The US Food and Drug Administration has approved AstraZeneca’s Movantik for opioid-induced constipation in adults with chronic non-cancer pain.
Home » Posts tagged 'fda' (Page 4)
Tag Archives: fda
FDA Approves Blincyto (blinatumomab) for Precursor B-Cell Acute Lymphoblastic Leukemia
 Blinatumomab linking a T cell to a malignant B cell.
Blinatumomab linking a T cell to a malignant B cell.
FDA Approves Blincyto (blinatumomab) for Precursor B-Cell Acute Lymphoblastic Leukemia
December 3, 2014 — The U.S. Food and Drug Administration today
approved Blincyto (blinatumomab) to treat patients with Philadelphia
chromosome-negative precursor B-cell acute lymphoblastic leukemia
(B-cell ALL), an uncommon form of ALL.

Blinatumomab (AMG103) is a drug that has anti-cancer properties. It belongs to a new class of constructed monoclonal antibodies,bi-specific T-cell engagers (BiTEs), that exert action selectively and direct the human immune system to act against tumor cells. Blinatumomab specifically targets the CD19 antigen present on B cells.[1]
The drug was developed by a German-American company Micromet, Inc. in cooperation with Lonza; Micromet was later purchases by Amgen, which has furthered the drug’s clinical trials. In July 2014, the FDA granted breakthrough therapy status to blinatumomab for the treatment of acute lymphoblastic leukemia (ALL).[2] In October 2014, Amgen’s Biologics License Application for blinatumomab was granted priority review designation by the FDA, thus establishing a deadline of May 19, 2015 for completion of the FDA review process.[3]
Structure and mechanism of action

Blinatumomab linking a T cell to a malignant B cell.
Blinatumomab enables a patient’s T cells to recognize malignant B cells. A molecule of blinatumomab combines two binding sites: a CD3site for T cells and a CD19 site for the target B cells. CD3 is part of the T cell receptor. The drug works by linking these two cell types andactivating the T cell to exert cytotoxic activity on the target cell.[4] CD3 and CD19 are expressed in both pediatric and adult patients, making blinatumomab a potential therapeutic option for both pediatric and adult populations.[5]
Therapeutic use
Clinical trials
In a phase 1 clinical study with blinatumomab, patients with non-Hodgkin’s lymphoma showed tumor regression, and in some cases complete remission.[6] There are ongoing phase 1 and phase 2 clinical trials of blinatumomab in patients with acute lymphoblastic leukemia (ALL).[7] One phase II trial for ALL reported good results in 2010 and another is starting.[8]
Adverse effects
Common side effects observed in Phase 2 trials are listed below; they were temporary and typically occurred during the first treatment cycle:[5]
- Flu-like symptoms (i.e. fever, headache, and fatigue)
- Tremor
- Weight increase
- Hypokalemia
- Decrease of blood immunoglobulin
CNS effects were also observed during clinical trials and were treated via a lower dose of blinatumomab, administration of dexamethasone, or treatment discontinuation. Because the side effects were reversible, early monitoring for the CNS symptoms listed below is important:[5]
- Seizure
- Encephalopathy
- Tremor
- Apraxia
- Speech disorders
- Disorientation
Less common side effects include cytokine release syndrome and immunogenicity.[5]
References
- Statement on a Nonproprietary Name adopted by the USAN Council: Blinatumomab
- Amgen Receives FDA Breakthrough Therapy Designation For Investigational BiTE® Antibody Blinatumomab In Acute Lymphoblastic Leukemia
- Amgen’s BiTE® Immunotherapy Blinatumomab Receives FDA Priority Review Designation In Acute Lymphoblastic Leukemia
- Mølhøj, M; Crommer, S; Brischwein, K; Rau, D; Sriskandarajah, M; Hoffmann, P; Kufer, P; Hofmeister, R; Baeuerle, PA (March 2007). “CD19-/CD3-bispecific antibody of the BiTE class is far superior to tandem diabody with respect to redirected tumor cell lysis”. Mol Immunol 44 (8): 1935–43. doi:10.1016/j.molimm.2006.09.032. PMID 17083975.
- Background Information for the Pediatric Subcommittee of the Oncologic Drugs Advisory Committee Meeting 04 December 2012
- Bargou, R; et al. (2008). “Tumor regression in cancer patients by very low doses of a T cell-engaging antibody”. Science 321 (5891): 974–977. doi:10.1126/science.1158545.PMID 18703743.
- ClinicalTrials.gov NCT00560794 Phase II Study of the BiTE Blinatumomab (MT103) in Patients With Minimal Residual Disease of B-precursor Acute ALL
- “Micromet initiates MT103 phase 2 trial in adult ALL patients”. 20 Sep 2010.
External links
| Monoclonal antibody | |
|---|---|
| Type | Bi-specific T-cell engager |
| Source | Mouse |
| Target | CD19, CD3 |
| Clinical data | |
| Legal status |
?
|
| Identifiers | |
| CAS number | 853426-35-4 |
| ATC code | None |
| UNII | 4FR53SIF3A |
| Chemical data | |
| Formula | C2367H3577N649O772S19 |
| Mol. mass | 54.1 kDa |
Regeneron and Sanofi’s dupilumab gets FDA breakthrough therapy status for atopic dermatitis
// // //
Regeneron Pharmaceuticals and Sanofi’s dupilumab has received breakthrough therapy designation from US Food and Drug Administration (FDA) to treat adults with moderate-to-severe atopic dermatitis (AD).
ROFECOXIB

ROFECOXIB
MK-966, MK-0966, Vioxx
162011-90-7
Rofecoxib /ˌrɒfɨˈkɒksɪb/ is a nonsteroidal anti-inflammatory drug (NSAID) that has now been withdrawn over safety concerns. It was marketed by Merck & Co. to treat osteoarthritis, acute pain conditions, and dysmenorrhoea. Rofecoxib was approved by the Food and Drug Administration (FDA) on May 20, 1999, and was marketed under the brand names Vioxx, Ceoxx, and Ceeoxx.
No Exclusivity found
| Patent No | Expirey Date | patent use code |
|---|---|---|
| 5474995 | Jun 24, 2013 | U-602 |
| 5474995*PED | Dec 24, 2013 | |
| 5691374 | May 18, 2015 | |
| 5691374*PED | Nov 18, 2015 | |
| 6063811 | May 6, 2017 | U-602 |
| 6063811*PED | Nov 6, 2017 | |
| 6239173 | Jun 24, 2013 | U-602 |
| 6239173*PED | Dec 24, 2013 |
 |
|
 |
|
| Systematic (IUPAC) name | |
|---|---|
| 4-(4-methylsulfonylphenyl)-3-phenyl-5H-furan-2-one | |
| Clinical data | |
| Pregnancy cat. | C (AU) |
| Legal status | Prescription Only (S4) (AU)withdrawn |
| Routes | oral |
| Pharmacokinetic data | |
| Bioavailability | 93% |
| Protein binding | 87% |
| Metabolism | hepatic |
| Half-life | 17 hours |
| Excretion | biliary/renal |
| Identifiers | |
| CAS number | 162011-90-7 |
| ATC code | M01AH02 |
| PubChem | CID 5090 |
| DrugBank | DB00533 |
| ChemSpider | 4911 |
| UNII | 0QTW8Z7MCR |
| Chemical data | |
| Formula | C17H14O4S |
| Mol. mass | 314.357 g/mol |
Rofecoxib gained widespread acceptance among physicians treating patients with arthritis and other conditions causing chronic or acute pain. Worldwide, over 80 million people were prescribed rofecoxib at some time.[1]
On September 30, 2004, Merck withdrew rofecoxib from the market because of concerns about increased risk of heart attack and stroke associated with long-term, high-dosage use. Merck withdrew the drug after disclosures that it withheld information about rofecoxib’s risks from doctors and patients for over five years, resulting in between 88,000 and 140,000 cases of serious heart disease.[2] Rofecoxib was one of the most widely used drugs ever to be withdrawn from the market. In the year before withdrawal, Merck had sales revenue of US$2.5 billion from Vioxx.[3] Merck reserved $970 million to pay for its Vioxx-related legal expenses through 2007, and have set aside $4.85bn for legal claims from US citizens.
Rofecoxib was available on prescription in both tablet-form and as an oral suspension. It was available by injection for hospital use.

Mode of action
Cyclooxygenase (COX) has two well-studied isoforms, called COX-1 and COX-2. COX-1 mediates the synthesis of prostaglandinsresponsible for protection of the stomach lining, while COX-2 mediates the synthesis of prostaglandins responsible for pain and inflammation. By creating “selective” NSAIDs that inhibit COX-2, but not COX-1, the same pain relief as traditional NSAIDs is offered, but with greatly reduced risk of fatal or debilitating peptic ulcers. Rofecoxib is a selective COX-2 inhibitor, or “coxib”.
Others include Merck’s etoricoxib (Arcoxia), Pfizer’s celecoxib (Celebrex) and valdecoxib (Bextra). Interestingly, at the time of its withdrawal, rofecoxib was the only coxib with clinical evidence of its superior gastrointestinal adverse effect profile over conventional NSAIDs. This was largely based on the VIGOR (Vioxx GI Outcomes Research) study, which compared the efficacy and adverse effect profiles of rofecoxib and naproxen.[4]
Pharmacokinetics
The therapeutic recommended dosages were 12.5, 25, and 50 mg with an approximate bioavailability of 93%.[5][6][7] Rofecoxib crossed the placenta and blood–brain barrier,[5][6][8]and took 1–3 hours to reach peak plasma concentration with an effective half-life (based on steady-state levels) of approximately 17 hours.[5][7][9] The metabolic products are cis-dihydro and trans-dihydro derivatives of rofecoxib[5][9] which are primarily excreted through urine.
Fabricated efficacy studies
On March 11, 2009, Scott S. Reuben, former chief of acute pain at Baystate Medical Center, Springfield, Mass., revealed that data for 21 studies he had authored for the efficacy of the drug (along with others such as celecoxib) had been fabricated in order to augment the analgesic effects of the drugs. There is no evidence that Reuben colluded with Merck in falsifying his data. Reuben was also a former paid spokesperson for the drug company Pfizer (which owns the intellectual property rights for marketing celecoxib in the United States). The retracted studies were not submitted to either the FDA or the European Union’s regulatory agencies prior to the drug’s approval. Drug manufacturer Merckhad no comment on the disclosure.[10]
Adverse drug reactions
Aside from the reduced incidence of gastric ulceration, rofecoxib exhibits a similar adverse effect profile to other NSAIDs.
Prostaglandin is a large family of lipids. Prostaglandin I2/PGI2/prostacyclin is just one member of it. Prostaglandins other than PGI2 (such as PGE2) also play important roles in vascular tone regulation. Prostacyclin/thromboxane are produced by both COX-1 and COX-2, and rofecoxib suppresses just COX-2 enzyme, so there is no reason to believe that prostacyclin levels are significantly reduced by the drug. And there is no reason to believe that only the balance between quantities of prostacyclin and thromboxane is the determinant factor for vascular tone.[11] Indeed Merck has stated that there was no effect on prostacyclin production in blood vessels in animal testing.[12] Other researchers have speculated that the cardiotoxicity may be associated with maleic anhydride metabolites formed when rofecoxib becomes ionized under physiological conditions. (Reddy & Corey, 2005)
Adverse cardiovascular events
VIGOR study and publishing controversy
The VIGOR (Vioxx GI Outcomes Research) study, conducted by Bombardier, et al., which compared the efficacy and adverse effect profiles of rofecoxib and naproxen, had indicated a significant 4-fold increased risk of acute myocardial infarction (heart attack) in rofecoxib patients when compared with naproxen patients (0.4% vs 0.1%, RR 0.25) over the 12 month span of the study. The elevated risk began during the second month on rofecoxib. There was no significant difference in the mortality from cardiovascular events between the two groups, nor was there any significant difference in the rate of myocardial infarction between the rofecoxib and naproxen treatment groups in patients without high cardiovascular risk. The difference in overall risk was by the patients at higher risk of heart attack, i.e. those meeting the criteria for low-dose aspirin prophylaxis of secondary cardiovascular events (previous myocardial infarction, angina, cerebrovascular accident, transient ischemic attack, or coronary artery bypass).
Merck’s scientists interpreted the finding as a protective effect of naproxen, telling the FDA that the difference in heart attacks “is primarily due to” this protective effect (Targum, 2001). Some commentators have noted that naproxen would have to be three times as effective as aspirin to account for all of the difference (Michaels 2005), and some outside scientists warned Merck that this claim was implausible before VIGOR was published.[13] No evidence has since emerged for such a large cardioprotective effect of naproxen, although a number of studies have found protective effects similar in size to those of aspirin.[14][15] Though Dr. Topol’s 2004 paper criticized Merck’s naproxen hypothesis, he himself co-authored a 2001 JAMA article stating “because of the evidence for an antiplatelet effect of naproxen, it is difficult to assess whether the difference in cardiovascular event rates in VIGOR was due to a benefit from naproxen or to a prothrombotic effect from rofecoxib.” (Mukherjee, Nissen and Topol, 2001.)
The results of the VIGOR study were submitted to the United States Food and Drug Administration (FDA) in February 2001. In September 2001, the FDA sent a warning letter to the CEO of Merck, stating, “Your promotional campaign discounts the fact that in the VIGOR study, patients on Vioxx were observed to have a four to five fold increase in myocardial infarctions (MIs) compared to patients on the comparator non-steroidal anti-inflammatory drug (NSAID), Naprosyn (naproxen).”[16] This led to the introduction, in April 2002, of warnings on Vioxx labeling concerning the increased risk of cardiovascular events (heart attack and stroke).
Months after the preliminary version of VIGOR was published in the New England Journal of Medicine, the journal editors learned that certain data reported to the FDA were not included in the NEJM article. Several years later, when they were shown a Merck memo during the depositions for the first federal Vioxx trial, they realized that these data had been available to the authors months before publication. The editors wrote an editorial accusing the authors of deliberately withholding the data.[17] They released the editorial to the media on December 8, 2005, before giving the authors a chance to respond. NEJM editor Gregory Curfman explained that the quick release was due to the imminent presentation of his deposition testimony, which he feared would be misinterpreted in the media. He had earlier denied any relationship between the timing of the editorial and the trial. Although his testimony was not actually used in the December trial, Curfman had testified well before the publication of the editorial.[18]
The editors charged that “more than four months before the article was published, at least two of its authors were aware of critical data on an array of adverse cardiovascular events that were not included in the VIGOR article.” These additional data included three additional heart attacks, and raised the relative risk of Vioxx from 4.25-fold to 5-fold. All the additional heart attacks occurred in the group at low risk of heart attack (the “aspirin not indicated” group) and the editors noted that the omission “resulted in the misleading conclusion that there was a difference in the risk of myocardial infarction between the aspirin indicated and aspirin not indicated groups.” The relative risk for myocardial infarctions among the aspirin not indicated patients increased from 2.25 to 3 (although it remained statitistically insignificant). The editors also noted a statistically significant (2-fold) increase in risk for serious thromboembolic events for this group, an outcome that Merck had not reported in the NEJM, though it had disclosed that information publicly in March 2000, eight months before publication.[19]
The authors of the study, including the non-Merck authors, responded by claiming that the three additional heart attacks had occurred after the prespecified cutoff date for data collection and thus were appropriately not included. (Utilizing the prespecified cutoff date also meant that an additional stroke in the naproxen population was not reported.) Furthermore, they said that the additional data did not qualitatively change any of the conclusions of the study, and the results of the full analyses were disclosed to the FDA and reflected on the Vioxx warning label. They further noted that all of the data in the “omitted” table were printed in the text of the article. The authors stood by the original article.[20]
NEJM stood by its editorial, noting that the cutoff date was never mentioned in the article, nor did the authors report that the cutoff for cardiovascular adverse events was before that for gastrointestinal adverse events. The different cutoffs increased the reported benefits of Vioxx (reduced stomach problems) relative to the risks (increased heart attacks).[19]
Some scientists have accused the NEJM editorial board of making unfounded accusations.[21][22] Others have applauded the editorial. Renowned research cardiologist Eric Topol,[23] a prominent Merck critic, accused Merck of “manipulation of data” and said “I think now the scientific misconduct trial is really fully backed up”.[24] Phil Fontanarosa, executive editor of the prestigious Journal of the American Medical Association, welcomed the editorial, saying “this is another in the long list of recent examples that have generated real concerns about trust and confidence in industry-sponsored studies”.[25]
On May 15, 2006, the Wall Street Journal reported that a late night email, written by an outside public relations specialist and sent to Journal staffers hours before the Expression of Concern was released, predicted that “the rebuke would divert attention to Merck and induce the media to ignore the New England Journal of Medicine‘s own role in aiding Vioxx sales.”[26]
“Internal emails show the New England Journal’s expression of concern was timed to divert attention from a deposition in which Executive Editor Gregory Curfman made potentially damaging admissions about the journal’s handling of the Vioxx study. In the deposition, part of the Vioxx litigation, Dr. Curfman acknowledged that lax editing might have helped the authors make misleading claims in the article.” The Journal stated that NEJM‘s “ambiguous” language misled reporters into incorrectly believing that Merck had deleted data regarding the three additional heart attacks, rather than a blank table that contained no statistical information; “the New England Journal says it didn’t attempt to have these mistakes corrected.”[26]
Alzheimer’s studies
In 2000 and 2001, Merck conducted several studies of rofecoxib aimed at determining if the drug slowed the onset of Alzheimer’s disease. Merck has placed great emphasis on these studies on the grounds that they are relatively large (almost 3000 patients) and compared rofecoxib to a placebo rather than to another pain reliever. These studies found an elevated death rate among rofecoxib patients, although the deaths were not generally heart-related. However, they did not find any elevated cardiovascular risk due to rofecoxib.[27] Before 2004, Merck cited these studies as providing evidence, contrary to VIGOR, of rofecoxib’s safety.
APPROVe study
In 2001, Merck commenced the APPROVe (Adenomatous Polyp PRevention On Vioxx) study, a three-year trial with the primary aim of evaluating the efficacy of rofecoxib for theprophylaxis of colorectal polyps. Celecoxib had already been approved for this indication, and it was hoped to add this to the indications for rofecoxib as well. An additional aim of the study was to further evaluate the cardiovascular safety of rofecoxib.
The APPROVe study was terminated early when the preliminary data from the study showed an increased relative risk of adverse thrombotic cardiovascular events (includingheart attack and stroke), beginning after 18 months of rofecoxib therapy. In patients taking rofecoxib, versus placebo, the relative risk of these events was 1.92 (rofecoxib 1.50 events vs placebo 0.78 events per 100 patient years). The results from the first 18 months of the APPROVe study did not show an increased relative risk of adverse cardiovascular events. Moreover, overall and cardiovascular mortality rates were similar between the rofecoxib and placebo populations.[28]
In summary, the APPROVe study suggested that long-term use of rofecoxib resulted in nearly twice the risk of suffering a heart attack or stroke compared to patients receiving a placebo.
Other studies
Pre-approval Phase III clinical trials, like the APPROVe study, showed no increased relative risk of adverse cardiovascular events for the first eighteen months of rofecoxib usage (Merck, 2004). Others have pointed out that “study 090,” a pre-approval trial, showed a 3-fold increase in cardiovascular events compared to placebo, a 7-fold increase compared to nabumetone (another [NSAID]), and an 8-fold increase in heart attacks and strokes combined compared to both control groups.[29][30] Although this was a relatively small study and only the last result was statistically significant, critics have charged that this early finding should have prompted Merck to quickly conduct larger studies of rofecoxib’s cardiovascular safety. Merck notes that it had already begun VIGOR at the time Study 090 was completed. Although VIGOR was primarily designed to demonstrate new uses for rofecoxib, it also collected data on adverse cardiovascular outcomes.
Several very large observational studies have also found elevated risk of heart attack from rofecoxib. For example, a recent retrospective study of 113,000 elderly Canadians suggested a borderline statistically significant increased relative risk of heart attacks of 1.24 from Vioxx usage, with a relative risk of 1.73 for higher-dose Vioxx usage. (Levesque, 2005). Another study, using Kaiser Permanente data, found a 1.47 relative risk for low-dose Vioxx usage and 3.58 for high-dose Vioxx usage compared to current use of celecoxib, though the smaller number was not statistically significant, and relative risk compared to other populations was not statistically significant. (Graham, 2005).
Furthermore, a more recent meta-study of 114 randomized trials with a total of 116,000+ participants, published in JAMA, showed that Vioxx uniquely increased risk of renal (kidney) disease, and heart arrhythmia.[31]
Other COX-2 inhibitors
Any increased risk of renal and arrhythmia pathologies associated with the class of COX-2 inhibitors, e.g. celecoxib (Celebrex), valdecoxib (Bextra), parecoxib (Dynastat),lumiracoxib, and etoricoxib is not evident,[31] although smaller studies[32][33] had demonstrated such effects earlier with the use of celecoxib, valdecoxib and parecoxib.
Nevertheless, it is likely that trials of newer drugs in the category will be extended in order to supply additional evidence of cardiovascular safety. Examples are some more specific COX-2 inhibitors, including etoricoxib (Arcoxia) and lumiracoxib (Prexige), which are currently (circa 2005) undergoing Phase III/IV clinical trials.
Besides, regulatory authorities worldwide now require warnings about cardiovascular risk of COX-2 inhibitors still on the market. For example, in 2005, EU regulators required the following changes to the product information and/or packaging of all COX-2 inhibitors:[34]
- Contraindications stating that COX-2 inhibitors must not be used in patients with established ischaemic heart disease and/or cerebrovascular disease (stroke), and also in patients with peripheral arterial disease
- Reinforced warnings to healthcare professionals to exercise caution when prescribing COX-2 inhibitors to patients with risk factors for heart disease, such as hypertension, hyperlipidaemia (high cholesterol levels), diabetes and smoking
- Given the association between cardiovascular risk and exposure to COX-2 inhibitors, doctors are advised to use the lowest effective dose for the shortest possible duration of treatment
Other NSAIDs
Since the withdrawal of Vioxx it has come to light that there may be negative cardiovascular effects with not only other COX-2 inhibitiors, but even the majority of other NSAIDs. It is only with the recent development of drugs like Vioxx that drug companies have carried out the kind of well executed trials that could establish such effects and these sort of trials have never been carried out in older “trusted” NSAIDs such as ibuprofen, diclofenac and others. The possible exceptions may be aspirin and naproxen due to their anti-platelet aggregation properties.
Withdrawal
Due to the findings of its own APPROVe study, Merck publicly announced its voluntary withdrawal of the drug from the market worldwide on September 30, 2004.[35]
In addition to its own studies, on September 23, 2004 Merck apparently received information about new research by the FDA that supported previous findings of increased risk of heart attack among rofecoxib users (Grassley, 2004). FDA analysts estimated that Vioxx caused between 88,000 and 139,000 heart attacks, 30 to 40 percent of which were probably fatal, in the five years the drug was on the market.[36]
On November 5, the medical journal The Lancet published a meta-analysis of the available studies on the safety of rofecoxib (Jüni et al., 2004). The authors concluded that, owing to the known cardiovascular risk, rofecoxib should have been withdrawn several years earlier. The Lancet published an editorial which condemned both Merck and the FDA for the continued availability of rofecoxib from 2000 until the recall. Merck responded by issuing a rebuttal of the Jüni et al. meta-analysis that noted that Jüni omitted several studies that showed no increased cardiovascular risk. (Merck & Co., 2004).
In 2005, advisory panels in both the U.S. and Canada encouraged the return of rofecoxib to the market, stating that rofecoxib’s benefits outweighed the risks for some patients. The FDA advisory panel voted 17-15 to allow the drug to return to the market despite being found to increase heart risk. The vote in Canada was 12-1, and the Canadian panel noted that the cardiovascular risks from rofecoxib seemed to be no worse than those from ibuprofen—though the panel recommended that further study was needed for all NSAIDs to fully understand their risk profiles. Notwithstanding these recommendations, Merck has not returned rofecoxib to the market.[37]
In 2005, Merck retained Debevoise & Plimpton LLP to investigate Vioxx study results and communications conducted by Merck. Through the report, it was found that Merck’s senior management acted in good faith, and that the confusion over the clinical safety of Vioxx was due to the sales team’s overzealous behavior. The report that was filed gave a timeline of the events surrounding Vioxx and showed that Merck intended to operate honestly throughout the process. Any mistakes that were made regarding the mishandling of clinical trial results and withholding of information was the result of oversight, not malicious behavior. The Martin Report did conclude that the Merck’s marketing team exaggerated the safety of Vioxx and replaced truthful information with sales tactics.[citation needed] The report was published in February 2006, and Merck was satisfied with the findings of the report and promised to consider the recommendations contained in the Martin Report. Advisers to the US Food and Drug Administration (FDA) have voted, by a narrow margin, that it should not ban Vioxx — the painkiller withdrawn by drug-maker Merck.
They also said that Pfizer’s Celebrex and Bextra, two other members of the family of painkillers known as COX-2 inhibitors, should remain available, despite the fact that they too boost patients’ risk of heart attack and stroke. url = http://www.nature.com/drugdisc/news/articles/433790b.html The recommendations of the arthritis and drug safety advisory panel offer some measure of relief to the pharmaceutical industry, which has faced a barrage of criticism for its promotion of the painkillers. But the advice of the panel, which met near Washington DC over 16–18 February, comes with several strings attached.
For example, most panel members said that manufacturers should be required to add a prominent warning about the drugs’ risks to their labels; to stop direct-to-consumer advertising of the drugs; and to include detailed, written risk information with each prescription. The panel also unanimously stated that all three painkillers “significantly increase the risk of cardiovascular events”.
The panel voted 17 to 15 against banning Vioxx (rofecoxib) entirely; the vote on Bextra (valdecoxib) was 17 to 13 with 2 abstentions; Celebrex (celecoxib) was endorsed 31 to 1. Shares of Merck, based in Whitehouse Station, New Jersey, and New York-based Pfizer closed up 13% and 7% respectively on 18 February, 2013, the day of the votes.
The FDA is expected to act on the recommendations within weeks. Although the agency usually follows the recommendations of its outside advisers, it is not bound to do so. A top official said that, in light of the closeness of some of the votes, the agency will examine the panel members’ comments in detail before deciding what to do.
An official from Merck said during the meeting that it would consider reintroducing Vioxx, which it withdrew in September 2004. On April 7, 2005, Pfizer withdrew Bextra from the U.S. market on recommendation by the FDA. Pfizer’s other painkiller, Celebrex, is still on the market.
Litigation
As of March 2006, there had been over 10,000 cases and 190 class actions filed against Merck[citation needed] over adverse cardiovascular events associated with rofecoxib and the adequacy of Merck’s warnings. The first wrongful death trial, Rogers v. Merck, was scheduled in Alabama in the spring of 2005, but was postponed after Merck argued that the plaintiff had falsified evidence of rofecoxib use.[1]
On August 19, 2005, a jury in Texas voted 10-2 to hold Merck liable for the death of Robert Ernst, a 59-year-old man who allegedly died of a rofecoxib-induced heart attack. The plaintiffs’ lead attorney was Mark Lanier. Merck argued that the death was due to cardiac arrhythmia, which had not been shown to be associated with rofecoxib use. The jury awarded Carol Ernst, widow of Robert Ernst, $253.4 million in damages. This award will almost certainly be capped at no more than US$26.1 million because of punitive damages limits under Texas law.[2] As of March 2006, the plaintiff had yet to ask the court to enter a judgment on the verdict; Merck has stated that it will appeal.
On November 3, 2005, Merck won the second case Humeston v. Merck, a personal injury case, in Atlantic City, New Jersey. The plaintiff experienced a mild myocardial infarction and claimed that rofecoxib was responsible, after having taken it for two months. Merck argued that there was no evidence that rofecoxib was the cause of Humeston’s injury and that there is no scientific evidence linking rofecoxib to cardiac events with short durations of use. The jury ruled that Merck had adequately warned doctors and patients of the drug’s risk.[3]
The first federal trial on rofecoxib, Plunkett v. Merck, began on November 29, 2005 in Houston. The trial ended in a hung jury and a mistrial was declared on December 12, 2005. According to the Wall Street Journal, the jury hung by an eight to one majority, favoring the defense. Upon retrial in February 2006 in New Orleans, where the Vioxx multidistrict litigation (MDL) is based, a jury found Merck not liable, even though the plaintiffs had the NEJM editor testify as to his objections to the VIGOR study.
On January 30, 2006, a New Jersey state court dismissed a case brought by Edgar Lee Boyd, who blamed Vioxx for gastrointestinal bleeding that he experienced after taking the drug. The judge said that Boyd failed to prove the drug caused his stomach pain and internal bleeding.
In January 2006, Garza v. Merck began trial in Rio Grande City, Texas. The plaintiff, a 71-year-old smoker with heart disease, had a fatal heart attack three weeks after finishing a one-week sample of rofecoxib. On April 21, 2006 the jury awarded the plaintiff $7 million compensatory and $25 million punitive. The Texas state court of appeals in San Antonio later rules Garza’s fatal heart attack probably resulted from pre-existing health conditions unrelated to his taking of Vioxx, thus reversing the $32 million jury award.[4]
On April 5, 2006, the jury held Merck liable for the heart attack of 77-year-old John McDarby, and awarded Mr McDarby $4.5 million in compensatory damages based on Merck’s failure to properly warn of Vioxx safety risks. After a hearing on April 11, 2006, the jury also awarded Mr McDarby an additional $9 million in punitive damages. The same jury found Merck not liable for the heart attack of 60-year-old Thomas Cona, a second plaintiff in the trial, but was liable for fraud in the sale of the drug to Cona.
Merck has reserved $970 million to pay for its Vioxx-related legal expenses through 2007, and have set aside $4.85bn for legal claims from US citizens. Patients who claim to have suffered as a result of taking Vioxx in countries outside the US are campaigning for this to be extended.
In March 2010, an Australian class-action lawsuit against Merck ruled that Vioxx doubled the risk of heart attacks, and that Merck had breached the Trade Practices Act by selling a drug which was unfit for sale.[38]
In November 2011, Merck announced a civil settlement with the US Attorney’s Office for the District of Massachusetts, and individually with 43 US states and the District of Columbia, to resolve civil claims relating to Vioxx.[5] Under the terms of the settlement, Merck agreed to pay two-thirds of a previously recorded $950 million reserve charge in exchange for release from civil liability. Litigation with seven additional states remains outstanding. Under separate criminal proceedings, Merck plead guilty to a federal misdemeanor charge relating to the marketing of the drug across state lines, incurring a fine of $321.6 million.[6]
Other effects
Rofecoxib was shown to improve premenstrual acne vulgaris in a placebo controlled study.[39]
Synthesis
Rofecoxib synthesis.[40]
,,,,,,,,,,,,,,,,,
The oxidation of 4- (methylsulfanyl) acetophenone (X) with monoperoxyphthalic acid (MMPP) in dichloro-methane / methanol gives the corresponding sulfone (XI), which is brominated with Br2 / AlCl3 in chloroform, yielding the expected phenacyl bromide ( XII). Finally, this compound is cyclocondensed with phenylacetic acid (I) by means of 1,8-diazabicyclo [5.4.0] undec-7-ene (DBU) and triethylamine in acetonitrile. 5) Reaction of [4- (methylsulfonyl ) phenyl] phenylacetyl-ene (XIII) with CO catalyzed by Rh4 (CO) 12 in THF at 100 C in a stainless steel autoclave at 100 Atm pressure, followed by a chromatographic separation in a silicagel column to eliminate the undesired regioisomer.

……………….
The synthesis of rofecoxib can be performed by several different ways: 1) The condensation of phenylacetic acid (I) with ethyl bromoacetate (II) by means of triethylamine in THF yields 2- (phenylacetoxy) acetic acid ethyl ester (III), which is cyclized to the hydroxyfuranone (IV) by means of potassium tert-butoxide in tert-butanol. The reaction of (IV) with triflic anhydride and diisopropylethylamine in dichloro-methane affords the corresponding triflate (V), which by reaction with LiBr in hot acetone yields the bromofuranone (VI) The condensation of (VI) with 4- (methylsulfanyl) phenylboronic acid (VII) by means of Na2CO3 and Pd (Ph3P) 4 in hot toluene gives 4- [4- (methylsulfanyl) -phenyl]. – 3-phenylfuran-2 (5H) -one (VIII), which is finally oxidized with 2KHSO5.KHSO4.K2SO4 (oxone). 2) The intermediate (VIII) can also be obtained by condensation of triflate (V) with boronic acid ( VII) by means of Na2CO3 and Pd (Ph3P) 4 in hot toluene. 3) The intermediate (VIII) can also be synthesized by the reaction of triflate (V) with tetramethylammonium chloride, giving the chlorofuranone (IX), which is then condensed with boronic acid (VII) as before.

Footnotes
- http://www.npr.org/templates/story/story.php?storyId=4054991
- “Up to 140,000 heart attacks linked to Vioxx.”. New Scientist. 2005-01-25. p. 1.
- “Merck Sees Slightly Higher 2007 Earnings”. New York Times. Reuters. 2006-12-07. p. A1.
- Bombardier, C.; Laine, L.; Reicin, A.; Shapiro, D.; Burgos-Vargas, R.; Davis, B.; Day, R.; Ferraz, M. B.; Hawkey, C. J.; Hochberg, M. C.; Kvien, T. K.; Schnitzer, T. J.; Vigor Study, G. (2000). “Comparison of Upper Gastrointestinal Toxicity of Rofecoxib and Naproxen in Patients with Rheumatoid Arthritis”. New England Journal of Medicine 343 (21): 1520–1528, 2 1528 following 1528. doi:10.1056/NEJM200011233432103. PMID 11087881. edit
- Merck & Co. VIOXX (rofecoxib tablets and oral suspension). Accessed at: http://www.merck.com/product/usa/pi_circulars/v/vioxx/vioxx_pi.pdf 01 Feb 2010
- Gold Standard Inc. Rofecoxib Vioxx Accessed at: http://www.mdconsult.com/das/pharm/body/181267313-3/946823742/full/2399 01 Feb 2010
- ^ Jump up to:a b Davies, N. M.; Teng, X. W.; Skjodt, N. M. (2003). “Pharmacokinetics of rofecoxib: a specific cyclo-oxygenase-2 inhibitor”. Clinical pharmacokinetics 42 (6): 545–556.PMID 12793839. edit
- Padi, S.; Kulkarni, S. (2004). “Differential effects of naproxen and rofecoxib on the development of hypersensitivity following nerve injury in rats”. Pharmacology, Biochemistry, and Behavior 79 (2): 349–358. doi:10.1016/j.pbb.2004.08.005. PMID 15501312. edit
- Scott, L. J.; Lamb, H. M. (1999). “Rofecoxib”. Drugs 58 (3): 499–505; discussion 506–7. doi:10.2165/00003495-199958030-00016. PMID 10493277. edit
- Winstein, Keith J. (March 11, 2009). “Top Pain Scientist Fabricated Data in Studies, Hospital Says”. The Wall Street Journal.
- Vane, J.; Bakhle, Y.; Botting, R. (1998). “Cyclooxygenases 1 and 2”. Annual review of pharmacology and toxicology 38: 97–120. doi:10.1146/annurev.pharmtox.38.1.97.PMID 9597150. edit
- sfgate.com
- Jump up^ www.saferdrugsnow.org
- Karha, J.; Topol, E. J. (2004). “The sad story of Vioxx, and what we should learn from it”. Cleveland Clinic journal of medicine 71 (12): 933–934, 936, 934–9.doi:10.3949/ccjm.71.12.933. PMID 15641522. edit
- Solomon, D. H.; Glynn, R. J.; Levin, R.; Avorn, J. (2002). “Nonsteroidal anti-inflammatory drug use and acute myocardial infarction”. Archives of Internal Medicine 162 (10): 1099–1104.doi:10.1001/archinte.162.10.1099. PMID 12020178. edit
- http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/EnforcementActivitiesbyFDA/WarningLettersandNoticeofViolationLetterstoPharmaceuticalCompanies/UCM166383.pdf
- Curfman, G.; Morrissey, S.; Drazen, J. (2005). “Expression of concern: Bombardier et al., “Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis,” N Engl J Med 2000;343:1520-8″. The New England Journal of Medicine 353 (26): 2813–2814. doi:10.1056/NEJMe058314. PMID 16339408. edit
- http://www.forbes.com/work/feeds/ap/2006/02/13/ap2523250.html. Missing or empty
|title=(help)[dead link] - Curfman, G.; Morrissey, S.; Drazen, J. (2006). “Expression of concern reaffirmed”. The New England Journal of Medicine 354 (11): 1193. doi:10.1056/NEJMe068054.PMID 16495386. edit
- Jump up^ Bombardier, C.; Laine, L.; Burgos-Vargas, R.; Davis, B.; Day, R.; Ferraz, M.; Hawkey, C.; Hochberg, M.; Kvien, T.; Schnitzer, T. J.; Weaver, A. (2006). “Response to expression of concern regarding VIGOR study”. The New England Journal of Medicine 354 (11): 1196–1199. doi:10.1056/NEJMc066096. PMID 16495387. edit
- http://pipeline.corante.com/archives/2006/02/22/nejm_vs_its_contributors_round_two.php
- http://dimer.tamu.edu/simplog/archive.php?blogid=3&pid=3293
- http://genetics.case.edu/faculty2.php?fac=ejt9
- Jump up^ http://www.medicinenet.com/script/main/art.asp?articlekey=56384&page=2
- http://www.beasleyallen.com/news/vioxx-plaintiffs-seek-mistrial-after-allegation-on-merck-study/
- David Armstrong (2006-05-15). “How the New England Journal Missed Warning Signs on Vioxx”. Wall Street Journal. p. A1.
- Konstam, M. A.; Weir, M. R.; Reicin, A.; Shapiro, D.; Sperling, R. S.; Barr, E.; Gertz, B. J. (2001). “Cardiovascular thrombotic events in controlled, clinical trials of rofecoxib”. Circulation104 (19): 2280–2288. doi:10.1161/hc4401.100078. PMID 11696466. edit
- Bresalier, R.; Sandler, R.; Quan, H.; Bolognese, J.; Oxenius, B.; Horgan, K.; Lines, C.; Riddell, R.; Morton, D.; Lanas, A.; Konstam, M. A.; Baron, J. A.; Adenomatous Polyp Prevention on Vioxx (APPROVe) Trial Investigators (2005). “Cardiovascular events associated with rofecoxib in a colorectal adenoma chemoprevention trial”. The New England Journal of Medicine 352(11): 1092–1102. doi:10.1056/NEJMoa050493. PMID 15713943. edit
- http://www.fda.gov/ohrms/dockets/ac/01/briefing/3677b2_06_cardio.pdf
- Jump up^ Wolfe, M. M. (2004). “Rofecoxib, Merck, and the FDA”. The New England Journal of Medicine 351 (27): 2875–2878; author 2878 2875–2878. doi:10.1056/NEJM200412303512719.PMID 15625749. edit
- Zhang, J.; Ding, E.; Song, Y. (2006). “Adverse effects of cyclooxygenase 2 inhibitors on renal and arrhythmia events: meta-analysis of randomized trials”. Journal of the American Medical Association 296 (13): 1619–1632. doi:10.1001/jama.296.13.jrv60015. PMID 16968832. edit
- Solomon, S.; McMurray, J.; Pfeffer, M.; Wittes, J.; Fowler, R.; Finn, P.; Anderson, W.; Zauber, A.; Hawk, E.; Bertagnolli, M.; Adenoma Prevention with Celecoxib (APC) Study Investigators (2005). “Cardiovascular risk associated with celecoxib in a clinical trial for colorectal adenoma prevention”. The New England Journal of Medicine 352 (11): 1071–1080.doi:10.1056/NEJMoa050405. PMID 15713944. edit
- Nussmeier, N.; Whelton, A.; Brown, M.; Langford, R.; Hoeft, A.; Parlow, J.; Boyce, S.; Verburg, K. (2005). “Complications of the COX-2 inhibitors parecoxib and valdecoxib after cardiac surgery”. The New England Journal of Medicine 352 (11): 1081–1091. doi:10.1056/NEJMoa050330. PMID 15713945. edit
- “European Medicines Agency concludes action on COX-2 inhibitors” (pdf). European Medicines Agency. Retrieved 2008-04-16.
- “Merck Announces Voluntary Worldwide Withdrawal of VIOXX” (pdf). Retrieved 2008-04-16.
- “Congress Questions Vioxx, FDA”. PBS NewsHour. 2004-11-18. Retrieved 2013-06-03.
- “SUMMARY: Report of the Expert Advisory Panel on the Safety of Cox-2 Selective Non-steroidal Anti-Inflammatory Drugs (NSAIDs)”. Health Canada. 2005-07-06. Retrieved 2011-06-04.
- Drug unfit for sale, says judge in compo case The Age, March 6, 2010
- http://bioline.utsc.utoronto.ca/archive/00002693/01/dv04120.pdf#search=%22acne%20rofecoxib%22
- http://vioxxlawyer.org/rofecoxib-synthesis/
References
- FDA (2005). “Summary minutes for the February 16, 17 and 18, 2005, Joint meeting of the Arthritis Advisory Committee and the Drug Safety and Risk Management Advisory Committee.” Published on the internet, March 2005. Link
- Fitzgerald GA, Coxibs and Cardiovascular Disease, N Engl J Med 2004;351(17): 1709–1711. PMID 15470192.
- Grassley CE (15 Oct 2004). Grassley questions Merck about communication with the FDA on Vioxx. Press Release.
- Jüni P, Nartey L, Reichenbach S, Sterchi R, Dieppe PA, Egger M (2004). Risk of cardiovascular events and rofecoxib: cumulative meta-analysis. Lancet (published online; see also Merck response below)
- Karha J and Topol EJ. The sad story of Vioxx, and what we should learn from it Cleve Clin J Med 2004; 71(12):933-939. PMID 15641522
- Michaels, D. (June 2005) DOUBT Is Their Product, Scientific American, 292 (6).
- Merck & Co., (5 Nov 2004). Response to Article by Juni et al. Published in The Lancet on Nov. 5. Press Release.
- Merck & Co (30 Sep 2004) Merck Announces Voluntary Worldwide Withdrawal of VIOXX. Press release [7].
- D. M. Mukherjee, S. E. Nissen, and E. J. Topol, “Risk of Cardiovascular Events Associated with Selective COX-2 Inhibitors,” Journal of the American Medical Association 186 (2001): 954–959.
- Nussmeier NA, Whelton AA, Brown MT, Langford RM, Hoeft A, Parlow JL, et al. Complications of the COX-2 inhibitors parecoxib and valdecoxib after cardiac surgery. N Engl J Med 2005;352(11):1081-91. PMID 15713945
- Okie, S (2005) “Raising the safety bar–the FDA’s coxib meeting.” N Engl J Med. 2005 Mar 31;352(13):1283-5. PMID 15800221.
- Leleti Rajender Reddy, Corey EJ. Facile air oxidation of the conjugate base of rofecoxib (Vioxx), a possible contributor to chronic human toxicity Tetrahedron Lett 2005, 46: 927. doi:10.1016/j.tetlet.2004.12.055
- Swan SK et al., Effect of Cyclooxygenase-2 Inhibition on Renal Function in Elderly Persons Receiving a Low-Salt Diet. Annals of Int Med 2000; 133:1–9
- Targum, SL. (1 Feb. 2001) Review of cardiovascular safety database. FDA memorandum. [8]
- Wolfe, MM et al., Gastrointestinal Toxicity of Nonsteroidal Anti-anflamattory Drugs, New England Journal of Medicine. 1999; 340; 1888-98.
External links
- National Public Radio 2004 Q&A on the case, following withdrawal announcement
- Court TV’s full coverage of the Vioxx civil trials
- Merck website on Vioxx litigation
- FDA Public Health Advisory on Vioxx
- David Michaels. Doubt is Their Product Scientific American, June 2004, p. 96-101
- JURIST, Much Pain, Much Gain: Skeptical Ruminations on the Vioxx Litigation
- Ted Frank, American Enterprise Institute, The Vioxx Litigation, Part I and Part II, December 2005
- briandeer.com – Vioxx: the UK connection
- Campaign for compensation for Vioxx victims outside the US
Literature References:
Selective cyclooxygenase-2 (COX-2) inhibitor. Prepn: Y. Ducharme et al., WO 9500501; eidem, US5474995 (both 1995 to Merck Frosst).
HPLC determn in plasma: C. M. Chavez-Eng et al., J. Chromatogr. B 748, 31 (2000).
Enzyme inhibition and clinical evaluation in dental pain: E. W. Ehrich et al., Clin. Pharmacol. Ther. 65, 336 (1999).
Evaluation of risk of gastrointestinal effects in patients with osteoarthritis: M. J. Langman et al., J. Am. Med. Assoc. 282, 1929 (1999); with rheumatoid arthritis: C. Bombardier et al., N. Engl. J. Med. 343, 1520 (2000).
Review of pharmacology and clinical experience: A. J. Matheson, D. P. Figgitt, Drugs 61, 833-865 (2001).
Keywords: Cyclooxygenase-2 Selective Inhibitor, Anti-inflammatory (Nonsteroidal), Analgesic (Non-Narcotic), rofecoxib, MK-0966, Vioxx
Nabriva’s lefamulin, BC 3781 receives FDA fast-track status to treat CABP and ABSSSI
Nabriva’s lefamulin receives FDA fast-track status to treat CABP and ABSSS
Austria-based Nabriva Therapeutics has received qualified infectious disease product (QIDP) and fast-track status designation from the US Food and Drug Administration for its lefamulin (BC 3781).
read

BC-3781
Topical pleuromutilin antibiotic agent
Gram-positive, including MRSA, PHASE 2 COMPLETED,Infection, acute bacterial skin and skin structure (ABSSSI)
Nabriva (Austria), Nabriva Therapeutics AG
BC-3781
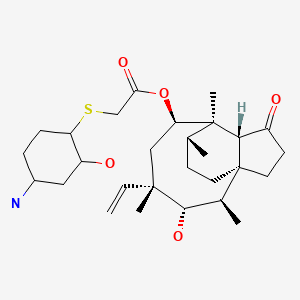
cas 1061872-97-6
UNII-61H04Z5F9K
(3aS,4R,5S,6S,8R,9R,9aR,10R)-5-Hydroxy-4,6,9,10-tetramethyl-1-oxo-6-vinyldecahydro-3a,9-propanocyclopenta[8]annulen-8-yl [[(1R,2R,4R)-4-amino-2-hydroxycyclohexyl]sulfanyl]acetate;
14-O-[2-[(1R,2R,4R)-4-Amino-2-hydroxycyclohexylsulfanyl]acetyl]mutilin
BC-3781 is a pleuromutilin antibiotic in early clinical development at Nabriva for the treatment of community acquired pneumonia and for the treatment of patients with acute bacterial skin and skin structure infections (ABSSSI). Pleuromutilin antibiotics interfere with bacterial protein synthesis via a specific interaction with the 23S rRNA of the 50S bacterial ribosome subunit. They have a distinct antibacterial profile and show no cross-resistance with any other class of antibiotics. In 2012, a codevelopment agreement was signed between Forest and Nabriva, but, in 2014, this agreement terminated and Nabriva retained all rights.
The pleuromutilin BC-3781 belongs to the first generation of pleuromutilins to combine excellent oral
bioavailability with substantial activity against Gram-positive pathogens and atypicals as well as some
Gram-negative pathogens. In particular, BC-3781 is highly active against multi-drug resistant (MDR)
pathogens including methicillin resistant Staphylococcus aureus (MRSA), MDR Streptococcus pneumonia
(i.e. macrolide and quinolone resistance), and vancomycin resistant Enterococcus faecium. It is
characterized by excellent in vivo activities (e.g. pneumonia model), outstanding PK/PD parameters,
allowing once a day dosing, and a novel mode of action. BC-3781 is being developed for both oral and IV
administration and is intended for the treatment of serious multi-drug resistant skin & skin structure
infections (CSSI) and moderate to severe pneumonia (CAP, HAP etc).
Pleuromutilins have been known since 1951, but only entered the market in 2007 with the approval of retapamulin for topical use. Until today, there are no pleuromutilins for systemic use approved in human clinical practice.
in 2007 with the approval of retapamulin for topical use. Until today, there are no pleuromutilins for systemic use approved in human clinical practice.
Nabriva is currently working on the development of new compounds is this class. The lead compound, BC-3781, if approved, will be the first pleuromutilin for systemic use in humans.
The compound shows potent in vitro activity against a large collection of staphylococci, streptococci, andE. faecium. When compared to linezolid and vancomycin, the compound shows greater overall potency againstS. aureus [121]. BC-3781 shows improved activity against most bacteria commonly associated with community-acquired respiratory tract infections, the compound is especially potent against S. pneumoniaincluding penicillin resistant strains. It also shows improved activity against H. influenza, M. catarrhalis, M. pneumoniae and C. pneumoniae.
BC-3781 is undergoing Phase I clinical trials for CAP and in March of 2011 has completed a Phase II clinical study comparing it to vancomycin for treatment of aBSSSI [119,120,121,122,123]. Nabriva Therapeutics AG announced that the cooperation with Forest Laboratories to develop the compound had elapsed, and that Nabriva retained all rights in BC-3781. The company informed that the product was Phase III ready and that it was seeking partners to continue further development [203].
Nabriva is also developing BC-7013 for topical use against Gram-positive infections and working on the discovery of new pleuromutilins [119,124].
Dr William Prince, CMO Nabriva Therapeutics commented:
“This is the first patient study with a systemic pleuromutilin. It will be an important proof of concept
for an exciting new class of antibiotics. The phase II study builds on our extensive preclinical and
phase I data which have demonstrated that BC-3781 can achieve therapeutically relevant blood and
tissue levels in man with excellent tolerability when administered by either oral or intravenous
routes.”
Dr. David Chiswell, CEO Nabriva Therapeutics commented:
“With a worldwide problem due to antibiotic resistant bacteria, there is a very significant need for
new classes of antibiotics with unique modes of action such as the pleuromutilins. The commercial
prospects for BC-3781 as the leading compound of an exciting new class are excellent, especially as it
has an ideal anti-bacterial spectrum for both skin and respiratory infections and is being developed
with both oral and intravenous formulations”
BC-3781 is highly active against key pathogens, including MRSA, associated with skin infections and
community and hospital acquired pneumonia and is more potent than Linezolid and vancomycin. The
compound’s novel mode of action ensures that it overcomes resistance mechanisms affecting all
approved classes of antibiotics. BC-378
About Nabriva Therapeutics
Nabriva Therapeutics is a biotechnology company focused on developing a new class of antibiotics for
the treatment of serious infections caused by resistant pathogens. Nabriva’s lead systemic product,
BC-3781, is being developed for the treatment of serious skin infections and bacterial pneumonia
caused by S. aureus, , S. pneumoniae, H. influenza, Mycoplasma, Legionella and other bacteria,
including drug resistant strains such as MRSA and vancomycin resistant E. faecium. In addition,
Nabriva Therapeutics’ topical pleuromutilin product candidate, BC-7013, is in clinical phase I. Nabriva
Therapeutics has a proven track record in world-class medicinal chemistry, clinical expertise, a
seasoned management team and solid IP. Nabriva Therapeutics is located in Vienna, Austria.
For more information on Nabriva please visit http://www.nabriva.com. Nabriva Therapeutics AG
…………………………………………
EP 2390245
http://www.google.com/patents/EP2390245A1?cl=en
……………………………………………..
http://www.google.im/patents/US20090118366?cl=es
The trivial name mutilin refers to the IUPAC systematic name (1S, 2R, 3S, 4S, 6R, 7R, 8R, 14R)-3,6-dihydroxy-2,4,7,14-tetramethyl-4-vinyl-tricyclo[5.4.3.01,8]tetradecan-9-one. In the examples, pleuromutilin derivatives are numbered in analogy to the mutilin numbering system described by H. Berner (Berner, H.; Schulz, G.; Schneider H. Tetrahedron 1980, 36, 1807-1811.):
…………………………………………………….
http://www.google.com/patents/WO2008113089A1?cl=en
Pleuromutilin, a compound of formula A
is a naturally occurring antibiotic, e.g. produced by the basidomycetes Pleurotus mutilus and P. passeckerianus, see e.g. The Merck Index, 13th edition, item 7617. A number of further pleuromutilins having the principle ring structure of pleuromutilin and being substituted at the hydroxy group have been developed, e.g. as antimicrobials.
From WO 02/04414 Al pleuromutilin derivatives, e.g. 14-O-[(Aminocyclohexan-2-yl (and – 3-yl)-sulfanyl)-acetyl]-mutilins; from WO 07/014409 Al e.g. 14-O-[((Mono- or dialkylamino)-cycloalkylsulfanyl)-acetyl]-mutilins and from WO 07/000004 Al e.g. [((Acyl- hydroxy-amino)-cycloalkylsulfanyl)-acetyl]-mutilins, are known.
14-O-{[(1R, 2R, 4R)-4-Amino-2-hydroxy-cyclohexylsulfanyl]-acetyl}- mutilin hydrochloride
Example 1 – 14-O-{[(1R, 2R, 4R)-4-Amino-2-hydroxy-cyclohexylsulfanyl]-acetyl}- mutilin hydrochloride + (IS, 2S, 4S) diastereomer hydrochloride
Step Al. 14-O-{[(1R, 2R, 4R)-4-tert-Butoxycarbonylamino-2-hydroxy- cyclohexylsulfanyl]-acetyl}-mutilin + (IS, 2S, 4S) diastereomer and 14-O-{[(lR, 2R, 5S)-5-i’eri’-Butoxycarbonylamino-2-hydroxy-cyclohexylsulfanyl]-acetyl}- mutilin + (IS, 2S, 5R) diastereomer and
14-0-{[(lR, 2R, 4S)-4-tert-Butoxycarbonylamino-2-hydroxy-cyclohexylsuIfanyl]-acetyl}- mutilin + (IS, 2S, 4R) diastereomer
To a solution of 3,4-epoxycyclohexyl-carbamic acid tert-butyl ester (Gomez-Sanchez, E.; Marco-Contelles J. Tetrahedron 2005, 61, 1207-1219.) (4.27g, 20mmol) and pleuromutilin thiol (Nagarajan, R. Eli Lilly and Company 1978, US4, 130,709) (7.10 g, 18 mmol) in 200 ml of tetrahydrofuran was added aluminum oxide (40 g, Brockmann activity I, neutral) and the resulting mixture was stirred for 40 hours at room temperature. The suspension was filtered and concentrated under reduced pressure. The residue was subjected to chromatography (silica, cyclohcxane / ethyl acetate = 1/1) to yield 14-O-{[(1R, 2R, 4R)-4-ler(- butoxycarbonylamino-2-hydroxy-cyclohcxylsulfanyl]-acctyl}-mutilin + (IS, 2S, 4S) diastereomer (a) (Rf = 0.38, 1.34g, 12%) as well as a mixture of 14-O-{[(1R, 2R, 5S)-5-tert- butoxycarbonylumino-2-hy(lroxy-cyclohcxylsulfnnyl]-ncctyl}-niυtilin + (I S, 2S, 5R) diastereomer and 14-O-{[(1R, 2R, 4S)-4-tert-butoxycarbonylamino-2-hydroxy- cyclυhexylsulfanyl]-acetyl}-mutilin + (IS, 2S, 4R) diastereomer (b) (Rf = 0.26, 2.81 g, 25%) as colorless amorphous foams. (a): 1H NMR (400MHz, DMSOd6, δ, ppm, inter alia): 6.74 (d, IH, NH, J = 7Hz), 6.13 (dd, IH, 19-H, J – I lHz and 18Hz), 5.54 (d, IH, 14-H, J = 8Hz), 5.05 (m, 2H, 20-H), 4.90 (d, IH, 2′-OH, J = 5Hz), 4.48 (d, IH, 11-OH, J = 6Hz), 3.55 – 3.20 (m, 6H, 1 ‘-H, 2‘-H, 4′-H, 11-H, 22-H), 2.40 (bs, IH, 4-H), 1.36 (s, 3H, 15-CH3), 1.35 (s, 9H, tert-butyl), 1.06 (s, 3H, 18-CH3), 0.81 (d, 3H, 17-CH3, J = 7Hz), 0.62 (d, 3H, 16-CH3, J = 7Hz). MS-ESI (m/z): 630 (MNa+), 1237 (2MNa+).
(b): 1H NMR (400MHz, DMSO-de, δ, ppm, inter alia): 6.70 (d, IH, NH, J = 7Hz), 6.12 (dd, IH, 19-H, J = HHz and 18Hz), 5.34 (d, IH, 14-H, J = 8Hz), 5.05 (m, 2H, 20-H), 4.82, 4.78 (d, IH, 2′-OH, J = 4Hz), 4.48 (d, IH, 11-OH, J = 6Hz), 3.55 – 3.20 (m, 5H, 2′-H, 475′-H, 11- H, 22-H), 2.97 (m, IH, 1 ‘-H), 2.40 (bs, IH, 4-H), 1.35 (s, 12H, 15-CH3, tert-butyl), 1.05 (s, 3H, 18-CH3), 0.82 (d, 3H, 17-CH3, J = 7Hz), 0.62 (d, 3H, 16-CH3, J = 7Hz). MS-ESI (m/z): 630 (MNa+), 1237 (2MNa+).
or Step A2. 14-O-{[(1R, 2R, 4R)-4-tert-Butoxycarbonylamino-2-liydroxy- cyclohexylsulfanyl]-acetyl}-mutilin + (IS, 2S, 4S) diastereomer and
14-O-{[(1R, 2R, 5S)-5-tert-Butoxycarbonylamino-2-hydroxy-cyclohexylsulfanyl]-acetyl}- mutilin + (IS, 2S, 5R) diastereomer and
14-O-{[(1R, 2R, 4S)-4-rerf-Butoxycarbonylamino-2-hydroxy-cyclohexylsulfanyl]-acetyl}- mutilin + (IS, 2S, 4R) diastereomer
To a solution of 3,4-epoxycyclohexyl-carbamic acid tert-butyl ester (10 g, 47 mmol) and pleuromutilin thiol (16.6 g, 42 mmol) in 200 ml of methanol and 20 ml of dioxane was added 2N NaOH (21 ml, 42 mmol) and the resulting mixture was stirred for 16 hours at room temperature. After completion of the reaction the pH was set to 7 with diluted HCl and the reaction mixture was concentrated under reduced pressure. The residue was diluted with water and brine and extracted three times with ethyl acetate. The organic layers were dried over sodium sulfate and filtered. The filtrate was concentrated under reduced pressure and after chromatography (silica, cyclohexane / ethyl acetate = 1/1) 14-O-{[(1R, 2R, 4R) A-tert- butoxycarbonylamino-2-hydroxy-cyclohexylsulfanyl] -acetyl }-mutilin + (IS, 2S, 4S) diastereomer (Rf = 0.40, 3.1g, 12% yield) as well as a mixture of 14-O-{[(1R, 2R, 5S)-5-tert- butoxycarbonylamino-2-hydroxy-cyclohexylsulfanyl]-acetyl}-mutilin + (IS, 2S, 5R) diastereomer and 14-O-{[(1R, 2R, 4S)-4-tert-butoxycarbonylamino-2-hydroxy- cyclohexylsulfanyl]-acetyl}-mutilin + (IS, 2S, 4R) diastereomer (Rf = 0.25, 6.35 g, 25%) were obtained as colorless amorphous foams. or Step A3. 14-O-{[(1R, 2R, 4R)-4-tert-Butoxycarbonylamino-2-hydroxy- cyclohexylsulfanyl]-acetyl}-mutilin + (IS, 2S, 4S) diastereomer and 14-O-{ [(1R, 2R, 5S)-5-tert-Butoxycarbonylamino-2-hydroxy-cyclohexylsulfanyl]-acetyl}- mutilin + (IS, 2S, 5R) diastereomer
To a solution of Pleuromutilin thiol (9.25 g, 23.5 mmol) in 100 ml of acetonitrile (dried over 4A molecular sieve) was added l,5-diazabicyclo[4.3.0]non-5-ene (DBN, 2.9 μl, 23.5 mmol) and after 1 hour of stirring at room temperature under argon atmosphere the mixture was ^ charged with syn-3,4-epoxycyclohexyl-carbamic acid tert-butyl ester (4.17 g, 19.5 mmol) and stirred for further 16 hours at room temperature. The reaction mixture was concentrated under reduced pressure. The residue was charged with water and brine and extracted three times with dichloromethane. The organic layers were dried over sodium sulphate and filtered. The filtrate was concentrated under reduced pressure and subjected to chromatography (silica, cyclohexane / ethyl acetate = 1/1) to yield 14-O-{[(1R, 2R, 4R)-4-teAY-butoxycarbonylamino- 2-hydroxy-cyclohexylsulfanyl]-acetyl}-mutilin + (IS, 2S, 4S) diastereomer (Rf = 0.38, 5.07g, 43%) as well as 14-O-{[(1R, 2R, 5S)-5-tert-butoxycarbonylamino-2-hydroxy- cyclohexylsulfanyl]-acetyl}-mutilin + (IS, 2S, 5R) diastereomer (Rf = 0.25, 2.95 g, 16.5%) as colorless amorphous foams.
Step B. 14-O-{[(1R, 2R, 4R)-4-Amino-2-hydroxy-cyclohexylsulfanyl]-acetyl}-mutilin + (IS, 2S, 4S) diastereomer
To a solution of 14-O-{[(1R, 2R, 4R)-4-teΛ-t-butoxycarbonylamino-2-hydroxy- cyclohexylsulfanyl]-acetyl}-mutilin + (IS, 2S, 4S) diastereomer (1.34 g, 2.20 mmol) in 75 ml of dichloromethane was added trifiuoroacetic acid (4 ml) at 4°C and stirred for 5 hours at room temperature. The reaction mixture was diluted with dichloromethane and cautiously poured into a saturated NaHCO3 solution. The phases were separated and the aqueous layer was washed two times with dichloromethane. The combined organic layers are dried over sodium sulfate and filtered. After chromatography (silica, ethyl acetate/methanol/35% ammonia solution = 50/50/1) 14-O-{[(1R, 2R, 4R)-4-amino-2-hydroxy-cyclohexylsulfanyl]- acetyl}-mutilin + (IS, 2S, 4S) diastereomer (745 mg, 67% yield) was obtained as colorless amorphous foam.
1H NMR (400MHz, DMSO-de, δ, ppm, inter alia): 6.14 (dd, IH, 19-H, J = 1 IHz and 18Hz), 5.54 (d, IH, 14-H, J = 8Hz), 5.05 (m, 2H, 20-H), 4.50 (d, IH, 11-OH, J = 6Hz), 3.50 – 3.20 (m, 5H, 2′-H, 4′-H, H-H, 22-H), 2.55 (m, IH, l ‘-H), 2.40 (bs, IH, 4-H), 1.35 (s, 3H, 15- CH3), 1.06 (s, 3H, 18-CH3), 0.82 (d, 3H, 17-CH3, J = 7Hz), 0.62 (d, 3H, 16-CH3, J = 7Hz). MS-ESI (m/z): 508 (MH+), 530 (MNa+), 1015 (2MH+), 1037 (2MNa+).
Step C. 14-O-{[(1R, 2R, 4R)-4-Amino-2-hydroxy-cyclohexylsulfanyI]-acetyl}- mutilin hydrochloride + (IS, 2S, 4S) diastereomer hydrochloride
A solution of 14-O-{[(1R, 2R, 4R)-4-amino-2-hydroxy-cyclphexylsulfanyl] -acetyl }-mutilin + (IS, 2S, 4S) diastereomer (325 mg, 0.64 mmol) in 20 ml of dioxane was treated with IN HCl (0.64ml, 0.64 mmol). After stirring at room temperature for 30 minutes the solution was lyophilized to obtain 14-O-{[(1R, 2R, 4R)-4-amino-2-hydroxy-cyclohexylsulfanyl] -acetyl }- mutilin hydrochloride + (IS, 2S, 4S) diastereomer hydrochloride (quantitative yield) as colorless amorphous solid.
1H NMR (500MHz, DMSO-Cl6, δ, ppm, inter alia): 7.6 (bs, 3H, NH3 +), 6.14 (dd, IH, 19-H, J = 1 IHz and 18Hz), 5.55 (d, IH, 14-H, J = 8Hz), 5.05 (m, 2H, 20-H), 4.52 (d, IH, H-OH, J = 6Hz), 3.50 – 3.20 (m, 4H, 2′-H, H-H, 22-H), 3.03 (m, IH, 4′-H), 2.53 (m, IH, 1 ‘-H), 2.40 (bs, IH, 4-H), 1.37 (s, 3H, 15-CH3), 1.06 (s, 3H, 18-CH3), 0.82 (d, 3H, 17-CH3, J = 7Hz), 0.62 (d, 3H, 16-CH3, J = 7Hz). MS-ESI (m/z): 508 (MH+), 530 (MNa+), 1015 (2MH+), 1037 (2MNa+), 542 (MCl“).
Example IA – 14-O-{[(1S, 2S, 4S)-4-Amino-2-hydroxy-cyclohexylsulfanyl]-acetyl}- mutilin and 14-O-{[(1R, 2R, 4R)-4-Amino-2-hydroxy-cyclohexylsuIfanyl]-acetyl}-mutilin
The mixture of 14-O-{[(1R, 2R, 4R)-4-Amino-2-hydroxy-cyclohexylsulfanyl]-acetyl}-mutilin + (IS, 2S, 4S) diastereomer (12 g, 23.6 mmol) from Example 1 Step B was separated on a cbiral column (250 x 20 mm CHIRALCEL OD-H, n-heptane / ethanol / diethylamine = 80/20/0.1) to yield 14-O-{[(1S*, 2S*, 4S*)-4-amino-2-hydroxy-cyclohexylsulfanyl]-acetyl}- mutilin (a) (early eluting compound, 4.76 g, 37% yield, uncorrected) and 14-O-{[(1R*, 2R*, 4R*)-4-amino-2-hydroxy-cyclohexylsulfanyl]-acetyl}-mutilin (b) (late eluting compound, 3.63 g, 30% yield, uncorrected) as colorless amorphous foams.
(a): 1H NMR (400MHz, DMSO-(I6, δ, ppm, inter alia): 6.13 (dd, IH, 19-H, J = 1 IHz and 18Hz), 5.54 (d, IH, 14-H, J = 8Hz), 5.05 (m, 2H, 20-H), 4.50 (d, IH, H-OH, J = 6Hz), 3.50 – 3.20 (m, 5H, 2′-H, 4′-H, H-H, 22-H), 2.55 (m, IH, l ‘-H), 2.40 (bs, IH, 4-H), 1.35 (s, 3H, 15- CH3), 1.05 (s, 3H, 18-CH3), 0.82 (d, 3H, 17-CH3, J = 7Hz), 0.62 (d, 3H, 16-CH3, J = 7Hz). MS-ESI (m/z): 508 (MH+), 530 (MNa+), 1015 (2MH+), 1037 (2MNa+), 506 (M-H) “, 542 (MCl“).
(b): 1H NMR (400MHz, DMSO-d6> δ, ppm, inter alia): 6.13 (dd, IH, 19-H, J = 1 IHz and 18Hz), 5.54 (d, IH, 14-H, J = 8Hz), 5.05 (m, 2H, 20-H), 4.50 (d, IH, H-OH, J = 6Hz), 3.50 – 3.20 (m, 5H, 2′-H, 4′-H, 11-H, 22-H), 2.55 (m, IH, 1 ‘-H), 2.40 (bs, IH, 4-H), 1.35 (s, 3H, 15- CH3), 1.05 (s, 3H, 18-CH3), 0.82 (d, 3H, 17-CH3, J = 7Hz), 0.62 (d, 3H, 16-CH3, J = 7Hz). MS-ESI (m/z): 508 (MH+), 530 (MNa+), 1015 (2MH+), 1037 (2MNa+), 506 (M-H) “, 542 (MCl“).
…………………………………………………….
WO 2011146954
http://www.google.com/patents/WO2011146954A1?cl=en
The present invention relates to crystalline 14-0-{[(4-amino-2-hydroxy-cyclohexyl)- sulfanyl] -acetyl }-mutilin, new processes for its preparation and crystalline salts thereof.
Pleuromutilin, a compound of formula
Pleuromutilin
is a naturally occurring antibiotic, e.g. produced by the basidiomycetes Pleurotus mutilus and P. passeckerianus, see e.g. The Merck Index, 12th edition, item 7694.
A number of further pleuromutilins having the principle ring structure of pleuromutilin and being substituted at the primary hydroxy group have been developed, e.g. as antimicrobials. Due to their pronounced antimicrobial activity, a group of pleuromutilin derivatives, amino- hydroxy-substituted cyclohexylsulfanylacetylmutilins, as disclosed in WO 2008/113089, have been found to be of particular interest. As described in WO2008/11089 14-0-{[(4- Amino-2-hydroxy-cyclohexyl)-sulfanyl] -acetyl }-mutilins are particularly useful compounds because they demonstrate activity against Gram-positive and Gram-negative pathogens e.g. associated with respiratory tract and skin and skin structure infections. For the production of substantially pure isomers/diastereomers of this group of compounds, there is a need for a production process which is convenient for use on an industrial scale and which also avoids the use of costly starting materials, environmentally hazardous reagents and solvents or time consuming and laborious purification steps. The production process described in WO 2008/113089 involves chromatographic purification of the compounds prepared according to individual synthesis steps and the final diastereomers are separated by chiral HPLC chromatography which cannot be used on industrial scale. Surprisingly, crystalline intermediates have been found which on the one hand have unexpected chemical purification potential which is important for the production processes for pure amino-hydroxy-substituted cyclohexylsulfanylacetylmutilins avoiding
chromatographic purification and separation steps.
It has to be pointed out that 14-0-{[(4-amino-2-hydroxy-cyclohexyl)-sulfanyl]-acetyl}- mutilins are potential new drug substances for the human market with regulatory
requirements defined in the corresponding ICH guidelines (International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use). The ICH guideline on impurities in new drug substances (Q3 A(R2)) includes the following thresholds:
As can be seen from the ICH thresholds above it is desirable to have all individual unknown impurities below 0.10% area and the structure elucidated impurities below 0.15%, respectively. Processes provided according to the present invention enable to produce APIs (Active Pharmaceutical Ingredients) within the desired specifications and fulfilling ICH requirements.
On the other hand, even more surprisingly, the crystalline intermediates yields to significant chiral enrichment which has a huge benefit in the production of the pure stereoisomers starting from cheaper racemic materials or less chirally pure starting materials. The described processes do not involve any chromatographic purification neither normal nor chiral phase in contrast to the synthetic procedures described in WO2008/113089 wherein is disclosed e.g. in Example 1, Step B that 14-0-{[(4-amino-2-hydroxy-cyclohexyl)-sulfanyl]- acetyl}-mutilins was isolated in the form of diastereomeric mixtures as colorless amorphous foams after normal phase chromatography. The chiral pure diastereomers are described to have been received in WO2008/113089, e.g. in Example 1 A after subjecting the mixture to chiral chromatography whereafter the separated pure diastereomers were isolated in the form of colorless amorphous foams.
Chiral chromatography, however is not a technology which can be applied on industrial large scale, and moreover no crystalline salts of 14-0-{[(4-amino-2-hydroxy-cyclohexyl)- sulfanyl]-acetyl}-mutilins were obtained according to WO2008/113089. In contrast to that, according to the present invention crystalline pharmaceutical acceptable salts of 14-0-{[(4-amino-2-hydroxy-cyclohexyl)-sulfanyl]-acetyl}-mutilins having surprising and superior properties over the amorphic prior art salts disclosed in
WO2008/113089 have been found; e.g. surprisingly the chemical stability of the crystalline salts of the present invention is improved over the amorphic salt forms; and also and in addition the crystalline salts of the present invention show a surprising low hygroscopicity.
Processes for the preparation of such crystalline salts wherein the salts may be obtained in a single stereoisomeric form from 14-0-{[(4-amino-2-hydroxy-cyclohexyl)-sulfanyl]-acetyl}- mutilins and processes for the preparation of stereoisomerically pure 14-0-{[(4-amino-2- hydroxy-cyclohexyl)-sulfanyl]-acetyl}-mutilins in crystalline form as a basis for the crystalline salts have also been found.
In one aspect the present invention provides a process for the preparation of a compound of formula I
in the form of a single stereoisomer in crystalline form, comprising
deprotecting the amine group
either in a compound of formula Ila
in a mixture of a compound of formula Ila with a compound of formula lib
wherein R is an amine protecting group, and isolating a compound of formula I obtained in the form of a single diastereomer in crystalline form either directly from the reaction mixture or via recrystallization in organic solvent.
In another aspect the present invention provides a compound of formula I as defined above in the form of a single stereoisomer in crystalline form.
Compounds of formula Ila are new and also form part of the present invention.
In another aspect the present invention provides a compound of formula Ha.
In a compound of formula I, or Ha, respectively, the carbon atoms of the cyclohexyl ring to which the hydroxy group, the amine group and the sulfanyl-acetyl-mutilin group are attached are all in the R configuration and thus a compound of formula I, or Ila represents an optionally amine protected 14-0-{[(l ?,2i?,4 ?)-4-amino-2-hydroxy-cyclohexylsulfanyl]- acetyl}-mutilin. In contrast to that, in a compound of formula lb
or lib the carbon atoms of the cyclohexyl ring to which the hydroxy group, the amine group and the sulfanyl-acetyl-mutilin group are attached are all in the S configuration and thus a compound of formula lib represents an optionally amino protected 14-0-{[(lS,2S,4S)-4-Amino-2-hydroxy- cyclohexylsulfanyl] -acetyl } -mutilin. An amine protecting group includes protecting groups known to a skilled person and which are removable under acidic, basic, hydrogenating, oxidative or reductive methods, e.g. by hydrogenolysis, treatment with an acid, a base, a hydride, a sulfide. Appropriate amine protecting groups e.g. are described in T. W. Greene, P. G. M. Wuts, Protective Groups in Organic Synthesis, Wiley-Interscience, 4th edition, 2007, particularly p. 696-868.
Example 1
tert-Butyl [(lR3Ri4R)-3-hydroxy-4-mercapto-cyclohexyl]-carbamate
3.94 Kg of {(li?,2J?,4i?)-4-[(tert-Butoxycarbonyl)-amino]-2-hydroxy-cyclohexyl}-benzene- carbothioate and 37 L of CH2C12 were charged to a vessel and the mixture obtained was stirred at 15-25°C. 0.39 Kg of 1,4-dithio-DL-threitol (10% wt) was added to the mixture and rinsed through with 2 L of CH2C12. To the mixture obtained 0.84 Kg of hydrazine monohydrate was added. The mixture obtained was stirred at 18 to 22°C for 3 h and the reaction was followed by HPLC. Upon completion of the reaction, 39 L of 1 M phosphoric acid solution was added and the mixture obtained was stirred for a further 15-30 min. Two phases formed were separated and the organic phase obtained was washed with 39 L of of 1 M phosphoric acid solution followed by 39 L 1% aqueous NaCl solution. The organic layer obtained was concentrated in vacuo at <40°C, to the concentration residue 20 L of CH2C12 was added and the mixture obtained again was concentrated. To the concentration residue obtained a further 8 L of CH2C12 was added and the mixture obtained was concentrated to dryness.
2.89 Kg of tert-Butyl [(l ?,3/?,4i?)-3-hydroxy-4-mercapto-cyclohexyl]-carbamate in the form of a white solid was obtained.
1H NMR (200 MHz, DMSO-de, ppm) δ 6.79 (d, J=7.8Hz, 1H), 4.99 (d, J=5.8Hz, 1H), 3.34 – 3.24 (m, 1H), 3.14 – 3.04 (m, 1H), 2.37 (d, J=3.8 Hz, 1H), 2.00 -1.89 (m, 1H), 1.87 – 1.82 (m, 1H), 1.73 – 1.67 (m, 1H), 1.47 – 1.04 (m, 12H)
Example 2
22-0-TosylpIeuromutilin
22-O-Tosylpleuromutilin is a known compound from literature. However a preparation procedure is outlined below.
A solution of 13.0 kg of pleuromutilin and 6.57 kg of 4-toluenesulfonyl chloride in 42.1 L of CH2CI2 at 10 to 15 °C was treated with 9.1 L of 5.7 M aqueous NaOH over 20 min, maintaining a temperature < 25 °C. The resulting off-white suspension was heated to reflux for 20 h and the reaction was followed until completion determined by HPLC. Upon reaction completion the mixture obtained was cooled to 20 to 30 °C, diluted with 52 L of CH2C12, stirred at 15 to 25 °C for 10 min, and the layers obtained were separated. The organic phase obtained was washed several times with 52 L of water until a pH of the aqueous layer was adjusted to < 9. The organic layer obtained was concentrated to 4 volumes and
azeotropically dried twice with 52 L of CH2C12. To the solution obtained 52 L of heptane were added dropwise and the solution obtained was concentrated at < 40 °C to
approximately 4 volumes. To the concentrate obtained 52 L of heptane was added and the resulting suspension was stirred at 20 to 25 °C for 2 to 2.5 h, filtered, the filter cake obtained was washed with 39 L of heptane and pulled dry on the filter.
The solid was dried under vacuum at < 40 °C for at least 12 h.
16.9 kg of 22-O-tosylpleuromutilin in the form of a white solid was obtained.
1H NMR (200 MHz, DMSO-d6, ppm, inter alia) δ 7.81 (d, 2H), 7.47 (d, 2H), 6.14 – 6.0 (m, 1H), 5.54 (d, J=7.8Hz, 1H), 5.08 – 4.99 (m, 2H), 4.70 (AB, J=16.2Hz, 2H), 3.41 (d, J=5.2Hz, 1H), 2.41(s, 4H), 1.04(s, 3H), 0.81 (d, 3H), 0.51 (d, 3H)
Example 3
14-0-{[(l/?,2R,4R)-4-ter/-Butoxycarbonylamino-2-hydroxy-cyclohexyI-sulfanyl]-acetyl}- mutilin
4.75 Kg of Pleuromutilin tosylate (Tos-PLEU) and 44.4 L of MTBE were charged into a vessel and to the mixture obtained 0.31 Kg of benzyl-tri-«-butylammonium chloride was added and rinsed through with 2.4 L of MTBE. To the mixture obtained 20 L of IM aqueous NaOH solution and 2.84 Kg of tert-Butyl [(lif,3i?,4^)-3-hydroxy-4-mercapto-cyclohexyl]- carbamate were added and the mixture obtained was stirred at 17 to 23 °C for 3 h. Upon completion of the reaction (determined by HPLC) two layers formed were separated and the lower aqueous layer was removed. The organic phase obtained was washed with 19 L of IM aqueous NaOH solution, twice with 20 L of 0.1 M phosphoric acid, 20 L of 10% aqueous NaHC03 solution and twice with 20 L of water. The organic liquors obtained were concentrated, the concentrate obtained was taken up in 7.46 Kg of 2-propanol, the mixture obtained was concentrated again and dried in vacuo at <40°C. 6.66 Kg of 14-O- { [( 1 -¾,2i?,4i?)-4-/ert-Butoxycarbonylamino-2-hydroxy-cyclohexyl-sulfanyl]-acetyl } -mutilin in the form of a white foam was obtained.
Ή NMR (200 MHz, DMSO-d6, ppm, inter alia) δ 6.78 (d, J=7.8Hz, 1H), 6.22 – 6.08 (m,lH), 5.55 (d, J=7.8Hz, 1H), 5.13 – 5.02 (m, 2H), 4.95 (d, J=5Hz, 1H), 4.52 (d, J=6Hz, 1H), 3.36 (AB, J=15Hz, 2H), 2.40 (s, broad, 1H), 2.15 – 2.0 (m, 3H), 1.9 – 1.8 (m, 1H), 1.35 (s, 9H), 0.81 (d, J=7Hz, 3H), 0.62 (d, J=6.6Hz, 3H)
MS (ESI, g/mol): m/z 653 [M+2Na] +
Example 4
14-0-{[(lR,2R,4R)-4-Amino-2-hydroxy-cyclohexyIsulfanyI]-acetyl}-mutilin, crystalline Form 2
Step A: 14-O-{[(li?.2i?,4i?)-4-Amino-2Thvdroxy-cyclohexylsulfanvn-acetvU-mutilin in crystalline Form 1
6.6 Kg of 14-O-{[(li?,2if,4/?)-4-tert-Butoxycarbonylamino-2-hydroxy-cyclohexyl-sulfanyl]- acetyl}-mutilin and 13.2 L of isopropanol were charged into a vessel and stirred at 20 to 25°C. 11.20 kg of 85% phosphoric acid was added and the mixture obtained was heated to approximately 50°C for at least 16 h. The mixture obtained was analyzed for reaction completion by HPLC. Upon completion of the reaction the mixture was cooled to 20 to 25°C and 52 L of CH2C12 was added. The mixture obtained was cooled to 0 to 5°C and 51 L of 30% aqueous K2CO3 solution was added over 1 h at <25°C. The mixture obtained was warmed to rt, stirred for 30 min and the pH of the aqueous layer was determined. To the mixture obtained a further 15 L of 30% aqueous K2C03 solution was added at <25°C, the mixture obtained was stirred at 15°C to 25 °C for 30 min and the two phases obtained were separated. The aqueous phase obtained was extracted with 51 L of CH2CI2 and the combined organic phases were washed with 51 L of purified water. The mixture obtained was concentrated to a volume of 25 L, 33.6 Kg of CH2C12 was added and the mixture obtained was concentrated to 25 L. To the concentrate obtained 33.6 Kg of CH2C12 was added and the mixture obtained was concentrated to 10 L. The concentration residue obtained was cooled to 18 to 22°C and 50 L of di-wopropyl ether was added over a period of 1 h. The slurry obtained was stirred at 15 to 25°C for a minimum of 2 h, filtered and the solid obtained was washed with 10 L of di-wopropyl ether and was dried.
3.79 Kg of 14-0-{[(li?,2i?,4if)-4-Amino-2-hydroxy-cyclohexylsulfanyl]-acetyl}-mutilin in crystalline Form 1 was obtained.
Step B: 14-O-{r(l-R.2i?,4j?)-4-amino-2-hvdroxy-cvclohexylsulfanyl1-acetv -mutilin. in crystalline Form 2
For further purification 14-O-{[(l ?,2 ?,4i?)-4-Amino-2-hydroxy-cyclohexylsulfanyl]- acetyl}-mutilin from Step A and 18.75 L of n-butanol were heated to 88 to 92°C until complete dissolution and stirred for 30 to 60 min. The mixture obtained was allowed to cool to 40 to 45°C over at least 2 h and further stirred at this temperature for 2 h. The mixture obtained was filtered and the precipitate obtained was washed with 3.75 L of «-butanol followed by 3.75 L of MTBE. That purification procedure was repeated and the resultant product was dried in vacuo at <40°C.
3.27 Kg of crystalline 14-0-{[(li?,2if,4i?)-4-amino-2-hydroxy-cyclohexylsulfanyl]-acetyl}- mutilin in crystalline Form 2 was obtained in the form of a white solid.
lH NMR (400 MHz, CDC13, ppm, inter alia) δ 6.51 – 6.44 (m, 1H), 5.78 (d, J=8Hz, 1H), 5.38 – 5.20 (m, 2H), 3.48 – 3.40 (m, 1H), 3.36 (d, J=7Hz, 1H), 3.25 (AB, J=15Hz, 2H), 2.92 – 2.82 (m, 1H), 2.6 – 2.5 (m, 1H), 1.45 (s, 3H), 1.20 (s, 3H), 0.88 (d, J=7Hz, 3 H), 0.73 (d, J=8Hz, 3H)
MS (ESI, g/mol): m/z 508 [M+H] +
Example 5
14-0-{[(lR^/f,4R)-4-Amino-2-hydroxy-cyclohexylsulfanyl]-acetyl}-mutilin, crystalline
To a solution of 900 g of 14-0-{[(li?,2i?,4i?)-4-tert-butoxycarbonylamino-2-hydroxy- cyclohexyl-sulfanyl]-acetyl}-mutilin in 9 L of CH2C12 at 15 to 25°C was added 1.8 L of TFA at 15 to 25°C and the resulting solution was stirred for 2 h. Following reaction completion the reaction mixture was concentrated under vacuum and the concentration residue obtained was azeo-dried with a total of 9 L of CH2C12. The concentrate obtained was dissolved in 4.5 L of CH2C12, the solution obtained cooled to 0 to 5°C and the pH was adjusted to pH 11 with aqueous 3.6 L 2CO3 (2.5M) solution. The biphasic mixture obtained was warmed to 15 to 20°C and stirred for 5 to 10 minutes. The layers obtained were separated, the aqueous phase obtained was extracted with 1.8 L of CH2C12, the organic phases obtained were combined, washed with 2.3 L of H20, dried over Na2S04 and concentrated to dryness under vacuum at <40°C. Crude 14-0- { [( 1 R,2R,4R)-4- Amino-2-hydroxy-cyclohexyl-sulfanyl]-acetyl } -mutilin was obtained. Yield: 744 g
For further purification the following procedure was applied:
To 744 g of crude 14-O-{[(li?,2i?,4i-)-amino-2-hydroxy-cyclohexyl-sulfanyl]-acetyl}- mutilin was added 2.23 L of THF and the resulting suspension was stirred at 15 to 25°C for 60 min. To the mixture obtained 7.44 L of MTBE was added over 15 to 30 min, the suspension obtained was aged for 60 min and filtered under nitrogen. The collected solids were washed with a total of 3 L of MTBE and pulled dry on the filter under nitrogen for 1.5 h.
626 g of 14-0-{[(li?,2i?,4i?)-4-Amino-2-hydroxy-cyclohexyl-sulfanyl]-acetyl}-mutilin in crystalline Form 1 was obtained.
The Ή NMR pattern confirms the structure of 14-O-{[(li?,2i?,4i?)-4-amino-2-hydroxy- cyclohexylsulfanyl] -acetyl} -mutilin. The NMR pattern for 14-O-{[(l ?,2i?,4/?)-4-amino-2- hydroxy-cyclohexylsulfanyl]-acetyl}-mutilin is described in example 4.
…………………………………………………………
REF
http://www.phase4-partners.com/wp-content/uploads/2013/09/100412.pdf
http://www.glsv-vc.com/downloads/2010-06-02_First%20Patient_PressRelease.pdf
119
Nabriva. Pleuromutilins. Available online: http://www.nabriva.com/programs/pleuromutilins/ (accessed on 7 December 2012).
120
Forest Laboratories. Our pipeline: Solid, and set for further growth. Available online: http://www.frx.com/research/pipeline.aspx (accessed on 13 April 2013).
121
Sader, H.S.; Biedenbach, D.J.; Paukner, S.; Ivezic-Schoenfeld, Z.; Jones, R.N. Antimicrobial activity of the investigational pleuromutilin compound BC-3781 tested against Gram-positive organisms commonly associated with acute bacterial skin and skin structure infections. Antimicrob. Agents Chemother. 2012,56, 1619–1623, doi:10.1128/AAC.05789-11.
122
Sader, H.S.; Paukner, S.; Ivezic-Schoenfeld, Z.; Biedenbach, D.J.; Schmitz, F.J.; Jones, R.N. Antimicrobial activity of the novel pleuromutilin antibiotic BC-3781 against organisms responsible for community-acquired respiratory tract infections (CARTIs). J. Antimicrob. Chemother. 2012, 67, 1170–1175, doi:10.1093/jac/dks001.
123
Nabriva Therapeutics AG. Study comparing the safety and efficacy of two doses of BC-3781 vs. vancomycin in patients with acute bacterial skin and skin structure infection (ABSSSI). Available online: http://www.clinicaltrials.gov/ct2/show/NCT01119105 (accessed on 13 April 2013).
124
Novak, R. Are pleuromutilin antibiotics finally fit for human use? Ann. NY Acad. Sci. 2011, 1241, 71–81, doi:10.1111/j.1749-6632.2011.06219.x.
 valnemulin
valnemulin
 retapamulin
retapamulin
| WO2002004414A1 * | Jul 9, 2001 | Jan 17, 2002 | Gerd Ascher | Pleuromutilin derivatives having antibacterial activity |
| WO2007000004A1 * | Jun 26, 2006 | Jan 4, 2007 | Nabriva Therapeutics Forschung | Pleuromutilin derivatives containing a hydroxyamino- or acyloxyaminocycloalkyl group |
| WO2007014409A1 * | Jul 26, 2006 | Feb 8, 2007 | Nabriva Therapeutics Forschung | Pleuromutilin derivatives useful as antibacterials |
| WO2008011089A2 | Jul 19, 2007 | Jan 24, 2008 | Mark B Gagner | Wagering game with special-event eligibility feature based on passive game play |
| WO2008113089A1 | Mar 19, 2008 | Sep 25, 2008 | Nabriva Therapeutics Ag | Pleuromutilin derivatives for the treatment of diseases mediated by microbes |
| US20060276503 * | Aug 30, 2004 | Dec 7, 2006 | Glaxo Group Limited | Novel process salts compositions and use |
FDA Approves Vitekta (elvitegravir) for HIV-1 Infection
FDA Approves Vitekta (elvitegravir) for HIV-1 Infection
September 24, 2014 — The U.S. Food and Drug Administration (FDA) has approved Vitekta (elvitegravir), an integrase strand transfer inhibitor for the combination treatment of human immunodeficiency virus type 1 (HIV-1) infection in treatment-experienced adults.

Elvitegravir
697761-98-1 CAS

Elvitegravir (EVG, formerly GS-9137) is a drug used for the treatment of HIV infection. It acts as an integrase inhibitor. It was developed[1] by the pharmaceutical company Gilead Sciences, which licensed EVG from Japan Tobacco in March 2008.[2][3][4] The drug gained approval by U.S. Food and Drug Administration on August 27, 2012 for use in adult patients starting HIV treatment for the first time as part of the fixed dose combination known as Stribild.[5]
According to the results of the phase II clinical trial, patients taking once-daily elvitegravir boosted by ritonavir had greater reductions in viral load after 24 weeks compared to individuals randomized to receive a ritonavir-boosted protease inhibitor.[6]
Human immunodeficiency virus type 1 (HIV-1) is the causative agent of acquired immunodeficiency disease syndrome (AIDS). After over 26 years of efforts, there is still not a therapeutic cure or an effective vaccine against HIV/AIDS. The clinical management of HIV-1 infected people largely relies on antiretroviral therapy (ART). Although highly active antiretroviral therapy (HAART) has provided an effective way to treat AIDS patients, the huge burden of ART in developing countries, together with the increasing incidence of drug resistant viruses among treated people, calls for continuous efforts for the development of anti-HIV-1 drugs. Currently, four classes of over 30 licensed antiretrovirals (ARVs) and combination regimens of these ARVs are in use clinically including: reverse transcriptase inhibitors (RTIs) (e.g. nucleoside reverse transcriptase inhibitors, NRTIs; and non-nucleoside reverse transcriptase inhibitors, NNRTIs), protease inhibitors (PIs), integrase inhibitors and entry inhibitors (e.g. fusion inhibitors and CCR5 antagonists).
- Gilead Press Release Phase III Clinical Trial of Elvitegravir July 22, 2008
- Gilead Press Release Gilead and Japan Tobacco Sign Licensing Agreement for Novel HIV Integrase Inhibitor March 22, 2008
- Shimura K, Kodama E, Sakagami Y, et al. (2007). “Broad Anti-Retroviral Activity and Resistance Profile of a Novel Human Immunodeficiency Virus Integrase Inhibitor, Elvitegravir (JTK-303/GS-9137)”. J Virol 82 (2): 764. doi:10.1128/JVI.01534-07. PMC 2224569. PMID 17977962.
- Stellbrink HJ (2007). “Antiviral drugs in the treatment of AIDS: what is in the pipeline ?”. Eur. J. Med. Res. 12 (9): 483–95. PMID 17933730.
- Sax, P. E.; Dejesus, E.; Mills, A.; Zolopa, A.; Cohen, C.; Wohl, D.; Gallant, J. E.; Liu, H. C.; Zhong, L.; Yale, K.; White, K.; Kearney, B. P.; Szwarcberg, J.; Quirk, E.; Cheng, A. K.; Gs-Us-236-0102 Study, T. (2012). “Co-formulated elvitegravir, cobicistat, emtricitabine, and tenofovir versus co-formulated efavirenz, emtricitabine, and tenofovir for initial treatment of HIV-1 infection: A randomised, double-blind, phase 3 trial, analysis of results after 48 weeks”.The Lancet 379 (9835): 2439–2448. doi:10.1016/S0140-6736(12)60917-9. PMID 22748591. edit
- Thaczuk, Derek and Carter, Michael. ICAAC: Best response to elvitegravir seen when used with T-20 and other active agents Aidsmap.com. 19 Sept. 2007.

The life cycle of HIV-1. 1. HIV-1 gp120 binds to CD4 and co-receptor CCR5/CXCR4 on target cell; 2. HIV-1 gp41 mediates fusion with target cell; 3. Nucleocapsid containing viral genome and enzymes enters cells; 4. Viral genome and enzymes are released; 5. Viral reverse transcriptase catalyzes reverse transcription of ssRNA, forming RNA-DNA hybrids; 6. RNA template is degraded by ribonuclease H followed by the synthesis of HIV dsDNA; 7. Viral dsDNA is transported into the nucleus and integrated into the host chromosomal DNA by the viral integrase enzyme; 8. Transcription of proviral DNA into genomic ssRNA and mRNAs formation after processing; 9. Viral RNA is exported to cytoplasm; 10. Synthesis of viral precursor proteins under the catalysis of host-cell ribosomes; 11. Viral protease cleaves the precursors into viral proteins; 12. HIV ssRNA and proteins assemble under host cell membrane, into which gp120 and gp41 are inserted; 13. Membrane of host-cell buds out, forming the viral envelope; 14. Matured viral particle is released
Elvitegravir, also known as GS 9137 or JTK 303, is an investigational new drug and a novel oral integrase inhibitor that is being evaluated for the treatment of HIV-1 infection. After HIVs genetic material is deposited inside a cell, its RNA must be converted (reverse transcribed) into DNA. A viral enzyme called integrase then helps to hide HIVs DNA inside the cell’s DNA. Once this happens, the cell can begin producing genetic material for new viruses. Integrase inhibitors, such as elvitegravir, are designed to block the activity of the integrase enzyme and to prevent HIV DNA from entering healthy cell DNA. Elvitegravir has the chemical name: 6-(3-chloro-2-fluorobenzyl)-1-[(S)-1 -hydroxy -methyl-2- methylpropyl]-7-methoxy-4-oxo-1, 4-dihydroquinoline-3-carboxylic acid and has the following structural formula:
WO 2000040561 , WO 2000040563 and WO 2001098275 disclose 4-oxo-1 , 4-dihydro-3- quinoline which is useful as antiviral agents. WO2004046115 provides certain 4- oxoquinoline compounds that are useful as HIV Integrase inhibitors.
US 7176220 patent discloses elvitegravir, solvate, stereoisomer, tautomer, pharmaceutically acceptable salt thereof or pharmaceutical composition containing them and their method of treatment. The chemistry involved in the above said patent is depicted below in the Scheme A. Scheme-A
Toluene, DIPEA
SOCl2 ,COCl (S)-(+)-Valinol
Toluene
,4-Difluoro-5-iodo- benzoic acid
THF
dichlorobis(triphenylphosphine)
palladium argon stream,
Elvitegravir Form ] Elvitegravir (residue) US 7635704 patent discloses certain specific crystalline forms of elvitegravir. The specific crystalline forms are reported to have superior physical and chemical stability compared to other physical forms of the compound. Further, process for the preparation of elvitegravir also disclosed and is depicted below in the Scheme B. The given processes involve the isolation of the intermediates at almost all the stages.
Scheme B
2,
–
Zn THF,
CK Br THF CU “ZnBr dιchlorobis(trιphenylphos
phine)palladium
Elvitegravir WO 2007102499 discloses a compound which is useful as an intermediate for the synthesis of an anti-HIV agent having an integrase-inhibiting activity; a process for production of the compound; and a process for production of an anti-HIV agent using the intermediate.
WO 2009036161 also discloses synthetic processes and synthetic intermediates that can be used to prepare 4-oxoquinolone compounds having useful integrase inhibiting properties.
The said processes are tedious in making and the purity of the final compound is affected because of the number of steps, their isolation, purification etc., thus, there is a need for new synthetic methods for producing elvitegravir which process is cost effective, easy to practice, increase the yield and purity of the final compound, or that eliminate the use of toxic or costly reagents.
US Patent No 7176220 discloses Elvitegravir, solvate, stereoisomer, tautomer, pharmaceutically acceptable salt thereof or pharmaceutical composition containing them and ■ their method of treatment. US Patent No 7635704 discloses Elvitegravir Form II, Form III and processes for their preparation. The process for the preparation of Form Il disclosed in the said patent is mainly by three methods – a) dissolution of Elvitegravir followed by seeding with Form II, b) recrystallisation of Elvitegravir, and c) anti-solvent method.
The process for the preparation of Form III in the said patent is mainly by three methods – a) dissolution of Form Il in isobutyl acetate by heating followed by cooling the reaction mass, b) dissolution of Form Il in isobutyl acetate by heating followed by seeding with Form III, and c) dissolving Form Il in 2-propanol followed by seeding with Form III.
Amorphous materials are becoming more prevalent in the pharmaceutical industry. In order to overcome the solubility and potential bioavailability issues, amorphous solid forms are becoming front-runners. Of special importance is the distinction between amorphous and crystalline forms, as they have differing implications on drug substance stability, as well as drug product stability and efficacy.
An estimated 50% of all drug molecules used in medicinal therapy are administered as salts. A drug substance often has certain suboptimal physicochemical or biopharmaceutical properties that can be overcome by pairing a basic or acidic drug molecule with a counter- ion to create a salt version of the drug. The process is a simple way to modify the properties of a drug with ionizable functional groups to overcome undesirable features of the parent drug. Salt forms of drugs have a large effect on the drugs’ quality, safety, and performance. The properties of salt-forming species significantly affect the pharmaceutical properties of a drug and can greatly benefit chemists and formulators in various facets of drug discovery and development.



chemical synthesis from a carboxylic acid 1 starts after conversion to the acid chloride iodide NIS 2 , and with three condensation 4 . 4 and the amino alcohol 5 addition-elimination reaction occurs 6 , 6 off under alkaline conditions with TBS protected hydroxy get the ring 7 , 7 and zinc reagent 8 Negishi coupling occurs to get 9 , the last 9 hydrolysis and methoxylated
Elvitegravir dimer impurity, WO2011004389A2
Isolation of 1-[(2S)-1-({3-carboxy-6-(3-chloro-2-fluorobenzyl)-1 -[(2S)-I- hydroxy-3-methylbutan-2-yl]-4-oxo-1 , 4-dihydroquinolin-7-yl}oxy)-3- methylbutan-2-yl 6-(3-chloro-2-fluorobenzyl)-7-methoxy-4-oxo-1 , 4-dihydroquinoline-3-carboxylic acid (elvitegravir dimer impurity, 13)
After isolation of the elvitegravir from the mixture of ethyl acetate-hexane, solvent from the filtrate was removed under reduced pressure. The resultant residue purified by column chromatography using a mixture of ethyl acetate-hexane (gradient, 20-80% EtOAc in hexane) as an eluent. Upon concentration of the required fractions, a thick solid was obtained which was further purified on slurry washing with ethyl acetate to get pure elvitegravir dimer impurity (13). The 1H-NMR, 13C-NMR and mass spectral data complies with proposed structure.
1H-NMR (DMSO-Cf6, 300 MHz, ppm) – δ 0.79 (m, d=6.3 Hz, 6H, 20 & 2O’)\ 1.18 & 1.20 (d, J=6.3 Hz & J=6.2 Hz, 6H, 21 & 21′)1, 2.42-2.49 (m, 2H, 19 & 19′), 3.81-3.89 (m, 3H, T & 17’Ha), 3.94-4.01 (m, 1 H, 17’Hb), 4.01 (s, 3H, 23), 4.11 (s, 2H, 7), 4.83-4.85 (m, 3H, 17 & 18′), 5.22 (t, J=4.7 Hz, 1H, OH), 5.41-5.44 (m, 1 H, 18), 6.73-6.78 (t, J=7.1 Hz, 1 H, 11)1‘ 2, 6.92-6.98 (t, J=8.0 Hz, 1H, 3′) 1‘2, 7.12-7.22 (m, 2H, 1 & 3), 7.34-7.39 (m, 1H, 2′),
7.45-7.48 (m, 1 H, 2), 7.49, 7.56 (s, 2H, 15 & 15′), 7.99, 8.02 (s, 2H, 9 & 9′), 8.89, 9.01 (s, 2H, 13 & 13′), 15.30, 15.33 (s, 2H, COOH’ & COOH”).
13C-NMR (DMSO-Cf6, 75 MHz, ppm)- δ 18.87, 19.03 (2OC, 20’C), 19.11 , 19.24 (21 C, 21 ‘C), 27.94 (7’C), 28.40 (7C), 28.91 , 30.08 (19C, 19’C), 56.80(23C), 60.11 (171C), 63.59 (18C), 66.52 (18’C), 68.53 (17C), 97.86, 98.97 (15, 15′), 107.43, 108.16 (12C, 12’C),
118.77, 119.38 (1OC, 10’C), 119.57 (d, J=17.6 Hz, 41C), 119.61 (d, J=17.9 Hz, 4C),
124.88 (d, J=4.3 Hz, 31C), 125.18 (d, J=4.2 Hz, 3C), 126.59, 126.96 (9C1 9’C), 127.14 (8’C), 127.62 (d, J=15.9 Hz, 61C), 127.73 (8C), 127.99 (d, J=15.2 Hz, 6C), 128.66 (2’C),
128.84 (11C), 128.84 (2C), 130.03 (d, J=3.4 Hz, 1C), 142.14, 142.44 (14C, 14’C), 144.37, 145.56 (13C, 131C), 155.24 (d, J=245.1 Hz, 5’C)1 155.61 (d, J=245.1 Hz, 5C),
160.17 (16’C), 162.04 (16C), 166.00, 166.14 (22C, 22’C), 176.17, 176.22 (11C, 111C).
DIP MS: m/z (%)- 863 [M+H]+, 885 [M+Na]+.
MAKE IN INDIA
http://makeinindia.com/sector/pharmaceuticals/

FDA Approves Trulicity (dulaglutide) for Type 2 Diabetes
FDA Approves Trulicity (dulaglutide) for Type 2 Diabetes

DULAGLUTIDE
PRONUNCIATION doo” la gloo’ tide
THERAPEUTIC CLAIM Treatment of type II diabetes
CHEMICAL NAMES
1. 7-37-Glucagon-like peptide I [8-glycine,22-glutamic acid,36-glycine] (synthetic
human) fusion protein with peptide (synthetic 16-amino acid linker) fusion protein with immunoglobulin G4 (synthetic human Fc fragment), dimer
2. [Gly8,Glu22,Gly36]human glucagon-like peptide 1-(7-37)-peptidyltetraglycyl-Lseryltetraglycyl-L-seryltetraglycyl-L-seryl-L-alanyldes-Lys229-[Pro10,Ala16,Ala17]human immunoglobulin heavy constant γ4 chain H-CH2-CH3 fragment, (55-55′:58-58′)-bisdisulfide dimer
- Dulaglutide
- LY 2189265
- LY-2189265
- LY2189265
- UNII-WTT295HSY5
| GLP-1 immunoglobulin G (IgG4) Fc fusion protein with extended activity; a hypoglycemic agent. |
-
7-37-Glucagon-like peptide I (8-glycine,22-glutamic acid,36-glycine) (synthetic human) fusion proteinwith peptide (synthetic 16-amino acid linker) fusion protein with immunoglobulin G4 (synthetic human Fc fragment), dimer
sept 18 2014
The US Food and Drug Administration (FDA) has approved dulaglutide (Trulicity, Eli Lilly & Co), as a once-weekly injection for the treatment of type 2 diabetes.
A member of the glucagon-like peptide-1 receptor agonist class, dulaglutide joins liraglutide (Victoza, Novo Nordisk), exenatide (Byetta, AstraZeneca/Bristol-Myers Squibb), and albiglutide (Tanzeum, GlaxoSmithKline), on the US market.
Once-weekly dulaglutide was approved based on 6 clinical trials involving a total of 3342 patients who received the drug. It was studied as a stand-alone therapy and in combination withmetformin, sulfonylurea, thiazolidinedione, and prandial insulin.
In one trial the once-weekly dulaglutide was non-inferior to daily liraglutide and in another it topped the oral dipeptidyl peptidase-4 (DPP-4) inhibitor sitagliptin (Januvia, Merck).
The most common side effects observed in patients treated with dulaglutide were nausea, diarrhea, vomiting, abdominal pain, and decreased appetite.
Dulaglutide should not be used to treat people with type 1 diabetes, diabetic ketoacidosis, or severe abdominal or intestinal problems, or as first-line therapy for patients who cannot be managed with diet and exercise.
As with others in its class, dulaglutide’s label will include a boxed warning that thyroid C-cell tumors have been observed in rodents but the risk in humans is unknown. The drug should not be used in patients with a personal or family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia type 2.
The FDA is requiring Lilly to conduct the following postmarketing studies for dulaglutide:
• A clinical trial to evaluate dosing, efficacy, and safety in children
• A study to assess potential effects on sexual maturation, reproduction, and central nervous system development and function in immature rats
• An MTC case registry of at least 15 years duration to identify any increase in MTC incidence with the drug
• A clinical trial comparing dulaglutide with insulin glargine on glycemic control in patients with type 2 diabetes and moderate or severe renal impairment
• A cardiovascular outcomes trial to evaluate the drug’s cardiovascular risk profile in patients with high baseline risk for cardiovascular disease.
The FDA approval also comes with a Risk Evaluation and Mitigation Strategy, including a communication plan to inform healthcare professionals about the serious risks associated with the drug.
STRUCTURAL FORMULA
Monomer
HGEGTFTSDV SSYLEEQAAK EFIAWLVKGG GGGGGSGGGG SGGGGSAESK 50
YGPPCPPCPA PEAAGGPSVF LFPPKPKDTL MISRTPEVTC VVVDVSQEDP 100
EVQFNWYVDG VEVHNAKTKP REEQFNSTYR VVSVLTVLHQ DWLNGKEYKC 150
KVSNKGLPSS IEKTISKAKG QPREPQVYTL PPSQEEMTKN QVSLTCLVKG 200
FYPSDIAVEW ESNGQPENNY KTTPPVLDSD GSFFLYSRLT VDKSRWQEGN 250
VFSCSVMHEA LHNHYTQKSL SLSLG 275
Disulfide bridges location
55-55′ 58-58′ 90-150 90′-150′ 196-254 196′-254′
MOLECULAR FORMULA C2646H4044N704O836S18
MOLECULAR WEIGHT 59.67 kDa
MANUFACTURER Eli Lilly and Company
CODE DESIGNATION LY2189265
CAS REGISTRY NUMBER 923950-08-7
http://www.ama-assn.org/resources/doc/usan/dulaglutide.pdf
LY2189265 (dulaglutide), a glucagon-like peptide-1 analog, is a biologic entity being studied as a once-weekly treatment for type 2 diabetes.
Dulaglatuide works by stimulating cells to release insulin only when blood sugar levels are high.
Gwen Krivi, Ph.D., vice president, product development, Lilly Diabetes, said of the drug, “We believe dulaglutide, if approved, can bring significant benefits to people with type 2 diabetes.”
In fact, it might help to control both diabetics’ blood sugar and their high blood pressure.
Eli Lilly CEO John Lechleiter believes the drug has the potential to be a blockbuster. Lilly could be ready to seek approval by 2013.
For more information on dulaglutide clinical studies, click here.
PRESS RELEASES
Data Preseted at 49th EASD Annual Meeting Show Treatment with Lilly’s Investigational Dulaglutide Resulted in Improved Patient-Reported Health Outcomes – September 26, 2013
Lilly Announces Positive Results of Phase III Trials of Dulaglutide in Type 2 Diabetes – April 16, 2013
Lilly Diabetes Announces Positive Results of Phase III Trials of Dulaglutide in Type 2 Diabetes – October 22, 2012
FDA approves AstraZeneca’s constipation drug Movantik
Read more at: http://www.pharmatimes.com/Article/14-09-16/FDA_approves_AstraZeneca_s_constipation_drug_Movantik.aspx#ixzz3DdGiFse8
FDA approves Keytruda for advanced melanoma, First PD-1 blocking drug to receive agency approval

September 4, 2014
FDA Release
The U.S. Food and Drug Administration today granted accelerated approval to Keytruda (pembrolizumab) for treatment of patients with advanced or unresectable melanoma who are no longer responding to other drugs.
Melanoma, which accounts for approximately 5 percent of all new cancers in the United States, occurs when cancer cells form in skin cells that make the pigment responsible for color in the skin. According to the National Cancer Institute, an estimated 76,100 Americans will be diagnosed with melanoma and 9,710 will die from the disease this year.
Keytruda is the first approved drug that blocks a cellular pathway known as PD-1, which restricts the body’s immune system from attacking melanoma cells. Keytruda is intended for use following treatment with ipilimumab, a type of immunotherapy. For melanoma patients whose tumors express a gene mutation called BRAF V600, Keytruda is intended for use after treatment with ipilimumab and a BRAF inhibitor, a therapy that blocks activity of BRAF gene mutations.
“Keytruda is the sixth new melanoma treatment approved since 2011, a result of promising advances in melanoma research,” said Richard Pazdur, M.D., director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Many of these treatments have different mechanisms of action and bring new options to patients with melanoma.”
The five prior FDA approvals for melanoma include: ipilimumab (2011), peginterferon alfa-2b (2011), vemurafenib (2011), dabrafenib (2013), and trametinib (2013).
The FDA granted Keytruda breakthrough therapy designation because the sponsor demonstrated through preliminary clinical evidence that the drug may offer a substantial improvement over available therapies. It also received priority review and orphan product designation. Priority review is granted to drugs that have the potential, at the time the application was submitted, to be a significant improvement in safety or effectiveness in the treatment of a serious condition. Orphan product designation is given to drugs intended to treat rare diseases.
The FDA action was taken under the agency’s accelerated approval program, which allows approval of a drug to treat a serious or life-threatening disease based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients. This program provides earlier patient access to promising new drugs while the company conducts confirmatory clinical trials. An improvement in survival or disease-related symptoms has not yet been established.
Keytruda’s efficacy was established in 173 clinical trial participants with advanced melanoma whose disease progressed after prior treatment. All participants were treated with Keytruda, either at the recommended dose of 2 milligrams per kilogram (mg/kg) or at a higher dose of 10 mg/kg. In the half of the participants who received Keytruda at the recommended dose of 2 mg/kg, approximately 24 percent had their tumors shrink. This effect lasted at least 1.4 to 8.5 months and continued beyond this period in most patients. A similar percentage of patients had their tumor shrink at the 10 mg/kg dose.
Keytruda’s safety was established in the trial population of 411 participants with advanced melanoma. The most common side effects of Keytruda were fatigue, cough, nausea, itchy skin (pruritus), rash, decreased appetite, constipation, joint pain (arthralgia) and diarrhea. Keytruda also has the potential for severe immune-mediated side effects. In the 411 participants with advanced melanoma, severe immune-mediated side effects involving healthy organs, including the lung, colon, hormone-producing glands and liver, occurred uncommonly.
Keytruda is marketed by Merck & Co., based in Whitehouse Station, New Jersey.


Pembrolizumab, Lambrolizumab, MK-3475
STRUCTURAL FORMULA
Heavy chain
QVQLVQSGVE VKKPGASVKV SCKASGYTFT NYYMYWVRQA PGQGLEWMGG 50
INPSNGGTNF NEKFKNRVTL TTDSSTTTAY MELKSLQFDD TAVYYCARRD 100
YRFDMGFDYW GQGTTVTVSS ASTKGPSVFP LAPCSRSTSE STAALGCLVK 150
DYFPEPVTVS WNSGALTSGV HTFPAVLQSS GLYSLSSVVT VPSSSLGTKT 200
YTCNVDHKPS NTKVDKRVES KYGPPCPPCP APEFLGGPSV FLFPPKPKDT 250
LMISRTPEVT CVVVDVSQED PEVQFNWYVD GVEVHNAKTK PREEQFNSTY 300
RVVSVLTVLH QDWLNGKEYK CKVSNKGLPS SIEKTISKAK GQPREPQVYT 350
LPPSQEEMTK NQVSLTCLVK GFYPSDIAVE WESNGQPENN YKTTPPVLDS 400
DGSFFLYSRL TVDKSRWQEG NVFSCSVMHE ALHNHYTQKS LSLSLGK 447
Light chain
EIVLTQSPAT LSLSPGERAT LSCRASKGVS TSGYSYLHWY QQKPGQAPRL 50′
LIYLASYLES GVPARFSGSG SGTDFTLTIS SLEPEDFAVY YCQHSRDLPL 100′
TFGGGTKVEI KRTVAAPSVF IFPPSDEQLK SGTASVVCLL NNFYPREAKV 150′
QWKVDNALQS GNSQESVTEQ DSKDSTYSLS STLTLSKADY EKHKVYACEV 200′
THQGLSSPVT KSFNRGEC 218′
Disulfide bridges
22-96 22”-96” 23′-92′ 23”’-92”’ 134-218′ 134”-218”’ 138′-198′ 138”’-198”’
147-203 147”-203” 226-226” 229-229” 261-321 261”-321” 367-425 367”-425”
Glycosylation sites (N)
Asn-297 Asn-297”
lambrolizumab, or MK-3475
| C6504H10004N1716O2036S46 (peptide) | |
| MOL. MASS | 146.3 kDa (peptide) |
Pembrolizumab, Lambrolizumab (also known as MK-3475) is a drug in development by Merck that targets the PD-1 receptor. The drug is intended for use in treating metastatic melanoma.
http://www.ama-assn.org/resources/doc/usan/lambrolizumab.pdf structureof lambrolizumab, or MK-3475
https://download.ama-assn.org/resources/doc/usan/x-pub/pembrolizumab.pdf
Statement on a Nonproprietary Name Adopted by the USAN Council. November 27, 2013.
see above link for change in name
may 2, 2013,
An experimental drug from Merck that unleashes the body’s immune system significantly shrank tumors in 38 percent of patients with advanced melanoma, putting the company squarely in the race to bring to market one of what many experts view as the most promising class of drugs in years.
The drugs are attracting attention here at the annual meeting of the American Society of Clinical Oncology, even though they are still in the early stage of testing. Data from drugs developed by Bristol-Myers Squibb and by Roche had already been released.
The drugs work by disabling a brake that prevents the immune system from attacking cancer cells. The brake is a protein on immune system cells called programmed death 1 receptor, or PD-1.
Merck’s study, which was presented here Sunday and also published in the New England Journal of Medicine, involved 135 patients. While tumors shrank in 38 percent of the patients over all, the rate was 52 percent for patients who got the highest dose of the drug, which is called lambrolizumab, or MK-3475.
But that is what is disclosed tonight, as to pembrolizumab, or MK-3475. Wow. With over $44 billion in 2013 worldwide revenue, that disclosure implies (to seasoned SEC lawyers) that spending on this one drug (or, biologic, to be more technical about it — but remember 40 years ago, Merck had no protein chain biologics research & development programs in its pipe — only chemical drug compounds). . . is material, to that number. Normally that would, in turn, mean that the spending is approaching 5 per cent of revenue. So — Merck may be spending $2.2 billion over the next 12 rolling months, on MK-3475. That’s one BIGhairy science bet, given that Whitehouse Station likely already had over $2 billion invested in the program, at year end 2013.


About Pembrolizumab
Pembrolizumab (MK-3475) is an investigational selective, humanized monoclonal anti-PD-1 antibody designed to block the interaction of PD-1 on T-cells with its ligands, PD-L1 and PD-L2, to reactivate anti-tumor immunity. Pembrolizumab exerts dual ligand blockade of PD-1 pathway.
Today, pembrolizumab is being evaluated across more than 30 types of cancers, as monotherapy and in combination. It is anticipated that by the end of 2014, the pembrolizumab development program will grow to more than 24 clinical trials across 30 different tumor types, enrolling an estimated 6,000 patients at nearly 300 clinical trial sites worldwide, including new Phase 3 studies in head and neck and other cancers. For information about Merck’s oncology clinical studies, please click here.
The Biologics License Application (BLA) for pembrolizumab is under priority review with the U.S. Food and Drug Administration (FDA) for the proposed indication for the treatment of patients with advanced melanoma previously-treated with ipilimumab; the PDUFA date is October 28, 2014. Pembrolizumab has been granted FDA’s Breakthrough Therapy designation for advanced melanoma. If approved by the FDA, pembrolizumab has the potential to be the first PD-1 immune checkpoint modulator approved in this class. The company plans to file a Marketing Authorization Application in Europe for pembrolizumab for advanced melanoma in 2014.
About Head and Neck Cancer
Head and neck cancers are a related group of cancers that involve the oral cavity, pharynx and larynx. Most head and neck cancers are squamous cell carcinomas that begin in the flat, squamous cells that make up the thin surface layer (epithelium) of the head and neck (called the). The leading risk factors for head and neck cancer include tobacco and alcohol use. Infection with certain types of HPV, also called human papillomaviruses, is a risk factor for some types of head and neck cancer, specifically cancer of the oropharynx, which is the middle part of the throat including the soft palate, the base of the tongue, and the tonsils. Each year there are approximately 400,000 cases of cancer of the oral cavity and pharynx, with 160,000 cancers of the larynx, resulting in approximately 300,000 deaths.

About Merck Oncology: A Focus on Immuno-Oncology
At Merck Oncology, our goal is to translate breakthrough science into biomedical innovations to help people with cancer worldwide. Harnessing immune mechanisms to fight cancer is the priority focus of our oncology research and development program. The Company is advancing a pipeline of immunotherapy candidates and combination regimens. Cancer is one of the world’s most urgent unmet medical needs. Helping to empower people to fight cancer is our passion. For information about Merck’s commitment to Oncology visit the Oncology Information Center at http://www.mercknewsroom.com/oncology-infocenter.
About Merck
Today’s Merck is a global healthcare leader working to help the world be well. Merck is known as MSD outside the United States and Canada. Through our prescription medicines, vaccines, biologic therapies, and consumer care and animal health products, we work with customers and operate in more than 140 countries to deliver innovative health solutions. We also demonstrate our commitment to increasing access to healthcare through far-reaching policies, programs and partnerships. For more information, visit http://www.merck.com and connect with us on Twitter, Facebook and YouTube.
Hamid, O; Robert, C; Daud, A; Hodi, F. S.; Hwu, W. J.; Kefford, R; Wolchok, J. D.; Hersey, P; Joseph, R. W.; Weber, J. S.; Dronca, R; Gangadhar, T. C.; Patnaik, A; Zarour, H; Joshua, A. M.; Gergich, K; Elassaiss-Schaap, J; Algazi, A; Mateus, C; Boasberg, P; Tumeh, P. C.; Chmielowski, B; Ebbinghaus, S. W.; Li, X. N.; Kang, S. P.; Ribas, A (2013). “Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma”. New England Journal of Medicine 369 (2): 134–44. doi:10.1056/NEJMoa1305133. PMID 23724846
key words
FDA, approved, Keytruda, advanced melanoma, PD-1 blocking drug, pembrolizumab, Lambrolizumab, MK-3475, Monoclonal antibody

Aripiprazole lauroxil ……….Alkermes submits new drug application


Aripiprazole
7-[4-[4-(2,3-dichlorophenyl)-1- piperazinyl]butoxy]- 3,4-dihydro-2(1H)-quinolinone.
END AUG 2014
The US Food and Drug Administration (FDA) has received a new drug application (NDA) from Ireland-based Alkermes for its aripiprazole lauroxil to treat schizophrenia.
Aripiprazole lauroxil is an injectable atypical antipsychotic with one-month and two-month formulations, developed for the treatment of schizophrenia, which is a chronic, severe and disabling brain disorder.
The company has submitted the application based on positive results from the pivotal phase three study that assessed the efficacy and safety of aripiprazole lauroxil, where the drug demonstrated significant improvements in schizophrenia symptoms when compared to a placebo.
Alkermes CEO Richard Pops said: “We have designed aripiprazole lauroxil to be a differentiated treatment option for schizophrenia, with a ready-to-use format with multiple dosing options, to help meet the individual needs of patients and their healthcare providers.
“These attributes, together with the robust clinical data observed in the pivotal study, position aripiprazole lauroxil to be a meaningful new entrant in the growing long-acting injectable antipsychotic market, and we look forward to working with the FDA to bring this important new medication to patients and physicians as quickly as possible.”
The study, in which both doses of aripiprazole lauroxil tested, including 441mg and 882mg, reached the primary endpoint with statistically significant and clinically meaningful reductions in positive and negative syndrome scale (PANSS) scores, according to the company.
In addition, it met all secondary endpoints and demonstrated significant improvements in schizophrenia symptoms against the placebo.
- ALKS 9070
- ALKS 9072
- Aripiprazole lauroxil
- RDC 3317
- RDC-3317
- UNII-B786J7A343
Aripiprazole lauroxil [USAN] CAS 1259305-29-7

| Systematic (IUPAC) name | |
|---|---|
| 7-{4-[4-(2,3-Dichlorophenyl)piperazin-1-yl]butoxy}-3,4-dihydroquinolin-2(1H)-one | |
| Clinical data | |
| Trade names | Abilify |
| AHFS/Drugs.com | monograph |
| MedlinePlus | a603012 |
| Licence data | EMA:Link, US FDA:link |
| Pregnancy cat. | B3 (AU) C (US) |
| Legal status | Prescription Only (S4) (AU) ℞-only (CA) POM (UK) ℞-only (US) |
| Routes | Oral (via tablets, orodispersable tablets, and oral solution); intramuscular (including as a depot) |
| Pharmacokinetic data | |
| Bioavailability | 87%[1][2][3][4] |
| Protein binding | >99%[1][2][3][4] |
| Metabolism | Hepatic (liver; mostly via CYP3A4 and CYP2D6[1][2][3][4]) |
| Half-life | 75 hours (active metabolite is 94 hours)[1][2][3][4] |
| Excretion | Renal (27%; <1% unchanged), Faecal (60%; 18% unchanged)[1][2][3][4] |
| Identifiers | |
| CAS number | 129722-12-9 |
| ATC code | N05AX12 |
| PubChem | CID 60795 |
| IUPHAR ligand | 34 |
| DrugBank | DB01238 |
| ChemSpider | 54790 |
| UNII | 82VFR53I78 |
| KEGG | D01164 |
| ChEBI | CHEBI:31236 |
| ChEMBL | CHEMBL1112 |
| Chemical data | |
| Formula | C23H27Cl2N3O2 |
| Mol. mass | 448.385 |
Aripiprazole (/ˌɛərɨˈpɪprəzoʊl/ AIR-i-PIP-rə-zohl; brand names: Abilify, Aripiprex) is a partial dopamine agonist of the second generation (or atypical) class of antipsychotics that is primarily used in the treatment of schizophrenia, bipolar disorder, major depressive disorder (as an add on to other treatment), tic disorders, and irritability associated with autism.[5]
It was approved by the U.S. Food and Drug Administration (FDA) for schizophrenia on November 15, 2002 and the European Medicines Agency on 4 June 2004; for acute manic and mixed episodes associated with bipolar disorder on October 1, 2004; as an adjunct for major depressive disorder on November 20, 2007;[6] and to treat irritability in children with autism on 20 November 2009.[7] Likewise it was approved for use as a treatment for schizophrenia by the TGA of Australia in May 2003.[1]
Aripiprazole was developed by Otsuka in Japan, and in the United States, Otsuka America markets it jointly with Bristol-Myers Squibb.
Regulator status
In the United States, the FDA has approved aripiprazole for the treatment of schizophrenia in adults and adolescents (aged 13–17), of manic and mixed episodes associated with Bipolar I (One) Disorder with or without psychotic features in adults, children and adolescents (aged 10–17),[59] of irritability associated with autism in pediatric patients (aged 6–17),[60] and of depression when used along with antidepressants in adults.[61]
Aripiprazole has been approved by the FDA for the treatment of acute manic and mixed episodes, in both pediatric patients aged 10–17 and in adults.[62]
In 2007, aripiprazole was approved by the FDA for the treatment of unipolar depression when used adjunctively with an antidepressant medication.[63] It has not been FDA-approved for use as monotherapy in unipolar depression.
Patent status
Otsuka’s US patent on aripiprazole expires on October 20, 2014;[64] however, due to a pediatric extension, a generic will not become available until at least April 20, 2015.[62] Barr Laboratories (now Teva Pharmaceuticals) initiated a patent challenge under the Hatch-Waxman Act in March 2007.[65] On November 15, 2010, this challenge was rejected by a United States district court in New Jersey.[1][2]
Dosage forms
Abilify 2mg tablets (US)
- Intramuscular injection, solution: 9.75 mg/mL (1.3 mL)
- Solution, oral: 1 mg/mL (150 mL) [contains propylene glycol, sucrose 400 mg/mL, and fructose 200 mg/mL; orange cream flavor]
- Tablet: 2 mg, 5 mg, 10 mg, 15 mg, 20 mg, 30 mg
- Tablet, orally disintegrating: 10 mg [contains phenylalanine 1.12 mg; creme de vanilla flavor]; 15 mg [contains phenylalanine 1.68 mg; creme de vanilla flavor]
Synthesis
Aripiprazole can be synthesized beginning with a dichloroaniline and bis(2-chloroethyl)amine:[66]

- U.S. Patent No.4, 734, 416 and U.S. Patent No.5,006,528 discloses the Aripiprazole, 7-{4- [4- (2, 3-dichlorophenyl) -1-piperazinyl] butoxy}- 3,4-dihydro-2 (IH) -quinolinone or 7-{4-[4- (2, 3-dichlorophenyl) -1- piperazinyl] butoxy}-3, 4-dihydro carbostyril, is a typical antipsychotic agent useful for the treatment of Schizophrenia, having the formula as given below.
Aripiprazole
U.S. patent No.5,006,528 discloses preparation of Aripiprazole and its pharmaceutically acceptable acid-addition salts. The process for the preparation of acid salts involves reaction of Aripiprazole with a pharmaceutically acceptable inorganic acids such as hydrochloric acid, sulfuric acid, phosphoric acid, hydrobromic acid, and the like; organic acids such as oxalic acid, maleic acid, fumaric acid, maleic acid, tartaric acid, citric acid, . benzoic acid and the like as per Scheme-1. Scheme- 1
a. K2CO3, Water K CH2CI2 c. Column chromatographic purification d. n-Hexane – Ethaπol
ARIPIPRAZOLE ACID SALT
The product Aripiprazole .obtained by the above process has melting point of 139.0° – 139.5°C.
The process involves purification of the intermediate, 7-(4- bromobutoxy) -3, 4-dihydrocarbostyril (III) by silica gel column chromatography to remove impurities formed during the reaction. The process further involves two recrystallizations of Aripiprazole from ethanol to obtain the pure Aripiprazole though compromising on yields by increasing the operational cost of the product. PCT publication WO 03/026659 discloses low hygroscopic forms of
Aripiprazole and the process for their preparation from the Aripiprazole hydrate Form SA’ . It further states that the anhydrous
Aripiprazole made by the Japanese patent publication No. 191256/1990, yields the Aripiprazole, which is significantly hygroscopic. As per PCT publication WO 03/026659 anhydrous crystals of Aripiprazole exist as type-I crystals and type-II crystals. Further discloses that the type-I crystals are prepared -by recrsytallization from ethanol solution of
Aripiprazole or by heating Aripiprazole hydrate at 800C and type-II crystals by heating type-I crystals at 130 to 1400C for 15 hrs.
PCT application Publication WO 03/026659 discloses process for the Aripiprazole polymorphic form-B by heating the Aripiprazole hydrate
‘A’ at 90 – 125°C for about 3 – 50 hrs. The process for Polymorphic
Form-C is by heating the Aripiprazole anhydrous to a temperature of 140
– 1500C. The process for Form-D is recrystallization from toluene; process for Form-E is heating with acetonitrile or by recrystallization from acetonitrile and the process for Form-F is by heating the suspension of anhydrous Aripiprazole in acetone. The polymorphic Form-G is by heating to 1700C for at least 2 weeks in a sealed tube, which is a glassy mass.
PCT publication WO 03/026659 further discloses the characterization data X-ray diffraction pattern; IR absorption and DSC of Form B, Form C, Form-D, Form-E, Form-F and Form-G.It further reported the melting point of Aripiprazole anhydrous Form B as 139.7°C-
Research
Perhaps owing to its mechanism of action relating to dopamine receptors, there is some evidence to suggest that aripiprazole blocks cocaine-seeking behavior in animal models without significantly affecting other rewarding behaviors (such as food self-administration).[67] Aripiprazole may be counter-therapeutic as treatment for methamphetamine dependency because it increased methamphetamine’s stimulant and euphoric effects, and increased the baseline level of desire for methamphetamine.[68]
http://www.google.com/patents/WO2006030446A1?cl=en

Scheme-3
Aripiprazole Acid addition salt
Form-A, B, C , D , E , F Type-I & Type-II Aripiprazole acid salts used for the preparation of polymorphs
…………………………….
| United States | 5006528 | 1994-10-20 | 2014-10-20 |
| United States | 7115587 | 2005-01-21 | 2025-01-21 |

Aripiprazole, 7-{4-[4-(2,3-dichlorophenyl)-1-piperazinyl]-butoxy}-3,4-dihydro carbostyril or 7-{4-[4-(2,3-dichlorophenyl)-1-piperazinyl]-butoxy}-3,4-dihydro-2 (1H)-quinolinone, is an atypical antipsychotic agent useful for the treatment of schizophrenia (U.S. Pat. No. 4,74,416 and U.S. Pat. No. 5,006,528). Schizophrenia is a common type of psychosis characterized by delusions, hallucinations and extensive withdrawal from others. Onset of schizophrenia typically occurs between the age of 16 and 25 and affects 1 in 100 individuals worldwide. It is more prevalent, than Alzheimer’s disease, multiple sclerosis, insulin-dependent diabetes and muscular dystrophy. Early diagnosis and treatment can lead to significantly improved recovery and outcome. Moreover, early therapeutic intervention can avert costly hospitalization.
Aripiprazole (Aripiprazole) is an atypical antipsychotic, on 15 November 2002 by the U.S. FDA clearance to market, its efficacy is through the dopamine D2 receptor and serotonin 5HT1A receptor partial agonist activity and serotonin 5HT2A receptor antagonism activity mediated common. With its unique mechanism of action and safety assessment, aripiprazole known as third-generation antipsychotic drugs.
[0003] Aripiprazole is a quinolinone derivative, developed by the Japanese company Otsuka Pharmaceutical, the chemical name
Is: 7 – {4 – [4 – (2,3 – dichlorophenyl)-1_ piperazinyl] butoxy} -3,4 – dihydro-quinolone, the following structural formula:
[0004]
[0005] For the preparation of aripiprazole, Japanese OtsukaPharmaceutical’s patent EP 0367141A2, and related patents US4234585, CN89108934 preparation methods described in 5. In addition, the patent CN1450056A, CN1562973A, CN1784385A, CN1680328A, CN1576273A, etc. describe some of these five Preparation
Method is very similar way. These preparation methods are direct or indirect use of 7 – hydroxy -3,4 – dihydro – quinolin-2 – one (HCS) that the key to higher prices of raw materials, and some methods involve harsh reaction conditions, poor selectivity, low yield, but also increases the cost of industrial production of the product.
[0006] Chinese patent CN1304373C preparation method is not described in the 7 – hydroxy-3 ,4 _ dihydro-2_ (1H) – quinoline
Quinolone intermediates for their preparation of the core reaction is as follows:
[0007]
[0008] This reaction is Friedel-Crafts alkylation reaction, there is a harsh reaction conditions, the yield is low, the reaction selectivity is poor, the shortcomings of high emissions, is not conducive to industrial mass production. SUMMARY OF THE INVENTION
[0009] In order to solve the above problems, the present invention provides a simple, high selectivity, high yield, low cost, environmentally friendly, easy to prepare industrialization aripiprazole and intermediates thereof.
[0010] The technical solution of the present invention, the present invention provides in one aspect a process for preparingaripiprazole novel intermediates.
[0011] The present invention, on the other hand provides a method for the preparation of intermediates.
[0012] The present invention provides the use of the other intermediates for preparing aripiprazole two new preparation methods.
[0013] Specifically, the present invention relates to novel intermediates, compounds of formula ⑴:
[0014]
[0015] wherein, R is selected from methyl, ethyl, propyl, isopropyl, butyl, t-butyl, benzyl and other common alkyl groups in any one, and preferably is ethyl.
[0016] Compound of formula ⑴: 3 – (4 – (4 – (4 – (2,3 _-dichlorophenyl)-piperazinyl) butoxy) _2_ nitrophenyl) propionate, is the following prepared by the procedure:
[0017] Step one, the acylation reaction: with 4 – methyl – 3 – nitro-phenol (VIII) and acetic anhydride as the raw material, DMAP as catalyst, to give 4 – methyl – 3 – nitrophenyl acetate ( VII).
[0018] wherein 4 – methyl – 3 – nitro-phenol (VIII), acetic anhydride, DMAP molar ratio is preferably 1: 1.0 to 1.4: 0.05, at room temperature, the reaction time is preferably 0.5 to 3 hours.
[0019] Step two, the bromination reaction: The resulting product, 4 to Step one – methyl – 3 – nitrophenyl acetate (VII), N-bromosuccinimide and benzoyl peroxide as a raw material , carbon tetrachloride solvent reflux, to give 4 – bromomethyl-3 – nitrophenyl acetate (VI).
[0020] wherein 4 – methyl – 3 – nitrophenyl acetate (VII), N-bromosuccinimide, benzoyl peroxide molar ratio is preferably 1: 1 to 1.2: 0.05, reaction time is preferably 4-18 hours.
[0021] Step three, instead of the reaction: in an appropriate solvent, adding an alkaline agent and diethyl malonate was stirred in an ice bath, was added dropwise step two the resulting product, 4 – bromomethyl-3 – nitrophenyl yl acetate (VI) solution after completion of the addition reaction of 1 to 3 hours to obtain a brown liquid product, 2 – (4_ acetoxy-2 – nitrobenzyl) malonate (V).
[0022], wherein the alkali agent is a common organic or inorganic base selected from sodium methoxide, sodium ethoxide, sodium hydride, sodium tert-butoxide or potassium tert-butoxide, preferably sodium tert-butoxide; the solvent is selected from tetrahydrofuran, methanol, ethanol, butanol, tert-butanol, toluene or N, N-dimethylformamide; 4 – bromomethyl-3 – nitrophenyl acetate (VI), alkaline agent and lipid diethyl molar ratio is preferably 1: 1.0 to 1.8: 1.0 to 1.4.
[0023] Step 4 Hydrolysis decarboxylation: the product obtained in Step Three 2 – (4_ acetoxy-2 – nitro-benzyl)-malonic acid diethyl ester (V) was added concentrated hydrochloric acid and a suitable solvent, heating and stirring reflux, to give a yellow solid product 3 – (4_ hydroxy-2 – nitrophenyl) propionic acid (IV).
[0024] wherein the solvent is selected from water, methanol, ethanol or acetic acid, water soluble solvent, was heated with stirring under reflux time is preferably 3 to 18 hours. [0025] Step five, the esterification reaction: the product obtained in step 4, 3 – (4 – hydroxy-2 – nitrophenyl) propionic acid (IV) was added to an appropriate solvent, the mixture was stirred in an ice bath, was added dropwise thionyl sulfone, after completion of the addition reaction of 1 to 3 hours, to give a pale brown liquid product 3 – (4 – hydroxy-2 – nitrophenyl) propionate (III).
[0026] wherein the solvent is selected from anhydrous methanol, ethanol, propanol, isopropanol, butanol, t-butanol, benzyl alcohol, alcohol and other common solvents.
[0027] Step VI substitution reaction: 1,4 – dibromobutane was added to an appropriate solvent and an alkaline reagent, heated to 50 ~ 100 ° C, the product obtained was added dropwise Step Five 3 – (4_ hydroxy – nitrophenyl) propionate (III) solution, after the addition was complete the reaction was kept 2 to 4 hours to obtain a brown liquid product 3 – (4 – (4 – bromo-butoxy)-2 – nitrophenyl) propionate (II).
[0028] wherein the solvent is selected from methanol, 95% ethanol, ethanol, acetonitrile and N, N-dimethylformamide, and the like; said alkaline agent is a common organic or inorganic weak base, such as triethylamine, pyridine, potassium carbonate, sodium carbonate, etc..
[0029] Step 7 condensation reaction: the product obtained in Step Six 3 – (4 – (4 – bromo-butoxy)-2 – nitrophenyl) propionate (II) adding a suitable solvent, (2,3 – dichlorophenyl)-piperazine hydrochloride 1_, alkaline reagents and catalysts, to obtain
The intermediate product 3 – (4 – (4 – (4 – (2,3 – dichlorophenyl)-piperazin-1 – yl) butoxy)-2 – nitrophenyl) propionate ⑴.
[0030] Among them, 3 – (4 – (4 – (4 – (2,3 _-dichlorophenyl)-piperazinyl) butoxy) _2_ nitrophenyl) propionate (I), (2, 3 – dichloro-phenyl)-piperazine hydrochloride 1_, alkaline reagents and catalysts, the four molar ratio is preferably 1: 0.9 to 1.0: 2.0 to 2.2: 0.05 to 0.5. The solvent is selected from methanol, ethanol and N, N-dimethylformamide, acetonitrile and the like. Step six of the alkaline reagent and alkaline reagent used in the same, said catalyst is a common low-iodine salts, such as sodium iodide, potassium iodide.
[0031] The present invention provides two other hand, the use of a compound of formula ⑴ preparing aripiprazole new method.
[0032] Method one: ⑴ intermediate compound of formula in an appropriate solvent in the acid or salt or a base in the presence of a reducing agent under the action of restoring ring closure reaction to obtain aripiprazole.
[0033] Method one reductive cyclization of the reducing agent used is iron, zinc, sodium sulfide, stannous chloride, and preferably iron; reaction solvent is selected from water, methanol, ethanol, ethyl acetate or in one or more of the mixed solvent; said acid is a common organic or inorganic acid, preferably acetic acid or hydrochloric acid; said salt is a common inorganic or organic salts selected from chloride, ferrous chloride, , ammonium sulfate, calcium chloride, zinc chloride, sodium chloride, sodium bromide or sodium acetate and the like; common said base is an inorganic base selected from sodium hydroxide, potassium hydroxide or sodium bicarbonate; the reduction ring-closing reaction temperature range of 30 ~ 140 ° C, preferably about 80 ° C; reaction time ranges from about 0.5 to 8 hours, preferably 2 hours.
[0034] Method two: ⑴ intermediate compound of formula in an appropriate solvent in the first catalyst, the reduction reaction, and then carried out in a suitable solvent can be prepared by cyclization of aripiprazole.
[0035] The reduction reaction of the second approach, the reducing agent is hydrogen or a carboxylic acid; the catalyst is selected from molybdenum, molybdenum dioxide or Raney nickel, preferably Raney nickel; the solvent is selected from methanol, ethanol, ethyl acetate or acetic acid, preferably ethanol; said ring-closing reaction of the solvent is selected from N, N-dimethylformamide, trichlorobenzene or xylene; reaction temperature range of 50 ~ 180 ° C, preferably about 70 ~ 150 ° C; reaction time the range of about 1 to 8 hours.
[0036] In summary, the present invention is described for preparing aripiprazole method in 4– methyl – 3 – nitro-phenol (VIII) as a starting material, by acetylation protected hydroxy, radical instead of 4 – bromomethyl-3 – nitrophenyl acetate (VI), the diethyl malonate and a nucleophilic substitution reaction to obtain 2 – (4_ acetoxy-2 – nitrobenzyl ) malonic acid diethyl ester (V), which is decarboxylated by hydrolysis, esterification, to give 3 – (4 – hydroxy-2 – nitrophenyl) propionate (III), the reaction product with dibromobutane an ether compounds, and with (2,3 – dichlorophenyl)-piperazine hydrochloride 1_ condensation, to give 3 – (4 – (4 – (4 – (2,3 – dichlorophenyl) piperazine -1 – yl) butoxy) -2 – nitrophenyl) propionate (I), and then by reductive cyclization step, or first reduced and then ring-closing reaction of aripiprazole. The synthetic route of the present invention is as follows: [0037]
According to Example 1 of Japanese Unexamined Patent Publication No. 191256/1990, anhydrous aripiprazole crystals are manufactured for example by reacting 7-(4-bromobutoxy)-3,4-dihydrocarbostyril with 1-(2,3-dichlorophenylpiperadine and recrystallizing the resulting raw anhydrousaripiprazole with ethanol. Also, according to the Proceedings of the 4th Japanese-Korean Symposium on Separation Technology (Oct. 6-8, 1996), anhydrousaripiprazole crystals are manufactured by heating aripiprazole hydrate at 80° C. However, the anhydrous aripiprazole crystals obtained by the aforementioned methods have the disadvantage of being significantly hygroscopic.
The hygroscopicity of these crystals makes them difficult to handle since costly and burdensome measures must be taken in order ensure they are not exposed to moisture during process and formulation. Exposed to moisture, the anhydrous form can take on water and convert to a hydrous form. This presents several disadvantages. First, the hydrous forms of aripiprazole have the disadvantage of being less bioavailable and less dissoluble than the anhydrous forms ofaripiprazole. Second, the variation in the amount of hydrous versus anhydrousaripiprazole drug substance from batch to batch could fail to meet specifications set by drug regulatory agencies. Third, the milling may cause the drug substance, Conventional Anhydrous Aripiprazole, to adhere so manufacturing equipment which may further result in processing delay, increased operator involvement, increased cost, increased maintenance, and lower production yield. Fourth, in addition to problems caused by introduction of moisture during the processing of these hygroscopic crystals, the potential for absorbance of moisture during storage and handling would adversely affect the dissolubility of aripiprazole drug substance. Thus shelf-life of the product could be significantly decreased and/or packaging costs could be significantly increased. It would be highly desirable to discover a form of aripiprazole that possessed low hygroscopicity thereby facilitating pharmaceutical processing and formulation operations required for producing dosage units of an aripiprazole medicinal product having improved shelf-life, suitable dissolubility and suitable bioavailability.
Also, Proceedings of the 4 the Japanese-Korean Symposium on Separation Technology (Oct. 6-8, 1996) state that, anhydrous aripiprazole crystals exist as type-I crystals and type-II crystals; the type-I crystals of anhydrous aripiprazolecan be prepared by recrystallizing from an ethanol solution of aripiprazole, or by heating aripiprazole hydrate at 80° C.; and the type-II crystals of anhydrousaripiprazole can be prepared by heating the type-I crystals of anhydrousaripiprazole at 130 to 140° C. for 15 hours.
By the aforementioned methods, anhydrous aripiprazole type-II crystals having high purity can not be easily prepared in an industrial scale with good repeatability.
Chemical Synthesis of Aripiprazole (active ingredient for Abilify)
Experimental Procedures for the preparation of Aripiprazole (Abilify, aripiprazole)
US 5,006,528 discloses process for the preparation of Aripiprazole in two steps The first step comprises synthesis of 7 -. (4-bromobutoxy) -3,4-dihydrocarbostyril (7-BBQ) by alkylating the hydroxy group of 7-hydroxy-3, 4 -dihydrocarbostyril (7-HQ) with 1 ,4-dibromobutane using potassium carbonate in water at reflux temperature for 3 hours to obtain 7-BBQ in 68% yield The resulting 7-BBQ is further reacted with 1 -. (2,3 – dichlorophenyl)-piperazine to obtain Aripiprazole.
Preparation of 7 – (4-Bromobutoxy) 3 ,4-dihydro-2 (1H) quinolinon ( 7 – (4-Bromobutoxy) 3 ,4-dihydrocarbostyril; 7-BBQ)
7-Hydroxy-3 ,4-dihydro-2 (1H)-quinolinone (aka 7-Hydroxy-3 ,4-dihydrocarbostyril, 60gm) and potassium carbonate (76.3 gm) were taken in acetonitrile (1200ml) at room temperature. To this tetra butyl ammonium iodide (13.7 gm) and 1 ,4-dibromobutane (238.5gm) were added and heated at 40 – 45 ° C for 24 hours Reaction mass was cooled upto room temperature and was filtered off The resulting filtrate was distilled off.. under vacuum. The resultant mass was cooled to 25-30 ° C and cyclohexane (300 ml) was added under stirring. The resulting solid was filtered off and was dried. The resulting solid was taken in water and was stirred for few minutes. The . solid was filtered and dried under vacuum at 55-60 ° C for 20 hours to obtain title compound mp 110.5-111 ° C; 1H NMR (DMSO-d6) ä 1.81 (2H, m,-CH2-), 1.95 (2H , m,-CH2-), 2.41 (2H, t, J) 7 Hz,-CH2CO-), 2.78 (2H, t, J) 7 Hz,-CH2-C-CO-), 3.60 (2H, t, J) 6 Hz,-CH2Br), 3.93 (2H, t, J) 6 Hz, O-CH2-), 6.43 (1H, d, J) 2.5 Hz), 6.49 (1H, dd, J) 2.5, 8 Hz ), 7.04 (1H, d, J) 8 Hz), 9.98 (1H, s, NHCO). Anal. (C13H16NO2Br) C, H, N.
Yield: 73-75%; Purity: 93-95%
Preparation of Aripiprazole (7 – {4 – [4 – (2,3-Dichlorophenyl) piperazin-1-yl] butoxy} 3 ,4-dihydroquinolin-2 (1H)-One)
7 – (4-Bromobutoxy)-l ,2,3,4-tetrahydroquinolin-2-one (50 gm) was taken in acetonitrile (500 ml) at 25-30 ° C. To this potassium carbonate (67.2 gm) and l – (2,3 – dichlorophenyl). piperazine hydrochloride (44.9gm) were added under stirring The reaction mixture was refluxed at 80-85 ° C for 8 hours The reaction mass was cooled to room temperature, filtered and the resulting solid was washed. with acetonitrile. To the resulting solid, water was added and was stirred. The solid was filtered off, washed with water and dried under vacuum at 75-80 ° C for 15 hrs. The resulting crude aripiprazole was crystallized from isopropyl alcohol and water to . obtain title compound Yield: 75-80%; Dimer Impurity: <0.1% 1H NMR:. DMSO-d6 d 9.96 [1H, s, NH]; 7.29 [2H, m, Ar]; 7.13 [1H, q, Ar ]; 7.04 [1H, d, Ar]; 6.49 [1H, dd, Ar]; 6.45 [1H, d, Ar]; 3.92 [2H, t,-CH2-O-]; 2.97 [4H, bb, 2 ( -CH2-)]; 2.78 [2H, t,-CH2-N2-)]; 2.39 [4H, m, 2 (-CH2-)]; 1.73 [2H, m, – CH2-]; 1.58 [2H, m .,-CH2-] IR: cm-1 3193; 2939; 2804; 1680; 1627; 1579; 1520; 1449; 1375; 1270; 1245; 1192; 1169; 1045; 965; 649; 869; 780; 712; 588 .
For the Process of references Aripiprazole (Abilify, Japanese: Oh, Bldg re phi, Ann reピplastic AKZO have suitable; Chinese: Ann-law who, aripiprazole)
Yasuo Oshiro, Seiji Sato, Nobuyuki Kurahashi, Tatsuyoshi Tanaka, Tetsuro Kikuchi, Katsura Tottori, Yasufumi Uwahodo, and Takao Nishi; Novel Antipsychotic Agents with Dopamine autoreceptor Agonist Properties: Synthesis and Pharmacology of 7 – [4 – (4-Phenyl-1- piperazinyl) butoxy] – 3,4-dihydro-2 (1H)-quinolinone Derivatives ; J. Med Chem. 1998, 41, 658-667.
Yasuo Oshiro, Seiji Sato, Nobuyuki Kurahashi; Carbostyril Derivatives , Otsuka Pharmaceutical Co., Ltd.;. U.S. Patent 5006528 ; Issue Date: Apr 9, 1991
BANDO, Takuji, YANO, Katsuhiko, FUKANA, Makoto, AOKI, Satoshi; Method for producing fine particles of aripiprazole anhydride crystals b; OTSUKA PHARMACEUTICAL CO, LTD, WO 2013002420 A1..
Yuanqiu Hui, Chen Hongwen, Qian Wen, firewood rain column, Xu Dan, Yang Zhimin, Tian Zhoushan; method for preparing high purity of aripiprazole; NJCTT Pharmaceutical Co., Ltd.; application number: 201210292382.0; Publication Number: CN102863377A; Publication date: 2013.01.09 After (The invention relates to the field of medicine and chemical industry, in particular to a method for preparing high purity of aripiprazole would join aripiprazole A solvent is heated, filtered, and the filtrate was added to a solvent B, low temperature mixing, filtration, the filter cake is suspended in water, adjusted to alkaline pH of the aqueous solution, filtration, high temperature vacuum dried to obtain a high-purity refined product Aripiprazole This method is simple, high purity, suitable for the industrial the large-scale application)
ZHENG Siji, LIU Xiaoyi, FU Linyong, TAN Bo, ZHOU Min:.. ARIPIPRAZOLE MEDICAMENT FORMULATION AND PREPARATION METHOD THEREFOR / FORMULATION DE MÉDICAMENT ARIPIPRAZOLE ET SON PROCÉDÉ DE PRÉPARATION / a aripiprazole pharmaceutical formulation and preparation method SHANGHAI ZHONGXI. PHARMACEUTICAL January 2013: WO 2013/000391
Zheng Si Ji, Liu Xiaoyi, Fulin Yong, Tan Bo, Zhou Min: A aripiprazole pharmaceutical formulation and preparation method; Shanghai Pharmaceutical Co., Ltd. and Western; Publication date: 2013.01.02: Application Number: CN 201210235157.3; Publication Number: CN102846543A (the invention provides a method for preparing aripiprazole pharmaceutical formulation, comprising the steps of: an acidic solution containing aripiprazole is dissolved in the acidulant, to obtain an acidic solution containing the drug; Thereafter, the resulting drug-containing acidic solution alkalizing agents and materials prepared by wet granulation or suspension to give aripiprazole pharmaceutical formulation; said excipients include antioxidants)
Zheng Si Ji; Tan wave; Fulin Yong; Liu Xiaoyi; Yuanshao Qing; Cao Zhihui; aripiprazole Ⅰ type microcrystalline, aripiprazole solid preparation and preparation methods; application number: 201110180032.0; Publication Number: CN102850268A; Publication Date: 2013.01.02
Cai Fu Bo, Qin Xinrong, Du Xiaochun, Li Ling; kind of aripiprazole improved method of synthesis; Chengdu Nakasone Pharmaceutical Group Co., Ltd.; Application Number: 200910058148.X; Publication Number: CN101781246A; Publication date: 2010.07.21 (the invention provides a method of synthesis of aripiprazole improved method according to the modified method of the present invention, aripiprazole into the etherification reaction and condensation reaction of two-step synthesis, by an etherification reaction in the quinolone compound and at least 6-fold molar equivalents of 1,4 – dihalo-butane reacted with a non-polar solvent ether aripiprazole precipitate, and recovering 1,4 – dihalo-butane recycling; azeotropic condensation reaction of a ketone to be / water mixture as solvent, aripiprazole etherified with a piperazine compound or a salt thereof in the presence of a base under reflux and alkaline metal iodide compound conditions, the amount of water added to the end of the reaction, cooling crystallization, filtration, and dried to give aripiprazole. improved high yield synthesis of high purity, step simple, low cost, suitable for industrial production.)
GUPTA, Vijay Shankar, KUMAR, Pramod, VIR, Dharam; Process for producing aripiprazole in anhydrous type i crystals; JUBILANT LIFE SCIENCES LIMITED; WO 2012131451 A1
SRIVASTAVA JAYANT GUPTA Vijay Shankar;. Improved process for the preparation of 7 (4-bromobutoxy) 3,4-dihydrocarbostyril, a precursor of aripiprazole; wo2011030213 A1
No Generic Abilify in the US until April 2015
On May 7, 2012, The US Court of Appeals for the Federal Circuit ruled in favor of Otsuka Pharmaceutical Co., Ltd. In its patent litigation against several companies including Israel-based Teva and Weston, Ontario-based Apotex seeking FDA approval to market generic copies of Abilify ®.. The Federal Circuit Affirmed a Decision of the U.S. District Court for the District of New Jersey Holding that the asserted claims ofU.S. Patent No. 5,006,528 Covering aripiprazole, the active Ingredient in Abilify ®, are Valid, THUS Maintaining Patent and Regulatory Protection for Abilify ® in the U.S. until at least April 20, 2015 . The Case is Otsuka Pharma Co.. V. sand Inc.., 2011-1126 and 2011-1127, US Court of Appeals for the Federal Circuit (Washington). The lower court case is Otsuka Pharmaceutical Co. v. Sandoz Inc., 07cv1000, US District Court for the District of New Jersey (Trenton).
Chemical Name for Aripiprazole (Abilify for active Ingredient): 7 – {4 – [4 – (2,3-Dichlorophenyl) piperazin-1-yl] butoxy} 3 ,4-dihydroquinolin-2 (1H)-One
CAS Number 129722 -12-9
aripiprazole chemical name 7 – [4 – [4 – (2,3 – dichlorophenyl) -1 – piperazinyl] butoxy] -3,4 – dihydro-2 ( 1H) – quinolinone
Aripiprazole (, Aripiprazole, Abilify) is an atypical antipsychotic medication for the quinoline derivatives, aripiprazole is a dopamine system stabilizer first, positive and schizophrenia negative symptoms have a significant effect. For the treatment of schizophrenia, the development of Otsuka Pharmaceutical Co., Ltd., in November 15, 2002 by the U.S. Food and Drug Administration (FDA) approval in the U.S., domestic aripiprazole has (Booz clear (brisking, manufacturers : Chengdu Nakasone Pharmaceutical), Austrian (Manufacturer: Shanghai Pharmaceutical Co., Ltd. and Western)) have been approved by the listing in China. On sale in the United States where the law by Bristol-Myers Squibb is responsible. An law where the main patent protection in the United States, and more than three-quarters of its sales from the U.S., patent will expire in April 2015.
Aripiprazole synthetic route
7 – hydroxy-3 ,4. Dihydro -2 (1H) – quinolinone as a starting material, 1,4. Dibromobutane ether to give 7 – (4 – Bromo-butoxy) -3,4 – dihydro – 2 (1H) quinolinone, and then with 1 – (2,3 – dichlorophenyl) piperazine acid condensation aripiprazole (7 – [4 – [4 – (2,3 – dichlorophenyl) -1 – piperazinyl] butoxy] -3,4 – dihydro -2 (1H) – quinolinone)
Aripiprazole preparation method
7 – (4 – Bromo-butoxy) -3,4 – dihydro -2 (1H) – quinolone
A reaction flask was added 7 – hydroxy – 3,4 – dihydro -2 (1H) – quinolone 32.6 g (0.2mol), 1,4 – dibromo butane 129.5g (0.6mol), 11.2% KOH solution 250ml (0.5mol) and DMF975ml, was heated to 60 º C for 2h diluted with 1L water, the aqueous layer with ethyl acetate. acetate (300ml × 2) and the combined organic layers were washed with water, dried over anhydrous sodium sulfate, filtered, and the filtrate was concentrated under reduced pressure to recover the solvent, the residue was recrystallized from isopropanol, to give 7 – (4 – Bromo-butoxy) – 3,4 – dihydro -2 (1H) – quinolone 38.7g, yield 68%, mp108 ~ 110 º C.
Synthesis of aripiprazole
in the reaction flask was added 7 – (4 – Bromo-butoxy) -3,4 – dihydro -2 (1H) – quinolone, 29.8g (0.1mol), KI25g (0.15mol) 95% Ethanol 596ml, stirred and heated to 60 º C, was added N-2 30min after 3 – dichlorophenyl piperazine 23.1g (0.1mol) and triethylamine 20ml (0.15mol), stirred for 8h at 60 º C the mixture is filtered. crystallization filtrate was cooled, filtered and the filter cake was recrystallized twice from ethanol and dried to obtain aripiprazole 25.6g, yield 57%, mp138.9 ~ 139.6 º C.
References
- “Product Information for ABILIFYTM Aripiprazole Tablets & Orally Disintegrating Tablets”. TGA eBusiness Services. Bristol-Myers Squibb Australia Pty Ltd. 1 November 2012. Retrieved 22 October 2013.
- “ABILIFY (aripiprazole) tablet ABILIFY (aripiprazole) solution ABILIFY DISCMELT (aripiprazole) tablet, orally disintegrating ABILIFY (aripiprazole) injection, solution [Otsuka America Pharmaceutical, Inc.]”. DailyMed. Otsuka America Pharmaceutical, Inc. April 2013. Retrieved 22 October 2013.
- “Abilify Tablets, Orodispersible Tablets, Oral Solution – Summary of Product Characteristics (SPC)”. electronic Medicines Compendium. Otsuka Pharmaceuticals (UK) Ltd. 20 September 2013. Retrieved 22 October 2013.
- “ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS”. European Medicines Agency. Otsuka Pharmaceutical Europe Ltd. Retrieved 22 October 2013.
- http://www.webmd.com/drugs/drug-64439-Abilify+Oral.aspx?drugid=64439&drugname=Abilify+Oral&source=1
- Hitti, Miranda (20 November 2007). “FDA OKs Abilify for Depression”. WebMD. Archived from the original on 5 December 2008. Retrieved 8 December 2008.
- Keating, Gina (23 November 2009). “FDA OKs Abilify for child autism irritability”. Reuters. Retrieved 22 September 2010.
- “abilify”. The American Society of Health-System Pharmacists. Retrieved 3 April 2011.
- Belgamwar RB, El-Sayeh HG (Aug 10, 2011). “Aripiprazole versus placebo for schizophrenia.”. The Cochrane database of systematic reviews (8): CD006622. PMID 21833956.
- Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, Samara M, Barbui C, Engel RR, Geddes JR, Kissling W, Stapf MP, Lässig B, Salanti G, Davis JM (2013). “Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis”. Lancet 382 (9896): 951–62. doi:10.1016/S0140-6736(13)60733-3. PMID 23810019.
- Hasan A, Falkai P, Wobrock T, Lieberman J, Glenthoj B, Gattaz WF, Thibaut F, Möller HJ (2013). “World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, part 2: update 2012 on the long-term treatment of schizophrenia and management of antipsychotic-induced side effects”. World J. Biol. Psychiatry 14 (1): 2–44. doi:10.3109/15622975.2012.739708. PMID 23216388.
- El-Sayeh HG, Morganti C (Apr 19, 2006). “Aripiprazole for schizophrenia.”. Cochrane database of systematic reviews (Online) (2): CD004578. doi:10.1002/14651858.CD004578.pub3. PMID 16625607.
- Belgamwar RB, El-Sayeh HG (Aug 10, 2011). “Aripiprazole versus placebo for schizophrenia.”. Cochrane database of systematic reviews (Online) (8): CD006622. doi:10.1002/14651858.CD006622.pub2. PMID 21833956.
- Bhattacharjee J, El-Sayeh HG (Jan 23, 2008). “Aripiprazole versus typicals for schizophrenia.”. Cochrane database of systematic reviews (Online) (1): CD006617. doi:10.1002/14651858.CD006617.pub2. PMID 18254107.
- Khanna P, Komossa K, Rummel-Kluge C, Hunger H, Schwarz S, El-Sayeh HG, Leucht S (Feb 28, 2013). “Aripiprazole versus other atypical antipsychotics for schizophrenia.”. Cochrane database of systematic reviews (Online) 2: CD006569. doi:10.1002/14651858.CD006569.pub4. PMID 23450570.
- “Psychosis and schizophrenia in adults: treatment and management | Guidance and guidelines | NICE”. National Institute for Health and Care Excellence.
- Barnes TR (2011). “Evidence-based guidelines for the pharmacological treatment of schizophrenia: recommendations from the British Association for Psychopharmacology”. J. Psychopharmacol. (Oxford) 25 (5): 567–620. doi:10.1177/0269881110391123. PMID 21292923.
- Hasan A, Falkai P, Wobrock T, Lieberman J, Glenthoj B, Gattaz WF, Thibaut F, Möller HJ (2013). “World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, part 2: update 2012 on the long-term treatment of schizophrenia and management of antipsychotic-induced side effects”. World J. Biol. Psychiatry 14 (1): 2–44. doi:10.3109/15622975.2012.739708. PMID 23216388.
- De Fruyt J, Deschepper E, Audenaert K, Constant E, Floris M, Pitchot W, Sienaert P, Souery D, Claes S (May 2012). “Second generation antipsychotics in the treatment of bipolar depression: a systematic review and meta-analysis.”. Journal of psychopharmacology (Oxford, England) 26 (5): 603–17. doi:10.1177/0269881111408461. PMID 21940761.
- Gitlin M, Frye MA (May 2012). “Maintenance therapies in bipolar disorders.”. Bipolar disorders. 14 Suppl 2: 51–65. doi:10.1111/j.1399-5618.2012.00992.x. PMID 22510036.
- de Bartolomeis A, Perugi G (October 2012). “Combination of aripiprazole with mood stabilizers for the treatment of bipolar disorder: from acute mania to long-term maintenance.”. Expert opinion on pharmacotherapy 13 (14): 2027–36. doi:10.1517/14656566.2012.719876. PMID 22946707.
- Komossa K, Depping AM, Gaudchau A, Kissling W, Leucht S (Dec 8, 2010). “Second-generation antipsychotics for major depressive disorder and dysthymia.”. Cochrane database of systematic reviews (Online) (12): CD008121. doi:10.1002/14651858.CD008121.pub2. PMID 21154393.
- Spielmans GI, Berman MI, Linardatos E, Rosenlicht NZ, Perry A, Tsai AC (Mar 12, 2013). “Adjunctive atypical antipsychotic treatment for major depressive disorder: a meta-analysis of depression, quality of life, and safety outcomes”. Cochrane database of systematic reviews (Online) 10 (3): CD008121. doi:10.1371/journal.pmed.1001403. PMID 23554581.
- Nelson JC, Papakostas GI (2009). “Atypical antipsychotic augmentation in major depressive disorder: a meta-analysis of placebo-controlled randomized trials”. Am J Psychiatry 166 (9): 980–91. doi:10.1176/appi.ajp.2009.09030312. PMID 19687129.
- Komossa K, Depping AM, Gaudchau A, Kissling W, Leucht S (2010). “Second-generation antipsychotics for major depressive disorder and dysthymia”. Cochrane Database Syst Rev (12): CD008121. doi:10.1002/14651858.CD008121.pub2. PMID 21154393.
- Ching H, Pringsheim T (May 16, 2012). “Aripiprazole for autism spectrum disorders (ASD).”. Cochrane database of systematic reviews (Online) 5: CD009043. doi:10.1002/14651858.CD009043.pub2. PMID 22592735.
- Joint Formulary Committee. British National Formulary (BNF) 65. Pharmaceutical Pr; 2013.
- Australian Medicines Handbook 2013 [Internet]. [cited 2013 Sep 30]. Available from: http://www.psa.org.au/shop/amh
- Truven Health Analytics, Inc. DRUGDEX® System (Internet) [cited 2013 Jun 25]. Greenwood Village, CO: Thomsen Healthcare; 2013.
- “Abilify Discmelt, Abilify Maintena (aripiprazole) dosing, indications, interactions, adverse effects, and more”. Medscape Reference. WebMD. Retrieved 22 October 2013.
- Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, Samara M, Barbui C, Engel RR, Geddes JR, Kissling W, Stapf MP, Lässig B, Salanti G, Davis JM (September 2013). “Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis.”. Lancet 382 (9896): 951–962. doi:10.1016/S0140-6736(13)60733-3. PMID 23810019.
- Abbasian C, Power P (March 2009). “A case of aripiprazole and tardive dyskinesia”. J Psychopharmacol (Oxford) 23 (2): 214–5. doi:10.1177/0269881108089591. PMID 18515468.
- Zaidi SH, Faruqui RA (January 2008). “Aripiprazole is associated with early onset of Tardive Dyskinesia like presentation in a patient with ABI and psychosis”. Brain Inj 22 (1): 99–102. doi:10.1080/02699050701822493. PMID 18183513.
- Maytal G, Ostacher M, Stern TA (June 2006). “Aripiprazole-related tardive dyskinesia”. CNS Spectr 11 (6): 435–9. PMID 16816781.
- http://www.medicines.org.uk/EMC/pdfviewer.aspx?isAttachment=true&documentid=16161
- “ABILIFY (aripiprazole) [package insert].”. Otsuka Pharmaceutical Co, Ltd. Retrieved 18 October 2012.
- Group, BMJ, ed. (March 2009). “4.2.1”. British National Formulary (57 ed.). United Kingdom: Royal Pharmaceutical Society of Great Britain. p. 192. ISBN 978-0-85369-845-6. “Withdrawal of antipsychotic drugs after long-term therapy should always be gradual and closely monitored to avoid the risk of acute withdrawal syndromes or rapid relapse.”
- Moncrieff J (Jul 2006). “Does antipsychotic withdrawal provoke psychosis? Review of the literature on rapid onset psychosis (supersensitivity psychosis) and withdrawal-related relapse”. Acta Psychiatr Scand 114 (1): 3–13. doi:10.1111/j.1600-0447.2006.00787.x. PMID 16774655.
- R. Baselt, Disposition of Toxic Drugs and Chemicals in Man, 8th edition, Biomedical Publications, Foster City, CA, 2008, pp. 105-106.
- “Abilify (Aripiprazole) – Warnings and Precautions”. DrugLib.com. 14 February 2007. Archived from the original on 4 December 2008. Retrieved 8 December 2008.
- http://www.drugs.com/cons/abilify-intramuscular.html
- http://www.drugs.com/pro/abilify.html
- Starrenburg FC, Bogers JP (April 2009). “How can antipsychotics cause diabetes mellitus? Insights based on receptor-binding profiles, humoral factors and transporter proteins”. European Psychiatry 24 (3): 164–170. doi:10.1016/j.eurpsy.2009.01.001. PMID 19285836.
- “Abilify (Aripiprazole) – Clinical Pharmacology”. DrugLib.com. 14 February 2007. Retrieved 8 December 2008.
- Brunton, Laurence (2011). Goodman & Gilman’s The Pharmacological Basis of Therapeutics 12th Edition. China: McGraw-Hill. pp. 406–410. ISBN 978-0-07-162442-8.
- “PDSP Ki Database”. National Institute of Mental Health. Retrieved 30 June 2013.
- Nguyen CT, Rosen JA, Bota RG (2012). “Aripiprazole partial agonism at 5-HT2C: a comparison of weight gain associated with aripiprazole adjunctive to antidepressants with high versus low serotonergic activities”. Prim Care Companion CNS Disord 14 (5). doi:10.4088/PCC.12m01386. PMC 3583771. PMID 23469329.
- Newman-Tancredi A, Heusler P, Martel JC, Ormière AM, Leduc N, Cussac D (2008). “Agonist and antagonist properties of antipsychotics at human dopamine D4.4 receptors: G-protein activation and K+ channel modulation in transfected cells”. Int. J. Neuropsychopharmacol. 11 (3): 293–307. doi:10.1017/S1461145707008061. PMID 17897483.
- Burstein ES, Ma J, Wong S, Gao Y, Pham E, Knapp AE, Nash NR, Olsson R, Davis RE, Hacksell U, Weiner DM, Brann MR (2005). “Intrinsic efficacy of antipsychotics at human D2, D3, and D4 dopamine receptors: identification of the clozapine metabolite N-desmethylclozapine as a D2/D3 partial agonist”. J. Pharmacol. Exp. Ther. 315 (3): 1278–87. doi:10.1124/jpet.105.092155. PMID 16135699.
- Davies MA, Sheffler DJ, Roth BL (2004). “Aripiprazole: a novel atypical antipsychotic drug with a uniquely robust pharmacology”. CNS Drug Rev 10 (4): 317–36. doi:10.1111/j.1527-3458.2004.tb00030.x. PMID 15592581.
- Lawler CP, Prioleau C, Lewis MM, Mak C, Jiang D, Schetz JA, Gonzalez AM, Sibley DR, Mailman RB (1999). “Interactions of the novel antipsychotic aripiprazole (OPC-14597) with dopamine and serotonin receptor subtypes”. Neuropsychopharmacology 20 (6): 612–27. doi:10.1016/S0893-133X(98)00099-2. PMID 10327430.
- Burstein ES, Ma J, Wong S, Gao Y, Pham E, Knapp AE, Nash NR, Olsson R, Davis RE, Hacksell U, Weiner DM, Brann MR (December 2005). “Intrinsic Efficacy of Antipsychotics at Human D2, D3, and D4 Dopamine Receptors: Identification of the Clozapine Metabolite N-Desmethylclozapine as a D2/D3 Partial Agonist”. J Pharmacol Exp Ther 315 (3): 1278–87. doi:10.1124/jpet.105.092155. PMID 16135699.
- Jordan S, Koprivica V, Chen R, Tottori K, Kikuchi T, Altar CA (2002). “The antipsychotic aripiprazole is a potent, partial agonist at the human 5-HT1A receptor”. Eur J Pharmacol 441 (3): 137–140. doi:10.1016/S0014-2999(02)01532-7. PMID 12063084.
- Shapiro DA, Renock S, Arrington E, Chiodo LA, Liu LX, Sibley DR, Roth BL, Mailman R (2003). “Aripiprazole, A Novel Atypical Antipsychotic Drug with a Unique and Robust Pharmacology”. Neuropsychopharmacology 28 (8): 1400–1411. doi:10.1038/sj.npp.1300203. PMID 12784105.
- Zhang JY, Kowal DM, Nawoschik SP, Lou Z, Dunlop J (February 2006). “Distinct functional profiles of aripiprazole and olanzapine at RNA edited human 5-HT2C receptor isoforms”. Biochem Pharmacol 71 (4): 521–9. doi:10.1016/j.bcp.2005.11.007. PMID 16336943.
- Kegeles LS, Slifstein M, Frankle WG, Xu X, Hackett E, Bae SA, Gonzales R, Kim JH, Alvarez B, Gil R, Laruelle M, Abi-Dargham A (2008). “Dose–Occupancy Study of Striatal and Extrastriatal Dopamine D2 Receptors by Aripiprazole in Schizophrenia with PET and [18F]Fallypride”. Neuropsychopharmacology 33 (13): 3111–3125. doi:10.1038/npp.2008.33. PMID 18418366.
- Yokoi F, Gründer G, Biziere K, Stephane M, Dogan AS, Dannals RF, Ravert H, Suri A, Bramer S, Wong DF (August 2002). “Dopamine D2 and D3 receptor occupancy in normal humans treated with the antipsychotic drug aripiprazole (OPC 14597): a study using positron emission tomography and [11C]raclopride”. Neuropsychopharmacology 27 (2): 248–59. doi:10.1016/S0893-133X(02)00304-4. PMID 12093598.
- “In This Issue”. Am J Psychiatry 165 (8): A46. August 2008. doi:10.1176/appi.ajp.2008.165.8.A46.
- “Abilify Receives Approval for Expanded Use in Children, Teens”. Psych Central. Retrieved 2012-07-16.
- “Abilify Gets FDA Approval For Autism Irritability”. Furious Seasons. Retrieved 2012-07-16.
- “FDA OKs Abilify for Depression : Antipsychotic Drug Approved for Use in Addition to Antidepressants for Treating Depression”. WebMD. Retrieved 2012-07-16.
- “Patent and Exclusivity Search Results”. Electronic Orange Book. US Food and Drug Administration. Retrieved 8 December 2008.
- http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/021436s21,021713s16,021729s8,021866s8lbl.pdfSection 2.3 pp 7-8
- US 5006528, Oshiro, Yasuo; Seiji Sato & Nobuyuki Kurahashi, “Carbostyril derivatives”, published October 20, 1989
- “Barr Confirms Filing an Application with a Paragraph IV Certification for ABILIFY(R) Tablets” (Press release). Barr Pharmaceuticals, Inc. 2007-03-20. Retrieved 2008-12-23.
- U.S. Patent 5,006,528
- Feltenstein MW, Altar CA, See RE (2007). “Aripiprazole blocks reinstatement of cocaine seeking in an animal model of relapse”. Biol. Psychiatry 61 (5): 582–90. doi:10.1016/j.biopsych.2006.04.010. PMID 16806092.
- Roache JD (2013). “Role of the human laboratory in the development of medications for alcohol and drug dependence”. In Johnson BA. Addiction medicine: science and practice. New York: Springer. p. 145. ISBN 978-1461439899.
External links
- Abilify website
- Abilify Full Prescribing Information (for Health Care Professionals)
- U.S. National Library of Medicine: Drug Information Portal – Aripiprazole
- Abilify adverse events reported to the FDA
- Mechanism of Action Of Aripiprazole
| WO2006079548A1 * | Jan 27, 2006 | Aug 3, 2006 | Sandoz Ag | Organic compounds |
| WO2006079549A1 | Jan 27, 2006 | Aug 3, 2006 | Sandoz Ag | Salts of aripiprazole |
| WO2014060324A1 | Oct 11, 2013 | Apr 24, 2014 | Sanovel Ilac Sanayi Ve Ticaret A.S | Aripiprazole formulations |
| EP1844036A1 * | Jan 27, 2006 | Oct 17, 2007 | Sandoz AG | Salts of aripiprazole |
| EP2093217A1 * | Jan 27, 2006 | Aug 26, 2009 | Sandoz AG | Polymorph and solvates of aripiprazole |
| EP2233471A1 * | Feb 6, 2009 | Sep 29, 2010 | Adamed Sp. z o.o. | A salt of 7-{4-[4-(2,3-dichlorophenyl)-1-piperazinyl]butoxy}-3,4.dihydro-2(1h)-quinolinone with 5-sulfosalicylic acid and its preparation process |
| EP2359816A1 | Feb 8, 2011 | Aug 24, 2011 | Sanovel Ilac Sanayi ve Ticaret A.S. | Aripiprazole formulations |
| US7504504 | Dec 16, 2004 | Mar 17, 2009 | Teva Pharmaceutical Industries Ltd. | Methods of preparing aripiprazole crystalline forms |
| US7714129 | Sep 29, 2006 | May 11, 2010 | Teva Pharmaceutical Industries Ltd. | Methods of preparing anhydrous aripiprazole form II |
| US8008490 | Jan 27, 2006 | Aug 30, 2011 | Sandoz Ag | Polymorphic forms of aripiprazole and method |
| US8188076 | Feb 26, 2010 | May 29, 2012 | Reviva Pharmaceuticals, Inc. | Compositions, synthesis, and methods of utilizing arylpiperazine derivatives |
| US8207163 | May 27, 2009 | Jun 26, 2012 | Reviva Pharmaceuticals, Inc. | Compositions, synthesis, and methods of using piperazine based antipsychotic agents |
| US8247420 | May 21, 2008 | Aug 21, 2012 | Reviva Pharmaceuticals, Inc. | Compositions, synthesis, and methods of using quinolinone based atypical antipsychotic agents |
| US8431570 | May 7, 2012 | Apr 30, 2013 | Reviva Pharmaceuticals, Inc. | Methods of utilizing arylpiperazine derivatives |
| US8461154 | May 7, 2012 | Jun 11, 2013 | Reviva Pharmaceuticals, Inc. | Methods of utilizing arylpiperazine derivatives |
| US8575185 | Feb 26, 2010 | Nov 5, 2013 | Reviva Pharmaceuticals, Inc. | Compositions, synthesis, and methods of utilizing quinazolinedione derivatives |
FDA expands approval of drug to treat Pompe disease to patients of all ages; removes risk mitigation strategy requirements

Human glucosidase, prepro-α-[199-arginine,223-histidine] [1]
Alglucosidase alfa
C4435H6739N1175O1279S32
105270.8020
August 1, 2014
The U.S. Food and Drug Administration today announced the approval of Lumizyme (alglucosidase alfa) for treatment of patients with infantile-onset Pompe disease, including patients who are less than 8 years of age. In addition, the Risk Evaluation and Mitigation Strategy (REMS) known as the Lumizyme ACE (Alglucosidase Alfa Control and Education) Program is being eliminated.
Pompe disease is a rare genetic disorder and occurs in an estimated 1 in every 40,000 to 300,000 births. Its primary symptom is heart and skeletal muscle weakness, progressing to respiratory weakness and death from respiratory failure.
The disease causes gene mutations to prevent the body from making enough of the functional form of an enzyme called acid alpha-glucosidase (GAA). This enzyme is necessary for proper muscle functioning. GAA is used by the heart and muscle cells to convert a form of sugar called glycogen into energy. Without the enzyme action, glycogen builds up in the cells and, ultimately, weakens the heart and muscles. Lumizyme is believed to work by replacing the deficient GAA, thereby reducing the accumulated glycogen in heart and skeletal muscle cells.
Lumizyme, a lysosomal glycogen-specific enzyme, was approved by the FDA in 2010 with a REMS to restrict its use to treatment of patients with late (non-infantile) onset Pompe disease who are 8 years of age and older. The REMS was required to mitigate the potential risk of rapid disease progression in the infantile-onset Pompe disease patients and patients with late onset disease less than 8 years of age, and to communicate the risks of anaphylaxis, severe allergic reactions and severe skin and systemic immune mediated reactions to prescribers and patients.
At the time of Lumizyme’s approval, there were insufficient data to support the safety and efficacy of Lumizyme in the infantile-onset Pompe population, so Lumizyme was approved for use only in late onset Pompe disease patients who are at least 8 years of age. Pompe patients with infantile-onset disease and patients younger than 8 years of age continued treatment with Myozyme, which was already approved. Myozyme and Lumizyme, both manufactured by Genzyme Corporation, are produced from the same cell line at different production scales.
This approval provides access to Lumizyme for all Pompe disease patients, regardless of their age.
The FDA reviewed newly available information and determined that Lumizyme and Myozyme are chemically and biochemically comparable. Consequently, the safety and effectiveness of Lumizyme and Myozyme are expected to be comparable. In addition, a single-center clinical study of 18 infantile-onset Pompe disease patients, aged 0.2 to 5.8 months at the time of first infusion, provides further support that infantile-onset patients treated with Lumizyme will have a similar improvement in ventilator-free survival as those treated with Myozyme.
Because data were submitted supporting approval of Lumizyme for all Pompe patients, a REMS restricting its use to a specific age group is no longer necessary. While the risk of anaphylaxis, severe allergic reactions, and severe cutaneous and immune mediated reactions for Lumizyme still exist, these risks are comparable to Myozyme and are communicated in labeling through the Warnings and Precautions, and a Boxed Warning.
“REMS continue to be vital tools for the agency to employ as we work with companies to address the serious risks associated with drugs and monitor their appropriate and safe use in various health care settings,” said Janet Woodcock, M.D., director of the FDA’s Center for Drug Evaluation and Research. “The agency remains committed to exercising a flexible and responsible regulatory approach that ensures REMS programs are being effectively and efficiently used and not resulting in an unnecessary burden on health care professionals and patients.”
Health care professionals and patients should also be aware:
- The Warnings and Precautions section of the Lumizyme product label and the Clinical Studies section of the Lumizyme label have been updated to include the safety information of the drug in infantile-onset Pompe disease patients. This includes information from the currently approved Myozyme label and information from a new, uncontrolled study in which patients with infantile onset disease were treated with Lumizyme.
- Lumizyme is approved with a Boxed Warning because of the risk of anaphylaxis, severe allergic reactions, immune-mediated reactions and cardiorespiratory failure.
- Health care professionals should continue to refer to the drug prescribing information for the latest recommendations on prescribing Lumizyme and report adverse events to the FDA’s MedWatch program (http://www.fda.gov/Safety/MedWatch/default.htm).
- Distribution of Lumizyme will no longer be restricted. Health care professionals, healthcare facilities, and patients will no longer be required to enroll in the Lumizyme REMS program (Lumizyme ACE Program) to be able to prescribe, dispense, or receive Lumizyme.
The most commonly reported side effects for Lumizyme were infusion-related reactions and included severe allergic reactions, hives, diarrhea, vomiting, shortness of breath, itchy skin, skin rash, neck pain, partial hearing loss, flushing, pain in extremities, and chest discomfort.
Myozyme and Lumizyme are marketed by Cambridge, Massachusetts-based Genzyme.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.
| Country | Patent Number | Approved | Expires (estimated) |
|---|---|---|---|
| Canada | 2416492 | 2008-04-29 | 2021-07-10 |

>Alglucosidase alfa AHPGRPRAVPTQCDVPPNSRFDCAPDKAITQEQCEARGCCYIPAKQGLQGAQMGQPWCFF PPSYPSYKLENLSSSEMGYTATLTRTTPTFFPKDILTLRLDVMMETENRLHFTIKDPANR RYEVPLETPHVHSRAPSPLYSVEFSEEPFGVIVRRQLDGRVLLNTTVAPLFFADQFLQLS TSLPSQYITGLAEHLSPLMLSTSWTRITLWNRDLAPTPGANLYGSHPFYLALEDGGSAHG VFLLNSNAMDVVLQPSPALSWRSTGGILDVYIFLGPEPKSVVQQYLDVVGYPFMPPYWGL GFHLCRWGYSSTAITRQVVENMTRAHFPLDVQWNDLDYMDSRRDFTFNKDGFRDFPAMVQ ELHQGGRRYMMIVDPAISSSGPAGSYRPYDEGLRRGVFITNETGQPLIGKVWPGSTAFPD FTNPTALAWWEDMVAEFHDQVPFDGMWIDMNEPSNFIRGSEDGCPNNELENPPYVPGVVG GTLQAATICASSHQFLSTHYNLHNLYGLTEAIASHRALVKARGTRPFVISRSTFAGHGRY AGHWTGDVWSSWEQLASSVPEILQFNLLGVPLVGADVCGFLGNTSEELCVRWTQLGAFYP FMRNHNSLLSLPQEPYSFSEPAQQAMRKALTLRYALLPHLYTLFHQAHVAGETVARPLFL EFPKDSSTWTVDHQLLWGEALLITPVLQAGKAEVTGYFPLGTWYDLQTVPVEALGSLPPP PAAPREPAIHSEGQWVTLPAPLDTINVHLRAGYIIPLQGPGLTTTESRQQPMALAVALTK GGEARGELFWDDGESLEVLERGAYTQVIFLARNNTIVNELVRVTSEGAGLQLQKVTVLGV ATAPQQVLSNGVPVSNFTYSPDTKVLDICVSLLMGEQFLVSWC
| Systematic (IUPAC) name | |
|---|---|
| Human glucosidase, prepro-α-[199-arginine,223-histidine] [1] | |
| Clinical data | |
| AHFS/Drugs.com | monograph |
| Legal status | FDA approved for children[2] |
| Routes | Intravenous[2] |
| Identifiers | |
| CAS number | 420794-05-0 |
| ATC code | A16AB07 |
| DrugBank | DB01272 |
| UNII | DTI67O9503 |
| KEGG | D03207 |
| Chemical data | |
| Formula | C4758H7262N1274O1369S35[1] |
| Mol. mass | 105338 [1] |
Alglucosidase alfa (Lumizyme, Myozyme, Genzyme) is an enzyme replacement therapy (ERT) orphan drug for treatment of Pompe disease (Glycogen storage disease type II), a rare lysosomal storage disorder (LSD).[3] Chemically speaking, the drug is ananalog of the enzyme that is deficient in patients affected by Pompe disease, alpha-glucosidase. It is the first drug available to treat this disease.[2]
Status
Orphan drug pharmaceutical company, Genzyme, markets alglucosidase alfa as “Myozyme”. In 2006, the U.S. Food and Drug Administration (FDA) approved Myozyme as a suitable ERT treatment for children.[2] Some health plans have refused to subsidize Myozyme for adult patients because it lacks approval for treatment in adults, as well as its high cost (US$300,000/yr for life).[4]
On August 1, 2014 the U.S. Food and Drug Administration announced the approval of Lumizyme (alglucosidase alfa) for treatment of patients with infantile-onset Pompe disease, including patients who are less than 8 years of age. In addition, the Risk Evaluation and Mitigation Strategy (REMS) known as the Lumizyme ACE (Alglucosidase Alfa Control and Education) Program is being eliminated. [5]
Side effects
Common observed adverse reactions to alglucosidase alfa treatment are pneumonia, respiratory complications, infections and fever. More serious reactions reported includeheart and lung failure and allergic shock. Myozyme boxes carry warnings regarding the possibility of life-threatening allergic response.[2]
References
- ^ Jump up to:a b c American Medical Association (USAN). “Alglucosidase alfa” (Microsoft Word). STATEMENT ON A NONPROPRIETARY NAME ADOPTED BY THE USAN COUNCIL. Retrieved 18 December 2007.
- ^ Jump up to:a b c d e “FDA Approves First Treatment for Pompe Disease” (Press release). FDA. 2006-04-28. Retrieved 2008-07-07.
- Jump up^ Kishnani PS, Corzo D, Nicolino M et al. (2007). “Recombinant human acid [alpha]-glucosidase: major clinical benefits in infantile-onset Pompe disease”. Neurology 68 (2): 99–109.doi:10.1212/01.wnl.0000251268.41188.04. PMID 17151339.
- Jump up^ Geeta Anand (2007-09-18). “As Costs Rise, New Medicines Face Pushback”. Wall Street Journal (Dow Jones & Company). Retrieved 2008-07-07.
- Jump up^ cite press release |title=FDA expands approval of drug to treat Pompe disease to patients of all ages; removes risk mitigation strategy requirements |publisher=FDA |date=2014-08-14 |url=http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm407563.htm
External links
- Myozyme (alglucosidase alfa), Genzyme official website
- MTAP (Myozyme Temporary Access Program), Genzyme official website
MYOZYME (alglucosidase alfa), a lysosomal glycogen-specific enzyme, consists of the human enzyme acid α-glucosidase (GAA), encoded by the most predominant of nine observed haplotypes of this gene. MYOZYME is produced by recombinant DNA technology in a Chinese hamster ovary cell line. The MYOZYME manufacturing process differs from that for LUMIZYME®, resulting in differences in some product attributes. Alglucosidase alfa degrades glycogen by catalyzing the hydrolysis of α-1,4- and α-1,6- glycosidic linkages of lysosomal glycogen.
Alglucosidase alfa is a glycoprotein with a calculated mass of 99,377 daltons for the polypeptide chain, and a total mass of approximately 110 kilo Daltons, including carbohydrates. Alglucosidase alfa has a specific activity of 3 to 5 U/mg (one unit is defined as that amount of activity that results in the hydrolysis of 1 μmole of synthetic substrate per minute under the specified assay conditions). MYOZYME is intended for intravenous infusion. It is supplied as a sterile, nonpyrogenic, white to off-white, lyophilized cake or powder for reconstitution with 10.3 mL
Sterile Water for Injection, USP. Each 50 mg vial contains 52.5 mg alglucosidase alfa, 210 mg mannitol, 0.5 mg polysorbate 80, 9.9 mg sodium phosphate dibasic heptahydrate, 31.2 mg sodium phosphate monobasic monohydrate. Following reconstitution as directed, each vial contains 10.5 mL reconstituted solution and a total extractable volume of 10 mL at 5.0 mg/mL alglucosidase alfa. MYOZYME does not contain preservatives; each vial is for single use only.

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....