Home » Posts tagged 'NEW DRUGS' (Page 25)
Tag Archives: NEW DRUGS
Sinovac Reports Preliminary Top-Line Results from Phase III Clinical Trial for EV71 Vaccine Candidate Against Hand, Foot and Mouth Disease

BEIJING, March 14, 2013
Sinovac Biotech Ltd. a leading provider of vaccines in China, announced today preliminary top-line data from its Phase III clinical trial assessing the efficacy, immunogenicity and safety of the Company’s proprietary Enterovirus 71 (“EV71”) vaccine against hand, foot and mouth disease (“HFMD”).
The primary objective of the study was to evaluate the efficacy of the EV71 vaccine in the prevention of HFMD caused by EV71 in infants of 6 to 35 months old. The preliminary Phase III data showed that Sinovac’s EV71 vaccine was 95.4% (95% CI: 87.5%, 98.3%) efficacious against HFMD caused by EV71.
The Phase III trial showed good immunogenicity and safety for Sinovac’s EV71 vaccine. The overall incidence of serious adverse events in this trial was 2.2% among the EV71 candidate vaccine recipients and 2.6% among those receiving a control vaccine during the fourteen months observation period. The difference in rates of serious adverse events (“SAEs”) is not statistically significant. Most of the SAEs were considered unlikely to be vaccine-related.
The double-blinded, randomized, placebo controlled Phase III clinical trial was conducted at three sites across China’s Jiangsu province. Approximately 10,000 healthy infants completed the two dose vaccination schedule (at 0 and 28 days) in the first quarter of 2012, prior to the HFMD epidemic season in China, followed by active monitoring period.
In parallel, Sinovac conducted another clinical study that was comprised of 1,400 volunteers and designed to evaluate the consistency of three consecutive lots of EV71 vaccine manufactured by the Company. The trial was conducted in children from 6 month to 5 years old. After receiving the vaccine, the ratios of neutralizing antibody GMTs on the 56th day of any two groups were calculated and the 95% confidence intervals of the ratios are all between 0.67 and1.5, which indicates the immunogenicity of the three vaccine lots is equivalent. The study results showed consistent immune response for all three lots and a good safety profile. With immunogenicity equivalent across the three consecutive lots, the results showed Sinovac’s vaccine production process and quality are stable.
In March 2008, an EV71 outbreak in Fuyang City of China’s Anhui Province caused 23 fatalities, and attracted significant attention from the government and medical communities. In May 2008, the PRC Ministry of Health identified EV71 as a Class C infectious disease according to prevention and control regulations. EV71 outbreaks have increased over the last five years, with over 1 million cases identified and 500 to 900 reported fatalities each year.
Dr. Weidong Yin , Chairman, President and CEO of Sinovac, commented, “We are excited to report an over 95% efficacy rate from the Phase III trial on our proprietary EV71 vaccine candidate. The conclusion of this trial marks an important milestone in the development of our proprietary vaccine. Hand, foot, and mouth disease continues to represent a significant unmet public health need and economic burden in China, as well as several other Asian countries. Our EV71 vaccine is poised to provide an effective solution to prevent hand, food and mouth disease caused by EV71, a much needed resource given the current limited prevention and EV71 specific treatment methods. At Sinovac, we are committed to our stated mission to develop and supply vaccines to eliminate human diseases.”
Professor Hua Wang, Lead Principal Investigator, stated, “The Phase III study for Sinovac’s EV71 vaccine candidate met its primary objective. The trial results demonstrated that the vaccine is not only safe, but shows significant efficacy in subjects.”
The Company’s next step is to finalize the clinical report, which will become an important part of documents to be filed with the PRC State Food and Drug Administration (“SFDA”) for the application of new drug certificate, GMP certification, and the production license in order to commence the commercial production of the vaccine. In parallel, Sinovac’s dedicated EV71 vaccine manufacturing facility has been completed and is ready for the GMP inspection by SFDA.
Sinovac obtained clinical research approval for its proprietary EV71 vaccine candidate from the SFDA in December 2010, and completed Phase I and II clinical trials in 2011. The preliminary results of the Phase I and Phase II studies confirmed that Sinovac’s vaccine candidate has good safety and immunogenicity profile.
About Sinovac
Sinovac Biotech Ltd. is a China-based biopharmaceutical company that focuses on research, development, manufacturing and commercialization of vaccines that protect against human infectious diseases including hepatitis A and B, seasonal influenza, H5N1 pandemic influenza and mumps, as well as animal rabies vaccine. In 2009, Sinovac was the first company worldwide to receive approval for its H1N1 influenza vaccine, Panflu.1, and has manufactured it for the Chinese Central Government, pursuant to the government-stockpiling program. The Company is also the only supplier of the H5N1 pandemic influenza vaccine to the government-stockpiling program. Sinovac is developing a number of new pipeline vaccines including vaccines for enterovirus 71 (against hand, foot, and mouth disease), pneumococcal conjugate, pneumococcal polysaccharides, varicella and rubella. Sinovac sells its vaccines mainly in China and exports selected vaccines to Mongolia, Nepal, and the Philippines.

A sensor-adaptor mechanism for enterovirus uncoating from structures of EV71
Xiangxi Wang, Wei Peng, Jingshan Ren, Zhongyu Hu, Jiwei Xu, Zhiyong Lou, Xumei Li, Weidong Yin, Xinliang Shen, Claudine Porta, Thomas S Walter, Gwyndaf Evans, Danny Axford, Robin Owen, David J Rowlands, Junzhi Wang*, David I Stuart*, Elizabeth E Fry* & Zihe Rao*
Enterovirus 71 1 (EV71) is a major agent of hand, foot and mouth disease in children that can cause severe central nervous system disease and death. No vaccine or antiviral therapy is available. High-resolution structural analysis of the mature virus and natural empty particles shows that the mature virus is structurally similar to other enteroviruses. In contrast, the empty particles are markedly expanded and resemble elusive enterovirus-uncoating intermediates not previously characterized in atomic detail. Hydrophobic pockets in the EV71 1 capsid are collapsed in this expanded particle, providing a detailed explanation of the mechanism for receptor-binding triggered virus uncoating. These structures provide a model for enterovirus uncoating in which the VP1 1 GH loop acts as an adaptor-sensor for cellular receptor attachment, converting heterologous inputs to a generic uncoating mechanism, highlighting new opportunities for therapeutic intervention. [ Nat Struct Mol Biol. 2012 Mar 4. doi: 10.1038/nsmb.2255. Epub ahead of print. PMID: 22388738 ][ PDF ]
Biogen submits haemophilia A drug to FDA

Mar 14 2013
Biogen Idec has filed the first long-lasting Factor VIII treatment for haemophilia A with the US Food and Drug Administration.
The US biotech major has submitted recombinant factor VIII Fc fusion protein (rFVIIIFc), the first haemophilia A product candidate “in a new class of long-lasting clotting factor therapies being developed with the goal of reducing the burden of treatment for this condition”. If approved, rFVIIIFc will be the first major advance in haemophilia A treatment in more than two decades, Biogen claims.
The regulatory submission is based on results from A-LONG, the largest Phase III study in haemophilia A to date. Glenn Pierce, Biogen’s head of global medical affairs, noted that in that trial, patients were able to inject rFVIIIFc once-weekly to twice-weekly, “which creates the potential for those currently on prophylactic treatment to reduce injections by 50 to 100 per year”. Moreover, patients currently treating bleeding episodes could potentially dose once per week “and maintain significant protection from bleeding with about the same total number of injections each year they use to treat bleeding episodes today”, he added.
Earlier this month, the FDA accepted for review the company’s BLA for its factor IX candidate, rFIXFc, for use in patients with haemophilia B.
Links
Phase III trial of Merck’s Vytorin passes vital safety test
mar 13 2013
Merck & Co’s stock enjoyed a boost yesterday after it revealed it has been given permission to continue a late-stage trial of its cholesterol buster Vytorin.
The Whitehouse Station, New Jersey-based firm must have a breathed a sigh of relief when the Data Safety Monitoring Board issued a green light for the Phase III IMPROVE for a second time, having found no significant safety concerns raised by the data.
After an earlier planned review of data last year, the Board, rather unusually, said it would undertake a second interim analysis at a later date, which had led to some concerns that there may be issues that could lead to the trial being halted, according to media reports.
However, it seems these fears are unfounded at this point, as the18,000-plus patient study – which is designed to determine whether Vytorin is more effective at reducing the risk of heart attack, stroke and death in patients with heart disease than simvastatin alone – has been cleared to conclude.
The drugmaker said the trial should finish in September next year, and it will no doubt be hoping for a positive outcome to prove the benefits of Vytorin – a combination of the generic simvastatin and the still-patented Zetia (ezetimibe) – and breathe a little new life into its heart franchise.
Citi Investment Research analyst Andrew Baum, however, expressed doubt in a research note the final analysis will show Merck’s drug is more effective than generic competition, according to the Associated Press.
 |
|
|---|---|
 |
|
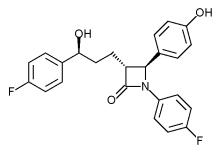
| Combination of | |
| Ezetimibe | via Niemann-Pick C1-Like 1 protein |
| Simvastatin | Statin HMG-CoA reductase inhibitor |
Health Canada approval-aHUS Canada applauds approval of Soliris® (eculizumab) first treatment for fatal, ultra-rare disease affecting children and adults


CAS number 219685-50-4
Soliris is a formulation of eculizumab which is a recombinant humanized monoclonal IgG2/4;κ antibody produced by murine myeloma cell culture and purified by standard bioprocess technology. Eculizumab contains human constant regions from human IgG2 sequences and human IgG4 sequences and murine complementarity-determining regions grafted onto the human framework light- and heavy-chain variable regions. Eculizumab is composed of two 448 amino acid heavy chains and two 214 amino acid light chains and has a molecular weight of approximately 148 kDa.
TORONTO, March 7, 2013
Atypical Hemolytic Uremic Syndrome (aHUS) Canada is thrilled by Health Canada’s recent approval of Soliris® (eculizumab) for the treatment of patients with atypical Hemolytic Uremic Syndrome (aHUS), 1 a very rare, chronic and life-threatening genetic condition affecting fewer than 60 patients in Canada.
aHUS leaves a part of the immune system (known as the complement system) uncontrolled and always active. As a result, the immune system attacks the body’s unhealthy and healthy cells which can cause blood vessel damage, abnormal blood clotting 2,3 and progressive damage to the body’s major organs, leading to heart attack, stroke, kidney failure and death.4
The management of aHUS has relied on plasma infusion and plasma exchange therapies with variable results.5 These lifelong therapies are costly, painful and time-consuming, and have not been studied or approved for the treatment of aHUS.6 If kidney failure has already occurred as a result of aHUS, dialysis is required, though it is not a curative treatment.7 Within a year of diagnosis, over half of patients will need dialysis, will have irreversible kidney damage, or will not survive.6 The majority of patients progress to end-stage kidney failure within three years of diagnosis.8,9
With the approval of Soliris, aHUS patients and their families finally have a reason for hope.
Sonia DeBortoli knows all too well the destructive force of the disease. Sonia’s 11-year-old son Joshua was diagnosed with aHUS in March 2012 and experienced kidney failure, internal bleeding and a blood clot in his groin as a result. He endured several painful hours of daily dialysis and plasma therapy, and was on prednisone and oxygen. Then, a chance to join a clinical trial for Soliris restored Joshua’s health so that he no longer needed the other therapies.
“Our whole world changed when Joshua was given Soliris – we now believe he has a long and healthy future. He is back at school, taking karate lessons and playing soccer,” Sonia says. “We got our little boy back, he got his life back, and we want the same for anyone who has to deal with this rare and devastating disease.”
A groundbreaking treatment advance for aHUS patients
Soliris (eculizumab) is the first and only pharmaceutical treatment for aHUS, and is being hailed by experts worldwide as a critical breakthrough in treating the disease. It has been shown to significantly improve patients’ health and quality of life.10 In clinical trials, Soliris has been proven effective in preventing blood vessel damage and abnormal blood clotting,11,12 leading to remission and significant improvement in kidney function.5,4 Soliris has also allowed patients to discontinue dialysis and plasma exchange therapies.10
Soliris is also indicated, and proven safe and effective, for the treatment of another rare and life-threatening disorder called paroxysmal nocturnal hemoglobinuria (PNH).13 Canadians living with PNH already have access to Soliris through private health insurance and provincial drug plans.
Immediate and sustained access to treatment urgently needed
Now that this new treatment option has been approved for the small number of Canadians living with the devastating symptoms of aHUS, Soliris must be made immediately accessible to all aHUS patients whose lives depend on this treatment.
“We are so hopeful that the Common Drug Review will recognize the urgent need for access to Soliris, and that provincial governments will act swiftly to provide reimbursement to patients who are in urgent need of this life-saving treatment,” says Tracy MacIntyre, a founder of aHUS Canada whose daughter is living with aHUS. “Immediate access to the drug would have a profoundly positive impact on the few Canadians living with aHUS, while any delay in funding treatment could lead to devastating consequences.”
About aHUS Canada
aHUS Canada was formed in November 2012 to support Canadian patients and families living with aHUS. In addition to establishing a Canadian aHUS community, the group is committed to building public awareness and understanding of aHUS and advocating for the best possible care and treatment for patients. For more information, please visit http://www.ahuscanada.org.
Eculizumab (INN and USAN; trade name Soliris®) is a humanized monoclonal antibody that is a first-in-class terminal complement inhibitor and the first therapy approved for the treatment of paroxysmal nocturnal hemoglobinuria (PNH), a rare, progressive, and sometimes life-threatening disease characterized by excessive destruction of red blood cells (hemolysis).[1] It costs £400,000 ($US 600,000) per year per patient.[1]
Eculizumab also is the first agent approved for the treatment of atypical hemolytic uremic syndrome (aHUS), an ultra-rare genetic disease that causes abnormal blood clots to form in small blood vessels throughout the body, leading to kidney failure, damage to other vital organs and premature death.[2][3]
In clinical trials in patients with PNH, eculizumab was associated with reductions in chronic hemolysis, thromboembolic events, and transfusion requirements, as well as improvements in PNH symptoms, quality of life, and survival.[1][4][5][6] Clinical trials in patients with aHUS demonstrated inhibition of thrombotic microangiopathy (TMA),[7] the formation of blood clots in small blood vessels throughout the body,[1][3][4] including normalization of platelets and lactate dehydrogenase (LDH), as well as maintenance or improvement in renal function.[7]
Eculizumab was discovered and developed by Alexion Pharmaceuticals and is manufactured by Alexion. It was approved by the United States Food and Drug Administration (FDA) on March 16, 2007 for the treatment of PNH, and on September 23, 2011 for the treatment of aHUS. It was approved by the European Medicines Agency for the treatment of PNH on June 20, 2007, and on November 24, 2011 for the treatment of aHUS. Eculizumab is currently being investigated as a potential treatment for other severe, ultra-rare disorders
- Hillmen, Young, Schubert, P, N, J, et al (2006). “The complement inhibitor eculizumab in paroxysmal nocturnal hemoglobinuria”. N Engl J Med 355 (12): 1233–1243. doi:10.1056/NEJMMoa061648. PMID 16990386.
- Noris, Caprioli, Bresin, M, J, E, et al. (2010). “Relative role of genetic complement abnormalities in sporadic and familial aHUS and their impact on clinical phenotype”. Clin J Am Soc Nephrol 5: 1844–1859.
- Caprioli, Noris, Brioschi, J, M, S, et al (2006). “Genetics of HUS: the impact of MPC, CFH, and IF mutations on clinical presentation, response to treatment, and outcome”. Blood 108: 1267–1279.
- Hillman, Hall, Marsh, P, C, JC, et al (2004). “Effect of eculizumab on hemolysis and transfusion requirements in patients with paroxysmal nocturnal hemoglobinuria”. N Eng J Med 350: 552–559.
- Ray, Burrows, Ginsberg, Burrows, JG, RF, JS, EA (2000). “Paroxysmal nocturnal hemoglobinuria and the risk of venous thrombosis: review and recommendations for management of the pregnant and nonpregnant patient”. Haemostasis 30: 103–107.
- Kelly, Hill, Arnold, RJ, A, LM, et al (2011). “Long-term treatment with eculizumab in paroxysmal nocturnal hemoglobinuria: sustained efficacy and improved survival”. Blood 117: 6786–6792.
- .Soliris® (eculizumab) prescribing information (2011). Cheshire, CT: Alexion Pharmaceuticals. http://www.soliris.net/sites/default/files/assets/soliris)pi.pdf.
Phase 2, Sarepta Therapeutics, Efficacy, Safety, and Tolerability Rollover Study of Eteplirsen in Subjects With Duchenne Muscular Dystrophy
Eteplirsen, also called AVI-4658, is an experimental drug, currently in clinical trials. It is designed for treatment of some mutations which cause Duchenne muscular dystrophy (DMD), a genetic degenerative muscle disease. Eteplirsen is a product of Sarepta Therapeutics Inc.
s excision of exon 51 during pre-mRNA splicing of the dystrophin RNA transcript. Skipping exon 51 changes the downstream reading frame of dystrophin;[1] giving eteplirsen to a healthy person would result in production of dystrophin mRNA which would not code for functional dystrophin protein but, for DMD patients with particular frameshifting mutations, giving eteplirsen can restore the reading frame of the dystrophin mRNA and result in production of functional (though internally-truncated) dystrophin.[2] Eteplirsen is given by intravenous infusion for systemic treatment of DMD.
Clinical studies
Several clinical trials have been conducted to test eteplirsen, one in the UK involving local injection to the foot,[3][4] one in the UK involving systemic injection at low doses[5][6] and one in the USA at higher systemic doses[7] that progressed to a rollover extension study.[8]
References
- “Exon Skipping Quantification by qRT-PCR in Duchenne Muscular Dystrophy Patients Treated with the Antisense Oligomer Eteplirsen”. Hum Gene Ther Methods.. 17 Oct 2012.
- “Morpholinos and Their Peptide Conjugates: Therapeutic Promise and Challenge for Duchenne Muscular Dystrophy.”. Biochim Biophys Acta. 1798 (12): 2296–303.. 17 Feb 2010.
- Gary Roper/Manager Clinical Research Governance Organisation, Imperial College London. “Safety and Efficacy Study of Antisense Oligonucleotides in Duchenne Muscular Dystrophy”. ClinicalTrials.gov. US Government, NIH. Retrieved 30 October 2012.
- Lancet Neurol. 8 (10): 918–28. 25 Aug 2009.
- Professor Francesco Muntoni, University College of London Institute of Child Health. “Dose-Ranging Study of AVI-4658 to Induce Dystrophin Expression in Selected Duchenne Muscular Dystrophy (DMD) Patients”. ClinicalTrials.gov. US Government, NIH. Retrieved 30 October 2012.
- “Exon skipping and dystrophin restoration in patients with Duchenne muscular dystrophy after systemic phosphorodiamidate morpholino oligomer treatment: an open-label, phase 2, dose-escalation study.”. Lancet. 378 (9791): 595–605. 23 Jul 2011.
- Sarepta Therapeutics. “Efficacy Study of AVI-4658 to Induce Dystrophin Expression in Selected Duchenne Muscular Dystrophy Patients”. ClinicalTrials.gov. US Government, NIH. Retrieved 30 October 2012.
- Sarepta Therapeutics. “Efficacy, Safety, and Tolerability Rollover Study of Eteplirsen in Subjects With Duchenne Muscular Dystrophy”. ClinicalTrials.gov. US Government, NIH. Retrieved 30 October 2012.
Phase 2 Drug: Ustekinumab A monoclonal antibody against the p40 subunit of IL-12/23 Other Name: Stelara
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Human |
| Target | IL-12 and IL-23
|

Ustekinumab, CAS number 815610-63-0, is also known by it’s brand name Stelara, which is marketed by Janssen Biotech, Inc. Developed as a treatment for adults with moderate to severe plaque psoriasis
Rockefeller University, MAR 2013
http://clinicaltrials.gov/ct2/show/NCT01806662
Atopic dermatitis (AD) is a chronic disease associated with intense itching, which affects most aspects of everyday life in the majority of patients. Acute inflammation and extensor/facial involvement is common in infants, whereas chronic inflammation increases in prevalence with age, as do localization to flexures. AD has a complex background characterized by immune activation, increased epidermal thickness in chronic diseased skin, and defective barrier function. In normal, healthy skin, the outer layer of the epidermis, the stratum corneum is made up flattened dead cells called corneocytes held together by a mixture of lipids and proteins. The stratum corneum and, in particular, the lipid layer are vital in providing a natural barrier function that locks water inside the skin and keeps allergens and irritants out. In people with AD, the barrier function is defective, which leads to dry skin. As the skin dries out, it cracks allowing allergens and irritants to penetrate.
Mild AD can be controlled with emollients and topical medications. However, moderate to severe AD is extremely difficult to control and requires systemic treatment that is often unsatisfactory due to impracticality and lack of effectiveness. Only three therapeutic options exist for moderate to severe AD, including: 1) oral steroids 2) cyclosporine A (CsA), that is not widely used in the US as it is not FDA approved for AD and 3) ultraviolet phototherapy. Oral steroids and CsA treatments have major side effects and UV radiation therapy is highly inconvenient for patients. Several biologic medications, such as TNF-alpha inhibitors, are effective, convenient, and relatively safe therapies for psoriasis, but have thus far not shown efficacy in AD. Ustekinumab is a unique biologic medication that may specifically target AD.
The investigators study will determine whether there is a reversal of the skin thickness and the immune pathways involved in the disease during treatment with Ustekinimab and what specific immune cells are involved. The investigators are also interested to understand how the clinical reversal of the disease will correlate with tissue reversal of the disease.
Detailed Description:
In psoriasis, epidermal hyperplasia is driven by underlying immune activation, whether as a direct response to IL-20 family cytokines that induces hyperplasia and inhibits keratinocyte terminal differentiation or as an indirect response to immune-mediated injury to keratinocytes. The epidermal reaction in psoriasis is largely restored to normal with selective immune suppression. Hence, one might hypothesize that similar epidermal responses should occur in the presence of “generalized” cellular immune activation, in diseases with similar inflammatory infiltrate and epidermal hyperplasia, such as AD. In fact, psoriasis and AD share features of dense T-cells and dentritic cell infiltrates, as well as over-expression of IL-22 in skin lesions. These diseases also share similar epidermal hyperplasia in their chronic phases.
Work from the investigators group showed that IL-22 is a key cytokine in the pathogenesis of both AD and psoriasis. The investigators have demonstrated that in psoriasis, ustekinumab suppresses the production of IL-12, IL-23, and IL-22. Additionally, by RT-PCR the investigators demonstrated that the mRNA expression of p40 cytokine and the IL23R is up-regulated in AD as compared to both normal skin and psoriasis. The investigators therefore hypothesize that ustekinumab will suppress IL-22 and possibly also p40 production in AD lesions and reverse both the epidermal growth/differentiation defects and the underlying immune activation, and hence will suppress disease activity. Interestingly, p40 was also found to be significantly up-regulated in non-lesional AD skin as compared with normal skin.
Although AD is thought to be predominately a disease of Th2-type cells, in the chronic stage, there is large Th1 component. To date, the precise mechanism by which sequential activation of Th2 and Th1 cells in AD is achieved remains unknown. IL-12 induces the differentiation and maturation of human Th cells into Th1-type cells. Recent circumstantial evidence suggests that in AD patients IL-12 may facilitate a change from the Th2-type to a Th1 cytokine profile. IL-12 was recently shown to be highly elevated in pediatric AD and its levels were strongly associated with disease severity.
Expression of IL-12 p40 mRNA is significantly enhanced in lesional skin from AD, suggesting that the enhanced local production of IL-12 in dendritic cells and macrophages may be responsible for the increased production of IFN-γ in chronic lesions potentially suggesting that IL-12 may have a pivotal role in promoting inflammation in atopic dermatitis. Topical steroids which constitute a mainstay of therapy in AD are known to strongly down-regulate IL-12 expression, possibly also indicating that targeted anti IL-12 therapy might important role in treating AD.
Recently, the Th1/Th2 paradigm in autoimmunity and allergy has been revisited to include a role for a new population of IL-17-producing Th cells known as Th17. Th17 cells are characterized by the production of inflammatory cytokines such as IL-17A, IL-17F, IL-22, and IL-26. One of the key factors involved in naive Th-cell commitment to a Th17 phenotype is IL-23.
Patients with acute AD were found to have increased Th17 T-cells in peripheral blood by flow cytometry and intracellular cytokine staining 26 as well as by immunohistochemistry (IHC) in lesions. Since IL-23 is the major inducer of Th17 T-cells, as well as “T22” T-cells, neutralization of IL-23 could potentially result in both decreased Th17 signal in acute AD as well as decreased “T22/IL22″ signal. Therefore the investigators postulate that ustekinumab in AD will act both inhibiting the IL-12-dependent Th1 shift in chronic AD stage as well as the pathogenic IL-22/”T22” axis in this disease.
Ustekinumab [1] (INN, experimental name CNTO 1275, proprietary commercial name Stelara,[2] Centocor) is a human monoclonal antibody. It is directed against interleukin 12 and interleukin 23, naturally occurring proteins that regulate the immune system and immune-mediated inflammatory disorders.[3]
In two Phase III trials for moderate to severe psoriasis, the longest >76 weeks, ustekinumab was safe and effective.[4][5]
A third Phase III trial, ACCEPT, compared the efficacy and safety of ustekinumab with etanercept in the treatment of moderate to severe plaque psoriasis.[6] This trial found a significantly higher clinical response with ustekinumab over the 12-week study period compared to high-dose etanercept.[6] It also demonstrated the clinical benefit of ustekinumab among patients who failed to respond to etanercept.[6]
Ustekinumab is approved in Canada, Europe and the United States to treat moderate to severe plaque psoriasis.[7]
As of November 2009, the drug is being investigated for the treatment of psoriatic arthritis.[8][9] It has also been tested in Phase II studies for multiple sclerosis[10] and sarcoidosis, the latter versus golimumab (Simponi).[11]
- Cingoz, Oya (2009). “Ustekinumab”. MAbs 1 (3): 216–221. doi:10.4161/mabs.1.3.8593. PMC 2726595. PMID 20069753.
- ^ European Medicines Agency, 20 November 2008, http://www.emea.europa.eu/pdfs/human/opinion/Stelara_58227008en.pdf
- ^ Reddy M, Davis C, Wong J, Marsters P, Pendley C, Prabhakar U (May 2007). “Modulation of CLA, IL-12R, CD40L, and IL-2Ralpha expression and inhibition of IL-12- and IL-23-induced cytokine secretion by CNTO 1275”. Cell. Immunol. 247 (1): 1–11. doi:10.1016/j.cellimm.2007.06.006. PMID 17761156.
- ^ Leonardi CL, Kimball AB, Papp KA, et al. (May 2008). “Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 76-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 1)”. Lancet 371 (9625): 1665–74. doi:10.1016/S0140-6736(08)60725-4. PMID 18486739.
- ^ Papp KA, Langley RG, Lebwohl M, et al. (May 2008). “Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 52-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 2)”. Lancet 371 (9625): 1675–84. doi:10.1016/S0140-6736(08)60726-6. PMID 18486740.
- ^ a b c Griffiths C, Strober B, van de Kerkhof P et al. (2010). “Comparison of Ustekinumab and Etanercept for Moderate-to-Severe Psoriasis”. N Engl J Med 362 (2): 118–28. doi:10.1056/NEJMoa0810652. PMID 20071701.
- ^ Medarex to Receive Milestone Payment for Approval of STELARA(TM) (Ustekinumab) for the Treatment of Moderate to Severe Plaque Psoriasis
- ^ ClinicalTrials.gov NCT00267956 A Study of the Safety and Efficacy of CNTO 1275 in Patients With Active Psoriatic Arthritis
- ^ ClinicalTrials.gov NCT01009086 A Study of the Safety and Efficacy of Ustekinumab in Patients With Psoriatic Arthritis
- ^ ClinicalTrials.gov NCT00207727 A Safety and Efficacy Study of CNTO1275 in Patients With Multiple Sclerosis
- ^ ClinicalTrials.gov NCT00955279 A Study to Evaluate the Safety and Effectiveness of Ustekinumab or Golimumab Administered Subcutaneously (SC) in Patients With Sarcoidosis
- ^ http://www.empr.com/stelara-approved-for-moderate-to-severe-psoriasis/article/149760/
- ^ a b Centocor 12/19/08 Press Release, http://www.centocor.com/centocor/i/press_releases/FDA_ISSUES_COMPLETE_RESPONSE_LETTER_TO_CENTOCOR_FOR_USTEKINUMAB_BIOLOGIC_LICENSE_APPLICATION_
- ^ Johnson LL. “Study: Drug for serious psoriasis tops competition” The Associated Press. 18 Sept 2008.[dead link]
- ^ Wild, David (November 2011), “Novel IL-12/23 Antagonist Shows Potential in Severe Crohn’s”, Gastroenterology & Endoscopy News 62 (11), retrieved 2011-12-04
- ^ a b c Weber J, Keam SJ (2009). “Ustekinumab”. BioDrugs 23 (1): 53–61. doi:10.2165/00063030-200923010-00006. PMID 19344192.
- ^ Segal BM, Constantinescu CS, Raychaudhuri A, Kim L, Fidelus-Gort R, Kasper LH (September 2008). “Repeated subcutaneous injections of IL12/23 p40 neutralising antibody, ustekinumab, in patients with relapsing-remitting multiple sclerosis: a phase II, double-blind, placebo-controlled, randomised, dose-ranging study”. Lancet Neurol 7 (9): 796–804. doi:10.1016/S1474-4422(08)70173-X. PMID 18703004.
- ^ “Important Safety Information”. STELARA® (ustekinumab). Janssen Biotech.
External links
- Centocor Ortho Biotech official site
- CNTO 1275 research studies registered with U.S. National Institutes of Health:
- ClinicalTrials.gov NCT00207727 Phase II Study on Multiple Sclerosis
- ClinicalTrials.gov NCT00320216 Phase II Study on Psoriasis
- ClinicalTrials.gov NCT00267969 Phase III Study on Psoriasis
- ClinicalTrials.gov NCT00307437 Phase III Study on Psoriasis
- ClinicalTrials.gov NCT00267956 Phase II Study on Psoriatic Arthritis
- Sylvester, Bruce (2006-03-06). “CNTO 1275 Shows Efficacy for Psoriasis: Presented at AAD”. Doctor’s Guide Publishing. Retrieved 2007-01-25.
MAA EU -GSK submits diabetes drug Eperzan, albiglutide in EU

MAA EU =marketing authorisation application EU
MAR 08 2013
GlaxoSmithKline has announced the submission of a marketing authorisation application for albiglutide, which will have the brand name Eperzan, to the European Medicines Agency.
The filing of albiglutide, a once-weekly treatment for type 2 diabetes, comes almost two months after it was filed in the USA. The drug is a GLP-1 receptor agonist, the same class of injectable treatments dominated by Novo Nordisk’s once-a-day Victoza (liraglutide), twice-daily Byetta (exenatide) and an extended-release formulation of the latter, Bydureon. They were developed and sold by Amylin, which was then acquired by Bristol-Myers Squibb and AstraZeneca.
The filing is based in part on a study which assessed albiglutide against Merck & Co’s DPP-4 inhibitor Januvia (sitagliptin) which showed that GSK’s drug showed clinically and statistically significant reductions in HbA1c from baseline and superiority versus the US firm’s diabetes blockbuster. However in data from a late-stage study released in November 2011, albiglutide failed to show non-inferiority to Victoza and a number of analysts believe GSK will have its work cut out to grab a decent share of the GLP-1 market.
Albiglutide is a glucagon-like peptide-1 agonist (GLP-1 agonist) drug under investigation by GlaxoSmithKline for treatment of type 2 diabetes. It is a dipeptidyl peptidase-4-resistant glucagon-like peptide-1 dimer fused to human albumin.
Albiglutide has a half-life of four to seven days, which is considerably longer than the other two GLP-1 analogs approved for market use, exenatide (Byetta) and liraglutide (Victoza).[1] [2] GLP-1 drugs are currently only available for subcutaneous administration on a daily basis, so a GLP-1 drug with a longer half-life is desirable. Such a drug would only need to be injected biweekly or weekly instead of daily, reducing the discomfort and inconvenience of GLP-1 administration considerably.
It has not yet been determined whether albiglutide is as effective an antidiabetic agent as GLP-1 drugs currently on the market, and final data remain to be published regarding the incidence of adverse effects related to the drug. To evaluate the efficacy and safety of the drug, albiglutide is undergoing eight Phase III clinical trials. Four of these trials should report useful data by end 2010.[3]
- Matthews JE, Stewart MW, De Boever EH, et al. (December 2008). “Pharmacodynamics, Pharmacokinetics, Safety, and Tolerability of Albiglutide, a Long-Acting Glucagon-Like Peptide-1 Mimetic, in Patients with Type 2 Diabetes”. J. Clin. Endocrinol. Metab. 93 (12): 4810–4817. doi:10.1210/jc.2008-1518. PMID 18812476.
- Baggio et al. (2008). “Glucagon-like Peptide-1 Analogs Other Than Exenatide”.
- “Phase III clinical trials of Albiglutide”.
Phase 2 SMP-986(afacifenacin fumarate) Overactive bladder/ Dainippon Sumitomo Pharma and Nippon Shinyaku conclude a license agreement for SMP-986, a therapeutic agent for urology
877606-63-8 cas no of afacifenacin
any str error, mail to amcrasto@gmail.com
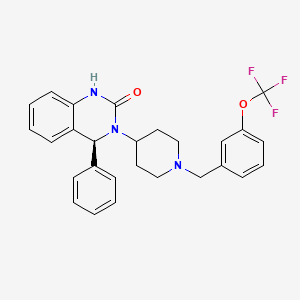
SMP-986 (afacifenacin fumarate)
(4S)-4-phenyl-3-(1-{[3-(trifluoromethoxy)phenyl]methyl}piperidin- 4-yl)-3,4-dihydroquinazolin-2(1H)-one muscarinic receptor antagonist

- Developed in-house
- SMP-986 possesses the dual pharmacological actions of muscarinic receptor antagonism (non-selective) and inhibition of the bladder afferent pathway through Na+-channel blockade. This compound is being evaluated for its ability to ease urinary urgency and reduce the frequency of both urination and incontinence. The compound has also exhibited the potential to have lower incidence of side effects related to muscarinic receptor antagonism, such as dry mouth.
- Development stage: Phase II in the U.S. and Europe. Phase II in Japan
7 mar 2013
Dainippon Sumitomo Pharma Co., Ltd. (DSP) and Nippon Shinyaku Co., Ltd. Announce they have concluded a license agreement for exclusive rights to develop, manufacture and commercialize SMP-986 in Japan, a new therapeutic agent for overactive bladder created by DSP.
DCVax®-Direct Phase I/II Trial For All Inoperable Solid Tumors Is Expected To Produce Ongoing Results In 2013

BETHESDA, Md., \
March 5, 2013 Northwest Biotherapeutics (NW Bio), a biotechnology company developing DCVax® personalized immune therapies for solid tumor cancers, announced today that its Phase I/II DCVax-Direct clinical trial for all inoperable solid tumor cancers is planned to begin within approximately the next sixty days. As a Phase I/II trial, this trial is not blinded and the results will be seen as the trial proceeds. With an efficacy endpoint of tumor regression (i.e., tumor shrinkage or elimination), this innovative trial is expected to yield meaningful ongoing results by the second half of 2013.
This clinical trial is approved by the FDA for all types of solid tumor cancers (i.e., cancers in any tissues of the body), and is configured to provide rapid results. In the Phase I portion, it will test both safety and a variety of dosing regimes, and will do so in multiple different cancers – avoiding the need to conduct separate Phase I studies in each such cancer, as is usually the case. Then, the trial will go directly into the Phase II portion, testing for efficacy, without the need for another FDA review.
DCVax®
All immune responses start in the same way that involves initially a single cell type, the dendritic cell (DC). This cell functions like the General of an army, in that it directs all ensuing activities of the immune response. The immune system is like an army with many divisions, and multiple soldiers with various types of weapons. When an invader, which could be a virus, bacteria, or a cancer cell, encounters a DC the result is that the DC consumes or eats the invader and chops it into small pieces. In the process, the DC becomes activated and starts traveling to the lymph node. In the lymph nodes the DC elicits a cascade of events eventually involving the entire army that leads to a full-blown immune response. Importantly, the nature of the invader and the nature of the DC activation dictate the type of immune response: the DC is the general of the army who directs all the soldiers to work in synchrony, and who determines which weapons to use to best defeat the enemy. We believe that preparing the DC outside the body, as done for DCVax® products, allows the greatest degree of control and begins the immune response in the natural fashion leading to the most complete attack on the foreign invader.
Different Approaches
We believe that the optimal way to arrive at the most effective immune response is through the control of the DC. Most traditional immunization approaches, including traditional virus, specific antigen or peptide vaccines as well as some that are used for immunotherapy of cancer, try to control the already existing DC in the body, or they try to modulate only one arm of the immune system. The immunogen, i.e. the virus, specific antigen, peptide or the cancer cells used to prepare the vaccine, is in those cases injected into the body in a formulation that aims at targeting and activating local DC. Examples are viral, specific antigen or peptide vaccines formulated with adjuvant, or killed tumor cells alone or modified to produce the DC mobilizing protein GM-CSF. In these instances, it is left to chance as to whether the immunogen arrives at the DC, whether the DC are properly activated, and effectively migrate to lymph nodes to produce an effective immune response. We believe that the failure of several recent clinical trials may be the result of the inability of these other approaches to effectively mount a natural and robust immune response.
Treatments that use only a single division of the immune system may employ only large amounts of T cells, or a single (monoclonal) antibody. DCVax® products are being developed to activate all aspects of the immune response, both cellular and antibody, thus potentially providing a broader and longer lasting immune and clinical response. Northwest Biotherapeutics’ products are deigned as pure, activated DC loaded with the immunogen as would naturally occur, and that are capable of migrating to lymph nodes. The intended result is a very robust, and full immune response consisting of both a specific cellular T cell response and a specific antibody response against the cancer associated antigen. Data obtained in our Phase I and Phase II clinical trials suggest that such response may occur and may translate into a clinical benefit.
Cancer and the Immune System
Cancer cells produce many substances that shut down the immune response, as well as substances that paralyze the DC that are resident in the body. We believe therefore that the optimal time for controlling cancer growth by activating the immune system is at the time when tumor burden is low. Northwest Biotherapeutics targets patients with brain cancer following surgery, radiation and chemotherapy, and hormone independent prostate cancer patients with no detectable tumor growth. This approach aims at inducing powerful immune responses to control progression of the disease.
Manufacturing
Northwest Biotherapeutics has focused on solving many of the challenges that are typically associated with producing personalized products that consist of living cells. The Company’s new automated cell processing system allows high-throughput production of products for a fraction of the historical cost.
- DCVax® products contain pure DC
- The DC in DCVax® are prepared outside the body, which eliminates many uncontrollable variables, and are subjected to a potency test designed to ensure that the DC administered to the patient are capable of eliciting an immune response
- DCVax® is used in patients with low tumor burden
- DCVax® products can be manufactured in a cost-efficient manner
ViiV Healthcare presents phase III SAILING study data of dolutegravir vs raltegravir in treatment-experienced adults with HIV-1

Dolutegravir
| Identifiers | |
|---|---|
| CAS number | 1051375-16-6 |
8 TH MATCH 2013
ViiV Healthcare, a global specialist HIV company established in November 2009 by GSK and Pfizer dedicated to delivering advances in treatment and care for people living with HIV, has announced 24-week data from the phase III SAILING (ING111762) study evaluating the investigational integrase inhibitor dolutegravir in patients with HIV-1 who are failing on current therapy, but had not been treated with an integrase inhibitor.
At 24 weeks, 79% of study participants receiving the once-daily dolutegravir regimen were virologically suppressed (HIV-1 RNA <50 c/mL) vs. 70% of participants on the twice-daily raltegravir regimen. This difference in response was statistically significant with a 95% confidence interval for the difference of 3.4% to 15.9% (p=0.003).
The SAILING study was designed to demonstrate non-inferiority of a regimen containing dolutegravir versus raltegravir (both with up to two background agents) and the analysis met this criterion; statistical superiority was concluded as part of a pre-specified testing procedure. These data were presented at the 20th Conference on Retroviruses and Opportunistic Infections (CROI) in Atlanta, Georgia.
Differences in treatment outcome in favour of the dolutegravir arm were driven by greater virologic response: at Week 24, 15% of patients receiving the dolutegravir regimen had virologic non-response vs. 24% of patients receiving the raltegravir regimen. In addition, fewer subjects failed therapy with integrase inhibitor resistance on dolutegravir (n=2) than on raltegravir (n=10, p=0.016).
Overall, the tolerability of dolutegravir (DTG) was similar to that of raltegravir (RAL). At 24 weeks, 2% of subjects on the dolutegravir regimen discontinued due to adverse events (AEs) vs. 4% of subjects on the raltegravir regimen. The rate of drug-related AEs was similar for both arms (DTG 20%, RAL 23%) and commonly reported AEs (defined as events that occurred in more than 10% of subjects) were similar on both arms, namely diarrhoea (20% DTG, 17% RAL) and upper respiratory tract infection (11% DTG, 8% RAL).
“People living with HIV who have developed resistance to more than one antiretroviral drug class face increasingly narrow treatment options and clinical decisions become increasingly complex. We welcome these initial results supporting the efficacy and tolerability of dolutegravir as a potentially useful addition in the management of HIV in treatment-experienced patients.” said John Pottage, chief scientific and medical officer, ViiV Healthcare. “These encouraging data were included as part of the comprehensive clinical data package supporting recent regulatory submissions for dolutegravir and we look forward to receiving the primary analysis at 48 weeks in due course.”
The primary objective of the ongoing double-blind, double-dummy phase III SAILING study is to demonstrate the antiviral activity of once-daily dolutegravir 50mg compared to twice-daily raltegravir 400mg over 48 weeks in HIV-1 infected, antiretroviral-experienced, integrase inhibitor-naïve adults. At baseline, 715 study participants were randomised 1:1 to receive either dolutegravir or raltegravir plus investigator-selected background regimen of no more than 2 agents, one of which was fully active. All subjects had documented genotypic or phenotypic resistance to agents from at least two antiretroviral therapy drug classes, and ongoing virologic replication. Median baseline HIV-1 RNA levels were 4.18 log10 c/mL and median baseline CD4+ cell counts were 200 cells/mm3. The study population included 32% women, 42% were of African American/African heritage, and 46% of study participants were classified as CDC Class C (patients who have one or more AIDS-defining illness). The 48-week primary analysis of this study will be presented at a future scientific meeting.
S/GSK1349572 (dolutegravir, DTG) is an investigational integrase inhibitor currently in development for the treatment of HIV; it does not require an additional pharmacokinetic boosting drug to be added to the regimen. Integrase inhibitors block HIV replication by preventing the viral DNA from integrating into the genetic material of human immune cells (T-cells). This step is essential in the HIV replication cycle and is also responsible for establishing chronic infection.
SAILING is the fourth phase III dolutegravir study reporting in 2012 and 2013. Data from the two studies in treatment-naïve populations, SPRING-2 (ING113086) and SINGLE (ING114467), were announced in April and July of 2012 respectively. Data from VIKING-3 (ING112574) in integrase inhibitor-resistant patients were announced in November 2012. Dolutegravir is not yet approved as a treatment for HIV or any other indication anywhere in the world.
Dolutegravir[1] is an experimental new drug under investigation for the treatment of HIV infection. Dolutegravir is an integrase inhibitor. Also known as S/GSK1349572 or just “572”, the drug is under development by GlaxoSmithKline (GSK). Studies have shown dolutegravir to be effective in patients with resistance to the integrase inhibitor, raltegravir.[2] Clinical trials are underway to support dolutegravir in combination with abacavir and lamivudine, in a new new fixed dose combination called 572-Trii.[3] In February, 2013 the Food and Drug Administration announced that it would fast track dolutegravir’s approval process.[4]
Results from the 96-week comparison with efavirenz, SPRING-1, showed dolutegravir 50mg orally to be effective at reducing HIV viral load and raising CD4 counts in integrase-naive patients. [5]
References
- [1] American Medical Association (AMA), STATEMENT ON A NONPROPRIETARY NAME ADOPTED BY THE USAN COUNCIL (Dolutegravir) Accessed 3 December 2011.
- Dolutegravir (“572”) Holds Up in Heavily Raltegravir-Resistant Patients, Phase 2B Study Finds Nelson Vergel. The Body PRO. Accessed 23 April 2011.
- Shionogi-ViiV Healthcare Starts Phase 3 Trial for “572-Trii” Test positive airwave. The Body PRO. Accessed 23 April 2011.
- “GSK wins priority status for new HIV drug in U.S”. Reuters. 16 February 2013. Retrieved 18 February 2013.
- Horn, Tim. ViiV’s Dolutegravir Continues to Show Well After 96 Weeks, Versus Sustiva, for First-Time Treatment. AIDSmeds.com 7 Mar 2012. Accessed 14 Mar 2012.

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....










