Home » Uncategorized (Page 167)
Category Archives: Uncategorized
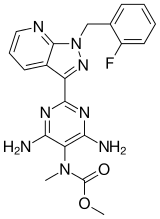
Malaria Drug (Furamidine) to Treat Cancer
View original post 260 more words
Pramlintide
Pramlintide (Symlin), a synthetic version of amylin, is a 37-amino acid peptide that is co-secreted with insulin by pancreatic β-cells. It was developed and approved in 2005 by the FDA for use in US patients with type I and II diabetes in conjunction with the administration of prandial insulin to improve postprandial glycemic control
 |
|---|
Pramlintide (Symlin) is a relatively new adjunct for diabetes (both type 1 and 2), developed by Amylin Pharmaceuticals (now a wholly owned subsidiary of Bristol Myers-Squibb). Pramlintide is delivered as an acetate salt.
Pramlintide is an analogue of amylin, a small peptide hormone that is released into the bloodstream by the β-cells of the pancreas along with insulin, after a meal.[1] Like insulin, amylin is completely absent in individuals with Type I diabetes.[2]
Reduction in glycated hemoglobin and weight loss have been shown in insulin-treated patients with type 2 diabetes taking pramlintide as an adjunctive therapy.[3]
By augmenting endogenous amylin, pramlintide aids in the absorption of glucose by slowing gastric emptying, promoting satiety via hypothalamic receptors (different receptors than for GLP-1), and inhibiting inappropriate secretion of glucagon, a catabolic hormone that opposes the effects of insulin and amylin. Pramlintide also has effects in raising the acute first-phase insulin response threshold following a meal.
Pramlintide has been approved by the FDA, for use by Type 1 and Type 2 Diabetics who use insulin.[4]Pramlintide allows patients to use less insulin, lowers average blood sugar levels, and substantially reduces what otherwise would be a large unhealthy rise in blood sugar that occurs in diabetics right after eating. Apart from insulin analogs, pramlintide is the only drug approved by the FDA to lower blood sugar in type 1 diabetics since insulin in the early 1920s.
Design and structure
Since native human amylin is highly amyloidogenic and potentially toxic, the strategy for designing pramlintide was to substitute residues from rat amylin, which is not amyloidogenic (but would presumably retain clinical activity). Proline residues are known to be structure-breaking residues, so these were directly grafted into the human sequence.
Amino acid sequences:
Pramlintide: KCNTATCATQRLANFLVHSSNNFGPILPPTNVGSNTY-(NH2)
Amylin: KCNTATCATQRLANFLVHSSNNFGAILSSTNVGSNTY-(NH2)
Rat amylin: KCNTATCATQRLANFLVRSSNNLGPVLPPTNVGSNTY-(NH2)
Pramlintide as protein is (positively charged).
- Jones MC (2007). “Therapies for diabetes: pramlintide and exenatide” (pdf). American Family Physician 75 (12): 1831–5. PMID 17619527.
- Edelman, Steve; Maier, Holly; Wilhelm, Ken (2008). “Pramlintide in the Treatment of Diabetes Mellitus”.BioDrugs 22 (6): 375–386. doi:10.2165/0063030-200822060-00004. ISSN 1173-8804.
- Hollander, Priscilla; Maggs, David G.; Ruggles, James A.; Fineman, Mark; Shen, Larry; Kolterman, Orville G.; Weyer, Christian (2004). “Effect of Pramlintide on Weight in Overweight and Obese Insulin-Treated Type 2 Diabetes Patients” (pdf). Obesity 12 (4): 661–668. doi:10.1038/oby.2004.76.ISSN 1930-7381.
- Ryan GJ, Jobe LJ, Martin R (2005). “Pramlintide in the treatment of type 1 and type 2 diabetes mellitus”. Clinical therapeutics 27 (10): 1500–12. doi:10.1016/j.clinthera.2005.10.009. PMID 16330288.
- www.symlin.com – product website
- www.amylin.com – Symlin page on the Amylin Pharmaceuticals website
| Pramlintide Acetate | |
| Pramlintide acetate is a relatively new adjunct treatment for diabetes (both type 1 and 2). |
Pramlintide Acetate, 196078-30-5,
| Synonym | Pramlintide Acetate,Pramlintide acetate hydrate |
| Molecular Formula | C171H267N51O53S2.X(C2H4O2).X(H2O) |
| Molecular Weight | 3949.39 |

Big boost for Incyte as Jakafi shines in PhII


ruxolitinib
Top-line results from a Phase II trial showed that its JAK inhibitor Jakafi (ruxolitinib), in combination with Roche’s Xeloda (capecitabine), improved survival in some patients with recurrent or treatment refractory advanced pancreatic cancer
http://www.pharmatimes.com/Article/13-08-
22/Big_boost_for_Incyte_as_Jakafi_shines_in_PhII.aspx
Ruxolitinib (trade names Jakafi and Jakavi, by Incyte Pharmaceuticals and Novartis) is a drug for the treatment of intermediate or high-risk myelofibrosis, a type of bone marrow cancer.It is also being investigated for the treatment of other types of cancer (such as lymphomas and pancreatic cancer), for polycythemia vera, and for plaque psoriasis.
The phase III Controlled Myelofibrosis Study with Oral JAK Inhibitor-I (COMFORT-I) and COMFORT-II trials showed significant benefits by reducing spleen size, relieving debilitating symptoms, and improving overall survival.
Mechanism of action
Ruxolitinib is a Janus kinase inhibitor with selectivity for subtypes 1 and 2 of this enzyme.
Side effects
Immunologic side effects have included herpes zoster (1.9%) and case reports of…
View original post 638 more words
QbD: new Guidance from EMA and FDA
DRUG REGULATORY AFFAIRS INTERNATIONAL

QbD: new Guidance from EMA and FDA
The European Medicine Agency (EMA) and the U.S. Food and Drug Agency (FDA) have published a joint question-and-answer document that provides further guidance on the quality-by-design concept. Read more.
http://www.gmp-compliance.org/ecanl_654_0_news_4015_8280,8356,Z-PDM_n.html
The Quality by Design (QbD) concept has been introduced by the International Conference on Harmonisation (ICH) document Q8, supported by Q9, Q10 and also Q11. In the meantime it is well-known within the pharmaceutical industry. However many companies still struggle with the implementation. Both the European Medicine Agency (EMA) and the U.S. Food and Drug Agency (FDA) are supporting the pharmaceutical industry in the employment of the paradigm. Now, EMA and FDA have published a second joint question-and-answer document that provides further guidance on the quality-by-design concept.
The new document focuses on ‘design space verification’ and reflects conclusions reached in the on-going parallel assessment, which was launched in 2011. The objective of the parallel…
View original post 388 more words
Chugai Pharma to commercialize Helsinn’s Anamorelin for anorexia-cachexia syndrome in Germany, France, Benelux, UK and Ireland

LUGANO, Switzerland, November 12, 2013 /PRNewswire/ —
Swiss Pharma Group Helsinn seals an alliance with Japanese company Chugai by granting exclusive distribution & licensing rights to commercialize its innovative phase III ghrelin receptor agonist in Germany, France, Benelux, UK andIreland
Swiss-based Helsinn group has granted Chugai Pharma Marketing Ltd., a wholly-owned subsidiary of Chugai Pharmaceutical Co., Ltd., exclusive commercialization rights to their innovative ghrelin receptor agonist, anamorelin, for the three major European pharma markets.
Anamorelin is a new first-in-class, oral, once daily drug, currently in phase III for the treatment of anorexia-cachexia in NSCLC, a detrimental multifactorial disorder that affects over 50% of people with cancer and in which systemic inflammation, reduced food intake and altered metabolism contribute to loss of muscle mass and reduction of body weight leading to reduced quality of life, functional impairment and decreased survival.
- Anamorelin is a synthetic orally active ghrelin receptor agonist which is under development for the management of non-small lung cancer associated cachexia/anorexia.
- Development status: Phase 3
- Appetite loss; Aging; Bone injury; Cachexia

Anamorelin HCl
| M. Wt | 583.16 |
|---|---|
| Formula | C31H43ClN6O3 |
| CAS No. | 861998-00-7 |
| Synonyms | RC 1291; RC1291; RC 1291-HCl; ONO-7643; ONO7643; ONO 7643. |
| Chemical Name | 2-amino-N-((R)-1-((R)-3-benzyl-3-(1,2,2-trimethylhydrazinecarbonyl)piperidin-1-yl)-3-(1H-indol-3-yl)-1-oxopropan-2-yl)-2-methylpropanamide hydrochloride |
Necitumumab

Necitumumab
Necitumumab is a fully human IgG1 monoclonal antibody designed to block the ligand binding site of the human epidermal growth factor receptor (EGFR), which is a target in several anti-cancer treatments because it sparks cancer progression, both by promoting angiogenesis, or the formation of new blood vessels for tumors, and by inhibiting apoptosis, or cell death. Recently approved therapies for non-squamous NSCLC, including afatinib and erlotinib, target specific EGFR mutations, but those drugs are used to treat patients with nonsquamous histology.Lilly did not provide specific data regarding the results of the trial, but the company announced that it plans to present that data at a scientific meeting next year, and to request a review of the drug by regulatory authorities before the end of 2014.
Necitumumabis one of three monoclonal antibodies in Phase III
development that targets EGFR, the target of the approved antibodies
cetuximab and panitumumab. However, necitumumab is a fully human
IgG1 antibody, distinguishing it from both the approved agents.
Necitumumab is directed against the ligand binding site of EGFR and is
being co-developed by Eli Lilly and Bristol-Myers Squibb in the United
States, Canada, and Japan, while Eli Lilly alone is developing it for other
markets. Necitumumabfirst entered clinical development in 2004 and
is now in Phase III development for the treatment of non–small-cell
lung cancer and Phase II for the treatment of colorectal cancer. The
primary indication chosen further distinguishes necitumumabfrom both
cetuximab and panitumumab, but it is an indication for which EGFR
kinase inhibitors such as erlotinib are approved.
In December 2009, Eli Lilly stressed the long half-life of necitumumab
(7–10 days, which permits dosing at 2–3 week intervals) and its potential
both for reduced hypersensitivity reactions (i.e., better tolerability) and
for induced host-mediated anticancer activity. In addition, it highlighted
that necitumumabdisplays similar or superior activity to cetuximab
in anticancer models. Preliminary data were presented from the Phase
II study in colorectal cancer showing antitumor activity in 73% of 44
patients treated with necitumumabplus FOLFOX.
Both Phase III studies in non–small-cell lung cancer are in stage IV
disease and in groups of 947 patients treated with necitumumabplus
cisplatin and a second agent. The INSPIRE study in non-squamous
disease began in November 2009 and uses pemetrexed as the second
drug, while the SQUIRE study commenced in January 2010 in
squamous disease and uses gemcitabine. Both studies have primary
completion dates in late 2011 and study completion dates of mid-2012,
which points to BLA submission in 2013.

A Phase I study in patients with solid tumors suggested that skin
toxicity was the dose-limiting toxicity and suggested that 800 mg of
necitumumab (at weekly or fortnightly intervals) be the maximum dose
(Kuenen et al. 2010).16 This dose was employed in the initial colorectal
cancer study, at 14-day intervals, which revealed a 60% partial response
(Taberno et al. 2008).17
The development strategy for necitumumab appears to have been
designed to establish it initially in a major indication where it will not
be competing with established antibody products, while seeking
to exploit the reported advantages over cetuximab appears to be
a secondary priority. While the reported Phase II data are very
encouraging, it will be some time before a better assessment of the
commercial prospects of necitumumab can be made. However, it does
appear to have significant potential.
Necitumumab (proposed INN) is a monoclonal antibody and an antineoplastic. It binds to the epidermal growth factor receptor(EGFR).[1] As of October 2009, two Phase III clinical trials are planned to investigate its effects on non-small cell lung carcinoma.[2][3]
- International Nonproprietary Names for Pharmaceutical Substances (INN, prepublication copy), World Health Organization.
- ClinicalTrials.gov NCT00981058 Squamous Non-Small Cell Lung Cancer (NSCLC) Treatment With the Inhibitor of Epidermal Growth Factor Receptor (EGFR) (SQUIRE)
- ClinicalTrials.gov NCT00982111 NonSquamous Non-Small Cell Lung Cancer Treatment With the Inhibitor of Epidermal Growth Factor Receptor (INSPIRE)
Possible Efficacy Of Lilly’s Necitumumab (IMC-11F8) In Lung Cancer Subset
18.4 2013
Eli Lilly announced yesterday their very preliminary and non-quantitative conclusions on the SQUIRE study, a 1093-patient Phase III trial of their anti-epidermal growth factor receptor (EGFR) antibody, necitumumab (IMC-11F8), against Stage IV squamous, non-small cell lung carcinoma (NSCLC).http://www.forbes.com/sites/davidkroll/2013/08/14/possible-efficacy-of-necitumumab-imc-11f8-in-squamous-nsclc-lung-cancer-subset/

The U.S. Food and Drug Administration approved Adempas (riociguat) to treat adults with two forms of pulmonary hypertension.
October 8, 2013 — The U.S. Food and Drug Administration today approved Adempas (riociguat) to treat adults with two forms of pulmonary hypertension.
Pulmonary hypertension is caused by abnormally high blood pressure in the arteries of the lungs. It makes the right side of the heart work harder than normal. In its various forms, pulmonary hypertension is a chronic, progressive, debilitating disease, often leading to death or need for lung transplantation
read all at
http://www.drugs.com/newdrugs/fda-approves-adempas-pulmonary-hypertension-3927.html
In the area of pulmonary hypertension Adempas (Riociguat) is the first member of a novel class of compounds – so-called ‘soluble guanylate cyclase (sGC) stimulators’ – being investigated as a new and specific approach to treating different types of pulmonary hypertension (PH). Adempas has the potential to overcome a number of limitations of currently approved treatments for pulmonary arterial hypertension (PAH) and addresses the unmet medical need in patients with chronic thromboembolic pulmonary hypertension (CTEPH)…
View original post 820 more words
Reslizumab
Reslizumab(CINQUIL) is a humanized monoclonal antibody
targeted against IL-5 that is being developed by Cephalon for the
treatment of eosinophilic asthma. In September 2010, Cephalon
indicated that it hopes to file a BLA in 2013, focusing on this subset of
severe asthmatics. Such patients are ca. 30% of the asthmatic population,
with the 750,000 patients in the United States suggested to offer the potential for peak market sales of $1 billion. However, previous
attempts to develop recombinant IL-5 antagonists for the treatment of asthma saw very disappointing clinical results with both mepolizumab
(GlaxoSmithKline) and reslizumab (Schering-Plough and Celltech).
Schering-Plough (now Merck) had been developing reslizumab in
partnership with Celltech (now UCB), utilizing the latter’s antibody
technology, but terminated development in 2002 after disappointing
clinical results. The rights were acquired by Ception Therapeutics in
2007, with development reinitiated for both pediatric eosinophilic
esophagitis and eosinophilic asthma. Cephalon acquired an option to
acquire Ception in January 2009 and exercised this option in April 2010
despite unpromising results in the Phase II/III study of reslizumab in
pediatric eosinophilic esophagitis patients.
In its November 2009 R&D presentation, Cephalon presented data
(from Schering-Plough) showing that reslizumab treatment of asthmatics
results in a sustained suppression of eosinophil levels; the protocols
employed in the Phase II/III study in pediatric eosinophilic esophagitis
and a Phase II study in eosinophilic asthma were described. The Phase
III study in asthmatics has yet to commence, but a 190-patient openlabel Phase III extension study in eosinophilic esophagitis is ongoing.
The Phase II/III study showed no discernable symptom improvement
despite suppression of eosinophil levels at all three doses tested (see
Walsh 2010).43 The outcome of the 106-patient Phase II study, in
February 2009, in asthmatics prompted Cephalon to acquire Ception.
Reslizumab treatment produced significant improvement in lung
function and reduced airway inflammation.
Reslizumab is currently the most advanced of three anti–IL-5monoclonal antibodies in development, but the 2013 submission date for a BLA seems optimistic given that Phase III studies have yet to start.
Mepolizumab is now in Phase II studies for the treatment of severe
asthma and nasal polyposis (having previously been filed for approval
in Europe for the treatment of hypereosinophilic syndrome), but the
filing was withdrawn and development for that indication discontinued
in late 2009. MedImmune and Kyowa Hakko Kirin’s benralizumab has
successfully completed a Phase IIa study in asthma with data presented
in September 2010, and a 108-patient study in asthma was completed
in October 2010. A similar-size Phase II study in COPD commenced in
November 2010.
Reslizumab is a humanized monoclonal antibody intended for the treatment of eosinophil-meditated inflammations of the airways, skin and gastrointestinal tract.[1] As of September 2009, the drug is undergoing Phase II/III clinical trials.[2]
- Walsh, GM (2009). “Reslizumab, a humanized anti-IL-5 mAb for the treatment of eosinophil-mediated inflammatory conditions”. Current opinion in molecular therapeutics11 (3): 329–36. PMID 19479666.
- ClinicalTrials.gov
Ixabepilone for breast cancer

Ixabepilone, 219989-84-1 cas
(1R,5S,6S,7R,10S,14S,16S)-6,10-dihydroxy-1,5,7,
9,9-pentamethyl-14-[(E)-1-(2-methyl-1,3-thiazol-
4-yl)prop-1-en-2-yl]-17-oxa-13-azabicyclo[14.1.0]
heptadecane-8,12-dione
Ixabepilone (INN; also known as azaepothilone B, codenamed BMS-247550) is an epothilone B analog developed byBristol-Myers Squibb as a chemotherapeutic medication for cancer.
It is produced by Sorangium cellulosum.
It acts to stabilize microtubules. It is highly potent agent, capable of damaging cancer cells in very low concentrations, and retains activity in cases where tumor cells are insensitive to paclitaxel.
On October 16, 2007, the U.S. Food and Drug Administration approved ixabepilone for the treatment of aggressive metastaticor locally advanced breast cancer no longer responding to currently available chemotherapies. In November 2008, the EMEAhas refused a marketing authorisation for Ixabepilone.
Ixabepilone is administered through injection, and is marketed under the trade name Ixempra.
patent approval expiry
| United States | 7312237 | 2004-08-21 | 2024-08-21 |
| United States | 6605599 | 1998-05-26 | 2018-05-26 |
| Applicant | Tradename | Generic Name | Dosage | NDA | Approval Date | Type | RLD | US Patent No. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Bristol Myers Squibb
|
IXEMPRA KIT
|
ixabepilone
|
INJECTABLE;IV (INFUSION) | 022065 | Oct 16, 2007 | RX | Yes | RE41911*PED | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Bristol Myers Squibb
|
IXEMPRA KIT
|
ixabepilone
|
INJECTABLE;IV (INFUSION) | 022065 | Oct 16, 2007 | RX | Yes | RE41393*PED | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Bristol Myers Squibb
|
IXEMPRA KIT
|
ixabepilone
|
INJECTABLE;IV (INFUSION) | 022065 | Oct 16, 2007 | RX | Yes | 7,312,237*PED | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Bristol Myers Squibb
|
IXEMPRA KIT
|
ixabepilone
|
INJECTABLE;IV (INFUSION) | 022065 | Oct 16, 2007 | RX | Yes | 7,125,899*PED | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Patent No | Patent Expiry | patent use code |
|---|---|---|
| 6670384 | Jan 23, 2022 | U-959 |
| 6670384 | Jan 23, 2022 | U-960 |
| 6670384*PED | Jul 23, 2022 | |
| 7022330 | Jan 23, 2022 | U-958 |
| 7022330*PED | Jul 23, 2022 | |
| 7125899 | May 26, 2018 | U-957 |
| 7125899*PED | Nov 26, 2018 | |
| 7312237 | Aug 21, 2024 | U-965 |
| 7312237*PED | Feb 21, 2025 | |
| RE41393 | Feb 8, 2022 | U-961 |
| RE41393*PED | Aug 8, 2022 | |
| RE41911 | Sep 28, 2020 | U-961 |
| RE41911*PED | Mar 28, 2021 |
| Exclusivity Code | ExclusivityDate |
|---|---|
| NCE | Oct 16, 2012 |
| PED | Apr 18, 2015 |
| M-61 | Oct 18, 2014 |
| PED | Apr 16, 2013 |
| Exclusivity Code | ExclusivityDate |
|---|---|
| NCE | Oct 16, 2012 |
Ixabepilone, in combination with capecitabine, has demonstrated effectiveness in the treatment of metastatic or locally advanced breast cancer in patients after failure of an anthracycline and a taxane.
It has been investigated for use in treatment of non-Hodgkin’s lymphoma. In pancreatic cancer phase two trial it showed some promising results (used alone). Combination therapy trials are ongoing.
Ixabepilone is an anti cancer agent acting as a microtubule inhibitor, and which in particular are efficient in the treatment of cancer not reacting to other anti cancer agents, such as e.g. paclitaxel. Ixabepilone is marketed under the trade name Ixempra® and are approved for the treatment of aggressive metastatic or locally advanced breast cancer which not responding to the current prevailing chemotherapies.
Ixabepilone known under the CAS no. 219989-84-1 has the following structure:
Ixabepilone
Ixabepilone may be prepared from a starting material named epothilone B having the structural formula:
Epothilone B Ixabepilone as a compound is described in the USRE4191 1. USRE4191 1 furthermore disclose a process for synthesizing Ixabepilone.
The US 6,365,749 describes a process for making ixabepilone by reacting epothilone B with a palladium catalyst in the presence of a nucleophilic donor.
The USRE39356 do also describe a process for making Ixabepilone by reacting epothilone B with an azide donor agent and a reducing agent in the presence of a phase transfer catalyst and a palladium catalyst.

Ixabepilone is the treatment of metastatic and advanced breast cancer drugs.Ixabepilone as anticancer drugs alone or in combination with capecitabine (Capecitabine) in combination. October 16, 2007 approved for marketing by the FDA, trade name Ixempra, by the Bristol-Myers Squibb Company’s development.
Ixabepilone is an anti-mitotic drugs that are inhibitors of tubulin, the mechanism and paclitaxel (Taxol) the same class of drugs. Epothilone (Epothilone) by colistin (myxobacterium) Sorangium cellulosum fermentation of several macrolide metabolites in general. Anticancer activity in vitro experiments, epothilone A and epothilone B showed good activity, even in the paclitaxel-resistant cells also showed good activity. But its activity in vivo experiments in general, this is probably due to the body of the ester hydrolases that macrolide ring opening induced inactivation. In a series of epothilone derivatives activity test, it was found with the lactam bond instead of the original product of ester bonds – ixabepilone anticancer activity can be well retained.
Ixabepilone is epothilone B semi-synthetic derivatives. Epothilone B is a macrocyclic lactone, a hydroxyl moiety is allyl alcohol, the Pd catalyst can be obtained by ring-opening Pd complexes 1 , 1 received azide nucleophile attacking the anion generated with three azide product phosphorus reduction to give methyl amino acids 2 . Here we must point out that the attack was completely azide stereoselectivity, which is determined by two consecutive trans-attack lead, Pd (0)-trans lactone generate offensive allyl Pd complexes, to accept anti-azide anion type attack, to maintain the configuration of the product obtained. Amino acids 2 HoBt and EDCI generated by an amide bond to get ixabepilone.

IXEMPRA (ixabepilone) is a microtubule inhibitor belonging to a class of antineoplastic agents, the epothilones and their analogs. The epothilones are isolated from the myxobacterium Sorangium cellulosum. Ixabepilone is a semisynthetic analog of epothilone B, a 16-membered polyketide macrolide, with a chemically modified lactam substitution for the naturally existing lactone.
The chemical name for ixabepilone is (1S,3S,7S,10R,11S,12S,16R)-7,11dihydroxy-8,8,10,12,16-pentamethyl-3-[(1E)-1-methyl-2-(2-methyl-4-thiazolyl)ethenyl]17-oxa-4-azabicyclo[14.1.0] heptadecane-5,9-dione, and it has a molecular weight of 506.7. Ixabepilone has the following structural formula:
 |
IXEMPRA (ixabepilone) for injection is intended for intravenous infusion only after constitution with the supplied DILUENT and after further dilution with a specified infusion fluid . IXEMPRA (ixabepilone) for injection is supplied as a sterile, non-pyrogenic, single-use vial providing 15 mg or 45 mg ixabepilone as a lyophilized white powder. The DILUENT for IXEMPRA is a sterile, non-pyrogenic solution of 52.8% (w/v) purified polyoxyethylated castor oil and 39.8% (w/v) dehydrated alcohol, USP. The IXEMPRA (ixabepilone) for injection and the DILUENT for IXEMPRA are co-packaged and supplied as IXEMPRA Kit.
….

back to home for more updates
![]()

DR ANTHONY MELVIN CRASTO Ph.D
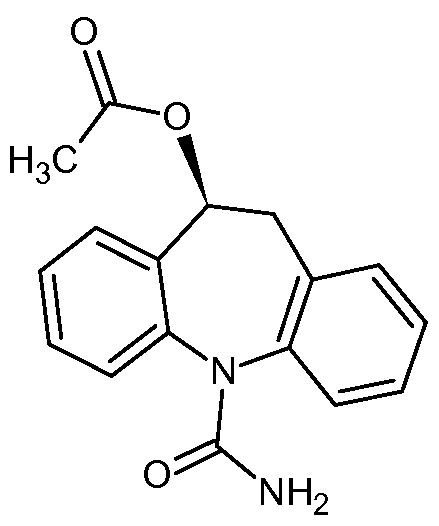
Aptiom (eslicarbazepine acetate) has been approved by the U.S. Food and Drug Administration as an add-on drug to help treat adults with partial epileptic seizures.
Eslicarbazepine acetate, 236395-14-5 cas no
(S)-10-Acetoxy- 10,11-dihydro- 5H-dibenz[b,f]azepine- 5-carboxamide
Sunovion Pharmaceuticals Inc. A US-based subsidiary of Japanese drugmaker Dainippon Sumitomo Pharma Announces FDA Approval of Aptiom® (eslicarbazepine acetate) as Once-Daily Adjunctive Treatment of Partial-Onset Seizures
MONDAY Nov. 11, 2013 — Aptiom (eslicarbazepine acetate) has been approved by the U.S. Food and Drug Administration as an add-on drug to help treat adults with partial epileptic seizures.
Epilepsy, caused by abnormal activity in the brain’s nerve cells, is diagnosed in some 200,000 people annually in the United States, the agency said in a news release. So-called “partial” seizures are the most common type of seizure among people with epilepsy, triggering possible symptoms including repetitive movement of limbs, unusual behavior and convulsions.http://www.drugs.com/news/aptiom-approved-seizures-48845.html
The FDA has determined that APTIOM will not be classified as a controlled substance. Sunovion expects APTIOM to be available in U.S. pharmacies in the second quarter (April – June) of 2014
APTIOM, a voltage-gated sodium channel inhibitor, is a prescription medicine approved for use as adjunctive treatment of partial-onset seizures. Treatment with APTIOM should be initiated at 400 mg once daily. After one week, dosage may be increased to the recommended maintenance dosage of 800 mg once daily. Some patients may benefit from the maximum recommended maintenance dosage of 1,200 mg once daily, although this dosage is associated with an increase in adverse reactions. The maximum dose of 1,200 mg daily should only be initiated after the patient has tolerated 800 mg daily for at least a week. For some patients, treatment may be initiated at 800 mg once daily if the need for additional seizure reduction outweighs an increased risk of adverse reactions during initiation.
The initial research and development of eslicarbazepine acetate was performed by BIAL, a privately held Portuguese research-based pharmaceutical company. Subsequently, Sunovion acquired the rights under an exclusive license to further develop and commercialize eslicarbazepine acetate in the U.S. and Canadian markets from BIAL. In February 2009, Eisai Europe Limited, a European subsidiary of Eisai Co., Ltd. (Eisai), entered into a license and co-promotion agreement with BIAL, which gave the rights to Eisai to sell eslicarbazepine acetate under the trade name Zebinix® in Europe. Zebinix was approved by the European Commission on April 21, 2009 as adjunctive therapy in adult patients with partial-onset seizures with or without secondary generalization and is currently marketed in Europe under the agreement.
Eslicarbazepine acetate (BIA 2-093) is an antiepileptic drug. It is a prodrug which is activated to eslicarbazepine (S–licarbazepine), an active metabolite of oxcarbazepine.[1]
It is being developed by Bial[2] and will be marketed as Zebinix or Exalief by Eisai Co. in Europe and as Stedesa by Sepracor[3] in America.
The European Medicines Agency (EMA) has recommended granting marketing authorization in 2009 for adjunctive therapy for partial-onset seizures, with or without secondary generalisation, in adults with epilepsy.[1] The U.S. Food and Drug Administration (FDA) announced on 2 June 2009 that the drug has been accepted for filing.[3]
Eslicarbazepine acetate is a prodrug for S(+)-licarbazepine, the major active metabolite of oxcarbazepine.[4] Its mechanism of action is therefore identical to that of oxcarbazepine. [5] There may, however, be pharmacokinetic differences. Eslicarbazepine acetate may not produce as high peak levels of (S)-(+)-licarbazepine immediately after dosing as does oxcarbazepine which could theoretically improve tolerability.
Like oxcarbazepine, eslicarbazepine may be used to treat bipolar disorder and trigeminal neuralgia.
The first European patent to protect this drug is EP 0751129 . The priority of this European patent is the Portuguese patent application PT 101732 .
- Dulsat, C., Mealy, N., Castaner, R., Bolos, J. (2009). “Eslicarbazepine acetate”. Drugs of the Future 34 (3): 189. doi:10.1358/dof.2009.034.03.1352675.
- Community register of medicinal products for human use: Exalief
- Medical News Today: Sepracor’s STEDESA (Eslicarbazepine Acetate) New Drug Application Formally Accepted For Review By The FDA
- Rogawski, MA (Jun 2006). “Diverse Mechanisms of Antiepileptic Drugs in the Development Pipeline”. Epilepsy Res 69 (3): 273–294. doi:10.1016/j.eplepsyres.2006.02.004. PMC 1562526. PMID 16621450.
- Rogawski MA, Löscher W (July 2004). “The neurobiology of antiepileptic drugs”. Nature Reviews Neuroscience 5 (7): 553–64. doi:10.1038/nrn1430. PMID 15208697.
- https://newdrugapprovals.wordpress.com/2013/03/11/sunovion-announces-fda-acceptance-for-review-of-new-drug-application-resubmission-for-stedesa-eslicarbazepine-acetate/
Eslicarbazepine acetate of Formula A, chemically known as (10S)-5-carbamoyl- 10,1 l-dihydro-5H-dibenzo[Z?,/]azepin- 10-yl acetate is indicated as adjunctive therapy in adults with partial-onset seizures with or without secondary generalisation.
Formula A
lO-oxo-10,1 l-dihydro-5H-dibenzo[Z?/]azepine-5-carboxamide of Formula 1, commonly known as oxcarbazepine, is an antiepileptic drug marketed under the trade name Trileptal®and is indicated for use as monotherapy or adjunctive therapy in the treatment of partial seizures in adults and as monotherapy in the treatment of partial seizures in children aged 4 years and above with epilepsy, and as adjunctive therapy in children aged 2 years and above with epilepsy. Oxcarbazepine is an intermediate for the preparation of eslicarbazepine.
Formula 1
Several processes are known in the literature for making and purifying eslicarbazepine acetate, for example, U.S. Patent No 5,753,646; and PCT Publications WO 2006/005951 ; WO 2007/1 17166; and WO 2010/1 13179.
U.S. Patent No. 5,753,646 provides a process for the preparation of eslicarbazepine acetate which involves adding dropwise a solution of acetyl chloride in dichloromethane to a suspension of (-)- 10-hydroxy-10,l l-dihydro-5H-dibenz/b,f/azepine-5-carboxamide in dichloromethane and pyridine at a temperature of less than 10°C under stirring. The residue obtained after workup was crystallized from a mixture of dichloromethane and ethyl acetate to give the eslicarbazepine acetate as white crystals.
U.S Publication No. 2009/0203902 provides preparation of eslicarbazepine acetate which involves the acylation of (S)-(+)-10,l l-dihydro-10-hydroxy-5H-dibenz/b,f/azepine- 5-carboxamide with acetic anhydride in presence of 4-(N,N-dimethylamino)pyridine and pyridine in dichloromethane at reflux temperature. The resulting solid obtained after work-up was slurried with isopropanol at reflux to obtain a solution. The solution was cooled to 1°C to 5°C and eslicarbazepine acetate was isolated from the reaction mass by filtration followed by washing with isopropanol.
PCT Publication No. WO 2010/1 13179 provides various purification methods of eslicarbazepine acetate which involve the use of acetonitrile/methyl tertiary butyl ether, tetrahydrofuran/n-hexane, tetrahydrofuran/methyl tertiary butyl methyl ether;
tetrahydrofuran, methyl ethyl ketone/n-hexane.
Several processes are known in the literature for making oxcarbazepine, for example, U.S. Patent Nos. 4,452,738 and 7,459,553; PCT Publication Nos. WO
2010/000196; WO 2008/012837; WO 2007/141798; WO 2006/075925; WO 2005/122671 ; WO 2005/1 18550; WO 2005/096709; WO 2005/092862; WO
2005/066133; WO 02/096881 ; WO 00/55138; and WO 96/21649.
PCT Publication No. WO 02/096881 provides a process for the preparation of oxcarbazepine which involves oxidation of 10,1 1 -dihydro- 10-hydroxy-5H- dibenz/b,f/azepine-5-carboxamide with peroxyacetic acid in presence of potassium dichromate adsorbed on silica gel at room temperature.
Japanese Patent Publication No. JP 2004- 175761 provides a process for the preparation of oxcarbazepine which involves oxidation of 10, 1 1 -dihydro- 10-hydroxy-5H- dibenzo[b,f]azepine-5-carboxamide with dimethyl sulfoxide and an activator such as sulfur trioxide-pyridine complex.
Chinese Publication No. CN 101302198 provides a process for the preparation of oxcarbazepine which involves oxidation of 10-hydroxy- 10, l 1 -dihydro-5H- dibenzo[Z?/]azepine-5-carbonitrile with TEMPO and sodium hypochlorite to provide 10- oxo- 10,1 l-dihydro-5H-dibenzo[Z?/]azepine-5-carbonitrile which was further hydrolysed with sulfuric acid to obtain oxcarbazepine.
-
Eslicarbazepine acetate, (S)-(-)-10-acetoxy-10,11-dihydro-5H-dibenz/b,f/azepine-5-carboxamide (“BIA 2-093”), is a new drug currently being developed which is useful for the treatment of various conditions, such as, for example, epilepsy and affective brain disorders, as well as pain conditions and nervous function alterations in degenerative and post-ischemic diseases. Although chemically related to carbamazepine and oxcarbazepine, eslicarbazepine acetate is believed to avoid the production of certain toxic metabolites (such as, for example, epoxides) and to avoid the unnecessary production of enantiomers or diastereoisomers of metabolites and conjugates, without losing pharmacological activity. See Benes et al., “Anticonvulsant and Sodium Channel-Blocking Properties of Novel 10,11-Dihydro-5H-dibenz[b,f]azepine-5-carboxamide Derivatives,” J. Med. Chem., 42, 2582-2587 (1999).
-
Like carbamazepine and oxcarbazepine, eslicarbazepine acetate is believed to be a voltage-gated sodium channel (VGSC) blocker that competitively interacts with site 2 of the inactivated state of the sodium channel. The affinity for this state of the channel is similar to that of carbamazepine, while the affinity for the resting state of the channel is about 3-fold lower than that of carbamazepine. This profile may suggest an enhanced inhibitory selectivity of eslicarbazepine acetate for rapidly firing neurons over those displaying normal activity. See Bonifacio et al., “Interaction of the Novel Anticonvulsant, BIA 2-093, with Voltage-Gated Sodium Channels: Comparison with Carbamazepine,” Epilepsia, 42, 600-608(2001).
-
Evaluation of the metabolic profile of eslicarbazepine acetate, following chiral analysis, in liver microsomes from rats, dogs, monkeys and humans was found to give the S(+) enantiomer of licarbazepine, (S)-(+)-10,11-dihydro-10-hydroxy-5H dibenz/b,f/azepine-5-carboxamide (also known as “eslicarbazepine”), and not the R(-) form of licarbazepine, (R)-(-)-10,11-dihydro-10-hydroxy-5H dibenz/b,f/azepine-5-carboxamide (also known as “R-licarbazepine”).
-
Studies in humans have shown that, after oral administration, eslicarbazepine acetate appears to be rapidly and extensively metabolized to the active metabolite eslicarbazepine and, in a minor extent, to R-licarbazepine. See Silveira et al., “BIA 2-093 Pharmacokinetics in Healthy Elderly Subjects,” Epilepsia, 45 (suppl. 3), 157 (2004). For example, the plasma concentrations of the parent drug (eslicarbazepine acetate) have been systematically found below the limit of quantification (LOQ) of the assay (10 ng/mL). See Almeida I; Almeida, L. & Soares-da-Silva, P., “Safety, Tolerability and Pharmacokinetic Profile of BIA 2-093, a Novel Putative Antiepileptic Agent, during First Administration to Humans,” Drugs R&D, 4, 269-284 (2003) (herein referred to as “Almeida II“). When a non-chiral method is used, the assay does not distinguish between eslicarbazepine and the R-enantiomer, and the mixture was reported as “BIA 2-005” or “racemic licarbazepine.”
-
The inventors performed entry-into-man studies in healthy subjects, the results of which they described in the Almeida I and Almeida II articles, both of which are hereby incorporated by reference. In these studies, the healthy subjects received a single oral dose of eslicarbazepine acetate wherein the dose ranged from 20 mg to 1200 mg (see Almeida II), and multiple daily-doses of eslicarbazepine acetate ranging from 200 mg twice-daily to 1200 mg once-daily (see Almeida I). Further studies (not yet published) by the inventors have investigated higher doses of eslicarbazepine acetate, including, for example, doses ranging up to 2400 mg once-daily. The studies showed that BIA 2-005 maximum observed plasma concentration (Cmax) was attained at about 1 hour to about 4 hours post-dose (tmax), the extent of systemic exposure to BIA 2-005 was approximately dose-proportional, and steady-state of BIA 2-005 plasma concentrations was attained at about 4 to 5 days. The mean renal clearance of BIA 2-005 from plasma was about 20-30 mL/min, and the total amount of BIA 2-005 recovered in the urine was approximately 20% and 40% within 12 hours and 24 hours post-dose, respectively.
-
The studies also showed that the apparent terminal half-life of BIA 2-005 ranged from about 8 hours to about 17 hours. See, e.g., Almeida II.
-
U.S. Patent No. 6,296,873 discloses a sustained release delivery system for carbamazepine, which has a half-life ranging from 25 hours to 85 hours. To avoid adverse effects, U.S. Patent No. 6,296,873 teaches that the carbamazepine should be administered in tablet form up to two or more times daily to slowly release the compound to maintain concentration levels between 4-12 µg/mL. Such a delivery system requires a form that is capable of delivering the compound over an extended period of time, such as a tablet form.

http://www.sciencedirect.com/science/article/pii/S0040403913005030

ESLICARBAZEPINE ACETATE
Physiochemical Pr operties:
| Molecular weight | : | 296.32 |
| Category | : | Anti-epileptic |
| Molecular formula | : | C17H16N2O5 |
| Chemical Name | : | (S)-(-)-10-acetoxy-10,11-dihydro-5H-dibenz [b, f] |
| azepine-5-carboxamide. | ||
| Description | : | White to off-White, odourless, non-hygroscopic, |
| crystalline powder. | ||
| Solubility | : | Freely soluble in dichloromethane, sparingly soluble |
| in acetone, acetonitrile, methanol, tetrahydrofuran and | ||
| slightly soluble in ethanol and 2-propanol, insoluble in | ||
| water | ||
| Melting Point | : | 184-187°C |
| Storage | : | Can be easily stored at temperatures up to 30°C |
HPLC, NMR

NMR NUMBERING

http://www.sciencedirect.com/science/article/pii/S0731708511006753

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....