Vortioxetine
ボルチオキセチン 臭化水素酸塩
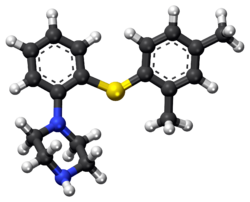
1-[2-(2,4-dimethylphenyl)sulfanylphenyl]piperazine
Lu AA21004
| VORTIOXETINE; CAS 508233-74-7;
1-(2-((2,4-Dimethylphenyl)thio)phenyl)piperazine; Lu AA21004; UNII-3O2K1S3WQV; C18H22N2S; |
| Molecular Formula: |
C18H22N2S |
| Molecular Weight: |
298.44568 g/mol |
Vortioxetine Hydrobromide

C18H22N2S.HBr : 379.36
[960203-27-4] HYDROBROMIDE
Vortioxetine is an atypical antipsychotic and antidepressant indicated for the treatment of major depressive disorder (MDD). It is classified as a serotonin modulator and simulator (SMS) as it has a multimodal mechanism of action towards the serotonin neurotransmitter system whereby it simultaneously modulates one or more serotonin receptors and inhibits the reuptake of serotonin. More specifically, vortioxetine acts via the following biological mechanisms: as a serotonin reuptake inhibitor (SRI) through inhibition of the serotonintransporter, as a partial agonist of the 5-HT1B receptor, an agonist of 5-HT1A, and an antagonist of the 5-HT3, 5-HT1D, and 5-HT7 receptors. SMSs were developed because there are many different subtypes of serotonin receptors, however, not all of these receptors appear to be involved in the antidepressant effects of SRIs. Some serotonin receptors seem to play a relatively neutral or insignificant role in the regulation of mood, but others, such as 5-HT1A autoreceptors and 5-HT7 receptors, appear to play an oppositional role in the efficacy of SRIs in treating depression.
Sept. 30, 2013 — The U.S. Food and Drug Administration today approved Brintellix (vortioxetine) to treat adults with major depressive disorder.
Major depressive disorder (MDD),
 Commonly referred to as depression, is a mental disorder characterized by mood changes and other symptoms that interfere with a person’s ability to work, sleep, study, eat and enjoy once-pleasurable activities. Episodes of depression often recur throughout a person’s lifetime, although some may experience a single occurrence.
Commonly referred to as depression, is a mental disorder characterized by mood changes and other symptoms that interfere with a person’s ability to work, sleep, study, eat and enjoy once-pleasurable activities. Episodes of depression often recur throughout a person’s lifetime, although some may experience a single occurrence.
READ ALL AT
http://www.drugs.com/newdrugs/fda-approves-brintellix-major-depressive-disorder-3918.html
Lu AA21004/vortioxetine
The disease: Major depression
The developers: Lundbeck, Takeda
Vortioxetine (vor-tye-OX-e-teen, code name Lu AA21004) is an experimental drug currently under development by Lundbeck and Takeda for the treatment of major depressive disorder (MDD) and generalized anxiety disorder (GAD).Commercial names chosen are Brintellix and Rexulti.
Regulatory approval for the treatment of MDD for the European market has been filed in September 2012, for the United States in October 2012, and filing for Canada should follow. Filing for the Japanese market is expected in 2013.
Depression
In May 22 2011, Lundbeck presented the results of four phase III trials on vortioxetine at the 2011 Annual Meeting of the American Psychiatric Association. A statistically significant effect was shown in two of the studies (one for active treatment using the Hamilton Depression Rating Scale (HAM-D), the second as a maintenance treatment), vortioxetine failed to prove superiority over placebo in a third (again using the HAM-D) and the fourth was nullified by an exceptionally high placebo response (according to the Montgomery-Åsberg Depression Rating Scale (MADRS)).
In July 2011, Lundbeck published the results of a double-blind, randomized, placebo-controlled clinical trial with venlafaxine as an active reference. It was found to be superior to placebo in treating MDD while having fewer side effects than venlafaxine. Similarly, in May 2012, Lundbeck published the results of a double-blind, randomized, placebo-controlled clinical trial with duloxetine evaluating vortioxetine in elderly depressed patients, and it was found superior to placebo, with fewer side effects than duloxetine.
In May 2012, Lundbeck disclosed the results of three phase III clinical trials, showing vortioxetine’s superiority over placebo according to the MADRS.
In August 2012, a randomized, double-blind trial confirms the superiority of vortioxetine over placebo according to all measures, excepted the Sheehan Disability scale.
In September 2012, a randomised, double-blind trial reveals that a dose of 5mg shows superiority over placebo only in patients that suffer from comorbid anxiety.This is consistent with results from another trial published in December 2012, demonstrating that 2.5 mg and 5 mg doses are ineffective.
Anxiety
August 2012, contradictory results of two randomized, double-blind trial were published. While the first demonstrated vortioxetine’s superiority over the placebo, the second showed that the drug had no efficacy, leading the authors to question the designs of the different trials.

United States Patent Number: 7,144,884 , 8,476,279
related to Chinese patent: CN1319958 C , CN1561336 A; CN1319958C, CN1561336A
patent validity: January 9, 2023 (U.S. Patent Number: 7,144,884), October 2, 2022 (U.S. Patent No.: 8,476,279)
peak annual sales (estimated): $ 2 billion
drug companies: Lundbeck (Lundbeck), Takeda (Takeda)
Wal antidepressant drug Paxil (Brintellix, Vortioxetine) for – 1 – Preparation – [2 – (2,4 methyl) phenyl] piperazine process
Method II:
815g of the NaOBut (8,48 mo1), 844 g of piperazine Qin (9,8 mol), 6,6 g of Pd (dba) 2 (11,48 mmol) and 13,6 g of rac-BINAP (21, 84 mmol) was stirred for 50 minutes with 4L ofbenzene. Then, 840 g 2 – bromo – iodobenzene (2,97 mol) and 1.5L of Yue added to the mixture with benzene, and the stirring was continued for 30 minutes. Finally, 390.8g of 2,4 -thiophenol (2,83 mol) was added together with 1.5L toluene. The resulting suspension was heated to reflux and reflux was continued for 5 hours. The reaction mixture was cooled overnight. 2L of water was added and stirred for l hour and then filtered through a filter aid, the resulting mixture. Then, the filtrate was washed with brine 3xlL. Subsequently, the combined aqueous phase extracted with 600ml of benzene. Then, Yue The combined benzene phase was heated to 70 ° C, then adding 329.2ml 48-wt. / HBr (aq.) and 164.6ml water o’s. The mixture was cooled to room temperature overnight. Final product was collected by filtration (l-[2 – (2,4 – di曱group – phenylsulfanyl) – phenyl] – piperazine hydrobromide Qin), and dried under vacuum (60 0 C), to give 895g of product (84% yield).
Method III:
The benzene is placed 500ml three-necked 1L round bottom flask equipped with a mechanical stirrer and add 809mg Pd2dba3 (0.88mmol; 0.5 mol%) and 952 mg DPEPhos (1.77 mmol; 0.5mol-%). The deep red solution was purged with nitrogen for 5 minutes, then add 100g2-bromo-iodobenzene (353 mmol) and 48.9 g 2,4 – bis thiophenol (353 mmol). Add 43.6g KOBut (389 mmol) caused an exothermic reaction, so that the temperature rise of 20 ° C 42 ° C, while forming a non-uniform mixture, and the color changed from deep red to orange / brown. The force of the suspension under nitrogen was heated to port 100 ° C. After only 20 minutes, HPLC showed complete conversion to have l-(2 – bromo – phenylsulfanyl) -2,4 – Yue group – benzene. The mixture was cooled to 40 ° C, was added to 600ml 15-wt% NaCl, and stirred for 5 minutes. The organic phase was separated, and the aqueous phase was washed 2xl00mwith benzene. The combined organic phase was washed with HCl (aq) NaCl and washed with 100ml 2M 100ml 15-wt%, and then Na 2 S04 dried by activated charcoal (10 g) at reflux for 15 minutes, filtered twice and evaporated to 107.3 g of orange-red oil (103%), the oil was found by HPLC purity of 98%.
To 90 g of the orange-red oil (307 mmol) in 500ml of anhydrous toluene was added 57 g boc-piperazine Qin (307 mmol), degassed with nitrogen for 5 minutes, was added 1.4g Pd2dba3 (1.53 mmol- %; 0.5 mol%) and 2.9g mc-BINAP (4.6 mmol; 1.5 mol-%), degassed and then another 2 minutes, then add 35.4 g of NaOtBu (368 mmol), and heated to 80 ° C for 18 hours. HPLC showed complete conversion to have the reaction mixture was cooled to RT, filtered, and the filter cake was washed with 2 x 100ml of曱benzene. % NaCl, washed twice in Na2S04 dried, added charcoal, refluxed for 30 minutes, filtered twice and evaporated to 140.7 g of a brown oil (4 – – The combined filtrates with 2 x 150ml 15 [2 – (2, 4 – di曱group – phenylsulfanyl) -. phenyl]-BOC-piperazine Qin). The resulting crude oil was dissolved in 300ml MeOH and 200ml 6MHCl (aq.) and refluxed for l hour, after which HPLC showed complete deprotection. After cooling to RT, the vacuum on a rotary evaporator to remove曱alcohol was added 20ml of concentrated NaOH (pH was measured to 13-14), after which the mixture with 1000ml EtOAc – 15 minutes from stirring. The organic phase was collected and dried 300ml 15wtQ /. Saline extraction in Na2S04 dried, and added 46.3 g of fumaric acid in 300mlMeOH (399 mmol) was added. The mixture was heated to reflux, cooled to room temperature and then placed in the tank (-18. C) overnight. The precipitate was collected, washed with 100ml and 100ml of acetone with EtOAc, and dried in vacuo (50 ° C), to give 103.2g of l-[2 – (2,4 – di group – phenylsulfanyl) – phenyl] – piperazine. Qin fumarate (249mmo1), as a white powder, overall yield 81%, determined by LC-MS and the purity was 99% fumarate. Use EtOAc/H20 / concentrated NaOH to the fumarate salt into the free base (l-[2 – (2,4 – dimethyl – phenylsulfanyl) – phenyl] – piperazine Qin), The organic phase was washed with brine, dried over Na 2 S04 sulfate, filtered and to the filtrate was added 34ml48-wto / o of HBr (aq.), to form a white solid precipitated. The solid was collected, and the solid was washed with 1000ml H20 boiling process, the resultant was cooled to room temperature and purified by forming a slurry. The final product was collected by filtration (l-[2 – (2,4 – digroup – phenylsulfanyl) – phenyl] – piperazine hydrobromide Qin Kr), and dried in vacuo (50 ° C), to produce 83g of white powder (total yield 71%).
Source:
1) Bang-Andersen B, Ruhland T, Jørgensen M, Smith G, Frederiksen K, Jensen KG, Zhong H, Nielsen SM, Hogg S, Mørk A, Stensbøl TB “Discovery of 1 -. [2 – (2,4 – dimethylphenylsulfanyl) phenyl] PIPERAZINE (Lu AA21004): a novel multimodal Major Compound for the treatment of depressive disorder. ” Journal of Medicinal Chemistry 54 (9): 3206-21.
2) Thomas Ruhland, Garrick Paul Smith, Benny Bang-Andersen, Ask Puschl, Ejner Knud Moltzen, Kim Andersen,; Phenyl-piperazine derivatives as serotonin reuptake inhibitors; US patent number 7144884 ; also published as CA2462110A1, CA2462110C , CN1319958C, CN1561336A, DE60225162D1, DE60225162T2, DE60233608D1, EP1436271A1, EP1436271B1, EP1749818A2, EP1749818A3, EP1749818B1, US7138407, US7148238, US7683053, US8110567, US8476279, US20050014740, US20060084662, US20060089368, US20070060574, US20110009423, US20120302553, WO2003029232A1; H. Lundbeck A / S;
T · Rouland, G · P · Smith, B · Bang – Anderson, A · Pi Shier, E · K · Moore Cen, K · Anderson; as serotonin reuptake inhibitors phenyl piperazine derivatives matter; CN 1319958 C
T · Rouland, G · P · Smith, B · Bang – Anderson, A · Pi Shier, E · K · Moore Cen, K · Anderson; as serotonin reuptake inhibitors phenyl piperazine derivatives; CN 1561336 A
3) Benny Bang-Andersen; Phenyl-piperazine derivatives as serotonin reuptake inhibitors; US patent number 8476279 B2 ; Also published as CA2462110A1, CA2462110C, CN1319958C, CN1561336A, DE60225162D1, DE60225162T2, DE60233608D1, EP1436271A1, EP1436271B1, EP1749818A2, EP1749818A3, EP1749818B1, US7138407, US7144884, US7148238, US7683053, US8110567, US20050014740, US20060084662, US20060089368, US20070060574, US20110009423, US20120302553, WO2003029232A1; H. Lundbeck A / S;
4) Kim Lasse Christensen; Process for the manufacture of 1 – [2 – (2,4-dimethyl-phenylsulfanyl)-phenyl]-piperazine; PCT application, WO2013102573 A1
5) Benny Bang-Andersen, Joergen Brodersen, Andre Faldt, Rene Holm, Morten Joergensen, De Diego Heidi Lopez, Michael J Mealy, Arne Moerk, Nicholas Moore, Lone Munch Ringgaard, Michael Harold Rock, Tine Bryan Stensboel; 1 – [2 – (2, 4-dimethylphenylsulfanyl)-phenyl] piperazine as a compound with combined serotonin reuptake, 5-ht3 and 5-ht1a activity for the treatment of cognitive impairment; WO2007144005 A1
Updated oct 2015…………….

Vortioxetine (vor-tye-oks-e-teen, trade name Trintellix) is an atypical antidepressant (a serotonin modulator and stimulator) made by Lundbeck and Takeda.[1]
Vortioxetine [1-[2-(2,4-Dimethylphenyl-sulfanyl)-phenyl]-piperazine] is an orally administered small molecule developed as once-daily treatment of major depressive disorder (MDD) and generalized anxiety disorder (GAD). As a drug, Vortioxetine is a bis-aryl-sulphanyl amine compound that combines serotonin (5-HT) reuptake inhibition with other characteristics, including receptor activity modulation.
Vortioxetine binds to the human serotonin (5-HT) transporter (SERT) with high affinity (Ki = 1.6 nM) and is a potent inhibitor of serotonin reuptake (IC50 = 5.4 nM), whereas its affinity for transporters of noradrenaline (Ki = 113 nM) and dopamine (Ki greater than 1000 nM) is much lower or negligible. The drug also has a broad receptor-binding profile, binding to the 5-HT1A receptor (Ki = 15 nM) where it acts as an agonist, the 5-HT1B receptor (Ki = 33 nM) where it acts as a partial agonist, and the 5-HT1D, 5-HT3 and 5-HT7 receptors (Ki = 54, 3.7 and 19 nM, respectively) where it displays antagonistic properties [1, 2].
Animal and in vitro studies indicate that several neurotransmitter systems may be impacted by vortioxetine, with the drug enhancing levels of 5-HT, noradrenaline, dopamine, acetylcholine and histamine in certain areas of the brain, as well as modulating γ-aminobutyric acid and glutamate neurotransmission. Results from additional animal models suggest vortioxetine may also improve measures of cognitive function, such as memory. In healthy volunteers, single or repeated administration of vortioxetine (10 mg) did not impair cognitive function, psychomotor performance or driving ability in a placebo-controlled study.
In September 2013, Vortioxetine was approved as Brintellix for the once-daily treatment of adults with MDD in the USA and one month later, EMA approved it as it first in line treatment for Europeans with MDD. It is marketed as Trintellix in Canada.
Vortioxetine was discovered by scientists at Lundbeck, where it was known as Lu AA21004. Takeda and Lundbeck entered into a strategic alliance to co-develop and co-commercialise vortioxetine and tedatioxetine in Japan and the USA in September 2007. The two companies will jointly complete product development, which will be funded primarily by Takeda, and the companies will share revenue generated in the USA and Japan.
Vortioxetine is administered orally at a starting dosage of 10 mg/day, with the dosage increased to 20 mg/day, as tolerated; 5 mg/ day may be considered if higher dosages are not tolerated. Dosages greater than 20 mg/day have not been assessed for efficacy or safety in controlled trials.
Medical use
Vortioxetine is used as first-line treatment for major depressive disorder.[1][2][3][4][5]
Pharmacokinetics
Vortioxetine reaches peak plasma concentration (Cmax) within 7 to 11 hours post-administration (Tmax), and its mean terminal half-life (t½) is ≈ 66 hours. Steady-state plasma concentrations are typically reached within two weeks.[1] It has no active metabolites (i.e. it is not a prodrug).[1]
Research
Vortioxetine has been studied in several clinical trials as a potential treatment for general anxiety disorder but results were inconsistent.[9][10]
History
Vortioxetine was discovered by scientists at Lundbeck who reported the rationale and synthesis for the drug (then called Lu AA21004) in a 2011 paper.[7][11]
In 2007, the compound was in Phase II clinical trials, and Lundbeck and Takeda entered into a partnership in which Takeda paid Lundbeck $40 million upfront, with promises of up to $345 million in milestone payments, and Takeda agreed to pay most of the remaining cost of developing the drug. The companies agreed to co-promote the drug in the US and Japan, and that Lundbeck would receive a royalty on all such sales. The deal included another drug candidate, tedatioxetine (Lu AA24530), and could be expanded to include two other Lundbeck compounds.[12]
Vortioxetine was approved by the U.S. FDA for the treatment of major depressive disorder (MDD) in adults in September, 2013,[13] and it was approved in Europe later that year.[14]
Vortioxetine was previously trademarked as Brintellix in the United States, but on May 2, 2016, the US FDA approved a name change to Trintellix in order to avoid confusion with the blood-thinning medication ticagrelor (Brilinta).[15]
WO2015155153, SYNTHESIS OF VORTIOXETINE VIA (2,4-DIMETHYLPHENYL)(2-IODOPHENYL)SULFANE INTERMEDIATE
Vortioxetine is disclosed as Example 1 e in WO 2003/029232 A1 and is described as being prepared analogously to Example 1 . The process used to prepare Example 1 involves the preparation of 1 -(2-((2-(trifluoromethyl)phenyl)thio)phenyl)piperazine on a solid polystyrene support, followed by decomplexation using visible light irradiation, and purification by preparative LC-MS and ion-exchange chromatography. The overall yield for the preparation of vortioxetine is described as 17%.
Several alternative palladium catalyzed processes for the preparation of vortioxetine are described in Examples 17 to 25 of WO 2007/144005 A1 . These processes describe the preparation of vortioxetine from 2,4-dimethylthiophenol and 2-bromoiodobenzene (or 1 ,2-dibromobenzene) starting materials via a 1 -(2-bromo-phenylsulfanyl)-2,4-dimethyl-benzene intermediate. Each of these processes involves the use of a palladium catalyst and a phosphine ligand.
The preparation of vortioxetine is also described by Bang-Andersen et al. in J. Med. Chem. (201 1 ), Vol. 54, 3206-3221 . Here, in a first step, te/t-butyl 4-(2-bromophenyl)piperazine-1 -carboxylate intermediate is prepared from Boc-piperazine and 2-bromoiodobenzene in a palladium catalyzed coupling reaction. te/t-Butyl 4-(2-bromophenyl)piperazine-1 -carboxylate is then reacted with 2,4-dimethylthiophenol, again in the presence of palladium catalyst and a phosphine ligand, to provide Boc-protected vortioxetine. In the final step, vortioxetine is deprotected using hydrochloric acid to give vortioxetine hydrochloride.
WO 2013/102573 A1 describes a reaction between 1 -halogen-2,4-dimethyl-phenyl, 2-halogen-thiophenol and an optionally protected piperazine in the presence of a base and a palladium catalyst consisting of a palladium source and a phosphine ligand.
Each of the above processes has disadvantages. The process described in WO 2003/029232 is low yielding and unsuitable for the large scale production of vortioxetine, whereas the processes described in WO 2007/144005 A1 , WO 2013/102573 A1 and by Bang-Andersen et al. require the use of expensive starting materials, palladium catalyst and phosphine ligand. In addition, the toxicity of palladium is well known, Liu et al. Toxicity of Palladium, Toxicology Letters, 4 (1979) 469-473, and the European Medicines Agency’ s Guideline on the Specification for Residues of Metal Catalysts sets clear limits on the permitted daily exposure to palladium arising from palladium residue within drug substances, http://www.ema.europa.eu. Thus it would be desirable to avoid the use of a palladium catalyst in the synthesis of vortioxetine and the subsequent purification steps required to remove palladium residue from the final pharmaceutical product.
The invention is described below in further detail by embodiments, without being limited thereto.
A general concept of the process of the present invention may be represented in Scheme 1 .

Scheme 1 : General representation of the basic synthetic concept of the present invention.
Scheme 2.

X = NH2: lb
Scheme 2: Representation of a particular synthetic embodiment of the present invention.
Compound III can also be prepared from 2,4-dimethylbenzenethiol (II) and 1 -fluoro-2-nitrobenzene (l”‘a) or 1 -chloro-2-nitrobenzene (l'”b). In the first step (2,4-dimethylphenyl)(2- nitrophenyl)sulfane (III’) is formed and in the second reaction step nitro group is reduced to ami

Z = F: l”‘a
Z = CI: l”‘b
Scheme 3: Representation of a particular synthetic embodiment of the present invention.
Example 7: Preparation of 1 -(2-((2,4-dimethylphenyl)thio)phenyl)piperazine vortioxetine, VII)

Mixture of (2,4-dimethylphenyl)(2-iodophenyl)sulfane V (0.34 g, 1 .0 mmol), piperazine VI (0.13 g, 1 .5 mmol), K3P03 (0.42 g, 2.0 mmol), Cul (19 mg, 0.1 mmol), and 2-phenylphenol (68 mg, 0.4 mmol) in dry and degassed DMSO (2 mL) was heated under nitrogen atmosphere at 120°C for 20 h. Water (10 mL) is then added and product is extracted to EtOAc (3 x 10 mL). Combined organic layers were washed with water (3 x 10 mL) and brine (2 x 10 mL) and dried over Na2S04. After evaporation of the solvent crude product is purified by chromatography to afford title compound: H NMR (CDCI3, 500 MHz) δ 1 .63 (br s, 1 H), 2.33 (s, 3H), 2.37 (s, 3H), 3.02-
3.09 (m, 8H), 6.52 (m, 1 H), 6.87 (m, 1 H), 7.04 (m, 1 H), 7.06-7.10 (m, 2H), 7.16 (m, 1 H), 7.39 (d, J= 7.8 Hz, 1 H); MS (ESI) m/z: 299 [MH]+.
Example 8: Preparation of 1 -(2-((2,4-dimethylphenyl)thio)phenyl)piperazine (vortioxetine, VII)

Mixture of (2,4-dimethylphenyl)(2-iodophenyl)sulfane V (0.34 g, 1 .0 mmol), piperazine VI (0.13 g, 1 .5 mmol), K3P03 (0.42 g, 2.0 mmol), Cul (19 mg, 0.1 mmol), and N,N-diethyl-2-hydroxybenzamide (39 mg, 0.2 mmol) in dry and degassed DMSO (2 mL) was heated under nitrogen atmosphere at 120 ^ for 20 h. Water (10 mL) is then added and product is extracted to EtOAc (3 x 10 mL). Combined organic layers were washed with water (3 x 10 mL) and brine (2 x 10 mL) and dried over Na2S04. After evaporation of the solvent crude product is purified by chromatography to afford title compound: H NMR (CDCI3, 500 MHz) δ 1 .63 (br s, 1 H), 2.33 (s, 3H), 2.37 (s, 3H), 3.02-3.09 (m, 8H), 6.52 (m, 1 H), 6.87 (m, 1 H), 7.04 (m, 1 H), 7.06-7.10 (m, 2H), 7.16 (m, 1 H), 7.39 (d, J= 7.8 Hz, 1 H); MS (ESI) m/z: 299 [MH]+.
Example 9: Preparation of 1 -(2-((2,4-dimethylphenyl)thio)phenyl)piperazine hydrobromide
(vortioxetine HBr, VII.HBr)

To a solution of vortioxetine VII (1 .80 g, 6.03 mmol) in iPrOAc (20 mL) at room temperature 48% HBr (0.68 mL, 6.03 mmol) was slowly added. Obtained mixture was stirred at room temperature for 1 h, white precipitate was then filtered off, washed with acetone (2 x 20 mL), and dried to afford title compound VII.HBr as a white powder (2.15 g, 94% yield): H NMR (DMSO-d6, 500 MHz) δ 2.23 (s, 3H), 2.32 (s, 3H), 3.15-3.27 (m, 8H), 6.40 (m, 1 H), 6.96 (m, 1 H), 7.08-7.17 (m, 3H), 7.24 (m, 1 H), 7.32 (d, J= 7.8 Hz, 1 H), 8.85 (br, 2H).
Reference Example 1 : Preparation of 1 -(2-((2,4-dimethylphenyl)thio)phenyl)piperazine
(vortioxetine, VII)

Mixture of piperazine (1 .0 g, 1 1 .6 mmol), NaOtBu (1 .37 g, 13.8 mmol), Pddba2 (40 mg, 0.07 mmol), and 1 ,3-bis(2,6-di-i-propylphenyl)imidazolium chloride (24 mg, 0,07 mmol) in dry and degassed toluene (10 mL) is stirred at room temperature for 1 h. (2,4-Dimethylphenyl)(2-iodophenyl)sulfane V (1 .32 g, 3.86 mmol) is then added, reaction mixture is heated to l OO’C and stirred for 24 h. After cooling to room temperature to the reaction mixture water (5 mL) and Celite (0.4 g) is added. After stirring for 20 min salts are filtered off, organic layer is separated, washed with brine (2 x 10 mL), dried over Na2S04 and solvent is evaporated to afford crude product, which is then purified by chromatography to afford title compound as yellowish crystals: H NMR (CDCI3, 500 MHz) δ 1 .63 (br s, 1 H), 2.33 (s, 3H), 2.37 (s, 3H),
Reference Example 2: Preparation of 1 -(2-((2,4-dimethylphenyl)thio)phenyl)piperazine
(vortioxetine, VII)

Mixture of piperazine (1 .29 g, 15.0 mmol), NaOtBu (1 .77 g, 17.8 mmol), Pddba2 (52 mg, 0.09 mmol), and rac-BINAP (93 mg, 0,15 mmol) in dry and degassed toluene (10 mL) was stirred at room temperature for 1 h. (2,4-Dimethylphenyl)(2-iodophenyl)sulfane V (1 .70 g, 5.0 mmol) was then added, reaction mixture was heated to 100°C and stirred for 24 h. After cooled to room temperature to the reaction mixture water (5 mL) and Celite (0.4 g) were added. After stirring for 20 min salts were filtered off, organic layer was separated, washed with brine (2 x 10 mL), dried over Na2S04 and solvent was evaporated to afford product as an orange oil (1 .41 g, 95% yield): H NMR (CDCI3, 500 MHz) δ 1 .63 (br s, 1 H), 2.33 (s, 3H), 2.37 (s, 3H), 3.02-3.09 (m, 8H), 6.52 (m, 1 H), 6.87 (m, 1 H), 7.04 (m, 1 H), 7.06-7.10 (m, 2H), 7.16 (m, 1 H), 7.39 (d, J = 7.8 Hz, 1 H); MS (ESI) m/z: 299 [MH]+.
Comparative Example 1 : Preparation of 1 -(2-((2,4-dimethylphenyl)thio)phenyl)piperazine
(vortioxetine, VII)

Mixture of (2,4-dimethylphenyl)(2-bromohenyl)sulfane V” (0.29 g, 1 .0 mmol), piperazine VI (0.13 g, 1 .5 mmol), K3P03 (0.42 g, 2.0 mmol), Cul (19 mg, 0.1 mmol), and 2-phenylphenol (68 mg, 0.4 mmol) in dry and degassed DMSO (2 mL) was heated under nitrogen atmosphere at 120°C for 20 h. Vortioxetine VII was not formed.
Comparative Example 2: Preparation of 1 -(2-((2,4-dimethylphenyl)thio)phenyl)piperazine
(vortioxetine, VII)

Mixture of (2,4-dimethylphenyl)(2-bromophenyl)sulfane V (0.29 g, 1 .0 mmol), piperazine VI (0.13 g, 1 .5 mmol), K3P03 (0.42 g, 2.0 mmol), Cul (19 mg, 0.1 mmol), and N,N-diethyl-2-hydroxybenzamide (39 mg, 0.2 mmol) in dry and degassed DMSO (2 mL) was heated under nitrogen atmosphere at 120 ^ for 20 h. Vortioxetine VII was not formed.
Vortioxetine Synthesis
WO2007144005A1: Industrial process
J Med Chem 2011, 54(9), 3206-3221: (also see Ref. 3; it has same details)
Identifications:
PAPER
Discovery of 1-[2-(2,4-Dimethylphenylsulfanyl)phenyl]piperazine (Lu AA21004): A Novel Multimodal Compound for the Treatment of Major Depressive Disorder
Benny Bang-Andersen*†, Thomas Ruhland†, Morten Jørgensen†, Garrick Smith†, Kristen Frederiksen†, Klaus Gjervig Jensen†, Huailing Zhong‡, Søren Møller Nielsen†, Sandra Hogg†, Arne Mørk†, and Tine Bryan Stensbøl†
† Neuroscience Drug Discovery Denmark, H. Lundbeck A/S, 9 Ottiliavej, DK-2500 Copenhagen-Valby, Denmark
‡ Lundbeck Research USA, 215 College Road, Paramus, New Jersey 07652-1431, United States
J. Med. Chem., 2011, 54 (9), pp 3206–3221
DOI: 10.1021/jm101459g

The synthesis and structure−activity relationship of a novel series of compounds with combined effects on 5-HT3A and 5-HT1A receptors and on the serotonin (5-HT) transporter (SERT) are described. Compound 5m (Lu AA21004) was the lead compound, displaying high affinity for recombinant human 5-HT1A (Ki = 15 nM), 5-HT1B (Ki = 33 nM), 5-HT3A (Ki = 3.7 nM), 5-HT7 (Ki = 19 nM), and noradrenergic β1 (Ki = 46 nM) receptors, and SERT (Ki = 1.6 nM). Compound 5mdisplayed antagonistic properties at 5-HT3A and 5-HT7 receptors, partial agonist properties at 5-HT1B receptors, agonistic properties at 5-HT1A receptors, and potent inhibition of SERT. In conscious rats, 5m significantly increased extracellular 5-HT levels in the brain after acute and 3 days of treatment. Following the 3-day treatment (5 or 10 (mg/kg)/day) SERT occupancies were only 43% and 57%, respectively. These characteristics indicate that 5m is a novel multimodal serotonergic compound, and 5m is currently in clinical development for major depressive disorder.
1-[2-(2,4-Dimethylphenylsulfanyl)phenyl]piperazine Hydrochloride (5m)
ALERT HYDROCHLORIDE DATA
5m was prepared according to general procedure 3 starting from intermediate 12m in a yield of 78%.
1H NMR (500 MHz, DMSO-d6) δ 9.39 (s, 2H), 7.33 (d, J = 7.7, 1H), 7.24 (s, 1H), 7.17−7.07 (m, 3H), 6.96 (dd, J = 7.6, 6.0, 1H), 6.41 (d, J = 7.8, 1H), 3.21 (broad s, 8H), 2.31 (s, 3H), 2.24 (s, 3H).
13C NMR (126 MHz, DMSO-d6) δ 148.22, 142.04, 139.68, 136.11, 133.74, 132.14, 128.46, 127.19, 126.40, 126.13, 125.46, 120.64, 48.47 (2C), 43.67 (2C), 21.10, 20.47.
HRMS calcd for C18H22N2S + H, 299.1576; found, 299.1584.
LC/MS (method 1): tR = 1.02 min, UV purity 97%, ELS purity 100%.
Anal. (C18H22N2S·HCl) C, H, N.
References
- US Label Last updated July 2014 after review in September, 2014. Versions of label are available at FDA index page Page accessed January 19, 2016
- [No authors listed] Vortioxetine. Aust Prescr. 2015 Jun;38(3):101-2. PMID 26648632Free full text
- “Relative efficacy and tolerability of vortioxetine versus selected antidepressants by indirect comparisons of similar clinical studies.”. Curr Med Res Opin 30: 2589–606. Oct 10, 2014. doi:10.1185/03007995.2014.969566. PMID 25249164.
- Köhler S, Cierpinsky K, Kronenberg G, Adli M. The serotonergic system in the neurobiology of depression: Relevance for novel antidepressants. J Psychopharmacol. 2016 Jan;30(1):13-22. PMID 26464458
- Kelliny M, Croarkin PE, Moore KM, Bobo WV. Profile of vortioxetine in the treatment of major depressive disorder: an overview of the primary and secondary literature. Ther Clin Risk Manag. 2015 Aug 12;11:1193-212. PMID 26316764 Free full text
- “Lundbeck’s “Serotonin Modulator and Stimulator” Lu AA21004: How Novel? How Good? – GLG News”.
- ^ Jump up to:a b c Bang-Andersen B, Ruhland T, Jørgensen M, et al. (May 2011). “Discovery of 1-[2-(2,4-dimethylphenylsulfanyl)phenyl]piperazine (Lu AA21004): a novel multimodal compound for the treatment of major depressive disorder”. Journal of Medicinal Chemistry 54 (9): 3206–21. doi:10.1021/jm101459g. PMID 21486038.
- N. Moore; B. Bang-Andersen; L. Brennum; K. Fredriksen; S. Hogg; A. Mork; T. Stensbol; H. Zhong; C. Sanchez; D. Smith (August 2008). “Lu AA21004: a novel potential treatment for mood disorders”. European Neuropsychopharmacology 18 (Supplement 4): S321.doi:10.1016/S0924-977X(08)70440-1.
- Pae CU et al. Vortioxetine, a multimodal antidepressant for generalized anxiety disorder: a systematic review and meta-analysis. J Psychiatr Res. 2015 May;64:88-98. PMID 25851751
- Reinhold JA, Rickels K. Pharmacological treatment for generalized anxiety disorder in adults: an update. Expert Opin Pharmacother. 2015;16(11):1669-81. PMID 26159446
- Sanchez C, Asin KE, Artigas F Vortioxetine, a novel antidepressant with multimodal activity: review of preclinical and clinical data. Pharmacol Ther. 2015 Jan;145:43-57. PMID 25016186 Free full text
- Daniel Beaulieu for First Word Pharma. September 5th, 2007 Lundbeck, Takeda enter strategic alliance for mood disorder, anxiety drugs
- FDA approves new drug to treat major depressive disorder, U.S. Food and Drug Administration Press Announcement.
- EMA Brintellix page at EMA site Page accessed January 19, 2016
- Commissioner, Office of the. “Safety Alerts for Human Medical Products – Brintellix (vortioxetine): Drug Safety Communication – Brand Name Change to Trintellix, to Avoid Confusion With Antiplatelet Drug Brilinta (ticagrelor)”. http://www.fda.gov. Retrieved2016-05-02.
References:
1. Gibb, A.; et. al. Vortioxetine: first global approval. Drugs 2014, 74(1), 135-145.
2. Bang-Andersen, B.; et. al. Discovery of 1-[2-(2,4-dimethylphenylsulfanyl)phenyl]piperazine (Lu AA21004): a novel multimodal compound for the treatment of major depressive disorder. J Med Chem 2011, 54(9), 3206-3221.
3. Bang-Andersen, B.; et. al. 1-[2-(2,4-dimethylphenylsulfanyl)-phenyl] piperazine as a compound with combined serotonin reuptake, 5-ht3 and 5-ht1a activity for the treatment of cognitive impairmentWO2007144005A1
| Patent ID |
Date |
Patent Title |
| US7683053 |
2010-03-23 |
PHENYL-PIPERAZINE DERIVATIVES AS SEROTONIN REUPTAKE INHIBITORS |
| US7148238 |
2006-12-12 |
Phenyl-piperazine derivatives as serotonin reuptake inhibitors |
| US7144884 |
2006-12-05 |
Phenyl-piperazine derivatives as serotonin reuptake inhibitors |
| US7138407 |
2006-11-21 |
Phenyl-piperazine derivatives as serotonin reuptake inhibitors |
| Patent ID |
Date |
Patent Title |
| US2013184291 |
2013-07-18 |
THERAPEUTIC USES OF 1-[2-(2,4-DIMETHYL-PHENYLSUFLANYL)PHENYL]PIPERAZINE |
| US8476279 |
2013-07-02 |
Phenyl-piperazine derivatives as serotonin reuptake inhibitors |
| US2013115292 |
2013-05-09 |
ENTERIC TABLET |
| US2012189697 |
2012-07-26 |
COMPOSITIONS OF 1-[2-(2,4-DIMETHYL-PHENYLSULFANYL)-PHENYL]PIPERAZINE |
| US2012035188 |
2012-02-09 |
LIQUID FORMULATIONS OF SALTS OF 1-[2-(2,4-DIMETHYLPHENYLSULFANYL)PHENYL]-PIPERAZINE |
| US8110567 |
2012-02-07 |
PHENYL-PIPERAZINE DERIVATIVES AS SEROTONIN REUPTAKE INHIBITORS |
| US2012004409 |
2012-01-05 |
Purification of 1-[2-(2,4-dimethylphenylsulfanyl)phenyl]piperazine |
| US2011201617 |
2011-08-18 |
Therapeutic Uses Of Compounds Having Combined SERT, 5-HT3 And 5-HT1A Activity |
| US2011009422 |
2011-01-13 |
1- [2-(2,4-DIMETHYLPHENYLSULFANYL)-PHENYL] PIPERAZINE AS A COMPOUND WITH COMBINED SEROTONIN REUPTAKE, 5-HT3 AND 5-HT1A ACTIVITY FOR THE TREATMENT OF PAIN OR RESIDUAL SYMPTOMS IN DEPRESSION RELATING TO SLEEP AND COGNITION |
| US2010297240 |
2010-11-25 |
1- [2- (2,4-DIMETHYLPHENYLSULFANYL)-PHENYL] PIPERAZINE AS A COMPOUND WITH COMBINED SEROTONIN REUPTAKE, 5-HT3 AND 5-HT1A ACTIVITY FOR THE TREATMENT OF COGNITIVE IMPAIRMENT |
| Patent ID |
Date |
Patent Title |
| US2015094316 |
2015-04-02 |
LIQUID FORMULATIONS OF SALTS OF 1-[2-(2,4-DIMETHYLPHENYLSULFANYL)PHENYL]PIPERAZINE |
| US8969355 |
2015-03-03 |
1-[2-(2,4 dimethylphenylsulfanyl)-phenyl]piperazine as a compound with combined serotonin reuptake, 5-HT3 and 5-HT1a activity for the treatment of cognitive impairment |
| US2015005318 |
2015-01-01 |
1-[2-(2,4-Dimethylphenylsulfanyl)-Phenyl]Piperazine As A Compound With Combined Serotonin Reuptake, 5-HT3 And 5-HT1a Activity For The Treatment Of Cognitive Impairment |
| US2014371453 |
2014-12-18 |
1-[2-(2,4-Dimethylphenylsulfanyl)-Phenyl]Piperazine As A Compound With Combined Serotonin Reuptake, 5-HT3 And 5-HT1a Activity For The Treatment Of Cognitive Impairment |
| US2014343287 |
2014-11-20 |
Process for the Manufacture of 1-[2-(2,4-Dimethyl-Phenylsulfanyl)-Phenyl]-Piperazine |
| US2014315921 |
2014-10-23 |
1-[2-(2,4-Dimethylphenylsulfanyl)-Phenyl]Piperazine As A Compound With Combined Serotonin Reuptake, 5-HT3 And 5-HT1a Activity For The Treatment Of Cognitive Impairment |
| US2014256943 |
2014-09-11 |
1-[2-(2,4-Dimethylphenylsulfanyl)-Phenyl]Piperazine As A Compound With Combined Serotonin Reuptake, 5-HT3 And 5-HT1a Activity For The Treatment Of Cognitive Impairment |
| US2014248355 |
2014-09-04 |
1-[2-(2,4-Dimethylphenylsulfanyl)-Phenyl]Piperazine As A Compound With Combined Serotonin Reuptake, 5-HT3 And 5-HT1a Activity For The Treatment Of Cognitive Impairment |
| US2014248356 |
2014-09-04 |
1-[2-(2,4-Dimethylphenylsulfanyl)-Phenyl]Piperazine As A Compound With Combined Serotonin Reuptake, 5-HT3 And 5-HT1a Activity For The Treatment Of Cognitive Impairment |
| US2014163043 |
2014-06-12 |
PHENYL-PIPERAZINE DERIVATIVES AS SEROTONIN REUPTAKE INHIBITORS |
| Patent ID |
Date |
Patent Title |
| US2016083359 |
2016-03-24 |
1-[2-(2,4-DIMETHYLPHENYLSULFANYL)-PHENYL]PIPERAZINE AS A COMPOUND With COMBINED SEROTONIN REUPTAKE, 5-HT3 AND 5-HT1A ACTIVITY FOR THE TREATMENT OF COGNITIVE IMPAIRMENT |
| US2016060215 |
2016-03-03 |
New Process For The Synthesis Of 1-(2-((2,4-Dimethylphenyl)Thio)Phenyl)Piperazine |
| US2016015706 |
2016-01-21 |
CRYSTALLINE FORMS OF AN ANTIDEPRESSANT COMPOUND |
| US2016009670 |
2016-01-14 |
VORTIOXETINE MANUFACTURING PROCESS |
| US9211288 |
2015-12-15 |
Compositions comprising vortioxetine and donepezil |
| US2015297585 |
2015-10-22 |
COMPOSITIONS COMPRISING VORTIOXETINE AND DONEPEZIL |
| US2015266841 |
2015-09-24 |
Novel Crystalline Form Of Vortioxetine Hydrobromide |
| US2015150867 |
2015-06-04 |
COMPOSITIONS OF 1-[2-(2,4-DIMETHYL-PHENYLSULFANYL)-PHENYL]PIPERAZINE |
| US2015110873 |
2015-04-23 |
ENTERIC TABLET |
| US2015094316 |
2015-04-02 |
LIQUID FORMULATIONS OF SALTS OF 1-[2-(2,4-DIMETHYLPHENYLSULFANYL)PHENYL]PIPERAZINE |
/////////////
-
CC(C=C(C)C=C1)=C1SC2=C(N3CCNCC3)C=CC=C2


 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....












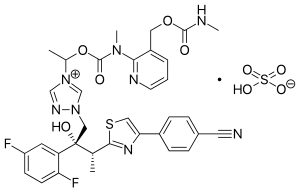
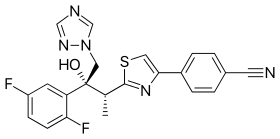
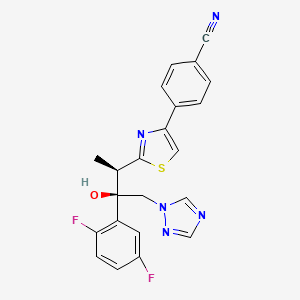 ISAVUCONAZOLE
ISAVUCONAZOLE









































 DACLIZUMAB,
DACLIZUMAB,