Home » cancer
Category Archives: cancer
Amcenestrant (SAR 439859)
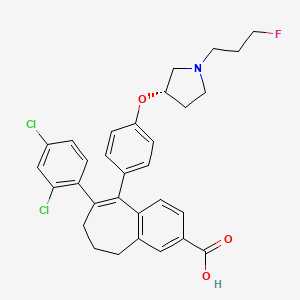
Amcenestrant (SAR 439859)
アムセネストラント
| Molecular Weight | 554.48 |
|---|---|
| Formula | C31H30Cl2FNO3 |
| CAS No. | 2114339-57-8 |
6-(2,4-dichlorophenyl)-5-[4-[(3S)-1-(3-fluoropropyl)pyrrolidin-3-yl]oxyphenyl]-8,9-dihydro-7H-benzo[7]annulene-2-carboxylic acid
8-(2,4-dichlorophenyl)-9-(4-{[(3 S )-1-(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro – 5H- Benzo[7]annulene-3-carboxylic acid
8-(2,4-Dichlorophenyl)-9-(4-{[(3 S )-1-(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5 H -benzo [7]annulene-3-carboxylic acid
C31H30Cl2FNO3 : 554.48 [ 2114339-57-8 ] _ _ _ _ _ _
| Efficacy | Antineoplastic, Selective estrogen receptor downregulator |
|---|---|
| Comment | Selective estrogen receptor downregulator (SERD) Treatment of breast cancer |
SAR439859 (compound 43d) is an orally active, nonsteroidal and selective estrogen receptor degrader (SERD). SAR439859 is a potent ER antagonist and has ER degrading activity with an EC50 of 0.2 nM for ERα degradation. SAR439859 demonstrates robust antitumor efficacy and limited cross-resistance in ER+ breast cancer.
Amcenestrant is an orally available, nonsteroidal selective estrogen receptor degrader/downregulator (SERD), with potential antineoplastic activity. Upon oral administration, amcenestrant specifically targets and binds to the estrogen receptor (ER) and induces a conformational change that promotes ER degradation. This prevents ER-mediated signaling and inhibits both the growth and survival of ER-expressing cancer cells.
Amcenestrant is reported to be a selective estrogen receptor degrader (SERD) which has estrogen receptor antagonist properties and accelerates the proteasomal degradation of the estrogen receptor. Amcenestrant is under clinical investigation as an anticancer agent, in particular for treatment of breast cancer.
The compound and processes for preparation thereof are described in International Publication No. WO 2017/140669.
Crystalline forms are described in International Publication No. WO 2021/116074.
PAPER
Journal of Medicinal Chemistry (2020), 63(2), 512-52
https://pubs.acs.org/doi/10.1021/acs.jmedchem.9b01293
6-(2,4-Dichlorophenyl)-5-[4-[(3S)-1-(3-fluoropropyl)pyrrolidin-3- yl]oxyphenyl]-8,9-dihydro-7H-benzo[7]annulene-2-carboxylic Acid (43d).
To a solution of 6-(2,4-dichloro-phenyl)-5-[4-[1-(3-fluoropropyl)-pyrrolidin-3-yloxy]-phenyl]-8,9-dihydro-7H-benzocycloheptene-2-carboxylic acid methyl ester (42d) (80 mg, 140.72 μmol) in methanol (5 mL) was added 5 N NaOH (562.88 μL), the reaction mixture was heated to 60 °C for 5 h, and the solvent was removed under reduced pressure. The residue was taken up in water (10 mL), and aqueous HCl (5 M) was added to pH 7. The slurry was extracted with dichloromethane, dried over magnesium sulfate, filtered, and concentrated under reduced pressure. The solid was purified by column chromatography eluting with a mixture of dichloromethane, acetonitrile, and methanol (90/5/5 v/v/v) to give 60 mg (77%) of 6- (2,4-dichlorophenyl)-5-[4-[(3S)-1-(3-fluoropropyl)pyrrolidin-3-yl]- oxyphenyl]-8,9-dihydro-7H-benzo[7]annulene-2-carboxylic acid (43d). 1 H NMR (400 MHz, DMSO-d6): 1.68 (m, 1H), 1.79 (dm, J = 25.3 Hz, 2 H), 2.07 to 2.23 (m, 5H), 2.38 (m, 1H), 2.46 (t, J = 7.2 Hz, 2H), 2.52 (m, 1H), 2.62 (m, 1H), 2.55 to 2.89 (m, 3H), 4.47 (td, J = 6.2 and 47.6 Hz, 2H), 4.72 (m, 1H), 6.63 (d, J = 8.9 Hz, 2H), 6.71 (m, 3H), 7.18 (d, J = 8.4 Hz, 1H), 8.26 (dd, J = 2.0 and 8.4 Hz, 1H), 7.58 (d, J = 2.0 Hz, 1H), 7.63 (d, J = 8.4 Hz, 1H), 7.79 (s, 1H), 12.3 (m, 1H). LCMS: 554 (M + H)+ .
PATENT
Amcenestrant can be prepared according to methods known from the literature, for example U.S. Patent No. 9,714,221.
Example 1: Preparation of amorphous Amcenestrant
[00164] Amcenestrant (20 mg, prepared according to U.S. Patent No. 9,714,221) was dissolved in ethyl acetate (0.2 mL) at room temperature (25°C). Solution was left in opened flask at RT for 16 days, until all the solvent evaporated. Obtained solid was analyzed by XRPD.
PATENT
U.S. Patent No. 9,714,221
https://patents.google.com/patent/US9714221B1/en
PATENT
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2017140669
Example 51. 6-(2,4-dichlorophenyl)-5-[4-[(3S)-1-(3-fluoropropyl)pyrrolidin-3-yl]oxyphenyl]-8,9-dihydro-7H-benzo[7]annulene-2-carboxylic acid
Methode B:
Step 1 : 6-(2,4-dichloro-phenyl)-5-{4-[1-(3-fluoro-propyl)-pyrrolidin-3-yloxy]-phenyl}-8,9-dihydro-7H-benzocycloheptene-2-arboxylic acid methyl ester.
To a solution of methyl 8-bromo-9-(4-{[(3S)-1-(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulene-3-carboxylate hydrobromide (D5) (150 mg, 298.56 μιηοΙ), in dioxane (12 ml) and water (2 ml), was added 2,4-dichlorophenyl-boronic acid (62.67 mg, 328.41 μηηοΙ), Cs2C03 (204.48 mg, 626.97 μηιοΙ), and Pd(dppf)CI2 (14.63 mg, 17.91 μιηοΙ). The reaction mixture was heated at 90°C for 3 hours, and partitioned between AcOEt and water. The phases were separated and the organic phase washed with brine, dried over MgS04 and concentrated under reduced pressure. The residue was purified by column chromatography eluting with a mixture of DCM, acetonitrile and MeOH (96/2/2; V/V/V) to give 80 mg (47%) of 6-(2,4-dichloro-phenyl)-5-{4-[1-(3-fluoro-propyl)-pyrrolidin-3-yloxy]-phenyl}-8,9-dihydro-7H-benzocycloheptene-2-arboxylic acid methyl ester.
LC/MS (m/z, MH+): 568
Step 2 : 6-(2,4-dichlorophenyl)-5-[4-[(3S)-1-(3-fluoropropyl)pyrrolidin-3-yl]oxyphenyl]-8,9-dihydro-7H-benzo[7]annulene-2-carboxylic acid
To a solution of 6-(2,4-dichloro-phenyl)-5-{4-[1-(3-fluoro-propyl)-pyrrolidin-3-yloxy]-phenyl}-8,9-dihydro-7H-benzocycloheptene-2-arboxylic acid methyl ester (80 mg, 140.72μιηο!) in MeOH (5 ml) was added a solution of NaOH (562.88 μΙ, 5 M) and the reaction mixture was heated at 60°C for 5 hours and the solvent removed under reduced pressure. The residue was taken up in water (10 ml) and aqueous HCI (5 M) added to pH
7. The slurry was extracted with DCM, dried over MgS04 and concentrated under reduced pressure. The solid was purified by column chromatography eluting with a mixture of DCM, acetonitrile and MeOH (90/5/5; V/V/V) to give 60 mg (77%) of 6-(2,4-dichlorophenyl)-5-[4-[(3S)-1-(3-fluoropropyl)pyrrolidin-3-yl]oxyphenyl]-8,9-dihydro-7H-benzo[7]annulene-2-carboxylic acid.
PATENT
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2019020559
Intermediate (c). Tert-butyl (3S)-3-[4-(4,4!5!5-tetramethyl-1 !3,2-dioxaborolan-2yl)phenoxy]pyrrolidine-1 -carboxylate
To a solution of commercially available 4-(4,4,5,5-tetramethyl-1 ,3,2-dioxaborolan-2-yl)phenol (a) (82.7 g, 364.51 mmol) in THF (2 L) was added under argon (R)-1 -N-Boc-3-hydroxypyrrolidine (b) (84.43 g, 437.41 mmol) followed by Ν,Ν,Ν’,Ν’-tetramethylazodicarboxamide (99.1 g, 546.77 mmol). The clear reaction mixture turned orange and triphenylphosphine (143.41 g, 546.77 mmol) was added. The reaction mixture was stirred at room temperature for 24 hours, meanwhile a precipitate of triphenylphosphine oxide formed (Ph3P=0). The reaction mixture was poured in water (1 .5 L) and extracted with ethyl acetate (AcOEt) (3×1 .5 L). Gathered organic phases were dried over magnesium sulfate (MgS04), filtered and concentrated under reduced pressure. The residue was taken up into diisopropylether (1 .5 L) and the solid formed (Ph3P=0) was filtered. The solvent was concentrated under reduced pressure and the residue purified by column chromatography eluting with a mixture of heptane with AcOEt (90/10; v/v) to give 145 g (100%) of tert-butyl (3S)-3-[4-(4,4,5,5-tetramethyl-1 ,3,2-dioxaborolan-2-yl)phenoxy]pyrrolidine-1 -carboxylate (c) as a colorless oil.
1H NMR (400 MHz, DMSO-d6, δ ppm): 1 .27 (s : 12H); 1 .39 (s : 9H); 2.05 (m : 1 H); 2.14 (m : 1 H); 3.37 (3H); 3.55 (m : 1 H); 5.05 (s : 1 H); 6.94 (d, J = 8.4 Hz : 2H); 7.61 (d, J = 8.4 Hz : 2H)
Intermediate (d). (3S)-3-[4-(4,4,5,5-tetramethyl-1 ,3,2-dioxaborolan-2yl)phenoxy]pyrrolidine, hydrochloride
To a solution of (S)-tert-butyl 3-(4-(4,4,5,5-tetramethyl-1 ,3,2-dioxaborolan-2-yl)phenoxy)pyrrolidine-1 -carboxylate (c) (80 g, 195.23 mmol) in MeOH (450 ml) was added slowly HCI 4N in dioxane (250 ml).
After 1 .5 hours, the reaction mixture was concentrated under reduced pressure and the residue was taken up into Et20 with stirring to give a solid which then was filtered and dried under vacuum to give 61.8 g (95%) of (3S)-3-[4-(4,4,5,5-tetramethyl-1 ,3,2-dioxaborolan-2yl)phenoxy]pyrrolidine, hydrochloride (d) as a white powder.
1H NMR (400 MHz, DMSO-d6, δ ppm): 1.28 (s : 12H); 2.10 (m : 1 H); 2.21 (m : 1 H); 3.31 (3H); 3.48 (m : 1 H); 5.19 (m : 1 H); 6.97 (d, J = 8.4 Hz : 2H); 7.63 (d, J = 8.4 Hz : 2H); 9.48 (s : 1 H); 9.71 (s : 1 H).
LC/MS (m/z, MH+): 290
Intermediate (e). (3S)-1 -(3-fluoropropyl)-3-[4-(4,4,5,5-tetramethyl-1 ,3,2-dioxaborolan-2-yl)phenoxy]pyrrolidine
To a suspension of (S)-3-(4-(4,4,5,5-tetramethyl-1 ,3,2-dioxaborolan-2-yl)phenoxy)pyrrolidine hydrochloride (d) (20 g, 61.42 mmol) in acetonitrile (100 ml), was added K2C03 (21 .22 g, 153.54 mmol) and 1 -iodo-3-fluoropropane (12.15 g, 61.42 mmol), under argon. The reaction
mixture was stirred at 40°C for 24 hours. After cooling to room temperature, the reaction mixture was filtered and washed with acetonitrile. The filtrate was concentrated under reduced pressure and the residue was taken up in DCM and the solid formed was filtered and washed with DCM. The filtrate was concentrated to give 21.5 g (100%) of (3S)-1 -(3-fluoropropyl)-3-[4-(4,4,5,5-tetramethyl-1 ,3,2-dioxaborolan-2-yl)phenoxy]pyrrolidine (e) as a yellow foam.
1H NMR (400 MHz, DMSO-d6, δ ppm): 1.27 (s : 12H); 1 .77 (m : 2H); 1 .84 (m : 1 H); 2.27 (m : 1 H); 2.41 (m : 1 H); 2.49 (2H); 2.62 (dd, J = 2.6 and 10.4Hz : 1 H); 2.69 (m : 1 H); 2.83 (dd, J = 6.2 and 10.4Hz : 1 H); 4.47 (td, J = 6.2 and 47Hz : 2H) ; 4.99 (m : 1 H); 6.77 (d , J = 8.4 Hz : 2H); 7.58 (d, J = 8.4 Hz : 2H).
LC/MS (m/z, MH+): 350
Intermediate (B). 5-oxo-6,7,8,9-tetrahydro-5H-benzo[7]annulen-2-yl 2,2-dimethylpropanoate
To a solution of 2-hydroxy-6,7,8,9-tetrahydro-5H-benzo[7]annulen-5-one (A) (1 .52 g, 8.63 mmol), in acetone (60 ml), was added K2C03 (1 .19 g, 8.63 mmol) and pivaloyl chloride (1.06 ml, 8.63 mmol). The reaction mixture was stirred at room temperature for 16 hours, filtered and concentrated under reduced pressure. The residue was purified by flash chromatography eluting with a gradient of heptane in AcOEt (100/0 to 85/15, v/v) to give 1.55 g (69%) of 5-oxo-6,7,8,9-tetrahydro-5H-benzo[7]annulen-2-yl 2,2-dimethylpropanoate (B) as a colorless oil.
1H NMR (400 MHz, DMSO-d6, δ ppm): 7.65 (d, 1 H); 7.10-7.04 (m, 2H); 2.95 (t, 2H); 2.68 (t, 2H); 1 .85-1 .65 (m, 4H).
LC/MS (m/z, MH+): 261
Intermediate (C). 9-(trifluoromethanesulfonyloxy)-6,7-dihydro-5H-benzo[7]annulen-3-yl 2,2-dimethylpropanoate
To a solution of 5-oxo-6,7,8,9-tetrahydro-5H-benzo[7]annulen-2-yl 2,2-dimethylpropanoate (B) (15 g, 57.62 mmol) in DCM (500 ml) was added dropwise under argon pyridine (7.28 ml, 86.43 mmol) and trifluoromethanesulfonic anhydride (19.58 ml, 1 15.24 mmol). The reaction mixture was stirred at room temperature for 2 hours and ice (200 g) was added. The phases were separated, the aqueous phase was washed with DCM and the gathered organic phases were dried over MgS04, filtered and evaporated under reduced pressure to give 22 g (97%) of 9-(trifluoromethanesulfonyloxy)-6,7-dihydro-5H-benzo[7]annulen-3-yl 2,2-dimethylpropanoate (C) as a white solid.
LC/MS (m/z, MH-): 391
Intermediate (D). 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulen-3-yl-2,2-dimeth lpropanoate
To a solution of 9-(trifluoromethanesulfonyloxy)-6,7-dihydro-5H-benzo[7]annulen-3-yl-2,2-dimethylpropanoate (C) (22 g, 56.07 mmol) and (3S)-1 -(3-fluoropropyl)-3-[4-(tetramethyl-1 ,3,2-dioxaborolan-2-yl)phenoxy]pyrrolidine (e) (20.56 g, 58.87 mmol) in dioxane (420 ml) and water (120 ml) was added under argon Pd(dppf)CI2 (2.75 g, 3.36 mmol) and Cs2C03 (36.57 g, 1 12.13 mmol). The reaction mixture was stirred for 1 hour at room temperature and was partitioned between water and DCM. The aqueous phase was washed with DCM and the gathered organic phases dried over MgS04, filtered and concentrated under reduced pressure. The residue was purified by column chromatography eluting with a gradient of MeOH in DCM (0 to 5%; V/V) to give 31 g (100 %) of 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulen-3-yl-2,2-dimethylpropanoate (D).
LC/MS (m/z, MH+): 466
Intermediate (E). 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulen-3-ol
To a solution under argon of 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulen-3-yl-2,2-dimethylpropanoate (D) (24.8 g, 53.26 mmol) in MeOH (300 ml), was added NaOH 5M (23 ml, 1 15.00 mmol). The reaction mixture was stirred for 2 hours at room temperature. pH was then adjusted to 7 by addition of 6N aqueous HCI solution. The MeOH was concentrated under reduced pressure, then DCM was added. The organic phase was dried over MgS04, and concentrated under reduced pressure. The residue was purified by flash chromatography eluting with a gradient of DCM/ MeOH from 100/0 to 95/05 to give 18.8 g (93%) of 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulen-3-ol (E) as a beige solid.
LC/MS (m/z, MH+): 382
Intermediate (F). 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulen-3-yl trifluoromethanesulfonate
To a solution of 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulen-3-ol (E) (20.6 g, 54.00 mmol) in DCM (200 ml) and pyridine (6.55 ml, 81 .00 mmol), cooled to 5°C (ice bath), was added dropwise trifluoromethanesulfonic anhydride (18.93 ml, 108.00 mmol) under argon, and the reaction temperature was maintained <15°C. The ice bath was removed, and the brown suspension was stirred at room temperature for 2 hours. Ice (200 g) and DCM (200 ml) were added and the phases separated. The organic phase was dried over MgS04, and concentrated under reduced pressure. The residue was
purified by flash chromatography eluting with a gradient of DCM/MeOH from 100/0 to 95/05 to give 24.7 g (89.1 %) of 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulen-3-yl trifluoromethanesulfonate (F) as a brown oil.
LC/MS (m/z, MH+): 514
Intermediate (G). Methyl 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulene-3-carboxylate
To a solution of 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulen-3-yl trifluoromethanesulfonate (F) (10.1 g, 19.67 mmol) in DMF (66 ml) and MeOH (33 ml), were added Pd(dppf)CI2 (909 mg, 1.18 mmol) and diisopropylethylamine (7.21 ml). The black suspension was carbonylated in an autoclave at 70°C under 5 bars of CO for 5 hours. The reaction mixture was filtered, then the filtrate was partially concentrated under reduced pressure. The residue was partitioned between AcOEt and water. The organic phase was washed with water (2x 100 ml), dried over MgS04, and concentrated under reduced pressure. The residue was purified by flash chromatography eluting with a gradient of DCIW MeOH from 100/0 to 95/05 to give 7.13 g (86%) of methyl 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulene-3-carboxylate (G) as a brown gum.
LC/MS (m/z, MH+): 424
Intermediate (A1 ). 5-oxo-6,7,8,9-tetrahydro-5H-benzo[7]annulen-2-yltrifluoromethanesulfonate
To a solution of commercially available 2-hydroxy-6,7,8,9-tetrahydro-5H-benzo[7]annulen-5-one (A) (18.5 g, 105 mmol) in DCM (185 ml) and lutidine (13.35 ml, 1 13.505 mmol), cooled at 5°C under argon, was added dropwise trifluoromethanesulfonic anhydride (20.22 ml,
123.29 mmol) while keeping temperature between 10 and 20°C. The reaction mixture was stirred for 1 hour at 5°C then at room temperature for 1 hour.
Then, ice (200 g) was added and the slurry partitioned between water and DCM. The organic phase was washed with aqueous NaHC03 solution, dried over MgS04, filtered off and concentrated under reduced pressure. The residue was purified by flash chromatography eluting with a gradient of heptane/AcOEt from 100 to 90/10 to give 28.2 g (87%) of 5-oxo-6,7,8,9-tetrahydro-5H-benzo[7]annulen-2-yl trifluoromethanesulfonate (A1 ) as an orange oil. LC/MS (m/z, MH+): 309
Intermediate (B1 ). Methyl 5-oxo-6,7,8,9-tetrahydro-5H-benzo[7]annulene-2-carboxylate
To a solution of 5-oxo-6,7,8,9-tetrahydro-5H-benzo[7]annulen-2-yl trifluoromethanesulfonate (A1 ) (5.03 g, 16.32 mmol) in DMF (24 ml) and MeOH (12 ml), were added Pd(dppf)CI2 (754 mg, 0.98 mmol) and diisopropylethylamine (6 ml). The black suspension was carbonylated in an autoclave at 70°C under 5 bars of CO for 2.5 hours. The reaction mixture was filtered, then the filtrate was partially concentrated under reduced pressure, and the residue, was partitioned between AcOEt and water. The organic phase was washed with water (2x 75 ml) and aqueous HCI 0.5 N, dried over MgS04 and concentrated under reduced pressure. The residue was purified by flash chromatography eluting with a gradient of heptane/AcOEt from 100/0 to 90/10 to give 3.4 g (95%) of methyl 5-oxo-6,7,8,9-tetrahydro-5H-benzo[7]annulene-2-carboxylate (B1 ) as a colorless oil.
LC/MS (m/z, MH+): 219
Intermediate (C1 ). Methyl 9-(trifluoromethanesulfonyloxy)-6,7-dihydro-5H-benzo[7]annulene-3-carboxylate
To a solution of methyl 5-oxo-6,7,8,9-tetrahydro-5H-benzo[7]annulene-2-carboxylate (B1 ) (18,19 g, 83,34 mmol) in DCM (500 ml) and anhydrous pyridine (1 1 ml, 130,56 mmol), cooled at 5°C under argon, was added dropwise trifluoromethanesulfonic anhydride (30 ml, 176,54 mmol). The reaction mixture, a thick suspension, was stirred at room temperature for 24 hours, then ice was added and partitioned between water and DCM. The organic phase was dried over MgS04, filtered off and concentrated under reduced pressure to give 29 g (100%) of methyl 9-(trifluoromethanesulfonyloxy)-6,7-dihydro-5H-benzo[7]annulene-3-carboxylate (C1 ) as a yellow gum.
LC/MS (m/z, MH+): 351
Intermediate (G). Methyl 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulene-3-carboxylate
To a solution of methyl 9-(trifluoromethanesulfonyloxy)-6,7-dihydro-5H-benzo[7]annulene-3-carboxylate (C1 ) (29 g, 82.9 mmol), (3S)-1 -(3-fluoropropyl)-3-[4-(tetramethyl-1 ,3,2-dioxaborolan-2-yl)phenoxy]pyrrolidine (e) (28.9 g, 82.9 mmol), in dioxane (225 ml) were added Pd(dppf)CI2 under argon, complex with DCM (3.73 g, 4.57 mmol) and Cs2C03 1 .5 M aqueous solution (1 1 1.12 ml, 166.68 mmol). The reaction mixture was stirred at 60°C for 1 hour.
After cooling to room temperature, the reaction mixture was poured into a mixture of water (500 ml) and AcOEt (400ml). The organic phase was washed with brine, dried over MgS04, filtered on celite and concentrated under reduced pressure. The residue was purified by flash chromatography eluting with a gradient of DCM/MeOH from 100/0 to 95/05 to give 23 g (65%) of methyl 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulene-3-carboxylate (G) as a brown gum.
LC/MS (m/z, MH+): 424
Intermediate (H). Methyl 8-bromo-9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro-5H-benzo[7]annulene-3-carboxylate hydrobromide
To a solution of methyl 9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro- 5H-benzo[7]annulene-3-carboxylate (G) (13.93 g, 32.89 mmol), in DCM (150 ml) was added under argon pyridinium tribromide (15.78 g, 44.41 mmol). The reaction mixture was stirred for 1 hour at room temperature. Water (200 ml) was added, organic phase was then dried over MgS04, and concentrated under reduced pressure. The residue was purified by flash chromatography eluting with a gradient of DCM/MeOH from 100/0 to 95/05 to give 16.4 g (85%) of methyl 8-bromo-9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7-dihydro- 5H-benzo[7]annulene-3-carboxylate hydrobromide (H) as a yellow meringue.
LC/MS (m/z, MH+): 502
Intermediate (I). 6-(2,4-dichloro-phenyl)-5-{4-[1 -(3-fluoro-propyl)-pyrrolidin-3-yloxy]-phenyl}- -dihydro-7H-benzocycloheptene-2-arboxylic acid methyl ester.
To a solution of methyl 8-bromo-9-(4-{[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxy}phenyl)-6,7- dihydro-5H-benzo[7]annulene-3-carboxylate hydrobromide (H) (150 mg, 298.56 μηηοΙ), in dioxane (12 ml) and water (2 ml), was added 2,4-dichlorophenyl-boronic acid (62.67 mg, 328.41 μηιοΙ), Cs2C03 (204.48 mg, 626.97 μπιοΙ), and Pd(dppf)CI2 (14.63 mg, 17.91 mol). The reaction mixture was heated at 90°C for 3 hours, and partitioned between AcOEt and water. The phases were separated and the organic phase washed with brine, dried over MgS04 and concentrated under reduced pressure. The residue was purified by column
chromatography eluting with a mixture of DCM, acetonitrile and MeOH (96/2/2; V/V/V) to give 80 mg (47%) of 6-(2,4-dichloro-phenyl)-5-{4-[1 -(3-fluoro-propyl)-pyrrolidin-3-yloxy]-phenyl}-8,9-dihydro-7H-benzocycloheptene-2-arboxylic acid methyl ester (I).
LC/MS (m/z, MH+): 568
Compound (1 ). 6-(2,4-dichlorophenyl)-5-[4-[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxyphenyl]-8,9-dihydro-7H-benzo[7]annulen -2-carboxylic acid
To a solution of 6-(2,4-dichloro-phenyl)-5-{4-[1 -(3-fluoro-propyl)-pyrrolidin-3-yloxy]-phenyl}-8,9-dihydro-7H-benzocycloheptene-2-arboxylic acid methyl ester (I) (80 mg, 140.72 μηηοΙ) in MeOH (5 ml) was added a solution of NaOH (562.88 μΙ, 5 M) and the reaction mixture was heated at 60°C for 5 hours and the solvent removed under reduced pressure. The residue was taken up in water (10 ml) and aqueous HCI (5 M) added to pH 7. The slurry was extracted with DCM, dried over MgS04 and concentrated under reduced pressure. The solid was purified by column chromatography eluting with a mixture of DCM, acetonitrile and MeOH (90/5/5; V/V/V) to give 60 mg (77%) of 6-(2,4-dichlorophenyl)-5-[4-[(3S)-1 -(3-fluoropropyl)pyrrolidin-3-yl]oxyphenyl]-8,9-dihydro-7H-benzo[7]annulene-2-carboxylic acid. 1H NMR (400 MHz, DMSO-d6, δ ppm): 1 .68 (m, 1 H); 1 ,79 (dm, J=25.3 Hz, 2 H); 2.07 to 2.23 (m, 5 H); 2.38 (m, 1 H); 2.46 (t, J=7.2 Hz, 2 H); 2.52 (m, 1 H); 2.62 (m, 1 H); 2.55 to 2.89 (m, 3 H); 4.47 (td, J=6.2 and 47.6 Hz, 2 H); 4.72 (m, 1 H); 6.63 (d, J=8.9 Hz, 2 H); 6.71 (m, 3 H); 7.18 (d, J=8.4 Hz, 1 H); 8.26 (dd, J=2.0 and 8.4 Hz, 1 H); 7.58 (d, J=2,0 Hz, 1 H); 7.63 (d, J=8.4 Hz, 1 H); 7.79 (s, 1 H); 12.3 (m, 1 H)
LC/MS (m/z, MH+): 554
//////////////
Admin note for myself . I am up for Grabs
I myself Dr Anthony Melvin Crasto Looking for a post retirement assignment as Advisor API & INT, Chem.
With 36 yrs rich experience, about dozen patents, 10000plus steps covered, 200 API targets, 30 plus products commercialization in plant in full career. Hands on knowledge of Synthesis, Process, scaleup, cost reduction, DOE , softwares etc
Kindly contact me
Dr Anthony Melvin Crasto
+919321316780
amcrasto@gmail.com
About myself
Dr Anthony Crasto
click on my website to know about me
Read http://amcrasto.weebly.com/
Also http://amcrasto.weebly.com/awards.html
Also
http://amcrasto.weebly.com/felicitations.html
1000 lakh google hits, 100lakh blog views, 10 lakh viewers in USA alone, all in 7 continents, 226 countries, 30 Indian and International awards, helping millions across the world

////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
/////Amcenestrant, SAR439859, アムセネストラント , Antineoplastic, CANCER
C1CC2=C(C=CC(=C2)C(=O)O)C(=C(C1)C3=C(C=C(C=C3)Cl)Cl)C4=CC=C(C=C4)OC5CCN(C5)CCCF
LORPUCITINIB

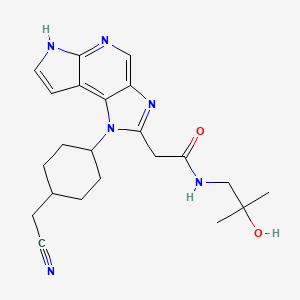
LORPUCITINIB
JNJ 64251330
2230282-02-5
UNII-OE1QTY7C25
| Molecular Weight | 408.50 |
|---|---|
| Formula | C22H28N6O2 |
| 1-(TRANS-4-(CYANOMETHYL)CYCLOHEXYL)-1,6-DIHYDRO-N-(2-HYDROXY-2-METHYLPROPYL)IMIDAZO(4,5-D)PYRROLO(2,3-B)PYRIDINE-2-ACETAMIDE |
2-[3-[4-(cyanomethyl)cyclohexyl]-3,5,8,10-tetrazatricyclo[7.3.0.02,6]dodeca-1,4,6,8,11-pentaen-4-yl]-N-(2-hydroxy-2-methylpropyl)acetamide
is a Gut-Restricted JAK Inhibitor for the research of Inflammatory Bowel Disease.
Lorpucitinib is an orally bioavailable pan-inhibitor of the Janus associated-kinases (JAKs), with potential immunomodulatory and anti-inflammatory activities. Upon oral administration, lorpucitinib works in the gastrointestinal (GI) tract where it targets, binds to and inhibits the activity of the JAKs, thereby disrupting JAK-signal transducer and activator of transcription (STAT) signaling pathways and the phosphorylation of STAT proteins. This may inhibit the release of pro-inflammatory cytokines and chemokines, reducing inflammatory responses and preventing inflammation-induced damage. The Janus kinase family of non-receptor tyrosine kinases, which includes tyrosine-protein kinase JAK1 (Janus kinase 1; JAK1), tyrosine-protein kinase JAK2 (Janus kinase 2; JAK2), tyrosine-protein kinase JAK3 (Janus kinase 3; JAK3) and non-receptor tyrosine-protein kinase TYK2 (tyrosine kinase 2), plays a key role in cytokine signaling and inflammaton.
PATENT
WO2019239387
WO2018112379
WO2018112382
PATENT
WO/2022/189496LORPUCITINIB FOR USE IN THE TREATMENT OF JAK MEDIATED DISORDERS
Example 1
[0117] 2-(1-((1r,4r)-4-(Cyanomethyl)cyclohexyl)-1,6-dihydroimidazo[4,5-d]pyrrolo[2,3-b]pyridin-2-yl)-N-(2-hydroxy-2-methylpropyl)acetamide
Step A: 2-(1-((1r,4r)-4-(Cyanomethyl)cyclohexyl)-6-(phenylsulfonyl)-1,6-dihydroimidazo[4,5-d]pyrrolo[2,3-b]pyridin-2-yl)-N-(2-hydroxy-2-methylpropyl)acetamide. To ensure dry starting material, ethyl 2-(1-((1r,4r)-4-(cyanomethyl)cyclohexyl)-6-(phenylsulfonyl)-1,6-dihydroimidazo[4,5-d]pyrrolo[2,3-b]pyridin-2-yl)acetate (Intermediate 3) was heated under vacuum at 50 °C for 18 h prior to the reaction. In a 1 L flask, ethyl 2-(1-((1r,4r)-4-(cyanomethyl)cyclohexyl)-6-(phenylsulfonyl)-1,6-dihydroimidazo[4,5-d]pyrrolo[2,3-b]pyridin-2-yl)acetate (Intermediate 3, 52.585 g, 104.01 mmol) was suspended in DMA (50 mL). 1-Amino-2-methylpropan-2-ol (50 mL) was added and the reaction was heated to 110 °C for 45 minutes, then to 125 °C for 5 hours. The reaction was cooled to room temperature and diluted with EtOAc (800 mL). The organic layer was extracted three times with a solution of water/ brine wherein the solution was made up of 1 L water plus 50 mL brine. The aqueous layers were back extracted with EtOAc (2 × 600 mL). The combined organic layers were dried over anhydrous MgSO4,
concentrated to dryness, and then dried for 3 days under vacuum to provide the title compound (65.9 g, 98% yield) as a yellow foam. The product was taken to the next step with no further purification. MS (ESI): mass calcd. for C28H32N6O4S, 548.22; m/z found, 549.2 [M+H]+.1H NMR (400 MHz, CDCl3): δ 8.76 (s, 1H), 8.26 – 8.19 (m, 2H), 7.84 (d, J = 4.1 Hz, 1H), 7.60 – 7.53 (m, 1H), 7.50 – 7.44 (m, 2H), 6.84 (d, J = 4.2 Hz, 1H), 4.76 – 4.61 (m, 1H), 3.97 (s, 2H), 3.45 (s, 1H), 3.27 (d, J = 5.9 Hz, 2H), 2.41 (d, J = 6.5 Hz, 2H), 2.38 – 2.25 (m, 2H), 2.23 – 2.12 (m, 2H), 2.09 -1.94 (m, 4H), 1.48 (qd, J = 13.6, 4.0 Hz, 2H), 1.21 (s, 6H).
[0118] Step B: 2-(1-((1r,4r)-4-(Cyanomethyl)cyclohexyl)-1,6-dihydroimidazo[4,5-d]pyrrolo[2,3-b]pyridin-2-yl)-N-(2-hydroxy-2-methylpropyl)acetamide. 2-(1-((1r,4r)-4-(Cyanomethyl)cyclohexyl)-6-(phenylsulfonyl)-1,6-dihydroimidazo[4,5-d]pyrrolo[2,3-b]pyridin-2-yl)-N-(2-hydroxy-2-methylpropyl)acetamide (65.90 g, 102.1 mmol) was added to a 1 L flask containing a stir bar. 1,4-dioxane (300 mL) was added, followed by aq KOH (3 M, 150 mL). The reaction was heated at 80 °C for 2 h. The reaction was cooled to room temperature and the solvent volume was reduced to about 200 mL on a rotovap. The residue was treated with a solution of water/brine (100 mL/100mL), then extracted with 10% MeOH in CH2Cl2 (2 x 1L). The organic layers were combined, dried over anhydrous MgSO4, and concentrated to dryness to provide a yellow solid. The solid was suspended in CH2Cl2 (200 mL), stirred vigorously for 30 minutes, and then collected by filtration. The solid was rinsed with CH2Cl2 (100 mL), dried by pulling air through the filter, and then further dried under vacuum at room temperature for 16 h to provide the title compound (41.59 g, 89% yield) as a white solid. MS (ESI): mass calcd. for C22H28N6O2, 408.23; m/z found, 409.2 [M+H]+. 1H NMR (600 MHz, DMSO-d6): δ 11.85 (s, 1H), 8.50 (s, 1H), 8.21 – 8.10 (m, 1H), 7.49 – 7.43 (m, 1H), 6.74 – 6.65 (m, 1H), 4.53 – 4.42 (m, 2H), 4.07 (s, 2H), 3.08 (d, J = 6.0 Hz, 2H), 2.58 (d, J = 6.1 Hz, 2H), 2.41 – 2.28 (m, 2H), 2.09 – 1.92 (m, 5H), 1.42 – 1.31 (m, 2H), 1.09 (s, 6H). The synthesis and active compound characterization of each of the aspects of this invention are provided herein in the form of examples. Due to the crystal structure of some of the aspects of this invention, polymorph screening may be pursued to further characterize specific forms of any such compound. This is illustrated in a non-limiting manner for compound of Formula I by the example under the heading polymorph screening.
[0119] The following compounds were prepared in reference to the foregoing synthesis:
Intermediate 1
[0120] 2-((1r,4r)-4-((5-Nitro-1-(phenylsulfonyl)-1H-pyrrolo[2,3-b]pyridin-4-yl)amino)cyclohexyl)acetonitrile
[0121] Step A: tert-butyl N-[(1r,4r)-4-(Hydroxymethyl)cyclohexyl]carbamate. To a 20-L 4-necked round-bottom flask purged and maintained with an inert atmosphere of nitrogen was placed (1r,4r)-4-[[(tert-butoxy)carbonyl]amino]cyclohexane-1-carboxylic acid (1066 g, 4.38 mol, 1.00 equiv) and THF (10 L). This was followed by the dropwise addition of BH3-Me2S (10 M, 660 mL) at -10 °C over 1 h. The resulting solution was stirred for 3 h at 15 °C. This reaction was performed three times in parallel and the reaction mixtures were combined. The reaction was then quenched by the addition of methanol (2 L). The resulting mixture was concentrated under vacuum. This resulted in of tert-butyl N-[(1r,4r)-4-(hydroxymethyl)cyclohexyl]carbamate (3000 g, 99.6%) as a white solid. MS (ESI): mass calcd. for C12H23NO3, 229.32; m/z found, 215.2 [M-tBu+MeCN+H]+; 1H NMR: (300 MHz, CDCl3): δ 4.40 (s, 1H), 3.45 (d, J = 6.3 Hz, 2H), 3.38 (s, 1H), 2.05-2.02 (m, 2H), 1.84-1.81 (m, 2H), 1.44 (s, 11H), 1.17-1.01 (m, 4H).
[0122] Step B: tert-butyl N-[(1r,4r)-4-[(Methanesulfonyloxy)methyl]cyclohexyl]carbamate. To a 20 L 4-necked round-bottom flask purged and maintained with an inert atmosphere of nitrogen, was placed tert-butyl N-[(1r,4r)-4-(hydroxymethyl)cyclohexyl]carbamate (1000 g, 4.36 mol, 1.00 equiv.), dichloromethane (10 L), pyridine (1380 g, 17.5 mol, 4.00 equiv.). This was followed by the dropwise addition of MsCl (1000 g, 8.73 mol, 2.00 equiv.) at -15 °C. The resulting solution was stirred overnight at 25 °C. This reaction was performed in parallel for 3 times and the reaction mixtures were combined. The reaction was then quenched by the addition of 2 L of water. The
water phase was extracted with ethyl acetate (1 x 9 L). The organic layer was separated and washed with 1 M HCl (3 x 10 L), NaHCO3 (saturated aq.) (2 x 10 L), water (1 x 10 L) and brine (1 x 10 L). The mixture was dried over anhydrous sodium sulfate, filtered and concentrated under vacuum. This resulted in of tert-butyl N-[(1r,4r)-4-[(methanesulfonyloxy)methyl]cyclohexyl]carbamate (3300 g, 82%) as a white solid. LC-MS: MS (ESI): mass calcd. for C13H25NO5S, 307.15; m/z found 292.1, [M-tBu+MeCN+H]+; 1H NMR: (300 MHz, CDCl3): δ 4.03 (d, J = 6.6 Hz, 2H), 3.38 (s, 1H), 3.00 (s, 3H), 2.07-2.05 (m, 2H), 1.87-1.84 (m, 2H), 1.72-1.69 (m, 1H), 1.44 (s, 9H), 1.19-1.04 (m, 4H).
[0123] Step C: tert-butyl N-[(1r,4r)-4-(Cyanomethyl)cyclohexyl]carbamate. To a 10 L 4-necked round-bottom flask, was placed tert-butyl N-[(1r,4r)-4-[(methanesulfonyloxy)methyl]cyclohexyl]carbamate (1100 g, 3.58 mol, 1.00 equiv.), DMSO (5500 mL) and NaCN (406 g, 8.29 mol, 2.30 equiv.). The resulting mixture was stirred for 5 h at 90 °C. This reaction was performed in parallel 3 times and the reaction mixtures were combined. The reaction was then quenched by the addition of 15 L of water/ice. The solids were collected by filtration. The solids were washed with water (3 x 10 L). This resulted in tert-butyl N-[(1r,4r)-4-(cyanomethyl)cyclohexyl]carbamate (2480 g, 97%) as a white solid. MS (ESI): mass calcd. for C13H22N2O2, 238.17; m/z found 224 [M-tBu+MeCN+H]+; 1H NMR: (300 MHz, CDCl3): δ 4.39 (s, 1H), 3.38 (s, 1H), 2.26 (d, J = 6.9 Hz, 2H), 2.08-2.04 (m, 2H), 1.92-1.88 (m, 2H), 1.67-1.61 (m, 1H), 1.44 (s, 9H), 1.26-1.06 (m, 4H).
[0124] Step D: 2-[(1r,4r)-4-Aminocyclohexyl]acetonitrile hydrochloride. To a 10-L round-bottom flask was placed tert-butyl N-[(1r,4r)-4-(cyanomethyl)cyclohexyl]carbamate (620 g, 2.60 mol, 1.00 equiv.), and 1,4-dioxane (2 L). This was followed by the addition of a solution of HCl in 1,4-dioxane (5 L, 4 M) dropwise with stirring at 10 °C. The resulting solution was stirred overnight at 25 °C. This reaction was performed for 4 times and the reaction mixtures were combined. The solids were collected by filtration. The solids were washed with 1,4-dioxane (3 x 3 L), ethyl acetate (3 x 3 L) and hexane (3 x 3 L). This resulted in 2-[(1r,4r)-4-aminocyclohexyl]acetonitrile hydrochloride (1753 g, 96%) as a white solid. MS (ESI): mass calcd. for C8H14N2, 138.12; m/z found 139.25, [M+H]+; 1H NMR: (300 MHz, DMSO-d6): δ 8.14 (s, 3H), 2.96-2.84 (m, 1H), 2.46 (d, J = 6.3 Hz, 2H), 1.98 (d, J = 11.1 Hz, 2H), 1.79 (d, J = 12.0 Hz, 2H), 1.64-1.49 (m, 1H), 1.42-1.29 (m, 2H), 1.18-1.04 (m, 2H).
[0125] Step E: 2-((1r,4r)-4-((5-Nitro-1-(phenylsulfonyl)-1H-pyrrolo[2,3-b]pyridin-4-yl)amino)cyclohexyl)acetonitrile. To a 1000 mL round bottom flask containing 2-[(1r,4r)-4-aminocyclohexyl]acetonitrile hydrochloride (29.10 g, 166.6 mmol) was added DMA (400 mL). The resulting suspension was treated with 4-chloro-5-nitro-1-(phenylsulfonyl)-1H-pyrrolo[2,3-b]pyridine (51.53 g, 152.6 mmol), followed by DIPEA (63.0 mL, 366 mmol). The reaction mixture was placed under N2 and heated at 80 °C for 4 h. The crude reaction mixture was cooled to room temperature and slowly poured into a vigorously stirred 2 L flask containing 1.6 L water. The resulting suspension was stirred for 15 minutes at room temperature, then filtered and dried for 16 h in a vacuum oven with heating at 70 °C to provide the title compound (63.37 g, 95%) as a yellow solid. MS (ESI): mass calcd. for C21H21N5O4S, 439.1; m/z found, 440.1 [M+H]+. 1H NMR (500 MHz, CDCl3): δ 9.10 (s, 1H), 8.99 (d, J = 7.8 Hz, 1H), 8.23 – 8.15 (m, 2H), 7.66 – 7.59 (m, 2H), 7.56 – 7.49 (m, 2H), 6.67 (d, J = 4.2 Hz, 1H), 3.95 – 3.79 (m, 1H), 2.38 (d, J = 6.2 Hz, 2H), 2.32 -2.21 (m, 2H), 2.08 – 1.98 (m, 2H), 1.88 – 1.76 (m, 1H), 1.60 – 1.32 (m, 4H).
Intermediate 2
[0126] 2-((1r,4r)-4-((5-Amino-1-(phenylsulfonyl)-1H-pyrrolo[2,3-b]pyridin-4-yl)amino)cyclohexyl)acetonitrile
[0127] 2-((1r,4r)-4-((5-Nitro-1-(phenylsulfonyl)-1H-pyrrolo[2,3-b]pyridin-4-yl)amino)cyclohexyl)acetonitrile (Intermediate 1, 58.60 g, 133.3 mmol) was dissolved in THF/MeOH (1:1, 4800 mL). The mixture was passed through a continuous-flow hydrogenation reactor (10% Pd/C), such as a Thales Nano H-Cube®, at 10 mL/min with 100 % hydrogen (atmospheric pressure, 80 °C), then the solution was concentrated to provide the product as a purple solid. The solid was triturated with EtOAc (400 mL) and then triturated again with MeOH (200 mL) then filtered and dried under vacuum to provide the title compound (50.2 g, 91.9% yield).
MS (ESI): mass calcd. for C21H23N5O2S, 409.2; m/z found, 410.2 [M+H]+. 1H NMR (400 MHz, CDCl3) δ 8.10 – 8.03 (m, 2H), 7.76 (s, 1H), 7.51 – 7.43 (m, 1H), 7.43 – 7.34 (m, 3H), 6.44 (d, J = 4.2 Hz, 1H), 4.61 (d, J = 8.5 Hz, 1H), 3.65 – 3.51 (m, 1H), 2.74 (s, 2H), 2.26 (d, J = 6.4 Hz, 2H), 2.19 – 2.05 (m, 2H), 1.97 – 1.86 (m, 2H), 1.76 – 1.59 (m, 1H), 1.33 – 1.12 (m, 4H).
Intermediate 3
[0128] Ethyl 2-(1-((1r,4r)-4-(cyanomethyl)cyclohexyl)-6-(phenylsulfonyl)-1,6-dihydroimidazo[4,5-d]pyrrolo[2,3-b]pyridin-2-yl)acetate
[0129] To a 1L round bottom flask containing a stir bar and 2-((1r,4r)-4-((5-amino-1-(phenylsulfonyl)-1H-pyrrolo[2,3-b]pyridin-4-yl)amino)cyclohexyl)acetonitrile (Intermediate 2, 58.31 g, 142.4 mmol) was added ethyl 3-ethoxy-3-iminopropanoate (60.51 g, 309.3 mmol), followed by EtOH (600 mL, dried over 3Å molecular sieves for 48 h). A reflux condenser was attached to the reaction flask, the reaction was purged with N2, and was heated at 90 °C for 9 h. The reaction mixture was cooled to room temperature and left to stand for 30 h where the product crystallized out as brown needles. The solids were broken up with a spatula and the reaction mixture was transferred to a 2 L flask. Water (1.4 L) was added slowly via separatory funnel with vigorous stirring. After addition of the water was complete, the suspension was stirred for 30 minutes. The brown needles were isolated by filtration and then dried by pulling air through the filter for 1 h. The product was transferred to a 500 mL flask and treated with EtOAc (200 mL). A small quantity of seed crystals were added, which induced the formation of a white solid precipitate. The suspension was stirred for 30 minutes at room temperature, filtered, rinsed with EtOAc (25 mL), and dried under vacuum to provide the product as a white solid (48.65 g, 68% yield). MS (ESI): mass calcd. for C26H27N5O4S, 505.2; m/z found, 506.2 [M+H]+. 1H NMR (400
MHz, CDCl3) δ 8.85 (s, 1H), 8.28 – 8.19 (m, 2H), 7.84 (d, J = 4.0 Hz, 1H), 7.61 – 7.53 (m, 1H), 7.52 – 7.43 (m, 2H), 6.84 (d, J = 4.1 Hz, 1H), 4.32 (s, 1H), 4.20 (q, J = 7.1 Hz, 2H), 4.09 (s, 2H), 2.44 (d, J = 6.2 Hz, 2H), 2.40 – 2.27 (m, 2H), 2.16 (d, J = 13.3 Hz, 2H), 2.12 – 1.96 (m, 3H), 1.54 – 1.38 (m, 2H), 1.27 (t, J = 7.1 Hz, 3H).
Polymorph screening example
[0130] Some embodiments of compound of Formula I as free bases present multiple crystalline configurations that have a complex solid-state behavior, some of which in turn can present distinguishing features among themselves due to different amounts of incorporated solvent. Some embodiments of compound of Formula I are in the form of pseudopolymorphs, which are embodiments of the same compound that present crystal lattice compositional differences due to different amounts of solvent in the crystal lattice itself. In addition, channel solvation can also be present in some crystalline embodiments of compound of Formula I, in which solvent is incorporated within channels or voids that are present in the crystal lattice. For example, the various crystalline configurations given in Table 2 were found for compound of Formula I. Because of these features, non-stoichiometric solvates were often observed, as illustrated in Table 2. Furthermore, the presence of such channels or voids in the crystal structure of some embodiments according to this invention enables the presence of water and/or solvent molecules that are held within the crystal structure with varying degrees of bonding strength. Consequently, changes in the specific ambient conditions can readily lead to some loss or gain of water molecules and/or solvent molecules in some embodiments according to this invention. It is understood that “solvation” (third column in Table 2) for each of the embodiments listed in Table 2 is the formula solvation, and that the actual determination of the same as a stoichiometry number (fourth column in Table 2) can slightly vary from the formula solvation depending on the actual ambient conditions when it is experimentally determined. For example, if about half of the water molecules in an embodiment may be present as hydrogen-bonded to the active compound in the crystal lattice, while about the other half of water molecules may be in channels or voids in the crystal lattice, then changes in ambient conditions may alter the amount of such loosely contained water molecules in voids or channels, and hence lead to a slight difference between the formula solvation that is assigned according to, for example, single crystal diffraction, and the
stoichiometry that is determined by, for example, thermogravimetric analysis coupled with mass spectroscopy.
Table 2. Embodiments of crystalline forms of compound of Formula I
[0131] The compound that was obtained as described in Example 1 was further crystallized by preparing a slurry in DCM (1:3, for example 10 g of compound in 30 ml DCM) that was stirred at 40oC for 4 hours, and further stirred for 14 hours at 25oC, then heptane was slowly added (1:2, for example 20 ml of heptane into the compound/DCM slurry/solution) at 25oC, stirred at 40oC for 4 hours, cooled to 25oC and stirred for further 14 hours at 25oC. Subsequent filtration led to compound of Formula I in the form of an off-white solid, that was identified as a monohydrate, a 1s embodiment.
CLIP
Journal of Medicinal Chemistry (2020), 63(6), 2915-2929

/////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Clip
https://clinicaltrials.gov/ct2/show/NCT04552197
The purpose of this study is to evaluate: systemic and local gut (rectum and sigmoid colon) exposure to JNJ-64251330, local tissue Pharmacodynamics (PD) using gut (rectum and sigmoid colon) biopsies (Part 1) and the effect of food on the rate and extent of absorption of JNJ-64251330 from oral tablet dosed with or without food (Part 2).
Familial adenomatous polyposis (FAP) is the most common polyposis syndrome. It is an autosomal dominant inherited disorder characterized by the early onset of hundreds to thousands of adenomatous polyps throughout the colon. JNJ-64251330 (lorpucitinib) is an oral, small molecule, potent pan-janus kinase (JAK) inhibitor that blocks phosphorylation of Signal Transducer and Activator of Transcription (STAT) proteins. pSTAT induces transcription of multiple genes involved in the progression of inflammatory disease. JNJ-64251330 has chemical properties that limits the amount of drug in the blood while delivering the drug to the tissues of the gut. Local inhibition of JAK in the gut may present a promising method to treat inflammatory diseases of the intestinal tract, such as FAP. The study consists of 3 phases: screening phase (30 days) a treatment phase (24 weeks), and follow-up visit (up to 30 days after last dose of study drug). The total duration of the study will be up to 32 weeks. Study evaluations will include efficacy via endoscopies, safety (monitoring of adverse events (AE), serious adverse events (SAEs), events of infections including tuberculosis (TB), clinical laboratory blood tests (complete blood count and serum chemistries), vital signs, and concomitant medication review), pharmacokinetics, pharmacodynamic and biomarkers evaluations.
Adenomatous polyposis coli (APC) also known as deleted in polyposis 2.5 (DP2.5) is a protein that in humans is encoded by the APC gene.[4] The APC protein is a negative regulator that controls beta-catenin concentrations and interacts with E-cadherin, which are involved in cell adhesion. Mutations in the APC gene may result in colorectal cancer.[5]
APC is classified as a tumor suppressor gene. Tumor suppressor genes prevent the uncontrolled growth of cells that may result in cancerous tumors. The protein made by the APC gene plays a critical role in several cellular processes that determine whether a cell may develop into a tumor. The APC protein helps control how often a cell divides, how it attaches to other cells within a tissue, how the cell polarizes and the morphogenesis of the 3D structures,[6] or whether a cell moves within or away from tissue. This protein also helps ensure that the chromosome number in cells produced through cell division is correct. The APC protein accomplishes these tasks mainly through association with other proteins, especially those that are involved in cell attachment and signaling. The activity of one protein in particular, beta-catenin, is controlled by the APC protein (see: Wnt signaling pathway). Regulation of beta-catenin prevents genes that stimulate cell division from being turned on too often and prevents cell overgrowth.
The human APC gene is located on the long (q) arm of chromosome 5 in band q22.2 (5q22.2). The APC gene has been shown to contain an internal ribosome entry site. APC orthologs[7] have also been identified in all mammals for which complete genome data are available.
////////////////JNJ-64251330, JNJ 64251330, LORPUCITINIB, PHASE 1, CANCER, Adenomatous Polyposis Coli
O=C(NCC(C)(O)C)CC1=NC2=CN=C(NC=C3)C3=C2N1[C@H]4CC[C@H](CC#N)CC4

NEW DRUG APPROVALS
ONE TIME
$10.00
Camizestrant, AZD 9833


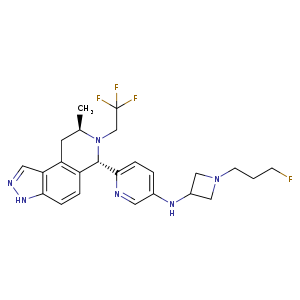
Camizestrant, AZD 9833
AZ 14066724
PHASE 2
CAS: 2222844-89-3
Chemical Formula: C24H28F4N6
Exact Mass: 476.2312
Molecular Weight: 476.5236
Elemental Analysis: C, 60.49; H, 5.92; F, 15.95; N, 17.64
N-(1-(3-fluoropropyl)azetidin-3-yl)-6-((6S,8R)-8-methyl-7-(2,2,2-trifluoroethyl)-6,7,8,9-tetrahydro-3H-pyrazolo[4,3-f]isoquinolin-6-yl)pyridin-3-amine
- AZ14066724
- AZD-9833
- AZD9833
- Camizestrant
- UNII-JUP57A8EPZ
- WHO 11592
- OriginatorAstraZeneca
- ClassAmines; Antineoplastics; Azetidines; Fluorinated hydrocarbons; Isoquinolines; Pyrazolones; Pyridines; Small molecules
- Mechanism of ActionSelective estrogen receptor degraders
- Phase IIIBreast cancer
- 13 Jun 2022AstraZeneca initiates a phase I drug-drug interaction trial of AZD 9833 Healthy postmenopausal female volunteers, in USA (NCT05438303)
- 10 Jun 2022AstraZeneca and Quotient Sciences complete the phase I QSC205863 trial in Breast cancer (In volunteers) in United Kingdom (PO, Liquid) (NCT05364255)
- 03 Jun 2022Safety, efficacy and pharmacokinetics data from the phase I SERENA 1 trial for Breast cancer presented at the 58th Annual Meeting of the American Society of Clinical Oncology (ASCO-2022)
- Mechanism:selective estrogen receptor degrader
- Area under investigation:estrogen receptor +ve breast cancer
- Date commenced phase:Q1 2019
- Estimated Filing Acceptance:
- CountryDateUS: EU: Japan: China:
AZD9833 is an orally available selective estrogen receptor degrader (SERD), with potential antineoplastic activity. Upon administration, SERD AZD9833 binds to the estrogen receptor (ER) and induces a conformational change that results in the degradation of the receptor. This prevents ER-mediated signaling and inhibits the growth and survival of ER-expressing cancer cells
Camizestrant is an orally available selective estrogen receptor degrader (SERD), with potential antineoplastic activity. Upon administration, camizestrant binds to the estrogen receptor (ER) and induces a conformational change that results in the degradation of the receptor. This prevents ER-mediated signaling and inhibits the growth and survival of ER-expressing cancer cells
SYN
https://www.thieme-connect.de/products/ejournals/abstract/10.1055/s-0040-1719368
Discovery of AZD9833, a Potent and Orally Bioavailable Selective Estrogen Receptor Degrader and Antagonist J. Med. Chem. 2020, 63, 14530–14559, DOI: 10.1021/acs.jmedchem.0c01163.

SYN
doi: 10.1021/acs.jmedchem.0c01163.

aReagents and Conditions: (a) n-BuLi, THF, −78 oC to 0 oC, 1 h, then 4 N HCl/dioxane, RT, 1 h, 60%; (b) alkyl triflate, DIPEA, 1,4-dioxane, 90 oC, 63-74% or isobutyrylaldehyde, Na(OAc)3BH, THF, 0 oC, 56%; (c) benzophenone imine, Pd2dba3, Rac-BINAP, NaOtBu, toluene, 90 oC, then 1 N aq. HCl, 71-85%; (d) nBuLi, THF, −78 oC to 0 oC, 1 h, then 4 N HCl/dioxane, RT, 4 h; e) NH2OH, NH2OH.HCl, EtOH, reflux. 84% over 2 steps; (f) alkyl triflate, DIPEA, 1,4-dioxane, 90 oC, 44-100% or 1-fluorocyclopropane-1- carboxylic acid, HATU, Et3N, DMF, RT, 61%, then BH3.THF, THF, 65 oC, 82%.

[α]26 D -147 (c 2.3, MeOH); 1H NMR (500 MHz, DMSO-d6, 27 °C) 1.08 (d, J = 6.6 Hz, 3H), 1.64 (dp, J = 25.0, 6.3 Hz, 2H), 2.45 (t, J = 6.9 Hz, 2H), 2.73(t, J = 6.8 Hz, 2H), 2.84 (dd, J = 17.1, 8.2 Hz, 1H), 2.96 (dt, J = 19.6, 9.8 Hz, 1H), 3.07 (dd, J = 17.2, 4.6 Hz, 1H), 3.49 (m, 1H), 3.50 – 3.58 (m, 1H), 3.58 – 3.66 (m, 2H), 3.92 (h, J = 6.5 Hz, 1H), 4.44 (dtd, J = 47.4, 6.1, 1.3 Hz, 2H), 4.93 (s, 1H), 6.23 (d, J = 6.9 Hz, 1H), 6.80 (d, J = 8.6 Hz, 1H), 6.83 (dt, J = 8.8, 2.0 Hz, 1H), 6.97 (d, J = 8.5 Hz, 1H), 7.22 (d, J = 8.6 Hz, 1H), 7.73 (d, J = 2.8 Hz, 1H), 8.05 (d, J = 1.3 Hz, 1H), 12.97 (s, 1H); 13C NMR (125 MHz, DMSO-d6, 27 °C) 16.2, 28.2 (d, J = 19.4 Hz), 30.1, 43.0, 47.3, 48.7 (q, J = 30.1 Hz), 54.8 (d, J = 5.6 Hz), 61.3 (2C), 67.1, 82.0 (d, J = 161.3 Hz), 107.5, 119.0, 122.4, 123.7, 126.1, 126.2 (q, J = 278.5 Hz), 126.4, 127.5, 131.7, 132.9, 138.5, 142.3, 150.0; 19F NMR (376 MHz, DMSO-d6, 27 °C) -218.1 (1F), -69.7 (3F); m/z (ES+), [M+H]+ = 477, HRMS (ESI) (MH+ ); calcd, 477.2408; found, 477.2390




/////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
AZD9833 is selective oestrogen receptor degrader (SERD). It works by breaking down the site where oestrogen attaches to the cancer cell. This can help stop or slow the growth of hormone receptor breast cancer. Researchers think that AZD9833 with palbociclib might work better than anastrozole and palbociclib.
AZD9833 + palbociclib
The patients will receive AZD9833 (75 mg, PO, once daily) + palbociclib (PO, once daily, 125 mg for 21 consecutive days followed by 7 days off treatment) + anastrozole placebo (1 mg, PO, once daily)
SERENA-1: Study of AZD9833 Alone or in Combination in Women With Advanced Breast Cancer. (clinicaltrials.gov)…..https://veri.larvol.com/news/azd9833/drug
P1, N=305, Recruiting, AstraZeneca | Trial primary completion date: Dec 2022 –> Oct 2023
2 months ago
Trial primary completion date
|
HER-2 (Human epidermal growth factor receptor 2) • ER (Estrogen receptor) • PGR (Progesterone receptor)
|
HER-2 negative
Ibrance (palbociclib) • everolimus • Verzenio (abemaciclib) • capivasertib (AZD5363) • camizestrant (AZD9833)
| Description | Camizestrant (AZD-9833) is a potent and orally active estrogen receptor (ER) antagonist. Camizestrant is used for the study of ER+ HER2-advanced breast cancer[1]. |
|---|---|
| IC50 & Target | IC50: estrogen receptor (ER)[1] |
| In Vitro | Camizestrant is extracted from patent US20180111931A1, example 17[1].MCE has not independently confirmed the accuracy of these methods. They are for reference only. |
| In Vivo | Camizestrant (oral administration; 0.2-50 mg/kg; 20 days) exhibits anti-tumour efficacy as a dose-dependent manner in human parental MCF7 mice xenograft[1]. Camizestrant (oral administration; 0.8-40 mg/kg; 30 days) decreases tumor growth as a dose-dependent manner. It gives almost complete tumour growth inhibition at the doses >10 mg/kg in mice[1]. MCE has not independently confirmed the accuracy of these methods. They are for reference only.Animal Model:Human ESR1 mutant breast cancer patient derived xenograft with CTC174 cells in female NSG mice[1]Dosage:0.8 mg/kg, 3 mg/kg, 10 mg/kg, 20 mg/kg, 40 mg/kgAdministration:Oral administration; 30 days; once dailyResult:Inhibited tumor growth in a dose-dependent manner. |
| Clinical Trial | NCT NumberSponsorConditionStart DatePhaseNCT04711252AstraZenecaER-Positive HER2-Negative Breast CancerJanuary 28, 2021Phase 3NCT04964934AstraZenecaER-Positive HER2-Negative Breast CancerJune 30, 2021Phase 3NCT04214288AstraZenecaAdvanced ER-Positive HER2-Negative Breast CancerApril 22, 2020Phase 2NCT04588298AstraZenecaHER2-negative Breast CancerNovember 2, 2020Phase 2NCT04541433AstraZenecaER&addition; HER2- Advanced Breast CancerSeptember 29, 2020Phase 1NCT03616587AstraZenecaER&addition; HER2- Advanced Breast CancerOctober 11, 2018Phase 1NCT04546347AstraZeneca|Quotient SciencesHealthy VolunteersSeptember 17, 2020Phase 1NCT04818632AstraZenecaER&addition;, HER2-, Metastatic Breast CancerOctober 11, 2021Phase 1 |
////////////Camizestrant, AZD 9833, AZ 14066724, UNII-JUP57A8EPZ, WHO 11592, PHASE 2, ASTRA ZENECA, CANCER
C[C@@H]1CC2=C3C(NN=C3)=CC=C2[C@@H](C4=NC=C(NC5CN(CCCF)C5)C=C4)N1CC(F)(F)F

NEW DRUG APPROVALS
ONE TIME
$10.00
GEMCITABINE
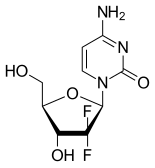
GEMCITABINE
95058-81-4
WeightAverage: 263.1981
Monoisotopic: 263.071762265
Chemical FormulaC9H11F2N3O4
4-amino-1-[(2R,4R,5R)-3,3-difluoro-4-hydroxy-5-(hydroxymethyl)oxolan-2-yl]-1,2-dihydropyrimidin-2-one
Product Ingredients
| INGREDIENT | UNII | CAS | INCHI KEY |
|---|---|---|---|
| Gemcitabine hydrochloride | U347PV74IL | 122111-03-9 | OKKDEIYWILRZIA-OSZBKLCCSA-N |
- LY-188011
- LY188011
Gemcitabine
CAS Registry Number: 95058-81-4
CAS Name: 2¢-Deoxy-2¢,2¢-difluorocytidine
Additional Names: 1-(2-oxo-4-amino-1,2-dihydropyrimidin-1-yl)-2-deoxy-2,2-difluororibose; dFdC; dFdCyd
Manufacturers’ Codes: LY-188011
Trademarks: Gemzar (Lilly)
Molecular Formula: C9H11F2N3O4
Molecular Weight: 263.20
Percent Composition: C 41.07%, H 4.21%, F 14.44%, N 15.97%, O 24.32%
Literature References: Prepn: L. W. Hertel, GB2136425; idem,US4808614 (1984, 1989 both to Lilly); L. W. Hertel et al.,J. Org. Chem.53, 2406 (1988); T. S. Chou et al.,Synthesis1992, 565. Antitumor activity: L. W. Hertel et al.,Cancer Res.50, 4417 (1990). Mode of action study: V. W. T. Ruiz et al.,Biochem. Pharmacol.46, 762 (1993). Clinical pharmacokinetics and toxicity: J. L. Abbruzzese et al.,J. Clin. Oncol.9, 491 (1991). Review of clinical studies: B. Lund et al.,Cancer Treat. Rev.19, 45-55 (1993).
Properties: Crystals from water, pH 8.5. [a]365 +425.36°; [a]D +71.51° (c = 0.96 in methanol). uv max (ethanol): 234, 268 (e 7810, 8560). LD10 i.v. in rats: 200 mg/m2 (Abbruzzese).
Optical Rotation: [a]365 +425.36°; [a]D +71.51°
Absorption maximum: uv max (ethanol): 234, 268 (e 7810, 8560)
Toxicity data: LD10 i.v. in rats: 200 mg/m2 (Abbruzzese)
Derivative Type: Hydrochloride
CAS Registry Number: 122111-03-9
Molecular Formula: C9H11F2N3O4.HCl
Molecular Weight: 299.66
Percent Composition: C 36.07%, H 4.04%, F 12.68%, N 14.02%, O 21.36%, Cl 11.83%
Properties: Crystals from water-acetone, mp 287-292° (dec). [a]D +48°; [a]365 +257.9° (c = 1.0 in deuterated water). uv max (water): 232, 268 nm (e 7960, 9360).
Melting point: mp 287-292° (dec)
Optical Rotation: [a]D +48°; [a]365 +257.9° (c = 1.0 in deuterated water)
Absorption maximum: uv max (water): 232, 268 nm (e 7960, 9360)
Therap-Cat: Antineoplastic.
Keywords: Antineoplastic; Antimetabolites; Pyrimidine Analogs.
Gemcitabine is a nucleoside metabolic inhibitor used as adjunct therapy in the treatment of certain types of ovarian cancer, non-small cell lung carcinoma, metastatic breast cancer, and as a single agent for pancreatic cancer.
Gemcitabine hydrochloride was first approved in ZA on Jan 10, 1995, then approved by the U.S. Food and Drug Administration (FDA) on May 15, 1996, and approved by Pharmaceuticals and Medicals Devices Agency of Japan (PMDA) on Aug 31, 2001. It was developed and marketed as Gemzar® by Eli Lilly.
Gemcitabine hydrochloride is a nucleoside metabolic inhibitor. It kills cells undergoing DNA synthesis and blocks the progression of cells through the G1/S-phase boundary. It is indicated for the treatment of advanced ovarian cancer that has relapsed at least 6 months after completion of platinum-based therapy, in combination with paclitaxel, for first-line treatment of metastatic breast cancer after failure of prior anthracycline-containing adjuvant chemotherapy, unless anthracyclines were clinically contraindicated, and it is also indicated in combination with cisplatin for the treatment of non-small cell lung cancer, and treated as a single agent for the treatment of pancreatic cancer.
Gemzar® is available as injection of lyophilized powder for intravenous use, containing 200 mg or 1000 mg of free Gemcitabine per vial. The recommended initial dosage is 1000 mg/m2 over 30 minutes on days 1 and 8 of each 21 day cycle for ovarian cancer, 1250 mg/m2 over 30 minutes on days 1 and 8 of each 21 day cycle for breast cancer, 1000 mg/m2 over 30 minutes on days 1, 8, and 15 of each 28 day cycle or 1250 mg/m2 over 30 minutes on days 1 and 8 of each 21 day cycle for non-small cell lung cancer, and 1000 mg/m2 over 30 minutes once weekly for the first 7 weeks, then one week rest, then once weekly for 3 weeks of each 28 day cycle for pancreatic cancer.
Approved Countries or AreaUpdate US, JP, CN, ZA
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 1996-05-15 | First approval | Gemzar | Ovarian cancer,Breast cancer,Non small cell lung cancer (NSCLC),Pancreatic cancer | Injection, Lyophilized powder, For solution | Eq. 200 mg/1000 mg Gemcitabine/vial | Lilly | Priority |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2013-02-01 | New indication | Gemzar | Relapsed or refractory malignant lymphoma | Injection, Lyophilized powder, For solution | 200 mg; 1 g | Lilly | |
| 2011-02-23 | New indication | Gemzar | Advanced ovarian cancer | Injection, Lyophilized powder, For solution | 200 mg; 1 g | Lilly | |
| 2010-02-05 | New indication | Gemzar | Advanced breast cancer | Injection, Lyophilized powder, For solution | 200 mg; 1 g | Lilly | |
| 2008-11-25 | New indication | Gemzar | Urothelial cancer | Injection, Lyophilized powder, For solution | 200 mg; 1 g | Lilly | |
| 2006-06-15 | New indication | Gemzar | Biliary cancer | Injection, Lyophilized powder, For solution | 200 mg; 1 g | Lilly | |
| 2001-08-31 | First approval | Gemzar | Pancreatic cancer,Non small cell lung cancer (NSCLC) | Injection, Lyophilized powder, For suspension | 200 mg; 1 g | Lilly |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2014-04-15 | Marketing approval | Ovarian cancer,Breast cancer,Non small cell lung cancer (NSCLC),Pancreatic cancer | Injection | Eq. 1000 mg Gemcitabine per vial | 湖北一半天制药 | ||
| 2014-04-15 | Marketing approval | Ovarian cancer,Breast cancer,Non small cell lung cancer (NSCLC),Pancreatic cancer | Injection | Eq. 200 mg Gemcitabine per vial | 湖北一半天制药 | 6类 | |
| 2014-04-08 | Marketing approval | Ovarian cancer,Breast cancer,Non small cell lung cancer (NSCLC),Pancreatic cancer | Injection | Eq.1000 mg Gemcitabine per vial | 南京正大天晴制药 | 6类 | |
| 2011-12-02 | Marketing approval | 健择/Gemzar | Ovarian cancer,Breast cancer,Non small cell lung cancer (NSCLC),Pancreatic cancer | Injection | Eq. 200 mg/1000 mg Gemcitabine per vial | Lilly | |
| 2010-08-31 | Marketing approval | Ovarian cancer,Breast cancer,Non small cell lung cancer (NSCLC),Pancreatic cancer | Injection | 1000 mg/200 mg | 北京协和药厂 | 6类 |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 1995-01-10 | First approval | Gemzar | Ovarian cancer,Breast cancer,Non small cell lung cancer (NSCLC),Pancreatic cancer | Injection, Lyophilized powder, For solution | Eq. 200 mg/1000 mg Gemcitabine per vial | Lilly |
Gemcitabine, with brand names including Gemzar,[1] is a chemotherapy medication.[2] It treats cancers including testicular cancer,[3]breast cancer, ovarian cancer, non-small cell lung cancer, pancreatic cancer, and bladder cancer.[2][4] It is administered by intravenous infusion.[2] It acts against neoplastic growth, and it inhibits the replication of Orthohepevirus A, the causative agent of Hepatitis E, through upregulation of interferon signaling.[5]
Common side effects include bone marrow suppression, liver and kidney problems, nausea, fever, rash, shortness of breath, mouth sores, diarrhea, neuropathy, and hair loss.[2] Use during pregnancy will likely result in fetal harm.[2] Gemcitabine is in the nucleoside analog family of medication.[2] It works by blocking the creation of new DNA, which results in cell death.[2]
Gemcitabine was patented in 1983 and was approved for medical use in 1995.[6] Generic versions were introduced in Europe in 2009 and in the US in 2010.[7][8] It is on the WHO Model List of Essential Medicines.[9]
Medical uses
Gemcitabine treats various carcinomas. It is used as a first-line treatment alone for pancreatic cancer, and in combination with cisplatin for advanced or metastatic bladder cancer and advanced or metastatic non-small cell lung cancer. It is used as a second-line treatment in combination with carboplatin for ovarian cancer and in combination with paclitaxel for breast cancer that is metastatic or cannot be surgically removed.[10][11][12]
It is commonly used off-label to treat cholangiocarcinoma[13] and other biliary tract cancers.[14]
It is given by intravenous infusion at a chemotherapy clinic.[2]
Contraindications and interactions
Taking gemcitabine can also affect fertility in men and women, sex life, and menstruation. Women taking gemcitabine should not become pregnant, and pregnant and breastfeeding women should not take it.[15]
As of 2014, drug interactions had not been studied.[11][10]
SYN
. Hertel, L. W.; Kroin, J. S.; Misner, J. W.; Tustin, J. M. J. Org. Chem. 1988, 53, 2406– 2409.


NEXT
a) Noe, C. R.; Jasic, M.; Kollmann, H.; Saadat, K. WO009147, 2007.; b) Noe, C. R.; Jasic, M.; Kollmann, H.; Saadat, K. US0249119, 2008. Note: no stereochemistry was indica


NExT
15. Hanzawa, Y.; Inazawa, K.; Kon, A.; Aoki, H.; Kobayashi, Y. Tetrahedron Lett. 1987, 28, 659–662. 16. Wirth, D. D. EP0727432, 1996


Synthesis Reference
John A. Weigel, “Process for making gemcitabine hydrochloride.” U.S. Patent US6001994, issued May, 1995.US6001994Route 1
Reference:1. J. Org. Chem. 1988, 53, 2406-2409.
2. US4808614A.Route 2
Reference:1. CN102417533A.Route 3
Reference:1. Nucleosides, Nucleotides and Nucleic Acids 2010, 29, 113-122.Route 4
Reference:1. CN102617677A.Route 5
Reference:1. CN103012527A.
SYN
U.S. Patent No. 4,808,614 (the ‘614 patent) describes a process for synthetically producing gemcitabine, which process is generally illustrated in Scheme Scheme 1

5

SYN
U.S. Patent No. 4,965,374 (the ‘374 patent) describes a process for producing gemcitabine from an intermediate 3,5-dibenzoyl ribo protected lactone of the formula:

11 where the desired erythro isomer can be isolated in a crystalline form from a mixture of erythro and threo isomers. The process described in the ‘374 patent is generally outlined in Scheme 2.
Scheme 2

mixture of α and β anomers
SYN
U.S. Patent No. 5,521,294 (the ‘294 patent) describes l-alkylsulfonyl-2,2- difluoro-3 -carbamoyl ribose intermediates and intermediate nucleosides derived therefrom. The compounds are reportedly useful in the preparation of 2′-deoxy-2′,2’- difluoro-β-cytidine and other β-anomer nucleosides. The ‘294 patent teaches, inter alia, that the 3-hydroxy carbamoyl group on the difluororibose intermediate may enhance formation of the desired β-anomer nucleoside derivative. The ‘294 patent describes converting the lactone 4 to the dibenzoyl mesylate 13, followed by deprotection at the 3 position to obtain the 5-monobenzoyl mesylate intermediate 15, which is reacted with various isocyanates to obtain the compounds of formula 16. The next steps involve coupling and deprotection using methods similar to those described in previous patents. The process and the intermediates 15 and 16 are illustrated by scheme 3 below: Scheme 3

13 15
PhCOCK
PhNCO/TEA -o. -~- j*«0Ms
PhNHCOO -r F
16
1 coupling 2 deprotection


16 gemcitabine
CLIP
https://www.sciencedirect.com/science/article/abs/pii/S0008621514000500

PATENT
https://patents.google.com/patent/WO2008129530A1/en
Scheme 4

e3
13A deprotection isomer separation

deprotection


EXAMPLE 1
[0045] This example demonstrates the preparation of 2-deoxy-2,2-difluoro-D- ribofuranose-3,5-dicinnamate-l-p-toluenesulfonate.
[0046] Crude 2-deoxy-2,2-difluoro-D-riboufuranose-3,5-dicinnamate (2.5g, 6 mmol) was dissolved in dichloromethane (20 ml) in a round flask, and diethylamine (0.7g, 9.6 mmol) was added followed by p-toluenesulfonyl chloride (1.32 g, 6.92 mmol), which was added drop wise while cooling to 0-50C. The mixture was stirred for 1 hour, and washed with IN HCl (15 ml), concentrated solution OfNaHCO3 (15 ml), and dried over MgSO4. The solvent was distilled off under reduced pressure to obtain crude 2-deoxy-2,2-difluoro-D-ribofuranose-3,5-dicinnamate-l-p- toluenesulfonate as light oil. Yield: 3.22 g, (5.6 mmol), 93%.
EXAMPLE 2
[0047] This example demonstrates the preparation of 3′,5′-dicinnamoyl-2′-deoxy- 2′,2′-difluorocytidine.
[0048] Dry 1 ,2-dichloroethane (800 ml) was added to N,O-bis(trimethylsilyl)- cytosine (136 g, 487 mmol) under nitrogen blanket to produce a clear solution, followed by adding trimethylsilyl triflate (Me3SiOTf), (100 ml, 122.8 g, 520 mmol) and stirred for 30 minutes. A solution of 2-deoxy-2,2-difluoro-D-ribofuranose-3,5- dicinnamate-1-p-toluenesulfonate (128 g, 224 mmol) in 1 ,2-dichloroethane (400 ml) was added drop wise, and the mixture was refluxed overnight. After cooling, the solvent was distilled off to obtain crude 3,5-dicinnamoyl-N4-trimethylsilyl-2′-deoxy- 2′,2′-difluorocytidine as a light yellow solid. The residue was dissolved in ethyl acetate (1600 ml) and washed 3 times with water (3X400 ml). The ethyl acetate phase was mixed with concentrated solution OfNaHCO3 (800 ml) for about 5 minutes, and then the mixture was set aside for about 20 minutes without stirring. The thus formed solid, which was precipitated in the inter-phase of the two layers, was filtered off and washed with 60 ml of ethyl acetate. The solid was dried under reduced pressure to obtain 116.7 g (223 mmol, 99.5%) of the crude 3′,5′-dicinnamoyl- 2′-deoxy-2′,2′- difluorocytidine containing 73.3 % of the β-anomer and 11.8 % of the α-anomer.
EXAMPLE 3
[0049] This example demonstrates the preparation of 3′,5′-dicinnamoyl-2′-deoxy- 2′,2′-difluorocytidine.
[0050] Dry 1,2-dichloroethane (1.5 L) was added to bis(trimethylsilyl)cytosine (417 g, 1.49 mol) under nitrogen blanket to produce a clear solution followed by adding trimethylsilyl triflate (Me3SiOTf), (300 ml, 368.4 g, 1.56 mol) and stirred for 30 minutes. A solution of 2-deoxy-2,2-difluoro-D-ribofuranose-3,5-dicinnamate-l-p- toluenesulfonate (384 g, 673 mmol) in 1,2-dichloroethane (1.2 L) was added drop wise, and the mixture was refluxed overnight. After cooling, the solvent was distilled off to obtain crude 3,5-dicinnamoyl-N4-trimethylsilyl-2l-deoxy-2′,2′-difluorocytidine as a light yellow solid. The residue was dissolved in ethyl acetate (2.4 L) and washed 3 times with water (3X1.2 L). The ethyl acetate phase was mixed with concentrated solution OfNaHCO3 (1.34 L) for about 20 minutes. The thus formed solid, which was precipitated in the inter-phase of the two layers, was filtered off and washed with 180 ml of ethyl acetate. The solid was dried under reduced pressure to obtain 346.5 g (0.66 mol, 99.9% yield) of the crude 3l,5l-dicinnamoyl-2′-deoxy-2′,2′-difluorocytidine containing 43 % of the β-anomer and 52 % of the α-anomer.
EXAMPLE 4
[0051] This example demonstrates the preparation of gemcitabine hydrochloride. [0052] To a solution of ammonia-methanol (15.8 %, 4.57 L), the crude 3,5- dicirmamoyl-2′-deoxy-2′,2′-difluorocytidine of example 3 was added (346.5 g, 0.66 mol), and stirred at ambient temperature for 6 hours. The mixture was concentrated to afford a light yellow solid (306 g). Purified water (3 L) was added to the solid, followed by addition of ethyl acetate (1.8 L), and stirring was maintained for about 10 minutes. The aqueous layer was separated and the organic layer was extracted with water (1.05 L). The aqueous layers were combined and water was removed by evaporation under reduced pressure to obtain an oil (154.7 g). Water was added (660 ml) and the mixture was heated to 50-550C to dissolve the solid. The mixture was cooled to 5-1O0C during about one hour and mixed for about 16 hours at that temperature. The thus formed solid was filtered and dried to afford 46.75 g (0.177 mol), containing 98 % of the β-anomer and 1.3 % of the α-anomer. 0.5N HCl (936 ml) was added followed by addition of dichloromethane (300 ml) with stirring. The water phase was separated and the aqueous phase was washed with dichloromethane (300 ml). After filtration, the aqueous phase was concentrated to dryness under reduced pressure to obtain gemcitabine hydrochloride as a solid (46.9 g). The solid was dissolved in water (187 ml) at ambient temperature and the mixture was heated to 500C to afford a clear solution and cooled to ambient temperature. Acetone (1.4 L) was added and stirring was maintained for about one hour. Then, the precipitate was collected by filtration and washed twice with acetone (2X30 ml) and dried at 450C under vacuum to obtain 39.2 g of gemcitabine hydrochloride, containing 99.9% of the β-anomer
EXAMPLE 5
[0053] This example demonstrates the preparation of gemcitabine hydrochloride. [0054] To a solution of ammonia-methanol (about 15.8 %, 1.35 L), the crude 3′,5′- dicinnamoyl-2′-deoxy-2′,2′-difluorocytidine prepared as described in example 2 was added (96 g, 183.4 mmol), and stirred at ambient temperature for 4 hours. The mixture was concentrated to afford a light yellow solid (80.5 g). Purified water (1 L) was added to the solid, followed by addition of ethyl acetate (600 ml), and stirring was maintained for about 10 minutes. The aqueous layer was separated and the organic layer was extracted with water (350 ml). The aqueous layers were combined and water was removed by evaporation under reduced pressure to obtain an oil (46.4 g). Water was added (220 ml) and the mixture was heated to 50-550C to dissolve the solid. The mixture was cooled to 0-50C during about one hour and mixed for about 16 hours at that temperature. The thus formed solid was filtered and dried to afford 11.1 g of gemcitabine free base. 0.5N HCl (240 ml) was added followed by addition of dichloromethane (100 ml) with stirring. The water phase was separated and the aqueous phase was washed with dichloromethane (300 ml). After filtration, the aqueous phase was concentrated to dryness under reduced pressure to obtain gemcitabine hydrochloride as a solid (12.0 g). The solid was dissolved in water (48 ml) at ambient temperature and the mixture was heated to 5O0C to afford a clear solution and cooled to ambient temperature. Acetone (360 ml) was added and stirring was maintained for about one hour. Then, the precipitate was collected by filtration and washed twice with acetone (2X30 ml) and dried at 450C under vacuum to obtain 9.9 g of gemcitabine hydrochloride, containing 99.6% of the β-anomer.
EXAMPLE 6
[0055] This example demonstrates the slurrying procedure of the 3 ‘,5′- dicinnamoyl-2′-deoxy-2’,2l-difluorocytidine in different solvents. [0056] 1 g of the crude 3′,5′-dicinnamoyl-2′-deoxy-2l,2′-difluorocytidine, containing 73.7 % of the β-anomer and 17.5 % of the α-anomer, was placed in flask and 10 ml of a solvent was added and the mixture was mixed at ambient temperature for one hour. Then, the solid was obtained by filtration, washed with 5 ml of the solvent and dried. The liquid obtained after filtering the solid and the liquid obtained after washing the solid were combined (hereinafter the mother liquor). The ratio between the β-anomer and the α-anomer in the solid and in the mother liquor was determined by HPLC and the results are summarized in Table 1.
Table 1

/////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Adverse effects
Gemcitabine is a chemotherapy drug that works by killing any cells that are dividing.[10] Cancer cells divide rapidly and so are targeted at higher rates by gemcitabine, but many essential cells also divide rapidly, including cells in skin, the scalp, the stomach lining, and bone marrow, resulting in adverse effects.[16]: 265
The gemcitabine label carries warnings that it can suppress bone marrow function and cause loss of white blood cells, loss of platelets, and loss of red blood cells, and that it should be used carefully in people with liver, kidney, or cardiovascular disorders. People taking it should not take live vaccines. The warning label also states it may cause posterior reversible encephalopathy syndrome, that it may cause capillary leak syndrome, that it may cause severe lung conditions like pulmonary edema, pneumonia, and adult respiratory distress syndrome, and that it may harm sperm.[10][17]
More than 10% of users develop adverse effects, including difficulty breathing, low white and red blood cells counts, low platelet counts, vomiting and nausea, elevated transaminases, rashes and itchy skin, hair loss, blood and protein in urine, flu-like symptoms, and edema.[10][15]
Common adverse effects (occurring in 1–10% of users) include fever, loss of appetite, headache, difficulty sleeping, tiredness, cough, runny nose, diarrhea, mouth and lip sores, sweating, back pain, and muscle pain.[10]
Thrombotic thrombocytopenic purpura (TTP) is a rare but serious side effect that been associated with particular chemotherapy medications including gemcitabine. TTP is a blood disorder and can lead to microangipathic hemolytic anemia (MAHA), neurologic abnormalities, fever, and renal disease.[18]
Pharmacology
Gemcitabine is hydrophilic and must be transported into cells via molecular transporters for nucleosides (the most common transporters for gemcitabine are SLC29A1 SLC28A1, and SLC28A3).[19][20] After entering the cell, gemcitabine is first modified by attaching a phosphate to it, and so it becomes gemcitabine monophosphate (dFdCMP).[19][20] This is the rate-determining step that is catalyzed by the enzyme deoxycytidine kinase (DCK).[19][20] Two more phosphates are added by other enzymes. After the attachment of the three phosphates gemcitabine is finally pharmacologically active as gemcitabine triphosphate (dFdCTP).[19] [21]
After being thrice phosphorylated, gemcitabine can masquerade as deoxycytidine triphosphate and is incorporated into new DNA strands being synthesized as the cell replicates.[2][19][20]
When gemcitabine is incorporated into DNA it allows a native, or normal, nucleoside base to be added next to it. This leads to “masked chain termination” because gemcitabine is a “faulty” base, but due to its neighboring native nucleoside it eludes the cell’s normal repair system (base-excision repair). Thus, incorporation of gemcitabine into the cell’s DNA creates an irreparable error that leads to inhibition of further DNA synthesis, and thereby leading to cell death.[2][19][20]
The form of gemcitabine with two phosphates attached (dFdCDP) also has activity; it inhibits the enzyme ribonucleotide reductase (RNR), which is needed to create new DNA nucleotides. The lack of nucleotides drives the cell to uptake more of the components it needs to make nucleotides from outside the cell, which also increases uptake of gemcitabine.[2][19][20][22]
Chemistry
Gemcitabine is a synthetic pyrimidine nucleoside prodrug—a nucleoside analog in which the hydrogen atoms on the 2′ carbon of deoxycytidine are replaced by fluorine atoms.[2][23][24]
The synthesis described and pictured below is the original synthesis done in the Eli Lilly Company labs. Synthesis begins with enantiopure D-glyceraldehyde (R)-2 as the starting material which can made from D-mannitol in 2–7 steps. Then fluorine is introduced by a “building block” approach using ethyl bromodifluroacetate. Then, Reformatsky reaction under standard conditions will yield a 3:1 anti/syn diastereomeric mixture, with one major product. Separation of the diastereomers is carried out via HPLC, thus yielding the anti-3 gemcitabine in a 65% yield.[23][24] At least two other full synthesis methods have also been developed by different groups.[24]

Illustration of the original synthesis process used and published by Hertel et al. in 1988 of Lilly laboratories.
History[
Gemcitabine was first synthesized in Larry Hertel’s lab at Eli Lilly and Company during the early 1980s. It was intended as an antiviral drug, but preclinical testing showed that it killed leukemia cells in vitro.[25]
During the early 1990s gemcitabine was studied in clinical trials. The pancreatic cancer trials found that gemcitabine increased one-year survival time significantly, and it was approved in the UK in 1995[10] and approved by the FDA in 1996 for pancreatic cancers.[4] In 1998, gemcitabine received FDA approval for treating non-small cell lung cancer and in 2004, it was approved for metastatic breast cancer.[4]
European labels were harmonized by the EMA in 2008.[26]
By 2008, Lilly’s worldwide sales of gemcitabine were about $1.7 billion; at that time its US patents were set to expire in 2013 and its European patents in 2009.[27] The first generic launched in Europe in 2009,[7] and patent challenges were mounted in the US which led to invalidation of a key Lilly patent on its method to make the drug.[28][29] Generic companies started selling the drug in the US in 2010 when the patent on the chemical itself expired.[29][8] Patent litigation in China made headlines there and was resolved in 2010.[30]
Society and culture
As of 2017, gemcitabine was marketed under many brand names worldwide: Abine, Accogem, Acytabin, Antoril, axigem, Bendacitabin, Biogem, Boligem, Celzar, Citegin, Cytigem, Cytogem, Daplax, DBL, Demozar, Dercin, Emcitab, Enekamub, Eriogem, Fotinex, Gebina, Gemalata, Gembin, Gembine, Gembio, Gemcel, Gemcetin, Gemcibine, Gemcikal, Gemcipen, Gemcired, Gemcirena, Gemcit, Gemcitabin, Gemcitabina, Gemcitabine, Gemcitabinum, Gemcitan, Gemedac, Gemflor, Gemful, Gemita, Gemko, Gemliquid, Gemmis, Gemnil, Gempower, Gemsol, Gemstad, Gemstada, Gemtabine, Gemtavis, Gemtaz, Gemtero, Gemtra, Gemtro, Gemvic, Gemxit, Gemzar, Gentabim, Genuten, Genvir, Geroam, Gestredos, Getanosan, Getmisi, Gezt, Gitrabin, Gramagen, Haxanit, Jemta, Kalbezar, Medigem, Meditabine, Nabigem, Nallian, Oncogem, Oncoril, Pamigeno, Ribozar, Santabin, Sitagem, Symtabin, Yu Jie, Ze Fei, and Zefei.[1]
Research
Because it is clinically valuable and is only useful when delivered intravenously, methods to reformulate it so that it can be given by mouth have been a subject of research.[31][32][33]
Research into pharmacogenomics and pharmacogenetics has been ongoing. As of 2014, it was not clear whether or not genetic tests could be useful in guiding dosing and which people respond best to gemcitabine.[19] However, it appears that variation in the expression of proteins (SLC29A1, SLC29A2, SLC28A1, and SLC28A3) used for transport of gemcitabine into the cell lead to variations in its potency. Similarly, the genes that express proteins that lead to its inactivation (deoxycytidine deaminase, cytidine deaminase, and NT5C) and that express its other intracellular targets (RRM1, RRM2, and RRM2B) lead to variations in response to the drug.[19] Research has also been ongoing to understand how mutations in pancreatic cancers themselves determine response to gemcitabine.[34]
It has been studied as a treatment for Kaposi sarcoma, a common cancer in people with AIDS which is uncommon in the developed world but not uncommon in the developing world.[35]
References
- ^ Jump up to:a b c “Gemcitabine International Brands”. Drugs.com. Archived from the original on 25 May 2014. Retrieved 6 May 2017.
- ^ Jump up to:a b c d e f g h i j k l “Gemcitabine Hydrochloride”. The American Society of Health-System Pharmacists. Archived from the original on 2 February 2017. Retrieved 8 December 2016.
- ^ “Drug Formulary/Drugs/ gemcitabine – Provider Monograph”. Cancer Care Ontario. Retrieved 6 December 2020.
- ^ Jump up to:a b c National Cancer Institute (2006-10-05). “FDA Approval for Gemcitabine Hydrochloride”. National Cancer Institute. Archived from the original on 5 April 2017. Retrieved 22 April 2017.
- ^ Li Y, Li P, Li Y, Zhang R, Yu P, Ma Z, Kainov DE, de Man RA, Peppelenbosch MP, Pan Q (December 2020). “Drug screening identified gemcitabine inhibiting hepatitis E virus by inducing interferon-like response via activation of STAT1 phosphorylation”. Antiviral Research. 184: 104967. doi:10.1016/j.antiviral.2020.104967. PMID 33137361.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 511. ISBN 9783527607495.
- ^ Jump up to:a b Myers, Calisha (13 March 2009). “Gemcitabine from Actavis launched on patent expiry in EU markets”. FierceBiotech. Archived from the original on 11 September 2017.
- ^ Jump up to:a b “Press release: Hospira launches two-gram vial of gemcitabine hydrochloride for injection”. Hospira via News-Medical.Net. 16 November 2010. Archived from the original on 2 October 2015.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ Jump up to:a b c d e f g “UK label”. UK Electronic Medicines Compendium. 5 June 2014. Archived from the original on 10 July 2017. Retrieved 6 May 2017.
- ^ Jump up to:a b “US formLabel” (PDF). FDA. June 2014. Archived (PDF) from the original on 16 February 2017. Retrieved 6 May 2017. For label updates see FDA index page for NDA 020509 Archived 2017-04-29 at the Wayback Machine
- ^ Zhang XW, Ma YX, Sun Y, Cao YB, Li Q, Xu CA (June 2017). “Gemcitabine in Combination with a Second Cytotoxic Agent in the First-Line Treatment of Locally Advanced or Metastatic Pancreatic Cancer: a Systematic Review and Meta-Analysis”. Targeted Oncology. 12 (3): 309–321. doi:10.1007/s11523-017-0486-5. PMID 28353074. S2CID 3833614.
- ^ Plentz RR, Malek NP (December 2016). “Systemic Therapy of Cholangiocarcinoma”. Visceral Medicine. 32 (6): 427–430. doi:10.1159/000453084. PMC 5290432. PMID 28229078.
- ^ Jain A, Kwong LN, Javle M (November 2016). “Genomic Profiling of Biliary Tract Cancers and Implications for Clinical Practice”. Current Treatment Options in Oncology. 17 (11): 58. doi:10.1007/s11864-016-0432-2. PMID 27658789. S2CID 25477593.
- ^ Jump up to:a b Macmillan Cancer Support. “Gemcitabine”. Macmillan Cancer Support. Archived from the original on 25 March 2017. Retrieved 6 May 2017.
- ^ Rachel Airley (2009). Cancer Chemotherapy. Wiley-Blackwell. ISBN 978-0-470-09254-5.
- ^ Siddall E, Khatri M, Radhakrishnan J (July 2017). “Capillary leak syndrome: etiologies, pathophysiology, and management”. Kidney International. 92 (1): 37–46. doi:10.1016/j.kint.2016.11.029. PMID 28318633.
- ^ Kasi PM (January 2011). “Thrombotic thrombocytopenic purpura and gemcitabine”. Case Reports in Oncology. 4 (1): 143–8. doi:10.1159/000326801. PMC 3114619. PMID 21691573.
- ^ Jump up to:a b c d e f g h i Alvarellos ML, Lamba J, Sangkuhl K, Thorn CF, Wang L, Klein DJ, Altman RB, Klein TE (November 2014). “PharmGKB summary: gemcitabine pathway”. Pharmacogenetics and Genomics. 24 (11): 564–74. doi:10.1097/fpc.0000000000000086. PMC 4189987. PMID 25162786.
- ^ Jump up to:a b c d e f Mini E, Nobili S, Caciagli B, Landini I, Mazzei T (May 2006). “Cellular pharmacology of gemcitabine”. Annals of Oncology. 17 Suppl 5: v7-12. doi:10.1093/annonc/mdj941. PMID 16807468.
- ^ Fatima, M., Iqbal Ahmed, M. M., Batool, F., Riaz, A., Ali, M., Munch-Petersen, B., & Mutahir, Z. (2019). Recombinant deoxyribonucleoside kinase from Drosophila melanogaster can improve gemcitabine based combined gene/chemotherapy for targeting cancer cells. Bosnian Journal of Basic Medical Sciences, 19(4), 342-349. https://doi.org/10.17305/bjbms.2019.4136
- ^ Cerqueira NM, Fernandes PA, Ramos MJ (2007). “Understanding ribonucleotide reductase inactivation by gemcitabine”. Chemistry. 13 (30): 8507–15. doi:10.1002/chem.200700260. PMID 17636467.
- ^ Jump up to:a b Brown K, Weymouth-Wilson A, Linclau B (April 2015). “A linear synthesis of gemcitabine”. Carbohydrate Research. 406: 71–5. doi:10.1016/j.carres.2015.01.001. PMID 25681996.
- ^ Jump up to:a b c Brown K, Dixey M, Weymouth-Wilson A, Linclau B (March 2014). “The synthesis of gemcitabine”. Carbohydrate Research. 387: 59–73. doi:10.1016/j.carres.2014.01.024. PMID 24636495.
- ^ Sneader, Walter (2005). Drug discovery: a history. New York: Wiley. p. 259. ISBN 978-0-471-89979-2.
- ^ “Gemzar”. European Medicines Agency. 24 September 2008. Archived from the original on 11 September 2017.
- ^ Myers, Calisha (18 August 2009). “Patent for Lilly’s cancer drug Gemzar invalidated”. FiercePharma. Archived from the original on 11 September 2017.
- ^ Holman, Christopher M. (Summer 2011). “Unpredictability in Patent Law and Its Effect on Pharmaceutical Innovation” (PDF). Missouri Law Review. 76 (3): 645–693. Archived from the original (PDF) on 2017-09-11. Retrieved 2017-05-06.
- ^ Jump up to:a b Ravicher, Daniel B. (28 July 2010). “On the Generic Gemzar Patent Fight”. Seeking Alpha. Archived from the original on 9 December 2012.
- ^ Wang M, Alexandre D (2015). “Analysis of Cases on Pharmaceutical Patent Infringement in Great China”. In Rader RR, et al. (eds.). Law, Politics and Revenue Extraction on Intellectual Property. Cambridge Scholars Publishing. p. 119. ISBN 9781443879262. Archived from the original on 2017-09-11.
- ^ Dyawanapelly S, Kumar A, Chourasia MK (2017). “Lessons Learned from Gemcitabine: Impact of Therapeutic Carrier Systems and Gemcitabine’s Drug Conjugates on Cancer Therapy”. Critical Reviews in Therapeutic Drug Carrier Systems. 34 (1): 63–96. doi:10.1615/CritRevTherDrugCarrierSyst.2017017912. PMID 28322141.
- ^ Birhanu G, Javar HA, Seyedjafari E, Zandi-Karimi A (April 2017). “Nanotechnology for delivery of gemcitabine to treat pancreatic cancer”. Biomedicine & Pharmacotherapy. 88: 635–643. doi:10.1016/j.biopha.2017.01.071. PMID 28142120.
- ^ Dubey RD, Saneja A, Gupta PK, Gupta PN (October 2016). “Recent advances in drug delivery strategies for improved therapeutic efficacy of gemcitabine”. European Journal of Pharmaceutical Sciences. 93: 147–62. doi:10.1016/j.ejps.2016.08.021. PMID 27531553.
- ^ Pishvaian MJ, Brody JR (March 2017). “Therapeutic Implications of Molecular Subtyping for Pancreatic Cancer”. Oncology. 31 (3): 159–66, 168. PMID 28299752. Archived from the original on 3 July 2017.
- ^ Krown SE (September 2011). “Treatment strategies for Kaposi sarcoma in sub-Saharan Africa: challenges and opportunities”. Current Opinion in Oncology. 23 (5): 463–8. doi:10.1097/cco.0b013e328349428d. PMC 3465839. PMID 21681092.
External links
- “Gemcitabine”. Drug Information Portal. U.S. National Library of Medicine.
| Clinical data | |
|---|---|
| Pronunciation | /dʒɛmˈsaɪtəbiːn/ |
| Trade names | Gemzar, others[1] |
| Other names | 2′, 2′-difluoro 2’deoxycytidine, dFdC |
| AHFS/Drugs.com | Monograph |
| Pregnancy category | AU: D |
| Routes of administration | Intravenous |
| ATC code | L01BC05 (WHO) |
| Legal status | |
| Legal status | AU: S4 (Prescription only)UK: POM (Prescription only)US: ℞-onlyIn general: ℞ (Prescription only) |
| Pharmacokinetic data | |
| Protein binding | <10% |
| Elimination half-life | Short infusions: 32–94 minutes Long infusions: 245–638 minutes |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 95058-81-4 |
| PubChem CID | 60750 |
| IUPHAR/BPS | 4793 |
| DrugBank | DB00441 |
| ChemSpider | 54753 |
| UNII | B76N6SBZ8R |
| KEGG | D02368 |
| ChEBI | CHEBI:175901 |
| ChEMBL | ChEMBL888 |
| CompTox Dashboard (EPA) | DTXSID3040487 |
| ECHA InfoCard | 100.124.343 |
| Chemical and physical data | |
| Formula | C9H11F2N3O4 |
| Molar mass | 263.201 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (verify) |
/////////////GEMCITABINE, LY 188011, LY188011, CANCER
NC1=NC(=O)N(C=C1)[C@@H]1O[C@H](CO)[C@@H](O)C1(F)F
Patent
Publication numberPriority datePublication dateAssigneeTitle
EP0577303A1 *1992-06-221994-01-05Eli Lilly And CompanyStereoselective glycosylation process
WO2006070985A1 *2004-12-302006-07-06Hanmi Pharm. Co., Ltd.METHOD FOR THE PREPARATION OF 2#-DEOXY-2#,2#-DIFLUOROCYTIDINE
WO2007027564A2 *2005-08-292007-03-08Chemagis Ltd.Process for preparing gemcitabine and associated intermediates
WO2007069838A1 *2005-12-142007-06-21Dong-A Pharm.Co., Ltd.A manufacturing process of 2′,2′-difluoronucleoside and intermediate
Family To Family Citations
JPS541315B2 *1974-11-221979-01-23
US4526988A *1983-03-101985-07-02Eli Lilly And CompanyDifluoro antivirals and intermediate therefor
US4751221A *1985-10-181988-06-14Sloan-Kettering Institute For Cancer Research2-fluoro-arabinofuranosyl purine nucleosides
US5223608A *1987-08-281993-06-29Eli Lilly And CompanyProcess for and intermediates of 2′,2′-difluoronucleosides
US4965374A *1987-08-281990-10-23Eli Lilly And CompanyProcess for and intermediates of 2′,2′-difluoronucleosides
US5256798A *1992-06-221993-10-26Eli Lilly And CompanyProcess for preparing alpha-anomer enriched 2-deoxy-2,2-difluoro-D-ribofuranosyl sulfonates
US5371210A *1992-06-221994-12-06Eli Lilly And CompanyStereoselective fusion glycosylation process for preparing 2′-deoxy-2′,2′-difluoronucleosides and 2′-deoxy-2′-fluoronucleosides
US5256797A *1992-06-221993-10-26Eli Lilly And CompanyProcess for separating 2-deoxy-2,2-difluoro-D-ribofuranosyl alkylsulfonate anomers
US5480992A *1993-09-161996-01-02Eli Lilly And CompanyAnomeric fluororibosyl amines
US5521294A *1995-01-181996-05-28Eli Lilly And Company2,2-difluoro-3-carbamoyl ribose sulfonate compounds and process for the preparation of beta nucleosides
US5559222A *1995-02-031996-09-24Eli Lilly And CompanyPreparation of 1-(2′-deoxy-2′,2′-difluoro-D-ribo-pentofuranosyl)-cytosine from 2-deoxy-2,2-difluoro-β-D-ribo-pentopyranose
US5602262A *1995-02-031997-02-11Eli Lilly And CompanyProcess for the preparation of 2-deoxy-2,2-difluoro-β-D-ribo-pentopyranose
US5633367A *1995-03-241997-05-27Eli Lilly And CompanyProcess for the preparation of a 2-substituted 3,3-difluorofuran
GB9514268D0 *1995-07-131995-09-13Hoffmann La RochePyrimidine nucleoside
US5756775A *1995-12-131998-05-26Eli Lilly And CompanyProcess to make α,α-difluoro-β-hydroxyl thiol esters
CA2641719A1 *2006-02-072007-08-16Chemagis Ltd.Process for preparing gemcitabine and associated intermediates
US20070249823A1 *2006-04-202007-10-25Chemagis Ltd.Process for preparing gemcitabine and associated intermediates
Publication numberPriority datePublication dateAssigneeTitle
CN102617483A *2011-06-302012-08-01江苏豪森药业股份有限公司Process for recycling cytosine during preparing process of gemcitabine hydrochloride
WO2013164798A12012-05-042013-11-07Tpresso AgPackaging of dry leaves in sealed capsules
CN105566418A *2014-10-092016-05-11江苏笃诚医药科技股份有限公司2′,3′-di-O-acetyl-5′-deoxy-5-fluorocytidine synthesis method
EP3817732A4 *2018-08-032022-06-08Cellix Bio Private LimitedCompositions and methods for the treatment of cancer
Family To Family Citations
CA2641719A1 *2006-02-072007-08-16Chemagis Ltd.Process for preparing gemcitabine and associated intermediates
US20070249823A1 *2006-04-202007-10-25Chemagis Ltd.Process for preparing gemcitabine and associated intermediates
IT1393062B1 *2008-10-232012-04-11Prime Europ TherapeuticalsPROCEDURE FOR THE PREPARATION OF GEMCITABINE CHLORIDRATE
PublicationPublication DateTitle
CA2509687C2012-08-14Process for the production of 2'-branched nucleosides
WO2008129530A12008-10-30Gemcitabine production process
AU2005328519B22012-03-01Intermediate and process for preparing of beta- anomer enriched 21deoxy, 21 ,21-difluoro-D-ribofuranosyl nucleosides
EP1931693A22008-06-18Process for preparing gemcitabine and associated intermediates
EP2164856A12010-03-24Processes related to making capecitabine
US8193354B22012-06-05Process for preparation of Gemcitabine hydrochloride
EP3638685A12020-04-22Synthesis of 3'-deoxyadenosine-5'-0-[phenyl(benzyloxy-l-alaninyl)]phosphate (nuc-7738)
EP2456778A12012-05-30Process for producing flurocytidine derivatives
US20090221811A12009-09-03Process for preparing gemcitabine and associated intermediates
JP5114556B22013-01-09A novel highly stereoselective synthetic process and intermediate for gemcitabine
EP0350292B11994-05-04Process for preparing 2'-deoxy-beta-adenosine
KR100908363B12009-07-20Stereoselective preparation method of tri-O-acetyl-5-deoxy-β-D-ribofuranose and separation method thereof
US20070249823A12007-10-25Process for preparing gemcitabine and associated intermediates
WO2007070804A22007-06-21Process for preparing gemcitabine and associated intermediates
KR101259648B12013-05-09A manufacturing process of 2′,2′-difluoronucloside and intermediate
US8338586B22012-12-25Process of making cladribine
WO2010029574A22010-03-18An improved process for the preparation of gemcitabine and its intermediates using novel protecting groups and ion exchange resins
KR20080090950A2008-10-09Process for preparing gemcitabine and associated intermediates
WO2012115578A12012-08-30Synthesis of flg

NEW DRUG APPROVALS
ONE TIME
$9.00
OTERACIL POTTASIUM
OTERACIL
UNII4R7FFA00RX, CAS Number2207-75-2, WeightAverage: 195.175, Monoisotopic: 194.96823705, Chemical FormulaC4H2KN3O4
[K+].OC1=NC(=NC(=O)N1)C([O-])=O
1,3,5-Triazine-2-carboxylic acid, 1,4,5,6-tetrahydro-4,6-dioxo-, potassium salt (1:1)
218-627-5[EINECS]
2207-75-2[RN]
4,6-Dihydroxy-1,3,5-triazine-2-carboxylic acid potassium salt
- KOX
- NSC 28841
- Oxonate
- Oxonate, potassium
CDSCO APPROVED,01.02.2022

Gimeracil bulk & Oteracil potassium bulk and Tegafur 15mg/20mg, Gimeracil 4.35mg/5.8mg and Oteracil 11.8mg/15.8mg capsules
indicated in adults for the treatment of advanced gastric cancer when given in combination with cisplatin.
Oteracil Potassium is the potassium salt of oxonate, an enzyme inhibitor that modulates 5- fluorouracil (5-FU) toxicity. Potassium oxonate inhibits orotate phosphoribosyltransferase, which catalyzes the conversion of 5-FU to its active or phosphorylated form, FUMP. Upon oral administration, Oxonate is selectively distributed to the intracellular sites of tissues lining the small intestines, producing localized inhibitory effects within the gastrointestinal tract. As a result, 5-FU associated gastrointestinal toxic effects are reduced and the incidence of diarrhea or mucositis is decreased in 5-FU related therapy.
Oteracil is an adjunct to antineoplastic therapy, used to reduce the toxic side effects associated with chemotherapy. Approved by the European Medicines Agency (EMA) in March 2011, Oteracil is available in combination with Gimeracil and Tegafur within the commercially available product “Teysuno”. The main active ingredient in Teysuno is Tegafur, a pro-drug of Fluorouracil (5-FU), which is a cytotoxic anti-metabolite drug that acts on rapidly dividing cancer cells. By mimicking a class of compounds called “pyrimidines” that are essential components of RNA and DNA, 5-FU is able to insert itself into strands of DNA and RNA, thereby halting the replication process necessary for continued cancer growth.
Oteracil’s main role within Teysuno is to reduce the activity of 5-FU within normal gastrointestinal mucosa, and therefore reduce’s gastrointestinal toxicity 1. It functions by blocking the enzyme orotate phosphoribosyltransferase (OPRT), which is involved in the production of 5-FU.
/////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
SYNTHESIS
https://patents.google.com/patent/CN103435566A/zh



SYN
https://europepmc.org/article/pmc/pmc7717319
Poje et al. reported a two-step, gram-scale preparation of the TS-1 additive oteracil 21 (Scheme 16).226 Iodine-mediated-oxidation of uric acid 116 produced dehydroallantoin 117 as the major product, and subsequent treatment with potassium hydroxide resulted in the rearranged product oteracil 21.227

Synthesis of Oteracil 21a
aReagents and conditions: (a) LiOH, I2, H2O, 5 °C, 5 min, then AcOH, 75%; (b) aq KOH, 20 min, rt, 82%.
(226) Poje M; Sokolić-Maravić L The mechanism for the conversion of uric acid into allantoin and dehydro-allantoin: A new look at an old problem. Tetrahedron 1986, 42 (2), 747–751. [Google Scholar]
(227) Sugi M; Igi M EP Patent 0957096, 1999.
EP0957096A1 *1998-05-111999-11-17SUMIKA FINE CHEMICALS Co., Ltd.Method for producing potassium oxonate
CN101475539A *2009-02-112009-07-08鲁南制药集团股份有限公司Refining method for preparing high-purity oteracil potassium
CN102250025A *2011-05-182011-11-23深圳万乐药业有限公司Preparation method suitable for industrially producing oteracil potassium
CN102746244A *2012-07-272012-10-24南京正大天晴制药有限公司Refining method of oteracil potassium
//////////OTERACIL POTTASIUM, KOX, NSC 28841, Oxonate, Oxonate potassium, INDIA 2022, APPROVALS 2022, CANCER
[K+].OC1=NC(=NC(=O)N1)C([O-])=O

NEW DRUG APPROVALS
ONE TIME
$10.00
GIMERACIL
GIMERACIL
C5H4ClNO2, 145.54
5-chloro-4-hydroxy-1H-pyridin-2-one
5-Chloro-2,4-dihydroxypyridine
5-Chloro-4-hydroxy-2(1H)-pyridone
CDSCO APPROVED,01.02.2022

Gimeracil bulk & Oteracil potassium bulk and Tegafur 15mg/20mg, Gimeracil 4.35mg/5.8mg and Oteracil 11.8mg/15.8mg capsules
indicated in adults for the treatment of advanced gastric cancer when given in combination with cisplatin.
| Combination of | |
|---|---|
| Tegafur | Antineoplastic drug |
| Gimeracil | Enzyme inhibitor |
| Oteracil | Enzyme inhibitor |
| Clinical data | |
| Trade names | Teysuno, TS-1 |
| Other names | S-1[1] |
| AHFS/Drugs.com | UK Drug Information |
| License data | EU EMA: by Tegafur |
| Pregnancy category | Contraindicated |
| Routes of administration | By mouth |
| ATC code | L01BC53 (WHO) |
| Legal status | |
| Legal status | UK: POM (Prescription only) [2]EU: Rx-only [3]In general: ℞ (Prescription only) |
| Identifiers | |
| CAS Number | 150863-82-4 |
| PubChem CID | 54715158 |
Tegafur/gimeracil/oteracil, sold under the brand names Teysuno and TS-1,[3][4] is a fixed-dose combination medication used for the treatment of advanced gastric cancer when used in combination with cisplatin,[3] and also for the treatment of head and neck cancer, colorectal cancer, non–small-cell lung, breast, pancreatic, and biliary tract cancers.[5]: 213
The most common severe side effects when used in combination with cisplatin include neutropenia (low levels of neutrophils, a type of white blood cell), anaemia (low red blood cell counts) and fatigue (tiredness).[3]
Tegafur/gimeracil/oteracil (Teysuno) was approved for medical use in the European Union in March 2011.[3] It has not been approved by the U.S. Food and Drug Administration (FDA).[5]: 213
Medical uses
In the European Union tegafur/gimeracil/oteracil is indicated in adults for the treatment of advanced gastric cancer when given in combination with cisplatin.[3]
Contraindications
In the European Union, tegafur/gimeracil/oteracil must not be used in the following groups:
- people receiving another fluoropyrimidine (a group of anticancer medicines that includes tegafur/gimeracil/oteracil) or who have had severe and unexpected reactions to fluoropyrimidine therapy;[3]
- people known to have no DPD enzyme activity, as well as people who, within the previous four weeks, have been treated with a medicine that blocks this enzyme;[3]
- pregnant or breastfeeding women;[3]
- people with severe leucopenia, neutropenia, or thrombocytopenia (low levels of white cells or platelets in the blood);[3]
- people with severe kidney problems requiring dialysis;[3]
- people who should not be receiving cisplatin.[3]
Mechanism of action
Tegafur is the actual chemotherapeutic agent. It is a prodrug of the active substance fluorouracil (5-FU).[3] Tegafur, is a cytotoxic medicine (a medicine that kills rapidly dividing cells, such as cancer cells) that belongs to the ‘anti-metabolites’ group. Tegafur is converted to the medicine fluorouracil in the body, but more is converted in tumor cells than in normal tissues.[3] Fluorouracil is very similar to pyrimidine.[3] Pyrimidine is part of the genetic material of cells (DNA and RNA).[3] In the body, fluorouracil takes the place of pyrimidine and interferes with the enzymes involved in making new DNA.[3] As a result, it prevents the growth of tumor cells and eventually kills them.[3]
Gimeracil inhibits the degradation of fluorouracil by reversibly blocking the dehydrogenase enzyme dihydropyrimidine dehydrogenase (DPD). This results in higher 5-FU levels and a prolonged half-life of the substance.[6]
Oteracil mainly stays in the gut because of its low permeability, where it reduces the production of 5-FU by blocking the enzyme orotate phosphoribosyltransferase. Lower 5-FU levels in the gut result in a lower gastrointestinal toxicity.[6]
Within the medication, the molar ratio of the three components (tegafur:gimeracil:oteracil) is 1:1:0.4.[7]
The maximum tolerated dose differed between Asian and Caucasian populations (80 mg/m2 and 25 mg/m2 respectively), perhaps due to differences in CYP2A6 genotype.[5]: 213
Research
It is being developed for the treatment of hepatocellular carcinoma.[8] and has activity in esophageal,(Perry Chapter 33) breast,[citation needed] cervical,[citation needed] and colorectal cancer.[9]
References
- ^ Liu TW, Chen LT (201). “S-1 with leucovorin for gastric cancer: how far can it go?”. Lancet Oncol. 17 (1): 12–4. doi:10.1016/S1470-2045(15)00478-7. PMID 26640038.
- ^ “Teysuno 20mg/5.8mg/15.8mg hard capsules – Summary of Product Characteristics (SmPC)”. (emc). Retrieved 30 July 2020.
- ^ Jump up to:a b c d e f g h i j k l m n o p q r “Teysuno EPAR”. European Medicines Agency (EMA). Retrieved 30 July 2020. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ “ティーエスワン 患者さん・ご家族向け総合情報サイト | 大鵬薬品工業株式会社”.
- ^ Jump up to:a b c DeVita, DeVita; Lawrence, TS; Rosenberg, SA (2015). DeVita, Hellman, and Rosenberg’s Cancer: Principles and Practice of Oncology (10th ed.). LWW. ISBN 978-1451192940.
- ^ Jump up to:a b A. Klement (22 July 2013). “Dreier-Kombination gegen Magenkrebs: Teysuno”. Österreichische Apothekerzeitung (in German) (15/2013): 23.
- ^ Peters GJ, Noordhuis P, Van Kuilenburg AB et al. (2003). “Pharmacokinetics of S-1, an oral formulation of ftorafur, oxonic acid and 5-chloro-2,4-dihydroxypyridine (molar ratio 1:0.4:1) in patients with solid tumors”. Cancer Chemother. Pharmacol. 52 (1): 1–12. doi:10.1007/s00280-003-0617-9. PMID 12739060. S2CID 10858817.
- ^ “BCIQ”.
- ^ Miyamoto Y, Sakamoto Y, Yoshida N, Baba H (2014). “Efficacy of S-1 in colorectal cancer”. Expert Opin Pharmacother. 15 (12): 1761–70. doi:10.1517/14656566.2014.937706. PMID 25032886. S2CID 23637808.
External links
- “Tegafur”. Drug Information Portal. U.S. National Library of Medicine.
- “Gimeracil”. Drug Information Portal. U.S. National Library of Medicine.
- “Oteracil”. Drug Information Portal. U.S. National Library of Medicine.
Gimeracil is an adjunct to antineoplastic therapy, used to increase the concentration and effect of the main active componets within chemotherapy regimens. Approved by the European Medicines Agency (EMA) in March 2011, Gimeracil is available in combination with Oteracil and Tegafur within the commercially available product “Teysuno”. The main active ingredient in Teysuno is Tegafur, a pro-drug of Fluorouracil (5-FU), which is a cytotoxic anti-metabolite drug that acts on rapidly dividing cancer cells. By mimicking a class of compounds called “pyrimidines” that are essential components of RNA and DNA, 5-FU is able to insert itself into strands of DNA and RNA, thereby halting the replication process necessary for continued cancer growth.
Gimeracil’s main role within Teysuno is to prevent the breakdown of Fluorouracil (5-FU), which helps to maintin high enough concentrations for sustained effect against cancer cells 2. It functions by reversibly and selectively blocking the enzyme dihydropyrimidine dehydrogenase (DPD), which is involved in the degradation of 5-FU 1. This allows higher concentrations of 5-FU to be achieved with a lower dose of tegafur, thereby also reducing toxic side effects.
/////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////


SYNTHESIS

SYN
https://europepmc.org/article/pmc/pmc7717319
Synthesis of Gimeracil 20a
aReagents and conditions: (a) CH3C(OCH3)3, MeOH, then (CH3)2NHCH(OCH3)2, reflux, 92%; (b) aq AcOH, 130 °C, 2 h, 95%; (c) SO2Cl2, HOAc, 50 °C, 0.5 h, 91%; (d) 40% H2SO4, 130 °C, 4 h, 91%; (e) SO2Cl2, HOAc, 50 °C, 45 min, 86%; (f) 75% H2 SO4, 140 °C, 3 h, then NaOH, then pH 4–4.5, 89%


In 1953, Kolder and Hertog reported a synthesis of the TS-1 additive gimeracil 20, which was completed in seven steps using 4-nitropyridine N-oxide as starting material.222 Later, Yano et al. reported an alternative gram-scale synthesis (Scheme 15).223 The one-pot, three component condensation of malononitrile 111, 1,1,1-trimethoxyethane, and 1,1-dimethyoxytrimethylamine generated the dicyano intermediate 112, which was into 2(1H)-pyridinone 113.224 Selective chlorination of 113 was followed by acid-mediated demethylation, hydrolysis, and decarboxylation, to afford gimeracil 20. Interestingly, Xu et al. found that treatment of intermediate 113 with sulfuryl chloride resulted in dichloro 115 formation, which could still be converted to gimeracil 20 by treatment with sulfuric acid.225
(222) Kolder CR; den Hertog HJ Synthesis and reactivity of 5-chloro-2,4-dihydroxypyridine. Rec. Trav. Chim 1953, 72, 285–295. [Google Scholar]
(223) Yano S; Ohno T; Ogawa K Convenient and practical synthesis of 5-chloro-4-hydroxy-2(1H)-pyridinone. Heterocycles 1993, 36, 145–148. [Google Scholar]
(224) Mittelbach M; Kastner G; Junek H Synthesen mit Nitrilen, 71. Mitt. Zur Synthese von 4-Hydroxynicotinsaure aus Butadiendicarbonitrilen. Arch. Pharm 1985, 318 (6), 481–486. [Google Scholar]
(225) Xu Y; Mao D; Zhang F CN Patent 1915976, 2007.

NEW DRUG APPROVALS
THIS MAY NOT RUN WITHOUT SUBSCRIPTION HELP. AVOID CLOSURE OF THIS BLOG
$10.00
//////////GIMERACIL, APPROVALS 2022, INDIA 2022
OC1=CC(=O)NC=C1Cl
IMIPRIDONE

![7-Benzyl-4-(2-methylbenzyl)-1,2,6,7,8,9-hexahydroimidazo[1,2-A]pyrido[3,4-E]pyrimidin-5(4H)-one.png](https://pubchem.ncbi.nlm.nih.gov/image/imgsrv.fcgi?cid=73777259&t=l)
IMIPRIDONE
CAS No. : 1616632-77-9
Molecular Weight, 386.4964
Related CAS #: 41276-02-2 (TIC10 isomer) 1616632-77-9 (free base) 1638178-82-1 (HCl) 1777785-71-3 (HBr) 2007141-57-1 (2HBr)
TIC 10, 0NC 201, OP 10
Synonym: ONC201; ONC 201; ONC-201; NSC350625; NSC-350625; NSC 350625; TIC10; TIC 10; TIC-10; TRAIL inducing compound 10; imipridone
7-benzyl-4-(2-methylbenzyl)-1,2,6,7,8,9-hexahydroimidazo[1,2-a]pyrido[3,4-e]pyrimidin-5(4H)-one
2,4,6,7,8,9-Hexahydro-4-((2-methylphenyl)methyl)-7-phenylmethyl)imidazo)(1,2-a)pyrido(3,4-e)pyrimidin-5(1H)-one
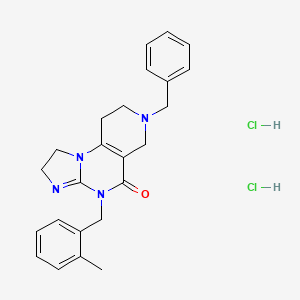
ONC-201 Dihydrochloride
459.4
UNII-53VG71J90J
53VG71J90J
Q27896336
1638178-82-1
- A TRAIL-dependent antitumor agent.
TIC10 (ONC-201) is a potent, orally active, and stable tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) inducer which acts by inhibiting Akt and ERK, consequently activating Foxo3a and significantly inducing cell surface TRAIL. TIC10 can cross the blood-brain barrier.
ONC-201, also known as TIC10, is a potent, orally active, and stable small molecule that transcriptionally induces TRAIL in a p53-independent manner and crosses the blood-brain barrier. TIC10 induces a sustained up-regulation of TRAIL in tumors and normal cells that may contribute to the demonstrable antitumor activity of TIC10. TIC10 inactivates kinases Akt and extracellular signal-regulated kinase (ERK), leading to the translocation of Foxo3a into the nucleus, where it binds to the TRAIL promoter to up-regulate gene transcription. TIC10 is an efficacious antitumor therapeutic agent that acts on tumor cells and their microenvironment to enhance the concentrations of the endogenous tumor suppressor TRAIL.
Akt/ERK Inhibitor ONC201 is a water soluble, orally bioavailable inhibitor of the serine/threonine protein kinase Akt (protein kinase B) and extracellular signal-regulated kinase (ERK), with potential antineoplastic activity. Upon administration, Akt/ERK inhibitor ONC201 binds to and inhibits the activity of Akt and ERK, which may result in inhibition of the phosphatidylinositol 3-kinase (PI3K)/Akt signal transduction pathway as well as the mitogen-activated protein kinase (MAPK)/ERK-mediated pathway. This may lead to the induction of tumor cell apoptosis mediated by tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL)/TRAIL death receptor type 5 (DR5) signaling in AKT/ERK-overexpressing tumor cells. The PI3K/Akt signaling pathway and MAPK/ERK pathway are upregulated in a variety of tumor cell types and play a key role in tumor cell proliferation, differentiation and survival by inhibiting apoptosis. In addition, ONC201 is able to cross the blood-brain barrier.
SYN
Organic & Biomolecular Chemistry, 19(39), 8497-8501; 2021
Herein, we present a copper-catalyzed tandem reaction of 2-aminoimidazolines and ortho-halo(hetero)aryl carboxylic acids that causes the regioselective formation of angularly fused tricyclic 1,2-dihydroimidazo[1,2-a]quinazolin-5(4H)-one derivatives. The reaction involved in the construction of the core six-membered pyrimidone moiety proceeded via regioselective N-arylation–condensation. The presented protocol been successfully applied to accomplish the total synthesis of TIC10/ONC201, which is an active angular isomer acting as a tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL): a sought after anticancer clinical agent.

7-Benzyl-4-(2-methylbenzyl)-1,2,6,7,8,9-hexahydroimidazo[1,2-a]pyrido[3,4-e]pyrimidin-5(4H)-one (6): Pale orange semi-solid, 202 mg (0.521 mmol), 52 % Rf = 0.25 (CH3OH/CHCl3 5:95); IR 1490, 1610, 1644, 2882, 2922 cm-1 ; 1H-NMR (500 MHz, CDCl3) δ = 2.39 (s, 3H), 2.54 (t, J = 5.5 Hz, 2H), 2.72 (t, J = 5.7 Hz, 2H), 3.31 (s, 2H), 3.67 (s, 2H), 3.84-3.91 (m, 4H), 5.04 (s, 2H), 7.02-7.04 (m, 1H), 7.08-7.12 (m, 3H), 7.26- 7.34 (m, 5H). 13C{1H}-NMR (101 MHz, CDCl3) δ = 19.3, 26.8, 43.4, 46.9, 48.2, 49.6, 50.45, 62.3, 102.1, 125.2, 125.9, 126.8, 127.4, 128.45, 129.2, 130.2, 134.2, 135.6, 137.9, 145.7, 153.3, 161.4; MS (ESI, m/z): [M+H]+ 387; HRMS (ESI, m/z): calcd for C24H27N4O [M+H]+ found 387.2183.



PATENT
https://patents.google.com/patent/WO2017132661A2/en
Scheme 1.


Scheme 2.


NEW DRUG APPROVALS
ONE TIME
$10.00
//////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
CLIP
https://mdanderson.elsevierpure.com/en/publications/discovery-and-clinical-introduction-of-first-in-class-imipridone-Discovery and clinical introduction of first-in-class imipridone ONC201
Abstract
ONC201 is the founding member of a novel class of anti-cancer compounds called imipridones that is currently in Phase II clinical trials in multiple advanced cancers. Since the discovery of ONC201 as a p53-independent inducer of TRAIL gene transcription, preclinical studies have determined that ONC201 has anti-proliferative and pro-apoptotic effects against a broad range of tumor cells but not normal cells. The mechanism of action of ONC201 involves engagement of PERK-independent activation of the integrated stress response, leading to tumor upregulation of DR5 and dual Akt/ERK inactivation, and consequent Foxo3a activation leading to upregulation of the death ligand TRAIL. ONC201 is orally active with infrequent dosing in animals models, causes sustained pharmacodynamic effects, and is not genotoxic. The first-in-human clinical trial of ONC201 in advanced aggressive refractory solid tumors confirmed that ONC201 is exceptionally well-tolerated and established the recommended phase II dose of 625 mg administered orally every three weeks defined by drug exposure comparable to efficacious levels in preclinical models. Clinical trials are evaluating the single agent efficacy of ONC201 in multiple solid tumors and hematological malignancies and exploring alternative dosing regimens. In addition, chemical analogs that have shown promise in other oncology indications are in pre-clinical development. In summary, the imipridone family that comprises ONC201 and its chemical analogs represent a new class of anti-cancer therapy with a unique mechanism of action being translated in ongoing clinical trials.
////////////IMIPRIDONE, TIC 10, ONC 201, NSC 350625, OP 10, Fast Track Designation, Orphan Drug Designation, Rare Pediatric Disease Designation, PHASE 3, GLIOMA, CHIMERIX
O=C1N(CC2=CC=CC=C2C)C3=NCCN3C4=C1CN(CC5=CC=CC=C5)CC4
Pafolacianine

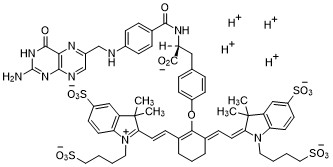
Pafolacianine
OTL-38
- Molecular FormulaC61H67N9O17S4
- Average mass1326.495 Da
FDA APPROVED NOV 2021
2-{(E)-2-[(3E)-2-(4-{2-[(4-{[(2-Amino-4-oxo-3,4-dihydro-6-pteridinyl)methyl]amino}benzoyl)amino]-2-carboxyethyl}phenoxy)-3-{(2E)-2-[3,3-dimethyl-5-sulfo-1-(4-sulfobutyl)-1,3-dihydro-2H-indol-2-ylidene ]ethylidene}-1-cyclohexen-1-yl]vinyl}-3,3-dimethyl-1-(4-sulfobutyl)-3H-indolium-5-sulfonate OTL-38Tyrosine, N-[4-[[(2-amino-3,4-dihydro-4-oxo-6-pteridinyl)methyl]amino]benzoyl]-O-[(6E)-6-[(2E)-2-[1,3-dihydro-3,3-dimethyl-5-sulfo-1-(4-sulfobutyl)-2H-indol-2-ylidene]ethylidene]-2-[(E)-2-[3,3-dimethy l-5-sulfo-1-(4-sulfobutyl)-3H-indolium-2-yl]ethenyl]-1-cyclohexen-1-yl]-, inner salt
2-(2-(2-(4-((2S)-2-(4-(((2-amino-4-oxo-3,4-dihydropteridin-6-yl)methyl)amino)benzamido)-2-carboxyethyl)phenoxy)-3-(2-(3,3-dimethyl-5-sulfo-1-(4-sulfobutyl)-1,3-dihydro-2H-indol-2-ylidene)ethylidene)cyclohex-1-en-1-yl)ethenyl)-3,3-dimethyl-5-sulfo-1-(4-sulfobutyl)-3H-indolium inner salt,sodium salt (1:4)
- 3H-Indolium, 2-(2-(2-(4-((2S)-2-((4-(((2-amino-3,4-dihydro-4-oxo-6-pteridinyl)methyl)amino)benzoyl)amino)-2-carboxyethyl)phenoxy)-3-(2-(1,3-dihydro-3,3-dimethyl-5-sulfo-1-(4-sulfobutyl)-2H-indol-2-ylidene)ethylidene)-1-cyclohexen-1-yl)ethenyl)-3,3-dimethyl-5-sulfo-1 (4-sulfobutyl)-, inner salt,sodium salt (1:4)
1628423-76-6 [RN]
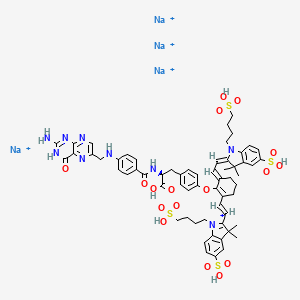
Pafolacianine sodium [USAN]
RN: 1628858-03-6
UNII: 4HUF3V875C
C61H68N9Na4O17S4+5
- Intraoperative Imaging and Detection of Folate Receptor Positive Malignant Lesions
Pafolacianine, sold under the brand name Cytalux, is an optical imaging agent.[1][2]
The most common side effects of pafolacianine include infusion-related reactions, including nausea, vomiting, abdominal pain, flushing, dyspepsia, chest discomfort, itching and hypersensitivity.[2]
It was approved for medical use in the United States in November 2021.[2][3]
Pafolacianine is a fluorescent drug that targets folate receptor (FR).[1]
Medical uses
Pafolacianine is indicated as an adjunct for intraoperative identification of malignant lesions in people with ovarian cancer.[1][2]
History
The safety and effectiveness of pafolacianine was evaluated in a randomized, multi-center, open-label study of women diagnosed with ovarian cancer or with high clinical suspicion of ovarian cancer who were scheduled to undergo surgery.[2] Of the 134 women (ages 33 to 81 years) who received a dose of pafolacianine and were evaluated under both normal and fluorescent light during surgery, 26.9% had at least one cancerous lesion detected that was not observed by standard visual or tactile inspection.[2]
The U.S. Food and Drug Administration (FDA) granted the application for pafolacianine orphan drug, priority review, and fast track designations.[2][4] The FDA granted the approval of Cytalux to On Target Laboratories, LLC.[2]

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////////////////////////////
SYN

WO 2014149073
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2014149073
In another aspect of the invention, this disclosure provides a method of synthesizing a compound having the formula
[0029] In a fourth embodiment of the invention, this disclosure provides a method of synthesizing a compound having the formula
[0030]
[0032] wherein C is any carbon isotope. In this embodiment, the amino acid linker is selected from a group consisting of methyl 2-di-tert-butyl dicarbonate-amino-3-(4-phenyl)propanoate, 3-(4-hydroxyphenyl)-2-(di-tert-butyl-dicarbonate methylamino)propanoic acid, 2-amino-4-(4-hydroxyphenyl)butanoic acid, and Tert-butyl (2-di-tert-butyl dicarbonate- amino)-3-(4-hydroxyphenyl)propanoate . In a particular embodiment, the aqueous base is potassium hydroxide (KOH). The method of this embodiment may also further include purifying the compound by preparatory HPLC.
EXAMPLE 1 : General synthesis of Pte – L Tyrosine – S0456 (OTL-0038)
[0088] Scheme:
C33H37CIF3N
Reactants for Step I:
[0089] A 500 mL round bottom flask was charged with a stirring bar, pteroic acid
(12.0 g, 29.40 mmol, 1 equiv), (L)-Tyr(-OfBu)-OfBu- HCI (1 1 .63 g, 35.28 mmol, 1 .2
equiv) and HATU (13.45 g, 35.28 mmol, 1 .2 equiv) then DMF (147 mL) was added to give a brown suspension [suspension A]. DIPEA (20.48 mL, 1 17.62 mmol, 4.0 equiv) was added slowly to suspension A at 23 °C, over 5 minutes. The suspension turned in to a clear brown solution within 10 minutes of addition of DIPEA. The reaction was stirred at 23 °C for 2.5 h. Reaction was essentially complete in 30 minutes as judged by LC/MS but was stirred further for 2.5 h. The formation of Pte_N10(TFA)_L_Tyr(-OfBu)-OfBu HCI (Figure 12) was confirmed by LC/MS showing m/z 409→m/z 684. LC/MS method: 0-50% acetonitrile in 20 mM aqueous NH4OAc for 5 min using Aquity UPLC-BEH C18, 1 .7μιη 2.1 * 50 mm column . The reaction mixture was cannulated as a steady stream to a stirred solution of aq. HCI (2.0 L, 0.28 M) over the period of 30 minutes to give light yellow precipitate of Pte_N10(TFA)_L_Tyr(-OfBu)-OfBu HCI. The precipitated Pte_N 10(TFA)_L_Tyr(- OfBu)-OfBu HCI was filtered using sintered funnel under aspirator vacuum, washed with water (8 * 300 mL) until the pH of the filtrate is between 3 and 4. The wet solid was allowed to dry under high vacuum for 12 hours on the sintered funnel. In a separate batch, where this wet solid (3) was dried under vacuum for 48 hours and then this solid was stored at -20 0 C for 48 h. However, this brief storage led to partial decomposition of 3. The wet cake (58 g) was transferred to a 500 mL round bottom flask and was submitted to the next step without further drying or purification.
Reactants for Step II:
The wet solid (58 g) was assumed to contain 29.40 mmol of the desired compound (3) (i. e. quantitative yield for the step I ).
[0090] A 500 mL round bottom flask was charged with a stirring bar, Pte_N10(TFA)_L_Tyr(-OfBu)-OfBu HCI as a wet cake (58 g, 29.40 mmol, 1 equiv). A solution of TFA:TIPS:H20 (95:2.5:2.5, 200 mL) was added at once to give a light brown suspension. The reaction content was stirred at 23°C for 1 .5 hours and was monitored by LC/MS. The suspension became clear dull brown solution after stirring for 5 minutes. LC/MS method: 0-50% acetonitrile in 20 mM aqueous NH4OAc for 5 min using Aquity UPLC-BEH C18, 1 .7μιη 2.1 * 50 mm column. The formation of Pte_TFA_L_Tyr (Figure 12) was confirmed by showing m/z 684→m/z 572. Reaction time varies from 30 min to 1 .5 hours depending on the water content of Pte_N10(TFA)_L_Tyr(-OfBu)-OfBu HCI. The reaction mixture was cannulated as a steady stream to a stirred MTBE (1 .8 L) at 23 °C or 100 °C to give light yellow precipitate of Pte_TFA_L_Tyr. The precipitated Pte_TFA_L_Tyr was filtered using sintered funnel under aspirator vacuum, washed with MTBE (6 * 300 mL) and dried under high vacuum for 8 hours to obtain Pte_TFA_L_Tyr (14.98 g, 83.98% over two steps) as a pale yellow solid. The MTBE washing was tested for absence of residual TFA utilizing wet pH paper (pH between 3-4). The yield of the reaction was between 80-85% in different batches. The deacylated side product was detected in 3.6% as judged by LC/MS. For the different batches this impurity was never more than 5%.
Reactants for Step III:
[0091] A 200 mL round bottom flask was charged with a stirring bar and Pte_TFA_L_Tyr (13.85 g, 22.78 mmol, 1 equiv), then water (95 mL) was added to give a yellow suspension [suspension B]. A freshly prepared solution of aqueous 3.75 M NaOH (26.12 mL, 97.96 mmol, 4.30 equiv), or an equivalent base at a corresponding temperature using dimethylsulfoxide (DMSO) as a solvent (as shown in Table 1 ), was added dropwise to suspension B at 23 °C, giving a clear dull yellow solution over 15 minutes [solution B]. The equivalence of NaOH varied from 3.3 to 5.0 depending on the source of 4 (solid or liquid phase synthesis) and the residual TFA. Trianion 5 (Figure 12) formation was confirmed by LC/MS showing m/z 572→m/z 476 while the solution pH was 9-10 utilizing wet pH paper. The pH of the reaction mixture was in the range of 9-10. This pH is crucial for the overall reaction completion. Notably, pH more than 10 leads to hydrolysis of S0456. Excess base will efficiently drive reaction forward with potential hydrolysis of S0456. The presence of hydrolysis by product can be visibly detected by the persistent opaque purple/blue to red/brown color.
TABLE 1 : Separate TFA deprotection via trianion formation; S0456
[0092] The precipitated OTL-0038 product could also be crashed out by adding the reaction solution steady dropwise to acetone, acetonitrile, isopropanol or ethyl acetate/acetone mixture. Acetone yields optimal results. However, viscous reactions could be slower due to partial insolubility and/or crashing out of S0456. In this reaction, the equivalence of the aqueous base is significant. Excess base will efficiently drive reaction forward with potential hydrolysis of S0456. This solution phase synthesis provides Pte_N10(TFA)_Tyr-OH »HCI salt and desires approximately 4.1 to approximately 4.8 equiv base as a source to hydrolyze the product. Particularly, precipitation of Pte_Tyr_S0456 was best achieved when 1 mL of reaction mixture is added dropwise to the stirred acetone (20 mL). Filtration of the precipitate and washing with acetone (3 x10 mL) gave the highest purity as judged from LC/MS chromatogram.
[0093] During experimentation of this solution-phase synthesis of Pte – L Tyrosine -S0456 (OTL-0038) at different stages, some optimized conditions were observed:
Mode of addition: Separate TFA deprotection via trianion formation; S0456 @ 23 °C; reflux.
Stability data of Pte – L Tyrosine – S0456 (OTL-0038):
Liquid analysis: At 40 °C the liquid lost 8.6% at 270 nm and 1 % at 774 nm. At room temperature the liquid lost about 1 .4% at 270 nm and .5% at 774 nm. At 5 °C the
270 nm seems stable and the 774 nm reasonably stable with a small degradation purity.
Source Purity Linker S0456 Base Solvent Duration % Conversion
4.3-4.6
Solution 0.95
95% 1 equiv equiv H20 15 min 100% phase equiv
K2C03
PATENT
US 20140271482
FDA approves pafolacianine for identifying malignant ovarian cancer lesions
On November 29, 2021, the Food and Drug Administration approved pafolacianine (Cytalux, On Target Laboratories, LLC), an optical imaging agent, for adult patients with ovarian cancer as an adjunct for interoperative identification of malignant lesions. Pafolacianine is a fluorescent drug that targets folate receptor which may be overexpressed in ovarian cancer. It is used with a Near-Infrared (NIR) fluorescence imaging system cleared by the FDA for specific use with pafolacianine.
Efficacy was evaluated in a single arm, multicenter, open-label study (NCT03180307) of 178 women diagnosed with ovarian cancer or with high clinical suspicion of ovarian cancer scheduled to undergo primary surgical cytoreduction, interval debulking, or recurrent ovarian cancer surgery. All patients received pafolacianine. One hundred and thirty-four patients received fluorescence imaging evaluation in addition to standard of care evaluation which includes pre-surgical imaging, intraoperative palpation and normal light evaluation of lesions. Among these patients, 36 (26.9%) had at least one evaluable ovarian cancer lesion detected with pafolacianine that was not observed by standard visual or tactile inspection. The patient-level false positive rate of pafolacianine with NIR fluorescent light with respect to the detection of ovarian cancer lesions confirmed by central pathology was 20.2% (95% CI 13.7%, 28.0%).
The most common adverse reactions (≥1%) occurring in patients were nausea, vomiting, abdominal pain, flushing, dyspepsia, chest discomfort, pruritus, and hypersensitivity.
The recommended pafolacianine dose is 0.025 mg/kg administered intravenously over 60 minutes, 1 to 9 hours before surgery. The use of folate, folic acid, or folate-containing supplements should be avoided within 48 hours before administration of pafolacianine.
View full prescribing information for Cytalux.
This application was granted priority review, fast track designation, and orphan drug designation. A description of FDA expedited programs is in the Guidance for Industry: Expedited Programs for Serious Conditions-Drugs and Biologics.
USFDA approves new drug to help identify cancer lesions
This drug is indicated for use in adult patients with ovarian cancer to help identify cancerous lesions during surgery.By The Health Master -December 2, 2021
The U.S. Food and Drug Administration (USFDA) has approved Cytalux (pafolacianine), an imaging drug intended to assist surgeons in identifying ovarian cancer lesions. The drug is designed to improve the ability to locate additional ovarian cancerous tissue that is normally difficult to detect during surgery.
Cytalux is indicated for use in adult patients with ovarian cancer to help identify cancerous lesions during surgery. The drug is a diagnostic agent that is administered in the form of an intravenous injection prior to surgery.
Alex Gorovets, M.D., deputy director of the Office of Specialty Medicine in the FDA’s Center for Drug Evaluation and Research said, “The FDA’s approval of Cytalux can help enhance the ability of surgeons to identify deadly ovarian tumors that may otherwise go undetected.
By supplementing current methods of detecting ovarian cancer during surgery, Cytalux offers health care professionals an additional imaging approach for patients with ovarian cancer.”
The American Cancer Society estimates there will be more than 21,000 new cases of ovarian cancer and more than 13,000 deaths from this disease in 2021, making it the deadliest of all female reproductive system cancers.
Conventional treatment for ovarian cancer includes surgery to remove as many of the tumors as possible, chemotherapy to stop the growth of malignant cells or other targeted therapy to identify and attack specific cancer cells.
Ovarian cancer often causes the body to overproduce a specific protein in cell membranes called a folate receptor. Following administration via injection, Cytalux binds to these proteins and illuminates under fluorescent light, boosting surgeons’ ability to identify the cancerous tissue.
Currently, surgeons rely on preoperative imaging, visual inspection of tumors under normal light or examination by touch to identify cancer lesions. Cytalux is used with a Near-Infrared fluorescence imaging system cleared by the FDA for specific use with pafolacianine.
The safety and effectiveness of Cytalux was evaluated in a randomized, multi-center, open-label study of women diagnosed with ovarian cancer or with high clinical suspicion of ovarian cancer who were scheduled to undergo surgery.
Of the 134 women (ages 33 to 81 years) who received a dose of Cytalux and were evaluated under both normal and fluorescent light during surgery, 26.9% had at least one cancerous lesion detected that was not observed by standard visual or tactile inspection.
The most common side effects of Cytalux were infusion-related reactions, including nausea, vomiting, abdominal pain, flushing, dyspepsia, chest discomfort, itching and hypersensitivity. Cytalux may cause fetal harm when administered to a pregnant woman.
The use of folate, folic acid, or folate-containing supplements should be avoided within 48 hours before administration of Cytalux. There is a risk of image interpretation errors with the use of Cytalux to detect ovarian cancer during surgery, including false negatives and false positives.
References
- ^ Jump up to:a b c d https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/214907s000lbl.pdf
- ^ Jump up to:a b c d e f g h i “FDA Approves New Imaging Drug to Help Identify Ovarian Cancer Lesions”. U.S. Food and Drug Administration (FDA) (Press release). 29 November 2021. Retrieved 30 November 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ “On Target Laboratories Announces FDA Approval of Cytalux (pafolacianine) injection for Identification of Ovarian Cancer During Surgery”. On Target Laboratories. 29 November 2021. Retrieved 30 November 2021 – via PR Newswire.
- ^ “Pafolacianine Orphan Drug Designations and Approvals”. U.S. Food and Drug Administration (FDA). 23 December 2014. Retrieved 30 November 2021.
External links
- “Pafolacianine”. Drug Information Portal. U.S. National Library of Medicine.
| Clinical data | |
|---|---|
| Trade names | Cytalux |
| Other names | OTL-0038 |
| License data | US DailyMed: Pafolacianine |
| Pregnancy category | Not recommended |
| Routes of administration | Intravenous |
| ATC code | None |
| Legal status | |
| Legal status | US: ℞-only [1][2] |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 1628423-76-6 |
| PubChem CID | 135565623 |
| DrugBank | DB15413 |
| ChemSpider | 64880249 |
| UNII | F7BD3Z4X8L |
| ChEMBL | ChEMBL4297412 |
| Chemical and physical data | |
| Formula | C61H67N9O17S4 |
| Molar mass | 1326.49 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI |
////////////Pafolacianine, FDA 2021, APPROVALS 2021, Cytalux, OVARIAN CANCER, OTL 38,
[Na+].[Na+].[Na+].[Na+].CC1(C)\C(=C/C=C/2\CCCC(=C2Oc3ccc(C[C@H](NC(=O)c4ccc(NCc5cnc6N=C(N)NC(=O)c6n5)cc4)C(=O)O)cc3)\C=C\C7=[N](CCCCS(=O)(=O)O)c8ccc(cc8C7(C)C)S(=O)(=O)O)\N(CCCCS(=O)(=O)O)c9ccc(cc19)S(=O)(=O)O

NEW DRUG APPROVALS
ONE TIME
$10.00
TNO 155
TNO 155
2-Oxa-8-azaspiro[4.5]decan-4-amine, 8-[6-amino-5-[(2-amino-3-chloro-4-pyridinyl)thio]-2-pyrazinyl]-3-methyl-, (3S,4S)-
- (3S,4S)-8-[6-Amino-5-[(2-amino-3-chloro-4-pyridinyl)thio]-2-pyrazinyl]-3-methyl-2-oxa-8-azaspiro[4.5]decan-4-amine
- (3S,4S)-8-(6-amino-5-((2-amino-3-chloropyridin-4-yl)thio)pyrazin-2-yl)-3-methyl-2-oxa-8-azaspiro[4.5]decan-4-amine
| Molecular Weight |
421.95 |
|---|---|
| Formula |
C₁₈H₂₄ClN₇OS |
| CAS No. |
- PTPN11 inhibitor TNO155
- SHP2 inhibitor TNO155
- TNO-155
- TNO155
- UNII-FPJWORQEGI
TNO155 is a potent selective and orally active allosteric inhibitor of wild-type SHP2 (IC50=0.011 µM). TNO155 has the potential for the study of RTK-dependent malignancies, especially advanced solid tumors.
- Originator Novartis
- Developer Mirati Therapeutics; Novartis
- Class Antineoplastics
- Mechanism of ActionProtein tyrosine phosphatase non receptor antagonists
- Phase I/IISolid tumours
- Phase IColorectal cancer
- 11 Jul 2021Phase I trial in Solid tumours is still ongoing in USA, Canada, Japan, South Korea, Netherlands, Singapore, Spain, Taiwan (NCT03114319)
- 04 Jun 2021Efficacy, safety and pharmacokinetics data from phase I trial in Solid tumours presented at 57th Annual Meeting of the American Society of Clinical Oncology (ASCO-2021)
- 08 Jan 2021Novartis plans a phase Ib/II trial for Solid tumours (Combination therapy, Inoperable/Unresectable, Late-stage disease, Metastatic disease, Second-line therapy or greater) in February 2021 (NCT04699188)
CLIP
Combinations with Allosteric SHP2 Inhibitor TNO155 to Block Receptor Tyrosine Kinase Signaling
//////////TNO 155, CANCER

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....















