Home » Posts tagged 'CANCER' (Page 10)
Tag Archives: CANCER
Garden Cress Extract Kills 97% of Breast Cancer Cells in Vitro

Garden Cress Extract Kills 97% of Breast Cancer Cells in Vitro: Garden cress, like broccoli, is a cruciferous-family vegetable but is unique because it contains very high amounts of BITC (benzyl isothiocyanate) which has emerged as a powerful anti-cancer compound. In this study, BITC was seen to kill 97% of ER- breastcancer cells (MDA-MB-231) after 24 hours of treatment. For comparison, the same dose of sulforaphane from broccoli killed only 75% of the cancer cells.

In other research, BITC has been found to slow the rate of breast cancer metastasizing by 86% and when given to mice, resulted in breast tumors 53% smaller than in untreated mice. BITC is now being intensively studied for a variety of cancers and has been shown in lab studies to be active against melanoma, glioma, prostate cancer, lung cancer, ovarian cancer, pancreatic cancer and others. Garden cress is one of the best sources of BITC. Other good sources include cabbage, Indian cress, Japanese radish (in particular Karami daikon) and, quite surprisingly, papaya seeds. As with othercruciferous vegetables, the best way to eat cress is raw in order to maximize the delivery of BITC.
http://www.ncbi.nlm.nih.gov/pubmed/17121941
http://extension.usu.edu/files/publications/publication/HG_Garden_2006-05.pdf
and
http://nopr.niscair.res.in/bitstream/123456789/12732/1/IJNPR%202(3)%20292-297.pdf
BITC

Botanical name: Lepidium sativum L.
Family: Brassicaceae = Cruciferae
Common names. English: cress, common cress, garden cress, land cress, pepper cress; Spanish: mastuerzo, mastuerzo hortense, lepidio, berro de jardín (Spain), berro de sierra, berro hortense (Argentina), escobilla (Costa Rica); Catalan: morritort, morrisà, Portuguese and Galician: masturco, mastruco, agrião-mouro, herba do esforzo; Portuguese: mastruco do Sul, agrião (Brazil); Basque: buminka, beatzecrexu
Synonyms/Common Names/Related Substances:
- Alpha-linolenic acid (ALA), agrião (Portuguese), agrião-mouro (Portuguese, Galician), beatzecrexu (Basque), berro de jardín (Spanish), berro de tierra (Spanish), berro hortense (Spanish), benzyl isothiocyanate (BITC), Brassicaceae (family), bran, buminka (Basque), common cress, cress, docosahexaenoic acid (DHA), eicosapentaenoic acid (EPA), escobilla (Spanish), endosperm, fiber, garden cress seed oil (GCO), garden pepper grass, glucosinolates, glutamic acid, herba do esforzo (Portuguese, Galician), hurf (Arabic), indoles, isothiocyanates, kardamon (Greek), land cress, linoleic acid (LA), lectin, lepidio (Spanish), Lepidium sativium, Lepidium sativum, leucine, mastruco (Portuguese, Galician), mastruco do sul (Portuguese), mastuerzo (Spanish), mastuerzo hortense (Spanish), methanol, morrisá (Catalan), morritort (Catalan), nasturtium (Latin), nasum torcere (Latin), omega-3 fatty acid, pepper cress, pepper grass, pepperwort, sulforaphane, tuffa’ (Arabic), turehtezuk (Persian), water cress, whole meal.
- Combination product example: SulforaWhite (a liposomal preparation that contains Lepidium sativum sprout extract, glycerin, lecithin, phenoxyethanol, and water).
Garden cress [commonly known as aliv in Marathi or halim in Hindi] is a green, cool-season perennial plant used as a leafy vegetable, typically used as a garnish. Undisturbed, the plant can grow to a height of two feet with minimal maintenance. When mature, garden cress produces white or light-pink flowers, and small seed pods. It has long leaves at the bottom of the stem and small, bright-green, feather-like leaves arranged on opposite sides of its stalks at the top.
Garden Cress, also called Pepper Wort, is an herb that is botanically known as Lepidium Sativum. It is referred to as ‘Aliv’ in Marathi and ‘Halim’ in Hindi. Belonging to the family Cruciferae, it is grown in all parts of India and is often used in the Indian cuisine. The leaves, roots, as well as seeds of this plant are used in cooking as they are extremely nutritious and also therapeutic in nature. The flowers of this plant are either white or light-pink in color.
This herb is the best source of iron and is hence recommended in the treatment of iron-deficiency anemia. It is also rich in folate, calcium, ascorbic acid, tocopherol, and beta-carotene. Garden Cress seeds are loaded with not just protein, but also linoleic and arachidic fatty acids. Since they contain phytochemicals that mimic estrogen to some extent, intake of these seeds is known to regulate menstruation and stimulate milk production in lactating mothers. That is precisely why women are given foods containing Garden Cress following childbirth.
The blood-purifying as well as antioxidant properties of this amazing plant are well documented. Hence, its regular consumption can greatly help to boost one’s immunity and prevent a gamut of diseases. It acts as a general tonic and can also help to increase the libido naturally. Since the testae of these seeds contain mucilage, they are invaluable in the management of both dysentery and constipation. The whole plant, along with its seeds, is said to be good for the eyes too. Hence, it is advisable to add it raw to salads, sandwiches, and chutneys, or to simply use it as a garnish along with coriander leaves for any food item.
Pregnant women should avoid taking Garden Cress in any form because it has the ability to induce uterine contractions and thereby trigger a spontaneous abortion. Also, since it is goitrogenic in nature, it may not be suitable for patients suffering from hypothyroidism. The oil derived from Garden Cress seeds is edible and can therefore be used as a cooking medium; however, some people may experience symptoms of indigestion due to its use. Such individuals should discontinue using this oil or mix it with some other edible oil, so as to dilute it and reduce its adverse effects.
Cress (Lepidium sativum), sometimes referred to as garden cress to distinguish it from similar plants also referred to as cress, is a rather fast-growing, edible herb. Garden cress is genetically related to watercress and mustard, sharing their peppery, tangy flavor and aroma. In some regions, garden cress is known as mustard and cress, garden pepper cress, pepperwort pepper grass, or poor man’s pepper.[1][2]
This annual plant can reach a height of 60 cm (~24 inches), with many branches on the upper part. The white to pinkish flowers are only 2 mm (1/12 of an inch) across, clustered in branched racemes.[3][4]
Origin of the name
Cultivation of this species, which is native to Southwest Asia (perhaps Persia) and which spread many centuries ago to western Europe, is very old, as is shown by the philological trace of its names in different Indo-European languages. These include the Persian word turehtezuk, the Greek kardamon, the Latin nasturtium and Arabic tuffa’ and hurf. In some languages there is a degree of confusion with watercress. It seems that the meaning of the word nasturtium (nasum torcere, because its smell causes the nose to turn up) must have been applied initially to garden cress, as both Pliny and Isidoro de Sevilla explain. The confusion remains with the terms used by the Hispano-Arabs. The word hurf is applied without distinction to watercress and garden cress (several species certainly of up to three different genera: Nasturtium, Lepidium and Cardaria). Thus the medieval agronomists of Andalusia went as far as differentiating between several hurf, such as hurf abyad, hurf babili, hurf madani….
Garden cress in agriculture
Garden cress is commercially grown in England, France, the Netherlands and Scandinavia.[5]
Cultivation of garden cress is practical on both mass scales and on the individual scale. Garden cress is suitable for hydroponic cultivation and thrives in slightly alkaline water. In many local markets, the demand for hydroponically grown cress can exceed available supply, partially because cress leaves are not suitable for distribution in dried form, so can be only partially preserved. Consumers commonly acquire cress as seeds or (in Europe) from markets as boxes of young live shoots.[5]
Edible shoots are typically harvested in one to two weeks after planting, when they are 5–13 cm (2 – 5 inches) tall.[6]
Properties, uses and cultivation
Xenophon (400 BC) mentions that the Persians used to eat this plant even before bread was known. It was also familiar to the Egyptians and was very much appreciated by the Greeks and Romans, who were very fond of banquets rich in spices and spicy salads. Columela (first century) makes direct reference to the cultivation of garden cress. In Los doce libros de Agricultura, he writes: ” …immediately after the calends of January, garden cress is sown out… when you have transplanted it before the calends of March, you will be able to harvest it like chives, but less often… it must not be cut after the calends of November because it dies from frosts, but can resist for two years if it is hoed and manured carefully… there are also many sites where it lives for up to ten years” (Book XI). The latter statements seem to indicate that he is also speaking of the perennial species L. Iatifolium, as L. sativum is an annual.
Almost all of the Andalusian agronomists of the Middle Ages (Ibn Hayyay, Ibn Wafid, Ibn al-Baytar, Ibn Luyun, Ibn al-Awwam) and many of the doctors, such as Maimonides, mention garden cress. Ibn al-Awwam also includes references from Abu al-Jair, Abu Abdalah as well as from Nabataean agriculture and, among other comments, he says: “Garden cress is sown between February and April (in January in Seville). It has small seeds which are mixed with earth for sowing to prevent the wind carrying them away…. It is harvested in May and is grown between ridges, in combination/conjunction with flax cultivation.”
Many of the authors of the old oriental and Mediterranean cultures emphasized the medicinal properties of cress, especially as an antiscorbutic, depurative and stimulant. Columela notes its vermifugal powers. Ibn al-Awwam refers to certain apparently antihistaminic properties, since it was used against insect bites and also as an insect repellent, in the form of a fumigant. It was perhaps Ibn al-Baytar, an Andalusian botanist (eighth century), who collected most information on its properties, summarizing the opinions of other authors such as El Farcy, who says that it incites coitus and stimulates the appetite; Ibn Massa, according to whom it dissipates colic and gets rid of tapeworms and other intestinal worms; or Ibn Massouih, who mentions that it eliminates viscous humours. Ibn al-Baytar also says that it is administered against leprosy, is useful for renal “cooling” and that, if hair is washed with garden cress water, it is “purified” and any loss is arrested.
In Iran and Morocco, the seeds are used as an aphrodisiac. In former Abyssinia, an edible oil was obtained from the seeds. In Eritrea, it was used as a dyestuff plant. Some Arab scholars have attributed garden cress’s reputation among Muslims to the fact that it was directly recommended by the Prophet.
Garden cress’s main use was always as an aromatic and slightly pungent plant. Not only in antiquity but also in the Middle Ages it enjoyed considerable prestige on royal tables. The young leaves were used for salads. The ancient Spartans ate them with bread. This use still continues and they are also eaten with bread and butter or with bread to which lemon, vinegar or sugar is added. However, it is mainly used nowadays in the seedling stage, the succulent hypocotyls being added to salads and as a garnish and decoration for dishes.
The roots, seeds and leaves have been used as a spicy condiment. Columela explains how oxygala, a type of curd cheese with herbs, was prepared: “Some people, after collecting cultivated or even wild garden cress, dry it in the shade and then, after removing the stem, add its leaves to brine, squeezing them and placing them in milk without any other seasoning, and adding the amount of salt they consider sufficient…. Others mix fresh leaves of cultivated cress with sweetened milk in a pot…”.
L. Iatifolium L. stands out for its horticultural interest; although it grows spontaneously on the edges of rivers and lakes, it is also occasionally grown in the same way as L. sativum. Its young leaves can be used for salads; the ancient Greeks and Romans used to grow it for this purpose. Its leaves and seeds were also used as a spicy condiment. Several sauces are prepared with its leaves, including in particular the bitter sauce of the paschal lamb of the Jews. The seeds of this species were known in England as the poor people’s pepper. The roots have been used on occasion as a substitute for radish.
In the fifteenth century, we know through Alonso de Herrera that garden cress was one of the vegetables most widely eaten in Castile. During the sixteenth century, obstinate attempts were made to introduce it into America. Right up to the beginning of the nineteenth century, its cultivation in Spain continued to be important, since Boutelou and Boutelou (1801) deal specifically with this crop in their Tratado de la huerta, commenting on the existence of several cultivars. At present, the cultivation of cress is very occasional in countries such as Spain and France. Water cress, in competition with garden cress, has eclipsed the cultivation of the latter. However, this is not the case in other central European countries or the United Kingdom, where its use is normal and the system of cultivation has changed substantially.
Botanical description
Cress is an annual, erect herbaceous plant, growing up to 50 cm. The basal leaves have long petioles and are lyrate-pinnatipartite; the caulinar leaves are laciniate-pinnate while the upper leaves are entire. The inflorescences are in dense racemes. The flowers have white or slightly pink petals, measuring 2 mm. The siliquae measure 5 to 6 x 4 mm, are elliptical, elate from the upper half, and glabrous. Cress flowers in the wild state between March and June.
It is an allogamous plant with self-compatible and self-incompatible forms and with various degrees of tolerance to prolonged autogamy. There are diploid forms, 2n = 2x = 16, and tetraploid forms, 2n = 4x =32. A degree of variability is noted in the character of the basal leaves which are cleft or split to a greater or lesser degree, a character which is controlled by a single incompletely dominant gene.
Ecology and phytogeography
Cress is a plant that is well suited to all soils and climates, although it does not tolerate frosts. In temperate conditions, it has a very rapid growth rate. It grows subspontaneously in areas transformed by humans, close to crops or human settlements. It appears in this way on the Iberian peninsula, mainly in the eastern regions.
Wild cress extends from the Sudan to the Himalayas. Most authors consider it to be a native of western Asia, whence it passed very quickly to Europe and the rest of Asia as a secondary crop, probably associated with cultivars of flax. Vavilov considers its main centre to be Ethiopia, where he found the widest variability; the Near East, central Asia and the Mediterranean are considered secondary centres. It is now naturalized in numerous parts of Europe, including the British Isles.
Cress in cookery
Genetic diversity
The genus Lepidium is made up of about 150 species, distributed throughout almost all temperate and subtropical regions of the world. On the Iberian peninsula and the Balearic Islands, at least 20 species or subspecies exist among the autochthonous and allochthonous taxa, some genetically close to L. sativum. Seven of them are exclusively endemic to the peninsula or, at the very most, are common with North Africa. Other close species are L. campestre (L.) R. Br. and L. ruderale L. which also have edible leaves. The leaves of L. campestre are used to prepare excellent sauces for fish.
Common cress (L. sativum L.), with regard to the anatomy of the leaf, stem and root, has been divided into three botanical varieties: vulgare, crispum and latifolium. The latter is the most mesomorphic, crispum the most xeromorphic and vulgare intermediate.
At present, most of the studies on the variability and development of new cultivars are being carried out in liaison with the VIR of St Petersburg, where there is a good collection of material. Of the 350 forms of garden cress studied in the Ukraine, Uzkolistnyti 3 was the best, being highly productive and of good quality. It is being used as the basis of improvement programmes, as it appreciably surpasses the best Soviet varieties in production and quality. Other cultivars well suited to European Russia are Tuikers Grootbladige (broad-leaved) and the lines Mestnyi k 137, k 106 and k 115. Of the types most cultivated in Europe, Early European, Eastern, Dagestan and Entire Leaved stand out, being distinguished by the length and shape of the leaf, earliness and susceptibility to cold. In Western Europe, one broad leaved type is especially appreciated (Broad Leaved French) as are curly types (Curly Leaved), the latter being used extensively to garnish dishes. In Africa, there are red, white and black varieties.
This crop is also arousing interest in Japan, and collecting expeditions to Nepal have been organized. Some specimens collected during an expedition to Iraq in 1986 are now stored in Abu Ghraib and in Gratersleben, Germany. There are also small collections of L. sativum in the PGRC in Addis Ababa (Ethiopia), at the ARARI of Izmir in Turkey and in Bari, Italy. At the Universidad Politécnica de Madrid there are accessions of 20 species of Lepidium, while the BGV of the Córdoba Botanical Garden keeps germplasm of the southern Iberian species of the genus.
| Nutritional value per 100 g (3.5 oz) | |
|---|---|
| Energy | 134 kJ (32 kcal) |
| Carbohydrates | 5.5 g |
| – Sugars | 4.4 g |
| – Dietary fiber | 1.1 g |
| Protein | 2.6 g |
| Vitamin A equiv. | 346 μg (43%) |
| – beta-carotene | 4150 μg (38%) |
| – lutein and zeaxanthin | 12500 μg |
| Thiamine (vit. B1) | 0.08 mg (7%) |
| Riboflavin (vit. B2) | 0.26 mg (22%) |
| Niacin (vit. B3) | 1 mg (7%) |
| Pantothenic acid (B5) | 0.247 mg (5%) |
| Vitamin B6 | 0.247 mg (19%) |
| Folate (vit. B9) | 80 μg (20%) |
| Vitamin C | 69 mg (83%) |
| Vitamin E | 0.7 mg (5%) |
| Vitamin K | 541.9 μg (516%) |
| Calcium | 81 mg (8%) |
| Iron | 1.3 mg (10%) |
| Magnesium | 38 mg (11%) |
| Manganese | 0.553 mg (26%) |
| Phosphorus | 76 mg (11%) |
| Potassium | 606 mg (13%) |
| Link to USDA Database entry Percentages are roughly approximated using US recommendations for adults. Source: USDA Nutrient Database |
|
Garden cress is added to soups, sandwiches and salads for its tangy flavor.[6] It is also eaten as sprouts, and the fresh or dried seed pods can be used as a peppery seasoning (haloon).[5] In England, cut cress shoots are commonly used in sandwiches with boiled eggs, mayonnaise and salt.

Garden cress can grow almost anywhere.
Nutrition profile
Garden cress is an important source of iron, folic acid, calcium, vitamins C, E and A. The seed contains arachidic and linoleic fatty acids. The seeds are high in calories and protein, whereas the leaves are an excellent source of vitamin A, C and folate.
| Energy | 30 Kcal |
| Carbohydrates | 5.5 g |
| Dietary fibre | 1.1 g |
| Protein | 2.6 g |
| Fat | 0.7 g |
| Vitamin A | 346 mcg |
| Folate | 80 mcg |
| Vitamin C | 69 mg |
| Calcium | 81 mg |
| Iron | 1.3 mg |

Both the leaves and stems of cress can be eaten raw in salads or sandwiches, and are sometimes called cress sprouts. When buying cress, look for firm, evenly coloured, rich green leaves. Avoid cress with any signs of slime, wilting, or discoloration. If stored in plastic, it can last up to five days in a refrigerator. To prolong the life of cress, place the stems in a glass container with water and cover them, refrigerating the cress until it is needed.
Cultivation practices
Cress is an easily grown plant with few requirements. It can be broadcast after the winter frosts or throughout the year in temperate climates. However, Boutelou and Boutelou (1801) were already recommending sowing in shallow furrows, which enables surplus plants to be thinned out and facilitates hoeing. Sowing has to be repeated every 15 to 20 days so that there is no shortage of young shoots and new leaves for salads – the leaves of earlier sowings begin to get tough and are no longer usable. The seed sprouts four or six days after sowing, depending on the season, and the leaves are ready for consumption after two or three weeks.
The usual form of cultivation continues to be as described, with 15 to 20 cm between rows and the use of irrigation in the summer, since they are lightly rooted seedlings which can dry up in a few days. Its growth is very rapid and harvesting can begin in the same month as sowing, with yields reaching 6 tonnes per hectare.
Health benefits of garden cress
For women’s health
Emenagogue: Garden cress has mild oestrogenic properties. It helps to regulate the menstrual cycle.
Galactogogue: Kheer made of garden cress seeds increases milk production and secretion in lactating mothers. Because of its high iron and protein content, it is often given post-partum to lactating mothers.
Aphrodisiac: Garden cress helps to improve libido.
For the gastro intestinal tract
Garden cress helps purify blood and stimulate appetite. It is used during constipation as a laxative and a purgative. Paste made of the seeds can be taken internally with honey to treat amoebic dysentery. The mucilage of the germinating seeds allays the irritation of the intestines in dysentery and diarrhoea. Garden cress crushed and drunk with hot water is beneficial to treat colic especially in infants.
For the respiratory tract
Garden cress seeds are good expectorants and when chewed they treat sore throat, cough, asthma and headache. The aerial parts are used in the treatment of asthma and cough.
For anaemia
Garden cress seeds being the richest source of non-haeme iron [iron found in haemoglobin which is an easily absorbed dietary iron.] help to increase the haemoglobin levels. When taken regularly, it helps to alleviate anaemia. It is advisable to have vitamin C half an hour after consumption of these seeds as it enhances iron absorption.

For diabetes
The seed coat of germinating seeds contains mucilage, which has a phytochemical called lepidimoide. Studies show that seeds of the plant lower the glycemic response to a test meal.
note sodium 2-O-rhamnopyranosyl-4-deoxy-threo-hex-4-enopyranosiduronate (designated lepidimoide)
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1075667/
epi-Lepidimoide
Sodium 6-deoxy-2-O-(4-deoxy-β-L-threo-hex-4-enopyranuronosyl)-α-L-glucopyranose
 cas 145039-76-5 and 157676-09-0
cas 145039-76-5 and 157676-09-0
The total synthesis of the unsaturated disaccharide, lepidimoide 4-deoxy--l-threo-hex-4-enopyranuronosyl-(1->2)-l-rhamnopyranose sodium salt, has been carried out from d-glucose and l-rhamnose (Tetrahedron Lett. 1993, 34, 2653), but the process is very long and complicated. A method for more easily producing this compound and in large quantities is necessary for further research. We have succeeded in conveniently synthesizing lepidimoide from okra (Hibiscus esculentus L.) fruit mucilage. At the same time, the isomer (epi-lepidimoide) was obtained as a byproduct. The structure was determined as the 4-deoxy--l-threo-hex-4-enopyranuronosyl-(1->2)-6-deoxy-l-glucopyranose sodium salt by spectral analysis. We found that lepidimoide easily epimerized to epi-lepidimoide in alkaline media. Both lepidimoide and epi-lepidimoide exhibited the same high activity in the cockscomb hypocotyls elongation test….Carbohydrate Research, Volume 339, Number 1, 2 January 2004 , pp. 9-19(11)
-
Dictionary of Natural Products, Supplement 3
books.google.co.in/books?isbn=0412604302John Buckingham – 1996 – ScienceLepidimoide. L-30020. 6-Deoxy-2-0-(4-deoxy-fi-L-lhreo-hex-4-enopyranuronosyl)-L- mannose, 9CI [157676-09-0] HOA—O …
lepidimoide
Sodium 2-O-L-rhamnopyranosyl-4-deoxy-alpha-L-threo-hex-4-eno-pyranosiduronateMolecular Formula: C12H17NaO10 Molecular Weight: 344.247149sodium;(2S,3R,4S)-3,4-dihydroxy-2-[(2S,3R,4R,5R,6S)-2,4,5-trihydroxy-6-methyloxan-3-yl]oxy-3,4-dihydro-2H-pyran-6-carboxylateSodium2-O-L-rhamnopyranosyl-4-deoxy-α-L-threo-hex-4-eno-pyranosiduronate
For cancer
Garden cress seeds contain antioxidants like vitamin A and E which help protect cells from damage by free radicals. Hence, these seeds have a chemoprotective [drugs which protect healthy tissue from the toxic effects of anticancer drugs] nature.
Anti-Cancer:
Being a family of Brassica family it has good anti cancer property. Garden cress seeds contain antioxidants like vitamin A and E which help protect cells from damage by free radicals. Hence, these seeds have a chemo protective nature.
Few years back garden cress seeds/ halim/ aliv was not a common food item or a familiar to be heard. But as years passed it’s popularity and it’s importance have been realized and now people are aware of some of the facts of these seeds. Though these facts are also accompanied by some myths. So I chose to write and clear few myths and doubts of these seeds so that maximum people can make use of it in their lives and improve quality of their diet and nutrition.
Nutritive value of these seeds is very high. It is available in almost all parts of the world. Its high nutritive value and cheaper availability makes it possible for people of all the sections of society to include in the diet and increase nutritive value of their meals. Garden cress seeds are very high in Iron and Folic acid content. These seeds are use as herbal medicine to treat iron deficiency anemia. People consuming 2tsp/day have seen to have good increased levels of hemoglobin over a period of 1-2 months. Garden cress seeds also contains calcium, ascorbic acid, tocopherol, and beta-carotene which helps to improve body’s immunity.Garden Cress seeds are loaded with not just protein, but also linoleic and arachidic fatty acids. Since they contain phytochemicals that resemble estrogen to some extent, intake of these seeds helps to regulate menstruation and stimulate milk production in lactating mothers. That is why women are given foods containing Garden Cress following childbirth.
Traditionally garden cress seeds were considered to be useful only during last few weeks of gestation and post delivery. It is considered to be hot food. But the truth is that these seeds have ability too increase uterine contraction. So in later stages of pregnancy it helps in inducing labour but if in case consumed in early stage of pregnancy (1st trimester) it leads to spontaneous abortion. It is also very carefully prescribed to a hypothyroid patients because it belongs to cruciferous family and is a goitrogen that prevent iodine absorption.
How to eat:
1. Roasted slightly with added salt.
2. Soaked in water then added to milk or juice.
3. Chikki or laddoo can be made. (preparation similar to til laddoo/chikki).
How much to eat:
Start with 1 tsp/day and then an be taken 1 tsp/2c a day.
Cress seeds have many more medicinal properties and researches are still on to find its benefits on health. Garden cress should be eaten in moderation. Excess consumption of these seeds may hv adverse effect on health.
For other things
Garden cress seeds are memory boosters because they contain arachidic and linoleic acids. They help gaining lean body mass because they are a good source of iron and protein. Research has proved that 60 per cent women have hair loss due to low iron levels and poor protein. A teaspoon of garden cress seeds soaked in lime water helps in iron absorption, which in turn strengthens hair. The plant is also used in treating bleeding piles. The leaves are mildly stimulant and diuretic, useful in scorbutic [related to or resembling scurvy] diseases and liver complaints. A paste of the seeds with water is applied to chapped lips, and against sunburn.
Side-effects
It is an abortifacient [substance that induces abortion], if had in excess. It contains goitrogens that prevent iodine absorption in thyroids and hence can lead to hypothyroidism. If large quantities of garden cress are consumed, the mustard oil it contains may cause digestive difficulties in some people who are sensitive to it. Therefore, garden cress should be eaten in moderation.
Other uses
Garden cress, known as chandrashoor, and the seeds, known as halloon[7] in India, are commonly used in the system of Ayurveda to prevent postnatal complications.[citation needed]
Garden cress seeds, since ancient times, have been used in local traditional medicine of India.[8] Garden cress seeds are bitter, thermogenic, depurative, rubefacient, galactogogue, tonic, aphrodisiac, ophthalmic, antiscorbutic, antihistaminic and diuretic. They are useful in the treatment ofasthma, coughs with expectoration, poultices for sprains, leprosy, skin disease, dysentery, diarrhoea, splenomegaly, dyspepsia, lumbago, leucorrhoea, scurvy and seminal weakness. Seeds have been shown to reduce the symptoms of asthma and improve lung function in asthmatics.[9]The seeds have been reported as possessing a hypoglycemic property[10] and the seed mucilage is used as a substitute for gum arabic and tragacanth.
Cress may be given to budgerigars.[11] The seeds are employed as poultice for removing pain, swelling etc.Some use it in the belief that it can cure asthma, bronchitis bleeding piles.[12]
Some use Lepidium sativum seeds for indigestion and constipation.[13]
Prospects for improvement
Most of the genetic improvement work on garden cress is being carried out in the CIS, with little or no work being done at present in the countries of western Europe. Mainly early cultivars with a prolonged production period and better cold tolerance are being developed.
Cress can be grown and used like white mustard. It germinates more slowly at low temperatures, the emergence period being three or four days longer. Shortening this period is an interesting improvement objective.
However, cress’s recovery and its greater presence on markets mainly depends on a modification of cultivation and marketing techniques. In countries such as the United Kingdom, where this vegetable is normally to be found at the markets, cultivation takes place in greenhouses throughout the year. The whole succulent hypocotyls of the very young seedlings are eaten. The seed is placed on the soil surface on soft, level beds. It is finely sprinkled with water and then covered with sackcloth which has been steam-sterilized and moistened. The latter is frequently wetted to maintain moisture and is removed when the seedlings reach 4 to 5 cm in height (after approximately seven days in spring and autumn and ten days in winter). The yellowish leaves turn green after two to three days.
The cress is harvested when the first pair of cotyledon leaves have developed and it is marketed in small bags or trays, sometimes together with seedlings of white mustard.
Garden cress and white pepper are sometimes sown in the plastic trays or bags in which they will be sold, generally in peat with a nutrient solution.
References
- Cassidy, Frederic Gomes and Hall, Joan Houston. Dictionary of American regional English, Harvard University Press, 2002. Page 97. ISBN 0-674-00884-7, ISBN 978-0-674-00884-7
- Staub, Jack E, Buchert, Ellen. 75 Exceptional Herbs for Your Garden Published by Gibbs Smith, 2008. ISBN 1-4236-0251-X, 9781423602514
- Vegetables of Canada. Published by NRC Research Press. ISBN 0-660-19503-8, ISBN 978-0-660-19503-2
- Boswell, John T. and Sowerby, James. English Botany: Or, Coloured Figures of British Plants. Robert Hardwicke, 1863. Page 215.
- Vegetables of Canada. NRC Research Press. ISBN 0-660-19503-8, ISBN 978-0-660-19503-2
- Hirsch, David P.. The Moosewood Restaurant kitchen garden: creative gardening for the adventurous cook. Ten Speed Press, 2005. ISBN 1-58008-666-7, ISBN 978-1-58008-666-0
- http://www.organicindia.com/PR_OH_chandrashoor.php
- The Wealth of Indian Raw Materials ,. New Delhi: Publication and information Directorate. 1979. pp. CSIR Vol 9, Page 71–72.
- NP, Archana; Anita, AM (2006). “A study on clinical efficacy of Lepidium sativum seeds in treatment of bronchial asthma”. Iran J Pharmacol Ther 5: 55–59.
- M, Eddouks; Maghrani M, Zeggwagh NA, Michel JB (2005). “Study of the hypoglycaemic activity of Lepidium sativum L. aqueous extract in normal and diabetic rats”. J Ethnopharmacol 97: 391–395.
- Budgerigars – Diets, PDSA.
- Bhatiya, KN (1996). Modern Approach to Batany. India: Surya publications. p. 516.
- Najeeb-Ur-Rehman, Mehmood MH, Alkharfy KM, Gilani AU, “Prokinetic and laxative activities of Lepidium sativum seed extract with species and tissue selective gut stimulatory actions. J Ethnopharmacol. 2011 Feb 2;
MARIZOMIB, Salinosporamide A
MARIZOMIB
http://www.ama-assn.org/resources/doc/usan/marizomib.pdf
THERAPEUTIC CLAIM Antineoplastic
CHEMICAL NAMES
1. 6-Oxa-2-azabicyclo[3.2.0]heptane-3,7-dione, 4-(2-chloroethyl)-1-[(S)-(1S)-2-
cyclohexen-1-ylhydroxymethyl]-5-methyl-, (1R,4R,5S)-
2. (1R,4R,5S)-4-(2-chloroethyl)-1-{(S)-[(1S)-cyclohex-2-en-1-yl]hydroxymethyl}-5-methyl-
6-oxa-2-azabicyclo[3.2.0]heptane-3,7-dione
MOLECULAR FORMULA C15H20ClNO4
MOLECULAR WEIGHT 313.8
MANUFACTURER Nereus Pharmaceuticals, Inc.
NOTE….Nereus Pharmaceuticals was acquired by Triphase Research and Development in 2012.
CODE DESIGNATION NPI-0052
CAS REGISTRY NUMBER 437742-34-2
Scripps Institution of Oceanography (Originator)
mp, 168–170° C. (authentic sample: 168–170° C., 169–171° C. in Angew. Chem. Int. Ed., 2003, 42, 355–357); mixture mp, 168–170C.
[α]23 D −73.2 (c 0.49, MeOH), −72.9 (c 0.55, MeOH, in Angew. Chem. Int. Ed., 2003, 42, 355–357);
FTIR (film) νmax: 3406, 2955, 2920, 2844, 1823, 1701, 1257, 1076, 1012, 785, 691 cm−1;
1H NMR (CDCl3, 500 MHz): δ 10.62 (1H, br), 6.42 (1H, d, J=10.5 Hz), 5.88 (1H, m), 4.25 (1H, d, J=9.0 Hz), 4.14 (1H, m), 4.01 (1H, m), 3.17 (1H, t, J=7.0 Hz), 2.85 (1H, m), 2.48 (1H, m), 2.32 (2H, m), 2.07 (3H, s), 1.91 (2H, m), 1.66 (2H, m), 1.38 (1H, m);
13C NMR (CDCl3, 125 MHz): δ 176.92, 169.43, 129.08, 128.69, 86.32, 80.35, 70.98, 46.18, 43.28, 39.31, 29.01, 26.47, 25.35, 21.73, 20.00;
HRMS (ESI) calcd. for (M−H)− C15H19ClNO4 312.1003, found 312.1003.
Marizomib, a highly potent proteasome inhibitor, is in early clinical development at Triphase Research and Development I Corp for the treatment of relapsed or relapsed/refractory multiple myeloma. Phase I clinical trials have also been carried out for the treatment of solid tumors and lymphoma; however, no recent developments have been reported for these studies.
HDAC inhibitors halt tumor cell differentiation and growth, and when combined with marizomib in preclinical in vitro and in vivo studies, show additive and synergistic antitumor activities.
The compound was discovered from a new marine-obligate gram-positive actinomycete (Salinispora tropica). Preclinical studies suggest that this next-generation compound may be superior to other proteasome inhibitors, with broader target inhibition, faster onset and longer duration of action, higher potency, and oral and intravenous availability. By inhibiting proteasomes, marizomib prevents the breakdown of proteins involved in signal transduction, which blocks growth and induces apoptosis in cancer cells.
In 2013, orphan drug designation was assigned in the U.S. for the treatment of multiple myeloma.
The compound was originally developed by Nereus Pharmaceuticals, which was acquired by Triphase Research and Development in 2012.
marizomib is a naturally-occurring salinosporamide, isolated from the marine actinomycete Salinospora tropica, with potential antineoplastic activity. Marizomib irreversibly binds to and inhibits the 20S catalytic core subunit of the proteasome by covalently modifying its active site threonine residues; inhibition of ubiquitin-proteasome mediated proteolysis results in an accumulation of poly-ubiquitinated proteins, which may result in the disruption of cellular processes, cell cycle arrest, the induction of apoptosis, and the inhibition of tumor growth and angiogenesis. This agent more may more potent and selective than the proteasome inhibitor bortezomib
Marizomib (NPI-0052) is an oral, irreversible ββ-lactone derivative that binds selectively to the active proteasomal sites. In vivo studies with marizomib demonstrate reduced tumor growth without significant toxicity in myeloma xenograft models. A phase I trial in refractory and relapsed MM is under way.
Salinosporamide A is a potent proteasome inhibitor used as an anticancer agent that recently entered phase I human clinical trials for the treatment of multiple myeloma only three years after its discovery.[1][2] This novel marine natural product is produced by the recently described obligate marine bacteria Salinispora tropica and Salinispora arenicola, which are found in ocean sediment. Salinosporamide A belongs to a family of compounds, known collectively as salinosporamides, which possess a densely functionalized γ-lactam-β-lactone bicyclic core.
Salinosporamide A was discovered by William Fenical and Paul Jensen from Scripps Institution of Oceanography in La Jolla, CA. In preliminary screening, a high percentage of the organic extracts of cultured Salinospora strains possessed antibiotic and anticancer activities, which suggests that these bacteria are an excellent resource for drug discovery.Salinospora strain CNB-392 was isolated from a heat-treated marine sediment sample and cytotoxicity-guided fractionation of the crude extract led to the isolation of salinosporamide A. Although salinosporamide A shares an identical bicyclic ring structure with omuralide, it is uniquely functionalized. Salinosporamide A displayed potent in vitro cytotoxicity against HCT-116 human colon carcinoma with an IC50 value of 11 ng mL-1. This compound also displayed potent and highly selective activity in the NCI’s 60-cell-line panel with a mean GI50 value (the concentration required to achieve 50% growth inhibition) of less than 10 nM and a greater than 4 log LC50 differential between resistant and susceptible cell lines. The greatest potency was observed against NCI-H226 non-small cell lung cancer, SF-539 CNS cancer, SK-MEL-28 melanoma, and MDA-MB-435 breast cancer (all with LC50 values less than 10 nM). Salinosporamide A was tested for its effects on proteasome function because of its structural relationship to omuralide. When tested against purified 20S proteasome, salinosporamide A inhibited proteasomal chymotrypsin-like proteolytic activity with an IC50 value of 1.3 nM.[3] This compound is approximately 35 times more potent than omuralide which was tested as a positive control in the same assay. Thus, the unique functionalization of the core bicyclic ring structure of salinosporamide A appears to have resulted in a molecule that is a significantly more potent proteasome inhibitor than omuralide.[1]
Salinosporamide A inhibits proteasome activity by covalently modifying the active site threonine residues of the 20S proteasome.
Biosynthesis
It was originally hypothesized that salinosporamide B was a biosynthetic precursor to salinosporamide A due to their structural similarities.
It was thought that the halogenation of the unactivated methyl group was catalyzed by a non-heme iron halogenase.[4][5]Recent work using 13C-labeled feeding experiments reveal distinct biosynthetic origins of salinosporamide A and B.[4][6]
While they share the biosynthetic precursors acetate and presumed β-hydroxycyclohex-2′-enylalanine (3), they differ in the origin of the four-carbon building block that gives rise to their structural differences involving the halogen atom. A hybrid polyketide synthase-nonribosomal peptide synthetase (PKS-NRPS) pathway is most likely the biosynthetic mechanism in which acetyl-CoA and butyrate-derived ethylmalonyl-CoA condense to yield the β-ketothioester (4), which then reacts with (3) to generate the linear precursor (5).
The first stereoselective synthesis was reported by Rajender Reddy Leleti and E. J.Corey.[7] Later several routes to the total synthesis of salinosporamide A have been reported.[7][8][9][10]
In vitro studies using purified 20S proteasomes showed that salinosporamide A has lower EC50 for trypsin-like (T-L) activity than does Bortezomib. In vivo animal model studies show marked inhibition of T-L activity in response to salinosporamide A, whereas bortezomib enhances T-L proteasome activity.
Initial results from early-stage clinical trials of salinosporamide A in relapsed/refractory multiple myeloma patients were presented at the 2011 American Society of Hematology annual meeting.[11] Further early-stage trials of the drug in a number of different cancers are ongoing.[12]
- Feling RH, Buchanan GO, Mincer TJ, Kauffman CA, Jensen PR, Fenical W (2003). “Salinosporamide A: a highly cytotoxic proteasome inhibitor from a novel microbial source, a marine bacterium of the new genus salinospora”. Angew. Chem. Int. Ed. Engl. 42 (3): 355–7.doi:10.1002/anie.200390115. PMID 12548698.
- Chauhan D, Catley L, Li G et al. (2005). “A novel orally active proteasome inhibitor induces apoptosis in multiple myeloma cells with mechanisms distinct from Bortezomib”. Cancer Cell 8 (5): 407–19.doi:10.1016/j.ccr.2005.10.013. PMID 16286248.
- K. Lloyd, S. Glaser, B. Miller, Nereus Pharmaceuticals Inc.
- Beer LL, Moore BS (2007). “Biosynthetic convergence of salinosporamides A and B in the marine actinomycete Salinispora tropica”. Org. Lett. 9 (5): 845–8.doi:10.1021/ol063102o. PMID 17274624.
- Vaillancourt FH, Yeh E, Vosburg DA, Garneau-Tsodikova S, Walsh CT (2006). “Nature’s inventory of halogenation catalysts: oxidative strategies predominate”. Chem. Rev.106 (8): 3364–78. doi:10.1021/cr050313i.PMID 16895332.
- Tsueng G, McArthur KA, Potts BC, Lam KS (2007). “Unique butyric acid incorporation patterns for salinosporamides A and B reveal distinct biosynthetic origins”. Applied Microbiology and Biotechnology 75 (5): 999–1005. doi:10.1007/s00253-007-0899-7.PMID 17340108.
- Reddy LR, Saravanan P, Corey EJ (2004). “A simple stereocontrolled synthesis of salinosporamide A”. J. Am. Chem. Soc. 126 (20): 6230–1. doi:10.1021/ja048613p.PMID 15149210.
- Ling T, Macherla VR, Manam RR, McArthur KA, Potts BC (2007). “Enantioselective Total Synthesis of (-)-Salinosporamide A (NPI-0052)”.Org. Lett. 9 (12): 2289–92. doi:10.1021/ol0706051. PMID 17497868.
- Ma G, Nguyen H, Romo D (2007). “Concise Total Synthesis of (±)-Salinosporamide A, (±)-Cinnabaramide A, and Derivatives via a Bis-Cyclization Process: Implications for a Biosynthetic Pathway?”. Org. Lett. 9 (11): 2143–6. doi:10.1021/ol070616u. PMC 2518687.PMID 17477539.
- Endo A, Danishefsky SJ (2005). “Total synthesis of salinosporamide A”. J. Am. Chem. Soc. 127 (23): 8298–9.doi:10.1021/ja0522783. PMID 15941259.
- “Marizomib May Be Effective In Relapsed/Refractory Multiple Myeloma (ASH 2011)”. The Myeloma Beacon. 2012-01-23. Retrieved 2012-06-10.
- ClinicalTrials.gov: Marizomib
……………………………………………………
IMPORTANT PAPERS
Total synthesis of salinosporamide A
Org Lett 2008, 10(19): 4239
Entry to heterocycles based on indium-catalyzed conia-ene reactions: Asymmetric synthesis of (-)-salinosporamide A
Angew Chem Int Ed 2008, 47(33): 6244
A concise and straightforward total synthesis of (+/-)-salinosporamide A, based on a biosynthesis model
Org Biomol Chem 2008, 6(15): 2782
Formal synthesis of salinosporamide A starting from D-glucose
Synthesis (Stuttgart) 2009, 2009(17): 2983
Stereoselective functionalization of pyrrolidinone moiety towards the synthesis of salinosporamide A
Tetrahedron 2012, 68(32): 6504
………………
Salinosporamide A(1) was recently discovered by Fenical et al. as a bioactive product of a marine microorganism that is widely distributed in ocean sediments. Feeling, R. H.; Buchanan, G. O.; Mincer, T. J.; Kauffman, C. A.; Jensen, P. R.; Fenical, W., Angew. Chem. Int. Ed., 2003, 42, 355–357.
Structurally Salinosporamide A closely resembles the terrestrial microbial product omuralide (2a) that was synthesized by Corey et al. several years ago and demonstrated to be a potent inhibitor of proteasome function. See, (a) Corey, E. J.; Li, W. D., Z. Chem. Pharm. Bull., 1999, 47, 1–10; (b) Corey, E. J., Reichard, G. A.; Kania, R., Tetrahedron Lett., 1993, 34, 6977–6980; (c) Corey, E. J.; Reichard, G. A., J. Am. Chem. Soc., 1992, 114, 10677–10678; (d) Fenteany, G.; Standaert, R. F.; Reichard, G. A.; Corey, E. J.; Schreiber, S. L., Proc. Natl. Acad. Sci. USA, 1994, 91, 3358–3362.
Omuralide is generated by β-lactonization of the N-acetylcysteine thiolester lactacystin (2b) that was first isolated by the Omura group as a result of microbial screening for nerve growth factor-like activity. See, Omura, S., Fujimoto, T., Otoguro, K., Matsuzaki, K., Moriguchi, R., Tanaka, H., Sasaki, Y., Antibiot., 1991, 44, 113–116; Omura, S., Matsuzaki, K., Fujimoto, T., Kosuge, K., Furuya, T., Fujita, S., Nakagawa, A., J. Antibiot., 1991, 44, 117–118.
Salinosporamide A, the first compound Fenical’s group isolated from Salinospora, not only had a never-before-seen chemical structure 1, but is also a highly selective and potent inhibitor of cancer-cell growth. The compound is an even more effective proteasome inhibitor than omuralide and, in addition, it displays surprisingly high in vitro cytotoxic activity against many tumor cell lines (IC50values of 10 nM or less). Fenical et al. first found the microbe, which they’ve dubbed Salinospora, off the coasts of the Bahamas and in the Red Sea. See,Appl. Environ. Microbiol., 68, 5005 (2002).
Fenical et al. have shown that Salinospora species requires a salt environment to live. Salinospora thrives in hostile ocean-bottom conditions: no light, low temperature, and high pressure. The Fenical group has now identified Salinosporain five oceans, and with 10,000 organisms per cm3 of sediment and several distinct strains in each sample; and according to press reports, they’ve been able to isolate 5,000 strains. See, Chemical & Engineering News, 81, 37 (2003).
A great percentage of the cultures Fenical et al. have tested are said to have shown both anticancer and antibiotic activity. Like omuralide 2a, salinosporamide A inhibits the proteasome, an intracellular enzyme complex that destroys proteins the cell no longer needs. Without the proteasome, proteins would build up and clog cellular machinery. Fast-growing cancer cells make especially heavy use of the proteasome, so thwarting its action is a compelling drug strategy. See, Fenical et al., U.S. Patent Publication No. 2003-0157695A1
PATENTS
WO 2005113558
http://www.google.com/patents/US7183417
Part I. Synthesis of the Salinosporamide A(1)
EXAMPLE 1
(4S, 5R) Methyl 4,5-dihydro-2 (4-methoxyphenyl)-5-methyloxazole-4-carboxylate (4)
A mixture of (2S, 3R)-methyl 2-(4-methoxybenzamido)-3-hydroxybutanoate (3) (35.0 g, 131 mmol) and p-TsOH.H2O (2.5 g, 13.1 mmol) in toluene (400 mL) was heated at reflux for 12 h. The reaction mixture was diluted with water (200 mL) and extracted with EtOAc (3×200 mL). The combined organic layers were washed with water, brine and dried over Na2SO4. The solvent was removed in vacuo to give crude oxazoline as yellow oil. Flash column chromatography on silica gel (eluent 15% EtOAc-Hexanes) afforded the pure oxazoline (26.1 g, 80%) as solid.
Rf=0.51 (50% ethyl acetate in hexanes), mp, 86–87° C.; [α]23 D+69.4 (c 2.0, CHCl3); FTIR (film) νmax: 2955, 1750, 1545, 1355, 1187, 1011, 810 cm−1; 1HNMR(CDCl3, 400 MHz): δ 7.87 (2H, d, J=9.2 Hz), 6.84 (2H, d, J=8.8 Hz), 4.90 (1H, m), 4.40 (1H, d, J=7.6 Hz), 3.79 (3H,s), 3.71 (3H, s), 1.49 (3H, d, J=6.0 Hz); 13C NMR (CDCl3, 100 MHz): δ 171.93, 165.54, 162.64, 130.52, 119.80, 113.85, 78.91, 75.16, 55.51, 52.73, 21.14; HRMS (ESI) calcd for C13H16NO4 (M+H)+.250.1079, found 250.1084.
EXAMPLE 2
(4R, 5R)-Methyl 4-{(benzyloxy) methyl)}-4,5-dihydro-2-(4-methoxyphenyl)-5-methyloxazole-4-carboxylate (5)
To a solution of LDA (50 mmol, 1.0 M stock solution in THF) was added HMPA (24 mL, 215 mmol) at −78° C. and then oxazoline 4 (12.45 g, 50 mmol, in 20 mL THF) was added dropwise with stirring at −78° C. for 1 h to allow complete enolate formation. Benzyloxy chloromethyl ether (8.35 mL, 60 mmol) was added at this temperature and after stirring the mixture at −78° C. for 4 h, it was quenched with water (50 mL) and warmed to 23° C. for 30 min. Then the mixture was extracted with ethyl acetate (3×50 mL) and the combined organic phases were dried (MgSO4) and concentrated in vacuo. The crude product was purified by column chromatography (silica gel, ethyl acetate/hexanes, 1:4 then 1:3) to give the benzyl ether 5 (12.7 g, 69%).
Rf=0.59 (50% ethyl acetate in hexanes). [α]23 D−6.3 (c 1.0, CHCl3); FTIR (film) (νmax; 3050, 2975, 1724, 1642, 1607, 1252, 1027, 745, 697 cm−1; 1H NMR (CDCl3, 400 MHz): δ 7.96 (2H, d, J=9.2 Hz), 7.26 (5H, m), 6.90 (2H, J=8.8 Hz), 4.80 (1H, m), 4.61 (2H, s), 3.87 (3H, m), 3.81 (3H, s), 3.73 (3H, s), 1.34 (3H, d, J=6.8 Hz); 13C NMR (CDCl3, 100 MHZ): 6171.23, 165.47, 162.63, 138.25, 130.64, 128.52, 127.87, 127.77, 120.15, 113.87, 81.40, 79.92, 73.91, 73.43, 55.58, 52.45, 16.92; HRMS (ESI) calcd for C21H24O5 (M+H)+370.1654, found 370.1644.
EXAMPLE 3
(2R,3R)-Methyl 2-(4-methoxybenzylamino)-2-((benzyloxy)methyl)-3hydroxybutanoate (6)
To a solution of oxazoline 5 (18.45 g, 50 mmol) in AcOH (25 mL) at 23° C. was added in portions NaCNBH3 (9.3 g, 150 mmol). The reaction mixture was then stirred at 40° C. for 12 h to allow complete consumption of the starting material. The reaction mixture was diluted with water (100 mL), neutralized with solid Na2CO3 and the aqueous layer was extracted with ethyl acetate (3×100 mL). The combined organic phases were dried over NaSO4 and concentrated in vacuo. The crude product was purified by column chromatography (silica gel, ethyl acetate/hexanes, 1:5) to give the N-PMB amino alcohol 6 (16.78 g, 90%).
Rf=0.50 (50% ethyl acetate in hexanes). [α]23 D−9.1(c 1.0, CHCl3); FTIR (film) νmax; 3354, 2949, 1731, 1511, 1242, 1070, 1030, 820, 736, 697 cm−1; 1H NMR (CDCl3, 400 MHz): δ 7.32 (7H, m), 6.87 (2H, d, J=8.8 Hz), 4.55 (2H, m), 4.10 (1H, q, J=6.4 Hz), 3.85 (2H, dd, J=17.2, 10.0 Hz), 3.81 (3H, s,), 3.77 (3H, s), 3. 69 (2H, dd, J=22.8, 11.6 Hz), 3.22 (2H, bs), 1.16 (3H, d, J=6.0 Hz); 13C NMR (CDCl3, 100 MHz): δ 173.34, 159.03, 137.92, 132.51, 129.78, 128.67, 128.07, 127.98, 114.07, 73.80, 70.55, 69.82, 69.65, 55.51, 55.29, 47.68, 18.15; HRMS (ESI) calcd. for C21H28NO5 (M+H)+ 374.1967, found 374.1974.
EXAMPLE 4
(2R,3R)-Methyl-2-(N-(4-methoxybenzyl)acrylamido)-2-(benzyloxy)methyl)-3-hydroxybutanoate (7)
A solution of amino alcohol 6 (26.2 g, 68.5 mmol) in Et2O (200 mL) was treated with Et3N (14.2 mL, 102.8 mmol) and trimethylchlorosilane (10.4 mL, 82.2 mmol) at 23° C. and stirred for 12 h. After completion, the reaction mixture was diluted with ether (200 mL) and then resulting suspension was filtered through celite. The solvent was removed to furnish the crude product (31.2 g, 99%) in quantitative yield as viscous oil. A solution of this crude trimethylsilyl ether (31.1 g) in CH2Cl2 (200 mL) was charged with diisopropylethylamine (14.2 mL, 81.6 mmol) and then cooled to 0° C. Acryloyl chloride (6.64 mL, 82.2 mmol) was added dropwise with vigorous stirring and the reaction temperature was maintained at 0° C. until completion (1 h). The reaction mixture was then diluted with CH2Cl2 (100 mL) and the organic layer was washed with water and brine. The organic layer was separated and dried over Na2SO4. The solvent was removed to afford the crude acrylamide 7 as a viscous oil. The crude product was then dissolved in Et2O (200 mL) and stirred with 6N HCl (40 mL) at 23° C. for 1 h. The reaction mixture was diluted with water (100 mL) and concentrated to provide crude product. The residue was purified by column chromatography (silica gel, ethyl acetate/hexanes, 1:5 to 1:1) to give pure amide 7 (28.3 g, 96%) as colorless solid, mp 88–89° C.
Rf=0.40 (50% ethyl acetate in hexanes), [α]23 D−31.1 (c 0.45, CHCl3), FTIR (film) νmax; 3435, 2990, 1725, 1649, 1610, 1512, 1415, 1287, 1242, 1175, 1087, 1029, 732, 698 cm−1; 1H NMR (CDCl3, 500 MHz): δ 7.25 (5H, m), 7.15 (2H, d, J=6.0 Hz), 6.85 (2H, d, J=7.5 Hz), 6.38 (2H, d, J=6.0 Hz), 5.55 (1H, t, J=6.0 Hz), 4.81 (2H, s), 4.71 (1H, q, J=6.5 Hz), 4.35 (2H, s), 4.00 (1H, d, J=10.0 Hz), 3.80 (1H, d, J=10.0 Hz), 3.76 (3H, s), 3.75 (3H, s), 3.28 (1H, bs), 1.22 (3H, d, J=6.0 Hz); 13C NMR (CDCl3, 125 MHz): δ 171.87, 168.74, 158.81, 137.73, 131.04, 129.68, 128.58, 128.51, 127.94, 127.72, 127.20, 127.14, 114.21, 73.71, 70.42, 69.76, 67.65, 55.45, 52.52, 49.09, 18.88; HRMS (ESI) calcd. for C24H30NO6 (M+H)+428.2073, found 428.2073.
EXAMPLE 5
(R)-Methyl-2-(N-(4-methoxybenzyl)acrylamido)-2-(benzyloxy)methyl)-3-oxybutanoate (8)
To a solution of amide 7 (10.67 g, 25.0 mmol) in CH2Cl2 (100 mL) was added Dess-Martin periodinane reagent (12.75 g, 30.0 mmol, Aldrich Co.) at 23° C. After stirring for 1 h, the reaction mixture was quenched with aq NaHCO3—Na2S2O3 (1:1, 50 mL) and extracted with ethyl acetate (3×50 mL). The organic phase was dried and concentrated in vacuo to afford the crude ketone. The crude product was purified by column chromatography (silica gel, ethyl acetate/hexanes) to give pure keto amide 8 (10.2 g, 96%).
Rf=0.80 (50% ethyl acetate in hexanes), mp 85 to 86° C.; [α]23 D−12.8 (c 1.45, CHCl3); FTIR (film) νmax: 3030, 2995, 1733, 1717, 1510, 1256, 1178, 1088, 1027, 733, 697 cm−1; 1H NMR (CDCl3, 500 MHz): δ 7.30 (2H, d, J=8.0), 7.25 (3H, m), 7.11 (2H, m), 6.88 (2H, d, J=9.0 Hz), 6.38 (2H, m), 5.63 (1H, dd, J=8.5, 3.5 Hz), 4.93 (1H, d, J=18.5 Hz), 4.78 (1H, d, J=18.5, Hz), 4.27 (2H, m), 3.78 (3H, s), 3.76 (3H, s), 2.42 (3H, s); 13C NMR (CDCl3, 125 MHz): δ 198.12, 169.23, 168.62, 158.01, 136.95, 130.64, 130.38, 128.63, 128.13, 127.77, 127.32, 114.33, 77.49, 73.97, 70.66, 55.49, 53.09, 49.03, 28.24; HRMS (ESI) calcd. for C24H28NO6 (M+H)+ 426.1916, found 426.1909.
EXAMPLE 6
(2R,3S)-Methyl-1-(4-methoxybenzyl)-2-((benzyloxy)methyl)-3-hydroxy-3-methyl-4-methylene-5-oxopyrrolidine-2-carboxylate (9+10)
A mixture of keto amide 8 (8.5 g, 20.0 mmol) and quinuclidine (2.22 g, 20.0 mmol) in DME (10 mL) was stirred for 5 h at 23° C. After completion, the reaction mixture was diluted with ethyl acetate (50 mL) washed with 2N HCl, followed by water and dried over Na2SO4. The solvent was removed in vacuo to give the crude adduct (8.03 g, 94.5%, 3:1 ratio of 9 to 10 dr) as a viscous oil. The diastereomeric mixture was separated at the next step, although small amounts of 9 and 10 were purified by column chromatography (silica gel, ethyl acetate/hexanes, 1:10 to 1:2) for analytical purposes.
Major Diastereomer (9).
[α]23 D−37.8 (c 0.51, CHCl3); FTIR (film) vmax: 3450, 3055, 2990, 1733, 1683, 1507, 1107, 1028, 808,734 cm−1; 1H NMR (CDCl3, 500 MHz): δ 7.29 (5H, m), 7.15 (2H, d, J=7.5 Hz), 6.74 (2H, d, J=8.5 Hz), 6.13 (1H, s), 5.57 (1H, s), 4.81 (1H, d, J=14.5 Hz), 4.45(1H, d, J=15.0 Hz), 4.20 (1H, d, J=12.0 Hz), 4.10 (1H, d, J=12.0 Hz) 3.75 (3H, s), 3.70 (1H, d, J=10.5 Hz), 3.64 (3H, s), 3.54 (1H, d, J=10.5 Hz), 2.55 (1H, bs, OH), 1.50 (3H, s); 13C NMR (CDCl3, 125 MHz): δ 169.67, 168.42, 158.97, 145.96, 137.57, 130.19, 130.12, 128.53, 127.83, 127.44, 116.79, 113.71, 76.32, 76.00, 73.16, 68.29, 55.45, 52.63, 45.36, 22.64; HRMS (ESI) calcd. for C24H28NO6 (M+H)+ 426.1916, found 426.1915.
Minor Diastereomer (10).
[α]23 D−.50.1 (c 0.40, CHCl3); FTIR (film) νmax: 3450, 3055, 2990, 1733, 1683, 1507, 1107, 1028, 808, 734 cm−1; 1H NMR (CDCl3, 500 MHz): δ 7.29 (5H, m), 7.12 (2H, d, J=7.5 Hz), 6.73 (2H, d, J=8.5 Hz), 6.12 (1H, s), 5.57 (1H, s), 4.88 (1H, d, J=15.5 Hz), 4.31 (1H, d, J=15.0 Hz), 4.08 (3H, m), 3.99 (1H, d, J=12.0 Hz) 3.73 (3H, s), 3.62 (3H, s), 3.47 (1H, bs, OH), 3.43 (1H, d, J=10.0 Hz), 1.31 (3H, s); 13C NMR (CDCl3, 125 MHz): δ 169.65, 167.89, 159.13, 147.19, 136.95, 130.29, 129.76, 128.74, 128.19, 127.55, 116.80, 113.82, 76.21, 75.66, 73.27, 68.02, 55.45, 52.52, 45.24, 25.25; HRMS (ESI) calcd. for (M+H)+ C24H28NO6 426.1916, found 426.1915.
EXAMPLE 7
Silylation of 9 and 10 and Purification of 11.
To a solution of lactams 9 and 10 (7.67 g, 18 mmol) in CH2Cl2 (25 ml) was added Et3N (7.54 ml, 54 mmol), and DMAP (2.2 g, 18 mmol) at 0° C., and then bromomethyl-dimethylchlorosilane (5.05 g, 27 mmol) (added dropwise). After stirring the mixture for 30 min at 0° C., it was quenched with aq NaHCO3 and the resulting mixture was extracted with ethyl acetate (3×50 mL). The combined organic layers were washed with water, brine and dried over Na2SO4. The solvent was removed in vacuo to give a mixture of the silated derivatives of 9 and 10 (9.83 g, 95%). The diastereomers were purified by column chromatography (silica gel, ethyl acetate/hexanes, 1:5 to 1:4) to give pure diastereomer 11 (7.4 g, 72%) and its diastereomer (2.4 g, 22%).
Silyl Ether (11).
Rf=0.80 (30% ethyl acetate in hexanes). [α]23 D−58.9 (c 0.55, CHCl3); FTIR (film) νmax; 3050, 2995, 1738, 1697, 1512, 1405, 1243, 1108, 1003, 809, 732 cm−1; 1H NMR (CDCl3, 500 MHz): δ 7.27 (5H, m), 7.05 (2H, d, J=7.0 Hz), 6.71 (2H, d, J=8.5 Hz), 6.18 (1H, s), 5.53 (1H, s), 4.95 (1H, d, J=15.5 Hz), 4.45 (1H, d, J=15.0 Hz), 4.02 (1H, J=12.0 Hz), 3.86 (1H, d, J=11.5 Hz) 3.72 (3H, s), 3.68 (3H, s), 3.65 (1H, d, J=10.5 Hz), 3.30 (1H, d, J=10.0 Hz), 2.34 (2H, d, J=2.0 Hz), 1.58 (3H, s), 0.19 (3H, s), 0.18 (3H, s); 13C NMR (CDCl3, 125 MHz): δ 168.62, 168.12, 158.93, 145.24, 137.53, 130.32, 130.30, 128.49, 127.76,127.22, 117.26, 113.60, 78.55, 78.03, 72.89, 68.45, 55.43, 52.37, 45.74, 21.87, 17.32, −0.72, −0.80; HRMS (ESI) Calcd. for C27H35BrNO6Si (M+H)+ 576.1417, found 576.1407.
EXAMPLE 8
Conversion of (11) to (12).
To a solution of compound 11 (5.67 g 10 mmol) in benzene (250 mL) at 80° C. under nitrogen was added a mixture of tributyltin hydride (4.03 ml, 15 mmol) and AIBN (164 mg, 1 mmol) in 50 ml benzene by syringe pump over 4 h. After the addition was complete, the reaction mixture was stirred for an additional 4 h at 80° C. and the solvent was removed in vacuo. The residue was dissolved in hexanes (20 mL) and washed with saturated NaHCO3 (3×25 mL), water and dried over Na2SO4. The solvent was removed in vacuo to give crude product. The crude product was purified by column chromatography (silica gel, ethyl acetate/hexanes, 1:5) to afford the pure 12 (4.42 g, 89%).
Rf=0.80 (30% ethyl acetate in hexanes). [α]23 D−38.8 (c 0.25, CHCl3); FTIR (film) νmax; 3025, 2985, 1756, 1692, 1513, 1247, 1177, 1059, 667 cm−1; 1H NMR (CDCl3, 500 MHz): δ 7.28 (5H, m), 7.09 (2H, d, J=7.0 Hz), 6.73 (2H, d, J=9.0 Hz), 4.96(1H, d, J=15.0 Hz), 4.35 (1H, d, J=15.5 Hz), 3.97 (1H, d, J=12.5 Hz), 3.86 (1H, d, J=12.0 Hz), 3.80 (1H, d, J=10.0 Hz), 3.72 (3H, s), 3.65 (3H, s), 3.27 (1H, d, J=10.5 Hz), 2.67 (1H, t, J=4.0 Hz), 2.41 (1H, m), 1.79 (1H, m), 1.46 (3H, s), 0.77 (1H, m), 0.46 (1H, m), 0.10 (3H, s), 0.19 (3H, s); 13C NMR (CDCl3, 125 MHz): δ 175.48, 169.46, 158.76, 137.59, 131.04, 129.90, 128.58, 127.88, 127.52, 113.59, 113.60, 81.05, 78.88, 73.12, 69.03, 55.45, 51.94, 48.81, 45.50, 22.79, 17.06, 7.76, 0.54; HRMS (ESI) calcd. for (M+H)+ C27H36NO6Si 498.2312, found 498.2309.
EXAMPLE 9
Debenzylation of (12).
A solution of 12 (3.98 g, 8 mmol) in EtOH (50 ml) at 23° C. was treated with 10% Pd—C (˜1 g) under an argon atmosphere. The reaction mixture was evacuated and flushed with H2 gas (four times) and then stirred vigorously under an atmosphere of H2 (1 atm, H2 balloon) at 23° C. After 12 h, the reaction mixture was filtered through Celite and concentrated in vacuo to give the crude debenzylation product (3.08 g, 95%) which was used for the next step. A small amount crude product was purified by column chromatography (silica gel, ethyl acetate/hexanes, 1:3) for analytical purposes. Rf=0.41 (50% ethyl acetate in hexanes).
mp, 45–47° C.; [α]23 D−30.9 (c 0.55, CHCl3); FTIR (film) νmax: 3432, 3020, 2926, 1735, 1692, 1512, 1244, 1174, 1094, 1024, 870, 795 cm−1; 1H NMR (CDCl3, 400 MHz): δ 7.36 (2H, d, J=8.5 Hz), 6.83 (2H, d, J=8.5 Hz), 5.16 (1H, d, J=15.0 Hz), 4.29 (1H, d, J=15.0 Hz), 3.92 (1H, m), 3.78 (3H, s), 3.68 (3H, s), 3.45 (1H, m), 2.53 (1H, t, J=4.0 Hz), 2.42 (1H, m), 1.82 (1H, m), 1.50 (3H, s), 1.28 (1H, m), 0.75 (1H, m), 0.47 (1H, m), 0.11 (3H, s), 0.02 (3H, s); 13C NMR (CDCl3, 125 MHz): δ 175.82, 169.51, 159.32, 131.00, 129.72, 114.52, 80.79, 80.13, 61.85, 55.48, 51.99, 49.29, 45.06, 23.11, 17.03, 7.44, 0.54; HRMS (ESI) calcd. for C20H30NO6Si (M+H)+ 408.1842, found 408.1846.
EXAMPLE 10
Oxidation to Form Aldehyde (13).
To a solution of the above alcohol from debenzylation of 12 (2.84 g, 7 mmol) in CH2Cl2 (30 mL) was added Dess-Martin reagent (3.57 g, 8.4 mmol) at 23° C. After stirring for 1 h at 23° C., the reaction mixture was quenched with aq NaHCO3—Na2S2O3 (1:1, 50 mL) and extracted with ethyl acetate (3×50 mL). The organic phase was dried and concentrated in vacuo to afford the crude aldehyde. The crude product was purified by column chromatography (silica gel, ethyl acetate/hexanes, 1:5) to give pure aldehyde 13 (2.68 g, 95%). Rf=0.56 (50% ethyl acetate in hexanes).
mp, 54–56° C.; [α]23 D−16.5 (c 0.60, CHCl3); FTIR (film) νmax: 3015, 2925, 1702 1297, 1247, 1170, 1096, 987, 794 cm−1; 1H NMR (CDCl3, 500 MHz): δ 9.62 (1H, s), 7.07 (2H, d, J=8.0 Hz), 6.73 (2H, d, J=8.5 Hz), 4.49 (1H, quart, J=8.5 Hz), 3.70 (3H, s), 3.67 (3H, s), 2.36 (2H, m), 1.75 (1H, m), 1.37 (3H, s), 0.73 (1H, m), 0.48 (1H, m), 0.07 (3H, s), 0.004 (3H, s); 13C NMR (CDCl3, 125 MHz): δ 197.26, 174.70, 167.36, 158.07, 130.49, 128.96, 113.81, 83.97, 82.36, 55.34, 52.43, 47.74, 46.32, 23.83, 16.90, 7.52, 0.56, 0.45; HRMS (ESD calcd. for C20H28NO6Si (M+H)+ 406.1686, found 406.1692.
EXAMPLE 11
Conversion of (13) to (14).
To a solution of freshly prepared cyclohexenyl zinc chloride (10 mL, 0.5 M solution in THF, 5 mmol) (see Example 15 below) at −78° C. under nitrogen was added a −78° C. solution of aldehyde 13 (1.01 g, in 3 ml of THF, 2.5 mmol). After stirring for 5 h at −78° C. reaction mixture was quenched with water (10 mL) then extracted with ethyl acetate (3×10 mL). The combined organic layers were dried over Na2SO4 and solvent was removed in vacuo to give crude product (20:1 dr). The diastereomers were purified by column chromatography (silica gel, ethyl acetate/hexanes, 1:10 to 1:2 affords the pure major diastereomer 14 (1.0 g, 83%) and a minor diastereomer (50 mg 5%). For 14: Rf=0.56 (50% ethyl acetate in hexanes).
mp, 79–81° C.; [a]23 D−28.5 (c 1.45, CHCl3); FTIR (film) νmax: 3267, 2927, 2894, 2829, 1742, 1667, 1509, 1248, 1164, 1024, 795 cm−1; 1H NMR (CDCl3, 500 MHz): δ 7.34 (2H, d, J=8.5 Hz), 6.81 (2H, d, J=9.0 Hz), 5.84 (1H, m), 5.73 (1H, m), 4.88 (1H, d, J=15.5 Hz), 4.39 (1H, d, J=14.5 Hz), 4.11 (1H, t, J=6.5 Hz), 3.77 (3H, s), 3.58 (3H, s), 3.00 (1H, m), 2.95 (1H, d, J=9.0 Hz), 2.83 (1H, t, J=3.5 Hz), 3.36 (1H, m), 2.27 (1H, m), 1.98 (2H, m), 1.74 (3H, m), 1.62 (3H, s), 1.14 (2H, m), 0.59 (1H, m), 0.39 (11H, m), 0.13 (3H, s), 0.03 (3H, s); 13C NMR (CDCl3, 125 MHz): δ 176.80, 170.03, 158.27, 131.86, 131.34, 128.50, 126.15, 113.40, 83.96, 82.45, 77.17, 55.45, 51.46, 48.34, 48.29, 39.08, 28.34, 25.29, 22.45, 21.09, 17.30, 7.75, 0.39, 0.28; HRMS (ESI) calcd. for C26H38NO6Si (M+H)+ 488.2468, found 488.2477.
EXAMPLE 12
Tamao-Fleming Oxidation of (14) to (15).
To a solution of 14 (0.974 g, 2 mmol) in THF (5 mL) and MeOH (5 mL) at 23° C. was added KHCO3 (0.8 g, 8 mmol) and KF (0.348 g, 6 mmol). Hydrogen peroxide (30% in water, 5 mL) was then introduced to this mixture. The reaction mixture was vigorously stirred at 23° C. and additional hydrogen peroxide (2 ml) was added after 12 h. After 18 h, the reaction mixture was quenched carefully with NaHSO3 solution (15 mL). The mixture was extracted with ethyl acetate (3×25 mL) and the combined organic layers were washed with water and dried over Na2SO4. The solvent was removed in vacuo to give the crude product. The crude product was purified by column chromatography (silica gel, ethyl acetate) to give the pure triol 15 (0.82 g, 92%).
Rf=0.15 (in ethyl acetate). mp, 83–84° C.; [α]23 D: +5.2 (c 0.60, CHCl3); FTIR (film) νmax; 3317, 2920, 2827, 1741, 1654, 1502, 1246, 1170, 1018, 802 cm−1; 1HNMR(CDCl3, 500 MHz): δ 7.77 (2H, d, J=8.0 Hz), 6.28 (2H, d, J=8.0 Hz), 5. 76 (1H, m), 5.63 (1H, d, J=10.0 Hz), 4.74 (1H, d, J=15.5 Hz), 4.54 (1H, d, J=15.0 Hz), 4.12 (1H, d, J=2.5 Hz), 3.80 (1H, m), 3.76 (3H, s), 3.72 (1H, m), 3.68 (3H, s), 3.00 (1H, m), 2.60 (1H, br), 2.20 (1H, m), 1.98 (2H, s), 1.87 (1H, m), 1.80 (1H, m), 1.71 (2H, m), 1.61 (3H, s), 1.14 (2H, m); 13C NMR (CDCl3, 125 MHz): δ 178.99, 170.12, 158.27, 131.30, 130.55, 128.13, 126.39, 113.74, 81.93, 80.75, 76.87, 61.61, 55.45, 51.97, 51.32, 48.07, 39.17, 27.71, 27.13, 25.22, 21.35, 21.22; HRMS (ESI) calcd. for C24H34NO7 (M+H)+ 448.2335, found 448.2334.
EXAMPLE 13
Deprotection of (15) to (16).
To a solution of 15 (0.670 g, 1.5 mmol) in acetonitrile (8 mL) at 0° C. was added a pre-cooled solution of ceric ammonium nitrate (CAN) (2.46 g 4.5 mmol in 2 mL H2O). After stirring for 1 h at 0° C. the reaction mixture was diluted with ethyl acetate (50 mL), washed with saturated NaCl solution (5 mL) and organic layers was dried over Na2SO4. The solvent was removed in vacuo to give the crude product which was purified by column chromatography (silica gel, ethyl acetate) to give the pure 16 (0.4 g, 83%).
Rf=0.10 (5% MeOH in ethyl acetate). mp, 138 to 140° C.; [α]23 D+14.5 (c 1.05, CHCl3); FTIR (film) νmax 3301, 2949, 2911, 2850, 1723, 1673, 1437, 1371, 1239, 1156, 1008, 689 cm−1; 1H NMR (CDCl3, 600 MHz): δ 8.48 (1H, br), 6.08 (1H, m), 5. 75 (1H, d, J=9.6 Hz), 5.29 (1H, br), 4.13 (1H, d, J=6.6 Hz), 3.83 (3H, m), 3.79 (1H, m), 3.72 (1H, m), 2.84 (1H, d, J=10.2 Hz), 2.20 (1H, m), 2.16 (1H, br), 1.98 (3H, m), 1.77 (3H, m), 1.59 (1H, m), 1.54 (3H, s), 1.25 (1H, m). 13C NMR (CDCl3, 125 MHz): δ 180.84, 172.95, 135.27, 123.75, 82.00, 80.11, 75.56, 62.39, 53.14, 51.78, 38.95, 28.79, 26.48, 25.04, 20.66, 19.99; HRMS (ESI) calcd. (M+H)+ for C16H26NO6 328.1760, found 328.1752.
EXAMPLE 14
Conversion of (16) to Salinosporamide A(1).
A solution of triol ester 16 (0.164 g, 0.5 mmol) in 3 N aq LiOH (3 mL) and THF (1 mL) was stirred at 5° C. for 4 days until hydrolysis was complete. The acid reaction mixture was acidified with phosphoric acid (to pH 3.5). The solvent was removed in vacuo and the residue was extracted with EtOAc, separated, and concentrated in vacuo to give the crude trihydroxy carboxylic acid 16a (not shown). The crude acid was suspended in dry CH2Cl2 (2 mL), treated with pyridine (0.5 mL) and stirred vigorously at 23° C. for 5 min. To this solution was added BOPCl (152 mg, 0.6 mmol) at 23° C. under argon, and stirring was continued for 1 h. The solvent was removed under high vacuum and the residue was suspended in dry CH3CN (1 mL) and treated with pyridine (1 mL). To this solution was added PPh3Cl2 (333 mg, 1.0 mmol) at 23° C. under argon with stirring. After 1 h the solvent was removed in vacuo. The crude product was purified by column chromatography (silica gel, ethyl acetate-CH2Cl2, 1:5) to give the pure β-lactone 1 (100 mg, 64%) as a colorless solid.
Rf=0.55 (50% ethyl acetate in hexane). mp, 168–170° C. (authentic sample: 168–170° C., 169–171° C. in Angew. Chem. Int. Ed., 2003, 42, 355–357); mixture mp, 168–170C. [α]23 D −73.2 (c 0.49, MeOH), −72.9 (c 0.55, MeOH, in Angew. Chem. Int. Ed., 2003, 42, 355–357); FTIR (film) νmax: 3406, 2955, 2920, 2844, 1823, 1701, 1257, 1076, 1012, 785, 691 cm−1; 1H NMR (CDCl3, 500 MHz): δ 10.62 (1H, br), 6.42 (1H, d, J=10.5 Hz), 5.88 (1H, m), 4.25 (1H, d, J=9.0 Hz), 4.14 (1H, m), 4.01 (1H, m), 3.17 (1H, t, J=7.0 Hz), 2.85 (1H, m), 2.48 (1H, m), 2.32 (2H, m), 2.07 (3H, s), 1.91 (2H, m), 1.66 (2H, m), 1.38 (1H, m);13C NMR (CDCl3, 125 MHz): δ 176.92, 169.43, 129.08, 128.69, 86.32, 80.35, 70.98, 46.18, 43.28, 39.31, 29.01, 26.47, 25.35, 21.73, 20.00; HRMS (ESI) calcd. for (M−H)− C15H19ClNO4 312.1003, found 312.1003.
| 544814 | Oct 1, 2007 | Jun 9, 2009 | Nereus Pharmaceuticals, Inc. | [3.2.0] Heterocyclic compounds and methods of using the same |
| US7579371 | Jun 15, 2006 | Aug 25, 2009 | Nereus Pharmaceuticals, Inc. | Methods of using [3.2.0] heterocyclic compounds and analogs thereof |
| US7824698 | Feb 4, 2008 | Nov 2, 2010 | Nereus Pharmaceuticals, Inc. | Lyophilized formulations of Salinosporamide A |
| US7842814 | Apr 6, 2007 | Nov 30, 2010 | Nereus Pharmaceuticals, Inc. | Total synthesis of salinosporamide A and analogs thereof |
| US7910616 | May 12, 2009 | Mar 22, 2011 | Nereus Pharmaceuticals, Inc. | Proteasome inhibitors |
| US8003802 | Mar 6, 2009 | Aug 23, 2011 | Nereus Pharmaceuticals, Inc. | Total synthesis of Salinosporamide A and analogs thereof |
| US8067616 | Oct 27, 2010 | Nov 29, 2011 | Nereus Pharmaceuticals, Inc. | Total synthesis of salinosporamide A and analogs thereof |
| US8168803 | Jun 10, 2008 | May 1, 2012 | Nereus Pharmaceuticals, Inc. | Methods of using [3.2.0] heterocyclic compounds and analogs thereof |
| US8217072 | Jun 18, 2004 | Jul 10, 2012 | The Regents Of The University Of California | Salinosporamides and methods for use thereof |
| US8222289 | Dec 15, 2009 | Jul 17, 2012 | The Regents Of The University Of California | Salinosporamides and methods for use thereof |
| US8227503 | Mar 21, 2011 | Jul 24, 2012 | Nereus Pharmaceuticals, Inc. | Proteasome inhibitors |
| US8314251 | Jul 15, 2011 | Nov 20, 2012 | Nereus Pharmaceuticals, Inc. | Total synthesis of salinosporamide A and analogs thereof |
| US8389564 | May 14, 2012 | Mar 5, 2013 | Venkat Rami Reddy Macherla | Proteasome inhibitors |
| US8394816 | Dec 5, 2008 | Mar 12, 2013 | Irene Ghobrial | Methods of using [3.2.0] heterocyclic compounds and analogs thereof in treating Waldenstrom’s Macroglobulinemia |
| Name: | Marizomib | |
| Synonyms: | 6-Oxa-2-azabicyclo[3.2.0]heptane-3,7-dione, 4-(2-chloroethyl)-1-[(S)-(1S)-2-cyclohexen-1-ylhydroxymethyl]-5-methyl-, (1R,4R,5S)-; Other Names: (-)-Salinosporamide A; ML 858; Marizomib; NPI 0052; Salinosporamide A | |
| CAS Registry Number: | 437742-34-2 | |
| Molecular Formula: | C15H20ClNO4 | |
| Molecular Weight: | 313.1 | |
| Molecular Structure: |  |
DARUNAVIR


DARUNAVIR
206361-99-1 CAS NO
[(1S,2R)-3-[[(4-Aminophenyl)sulfonyl] (2-methylpropyl)amino]-2-hydroxy-1-(phenylmethyl)propyl]carbamic acid (3R,3aS,6aR)-hexahydrofuro[2,3-b]furan-3-yl ester
M. P.:- 72-74 °C (dec)
MW: 547.66
Darunavir and processes for its preparation are disclosed in EP0715618, W09967417, EP1725566 and Bioorganic & Medicinal Chemistry Letters (2004), 14(4), 959-963.
J Med Chem. 2013 May 23;56(10):4017-27. doi: 10.1021/jm400231v
US20050250845 discloses various pseudopolymorphs of darunavir and processes for their preparation. According to this application, “pseudopolymorph” is defined as a crystalline form of a compound in which solvent molecules are incorporated in the lattice structure. The Form B disclosed in the patent application is a pseudopolymorph wherein water is used as solvent. The thermogravimetric experiments of the Form B shows weight loss of 3.4% in the temperature range 25-78°C (water), 5.1% in the temperature range 25-1 10°C (ethanol and water) and further 1.1% weight loss (ethanol) in temperature range 110-200° C. Further at the drying step the Form B showed about 5.6% weight loss. The obtained dried product was hygroscopic and it adsorbed up to 6.8% water at high relative humidity. Amorphous form of darunavir is disclosed in US20050250845 and the publication in J.Org. Chem. 2004, 69, 7822 – 7829.
US 7700645 patent disclosed amorphous Darunavir, various solvates of Darunavir including ethanolate and method for their preparation as well as their use as a medicament. Journal of Organic Chemistry 2004, 69, 7822-7829 disclosed amorphous Darunavir is obtained by purification with column chromatography in 2% methanol in chloroform as eluent. PCT publication WO2010086844A1 disclosed crystalline dimethylsulfoxide solvate and crystalline tetrahydrofuran solvate of darunavir. The publication also disclosed the amorphous darunavir having the IR spectrum with characteristic peaks at about 1454 and 1365 cm“1
PCT publication WO201 1083287A2 disclosed crystalline darunavir hydrate substantially free of any non aqueous solvent.
Drug information:- Darunavir is an Anti-microbial drug further classified as anti-viral agent of the class protease inhibitor. It is used either single or in combination with other drugs for the treatment of human immunodeficiency virus.
Darunavir (brand name Prezista, formerly known as TMC114) is a drug used to treat HIV infection. It is in the protease inhibitor class. Prezista is an OARAC recommended treatment option for treatment-naïve and treatment-experienced adults and adolescents.Developed by pharmaceutical company Tibotec, darunavir is named after Arun K. Ghosh, the chemist who discovered the molecule at the University of Illinois at Chicago. It was approved by the Food and Drug Administration (FDA) on June 23, 2006.[2]
Darunavir is a second-generation protease inhibitor (PIs), designed specifically to overcome problems with the older agents in this class, such as indinavir. Early PIs often have severe side effects and drug toxicities, require a high therapeutic dose, are costly to manufacture, and show a disturbing susceptibility to drug resistant mutations. Such mutations can develop in as little as a year of use, and effectively render the drugs useless.
Darunavir was designed to form robust interactions with the protease enzyme from many strains of HIV, including strains from treatment-experienced patients with multiple resistance mutations to PIs.
Darunavir received much attention at the time of its release, as it represents an important treatment option for patients with drug-resistant HIV. Patient advocacy groups pressured developer Tibotec not to follow the previous trend of releasing new drugs at prices higher than existing drugs in the same class. Darunavir was priced to match other common PIs already in use, such as the fixed-dose combination drug lopinavir/ritonavir.
PREZISTA (darunavir) is an inhibitor of the human immunodeficiency virus (HIV-1) protease.
PREZISTA (darunavir), in the form of darunavir ethanolate, has the following chemical name: [(1S,2R)-3-[[(4-aminophenyl)sulfonyl](2-methylpropyl)amino]-2-hydroxy-1-(phenylmethyl)propyl]-carbamic acid (3R,3aS,6aR)-hexahydrofuro[2,3-b]furan-3-yl ester monoethanolate. Its molecular formula is C27H37N3O7S • C2H5OH and its molecular weight is 593.73. Darunavir ethanolate has the following structural formula:
 |
Darunavir ethanolate is a white to off-white powder with a solubility of approximately 0.15 mg/mL in water at 20°C.
|
|
4-11-2012
|
METHODS FOR THE PREPARATION OF HEXAHYDROFURO[2,3-b]FURAN-3-OL
|
|
|
12-28-2011
|
Substituted Aminophenylsulfonamide Compounds as Hiv Protease Inhibitor
|
|
|
12-23-2011
|
POLYMORPHS OF DARUNAVIR
|
|
|
12-14-2011
|
METHODS FOR THE PREPARATION OF N-ISOBUTYL-N-(2-HYDROXY-3-AMINO-4-PHENYLBUTYL)-P-NITROBENZENESULFONYLAMIDE DERIVATIVES
|
|
|
11-30-2011
|
Protease inhibitor precursor synthesis
|
|
|
6-31-2011
|
PROCESS FOR THE PREPARATION OF (3R,3AS,6AR)-HEXAHYDROFURO [2,3-B] FURAN-3-YL (1S,2R)-3-[[(4-AMINOPHENYL) SULFONYL] (ISOBUTYL) AMINO]-1-BENZYL-2-HYDROXYPROPYLCARBAMATE
|
|
|
9-29-2010
|
Aminophenylsulfonamide Derivatives as Hiv Protease Inhibitor
|
|
|
8-11-2010
|
Process for the preparation of (3R,3aS,6aR)-hexahydrofuro [2,3-b] furan-3-yl (1S,2R)-3[[(4-aminophenyl) sulfonyl] (isobutyl) amino]-1-benzyl-2-hydroxypropylcarbamate
|
|
|
7-30-2010
|
RELATING TO ANTI-HIV TABLET FORMULATIONS
|
|
|
7-30-2010
|
COMBINATION FORMULATIONS
|
|
7-2-2010
|
METHODS AND INTERMEDIATES USEFUL IN THE SYNTHESIS OF HEXAHYDROFURO [2,3-B]FURAN-3-OL
|
|
|
5-7-2010
|
METHODS AND COMPOSITIONS FOR TREATING HIV INFECTIONS
|
|
|
4-21-2010
|
Pseudopolymorphic forms of a hiv protease inhibitor
|
|
|
9-21-2007
|
Immunoassays, Haptens, Immunogens and Antibodies for Anti-HIV Therapeutics
|
|
|
6-23-2006
|
Method for treating HIV infection through co-administration of tipranavir and darunavir
|
|
|
6-3-2005
|
Combination of cytochome p450 dependent protease inhibitors
|
| Cited Patent | Filing date | Publication date | Applicant | Title |
|---|---|---|---|---|
| WO2010086844A1 | Dec 8, 2009 | Aug 5, 2010 | Mapi Pharma Hk Limited | Polymorphs of darunavir |
| WO2011048604A2 * | Sep 16, 2010 | Apr 28, 2011 | Matrix Laboratories Limited | An improved process for the preparation of darunavir |
| WO2011083287A2 | Oct 6, 2010 | Jul 14, 2011 | Cipla Limited | Darunavir polymorph and process for preparation thereof |
| CN102584844A * | Jan 11, 2011 | Jul 18, 2012 | 浙江九洲药业股份有限公司 | Darunavir crystal form and method for preparing same |
| US6248775 | Apr 8, 1999 | Jun 19, 2001 | G. D. Searle & Co. | α- and β-amino acid hydroxyethylamino sulfonamides useful as retroviral protease inhibitors |
| US7700645 | May 16, 2003 | Apr 20, 2010 | Tibotec Pharmaceuticals Ltd. | Pseudopolymorphic forms of a HIV protease inhibitor |
| Reference | ||
|---|---|---|
| 1 | JOURNAL OF ORGANIC CHEMISTRY vol. 69, 2004, pages 7822 – 7829 | |
| 2 | * | VAN GYSEGHEM E ET AL: “Solid state characterization of the anti-HIV drug TMC114: Interconversion of amorphous TMC114, TMC114 ethanolate and hydrate“, EUROPEAN JOURNAL OF PHARMACEUTICAL SCIENCES, ELSEVIER, AMSTERDAM, NL, vol. 38, no. 5, 8 December 2009 (2009-12-08), pages 489-497, XP026764329, ISSN: 0928-0987, DOI: 10.1016/J.EJPS.2009.09.013 [retrieved on 2009-09-24] |
Virus-encoded proteases, which are essential for viral replication, are required for the processing of viral protein precursors. Interference with the processing of protein precursors inhibits the formation of infectious virions. Accordingly, inhibitors of viral proteases may be used to prevent or treat chronic and acute viral infections. Darunavir has HIV protease inhibitory activity and is particularly well suited for inhibiting HIV-I and HIV -2 viruses. Darunavir, chemically (1 S^R.S’R.S’aS.e’aRJ-fS’he ahydrofuro^.S-b ]furanyl-[3-( 4-aminobenzenesulfonyl)isobutylamino [- 1-benzyl-zhydroxypropyl]carbamate. Darunavir is represented by the following structure:
Darunavir and its pharmaceutically acceptable salts were disclosed in US 6248775 patent, wherein Darunavir is prepared by condensing 2R-hydroxy-3-[[(4-aminophenyl)sulfonyl](2- methylpropyl)amino]-1S(phenylmethyl)propylamine with hexahydro-furo[2,3-b]furan-3-ol in anhydrous acetonitrile in the presence of anhydrous pyridine and Ν,Ν’-disuccinimidyl carbonate at ambient temperature.
US 7700645 patent disclosed amorphous Darunavir, various solvates of Darunavir including ethanolate and method for their preparation as well as their use as a medicament. Journal of Organic Chemistry 2004, 69, 7822-7829 disclosed amorphous Darunavir is obtained by purification with column chromatography in 2% methanol in chloroform as eluent. PCT publication WO2010086844A1 disclosed crystalline dimethylsulfoxide solvate and crystalline tetrahydrofuran solvate of darunavir. The publication also disclosed the amorphous darunavir having the IR spectrum with characteristic peaks at about 1454 and 1365 cm“1
PCT publication WO201 1083287A2 disclosed crystalline darunavir hydrate substantially free of any non aqueous solvent.
Darunavir Ethanolate, has the chemical name: [(1 S, 2R)-3-[[(4-aminophenyl) sulfonyl](2- methylpropyl)amino]-2-hydroxy-1-(phenylmethyl)propyl]carbamic acid (3/?, 3aS, 6a/?)- hexahydrofuro[2,3-i>]furan-3-yl ester monoethanolate and has the following structural formula:
Darunavir and its process are first disclosed in US 6248775, wherein 2 ?-hydroxy-3-[[(4- aminophenyl)sulfonyl](2-methylpropyl)amino]-1 S(phenylmethyl) propylamine (4) is reacted with (3R, 3aS, 6aR)-hexahydrofuro[2,3- >]furan-3-ol in anhydrous acetonitrile in the presence of N, W-disuccinimidyl carbonate, anhydrous pyridine at ambient temperature followed by workup to get Darunavir (Scheme A).
Scheme A
Darunavir
US 20050250845 disclosed the various solvates of Darunavir including ethanolate and method for their preparation as well as their use as a medicament. The same application disclosed the amorphous Darunavir by Raman spectra without process details.
WO 2005063770 discloses process for the preparation of Darunavir ethanolate, wherein 2R-hydroxy-3-[[(4-aminophenyl)sulfonyl](2-methylpropyl)amino]-1 S-(phenylmethyl)propyl amine (4) is reacted with (3R, 3aS, 6a ?)-hexahydrofuro[2,3-b]furan-3-ol in the presence of N, /V-disuccinimidyl carbonate, triethylamine, 41% methylamine in ethanol in a mixture of ethyl acetate and acetonitrile followed by workup and crystallization from ethanol to get Darunavir ethanolate (Scheme B).
Scheme B
In the prior art process, compound of formula 4 condensed with (3/?, 3aS, 6aR)- hexahydrofuro[2,3-6]furan-3-ol in large excess of solvent or solvent mixture containing large excess of base or mixture of bases to get Darunavir. Further, the obtained products by the processes described in the prior art are not satisfactory, from purity point of view. We have repeated the Darunavir synthetic procedures as described in the prior art and found that relatively large amounts of impurities were obtained along with Darunavir (Table-1) which need repeated crystallizations in different solvents to get desired quality of the final product resulting in poor yields. Among other impurities, the carbonic acid [(1/?,2S)-1-{((4-amino-benzenesulfonyl)-isobutyl-amino)-methyl}-2-((3R,3aSI6aR)- hexahydro-furot2,3-/3]furan-3-yloxycarbonylamino)-3-phenyl-propylester (3R,3aS,6aR)- hexahydro-furo[2,3-ft]furan-3-yl ester (difuranyl impurity of formula 1) is identified.

Conditions:-
i. Phenyl magnesium bromide, Cuprous cyanide, tetrahydrofuran, 23 °C, 1 h,
ii. t-Butyl hydroperoxide, titanium tetraisopropoxide, diethyl D-tartrate, dichloromethane, -22 °C, 24 h,
iii. Azidotrimethylsilane, titanium tetraisopropoxide, Benzene, reflux, 25 min,
iv. 2-Acetoxyisobutyryl chloride, Chloroform, 23 °C, 8 h,
v. Isobutyl amine, isopropanol, 80 °C, 12 h,
vi 4-aminobenzenesulfonyl chloride, aq. Sodium bicarbonate, dichloromethane, 23 °C, 12 h,
vii. 10% palladium on carbon, hydrogen gas (50 psi), methanol, acetic acid, tetrahydrofuran, room temperature, 2 h,
viii. [3R, 3aS,6aS]-3-hydroxyhexahydrofuro[2,3-b]-furan, disuccanamidyl carbonate, triethylamine, acetonitrile, 23 °C, 12 h
Schematic Representation for Synthesis of Darunavir
Preparation of Darunavir is described in US patent 05,158,713, and also in WO9967417 and WO9967254. Accordingly, 2-vinyloxirane 1 on reacting with phenyl magnesium bromide in presence of tetrahydrofuran solvent and cuprous cyanide catalyst give 4-phenylbut-2-ene-1-ol 2. Oxidizing 2 with t-Butyl hydroperoxide in presence of titanium tetraisopropoxide and diethyl D-tartrate using dichloromethane as solvent give [(3S)-3-benzyloxiran-2-yl]methanol 3.
Heating 3 with azidotrimethylsilane in presence of titanium tetraisopropoxide using benzene as solvent give (2S,3S)-3-azido-4-phenyl-butane-1,2-diol 4. The 1,2-dipl compound 4 underwent cyclization when treated with 2-acetoxyisobutyryl chloride in chloroform give (2S)-2-[(1S)-1-azido-2-phenyl-ethyl]oxirane 5, which was further heating with isobutylamine and isopropanol at higher temperature give (2R,3S)-3-azido-1-(isobutylamino)-4-phenyl-butan-2-ol 6. Compound 6 was reacted with 4-aminobenzenesulfonyl chloride in presence of aq. Sodium bicarbonate as base and dichloromethane as solvent resulting in to 4-amino-N-[(2R,3S)-3-azido-2-hydroxy-4-phenyl-butyl]-N-isobutyl-benzenesulfonamide 7.
Hydrogenating 7 with 10% palladium on carbon catalyst using hydrogen gas (50 psi) in methanol and tetrahydrofuran solvent in presence of small amount of acetic acid at ambient temperature resulted in to 4-amino-N-[(2R,3S)-3-amino-2-hydroxy-4-phenyl-butyl]-N-isobutyl-benzenesulfonamide 8. The final step involves reacting 8 with [3R,3aS,6aS]-3-hydroxyhexahydrofuro[2,3-b]-furan and disuccanamidyl carbonate in presence of triethylamine base and acetonitrile as solvent afford [(1S,2R)-3-[[(4-Aminophenyl)sulfonyl] (2-methylpropyl)amino]-2-hydroxy-1-(phenylmethyl)propyl]carbamic acid (3R,3aS,6aR)-hexahydrofuro[2,3-b]furan-3-yl ester also called Darunavir 9.
…………………………
http://www.google.com/patents/WO2013114382A1?cl=en
process for the preparation of amorphous Darunavir is as
Process for the preparation of intermediate 2 is as shown in below scheme.
Examples
Example -1 : Preparation of [(1S, 2S)-3-chloro-2-hydroxy-1-(phenyl methyl) propyl] carbamic acid tert-butyl ester (5).
The solution of (3S)-3-(tert-butoxycarbonyl) amino-1-chloro-4-phenyl-2-butanone (Chloromethyl ketone 6,100 g) and aluminium isopropoxide (35 g) in isoprpylalcohol was heated to mild reflux and maintained for 3 hours. After completion of reaction distilled off isopropyl alcohol up to 50 % under vacuum and the resultant mass was cooled to 25-35°C. Water was added to the distillate, pH was adjusted to 3.0-4.0 with acetic acid and maintained the stirring for 2 hours at 25-35°C. The obtained solid was filtered and washed with water. The wet cake was taken into isopropyl alcohol (400mL) and heated to reflux for 60minutes, the mass was cooled to 25-35°C again maintain the stirring for 60minutes, the obtained solid was filtered and washed with isopropyl alcohol. The wet product was dried under normal drying to get title compound 5 (yield 80 g). Example -2: Preparation of [(1 S, 2R)-3-[(2-methylpropyl) amino]-2-hydroxy-1- (phenylmethyl) propyl] carbamic acid tert-butyl ester (4).
The mixture of [(1S, 2S)-3-chloro-2-hydroxy-1-(phenylmethyl) propyl] carbamic acid tert-butyl ester (5,100 g), isobutyl amine (294 g), sodium carbonate (31.3 g) and water was heated to 60 – 65°C and maintained for 3hours. After completion of reaction water (200 mL) was added and distilled out excess isobutyl amine under vacuum at below 75°C. Water (800 mL) was added to the distillate, cooled to 25-35°C and stirred for 2 hours. The obtained solid was filtered and washed with water to get title compound 4 (yield 105 g).
Example -3: Preparation of [(1S, 2R)-3-[[(4-nitrophenyl) sulfonyl] (2-methylpropyl) amino]- 2-hydroxy-1-(phenylmethyl) propyl] carbmic acid tert-butylester (3).
[(1 S, 2R)-3-[(2-methylpropyl) amino]-2-hydroxy-1 -(phenyl methyl) propyl] carbamic acid tert-butyl ester (4, 100 gm) and triethylamine (39.04 g) was added to methylenedichloride (1200 mL) and the temperature was raised to 40°C. p-nitro benzene sulfonyl chloride solution (72.3g of p-NBSC dissolve in 300mL methylenedichloride) was added slowly at 40-45°C for 2-3 hrs. The reaction was maintained for 3hours at 40 – 45°C. After completion of the reaction, water (500 mL) was added, separated the organic layer and distilled out methylene dichloride at atmospheric pressure. Finally, strip out the methylene dichloride by using isopropyl alcohol (200 mL). Isopropyl alcohol (1000 mL) was added to the distillate and maintained the stirring for 60 minutes at 70- 80°C. Cooled the mass to 30 – 35°C, filtered and washed with Isopropyl alcohol to get title compound 3 (yield 145 g). Example – 4: Preparation of 4-Amino-N-(2R, 3S) (3-amino-2-hydroxy-4-phenylbutyl)-N- isobutyl-benzene sulfonamide (1).
(1S, 2R)-{1-benzyl-2-hydroxy-3-[isobutyl-(4-nitro-benzenesulfonyl)-amino]-propyl}-carbamic acid tert-butyl ester (3, 100g), 10% palladium carbon (10gm) and triethanolamine (2gm) were suspended in isopropyl alcohol. The reaction was heated to 40 – 45°C and maintained under 4 – 6kg/cm2 of hydrogen pressure for 3 hours. After completion of reaction, the mass was filtered and hydrochloric acid (70mL) was added to the filtered mass. The solution was heated to reflux and maintained for 2-3hours. After completion of reaction the mass was cooled to 25-35°C, the reaction mass pH was adjusted to 6.0 – 7.0 with 20% sodium hydroxide solution and distilled out isopropyl alcohol under vacuum at below 55°C. Ethanol (200mL) and water (400mL) was added to the distillate, the mass pH was adjusted to 9.0 – 10.0 with 20% sodium hydroxide solution at 25-35°C and maintained the stirring for 2 hours at 25-35°C. The mass was cooled to 0 – 5°C, filtered and wash with water. The wet product was taken into ethanol (350mL), maintained the stirring for 30minutes at reflux temperature. The mass was cooled to 2 – 4°C, stirred for 2 hours, filtered and washed with ethanol (50 mL). The wet product was dried under normal drying to get title compound 1 (Yield 60 g).
Example-5: Preparation of ethyl-2-(4,5-dihydrofuran-3-yl)-2-oxoacetate (VI).
2, 3-Dihydrofuran (250 g) was taken in toluene (2000 mL) and triethyl amine (505 g) was added to above solution. Ethyl oxalyl chloride (536.5 g) was slowly added to the above mixture by maintaining temperature at 25-30°C and maintained the stirring for 5 hours. After completion of reaction separated the organic layer, washed the organic layer with 8% sodium bicarbonate solution (2x500mL). Organic layer was distilled completely under vacuum to get title compound VI (Yield 560g).
1 H NMR : 1.38 (t, 3H), 2.93 (t, 2H), 4.34 (q, 2H), 4.63 (t, 2H), 8.02 (s, 1 H).
Example-6: Preparation of ethyl-2-(3-bromo-2-ethoxytetrahydrofuran-3-yl)-2-oxoacetate (V).
Ethyl-2-(4,5-dihydrofuran-3-yl)-2-oxoacetate (Vl, 100g) was dissolved in dichloromethane (500ml) and Ethanol (150mL) was added. The reaction mass was cooled to 5 to 10°C. N- bromosuccinimide (1 15 g) was added lot wise by maintaining temp below 10°C. Reaction mass was then stirred at 20-30°C till completion of reaction. Reaction mass was washed with sodium bicarbonate solution (2%, 3x400mL) and the organic layer was used for the next step.
Example-7: Preparation of hexahydrofuro [2, 3-b] furan-3-ol (IV).
To the solution of Ethyl-2-(3-bromo-2-ethoxy tetra hydrofuran-3-yl)-2-oxoacetate in dichloromethane (V, 500mL) as prepared in above example, sodium sulphite solution (225g was dissolved in 1700mL of water) was added at 25-35°C. Reaction mass was stirred for 5-8hours at the same temperature and separated the organic and aqueous layers. Organic layer was washed with water (340mL). Distilled out the solvent completely get ethyl-2-(2-ethoxy tetra hydrofuran-3- yl)-2-oxoacetate. Sodium borohydride (35.5g)was dissolved in ethanol (400mL) under nitrogen atmosphere, ethyl-2-(2-ethoxytetra hydrofuran-3-yl)-2-oxoacetate was dissolved in ethanol (100mL) and slowly added to above solution at 15-30°C. Reaction mass was heated to 30-45X, maintained for 5-8 hours, the reaction mass temperature was raised to 55°C and stirred for 8 hours. The reaction mass was cooled to 20-30°C, ammonium chloride solution (1 5g in 200mL water) was slowly added and stirred for 1-2hours. The reaction mass was filtered and filtrate was distilled out under vacuum to get residue. Dichloromethane (600mL) was added to residue and cooled to -10°C. Hydrochloric acid (85mL) was added slowly drop wise in 2 hours by maintaining temp -5 to 0°C, reaction mass was stirred for 60minutes at -5 to 0°C and distilled the solvent completely. The obtained residue was stripped out with isopropyl alcohol (2x200mL, 1x100mL), ethyl acetate (500mL) was added to the resultant residue, stirred for 30-60minutes and cooled to 10-15°C. The solution was filtered and filtrate was concentrated to get title compound IV (yield 56 g).
Example-8: Preparation of Hexahydrofuro [2, 3-b] furan-3-yl acetate (III).
Hexahydrofuro [2, 3-b] furan-3-ol (IV, 60g) was dissolved in dichloromethane (300mL) and cooled to 0-5°C. To the cooled solution triethylamine (58.2 g), N, N-dimethylaminopyridine (1.12g) was added, acetic anhydride (56.5g) was added for 30-60 minutes at the same temperature, the mass temperature was raised to 25-35°C and stirred for 2-4hours. After completion of reaction the mass was cooled to 10-20°C, water (120mL) was added, stirred for 30minutes, separated the organic layer, washed with 10% sodium chloride solution (120mL) and distilled out dichloromethane to get title compound (yield 72g). Further, the product was purified by fractional distillation to get pure Hexahydrofuro [2, 3-b] furan-3-yl acetate III (yield 54g).
1 H NMR : 1.9-2.09(m, 2H), 2.10(s, 3H), 3.0-3.1 (m, 1 H), 3.86-4.03(m, 2H), 3.73(dd, 1 H), 4.10(dd, 1 H), 5.19(m, 1 H), 5.72 (d, 1 H)
Example-9: Preparation of (3R, 3aS, 6aR)-Hexahydrofuro [2, 3-b] furan-3-yl acetate (II). To the buffer solution (104.3g of sodium dihydrogen orthophosphate dissolved in 530mL of water & pH adjusted to 6.0-6.5 with saturated sodium bicarbonate solution(68g in 680 mL water) solution) hexahydrofuro [2, 3-b] furan-3-yl acetate (111,115g) and CAL-B (17.25g) was added at 25-35°C, heated to 38-45°C and stirred for 24 hours. CAL-B (17.25g) was added stirred for 16 hours, again CAL- B (11.5g) was added at 38-45°C and stirred for 16 hours (pH should maintain 6.0-6.5). The reaction mass was cooled to 20-30°C, methylenedichloride (1 150mL) was added to the mass and stirred for 30 minutes. The reaction mass was filtered through hyflowbed then separated the organic layer and washed with 10%sodiumchloride solution (575mL). Organic layer was distilled completely under vacuum to get title compound II (yield 40. Og). Example-10: Preparation of (3R, 3aS, 6aR)-Hexahydrofuro [2, 3-b] furan-3-ol (I).
(3R, 3aS, 6aR)-Hexahydrofuro [2, 3-b] furan-3-yl acetate (II, 14.0g) was dissolved in methanol (42mL). Potassium carbonate (0.34g) was added and stirred at 25-35°C for 6-8hours. Methanol was distilled out completely under vacuum, to the distillate methylenedichloride (28mL) was added, stirred the mass for 30 minutes and again distilled the solvent to get residue. Dissolved the residue in dichloromethane (56mL), the resultant solution was treated with carbon and the solvent was completely distilled out get title compound I (yield 10.5g). Example-11 : Preparation of (3R, 3aS, 6aR)-Hexahydrofuro [2, 3-b]-furan-3-yl-4-nitrophenyl carbonate (2).
To the solution of (3R, 3aS, 6aR)-Hexahydrofuro [2, 3-b] furan-3-ol (l,100g) and Bis-nitrophenyl carbonate (257.2g) in methylene dichloride (1200mL), triethylamine solution (132 g in 300 mL of methylene dichloride) was added slowly at 20-30°C for 2-3hours. Maintained the reaction at the same temperature for 8-10hours, after completion of reaction water (500mL) was added for 30- 60minut.es and settled the reaction mass then separated the organic layer. Organic layer was washed with 10% acetic acid (100mL) and 10% sodium chloride solution (500mL), distilled the organic layer and co distilled with ethyl acetate (100mL). Ethyl acetate (300mL) was added to the distillate and heated to 50-55°C for 30-45minut.es to get clear solution, the solution was cooled to 5-10°C and maintained at the same temperature for 60 minutes. The obtained solid was filtered, washed with ethanol (100mL) and dried the wet material at 40-45°C for 10-14 hours to get title compound 2 (yield 160g). Example-12: Preparation of dimethylformamide solvate of Darunavir.
To a mixture of 4-amino-N-(2r,3S)(3-amino-2-hydroxy-4-phenylbutyl)-N-lsobutyl- benzenesulfonamide (1 ,25g) and N-methyl-2-pyrrolidinone (NMPO, 50mL), a solution of (3R,3aS,6aR)-Hexahydrofuro[2,3-b]-furan-3-yl-4-nitrophenyl carbonate (2, 8.85g) and N-methyl- 2-pyrrolidinone (75mL) was added at -5 to 0°C for 2 to 3 hours under nitrogen atmosphere. The mass temperature was slowly raised to 25 to 30°C and stirred for 6 to 8 hours. The reaction mass was quenched in to the solution of methylene chloride (125mL) and water (250mL) at 25-35°C for 30 to 45 minutes. Separated the organic layer followed by washed with 10% sodium carbonate solution (150mL), 10% sodium chloride solution (150mL) and with water (6x150mL). Organic layer was dried over sodium sulphate and distill off the solvent under vacuum at below 50°C to obtain darunavir as a residue. To the residue Ν,Ν-dimethyl formamide (50mL) was added and cooled to 0 to -5°C, water (25mL) was added to the solution and maintained for 12hours at 0 to -5 °C, the obtained solid was filtered and washed with pre-cooled mixture of N,N-dimethyl formamide & water (25mL+25mL) to get dimethylformamide solvate of darunavir.
Example-13: Preparation of non-solvated crystalline Darunavir.
To a mixture of 4-amino-N-(2r,3S)(3-amino-2-hydroxy-4-phenylbutyl)-N-lsobutyl- benzenesulfonamide (1, 25g) and N-methyl-2-pyrrolidinone (NMPO, 50mL), a solution of (3R,3aS,6aR)-Hexahydrofuro[2,3-b]-furan-3-yl-4-nitrophenyl carbonate (2, 18.85g) and N- methyl-2-pyrrolidinone (75mL) was added at -5 – 0°C for 2 to 3 hours under nitrogen atmosphere. The mass temperature was slowly raised to 25 – 30°C and stirred for 6 to 8 hours. The reaction mass was quenched in to the solution of methylene chloride (250mL) and water (250mL) at 25- 35°C for 30 – 45 minutes. Separated the organic layer followed by washed with 10% potassium carbonate solution (5x125mL), water (5x125mL), 20% sodium chloride solution (25mL), finally washed with 20% citric acid solution (125mL). The organic layer was treated with carbon and distilled off the solvent under vacuum at below 50°C to obtain darunavir as a residue. To the residue ethylacetate (250mL) was added and cooled to 0 to -5°C, to the cooled solution hexane (225mL) was added and maintained for 12hours at 0 to -5 °C, the obtained solid was filtered, washed with pre-cooled mixture of ethylacetate and hexane (25mL+25mL) and dried the compound to get non-solvated crystalline darunavir(yield 25g).
Example -14: Preparation of Amorphous Darunavir.
Darunavir (200g) as obtained in above example was dissolved in methylene dichloride (10L) and washed with water (3×1000 mL). Organic layer was taken into agitated thin film dryer (ATFD) feed tank. Applied initial temperature about 36 – 40°C and high vacuum (580mm/Hg) to the vessel. Slowly feed the solution to the Vessel (feed rate 5L r) over 1hour finally given the methylene chloride (3L) flushing. The material is collected in the material collecter. Dried at 58 -62°C for 40 hours to get amorphous darunavir (yield 160g).
………………..
http://www.google.com/patents/WO2011048604A2?cl=en

Preparation of Durumvir ethanolate
A solution of (3R,3aS,6a ?)-hexahydrofuro[2,3-D]furan-3-yl 4-nitrophenyl carbonate (5b, 75.4 g) in A -methyl-2-pyrrolidinone (300 mL) was added to a pre-cooled (-2 ± 2°C) solution of the compound of formula 4 (100 g) in W-methyl-2-pyrrolidinone (200 mL) at -4 to 0°C over a period of 2 h. The temperature of the reaction mass was slowly raised to 25 – 30°C and maintained for 8 h. After completion of the reaction (TLC monitoring), ethyl acetate (1000 mL) and purified water (500 mL) were added to the reaction mass. The layers were separated; organic layer was washed with sodium carbonate solution (2 X 500 mL) followed by sodium chloride solution. The organic layer was concentrated; ethanol (300 mL) was added, heated to 45 – 50°C, maintained for 1 h, filtered and washed with ethanol. The wet compound was taken into a mixture of ethyl acetate- ethanol (7:93, 600 mL), heated to reflux, charcoal was added and filtered. The resultant filtrate was cooled to 0 – 5°C, filtered the separated solid and washed with ethanol. The wet compound was dried at 45°C to obtain the in 124.3 g (yield-82.5%). The obtained Darunavir ethanolate had purity of 99.79% on area by HPLC and contained 0.08% on area by HPLC of the difuranyl impurity. Preparation of Amorphous Darunavir
Example – 4
A solution of Darunavir ethanolate (200 g) in dichloromethane (10 L) was taken into ATFD Feed tank. The solvent was evaporated by fed the solution slowly to the ATFD Vessel (feed rate 5 L /h) at 36 – 40°C and high vacuum (580 mm/Hg) over 2 h and then flushed with dichloromethane (3 L). The material is collected in the material collector in 160g with the HPLC Purity of 99.60% and particle size D50 of approximately 50 micrometers and Dgo of approximately 100 to 180 micrometers. Example-5
Darunavir Ethanolate (200 gm) was dissolved in Methylene chloride (1000 ml) and solvent was evaporated by applying vacuum followed by isolation of amorphous Darunavir as a solid as such or by charging n-Heptane or Isopropyl ether. Example – 6
Darunavir Ethanolate (10 g) was dissolved in ethyl acetate (50 mL). The solution was heated to 40 – 45°C and maintained for 30 min. Ethyl acetate was distilled off under vacuum completely to get residue in the form of semisolid. n-Heptane (50 mL) was added to the residue and stirred for 30 min. at ambient temperature. The separated solid was filtered, washed the wet cake with n-heptane (5 mL) and dried at 40 – 45°C under vacuum to get 8.0 g of amorphous Darunavir.
Example – 7
Darunavir Ethanolate (10 g) was placed into a dry round bottom flask and heated to 110 – 120°C to melt and maintained under vacuum for 4 h. The reaction mass was slowly cooled to 25 – 35°C. The obtained glass type crystal was broken into powder to afford 8.5 g of amorphous Darunavir.
Example – 8
Darunavir Ethanolate (5.0 g) was suspended into glycerol (25 g), heated to 110 – 120°C under vacuum and maintained for 30min. Water (50 mL) was added to the cooled reaction mass at 25 – 35°C under stirring and the obtained suspension was stirred for 30 min at 25 – 35°C. The separated solid was filtered and dried at 40 – 45°C under vacuum to yield 3.5 g of amorphous Darunavir. Example – 9
Carbonic acid [(1 R,2S)-1-{((4-amino-benzenesulfonyl)-isobutyl-amino)-methyl}-2- ((3/?,3aS,6aR)-hexahydro-furo[2,3-ft]furan-3-yloxycarbonylamino)-3-phenyl-propylester (3R,3aS,6a ?)-hexahydro-furo[2,3- )]furan-3-yl ester (difuranyl impurity, 1).
The difuranyl impurity (1) isolated from the mother liquor by preparative HPLC using a mixture of formic acid-water (1 :99) as eluent. The 1H-NMR, 13C-NMR and mass spectral data complies with proposed structure.
1H-NMR (DMSO-cfe, 300 MHz, ppm) – δ 0.79 (d, J=6.6 Hz, 6H, 15 & 15′), 1.14-1.20 (m, 1 H, 20Ha), 1.34-1.42 (m, 1 H, 20Hb), 1.75-1.85 (m, 2H, 20’Ha & 14), 1.94-2.01(m, 1 H, 20’Hb), 2.54-2.64 (m, 2H, 8Ha & 13Ha), 2.74-2.89 (m, 3H, 8Hb, 13Hb & 19), 3.00-3.11 (m, 2H, 5Ha & 19′), 3.34-3.39 (m, 1H, 5Hb), 3.54-2.63 (m, 3H, 21 Ha & 17Ha), 3.65-3.74 (m, 3H, 21’Ha, 21 Hb &17Hb), 3.81-3.89 (m, 2H, 21’Hb & 17’Ha), 3.94-4.04 (m, 2H, 7 & 17’Hb), 4.81-4.88 (m, 1 H, 6), 4.92-4.96 (m, 1 H, 18′), 5.03-5.10 (m, 1 H, 18), 5.11 (d, J=5.4 Hz, 1 H, 22′), 5.61 (d, J=5.1 Hz, 1 H, 22), 6.03 (brs, 2H, NH2, D20 exchangeable), 6.63 (d, J=8.7 Hz, 2H, 2 & 2″), 7.15-7.28 (m, 5H, 10H, 10Ή, 11 H, 11′ & 12), 7.40 (d, J=8.7 Hz, 2H, 3 & 3′), 7.55 (d, J=9.3 Hz, 1 H, NH, D20 exchangeable).
“H-NMR (DMSO-d6, 75 MHz, ppm)- δ 19.56 & 19.81 (15C & 15’C), 25.42 (20 ), 25.47 (20C), 26.28 (14C), 35.14 (8C), 44.45(19’C), 45.01 (19C), 49.21 (5C), 53.39 (7C), 57.55 (13C), 68.70 (21 ‘C), 68.74 (21C), 69.95 (17’C), 70.20(17C), 72.65 (6C), 76.27 (18C), 79.59 (18’C), 108.70 (22’C), 108.75 (22C), 112.69 (2C), 122.56 (4C), 126.12 (12C), 128.04 (11 C & 11’C), 129.03 (10C & 10’C), 129.08 (3C), 138.03 (9C), 152.99 (1C), 153.55 (16’C), 155.32 (16C).
DIP MS: m/z (%) 1108 [M+Hf, 1131 [M+Naf
……………
http://www.google.com/patents/US20130244297

According to the present invention Darunavir having the below impurity not more than 0.1, preferably 0.05%.
………….
DARUNAVIR
Necitumumab

Necitumumab
Necitumumab is a fully human IgG1 monoclonal antibody designed to block the ligand binding site of the human epidermal growth factor receptor (EGFR), which is a target in several anti-cancer treatments because it sparks cancer progression, both by promoting angiogenesis, or the formation of new blood vessels for tumors, and by inhibiting apoptosis, or cell death. Recently approved therapies for non-squamous NSCLC, including afatinib and erlotinib, target specific EGFR mutations, but those drugs are used to treat patients with nonsquamous histology.Lilly did not provide specific data regarding the results of the trial, but the company announced that it plans to present that data at a scientific meeting next year, and to request a review of the drug by regulatory authorities before the end of 2014.
Necitumumabis one of three monoclonal antibodies in Phase III
development that targets EGFR, the target of the approved antibodies
cetuximab and panitumumab. However, necitumumab is a fully human
IgG1 antibody, distinguishing it from both the approved agents.
Necitumumab is directed against the ligand binding site of EGFR and is
being co-developed by Eli Lilly and Bristol-Myers Squibb in the United
States, Canada, and Japan, while Eli Lilly alone is developing it for other
markets. Necitumumabfirst entered clinical development in 2004 and
is now in Phase III development for the treatment of non–small-cell
lung cancer and Phase II for the treatment of colorectal cancer. The
primary indication chosen further distinguishes necitumumabfrom both
cetuximab and panitumumab, but it is an indication for which EGFR
kinase inhibitors such as erlotinib are approved.
In December 2009, Eli Lilly stressed the long half-life of necitumumab
(7–10 days, which permits dosing at 2–3 week intervals) and its potential
both for reduced hypersensitivity reactions (i.e., better tolerability) and
for induced host-mediated anticancer activity. In addition, it highlighted
that necitumumabdisplays similar or superior activity to cetuximab
in anticancer models. Preliminary data were presented from the Phase
II study in colorectal cancer showing antitumor activity in 73% of 44
patients treated with necitumumabplus FOLFOX.
Both Phase III studies in non–small-cell lung cancer are in stage IV
disease and in groups of 947 patients treated with necitumumabplus
cisplatin and a second agent. The INSPIRE study in non-squamous
disease began in November 2009 and uses pemetrexed as the second
drug, while the SQUIRE study commenced in January 2010 in
squamous disease and uses gemcitabine. Both studies have primary
completion dates in late 2011 and study completion dates of mid-2012,
which points to BLA submission in 2013.

A Phase I study in patients with solid tumors suggested that skin
toxicity was the dose-limiting toxicity and suggested that 800 mg of
necitumumab (at weekly or fortnightly intervals) be the maximum dose
(Kuenen et al. 2010).16 This dose was employed in the initial colorectal
cancer study, at 14-day intervals, which revealed a 60% partial response
(Taberno et al. 2008).17
The development strategy for necitumumab appears to have been
designed to establish it initially in a major indication where it will not
be competing with established antibody products, while seeking
to exploit the reported advantages over cetuximab appears to be
a secondary priority. While the reported Phase II data are very
encouraging, it will be some time before a better assessment of the
commercial prospects of necitumumab can be made. However, it does
appear to have significant potential.
Necitumumab (proposed INN) is a monoclonal antibody and an antineoplastic. It binds to the epidermal growth factor receptor(EGFR).[1] As of October 2009, two Phase III clinical trials are planned to investigate its effects on non-small cell lung carcinoma.[2][3]
- International Nonproprietary Names for Pharmaceutical Substances (INN, prepublication copy), World Health Organization.
- ClinicalTrials.gov NCT00981058 Squamous Non-Small Cell Lung Cancer (NSCLC) Treatment With the Inhibitor of Epidermal Growth Factor Receptor (EGFR) (SQUIRE)
- ClinicalTrials.gov NCT00982111 NonSquamous Non-Small Cell Lung Cancer Treatment With the Inhibitor of Epidermal Growth Factor Receptor (INSPIRE)
Possible Efficacy Of Lilly’s Necitumumab (IMC-11F8) In Lung Cancer Subset
18.4 2013
Eli Lilly announced yesterday their very preliminary and non-quantitative conclusions on the SQUIRE study, a 1093-patient Phase III trial of their anti-epidermal growth factor receptor (EGFR) antibody, necitumumab (IMC-11F8), against Stage IV squamous, non-small cell lung carcinoma (NSCLC).http://www.forbes.com/sites/davidkroll/2013/08/14/possible-efficacy-of-necitumumab-imc-11f8-in-squamous-nsclc-lung-cancer-subset/

Ixabepilone for breast cancer

Ixabepilone, 219989-84-1 cas
(1R,5S,6S,7R,10S,14S,16S)-6,10-dihydroxy-1,5,7,
9,9-pentamethyl-14-[(E)-1-(2-methyl-1,3-thiazol-
4-yl)prop-1-en-2-yl]-17-oxa-13-azabicyclo[14.1.0]
heptadecane-8,12-dione
Ixabepilone (INN; also known as azaepothilone B, codenamed BMS-247550) is an epothilone B analog developed byBristol-Myers Squibb as a chemotherapeutic medication for cancer.
It is produced by Sorangium cellulosum.
It acts to stabilize microtubules. It is highly potent agent, capable of damaging cancer cells in very low concentrations, and retains activity in cases where tumor cells are insensitive to paclitaxel.
On October 16, 2007, the U.S. Food and Drug Administration approved ixabepilone for the treatment of aggressive metastaticor locally advanced breast cancer no longer responding to currently available chemotherapies. In November 2008, the EMEAhas refused a marketing authorisation for Ixabepilone.
Ixabepilone is administered through injection, and is marketed under the trade name Ixempra.
patent approval expiry
| United States | 7312237 | 2004-08-21 | 2024-08-21 |
| United States | 6605599 | 1998-05-26 | 2018-05-26 |
| Applicant | Tradename | Generic Name | Dosage | NDA | Approval Date | Type | RLD | US Patent No. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Bristol Myers Squibb
|
IXEMPRA KIT
|
ixabepilone
|
INJECTABLE;IV (INFUSION) | 022065 | Oct 16, 2007 | RX | Yes | RE41911*PED | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Bristol Myers Squibb
|
IXEMPRA KIT
|
ixabepilone
|
INJECTABLE;IV (INFUSION) | 022065 | Oct 16, 2007 | RX | Yes | RE41393*PED | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Bristol Myers Squibb
|
IXEMPRA KIT
|
ixabepilone
|
INJECTABLE;IV (INFUSION) | 022065 | Oct 16, 2007 | RX | Yes | 7,312,237*PED | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Bristol Myers Squibb
|
IXEMPRA KIT
|
ixabepilone
|
INJECTABLE;IV (INFUSION) | 022065 | Oct 16, 2007 | RX | Yes | 7,125,899*PED | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Patent No | Patent Expiry | patent use code |
|---|---|---|
| 6670384 | Jan 23, 2022 | U-959 |
| 6670384 | Jan 23, 2022 | U-960 |
| 6670384*PED | Jul 23, 2022 | |
| 7022330 | Jan 23, 2022 | U-958 |
| 7022330*PED | Jul 23, 2022 | |
| 7125899 | May 26, 2018 | U-957 |
| 7125899*PED | Nov 26, 2018 | |
| 7312237 | Aug 21, 2024 | U-965 |
| 7312237*PED | Feb 21, 2025 | |
| RE41393 | Feb 8, 2022 | U-961 |
| RE41393*PED | Aug 8, 2022 | |
| RE41911 | Sep 28, 2020 | U-961 |
| RE41911*PED | Mar 28, 2021 |
| Exclusivity Code | ExclusivityDate |
|---|---|
| NCE | Oct 16, 2012 |
| PED | Apr 18, 2015 |
| M-61 | Oct 18, 2014 |
| PED | Apr 16, 2013 |
| Exclusivity Code | ExclusivityDate |
|---|---|
| NCE | Oct 16, 2012 |
Ixabepilone, in combination with capecitabine, has demonstrated effectiveness in the treatment of metastatic or locally advanced breast cancer in patients after failure of an anthracycline and a taxane.
It has been investigated for use in treatment of non-Hodgkin’s lymphoma. In pancreatic cancer phase two trial it showed some promising results (used alone). Combination therapy trials are ongoing.
Ixabepilone is an anti cancer agent acting as a microtubule inhibitor, and which in particular are efficient in the treatment of cancer not reacting to other anti cancer agents, such as e.g. paclitaxel. Ixabepilone is marketed under the trade name Ixempra® and are approved for the treatment of aggressive metastatic or locally advanced breast cancer which not responding to the current prevailing chemotherapies.
Ixabepilone known under the CAS no. 219989-84-1 has the following structure:
Ixabepilone
Ixabepilone may be prepared from a starting material named epothilone B having the structural formula:
Epothilone B Ixabepilone as a compound is described in the USRE4191 1. USRE4191 1 furthermore disclose a process for synthesizing Ixabepilone.
The US 6,365,749 describes a process for making ixabepilone by reacting epothilone B with a palladium catalyst in the presence of a nucleophilic donor.
The USRE39356 do also describe a process for making Ixabepilone by reacting epothilone B with an azide donor agent and a reducing agent in the presence of a phase transfer catalyst and a palladium catalyst.

Ixabepilone is the treatment of metastatic and advanced breast cancer drugs.Ixabepilone as anticancer drugs alone or in combination with capecitabine (Capecitabine) in combination. October 16, 2007 approved for marketing by the FDA, trade name Ixempra, by the Bristol-Myers Squibb Company’s development.
Ixabepilone is an anti-mitotic drugs that are inhibitors of tubulin, the mechanism and paclitaxel (Taxol) the same class of drugs. Epothilone (Epothilone) by colistin (myxobacterium) Sorangium cellulosum fermentation of several macrolide metabolites in general. Anticancer activity in vitro experiments, epothilone A and epothilone B showed good activity, even in the paclitaxel-resistant cells also showed good activity. But its activity in vivo experiments in general, this is probably due to the body of the ester hydrolases that macrolide ring opening induced inactivation. In a series of epothilone derivatives activity test, it was found with the lactam bond instead of the original product of ester bonds – ixabepilone anticancer activity can be well retained.
Ixabepilone is epothilone B semi-synthetic derivatives. Epothilone B is a macrocyclic lactone, a hydroxyl moiety is allyl alcohol, the Pd catalyst can be obtained by ring-opening Pd complexes 1 , 1 received azide nucleophile attacking the anion generated with three azide product phosphorus reduction to give methyl amino acids 2 . Here we must point out that the attack was completely azide stereoselectivity, which is determined by two consecutive trans-attack lead, Pd (0)-trans lactone generate offensive allyl Pd complexes, to accept anti-azide anion type attack, to maintain the configuration of the product obtained. Amino acids 2 HoBt and EDCI generated by an amide bond to get ixabepilone.

IXEMPRA (ixabepilone) is a microtubule inhibitor belonging to a class of antineoplastic agents, the epothilones and their analogs. The epothilones are isolated from the myxobacterium Sorangium cellulosum. Ixabepilone is a semisynthetic analog of epothilone B, a 16-membered polyketide macrolide, with a chemically modified lactam substitution for the naturally existing lactone.
The chemical name for ixabepilone is (1S,3S,7S,10R,11S,12S,16R)-7,11dihydroxy-8,8,10,12,16-pentamethyl-3-[(1E)-1-methyl-2-(2-methyl-4-thiazolyl)ethenyl]17-oxa-4-azabicyclo[14.1.0] heptadecane-5,9-dione, and it has a molecular weight of 506.7. Ixabepilone has the following structural formula:
 |
IXEMPRA (ixabepilone) for injection is intended for intravenous infusion only after constitution with the supplied DILUENT and after further dilution with a specified infusion fluid . IXEMPRA (ixabepilone) for injection is supplied as a sterile, non-pyrogenic, single-use vial providing 15 mg or 45 mg ixabepilone as a lyophilized white powder. The DILUENT for IXEMPRA is a sterile, non-pyrogenic solution of 52.8% (w/v) purified polyoxyethylated castor oil and 39.8% (w/v) dehydrated alcohol, USP. The IXEMPRA (ixabepilone) for injection and the DILUENT for IXEMPRA are co-packaged and supplied as IXEMPRA Kit.
….

back to home for more updates
![]()

DR ANTHONY MELVIN CRASTO Ph.D
BAYER 2013 AND BEYOND
http://www.bayer.com/
Bayer
With 11 treatments in Phase I trials, 8 in Phase II, and 13 in Phase III, Bayer has a strong pipeline.
By far the most interest currently, given that the latest reports came out October 21st, is riociguat (BAY 63-2521),

which has had good news from its ongoing Phase III clinical trials of the treatment for pulmonary arterial hypertension, also known as PAH. PAH is a progressive condition that overburdens the heart.
Trials indicate subjects had improved heart function and could better tolerate physical exercise. Patients on riociguat improved their walking distance by 36 meters on average, while those on placebo showed no improvement.
Professor Hossein Ardeschir Ghofrani of University Hospital Giessen, the principal investigator, was quite pleased with the results and explained the value of the measurement. “The six-minute walk distance test is a well-validated clinical measure in patients with PAH, and therefore, the results of the PATENT-1 trial are encouraging. . .These data from the PATENT study suggest that riociguat may be a potential treatment option both for patients who have never been treated for PAH as well as for those who have received prior treatment.”
Hossein A. Ghofrani
Associate Professor of Internal Medicine,
MD (University of Giessen) 1995 Research interests: pulmonary hypertension, ischaemia-reperfusion, experimental therapeutics, clinical trials
http://www.uni-giessen.de/cms/fbz/fb11/forschung/graduierte/mbml/faculty
Although Bayer put forth no sales estimate for the treatment, analysts predicted 2017 sales from riociguat of $480 million

BAYER PIPELINE AS ON OCT 25 2013
phase 1
| Project | Indication |
|---|---|
| CDK-Inhibitor (BAY 1000394) | Cancer |
| Mesothelin-ADC (BAY 94-9343) | Cancer |
| PSMA Bi TE Antibody (BAY 2010112) | Cancer |
| PI3K-Inhibitor (BAY 1082439) | Cancer |
| FGFR2 Antibody (BAY 1179470) | Cancer |
| HIF-PH (BAY 85-3934) | Anemia |
| Partial Adenosine A1 Agonist(BAY 1067197) | Heart Failure |
| Vasopressin Receptor Antagonist(BAY 86-8050) | Heart Failure |
| sGC Stimulator (BAY 1021189) | Heart Failure |
| S-PRAnt (BAY 1002670) | Symptomatic uterine fibroids |
| BAY 1026153 | Endometriosis |
phase2
| Project | Indication |
|---|---|
| PI3K-Inhibitor (BAY 80-6946) | Cancer |
| Regorafenib | Cancer |
| Refametinib (MEK-Inhibitor) | Cancer |
| Radium-223-Dichloride | Cancer |
| Sorafenib | Additional Indications |
| MR-Antagonist (BAY 94-8862) | Congestive Heart Failure (CHF) |
| MR-Antagonist (BAY 94-8862) | Diabetic Nephopathy |
| Riociguat (sGC Stimulator) | Pulmonary Hypertension |
| Neutrophil Elastase Inhibitor(BAY 85-8501) | Bronchiectasis |
phase 3
| Project | Indication |
|---|---|
| Sorafenib | Breast Cancer |
| Sorafenib | Adjuvant HCC |
| Sorafenib | Adjuvant RCC |
| Regorafenib | HCC 2nd line |
| Rivaroxaban | Major Adverse Cardiac Events |
| Rivaroxaban | CHF and CAD |
| peg rFVIII(BAY 94-9027) | Hemophilia |
| Aflibercept | Myopic choroidal neovascularization (mCNV) |
| Aflibercept | Diabetic Macular Edema (DME) |
| LCS 16 | Contraception |
| Vaginorm | Vulvovaginal atrophy (VVA) |
| Sodium Deoxycholate | Submental fat removal |
| Cipro DPI | Lung infection |
| Tedizolid | Skin and Lung Infections |
| Amikacin Inhale | Gram-negative pneumonia |
Information for Download from bayer
Sorafenib tosylate
https://newdrugapprovals.wordpress.com/2013/07/16/nexavar-sorafenib/
TEDIZOLID PHOSPHATE
![]()
Leverkusen, October 8, 2013 – Following the recent commercial introduction of five new drugs to address the medical needs of patients with various diseases, Bayer is now accelerating the development of further five promising drug candidates which are currently undergoing phase I and II clinical studies. The company today announced that it plans to progress these five new highly innovative drug candidates in the areas of oncology, cardiology, and women’s health into phase III clinical studies by 2015.
“Our Pharma research and development has done a tremendous job of bringing five new products to the market offering physicians and patients new treatment alternatives for serious diseases”, said Bayer CEO Dr. Marijn Dekkers. “Following our mission statement ‘Science For A Better Life’, the five chosen further drug candidates all have the potential to impact the way diseases are treated for the benefit of patients.”

Bayer CEO Dr. Marijn Dekkers
“Our research and development activities are strongly focused on areas where treatment options are not available today or where true breakthrough innovations are missing”, said Prof. Andreas Busch, member of the Bayer HealthCare Executive Committee and Head of Global Drug Discovery at Bayer HealthCare. “Our drug development pipeline holds a number of promising candidates which we want to bring to patients who need them urgently”, said Kemal Malik, member of the Bayer HealthCare Executive Committee, Chief Medical Officer and Head of Pharmaceutical Development at Bayer HealthCare. “Furthermore we are continuing to expand the range of indications for all our recently launched products Xarelto, Stivarga, Xofigo, Riociguat as well as Eylea and further refine the profile of these drugs in specific patient populations.”
Cl 223Ra Cl
Xofigo
https://newdrugapprovals.wordpress.com/2013/09/21/xofigo-injection-recommended-for-approval-in-eu/
The five mid-stage candidates have been selected for accelerated development based on positive “proof-of-concept” data from early clinical studies. Three of them are development compounds in the area of cardiology or the cardio-renal syndrome: Finerenone (BAY 94-8862) is a next generation oral, non-steroidal Mineralocorticoid Receptor antagonist which blocks the deleterious effects of aldosterone. Currently available steroidal MR antagonists have proven to be effective in reducing cardiovascular mortality in patients with heart failure but have significant side effects that limit their utilization. Finerenone is currently in clinical Phase IIb development for the treatment of worsening chronic heart failure, as well as diabetic nephropathy.
Finerenone (BAY 94-8862)
The second drug candidate in the area of cardiology is an oral soluble guanylate cyclase (sGC) stimulator (BAY 1021189). The start of a Phase IIb study in patients with worsening chronic heart failure is expected later this year.
For the cardio-renal syndrome, a Phase IIb program with the investigational new drug Molidustat (BAY 85-3934) is under initiation in patients with anemia associated with chronic kidney disease and/or end-stage renal disease. Molidustat is a novel inhibitor of hypoxia-inducible factor (HIF) prolyl hydroxylase (PH) which stimulates erythropoietin (EPO) production and the formation of red blood cells. Phase I data have shown that inhibition of HIF-PH by Molidustat results in an increase in endogenous production of EPO.
Molidustat (BAY 85-3934)
In oncology, Copanlisib (BAY 80-6946), a novel, oral phosphatidylinositol-3 kinases (PI3K) inhibitor, was selected for accelerated development. Copanlisib demonstrated a broad anti-tumor spectrum in preclinical tumor models and promising early clinical signals in a Phase I study in patients with follicular lymphoma. A Phase II study in patients with Non-Hodgkin’s lymphoma is currently ongoing.
Bayer has also made good progress in the development of new treatment options for patients with gynecological diseases: sPRM (BAY 1002670) is a novel oral progesterone receptor modulator that holds the promises of long-term treatment of patients with symptomatic uterine fibroids. Based on promising early clinical data the initiation of a Phase III study is planned for mid-2014.
Initiation of further studies with recently launched products
Bayer has successfully launched five new pharmaceutical products, namely Xarelto™, Stivarga™, Xofigo™, Eylea™, and Riociguat, which has very recently been approved in Canada under the trade name Adempas™.


Regorafenib, stivarga
Bayer’s Eylea (aflibercept),
https://newdrugapprovals.wordpress.com/2013/06/01/lucentis-rival-one-step-away-from-nhs-approval/
Xarelto has been approved globally for five indications across seven distinct areas of use, allowing doctors to treat patients in a greater variety of venous and arterial thromboembolic conditions than any other novel oral anticoagulant. The company continues to study the use of Xarelto for the treatment of further cardiovascular diseases. Ongoing clinical Phase III studies include COMPASS and COMMANDER-HF. The COMPASS study will assess the potential use of Xarelto in combination with aspirin, or as a single treatment to prevent major adverse cardiac events (MACE) in nearly 20,000 patients with atherosclerosis related to coronary or peripheral artery disease. The COMMANDER-HF study will evaluate the potential added benefit of Xarelto in combination with single or dual-antiplatelet therapy to help reduce the risk of death, heart attack and stroke in approximately 5,000 patients with chronic heart failure and coronary artery disease, following hospitalization for exacerbation of their heart failure.
In order to answer medically relevant questions for specific patient populations Bayer has initiated a range of additional Xarelto studies in patients with atrial fibrillation (AF) undergoing percutaneous coronary intervention with stent placement (PIONEER-AF-PCI), cardioversion (X-VERT) or an AF ablation procedure (VENTURE-AF).
As an extension to the Xarelto clinical trial programme, a number of real-world studies are designed to observe and further evaluate Xarelto in everyday clinical practice. These include the XAMOS study of more than 17,000 orthopaedic surgery patients, which confirmed the clinical value of oral, once-daily Xarelto in routine clinical practice in adults following orthopaedic surgery of the hip or knee. XANTUS is designed to collate data on real-world protection with Xarelto in over 6,000 adult patients in Europe with non-valvular AF at risk of stroke while XANAP is designed to collate data on real-world protection with Xarelto in over 5,000 adult patients in Europe and Asia with non-valvular AF at risk of stroke. XALIA will generate information from over 4,800 patients treated for an acute DVT with either Xarelto or standard of care.
In the area of oncology, Stivarga has been approved in 42 countries for use against metastatic colorectal cancer that is refractory to standard therapies, and additionally for gastrointestinal stromal tumor (GIST) in the US and Japan. Bayer is now planning to assess Stivarga in earlier stages of colorectal cancer as well as other cancer types. A Phase III trial in patients with colorectal cancer after resection of liver metastases is currently under initiation. Based on early clinical data Bayer has also initiated a Phase III study in liver cancer in patients who have progressed on sorafenib treatment.
Furthermore, the anti-cancer drug Xofigo (radium 223 dichloride) is a first-in-class alpha-pharmaceutical which is designed for use in prostate cancer patients with ‘bone metastases’ (secondary cancers in the bone) to treat the cancer in the bone and to help extend their lives. Xofigo is approved in the US for the treatment of patients with advanced castrate-resistant prostate cancer with symptomatic bone metastases. In addition, the European CHMP recently gave a positive opinion for radium 223 dichloride for the same use. The decision of the European Commission on the approval is expected in the fourth quarter of 2013.
Based on the excellent Phase III results for Xofigo in patients with castration resistant prostate cancer and symptomatic bone metastases Bayer is looking to expand the use of Xofigo to earlier stages of the disease, and plans to initiate a Phase III study in combination with the novel anti-hormonal agent abiraterone. In addition, early stage signal-generating studies in other cancer forms where bone metastases are important causes of morbidity and mortality are planned.
In the area of pulmonary hypertension Adempas (Riociguat) is the first member of a novel class of compounds – so-called ‘soluble guanylate cyclase (sGC) stimulators’ – being investigated as a new and specific approach to treating different types of pulmonary hypertension (PH). Adempas has the potential to overcome a number of limitations of currently approved treatments for pulmonary arterial hypertension (PAH) and addresses the unmet medical need in patients with chronic thromboembolic pulmonary hypertension (CTEPH). It was approved for the treatment of CTEPH in Canada in September 2013, making it the world’s first drug approved in this deadly disease.
Riociguat has already shown promise as a potential treatment option beyond these two PH indications. An early clinical study was conducted in PH-ILD (interstitial lung disease), a disease characterized by lung tissue scarring (fibrosis) or lung inflammation which can lead to pulmonary hypertension, and, based on positive data, the decision was taken to initiate Phase IIb studies in PH-IIP (idiopathic pulmonary fibrosis), a subgroup of PH-ILD. Moreover, scientific evidence was demonstrated in preclinical models that the activity may even go beyond vascular relaxation. To prove the hypothesis Bayer is initiating clinical studies in the indication of systemic sclerosis (SSc), an orphan chronic autoimmune disease of the connective tissue affecting several organs and associated with high morbidity and mortality. If successful, Riociguat has the potential to become the first approved treatment for this devastating disease.
In the area of ophthalmology, Eylea (aflibercept solution for injection) is already approved in Europe and several additional countries for the treatment of neovascular (wet) age-related macular degeneration and for macular edema following central retinal vein occlusion. In September, Bayer HealthCare and Regeneron Pharmaceuticals presented data of the two phase III clinical trials VIVID-DME and VISTA-DME of VEGF Trap-Eye for the treatment of diabetic macular edema (DME) at the annual meeting of the Retina Society in Los Angeles and at the EURetina Congress in Hamburg, Germany. Both trials achieved the primary endpoint of significantly greater improvements in best-corrected visual acuity from baseline compared to laser photocoagulation at 52 weeks. Bayer plans to submit an application for marketing approval for the treatment of DME in Europe in 2013.
About Bayer HealthCare
The Bayer Group is a global enterprise with core competencies in the fields of health care, agriculture and high-tech materials. Bayer HealthCare, a subgroup of Bayer AG with annual sales of EUR 18.6 billion (2012), is one of the world’s leading, innovative companies in the healthcare and medical products industry and is based in Leverkusen, Germany. The company combines the global activities of the Animal Health, Consumer Care, Medical Care and Pharmaceuticals divisions. Bayer HealthCare’s aim is to discover, develop, manufacture and market products that will improve human and animal health worldwide. Bayer HealthCare has a global workforce of 54,900 employees (Dec 31, 2012) and is represented in more than 100 countries. More information at www.healthcare.bayer.com.
![]()
Current Oncology Pipeline Trends

Oncology drug development far outpaces drug development for other therapeutic areas and the magnitude of that difference is significant. Here’s a current review of what is in the pipeline and an analysis of where oncology research is headed.

Stacey Ness, PharmD, RPh, MSCS, AAHIVP, has worked in both national specialty pharmacy and payer organizations and has experience in clinical management, adherence, and persistency programs, as well as chronic disease cost optimization strategies. Dr. Ness is active in the Consortium of Multiple Sclerosis Centers, Academy of Managed Care Pharmacy, National Home Infusion Association, National Association of Specialty Pharmacy, Specialty Pharmacy Certification Board, and Hematology and Oncology Pharmacy Association, and has served on the Minnesota Medicaid Drug Formulary Committee since 2008. She is a multiple sclerosis certified specialist, a credentialed HIV pharmacist, and currently serves as the director of specialty clinical services at Managed Health Care Associates, Inc, a health care services organization based in Florham Park, New Jersey.
FDA Approves Perjeta for Neoadjuvant Breast Cancer Treatment
pertuzumab
Sept. 30, 2013 — The U.S. Food and Drug Administration today granted accelerated approval to Perjeta (pertuzumab) as part of a complete treatment regimen for patients with early stage breast cancer before surgery (neoadjuvant setting). Perjeta is the first FDA-approved drug for the neoadjuvant treatment of breast cancer.
Perjeta was approved in 2012 for the treatment of patients with advanced or late-stage (metastatic) HER2-positive breast cancer. HER2-positive breast cancers have increased amounts of the HER2 protein that contributes to cancer cell growth and survival
cut paste of my old article
he European Medicines Agency (EMA) has approved Roche’s PERJETA (pertuzumab) for patients with previously untreated HER2-positive metastatic breast cancer (mBC)
MARCH 5, 2013 8:59 AM / 4 COMMENTS /

Pertuzumab (also called 2C4, trade name Perjeta) is a monoclonal antibody. The first of its class in a line of agents called “HER dimerization inhibitors”. By binding to HER2, it inhibits the dimerization of HER2 with other HER receptors, which is hypothesized to result in slowed tumor growth.[1] Pertuzumab received US FDA approval for the treatment of HER2-positive metastatic breast cancer on June 8, 2012.[2] Pertuzumab was developed at Genentech and is now owned by Roche which acquired Genentech in 2009.
Clinical trials
Early clinical trials of pertuzumab in prostate, breast, and ovarian cancers have been met with limited success.[3]
The dosage of pertuzumab used in the pivotal phase III CLEOPATRA (Clinical Evaluation of Pertuzumab and Trastuzumab) trial was as follows: IV 840 mg loading dose followed by IV 420 mg every three weeks.[4]
The pharmacokinetics of intravenous pertuzumab appear to be unaffected by age and no drug-drug interaction has been reported with docetaxel. The pharmacokinetics and pharmacodynamics of pertuzumab were summarized in a Feb 2012 review by Gillian Keating.[4]
The combination of pertuzumab plus trastuzumab plus docetaxel, as compared with placebo plus trastuzumab plus docetaxel, when used as first-line treatment for HER2-positive metastatic breast cancer, significantly prolonged progression-free survival, with no increase in cardiac toxic effects in the randomized, double-blind, multinational, phase III CLEOPATRA trial.[5]
Intravenous pertuzumab is currently being evaluated in patients with breast cancer in the following trials: MARIANNE (advanced breast cancer), NEOSPHERE (early breast cancer), TRYPHAENA (HER2-positive stage II/III breast cancer) and APHINITY (HER2-positive nonmetastatic breast cancer).[4]
References
- de Bono, Johann S.; Bellmunt, J; Attard, G; Droz, JP; Miller, K; Flechon, A; Sternberg, C; Parker, C et al. (20 January 2007). “Open-Label Phase II Study Evaluating the Efficacy and Safety of Two Doses of Pertuzumab in Castrate Chemotherapy-Naive Patients With Hormone-Refractory Prostate Cancer”. Journal of Clinical Oncology 25 (3): 257–262.doi:10.1200/JCO.2006.07.0888. PMID 17235043.
- “FDA Approves Perjeta (Pertuzumab) for People With HER2-Positive Metastatic Breast Cancer” (Press release). Genentech. Retrieved 2012-06-09.
- Genentech press release – May 15, 2005
- Keating GM. Pertuzumab: in the first-line treatment of HER2-positive metastatic breast cancer. Drugs 2012 Feb 12; 72 (3): 353-60.Link text
- Baselga J, Cortés J, Kim SB, and the CLEOPATRA Study Group. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med 2012 Jan 12; 366 (2): 109-19. Link text
Daclizumab
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Humanized (from mouse) |
| Target | CD25 |

Daclizumab is a humanized monoclonal antibody indicated in the United States for prophylaxis of acute organ rejection in patients receiving renal transplants.
It was marketed as Zenepax, but discontinued by Roche in 2009 due to diminishing market demand for that indication. Biogen Idec is currently conducting phase III trials for daclizumab in MS. A phase III trial started in March 2010 is being conducted to determine efficacy of preventing MS relapse.
Study dosing of daclizumab is 150 mg subcutaneously once every 4 weeks versus interferon beta-1a (Avonex) 30 mg intramuscularly given once weekly for 96 to 144 weeks.
Daclizumab (Zenapax®) (molecular wt = 144 kd.) is a humanized monoclonal antibody (IgG1) produced by recombinant DNA technology. It gained FDA approval in Dec 1997. It is known by several other names including HAT (Humanized Anti-Tac), SMART anti-Tac, anti-CD25, and humanized anti-IL2-receptor. It was developed and patented by Protein Design Laboratories (Mountain View, CA) and it is marketed by Hoffman LaRoche (Nutley, NJ ).
Daclizumab is a composite of human (90%) and murine (10%) antibody sequences. In the model below, the murine portions are shown in red and dark blue; the rest of the molecule (gray color) represents the human sequence
The study is aiming for enrollment of 1500 patients and is expected to be complete in January 2014.
more info
Daclizumab (trade name Zenapax) is a therapeutic humanized monoclonal antibody. It is used to prevent rejection in organ transplantation, especially in kidney transplants. The drug is also under investigation for the treatment of multiple sclerosis.
Daclizumab works by binding to CD25, the alpha subunit of the IL-2 receptor of T cells. The drug is marketed in the US, but not in Europe.
Uses
Prevention of organ transplants
Daclizumab is given in multiple doses, the first 1 hour before the transplant operation and 5 further doses given at two week intervals after the transplant. These saturate the receptors and prevent T cell activation and thus prevent formation of antibodiesagainst the transplant.
Like the similar drug basiliximab, daclizumab reduces the incidence and severity of acute rejection in kidney transplantation without increasing the incidence of opportunistic infections.
Daclizumab usage may also be indicated in place of a calcineurin-inhibitor (ciclosporin or tacrolimus) during the early phase after kidney transplantation, when the kidney is recovering and vulnerable to calcineurin-inhibitor toxicity. This has been shown to be beneficial in non-heart beating donor kidney transplantation.
In the United Kingdom, the National Institute for Health and Clinical Excellence (NICE) has recommended its use be considered for all kidney transplant recipients.[citation needed]
Multiple sclerosis
In 2006 it began a Phase II clinical trial that finished in 2007 as a possible multiple sclerosis (MS) treatment. Participants were nine patients with multiple sclerosis not controlled with interferon. Daclizumab was effective in reducing lesions and improving clinical scores.[1] As of June 2013, the drug is in Phase III trials for this indication.[2]
Autoimmune diseases
Daclizumab has also been used to slow the progression of autoimmune diseases, particularly that of birdshot chorioretinopathy.[3]
Common side effects with a frequency of at least 10% include sleeplessness, tremor, headache, arterial hypertension, dyspnoea, gastrointestinal side effects and oedema. In rare cases, the drug can cause severe anaphylaxis.[4]
Daclizumab must not be administered to lactating women.[4]
History
Daclizumab was developed by PDL Biopharma, building on research at the National Institutes of Health (NIH).[5] Since December 1997, it is marketed by Hoffmann-La Roche in the US.
In April 2008, Hoffmann-La Roche submitted an application to have its marketing authorisation withdrawn in the EU for commercial reasons. The drug faced diminishing market demand, according to the company. There were no safety concerns with its use. As of January 2009, its marketing authorisation has been withdrawn and the product discontinued completely.[6][7]
- Rose JW, Burns JB, Bjorklund J, Klein J, Watt HE, Carlson NG (2007). “Daclizumab phase II trial in relapsing and remitting multiple sclerosis: MRI and clinical results”.Neurology 69 (8): 785–789. doi:10.1212/01.wnl.0000267662.41734.1f.PMID 17709711.
- ClinicalTrials.gov NCT01462318 An Immunogenicity and Pharmacokinetics (PK) Study of DAC HYP Prefilled Syringe in Relapsing Remitting Multiple Sclerosis (RRMS) (OBSERVE)
- Sobrin L, Huang JJ, Christen W, Kafkala C, Choopong P, Foster CS (2008). “Daclizumab for treatment of birdshot chorioretinopathy”. Arch Ophthalmol. 126 (2): 186–191. doi:10.1001/archophthalmol.2007.49. PMID 18268208.
- “EPAR for Zenapax”. European Medicines Agency. 2007.
- Tsurushita, N.; Hinton, P. R.; Kumar, S. (2005). “Design of humanized antibodies: From anti-Tac to Zenapax”. Methods 36 (1): 69–83.doi:10.1016/j.ymeth.2005.01.007. PMID 15848076. edit
- British National Formulary, Edition 57
- EMEA: Withdrawal of the marketing authorisation in the European Union
Ipilimumab – Yervoy Battles Melanoma, but Can It Become a Blockbuster?

Ipilimumab
by Todd Campbell, The Motley Fool Sep 28th 2013 1:00PM
Updated Sep 28th 2013 1:02PM
In early 2011, the Food and Drug Administration approved Bristol-Myers Squibb‘s drug Yervoy as a treatment for skin cancer melanoma. The drug marked the first approved treatment proven to extend the life of a person diagnosed with the disease. It marked a big leap forward in medicine as an early leader in immunotherapy, or the unleashing of the body’s immune system on cancer.
read all at
http://www.dailyfinance.com/2013/09/28/yervoy-battles-melanoma-but-can-it-become-a-blockb/

Ipilimumab’s molecular target is CTLA-4 (Uniprot: P16410; canSAR ; PFAM: P16410), a negative regulator of T-cell activation. Ipilimumab augments T-cell activation and proliferation by binding to CTLA-4 and preventing its interaction with its ligands (CD80 and CD86). CTLA-4 is a membrane-bound, 223 amino acid long, T-cell protein. It contains an immunoglobulin V-type domain (PFAM:PF07686). The structure of CTLA-4 is determined (see e.g. PDBe:3osk)
Ipilimumab (i pi lim′ ue mab; also known as MDX-010 and MDX-101), marketed asYervoy, is a drug used for the treatment of melanoma, a type of skin cancer. It is a U.S. Food and Drug Administration (FDA) approved human monoclonal antibody developed byBristol-Myers Squibb, and works by activating the immune system by targeting CTLA-4.
Cytotoxic T lymphocytes (CTLs) can recognize and destroy cancer cells. However, there is also an inhibitory mechanism that interrupts this destruction. Ipilimumab turns off this inhibitory mechanism and allows CTLs to continue to destroy cancer cells.
In addition to melanoma, ipilimumab is undergoing clinical trials for the treatment of non-small cell lung carcinoma (NSCLC), small cell lung cancer (SCLC) and metastatic hormone-refractory prostate cancer.
Yervoy is a monoclonal antibody drug indicated for treating metastatic melanoma. The drug was developed by Bristol-Myers Squibb.
In March 2011, The US Food and Drug Administration (FDA) approved Yervoy to treat patients with newly diagnosed or previously-treated unresectable or metastatic melanoma. Yervoy is the first drug approved vor the treatment of metastatic melanoma in the US.
Bristol-Myers Squibb submitted a marketing authorisation application to the European Medicines Agency in May 2010. The drug received approval from the European Commission in July 2011.
Approval from Australia’s Therapeutic Goods Association was received in July 2011. The drug is currently being reviewed by Health Canada.
Metastatic melanoma
Melanoma responsible for majority of skin cancer deaths in the US. In metastatic melanoma the cancer spreads to other parts of the body from its starting point. It becomes difficult to treat the disease once it spreads beyond the skin to other parts of the body. The disease is also known as stage IV melanoma.
If the melanoma spreads to the lungs then the patient faces breathing problems. The patients with metastatic melanoma may feel symptoms of fatigue, loss of weight, and appetite and bowel problems.
The incidence of the disease has increased steadily in the US after 1970s. The American Cancer Society (ACS) estimated that more than 68,000 new cases of melanoma were registered in the US in 2009. The ACS estimated that the number of deaths occurred due to melanoma in 2010 was more than 8,700.
Yervoy mechanism
Yervoy treats metastatic melanoma by activating the immune system. The drug works by binding or inhibiting cytotoxic T lymphocyte-associated antigen 4 (CTLA-4), a molecule that plays vital role in relating natural immune responses. The presence or absence of CTLA-4 can curb or increase the immune system’s T-cell response in fighting disease.
The drug also works by blocking a complex set of interactions in the immune system. It is designed to inhibit the activity of CTLA-4, thereby sustaining an active immune response in its attack on cancer cells.
Approvals and indications
Ipilimumab was approved by the FDA in March 2011 to treat patients with late-stage melanoma that has spread or cannot be removed by surgery. On February 1, 2012, Health Canada approved ipilimumab for “treatment of unresectable or metastatic melanoma in patients who have failed or do not tolerate other systemic therapy for advanced disease.” Additionally Ipilimumab was approved in the European Union (EU), for second line treatment of metastatic melanoma, November 2012


 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
















































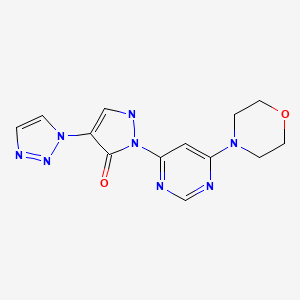
 DACLIZUMAB,
DACLIZUMAB,
