Home » Articles posted by DR ANTHONY MELVIN CRASTO Ph.D (Page 412)
Author Archives: DR ANTHONY MELVIN CRASTO Ph.D
The U.S. Food and Drug Administration today announced that it has approved an amended application submitted by Teva Women’s Health, Inc. to market Plan B One-Step (active ingredient levonorgestrel) for use without a prescription by women 15 years of age and older
April 30, 2013 — The U.S. Food and Drug Administration today announced that it has approved an amended application submitted by Teva Women’s Health, Inc. to market Plan B One-Step (active ingredient levonorgestrel) for use without a prescription by women 15 years of age and older.
After the FDA did not approve Teva’s application to make Plan B One-Step available over-the-counter for all females of reproductive age in December 2011, the company submitted an amended application to make the product available for women 15 years of age and older without a prescription.
FDA Approves Procysbi for Nephropathic Cystinosis

Cysteamine bitartrate
April 30, 2013 — The U.S. Food and Drug Administration today approved Procysbi (cysteamine bitartrate) for the management of nephropathic cystinosis in children and adults. Procysbi was granted orphan product designation because it is intended to treat a rare disease or condition.
Cystinosis is a rare genetic condition that affects an estimated 500 patients in the United States and about 3,000 patients worldwide. Fatal if not treated in early childhood, cystinosis causes a protein building block called cystine to build up in every cell of the body. The buildup of cystine causes kidney problems, which can cause the body to lose too much sugar, proteins and salts through the urine. Cystinosis may lead to slow body growth and small stature, weak bones and developing and worsening kidney failure. There are three types of cystinosis, the most severe being nephropathic cystinosis, which severely damages the kidneys.
Currently the FDA approved drugs used to treat cystinosis include Cystagon (cysteamine bitartrate), an immediate-release tablet that was approved in 1994, and Cystaran (cysteamine ophthalmic solution) eye drops, approved last year to treat corneal cystine crystal accumulation.
Procysbi is a delayed-release capsule intended for patients ages 6 years and older. While Cystagon is taken every six hours around the clock to control cystine levels, Procysbi is a long-acting formulation that is taken every 12 hours.
“Procysbi is the only delayed-release product approved by FDA to treat nephropathic cystinosis, offering patients with this rare disease an important new treatment option,” said Andrew E. Mulberg, M.D., deputy director, Division of Gastroenterology and Inborn Errors Products, Center for Drug Evaluation and Research, FDA.
The major study supporting Procysbi’s safety and effectiveness involved 43 adult and pediatric patients with nephropathic cystinosis. Patients were randomly assigned to receive Cystagon or Procysbi for three weeks before being switched to the other product for an additional three weeks. Blood testing showed Procysbi was as effective as Cystagon in controlling cystine levels.
The most common side effects in patients treated with cysteamine products include nausea, bad breath, abdominal pain, constipation, indigestion or upset stomach, headache, drowsiness and dizziness. Other uncommon but serious side effects include ulcers or bleeding of the stomach or intestine, altered mental state, seizures, severe skin rashes and allergic reactions.
Procysbi is marketed by Novato, Calif.-based Raptor Pharmaceuticals. Cystagon is marketed by Canonsburg, Pa.-based Mylan Inc. Cystaran is marketed by Gaithersburg, Md.-based Sigma-Tau Pharmaceuticals, Inc.
FDA Approves Actemra for Children with Polyarticular Juvenile Idiopathic Arthritis
tocilizumab
April 30, 2013
Roche announced today that the U.S. Food and Drug Administration (FDA) has approved Actemra (tocilizumab) for the treatment of polyarticular juvenile idiopathic arthritis (PJIA). The medicine can be used in children two years of age and older with active disease. Actemra can be given alone or in combination with methotrexate (MTX) in people with PJIA.
PJIA is a form of juvenile idiopathic arthritis (JIA), also known as juvenile rheumatoid arthritis, a chronic disease of childhood.1 JIA affects approximately 100 in every 100,000 children2 of which PJIA accounts for around 30 percent.3 PJIA is characterised by inflammation in five or more joints within the first six months of the disease and most commonly affects the small joints in the body such as the hands and feet.3
“Polyarticular juvenile idiopathic arthritis is a rare debilitating condition in children that worsens over time,” said Hal Barron, M.D., chief medical officer and head, Global Product Development. “We are pleased to offer Actemra to doctors and parents of children aged two or older to help improve the signs and symptoms of this often painful disease.”
This FDA approval marks the second Actemra indication in children and is the first FDA approval for the treatment of PJIA in approximately five years. The EU Committee for Medicinal Products for Human Use (CHMP) also announced a positive opinion for this indication on Friday, April 26. The final approval from the European Medicines Agency (EMA) is expected this summer.
The expanded indication for Actemra was based on positive data from the Phase III CHERISH study in children with PJIA, which had an open label phase, followed by a randomised double-blind placebo-controlled withdrawal phase. The study demonstrated that patients treated with Actemra experienced clinically meaningful improvement in signs and symptoms of PJIA. A total of 91 percent of patients taking Actemra plus MTX and 83 percent of patients taking Actemra alone achieved an ACR 30 response at week 16 compared to baseline. In the randomised double-blind placebo-controlled withdrawal phase of the trial, Actemra-treated patients experienced significantly fewer disease flares compared to placebo-treated patients [26 percent (21/82) vs. 48 percent (39/81)].
The safety data collected to date for Actemra in PJIA patients is consistent with that observed in previous studies in Actemra-treated patients.4 In the CHERISH study, infections were the most common adverse events (AEs) and serious adverse events (SAEs) over 40-weeks. Laboratory abnormalities known to occur with Actemra were also observed in this study, including decreases in white blood cell counts and platelet counts, and elevation in ALT and AST liver enzyme levels.
About Actemra (tocilizumab)
Actemra is the first humanised interleukin-6 (IL-6) receptor antagonist approved for the treatment of adult patients with moderately to severely active rheumatoid arthritis (RA) who have had an inadequate response to one or more disease-modifying antirheumatic drugs (DMARDs). The extensive Actemra clinical development programme included five Phase III clinical studies and enrolled more than 4,000 people with RA in 41 countries, including the United States. In addition, Actemra is also approved for the treatment of active systemic juvenile idiopathic arthritis (SJIA) in patients two years of age and older and polyarticular juvenile idiopathic arthritis (PJIA) in patients two years of age and older who have responded inadequately to previous therapy with MTX.
Actemra is part of a co-development agreement with Chugai Pharmaceutical Co. and has been approved in Japan since June 2005. Actemra is approved in the European Union, where it is known as RoActemra, and several other countries, including China, India, Brazil, Switzerland and Australia.
Headquartered in Basel, Switzerland, Roche is a leader in research-focused healthcare with combined strengths in pharmaceuticals and diagnostics. Roche is the world’s largest biotech company, with truly differentiated medicines in oncology, infectious diseases, inflammation, metabolism and neuroscience. Roche is also the world leader in in vitro diagnostics and tissue-based cancer diagnostics, and a frontrunner in diabetes management. Roche’s personalised healthcare strategy aims at providing medicines and diagnostic tools that enable tangible improvements in the health, quality of life and survival of patients. In 2012 Roche had over 82,000 employees worldwide and invested over 8 billion Swiss francs in R&D. The Group posted sales of 45.5 billion Swiss francs. Genentech, in the United States, is a wholly owned member of the Roche Group. Roche is the majority shareholder in Chugai Pharmaceutical, Japan. For more information, please visit www.roche.com.
Tocilizumab (INN, or atlizumab, developed by Hoffmann–La Roche and Chugai and sold under the trade names Actemra and RoActemra) is an immunosuppressive drug, mainly for the treatment of rheumatoid arthritis (RA) and systemic juvenile idiopathic arthritis, a severe form of RA in children. It is a humanized monoclonal antibody against the interleukin-6 receptor (IL-6R). Interleukin 6 (IL-6) is a cytokine that plays an important role in immune response and is implicated in the pathogenesis of many diseases, such as autoimmune diseases, multiple myeloma and prostate cancer.
Merck & Co and Pfizer join forces on diabetes pill
ertugliflozin
PF04971729
(1S,2S,3S,4R,5S)-5-[4-Chloro-3-(4-ethoxybenzyl)phenyl]-1-(hydroxymethyl)-6,8-dioxabicyclo[3.2.1]octane-2,3,4-triol
Drug giants Merck & Co and Pfizer have formed a new alliance to jointly develop and commercialise the latter’s ertugliflozin for the treatment of type II diabetes.
The drug is an investigational oral sodium glucose cotransporter (SGLT2) inhibitor, which is on the verge of entering Phase III trials, scheduled for later this year.
read more
http://www.pharmatimes.com/Article/13-04-30/Merck_Co_and_Pfizer_join_forces_on_diabetes_pill.aspx
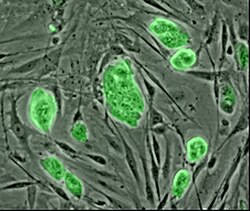
Regenerative Medicine: Polymer coating could help stem cells target inflamed blood vessels to regrow healthy tissue
People with chronic diseases like diabetes and multiple sclerosis have inflamed, leaky blood vessels, heightening their risk of heart attack and stroke. Some scientists envision using a patient’s own stem cells to regrow healthy tissue to plug the leaks and calm inflammation. A new polymer coating could help these stem cells find and adhere to inflamed endothelial tissue (J. Am. Chem. Soc., DOI: 10.1021/ja400636d).
read all at
http://cen.acs.org/articles/91/web/2013/04/Putting-Stem-Cells-Place.html
 Serving The Chemical, Life Sciences & Laboratory Worlds
Serving The Chemical, Life Sciences & Laboratory Worlds
Scioderm’s SD-101 Receives Breakthrough Therapy Designation from FDA for Treatment of Epidermolysis Bullosa
DURHAM, N.C., April 29, 2013 Scioderm announced its investigational product SD-101 has received Breakthrough Therapy designation by the U.S. Food and Drug Administration (FDA) for the treatment of patients with inherited Epidermolysis Bullosa (EB). SD-101 is Scioderm’s investigational therapy that is being evaluated for the treatment of skin blistering and erosions associated with this disease, including facilitation of healing of skin lesions and reduction of the incidence and/or severity of new lesions.
read all at

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....