Home » 2021 (Page 5)
Yearly Archives: 2021
POLIDOCANOL


POLIDOCANOL
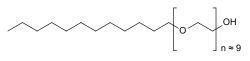
Synonym: Polidocanol; C12E9, Dodecyl nonaethylene glycol ether, Dodecylnonaglycol, Polidocanol, Polyoxyethylene (9) lauryl ether; trade names: Asclera, Aethoxysklerol and Varithena; Laureth-9; Dodecylnonaoxyethylene glycol monoether
IUPAC/Chemical Name: 3,6,9,12,15,18,21,24,27-nonaoxanonatriacontan-1-ol
3055-99-0
Chemical Formula: C30H62O10
Exact Mass: 582.4343Polidocanol
CAS Registry Number: 9002-92-0
CAS Name: a-Dodecyl-w-hydroxypoly(oxy-1,2-ethanediyl)
Additional Names: polyethylene glycol (9) monododecyl ether; dodecyl alcohol polyoxyethylene ether; hydroxypolyethoxydodecane; laureth 9; polyoxyethylene lauryl ether
Trademarks: Aethoxysklerol (Kreussler); Aetoxisclerol (Dexo); Atlas G-4829 (ICI); Hetoxol L-9 (Heterene Chem.)Line Formula: C12H25(OCH2CH2)nOH
Literature References: Contains an average of nine ethylene oxide units and has an average mol wt ~600. Prepd by reaction of ethylene oxide and dodecyl alcohol: Pertsemlides, Soehring, Arzneim.-Forsch.10, 990 (1960). Toxicology: H. S. Zipf et al.,ibid.7, 162 (1957). Review of clinical experience: P. M. Goldman, J. Dermatol. Surg. Oncol.15, 204-209 (1989).
Properties: Sol in water, ethanol, toluene. Miscible with hot mineral, natural and synthetic oils; with fats and fatty alcohols. LD50 in mice (mg/kg): 1170 orally, 125 i.v. (Zipf).
Toxicity data: LD50 in mice (mg/kg): 1170 orally, 125 i.v. (Zipf)
Use: Solvent; nonionic emulsifier; pharmaceutic aid (surfactant); spermaticide.
Therap-Cat: Anesthetic (topical); antipruritic; sclerosing agent.
Keywords: Anesthetic (Local); Antipruritic; Sclerosing Agent.
| EINECS | 221-284-4 | ||
| CAS No. | 3055-99-0 | Density | 1.007 g/cm3 |
| PSA | 103.30000 | LogP | 4.04900 |
| Solubility | Melting Point | 33-36 °C | |
| Formula | C30H62O10 | Boiling Point | 615.857 °C at 760 mmHg |
| Molecular Weight | 582.43 | Flash Point | 326.259 °C |
Polidocanol is a local anaesthetic and antipruritic component of ointments and bath additives. It relieves itching caused by eczema and dry skin.[1] It has also been used to treat varicose veins,[2] hemangiomas, and vascular malformations.[3] It is formed by the ethoxylation of dodecanol.
Polidocanol is a local anaesthetic and antipruritic component of ointments and bath additives. It relieves itching caused by eczema and dry skin. It is formed by the ethoxylation of dodecanol. The substance is also used as a sclerosant, an irritant injected to treat varicose veins, under the trade names Asclera, Aethoxysklerol and Varithena. Polidocanol causes fibrosis inside varicose veins, occluding the lumen of the vessel, and reducing the appearance of the varicosity. The FDA has approved polidocanol injections for the treatment of small varicose (less than 1 mm in diameter) and reticular veins (1 to 3 mm in diameter). Polidocanol works by damaging the cell lining of blood vessels, causing them to close and eventually be replaced by other types of tissue.

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////////////////////////////
SYN

Yu, Zeqiong; Bo, Shaowei; Wang, Huiyuan; Li, Yu; Yang, Zhigang; Huang, Yongzhuo; Jiang, Zhong-Xing. Application of Monodisperse PEGs in Pharmaceutics: Monodisperse Polidocanols. Molecular Pharmaceutics. Volume 14. Issue 10. Pages 3473-3479. 2017.
SYN 2

Jiang, Zhongxing; Yu, Zeqiong. Process for preparation of monodisperse nona-polyethylene glycol dodecyl alcohol monoether and sulfate. Assignee Wuhan University, Peop. Rep. China. CN 106316802. (2017).
Sclerotherapy
Polidocanol is also used as a sclerosant, an irritant injected to treat varicose veins, under the trade names Asclera, Aethoxysklerol[4] and Varithena.[5] Polidocanol causes fibrosis inside varicose veins, occluding the lumen of the vessel, and reducing the appearance of the varicosity.
The FDA has approved polidocanol injections for the treatment of small varicose (less than 1 mm in diameter) and reticular veins (1 to 3 mm in diameter). Polidocanol works by damaging the cell lining of blood vessels, causing them to close and eventually be replaced by other types of tissue.[6][7] Polidocanol in the form of Varithena injected in the greater saphenous vein can cause the eruption of varicose and spider veins throughout the lower leg. This procedure should be done with caution and with the knowledge that the appearance of the leg may be forever compromised.

Pure polidocanol for pharmaceutical use
On March 30th,2010 the FDA approved Polidocanol under the trade name Asclera. Polidocanol is a sclerosing agent indicated to treat uncomplicated spider veins (varicose veins ≤1 mm in diameter) and uncomplicated reticular veins (varicose veins 1 to 3 mm in diameter) in the lower extremities. Varicose veins develop when the small valves inside the veins no longer work properly, allowing the blood to flow backwards and then pool in the vein.
When injected intravenously, Polidocanol works by locally damaging the endothelium of the blood vessel, causing platelets to aggregate at the site of damage and attach to the venous wall. Eventually, a dense network of platelets, cellular debris and fibrin occludes the vessel, which is then replaced with connective fibrous tissue. As one would expect for this type of molecule and also the mechanism of action, there is believed to be no specific molecular target for Polidocanol.
Polidocanol is a large ‘small molecule’ drug (Molecular Weight of 583 g.mol-1), with a mean half-life of 1.5 hr. Polidocanol is administrated intravenously and the strength of the solution and the volume injected depend on the size and extent of the varicose veins. Thus, the recommended dosage is 0.1 to 0.3 mL for each injection (Asclera 0.5% for spider veins and Asclera 1% for reticular veins) into each varicose vein, and a maximum recommended volume per treatment session of 10 mL.
Polidocanol’s chemical structure is 2-[2-[2-[2-[2-[2-[2-[2-[2-(dodecyloxy)ethoxy]ethoxy]ethoxy]ethoxy]ethoxy]ethoxy]ethoxy]ethoxy]ethanol. It is a non-ionic detergent, similar to polyethylene glycol (PEG) in structure, consisting of two components, a polar hydrophilic (dodecyl alcohol) and an apolar hydrophobic (polyethylene oxide – the part in brackets in the chemical structure) chain.
References
- ^ “E45 itch relief cream”. netdoctor.co.uk. Retrieved 2007-07-12.
- ^ Star P, Connor DE, Parsi K (April 2018). “Novel developments in foam sclerotherapy: Focus on Varithena® (polidocanol endovenous microfoam) in the management of varicose veins”. Phlebology. 33 (3): 150–162. doi:10.1177/0268355516687864. PMID 28166694.
- ^ Gao Z, Zhang Y, Li W, Shi C (January 2018). “Effectiveness and safety of polidocanol for the treatment of hemangiomas and vascular malformations: A meta-analysis”. Dermatologic Therapy. 31 (1). doi:10.1111/dth.12568. PMID 29082587.
- ^ Sclerotherapy, Laurence Z Rosenberg, MD, eMedicine.com
- ^ “Varithena™ (polidocanol injectable foam) For Intravenous Use. Full Prescribing Information” (PDF). Biocompatibles, Inc. Archived from the original (PDF) on 4 August 2016. Retrieved 1 October 2015.
- ^ Facts and Companies: Varicose Vein Treatment Approved
- ^ “Asclera Full Prescribing Information in Drug Reference Encyclopedia”. Retrieved 2010-04-11.
| Clinical data | |
|---|---|
| Other names | PolydocanolLaureth 9Macrogol lauryl etherLauromacrogolPEG-9 lauryl alcoholPOE-9 lauryl alcoholDodecylpolyethyleneglycoletherHydroxyl polyethoxy dodecaneOxypolyethoxydodecane |
| AHFS/Drugs.com | International Drug Names |
| Pregnancy category | Topical: allowed Injection: contraindication in months 1–3 and after week 36 |
| Routes of administration | topical, subcutaneous injection |
| ATC code | C05BB02 (WHO) |
| Legal status | |
| Legal status | OTC (topical), ℞ (injection) |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 9002-92-0 3055-99-0 |
| PubChem CID | 656641 |
| ChemSpider | 570993 |
| UNII | 0AWH8BFG9A |
| KEGG | D01993 |
| ChEMBL | ChEMBL1201751 |
| ECHA InfoCard | 100.019.351 |
| Chemical and physical data | |
| Formula | C30H62O10 |
| Molar mass | 582.816 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (what is this?) (verify) |
////////POLIDOCANOL, Anesthetic , Antipruritic, Sclerosing Agent,
CCCCCCCCCCCCOCCOCCOCCOCCOCCOCCOCCOCCOCCO

NEW DRUG APPROVALS
ONE TIME
$10.00
DOCUSATE
DOCUSATE
1,4-Bis(2-ethylhexyl) sulfosuccinate
- Molecular FormulaC20H38O7S
- Average mass422.577 Da
1,4-Bis[(2-ethylhexyl)oxy]-1,4-dioxobutane-2-sulfonic acid
10041-19-7[RN]
233-124-0[EINECS]
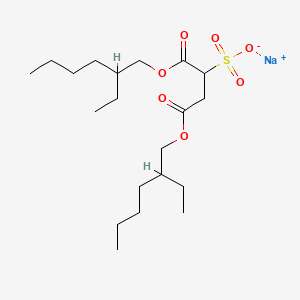
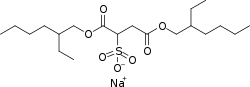
Docusate Sodium
Dioctyl sodium sulfosuccinate
sodium;1,4-bis(2-ethylhexoxy)-1,4-dioxobutane-2-sulfonate
CAS Registry Number: 577-11-7
CAS Name: Sulfobutanedioic acid 1,4-bis(2-ethylhexyl) ester sodium salt
Additional Names: sulfosuccinic acid 1,4-bis(2-ethylhexyl) ester S-sodium salt; bis(2-ethylhexyl)sodium sulfosuccinate; dioctyl sodium sulfosuccinate; sodium dioctyl sulfosuccinate; DSS
Trademarks: Aerosol OT (Cyanamid); Colace (Roberts); Comfolax (Searle); Coprola (Dunster); Dioctylal (Continental Pharma); Dioctyl (Medo); Diotilan (Chinoin); Disonate (Lannett); Doxinate (Hoechst); Doxol (Blair); Dulcivac (Harvey); Jamylène (Thaplix); Molatoc; Molcer (Wallace); Nevax; Regutol (Schering-Plough); Soliwax (Concept Pharm.); Velmol (Berlex); Waxsol (Norgine); Yal (Ritter)
Molecular Formula: C20H37NaO7S
Molecular Weight: 444.56
Percent Composition: C 54.03%, H 8.39%, Na 5.17%, O 25.19%, S 7.21%
Literature References: Prepn: Jaeger, US2028091; US2176423 (1936, 1939, both to Am. Cyanamid). Structure and wetting power: Caryl, Ind. Eng. Chem.33, 731 (1941). Comprehensive description: S. Ahuja, J. Cohen, Anal. Profiles Drug Subs.2, 199-219 (1973); 12, 713-720 (1983). For structure see Docusate calcium.
Properties: Available as wax-like solid, usually in rolls of tissue-thin material; also as 50-75% solns in various solvents. Soly in water (g/l): 15 (25°), 23 (40°), 30 (50°), 55 (70°). Sol in CCl4, petr ether, naphtha, xylene, dibutyl phthalate, liq petrolatum, acetone, alcohol, vegetable oils. Very sol in water + alcohol, water + water-miscible organic solvents. Stable in acid and neutral solns; hydrolyzes in alkaline solns.
Derivative Type: Docusate potassium
CAS Registry Number: 7491-09-0
Trademarks: Rectalad (Carter-Wallace)
Molecular Formula: C20H37KO7S
Molecular Weight: 460.67
Percent Composition: C 52.14%, H 8.10%, K 8.49%, O 24.31%, S 6.96%
NOTE: Ingredient of the laxative Peri-Colace (Roberts) which also contains casanthranol.Use: Sodium salt as pharmaceutic aid (surfactant); as wetting agent in industrial, pharmaceutical, cosmetic and food applications; dispersing and solubilizing agent in foods; adjuvant in tablet formation.
Therap-Cat: Stool softener.
Therap-Cat-Vet: Stool softener.
Keywords: Laxative/Cathartic.
Docusate Calcium
CAS Registry Number: 128-49-4
CAS Name: Sulfobutanedioic acid 1,4-bis(2-ethylhexyl)ester calcium salt
Additional Names: bis[2-ethylhexyl]calcium sulfosuccinate; calcium dioctyl sulfosuccinate; dioctyl calcium sulfosuccinate
Trademarks: Surfak (HMR)
Molecular Formula: C40H74CaO14S2
Molecular Weight: 883.22
Percent Composition: C 54.40%, H 8.44%, Ca 4.54%, O 25.36%, S 7.26%
Literature References: Prepd from dioctyl sodium sulfosuccinate dissolved in isopropanol and from calcium chloride dissolved in methanol: Klotz, US3035973 (1962 to Lloyd Brothers).
Properties: White precipitate. Sol in mineral and vegetable oils, liq polyethylene glycol. Practically insol in glycerol. Claimed to have greater surface-active wetting properties than the sodium salt.
NOTE: Ingredient of Doxidan (HMR) which also contains phenolphthalein.
Therap-Cat: Stool softener.
Keywords: Laxative/Cathartic.
Derivatives
free acid
- Formula:C20H38O7S
- MW:422.58 g/mol
- CAS-RN:10041-19-7
- EINECS:233-124-0
calcium salt
- Formula:C40H74CaO14S2
- MW:883.23 g/mol
- CAS-RN:128-49-4
- EINECS:204-889-8
potassium salt
- Formula:C20H37KO7S
- MW:460.67 g/mol
- CAS-RN:7491-09-0
- EINECS:231-308-5
SYN
| CAS-RN | Formula | Chemical Name | CAS Index Name |
|---|---|---|---|
| 141-02-6 | C20H36O4 | bis(2-ethylhexyl) fumarate | 2-Butenedioic acid (E)-, bis(2-ethylhexyl) ester |
| C4H4O4 | (E)-2-butenedioic acid | ||
| 104-76-7 | C8H18O | 2-ethyl-1-hexanol | 1-Hexanol, 2-ethyl- |
SYN
https://scialert.net/fulltext/?doi=jas.2011.1396.1400
 | |
| Fig. 1: | Synthesis of Trihexyltetradecylphosphonium octylsulfosuccinate [P6, 6, 6, 14][docusate] |
SYN

Docusate is the common chemical and pharmaceutical name of the anionbis(2-ethylhexyl) sulfosuccinate, also commonly called dioctyl sulfosuccinate (DOSS).[2][3][4]
Salts of this anion, especially docusate sodium, are widely used in medicine as laxatives and as stool softeners, by mouth or rectally.[1] It is on the World Health Organization’s List of Essential Medicines.[5][6] Some studies claim that docusate is not more effective than a placebo for improving constipation.[7][8][9][10] Other docusate salts with medical use include those of calcium and potassium.[11][1][2]
Docusate salts are also used as food additives, emulsifiers, dispersants, and wetting agents, among other uses.[12]
History
Sodium docusate was patented in 1937 by Coleman R. Caryl and Alphons O. Jaeger for American Cyanamid,[3] which commercialized it for many years as a detergent under the brand name Aerosol OT.
Its use for the treatment of constipation was first proposed in 1955 by James L. Wilson and David G. Dickinson,[4] and quicky popularized under the name Doxinate.[13]
Medical use
Constipation
The main medical use of docusate sodium is to treat constipation, acting as a laxative and stool softener. In painful anorectal conditions such as hemorrhoid and anal fissures, it can help avoid pain caused by straining during bowel movements.
When administered by mouth, a bowel movement often occurs in 1 to 3 days,[1] while rectal use may be effective within 20 minutes.[14]
Sodium docusate is recommended as a stool softener for children.[1]
However, its effectiveness for constipation is poorly supported by evidence.[7][8] Multiple studies have found docusate to be no more effective than a placebo for improving constipation.[7][8][9][10] Others have found it to be less useful for the treatment of chronic constipation than psyllium.[10][15][16]
The medication may be given to people who are receiving opioid medication, although prolonged use may cause irritation of the gastrointestinal tract.[10][16]
Other medical uses
Docusate sodium, when used with ear syringing, may help with earwax removal, particularly in the case of impaction.[17]
Sodium docusate is also used as a lubricant in the production of tablets and as an emulsifier in topical preparations and other suspensions.[18]
Precautions and contraindications
Docusate sodium is approved and recommended as safe during pregnancy and breastfeeding.[19][20]
Docusate is not recommended in people with appendicitis, acute abdomen, or ileus.[16]
When taken by mouth it should be ingested with plenty of water.
Side effects
Side effects are uncommon and typically mild,[1] and may include stomach pain, abdominal cramps or diarrhea,[1] Efficacy decreases with long-term use, and may cause poor bowel function.[11]
Serious allergic reactions may occur with the drug. The most severe side effect of docusate, although very rare, is rectal bleeding.[21]
Interactions
Docusate might increase resorption of other drugs, for example, dantron (1,8-dihydroxyanthraquinone).[16]
Mechanism of action
Docusate sodium works by allowing more water to be absorbed by the stool.[11][22]
Docusate does not stay in the gastrointestinal tract, but is absorbed into the bloodstream and excreted via the gallbladder[16] after undergoing extensive metabolism.
The effect of docusate may not necessarily be all due to its surfactant properties. Perfusion studies suggest that docusate inhibits fluid absorption or stimulates secretion in the portion of the small intestine known as the jejunum.
Pharmaceutical brand names
In the U.S., docusate sodium for pharmaceutical use is available under multiple brand names: Aqualax, Calube, Colace, Colace Micro-Enema, Correctol Softgel Extra Gentle, DC-240, Dialose, Diocto, Dioctocal, Dioctosoftez, Dioctyn, Dionex, Doc-Q-Lace, Docu Soft, Docucal, Doculax, Docusoft S, DOK, DOS, Doss-Relief, DSS, Dulcolax – Stool Softener (not to be confused with another drug marketed under the Dulcolax brand, bisacodyl, which is a stimulant laxative), Ex-Lax Stool Softener, Fleet Sof-Lax, Genasoft, Kasof, Laxa-basic, Modane Soft, Octycine-100, Pedia-Lax, Preferred Plus Pharmacy Stool Softener, Regulax SS, Sulfalax Calcium, Sur-Q-Lax, Surfak Stool Softener, and Therevac-SB. Generic preparations are also available.
In the UK, dioctyl sodium sulfosuccinate is sold under the brand name Docusol (Typharm Ltd) and DulcoEase (Boehringer Ingelheim).
In Australia, dioctyl sodium sulfosuccinate is sold as Coloxyl and Coloxyl with senna.
In India, preparations include Laxatin by Alembic, Doslax by Raptakos Laboratories, Cellubril by AstraZeneca, and Laxicon by Stadmed.
Other uses
Dioctyl sodium sulfosuccinate is used as a surfactant in a wide range of applications, often under the name Aerosol-OT.[4][23] It is unusual in that it is able to form microemulsions without the use of co-surfactants, and it has a rich variety of aqueous-phase behavior including multiple liquid crystalline phases.[24]
Food additive
Dioctyl sodium sulfosuccinate has been approved by the US FDA as a “generally recognized as safe” (GRAS) additive.[25] It is used in a variety of food products, as a surface active agent, stabilizer, thickener, wetting agent, processing aid, solubilizing agent, emulsifier, and dispersant. The highest amount found in food products is 0.5% by weight, which include pasteurized cheese spreads, cream cheeses and salad dressings.[26] The FDA also approved its use as a wetting agent or solubilizer for flavoring agents in carbonated and non-carbonated drinks at levels up to 10 parts per million.[25]
Microencapsulation
Sodium docusate is the most widely used surfactant in reverse micelleencapsulation studies.[27]
Non-medical brand names
As a surfactant, docusate sodium is or has been commercialized under many brand names, including DSSj Aerosol OT, Alphasol OT, Colace, Complemix, Coprol, Dioctylal, Dioctyl-Medo Forte, Diotilan, Diovac, Disonate, Doxinate, Doxol, Dulsivac, Molatoc, Molofac, Nevax, Norval, Regutol, Softili, Solusol, Sulfimel DOS, Vatsol OT, Velmol, and Waxsol[28]
Chemistry
Structure and properties
The structural formula of the docusate anion is R−O−C(=O)−CH(SO−
3)−CH
2−C(=O)−O−R, where R is the 2-ethylhexyl groupH
3C−(CH
2)
3−C(−CH
2−CH
3)H−CH
2−. The conjugate acid can be described as the twofold carboxylate ester of sulfosuccinic acid with 2-ethylhexanol.
The compound is a white, wax-like, plastic solid, with an odor suggestive of octyl alcohol. It starts to decompose at about 220 °C.[28]
Solubility of dioctyl sodium sulfosuccinate in water is 14 g/L at 25 °C, increasing to 55 g/L at 70 °C.[28] Solubility is better in less polar solvents: 1:30 in ethanol, 1:1 in chloroform and diethylether, and practically unlimited in petroleum ether (25 °C). It also is highly soluble in glycerol, although this is a rather polar solvent. It is also highly soluble in xylene, oleic acid, acetone, diacetone alcohol, methanol, isopropanol, 2-butanol, methyl acetate, ethyl acetate, furfurol, and vegetable oils.[28]
The ester groups are easily cleaved under basic conditions, but are stable against acids.[16]
Synthesis
Sodium dioctyl sulfosuccinate can be obtained by treating dioctyl maleate with sodium bisulfite. The bisulfite anion adds to the double bond:−CH=CH− + HSO−
3 → −CH(−SO−
3)−CH
2−
Toxicity
Ingestion may cause the side effects described above, such as diarrhea, intestinal bloating, and occasionally cramping pains. Dioctyl sodium sulfosuccinate is not known to be carcinogenic, mutagenic, or teratogenic.[29]
Marine species
Dioctyl sodium sulfosuccinate is of low toxicity for crustaceans such as the hermit crabClibanarius erythropus and the shrimp Crangon crangon. Toxicity for molluscs varies widely, with 48-hour LD50 found between 5 mg/l for the common limpet and 100 mg/l for the common periwinkle. Various species of phytoplankton have an LD50 around 8 mg/l.
In a 2010 study, dioctyl sodium sulfosuccinate exhibited higher toxicity against bacteria (Vibrio fischeri, Anabaena sp.) and algae (Pseudokirchneriella subcapitata) than did a number of fluorinated surfactants (PFOS, PFOA, or PFBS). Measuring bioluminescence inhibition of the bacteria and growth inhibition of the algae, the LD50 were in the range of 43–75 mg/l. Combinations of the fluorinated compounds with dioctyl sodium sulfosuccinate showed mid to highly synergistic effects in most settings, meaning that such combinations are significantly more toxic than the individual substances.[30]
Freshwater species
The substance is highly toxic for rainbow trout with a median lethal concentration (LC50) of 0.56 mg/l after 48 hours for the pure substance. It is only slightly to moderately toxic for rainbow trout fingerlings, and slightly toxic for harlequin rasboras (LC50 27 mg/l of a 60% formulation after 48 hours).

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////////////////////////////
References
- ^ Jump up to:a b c d e f g h “Docusate Salts”. The American Society of Health-System Pharmacists. Archived from the original on 23 September 2015. Retrieved 11 August 2015.
- ^ Jump up to:a b American Society of Health-System Pharmacists (15 August 2011). “Stool Softeners”. Archived from the original on 5 September 2015.
- ^ Jump up to:a b US 2181087, Caryl CR, Jaeger AO, “Detergent composition”, issued 21 November 1939, assigned to American Cyanamid
- ^ Jump up to:a b c Wilson JL, Dickinson DG (May 1955). “Use of dioctyl sodium sulfosuccinate (aerosol O.T.) for severe constipation”. Journal of the American Medical Association. 158 (4): 261–3. doi:10.1001/jama.1955.02960040019006a. PMID 14367076.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06.
- ^ “Docusate – Drug Usage Statistics”. ClinCalc. Retrieved 18 February 2021.
- ^ Jump up to:a b c Fakheri RJ, Volpicelli FM (February 2019). “Things We Do for No Reason: Prescribing Docusate for Constipation in Hospitalized Adults”. Journal of Hospital Medicine. 14 (2): 110–113. doi:10.12788/jhm.3124. PMID 30785419.
- ^ Jump up to:a b c “Dioctyl Sulfosuccinate or Docusate (Calcium or Sodium) for the Prevention or Management of Constipation: A Review of the Clinical Effectiveness”. CADTH Rapid Response Reports. 26 June 2014. PMID 25520993.
- ^ Jump up to:a b Candy B, Jones L, Larkin PJ, Vickerstaff V, Tookman A, Stone P (May 2015). “Laxatives for the management of constipation in people receiving palliative care” (PDF). The Cochrane Database of Systematic Reviews. 13 (5): CD003448. doi:10.1002/14651858.CD003448.pub4. PMC 6956627. PMID 25967924.
- ^ Jump up to:a b c d Ramkumar D, Rao SS (April 2005). “Efficacy and safety of traditional medical therapies for chronic constipation: systematic review”. The American Journal of Gastroenterology. 100 (4): 936–71. PMID 15784043.
- ^ Jump up to:a b c 2013 Nurse’s Drug Handbook. Burlington, MA: Jones & Bartlett Learning. 2013. p. 366. ISBN 9781449642846.
- ^ Ash M, Ash I (2004). Handbook of preservatives. Endicott, N.Y.: Synapse information resources. p. 375. ISBN 9781890595661.
- ^ Friedman M (October 1956). “Dioctyl sodium sulfosuccinate (doxinate) in chronic functional constipation”. American Practitioner and Digest of Treatment. 7 (10): 1588–91. PMID 13362832.
- ^ “Docusate sodium”. 18 December 2004. Archived from the original on 21 July 2011. Retrieved 6 March 2019.
- ^ Portalatin M, Winstead N (March 2012). “Medical management of constipation”. Clinics in Colon and Rectal Surgery. 25 (1): 12–9. doi:10.1055/s-0032-1301754. PMC 3348737. PMID 23449608.
- ^ Jump up to:a b c d e f Dinnendahl V, Fricke U, eds. (2010). Arzneistoff-Profile(in German). 2 (23 ed.). Eschborn, Germany: Govi Pharmazeutischer Verlag. ISBN 978-3-7741-9846-3.
- ^ “How effective is docusate as a cerumenolytic agent?”. GlobalRPH.com. Archived from the original on 23 November 2010.
- ^ Jasek W, ed. (2008). Austria-Codex Stoffliste (in German) (41 ed.). Vienna: Österreichischer Apothekerverlag. p. 316. ISBN 978-3-85200-190-6.
- ^ Yaffe SJ (2011). Drugs in pregnancy and lactation : a reference guide to fetal and neonatal risk (9 ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 1651. ISBN 9781608317080.
- ^ Mahadevan U, Kane S (July 2006). “American gastroenterological association institute medical position statement on the use of gastrointestinal medications in pregnancy”. Gastroenterology. 131(1): 278–82. doi:10.1053/j.gastro.2006.04.048. PMID 16831610.
- ^ drugs.com: Docusate Archived 16 July 2010 at the Wayback Machine
- ^ Hamilton RJ (2013). Tarascon pocket pharmacopoeia : 2013 classic shirt-pocket edition (27 ed.). Burlington, Ma.: Jones & Bartlett Learning. p. 112. ISBN 9781449665869.
- ^ Whiffen AJ (1946). “Aerosol OT in the preparation of microscopic mounts of fungi”. Mycologia. 38: 346. doi:10.1080/00275514.1946.12024063. PMID 20983186.
- ^ Nave S, Eastoe J, Penfold J (November 2000). “What Is So Special about Aerosol-OT? 1. Aqueous Systems”. Langmuir. 16(23): 8733–8740. doi:10.1021/la000341q.
- ^ Jump up to:a b “GRAS Notice Inventory Agency Response Letter GRAS Notice No. GRN 000006”. Center for Food Safety and Applied Nutrition. 20 July 1998. Archived from the original on 31 October 2017. Retrieved 24 January 2020.
- ^ “CFR – Code of Federal Regulations Title 21”. http://www.accessdata.fda.gov. Retrieved 29 January 2020.
- ^ Flynn PF (2004). “Multidimensional multinuclear solution NMR studies of encapsulated macromolecules”. Prog. Nucl. Magn. Reson. Spectrosc. 45 (1–2): 31–51. doi:10.1016/j.pnmrs.2004.04.003.
- ^ Jump up to:a b c d Ahuja S, Cohen J (January 1973). “Dioctyl Sodium Sulfosuccinate”. InAnalytical Profiles of Drug Substances. Analytical Profiles of Drug Substances. 2. Academic Press. pp. 199–219. doi:10.1016/S0099-5428(08)60040-4. ISBN 9780122608025.
- ^ ScienceLab.com: Docusate sodium Material Safety Data SheetArchived 2006-10-17 at the Wayback Machine
- ^ Rosal R, Rodea-Palomares I, Boltes K, Fernández-Piñas F, Leganés F, Petre A (September 2010). “Ecotoxicological assessment of surfactants in the aquatic environment: combined toxicity of docusate sodium with chlorinated pollutants”. Chemosphere. 81 (2): 288–93. Bibcode:2010Chmsp..81..288R. doi:10.1016/j.chemosphere.2010.05.050. PMID 20579683.
External links
- “Docusate”. Drug Information Portal. U.S. National Library of Medicine.
- “Docusate sodium”. Drug Information Portal. U.S. National Library of Medicine.
- Stool Softeners at the N.I.H.PubMed Health resource.
//////////DOCUSATE, Stool softener, Laxative, Cathartic,
CCCC(CC)COC(=O)CC(C(=O)OCC(CC)CCCC)S(=O)(=O)[O-].[Na+]

NEW DRUG APPROVALS
one time
$10.00
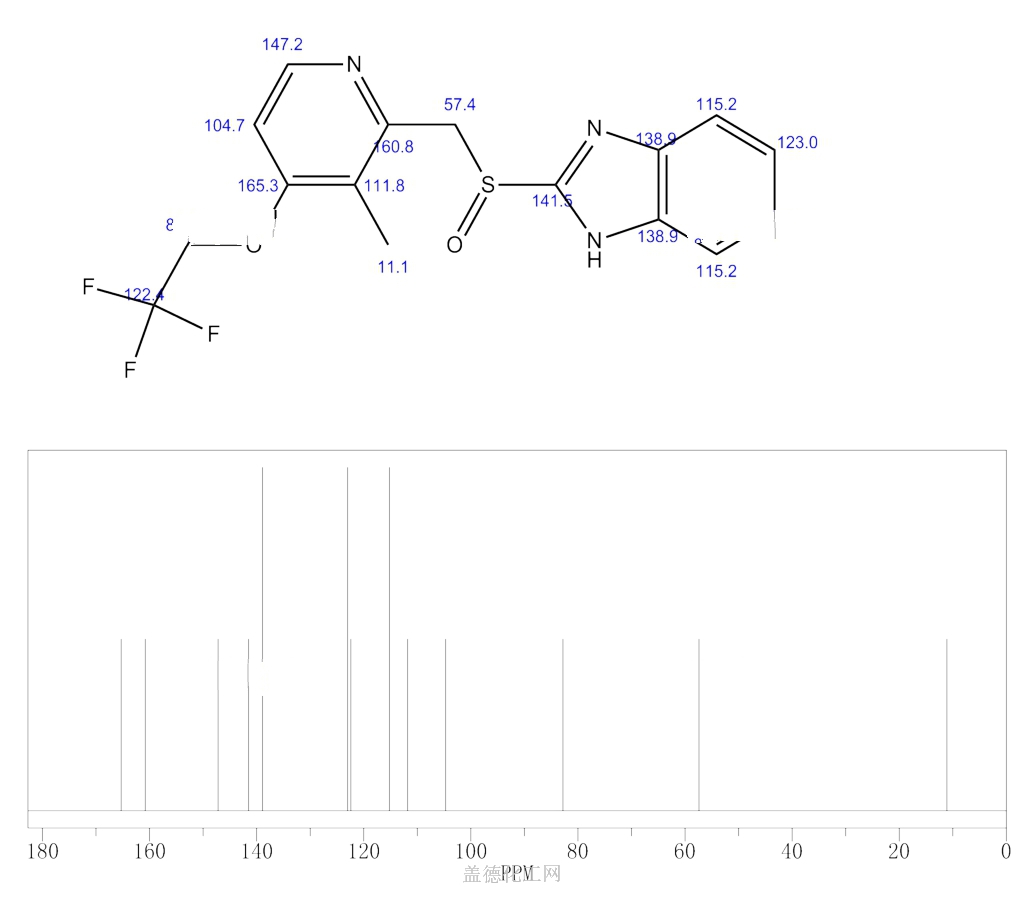
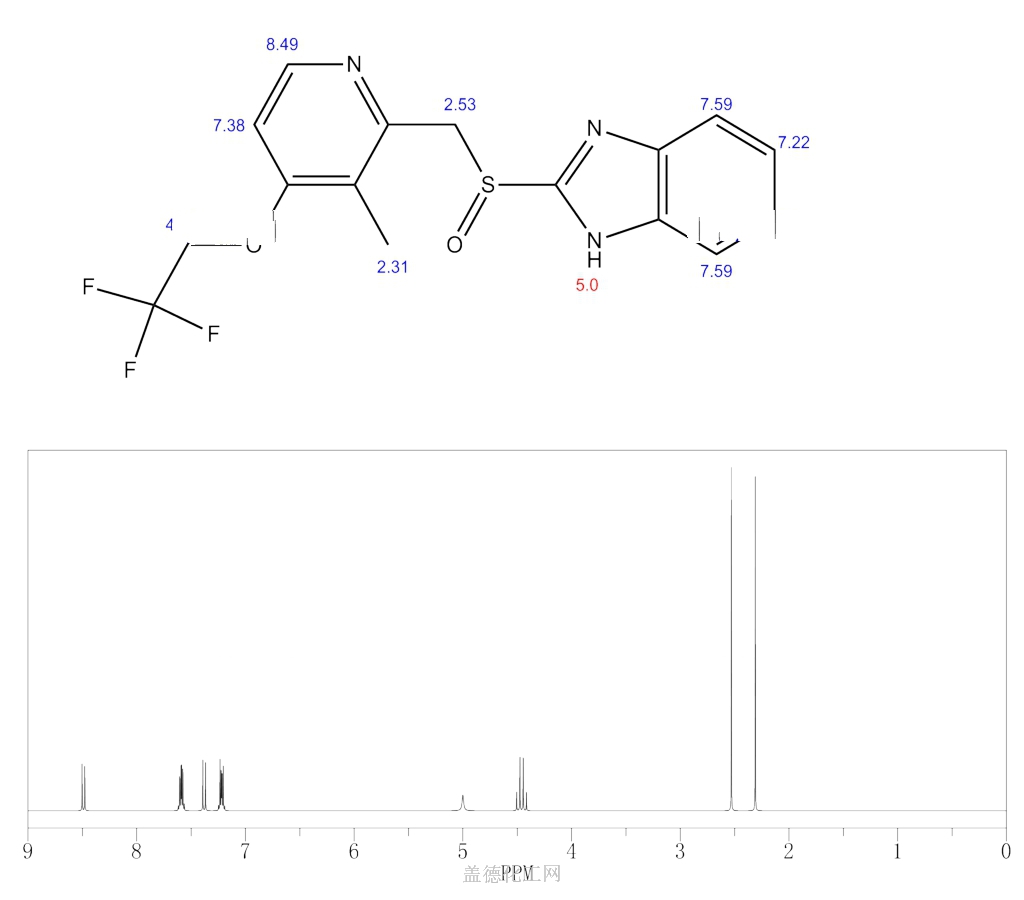
LANSOPRAZOLE

Lansoprazole
- Molecular FormulaC16H14F3N3O2S
- Average mass369.362 Da
Lansoprazole, AG-1749, ABT-006, CG-4801, A-65006, Ogast, Lanzor, Lanzo, Agopton, Opiren, Bamalite, Takepron, Lansox, Lansox, Ogastro, Monolitum, Prevacid, Zoton103577-45-3[RN]
1H-Benzimidazole, 2-[[[3-methyl-4-(2,2,2-trifluoroethoxy)-2-pyridinyl]methyl]sulfinyl]-
лансопразол [Russian] [INN], لانسوبرازول [Arabic] [INN], 兰索拉唑 [Chinese] [INN]
CAS Registry Number: 103577-45-3
CAS Name: 2-[[[3-Methyl-4-(2,2,2-trifluoro-ethoxy)-2-pyridinyl]methyl]sulfinyl]-1H-benzimidazole
Additional Names: 2-(2-benzimidazolylsulfinylmethyl)-3-methyl-4-(2,2,2-trifluoroethoxy)pyridine
Manufacturers’ Codes: A-65006; AG-1749
Trademarks: Agopton (Takeda); Lansox (Takeda); Lanzor (Aventis); Limpidex (Sigma-Tau); Ogast (Takeda); Prevacid (TAP); Takepron (Takeda); Zoton (Wyeth)
Molecular Formula: C16H14F3N3O2S, Molecular Weight: 369.36
Percent Composition: C 52.03%, H 3.82%, F 15.43%, N 11.38%, O 8.66%, S 8.68%
Literature References: Gastric proton-pump inhibitor. Prepn: A. Nohara, Y. Maki, EP174726; eidem,US4628098 (both 1986 to Takeda).HPLC determn in plasma: T. Uno et al., J. Chromatogr. B816, 309 (2005). Pharmacology: H. Satoh et al.,J. Pharmacol. Exp. Ther.248, 806 (1989). Mechanism of action study: H. Nagaya et al.,ibid.252, 1289 (1990). Clinical pharmacology and effect on human gastric acid secretion: P. Müller et al.,Aliment. Pharmacol. Ther.3, 193 (1989). Review of pharmacology and clinical experience: H. D. Langtry, M. I. Wilde, Drugs54, 473-500 (1997). Comparative clinical trial with esomeprazole in erosive esophagitis: C. W. Howden et al., Clin. Drug Invest.22, 99 (2002).
Properties: mp 178-182° (dec).
Melting point: mp 178-182° (dec)
Therap-Cat: Antiulcerative., Keywords: Antiulcerative; Gastric Proton Pump Inhibitor.
Lansoprazole, sold under the brand name Selanz SR among others, is a medication which reduces stomach acid.[2] It is used to treat peptic ulcer disease, gastroesophageal reflux disease, and Zollinger–Ellison syndrome.[3] Effectiveness is similar to other proton pump inhibitors (PPIs).[4] It is taken by mouth.[2] Onset is over a few hours and effects last up to a couple of days.[2]
Common side effects include constipation, abdominal pain, and nausea.[2][5] Serious side effects may include osteoporosis, low blood magnesium, Clostridium difficile infection, and pneumonia.[2][5] Use in pregnancy and breastfeeding is of unclear safety.[1] It works by blocking H+/K+-ATPase in the parietal cells of the stomach.[2]
Lansoprazole was patented in 1984 and came into medical use in 1992.[6] It is available as a generic medication.[3] In 2017, it was the 188th most commonly prescribed medication in the United States, with more than three million prescriptions.[7][8]
Medical uses
Lansoprazole is used for treatment of:[5]
- Ulcers of the stomach and duodenum, and NSAID-induced ulcers
- Helicobacter pylori infection, alongside antibiotics (adjunctive treatment), treatment to kill H. pylori causing ulcers or other problems involves using two other drugs besides lansoprazole known as “triple therapy“, and involves taking twice daily for 10 or 14 days lansoprazole, amoxicillin, and clarithromycin
- Gastroesophageal reflux disease
- Zollinger-Ellison syndrome[9]
There is no good evidence that it works better than other PPIs.[4]
Side effects
Side effects of PPIs in general[10] and lansoprazole in particular[11] may include:[5]
- Common: diarrhea, abdominal pain[12]
- Infrequent: dry mouth, insomnia, drowsiness, blurred vision, rash, pruritus
- Rarely and very rarely: taste disturbance, liver dysfunction, peripheral oedema, hypersensitivity reactions (including bronchospasm, urinary, angioedema, anaphylaxis), photosensitivity, fever, sweating, depression, interstitial nephritis, blood disorders (including leukopenia, leukocytosis, pancytopenia, thrombocytopenia), arthralgia, myalgia, skin reactions[13] including (erythroderma[14] Stevens–Johnson syndrome, toxic epidermal necrolysis, bullous eruption)
PPIs may be associated with a greater risk of hip fractures and Clostridium difficile-associated diarrhea.[5]: 22
Interactions
Lansoprazole interacts with several other drugs, either due to its own nature or as a PPI.[15]
- PPIs reduce absorption of antifungals (itraconazole and ketoconazole) [16] and possibly increase digoxin in plasma
- Increases plasma concentrations of cilostazol (risk of toxicity)
Lansoprazole possibly interacts with, among other drugs:
- sucralfate
- ampicillin
- bisacodyl
- clopidogrel
- delavirdine
- fluvoxamine
- iron salts
- voriconazole
- aminophylline and theophylline
- astemizole
Chemistry
It is a racemic 1:1 mixture of the enantiomers dexlansoprazole and levolansoprazole.[17] Dexlansoprazole is an enantiomerically pure active ingredient of a commercial drug as a result of the enantiomeric shift. Lansoprazole’s plasma elimination half-life (1.5 h) is not proportional to the duration of the drug’s effects to the person (i.e. gastric acid suppression).[18]
History
Main article: Discovery and development of proton pump inhibitors
Lansoprazole , available in the name of Selanz SR, was originally synthesized at Takeda and was given the development name AG 1749.[19] Takeda patented it in 1984 and the drug launched in 1991.[20] In the United States, it was approved for medical use in 1995.[21]
Society and culture

Prevacid 30 mg
Patents
The lansoprazole molecule is off-patent and so generic drugs are available under many brand names in many countries;[22] there are patents covering some formulations in effect as of 2015.[23] Patent protection expired on 10 November 2009.[24][25]
Availability
Since 2009, lansoprazole has been available over the counter (OTC) in the U.S. as Prevacid 24HR[26][27] and as Lansoprazole 24HR.[28] In Australia, it is marketed by Pfizer as Zoton.[citation needed]
Research
In vitro experiments have shown that lansoprazole binds to the pathogenic form of tau protein.[29] As of 2015 laboratory studies were underway on analogs of lansoprazole to explore their use as potential PET imaging agents for diagnosing tauopathies including Alzheimer’s disease.[29]
SYN
English: doi: 10.1248/cpb.38.2853
SYN
Method of synthesis
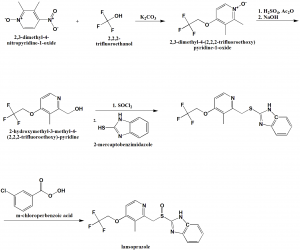
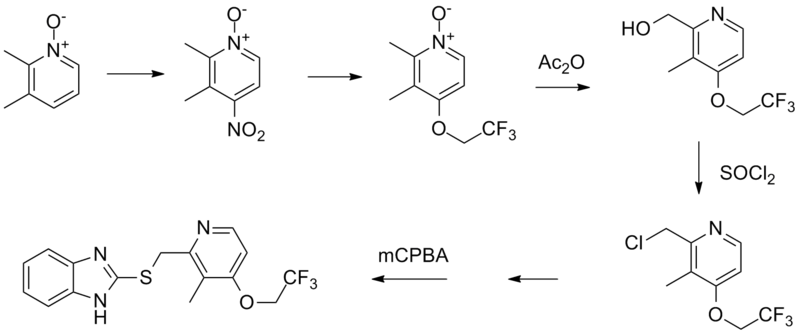
i. 2,3-dimethyl-4-nitropyridine-1-oxide is reacted with 2,2,2-trifluoroethanol in presence of potassium carbonate to give 2,3-dimethyl-4-(2,2,2-trifluoro-ethoxy)pyridine-1-oxide.
ii. The compound so formed is treated with acetic anhydride in acidic conditions followed by nutrilizing with sodium hydroxide solution to get 2-hydroxymethyl-3-methyl-4-(2,2,2-trifluoroethoxy)-pyridine
iii. Last is treated with thionyl chloride followed by reaction with 2-mercaptobenzimidazole to get 2-[3-methyl-4-(2,2,2-trifluoroethoxy)pyrid-2-ylmethylthio]benzimidazole.
iv. Above formed compound is reacted with m-chloro-perbenzoic acid to get lansoprazole.[2]
SYN
Proton Pump Inhibitors
Ruben Vardanyan, Victor Hruby, in Synthesis of Best-Seller Drugs, 2016
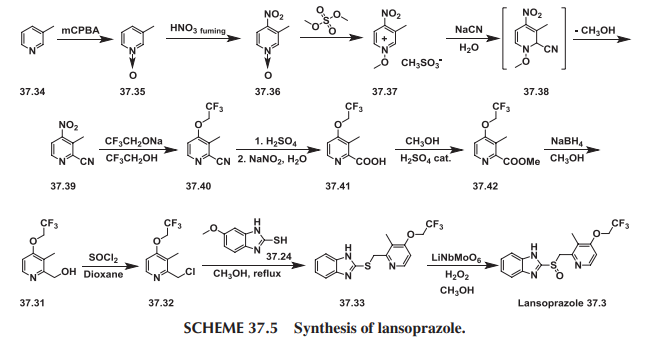
Lansoprazole–Prevacid
Lansoprazole (37.3) is the second approved gastric acid pump inhibitor. The common approach for the synthesis of lansoprazole involves coupling of mercapto-benzimidazole (37.24) with a new 2-chloromethylpyridine derivative (37.32) followed by oxidation of the prochiral sulfide group with m-chloroperbenzoic acid or hydrogen peroxide was first disclosed by Nohara and Maki [73], with followed improvements in patents [74-78] and briefly summed up in papers [79-80].
Lansoprazole synthesis is represented on the Scheme 37.4.

In principle it repeats the synthesis Scheme of omeprazole, differing in details and characteristics, for example, in place of 2,3,5-collidine (37.15) as a starting material, 2,3-lutidine (37.27) was selected, and the methoxy group in the fourth position of pyridine ring was replaced by the 2,2,2-trifluoroethoxy group.
Another interesting approach has been demonstrated [81]. In this case, 2-chloromethyl-3-methyl-4-(2,2,2-trifluoroethoxy)pyridine (37.32) was prepared starting with 3-picoline (37.34), which was oxidized using peracids (i.e., m-chloroperoxybenzoic acid) to produce 3-methylpyridineN-oxide (37.35). The obtained product was nitrated with fuming nitric acid to produce 3-methyl-4-nitropyridine N-oxide (37.36). The prepared N-oxide was treated with dimethylsulfate at 65 to 70°C to form N-methoxypyridinium salt (37.37), the aqueous solution of which on cooling was treated with sodium cyanide to produce an after formation of intermediate (37.38) and elimination of methanol 2-cyano-3-methyl-4-nitropyridine (37.39). This method for the synthesis of 2-cyanopyridines via addition of cyanide ion to N-alkoxy-quaternary salts of pyridines, supplements the plethora of Reissert-Kaufmann reactions in the quinoline and isoquinoline series previously described [82]. The nitro group in (37.39) was replaced by the 2,2,2-trifluoroethoxy group by a direct reaction with sodium trifluoroethoxide in trifluoroethanol that produced ether (37.40). The next step—transformation of nitrile group in prepared 2-cyanopyridine (37.40) to 2-carboxypyridine (37.41)—was carried out in a one-pot procedure by heating the 2-cyano compound in the presence of concentrated sulfuric acid followed by reaction of the intermediate amide with sodium nitrite under aqueous acidic conditions [83,84]. The obtained acid was esterified in methanol with a catalytic amount of sulfuric acid to produce ester (37.42). The ester (37.42) was reduced by NaBH4, producing the above-described 2-hydroxymethyl- pyridine derivative (37.31) followed by a reaction with thionyl chloride in dioxane that produced the required 2-chloromethylpyridine compound (37.32). Direct reaction of the last with 2-mercaptobenzimidazole (37.34) in methanol, even without use of any base, produced a sulfide (37.33) in high yield. The oxidation of the last to lansoprazole (37.3) has been carried out by various oxidants and catalysts, which, together with the desired sulfoxide, produced a certain amount of overoxidized product. Oxidizing sulfide (37.33) with a new oxidation method made up of the use of the composite metal oxide catalyst, LiNbMoO6, in methanol and 35% H2O2 as an oxidant sulfide (37.33) was successfully oxidized to desired lansoprazole (37.3) (Scheme 37.5.).

Lansoprazole is the second inhibitor of the gastric H+/K+-ATPase to be marketed for the treatment of peptic ulcer disease and reflux esophagitis, erosive esophagitis, and Zollinger-Ellison syndrome. It is an inhibitor of gastric acid secretion and also exhibits antibacterial activity against H. pylori in vitro. More common side effects of lansoprazole are diarrhea and skin rash or itching. Less-common side effects are abdominal pain, joint pain, nausea, vomiting, and increased or decreased appetite [85-91].
SYN
| AU 8545895; EP 0174726; ES 8607288; JP 1986050978; US 4628098; US 4689333 |
The condensation of 2,3-dimethyl-4-nitropyridine N-oxide (I) with 2,2,2-trifluoroethanol (II) by means of K2CO3 in hot HMPT gives 2,3-dimethyl-4-(2,2,2-trifluoroethoxy)pyridine N-oxide (III), which by isomerization in acetic anhydride at 100 C is converted to 2-(hydroxymethyl)-3-methyl-4-(2,2,2-trifluoroethoxy)pyridine (IV). The reaction of (IV) with SOCl2 in refluxing CHCl3 affords the corresponding chloromethyl derivative (V), which is condensed with 2-mercaptobenzimidazole (VI) by means of sodium methoxide in refluxing methanol to yield 2-(2-benzimidazolylthiomethyl)-3-methyl-4-(2,2,2-trifluoroethoxy)pyridin (VII). Finally, this compound is oxidized with m-chloroperbenzoic acid in CHCl3.
SYN
SYN
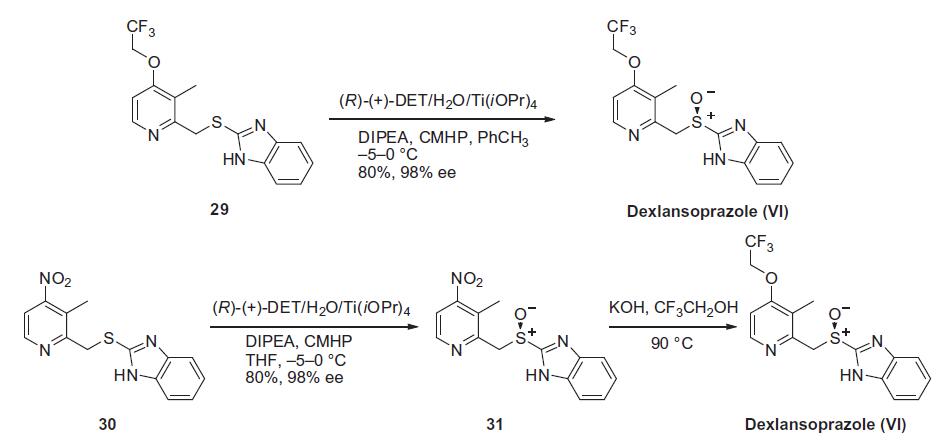
Chemical Synthesis
Similar to the synthesis of the chiral sulfoxide of armodafinil vide supra, the preparation of the chiral sulfoxide of lansoprazole utilized the catalytic oxidation method developed by Kagan and co-workers (the Scheme). Two routes have been reported that describe the preparation of dexlansoprazole on large scale. The first route developed by Takeda reacts commercially available thioether 29, also used to make lansoprazole, under the Kagan asymmetric oxidation conditions and the alternative route utilizes the cheaper commercial intermediate nitrosulfide 30 in the analogous asymmetric oxidation by Kagan). Thus, the catalyst complex consisting of (+)-DET, Ti(OiPr)4 and water was formed in the presence of thioether 29 in toluene at 30–40°C. The reaction mixture was then cooled to 5 °C and DIPEA and cumene hydroperoxide (CMHP) were added to give, after aqueous work-up and in situ crystallization from the organic layer, dexlansoprazole (VI) in 98% ee. No yield was given in the patent. An alternate, but similar, sequence was also described wherein the nitrosulfide intermediate 30 was subjected to similar oxidative conditions that gave intermediate nitro compound 31 in 80% yield and 98% ee. Compound 31 was treated with KOH and trifluoroethanol to provide dexlansoprazole (VI).
R-(+)-Lansoprazole Preparation Products And Raw materials
PATENT
https://patents.google.com/patent/WO2008087665A2/enA number of substituted 2-(2-pyridylmethyl) sulfinyl-lH-benzimidazole derivatives are reported as gastric proton pump inhibitors. These benzimidazole derivatives include lansoprazole, omeprazole, pantoprazole, and rabeprazole. The Lansoprazole is generally represented by the following chemical formula I

US 4,628,098 & 4,689,333 describes lansoprazole having its chemical name (2-[[[3-methyl-4-(2, 2, 2-trifluoro-ethoxy)-2-pyridinyl] methyl] sulfinyl]-lH-benzimidazole. As a characteristic shared with other benzimidazole derivatives (e.g., omeprazole and pantoprazole), lansoprazole can inhibit gastric acid secretion, and thus commonly used as an antiulcer agent. Several methods for preparing Lansoprazole are known. The majority of these methods involve the use of a lansoprazole precursor that contains a thioether group. The thioether group is oxidized in the last step of preparation to form the lansoprazole. These patents (‘098 and ‘333) further describes the oxidation of the thioether group using m-chloroperbenzoic acid, per acid, sodium bromite, sodium hypochlorite, or hydrogen peroxide as the oxidizing agent and the reaction solvent is halogenated hydrocarbon, ether, amide, alcohol, or water.US 6,002,011 describe the crystallization of Lansoprazole from the same ethanol: water system, containing traces of ammonia. This patent discloses a reslurry method in water, which permits to obtain more stable “solvent free” Lansoprazole. This patent fails to disclose the level of purity for Lansoprazole. In addition, the ethanol and water are difficult to eliminate. Even after intensive drying, Lansoprazole still contains solvent and is unstable under storage. US 6,180,652 describe the presence of sulfone derivative. Formation of sulfone derivative brings about the drawback of low yield of the desired sulfoxide. Although attempts have been made to separate the sulfone derivative from Lansoprazole, it is not a simple task, given their very similar structures and physicochemical properties. This patent also describes a method for separation of Lansprazole from its sulfone derivative, by converting to an acetone complex of the Lansoprazole salt & hence is purified in this method. Lansoprazole and other 2-(2- pyridylmethyl) sulfinylbenzimidazole derivatives tend to lose stability and undergo decomposition when contaminated with traces of a solvent, particularly water, in their crystal structure. It is desirable that the benzimidazole crystals be solvent free (i.e., residual solvent should be reduced to a minimum).US 6,909,004 describes the method of purifying Lansoprazole, comprising the steps of: a) providing a solution of lansoprazole in a solvent selected from an organic solvent or a mixture of organic solvent and water in the presence of an amine compound; b) combining the provided solution with an acid, and c)isolating the purified Lansoprazole. The amine compound is present in 1:1, mole: mole, ratio relative to the lansoprazole. Solution is in an organic solvent selected from the group consisting of alcohols, acetone, 2-butanone, dimethylformamide and tetrahydrofuran. The alcohol consisting of ethanol, methanol, n-propanol, & iso-propanol.US 7022859 & US 7060837 provides a method for preparing a substantially pure Lansoprazole containing less than about 0.2% (wt/wt) impurities including sulfone/sulfide derivatives. The present invention also provides a process for recrystallizing Lansoprazole to obtain a Lansoprazole containing less than about 0.1% (wt/wt) water.US 2004/010151 disclose a method of preparing crystalline Lansoprazole form A, comprising the steps of: a) preparing a solution of Lansoprazole in a solvent selected from the group consisting of methanol, n-butanol, acetone, methylethylketone, ethyl acetate, dimethyl sulfoxide, dimethylforniamide and their mixtures optionally with water; and b) isolating crystalline Lansoprazole form A.US 2005/020638 describe the process of preparing a stable Lansoprazole, comprising the steps of: a) crystallizing a Lansoprazole from an organic solvent or a mixture of organic solvent and water in the presence of a weak base; and b) isolating a stable Lansoprazole. An amorphous form of Lansoprazole prepared by spray drying method has been described (Farm. Vest. vol. 50, p. 347 (1999)). Curin et al. describe an ethanole solvate form and an ethanole-hydrate form of Lansoprazole (Farm. Vest. vol. 48, pp. 290-291 (1997). Kotar et al. describe two lansoprazole polymorphs, designated as crystalline Lansoprazole forms A and B, (Eur. J. Pharm. Sci. vol. 4, p. 182 (1996 Supp). According to Kotar, each of the crystalline Lansoprazole forms A and B exhibits a different DSC curve. In fact, crystalline Lansoprazole form B is unstable and can undergo a solid-solid transition to form crystalline Lansoprazole form A. No XRD data for crystalline Lansoprazole forms A and B, and fails to disclose processes for preparing these crystalline forms. No indication was found in the literature regarding the existence of other crystalline Lansoprazole forms other than the known forms A, B, ethanolate and ethanolate- hydrate.WO 00/78729 is discloses a phenomenon of polymorphism in Lansoprazole. The crystalline forms , I and II. The form I find application as an active ingredient of pharmaceutical compositions.WO 03/082857 disclose a method of preparing crystalline Lansoprazole form A, comprising the steps of: a) preparing a solution of Lansoprazole in a solvent selected from the group consisting of methanol, n-butanol, acetone, methylethylketone, ethyl acetate, dimethyl sulfoxide, dimethylformamide and their mixtures optionally with water; and b) isolating crystalline Lansoprazole form A.WO 2004/046135 describe the process for preparing a stable Lansoprazole compound, comprising the steps of: a) crystallizing a Lansoprazole from an organic solvent or a mixture of organic solvent and water in the presence of an amine; and b) isolating a stable Lansoprazole compound, wherein the stable Lansoprazole compound comprises greater than 500 ppm and not more than about 3,000 ppm water.Since proton pump inhibitors of the benzimidazole-type are very susceptible to degradation under acidic or neutral conditions, the reaction mixture is usually worked-up under basic conditions. These basic conditions may decompose any unwanted oxidizing agent still present in the reaction mixture and may also neutralize any acid formed when the oxidizing agent is consumed in the oxidation reaction. The main problem with the oxidation reaction to convert the sulfide intermediates of formula (II) into the sulfoxide compounds of formula (I) is over- oxidation, i.e. oxidation from sulfoxides of formula (I) to sulfones of formula (III) ; N-oxide of formula (IV) & chlorinating impurities ( V).The formation of sulfones of formula (III) due to over-oxidation is almost impossible to avoid and can be kept to a minimum by performing the oxidation reaction at a low temperature and restricting the amount of oxidizing agent. Typically the amount of oxidizing agent is less than 1 molar equivalent of the starting material, i.e. sulfide intermediates of formula (II), which inevitably results in a less than 100% conversion of starting material. Usually the amount of oxidizing agent is a compromise between maximum conversion of starting material, maximum formation of sulfoxides of formula (I) and minimum formation of unwanted sulfones of formula (III). Chlorinating impurities (V) are observed when chlorinating oxidizing agent such as sodium hypochlorite is used for oxidation reaction. Furthermore removal of the sulfones of formula (III) & chlorinating impurities (V) has often proved to be difficult, time-consuming and costly, in particular when high performance chromatography on an industrial scale is needed. Another problem with the benzimidazole-type is very susceptible to degradation when exposed to high temperatures for removal of solvents during distillation.Thus, there is continuing need to obtain 2-(2-pyridylmethyl) sulfϊnyl-lH-benzirnidazoles (e.g., Lansoprazole) that are free of contaminants including sulfone and sulfide derivatives. There has also -been a long-felt need for a method to prepare Lansoprazole having reduced water content (<0.1% wt/wt water).SCHEME : ]

LANSOPRAZOLE (I) SULPHONE (III)

N-OXIDE (IV)

SULPHIDE (II)+ Chlorinated Impurities(V)General Example10 g of 2- [3-methyl-4-(2,2,2-trifluoroethoxy)-2-pyridyl] methylthio-lH-benzimidazole was suspended in 100 ml chloroform and cooled to -100C. To the above suspension 3.4 g m- chloroperbenzoic acid solution in chloroform was added over a period of 2 hrs at -10 C. After completion of reaction, reaction mass was added to sodium bicarbonate solution (500 ml) and both layers were separated. Organic layer was washed with 2 x 50 ml of hypo solution followed by washing with 3 x 200 ml sodium bicarbonate solution. Both the layers were separated. Chloroform layer was washed with sodium bicarbonate solution (0.5%; 500 ml) at room temperature. Various co-solvents mentioned in Table- 1 were added to organic layer cool slowly to -10 to 100C. Filtered and washed with chilled chloroform (10 ml) followed by sodium bicarbonate solution (0.5%, 100 ml) & dried to get pure Lansoprazole.SYNhttp://www.ijmca.com/File_Folder/116-120.pdf



join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////////////////////////////
Literatures:
Chemical and Pharmaceutical Bulletin, , vol. 38, # 10 p. 2853 – 2858
Literatures:
RECORDATI INDUSTRIA CHIMICA E FARMACEUTICA SPA Patent: WO2008/77866 A1, 2008 ; Location in patent: Page/Page column 16-17; 19 ;
Yield: ~92%
Patent
Publication numberPriority datePublication dateAssigneeTitleUS4628098A *1984-08-161986-12-09Takeda Chemical Industries, Ltd.2-[2-pyridylmethylthio-(sulfinyl)]benzimidazolesWO2004018454A1 *2002-08-212004-03-04Teva Pharmaceutical Industries Ltd.A method for the purification of lansoprazoleUS20040049045A1 *2000-12-012004-03-11Hideo HashimotoProcess for the crystallization of (r)-or (s)-lansoprazole
Publication numberPriority datePublication dateAssigneeTitleWO2012004802A12009-07-072012-01-12Council Of Scientific & Industrial ResearchContinuous flow process for the preparation of sulphoxide compoundsCN107964005A *2017-11-102018-04-27扬子江药业集团江苏海慈生物药业有限公司A kind of preparation method of Lansoprazole
References
- ^ Jump up to:a b c “Lansoprazole Use During Pregnancy”. Drugs.com. Retrieved 3 March 2019.
- ^ Jump up to:a b c d e f “Lansoprazole Monograph for Professionals”. Drugs.com. American Society of Health-System Pharmacists. Retrieved 3 March 2019.
- ^ Jump up to:a b British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 79–80. ISBN 9780857113382.
- ^ Jump up to:a b “[99] Comparative effectiveness of proton pump inhibitors | Therapeutics Initiative”. 28 June 2016. Retrieved 14 July 2016.
- ^ Jump up to:a b c d e “Lansoprazole capsule, delayed release pellets”. DailyMed. 11 October 2016. Retrieved 31 December 2019.
- ^ Fischer, Jnos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 445. ISBN 9783527607495.
- ^ “The Top 300 of 2020”. ClinCalc. Retrieved 11 April 2020.
- ^ “Lansoprazole – Drug Usage Statistics”. ClinCalc. Retrieved 11 April 2020.
- ^ Hirschowitz BI, Mohnen J, Shaw S (August 1996). “Long-term treatment with lansoprazole for patients with Zollinger-Ellison syndrome”. Aliment. Pharmacol. Ther. 10 (4): 507–22. doi:10.1046/j.1365-2036.1996.10152000.x. PMID 8853754. S2CID 10668517.
- ^ British National Formulary (Free registration required) 1.3.5 Proton pump inhibitors
- ^ British National Formulary (Free registration required) Lansoprazole
- ^ “Prevacid (Lansoprazole) Drug Information: Side Effects and Drug Interactions – Prescribing Information at RxList”. RxList. Retrieved 9 February 2016.
- ^ K C Singhal & S Z Rahman, Lansoprazole Induced Adverse Effects on the Skin, Indian Medical Gazette, July 2001, Vol. CXXXV. N0. 7: 223-225
- ^ Sterry W, Assaf C (2007). “Erythroderma”. In Bolognia JL (ed.). Dermatology. St. Louis: Mosby. p. 154. ISBN 978-1-4160-2999-1..
- ^ British National Formulary (Free registration required) Lansoprazole interactions
- ^ Piscitelli, S. C.; Goss, T. F.; Wilton, J. H.; d’Andrea, D. T.; Goldstein, H; Schentag, J. J. (1991). “Effects of ranitidine and sucralfate on ketoconazole bioavailability”. Antimicrobial Agents and Chemotherapy. 35 (9): 1765–1771. doi:10.1128/aac.35.9.1765. PMC 245265. PMID 1952845.
- ^ “Pharmacy Benefit Update”. Retrieved 2 July 2014.
- ^ “Prevacid Pharmacology, Pharmacokinetics, Studies, Metabolism”. RxList.com. 2007. Archived from the original on 16 August 2000. Retrieved 14 April 2007.
- ^ Fischer, Janos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 102. ISBN 9783527607495.
- ^ Chorghade, Mukund S. (2006). Drug Discovery and Development, Volume 1: Drug Discovery. John Wiley & Sons. p. 201. ISBN 9780471780090.
- ^ Mosby’s Drug Consult: Lansoprazole
- ^ drugs.com International availability of lansoprazole Page accessed 3 February 2015
- ^ drugs.com Generic lansoprazole Page accessed 3 February 2015
- ^ “Prevacid Drug Profile”. Drugpatentwatch.com. Retrieved 30 April 2020.
- ^ Teva to release Prevacid version when patent expires
- ^ “Prevacid 24 HR- lansoprazole capsule, delayed release”. DailyMed. 7 August 2019. Retrieved 31 December 2019.
- ^ “Prevacid 24 HR- lansoprazole capsule, delayed release”. DailyMed. 11 December 2019. Retrieved 31 December 2019.
- ^ “Lansoprazole 24 HR- lansoprazole capsule, delayed release”. DailyMed. 21 December 2017. Retrieved 31 December 2019.
- ^ Jump up to:a b Villemagne, VL; Fodero-Tavoletti, MT; Masters, CL; Rowe, CC (January 2015). “Tau imaging: early progress and future directions”. The Lancet. Neurology. 14 (1): 114–24. doi:10.1016/s1474-4422(14)70252-2. PMID 25496902. S2CID 10502833.
External links
- “Lansoprazole”. Drug Information Portal. U.S. National Library of Medicine.
| Clinical data | |
|---|---|
| Pronunciation | /lænˈsoʊprəzoʊl/ lan-SOH-prə-zohl |
| Trade names | Prevacid, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a695020 |
| License data | EU EMA: by INNUS DailyMed: LansoprazoleUS FDA: Lansoprazole |
| Pregnancy category | AU: B3[1] |
| Routes of administration | By mouth, intravenous (IV) |
| Drug class | Proton pump inhibitor |
| ATC code | A02BC03 (WHO) |
| Legal status | |
| Legal status | AU: S2, S3, & S4UK: POM (Prescription only)US: OTC / Rx-only |
| Pharmacokinetic data | |
| Bioavailability | 80% or more |
| Protein binding | 97% |
| Metabolism | Liver (CYP3A4– and CYP2C19-mediated) |
| Elimination half-life | 1.0–1.5 hours |
| Excretion | Kidney and fecal |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 103577-45-3 |
| PubChem CID | 3883 |
| IUPHAR/BPS | 7208 |
| DrugBank | DB00448 |
| ChemSpider | 3746 |
| UNII | 0K5C5T2QPG |
| KEGG | D00355 |
| ChEBI | CHEBI:6375 |
| ChEMBL | ChEMBL480 |
| CompTox Dashboard (EPA) | DTXSID4023200 |
| ECHA InfoCard | 100.173.220 |
| Chemical and physical data | |
| Formula | C16H14F3N3O2S |
| Molar mass | 369.36 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| Chirality | Racemic mixture |
| showSMILES | |
| showInChI | |
| (verify) |
////LANSOPRAZOLE, A-65006, AG-1749, A 65006, AG 1749, лансопразол , لانسوبرازول , 兰索拉唑 , Antiulcerative, Gastric Proton Pump Inhibitor,

NEW DRUG APPROVALS
ONE TIME
$10.00
PRILOCAINE

PRILOCAINE
- Molecular FormulaC13H20N2O
- Average mass220.311 Da
Propanamide, N-(2-methylphenyl)-2-(propylamino)-
прилокаин [Russian] [INN]
بريلوكائين [Arabic] [INN]
丙胺卡因 [Chinese] [INN]
1641
211-957-0[EINECS]
721-50-6[RN]
N-(2-Methylphenyl)-2-(propylamino)propanamid
N-(2-méthylphényl)-2-(propylamino)propanamide
PrilocaineCAS Registry Number: 721-50-6
CAS Name:N-(2-Methylphenyl)-2-(propylamino)propanamide
Additional Names: 2-(propylamino)-o-propionotoluidide; N-(a-propylaminopropionyl)-o-toluidine; a-propylamino-2-methylpropionanilide; propitocaine
Molecular Formula: C13H20N2O
Molecular Weight: 220.31
Percent Composition: C 70.87%, H 9.15%, N 12.72%, O 7.26%
Literature References: Prepn: N. Löfgren, C. Tegner, Acta Chem. Scand.14, 486 (1960); GB839943; N. Löfgren, C. Tegner, US3160662 (1960, 1964 both to Astra).
Properties: Needles, mp 37-38°. bp0.1 159-162°. nD20 1.5298.
Melting point: mp 37-38°
Boiling point: bp0.1 159-162°
Index of refraction:nD20 1.5298 Derivative Type: Hydrochloride
CAS Registry Number: 1786-81-8
Manufacturers’ Codes: L-67
Trademarks: Citanest (AstraZeneca); Xylonest (AstraZeneca)
Molecular Formula: C13H20N2O.HCl
Molecular Weight: 256.77
Percent Composition: C 60.81%, H 8.24%, N 10.91%, O 6.23%, Cl 13.81%
Properties: Crystals from ethanol + isopropyl ether, mp 167-168°. Readily sol in water.
Melting point: mp 167-168° Therap-Cat: Anesthetic (local).Keywords: Anesthetic (Local).
- ASTRA 1512
- ASTRA 1515
- ASTRA-1512
- ASTRA-1515
- L 67
| INGREDIENT | UNII | CAS | INCHI KEY |
|---|---|---|---|
| Prilocaine hydrochloride | MJW015BAPH | 1786-81-8 | BJPJNTKRKALCPP-UHFFFAOYSA-N |
Agoneaze, Anodyne Lpt, Citanest, Citanest Forte, Dermacinrx Prikaan, Dermacinrx Prizopak, Emla, Fortacin, Lido Bdk, Lido-prilo Caine Pack, Lidopril, Oraqix, Prilolid, Prizotral, Relador
Prilocaine is a local anesthetic used in dental procedures.
A local anesthetic that is similar pharmacologically to lidocaine. Currently, it is used most often for infiltration anesthesia in dentistry. (From AMA Drug Evaluations Annual, 1992, p165)
Prilocaine (/ˈpraɪləˌkeɪn/[1]) is a local anesthetic of the amino amide type first prepared by Claes Tegner and Nils Löfgren. In its injectable form (trade name Citanest), it is often used in dentistry. It is also often combined with lidocaine as a topical preparation for dermal anesthesia (lidocaine/prilocaine or EMLA), for treatment of conditions like paresthesia. As it has low cardiac toxicity, it is commonly used for intravenous regional anaesthesia (IVRA).
Contraindications
In some patients, ortho-toluidine, a metabolite of prilocaine, may cause methemoglobinemia, which may be treated with methylene blue. Prilocaine may also be contraindicated in people with sickle cell anemia, anemia, or symptomatic hypoxia.[2]
Combinations
It is given as a combination with the vasoconstrictor epinephrine under the trade name Citanest Forte. It is used as an eutectic mixture with lidocaine, 50% w/w, as lidocaine/prilocaine. The mixture is an oil with a melting point of 18 °C (64 °F). A 5% emulsion preparation, containing 2.5% each of lidocaine/prilocaine, is marketed by APP Pharmaceuticals under the trade name EMLA (an abbreviation for eutectic mixture of local anesthetics).[3]
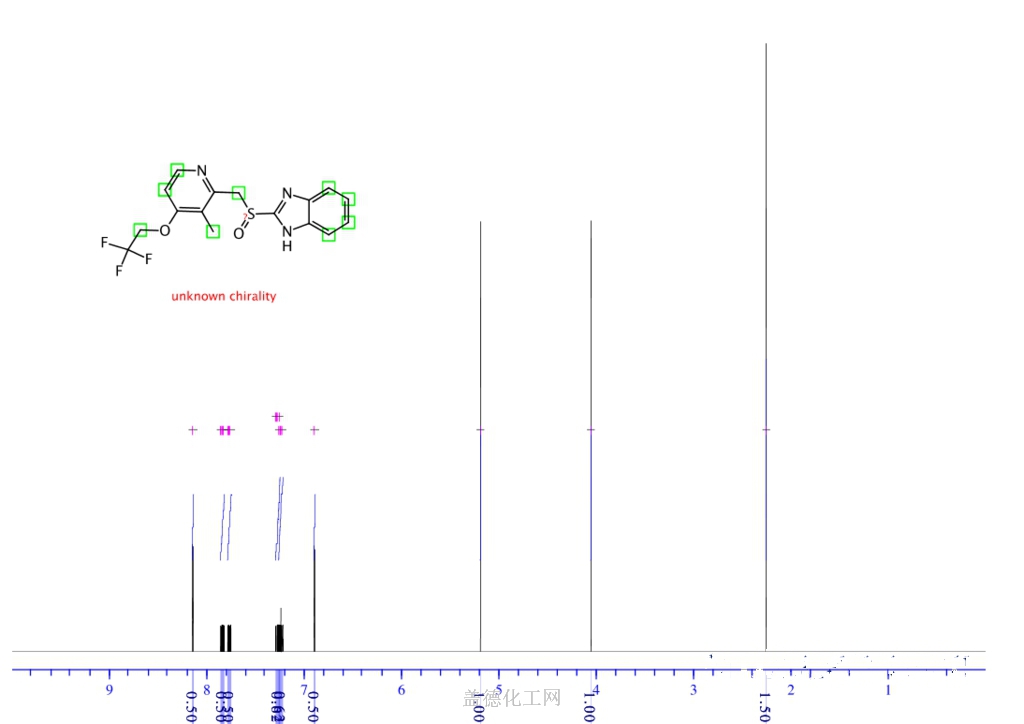
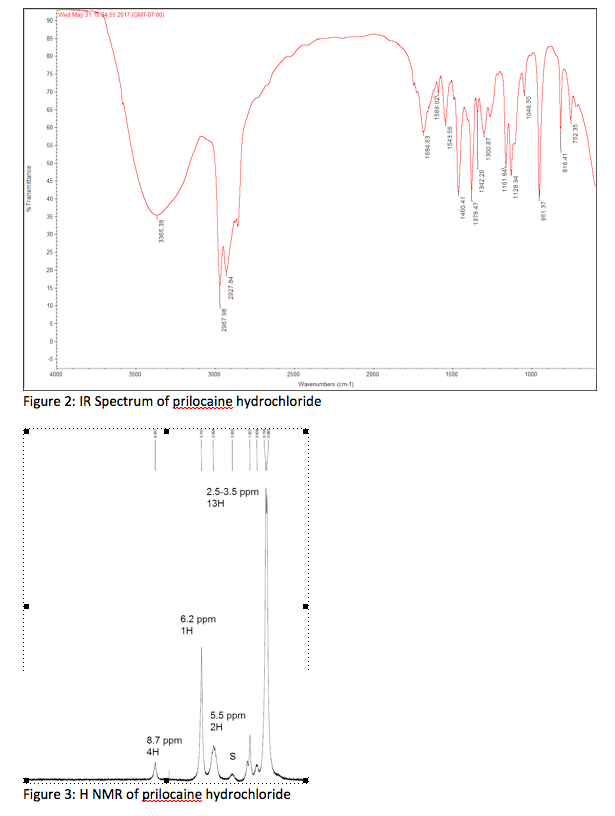
NMR
![1 H-nuclear magnetic resonance ( 1 H-NMR) spectra of prilocaine solution after sterilization with the assignment of the prilocaine hydrogens. [Prilocaine] = 5 mM, 20°C, 500 MHz.](https://www.researchgate.net/profile/Francisco-Groppo/publication/23458262/figure/fig3/AS:394557704425486@1471081295276/1-H-nuclear-magnetic-resonance-1-H-NMR-spectra-of-prilocaine-solution-after.png) 1 H-nuclear magnetic resonance ( 1 H-NMR) spectra of prilocaine solution after sterilization with the assignment of the prilocaine hydrogens. [Prilocaine] = 5 mM, 20°C, 500 MHz.
1 H-nuclear magnetic resonance ( 1 H-NMR) spectra of prilocaine solution after sterilization with the assignment of the prilocaine hydrogens. [Prilocaine] = 5 mM, 20°C, 500 MHz.
Compendial status

Table 1 The common types of local anesthetics
| COMPOUND | STRUCTURE | TIME TO MARKET | APPLICATION METHODS |
|---|---|---|---|
| Procaine | 1904 | Infiltration anesthesia, conduction anesthesia, subarachnoid anesthesia and epidural anesthesia | |
| Chloroprocaine | 1952 | Infiltration anesthesia, epidural anesthesia and conduction anesthesia | |
| Hydroxyprocaine | 1960 | Infiltration anesthesia | |
| Tetracaine | 1988 | Conduction anesthesia, subarachnoid anesthesia and epidural anesthesia | |
| Oxybuprocaine | 1975 | Topical anesthesia | |
| Tutocaine | 1976 | Topical anesthesia and infiltration anesthesia | |
| Butacaine | 1976 | Topical anesthesia and infiltration anesthesia | |
| Dimethocaine | 1938 | Topical anesthesia and infiltration anesthesia | |
| Thiocaine | Halt sales | Topical anesthesia and infiltration anesthesia | |
| Lidocaine | 1948 | Conduction anesthesia and epidural anesthesia | |
| Mepivacaine | 1986 | Infiltration anesthesia, conduction anesthesia, epidural anesthesia and topical anesthesia | |
| Bupivacaine | 2000 | Infiltration anesthesia, conduction anesthesia and epidural anesthesia | |
| Ropivacaine | 1996 | Infiltration anesthesia, conduction anesthesia and epidural anesthesia | |
| Trimecaine | 1965 | Infiltration anesthesia, surface anesthesia and epidural anesthesia | |
| Prilocaine | 1993 | Infiltration anesthesia, topical anesthesia and epidural anesthesia | |
| Etidocaine | 1976 | Epidural anesthesia | |
| Pyrrocaine | 1964 | Conduction anesthesia and epidural anesthesia | |
| Butanilicaine | 1982 | Infiltration anesthesia and conduction anesthesia | |
| Cinchocaine | 1985 | Topical anesthesia, subarachnoid anesthesia and epidural anesthesia | |
| Articaine | 2002 | Infiltration anesthesia and subarachnoid anesthesia | |
| Dyclonine | 1956 | Topical anesthesia | |
| Falicaine | 1957 | Topical anesthesia | |
| Quinisocaine | 1957 | Topical anesthesia | |
| Pramocaine | 1977 | Topical anesthesia | |
| Diperodon | 1980 | Topical anesthesia | |
| Heptacaine | 1984 | Infiltration anesthesia |

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////////////////////////////
Synthesis Reference
SYN
English: N. Lofgren and C. Tegner, Acta Chem. Scand., 14, 486 (1960). DOI number: 10.3891/acta.chem.scand.14-0486
SYN
SUN
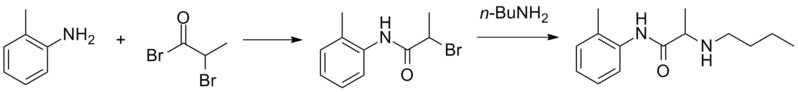
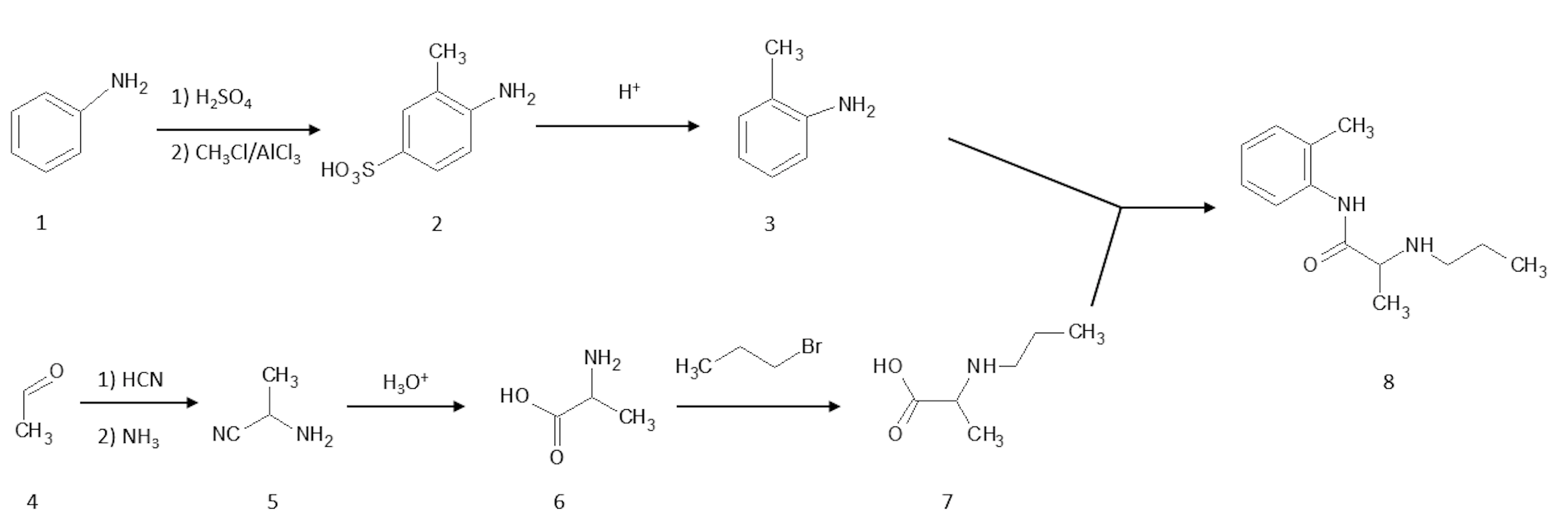
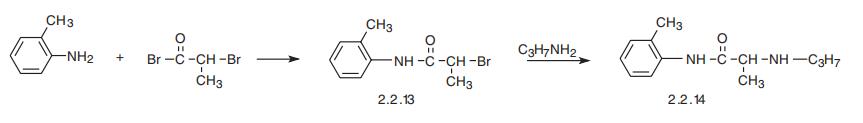
Prilocaine, 2-(propylamino)-o-propiontoluidine (2.2.14), is structurally related to the exact same group as ethidocaine, yet it differs structurally in that during synthesis, o-toluidine is used instead of 2,6-dimethylaniline, and instead of a butyric acid, a fragment of propionic acid, and a terminal propylethylamine group is replaced with a propylamine group. In order to synthesize prilocaine, o-toluidine is reacted with bromopropionyl bromide, and the resulting bromopropionyltoluidide (2.2.13) is then reacted with propylamine, which gives prilocaine [22,23].
SYN

SYN
| Clinical data | |
|---|---|
| Trade names | Citanest |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a603026 |
| License data | EU EMA: by INNUS DailyMed: Prilocaine |
| Pregnancy category | AU: A |
| Routes of administration | Subcutaneous |
| ATC code | N01BB04 (WHO) |
| Legal status | |
| Legal status | AU: S4 (Prescription only)US: ℞-only |
| Pharmacokinetic data | |
| Protein binding | 55% |
| Metabolism | Liver and kidney |
| Elimination half-life | 10-150 minutes, longer with impaired liver or kidney function |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 721-50-6 |
| PubChem CID | 4906 |
| IUPHAR/BPS | 7276 |
| DrugBank | DB00750 |
| ChemSpider | 4737 |
| UNII | 046O35D44R |
| KEGG | D00553 as HCl: D01243 |
| ChEBI | CHEBI:8404 |
| ChEMBL | ChEMBL1194 |
| CompTox Dashboard (EPA) | DTXSID7031955 |
| ECHA InfoCard | 100.010.871 |
| Chemical and physical data | |
| Formula | C13H20N2O |
| Molar mass | 220.316 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| Chirality | Racemic mixture |
| Melting point | 37 to 38 °C (99 to 100 °F) |
| showSMILES | |
| showInChI | |
| (verify) |
References
- ^ “Prilocaine”. Merriam-Webster Dictionary. Retrieved 2016-01-21.
- ^ Patel V, Morrissey J (2011-09-15). Practical and Professional Clinical Skills. Oxford University Press. p. 267. ISBN 9780199585618.
- ^ “Topical Anesthesia Use in Children: Eutectic Mixture of Local Anesthetics”. Medscape.com. Retrieved 2014-01-07.
- ^ The United States Pharmacopeial Convention, Revision Bulletin: Lidocaine and Prilocaine Cream–Revision to Related Compounds Test, archived from the original on 5 July 2010, retrieved 10 July 2009
External links
- “Prilocaine”. Drug Information Portal. U.S. National Library of Medicine.
- “Prilocaine hydrochloride”. Drug Information Portal. U.S. National Library of Medicine.
//////////PRILOCAINE, Anesthetic, ASTRA 1512, ASTRA 1515, ASTRA-1512, ASTRA-1515, L 67,
CCCNC(C)C(=O)NC1=CC=CC=C1C

NEW DRUG APPROVALS
ONE TIME
$10.00
CEFOPERAZONE
Cefoperazone
- Molecular FormulaC25H27N9O8S2
- Average mass645.667 Da
Product Ingredients
| INGREDIENT | UNII | CAS | INCHI KEY |
|---|---|---|---|
| Cefoperazone sodium | 5FQG9774WD | 62893-20-3 | NCFTXMQPRQZFMZ-WERGMSTESA-M |
(6R,7R)-7-{[(2R)-2-{[(4-ethyl-2,3-dioxopiperazin-1-yl)carbonyl]amino}-2-(4-hydroxyphenyl)acetyl]amino}-3-{[(1-methyl-1H-tetrazol-5-yl)thio]methyl}-8-oxo-5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid
(6R,7R)-7-[(2R)-2-[(4-ethyl-2,3-dioxopiperazine-1-carbonyl)amino]-2-(4-hydroxyphenyl)acetamido]-3-{[(1-methyl-1H-1,2,3,4-tetrazol-5-yl)sulfanyl]methyl}-8-oxo-5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid
263-749-4[EINECS], 4742
5-Thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid, 7-[[(2R)-2-[[(4-ethyl-2,3-dioxo-1-piperazinyl)carbonyl]amino]-2-(4-hydroxyphenyl)acetyl]amino]-3-[[(1-methyl-1H-tetrazol-5-yl)thio]methyl]-8-oxo- , (6R,7R)- [ACD/Index Name]
5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid, 7-[[(2R)-2-[[(4-ethyl-2,3-dioxo-1-piperazinyl)carbonyl]amino]-2-(4-hydroxyphenyl)acetyl]amino]-3-[[(1-methyl-1H-tetrazol-5-yl)thio]methyl]-8-oxo-, (6R,7R)-
62893-19-0[RN]
7-[D-(-)-a-(4-Ethyl-2,3-dioxo-1-piperazinecarboxamido)-a-(4-hydroxyphenyl)acetamido]-3-[[(1-methyl-1H-tetrazol-5-yl)thio]methyl]-3-cephem-4-carboxylic Acid
7U75I1278D
Experimental Properties
| PROPERTY | VALUE | SOURCE |
|---|---|---|
| melting point (°C) | 188-190 | Saikawa, I., Takano, S., Yoshida, C., Takashima, 0..Momonoi, K., Kuroda, S., Komatsu, M., Yasuda, T.and Kodama, Y.; British Patent 1,508,071; April 19,1978; assigned to Toyama Chemical Co., Ltd. and U.S. Patent 4,110,327; August 29,1978; also assigned to Toyama Chemical Co., Ltd. |
| logP | -0.74 | HANSCH,C ET AL. (1995) |
Cefoperazone
CAS Registry Number: 62893-19-0
CAS Name: (6R,7R)-7-[[(2R)-[[(4-Ethyl-2,3-dioxo-1-piperazinyl)carbonyl]amino](4-hydroxyphenyl)acetyl]amino]-3-[[(1-methyl-1H-tetrazol-5-yl)thio]methyl]-8-oxo-5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acidAdditional Names: 7-[D-(-)-a-(4-ethyl-2,3-dioxo-1-piperazinecarboxamido)-a-(4-hydroxyphenyl)acetamido]-3-[[(1-methyl-1H-tetrazol-5-yl)thio]methyl]-3-cephem-4-carboxylic acid
Molecular Formula: C25H27N9O8S2
Molecular Weight: 645.67
Percent Composition: C 46.50%, H 4.21%, N 19.52%, O 19.82%, S 9.93%
Literature References: Broad spectrum third generation cephalosporin antibiotic. Prepn: I. Saikawa et al.,BE837682; eidem,US4410522 (1976, 1983 both to Toyama); eidem,Yakugaku Zasshi99, 929 (1979). Stability in aq soln: eidem,ibid. 1207. In vitro activity: M. V. Borobio et al.,Antimicrob. Agents Chemother.17, 129 (1980). Kinetics in rats: J. Fabre et al.,Schweiz. Med. Wochenschr.110, 264 (1980); in humans: A. F. Allaz, ibid.109, 1999 (1979). Review of pharmacology and therapeutic efficacy: R. N. Brogden et al.,Drugs22, 423-460 (1981). Symposium on clinical studies: ibid. Suppl. 1, 1-124.
Properties: Crystals from acetonitrile/water, mp 169-171° (hydrated). Stable at pH 4.0-7.0; slightly unstable in acid; highly unstable in alkaline soln.
Melting point: mp 169-171° (hydrated)
Derivative Type: Sodium salt
CAS Registry Number: 62893-20-3
Manufacturers’ Codes: CP-52640-2; T-1551
Trademarks: Bioperazone (Biopharma); Cefazone (Firma); Cefobid (Pfizer); Cefobine (Pfizer); Cefobis (Pfizer); Cefogram (Metapharma); Cefoneg (Tosi); Cefosint (Proter); Dardum (Lisapharma); Farecef (Lafare); Kefazon (Esseti); Novobiocyl (Francia); Pathozone (Pfizer); Peracef (Pfizer); Perocef (Pulitzer); Tomabef (Aandersen)
Molecular Formula: C25H26N9NaO8S2
Molecular Weight: 667.65
Percent Composition: C 44.97%, H 3.93%, N 18.88%, Na 3.44%, O 19.17%, S 9.61%
Therap-Cat: Antibacterial., Therap-Cat-Vet: Antibacterial.
Keywords: Antibacterial (Antibiotics); ?Lactams; Cephalosporins.
Cefoperazone is a third-generation cephalosporin antibiotic, marketed by Pfizer under the name Cefobid. It is one of few cephalosporin antibiotics effective in treating Pseudomonas bacterial infections which are otherwise resistant to these antibiotics.
It was patented in 1974 and approved for medical use in 1981.[1] Cefoperazone/sulbactam (Sulperazon) is a co-formulation with sulbactam.
Cefoperazone is a broad-spectrum cephalosporin antibiotic used for the treatment of bacterial infections in various locations, including the respiratory tract, abdomen, skin, and female genital tracts.
Cefoperazone is a semisynthetic broad-spectrum cephalosporin proposed to be effective against Pseudomonas infections. It is a third-generation antiobiotic agent and it is used in the treatment of various bacterial infections caused by susceptible organisms in the body, including respiratory tract infections, peritonitis, skin infections, endometritis, and bacterial septicemia. While its clinical use has been discontinued in the U.S., cefoperazone is available in several European countries most commonly under the product name, Sulperazon.

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////////////////////////////
SYN

English: I. Saikawa, S. Takano, Y. Shuntaro, C. Yoshida, 0.
Takashima, K. Momonoi, S. Kuroda, M. Komatsu, T. Yasuda, and Y. Kodama, German Offen., DE 2,600,880 (1977); Chem.
Abstr., 87_, 184533b (1977).
SYN
Following is one of the synthesis routes:
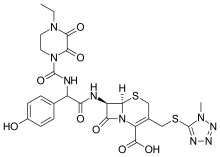
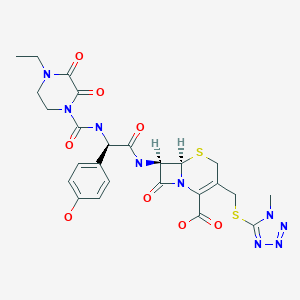
alpha-(4-Ethyl-2,3-dioxo-1-piperazinocarbonylamino)-p-hydroxyphenylacetic acid (I) is condensed with 7-amino-3-[(1-methyl-1H-tetrazol-5-yl)thiomethyl]-3-cephem-4-carboxylic acid (II) in the presence of ethyl chlorocarbonate and N,O-bis(trimethylsilyl)acetamide in acetonitrile to produce Cefoperazone sodium.

SYN
Antibiotics
R.S. Vardanyan, V.J. Hruby, in Synthesis of Essential Drugs, 2006
Cefoperazone
Cefoperazone, (6R,7R)-7-[(R)-2-(4-ethyl-2,3-dioxo-1-piperazincarboxamido)-2-(p-hydroxyphenyl)acetamido]-3-[[(1-methyl-1 H-tetrazol-5-yl)thio]methyl]-8-oxo-5-thia-1-azabicyclo[4.2.0]oct-2-en-2-carboxylic acid (32.1.2.84), is synthesized by acylating 7-amino-3-(1-methyl-1,2,3,4-tetrazol-5-yl)-thiomethyl-3-cefem-4-carboxylic acid (32.1.2.24) with a mixed anhydride synthesized from ethyl chloroformate and α-(4-ethylpiperazin-2, 3-dion-1-carbonylamino)-4-hydroxyphenylacetic acid (32.1.2.83), which in turn is synthesized from 4-ethylpiperazin-2,3-dion-1-carboxylic acid (32.1.1.29) and the sodium salt of 4-hydroxyphenylglycine [163–168].


Cefoperazone also has a broad spectrum of antimicrobial action, including most clinically significant microorganisms: Gram-positive, Gram-negative, aerobic, and anaerobic. It is stable with respect to most beta-lactamases of Gram-positive and Gram-negative bacteria.
Cefoperazone is used for bacterial infections of the lower respiratory tract, urinary and sexual tracts, bones, joints, skin, soft tissues, abdominal, and gynecological infections. Synonyms of this drug are cefazon, cefobid, cefobis, and many others.
Spectrum of bacterial susceptibility
Cefoperazone has a broad spectrum of activity and has been used to target bacteria responsible for causing infections of the respiratory and urinary tract, skin, and the female genital tract. The following represents MIC susceptibility data for a few medically significant microorganisms.
- Haemophilus influenzae: 0.12 – 0.25 µg/ml
- Staphylococcus aureus: 0.125 – 32 µg/ml
- Streptococcus pneumoniae: ≤0.007 – 1 µg/ml[2]
Adverse effects
Cefoperazone contains an N-methylthiotetrazole (NMTT or 1-MTT) side chain. As the antibiotic is broken down in the body, it releases free NMTT, which can cause hypoprothrombinemia (likely due to inhibition of the enzyme vitamin K epoxide reductase) and a reaction with ethanol similar to that produced by disulfiram (Antabuse), due to inhibition of aldehyde dehydrogenase.[3]
Mechanism of action
Cefoperazone exerts its bactericidal effect by inhibiting the bacterial cell wall synthesis, and sulbactam acts as a beta-lactamase inhibitor, to increase the antibacterial activity of cefoperazone against beta-lactamase-producing organisms.
References
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 494. ISBN 9783527607495.
- ^ “Cefoperazone (Cefobid) – The Antimicrobial Index Knowledgebase – TOKU-E”. antibiotics.toku-e.com.
- ^ Stork CM (2006). “Antibiotics, antifungals, and antivirals”. In Nelson LH, Flomenbaum N, Goldfrank LR, Hoffman RL, Howland MD, Lewin NA (eds.). Goldfrank’s toxicologic emergencies. New York: McGraw-Hill. p. 847. ISBN 0-07-143763-0. Retrieved 2009-07-03.
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| MedlinePlus | a601206 |
| ATC code | J01DD12 (WHO) QJ51DD12 (WHO) |
| Pharmacokinetic data | |
| Excretion | Hepatic |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 62893-19-0 |
| PubChem CID | 44185 |
| DrugBank | DB01329 |
| ChemSpider | 40206 |
| UNII | 7U75I1278D |
| KEGG | D07645 |
| ChEMBL | ChEMBL507674 |
| CompTox Dashboard (EPA) | DTXSID2022759 |
| ECHA InfoCard | 100.057.936 |
| Chemical and physical data | |
| Formula | C25H27N9O8S2 |
| Molar mass | 645.67 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (verify) |
//////////cefoperazone, Antibacterial, Antibiotics, Lactams, Cephalosporins, CP-52640-2, T-1551, CP 52640-2, T 1551
[H][C@]12SCC(CSC3=NN=NN3C)=C(N1C(=O)[C@@]2([H])NC(=O)[C@H](NC(=O)N1CCN(CC)C(=O)C1=O)C1=CC=C(O)C=C1)C(O)=O

NEWDRUG APPROVALS
one time
$10.00
CICLOPIROX

- Molecular FormulaC12H17NO2
- Average mass207.269 Da
CICLOPIROX(6-Cyclohexyl-1-hydroxy-4-methyl-2(1H)-pyridone)
2(1H)-Pyridinone, 6-cyclohexyl-1-hydroxy-4-methyl-
249-577-2[EINECS]
29342-05-0[RN]
KS-5085, циклопирокс , سيكلوبيروكس , 环吡酮 ,
Ciclopirox
CAS Registry Number: 29342-05-0
CAS Name: 6-Cyclohexyl-1-hydroxy-4-methyl-2(1H)-pyridinone
Molecular Formula: C12H17NO2
Molecular Weight: 207.27
Percent Composition: C 69.54%, H 8.27%, N 6.76%, O 15.44%
Literature References: Broad spectrum antimycotic agent with some antibacterial activity. Prepn: G. Lohaus, W. Dittmar, ZA6906039; eidem,US3883545 (1970, 1975 both to Hoechst). In vitro study: eidem,Arzneim.-Forsch.23, 670 (1973). Series of articles on pharmacokinetics, pharmacology, teratology, toxicity studies: Oyo Yakuri9, 57-115 (1975), C.A.83, 53159d, 53538b, 53539c, 71844c, 90833q (1975). Series of articles on chemistry, mechanism of action, toxicology, clinical trials: Arzneim.-Forsch.31, 1309-1386 (1981). Toxicity data: H. G. Alpermann, E. Schutz, ibid. 1328. Review: S. G. Jue et al.,Drugs29, 330-341 (1985). Review of clinical experience in seborrheic dermatitis: A. Starova, R. Aly, Expert Opin. Drug Saf.4, 235-239 (2005).
Properties: Solid, mp 144°.
Melting point: mp 144°
Derivative Type: Ethanolamine salt (1:1)
CAS Registry Number: 41621-49-2
Additional Names: Ciclopirox olamine
Manufacturers’ Codes: HOE-296
Trademarks: Batrafen (HMR); Brumixol (Bruschettini); Ciclochem (Novag); Dafnegin (Poli); Loprox (HMR); Micoxolamina (Domp?; Mycoster (Fabre)
Molecular Formula: C14H24N2O3
Molecular Weight: 268.35
Percent Composition: C 62.66%, H 9.01%, N 10.44%, O 17.89%
Properties: LD50 in mice, rats (mg/kg): 2898, 3290 orally (Alpermann, Schutz).
Toxicity data: LD50 in mice, rats (mg/kg): 2898, 3290 orally (Alpermann, Schutz)
- EINECS:255-464-9
- LD50:71 mg/kg (M, i.v.); 1740 mg/kg (M, p.o.);
72 mg/kg (R, i.v.); 2350 mg/kg (R, p.o.)
Therap-Cat: Antifungal.
Keywords: Antifungal (Synthetic).

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////////////////////////////
Ciclopirox (sometimes known by the abbreviation CPX[2]) is a synthetic antifungal agent for topical dermatologic treatment of superficial mycoses. It is most useful against Tinea versicolor. It is sold under many brand names worldwide.[1]
Medical uses
Ciclopirox is indicated for the treatment of tinea pedis and tinea corporis due to Trichophyton rubrum, Trichophyton mentagrophytes and Epidermophyton floccosum, as well as seborrheic dermatitis. It is not to be used in the eyes or vagina, and nursing women should consult their doctors before use, since it is not known whether ciclopirox passes into human milk. A burning sensation may be felt when first applying ciclopirox on the skin.[3]
Nail infections
In addition to other formulations, ciclopirox is used in lacquers for topical treatment of onychomycosis (fungal infections of the nails). A meta-analysis of the six trials of nail infections available in 2009 concluded that they provided evidence that topical ciclopirox had poor cure rates and that amorolfine might be substantially more effective, but more research was required.
“Combining data from 2 trials of ciclopiroxolamine versus placebo found treatments failure rates of 61% and 64% for ciclopiroxolamine. These outcomes followed long treatment times (48 weeks) and this makes ciclopiroxolamine a poor choice for nail infections. Better results were observed with the use of amorolfine lacquer; 6% treatment failure rates were found after 1 month of treatment but these data were collected on a very small sample of people and these high rates of success might be unreliable.”[4]
Pharmacology
Pharmacodynamics
In contrast to the azoles and other antimycotic drugs, the mechanism of action of ciclopirox is poorly understood.[5] However, loss of function of certain catalase and peroxidase enzymes has been implicated as the mechanism of action, as well as various other components of cellular metabolism. In a study conducted to further elucidate ciclopirox’s mechanism, several Saccharomyces cerevisiae mutants were screened and tested. Results from interpretation of the effects of both the drug treatment and mutation suggested that ciclopirox may exert its effect by disrupting DNA repair, cell division signals and structures (mitotic spindles) as well as some elements of intracellular transport.[6]
It is currently being investigated as an alternative treatment to ketoconazole for seborrhoeic dermatitis as it suppresses growth of the yeast Malassezia furfur. Initial results show similar efficacy to ketoconazole with a relative increase in subjective symptom relief due to its inherent anti-inflammatory properties.[7]
Chemistry
Ciclopirox is a considered a hydroxypyrimidine (sic) antifungal agent.[citation needed] Structurally, ciclopirox is the N-oxide of a 2-hydroxypyridine derivative and therefore ought to be termed a hydroxypyridine antifungal agent. Additionally, the structure as drawn above is the lactam tautomer and indicates the molecule being an N-Hydroxy-2-pyridone. Hence the classification of ciclopirox as a 2-pyridone antifungal agent.
Ciclopirox is used clinically as ciclopirox olamine, the olamine salt of ciclopirox.
Literatures:
Lohaus; Dittmar Arzneimittel-Forschung/Drug Research, 1981 , vol. 31, # 8 a p. 1311 – 1316
Literatures:
Hoechst Aktiengesellschaft Patent: US3972888 A1, 1976 ;
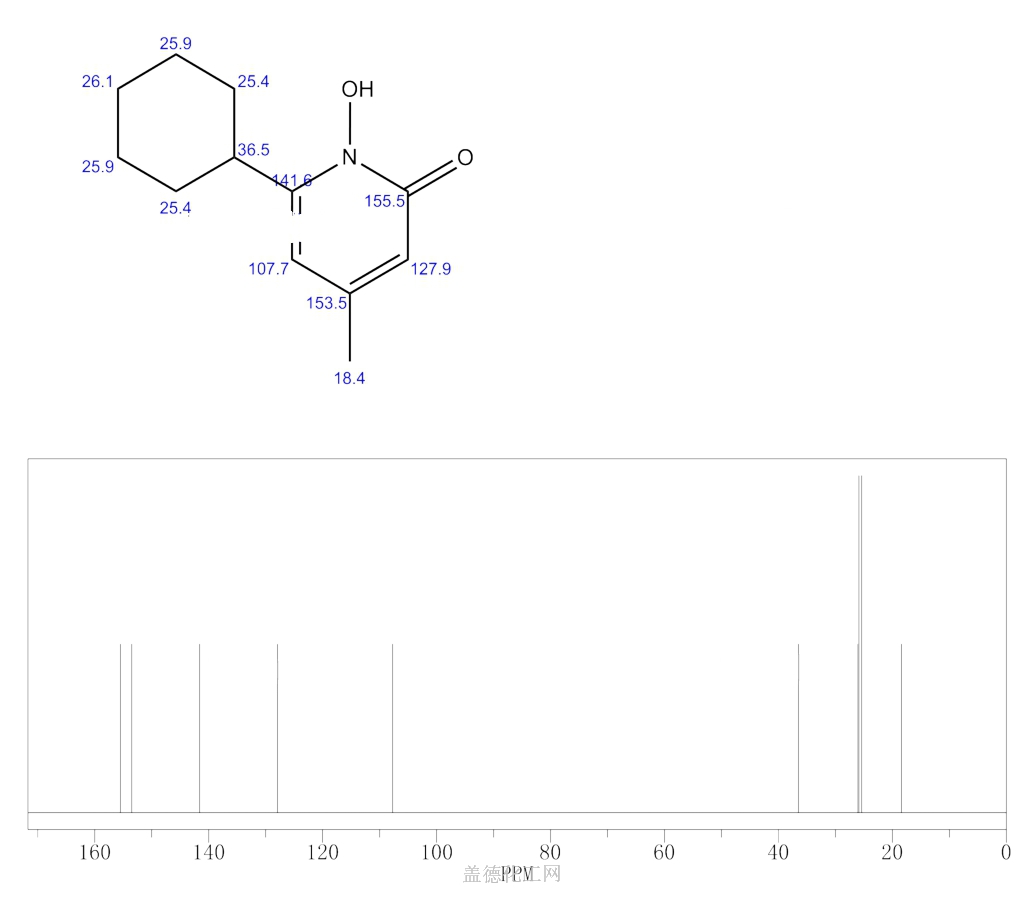
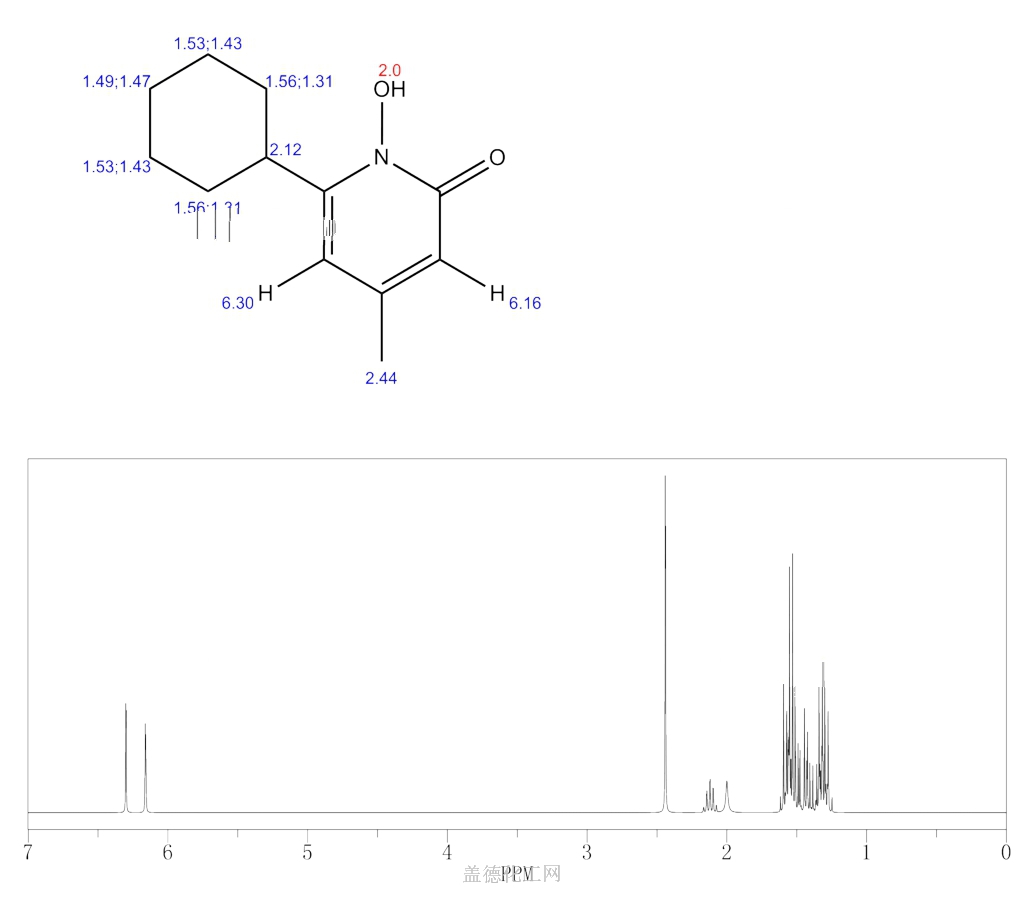
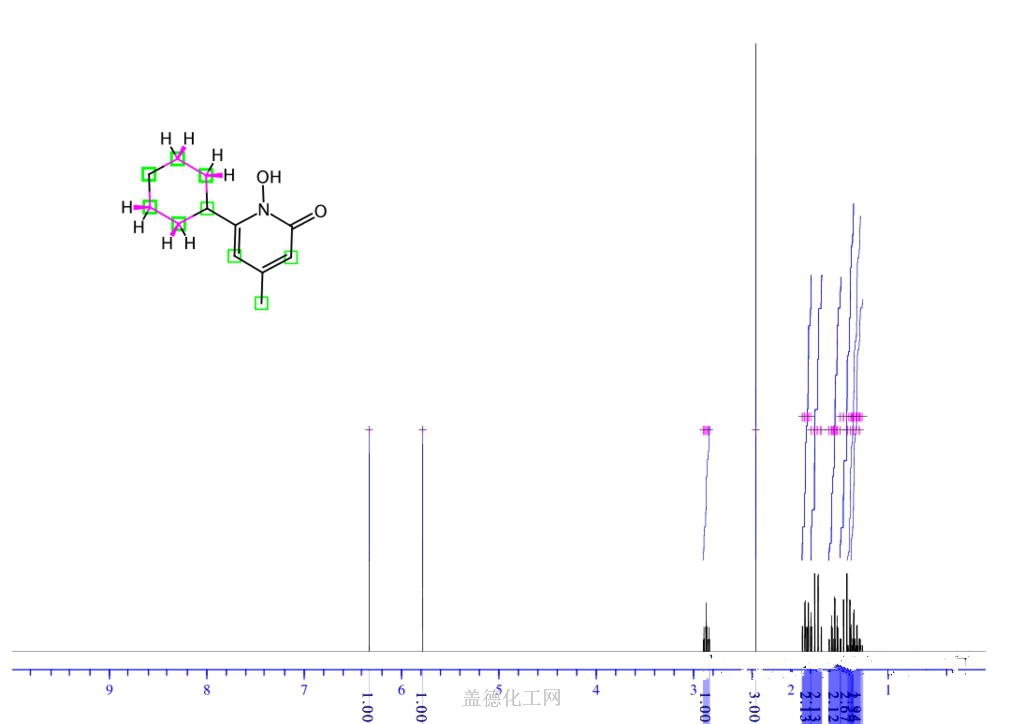
SYNTHESIS
SYN

SYN
W. Dittmar, E. Druckrey andBroad spectrum antimycotic agent with some antibacterial activity. Prepn: G. Lohaus, W. Dittmar, ZA 6906039; eidem, US 3883545 (1970, 1975 both to Hoechst). In vitro study: eidem, Arzneim.-Forsch. 23, 670 (1973).
H. Urbach, J. Med. Chem., 17, 753 (1974); W. Dittmar and G. Lohaus,
German Patent 2,214,608 (1973); Chem. Abstr., 79: 146419w (1973).

SYN
ethanolamine (CAS NO.: ), with other names as 6-Cyclohexyl-1-hydroxy-4-methyl-2(1H)-pyridinone 2-aminoethanol, could be produced through the following synthetic routes.
.jpg)
Compound can be prepared in two different ways: 1) The reaction of methyl 5-oxo-5-cyclohexyl-3-methylpentenoate (I) with NH2OH gives the corresponding oxime (II), which is then cyclized to 6-cyclohexyl-1-hydroxy-4-methyl-2(1H)-pyridone (III). Finally, this compound is salified with ethanolamine (IV). 2) Compound (III) can also be obtained by reaction of 6-cyclohexyl-4-methyl-2-pyron (V) with hydroxylamine hydrochloride in hot 2-aminopyridine.
SYN
| CAS-RN | Formula | Chemical Name | CAS Index Name |
|---|---|---|---|
| 14818-35-0 | C12H16O2 | 6-cyclohexyl-4-methyl-2-pyrone | 2H-Pyran-2-one, 6-cyclohexyl-4-methyl- |
| 141-43-5 | C2H7NO | ethanolamine | Ethanol, 2-amino- |
| 7803-49-8 | H3NO | hydroxylamine | Hydroxylamine |
PATENT
https://patents.google.com/patent/US9545413B2/en
The molecule 6-cyclohexyl-1-hydroxy-4-methylpyridin-2(1H)-one, also known as Ciclopirox, is a commercially available antifungal agent as an olamine salt. Ciclopirox olamine has been used to treat superficial mycoses and Tinea versicolor following topical application to the skin. Following enteral administration, ciclopirox undergoes significant first-pass effect resulting in low oral bioavailability. The oral route of administration is also associated with gastrointestinal toxicities observed in animals and humans limiting its benefit in animal and human health applications. Ciclopirox olamine has poor solubility, limiting opportunities to deliver the antifungal agent via parenteral administration of suitably potent solutions and suspensions. As such, it would be beneficial to configure ciclopirox for improved water solubility in order to deliver the drug by parenteral routes of administration.
References
- ^ Jump up to:a b Drugs.com International brand names for ciclopirox Page accessed January 201, 2016
- ^ Ciclopirox
- ^ “Ciclopirox Olamine Antifungal Shampoo”. Okdermo. Retrieved 2019-08-06.
- ^ Crawford F (2007). “Topical treatments for fungal infections of the skin and nails of the foot”. The Cochrane Database of Systematic Reviews. 2007 (3): CD001434. doi:10.1002/14651858.CD001434.pub2. PMC 7073424. PMID 17636672.
- ^ Niewerth M, Kunze D, Seibold M, Schaller M, Korting HC, Hube B (June 2003). “Ciclopirox Olamine Treatment Affects the Expression Pattern of Candida albicans Genes Encoding Virulence Factors, Iron Metabolism Proteins, and Drug Resistance Factors”. Antimicrobial Agents and Chemotherapy. 47 (6): 1805–1817. doi:10.1128/AAC.47.6.1805-1817.2003. PMC 155814. PMID 12760852.
- ^ Leem SH, Park JE, Kim IS, Chae JY, Sugino A, Sunwoo Y (2003). “The possible mechanism of action of ciclopirox olamine in the yeast Saccharomyces cerevisiae”. Mol. Cells. 15 (1): 55–61. PMID 12661761.
- ^ Ratnavel RC, Squire RA, Boorman GC (2007). “Clinical efficacies of shampoos containing ciclopirox olamine (1.5%) and ketoconazole (2.0%) in the treatment of seborrhoeic dermatitis”. J Dermatolog Treat. 18 (2): 88–96. doi:10.1080/16537150601092944. PMID 17520465. S2CID 34852507.
| Clinical data | |
|---|---|
| Trade names | Many brand names worldwide[1] |
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| MedlinePlus | a604021 |
| Pregnancy category | B |
| Routes of administration | Topical (applied as a nail lacquer, skin cream or shampoo) |
| ATC code | D01AE14 (WHO) G01AX12 (WHO) |
| Legal status | |
| Legal status | US: ℞-onlyRx-only (CA) |
| Pharmacokinetic data | |
| Bioavailability | <5% with prolonged use |
| Protein binding | 94 to 97% |
| Elimination half-life | 1.7 hours |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 29342-05-0 |
| PubChem CID | 2749 |
| DrugBank | DB01188 |
| ChemSpider | 2647 |
| UNII | 19W019ZDRJ |
| KEGG | D03488 |
| ChEBI | CHEBI:453011 |
| ChEMBL | ChEMBL1413 |
| CompTox Dashboard (EPA) | DTXSID9048564 |
| ECHA InfoCard | 100.045.056 |
| Chemical and physical data | |
| Formula | C12H17NO2 |
| Molar mass | 207.269 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (verify) |
////////CICLOPIROX OLAMINE

NEW DRUG APPROVALS
ONE TIME
$10.00
RITONAVIR
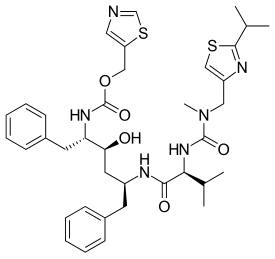
RITONAVIR
- Molecular FormulaC37H48N6O5S2
- Average mass720.944 Da
1,3-Thiazol-5-ylmethyl-[(1S,2S,4S)-1-benzyl-2-hydroxy-4-({(2S)-3-methyl-2-[(methyl{[2-(1-methylethyl)-1,3-thiazol-4-yl]methyl}carbamoyl)amino]butanoyl}amino)-5-phenylpentyl]carbamat
155213-67-5[RN]
7449Abbott 84538
UNII-O3J8G9O825
ритонавир
ريتونافير
利托那韦
(1E,2S)-N-[(2S,4S,5S)-4-Hydroxy-5-{(E)-[hydroxy(1,3-thiazol-5-ylmethoxy)methylene]amino}-1,6-diphenyl-2-hexanyl]-2-[(E)-(hydroxy{[(2-isopropyl-1,3-thiazol-4-yl)methyl](methyl)amino}methylene)amino]-3- methylbutanimidic acid
(2S,3S,5S)-5-[N-[N-[[N-methyl-N-[(2-isopropyl-4-thiazolyl)methyl]amino]carbonyl]valinyl]amino]-2-[N-[(5-thiazolyl)methoxycarbonyl]amino]-1,6-diphenyl-3-hydroxyhexane
- A-84538
- Abbott 84538
- ABBOTT-84538
- ABT 538
- ABT-538
- DRG-0244
- NSC-693184
- TMC 114r
Ritonavir
CAS Registry Number: 155213-67-5
CAS Name: (5S,8S,10S,11S)-10-Hydroxy-2-methyl-5-(1-methylethyl)-1-[2-(1-methylethyl)-4-thiazolyl]-3,6-dioxo-8,11-bis(phenylmethyl)-2,4,7,12-tetraazatridecan-13-oic acid 5-thiazolylmethyl ester
Additional Names: (2S,3S,5S)-5-[N-[N-[[N-methyl-N-[(2-isopropyl-4-thiazolyl)methyl]amino]carbonyl]valinyl]amino]-2-[N-[(5-thiazolyl)methoxycarbonyl]amino]-1,6-diphenyl-3-hydroxyhexane
Manufacturers’ Codes: A-84538; Abbott 84538; ABT-538
Trademarks: Norvir (Abbott)
Molecular Formula: C37H48N6O5S2
Molecular Weight: 720.94
Percent Composition: C 61.64%, H 6.71%, N 11.66%, O 11.10%, S 8.90%
Literature References: Peptidomimetic HIV-1 protease inhibitor. Prepn: D. J. Kempf et al.,WO9414436; eidem,US5541206 (1994, 1996 both to Abbott). Antiretroviral spectrum, pharmacokinetics: idemet al.,Proc. Natl. Acad. Sci. USA92, 2484 (1995). Structural model for drug resistance: M. Markowitz et al.,J. Virol.69, 701 (1995). HPLC determn in biological fluids: R. M. W. Hoetelmans et al.,J. Chromatogr. B705, 119 (1998). Review of clinical experience: A. P. Lea, D. Faulds, Drugs52, 541-546 (1996). Clinical trial with nucleoside analogs in HIV-infected children: S. A. Nachman et al.,J. Am. Med. Assoc.283, 492 (2000). Clinical trial with lopinavir, q.v., in HIV infection: S. Walmsley et al.,N. Engl. J. Med.346, 2039 (2002).
Therap-Cat: Antiviral.
Keywords: Antiviral; Peptidomimetics; HIV Protease Inhibitor.Company:Abbvie (Originator)Sales:$389 Million (Y2012); 
$419 Million (Y2011);ATC Code:J05AE03
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2010-02-10 | New dosage form | Norvir | HIV infection | Tablet | 100 mg | Abbvie | |
| 1999-06-29 | Additional approval | Norvir | HIV infection | Capsule | 100 mg | Abbvie | |
| 1996-03-01 | New dosage form | Norvir | HIV infection | Capsule | 100 mg | Abbvie | Priority |
| 1996-03-01 | First approval | Norvir | HIV infection | Solution | 80 mg/mL | Abbvie |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 1996-08-26 | First approval | Norvir | HIV infection | Capsule | 100 mg | Abbvie | |
| 1996-08-26 | First approval | Norvir | HIV infection | Tablet, Film coated | 100 mg | Abbvie | |
| 1996-08-26 | First approval | Norvir | HIV infection | Solution | 80 mg/mL | Abbvie |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2011-02-28 | New dosage form | Norvir | HIV infection | Tablet | 100 mg | Abbvie | |
| 1998-09-25 | First approval | Norvir | HIV infection | Solution | 80 mg/mL | Abbvie |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2013-10-15 | Marketing approval | HIV infection | Tablet | 100 mg | Abbvie | ||
| 2010-07-29 | Marketing approval | 爱治威/Norvir | HIV infection | Capsule | 100 mg | Abbott | |
| 2010-07-13 | Marketing approval | 迈可欣 | HIV infection | Solution | 75 ml:6 g | 美吉斯制药(厦门) | 3.1类 |
Ritonavir was first approved by the U.S. Food and Drug Administration (FDA) on March 1, 1996, then approved by European Medicine Agency (EMA) on August 26, 1996, and approved by Pharmaceuticals and Medical Devices Agency of Japan (PMDA) on September 25, 1998. It was developed and marketed as Norvir® by Abbvie.
Ritonavir is an HIV protease inhibitor. It is indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection.
Norvir® is available as solution for oral use, containing 80 mg of free Ritonavir per mL. The recommended dose is 600 mg twice-day with meals for adult patients.
Ritonavir is an HIV protease inhibitor used in combination with other antivirals in the treatment of HIV infection.
Ritonavir (RTV), sold under the brand name Norvir, is an antiretroviral medication used along with other medications to treat HIV/AIDS.[2] This combination treatment is known as highly active antiretroviral therapy (HAART).[2] Often a low dose is used with other protease inhibitors.[2] It may also be used in combination with other medications for hepatitis C.[3] It is taken by mouth.[2] The capsules of the medication do not work the same as the tablets.[2]
Common side effects include nausea, vomiting, loss of appetite, diarrhea, and numbness of the hands and feet.[2] Serious side effects include liver problems, pancreatitis, allergic reactions, and arrythmias.[2] Serious interactions may occur with a number of other medications including amiodarone and simvastatin.[2] At low doses it is considered to be acceptable for use during pregnancy.[4] Ritonavir is of the protease inhibitor class.[2] Typically, however, it is used to inhibit the enzyme that metabolizes other protease inhibitors.[5] This inhibition allows lower doses of these latter medication to be used.[5]
Ritonavir was patented in 1989 and came into medical use in 1996.[6][7] It is on the World Health Organization’s List of Essential Medicines.[8] Ritonavir capsules were approved as a generic medication in the United States in 2020.[9]

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////////////////////////////
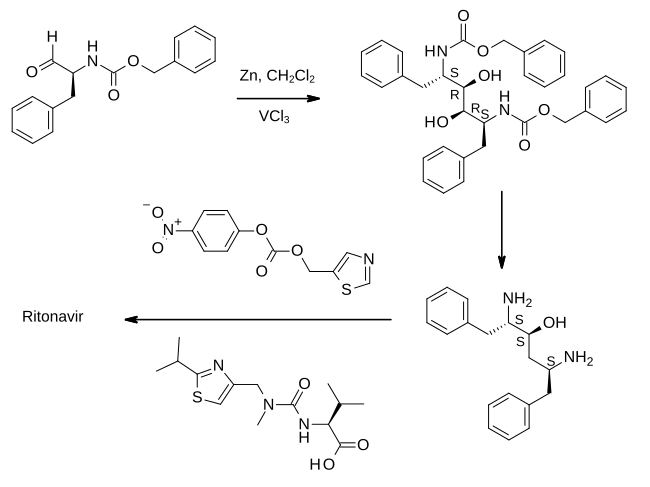
In the first step shown, an aldehyde derived from phenylalanine is treated with zinc dust in the presence of vanadium(III) chloride. This results in a pinacol coupling reaction which dimerises the material to provide an intermediate which is converted to its epoxide and then reduced to (2S,3S,5S)-2,5-diamino-1,6-diphenylhexan-3-ol. Importantly, this retains the absolute stereochemistry of the amino acid precursor. The diamine is then treated sequentially with two thiazole derivatives, each linked by an amide bond, to provide ritonavir.[23][24]
REF 23, 24 BELOW
- WO patent 1994014436, Kempf, Dale J.; Norbeck, Daniel W.; Sham, Hing Leung; Zhao, Chen; Sowin, Thomas J.; Reno, Daniel S.; Haight, Anthony R. and Cooper, Arthur J., “Retroviral protease inhibiting compounds”, published 1994-07-07, assigned to Abbott Laboratories
- ^ Vardanyan, Ruben; Hruby, Victor (2016). “34: Antiviral Drugs”. Synthesis of Best-Seller Drugs. pp. 698–701. doi:10.1016/B978-0-12-411492-0.00034-1. ISBN 9780124114920. S2CID 75449475.
SYN
EP 0674513; EP 0727419; JP 1996505844; JP 1997118679; JP 1998087639; WO 9414436 |
The oxidation of N-(benzyloxycarbonyl)-L-phenylalaninol (I) with oxalyl chloride in DMSO gives the corresponding aldehyde (II), which by dimerization with Zn dust in dichloromethane yields (2S,3R,4R,5S)-2,5-bis(benzyloxycarbonylamino)-1,6-diphenylhexane-3,4-diol (III) [along with the (2S,3S,4S,5S)-isomer]. The reaction of (III) with alpha-acetoxyisobutyryl bromide (IV) in hexane/dichloromethane affords (2S,3R,4R,5S)-2,5-bis(benzyloxycarbonylamino)-4-bromo-1,6-diphenylhexan-3-ol acetate ester (V), which is converted into the corresponding epoxide (VI) with NaOH in dioxane/water. The reduction of the epoxide (VI) with NaBH4 in THF affords (2S,3S,5S)-2,5-bis(benzyloxycarbonylamino)-1,6-diphenylhexan-3-ol (VII), which is deprotected with Ba(OH)2 in refluxing dioxane/water yielding the corresponding diamine (VIII). The cyclization of (VIII) with phenylboronic acid (IX) in refluxing toluene gives (4S,6S)-6-[1(S)-amino-2-phenylethyl]-4-benzyl-2-phenyl-1,3,2-oxaazaborinane (X), which is condensed with (5-thiazolylmethyl)(4-nitrophenyl)carbonate (XI) in THF to afford (2S,3S,5S)-5-amino-1,6-diphenyl-2-(5-thiazolylmethoxycarbonylamino) hexan-3-ol (XII). Finally, this compound is condensed with N-[N-(2-isopropylthiazol-4-ylmethyl)-N-methylaminocarbonyl]-L-valine (XIII) by means of 1-hydroxybenzotriazole (HBT) and N-[3-(dimethylamino)propyl]-N’-ethylcarbodiimide (DEC) in THF.
SYN
The thiazolyl carbonate (XI) has been synthesized as follows: The reaction of formamide (XIV) with P2S5 in ethyl ether gives thioformamide (XV), which is cyclized with 2-chloro-3-oxopropionic acid ethyl ester (XVI) [obtained by condensation of ethyl chloroacetate (XVII) with ethyl formate (XVIII) by means of t-BuOK in THF] yielding thiazol-5-carboxylic acid ethyl ester (XIX). The reduction of (XIX) with LiAlH4 in THF affords 5-thiazolylmethanol (XX), which is then esterified with 4-nitrophenyl chloroformate (XXI) by means of 4-methylmorpholine (MPH) in dichloromethane to give the desired product (XI).
SYN
The N-substituted valine (XIII) has been synthesized as follows: The reaction of isobutyramide (XXII) with phosphorus pentasulfide (P4S10) in ethyl ether gives the corresponding thioamide (XXIII), which is cyclized with 1,3-dichloroacetone (XXIV) by means of MgSO4 in refluxing acetone yielding 4-(chloromethyl)-2-isopropylthiazole (XXV). The reaction of (XXV) with methylamine in water affords N-(2-isopropylthiazol-4-ylmethyl)-N-methylamine (XXVI), which is condensed with N-(4-nitrophenoxycarbonyl)-L-valine methyl ester (XXVII) by means of 4-(dimethylamino)pyridine (DMAP) and triethylamine in refluxing THF to give the thiazol-substituted L-valine ester (XXVIII). Finally, this compound is converted into the corresponding free acid with LiOH in dioxane/water. The N-(4-nitrophenoxycarbonyl)-L-valine methyl ester (XXVII) has been synthesized by reaction of chloroformate (XXI) with L-valine methyl ester (XXIX) by means of 4-methylmorpholine (MPH) in dichloromethane.
SYN
Org Process Res Dev 1999,3(2),94 |
A new method for the preparation of a key diaminoalcohol intermediate in the synthesis of ritonavir has been described: The reaction of L-phenylalanine (XXIX) with benzyl chloride by means of K2CO3 and KOH in hot water gives N,N-dibenzyl-L-phenylalanine benzyl ester (XXX), which is condensed first with acetonitrile by means of NaNH2 and then with benzylmagnesium chloride, both reactions in methyl tert-butyl ether, yielding 5-amino-2-(dibenzylamino)-1,6-diphenylhex-4-en-3-one (XXXI). The reduction of (XXXI) with NaBH4 with an accurate control of the solvent and acidity, results in an enhanced enantioselectivity towards the desired (S,S,S)-enantiomer of 5-amino-2-(dibenzylamino)-1,6-diphenyl-3-hexanol (XXXII). Finally, this compound is deprotected by hydrogenation with ammonium formate over Pd/C in methanol/water to provide the target chiral diaminoalcohol (VIII).
SYN
Chem Commun (London) 2001,(2),203 |
he reaction of N-(tert-butoxycarbonyl)-L-phenylalanine methyl ester (I) with trimethylphosphonate lithium salt (II) in THF gives the dimethyl L-phenylalanylmethylphosphonate (III), which is condensed with 2-phenylacetaldehyde (IV) by means of Na2CO3 in ethanol yielding the diphenylhexenone (V). The reduction of the carbonyl group of (V) with NaBH4 in methanol affords a diastereomeric mixture of alcohols (VI) and (VII) from which the desired major isomer (VII) is separated by column chromatography.. The epoxidation of the double bond of (VII) with MCPBA in dichloromethane gives the epoxide (VIII) (1), which is cleaved with Red-Al in THF providing the diol (IX). The reaction of (IX) with Ms-Cl and DIEA yields the intermediate dimesylate (X) which, without isolation, affords oxazolidinone (XI). The reaction of (XI) with sodium azide and 18-C-6 in DMSO gives the azide (XII), which is treated with NaH and Boc2O in THF in order to cleave the oxazolidine ring and furnish the protected aminoalcohol (XIII). Finally the azido group of (XIII) is hydrogenate with H2 over Pd/C in methanol to afford the monoprotected diaminoalcohol (XIV) the target compound.
SYN
https://www.scielo.br/j/mioc/a/FT4WXwhbCPCkm7W6XdX4GHm/?lang=en
Ritonavir (2) – The first disclosure of ritonavir (2) is presented in a patent from 1994, assigned to Abbott Laboratories. Even though the patent consists of a range of Markush structures, among which is found (2), its synthesis is not presented.249 The synthetic pathway to obtain (2) was disclosed for the first time in a second-generation patent in 1995, by the same company.250,251 Some drawbacks related to the synthesis presented by Abbott include the employment of expensive condensing agents, as 1-Ethyl-3-(3-dimethylaminopropyl) carbodiimide (EDC) and poor reaction yields on the first steps of the synthetic pathway, making this strategy too expensive and not suitable for scale-up production. Considering the above deficiencies, a recent Chinese patent concerning the synthesis of ritonavir (2) has been released.
The synthetic pathway described in the patent starts with a nucleophilic addition-elimination reaction between the starting material (2-isopropylthiazol-4-yl)- nitro-methylamine (71) and N-[(2,2,2-trichloroethoxy)carbonyl]-L-valine (72), generating intermediate (73). The intermediate is mixed with p-toluenesulfonyl chloride and triethylamine to activate the acid function, followed by the addition of reagent (74) in a one-pot procedure. The condensation allows the formation of intermediate (75), which is submitted to acidic conditions for a Boc deprotection, followed by another nucleophilic addition-elimination reaction with reagent (76), thus obtaining the final product ritonavir (2) (Fig. 16).252 When comparing both patents, it is possible to highlight important advantages present in the latest one, including the use of cheap and easily available reagents, for instance, the use of p-toluenesulfonyl chloride as an amide condensing agent, the synthetic pathway has a high yield (79% overall), low cost and it is ease to scale-up the production.

SYN
US5543551

Reference:1. US5541206A / EP0402646B1.
Reference:1. Org. Process Res. Dev. 1999, 3, 94-100.
https://pubs.acs.org/doi/abs/10.1021/op9802071
Patent
2. WO2006090264A1.
Reference:1. Tetrahedron Lett. 2011, 52, 6968-6970.
SYN
Synthesis ReferenceUS5484801
SYN
Method of synthesis
i. Valine condensed with bis-trichloromethyl carbonate to give an intermediate compound 4-isopropyloxazolidine-2,5-dione.
ii. The intermediate compound is reacted with compound (1) to give compound (2).
ii. (2) reacts with bis-trichloromethyl carbonate followed by reaction with (2-isopropylthiazol-4-yl)-N-methylmethanamine to give compound (3).
iv. Primary amine group of (3) is subjected to deprotection by the removal of two benzyl groups to give compound (4).
v. (4) reacts with (5) to give Ritonavir in good yield.
CLICK ON BELOW IMAGE
CLIP
SYN
US5543551

SYN
Ruben Vardanyan, Victor Hruby, in Synthesis of Best-Seller Drugs, 2016
Lopinavir–Kaletra
The first report of a new protease inhibitor candidate lopinavir (34.1.21) seems to be Abbott’s patent [134].
The core of lopinavir is identical to that of ritonavir. The 5-thiazolyl end group in ritonavir was replaced by the phenoxyacetyl group, and the 2-isopropylthiazolyl group in ritonavir was replaced by a modified valine in which the amino terminus had a six-membered cyclic urea attached.
Synthetic strategy employed for the synthesis of multikilogram quantities of lopinavir is very similar to that implemented for ritonavir (34.1.22), but using the protected version (34.1.79) of the “core” diamino alcohol (34.1.55), which was sequentially acylated with the acid chlorides of (S)-3-methyl-2-(2-oxotetrahydropyrimidin-1(2H)-yl)butanoic acid (34.1.89) and 2-(2,6-dimethylphenoxy)acetic acid (34.1.94) [135,136].
The bulk synthesis of protected diamino alcohol (34.1.79) was proposed [137,138] by a method closely related to the method [122,123] for ritonavir. For that purpose L-phenylalanine (34.1.74) was sequentially trialkylated with benzyl chloride using a K2CO3/water system at reflux to produce a tribenzylated product (34.1.75). A solution with generated acetonitrile anion in THF was added to the benzylated product (34.1.75) at less than −40°C to yield the cyanomethylketone (34.1.76), which was exposed to Grignard reagent–benzyl magnesium chloride to produce an enaminone (34.1.77). No racemization was observed in these two steps. The addition of the obtained enaminone (34.1.77) in THF/PrOH to a solution of NaBH4 and MsOH in THF at 5°C produced an intermediate aminoketone (34.1.78). No further reduction of the keto group occurs under these conditions. Reduction of the keto group could proceed by addition of a preformed solution of sodium tris(trifluoroacetoxy)borohydride in tetrahydrofuran [NaBH3(OTFA)], which produces a mixture of amino alcohols composed of 93% of the desired (2S)-5-amino-2-(dibenzylamino)-1,6-diphenylhexan-3-ol (34.1.79) along with 7% of the three undesired diastereomers. The crude mixture was debenzylated (Pd-C, HCONH4), and the product was purified by precipitation from iPrOH/HCl (aq) to produce (34.1.55) in greater than 99% purity and in high yield (Scheme 34.8.).

An efficient synthesis of each of the side chain moieties and their coupling with the “core” diamino alcohol derivatives was developed as follows: (S)-3-methyl-2-(2-oxotetrahydropyrimidin-1(2H)-yl)butanoic acid (34.1.85) was prepared starting from L-valine (34.1.80), which was first converted to N-phenoxycarbonyl-L-valine (34.1.82) with phenylchloroformate (34.1.81). Accurate pH monitoring (pH 9.5 to 10.2) was necessary and LiOH was found to be a superior base. Control of pH was essential as the valine dimer and its derivatives were formed as reaction byproducts outside of this pH margin. LiCl was added to provide a lower freezing point to the aqueous solution and neutral Al2O3 was added to prevent gumming and emulsion formation during the course of the reaction.
Treatment of N-phenoxycarbonyl-L-valine (34.1.82) with 3-chloropropylamine hydrochloride (34.1.3) and solid NaOH in THF produced the unisolated salt of chloropropylurea (34.1.84), which was then treated with t-BuOK, effecting cyclization to produce the desired acid (34.1.85) in 75 to 85% yield and in greater than 99% enantiomeric excess. Acylation of (34.1.79) with synthesized acid (34.1.85) was initially achieved by well-known peptide coupling methods. Optimization of this transformation allowed the discovery of a more cost-effective method for implementing acyl chloride (34.1.86), which was easily prepared using thionyl chloride in THF at room temperature.
The reaction of dibenzylamino alcohols (34.1.79) with acyl chloride (34.1.86) in the presence of 3.0 equivalents of imidazole in EtOAc and DMF produced acylated intermediate (34.1.87) as a mixture of diastereomers, which, without any further purification, was subjected to debenzylation with Pd/C and HCO2NH4 in MeOH at 50°C, which proceeded without significant complications to produce (34.1.88).
Exposure of crude (34.1.88) to L-pyroglutamic acid (34.1.89) in dioxane at 50°C followed by cooling, allowed for the isolation of (S)-N-((2S,4S,5S)-5-amino-4-hydroxy-1,6-diphenylhexan-2-yl)-3-methyl-2-(2-oxotetrahydropyrimidin-1(2H)-yl)butanamide (34.1.90) pyroglutamic salt as virtually a single diastereomer in high yield (Scheme 34.9.).

Acyl chloride (34.1.92) was prepared by the reaction of 2-(2,6-dimethylphenoxy)acetic acid (34.1.91) with thionyl chloride in EtOAc, at room temperature adding a single drop of DMF, and warming the slurry to 50°C, which produced a clear solution of (34.1.92) that was used in the subsequent acylation of amine (34.1.90). Reaction of pyroglutamate salt (34.1.90) with acyl chloride (34.1.95) in ethyl acetate under Schotten-Baumann reaction conditions (use of a two-phase solvent system) in the presence of a water solution of NaHCO3 for liberation of free amine, produced the desired lopinavir (34.1.21) in high yield and purity (Scheme 34.10.).

Lopinavir is a novel and strong protease inhibitor developed from ritonavir with high specificity for HIV-1 protease [139-141]. It is indicated, in combination with other antiretroviral agents, for the treatment of HIV-1 infection. Numerous clinical trials have shown that lopinavir/ritonavir (Kaletra) is highly effective as a component of highly active antiretroviral therapy [142,143].
Ritonavir is indicated in combination with other antiretroviral agents for the treatment of HIV-1-infected patients (adults and children of two years of age and older).[1][2]
PATENT
https://patents.google.com/patent/EP1133485B1/en
- Ritonavir (CAS Number [155213-67-5]), the structural formula of which is given below,is an inhibitor of human HIV protease which was described for the first time by Abbott in International Patent Application WO 94/14436, together with the process for the preparation thereof.
- [0002]
In the synthesis scheme given in WO 94/14436, Ritonavir is manufactured starting from valine and from compounds 1, 4 and 7, the structural formulae of which are also given below. - [0003]
The synthesis process in question was subsequently optimised in its various parts by Abbot, who then described and claimed the individual improvements in the patent documents listed below: US 5,354,866, US 5,541,206, US 5,491,253, WO98/54122, WO 98/00393 and WO 99/11636. - [0004]
The process for the synthesis of Ritonavir carried out on the basis of the above-mentioned patent documents requires, however, a particularly large number of intermediate stages; it is also unacceptable from the point of view of so-called “low environmental impact chemical synthesis” (B.M.Trost Angew. Chem. Int. Ed. Engl. (1995) 34, 259-281) owing to the increased use of activating groups and protective groups which necessitate not inconsiderable additional work in disposing of the by-products of the process, with a consequent increase in the overall manufacturing costs. - [0005]
The object of the present invention is therefore to find a process for the synthesis of Ritonavir which requires a smaller number of intermediate stages and satisfies the requirements of low environmental impact chemical synthesis, thus limiting “waste of material”. - [0006]
A process has now been found which, by using as starting materials the same compounds as those used in WO 94/14436, leads to the formation of Ritonavir in only five stages and with a minimum use of carbon atoms that are not incorporated in the final molecule.
EXAMPLESStage 1
- [0014]
ReagentMolecular weightAmountMmolEq.Amine 1464.6515 g32.2821Val-NCA 2142.136.9 g48.5471.5Triethylamine101.194.5 ml32.2831 (d = 0.726) Dichloromethane 108 ml Sol. 0.3 M - [0015]
Compound Val-NCA 2 was added to a solution of amine 1 (note 1, 2) in dichloromethane (60 ml) at -15°C under nitrogen followed by a solution of triethylamine in dichloromethane (48 ml) (note 3). The reaction mixture was maintained under agitation at from -15° to -13°C for two hours (note 4). The solution was used directly for the next stage without further purification.
- Note 1. Amine 1 was prepared using the procedure described in A.R. Haight et al. Org. Proc. Res. Develop. (1999) 3, 94-100.
- Note 2. Amine 1 was a mixture of stereoisomers with a ratio of 80 : 3.3 : 2.1 : 1.9.
- Note 3. This solution was added dropwise over a period of 25 minutes.
- Note 4. HPLC analysis after 2 hours: Amide 3 70.2 % – starting material 4.3 %
Stage 2
- [0016]
ReagentMolecular weightAmountMmolEq.Amine 3 Solution from stage 1563.78 32.2821Triethylamine101.19 (d = 0.726)2.6 ml18.6540.6Bis(trichloromethyl) carbonate (BTC)296.753.5 g11.7940.36dichloromethane 65 ml N-Methyl-4-aminomethyl-2-isopropylthiazole 4170.275.5 g32.2821triethylamine101.196.9 ml49.5041.5 (d = 0.726) Dichloromethane 52 ml - [0017]
The triethylamine was added slowly to the solution of amine 3 resulting from stage 1 and this mixture was in turn added slowly to a solution of BTC in dichloromethane (65 ml) at from -15° to -13°C and the reaction mixture was maintained under agitation at that temperature for 1.5 hours (note 1). A solution of amine 4 and triethylamine in dichloromethane (52 ml) was then added slowly to the reaction mixture (note 2) and maintained under agitation at that temperature for one hour (note 3). The reaction was stopped with water (97 ml) and the two phases were separated. The organic phase was washed with a 10% aqueous citric acid solution, filtered over Celite and evaporated with a yield of 25 g of crude urea 5 which was purified by flash chromatography on silica gel (eluant: toluene – ethyl acetate 6:4) to give 9.4 g of pure compound 5 (total yield of the two stages 38%) (note 4).
- Note 1. HPLC analysis after 1.5 hours of the reaction stopped in tert-butylamine: Amide 3 = 0.41 % – intermediate isocyanate = 61.3 %
- Note 2. The solution of amine 4 was added over a period of approximately 20 minutes.
- Note 3. HPLC analysis after 1 hour: Amide 3 = 7 % – Urea 5 = 54 %
- Note 4. 1H-NMR (CDCl3, 600 MHz) δ 7.31 (m, 4H), 7.28-7.24 (m, 4H), 7.21-7.14 (m, 8H), 7.11 (d, 2H), 7.05 (d, 2H), 6.96 (s, 1H), 6.75 (bd, 1H), 5.96 (bs, 1H), 4.48 (d, 1H), 4.39 ( d, 1H), 4.13 (dd, 1H), 4.09 (m, 1H), 3.93 (bd, 2H), 3.56 (bt, 1H), 3.39 (d, 2H), 3.28 (m, 1H), 3.04 (dd, 1H), 2.97 (s, 3H), 2.89 (m, 1H), 2.74 (q, 1H), 2.61 (m, 2H), 2.25 (m, 1H), 1.53 ( ddd, 1H), 1.38 (d, 6H), 1.28 (dt, 1H), 0.98 (d, 3H), 0.91 (d, 3H).
Stage 3
- [0018]
ReagentMolecular weightAmountMmolEq.Urea 5760.053.5 g4.6051Pd(OH)2/C 20% 5.25 g 30% w/wAcetic acid 31 ml Sol. 0.15 M - [0019]
The Pearlman catalyst (note 1) was added to a solution of urea 5 in acetic acid and the mixture was hydrogenated for 5 hours at from 4 to 4.5 bar and from 78 to 82°C (note 2). The catalyst was filtered and the solvent was removed under reduced pressure. The crude product was dissolved in water (35 ml), the pH was adjusted to a value of 8 with NaOH, and extracted with CH2Cl2 (2×15 ml). The organic phase was washed with water (10 ml) and the solvent was evaporated under reduced pressure with a yield of 1.8 g of amine 6 as a free base which was used for the next stage without further purification (note 3, 4).
- Note 1. Of the various reaction conditions tested, such as HCOONH4/Pd-C in MeOH, H2/Pd-C in methanol, H2Pd-C/CH3SO3H in methanol, H2/Pd(OH)2/C in methanol, etc., the best conditions we have found hitherto are those described in this Example.
- Note 2. HPLC analysis after 5 hours: amine 6 = 52 % – monobenzyl derivative = 9.3%.
- Note 3. HPLC analysis on the free base: amine 6 = 54 % – monobenzyl derivative = 6%.
- Note 4. 1H-NMR (CDCl3, 600 MHz) δ 7.29 (m, 4H), 7.22-7.14 (m, 6H), 7.00 (s, 1H), 6.83 (bd, 1H), 6.15 (bs, 1H), 4.49 (d, 1H), 4.41 ( d, 1H), 4.25 (m, 1H), 4.08 (m, 1H), 3.38 (m, 1H), 3.29 (m, 1H), 2.99 (s, 3H), 2.92 (dd 1H), 2.84 (m, 2H), 2.76 (m, 1H), 2.47 (m, 1H), 2.28 (m, 1H), 1.76 ( dt, 1H), 1.61 (dt, 1H), 1.38 (d, 6H), 0.95 (d, 3H), 0.89 (d, 3H).
Stage 4
- [0020]
ReagentMolecular weightAmountMmolEq.Amine 6579.801.8 g3.101Compound 7.HCl316.701.28 g4.031.3NaHCO384.00370 mg4.401.4Ethyl acetate 31 ml Sol. 0.1M - [0021]
A solution of the chloride of compound 7 in ethyl acetate was treated with an aqueous sodium bicarbonate solution. The phases were separated and the organic phase was added to a solution of amine 6 in ethyl acetate. The reaction mixture was heated at 60°C for 12 hours, then concentrated; ammonia was added and the solution was maintained under agitation for 1 hour. The organic phase was washed with a 10% aqueous potassium carbonate solution (3x5ml) and with a saturated sodium chloride solution (5 ml); the solvent was removed under reduced pressure. The crude product was purified by flash chromatography on silica gel (eluant ethyl acetate) to give 900 mg of pure Ritonavir (total yield of the two stages 27 %) (note 1).
- Note 1. 1H-NMR (DMSO, 600 MHz) δ 9.05(s, 1H), 7.86 (s, 1H), 7.69 (d, 1H), 7.22-7.10 (m,11H), 6.88 (d, 1H), 6.02 (d, 1H), 5.16 (d, 1H), 5.12 (d, 1H), 4.60 (bs, 1H), 4.48 (d, 1H), 4.42 (d, 1H), 4.15 (m, 1H), 3.94 (dd, 1H), 3.83 (m, 1H), 3.59 (bt, 1H), 3.23 (m, 1H), 2.87 (s, 3H), 2.69-2.63 (m, 3H), 2.60 (m, 1H), 1.88 (m, 1H), 1.45 (m, 2H), 1.30 (d, 6H), 0.74 (d, 6H).
Side effects
When administered at the initially tested higher doses effective for anti-HIV therapy, the side effects of ritonavir are those shown below.[10]
- asthenia, malaise
- diarrhea
- nausea and vomiting
- abdominal pain
- dizziness
- insomnia
- sweating
- taste abnormality
- metabolic effects, including
- hypercholesterolemia
- hypertriglyceridemia
- elevated transaminases
- elevated creatine kinase
One of ritonavir’s side effects is hyperglycemia, through inhibition of the GLUT4 insulin-regulated transporter, thus keeping glucose from entering fat and muscle cells.[medical citation needed] This can lead to insulin resistance and cause problems for people with type 2 diabetes.[medical citation needed]
Drug interactions
Ritonavir induces CYP 1A2 and inhibits the major P450 isoforms 3A4 and 2D6.[according to whom?][medical citation needed] Concomitant therapy of ritonavir with a variety of medications may result in serious and sometimes fatal drug interactions.[11] The list of clinically significant interactions of ritonavir includes the following drugs:
Mechanism of action
Ritonavir was originally developed as an inhibitor of HIV protease, one of a family of pseudo-C2-symmetric small molecule inhibitors.
Ritonavir (center) bound to the active site of HIV protease.[medical citation needed]
Ritonavir is now rarely used for its own antiviral activity but remains widely used as a booster of other protease inhibitors. More specifically, ritonavir is used to inhibit a particular enzyme, in intestines, liver, and elsewhere, that normally metabolizes protease inhibitors, cytochrome P450-3A4 (CYP3A4).[16] The drug binds to and inhibits CYP3A4, so a low dose can be used to enhance other protease inhibitors. This discovery drastically reduced the adverse effects and improved the efficacy of protease inhibitors and HAART. However, because of the general role of CYP3A4 in xenobiotic metabolism, dosing with ritonavir also affects the efficacy of numerous other medications, adding to the challenge of prescribing drugs concurrently.[medical citation needed][17][better source needed]
Pharmocodymanics and pharmacokinetics
The capsules of the medication do not have the same bioavailability as the tablets.[2]
History
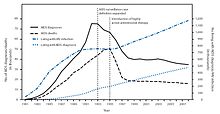
New HIV infections and deaths, before and after the FDA approval of “highly active antiretroviral therapy”,[18] of which saquinavir and ritonavir were key as the first two protease inhibitors.[medical citation needed] As a result of the new therapies, HIV deaths in the United States fell dramatically within two years.[18]
Ritonavir is manufactured as Norvir by AbbVie, Inc..[citation needed] The US Food and Drug Administration (FDA) approved ritonavir on March 1, 1996,[19] making it the seventh U.S.-approved antiretroviral drug and the second U.S.-approved protease inhibitor (after saquinavir four months earlier).[citation needed] As a result of the introduction of new “highly active antiretroviral thearap[ies]”—of which the protease inhibitors ritonavir and saquinavir were critical[citation needed]—the annual U.S. HIV-associated death rate fell from over 50,000 to about 18,000 over a period of two years.[20][21]
In 2003, Abbott (now AbbVie, Inc.) raised the price of a Norvir course from US$1.71 per day to US$8.57 per day, leading to claims of price gouging by patients’ groups and some members of Congress. Consumer group Essential Inventions petitioned the NIH to override the Norvir patent, but the NIH announced on August 4, 2004, that it lacked the legal right to allow generic production of Norvir.[22]
In 2014, the FDA approved a combination of ombitasvir/paritaprevir/ritonavir for the treatment of hepatitis C virus (HCV) genotype 4,[3] where the presence of ritonavir again capitalizes on its inhibitory interaction with the human drug metabolic enzyme CYP3A4.
Polymorphism and temporary market withdrawal
Ritonavir was originally dispensed as an ordinary capsule that did not require refrigeration. This contained a crystal form of ritonavir that is now called form I.[23] However, like many drugs, crystalline ritonavir can exhibit polymorphism, i.e., the same molecule can crystallize into more than one crystal type, or polymorph, each of which contains the same repeating molecule but in different crystal packings/arrangements. The solubility and hence the bioavailability can vary in the different arrangements, and this was observed for forms I and II of ritonavir.[24]
During development—ritonavir was introduced in 1996—only the crystal form now called form I was found; however, in 1998, a lower free energy,[25] more stable polymorph, form II, was discovered. This more stable crystal form was less soluble, which resulted in significantly lower bioavailability. The compromised oral bioavailability of the drug led to temporary removal of the oral capsule formulation from the market.[24] As a consequence of the fact that even a trace amount of form II can result in the conversion of the more bioavailable form I into form II, the presence of form II threatened the ruin of existing supplies of the oral capsule formulation of ritonavir; and indeed, form II was found in production lines, effectively halting ritonavir production.[23] Abbott (now AbbVie) withdrew the capsules from the market, and prescribing physicians were encouraged to switch to a Norvir suspension.[citation needed]
The company’s research and development teams ultimately solved the problem by replacing the capsule formulation with a refrigerated gelcap.[when?][citation needed] In 2000, Abbott (now AbbVie) received FDA-approval for a tablet formulation of lopinavir/ritonavir (Kaletra) which contained a preparation of ritonavir that did not require refrigeration.[26]
Research
In 2020, the fixed-dose combination of lopinavir/ritonavir was found not to work in severe COVID-19.[27] In the trial the medication was started around thirteen days after the start of symptoms.[27] Virtual screening of the 1930 FDA-approved drugs followed by molecular dynamics analysis predicted ritonavir blocks the binding of the SARS-CoV-2 spike (S) protein to the human angiotensin-converting enzyme-2 (hACE2) receptor, which is critical for the virus entry into human cells.[28]
References
- ^ Jump up to:a b “Norvir EPAR”. European Medicines Agency (EMA). Retrieved 20 August 2020. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ Jump up to:a b c d e f g h i j k “Ritonavir”. The American Society of Health-System Pharmacists. Archived from the original on 2015-10-17. Retrieved Oct 23, 2015.
- ^ Jump up to:a b “FDA approves Viekira Pak to treat hepatitis C”. Food and Drug Administration. December 19, 2014. Archived from the original on October 31, 2015.
- ^ “Ritonavir Pregnancy and Breastfeeding Warnings”. drugs.com. Archived from the original on 7 September 2015. Retrieved 23 October 2015.
- ^ Jump up to:a b British National Formulary 69 (69 ed.). Pharmaceutical Pr. March 31, 2015. p. 426. ISBN 9780857111562.
- ^ Hacker, Miles (2009). Pharmacology principles and practice. Amsterdam: Academic Press/Elsevier. p. 550. ISBN 9780080919225.
- ^ Fischer, Jnos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 509. ISBN 9783527607495.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ “First Generic Drug Approvals”. U.S. Food and Drug Administration (FDA). Retrieved 13 February 2021.
- ^ “Norvir side effects (Ritonavir) and drug interactions – prescription drugs and medications at RxList”. June 27, 2007. Archived from the original on 2007-06-27.
- ^ “Ritonavir: Drug Information Provided by Lexi-Comp: Merck Manual Professional”. April 30, 2008. Archived from the originalon 2008-04-30.
- ^ Henry, J. A.; Hill, I. R. (1998). “Fatal interaction between ritonavir and MDMA”. Lancet. 352 (9142): 1751–1752. doi:10.1016/s0140-6736(05)79824-x. PMID 9848354. S2CID 45334940.
- ^ Papaseit, E.; Vázquez, A.; Pérez-Mañá, C.; Pujadas, M.; De La Torre, R.; Farré, M.; Nolla, J. (2012). “Surviving life-threatening MDMA (3,4-methylenedioxymethamphetamine, ecstasy) toxicity caused by ritonavir (RTV)”. Intensive Care Medicine. 38 (7): 1239–1240. doi:10.1007/s00134-012-2537-9. PMID 22460853. S2CID 19375709.
- ^ Nieminen, Tuija H.; Hagelberg, Nora M.; Saari, Teijo I.; Neuvonen, Mikko; Neuvonen, Pertti J.; Laine, Kari; Olkkola, Klaus T. (2010). “Oxycodone concentrations are greatly increased by the concomitant use of ritonavir or lopinavir/ritonavir”. European Journal of Clinical Pharmacology. 66 (10): 977–985. doi:10.1007/s00228-010-0879-1. ISSN 0031-6970. PMID 20697700. S2CID 25770818.
- ^ Hsieh, Yi-Ling; Ilevbare, Grace A.; Van Eerdenbrugh, Bernard; Box, Karl J.; Sanchez-Felix, Manuel Vincente; Taylor, Lynne S. (2012-05-12). “pH-Induced Precipitation Behavior of Weakly Basic Compounds: Determination of Extent and Duration of Supersaturation Using Potentiometric Titration and Correlation to Solid State Properties”. Pharmaceutical Research. 29 (10): 2738–2753. doi:10.1007/s11095-012-0759-8. ISSN 0724-8741. PMID 22580905. S2CID 15502736.
- ^ Zeldin RK, Petruschke RA (2004). “Pharmacological and therapeutic properties of ritonavir-boosted protease inhibitor therapy in HIV-infected patients”. Journal of Antimicrobial Chemotherapy. 53 (1): 4–9. doi:10.1093/jac/dkh029. PMID 14657084.
- ^ “Drug Development and Drug Interactions: Table of Substrates, Inhibitors and Inducers”. U.S. Food and Drug Administration(FDA). December 3, 2019.
- ^ Jump up to:a b (PDF)https://web.archive.org/web/20150924044850/http://www.cdc.gov/mmwr/PDF/wk/mm6021.pdf. Archived from the original (PDF)on 2015-09-24. Retrieved 2020-02-17. Missing or empty
|title=(help) - ^ “Ritonavir FDA approval package” (PDF). 1 March 1996.
- ^ “HIV Surveillance—United States, 1981-2008”. Archived from the original on 9 November 2013. Retrieved 8 November 2013.
- ^ The CDC, in its Morbidity and Mortality Weekly Report, ascribes this to “highly active antiretroviral therapy”, without mention of either of these drugs, see the preceding citation. A further citation is needed to make this accurate connection between this drop and the introduction of the protease inhibitors.
- ^ Ceci Connolly (2004-08-05). “NIH Declines to Enter AIDS Drug Price Battle”. The Washington Post. Archived from the original on 2008-08-20. Retrieved 2006-01-16.
- ^ Jump up to:a b Bauer J; et al. (2001). “Ritonavir: An Extraordinary Example of Conformational Polymorphism”. Pharmaceutical Research. 18 (6): 859–866. doi:10.1023/A:1011052932607. PMID 11474792. S2CID 20923508.
- ^ Jump up to:a b S. L. Morissette; S. Soukasene; D. Levinson; M. J. Cima; O. Almarsson (2003). “Elucidation of crystal form diversity of the HIV protease inhibitor ritonavir by high-throughput crystallization”. Proc. Natl. Acad. Sci. USA. 100 (5): 2180–84. doi:10.1073/pnas.0437744100. PMC 151315. PMID 12604798.
- ^ Lüttge, Andreas (February 1, 2006). “Crystal dissolution kinetics and Gibbs free energy”. Journal of Electron Spectroscopy and Related Phenomena. 150 (2): 248–259. doi:10.1016/j.elspec.2005.06.007.
- ^ “Kaletra FAQ”. AbbVie’s Kaletra product information. AbbVie. 2011. Archived from the original on 7 July 2014. Retrieved 5 July2014.
- ^ Jump up to:a b Cao, Bin; Wang, Yeming; Wen, Danning; Liu, Wen; Wang, Jingli; Fan, Guohui; et al. (18 March 2020). “A Trial of Lopinavir–Ritonavir in Adults Hospitalized with Severe Covid-19”. New England Journal of Medicine. 382 (19): 1787–1799. doi:10.1056/NEJMoa2001282. PMC 7121492. PMID 32187464.
- ^ Bagheri, Milad; Niavarani, Ahmadreza (2020-10-08). “Molecular dynamics analysis predicts ritonavir and naloxegol strongly block the SARS-CoV-2 spike protein-hACE2 binding”. Journal of Biomolecular Structure and Dynamics: 1–10. doi:10.1080/07391102.2020.1830854. ISSN 0739-1102. PMID 33030105. S2CID 222217607.
Further reading
- Chemburkar, Sanjay R.; Bauer, John; Deming, Kris; Spiwek, Harry; Patel, Ketan; Morris, John; Henry, Rodger; Spanton, Stephen; et al. (2000). “Dealing with the Impact of Ritonavir Polymorphs on the Late Stages of Bulk Drug Process Development”. Organic Process Research & Development. 4 (5): 413–417. doi:10.1021/op000023y.
External links
- “Ritonavir”. Drug Information Portal. U.S. National Library of Medicine.
| Clinical data | |
|---|---|
| Trade names | Norvir |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a696029 |
| License data | EU EMA: by INNUS DailyMed: Ritonavir |
| Pregnancy category | AU: B3 |
| Routes of administration | By mouth |
| ATC code | J05AE03 (WHO) |
| Legal status | |
| Legal status | AU: S4 (Prescription only)CA: ℞-onlyUK: POM (Prescription only)US: ℞-onlyEU: Rx-only [1] |
| Pharmacokinetic data | |
| Protein binding | 98-99% |
| Metabolism | Liver |
| Elimination half-life | 3-5 hours |
| Excretion | mostly fecal |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 155213-67-5 |
| PubChem CID | 392622 |
| DrugBank | DB00503 |
| ChemSpider | 347980 |
| UNII | O3J8G9O825 |
| KEGG | D00427 |
| ChEBI | CHEBI:45409 |
| ChEMBL | ChEMBL163 |
| NIAID ChemDB | 028478 |
| PDB ligand | RIT (PDBe, RCSB PDB) |
| CompTox Dashboard (EPA) | DTXSID1048627 |
| ECHA InfoCard | 100.125.710 |
| Chemical and physical data | |
| Formula | C37H48N6O5S2 |
| Molar mass | 720.95 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (what is this?) (verify) |
/////////////RITONAVIR, Antiviral, Peptidomimetics, HIV Protease Inhibitor, A-84538, Abbott 84538, ABBOTT-84538, ABT 538, ABT-538, DRG-0244, NSC-693184, TMC 114r
CC(C)[C@H](NC(=O)N(C)CC1=CSC(=N1)C(C)C)C(=O)N[C@H](C[C@H](O)[C@H](CC1=CC=CC=C1)NC(=O)OCC1=CN=CS1)CC1=CC=CC=C1

NEW DRUG APPROVALS
ONE TIME
$10.00
BUPIVACAINE
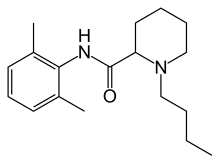
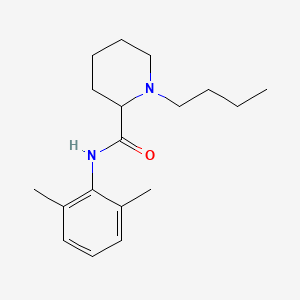
Bupivacaine
cas 38396-39-3, MF C18H28N2O, Average: 288.4277
1-butyl-N-(2,6-dimethylphenyl)piperidine-2-carboxamide
- AH 250
- DUR-843
- LAC-43
- SKY 0402
- SKY-0402
- SKY0402
- Win 11318
2-Piperidinecarboxamide, 1-butyl-N-(2,6-dimethylphenyl)-, hydrochloride, hydrate (1:1:1), cas 73360-54-0
Molecular Formula, C18H28N2O.ClH.H2O
Bupivan (Sun) / Carbostesin (AstraZeneca) / Marcain (AstraZeneca) / Marcaina (AstraZeneca) / Posimir (Durect) / Sensorcaine-MPF (Astra Zeneca) / Xaracoll (Innocoll Holdings Limited)
Product Ingredients
| INGREDIENT | UNII | CAS | INCHI KEY |
|---|---|---|---|
| Bupivacaine hydrochloride | 7TQO7W3VT8 | 73360-54-0 | HUCIWBPMHXGLFM-UHFFFAOYSA-N |
| Bupivacaine hydrochloride anhydrous | AKA908P8J1 | 18010-40-7 | SIEYLFHKZGLBNX-UHFFFAOYSA-N |
BupivacaineCAS Registry Number: 2180-92-9
CAS Name: 1-Butyl-N-(2,6-dimethylphenyl)-2-piperidinecarboxamide
Additional Names:dl-1-butyl-2¢,6¢-pipecoloxylidide; 1-n-butyl-2¢,6¢-dimethyl-2-piperidinecarboxanilide; dl-N-n-butylpipecolic acid 2,6-xylidide; 1-butyl-2-(2,6-xylylcarbamoyl)piperidine; dl-1-n-butylpiperidine-2-carboxylic acid 2,6-dimethylanilide
Molecular Formula: C18H28N2O
Molecular Weight: 288.43
Percent Composition: C 74.95%, H 9.78%, N 9.71%, O 5.55%
Literature References: Prepn: B. Ekenstam et al.,Acta Chem. Scand.11, 1183 (1957); B. T. Ekenstam, B. G. Pettersson, US2955111 (1960 to AB Bofors). Resolution of isomers: B. F. Tullar, J. Med. Chem.14, 891 (1971). Stereospecific synthesis: B. Adger et al.,Tetrahedron Lett.37, 6399 (1996).Pharmacology of racemate: F. Henn, R. Brattsand, Acta Anaesthesiol. Scand. Suppl.21, 9 (1966), C.A.66, 17863u (1967); of isomers: F. P. Luduena et al.,Arch. Int. Pharmacodyn.200, 359 (1972). Clinical pharmacokinetics: D. W. Blake et al.,Anaesth. Intensive Care22, 522 (1994). Comprehensive description: T. D. Wilson, Anal. Profiles Drug Subs.19, 59-94 (1990). Review of use in spinal anesthesia: Acta Anaesthesiol. Scand.35, 1-10 (1991). Review of pharmacology and clinical efficacy of levobupivacaine: K. J. McClellan, C. M. Spencer, Drugs56, 355-362 (1998).Properties: mp 107.5-108°. pKa 8.09; also reported as 8.17. Partition coefficient: (oleyl alcohol/water) 1565; (n-heptane/pH 7.4 buffer) 27.5.
Melting point: mp 107.5-108°
pKa: pKa 8.09; also reported as 8.17
Log P: Partition coefficient: (oleyl alcohol/water) 1565; (n-heptane/pH 7.4 buffer) 27.5
Derivative Type: Hydrochloride monohydrate
CAS Registry Number: 14252-80-3
Manufacturers’ Codes: AH-2250; LAC-43
Trademarks: Carbostesin (AstraZeneca); Marcaine (AstraZeneca); Sensorcaine (AstraZeneca)
Molecular Formula: C18H28N2O.HCl.H2O
Molecular Weight: 342.90
Percent Composition: C 63.05%, H 9.11%, N 8.17%, O 9.33%, Cl 10.34%
Properties: White, odorless crystalline powder. mp 258.5°. Slightly sol in acetone, chloroform, ether. Soly (mg/ml): water 40; alcohol 125. LD50 in mice (mg/kg): 7.8 i.v., 82 s.c. (Henn, Brattsand).
Melting point: mp 258.5°
Toxicity data: LD50 in mice (mg/kg): 7.8 i.v., 82 s.c. (Henn, Brattsand)
Derivative Type: (-)-Form
CAS Registry Number: 27262-47-1
Additional Names: Levobupivacaine; (S)-bupivacaine
Properties: Crystals from isopropanol, mp 135-137°. [a]D25 -80.9° (c = 5 in methanol).
Melting point: mp 135-137°
Optical Rotation: [a]D25 -80.9° (c = 5 in methanol)
Derivative Type: (-)-Form hydrochloride
CAS Registry Number: 27262-48-2
Trademarks: Chirocaine (Abbott)
Molecular Formula: C18H28N2O.HCl
Molecular Weight: 324.89
Percent Composition: C 66.54%, H 9.00%, N 8.62%, O 4.92%, Cl 10.91%
Properties: mp 255-257°. [a]D25 -12.3° (c = 2 in water).
Melting point: mp 255-257°
Optical Rotation: [a]D25 -12.3° (c = 2 in water)
Therap-Cat: Anesthetic (local).
Keywords: Anesthetic (Local).
Other Names for this Substance
- 2-Piperidinecarboxamide, 1-butyl-N-(2,6-dimethylphenyl)-, hydrochloride, hydrate (1:1:1)
- 2-Piperidinecarboxamide, 1-butyl-N-(2,6-dimethylphenyl)-, monohydrochloride, monohydrate
- Bupivacaine hydrochloride monohydrate
- Marcain Heavy
- Marcain
(-)-Bupivacaine hydrochloride, Levobupivacaine hydrochloride, Chirocaine
Synthesis Reference
Thuresson, B. and Egner, B.P.H.; U.S. Patent 2,792,399; May 14, 1957; assigned to AB Bofors, Sweden. Thuresson, B. and Pettersson, B.G.; US. Patent 2,955.1 11; October 4,1960; assigned to AB Bofors, Sweden., US2955111
SYN
British Patent 869,978 (1959).

SYN
Bupivacaine, N-2,6-(dimethyl)1-butyl-2-piperidincarboxamide (2.2.7), is chemically similar to mepivacaine and only differs in the replacement of the N-methyl substituent on the piperidine ring with an N-butyl substituent. There are also two suggested methods of synthesis. The first comes from α-picolin-2,6-xylidide (2.2.4). The alkylation of the last with butyl bromide gives the corresponding pyridine salt (2.2.6). Finally, it is reduced by hydrogen using platinum oxide as a catalyst into a piperidine derivative—bupivacaine [13,16].

The other method results directly from the piperidine-2-carboxylic acid chloride, which is reacted with 2,6-dimethylaniline. The resulting amide (2.2.8) is further alkylated with butyl bromide to bupivacaine [17–19].

Like lidocaine and mepivacaine, bupivacaine is used in infiltration, spinal, and epidural anesthesia in blocking nerve transmission. Its most distinctive property is its long-lasting action. It is used for surgical intervention in urology and in lower thoracic surgery from 3 to 5 h in length, and in abdominal surgery lasting from 45 to 60 min. It is used to block the trifacial nerve, the sacral and brachial plexuses, in resetting dislocations, in epidural anesthesia, and during Cesarian sections. The most common synonym for bupivacaine is marcaine.
SYN
3.7 Bupivacaine (21293) and Levobupivacaine (1976)
Bupivacaine (3.1.41) (Marcaine) is a local anesthetic of great potency and long duration that has been widely used for years, but it has cardio and CNS toxic sideeffects. For many years it was nearly the only local anesthetic applicable to almost all kinds of loco-regional anesthetic techniques, and nowadays, in many occasions, it is still the only alternative available [61–64].
Bupivacaine is currently used in racemic form. At high doses, however, the racemate is potentially hazardous due to toxicity problems.
Currently, racemic bupivacaine (3.1.41) is produced from picolinic acid (3.1.38) either by reduction to pipecolic acid (3.1.39) and then, after conversion to corresponding acid chloride (3.1.40) coupling with 2,6-xylidine to give pipecolic acid-2,6-xylidide (3.1.33), or by reducing the pyridyl amide (3.1.43) prepared from picolinic acid chloride (3.1.42) over platinum oxide. The amide intermediate (3.1.33), which can also be used to prepare the anesthetics ropivacaine (3.1.37) and mepivacaine (3.1.31), was transformed to desired bupivacaine (3.1.41) either by direct alkylation using butyl bromide and potassium carbonate or by reductive amination using butyraldehyde [45,59,65–69] (Scheme 3.7).

Enantiomers of bupivacaine can be prepared via diastereomeric salt resolution with tartaric acid or by resolution of the amide (3.1.33) with O,O-dibenzoyl tartaric acid followed by alkylation [47,70].
One of enantiomers, S(–) isomer of the racemic bupivacaine (levobupivacaine), has equal potency but less cardiotoxic and CNS effects in comparison with both R(+) bupivacaine and bupivacaine racemate. The reduced toxicity of levobupivacaine (3.1.48) gives a wider safety margin in clinical practice [71,72].
Stereospecific synthesis of levobupivacaine from (S)-lysine have been proposed (Scheme 3.8).

Treatment of N-CBZ (S)-lysine (3.1.44) with sodium nitrite in acetic acid yields the acetate (3.1.45). The prepared acetate (3.1.45) was then coupled with dimethyl aniline using N,N′-dicyclohexylcarbodiimide to give the amide (3.1.46) in good yield. The acetate group was then converted into the tosylate (3.1.47), which was deprotected and cyclized stereospecifically in one-pot reaction to give the amide (3.1.33) in high yield. Alkylation is easily achieved using an alkyl bromide and K2CO3 without any racemization. Alkylation can also be carried out using butyraldehyde/formic acid although the former is a much simpler process [73] (Scheme 3.8).
SYN
WO 9611181
Levobupivacaine has been obtained by two different ways: 1) The deamination of N-benzoyloxycarbonyl-L-lysine (I) with NaNO2/acetic acid gives 6-acetoxy-2(S)-(benzyl-oxycarbonylamino)hexanoic acid (II), which is amidated with 2,6-dimethylaniline (III) and dicyclohexylcarbodiimide (DCC) to the expected amide (IV). The deacetylation of (IV) with K2CO3 in methanol affords compound (V), which is tosylated as usual with tosyl chloride giving intermediate (VI), which is stereospecifically cyclized by means of K2CO3 in ethanol yielding N-(2,6-dimethyl-phenyl)piperidine-2 (S)-carboxamide (VII). Finally, this compound is alkylated with butyl bromide and K2CO3 or by reductoalkylation with butyraldehyde. 2) The amidation of piperidine-2-carboxylic acid (VIII) with 2,6-dimethylaniline (III) by means of SOCl2 in toluene gives the corresponding amide (IX), which is alkylated with butyl bromide as before yielding racemic bupivacaine (X) (3). This compound is then submitted to optical resolution by treatment with (S,S)-(?-tartaric acid followed by crystallization of the resulting tartrate and acidification with HCl in isopropanol.
SYN
| Org Process Res Dev 2000,4(6),530 |
Improved yield in the synthesis of levobupivacaine. An improved yield in the synthesis of levobupivacaine can be obtained by recovering the unwanted (R)-enantiomer side product in the optical resolution of the racemic bupivacaine. The treatment of (R)-(I) with refluxing propionic acid causes its racemization, yielding racemic-(I) (bupivacaine), which is then submitted to a new optical resolution process using dibenzoyl-L-tartaric acid.
Literatures:
Acta Chemica Scandinavica (1947-1973), , vol. 11, p. 1183,1184
Literatures:
BRIDGE PHARMA, INC. Patent: WO2008/88756 A1, 2008 ; Location in patent: Page/Page column 30-31 ;
Yield: ~94%
nmr
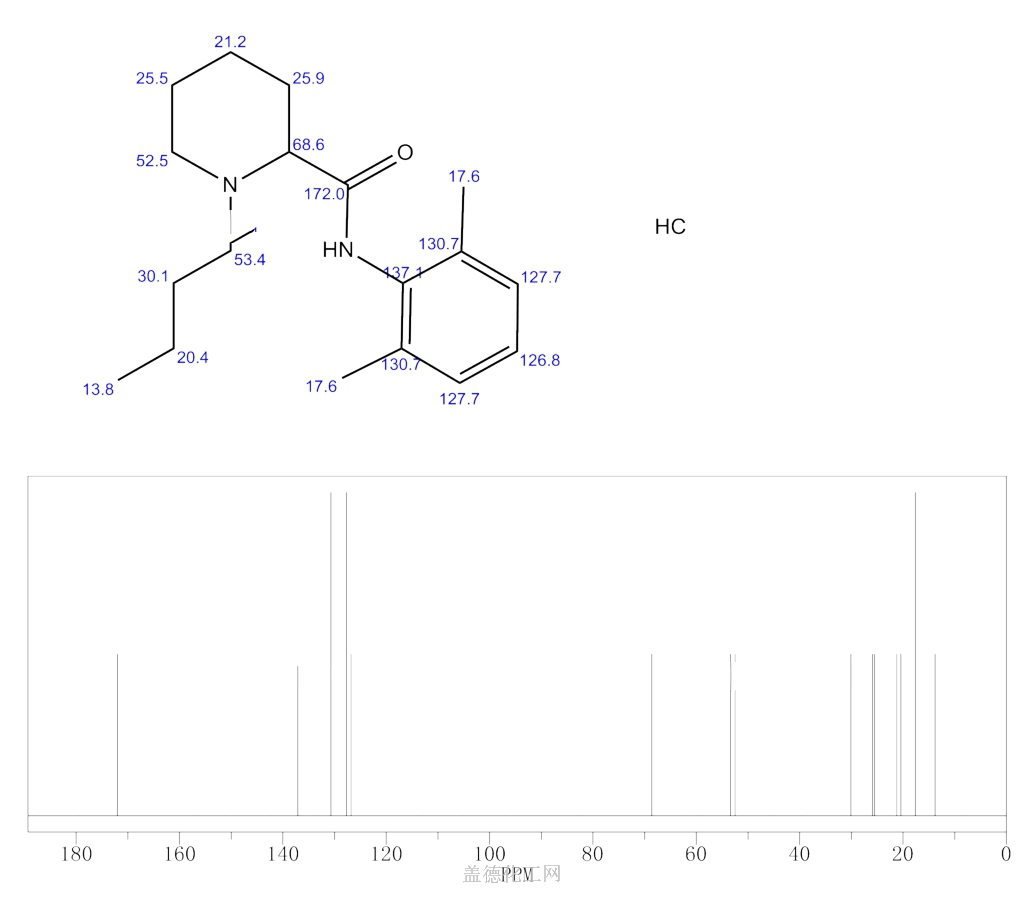
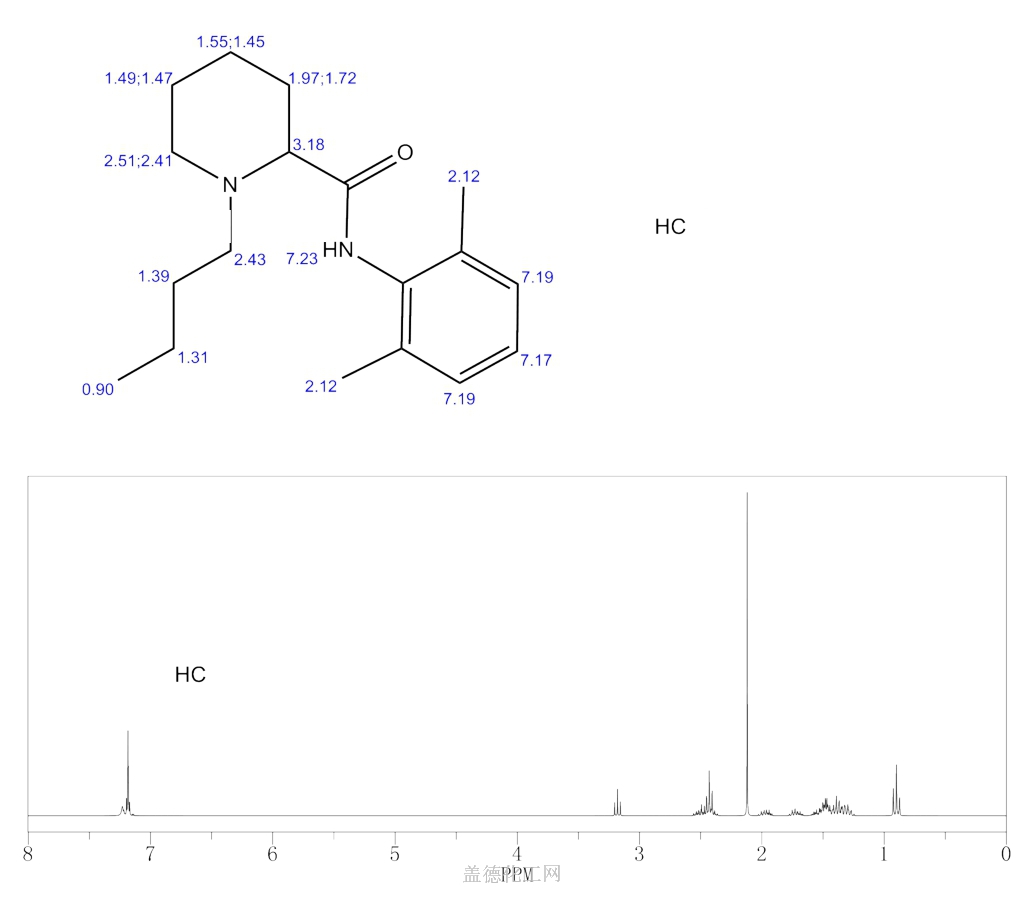
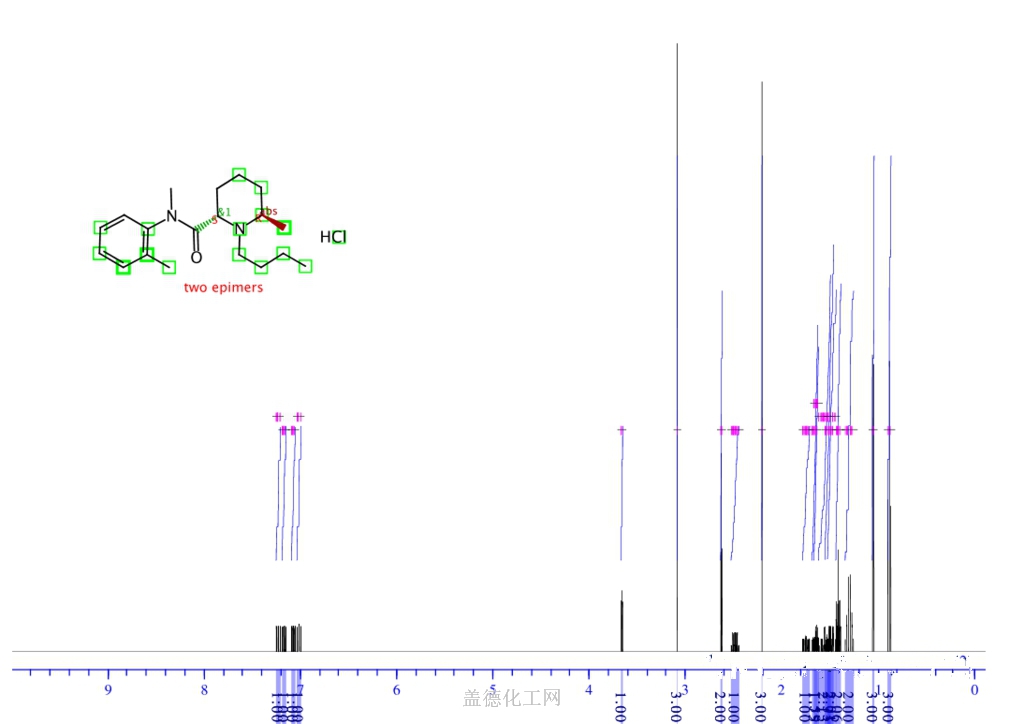
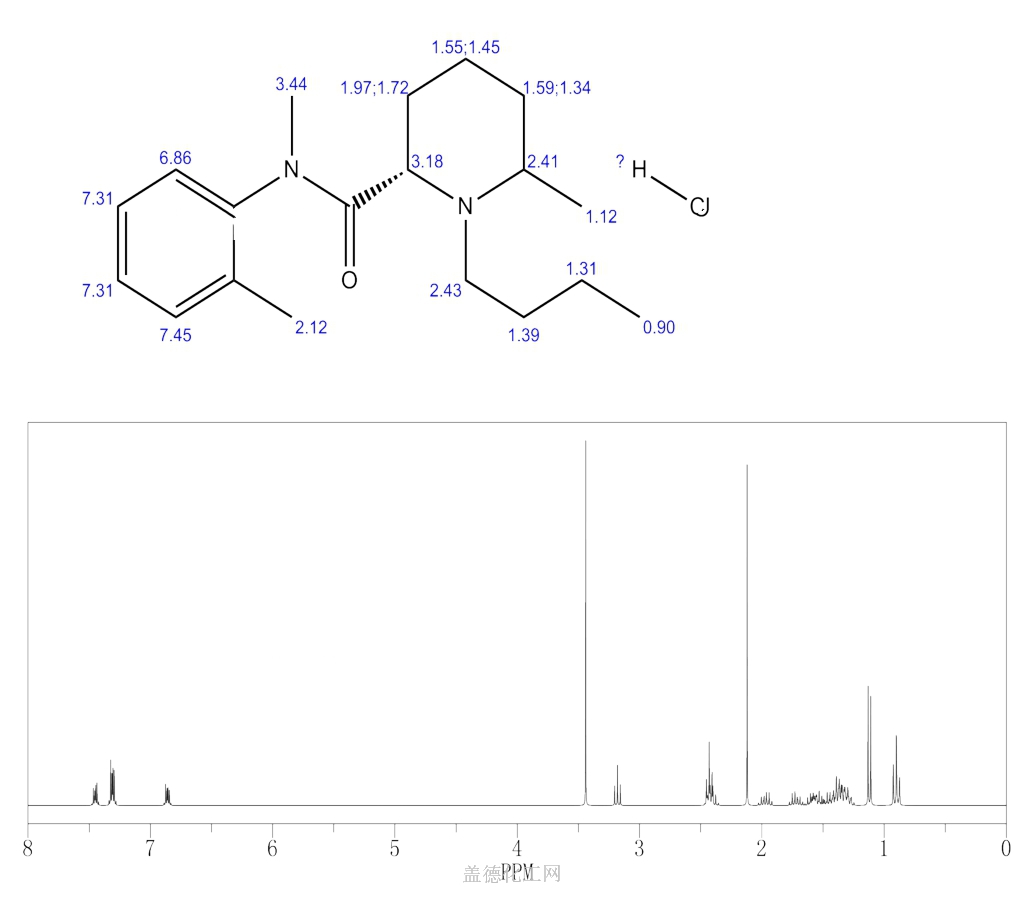
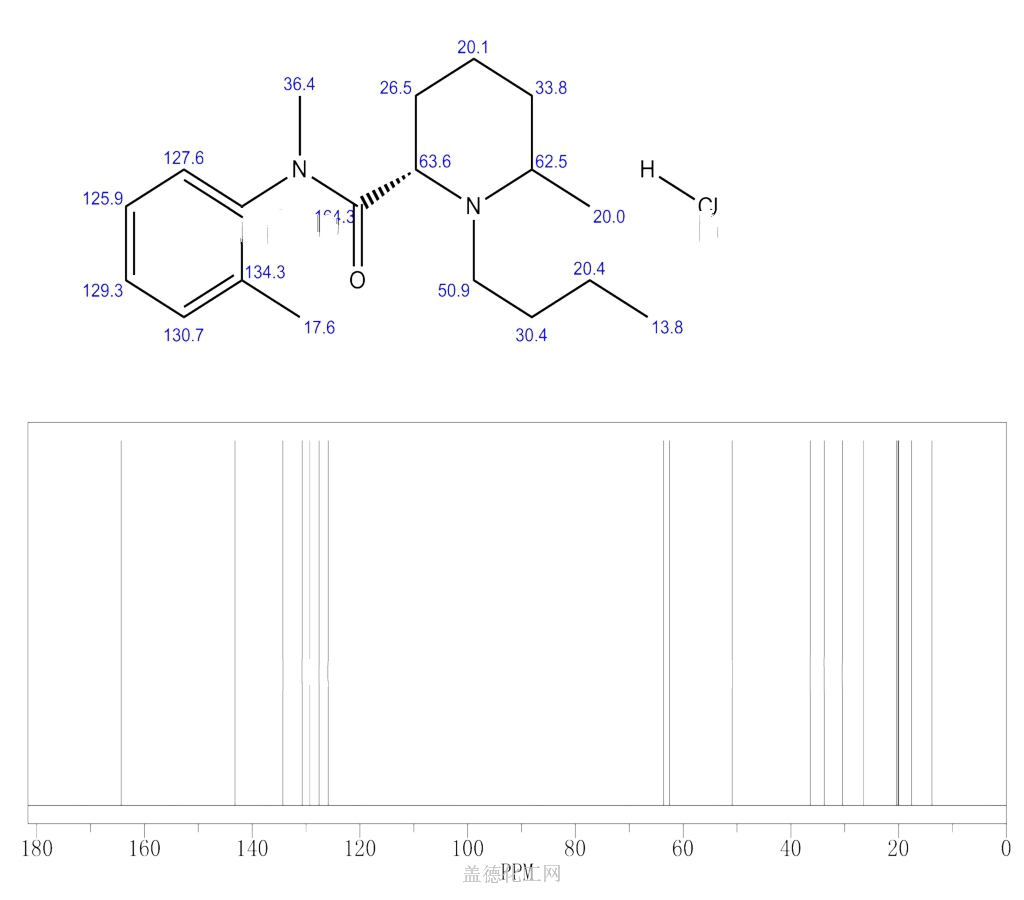

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////////////////////////////
Bupivacaine is a local anesthetic used in a wide variety of superficial and invasive procedures.
Bupivacaine, marketed under the brand name Marcaine among others, is a medication used to decrease feeling in a specific area.[4] In nerve blocks, it is injected around a nerve that supplies the area, or into the spinal canal’s epidural space.[4] It is available mixed with a small amount of epinephrine to increase the duration of its action.[4] It typically begins working within 15 minutes and lasts for 2 to 8 hours.[4][5]
Possible side effects include sleepiness, muscle twitching, ringing in the ears, changes in vision, low blood pressure, and an irregular heart rate.[4] Concerns exist that injecting it into a joint can cause problems with the cartilage.[4] Concentrated bupivacaine is not recommended for epidural freezing.[4] Epidural freezing may also increase the length of labor.[4] It is a local anaesthetic of the amide group.[4]
Bupivacaine was discovered in 1957.[6] It is on the World Health Organization’s List of Essential Medicines.[7] Bupivacaine is available as a generic medication.[4][8] An implantable formulation of bupivacaine (Xaracoll) was approved for medical use in the United States in August 2020.[9][10][11]
Medical uses
Bupivacaine is indicated for local infiltration, peripheral nerve block, sympathetic nerve block, and epidural and caudal blocks. It is sometimes used in combination with epinephrine to prevent systemic absorption and extend the duration of action. The 0.75% (most concentrated) formulation is used in retrobulbar block.[12] It is the most commonly used local anesthetic in epidural anesthesia during labor, as well as in postoperative pain management.[13] Liposomal formulations of bupivacaine (brand name EXPAREL) have shown to be more effective in providing pain relief than plain solutions of bupivacaine.[14][15]
The fixed-dose combination of bupivacaine with Type I collagen (brand name Xaracoll) is indicated for acute postsurgical analgesia (pain relief) for up to 24 hours in adults following open inguinal hernia repair.[10][11]
Bupivacaine (Posimir) is indicated in adults for administration into the subacromial space under direct arthroscopic visualization to produce post-surgical analgesia for up to 72 hours following arthroscopic subacromial decompression.[16][17]
Contraindications
Bupivacaine is contraindicated in patients with known hypersensitivity reactions to bupivacaine or amino-amide anesthetics. It is also contraindicated in obstetrical paracervical blocks and intravenous regional anaesthesia (Bier block) because of potential risk of tourniquet failure and systemic absorption of the drug and subsequent cardiac arrest. The 0.75% formulation is contraindicated in epidural anesthesia during labor because of the association with refractory cardiac arrest.[18]
Adverse effects
Compared to other local anaesthetics, bupivacaine is markedly cardiotoxic.[19] However, adverse drug reactions (ADRs) are rare when it is administered correctly. Most ADRs are caused by accelerated absorption from the injection site, unintentional intravascular injection, or slow metabolic degradation. However, allergic reactions can rarely occur.[18]
Clinically significant adverse events result from systemic absorption of bupivacaine and primarily involve the central nervous system (CNS) and cardiovascular system. CNS effects typically occur at lower blood plasma concentrations. Initially, cortical inhibitory pathways are selectively inhibited, causing symptoms of neuronal excitation. At higher plasma concentrations, both inhibitory and excitatory pathways are inhibited, causing CNS depression and potentially coma. Higher plasma concentrations also lead to cardiovascular effects, though cardiovascular collapse may also occur with low concentrations.[20] Adverse CNS effects may indicate impending cardiotoxicity and should be carefully monitored.[18]
- CNS: circumoral numbness, facial tingling, vertigo, tinnitus, restlessness, anxiety, dizziness, seizure, coma
- Cardiovascular: hypotension, arrhythmia, bradycardia, heart block, cardiac arrest[13][18]
Toxicity can also occur in the setting of subarachnoid injection during high spinal anesthesia. These effects include: paresthesia, paralysis, apnea, hypoventilation, fecal incontinence, and urinary incontinence. Additionally, bupivacaine can cause chondrolysis after continuous infusion into a joint space.[18]
Bupivacaine has caused several deaths when the epidural anaesthetic has been administered intravenously accidentally.[21]
Treatment of overdose
Further information: Lipid rescue
Animal evidence[22][23] indicates intralipid, a commonly available intravenous lipid emulsion, can be effective in treating severe cardiotoxicity secondary to local anaesthetic overdose, and human case reports of successful use in this way.[24][25] Plans to publicize this treatment more widely have been published.[26]
Pregnancy and lactation
Bupivacaine crosses the placenta and is a pregnancy category C drug. However, it is approved for use at term in obstetrical anesthesia. Bupivacaine is excreted in breast milk. Risks of discontinuing breast feeding versus discontinuing bupivacaine should be discussed with the patient.[18]
Postarthroscopic glenohumeral chondrolysis
Bupivacaine is toxic to cartilage and its intra-articular infusions may lead to postarthroscopic glenohumeral chondrolysis.[27]
Pharmacology
Pharmacodynamics
Bupivacaine binds to the intracellular portion of voltage-gated sodium channels and blocks sodium influx into nerve cells, which prevents depolarization. Without depolarization, no initiation or conduction of a pain signal can occur.
Pharmacokinetics
The rate of systemic absorption of bupivacaine and other local anesthetics is dependent upon the dose and concentration of drug administered, the route of administration, the vascularity of the administration site, and the presence or absence of epinephrine in the preparation.[28]
- Onset of action (route and dose-dependent): 1-17 min
- Duration of action (route and dose-dependent): 2-9 hr
- Half life: neonates, 8.1 hr, adults: 2.7 hr
- Time to peak plasma concentration (for peripheral, epidural, or caudal block): 30-45 min
- Protein binding: about 95%
- Metabolism: hepatic
- Excretion: renal (6% unchanged)[18]
Chemical structure
Like lidocaine, bupivacaine is an amino-amide anesthetic; the aromatic head and the hydrocarbon chain are linked by an amide bond rather than an ester as in earlier local anesthetics. As a result, the amino-amide anesthetics are more stable and less likely to cause allergic reactions. Unlike lidocaine, the terminal amino portion of bupivacaine (as well as mepivacaine, ropivacaine, and levobupivacaine) is contained within a piperidine ring; these agents are known as pipecholyl xylidines.[13]
Society and culture
Legal status
On 17 September 2020, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) adopted a positive opinion, recommending the granting of a marketing authorization for the medicinal product Exparel, intended for the treatment of post-operative pain.[29] The applicant for this medicinal product is Pacira Ireland Limited.[29] Exparel liposomal was approved for medical use in the European Union in November 2020.[30]
Economics
Bupivacaine is available as a generic medication.[4][8]
Research
Levobupivacaine is the (S)-(–)-enantiomer of bupivacaine, with a longer duration of action, producing less vasodilation. Durect Corporation is developing a biodegradable, controlled-release drug delivery system for after surgery. It has currently[when?] completed a phase-III clinical trial.[31]
References
- ^ “Bupivacaine Use During Pregnancy”. Drugs.com. 13 April 2020. Retrieved 21 September 2020.
- ^ “Marcaine- bupivacaine hydrochloride injection, solution Marcaine with epinephrine- bupivacaine hydrochloride and epinephrine bitartrate injection, solution”. DailyMed. Retrieved 13 February2021.
- ^ “Sensorcaine MPF- bupivacaine hydrochloride injection, solution”. DailyMed. Retrieved 13 February 2021.
- ^ Jump up to:a b c d e f g h i j k l m n “Bupivacaine Hydrochloride”. The American Society of Health-System Pharmacists. Archived from the original on 2015-06-30. Retrieved August 1, 2015.
- ^ Jump up to:a b Whimster, David Skinner (1997). Cambridge textbook of accident and emergency medicine. Cambridge: Cambridge University Press. p. 194. ISBN 9780521433792. Archived from the original on 2015-10-05.
- ^ Egan, Talmage D. (2013). Pharmacology and physiology for anesthesia : foundations and clinical application. Philadelphia, PA: Elsevier/Saunders. p. 291. ISBN 9781437716795. Archivedfrom the original on 2016-05-12.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06.
- ^ Jump up to:a b Hamilton, Richart (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. p. 22. ISBN 9781284057560.
- ^ “Xaracoll: FDA-Approved Drugs”. U.S. Food and Drug Administration (FDA). Retrieved 2 September 2020.
- ^ Jump up to:a b “FDA approval letter” (PDF). U.S. Food and Drug Administration (FDA). 28 August 2020. Retrieved 2 September2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ Jump up to:a b “FDA Approves Xaracoll (bupivacaine HCl) Implant, a Non-opioid, Drug-device Treatment Option for Acute Postsurgical Pain Relief for up to 24 Hours Following Open Inguinal Hernia Repair in Adults” (Press release). Innocoll Pharmaceuticals. 31 August 2020. Retrieved 2 September 2020 – via PR Newswire.
- ^ Lexicomp. “Bupivacaine (Lexi-Drugs)”. Archived from the original on 2014-04-10. Retrieved 20 April 2014.
- ^ Jump up to:a b c Miller, Ronald D. (November 2, 2006). Basics of Anesthesia. Churchill Livingstone.
- ^ Ma, Ting-Ting, et al. (2017). “Liposomal bupivacaine versus traditional bupivacaine for pain control after total hip arthroplasty: A meta-analysis”. Medicinevol. 96 (96, 25 (2017): e7190): e7190. doi:10.1097/MD.0000000000007190. PMC 5484209. PMID 28640101.
- ^ Mont, M. A., Beaver, W. B., Dysart, S. H., Barrington, J. W., & Gaizo, D. J. (2018). “Local Infiltration Analgesia With Liposomal Bupivacaine Improves Pain Scores and Reduces Opioid Use After Total Knee Arthroplasty: Results of a Randomized Controlled Trial”. The Journal of Arthroplasty. 33 (1): 33(1), 90–96. doi:10.1016/j.arth.2017.07.024. PMID 28802777.
- ^https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2021/204803Orig1s000ltr.pdf
- ^ “Durect Corporation Announces U.S. FDA Approval of Posimir For Post-Surgical Pain Reduction for up to 72 Hours Following Arthroscopic Subacromial Decompression” (Press release). Durect Corporation. 2 February 2021. Retrieved 13 February 2021 – via PR Newswire.
- ^ Jump up to:a b c d e f g “Bupivacaine (Lexi-Drugs)”. Archived from the original on 2014-04-10. Retrieved 20 April 2014.
- ^ de La Coussaye, J. E.; Eledjam, J. J.; Brugada, J.; Sassine, A. (1993). “[Cardiotoxicity of local anesthetics]”. Cahiers d’Anesthésiologie. 41 (6): 589–598. ISSN 0007-9685. PMID 8287299.
- ^ Australian Medicines Handbook. Adelaide. 2006. ISBN 978-0-9757919-2-9.
- ^ ABS-CBN Interactive: Filipino nurse dies in UK due to wrong use of anaesthetic
- ^ Weinberg, GL; VadeBoncouer, T; Ramaraju, GA; Garcia-Amaro, MF; Cwik, MJ. (1998). “Pretreatment or resuscitation with a lipid infusion shifts the dose-response to bupivacaine-induced asystole in rats”. Anesthesiology. 88 (4): 1071–5. doi:10.1097/00000542-199804000-00028. PMID 9579517. S2CID 1661916.
- ^ Weinberg, G; Ripper, R; Feinstein, DL; Hoffman, W. (2003). “Lipid emulsion infusion rescues dogs from bupivacaine-induced cardiac toxicity”. Regional Anesthesia and Pain Medicine. 28 (3): 198–202. doi:10.1053/rapm.2003.50041. PMID 12772136. S2CID 6247454.
- ^ Rosenblatt, MA; Abel, M; Fischer, GW; Itzkovich, CJ; Eisenkraft, JB (July 2006). “Successful use of a 20% lipid emulsion to resuscitate a patient after a presumed bupivacaine-related cardiac arrest”. Anesthesiology. 105 (1): 217–8. doi:10.1097/00000542-200607000-00033. PMID 16810015.
- ^ Litz, RJ; Popp, M; Stehr, S N; Koch, T. (2006). “Successful resuscitation of a patient with ropivacaine-induced asystole after axillary plexus block using lipid infusion”. Anaesthesia. 61 (8): 800–1. doi:10.1111/j.1365-2044.2006.04740.x. PMID 16867094. S2CID 43125067.
- ^ Picard, J; Meek, T (February 2006). “Lipid emulsion to treat overdose of local anaesthetic: the gift of the glob”. Anaesthesia. 61(2): 107–9. doi:10.1111/j.1365-2044.2005.04494.x. PMID 16430560. S2CID 29843241.
- ^ Gulihar, Abhinav; Robati, Shibby; Twaij, Haider; Salih, Alan; Taylor, Grahame J.S. (December 2015). “Articular cartilage and local anaesthetic: A systematic review of the current literature”. Journal of Orthopaedics. 12 (Suppl 2): S200–S210. doi:10.1016/j.jor.2015.10.005. PMC 4796530. PMID 27047224.
- ^ “bupivacaine hydrochloride (Bupivacaine Hydrochloride) injection, solution”. FDA. Archived from the original on 21 April 2014. Retrieved 20 April 2014.
- ^ Jump up to:a b “Exparel: Pending EC decision”. European Medicines Agency (EMA). 17 September 2020. Retrieved 21 September 2020.Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ “Exparel liposomal EPAR”. European Medicines Agency (EMA). 15 September 2020. Retrieved 11 December 2020.
- ^ “Bupivacaine Effectiveness and Safety in SABER Trial (BESST)”. ClinicalTrials.gov. 20 January 2010. Archived from the original on 2011-12-27. Retrieved 2012-03-01.
External links
- “Bupivacaine”. Drug Information Portal. U.S. National Library of Medicine.
///////////Bupivacaine, AH 250, DUR-843, LAC-43, SKY 0402, SKY-0402, SKY0402, Win 11318, ANAESTHETIC
- CCCCN1CCCCC1C(=O)NC1=C(C)C=CC=C1C

NEW DRUG APPROVALS
ONE TIME
$10.00
ROPIVACAINE

Ropivacaine
CAS No.84057-95-4 (Ropivacaine);
- Molecular FormulaC17H26N2O
- Average mass274.401 Da
HCL SALTCAS Registry Number: 98717-15-8
HCL MONOHYDRATE
Molecular Weight328.88, FormulaC17H26N2O • HCl • H2O
132112-35-7 (Ropivacaine HCl Monohydrate);
Chemical Name S-(-)-1-propyl-2′,6′-pipecoloxylidide hydrochloride monohydrate(S)-(-)-1-Propyl-2′,6′-pipecoloxylidide
(S)-N-(2,6-dimethylphenyl)-1-propyl-2-piperidinecarboxamide
2-Piperidinecarboxamide, N-(2,6-dimethylphenyl)-1-propyl-, (2S)-
5376
5421606[Beilstein]
7IO5LYA57N
84057-95-4[RN]
854056-07-8[RN]
(S)-ropivacaine
(2S)-N-(2,6-Dimethylphenyl)-1-propyl-2-piperidinecarboxamide
ропивакаин [Russian] [INN]
روبيفاكائين [Arabic] [INN]
罗哌卡因 [Chinese] [INN]
Drug Name:Ropivacaine Hydrochloride Hydrate
Research Code:LEA-103; NA-001; (-)-LEA-103;
Trade Name:Naropin® / Anapeine®
MOA:Sodium channels blockers
Indication:Anaesthetic
Company:AstraZeneca (Originator) , Fresenius Kabi
ATC Code:N01BB09APPROVED
- US
- JP
- CN
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 1996-09-26 | First approval | Naropin | Anaesthetic | Injection | 2 mg/ml; 5 mg/ml; 7.5 mg/ml; 10 mg/ml | APP Pharmaceuticals |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2001-04-04 | First approval | Anapeine | Anaesthetic | Injection | 2 mg/ml; 7.5 mg/ml; 10 mg/ml | AstraZeneca |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2010-02-11 | Marketing approval | 耐乐品/Naropin | Anaesthetic | Injection | 20 mg/10 ml;100 mg/10 ml; 75 mg/10 ml; 50 mg/10 ml | AstraZeneca | |
| 2010-02-03 | Marketing approval | 耐乐品/Naropin | Anaesthetic | Injection | 2 mg/mL | AstraZeneca |
| No. | NDA No. | Major Technical Classification | Patent No. | Estimated Expiry Date | Drug Substance Claim | Drug Product Claim | Patent Use Code (All list) |
| 1 | N020533 | Uses(Indication) | 5670524 | 2014-09-23 | Y | Y | U – 833 |
| 2 | N020533 | Device | 7828787 | 2025-10-18 | Y | ||
| 3 | N020533 | Device | 7857802 | 2026-11-28 | Y | ||
| 4 | N020533 | Device | 8118802 | 2023-05-18 | Y | ||
| 5 | N020533 | Device | 8162915 | 2024-05-23 | Y |
Ropivacaine
CAS Registry Number: 84057-95-4
CAS Name: (2S)-N-(2,6-dimethylphenyl)-1-propyl-2-piperidinecarboxamide
Additional Names: (S)-(-)-1-propyl-2¢,6¢-pipecoloxylidide; l-N-n-propylpipecolic acid-2,6-xylidide
Manufacturers’ Codes: LEA-103
Molecular Formula: C17H26N2O, Molecular Weight: 274.40
Percent Composition: C 74.41%, H 9.55%, N 10.21%, O 5.83%
Literature References: Prepn: A. F. Thuresson, C. Bovin, WO8500599 (1985 to Apothekernes); H.-J. Federsel et al.,Acta Chem. Scand.B41, 757 (1987).Physicochemical properties: G. R. Strichartz et al.,Anesth. Analg.71, 158 (1990).HPLC determn in human plasma: Z. Yu et al.,J. Chromatogr. B654, 221 (1994). In vitro metabolism: Y. Oda et al.,Anesthesiology82, 214 (1995). Clinical pharmacokinetics: D. J. Kopacz et al.,ibid.81, 1139 (1994). Toxicity study in sheep: A. C. Santos et al.,ibid.82, 734 (1995). Clinical evaluation in relief of surgical pain: I. Cederholm et al.,Reg. Anesth.19, 18 (1994); B. Johansson et al.,Anesth. Analg.78, 210 (1994); labor pain: R. Stienstra et al.,ibid.80, 285 (1995).
Properties: Crystals from toluene, mp 144-146°. [a]D25 -82.0° (c = 2 in methanol). pKa 8.16. Distribution coefficient (1-octanol/aq buffer, pH 7.4): 115.0.
Melting point: mp 144-146°
pKa: pKa 8.16
Optical Rotation: [a]D25 -82.0° (c = 2 in methanol)
Derivative Type: Hydrochloride
CAS Registry Number: 98717-15-8
Trademarks: Naropin (AstraZeneca)
Molecular Formula: C17H26N2O.HCl, Molecular Weight: 310.86
Percent Composition: C 65.68%, H 8.75%, N 9.01%, O 5.15%, Cl 11.40%
Properties: Crystals from isopropyl alcohol, mp 260-262°. [a]D25 -6.6° (c = 2 in water).
Melting point: mp 260-262°
Optical Rotation: [a]D25 -6.6° (c = 2 in water)
Derivative Type: Hydrochloride monohydrate
CAS Registry Number: 132112-35-7
Properties: Crystals from acetone + water, mp 269.5-270.6°. [a]D20 -7.28° (c = 2 in water).
Melting point: mp 269.5-270.6°
Optical Rotation: [a]D20 -7.28° (c = 2 in water)
Therap-Cat: Anesthetic (local).
Keywords: Anesthetic (Local).Product Ingredients
| INGREDIENT | UNII | CAS | INCHI KEY |
|---|---|---|---|
| Ropivacaine hydrochloride | V910P86109 | 132112-35-7 | VSHFRHVKMYGBJL-CKUXDGONSA-N |
| Ropivacaine hydrochloride anhydrous | 35504LBE2T | 98717-15-8 | NDNSIBYYUOEUSV-RSAXXLAASA-N |
Ropivacaine is an analgesic drug used for local or regional anesthesia for surgery and short-term management of pain.Ropivacaine is an aminoamide local anaesthetic drug commonly marketed by AstraZeneca under the trade name Naropin. It is present as a racemic mixture of the enantiomers containing equal proportions of the “S” and “R” forms. The marketed form contains the single S-enantiomer as the active ingredient.
Ropivacaine hydrochloride hydrate was first approved by the U.S. Food and Drug Administration (FDA) on September 26, 1996, then approved by Pharmaceuticals and Medical Devices Agency of Japan (PMDA) in April 4, 2001. It was developed by AstraZeneca, then marketed as Naropin® by APP Pharmaceuticals, LLC. in the US and as Anapeine® by AstraZeneca in JP.
Ropivacaine is a local anaesthetic drug belonging to the amino amide group. It is indicated for the production of local or regional anesthesia for surgery and for acute pain management.
Naropin® is available as injection solution for intravenous use, containing 2, 5, 7.5 or 10 mg of Ropivacaine hydrochloride one mL. Common concentration is 7.5 mg/mL, and the maximum single dose is 200 mg.
Ropivacaine (rINN) /roʊˈpɪvəkeɪn/ is a local anaesthetic drug belonging to the amino amide group. The name ropivacaine refers to both the racemate and the marketed S–enantiomer. Ropivacaine hydrochloride is commonly marketed by AstraZeneca under the brand name Naropin.

Table 1 The common types of local anesthetics
Syn
Synthesis Reference
Peter Jaksch, “Process for the preparation of ropivacaine hydrochloride monohydrate.” U.S. Patent US5959112, issued February, 1970.
US5959112Route 1
Reference:1. US2799679A.
Reference:1. WO8500599A1.
https://patents.google.com/patent/WO1985000599A1/enA large variety of N-alkyl-pipecolic acid amides have been synthesized. A number of these compounds have found use as local anesthetics, such as Mepivacaine, namely the racemate of N-methylpipecolic–acid-2,6-xylidide:

and Bupivacaine, namely the racemate of N-butylpipecolic- acid-2,6-xylidide:

References disclosing homologs of this series of compounds include U.S. Patent 2,799,679; British Patent 775,749; British Patent 775,750; British Patent 800,565; British Patent 824,542; British Patent 869,978; British Patent 949,729; U.S. Patent 4,110,331; and U.S. Patent 4,302,465.There is a summary paper dealing with these types of anesthetics, and related compounds in a paper in Acta Che ica Scandinavica 11, (1957) No. 7 pp. 1183-1190 by Bo Thuresson af Ekenstam et al.There is a discussion of the“ effect of optical isomers in related compounds in J. Med. Chem., 14 (1971) pp. 891-892 entitled “Optical Isomers Of Mepivacaine And Bupivacaine” by Benjamin F. Tullar; Acta Pha m. Suecica, 8 (1971) pp. 361- 364 entitled “Some Physicochemical Properties Of The Racemates And The Optically Active Isomers Of Two Local Anaesthetic Compounds”, by . Friberger et al -.; Acta Pharmacol et Toxicol, 31 (1972). pp. 273-286 entitled “Toxicological And Local Anaesthetic Effects Of Optically Active Isomers Of Two Local Anaesthetic Compounds”, by G. Aberg; Annual Review Of Pharmacology, 9 (1969) pp. 5Q3-520 entitled “Duration Of Local Anaesthesia”, by F.P. Luduena and Acta Pharmacol, et Toxicol, 41 (1977). pp. 432-443 entitled “Studies On The Duration Of Local Anaesthesia: Structure/Activity Relationships In A Series Of Homologous Local Anaesthetics”, by G. Aberg et al.

Reference:1. J. Labelled Compd. Rad. 1987, 24, 521-528.Route 4
Reference:1. CN104003930A.
https://patents.google.com/patent/CN104003930A/enRopivacaine (Ropivacaine) is the long-acting local anesthetics of amide derivatives of Novel pure levo form of Astra drugmaker of Sweden listing in 1996, there is analgesia and anesthesia dual function, be widely used in nerve block anesthesia, local infiltration anesthesia and epidural anesthesia , be particularly useful for Postoperative Analgesia After and obstetrical analgesia.On piperidine ring in ropivacaine structure, having a chiral carbon atom, is chipal compounds, and levoisomer is low compared with dextrorotatory isomer toxicity, and action effect is good.Ropivacaine HCL is the hydrochloride of ropivacaine, and chemistry is by name: (-)-(S)-N-(2,6-3,5-dimethylphenyl)-1-n-propyl piperidines-2-carboxamide hydrochloride, molecular formula is C 17 h 26 n 2 oHCl, structural formula:At present, in prior art, the synthetic method of ropivacaine mainly contains:Taking L-2-piperidine formyl chlorine as starting raw material, through phosphorus pentachloride or sulfur oxychloride acidylate, then with the condensation of 2,6-xylidine, and then react and obtain ropivacaine with n-propyl bromide.Although this method production technique is simple, reactions steps is also shorter, but commercially available L-2-piperidine carboxylic acid average price is 4~5 times of racemization Pipecolic Acid, raw materials cost is too high, and may there is racemization phenomenon in subsequent reactions process, affect optical purity of products, for example US Patent No. 4695576 and “Chinese Medicine magazine” o. 11th in 2012 “Ropivacaine HCL a synthetic” literary composition and Chinese patent CN201310041390.2 all adopt this kind of method.”synthetic chemistry” the 14th the 4th phase of volume “Synthesis of Ropivacaine Hydrochloride by Triphosgene” in 2006 and Hunan University’s Master’s thesis “synthesising process research of Ropivacaine HCL and” disclose the synthetic method of another ropivacaine, the Pipecolic Acid that adopts inexpensive racemization is raw material, prepare Ropivacaine HCL through reactions such as amidation, alkylations, use triphosgene or thionyl chloride to prepare acyl chlorides, but triphosgene danger in the time of storage and aftertreatment is larger, is not suitable for suitability for industrialized production; And partial condition in the latter’s method (reagent that the pH separating as intermediate (I) and reagent, catalyzer and recrystallization are used etc.) haves much room for improvement,under its test conditions, be difficult to take into account high purity and high yield simultaneously, according to prior art, the separation of ropivacaine raceme is also not ideal.The preparation method of embodiment 1, a kind of Ropivacaine HCL, comprises the steps:(1) preparation of intermediate (I) N-(2,6-dimethyl benzene)-2-piperidyl urea10.0g2-piperidine carboxylic acid, 160ml toluene are added in 500ml reaction flask.Pass into HCl gas, to pH2, be warming up to 48 ± 2 DEG C, add 1.5mlDMF, drip 11.2g (1.2 equivalent) sulfur oxychloride and 20ml toluene mixture liquid, drip and finish, be incubated 48 ± 2 DEG C of reaction 3h.Drip 2 of 4.0 equivalents, 6-xylidine and 20ml toluene mixture liquid, be incubated 58 ± 2 DEG C of reaction 3h.Filter, obtain yellow-green colour wet product 65g, dry to obtain gray solid 56g, solid is added in 280ml purified water, stir the molten reaction solution that obtains; 10%NaOH solution is slowly dropped in reaction solution, adjust pH to 4.5-5.0, use 100ml toluene wash , layering, retains water layer, continues to adjust pH to 9-10 with 10%NaOH solution, adds 100ml methylene dichloride.Layering, gets organic layer,and water layer continues to use 50ml dichloromethane extraction, merges organic layer, adds anhydrous sodium sulfate dehydration, 40 DEG C of concentrating under reduced pressure.Obtain pale yellow oily liquid body 15.5g, yield 86.2%, is intermediate (I) N-( 2,6-dimethyl benzene)-2-piperidyl urea.(2) preparation of intermediate (II) N-(2,6-3,5-dimethylphenyl)-1-n-propyl piperidines-2-methane amideIntermediate 15.5 g of (the I) Dissolved in 60mlDMF IS, ADDS 8.9gK 2 cO . 3 , 8.2 g of drip (1.0 equivalent)-n-propyl bromide, and drip BE Finishing After Warming up to 78 ± 2 of DEG C, Insulation Reaction 2H; Ice Bath is down to room temperature, filters, and filtrate is added in 150ml frozen water, separates out a large amount of white solids, filter, dry, obtain white solid 17.4g, yield 95.0%, is intermediate (II) N-(2, 6-3,5-dimethylphenyl)-1-n-propyl piperidines-2-methane amide.(3) preparation of left-handed ropivacaine tartrate17.4g intermediate (II) is dissolved in 100ml Virahol, heats up 40 DEG C and stir molten; Treat entirely moltenly, add successively 1.80g (0.1 equivalent) titanium isopropylate, 1.91g (0.2 equivalent) D-tartrate, be warming up to backflow, after solution clarification, continue reaction 2h; Be cooled to 30 DEG C of crystallizatioies, filter, 75 DEG C of oven dry, obtain white solid 8.7g, and yield 39.2% is left-handed ropivacaine tartrate; After testing, ropivacaine purity 99.02%, dextrorotatory isomer per-cent 0.98%.(4) preparation of Ropivacaine HCL crude productLeft-handed 8.7g ropivacaine tartrate is joined in 50ml Virahol, be warming up to 50 DEG C, drip concentrated hydrochloric acid, surveying pH is 1~2, insulation reaction 2h.Be cooled to 0 DEG C of crystallization, separate out a large amount of white solids, filter, dry, obtain white solid 6.6g, yield 85.5%, is Ropivacaine HCL crude product.After testing, ropivacaine purity 99.11%, dextrorotatory isomer per-cent 0.89%.(5) refining6.6g crude product and 40ml dehydrated alcohol-concentrated hydrochloric acid mixed solution (20:1) are added in reaction flask, be heated to 50 DEG C and make to dissolve; Complete molten after, naturally cool to room temperature, ice-water bath is cooled to 0 DEG C, crystallization 2h; Filter, 5ml mixed solution washing for filter cake, obtains wet product, dries, and obtains white solid 6.0g, and yield 91.7%, is Ropivacaine HCL fine work.After testing, ropivacaine purity 99.91 %, dextrorotatory isomer per-cent 0.09%.The preparation method of embodiment 2, a kind of Ropivacaine HCLStep is as follows:(1) preparation of intermediate (I) N-(2,6-dimethyl benzene)-2-piperidyl urea100.0g2-piperidine carboxylic acid, 1600ml toluene are added in 3000ml reaction flask.Pass into HCl gas, to pH2 left and right, be warming up to 45~50 DEG C, add 15mlDMF, drip 111.5g (1.2 equivalent) sulfur oxychloride and 200ml toluene mixture liquid, drip and finish, be incubated 50-55 DEG C of reaction 3h.Drip 2 of 4.0 equivalents, 6-xylidine and 200ml toluene mixture liquid, be incubated 55~60 DEG C of reaction 2h.Filter, obtain the about 660g of yellow-green colour wet product, dry to obtain gray solid 545g, solid is added in 3000ml purified water, stir the molten reaction solution that obtains; 10%NaOH solution is slowly dropped in reaction solution, adjust pH to 4.5~5.0 , use 1000ml toluene wash, layering, retains water layer, continues to adjust pH to 9~10 with 10%NaOH solution, adds 1000ml methylene dichloride.Layering, gets organic layer,and water layer continues to use 750ml dichloromethane extraction, merges organic layer, adds anhydrous sodium sulfate dehydration, 40 DEG C of concentrating under reduced pressure.Obtain the about 151.8g of pale yellow oily liquid body, yield 84.5%, is intermediate (I) N-(2,6-dimethyl benzene)-2-piperidyl urea.(2) preparation of intermediate (II) N-(2,6-3,5-dimethylphenyl)-1-n-propyl piperidines-2-methane amideIntermediate 150.0 g (the I) Dissolved in 600mlDMF IS, ADDS 86.5gK 2 cO . 3 , drip 95.4 g (1.2 equivalent)-n-propyl bromide, and drip BE Finishing After Warming up to 85 ~ 90 of DEG C, Insulation Reaction 2H; of Be Down to room temperature, filter, filtrate is added in 1500ml frozen water, separate out a large amount of white solids, filter, dry, obtain the about 167.6g of white solid, yield 94.6%, is intermediate (II) N-(2, 6-3,5-dimethylphenyl)-1-n-propyl piperidines-2-methane amide.(3) preparation of left-handed ropivacaine tartrate160.0g intermediate (II) is dissolved in 1000ml Virahol, heats up 50 DEG C and stir molten; Treat entirely moltenly, add successively 16.58g (0.1 equivalent) titanium isopropylate, 43.8g (0.5 equivalent) D-tartrate, be warming up to backflow, after solution clarification, continue reaction 3h; Cooling, is down to 30-35 DEG C of crystallization, filters, and 75 DEG C of oven dry, obtain white solid 84.2g, and yield 41.3% is left-handed ropivacaine tartrate; After testing, ropivacaine purity 98.97%, dextrorotatory isomer per-cent 1.03%.(4) preparation of Ropivacaine HCL crude productLeft-handed 80.0g ropivacaine tartrate is joined in 500ml Virahol, be warming up to 50 DEG C, drip concentrated hydrochloric acid, surveying pH is 1~2, insulation reaction 4h.Be cooled to 0~5 DEG C of crystallization, separate out a large amount of white solids, filter, dry, obtain the about 61.6g of white solid, yield 86.5%, is Ropivacaine HCL crude product.After testing, ropivacaine purity 99.07%, dextrorotatory isomer per-cent 0.93%.(5) refining60.0g crude product and 500ml dehydrated alcohol-concentrated hydrochloric acid mixed solution (20:1) are added in reaction flask, be heated to 50 DEG C and make to dissolve; Complete molten after, cooling crystallization, ice-water bath is cooled to 0-5 DEG C, crystallization 4h; Filter, a small amount of cold mixed solution washing for filter cake, obtains wet product, dries, and obtains white solid 55.6g, and yield 92.7%, is Ropivacaine HCL fine work.After testing, ropivacaine purity 99.87%, dextrorotatory isomer per-cent 0.13%.The preparation method of embodiment 3, a kind of Ropivacaine HCLStep is as follows:(1) preparation of intermediate (I) N-(2,6-dimethyl benzene)-2-piperidyl urea10.0g2-piperidine carboxylic acid, 160ml toluene are added in 500ml reaction flask.Pass into HCl gas, to pH3 left and right, be warming up to 48 ± 2 DEG C, add 1.5mlDMF, drip 9.3g (1.0 equivalent) sulfur oxychloride and 20ml toluene mixture liquid, drip and finish, be incubated 48 ± 2 DEG C of reaction 2h.Drip 2 of 4.0 equivalents, 6-xylidine and 20ml toluene mixture liquid, be incubated 58 ± 2 DEG C of reaction 3h.Filter, obtain yellow-green colour wet product 63.6g, dry to obtain gray solid 55g, solid is added in 280ml purified water, stir the molten reaction solution that obtains; 10%NaOH solution is slowly dropped in reaction solution, adjust pH to 4.5-5.0, use 100ml toluene wash, layering, retains water layer, continues to adjust pH to 9-10 with 10%NaOH solution, adds 100ml methylene dichloride.Layering, gets organic layer,and water layer continues to use 50ml dichloromethane extraction, merges organic layer, adds anhydrous sodium sulfate dehydration, 40 DEG C of concentrating under reduced pressure.Obtain the about 14.8g of pale yellow oily liquid body, yield 82.4%, is intermediate (I) N-(2,6-dimethyl benzene)-2-piperidyl urea.(2) preparation of intermediate (II) N-(2,6-3,5-dimethylphenyl)-1-n-propyl piperidines-2-methane amideIntermediate 14.8 g of (the I) Dissolved in 60mlDMF IS, ADDS 8.5gK 2 cO . 3 , 7.8 g of drip (1.0 equivalent)-n-propyl bromide, and drip After Finishing of DEG BE Warming up to 75 C, Reaction Insulation 2H; IS Down Ice Bath to room temperature, filters, and filtrate is added in 150ml frozen water, separates out a large amount of white solids, filter, dry, obtain the about 16.0g of white solid, yield 91.5%, is intermediate (II) N-(2 ,6-3,5-dimethylphenyl)-1-n-propyl piperidines-2-methane amide.(3) preparation of left-handed ropivacaine tartrate15g intermediate (II) is dissolved in 100ml Virahol, heats up 40 DEG C and stir molten; Treat entirely moltenly, add successively 1.72g (0.1 equivalent) titanium isopropylate, 1.82g (0.2 equivalent) D-tartrate, be warming up to backflow , after solution clarification, continue reaction 1h; Be cooled to 32 DEG C of crystallizatioies, filter, 75 DEG C of oven dry, obtain white solid 7.5g, and yield 39.2% is left-handed ropivacaine tartrate; After testing, ropivacaine purity 98.92 %, dextrorotatory isomer per-cent 0.99%.(4) preparation of Ropivacaine HCL crude productLeft-handed 7.5g ropivacaine tartrate is joined in 50ml Virahol, be warming up to 40 DEG C, drip concentrated hydrochloric acid, surveying pH is 1~2, insulation reaction 1h.Be cooled to 0 DEG C of crystallization, separate out a large amount of white solids, filter, dry, obtain the about 5.7g of white solid, yield 85.3%, is Ropivacaine HCL crude product.After testing, ropivacaine purity 99.12%, dextrorotatory isomer per-cent 0.96%.(5) refining5.7g crude product and 40ml dehydrated alcohol-concentrated hydrochloric acid mixed solution (20:1) are added in reaction flask, be heated to 50 DEG C and make to dissolve; Complete molten after, naturally cool to room temperature, ice-water bath is cooled to 0 DEG C, crystallization 2h; Filter, 10ml mixed solution washing for filter cake, obtains wet product, dries, and obtains white solid 5.5g, and yield 92.1%, is Ropivacaine HCL fine work.After testing, ropivacaine purity 99.92 %, dextrorotatory isomer per-cent 0.15%.The preparation method of embodiment 4, a kind of Ropivacaine HCLStep is as follows:(1) preparation of intermediate (I) N-(2,6-dimethyl benzene)-2-piperidyl urea10.0g2-piperidine carboxylic acid, 160ml toluene are added in 500ml reaction flask.Pass into HCl gas, to pH3 left and right, be warming up to 48 ± 2 DEG C, add 1.5mlDMF, drip 10.2g (1.1 equivalent) sulfur oxychloride and 20ml toluene mixture liquid, drip and finish, be incubated 48 ± 2 DEG C of reaction 6h.Drip 2 of 4.0 equivalents, 6-xylidine and 20ml toluene mixture liquid, be incubated 58 ± 2 DEG C of reaction 8h.Filter, obtain yellow-green colour wet product 64.2g, dry to obtain gray solid 55.6g, solid is added in 280ml purified water, stir the molten reaction solution that obtains; 10%NaOH solution is slowly dropped in reaction solution, adjust pH to 4.5-5.0 , use 100ml toluene wash, layering, retains water layer, continues to adjust pH to 9-10 with 10%NaOH solution, adds 100ml methylene dichloride.Layering, gets organic layer,and water layer continues to use 50ml dichloromethane extraction, merges organic layer, adds anhydrous sodium sulfate dehydration, 40 DEG C of concentrating under reduced pressure.Obtain the about 14.9g of pale yellow oily liquid body, yield 82.9%, is intermediate (I) N-(2,6-dimethyl benzene)-2-piperidyl urea.(2) preparation of intermediate (II) N-(2,6-3,5-dimethylphenyl)-1-n-propyl piperidines-2-methane amideIntermediate 14.9 g of (the I) Dissolved in 60mlDMF IS, ADDS 8.5gK 2 cO . 3 , 7.8 g of drip (1.0 equivalent)-n-propyl bromide, and drip After Finishing of DEG BE Warming up to 75 C, Reaction Insulation 2H; IS Down Ice Bath to room temperature, filters, and filtrate is added in 150ml frozen water, separates out a large amount of white solids, filter, dry, obtain the about 16.1g of white solid, yield 92.0%, is intermediate (II) N-(2 ,6-3,5-dimethylphenyl)-1-n-propyl piperidines-2-methane amide.(3) preparation of left-handed ropivacaine tartrate15g intermediate (II) is dissolved in 100ml Virahol, heats up 60 DEG C and stir molten; Treat entirely moltenly, add successively 1.72g (0.1 equivalent) titanium isopropylate, 1.82g (0.2 equivalent) D-tartrate, be warming up to backflow , after solution clarification, continue reaction 4h; Be cooled to 30 DEG C of crystallizatioies, filter, 75 DEG C of oven dry, obtain white solid 7.6g, and yield 39.7% is left-handed ropivacaine tartrate; After testing, ropivacaine purity 99.01 %, dextrorotatory isomer per-cent 1.05%.(4) preparation of Ropivacaine HCL crude productLeft-handed 7.6g ropivacaine tartrate is joined in 50ml Virahol, be warming up to 40 DEG C, drip concentrated hydrochloric acid, surveying pH is 1~2, insulation reaction 4h.Be cooled to 5 DEG C of crystallizatioies, separate out a large amount of white solids, filter, dry, obtain the about 5.7g of white solid, yield 85.3%, is Ropivacaine HCL crude product.After testing, ropivacaine purity 99.06%, dextrorotatory isomer per-cent 0.95%.(5) refining5.7g crude product and 40ml dehydrated alcohol-concentrated hydrochloric acid mixed solution (volume ratio 20:1) are added in reaction flask, be heated to 80 DEG C and make to dissolve; Complete molten after, naturally cool to room temperature, ice- water bath is cooled to 5 DEG C, crystallization 2h; Filter, 10ml mixed solution washing for filter cake, obtains wet product, dries, and obtains white solid 5.2g, and yield 91.2%, is Ropivacaine HCL fine work.After testing, ropivacaine purity 99.81%, dextrorotatory isomer per-cent 0.11%.The optical isomer method for detecting purity of left-handed ropivacaine tartrate, Ropivacaine HCL crude product and the Ropivacaine HCL purified product obtaining in above-described 1-4 is: measure according to high performance liquid chromatography (annex VD), with alpha- acid glycoprotein post (AGP, 100mm × 4.0mm, 5 μ m are suitable for); Agilent-1260 type high performance liquid chromatograph; (get potassium primary phosphate 2.72g with Virahol-phosphate buffered saline buffer, the 800ml that adds water dissolves, regulating pH value with 0.1mol/L sodium hydroxide solution is 7.1, be diluted with water to 1000ml) be (10:90) moving phase, detection wavelength is: 210nm, column temperature: 30 DEG C, flow velocity 1.0ml/min, limit is: dextrorotatory isomer must not be greater than 0.5%.
PATENThttps://patents.google.com/patent/CN109503465A/enThe embodiment of 1 intermediate (-) of-(2S)-N- (2,6- 3,5-dimethylphenyl) piperidines -2- formamideL- piperidinecarboxylic acid hydrochloride (30.00g, 0.18mol), toluene are sequentially added in three mouthfuls of reaction flasks of 500ml cleaning N,N-Dimethylformamide (1ml), thionyl chloride (25.85g, 0.2 2mol) is added in (300ml) , stirring.It finishes, is warming up to 50~55 DEG C insulation reaction 3 hours.Snubber device is added to vacuumize 1 hour.The toluene solution of 2,6- dimethylaniline is added dropwise (2,6- dimethylanilines (109.75g , 0.91mol) are mixed with toluene (60ml)).It finishes, 60 DEG C of insulation reaction 2.0h.Cooling It to 20~30 DEG C, is added purified water (300ml), water phase is collected in layering; Fresh toluene (300ml), 10% hydrogen-oxygen is added in water phase Change sodium regulation system pH=6- 7, water phase is collected in layering; Water phase 10% sodium hydroxide regulation system pH=11~12,room temperature Stirring 4 hours, filter, purified water (150ml) elute filter cake, filter cake in 60 DEG C of air dry ovens it is dry 35.88g (yield 85%, HPLC purity 94.023% is calculated by areas of peak normalization method) .The purification of 2 intermediate (-) of-(2S)-N- (2,6- 3,5-dimethylphenyl) piperidines -2- formamide1 gained intermediate (-) of embodiment-(2S)-N- (2,6- diformazan is sequentially added in three mouthfuls of reaction flasks of 100ml cleaning Base phenyl) piperidines -2- formamide (5.00g, 21.52mmol), ether (50ml), stir and are warming up to reflux, flow back insulated and stirred 1 Hour, it is cooled to room temperature, insulated and stirred 1 hour, is filtered, ether (10ml) elutes filter cake, and filter cake is dry in 50 DEG C of air dry ovens Dry 2 hours 2.66g (yield 53.2% calculates HPLC purity 99.837% by areas of peak normalization method), map is shown in attached drawing 1.The purification of 3 intermediate (-) of-(2S)-N- (2,6- 3,5-dimethylphenyl) piperidines -2- formamide1 gained intermediate (-) of embodiment-(2S)-N- (2,6- diformazan is sequentially added in three mouthfuls of reaction flasks of 100ml cleaning Base phenyl) piperidines -2- formamide (5.00g, 21.52mmol), isopropyl ether (50ml), stir and are warming up to reflux, reflux heat preservation is stirred It mixes 1 hour, is cooled to room temperature, insulated and stirred 1 hour, filters, isopropyl ether (10m l) elutes filter cake, and filter cake is dry in 50 DEG C of air blast Dry 2 hours 3.45g of dry case (yield 69.0% calculates HPLC purity 99.332% by areas of peak normalization method).Map is shown in attached Fig. 2.The purification of 4 intermediate (-) of-(2S)-N- (2,6- 3,5-dimethylphenyl) piperidines -2- formamide1 gained intermediate (-) of embodiment-(2S)-N- (2,6- diformazan is sequentially added in three mouthfuls of reaction flasks of 100ml cleaning Base phenyl) piperidines -2- formamide (5.00g, 21.52mmol), methyl tertiary butyl ether(MTBE) (50ml), stir and are warming up to reflux, flow back Insulated and stirred 1 hour, be cooled to room temperature, insulated and stirred 1 hour, filter, methyl tertiary butyl ether(MTBE) (10ml) elutes filter cake, filter cake in Dry 2 hours 4.75g (yield 95% calculates HPLC purity 99.709% by areas of peak normalization method) of 50 DEG C of air dry ovens, Map is shown in attached drawing 3.5 intermediate (-) of embodiment-(2S)-N- (2,6- 3,5-dimethylphenyl) piperidines -2- formamide preparation and purificationA) the preparation of intermediate (-)-(2S)-N- (2,6- 3,5-dimethylphenyl) piperidines -2- formamideL- piperidinecarboxylic acid hydrochloride (3kg, 18.1mol), toluene (30L) are added in 50L reaction kettle, N, N- is added in stirring Dimethylformamide (1L), thionyl chloride (2.59kg, 21.8mol). It finishes, is warming up to 50~55 DEG C of insulation reactions 3 hours. Snubber device is added to vacuumize 6 hours.Be added dropwise 2,6- dimethylaniline toluene solution (2,6- dimethylanilines (11kg, It 90.8mol) is mixed with toluene (6L)).It finishes, 60 DEG C of insulation reaction 2.0h. 20~30 DEG C are cooled to, is added purified water (30L), Water phase is collected in layering; Water phase is added fresh toluene (30L) , 10% sodium hydroxide regulation system pH=6-7, and water is collected in layering Phase; 10% sodium hydroxide regulation system pH=11~12 of water phase, are stirred at room temperature 4 hours, filter,purified water (15L) elution filter Cake, filter cake in 60 DEG C of air dry ovens it is dry 3.52kg (yield 84%, by areas of peak normalization method calculate HPLC purity 98.092%), map is shown in attached drawing 4.B) the purification of intermediate (-)-(2S)-N- (2,6- 3,5-dimethylphenyl) piperidines -2- formamideIntermediate (-)-(2S)-N- (2,6- 3,5-dimethylphenyl) piperidines -2- formamide (3. is sequentially added in 50L reaction kettle 5kg, 15.1mol), methyl tertiary butyl ether(MTBE) (35L), stirring is warming up to reflux, flows back insulated and stirred 1 hour, be cooled to room temperature, guarantor Temperature stirring 1 hour, filters, and methyl tertiary butyl ether(MTBE) (7L) elutes filter cake, and filter cake is in the dry 8 hours 3.3kg of 50 DEG C of air dry ovens (yield 94% calculates HPLC purity 99.889% by areas of peak normalization method), map is shown in attached drawing 5.
Literatures:
Navinta LLC Patent: US2006/276654 A1, 2006 ; Location in patent: Page/Page column 5 ;
Yield: ~82%
Literatures:
US2006/276654 A1, ; Page/Page column 5 ;
Yield: null
SYN
https://pubs.rsc.org/en/content/articlehtml/2019/ra/c9ra09287k
Ropivacaine is the S-enantiomer of an N-alkyl pipecoloxylidine derivative, which is the first local anesthetic with chiral activity, and is widely used in clinical infiltration anesthesia, conduction anesthesia and epidural anesthesia. It has a long of local anesthesia and analgesic effect. However, ropivacaine also has serious safety risks in clinical practice. When the concentration of ropivacaine in human blood is too high, it may cause toxicity to the cardiovascular and central nervous system, and even cause allergic reactions in some patients. Thus far, the mechanism of the effect of ropivacaine on local anesthesia is not clear. Ropivacaine is a multitarget drug that acts on the gamma-aminobutyric acid a receptor (GABAA-R) and N-methyl-D-aspartate acid receptor (NDMA-R). Sodium (Na+) channels are a key target of local anesthetics and these two receptors regulate sodium channels. Previous studies on the structural modification of ropivacaine mainly focused on the substitution of –CH3 on the phenyl group or the substitution of –CH2CH2CH3 on piperidine with different alkyl groups. In 2017, Wen L. et al.69 reported the design and synthesis of ropivacaine analogues for local anesthesia. In the process of structural design, they used ropivacaine as the lead compound to design two series of compounds, 4a–4q (17 new substituted imines). In the first series of compounds, 4a–4i, different substituents were selected to replace –CH2CH2CH3 on piperidine. In the second series of compounds, 4j–4q, the methyl groups were replaced by –CF3 at the o-positions, m-positions and p-positions. Meanwhile, the –CH2CH2CH3 on piperidine ring was also substituted and modified. The process for the synthesis of the target compounds is shown in Scheme 8. The synthetic route takes piperic acid (compound 1) as the starting material, hydrochloric acid and sulfoxide chloride as additives, and toluene as the reaction solvent to convert compound 1 into acyl chloride salt (compound 2). Compound 2 was then treated with substituted aniline and reacted at 58 °C for 5 h to form compounds 3a–3i and 3j–3q. Finally, bromoalkyl and hydrochloric acid were used to treat compounds 3a–3i and 3j–3q. Potassium carbonate (K2CO3) was used as an acid dressing agent and dimethylformamide (DMF) as the reaction solvent in N-alkylation reaction. The N-alkylation reaction lasted 10 h at 80 °C, and the salt reaction lasted 5 min at room temperature to obtain the final target compounds 4a–4q. The total yield of the target compounds ranged from 17.5% to 87.7%. The synthetic route has the advantages of mild reaction conditions, cheap reagents and simple operation. However, using this synthetic route, the total yield of some products is too low, and too low yield will bring great problems to the synthesis cost, which needs to be further optimized in follow-up work. In the evaluation of the local anesthesia effect, sciatic nerve block activity, infiltration anesthesia activity, corneal anesthesia activity and spinal cord anesthesia activity were used as evaluation indexes. Ropivacaine was used as a positive control substance to test the local anesthesia activity in vitro. Firstly, the local anesthesia effect of all the target compounds 4a–4q was screened by a sciatic nerve block test in toads in vitro (Table 6). The preliminary screening results in vitro showed that these compounds increased the blocking effect of the sciatic nerve on electrical stimulation, with ED50 values ranging from 0.012 to 0.64 (positive control for ropivacaine was 0.013), with the highest activity shown by compound 4b. In terms of latent period, that of target compounds 4a–4q ranged from 27.7 to 59.4 min. Based on the results of the preliminary in vitro screening, compounds 4a, 4b, 4c, 4j and 4l were selected to test the efficacy of invasive anesthesia in guinea pigs. The results of the infiltration anesthesia test showed that the local anesthetic effect of compounds 4c and 4l was similar to that of the positive control ropivacaine, and the local anesthetic activity of other compounds was lower than that of the positive control. Furthermore, compounds 4a, 4b, 4c, 4j and 4l were used to test the local surface anesthesia effect of these compounds (Table 7). The results of the surface anesthesia test showed that compound 4l had a similar local anesthetic effect as the positive control ropivacaine, while the effect of the other compounds was poor in comparison with the positive control. Finally, compounds 4a, 4b, 4c, 4j and 4l were tested for spinal anesthesia in order to further study their local surface anesthesia effect. The experimental results showed that the ED50 produced by compounds 4l and 4b was 5.02 and 7.87, respectively, while the effects of compounds 4a, 4c and 4j were poor. The evaluation of local anesthesia in vitro found that compound 4l had the best activity, and thus molecular docking of compound 4l and ropivacaine was conducted to further study its local anesthesia mechanism. The molecular docking results showed that compound 4l interacts with receptor proteins of VGSC, GABAA-R and NDMA-R, which may help optimize and predict the activity of these ropivacaine analogues as potential local anesthetics.
| Scheme 8 Reagents and conditions: (a) (i) HCl,PhCH3, r.t., 1 h; (ii) PhCH3, SOCl2, 55 °C, 1 h; (b) substituted anilines, 58 °C, 5 h; and (c) (i) RBr, K2CO3, DMF, 80 °C, 10 h; (ii) HCl, r.t., 5 min. |
SYN
Prepn: A. F. Thuresson, C. Bovin, WO 8500599 (1985 to Apothekernes); H.-J. Federsel et al., Acta Chem. Scand. B41, 757 (1987).

CLIP
Ropivacaine hydrochloride was synthesized from L-2-pipecolic acid by successive reaction with SOCl2 and 2,6-dimethylaniline at 40 °C under ultrasonic irradiation to yield L-N-(2,6-dimethylphenyl)piperidin-2-carboxamide (4), and 4 was reacted with 1-bromopropane at 50 °C for 1 h under ultrasonic irradiation. The effects of reaction solvent, temperature and time under ultrasonic irradiation were investigated. Compared with conventional methods, present procedures have the advantages in milder conditions, shorter reaction time and higher yields. The total yield was 67.5%, [α]25 D= – 6.6°(c = 2, H2O).

SYN
Ropivacaine (3.1.37) (Naropin) is the pure S(–)-enantiomer of propivacaine released for clinical use in 1996. It is a long-acting, well tolerated local anesthetic agent and first produced as a pure enantiomer. Its effects and mechanism of action are similar to other local anesthetics working via reversible inhibition of sodium ion influx in nerve fibers. It may be a preferred option among other drugs among this class of compounds because of its reduced CNS and cardiotoxic potential and its lower propensity for motor block in the management of postoperative pain and labor pain [48–58].
The synthesis of ropivacaine (3.1.37) was carried out starting with l-pipecolic acid (3.1.34), prepared by a resolution of (±)-pipecolic acid with (+)-tartaric acid, which was dissolved in acetyl chloride and converted to acid chloride (3.1.35) with phosphorus pentachloride. The obtained compound (3.1.35) dissolved in toluene a solution of 2,6-xylidine (3.1.28) dissolved in the mixture of equal volumes of acetone, and N-methyl-2-pyrrolidone was added at 70°C to give (+)-l-pipecolic acid-2,6-xylidide (3.1.36). Reaction of this compound with propyl bromide in presence of potassium carbonate in i-PrOH/H2O gave the desired ropivacaine (3.1.37) [59] (Scheme 3.6).

Another approach for the synthesis of ropivacaine (3.1.37) was proposed via a resolution of enantiomers of chiral pipecolic acid-2,6-xylidide [60].
SYN

Scheme 21. Generation of ‘cation pool’ and its applications.
Reproduced from Yoshida, J.; Suga, S.; Suzuki, S.; et al. J. Am. Chem. Soc. 1999, 121, 9546–9549, and Shankaraiah, N.; Pilli, R. A.; Santos, L. S. Tetrahedron Lett. 2008, 49, 5098–5100.
CLIP
Process R&D under the magnifying glass: Organization, business model, challenges, and scientific context
Hans-Jürgen Federsel, in Bioorganic & Medicinal Chemistry, 2010
The synthesis of ropivacaine is achieved in only three steps, as in the previous example, comprised of a resolution of a racemic, commercially available starting material (pipecoloxylidide) followed by an N-alkylation and the final precipitation of the product as its HCl salt.14,24 Focusing on the middle step—the attachment of a propyl moiety onto the piperidine nitrogen—this reaction when developed in the laboratory and scaled up to maximum pilot plant volume (1000 L) behaved very well (Scheme 3). Thus, boiling the reaction mixture (reactants in a H2O/organic solvent mixture in the presence of a solid inorganic base) for an extended period of time (6 h) at high temperature (100 °C), the transformation was considered complete once a sample of the process solution showed <1% of remaining starting material. In preparation for launch, the method that had been thoroughly investigated and tested over a number of years and proven reliable on scale up had to be validated in the authentic 4000 L production equipment. Much to our surprise (and shock) we, however, found that the reaction came to a complete stand still long before reaching the expected end point. With a large amount of un-reacted starting material (30–40%) we were facing a situation that had never occurred during the lengthy development phase and this put the whole project in a very critical state as we were not able to reproduce the manufacturing method.


join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////////////////////////////
History
Ropivacaine was developed after bupivacaine was noted to be associated with cardiac arrest, particularly in pregnant women. Ropivacaine was found to have less cardiotoxicity than bupivacaine in animal models.
Clinical use
Contraindications
Ropivacaine is contraindicated for intravenous regional anaesthesia (IVRA). However, new data suggested both ropivacaine (1.2-1.8 mg/kg in 40ml) and levobupivacaine (40 ml of 0.125% solution) be used, because they have less cardiovascular and central nervous system toxicity than racemic bupivacaine.[1]
Adverse effects
Adverse drug reactions (ADRs) are rare when it is administered correctly. Most ADRs relate to administration technique (resulting in systemic exposure) or pharmacological effects of anesthesia, however allergic reactions can rarely occur.
Systemic exposure to excessive quantities of ropivacaine mainly result in central nervous system (CNS) and cardiovascular effects – CNS effects usually occur at lower blood plasma concentrations and additional cardiovascular effects present at higher concentrations, though cardiovascular collapse may also occur with low concentrations. CNS effects may include CNS excitation (nervousness, tingling around the mouth, tinnitus, tremor, dizziness, blurred vision, seizures followed by depression (drowsiness, loss of consciousness), respiratory depression and apnea). Cardiovascular effects include hypotension, bradycardia, arrhythmias, and/or cardiac arrest – some of which may be due to hypoxemia secondary to respiratory depression.[2]
Postarthroscopic glenohumeral chondrolysis
Ropivacaine is toxic to cartilage and their intra-articular infusions can lead to Postarthroscopic glenohumeral chondrolysis.[3]
Treatment of overdose
As for bupivacaine, Celepid, a commonly available intravenous lipid emulsion, can be effective in treating severe cardiotoxicity secondary to local anaesthetic overdose in animal experiments[4] and in humans in a process called lipid rescue.[5][6][7]
References
- ^ (Basic of Anesthesia, Robert Stoelting, page 289)
- ^ Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006. ISBN 0-9757919-2-3
- ^ Gulihar A, Robati S, Twaij H, Salih A, Taylor GJ (December 2015). “Articular cartilage and local anaesthetic: A systematic review of the current literature”. Journal of Orthopaedics. 12 (Suppl 2): S200-10. doi:10.1016/j.jor.2015.10.005. PMC 4796530. PMID 27047224.
- ^ Weinberg G, Ripper R, Feinstein DL, Hoffman W (2003). “Lipid emulsion infusion rescues dogs from bupivacaine-induced cardiac toxicity”. Regional Anesthesia and Pain Medicine. 28 (3): 198–202. doi:10.1053/rapm.2003.50041. PMID 12772136. S2CID 6247454.
- ^ Picard J, Meek T (February 2006). “Lipid emulsion to treat overdose of local anaesthetic: the gift of the glob”. Anaesthesia. 61 (2): 107–9. doi:10.1111/j.1365-2044.2005.04494.x. PMID 16430560. S2CID 29843241.
- ^ Rosenblatt MA, Abel M, Fischer GW, Itzkovich CJ, Eisenkraft JB (July 2006). “Successful use of a 20% lipid emulsion to resuscitate a patient after a presumed bupivacaine-related cardiac arrest”. Anesthesiology. 105 (1): 217–8. doi:10.1097/00000542-200607000-00033. PMID 16810015.
- ^ Litz RJ, Popp M, Stehr SN, Koch T (August 2006). “Successful resuscitation of a patient with ropivacaine-induced asystole after axillary plexus block using lipid infusion”. Anaesthesia. 61 (8): 800–1. doi:10.1111/j.1365-2044.2006.04740.x. PMID 16867094. S2CID 43125067.
External links
- “Ropivacaine”. Drug Information Portal. U.S. National Library of Medicine.
- “Ropivacaine hydrochloride”. Drug Information Portal. U.S. National Library of Medicine.
| Clinical data | |
|---|---|
| Trade names | Naropin |
| AHFS/Drugs.com | Monograph |
| Pregnancy category | AU: B1 |
| Routes of administration | Parenteral |
| ATC code | N01BB09 (WHO) |
| Legal status | |
| Legal status | AU: S4 (Prescription only) |
| Pharmacokinetic data | |
| Bioavailability | 87%–98% (epidural) |
| Metabolism | Liver (CYP1A2-mediated) |
| Elimination half-life | 1.6–6 hours (varies with administration route) |
| Excretion | Kidney 86% |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 84057-95-4 |
| PubChem CID | 175805 |
| IUPHAR/BPS | 7602 |
| DrugBank | DB00296 |
| ChemSpider | 153165 |
| UNII | 7IO5LYA57N |
| KEGG | D08490 as HCl: D04048 |
| ChEBI | CHEBI:8890 |
| ChEMBL | ChEMBL1077896 |
| CompTox Dashboard (EPA) | DTXSID4040187 |
| ECHA InfoCard | 100.128.244 |
| Chemical and physical data | |
| Formula | C17H26N2O |
| Molar mass | 274.408 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| Melting point | 144 to 146 °C (291 to 295 °F) |
| showSMILES | |
| showInChI | |
| (verify) |
Patent
Publication numberPriority datePublication dateAssigneeTitleUS4695576A *1984-07-091987-09-22Astra Lake Medel AktiebolagLNn-propylpipecolic acid-2,6-xylidideUS20050065345A1 *2001-09-102005-03-24Toshio TsuchidaMethod for producing pipecolamide derivativeCN103086954A *2013-02-042013-05-08Shandong Pharmaceutical Industry Research InstituteMethod for preparing ropivacaineCN104003930A *2014-06-132014-08-27Shandong Alura Pharmaceutical Research and Development Co., Ltd.Method for preparing hydrochloric acid ropivacaineCN107325041A *2017-06-202017-11-07Guangzhou Tonghui Pharmaceutical Co., Ltd.A kind of preparation method of Ropivacaine HCL
Non-Patent
TitleNAGULA SHANKARAIAH, etc.: “Enantioselective total syntheses of ropivacaine and its analogues”, “TETRAHEDRON LETTERS” *Liu Yi, et al.: “Synthesis of Ropivacaine Hydrochloride”, “Chinese Journal of Pharmaceutical Industry” *Ye Jiao, et al.: “Synthesis of Ropivacaine Hydrochloride by Triphosgene Method”, “Synthetic Chemistry” *Jiang Yao: “Study on the Synthetic Process of Ropivacaine Hydrochloride and Bupivacaine Hydrochloride”, “Engineering Science and Technology Series Ⅰ” *
/////////////Ropivacaine, Anesthetic, ропивакаин , روبيفاكائين , 罗哌卡因 , DRopivacaine Hydrochloride Hydrate, LEA-103, NA-001, (-)-LEA-103
CCCN1CCCC[C@H]1C(=O)NC1=C(C)C=CC=C1C

NEW DRUG APPROVALS
ONE TIME
$10.00
LIDOCAINE
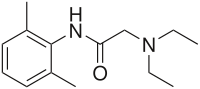
LIDOCAINE
CAS Registry Number: 137-58-6
CAS Name: 2-(Diethylamino)-N-(2,6-dimethylphenyl)acetamide
Additional Names: 2-diethylamino-2¢,6¢-acetoxylidide; w-diethylamino-2,6-dimethylacetanilide; lignocaine
Trademarks: Cuivasil (IDC); Lidoderm (Hind); LidoPosterine (Kade); Vagisil (Combe)
Molecular Formula: C14H22N2O
Molecular Weight: 234.34
Percent Composition: C 71.75%, H 9.46%, N 11.95%, O 6.83%
Literature References: Long-acting, membrane stabilizing agent against ventricular arrhythmia. Originally developed as a local anesthetic. Prepn: N. M. Löfgren, B. J. Lundqvist, US2441498 (1948 to Astra); A. D. H. Self, A. P. T. Easson, GB706409 (1954 to May & Baker); I. P. S. Hardie, E. S. Stern, GB758224 (1956 to J. F. Macfarlane & Co.); Zhuravlev, Nikolaev, Zh. Obshch. Khim.30, 1155 (1960). Toxicity studies: E. R. Smith, B. R. Duce, J. Pharmacol. Exp. Ther.179, 580 (1971); G. H. Kronberg et al.,J. Med. Chem.16, 739 (1973). Review of pharmacokinetics: N. L. Benowitz, W. Meister, Clin. Pharmacokinet.3, 177 (1978). Review of action as local anesthetic: Löfgren, Studies on Local Anesthetics: Xylocaine, A New Synthetic Drug (Hoeggstroms, Stockholm, 1948); Cooper, Pharm. J.171, 68 (1953). Reviews of anti-arrhythmic agents: J. L. Anderson et al.,Drugs15, 271 (1978); L. H. Opie, Lancet1, 861 (1980); E. Carmeliet, Ann. N.Y. Acad. Sci.427, 1 (1984). Comprehensive description: K. Groningsson et al.,Anal. Profiles Drug Subs.14, 207-243 (1985); M. F. Powell, ibid.15, 761-779 (1986). Review of use in treatment of postherpetic neuralgia: P. S. Davies, B. S. Galer, Drugs64, 937-947 (2004).Properties: Needles from benzene or alcohol, mp 68-69°. bp4 180-182°; bp2 159-160°. Insol in water. Sol in alcohol, ether, benzene, chloroform, oils. Partition coefficient (octanol/water, pH 7.4): 43.
Melting point: mp 68-69°
Boiling point: bp4 180-182°; bp2 159-160°
Log P: Partition coefficient (octanol/water, pH 7.4): 43
Derivative Type: Hydrochloride
CAS Registry Number: 73-78-9; 6108-05-0 (monohydrate)
Trademarks: Basicaina (Galenica); Batixim (So.Se.); Dynexan (Kreussler); Heweneural (Hevert); Licain (DeltaSelect); Lidesthesin (Ritsert); Lidofast (Angelini); Lidoject (Hexal); Lidrian (Baxter); Odontalg (Giovanardi); Sedagul (Wild); Xylocaine (AstraZeneca); Xylocard (AstraZeneca); Xylocitin (Jenapharm); Xyloneural (Strathmann)
Molecular Formula: C14H22N2O.HCl
Molecular Weight: 270.80
Percent Composition: C 62.09%, H 8.56%, N 10.34%, O 5.91%, Cl 13.09%
Properties: Crystals, mp 127-129°; monohydrate, mp 77-78°. Very sol in water, alcohol; sol in chloroform. Insol in ether. pH of 0.5% aq soln: 4.0-5.5. LD50 in mice (mg/kg): 292 orally (Smith, Duce); 105 i.p.; 19.5 i.v. (Kronberg).
Melting point: mp 127-129°; mp 77-78°
Toxicity data: LD50 in mice (mg/kg): 292 orally (Smith, Duce); 105 i.p.; 19.5 i.v. (Kronberg)
Therap-Cat: Anesthetic (local); antiarrhythmic (class IB).
Therap-Cat-Vet: Anesthetic (local).
Keywords: Anesthetic (Local); Antiarrhythmic.

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////////////////////////////
CLIP
https://pubs.acs.org/doi/10.1021/ed076p1557
http://www.asianjournalofchemistry.co.in/User/ViewFreeArticle.aspx?ArticleID=19_7_12
PATENT
https://patents.google.com/patent/CN102070483B/en#:~:text=The%20method%20comprises%20the%20following,as%20solvent%20and%20carbonate%20isPreparation method of the present invention, it can be two-step approach, comprises the steps:1) 2,6-xylidine is dissolved in the acetone, adds carbonate then, the back that stirs drips chloroacetyl chloride, and 20~35 ℃ (room temperature) be stirring reaction 3h down; After-filtration is finished in reaction, and after filter cake was washed with water to filtrate and is neutrality, drying made intermediate chloracetyl-2, the 6-xylidine, and yield is about about 94%;
2) intermediate that step 1) is made is dissolved in the acetone, adds carbonate then, and the back that stirs drips diethylamine, back flow reaction 8h; After-filtration is finished in reaction, and filtrate is recrystallization, drying after removing solvent under reduced pressure, makes lignocaine.Wherein, in the step 1) 2, the mol ratio of 6-xylidine, chloroacetyl chloride and carbonate is 1: 1.2~1.7: 1.3~2.0, is preferably 1: 1.5: 1.6.
Step 2) intermediate chloracetyl-2 in, the mol ratio of 6-xylidine, diethylamine and carbonate is 1: 1.5~2.5: 1.2~2.0, is preferably 1: 2: 1.5.In addition, preparation method of the present invention owing to all be that solvent, carbonate are catalyzer with acetone in the two-step reaction, therefore can further optimize reaction process on the basis of two-step approach, namely the intermediate of Sheng Chenging needn’t pass through aftertreatment, prepares lignocaine by one kettle way.Described one kettle way comprises the steps: 2,6-xylidine is dissolved in the acetone, adds carbonate then, after stirring, drips chloroacetyl chloride, and 20~35 ℃ (room temperature) be reaction 3h down; After reaction is finished, without processing, directly drip diethylamine, back flow reaction 8h, after-filtration is finished in reaction, and filtrate is recrystallization, drying after removing solvent under reduced pressure, makes lignocaine.Wherein, described 2, the mol ratio of 6-xylidine, chloroacetyl chloride, diethylamine and carbonate is 1: 1.2~1.7: 1.5~2.5: 2.5~3.5, is preferably 1: 1.5: 2: 2.5.
In addition, preparation method of the present invention adopts TLC monitoring reaction progress, and the developping agent of TLC is sherwood oil: ethyl acetate (V/V)=3: 1.The invention has the advantages that, the method synthesis technique for preparing lignocaine of the present invention is simple, do not need in the intermediate aftertreatment first pickling numerous and diverse step of alkali cleaning again, avoided unnecessary loss, therefore the yield of the intermediate that makes of the inventive method and lignocaine is all higher, and the lignocaine purity that makes is good, reaches more than 99%, has favorable industrial application prospect; In addition, the inventive method uses acetone to make solvent, and this solvent is nontoxic substantially non-stimulated, and can recycle, and is environmentally friendly.
EmbodimentBelow further specify the present invention by specific embodiment, but be not used for limiting the scope of the invention.
Embodiment 1 two-step approach prepares lignocaine1) intermediate chloracetyl-2, the preparation of 6-xylidineAdd 102g 2 in the 1000mL there-necked flask, the 6-xylidine is made solvent with 400mL acetone, adds 200g salt of wormwood again, and mechanical stirring evenly back drips 100mL chloroacetyl chloride (1.5h drips off), (20 ℃) stirring reaction 3h under the room temperature; Reaction finishes the back suction filtration, and filter cake is washed with water to filtrate and is neutral, and under 100 ℃ of temperature dry 1 hour then, make the 156g white powder, be intermediate chloracetyl-2,6-xylidine, yield are 94%, fusing point is 145.0~147.0 ℃.2) preparation of lignocaineAdd 80g intermediate chloracetyl-2 in the 1000mL there-necked flask, the 6-xylidine is made solvent with 400mL acetone, and the dissolving back adds 112g salt of wormwood, drips the 60g diethylamine fast, back flow reaction 8h; Reaction finishes the back suction filtration, and filtrate is removal of solvent under reduced pressure under 40 ℃ of temperature, uses 150mL sherwood oil recrystallization then, suction filtration, vacuum-drying 6h under 40 ℃ of temperature makes the 90g white powder, is lignocaine, yield is 95%, and fusing point is 67.0~68.0 ℃, and content is 99.05%.
Embodiment 2 two-step approachs prepare lignocaine1) intermediate chloracetyl-2, the preparation of 6-xylidineAdd 102g 2 in the 1000mL there-necked flask, the 6-xylidine is made solvent with 400mL acetone, adds 163g salt of wormwood again, and mechanical stirring evenly back drips 80mL chloroacetyl chloride (1.5h drips off), (20 ℃) stirring reaction 3h under the room temperature; Reaction finishes the back suction filtration, and filter cake is washed with water to filtrate and is neutral, and under 100 ℃ of temperature dry 1 hour then, make the 136g white powder, be intermediate chloracetyl-2,6-xylidine, yield are 82%, fusing point is 145~146 ℃.
2) preparation of lignocaineAdd 80g intermediate chloracetyl-2 in the 1000mL there-necked flask, the 6-xylidine is made solvent with 400mL acetone, and the dissolving back adds 90g salt of wormwood, drips the 45g diethylamine fast, back flow reaction 8h; Reaction finishes the back suction filtration, and filtrate is removal of solvent under reduced pressure under 40 ℃ of temperature, uses 150mL sherwood oil recrystallization then, suction filtration, vacuum-drying 6h under 40 ℃ of temperature makes the 84g white powder, is lignocaine, yield is 89%, and fusing point is 66~67 ℃, and content is 99.15%.
Embodiment 3 two-step approachs prepare lignocaine1) intermediate chloracetyl-2, the preparation of 6-xylidineAdd 102g 2 in the 1000mL there-necked flask, the 6-xylidine is made solvent with 400mL acetone, adds 250g salt of wormwood again, and mechanical stirring evenly back drips 113mL chloroacetyl chloride (1.5h drips off), (20 ℃) stirring reaction 3h under the room temperature; Reaction finishes the back suction filtration, and filter cake is washed with water to filtrate and is neutral, and under 100 ℃ of temperature dry 1 hour then, make the 150g white powder, be intermediate chloracetyl-2,6-xylidine, yield are 90%, fusing point is 147~148 ℃.
2) preparation of lignocaineAdd 80g intermediate chloracetyl-2 in the 1000mL there-necked flask, the 6-xylidine is made solvent with 400mL acetone, and the dissolving back adds 150g salt of wormwood, drips the 75g diethylamine fast, back flow reaction 8h; Reaction finishes the back suction filtration, and filtrate is removal of solvent under reduced pressure under 40 ℃ of temperature, uses 150mL sherwood oil recrystallization then, suction filtration, vacuum-drying 6h under 40 ℃ of temperature makes the 88g white powder, is lignocaine, yield is 93%, and fusing point is 68~69 ℃, and content is 98.75%.
Embodiment 4 one kettle ways prepare lignocaineIn the 5000mL there-necked flask, add 305g 2, the 6-xylidine, make solvent with 2000mL acetone, add 700g salt of wormwood again, mechanical stirring evenly back slowly drips 230mL chloroacetyl chloride (1.5h drips off), room temperature (35 ℃) is stirring reaction 3h down, and TLC point plate (use sherwood oil: ethyl acetate (V/V)=3: 1 is made developping agent) demonstration reacts completely; Dropwise 5 50g diethylamine then, the back back flow reaction 8h that stirs, TLC monitoring (developping agent is the same) shows and reacts completely; The reaction solution suction filtration, filtrate is removal of solvent under reduced pressure under 40 ℃ of temperature, gets light yellow solid, uses sherwood oil recrystallization secondary then, makes 482g white lignocaine crystal, and total recovery is 82%, and fusing point is 68.0~69.0 ℃, and content is 99.75%.
Comparative example 1 existing method prepares lignocaine1) intermediate chloracetyl-2, the preparation of 6-xylidineIn the 1000mL there-necked flask, with 102g 2, the 6-xylidine is dissolved in the 400mL glacial acetic acid, stirs slowly to add the 100mL chloroacetyl chloride down, is heated to 45 ℃, adds 200g solid sodium acetate (containing crystal water) then, reaction 2h; After reaction finished, ice bath was cooled to below 10 ℃, suction filtration, filter cake is washed with water to filtrate and is neutral, and drying is 1 hour under 100 ℃ of temperature, makes the 111g white powder, be intermediate chloracetyl-2,6-xylidine, yield are that 67% fusing point is 145.0~148.0 ℃.
2) preparation of lignocaineAdd 80g intermediate chloracetyl-2 in the 1000mL there-necked flask, the 6-xylidine is made solvent with 400mL toluene, and the dissolving back drips 60g diethylamine, back flow reaction 3.5h fast; After reaction finished, ice bath was cooled to 5 ℃, suction filtration, filtrate is used the 3mol/L hcl as extraction agent, and the acid solution that extraction is obtained is cooled to 10 ℃ then, stirs slowly to add 6mol/L KOH solution down, be alkalescence (pH8~9) to solution, with pentane extraction, organic layer was after washing, Anhydrous potassium carbonate drying after ice bath was cooled to 20 ℃, vapor bath is steamed and is desolventized, make the 74g white powder, be lignocaine, yield is 78%, fusing point is 66.0~67.0 ℃, and content is 97.15%.Embodiment 1 compares with comparative example 1, its intermediate chloracetyl-2, and the yield of 6-xylidine obviously improves, and reaches 94%, and the total recovery of final product lignocaine also is significantly improved, and the content of lignocaine is brought up to about 99%.Embodiment 4 compares with comparative example 1, and the total recovery of lignocaine is significantly improved, and reach 82%, and content is brought up to more than 99%.
Though above with a general description of the specific embodiments, the present invention is described in detail, on basis of the present invention, can make some modifications or improvements it, this will be apparent to those skilled in the art.Therefore, these modifications or improvements all belong to the scope of protection of present invention without departing from theon the basis of the spirit of the present invention.
CLIPhttps://www.cerritos.edu/chemistry/chem_212/Documents/Lab/10_lidocaine.pdf

Procedure: (1st week)A: Synthesis of 2,6-Dimethylaniline via Reduction of 2,6-Dimethylnitrobenzene 1. Dissolve1.0 g of 2,6-dimethylnitrobenzene in 10 mL of glacial acetic acid in a 50 mL Erlenmeyer flask. 2. In a 25 mL flask, dissolve 4.6 grams of SnCl2 · 2H2O in 8 mL of concentrated HCl, inside the fume hood. 3. Add the SnCl2 solution in one portion to the nitroxylene solution, magnetically swirl and mix, and let the mixture stand for 15 minutes. 4. Cool the mixture and collect the crystalline salt (dimethylaniline in the salt form: C6H5NH3 +Cl- ) in a Buchner funnel. 5. Transfer the moist crystals to an Erlenmeyer flask, add 5-10 mL of water, and make the solution strongly basic (to remove the acid and change C6H5NH3 +Clback intoC6H5NH2) by adding 30% KOH solution (12 to 17 mL required). 6. After cooling extract with three 10 mL portions of ether, rinse the ether extracts twice with 10 mL of water, and dry over K2CO3. 7. Evaporate the dried and filtered solution to an oil, transfer and rinse into a 50 mL Erlenmeyer flask, complete evaporation, weigh, and calculate the %yield of 2,6-dimethylaniline.
B: Synthesis of α-Chloro-2,6-dimethylacetanilide (prepare for a steam bath ahead of time) 1. For every 7 grams (from this step on, you need to calculate proportionally how much you need to add according to the actual weight that you got) of dimethylaniline from the previous step, add 50 mL of glacial acetic acid, and 7.2 g (or 5.2 mL) of chloroacetyl chloride, in that order. 2. Warm the solution on a steam bath to (40–50)ºC, remove, and add a solution of 1 gram of sodium acetate in 100 mL of water. 3. Cool the mixture and collect the product in a Buchner funnel. 4. Transfer the product to a disk of medium–sized filter paper, finely divide it with a spatula, and let air dry until the next laboratory period. 5. Upon drying, measure the mass and the melting point. Also, calculate the % yield.
B: Synthesis of α-Chloro-2,6-dimethylacetanilide (prepare for a steam bath ahead of time) 1. For every 7 grams (from this step on, you need to calculate proportionally how much you need to add according to the actual weight that you got) of dimethylaniline from the previous step, add 50 mL of glacial acetic acid, and 7.2 g (or 5.2 mL) of chloroacetyl chloride, in that order. 2. Warm the solution on a steam bath to (40–50)ºC, remove, and add a solution of 1 gram of sodium acetate in 100 mL of water. 3. Cool the mixture and collect the product in a Buchner funnel. 4. Transfer the product to a disk of medium–sized filter paper, finely divide it with a spatula, and let air dry until the next laboratory period. 5. Upon drying, measure the mass and the melting point. Also, calculate the % yield.
D. Synthesis of the bisulfate salt of lidocaine 1. Dissolve the lidocaine in ether (10 mL per gram of lidocaine) and add 2 mL of 2.2 M sulfuric acid in ethanol per gram of lidocaine. 2. Stir and scratch with a glass rod to mix and induce crystallization. 3. Dilute the mixture with an equal volume of acetone to aid filtration and collect the salt in a small Buchner funnel. 4. Rinse the solid on the funnel with a few milliliters of acetone and air dry and weigh the product. 5. Calculate the % yield of this step. *** Overall % Yield The overall % YCLIPhttp://home.sandiego.edu/~khuong/chem302L/Handouts/Lidocaine_handout_Su07.pdfSynthetic Strategy Lidocaine will be prepared via a three-step linear synthesis starting from 2,6-dimethylnitrobenzene. The reduction of 2,6-dimethylnitrobenzene 1 with three equivalents of stannous chloride (SnCl2) yields the ammonium salt 2. It is very important that the reaction mixture is strongly acidic during this reaction because the reduction of nitrobenzene using different reducing reagents and conditions can afford a variety of functional groups: nitroso, hydroxylamine (zinc dust, pH 4), azoxy (sodium arsenite), azo (zinc, weakly basic), or hydrazo (zinc, strongly basic). In industrial settings, often iron or tin with hydrochloric acid is used instead of stannous chloride because iron and tin are cheaper, but the reduction takes much longer. In the workup portion of the reaction, the ammonium salt 2 is reacted with an aqueous potassium hydroxide solution, liberating the free 2,6-dimethylaniline 3 in an acid-base reaction.

The reaction of 3 with the bifunctional α-chloroacetyl chloride leads to α-chloro-2,6-dimethylacetanilide 4. A slight excess of the acid chloride is used to ensure the complete conversion of the amine to the amide. The formation of the amide is a result of the significantly higher reactivity (~106 times) of the acyl chloride over the alkyl chloride. The addition of sodium acetate solution avoids the formation of HCl which would protonate unreacted 3 causing it to co-precipitate with the desired product 4.

In the last step, diethylamine performs a nucleophilic substitution (SN2) on the remaining alkyl chloride. Diethylamine serves both as a nucleophile to form lidocaine 5, and as acid scavenger, leading to formation of NH2Et2 + Cl- in this reaction. Since diethylamine is not a very strong nucleophile, it is used in excess here to improve the yield and speed up the reaction. The unreacted amine is later removed by extraction with water. The aqueous extraction of lidocaine with acid separates the unreacted chloroanilide 4 and the lidocaine. After addition of a strong base like aqueous potassium hydroxide, crude lidocaine is obtained.

Procedure Synthesis of 2,6-dimethylaniline (3) Dissolve 15 g of SnCl2•2H2O in 27 mL of concentrated hydrochloric acid. If necessary, heat the mixture gently. Add this solution in one portion to a solution of 3 mL of 2,6-dimethylnitrobenzene in 34 mL of glacial acetic acid. Swirl the resulting mixture and then allow it to stand for 15 minutes before placing the mixture in an ice bath. Collect the formed precipitate by vacuum filtration. Place the wet precipitate obtained above in a beaker and add 20 mL of water. Neutralize the acidic mixture by carefully adding an 8 M aqueous potassium hydroxide with continuous stirring until basic to litmus. Place the mixture in an ice bath. Upon cooling to room temperature, extract the mixture three times with diethyl ether. Combine the organic layers and wash them twice with water and once with brine. Dry the organic layer over anhydrous potassium carbonate. Decant away from the drying agent and evaporate the diethyl ether from a dry, preweighed flask using a rotary evaporator. The oily residue will be your crude product 3. Obtain and record the following information: 1. crude product description (co2. crude weight/percent yieldSynthesis of α-chloro-2,6-dimethylacetanilide (4) Dissolve 3 in 17 mL of glacial acetic acid. Add 1.1 equivalents (based on the moles of 3) of α-chloroacetyl chloride to this solution. Heat the solution to 40-50 o C for ten minutes to complete the reaction. Upon cooling, add a solution of ~3.3 g sodium acetate trihydrate in 67 mL water and then place the resulting mixture in an ice bath. Collect the precipitate by vacuum filtration. Rinse the filter cake with copious amounts of water in order to remove the acetic acid. It is important that the product be completely free of acetic acid after this step (why?). The pH of the individual water rinses can be checked with litmus paper to determine if the product is acid free. Allow for the product to air-dry on a watch glass until the next meeting. There is a reasonable chance that you will not obtain a precipitate as described above. If this is the case, you can try “seeding” using a small sample of authentic product from a classmate. If this does not work, check the TLC to be sure that you have formed product and devise an extractive workup that will separate the unreacted aniline 3 from the desired product 4. (Make sure you understand how to do this even if you obtain a precipitate in the first place). After the aqueous workup and following removal of solvent, you should obtain a solid. If not, check the TLC, using a sample of authentic product from a classmate as a standard. If the product appears relatively pure, you can continue even though the material is not a solid. Obtain and record the following information: 1. crude product description (color, physical state, etc.) 2. crude weight/percent yield 3. mp (if a solid)
4. TLC analysis 5. IR (check for presence of amide functional group) Synthesis of lidocaine; α-(N,N-diethylamino)-2,6-dimethylacetanilide (5). In a round bottom flask, dissolve α-chloro-2,6-dimethylacetanilide 4 in 17 mL of toluene. Before continuing, spot several (4 to 5) TLC plates in advance with this solution of 4. Provide three lanes and spot the 4 on the “SM” and “CO-SPOT” lanes. You will use these plates to monitor the progress of this reaction. Add three equivalents of diethylamine to the round bottom flask, and reflux the mixture vigorously until the reaction is complete. The amount of time required for complete reaction depends on many factors but it will likely take anywhere from more than a few minutes up to several hours. If the reaction is not complete when your lab period ends, you can stopper the reaction and reflux it for additional time at the next period. Usually a white precipitate forms during the reflux. Upon cooling, transfer the reaction mixture to a separatory funnel and extract the mixture three times with water. Next, extract the organic layer with two portions of 3 M hydrochloric acid. Cool the combined acidic aqueous extracts in an ice bath and then add 8 M aqueous potassium hydroxide slowly until the mixture is strongly basic again. The formation of a thin, dark yellow oily layer on top or a white solid is observed at this point. Place the mixture in an ice bath. Once the mixture is chilled, try to initiate the crystallization of the final product if no solid has formed at this point. Collect the obtained precipitate by filtration using a Büchner funnel. Wash it with twice with water and then press it as dry as possible. Obtain and record the following information: 1. crude product description (color, physical state, etc.) 2. crude weight/percent yield 3. TLC analysis Recrystallize the crude product from hexanes. Regardless of the final physical state of your product (solid or oil), obtain and record the following: 1. pure product description (color, physical state, etc.) 2. pure product weight/percent yield 3. overall (three-step) percent yield (from starting material 1) 4. TLC analysis 5. melting point (if a solid) 6. IR 7. 1 H and 13C NMR spectra of lidocaine will be given to you. Turn in a sample of your final product.
1H NMR
13C NMR
MS
IR KBR
Lidocaine is an antiarrhythmic medicine and also serves as a local anaesthetic drug. It is utilized in topical application to relieve pain, burning and itching sensation caused from skin inflammations. This drug is mainly used for minor surgeries. Figure 1 shows the 1H NMR spectrum of 200 mM lidocaine in CDCl3.
.jpg)
Figure 1. Proton NMR spectrum of 200 mM lidocaine in CDCl3.
1H NMR Relaxation
Figures 2, 3 and 4 show the relaxation time measurements. It can be seen that the relaxation times are shortest for the CH2 protons and longest for the CH protons. The first data point amplitude increases with the number of protons for the related peak.
.jpg)
Figure 2. Proton T1 relaxation time measurement of 200 mM lidocaine in CDCl3.
.jpg)
Figure 3. Proton T2 relaxation time measurement of 200 mM lidocaine in CDCl3.
.jpg)
Figure 4. COSY spectrum of 200 mM lidocaine in CDCl3. The cross-peaks and corresponding exchanging protons are labeled by colour-coded arrows and ellipses.
2D COSY
Figure 4 shows the 2D COSY spectrum where two spin systems (6,7,8) to (10,11) can be clearly seen. For instance, the methyl groups at 10 and 11 positions bond to aromatic protons at 6 and 8 positions, while the methyl groups at 16 and 17 positions bond to the ethylene groups at 14 and 15 positions. No coupling occurs at positions (6,7,8) to (16,17) or (14,15).
2D Homonuclear J-Resolved Spectroscopy
The chemical shift in the 2D homonuclear j-resolved spectrum appears along the direct (f2) direction and the effects of coupling between protons appear along the indirect (f1) dimension. This enables the assignment of chemical shifts of multiplets and may help in measuring unresolved couplings. Also, a decoupled 1D proton spectrum is produced by the projection along the f1 dimension. The 2D homonuclear j-resolved spectrum of lidocaine, plus the 1D proton spectrum (blue line) are shown in Figure 5.
.jpg)
Figure 5. Homonuclear j-resolved spectrum of 200 mM lidocaine in CDCl3. The multiplet splitting frequencies for different couplings are colour- coded.
The projection which is vertical reveals how the multiplets disintegrate into a single peak, which makes the 1D spectrum more simplified. Peak multiplicities are produced by vertical traces from peaks in the 2D spectrum and help in determining the frequencies of proton-proton coupling. When coupling frequencies are compared between different peaks, information can be obtained regarding which peaks are bonded to each other. Also, Information regarding the coupling strength can be obtained from the size of the coupling frequencies. These couplings substantiate the results of the COSY experiment.
However, in this experiment, the effects of second order coupling appear in the f1 direction as additional peaks which are equidistant from the coupling partners detached from the zero frequency in the f1 dimension. These peaks provide proof of second order coupling partners, but are generally considered as artifacts. Figure 6 shows these coupling partners and additional peaks marked by colour-coded arrows and ellipses.
.jpg)
Figure 6. Homonuclear j-resolved spectrum of 200 mM lidocaine in CDCl3 showing the extra peaks due to strong couplings.
1D 13C Spectra
Figure 7 shows the 13C NMR spectra of 1 M lidocaine in CDCl3. Since the 1D Carbon experiment is highly susceptible to the 13C nuclei in the specimen, it easily and clearly resolves 9 resonances. In this experiment, only carbons coupled to protons are seen.
.jpg)
Figure 7. Carbon spectra of 1 M lidocaine in CDCl3.
Given the fact that the DEPT spectra do not display the peaks at 170 and 135ppm, they must be part of quaternary carbons. The DEPT-135 and the DEPT-45 experiments provide signals of CH3, CH2 and CH groups, while the DEPT-90 experiment provides only the signal of CH groups. However, in DEPT-135 the CH2 groups occur as negative peaks. It can thus be summed up that the peaks between 45 and 60ppm belong to ethylene groups; the peaks between 10 and 20ppm are part of the methyl groups; and the peaks between 125 and 130ppm belong to methyne groups. A similar study can be carried out on the C and CH peaks.
Heteronuclear Correlation
The Heteronuclear Correlation (HETCOR) experiment identifies the proton signal that appears along the indirect dimension and the carbon signal along the direct dimension. Figure 8 shows the HETCOR spectrum of 1 M lidocaine in CDCl3. in the 2D spectrum, the peaks reveal which proton is attached to which carbon. This experiment helps in resolving assignment uncertainty from the ID carbon spectra.
.jpg)
Figure 8. HETCOR spectrum of 1 M lidocaine in CDCl3.
Heteronuclear Multiple Quantum Coherence
Heteronuclear Multiple Quantum Coherence (HMQC) is similar to the HETCOR experiment and is utilized to associate proton resonances to the carbons that are coupled directly to those protons. But in the HMQC experiment, the proton signal appears along the direct dimension and the carbon signal along the indirect dimension. Figure 9 shows the HMQC spectrum of 1 M lidocaine in CDCl3. In the 2D spectrum, the peaks show which proton is attached to which carbon. For conclusive peak assignment, a similar study with the HETCOR spectrum can be carried out.
.jpg)
Figure 9. HMQC spectrum of 1 M lidocaine in CDCl3.
Heteronuclear Multiple Bond Correlation
The Heteronuclear Multiple Bond Correlation (HMBC) experiment can be employed to achieve long-range correlations of proton and carbon via two or three bond couplings. Similar to the HMQC experiment, the proton signal appears along the direct dimension and the carbon signal along the indirect dimension. Figure 10 shows the HMBC spectrum of 1 M lidocaine in CDCl3.
.jpg)
Figure 10. HMBC spectrum of 1 M lidocaine in CDCl3, with some of the long-range couplings marked.
The couplings amid the molecular positions appear analogous to the couplings seen in the COSY spectrum; however, the HMBC also displays couplings to quaternary carbons, which are not seen either in HMQC or COSY experiments. In addition, there is a correlation between protons and carbons. This is attributed to three-bond bonding from 14 and 15 and vice versa, as shown in light green in Figure 1.
SYN
Synthesis of lidocaine T. J. Reilly (1999). “The Preparation of Lidocaine”. J. Chem. Ed. 76 (11): 1557.
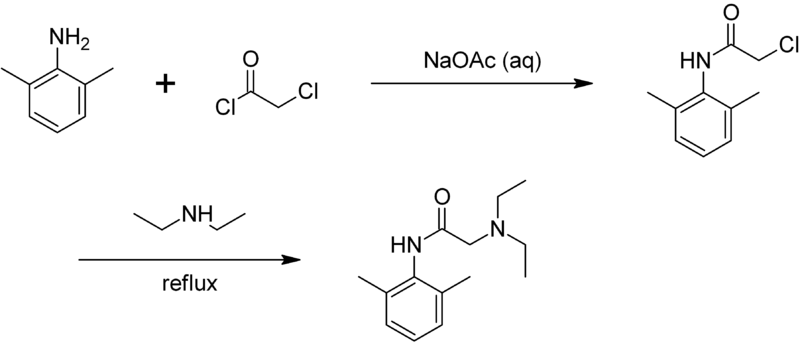
CLIP
The Present Synthesis Of Lidocaine Begins With 2,6-Dimethylnitrobenzene (1). This Compound Can Be Made From 1,3-Dimethylbenzene, Also Known As M-Xylene, Which Is More Difficult To Make. Luckily,
This problem has been solved!
See the answer
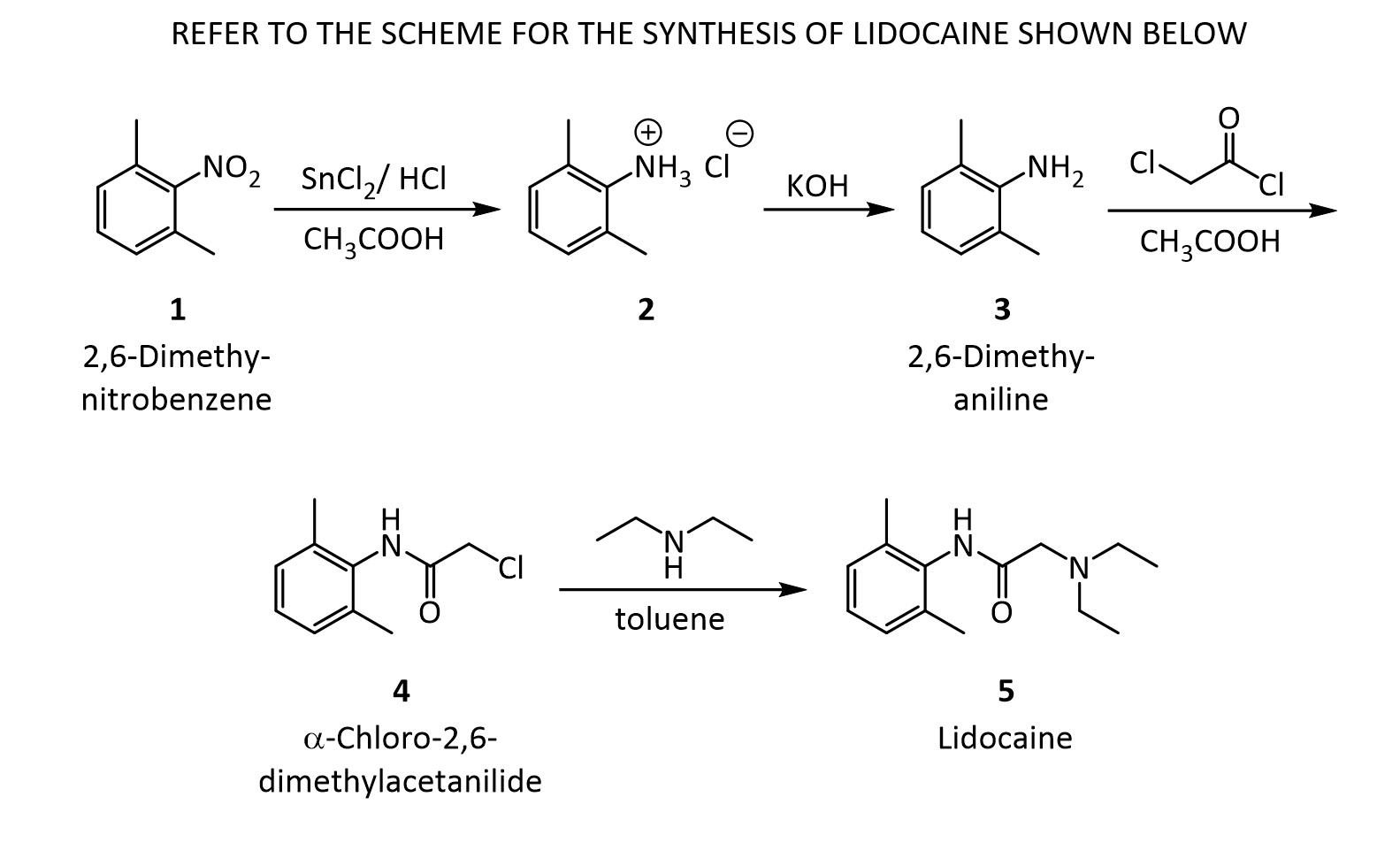
- The present synthesis of lidocaine begins with 2,6-dimethylnitrobenzene (1). This compound can be made from 1,3-dimethylbenzene, also known as m-xylene, which is more difficult to make. Luckily, m-xylene is commercially available, so a synthesis of 1 from m-xylene is a practical alternative if one wants to begin the synthesis of lidocaine with m-xylene. Suppose you want to prepare 1 from m-xylene. Show with chemical equations the reagents that you would use, and the possible isomers that would result.
2. The practical transformation of 1 into 3 is carried out by the following scheme:
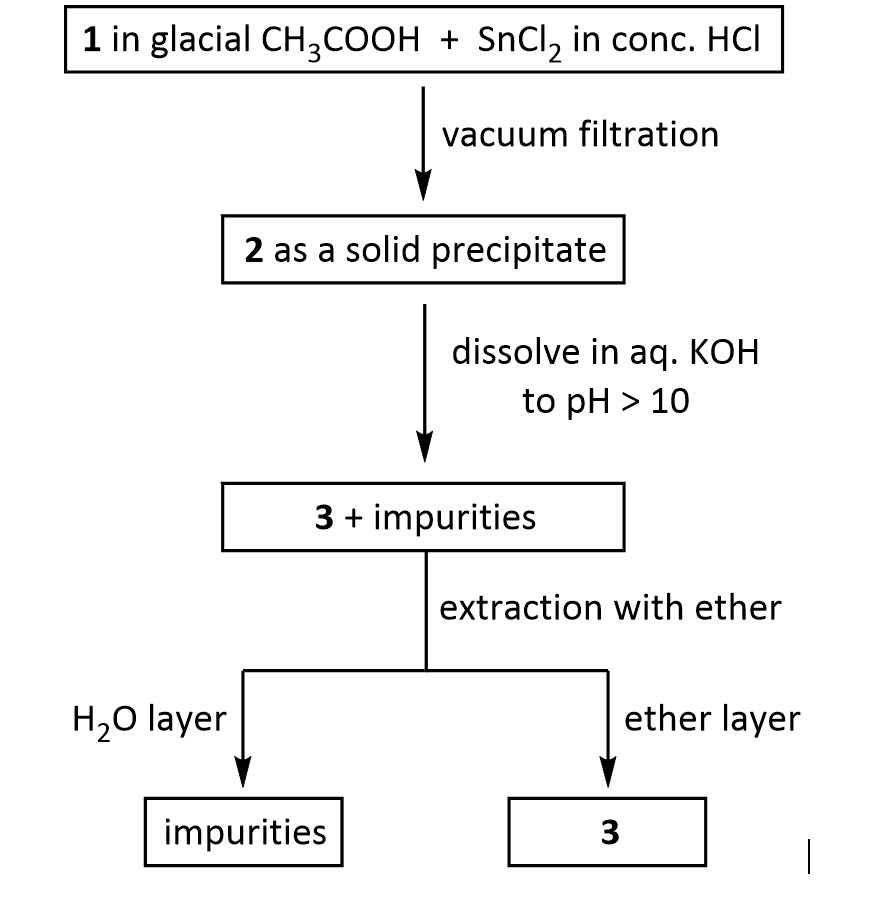
Suppose you dissolve the solid precipitate of 2 in water, but forget to include the KOH in the second step above. What would happen after the extraction with ether? Give your answer in terms of what would be found in the ether layer, and in the aqueous layer.
3. Suppose you’re out of acetic acid (CH3COOH) and decide to use ethanol (CH3 CH2OH) as the solvent in the transformation of 3 into 4. Would this be a wise choice, and why?
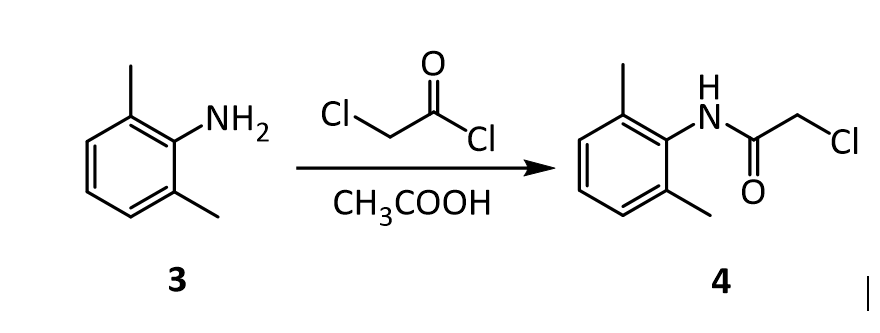
4.The amide 4 has a nitrogen attached to the benzene ring, and a chlorine attached to a primary carbon. Yet, it doesn’t react with itself in a nucleophilic displacement. Why is the nitrogen in the amide not nucleophilic? Give your answer in terms of the resonance forms of amides in general:
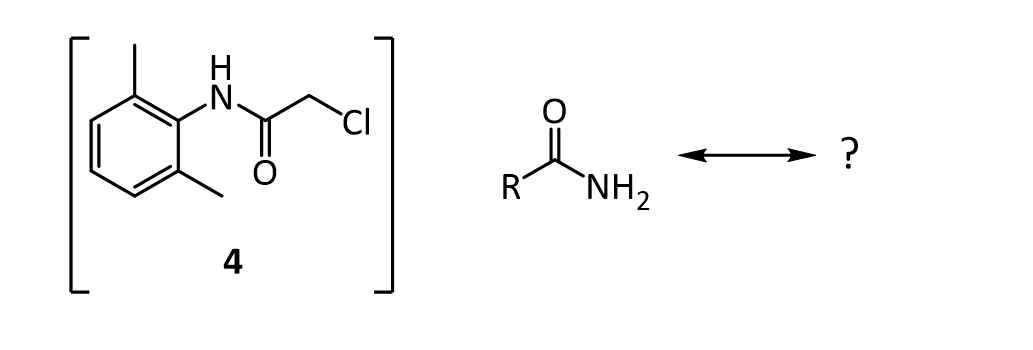
5. In the reaction below, what factors come into play to favor attack of the aniline 3 on the carbonyl carbon of the acid chloride (carbon 1 in red), rather than at the a-carbon (carbon 2 in red)?
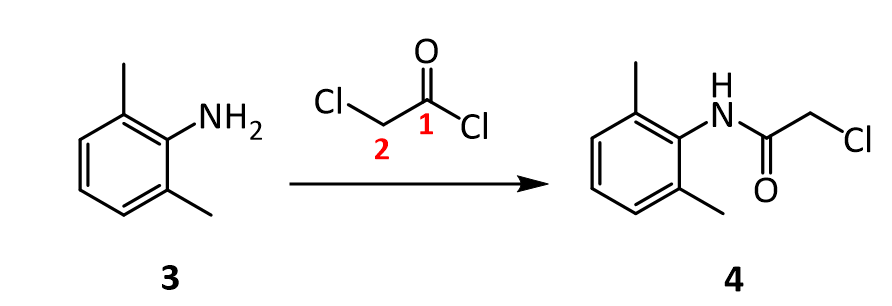
6. Before carrying out the transformation below, compound 4 and the glassware used must be oven-dried. What would happen if the reaction was attempted using wet 4?
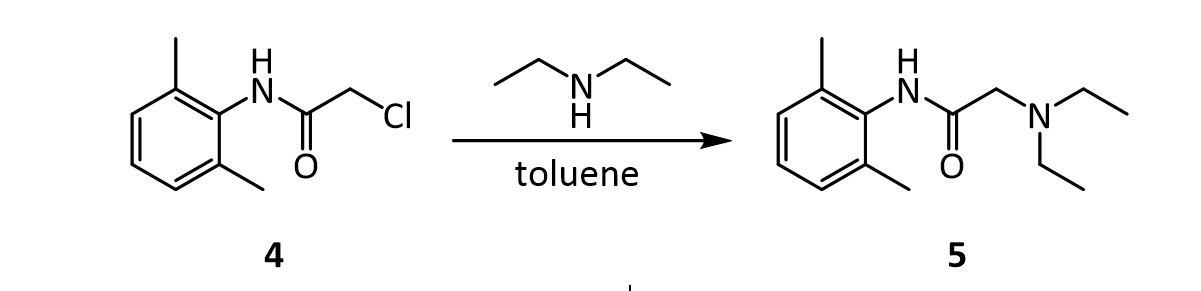
7.In the reaction below, what factors come into play to favor attack of diethylamine on the a-carbon (carbon 1 in red), rather than on the amide C=O carbon (carbon 2 in red)?
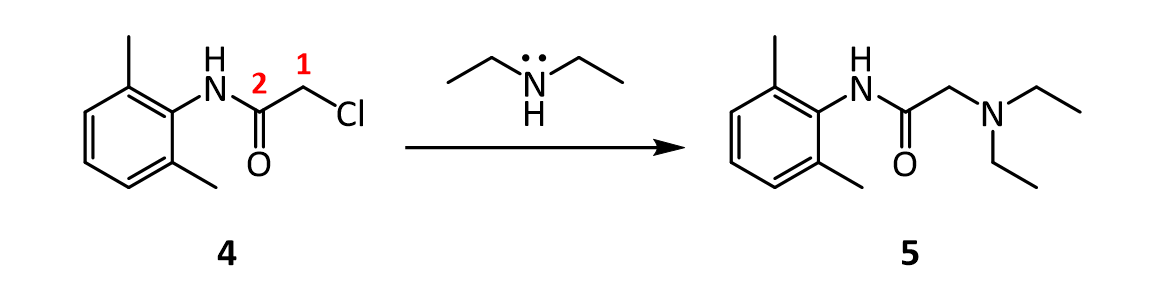
8. In the reaction below, why does the amine nitrogen (#1 in red) undergo protonation with H2SO4 preferentially over the amide nitrogen (#2 in red)? In other words, why is nitrogen 1 basic, but nitrogen 2 is not?
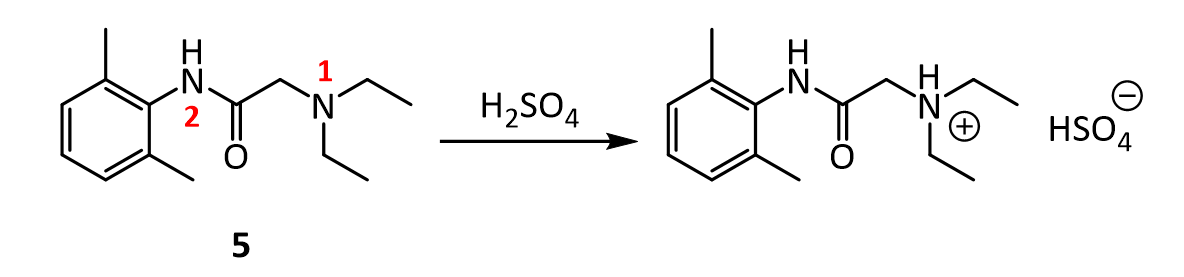
9.Lidocaine and other drugs containing amino groups are usually marketed as their hydrochloride or hydrogen sulfate salts, rather than as “free amines.” Provide two reasons why this practice makes sense.
10.Although lidocaine is marketed as its hydrochloride salt, it doesn’t exhibit the same level of physiological activity as the free amine. The free amine is more lipophilic and diffuses across a neuron cell membrane more rapidly than the ionic salt, resulting in a more rapid onset of anesthesia. Therefore, sodium bicarbonate (NaHCO3) is added to a solution of lidocaine prior to injection. How does the addition of sodium bicarbonate promote a faster anesthetic effect?
CLIP
CLIP
Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia.[7][8] When used for local anaesthesia or in nerve blocks, lidocaine typically begins working within several minutes and lasts for half an hour to three hours.[8][9] Lidocaine mixtures may also be applied directly to the skin or mucous membranes to numb the area.[8] It is often used mixed with a small amount of adrenaline (epinephrine) to prolong its local effects and to decrease bleeding.[8]
If injected intravenously, it may cause cerebral effects such as confusion, changes in vision, numbness, tingling, and vomiting.[7] It can cause low blood pressure and an irregular heart rate.[7] There are concerns that injecting it into a joint can cause problems with the cartilage.[8] It appears to be generally safe for use in pregnancy.[7] A lower dose may be required in those with liver problems.[7] It is generally safe to use in those allergic to tetracaine or benzocaine.[8] Lidocaine is an antiarrhythmic medication of the class Ib type.[7] This means it works by blocking sodium channels and thus decreasing the rate of contractions of the heart.[7] When injected near nerves, the nerves cannot conduct signals to or from the brain.[8]
Lidocaine was discovered in 1946 and went on sale in 1948.[10] It is on the World Health Organization’s List of Essential Medicines.[11] It is available as a generic medication.[8][12] In 2018, it was the 233rd most commonly prescribed medication in the United States, with more than 2 million prescriptions.[13][14]
Medical uses
Local numbing agent
The efficacy profile of lidocaine as a local anaesthetic is characterized by a rapid onset of action and intermediate duration of efficacy. Therefore, lidocaine is suitable for infiltration, block, and surface anaesthesia. Longer-acting substances such as bupivacaine are sometimes given preference for spinal and epidural anaesthesias; lidocaine, though, has the advantage of a rapid onset of action. Adrenaline vasoconstricts arteries, reducing bleeding and also delaying the resorption of lidocaine, almost doubling the duration of anaesthesia.
Lidocaine is one of the most commonly used local anaesthetics in dentistry. It can be administered in multiple ways, most often as a nerve block or infiltration, depending on the type of treatment carried out and the area of the mouth worked on.[15]
For surface anaesthesia, several formulations can be used for endoscopies, before intubations, etc. Buffering the pH of lidocaine makes local numbing less painful.[16] Lidocaine drops can be used on the eyes for short ophthalmic procedures. There is tentative evidence for topical lidocaine for neuropathic pain and skin graft donor site pain.[17][18] As a local numbing agent, it is used for the treatment of premature ejaculation.[19]
An adhesive transdermal patch containing a 5% concentration of lidocaine in a hydrogel bandage, is approved by the US FDA for reducing nerve pain caused by shingles.[20] The transdermal patch is also used for pain from other causes, such as compressed nerves and persistent nerve pain after some surgeries.
Heart arrhythmia
Lidocaine is also the most important class-1b antiarrhythmic drug; it is used intravenously for the treatment of ventricular arrhythmias (for acute myocardial infarction, digoxin poisoning, cardioversion, or cardiac catheterization) if amiodarone is not available or contraindicated. Lidocaine should be given for this indication after defibrillation, CPR, and vasopressors have been initiated. A routine preventive dose is no longer recommended after a myocardial infarction as the overall benefit is not convincing.[21]
Epilepsy
A 2013 review on treatment for neonatal seizures recommended intravenous lidocaine as a second-line treatment, if phenobarbital fails to stop seizures.[22]
Other
Intravenous lidocaine infusions are also used to treat chronic pain and acute surgical pain as an opiate sparing technique. The quality of evidence for this use is poor so it is difficult to compare it to placebo or an epidural.[23]
Inhaled lidocaine can be used as a cough suppressor acting peripherally to reduce the cough reflex. This application can be implemented as a safety and comfort measure for patients who have to be intubated, as it reduces the incidence of coughing and any tracheal damage it might cause when emerging from anaesthesia.[24]
Lidocaine, along with ethanol, ammonia, and acetic acid, may also help in treating jellyfish stings, both numbing the affected area and preventing further nematocyst discharge.[25][26]
For gastritis, drinking a viscous lidocaine formulation may help with the pain.[27]
Adverse effects
Adverse drug reactions (ADRs) are rare when lidocaine is used as a local anesthetic and is administered correctly. Most ADRs associated with lidocaine for anesthesia relate to administration technique (resulting in systemic exposure) or pharmacological effects of anesthesia, and allergic reactions only rarely occur.[28] Systemic exposure to excessive quantities of lidocaine mainly result in central nervous system (CNS) and cardiovascular effects – CNS effects usually occur at lower blood plasma concentrations and additional cardiovascular effects present at higher concentrations, though cardiovascular collapse may also occur with low concentrations. ADRs by system are:
- CNS excitation: nervousness, agitation, anxiety, apprehension, tingling around the mouth (circumoral paraesthesia), headache, hyperesthesia, tremor, dizziness, pupillary changes, psychosis, euphoria, hallucinations, and seizures
- CNS depression with increasingly heavier exposure: drowsiness, lethargy, slurred speech, hypoesthesia, confusion, disorientation, loss of consciousness, respiratory depression and apnoea.
- Cardiovascular: hypotension, bradycardia, arrhythmias, flushing, venous insufficiency, increased defibrillator threshold, edema, and/or cardiac arrest – some of which may be due to hypoxemia secondary to respiratory depression.[29]
- Respiratory: bronchospasm, dyspnea, respiratory depression or arrest
- Gastrointestinal: metallic taste, nausea, vomiting
- Ears: tinnitus
- Eyes: local burning, conjunctival hyperemia, corneal epithelial changes/ulceration, diplopia, visual changes (opacification)
- Skin: itching, depigmentation, rash, urticaria, edema, angioedema, bruising, inflammation of the vein at the injection site, irritation of the skin when applied topically
- Blood: methemoglobinemia
- Allergy
ADRs associated with the use of intravenous lidocaine are similar to toxic effects from systemic exposure above. These are dose-related and more frequent at high infusion rates (≥3 mg/min). Common ADRs include: headache, dizziness, drowsiness, confusion, visual disturbances, tinnitus, tremor, and/or paraesthesia. Infrequent ADRs associated with the use of lidocaine include: hypotension, bradycardia, arrhythmias, cardiac arrest, muscle twitching, seizures, coma, and/or respiratory depression.[29]
It is generally safe to use lidocaine with vasoconstrictor such as adrenaline, including in regions such as the nose, ears, fingers, and toes.[30] While concerns of tissue death if used in these areas have been raised, evidence does not support these concerns.[30]
Interactions
Any drugs that are also ligands of CYP3A4 and CYP1A2 can potentially increase serum levels and potential for toxicity or decrease serum levels and the efficacy, depending on whether they induce or inhibit the enzymes, respectively. Drugs that may increase the chance of methemoglobinemia should also be considered carefully. Dronedarone and liposomal morphine are both absolutely a contraindication, as they may increase the serum levels, but hundreds of other drugs require monitoring for interaction.[31]
Contraindications
Absolute contraindications for the use of lidocaine include:
- Heart block, second or third degree (without pacemaker)
- Severe sinoatrial block (without pacemaker)
- Serious adverse drug reaction to lidocaine or amide local anesthetics
- Hypersensitivity to corn and corn-related products (corn-derived dextrose is used in the mixed injections)
- Concurrent treatment with quinidine, flecainide, disopyramide, procainamide (class I antiarrhythmic agents)
- Prior use of amiodarone hydrochloride
- Adams-Stokes syndrome[32]
- Wolff-Parkinson-White syndrome[32]
- Lidocaine viscous is not recommended by the FDA to treat teething pain in children and infants.[33]
Exercise caution in patients with any of these:
- Hypotension not due to arrhythmia
- Bradycardia
- Accelerated idioventricular rhythm
- Elderly patients
- Ehlers-Danlos Syndrome
- Pseudocholinesterase deficiency
- Intra-articular infusion (this is not an approved indication and can cause chondrolysis)
- Porphyria, especially acute intermittent porphyria; lidocaine has been classified as porphyrogenic because of the hepatic enzymes it induces,[34] although clinical evidence suggests it is not.[35] Bupivacaine is a safe alternative in this case.
- Impaired liver function – people with lowered hepatic function may have an adverse reaction with repeated administration of lidocaine because the drug is metabolized by the liver. Adverse reactions may include neurological symptoms (e.g. dizziness, nausea, muscle twitches, vomiting, or seizures).[36]
Overdosage
Overdoses of lidocaine may result from excessive administration by topical or parenteral routes, accidental oral ingestion of topical preparations by children (who are more susceptible to overdose), accidental intravenous (rather than subcutaneous, intrathecal, or paracervical) injection, or from prolonged use of subcutaneous infiltration anesthesia during cosmetic surgery.
Such overdoses have often led to severe toxicity or death in both children and adults. Lidocaine and its two major metabolites may be quantified in blood, plasma, or serum to confirm the diagnosis in potential poisoning victims or to assist forensic investigation in a case of fatal overdose.
Lidocaine is often given intravenously as an antiarrhythmic agent in critical cardiac-care situations.[37] Treatment with intravenous lipid emulsions (used for parenteral feeding) to reverse the effects of local anaesthetic toxicity is becoming more common.[38]
Postarthroscopic glenohumeral chondrolysis
Lidocaine in large amounts may be toxic to cartilage and intra-articular infusions can lead to postarthroscopic glenohumeral chondrolysis.[39]
Pharmacology
Mechanism of action
Lidocaine alters signal conduction in neurons by prolonging the inactivation of the fast voltage-gated Na+ channels in the neuronal cell membrane responsible for action potential propagation.[40] With sufficient blockage, the voltage-gated sodium channels will not open and an action potential will not be generated. Careful titration allows for a high degree of selectivity in the blockage of sensory neurons, whereas higher concentrations also affect other types of neurons.
The same principle applies for this drug’s actions in the heart. Blocking sodium channels in the conduction system, as well as the muscle cells of the heart, raises the depolarization threshold, making the heart less likely to initiate or conduct early action potentials that may cause an arrhythmia.[41]
Pharmacokinetics
When used as an injectable it typically begins working within four minutes and lasts for half an hour to three hours.[8][9] Lidocaine is about 95% metabolized (dealkylated) in the liver mainly by CYP3A4 to the pharmacologically active metabolites monoethylglycinexylidide (MEGX) and then subsequently to the inactive glycine xylidide. MEGX has a longer half-life than lidocaine, but also is a less potent sodium channel blocker.[42] The volume of distribution is 1.1 L/kg to 2.1 L/kg, but congestive heart failure can decrease it. About 60% to 80% circulates bound to the protein alpha1 acid glycoprotein. The oral bioavailability is 35% and the topical bioavailability is 3%.
The elimination half-life of lidocaine is biphasic and around 90 min to 120 min in most patients. This may be prolonged in patients with hepatic impairment (average 343 min) or congestive heart failure (average 136 min).[43] Lidocaine is excreted in the urine (90% as metabolites and 10% as unchanged drug).[44]
History
Lidocaine, the first amino amide–type local anesthetic, was first synthesized under the name ‘xylocaine’ by Swedish chemist Nils Löfgren in 1943.[45][46][47] His colleague Bengt Lundqvist performed the first injection anesthesia experiments on himself.[45] It was first marketed in 1949.
Society and culture
Dosage forms
Lidocaine, usually in the form of its hydrochloride salt, is available in various forms including many topical formulations and solutions for injection or infusion.[48] It is also available as a transdermal patch, which is applied directly to the skin.
- Lidocaine hydrochloride 2% epinephrine 1:80,000 solution for injection in a cartridge
- Lidocaine hydrochloride 1% solution for injection
- Topical lidocaine spray
- 2% viscous lidocaine
Names
Lidocaine is the International Nonproprietary Name (INN), British Approved Name (BAN), and Australian Approved Name (AAN),[49] while lignocaine is the former BAN[citation needed] and AAN. Both the old and new names will be displayed on the product label in Australia until at least 2023.[50]
Xylocaine is a brand name.
Recreational use
As of 2021, lidocaine is not listed by the World Anti-Doping Agency as a substance whose use is banned in sport.[51] It is used as an adjuvant, adulterant, and diluent to street drugs such as cocaine and heroin.[52] It is one of the three common ingredients in site enhancement oil used by bodybuilders.[53]
Adulterant in cocaine
Lidocaine is often added to cocaine as a diluent.[54][55] Cocaine and lidocaine both numb the gums when applied. This gives the user the impression of high-quality cocaine, when in actuality the user is receiving a diluted product.[56]
Compendial status
Veterinary use
It is a component of the veterinary drug Tributame along with embutramide and chloroquine used to carry out euthanasia on horses and dogs.[58][59]
References
- ^ “Lidocaine”. Merriam-Webster Dictionary.
- ^ “Lidocaine”. Dictionary.com Unabridged. Random House.
- ^ “Poisons Standard February 2021”. Federal Register of Legislation. 1 January 2021. Retrieved 11 April 2021.
- ^ “Lidocaine Hydrochloride Injection BP 1% w/v – Summary of Product Characteristics (SmPC)”. (emc). 29 June 2020. Retrieved 11 April 2021.
- ^ “Xylocaine MPF- lidocaine hydrochloride injection, solution Xylocaine- lidocaine hydrochloride injection, solution Xylocaine- lidocaine hydrochloride,epinephrine bitartrate injection, solution”. DailyMed. Retrieved 11 April 2021.
- ^ “Ztlido- lidocaine patch”. DailyMed. Retrieved 11 April 2021.
- ^ Jump up to:a b c d e f g h i j k “Lidocaine Hydrochloride (Antiarrhythmic)”. The American Society of Health-System Pharmacists. Archivedfrom the original on 2015-08-10. Retrieved Aug 26, 2015.
- ^ Jump up to:a b c d e f g h i j “Lidocaine Hydrochloride (Local)”. The American Society of Health-System Pharmacists. Archived from the original on 2015-09-06. Retrieved Aug 26, 2015.
- ^ Jump up to:a b c J. P. Nolan; P. J. F. Baskett (1997). “Analgesia and anaesthesia”. In David Skinner; Andrew Swain; Rodney Peyton; Colin Robertson (eds.). Cambridge Textbook of Accident and Emergency Medicine. Project co-ordinator, Fiona Whinster. Cambridge, UK: Cambridge University Press. p. 194. ISBN 9780521433792. Archived from the original on 2017-09-08.
- ^ Scriabine, Alexander (1999). “Discovery and development of major drugs currently in use”. In Ralph Landau; Basil Achilladelis; Alexander Scriabine (eds.). Pharmaceutical Innovation: Revolutionizing Human Health. Philadelphia: Chemical Heritage Press. p. 211. ISBN 9780941901215. Archived from the original on 2017-09-08.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06.
- ^ Hamilton, Richart (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. p. 22. ISBN 9781284057560.
- ^ “The Top 300 of 2021”. ClinCalc. Retrieved 18 February 2021.
- ^ “Lidocaine – Drug Usage Statistics”. ClinCalc. Retrieved 18 February 2021.
- ^ “Local anaesthetic drugs”.
- ^ Cepeda MS, Tzortzopoulou A, Thackrey M, Hudcova J, Arora Gandhi P, Schumann R (December 2010). Tzortzopoulou A (ed.). “Adjusting the pH of lidocaine for reducing pain on injection”. The Cochrane Database of Systematic Reviews (12): CD006581. doi:10.1002/14651858.CD006581.pub2. PMID 21154371.(Retracted, see doi:10.1002/14651858.cd006581.pub3. If this is an intentional citation to a retracted paper, please replace
{{Retracted}}with{{Retracted|intentional=yes}}.) - ^ Derry S, Wiffen PJ, Moore RA, Quinlan J (July 2014). Derry S (ed.). “Topical lidocaine for neuropathic pain in adults”. The Cochrane Database of Systematic Reviews. 7 (7): CD010958. doi:10.1002/14651858.CD010958.pub2. PMC 6540846. PMID 25058164.
- ^ Sinha S, Schreiner AJ, Biernaskie J, Nickerson D, Gabriel VA (November 2017). “Treating pain on skin graft donor sites: Review and clinical recommendations”. The Journal of Trauma and Acute Care Surgery. 83 (5): 954–964. doi:10.1097/TA.0000000000001615. PMID 28598907. S2CID 44520644.
- ^ “Lidocaine/prilocaine spray for premature ejaculation”. Drug and Therapeutics Bulletin. 55 (4): 45–48. April 2017. doi:10.1136/dtb.2017.4.0469. PMID 28408390. S2CID 19110955.
- ^ Kumar M, Chawla R, Goyal M (2015). “Topical anesthesia”. Journal of Anaesthesiology Clinical Pharmacology. 31 (4): 450–6. doi:10.4103/0970-9185.169049. PMC 4676230. PMID 26702198.
- ^ Martí-Carvajal AJ, Simancas-Racines D, Anand V, Bangdiwala S (August 2015). “Prophylactic lidocaine for myocardial infarction”. The Cochrane Database of Systematic Reviews. 8 (8): CD008553. doi:10.1002/14651858.CD008553.pub2. PMC 8454263. PMID 26295202.
- ^ Slaughter LA, Patel AD, Slaughter JL (March 2013). “Pharmacological treatment of neonatal seizures: a systematic review”. Journal of Child Neurology. 28 (3): 351–64. doi:10.1177/0883073812470734. PMC 3805825. PMID 23318696.
- ^ Weibel S, Jelting Y, Pace NL, Helf A, Eberhart LH, Hahnenkamp K, et al. (June 2018). “Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery in adults”. The Cochrane Database of Systematic Reviews. 2018 (6): CD009642. doi:10.1002/14651858.cd009642.pub3. PMC 6513586. PMID 29864216.
- ^ Biller JA (2007). “Airway obstruction, bronchospasm, and cough”. In Berger AM, Shuster JL, Von Roenn JH (eds.). Principles and practice of palliative care and supportive oncology. Hagerstwon, MD: Lippincott Williams & Wilkins. pp. 297–307. ISBN 978-0-7817-9595-1.
Inhaled lidocaine is used to suppress cough during bronchoscopy. Animal studies and a few human studies suggest that lidocaine has an antitussive effect…
- ^ Birsa LM, Verity PG, Lee RF (May 2010). “Evaluation of the effects of various chemicals on discharge of and pain caused by jellyfish nematocysts”. Comp. Biochem. Physiol. C. 151 (4): 426–30. doi:10.1016/j.cbpc.2010.01.007. PMID 20116454.
- ^ Morabito R, Marino A, Dossena S, La Spada G (Jun 2014). “Nematocyst discharge in Pelagia noctiluca (Cnidaria, Scyphozoa) oral arms can be affected by lidocaine, ethanol, ammonia and acetic acid”. Toxicon. 83: 52–8. doi:10.1016/j.toxicon.2014.03.002. PMID 24637105.
- ^ James G. Adams (2012). “32”. Emergency Medicine: Clinical Essentials. Elsevier Health Sciences. ISBN 9781455733941. Archived from the original on 2017-09-08.
- ^ Jackson D, Chen AH, Bennett CR (October 1994). “Identifying true lidocaine allergy”. J Am Dent Assoc. 125 (10): 1362–6. doi:10.14219/jada.archive.1994.0180. PMID 7844301.
- ^ Jump up to:a b Australian Medicines Handbook. Adelaide, S. Aust: Australian Medicines Handbook Pty Ltd. 2006. ISBN 978-0-9757919-2-9.[page needed]
- ^ Jump up to:a b Nielsen LJ, Lumholt P, Hölmich LR (October 2014). “[Local anaesthesia with vasoconstrictor is safe to use in areas with end-arteries in fingers, toes, noses and ears]”. Ugeskrift for Laeger. 176(44). PMID 25354008.
- ^ “Lidocaine”. Epocrates. Archived from the original on 2014-04-22.
- ^ Jump up to:a b “Lidocaine Hydrochloride and 5% Dextrose Injection”. Safety Labeling Changes. FDA Center for Drug Evaluation and Research (CDER). January 2014. Archived from the original on 2013-04-03.
- ^ “Lidocaine Viscous: Drug Safety Communication – Boxed Warning Required – Should Not Be Used to Treat Teething Pain”. FDA Center for Drug Evaluation and Research (CDER). June 2014. Archived from the original on 2014-07-14.
- ^ “Table 96–4. Drugs and Porphyria” (PDF). Merck Manual. Merck & Company, Inc. 2011. Archived from the original on 2014-04-20.
- ^ “Lidocaine – N01BB02”. Drug porphyrinogenicity monograph. The Norwegian Porphyria Centre and the Swedish Porphyria Centre. Archived from the original on 2014-04-20.
strong clinical evidence points to lidocaine as probably not porphyrinogenic
- ^ Khan, M. Gabriel (2007). Cardiac Drug Therapy (7th ed.). Totowa, NJ: Humana Press. ISBN 9781597452380.
- ^ Baselt R (2008). Disposition of Toxic Drugs and Chemicals in Man(8th ed.). Foster City, CA: Biomedical Publications. pp. 840–4. ISBN 978-0-9626523-7-0.
- ^ Picard J, Ward SC, Zumpe R, Meek T, Barlow J, Harrop-Griffiths W (February 2009). “Guidelines and the adoption of ‘lipid rescue’ therapy for local anaesthetic toxicity”. Anaesthesia. 64 (2): 122–5. doi:10.1111/j.1365-2044.2008.05816.x. PMID 19143686. S2CID 25581037.
- ^ Gulihar A, Robati S, Twaij H, Salih A, Taylor GJ (December 2015). “Articular cartilage and local anaesthetic: A systematic review of the current literature”. Journal of Orthopaedics. 12 (Suppl 2): S200-10. doi:10.1016/j.jor.2015.10.005. PMC 4796530. PMID 27047224.
- ^ Carterall, William A. (2001). “Molecular mechanisms of gating and drug block of sodium channels”. Sodium Channels and Neuronal Hyperexcitability. Novartis Foundation Symposia. 241. pp. 206–225. doi:10.1002/0470846682.ch14. ISBN 9780470846681.
- ^ Sheu SS, Lederer WJ (Oct 1985). “Lidocaine’s negative inotropic and antiarrhythmic actions. Dependence on shortening of action potential duration and reduction of intracellular sodium activity”. Circulation Research. 57 (4): 578–90. doi:10.1161/01.res.57.4.578. PMID 2412723.
- ^ Lewin NA, Nelson LH (2006). “Chapter 61: Antidysrhythmics”. In Flomenbaum N, Goldfrank LR, Hoffman RL, Howland MD, Lewin NA, Nelson LH (eds.). Goldfrank’s Toxicologic Emergencies(8th ed.). New York: McGraw-Hill. pp. 963–4. ISBN 978-0-07-143763-9.
- ^ Thomson PD, Melmon KL, Richardson JA, Cohn K, Steinbrunn W, Cudihee R, Rowland M (April 1973). “Lidocaine pharmacokinetics in advanced heart failure, liver disease, and renal failure in humans”. Ann. Intern. Med. 78 (4): 499–508. doi:10.7326/0003-4819-78-4-499. PMID 4694036.
- ^ Collinsworth KA, Kalman SM, Harrison DC (1974). “The clinical pharmacology of lidocaine as an antiarrhythymic drug”. Circulation. 50 (6): 1217–30. doi:10.1161/01.CIR.50.6.1217. PMID 4609637.
- ^ Jump up to:a b Löfgren N (1948). Studies on local anesthetics: Xylocaine: a new synthetic drug (Inaugural dissertation). Stockholm, Sweden: Ivar Heggstroms. OCLC 646046738.[page needed]
- ^ Löfgren N, Lundqvist B (1946). “Studies on local anaesthetics II”. Svensk Kemisk Tidskrift. 58: 206–17.
- ^ Wildsmith JAW (2011). “Lidocaine: A more complex story than ‘simple’ chemistry suggests” (PDF). The Proceedings of the History of Anaesthesia Society. 43: 9–16. Archived (PDF) from the original on 2014-04-22.
- ^ “Lidocaine international forms and names”. Drugs.com. Retrieved 29 October 2017.
- ^ “Lidocaine Ingredient Summary”. Therapeutic Goods Administration. Retrieved 20 September 2018.
- ^ “Updating medicine ingredient names – list of affected ingredients”. Therapeutic Goods Administration. 24 June 2019. Retrieved 16 February 2020.
- ^ “The 2021 Prohibited List International Standard” (PDF). The World Anti-Doping Code. World Anti-Doping Agency (WADA). 1 January 2021. Archived from the original (PDF) on 13 May 2021. Retrieved 18 May 2021.
- ^ “New York Drug Threat Assessment”. National Drug Intelligence Center. November 2002. Archived from the original on 2012-08-12.
- ^ Pupka A, Sikora J, Mauricz J, Cios D, Płonek T (2009). “[The usage of synthol in the body building]”. Polimery W Medycynie. 39(1): 63–5. PMID 19580174.
- ^ Bernardo NP; Siqueira MEPB; De Paiva MJN; Maia PP (2003). “Caffeine and other adulterants in seizures of street cocaine in Brazil”. International Journal of Drug Policy. 14 (4): 331–4. doi:10.1016/S0955-3959(03)00083-5.
- ^ “UNITED STATES of America, Plaintiff-Appellee, v. Luis A. CUELLO, Alvaro Bastides-Benitez, John Doe, a/k/a Hugo Hurtado, and Alvaro Carvajal, Defendants-Appellants”. Docket No. 78-5314. United States Court of Appeals, Fifth Circuit. 1979-07-25. Archived from the original on 2012-05-24.
- ^ Winterman, Denise (2010-09-07). “How cutting drugs became big business”. BBC News Online. BBC News Magazine. Archivedfrom the original on 2 February 2017. Retrieved 20 January 2017.
- ^ “Revision Bulletin: Lidocaine and Prilocaine Cream–Revision to Related Compounds Test”. The United States Pharmacopeial Convention. November 30, 2007. Archived from the original on May 1, 2013.
- ^ Peterson, Michael E.; Talcott, Patricia A. (2013-08-07). Small Animal Toxicology. Elsevier Health Sciences. ISBN 978-0323241984. Archived from the original on 2017-09-08.
- ^ “FDA Freedom of Information Summary – Tributame” (PDF). Archived from the original (PDF) on 2015-05-18.
External links
- “Lidocaine”. Drug Information Portal. U.S. National Library of Medicine.
- “Lidocaine Transdermal Patch”. MedlinePlus.
- US patent 2441498, Nils Magnus Loefgren & Bengt Josef Lundqvist, “Alkyl glycinanilides”, published 1948-05-11, issued 1948-05-11, assigned to ASTRA APOTEKARNES KEM FAB
| IUPAC name2-(diethylamino)- N-(2,6-dimethylphenyl)acetamide | |
| CAS Number | 137-58-6 as HCl: 73-78-9 |
|---|---|
| PubChem CID | 3676as HCl: 6314 |
| IUPHAR/BPS | 2623 |
| DrugBank | DB00281 as HCl: DBSALT001508 |
| ChemSpider | 3548 as HCl: 6075 |
| UNII | 98PI200987as HCl: EC2CNF7XFP |
| KEGG | D00358 as HCl: D02086 |
| ChEBI | CHEBI:6456 as HCl: CHEBI:50512 |
| ChEMBL | ChEMBL79 as HCl: ChEMBL541521 |
| PDB ligand | LQZ (PDBe, RCSB PDB) |
| CompTox Dashboard (EPA) | DTXSID1045166 |
| ECHA InfoCard | 100.004.821 |
| Chemical and physical data | |
| Formula | C14H22N2O |
| Molar mass | 234.343 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| Melting point | 68 °C (154 °F) |
| showSMILES | |
| showInChI |
////////LIDOCAINE, lignocaine

NEW DRUG APPROVALS
ONE TIME
$10.00

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....