Home » Articles posted by DR ANTHONY MELVIN CRASTO Ph.D (Page 229)
Author Archives: DR ANTHONY MELVIN CRASTO Ph.D
Aplaviroc, AK602, GSK-873140

Aplaviroc
4-(4-{[(3R)-1-butyl-3-[(R)-cyclohexylhydroxymethyl]-2,5-dioxo- 1,4,9-triazaspiro[5.5]undecan-9-yl]methyl}phenoxy)benzoic acid
for the treatment of HIV infection
461023-63-2 of hydrochloride
461443-59-4 (free base)
873140
AK-602
GW-873140
ONO-4128
ono…….innovator
| Ono Pharmaceutical Co., Ltd. |
| Identifiers | |
|---|---|
| CAS number | 461023-63-2 |
| ATC code | None |
| PubChem | CID 3001322 |
| ChemSpider | 2272720 |
| UNII | 98B425P30V |
| KEGG | D06557 |
| ChEMBL | CHEMBL1255794 |
| Chemical data | |
| Formula | C33H43N3O6 |
| Mol. mass | 577.711 g/mol |
Aplaviroc (INN, codenamed AK602 and GSK-873140) is a CCR5 entry inhibitor developed for the treatment of HIV infection.[1][2] It is developed by GlaxoSmithKline.
In October 2005, all studies of aplaviroc were discontinued due to liver toxicity concerns.[3][4] Some authors have claimed that evidence of poor efficacy may have contributed to termination of the drug’s development;[5] the ASCENT study, one of the discontinued trials, showed aplaviroc to be under-effective in many patients even at high concentrations.[6]
Aplaviroc hydrochloride, an orally-effective, long-acting chemokine CCR5 receptor antagonist, had been under development by Ono and GlaxoSmithKline for the treatment of HIV infection. In early 2006, the companies discontinued development of the antagonist based on reports of elevated liver function test values from clinical studies.
Originally developed at Ono, aplaviroc was licensed to GlaxoSmithKline in 2003 for development, manufacturing and marketing. GlaxoSmithKline also obtained rights to evaluate the agent in non-HIV conditions worldwide with the exception of Japan, South Korea and Taiwan.
A low-molecular-weight compound, aplaviroc prevents HIV viral infection by blocking the binding of the virus to the CCR5 receptor
……………….
WO 2002074770
0r
http://www.google.com/patents/EP1378510A1?cl=en
Reference example 3(3)
- (3R)-1-butyl-2,5-dioxo-3-((1R)-1-hydroxy-1-cyclohexyl)-1,4,9-triazaspiro[5.5]undecane • hydrochloride
-
[0136]
TLC:Rf 0.32 (butanol:acetic acid:water = 4:2:1);
NMR (CD3OD): δ 4.16 (d, J = 2.0 Hz, 1H), 3.95 (m, 1H), 3.70 (m, 1H), 3.52 (m, 1H), 3.37 (m, 1H), 3.28 (m, 1H), 3.22-3.13 (m, 2H), 2.46-1.93 (m, 6H), 1.80-1.64 (m, 5H), 1.48-1.15 (m, 6H), 1.02-0.87 (m, 5H);
Optical rotation:[α]D +1.22 (c 1.04, methanol, 26°C).
Example 9(54)
- (3R)-1-butyl-2,5-dioxo-3-((1R)-1-hydroxy-1-cyclohexylmethyl)-9-(4-(4-carboxyphenyloxy)phenylmethyl)-1,4,9-triazaspiro[5.5]undecane • hydrochloride
-
[0359]
TLC:Rf 0.43(chloroform:methanol = 5:1);
NMR (CD3OD):δ 8.05 (d, J = 9.0 Hz, 2H), 7.61 (d, J = 9.0 Hz, 2H), 7.19 (d, J = 9.0 Hz, 2H), 7.08 (d, J = 9.0 Hz, 2H), 4.38 (s, 2H), 4.17 (d, J = 2.1 Hz, 1H), 4.02 (m, 1H), 3.78 (m, 1H), 3.60-3.40 (m, 3H), 3.30-3.10 (m, 2H), 2.56-1.86 (m, 6H), 1.82-1.60 (m, 5H), 1.52-1.16 (m, 6H), 1.06-0.82 (m, 2H), 0.97 (t, J = 7.2 Hz, 3H).
………………….
http://www.beilstein-journals.org/bjoc/single/articleFullText.htm?publicId=1860-5397-9-265
Owing to the special properties of piperazines (increased solubility and H-bond acceptor capability etc.) it is often considered to be a privileged structure and therefore occurs widely, for instance in GlaxoSmithKlines investigational anti-HIV drug aplaviroc (4.37) which, despite being a promising CCR5 receptor antagonist, was discontinued due to hepatotoxicity concerns. In this compound the spirodiketopiperazine unit (4.35) was designed to mimic a type-1 β-turn (4.36) as present in G-protein coupled receptors (Figure 14) [117].
The synthesis of aplaviroc and its analogues can be accomplished via the use of an Ugi multicomponent reaction (Ugi-MCR) [118]. The procedure involved the condensation of piperidone 4.38 and butylamine (4.39) followed by reaction of the resulting imine with isocyanide 4.41 and interception of the nitrilium intermediate with the amino acid4.40 (Scheme 47) [119]. This sequence was completed by structural rearrangement and acid-mediated ring closure to produce the spirocyclic diketopiperazine 4.43. Following debenzylation this material was subjected to a reductive amination finally affording aplaviroc analogues (Scheme 47).
- 117 Habashita, H.; Kokubo, M.; Hamano, S.; Hamanaka, N.; Toda, M.; Shibayama, S.; Tada, H.; Sagawa, K.; Fukushima, D.; Maeda, K.; Mitsuya, H. J. Med. Chem. 2006, 49, 4140–4152. doi:10.1021/jm060051s
- Dömling, A.; Huang, Y. Synthesis 2008, 2859–2883. doi:10.1055/s-0030-1257906
ref 118 - Nishizawa, R.; Nishiyama, T.; Hisaichi, K.; Matsunaga, N.; Minamoto, C.; Habashita, H.; Takaoka, Y.; Toda, M.; Shibayama, S.; Tada, H.; Sagawa, K.; Fukushima, D.; Maeda, K.; Mitsuya, H.Bioorg. Med. Chem. Lett. 2007, 17, 727–731. doi:10.1016/j.bmcl.2006.10.084
ref 119
| Patent | Submitted | Granted |
|---|---|---|
| Triazaspiro[5.5]undecane derivative and pharmaceutical composition comprising the same as active ingredient [US7262193] | 2005-09-29 | 2007-08-28 |
| Drugs containing triazaspiro[5.5]undecane derivatives as the active ingredient [US7285552] | 2004-06-03 | 2007-10-23 |
| Triazaspiro[5.5]undecane derivatives and drugs containing the same as the active ingredient [US7053090] | 2004-04-29 | 2006-05-30 |
| WO1998031364A1 * | Jan 20, 1998 | Jul 23, 1998 | Timothy Harrison | 3,3-disubstituted piperidines as modulators of chemokine receptor activity |
| WO2000014086A1 * | Jan 21, 1999 | Mar 16, 2000 | Kyowa Hakko Kogyo Kk | Chemokine receptor antagonists and methods of use therefor |
| WO2002074769A1 * | Mar 18, 2002 | Sep 26, 2002 | Kenji Maeda | Drugs containing triazaspiro[5.5]undecane derivatives as the active ingredient |
References
- Maeda, Kenji; Ogata, Hiromi; Harada, Shigeyoshi et al. (2004). “Determination of binding sites of a unique CCR5 inhibitor AK602 / ONO-4128/ GW873140 on human CCR5” (PDF). Conference on Retroviruses and Opportunistic Infections. Archived from the original on November 3, 2005.
- Nakata, Hirotomo; Maeda, Kenji; Miyakawa, Toshikazu et al. (February 2005). “Potent Anti-R5 Human Immunodeficiency Virus Type 1 Effects of a CCR5 Antagonist, AK602/ONO4128/GW873140, in a Novel Human Peripheral Blood Mononuclear Cell Nonobese Diabetic-SCID, Interleukin-2 Receptor γ-Chain-Knocked-Out AIDS Mouse Model”. Journal of Virology 79 (4): 2087–96.doi:10.1128/jvi.79.4.2087-2096.2005.
- “Aplaviroc (GSK-873,140)”. AIDSmeds.com. October 25, 2005. Retrieved September 5, 2008.[dead link]
- Nichols WG, Steel HM, Bonny T et al. (March 2008). “Hepatotoxicity Observed in Clinical Trials of Aplaviroc (GW873140)”.Antimicrobial Agents and Chemotherapy 52 (3): 858–65. doi:10.1128/aac.00821-07. PMC 2258506. PMID 18070967.
- Moyle, Graeme (December 19, 2006). “The Last Word on Aplaviroc: A CCR5 Antagonist With Poor Efficacy”. The Body.Archived from the original on 6 October 2008. Retrieved September 5, 2008.
- Currier, Judith; Lazzarin, Adriano; Sloan, Louis et al. (2008). “Antiviral activity and safety of aplaviroc with lamivudine/zidovudine in HIV-infected, therapy-naive patients: the ASCENT (CCR102881) study”. Antiviral Therapy (Lond.) 13 (2): 297–306.PMID 18505181.
Further reading
- Horster, S; Goebel, FD (April 2006). “Serious doubts on safety and efficacy of CCR5 antagonists: CCR5 antagonists teeter on a knife-edge”. Infection 34 (2): 110–13. doi:10.1007/s15010-006-6206-1. PMID 16703305.
FAMOTIDINE


FAMOTIDINE
76824-35-6
3-(2-Guanidinothiazol-4-ylmethylthio)-N-sulfamoylpropanamidine
MK-208
YM-11170
YM-1170
Histamine H2 Receptor Antagonists
Gastroesophageal Reflux Disease,
Agents forGastric Antisecretory Drugs (GERD)
Astellas Pharma (Innovaator)Launched – 1985

| Systematic (IUPAC) name | |
|---|---|
| 3-[({2-[(diaminomethylidene)amino]-1,3-thiazol-4-yl}methyl)sulfanyl]-N’-sulfamoylpropanimidamide | |
| Clinical data | |
| Trade names | Pepcid |
| AHFS/Drugs.com | monograph |
| MedlinePlus | a687011 |
| Licence data | US FDA:link |
| Pregnancy cat. | |
| Legal status | |
| Routes | Oral (tablet form) |
| Pharmacokinetic data | |
| Bioavailability | 40-45% (Oral)[1] |
| Protein binding | 15-20%[1] |
| Metabolism | hepatic |
| Half-life | 2.5-3.5 hours[1] |
| Excretion | Renal (25-30% unchanged [Oral])[1] |
| Identifiers | |
| CAS number | 76824-35-6 |
| ATC code | A02BA03 |
| PubChem | CID 3325 |
| DrugBank | DB00927 |
| ChemSpider | 3208 |
| UNII | 5QZO15J2Z8 |
| Chemical data | |
| Formula | C8H15N7O2S3 |
| Mol. mass | 337.449 g/mol |
Famotidine is an H2-histamine antagonist that was first launched by Astellas Pharma (formerly Yamanouchi) in Japan in 1985 as an injectable for the treatment of upper gastrointestinal hemorrhage and for the treatment of Zollinger-Ellison syndrome. In 1986, the drug was launched pursuant to a collaboration between Merck Sharp & Dohme and Sigma-Tau for the oral prevention and treatment of gastroesophageal reflux disease (GERD).
Famotidine (INN) /fəˈmɒtɪdiːn/ is a histamine H2-receptor antagonist that inhibits stomach acid production, and it is commonly used in the treatment of peptic ulcer disease (PUD) and gastroesophageal reflux disease (GERD/GORD). It is commonly marketed byJohnson & Johnson/Merck under the trade names Pepcidine and Pepcid and by Astellas under the trade name Gaster. Unlikecimetidine, the first H2 antagonist, famotidine has no effect on the cytochrome P450 enzyme system, and does not appear to interact with other drugs.[2]
Medical use
Certain preparations of famotidine are available over the counter (OTC) in various countries. In the US 20 or more mg, sometimes in combination with a more traditional antacid, are available OTC. Larger doses still require a prescription.

Famotidine is given to surgery patients before operations to prevent postoperative nausea and to reduce the risk of aspiration pneumonitis. Famotidine is also given to some patients taking NSAIDs, to prevent peptic ulcers.[3] It serves as an alternative toproton-pump inhibitors.[4]
It is also given to dogs and cats with acid reflux.
Famotidine has also been used in combination with an H1 antagonist to treat and prevent urticaria caused by an acute allergic reaction.[5]
Side-effects
Side-effects are associated with famotidine use. In clinical trials, the most common adverse effects were headache, dizziness, andconstipation or diarrhea.[6]
History
Famotidine was developed by Yamanouchi Pharmaceutical Co.[7] It was licensed in the mid-80s by Merck & Co.[8] and is marketed by a joint venture between Merck and Johnson & Johnson. The imidazole-ring of cimetidine was replaced with a 2-guanidinothiazole ring. Famotidine proved to be 30 times more active than cimetidine.[citation needed]
It was first marketed in 1981. Pepcid RPD orally-disintegrating tablets were released in 1999. Generic preparations became available in 2001, e.g.Fluxid (Schwarz) or Quamatel (Gedeon Richter Ltd.).
In the United States and Canada, a product called Pepcid Complete, which combines famotidine with an antacid in a chewable tablet to quickly relieve the symptoms of excess stomach acid, is available. In the UK, this product is known as Pepcidtwo.
Famotidine suffers from poor bioavailability (50%), as it is poorly soluble in the low pH of the stomach. Famotidine used in combination with antacids promotes local delivery of these drugs to the receptor of the parietal cell wall. Therefore, researchers are developing innovative formulations of tablets, such as gastroretentive drug delivery systems. Such tablets are retained in the stomach for a longer period of time, thereby improving the bioavailability of drugs. Local delivery also increases bioavailability at the stomach wall receptor site and increases the efficacy of drugs to reduce acid secretion.[9]
Research
Famotidine has been investigated as an adjunct in treatment-resistant schizophrenia. In one trial it caused a 10% reduction in schizophrenic symptom severity in treatment-resistant patients.[10]
Famotidine is also indicated in the treatment of duodenal and benign gastric ulcers, for the prevention of relapse of duodenal ulceration, for the treatment of gastric mucosal lesions associated with acute gastritis and acute exacerbation of chronic gastritis, for the treatment of heartburn associated with acid indigestion and sour stomach, for the prevention of meal-induced heartburn, and for the treatment of reflux esophagitis due to GERD, including ulcerative disease as diagnosed by endoscopy. The drug is currently marketed in tablet, film-coated tablet, orally-disintegrating tablet, powder, lyophilized powder for injection solution and injectable formulations. The compound had been in development for the treatment of non-erosive reflux disease (NERD), however, Astellas Pharma discontinued development for this indication in 2007.

Famotidine was developed by replacing the imidazole ring of GlaxoSmithKline’s cimetidine with a 2-guanidinothiazole ring, a modification proven to increase the activity of the drug 30-fold. Famotidine competitively inhibits the action of histamine at the histamine H2 receptors of the parietal cells. It suppresses the normal secretion of acid by parietal cells and the meal-stimulated secretion of acid by two mechanisms: by blocking histamine released by enterochromaffin-like (ECL) cells in the stomach from binding to H2 receptors and stimulating acid secretion, and by reducing the effect that other compounds (such as gastrin, pentagastrin, caffeine, insulin and acetylcholine) have on the promotion of acid secretion due to H2 receptor blockade.
Famotidine was originally developed at Astellas Pharma. It was subsequently licensed in the U.S. to Merck & Co., known outside the U.S. and Canada as Merck Sharp & Dohme. In 2007, Salix acquired the U.S. rights to famotidine oral solution (Pepcid[R]) for the treatment of GERD and peptic ulcer. Sigma-Tau holds rights to the drug and is responsible for marketing activities in Italy. Famotidine is sold in over 110 countries worldwide, including France, Germany, Italy, Japan, the U.S. and the U.K.

……………………………..
US 4283408
http://www.google.co.in/patents/US4283408


The reaction ot S-(2-aminothiazol-4-ylmethyl)isothiourea (I) with 3-chloropropionitrile (II) by means of NaOH in ethanol – water gives 3-(2-aminothiazol-4-ylmethylthio)propionitrile (III), which is condensed with benzoyl isothiocyanate (IV) in refluxing acetone to afford 3-[2-(3-benzoylthioureido)thiazol-4-ylmethylthio]propionitrile (V). The hydrolysis of (V) with K2CO3 in acetone – methanol – water yields 3-(2-thioureidothiazonl-4-ylmethylthio)propionitrile (VI), which by methylation with methyl iodide in refluxing ethanol is converted into 3-[2-(S-methylisothioureido)thiazol-4-ylmethylthio]propionitrile hydroiodide (VII). The reaction of (VII) with NH3 and NH4Cl in methanol at 90 C in a pressure vessel affords 3-(2-guanidinothiazol-4-ylmethylthio)propionitrile (VIII), which by partial alcoholysis with methanol by means of dry HCl in CHCl3 is converted into methyl 3-(2-guanidinothiazol-4-ylmethylthio)propionimidate (IX). Finally, this compound is treated with sulfamide in refluxing methanol.
Drugs Fut 1983, 8, 1, 14
US 4283408
DOS 2 951 675 (Yamanouchi; appl. 21.12.1979; J-prior. 2.8.1979).
DOS 3 008 056 (Yamanouchi; appl. 3.3.1980; J-prior. 6.3.1979, 23.6.1979).
GB 2 052 478 (Yamanouchi; appl. 6.3.1980; J-prior. 6.3.1979, 23.6.1979).
GB 2 055 800 (Yamanouchi; appl. 20.12.1979; J-prior. 2.8.1979).
synthesis of S-[2-aminothiazol-4-ylmethyl]isothiourea:
Spragne, J.M.; Lund, A.H.; Ziegler, C.: J. Am. Chem. Soc. (JACSAT) 68, 2155 (1946).

FT IR OF FAMOTIDINE

http://link.springer.com/article/10.1007%2Fs00216-011-5599-6

[1H,13C] 2D NMR Spectrum
………………………..
DSC OF FAMOTIDINE
WILL BE ADDED
……………………………
…………………..
UV – range
 |
||||
| Conditions : Concentration – 1 mg / 100 ml | ||||
| The solvent designation graphics | Methanol |
Water |
0.1М HCl |
0.1M NaOH |
|---|---|---|---|---|
| Maximum absorption | 287 nm | – | 265 nm | 286 nm |
 |
465 | – | 309 | 440 |
| e | 15700 | – | 10400 | 14850 |
FIG WILL BE ADDED
IR – spectrum
…………..
Synthesis pathway
Trade names
| Country | Trade name | Manufacturer |
|---|---|---|
| Germany | Fadul | Hexal |
| Famobeta | betapharm | |
| Famonerton | Dolorgiet | |
| Pepdul | TEOFARMA | |
| various generic drugs | ||
| France | Peptsidak | McNeil |
| Peptsidduo | McNeil | |
| Pepdin | Merck Sharp & Dohme-Chibret | |
| Great Britain | Peptsid | Merck Sharp & Dohme |
| Italy | Famoudou | Sigma-Tau |
| Gastridin | Merck Sharp & Dohme | |
| Motiaks | Neopharmed | |
| Japan | Gaster | Astellas |
| United States | Peptsid | Merck, 1986 |
| – “- | Johnson & Johnson; Merck | |
| Ukraine | Ulfamid | Krka, dd, Novo mesto, Slovenia |
| Kvamatel | JSC “Gedeon Richter”, Hungary | |
| Famasan | ABM. MED. CA AT Prague, Czech Republic | |
| FamodinGeksal | Salyutas Pharma GmbH, Germany, venture hexane AG, Germany | |
| various generic drugs | ||
Formulations
-
ampoule 10 mg, 20 mg;
-
Tablets coated with 10 mg, 20 mg, 40 mg;
-
oral suspension, 40 mg / 5 ml;
-
2% powder, 10%;
-
10 mg tablets, 20 mg;
-
vials (lyophilisate) 20 mg
Reference for above
-
DOS 2,951,675 (Yamanouchi; appl. 21.12.1979; J-prior. 2.8.1979).
-
DOS 3,008,056 (Yamanouchi; appl. 3.3.1980; J-prior. 6.3.1979, 23.6.1979).
-
GB 2052478 (Yamanouchi; appl. 6.3.1980; J-prior. 6.3.1979, 23.6.1979).
-
GB 2055800 (Yamanouchi; appl. 20.12.1979; J-prior. 2.8.1979).
-
US 4,283,408 (Yamanouchi; 11.8.1981; J-prior. 2.8.1979).
References
- Truven Health Analytics, Inc. DRUGDEX® System (Internet) [cited 2013 Oct 10]. Greenwood Village, CO: Thomsen Healthcare; 2013.
- Humphries TJ, Merritt GJ (August 1999). “Review article: drug interactions with agents used to treat acid-related diseases” (pdf). Aliment. Pharmacol. Ther. 13 (Suppl 3): 18–26.doi:10.1046/j.1365-2036.1999.00021.x. PMID 10491725.
- “Horizon Pharma, Inc. Announces FDA Approval of DUEXIS(R) for the Relief of the Signs and Symptoms of Rheumatoid Arthritis and Osteoarthritis and to Decrease the Risk of Developing Upper Gastrointestinal Ulcers” (Press release). Horizon Pharma. 2011-04-25.
- Brauser D (Jul 13, 2009). “Famotidine May Prevent Peptic Ulcers, Esophagitis in Patients Taking Low-Dose Aspirin”. Medscape.
- Fogg TB, Semple D (29 November 2007). “Combination therapy with H2 and H1 antihistamines in acute, non compromising allergic reactions”. BestBets. Manchester, England: Manchester Royal Infirmary. Retrieved 26 April 2011.
- “Pepcid Side Effects & Drug Interactions”. RxList.com. 2008. Retrieved 2008-07-31.
- US patent 4283408, HIRATA YASUFUMI; YANAGISAWA ISAO; ISHII YOSHIO; TSUKAMOTO SHINICHI; ITO NORIKI; ISOMURA YASUO; TAKEDA MASAAKI, “Guanidinothiazole compounds, process for preparation and gastric inhibiting compositions containing them”, issued 1981-08-11
- “Sankyo Pharma”. Skyscape Mediwire. 2002. Retrieved 2009-10-30.[dead link]
- “Formulation and Evaluation of Gastroretentive Floating Tablets of Famotidine”. Farmavita.Net. 2008. Retrieved 2009-01-30.
- Meskanen, K; Ekelund, H; Laitinen, J; Neuvonen, PJ; Haukka, J; Panula, P; Ekelund, J (August 2013). “A randomized clinical trial of histamine 2 receptor antagonism in treatment-resistant schizophrenia.”. Journal of Clinical Psychopharmacology 33 (4): 472–478. doi:10.1097/JCP.0b013e3182970490. PMID 23764683.
Esoxybutynin, (S)-Oxybutynin

Drug name, 药物名称….. Esoxybutynin, (S)-Oxybutynin

| CAS No. | 119618-22-3 |
| Chemical Name: | (S)-Oxybutynin |
| Synonyms: | Esoxybutynin;(S)-Oxybutynin;(S)-OXYBUTYNIN HCL;(S)-OXYBUTYNIN CHLORIDE;(S)-OXYBUTYNIN HYDROCHLORIDE;(S)-Hydroxycyclohexylphenylacetic acid 4-(diethylamino)-2-butynyl ester;(S)-CYCLOHEXYL-HYDROXY-PHENYL-ACETIC ACID 4-DIETHYLAMINO-BUT-2-YNYL ESTER;(αS)-α-Cyclohexyl-α-hydroxybenzeneacetic acid 4-(diethylamino)-2-butin-1-yl ester;Benzeneacetic acid, a-cyclohexyl-a-hydroxy-, 4-(diethylamino)-2-butynyl ester, (S)-;(S)-α-Phenylcyclohexaneglycolic Acid 4-(Diethylamino)-2-butynyl Ester, Hydrochloride |
| CBNumber: | CB1746039 |
| Molecular Formula: | C22H31NO3 |
| Formula Weight: | 357.49 |
Oxybutynin and its derivatives are applicable as a bronchodilator or a remedy for pollakisuria. Also, oxybutynin exerts a direct antispasmodic effect on various forms of smooth muscle, mainly by inhibiting the action of acetylcholine on smooth muscle as an anti-cholinergic drug and the like. Oxybutynin is marketed in hydrochloride form. Oxybutynin known as [α-cyclohexyl-hydroxy-benzeneaceticacid- 4-(diethyl amino)-2-butynyl ester] he US Patent No. 3,176,019 (‘019) discloses about 4-amino-2-butynol esters and their derivatives, particularly about oxybutynin hydrochloride. It also reveals about the synthesis of oxybutynin, wherein, the methyl phenyl cyclohexyl glycolate is reacted with 4-diethylamino-2-butynylacetate in presence of base to yield oxybutynin followed by further workup. Further, it is treated with 2N HCl solution to form hydrochloride salt. It is recrystallised by employing ethyl acetate or water to obtain pure oxybutynin hydrochloride. Further, the US Patent ‘019 unveils about the reaction of propargyl-2-cyclohexyl-2-hydroxy-2-phenyl acetate, /^-formaldehyde and diethyl amine in dry dioxane to obtain crude product of oxybutynin. The dry hydrogen chloride gas is passed through the ether solution of oxybutynin to yield the oxybutynin chloride as precipitate.
According to the prior art process oxybutynin is obtained as oil, which contains lot of impurities, therefore, it needs to purify high vacuum distillation. Also, the resultant oxybutynin base is having a low melting point, which may decompose during high vacuum distillation. Further, the existence of any polymorphism in oxybutynin is not disclosed in prior arts. In light of the foregoing, a need exists in the art for inventing a new form and the process thereof. Objects and Summary of the Invention
It is a principal object of the present invention is to provide a novel crystalline oxybutynin base in a solid state having improved quality.
Another object of the present invention is to provide a process for the preparation of novel crystalline oxybutynin base as a solid state. Further, object of the present invention is to provide a process for preparing an acid addition salt of oxybutynin employing crystalline oxybutynin base
In accordance with one preferred embodiment of the present invention, there is provided a crystalline oxybutynin base characterized by using different analytical tools including X-ray powder diffraction pattern, Thermo Gravimetric Analysis (TGA), and Differential Scanning Calorimetry (DSC).
Oxybutynin is used therapeutically in the treatment of intestinal hypermotility and in the treatment of urinary incontinence due to detrusor instability. Oxybutynin is sold for this purpose under the trade name of Ditropan®. Chemical names for oxybutynin are 4- (diethylamino)-2-butynyl-α-cyclohexyl-α-hydroxy benzeneacetate, and 4-(diethylamino)-2- butynylphenylcyclohexyl-glycolate. It is a racemic mixture of the R-enantiomer, R- oxybutynin, and the S-enantiomer, S-oxybutynin.
Use of the S-enantiomer of oxybutynin, S-oxybutynin, for the treatment of urinary incontinence has been described in U.S. Patent Numbers 5,532,278, and 5,736,577. The structure of S-oxybutynin (Registry Number 1 19618-22-3) is shown in formula I. S- oxybutynin is not commercially available at the present time.
Administration of racemic oxybutynin may result in a number of adverse effects. These adverse effects include, but are not limited to, xerostomia, mydriasis, drowsiness, nausea, constipation, palpitations and tachycardia. The amelioration of cardiovascular side effects of racemic oxybutynin, such as tachycardia and palpitations, is of particular therapeutic value.
The synthesis of S-oxybutynin has been described in the literature by Kacher et al, J. Pharmacol. Exp. Ther., 247, 867-872 (1988). An improved synthetic method is disclosed in copending U.S. patent application, serial number 09/21 1,646, the contents of which are incorporated in their entirety. In this method, an activated derivative of cyclohexylphenylglycolic acid (CHPGA), the mixed anhydride I, is prepared.
isobutylchloroforrnate
The mixed anhydride I is coupled with the propargyl alcohol derivative 4-N,N-diethylamino butynol (4-N,N-DEB)( III where R1 is -CH2R2; R2 is -ΝR3R4; and R3 and R4 are each ethyl.) Reaction of the optically active mixed anhydride with 4-NN-DEB produces a single enantiomer of oxybutynin, in this case, (S)-4-diethylamino-2- butynylphenylcyclohexylglycolate.
Improved syntheses of starting material CHPGA have been described in two copending U.S. Patent Applications, Serial Numbers 09/050,825 and 09/050,832. The contents of both are incorporated by reference in their entirety. In the first (09/050,825), phenylglyoxylic acid or cyclohexylglyoxylic acid is condensed with a single enantiomer of a cyclic vicinal aminoalcohol to form an ester of the phenylglyoxylic acid or the cyclohexylglyoxylic acid. The ester is reacted with an appropriate Grignard reagent to provide an α-cyclohexylphenylglycolate ester. A single diastereomer of the product ester is separated from the reaction mixture, and hydrolyzed to provide S-α- cyclohexylphenylglycolic acid (S-CHPGA). The second (09/050,832) discloses an alternate stereoselective process for preparing CHPGA. A substituted acetaldehyde is condensed with mandelic acid to provide a 5-phenyl-l,3-dioxolan-4-one, which is subsequently reacted with cyclohexanone to provide a 5-(l-hydroxy cyclohexyl)-5-phenyl-l,3-dioxolan-4-one. The product is dehydrated to a 5-(l-cyclohexenyl)-5-phenyl-l,3-dioxolan-4-one, hydrolyzed and reduced to CHPGA.
……………………………..
SYNTHESIS

Racemic cyclohexylphenyl glycolic acid (CHPGA) (I) is dissolved with (L)-tyrosine methyl ester (II) in refluxing acetonitrile/water to yield a mixture of diastereomeric salts, which is resolved by crystallization to afford the desired diastereomeric salt [(S)-CHPGA-(L)-TME] (III). Finally, the hydrolysis of salt (III) with HCl or H2SO4 at 40-50篊 in toluene yields the enantiomer (IV). Alternatively intermediate (IV) can be obtained as follows: acetalization of (S)-mandelic acid (V) with pivaldehyde (VI) in pentane and catalytic TfOH provides derivative (VII), which is then treated with LHMDS and then condensed with cyclohexanone (VIII) in THF to furnish aldol adduct (IX). Elimination of tertiary alcohol in (IX) with SOCl2 and pyridine in THF gives derivative (X), which is then converted into intermediate (IV) either by first hydrolysis of lactone (X) with KOH in MeOH and subsequent hydrogenation of the obtained derivative (XI) over Pd/C in MeOH, or by first hydrogenation of (X) over Pd/C in MeOH to give (XII), followed by hydrolysis with KOH in MeOH. On turn, derivative (XII) can alternatively be synthesized by treatment of derivative (VII) with LHMDS, followed by reaction with 3-bromocyclohexene (XIII) in THF to provide derivative (XIV), which is then hydrogenated over Pd/C.
US 5973182; US 6140529; WO 0023414
……………………………………………………………

The desired product is finally obtained by first formation of a mixed anhydride (XVI) by reaction of the cyclohexylphenyl glycolic acid (IV) with isobutylchloroformate (XV) in cyclohexane in the presence of Et3N, followed by treatment with 4-N,N-diethylamino butynol (XVII) (obtained on turn from reaction of propargyl alcohol (XVIII) with diethylamine (XIX) in the presence of paraformaldehyde and CuCl.

J Org Chem 2000,65(19),6283
Racemic cyclohexylphenyl glycolic acid (CHPGA) (I) is dissolved with (L)-tyrosine methyl ester (II) in refluxing acetonitrile/water to yield a mixture of diastereomeric salts, which is resolved by crystallization to afford the desired diastereomeric salt [(S)-CHPGA-(L)-TME] (III). Finally, the hydrolysis of salt (III) with HCl or H2SO4 at 40-50篊 in toluene yields the enantiomer (IV). Alternatively intermediate (IV) can be obtained as follows: acetalization of (S)-mandelic acid (V) with pivaldehyde (VI) in pentane and catalytic TfOH provides derivative (VII), which is then treated with LHMDS and then condensed with cyclohexanone (VIII) in THF to furnish aldol adduct (IX). Elimination of tertiary alcohol in (IX) with SOCl2 and pyridine in THF gives derivative (X), which is then converted into intermediate (IV) either by first hydrolysis of lactone (X) with KOH in MeOH and subsequent hydrogenation of the obtained derivative (XI) over Pd/C in MeOH, or by first hydrogenation of (X) over Pd/C in MeOH to give (XII), followed by hydrolysis with KOH in MeOH. On turn, derivative (XII) can alternatively be synthesized by treatment of derivative (VII) with LHMDS, followed by reaction with 3-bromocyclohexene (XIII) in THF to provide derivative (XIV), which is then hydrogenated over Pd/C.
CLIP

Tetrahedron Lett 2002,43(48),8647
The catalytic enantioselective cyanosilylation of the ketone (I) by means of Tms-CN catalyzed by gadolinium isopropoxide and the chiral ligand (II) in THF/propionitrile gives the silylated cyanohydrin (III), which is reduced by means of DIBAL in toluene to yield the carbaldehyde (IV). The desilylation of (IV) by means of HCl in aqueous THF affords the hydroxyaldehyde (V), which is finally oxidized by means of NaClO2 in tert-butanol/water to provide the target (S)-2-cyclohexyl-2-hydroxy-2-phenylacetic acid intermediate (VI) (see Scheme no. 23604001a, intermediate (IV)).
PATENT
http://www.google.com/patents/WO2009122429A2?cl=en
Example-1 Preparation of 4-diethylamino-2-butyne-ol
A mixture of para formaldehyde (105.Og), N,N-diethyl amine(300g) and copper(II) acetate (7.5g) in 1,4 dioxane (900ml) was heated to 60-65° C. After 1.5 h, 2-propyne-l-ol (150g, 2.7 moles) was added and the mixture was heated at 90-95° C. after 2 hrs; excess solvent, 1,4 dioxane, evaporated at reduced pressure to afford 315g
(84%) of the product as an oil. Example-2
Preparation of diethylamino-2-butvnylacetate
A mixture of 4-diethylamino-2-butyne-l-ol (30Og), acetic acid (600ml); acetic anhydride (300ml) and con.sulphuric acid (15ml) was heated to 65-70° C. After 2hrs.of maintenance excess solvent mixture was evaporated at reduced pressure. The residue was cooled and poured in a mixture of dichloromethane (1800ml) and DM water (3000ml).The reaction mass was saturated with sodium bicarbonate (300g) solid slowly controlling effervescences. The organic layer was separated and washed with 2% sodium bicarbonate and 1% EDTA solution to afford 318g (81%) of product as oil.
Example-3
Preparation of 4-diethylamino-2-butvnyl phenyl cvclohexyl alveolate hydrochloride (Oxybutynin Hydrochloride)
A mixture of 150g of methyl phenyl cyclohexyl glycolate, 133g of 4- diethylamino-2-butynyl acetate was dissolved in 1.8 ltr of n-heptane. The solution was added with 1.2 g of sodium methoxide. The solution was heated with stirring to a temperature of 95-100° C and distillate was collected. After 30min of maintenance at 95-100° C, the solution was cooled to 65-70° C under nitrogen. The solution was added with 3.24 g of sodium methoxide. The solution was heated with stirring to a temperature of 95-100° C and distillate was collected. After 1 hr. maintenance at 95- 100° C, reaction mass cooled to room temperature, washed with water. n-Heptane layer was separated and added 300 ml of 2N Hydrochloric acid to give oxybutynin hydrochloride. The crude was recrystallised from ethyl acetate.
Example-4 Preparation of Oxybutvnin base
A mixture of 150g of methyl phenyl cyclohexyl glycolate, 133g of 4- diethylamino-2-butynyl acetate was dissolved in 1.8 ltr of n-heptane. The solution was added with 1.2 g of sodium methoxide. The solution was heated with stirring to a temperature of 95-100° C and distillate was collected. After 30min of maintenance at 95-100° C, the solution was cooled to 65-70° C under nitrogen. The solution was added with 3.24 g of sodium methoxide. The solution was heated with stirring to a temperature of 95-100° C and distillate was collected. After 1 hr. maintenance at 95-
100° C, reaction mass cooled to room temperature, washed with ‘water. n-Heptane layer was separated, concentrated under reduced pressure to give residue. n-Pentane (250ml) was added to the residue and stirred under nitrogen atmosphere at 25-30° C. The solid product was filtered and washed with chilled n-pentane. Wet cake was dried at 40-42° C. Dry weight = 160.O g
Example-5 Preparation of Oxybutvnin (Base)
Oxybutynin chloride (lOOgm) was treated with DM water (500ml) at 25-30° C and heated to 40-45° C to observe clear solution. n-Heptane (500ml) was added to the solution and adjusted the pH of the mass to 10.0-11.0 using 5% sodium hydroxide solution at 20-25° C. Layers obtained were separated and aqueous layer was extracted with heptane. Organic layers were combined and concentrated under vacuum at 40- 45° C to, give residue. n-Pentane (250ml) was added to the residue and stirred under nitrogen atmosphere at 25-30° C. The solid product was filtered and washed with chilled n-pentane. Wet cake was dried at 40-42° C. Dry weight = 85.0 gm
PATENT
http://www.google.com/patents/US3176019
Example XIX 4-diethylamino-2-butynyl phenylcyclohexylglycolate hydrochl0ride.-A mixture of 394.2 g. of methyl phenylcyclohexylglycolate, 293.1 g. of 4-diethylamino-2-butynyl acetate was dissolved with Warming in 2.6 l. of n-heptane. The solution was heated with stirring to a temperature of 60-70 C. and 8.0 g. of sodium methoxide were added. The temperature of the mixture was then raised until the solvent began to distill. Distillation was continued at a gradual rate and aliquots of the distillate were successively collected and analyzed for the presence of methyl acetate by measurement of the refractive index. The reaction was completed when methyl acetate no longer distilled, and the refractive index observed was that of pure heptane (11 1.3855). About three and one-half hours were required for the reaction to be completed. The reaction mixture was then allowed to cool to room temperature, washed with Water, and extracted with four ml. portions of 2 N hydrochloric acid. The aqueous extracts Were combined and stirred at room temperature to permit crystallization of the hydrochloride salt of the desired product. Crystallization was completed by cooling the slurry in an ice bath, and the product was collected by filtration, pressed dry, and recrystallized from 750 ml. of water. Yield of pure crystalline material, 323 g.
PATENT
http://www.google.com/patents/EP1185498A2?cl=en
Background of the Invention Cyclohexylphenyl glycolic acid (also referred to herein as “CHPGA”) is used as a starting material for manufacturing compounds that have important biological and therapeutic activities. Such compounds include, for example, oxphencyclimine, oxyphenonium bromide, oxypyrronium bromide, oxysonium iodide, oxybutynin (4- diethylamino-2-butynyl phenylcyclohexylglycolate) and its metabolites, such as desethyloxybutynin (4-ethylamino-2-butynyl phenylcyclohexylglycolate). The important relation between stereochemistry and biological activity is well known. For example, the (S)-enantiomers of oxybutynin and desethyloxybutynin have been shown to provide a superior therapy in treating urinary incontinence, as disclosed in U.S. Patent Nos. 5,532,278 and 5,677,346. The (R) enantiomer of oxybutynin has also been suggested to be a useful drug candidate. [Noronha-Blob et al., J. Pharmacol. Exp. Ther. 256, 562-567 (1991)]. Racemic CHPGA is generally prepared by one of two methods: (1) selective hydrogenation of phenyl mandelic acid or of phenyl mandelate esters, as shown in Scheme 1; or (2) cyclohexyl magnesium halide addition to phenylglyoxylate as shown in Scheme 2. Scheme 1.
R is hydrogen or lower alkyl.
Scheme 2.
Asymmetric synthesis of individual enantiomers of CHPGA has been approached along the lines of Scheme 2, by Grignard addition to a chiral auxiliary ester of glyoxylic acid to give a diastereomeric mixture of esters. In addition, multiple step asymmetric synthesis of (R)-CHPGA from fDJ-arabinose using Grignard reagents has been reported. In general, simple primary alkyl or phenyl Grignard (or alkyllithium) reagents are used for the addition, and the addition of inorganic salts (e.g. ZnCl2) appears to increase the diastereoselectivity of the products.
As outlined in Scheme 3 below, the simple chiral ester wherein R* is the residue of a chiral alcohol, can be directly converted to chiral drugs or drug candidates by trans-esterification (R’=acetate), or hydrolyzed to yield chiral CHPGA (R’=H).
Scheme 3
esterification
(S) or (R)-Oxybutynin
(S) or (R)-CYLOHEXYLPHENYL GLYCOLIC ACID VIA RESOLUTION The resolution process of the present invention provides an inexpensive and efficient method for preparing a single enantiomer from racemic CHPGA via the formation of the diastereomeric salt with (L) or (D) -tyrosine methyl ester, also referred to herein as “(Z) or (D)-TME”. The process consists of three parts, which are depicted and described below: Part 1: Preparation of (S)-CHPGA-(Z)-TME diastereomeric salt or (R)-CHPGA-(D)-TME diastereomeric salt; Part 2:
Preparation of (S) or (R) CHPGA; and Part 3 – Recovery of (L) or (D)-tyrosine methyl ester. The ability to recover the resolving agent in high yield is an advantageous feature of the process of the invention. It greatly reduces cost by allowing recycling of the resolving agent. For ease in understanding, the diastereomeric salt, (<S)-CHPGA-(E)-TME, and the pure enantiomer (S)-CHPGA are depicted in the reactions below. However, the (R) enantiomeric series could instead be depicted and is similarly produced using the opposite enantiomer of TME.
Part 1 : Preparation of (5VCHPGA-(XVTyrosine Methyl Ester Diastereomer Salt
* ( )-TME
(S, R)-CHPGA (S)-CHPGA – (J)-TME (MW= 234.3) (MW = 429.5)
For use in the process of Part 1, the racemic starting material, (S, R)- cyclohexylphenyl glycolic acid (CHPGA) can be prepared by the process described above, i.e. (1) selective hydrogenation of phenyl mandelic acid or of phenyl mandelate esters or (2) cyclohexyl magnesium halide addition to phenylglyoxylate. Mandelic acid and phenylglyoxylic acid, also known as benzoylformic acid, are commercially available. Phenyl mandelic acid may be prepared by Grignard addition of phenyl magnesium bromide to diethyl oxalate followed by hydrolysis. The (L) enantiomer of tyrosine methyl ester is also readily available from commercial sources, as is (Z))-tyrosine, which can then be esterified to produce (_9)-tyrosine methyl ester using conventional techniques, such as acid-catalyzed esterification with methanol. The diastereomer of the present process is produced by dissolving racemic
CHPGA and an appropriate amount of an enantiomer of tyrosine methyl ester in a suitable solvent and then bringing about the insolubilization of one diastereomer. For example, racemic CHPGA and about 0.5 molar equivalents of (Z)-tyrosine methyl ester or (Z))-tyrosine methyl ester can be dissolved in a mixture of acetonitrile and water. When the solvent is about 10 wt % water in acetonitrile, solution may be achieved by heating, preferably by heating to reflux (approximately 78° C). After heating the solution for a sufficient time to achieve complete dissolution, usually about 5 minutes at reflux, followed by cooling, preferably to about 0-5° C, the diastereomeric salt (S)-CHPGA – (E)-TME or (R)-CHPGA – (£>)- TME, depending on the TME enantiomer used, crystallizes from solution. Better yields are obtained when the cooling temperature is maintained until crystallization of the diastereomer salt is complete, typically a period of about four hours. The salt crystals are then separated from the solution, for example by filtration. The crystalline product may be washed with solvent and dried. When the solvent is water/acetonitrile, drying under vacuum at about 40-50° C is effective. The mother liquor stream may be saved for later racemization and recovery of residual CHPGA. Racemization may be effected with aqueous mineral acids, particularly aqueous sulfuric acid in ethanol. Part 2: Preparation of (S.-CHPGA
(S)-CHPGA – (Z)-TME (S)-CHPGA
(MW = 429.5) (MW= 234.3)
In Part 2, the CHPGA enantiomer produced, (S) or (R)-CHPGA, is liberated from the diastereomeric salt. For the preparation of (S)-CHPGA, the (S)-CHPGA-(E)- TME salt from Part 1 is added to and dissolved to form a solution which is about 15 wt % substrate in toluene. The solution is treated with an excess of dilute mineral acid, such as 1.1 equivalents of 0.5 M HC1 or H2SO4. Upon dissolution of the diastereomeric salt, essentially all the TME enantiomer is converted to the hydrochloride salt. The diastereomeric salt mixture may be heated to about 40-50° C for about 10 minutes to facilitate dissolution of the solids. A phase split yields an aqueous solution containing (Z)-TME-HCl and an organic solution of (S)-CHPGA in toluene. The aqueous phase is separated from the organic solution and saved for recovery of the tryrosine methyl ester in Step 3 below. A common method of separation, which may be used throughout the processes described herein, is gravitational settling followed by drainage of the aqueous phase through a tap in the bottom of the reaction vessel.
The toluene organic phase containing (S)-CHPGA may be washed a second time with mineral acid, as specified above, and heated. The organic phase and aqueous phase are then separated, and the aqueous phase is discarded along with the rag layer, i.e. the layer separating the two phases. The retained toluene organic phase is then preferably concentrated, typically by vacuum distillation, to a weight that is about 2.1 to 2.3 times the weight of the diastereomeric salt originally present, followed by gradual cooling to 0-5° C to initiate crystallization of the single (S) enantiomer of CHPGA, as indicated by the formation of a thick slurry. The slurry is cooled for at least an hour to ensure that crystallization is complete, then filtered to isolate (S)-CHPGA. The (S)-CHPGA cake is then dried under vacuum while heating to a temperature of about (40-45° C).
Part 3 : Recovery of (X -Tyrosine Methyl Ester The aqueous phase containing (Z)-TME-HCl or (D)-TME-HCl saved from
Part 2 is cooled, preferably to about 0-5° C. While maintaining the cooling temperature, the aqueous solution is titrated with 0.5M NaOH to a pH of approximately 9.0. Typically, a thin slurry will form as the TME enantiomer precipitates. The TME enantiomer is isolated by filtration, washing with deionized water, and drying under vacuum at a temperature of about (40-50° C).
The resolution process of the present invention set forth above is illustrated by, but not limited to, the following example:
Example 1 Part 1 : Preparation of (S)-CHPGA-(E -Tyrosine Methyl Ester Diastereomer Salt A 2-liter reactor was charged with 100.0 g racemic CHPGA, 41.7 g (L)-
TME (0.5 equiv.), 549.2 g CH3CN, and 54.8 g deionized water. The reaction mixture was heated to reflux at approximately 78° C for about 5 min. The solution was then cooled to a temperature between 0-5° C over a period of 2 hours and remained cooling (0-5 ° C) for about 2 hours. The solution was filtered to isolate the (S)-CHPGA-(Z)-TME diastereomeric salt, and the salt cake was washed with 130 g chilled ( 0-5° C) CH3CN. The salt cake was dried in vacuo at 40-50° C , and the residual solvent remaining in the cake was < 0.5%. Yield = 77.1 g (42.1 mole %); ee > 99.0% (S).
Part 2: Preparation of .S.-CHPGA A 1000 mL reactor was charged with 77. 1 g (S)-CHPGA-(E)-TME from
Part 1, 447.0 g toluene, 339.2 g 0.5M HC1 (1.1 equiv.) and heated to 40-50°C while stirring until the solids dissolved (about 10 min). While maintaining the temperature at 40-50° C, the organic and aqueous phases separated after about 10 minutes. The phases were divided, and the aqueous (bottom) phase containing (L)- TME-HC1 was saved for recovery in Part 3 below. Approximately 370 g aqueous phase was recovered.
To the toluene organic phase an additional 169.6 g 0.5M HC1 (0.6 equiv.) were added, and the solution was heated to a temperature between 40-50° C while stirring for about 10 minutes. The toluene and aqueous phases were allowed to separate (~ 10 min.), while maintaining the temperature between 40-50° C. The phases were divided, and the aqueous (bottom) phase and rag layer were discarded. The organic phase was concentrated by vacuum distillation to a final weight of 168.0 g, then cooled to 0-5 °C over a period of about one hour during which time a thick slurry formed spontaneously. Agitation was adjusted as necessary. The slurry was cooled at 0-5 °C for an additional one hour. The slurry was filtered to recover the (S)-CHPGA. The (S)-CHPGA filter cake was dried in vacuo at 40-45° C , and the residual solvent remaining in the cake was < 0.2%. Yield = 35.8 g (85 mole %); ee > 99.0%; chemical purity (% HPLC area) > 99.0%.
Part 3: Recovery of (Z)-Tyrosine Methyl Ester
A 2-liter vessel was charged with the aqueous phase saved from Part 2 (370 g). The solution was cooled to 0-5 °C, and the cooling temperature was maintained while titrating with 0.5 M NaOH to a pH of 9.0 ±0.5 over approximately 30 min. A thin slurry formed as (Z)-TME precipitated. The slurry was filtered, and the (L)-
TME cake was washed with 154 g deionized water. The cake was dried in vacuo at 40-50°C , and the residual solvent remaining in the cake was < 1.0%. Yield = 30.5 g (E)-TME (87 mole %).
(S) OR fRVOXYBUTYNIN AND RELATED COMPOUNDS VIA DIRECT COUPLING
The synthesis of a single enantiomer of oxybutynin and oxybutynin analogs according to the present invention comprises coupling an enantiomer of cyclohexylphenyl glycolic acid with a propargyl alcohol derivative utilizing carboxylic acid activation. Optically active CHPGA may be prepared either by the resolution process described above or by asymmetric methods. The present invention also provides a process for converting the aforementioned enantiomers of oxybutynin and oxybutynin analogs to their corresponding hydrochloride salts. The synthetic process consists of two reactions, which are depicted and described below: Part 1: Formation of the Mixed Anhydride; Part 2: Formation of (S) or (R) oxybutynin and its related compounds. Again for ease in understanding, the (S) enantiomeric series is depicted, although the (R) series is produced similarly.
Part 1 : Formation of the Mixed Anhydride
isobut lchloroformate
(S)-CHPGA Mixed Anhydride MW=234.29
In Part 1, (S) or (R) cyclohexylphenyl glycolic acid (CHPGA) is reacted with an alkyl chloroformate in an organic solvent to form a mixed anhydride enantiomer, as shown above, which can then react to form the desired chiral product in Part 2 below.
It should be noted that, while mixed anhydrides are often employed for the synthesis of amides, their use for ester synthesis is quite unusual. It should also be noted that a surprising and unexpected aspect of the present process is that the mixed anhydride intermediate proceeds to a chiral product without affecting the tertiary carbinol of CHPGA, which would lead to impurity formation or racemization. One would expect reaction with an acyl halide at the benzylic hydroxyl resulting in the formation of a stable, but undesired compound, such as an ester. Alternatively, if the hydroxyl were activated (unintentionally) to form a good leaving group, as, for example, under acidic conditions, the dissociation of the leaving group would form a benzylic carbonium ion, leading to racemization. One would therefore expect a loss in optical activity of the oxybutynin or the extensive production of by-products. Surprisingly, the present process produces a high purity product, and no racemization is observed.
In the preparation of the mixed anhydride, two intermediates, in addition to the mixed anhydride shown above, were detected. The two were isolated and their structures were determined by NMR to be
carbonate-anhydride A carbonate-acid B wherein R5 was isobutyl. Both intermediates were smoothly converted to oxybutynin upon treatment with 4-N,N-DEB.
The reaction is preferably carried out in an inert atmosphere, such as nitrogen or argon, and the reaction solution is stirred using conventional techniques. In the depiction above, isobutyl chloroformate (IBCF) is shown as the preferred alkyl chloroformate for reaction with (S)-CHPGA forming the isobutyloxy mixed anhydride. However, other alkyl chloroformates, such as isopropenylchloroformate and 2-ethylhexylchloroformate, for example, may instead be used. The amount of alkyl chloroformate used in the reaction is preferably about 1.2 equivalents with respect to the CHPGA enantiomer.
Preferably, the reaction proceeds in the presence of a tertiary amine (2.5 equiv.), such as triethylamine (TEA), 4-N,N-dimethylaminopyridine (DMAP), pyridine, diisopropylethylamine, diethylmethylamine, Ν-methylpiperidine or Ν- methylmorpholine, which scavenges the HC1 produced. Organic solvents that may be used include, but are not limited to cyclohexane, heptane, toluene, tetrahydrofuran (THF), ethylene glycol dimethyl ether (DME), diethoxy methane (DEM), and methyl t-butyl ether (MTBE). Part 2: Formation of (S) or (R -Oxybutynin and its Analogs
Mixed Anhydride (S)-Oxybutynin or Analog
A sidechain propargyl alcohol derivative of formula (III), wherein R1 is as previously defined, is added to the mixed anhydride contained in the reaction mixture to produce the single enantiomer of oxybutynin or analog thereof (II). About 1.3 equivalents of the formula (III) compound relative to (S) or (R)-CHPGA is sufficient. Typically, the reaction mixture is heated to reflux at a temperature of about 65-80° C, but more preferably about 70-75° C, until the reaction is complete, as determined by HPLC.
Most preferably, the propargyl alcohol derivative of formula (III) is a 4- amino propargyl alcohol derivative, wherein R1 is represented as -CH2R2; R2 is – NR3R4; and R3 and R4 are each independently lower alkyl, benzyl or methoxybenzyl. For example, the compound of formula (III) is most preferably 4-N,N-diethylamino butynol (4-N,N-DEB), where R3 and R4 are each ethyl. Reaction of the mixed anhydride with 4-N.N-DEB produces the single enantiomer of oxybutynin, i.e. (S) or (R)-4-diethylamino-2-butynyl phenylcyclohexylglycolate. Another preferred embodiment is the reaction using an Ν-protected 4-N-ethylamino butynol, such as Ν-ethyl-Ν-(4-methoxybenzyl)butynol, as the propargyl alcohol derivative and then cleaving the protecting group (by methods well known in the art) to produce (S) or (R)-4-ethylamino-2-butynyl phenylcyclohexylglycolate, also known as desethyloxybutynin. In that case, R3 is ethyl, and R4 is converted to hydrogen in formula (III). Suitable protecting groups are described in Greene and Wuts Protecting Groups in Organic Synthesis. Second Edition Wiley, New York 1991, p. 362-371, which is incorporated herein by reference. In another preferred embodiment, the propargyl alcohol derivative of formula (III) is 4-N,N- ethylmethylamino butynol, which results in the formation of (Sf) or (R)-4- ethylmethylamino-2-butynyl phenylcyclohexylglycolate. In this case, R3 is ethyl, and R4 is methyl.
Other useful sidechain propargyl alcohol compounds in which R1 is -CH2R2 are those wherein R2 is azide, hydroxy, or halo. In addition, propargyl alcohol itself, also known as 2-propyn-l-ol, may be reacted with the mixed anhydride. In this case, R1 is hydrogen in formula (III). 4-N,N-Diethylamino butynol for use as the sidechain propargyl alcohol in the present invention may be prepared by reacting propargyl alcohol, paraformaldehyde, and diethylamine under standard Mannich conditions. Other amino and alkyl amino propargyl alcohol derivatives of structure (III) can be formed by the process disclosed in U.S. Patent No. 5,677,346. Briefly, a secondary amine, in which one or more substituents may be a protecting group, such as N-ethyl-4- methoxybenzenemethanamine for example, is reacted with propargyl alcohol and paraformaldehyde in the presence of cuprous chloride. After condensation with the activated CHPGA, the addition of α-chloroethyl carbonochloridate removes the protecting group. In this example, the 4-N-ethylaminobutynyl ester is the ultimate product. The remaining propargyl alcohol derivatives for use in the present invention are commercially available or can be synthesized by methods known in the art.
As stated above, the progress of the condensation of the mixed anhydride with the propargyl alcohol may be conveniently monitored by periodic HPLC analyses of the reaction mixture until the desired extent of conversion is reached. At >80% conversion, the reaction is preferably quenched by washing with 10-12% aqueous monobasic sodium phosphate and water. About 8.5 g of the phosphate per gram of enantiomeric CHPGA used is typical. After separation of the organic phase, the aqueous washes are then discarded. A final wash using deionized water may then be performed, after which the bottom aqueous phase is discarded. The retained organic phase containing the enantiomer of structure (II) in solution with the organic solvent can then be concentrated to remove most of the solvent, typically by vacuum distillation.
Formation of the Hvdrochloride Salt
(S)-Oxybutynin or Analog (S)-Oxybutynin or Analog-HCl
To promote crystallization, the organic solvent containing the enantiomer of oxybutynin or one of its analogs (II) produced by the process outlined above (also referred to herein as “free base enantiomer (II)”) is exchanged with ethyl acetate (EtOAc). Typically, the organic solvent is removed by vacuum distillation to contain about 20-25 wt % (S) or (R) enantiomer of structure (II), which is based on the theoretical amount of free base (II) formed from the coupling process above. Ethyl acetate is then added to obtain the original solution volume or weight. This step may be repeated substituting the removal of EtOAc for the organic solvent. The EtOAc solution may be filtered through a filtering agent, such as diatomaceous earth. The filter cake is washed with EtOAc as needed.
The filtrate is then concentrated by vacuum distillation, for example, to contain about 20-25 wt % (theoretical) of free base enantiomer (II) and < 0.3 wt % water. To maximize product yield and purity and to encourage crystallization, most of the water should be removed from the solution. If the foregoing concentration processes are insufficient to reduce the water to < 0.3%, the vacuum distillation may be repeated with fresh solvent or a drying agent, such as magnesium sulfate may be employed. Water content can be determined by KF (Karl Fisher method). Methyl t-butyl ethyl (MTBE) is then added to the concentrated EtOAc solution to a volume that reduces the concentration by weight of the free base enantiomer (II) by about one third, or optimally to between about 6.5 and 8.5 wt %. The hydrochloride salt is then formed by the addition of HC1, while stirring. A slight excess of HC1 in ethanol, for example about 1.1 equivalents of 35-40 wt % HC1, is generally sufficient. The temperature may be increased to 35-45° C. To initiate recrystallization, the solution may be seeded with the hydrochloride salt of the enantiomer of structure (II). After about an hour of stirring, which may be done at 35-45° C, a slurry forms. If the slurry is cooled to about 0-5° C and this temperature maintained for about two hours, filtration provides a very good recovery of the hydrochloride salt of the enantiomer of structure (II). The filter cake is typically a white to off-white crystalline solid, which can then be washed with ambient temperature methyl t-butyl ether (at least 2.2 g MTBE per gram free base enantiomer (II)), followed by vacuum drying at 40- 50° C.
The following example is illustrative, but the present invention is not limited to the embodiment described therein:
Example 2 Preparation of (S)-Oxybutvnin-HCl
A 3-neck round bottomed flask was charged with 50.0 g (S)-CHPGA (213.0 mmol) and 780 g (1000 mL) cyclohexane under nitrogen. While stirring, 54 g triethylamine (2.5 equiv.) and 35 g isobutyl chloroformate (IBCF)(1.2 equiv.) were slowly added while maintaining the temperature at 20-30° C. After about 0.5 hour, while continuing to stir the reaction mixture, 39.15 g 4-N,N-DEB (1.3 equiv.) were added, and the mixture was heated to 65 °C to reflux . Mixing continued at reflux until the formation of (S)-oxybutynin was complete by HPLC area normalization. Heating was discontinued, and the reaction mixture was cooled to between
20-30° C. At this time, 425 g of 11.5% ΝaH2PO4Η20 aqueous solution were added to the mixture, and the mixture was stirred for 10 min. Stirring was discontinued, and the organic and aqueous phases separated after about 15 minutes. The aqueous (bottom) phase was discarded. 425 g of 11.5% NaH2PO4Η20 aqueous solution were again added to the retained organic phase, and the mixture was stirred for about 10 min. The phases were then permitted to separate, which took about 15 minutes. The aqueous (bottom) phase was again discarded. To the remaining organic phase, deionized water (400 g) was added. The mixture was stirred for about 10 min, followed by phase separation after about 15 minutes. The aqueous (bottom) phase was discarded.
Cyclohexane was removed from the organic phase by vacuum distillation to about 350 g (~ 22 wt % (S)-oxybutynin based on the theoretical amount (76.29 g) of (S)-oxybutynin free base formed). Ethyl acetate (EtOAc) was added to obtain the original solution volume of about 1000 mL (or about 83 Og), followed by vacuum distillation to 20-25 wt % (S)-oxybutynin. EtOAc was then added a second time to a volume of about 1000 mL (or about 830g). The batch was then polish filtered through about 5.0 g CELITE® while washing the filter cake with EtOAc as needed. The filtered mixture was concentrated and dried by vacuum distillation to 339 g (~ 22.5 wt % (S)-oxybutynin) and < 03 wt % water, as measured by KF. Based on the theoretical amount of (S)-oxybutynin free base (76.29 g), methyl t-butyl ether was added to adjust the (S)-oxybutynin free base concentration to 8.0 wt % (953 g). With agitation, 23 g of 37 wt % HC1 in EtOH (1.1 equiv.) were slowly added to the solution, while maintaining the temperature between 20 and 45° C. The temperature of the solution was then adjusted to 35-45° C, and the solution was seeded with about 500 mg (S)-oxybutynin-HCl crystals (approximately 10 mg of seeds per g (S)-CHPGA ). The temperature was maintained, and the solution was stirred for about one hour. A slurry formed, which was then cooled to 0-5 °C over a minimum of 1 hour and held for 2 hours. The slurry was then filtered to recover the (S)-oxybutynin-HCl. The filter cake was a white to off-white crystalline solid. After washing with MTBE (a minimum of 167.84 g MTBE (2.2 g MTBE/g (S)-oxybutynin free base), the cake was dried in vacuo at 40-45 °C. The residual solvent remaining in the cake was < 0.5%. Dry weight = 57.9 g. Overall yield = 68.9%.
Example 3 Isolation of the two carbonate intermediates A and B To a racemic mixture of cyclohexylphenylglycolic acid [CHPGA] (5.0 g, 0.0213mol) in cyclohexane (100 mL) was added triethylamine (7.4 mL, 0.053 mol) and isobutylchloroformate (5.5mL, 0.0426mol). The slurry was allowed to stir at ambient temperature for approximately 0.5 h, at which time the reaction was quenched with a 10% aq. NaH2PO4 (50 ml). The organic phase was separated from the aqueous phase and washed with 10% aq. NaH2PO4 (50mL) followed by DI water (50mL). The organic phase was dried over anhydrous MgSO4 and concentrated in vacuo to afford a colorless oil. The product was purified by flash chromatography eluting with 95:5 hexane-EtOAc [Rf = 0.2] to afford pure carbonate-anhydride A. The structure was confirmed by H and 13C NMR, IR, in sttw IR and MS.
To a racemic mixture of cyclohexylphenylglycolic acid [CHPGA] (5.0 g, 0.0213 mol) in cyclohexane (100 mL) was added triethylamine (7.4 mL, 0.053mol) or preferably 1-methyl piperidine (O.053mol), and isobutylchloroformate (3.3 mL, 0.026mol). The slurry was allowed to stir at ambient temperature for approximately 0.5 h, at which time the reaction was quenched with a 10% aq. solution of NaH2PO4 (50 mL) followed by DI water (50mL). The organic phase was dried over anhydrous MgSO4 and concentrated in vacuo to afford a colorless oil as a 4:1 mixture of A and B by HPLC. The crude product was purified by passing the mixture through a plug of neutral alumina. Compound A was eluted first using
CHClj B was then washed off the alumina with acetone and concentrated in vacuo to afford pure carbonate-acid B. The structure was confirmed by H and 13C NMR, IR, in situ IR and MS.
PATENT
http://www.google.com/patents/US6294582
The synthesis of S-oxybutynin has been described in the literature by Kacher et al., J. Pharmacol. Exp. Ther., 247, 867-872 (1988). An improved synthetic method is disclosed in copending U.S. patent application, Ser. No. 09/211,646, now U.S. Pat. No. 6,140,529, the contents of which are incorporated in their entirety. In this method, an activated derivative of cyclohexylphenylglycolic acid (CHPGA), the mixed anhydride I, is prepared.
The mixed anhydride I is coupled with the propargyl alcohol derivative 4-N,N-diethylamino butynol (4-N,N-DEB)(III where R1 is —CH2R2; R2 is —NR3R4; and R3 and R4 are each ethyl.) Reaction of the optically active mixed anhydride with 4-N,N-DEB produces a single enantiomer of oxybutynin, in this case, (S)-4-diethylamino-2-butynylphenylcyclohexylglycolate.
Improved syntheses of starting material CHPGA have been described in two copending U.S. patent applications, Ser. No. 09/050,825, now U.S. Pat. No. 6,013,830, and 09/050,832. The contents of both are incorporated by reference in their entirety. In the first (09/050,825, now U.S. Pat. No. 6,013,830), phenylglyoxylic acid or cyclohexylglyoxylic acid is condensed with a single enantiomer of a cyclic vicinal aminoalcohol to form an ester of the phenylglyoxylic acid or the cyclohexylglyoxylic acid. The ester is reacted with an appropriate Grignard reagent to provide an a-cyclohexylphenylglycolate ester. A single diastereomer of the product ester is separated from the reaction mixture, and hydrolyzed to provide S-α-cyclohexylphenylglycolic acid (S-CHPGA). The second (09/050,832) discloses an alternate stereoselective process for preparing CHPGA. A substituted acetaldehyde is condensed with mandelic acid to provide a 5-phenyl-1,3-dioxolan-4-one, which is subsequently reacted with cyclohexanone to provide a 5-(1-hydroxy cyclohexyl)-5-phenyl-1,3-dioxolan-4-one. The product is dehydrated to a 5-(1-cyclohexenyl)-5-phenyl-1,3-dioxolan-4-one, hydrolyzed and reduced to CHPGA.
The magnitude of a prophylactic or therapeutic dose of S-oxybutynin in the acute or chronic management of disease will vary with the severity of the condition to be treated, and the route of administration. The dose, and perhaps the dose frequency will also vary according to the age, body weight, and the response of the individual patient. In general, the daily dose ranges when administered by inhalation, for the conditions described herein, are from about 0.1 mg to about 100 mg in single or divided dosages. Preferably a daily dose range should be between about 10 mg to about 25 mg, in single or divided dosages, preferably in from 2-4 divided dosages. In managing the patient the therapy should be initiated at a lower dose, perhaps from 5 mg to about 10 mg, and increased up to about 2×20 mg or higher depending on the patient’s global response. When administered orally, preferably as a soft elastic gelatin capsule, the preferred dose range is from about 1 mg to about 1 g per day, more preferably, from about 25 mg to about 700 mg per day, and most preferably, from about 100 mg to about 400 mg per day. It is further recommended that children and patients over 65 years and those with apaired renal, or hepatic function, initially receive low dosages and that they be titrated based on individual responses and blood levels. It may be necessary to use dosages outside these ranges in some cases, as will be apparent to those skilled in the art. Further, it is noted that the clinician or treating physician possesses knowledge of how and when to interrupt, adjust, or terminate therapy in conjunction with individual patient response. The terms “a therapeutically effective quantity”, and “a quantity sufficient to alleviate bronchospasms” are encompassed by the above described dosage amounts and dose frequency schedule.
The methods of the present invention utilize S-oxybutynin, or a pharmaceutically acceptable salt thereof. The term “pharmaceutically acceptable salt” or “a pharmaceutically acceptable salt thereof” refer to salts prepared from pharmaceutically acceptable nontoxic acids including both inorganic and organic acids. Suitable pharmaceutically acceptable acid addition salts for the compound of the present invention include acetic, benzenesulfonic (besylate), benzoic, camphorsulfonic, citric, ethanesulfonic, fumaric, gluconic, glutamic, hydrobromic, hydrochloric, isethionic, lactic, maleic, malic, mandelic, methanesulfonic, mucic, nitric, pamoic, pantothenic, phosphoric, succinic, sulfuric, tartaric, and p-toluene sulfonic. The hydrochloride has particular utility.
Preferred unit dosage formulations are those containing an effective dose, as recited, or an appropriate fraction thereof, of S-oxybutynin or pharmaceutically acceptable salts thereof. The formulations of this invention may include other agents conventional in the art having regard to the type of formulation in question. For example, formulations for oral administration may include carriers such as starches, sugars, microcystalline cellulose, diluents, granulating agents, flavoring agents and the like. Formulations suitable for oral, rectal and parenteral administration (including subcutaneous, transdermal, intramuscular, and intravenous) and inhalation may be used for treatment according to the present invention.
Any suitable route of administration may be employed for providing the patient with an effective dosage of S-oxybutynin. For example, oral, rectal, parenteral (subcutaneous, intramuscular, intravenous), transdermal, and like forms of administration may be employed. Transdermal administration may be improved by the inclusion of a permeation enhancer in the transdermal delivery device, for example as described in PCT application WO 92/20377. Dosage forms include troches, dispersions, suspensions, solutions, aerosols, patches, syrups, tablets and capsules, including soft elastic gelatin capsules. Oral and parenteral sustained release dosage forms may also be used.
Because of their ease of administration, tablets and capsules represent one of the more advantageous oral dosage unit forms, in which case solid pharmaceutical carriers are employed. If desired, tablets may be coated by standard aqueous or nonaqueous techniques. Soft elastic gel capsules are a preferred form of administration of S-oxybutynin.
Soft elastic gelatin capsules may be prepared by mixing S-oxybutynin with a digestible oil such as soybean oil, lecithin, cottonseed oil, or olive oil. The mixture is then injected into gelatin by means of a positive pressure pump, such that each dosage unit contains an effective dose of S-oxybutynin. The capsules are subsequently washed and dried.
Oral syrups, as well as other oral liquid formulations, are well known to those skilled in the art, and general methods for preparing them are found in most standard pharmacy school textbooks. An exemplary source is Remington: The Science and Practice of Pharmacy. Chapter 86 of the 19th edition of Remington entitled “Solutions, Emulsions, Suspensions and Extracts” describes in complete detail the preparation of syrups (pages 1503-1505) and other oral liquids. Similarly, sustained release formulation is well known in the art, and Chapter 94 of the same reference, entitled “Sustained-Release Drug Delivery Systems”, describes the more common types of oral and parenteral sustained-release dosage forms (pages 1660-1675.) The relevant disclosure, Chapters 86 and 94, is incorporated herein by reference.
Controlled release means and delivery devices are also described in U.S. Pat. Nos. 3,845,770; 3,916,899; 3,536,809; 3,598,123; and 4,008,719, and in PCT application WO 92/20377. Because they reduce peak plasma concentrations, controlled release dosage forms are particularly useful for providing a therapeutic plasma concentration of S-oxybutynin while avoiding the side effects associated with peak plasma concentrations.
Formulations suitable for inhalation include sterile solutions for nebulization comprising a therapeutically effective amount of S-oxybutynin or a pharmaceutically acceptable salt thereof, dissolved in aqueous saline solution and optionally containing a preservative such as benzalkonium chloride or chlorobutanol, and aerosol formulations comprising a therapeutically effective amount of S-oxybutynin, or a pharmaceutically acceptable salt thereof, dissolved or suspended in an appropriate propellant (e.g., HFA-134a, HFA-227, or a mixture thereof, or a chlorofluorocarbon propellant such as a mixture of Propellants 11, 12 and/or 114) optionally containing a surfactant. Aerosols may be conveniently presented in unit dosage form and prepared by any of the methods well-known in the art of pharmacy. The preparation of a particularly desirable aerosol formulation is described in European Patent No. 556239, the disclosure of which is incorporated herein by reference. Also suitable are dry powder formulations comprising a therapeutically effective amount of S-oxybutynin or a pharmaceutically acceptable salt thereof, blended with an appropriate carrier and adapted for use in connection with a dry-powder inhaler.
……………………….
| CZ20013826A3 * | Title not available | |||
| US3176019 * | Jun 20, 1961 | Mar 30, 1965 | Mead Johnson & Co | Substituted aminobutynyl acetates |
| Reference | ||
|---|---|---|
| 1 | * | DATABASE CAPLUS [Online] 13 November 2010 STN Database accession no. 2006:220682 & CZ 20 013 826 A3 18 June 2003 |
| 2 | * | DATABASE CAPLUS 13 January 2010 STN: ‘Syntheses of oxybutynin hydrochloride‘ Database accession no. 1997:395370 & ZHONGGUO YIYAO GONGYE ZAZHI vol. 27, no. 9, pages 387 – 389 |

CLIP
Racemic
 |
|
 |
|
| Systematic (IUPAC) name | |
|---|---|
| 4-Diethylaminobut-2-ynyl 2-cyclohexyl-2-hydroxy-2-phenylethanoate | |
| Clinical data | |
| Trade names | Ditropan |
| AHFS/Drugs.com | monograph |
| MedlinePlus | a682141 |
| Pregnancy cat. | |
| Legal status | |
| Routes | oral, transdermal gel, transdermal patch |
| Pharmacokinetic data | |
| Protein binding | 91%-93% |
| Half-life | 12.4-13.2 hours |
| Identifiers | |
| CAS number | 5633-20-5 |
| ATC code | G04BD04 |
| PubChem | CID 4634 |
| IUPHAR ligand | 359 |
| DrugBank | DB01062 |
| ChemSpider | 4473 |
| UNII | K9P6MC7092 |
| KEGG | D00465 |
| ChEBI | CHEBI:7856 |
| ChEMBL | CHEMBL1231 |
| Chemical data | |
| Formula | C22H31NO3 |
| Mol. mass | 357.486 g/mol |
Oxybutynin (Ditropan, Lyrinel XL, Lenditro (South Africa)) is an anticholinergic medication used to relieve urinary and bladder difficulties, including frequent urination and inability to control urination (urge incontinence), by decreasing muscle spasms of the bladder.[1]
It competitively antagonizes the M1, M2, and M3 subtypes of the muscarinic acetylcholine receptor. It also has direct spasmolytic effects on bladder smooth muscle as a calcium antagonist and local anesthetic, but at concentrations far above those used clinically.
Oxybutynin is also a possible treatment of hyperhidrosis (hyper-active sweating).[2][3][4]
Chemistry
Oxybutynin contains one stereocenter. Commercial formulations are sold as the racemate. The (R)-enantiomer is a more potent anticholinergic than either the racemate or the (S)-enantiomer, which is essentially without anticholinergic activity at doses used in clinical practice.[5][6] However, (R)-oxybutynin administered alone offers little or no clinical benefit above and beyond the racemic mixture. The other actions (calcium antagonism, local anesthesia) of oxybutynin are not stereospecific. (S)-Oxybutynin has not been clinically tested for its spasmolytic effects, but may be clinically useful for the same indications as the racemate, without the unpleasant anticholinergic side effects.
Clinical efficacy
In two trials of patients with overactive bladder, transdermal oxybutynin 3.9 mg/day decreased the number of incontinence episodes and increased average voided volume to a significantly greater extent than placebo. There was no difference in transdermal oxybutynin and extended-release oral tolterodine.[7]
Adverse effects
Common adverse effects associated with oxybutynin and other anticholinergics include: dry mouth, difficulty in urination, constipation, blurred vision, drowsiness, and dizziness.[8] Anticholinergics have also been known to induce delirium.[9]
These are dose-related and sometimes severe. In one population studied—after six months, more than half of the patients had stopped taking the medication because of side effects and calcium defects. An intake of calcium of 800 to 1000 mg is suggested.Dry mouth may be particularly severe; one estimate is that over a quarter of patients who begin oxybutynin treatment may have to stop because of dry mouth.
N-Desethyloxybutynin is an active metabolite of oxybutynin that is thought responsible for much of the adverse effects associated with the use of oxybutynin.[10] N-Desethyloxybutynin plasma levels may reach as much as six times that of the parent drug after administration of the immediate-release oral formulation.[11] Alternative dosage forms have been developed in an effort to reduce blood levels of N-desethyloxybutynin and achieve a steadier concentration of oxybutynin than is possible with the immediate release form. The long-acting formulations also allow once-daily administration instead of the twice-daily dosage required with the immediate-release form. The transdermal patch, in addition to the benefits of the extended-release oral formulations, bypasses the first-pass hepatic effect that the oral formulations are subject to.[12] In those with overflow incontinence because of diabetes or neurological diseases like multiple sclerosis or spinal cord trauma, oxybutynin can worsen overflow incontinence since the fundamental problem is that the bladder is not contracting.
Clinical pharmacology
Oxybutynin chloride exerts direct antispasmodic effect on smooth muscle and inhibits the muscarinic action of acetylcholine on smooth muscle. It exhibits one-fifth of the anticholinergic activity of atropine on the rabbit detrusor muscle, but four to ten times the antispasmodic activity. No blocking effects occur at skeletal neuromuscular junctions or autonomic ganglia (antinicotinic effects).
Sources say the drug is absorbed within one hour and has an elimination half-life of 2 to 5 hours.[13][14][15] There is a wide variation among individuals in the drug’s concentration in blood. This, and its low concentration in urine, suggest that it is eliminated through the liver.[14]
Contraindications
Oxybutynin chloride is contraindicated in patients with untreated angle closure glaucoma, and in patients with untreated narrow anterior chamber angles—since anticholinergic drugs may aggravate these conditions. It is also contraindicated in partial or complete obstruction of the gastrointestinal tract, hiatal hernia, gastroesophageal reflux disease, paralytic ileus, intestinal atony of the elderly or debilitated patient, megacolon, toxic megacolon complicating ulcerative colitis, severe colitis, and myasthenia gravis. It is contraindicated in patients with obstructive uropathy and in patients with unstable cardiovascular status in acute hemorrhage. Oxybutynin chloride is contraindicated in patients who have demonstrated hypersensitivity to the product.
Formulations
It is available orally in generic formulation or as the brand-names Ditropan, Lyrinel XL, or Ditrospam, as a transdermal patch under the brand name Oxytrol, and as a topical gel under the brand name Gelnique.
A 2009 Weill Cornell Medical College study concluded that patients switched to generic oxybutynin experienced a degradation in therapeutic value: “In women, there was a doubling of daytime frequency of urination, a slight 20% increase in nocturia, and a 46.3% increase in urge incontinence. In men, there was a 2.4-fold increase in daytime frequency, a 40% increase in nocturia, and a 40.6% increase in urge incontinence”.[16]
PATENT
http://www.google.com/patents/US3176019
Example XIX 4-diethylamino-2-butynyl phenylcyclohexylglycolate hydrochl0ride.-A mixture of 394.2 g. of methyl phenylcyclohexylglycolate, 293.1 g. of 4-diethylamino-2-butynyl acetate was dissolved with Warming in 2.6 l. of n-heptane. The solution was heated with stirring to a temperature of 60-70 C. and 8.0 g. of sodium methoxide were added. The temperature of the mixture was then raised until the solvent began to distill. Distillation was continued at a gradual rate and aliquots of the distillate were successively collected and analyzed for the presence of methyl acetate by measurement of the refractive index. The reaction was completed when methyl acetate no longer distilled, and the refractive index observed was that of pure heptane (11 1.3855). About three and one-half hours were required for the reaction to be completed. The reaction mixture was then allowed to cool to room temperature, washed with Water, and extracted with four ml. portions of 2 N hydrochloric acid. The aqueous extracts Were combined and stirred at room temperature to permit crystallization of the hydrochloride salt of the desired product. Crystallization was completed by cooling the slurry in an ice bath, and the product was collected by filtration, pressed dry, and recrystallized from 750 ml. of water. Yield of pure crystalline material, 323 g.

References
- Chapple CR. “Muscarinic receptor antagonists in the treatment of overactive bladder”. Urology (55)5, Supp. 1:33-46, 2000.
- Tupker RA, Harmsze AM, Deneer VH (2006). “Oxybutynin therapy for generalized hyperhidrosis.”. Arch Dermatol 142 (8): 1065–6. doi:10.1001/archderm.142.8.1065. PMID 16924061.
- Mijnhout GS, Kloosterman H, Simsek S, Strack van Schijndel RJ, Netelenbos JC. (2006). “Oxybutynin: dry days for patients with hyperhidrosis.”. Neth J Med 64 (9): 326–8. PMID 17057269.
- Schollhammer M, Misery L. (2007). “Treatment of hyperhidrosis with oxybutynin.”. Arch Dermatol. 143 (4): 544–5. doi:10.1001/archderm.143.4.544. PMID 17438194.
- Kachur JF, et al. “R and S enantiomers of oxybutynin: pharmacological effects in guinea pig bladder and intestine.” Journal of Pharmacology and Experimental Therapeutics 247:867-72, 1988.
- Noronha-Blob L, Kachur JF. “Enantiomers of oxybutynin: in vitro pharmacological characterization at M1, M2 and M3 muscarinic receptors and in vivo effects on urinary bladder contraction, mydriasis and salivary secretion in guinea pigs.” Journal of Pharmacology and Experimental Therapeutics 256:562-7, 1991.
- Baldwin C, Keating GM.[1].Drugs 2009;69 (3):327-337. doi:10.2165/00003495-200969030-00008.
- Mehta D (Ed.) 2006. British National Formulary 51. Pharmaceutical Press. ISBN 0-85369-668-3
- Andreasen NC and Black DW, “Introductory Textbook of Psychiatry.” American Psychiatric Publishing Inc. 2006
- Allen B. Reitz, Suneel K. Gupta, Yifang Huang, Michael H. Parker, and Richard R. Ryan (2007). “The preparation and human muscarinic receptor profiling of oxybutynin and N-desethyloxybutynin enantiomers”. Med Chem 3 (6): 543–5. doi:10.2174/157340607782360353. PMID 18045203.
- Zobrist RH, et al. “Pharmacokinetics of the R- and S-Enantiomers of Oxybutynin and N-Desethyloxybutynin Following Oral and Transdermal Administration of the Racemate in Healthy Volunteers”. Pharmaceutical Research 18:1029-1034, 2001.
- Oki T, et al. “Advantages for Transdermal over Oral Oxybutynin to Treat Overactive Bladder: Muscarinic Receptor Binding, Plasma Drug Concentration, and Salivary Secretion”. Journal of Pharmacology and Experimental Therapeutics Fast Forward 316:1137-1145, 2006.
- [2] “Oxybutynin” Retrieved on 30 August 2012.
- [3] “The pharmacokinetics of oxybutynin in man. (Abstract)” Retrieved on 30 August 2012.
- [4] “Oxybutynin” Retrieved on 30 August 2012.
- Kerr, Martha (2009-05-03). “AUA 2009: Generics Not Equal to Brand-Name Drugs for Overactive Bladder”. American Urological Association (AUA) 104th Annual Scientific Meeting (Medscape). Retrieved 2013-04-20.
External links
- http://health.yahoo.com/urinary-medications/oxybutynin-oral/healthwise–d00328a1.html
- http://www.mayoclinic.com/health/drug-information/DR601047
- http://www.medicinenet.com/oxybutynin_er-oral/article.htm
| Title: OxybutyninCAS Registry Number: 5633-20-5CAS Name: a-Cyclohexyl-a-hydroxybenzeneacetic acid 4-(diethylamino)-2-butynyl esterAdditional Names: a-phenylcyclohexaneglycolic acid 4-(diethylamino)-2-butynyl ester; 4-diethylamino-2-butynyl phenylcyclohexylglycolate; oxibutininaMolecular Formula: C22H31NO3Molecular Weight: 357.49Percent Composition: C 73.91%, H 8.74%, N 3.92%, O 13.43%Literature References: Muscarinic receptor antagonist. Prepn: GB 940540 (1963 to Mead Johnson). Physico-chemical properties: E. Miyamoto et al., Analyst 119, 1489 (1994). GC-MS determn in plasma: K. S. Patrick et al., J. Chromatogr. 487, 91 (1989). Toxicity: E. I. Goldenthal, Toxicol. Appl. Pharmacol. 18, 185 (1971). Review of pharmacodynamics and therapeutic use: Y. E. Yarker et al., Drugs Aging 6, 243-262 (1995).Properties: pKa 8.04. Log P (n-octanol/water): 2.9 (pH 6). Soly in water (mg/ml): 77 (pH 1); 0.8 (pH 6); 0.012 (pH >9.6).pKa: pKa 8.04Log P: Log P (n-octanol/water): 2.9 (pH 6)Derivative Type: HydrochlorideCAS Registry Number: 1508-65-2
Additional Names: Oxybutynin chloride Manufacturers’ Codes: MJ-4309-1 Trademarks: Cystrin (Sanofi-Synthelabo); Ditropan (Sanofi-Synthelabo); Dridase (Sanofi-Synthelabo); Kentera (UCB); Pollakisu (Kodama); Tropax (BMS) Molecular Formula: C22H31NO3.HCl Molecular Weight: 393.95 Percent Composition: C 67.07%, H 8.19%, N 3.56%, O 12.18%, Cl 9.00% Properties: Crystals, mp 129-130°. Sol in water, acids. Practically insol in alkali. LD50 orally in rats: 1220 mg/kg (Goldenthal). Melting point: mp 129-130° Toxicity data: LD50 orally in rats: 1220 mg/kg (Goldenthal)
Therap-Cat: In treatment of urinary incontinence. Keywords: Antimuscarinic. |
Launching new Blog……DRUG PATENTS INTERNATIONAL
Beta carotene may protect people with common genetic risk factor for type-2 diabetes
25 JAN 2013
STANFORD, Calif. — Stanford University School of Medicine investigators have found that for people harboring a genetic predisposition that is prevalent among Americans, beta carotene, which the body converts to a close cousin of vitamin A, may lower the risk for the most common form of diabetes, while gamma tocopherol, the major form of vitamin E in the American diet, may increase risk for the disease.
The scientists used a “big data” approach to hunt down interactions between gene variants previously associated with increased risk for type-2 diabetes and blood levels of substances previously implicated in type-2 diabetes risk. In people carrying a double dose of one such predisposing gene variant, the researchers pinpointed a highly statistically significant inverse association of beta carotene blood levels with type-2 diabetes risk, along with a suspiciously high positive association of gamma tocopherol with risk for the disease.
“Type-2 diabetes affects…
View original post 1,081 more words
Tagged Phosphine Reagents to Assist Reaction Work-up by Phase-Switched Scavenging Using a Modular Flow Reactor Process
The use of three orthogonally tagged phosphine reagents to assist chemical work-up via phase-switch scavenging in conjunction with a modular flow reactor is described. These techniques (acidic, basic and Click chemistry) are used to prepare various amides and tri-substitutedguanidines from in situ generated iminophosphoranes.
Tagged Phosphine Reagents to Assist Reaction Work-up by Phase-Switched Scavenging Using a Modular Flow Reactor Process
C.D. Smith, I.R. Baxendale, G.K. Tranmer, M. Baumann, S.C. Smith, R.A. Lewthwaite and S.V. Ley, Org. Biomol. Chem., 2007, 5, 1562-1568.
http://pubs.rsc.org/en/content/articlelanding/2007/ob/b703033a/unauth#!divAbstract
New USP Requirements on Plastic Packaging Systems
DRUG REGULATORY AFFAIRS INTERNATIONAL

New USP Requirements on Plastic Packaging Systems |
| The USP describes in an article of the Pharmacopeial Forum the future requirements for plastic packaging systems. Here, the importance is laid on the selection of suitable, safe plastic materials and the verification of potential interactions. More information can be found here in the News. |
GMP News: New USP Requirements on Plastic Packaging Systems
An interesting article from the USP on the future requirements for plastic packaging systems has been published in the Pharmacopoeial Forum 39(6).
In this article, the USP’s experts group provides an overview of the already existing and also the planned General Chapters on pharmaceutical plastic packaging systems. Together both chapters aim to describe a general and chemistry-based approach for the quality and safety of packaging systems and their starting materials for the construction of these packaging systems.
Among the key topics which are discussed, you can find:
- a. The…
View original post 160 more words
Ламотрижин, Lamotrigine an antiepileptic

| Patent No | Expiry Date | |
|---|---|---|
| 5698226*PED | Jul 29, 2012 |
Lamotrigine /ləˈmoʊtrɨˌdʒiːn/, marketed in most of the world as Lamictal /ləˈmɪktəl/ by GlaxoSmithKline, is an anticonvulsant drug used in the treatment of epilepsy and bipolar disorder. It is also used off-label as an adjunct in treating clinical depression.[1] For epilepsy, it is used to treat focal seizures, primary and secondary tonic-clonic seizures, and seizures associated with Lennox-Gastaut syndrome.
Like many other anticonvulsant medications, lamotrigine also seems to act as an effective mood stabilizer, and has been the first US Food and Drug Administration (FDA)-approved drug for this purpose since lithium, a drug approved almost 30 years earlier.
It is approved for the maintenance treatment of bipolar type I. Chemically unrelated to other anticonvulsants (due to lamotrigine being a phenyltriazine), lamotrigine has many possible side-effects.
Lamotrigine is generally accepted to be a member of the sodium channel blocking class of antiepileptic drugs,[2] but it could have additional actions since it has a broader spectrum of action than other sodium channel antiepileptic drugs such as phenytoin and carbamazepine and is effective in the treatment of the depressed phase of bipolar disorder, where as other sodium channel blocking antiepileptic drugs are not.
In addition, lamotrigine shares few side-effects with other, unrelated anticonvulsants known to inhibit sodium channels, which further emphasises its unique properties.[3] Lamotrigine is inactivated by hepatic glucuronidation.[4]
Ламотрижин (Lamotrigine)
UV – range
IR – spectrum
Reference
-
UV and IR Spectra. H.-W. Dibbern, R.M. Muller, E. Wirbitzki, 2002 ECV
-
NIST / EPA / NIH Mass Spectral Library 2008
-
Handbook of Organic Compounds. NIR, IR, Raman, and UV-Vis Spectra Featuring Polymers and Surfactants, Jr., Jerry Workman. Academic Press, 2000.
-
Handbook of ultraviolet and visible absorption spectra of organic compounds, K. Hirayama. Plenum Press Data Division, 1967.
Brief background information
| Salt | ATC | Formula | MM | CAS |
|---|---|---|---|---|
| – | N03AX09 | C9H7Cl2N5 | 256.10 g / mol | 84057-84-1 |
Application
-
anticonvulsant
-
ingibitor glutamat
-
Lamotrigine is the common name for 3,5-diamino-6-(2,3-dichlorophenyl)-1,2,4-triazine which is a commercially marketed, pharmaceutically active substance known to be useful for the treatment of epilepsy and bipolar disorder. Lamotrigine (Formula I. below) has an empirical formula of C9H7N5Cl2 and a molecular weight of 256.09.
-
Lamotrigine is currently available in its anhydrous crystalline form which is characterized by the X-ray Powder Diffraction (XRD) spectrum shown in Figure 2.
-
Lamotrigine and its pharmaceutically acceptable acid addition salts are generally described in U.S. Patent No. 4,560,687 (“the ‘687 patent”). The ‘687 patent, however, provides no examples for preparing lamotrigine.
-
U.S. Patent No. 4,602,017 (“the `017 patent”) discloses a process for preparing lamotrigine by cyclizing the intermediate 2-(2,3-dichlorophenyl)-2-guanidinylimino acetonitrile (Formula VI, below) by refluxing it in an alkanol in the presence of a strong base. The product is then treated with ice water, stirred for 30 minutes, filtered, and recrystallized to produce a residue, which is treated with isopropanol to yield lamotrigine. The process described in the ‘017 patent for preparing lamotrigine is illustrated in Scheme 1.
-
Various references disclose other different processes for producing lamotrigine. For example, WO 00/35888 discloses a process for preparing the intermediate of Formula IV, and describes preparing lamotrigine using this intermediate by a process similar to the one shown in Scheme 1 but using, in the last step, an aqueous solution of potassium hydroxide instead of the methanolic solution.
-
U.S. Patent No. 5,912,345 discloses cyclizing the intermediate of Formula VI using ultraviolet or visible radiation and heating to reflux temperature.
-
WO 01/49669 discloses the reaction of intermediates of Formula IV and Formula V to give intermediate Formula VI using sulfuric acid and p-toluenesulfonic acid. Cyclization is then performed by refluxing in an aliphatic alkanol in the presence of a base. The obtained lamotrigine is then purified by recrystallization or chromatographic separation to produce lamotrigine with a purity of 99.70 (calculated by HPLC).
-
U.S. Patent No. 5,925,755 discloses preparing lamotrigine from 6-(2,3-dichlorophenyl)-5-chloro-3-thiomethyl-1,2,4-triazine that has been dissolved in ethanol saturated with ammonia gas, by heating in a sealed glass tube in an autoclave at 180° C/1930 kPa for 72 hours followed by recrystallizing from methanol.
-
Lamotrigine is known to form solvates with different alcohols. For example, according to an article published in 1989 by Robert W. Janes et al- in Acta Cryst. (1989), C45, 129-132, entitled “Structure of Lamotrigine Methanol Solvate: 3,5-Diamino-6-(2,3-dichlorophenyl)-1,2,4-triazine-Methanol, A Novel Anticonvulsant Drug,” the crystal structure of a sample of “lamotrigine methanol solvate” was provided by the Wellcome Research Laboratories, UK, and a second form of lamotrigine was crystallized from absolute ethanol. According toEP 0 800 520 B 1, published on October 15, 1997, “lamotrigine ethanolate” can be obtained by crystallization of lamotrigine from ethanol (see Examples 5 and 6). Similarly, EP 0 021 121 teaches that “lamotrigine isoproponate” can be obtained by recrystallization from isopropanol (see Example 1). Lamotrigine alcohol solvates can be dried to yield anhydrous lamotrigine. For example, WO 96/20935 describes the drying and recystallization from methanol of anhydrous lamotrigine having a meriting point of 218° C (see Example 6).
-
Most of the known processes for preparing lamotrigine do so only in low yields and by using drastic conditions (e.g., temperature and pressure) or by using dangerous reagents or expensive equipment. Moreover, the known processes only describe preparing lamotrigine as a crude product that is then purified by recrystallization from a solvent and fail to disclose any other processes for purifying lamotrigine.
Synthesis pathway
Trade names
| Country | Trade name | Manufacturer |
|---|---|---|
| Germany | Elmendos | GlaxoSmithKline |
| Lamictal | -»- | |
| various generic drugs | ||
| France | Lamikstart | GlaxoSmithKline |
| Lamictal | Novartis | |
| UK | -»- | GlaxoSmithKline |
| Italy | -»- | -»- |
| United States | -»- | -»- |
| Ukraine | Lamictal | GlaxoSmithKline Pharmaceuticals SA, Poland |
| Herolamyk | Gerota Farmatseutika GmbH (manufacturer responsible for batch release), Austria Deksel Ltd., Israel |
|
| Lamotrin | OOO «Pharma Home» Ukraine | |
| Lamitrin | Farmasayns Inc., Canada | |
| various generic drugs | ||
Formulations
-
Tablets 5 mg, 25 mg, 50 mg, 100 mg, 200 mg
Reference
-
Синтез a)
-
US 4 602 017 (Wellcome; 22.7.1986; appl. 27.2.1984; prior. 15.9.1981, 29.5.1980; GB-prior. 1.6.1979).
-
US 4 847 249 (Wellcome; 11.7.1989; appl. 29.5.1987; GB-prior. 30.5.1986).
-
EP 21 121 (Wellcome; appl. 30.5.1980; GB-prior. 1.6.1979).
-
EP 59 987 (Wellcome; appl. 30.5.1980; GB-prior. 1.6.1979).
-
WO 2 008 019 798 (Lonza; 21.02.2008; USA-prior. 17.11.2006; EP-prior. 14.8.2006).
-
-
Синтез b)
-
US 6 683 182 (Helm AG; 27.1.2004; appl. 9.10.2003; PCT-prior. 4.7.2002; DE-prior. 17.7.2001).
-
EP 1 311 492 (Helm AG; appl. 4.7.2002; DE-prior. 17.7.2001).
-

http://www.google.com/patents/EP2128145A2?cl=en


EXAMPLES
-
[0047]The following examples are for illustrative purposes only and are not intended, nor should they be interpreted to, limit the scope of the invention.
General Experimental Conditions:I. HPLC Assay Method:
-
[0048]The chromatographic separation was carried out at room temperature (20-25° C) using a Lichrosphere RP-select B, 5 µm,4.0 x 250 mm I.D. column.
-
[0049]The mobile phase was prepared by mixing 320 mL of acetonitrile with 680 mL of buffer (pH = 5.6) prepared from 3.85 g of ammonium acetate dissolved in 1000 mL of water and by adjusting the pH to 5.6 with glacial acetic acid. The mobile phase was mixed and filtered through a 0.22 µm nylon filter under vacuum.
-
[0050]The chromatograph was equipped with a 306 nm detector, and the flow rate was 1.0 mL per minute. Test samples (20 µL) were prepared by dissolving the appropriate amount of sample in order to obtain 1 mg/mL of acetonitrile.
Example 1: Preparation of 3,5-diamino-6-(2,3-dichlorophenyl)-1,2,4-triazineStep 1. Preparation of Lamotrigine
-
[0051]In a 800 L reactor, 38 kg of 2-(2,3-dichlorophenyl)-2-guanidinyliminoacetonitrile (0.148 kmoles) and 298 kg of isopropanol were combined. The mixture was then heated to reflux temperature (approximately 82° C) and maintained at 82 ± 3° C for 6 hours. Thereafter, the mixture was cooled to 20-25° C and stirred for 1 hour at this temperature. The suspension was then filtered and washed with 8 kg of isopropanol.
Step 2. Removal of Mechanical Impurities
-
[0052]The crude lamotrigine obtained in Step I and 335 kg of deionized water were combined in the 800 L reactor, and the temperature was adjusted to between 35 and 40° C. Methanesulfonic acid was then added to the mixture until the pH was between 1.5 and 2.0 while maintaining the temperature between 35 to 40° C. The resulting aqueous solution of lamotrigine methane sulfonate was then filtered, and the filter and reactor were washed with 4 kg of deionized water.
-
[0053]The solution of lamotrigine methanesulfonate was then added to the 800 L reactor, and the pH was adjusted to 6.5 to 7.5 by adding a 50% solution of sodium hydroxide. Next, the temperature was adjusted at 20 to 25° C, and the mixture was stirred at this temperature for 1 hour. Thereafter, the suspension was filtered and washed with 20 kg of deionized water followed by 8 kg of methanol, to obtain wet lamotrigine monohydrate.
Step 3. Conversion of Lamotrigine Hydrate to Anhydrous Lamotrigine
-
[0054]In the 800 L reactor, the wet lamotrigine hydrate obtained in Step 2 and 255 kg of filtered methanol were combined, and the mixture was heated to reflux temperature. The mixture was then cooled to 20-25° C and stirred at this temperature for 1 hour. Thereafter, the suspension was filtered and washed with 8 kg of methanol.
-
[0055]The wet product obtained was dried under vacuum for 16 hours at 85 ± 5° C and then was milled and sieved (500 µm to yield 29.11 kg (0.114 kmoles) of lamotrigine (Yield: 76.8%; Purity (HPLC analysis): 99.9%; Melting Point = 216° C).
Example 2: Preparation of Lamotrigine Monohydrate
-
[0056]Lamotrigine (46 g) and 460 mL of deionized water were combined, and the temperature of the mixture was adjusted at 3 5 to 40° C. Initially, the pH of the mixture was 4.11. Methanesulfonic acid was then added to the mixture until the pH was 1.4 while maintaining the temperature of the mixture at or below 30° C. A light, opaline solution was obtained following addition of the methanesulfonic acid. The obtained solution of lamotrigine methanesulfonate was then filtered and the filter was washed with 4.6 mL of deionized water.
-
[0057]The pH of the solution of lamotrigine methanesulfonate was next adjusted to 6.8-7.2 by adding a 50% solution of sodium hydroxide while maintaining the temperature at or below 30° C. The temperature was then adjusted to between 20° C and 25° C, and the mixture was stirred at this temperature for 1 hour. Thereafter, the suspension was filtered, and the obtained product was washed with deionized water and dried at 40° C to yield 49.23 g of lamotrigine monohydrate. Analysis: titration (perchloric acid): 99.23%; purity (HPLC analysis): 99%; Water (Karl Fischer) = 6.68%.
……………………………………
Example 6: Preparation of lamotrigine
The 6- (2,3, -dichlorophenyl) -5-chloro-3-thiomethyl-
1, 2,4-triazine prepared in Example 5 was dissolved in ethanol (100 ml) saturated with ammonia gas and heated in a sealed glass tube in an autoclave at 180°C/1930 kPa
(280 p.s.i.) for 72 hours.
The total contents of the tube was evaporated down to give a dark brown crude product. The crude product was recrystallised from methanol and identified as compound (I) , 3, 5-diamino-6- (2,3-dichlorophenyl) -1-2,4-triazine
(lamotrigine) by TLC (Rf = 0.20) . Melting point = 218°C.
http://www.google.com/patents/WO1996020935A1?cl=en
……………….
3,5-diamino-6-(2,3-dichlorophenyl)-1,2,4-triazine of the Formula (I)
also known as lamotrigine, is the active ingredient of several pharmaceutical compositions used for the treatment of different diseases of the central nervous system (e.g. epilepsy).
The synthesis of substituted 3,5-diamino-1,2,4-triazine derivatives is known from the literature. In the following publications the general synthesis of substituted derivatives is described—Agr. Res. Serif. 3 188 (1966) and J. Med. Chem. 859 (1972)—according to which benzoyl cyanide is reacted with aminoguanidine in acidic medium and the so obtained adduct is cyclized under basic conditions. According to the process described in the European Patent No. 21121—analogously to the method described above—2,3-dichlorobenzoyl cyanide is reacted with the hydrogencarbonate salt of aminoguanidine in dimethyl sulfoxide as solvent, in the presence of 8 N nitric acid for 7 days. The obtained adduct is cyclized with methanolic potassium-hydroxide solution to the final product in 15% yield—calculated on the starting material. Basically similar process is described in the European Patent No. 142306. The disadvantages of the above processes are the extremely aggressive reaction medium, the long reaction time as well as the very low yield.
The European Patent No. 247842 describes a process in which 8 M solution of sulfuric acid is used instead of 8 N nitric acid in the condensation reaction, and the reaction time is 48 h. The cyclization reaction is carried out in n-propanol at reflux temperature. The yield is 41%. The disadvantages of this process are the low yield and the aggressive reaction medium.
Basically similar process is described in the U.S. Pat. No. 6,111,101, in which the condensation is carried out in a mixture of diluted sulfuric acid and acetonitrile for 60 h, then the cyclization is carried out with 1% aqueous potassium hydroxide solution. The yield is 44%. The crude product is purified by recrystallization from methanol with the help of clarifier. The disadvantages of the process are the aggressive medium, the low yield and the very long reaction time.
The modification of the above process is described in the European Patent No. 963980, in which the cyclization reaction is carried out in n-propanol at reflux temperature. The yield is 60%. The product is purified by recrystallization from n-propano 1. The disadvantages of this process are also the long reaction time and the aggressive reaction medium.
According to the International Patent Application No. WO96120934 an intermediate, which is prepared with great difficulty, is converted into lamotrigine by cyclizing in a photo-chemical reactor in 80% yield. The disadvantage of the process is that it can not be applied on industrial scale.
The International Patent Application No. WO96120935 describes a six-step synthesis, which is difficult to carry out and hardly realizable on industrial scale, as well as the yield of the final product is very low. The disadvantages of the process are the complicated synthesis, the applied hazardous reagents and the low yield.
http://www.google.com/patents/US7390899
EXAMPLE 23,5-diamino-6-(2,3-diehlorophenyl)-1,2,4-triazine
A suspension of 24.0 g of methanesulfonic acid and 21.0 g (0.079 mol) of aminoguanidine dimesylate is warmed to 65-70° C. in a 500 ml round bottom flask, equipped with a stirrer, a thermometer and a dropping funnel. The mixture becomes homogenous after 15 min, then a solution of 12.0 g (0.06 mol) of 2,3-dichlorobenzoyl cyanide in 10 ml of acetonitrile is added dropwise. The obtained mixture is stirred at 65-70° C. for 1 h. A mixture of 9 g (0.223 mol) of magnesium oxide and 60 ml of water is stirred for 5 min and the obtained suspension is added to the reaction mixture over a period of 10 min.
The temperature of the reaction mixture is raised to 70° C. and kept at this temperature for 3 h. The hot reaction mixture is filtered, 90 ml of water is added to the filtrate and concentrated. 60 ml of water is added to the residue, the suspension is stirred at 0-5° C., then filtered off. The product is washed with water and dried at 60-70° C. to yield 14.3 g (93.1%) of the crude title compound. Melting point: 212-216° C.
EXAMPLE 3Crystallization of 3,5-diamino-6-(2,3-diehlorophenyl)-1,2,4-triazine
10 g of 3,5-diamino-6-(2,3-dichlorophenyl)-1,2,4-triazine is dissolved in 400 ml of acetone at reflux temperature, then 0.5 g of charcoal is added and the mixture is refluxed for 5 min. The clarifier is filtered off and the filtrate is cooled to 0-5° C. The precipitated crystals are filtered off and dried at 90° C. in vacuum to yield 7.0 g (70%) of the product. Melting point: 215-219° C.
………………………………………….
Lamotrigine 3,5-diamino-6-(2,3-dichlorophenyl)-l,2,4-triazine, is an antiepileptic drug, and its analogues were first disclosed in British Patent No. 759,014 (1956). Subsequently, Lamotrigine and its analogues were described in Canadian Patent Nos. 1,112,643 and 1,133,938, and in United States Patent No. 4,602,017. Processes for the preparation of Lamotrigine are also disclosed in international publications and patents WO 96/20934, WO 96/20935, WO 00/35888 and European Patent No. 963,980.
Lamotrigine 1
The process (as disclosed in Canadian Patent Nos. 1,112,643 and 1,133,938, United States Patent No. 4,602,017 and in British Patent No. 759,014) for the preparation of Lamotrigine involves reaction of 2,3-dichlorobenzoyl cyanide 2 and aminoguanidine bicarbonate in dimethylsulfoxide and 8N aqueous nitric acid (scheme 1). The above process uses drastic conditions (20 eq. 8N HNO3), excess reagents and requires 7 days for completion of the reaction. The overall yield of the process from 2,3-dichlorobenzoyl cyanide is 15.6%.
Scheme 1
2. MeOH, KOH, heat Lamotrigine 1 15.6% yield
The process reported in WO 00/35888 for this reaction uses H2S04 instead of 8N HNO3. However, it also suffers from lower yield (40%) and longer reaction time (2.5 days). The process also uses a large excess (-11 times) of sulfuric acid.
It is accordingly an object of the present invention to provide an improved process for the manufacture of lamotrigine which overcome the problems associated with poor efficiency described in the prior art. More broadly, it is an object of the present invention to provide novel processes for the production of 3,5-diamino-6-substituted-l,2,4-triazines.
SUMMARY OF THE INVENTION
In accordance with one aspect of the present invention, there is provided a process for the manufacture of an intermediate compound of formula IV
formula IV useful for manufacturing 3,5-diamino-6-substituted-l,2,4-triazines, wherein R is an optionally substituted C1-C4 alkyl or aryl group, which process comprises reacting a compound of formula II:
formula II
with aminoguanidine in the presence of an acid in an organic solvent under anhydrous conditions followed by treatment with a dehydrating reagent.
In accordance with another aspect of the present invention there is provided a process for the manufacture of 3,5-diamino-6-substituted-l,2,4-triazines of formula I:
formula I
comprising the steps of:
(a) reacting a compound of formula (II):
formula II
with aminoguanidine salts, or equivalent thereof, in the presence of an acid in an organic solvent under anhydrous conditions to form a cyanohydrin of formula III:
formula III
(b) dehydrating the cyanohydrin of formula III to form a compound of formula IV by treatment with a dehydrating reagent,
formula IV
and
(c) cyclization of the compound of formula IV into a 3,5-diamino-6- substituted-l,2,4-triazine of compound of formula I or into a hydrated form thereof.
Suitably the substituted Ci-Q alkyl group is methyl, ethyl, propyl or butyl and the substituted aryl group is preferably 2,3-dichlorophenyl.
The process of the present invention provides a high yielding and cost- effective process for the preparation of 3,5-diamino-6-substituted-l,2,4- triazines in general and Lamotrigine in particular. This result is obtained through the use of an additive, namely a dehydrating agent, such as thionyl chloride, POCI3 or PCI5, and by employing organic acid in combination with a polar organic solvent, which stabilizes the cyanohydrin of formula III. The cyanohydrin of formula III upon addition of a dehydrating agent affords the intermediate iminoguanidine of formula IV (scheme 2). The acid used in this process can be dry organosulfonic acids such as methanesulfonic acid or para-toluenesulfonic acid, either in combination with dry polar organic solvents, such as dimethylformamide (DMF), N-methyl-2- pyrrolidinone (NMP) or dimethylsulfoxide (DMSO), or combinations of a polar solvent with nonpolar solvents such as tetrahydrofuran (THF). The dehydrating reagents used in the process can be SOCl2, POCI3 or PCI5, oxalyl chloride, phosgene or equivalents thereof.
Scheme 2
dehydration ,
f
ormula II formula III
cyclisation
formula IV
The process, as shown in Scheme 2, involves the reaction of aryl cyanide, preferably 2,3-dichlorobenzoyl cyanide 2 (in which R = 2,3-dichlorophenyl), with an organic acid, for example para-toluenesulfonic acid or methanesulfonic acid, and dry organic solvents, for example DMSO, NMP or DMF, at suitable temperatures to form an intermediate of formula III. The reaction mixture is treated with dehydrates for example SOCl2, POCI3 or PCI5, oxalyl chloride, phosgene or equivalent thereof at a suitable temperature to form the iminoguanidine of formula IV. The iminoguanidine salt in the reaction mixture is cyclized upon basification and heating. The in inoguanidine salt can be basified and isolated by filtration. The isolated iminoguanidine can be cyclized to form Lamotrigine using a base (such as NaOH, NH3 or KOH) in a protic solvent (such as methanol, ethanol, isopropanol or water). Lamotrigine 1 can be isolated as the monohydrate when the cyclization of the intermediate is carried out using base and isopropanol/ water mixture or NMP/ water. The lamotrigine monohydrate is a new compound and is further characterized in having the following peaks in powder X-ray diffraction pattern at an angle of two theta (2Θ) is found to be: 10.34, 11.53, 12.46, 13.36, 13.86, 14.15, 14.94, 16.43, 16.65, 17.44, 17.97, 18.77, 18.91, 19.11, 19.52, 20.58, 22.11, 22.31, 23.09, 23.61, 24.18, 24.99, 25.52, 26.31, 26.83, 27.68, 28.53, 29.07, 29.24, 29.86, 30.09, 30.63, 31.01, 31.37, 31.78, 32.82, 33.25, 34.35, 34.96, 36.23, 36.92, 37.97, 38.60, 38.90. The positions of the peaks in powder X-ray diffraction pattern studies of anhydrous lamotrigine at an angle of two theta (2Θ) to be 9.80, 11.39, 12,46, 13.29, 13.86, 14.13, 15.62, 16.66, 17.44, 17.97, 19.54, 20.56, 22.30, 22.89, 23.61, 24.81, 25.50, 26.31, 26.74, 27.87, 28.42, 28.86, 29.38, 29.66, 30.95, 31.66, 32.59, 33.23, 33.61, 33.83, 34.21, 35.20, 36.27, 37.16, 37.90, 38.35, 38.92, 39.17, 39.45.
The overall yield of lamotrigine is high (molar yield: 80 – 85%). The above described process is very cost-effective, operationally simple and completed in a short time period (6 to 10 hours).
BRIEF DESCRIPTION OF THE DRAWINGS
Figure 1 is the powder X-ray diffraction pattern of lamotrigine monohydrate.
Figure 2 is a differential scanning calorimetry thermogram (DSC) of lamotrigine monohydrate.
Figure 3 is a Fourier transform infrared spectrum (FTIR) of lamotrigine monohydrate.
Figure 4 is the powder X-ray diffraction pattern of anhydrous lamotrigine. Figure 5 is a differential scanning calorimetry thermogram (DSC) of anhydrous lamotrigine.
Figure 6 is a Fourier transform infrared spectrum (FTIR) of anhydrous lamotrigine.
The following examples serve to illustrate embodiments of the present invention in a manner in which they can be practiced but, as such, should not be considered in a limiting sense.
EXAMPLES
Procedure I
To a round bottomed flask was added aminoguanidine hydrochloride (116.1 g, 1.05 mol) and dimethylformamide (900 mL). To this mixture was added methanesulfonic acid (130.4 g, 1.36 mol) followed by adding 2,3- dichlorobenzoylcyanide (150.0 g, 0.75 mol). The reaction mixture was stirred for 1 hour and then the dehydrating reagent, thionyl chloride, (45.2g, 0.38 mol) was added. The reaction mixture was stirred for another hour and then basified with KOH solution (4N). The precipitate was filtered and washed with water.
Yield: 401.3 g damp cake (KF = 39.2%).
Analytically pure sample of the intermediate is prepared as following:
20.0 g of the damp cake was suspended in 60 ml MeOH and stirred at room temperature for 3 hours. The solid was filtered and dried in vacuum at room temperature to give 5.4 g analytic pure iminoguanidine as a yellow solid.
m.p.: 179 ~ 180° C (corrected).
MS (m/z): 256.3 [M+] IR: 3491.8; 3457.1 (Amine N-H stretching); 2207.5 (CN stretching); 1681.9 (Imine C=N stretching); 1055.5 (Caryi-Cl stretching).
Η-NMR (300 MHz, DMSO-D6): 7.66 (ad, J = 7.9 Hz, 2H), 7.41 (dd, J = 7.9; 7.9 Hz, 1H), 6.70 (br s, NH2).
^C-NMR (75 MHz, DMSO-D6): 163.6, 135.3, 132.4, 130.0, 129.5, 129.0, 128.2, 114.4, 113.8.
Elemental analysis: C H N
Calculated: 42.21 2.76 27.35
Found: 42.10 2.49 27.69
Procedure II:
A round bottomed flask was charged with iminoguanidine (401.3 g from procedure I), isopropanol (1000.0 ml) and KOH (85%, 12.0 g, 0.18 mol). The reaction mixture was refluxed for 3 hours. Isopropanol was distilled and water (800 ml) was added. The reaction mixture was stirred for 3 hours, the solid was filtered and washed with water. The damp cake is dried under vacuum to yield 168.5 grams of lamotrigine monohydrate as crystalline solid (82% based on 2,3-dichlorobenzoyl cyanide).
Procedure III (without isolation of intermediate of formula IV):
To a round bottomed flask was added aminoguanidine hydrochloride (116.1 g, 1.05 mol) and dimethylformamide (900 ml). To this mixture was added methanesulfonic acid (130.4 g, 1.36 mol) followed by 2,3-dichlorobenzoyl cyanide (150.0 g, 0.75 mol). The reaction mixture was stirred for 1 hour and then dehydrating reagent thionyl chloride (45.2g, 0.38 mol) was added slowly. The reaction mixture was stirred for another hour and then basified with KOH solution (4 N). The Reaction mixture was heated under reflux (100 ~ 105° C) for 3 ~ 4 hours and cooled slowly to room temperature. The solid was filtered and washed with water. After drying, 160.7g of lamotrigine monohydrate as a crystalline solid (78% based on 2,3-dichlorobenzoyl cyanide) was obtained.
See also FIG. 1, 2, 3.
Karl Fischer (water content): 5.92 – 6.03%
DSC: 106.86, 216.65° C (onset).
MS (m/z): 256.3 [M+]
IR: 3496.9; 3450.3; 3338.5; 3211.0; 1658.7; 1524.0; 1328.8; 1027.1.
iH-NMR (300 MHz, DMSO-D6): 7.66 (ad, J = 7.9 Hz, 2H), 7.41 (dd, J = 7.9; 7.9 Hz, 1H), 6.70 (br s, NH2).
13C-NMR (75 MHz, DMSO-D6): 163.6, 135.3, 132.4, 130.0, 129.5, 129.0, 128.2, 114.4, 113.8.
Procedure IV (preparation of anhydrous lamotrigine from lamotrigine monohydrate):
150 g lamotrigine monohydrate (from procedure II or III) was recrystallized in 900 mL isopropanol giving 132 g (94%) of anhydrous lamotrigine as a crystalline solid.
See also FIG. 4, 5, 6.
m.p.: 216 – 217° C (corrected).
MS (m/z): 256.3 [M+]
Η-NMR (300 MHz, DMSO-D6): 7.69 (dd, J = 1.7; 7.9 Hz, 1H), 7.43 (dd, J = 7.9; 7.6 Hz, 1H), 7.35 (dd, J = 1.7; 7.6 Hz, 1H), 6.70 (br s, NH2), 6.44 (br s, NH2).
13C-NMR (75 MHz, DMSO-D6): 162.1, 154.1, 138.3, 136.8, 132.0, 131.6, 130.6, 128.5. Elemental analysis: C H N
Calculated: 42.21 2.76 27.35
Found: 42.10 2.58 27.46
http://www.google.com/patents/WO2003078407A1?cl=en
 |
|
 |
|
| Systematic (IUPAC) name | |
|---|---|
| 6-(2,3-Dichlorophenyl)-1,2,4-triazine-3,5-diamine | |
| Clinical data | |
| Trade names | Lamictal |
| AHFS/Drugs.com | monograph |
| MedlinePlus | a695007 |
| Licence data | US FDA:link |
| Pregnancy cat. | |
| Legal status | |
| Routes | Oral |
| Pharmacokinetic data | |
| Bioavailability | 98% |
| Protein binding | 55% |
| Metabolism | Hepatic (mostly UGT1A4-mediated) |
| Half-life | 29 hours |
| Excretion | Urine (65%), faeces (2%) |
| Identifiers | |
| CAS number | 84057-84-1 |
| ATC code | N03AX09 |
| PubChem | CID 3878 |
| IUPHAR ligand | 2622 |
| DrugBank | DB00555 |
| ChemSpider | 3741 |
| UNII | U3H27498KS |
| KEGG | D00354 |
| ChEBI | CHEBI:6367 |
| ChEMBL | CHEMBL741 |
| Chemical data | |
| Formula | C9H7Cl2N5 |
| Mol. mass | 256.091 g/mol |
History
- December 1994 — Lamotrigine was approved for the treatment of partial seizures.[5]
- August 1998 — for use as adjunctive treatment of Lennox-Gastaut syndrome in pediatric and adult patients, new dosage form: chewable dispersible tablets.
- December 1998 — for use as monotherapy for treatment of partial seizures in adult patients when converting from a single enzyme-inducing anti-epileptic drug (EIAED).
- January 2003 — for use as adjunctive therapy for partial seizures in pediatric patients as young as two years of age.
- June 2003 — approved for maintenance treatment of Bipolar I disorder; the first such medication since lithium.[10]
- January 2004 — for use as monotherapy for treatment of partial seizures in adult patients when converting from the anti-epileptic drug valproate [including valproic acid (Depakene); sodium valproate (Epilim) and divalproex sodium (Depakote)].
Availability
GlaxoSmithKline’s trademarked brand of lamotrigine, Lamictal, is manufactured in scored tablets (25 mg, 50 mg, 100 mg, 150 mg and 200 mg) and chewable dispersible tablets (2 mg, 5 mg and 25 mg). Five-week sample kits are also available; these include titration [66]instructions and scored tablets (25 mg for patients taking valproate, 25 mg and 100 mg for patients not taking valproate). Lamotrigine is also available in un-scored tablet form. In 2005, Teva Pharmaceutical Industries Ltd. began selling generic lamotrigine in the United States, but only in 5 mg and 25 mg chewable dispersible tablets.[67] On 23 July 2008 Teva began offering the full line of generic lamotrigine in the US.[68]Lamotrigine is also available in generic form[69] in the United States, the United Kingdom, Canada and Australia. It should be noted that brand name Lamictal is not available in 200 mg tablets in Canada, at all registered pharmacies (while 25, 100, and 150 mg are all offered). Starter kits are also not available in Canada.
Lamotrigine is marketed as Lamotrine in Egypt, Lamitrin in Bangladesh [1], Lamictin in South Africa, למוג’ין (Lamogine)[70] in Israel, and 라믹탈 in South Korea and generally named as Lamitor.
Lamictal XR
In 2009 GlaxoSmithKline received FDA Approval for an extended-release version of lamotrigine branded Lamictal XR.[71] Lamictal XR tablets are a novel preparation of lamotrigine, delivered in a tablet with an enteric coating that GlaxoSmithKline has branded DiffCORE. The extended release formulation is analogous to the instant release version, such that treatment may begin without titration[66] or recalibration of the dosage.
References
- ^ Jump up to:a b Barbosa L, Berk M, Vorster M (April 2003). “A double-blind, randomised, placebo-controlled trial of augmentation with lamotrigine or placebo in patients concomitantly treated with fluoxetine for resistant major depressive episodes”. J Clin Psychiatry 64 (4): 403–7. doi:10.4088/JCP.v64n0407. PMID 12716240.
- Jump up^ Rogawski MA, Löscher W (July 2004). “The neurobiology of antiepileptic drugs”. Nat Rev Neurosci 5 (7): 553–564. doi:10.1038/nrn1430. PMID 15208697.
- Jump up^ Lees G, Leach MJ (May 1993). “Studies on the mechanism of action of the novel anticonvulsant lamotrigine (Lamictal) using primary neurological cultures from rat cortex”.Brain Research 612 (1–2): 190–9. doi:10.1016/0006-8993(93)91660-K.PMID 7687190.
- Jump up^ Werz MA (October 2008). “Pharmacotherapeutics of epilepsy: use of lamotrigine and expectations for lamotrigine extended release”. Ther Clin Risk Manag 4 (5): 1035–46.doi:10.2147/TCRM.S3343. PMID 19209284.
- ^ Jump up to:a b anonymous (19 March 2004). “EFFICACY SUPPLEMENTS APPROVED IN CALENDAR YEAR 2003”. FDA/Center for Drug Evaluation and Research. Retrieved 2008-04-09.
- Jump up^ Kasper, D (2005). Fauci AS, Braunwald E, et al, ed. eds. Harrison’s Principles of Internal Medicine, 16th ed. McGraw-Hill. pp. 3–22. ISBN 9780071466332.
- Jump up^ Tierny, LM Jr (2006). McPhee SJ, Papadakis MA, ed. Current Medical Diagnosis and Treatment, 45th ed. McGraw-Hill. ISBN 0071454101.
- Jump up^ French JA, Kanner AM, Bautista J, et al. (April 2004). “Efficacy and tolerability of the new antiepileptic drugs II: treatment of refractory epilepsy: report of the Therapeutics and Technology Assessment Subcommittee and Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society”. Neurology 62 (8): 1261–73. doi:10.1212/01.WNL.0000123695.22623.32. PMID 15111660.
- Jump up^ Pellock JM (November 1999). “Managing pediatric epilepsy syndromes with new antiepileptic drugs”. Pediatrics 104 (5 Pt 1): 1106–16. doi:10.1542/peds.104.5.1106.PMID 10545555.
- ^ Jump up to:a b GlaxoSmithKline, 2003
- ^ Jump up to:a b Ghaemi, S.N., Shirzadi, A.A., Filkowski, M. (2008). “Publication Bias and the Pharmaceutical Industry: The Case of Lamotrigine in Bipolar Disorder”. Medscape J Med10 (9): 211. PMC 2580079. PMID 19008973.
- Jump up^ Goldberg JF, Calabrese JR, Saville BR, Frye MA, Ketter TA, Suppes T, Post RM, Goodwin FK. (2009). “Mood stabilization and destabilization during acute and continuation phase treatment for bipolar I disorder with lamotrigine or placebo”. Clinical Psychiatry 70(9): 1273–80. doi:10.4088/JCP.08m04381. PMID 19689918.
- Jump up^ Goldsmith DR, Wagstaff AJ, Ibbotson T, Perry CM (2003). “Lamotrigine: a review of its use in bipolar disorder”. Drugs 63 (19): 2029–50. doi:10.2165/00003495-200363190-00009. PMID 12962521.
- Jump up^ Geddes JR (May 2011). “Treatment of bipolar disorder”. = Lancet 11 (9878): 1672–82.doi:10.1016/S0140-6736(13)60857-0. PMID 23663953.
- Jump up^ “Acute Treatment — Formula and Implementation of a Treatment Plan”. Practice Guideline for the Treatment of Patients With Bipolar Disorder Second Edition. American Psychiatric Association. Retrieved 15 August 2010.
- Jump up^ “Main page”. Practice Guideline for the Treatment of Patients With Bipolar Disorder Second Edition. American Psychiatric Association. Retrieved 15 August 2010.
- Jump up^ Calabrese JR, Huffman RF, White RL, Edwards S, Thompson TR, Ascher JA, Monaghan ET, Leadbetter RA (2008). “Lamotrigine in the acute treatment of bipolar depression: results of five double-blind, placebo-controlled clinical trials”. Bipolar disorders 10 (2): 323–333. doi:10.1111/j.1399-5618.2007.00500.x. PMID 18271912.
- Jump up^ Calabrese JR, Geddes JR, Goodwin GM (2009). “Lamotrigine for treatment of bipolar depression: independent meta-analysis and meta-regression of individual patient data from five randomised trials”. British Journal of Psychiatry 194 (1): 4–9.doi:10.1192/bjp.bp.107.048504. PMID 19118318.
- Jump up^ Reid, JG; Gitlin MJ; Altshuler LL (July 2013). “Lamotrigine in psychiatric disorders”. J Clin Psychiatry 74 (7): 675–84. doi:10.4088/JCP.12r08046. PMID 23945444.
- Jump up^ Backonja M (June 2004). “Neuromodulating drugs for the symptomatic treatment of neuropathic pain”. Curr Pain Headache Rep 8 (3): 212–6. doi:10.1007/s11916-004-0054-4. PMID 15115640.
- Jump up^ Jensen, T. S. (2002). “Anticonvulsants in neuropathic pain: Rationale and clinical evidence”. European Journal of Pain 6: 61–68. doi:10.1053/eujp.2001.0324.PMID 11888243.
- Jump up^ Pappagallo M (October 2003). “Newer antiepileptic drugs: possible uses in the treatment of neuropathic pain and migraine”. Clin Ther 25 (10): 2506–38. doi:10.1016/S0149-2918(03)80314-4. PMID 14667954.
- Jump up^ Medford, N. (2005). “Understanding and treating depersonalisation disorder”. Advances in Psychiatric Treatment 11 (2): 92–100. doi:10.1192/apt.11.2.92.
- Jump up^ Hermle, L.; Simon, M.; Ruchsow, M.; Geppert, M. (2012). “Hallucinogen-persisting perception disorder”. Therapeutic Advances in Psychopharmacology 2 (5): 199–205.doi:10.1177/2045125312451270. PMC 3736944. PMID 23983976.
- Jump up^ Erfurth, A.; Walden, J. O. R.; Grunze, H. (1998). “Lamotrigine in the Treatment of Schizoaffective Disorder”. Neuropsychobiology 38 (3): 204–205. doi:10.1159/000026540.PMID 9778612.
- Jump up^ Lieb, K.; Völlm, B.; Rücker, G.; Timmer, A.; Stoffers, J. M. (2009). “Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials”. The British Journal of Psychiatry 196 (1): 4–12. doi:10.1192/bjp.bp.108.062984.PMID 20044651.
- Jump up^ Stein, D. J.; Zungu-Dirwayi, N.; Van Der Linden, G. J. H.; Seedat, S. (2000). “Pharmacotherapy for post traumatic stress disorder (PTSD)”. In Stein, Dan. “Cochrane Database of Systematic Reviews”. doi:10.1002/14651858.CD002795.
- Jump up^ Öncü, B; Er, O; Çolak, B; Nutt, DJ (Mar 2014). “Lamotrigine for attention deficit-hyperactivity disorder comorbid with mood disorders: a case series.”. Journal of psychopharmacology (Oxford, England) 28 (3): 282–3. PMID 23784736.
- Jump up^ Hancock EC, Cross JH. (2013). “Treatment of Lennox-Gastaut syndrome.”. Cochrane Database of Systematic Reviews (2). doi:10.1002/14651858.CD003277.pub3.
- ^ Jump up to:a b c d e “Lamictal Prescribing Information” (PDF). GlaxoSmithKline. May 2007. Retrieved 2008-04-09.
- Jump up^ Serrani Azcurra, DJ (Jun 2012). “Lamotrigine rechallenge after a skin rash. A combined study of open cases and a meta-analysis.”. Revista de psiquiatria y salud mental 6 (4): 144–9. doi:10.1016/j.rpsm.2012.04.002. PMID 23084805.
- ^ Jump up to:a b c http://www.drugs.com/monograph/lamotrigine.html
- ^ Jump up to:a b c unknown, unknown. National Institute of Healthhttp://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=d7e3572d-56fe-4727-2bb4-013ccca22678#nlm34070-3. Retrieved 8 May 2014. Missing or empty
|title=(help) - Jump up^ Nicholson, R J; Kelly, K P; Grant, I S (25 February 1995). “Leucopenia associated with lamotrigine”. BMJ. Retrieved 16 June 2010.
- Jump up^ Lamotrigine does not prolong QTc in a thorough QT/QTc study in healthy subjectsDixon, Ruth; Job, S., Oliver, R., Tompson, D., Wright, J. G., Maltby, K., Lorch, U. and Taubel, J. (2008). (July 2008). “Lamotrigine does not prolong QTc in a thorough QT/QTc study in healthy subjects”. Br J Clin Pharmacol 2008 66 (3): 396–404.doi:10.1111/j.1365-2125.2008.03250.x.
- Jump up^ Motomura, E; Tanii, H; Usami, A; Ohoyama, K; Nakagawa, M; Okada, M (March 2012). “Lamotrigine-Induced Neuroleptic Malignant Syndrome Under Risperidone Treatment: A Case Report”. The Journal of Neuropsychiatry and Clinical Neurosciences 24 (2): E38-E39.doi:10.1176/appi.neuropsych.11040093. PMID 22772697.
- Jump up^ Ishioka, M; Yasui-Furukori, N; Hashimoto, K; Sugawara, N (July–August 2013). “Neuroleptic malignant syndrome induced by lamotrigine.”. Clinical Neuropharmacology 36(4): 131–132. doi:10.1097/WNF.0b013e318294799a. PMID 23783003.
- ^ Jump up to:a b c d unknown, unknown. “Lamictal”. National Institute of Health. Retrieved 8 May 2014.
- Jump up^ Reimers A, A; Helde G; Brodtkorb E (September 2005). “Ethinyl estradiol, not progestogens, reduces lamotrigine serum concentrations”. Epilepsia (Blackwell Science) 46(9): 1414–7. doi:10.1111/j.1528-1167.2005.10105.x. PMID 16146436.
- ^ Jump up to:a b Sidhu J, J; Job S; Singh S; Philipson R (February 2006). “The pharmacokinetic and pharmacodynamic consequences of the co-administration of lamotrigine and a combined oral contraceptive in healthy female subjects”. Br J Clin Pharmacol. 61 (2): 191–9.doi:10.1111/j.1365-2125.2005.02539.x. PMC 1885007. PMID 16433873.
- Jump up^ FDA: Safety Alerts: Lamotrigine
- Jump up^ Berwaerts, K; Sienaert P; De Fruyt J (2009). “Teratogenic effects of lamotrigine in women with bipolar disorder”. Tijdschr Psychiatr (in Dutch) 51 (10): 741–50.PMID 19821242.
- Jump up^ Prakash; Prabhu LV, Nasar MA et al. (October 2007). “Lamotrigine in pregnancy: safety profile and the risk of malformations”. Singapore Med J 48 (10): 880–3. PMID 17909669.
- Jump up^ McVearry, KM; Gaillard WD; VanMeter J; Meador KJ (December 2009). “A prospective study of cognitive fluency and originality in children exposed in utero to carbamazepine, lamotrigine, or valproate monotherapy”. Epilepsy Behav 16 (4): 609–16.doi:10.1016/j.yebeh.2009.09.024. PMID 19892603.
- Jump up^ Hale, TW (2008). Medications and Mothers’ Milk (13th ed.). Hale Publishing. p. 532.ISBN 978-0-9815257-2-3.
- Jump up^ anonymous. “Lamictal, Warnings & Precautions”. RxList Inc. Retrieved 2008-04-09.
- Jump up^ “The mechanisms by which AEDs affect cognition and the measures to prevent the adverse effects in immature rats”.
- Jump up^ Glaxo Smith Klein Clinical Study Register, Study No. LAM40120: Lamotrigine (Lamictal®) Treatment in adults with Attention Deficit Hyperactivity Disorder (ADHD), A pilot study
- Jump up^ Oncü B, Er O, Colak B, Nutt DJ (2014). “Lamotrigine for attention deficit-hyperactivity disorder comorbid with mood disorders: a case series.”. J Psychopharmacol 28 (3): 282–3.doi:10.1177/0269881113493365. PMID 23784736.
- Jump up^ Foldvary, N; Perry M, Lee J et al. (December 2001). “The effects of lamotrigine on sleep in patients with epilepsy”. Epilepsia 42 (12): 1569–73. doi:10.1046/j.1528-1157.2001.46100.x. PMID 11879368.
- Jump up^ Bonanni, E; Galli R, Gori S et al. (June 2001). “Neurophysiological evaluation of vigilance in epileptic patients on monotherapy with lamotrigine”. Clin Neurophysiol 112 (6): 1018–22. doi:10.1016/S1388-2457(01)00537-5. PMID 11377260.
- Jump up^ Placidi, F; Marciani MG, Diomedi M et al. (August 2000). “Effects of lamotrigine on nocturnal sleep, daytime somnolence and cognitive functions in focal epilepsy”. Acta Neurol Scand 102 (2): 81–6. doi:10.1034/j.1600-0404.2000.102002081.x.PMID 10949523.
- Jump up^ Sadler, M (March 1999). “Lamotrigine associated with insomnia”. Epilepsia 40 (3): 322–5.doi:10.1111/j.1528-1157.1999.tb00712.x. PMID 10080513.
- Jump up^ http://www.ehealthme.com/ds/lamictal/myoclonic+jerks Retrieved August 19, 2010. Myoclonic Jerk in the use of Lamictal.
- Jump up^ Rogawski, M (2002). “Chapter 1: Principles of antiepileptic drug action”. In Levy RH, Mattson RH, Meldrum BS, Perucca E. Antiepileptic Drugs, Fifth Edition. Lippincott Williams & Wilkins. pp. 3–22. ISBN 9780781723213.
- Jump up^ Thomas, SP; Nandhra HS; Jayaraman A (April 2010). “Systematic review of lamotrigine augmentation of treatment resistant unipolar depression (TRD)”. J Ment Health 19 (2): 168–75. doi:10.3109/09638230903469269. PMID 20433324.
- Jump up^ Ketter, TA; Manji HK; Post RM (October 2003). “Potential mechanisms of action of lamotrigine in the treatment of bipolar disorders”. J Clin Psychopharmacol 23 (5): 168–75.doi:10.1097/01.jcp.0000088915.02635.e8. PMID 14520126.
- Jump up^ Braga, MF; Aroniadou-Anderjaska V; Post RM; Li H (March 2002). “. Lamotrigine reduces spontaneous and evoked GABAA receptor-mediated synaptic transmission in the basolateral amygdala: implications for its effects in seizure and affective disorders”.Neuropharmacology 42 (4): 522–9. doi:10.1016/s0028-3908(01)00198-8.PMID 11955522.
- Jump up^ Shiah, IS; Yatham LN; Gau YC; Baker GB (May 2003). “. Potential mechanisms of action of lamotrigine in the treatment of bipolar disorders”. Prog Neuropsychopharmacol Biol Psychiatry 27 (3): 419–23. doi:10.1016/S0278-5846(03)00028-9. PMID 12691776.
- Jump up^ Southam, E; Kirkby D; Higgins GA; Hagan RM (Sep 1998). “Lamotrigine inhibits monoamine uptake in vitro and modulates 5-hydroxytryptamine uptake in rats”. Eur J Pharmacol 25 (358(1)): 19–24. PMID 9809864.
- ^ Jump up to:a b “LAMICTAL (lamotrigine) tablet”. Daily Med. U.S. National Library of Medicine. Retrieved 2013-12-26.
- Jump up^ Ramsay RE, Pellock JM, Garnett WR, et al. (1991). “Pharmacokinetics and safety of lamotrigine (Lamictal) in patients with epilepsy”. Epilepsy Res. 10 (2–3): 191–200.doi:10.1016/0920-1211(91)90012-5. PMID 1817959.
- Jump up^ Cohen, AF; Land GS; Breimer DD; Yuen WC; Winton C; Peck AW (Nov 1987). “Lamotrigine, a new anticonvulsant: pharmacokinetics in normal humans”. Clin Pharmacol Ther 42 (5): 535–41. PMID 3677542.
- Jump up^ Goa, KL; Ross SR; Chrisp P (Jul 1993). “A review of its pharmacological properties and clinical efficacy in epilepsy”. Drugs 46 (1): 152–76. doi:10.2165/00003495-199346010-00009. PMID 7691504.
- Jump up^ Anderson, GD (May 1998). “A mechanistic approach to antiepileptic drug interactions.”.Pharmacother 32 (5): 554–63. doi:10.1345/aph.17332. PMID 9606477.
- ^ Jump up to:a b In medicine, titration is the process of gradually adjusting the dose of a medication until optimal results are reached.
- Jump up^ anonymous (17 February 2005). “Press Release, Teva Announces Settlement Of Lamictal Litigation With Glaxosmithkline”. Teva Pharmaceutical Industries Ltd. Retrieved 2008-04-09.
- Jump up^ http://www.tevapharm.com/pr/2008/pr_779.asp
- Jump up^ anonymous (2 March 2005). “Treatment for epilepsy: generic lamotrigine”. Department of Health (UK). Retrieved 2008-04-09.
- Jump up^ anonymous (2007). “LAMOTRIGINE”. http://www.drug.co.il. Retrieved 2008-04-14.
- Jump up^ Waknine Y (2009). “FDA Approves Extended-Release Lamotrigine for Adjunctive Treatment of Epilepsy”. MedScape. Retrieved 2010-05-18.
External links
- FAQ: Psychiatric Uses of Lamotrigine (Lamictal), by Ivan K. Goldberg, MD. Includes many references from the medical literature.
- Center for Drug Evaluation and Research: Lamictal — documents related to the FDA approval process, including medical reviews and correspondence letters.
- Epilepsy South Africa: MEDICATION FOR EPILEPSY — an Epilepsy FAQ with a list of medicines for treatment thereof, includes lamotrigine with South African trade name Lamictin
- Adverse Reactions — Reported adverse reactions and side-effects.
- U.S. National Library of Medicine: Drug Information Portal — Lamotrigine
| Cited Patent | Filing date | Publication date | Applicant | Title | |
|---|---|---|---|---|---|
| EP0021121A1 | May 30, 1980 | Jan 7, 1981 | The Wellcome Foundation Limited | 1,2,4-Triazine derivatives, process for preparing such compounds and pharmaceutical compositions containing them | |
| EP0800520B1 | Dec 29, 1995 | Jun 19, 2002 | The Wellcome Foundation Limited | Process for the preparation of lamotrigine | |
| US4560687 | Mar 5, 1984 | Dec 24, 1985 | Baxter Martin G | Substituted aromatic compounds | |
| US4602017 | Feb 27, 1984 | Jul 22, 1986 | Sawyer David A | Substituted aromatic compounds | |
| US5912345 | Dec 29, 1995 | Jun 15, 1999 | Glaxo Wellcome Inc. | Process for the preparation of lamotrigine | |
| US5925755 | Dec 29, 1995 | Jul 20, 1999 | Glaxo Wellcome Inc. | Process for the preparation of lamotrigine | |
| US60834821 | Title not available | ||||
| WO1996020935A1 | Dec 29, 1995 | Jul 11, 1996 | Grahame Roy Lee | Process for the preparation of lamotrigine | |
| WO1997000681A1 * | Jun 20, 1996 | Jan 9, 1997 | Alison Green Floyd | Pharmaceutical composition containing lamotrigine | |
| WO2000035888A1 | Dec 7, 1999 | Jun 22, 2000 | Sharad Kumar Vyas | An improved process for the preparation of 3,5-diamino-6-(2,3-dichlorophenyl)-1,2,4-triazine | |
| WO2001049669A1 | Jan 3, 2000 | Jul 12, 2001 | Tarur Venkatasub Radhakrishnan | A process for the preparation of 6-(2,3-dichlorophenyl)-1,2,4-triazine-3,5-diamine, commonly known as lamotrigine | |
| WO2002068398A1 * | Feb 27, 2002 | Sep 6, 2002 | Judith Aronhime | New crystal forms of lamotrigine and processes for their preparations | |
| WO2003078407A1 * | Dec 18, 2002 | Sep 25, 2003 | Brantford Chem Inc | A new and efficient process for the preparation of lamotrigine and related 3,5-diamino-6-substituted-1,2,4-triazines | |
| WO2005003104A2 * | Jun 28, 2004 | Jan 13, 2005 | Jubilant Organosys Ltd | Crystalline forms of lamotrigine monohydrate and anhydrous lamotrigine and a process for their preparation | |
| WO2009061513A1 * | Nov 10, 2008 | May 14, 2009 | Miranda L Cheney | Crystalline forms of lamotrigine |
| Reference | ||
|---|---|---|
| 1 | * | KUBICKI, M. ET AL: “Hydrogen bonding patterns in 3,5-diamino-6-aryl triazines” JOURNAL OF MOLECULAR STRUCTURE , 570(1-3), 53-60 CODEN: JMOSB4; ISSN: 0022-2860, 2001, XP002545066 |
| 2 | ROBERT W. JANES ACTA CRYST. vol. C45, 1989, pages 129 – 132 | |
SURAMIN

Suramin
A polyanionic compound with an unknown mechanism of action. It is used parenterally in the treatment of African trypanosomiasis and it has been used clinically with diethylcarbamazine to kill the adult Onchocerca. (From AMA Drug Evaluations Annual, 1992, p1643) It has also been shown to have potent antineoplastic properties.
A polyanionic compound with an unknown mechanism of action. It is used parenterally in the treatment of African trypanosomiasis and it has been used clinically with diethylcarbamazine to kill the adult Onchocerca. (From AMA Drug Evaluations Annual, 1992, p1643) It has also been shown to have potent antineoplastic properties. Suramin is manufactured by Bayer in Germany as Germanin®.
Also known as: Naphuride, Germanin, Naganol, Belganyl, Fourneau, Farma, Antrypol, Suramine, Naganin
8,8′-{Carbonylbis[imino-3,1-phenylenecarbonylimino(4-methyl-3,1-phenylene)carbonylimino]}di(1,3,5-naphthalenetrisulfonic acid) …FREE FORM
8,8′-[Ureylenebis[m-phenylenecarbonylimino(4-methyl-m-phenylene)carbonylimino]]di(1,3,5-naphthalenetrisulfonic acid) hexasodium salt
CAS 145-63-1 FREE FORM
129-46-4 of hexa sodium
LAUNCHED 1940 BAYER
| Formula | C51H40N6O23S6 |
|---|---|
| Mol. mass | 1297.29 |
The molecular formula of suramin is C51H34N6O23S6. It is a symmetric molecule in the center of which lies urea, NH-CO-NH. Suramin contains eightbenzene rings, four of which are fused in pairs (naphthalene), four amide groups in addition to the one of urea and six sulfonate groups. When given as drug it usually contains six sodium ions that form a salt with the six sulfonate groups.
Suramin is a drug developed by Oskar Dressel and Richard Kothe of Bayer, Germany in 1916, and is still sold by Bayer under the brand nameGermanin.
Suramin sodium is a heparanase inhibitor that was first launched in 1940 by Bayer under the brand name Antrypol for the treatment of helminthic infection. It was later launched by Bayer for the treatment of trypanosomiasis (African sleeping sickness).
More recently, the product has entered early clinical development at Ohio State University for the treatment of platinum-pretreated patients with stage IIIB/IV non-small cell lung cancer, in combination with docetaxel or gemcitabine.
The National Cancer Institute (NCI) is conducting phase II clinical studies for the treatment of glioblastoma multiforme and for the treatment of adrenocortical carcinoma.
According to the National Cancer Institute there are no active clinical trials (as of April 1, 2008). Completed and closed clinical trials are listed here:[1]
In addition to Germanin, the National Cancer Institute also lists the following “Foreign brand names”: 309 F or 309 Fourneau,[1] Bayer 205, Moranyl, Naganin, Naganine.

It is used for treatment of human sleeping sickness caused by trypanosomes.[2]
It has been used in the treatment of onchocerciasis.[3]
It has been investigated as treatment for prostate cancer.[4]
Also, suramin as treatment for autism is being evaluated. [5]
Suramin is administered by a single weekly intravenous injection for six weeks. The dose per injection is 1 g.
The most frequent adverse reactions are nausea and vomiting. About 90% of patients will get an urticarial rash that disappears in a few days without needing to stop treatment. There is a greater than 50% chance of adrenal cortical damage, but only a smaller proportion will require lifelongcorticosteroid replacement. It is common for patients to get a tingling or crawling sensation of the skin with suramin. Suramin will cause clouding of the urine which is harmless: patients should be warned of this to avoid them becoming alarmed.
Kidney damage and exfoliative dermatitis occur less commonly.
Suramin has been applied clinically to HIV/AIDS patients resulting in a significant number of fatal occurrences and as a result the application of this molecule was abandoned for this condition. http://www.ncbi.nlm.nih.gov/pubmed/3548350
Suramin is also used in research as a broad-spectrum antagonist of P2 receptors[6][7] and agonist of Ryanodine receptors.[8]
![ChemSpider 2D Image | 8,8'-{Carbonylbis[imino-3,1-phenylenecarbonylimino(4-methyl-3,1-phenylene)carbonylimino]}di(1,3,5-naphthalenetrisulfonic acid) | C51H40N6O23S6](https://images-blogger-opensocial.googleusercontent.com/gadgets/proxy?url=http%3A%2F%2Fwww.chemspider.com%2FImagesHandler.ashx%3Fid%3D5168%26w%3D200%26h%3D200&container=blogger&gadget=a&rewriteMime=image%2F*)
Its effect on telomerase has been investigated.[9]
It may have some activity against RNA viruses.[10]
In addition to antagonism of P2 receptors, Suramin inhibits the acitivation of heterotrimeric G proteins in a variety of other GPCRs with varying potency. It prevents the association of heteromeric G proteins and therefore the receptors Guanine exchange functionality (GEF). With this blockade the GDP will not release from the Gα subunit so it can not be replaced by a GTP and become activated. This has the effect of blocking downstream G protein mediated signaling of various GPCR proteins including Rhodopsin, the A1 Adenosine receptor, and the D2 dopamine receptor.[11]
A polyanionic compound with an unknown mechanism of action. It is used parenterally in the treatment of African trypanosomiasis and it has been used clinically with diethylcarbamazine to kill the adult Onchocerca. (From AMA Drug Evaluations Annual, 1992, p1643) It has also been shown to have potent antineoplastic properties. Suramin is manufactured by Bayer in Germany as Germanin®.
|
8-1-2012 |
InCl3-catalysed synthesis of 2-aryl quinazolin-4(3H)-ones and 5-aryl pyrazolo[4,3-d]pyrimidin-7(6H)-ones and their evaluation as potential anticancer agents. |
Bioorganic & medicinal chemistry letters |
|
9-1-2012 |
Identification of a sirtuin 3 inhibitor that displays selectivity over sirtuin 1 and 2. |
European journal of medicinal chemistry |
|
1-1-2013 |
Inhibition of the human deacylase Sirtuin 5 by the indole GW5074. |
Bioorganic & medicinal chemistry letters |
|
5-9-2013 |
Discovery of thieno[3,2-d]pyrimidine-6-carboxamides as potent inhibitors of SIRT1, SIRT2, and SIRT3. |
Journal of medicinal chemistry |
- The formula of suramin was kept secret by Bayer for commercial reasons. But it was elucidated and published in 1924 by Fourneau and his team of the Pasteur Institute, and it is only on this date that its exact chemical composition was known. (E. Fourneau, J. and Th. Tréfouël and J. Vallée (1924). “Sur une nouvelle série de médicaments trypanocides”, C. R. Séances Acad. Sci. 178: 675.)
- Darsaud A, Chevrier C, Bourdon L, Dumas M, Buguet A, Bouteille B (January 2004). “Megazol combined with suramin improves a new diagnosis index of the early meningo-encephalitic phase of experimental African trypanosomiasis”. Trop. Med. Int. Health 9 (1): 83–91.doi:10.1046/j.1365-3156.2003.01154.x. PMID 14728611.
- Anderson J, Fuglsang H (July 1978). “Further studies on the treatment of ocular onchocerciasis with diethylcarbamazine and suramin”. Br J Ophthalmol 62 (7): 450–7.doi:10.1136/bjo.62.7.450. PMC 1043255. PMID 678497.
- Ahles TA, Herndon JE, Small EJ, et al. (November 2004). “Quality of life impact of three different doses of suramin in patients with metastatic hormone-refractory prostate carcinoma: results of Intergroup O159/Cancer and Leukemia Group B 9480”. Cancer 101 (10): 2202–8.doi:10.1002/cncr.20655. PMID 15484217.
- http://medicalxpress.com/news/2013-03-drug-treatment-autism-symptoms-mouse.html
- Abbracchio MP, Burnstock G, Boeynaems JM, Barnard EA, Boyer JL, Kennedy C, Knight GE, Fumagalli M, Gachet C, Jacobson KA, Weisman GA. (september 2006). “International Union of Pharmacology LVIII: update on the P2Y G protein-coupled nucleotide receptors: from molecular mechanisms and pathophysiology to therapy”. Pharmacol Rev. 58 (3): 281–341.doi:10.1124/pr.58.3.3. PMID 16968944.
- Khakh BS, Burnstock G, Kennedy C, King BF, North RA, Séguéla P, Voigt M, Humphrey PP. (march 2001). “International union of pharmacology. XXIV. Current status of the nomenclature and properties of P2X receptors and their subunits”. Pharmacol Rev. 53 (1): 107–118.PMID 11171941.
- Wolner I, Kassack MU, Ullmann H, Karel A, Hohenegger M (October 2005). “Use-dependent inhibition of the skeletal muscle ryanodine receptor by the suramin analogue NF676”. Br. J. Pharmacol. 146 (4): 525–33. doi:10.1038/sj.bjp.0706359. PMC 1751178.PMID 16056233.
- Erguven M, Akev N, Ozdemir A, Karabulut E, Bilir A (August 2008). “The inhibitory effect of suramin on telomerase activity and spheroid growth of C6 glioma cells”. Med. Sci. Monit. 14(8): BR165–73. PMID 18667993.
- Mastrangelo E, Pezzullo M, Tarantino D, Petazzi R, Germani F, Kramer D, Robel I, Rohayem J, Bolognesi M, Milani M (2012) Structure-based inhibition of norovirus RNA-dependent RNA-polymerases. J Mol Biol
- Beindl W, Mitterauer T, Hohenegger M, Ijzerman AP, Nanoff C, Freissmuth M. (August 1996).“Inhibition of receptor/G protein coupling by suramin analogues”. ol. Pharmacology. 50 (2): 415–23. PMID 8700151.
- Drugs Fut 1986, 11(10): 860
- WO 2012159107
- WO 2012087336
- US 2011257109
- WO 2009022897
- WO 2009020613
- WO 2008094027
- EP 0486809
- US 5158940
- US 5173509
- WO 1993007864
- WO 1994008574
SURAMIN
- Suramin bound to proteins in the PDB
- Drug information
- Suramin, drug information by JBC Online
- Suramin in treating patients with recurrent bladder cancer
- National Cancer Institute
Enterovirus-71 (EV71) is one of the major causative reagents for hand-foot-and-mouth disease. In particular, EV71 causes severe central nervous system infections and leads to numerous dead cases. Although several inactivated whole-virus vaccines have entered in clinical trials, no antiviral agent has been provided for clinical therapy. In the present work, we screened our compound library and identified that suramin, which has been clinically used to treat variable diseases, could inhibit EV71 proliferation with an IC50 value of 40μM. We further revealed that suramin could block the attachment of EV71 to host cells to regulate the early stage of EV71 infection, as well as affected other steps of EV71 life cycle. Our results are helpful to understand the mechanism for EV71 life cycle and provide a potential for the usage of an approved drug, suramin, as the antiviral against EV71 infection.
- Suramin Hexasodium
- 129-46-4
Synonyms
- 309 F
- Antrypol
- BAY 205
- Bayer 205
- CI-1003
- EINECS 204-949-3
- Fourneau 309
- Germanin
- Moranyl
- Naganin
- Naganine
- Naganinum
- Naganol
- Naphuride sodium
- NF060
- NSC 34936
- SK 24728
- Sodium suramin
- Suramin Hexasodium
- Suramin sodium
- Suramina sodica
- Suramina sodica [INN-Spanish]
- Suramine sodique
- Suramine sodique [INN-French]
- Suramine sodium
- Suraminum natricum
- Suraminum natricum [INN-Latin]
- UNII-89521262IH
Suramin Sodium, is an anticancer agent with a wide variety of activities.
Recently suramin was shown to inhibit FSH binding to its receptor (Daugherty, R. L.; Cockett, A. T. K.; Schoen, S. R. and Sluss, P. M. “Suramin inhibits gonadotropon action in rat testis: implications for treatment of advanced prostate cancer” J. Urol. 1992, 147, 727-732).
This activity causes, at least in part, the decrease in testosterone production seen in rats and humans that were administered suramin(Danesi, R.; La Rocca, R. V.; Cooper, M. R.; Ricciardi, M. P.; Pellegrini, A.; Soldani, P.; Kragel, P. J.; Paparelli, A.; Del Tacca, M.; Myers, C. E, “Clinical and experimental evidence of inhibition of testosterone production by suramin.” J. Clin. Endocrinol. Metab. 1996, 81, 2238-2246).
Suramin is the only non-peptidic small molecule that has been reported to be an FSH receptor binding antagonist.
Suramin is 8,8′ – (carbonylbis(imino-3,1-phenylenecarbonylimino (4-methyl-3,1-phenylene) carbonylimino)) bis-1,3 ,5-naphthalenetrisulfonic acid (GB Patent No. 224849). This polyanionic compound has been used for many decades as a prophylactic and therapeutic agent for try- panosomiasis. It was subsequently shown that suramin is able to block the activity of a variety of proteins like cellular and viral enzymes and growth factors (Mitsuya, M. et al. Science 226 : 172 (1984), Hosang, M. J. Cell. Biochem. 29 : 265 (1985), De Clercq, E. Cancer Lett. 8 : 9 (1979)).
![]()
|
5-32-1977 |
Complement inhibitors |
|
|
5-25-1977 |
Aromatic amidines as antiviral agents in animals |
|
|
5-4-1977 |
Complement inhibitors |
|
|
5-4-1977 |
Complement inhibitors |
|
|
4-27-1977 |
Cyclodextrin sulfate salts as complement inhibitors |
|
|
4-20-1977 |
Ureylenebis methyl-phenylene-carbonyl-bis-dihydro-2-oxo-naphthoxazine disultonic acids |
|
|
3-30-1977 |
Water treatment for controlling the growth of algae employing biguanides |
|
|
3-2-1977 |
Isoxazole substituted nitroimidazoles |
|
|
2-16-1977 |
Amidophenyl-azo-naphthalenesulfonic complement inhibitors and method of use thereof |
|
|
2-9-1977 |
Complement inhibitors |
|
2-10-2011 |
MODULATION OF HUMAN MAST CELL ACTIVATION MODULATION OF HUMAN MAST CELL ACTIVATION |
|
|
11-18-2010 |
Admixtures for inorganic binders based on a hydrogenated disaccharide, inorganic binders containing these admixtures and process for their preparation Admixtures for inorganic binders based on a hydrogenated disaccharide, inorganic binders containing these admixtures and process for their preparation |
|
|
10-28-2010 |
THERAPEUTIC INHIBITORS OF VASCULAR SMOOTH MUSCLE CELLS |
|
|
9-9-2010 |
APPARATUS FOR USING ELECTROPORATION MEDIATED DELIVERY OF DRUGS AND GENES |
|
|
4-8-2010 |
PREPARATION AND USE OF SULFATED OLIGOSACCHARIDES |
|
|
10-29-2009 |
THERAPEUTIC INHIBITOR OF VASCULAR SMOOTH MUSCLE CELLS THERAPEUTIC INHIBITOR OF VASCULAR SMOOTH MUSCLE CELLS |
|
|
8-20-2009 |
METHOD OF MAKING MINERAL FIBRES METHOD OF MAKING MINERAL FIBRES |
|
|
6-25-2009 |
OXYGEN-FUEL BOOST REFORMER PROCESS AND APPARATUS |
|
|
4-23-2009 |
METHODS OF TREATING VASCULAR DISEASE WITH TNF ANTAGONISTS METHODS OF TREATING VASCULAR DISEASE WITH TNF ANTAGONISTS |
|
|
3-26-2009 |
COPOLYMER COMPOSITIONS FOR ORAL DELIVERY |
|
5-3-1978 |
1,3,5- Or 1,3,6-naphthalenetriyltris(sulfonylimino)aryl acids and salts |
|
|
3-22-1978 |
Nitroimidazoles |
|
|
2-15-1978 |
Treatment of rheumatoid arthritis and related diseases |
|
|
1-4-1978 |
AROMATIC AMIDINES AS ANTIVIRAL AGENTS IN ANIMALS |
|
|
1-4-1978 |
Malto-dextrin poly(H-)sulfates |
|
|
12-14-1977 |
Disazo compounds useful as complement inhibitors |
|
|
12-7-1977 |
Bis-substituted naphthalene-azo phenyleneazo-stilbene-disulfonic and naphthalene-sulfonic acid |
|
|
9-28-1977 |
UREIDOPHENYLENEBIS(CARBONYLIMINO)DINAPHTHALENETRISULFONIC ACID COMPOUNDS |
|
|
9-21-1977 |
Substituted bisnaphthylazo diphenyl ureido complement inhibitors |
|
|
9-7-1977 |
Substituted-hydroxy-naphthalenedisulfonic acid compounds |
|
1-12-1977 |
Complement inhibitors |
|
|
12-22-1976 |
Complement inhibitors |
|
|
10-13-1976 |
Complement inhibitors |
![]()
| EP0183352A2 * | Sep 27, 1985 | Jun 4, 1986 | THE UNITED STATES OF AMERICA as represented by the Secretary United States Department of Commerce | Use of suramin for clinical treatment of infection with any of the members of the family of human-t-cell leukemia (htvl) viruses including lymphadenopathy virus (lav) |
| EP0205077A2 * | Jun 3, 1986 | Dec 17, 1986 | Bayer Ag | Suramin sodium for use as an immunostimulant |
![]()
| EP0515523A1 * | Feb 13, 1991 | Dec 2, 1992 | THE UNITED STATES OF AMERICA as represented by the Secretary United States Department of Commerce | Use of suramin to treat rheumatologic diseases |
| EP0755254A1 * | Mar 24, 1995 | Jan 29, 1997 | The Trustees Of The University Of Pennsylvania | Prevention and treatment of ischemia-reperfusion and endotoxin-related injury using adenosine and purino receptor antagonists |
| EP1460087A1 * | Feb 17, 1997 | Sep 22, 2004 | The Kennedy Institute Of Rheumatology | Methods of treating vascular disease with TNF antagonists |
| EP1940376A2 * | Oct 3, 2006 | Jul 9, 2008 | Rottapharm S.P.A. | Use of neboglamine in the treatment of toxicodependency |
| EP1945204A2 * | Oct 27, 2006 | Jul 23, 2008 | Brane Discovery S.R.L. | V-atpase inhibitors for use in the treatment of septic shock |
| US5453444 * | Oct 6, 1994 | Sep 26, 1995 | Otsuka Pharmaceutical Co., Ltd. | Method to mitigate or eliminate weight loss |
| US5534539 * | Jun 12, 1995 | Jul 9, 1996 | Farmitalia Carlo Erba S.R.L. | Biologically active ureido derivatives useful as anit-metastic agenst |
| US5596105 * | Jan 13, 1995 | Jan 21, 1997 | Farmitalia Carlo Erba S.R.L. | Therapeutically active naphthalenesulfonic pyrrolecarboxamido derivatives |
| US7476693 | Mar 26, 2003 | Jan 13, 2009 | Eastern Virginia Medical School | Suramin and derivatives thereof as topical microbicide and contraceptive |
| US7608262 | Feb 16, 1996 | Oct 27, 2009 | The Kennedy Institute Of Rheumatology | Methods of preventing or treating thrombosis with tumor necrosis factor antagonists |
| US8552064 | Dec 19, 2008 | Oct 8, 2013 | Eastern Virginia Medical School | Suramin and derivatives thereof as topical microbicide and contraceptive |
| WO1994008574A1 * | Oct 12, 1993 | Apr 28, 1994 | Otsuka America Pharmaceutical | Treatment of cachexia and inhibition of il-6 activity |
| WO1994010990A1 * | Nov 12, 1993 | May 26, 1994 | British Bio Technology | Inhibition of tnf production |
| WO1997030088A2 * | Feb 17, 1997 | Aug 21, 1997 | Kennedy Inst Of Rheumatology | Methods of treating vascular disease with tnf antagonists |
| WO2004113920A1 * | Jun 18, 2004 | Dec 29, 2004 | Babon Jeff James | Screening method for substances binding to merozoite surface protein-1/42 |
| WO2008138943A2 * | May 14, 2008 | Nov 20, 2008 | Mara Galli | Prophylactic and therapeutic use of sirtuin inhibitors in tnf-alpha mediated pathologies |
| WO2009137471A2 * | May 5, 2009 | Nov 12, 2009 | University Of Miami | Azo dye related small molecule modulators of protein-protein interactions |
| WO2010016628A1 * | Jul 10, 2009 | Feb 11, 2010 | Sammy Opiyo | Conjugated suramin amino compounds for medical conditions |
| WO2012159107A1 * | May 21, 2012 | Nov 22, 2012 | Rhode Island Hospital | Inhibition of renal fibrosis |
Title: Suramin Sodium
CAS Registry Number: 129-46-4
CAS Name: 8,8¢-[Carbonylbis[imino-3,1-phenylenecarbonylimino(4-methyl-3,1-phenylene)carbonylimino]]bis-1,3,5-naphthalenetrisulfonic acid hexasodium salt
Additional Names: hexasodium sym-bis(m-aminobenzoyl-m-amino-p-methylbenzoyl-1-naphthylamino-4,6,8-trisulfonate) carbamide
Manufacturers’ Codes: Bayer 205; Fourneau 309
Trademarks: Antrypol (AstraZeneca); Germanin (Bayer); Moranyl (Specia); Naganol; Naphuride
Molecular Formula: C51H34N6Na6O23S6
Molecular Weight: 1429.17
Percent Composition: C 42.86%, H 2.40%, N 5.88%, Na 9.65%, O 25.75%, S 13.46%
Literature References: Discovered in 1917 by O. Dressel and R. Kothe: J. Dressel, J. Chem. Educ. 38, 620 (1961). Prepn: E. Fourneau et al., Compt. Rend. 178, 675 (1924); J. Trefouel, E. Fourneau, GB 224849 (1923); B. Heymann, Angew. Chem. 37, 585 (1924). Pharmacology, toxicology and clinical antiparasitic activity: F. Hawking, Adv. Pharmacol. Chemother. 15, 289-322 (1978). Inhibition of reverse transcriptase in vitro: E. De Clercq, Cancer Lett. 8, 9 (1979); vs HIV: H. Mitsuya et al., Science 226, 172 (1984). HPLC determn in plasma: R. W. Klecker, J. M. Collins, J. Liq. Chromatogr. 8, 1685 (1985). Pharmacokinetics: J. M. Collins et al., J. Clin. Pharmacol. 26, 22 (1986). Pharmacology and virustatic effect in AIDS: S. Broder et al., Lancet 2, 627 (1985); A. M. Levine et al., Ann. Intern. Med. 105, 32 (1986). Clinical trial in onchocerciasis: H. Schultz-Key et al., Trop. Med. Parasitol. 36, 244 (1985); in prostate cancer: C. Myers et al., J. Clin. Oncol. 10, 881 (1992). Review: Olenick in Antibiotics vol. 3,J. W. Corcoran, F. E. Hahn, Eds. (Springer-Verlag, New York, 1975) pp 699-703; R. La Rocca et al., Cancer Cells 2, 106-115 (1990).
Properties: White or slightly pink or cream-colored powder. Slightly bitter taste. Hygroscopic. Freely sol in water, in physiological saline; sparingly sol in 95% alcohol. Insol in benzene, ether, petr ether, chloroform. Aq solns are neutral to litmus. LD50 in mice (mg/kg): ~620 i.v. (Hawking).
Toxicity data: LD50 in mice (mg/kg): ~620 i.v. (Hawking)
Therap-Cat: Anthelmintic (Nematodes); antiprotozoal (Trypanosoma).
Therap-Cat-Vet: Antiprotozoal (Trypanosoma).
Keywords: Anthelmintic (Nematodes); Antiprotozoal (Trypanosoma); Reverse Transcriptase Inhibitor.

![]()

THANKS AND REGARD’S
DR ANTHONY MELVIN CRASTO Ph.D
GLENMARK SCIENTIST , NAVIMUMBAI, INDIA
did you feel happy, a head to toe paralysed man’s soul in action for you round the clock
need help, email or call me
MOBILE-+91 9323115463
web link
I was paralysed in dec2007, Posts dedicated to my family, my organisation Glenmark, Your readership keeps me going and brings smiles to my family
Summary of Metabolomics
Leaders in Pharmaceutical Business Intelligence Group, LLC, Doing Business As LPBI Group, Newton, MA
Summary of Metabolomics
Author and Curator: Larry H. Bernstein, MD, FCAP
This concludes the series on metabolomics, a rapidly developing science that is interconnected with a group termed – OMICS: proteomics, transcriptomics, genomics, and metabolomics. This chapter is most representative of the many important studies being done in the field, which ranges most widely because it has opened doors into nutrition and nutritional supplements, plant biochemistry, agricultural crops and breeding, animal breeding, worldwide malnutrition, diabetes, cancer, neurosciences, circulatory, respiratory, and musculosletal disorders, infectious diseases and immune system disorders. Obviously, it is not possible to cover the full range of activity, but metabolomics is most comprehensive in exploring the full range of metabolic changes that occur in health during the full age range from development to the geriatric years. It can be integrated well with gene expression, proteomics studies, and epidemiological investigations.
The subchapters are given here:
7.1 Extracellular evaluation of intracellular flux in yeast cells
View original post 1,051 more words

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....










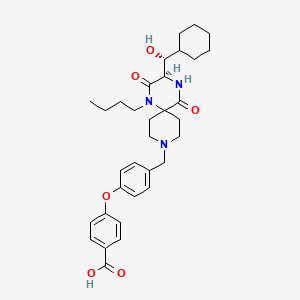


![[1860-5397-9-265-14]](https://i0.wp.com/www.beilstein-journals.org/bjoc/content/figures/1860-5397-9-265-14.png)
![[1860-5397-9-265-i47]](https://i0.wp.com/www.beilstein-journals.org/bjoc/content/inline/1860-5397-9-265-i47.png)





![Chemical structure for Esoxybutynin [INN]](https://pubchem.ncbi.nlm.nih.gov/image/imgsrv.fcgi?t=l&deposited=t&sid=135253519)




























