RELACORILANT
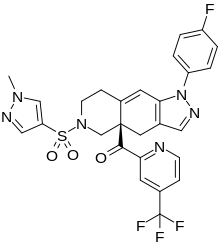
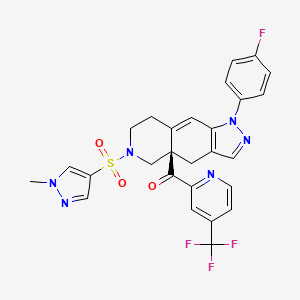
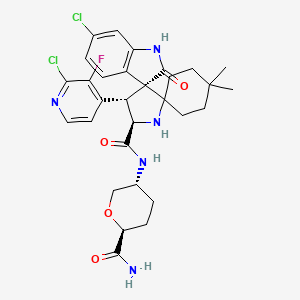
Relacorilant
- Molecular FormulaC27H22F4N6O3S
- Average mass586.561 Da
CAS 1496510-51-0
Phase III
[(4aR)-1-(4-fluorophenyl)-6-(1-methylpyrazol-4-yl)sulfonyl-4,5,7,8-tetrahydropyrazolo[3,4-g]isoquinolin-4a-yl]-[4-(trifluoromethyl)pyridin-2-yl]methanone
релакорилант[Russian][INN]
ريلاكوريلانت[Arabic][INN]
瑞拉可兰[Chinese][INN]
- OriginatorCorcept Therapeutics
- ClassAntineoplastics; Fluorine compounds; Isoquinolines; Ketones; Organic sulfur compounds; Pyrazoles; Pyridines; Small molecules
- Mechanism of ActionGlucocorticoid receptor antagonists
- Orphan Drug StatusYes – Pancreatic cancer; Cushing syndrome
- Phase IIICushing syndrome; Ovarian cancer; Pancreatic cancer
- Phase IIFallopian tube cancer; Peritoneal cancer; Prostate cancer
- Phase I/IISolid tumours
- Phase IAdrenocortical carcinoma
Most Recent Events
- 09 Sep 2022Subgroup analysis efficacy data from a phase-II trial in Ovarian cancer presented at the 47th European Society for Medical Oncology Congress (ESMO-2022)
- 29 Jun 2022Phase-III clinical trials in Ovarian cancer (Combination therapy, Recurrent, Second-line therapy or greater) in USA (PO)
- 06 Jun 2022Corcept Therapeutics announces intentions to submit a NDA for Ovarian cancer
Relacorilant (developmental code name CORT-125134) is an antiglucocorticoid which is under development by Corcept Therapeutics for the treatment of Cushing’s syndrome.[1] It is also under development for the treatment of solid tumors and alcoholism.[1][2] The drug is a nonsteroidal compound and acts as an antagonist of the glucocorticoid receptor.[1] As of December 2017, it is in phase II clinical trials for Cushing’s syndrome and phase I/II clinical studies for solid tumors, while the clinical phase for alcoholism is unknown.[1]
Relacorilant is an orally available antagonist of the glucocorticoid receptor (GR), with potential antineoplastic activity. Upon administration, relacorilant competitively binds to and blocks GRs. This inhibits the activity of GRs, and prevents both the translocation of the ligand-GR complexes to the nucleus and gene expression of GR-associated genes. This decreases the negative effects that result from excess levels of endogenous glucocorticoids, like those seen when tumors overproduce glucocorticoids. In addition, by binding to GRs and preventing their activity, inhibition with CORT125134 also inhibits the proliferation of GR-overexpressing cancer cells. GRs are overexpressed in certain tumor cell types and promote tumor cell proliferation.
CLIP
https://europepmc.org/article/pmc/pmc8175224
Relacorilant (CORT125134)118) is being developed by Corcept Therapeutics, Inc. It is an orally active, high-affinity, selective antagonist of the glucocorticoid receptor that may benefit from the modulation of cortisol activity. In structural optimization, the introduction of a trifluoromethyl group to the 4-position on the pyridyl moiety was found to increase HepG2 tyrosine amino transferase assay potency by a factor of four. Relacorilant is currently being evaluated in a phase II clinical study in patients with Cushing’s syndrome.119)
2-Bromo-4-(trifluoromethyl)pyridine (17) prepared from (E)-4-ethoxy-1,1,1-trifluorobut-3-en-2-one is employed as a key intermediate for the preparation of relacorilant as shown in Scheme 31.120)

Scheme31. Synthesis of relacorilant.118)
118) H. Hunt, T. Johnson, N. Ray and I. Walters (Corcept Therapeutics, Inc.): PCT Int. Appl. WO2013/177559 (2013).
119) H. J. Hunt, J. K. Belanoff, I. Walters, B. Gourdet, J. Thomas, N. Barton, J. Unitt, T. Phillips, D. Swift and E. Eaton: Identification of the Clinical Candidate (R)-(1-(4-Fluorophenyl)-6-((1-methyl-1H-pyrazol-4-yl)sulfonyl)-4,4a,5,6,7,8-hexahydro-1H-pyrazolo[3,4-g]isoquinolin-4a-yl)(4-(trifluoromethyl)pyridin-2-yl)methanone (CORT125134): A Selective Glucocorticoid Receptor (GR) Antagonist. J. Med. Chem. 60, 3405–3421 (2017). [Abstract] [Google Scholar]
120) B. Lehnemann, J. Jung and A. Meudt (Archimica GmbH): PCT Int. Appl. WO 2007/000249 (2007).
PAPER
https://pubs.acs.org/doi/abs/10.1021/acs.jmedchem.7b00162
The nonselective glucocorticoid receptor (GR) antagonist mifepristone has been approved in the U.S. for the treatment of selected patients with Cushing’s syndrome. While this drug is highly effective, lack of selectivity for GR leads to unwanted side effects in some patients. Optimization of the previously described fused azadecalin series of selective GR antagonists led to the identification of CORT125134, which is currently being evaluated in a phase 2 clinical study in patients with Cushing’s syndrome.

PATENT
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2013177559


SYN

////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Cushing’s syndrome (CS) is a metabolic disorder caused by chronic hypercortisolism. CS is associated with cardiovascular, metabolic, skeletal and psychological dysfunctions and can be fatal if left untreated. The first-line treatment for all forms of CS is a surgery. However, medical therapy has to be chosen if surgical resection is not an option or is deemed ineffective. Currently available therapeutics are either not selective and have side effects or are only available as an injection (pasireotide).
References
- ^ Jump up to:a b c d “Relacorilant – Corcept Therapeutics – AdisInsight”.
- ^ Veneris JT, Darcy KM, Mhawech-Fauceglia P, Tian C, Lengyel E, Lastra RR, Pejovic T, Conzen SD, Fleming GF (2017). “High glucocorticoid receptor expression predicts short progression-free survival in ovarian cancer”. Gynecol. Oncol. 146 (1): 153–160. doi:10.1016/j.ygyno.2017.04.012. PMC 5955699. PMID 28456378.
External links
| Clinical data | |
|---|---|
| Other names | CORT-125134 |
| Routes of administration | By mouth |
| Drug class | Antiglucocorticoid |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 1496510-51-0 |
| PubChem CID | 73051463 |
| ChemSpider | 57617720 |
| UNII | 2158753C7E |
| KEGG | D11336 |
| Chemical and physical data | |
| Formula | C27H22F4N6O3S |
| Molar mass | 586.57 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI |
//////////////Relacorilant, Phase III , Orphan Drug, Cushing syndrome, Ovarian cancer, Pancreatic cancer, релакорилант , ريلاكوريلانت , 瑞拉可兰 ,
CN1C=C(C=N1)S(=O)(=O)N2CCC3=CC4=C(CC3(C2)C(=O)C5=NC=CC(=C5)C(F)(F)F)C=NN4C6=CC=C(C=C6)F

NEW DRUG APPROVALS
ONE TIME
$10.00
Tremelimumab
(Light chain)
DIQMTQSPSS LSASVGDRVT ITCRASQSIN SYLDWYQQKP GKAPKLLIYA ASSLQSGVPS
RFSGSGSGTD FTLTISSLQP EDFATYYCQQ YYSTPFTFGP GTKVEIKRTV AAPSVFIFPP
SDEQLKSGTA SVVCLLNNFY PREAKVQWKV DNALQSGNSQ ESVTEQDSKD STYSLSSTLT
LSKADYEKHK VYACEVTHQG LSSPVTKSFN RGEC
(Heavy chain)
QVQLVESGGG VVQPGRSLRL SCAASGFTFS SYGMHWVRQA PGKGLEWVAV IWYDGSNKYY
ADSVKGRFTI SRDNSKNTLY LQMNSLRAED TAVYYCARDP RGATLYYYYY GMDVWGQGTT
VTVSSASTKG PSVFPLAPCS RSTSESTAAL GCLVKDYFPE PVTVSWNSGA LTSGVHTFPA
VLQSSGLYSL SSVVTVPSSN FGTQTYTCNV DHKPSNTKVD KTVERKCCVE CPPCPAPPVA
GPSVFLFPPK PKDTLMISRT PEVTCVVVDV SHEDPEVQFN WYVDGVEVHN AKTKPREEQF
NSTFRVVSVL TVVHQDWLNG KEYKCKVSNK GLPAPIEKTI SKTKGQPREP QVYTLPPSRE
EMTKNQVSLT CLVKGFYPSD IAVEWESNGQ PENNYKTTPP MLDSDGSFFL YSKLTVDKSR
WQQGNVFSCS VMHEALHNHY TQKSLSLSPG K
(Disulfide bridge: L23-L88, L134-L194, L214-H139, H22-H96, H152-H208, H265-H325, H371-H429, H227-H’227, H228-H’228, H231-H’231, H234-H’234)
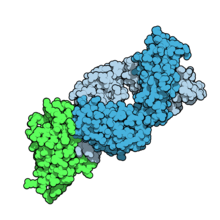
Fab fragment of tremelimumab (blue) binding CTLA-4 (green). From PDB entry 5GGV.
Tremelimumab
| Formula | C6500H9974N1726O2026S52 |
|---|---|
| CAS | 745013-59-6 |
| Mol weight | 146380.4722 |
FDA APPROVED2022/10/21, Imjudo
PEPTIDE, CP 675206
| Antineoplastic, Immune checkpoint inhibitor, Anti-CTLA4 antibody | |
| Disease | Hepatocellular carcinoma |
|---|
Tremelimumab (formerly ticilimumab, CP-675,206) is a fully human monoclonal antibody against CTLA-4. It is an immune checkpoint blocker. Previously in development by Pfizer,[1] it is now in investigation by MedImmune, a wholly owned subsidiary of AstraZeneca.[2] It has been undergoing human trials for the treatment of various cancers but has not attained approval for any.
Imjudo (tremelimumab) in combination with Imfinzi approved in the US for patients with unresectable liver cancer
PUBLISHED24 October 2022
24 October 2022 07:00 BST
Approval based on HIMALAYA Phase III trial results which showed single priming dose of Imjudo added to Imfinzi reduced risk of death by 22% vs. sorafenib
AstraZeneca’s Imjudo (tremelimumab) in combination with Imfinzi (durvalumab) has been approved in the US for the treatment of adult patients with unresectable hepatocellular carcinoma (HCC), the most common type of liver cancer. The novel dose and schedule of the combination, which includes a single dose of the anti-CTLA-4 antibody Imjudo 300mg added to the anti-PD-L1 antibody Imfinzi 1500mg followed by Imfinzi every four weeks, is called the STRIDE regimen (Single Tremelimumab Regular Interval Durvalumab).
The approval by the US Food and Drug Administration (FDA) was based on positive results from the HIMALAYA Phase III trial. In this trial, patients treated with the combination of Imjudo and Imfinzi experienced a 22% reduction in the risk of death versus sorafenib (based on a hazard ratio [HR] of 0.78, 95% confidence interval [CI] 0.66-0.92 p=0.0035).1 Results were also published in the New England Journal of Medicine Evidence showing that an estimated 31% of patients treated with the combination were still alive after three years, with 20% of patients treated with sorafenib still alive at the same duration of follow-up.2
Liver cancer is the third-leading cause of cancer death and the sixth most commonly diagnosed cancer worldwide.3,4 It is the fastest rising cause of cancer-related deaths in the US, with approximately 36,000 new diagnoses each year.5,6
Ghassan Abou-Alfa, MD, MBA, Attending Physician at Memorial Sloan Kettering Cancer Center (MSK), and principal investigator in the HIMALAYA Phase III trial, said: “Patients with unresectable liver cancer are in need of well-tolerated treatments that can meaningfully extend overall survival. In addition to this regimen demonstrating a favourable three-year survival rate in the HIMALAYA trial, safety data showed no increase in severe liver toxicity or bleeding risk for the combination, important factors for patients with liver cancer who also have advanced liver disease.”
Dave Fredrickson, Executive Vice President, Oncology Business Unit, AstraZeneca, said: “With this first regulatory approval for Imjudo, patients with unresectable liver cancer in the US now have an approved dual immunotherapy treatment regimen that harnesses the potential of CTLA-4 inhibition in a unique combination with a PD-L1 inhibitor to enhance the immune response against their cancer.”
Andrea Wilson Woods, President & Founder, Blue Faery: The Adrienne Wilson Liver Cancer Foundation, said: “In the past, patients living with liver cancer had few treatment options and faced poor prognoses. With today’s approval, we are grateful and optimistic for new, innovative, therapeutic options. These new treatments can improve long-term survival for those living with unresectable hepatocellular carcinoma, the most common form of liver cancer. We appreciate the patients, their families, and the broader liver cancer community who continue to fight for new treatments and advocate for others.”
The safety profiles of the combination of Imjudo added to Imfinzi and for Imfinzi alone were consistent with the known profiles of each medicine, and no new safety signals were identified.
Regulatory applications for Imjudo in combination with Imfinzi are currently under review in Europe, Japan and several other countries for the treatment of patients with advanced liver cancer based on the HIMALAYA results.
Notes
Liver cancer
About 75% of all primary liver cancers in adults are HCC.3 Between 80-90% of all patients with HCC also have cirrhosis.7 Chronic liver diseases are associated with inflammation that over time can lead to the development of HCC.7
More than half of patients are diagnosed at advanced stages of the disease, often when symptoms first appear.8 A critical unmet need exists for patients with HCC who face limited treatment options.8 The unique immune environment of liver cancer provides clear rationale for investigating medications that harness the power of the immune system to treat HCC.8
HIMALAYA
HIMALAYA was a randomised, open-label, multicentre, global Phase III trial of Imfinzi monotherapy and a regimen comprising a single priming dose of Imjudo 300mg added to Imfinzi 1500mg followed by Imfinzi every four weeks versus sorafenib, a standard-of-care multi-kinase inhibitor.
The trial included a total of 1,324 patients with unresectable, advanced HCC who had not been treated with prior systemic therapy and were not eligible for locoregional therapy (treatment localised to the liver and surrounding tissue).
The trial was conducted in 181 centres across 16 countries, including in the US, Canada, Europe, South America and Asia. The primary endpoint was overall survival (OS) for the combination versus sorafenib and key secondary endpoints included OS for Imfinzi versus sorafenib, objective response rate and progression-free survival (PFS) for the combination and for Imfinzi alone.
Imfinzi
Imfinzi (durvalumab) is a human monoclonal antibody that binds to the PD-L1 protein and blocks the interaction of PD-L1 with the PD-1 and CD80 proteins, countering the tumour’s immune-evading tactics and releasing the inhibition of immune responses.
Imfinzi was recently approved to treat patients with advanced biliary tract cancer in the US based on results from the TOPAZ-1 Phase III trial. It is the only approved immunotherapy in the curative-intent setting of unresectable, Stage III non-small cell lung cancer (NSCLC) in patients whose disease has not progressed after chemoradiotherapy and is the global standard of care in this setting based on the PACIFIC Phase III trial.
Imfinzi is also approved in the US, EU, Japan, China and many other countries around the world for the treatment of extensive-stage small cell lung cancer (ES-SCLC) based on the CASPIAN Phase III trial. In 2021, updated results from the CASPIAN trial showed Imfinzi plus chemotherapy tripled patient survival at three years versus chemotherapy alone.
Imfinzi is also approved for previously treated patients with advanced bladder cancer in several countries.
Since the first approval in May 2017, more than 100,000 patients have been treated with Imfinzi.
As part of a broad development programme, Imfinzi is being tested as a single treatment and in combinations with other anti-cancer treatments for patients with SCLC, NSCLC, bladder cancer, several gastrointestinal (GI) cancers, ovarian cancer, endometrial cancer, and other solid tumours.
Imfinzi combinations have also demonstrated clinical benefit in metastatic NSCLC in the POSEIDON Phase III trial.
Imjudo
Imjudo (tremelimumab) is a human monoclonal antibody that targets the activity of cytotoxic T-lymphocyte-associated protein 4 (CTLA-4). Imjudo blocks the activity of CTLA-4, contributing to T-cell activation, priming the immune response to cancer and fostering cancer cell death.
Beyond HIMALAYA, Imjudo is being tested in combination with Imfinzi across multiple tumour types including locoregional HCC (EMERALD-3), SCLC (ADRIATIC) and bladder cancer (VOLGA and NILE).
Imjudo is also under review by global regulatory authorities in combination with Imfinzi and chemotherapy in 1st-line metastatic NSCLC based on the results of the POSEIDON Phase III trial, which showed the addition of a short course of Imjudo to Imfinzi plus chemotherapy improved both overall and progression-free survival compared to chemotherapy alone.
AstraZeneca in GI cancers
AstraZeneca has a broad development programme for the treatment of GI cancers across several medicines spanning a variety of tumour types and stages of disease. In 2020, GI cancers collectively represented approximately 5.1 million new diagnoses leading to approximately 3.6 million deaths.9
Within this programme, the Company is committed to improving outcomes in gastric, liver, biliary tract, oesophageal, pancreatic, and colorectal cancers.
Imfinzi (durvalumab) is being assessed in combinations in oesophageal and gastric cancers in an extensive development programme spanning early to late-stage disease across settings.
The Company aims to understand the potential of Enhertu (trastuzumab deruxtecan), a HER2-directed antibody drug conjugate, in the two most common GI cancers, colorectal and gastric cancers. Enhertu is jointly developed and commercialised by AstraZeneca and Daiichi Sankyo.
Lynparza (olaparib) is a first-in-class PARP inhibitor with a broad and advanced clinical trial programme across multiple GI tumour types including pancreatic and colorectal cancers. Lynparza is developed and commercialised in collaboration with MSD (Merck & Co., Inc. inside the US and Canada).
AstraZeneca in immuno-oncology (IO)
Immunotherapy is a therapeutic approach designed to stimulate the body’s immune system to attack tumours. The Company’s immuno-oncology (IO) portfolio is anchored in immunotherapies that have been designed to overcome evasion of the anti-tumour immune response. AstraZeneca is invested in using IO approaches that deliver long-term survival for new groups of patients across tumour types.
The Company is pursuing a comprehensive clinical trial programme that includes Imfinzi as a single treatment and in combination with Imjudo (tremelimumab) and other novel antibodies in multiple tumour types, stages of disease, and lines of treatment, and where relevant using the PD-L1 biomarker as a decision-making tool to define the best potential treatment path for a patient.
In addition, the ability to combine the IO portfolio with radiation, chemotherapy, and targeted small molecules from across AstraZeneca’s oncology pipeline, and from research partners, may provide new treatment options across a broad range of tumours.
AstraZeneca in oncology
AstraZeneca is leading a revolution in oncology with the ambition to provide cures for cancer in every form, following the science to understand cancer and all its complexities to discover, develop and deliver life-changing medicines to patients.
The Company’s focus is on some of the most challenging cancers. It is through persistent innovation that AstraZeneca has built one of the most diverse portfolios and pipelines in the industry, with the potential to catalyse changes in the practice of medicine and transform the patient experience.
AstraZeneca has the vision to redefine cancer care and, one day, eliminate cancer as a cause of death.
////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Mechanism of action
Tremelimumab aims to stimulate an immune system attack on tumors. Cytotoxic T lymphocytes (CTLs) can recognize and destroy cancer cells. However, there is also an inhibitory mechanism (immune checkpoint) that interrupts this destruction. Tremelimumab turns off this inhibitory mechanism and allows CTLs to continue to destroy the cancer cells.[3] This is immune checkpoint blockade.
Tremelimumab binds to the protein CTLA-4, which is expressed on the surface of activated T lymphocytes and inhibits the killing of cancer cells. Tremelimumab blocks the binding of the antigen-presenting cell ligands B7.1 and B7.2 to CTLA-4, resulting in inhibition of B7-CTLA-4-mediated downregulation of T-cell activation; subsequently, B7.1 or B7.2 may interact with another T-cell surface receptor protein, CD28, resulting in a B7-CD28-mediated T-cell activation unopposed by B7-CTLA-4-mediated inhibition.
Unlike Ipilimumab (another fully human anti-CTLA-4 monoclonal antibody), which is an IgG1 isotype, tremelimumab is an IgG2 isotype.[4][5]
Clinical trials
Melanoma
Phase 1 and 2 clinical studies in metastatic melanoma showed some responses.[6] However, based on early interim analysis of phase III data, Pfizer designated tremelimumab as a failure and terminated the trial in April 2008.[1][7]
However, within a year, the survival curves showed separation of the treatment and control groups.[8] The conventional Response Evaluation Criteria in Solid Tumors (RECIST) may underrepresent the merits of immunotherapies. Subsequent immunotherapy trials (e.g. ipilimumab) have used the Immune-Related Response Criteria (irRC) instead.
Mesothelioma
Although it was designated in April 2015 as orphan drug status in mesothelioma,[9] tremelimumab failed to improve lifespan in the phase IIb DETERMINE trial, which assessed the drug as a second or third-line treatment for unresectable malignant mesothelioma.[10][11]
Non-small cell lung cancer
In a phase III trial, AstraZeneca paired tremelimumab with a PD-L1 inhibitor, durvalumab, for the first-line treatment of non-small cell lung cancer.[12] The trial was conducted across 17 countries, and in July 2017, AstraZeneca announced that it had failed to meet its primary endpoint of progression-free survival.[13]
References
- ^ Jump up to:a b “Pfizer Announces Discontinuation of Phase III Clinical Trial for Patients with Advanced Melanoma”. Pfizer.com. 1 April 2008. Retrieved 5 December 2015.
- ^ Mechanism of Pathway: CTLA-4 Inhibition[permanent dead link]
- ^ Antoni Ribas (28 June 2012). “Tumor immunotherapy directed at PD-1”. New England Journal of Medicine. 366 (26): 2517–9. doi:10.1056/nejme1205943. PMID 22658126.
- ^ Tomillero A, Moral MA (October 2008). “Gateways to clinical trials”. Methods Find Exp Clin Pharmacol. 30 (8): 643–72. doi:10.1358/mf.2008.30.5.1236622. PMID 19088949.
- ^ Poust J (December 2008). “Targeting metastatic melanoma”. Am J Health Syst Pharm. 65 (24 Suppl 9): S9–S15. doi:10.2146/ajhp080461. PMID 19052265.
- ^ Reuben, JM; et al. (1 Jun 2006). “Biologic and immunomodulatory events after CTLA-4 blockade with tremelimumab in patients with advanced malignant melanoma”. Cancer. 106 (11): 2437–44. doi:10.1002/cncr.21854. PMID 16615096. S2CID 751366.
- ^ A. Ribas, A. Hauschild, R. Kefford, C. J. Punt, J. B. Haanen, M. Marmol, C. Garbe, J. Gomez-Navarro, D. Pavlov and M. Marsha (May 20, 2008). “Phase III, open-label, randomized, comparative study of tremelimumab (CP-675,206) and chemotherapy (temozolomide [TMZ] or dacarbazine [DTIC]) in patients with advanced melanoma”. Journal of Clinical Oncology. 26 (15S): LBA9011. doi:10.1200/jco.2008.26.15_suppl.lba9011.[permanent dead link]
- ^ M.A. Marshall, A. Ribas, B. Huang (May 2010). “Evaluation of baseline serum C-reactive protein (CRP) and benefit from tremelimumab compared to chemotherapy in first-line melanoma”. Journal of Clinical Oncology. 28 (15S): 2609. doi:10.1200/jco.2010.28.15_suppl.2609.[permanent dead link]
- ^ FDA Grants AstraZeneca’s Tremelimumab Orphan Drug Status for Mesothelioma [1]
- ^ “Tremelimumab Fails Mesothelioma Drug Trial”. Archived from the original on 2016-03-06. Retrieved 2016-03-06.
- ^ AZ’ tremelimumab fails in mesothelioma trial
- ^ “AstraZeneca’s immuno-oncology combo fails crucial Mystic trial in lung cancer | FierceBiotech”.
- ^ “AstraZeneca reports initial results from the ongoing MYSTIC trial in Stage IV lung cancer”.
///////////Tremelimumab, Imjudo, APPROVALS 2022, FDA 2022, PEPTIDE, CP 675206, Antineoplastic, Immune checkpoint inhibitor, Anti-CTLA4 antibody

NEW DRUG APPROVALS
ONE TIME
$10.00
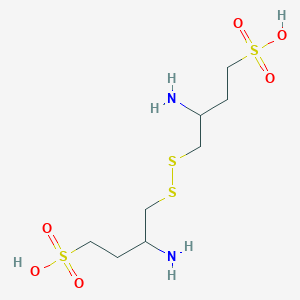
MILADEMETAN

Milademetan
| Molecular Weight | 618.53 |
|---|---|
| Formula | C30H34Cl2FN5O4 |
| CAS No. | 1398568-47-2 |
Milademetan. hcl
Chemical Formula: C30H35Cl3FN5O4
Exact Mass: 617.1972
Molecular Weight: 654.99
Elemental Analysis: C, 55.01; H, 5.39; Cl, 16.24; F, 2.90; N, 10.69; O, 9.77
1398568-47-2 (free base) 1398569-75-9 (tosylate) 2095625-97-9 (tosylate hydrate) Milademetan HCl
DS3032b; DS-3032b; DS 3032b; DS3032; DS-3032; DS 3032; DS-3032b tosylate; Milademetan tosylate; Milademetan HCl
(3’R,4’S,5’R)-N-[(3R,6S)-6-carbamoyloxan-3-yl]-6”-chloro-4′-(2-chloro-3-fluoropyridin-4-yl)-4,4-dimethyl-2”-oxo-1”,2”-dihydrodispiro[cyclohexane-1,2′-pyrrolidine-3′,3”-indole]-5′-carboxamide hydrochloride
orphan drug, UNII:R3I80TLN7S, миладеметан , ميلاديميتان , 米拉美坦
(3’R,4’S,5’R)-N-((3R,6S)-6-Carbamoyltetrahydro-2H-pyran-3-yl)-6”-chloro-4′-(2-chloro-3-fluoro-4-pyridinyl)-4,4-dimethyl-2”-oxo-1”,2”-dihydrodispiro(cyclohexane-1,2′-pyrrolidine-3′,3”-indole)-5′-carboxamide
milademetan
rolontis
SPI-2012
Milademetan, also known as DS-3032b or DS-3032, is a potent and selective MDM2 inhibitor with potential antineoplastic activity. Upon oral administration, MDM2 inhibitor DS-3032b binds to, and prevents the binding of MDM2 protein to the transcriptional activation domain of the tumor suppressor protein p53. By preventing this MDM2-p53 interaction, the proteosome-mediated enzymatic degradation of p53 is inhibited and the transcriptional activity of p53 is restored. This results in the restoration of p53 signaling and leads to the p53-mediated induction of tumor cell apoptosis.
DS-3032 (Milademetan) is an orally available, potent and selective inhibitor of the p53-MDM2 (murine double minute 2) interaction. Milademetan binds to, and prevents the binding of MDM2 protein to the transcriptional activation domain of the tumor suppressor protein p53. Milademetan is 10-fold more potent than the first-generation inhibitor nutlin-3a. By preventing this MDM2-p53 interaction, the proteasome-mediated enzymatic degradation of p53 is inhibited and the transcriptional activity of p53 is restored. This results in the restoration of p53 signaling and leads to the p53-mediated induction of tumor cell apoptosis. DS-3032 is currently being evaluated in three phase 1 clinical trials for solid and hematological malignancies, including acute myeloid leukemia (AML), acute lymphocytic leukemia (ALL), chronic myeloid leukemia (CML) in blast phase, lymphoma and myelodysplastic syndrome (MDS).
- OriginatorRigel Pharmaceuticals
- DeveloperDaiichi Sankyo Inc; National Cancer Center Hospital East; Rain Therapeutics; University of Texas M. D. Anderson Cancer Center
- ClassAntineoplastics; Cyclohexanes; Indoles; Pyrrolidines; Small molecules
- Mechanism of ActionProto-oncogene protein c mdm2 inhibitors
- Orphan Drug StatusYes – Liposarcoma
- Phase IIILiposarcoma
- Phase IISarcoma; Solid tumours
- Phase I/IIAcute myeloid leukaemia
- Phase ILymphoma; Myelodysplastic syndromes
- PreclinicalMesothelioma
- No development reportedMultiple myeloma
- 10 Aug 2022Rain Therapeutics completes enrolment in phase-III clinical trials in Liposarcoma in (Inoperable/Unresectable, Metastatic disease, Second-line therapy or greater) in United Kingdom, Taiwan, Spain, Poland, South Korea, Italy, Hong Kong, Germany, Georgia, France, Canada, Belgium, Austria (PO) (NCT04979442)
- 09 Jun 2022Efficacy, adverse events and pharmacodynamics data from phase I/II trial in Acute myeloid leukemia presented at the 27th Congress of the European Haematology Association(EHA-2022)
- 04 May 2022Rain Therapeutics plans a phase I/II MANTRA-4 trial in Solid tumours (Combination therapy, Late-stage disease) in Second half of 2022
PATENT
WO2015033974

[Example 2]
Ethyl (3’R,4’S,5’R)-6”-chloro-4′-(3-chloro-2-fluorophenyl)-4,4-dimethyl-2”-oxo 1″,2″-dihydrodispiro[cyclohexane-1,2′-pyrrolidine-3′,3″-indole]-5′-carboxylate
[0202]
[Chem. 58]
[0203]
(3E/Z)-6-chloro-3-(3-chloro-2-fluorobenzylidene)-1,3-dihydro-2H-indol-2-one ( WO 2006/091646) (98.7) under nitrogen atmosphere mg), (R)-BINAP (12.1 mg, 0.019 mmol), CuOAc (2.0 mg, 0.016 mmol), 4,4-dimethylcyclohexanone (61.4 mg, 0.48 mmol), glycine ethyl ester. (39.5 μL, 0.39 mmol) and a solution of triethylamine (6.8 μL, 0.049 mmol) in N,N-dimethylacetamide (2.0 mL) were added and stirred at room temperature for 22 hours. Ethyl acetate (2 mL), water (1 mL), and 20% aqueous ammonium chloride solution (1 mL) were added to the reaction mixture, and the mixture was vigorously stirred to separate the organic layer. The aqueous layer was extracted twice with ethyl acetate (2 mL each) and all the organic layers were combined and then washed with water three times (5 mL each). The obtained organic layer was concentrated under reduced pressure, ethyl acetate (6 mL) and silica gel (500 mg) were added to the residue, and the silica gel was separated by filtration. The filtrate was concentrated under reduced pressure, ethanol (1.0 mL) was added to the residue, water (1 mL) was added dropwise, and the mixture was stirred overnight at room temperature. The precipitated solid was filtered and dried under reduced pressure at 40° C. to obtain the title compound (137 mg, yield 82%, 94% ee) as a solid.
1H NMR (500 MHz, CDCl3): δ = 0.67 (s, 3H), 0.91 (s, 3H), 1.10-1.19 (m, 2H), 1.17 (t, J=7.3 Hz, 3H), 1.25-1.33 (m, 1H), 1.44- 1.72 (m, 3H), 1.87-2.01 (m, 1H), 3.16 (s, 1H), 4.07-4.21 (m, 2H), 4.52 (d, J = 8.5 Hz, 1H), 4.83 (d, J = 8.5 Hz, 1H), 6.74 (d, J = 1.5Hz, 1H), 6.81-6.86 (m, 1H), 7.06 (dd, J = 8.3, 2.8 Hz, 1H), 7.10-7.16 (m, 1H), 7.37 (dd, J = 8.3, 1.8 Hz, 1H), 7.48-7.54 (m, 1H), 7.81 (s, 1H).
(HPLC conditions for optical purity determination)
カラム: CHIRALPAK OD-3R 4.6 × 150 mm, 3μm
Moving layer: 10mM Rinic acid buffer: MeCN = 40:60
Flow rate: 1.0 min/min
カラム Temperature: 40°C
Exhaust wavelength: 254 nm
Injection volume: 5 μL
Hold time: Labeling compound = 13.8 min, エナンチオマー= 12.9 min
[Example 11]
11-1) Effects of various asymmetric catalysts
[0230]
[Chem. 67]
[0231]
(3E/Z)-6-chloro-3-[(2-chloro-3-fluoropyridin-4-yl)methylene]-1,3-dihydro-2H-indol-2-one ( WO 2012 / 121361), 4,4-dimethylcyclohexanone (1.5 eq.), glycine ethyl ester (1.2 eq.), triethylamine (15 mol%) in THF solution (10 times the volume), separately, Lewis acid (5 mol%) , an asymmetric ligand (6 mol %) and THF (10 times the amount) were stirred for 1 hour under a nitrogen atmosphere, a catalyst solution prepared was added, and the mixture was stirred at room temperature for 12 to 16 hours. After that, the resulting trans1 compound ((ethyl (3′S,4′R,5′S)-6″-chloro-4′-(2-chloro-3-fluoropyridin-4-yl) -4,4-dimethyl-2”-oxo-1”,2”-dihydrodispiro[cyclohexane-1,2′-pyrrolidine-3′,3”-indole]-5′-carboxylate) Optical purity and HPLC yield were measured.
(HPLC conditions for measuring optical purity)
Column: CHIRALPAK OD-3R 4.6 × 150 mm, 3 µm
Mobile phase: 10 mM phosphoric acid buffer: MeCN = 40:60
Flow rate: 1.0 min/min
column Temperature: 40°C
Detection wavelength: 254 nm
Injection volume: 5 µL
Retention time: Title compound = 13.8 min, enantiomer = 12.9 min
Main results are shown in Table 1.
[0232]
[Table 1-1]
[Table 1-2]
[0233]
11-2) Effects of various solvents
[0234]
[Chem. 68]
[0235]
(3E/Z)-6-chloro-3-[(2-chloro-3-fluoropyridin-4-yl)methylene]-1,3-dihydro-2H-indol-2-one ( WO 2012 / 121361), 4,4-dimethylcyclohexanone (1.5 eq.), glycine ethyl ester (1.2 eq.), triethylamine (15 mol%), a solvent (10 times the amount), CuOAc (5 mol%), ( A catalyst solution prepared by stirring S)-BINAP (6 mol %) and a solvent (10 times the amount) under a nitrogen atmosphere for 1 hour was added, followed by stirring at room temperature for 21.5 hours. After that, by HPLC, the resulting trans2 compound (ethyl (3’S,4’R,5’S)-6”-chloro-4′-(2-chloro-3-fluoropyridin-4-yl)- HPLC of 4,4-dimethyl-2″-oxo-1″,2″-dihydrodispiro[cyclohexane-1,2′-pyrrolidine-3′,3″-indole]-5′-carboxylate) Yields and optical purities were determined.
Table 2 shows the main results.
[0236]
[Table 2]
11-3) Examination of Cu(I) Lewis acid
PATENT
WO2014038606
WO2014038606 CLICK HERE
Example 1
[0062]
[Chem.3]
[0063]
(3′R,4′S,5′R)-N-[(3R,6S)-6-carbamoyltetrahydro-2H-pyran-3-yl]-6″-chloro-4′-(2-chloro- 3-fluoropyridin-4-yl)-4,4-dimethyl-2″-oxo-1″,2″-dihydrodispiro[cyclohexane-1,2′-pyrrolidine-3′,3″-indole]-5 ‘
-Carboxamide The compound (35 mg, 0.24 mmol) obtained in Reference Example 2, Step 3 was added to a solution of the compound (100 mg, 0.20 mmol) obtained in Step 3 of Reference Example 1 in N,N-dimethylformamide (4 ml). , triethylamine (0.04 ml, 0.30 mmol), 1-hydroxybenzotriazole (27 mg, 0.20 mmol) and 1-ethyl-3-(3-dimethylaminopropyl)carbodiimide hydrochloride (46 mg, 0.24 mmol) were added. , and stirred for 1 hour at 50° C. After allowing to cool, the reaction solution was diluted with ethyl acetate, washed successively with water, saturated aqueous sodium hydrogencarbonate solution and saturated brine, and dried over anhydrous sodium sulfate. After evaporating the solvent under reduced pressure, the residue was purified by NH-silica gel column chromatography [chloroform:methanol=50:1 (v/v)]. After stirring for 24 hours at rt, the solvent was distilled off under reduced pressure to obtain 94 mg (76%) of the title compound as a solid.1H
– NMR (400 MHz, CDCl3 ) .) δ: 0.68 (3H, s), 0.95 (3H, s), 1.11-1.27 (2H, m), 1.35-1.81 (8H, m), 2.10-2.17 (1H, m), 2.25-2.32 (1H, m), 3.15(1H,t,J=10.5Hz), 3.27(1H,br s), 3.80(1H,dd,J=11.0,2.3Hz), 3.85-3.95(1H,m), 4.13(1H, ddd,J=10.8,4.5,1.3Hz),4.44(1H,d,J=9.2Hz),4.64(1H,d,J=9.2Hz),5.46(1H,d,J=3.7Hz),6.49( 1H,d,J=3.7Hz), 6.74(1H,d,J=1.8Hz), 7.07(1H,dd,J=8.2,1.8Hz), 7.31(1H,dd,J=8.2,2.3Hz), 7.48-7.52(2H,m),7.62(1H,s),8.05(1H,d,J=5.5Hz).MS
(ESI)m/z:618(M+H) +
Reference example 1
[0087]
[Chem.4]
[0088]
[Step 1] (3E/Z)-6-chloro-3-[(2-chloro-3-fluoropyridin-4-yl)methylene]-1,3-dihydro-2H-indol-2-one
6-chloro -1,3-dihydro-2H-indol-2-one (2.20 g, 13.11 mmol) and 2-chloro-3-fluoroisonicotinaldehyde (2.20 g, 13.8 mmol) in methanol (130 ml). , N,N-diisopropylethylamine (0.46 ml, 2.63 mmol) was added, and the mixture was heated under reflux for 16 hours. After standing to cool, the precipitate was collected by filtration, washed with cold methanol and dried to obtain 3.37 g (83%) of the title compound as a solid.
MS(APCI) m/z: 309(M+H) + .
[0089]
[Step 2] (3′S,4′R,7′S,8′S,8a′R)-6″-chloro-8′-(2-chloro-3-fluoropyridin-4-yl)-4 ,4-dimethyl-3′,4′-diphenyl-3′,4′,8′,8a′-tetrahydro-1′H-dispiro[cyclohexane-1,6′-pyrrolo[2,1-c][1 ,4]oxazine-7′,3″-indole]-1′,2″(1″H)
-dione Under a nitrogen atmosphere, the compound obtained in Step 1 (1.86 g, 6.00 mmol), (5R,6S )-5,6-diphenylmorpholin-2-one (1.67 g, 6.60 mmol) and 4,4-dimethylcyclohexanone (0.83 g, 6.60 mmol) in tetrahydrofuran (30 ml) was added with diethyl boron trifluoride. An ether complex (0.15 ml, 1.20 mmol) and molecular sieve 4A (powder) (3 g) were added, and the mixture was heated and stirred at 70° C. for 7 days. After allowing to cool, insoluble matter was removed by filtration through celite, and the filtrate was washed with saturated brine and dried over anhydrous sodium sulfate. The solvent was distilled off under reduced pressure and purified by silica gel column chromatography [n-hexane:ethyl acetate=4:1→1:1 (v/v)] to obtain 3.39 g (84%) of the title compound as a solid. rice field.
1 H-NMR (400 MHz, CDCl3) δ: 0.21 (3H, s), 0.53 (3H, s), 0.89-1.08 (3H, m), 1.28-1.43 (3H, m), 1.73-1.81 (1H, m), 2.23-2.33 (1H, m), 4.58 (1H, d, J = 11.0Hz), 4.86 (1H, d, J = 3.2Hz), 5.31 (1H, d, J = 11.0Hz), 6.25 (1H, d, J = 8.3Hz) ,6.67(1H,dd,J=8.3,1.8Hz),6.72-6.77(2H,m),6.93(1H,d,J=1.8Hz),7.04-7.17(6H,m),7.18-7.25(3H ,m),7.79(1H,t,J=4.6Hz),7.99(1H,s),8.29(1H,d,J=5.0Hz).MS
(APCI)m/z:670(M+H) + .
[0090]
[Step 3] (4′S,5′R)-6″-chloro-4′-(2-chloro-3-fluoropyridin-4-yl)-4,4-dimethyl-2″-oxo-1″ ,2″-dihydrodispiro[cyclohexane-1,2′-pyrrolidine-3′,3″-indole]-5′-carboxylic acid
The compound obtained in step 2 (630 mg, 0.94 mmol) was treated with acetonitrile (10 ml). Dissolve in water (4 ml), add potassium carbonate (130 mg, 0.94 mmol) and heat under reflux for 16 hours at 85° C. After allowing to cool, add anhydrous magnesium sulfate (113 mg, 0.94 mmol) and stir at room temperature for 15 minutes. After extraction with ethyl acetate, the organic layer was washed with saturated brine and dried over anhydrous magnesium sulfate. (2-chloro-3-fluoropyridin-4-yl)-1′-[(1R,2S)-2-hydroxy-1,2-diphenylethyl]-4,4-dimethyl-2″-oxo-1″ ,2″-dihydrodispiro[cyclohexane-1,2′-pyrrolidine-3′,3″-indole]-5′-carboxylic acid (650 mg, 100%) was obtained as a solid [MS (ESI) m/z :688(M+H) +]. The resulting carboxylic acid (650 mg, 0.94 mmol) was dissolved in methanol (30 ml) and water (8 ml), and diammonium cerium (IV) nitrate (1.55 g, 2.82 mmol) was added under ice-cooling. Stir at room temperature for 30 minutes. Potassium carbonate (780 mg, 5.64 mmol) was added under ice-cooling, and the mixture was stirred at the same temperature for 1 hour. After removing the insoluble matter by filtration through celite, the filtrate was concentrated under reduced pressure, water was added to the resulting residue, and the mixture was extracted with ethyl acetate. The organic layer was washed with saturated brine and dried over anhydrous sodium sulfate. The solvent was distilled off under reduced pressure, and the resulting residue was purified by silica gel column chromatography [chloroform:methanol=20:1→4:1 (v/v)] to obtain 152 mg (33%) of the title compound as a solid. .
1 H-NMR (500 MHz, CD 3 OD) δ: 0.74 (3H, s), 0.9 (3H, s), 1.29-1.44 (2H, m), 1.48-1.58 (2H, m), 1.64-1.76 (1H ,m),1.94-2.02(1H,m),2.11(1H,ddd,J=14.0,14.0,4.0Hz),2.43-2.53(1H,m),5.07(1H,d,J=10.3Hz), 5.32(1H,d,J=10.3Hz),6.84(1H,d,J=1.7Hz),7.16(1H,dd,J=8.3,2.0Hz),7.63(1H,dd,J=8.0,2.3Hz) ),7.75(1H,t,J=5.2Hz),8.15(1H,d,J=5.2Hz).
MS(ESI)m/z:492(M+H) + .
[0091]
Reference example 2
[0092]
[Chem.5]
[0093]
[Step 1] Methyl 2,6-anhydro-3,4,5-trideoxy-5-(dibenzylamino)-L-erythro
-hexonate 2,6-anhydro-3,4,5-trideoxy-5-( dibenzylamino)-L-erythro-hexonate methyl 2,6-anhydro-3,4,5-trideoxy-5-(dibenzylamino)-L-erythro-hexonate (1.60 g, 4.70 mmol) was The mixture was dissolved in methanol (30 ml), 1N aqueous sodium hydroxide solution (10 ml) was gradually added under ice-cooling, and the mixture was stirred at room temperature for 3 hours. Dowex 50W-X8 was added to the reaction mixture to adjust the pH to 5 to 6, insoluble materials were removed by filtration, and the filtrate was concentrated under reduced pressure to obtain 1.7 g (100%) of the title compound as a solid.
1 H-NMR (400 MHz, CDCl 3 ) δ: 1.18-1.26(1H,m), 1.36-1.48(1H,m), 1.79-1.97(2H,m), 2.62(1H,t,J=11.0Hz) ,3.18(1H,t,J=10.4Hz),3.40(1H,d,J=11.5Hz),3.51-3.61(4H,m),3.90-3.99(1H,m),7.12-7.38(10H,m ).
MS(ESI)m/z:326(M+H) + .
[0094]
[Step 2] (2S,5R)-5-(dibenzylamino)tetrahydro-2H-pyran-2-carboxamide
The compound (870 mg, 2.67 mmol) obtained in Step 1 above was dissolved in N,N-dimethylformamide (30 ml). 1-hydroxybenzotriazole (361 mg, 2.67 mmol) and 1-ethyl-3-(3-dimethylaminopropyl)carbodiimide hydrochloride (614 mg, 3.20 mmol) were added and stirred at room temperature for 15 minutes. Ammonium chloride (285 mg, 5.44 mmol) and N,N-diisopropylethylamine (1.86 ml, 10.7 mmol) were added and stirred at room temperature for 8 hours. After diluting with ethyl acetate, the organic layer was washed with saturated aqueous sodium hydrogencarbonate solution and saturated brine in that order, and dried over anhydrous sodium sulfate. The solvent was removed under reduced pressure to give 495 mg (57%) of the title compound as a solid.
1 H-NMR (400 MHz, CDCl 3 ) δ: 1.35-1.45 (1H, m), 1.60-1.70 (1 H, m), 2.10-2.18 (1 H, m), 2.21-2.28 (1 H, m), 2.76 ( 1H,tt,J=11.4,4.0Hz),3.44(1H,t,J=10.9Hz),3.67(4H,q,J=14.2Hz),3.71-3.73(1H,m),4.04(1H,dq ,J=11.0,2.1Hz),5.35(1H,s),6.40(1H,s),7.21-7.36(10H,m).MS
(ESI)m/z:325(M+H) + .
[0095]
[Step 3] (2S,5R)-5-aminotetrahydro-2H-pyran-2-carboxamide
The compound (490 mg, 1.51 mmol) obtained in Step 2 above was dissolved in ethanol (10 ml) and treated with 20% palladium hydroxide. (100 mg) was added, and the mixture was stirred at room temperature for 16 hours under a hydrogen atmosphere. After removing the catalyst by filtration through celite, the filtrate was distilled off under reduced pressure and dried to obtain 215 mg (99%) of the title compound as a solid.
1 H-NMR (400 MHz, DMSO-d 6 ) δ: 1.11-1.22(1H,m), 1.25-1.35(1H,m), 1.83-1.91(2H,m), 2.51-2.60(1H,m), 2.90(1H,t,J=10.5Hz),3.52(1H,d,J=11.9Hz),
3.78-3.84 (1H,m),6.99(1H,br s),7.09(1H,br s). (ESI) m/z: 145(M+H) + .
PATENT
WO2012121361
PATENT
WO2015033974
PAPER
https://pubs.acs.org/doi/10.1021/acs.oprd.2c00192
Abstract

Herein, we report the structure and synthesis of the potent MDM2-p53 inhibitor BI-0282. The complex spirooxindole scaffold bearing four stereocenters embedded in a rigid polycyclic ring-system was effectively prepared on a multi-gram scale in only five synthesis steps employing a three-component 1,3-dipolar cycloaddition and a late-stage Davis–Beirut reaction as key steps.
Compound 1
Intermediate 10 (28.8 g, 44.8 mmol) is dissolved in isopropanol (300 mL) and a solution of potassium hydroxide (39.0 g, 694.9 mmol) in water (95 mL) is slowly added. After stirring for 16 h at ambient temperature, the solvents are partially removed under reduced pressure. The residue is diluted with ethyl acetate and treated with a diluted aqueous solution of citric acid. After extraction of the aqueous layer with ethyl acetate, the organic layers are combined, dried with sodium sulfate, and the solvent is removed under reduced pressure. Purification by normal phase column chromatography using dichloromethane and methanol as solvents yields rac-1 (25.8 g, 43.5 mmol) in 70% yield as an amorphous white solid.
Chiral SFC and subsequent purification by reversed phase column chromatography using acetonitrile and methanol as solvents furnishes 1 (BI-0282).
Rac-1 (60 g, 93,3 mmol) was separated by chiral SFC and reversed phase column chromatography to obtain 1 (24.4 g, 40,0 mmol, 43%) as an amorphous white solid.
Chiral HPLC (CHIRALPAK, heptane/isopropanol/trifluoroacetic acid = 70/30/0.1, flow rate 1.0 mL/min, I = 240 mM) tR = 7.8 min (1), and 11.1 min (ent-1). Preparative SFC (CHIRALPAK, carbon dioxide/(isopropanol + 1% diethylamine) = 70/30, flow rate 300 g/min, I = 290 nM).
1H NMR (500 MHz, DMSO-d6): δ 12.64 (br s, 1H), 10.29 (s, 1H), 7.67 (s, 1H), 7.47 (d, J = 8.83 Hz, 2H), 7.29–7.36 (m, 1H), 7.26 (d, J = 7.88 Hz, 1H), 7.21 (dd, J = 1.26, 8.83 Hz, 1H), 7.12 (t, J = 8.04 Hz, 1H), 6.92 (dd, J = 1.89, 7.88 Hz, 1H), 6.48 (d, J = 1.89 Hz, 1H), 5.86 (t, J = 9.14 Hz, 1H), 4.59–4.68 (m, 1H), 4.52 (dd, J = 7.88, 11.35 Hz, 1H), 4.23–4.32 (m, 1H), 4.20 (d, J = 10.09 Hz, 1H), 2.27 (dd, J = 7.57, 13.08 Hz, 1H), 2.13 (dd, J = 5.83, 13.08 Hz, 1H), 0.47–0.62 (m, 1H), 0.26–0.37 (m, 1H), 0.11–0.20 (m, 1H), −0.04 to 0.04 (m, 1H), −0.25 (s, 1H).
13C{1H} NMR (125 MHz, DMSO-d6): δ 177.5, 168.1, 156.1 (d, 1JC,F = 248.7 Hz), 146.3, 145.3, 144.0, 134.1, 130.3, 129.7, 129.5, 126.8, 126.7, 125.4 (d, 3JC,F = 4.4 Hz), 123.5 (d, 2JC,F = 13.2 Hz), 122.5, 120.0, 119.9, 119.7 (d, 2JC,F = 18.3 Hz), 118.7, 110.0, 107.3, 76.4, 69.2, 57.5, 56.8, 54.2, 51.2, 11.6, 5.5, 4.1.
HRMS (ESI) m/z: [M + H]+ calcd for C30H24Cl2FN4O4, 593.1153; found, 593.1165.
////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Milademetan is under investigation in clinical trial NCT02319369 (Safety, Tolerability and Pharmacokinetics of Milademetan Alone and With 5-Azacitidine (AZA) in Acute Myelogenous Leukemia (AML) or High-Risk Myelodysplastic Syndrome (MDS)).
- [1]. ARYL SULFONOHYDRAZIDES. WO 2017069289 A1.[2]. M.M. Gounder, et al. Milademetan, an oral MDM2 inhibitor, in well-differentiated/dedifferentiated liposarcoma: results from a phase 1 study in patients with solid tumors or lymphomas. European Journal of Cancer 138S2 (2020) S1–S62.[3]. Li, Yangbing, et al. Development of novel PROTAC Small-Molecule Degraders of MDM2 Protein and Peptidomimetic Inhibitors Targeting WDR5-MLL1 Protein-Protein Interaction.[4]. Viktor Arnhold, et al. Reactivating TP53 signaling by the novel MDM2 inhibitor DS-3032b as a therapeutic option for high-risk neuroblastoma. ncotarget. 2018 Jan 5; 9(2): 2304–2319.
/////////Milademetan, DS3032b, DS-3032b, DS 3032b, DS3032, DS-3032, DS 3032, DS-3032b tosylate, Milademetan tosylate, Milademetan HCl, orphan drug, UNII:R3I80TLN7S, миладеметан , ميلاديميتان , 米拉美坦
CC1(C)CCC2(CC1)N[C@H]([C@H](C1=C(F)C(Cl)=NC=C1)[C@]21C(=O)NC2=CC(Cl)=CC=C12)C(=O)N[C@@H]1CC[C@H](OC1)C(N)=O
NEW DRUG APPROVALS
ONE TIME
$10.00
Daxibotulinumtoxin A

Daxibotulinumtoxin A
FDA APPROVED 2022 2022/9/7, Daxxify
| Formula | C6708H10359N1729O1995S32 |
|---|---|
| CAS | 93384-43-1 |
| Mol weight | 148171.4934 |
Daxibotulinumtoxin A-lanm
Treatment of galbellar lines, cervical dystonia, lateral canthal lines, migraine headaches and hyperhidrosis
- DeveloperRevance Therapeutics; Shanghai Fosun Pharmaceutical
- ClassAnalgesics; Anti-inflammatories; Antiarrhythmics; Antidepressants; Antimigraines; Antipruritics; Antispasmodics; Bacterial proteins; Bacterial toxins; Botulinum toxins; Eye disorder therapies; Foot disorder therapies; Muscle relaxants; Skin disorder therapies; Urologics; Vascular disorder therapies
- Mechanism of ActionAcetylcholine inhibitors; Glutamate antagonists; Membrane transport protein modulators; Neuromuscular blocking agents
- Orphan Drug StatusYes – Torticollis
- RegisteredGlabellar lines
- Phase IIITorticollis
- Phase IIMuscle spasticity
- No development reportedSkin disorders
- DiscontinuedPlantar fasciitis
- 19 Sep 2022Efficacy data from a phase IIa FHL trials in Glabellar-lines (crow’s feet) released by Revance
- 19 Sep 2022Updated efficacy and safety data from the phase III SAKURA 1, SAKURA 2 and SAKURA 3 trials in Glabellar lines released by Revance Therapeutics
- 18 Sep 2022Updated efficacy and safety data from the phase III SAKURA 1, SAKURA 2 and SAKURA 3 trials in Glabellar lines released by Revance Therapeutics
////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
DAXI Impresses; Approaches FDA Approval
March 2, 2021
Dermatology Times, Dermatology Times, February 2021 (Vol. 42, No. 2), Volume 42, Issue 2
The investigational neuromodulator, evaluated in clinical trials as a treatment for glabellar lines and as a combined therapy for glabellar, dynamic forehead, and lateral canthal lines, is quickly nearing an approval by the FDA.
The long-awaited, longer-lasting neuromodulator drug candidate DaxibotulinumtoxinA for Injection (DAXI), a botulinum toxin type A formulated with a novel peptide excipient, may be nearing FDA approval.
In mid-December 2020, Revance Therapeutics shared results from its phase 2 upper facial lines study (NCT04259086),1 in which investigators looked at DAXI for combined treatment of glabellar, dynamic forehead, and lateral canthal lines.
The authors reported on a multicenter study of 48 patients enrolled to receive 40, 32, and 48 U of DAXI for injection in the glabellar complex, forehead, and lateral canthal areas, respectively. At week 4, nearly 92% of patients achieved an Investigator Global Assessment (IGA) score indicating no or mild wrinkle severity with maximum contraction on their lateral canthal lines. Nearly 96% achieved similar results on their forehead and glabellar lines at week 4.
Wrinkle severity returned to baseline at a median of 7.6 months post treatment, according to the phase 2 study findings.
The treatment was well tolerated in all upper facial regions. The most common adverse event (AE) was injection site erythema, which occurred in 6.3% of patients. The authors reported no eyelid or brow ptosis.
This was Revance’s first DAXI study on not just glabellar lines but also on forehead and periocular lines, or crow’s-feet, according to Jeffrey S. Dover, MD, FRCPC, a phase 2 study investigator and a dermatologist at SkinCare Physicians in Chestnut Hill, Massachusetts. “I think this is yet more evidence that the Revance neuromodulator produces an impressive effect on lines of negative facial expression and lasts longer than any of the other neuromodulators approved by the FDA thus far,” said Dover.
Dermatologic Surgery published 2 papers on the investigational neuromodulator in January 2021. In one study,2 investigators evaluated the use of up to 3 DAXI treatments for moderate or severe glabellar lines. They focused on data from SAKURA 1 and 2 (NCT03014622 and NCT03014635), two identical phase 3, open label, multicenter studies in which investigators evaluated single and repeat treatment of the glabellar lines with 40 U of DAXI.
The authors reported on safety results for nearly 2700 patients, including 882 who received a second treatment and 568 who got DAXI a third time. Treatment-related AEs, which were generally mild and resolved, occurred in 17.8% of patients. Eyelid ptosis occurred in 0.9% of treatments.
Investigators of 2 other studies3,4 focused on DAXI efficacy among nearly 2700 subjects enrolled in Revance’s preceding pivotal trials. Participants received repeat treatments when they returned to baseline on the IGA–Frown Wrinkle Severity (FWS) and IGA–Patient Frown Winkle Severity (PFWS) scales at 12 weeks and up to 36 weeks after treatment.
More than 96% of patients achieved no or mild severity in glabellar wrinkles on the IGA- FWS scale after each of the 3 treatments, with peak responses between weeks 2 to 4, and about one-third or more saw no or mild severity at week 24. Response rates reached highs of 92% or more at weeks 2 to 4 on the IGA-PFWS scale.
“The median duration for return to moderate or severe severity was 24 weeks,” the authors said. “If approved, I believe daxibotulinumtoxinA will change the landscape of neuromodulators significantly. The approved ones all last 3 months. They all give nice results and have few adverse effects,” Dover said.
He and other investigators have seen no rise in AEs, and those that did occur lasted no longer than those of Botox, he said.
Revance appears to be preparing for approval. The company announced on December 22, 2020, that it has a strategic commercial manufacturing agreement with Ajinomoto Bio- Pharma Services for the supply of DAXI.5
As of November 24, 2020, the FDA had deferred a decision on the neuromodulator because the required factory inspection could not be conducted due to travel restrictions related to coronavirus disease 2019.6 The FDA did not indicate any other issues.
References:
- Green JB, Mariwalla K, Coleman K, et al. A large, open-label, phase 3 safety study of DaxibotulinumtoxinA for Injection in glabellar lines: a focus on safety from the SAKURA 3 study. Derm Surg. 2021;47(1):42-46. doi:10.1097/DSS.0000000000002463
- Carruthers JD, Jean D, Fagien S, et al; SAKURA 1 and SAKURA 2 Investigator Group. DaxibotulinumtoxinA for Injection for the treatment of glabellar lines: results from each of two multicenter, randomized, double-blind, placebo-controlled, phase 3 studies (SAKURA 1 and SAKURA 2).Plast Reconstr Surg. 2020;1(145):45-58.doi: 10.1097/PRS.0000000000006327
- Fabi SG, Cohen JL, Green LJ, et al. DaxibotulinumtoxinA for Injection for the treatment of glabellar lines: efficacy results from SAKURA 3, a large, open-label, phase 3 safety study. Derm Surg. 2021;47(1):48-54. doi:10.1097/DSS.0000000000002531
- https://investors.revance.com/news-releases/news-release-details/ajinomoto-bio-pharma-services-and-revance-therapeutics-announce. December 22, 2020. Accessed January 15, 2021.
- FDA defers approval of DaxibotulinumtoxinA for Injection in glabellar lines due to COVID-19 related travel restrictions impacting manufacturing site inspection. News release. Revance Therapeutics, Inc. November 25, 2020. Accessed January 13, 2021. https://www.businesswire.com/news/home/20201125005462/en/FDA-Defers-Approval-DaxibotulinumtoxinA-Injection-Glabellar-Lines
///////////Daxibotulinumtoxin A, FDA 2022, APPROVALS 2022, DAXI, Daxibotulinumtoxin-A, DaxibotulinumtoxinA for Injection, daxibotulinumtoxinA-lanm, DAXXIFY, RT-002, Orphan Drug

NEW DRUG APPROVALS
ONE TIME
$10.00
Ozoralizumab
Ozoralizumab
| Formula | C1682H2608N472O538S12 |
|---|---|
| CAS | 1167985-17-2 |
| Mol weight | 38434.3245 |
PMDA JAPAN APPROVED 2022 2022/9/26 Nanozora
anti-TNFα Nanobody®; ATN-103; Nanozora; PF-5230896; TS-152
Ozoralizumab is a humanized monoclonal antibody designed for the treatment of inflammatory diseases.[1]
Ozoralizumab was developed by Pfizer Inc, and now belongs to Ablynx NV. Ablynx has licensed the rights to the antibody in China to Eddingpharm.
Ozoralizumab has been used in trials studying the treatment of Rheumatoid Arthritis and Active Rheumatoid Arthritis.
Ozoralizumab is a 38 kDa humanized trivalent bispecific construct consisting of two anti-TNFα NANOBODIES® and anti-HSA NANOBODY® that was generated at Ablynx by a previously described method (23). Llamas were immunized with human TNFα and human muscle extract, which is rich in HSA, to induce the formation of anti-TNFα VHH and anti-HSA VHH. Both the anti-TNFα VHH and anti-HSA VHH were humanized by a complementary determining regions (CDR) grafting approach in which the CDR of the gene encoding llama VHH was grafted onto the most homologous human VHH framework sequence. Since binding to serum albumin prolongs the half-life of VHH (23, 26, 27), an anti-HSA VHH which efficiently binds murine serum albumin as well was incorporated into the two anti-TNFα VHHs. The three components were fused using a flexible Gly-Ser linker.
////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Humanized |
| Clinical data | |
| ATC code | none |
| Identifiers | |
| CAS Number | 1167985-17-2 |
| ChemSpider | none |
| UNII | 05ZCK72TXZ |
| KEGG | D09944 |
| Chemical and physical data | |
| Formula | C1682H2608N472O538S12 |
| Molar mass | 38434.85 g·mol−1 |
- OriginatorAblynx
- DeveloperAblynx; Eddingpharm; Pfizer; Taisho Pharmaceutical
- ClassAnti-inflammatories; Antirheumatics; Monoclonal antibodies; Proteins
- Mechanism of ActionTumour necrosis factor alpha inhibitors
- Orphan Drug StatusNo
- New Molecular EntityYes
- RegisteredRheumatoid arthritis
- DiscontinuedAnkylosing spondylitis; Crohn’s disease; Psoriatic arthritis
- 05 Oct 2022Sanofi’s affiliate Ablynx has worldwide patent pending for Nanobodies® (Sanofi website, October 2022)
- 05 Oct 2022Sanofi’s affiliate Ablynx has worldwide patent protection for Nanobodies® (Sanofi website, October 2022)
- 26 Sep 2022First global approval – Registered for Rheumatoid arthritis in Japan (SC)
References
- ^ Kratz F, Elsadek B (July 2012). “Clinical impact of serum proteins on drug delivery”. J Control Release. 161 (2): 429–45. doi:10.1016/j.jconrel.2011.11.028. PMID 22155554.
////////Ozoralizumab, Nanozora, Monoclonal antibody, nanobody, Treatment inflammation, ATN 103, APPROVALS 2022, JAPAN 2022

NEW DRUG APPROVALS
ONE TIME
$10.00
Firibastat
_648927-86-0.png)
Firibastat
- Molecular FormulaC8H20N2O6S4
- Average mass368.514 Da
368.5
RB 150
Qgc-001(racemate)
UNII-PD5EII1F9A
Firibastat, (+/-)-
PD5EII1F9A
3-amino-4-[(2-amino-4-sulfobutyl)disulfanyl]butane-1-sulfonic acid
1-Butanesulfonic acid, 4,4′-dithiobis(3-amino-
3-Amino-4-((2-amino-4-sulfo-butyl)disulfanyl)butane-1-sulfonic acid
cas 721392-96-7, RACEMIC
CAS 648927-86-0, (S)-3-amino-4-(((S)-2-amino-4-sulfobutyl)disulfaneyl)butane-1-sulfonic acid
фирибастат[Russian][INN]
فيريباستات[Arabic][INN]
(3S,3’S)-4,4′-Disulfanediylbis(3-aminobutane-1-sulfonic acid)
firibastatum
фирибастат
فيريباستات
非立巴司他[Chinese]
PAPER
Journal of Labelled Compounds & Radiopharmaceuticals (2004), 47(13), 997-1005
PATENT
https://patents.google.com/patent/WO2020084131A1/en
PATENT
WO2012045849


EXAMPLES
Example 1: Synthesis of compound I from (S) ethyl 2-(benzyloxycarbonylamino) 4-(neopentyloxysulfonyl)butanoate
Step (a): (S) neopentyl 3-(benzylox carbonylamino) 4-hydroxybutane 1-sulfonate B
B
(S) ethyl 2-(benzyloxycarbonylamino) 4-(neopentyloxysulfonyl)butanoate A (41.55g, 100.0 mmol, 1.0 eq.) is added dropwise onto a 2M solution of LiBH4 in THF (50 mL, 44.8 g, 100.0 mmol, 1.0 eq.). The addition is performed at room temperature over a 3 hrs period. At the end of the addition, the mixture is stirred at room temperature until conversion is complete (A<1%). Addition of toluene, followed by hydrolysis with HC1, washings of the organic layer with NaHC03 and water, and concentration under vacuum lead to the desired product as a pale yellow oil in quantitative yield (ee = 98%), which slowly crystallises at room temperature in 4 or 5 days.
As B was found to have a very low melting point by DSC analysis, it was not possible to isolate it as a solid by simple crystallisation. It was decided to let it in solution and use it without further purification in the following step.
Step (b): (S) neopentyl 3-(benzyloxycarbonylamino) 4-(methylsulfonyloxy)butane 1-sulfonate
C
C
A solution of B (57.64 g, 154.34 mmol, 1.0 eq.) in toluene (115 mL, 2.0 vol.) is diluted with MTBE (173 mL, 3.0 vol.) at room temperature. Mesyl chloride (17.9 mL, 26.5 g, 231.50 mmol, 1.5 eq.) is then added at room temperature and the homogeneous mixture is cooled to 10°C. The addition of triethylamine (43.0 mL, 31.2 g, 308.67 mmol, 2.0 eq.) is performed at T<20°C. At the end of the addition, the mixture is stirred at 10°C until conversion is complete (B<1%). After hydrolysis with diluted HCl, the organic layer is washed with NaHC03, water and brine, followed by a partial concentration under reduced pressure. The corresponding mesylate is then crystallised by addition of heptanes (5.0 vol.) at 40°C. After cooling, filtration and drying, the expected product is isolated as a whitish solid in 92.5% yield and with a very high chemical purity (98%).
Step (c): (S) 2-(benzyloxycarbonylamino) 4-(neopentyloxysulfonyl)butyl thioacetate D
D
A solution of mesylate C (81.3 g, 180.05 mmol, 1.0 eq.) in acetone (203 mL, 2.5 vol.) is added dropwise to a suspension of potassium thioacetate (41.1 g, 360.1 mmol, 2.0 eq.) in acetone (203 mL, 2.5 vol.) at room temperature and over a period of 2 hrs. The reaction mixture is stirred at room temperature until conversion is complete (C<1%). After filtration of the salts and addition of toluene (4.0 vol.), acetone is removed by distillation under reduced pressure at 25°C. The solution is then treated with active charcoal and concentrated to 2.0 volumes. Slow addition of heptane (5.0 vol.) at room temperature, followed by cooling at 0°C, filtration and drying at 45°C, provides the expected product as a whitish solid in 78.2% yield and with a very high chemical purity (98%).
Step (d): (3S,3S’) neopentyl 4,4′-disulfanediylbis(3-(benzyloxycarbonylamino)butane 1-sulfonate) E
E
A solution of D (59.16 g, 137.1 mmol, 1.0 eq.) suspended in ethanol (203 mL, 2.5 vol.) is cooled to 0°C. 20% sodium hydroxide (25.1 mL, 150.8 mmol, 1.1 eq.) diluted with water
(16.9 mL, 0.285 vol.) is then added dropwise to the suspension by keeping the temperature below 10°C. The reaction mixture is warmed to room temperature and stirred until conversion is complete (D<1%). The intermediate thiol reacts at room temperature with a solution of iodine (20.9 g, 82.3 mmol, 0.6 eq.) in ethanol (118 mL, 2.0 vol.). The reaction is complete at the end of the addition of the oxidizing agent. After addition of a Na2S205 (13.0 g, 68.5 mmol, 0.5 eq.) aqueous solution (118 mL, 2.0 vol.) to reduce the excess of residual iodine, ethanol is removed by distillation under reduced pressure at 40°C. Addition of water (3.0 vol.) at room temperature, followed by cooling at 0°C, filtration and drying at 45-50°C, provides the expected dimer as a white solid in 98.3% yield and with a very high chemical purity (97.0%). The amount of iodide ions, coming from the reduction of iodine, is checked in the sample by potentiometric assay.
E°(Ag+/Ag(s))=0.80V
KsAgi=1.5.10“16
[AgNO3]=0.1N
Electrode: E=E°(Ag+/Ag(s))+0.061og[Ag+]
E=E°(Ag+/Ag(s))+0.061og (Ksi/[L])
Assay: [T] decreases and E increases
LOD=l mg
Four further washings with water are performed until no more iodide ions are detected. The results are presented in table 2.
Table 2.
Step (e): (3S,3S’) 4,4′-disulfanediylbis(3-aminobutane 1-sulfonic acid) compound I
4
Compound I
A solution of E (44.0 g, 56.6 mmol, 1.0 eq.) in TFA (220 mL, 5.0 vol.) and anisole (44 mL, 1.0 vol.) is heated to reflux (75°C) and the reaction mixture is stirred in these conditions until conversion is complete (E<1%). TFA is removed by distillation under reduced pressure at 50°C. Slow addition of MTBE (5.0 vol.) at room temperature makes the expected product precipitate. After trituration, filtration and washing with MTBE (1.0 vol.), the crude solid is suspended in methanol (220 mL, 5.0 vol.). New trituration, filtration and washing with MTBE (1.0 vol.), followed by drying under reduced pressure, provides compound I as a white solid in 92.5% yield.
NMR: 1H (solvent D20, 400 MHz, ppm): 4.70 (s, 6H, ¾); 3.77 (m, 2H, H2); 3.14 (dd, 2H, Hi); 2.98 (dd, 4H, H4); 2.86 (dd, 2H, Hi); 2.13 (m, 4H, H3). 13C (solvent D20, 100 MHz, ppm): 49.4 (2C, C2); 46.6 (2C, C4); 38.3 (2C, C ; 26.9 (2C, C3).
////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
- OriginatorCNRS; INSERM; University Paris Descartes
- DeveloperQuantum Genomics
- ClassAmines; Aminopeptidases; Antihypertensives; Cardiovascular therapies; Disulfides; Heart failure therapies; Metalloexopeptidases; Small molecules; Sulfonic acids
- Mechanism of ActionGlutamyl aminopeptidase inhibitors
- Orphan Drug StatusNo
- New Molecular EntityYes
- Phase IIIHypertension
- Phase IIChronic heart failure; Left ventricular dysfunction
- 28 Mar 2022No recent reports of development identified for phase-I development in Hypertension(In volunteers) in United Kingdom (PO, Tablet)
- 25 Nov 2021Firibastat licensed to Teva in Israel
- 11 Oct 2021Quantum Genomics plans a phase III trial for Heart failure
////////Firibastat, фирибастат , فيريباستات , firibastatum, фирибастат ,فيريباستات ,非立巴司他 , rb 150, (+/-)-QGC-001, qgc 001,
C(CS(=O)(=O)O)C(CSSCC(CCS(=O)(=O)O)N)N

Futibatinib

Futibatinib
フチバチニブ
| Formula | C22H22N6O3 |
|---|---|
| CAS | 1448169-71-8 |
| Mol weight | 418.4485 |
2022/9/30 FDA APPROVED, Lytgobi
| Antineoplastic, Receptor tyrosine kinase inhibitor | |
| Disease | Cholangiocarcinoma (FGFR2 gene fusion) |
|---|
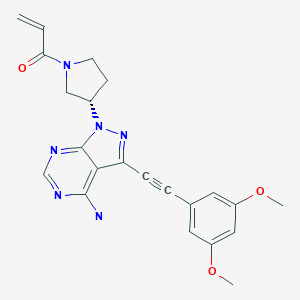
1-[(3S)-3-[4-amino-3-[2-(3,5-dimethoxyphenyl)ethynyl]-1H-pyrazolo[3,4-d]pyrimidin-1-yl]-1-pyrrolidinyl]-2-propen-1-one
TAS-120, TAS 120, TAS120; Futibatinib
Futibatinib, also known as TAS-120 is an orally bioavailable inhibitor of the fibroblast growth factor receptor (FGFR) with potential antineoplastic activity. FGFR inhibitor TAS-120 selectively and irreversibly binds to and inhibits FGFR, which may result in the inhibition of both the FGFR-mediated signal transduction pathway and tumor cell proliferation, and increased cell death in FGFR-overexpressing tumor cells. FGFR is a receptor tyrosine kinase essential to tumor cell proliferation, differentiation and survival and its expression is upregulated in many tumor cell types.

SYN
Patent Document 1: International Publication WO 2007/087395 pamphlet
Patent Document 2: International Publication WO 2008/121742 pamphlet
Patent Document 3: International Publication WO 2010/043865 pamphlet
Patent Document 4: International Publication WO 2011/115937 pamphlet
Unlicensed Document 1 : J. Clin. Oncol. 24, 3664-3671 (2006)
Non-licensed Document 2: Mol. Cancer Res. 3, 655-667 (2005)
Non-licensed Document 3: Cancer Res. 70, 2085-2094 (2010)
Non-licensed Document 4: Clin. Cancer Res. 17, 6130-6139 (2011)
Non-licensed Document 5: Nat. Med. 1, 27-31 (1995)
WO2020095452
WO2020096042
WO2020096050
WO2019034075
WO2015008844
WO2015008839
WO2013108809
SYN
US9108973
SYN
Reference Example 1: WXR1
Compound WXR1 was synthesized according to the route reported in patent WO2015008844. 1 H NMR(400MHz, DMSO-d 6 )δ8.40(d,J=3.0Hz,1H),6.93(d,J=2.5Hz,2H),6.74-6.52(m,2H),6.20-6.16( m,1H), 5.74-5.69(m,1H), 5.45-5.61(m,1H), 4.12-3.90(m,2H), 3.90-3.79(m,8H), 2.47-2.30(m,2H). MS m/z: 419.1[M+H] +
PAPER
Bioorg Med Chem, March 2013, Vol.21, No.5, pp.1180-1189
SYN
WO2015008844
PATENT
////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
| Clinical data | |
|---|---|
| Trade names | Lytgobi |
| Other names | TAS-120 |
| License data | US DailyMed: Futibatinib |
| Routes of administration | By mouth |
| Drug class | Antineoplastic |
| ATC code | L01EN04 (WHO) |
| Legal status | |
| Legal status | US: ℞-only [1] |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 1448169-71-8 |
| PubChem CID | 71621331 |
| IUPHAR/BPS | 9786 |
| DrugBank | DB15149 |
| ChemSpider | 58877816 |
| UNII | 4B93MGE4AL |
| KEGG | D11725 |
| ChEMBL | ChEMBL3701238 |
| PDB ligand | TZ0 (PDBe, RCSB PDB) |
| Chemical and physical data | |
| Formula | C22H22N6O3 |
| Molar mass | 418.457 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI |
Futibatinib, sold under the brand name Lytgobi, is a medication used for the treatment of cholangiocarcinoma (bile duct cancer).[1][2] It is a kinase inhibitor.[1][3] It is taken by mouth.[1]
Futibatinib was approved for medical use in the United States in September 2022.[1][2][4]
Medical uses
Futibatinib is indicated for the treatment of adults with previously treated, unresectable, locally advanced or metastatic intrahepatic cholangiocarcinoma harboring fibroblast growth factor receptor 2 (FGFR2) gene fusions or other rearrangements.[1][2]
Names
Futibatinib is the international nonproprietary name (INN).[5]
References
- ^ Jump up to:a b c d e f “Lytgobi (futibatinib) tablets, for oral use” (PDF). Archived (PDF) from the original on 4 October 2022. Retrieved 4 October 2022.
- ^ Jump up to:a b c https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2022/214801Orig1s000ltr.pdf Archived 4 October 2022 at the Wayback Machine
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ “Lytgobi (Futibatinib) FDA Approval History”. Archived from the original on 4 October 2022. Retrieved 4 October 2022.
- ^ “FDA Approves Taiho’s Lytgobi (futibatinib) Tablets for Previously Treated, Unresectable, Locally Advanced or Metastatic Intrahepatic Cholangiocarcinoma” (Press release). Taiho Oncology. 30 September 2022. Archived from the original on 4 October 2022. Retrieved 4 October 2022 – via PR Newswire.
- ^ World Health Organization (2019). “International nonproprietary names for pharmaceutical substances (INN): recommended INN: list 81”. WHO Drug Information. 33 (1). hdl:10665/330896.
External links
- “Futibatinib”. Drug Information Portal. U.S. National Library of Medicine.
//////////Futibatinib, Lytgobi, FDA 2022, APPROVALS 2022, フチバチニブ , ANTINEOPLASTIC, TAS 120
C=CC(N1C[C@@H](N2N=C(C#CC3=CC(OC)=CC(OC)=C3)C4=C(N)N=CN=C42)CC1)=O

NEW DRUG APPROVALS
ONE TIME
$10.00
Lutetium (177Lu) chloride
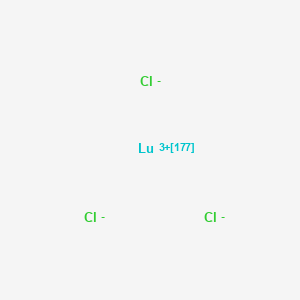
Lutetium (177Lu) chloride
塩化ルテチウム (177Lu)
| Formula | Lu. 3Cl |
|---|---|
| CAS | 16434-14-3 |
| Mol weight | 281.326 |
2022/9/15 EMA 2022, Illuzyce
EndolucinBeta
(177Lu)lutetium(3+) trichloride
| Diagnostic aid, Radioactive agent |
Lutetium 177 is an isotope of a rare-earth lanthanide metal lutetium. Radioactive decay of Lu 177 produces electrons with low energies making the isotope suitable for treatment of metastatic disease. A complex of Lu177 and somatostatin analog DOTA-TATE was approved by the FDA for the treatment of somatostatin receptor-positive gastroenteropancreatic neuroendocrine tumors, including foregut, midgut, and hindgut neuroendocrine tumors in adults. It is marketed under a tradename Lutathera. Lutetium in the complex with other carriers – phosphonates and monoclonal antibodies – was investigated in clinical trials as radiotherapy to prostate, ovarian, renal and other types of cancer.Lutetium (177Lu) chloride is a radioactive compound used for the radiolabeling of pharmaceutical molecules, aimed either as an anti-cancer therapy or for scintigraphy (medical imaging).[5][6] It is an isotopomer of lutetium(III) chloride containing the radioactive isotope 177Lu, which undergoes beta decay with a half-life of 6.65 days.
Medical uses
Lutetium (177Lu) chloride is a radiopharmaceutical precursor and is not intended for direct use in patients.[5] It is used for the radiolabeling of carrier molecules specifically developed for reaching certain target tissues or organs in the body. The molecules labeled in this way are used as cancer therapeutics or for scintigraphy, a form of medical imaging.[5] 177Lu has been used with both small molecule therapeutic agents (such as 177Lu-DOTATATE) and antibodies for targeted cancer therapy[8][9]
////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
| Clinical data | |
|---|---|
| Trade names | Lumark, EndolucinBeta, Illuzyce |
| AHFS/Drugs.com | Lumark UK Drug Information EndolucinBeta UK Drug Information |
| License data | EU EMA: by INN |
| Pregnancy category | AU: X (High risk)[1][2] |
| ATC code | None |
| Legal status | |
| Legal status | AU: Unscheduled [3][4]EU: Rx-only [5][6][7]In general: ℞ (Prescription only) |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 16434-14-3 |
| PubChem CID | 71587001 |
| DrugBank | DBSALT002634 |
| ChemSpider | 32700269 |
| UNII | 1U477369SN |
| KEGG | D10828 |
| CompTox Dashboard (EPA) | DTXSID20167745 |
| Chemical and physical data | |
| Formula | Cl3Lu |
| Molar mass | 281.32 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| hideSMILES[Cl-].[Cl-].[Cl-].[177Lu+3] |
Contraindications
Medicines radiolabeled with lutetium (177Lu) chloride must not be used in women unless pregnancy has been ruled out.[5]
Adverse effects
The most common side effects are anaemia (low red blood cell counts), thrombocytopenia (low blood platelet counts), leucopenia (low white blood cell counts), lymphopenia (low levels of lymphocytes, a particular type of white blood cell), nausea (feeling sick), vomiting and mild and temporary hair loss.[5]
Society and culture
Legal status
Lutetium (177Lu) chloride (Lumark) was approved for use in the European Union in June 2015.[5] Lutetium (177Lu) chloride (EndolucinBeta) was approved for use in the European Union in July 2016.[6]
On 21 July 2022, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) adopted a positive opinion, recommending the granting of a marketing authorization for the medicinal product Illuzyce, a radiopharmaceutical precursor.[10] Illuzyce is not intended for direct use in patients and must be used only for the radiolabelling of carrier medicines that have been specifically developed and authorized for radiolabelling with lutetium (177Lu) chloride.[10] The applicant for this medicinal product is Billev Pharma ApS.[10] Illuzyce was approved for medical use in the European Union in September 2022.[7]
References
- ^ “Lutetium (177Lu) Chloride”. Therapeutic Goods Administration (TGA). 21 January 2022. Archived from the original on 5 February 2022. Retrieved 5 February 2022.
- ^ “Updates to the Prescribing Medicines in Pregnancy database”. Therapeutic Goods Administration (TGA). 12 May 2022. Archived from the original on 3 April 2022. Retrieved 13 May 2022.
- ^ “TGA eBS – Product and Consumer Medicine Information Licence”. Archived from the original on 5 February 2022. Retrieved 5 February 2022.
- ^ http://www.ebs.tga.gov.au/servlet/xmlmillr6?dbid=ebs/PublicHTML/pdfStore.nsf&docid=1C7A40803A3A3F94CA2587D4003CE48A&agid=(PrintDetailsPublic)&actionid=1 Archived 30 July 2022 at the Wayback Machine[bare URL PDF]
- ^ Jump up to:a b c d e f g “Lumark EPAR”. European Medicines Agency (EMA). Archived from the original on 25 October 2020. Retrieved 7 May 2020. Text was copied from this source under the copyright of the European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ Jump up to:a b c “EndolucinBeta EPAR”. European Medicines Agency (EMA). Archived from the original on 28 October 2020. Retrieved 7 May 2020. Text was copied from this source under the copyright of the European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ Jump up to:a b “Illuzyce EPAR”. European Medicines Agency (EMA). 18 July 2022. Archived from the original on 22 September 2022. Retrieved 21 September 2022. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ Lundsten S, Spiegelberg D, Stenerlöw B, Nestor M (December 2019). “The HSP90 inhibitor onalespib potentiates 177Lu‑DOTATATE therapy in neuroendocrine tumor cells”. International Journal of Oncology. 55 (6): 1287–1295. doi:10.3892/ijo.2019.4888. PMC 6831206. PMID 31638190.
- ^ Michel RB, Andrews PM, Rosario AV, Goldenberg DM, Mattes MJ (April 2005). “177Lu-antibody conjugates for single-cell kill of B-lymphoma cells in vitro and for therapy of micrometastases in vivo”. Nuclear Medicine and Biology. 32 (3): 269–78. doi:10.1016/j.nucmedbio.2005.01.003. PMID 15820762.
- ^ Jump up to:a b c “Illuzyce: Pending EC decision”. European Medicines Agency. 21 July 2022. Archived from the original on 30 July 2022. Retrieved 30 July 2022. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
External links
- “Lutetium chloride Lu-177”. Drug Information Portal. U.S. National Library of Medicine.
.///////////Lutetium (177Lu) chloride, EMA 2022, EU 2022, APPROVALS 2022, Illuzyce, EndolucinBeta, 塩化ルテチウム (177Lu),

NEW DRUG APPROVALS
ONE TIME
$10.00

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....










