer. p. 581. ISBN 978-0-387-23180-8.
- ^ Capková K, Salzameda NT, Janda KD (October 2009). “Investigations into small molecule non-peptidic inhibitors of the botulinum neurotoxins”. Toxicon. 54 (5): 575–82. doi:10.1016/j.toxicon.2009.03.016. PMC 2730986. PMID 19327377.
- ^ Flanders M, Tischler A, Wise J, Williams F, Beneish R, Auger N (June 1987). “Injection of type A botulinum toxin into extraocular muscles for correction of strabismus”. Canadian Journal of Ophthalmology. 22 (4): 212–17. PMID 3607594.
- ^ “Botulinum toxin therapy of eye muscle disorders. Safety and effectiveness. American Academy of Ophthalmology”. Ophthalmology. Suppl: 37–41. September 1989. doi:10.1016/s0161-6420(89)32989-7. PMID 2779991.
- ^ Giesler M (2012). “How Doppelgänger Brand Images Influence the Market Creation Process: Longitudinal Insights from the Rise of Botox Cosmetic”. Journal of Marketing. 76(6): 55–68. doi:10.1509/jm.10.0406.
- ^ “BOTOX Cosmetic (onabotulinumtoxinA) Product Information”. Allergan. January 22, 2014.
- ^ Nayyar P, Kumar P, Nayyar PV, Singh A (December 2014). “BOTOX: Broadening the Horizon of Dentistry”. Journal of Clinical and Diagnostic Research : JCDR. 8 (12): ZE25–9. doi:10.7860/JCDR/2014/11624.5341. PMC 4316364. PMID 25654058.
- ^ Al-Fouzan AF, Mokeem LS, Al-Saqat RT, Alfalah MA, Alharbi MA, Al-Samary AE (June 2017). “Botulinum Toxin for the Treatment of Gummv Smile”. The Journal of Contemporary Dental Practice. 18 (6): 474–478. doi:10.5005/jp-journals-10024-2068. PMID 28621277.
- ^ Hwang WS, Hur MS, Hu KS, Song WC, Koh KS, Baik HS, Kim ST, Kim HJ, Lee KJ (January 2009). “Surface anatomy of the lip elevator muscles for the treatment of gummy smile using botulinum toxin”. The Angle Orthodontist. 79 (1): 70–7. doi:10.2319/091407-437.1. PMID 19123705.
- ^ Gracco A, Tracey S (May 2010). “Botox and the gummy smile”. Progress in Orthodontics. 11 (1): 76–82. doi:10.1016/j.pio.2010.04.004. PMID 20529632.
- ^ Mazzuco R, Hexsel D (December 2010). “Gummy smile and botulinum toxin: a new approach based on the gingival exposure area”. Journal of the American Academy of Dermatology. 63 (6): 1042–51. doi:10.1016/j.jaad.2010.02.053. PMID 21093661.
- ^ Walsh S (October 15, 2010). “FDA approves Botox to treat chronic migraine”. FDA Press Releases. Retrieved October 15, 2010.
- ^ Watkins T (October 15, 2010). “FDA approves Botox as migraine preventative”. CNN (US).
- ^ Dodick DW, Turkel CC, DeGryse RE, Aurora SK, Silberstein SD, Lipton RB, Diener HC, Brin MF (June 2010). “OnabotulinumtoxinA for treatment of chronic migraine: pooled results from the double-blind, randomized, placebo-controlled phases of the PREEMPT clinical program”. Headache. 50 (6): 921–36. doi:10.1111/j.1526-4610.2010.01678.x. PMID 20487038.
- ^ Ashkenazi A (March 2010). “Botulinum toxin type a for chronic migraine”. Current Neurology and Neuroscience Reports. 10 (2): 140–46. doi:10.1007/s11910-010-0087-5. PMID 20425239.
- ^ Magid M, Keeling BH, Reichenberg JS (November 2015). “Neurotoxins: Expanding Uses of Neuromodulators in Medicine – Major Depressive Disorder”. Plastic and Reconstructive Surgery. 136 (5 Suppl): 111S–19S. doi:10.1097/PRS.0000000000001733. PMID 26441090.
- ^ Jump up to:a b http://adisinsight.springer.com/drugs/800008810
External links
- A Poison That Can Heal from the U.S. Food and Drug Administration
- BotDB: extensive resources on BoNT structures, inhibitors, kinetics, and literature
- A consumer sociological investigation of Botox Cosmetic’s Rise
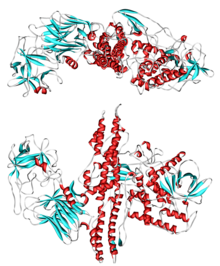 |
|
| Clinical data | |
|---|---|
| Routes of administration |
IM (approved), SC, intradermal, into glands |
| ATC code | |
| Legal status | |
| Legal status |
|
| Identifiers | |
| CAS Number | |
| DrugBank | |
| ChemSpider |
|
| ECHA InfoCard | 100.088.372 |
| Chemical and physical data | |
| Formula | C6760H10447N1743O2010S32 |
| Molar mass | 149 kg/mol (149,321g/mol) g·mol−1 |
| |
|
| Bontoxilysin | |
|---|---|
| Identifiers | |
| EC number | 3.4.24.69 |
| Databases | |
| IntEnz | IntEnz view |
| BRENDA | BRENDA entry |
| ExPASy | NiceZyme view |
| KEGG | KEGG entry |
| MetaCyc | metabolic pathway |
| PRIAM | profile |
| PDBstructures | RCSB PDB PDBe PDBsum |
| Gene Ontology | AmiGO / QuickGO |
////////////Prabotulinumtoxin A, プラボツリナムトキシンA ,APPROVED , FDA 2019, Jeuveau, AGN 191622, ANT-1207, ANT-1401, ANT-1403, NT 201
Triclabendazole, トリクラベンダゾール

Triclabendazole
トリクラベンダゾール
CGA-89317
| Formula |
C14H9Cl3N2OS
|
|---|---|
| CAS |
68786-66-3
|
| Mol weight |
359.6581
|
Anthelmintic
APPROVED, Egat, FDA 2019, 02/13/2019
Triclabendazole, sold under the brand name Egaten among others, is a medication used to treat liver flukes, specifically fascioliasisand paragonimiasis.[1] It is very effective for both conditions.[1] Treatment in hospital may be required.[1] It is taken by mouth with typically one or two doses being required.[1]
Side effects are generally few, but can include abdominal pain and headaches.[1] Biliary colic may occur due to dying worms.[2] While no harms have been found with use during pregnancy, triclabendazole has not been well studied in this population.[2] It is a member of the benzimidazole family of medications for worms.[1]
Triclabendazole was approved for medical use in the United States in 2019.[3] It is on the World Health Organization’s List of Essential Medicines, the most effective and safe medicines needed in a health system.[4] For human use it can also be obtained from the World Health Organization.[2] It is also used in other animals.[5]
Chemistry
It is a member of the benzimidazole family of anthelmintics. The benzimidazole drugs share a common molecular structure, triclabendazole being the exception in having a chlorinated benzene ring but no carbamate group. Benzimidazoles such as triclabendazole are generally accepted to bind to beta-tubulin therefore preventing the polymerization of microtubules.
History
Since late 1990s, triclabendazole became available as a generic drug, as patents expired in many countries. Many products were developed then. Among them, Trivantel 15, a 15% triclabendazole suspension, was launched by Agrovet Market Animal Health in the early 2000s. In 2009, the first triclabendazole injectable solution (combined with ivermectin) was developed and launched, also by Agrovet Market Animal Health. The product, Fasiject Plus, a triclabendazole 36% and ivermectin 0.6% solution, is designed to treat infections by Fasciola hepatica (both immature and adult liver flukes), roundworms and ectoparasites, as well.
Fasinex is a brandname for veterinary use while Egaten is a brandname for human use.
Patent
https://patents.google.com/patent/WO2012070068A2
Triclabendazole, chemically known as 5-chloro-6-(2,3-dichlorophenoxy)-2- (methylthio)-lH-benzimidazole represented by formula I,
is a halogenated benzimidazole compound that possesses high activity against immature and adult stages of the liver fluke, Faciola hepatica. The intensive use of Triclabendazole in endemic areas of facioliasis has resulted in the development of liver flukes resistant to this compound.
US 4, 197,307 discloses the process for the preparation of Triclabendazole, wherein 4- chloro-5-(2,3-dichlorophenoxy)-l,2-benzenediamine is reacted with carbondisulfide to give cyclic benzimidazole thione, which is further subjected to alkylation reaction with dimethyl sulfate to give Triclabendazole.
Chinese patent 10155523 ldescribes a process for the preparation of Triclabendazole by hydrolysing N-(4,5-dichloro-2-nitrophenyl)acetamide of formula VII to 4,5- dichloro-2-nitroaniline of formula VIII and condensing it with 2,3-dichlorophenol of formula VI in presence of a phase transfer catalyst to obtain 4-chloro-5(2,3- dichlorophenoxy)-2-nitroaniline of formula IV, which is further reduced in presence of Iron to obtain 4-chloro-5-(2,3-dichlorophenoxy)benzene-l ,2-diamine of formula III. The obtained diamine of formula III is cyclised in presence of carbondisulfide to obtain 6-chloro-5-(2,3-dichlorophenoxy)- lH-benzimidazole-2-thiol of formula II. The compound of formula II is methylated using dimethyl sulphate to obtain Triclabendazole of formula I. The process disclosed in this patent is illustrated in scheme 1 below:
Scheme 1
6-chloro-5-(2,3-dichlorophenoxy)-1H-benzimidazole-2-t ioi 4-chloro-5-(2,3-dichlorop enoxy)benzene-1 ,2-diamine
6-chloro-5-(2,3-dichlorophenoxy)-2-(methylthio)-1H-benzimidazole
I
However, the above prior art process is not preferred at a commercial scale because the hydrolysis of N-(4,5-dichloro-2-nitrophenyl)acetamide of formula VII is carried out before condensation with 2,3-dichlorophenol of formula VI, which is labile to formation of impurities and moreover the condensation is carried out in the presence of a phase transfer catalyst. Further, Iron is used as a catalyst for reduction which is riot environment friendly and involves tedious work-up. The final compound Triclabendazole is directly obtained by the methylating the compound of formula II using dimethylsulfate. The purity of thus obtained Triclabendazole is not high. Thus it is highly desirable to develop a process which overcomes most of the prior art drawbacks. The present inventors have developed a process for the preparation of Thiabendazole, which is environment friendly, technologically safe, simple and cost effective
Scheme 2
+ NH4CI + H20
Example 1: Preparation of 5-chIoro-6-(2,3-dichlorophenoxy)-2-(methylthio)-lH- benzimidazole (I)
(a) Preparation of 4-chloro-5(2,3-dichlorophenoxy)-2-nitroaniline;
2, 3-dichIorophenol (1 kg) in DMF (1.5 L), 2-nitro 4,5-dichloroacetanilide (1.52 kg), and potassium carbonate were heated into the flask for 12 hrs while maintaining the temperature at 90°C under vacuum and after that cooled to room temperature. Methanol (2 L), 48% caustic lye (0.3 kg) in 300 mL water were added to it and heated to 50°C for 4 hrs. Further water (4 L) was added, stirred, filtered and washed with water and with methanol.
Weight= 2 kg.
(b) Preparation of 4-chloro-5(2,3-dichlorophenoxy)-l,2-phenylenediamine;
Raney nickel (10.8 g) was added into a reaction mixture containing 4-chIoro- 5(2,3-dichlorophenoxy)-2-nitroaniline (900 g), methanol (3.4 L) at RT, caustic lye (2.72 g). Nitrogen was flushed into and charged with hydrogen. The reaction mixture was heated slowly to 100°C for 12 hrs, cooled to RT and filtered.
Weight: 819 g (c) Preparation of 6-chloro-5(2,,3-dichlorophenoxy)-lH- benzimidazole-2- thiol:
In the mixture of 4-chloro-5(2,3-dichlorophenoxy)-l ,2-phenylenediamine in methanol (800 g) and caustic lye (245 mL), carbondisulfide (259 g) was added slowly and the reaction mass was refluxed‘ for 6 hrs. After completion of the reaction water (2.5 L) and acetic acid was added over a period of 2hrs at 60°C. Water was added (2.5 litre) again and heated to 90°C for 2hrs, filtered and washed with hot water to obtain the title compound.
Weight: 863 g.
(d) Preparation of 6-chloro-5(2.3-dichlorophenoxy)-2-(metylthio)-lH- benzimidazole:
6-chloro-5(2,3-dichlorophenoxy)-l H- benzimidazole-2-thiol(400kg) was added to methanol (700 L) and heated to 40°C. Dimethyl sulphate was added slowly at 40°C to it. The reaction mass was heated to 60-65°C and maintain for 6hrs. After completion of the reaction the reaction mass was cooled to 15°C, centrifuged the material and washed with 75 L of methanol to obtain wet cake of Triclabendazole methanesulfonate (520-560 kg).
Triclabendazole methanesulfonate (200 g) and methanol (1.2 L) was refluxed, cooled and charcoal was added and refluxed again for 1 hr. The reaction mass was filtered and concentrated hydrochloric acid was added. The precipitate was‘ cooled to RT, stirred for 1 hr, filtered and Triclabendazole hydrochloride was isolated (250 g wet) .
The water was added to the above Triclabendazole hydrochloride and ammonia was charged and stired for 2-3 hrs. The reaction mass was filtered, washed with water and dried to obtain Triclabendazole.
Weight: 156 g.
Example 2:Preparation of 6-chloro-5(2,3-dichlorophenoxy)-2-(metylthio)-lH- benzimidazole In a RBF methanol (200 mL), 6-chloro-5(2,3-dichlorophenoxy)-lH- benzimidazole-2-thiol ((200 g) and dimethylsulfate (40 g) were heated to 60 ± 2°C and water (100 mL) was added and stirred for half an hr. Sodium carbonate solution (25 g Na2CC>3 in 200 mL water) was added slowly and temperature was raised to 60 °C and stirred for VA hr. After completion of reaction, the reaction mixture was cooled to 60°C, filtered, washed with water further washed with toluene and dried.
To the above wet crude 6-chloro-5(2,3-dichlorophenoxy)-2-(metylthio)-lH- benzimidazole, toluene (500 mL) was charged and water was removed azeotropically using Dean Stark apparatus. The mixture was heated to 100-1 12°C and 5 g charcoal was added, stirred for half an hr at 100-105°C. The reaction mixture was filtered through hyflow bed and washed with fresh toluene. The mother liquor was cooled to 70°C and isopropanol (7 mL) was added, cooled to room temperature to precipitate, filtered and washed with fresh toluene, dried at 75°C for 4 hrs to obtain pure Triclabendazole.
Yield of Triclabendazole is 85 gm. (81.7%).
Example 3: Purification of Triclabendazole:
The wet cake of Triclabendazole was heated to 90-100°C in toluene (1.92 litre). Water was removed azeotropically. The solution/mixture was cooled charcoal was added, refluxed and filtered. Again the obtained material was heated to 90-100°C, 180 ml of IPA was added, cooled to RT, filtered and dried for 24 hrs at 90-100°C.
Wt: 132 g (1st crop) and \2±\ g (2nd crop)
PATENT
https://patents.google.com/patent/CN103360323A/en

Example 1: Preparation of the present invention, the step of azole trichlorobenzene as follows:
[0020] The first step, 4-chloro-5- (2,3-dichlorophenoxy) -2-nitroaniline, i.e. a compound of formula III in the reaction:
[0021] 1,2,3-trichlorobenzene was added in the reaction kettle 43.5kg, 40kg of 50% aqueous potassium hydroxide solution, was heated at reflux for 7 hours, xylene was added 150L, 4,5- dichloro-2-nitro 41.4kg of aniline and a catalyst TBAB5kg, reacted for 8 hours, the reaction temperature is controlled at 125 ° C, slowly cooled to room temperature under stirring, to precipitate a large number of brown crystals, was filtered, washed with chilled xylene crystals paint IOkg, drained, washed with water to of drying to give 4-chloro-5- (2,3-dichlorophenoxy) -2_ nitroaniline 54kg, yield: 81%, melting point: 145 ° C~150 ° C, the substance pattern shown in Figure 1; wherein the compound is 1,2,3-trichlorobenzene of formula I in the reaction; 4,5-dichloro-2-nitroaniline reaction of a compound of formula II;
[0022] The second step, 5-chloro _6_ (2, 3_-dichlorophenoxy) _2_ mercapto – benzimidazole was prepared, i.e. a compound of formula V in the reaction:
[0023] obtained in the first step chlorine _5_ 4_ (2, 3_-dichlorophenoxy) _2_ nitroaniline 54kg Dad added to the reaction, and then added at a concentration of 80% ethanol 540L, was heated until dissolution was added Raney nickel catalyst 5kg, was heated to a boil, a solution prepared by the dropwise addition of hydrazine hydrate and 30L 12kg ethanol solution dropwise 4 ~ 6 hours, the yellow solution was gradually faded, TLC detection reaction end, Raney nickel catalyst was removed by filtration, dried the filter cake was washed several times with ethanol, containing 4-chloro-5- (2,3-dichlorophenoxy) 1,2_ phenylenediamine filtrate was used directly in the next step, the filtrate was added potassium hydroxide 11kg after stirring until the whole solution was slowly added 18kg of carbon disulfide in the range of 25 V~30 ° C, after the addition was stirred at room temperature for 2 hours and then heated to reflux for 10 hours, add decolorizing charcoal 2.5kg, refluxing was continued for I h, cooled to 30 ° C or below, filtered, the filter cake was washed with ethanol, the filtrate after recovery of ethanol by distillation, the residue was diluted IOOkg added water, adjusted to pH 2 to 3 with 5% aqueous hydrochloric acid, filtered, washed well with water to nearly neutral, and drying, to give an off-white solid, 5-chloro-6- (2,3-dichlorophenoxy) -2-mercapto – benzimidazole- 47.5kg, melting point 290. . ~300 ° C, 85% yield; the pattern shown in Figure 2, wherein _5_ chloro-4- (2,3-dichlorophenoxy) -2_ nitroaniline compound of formula III in the reaction ; 4-chloro-5- (2,3-dichlorophenoxy) I, 2- phenylenediamine compound of formula IV in the reaction; 5-chloro-6- (2,3-dichlorophenoxy) -2-mercapto – benzimidazole compound of the formula V in the reaction;
Preparation [0024] The third step, triclabendazole, i.e., the reaction of the compound of formula VI:
[0025] The first gas _ ■ 5- obtained in step -6_ (2,3- _ ■ gas phenoxy) _2- mercapto – benzo taste Jie sit 47.5kg, oxygen potassium 8.5kg, a concentration of 80% 285kg of methanol, added to the reaction kettle was cooled to ice bath 5~10 ° C, was added dropwise dimethyl sulfate 19kg, 3 hours dropwise, stirring continued for 3 hours to obtain a reaction solution containing triclabendazole, the conditions of room temperature under added dropwise to the reaction solution containing triclabendazole in dilute sulfuric acid to adjust the pH 8-9, 50kg of purified water was added dropwise, dropwise 2 hours, stirring was continued for 2 hours at the same temperature, as a large amount of white solid precipitated a thick paste; 80kg of deionized water was added, stirred sufficiently dispersing the paste solids, filtered off with suction, washed to neutrality with 80kg purified water immersion, drying centrifuge, drying, to give a crude product triclabendazole 42kg, close was 81.5% with a purity of 95%, recrystallized from ethanol to give the desired product triclabendazole 39kg, yield 92.8%, content 99.5%, of which 5-chloro-6- (2,3-dichloro phenoxy) _2_ mercapto – benzimidazole compound of the formula V in the reaction; triclabendazole a compound of formula VI in the reaction.
PATENTS
Non-Patent
Publication numberPriority datePublication dateAssigneeTitle
References
- ^ Jump up to:a b c d e f WHO Model Formulary 2008 (PDF). World Health Organization. 2009. pp. 94, 96. ISBN 9789241547659. Archived (PDF) from the original on 13 December 2016. Retrieved 8 December 2016.
- ^ Jump up to:a b c Wolfe, M. Michael; Lowe, Robert C. (2014). “Benzimidazoles”. Pocket Guide to GastrointestinaI Drugs. John Wiley & Sons. p. PT173. ISBN 9781118481554. Archived from the original on 2016-12-20.
- ^ “Egaten (triclabendazole)” (PDF). FDA. Retrieved 18 February 2019.
- ^ “WHO Model List of Essential Medicines (19th List)” (PDF). World Health Organization. April 2015. Archived (PDF) from the original on 13 December 2016. Retrieved 8 December 2016.
- ^ “Triclabendazole – Drugs.com”. http://www.drugs.com. Archived from the original on 20 December 2016. Retrieved 10 December 2016.
Further reading
- “Report of the WHO Informal Meeting on use of triclabendazole in fascioliasis control” (PDF). who.int. 2006. Retrieved 10 December 2016.
 |
|
| Clinical data | |
|---|---|
| Trade names | Fasinex, Egaten, others |
| AHFS/Drugs.com | International Drug Names |
| Routes of administration |
by mouth |
| ATC code | |
| Pharmacokinetic data | |
| Metabolism | Oxidation to sulfone and sulfoxide metabolites |
| Elimination half-life | 22–24 hs |
| Excretion | Feces (>95%), urine (2%), milk (<1%) |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| ECHA InfoCard | 100.127.414 |
| Chemical and physical data | |
| Formula | C14H9Cl3N2OS |
| Molar mass | 359.658 g·mol−1 |
| 3D model (JSmol) | |
////////////Triclabendazole, トリクラベンダゾール , Egat, CGA-89317 , CGA 89317 ,Anthelmintic, fda 2019