Home » Posts tagged 'fda' (Page 8)
Tag Archives: fda
GADODIAMIDE, OMNISCAN Drug Patent Expiration, 1 st oct 2013
GADODIAMIDE
GE HEALTHCARE, OMNISCAN
Drug Patent Expiration
1 st oct 2013, US5560903, CAS 122795-43-1
| GADODIAMIDE | INJECTABLE; INJECTION | 287MG/ML | RX | NDA 020123 |
Gadodiamide is a gadolinium-based MRI contrast agent, used in MR imaging procedures to assist in the visualization of blood vessels. It is commonly marketed under the trade name Omniscan.
For intravenous use in MRI to visualize lesions with abnormal vascularity (or those thought to cause abnormalities in the blood-brain barrier) in the brain (intracranial lesions), spine, and associated tissues.
Gadodiamide is a contrast medium for cranial and spinal magnetic resonance imaging (MRI) and for general MRI of the body after intravenous administration. The product provides contrast enhancement and facilitates visualisation of abnormal structures or lesions in various parts of the body including the central nervous system (CNS). It does not cross an intactblood brain barrier but might give enhancement in pathological conditions.
Based on the behavior of protons when placed in a strong magnetic field, which is interpreted and transformed into images by magnetic resonance (MR) instruments. Paramagnetic agents have unpaired electrons that generate a magnetic field about 700 times larger than the proton’s field, thus disturbing the proton’s local magnetic field. When the local magnetic field around a proton is disturbed, its relaxation process is altered. MR images are based on proton density and proton relaxation dynamics. MR instruments can record 2 different relaxation processes, the T1 (spin-lattice or longitudinal relaxation time) and the T2 (spin-spin or transverse relaxation time). In magnetic resonance imaging (MRI), visualization of normal and pathological brain tissue depends in part on variations in the radiofrequency signal intensity that occur with changes in proton density, alteration of the T1, and variation in the T2. When placed in a magnetic field, gadodiamide shortens both the T1 and the T2 relaxation times in tissues where it accumulates. At clinical doses, gadodiamide primarily affects the T1 relaxation time, thus producing an increase in signal intensity. Gadodiamide does not cross the intact blood-brain barrier; therefore, it does not accumulate in normal brain tissue or in central nervous system (CNS) lesions that have not caused an abnormal blood-brain barrier (e.g., cysts, mature post-operative scars). Abnormal vascularity or disruption of the blood-brain barrier allows accumulation of gadodiamide in lesions such as neoplasms, abscesses, and subacute infarcts.

1.Schenker MP, Solomon JA, Roberts DA. (2001). Gadolinium Arteriography Complicated by Acute Pancreatitis and Acute Renal Failure, Journal of vascular and interventional radiology 12(3):393.[1]
2 Unal O, Arslan H. (1999). Cardiac arrest caused by IV gadopentetate dimeglumine. AJR Am J Roentgenol 172:1141.[2]
3 Cacheris WP, Quay SC, Rocklage SM. (1990). The relationship between thermodynamics and the toxicity of gadolinium complexes, Magn Reson Imaging 8(6):467-81. doi:10.1016/0730-725X(90)90055-7
4 Canavese, C; Mereu, MC; Aime, S; Lazzarich, E; Fenoglio, R; Quaglia, M; Stratta, P (2008). “Gadolinium-associated nephrogenic systemic fibrosis: the need for nephrologists’ awareness”. Journal of nephrology 21 (3): 324–36. PMID 18587720.
COUNTRY PATENT APPROVED, EXPIRY
| United States | 5560903 | 1993-10-01 | 2013-10-01 |
| Canada | 1335819 | 1995-06-06 | 2012-06-06 |
| United States | 5362475 | 1994-11-08 | 2011-11-08 |
| Canada | 1335819 | 1995-06-06 | 2012-06-06 |
| United States | 5560903 | 1993-10-01 | 2013-10-01 |
Gadolinium contrast agents are used as contrast media to enhance magnetic resonance imaging as they are paramagnetic. This compound has a low incidence of adverse side effects, although there is a rare association with nephrogenic systemic fibrosis (NSF) when given to people with severe renal impairment (ie, GFRglomerular filtration rate <30mL/min/1·73m2).It seems to be related to the liberation of free gadolinium ions, and UK CHM advice is against using the least stable of the agents – Omniscan (gadodiamide) – in patients with severe renal impairment, and carefully considering whether to use others where renal function is impaired.
OMNISCAN (gadodiamide) Injection is the formulation of the gadolinium complex of diethylenetriamine pentaacetic acid bismethylamide, and is an injectable, nonionic extracellular enhancing agent for magnetic resonance imaging. OMNISCAN is administered by intravenous injection. OMNISCAN is provided as a sterile, clear, colorless to slightly yellow, aqueous solution. Each 1 mL contains 287 mg gadodiamide and 12 mg caldiamide sodium in Water for Injection.
The pH is adjusted between 5.5 and 7.0 with hydrochloric acid and/or sodium hydroxide. OMNISCAN contains no antimicrobial preservative. OMNISCAN is a 0.5 mol/L solution of aqua[5,8-bis(carboxymethyl)11-[2-(methylamino)-2-oxoethyl]-3-oxo-2,5,8,11-tetraazatridecan-13-oato (3-)-N5, N8, N11, O3, O5, O8, O11, O13] gadolinium hydrate, with a molecular weight of 573.66 (anhydrous), an empirical formula of C16H28GdN5O9•xH2O, and the following structural formula:
 |
Pertinent physicochemical data for OMNISCAN are noted below:
PARAMETER
| Osmolality (mOsmol/kg water) | @ 37°C | 789 |
| Viscosity (cP) | @ 20°C | 2 |
| @ 37°C | 1.4 | |
| Density (g/mL) | @ 25°C | 1.14 |
| Specific gravity | @ 25°C | 1.15 |
OMNISCAN has an osmolality approximately 2.8 times that of plasma at 37°C and is hypertonic under conditions of use.
gadodiamide, chemical name: [5,8 _ bis (carboxymethyl) -11 – [2_ (methylamino)-2_ ethyl] -3 – O 2 ,5,8, 11 – tetraazacyclododecane-decane -13 – oxo-(3 -)] gadolinium trihydrate. Its structure is shown in formula one.
[0003] Structural Formula:
[0004]
[0005] Magnetic resonance contrast agent gadodiamide resonance than ionic contrast agents safer generation of products, it is non-ionic structure significantly reduces the number of particles in solution, osmotic balance of body fluids is very small.Meanwhile, gadodiamide relatively low viscosity to bring the convenience of nursing staff, making it easier to bolus. In addition, gadodiamide pioneered the use of amide-substituted carboxyl part, not only reduces the toxicity of carboxyl groups and ensure the non-ionic nature of the product solution.
[0006] reported in the literature and their intermediates gadodiamide synthetic route is as follows:
[0007] 1. Compound III synthetic routes for its preparation in U.S. Patent No. US5508388 described as: In the synthesis process, the inventors using acetonitrile as solvent, acetic anhydride as dehydrating agent, pyridine as acid-binding agent, at 55 ~ 60 ° C, the reaction 18h. Anti-
See the reaction should be a process. The disadvantage of this synthesis are acetonitrile toxicity, not widely used.
[0008]
[0009] Reaction a
[0010] (2) Synthesis of Compound III in many articles are reported in the patent and its implementation method similar to the patent US5508388.
[0011] In US3660388, the diethylenetriamine pentaacetic acid (Compound II), pyridine, acetic anhydride, the mixture was reacted at 65 ° C or 20h at 125 ° C the reaction 5min, to give compound III.
[0012] In US4822594, the compounds II, pyridine, acetic anhydride mixture was reacted at 65 ° C 20h, to give compound III.
[0013] In US4698263, the compounds II, pyridine, acetic anhydride heated in a nitrogen or argon atmosphere under reflux for 18h, to give compound III. [0014] In the EPO183760B1, the compounds II, pyridine, acetic anhydride mixture was reacted at 55 ° C 24h, to give compound III.
[0015] In CN1894223A, the compounds II, pyridine, acetic anhydride, the mixture above 65 ° C the reaction mixture, and the pyridine of DTPA feed ratio is: 1: (0.5 to 3).
[0016] The above patents do not provide for the compound III is post-processing method.
[0017] 3 Synthesis of Compound IV.
[0018] In U.S. Patent US4859451, the diethylenetriamine pentaacetic acid dianhydride (compound III) and ammonia, methanol and the reaction of compounds IV, see Reaction Scheme II.
[0019]
[0020] Reaction two
[0021] In the patent US5087439, the compound III with methylamine in aqueous solution for several hours, or overnight reactions, see reaction formula III.
[0022]
[0023] Reactive three
[0024] These two patents using ammonia and methylamine, which can form explosive mixtures with air, in case of fire or high pressure can cause an explosion in the production process of great insecurity. Although raw material prices are lower, but higher production conditions (such as requiring sealed, low temperature, etc.). Compared to this synthesis process,
[0025] 4, gadodiamide (Compound I) synthesis.
[0026] In the patent US4859451, the use of gadolinium chloride with the compound IV is carried out under acidic conditions, complexing. Finally, tune
Section PH neutral, see reaction IV.
[0027]
[0028] Reaction formula tetrakis [0029] in the patent US5087439, the chlorides are used as reactants, and details of the post-processing method of Compound I.
[0030] In the patent US5508388, the use of gadolinium oxide with compound IV in acetonitrile, water with stirring, the resulting compound I.
[0032] The synthetic route is as follows:
[0033]
[0034] 1) Compound II (diethylenetriamine pentaacetic acid) in pyridine, acetic anhydride in the presence of a dehydration reaction into the acid anhydride, and the product was stirred with cold DMF, leaving the solid filtered, washed with ether reagents, drying , to obtain a white powdery solid compound III (diethylenetriamine pentaacetic acid anhydride);
[0035] 2) Compound III in DMF with methylamine hydrochloride, the reaction of the compound IV (5,8 _ bis carboxymethyl methyl-11 – [2 – (dimethylamino) -2 – oxoethyl] – 3 – oxo -2,5,8,11 – tetraazacyclododecane _13_ tridecyl acid); and the control compound III: MeNH2 · HCl molar ratio = 1: (1 to 4), control the temperature between 20 ~ 80 ° C, the reaction time is 4 ~ 6h, after the treatment, the method of distillation under reduced pressure to remove DMF, the product is dissolved in a polar solvent, methanol, and then adding a solvent polarity modulation, so that the target Compound IV from system completely precipitated;
[0036] 3) Compound IV with gadolinium oxide formed in the presence of hydrochloric acid of the complex, after the reaction, filtration and drying, to obtain a white powdery compound I, i.e. gadodiamide.
[0037] Existing gadodiamide Synthesis basically from the synthesis of Compound IV as a starting material, the present invention is first introduced to the compound II as a starting material to synthesize gadodiamide. Synthesis of the conventional method of gadodiamide, the present invention has the advantage of inexpensive starting materials, convenient and easy to get. In addition, the synthetic pathway intermediates are involved in the post-processing is simple, enabling continuous reaction, saving time and cost savings, the reaction becomes controlled step by step, and try to avoid the use of toxic reagents, reducing the possibility of operator injury , while also greatly reducing damage to the environment.
Bristol-Myers Squibb announced promising results from an expanded phase 1 dose-ranging study of its lung cancer drug nivolumab

NIVOLUMAB
Anti-PD-1;BMS-936558; ONO-4538
PRONUNCIATION nye vol’ ue mab
THERAPEUTIC CLAIM Treatment of cancer
CHEMICAL DESCRIPTION
A fully human IgG4 antibody blocking the programmed cell death-1 receptor (Medarex/Ono Pharmaceuticals/Bristol-Myers Squibb)
MOLECULAR FORMULA C6362H9862N1712O1995S42
MOLECULAR WEIGHT 143.6 kDa
SPONSOR Bristol-Myers Squibb
CODE DESIGNATION MDX-1106, BMS-936558
CAS REGISTRY NUMBER 946414-94-4
Bristol-Myers Squibb announced promising results from an expanded phase 1 dose-ranging study of its lung cancer drug nivolumab
Nivolumab (nye vol’ ue mab) is a fully human IgG4 monoclonal antibody designed for the treatment of cancer. Nivolumab was developed by Bristol-Myers Squibb and is also known as BMS-936558 and MDX1106.[1] Nivolumab acts as an immunomodulator by blocking ligand activation of the Programmed cell death 1 receptor.
A Phase 1 clinical trial [2] tested nivolumab at doses ranging from 0.1 to 10.0 mg per kilogram of body weight, every 2 weeks. Response was assessed after each 8-week treatment cycle, and were evaluable for 236 of 296 patients. Study authors concluded that:”Anti-PD-1 antibody produced objective responses in approximately one in four to one in five patients with non–small-cell lung cancer, melanoma, or renal-cell cancer; the adverse-event profile does not appear to preclude its use.”[3]
Phase III clinical trials of nivolumab are recruiting in the US and EU.[4]
- Statement On A Nonproprietary Name Adopted By The USAN Council – Nivolumab, American Medical Association.
- A Phase 1b Study of MDX-1106 in Subjects With Advanced or Recurrent Malignancies (MDX1106-03), NIH.
- Topalian SL, et al. (June 2012). “Safety, Activity, and Immune Correlates of Anti–PD-1 Antibody in Cancer”. New England Journal of Medicine 366. doi:10.1056/NEJMoa1200690. Lay summary – New York Times.
- Nivolumab at ClinicalTrials.gov, A service of the U.S. National Institutes of Health.
The PD-1 blocking antibody nivolumab continues to demonstrate sustained clinical activity in previously treated patients with advanced non-small cell lung cancer (NSCLC), according to updated long-term survival data from a phase I trial.
Survival rates at one year with nivolumab were 42% and reached 24% at two years, according to the median 20.3-month follow up. Additionally, the objective response rate (ORR) with nivolumab, defined as complete or partial responses by standard RECIST criteria, was 17% for patients with NSCLC. Results from the updated analysis will be presented during the 2013 World Conference on Lung Cancer on October 29.
“Lung cancer is very difficult to treat and there continues to be a high unmet medical need for these patients, especially those who have received multiple treatments,” David R. Spigel, MD, the program director of Lung Cancer Research at the Sarah Cannon Research Institute and one of the authors of the updated analysis, said in a statement.
“With nivolumab, we are investigating an approach to treating lung cancer that is designed to work with the body’s own immune system, and these are encouraging phase I results that support further investigation in larger scale trials.”
In the phase I trial, 306 patients received intravenous nivolumab at 0.1–10 mg/kg every-other-week for ≤12 cycles (4 doses/8 week cycle). In all, the trial enrolled patients with NSCLC, melanoma, renal cell carcinoma, colorectal cancer, and prostate cancer.
The long-term follow up focused specifically on the 129 patients with NSCLC. In this subgroup, patients treated with nivolumab showed encouraging clinical activity. The participants had a median age of 65 years and good performance status scores, and more than half had received three or more prior therapies. Across all doses of nivolumab, the median overall survival was 9.9 months, based on Kaplan-Meier estimates.
In a previous update of the full trial results presented at the 2013 ASCO Annual Meeting, drug-related adverse events of all grades occurred in 72% of patients and grade 3/4 events occurred in 15%. Grade 3/4 pneumonitis related to treatment with nivolumab emerged early in the trial, resulting in 3 deaths. As a result, a treatment algorithm for early detection and management was developed to prevent this serious side effect.
Nivolumab is a fully human monoclonal antibody that blocks the PD-1 receptor from binding to both of its known ligands, PD-L1 and PD-L2. This mechanism, along with early data, suggested an associated between PD-L1 expression and response to treatment.
In separate analysis presented at the 2013 World Conference on Lung Cancer, the association of tumor PD-L1 expression and clinical activity in patients with NSCLC treated with nivolumab was further explored. Of the 129 patients with NSCLC treated with nivolumab in the phase I trial, 63 with NSCLC were tested for PD-L1 expression by immunohistochemistry (29 squamous; 34 non-squamous).
Bristol-Myers Squibb announced promising results from phase 2b study of its rheumatoid arthritis drug clazakizumab
NONPROPRIETARY NAME ADOPTED BY THE USAN COUNCIL
CLAZAKIZUMAB
PRONUNCIATION klaz” a kiz’ ue mab
THERAPEUTIC CLAIM Autoimmune diseases, rheumatoid arthritis
CHEMICAL NAMES
1. Immunoglobulin G1, anti-(human interleukin 6) (human-Oryctolagus cuniculus monoclonal BMS-945429/ALD518 heavy chain), disulfide with human-Oryctolagus cuniculus monoclonal BMS-945429/ALD518 κ-chain, dimer
2. Immunoglobulin G1, anti-(human interleukin-6 (B-cell stimulatory factor 2, CTL differentiation factor, hybridoma growth factor, interferon beta-2)); humanized rabbit monoclonal BMS-945429/ALD518 [300-alanine(CH2-N67>A67)]1 heavy chain (223-217′)-disulfide with humanized rabbit monoclonal BMS-945429/ALD518 light chain dimer (229-229”:232-232”)-bisdisulfide, O-glycosylated
MOLECULAR FORMULA C6426H9972N1724O2032S42
MOLECULAR WEIGHT 145.2 kDa
SPONSOR Bristol-Myers Squibb
CODE DESIGNATION BMS-945429, ALD518
CAS REGISTRY NUMBER 1236278-28-6
Monoclonal antibody
Type Whole antibody
Source Humanized
Target IL6
CAS number 1236278-28-6
Clazakizumab is a humanized monoclonal antibody designed for the treatment of rheumatoid arthritis.[1]
Clazakizumab was developed by Alder Biopharmaceuticals and Bristol-Myers Squibb.
gamma1 heavy chain (1-450) [humanized VH (Homo sapiens IGHV3-66*01 (83.50%) -(IGHD)-IGHJ3*02 M123>L (115)) [8.8.14] (1-120) -Homo sapiens IGHG1*03 CH
Biosimilars-in-India
http://www.ibef.org/download/Biosimilars-in-India-30312.pdf
-
Biosimilars – India Brand Equity Foundation
www.ibef.org/download/Biosimilars-in-India-30312.pdfpatented/registered biotech products, but are manufactured by new companies after the patent expiry of the originator product. The global. Biosimilars market is …
Alexion obtains FDA breakthrough therapy status for cPMP to treat MoCD type A disorder

cyclic pyranopterin monophosphate (cPMP, ALXN1101)
Alexion Pharma International Sàrl has received a breakthrough therapy designation from the US Food and Drug Administration (FDA) for its cyclic pyranopterin monophosphate (cPMP, ALXN1101), an enzyme co-factor replacement therapy to treat patients with molybdenum cofactor deficiency (MoCD) type A.
Alexion obtains FDA breakthrough therapy status for cPMP to treat MoCD type A disorder
read all at
Cyclic pyranopterin monophosphate (cPMP) is an experimental treatment formolybdenum cofactor deficiency type A, which was developed by José Santamaría-Araujo and Schwarz at the German universities TU Braunschweig and the University of Cologne.[1][2]
cPMP is a precursor to molybdenum cofactor, which is required for the enyzme activity ofsulfite oxidase, xanthine dehydrogenase/oxidase and aldehyde oxidase.[3]
- Guenter Schwarz Laboratory, Institute for Biochemistry – University of Cologne (English, German)
- Günter Schwarz, José Angel Santamaria-Araujo, Stefan Wolf, Heon-Jin Lee, Ibrahim M. Adham, Hermann-Josef Gröne, Herbert Schwegler, Jörn Oliver Sass, Tanja Otte, Petra Hänzelmann, Ralf R. Mendel, Wolfgang Engel and Jochen Reiss (2004). “Rescue of lethal molybdenum cofactor deficiency by a biosynthetic precursor from Escherichia coli“. Human Molecular Genetics 13 (12): 1249–1255. doi:10.1093/hmg/ddh136.PMID 15115759.
- Doctors risk untried drug to stop baby’s brain dissolving, TimesOnline, November 5, 2009
- José Angel Santamaria-Araujo, Berthold Fischer, Tanja Otte, Manfred Nimtz, Ralf R. Mendel, Victor Wray and Günter Schwarz (2004). “The Tetrahydropyranopterin Structure of the Sulfur-free and Metal-free Molybdenum Cofactor Precursor”. The Journal of Biological Chemistry 279 (16): 15994–15999.doi:10.1074/jbc.M311815200. PMID 14761975.
Molybdenum cofactor (Moco) deficiency is a pleiotropic genetic disorder. Moco consists of molybdenum covalently bound to one or two dithiolates attached to a unique tricyclic pterin moiety commonly referred to as molybdopterin (MPT). Moco is synthesized by a biosynthetic pathway that can be divided into four steps, according to the biosynthetic intermediates precursor Z (cyclicpyranopterin monophosphate; cPMP), MPT, and adenylated MPT. Mutations in the Moco biosynthetase genes result in the loss of production of the molybdenum dependent enzymes sulfite-oxidase, xanthine oxidoreductase, and aldehyde oxidase. Whereas the activities of all three of these cofactor-containing enzymes are impaired by cofactor deficiency, the devastating consequences of the disease can be traced to the loss of sulfite oxidase activity. Human Moco deficiency is a rare but severe disorder accompanied by serious neurological symptoms including attenuated growth of the brain, unbeatable seizures, dislocated ocular lenses, and mental retardation. Until recently, no effective therapy was available and afflicted patients suffering from Moco deficiency died in early infancy.
It has been found that administration of the molybdopterin derivative precursor Z, a relatively stable intermediate in the Moco biosynthetic pathway, is an effective means of therapy for human Moco deficiency and associated diseases related to altered Moco synthesis {see U.S. Patent No. 7,504,095). As with most replacement therapies for illnesses, however, the treatment is limited by the availability of the therapeutic active agent.
WO 2012112922 A1
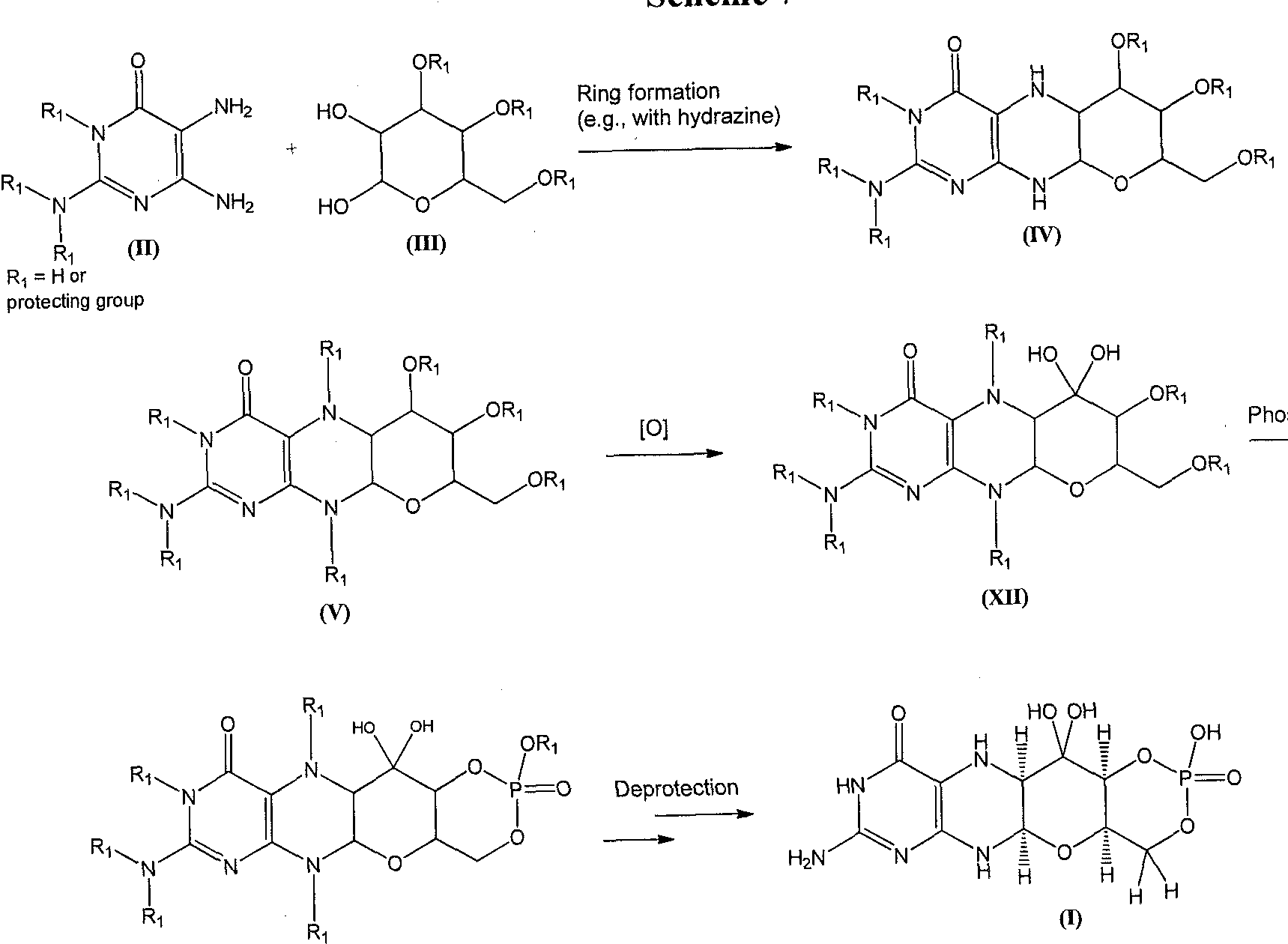
In this synthesis, the deprotection may involve, for example, either sequential or one-pot deprotection of certain amino and hydroxyl protecting groups on a compound of formula (VII) to furnish the compound of formula (I). Suitable reagents and conditions for the deprotection of a compound of formula (VII) can be readily determined by those of ordinary skill in the art. For example, compound (I) may be formed upon treatment of a compound of formula (VII) under conditions so that hydroxyl protecting groups, such as acetate, isopropylidine, and benzylidine protecting groups, are removed from the formula (VII) structure. The acetate group can be cleaved, for example, under Zemplen conditions using catalytic NaOMe as a base in methanol. The benzylidene and isopropylidene groups can be cleaved by hydrogenation or using acidic hydrolysis as reported by R.M. Harm et ah, J. Am. Chem. Soc, 72, 561 (1950). In yet another example, the deprotection can be performed so that amino protecting groups, such as 9- fluorenylmethyl carbamate (Fmoc), t-butyl carbamate (Boc), and carboxybenzyl carbamate (cbz) protecting groups are cleaved from the compound of formula (VII). 9-fluorenylmethyl carbamate (Fmoc) can be removed under mild conditions with an amine base (e.g. , piperidine) to afford the free amine and dibenzofulvene, as described by E. Atherton et al, “The
Fluorenylmethoxycarbonyl Amino Protecting Group,” in The Peptides, S. Udenfriend and J. Meienhofer, Academic Press, New York, 1987, p. 1. t-butyl carbamate (Boc) can be removed, as reported by G.L. Stahl et al., J. Org. Chem., 43, 2285 (1978), under acidic conditions (e.g., 3 M HC1 in EtOAc). Hydrogenation can be used to cleave the carboxybenzyl carbamate (cbz) protecting group as described by J. Meienhofer et al., Tetrahedron Lett., 29, 2983 (1988).
To prevent oxidation of formula (I) during the reaction, the deprotection may be performed under anaerobic conditions. The deprotection may also be performed at ambient temperature or at temperatures of from about 20 – 60 °C (e.g. , 25, 30, 35, 40, 45, 50, or 55 °C).
The compound of formula (I) may be isolated in the form of a pharmaceutically acceptable salt. For example, the compound of formula (I) may be crystallized in the presence of HC1 to form the HC1 salt form of the compound. In some embodiments, the compound of formula (I) may be crystallized as the HBr salt form of the compound. The compound of formula (I) may also be isolated, e.g., by precipitation as a sodium salt by treating with NaOH. The compound of formula (I) is labile under certain reaction and storage conditions. In some embodiments, the final solution comprising the compound of formula (I) may be acidified by methods known in the art. For example, the compound of formula (I), if stored in solution, can be stored in an acidic solution.
In some embodiments, the compound of formula (I) may be prepared, for example, by: reacting a compound of formula (II- A):
with a compound of formula (III- A):
in the presence of a hydrazine to produce a compound of formula (IV- A):
selectively protecting the compound of formula (IV-A) to prepare a compound of formula (V-A):
wherein:
Rj is a protecting group, as defined above;
phosphorylating the compound of formula (V-A) to prepare a compound of formula (VI- A):
oxidizing the compound of formula (VI-A) to prepare a compound of formula (VII- A):
; and deprotecting the compound of formula (VII-A) to prepare the compound of formula (I). For example, a compound of formula (I) can be prepared as shown in Scheme 3.
Scheme 3.
5 R = Fraoc
In another embodiment, the compound of formula (I) is prepared by:
reacting a compound of formula (II- A):
with a compound of formula (III- A):
in the presence of a hydrazine to produce a compound of formula (IV-A):
selectively protecting the compound of formula (IV-A) to prepare a compound of formula (V-B):
wherein:
each Ri is independently a protecting group, as defined above;
phosphorylating the compound of formula (V-B) to prepare a compound of formula (VI-B):
oxidizing the compound of formula (VI-B) to prepare a compound of formula (VII-B):
; and deprotecting the compound of formula (VII-B) to prepare the compound of formula (I), example, a compound of formula (I) can be prepared as shown in Scheme 4.
Scheme 4.
Alternatively, a compound of formula (I) can be formed as shown in Scheme 5. A diaminopyrimidinone compound of formula (II) can be coupled with a phosphorylated hexose sugar of formula (VIII), to give a compound of formula (IX). The piperizine ring nitrogen atoms can be protected to give a compound of formula (X) which can be oxidized to give a diol of formula (XI). The diol of formula (XI) can then be deprotected using appropriate conditions and converted to the compound of formula (I).
Scheme 5
In this embodiment, the phosphate may be introduced at the beginning of the synthesis to avoid undesirable equilibrium between the pyrano and furano isomers during subsequent steps of the synthesis. For example, a compound of formula (I) can be prepared as shown in Scheme 6.
Scheme 6.
ridine
A compound of formula (I) can also be formed as shown in Scheme 7. A diaminopyrimidinone compound of formula (II) can be coupled to a compound of formula (III) to afford the piperizine derivative of formula (IV). The piperizine ring nitrogen atoms of the compound of formula (IV) can be protected under standard conditions to give a derivative of formula (V). The formula (V) structure can be oxidized to afford compounds of formula (XII). Phosphorylation of a compound of formula (XII) gives a compound of formula (VII). Global deprotection of the compound of formula (VII) can afford the compound of formula (I).
Scheme 7
Piperizine ring protection
sphorylation
(VII)
For example, a compound of formula (I) can be prepared as shown in Scheme 8.
Scheme 8.
FDA In India: Going Global, Coming Home, Altaf Ahmed Lal, Ph.D. is the Director of FDA’s office in India.

Altaf Ahmed Lal, Ph.D. is the Director of FDA’s office in India.
http://blogs.fda.gov/fdavoice/index.php/2013/09/fda-in-india-going-global-coming-home/
By: Altaf Ahmed Lal, Ph.D.
What is it like to be starting my new position as director of FDA’s office in India?
It’s like coming home.
http://blogs.fda.gov/fdavoice/index.php/2013/09/fda-in-india-going-global-coming-home/
My new tenure at FDA began in June, but as a former health attaché in the U.S. Embassy, I played an enthusiastic role in helping to establish FDA in my native country. I was born in Kashmir, India, and though I left the country in 1980 to explore new professional opportunities in the United States, I have since been drawn back again and again.
http://blogs.fda.gov/fdavoice/index.php/2013/09/fda-in-india-going-global-coming-home/
BAYER 2013 AND BEYOND
http://www.bayer.com/
Bayer
With 11 treatments in Phase I trials, 8 in Phase II, and 13 in Phase III, Bayer has a strong pipeline.
By far the most interest currently, given that the latest reports came out October 21st, is riociguat (BAY 63-2521),

which has had good news from its ongoing Phase III clinical trials of the treatment for pulmonary arterial hypertension, also known as PAH. PAH is a progressive condition that overburdens the heart.
Trials indicate subjects had improved heart function and could better tolerate physical exercise. Patients on riociguat improved their walking distance by 36 meters on average, while those on placebo showed no improvement.
Professor Hossein Ardeschir Ghofrani of University Hospital Giessen, the principal investigator, was quite pleased with the results and explained the value of the measurement. “The six-minute walk distance test is a well-validated clinical measure in patients with PAH, and therefore, the results of the PATENT-1 trial are encouraging. . .These data from the PATENT study suggest that riociguat may be a potential treatment option both for patients who have never been treated for PAH as well as for those who have received prior treatment.”
Hossein A. Ghofrani
Associate Professor of Internal Medicine,
MD (University of Giessen) 1995 Research interests: pulmonary hypertension, ischaemia-reperfusion, experimental therapeutics, clinical trials
http://www.uni-giessen.de/cms/fbz/fb11/forschung/graduierte/mbml/faculty
Although Bayer put forth no sales estimate for the treatment, analysts predicted 2017 sales from riociguat of $480 million

BAYER PIPELINE AS ON OCT 25 2013
phase 1
| Project | Indication |
|---|---|
| CDK-Inhibitor (BAY 1000394) | Cancer |
| Mesothelin-ADC (BAY 94-9343) | Cancer |
| PSMA Bi TE Antibody (BAY 2010112) | Cancer |
| PI3K-Inhibitor (BAY 1082439) | Cancer |
| FGFR2 Antibody (BAY 1179470) | Cancer |
| HIF-PH (BAY 85-3934) | Anemia |
| Partial Adenosine A1 Agonist(BAY 1067197) | Heart Failure |
| Vasopressin Receptor Antagonist(BAY 86-8050) | Heart Failure |
| sGC Stimulator (BAY 1021189) | Heart Failure |
| S-PRAnt (BAY 1002670) | Symptomatic uterine fibroids |
| BAY 1026153 | Endometriosis |
phase2
| Project | Indication |
|---|---|
| PI3K-Inhibitor (BAY 80-6946) | Cancer |
| Regorafenib | Cancer |
| Refametinib (MEK-Inhibitor) | Cancer |
| Radium-223-Dichloride | Cancer |
| Sorafenib | Additional Indications |
| MR-Antagonist (BAY 94-8862) | Congestive Heart Failure (CHF) |
| MR-Antagonist (BAY 94-8862) | Diabetic Nephopathy |
| Riociguat (sGC Stimulator) | Pulmonary Hypertension |
| Neutrophil Elastase Inhibitor(BAY 85-8501) | Bronchiectasis |
phase 3
| Project | Indication |
|---|---|
| Sorafenib | Breast Cancer |
| Sorafenib | Adjuvant HCC |
| Sorafenib | Adjuvant RCC |
| Regorafenib | HCC 2nd line |
| Rivaroxaban | Major Adverse Cardiac Events |
| Rivaroxaban | CHF and CAD |
| peg rFVIII(BAY 94-9027) | Hemophilia |
| Aflibercept | Myopic choroidal neovascularization (mCNV) |
| Aflibercept | Diabetic Macular Edema (DME) |
| LCS 16 | Contraception |
| Vaginorm | Vulvovaginal atrophy (VVA) |
| Sodium Deoxycholate | Submental fat removal |
| Cipro DPI | Lung infection |
| Tedizolid | Skin and Lung Infections |
| Amikacin Inhale | Gram-negative pneumonia |
Information for Download from bayer
Sorafenib tosylate
https://newdrugapprovals.wordpress.com/2013/07/16/nexavar-sorafenib/
TEDIZOLID PHOSPHATE
![]()
Leverkusen, October 8, 2013 – Following the recent commercial introduction of five new drugs to address the medical needs of patients with various diseases, Bayer is now accelerating the development of further five promising drug candidates which are currently undergoing phase I and II clinical studies. The company today announced that it plans to progress these five new highly innovative drug candidates in the areas of oncology, cardiology, and women’s health into phase III clinical studies by 2015.
“Our Pharma research and development has done a tremendous job of bringing five new products to the market offering physicians and patients new treatment alternatives for serious diseases”, said Bayer CEO Dr. Marijn Dekkers. “Following our mission statement ‘Science For A Better Life’, the five chosen further drug candidates all have the potential to impact the way diseases are treated for the benefit of patients.”

Bayer CEO Dr. Marijn Dekkers
“Our research and development activities are strongly focused on areas where treatment options are not available today or where true breakthrough innovations are missing”, said Prof. Andreas Busch, member of the Bayer HealthCare Executive Committee and Head of Global Drug Discovery at Bayer HealthCare. “Our drug development pipeline holds a number of promising candidates which we want to bring to patients who need them urgently”, said Kemal Malik, member of the Bayer HealthCare Executive Committee, Chief Medical Officer and Head of Pharmaceutical Development at Bayer HealthCare. “Furthermore we are continuing to expand the range of indications for all our recently launched products Xarelto, Stivarga, Xofigo, Riociguat as well as Eylea and further refine the profile of these drugs in specific patient populations.”
Cl 223Ra Cl
Xofigo
https://newdrugapprovals.wordpress.com/2013/09/21/xofigo-injection-recommended-for-approval-in-eu/
The five mid-stage candidates have been selected for accelerated development based on positive “proof-of-concept” data from early clinical studies. Three of them are development compounds in the area of cardiology or the cardio-renal syndrome: Finerenone (BAY 94-8862) is a next generation oral, non-steroidal Mineralocorticoid Receptor antagonist which blocks the deleterious effects of aldosterone. Currently available steroidal MR antagonists have proven to be effective in reducing cardiovascular mortality in patients with heart failure but have significant side effects that limit their utilization. Finerenone is currently in clinical Phase IIb development for the treatment of worsening chronic heart failure, as well as diabetic nephropathy.
Finerenone (BAY 94-8862)
The second drug candidate in the area of cardiology is an oral soluble guanylate cyclase (sGC) stimulator (BAY 1021189). The start of a Phase IIb study in patients with worsening chronic heart failure is expected later this year.
For the cardio-renal syndrome, a Phase IIb program with the investigational new drug Molidustat (BAY 85-3934) is under initiation in patients with anemia associated with chronic kidney disease and/or end-stage renal disease. Molidustat is a novel inhibitor of hypoxia-inducible factor (HIF) prolyl hydroxylase (PH) which stimulates erythropoietin (EPO) production and the formation of red blood cells. Phase I data have shown that inhibition of HIF-PH by Molidustat results in an increase in endogenous production of EPO.
Molidustat (BAY 85-3934)
In oncology, Copanlisib (BAY 80-6946), a novel, oral phosphatidylinositol-3 kinases (PI3K) inhibitor, was selected for accelerated development. Copanlisib demonstrated a broad anti-tumor spectrum in preclinical tumor models and promising early clinical signals in a Phase I study in patients with follicular lymphoma. A Phase II study in patients with Non-Hodgkin’s lymphoma is currently ongoing.
Bayer has also made good progress in the development of new treatment options for patients with gynecological diseases: sPRM (BAY 1002670) is a novel oral progesterone receptor modulator that holds the promises of long-term treatment of patients with symptomatic uterine fibroids. Based on promising early clinical data the initiation of a Phase III study is planned for mid-2014.
Initiation of further studies with recently launched products
Bayer has successfully launched five new pharmaceutical products, namely Xarelto™, Stivarga™, Xofigo™, Eylea™, and Riociguat, which has very recently been approved in Canada under the trade name Adempas™.


Regorafenib, stivarga
Bayer’s Eylea (aflibercept),
https://newdrugapprovals.wordpress.com/2013/06/01/lucentis-rival-one-step-away-from-nhs-approval/
Xarelto has been approved globally for five indications across seven distinct areas of use, allowing doctors to treat patients in a greater variety of venous and arterial thromboembolic conditions than any other novel oral anticoagulant. The company continues to study the use of Xarelto for the treatment of further cardiovascular diseases. Ongoing clinical Phase III studies include COMPASS and COMMANDER-HF. The COMPASS study will assess the potential use of Xarelto in combination with aspirin, or as a single treatment to prevent major adverse cardiac events (MACE) in nearly 20,000 patients with atherosclerosis related to coronary or peripheral artery disease. The COMMANDER-HF study will evaluate the potential added benefit of Xarelto in combination with single or dual-antiplatelet therapy to help reduce the risk of death, heart attack and stroke in approximately 5,000 patients with chronic heart failure and coronary artery disease, following hospitalization for exacerbation of their heart failure.
In order to answer medically relevant questions for specific patient populations Bayer has initiated a range of additional Xarelto studies in patients with atrial fibrillation (AF) undergoing percutaneous coronary intervention with stent placement (PIONEER-AF-PCI), cardioversion (X-VERT) or an AF ablation procedure (VENTURE-AF).
As an extension to the Xarelto clinical trial programme, a number of real-world studies are designed to observe and further evaluate Xarelto in everyday clinical practice. These include the XAMOS study of more than 17,000 orthopaedic surgery patients, which confirmed the clinical value of oral, once-daily Xarelto in routine clinical practice in adults following orthopaedic surgery of the hip or knee. XANTUS is designed to collate data on real-world protection with Xarelto in over 6,000 adult patients in Europe with non-valvular AF at risk of stroke while XANAP is designed to collate data on real-world protection with Xarelto in over 5,000 adult patients in Europe and Asia with non-valvular AF at risk of stroke. XALIA will generate information from over 4,800 patients treated for an acute DVT with either Xarelto or standard of care.
In the area of oncology, Stivarga has been approved in 42 countries for use against metastatic colorectal cancer that is refractory to standard therapies, and additionally for gastrointestinal stromal tumor (GIST) in the US and Japan. Bayer is now planning to assess Stivarga in earlier stages of colorectal cancer as well as other cancer types. A Phase III trial in patients with colorectal cancer after resection of liver metastases is currently under initiation. Based on early clinical data Bayer has also initiated a Phase III study in liver cancer in patients who have progressed on sorafenib treatment.
Furthermore, the anti-cancer drug Xofigo (radium 223 dichloride) is a first-in-class alpha-pharmaceutical which is designed for use in prostate cancer patients with ‘bone metastases’ (secondary cancers in the bone) to treat the cancer in the bone and to help extend their lives. Xofigo is approved in the US for the treatment of patients with advanced castrate-resistant prostate cancer with symptomatic bone metastases. In addition, the European CHMP recently gave a positive opinion for radium 223 dichloride for the same use. The decision of the European Commission on the approval is expected in the fourth quarter of 2013.
Based on the excellent Phase III results for Xofigo in patients with castration resistant prostate cancer and symptomatic bone metastases Bayer is looking to expand the use of Xofigo to earlier stages of the disease, and plans to initiate a Phase III study in combination with the novel anti-hormonal agent abiraterone. In addition, early stage signal-generating studies in other cancer forms where bone metastases are important causes of morbidity and mortality are planned.
In the area of pulmonary hypertension Adempas (Riociguat) is the first member of a novel class of compounds – so-called ‘soluble guanylate cyclase (sGC) stimulators’ – being investigated as a new and specific approach to treating different types of pulmonary hypertension (PH). Adempas has the potential to overcome a number of limitations of currently approved treatments for pulmonary arterial hypertension (PAH) and addresses the unmet medical need in patients with chronic thromboembolic pulmonary hypertension (CTEPH). It was approved for the treatment of CTEPH in Canada in September 2013, making it the world’s first drug approved in this deadly disease.
Riociguat has already shown promise as a potential treatment option beyond these two PH indications. An early clinical study was conducted in PH-ILD (interstitial lung disease), a disease characterized by lung tissue scarring (fibrosis) or lung inflammation which can lead to pulmonary hypertension, and, based on positive data, the decision was taken to initiate Phase IIb studies in PH-IIP (idiopathic pulmonary fibrosis), a subgroup of PH-ILD. Moreover, scientific evidence was demonstrated in preclinical models that the activity may even go beyond vascular relaxation. To prove the hypothesis Bayer is initiating clinical studies in the indication of systemic sclerosis (SSc), an orphan chronic autoimmune disease of the connective tissue affecting several organs and associated with high morbidity and mortality. If successful, Riociguat has the potential to become the first approved treatment for this devastating disease.
In the area of ophthalmology, Eylea (aflibercept solution for injection) is already approved in Europe and several additional countries for the treatment of neovascular (wet) age-related macular degeneration and for macular edema following central retinal vein occlusion. In September, Bayer HealthCare and Regeneron Pharmaceuticals presented data of the two phase III clinical trials VIVID-DME and VISTA-DME of VEGF Trap-Eye for the treatment of diabetic macular edema (DME) at the annual meeting of the Retina Society in Los Angeles and at the EURetina Congress in Hamburg, Germany. Both trials achieved the primary endpoint of significantly greater improvements in best-corrected visual acuity from baseline compared to laser photocoagulation at 52 weeks. Bayer plans to submit an application for marketing approval for the treatment of DME in Europe in 2013.
About Bayer HealthCare
The Bayer Group is a global enterprise with core competencies in the fields of health care, agriculture and high-tech materials. Bayer HealthCare, a subgroup of Bayer AG with annual sales of EUR 18.6 billion (2012), is one of the world’s leading, innovative companies in the healthcare and medical products industry and is based in Leverkusen, Germany. The company combines the global activities of the Animal Health, Consumer Care, Medical Care and Pharmaceuticals divisions. Bayer HealthCare’s aim is to discover, develop, manufacture and market products that will improve human and animal health worldwide. Bayer HealthCare has a global workforce of 54,900 employees (Dec 31, 2012) and is represented in more than 100 countries. More information at www.healthcare.bayer.com.
![]()
LY2189265 (dulaglutide), a glucagon-like peptide-1 analog as once-weekly treatment for type 2 diabetes.

DULAGLUTIDE
PRONUNCIATION doo” la gloo’ tide
THERAPEUTIC CLAIM Treatment of type II diabetes
CHEMICAL NAMES
1. 7-37-Glucagon-like peptide I [8-glycine,22-glutamic acid,36-glycine] (synthetic
human) fusion protein with peptide (synthetic 16-amino acid linker) fusion protein with immunoglobulin G4 (synthetic human Fc fragment), dimer
2. [Gly8,Glu22,Gly36]human glucagon-like peptide 1-(7-37)-peptidyltetraglycyl-Lseryltetraglycyl-L-seryltetraglycyl-L-seryl-L-alanyldes-Lys229-[Pro10,Ala16,Ala17]human immunoglobulin heavy constant γ4 chain H-CH2-CH3 fragment, (55-55′:58-58′)-bisdisulfide dimer
STRUCTURAL FORMULA
Monomer
HGEGTFTSDV SSYLEEQAAK EFIAWLVKGG GGGGGSGGGG SGGGGSAESK 50
YGPPCPPCPA PEAAGGPSVF LFPPKPKDTL MISRTPEVTC VVVDVSQEDP 100
EVQFNWYVDG VEVHNAKTKP REEQFNSTYR VVSVLTVLHQ DWLNGKEYKC 150
KVSNKGLPSS IEKTISKAKG QPREPQVYTL PPSQEEMTKN QVSLTCLVKG 200
FYPSDIAVEW ESNGQPENNY KTTPPVLDSD GSFFLYSRLT VDKSRWQEGN 250
VFSCSVMHEA LHNHYTQKSL SLSLG 275
Disulfide bridges location
55-55′ 58-58′ 90-150 90′-150′ 196-254 196′-254′
MOLECULAR FORMULA C2646H4044N704O836S18
MOLECULAR WEIGHT 59.67 kDa
MANUFACTURER Eli Lilly and Company
CODE DESIGNATION LY2189265
CAS REGISTRY NUMBER 923950-08-7
http://www.ama-assn.org/resources/doc/usan/dulaglutide.pdf
LY2189265 (dulaglutide), a glucagon-like peptide-1 analog, is a biologic entity being studied as a once-weekly treatment for type 2 diabetes.
Dulaglatuide works by stimulating cells to release insulin only when blood sugar levels are high.
Gwen Krivi, Ph.D., vice president, product development, Lilly Diabetes, said of the drug, “We believe dulaglutide, if approved, can bring significant benefits to people with type 2 diabetes.”
In fact, it might help to control both diabetics’ blood sugar and their high blood pressure.
Eli Lilly CEO John Lechleiter believes the drug has the potential to be a blockbuster. Lilly could be ready to seek approval by 2013.
For more information on dulaglutide clinical studies, click here.
PRESS RELEASES
Data Preseted at 49th EASD Annual Meeting Show Treatment with Lilly’s Investigational Dulaglutide Resulted in Improved Patient-Reported Health Outcomes – September 26, 2013
Lilly Announces Positive Results of Phase III Trials of Dulaglutide in Type 2 Diabetes – April 16, 2013
Lilly Diabetes Announces Positive Results of Phase III Trials of Dulaglutide in Type 2 Diabetes – October 22, 2012
Phase 3-LY2439821 (ixekizumab) for psoriasis and psoriatic arthritis.
 |
|
|---|---|
http://www.ama-assn.org/resources/doc/usan/ixekizumab.pdf
USAN IXEKIZUMAB
PRONUNCIATION ix” e kiz’ ue mab
THERAPEUTIC CLAIM Treatment of autoimmune diseases
CHEMICAL NAMES
1. Immunoglobulin G4, anti-(human interleukin 17A) (human monoclonal LY2439821γ4-chain), disulfide with human monoclonal LY2439821 κ-chain, dimer
2. Immunoglobulin G4, anti-(human interleukin-17A (IL-17, cytotoxic
T-lymphocyte-associated antigen 8)); humanized mouse monoclonal LY2439821 des-Lys446-[Pro227]γ4 heavy chain {H10S>P,CH3107K>-} (133-219′)-disulfide with humanized mouse monoclonal LY2439821 κ light chain, dimer (225-225”:228-228”)-bisdisulfide
MOLECULAR FORMULA C6492H10012N1728O2028S46
MOLECULAR WEIGHT 146.2 kDa
SPONSOR Eli Lilly and Co.
CODE DESIGNATION LY2439821
CAS REGISTRY NUMBER 1143503-69-8
Ixekizumab is a humanized monoclonal antibody used in the treatment of autoimmune diseases.[1]
Ixekizumab was developed by Eli Lilly and Co.
Lilly’s Anti-IL-17 Monoclonal Antibody, Ixekizumab, Met Primary Endpoint in Phase II Study in Patients With Chronic Plaque Psoriasis – March 28, 2012
more info
Inflammation represents a key event of many diseases, such as psoriasis, inflammatory bowel diseases, rheumatoid arthritis, asthma, multiple sclerosis,
atherosclerosis, cystic fibrosis, and sepsis. Inflammatory cells, such as neutrophils, eosinophils, basophils, mast cells, macrophages, endothelial cells, and platelets, respond to inflammatory stimuli and foreign substances by producing bioactive mediators. These mediators act as autocrines and paracrines by interacting with many cell types to promote the inflammatory response. There are many mediators that can promote inflammation, such as cytokines and their receptors, adhesion molecules and their receptors, antigens involved in lymphocyte activation, and IgE and its receptors. [0004] Cytokines, for example, are soluble proteins that allow for communication between cells and the external environment. The term cytokines includes a wide range of proteins, such as lymphokines, monokines, interleukins, colony stimulating factors, interferons, tumor necrosis factors, and chemokines. Cytokines serve many functions, including controlling cell growth, migration, development, and differentiation, and mediating and regulating immunity, inflammation, and hematopoiesis. Even within a given function, cytokines can have diverse roles. For example, in the context of mediating and regulating inflammation, some cytokines inhibit the inflammatory response (anti-inflammatory cytokines), others promote the inflammatory response (pro-inflammatory cytokines). And certain cytokines fall into both categories, i.e., can inhibit or promote inflammation, depending on the situation. The targeting of proinflammatory cytokines to suppress their natural function, such as with antibodies, is a well-established strategy for treating various inflammatory diseases.
Many inflammatory diseases are treated by targeting proinflammatory cytokines with antibodies. Most (if not all) of the anti-proinflammatory cytokine antibodies currently on the market, and those currently in clinical trials, are of the IgG class. See, for example, Nature Reviews, vol. 10, pp. 301-316 (2010); Nature Medicine, vol. 18, pp. 736-749 (2012); Nature Biotechnology, vol. 30, pp. 475-477 (2012); Anti-Inflammatory & Anti- Allergy Agents in Medicinal Chemistry, vol. 8, pp. 51-71 (2009);
FlOOO.com/Reports/Biology/content/1/70, F 1000 Biology Reports, 1 :70 (2009); mAbs 4: 1, pp. 1-3 (2012); mAbs 3: 1, pp. 76-99 (2011); clinicaltrials.gov (generally), and
clinicaltrialsregister.eu/ (generally). These IgG antibodies are administered systemically and thus are often associated with unwanted side effects, which can include one or more of, for example, infusion reactions and immunogenicity, hypersensitivity reactions,
immunosuppression and infections, heart problems, liver problems, and others. Additionally the suppression of the target cytokines at non-diseased parts of the body can lead to unwanted effects.
In an attempt to reduce side effects associated with systemic treatment and to eliminate the inconvenience and expense of infusions, an article proposed an oral anti-TNF therapy that could be useful in treating Crohn’ s disease. Worledge et al. “Oral Administration of Avian Tumor Necrosis Factor Antibodies Effectively Treats Experimental Colitis in Rats.” Digestive Diseases and Sciences 45(12); 2298-2305 (December 2000). This article describes immunizing hens with recombinant human TNF and an adjuvant, fractionating polyclonal yolk antibody (IgY, which in chickens is the functional equivalent to IgG), and administering the unformulated polyclonal IgY (diluted in a carbonate buffer to minimize IgY acid hydrolysis in the stomach) to rats in an experimental rodent model of colitis. The rats were treated with 600mg/kg/day of the polyclonal IgY. The uses of animal antibodies and polyclonal antibodies, however, are undesirable.
In a similar attempt to avoid adverse events associated with systemic administration, another group, Avaxia Biologies Inc., describes a topical (e.g., oral or rectal) animal-dervied polyclonal anti-TNF composition that could be useful in treating
inflammation of the digestive tract, such as inflammatory bowel disease. WO2011047328. The application generally states that preferably the polyclonal antibody composition is prepared by immunizing an animal with a target antigen, and the preferably the polyclonal antibody composition is derived from milk or colostrum with bovine colostrums being preferred (e.g., p. 14). The application also generally states that the animal derived polyclonal antibodies could be specific for (among other targets) other inflammatory cytokines (e.g., pp. 6-7). This application describes working examples in which cows were immunized with murine TNF and the colostrum was collected post-parturition to generate bovine polyclonal anti-TNF antibodies (designated as AVX-470). The uses of animal-derived antibodies and polyclonal antibodies, however, are undesirable.
IgA molecular forms have been proposed as treatments for various diseases, most notably as treatments for pollen allergies, as treatments against pathogens, and as treatments for cancer.
For example, one article describes anti-AmbCtl (a ragweed pollen antigen) humanized monomelic IgA and dimeric IgA antibodies made in murine cells (NSO and Sp2/0 cells). The dimeric IgA contains a mouse J-chain. The article proposes that the antibodies may be applied to a mucosal surface or the lower airway to inhibit entry of allergenic molecules across the mucosal epithelium and therefore to prevent the development of allergic response. Sun et al. “Human IgA Monoclonal Antibodies Specific for a Major Ragweed Pollen Antigen.” Nature Biotechnology 13, 779-786 (1995).
Several other articles propose the use of IgA antibodies as a defense against pathogens.
Two articles proposed the use of an anti-streptococcal antigen I II secretory IgA-G hybrid antibody. Ma et al. “Generation and Assembly of Secretory Antibodies in Plants.” Science 268(5211), 716-719 (May 1995); Ma et al. “Characterization of a
Recombinant Plant Monoclonal Secretory Antibody and Preventive Immunotherapy in Humans.” Nature Medicine 4(5); 601-606 (May 1998). The hybrid antibody contains murine monoclonal kappa light chain, hybrid Ig A-G heavy chain, murine J- Chain, and rabbit secretory component. The antibody was made by successive sexual crossing between four transgenic N. tabacum plants and filial recombinants to form plant cells that expressed all four protein chains simultaneously. The parent antibody (the source of the antigen binding regions, is identified as the IgG antibody Guy’s 13. The group proposes that although slgA may provide an advantage over IgG in the mucosal environment, such is not always the case (1998 Ma at p. 604, right column).
A related article identifies the anti-streptococcal antigen I/II secretory IgA-G hybrid antibody, which was derived from Guy’s 13 IgA, as CaroRx. Wycoff. “Secretory IgA Antibodies from Plants.” Current Pharmaceutical Design 10(00); 1-9 (2004). Planet Biotechnology Inc. This related article states that the CaroRx antibody was designed to block adherence to teeth of the bacteria that causes cavities. Apparently, the CaroRx antibody was difficult to purify; the affinity of Protein A for the murine Ig domain was too low and protein G was necessary for sufficient affinity chromatography. Furthermore, the article states that several other chromatographic media had shown little potential as purification steps for the hybrid slgA-G from tobacco leaf extracts. The article also indicates that the authors were unable to control for human-like glycosylation in tobacco, but that such was not a problem because people are exposed to plant glycans every day in food without ill effect.
WO9949024, which lists Wycoff as an inventor, Planet Biotechnology Inc. as the applicant, describes the use of the variable regions of Guy’s 13 to make a secretory antibody from tobacco. The application contains only two examples – the first a working example and the second a prophetic example. Working Example 1 describes the transient production of an anti-S. mutans SA I/III (variable region from Guy’s 13) in tobacco. The tobacco plant was transformed using particle bombardment of tobacco leaf disks. Transgenic plants were then screened by Western blot “to identify individual transformants expressing assembled human slgA” (p. 25). Prophetic Example 2 states that in a transformation system for Lemna gibba (a monocot), bombardment of surface-sterilized leaf tissue with DNA- coated particles “is much the same as with” tobacco (a dicot). The prophetic example also stops at screening by immunoblot analysis for antibody chains and assembled slgA, and states that the inventors “expect to find fully assembled slgA.” [0014] Another article proposed the use of an anti-RSV glycoprotein F IgA antibodies (mlgA, dlgA, and slgA). Berdoz et al. “In vitro Comparison of the Antigen-Binding and Stability Properties of the Various Molecular Forms of IgA antibodies Assembled and Produced in CHO Cells.” Proc. Natl. Acad. Sci. USA 96; 3029-3034 (March 1999). The slgA antibody was made in CHO cells sequentially transfected with chimeric heavy and light chains, human J-Chain, and human secretory component, respectively. Single clones were generated to express the mlgA (clone 22), the dlgA (clone F), and the slgA (clone 6) (p. 3031).
Still other articles proposed, for example: (1) anti-HSV mlgA made in maize (Karnoup et al. Glycobiology 15(10); 965-981 (May 2005)) (which states that at that time there had been little success in the application of IgA class antibodies to therapeutic use because of the difficulty in producing the dimeric form in mammalian cells at economic levels); (2) anti-C. difficile toxin A chimeric mouse-human monomeric and dimeric IgA made in CHO cells (Stubbe et al. Journal of Immunology 164; 1952-1960 (2000)); (3) anti-N. meningitidis chimeric IgA antibodies were produced in BHK cells cotransfected with human J-Chain and/or human secretory component (Vidarsson et al., Journal of Immunology 166; 6250-6256 (2001)); (4) mti-Pseudomonas aeruginosa 06 lipopolysaccharide chimeric mouse/human mlgAl made in CHO cells (Preston et al. Infection and Immunity 66(9); 4137- 4142 (September 1998)); (5) anti-Plasmodium mlgA made in CHO cells (Pleass et al. Blood 102(13); 4424-4429 (December 2003)) (which states that unlike their parental mouse IgG antibodies, the mlgA antibodies failed to protect against parasitic challenge in vivo); and (5) ^^-Helicobacter pylori urease subunit A slgA and dlgA (Berdoz et al. Molecular
Immunology 41(10); 1013-1022 (August 2004)). [0016] For a review article discussing passive and active protection against pathogens at mucosal surfaces, see Corthesy. “Recombinant Immunoglobulin A: Powerful Tools for Fundamental and Applied Research.” Trends in Biotechnology 20(2); 65-71 (February 2002).
Still other articles propose the use of IgA antibodies as a treatment for cancer.
For example, one article describes a Phase la trial of a muring anti-transferrin receptor IgA antibody (Brooks et al. “Phase la Trial of Murine Immunoglobulin A
Antitransferrin Receptor Antibody 42/6.” Clinical Cancer Research 1(11); 1259-1265 (November 1995)). Another article describes a human anti-Ep-CAM mIgA made in BHK (baby hamster kidney) cells (Huls et al. “Antitumor Immune Effector Mechanisms Recruited by Phase Display-Derived Fully Human IgGl and IgAl Monoclonal Antibodies.” Cancer Research 59; 5778-5784 (November 1999)). Still another article describes an anti-HLA Class II chimeric mIgA antibody made in BHK cells (Dechant et al. “Chimeric IgA Antibodies Against HLA Class II Effectively Trigger Lymphoma Cell Killing.” Blood 100(13); 4574- 4580 (December 2002)). Yet other articles describe anti-EGFR mIgA or dlgA antibodies made in CHO, including Dechant et al. “Effector Mechanisms of Recombinant IgA
Antibodies Against Epidermal Growth Factor Receptor.” Journal of Immunology 179; 2936- 2943 (2007), Beyer et al. “Serum- Free Production and Purification of Chimeric IgA
Antibodies.” Journal of Immunology 346; 26-37 (2009) (stating that as of 2009, IgA antibodies have not been commercially explored for problems including lack of production and purification methods), and Lohse et al. “Recombinant Dimeric IgA Antibodies Against the Epidermal Growth Factor Receptor Mediate Effective Tumor Cell Killing.” Journal of Immunology 186; 3770-3778 (February 2011).
For a review article on anti-cancer IgA antibodies, see Dechant et al. “IgA antibodies for Cancer Therapy. ” Critical Reviews in Oncology/Hematology 39; 69-77 (2001); states that compared with infectious diseases, the role of IgA in cancer immunotherapy is even less investigated).
IL17 and IFN-garama inhibition for the treatment of autoimmune inflammation
The IL-17 family of cytokines has been associated with the pathogenesis of autoimmune diseases and is generally blamed for the pathogenic symptoms of autoimmune inflammation. Overexpression of IL-17 is a hallmark for autoimmune diseases like rheumatoid arthritis, systemic lupus erythematomatosus, inflammatory bowel disease, multiple sclerosis, and psoriasis (Yao Z et. al., J Immunol, 155(12), 1995, 5483-6. Chang S H, et.al, Cytokine, 46, 2009, 7-11; Hisakata Yamada et.al, Journal of Inflamm. Res., 3, 2010, 33-44)).
The IL-17 cytokine family comprises six members, out of which IL-17 A and IL-17F are the best characterized. IL-17A and IL-17F exist as homo- as well as as heterodimers (IL-17AA, IL-17AF, IL-17FF). IL-17A and IL-17F are clearly associated with inflammation (Gaffen S H, Cytokine, 43, 2008, 402-407; Torchinsky M B et al, Cell. Mol. Life Sci., 67, 2010, 1407- 1421).
The secretion of IL-17 is predominantly caused by a specific subtype of T helper cells termed TH-17 cells. IL-23, TGFp and IL-6 were shown to be important factors leading to conversion of nai‘ve CD4+ T-cells to THl 7 cells. It was also reported that TGF and IL-6 potently induce in synergy THl 7 differentiation. Important transcription factors for the secretion of IL-17 from TH17 cells are RORyt and STAT3 (IvanovJ et.al. Cell 126, 2006, 1121-1133). IL-17 induces pro-inflammatory cytokines (IL-6, TNF- and IL-lb) and Chemokines (CXCL1,GCP-2,CXCL8 or IL-8,CINC,MCP-1). It increases the production of nitric oxide prostaglandin E2 and matrix-metalloproteinases. As a consequence of these events neutrophil infiltration, tissue damage and chronic inflammation occurs (PECK A et.al, Clin Immunol., 132(3), 2009, 295-304).
Before the recognition of the importance of IL-17 in autoimmune inflammation, IFN-gamma derived from THl cells was believed to be an important cytokine that drives autoimmune disorders (Takayanagi H et. al. Nature, 408, 2000, 600-605. Huang W. et. al. Arthritis Res. Ther., 5, 2002, R49-R59) The secretion of IFN-gamma is a key feature of the THl effector cell lineage and the secretion is regulated by the transcription factors T-bet and STAT4 (Bluestone JA et. al. Nat Rev Immunol, 11, 2009, 811-6). Infiltration of activated T-cells and elevation of M-CSF, IL-10 and TNF support this notion (Yamanda H et.al Ann. Rheu. Dis., 67, 2008, 1299-1304; Kotake S et.al. Eur. J. Immunol, 35, 2005, 3353-3363).
Recently, a more complex situation was proposed, where hybrid TH17/TH1 cells induced by IL-23 and IL-6 in concert with IL-1 secrete IL-17 and IFN-gamma. These cells are under the control of the transcription factors RORyt and T-bet, confirming the notion, that these are true hybrids of THl and THl 7 cells. It was also demonstrated that these double producing cells are the pathogenic species in IBD and EAE (Buonocore S et.al. Nature, 464, 2010, 1371-5; Ghoreshi K. et. al. Nature, 467, 2010, 967-971).
Compounds which target and suppress both IL-17 and IFN-gamma are predisposed for the treatment of autoimmune disorders.
The effectiveness of blocking IL-17 signaling as therapeutic treatment in autoimmune diseases has already been proven in clinical trials with e.g. monoclonal antibodies against IL- 17A (AIN457, secukinumab; Ly2439821,ixekizumab; RG4934) and/or the IL-17 receptor IL- 17RA (AMG827, brodalumab).
Positive results have been reported for the treatment of rheumatoid arthritis, psoriasis and uveitis (Hueber W et al, Sci. Transl. Med., 2, 2010, 52ra72, DOI: 10.1126/scitranslmed.3001107; van den Berg W B e/ al, Nat. Rev. Rheumatol, 5, 2009, 549-553), ankylosing spondylitis and spondyloarthritides (Song I-H et al, Curr. Opin. Rheumatol., 23, 2011, 346-351).
Secukinumab is currently under investigation in clinical trials for psoriatic arthritis, Behcet disease, uveitits, inflammatory bowel disease, Crohn’s disease, multiple sclerosis (Kopf M et al., Nat. Rev. Drug Disc, 9, 2010, 703-718; Song I-H et al, Curr. Opin. Rheumatol., 23, 2011, 346-351).
Brodalumab, Ixekizumab and RG4934 are currently in clinical trials for the treatment of rheumatoid arthritis, psoriasis and/or psoriatic arthritis (Kopf M et al, Nat. Rev. Drug Disc, 9, 2010, 703-718; clinicaltrials.gov; Medicines in development for skin diseases, 201 1, published by PhRMA, www .phrma. com) .
With regard to blocking of IFN-gamma signaling as therapeutic treatment in autoimmune diseases, the IFN-gamma-specific monoclonal antibody AMG811 is currently under clinical investigations for the treatment of systemic lupus erythematosus (Kopf M et al., Nat. Rev. Drug Disc, 9, 2010, 703-718).
LASTACAFT, ALCAFTADINE.. Drug Patent Expiration, 21st Nov 2013
ALCAFTADINE
Alcaftadine is used to prevent eye irritation brought on by allergic conjunctivitis. It is a H1histamine receptor antagonist.
It was approved by the U.S. Food and Drug Administration in 2010 under the trade name Lastacaft.
LASTACAFT, ALLERGAN
Drug Patent Expiration and Exclusivity
| Active Ingredient | Form | Dosage | Drug Type | Application | Product | |
|---|---|---|---|---|---|---|
| ALCAFTADINE | SOLUTION/DROPS; OPHTHALMIC | 0.25% | RX | 022134 | 001 |
Patents
There are 1 patent(s) protecting ALLERGAN’s LASTACAFT.
The last patent expires on 2013-11-21.
| Patent | Expiration | |
|---|---|---|
| US5468743 | Imidazo[2,1-b]benzazepine derivatives, compositions and method of use
The present invention is concerned with novel imidazo[2, 1-b][3]benzazepines of formula ##STR1## the pharmaceutically acceptable addition salts and stereochemically isomeric forms thereof, wherein each of the dotted lines independently represents an optional bond; R.sup.1 represents hydrogen, halo, C.sub.1-4 alkyl or C.sub.1-4 alkyloxy; R.sup.2 represents hydrogen, halo, C.sub.1-4 alkyl or C.sub.1-4 alkyloxy; R.sup.3 represents hydrogen, C.sub.1-4 alkyl, ethenyl substituted with hydroxycarbonyl or C.sub.1-4 alkyloxycarbonyl, C.sub.1-4 alkyl substituted with hydroxycarbonyl or C.sub.1-4 alkyloxycarbonyl, hydroxyC.sub.1-4 alkyl, formyl or hydroxycarbonyl; R.sup.4 represents hydrogen, C.sub.1-4 alkyl, hydroxyC.sub.1-4 alkyl, phenyl or halo; R.sup.5 represents hydrogen, C.sub.1-4 alkyl or halo; L represents hydrogen; C.sub.1-6 alkyl; C.sub.1-6 alkyl substituted with one substituent selected from the group consisting of hydroxy, halo, C.sub.1-4 alkyloxy, hydroxycarbonyl, C.sub.1-4 alkyloxycarbonyl, C.sub.1-4 alkyloxycarbonyl-C.sub.1-4 alkyloxy, hydroxycarbonylC.sub.1-4 alkyloxy, C.sub.1-4 alkyloxycarbonylamino, C.sub.1-4 alkylaminocarbonyl, C.sub.1-4 alkylaminocarbonylamino, C.sub.1-4 alkylaminothiocarbonylamino, aryl, aryloxy and arylcarbonyl; C.sub.1-6 alkyl substituted with both hydroxy and aryloxy; C.sub.3-6 alkenyl; C.sub.3-6 alkenyl substituted with aryl; or, L represents a radical of formula –Alk–Y–Het.sup.1 (a-1),–Alk–NH–CO–Het.sup.2 (a-2)or –Alk–Het.sup.3 (a-3); provided that 6,11-dihydro-11-(4-piperidinylidene)-5H-imidazo[2,1-b][3]benzazepine is ecxluded, which are useful antiallergic compounds.Compositions comprising said compounds, methods of using and processes for preparing the same.
|
2013-11-21 |
Exclusivity
Exclusivity is marketing rights granted by the FDA to the ALLERGAN.
Exclusivity ends on 2015-07-28.
| Date | Supplement No. | Action | Documents |
|---|---|---|---|
| 2010-07-28 | 000 | Approval |

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....