Home » Articles posted by DR ANTHONY MELVIN CRASTO Ph.D (Page 45)
Author Archives: DR ANTHONY MELVIN CRASTO Ph.D
Anthony crasto is now Consultant Glenmark Lifesciences at Glenmark Life Sciences!

I’m happy to share that I’m starting a new position as Consultant Glenmark Lifesciences at Glenmark Life Sciences!
17th Jan 2022, A new innings
I retired 16th Jan 2022 at 58 yrs from Glenmark . completed 16 yrs 2 months
30 plus years in the field of Process research

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
///////////////
DIPYRIDAMOLE
Dipyridamole
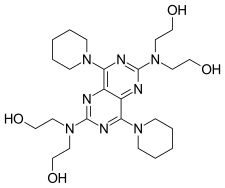
- Molecular FormulaC24H40N8O4
- Average mass504.626 Da
2,2′,2”,2”’-{[4,8-Di(piperidin-1-yl)pyrimido[5,4-d]pyrimidine-2,6-diyl]dinitrilo}tetraethanol
200-374-7[EINECS]
58-32-2[RN]
Ethanol, 2,2′,2”,2”’-[(4,8-di-1-piperidinylpyrimido[5,4-d]pyrimidine-2,6-diyl)dinitrilo]tetrakis-
дипиридамол [Russian] [INN]
ديبيريدامول [Arabic] [INN]
双嘧达莫 [Chinese] [INN]
0068373 [Beilstein]
DipyridamoleCAS Registry Number: 58-32-2
CAS Name: 2,2¢,2¢¢,2¢¢¢-[(4,8-Di-1-piperidinylpyrimido[5,4-d]pyrimidine-2,6-diyl)dinitrilo]tetrakisethanol
Additional Names: 2,6-bis(diethanolamino)-4,8-dipiperidinopyrimido-[5,4-d]pyrimidine
Manufacturers’ Codes: NSC-515776; RA-8
Trademarks: Anginal (Yamanouchi); Cardoxin (RAFA); Cleridium (Marcofina); Coridil (Delalande); Coronarine (NEGMA); Curantyl (Berlin-Chemie); Dipyridan (Hokuriku); Gulliostin (Taiyo); Natyl (Interdelta); Peridamol (Boehringer, Ing.); Persantine (Boehringer, Ing.); Piroan (Towa Yakuhin); Prandiol (Bottu); Protangix (Lefrancq)
Molecular Formula: C24H40N8O4
Molecular Weight: 504.63
Percent Composition: C 57.12%, H 7.99%, N 22.21%, O 12.68%
Literature References: Phosphodiesterase inhibitor that reduces platelet aggregation; also acts as a coronary vasodilator. Prepn: GB807826; F. G. Fischer, et al.,US3031450 (1959, 1962 both to Thomae). Activity studies: Saraf, Seth, Indian J. Physiol. Pharmacol.15, 135 (1971). Toxicological study: F. Takenaka et al.,Arzneim.-Forsch.22, 892 (1972). Symposium on pharmacology and clinical experience as antithrombotic: Thromb. Res.60, Suppl. 12, 1-99 (1990). Review of use as pharmacological stress agent in echocardiography: M. B. Buchalter et al.,Postgrad. Med. J.66, 531-535 (1990); in 201Tl cardiac imaging: S. G. Beer et al.,Am. J. Cardiol.67, Suppl., 18D-26D (1991).
Properties: Deep yellow needles from ethyl acetate, mp 163°. Bitter taste. Slightly sol in H2O; sol in dil acid having a pH of 3.3 or below; very sol in methanol, ethanol, chloroform; not too sol in acetone, benzene, ethyl acetate. Solns are yellow and show strong blue-green fluorescence. LD50 in rats: 8.4 g/kg orally; 208 mg/kg i.v. (Takenaka).Melting point: mp 163°
Toxicity data: LD50 in rats: 8.4 g/kg orally; 208 mg/kg i.v. (Takenaka)
Derivative Type: Combination with aspirin
Trademarks: Aggrenox (Boehringer, Ing.)
Literature References: Review of pharmacology and clinical efficacy in secondary prevention of stroke: P. S. Hervey, K. L. Goa, Drugs58, 469-475 (1999).
Therap-Cat: Antithrombotic; diagnostic aid (cardiac stress testing).
Keywords: Antithrombotic; Diagnostic Aid; Phosphodiesterase Inhibitor.
Dipyridamole (trademarked as Persantine and others) is a nucleoside transport inhibitor and a PDE3 inhibitor medication that inhibits blood clot formation[3] when given chronically and causes blood vessel dilation when given at high doses over a short time.
PATENT
https://patents.google.com/patent/WO2011151640A1/enDipyridamole, represented by structural formula (I), possesses platelet aggregation inhibiting, anti-thrombotic and vasodilator properties and it is marketed as an anti-platelet therapy for the treatment and prevention of disorders such as thrombo-embolisms.

A process for the preparation of dipyridamole, disclosed in patent US 3031450, involves the reaction of 2,6-dichloro-4,8-dipiperidino-pyrimido(5,4-d)pyrimidine with diethanolamine (see Scheme 1). The preparation of 2,6-dichloro-4,8-dipiperidino- pyrimido(5,4-d)pyrimidine is also reported in US 3031450 and is incorporated herein by reference. The reaction to prepare dipyridamole does not employ an additional reaction solvent and is a neat mixture of the two reactants carried out at a very high temperature of 190 to 195°C. The process also involves a cumbersome work-up to isolate dipyridamole, since the crude product obtained is a pasty mass which needs decantation of the mother liquor and further purification. This decantation process is not practical on commercial scale.

2,6-dichloro-4,8-dipiperidino- dipyridamole (Ί) pyflmido(5,4-d)pyrimidineScheme 1A similar process for the production of dipyridamole is described in patent DD 117456 wherein the reaction conditions exemplified are heating 2,6-dichloro-4,8-dipiperidino- pyrimido(5,4-d)pyrimidine and diethanolamine at 155 to 160°C under vacuum. However, this process again requires a high temperature which leads to the formation of impurities.A process for the preparation and purification of dipyridamole is disclosed in patent DE 1812918, wherein 2,6-dicMoro-4,8-dipiperidino-pyrimido(5,4-d)pyrimidine and diethanolamine are heated to 150 to 200°C. After completion of the reaction, the reaction mixture is dissolved in chloroform, which is further separated into an upper layer of diethanolamine and its hydrochloride and a chloroform solution. The chloroform solution obtained is separated and reduced to dryness after stirring with water. This process also requires a high temperature which can lead to the formation of impurities. In addition, the solvent used for the isolation of dipyridamole, chloroform, is inconvenient as it is a restricted solvent and its permitted limit in the final marketed dipyridamole is very low.A similar process, wherein dipyridamole is manufactured by the reaction of diethanolamine with 2,6-dichloro-4,8-dipiperidino-pyrimido(5,4-d)pyrimidine is disclosed in patent RO 104718. However, this process again requires high temperatures of 180 to 200°C which leads to the formation of impurities and, consequently, the yield of the final product is very low (58%) with a purity of less than 98%.A process is disclosed in patent DD 115670, wherein the purification of dipyridamole involves refluxing it in butyl acetate, AcOBu, for 2 hours in the presence of an equal amount of silica gel or column chromatography on silica gel at 60-100°C. However, purification by column chromatography is not economical and not feasible on industrial scale. Moreover, this purification process only removes one specific impurity, 2,4,6-tris- (diethanolamino) – 8 -pip eridino-pyrimido (5,4-d)pyrimidine .The processes described above to prepare dipyridamole do not employ an additional reaction solvent but involve neat mixtures of the two reactants, 2,6-dichloro-4,8- dipiperidino-pyrimido(5,4-d)pyrimidine and diethanolamine, which are heated at very high temperatures. The use of neat reaction mixtures and/ or high temperatures means that it is very difficult to control the levels of impurities formed.Another process for the preparation of dipyridamole, disclosed in patent application WO 2007/080463, involves reacting diethanolamine with 2,6-dichloro-4,8-dipiperidino- pyrimido(5,4-d)pyrimidine in a solvent selected from the group consisting of l-methyl-2- pyrrolidinone, sulpholane and polyethylene glycol. However, the exemplified reaction temperatures are very high at 190 to 200°C and the HPLC purity of the crude dipyridamole is reported to be only 90-94%. A purification method is disclosed using first a ketonic solvent and then an alcohol and water. Even though the process disclosed in this patent application uses a solvent in the reaction, the temperature of reaction is still very high and the purification in ketonic solvent is reported at high temperature (100 to 120°C). The HPLC purity after purification is reported as only 99.0-99.5%.As discussed above, all the processes disclosed in the prior art for the preparation of dipyridamole suffer from serious disadvantages with respect to commercial production. The prior art synthetic and purification processes employ high temperatures in the preparation of dipyridamole which leads to inefficiency and high processing costs. The high temperatures also lead to higher levels of impurities being formed during manufacture with the consequence that further cumbersome and expensive purification procedures are required.The high quality dipyridamole prepared by the processes according to the present invention can be used for the preparation of a pharmaceutical composition to use in the manufacture of a medicament for anti-platelet therapy. A preferred embodiment of the present invention, illustrated in Scheme 2, provides a process for the preparation of dipyridamole comprising reacting 2,6-dichloro-4,8- dipiperidino-pyrimido(5,4-d)pyrimidine with diethanolamine at 113-115°C. This reaction temperature is significantly lower than that used in the prior art processes to prepare dipyridamole.

Another preferred embodiment of the present invention, illustrated in Scheme 3, also provides a process for the preparation of dipyridamole by the reaction of 2,6-dichloro-4,8- dipiperidino-pyrimido(5,4-d)pyrimidine with diethanolamine in dimethylsulfoxide at 120- 125°C to afford the mono-substituted intermediate, 2-chloro-6-diethanolamino-4,8- dipiperidino-pyrimido(5,4-d)pyrimidine, which is isolated and then further converted to dipyridamole by heating in diethanolamine at 113-115°C.Although the solvent used in this preferred embodiment of the present invention is preferably dimethylsulfoxide (DMSO), other solvents can alternatively be used. Preferred alternative solvents are other polar aprotic solvents, such as dimethylformamide (DMF), dimethylacetamide (DMA) or N-methyl-2-pyrrolidinone (NMP). Alternatively, hydrocarbon solvents can be used. Preferred hydrocarbon solvents are aromatic hydrocarbon solvents such as toluene or xylene.


Example 1Preparation of crude dipyridamoleDiethanolamine (10 vol) and 2,6-dichloro-4,8-dipiperidino-pyrimido(5,4-d)pyrimidine (1 eq) were mixed at 25-30°C, stirred for 10 minutes and then heated at 113-115°C for 45-48 hours. After completion of the reaction, the mixture was cooled to 75-80°C. Ethanol (5 vol) was added at 75-80°C and the mixture was stirred at 75-80°C for 10 minutes. Toluene (10 vol) was added at 70-75°C and the mixture was stirred at 70-75°C for 15 minutes. Purified water (15 vol) was added at 70-75°C and the mixture was stirred at 60-65°C for 30 minutes. The mixture was then cooled and stirred at 25-30°C for 30 minutes. The precipitated solid was filtered and washed with purified water (2 x 5 vol) before drying at 75-80°C under reduced pressure afforded crude dipyridamole as a yellow crystalline solid. Yield (w/w) = 80-85%Yield (molar) = 58-62%HPLC purity > 98%Example 2Stage 1: Preparation of 2-chloro-6-diemanolamino-4,8-dipiperidino-pyrimido(5,4-d) pyrimidineDiethanolamine (3 eq) and 2,6-dichloro-4,8-dipiperidino-pyrimido(5,4-d)pyrimidine (1 eq) were added to dimefhylsulfoxide (10 vol) at 25-30°C, stirred for 10 minutes and then heated at 120-125°C for 4-5 hours. After completion of the reaction, the reaction mixture was cooled to 55-60°C. Acetone (5 vol) was added at 55-60°C and the mixture was stirred at 55-60°C for 10 minutes. Purified water (15 vol) was added at 55-60°C and the mixture was stirred at 50-55°C for 15 minutes. The mixture was cooled to 25-30°C and stirred at 25-30°C for 30 minutes. The precipitated solid was filtered, washed with purified water (2 x 5 vol) and dried at 75-80°C under reduced pressure to afford crude 2-chloro-6- diethanolamino-4,8-dipiperidino-pyrimido(5,4-d)pyrimidine as a yellow crystalline solid. Yield (w/w) = 110-120%Yield (molar) = 93-100%HPLC purity > 96%Stage 2: Preparation of crude dipyridamoleDiethanolamine (10 vol) and 2-chloro-6-diemanolamino-4,8-dipiperidino-pyrimido(5,4-d) pyrimidine (1 eq) were mixed at 25-30°C, stirred for 10 minutes and then heated at 113- 115°C for 45-48 hours. After completion of the reaction, the mixture was cooled to 75- 80°C. Ethanol (5 vol) was added and the mixture was stirred at 75-80°C for 10 minutes. Toluene (10 vol) was added and the mixture was stirred at 70-75°C for 15 minutes. Purified water (15 vol) was added and the mixture was stirred at 60-65°C for 30 minutes. The mixture was then cooled to 25-30°C and stirred for 30 minutes. The precipitated solid was filtered, washed with purified water (2 x 5 vol) and dried at 75-80°C under reduced pressure to afford crude dipyridamole as a yellow crystalline solid.Yield (w/w) = 95-97%Yield (molar) = 82-84%HPLC purity > 98%Example 3Crystallization of crude dipyridamoleCrude dipyridamole (1 eq) and diefhanolamine (8 vol) were stirred together at 25-30°C for 10 minutes and then heated to about 80°C for 10 minutes. The clear solution was cooled to 75-80°C, ethanol (5 vol) was added and the mixture was stirred at 75-80°C for 10 minutes. Toluene (10 vol) was added and the mixture was stirred at 70-75°C for 15 minutes. The mixture was cooled to 25-30°C, stirred at 25-30°C for 10 minutes and filtered. The filtrate was heated to 70-75°C for 10 minutes, purified water (15 vol) was added and the mixture was stirred at 60-65°C for 30 minutes before cooling to 25-30°C with stirring for 30 minutes. The precipitated solid was filtered, washed with purified water (2 x 5 vol) and dried at 75-80°C under reduced pressure to afford dipyridamole as a yellow crystalline solid.Yield (w/w and molar) = 90-95%HPLC purity > 99.9%
PATENT
https://patents.google.com/patent/WO2007080463A1/enDipyridamole which is chemically known as 4,8-Bis(piperidino)-N,N,N’,N’- tetra(2-hydroxyethyl)pyrimido[5,4-d]pyrimidine-2,6-diamine is a platelet adhesion inhibitor. It is useful in anti-platelet therapy and it is marketed as Persantin ® by Boehringer Ingelheim.The platelet aggregation inhibiting properties, anti-thrombotic and vasodilator properties of Dipyridamole is reported in US patent 3031450 which also describe a process for its preparation by reacting 2-chloro-6-diethanolamino-4, 8-dipiperidyl- pyrimido-pyrimidine with diethanolamine.German patent 117456 describes the process for the production of Dipyridamole from 2,6-dichloro-4,8-dipiperidinopyrimido[5,4-d]pyrimidine and diethanolamine at 130 to 200° C under vacuum. German patent 1812918 describes the process for the preparation and purification of Dipyridamole. According to this patent 2,6-dichloro-4,8,- dipiperidinopyrimido[5,4-d]pyrimidine and diethanolamine are heated to 150 to 2000C to obtain Dipyridamole. This is characterized by the fact that after the completion of the reaction, the reaction mixture is dissolved in chloroform, which is further separated into the upper layer of diethanolamine and its hydrochloride and the chloroform solution. Thus obtained chloroform solution is reduced to dryness after stirring with water.RO 104718 Bl describes a process where Dipyridamole is manufactured and purified by reaction of diethanolamine with 2,6-dichloro-4,8-dipiperidinopyrimido[5,4- d]pyrimidine. In this process the yield is very low (58%) and purity is only 98%.Another patent DDl 15670 Z describes a process for the purification of Dipyridamole by refluxing it in AcOBu for 2 h in the presence of an equal amount of silica gel or by column chromatography on silica gel at 60-1000C. The purification by column chromatography is not economical and feasible at industrial scale.All the above mentioned prior art are neat reaction in which it is difficult to control the impurity and is not easy to scale up. In the prior art process the obtained product is pasty which needs decanting the mother liquor and further purification.We focused our research to develop an improved and efficient process for the preparation and purification of Dipyridamole of formula (I) which will overcome the above mentioned prior art problems and will produce Dipyridamole in substantially good yield, high purity and with no mixture of solvents.Objectives of the InventionThe main objective of the present invention is to provide an improved process for the preparation and purification of compound of formula (I), which gives better purity and high yield of the product. Another objective of the present invention is to provide a process for the preparation and purification of compound of formula (I), which would be easy to scale up and implement at industrial level.Yet another objective of the present invention is to provide a process for the preparation and purification of compound of formula (I), which avoids, use of hazardous gas (SO2) and corrosive chemicals like HCl, H2SO4, acetic acid, NaOH, NH3 etc.Summary of the InventionAccordingly, the present invention provides a process for the preparation ofDipyridamole of formula (I) comprising reacting 2,6-Dichloro-4,8- dipiperidinopyrimido- (5,4-d)pyrimidine (DDH) of formula (II) with Diethanolamine (DEA) of formula (III) using a solvent. This process can be represented by the scheme given below:
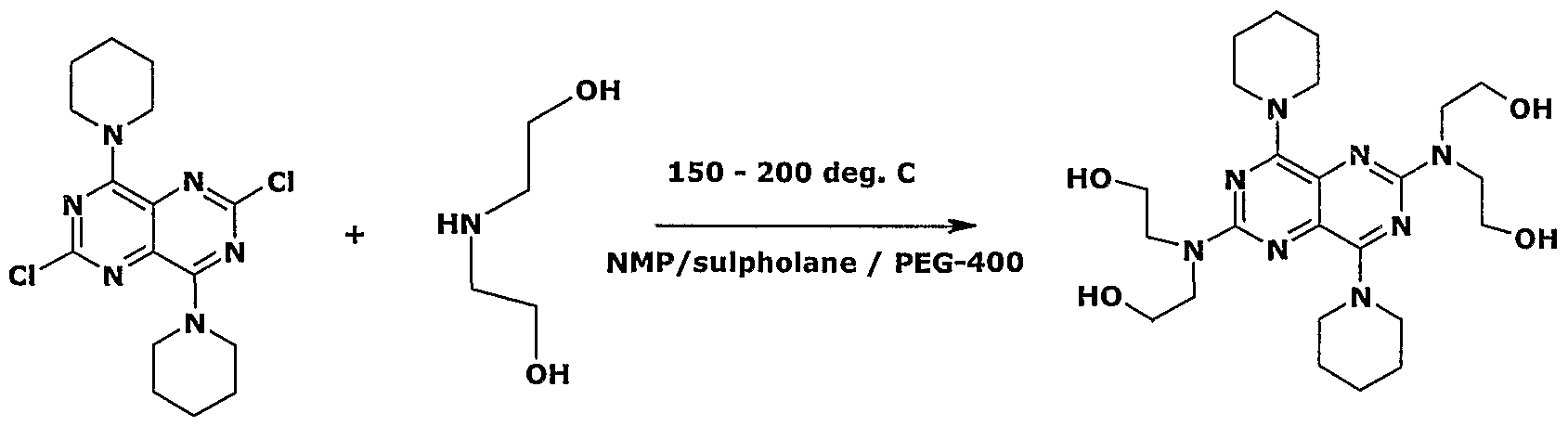
(II) (III) (I)The obtained wet or optionally dried crude Dipyridamole is purified by using ketonic solvent and aqueous alcoholic solvent or mixture thereof.Description of the InventionIn an embodiment of the present invention the solvent is selected from the group consisting of l-Methyl-2-pyrrolidinone, Sulpholane and Polyethylene glycol, preferably l-Methyl-2-pyrrolidinone (NMP). In another embodiment of the present invention, the polyethylene glycol used is PEG-20Q or PEG-400, preferably PEG-400.In yet another embodiment of the present invention, the reaction is carried out at a temperature of about 25° C to reflux temperature, preferably at a temperature of about 150° C to 2000C.In still another embodiment of the present invention the starting material of this invention is prepared according to the literature available in the prior art.In yet another embodiment the ketonic solvent is acetone, methyl ethyl ketone, methyl vinyl ketone or methyl isobutyl ketone (MIBK), preferably MIBK.In yet another embodiment the alcoholic solvent is selected from the group having Ci to C4 alkanol preferably isopropyl alcohol (IPA) or methanol.The present invention is illustrated with the following examples, which should not be construed for limiting the scope of the invention.Example 1Preparation of Dipyridamole (Crude)250 mL of l-Methyl-2-pyrrolidinone (NMP), 50g of 2,6-Dichloro-4,8 dipiperidinopyrimido(5,4-d)pyrimidine (DDH) and 136g of Diethanolamine (DEA) were charged into a 2.0 L four-necked RBF at 25-35 0C. The reaction mass was heated to 190 – 2000C and maintained for 1.5 to 2.5 hrs under stirring. The reaction mass was cooled to 25-350C and 450 mL of purified water was charged slowly into it and stirred for lhr. The solid reaction mass was filtered and washed with 500ml-purified water and dried the solid under vacuum at 50-550C for 8 to 10 hrs to get 55-60 g of crude Dipyridamole of 90-94% HPLC purity.Purification Of DipyridamoleMethyl isobutyl ketone (750 ml) and 50 g of Dipyridamole (crude) were charged into a clean 2.0 L four-necked RBF at 25-3O0C and heated to 100-1200C. It was stirred to dissolve and cooled to 25-350C and stirred for 30-60 min. The solid was Filtered and washed with 100 ml MIBK. The product was dried at 45-50 0C under vacuum. The obtained material was further purified as follows:Isopropyl alcohol (200 mL) and 40-45 g of Dipyridamole were charged into a clean 1.0 lit four-necked RBF at 25-350C. It was heated to 60-650C. Carbon (Ig) was added at 30-350C and filtered through celite and washed with 50 mL IPA. Water (500 mL) was charged slowly and stirred for 30 min. The solid was filtered and washed with a mixture of IPA : Water (1 :2) and dried the product at 45-50 0C under vacuum to obtain 43-5Og of Dipyridamole having HPLC purity 99.0 – 99.5%Example 2Sulpholane (15 mL), 5.0g of 2,6-Dichloro-4,8-dipiperidinopyrimido(5,4-d) pyrimidine (DDH) and 8.6g Diethanolamine (DEA) were charged into 100 mL four- necked RBF at 25-35°C. It was heated to 190-2000C and stirred for 2-3 hrs. The reaction mass was cooled to 25-35°C and 45 mL of water was added into it. The reaction mass was stirred. The solid was filtered and washed with water. The solid was purified with MIBK,IPA-Water as given in example 1.Example 3Polyethylene glycol-400 (15 mL), 5g of 2,6-Dichloro-4,8-dipiperidinopyrimido (5,4-d) pyrimidine (DDH) and 8.6 gm Diethanolamine (DEA) were charged into 10OmL four necked RBF at 25-35°C. The reaction mass was heated to 190-2000C and maintained for 2-3 hrs. The mixture was cooled to 25-350C. Water (45 mL) was added to the reaction mixture and stirred. The solid was filtered and washed with water. The solid was purified with MIBK,IPA- Water as given in example 1.Example 4 (Azeotrophic removal of water in MIBK purification)Preparation of Dipyridamole (Crude*) l-Methyl-2-pyrrolidinone (150 mL), 50g of 2,6-Dichloro-4,8-dipiperidinopyrimido(5,4-d)pyrimidine (DDH) and 136g Diethanolamine (DEA) was charged into a 2.0 L four-necked RBF at 25-35 0C. The reaction mass was stirred & heated to 190 – 2000C and stirring was continued for 1.5 to 2.5 hrs. The reaction mass was cooled to 25-350C and 450 mL of purified water was charged slowly into it and stirred for lhr. The solid reaction mass was filtered and washed with 500ml-purified water to obtain 110-13Og of wet crude Dipyridamole.Purification Of DipyridamoleMethyl isobutyl ketone (750 ml) and 65 g of Dipyridamole (wet crude) were charged into a clean 2.0 L four-necked RBF at 25-3O0C and heated to 100-1200C followed by azeotrophic separation of water. It was cooled to 25-350C and stirred for30-60 min. The solid was filtered and washed with 100 ml MIBK. The product was dried at 45-50 0C under vacuum. The obtained material was further purified as follows:Isopropyl alcohol (200 mL) and 45-48 g of Dipyridamole were charged into a clean 1.0 L four-necked RBF at 25-350C. It was heated to 60-650C and stirred to dissolve. Carbon (Ig) was added at 30-350C and filtered through celite and washed with 50 mL IPA. Water (500 mL) was charged slowly and stirred for 30 min. The solid was filtered and washed with a mixture of IPA : Water (1:2) and dried the product at 45-50 0C under vacuum to obtain 43-5Og of Dipyridamole having HPLC purity 99.0-99.5%Purification with Methaanol-waterMethanol (200 mL) and 45-48 g of Dipyridamole were charged into a clean 1.0 L four-necked RBF at 25-350C. It was heated to 60-650C and stirred to dissolve. Carbon (Ig) was added at 30-350C and filtered through celite and washed with 50 mL methanol. Water (500 mL) was charged slowly and stirred for 30 min. The solid was filtered and washed with a mixture of methanol : Water (1 :2) and dried the product at 45-50 0C under vacuum to obtain 45g of Dipyridamole having HPLC purity 99%.
PATENThttps://patents.google.com/patent/CN108069972A/enEmbodiment 1Weigh urea 120g(2mol), ethylene glycol 62g(1mol)120 DEG C are heated in a kettle, in Catalyzed by p-Toluenesulfonic Acid Effect is lower to carry out step(1)Reaction, generate compound 3;Then 2,3- diamino succinic acid 37g is weighed(0.25mol)With step The compound 3 generated in rapid 1 carries out the reaction generation compound 5 of step 2,220 DEG C, reaction time 3h of reaction temperature, catalyst For the nickel-base catalyst of support type, catalyst is filtered out after the completion of reaction;Exist in phosphorus oxychloride, phosphorus trichloride and lead to chlorine In the case of, compound 5 carries out chlorination reaction generation compound 6,110 DEG C of reaction temperature, reaction time 30h;Weigh piperidines 85g (1mol)Step is carried out with compound(4)Reaction, after reaction liquid hydrolysis, cooling filtering, be dried to obtain compound 9;Claim Take 105g(1mol)Diethanol amine and compound 9 carry out step(6)Reaction, 220 DEG C of reaction temperature, reaction time 3h fills 1.5 MPa of Hydrogen Vapor Pressure, catalyst are the crude product of the nickel-base catalyst, after reaction cold filtration of support type, and crude product passes through It is refining to obtain Dipyridamole finished product, quality 62.10g, purity 99.21%, product yield 48.74%(Yield is with 2,3- diamino fourths Diacid is calculating benchmark).Embodiment 2Weigh urea 120g(2mol), ethylene glycol 62g(1mol)120 DEG C are heated in a kettle, in Catalyzed by p-Toluenesulfonic Acid Effect is lower to carry out step(1)Reaction, generate compound 3;Then 2,3- diamino succinic acid 30g is weighed(0.2mol)With step The compound 3 generated in rapid 1 carries out the reaction generation compound 5 of step 2,220 DEG C, reaction time 3h of reaction temperature, catalyst For the nickel-base catalyst of support type, catalyst is filtered out after the completion of reaction;Exist in phosphorus oxychloride, phosphorus trichloride and lead to chlorine In the case of, compound 5 carries out chlorination reaction generation compound 6,110 DEG C of reaction temperature, reaction time 30h;Weigh piperidines 85g (1mol)Step is carried out with compound(4)Reaction, after reaction liquid hydrolysis, cooling filtering, be dried to obtain compound 9;Claim Take 105g(1mol)Diethanol amine and compound 9 carry out step(6)Reaction, 220 DEG C of reaction temperature, reaction time 3h fills 1.5 MPa of Hydrogen Vapor Pressure, catalyst are the crude product of the nickel-base catalyst, after reaction cold filtration of support type, and crude product passes through It is refining to obtain Dipyridamole finished product, quality 50.34g, purity 99.3%, product yield 49.53%(Yield is with 2,3- diamino fourth two Acid is calculating benchmark).Embodiment 3Other steps are the same as embodiment 2, step(6)In reaction temperature for 240 DEG C, product yield 50.31%.Comparative example 1Weigh urea 36g(0.6mol), ethyl acetoacetate 26g(0.2mol), add in ethanol-hydrogen chloride liquid(30% hydrochloric acid:95% second Alcohol=1:4)Then 200ml, drying and dehydrating after stirring add in sodium hydroxide solution and are warming up to 95 DEG C, then cool to 75 DEG C, add Hydrochloric acid adjusts PH=1, cold filtration, the 6- methyluracils of washing filtering;Nitric acid is added in reaction pot, is cooled to less than 10 DEG C, Stirring adds in 6- methyluracils, be warming up to 30 DEG C of heat preservations 1 it is small when the nitro whey liquid that filters;Take a policy powder in water, stirring After dissolving plus nitro whey liquid, temperature control keep the temperature 30min at 35 DEG C, add the static 3h of hydrochloric acid, stir 2h, filtration drying obtains amino breast Clear liquid;Again weigh urea 36g and add in reaction kettle with amino whey liquid, stirring is warming up to 100 DEG C of heat preservation 20min, cools to 90 DEG C add in 2mol/L sodium hydroxide solution, be warming up to 100 DEG C heat preservation dissolving 1h.Cool to 40 DEG C, filter tetrahydroxy pyrimidine- [4,5d] and pyrimidine sodium salt, adds water, 60 DEG C of heat preservation 30min add hydrochloric acid to adjust PH=4, is cooled to 15 DEG C of filterings, washing, dries 2,4,6,8- tetrahydroxys pyrimidine-[4,5d] and pyrimidine;Tetrahydroxy object, phosphorus oxychloride, phosphorus trichloride are added in reaction kettle, is stirred, 10 DEG C of similarly hereinafter chlorine are warming up to 110 DEG C of reflux for 24 hours, be cooled to 15 DEG C of filterings, washing, dry 2,4,6,8- tetrachloro-pyrimidines- [4,5d] and pyrimidine;Acetone, tetrachloride are sequentially added, piperidines-acetone mixture, 30 DEG C of heat preservations are added dropwise in 20 DEG C of heat preservation 30min 1h, adds water to stir 1h, and filtration drying obtains 2,6- bis- chloro- 4,8 ,-two piperidines-pyrimidine(Dichloride);Weigh diethanol amine 63g with Dichloride is mixed, and is warming up to 200 DEG C of heat preservation 15min, is cooled to less than 25 DEG C plus acetone and stirs 30min, then 30 DEG C 4h is kept the temperature, filtration drying obtains Dipyridamole crude product, then carries out refined Dipyridamole finished product 13.53, purity 98.5%, yield 13.21%(Using ethyl acetoacetate as calculating standard).It is found by being compared with comparative example:The method of the production Dipyridamole of the present invention is short with synthetic route, into The characteristics of product high income, production cost is low.
SYN
GB 807826 U.S. Patent 3,031,450

SYN

SYN
R.S. Vardanyan, V.J. Hruby, in Synthesis of Essential Drugs, 2006
Dipyridamole
Dipyridamole, 2,2′,2″,2′″-[(4,8-dipiperidinopirimido[5,4-d]pirimidin-2,6-diyl)-diimino]-tetraethanol (19.4.13), is easily synthesized from 5-nitroorotic acid (19.4.8), easily obtained, in turn, by nitrating of 2,4-dihydroxy-6-methylpyrimidine, which is usually synthesized by the condensation of urea with acetoacetic ether. Reduction of the nitro group in 5-nitroorotic acid by various reducing agents gives 5-aminoorotic acid (19.4.9), which is reacted with urea or with potassium cyanide to give 2,4,6,8-tetrahydroxypyrimido[5,4-d]pyrimidine (19.4.10). This undergoes a reaction with a mixture of phosphorous oxychloride and phosphorous pentachloride, which forms 2,4,6,8- tetra-chloropyrimido[5,4-d]pyrimidine (19.4.11). Reacting the resulting tetrachloride with piperidine replaces the chlorine atoms at C4 and C8 of the heterocyclic system with piperidine, giving 2,6-dichloropyrimido-4,8-dipiperidino[5,4-d]pyrimidine (19.4.12). Reacting the resulting product with diethanolamine gives dipyridamole (19.4.13) [32,33].

Dipyridamole increases coronary blood circulation, increases oxygen flow to the myocardium, potentiates adenosine activity, and impedes its metabolization. It inhibits aggregation of thrombocytes, blocks phosphodiesterase, increases microcirculation, and inhibits the formation of thrombocytes.
It is used for chronic coronary insufficiency, as well as for preventing and treating thrombosis. Synonyms of this drug are anginal, curantyl, stenocor, thrompresantin, and many others.SYN
Chemical Synthesis
Dipyridamole, 2,2′,2”,2”’-[(4,8-dipiperidinopirimido[5,4-d]pirimidin-2,6- diyl)-diimino]-tetraethanol (19.4.13), is easily synthesized from 5-nitroorotic acid (19.4.8), easily obtained, in turn, by nitrating of 2,4-dihydroxy-6-methylpyrimidine, which is usually synthesized by the condensation of urea with acetoacetic ether. Reduction of the nitro group in 5-nitroorotic acid by various reducing agents gives 5-aminoorotic acid (19.4.9), which is reacted with urea or with potassium cyanide to give 2,4,6,8- tetrahydroxypyrimido[5,4-d]pyrimidine (19.4.10). This undergoes a reaction with a mixture of phosphorous oxychloride and phosphorous pentachloride, which forms 2,4,6,8- tetrachloropyrimido[ 5,4-d]pyrimidine (19.4.11). Reacting the resulting tetrachloride with piperidine replaces the chlorine atoms at C4 and C8 of the heterocyclic system with piperidine, giving 2,6-dichloropyrimido-4,8-dipiperidino[5,4-d]pyrimidine (19.4.12). Reacting the resulting product with diethanolamine gives dipyridamole (19.4.13).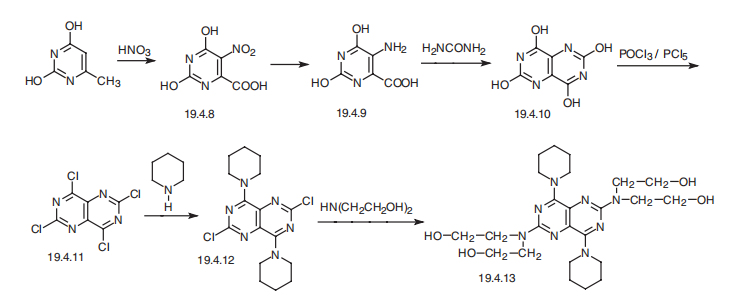
clipA general outline of the procedure for synthesizing dipyridamole is shown in Scheme 1. Reaction of the pyrimidino pyrimidine-2,4,6,8- tetraol (1) with a mixture of phosphorous oxychloride and phosphorous pentachloride gives the tetrachloro derivative (2). The halogens at the peri positions 4 and 8 are more reactive to substitution than are the remaining halogen pairs 2 and 6, which are in effect the two positions of the pyrimidines. Thus, reaction with piperidine at ambient temperature gives the 4, 8 diamine (3). Subsequent reaction with bis-2-hydroxy ethylamine under more strenuous conditions gives dipyridamole (4) [12, 13].12. F.G. Fischer, J. Roch, and A. Kottler, U.S. Patent 3, 031, 450 (1962). 13. D. Lednicer and L.A. Mitscher, The Organic Chemistry of Drug Synthessis Volume 1, John Wiley and Sons, New York, p. 428 (1977).






set 2







set 3




AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Medical uses
- Dipyridamole is used to dilate blood vessels in people with peripheral arterial disease and coronary artery disease[4]
- Dipyridamole has been shown to lower pulmonary hypertension without significant drop of systemic blood pressure
- It inhibits formation of pro-inflammatory cytokines (MCP-1, MMP-9) in vitro and results in reduction of hsCRP[clarification needed] in patients.
- It inhibits proliferation of smooth muscle cells in vivo and modestly increases unassisted patency of synthetic arteriovenous hemodialysis grafts.[5]
- It increases the release of tissue plasminogen activator from brain microvascular endothelial cells.
- It results in an increase of 13-hydroxyoctadecadienoic acid and decrease of 12-hydroxyeicosatetraenoic acid in the subendothelial matrix and reduced thrombogenicity of the subendothelial matrix.
- Pretreatment it reduced reperfusion injury in volunteers.
- It has been shown to increase myocardial perfusion and left ventricular function in patients with ischemic cardiomyopathy.
- It results in a reduction of the number of thrombin and PECAM-1 receptors on platelets in stroke patients.
- Cyclic adenosine monophosphate impairs platelet aggregation and also causes arteriolar smooth muscle relaxation. Chronic therapy did not show significant drop of systemic blood pressure.
- It inhibits the replication of mengovirus RNA.[6]
- It can be used for myocardial stress testing as an alternative to exercise-induced stress methods such as treadmills.
Stroke
A combination of dipyridamole and aspirin (acetylsalicylic acid/dipyridamole) is FDA-approved for the secondary prevention of stroke and has a bleeding risk equal to that of aspirin use alone.[4] Dipyridamole absorption is pH-dependent and concomitant treatment with gastric acid suppressors (such as a proton pump inhibitor) will inhibit the absorption of liquid and plain tablets.[7][8] Modified release preparations are buffered and absorption is not affected.[9][10]
However, it is not licensed as monotherapy for stroke prophylaxis, although a Cochrane review suggested that dipyridamole may reduce the risk of further vascular events in patients presenting after cerebral ischemia.[11]
A triple therapy of aspirin, clopidogrel, and dipyridamole has been investigated, but this combination led to an increase in adverse bleeding events.[12]
- Vasodilation occurs in healthy arteries, whereas stenosed arteries remain narrowed. This creates a “steal” phenomenon where the coronary blood supply will increase to the dilated healthy vessels compared to the stenosed arteries which can then be detected by clinical symptoms of chest pain, electrocardiogram and echocardiography when it causes ischemia.
- Flow heterogeneity (a necessary precursor to ischemia) can be detected with gamma cameras and SPECT using nuclear imaging agents such as Thallium-201, Tc99m–Tetrofosmin and Tc99m–Sestamibi. However, relative differences in perfusion do not necessarily imply any absolute decrease in blood supply in the tissue supplied by a stenosed artery.
Other uses
Dipyridamole also has non-medicinal uses in a laboratory context, such as the inhibition of cardiovirus growth in cell culture.[citation needed]
Drug interactions
Due to its action as a phosphodiesterase inhibitor, dipyridamole is likely to potentiate the effects of adenosine. This occurs by blocking the nucleoside transporter (ENT1) through which adenosine enters erythrocyte and endothelial cells.[13]
According to Association of Anaesthetists of Great Britain and Ireland 2016 guidelines, dipyridamole is considered to not cause risk of bleeding when receiving neuroaxial anaesthesia and deep nerve blocks. It does not therefore require cessation prior to anaesthesia with these techniques, and can continue to be taken with nerve block catheters in place.[14]
Overdose
Dipyridamole overdose can be treated with aminophylline[2]: 6 or caffeine which reverses its dilating effect on the blood vessels. Symptomatic treatment is recommended, possibly including a vasopressor drug. Gastric lavage should be considered. Since dipyridamole is highly protein bound, dialysis is not likely to be of benefit.
Mechanisms of action
Dipyridamole has two known effects, acting via different mechanisms of action:
- Dipyridamole inhibits the phosphodiesterase enzymes that normally break down cAMP (increasing cellular cAMP levels and blocking the platelet aggregation, response[4] to ADP) and/or cGMP.
- Dipyridamole inhibits the cellular reuptake of adenosine into platelets, red blood cells, and endothelial cells, leading to increased extracellular concentrations of adenosine.
Experimental studies[
Dipyridamole is currently undergoing repurposing for treatment of ocular surface disorders. These include pterygium and dry eye disease. The first report of topical dipyridamole’s benefit in treating pterygium was published in 2014.[15] A subsequent report of outcomes in 25 patients using topical dipyridamole was presented in 2016.[16]
See also
References
- ^ Nielsen-Kudsk, F; Pedersen, AK (May 1979). “Pharmacokinetics of Dipyridamole”. Acta Pharmacologica et Toxicologica. 44 (5): 391–9. doi:10.1111/j.1600-0773.1979.tb02350.x. PMID 474151.
- ^ Jump up to:a b “Aggrenox (aspirin/extended-release dipyridamole) Capsules. Full Prescribing Information” (PDF). Boehringer Ingelheim Pharmaceuticals, Inc. Retrieved 1 December 2016.
- ^ “Dipyridamole” at Dorland’s Medical Dictionary
- ^ Jump up to:a b c Brown DG, Wilkerson EC, Love WE (March 2015). “A review of traditional and novel oral anticoagulant and antiplatelet therapy for dermatologists and dermatologic surgeons”. Journal of the American Academy of Dermatology. 72 (3): 524–34. doi:10.1016/j.jaad.2014.10.027. PMID 25486915.
- ^ Dixon BS, Beck GJ, Vazquez MA, et al. (2009). “Effect of dipyridamole plus aspirin on hemodialysis graft patency”. N Engl J Med. 360 (21): 2191–2201. doi:10.1056/nejmoa0805840. PMC 3929400. PMID 19458364.
- ^ Dipyridamole in the laboratory: Fata-Hartley, Cori L.; Ann C. Palmenberg (2005). “Dipyridamole reversibly inhibits mengovirus RNA replication”. Journal of Virology. 79 (17): 11062–11070. doi:10.1128/JVI.79.17.11062-11070.2005. PMC 1193570. PMID 16103157.
- ^ Russell TL, Berardi RR, Barnett JL, O’Sullivan TL, Wagner JG, Dressman JB. pH-related changes in the absorption of “dipyridamole” in the elderly. Pharm Res (1994) 11 136–43.
- ^ Derendorf H, VanderMaelen CP, Brickl R-S, MacGregor TR, Eisert W. “Dipyridamole” bioavailability in subjects with reduced gastric acidity. J Clin Pharmacol (2005) 45, 845–50.
- ^ “Archived copy”. Archived from the original on 2009-07-05. Retrieved 2010-02-06.
- ^ Stockley, Ivan (2009). Stockley’s Drug Interactions. The Pharmaceutical Press. ISBN 978-0-85369-424-3.
- ^ De Schryver EL, Algra A, van Gijn J (2007). Algra A (ed.). “Dipyridamole for preventing stroke and other vascular events in patients with vascular disease”. Cochrane Database of Systematic Reviews (2): CD001820. doi:10.1002/14651858.CD001820.pub3. PMID 17636684.
- ^ Sprigg N, Gray LJ, England T, et al. (2008). Berger JS (ed.). “A randomised controlled trial of triple antiplatelet therapy (aspirin, clopidogrel and dipyridamole) in the secondary prevention of stroke: safety, tolerability and feasibility”. PLOS ONE. 3 (8): e2852. Bibcode:2008PLoSO…3.2852S. doi:10.1371/journal.pone.0002852. PMC 2481397. PMID 18682741.
- ^ Gamboa A, Abraham R, Diedrich A, Shibao C, Paranjape SY, Farley G, et al. Role of adenosine and nitric oxide on the mechanisms of action of dipyridamole. Stroke. 2005;36(10):2170-2175.
- ^ AAGBI Guidelines Neuraxial and Coagulation June 2016
- ^ Carlock, Beth H.; Bienstock, Carol A.; Rogosnitzky, Moshe (2014-03-25). “Pterygium: Nonsurgical Treatment Using Topical Dipyridamole – A Case Report”. Case Reports in Ophthalmology. 5 (1): 98–103. doi:10.1159/000362113. ISSN 1663-2699. PMC 3995373. PMID 24761148.
- ^ “Topical Dipyridamole for Treatment of Pterygium and Associated Dry Eye Symptoms: Analysis of User-Reported Outcomes”. ResearchGate. Retrieved 2019-05-19.
| Clinical data | |
|---|---|
| Trade names | Persantine, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682830 |
| Pregnancy category | B |
| Routes of administration | By mouth, IV |
| ATC code | B01AC07 (WHO) |
| Legal status | |
| Legal status | UK: POM (Prescription only)US: ℞-only |
| Pharmacokinetic data | |
| Bioavailability | 37–66%[1] |
| Protein binding | ~99% |
| Metabolism | Liver (glucuronidation)[2] |
| Elimination half-life | α phase: 40 min, β phase: 10 hours |
| Excretion | Biliary (95%), urine (negligible) |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 58-32-2 |
| PubChem CID | 3108 |
| IUPHAR/BPS | 4807 |
| DrugBank | DB00975 |
| ChemSpider | 2997 |
| UNII | 64ALC7F90C |
| KEGG | D00302 |
| ChEBI | CHEBI:4653 |
| ChEMBL | ChEMBL932 |
| CompTox Dashboard (EPA) | DTXSID6040668 |
| ECHA InfoCard | 100.000.340 |
| Chemical and physical data | |
| Formula | C24H40N8O4 |
| Molar mass | 504.636 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| hideSMILESOCCN(CCO)C(N=C1N2CCCCC2)=NC3=C1N=C(N(CCO)CCO)N=C3N4CCCCC4 | |
| showInChI | |
| (verify) |
Patent
Publication numberPriority datePublication dateAssigneeTitleUS3031450A1959-04-301962-04-24Thomae Gmbh Dr KSubstituted pyrimido-[5, 4-d]-pyrimidinesDE1812918A11968-04-251969-11-06Dresden Arzneimittel2,6-Bis (diethanolamino-4,8-dipiperidino-pyrimido (5,4-d)-pyrimidine – purification by simple procedure giving good yieldsDD115670A11974-02-191975-10-12DD117456A11975-02-131976-01-12DE2927539A1 *1979-07-071981-01-08Margineanu Dan Axente Dipl IngBis:di:ethanol-amino-di:piperidino-pyrimido-pyrimidine prepn. – from methyl acetoacetate and urea via amino-orotic acidRO104718B11989-08-091994-09-30Medicamente DePRODUCTION METHOD OF PURE 2,6-bis-(DIETHANOL AMIDE)-4,8-DI- PIPERIDINE-PYRIMIDO-(5,4-d)-PYRIMIDINEWO2007080463A12006-01-122007-07-19Orchid Chemicals & Pharmaceuticals LimitedAn improved process for the preparation of dipyridamoleFamily To Family CitationsDE115670C *JPS5191295A *1975-02-051976-08-10Jipiridamooruno kairyoseizohoJPS5757038B2 *1977-09-301982-12-02Yamanouchi Pharma Co LtdJPS57209291A *1981-06-171982-12-22Kyowa Hakko Kogyo Co LtdPurification of dipyridamoleUS6232312B1 *1995-06-072001-05-15Cell Pathways, Inc.Method for treating patient having precancerous lesions with a combination of pyrimidopyrimidine derivatives and esters and amides of substituted indenyl acetic acidesCN1425461A *2003-01-032003-06-25贵州益佰制药股份有限公司Injection preparation for resisting platelet aggregation and its producing methodCN1634085A *2004-11-242005-07-06崔晓廷Injectio of aspirin and dipyridamole and its preparing process
Non-Patent
TitleCURTIN, NICOLA J. ET AL: “Resistance-Modifying Agents of Pyrimido[5,4-d]pyrimidine Modulators of Antitumor Drug Activity. Synthesis and Structure-Activity Relationships for Nucleoside Transport Inhibition and Binding to .alpha.1-Acid Glycoprotein”, JOURNAL OF MEDICINAL CHEMISTRY , 47(20), 4905-4922 CODEN: JMCMAR; ISSN: 0022-2623, 26 August 2004 (2004-08-26), XP002651697 *
CN104710431B *2015-03-182017-03-01常州康普药业有限公司A kind of purifying process of dipyridamoleCN107782805B *2016-08-252021-02-02亚宝药业集团股份有限公司HPLC analysis method for key intermediate impurity synthesized by dipyridamoleCN106380471B *2016-08-312018-11-06广州市桐晖药业有限公司A kind of preparation method of DipyridamoleCN108069972A *2016-11-162018-05-25湖南尔康制药股份有限公司A kind of production method of Dipyridamole bulk pharmaceutical chemicalsCN106946887B *2017-03-242019-05-28大连万福制药有限公司A kind of preparation method introducing catalyst optimization synthesis Dipyridamole
/////////////////Dipyridamole, дипиридамол , ديبيريدامول , 双嘧达莫 , 0068373 , NSC-515776, RA-8
OCCN(CCO)C(N=C1N2CCCCC2)=NC3=C1N=C(N(CCO)CCO)N=C3N4CCCCC4

NEW DRUG APPROVALS
ONE TIME
$10.00
Racecadotril

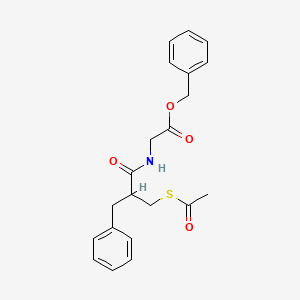

Racecadotril
- Molecular FormulaC21H23NO4S
- Average mass385.477 Da
(±)-Acetorphan
(RS)-Benzyl N-[3-(acetylthio)-2-benzylpropanoyl]glycinate
2-{[2-[(acetylthio)methyl]-1-oxo-3-phenylpropyl]amino}acetic acid (phenylmethyl) ester7378
76K53XP4TO
81110-73-8[RN]
Benzyl N-[3-(acetylsulfanyl)-2-benzylpropanoyl]glycinate [ACD/IUPAC Name]
Cadotril
Dexecadotril[INN]
Glycine, N-[3-(acetylthio)-1-oxo-2-(phenylmethyl)propyl]-, phenylmethyl ester
Hidrasec [Trade name]
рацекадотрил[Russian][INN]
راسيكادوتريل[Arabic][INN]
消旋卡多曲[Chinese][INN]
RacecadotrilCAS Registry Number: 81110-73-8
CAS Name:N-[2-[(Acetylthio)methyl]-1-oxo-3-phenylpropyl]glycine phenylmethyl ester
Additional Names:N-[(R,S)-3-acetylthio-2-benzylpropanoyl]glycine benzyl ester; acetorphan
Trademarks: Hidrasec (GSK); Tiorfan (Bioprojet)
Molecular Formula: C21H23NO4S, Molecular Weight: 385.48
Percent Composition: C 65.43%, H 6.01%, N 3.63%, O 16.60%, S 8.32%
Literature References: Antisecretory enkephalinase inhibitor. Prepn: B. Roques et al.,EP38758 (1981); eidem,US4513009 (1985 to Bioprojet). Pharmacology: J.-M. Lecomte et al.,J. Pharmacol. Exp. Ther.237, 937 (1986). Effect on intestinal transit: J. F. Bergmann et al.,Aliment. Pharmacol. Ther.6, 305 (1992). Clinical trial in acute diarrhea: P. Baumer et al.,Gut33, 753 (1992); in children: E. Salazar-Lindo et al.,N. Engl. J. Med.343, 463 (2000). Symposium on pharmacology and clinical experience: Aliment. Pharmacol. Ther.13, Suppl. 6, 1-32 (1999). Review of clinical development: J.-C. Schwartz, Int. J. Antimicrob. Agents14, 75-79 (2000); J. M. Lecomte, ibid. 81-87.
Properties: White crystals from ether mp 89°., Melting point: mp 89°
Derivative Type: (S)-Form
CAS Registry Number: 112573-73-6
Additional Names: Ecadotril; sinorphan
Manufacturers’ Codes: Bay-y-7432
Molecular Formula: C21H23NO4S, Molecular Weight: 385.48
Percent Composition: C 65.43%, H 6.01%, N 3.63%, O 16.60%, S 8.32%
Literature References: Prepn: P. Duhamel et al.,EP318377; eidem,US5208255 (1989, 1993 both to Bioprojet); and pharmacology: B. Giros et al.,J. Pharmacol. Exp. Ther.243, 666 (1987). Clinical effect on plasma ANP levels in CHF: J. C. Kahn et al.,Lancet335, 118 (1990); on renal function: F. Schmitt et al.,Am. J. Physiol.267, F20 (1994). Clinical trial in heart failure: C. M. O’Connor et al.,Am. Heart J.138, 1140 (1999); J. G. F. Cleland, K. Swedberg, Lancet351, 1657 (1998).
Properties: mp 71°. [a]D25 -24.1° (c = 1.3 in methanol). LD50 i.v. in mice: >100 mg/kg (Duhamel, 1993).
Melting point: mp 71°
Optical Rotation: [a]D25 -24.1° (c = 1.3 in methanol)
Toxicity data: LD50 i.v. in mice: >100 mg/kg (Duhamel, 1993)
Therap-Cat: Antidiarrheal.
Keywords: Antidiarrheal; Neutral Endopeptidase Inhibitor.

Racecadotril is an anti-secretory enkephalinase inhibitor useful in the treatment of diarrhea.Racecadotril has been investigated for the basic science and treatment of Diarrhea, Acute Diarrhea, and Acute Gastroenteritis.
Racecadotril, also known as acetorphan, is an antidiarrheal medication which acts as a peripheral enkephalinase inhibitor.[3] Unlike other opioid medications used to treat diarrhea, which reduce intestinal motility, racecadotril has an antisecretory effect — it reduces the secretion of water and electrolytes into the intestine.[3] It is available in France (where it was first introduced in ~1990) and other European countries (including Germany, Italy, the United Kingdom, Spain, Portugal, Poland, Finland, Russia and the Czech Republic) as well as most of South America and some South East Asian countries (including China, India and Thailand), but not in the United States. It is sold under the tradename Hidrasec, among others.[4] Thiorphan is the active metabolite of racecadotril, which exerts the bulk of its inhibitory actions on enkephalinases.[5]
Medical uses
Racecadotril is used for the treatment of acute diarrhea in children and adults and has better tolerability than loperamide, as it causes less constipation and flatulence.[6][7] Several guidelines have recommended racecadotril use in addition to oral rehydration treatment in children with acute diarrhea.[8]
Contraindications
Racecadotril has no contraindications apart from known hypersensitivity to the substance.[9][10]
There is insufficient data for the therapy of chronic diarrhea, for patients with renal or hepatic failure, and for children under three months. Additional contraindications for the children’s formulation are hereditary fructose intolerance, glucose-galactose malabsorption and saccharase deficiency, as it contains sugar.[7][9]
Racecadotril (CAS NO.: 81110-73-8), with its systematic name of Glycine, N-(2-((acetylthio)methyl)-1-oxo-3-phenylpropyl)-, phenylmethyl ester, (+-)-, could be produced through many synthetic methods.
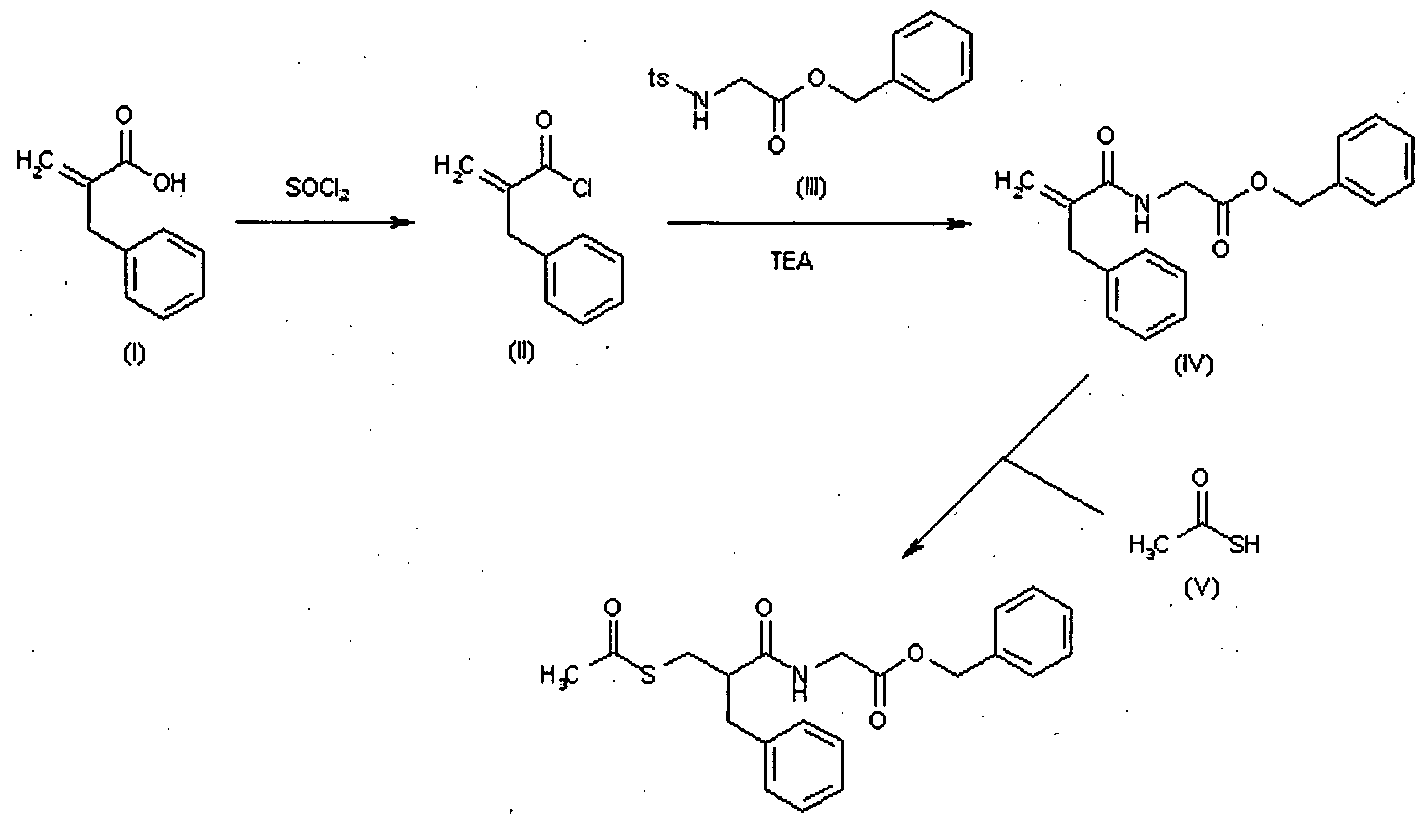
Following is one of the synthesis routes: 2-Benzylacrylic acid (I) reacts with SOCl2 in hot toluene to afford the acyl chloride (II), which is condensed with N-tosylglycine benzyl ester (III) in the presence of TEA in toluene to yield the corresponding amide (IV). Finally, this compound is condensed with thioacetic acid by heating at 80 °C to afford the target acylthio compound.
Racecadotril is a neutral endopeptidase inhibitor used as antidiarrheal in the treatment of chronic cardiac insufficiency and is available under the brand names Hidrasec and Tiorfan. Racecadotril is chemically known as N-[2-[(acetylthio) methyl]- l-oxo-3-phenylpropyl] glycine phenyl methyl ester, (herein after referred by its generic name racecadotril) and represented by the formula (I).

U.S. Patent No. US 4,513,009 describes amino acid derivatives including racecadotril, a pharmaceutical composition and a method of treatment.
The US’009 patent also discloses a process for the preparation of racecadotril which is illustrated by below scheme:

U.S. Patent No. US 6,835,851 B2 discloses a process for the preparation of racecadotril which is illustrated by scheme below:
European Patent No. EP 0501870B 1 discloses a process for the preparation of racec

Racecadotril
The use of coupling agents like hydroxyl benzotriazole (HOBT) and dicyclohexyl amine carbodiimide (DCC) generally induces the formation of side products such as dicyclohexylurea. These side products do lead to major problems, wherein purification by chromatography may be contemplated, but the side products are extremely difficult to remove on an industrial scale.
Consequently, efforts have been made to replace the peptidic coupling step
so as to avoid the formation of side products associated with the use of the coupling agents. Thus, it appears that, even if the preparation of N-(mercaptoacyl)amino acid derivatives from .alpha.-substituted acrylic acids by Michael addition of a thio acid and conversion of acid to acid chloride by using thionyl chloride and then coupling of an amino ester may be advantageous on a laboratory scale, such reactions are difficult to adapt on an industrial use.
The aforementioned processes described above involves expensive reagents such as hydroxyl benzotriazole (HOBT) and dicyclohexyl amine carbodiimide (DCC) and hazardous reagent like thionyl chloride thus rendering the processes expensive and not feasible on industrial scale.
SYNTHESIS BY WORLDDRUGTRACKER

Patent
https://www.google.com/patents/WO2013098826A1?cl=en
EXAMPLES
Example-1: Preparation of Racecadotril (I):
Step A) Preparation of 2-acetyIsulfanyI methyI-3-phenyI propionic acid (IV)
16.2 g of 2-benzylacrylic acid and 12.3 ml of thioacetic acid were were charged into a clean and dry R.B.flask and stirred at about 30°C for about 1 hour. The reaction mixture was heated to about 60°C and stirred for about 4 hours.The excess of thioacetic acid was distilled off completely to afford the title compound as residue. Yield: 23.8 g. Step B) Preparation of Racecadotril crude (la)
23.8 g. of 2-acetyl sulfanylmethyl-3-phenyl-propionic acid (IV), 200ml of methylene chloride and 16.7 ml of triethylamine were charged into a clean and dry R.B.flask. 10. 5 ml of ethylchloroformate was added at about -5°C. The resultant reaction mixture was stirred at about 0°C for about 30 min. 33.7 g of glycine benzyl ester p-tosyalte (II), 14 ml of triethylamine and 100ml of methylene chloride was added as a mixture to the reaction mass at about 0°C. Then the resultant reaction mixture was stirred at about 0°C for about 1 hr. followed by at about 30°C for about 30 min. After completion of the reaction as determined by TLC, the reaction mass was washed with 65 ml of distilled water, 65 ml 4% sodium bicarbonate solution and followed by 65 ml distilled water. The organic and aqueous phases were separated and the solvent was distilled completely, 2 x 50 ml Isopropyl alcohol was charged and again distilled off the solvent completely to give residue. The residue
obtained was triturated with a mixture of isopropyl alcohol 4 ml) and n-hexane (94 ml) at about 5°C to the title compound as crude. Yield: 34 g.
ExampIe-2: Purification of Racecadotril (Crude):
34 g. of crude Racecadotril and 35 ml of 20 % v/v aqueous .methanol were charged in a clean and dry R.B.flask and heated to about 65°C. 3g. of SP.carbon was charged and stirred at about 65°C for about 10 min. The reaction suspension was stirred at about 65°C for about 10 min. The reaction suspension was filtered on hyflow bed (diatomous earth) and washed the hyflow bed with 30 ml of aqueous methanol. The filtrate obtained was cooled to about 0°C for about 30 min. The solid separated was filtered and the solid obtained washed with 60 ml of precooled aqueous methanol to afford the pure racecadotril (I).
Yield: 29 g.; Purity by HPLC: 99.5 area %; The overall yield is 75.3%.
PATENT
https://www.google.com/patents/CN104356036A?cl=en
Example 1
The 40. 0g Racecadotril dissolved in 200ml of absolute ethanol and water bath heated to 40 ° C, and stir until the whole solution, stirring was stopped, the solution was placed in 15 ° C water bath was allowed to stand, when starting When there is precipitation of crystals, and then placed under the 0 ° C crystallization, after filtration, to 45 ° C under hot air drying cycle 6 hours to obtain 29. 2g, purity 99.6% of Racecadotril a polymorph crystals.
reflection angle X-ray powder diffraction pattern 20 at 4.3 °, 8.7 °, 13.2 °, 16.8 °, 17.8 ° and 20.0 ° at the show X-ray powder diffraction peaks. In 1135. 19CHT1,1551. 46CHT1,1644. 73CHT1,1687. 57CHT1, 1731. 35CHT1 and 3289. 20CHT1 displayed at an infrared absorption peak.
Clips
US 20020055645
PATENT
Racecadotril, chemical name N_ [(R, S) -3- acetyl-mercapto-2-benzyl-propionyl)] glycine benzyl ester, is a neprilysin inhibitor, selectively, reversible inhibition of neprilysin, so that the inner protection from degradation of endogenous enkephalins, prolong the physiological activity of endogenous enkephalins in the digestive tract, mainly used in clinical treatment of children and adults with acute diarrhea. Its structural formula is as follows:

Racecadotril as enkephalinase inhibitors, developed in France in 1993 Bioprojet listed acute diarrhea treatment, trade name Tiorfan.
In W02011116490A1, US5945548 and CN101768095A and other documents, documented racecadotril the synthesis process, but did not report the crystal form; therefore the present inventors have not reported Racecadotril crystalline polymorph conduct further
Example 1
[0032] The 40. 0g Racecadotril dissolved in 200ml of absolute ethanol and water bath heated to 40 ° C, and stir until the whole solution, stirring was stopped, the solution was placed in 15 ° C water bath was allowed to stand, when starting When there is precipitation of crystals, and then placed under the 0 ° C crystallization, after filtration, to 45 ° C under hot air drying cycle 6 hours to obtain 29. 2g, purity 99.6% of Racecadotril a polymorph crystals.
[0033] reflection angle X-ray powder diffraction pattern 20 at 4.3 °, 8.7 °, 13.2 °, 16.8 °, 17.8 ° and 20.0 ° at the show X-ray powder diffraction peaks. In 1135. 19CHT1,1551. 46CHT1,1644. 73CHT1,1687. 57CHT1, 1731. 35CHT1 and 3289. 20CHT1 displayed at an infrared absorption peak.
SYN
EP 0038758
Alternatively, the condensation of dimethyl malonate (VI) with benzaldehyde (VII) by means of piperidine in refluxing toluene gives dimethyl benzylidenemalonate (VIII), which is reduced with H2 over Pd/C in toluene to yield the corresponding benzyl derivative (IX). The hydrolysis of (IX) with NaOH in water affords the benzylmalonic acid (X). Alternatively, intermediate (X) can also be obtained starting from diethyl malonate (XI), which is condensed with with benzaldehyde (VII) by means of piperidine in refluxing toluene to give diethyl benzylidenemalonate (XII). Reduction of (XII) with H2 over Pd/C in toluene yields the corresponding benzyl derivative (XIII), which is then hydrolized with NaOH in water. The monodecarboxylation of (X) and its condensation with paraformaldehyde and diethylamine in refluxing ethyl acetate provides 2-benzylacrylic acid (XIV), which is condensed with thioacetic acid (V) by heating at 70 C to afford 2-(acetylsulfanylmethyl)-3-phenylpropionic acid (XV). Finally, this compound is condensed with N-tosylglycine benzyl ester (XVI) by means of HOBt, DCC and TEA in THF.
SYN
| EP 0729936 |
Reaction of benzaldehyde (I) with dimethyl malonate (II) in refluxing toluene in the presence of piperidine and HOAc provides dimethyl benzylidene malonate (III), which is then hydrogenated over Pd/C to afford dimethyl benzyl malonate (IV). Reduction of (IV) with LiAlH4 in refluxing THF furnishes 2-benzyl-1,3-propanediol (V), which is then subjected to reaction with vinyl acetate (VI) by means of Novozym 435 enzyme to yield diacetate (VII). Enantioselective removal of one acetyl group from (VII) by treatment with Pseudomonas fluorescens Lipase in acetone/phosphate buffer (pH = 7) at 30 C gives 3-acetoxy-2(S)-benzyl-propanol (S)-(VIII), which is then oxidized by means of Jones reagent in acetone/isopropanol to provide carboxylic acid (R)-(IX). The hydrolysis of (IX) with LiOH in THF/H2O gives 2(R)-benzyl-3-hydroxypropanoic acid (R)-(X). Alternatively, intermediate (X) can also be synthesized as follows: Condensation of benzaldehyde (I) with methyl acrylate (XV) by means of diaza-1,4-bicyclo[2.2.2.]octane affords methyl beta-hydroxy-alpha-methylene-benzenepropanoate (XVI), which is then subjected to hydrolysis with KOH in MeOH/H2O to yield carboxylic acid (XVII). Treatment of (XVII) with p-toluenesulfonic acid in refluxing HOAc gives (E)-2-(acetoxymethyl)-3-phenylpropionic acid (XVIII), which is finally converted into (X) by enantioselective hydrogenation in the presence of S-Binap and ruthenium catalyst [CodRu(all)2]. Derivative (R)-(X) is then converted into 3-(acetylsulfanyl)-2(S)-benzylpropionic acid (XI) by means of a Mitsunobu reaction with thioacetic acid, diisopropyl azodicarboxylate (DIAD) and triphenylphosphine (PPh3). Compound (XI) is then subjected to optical purification by formation and isolation of the corresponding salt with (-)-ephedrine and subsequent hydrolysis with HCl to furnish enantiomerically pure (S)-(XII). Finally, carboxylic acid (S)-(XII) is converted into ecadotril by its coupling with benzyl glycinate (XIV), either by means of Et3N, DCC and HOBt in CHCl3, or by first reaction with thionyl chloride to give acid chloride (S)-(XIII) and subsequent coupling with glycinate (XIV) by means of Et3N in CH2Cl2.
SYN
The reaction of 2-benzylacrylic acid (I) with SOCl2 in hot toluene gives the acyl chloride (II), which is condensed with N-tosylglycine benzyl ester (III) by means of TEA in toluene to yield the corresponding amide (IV). Finally, this compound is condensed with thioacetic acid by heating at 80 C to afford the target acylthio compound.
| FR 2816309; US 2002055645 |

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Side effects
The most common adverse effect is headache, which occurs in 1–2% of patients.[7] Rashes occur in fewer than 1% of patients. Other described skin reactions include itching, urticaria, angioedema, erythema multiforme, and erythema nodosum.[9][10]
Overdose
No cases of overdose are known. Adults have tolerated 20-fold therapeutic doses without ill effects.[10]
Interactions
No interactions in humans have been described. Combining racecadotril with an ACE inhibitor can theoretically increase the risk for angioedema.[9][10]
Racecadotril and its main metabolites neither inhibit nor induce the liver enzymes CYP1A2, CYP2C9, CYP2C19, CYP2D6, and CYP3A4. They also do not induce UGT enzymes.[10] This means that racecadotril has a low potential for pharmacokinetic interactions.
Pharmacology
Mechanism of action
Enkephalins are peptides produced by the body that act on opioid receptors with preference for the δ subtype.[11] Activation of δ receptors inhibits the enzyme adenylyl cyclase, decreasing intracellular levels of the messenger molecule cAMP.[7]
The active metabolite of racecadotril, thiorphan, inhibits enkephalinase enzymes in the intestinal epithelium with an IC50 of 6.1 nM, protecting enkephalins from being broken down by these enzymes. (Racecadotril itself is much less potent at 4500 nM.)[7][8] This reduces diarrhea related hypersecretion in the small intestine without influencing basal secretion. Racecadotril also has no influence on the time substances, bacteria or virus particles stay in the intestine.[10]
Pharmacokinetics

Some metabolites of racecadotril.
top left: precursor to the active metabolite
top right: active metabolite
bottom row: inactive metabolites
Racecadotril is rapidly absorbed after oral administration and reaches Cmax within 60 minutes. Food delays Cmax by 60 to 90 minutes but does not affect the overall bioavailability. Racecadotril is rapidly and effectively metabolized to the moderately active S-acetylthiorphan the main active metabolite thiorphan, of which 90% are bound to blood plasma proteins. In therapeutic doses, racecadotril does not pass the blood–brain barrier. Inhibition of enkephalinases starts 30 minutes after administration, reaches its maximum (75–90% inhibition with a therapeutic dose) two hours after administration, and lasts for eight hours. The elimination half-life, measured from enkephalinase inhibition, is three hours.[7][8][9]
Thiorphan is further metabolized to inactive metabolites such as the methyl thioether and the methyl sulfoxide. Both active and inactive metabolites are excreted, mostly via the kidney (81.4%), and to a lesser extent via the feces (8%).[10]
Society and culture
Brand names
In both France and Portugal it is sold as Tiorfan and in Italy as Tiorfix. In India it is available as Redotril and Enuff.[4]
See also
- Ecadotril, the (S)-enantiomer of racecadotril
- D/DL-Phenylalanine
- RB-101
References
- ^ https://www.ema.europa.eu/documents/psusa/racecadotril-list-nationally-authorised-medicinal-products-psusa/00002602/202003_en.pdf
- ^ Jump up to:a b c d “SPC-DOC_PL 39418-0003.PDF” (PDF). Medicines and Healthcare Products Regulatory Agency. Bioprojet Europe Ltd. 26 December 2012. Retrieved 7 May 2014.
- ^ Jump up to:a b Matheson AJ, Noble S (April 2000). “Racecadotril”. Drugs. 59 (4): 829–35, discussion 836–7. doi:10.2165/00003495-200059040-00010. PMID 10804038.
- ^ Jump up to:a b Brayfield, A, ed. (13 December 2013). “Racecadotril”. Martindale: The Complete Drug Reference. London, UK: Pharmaceutical Press. Retrieved 6 May 2014.
- ^ Spillantini MG, Geppetti P, Fanciullacci M, Michelacci S, Lecomte JM, Sicuteri F (June 1986). “In vivo ‘enkephalinase’ inhibition by acetorphan in human plasma and CSF”. European Journal of Pharmacology. 125 (1): 147–50. doi:10.1016/0014-2999(86)90094-4. PMID 3015640.
- ^ Fischbach, Wolfgang; Andresen, Viola; Eberlin, Marion; Mueck, Tobias; Layer, Peter (2016). “A Comprehensive Comparison of the Efficacy and Tolerability of Racecadotril with Other Treatments of Acute Diarrhea in Adults”. Frontiers in Medicine. 3: 44. doi:10.3389/fmed.2016.00044. ISSN 2296-858X. PMC 5064048. PMID 27790616.
- ^ Jump up to:a b c d e f Dinnendahl, V; Fricke, U, eds. (1982). Arzneistoff-Profile (in German). Eschborn, Germany: Govi Pharmazeutischer Verlag. ISBN 978-3-7741-9846-3.
- ^ Jump up to:a b c Eberlin, Marion; Mück, Thomas; Michel, Martin C. (2012). “A Comprehensive Review of the Pharmacodynamics, Pharmacokinetics, and Clinical Effects of the Neutral Endopeptidase Inhibitor Racecadotril”. Frontiers in Pharmacology. 3: 93. doi:10.3389/fphar.2012.00093. ISSN 1663-9812. PMC 3362754. PMID 22661949.
- ^ Jump up to:a b c d e Mediq.ch: racecadotril. Accessed 2019-12-30.
- ^ Jump up to:a b c d e f g Haberfeld, H, ed. (2019). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag. Hidrasec 100 mg-Hartkapseln.
- ^ Cumming, P (2019). “A Survey of Molecular Imaging of Opioid Receptors”. Molecules. 24 (22): 4190. doi:10.3390/molecules24224190. PMC 6891617. PMID 31752279.
External links
- “Racecadotril”. Drug Information Portal. U.S. National Library of Medicine.
| Clinical data | |
|---|---|
| Trade names | Hidrasec, Tiorfan, Zedott, others |
| Other names | Benzyl 2-[3-(acetylthio)-2-benzylpropanamido]acetate |
| AHFS/Drugs.com | International Drug Names |
| Routes of administration | By mouth |
| ATC code | A07XA04 (WHO) |
| Legal status | |
| Legal status | UK: POM (Prescription only)EU: Rx-only [1] |
| Pharmacokinetic data | |
| Protein binding | 90% (active metabolite thiorphan)[2] |
| Metabolism | Liver-mediated[2] |
| Onset of action | 30 min |
| Elimination half-life | 3 hours[2] |
| Excretion | Urine (81.4%), feces (8%)[2] |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 81110-73-8 |
| PubChem CID | 107751 |
| DrugBank | DB11696 |
| ChemSpider | 96913 |
| UNII | 76K53XP4TO |
| KEGG | D08464 |
| ChEMBL | ChEMBL2103772 |
| CompTox Dashboard (EPA) | DTXSID8045513 |
| ECHA InfoCard | 100.214.352 |
| Chemical and physical data | |
| Formula | C21H23NO4S |
| Molar mass | 385.48 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| Chirality | Racemic mixture |
| Melting point | 89 °C (192 °F) |
| showSMILES | |
| showInChI | |
| (what is this?) (verify) |

| CN101103960A * | Jul 14, 2006 | Jan 16, 2008 | 海南盛科生命科学研究院 | Dry mixed suspension containing racecadotril and preparation method thereof |
| CN101768095A * | Dec 26, 2008 | Jul 7, 2010 | 山东齐都药业有限公司 | Preparation method of racecadotril |
| WO2001097803A1 * | Jun 20, 2001 | Dec 27, 2001 | Laboratoire Glaxosmithkline | Pharmaceutical preparations comprising racecadotril (acetorphan) |
| WO2013098826A1 * | Dec 26, 2011 | Jul 4, 2013 | Symed Labs Limited | “a process for the preparation of n-[2-[(acetylthio) methyl]-1-oxo-3-phenylpropyl] glycine phenyl methyl ester and intermediates thereof” |
| Reference |
|---|
| Reference | ||||
|---|---|---|---|---|
| CN101103960A * | Jul 14, 2006 | Jan 16, 2008 | 海南盛科生命科学研究院 | Dry mixed suspension containing racecadotril and preparation method thereof |
| CN101768095A * | Dec 26, 2008 | Jul 7, 2010 | 山东齐都药业有限公司 | Preparation method of racecadotril |
| WO2001097803A1 * | Jun 20, 2001 | Dec 27, 2001 | Laboratoire Glaxosmithkline | Pharmaceutical preparations comprising racecadotril (acetorphan) |
| WO2013098826A1 * | Dec 26, 2011 | Jul 4, 2013 | Symed Labs Limited | “a process for the preparation of n-[2-[(acetylthio) methyl]-1-oxo-3-phenylpropyl] glycine phenyl methyl ester and intermediates thereof” |
| 1 | * | 金庆平 等: “神经内肽酶抑制剂消旋卡多曲(Racecadotril)的合成工艺研究“, 《中国现代应用药学杂志》, vol. 20, no. 7, 31 August 2003 (2003-08-31) |
| Reference | ||||
|---|---|---|---|---|
| Citing Patent | Filing date | Publication date | Applicant | Title |
| US6013829 * | Feb 4, 1997 | Jan 11, 2000 | Societe Civile Bioprojet | Process for the asymmetric synthesis of S-acyl derivatives of 2-mercaptomethyl -3- phenyl propanoic acid, application to the synthesis of N-(mercaptoacyl) amino acid derivatives |
| US20040009956 * | Apr 29, 2003 | Jan 15, 2004 | Dehua Pei | Inhibition of protein tyrosine phosphatases and SH2 domains by a neutral phosphotyrosine mimetic |
| 1 | * | MOHAMED A.O. ET AL.: ‘Stability-indicating methods for the determination of racecadotril in the presence of its degradation products‘ BIOSCIENCE TRENDS vol. 3, no. 6, 2009, pages 247 – 252, XP055074337 | ||
| CN104356036A * | Nov 7, 2014 | Feb 18, 2015 | 山东齐都药业有限公司 | Alpha crystal form of racecadotril and preparation method of alpha crystal form |
///////////Racecadotril, рацекадотрил , راسيكادوتريل , 消旋卡多曲 , Antidiarrheal, Neutral Endopeptidase Inhibitor, Cadotril, Dexecadotril ,
CC(=O)SCC(CC1=CC=CC=C1)C(=O)NCC(=O)OCC1=CC=CC=C1

NEW DRUG APPROVALS
ONE TIME
$10.00
CEFADROXIL

CEFADROXIL
- Molecular FormulaC16H17N3O5S
- Average mass363.388 Da
(6R,7R)-7-{[(2R)-2-Amino-2-(4-hydroxyphenyl)acetyl]amino}-3-methyl-8-oxo-5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid
256-555-6[EINECS]
50370-12-2[RN]
5-Thia-1-azabicyclo(4.2.0)oct-2-ene-2-carboxylic acid, 7-(((2R)-amino(4-hydroxyphenyl)acetyl)amino)-3-methyl-8-oxo-, (6R,7R)-
5-Thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid, 7-[[(2R)-2-amino-2-(4-hydroxyphenyl)acetyl]amino]-3-methyl-8-oxo-, (6R,7R)-
цефадроксил [Russian] [INN]
سيفادروكسيل [Arabic] [INN]
头孢羟氨苄 [Chinese] [INN]
Cephos
- Molecular FormulaC16H19N3O6S
- Average mass381.404 Da
5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid, 7-[[(2R)-2-amino-2-(4-hydroxyphenyl)acetyl]amino]-3-methyl-8-oxo-, (6R,7R)-, monohydrate
66592-87-8[RN]
(6R,7R)-7-{[(2R)-2-amino-2-(4-hydroxyphenyl)acetyl]amino}-3-methyl-8-oxo-5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid hydrate
(6R,7R)-7-{[(2R)-2-Amino-2-(4-hydroxyphenyl)acetyl]amino}-3-methyl-8-oxo-5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid hydrate (1:1)
Product Ingredients
| INGREDIENT | UNII | CAS | INCHI KEY |
|---|---|---|---|
| Cefadroxil hemihydrate | J9CMF6461M | 119922-85-9 | AJAMDISMDZXITN-QXBGZBSVSA-N |
| Cefadroxil monohydrate | 280111G160 | 66592-87-8 | NBFNMSULHIODTC-CYJZLJNKSA-N |
| Cefadroxil sodium | SSZ6380I0I | 42284-83-3 | GQOVFIUWRATNJC-CYJZLJNKSA-M |
CefadroxilCAS Registry Number: 66592-87-8
CAS Name: (6R,7R)-7-[[(2R)-Amino-(4-hydroxyphenyl)acetyl]amino]-3-methyl-8-oxo-5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid monohydrate
Additional Names: 7-[D-(-)-a-amino-a-(4-hydroxyphenyl)acetamido]-3-methyl-3-cephem-4-carboxylic acid monohydrate; p-hydroxycephalexine monohydrate
Manufacturers’ Codes: BL-S578; MJF-11567-3
Trademarks: Baxan (BMS); Bidocef (BMS); Cefa-Drops (Fort Dodge); Cefamox (BMS); Ceforal (Farmoffer); Cephos (CT); Duracef (BMS); Duricef (BMS); Kefroxil (Torre); Oracéfal (BMS); Sedral (BMS); Ultracef (BMS)
Molecular Formula: C16H17N3O5S.H2O
Molecular Weight: 381.40
Percent Composition: C 50.39%, H 5.02%, N 11.02%, O 25.17%, S 8.41%
Literature References: Semi-synthetic cephalosporin antibiotic. Prepn: NL6812382; L. B. Crast, Jr., US3489752 (1969, 1970 both to Bristol-Myers); T. Takahashi et al.,DE2216113; eidem,US3816253 (1972, 1974, both to Takeda). Prepn of crystalline monohydrate: D. Bouzard et al.,US4504657 (1985 to Bristol-Myers). Antimicrobial activity: R. E. Buck, K. E. Price, Antimicrob. Agents Chemother.11, 324 (1977). Pharmacology: M. Pfeffer et al.,ibid. 331; A. I. Hartstein et al.,ibid.12, 93 (1977). Review:J. Antimicrob. Chemother.10, Suppl. B, 1-162 (1982). Series of articles on clinical trials in respiratory tract infections: Drugs32, Suppl. 3, 1-56 (1986).Properties: White crystals, mp 197° (dec).
Melting point: mp 197° (dec)
Therap-Cat: Antibacterial.
Therap-Cat-Vet: Antibacterial.
Keywords: Antibacterial (Antibiotics); ?Lactams; Cephalosporins.
Cefadroxil is a cephalosporin antibiotic used in the treatment of various bacterial infections, such as urinary tract infections, skin and skin structure infections, and tonsillitis.
Cefadroxil (formerly trademarked as Duricef) is a broad-spectrum antibiotic of the cephalosporin type, effective in Gram-positive and Gram-negative bacterial infections. It is a bactericidal antibiotic.
It was patented in 1967 and approved for medical use in 1978.[1]
DURICEF (cefadroxil) is a semisynthetic cephalosporin antibiotic intended for oral administration. It is a white to yellowish-white crystalline powder. It is soluble in water and it is acid- stable. It is chemically designated as 5-Thia-l-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid, 7-[[amino(4-hydroxyphenyl)acetyl]amino]-3-methyl-8-oxo-, monohydrate[6R- [6α,7β(R*)]]-. It has the formula C16H17N3O5S•H20 and the molecular weight of 381.40. It has the following structural formula:
 |
DURICEF (cefadroxil) film-coated tablets, 1 g, contain the following inactive ingredients: microcrystalline cellulose, hydroxypropyl methylcellulose, magnesium stearate, polyethylene glycol, polysorbate 80, simethicone emulsion, and titanium dioxide.
DURICEF (cefadroxil) for Oral Suspension contains the following inactive ingredients: FD&C Yellow No. 6, flavors (natural and artificial), polysorbate 80, sodium benzoate, sucrose, and xanthan gum.
DURICEF (cefadroxil) capsules contain the following inactive ingredients: D&C Red No. 28, FD&C Blue No. 1, FD&C Red No. 40, gelatin, magnesium stearate, and titanium dioxide.
SYN

IR spectrum of pure cefadroxil drug.
Synthesis Reference
Leonardo Marsili, “Substantially anhydrous crystalline cefadroxil and method for producing it.” U.S. Patent US5329001, issued April, 1978.
SYN
Antibiotics
R.S. Vardanyan, V.J. Hruby, in Synthesis of Essential Drugs, 2006
Cefadroxil
Cefadroxil, [6R-[6α,7β(R)]]-3-methyl-8-oxo-7-[[amino(4-hydroxyphenyl) acetyl]amino]-5-thia-1-azabicyclo[4.2.0]oct-2-en-2-carboxylic acid (32.1.2.14), is an analog of cephalexin and differs only in the presence of a hydroxyl group in the fourth position of the phenyl ring of phenylglycine, and is synthesized by a scheme analogous to the scheme of cephradin synthesis [90–96].

Cefadroxil has a broad spectrum of antimicrobial action; it is active with respect to Gram-positive and Gram-negative microorganisms. Like all of the other drugs described above, it acts as a bactericide by disrupting the process of restoring the membranes of bacteria. Synonyms of this drug are bidocef, cefadril, duracef, ultracef, and others.SYN
Cefadroxil
- ATC:J01DA09
- MW:363.39 g/mol
- CAS-RN:50370-12-2
- InChI Key:BOEGTKLJZSQCCD-UEKVPHQBSA-N
- InChI:InChI=1S/C16H17N3O5S/c1-7-6-25-15-11(14(22)19(15)12(7)16(23)24)18-13(21)10(17)8-2-4-9(20)5-3-8/h2-5,10-11,15,20H,6,17H2,1H3,(H,18,21)(H,23,24)/t10-,11-,15-/m1/s1
- EINECS:256-555-6
- LD50:>1.5 g/kg (M, i.v.); >10 g/kg (M, p.o.);
>1 g/kg (R, i.v.); >10 g/kg (R, p.o.);
>2 g/kg (dog, p.o.)
Synthesis
Substances
| CAS-RN | Formula | Chemical Name | CAS Index Name |
|---|---|---|---|
| 22252-43-3 | C8H10N2O3S | 7-amino-3-deacetoxycephalosporanic acid | 5-Thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid, 7-amino-3-methyl-8-oxo-, (6R-trans)- |
| 53487-89-1 | C13H15NO5 | d(–)-4-hydroxy-N-(2-methoxycarbonyl-1-methylethenyl)phenylglycine | Benzeneacetic acid, 4-hydroxy-α-[(3-methoxy-1-methyl-3-oxo-1-propenyl)amino]-, (R)- |
PATENT
https://patents.google.com/patent/WO2005042543A1/enOral cephalosporin antibiotics, including cefprozil, cefatrizine, and cefadroxii, commonly have a 4-hydroxyphenylglycine group, as represented by the following formula:

The compound of the above formula is cefprozil when A is -C=CH-CH3, cefatrizine when A is 1 H-1 ,2,3-triazole-4-yl-thiomethyl, and cefadroxii when A is -CH3. Conventionally, there have been known various processes for preparing oral cephalosporin antibiotics, such as cefprozil, cefatrizine, and cefadroxii, by reacting reactive derivatives of 4-hydroxyphenylglycine with 3-cephem compounds. For example, U.S. Patent No. 3,985,741 discloses a process for preparing a cefadroxii, which includes reacting 4-hydroxyphenylglycine and ethylchloroformate inN-methylmorpholine to obtain an anhydride, followed by reaction with7-amino-deacetoxy-cephalosporanic acid (7-ADCA). However, the yield and quality of the product are poor. U.S. Patent Nos. 4,520,022, 4,591 ,641 , and 4,661 ,590 disclose a condensation reaction between 4-hydroxyphenylglycine with a protected amino group and a cephem compound in the presence of Λ/.Λ/’-dicyclohexylcarbodimide. However,Λ/,Λ/’-dicyclohexylurea produced after the condensation reaction is not easily removed, which restricts industrial applications. U.S. Patent No. 4,336,376 discloses a process for preparing a cefadroxii, which includes reacting a 4-hydroxyphenylglycine salt having a protected amino group with trimethylsilyl-2-oxazolidinone to protect a 4-hydroxyl group followed by reaction with acylchloride to obtain a 4-hydroxyphenylglycine anhydride and then reaction with 7-ADCA. However, silylation is prerequisite and these reactions are annoying, and thus, this process is not suitable for industrial application. U.S. Patent No. 4,708,825 discloses a technique of reacting4-hydroxyphenylglycine having a substituted amino group with thionyl chloride using a gaseous hydrogen chloride to obtain a 4-hydroxyphenylglycyl chloride hydrochloride followed by reaction with a cephem compound. However, handling property of the thionyl chloride and the gaseous hydrogen chloride is poor, and thus, this technique is not suitable for industrial application. U.S. Patent Nos. 3,925,418, 4,243,819, and 4,464,307 disclose a process for producing 4-hydroxyphenylglycine using excess phosgene. However, difficulty in handling of highly toxic phosgene, removal of excess residual phosgene, and control of reaction conditions renders mass production difficult. As a process for preparing a reactive anhydride of 4-hydroxyphenylglycine, there are reported a method for the preparation of acid chloride using phosphorus pentachloride, phosphorus oxychloride, or thionyl chloride, and a method for the preparation of active ester using imidazole, mercaptobenzothiazole, or hydroxybenzotriazole. However, an acid chloride of 4-hydroxyphenylglycine has poor reactivity due to a hydroxyl group and an active ester of 4-hydroxyphenylglycine has poor reactivity and involves a side reaction. In addition, Korean Patent Laid-Open Publication Nos. 2002-69431 , 2002-69432, 2002-69437, and 2002-69440 disclose a process for preparing a pivaloyl or succinimide derivative of 4-hydroxyphenylglycine and a process for preparing a cephem compound such as cefprozil using the pivaloyl or succinimide derivative of 4-hydroxyphenylglycine. Meanwhile, there have been known various preparation processes for 3-(Z)-propenyl cephem derivative which is a compound useful as an intermediate for preparation of cefprozil which is an oral cephalosporin antibiotic. WO93/16084 discloses a process of selectively separating a 3-(Z)-propenyl cephem compound by means of a hydrochloride, metal, or tertiary amine salt of7-amino-3-(1-propen-1-yl)-3-cephem-carboxylic acid or by adsorption chromatography. However, there is a disadvantage in that separation and purification are cost-ineffective. U.K. Patent No. 2,135,305 discloses a process for preparing cefprozil from a4-hydroxyphenylglycine compound with a t-butoxycarbonyl-protected amino group and a cephem compound with a benzhydryl-protected carboxyl group. However, incorporation of a 3-propenyl group after acylation lowers reaction efficiency and high-performance liquid chromatography is required for isomer separation, which render industrial application difficult. U.S. Patent No. 4,727,070 discloses a technique of removing an E-isomer cefprozil from a mixture of 27E cefprozil, which includes incorporating an active group such as sodium imidazolidinone into the mixture of 2VE cefprozil by reaction of the mixture of 27E cefprozil with acetone followed by deprotection. However, purification by chromatography incurs enormous costs. In view of the above problems, Korean Patent Laid-Open Publication No.2002-80838 discloses a process for preparing a 3-(Z)-propenyl cephem compound by reacting a phosphoranylidene cephem compound with acetaldehyde in a mixed solvent essentially consisting of ether in the presence of a base. According to a disclosure in this patent document, ether is essentially used. In this respect, in the case of using methylenechloride or tetrahydrofuran, even when other reaction conditions, for example, reaction temperature, reaction duration, base, catalyst, and the like are adjusted, it is very difficult to adjust the content of the Z-isomer to more than 83%.DETAILED DESCRIPTION OF THE INVENTION Technical Goal of the Invention The present invention provides a process for simply preparing a cephalosporin antibiotic in high yield and purity using a novel reactive intermediate, i.e., a 4-hydroxyphenylglycine derivative. The present invention also provides a novel reactive intermediate, i.e., a 4-hydroxyphenylglycine derivative which is used in simply preparing a cephalosphorin antibiotic in high yield and purity, and a preparation process thereof. While searching for a process for stereospecifically preparing a novel3-(Z)-propenyl cephem derivative, the present inventors found that use of a mixed solvent including methylenechloride, isopropylalcohol, and water in a predetermined ratio can stereospecifically and efficiently produce the 3-(Z)-propenyl cephem derivative, which is in contrary to the disclosure in Korean Patent Laid-Open Publication No. 2002-80838. Therefore, the present invention also provides a process for stereospecifically preparing a 3-(Z)-propenyl cephem derivative using a mixed solvent including methylenechloride, isopropylalcohol, and water in a predetermined ratio.



Example 9 Preparation of7-r2-amino-2-(4-hvdroxyphenyl)acetamido1-3-methyl-3-cephem-4-carboxylic acid(cefadroxii) The reaction solution obtained in step A of Example 1 was cooled to -40 °C and a solution obtained by dissolving 6.21 g (0.029mol) of 7-amino-3-methyl-3-cephem-4-carboxylic acid in 40 ml of methylenechloride, 10 ml of water, and 6.5 g of triethylamine was gradually dropwise added thereto for 1 hour. Then, the reaction mixture was incubated at the same temperature for 2 hours and cooled to 0°C to obtain an insoluble solid. The insoluble solid was filtered. A filtrate was sent to a reactor and then stirred for 1 hour after addition of 20 ml of 6N HCI. The reaction solution was adjusted to pH of 3.2 by addition of 10% NaOH, stirred at0°C for 2 hours, and filtered to give 9.1g (83%) of the titled compound as a white solid. H-NMR( δ , D20-d2) : 1.79(3H, d, 8.6Hz, -CH3), 3.22(1 H, d, 18Hz, 2-H),3.55(1 H. d. 18Hz, 2-H), 5.15(1 H, d, 4.6Hz, 6-H), 5.66(1 H, d, 4.6Hz, 7-H), 6.91 (2H, d,8.0Hz, phenyl-H), 7.38(2H, d, 8.0Hz, phenyl-H)
PAPER
Deshmukh, J. H.; Asian Journal of Chemistry 2010, V22(3), P1760-1768
Journal of the Chinese Chemical Society (Weinheim, Germany), 66(12), 1649-1657; 2019
Journal of the Indian Chemical Society, 93(6), 593-598; 2016
Biotechnology Letters, 34(9), 1719-1724; 2012
PATENT
WO 2011113486
By Gupta, Niranjan Lal et alFrom Indian, 184842, 30 Sep 2000
PAPER
European Journal of Organic Chemistry, (10), 1817-1820; 2001
PAPER
Organic Letters, 2(18), 2829-2831; 2000
The cephalosporin antibiotic Cefadroxil can be epimerized at the α-carbon of its amino acid side chain using pyridoxal as the mediator. By clathration with 2,7-dihydroxynaphthalene, the desired diastereomer can be selectively withdrawn from the equilibrating mixture of epimers. In this way, an asymmetric transformation of Cefadroxil can be accomplished. This opens the possibility of the production of Cefadroxil starting from racemic p-hydroxyphenylglycine, in contrast to the current industrial synthesis that employs the d-amino acid in enantiopure form.


AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Medical use
Cefadroxil is a first-generation cephalosporin antibacterial drug that is the para-hydroxy derivative of cephalexin, and is used similarly in the treatment of mild to moderate susceptible infections such as the bacterium Streptococcus pyogenes, causing the disease popularly called strep throat or streptococcal tonsillitis, urinary tract infection, reproductive tract infection, and skin infections.
Cefadroxil is used as an antibiotic prophylaxis before dental procedures, for patients allergic to penicillins.
Spectrum of bacterial resistance and susceptibility
Cefadroxil has a broad spectrum of activity and has been effective in treating bacteria responsible for causing tonsillitis, and infections of the skin and urinary tract. The following represents MIC susceptibility data for a few medically significant microorganisms.[2]
- Escherichia coli: 8 μg/ml
- Staphylococcus aureus: 1 – 2 μg/ml
- Streptococcus pneumoniae: ≤1 – >16 μg/ml
Side effects
The most common side effects of cefadroxil are diarrhea (which, less commonly, may be bloody), nausea, upset stomach, and vomiting. Other side effects include[3] rashes, hives, and itching.
Pharmacokinetics
Cefadroxil is almost completely absorbed from the gastrointestinal tract. After doses of 500 mg and 1 g by mouth, peak plasma concentrations of about 16 and 30 micrograms/ml, respectively, are obtained after 1.5 to 2.0 hours. Although peak concentrations are similar to those of cefalexin, plasma concentrations are more sustained. Dosage with food does not appear to affect the absorption of cefadroxil. About 20% of cefadroxil is reported to be bound to plasma proteins. Its plasma half-life is about 1.5 hours and is prolonged in patients with renal impairment.
Cefadroxil is widely distributed to body tissues and fluids. It crosses the placenta and appears in breast milk. More than 90% of a dose of cefadroxil may be excreted unchanged in the urine within 24 hours by glomerular filtration and tubular secretion; peak urinary concentrations of 1.8 mg/ml have been reported after a dose of 500 mg. Cefadroxil is removed by haemodialysis.
Dosage
Cefadroxil is given by mouth, and doses are expressed in terms of the anhydrous substance; 1.04 g of cefadroxil monohydrate is equivalent to about 1 g of anhydrous cefadroxil.
Veterinary use
It can be used for treating infected wounds on animals. Usually in powder form mixed with water, it has a color and smell similar to Tang. Given orally to animals, the amount is dependent on their weight and severity of infection.
References
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 493. ISBN 9783527607495.
- ^ “Cefadroxil, Free Acid Susceptibility and Minimum Inhibitory Concentration (MIC) Data” (PDF).
- ^ “Cefadroxil side effects”. Drugs.
| Clinical data | |
|---|---|
| Trade names | Duricef |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682730 |
| Routes of administration | Oral |
| ATC code | J01DB05 (WHO) |
| Legal status | |
| Legal status | In general: ℞ (Prescription only) |
| Pharmacokinetic data | |
| Protein binding | plasma protein |
| Metabolism | unknown |
| Elimination half-life | 1.5 hours |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 66592-87-8 |
| PubChem CID | 47964 |
| DrugBank | DB01140 |
| ChemSpider | 43629 |
| UNII | 280111G160 |
| KEGG | D02353 |
| ChEBI | CHEBI:53667 |
| ChEMBL | ChEMBL1644 |
| CompTox Dashboard (EPA) | DTXSID8022749 |
| ECHA InfoCard | 100.051.397 |
| Chemical and physical data | |
| Formula | C16H17N3O5S |
| Molar mass | 363.39 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (what is this?) (verify) |
////////////CEFADROXIL, цефадроксил , سيفادروكسيل , 头孢羟氨苄 , BL-S578; MJF-11567-3, BL S578, MJF 11567-3
[H][C@]12SCC(C)=C(N1C(=O)[C@H]2NC(=O)[C@H](N)C1=CC=C(O)C=C1)C(O)=O

NEW DRUG APPROVALS
ONE TIME
$10.00
MY NEW DRUG APPROVALS BLOG HAS CLOCKED 35 LAKH VIEWS IN 7 CONTINENTS, 226 COUNTRIES

MY NEW DRUG APPROVALS BLOG HAS CLOCKED 35 LAKH VIEWS IN 7 CONTINENTS, 226 COUNTRIES
Service to education is service to humanity, Taking free education to the world, Every difficulty an opportunity,In the dark but yet in light,proud of my disabilty, Taking industry experience to students, See the ability not the disabilty, The only disability in life is a bad attitude !!!, Dreamt a billion when hit by million, Mentor to the world
![]() All my awards, https://lnkd.in/fGxx9VF
All my awards, https://lnkd.in/fGxx9VF
Click on above links
Cabergoline
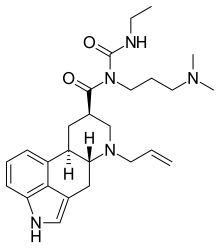
Cabergoline
Cabaser
- Molecular FormulaC26H37N5O2
- Average mass451.604 Da
1-Ethyl-3-(3′-dimethylaminopropyl)-3-(6′-allylergoline-8’β-carbonyl)urea
5860
81409-90-7[RN]
(6aR,9R,10aR)-N-[3-(dimethylamino)propyl]-N-(ethylcarbamoyl)-7-prop-2-en-1-yl-4,6,6a,7,8,9,10,10a-octahydroindolo[4,3-fg]quinoline-9-carboxamide
(8b)-N-[3-(Dimethylamino)propyl]-N-[(ethylamino)carbonyl]-6-(2-propenyl)ergoline-8-carboxamide
(8β)-6-Allyl-N-[3-(dimethylamino)propyl]-N-(ethylcarbamoyl)ergoline-8-carboxamide
Ergoline-8-carboxamide, N-[3-(dimethylamino)propyl]-N-[(ethylamino)carbonyl]-6-(2-propen-1-yl)-, (8β)-
ergoline-8-carboxamide, N-[3-(dimethylamino)propyl]-N-[(ethylamino)carbonyl]-6-(2-propenyl)-, (8β)-
KE6167600, LL60K9J05T, UNII-LL60K9J05T,
каберголин
كابارغولين
卡麦角林,
- FCE 21336
- FCE-21336
Cabergoline
CAS Registry Number: 81409-90-7
CAS Name:(8b)-N-[3-(Dimethylamino)propyl]-N-[(ethylamino)carbonyl]-6-(2-propenyl)ergoline-8-carboxamide
Additional Names: 1-ethyl-3-(3¢-dimethylaminopropyl)-3-(6¢-allylergoline-8¢b-carbonyl)urea; 1-[(6-allylergoline-8b-yl)carbonyl]-1-[3-(dimethylamino)propyl]-3-ethylurea
Manufacturers’ Codes: FCE-21336
Trademarks: Dostinex (Pharmacia & Upjohn)
Molecular Formula: C26H37N5O2, Molecular Weight: 451.60
Percent Composition: C 69.15%, H 8.26%, N 15.51%, O 7.09%
Literature References: Dopamine D2-receptor agonist. Prepn: P. Salvati et al.,BE888243; eidem,US4526892 (1981, 1985 both to Farmitalia Carlo Erba). Prepn and bioactivity: E. Brambilla et al.,Eur. J. Med. Chem.24, 421 (1989). Clinical pharmacology: C. Ferrari et al.,J. Clin. Endocrinol. Metab.63, 941 (1986). Veterinary trial as abortifacient in dogs: K. Post et al.,Theriogenology29, 1233 (1988). Clinical evaluation to prevent puerperal lactation: G. B. Melis et al.,Obstet. Gynecol.71, 311 (1988); in hyperprolactinemic disorders: C. Ferrari et al.,J. Clin. Endocrinol. Metab.68, 1201 (1989). Clinical trial in Parkinson’s disease: J. T. Hutton et al.,Neurology46, 1062 (1996).
Properties: White crystals from diethyl ether, mp 102-104°. Sol in ethyl alcohol, chloroform, DMF; slightly sol in 0.1 N HCl; very slightly sol in n-hexane. Insol in water. LD50 orally in male mice: >400 mg/kg (Brambilla).
Melting point: mp 102-104°
Toxicity data: Sol in ethyl alcohol, chloroform, DMF; slightly sol in 0.1 N HCl; very slightly sol in n-hexane. Insol in water. LD50 orally in male mice: >400 mg/kg (Brambilla)
Cabergoline diphosphate
85329-89-1
Derivative Type: Diphosphate
CAS Registry Number: 85329-89-1, Molecular Formula: C26H37N5O2.2H3PO4, Molecular Weight: 647.59
Percent Composition: C 48.22%, H 6.69%, N 10.81%, O 24.71%, P 9.57%
Properties: mp 153-155°., Melting point: mp 153-155°
Therap-Cat: Prolactin inhibitor; antiparkinsonian.
Therap-Cat-Vet: Prolactin inhibitor.
Keywords: Antiparkinsonian; Dopamine Receptor Agonist; Prolactin Inhibitor.
Cabergoline, sold under the brand name Dostinex among others, is a dopaminergic medication used in the treatment of high prolactin levels, prolactinomas, Parkinson’s disease, and for other indications. It is taken by mouth.
Cabergoline is an ergot derivative and a potent dopamine D2 receptor agonist.[1]
Cabergoline was patented in 1980 and approved for medical use in 1993.[2]
Cabergoline is a dopamine receptor agonist used for the treatment of hyperprolactinemic conditions due to various causes.
Cabergoline, an ergot derivative, is a long-acting dopamine agonist and prolactin inhibitor. It is used to treat hyperprolactinemic disorders and Parkinsonian Syndrome. Cabergoline possesses potent agonist activity on dopamine D2 receptors.
Synthesis Reference
PAPER
https://www.researchgate.net/publication/11103403_A_Practical_Synthesis_of_Cabergoline
N-[[(5R,8R,10R)-6-Allylergolin-8-yl]carbonyl]-N-[3-(di-methylamino)propyl]-N′-ethylurea (1). Compound 11 (40.13g, 72.7 mmol), H2O (200 mL), and 1 M aqueous hydrochloric acid(182 mL, 182 mmol) were combined and heated to 80 °C for 1 h.EtOAc (300 mL) was added to the light yellow solution. The pHwas adjusted to 10 with concentrated NH4OH (30 mL). Theorganic phase was separated and extracted with H2O(2×100mL). The aqueous layer was extracted with EtOAc (1 ×100 mL),and the combined organic layer was dried over Na2SO4, filtered,and concentrated to an amorphous solid. Cabergoline wasisolated in 94% yield (55% chemical yield overall from 8in highpurity (99 area % by HPLC): 1H NMR (CDCl3)δ1.18 (t, J)7.1 Hz, 3H), 1.76 (m, 2H), 1.85 (m, 2H), 2.23 (s, 6H), 2.34 (m,2H), 2.53-2.84 (m, 4H), 2.98 (m, 1H), 3.17 (m, 1H), 3.29-3.44(m, 4H), 3.55 (m, 1H), 3.83 (m, 2H), 5.19 (d, J)10.2 Hz, 1H),5.25 (d, J)16.8 Hz, 1H), 5.95 (m, 1H), 6.87 (m, 2H), 7.14 (m,2H), 8.88 (s, 1H), 9.45 (s, 1H); 13C NMR (100 MHz, CDCl3)δ14.7, 26.61, 31.31, 35.41, 40.04, 42.23, 43.21, 44.93, 55.61, 56.10,63.74, 108.7, 111.58, 113.10, 117.88, 118.36, 122.98, 126.02,132.67, 133.31, 133.83, 177.89.
1H AND 13 NMR IN CDCl3file:///C:/Users/Inspiron/Downloads/jo0203847_si_001.pdf
in dmso d6
SYN
DOI: 10.1016/0223-5234(89)90087-1

PATENT
https://patents.google.com/patent/EP1720869B1/en
- 6-Allyl-N-[3-(dimethylamino)propyl]-N-[(ethylamino)carbonyl]-ergoline-8β-carboxamide – international non-proprietary name cabergoline – of formula (I)is a potent dopamine agonist and is useful as anti-Parkinson drug and as prolactin inhibitor (Eur. J. Med. Chem. 1989, 24, 421-426 and United States Patent 5,382,669 ).
- [0003]
Cabergoline (I) was firstly prepared according to United States Patent 4,526,892 by reaction of 6-allyl-ergoline-8β-carboxylic acid (II) with 1-[3-(dimethylamino)propyl)-3-ethylcarbodiimide (EDC) (Scheme 1). - [0004]
In this case both regioisomers (I) and (III) were obtained and the yield of the isolated cabergoline (I) is only approx. 21% as a consequence of isolation difficulties, considering that the yield of compound (II) prepared from (XIII) according to the state of the art is 70%. - [0005]
Eur. J. Med. Chem. 1989, 24, 421-426 describes another method for the preparation of Cabergoline (I), which is based on the direct reaction of 6-allyl-N-[3-(dimethylamino)propyl]-ergoline-8β-carboxamide (IV) with ethyl isocyanate (EtNCO) (Scheme 2). - [0006]
Since this reaction leads to equilibrium, it requires the use of a large excess of ethyl isocyanate (up to 40 equivalents) for reasonable conversion and must be conducted at above 100°C in toluene for several hours. The use of large quantities of toxic ethyl isocyanate under drastic reaction conditions presents a serious hazard for the large-scale preparation of cabergoline (I). In addition, conversion to (I) is incomplete and competitive acylation of the indole nitrogen forming compounds (V) and (VI) occurs. This side reaction complicates the product purification and reduces the yield, which is only approx. 58%, considering that the yield of compound (IV) prepared from (XIII) according to the state of the art is 72%. - [0007]
The method proposed in United States Patent 5,382,669 and Syn. Lett. 1995, 605-606 showed that catalysis by copper salts in the presence of phosphine ligands permitted the ethyl isocyanate reaction to be run at room temperature with only 3 equivalents of ethyl isocyanate. However, despite of moderation in reaction conditions the conversion and the ratio of cabergoline (I) and the byproducts (V and VI) are not much different from the uncatalyzed thermal reaction. The yield is only approx. 48% and 57%, considering that the yield of compound (IV) prepared from (XIII) according to the state of the art is 72%. - [0008]
J. Org. Chem. 2002, 67, 7147-7150 describes an ethyl isocyanate-free method for the production of cabergoline (I) that solves the problem of completing acylation of indole nitrogen, too. - [0009]
The first step is the protection of indole nitrogen of amide (IV) preferably as tert-butyl carbamate (VII). - [0010]
Extension of the amide side chain is done by deprotonation of compound (VII) with sodium hexamethyldisilazide (NaHMDS) followed by trapping the anion with phenyl chloroformate (PhOCOCl) to yield the phenyl carbamate (VTII). - [0011]
Reaction of compound (VII) with ethylamine hydrochloride (EtNH2xHCl) gives BOC-cabergoline (IX) but also generates the ethylamide (X). The deprotection is done from the mixture of (IX) and (X) with 1N aqueous hydrochloric acid. The purified cabergoline (I) is then isolated by basification followed by chromatography on silica. (Scheme 3). - [0012]
In this approach the deprotonating step requires special cold reactor and strictly anhydrous circumstances. These requirements can hardly be satisfied in the course of large-scale preparation and the yield is only approx. 52%, considering that the yield of compound (VII) prepared from (XIII) according to the state of the art is 66%. - [0013]
According to US 2002/0177709 A1 Patent Application cabergoline (I) may be prepared by silylating amide (IV) with a silylating agent (e.g. trimethylsilyl trifluoromethane sulfonate – TMSOTf), reacting the obtained product (XI) with ethyl isocyanate (EtNCO) followed by desilylation of intermediate (XII) (Scheme 4). - [0014]
The disadvantage of this process is, that the silylating step requires strictly anhydrous circumstances. Otherwise, the reaction with ethyl isocyanate runs too long (24 hours) raising the safety hazard in the course of large-scale preparation and the yield is approx. 65%, considering that the yield of compound (IV) prepared from (XIII) according to the state of the art is 72%. - [0015]
Several crystalline forms of Cabergoline (I) are known. - [0016]
IL Farmaco 1995, 50 (3), 175-178 describes the preparation of crystalline form I. This solvated anhydrate product is crystallized from diethyl ether. - [0017]
WO 01/70740 A1 Patent Application describes a new process for the preparation of crystalline form I from the new crystalline form V. The form V – which is toluene solvate – is prepared from the mixture of the purified cabergoline (I) with toluene and diethyl ether by a long-lasting complicated process, at low reaction temperature, and the yield is only 45%. The crystalline form I is prepared by drying the form V in vacuum. - [0018]
WO 01/72746-A1 Patent Application describes the preparation of crystalline form VII from the crystalline form L By this process the suspension of form I in n-heptane or 1,4-dioxane is stirred for 48 hours, and then the suspension was filtered to obtain the crystalline form VII. The yield is 45.2%. - [0019]
WO 01/72747 A1 Patent Application describes the crystalline form II and a process for its preparation with approx. 70% yield by stirring the cabergoline (I) for several days in an organic solvent (eg. diethyl ether) at low temperature. - [0020]
Xenobiotica 1993, 23(12), 1377-1389, describes a comparison of the disposition and urinary metabolic pattern of 14C-cabergoline after single oral administration to rat, monkey and man. Among the potential metabolites of cabergoline a compound identified as FCE 27392 is disclosed, which corresponds to intermediate XIX of the preparation process of cabergoline according to the present invention.
The reaction procedure is shown in Scheme 5.

EXAMPLE 5Synthesis of 6-allyl-N-[3-(dimethylamino)propyl]-N-[(ethylamino)carbonyl]-ergoline-8β-carboxamide (I) (Cabergoline).
- [0077]
To a suspension of 9.0 g (21.87 mmol) N-[3-(dimethylamino)propyl]-N-[(ethylamino)carbonyl)-ergoline-8β-carboxamide (XIX) in 250 ml of toluene 0.5 g of tetrakis(triphenylphosphine)palladium(0) and 5 ml of allyl acetate was added, and the reaction mixture was stirred at ambient temperature for 2 hours. The resulting mixture was washed with 100 ml of water. The organic layer was dried over anhydrous sodium sulphate. The dried solution was concentrated in vacuum and the product was purified on a silica plug to give 9.1 g (92.3%) of the title compound.
1H NMR (DMSO-d6, TMS, 500MHz) δ 1.10 (t, 3H, J=7.2Hz, CONHCH2CH 3); 1.47 (q, 1H, J=12.4Hz, Hβ-9); 1.62-1.72 (m, 2H, CONCH2CH 2CH2N(CH3)2); 2.15 (s, 6H, CONCH2CH2CH2N(CH 3)2); 2.20-2.30 (m, 2H, CONHCH2CH2CH 2N(CH3)2); 2.32-2.40 (m, 2H, H-5, Hβ-7); 2.54 (dd, 1H, J=14.3Hz, 11.2Hz, Hα-4); 2.68-2.84 (m, 2H, Hα-9, H-10); 3.08 (ddd, 1H, J=11.3Hz, 3.1Hz, 1.8Hz, Hα-7); 3.14-3.22 (m, 2H, CONHCH 2CH3); 3.26 (dd, 1H, J=14.7Hz, 7.3Hz, Hx-N(6)CH 2CH=CH2); 3.28-3.38 (m, 2H, Hβ-4, H-8); 3.48 (dd, 1H, J=14.7Hz, 5.8Hz, Hy-N(6)CH 2CH=CH2); 3.58-3.68 (m, 2H, CONCH 2CH2CH2N(CH3)2); 5.15 (d, 1H, J=10.3Hz, Hx-N(6)CH2CH=CH 2); 5.24 (d, 1H, J=17.2Hz, Hy-N(6)CH2CH=CH 2); 5.88-5.98 (m, 1H, N(6)CH2CH=CH2); 6.75 (d, 1H, J=7.0Hz, H-12); 6.97 (s, 1H, H-2); 7.01 (t, 1H, J=7.5Hz, H-13); 7.13 (d, 1H, J=8.0Hz, H-14); 9.04 (t, 1H, J=5.0Hz, CONHCH2CH3); 10.60 (s, 1H, N(1)H).
EXAMPLE 6Production of amorphous form of Cabergoline (I)
- [0078]
- a) 10 g of chromatographically purified oily Cabergoline (I) was dissolved in 50 ml of acetone. The solution was concentrated in vacuum at 25-30°C to approx. 15 g. The obtained oily residue was dissolved in 40 ml of acetone, and the solution was concentrated in vacuum at 25-30°C to approx. 12 g. The obtained oily residue was dissolved in 30 ml of acetone again, and the solution was concentrated in vacuum at 25-30°C to 10 g. The obtained solid Cabergoline (I) was dried in vacuum at 25-30°C to solvent-free, to give 9.8 g (98%) of the title compound.
- b) The same as in Example 6a, but employing methyl acetate as solvent, 9.85 g (98.5%) of the title compound was obtained.
- c) The same as in Example 6a, but employing dichloromethane as solvent, 9.82 g (982%) of the title compound was obtained.
Patent
Publication numberPriority datePublication dateAssigneeTitleFamily To Family CitationsGB9205439D0 *1992-03-121992-04-22Erba Carlo SpaProcess for the synthesis of ergoline derivativesUS6696568B2 *2001-04-162004-02-24Finetech Ltd.Process and intermediates for production of cabergoline and related compoundsJP2004525187A *2001-04-162004-08-19フイネテク・リミテツドMethods and intermediates for the preparation of cabergoline and related compounds
Publication numberPriority datePublication dateAssigneeTitleFamily To Family CitationsEP1620101A4 *2003-05-082008-07-09Ivax Pharmaceuticals SroPolymorphs of cabergolineEP1925616A1 *2006-10-262008-05-28LEK Pharmaceuticals D.D.Process for the preparation of crystal forms of cabergoline via stable solvates of cabergolineWO2008104956A2 *2007-02-282008-09-04Ranbaxy Laboratories LimitedProcess for the preparation of amorphous cabergolineEP2083008A1 *2007-12-072009-07-29Axxonis Pharma AGErgoline derivatives as selective radical scavengers for neuronsWO2011154827A2 *2010-06-112011-12-15Rhodes TechnologiesTransition metal-catalyzed processes for the preparation of n-allyl compounds and use thereofCA2876321A1 *2012-06-222013-12-27Map Pharmaceuticals, Inc.Novel cabergoline derivatives
SYNBE 0894060; JP 58038282This compound can be obtained by two differents ways: 1) By condensation of 6-allyl-N-[3-(dimethylamino)propyl]ergolin-8-beta-caboxamide (I) with ethyl isocyanate (II) in refluxing toluene. 2) By condensation of 6-allylergolin-8-beta-carboxylic acid (III) with N-ethyl-N’-[3-(dimethylamino)propyl]carbodiimide (IV) in refluxing THF.
SYN
| J Label Compd Radiopharm 1991,29(5),519 |
The synthesis of tritiated cabergoline by two similar routes has been described: 1) The acylation of 6-nor-dihydrolysergic acid methyl ester (I) with propargyl bromide yields the corresponding 6-propargyl derivative (II), which is hydrogenated with tritium gas over Pd/C in the presence of quinoline to give the ditritiated 6-allyl derivative (III). This compound is treated with 3-(dimethylamino)propylamine at 120 C, yielding the amide (IV), which is finally treated with ethyl isocyanate. 2) The reaction of the propargyl derivative (II) with 3-(dimethylamino)propylamine as before gives the amide (V). The reaction of (V) with ethyl isocyanate gives compound (VI), which is then hydrogenated with tritium as before.
SYNThe synthesis of [14C]-cabergoline has also been described: The reaction of 6-allylergoline-8beta-carboxylic acid methyl ester (I) with hydrazine in refluxing methanol gives the hydrazide (II), which by reaction with NaNO2-HCl in water is converted to the amine (III). The reaction of (III) again with NaNO2-HCl in water, followed by reaction with SnCl2, affords the chloro derivative (IV), which is condensed with [14C]-CNK in refluxing ethanol-water yielding the nitrile (V). Hydrolysis of (V) with NaOH in refluxing ethanol affords the acid (VI), which is finally condensed with N-ethyl-N’-[3-(dimethylamino)propyl]carbodiimide in DMF.

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Medical uses
- Lactation suppression
- Hyperprolactinemia[3]
- Adjunctive therapy of prolactin-producing pituitary gland tumors (prolactinomas);
- Monotherapy of Parkinson’s disease in the early phase;
- Combination therapy, together with levodopa and a decarboxylase inhibitor such as carbidopa, in progressive-phase Parkinson’s disease;
- In some countries also: ablactation and dysfunctions associated with hyperprolactinemia (amenorrhea, oligomenorrhea, anovulation, nonpuerperal mastitis and galactorrhea);
- Treatment of uterine fibroids.[4][5]
- Adjunctive therapy of acromegaly, cabergoline has low efficacy in suppressing growth hormone levels and is highly efficient in suppressing hyperprolactinemia that is present in 20-30% of acromegaly cases; growth hormone and prolactin are similar structurally and have similar effects in many target tissues, therefore targeting prolactin may help symptoms when growth hormone secretion can not be sufficiently controlled by other methods;
Cabergoline is frequently used as a first-line agent in the management of prolactinomas due to its higher affinity for D2 receptor sites, less severe side effects, and more convenient dosing schedule than the older bromocriptine, though in pregnancy bromocriptine is often still chosen since there is less data on safety in pregnancy for cabergoline.
Off-label
It has at times been used as an adjunct to SSRI antidepressants as there is some evidence that it counteracts certain side effects of those drugs, such as reduced libido and anorgasmia. It also has been suggested that it has a possible recreational use in reducing or eliminating the male refractory period, thereby allowing men to experience multiple ejaculatory orgasms in rapid succession, and at least two scientific studies support those speculations.[6][7]: e28–e33 Additionally, a systematic review and meta-analysis concluded that prophylactic treatment with cabergoline reduces the incidence, but not the severity, of ovarian hyperstimulation syndrome (OHSS), without compromising pregnancy outcomes, in females undergoing stimulated cycles of in vitro fertilization (IVF).[8] Also, a study on rats found that cabergoline reduces voluntary alcohol consumption, possibly by increasing GDNF expression in the ventral tegmental area.[9] It may be used in the treatment of restless legs syndrome.[citation needed]
Pregnancy and lactation
Relatively little is known about the effects of this medication during pregnancy and lactation. In some cases the related bromocriptine may be an alternative when pregnancy is expected.[citation needed]
- Pregnancy: available preliminary data indicates a somewhat increased rate of congenital abnormalities in patients who became pregnant while treated with cabergoline.[citation needed]. However, one study concluded that “foetal exposure to cabergoline through early pregnancy does not induce any increase in the risk of miscarriage or foetal malformation.”[10]
- Lactation: In rats cabergoline was found in the maternal milk. Since it is not known if this effect also occurs in humans, breastfeeding is usually not recommended if/when treatment with cabergoline is necessary.
- Lactation suppression: In some countries cabergoline (Dostinex) is sometimes used as a lactation suppressant. It is also used in veterinary medicine to treat false pregnancy in dogs.
Contraindications
- Hypersensitivity to ergot derivatives
- Pediatric patients (no clinical experience)
- Severely impaired liver function or cholestasis
- Concomitant use with drugs metabolized mainly by CYP450 enzymes such as erythromycin and ketoconazole, because increased plasma levels of cabergoline may result (although cabergoline undergoes minimal CYP450 metabolism).
- Cautions: severe cardiovascular disease, Raynaud’s disease, gastroduodenal ulcers, active gastrointestinal bleeding, hypotension.
Side effects
Side effects are mostly dose dependent. Much more severe side effects are reported for treatment of Parkinson’s disease and (off-label treatment) for restless leg syndrome which both typically require very high doses. The side effects are considered mild when used for treatment of hyperprolactinemia and other endocrine disorders or gynecologic indications where the typical dose is one hundredth to one tenth that for Parkinson’s disease.[citation needed]
Cabergoline requires slow dose titration (2–4 weeks for hyperprolactinemia, often much longer for other conditions) to minimise side effects. The extremely long bioavailability of the medication may complicate dosing regimens during titration and require particular precautions.
Cabergoline is considered the best tolerable option for hyperprolactinemia treatment although the newer and less tested quinagolide may offer similarly favourable side effect profile with quicker titration times.
Approximately 200 patients with newly diagnosed Parkinson’s disease participated in a clinical study of cabergoline monotherapy.[11] Seventy-six (76) percent reported at least one side effect. These side effects were chiefly mild or moderate:
- GI tract: Side effects were extremely frequent. Fifty-three percent of patients reported side effects. Very frequent: Nausea (30%), constipation (22%), and dry mouth (10%). Frequent: Gastric irritation (7%), vomiting (5%), and dyspepsia (2%).
- Psychiatric disturbances and central nervous system (CNS): Altogether 51 percent of patients were affected. Very frequent: Sleep disturbances (somnolence 18%, insomnia 11%), vertigo (27%), and depression (13%). Frequent: dyskinesia (4%) and hallucinations (4%).
- Cardiovascular: Approximately 30 percent of patients experienced side effects. Most frequent were hypotension (10%), peripheral edema (14%) and non-specific edema (2%). Arrhythmias were encountered in 4.8%, palpitations in 4.3%, and angina pectoris in 1.4%.
In a combination study with 2,000 patients also treated with levodopa, the incidence and severity of side effects was comparable to monotherapy. Encountered side effects required a termination of cabergoline treatment in 15% of patients. Additional side effects were infrequent cases of hematological side effects, and an occasional increase in liver enzymes or serum creatinine without signs or symptoms.
As with other ergot derivatives, pleuritis, exudative pleura disease, pleura fibrosis, lung fibrosis, and pericarditis are seen. These side effects are noted in less than 2% of patients. They require immediate termination of treatment. Clinical improvement and normalization of X-ray findings are normally seen soon after cabergoline withdrawal. It appears that the dose typically used for treatment of hyperprolactinemia is too low to cause this type of side effects.
Valvular heart disease
In two studies published in the New England Journal of Medicine on January 4, 2007, cabergoline was implicated along with pergolide in causing valvular heart disease.[12][13] As a result of this, the FDA removed pergolide from the U.S. market on March 29, 2007.[14] Since cabergoline is not approved in the U.S. for Parkinson’s Disease, but for hyperprolactinemia, the drug remains on the market. The lower doses required for treatment of hyperprolactinemia have been found to be not associated with clinically significant valvular heart disease or cardiac valve regurgitation.[15][16]
Interactions
No interactions were noted with levodopa or selegiline. The drug should not be combined with other ergot derivatives. Dopamine antagonists such as antipsychotics and metoclopramide counteract some effects of cabergoline. The use of antihypertensive drugs should be intensively monitored because excessive hypotension may result from the combination.
Pharmacology
Pharmacodynamics
| Site | Affinity (Ki [nM]) | Efficacy (Emax [%]) | Action |
|---|---|---|---|
| D1 | 214–32,000 | ? | ? |
| D2S | 0.5–0.62 | 102 | Full agonist |
| D2L | 0.95 | 75 | Partial agonist |
| D3 | 0.80–1.0 | 86 | Partial agonist |
| D4 | 56 | 49 | Partial agonist |
| D5 | 22 | ? | ? |
| 5-HT1A | 1.9–20 | 93 | Partial agonist |
| 5-HT1B | 479 | 102 | Full agonist |
| 5-HT1D | 8.7 | 68 | Partial agonist |
| 5-HT2A | 4.6–6.2 | 94 | Partial agonist |
| 5-HT2B | 1.2–9.4 | 123 | Full agonist |
| 5-HT2C | 5.8–692 | 96 | Partial agonist |
| 5-HT3 | >10,000 | – | – |
| 5-HT4 | 3,000 | ? | ? |
| 5-HT6 | 1,300 | ? | ? |
| 5-HT7 | 2.5 | ? | Antagonist |
| α1A | 288–>10,000 | 0 | Silent antagonist |
| α1B | 60–1,000 | ? | ? |
| α1D | 166 | ? | ? |
| α2A | 12–132 | 0 | Silent antagonist |
| α2B | 17–72 | 0 | Silent antagonist |
| α2C | 22–364 | 0 | Silent antagonist |
| α2D | 3.6 | ? | ? |
| H1 | 1,380 | ? | ? |
| M1 | >10,000 | – | – |
| SERT | >10,000 | – | – |
| Notes: All sites are human except α2D-adrenergic, which is rat (no human counterpart).[17] Negligible affinity (>10,000 nM) for various other receptors (β1– and β2-adrenergic, adenosine, GABA, glutamate, glycine, nicotinic acetylcholine, opioid, prostanoid).[18] Sources: [17][19][20][18][21] |
Cabergoline is a long-acting dopamine D2 receptor agonist. In-vitro rat studies show a direct inhibitory effect of cabergoline on the prolactin secretion in the lactotroph cells of the pituitary gland and cabergoline decreases serum prolactin levels in reserpinized rats.[citation needed] Although cabergoline is commonly described principally as a D2 receptor agonist, it also possesses significant affinity for the dopamine D3, and D4, serotonin 5-HT1A, 5-HT2A, 5-HT2B, and 5-HT2C, and α2-adrenergic receptors, as well as moderate/low affinity for the dopamine D1, serotonin 5-HT7, and α1-adrenergic receptors.[17][18][22] Cabergoline functions as an partial or full agonist at all of these receptors except for the 5-HT7, α1-adrenergic, and α2-adrenergic receptors, where it acts as an antagonist.[19][20][18] Cabergoline has been associated with cardiac valvulopathy due to activation of 5-HT2B receptors.[23]
Pharmacokinetics
Following a single oral dose, resorption of cabergoline from the gastrointestinal (GI) tract is highly variable, typically occurring within 0.5 to 4 hours. Ingestion with food does not alter its absorption rate. Human bioavailability has not been determined since the drug is intended for oral use only. In mice and rats the absolute bioavailability has been determined to be 30 and 63 percent, respectively. Cabergoline is rapidly and extensively metabolized in the liver and excreted in bile and to a lesser extent in urine. All metabolites are less active than the parental drug or inactive altogether. The human elimination half-life is estimated to be 63 to 68 hours in patients with Parkinson’s disease and 79 to 115 hours in patients with pituitary tumors. Average elimination half-life is 80 hours.
The therapeutic effect in treatment of hyperprolactinemia will typically persist for at least 4 weeks after cessation of treatment.
History
Cabergoline was first synthesized by scientists working for the Italian drug company Farmitalia-Carlo Erba in Milan who were experimenting with semisynthetic derivatives of the ergot alkaloids, and a patent application was filed in 1980.[24][25][26] The first publication was a scientific abstract at the Society for Neuroscience meeting in 1991.[27][28]
Farmitalia-Carlo Erba was acquired by Pharmacia in 1993,[29] which in turn was acquired by Pfizer in 2003.[30]
Cabergoline was first marketed in The Netherlands as Dostinex in 1992.[24] The drug was approved by the FDA on December 23, 1996.[31] It went generic in late 2005 following US patent expiration.[32]
Society and culture
Brand names
Brand names of cabergoline include Cabaser, Dostinex, Galastop (veterinary), and Kelactin (veterinary), among others.[33]
Research
Cabergoline was studied in one person with Cushing’s disease, to lower adrenocorticotropic hormone (ACTH) levels and cause regression of ACTH-producing pituitary adenomas.[34]
References
- ^ J. Elks; C. R. Ganellin (1990). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 204–.
- ^ Fischer, Jnos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 533. ISBN 9783527607495.
- ^ UK electronic Medicines Compendium Dostinex Tablets Last Updated on eMC Dec 23, 2013
- ^ Sayyah-Melli, M; Tehrani-Gadim, S; Dastranj-Tabrizi, A; Gatrehsamani, F; Morteza, G; Ouladesahebmadarek, E; Farzadi, L; Kazemi-Shishvan, M (2009). “Comparison of the effect of gonadotropin-releasing hormone agonist and dopamine receptor agonist on uterine myoma growth. Histologic, sonographic, and intra-operative changes”. Saudi Medical Journal. 30 (8): 1024–33. PMID 19668882.
- ^ Sankaran, S.; Manyonda, I. (2008). “Medical management of fibroids”. Best Practice & Research Clinical Obstetrics & Gynaecology. 22 (4): 655–76. doi:10.1016/j.bpobgyn.2008.03.001. PMID 18468953. http://www.britishfibroidtrust.org.uk/journals/bft_Sankaran.pdf
- ^ Krüger TH, Haake P, Haverkamp J, et al. (December 2003). “Effects of acute prolactin manipulation on sexual drive and function in males”. Journal of Endocrinology. 179 (3): 357–65. CiteSeerX 10.1.1.484.4005. doi:10.1677/joe.0.1790357. PMID 14656205.
- ^ Hollander, Adam B.; Pastuszak, Alexander W.; Lipshultz, Larry I. (2016). “Cabergoline in the Treatment of Male Orgasmic Disorder—A Retrospective Pilot Analysis”. Journal of Sexual Medicine. 4 (4): e28–e33. doi:10.1016/j.esxm.2015.09.001. PMC 4822480. PMID 26944776.
- ^ Youssef MA, van Wely M, Hassan MA, et al. (March 2010). “Can dopamine agonists reduce the incidence and severity of OHSS in IVF/ICSI treatment cycles? A systematic review and meta-analysis”. Hum Reprod Update. 16 (5): 459–66. doi:10.1093/humupd/dmq006. PMID 20354100.
- ^ Carnicella, S.; Ahmadiantehrani, S.; He, D. Y.; Nielsen, C. K.; Bartlett, S. E.; Janak, P. H.; Ron, D. (2009). “Cabergoline Decreases Alcohol Drinking and Seeking Behaviors Via Glial Cell Line-Derived Neurotrophic Factor”. Biological Psychiatry. 66 (2): 146–153. doi:10.1016/j.biopsych.2008.12.022. PMC 2895406. PMID 19232578.
- ^ Colao, A; Abs R.; et al. (January 2008). “Pregnancy outcomes following cabergoline treatment: extended results from a 12-year observational study”. Clinical Endocrinology. 68 (1): 66–71. doi:10.1111/j.1365-2265.2007.03000.x. PMID 17760883. S2CID 38408935.
- ^ Rinne, U. K.; Bracco, F.; Chouza, C.; Dupont, E.; Gershanik, O.; Masso, J. F. M.; Montastruc, J. L.; Marsden, C. D.; Dubini, A.; Orlando, N.; Grimaldi, R. (1997-02-01). “Cabergoline in the treatment of early parkinson’s disease: Results of the first year of treatment in a double-blind comparison of cabergoline and levodopa”. Neurology. 48 (2): 363–368. doi:10.1212/WNL.48.2.363. ISSN 0028-3878. PMID 9040722. S2CID 34955541.
- ^ Schade, Rene; Andersohn, Frank; Suissa, Samy; Haverkamp, Wilhelm; Garbe, Edeltraut (2007-01-04). “Dopamine Agonists and the Risk of Cardiac-Valve Regurgitation”. New England Journal of Medicine. 356 (1): 29–38. doi:10.1056/NEJMoa062222. PMID 17202453.
- ^ Zanettini, Renzo; Antonini, Angelo; Gatto, Gemma; Gentile, Rosa; Tesei, Silvana; Pezzoli, Gianna (2007-01-04). “Valvular Heart Disease and the Use of Dopamine Agonists for Parkinson’s Disease”. New England Journal of Medicine. 356 (1): 39–46. doi:10.1056/NEJMoa054830. PMID 17202454.
- ^ “Food and Drug Administration Public Health Advisory”. Food and Drug Administration. 2007-03-29. Archived from the original on 2007-04-08. Retrieved 2007-04-27.
- ^ Bogazzi, F.; Buralli, S.; Manetti, L.; Raffaelli, V.; Cigni, T.; Lombardi, M.; Boresi, F.; Taddei, S.; Salvetti, A. (2008). “Treatment with low doses of cabergoline is not associated with increased prevalence of cardiac valve regurgitation in patients with hyperprolactinaemia”. International Journal of Clinical Practice. 62 (12): 1864–9. doi:10.1111/j.1742-1241.2008.01779.x. PMID 18462372. S2CID 7822137.
- ^ Wakil, A.; Rigby, A. S; Clark, A. L; Kallvikbacka-Bennett, A.; Atkin, S. L (2008). “Low dose cabergoline for hyperprolactinaemia is not associated with clinically significant valvular heart disease”. European Journal of Endocrinology. 159 (4): R11–4. doi:10.1530/EJE-08-0365. PMID 18625690.
- ^ Jump up to:a b c Millan MJ, Maiofiss L, Cussac D, Audinot V, Boutin JA, Newman-Tancredi A (November 2002). “Differential actions of antiparkinson agents at multiple classes of monoaminergic receptor. I. A multivariate analysis of the binding profiles of 14 drugs at 21 native and cloned human receptor subtypes”. J Pharmacol Exp Ther. 303 (2): 791–804. doi:10.1124/jpet.102.039867. PMID 12388666. S2CID 6200455.
- ^ Jump up to:a b c d Sharif NA, McLaughlin MA, Kelly CR, Katoli P, Drace C, Husain S, Crosson C, Toris C, Zhan GL, Camras C (March 2009). “Cabergoline: Pharmacology, ocular hypotensive studies in multiple species, and aqueous humor dynamic modulation in the Cynomolgus monkey eyes”. Experimental Eye Research. 88 (3): 386–97. doi:10.1016/j.exer.2008.10.003. PMID 18992242.
- ^ Jump up to:a b Newman-Tancredi A, Cussac D, Audinot V, Nicolas JP, De Ceuninck F, Boutin JA, Millan MJ (November 2002). “Differential actions of antiparkinson agents at multiple classes of monoaminergic receptor. II. Agonist and antagonist properties at subtypes of dopamine D(2)-like receptor and alpha(1)/alpha(2)-adrenoceptor”. J Pharmacol Exp Ther. 303 (2): 805–14. doi:10.1124/jpet.102.039875. PMID 12388667. S2CID 35238120.
- ^ Jump up to:a b Newman-Tancredi A, Cussac D, Quentric Y, Touzard M, Verrièle L, Carpentier N, Millan MJ (November 2002). “Differential actions of antiparkinson agents at multiple classes of monoaminergic receptor. III. Agonist and antagonist properties at serotonin, 5-HT(1) and 5-HT(2), receptor subtypes”. J Pharmacol Exp Ther. 303 (2): 815–22. doi:10.1124/jpet.102.039883. PMID 12388668. S2CID 19260572.
- ^ https://web.archive.org/web/20210413033753/https://pdsp.unc.edu/databases/pdsp.php?testFreeRadio=testFreeRadio&testLigand=Cabergoline&doQuery=Submit+Query
- ^ National Institute of Mental Health. PDSD Ki Database (Internet) [cited 2013 Jul 24]. ChapelHill (NC): University of North Carolina. 1998-2013. Available from: “Archived copy”. Archived from the original on 2013-11-08. Retrieved 2014-03-04.
- ^ Cavero I, Guillon JM (2014). “Safety Pharmacology assessment of drugs with biased 5-HT(2B) receptor agonism mediating cardiac valvulopathy”. J Pharmacol Toxicol Methods. 69 (2): 150–61. doi:10.1016/j.vascn.2013.12.004. PMID 24361689.
- ^ Jump up to:a b Council regulation (EEC) no 1768/92 in the matter of Application No SPC/GB94/012 for a Supplementary Protection Certificate in the name of Farmitalia Carlo Erba S. r. l.
- ^ Espace record: GB 202074566
- ^ US Patent 4526892 – Dimethylaminoalkyl-3-(ergoline-8′.beta.carbonyl)-ureas
- ^ Fariello, RG (1998). “Pharmacodynamic and pharmacokinetic features of cabergoline. Rationale for use in Parkinson’s disease”. Drugs. 55 (Suppl 1): 10–6. doi:10.2165/00003495-199855001-00002. PMID 9483165. S2CID 46973281.
- ^ Carfagna N, Caccia C, Buonamici M, Cervini MA, Cavanus S, Fornaretto MG, Damiani D, Fariello RG (1991). “Biochemical and pharmacological studies on cabergoline, a new putative antiparkinsonian drug”. Soc Neurosci Abs. 17: 1075.
- ^ Staff. News: Farmitalia bought by Kabi Pharmacia[permanent dead link]. Ann Oncol (1993) 4 (5): 345.
- ^ Staff, CNN/Money. April 16, 2003 It’s official: Pfizer buys Pharmacia
- ^ FDA approval history
- ^ “Drugs@FDA: FDA Approved Drug Products – ANDA 076310”. http://www.accessdata.fda.gov. FDA.gov. Retrieved 14 December 2018.
- ^ “Cabergoline Uses, Side Effects & Warnings”. Archived from the original on 2015-12-30.
- ^ Miyoshi, T.; et al. (2004). “Effect of cabergoline treatment on Cushing’s disease caused by aberrant adrenocorticotropin-secreting macroadenoma”. Journal of Endocrinological Investigation. 27 (11): 1055–1059. doi:10.1007/bf03345309. PMID 15754738. S2CID 6660262.
External links
| Clinical data | |
|---|---|
| Trade names | Dostinex, others |
| AHFS/Drugs.com | Monograph |
| License data | US FDA: CABERGOLINE |
| Routes of administration | Oral |
| ATC code | G02CB03 (WHO) N04BC06 (WHO) |
| Legal status | |
| Legal status | US: ℞-only |
| Pharmacokinetic data | |
| Bioavailability | First-pass effect seen; absolute bioavailability unknown |
| Protein binding | Moderately bound (40–42%); concentration-independent |
| Metabolism | Hepatic, predominately via hydrolysis of the acylurea bond or the urea moiety |
| Elimination half-life | 63–69 hours (estimated) |
| Excretion | Urine (22%), feces (60%) |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 81409-90-7 |
| PubChem CID | 54746 |
| IUPHAR/BPS | 37 |
| DrugBank | DB00248 |
| ChemSpider | 49452 |
| UNII | LL60K9J05T |
| KEGG | D00987 |
| ChEBI | CHEBI:3286 |
| ChEMBL | ChEMBL1201087 |
| CompTox Dashboard (EPA) | DTXSID6022719 |
| ECHA InfoCard | 100.155.380 |
| Chemical and physical data | |
| Formula | C26H37N5O2 |
| Molar mass | 451.615 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (what is this?) (verify) |
////////////////Cabergoline, UNII-LL60K9J05T, каберголин , كابارغولين ,卡麦角林 , FCE-21336
[H][C@@]12CC3=CNC4=CC=CC(=C34)[C@@]1([H])C[C@H](CN2CC=C)C(=O)N(CCCN(C)C)C(=O)NCC

NEW DRUG APPROVALS
one time
$10.00
Zuclopenthixol
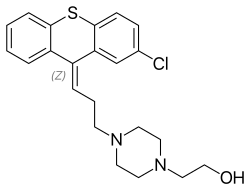
Zuclopenthixol
Clopenthixol
- Molecular FormulaC22H25ClN2OS
- Average mass400.965 Da
53772-83-1 [RN],
- N05AF05
1-Piperazineethanol, 4-[(3Z)-3-(2-chloro-9H-thioxanthen-9-ylidene)propyl]-
5443
2-{4-[(3Z)-3-(2-Chloro-9H-thioxanthen-9-ylidene)propyl]piperazin-1-yl}ethanol
258-758-5[EINECS]
Z)-Clopenthixol
1-piperazineethanol, 4-(3-(2-chloro-9h-thioxanthen-9-ylidene)propyl)-
1-Piperazineethanol, 4-(3-(2-chlorothioxanthen-9-ylidene)propyl)-
1-Piperazineethanol, 4-[(3Z)-3-(2-chloro-9H-thioxanthen-9-ylidene)propyl]-
- 1-Piperazineethanol, 4-[3-(2-chloro-9H-thioxanthen-9-ylidene)propyl]-, (Z)-
- 4-[(3Z)-3-(2-Chloro-9H-thioxanthen-9-ylidene)propyl]-1-piperazineethanol
- 9H-Thioxanthene, 1-piperazineethanol deriv.
- (Z)-Clopenthixol
- Acuphase
- Cisordinol
- Clopixol
- Clopixol depo
- Zuclopenthixol
- cis-(Z)-Clopenthixol
- cis-Clopenthixol
- α-Clopenthixol
Product Ingredients
| INGREDIENT | UNII | CAS | INCHI KEY |
|---|---|---|---|
| Zuclopenthixol acetate | 349S2ZHF05 | 85721-05-7 | OXAUOBQMCDIVPQ-IOXNKQMXSA-N |
| Zuclopenthixol decanoate | TSS9KIZ5OG | 64053-00-5 | QRUAPADZILXULG-WKIKZPBSSA-N |
| Zuclopenthixol dihydrochloride | 7042692VYN | 58045-23-1 | LPWNZMIBFHMYMX-MHKBYHAFSA-N |
Zuclopenthixol hydrochloride
58045-23-1, MW: 473.8933
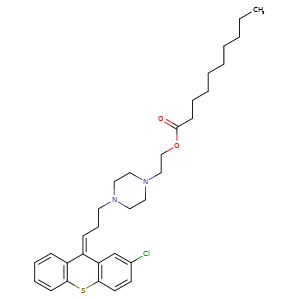
ZUCLOPENTHIXOL DECANOATE, CLOPENTHIXOL DECANOATE, CIS-
64053-00-5, Molecular Formula, C32-H43-Cl-N2-O2-S, Molecular Weight, 555.2227
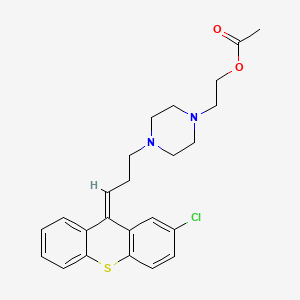
Zuclopenthixol acetate
85721-05-7, C24H27ClN2O2S, 443.0ClopenthixolCAS Registry Number: 982-24-1
CAS Name: 4-[3-(2-Chloro-9H-thioxanthen-9-ylidene)propyl]-1-piperazineethanol
Additional Names: 2-chloro-9-[3-[4-(2-hydroxyethyl)-1-piperazinyl]propylidene]thiaxanthene
Molecular Formula: C22H25ClN2OS
Molecular Weight: 400.96
Percent Composition: C 65.90%, H 6.28%, Cl 8.84%, N 6.99%, O 3.99%, S 8.00%
Literature References: Thioxanthene neuroleptic. Prepn (configuration not specified): BE585338; P. V. Petersen et al.,US3116291 (1960, 1963 both to Kefalas A/S). Prepn of the pharmacologically active cis-isomer: BE816855; N. Lassen, US3996211 (1974, 1976 both to Kefalas A/S). Pharmacology: Cazzullo, Andreola, Acta Neurol.20, 162 (1965); Weissman, Mod. Probl. Pharmacopsychiatry2, 15 (1969); Moeller Nielsen, ibid. 23. Metabolism: Khan, Acta Pharmacol. Toxicol.27, 202 (1969). HPLC determn of isomers in serum: T. Aaes-Jorgensen, J. Chromatogr.188, 239 (1980). Series of articles on pharmacology and clinical studies: Acta Psychiatr. Scand.64, Suppl. 294, 1-77 (1981).
Properties: Colorless syrup. Sparingly sol in ether. Readily sol in methanol.
Derivative Type: Dihydrochloride
CAS Registry Number: 633-59-0
Manufacturers’ Codes: AY-62021; N-746
Trademarks: Ciatyl (Troponwerke); Sordenac (Lundbeck); Sordinol (Ayerst)
Molecular Formula: C22H25ClN2OS.2HCl
Molecular Weight: 473.89
Percent Composition: C 55.76%, H 5.74%, Cl 22.44%, N 5.91%, O 3.38%, S 6.77%
Properties: Crystals from ethanol, mp 250-260° (dec). Freely sol in water; sparingly sol in alcohol. Practically insol in other organic solvents. LD50 in male mice (mg/kg): 111 i.v. (Lassen).
Melting point: mp 250-260° (dec)
Toxicity data: LD50 in male mice (mg/kg): 111 i.v. (Lassen)
Derivative Type:cis(Z)-Form
CAS Registry Number: 53772-83-1
Additional Names: a-Clopenthixol; zuclopenthixol
Properties: Crystals, mp 84-85°.
Melting point: mp 84-85°
Derivative Type:cis(Z)-Form dihydrochloride
CAS Registry Number: 58045-23-1
Trademarks: Cisordinol (Lundbeck); Clopixol (HMR)
Properties: Crystals, mp 250-260° (dec). LD50 in male mice (mg/kg): 105 i.v. (Lassen).
Melting point: mp 250-260° (dec)
Toxicity data: LD50 in male mice (mg/kg): 105 i.v. (Lassen)
Therap-Cat: Antipsychotic.
Keywords: Antipsychotic; Thioxanthenes.
Zuclopenthixol is an antipsychotic indicated for the management of schizophrenia. The acuphase formulation is indicated for initial treatment of acute psychosis or exacerbation of psychosis, while the depot formulation is best for maintenance.Zuclopenthixol, also known as Zuclopentixol or Zuclopenthixolum, is an antipsychotic agent. Zuclopenthixol is a thioxanthene-based neuroleptic with therapeutic actions similar to the phenothiazine antipsychotics. It is an antagonist at D1 and D2 dopamine receptors. Major brands of zuclopenthixol are Cisordinol, Acuphase, and Clopixol. This drug is a liquid. This compound belongs to the thioxanthenes. These are organic polycyclic compounds containing a thioxanthene moiety, which is an aromatic tricycle derived from xanthene by replacing the oxygen atom with a sulfur atom. Known drug targets of zuclopenthixol include 5-hydroxytryptamine receptor 2A, D(1B) dopamine receptor, D(2) dopamine receptor, D(1A) dopamine receptor, and alpha-1A adrenergic receptor. It is known that zuclopenthixol is metabolized by Cytochrome P450 2D6. Zuclopenthixol was approved for use in Canada in 2011, but is not approved for use in the United States.
Zuclopenthixol (brand names Cisordinol, Clopixol and others), also known as zuclopentixol, is a medication used to treat schizophrenia and other psychoses. It is classed, pharmacologically, as a typical antipsychotic. Chemically it is a thioxanthene. It is the cis–isomer of clopenthixol (Sordinol, Ciatyl).[1] Clopenthixol was introduced in 1961, while zuclopenthixol was introduced in 1978.
Zuclopenthixol is a D1 and D2 antagonist, α1-adrenergic and 5-HT2 antagonist.[2] While it is approved for use in Australia, Canada, Ireland, India, New Zealand, Singapore, South Africa and the UK it is not approved for use in the United States.[3][4]
Medical uses
Available forms
Zuclopenthixol is available in three major preparations:
- As zuclopenthixol decanoate (Clopixol Depot, Cisordinol Depot), it is a long-acting intramuscular injection. Its main use is as a long-acting injection given every two or three weeks to people with schizophrenia who have a poor compliance with medication and suffer frequent relapses of illness.[5] There is some evidence it may be more helpful in managing aggressive behaviour.[6]
- As zuclopenthixol acetate (Clopixol-Acuphase, Cisordinol-Acutard), it is a shorter-acting intramuscular injection used in the acute sedation of psychotic inpatients. The effect peaks at 48–72 hours providing 2–3 days of sedation.[7]
- As zuclopenthixol dihydrochloride (Clopixol, Cisordinol), it is a tablet used in the treatment of schizophrenia in those who are compliant with oral medication.[8]
It is also used in the treatment of acute bipolar mania.
Dosing
As a long-acting injection, zuclopenthixol decanoate comes in a 200 mg and 500 mg ampoule. Doses can vary from 50 mg weekly to the maximum licensed dose of 600 mg weekly. In general, the lowest effective dose to prevent relapse is preferred. The interval may be shorter as a patient starts on the medication before extending to 3 weekly intervals subsequently. The dose should be reviewed and reduced if side effects occur, though in the short-term an anticholinergic medication benztropine may be helpful for tremor and stiffness, while diazepam may be helpful for akathisia. 100 mg of zuclopenthixol decanoate is roughly equivalent to 20 mg of flupentixol decanoate or 12.5 mg of fluphenazine decanoate.
In acutely psychotic and agitated inpatients, 50 – 200 mg of zuclopenthixol acetate may be given for a calming effect over the subsequent three days, with a maximum dose of 400 mg in total to be given. As it is a long-acting medication, care must be taken not to give an excessive dose.
In oral form zuclopenthixol is available in 10, 25 and 40 mg tablets, with a dose range of 20–60 mg daily.
Side effects
Chronic administration of zuclopenthixol (30 mg/kg/day for two years) in rats resulted in small, but significant, increases in the incidence of thyroid parafollicular carcinomas and, in females, of mammary adenocarcinomas and of pancreatic islet cell adenomas and carcinomas. An increase in the incidence of mammary adenocarcinomas is a common finding for D2 antagonists which increase prolactin secretion when administered to rats. An increase in the incidence of pancreatic islet cell tumours has been observed for some other D2 antagonists. The physiological differences between rats and humans with regard to prolactin make the clinical significance of these findings unclear.
Withdrawal syndrome: Abrupt cessation of therapy may cause acute withdrawal symptoms (eg, nausea, vomiting, or insomnia). Symptoms usually begin in 1 to 4 days of withdrawal and subside within 1 to 2 weeks.[1][2]
Other permanent side effects are similar to many other typical antipsychotics, namely extrapyramidal symptoms as a result of dopamine blockade in subcortical areas of the brain. This may result in symptoms similar to those seen in Parkinson’s disease and include a restlessness and inability to sit still known as akathisia, a slow tremor and stiffness of the limbs.[8] Zuclopenthixol is thought to be more sedating than the related flupentixol, though possibly less likely to induce extrapyramidal symptoms than other typical depots.[5] As with other dopamine antagonists, zuclopenthixol may sometimes elevate prolactin levels; this may occasionally result in amenorrhoea or galactorrhoea in severe cases. Neuroleptic malignant syndrome is a rare but potentially fatal side effect. Any unexpected deterioration in mental state with confusion and muscle stiffness should be seen by a physician.
Zuclopenthixol decanoate induces a transient dose-dependent sedation. However, if the patient is switched to maintenance treatment with zuclopenthixol decanoate from oral zuclopenthixol or from i.m. zuclopenthixol acetate the sedation will be no problem. Tolerance to the unspecific sedative effect develops rapidly.[9]
SYN
Journal of the American Chemical Society (2019), 141(6), 2251-2256
https://pubs.acs.org/doi/10.1021/jacs.8b13907
Synthesis of Clopenthixol (4d)
Inside a nitrogen-filled glovebox, an oven-dried glass culture tube (Fischer Scientific part #14- 959-35A), equipped with a magnetic stirring bar, was charged with 2-chloro-9H-thioxanthen-9- one (245 mg, 1.0 mmol, 1 equiv), copper(II) acetate (0.91 mg, 0.0050 mmol, 0.0050 equiv), racBINAP (3.2 mg, 0.0050 mmol, 0.0050 equiv), and THF (1.0 mL). The tube was then fitted tightly with a Teflon-lined blow-out screw cap (Kimble-Chase part #73808-15425). The reaction tube was removed from the glovebox, and the mixture was stirred rapidly for 5 min. A balloon, connected to a 6 mL plastic syringe head, was filled with allene gas until its size was roughly 6 cm in diameter. A needle was attached to the head of the syringe. The reaction tube was evacuated by piercing the septum with a needle connected to a Schlenk line. Immediately after, the allene contained in the balloon was used to refill the reaction tube by piercing the septum with the needle. The balloon decreased to roughly half its original diameter during the refill process. The needle and balloon were left attached, and dimethoxy(methyl)silane (250 uL, 2.0 mmol, 2.0 equiv) was added to the reaction mixture using a 1 mL plastic syringe. The solution was then stirred overnight at rt. At this point, the flask was quickly evacuated by piercing the septum with a needle connected to a Schlenk line, and the headspace was refilled with dry nitrogen. This process was repeated a total of three times. THF (1 mL) solution containing 4e (367 mg, 1.2 mmol, 1.2 equiv), triphenylphosphine (11.5 mg, 0.044 mmol, 0.044 equiv), racDTBM-SEGPHOS (26.8 mg, 0.044 mmol, 0.044 equiv), and copper(II) acetate (3.6 mg, 0.040 mmol, 0.040 equiv) was added to the reaction mixture using a 1 mL plastic syringe. The reaction tube was heated to 40 °C by submersion in an oil bath overnight. After cooling to rt, the cap was removed and 4 M HCl in dioxane was slowly added to the reaction mixture (2.0 mL, WARNING: VIGOROUS HYDROGEN GAS EVOLUTION). The color of the reaction mixture turned to deep red, and after stirring for approximately 30 min, a tan precipitate evolved. After an additional 1 h, diethyl ether (10 mL) was added and the solids collected by filtration (950 mg). By LC/MS analysis, this solid contains mostly 4c (as the hydrochloride) with a trace amount of triphenylphosphine oxide. The entire solid was suspended in dry acetonitrile (1.0 mL) in another dry reaction tube, equipped with a magnetic stirring bar. Potassium carbonate (552 mg, 4 mmol) was added to the tube, which was then capped and placed under a nitrogen atmosphere using a needle connected to a Schlenk line. 2-bromoethanol (142 uL, 2 mmol) was added to the reaction mixture using a glass microsyringe, and the mixture was left to stir overnight at rt. After this time, the cap was removed, and the solution was diluted with water (10 mL). The mixture was extracted with dichloromethane (3 x 10 mL), and the combined organic phases was concentrated with the aid of a rotary evaporator. The mixture was purified by reverse phase preparative HPLC (C18 column, MeCN/water) to yield a 1.1:1 Z/E mixture of 4d as a yellow foamy solid (217 mg, 54% overall yield). The identity of 4d was confirmed by LC/MS analysis against a commercially available standard (Cayman Chemical) and by comparison of 1H NMR to the literature. 13 For further structural confirmation, a portion of 4d was repurified by HPLC to obtain pure (Z)-4d, the biologically active isomer, whose spectra have not been reported in the literature. 1H NMR (400 MHz, CDCl3) δ 7.43 (dd, J = 14.5, 6.2 Hz, 3H), 7.27 (q, J = 8.2 Hz, 4H), 7.17 (d, J = 8.3 Hz, 1H), 5.89 (t, J = 7.1 Hz, 1H), 3.60 (t, J = 5.4 Hz, 2H), 2.62 (t, J = 7.2 Hz, 2H), 2.58–2.35 (m, 12H); 13C NMR (101 MHz, CDCl3) δ 140.2, 135.7, 133.4, 133.2, 132.7, 130.9, 130.4, 128.6, 127.3, 126.9, 126.8, 126.7, 126.2, 125.6, 59.2, 58.3, 57.7, 53.1, 52.8, 27.3.
SYN
Chemical Engineering & Technology (2016), 39(10), 1821-1827.
https://onlinelibrary.wiley.com/doi/10.1002/ceat.201500673
SYN
European Journal of Pharmaceutics and Biopharmaceutics (2012), 82(2), 437-456.
https://www.sciencedirect.com/science/article/abs/pii/S0939641112002263?
SYN
Organic Process Research & Development (2013), 17(9), 1142-1148.
https://pubs.acs.org/doi/10.1021/op400069e
SUN
CN 103214453
https://patents.google.com/patent/CN103214453A/enDiuril ton (Clopenthixol), chemistry 2-chloro-9-[3 ‘ by name-(N ‘-the 2-hydroxyethyl piperazine-N)-allyl group]-thioxanthene, this product is a kind of Thiaxanthene derivative, has significant antipsycholic action and special sedative effect, is particularly useful for the schizophrenia patient.Its activeconstituents is its alpha-isomer, i.e. zuclopenthixol (structural formula is seen Fig. 1); Have the stereotypy effect that anti-Ritalin causes, and the effect of anti-Apomorphine is arranged, this product energy rejection condition avoiding reaction and catalepsy are stronger 10 times than chlorpromazine.A little less than the cholinolytic effect, and antihistamine effect is strong.Zuclopenthixol is applicable to that treatment has psychosis, class Paranoia-illusion type schizophrenia, hebephrenia, the manic and anxiety periodic psychosis of anxiety and illusion symptom; The uneasiness that mental element causes, excitement, psychiatric disorder, the encephalatrophy process, post-traumatic psychosis, the proverb of trembling are absurd etc.Be particularly useful for elderly patients.Recorded the quality standard of zuclopenthixol sheet, zuclopenthixol dihydrochloride, Ciatyl Depot and zuclopenthixol acetic ester etc. in the British Pharmacopoeia, wherein the zuclopenthixol quality standard has stipulated that its content should be 95%-105%.But in actual industrial production, guarantee that zuclopenthixol reaches pharmaceutically acceptable purity, and β-isomer (structural formula is seen Fig. 2) content being limited in 5%, is a very thing of difficulty.About the preparation method of zuclopenthixol, mainly containing of bibliographical information is following several:As if the general separation of having described diuril ton isomer can be undertaken by the fractional crystallization of dihydrochloride among the BE585338A of nineteen fifty-nine application, and still, this separation method yield is extremely low, and complicated operation does not also have actual industrial use.Described the preparation method of diuril ton isomer mixture among the US3116291, wherein alpha-isomer is that the content of zuclopenthixol is 30%-35%.Obtain purer zuclopenthixol by diuril ton alkali being carried out fractional separation in the literary composition with ether organic solvent, but, instructed crystallization to come the purifying zuclopenthixol can not obtain good result, especially in isomer mixture, had under the situation of a large amount of impurity existence by diuril ton alkali.Embodiment 1: the preparation of diuril ton base1) preparation of 2-chloro-9-allyl group-9-thioxanthene alcohol100.00g (0.405mol) 2-chloro-9-thioxanthone is dissolved in the 600mL tetrahydrofuran (THF), 20 ℃ of-30 ℃ of stirrings, add magnesium powder 26g then, iodine 1g, splash into chlorallylene 65g (0.855mol), 40 ℃-50 ℃ are reacted 2h down, and the cooling back drips 20% sodium chloride aqueous solution 1000ml in reaction solution, stir 10min, filter insolubles, use dichloromethane extraction then 2 times, each 500ml, merge organic phase, water 500ml washing is told organic layer, dry after-filtration, filtrate is concentrated except that desolvating, obtain 105.40g2-chloro-9-allyl group-9-thioxanthene alcohol.2) preparation of 2-chloro-9-(2-propenylidene) thioxanthene100.00g (0.346mol) 2-chloro-9-allyl group-9-thioxanthene alcohol is dissolved in the 100ml toluene, solution is heated to 40 ℃, the Acetyl Chloride 98Min. of 1.34g (0.017mol) is dissolved in the diacetyl oxide of 41.19g (0.403mol) and drops in the above-mentioned solution, temperature is controlled at about 40 ℃, dropwise, it is complete until the TLC monitoring reaction that heating makes temperature of reaction rise to 50 ℃ of-55 ℃ of reactions, and concentrating under reduced pressure steams solvent, obtains 94.01g2-chloro-9-(2-propenylidene) thioxanthene.3) preparation of clopenthixol baseN-(2-hydroxyethyl) piperazine of getting 90.00g (0.332mol) 2-chloro-9-(2-propenylidene) thioxanthene and 215.21g (1.65mol) adds in the 1L four-hole boiling flask, stirs and is warming up to 100 ℃ of reactions, and TLC monitors to reacting completely.Vacuum oil pump concentrating under reduced pressure excessive N-(2-hydroxyethyl) piperazine, temperature is controlled at 100 ℃-135 ℃, and oil pump vacuum tightness is at 0.2-1mmHg.Distillation finishes, and adds the benzene of 400ml and the water of 100ml in gained oily matter, and 70 ℃ are stirred 15min, and separatory is used the water washing organic phase of 100ml again, and simultaneous temperature is controlled at 60 ℃-70 ℃, separatory; With organic phase concentrate resistates.This resistates is dissolved in the 300ml methylene dichloride, after add 10% hydrochloric acid soln and transfer pH to 2-3, stirring 10min, separatory, water discard dichloromethane extraction liquid with the dichloromethane extraction of 150ml; Above-mentioned water adds ammoniacal liquor and regulates pH=9-10, extract with methylene dichloride (300ml * 2) after stirring 10min, merge organic phase, use anhydrous sodium sulfate drying, suction filtration, filtrate decompression concentrate 109.32g diuril ton base, isomer proportion α/β is that 45/55 (the HPLC area normalization method: analytical column is 4.6 * 250mmAgilent C18 post, moving phase is acetonitrile: methyl alcohol: phosphoric acid buffer=20: 30: 50, flow velocity are 1mL/min; With this understanding, the retention time of zuclopenthixol is 12min, and the retention time of β-isomer is 16min).Embodiment 2: the preparation of zuclopenthixol Chlorodracylic acid ester 2HCl100.00g (0.250mol) α/β-diuril ton is dissolved in the ethyl acetate of 500ml, under 40 ℃ of conditions, drips the 100ml ethyl acetate that is dissolved with 52.48g (0.30mol) parachlorobenzoyl chloride, dropwise the back back flow reaction, complete until the TLC monitoring reaction.Remove the 300ml solvent under reduced pressure, be cooled to 4 ℃, remove by filter precipitation.Mother liquor is heated to 40 ℃, drips the concentrated hydrochloric acid aqueous solution of 12.50g (0.125mol) 37%, react about 1h after, cool off, have solid to separate out, filter 56.27g zuclopenthixol Chlorodracylic acid ester 2HCl.Purity (HPLC is the same) is 97.11%, and productive rate is 36.82%.Embodiment 3: the preparation of zuclopenthixol2HCl is dissolved in the methanol aqueous solution of 300ml80% with 45.25g (0.074mol) zuclopenthixol Chlorodracylic acid ester, adds the potassium hydroxide of 16.83mol (0.30mol) then.With mixture heating up to 50 ℃, insulation reaction 1h.Underpressure distillation removes and desolvates, and with toluene (200ml * 2) and water extraction, merges organic phase, and concentrating under reduced pressure is removed toluene; Residue obtainedly carry out recrystallization with hexanaphthene, the 25.51g dried crystals.Purity is 99.7%, and productive rate is 86.17%. 1H?NMR(CDCl 3,400MHz),δ:7.10-7.46(7H,m),5.98(1H,t),3.41(2H,t),2.46-2.52(14H,m)。Embodiment 4: the preparation of Ciatyl Depot 2HClThe zuclopenthixol of 50.00g (0.125mol) is dissolved in the methylene dichloride of 500ml, and to wherein dripping 28.60g (0.150mol) decanoyl chloride, back flow reaction is complete to the TLC monitoring reaction after dropwising under the room temperature.Underpressure distillation removes and desolvates, and adds the ethyl acetate of 300ml in residue, drips the ethyl acetate solution that contains hydrogenchloride again, is transferred to 3-4 until pH.After the cooling, filter, vacuum-drying gets 70.63g Ciatyl Depot 2HCl.Productive rate is 90.12%.Embodiment 5: the preparation of Ciatyl DepotThe Ciatyl Depot 2HCl of 60g (0.0957mol) is suspended in the t-butyl methyl ether of 400ml, drips water (250ml) solution of 13.22g (0.0957mol) salt of wormwood, stirring reaction 0.5h.Two are separated, and use 100ml water washing organic phase again, use the anhydrous sodium sulfate drying organic phase, filter, and organic solvent is removed in underpressure distillation, get the 51.29g Ciatyl Depot.Productive rate is 96.58%. 1H?NMR(CDCl 3,400MHz),δ:7.12-7.50(7H,m),5.90(1H,t),4.35(2H,t),3.41(2H,t),2.97(2H,t),2.32-2.57(10H,m),2.06(2H,t),1.64(2H,m),1.30(12H,m),0.88(3H,t)。
SYN
https://patents.google.com/patent/WO2017121755A1/enPreparation of ZU3:9-(3-(4-(2-hydroxyethyl)piperazinyl)propylidene)-thioxanthene

ZU3To a solution of 9-oxothioxanthene (1.0 equiv.) in THF at reflux were added a solution of cyclopropylmagnesium bromide in THF (1.0 equiv.) and stirred during 2 hours. The mixture was cooled down at room temperature and a solution of hydrogen bromide in acetic acid (4 eq.) was added and stirred at room temperature. The reaction mixture was concentrated in vacuo and purified by silica gel column chromatography to obtain 9- (3bromopropylidene)thioxanthene in 30% yield.Then, to a solution of 9-(3bromopropylidene)thioxanthene in acetonitrile at reflux was added N-(2-hydroxyethyl)piperazine (1,5 eq.), potassium iodide (0.1 eq.) and potassium carbonate (3 eq.). The mixture was stirred at reflux then concentrated in vacuo and purified by silica gel column chromatography to afford ZU3 with 98% purity (HPLC). HPLC analysis (BEH C18 type, mobile phase: H20/ acetonitrile (HCOOH 0.1%)) : tR = 1.68 min. Preparation of ZUf:l-(3-(9H-thioxanthen-9-ylidene)propyl)piperidine-4-carboxylic acid), ZU4 (9-(3-(4- (ethylacetate) iperidine)propylidene)-thioxanthene

To a solution of 9-(3-bromopropylidene)thioxanthene in acetonitrile at reflux was added N-ethylacetate piperidine (1,5 eq.), potassium iodide (0.1 eq.) and potassium carbonate (3 eq.). The mixture was stirred at reflux then concentrated in vacuo and purified by silica gel column chromatography to afford ZU4 as a brown oil with a purity of 97% in HPLC analysis HPLC analysis (BEH C18 type, mobile phase: H20/acetonitrile (HCOOH 0.1%)) : tR = 2.07 min.The compound ZU4 was stirred during 2 hours at reflux in a mixture of THF and a solution of NaOH in water. After phase separation, the aqueous layer was extracted twice by diethyl ether. The global organic layer was, then, washed by a saturated solution of NaCl, dried over MgSC^, filtered and concentrated in vacuo to afford ZUf HPLC analysis (BEH CI 8 type, mobile phase: H20/acetonitrile (HCOOH 0.1%)) : tR = 2.24 min.Preparation of ZU5:(Z)-2-(4-(3-(2-chloro-9H-thioxanthen-9-ylidene)propyl)piperazin-l-yl)ethylacetate

To a solution of ZU (4-[3-(2-chloro-9H-thioxanthen-9-ylidene)propyl]-l- piperazineethanol) (leq.) in dichloromethane was added acetic anhydride (1.5 eq.), 4- dimethylaminopyridine (0,1 eq.) and trimethylamine (1 eq.). The mixture was stirred at room temperature and then concentrated in vacuo to afford ZU5 as a yellow oil with 97% of purity (HPLC). HPLC analysis {BEH C18 type, mobile phase: H20/acetonitrile (HCOOH 0.1%)): tR = 2.44 minPreparation of ZUe and ZU6:l-(3-(9H-xanthen-9-ylidene)propyl)piperidine-4-carboxylic acidand eth -(3-(9H-xanthen-9-ylidene)propyl)piperidine-4-carboxylate

To a solution of 9-oxoxanthene (1.0 equiv.) in THF at reflux were added a solution of cyclopropylmagnesium bromide in THF (1.0 equiv.) and stirred during 2 hours. The mixture was cooled down at room temperature and a solution of hydrogen bromide in acetic acid (4 eq.) was added and stirred at room temperature. The reaction mixture was concentrated in vacuo and purified by silica gel column chromatography to obtain 9- (3bromopropylidene)-oxoxanthene.Then, to a solution of 9-(3bromopropylidene)-oxoxanthene in acetonitrile at reflux was added Ethyl 4-piperidinecarboxylate (1,5 eq.), potassium iodide (0.1 eq.) and potassium carbonate (3 eq.). The mixture was stirred at reflux then concentrated in vacuo and purified by silica gel column chromatography to obtain ZU6 ZU6 is then dissolved in a mixture of THF and a solution of NaOH in water. After phase separation, the aqueous layer was extracted twice by diethyl ether. The global organic layer was, then, washed by a saturated solution of NaCl, dried over MgSC^, filtered and concentrated in vacuo to afford ZUe as a white solid with a purity up to 97% in HPLC. Preparation of ZUc:(Z)-2-(4-(3-(2-(trifluoromethyl)-9H-thioxanthen-9-ylidene)propyl)piperazin-l-yl) ethanamine

EtOH, reflux, 2hPurification withHCI buffer

To a solution of ZU1 (2-[4-[3-[2-(trifiuoromethyl)thioxanthen-9- ylidene]propyl]piperidin-l-yl] ethanol) (leq.) in THF was added diethylazodicarboxylate, phtalimide and triphenylphosphine. The solution was stirred at room temperature during 3 hours and then concentrated in vacuo. The crude oil was then dissolved in ethanol, hydrazine was added and the mixture was stirred at reflux during 2 hours. The crude product obtained after concentration was purified via a reversed phase chromatography using HCI as buffer to afford the compound ZUc as an hydrochloride salt (orange solid). [M+H]+ (ESI+) : 434. HPLC analysis (BEH C18 type, mobile phase: H20/acetonitrile (HCOOH 0.1%)): tR = 2.04 min Preparation of ZUd:(Z)-l-(2-fluoroethyl)-4-(3-(2-(trifluoromethyl)-9H-thioxanthen-9-ylidene)propyl) iperazine

To a solution of flupenthixol in dichloromethane was added at -10°C diethylamino sulfur trifluoride. The mixture was then stirred at room temperature. The crude product was purified via a reversed phase chromatography using HC1 as buffer to afford the compound ZUd as a hydrochloride salt (orange solid) with 97% purity in HPLC. HPLC analysis (BEH C18 type, mobile phase: H20/acetonitrile (HCOOH 0.1%)): tR = 3.59 min.Compounds ZU, ZUa, ZUb, ZU1, ZU2The following compounds can be easily found in commerce:

Example 2: Ebselen oxide derivatives

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Pharmacology
Pharmacodynamics

Cisordinol 10 mg tablet
Zuclopenthixol antagonises both dopamine D1 and D2 receptors, α1-adrenoceptors and 5-HT2 receptors with a high affinity, but has no affinity for cholinergic muscarine receptors. It weakly antagonises the histamine (H1) receptor but has no α2-adrenoceptor blocking activity[citation needed].
Evidence from in vitro work and clinical sources (i.e. therapeutic drug monitoring databases) suggests that both CYP2D6 and CYP3A4 play important roles in zuclopenthixol metabolism.[11]
Pharmacokinetics
History
Zuclopenthixol was introduced by Lundbeck in 1978.[22]
References
- ^ Sneader, Walter (2005). Drug discovery: a history. New York: Wiley. p. 410. ISBN 0-471-89980-1.
- ^ Pharmacological effects of a specific dopamine D-1 antagonist SCH 23390 in comparison with neuroleptics Life sciences 1984 Apr 16;34(16):1529-40.
- ^ Green, Alan I.; Noordsy, Douglas L.; Brunette, Mary F.; O’Keefe, Christopher (2008). “Substance abuse and schizophrenia: Pharmacotherapeutic intervention”. Journal of Substance Abuse Treatment. 34 (1): 61–71. doi:10.1016/j.jsat.2007.01.008. ISSN 0740-5472. PMC 2930488. PMID 17574793.
- ^ Sweetman, Sean C., ed. (2009). “Anxiolytic Sedatives Hypnotics and Antipsychotics”. Martindale: The complete drug reference (36th ed.). London: Pharmaceutical Press. pp. 1040–1. ISBN 978-0-85369-840-1.
- ^ Jump up to:a b da Silva Freire Coutinho E, Fenton M, Quraishi SN (1999). “Zuclopenthixol decanoate for schizophrenia”. The Cochrane Database of Systematic Reviews. John Wiley and Sons, Ltd. (2): CD001164. doi:10.1002/14651858.CD001164. PMC 7032616. PMID 10796607. Retrieved 2007-06-12.
- ^ Haessler F, Glaser T, Beneke M, Pap AF, Bodenschatz R, Reis O (2007). “Zuclopenthixol in adults with intellectual disabilities and aggressive behaviours”. British Journal of Psychiatry. 190 (5): 447–448. doi:10.1192/bjp.bp.105.016535. PMID 17470962.
- ^ Lundbeck P/L (1991). “Clopixol Acuphase 50 mg/mL Injection Clopixol Acuphase 100 mg / 2 mL Injection”. Lundbeck P/L. Retrieved 2007-06-12.
- ^ Jump up to:a b Bryan, Edward J.; Purcell, Marie Ann; Kumar, Ajit (16 November 2017). “Zuclopenthixol dihydrochloride for schizophrenia”. The Cochrane Database of Systematic Reviews. 2017 (11): CD005474. doi:10.1002/14651858.CD005474.pub2. ISSN 1469-493X. PMC 6486001. PMID 29144549.
- ^ “Summary of Product Characteristics” (PDF).
- ^ Jump up to:a b c d e “TGA eBS – Product and Consumer Medicine Information Licence”.
- ^ Davies SJ, Westin AA, Castberg I, Lewis G, Lennard MS, Taylor S, Spigset O (2010). “Characterisation of zuclopenthixol metabolism by in vitro and therapeutic drug monitoring studies”. Acta Psychiatrica Scandinavica. 122 (6): 445–453. doi:10.1111/j.1600-0447.2010.01619.x. PMID 20946203. S2CID 41869401.
- ^ Parent M, Toussaint C, Gilson H (1983). “Long-term treatment of chronic psychotics with bromperidol decanoate: clinical and pharmacokinetic evaluation”. Current Therapeutic Research. 34 (1): 1–6.
- ^ Jump up to:a b Jørgensen A, Overø KF (1980). “Clopenthixol and flupenthixol depot preparations in outpatient schizophrenics. III. Serum levels”. Acta Psychiatrica Scandinavica. Supplementum. 279: 41–54. doi:10.1111/j.1600-0447.1980.tb07082.x. PMID 6931472.
- ^ Jump up to:a b Reynolds JE (1993). “Anxiolytic sedatives, hypnotics and neuroleptics.”. Martindale: The Extra Pharmacopoeia (30th ed.). London: Pharmaceutical Press. pp. 364–623.
- ^ Ereshefsky L, Saklad SR, Jann MW, Davis CM, Richards A, Seidel DR (May 1984). “Future of depot neuroleptic therapy: pharmacokinetic and pharmacodynamic approaches”. The Journal of Clinical Psychiatry. 45 (5 Pt 2): 50–9. PMID 6143748.
- ^ Jump up to:a b Curry SH, Whelpton R, de Schepper PJ, Vranckx S, Schiff AA (April 1979). “Kinetics of fluphenazine after fluphenazine dihydrochloride, enanthate and decanoate administration to man”. British Journal of Clinical Pharmacology. 7 (4): 325–31. doi:10.1111/j.1365-2125.1979.tb00941.x. PMC 1429660. PMID 444352.
- ^ Young D, Ereshefsky L, Saklad SR, Jann MW, Garcia N (1984). Explaining the pharmacokinetics of fluphenazine through computer simulations. (Abstract.). 19th Annual Midyear Clinical Meeting of the American Society of Hospital Pharmacists. Dallas, Texas.
- ^ Janssen PA, Niemegeers CJ, Schellekens KH, Lenaerts FM, Verbruggen FJ, van Nueten JM, et al. (November 1970). “The pharmacology of fluspirilene (R 6218), a potent, long-acting and injectable neuroleptic drug”. Arzneimittel-Forschung. 20 (11): 1689–98. PMID 4992598.
- ^ Beresford R, Ward A (January 1987). “Haloperidol decanoate. A preliminary review of its pharmacodynamic and pharmacokinetic properties and therapeutic use in psychosis”. Drugs. 33 (1): 31–49. doi:10.2165/00003495-198733010-00002. PMID 3545764.
- ^ Reyntigens AJ, Heykants JJ, Woestenborghs RJ, Gelders YG, Aerts TJ (1982). “Pharmacokinetics of haloperidol decanoate. A 2-year follow-up”. International Pharmacopsychiatry. 17 (4): 238–46. doi:10.1159/000468580. PMID 7185768.
- ^ Larsson M, Axelsson R, Forsman A (1984). “On the pharmacokinetics of perphenazine: a clinical study of perphenazine enanthate and decanoate”. Current Therapeutic Research. 36 (6): 1071–88.
- ^ William Andrew Publishing (22 October 2013). Pharmaceutical Manufacturing Encyclopedia. Elsevier. pp. 1102–. ISBN 978-0-8155-1856-3.
External links
- Product information for Zuclopenthixol (CLOPIXOL), provided by the Therapeutic Goods Administration — https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2010-PI-05705-3
| Clinical data | |
|---|---|
| Trade names | Clopixol |
| AHFS/Drugs.com | International Drug Names |
| Pregnancy category | AU: C |
| Routes of administration | Oral, IM |
| Drug class | Typical antipsychotic |
| ATC code | N05AF05 (WHO) |
| Legal status | |
| Legal status | AU: S4 (Prescription only)UK: POM (Prescription only)In general: ℞ (Prescription only) |
| Pharmacokinetic data | |
| Bioavailability | 49% (oral) |
| Protein binding | 98% |
| Metabolism | Hepatic (CYP2D6 and CYP3A4-mediated) |
| Elimination half-life | 20 hours (oral), 19 days (IM) |
| Excretion | Feces |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 53772-83-1 85721-05-7 (acetate) 64053-00-5 (decanoate) |
| PubChem CID | 5311507 |
| DrugBank | DB01624 |
| ChemSpider | 4470984 |
| UNII | 47ISU063SG |
| KEGG | D03556 |
| ChEBI | CHEBI:51364 |
| ChEMBL | ChEMBL53904 |
| CompTox Dashboard (EPA) | DTXSID3048233 |
| ECHA InfoCard | 100.053.398 |
| Chemical and physical data | |
| Formula | C22H25ClN2OS |
| Molar mass | 400.97 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (what is this?) (verify) |
/////////zuclopenthixol, N05AF05, Clopenthixol, Cisordinol, Clopixol
OCCN1CCN(CC\C=C2\C3=C(SC4=C2C=C(Cl)C=C4)C=CC=C3)CC1

NEW DRUG APPROVALS
ONE TIME
$10.00
Aztreonam

Aztreonam
- Molecular FormulaC13H17N5O8S2
- Average mass435.433 Da
(2S,3S)-3-{[(2Z)-2-(2-Ammonio-1,3-thiazol-4-yl)-2-{[(2-carboxy-2-propanyl)oxy]imino}acetyl]amino}-2-methyl-4-oxo-1-azetidinesulfonate2-[[(Z)-[1-(2-amino-4-thiazolyl)-2-[[(2S,3S)-2-methyl-4-oxo-1-sulfo-3-azetidinyl]amino]-2-oxoethylidene]amino]oxy]-2-methyl-propanoic acid
278-839-9[EINECS]
5159
78110-38-0[RN]
UA2451400
азтреонам [Russian] [INN]
أزتريونام [Arabic] [INN]
氨曲南 [Chinese] [INN]
AztreonamCAS Registry Number: 78110-38-0
CAS Name: [2S-[2a,3b(Z)]]-2-[[[1-(2-Amino-4-thiazolyl)-2-[(2-methyl-4-oxo-1-sulfo-3-azetidinyl)amino]-2-oxoethylidene]amino]oxy]-2-methylpropanoic acid
Additional Names: azthreonam
Manufacturers’ Codes: SQ-26776
Trademarks: Azactam (BMS); Primbactam (Menarini)
Molecular Formula: C13H17N5O8S2, Molecular Weight: 435.43
Percent Composition: C 35.86%, H 3.94%, N 16.08%, O 29.40%, S 14.73%
Literature References: The first totally synthetic monocyclic b-lactam (monobactam) antibiotic. It has a high degree of resistance to b-lactamases and shows specific activity vs aerobic gram-negative rods.
Prepn: R. B. Sykes et al.,NL8100571 (1981 to Squibb), C.A.96, 181062x (1982).
Fast-atom-bombardment mass spectra: A. I. Cohen et al.,J. Pharm. Sci.71, 1065 (1982). Activity vs gram-negative bacteria: R. B. Sykes et al.,Antimicrob. Agents Chemother.21, 85 (1982). Series of articles on structure-activity, in vitro and in vivo properties, pharmacokinetics: J. Antimicrob. Chemother.8, Suppl. E, 1-148 (1981).
Toxicology: G. R. Keim et al.,ibid. 141. Mechanism of action study: A. D. Russell, J. R. Furr, ibid.9, 329 (1982). Comparative stability to renal dipeptidase: H. Mikami et al.,Antimicrob. Agents Chemother.22, 693 (1982). Human pharmacokinetics: E. A. Swabb et al.,ibid.21, 944 (1982).
Clinical evaluation in urinary tract infection: C. Donadio et al.,Drugs Exp. Clin. Res.13, 167 (1987). Clinical efficacy in neonatal sepsis: S. Sklavunu-Tsurutsoglu et al.,Rev. Infect. Dis.13, Suppl. 7, S591 (1991). Comprehensive description: K. Florey, Anal. Profiles Drug Subs.17, 1-39 (1988).
Properties: White crystalline, odorless powder, dec 227°. Very slightly sol in ethanol, slightly sol in methanol, sol in DMF, DMSO. Practically insol in toluene, chloroform, ethyl acetate.
Derivative Type: Disodium salt
Molecular Formula: C13H15N5Na2O8S2, Molecular Weight: 479.40
Percent Composition: C 32.57%, H 3.15%, N 14.61%, Na 9.59%, O 26.70%, S 13.38%
Properties: LD50 (mg/kg): 3300 i.v. in mice; 6600 i.p. in rats (Keim).
Toxicity data: LD50 (mg/kg): 3300 i.v. in mice; 6600 i.p. in rats (Keim)
Therap-Cat: Antibacterial.
Keywords: Antibacterial (Antibiotics); ?Lactams; Monobactams.
Aztreonam is a beta-lactam antibiotic used to treat select aztreonam sensitive gram negative bacteria.
Product Ingredients
| INGREDIENT | UNII | CAS | INCHI KEY |
|---|---|---|---|
| Aztreonam lysine | XNM7LT65NP | 827611-49-4 | KPPBAEVZLDHCOK-JHBYREIPSA-N |
A monocyclic beta-lactam antibiotic originally isolated from Chromobacterium violaceum. It is resistant to beta-lactamases and is used in gram-negative infections, especially of the meninges, bladder, and kidneys. It may cause a superinfection with gram-positive organisms.
Aztreonam, sold under the brand name Azactam among others, is an antibiotic used primarily to treat infections caused by gram-negative bacteria such as Pseudomonas aeruginosa.[1][2] This may include bone infections, endometritis, intra abdominal infections, pneumonia, urinary tract infections, and sepsis.[1] It is given by intravenous or intramuscular injection or by inhalation.[1]
Common side effects when given by injection include pain at the site of injection, vomiting, and rash.[1] Common side effects when inhaled include wheezing, cough, and vomiting.[1] Serious side effects include Clostridium difficile infection and allergic reactions including anaphylaxis.[1] Those who are allergic to other β-lactam have a low rate of allergy to aztreonam.[1] Use in pregnancy appears to be safe.[1] It is in the monobactam family of medications.[1] Aztreonam inhibits cell wall synthesis by blocking peptidoglycan crosslinking to cause bacterial death.[1]
Aztreonam was approved for medical use in the United States in 1986.[1] It was removed from the World Health Organization’s List of Essential Medicines in 2019.[3][4] It is available as a generic medication.[1] It is a manufactured version of a chemical from the bacterium Chromobacterium violaceum.[5]
Medical uses
Nebulized forms of aztreonam are used to treat infections that are complications of cystic fibrosis and are approved for such use in Europe and the US; they are also used off-label for non-CF bronchiectasis, ventilator-associated pneumonia, chronic obstructive pulmonary disease, mycobacterial disease, and to treat infections in people who have received lung transplants.[6]
Aztreonam has strong activity against susceptible Gram-negative bacteria, including Pseudomonas aeruginosa. It is resistant to some beta-lactamases, but is inactivated by extended-spectrum beta-lactamases.
It has no useful activity against Gram-positive bacteria or anaerobes. It is known to be effective against a wide range of bacteria including Citrobacter, Enterobacter, E. coli, Haemophilus, Klebsiella, Proteus, and Serratia species.[7] The following represents minimum inhibitory concentration (MIC) susceptibility data for a few medically significant microorganisms.
- Staphylococcus aureus 8 – >128 μg/ml
- Staphylococcus epidermidis 8 – 32 μg/ml
- Streptococcus pyogenes 8 – ≥128 μg/ml
Synergism between aztreonam and arbekacin or tobramycin against P. aeruginosa has been suggested.[9]
SYN
ACS Medicinal Chemistry Letters, 11(2), 162-165; 2020
https://pubs.acs.org/doi/10.1021/acsmedchemlett.9b00534

Aztreonam, first discovered in 1980, is an FDA approved, intravenous, monocyclic beta-lactam antibiotic. Aztreonam is active against Gram-negative bacteria and is still used today. The oral bioavailability of aztreonam in humans is less than 1%. Herein we describe the design and synthesis of potential oral prodrugs of aztreonam.
A stirring mixture of CES1 (20 mg, 2200 Units) in a 15 mM solution of sodium phosphate monobasic (enzyme grade) in acetonitrile-d3 / D2O (1 mL; ratio of 2.5 : 97.5) was heated at 37 °C for 5 min. 2-(((Z)-(1-(2-aminothiazol-4-yl)-2-(((2S,3S)-1-((2,2- dimethyl-4-(pivaloyloxy)butoxy)sulfonyl)-2-methyl-4-oxoazetidin-3-yl)amino)-2- oxoethylidene)amino)oxy)-2-methylpropanoic acid TFA salt 28c (10 mg, 14 µmol) was added, and the suspension was stirred for 70 min at 37 °C. Over the course of the reaction a fine precipitate formed. The mixture was filtered through a 25 mm, 0.45 µM glass fiber syringe filter (Pall Corporation Acrodisc). The filtrate was analyzed by 1H-NMR spectroscopy to reveal that 3,3-dimethyltetrahydrofuran was released as one of the products. The presence of 3,3-dimethyltetrahydrofuran was confirmed by 1H-NMR analysis of the same sample spiked with 2 µL of authentic materialSYN Faming Zhuanli Shenqing, 106520857,
SYN
Synthesis Reference
Neal G. Anderson, Carl F. Anderson, “Delta form of aztreonam and preparation thereof.” U.S. Patent US4826973, issued January, 1983.
SYN
https://patents.google.com/patent/US7145017B2/enAztreonam is a monobactam antibiotic disclosed in U.S. Pat. No. 4,775,670, which is incorporated by reference herein in its entirety. Aztreonam has the chemical name (Z)-2-[[[(2-amino-4-thiazolyl)[[(2S,-3S)-2-methyl-4-oxo-1-sulfo-3-azetidinyl]carbamoyl]methylene]amino]oxy]-2-methylpropionic acid. Aztreonam is also known as [3S-[3α(Z),4β]]-3-[[(2-amino-4-thiazolyl)[(1-carboxy-1-methylethoxy)imino]acetyl]amino]-4-methyl-2-oxo-1-azetidinesulfonic acid and (2S, 3S)-3-[[2-[2-amino-4-thiazolyl]-(Z)-2[(1-carboxy-1-methylethoxy)imino]acetyl]amino]-4-methyl-2-oxo-1-azetidine-1-sulfonic acid.Aztreonam has the structure:

Aztreonam is known to exist in various polymorphic forms including the α, β, δ, and γ forms.U.S. Pat. No. 4,775,670 discloses a process for making Aztreonam, a compound of formula I:

The process includes acylating a compound of formula IV:

The acylation entails reacting a compound of formula IV with a carboxylic acid or the corresponding carboxylic acid halide or carboxylic acid anhydride (R1—OH) in the presence of a carbodiimide such as dicyclohexylcarbodiimide and a substance capable of forming an active ester in situ such as N-hydroxybenzotriazole. U.S. Pat. No. 4,775,670 discloses that when the acyl group (R1) contains reactive functional groups, such as amino or carboxyl groups, it may be necessary to first protect those functional groups, then carry out the acylation reaction, and finally deprotect the resulting product. The deprotection is carried out by reaction of the acylation product with trifluoroacetic acid in the presence of anisole under anhydrous conditions.Similarly, U.S. Pat. No. 4,946,838 discloses a process for making crystalline anhydrous Aztreonam comprising reacting the diphenylmethyl ester of Aztreonam ([3S-[3β(Z),4α]]-3-[[(2-amino-4-thiazolyl)[(1-diphenylmethoxycarbonyl-1-methylethoxy)imino]acetyl]amino]-4-methyl-2-oxo-1-azetidinesulfonic acid) with trifluoroacetic acid in the presence of anisole under anhydrous conditions to produce the α-form of Aztreonam. The α-form is recrystallized from an anhydrous organic solvent to produce the β-form of Aztreonam. The β-form is anhydrous, substantially non-hygroscopic and more stable than the α-form.U.S. Pat. No. 5,254,681 discloses a process for preparing monobactams of formula (I):

wherein R is acyl. The process comprises acylating azetidin with 2-(2-amino-4-thiazolyl)-2-(Z)-(alkoxyimino) acetic acid in the presence of 1-hydroxy-benzotriazole and dicyclohexylcarbodiimide.U.S. Pat. No. 5,194,604 discloses a process and intermediates for making beta-lactams having aminothiazole(iminooxyacetic acid)acetic acid sidechains of formula (I), such as Aztreonam. The process comprises acylating a compound of formula III:

with a compound of formula (II):

in which R7 is

wherein

is a 4, 5, 6 or 7 membered heterocyclic ring having at least one nitrogen atom in the ring or such a group fused to a phenyl or substituted phenyl ring, to form a compound of formula (I):

wherein R1–R6 are as defined in U.S. Pat. No. 5,194,604.U.S. Pat. No. 4,652,651, which is incorporated by reference herein in its entirety, discloses a process for making 1-sulpho-2-oxoazetidine derivatives of the formula (I):

in which Het is an optionally amino-substituted, 5- or 6-membered, aromatic heterocycle containing 1 or 2 nitrogen atoms and optionally also an oxygen or sulphur atom, R1 may be lower alkoxycarbonyl-lower alkyl and R2 may be lower alkyl. The process entails acylating a compound of formula (II):

in which R20 equals R2 and R3 is hydrogen or sulpho, with a thioester of the formula (III):

in which Het is as above and R10 has any of the values of R1. U.S. Pat. No. 4,652,651 discloses that where R10 is a lower alkoxycarbonyl-lower alkyl group, for example the t-butoxycarbonylmethyl group, this can be converted, if desired, into the corresponding carboxylower alkyl group by treatment with a strong acid such as trifluoroacetic acid (optionally in the presence of anisole), hydrochloric acid or p-toluenesulphonic acid at a low temperature such as −10° C. to room temperature.There remains a need in the art for a process of making Aztreonam which does not require anhydrous reaction conditions and which also enables high yield and high purity. The present invention answers this need.
SUMMARY OF THE INVENTIONThe invention is based on the discovery that Aztreonam can be produced by reacting [3S-[3α(Z),4β]]-3-[[(2-amino-4-thiazolyl)[(1-t-butoxycarbonyl-1-methylethoxy)imino]acetyl]amino]-4-methyl-2-oxo-1-azetidinesulfonic acid with aqueous acid. The process of the invention, enables yields of between 70–75% and purities above 98%, preferably above 99%. The inventive aqueous process is advantageous over the prior art anhydrous processes in that the reaction conditions are more mild, there is no need to clean the final product and there is no need to keep the system dry. Thus, the aqueous process is less expensive than the anhydrous processes.The present invention is directed to a process for preparing [3S-[3α(Z),4β]]-3-[[(2-amino-4-thiazolyl)[(1-carboxy-1-methylethoxy)imino]acetyl]amino]-4-methyl-2-oxo-1-azetidinesulfonic acid by hydrolyzing the ester group of [3S-[3α(Z),4β]]-3-[[(2-amino-4-thiazolyl)[(1-t-butoxycarbonyl-1-methylethoxy)imino]acetyl]amino]-4-methyl-2-oxo-1-azetidinesulfonic acid. The hydrolysis may be effected by reacting the ester with aqueous acid, at elevated temperatures.One reaction scheme for carrying out the process is shown below:

EXAMPLE 15.4 g Azetidin is dissolved in 20 ml acetonitrile (or dimethyl formamide) with the assistance of 5 ml of triethylamine at room temperature. The solution is cooled to 0° C. A solution of 4 g TAEM in 25 ml THF is added with magnetic stirring. If the color disappears, 8 g TAEM in 50 ml THF is added. After 10 minutes, another 4.1 g TAEM in 25 ml THF is added. The solution is stirred at 0° C. for an additional hour. The pH is adjusted to about 4–5 with a freshly prepared TFA solution (TFA-THF 1:4, V/V). Being careful not to evaporate the acetonitrile, the THF is evaporated (weight loss is about 90 g) at 30° C. under vacuum. The remaining residue is diluted with 200 ml ethylacetate and then extracted with 100 ml and then 50 ml of distilled water. The aqueous extracts are combined and washed twice with 50 ml ethylacetate after readjustment of the pH to about 4–5. The dissolved ethylacetate is removed from the aqueous phase by vacuum at 30° C. 10–15 g KCl (or NaCl) is dissolved. The solution is acidified with HCl solution (cc. HCl-distilled water 1:4, V/V) with stirring (approx. 10 ml). The solution is cooled to 0° C. with slow stirring and crystallization occurs. The resulting suspension is refrigerated overnight (at about 5° C.). The suspension is filtered on a glass filter, and the crystals are washed with chilled water. The washed crystals are dried at room temperature. The product, Aztreonam t-butyl ester, is about 12.5–13 g white solid, which is sufficiently pure for the next step.
EXAMPLE 265 g Azetidine is dissolved in a mixture of 240 ml acetonitrile and 60 ml triethylamine. When dissolution is complete, TAEM is added in four portions. The suspension is stirred for 20–30 min, then diluted with 500 ml EtOAc and 500 ml water and stirred for 5–10 min. The pH of the emulsion is set to 5 with 2.4 M HCl solution. After the phases separate, the pH of the aqueous phase is checked. If the pH is between 4.20 and 5.30, the two phases are filtered and separated, otherwise more HCl is added. The upper phase is diluted with 900 ml ethylacetate and extracted with 2×500 ml water (faster phase separation). The combined aqueous phase is diluted with 500 ml water and washed with 2×500 ml ethylacetate. The dissolved ethylacetate is removed from the aqueous phase by vacuum. The aqueous phase is acidified further to pH 2 with 2.4 M HCl solution. The solution is stirred and cooled. Crystallization starts soon. The suspension is stirred and cooled to 0° C., stirring at this temperature overnight. The suspension is filtered, washed with chilled water, dried at 38° C. in air-circulated oven for 3 h. The yield is approx. 116–120 g of Aztreonam t-butyl ester.
EXAMPLE 3Aztreonam t-butyl ester (113.6 g, 0.231 mol) is suspended in 975 ml water at 60° C. with stirring and 325 ml trifluoroacetic acid is added. The solution is stirred for 60 min., then it is cooled slowly using an ice-water bath. After the product precipitates, the suspension is refrigerated overnight. The product is filtered on a glass-filter, suspended in 240 ml chilled water and filtered again. The filtrate is re-suspended in 360 ml cold acetone and filtered. The latter step is repeated and the product is dried at room temperature to yield 61.6 g Aztreonam (water content: 15–16%).
EXAMPLE 4Aztreonam t-butyl ester (18.0 g, 0.0366 mol) is suspended in 144 ml water at 60° C. with stirring and 40 ml aqueous hydrochloric acid (1:1, V/V) is added. The solution is stirred for 60 min, then 37 ml 5.4 M NaOH solution is added. The solution is cooled slowly using an ice-water bath. After the product precipitates, the suspension is refrigerated overnight. The product is filtered on a glass-filter, suspended in 50 ml chilled water and filtered again. The filtrate is re-suspended in 70 ml cold acetone and filtered. The latter step is repeated and the product is dried at room temperature to yield 8.3 g Aztreonam (water content: 15–16%). The crude Aztreonam is crystallized.
EXAMPLE 5Aztreonam t-butyl ester (100.00 g, Assay as is: 97.2%, 0.19796 mol)) is suspended in a mixture of 450 ml water and 5 ml trifluoroacetic acid. The suspension, which slowly becomes clear, is heated to 58° C. with stirring and 100 ml trifluoroacetic acid is added. The solution is stirred for 105 min at 60–63° C. The solution is added to chilled water (450 ml) with efficient stirring and the resulting slurry is cooled further to 25° C. After two hours it is cooled to 0° C. and stirred for 18 hours. The product is filtered on a glass-filter and washed with 300 ml chilled water. The product is suspended in 650 ml chilled water, then filtered and washed with 300 ml cold acetone. The product is suspended in 400 ml cold acetone and filtered and dried in an air-ventilation oven at 30° C. for 30 min. Yield: 66.6 g (63%, according to assays) Aztreonam (Assay: 100.5%, water content: 18.0%).HPLC Impurity Profile:
- Aztreonam: 99.22%
- Aztreonam t-butyl ester: 0.44%
HPLC Impurity Profile of Sample from Reaction Mixture: - Aztreonam: 82.20%
- Aztreonam t-butyl ester: 0.43%
- Aztreonam, open-chained: 7.22%
- Other main degradation product (RRT=0.56): 5.24%
EXAMPLE 6Aztreonam t-butyl ester (27.11 g, Assay as is: 96.5%, 0.05328 mol) is suspended in a mixture of 122 ml water and 1.35 ml cc. HCl. The suspension is heated to 62° C. with stirring and 30 ml cc. HCl is added. The suspension, which becomes clear after approx. 15 min, (then the product starts to precipitate), is stirred for 30 min at 63–65° C. Chilled water (162 ml) is added with efficient stirring and the resulting slurry is cooled further to 25° C. After two hours it is cooled to 0° C. and stirred for 2 hours. The product is filtered on a glass-filter, washed twice with 120 ml chilled water, twice with 125 ml cold acetone and filtered. The product is dried at room temperature overnight. Yield: 19.44 g (72%, according to assays) Aztreonam (Assay: 100.1%, water content: 14.4%).HPLC Impurity Profile:
- Aztreonam: 99.65%
- Aztreonam t-butyl ester: 0.21%
HPLC Impurity Profile of Sample from Reaction Mixture: - Aztreonam: 89.43%
- Aztreonam t-butyl ester: 0.26%
- Aztreonam, open-chained: 4.70%
- Other main degradation product (RRT=0.56): 1.47%
SYN
Manufacturing Process
This mixture was sterilized for 15 minutes at 121°C at 15 lbs/inch2 steam pressure prior to use. The fermentation flasks were incubated at 25°C for 40 to 45 hours on a of rotary shaker. A 250 liter batch of Agrobacterium radiobacter A.T.C.C. No. 31700 is fermented in a 100 gallon steel vessel with a media and operating conditions described below. Culture of Agrobacterium radiobacter grown out on agar slants, pH 7.3 consisted of yeast extract (1 g), beef extract (1 g), NZ amine A (2 g), glucose (10 g), agar (15 g) in 1000 ml distilled water. Loopful of surface growth from agar slant was used as the source of incolumn. Medium of oatmeal (20 g), tomato paste (20 g) tapped water to 1000 ml, pH 7, was sterilized for 15 min at 121°C at 15 lbs/inch2 steam pressure prior to use. 100 ml of the medium, containing incolumn is incubated at 25°C for about 24 hours on a rotary shaker. It was added to a mixture of yeast extract (5 g), glucose (10 g) in 1 L distilled water and incubated for about 42 hours at 25°C in 100 gallon stainless steel fermentation vessel.
During incubation, the broth is agitated at 155 r.p.m. and aerated at rate of 10.0 cubic feet per minute. An antifoam agent (Ucon LB625, Union Carbide) was added as needed. The fermentation beer was adjusted to pH 4 with aqueous HCl and calls separated by centrifugation. The supernatante (200 L) was extracted with 40 L of 0.05 m cetyldimethylbenzyl ammonium chloride in dichloromethane and extract concentrated in vacuo to 5.5 L. The concentrate was then extracted with solution of 177 g of sodium thiocyanate in 2 L of water, adjusting the mixture of pH 4.35 with phosphoric acid. The aqueous extract was concentrated in vacuo to 465 ml and added to 1840 ml of methanol. Solids are filtrated yielded 194 g of crude solid product. It was dissolved and chromatographed on a 5×106.5 cm column of Sephadex G-10 three times and after concentrating in vacuo gave 3.5 g of crude antibiotic M53 (azetreonam) which was chromatographed at first on QAE Sephadex A- 25 (liner gradient, prepared from 2.5 L of water and 2.5 L of 0.25 M sodium nitrate). Then the residue (fractions 26-75) gave M53 (natrium salt) after evaporation. It was triturated with methanol and the souble fraction, 0.40 g was chromatographed on a 2.5×20 cm column of Diaion HP20AG, eluting at 2 ml per minute with water and collecting 20 ml fractions. Fractions 26-75 gave 51.9 mg of antibiotic M53 (sodium salt).
Chemical Synthesis
Aztreonam, (Z)-2[[[(2-amino-4-thiazolyl)[[(2S,3S)-2-methyl-4-oxo-1-sulfo-3-azetidinyl]cabamoyl]methylen]amino]oxy]-2-methylpropionoic acid (32.1.4.9), is synthesized from tert-butyloxycarbonylthreonine, which is reacted with O-benzylhydroxylamine in the presence of dicyclohexylcarbodimide and 1-hydroxybenzotriazole, to form the benzyl hydroxamide derivative (32.1.4.1). This product undergoes a reaction with triphenylphosphine and ethyl azodicarboxylate, which results in the cyclodehydration of the product to (3S-trans)-N-benzyloxy-3-tert-butyloxycarbonylamino-4-methyl-azetidinone (32.1.4.2). Debenzylating this by hydrogen reduction using a palladium on carbon catalyst forms (3S-trans)-N-hydroxy-3-tertbutyloxycarbonyl-amino-4-methyl-azetidinone (32.1.4.3). The hydroxyl group in this compound is removed by reducing it with titanium trichloride, which forms azetidinone (32.1.4.4). Removing the tert-butyloxycarbonyl protection using trifluoroacetic acid and subsequent acylation of the resulting product with the benzyl chloroformate gives (3S-trans)-benzyloxycarbonylamino-4-methylazetidinone (32.1.4.5). Sulfonating this product with a mixture of sulfur trioxide and dimethylformamide gives the corresponding N-sulfonic acid. Turning the resulting Nsulfonic acid into a potassium salt by reacting it with potassium hydrophosphate, followed by replacing the potassium cation with a tetrabutylammonium cation by reacting it with tetrabutylammonium sulfate gives the product (32.1.4.6). Reducing this with hydrogen using a palladium on carbon catalyst gives 3-amino-4-methyl-monobactamic acid (32.1.4.7). Acylating this with (Z) 2-amino-α-[[2-(diphenylmethoxy)-1,1-dimethyl-2-oxoethoxy]imino] 4-thiazoleacetic acid in the presence of dicyclohexylcarbodiimide and 1-hydroxy-benzotriazole gives the diphenylmethyl ester of the desired aztreonam (32.1.4.8), which is hydrolyzed to aztreonam (32.1.4.9) using trifluoroacetic acid.
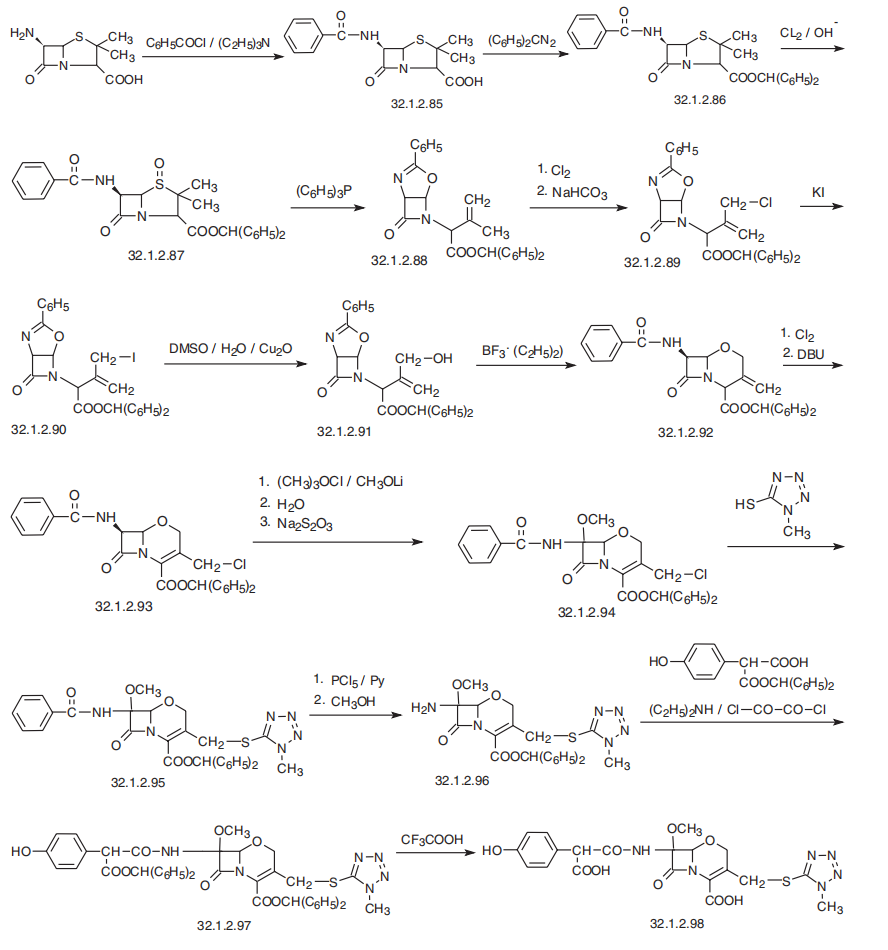
It is believed that the methyl group at position 4 increases the stability of the beta-lactam ring with respect to most beta-lactamases, and at the same time it does not induce formation of beta-lactamase as cephalosporins and imipenems do.

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Spectrum of activity
Acinetobacter anitratus, Escherichia coli, Pseudomonas aeruginosa, and Proteus mirabilis are generally susceptible to aztreonam, while some staphylococci, Staphylococcus aureus, Staphylococcus haemolyticus and Xanthomonas maltophilia are resistant to it. Furthermore, Aeromonas hydrophila, Citrobacter koseri (Citrobacter diversus), Pantoea agglomerans (Enterobacter agglomerans), Haemophilus spp. and Streptococcus pyogenes have developed resistance to aztreonam to varying degrees.[10]
Aztreonam is often used in people who are penicillin allergic or who cannot tolerate aminoglycosides.[medical citation needed]
Administration[edit]
Aztreonam is poorly absorbed when given orally, so it must be administered as an intravenous or intramuscular injection (trade name Azactam ), or inhaled (trade name Cayston) using an ultrasonic nebulizer. In the United States, the Food and Drug Administration (FDA) approved the inhalation form on 22 February 2010, for the suppression of P. aeruginosa infections in patients with cystic fibrosis.[11] It received conditional approval for administration in Canada and the European Union in September 2009,[11] and has been fully approved in Australia.[12]
Side effects
Reported side effects include injection site reactions, rash, and rarely toxic epidermal necrolysis. Gastrointestinal side effects generally include diarrhea and nausea and vomiting. There may be drug-induced eosinophilia. Because of the unfused beta-lactam ring there is somewhat lower cross-reactivity between aztreonam and many other beta-lactam antibiotics, and it may be safe to administer aztreonam to many patients with hypersensitivity (allergies) to penicillins and nearly all cephalosporins.[13] There is a much lower risk of cross-sensitivity between aztreonam and other beta-lactam antibiotics than within other beta-lactam antibiotics. However, there is a higher chance of cross-sensitivity if a person is specifically allergic to ceftazidime, a cephalosporin. Aztreonam exhibits cross-sensitivity with ceftazidime due to a similar side chain.[14]
Mechanism of action
Aztreonam is similar in action to penicillin. It inhibits synthesis of the bacterial cell wall, by blocking peptidoglycan crosslinking. It has a very high affinity for penicillin-binding protein-3 and mild affinity for penicillin-binding protein-1a. Aztreonam binds the penicillin-binding proteins of Gram-positive and anaerobic bacteria very poorly and is largely ineffective against them.[13] Aztreonam is bactericidal, but less so than some of the cephalosporins.[medical citation needed]
References
- ^ Jump up to:a b c d e f g h i j k l “Aztreonam”. The American Society of Health-System Pharmacists. Retrieved 8 December 2017.
- ^ British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. p. 381. ISBN 9780857111562.
- ^ World Health Organization (2019). Executive summary: the selection and use of essential medicines 2019: report of the 22nd WHO Expert Committee on the selection and use of essential medicines. Geneva: World Health Organization. hdl:10665/325773. WHO/MVP/EMP/IAU/2019.05. License: CC BY-NC-SA 3.0 IGO.
- ^ World Health Organization (2019). The selection and use of essential medicines: report of the WHO Expert Committee on Selection and Use of Essential Medicines, 2019 (including the 21st WHO Model List of Essential Medicines and the 7th WHO Model List of Essential Medicines for Children). Geneva: World Health Organization. hdl:10665/330668. ISBN 9789241210300. ISSN 0512-3054. WHO technical report series;1021.
- ^ Yaffe SJ, Aranda JV (2010). Neonatal and Pediatric Pharmacology: Therapeutic Principles in Practice. Lippincott Williams & Wilkins. p. 438. ISBN 9780781795388.
- ^ Quon BS, Goss CH, Ramsey BW (March 2014). “Inhaled antibiotics for lower airway infections”. Annals of the American Thoracic Society. 11 (3): 425–34. doi:10.1513/annalsats.201311-395fr. PMC 4028738. PMID 24673698.
- ^ Mosby’s Drug Consult 2006 (16th ed.). Mosby, Inc. 2006.
- ^ “Aztreonam Susceptibility and Minimum Inhibitory Concentration (MIC) Data” (PDF). toku-e.com. 3 February 2020.
- ^ Kobayashi Y, Uchida H, Kawakami Y (December 1992). “Synergy with aztreonam and arbekacin or tobramycin against Pseudomonas aeruginosa isolated from blood”. The Journal of Antimicrobial Chemotherapy. 30 (6): 871–2. doi:10.1093/jac/30.6.871. PMID 1289363.
- ^ “Aztreonam spectrum of bacterial susceptibility and Resistance” (PDF). Retrieved 15 May 2012.
- ^ Jump up to:a b Larkin C (22 February 2010). “Gilead’s Inhaled Antibiotic for Lungs Wins Approval”. BusinessWeek. Archived from the original on 2 March 2010. Retrieved 5 March 2010.
- ^ “FDA approves Gilead cystic fibrosis drug Cayston”. BusinessWeek. 23 February 2010. Retrieved 5 March 2010.
- ^ Jump up to:a b AHFS Drug Information 2006 (2006 ed.). American Society of Health-System Pharmacists. 2006.
- ^ Terico, AT; Gallagher, JC (December 2014). “Beta-lactam hypersensitivity and cross-reactivity”. Journal of Pharmacy Practice. 27 (6): 530–44. doi:10.1177/0897190014546109. PMID 25124380. S2CID 19275020.
External links
- “Aztreonam”. Drug Information Portal. U.S. National Library of Medicine.
| Clinical data | |
|---|---|
| Trade names | Azactam, Cayston, others |
| AHFS/Drugs.com | Monograph |
| License data | EU EMA: by INN |
| Pregnancy category | AU: B1 |
| Routes of administration | Intravenous, intramuscular, inhalation |
| ATC code | J01DF01 (WHO) |
| Legal status | |
| Legal status | UK: POM (Prescription only)US: ℞-onlyEU: Rx-only |
| Pharmacokinetic data | |
| Bioavailability | 100% (IM) 0.1% (by mouth in rats) Unknown (by mouth in humans) |
| Protein binding | 56% |
| Metabolism | Liver (minor %) |
| Elimination half-life | 1.7 hours |
| Excretion | Kidney |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 78110-38-0 |
| PubChem CID | 5742832 |
| DrugBank | DB00355 |
| ChemSpider | 4674940 |
| UNII | G2B4VE5GH8 |
| KEGG | D00240 |
| ChEBI | CHEBI:161680 |
| ChEMBL | ChEMBL158 |
| CompTox Dashboard (EPA) | DTXSID0022640 |
| ECHA InfoCard | 100.071.652 |
| Chemical and physical data | |
| Formula | C13H17N5O8S2 |
| Molar mass | 435.43 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| Melting point | 227 °C (441 °F) (dec.) |
| showSMILES | |
| showInChI | |
| (verify) |
Patent
Publication numberPriority datePublication dateAssigneeTitleEP0070024A11981-07-131983-01-19E.R. Squibb & Sons, Inc.The crystalline anhydrous form of (3S-(3 alpha(z),4 beta))-3-(((2-amino-4-thiazolyl)(1-carboxy-1-methylethoxy)-imino)-acetyl)-amino)-4-methyl-2-oxo-1-azetidinesulfonic acid, method for its preparation, mixture and pharmaceutical composition containing itUS4529698A1981-01-191985-07-16E. R. Squibb & Sons, Inc.Process for preparing a 2-oxo-1-azetidinesulfonic acid saltUS4652651A1983-05-311987-03-24Hoffmann-La Roche Inc.Process for the manufacture of 1-sulpho-2-oxoazetidine carboxylic acid intermediates via catalytic ester cleavageUS4775670A1980-09-291988-10-04E. R. Squibb & Sons, Inc.2-oxo-1-azetidinesulfonic acid saltsEP0297580A11987-07-011989-01-04E.R. Squibb & Sons, Inc.Amorphous form of aztreonamUS4826973A1984-07-201989-05-02E. R. Squibb & Sons, Inc.Delta form of aztreonam and preparation thereofUS4923998A1977-03-141990-05-08Fujisawa Pharmaceutical Company, Ltd.Cephem and cepham compounds and processes for preparation thereofUS4946838A1981-07-131990-08-07E. R. Squibb & Sons, Inc.Crystalline anhydrous aztreonamUS5194604A1990-06-291993-03-16E. R. Squibb & Sons, Inc.Process and intermediates for beta-lactams having aminothiazole(iminooxyacetic acid)acetic acid sidechainsUS5254681A1989-08-021993-10-19Consiglio Nazionale Delle RicercheProcess for preparing monobactames and their intermediate productPL165700B11991-10-151995-01-31PanMethod of obtaining z2/2-aminothiazolyl-4/-2/-t-butoxycarbonyl-1-methylethoxyimine/ acetic acidWO2002051356A22000-12-272002-07-04Salus Pharma, Inc.Inhalable aztreonam for treatment and prevention of pulmonary bacterial infectionsWO2003018578A12001-08-272003-03-06Aurobindo Pharma Ltd.Method for producing beta form of crystalline anhydrous aztreonamUS20040062721A12000-12-272004-04-01Montgomery Alan BruceInhalable aztreonam lysinate formulation for treatment and prevention of pulmonary bacterial infectionsWO2004052333A12002-12-112004-06-24Pari GmbhPharmaceutical compositions for the pulmonary delivery of aztreonamUS20050014739A12003-05-152005-01-20Viktor GyollaiAztreonam beta polymorph with very low residual solvent contentUS20050032775A12003-07-022005-02-10Viktor GyollaiAztreonam L-lysine and methods for the preparation thereof
Publication numberPriority datePublication dateAssigneeTitle
Family To Family CitationsCN1802371A2003-05-152006-07-12特瓦药厂有限公司Aztreonam beta-polymorph with very low residual solvent contentAU2004256124B2 *2003-07-022011-04-28Corus Pharma, Inc.Aztreonam L-lysine and methods for the preparation thereofWO2006122253A1 *2005-05-092006-11-16Sicor, Inc.Process for making aztreonamWO2007083187A2 *2006-01-162007-07-26Orchid Chemicals & Pharmaceuticals LimitedAn improved process for the preparation of monobactam antibioticCN101412715B *2008-12-162010-04-14海南百那医药发展有限公司Aztreonam compound and preparation thereofCN102127068B *2010-12-312012-08-29山西普德药业股份有限公司Method for synthesizing aztreonam compoundCN102311431B *2011-08-302014-12-10海南海药股份有限公司Method for preparing anhydrous beta-aztreonamCN105017241B *2015-06-242018-03-06山东罗欣药业集团股份有限公司A kind of aztreonam compound and its preparation
////////////////Aztreonam, SQ 26776, antibacterial, lactam, monobactam, UA2451400, азтреонам , أزتريونام , 氨曲南 ,
C[C@H]1[C@H](NC(=O)C(=N/OC(C)(C)C(=O)O)\C2=CSC([NH3+])=N2)C(=O)N1S([O-])(=O)=O

NEW DRUG APPROVALS
ONE TIME
$10.00
Tezepelumab-ekko

(Heavy chain)
QMQLVESGGG VVQPGRSLRL SCAASGFTFR TYGMHWVRQA PGKGLEWVAV IWYDGSNKHY
ADSVKGRFTI TRDNSKNTLN LQMNSLRAED TAVYYCARAP QWELVHEAFD IWGQGTMVTV
SSASTKGPSV FPLAPCSRST SESTAALGCL VKDYFPEPVT VSWNSGALTS GVHTFPAVLQ
SSGLYSLSSV VTVPSSNFGT QTYTCNVDHK PSNTKVDKTV ERKCCVECPP CPAPPVAGPS
VFLFPPKPKD TLMISRTPEV TCVVVDVSHE DPEVQFNWYV DGVEVHNAKT KPREEQFNST
FRVVSVLTVV HQDWLNGKEY KCKVSNKGLP APIEKTISKT KGQPREPQVY TLPPSREEMT
KNQVSLTCLV KGFYPSDIAV EWESNGQPEN NYKTTPPMLD SDGSFFLYSK LTVDKSRWQQ
GNVFSCSVMH EALHNHYTQK SLSLSPGK
(Light chain)
SYVLTQPPSV SVAPGQTARI TCGGNNLGSK SVHWYQQKPG QAPVLVVYDD SDRPSWIPER
FSGSNSGNTA TLTISRGEAG DEADYYCQVW DSSSDHVVFG GGTKLTVLGQ PKAAPSVTLF
PPSSEELQAN KATLVCLISD FYPGAVTVAW KADSSPVKAG VETTTPSKQS NNKYAASSYL
SLTPEQWKSH RSYSCQVTHE GSTVEKTVAP TECS
(Disulfide bridge: H22-H96, H136-L213, H149-H205, H224-H’224, H225-H’225, H228-H’228, H231-H’231, H262-H322, H368-H426, H’22-H’96, H’136-L’213, H’149-H’205, H’262-H’322, H’368-H’426, L22-L87, L136-L195, L’22-L’87, L’136-L’195)
Tezepelumab-ekko
テゼペルマブ (遺伝子組換え)
| Formula | C6400H9844N1732O1992S52 |
|---|---|
| CAS | 1572943-04-4 |
| Mol weight | 144588.4306 |
PEPTIDE
UD FDA APPROVED, 12/17/2021, To treat severe asthma as an add-on maintenance therapy , Tezspire
Monoclonal antibody
Treatment of asthma and atopic dermatitis
Tezepelumab, sold under the brand name Tezspire, is a human monoclonal antibody used for the treatment of asthma.[4][5]
It blocks thymic stromal lymphopoietin (TSLP),[2] an epithelial cytokine that has been suggested to be critical in the initiation and persistence of airway inflammation.[6]
It was approved for medical use in the United States in December 2021.[2][3]
Medical uses
Tezepelumab is indicated for the add-on maintenance treatment of people aged twelve years and older with severe asthma.[2]
Research
In Phase III trials, tezepelumab demonstrated efficacy compared to placebo for patients with severe, uncontrolled asthma.[7][8]
Structural studies by X-ray crystallography showed that Tezepelumab competes against a critical part of the TSLPR binding site on TSLP.[1]
It is being studied for the treatment of chronic obstructive pulmonary disease, chronic rhinosinusitis with nasal polyps, chronic spontaneous urticaria and eosinophilic esophagitis (EoE).[3]

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////

References
- ^ Jump up to:a b Verstraete K, Peelman F, Braun H, Lopez J, Van Rompaey D, Dansercoer A, et al. (April 2017). “Structure and antagonism of the receptor complex mediated by human TSLP in allergy and asthma”. Nature Communications. 8 (1): 14937. Bibcode:2017NatCo…814937V. doi:10.1038/ncomms14937. PMC 5382266. PMID 28368013.
- ^ Jump up to:a b c d https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/761224s000lbl.pdf
- ^ Jump up to:a b c “Tezspire (tezepelumab) approved in the US for severe asthma”. AstraZeneca (Press release). 17 December 2021. Retrieved 17 December 2021.
- ^ Marone G, Spadaro G, Braile M, Poto R, Criscuolo G, Pahima H, et al. (November 2019). “Tezepelumab: a novel biological therapy for the treatment of severe uncontrolled asthma”. Expert Opinion on Investigational Drugs. 28 (11): 931–940. doi:10.1080/13543784.2019.1672657. PMID 31549891. S2CID 202746054.
- ^ Matera MG, Rogliani P, Calzetta L, Cazzola M (February 2020). “TSLP Inhibitors for Asthma: Current Status and Future Prospects”. Drugs. 80 (5): 449–458. doi:10.1007/s40265-020-01273-4. PMID 32078149. S2CID 211194472.
- ^ “Tezepelumab granted Breakthrough Therapy Designation by US FDA”. AstraZeneca (Press release). 7 September 2018.
- ^ “Studies found for: Tezepelumab”. ClinicalTrials.Gov. National Library of Medicine, National Institutes of Health, U.S. Department of Health and Human Services.
- ^ Menzies-Gow A, Corren J, Bourdin A, Chupp G, Israel E, Wechsler ME, et al. (May 2021). “Tezepelumab in Adults and Adolescents with Severe, Uncontrolled Asthma”. New England Journal of Medicine. 384 (19): 1800–09. doi:10.1056/NEJMoa2034975. PMID 33979488. S2CID 234484931.
External links
- “Tezepelumab”. Drug Information Portal. U.S. National Library of Medicine.
- Clinical trial number NCT02054130 for “Study to Evaluate the Efficacy and Safety of MEDI9929 (AMG 157) in Adult Subjects With Inadequately Controlled, Severe Asthma” at ClinicalTrials.gov
- Clinical trial number NCT03347279 for “Study to Evaluate Tezepelumab in Adults & Adolescents With Severe Uncontrolled Asthma (NAVIGATOR)” at ClinicalTrials.gov
| Structural basis for inhibition of TSLP-signaling by Tezepelumab (PDB 5J13)[1] | |
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Human |
| Target | thymic stromal lymphopoietin (TSLP) |
| Clinical data | |
| Trade names | Tezspire |
| Other names | MEDI9929, AMG 157, tezepelumab-ekko |
| License data | US DailyMed: Tezepelumab |
| Routes of administration | Subcutaneous |
| ATC code | None |
| Legal status | |
| Legal status | US: ℞-only [2][3] |
| Identifiers | |
| CAS Number | 1572943-04-4 |
| DrugBank | DB15090 |
| ChemSpider | None |
| UNII | RJ1IW3B4QX |
| KEGG | D11771 |
| Chemical and physical data | |
| Formula | C6400H9844N1732O1992S52 |
| Molar mass | 144590.40 g·mol−1 |
////////////Tezepelumab-ekko, Tezspire, PEPTIDE, APPROVALS 2021, FDA 2021, Monoclonal antibody
, asthma, atopic dermatitis, ANTI INFLAMATORY, テゼペルマブ (遺伝子組換え)

NEW DRUG APPROVALS
ONE TIME
$10.00
Efgartigimod alfa-fcab
DKTHTCPPCP APELLGGPSV FLFPPKPKDT LYITREPEVT CVVVDVSHED PEVKFNWYVD
GVEVHNAKTK PREEQYNSTY RVVSVLTVLH QDWLNGKEYK CKVSNKALPA PIEKTISKAK
GQPREPQVYT LPPSRDELTK NQVSLTCLVK GFYPSDIAVE WESNGQPENN YKTTPPVLDS
DGSFFLYSKL TVDKSRWQQG NVFSCSVMHE ALKFHYTQKS LSLSPGK
(Disulfide bridge: 6-6′, 9-9′, 41-101, 147-205, 41′-101′, 147′-205′)
Efgartigimod alfa-fcab
| Formula | C2310H3554N602O692S14 |
|---|---|
| CAS | 1821402-21-4 |
| Mol weight | 51279.464 |
US FDA APPROVED 12/17/2021, To treat generalized myasthenia gravis
Press Release, Vyvgart, BLA 761195
| エフガルチギモドアルファ (遺伝子組換え) |
PEPTIDE
Treatment of IgG-driven autoimmune diseases

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
https://www.fda.gov/news-events/press-announcements/fda-approves-new-treatment-myasthenia-gravis
FDA Approves New Treatment for Myasthenia Gravis
Approval is the First of a New Class of Medication for this Rare, Chronic, Autoimmune, Neuromuscular DiseaseFor Immediate Release:December 17, 2021
The U.S. Food and Drug Administration today approved Vyvgart (efgartigimod) for the treatment of generalized myasthenia gravis (gMG) in adults who test positive for the anti-acetylcholine receptor (AChR) antibody.
Myasthenia gravis is a chronic autoimmune, neuromuscular disease that causes weakness in the skeletal muscles (also called voluntary muscles) that worsens after periods of activity and improves after periods of rest. Myasthenia gravis affects voluntary muscles, especially those that are responsible for controlling the eyes, face, mouth, throat, and limbs. In myasthenia gravis, the immune system produces AChR antibodies that interfere with communication between nerves and muscles, resulting in weakness. Severe attacks of weakness can cause breathing and swallowing problems that can be life-threatening.
“There are significant unmet medical needs for people living with myasthenia gravis, as with many other rare diseases,” said Billy Dunn, M.D., director of the Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research. “Today’s approval is an important step in providing a novel therapy option for patients and underscores the agency’s commitment to help make new treatment options available for people living with rare diseases.”
Vyvgart is the first approval of a new class of medication. It is an antibody fragment that binds to the neonatal Fc receptor (FcRn), preventing FcRn from recycling immunoglobulin G (IgG) back into the blood. The medication causes a reduction in overall levels of IgG, including the abnormal AChR antibodies that are present in myasthenia gravis.
The safety and efficacy of Vyvgart were evaluated in a 26-week clinical study of 167 patients with myasthenia gravis who were randomized to receive either Vyvgart or placebo. The study showed that more patients with myasthenia gravis with antibodies responded to treatment during the first cycle of Vyvgart (68%) compared to those who received placebo (30%) on a measure that assesses the impact of myasthenia gravis on daily function. More patients receiving Vyvgart also demonstrated response on a measure of muscle weakness compared to placebo.
The most common side effects associated with the use of Vyvgart include respiratory tract infections, headache, and urinary tract infections. As Vyvgart causes a reduction in IgG levels, the risk of infections may increase. Hypersensitivity reactions such as eyelid swelling, shortness of breath, and rash have occurred. If a hypersensitivity reaction occurs, discontinue the infusion and institute appropriate therapy. Patients using Vyvgart should monitor for signs and symptoms of infections during treatment. Health care professionals should administer appropriate treatment and consider delaying administration of Vyvgart to patients with an active infection until the infection is resolved.
The FDA granted this application Fast Track and Orphan Drug designations. The FDA granted the approval of Vyvgart to argenx BV.
///////////efgartigimod alfa-fcab, Vyvgart, FDA 2021,APPROVALS 2021, myasthenia gravis, argenx BV, Fast Track, Orphan Drug, PEPTIDE,
| エフガルチギモドアルファ (遺伝子組換え) |

NEW DRUG APPROVALS
one time
$10.00

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....











