Home » Uncategorized (Page 214)
Category Archives: Uncategorized
Potential diabetes breakthrough Harvard researchers discover hormone that spurs beta cell production
Betatrophin causes a specific increase in pancreatic β cell replication. Betatrophin is a secreted protein expressed in liver and fat. The increase in β cell replication and mass improves glycemic control. (Credit: Peng Yi, Ji-Sun Park, Douglas A. Melton/Cell)
Potential diabetes breakthrough
Researchers at the Harvard Stem Cell Institute (HSCI) have discovered a hormone that holds promise for a dramatically more effective treatment of type 2 diabetes, a metabolic illness afflicting an estimated 26 million Americans.
The researchers believe that the hormone might also have a role in treating type 1, or juvenile, diabetes.
The work was published by the journal Cell.
The hormone, called betatrophin, causes mice to produce insulin-secreting pancreatic beta cells at up to 30 times the normal rate. The new beta cells only produce insulin when called for by the body, offering the potential for the natural regulation of insulin and a great reduction in the complications associated with diabetes, the leading medical cause of amputations and non-genetic loss of vision.
The researchers who discovered betatrophin, HSCI co-director Doug Melton and postdoctoral fellow Peng Yi, caution that much work remains to be done before it could be used as a treatment in humans. But the results of their work, which was supported in large part by a federal research grant, already have attracted the attention of drug manufacturers.
“If this could be used in people,” said Melton, Harvard’s Xander University Professor and co-chair of the University’s Department of Stem Cell and Regenerative Biology, “it could eventually mean that instead of taking insulin injections three times a day, you might take an injection of this hormone once a week or once a month, or in the best case maybe even once a year.”
Type 2 diabetes, a disease associated with the national obesity epidemic, is usually caused by a combination of excess weight and lack of exercise. It causes patients to slowly lose beta cells and the ability to produce adequate insulin. One recent study has estimated that diabetes treatment and complications cost the United States $218 billion annually, or about 10 percent of the nation’s entire health bill.
“Our idea here is relatively simple,” Melton said. “We would provide this hormone, the type 2 diabetic will make more of their own insulin-producing cells, and this will slow down, if not stop, the progression of their diabetes. I’ve never seen any treatment that causes such an enormous leap in beta cell replication.”
EMA- Committee for Medicinal Products for Human Use (CHMP) adopted a positive opinion, recommending the granting of a marketing authorisation for Spedra, for the treatment of erectile dysfunction in adult men.
AVANAFIL, SPEDRA
On 25 April 2013, the Committee for Medicinal Products for Human Use (CHMP) adopted a positive opinion, recommending the granting of a marketing authorisation for the medicinal product Spedra, 50 mg, 100 mg, 200 mg, tablet intended for the treatment of erectile dysfunction in adult men.
The applicant for this medicinal product is VIVUS BV.
They may request a re-examination of any CHMP opinion, provided they notify the European Medicines Agency in writing of their intention within 15 days of receipt of the opinion. The active substance of Spedra is avanafil, a selective phosphodiesterase (PDE) type 5 inhibitor that leads to higher cyclic guanosine monophosphate (cGMP)-specific PDE5 levels. This enhances smooth muscle relaxation, which results in an inflow of blood into the penile tissues, thereby producing an erection. The benefit with Spedra is its effect on the ability of men with erectile dysfunction to achieve and maintain an erection sufficient for satisfactory sexual activity. It was observed in clinical trials that Spedra increased the percentage of sexual attempts resulting in successful intercourse by roughly 20-30% over placebo in the general population of adult men with erectile dysfunction. The most common side effects are headache, flushing, nasal and sinus congestion, dyspepsia and back pain. A pharmacovigilance plan for Spedra will be implemented as part of the marketing authorisation. The approved indication is: “Treatment of erectile dysfunction in adult men. In order for Spedra to be effective, sexual stimulation is required.” Detailed recommendations for the use of this product will be described in the summary of product characteristics (SmPC), which will be published in the European public assessment report (EPAR) and made available in all official European Union languages after the marketing authorisation has been granted by the European Commission. The CHMP, on the basis of quality, safety and efficacy data submitted, considers there to be a favourable benefit-to-risk balance for Spedra and therefore recommends the granting of the marketing authorisation.
Avanafil is a PDE5 inhibitor approved for erectile dysfunction on April 27, 2012.[1] Avanafil is known by the trademark name Stendra and was developed by Vivus Inc. It acts by inhibiting a specific phosphodiesterase type 5 enzyme which is found in various body tissues, but primarily in the corpus cavernosum penis, as well as the retina. Other similar drugs are sildenafil, tadalafil and vardenafil. The advantage of avanafil is that it has very fast onset of action compared with other PDE5 inhibitors.
Avanafil can be synthesized from a benzylamine derivative and a pyrimidine derivative:
“FDA approves Stendra for erectile dysfunction” (Press release). Food and Drug Administration (FDA). April 27, 2012.
Yamada, K.; Matsuki, K.; Omori, K.; Kikkawa, K.; 2004, U.S. Patent 6,797,709
A cutting that phenanthrene by a methylthio urea ( a ) and ethoxy methylene malonate ( 2 ) cyclization of 3 , chloride, phosphorus oxychloride get 4 , 4 with benzyl amine 5 occurred SNAr the reaction product after oxidation with mCPBA 6 . In pyrimidine, if the 2 – and 4 – positions are active simultaneously the same leaving group in the case, SNAr reaction occurs preferentially at 4 – position, but does not guarantee the 2 – side reaction does not occur. Here is an activity of the poor leaving group sulfide spans 2 – bit, and a good leaving group active chlorine occupy four – position, thus ensuring a high regioselectivity of the reaction. 4 – position after completion of the reaction, then the 2 – position of the group activation, where sulfide sulfoxide better than the leaving group. Amino alcohols 7 and 6 recurrence SNAr reaction 8 , 8 after alkaline hydrolysis and acid alpha amidation get that phenanthrene.
European Medicines Agency recommends approval of first treatment for pseudobulbar affect
26/04/2013
Dextromethorphan

Quinidine
European Medicines Agency recommends approval of first treatment for pseudobulbar affect
Medicine to help curb bouts of uncontrolled emotional expression in patients with certain neurological disorders
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended the granting of a marketing authorisation for Nuedexta, a medicine for the treatment of pseudobulbar affect in adults.
Pseudobulbar affect is a medical condition in which patients experience sudden and uncontrollable bouts of laughing or crying unrelated or disproportionate to their emotional state. It occurs when certain neurological disorders, such as multiple sclerosis (MS) and amyotrophic lateral sclerosis (ALS) or a stroke, damage areas of the brain that are involved in the control of normal expression of emotion. This damage can disrupt brain signalling, resulting in the alteration or loss of control of emotional expression.
Although pseudobulbar affect is a non-life-threatening condition, it can have a significant impact on an individual’s ability to interact normally in society and on their relationships with others. There is currently no treatment approved for pseudobulbar affect in the European Union.
Nuedexta is a combination of two known active substances, dextromethorphan hydrobromide and quinidine sulphate. In studies, treatment with these medicines significantly decreased episodes of involuntary, uncontrollable laughing or crying.
Pseudobulbar affect is observed in a number of neurological conditions. Nuedexta has currently only been studied in patients with MS and ALS. Nuedexta is not suitable for treating episodes of laughing or crying brought on by mood swings and not due to pseudobulbar affect.
The CHMP’s opinion on Nuedexta will now be sent to the European Commission for the adoption of a marketing authorisation.
Note
- The marketing authorisation holder for Nuedexta is Jenson Pharmaceutical Services Ltd.
Dextromethorphan/quinidine (trade name Nuedexta) is a combination drug containing the active ingredients dextromethorphan and quinidine. It was the first FDA-approved drug for the treatment of pseudobulbar affect (PBA).
In a 12 week randomized, double-blind trial, amyotrophic lateral sclerosis and multiple sclerosis patients with significant PBA were given either Nudexta 30/10 mg or placebo. In 326 randomized patients, the PBA-episode daily rate was 46.9% (p < 0.0001) lower for Nudexta than for placebo.
Nuedexta was approved in February 2011 and is marketed in the United States by Avanir Pharmaceuticals.
Celgene makes good start to 2013 as Revlimid hits $1 billion
April 26, 2013
Celgene Corp has posted a healthy set of financials for the first quarter despite a 4.1% decline in net income to $410.2 million, as product sales increased 15% to $1.43 billion. read more at————http://www.pharmatimes.com/Article/13-04-26/Celgene_makes_good_start_to_2013_as_Revlimid_hits_1_billion.aspx

(RS)-3-(4-amino-1-oxo 1,3-dihydro-2H-isoindol- 2-yl)piperidine-2,6-dione
Lenalidomide
REVLIMID® is an oral immunomodulatory drug marketed in the United States and many international markets, in combination with dexamethasone, for treatment of patients with multiple myeloma who have received at least one prior therapy. It is also marketed in the United States and certain international markets for the treatment of transfusion-dependent anemia due to low- or intermediate-1-risk myelodysplastic syndromes, or MDS, associated with a deletion 5q cytogenetic abnormality with or without additional cytogenetic abnormalitie.Revlimid Worldwide annual sales in 2011 was $3.2bLenalidomide (Revlimid) is a derivative of thalidomideintroduced in 2004.It was initially intended as a treatment for multiple myeloma, for which thalidomide is an accepted therapeutic treatment. Lenalidomide has also shown efficacy in the class of hematological disorders known as myelodysplastic syndromes (MDS). Lenalidomide has significantly improved overall survival in myeloma (which generally carries a poor prognosis), although toxicity remains an issue for users. [1]It costs $163,381 per year for the average patient.[2]
Lenalidomide has been used to successfully treat both inflammatory disorders and cancers in the past 10 years. There are multiple mechanisms of action, and they can be simplified by organizing them as mechanisms of action in vitro and in vivo.[3] In vitro, lenalidomide has three main activities: direct anti-tumor effect, inhibition of the microenvironment support for tumor cells, and immunomodulatory role. In vivo, lenalidomide induces tumor cell apoptosis directly and indirectly by inhibition of bone marrow stromal cell support, by anti-angiogenic and anti-osteoclastogenic effects, and by immunomodulatory activity. Lenalidomide has a broad range of activities that can be exploited to treat many hematologic and solid cancers.
- McCarthy; Philip L. McCarthy, Kouros Owzar, Craig C. Hofmeister, et al. (May 10, 2012). “Lenalidomide after Stem-Cell Transplantation for Multiple Myeloma”. N Engl J Med 366 (19): 1770–1781. doi:10.1056/NEJMoa1114083. PMID 22571201.
- Badros, Ashraf Z. Badros (May 10, 2012). “Lenalidomide in Myeloma — A High-Maintenance Friend”. N Engl J Med 366 (19): 1836–1838. doi:10.1056/NEJMe1202819. PMID 22571206.
- Vallet S, Palumbo A, Raje N, Boccadoro M, Anderson KC (July 2008). “Thalidomide and lenalidomide: Mechanism-based potential drug combinations”. Leukemia & Lymphoma 49 (7): 1238–45. doi:10.1080/10428190802005191. PMID 18452080.
TOXINS-Occurrence of ochratoxin A in Korean paprika

ochratoxin A
Occurrence of ochratoxin A in Korean red paprika

http://www.ncbi.nlm.nih.gov/pubmed/23605491
National Agricultural Products Quality Management Service, Seoul, 150-804, Korea, ahnjs@naqs.go.kr.
A large amount-260,000 tons-of red paprika is consumed annually in Korea, where the people prefer hot and pungent to sweet foods.
,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,
Occurrence of ochratoxin A in herbal drugs of Indian origin – a report.
Source
Medicinal Plant Research Laboratory, University Department of Botany, Bhagalpur University, 812 007, Bhagalpur, India.
Abstract
This paper contains a report of occurrence of ochratoxin A in some common herbal medicines collected from different store-houses and shop-keepers of Bihar, India. Of 129 samples of 9 plants, 55 were found to be contaminated with various levels of ochratoxin A. The level of ochratoxin A was found maximal in barks ofHolarrhena antidysenterica (1.14…
View original post 190 more words
DRUG SPOTLIGHT-Afinitor (everolimus) , Novartis:
Afinitor (everolimus)
40-O-(2-hydroxyethyl)-rapamycin
Company: Novartis
Approval Status: Approved July 2012
Treatment Area: hormone receptor-positive, HER2-negative breast cancer
Everolimus is a derivative of Rapamycin (sirolimus), and works similarly to Rapamycin as an mTOR (mammalian target of rapamycin) inhibitor. It is currently used as an immunosuppressant to prevent rejection of organ transplants. In a similar fashion to other mTOR inhibitors Everolimus’ effect is solely on the mTORC1 protein and not on the mTORC2 protein.
159351-69-6 CAS NO
BRANDS
| Afinitor | Novartis |
| Certican | Novartis |
| VOTUBIA | Novartis |
| Zortress | Novartis |
Afinitor (everolimus), an inhibitor of mTOR (mammalian target of rapamycin), is an antineoplastic agent.
Afinitor is specifically approved for the treatment of postmenopausal women with advanced hormone receptor-positive, HER2-negative breast cancer (advanced HR+ BC) in combination with exemestane, after failure of treatment with letrozole or anastrozole.
Afinitor is supplied as a tablet for oral administration. The recommended dose of Afinitor for breast cancer is 10 mg, to be taken once daily, at the same time every day, either consistently with food or consistently without food.
FDA Approval
The FDA approval of Afinitor for the treatment of advanced hormone receptor-positive, HER2-negative breast cancer was based on a randomized, double-blind, multicenter study in 724 postmenopausal women with estrogen receptor-positive, HER 2/neu-negative advanced breast cancer with recurrence or progression following prior therapy with letrozole or anastrozole.
Everolimus is indicated for the treatment of postmenopausal women with advanced hormone receptor-positive, HER2-negative breast cancer (advanced HR+ BC) in combination with exemestane, after failure of treatment with letrozole or anastrozole. Indicated for the treatment of adult patients with progressive neuroendocrine tumors of pancreatic origin (PNET) with unresectable, locally advanced or metastatic disease. Indicated for the treatment of adult patients with advanced renal cell carcinoma (RCC) after failure of treatment with sunitinib or sorafenib. Indicated for the treatment of adult patients with renal angiomyolipoma and tuberous sclerosis complex (TSC), not requiring immediate surgery. Indicated in pediatric and adult patients with tuberous sclerosis complex (TSC) for the treatment of subependymal giant cell astrocytoma (SEGA) that requires therapeutic intervention but cannot be curatively resected.
Everolimus (RAD-001) is the 40-O-(2-hydroxyethyl) derivative of sirolimus and works similarly to sirolimus as an inhibitor of mammalian target of rapamycin (mTOR).
It is currently used as an immunosuppressant to prevent rejection of organ transplants and treatment of renal cell cancer and other tumours. Much research has also been conducted on everolimus and other mTOR inhibitors for use in a number of cancers.
It is marketed by Novartis under the tradenames Zortress (USA) and Certican (Europe and other countries) in transplantation medicine, and Afinitor in oncology.
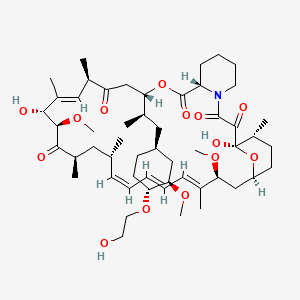
AFINITOR (everolimus), an inhibitor of mTOR, is an antineoplastic agent.
The chemical name of everolimus is (1R,9S,12S,15R,16E,18R,19R,21R,23S,24E,26E,28E,30S,32S,35R)-1,18- dihydroxy-12-{(1R)-2-[(1S,3R,4R)-4-(2-hydroxyethoxy)-3-methoxycyclohexyl]-1-methylethyl}-19,30-dimethoxy15,17,21,23,29,35-hexamethyl-11,36-dioxa-4-aza-tricyclo[30.3.1.04,9]hexatriaconta-16,24,26,28-tetraene-2,3,10,14,20pentaone.
The molecular formula is C53H83NO14 and the molecular weight is 958.2. The structural formula is:
 |
AFINITOR Tablets are supplied for oral administration and contain 2.5 mg, 5 mg, 7.5 mg, or 10 mg of everolimus. The tablets also contain anhydrous lactose, butylated hydroxytoluene, crospovidone, hypromellose, lactose monohydrate, and magnesium stearate as inactive ingredients.
AFINITOR DISPERZ (everolimus tablets for oral suspension) is supplied for oral administration and contains 2 mg, 3 mg, or 5 mg of everolimus. The tablets for oral suspension also contain butylated hydroxytoluene, colloidal silicon dioxide, crospovidone, hypromellose, lactose monohydrate, magnesium stearate, mannitol, and microcrystalline cellulose as inactive ingredients.

- R.N Formica Jra, K.M Lorberb, A.L Friedmanb, M.J Biaa, F Lakkisa, J.D Smitha, M.I Lorber (March 2004). “The evolving experience using everolimus in clinical transplantation”. Elsevier 36 (2): S495–S499.
- “Afinitor approved in US as first treatment for patients with advanced kidney cancer after failure of either sunitinib or sorafenib” (Press release). Novartis. 2009-03-30. Retrieved April 6, 2009.
- “Novartis receives US FDA approval for Zortress (everolimus) to prevent organ rejection in adult kidney transplant recipients” (Press release). Novartis. 2010-04-22. Retrieved April 26, 2010.
- “Novartis’ Afinitor Cleared by FDA for Treating SEGA Tumors in Tuberous Sclerosis”. 1 Nov 2010.
- http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm254350.htm
- “US FDA approves Novartis drug Afinitor for breast cancer”. 20 Jul 2012.
PATENTS

|
Country
|
Patent Number
|
Approved
|
Expires (estimated)
|
|---|---|---|---|
| United States | 6440990 | 1993-09-24 | 2013-09-24 |
| Canada | 2145383 | 2004-11-16 | 2013-09-24 |
| Canada | 2225960 | 2004-05-11 | 2016-07-12 |
| United States | 7297703 | 1999-12-06 | 2019-12-06 |
|
10-28-2011
|
METHODS OF TREATMENT
|
|
|
1-21-2011
|
ANTI-IGF1R
|
|
|
1-14-2011
|
HISTONE H2AX (HH2AX) BIOMARKER FOR FTI SENSITIVITY
|
|
|
3-24-2010
|
Thermal treatment of a drug eluting implantable medical device
|
|
|
1-13-2010
|
Therapeutic phosphonate compounds
|
|
|
10-21-2009
|
Processes for preparing water-soluble polyethylene glycol conjugates of macrolide immunosuppressants
|
|
|
10-16-2009
|
Heparin Prodrugs and Drug Delivery Stents Formed Therefrom
|
|
|
9-11-2009
|
PHOSPHONATE COMPOUNDS HAVING IMMUNO-MODULATORY ACTIVITY
|
|
|
12-31-2008
|
Phosphonate compounds having immuno-modulatory activity
|
|
|
10-8-2008
|
Anti-inflammatory phosphonate compounds
|
|
6-27-2008
|
Genes Involved in Neurodegenerative Conditions
|
|
|
10-24-2007
|
Fluid treatment of a polymeric coating on an implantable medical device
|
|
|
7-11-2007
|
Oxepane isomer of 42-O-(2-hydroxy)ethyl-rapamycin
|
|
|
2-9-2007
|
40-O-(2-hydroxy)ethyl-rapamycin coated stent
|
|
|
1-5-2007
|
Methods for treating neurofibromatosis 1
|
|
|
9-8-2006
|
Anti-inflammatory phosphonate compounds
|
| WO1994009010A1 | Sep 24, 1993 | Apr 28, 1994 | Sandoz Ag | O-alkylated rapamycin derivatives and their use, particularly as immunosuppressants |
| WO2007135397A1 * | May 18, 2007 | Nov 29, 2007 | Christoph Beckmann | 36 -des (3 -methoxy-4 -hydroxycyclohexyl) 36 – (3 -hydroxycycloheptyl) derivatives of rapamycin for the treatment of cancer and other disorders |
| EP0663916A1 | Sep 24, 1993 | Jul 26, 1995 | Novartis AG | O-alkylated rapamycin derivatives and their use, particularly as immunosuppressants |
| US5665772 | Sep 24, 1993 | Sep 9, 1997 | Sandoz Ltd. | O-alkylated rapamycin derivatives and their use, particularly as immunosuppressants |
| US20030125800 | Apr 24, 2002 | Jul 3, 2003 | Shulze John E. | Drug-delivery endovascular stent and method for treating restenosis |
…………………………………….
Rapamycin is a known macrolide antibiotic produced by Streptomvces hvgroscopicus. having the structure depicted in Formula A:
See, e.g., McAlpine, J.B., et al., J. Antibiotics (1991) 44: 688; Schreiber, S.L., et al., J. Am. Chem. Soc. (1991) J_13: 7433‘- US Patent No. 3 929 992. Rapamycin is an extremely potent immunosuppressant and has also been shown to have antitumor and antifungal activity. Its utility as a pharmaceutical, however, is restricted by its very low and variable bioavailabiiity as well as its high toxicity. Moreover, rapamycin is highly insoluble, making it difficult to formulate stable galenic compositions.
Everolimus, 40-O-(2-hydroxyethyl)-rapamycin of formula (1) is a synthetic derivative of rapamycin (sirolimus) of formula (2), which is produced by a certain bacteria strain and is also pharmaceutically active.
(1) (2)
Everolimus is marketed under the brand name Certican for the prevention of rejection episodes following heart and kidney transplantation, and under the brand name Afinitor for treatment of advanced kidney cancer.
Due to its complicated macrolide chemical structure, everolimus is, similarly as the parent rapamycin, an extremely unstable compound. It is sensitive, in particular, towards oxidation, including aerial oxidation. It is also unstable at temperatures higher than 25°C and at alkaline pH.
Everolimus and a process of making it have been disclosed in WO 94/09010
Synthesis

Alkylation of rapamycin (I) with 2-(tert-butyldimethylsilyloxy)ethyl triflate (II) by means of 2,6-lutidine in hot toluene gives the silylated target compound (III), which is deprotected by means of 1N HCl in methanol (1). (Scheme 21042401a) Manufacturer Novartis AG (CH). References 1. Cottens, S., Sedrani, R. (Sandoz-Refindungen VmbH; Sandoz-Patent GmbH; Sandoz Ltd.). O-Alkylated rapamycin derivatives and their use, particularly as immunosuppressants. EP 663916, EP 867438, JP 96502266, US 5665772, WO 9409010.EP 0663916; EP 0867438; JP 1996502266; JP 1999240884; US 5665772; WO 9409010
…………..
SYNTHESIS
https://www.google.com/patents/WO2012103960A1
(US 5,665,772, EP 663916). The process principle is shown in the scheme below, wherein the abbreviation RAP-OH has been used as an abbreviation for the rapamycin structure of formula (2) above, L is a leaving group and P is a trisubstituted silyl group serving as a OH- protective group.
RAP-OH + L-CH2-CH2-0-P — –> RAP-O-CH2-CH2-O-P — – > RAP-O-CH2-CH2-OH
(2) (4) (1)
Specifically, the L- group is a trifluoromethanesulfonate (triflate) group and the protective group P- is typically a tert-butyldimethylsilyloxy- group. Accordingly, the known useful reagent within the above general formula (3) for making everolimus from rapamycin is 2-(tert-butyldimethylsilyloxy)ethyl triflate of formula (3 A):
According to a known synthetic procedure disclosed in Example 8 of WO 94/09010 and in Example 1 of US application 2003/0125800, rapamycin (2) reacts in hot toluene and in the presence of 2,6-lutidine with a molar excess of the compound (3 A), which is charged in several portions, to form the t-butyldimethylsilyl-protected everolimus (4A). This compound is isolated and deprotected by means of IN aqueous HC1 in methanol. Crude everolimus is then purified by column chromatography. Yields were not reported.
(2) (3A) (4A) (1)
In an article of Moenius et al. (J. Labelled Cpd. Radiopharm. 43, 113-120 (2000)), which used the above process for making C14-labelled and tritiated everolimus, a diphenyl- tert.butylsilyloxy -protective group was used as the alkylation agent of formula (3B).
Only 8% yield of the corresponding compound (4B)
and 21% yield of the compound (1) have been reported.
Little is known about the compounds of the general formula (3) and methods of their preparation. The synthesis of the compound (3 A) was disclosed in Example 1 of US application 2003/0125800. It should be noted that specification of the reaction solvent in the key step B of this synthesis was omitted in the disclosure; however, the data about isolation of the product allow for estimation that such solvent is dichloromethane. Similarly also a second article of Moenius et al. (J. Labelled Cpd. Radiopharm.42, 29-41 (1999)) teaches that dichloromethane is the solvent in the reaction.
It appears that the compounds of formula (3) are very reactive, and thus also very unstable compounds. This is reflected by the fact that the yields of the reaction with rapamycine are very low and the compound (3) is charged in high molar extent. Methods how to monitor the reactivity and/or improve the stability of compounds of general formula (3), however, do not exist.
Thus, it would be useful to improve both processes of making compounds of formula (3) and, as well, processes of their application in chemical synthesis.
xample 6: 40-O-[2-((2,3-dimethylbut-2-yl)dimethylsilyloxy)ethyl]rapamycin
In a 100 mL flask, Rapamycin (6 g, 6.56 mmol) was dissolved in dimethoxyethane (4.2 ml) and toluene (24 ml) to give a white suspension and the temperature was raised to 70°C. After 20 min, N,N-diisopropylethylamine (4.56 ml, 27.6 mmol) and 2-((2,3-dimethylbutan-2- yl)dimethylsilyloxy)ethyl trifluoromethanesulfonate (8.83 g, 26.3 mmol) were added in 2 portions with a 2 hr interval at 70°C. The mixture was stirred overnight at room temperature, then diluted with EtOAc (40 ml) and washed with sat. NaHC03 (30 ml) and brine (30 ml). The organic layer was dried with Na2S04, filtered and concentrated. The cmde product was chromatographed on a silica gel column (EtOAc/heptane 1/1 ; yield 4.47 g).
Example 7: 40-O-(2-hydroxyethyl)-rapamycin [everolimus]
In a 100 mL flask, 40-O-[2-((2,3-dimethylbut-2-yl)dimethylsilyloxy)ethyl]rapamycin (4.47 g, 4.06 mmol) was dissolved in methanol (20 ml) to give a colorless solution. At 0°C, IN aqueous hydrochloric acid (2.0 ml, 2.0 mmol) was added and the mixture was stirred for 90 min. The reaction was followed by TLC (ethyl acetate/n-heptane 3 :2) and HPLC. Then 20 ml of saturated aqueous NaHC03 were added, followed by 20 ml of brine and 80 ml of ethyl acetate. The phases were separated and the organic layer was washed with saturated aqueous NaCl until pH 6/7. The organic layer was dried by Na2S04, filtered and concentrated to yield 3.3 g of the product.
……………………….
SYNTHESIS
https://www.google.co.in/patents/WO1994009010A1
Example 8: 40-O-(2-Hydroxy)ethyl-rapamycin
a) 40-O-[2-(t-Butyldimethylsilyl)oxy]ethyl-rapamycin
A solution of 9.14 g (10 mmol) of rapamycin and 4.70 mL (40 mmol) of 2,6-lutidine in 30 mL of toluene is warmed to 60°C and a solution of 6.17 g (20 mmol) of 2-(t-butyldimethylsilyl)oxyethyl triflate and 2.35 mL (20 mmol) of 2,6-lutidine in 20 mL of toluene is added. This mixture is stirred for 1.5h. Then two batches of a solution of 3.08 g (10 mmol) of triflate and 1.2 mL (10 mmol) of 2,6-lutidine in 10 mL of toluene are added in a 1.5h interval. After addition of the last batch, stirring is continued at 60°C for 2h and the resulting brown suspension is filtered. The filtrate is diluted with ethyl acetate and washed with aq. sodium bicarbonate and brine. The organic solution is dried over anhydrous sodium sulfate, filtered and concentrated. The residue is purified by column chromatography on silica gel (40:60 hexane-ethyl acetate) to afford 40-O-[2-(t-butyldimethylsilyl)oxy]ethyl-rapamycin as a white solid: 1H NMR (CDCl3) δ 0.06 (6H, s), 0.72 (1H, dd), 0.90 (9H, s), 1.65 (3H, s), 1.75 (3H, s), 3.02 (1H, m), 3.63 (3H, m), 3.72 (3H, m); MS (FAB) m/z 1094 ([M+Na]+), 1022 ([M-(OCH3+H2O)]+).
b) 40-O-(2-Hydroxy)ethyl-rapamycin
To a stirred, cooled (0°C) solution of 4.5 g (4.2 mmol) of 40-O-[2-(t-butyldimethylsilyl)oxy]ethyl-rapamycin in 20 mL of methanol is added 2 mL of IN HCl. This solution is stirred for 2h and neutralized with aq. sodium bicarbonate. The mixture is extracted with three portions of ethyl acetate. The organic solution is washed with aq.
sodium bicarbonate and brine, dried over anhydrous sodium sulfate, filtered and
concentrated. Purification by column chromatography on silica gel (ethyl acetate) gave the title compound as a white solid:1H NMR (CDCl3) δ 0.72 (1H, dd), 1.65 (3H, s), 1.75 (3H, s), 3.13 (5H, s and m), 3.52-3.91 (8H, m); MS (FAB) m/z 980 ([M+Na]+), 926 ([M-OCH3]+), 908 ([M-(OCH3+H2O)]+), 890 ([M-(OCH3+2H2O)]+), 876 ([M-(2CH3OH+OH)]+), 858 ([M-(OCH3+CH3OH+2H2O)]+).
MBA (rel. IC50) 2.2
IL-6 dep. prol. (rel. IC50) 2.8
MLR (rel. IC50) 3.4
…………………..
synthesis
Everolimus (Everolimus) was synthesized by the Sirolimus (sirolimus, also known as rapamycin Rapamycin) ether from. Sirolimus is from the soil bacterium Streptomyces hygroscopicus isolated metabolites. Activation end sirolimus (triflate, Tf) the other end of the protection (t-butyldimethylsilyl, TBS) of ethylene glycol 1 reaction of 2 , because the hydroxyl group 42 hydroxyl site over the 31-bit resistance is small, so the reaction only occurs in 42. Compound 2under acidic conditions TBS protection is removed everolimus.

DRUG SPOTLIGHT –CUBICIN, DAPTOMYCIN
Daptomycin

N-decanoyl-L-tryptophyl-L-asparaginyl-L-aspartyl-L-threonylglycyl-
L-ornithyl-L-aspartyl-D-alanyl-L-aspartylglycyl-D-seryl-threo-3-methyl-L-glutamyl-3-anthraniloyl-L-alanine[egr]1-lactone
Daptomycin is a lipopeptide antibiotic used in the treatment of systemic and life-threatening infections caused by Gram-positive organisms. It is a naturally occurring compound found in the soil saprotroph Streptomyces roseosporus. Its distinct mechanism of action makes it useful in treating infections caused by multi-resistant bacteria. It is marketed in the United States under the trade name Cubicin by Cubist Pharmaceuticals.

The compound LY 146032 was discovered by researchers at Eli Lilly and Company in the late 1980s.LY 146032 showed promise in Phase I/II clinical trials for treatment of infection caused by Gram-positive organisms. Lilly ceased development because high-dose therapy was associated with adverse effects on skeletal muscle, including myalgia and potential myositis.
The rights to LY 146032 were acquired by Cubist Pharmaceuticals in 1997, which following U.S. Food and Drug Administration (FDA) approval in September 2003 for use in people older than 18 years began marketing the drug under the trade name CUBICIN. Cubicin is marketed in the EU and in several other countries by Novartis following its purchase of Chiron Corporation, previous licensee.
Daptomycin has a distinct mechanism of action, disrupting multiple aspects of bacterial cell membrane function. It appears to bind to the membrane and cause rapid depolarization, resulting in a loss of membrane potential leading to inhibition of protein, DNA and RNA synthesis, which results in bacterial cell death
US HERBS- FIGHT CANCER WITH BROCCOLI
An example of the superfoods is the broccoli. Broccoli belongs to the cruciferous group of vegetables. Naturally, broccoli is an an excellent source of vitamins, minerals and fiber. These are elements from Nature that have been extensively studied.
Epidemiological studies provideevidence that the consumption of this vegetable protects against cancer. The protection against cancer is mainly derived from altering estrogen metabolism and antioxidant properties, enhancing detoxification, decreasing carcinogen coumpound activation, slowing tumor growth and inducing cancer cell apoptosis (death). Such attributes qualify broccoli as a superfood.
American Institute of Cancer Research estimates that a daily intake of three servings would potentially reduce cancer rates by 20%.
Broccoli contains certain chemicals that may reduce the risk of colorectal or other cancers, although it is not clear which individual compounds may be responsible for the protective effects. While research in this area continues, the best advice at this time to reduce cancer risk is to eat a wide variety of vegetables. It is reasonable to include broccoli as part of a balanced diet.
roccoli has been around for more than 2,000 years but has only been commercially grown in the United States since the 1920s. Today, more than 90% of the broccoli harvested in the United States comes from California, although it is also grown in other parts of the country.
About 2 decades ago, researchers first suggested a possible link between diets high in cruciferous vegetables (a group of plants including cauliflower, cabbage, broccoli, and Brussels sprouts)) and a lower risk of cancer. However, it was not until the 1990s that certain chemicals found in broccoli were identified as possible cancer-preventing compounds. In 1997, a study was published that noted broccoli sprouts had higher levels of one of these compounds than mature broccoli.
Broccoli is a plant in the cabbage family, whose large flower head is used as a vegetable. The word broccoli, from the Italian plural of broccolo, refers to “the flowering top of a cabbage”. Broccoli is usually boiled or steamed but may be eaten raw and has become popular as a raw vegetable in hors d’œuvre trays. The leaves may also be eaten.
Broccoli is classified in the Italica cultivar group of the species Brassica oleracea. Broccoli has large flower heads, usually green in color, arranged in a tree-like structure on branchessprouting from a thick, edible stalk. The mass of flower heads is surrounded by leaves. Broccoli most closely resembles cauliflower, which is a different cultivar group of the same species.
Broccoli was derived from cultivated leafy cole crops in the Northern Mediterranean in about the 6th century BCE. Since the Roman Empire, broccoli has been considered a uniquely valuable food among Italians. Broccoli was brought to England from Antwerp in the mid-18th century by Peter Scheemakers. Broccoli was first introduced to the United States by Italian immigrants but did not become widely known there until the 1920s
Broccoli is high in vitamin C and dietary fiber; it also contains multiple nutrients with potent anti-cancer properties, such as diindolylmethane and small amounts of selenium. A single serving provides more than 30 mg of vitamin C and a half-cup provides 52 mg of vitamin C. The 3,3′-Diindolylmethane found in broccoli is a potent modulator of theinnate immune response system with anti-viral, anti-bacterial and anti-cancer activity. Broccoli also contains the compound glucoraphanin, which can be processed into an anti-cancer compound sulforaphane, though the benefits of broccoli are greatly reduced if the vegetable is boiled. Broccoli is also an excellent source of indole-3-carbinol, a chemical which boosts DNA repair in cells and appears to block the growth of cancer cells.
Boiling broccoli reduces the levels of suspected anti-carcinogenic compounds, such as sulforaphane, with losses of 20–30% after five minutes, 40–50% after ten minutes, and 77% after thirty minutes. However, other preparation methods such as steaming,microwaving, and stir frying had no significant effect on the compounds.
Broccoli has the highest levels of carotenoids in the brassica family.[17] It is particularly rich in lutein and also provides a modest amount of beta-carotene.
A high intake of broccoli has been found to reduce the risk of aggressive prostate cancer. Broccoli consumption may also help prevent heart disease.
Broccoli sprouts are often suggested for their health benefits
| Nutritional value per 100 g (3.5 oz) | |
|---|---|
| Energy | 141 kJ (34 kcal) |
| Carbohydrates | 6.64 g |
| – Sugars | 1.7 g |
| – Dietary fiber | 2.6 g |
| Fat | 0.37 g |
| Protein | 2.82 g |
| Water | 89.3 g |
| Vitamin A equiv. | 31 μg (4%) |
| – beta-carotene | 361 μg (3%) |
| – lutein and zeaxanthin | 1403 μg |
| Thiamine (vit. B1) | 0.071 mg (6%) |
| Riboflavin (vit. B2) | 0.117 mg (10%) |
| Niacin (vit. B3) | 0.639 mg (4%) |
| Pantothenic acid (B5) | 0.573 mg (11%) |
| Vitamin B6 | 0.175 mg (13%) |
| Folate (vit. B9) | 63 μg (16%) |
| Vitamin C | 89.2 mg (107%) |
| Vitamin E | 0.78 mg (5%) |
| Vitamin K | 101.6 μg (97%) |
| Calcium | 47 mg (5%) |
| Iron | 0.73 mg (6%) |
| Magnesium | 21 mg (6%) |
| Manganese | 0.21 mg (10%) |
| Phosphorus | 66 mg (9%) |
| Potassium | 316 mg (7%) |
| Zinc | 0.41 mg (4%) |
| Link to USDA Database entry Percentages are relative to US recommendations for adults. Source: USDA Nutrient Database
Broccoli is considered a good source of nutrients because it is rich in vitamin C, carotenoids (vitamin A-like substances), fiber, calcium, and folate. Broccoli is also a source of many substances called phytochemicals, or plant chemicals, that may have anticancer properties. For example, broccoli contains several compounds called isothiocyanates, including sulforaphane and indole-3-carbinol (I3C), which have been touted as possible anti-cancer agents in recent years. Early studies have shown these substances may act as anti-oxidants and may boost detoxifying enzymes in the body. Some studies have also suggested they may alter the levels of estrogen in the body, which might affect breast cancer risk.The chemical composition of broccoli and other cruciferous vegetables is complex, which makes it hard to determine which compound or combination of compounds may provide protection against cancer. Eating a wide variety of plant-based foods may be the best way to get the necessary components.Some researchers suggest that small amounts of broccoli sprouts may protect against the risk of cancer as effectively as much larger amounts of the mature vegetable. We are not aware of any clinical studies that have been done in humans to verify this claim.Another substance in broccoli, indole-3-carbinol (I3C), seems to alter estrogen levels and may also raise levels of protective enzymes in the body. Several studies of cancer cells growing in laboratory dishes or flasks have shown it may slow or stop the growth of breast, prostate, and other cancer cells. Some early studies in animals have shown similar results. Small studies in humans have found it may prevent the development of pre-cancerous growths in the cervix, as well as growths called papillomas in the throat. Again, larger studies are needed to find out what benefits I3C may have against cancer. THE MOLECULES The active molecules are Indole-3-carbinol (1H-indol-3-ylmethanol IUPAC name) OR I3C and isothiocyanates (mostly sulforaphane: 1-Isothiocyanato-4-methylsulfinylbutane). Indole-3-carbinol has a indole with a hydroxymethyl group that represents the hydrophilic group. Sulfurofane is a isothiocyanate, it means that it has a –N=C=S chemical group, formed by substituting sulfur for oxygen in the isocyanate group, bounded to a big alkyl chain containing a sulfinyl S=O group. Both indole-3-carbinol and sulphoraphane derive from glucosinolates. Glucosinolates are a class of organic compounds that contain sulfur and nitrogen and are derived from glucose and an amino acid. They occur as secondary metabolites of almost all plants of the order Brassicales. GENERAL EFFECTS ON HEALTH I3C has been shown to have a chemopreventive action on several human cancers. The first and greatest effects concern breast and cervical estrogen-dependant cancer. Later, many researches managed to relate I3C with the prevention from colon, lung and prostate cancer too. The micronutrient indole-3-carbinol: implications for disease and chemoprevention, 2000 Sulforaphane, like I3C, is useful against many types of cancer. Moreover, it has antimicrobial properties, as it appears to help eradicate Helicobacter Pylori from the stomach. Molecular targets of dietary phenethyl isothiocyanate and sulforaphane for cancer |
|
DRUG SPOTLIGHT- Pemetrexed

Pemetrexed
(2S)-2-{[4-[2-(2-amino-4-oxo-1,7-dihydro
pyrrolo[2,3-d]pyrimidin-5-yl)ethyl]benzoyl]amino}
pentanedioic acid
N-[4-[2-(2-amino-4,7-dihydro-4-oxo-3H-pyrrolo[2,3-d]-pyrimidin-5-yl)ethyl] benzoyl]-L-glutamic acid or N-[4-[2-(2-amino-4,7-dihydro-4-oxo-1 H-pyrrolo [2,3-d]-pyrimidin-5-yl)ethyl] benzoyl]-L-glutamic acid
GENERIC LICENSING NEWSLETTER TODAY 23 APRIL 2013 REPORTED, SEE LINK BELOW
http://www.leadformix.com/ef1/preview_campaign.php?lf1=775434470d357512625317e6516156
 |
PEMETREXED
Pemetrexed is a chemotherapy drug used in the treatment of pleural mesothelioma as well as non-small cell lung cancer.Used in combination with cisplatin for the treatment of malignant pleural mesothelioma in adults whose disease is unresectable or who otherwise are not candidates for potentially curative surgery. Also used as a monotherapy for the treatment of locally advanced or metastatic non-small cell lung cancer (NSCLC) after prior chemotherapy.Click here to contact Logenex about this product.
|
Pemetrexed (brand name Alimta) is a chemotherapy drug manufactured and marketed by Eli Lilly and Company. Its indications are the treatment of pleural mesothelioma andnon-small cell lung cancer.
The molecular structure of pemetrexed was developed by Edward C. Taylor at Princeton University and clinically developed by Indianapolis based drug maker, Eli Lilly and Company in 2004.
 PEMETREXED
PEMETREXED
Pemetrexed is chemically similar to folic acid and is in the class of chemotherapy drugs called folate antimetabolites. It works by inhibiting three enzymes used in purine andpyrimidine synthesis—thymidylate synthase (TS), dihydrofolate reductase (DHFR), andglycinamide ribonucleotide formyltransferase[1][2] (GARFT). By inhibiting the formation of precursor purine and pyrimidine nucleotides, pemetrexed prevents the formation of DNAand RNA, which are required for the growth and survival of both normal cells and cancer cells.
Pemetrexed disodium is chemically described as L-Glutamic acid, N-[4-[2- (2-amino-4,7-dihydro-4-oxo-1 H-pyrrolo[2,3-d]pyrimidin-5-yl)ethyl]benzoyl]- disodium salt heptahydrate, represented by the chemical structure of Formula (I).
Formula I
Pemetrexed is an anti-folate anti-neoplastic agent that exerts its action by disrupting folate-dependent metabolic processes essential for cell replication. It is believed to work by inhibiting three enzymes that are required in purine and pyrimidine biosynthesis — thymidylate synthase (TS), dihydrofolate reductase (DHFR), and glycinamide ribonucleotide formyl transferase (GARFT). Pemetrexed is available in the market under the brand name ALIMTA®.
Taylor et al., in describe pemetrexed, its related compounds and pharmaceutically acceptable cation. Chelius et al., in WO 01/14379 A2 disclose pemetrexed disodium crystalline hydrate Form I and process for preparation thereof.
Chelius et al., in WO 01/62760 disclose pemetrexed disodium heptahydrate crystalline Form Il and process for the preparation thereof.
Journal of Organic Process Research & Development, Volume 3, 1999, page 184 describes a process for the preparation of pemetrexed diacid. Busolli et al., in WO200802141 1 disclose process for preparation of pharmaceutically acceptable salt of pemetrexed diacid.
Busolli et al., in WO2008021405A1 disclose seven crystalline forms of pemetrexed diacid designated as Form A, B, C, D, E, F, & G and processes for preparation thereof.
In February 2004, the Food and Drug Administration approved pemetrexed for treatment of malignant Pleural Mesothelioma, a type of tumor of the lining of the lung, in combination with cisplatin[3] for patients whose disease is either unresectable or who are not otherwise candidates for curative surgery.[4] In September 2008, the FDA granted approval as a first-line treatment, in combination with cisplatin, against locally-advanced and metastatic non-small cell lung cancer (NSCLC) in patients with non-squamous histology. A Phase III study showed benefits of maintenance use of pemetrexed for non-squamous NSCLC.Activity has been shown in malignant peritoneal mesothelioma.Trials are currently testing it against esophagus and other cancers.
MECHANISM

Pemetrexed is also recommended in combination with carboplatin for the first-line treatment of advanced non-small cell lung cancer.However, the relative efficacy or toxicity of pemetrexed-cisplatin versus pemetrexed-carboplatin has not been established beyond what is generally thought about cisplatin or carboplatin doublet drug therapy
In addition to the brand name Alimta, this drug is also marketed in India by Abbott Healthcare as Pleumet and by Cadila Healthcare asPemecad.
-
Pemetrexed disodium is a multitargeted antifolate agent approved as a single agent for the treatment of non-small cell lung cancer, and in combination with cisplatin for the treatment of patient with malignant pleural mesothelioma, under the trade name Alimta®.
Pemetrexed disodium is available in a number of crystalline forms. -
Barnett et al, Organic Process Research & Development, 1999, 3, 184-188 discloses synthesis and crystallization of pemetrexed disodium from water-ethanol. The product obtained by the process disclosed herein is the 2.5 hydrate of pemetrexed disodium.
-
United States patent number 7,138,521 discloses a crystalline heptahydrate form of pemetrexed disodium, which has enhanced stability when compared to the known 2.5 hydrate.
-
To date workers have concentrated on producing stable crystalline forms of pemetrexed disodium and there has been no disclosure of any non-crystalline form of this active.
-
We have now found a new form of pemetrexed disodium, which is an amorphous form, as characterized by powder X-ray diffraction. Surprisingly, we have found that it is possible to prepare an amorphous form of pemetrexed disodium and that this form is stable. The amorphous form of the invention is stable contrary to expectations. The amorphous form of pemetrexed disodium of the present invention is stable as it retains it’s amorphous character under a variety of storage conditions. The amorphous form of the present invention is particularly advantageously characterized by a bulk density in the range of 0.15 to 0.35 gm/ml.
N-[4-[2-(2-amino-4,7-dihydro-4-oxo-3H-pyrrolo[2,3-d]-pyrimidin-5-yl)ethyl] benzoyl]-L-glutamic acid or N-[4-[2-(2-amino-4,7-dihydro-4-oxo-1 H-pyrrolo [2,3-d]-pyrimidin-5-yl)ethyl] benzoyl]-L-glutamic acid (also known as
“Pemetrexed”)
R = H: Pemetrexed; I
R = Na: Pemetrexed Disodium; II is a known compound. Pemetrexed Disodium is an known anticancer agent. It is clinically active in several solid tumors and approved for treatment of malignant pleural mesothelioma (MPM) and metastatic non-small cell lung cancer (NSCLC). Pemetrexed Disodium is supplied as a sterile lyophilized powder for intravenous administration.
The compound of formula I including pharmaceutically salts thereof as well as a process for its preparation is at first and specifically disclosed in EP patent no. 0432677 B1. The preparation and isolation of Pemetrexed (compound of formula I) as its Disodium salt (compound of formula II) was described for the first time in WO patent no. 9916742 A1 and in Drugs of the future 1998, 23(5), 498-507 as well as by Charles J. Barnett et al. in Organic Process Research & Development, 1999, 3, 184-188 and by Peter Norman in Current Opinion in Investigational Drugs 2001 , 2(11 ), 1611-1622.
Detailed information about the crystalline form of Pemetrexed Disodium prepared according to the process as described above were not provided but it is reported by Charles J. Barnett et al. in Organic Process Research & Development, 1999, 3, 184-188 that the disodium salt II was obtained as a hygroscopic solid.
The first crystalline form of Pemetrexed Disodium has been described in WO patent no. 0114379 designated Disodium MTA Hydrate Form I (MTA = multi- targeted antifolate, disodium N-[4-[2-(2-amino-4,7-dihydro-4-oxo-3H- pyrrolo[2,3-d]-pyrimidin-5-yl)ethyl]benzoyl]-L-glutamic acid salt). The Disodium MTA Hydrate Form I obtained according to the Examples 2, 3 and 4 contained different amounts of water (Example 2: water = 9.1%; Example 3: water = 17.7%; Example 4: water = 11.7%). The Disodium MTA Hydrate Form I has a typical XRD pattern as shown in Figure 4 (the corresponding 2theta values have been calculated from the provided d-spacing values).
An improved crystalline form of Pemetrexed Disodium has been disclosed in WO patent no. 0162760. It is teached that Pemetrexed Disodium can exist in the form of a heptahydrate (Form II; theoretical amount of water: approx 21%) which is much more stable than the previously known 2.5 hydrate (Form I; theoretical amount of water: 8.7%). The Pemetrexed Disodium Heptahydrate Form (Form II) has a typical XRD pattern as shown in Figure 5 (the corresponding 2theta values have been calculated from the provided d- spacing values).
The Chinese patent no. 1778802 describes a hydrate or trihydrate form of Pemetrexed Disodium. The preparation of Pemetrexed Disodium hydrate or trihydrate includes crystallization from water and water soluble solvent. An overview of the X ray powder diffraction data for Pemetrexed Disodium Hydrate provided in Chinese patent no. 1778802 is shown in Figure 6.
The WO patent no. 2008124485 disclose besides crystalline Forms of the diacid Pemetrexed also amorphous Pemetrexed Disodium as well as a crystalline Form III thereof including a composition containing a major amount of amorphous Form and a minor amount of crystalline Form III of Pemetrexed Disodium. An overview of the X ray powder diffraction data for Pemetrexed Disodium crystalline Form 3 is shown in Figure 7.
EP patent application no. 2072518 disclose a stable amorphous form of Pemetrexed Disodium.
-
According to the more recent US 5,416,211 , which is incorporated herein by reference, pemetrexed can be synthesized from 4-[2-(2-amino-4,7-dihydro-4-oxo-1H-pyrrolo[2,3-d]pyrimidin-5-yl)ethyl]benzoic acid of formula 1, obtained from simple precursors, in accordance with the following Scheme 1:
-
This second method seems to be used also for the industrial preparation of the active ingredient. In fact, the same type of synthesis scheme is also described in C. J. Barnett, T. W. Wilson and M. E. Kobierski, Org. Proc. Res. & Develop., 1999, 3, 184-188, in which the experimental examples refer to a scale of the order of tens of kgs.



……………………….
Example 1 Preparation of crude pemetrexed disodium
[0023] N-[4-2-(2-Amino-4, 7-dihydro-4-oxo-
1 H-pyrrolo[2,3-d]pyrimidin-5-yl)ethyl]benzoyl]-L-glutamic Acid Diethyl Ester
4-Methylbenzenesulfonic Acid Salt and purified process water (PPW) (about 10 kg) are charged to a suitable vessel under nitrogen. The reactor is cooled to NMT 10Ό under nitrogen. Pre-cooled sodium hydroxide solution (about 1.5 kg )/PPW (about 11.4 kg) are added and the temperature is maintained at NMT 10Ό. The mixture is stirred at NMT 0 until the solid is dissolved. Pre-cooled isopropanol (about 62.8 kg) is added and the mixture temperature is maintained at NMT 5 . Pre-cooled 1 N hydrochloric acid in isopropanol is added to adjust the pH to 6.5 to 9.5, preferably between pH 7.5 to pH 8.5, at NMT 5 . The mixture is warmed to a room temperature (i.e., 15-30Ό, preferably 20-25″C) and stirred. The solids are filtered and washed with isopropanol/PPW. The wet cake is vacuum dried to provide crude pemetrexed disodium (about 2.30 kg).
Example 2 Purification of crude pemetrexed disodium to pemetrexed disodium
[0024] Crude pemetrexed disodium (about 2.1 kg) and PPW (about 23.3 kg) are charged under nitrogen to a suitable vessel at 15 to 30 . Isopropanol (about 28.3 kg) is added slowly to cloud point and stirred. Isopropanol (up to about 55 kg) is charged and stirred. The solids are filtered arid washed with isopropanol/PPW. The wet cake is vacuum dried to provide pemetrexed disodium (about 1.9 kg) (90% Yiled). 1 H NMR (D20): δ 7.51 (2H, d, J=8.0 Hz), 6.98 (2H, d, J=8.0 Hz), 6.12 (1 H, s), 4.26-4.23 (H, m), 3.60-3.54 (4H, m), 2.27-2.23 (2H, m), 2.13-2.08 (1 H, m), 2.00-1.94 (1 H, m)
HPLC
Example 7
HPLC Analysis method
-
Reagent: Water :milliQ,
Sodium perchlorate :AR Grade
Perchloric acid :AR Grade
Acetonitrile :J.T.Baker gradient
Trifluroacetic acid :AR Grade
Buffer solution: 6.1 g of sodium perchlorate into a 1000ml water. Adjust the pH to 3.0 (± 0.1) with perchloric acid.
Mobile phase A:
mixture of buffer and acetonitrile in the proportion of (90:10).
Mobile phase B:
mixture of buffer and acetonitrile in the proportion of (10 : 90).
Diluent -1 : mixture of water and acetonitrile in the ratio of 50 : 50.
Diluent -2: mixture of water and acetonitrile in the ratio of 90 : 10.
Standard Stock Solution:
Transfer accurately weighed 1.5 mg impurity-E RS and into a 200 ml volumetric flask. Dissolve in and dilute upto mark with diluent-1.
Blank solution
-
Add 10 ml diluent-2 and 50µl of 3% trifluro acetic acid to a 50 ml volumetric flask, and dilute upto mark with diluent-2.
System suitability solution
-
Transfer about 25 mg accurately weighed pemetrexed disodium sample in to a 50 ml volumetric flask. First add 10ml of diluent-2 and sonicate to dissolve the contents.Then add 50µl of 3% trifluro acetic acid (prepared in water) and add 5 ml of standard stock solution and dilute up to mark with diluent-2.
Sample preparation
-
Transfer about 25 mg accurately weighed pemetrexed disodium sample in to a 50 ml volumetric flask. First add 10ml of diluent-2 and sonicate to dissolve the contents.Then add 50µl of 3% trifluro acetic acid (prepared in water) and dilute up to mark with diluent-2 (500 µg/ml).
Chromatographic system :
-
Use a suitable high pressure liquid chromatography system equipped with Column: 250 mm x 4.6mm containing 5µ packing material (suggested column – Inertsil ODS 3V)
Detector: UV detector set to 240 nm
Cooler temp: 5°C.
Flow rate: about 1.5 ml/min. -
The system is also equipped to deliver the two phases in a programmed manner as shown in the following table :
Gradient programme :
-
[0082]
0 92 8 15 85 15 30 65 35 35 65 35 36 92 8 40 92 8
Procedure:
-
Inject 20µl of blank and system suitability solution into the chromatograph set to above conditions and record the chromatograms up to 40 min.
Calculate the resolution between pemetrexed disodium and impurity-E. The resolution should not be less than 3.0. Calculate the Number of theoretical plate and tailing factor for pemetrexed peak. Number of theoretical plate is NLT 4000 and tailing factor is NMT 2.0. -
Inject 20µl of test solution and calculate the chromatographic purity by area normalisation method.
……………………..
Synthetic Route for the Preparation of Pemetrexed Disodium
Starting from commercially available materials a novel synthetic route for the synthesis of Pemetrexed-IM8 (the dimethyl ester of Pemetrexed) was developed which was then used for the preparation of Pemetrexed Disodium (Scheme 1).
The current synthetic route for the preparation of Pemetrexed IM8 starts with an aldol-condensation reaction of Methyl-4-formylbenzoate (SM1) with 1,1-Dimethoxyacetone (SM2) to give Pemetrexed IM1a. As Pemetrexed IM1a irreversibly converts to its aldol-addition product Pemetrexed IM1b under reaction conditions the reaction mixture is directly submitted to hydrogenation (i.e. without isolation of Pemetrexed IM1a) over Pd/C to give Pemetrexed IM2. As under the hydrogenation conditions not only the double-bond of IM1a is hydrogenated but also some amount of Pemetrexed IM2 is converted to Pemetrexed IM3 (hydrogenation of the carbonyl function to the corresponding secondary alcohol) a solution of NaBH4 is added to the reaction mixture to ensure complete conversion to Pemetrexed IM3. The Pd-catalyst is removed by filtration and the reaction mixture is extracted with toluene. The combined organic layers are evaporated to give crude Pemetrexed IM3 as oil. This oil is dissolved in THF and the alcohol functionality is converted to a mesylate using MsCl and NEt3. The salts are removed by filtration, glacial acetic acid is added and THF is removed by distillation. Upon addition of water Pemetrexed IM4 crystallizes and is isolated by filtration. The dried Pemetrexed IM4 is dissolved in glacial acetic acid and gaseous HCl is added to cleave the dimethoxy acetale and liberate the aldehyde functionality of Pemetrexed IM5. Upon complete deprotection a solution of 2,6-diamino-4-hydroxypyrimidine in aq. NaOH and acetonitrile is added. Upon complete conversion the crystallized Pemetrexed IM6 is isolated by filtration. The saponification of the methyl ester of Pemetrexed IM6 to Pemetrexed IM7 is done using aqueous NaOH. Upon addition of aq. HCl first the Na-salt of Pemetrexed IM7 crystallizes from the reaction mixture. The salt is isolated by filtration, purified by slurry in a mixture of MeOH and water and then converted to Pemetrexed IM7 by pH adjustment in water using aq. HCl. Dried Pemetrexed IM7 (water content not more than 6.0%) is dissolved in DMF, activated using 1,1-carbonyldiimidazolide (CDI) and then reacted with dimethyl-L-glutamate hydrochlorid to give, upon addition of water and filtration, crude Pemetrexed IM8. This intermediate is purified by tosylate salt formation, followed by recrystallization and liberation to give pure Pemetrexed IM8. Starting with the saponification of Pemetrexed IM8 the preparation of different solid forms of Pemetrexed Disodium can be achieved.
Methods For Preparing Pemetrexed Disodium Form IV and Investigation of its Stability
An overview on the possible transformations of Pemetrexed IM8 to Pemetrexed Disodium Form IV is shown in FIG. 20.
Description of Possible Routes for the Preparation of Pemetrexed Disodium Form IV Starting from Pemetrexed IM8
All routes start with saponification of Pemetrexed IM8 in water at IT=20° C. to 30° C. using 3.25 eq of NaOH. Upon complete conversion an aqueous solution of Pemetrexed Disodium with a pH of 13.0 to 13.5 is obtained. Starting from this mixture the desired route can be accessed by addition of HCl to adjust the pH to a certain value (depending on the route, FIG. 20).
Structures of Pemetrexed (Compound I), Pemetrexed Disodium (Compound II) and Pemetrexed Monosodium (Compound IV)
Surprisingly we found that the crucial feature of all successful transformations to Pemetrexed Disodium Form IV is the presence of Pemetrexed Monosodium during the transformation. Routes starting from pure Pemetrexed Disodium Heptahydrate, Pemetrexed Disodium 2.5 hydrate or Pemetrexed Disodium Form A in the presence of seeding crystals of Pemetrexed Disodium Form IV were not successful and resulted in isolation of Pemetrexed Disodium Form A. The same transformations, if carried out in the presence of 0.15 eq of Pemetrexed Monosodium were successful and after addition of 0.15 eq NaOH allowed the isolation of pure Pemetrexed Disodium Form IV. The use of 0.15 eq HCl instead of 0.15 eq Pemetrexed Monosodium under the same conditions resulted in isolation of Pemetrexed Disodium Form A without any Pemetrexed Disodium Form IV. Transformations via isolated Pemetrexed Monosodium gave complete transformation to Pemetrexed Disodium Form IV if either 1.0 eq NaOH were added slowly (over a period of several hours) to Pemetrexed Monosodium or if initially only 0.85 eq of NaOH (based on Pemetrexed Monosodium) were added, followed by 0.15 eq once the transformation to Pemetrexed Disodium Form IV was complete. Very fast addition (<1 min) of 1.0 eq NaOH resulted in formation of Pemetrexed Disodium Form A containing traces of Pemetrexed Disodium Heptahydrate.
Starting from Pemetrexed (compound I) the transformation to Pemetrexed Disodium Form IV would be possible if initially 1.85 eq of NaOH were added followed by 0.15 eq once the transformation was complete. Alternatively, 2.0 eq of NaOH could be added over a long period of time (i.e several hours) to achieve formation of Pemetrexed Form IV. Fast addition (<1 min) of 2.0 eq of NaOH is assumed to result in formation of Pemetrexed Disodium Form A. All these experiments show the presence of Pemetrexed Monosodium to be crucial during the transformations. This presence can be achieved by either addition of catalytic amounts of Pemetrexed Monosodium to Pemetrexed Disodium, by slow addition over several hours of NaOH to Pemetrexed Monosodium or by portionwise addition of NaOH to Pemetrexed Monosodium. Addition of catalytic amounts of HCl to Pemetrexed Disodium (in situ preparation of Pemetrexed Monosodium) failed to give Pemetrexed Disodium Form IV.
Fast addition of NaOH to Pemetrexed Monosodium results in fast formation of Pemetrexed Disodium, thereby lacking the necessary catalytic amounts of Pemetrexed Monosodium to catalyze the transformation to Pemetrexed Disodium Form IV. EtOH as solvent and water content of EtOH were found to be crucial parameters for the transformation to Pemetrexed Disodium Form IV. So far the transformation has only been observed in EtOH containing 0-4% water (v/v). A water content>4% (v/v) results in formation of Pemetrexed Disodium Heptahydrate. Under the conditions used (EtOH containing 0-4% water (v/v)) both Pemetrexed Disodium Heptahydrate and Pemetrexed Disodium 2.5 hydrate are transformed to Pemetrexed Form A. Therefore the mechanism of the transformation to Pemetrexed Disodium Form IV is assumed to proceed via Pemetrexed Disodium Form A with Pemetrexed Monosodium acting as catalyst for the transformation.
Preparation of Pemetrexed Disodium Heptahydrate
a) Preparation of Pemetrexed Disodium Heptahydrate Starting from Pemetrexed IM8
Pemetrexed Disodium Heptahydrate was prepared by adjustment of the pH of the Pemetrexed Disodium solution after saponification from pH=13 to pH=8 using HCl followed by addition of EtOH (3 times the volume of water) to achieve crystallization. Precipitated Pemetrexed Disodium Heptahydrate was isolated by filtration, washed with a mixture of EtOH and water (4:1 v/v) followed by EtOH. The wet product was dried in vacuo at 200 mbar at 20° C. to 30° C. until water content of the dried product was 20.1% to 22.1%.
b) Conversion of Pemetrexed Disodium Form A to Pemetrexed Disodium Heptahydrate
To a suspension of Pemetrexed Disodium Form A in EtOH was added water until a mixture of EtOH containing 25% water (v/v) was obtained. The resulting suspension was stirred at 20° C. to 30° C. until conversion was complete according to PXRD. Pemetrexed Disodium Heptahydrate was isolated by filtration, washed with EtOH and dried in vacuo at 200 mbar at 20° C. to 30° C. until water content of the dried product was 20.1% to 22.1%.
………………………..

- REFERENCES
- McLeod, Howard L.; James Cassidy, Robert H. Powrie, David G. Priest, Mark A. Zorbas, Timothy W. Synold, Stephen Shibata, Darcy Spicer, Donald Bissett, Yazdi K. Pithavala, Mary A. Collier, Linda J. Paradiso, John D. Roberts (Jul-2000).“Pharmacokinetic and Pharmacodynamic Evaluation of the Glycinamide Ribonucleotide Formyltransferase Inhibitor AG2034”. Clinical Cancer Research 6 (7): 2677–84.PMID 10914709. More than one of
|work=and|journal=specified (help) - Avendano, Carmen; Menendez, J. Carlos (April 2008).Medicinal Chemistry of Anticancer Drugs. Amsterdam:Elsevier. p. 37. ISBN 0-444-52824-5.
- Manegold C (August 2003). “Pemetrexed (Alimta, MTA, multitargeted antifolate, LY231514) for malignant pleural mesothelioma”. Semin. Oncol. 30 (4 Suppl 10): 32–6.doi:10.1016/S0093-7754(03)00283-5. PMID 12917819.
- National Cancer Institute: FDA Approval for Pemetrexed Disodium
| US6090168 * | Oct 6, 1999 | Jul 18, 2000 | Eli Lilly And Company | Processes and intermediates useful to make antifolates |
| US7138521 | Feb 12, 2001 | Nov 21, 2006 | Eli Lilly And Company | Crystalline of N-[4-[2-(2-Amino-4,7-dihydro-4oxo-3H-pyrrolo[2,3-D]pyrimidin-5-YL)ethyl]benzoyl]-L-glutamic acid and process therefor |
| US20030216416 * | Feb 12, 2001 | Nov 20, 2003 | Chelius Erik Christopher | Novel crystalline of n-[4-[2-(2-amino-4,7-dihydro-4oxo-3h-pyrrolo[2,3-d]pyrimidin-5-yl)ethyl]benzoyl]-l-glutamic acid and process therefor |
| WO2001014379A2 * | Aug 15, 2000 | Mar 1, 2001 | Erik Christopher Chelius | A novel crystalline form of disodium n-[4-[2-(2-amino-4,7-dihydro-4-oxo-3h-pyrrolo[2,3-d]-pyrimidin-5-yl)ethyl]benzoyl]-l-glutamic acid salt and processes therefor |
| WO2008021405A1 * | Aug 14, 2007 | Feb 21, 2008 | Sicor Inc | Crystalline forms of pemetrexed diacid and processes for the preparation thereof |
| WO2008124485A2 * | Apr 3, 2008 | Oct 16, 2008 | Reddys Lab Ltd Dr | Solid forms of pemetrexed |
PHASE 2 -TetraLogic’s BIRINAPANT for treatment of acute myeloid leukemia, pancreatic cancer, or ovarian cancer
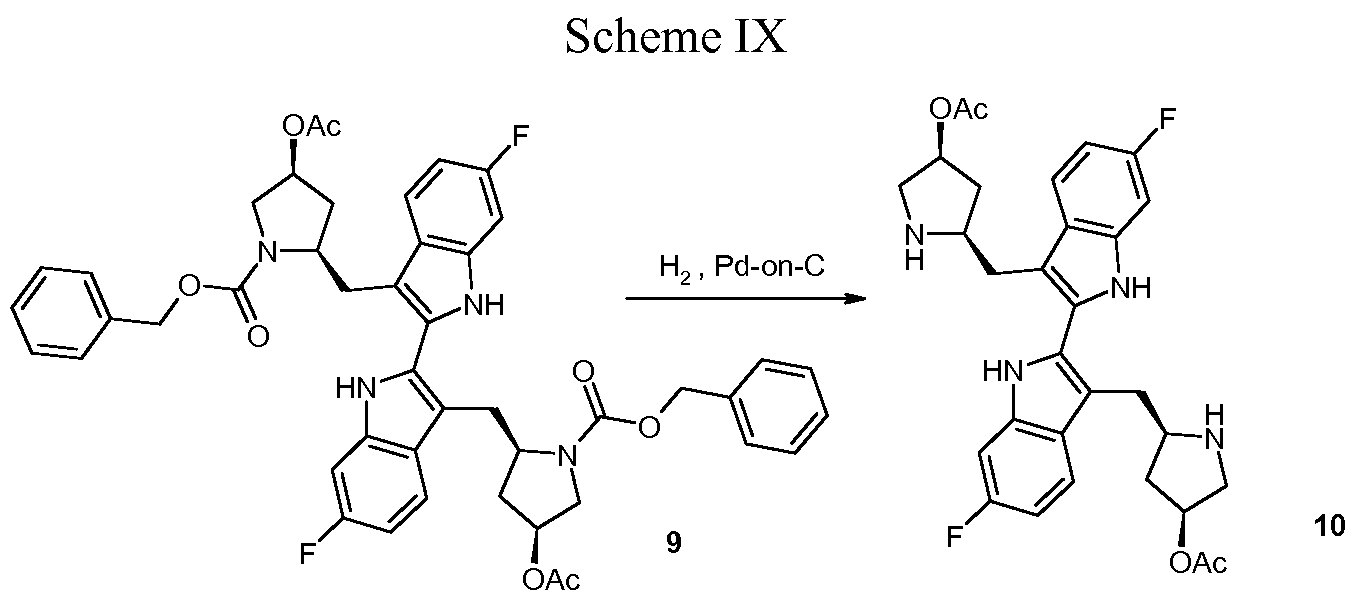
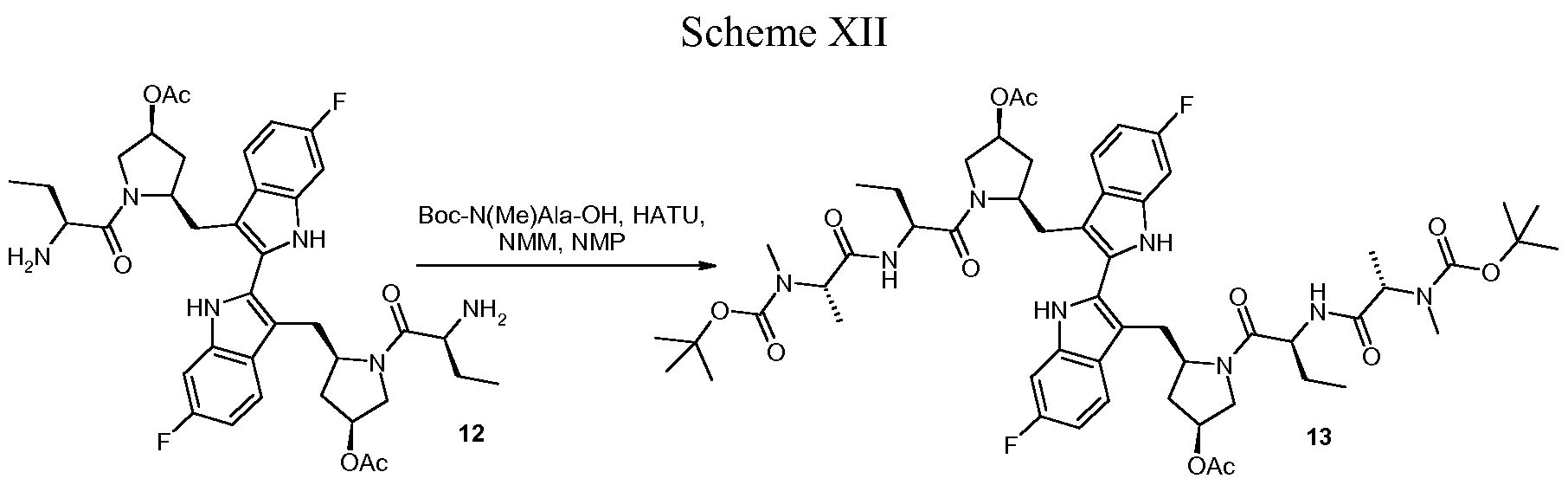
BIRINAPANT, Apoptosis inhibitor
(2S,2’S)-N,N’-((2S,2’S)-((3S,3’S,5R,5’R)-5,5′-((6,6′-difluoro-1H,1’H-[2,2′-biindole]-3,3′-diyl)bis(methylene))bis(3-hydroxypyrrolidine-5,1-diyl))bis(1-oxobutane-2,1-diyl))bis(2-(methylamino)propanamide)
1260251-31-7 cas no
Birinapant is an antagonist of XIAP and cIAP1 with Kd value of 45 nM and <1 nM, respectively.
US20110003877,WO 2013049350 A1
| Molecular Weight: | 806.94 |
| Birinapant Formula: | C42H56F2N8O6 |
Birinapant, also known as TL32711, is a synthetic small molecule and peptido mimetic of second mitochondrial-derived activator of caspases (SMAC) and inhibitor of IAP (Inhibitor of Apoptosis Protein) family proteins, with potential antineoplastic activity. As a SMAC mimetic and IAP antagonist, TL32711 binds to and inhibits the activity of IAPs, such as X chromosome-linked IAP (XIAP) and cellular IAPs 1 and 2. Since IAPs shield cancer cells from the apoptosis process, this agent may restore and promote the induction of apoptosis through apoptotic signaling pathways in cancer cells. IAPs are overexpressed by many cancer cell types and suppress apoptosis by binding and inhibiting active caspases-3, -7 and -9 via their baculoviral lAP repeat (BIR) domains
Birinapant is currently in Phase II clinical trials in patients with acute myeloid leukemia, pancreatic cancer, or ovarian cancer. Although these trials don’t have a control group, the emerging data are promising, TetraLogic chief executive officer John M. Gill told C&EN. (Early-stage cancer clinical trials are commonly run without placebo groups.) The birinapant trials show preliminary evidence both that the drug is having the desired effect and that this effect is associated with signs of clinical activity. Given these results, the company plans to launch randomized Phase II studies early in 2014
Birinapant, also called TL32711, is a potent antagonist for XIAP with Kd value of 45 nM and cIAP1 with Kd value <1 nM [1].
Birinapant not only binds to the isolated BIR3 domains of cIAP1, cIAP2, XIAP but the single BIR domain of ML-IAP with high affinity and degrades TRAF2-bound cIAP1 and cIAP2 rapidly accordingly inhibiting the activation of TNF-mediated NF- kB. Additionally, birinapantcan promote the formation of caspase-8: RIPK1 complex in response to TNF stimulation, which result in downstream caspasesactivation [4].
In the inorganic SUM149- and SUM190-derived cells, which with differential XIAP expression (SUM149 wtXIAP, SUM190 shXIAP) and other high cIAP1/2 but low XIAP binding affinity bivalent Smac mimetic GT13402, XIAP inhibition are needed for increasing TRAIL potency. Opposite, single agent efficacy of Birinapant is owing to pan-IAP antagonism. Rapid cIAP1 degradation was caused by birinapant, as well as NF-κB activation, PARP cleavage andcaspase activation. While combined withTNF-α, showing strong combination activity, the combination was more effective than individual. The response in spheroid models was conserved, whereas in vivo birinapant inhibited tumor growth without adding TNF-α in vitro to resistant cell lines. In a parental cell line, TNF-αcombined withbirinapantinhibited the growth of a melanoma cell line with acquired resistance to the same extent of BRAF inhibition [1, 2].
Drug treatment increased the mean [18F]ICMT-11 tumor uptake with a peak at 24 hours for CPA (40 mg/kg; AUC40-60: 8.04 ± 1.33 and 16.05 ± 3.35 %ID/mL × min at baseline and 24 hours, respectively) and 6 hours for birinapant (15 mg/kg; AUC40-60: 20.29 ± 0.82 and 31.07 ± 5.66 %ID/mL × min, at baseline and 6 hours, respectively). Voxel-based spatiotemporal analysis of tumor-intrinsic heterogeneity showed that [18F] ICMT-11 could detect the discrete pockets of caspase-3 activation. Caspase-3 activation that measured ex vivo associated with the increased tumor [18F] ICMT-11, and early radiotracer uptake predicted apoptosis, distinct from the glucose metabolism with [18F] fluorodeoxyglucose-PET, which depicted the continuous loss of cell viability [3].


Birinapant was designed to reinstate cancer cells’ ability to die. Many cancers that are resistant to conventional chemotherapy drugs have defects in the cell death pathway known as apoptosis. The human body uses apoptosis every day to clear away abnormal or unwanted cells.
Apoptosis is a tightly regulated process, Condon explains, with a network of proteins that activate or block the process. TetraLogic’s target is a family of proteins called the Inhibitor of Apoptosis proteins. As their name suggests, these proteins block apoptosis. They interfere with protease enzymes that carry out cellular dismantling.
TetraLogic’s aim is to lift that blockade to restart apoptosis in tumors. Many tumors have excesses of the apoptosis inhibitor proteins relative to normal cells, so targeting this process has the potential to be less toxic to normal cells compared with conventional chemotherapy.
It turns out nature has a way of negating the inhibitor proteins’ actions—a protein known as Smac. TetraLogic’s founders demonstrated that only a tiny portion of Smac is necessary to keep the inhibitor proteins at bay—the four amino acids at the protein’s N-terminus. “Once you can get a protein down to a tetrapeptide,” about the size of a small-molecule drug, “you start getting a lot of interest from the pharma community,” Condon told C&EN.
Peptides fall apart in the body too quickly to be drugs, so Condon’s team worked with molecular mimics of the Smac tetrapeptide. Their biggest advance was realizing that combining two copies of their tetrapeptide mimics into one molecule made their compounds highly effective at reinstating apoptosis in cancer cell lines. Many proteins in the apoptosis pathway function as dimers, so using these so-called bivalent mimics against them makes sense, Condon said.
However, several of the bivalent compounds were associated with pronounced body weight loss in mice. Condon’s team eventually learned that replacing a branched side chain on their peptide mimics and adding a hydroxyl group to a proline residue improved the tolerability for the animals without impacting the antitumor effect. With that, birinapant was born.
In mice, birinapant shrank tumors. The compound has been in clinical trials since 2009, both on its own and in combination with other chemotherapy drugs such as irinotecan and gemcitabine. On the basis of other biochemical work on the apoptosis pathway, TetraLogic thinks these drugs could act in synergy with birinapant to treat cancer, Condon said.
Birinapant is currently in Phase II clinical trials in patients with acute myeloid leukemia, pancreatic cancer, or ovarian cancer. Although these trials don’t have a control group, the emerging data are promising, TetraLogic chief executive officer John M. Gill told C&EN. (Early-stage cancer clinical trials are commonly run without placebo groups.) The birinapant trials show preliminary evidence both that the drug is having the desired effect and that this effect is associated with signs of clinical activity. Given these results, the company plans to launch randomized Phase II studies early in 2014.
1H NMR













spectral data
1H NMR (300 MHz, CDC13): 511.74 (s, 2H), 8.27 (d, J= 8.7 Hz, 2H), 7.71 (dd, J= 5.4, 8.4 Hz, 2H), 7.55 (dd, J =2.4, 9.6 Hz, 2H), 6.88 (ddd, J= 2.4, 9.3, 9.3 Hz, 2H), 4.62-4.78 (m, 4H), 4.43 (dd, J= 9.3, 9.9 Hz, 2H), 4.03 (dd, J= 4.8, 11.4 Hz, 2H), 3.80 (d, J = 11.4 Hz, 2H), 3.66 (dd, J= 2.7, 14.4 Hz, 2H), 3.53 (dd, J = 11.4, 14.4 Hz, 2H), 3.11 (q, J = 6.9 Hz, 2H), 2.56 (s, 6H), 2.45 (m, 2H), 2.19 (d, J= 14.4 Hz, 2H), 1.76-2.10 (m, 6H), 1.59 (br s, 2H), 1.39 (d, J= 6.9 Hz, 6H), 1.22-1.38 (m, 2H), 1.07 (t, J = 7.2 Hz, 6H) ppm;
13C NMR (75 MHz, d6– DMSO): 5175.2, 172.8, 161.6, 158.5, 137.3, 137.2, 128.4, 128.3, 126.4, 120.8, 120.6, 109.4, 108.7, 108.4, 98.4, 98.0, 70.8, 60.2, 59.9, 56.6, 51.8, 36.4, 35.3, 28.3, 25.6, 20.0, 10.6 ppm.
Mass spectrum (ESI), m/z 807.5 [(M)+; calcd for C42H56F2N806: 806.9].
Paper
Click to access op5b00390_si_001.pdf
Click to access op5b00390_si_001.pdf
Process Development and Synthesis of Birinapant: Large Scale Preparation and Acid-Mediated Dimerization of the Key Indole Intermediate

Birinapant/TL32711 (1) is a novel bivalent antagonist of the inhibitor of apoptosis (IAP) family of proteins which is currently in clinical development for the treatment of cancer and hepatitis B virus (HBV) infection. In this report, we present a detailed description of the 1 drug substance synthesis used to support our ongoing clinical studies. Key transformations in this process included the development of a scalable, high-yielding route to acyl indole 14 as well as a two-step dimerization/oxidation of indole 19 that afforded biindole 21 in excellent yield and purity (70% yield, 2 steps; >95 area% purity by HPLC analysis). In addition, partial defluorination of 21 was observed following hydrogen-mediated benzyloxycarbonyl (Cbz) protective group removal which was obviated by the use of HBr/HOAc for this transformation. The use of commercially available amino acid derivatives afforded related impurities which proved difficult to purge in subsequent steps. Thus, defining the impurity specification for these reagents was critical to providing 1 drug substance of >99 area% chemical purity. Using this process, we have successfully prepared 1 drug substance multiple times on >500-g-scale in support of our clinical development program.
References:
1.Allensworth JL, Sauer S, Lyerly HK, et al. Smac mimetic Birinapant induces apoptosis and enhances TRAIL potency in inflammatory breast cancer cells in an IAP-dependent and TNF-a-independent mechanism. Breast Cancer Research, 2013, 137:359-371.
2.Krepler C, Chunduru SK, Halloran MB, et al. The novel SMAC mimetic birinapant exhibits potent activity against human melanoma cells. Clinical Cancer Research, 2013, 19 (7): 1784-1794.
3.Nguyen QD, Lavdas I, Gubbins J, et al. Temporal and Spatial Evolution of Therapy-Induced Tumor Apoptosis Detected by Caspase-3–Selective Molecular Imaging. Clinical Cancer Research, 2013, 19 (14): 3914-3924.
4.Benetatos CA, Mitsuuchi Y, Burns JM, et al. Birinapant (TL32711), a Bivalent SMAC Mimetic, Targets TRAF2-Associated cIAPs, Abrogates TNF-Induced NF-kB Activation, and Is Active in Patient-Derived Xenograft Models. 2014, 13(4):867-879.


 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....

































