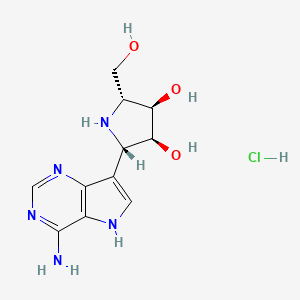
EIDD-2801 works similarly to Gilead Sciences’ remdesivir, an unapproved drug that was developed for the Ebola virus and is being studied in five Phase III trials against COVID-19. Both molecules are nucleoside analogs that metabolize into an active form that blocks RNA polymerase, an essential component of viral replication.
Home » 2020 (Page 6)
Yearly Archives: 2020
Desidustat

Ranjit Desai
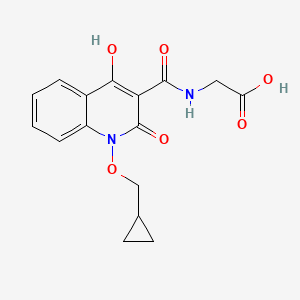
DESIDUSTAT
2-(1-(cyclopropylmethoxy)-4-hydroxy-2-oxo-1,2-dihydroquinoline-3-carboxamido)acetic acid
desidustat
Glycine, N-((1-(cyclopropylmethoxy)-1,2-dihydro-4-hydroxy-2-oxo-3-quinolinyl)carbonyl)-
N-(1-(Cyclopropylmethoxy)-4-hydroxy-2-oxo-1,2-dihydroquinoline-3-carbonyl)glycine
ZYAN1 compound
(1-(cyclopropylmethoxy)-4-hydroxy-2-oxo-1,2-dihydroquinoline-3-carbonyl) glycine in 98% yield, as a solid. MS (ESI-MS): m/z 333.05 (M+H) +. 1H NMR (DMSO-d 6): 0.44-0.38 (m, 2H), 0.62-0.53 (m, 2H), 1.34-1.24 (m, 1H), 4.06-4.04 (d, 2H), 4.14-4.13 (d, 2H), 7.43-7.39 (t, 1H), 7.72-7.70 (d, 1H), 7.89-7.85 (m, 1H), 8.11-8.09 (dd, 1H), 10.27-10.24 (t, 1H), 12.97 (bs, 1H), 16.99 (s, 1H). HPLC Purity: 99.85%
Oxemia (Desidustat) has received approval from the Drug Controller General of India. This was an incredible team effort by Zydans across the organization and I am so proud of what we have accomplished. Oxemia is a breakthrough treatment for Anemia associated with Chronic Kidney Disease in Patients either on Dialysis or Not on Dialysis, and will help improve quality of life for CKD patients. Team #zydus , on to our next effort!
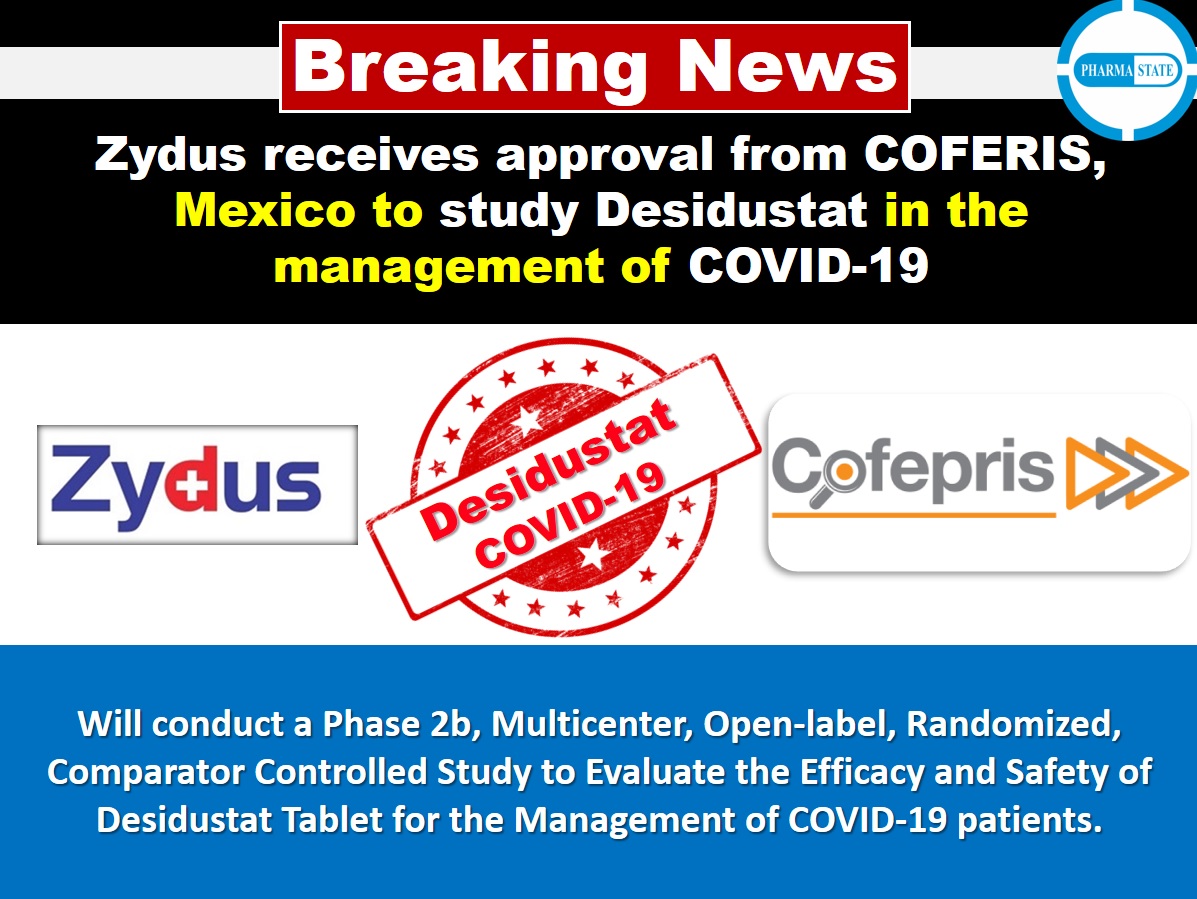
Desidustat (INN, also known as ZYAN1) is a drug for the treatment of anemia of chronic kidney disease. This drug with the brand name Oxemia is discovered and developed by Zydus Life Sciences.[1] The subject expert committee of CDSCO has recommended the grant of permission for manufacturing and marketing of Desidustat 25 mg and 50 mg tablets in India,based on some conditions related to package insert, phase 4 protocols, prescription details, and GCP.[2] Clinical trials on desidustat have been done in India and Australia.[3] In a Phase 2, randomized, double-blind, 6-week, placebo-controlled, dose-ranging, safety and efficacy study, a mean hemoglobin increase of 1.57, 2.22, and 2.92 g/dL in desidustat 100, 150, and 200 mg arms, respectively, was observed.[4] The Phase 3 clinical trials were conducted at additional lower doses as of 2019.[5] Desidustat is developed for the treatment of anemia as an oral tablet, where currently injections of erythropoietin and its analogues are drugs of choice. Desidustat is a HIF prolyl-hydroxylase inhibitor. In preclinical studies, effects of desidustat was assessed in normal and nephrectomized rats, and in chemotherapy-induced anemia. Desidustat demonstrated hematinic potential by combined effects on endogenous erythropoietin release and efficient iron utilization.[6][7] Desidustat can also be useful in treatment of anemia of inflammation since it causes efficient erythropoiesis and hepcidin downregulation.[8] In January 2020, Zydus entered into licensing agreement with China Medical System (CMS) Holdings for development and commercialization of desidustat in Greater China. Under the license agreement, CMS will pay Zydus an initial upfront payment, regulatory milestones, sales milestones and royalties on net sales of the product. CMS will be responsible for development, registration and commercialization of desidustat in Greater China.[9] It has been observed that desidustat protects against acute and chronic kidney injury by reducing inflammatory cytokines like IL-6 and oxidative stress [10] A clinical trial to evaluate the efficacy and safety of desidustat tablet for the management of Covid-19 patients is ongoing in Mexico, wherein desidustat has shown to prevent acute respiratory distress syndrome (ARDS) by inhibiting IL-6.[11] Zydus has also received approval from the US FDA to initiate clinical trials of desidustat in chemotherapy Induced anemia (CIA).[12]. Desidustat has met the primary endpoints in the phase 3 clinical trials and Zydus had filed the New Drug Application (NDA) to DCGI in November, 2021.[13]\
CLIP
Zydus receives DCGI approval for new drug Oxemia; what you need to know
The new drug is an oral, small molecule hypoxia-inducible factor-prolyl hydroxylase (HIF-PH) inhibitor, Zydus said in a statement.
Gujarat-based pharma company Zydus Lifesciences on Monday received the Drugs Controller General of India (DCGI) approval for its new drug application for a first-of-its-kind oral treatment for anemia associated with Chronic Kidney Disease (CKD) – Oxemia (Desidustat).
The new drug is an oral, small molecule hypoxia-inducible factor-prolyl hydroxylase (HIF-PH) inhibitor, the drug firm said in a statement.
Desidustat showed good safety profile, improved iron mobilization and LDL-C reduction in CKD patients in DREAM-D and DREAM-ND Phase III clinical trials, conducted in approximately 1,200 subjects. Desidustat provides CKD patients with an oral convenient therapeutic option for the treatment of anemia. The pharma major did not, however, declare the cost per dose if the drug is available in the market.
“After more than a decade of research and development into the science of HIF-PH inhibitors, results have demonstrated that Oxemia addresses this unmet need and additionally reduces hepcidin, inflammation and enables better iron mobilization. This advancement offers ease of convenience for the patient and will also reduce the disease burden by providing treatment at an affordable cost, thereby improving the quality of life for patients suffering from Chronic Kidney Disease,” Chairman of Zydus Lifesciences Pankaj Patel said.
Chronic Kidney Disease (CKD) is a progressive medical condition characterised by a gradual loss of kidney function and is accompanied by comorbidities like anemia, cardiovascular diseases (hypertension, heart failure and stroke), diabetes mellitus, eventually leading to kidney failure.
PATENT
|
Scheme 3:
|
Step 1′a Process for Preparation of ethyl 2-iodobenzoate (XI-a)
Step-2 Process for the Preparation of ethyl 2-((tert-butoxycarbonyl)(cyclopropylmethoxy)aminolbenzoate (XII-a)
Step 3 Process for the Preparation of ethyl 2-((cyclopropylmethoxy)amino)benzoate (XIII-a)
Step 4 Process for the Preparation of ethyl 24N-(cyclopropylinethoxy)-3-ethoxy-3-oxopropanamido)benzoate (XIV-a)
Step 5: Process for the Preparation of ethyl 1-(cyclopropylmethoxy)-4-hydroxy-2-oxo-1,2 dihydroquinolline-3-carboxylate (XY-a)
Purification
Step 6 Process for the Preparation of ethyl (1-(cyclopropylmethoxy)-4-hydroxy-2-oxo-1,2-dihydroquinoline-3-carbonyl)glycinate (XVI-a)
Purification
Step 7: Process for the Preparation of (1-(cyclopropylmethoxy)-4-hydroxy-2-oxo-1,2-dihydroquinoline-3-carbonyl)glycine (I-a)
Polymorphic Data (XRPD):
References[edit]
- ^ “Zydus receives DCGI approval for new drug Oxemia; what you need to know”.
- ^ CDSCO, SEC Committee. “SEC meeting to examine IND proposals, dated 29.12.2021”. CDSCO website Govt of India. CDSCO. Retrieved 19 January 2022.
- ^ Kansagra KA, Parmar D, Jani RH, Srinivas NR, Lickliter J, Patel HV, et al. (January 2018). “Phase I Clinical Study of ZYAN1, A Novel Prolyl-Hydroxylase (PHD) Inhibitor to Evaluate the Safety, Tolerability, and Pharmacokinetics Following Oral Administration in Healthy Volunteers”. Clinical Pharmacokinetics. 57 (1): 87–102. doi:10.1007/s40262-017-0551-3. PMC 5766731. PMID 28508936.
- ^ Parmar DV, Kansagra KA, Patel JC, Joshi SN, Sharma NS, Shelat AD, Patel NB, Nakrani VB, Shaikh FA, Patel HV; on behalf of the ZYAN1 Trial Investigators. Outcomes of Desidustat Treatment in People with Anemia and Chronic Kidney Disease: A Phase 2 Study. Am J Nephrol. 2019 May 21;49(6):470-478. doi: 10.1159/000500232.
- ^ “Zydus Cadila announces phase III clinical trials of Desidustat”. 17 April 2019. Retrieved 20 April 2019 – via The Hindu BusinessLine.
- ^ Jain MR, Joharapurkar AA, Pandya V, Patel V, Joshi J, Kshirsagar S, et al. (February 2016). “Pharmacological Characterization of ZYAN1, a Novel Prolyl Hydroxylase Inhibitor for the Treatment of Anemia”. Drug Research. 66 (2): 107–12. doi:10.1055/s-0035-1554630. PMID 26367279.
- ^ Joharapurkar AA, Pandya VB, Patel VJ, Desai RC, Jain MR (August 2018). “Prolyl Hydroxylase Inhibitors: A Breakthrough in the Therapy of Anemia Associated with Chronic Diseases”. Journal of Medicinal Chemistry. 61 (16): 6964–6982. doi:10.1021/acs.jmedchem.7b01686. PMID 29712435.
- ^ Jain M, Joharapurkar A, Patel V, Kshirsagar S, Sutariya B, Patel M, et al. (January 2019). “Pharmacological inhibition of prolyl hydroxylase protects against inflammation-induced anemia via efficient erythropoiesis and hepcidin downregulation”. European Journal of Pharmacology. 843: 113–120. doi:10.1016/j.ejphar.2018.11.023. PMID 30458168. S2CID 53943666.
- ^ Market, Capital (20 January 2020). “Zydus enters into licensing agreement with China Medical System Holdings”. Business Standard India. Retrieved 20 January 2020 – via Business Standard.
- ^ Joharapurkar, Amit; Patel, Vishal; Kshirsagar, Samadhan; Patel, Maulik; Savsani, Hardikkumar; Jain, Mukul (22 January 2021). “Prolyl hydroxylase inhibitor desidustat protects against acute and chronic kidney injury by reducing inflammatory cytokines and oxidative stress”. Drug Development Research. 82 (6): 852–860. doi:10.1002/ddr.21792. PMID 33480036. S2CID 231680317.
- ^ “Zydus’ trials of Desidustat shows positive results for Covid-19 management”. The Hindu Business Line. The Hindu. Retrieved 25 January 2021.
- ^ “Zydus receives approval from USFDA to initiate clinical trials of Desidustat in cancer patients receiving chemotherapy”. PipelineReview.com. La Merie Publishing. Retrieved 22 January 2021.
- ^ “Stock Share Price | Get Quote | BSE”.
 |
|
| Clinical data | |
|---|---|
| Other names | ZYAN1 |
| Identifiers | |
| CAS Number | |
| UNII | |
| Chemical and physical data | |
| Formula | C16H16N2O6 |
| Molar mass | 332.312 g·mol−1 |
| 3D model (JSmol) | |
Date
| CTID | Title | Phase | Status | Date |
|---|---|---|---|---|
| NCT04215120 | Desidustat in the Treatment of Anemia in CKD on Dialysis Patients | Phase 3 | Recruiting | 2020-01-02 |
| NCT04012957 | Desidustat in the Treatment of Anemia in CKD | Phase 3 | Recruiting | 2019-12-24 |
////////// DESIDUSTAT, ZYDUS CADILA, COVID 19, CORONA VIRUS, PHASE 3, ZYAN 1, OXEMIA, APPROVALS 2022, INDIA 2022
GST-HG-121
GST-HG-121
mw 431.4
C23 H29 N07
Fujian Cosunter Pharmaceutical Co Ltd
Preclinical for the treatment of hepatitis B virus infection
This compound was originally claimed in WO2018214875 , and may provide the structure of GST-HG-121 , an HBsAg inhibitor which is being investigated by Fujian Cosunter for the treatment of hepatitis B virus infection; in June 2019, an IND application was planned in the US and clinical trials of the combination therapies were expected in 2020. Fujian Cosunter is also investigating GST-HG-131 , another HBsAg secretion inhibitor, although this appears to be being developed only as a part of drug combination.
WO2017013046A1
PATENT
WO2018214875
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2018214875&_cid=P21-KB0QYA-12917-1
PATENT
WO-2020103924
Novel crystalline forms of 11-oxo-7,11-dihydro-6H-benzo[f]pyrido[1,2-d][1,4]azepine, a hepatitis B surface antigen and HBV replication inhibitor, useful for treating HBV infection.
Step H: Compound 9 (15.80 g, 35.95 mmol) was dissolved in dichloromethane (150.00 mL), and trifluoroacetic acid (43.91 mL, 593.12 mmol) was added. The reaction solution was stirred at 10 degrees Celsius for 3 hours. The reaction solution was concentrated under reduced pressure and spin-dried, sodium bicarbonate aqueous solution (100.00 mL) was added, and dichloromethane (100.00 mL) was extracted. The organic phase was dried over anhydrous sodium sulfate, filtered and concentrated under reduced pressure to obtain compound 10.
Step J: Compound 12 (875.00 mg, 1.90 mmol) was dissolved in toluene (20.00 mL) and ethylene glycol dimethyl ether (20.00 mL), and tetrachlorobenzoquinone (1.40 g, 5.69 mmol) was added. The reaction solution was stirred at 120 degrees Celsius for 12 hours. The reaction solution was cooled to room temperature, and a saturated aqueous sodium carbonate solution (50.00 ml) and ethyl acetate (60.00 ml) were added. The mixed solution was stirred at 10-15 degrees Celsius for 20 minutes, and the liquid was separated to obtain an organic phase. Add 2.00 mol/L aqueous hydrochloric acid solution (60.00 mL) to the organic phase, stir at 10-15 degrees Celsius for 20 minutes, and separate the liquid. Wash the organic phase with 2 mol/L aqueous hydrochloric acid solution (60.00 mL×2), separate the liquid, and separate the water phase A 2 mol/L aqueous sodium hydroxide solution (200.00 ml) and dichloromethane (200.00 ml) were added. The layers were separated, and the organic phase was dried over anhydrous sodium sulfate, filtered and concentrated under reduced pressure to obtain compound 13.
Step K: Compound 13 (600.00 mg, 1.31 mmol) was dissolved in methanol (6.00 mL), and 4.00 mol/L aqueous sodium hydroxide solution (2.00 mL, 6.39 equiv) was added. The reaction solution was stirred at 15 degrees Celsius for 0.25 hours. The reaction solution was adjusted to pH=3-4 with a 1.00 mol/L hydrochloric acid aqueous solution, and then extracted with dichloromethane (50.00 mL×3). The organic phases were combined, washed with saturated brine (50.00 mL), and dried over anhydrous sodium sulfate , Filtered and concentrated under reduced pressure to obtain the compound of formula (I). ee value (enantiomeric excess): 100%.
////////////GST-HG-121, Fujian Cosunter, Preclinical , hepatitis B, virus infection
O=C(O)C1=CN2C(=CC1=O)c3cc(OC)c(OCCCOC)cc3OC[C@H]2C(C)(C)C
O=C(O)C1=CN2C(=CC1=O)c3cc(OC)c(OCCCOC)cc3OC[C@H]2C(C)(C)C
NARONAPRIDE

NARONAPRIDE
860174-12-5
Average: 537.1
C27H41ClN4O5
ATI 7505 / ATI-7505
(3R)-1-azabicyclo[2.2.2]octan-3-yl 6-[(3S,4R)-4-(4-amino-5-chloro-2-methoxybenzamido)-3-methoxypiperidin-1-yl]hexanoate
| INGREDIENT | UNII | CAS | |
|---|---|---|---|
| Naronapride dihydrochloride | 898PE2W8US | 860169-57-9 |
860174-12-5 (free base) 860169-57-9 (HCl)
Naronapride (free base), also known as ATI-7505, is a highly selective, high-affinity 5-HT(4) receptor agonist for gastrointestinal motility disorders. ATI-7505 accelerates overall colonic transit and tends to accelerate GE and AC emptying and loosen stool consistency.
Investigated for use/treatment in gastroesophageal reflux disease (GERD) and gastroparesis.
Renexxion , presumed to have been spun-out from Armetheon , under license from ARYx Therapeutics is developing naronapride (ATI-7505; phase 2 clinical in February 2020), an analog of the gastroprokinetic 5-HT 4 agonist cisapride identified using ARYx’s RetroMetabolic platform technology (ARM), for the oral treatment of upper GI disorders. In September 2018, this was still the case . PATENT
WO2005068461
NEW PATENT
WO-2020096911
Process for preparing trihydrate salt of naronapride hydrochloride as 5-HT 4 receptor agonist useful for treating gastrointestinal disorders such as dyspepsia, gastroparesis, constipation, post-operative ileus. Appears to be the first filing from the assignee and the inventors on this compound,
In some aspects, provided herein is a method of making a trihydrate form of (3S, 4R, 3’R)-6-[4-(4-amino-5-chloro-2-methoxy-benzoylamino)-3-methoxy-piperidin-l-yl]-hexanoic acid l-azabicyclo[2.2.2]oct-3’-yl ester di-hydrochloride salt, which has the following formula:
Example 5: NMR Characterization of the Trihydrate
[0282] ^-Nuclear Magnetic Resonance Spectroscopy (‘H-NMR) : Approximately 6 mg of the trihydrate was dissolved in in 1 g of deuterated solvent (dimethylsulfoxide (DMSO)-C45 99.9% d, with 0.05% v/v tetramethyl silane (TMS)). A Varian Gemini 300 MHz FT-NMR spectrometer was used to obtain the ¾-NMK spectrum. A list of the peaks is provided in Table 1 below. A representative ‘H-NMR spectrum is provided in FIG. 6.
Table 1. ‘H-NMR peak list for trihydrate
[0283] 13 C-Nuclear Magnetic Resonance Spectroscopy ( 13C-NMR ): Approximately 46 mg of the trihydrate was dissolved in 1 mL of deuterated solvent (deuterium oxide, Aldrich, 99.9% D, TPAS 0.75%). The 13C-NMR spectrum was obtained using a Varian Gemini 300 MHz FT-NMR spectrometer. A list of the peaks is provided in Table 2 below. A representative 13C-NMR spectrum is provided in FIG. 7.
Table 2. 13C-NMR peak list for trihydrate
PATENT
US10570127 claiming composition (eg tablet) comprising a trihydrate form of naronapride.
patent
ARYX THERAPEUTICS, WO2005/68461, A1, (2005)
Methods
titanium tetraethoxide; toluene;
Reactants can be synthesized in 1 step.
ARYX THERAPEUTICS, WO2005/68461, A1, (2005) The ester (1 part by weight) and (R)-3-Quinuclidinol (about 1.12 part by weight) were suspended in toluene before slowly adding titanium (IV) ethoxide (about 0.5 part by weight) to the stirred suspens ion. The mixture was heated to about 91 °C under a stream of nitrogen, and partial vacuum was applie d to the flask through a distillation apparatus in order to azeotropically remove the ethanol. Addit ional toluene was added as needed to maintain a minimum solvent volume in the flask. The reaction was considered complete after about 33 hours. The mixture was cooled to about room temperature and ext racted five times with water. The organic layer was concentrated under reduced pressure and the resulting residue was redissolved in EtOH/iPrOH (about 1: 1 v/v) and then filtered through a 0.45 micron membrane filter to remove any particulates. Concentrated hydrochloric acid was added slowly to the stirred filtrate to precipitate out the desired product as the dihydrochloride salt. The resulting s uspension was stirred for several hours at room temperature and collected under vacuum filtration and rinsed with EtOH/tPrOH (1: 1; v/v) to provide 0.53 part by weight of the crude product salt. Crude dihydrochloride salt was resuspended in ethanol and heated to reflux before cooling to room temperature over about 1 hour. The product was collected under vacuum filtration and rinsed with ethanol an d then air-dried. The solids were resuspended in ethanol and warmed to about 55 °C to give a clear s olution before adding warm isopropanol and the product was allowed to precipitate by slow cooling to room temperature. The resulting suspension was stirred for several hours before vacuum filtering and rinsing with, e. g., isopropanol. The product was vacuum dried, initially at room temperature for several hours and then at about 55 °C until a constant weight was achieved.
Methods
dmap; 1-ethyl-(3-(3-dimethylamino)propyl)-carbodiimide hydrochloride; DMFA;
Reactants can be synthesized in 2 steps.
ARYX THERAPEUTICS, WO2007/28073, A2, (2007) Production of Compound IV and Compound VI[0394] A mixture of (+)-Comrhoound II (1 eq.), (R)-(-)-3-quinuclidinol HCl salt (1 eq.), EDAC (1 eq.) and DMAP (1 eq.) in DMF is heated at around 5OC overnight . After cooling and diluting with water, the mixture is purified by chromatography or by crystallization to provide Compound IV. Similarly, using (S)-(+)-quinuclidinol, Compound VI is obtained
REFERENCES
1: Jiang C, Xu Q, Wen X, Sun H. Current developments in pharmacological therapeutics for chronic constipation. Acta Pharm Sin B. 2015 Jul;5(4):300-9. doi: 10.1016/j.apsb.2015.05.006. Epub 2015 Jun 6. Review. PubMed PMID: 26579459; PubMed Central PMCID: PMC4629408.
2: Buchwald P, Bodor N. Recent advances in the design and development of soft drugs. Pharmazie. 2014 Jun;69(6):403-13. Review. PubMed PMID: 24974571.
3: Mozaffari S, Didari T, Nikfar S, Abdollahi M. Phase II drugs under clinical investigation for the treatment of chronic constipation. Expert Opin Investig Drugs. 2014 Nov;23(11):1485-97. doi: 10.1517/13543784.2014.932770. Epub 2014 Jun 24. Review. PubMed PMID: 24960333.
4: Shin A, Camilleri M, Kolar G, Erwin P, West CP, Murad MH. Systematic review with meta-analysis: highly selective 5-HT4 agonists (prucalopride, velusetrag or naronapride) in chronic constipation. Aliment Pharmacol Ther. 2014 Feb;39(3):239-53. doi: 10.1111/apt.12571. Epub 2013 Dec 5. Review. PubMed PMID: 24308797.
5: Stevens JE, Jones KL, Rayner CK, Horowitz M. Pathophysiology and pharmacotherapy of gastroparesis: current and future perspectives. Expert Opin Pharmacother. 2013 Jun;14(9):1171-86. doi: 10.1517/14656566.2013.795948. Epub 2013 May 11. Review. PubMed PMID: 23663133.
6: Tack J, Camilleri M, Chang L, Chey WD, Galligan JJ, Lacy BE, Müller-Lissner S, Quigley EM, Schuurkes J, De Maeyer JH, Stanghellini V. Systematic review: cardiovascular safety profile of 5-HT(4) agonists developed for gastrointestinal disorders. Aliment Pharmacol Ther. 2012 Apr;35(7):745-67. doi: 10.1111/j.1365-2036.2012.05011.x. Epub 2012 Feb 22. Review. PubMed PMID: 22356640; PubMed Central PMCID: PMC3491670.
7: Hoffman JM, Tyler K, MacEachern SJ, Balemba OB, Johnson AC, Brooks EM, Zhao H, Swain GM, Moses PL, Galligan JJ, Sharkey KA, Greenwood-Van Meerveld B, Mawe GM. Activation of colonic mucosal 5-HT(4) receptors accelerates propulsive motility and inhibits visceral hypersensitivity. Gastroenterology. 2012 Apr;142(4):844-854.e4. doi: 10.1053/j.gastro.2011.12.041. Epub 2012 Jan 4. PubMed PMID: 22226658; PubMed Central PMCID: PMC3477545.
8: Bowersox SS, Lightning LK, Rao S, Palme M, Ellis D, Coleman R, Davies AM, Kumaraswamy P, Druzgala P. Metabolism and pharmacokinetics of naronapride (ATI-7505), a serotonin 5-HT(4) receptor agonist for gastrointestinal motility disorders. Drug Metab Dispos. 2011 Jul;39(7):1170-80. doi: 10.1124/dmd.110.037564. Epub 2011 Mar 29. PubMed PMID: 21447732.
9: Tack J. Current and future therapies for chronic constipation. Best Pract Res Clin Gastroenterol. 2011 Feb;25(1):151-8. doi: 10.1016/j.bpg.2011.01.005. Review. PubMed PMID: 21382586.
10: Manabe N, Wong BS, Camilleri M. New-generation 5-HT4 receptor agonists: potential for treatment of gastrointestinal motility disorders. Expert Opin Investig Drugs. 2010 Jun;19(6):765-75. doi: 10.1517/13543784.2010.482927. Review. PubMed PMID: 20408739.
11: Sanger GJ. Translating 5-HT receptor pharmacology. Neurogastroenterol Motil. 2009 Dec;21(12):1235-8. doi: 10.1111/j.1365-2982.2009.01425.x. Review. PubMed PMID: 19906028.
12: Vakil N. New pharmacological agents for the treatment of gastroesophageal reflux disease. Rev Gastroenterol Disord. 2008 Spring;8(2):117-22. Review. PubMed PMID: 18641594.
13: Bayés M, Rabasseda X, Prous JR. Gateways to clinical trials. Methods Find Exp Clin Pharmacol. 2007 Jun;29(5):359-73. PubMed PMID: 17805439.
14: Camilleri M, Vazquez-Roque MI, Burton D, Ford T, McKinzie S, Zinsmeister AR, Druzgala P. Pharmacodynamic effects of a novel prokinetic 5-HT receptor agonist, ATI-7505, in humans. Neurogastroenterol Motil. 2007 Jan;19(1):30-8. PubMed PMID: 17187586.
////////////NARONAPRIDE, ATI 7505, ATI 7505,PHASE 2
CO[C@H]1CN(CCCCCC(=O)O[C@H]2CN3CCC2CC3)CC[C@H]1NC(=O)C1=C(OC)C=C(N)C(Cl)=C1
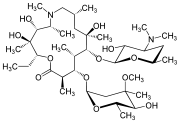
VOCLOSPORIN

Voclosporin
- Molecular FormulaC63H111N11O12
- Average mass1214.622 Da
VOCLOSPORIN
Aurinia Pharmaceuticals (following its merger with Isotechnika ), in collaboration with licensee Paladin Labs (a subsidiary of Endo International plc ), 3SBio ,and ILJIN , is developing a capsule formulation of the immunosuppressant calcineurin inhibitor peptide voclosporin for the treatment of psoriasis, the prevention of organ rejection after transplantation, autoimmune disease including systemic lupus erythematosus and lupus nephritis, and nephrotic syndrome including focal segmental glomerulosclerosis;
Voclosporin is an experimental immunosuppressant drug being developed by Aurinia Pharmaceuticals. It is being studied as a potential treatment for lupus nephritis (LN) and uveitis.[1] It is an analog of ciclosporin that has enhanced action against calcineurin and greater metabolic stability.[2] Voclosporin was discovered by Robert T. Foster and his team at Isotechnika in the mid 1990s.[3] Isotechnika was founded in 1993 and merged with Aurinia Pharmaceuticals in 2013.
Initially, voclosporin was a mixture of equal proporations of cis and trans geometric isomers of amino acid-1 modified cyclosporin. Later, in collaboration with Roche in Basel, Switzerland, voclosporin’s manufacturing was changed to yield the predominantly trans isomer which possesses most of the beneficial effect of the drug (immunosuppression) in the treatment of organ transplantation and autoimmune diseases.
Patent
WO-2020082061
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2020082061&_cid=P12-K9MDK8-59382-1
Novel crystalline forms of voclosporin which is a structural analog of cyclosporine A as calcineurin signal-transduction pathway inhibitor useful for treating lupus nephritis.
Voclosporin is a structural analog of cyclosporine A, with an additional single carbon extension that has a double-bond on one side chain. Voclosporin has the chemical name (3S,6S,9S,l2R,l5S,l8S,2lS,24S,30S,33S)-30-Ethyl-33-[(lR,2R,4E)-l-hydroxy-2-methyl-4,6-heptadien-l-yl]-6,9,l8,24-tetraisobutyl-3,2l-diisopropyl-l,4,7,l0,l2,l5,l9,25,28-nonamethyl-l,4,7,l0,l3,l6,l9,22,25,28,3 l-undecaazacyclotritriacontane-2,5,8,l l,l4,l7,20,23,26,29,32-undecone and the following chemical structure:
Voclosporin is reported to be a semisynthetic structural analogue of cyclosporine that exerts its immunosuppressant effects by inhibition of the calcineurin signal-transduction pathway and is in Phase 3 Clinical Development for Lupus Nephritis.
[0003] Voclosporin and process for preparation thereof are known from International Patent Application No. WO 1999/18120.
[0004] Certain mixtures of cis and trans-isomers of cyclosporin A analogs referred to as
ISATX247 in different ratios are known from U.S. Patent No. 6,998,385, U.S. Patent No. 7,332,472 and U.S. Patent No. 9,765,119.
[0005] Polymorphism, the occurrence of different crystal forms, is a property of some molecules and molecular complexes. A single compound, like Voclosporin, may give rise to a variety of polymorphs having distinct crystal structures and physical properties like melting point, thermal behaviors (e.g. measured by thermogravimetric analysis – “TGA”, or differential scanning calorimetry – “DSC”), powder X-ray diffraction (PXRD) pattern, infrared absorption fingerprint, Raman absorption fingerprint, and solid state (13C-) NMR spectrum. One or more of these techniques may be used to distinguish different polymorphic forms of a compound.
[0006] Different salts and solid state forms (including solvated forms) of an active
pharmaceutical ingredient may possess different properties. Such variations in the properties of different salts and solid state forms and solvates may provide a basis for improving formulation, for example, by facilitating better processing or handling characteristics, improving the dissolution profile, or improving stability (polymorph as well as chemical stability) and shelf-life. These variations in the properties of different salts and solid state forms may also provide improvements to the final dosage form, for instance, if they serve to improve bioavailability. Different salts and solid state forms and solvates of an active pharmaceutical ingredient may also give rise to a variety of polymorphs or crystalline forms, which may in turn provide additional opportunities to use variations in the properties and characteristics of a solid active pharmaceutical ingredient for providing an improved product.
[0007] Discovering new salts, solid state forms and solvates of a pharmaceutical product can provide materials having desirable processing properties, such as ease of handling, ease of processing, storage stability, and ease of purification or as desirable intermediate crystal forms that facilitate conversion to other salts or polymorphic forms. New salts, polymorphic forms and solvates of a pharmaceutically useful compound can also provide an opportunity to improve the performance characteristics of a pharmaceutical product (dissolution profile, bioavailability, etc.). It enlarges the repertoire of materials that a formulation scientist has available for formulation optimization, for example by providing a product with different properties, e.g., a different crystal habit, higher crystallinity or polymorphic stability which may offer better processing or handling characteristics, improved dissolution profile, or improved shelf-life.
[0008] For at least these reasons, there is a need for solid state forms (including solvated forms) of Voclosporin and salts thereof.
HPLC method:
Method description
Column: Zorbax SB C18, 1.8 pm, 100×2.1 mm
Mobile phase: A: 38 ACN : 7 TBME : 55 voda : 0.02 H3P04 (V/V/V/V)
B: 70 ACN : 7 TBME : 23 voda : 0.02 H P04 (V/V/V/V)
Flow rate: 0.5 mL/min
Gradient
Analysis time: 26 minutes + 3 minutes equilibration
Injection volume: 3.0 pL
Column temperature: 90 °C
Diluent: Ethanol
Detection: UV, 210 nm
EXAMPLES
[0095] The starting material Voclosporin crude may be obtained according to ET.S. Patent No. 6,998,385 ETnless otherwise indicated, the purity is determined by HPLC (area percent). The crude product contained according to HPLC analysis 42.6 % trans-Voclosporin (further only Voclosporin), 40.2 % cis-Voclosporin and 2.9 % Cyclosporin A. The crude Voclosporin was purified by column chromatography on silica gel using a mixture of toluene and acetone 82 : 18 (v/v) as mobile phase. The fractions were monitored by HPLC. The appropriate fractions were joined and evaporated, obtaining purified Voclosporin as a white foam. According to HPLC analysis it contained 85.7 % Voclosporin, 3.6 % cis-Voclosporin and 2.6 % Cyclosporin A (further only purified Voclosporin).
[0096] The Voclosporin crude (containing about 42.6 % of Voclosporin) was used for further optimization of the chromatographic separation of cis-Voclosporin and Voclosporin and the effort resulted in improved process for chromatographic separation which includes purification by column chromatography on silica gel using a mixture of toluene and methylisobutylketone 38 : 62 as mobile phase. The fractions were monitored by HPLC. The appropriate fractions were joined and evaporated to a dry residue, weighing 31.0 grams. This residue was not analyzed. The material was dissolved in 25 ml of acetone and then 50 ml of water was added and the solution was let to crystallize for 2 hours in the refrigerator. Then the crystalline product was separated by filtration and dried in vacuum dryer (40 °C, 50 mbar, 12 hours), obtaining 29.6 g of dry product containing 90.6 % of Voclosporin, 0.4 % cis-Voclosporin and 3.7 % Cyclosporin A (further mentioned as final Voclosporin).
Example 1: Preparation of Voclosporin Form A
4.1 grams of Purified Voclosporin was dissolved in acetone and the solution was evaporated to 8.0 grams and the concentrate was diluted by 6 ml of water. The solution was let to crystallize in refrigerator at about 2 °C for 12 hours. The crystalline product was filtered off, washed by a mixture of acetone and water 1 : 1 (v/v) and dried on open air obtaining 2.6 grams of crystalline product Form A. Voclosporin form A was confirmed by PXRD as presented in Figure 1.
Example 2: Preparation of Voclosporin Form B
[0097] 1.0 gram of Purified Voclosporin was dissolved in a mixture of 1.5 ml acetone and 3.0 ml n-hexane. The solution was let to crystallize in refrigerator at about 2 °C for 12 hours. The crystalline product was filtered off, washed by a mixture of acetone and hexane 1 : 2 (v/v) and dried on open air obtaining 0.5 grams of crystalline product Form B. Voclosporin form B was confirmed by PXRD as presented in Figure 2.
Example 3: Preparation of Amorphous Voclosporin
[0098] 2.0 grams of Purified Voclosporin was dissolved in 40 ml of hot cyclohexane and the solution was stirred for 12 hours at room temperature. Then the crystalline product was filtered off and washed with 5 ml of cyclohexane and dried on open air, obtaining 1.3 grams of amorphous powder. Amorphous Voclosporin was confirmed by PXRD as presented in Figure 3
Example 4: Preparation of Voclosporin Form C
[0099] Final Voclosporin (2 grams) was dissolved in acetonitrile (20 ml) at 50 °C, water (6 ml) was added with stirring, and the clear solution was allowed to crystallize 5 days at 20 °C. Colorless needle crystals were directly mounted to the goniometer head in order to define the crystal structure. Voclosporin form C was confirmed by X-ray crystal structure determination.
References
- ^ “Luveniq Approval Status”.
Luveniq (voclosporin) is a next-generation calcineurin inhibitor intended for the treatment of noninfectious uveitis involving the intermediate or posterior segments of the eye.
- ^ “What is voclosporin?”. Isotechnika. Retrieved October 19, 2012.
- ^ U.S. Patent 6,605,593
External links
 |
|
| Names | |
|---|---|
| IUPAC name
(3S,6S,9S,12R,15S,18S,21S,24S,30S,33S)-30-Ethyl-33-[(1R,2R,4E)-1-hydroxy-2-methyl-4,6-heptadien-1-yl]-6,9,18,24-tetraisobutyl-3,21-diisopropyl-1,4,7,10,12,15,19,25,28-nonamethyl-1,4,7,10,13,16,19,22,25,28,31-undecaazacyclotritriacontane-2,5,8,11,14,17,20,23,26,29,32-undecone
|
|
| Other names
VCS, ISA247, Luveniq
|
|
| Identifiers | |
|
3D model (JSmol)
|
|
| ChemSpider | |
|
PubChem CID
|
|
| Properties | |
| C63H111N11O12 | |
| Molar mass | 1214.646 g·mol−1 |
|
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
|
|
Synthesis
methanol; potassium carbonate;
Reactants can be synthesized in 7 steps.
Synthesis, vol. 44, 1, (2012), p. 63 – 68
sulfuric acid; tetrahydrofuran;
ISOTECHNIKA INC., WO2004/89960, A2, (2004) 20 ml of THF were added and the reaction mixture was cooled to 0 °C. 2.7 ML (48.69 mmol, 3 equiv. ) of concentrated sulfuric acid were added. The temperature was raised to RT. After completion of the reaction (ca 1 hour), 100 ml of water were added. The organic phase was separated and washed 2 times with 50 ml water. The water phases were re-extracted sequentially with 50 ml dichloromethane. The c ombined organic phases were dried over NA2SO4, filtered and concentrated under reduced pressure at 3 0°C. The resulting white foam was re-dissolved in 250 ml MTBE and after a few minutes, the crystalli zation started. After stirring 15 min. at RT and 2 hours at 0-2 C, THE SUSPENSION WAS FILTERED. THE crystals were washed with 50 ml cold MTBE (-20 °C) and dried at 40-50 °C under reduced pressure to p rovide 19.2 g of (E) -acetyl-ISA247 as white powder in >98percent isomeric purity (400MHZ LH NMR). (E)-ACETYL-ISA247 can be RECRYSTALLIZED by dissolving the solid in dichloromethane at room temperatur e and exchanging the solvent to MTBE (by adding MTBE, concentrating the solution to half its volume under reduced pressure at 40°C and repeating these operation 2 to three times). The solution is cool ed to room temperature and the crystallization then starts within a few minutes. The suspension is s tirred at room temperature for 2h and 30min at 0°C. The crystals of (E) -acetyl-ISA247 are isolated after filtration, washing with MTBE and drying under reduced pressure at 40°C.iii) Peterson eliminat ion The CRUDE-TRIMETHYLSILYALCOHOL diastereomers mixture (11 g, maximum 4.056 mmol) was dissolved in 25 ml THF. 0.679 ml (12.16 mmol, 3 equiv.) concentrated sulfuric were added dropwise maintaining th e temperature between 20 °C and 25 °C. After 2 hours at RT, 50 ml half saturated aqueous NaCl soluti on were added. The resulting mixture was extracted twice with 50 ML MTBE. The organic phases were washed with 50ML of a half saturated aqueous NACL solution, combined, dried over NA2SO4 and concentrat ed under reduce pressure at 40°C. The resulting crude E-acetyl-ISA247 was re-dissolved in 20 ml dich loromethane and concentrated under reduced pressure. The crude product was dissolved in 60 ml MTBE. The crystallization started within 10 min. The suspension was stirred for an additional 15 min. at R T and 2 hours AT-10 °C. The crystals were isolated by filtration, washed with 20 ml cold MTBE (-20 ° C) and dried under reduced pressure to provide 3. 6 G of (E)-ACETYL-ISA247 in ca 98percent isomeric purity by NMR.iii) Peterson elimination After overnight reaction, the organic layer was separated an d the water phase was discarded. 50 ML THF were added to the organic phase. The solution was concent rated under reduced pressure at 30 °C to half its volume. 100 ML THP were added and the solution was concentrated to 80 ML. The volume was adjusted to 100 ml with THF and the solution was cooled to 0- 2 °C. 1. 812 ML (32. 46 MMOL, 2 equiv.) concentrated sulfuric acid were added dropwise over 5 min., maintaining the temperature below 5 °C. After addition, the reaction cooling bath was removed and th e temperature was raised to RT. After 4 hours reaction, 40 ML water were added followed by 20 ml MTB E. The aqueous layer was separated and discarded. The organic phase was washed with 40 ml NAHCO3 Q, 20 ML saturated NACLAQ, 40 ml saturated NaClaq, dried over Na2SO4, filtered and concentrated at 40 ° C under reduced pressure. The crude E-acetyl-ISA247 was RE-DISSOLVED in 200 ml MTBE and crystallizat ion started within a few minutes. After 15 min. at RT and 2.5 hours at 0 °C, the suspension was filt ered, the crystals were washed with 50 ML MTBE and dried at 50 °C under reduced pressure to give 18. 45 g of (E) -acetyl-ISA247 as a white powder (>98percent isomeric purity by NMR).iii) Peterson elim ination 5 ml THF were added to the organic phase and the solution was cooled to 0- 2 °C. 181 UL (3.2 46, 2 equiv. ) concentrated sulfuric acid were added. The reaction mixture was warmed up to RT. Afte r stirring overnight, 20 ml water were added. The aqueous layer was separated and discarded. The organic phase was washed with 20 ml of 5percent aqueous NAHCO3 solution, dried over MGS04, filtered and concentrated under reduced pressure at 40 °C to give 2 g of (E) -acetyl-ISA247 as a white foam in > 98percent double bond isomeric purity (by NMR).ii) Peterson elimination The crude product was dissol ved in 11.15 ML THF and 268 P1 concentrated sulfuric acid were added. The reaction mixture was heate d at 33 °C for 1.5 hour and then cooled to RT. 22 ml water were added and the reaction mixture was e xtracted with 22 ml MTBE. The aqueous phase was RE-EXTRACTED with 11 ml MTBE. The organic layer were washed with 11 ml water, combined, dried over NA2SO4, filtered and concentrated at 40 °C under redu ced pressure to give 1.89 g of crude (E) -acetyl-ISA247 as a beige powder. The crude product was re-dissolved in 20 ml MTBE at RT. The crystallization started within a few minutes. The suspension was stirred 30 min. at RT, 45 min. at-10 °C and was filtered. The solid was washed with cold MTBE and dr ied at 40 °C under reduced pressure to give 1.02 g of (E)-acetylISA247 as a white powder in ca 98per cent double bond isomeric purity (NMR). ii) Peterson elimination The crude product was dissolved in 8 ML THF at RT. The solution was cooled to 0-5 °C and 200 UL of concentrated sulfuric acid were adde d dropwise. The temperature was raised to RT and the reaction mixture was stirred 10 hours. 40 ml MTBE and 15 ml of water were added. The water phase was separated and discarded. The organic phase was washed 15 ml of a 5percent aqueous NAHCO3 solution, 15 ml of a half saturated aqueous NACL solution, dried over NA2SO4, filtered and concentrated under reduced pressure to give 1. 8 g of crude E-acet yl- ISA247. The crude diene was dissolved in 20 ml dichloromethane. 20 ML MTBE were added, and the s olution was concentrated at 40 °C under reduced pressure to half its volume. The last two operations was repeated three times to in order to exchange the solvent from dichloromethane to MTBE. The solution was cooled to RT and the crystallization started within a few minutes. The suspension was stirr ed 2 hours at RT and 30 min. at 0 °C. The suspension was filtered. The solid was washed with 15 ml M TBE and dried under reduced pressure at 40 °C to give 1.1 g OF E-ACETYL-ISA247 in >95percent double bond isomeric purity (NMR), as a white powder.ii) Peterson elimination The crude product was dissolv ed in 10 ml THF at RT. The solution was cooled to 0-5 °C and 200 UL of concentrated sulfuric acid we re added dropwise. The temperature was raised to RT and the reaction mixture was stirred overnight. 40 ml MTBE and 15 ML of water were added. The water phase was separated and discarded. The organic p hase was washed with 15 ml water, 15 ml of a 5percent aqueous NAHCO3 solution, 15 ml of a half saturated aqueous NaCl solution, filtered and concentrated under reduced pressure to give 1.8 g of crude E-ACETYL-ISA247. The crude diene was redissolved in 35 ml of MTBE. The crystallization started withi n a few minutes. The suspension was stirred 2 hours at RT and 30 min. at 0 °C. The suspension was fi ltered. The solid was washed with 15 ml MTBE and dried under reduced pressure at 40 °C to gi ve 1 g of E-acetyl-ISA247 in >95percent double bond isomeric purity (NMR), as a white powder.
REFERENCES
1: Mok CC. Calcineurin inhibitors in systemic lupus erythematosus. Best Pract Res Clin Rheumatol. 2017 Jun;31(3):429-438. doi: 10.1016/j.berh.2017.09.010. Epub 2017 Oct 11. Review. PubMed PMID: 29224682.
2: Dang W, Yin Y, Wang Y, Wang W, Su J, Sprengers D, van der Laan LJW, Felczak K, Pankiewicz KW, Chang KO, Koopmans MPG, Metselaar HJ, Peppelenbosch MP, Pan Q. Inhibition of Calcineurin or IMP Dehydrogenase Exerts Moderate to Potent Antiviral Activity against Norovirus Replication. Antimicrob Agents Chemother. 2017 Oct 24;61(11). pii: e01095-17. doi: 10.1128/AAC.01095-17. Print 2017 Nov. PubMed PMID: 28807916; PubMed Central PMCID: PMC5655111.
3: Wong TC, Lo CM, Fung JY. Emerging drugs for prevention of T-cell mediated rejection in liver and kidney transplantation. Expert Opin Emerg Drugs. 2017 Jun;22(2):123-136. doi: 10.1080/14728214.2017.1330884. Epub 2017 May 22. Review. PubMed PMID: 28503959.
4: Chow C, Simpson MJ, Luger TA, Chubb H, Ellis CN. Comparison of three methods for measuring psoriasis severity in clinical studies (Part 1 of 2): change during therapy in Psoriasis Area and Severity Index, Static Physician’s Global Assessment and Lattice System Physician’s Global Assessment. J Eur Acad Dermatol Venereol. 2015 Jul;29(7):1406-14. doi: 10.1111/jdv.13132. Epub 2015 Apr 27. PubMed PMID: 25917315.
5: Simpson MJ, Chow C, Morgenstern H, Luger TA, Ellis CN. Comparison of three methods for measuring psoriasis severity in clinical studies (Part 2 of 2): use of quality of life to assess construct validity of the Lattice System Physician’s Global Assessment, Psoriasis Area and Severity Index and Static Physician’s Global Assessment. J Eur Acad Dermatol Venereol. 2015 Jul;29(7):1415-20. doi: 10.1111/jdv.12861. Epub 2015 Apr 27. PubMed PMID: 25917214.
6: Maya JR, Sadiq MA, Zapata LJ, Hanout M, Sarwar S, Rajagopalan N, Guinn KE, Sepah YJ, Nguyen QD. Emerging therapies for noninfectious uveitis: what may be coming to the clinics. J Ophthalmol. 2014;2014:310329. doi: 10.1155/2014/310329. Epub 2014 Apr 24. Review. PubMed PMID: 24868451; PubMed Central PMCID: PMC4020293.
7: Hardinger KL, Brennan DC. Novel immunosuppressive agents in kidney transplantation. World J Transplant. 2013 Dec 24;3(4):68-77. doi: 10.5500/wjt.v3.i4.68. Review. PubMed PMID: 24392311; PubMed Central PMCID: PMC3879526.
8: Ling SY, Huizinga RB, Mayo PR, Larouche R, Freitag DG, Aspeslet LJ, Foster RT. Cytochrome P450 3A and P-glycoprotein drug-drug interactions with voclosporin. Br J Clin Pharmacol. 2014 Jun;77(6):1039-50. doi: 10.1111/bcp.12309. PubMed PMID: 24330024; PubMed Central PMCID: PMC4093929.
9: Mayo PR, Ling SY, Huizinga RB, Freitag DG, Aspeslet LJ, Foster RT. Population PKPD of voclosporin in renal allograft patients. J Clin Pharmacol. 2014 May;54(5):537-45. doi: 10.1002/jcph.237. Epub 2013 Nov 30. PubMed PMID: 24243422.
10: Gubskaya AV, Khan IJ, Valenzuela LM, Lisnyak YV, Kohn J. Investigating the Release of a Hydrophobic Peptide from Matrices of Biodegradable Polymers: An Integrated Method Approach. Polymer (Guildf). 2013 Jul 8;54(15):3806-3820. PubMed PMID: 24039300; PubMed Central PMCID: PMC3770487.
11: Ling SY, Huizinga RB, Mayo PR, Freitag DG, Aspeslet LJ, Foster RT. Pharmacokinetics of voclosporin in renal impairment and hepatic impairment. J Clin Pharmacol. 2013 Dec;53(12):1303-12. doi: 10.1002/jcph.166. Epub 2013 Oct 8. PubMed PMID: 23996158.
12: Mayo PR, Huizinga RB, Ling SY, Freitag DG, Aspeslet LJ, Foster RT. Voclosporin food effect and single oral ascending dose pharmacokinetic and pharmacodynamic studies in healthy human subjects. J Clin Pharmacol. 2013 Aug;53(8):819-26. doi: 10.1002/jcph.114. Epub 2013 Jun 4. PubMed PMID: 23736966.
13: Schultz C. Voclosporin as a treatment for noninfectious uveitis. Ophthalmol Eye Dis. 2013 May 5;5:5-10. doi: 10.4137/OED.S7995. Print 2013. PubMed PMID: 23700374; PubMed Central PMCID: PMC3653814.
14: Gomes Bittencourt M, Sepah YJ, Do DV, Agbedia O, Akhtar A, Liu H, Akhlaq A, Annam R, Ibrahim M, Nguyen QD. New treatment options for noninfectious uveitis. Dev Ophthalmol. 2012;51:134-61. doi: 10.1159/000336338. Epub 2012 Apr 17. Review. PubMed PMID: 22517211.
15: Khan IJ, Murthy NS, Kohn J. Hydration-induced phase separation in amphiphilic polymer matrices and its influence on voclosporin release. J Funct Biomater. 2012 Oct 30;3(4):745-59. doi: 10.3390/jfb3040745. PubMed PMID: 24955746; PubMed Central PMCID: PMC4030927.
16: Roesel M, Tappeiner C, Heiligenhaus A, Heinz C. Oral voclosporin: novel calcineurin inhibitor for treatment of noninfectious uveitis. Clin Ophthalmol. 2011;5:1309-13. doi: 10.2147/OPTH.S11125. Epub 2011 Sep 13. PubMed PMID: 21966207; PubMed Central PMCID: PMC3180504.
17: Busque S, Cantarovich M, Mulgaonkar S, Gaston R, Gaber AO, Mayo PR, Ling S, Huizinga RB, Meier-Kriesche HU; PROMISE Investigators. The PROMISE study: a phase 2b multicenter study of voclosporin (ISA247) versus tacrolimus in de novo kidney transplantation. Am J Transplant. 2011 Dec;11(12):2675-84. doi: 10.1111/j.1600-6143.2011.03763.x. Epub 2011 Sep 22. PubMed PMID: 21943027.
18: Kuglstatter A, Mueller F, Kusznir E, Gsell B, Stihle M, Thoma R, Benz J, Aspeslet L, Freitag D, Hennig M. Structural basis for the cyclophilin A binding affinity and immunosuppressive potency of E-ISA247 (voclosporin). Acta Crystallogr D Biol Crystallogr. 2011 Feb;67(Pt 2):119-23. doi: 10.1107/S0907444910051905. Epub 2011 Jan 15. PubMed PMID: 21245533; PubMed Central PMCID: PMC3045272.
19: Kunynetz R, Carey W, Thomas R, Toth D, Trafford T, Vender R. Quality of life in plaque psoriasis patients treated with voclosporin: a Canadian phase III, randomized, multicenter, double-blind, placebo-controlled study. Eur J Dermatol. 2011 Jan-Feb;21(1):89-94. doi: 10.1684/ejd.2010.1185. PubMed PMID: 21227890.
20: Deuter CM. [Systemic voclosporin for uveitis treatment]. Ophthalmologe. 2010 Jul;107(7):672-5. doi: 10.1007/s00347-010-2217-5. German. PubMed PMID: 20571806.
//////////VOCLOSPORIN, Voclosporin, ISA247, ISAtx 247, ISAtx-247, ISAtx247, Luveniq, LX211,
CC[C@@H]1NC([C@@H](N(C([C@@H](N(C([C@@H](N(C([C@@H](N(C([C@H](NC([C@@H](NC([C@@H](N(C([C@H](C(C)C)NC([C@@H](N(C(CN(C1=O)C)=O)C)CC(C)C)=O)=O)C)CC(C)C)=O)C)=O)C)=O)C)CC(C)C)=O)C)CC(C)C)=O)C)C(C)C)=O)C)[C@@H]([C@@H](C/C=C/C=C)C)O)=O
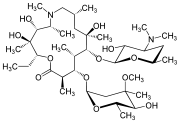
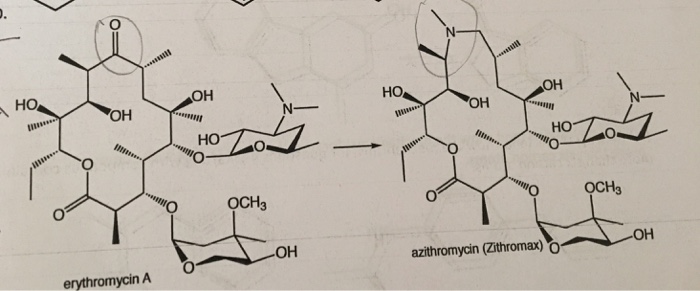
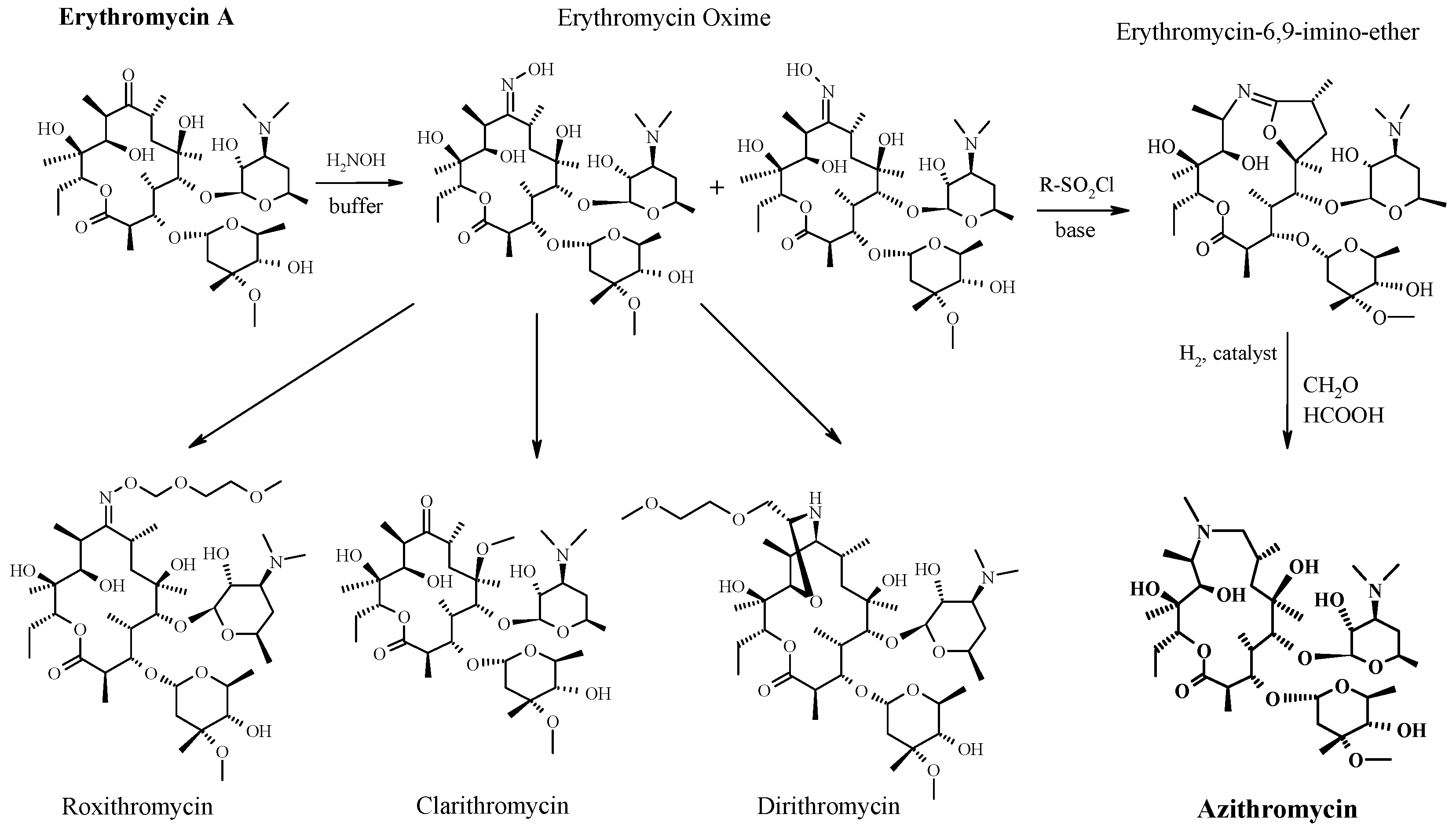
AZITHROMYCIN, アジスロマイシン;
AZITHROMYCIN
C38H72N2O12,
748.9845
アジスロマイシン;
| CAS: | 83905-01-5 |
| PubChem: | 51091811 |
| ChEBI: | 2955 |
| ChEMBL: | CHEMBL529 |
| DrugBank: | DB00207 |
| PDB-CCD: | ZIT[PDBj] |
| LigandBox: | D07486 |
| NIKKAJI: | J134.080H |
Azithromycin is an antibiotic used for the treatment of a number of bacterial infections.[3] This includes middle ear infections, strep throat, pneumonia, traveler’s diarrhea, and certain other intestinal infections.[3] It can also be used for a number of sexually transmitted infections, including chlamydia and gonorrhea infections.[3] Along with other medications, it may also be used for malaria.[3] It can be taken by mouth or intravenously with doses once per day.[3]
Common side effects include nausea, vomiting, diarrhea and upset stomach.[3] An allergic reaction, such as anaphylaxis, QT prolongation, or a type of diarrhea caused by Clostridium difficile is possible.[3] No harm has been found with its use during pregnancy.[3] Its safety during breastfeeding is not confirmed, but it is likely safe.[4] Azithromycin is an azalide, a type of macrolide antibiotic.[3] It works by decreasing the production of protein, thereby stopping bacterial growth.[3]
Azithromycin was discovered 1980 by Pliva, and approved for medical use in 1988.[5][6] It is on the World Health Organization’s List of Essential Medicines, the safest and most effective medicines needed in a health system.[7] The World Health Organization classifies it as critically important for human medicine.[8] It is available as a generic medication[9] and is sold under many trade names worldwide.[2] The wholesale cost in the developing world is about US$0.18 to US$2.98 per dose.[10] In the United States, it is about US$4 for a course of treatment as of 2018.[11] In 2016, it was the 49th most prescribed medication in the United States with more than 15 million prescriptions.[12]
Medical uses
Azithromycin is used to treat many different infections, including:
- Prevention and treatment of acute bacterial exacerbations of chronic obstructive pulmonary disease due to H. influenzae, M. catarrhalis, or S. pneumoniae. The benefits of long-term prophylaxis must be weighed on a patient-by-patient basis against the risk of cardiovascular and other adverse effects.[13]
- Community-acquired pneumonia due to C. pneumoniae, H. influenzae, M. pneumoniae, or S. pneumoniae[14]
- Uncomplicated skin infections due to S. aureus, S. pyogenes, or S. agalactiae
- Urethritis and cervicitis due to C. trachomatis or N. gonorrhoeae. In combination with ceftriaxone, azithromycin is part of the United States Centers for Disease Control-recommended regimen for the treatment of gonorrhea. Azithromycin is active as monotherapy in most cases, but the combination with ceftriaxone is recommended based on the relatively low barrier to resistance development in gonococci and due to frequent co-infection with C. trachomatis and N. gonorrhoeae.[15]
- Trachoma due to C. trachomatis[16]
- Genital ulcer disease (chancroid) in men due to H. ducrey
- Acute bacterial sinusitis due to H. influenzae, M. catarrhalis, or S. pneumoniae. Other agents, such as amoxicillin/clavulanate are generally preferred, however.[17][18]
- Acute otitis media caused by H. influenzae, M. catarrhalis or S. pneumoniae. Azithromycin is not, however, a first-line agent for this condition. Amoxicillin or another beta lactam antibiotic is generally preferred.[19]
- Pharyngitis or tonsillitis caused by S. pyogenes as an alternative to first-line therapy in individuals who cannot use first-line therapy[20]
Bacterial susceptibility
Azithromycin has relatively broad but shallow antibacterial activity. It inhibits some Gram-positive bacteria, some Gram-negative bacteria, and many atypical bacteria.
A strain of gonorrhea reported to be highly resistant to azithromycin was found in the population in 2015. Neisseria gonorrhoeae is normally susceptible to azithromycin,[21] but the drug is not widely used as monotherapy due to a low barrier to resistance development.[15] Extensive use of azithromycin has resulted in growing Streptococcus pneumoniae resistance.[22]
Aerobic and facultative Gram-positive microorganisms
- Staphylococcus aureus (Methicillin-sensitive only)
- Streptococcus agalactiae
- Streptococcus pneumoniae
- Streptococcus pyogenes
Aerobic and facultative Gram-negative microorganisms
- Haemophilus ducreyi
- Haemophilus influenzae
- Moraxella catarrhalis
- Neisseria gonorrhoeae
- Bordetella pertussis
- Legionella pneumophila
Anaerobic microorganisms
- Peptostreptococcus species
- Prevotella bivia
Other microorganisms
- Chlamydophila pneumoniae
- Chlamydia trachomatis
- Mycoplasma genitalium
- Mycoplasma pneumoniae
- Ureaplasma urealyticum
Pregnancy and breastfeeding
No harm has been found with use during pregnancy.[3] However, there are no adequate well-controlled studies in pregnant women.[23]
Safety of the medication during breastfeeding is unclear. It was reported that because only low levels are found in breast milk and the medication has also been used in young children, it is unlikely that breastfed infants would suffer adverse effects.[4] Nevertheless, it is recommended that the drug be used with caution during breastfeeding.[3]
Airway diseases
Azithromycin appears to be effective in the treatment of COPD through its suppression of inflammatory processes.[24] And potentially useful in asthma and sinusitis via this mechanism.[25] Azithromycin is believed to produce its effects through suppressing certain immune responses that may contribute to inflammation of the airways.[26][27]
Adverse effects
Most common adverse effects are diarrhea (5%), nausea (3%), abdominal pain (3%), and vomiting. Fewer than 1% of people stop taking the drug due to side effects. Nervousness, skin reactions, and anaphylaxis have been reported.[28] Clostridium difficile infection has been reported with use of azithromycin.[3] Azithromycin does not affect the efficacy of birth control unlike some other antibiotics such as rifampin. Hearing loss has been reported.[29]
Occasionally, people have developed cholestatic hepatitis or delirium. Accidental intravenous overdose in an infant caused severe heart block, resulting in residual encephalopathy.[30][31]
In 2013 the FDA issued a warning that azithromycin “can cause abnormal changes in the electrical activity of the heart that may lead to a potentially fatal irregular heart rhythm.” The FDA noted in the warning a 2012 study that found the drug may increase the risk of death, especially in those with heart problems, compared with those on other antibiotics such as amoxicillin or no antibiotic. The warning indicated people with preexisting conditions are at particular risk, such as those with QT interval prolongation, low blood levels of potassium or magnesium, a slower than normal heart rate, or those who use certain drugs to treat abnormal heart rhythms.[32][33][34]
Pharmacology
Mechanism of action
Azithromycin prevents bacteria from growing by interfering with their protein synthesis. It binds to the 50S subunit of the bacterial ribosome, thus inhibiting translation of mRNA. Nucleic acid synthesis is not affected.[23]
Pharmacokinetics
Azithromycin is an acid-stable antibiotic, so it can be taken orally with no need of protection from gastric acids. It is readily absorbed, but absorption is greater on an empty stomach. Time to peak concentration (Tmax) in adults is 2.1 to 3.2 hours for oral dosage forms. Due to its high concentration in phagocytes, azithromycin is actively transported to the site of infection. During active phagocytosis, large concentrations are released. The concentration of azithromycin in the tissues can be over 50 times higher than in plasma due to ion trapping and its high lipid solubility.[citation needed] Azithromycin’s half-life allows a large single dose to be administered and yet maintain bacteriostatic levels in the infected tissue for several days.[35]
Following a single dose of 500 mg, the apparent terminal elimination half-life of azithromycin is 68 hours.[35] Biliary excretion of azithromycin, predominantly unchanged, is a major route of elimination. Over the course of a week, about 6% of the administered dose appears as unchanged drug in urine.
History
A team of researchers at the pharmaceutical company Pliva in Zagreb, SR Croatia, Yugoslavia, — Gabrijela Kobrehel, Gorjana Radobolja-Lazarevski, and Zrinka Tamburašev, led by Dr. Slobodan Đokić — discovered azithromycin in 1980.[6] It was patented in 1981. In 1986, Pliva and Pfizer signed a licensing agreement, which gave Pfizer exclusive rights for the sale of azithromycin in Western Europe and the United States. Pliva put its azithromycin on the market in Central and Eastern Europe under the brand name Sumamed in 1988. Pfizer launched azithromycin under Pliva’s license in other markets under the brand name Zithromax in 1991.[36] Patent protection ended in 2005.[37]
Society and culture
Zithromax (azithromycin) 250 mg tablets (CA)
Cost
It is available as a generic medication.[9] The wholesale cost is about US$0.18 to US$2.98 per dose.[10] In the United States it is about US$4 for a course of treatment as of 2018.[11] In India, it is about US$1.70 for a course of treatment.[citation needed]
Available forms
Azithromycin is commonly administered in film-coated tablet, capsule, oral suspension, intravenous injection, granules for suspension in sachet, and ophthalmic solution.[2]
Usage
In 2010, azithromycin was the most prescribed antibiotic for outpatients in the US,[38] whereas in Sweden, where outpatient antibiotic use is a third as prevalent, macrolides are only on 3% of prescriptions.[39]
READ
References
- ^ Jump up to:ab “Azithromycin Use During Pregnancy”. Drugs.com. 2 May 2019. Retrieved 24 December 2019.
- ^ Jump up to:abcdef “Azithromycin International Brands”. Drugs.com. Archived from the original on 28 February 2017. Retrieved 27 February 2017.
- ^ Jump up to:abcdefghijklm “Azithromycin”. The American Society of Health-System Pharmacists. Archived from the original on 5 September 2015. Retrieved 1 August 2015.
- ^ Jump up to:ab “Azithromycin use while Breastfeeding”. Archived from the original on 5 September 2015. Retrieved 4 September 2015.
- ^ Greenwood, David (2008). Antimicrobial drugs : chronicle of a twentieth century medical triumph (1. publ. ed.). Oxford: Oxford University Press. p. 239. ISBN9780199534845. Archived from the original on 5 March 2016.
- ^ Jump up to:ab Fischer, Jnos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 498. ISBN9783527607495.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ World Health Organization (2019). Critically important antimicrobials for human medicine (6th revision ed.). Geneva: World Health Organization. hdl:10665/312266. ISBN9789241515528. License: CC BY-NC-SA 3.0 IGO.
- ^ Jump up to:ab Hamilton, Richart (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. ISBN9781284057560.
- ^ Jump up to:ab “Azithromycin”. International Drug Price Indicator Guide. Retrieved 4 September 2015.
- ^ Jump up to:ab “NADAC as of 2018-05-23”. Centers for Medicare and Medicaid Services. Retrieved 24 May 2018.
- ^ “The Top 300 of 2019”. clincalc.com. Retrieved 22 December2018.
- ^ Taylor SP, Sellers E, Taylor BT (2015). “Azithromycin for the Prevention of COPD Exacerbations: The Good, Bad, and Ugly”. Am. J. Med. 128 (12): 1362.e1–6. doi:10.1016/j.amjmed.2015.07.032. PMID26291905.
- ^ Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM, Musher DM, Niederman MS, Torres A, Whitney CG (2007). “Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults”. Clin. Infect. Dis. 44 Suppl 2: S27–72. doi:10.1086/511159. PMID17278083.
- ^ Jump up to:ab “Gonococcal Infections – 2015 STD Treatment Guidelines”. Archived from the original on 1 March 2016.
- ^ Burton M, Habtamu E, Ho D, Gower EW (2015). “Interventions for trachoma trichiasis”. Cochrane Database Syst Rev. 11 (11): CD004008. doi:10.1002/14651858.CD004008.pub3. PMC4661324. PMID26568232.
- ^ Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, Brook I, Ashok Kumar K, Kramper M, Orlandi RR, Palmer JN, Patel ZM, Peters A, Walsh SA, Corrigan MD (2015). “Clinical practice guideline (update): adult sinusitis”. Otolaryngol Head Neck Surg. 152 (2 Suppl): S1–S39. doi:10.1177/0194599815572097. PMID25832968.
- ^ Hauk L (2014). “AAP releases guideline on diagnosis and management of acute bacterial sinusitis in children one to 18 years of age”. Am Fam Physician. 89 (8): 676–81. PMID24784128.
- ^ Neff MJ (2004). “AAP, AAFP release guideline on diagnosis and management of acute otitis media”. Am Fam Physician. 69 (11): 2713–5. PMID15202704.
- ^ Randel A (2013). “IDSA Updates Guideline for Managing Group A Streptococcal Pharyngitis”. Am Fam Physician. 88 (5): 338–40. PMID24010402.
- ^ The Guardian newspaper: ‘Super-gonorrhoea’ outbreak in Leeds, 18 September 2015Archived 18 September 2015 at the Wayback Machine
- ^ Lippincott Illustrated Reviews : Pharmacology Sixth Edition. p. 506.
- ^ Jump up to:ab “US azithromycin label”(PDF). FDA. February 2016. Archived(PDF) from the original on 23 November 2016.
- ^ Simoens, Steven; Laekeman, Gert; Decramer, Marc (May 2013). “Preventing COPD exacerbations with macrolides: A review and budget impact analysis”. Respiratory Medicine. 107 (5): 637–648. doi:10.1016/j.rmed.2012.12.019. PMID23352223.
- ^ Gotfried, Mark H. (February 2004). “Macrolides for the Treatment of Chronic Sinusitis, Asthma, and COPD”. CHEST. 125 (2): 52S–61S. doi:10.1378/chest.125.2_suppl.52S. ISSN0012-3692. PMID14872001.
- ^ Zarogoulidis, P.; Papanas, N.; Kioumis, I.; Chatzaki, E.; Maltezos, E.; Zarogoulidis, K. (May 2012). “Macrolides: from in vitro anti-inflammatory and immunomodulatory properties to clinical practice in respiratory diseases”. European Journal of Clinical Pharmacology. 68 (5): 479–503. doi:10.1007/s00228-011-1161-x. ISSN1432-1041. PMID22105373.
- ^ Steel, Helen C.; Theron, Annette J.; Cockeran, Riana; Anderson, Ronald; Feldman, Charles (2012). “Pathogen- and Host-Directed Anti-Inflammatory Activities of Macrolide Antibiotics”. Mediators of Inflammation. 2012: 584262. doi:10.1155/2012/584262. PMC3388425. PMID22778497.
- ^ Mori F, Pecorari L, Pantano S, Rossi M, Pucci N, De Martino M, Novembre E (2014). “Azithromycin anaphylaxis in children”. Int J Immunopathol Pharmacol. 27 (1): 121–6. doi:10.1177/039463201402700116. PMID24674687.
- ^ Dart, Richard C. (2004). Medical Toxology. Lippincott Williams & Wilkins. p. 23.
- ^ Tilelli, John A.; Smith, Kathleen M.; Pettignano, Robert (2006). “Life-Threatening Bradyarrhythmia After Massive Azithromycin Overdose”. Pharmacotherapy. 26 (1): 147–50. doi:10.1592/phco.2006.26.1.147. PMID16506357.
- ^ Baselt, R. (2008). Disposition of Toxic Drugs and Chemicals in Man (8th ed.). Foster City, CA: Biomedical Publications. pp. 132–133.
- ^ Denise Grady (16 May 2012). “Popular Antibiotic May Raise Risk of Sudden Death”. The New York Times. Archived from the original on 17 May 2012. Retrieved 18 May 2012.
- ^ Ray, Wayne A.; Murray, Katherine T.; Hall, Kathi; Arbogast, Patrick G.; Stein, C. Michael (2012). “Azithromycin and the Risk of Cardiovascular Death”. New England Journal of Medicine. 366(20): 1881–90. doi:10.1056/NEJMoa1003833. PMC3374857. PMID22591294.
- ^ “FDA Drug Safety Communication: Azithromycin (Zithromax or Zmax) and the risk of potentially fatal heart rhythms”. FDA. 12 March 2013. Archived from the original on 27 October 2016.
- ^ Jump up to:ab “Archived copy”. Archived from the original on 14 October 2014. Retrieved 10 October 2014.
- ^ Banić Tomišić, Z. (2011). “The Story of Azithromycin”. Kemija U Industriji. 60 (12): 603–617. ISSN0022-9830. Archived from the original on 8 September 2017.
- ^ “Azithromycin: A world best-selling Antibiotic”. http://www.wipo.int. World Intellectual Property Organization. Retrieved 18 June 2019.
- ^ Hicks, LA; Taylor TH, Jr; Hunkler, RJ (April 2013). “U.S. outpatient antibiotic prescribing, 2010”. The New England Journal of Medicine. 368 (15): 1461–1462. doi:10.1056/NEJMc1212055. PMID23574140.
- ^ Hicks, LA; Taylor TH, Jr; Hunkler, RJ (September 2013). “More on U.S. outpatient antibiotic prescribing, 2010”. The New England Journal of Medicine. 369 (12): 1175–1176. doi:10.1056/NEJMc1306863. PMID24047077.
External links
Keywords: Antibacterial (Antibiotics); Macrolides.
- “Azithromycin”. Drug Information Portal. U.S. National Library of Medicine.
 |
|
 |
|
| Clinical data | |
|---|---|
| Trade names | Zithromax, Azithrocin, others[2] |
| Other names | 9-deoxy-9α-aza-9α-methyl-9α-homoerythromycin A |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a697037 |
| License data |
|
| Pregnancy category |
|
| Routes of administration |
By mouth (capsule, tablet or suspension), intravenous, eye drop |
| Drug class | Macrolide antibiotic |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 38% for 250 mg capsules |
| Metabolism | Liver |
| Elimination half-life | 11–14 h (single dose) 68 h (multiple dosing) |
| Excretion | Biliary, kidney (4.5%) |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| NIAID ChemDB | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.126.551 |
| Chemical and physical data | |
| Formula | C38H72N2O12 |
| Molar mass | 748.984 g·mol−1 g·mol−1 |
| 3D model (JSmol) | |
/////////AZITHROMYCIN, Antibacterial, Antibiotics, Macrolides, CORONA VIRUS, COVID 19, アジスロマイシン ,


Substances Referenced in Synthesis Path
CAS-RN Formula Chemical Name CAS Index Name
76801-85-9 C37H70N2O12 2-deoxo-9a-aza-9a-homoerythromycin A 1-Oxa-6-azacyclopentadecan-15-one,
13-[(2,6-dideoxy-3-C-methyl-3-O-methyl-α-L-ribo-hexopyranosyl)oxy]-2-eth- yl-3,4,10-trihydroxy-3,5,8,10,12,14-hexamethyl-11-[[3,4,6-trideoxy-3-(dimethylamino)-β-D-xylo-hexopyranosyl]oxy]-, [2R-(2
R*,3S*,4R*,5R*,8R*,10R*,11R*,12S*,13S*,1
4R*)]-
90503-04-1 C37H70N2O14 [2R-(2R*,3S*,4R*,5R*,8R*,10R*,11R*,12S*,
13S*,14R*)]-13-[(2,6-dideoxy-3-C-methyl3-O-methyl-α-L-ribo-hexopyranosyl)
oxy]-2-ethyl-3,4,6,10-tetrahydroxy3,5,8,10,12,14-hexamethyl-13-[[3,4,6-
trideoxy-3-(dimethyloxidoamino)-
β-D-xylo-hexopyranosyl] oxy]-1-oxa-6-azacyclopentadecan-15-one
1-Oxa-6-azacyclopentadecan-15-one,
13-[(2,6-dideoxy-3-C-methyl-3-Omethyl-α-L-ribo-hexopyranosyl)
oxy]-2-ethyl-3,4,6,10-tetrahydroxy3,5,8,10,12,14-hexamethyl-13-[[3,4,6-
trideoxy-3-(dimethyloxidoamino)-β-Dxylo-hexopyranosyl]oxy]-, [2R-(2R*,3S*,4R
*,5R*,8R*,10R*,11R*,12S*,13S*,14R*)]-
90503-05-2 C38H72N2O14 [2R-(2R*,3S*,4R*,5R*,8R*,10R*,11R*,12S*,
13S*,14R*)]-13-[(2,6-dideoxy-3-C-methyl3-O-methyl-α-L-ribo-hexopyranosyl) oxy]-2-ethyl-3,4,10-trihydroxy3,5,6,8,10,12,14-heptamethyl-11-[[3,4,6-
trideoxy-3-(dimethyloxidoamino)-
β-D-xylo-hexopyranosyl]
oxy]-1-oxa-6-azacyclopentadecan-15-one
6-oxide
1-Oxa-6-azacyclopentadecan-15-one,
13-[(2,6-dideoxy-3-C-methyl-3-Omethyl-α-L-ribo-hexopyranosyl)
oxy]-2-ethyl-3,4,10-trihydroxy3,5,6,8,10,12,14-heptamethyl-11-[[3,4,6-
trideoxy-3-(dimethyloxidoamino)-βD-xylo-hexopyranosyl]oxy]-, 6-oxide,
[2R-(2R*,3S*,4R*,5R*,8R*,10R*,11R*,12S*,1
3S*,14R*)]-
50-00-0 CH2O formaldehyde Formaldehyde
74-88-4 CH3I methyl iodide Methane, iodoTrade Names
Country Trade Name Vendor Annotation
D Ultreon Pfizer
Zithromax Pfizer Pharma/Gödecke/Parke-Davis
numerous generic preparations
F Azadose Pfizer
Monodose Pfizer
Zithromax Pfizer
GB Zithromax Pfizer
I Azitrocin Bioindustria
Ribotrex Pierre Fabre
Trocozina Sigma-Tau
Zithromax Pfizer
J Zithromac Pfizer
USA Azasite InSite Vision
Zithromax Pfizer as dihydrate
Formulations
cps. 100 mg, 250 mg; Gran. 10%; susp. 200 mg (as dihydrate); tabl. 250 mg
References
Djokic, S. et al.: J. Antibiot. (JANTAJ) 40, 1006 (1987).
a DOS 3 140 449 (Pliva; appl. 12.10.1981; YU-prior. 6.3.1981).
US 4 517 359 (Pliva; 14.5.1985; appl. 22.9.1981; YU-prior. 6.3.1981).
b EP 101 186 (Pliva; appl. 14.7.1983; USA-prior. 19.7.1982, 15.11.1982).
US 4 474 768 (Pfizer; 2.10.1984; prior. 19.7.1982, 15.11.1982).
educt by ring expansion of erythromycin A oxime by Beckmann rearrangement:
Djokic, S. et al.: J. Chem. Soc., Perkin Trans. 1 (JCPRB4) 1986, 1881-1890.
Bright, G.M. et al.: J. Antibiot. (JANTAJ) 41, 1029 (1988). US 4 328 334 (Pliva; 4.5.1982; YU-prior. 2.4.1979).
stable, non-hygroscopic dihydrate: EP 298 650 (Pfizer; appl. 28.6.1988).
medical use for treatment of protozoal infections:
US 4 963 531 (Pfizer; 16.10.1990; prior. 16.8.1988, 10.9.1987).
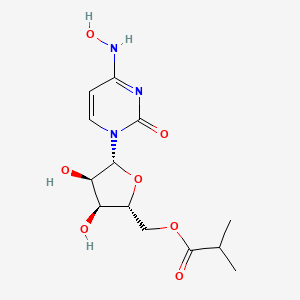
Molnupiravir, EIDD 2801
EIDD 2801
| Molecular Formula: | C13H19N3O7 |
|---|---|
| Molecular Weight: | 329.31 g/mol |
[(2R,3S,4R,5R)-3,4-dihydroxy-5-[4-(hydroxyamino)-2-oxopyrimidin-1-yl]oxolan-2-yl]methyl 2-methylpropanoate
UNII YA84KI1VEW
CAS 2349386-89-4
Molnupiravir (development codes MK-4482 and EIDD-2801) is an experimental antiviral drug which is orally active (can be taken orally) and was developed for the treatment of influenza. It is a prodrug of the synthetic nucleoside derivative N4-hydroxycytidine, and exerts its antiviral action through introduction of copying errors during viral RNA replication.[1][2] Activity has also been demonstrated against coronaviruses including SARS, MERS and SARS-CoV-2.[3]
The drug was developed at Emory University by the university’s drug innovation company, Drug Innovation Ventures at Emory (DRIVE). It was then acquired by Miami-based company Ridgeback Biotherapeutics, who later partnered with Merck & Co. to develop the drug further.
Safety Controversy
In April 2020, a whistleblower complaint by former Head of US Biomedical Advanced Research and Development Authority (BARDA) Rick Bright revealed concerns over providing funding for the further development of molnupiravir due to similar drugs having mutagenic properties (producing birth defects).[4] A previous company, Pharmasset, that had investigated the drug’s active ingredient had abandoned it. These claims were denied by George Painter, CEO of DRIVE, noting that toxicity studies on molnupiravir had been carried out and data provided to regulators in the US and UK, who permitted safety studies in humans to move forward in the spring of 2020. Also at this time, DRIVE and Ridgeback Biotherapeutics stated they planned future safety studies in animals.[5]
COVID-19
After being found to be active against SARS-CoV-2 in March 2020, molnupiravir was tested in a preliminary human study for “Safety, Tolerability, and Pharmacokinetics” in healthy volunteers in the UK and US.[6] In June 2020, Ridgeback Biotherapeutics announced it was moving to Phase II trials to test the efficacy of the drug as a treatment for COVID-19.[7] Two trials of small numbers of hospitalized and non-hospitalized patients in the US and the UK were underway in July.[8][9] In late July 2020, and without yet releasing any medical data, Merck, which had been partnering with Ridgeback Biotherapeutics on developing the drug, announced its intention to move molnupiravir to late stage trials beginning in September 2020.[10] On October 19 2020, Merck began a one year Stage 2/3 trial focused on hospitalized patients.[11]

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@gmail.com
PATENT
WO 2019113462
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2019113462
Example 10: Synthesis of EIDD-2801
A 1L round bottom flask was charged with uridine (25 g, 102.38 mmol) and acetone (700 mL). The reaction mixture was allowed to stir at rt. The slurry was then treated with sulfuric acid (0.27 mL, 5.12 mmol). Stirring was allowed to continue at rt for 18 hours. The reaction was quenched with 100 mL of trimethylamine and was used in the next step without further pruficication.
A 1L round bottom flask was charged with the reaction mixture from the previous reaction. Triethylamine (71.09 mL, 510.08 mmol) and 4-dimethylaminopyridine (0.62 g, 5.1 mmol) were then added. The flask was cooled using an ice bath and then 2-methylpropanoyl 2-methylpropanoate (17.75 g, 112.22 mmol) was slowly added. The reaction mixture was allowed to stir at rt until the reaction was complete. The reaction mixture was concentrated under reduced pressure, and the residue was dissolved in 600 mL ethyl acetate and washed with saturated aqueous bicarbonate solution x 2, water x 2 and brine x 2. The organics were dried over sodium sulfate and concentrated under reduced pressure to yield a clear colorless oil. The crude product was used in the next step without further purification.
A 1L round bottom flask was charged with the crude product from above (36 g, 101.59 mmol) and MeCN (406.37 mL). The reaction mixture was allowed to stir until all the starting material was dissolved. Next, 1,2, 4-triazole (50.52 g, 731.46 mmol) was added followed by the addition of N,N-diethylethanamine (113.28 mL, 812.73 mmol). The reaction mixture was allowed to stir at rt until all solids dissolved. The reaction was then cooled to 0°C using an ice bath. Phosphorous oxychloride (24.44 mL, 152.39 mmol) was added slowly. The slurry that formed was allowed to stir under argon while slowly warming to rt. The reaction was then allowed to stir until complete by TLC (EtOAc). The reaction was then quenched by the addition of lOOmL of water. The slurry then became a dark colored solution, which was
then concentrated under reduced pressure. The residue was dissolved in DCM and washed with water and brine. The organics were then dried over sodium sulfate, filtered, and concentrated under reduced pressure. The product was purified by silica gel chromatography (2 x 330 g columns). All fractions containing product were collected and concentrated under reduced pressure.
A 500 mL round bottom flask was charged with the product from the previous step (11.8 g, 29.11 mmol) and isopropyl alcohol (150 mL). The reaction mixture was allowed to stir at rt until all solids dissolved. Next, hydroxylamine (1.34 mL, 43.66 mmol) was added and stirring continued at ambient temperature. When the reaction was complete (HPLC) some solvent was removed under high vacuum at ambient temperature. The remaining solvent was removed under reduced pressure at 45°C. The resulting residue was dissolved in EtOAc and was washed with water and brine. The organics were dried over sodium sulfate, filtered, and concentrated under reduced pressure to yield oil. Crystals formed upon standing at rt. The crystals were collected by filtration, washed with ether x 3, and dried in vacuo to provide the product as a white solid.
A 200 mL round bottom flask was charged with the product from the previous step (6.5 g, 17.6 mmol) and formic acid (100 mL, 2085.6 mmol). The reaction mixture was allowed to stir at rt overnight. The progress of the reaction was monitored by HPLC. The reaction mixture was concentrated under reduced pressure at 42°C to yield a clear, pale pink oil. Next, 30 mL of ethanol was added. Solvent was then removed under reduced pressure. MTBE (50 mL) was added to the solid and heated. Next, isopropyl alcohol was added and heating was continued until all solid material dissolved (5 mL). The solution was then allowed to cool and stand at rt.
A solid started to form after about lhr. The solids were collected by filtration, washed with MTBE, and dried in vacuo to yield the EIDD-2801 as a white solid. The filtrate was concentrated under reduced pressure to yield a sticky solid, which was dissolved in a small amount of isopropyl alcohol with heating. The solution was allowed to stand at rt overnight. A solid formed in the flask, which was collected by filtration, rinsed with isopropyl alcohol and MTBE, and dried in vacuo to an additional crop of desired product.
EIDD-2801 (25 g) was dissolved in 250 mL of isopropyl alcohol by heating to 70°C to give a clear solution. The warm solution was polish filtered and filtrate transferred to 2L three neck flask with overhead stirrer. It was warmed back to 70°C and MTBE (250 mL) was slowly added into the flask. The clear solution was seeded and allowed to cool slowly to rt with stirring for 18 hrs. The EIDD-2801 solid that formed was filtered and washed with MTBE and dried at 50°C under vacuum for l8hours. The filtrate was concentrated, redissolved in 50 mL isopropyl alcohol and 40 mL MTBE by warming to give clear solution and allowed to stand at rt to give a second crop of EIDD-2801.
Example 11: General synthesis for Deuteration
389 390
The lactone 389 (0.0325 mol) was added to a dry flask under an argon atmosphere and was then dissolved in dry THF (250 mL). The solution as then cooled to -78°C and a DIBAL-D solution in toluene (0.065 mol) was dropwise. The reaction was allowed to stir at -78°C for 3-4 hours. The reaction was then quenched with the slow addition of water (3 mL). The reaction was then allowed to stir while warming to rt. The mixture was then diluted with two volumes of diethyl ether and was then poured into an equal volume of saturated sodium potassium tartrate solution. The organic layer was separated, dried over MgSCri. filtered, and concentrated under reduced pressure. The residue was purified on silica eluting with hexanes/ethyl acetate. The resulting lactol 390 was then converted to an acetate or benzolyate and subjected to cytosine coupling conditions and then further elaborated to N-hydroxycytidine.
PATENT
WO 2019173602
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2019173602
PAPER
ChemRxiv (2020), 1-3.
AND
ChemRxiv (2020), 1-2
PAPER
A Concise Route to MK-4482 (EIDD-2801) from Cytidine: Part 2
Synlett (2020), Ahead of Print.

A new route to MK-4482 was developed. The route replaces uridine with the more available and less expensive cytidine. Low-cost, simple reagents are used for the chemical transformations, and the yield is improved from 17% to 44%. A step is removed from the longest linear sequence, and these advancements are expected to expand access to MK-4482 should it become a viable drug substance.
To a 20 mL vial was added N-hydroxycytidine acetonide ester 5 (0.25 g, 96% purity) followed by formic acid (4 mL). The resultant solution was stirred at room temperature for 4 h 20 min. Solvent was removed under reduced pressure and fresh EtOH (5 mL) was added. The resultant solution was again concentrated under vacuum to afford an oil. Methyl tert-butyl ether and IPA (5 mL each) were successively added as described earlier for preparation of compound 4 and concentrated to give 0.205 g of crude material (77% assay yield, 79% purity). This material was purified by silica gel column chromatography in 8 % MeOH/ Chloroform to afford 130 mg of EIDD-2801 as a solid (60% isolated yield corrected for purity, 98% purity) 1H NMR (600 MHz, CD3OD): δ 6.91 (d, J = 8.2 Hz, 1H), 5.82 (d, J = 4.8 Hz, 1H), 5.61 (d, J = 8.2 Hz, 1H), 4.29 (d, J = 3.6 Hz, 2H), 4.14 (t, J = 4.9 Hz, 1H), 4.08 (p, J = 4.9 Hz, 2H), 2.62 (septet, J = 7.0 Hz, 1H), 1.19 (d, J = 7.0 Hz, 6H); 13C NMR (151 MHz, CD3OD): δ 178.6, 151.81, 146.44, 132.04, 99.84, 90.74, 82.88, 74.67, 71.80, 65.23, 35.45, 27.49, 19.65, 19.61.


One-Pot Transamination/Deprotection of 4 to EIDD-2801: To acetonide ester 4 (1.03 g, 77% Purity) in a 100 mL single neck round bottom flask was added hydroxylamine sulfate (1.09 g, 3.2 equiv.) followed by 40% IPA (20 mL prepared by mixing 12 mL of water and 8 mL of 99.5% IPA. The resultant solution was heated to 78˚C (internal temperature 72-73 ˚C) for 23 h upon which time HPLC showed the formation of EIDD-2801. Solvent was removed on a rotary evaporator and isopropanol (20 mL) was then added. The resulting slurry was sonicated for 5 minutes. The insoluble residue was then filtered and the filtrate concentrated under reduced pressure to afford crude material. (1.34 g, 38% purity, 69% assay yield). The resultant material was purified by silica gel chromatography (5-6% MeOH/DCM) to provide pure EIDD-2801 as two fractions (0.26 g, >99% purity, 36% corrected yield) as an yellow solid and 0.27 g (69.5% purity, 26% corrected yield) as a pinkish solid. The lower purity material was subjected to a second column purification again using 7% MeOH/ DCM to afford 0.137 g of material with 90% purity by NMR. The combined yield thus was estimated to be 53%. The 1H NMR spectrum of the product thus obtained matched the one obtained in the sequential approach as outlined above.
SYN
- A High‐Yielding Synthesis of EIDD‐2801 from Uridine,
Alexander Steiner, Desiree Znidar, Sándor B. Ötvös, David R. Snead, Doris Dallinger, C. Oliver Kappe,
Eur. J. Org. Chem. 2020.
https://doi.org/10.1002/ejoc.202001340





EIDD-2801 was isolated in 69% yield (307 mg) and ≥99% purity as a white
solid.
1H-NMR (300 MHz, MeOH-d4) δ 6.91 (d, J= 8.3 Hz, 1H), 5.82 (d, J= 4.8 Hz, 1H), 5.61 (d, J= 8.2 Hz, 1H), 4.29
(d, J= 3.6 Hz, 2H), 4.15-4.07 (m, 3H), 2.62 (sept, J= 7.0 Hz, 1H), 1.18 (d, J= 7.0 Hz 6H);
13C-NMR (75 MHz,
MeOH-d4Ϳ δ 178.2, 151.5, 146.1, 131.7, 99.5, 90.4, 82.5, 74.3, 71.5, 64.9, 35.1, 19.3, 19.3. The NMR data
is in agreement with previously published values.[2] HRMS (ESI, positive mode): m/z [M + H]+
Calcd for
[C13H20N3O7 +H]+
: 330.1296, found: 330.1297.


SYN
C. Oliver Kappe, Doris Dallinger, University of Graz, Austria, and colleagues have developed an improved synthesis of EIDD-2801 from uridine (pictured below) by strategically reordering the synthetic steps. The reaction sequence starts with the activation of uridine with 1,2,4-triazole and continues with a telescoped acetonide protection/esterification and a telescoped hydroxyamination/acetonide deprotection. Telescoped reaction sequences consist of two or more than one one-pot procedures that are performed back-to-back without a work-up step in-between. A continuous flow process was used for the final acetonide deprotection, which improved selectivity and reproducibility.
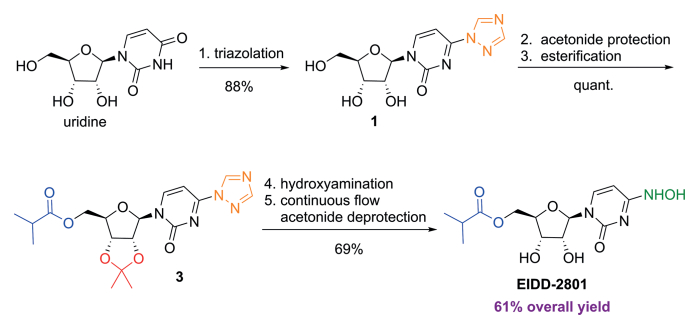
SYN
https://www.frontiersin.org/articles/10.3389/fphar.2020.01013/full
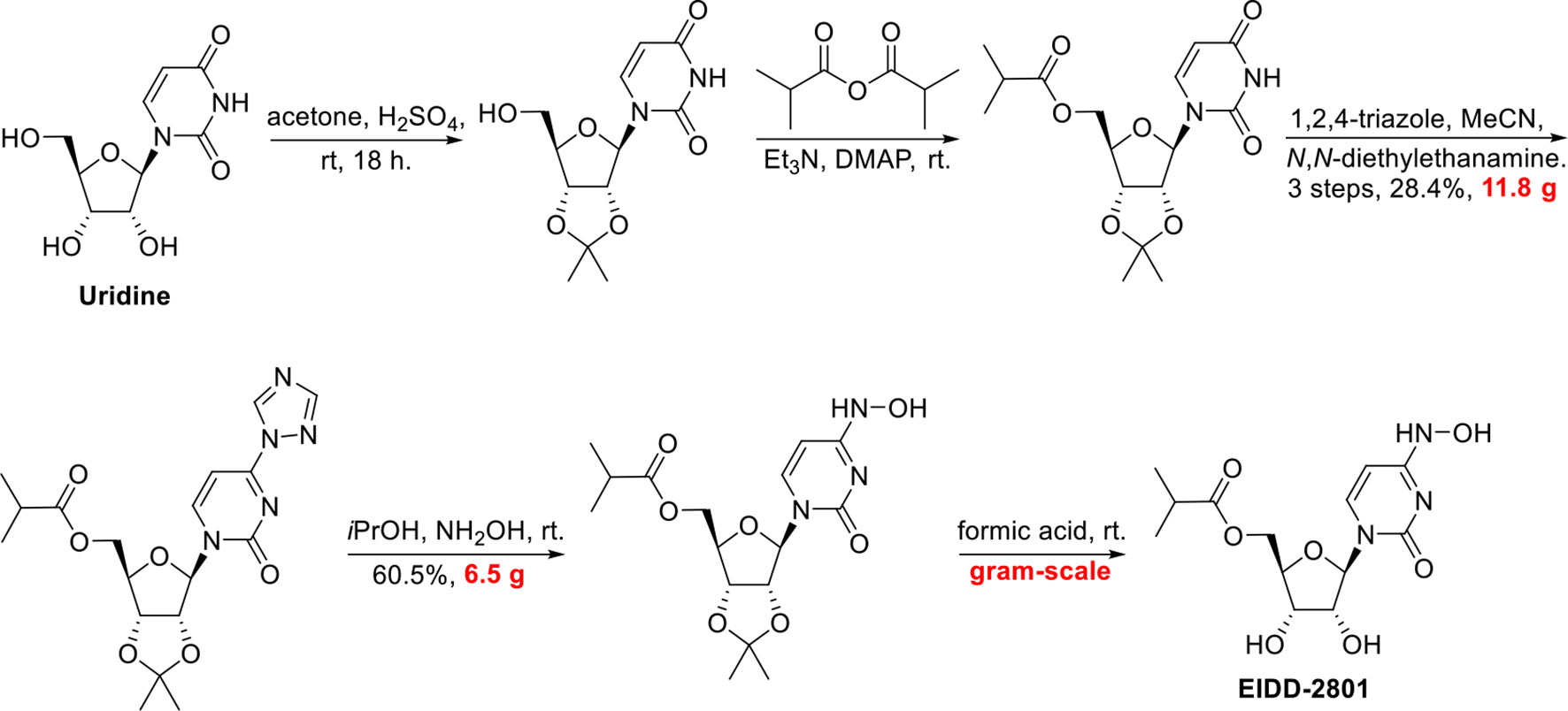
SYN
http://www.rsc.org/suppdata/d0/cc/d0cc05944g/d0cc05944g1.pdf
To a solution of 5’-O-isobutyrylcytidine 4 (1.0 g, 90% purity, 2.87 mmol, 1.0 eq) in 2-propanol (15 ml), hydroxylamine sulphate (2.12 g, 12.93 mmol, 4.5 eq.) was added and reaction was stirred for 20 h at 78 C. Upon completion, the reaction was cooled to room temperature. The organic layer (upper layer) was separated from biphasic reaction mixture. The aqueous layer was washed with 2-propanol (2 X 5 mL). The combined organic layer was concentrated using rotary evaporation and the crude was purified by column chromatography with a gradient of 2-15% methanol in dichloromethane to yield EIDD-2801 (1) as a white solid (963 mg, 94% purity, 96% yield). 1H NMR (600 MHz, D2O) δ 6.98 (d, J = 8.3 Hz, 1H), 5.87 (d, J = 5.0 Hz, 1H), 5.78 (d, J = 8.2 Hz, 1H), 4.39 – 4.33 (m, 3H), 4.28 (dd, J = 6.6, 3.4 Hz, 2H), 2.69 (hept, J = 7.0 Hz, 1H), 1.17 (d, J = 3.7 Hz, 3H), 1.16 (d, J = 3.7 Hz, 3H). 13C NMR (126 MHz, D2O) δ 18.1, 18.2, 33.9, 48.8, 63.6, 69.6, 72.5, 81.0, 88.5, 98.8, 131.1, 151.1, 179.8 ppm; LRMS: 330.1 [M+H]+ ; HRMS (ESI): calcd. for C13H19N3O7 [M+H]+ 330.1296, found 330.1302; Purity: 94% (assessed by qNMR).


https://pubs.rsc.org/en/content/articlehtml/2020/cc/d0cc05944g
 |
||
| Fig. 2 A new route to MK-4482 from cytidine. | ||
References
- ^ Toots M, Yoon JJ, Cox RM, Hart M, Sticher ZM, Makhsous N, et al. (October 2019). “Characterization of orally efficacious influenza drug with high resistance barrier in ferrets and human airway epithelia”. Science Translational Medicine. 11 (515): eaax5866. doi:10.1126/scitranslmed.aax5866. PMC 6848974. PMID 31645453.
- ^ Toots M, Yoon JJ, Hart M, Natchus MG, Painter GR, Plemper RK (April 2020). “Quantitative efficacy paradigms of the influenza clinical drug candidate EIDD-2801 in the ferret model”. Translational Research. 218: 16–28. doi:10.1016/j.trsl.2019.12.002. PMID 31945316.
- ^ Sheahan TP, Sims AC, Zhou S, Graham RL, Pruijssers AJ, Agostini ML, et al. (April 2020). “An orally bioavailable broad-spectrum antiviral inhibits SARS-CoV-2 in human airway epithelial cell cultures and multiple coronaviruses in mice”. Science Translational Medicine. 12 (541): eabb5883. doi:10.1126/scitranslmed.abb5883. PMC 7164393. PMID 32253226.
- ^ Halford, Bethany. “An emerging antiviral takes aim at COVID-19”. Retrieved 1 August 2020.
- ^ Cohen, Jon; Piller, Charles (13 May 2020). “Emails offer look into whistleblower charges of cronyism behind potential COVID-19 drug”. Science. Retrieved 1 August 2020.
- ^ “COVID-19 First In Human Study to Evaluate Safety, Tolerability, and Pharmacokinetics of EIDD-2801 in Healthy Volunteers”. ClinicalTrials.gov. Retrieved 1 June 2020.
- ^ “Ridgeback Biotherapeutics Announces Launch of Phase 2 Trials Testing EIDD-2801 as Potential Treatment for COVID-19”. Business Wire. Retrieved 4 July 2020.
- ^ “A Safety, Tolerability and Efficacy of EIDD-2801 to Eliminate Infectious Virus Detection in Persons With COVID-19”. ClinicalTrials.gov. Retrieved 4 July 2020.
- ^ “The Effect of EIDD-2801 on Viral Shedding of SARS-CoV-2 (COVID-19)”. ClinicalTrials.gov. Retrieved 4 July 2020.
- ^ Court, Emma (31 July 2020). “Merck pushes ahead on COVID-19 treatment, vaccines”. Retrieved 31 July 2020.
- ^ ClinicaL trials register : Efficacy and Safety of Molnupiravir (MK-4482) in Hospitalized Adult Participants With COVID-19 (MK-4482-001)
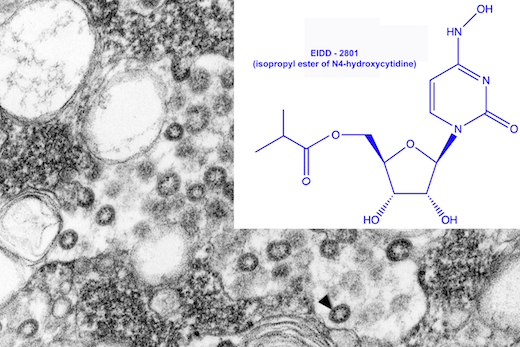
Electron microscope image of SARS virus in a tissue culture isolate, courtesy of CDC Public Health Image Library.
The drug EIDD-1931 was effective against SARS and MERS viruses in the laboratory, and a modified version (EIDD-2801) could potentially be valuable against 2019-nCoV.
https://news.emory.edu/stories/2020/02/coronavirus_eidd/index.html
Emory, collaborators testing antiviral drug as potential treatment for coronaviruses
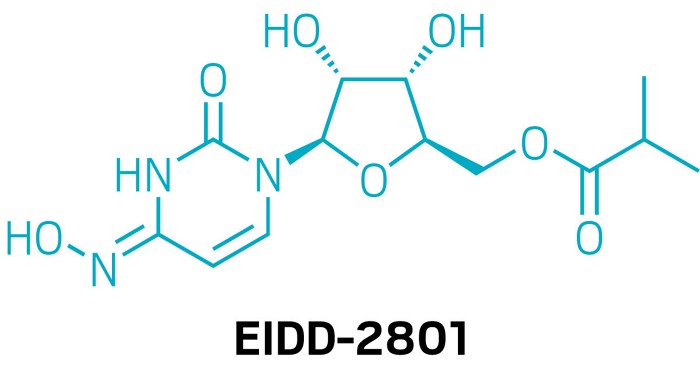
An antiviral compound discovered at Emory University could potentially be used to treat the new coronavirus associated with the outbreak in China and spreading around the globe. Drug Innovation Ventures at Emory (DRIVE), a non-profit LLC wholly owned by Emory, is developing the compound, designated EIDD-2801.
In testing with collaborators at the University of North Carolina at Chapel Hill and Vanderbilt University Medical Center, the active form of EIDD-2801, which is called EIDD-1931, has shown efficacy against the related coronaviruses SARS (Severe Acute Respiratory Syndrome)- and MERS-CoV (Middle East Respiratory Syndrome Coronavirus). Some of the data was recently published in Journal of Virology.
EIDD-2801 is an oral ribonucleoside analog that inhibits the replication of multiple RNA viruses, including respiratory syncytial virus, influenza, chikungunya, Ebola, Venezuelan equine encephalitis virus, and Eastern equine encephalitis viruses.
“We have been planning to enter human clinical tests of EIDD-2801 for the treatment of influenza, and recognized that it has potential activity against the current novel coronavirus,” says George Painter, PhD, director of the Emory Institute for Drug Development (EIDD) and CEO of DRIVE. “Based on the drug’s broad-spectrum activity against viruses including influenza, Ebola and SARS-CoV/MERS-CoV, we believe it will be an excellent candidate.”
“Our studies in the Journal of Virology show potent activity of the EIDD-2801 parent compound against multiple coronaviruses including SARS and MERS,” says Mark Denison, MD, the Stahlman Professor of Pediatrics and director of pediatric infectious diseases at Vanderbilt University School of Medicine. “It also has a strong genetic barrier to development of viral resistance, and its oral bioavailability makes it a candidate for use during an outbreak.”
“Generally speaking, seasonal flu is still a much more common threat than this coronavirus, however, novel emerging coronaviruses represent a considerable threat to global health as evidenced by the new 2019-nCoV,” said Ralph Baric, PhD, an epidemiology professor at the University of North Carolina’s Gillings School of Global Public Health. “But the reason the new coronavirus is so concerning is that it’s much more likely to be deadly than the flu – fatal for about one in 25 people versus one in 1,000 for the flu.”
The development of EIDD-2801 has been funded in whole or in part with Federal funds from the National Institute of Allergy and Infectious Diseases (NIAID), under contract numbers HHSN272201500008C and 75N93019C00058, and from the Defense Threat Reduction Agency (DTRA), under contract numbers HDTRA1-13-C-0072 and HDTRA1-15-C-0075, for the treatment of Influenza, coronavirus, chikungunya, and Venezuelan equine encephalitis virus.
About DRIVE: DRIVE is a non-profit LLC wholly owned by Emory started as an innovative approach to drug development. Operating like an early stage biotechnology company, DRIVE applies focus and industry development expertise to efficiently translate discoveries to address viruses of global concern. Learn more at: http://driveinnovations.org/
Emory-discovered antiviral is poised for COVID-19 clinical trials
The nucleoside inhibitor has advantages over Gilead’s remdesivir but has yet to be tested in humans
Asmall-molecule antiviral discovered by Emory University chemists could soon start human testing against COVID-19, the respiratory disease caused by the novel coronavirus. That’s the plan of Ridgeback Biotherapeutics, which licensed the compound, EIDD-2801, from an Emory nonprofit.
But remdesivir can only be given intravenously, meaning it would be difficult to deploy widely. In contrast, EIDD-2801 can be taken in pill form, says Mark Denison, a coronavirus expert and director of the infectious diseases division at Vanderbilt Medical School. Denison partnered with Emory and researchers at the University of North Carolina to test the compound against coronaviruses.
EIDD-2801 has other promising features. Many antivirals work by introducing errors into the viral genome, but, unlike other viruses, coronaviruses can fix some mistakes. In lab experiments, EIDD-2801 “was able to overcome the coronavirus proofreading function,” Denison says.
He also notes that while remdesivir and EIDD-2801 both block RNA polymerase, they appear to do it in different ways, meaning they could be complementary.
Unlike remdesivir, EIDD-2801 lacks human safety data. Ridgeback founder and CEO Wendy Holman says she expects the US Food and Drug Administration to give the green light for a Phase I study in COVID-19 infections within “weeks, not months.”
“weeks, not months.”
 |
|
| Clinical data | |
|---|---|
| Other names | MK-4482, EIDD-2801 |
| Legal status | |
| Legal status |
|
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| UNII | |
| Chemical and physical data | |
| Formula | C13H19N3O7 |
| Molar mass | 329.31 g·mol−1 |
| 3D model (JSmol) | |
////////EIDD 2801, EMORY, CORONA VIRUS, COVID 19, mk 4482, molnupiravir, merck
CC(C)C(=O)OC[C@H]2O[C@@H](N1C=CC(=NC1=O)NO)[C@H](O)[C@@H]2O

NEW DRUG APPROVALS
ONE TIME
$10.00



| Application Id | Application Number | Application Date | Country | Title |
| US333828014 | 17170172 | 08.02.2021 | US | N4-HYDROXYCYTIDINE AND DERIVATIVES AND ANTI-VIRAL USES RELATED THERETO |
| US305251595 | 16755779 | 07.12.2018 | US | N4-HYDROXYCYTIDINE AND DERIVATIVES AND ANTI-VIRAL USES RELATED THERETO |
| WO2021159044 | PCT/US2021/016984 | 07.02.2021 | WO | N4-HYDROXYCYTIDINE AND DERIVATIVES AND ANTI-VIRAL USES RELATED THERETO |
| WO2021137913 | PCT/US2020/054857 | 08.10.2020 | WO | 4′-HALOGEN CONTAINING NUCLEOTIDE AND NUCLEOSIDE THERAPEUTIC COMPOSITIONS AND USES RELATED THERETO |



CHLOROQUINE, クロロキン;Хлорохин , クロロキン , كلوروكين
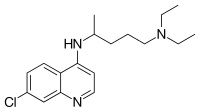
CHLOROQUINE
| Formula |
C18H26ClN3
|
|---|---|
| CAS |
54-05-7
|
| Mol weight |
319.8721
|
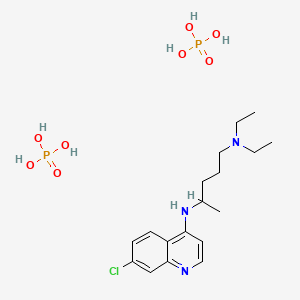
Chloroquine is a medication used primarily to prevent and to treat malaria in areas where that parasitic disease is known to remain sensitive to its effects.[1] A benefit of its use in therapy, when situations allow, is that it can be taken by mouth (versus by injection).[1] Controlled studies of cases involving human pregnancy are lacking, but the drug may be safe for use for such patients.[verification needed][1][2] However, the agent is not without the possibility of serious side effects at standard doses,[1][3] and complicated cases, including infections of certain types or caused by resistant strains, typically require different or additional medication.[1] Chloroquine is also used as a medication for rheumatoid arthritis, lupus erythematosus, and other parasitic infections (e.g., amebiasis occurring outside of the intestines).[1] Beginning in 2020, studies have proceeded on its use as a coronavirus antiviral, in possible treatment of COVID-19.[4]
Chloroquine, otherwise known as chloroquine phosphate, is in the 4-aminoquinoline class of drugs.[1] As an antimalarial, it works against the asexual form of the malaria parasite in the stage of its life cycle within the red blood cell.[1] In its use against rheumatoid arthritis and lupus erythematosus, its activity as a mild immunosuppressive underlies its mechanism.[1] Antiviral activities, established and putative, are attributed to chloroquines inhibition of glycosylation pathways (of host receptor sialylation or virus protein post-translational modification), or to inhibition of virus endocytosis (e.g., via alkalisation of endosomes), or other possible mechanisms.[5] Common side effects resulting from these therapeutic uses, at common doses, include muscle problems,[clarification needed] loss of appetite, diarrhea, and skin rash.[clarification needed][1] Serious side effects include problems with vision (retinopathy), muscle damage, seizures, and certain anemias.[1][6]
Chloroquine was discovered in 1934 by Hans Andersag.[7][8] It is on the World Health Organization’s List of Essential Medicines, the safest and most effective medicines needed in a health system.[9] It is available as a generic medication.[1] The wholesale cost in the developing world is about US$0.04.[10] In the United States, it costs about US$5.30 per dose.[1]
Medical uses
Malaria
Distribution of malaria in the world:[11]
♦ Elevated occurrence of chloroquine- or multi-resistant malaria
♦ Occurrence of chloroquine-resistant malaria
♦ No Plasmodium falciparum or chloroquine-resistance
♦ No malaria
Chloroquine has been used in the treatment and prevention of malaria from Plasmodium vivax, P. ovale, and P. malariae. It is generally not used for Plasmodium falciparum as there is widespread resistance to it.[12][13]
Chloroquine has been extensively used in mass drug administrations, which may have contributed to the emergence and spread of resistance. It is recommended to check if chloroquine is still effective in the region prior to using it.[14] In areas where resistance is present, other antimalarials, such as mefloquine or atovaquone, may be used instead. The Centers for Disease Control and Prevention recommend against treatment of malaria with chloroquine alone due to more effective combinations.[15]
Amebiasis
In treatment of amoebic liver abscess, chloroquine may be used instead of or in addition to other medications in the event of failure of improvement with metronidazole or another nitroimidazole within 5 days or intolerance to metronidazole or a nitroimidazole.[16]
Rheumatic disease
As it mildly suppresses the immune system, chloroquine is used in some autoimmune disorders, such as rheumatoid arthritis and lupus erythematosus.[1]
Side effects
Side effects include blurred vision, nausea, vomiting, abdominal cramps, headache, diarrhea, swelling legs/ankles, shortness of breath, pale lips/nails/skin, muscle weakness, easy bruising/bleeding, hearing and mental problems.[17][18]
- Unwanted/uncontrolled movements (including tongue and face twitching) [17]
- Deafness or tinnitus.[17]
- Nausea, vomiting, diarrhea, abdominal cramps[18]
- Headache.[17]
- Mental/mood changes (such as confusion, personality changes, unusual thoughts/behavior, depression, feeling being watched, hallucinating)[17][18]
- Signs of serious infection (such as high fever, severe chills, persistent sore throat)[17]
- Skin itchiness, skin color changes, hair loss, and skin rashes.[18][19]
- Chloroquine-induced itching is very common among black Africans (70%), but much less common in other races. It increases with age, and is so severe as to stop compliance with drug therapy. It is increased during malaria fever; its severity is correlated to the malaria parasite load in blood. Some evidence indicates it has a genetic basis and is related to chloroquine action with opiate receptors centrally or peripherally.[20]
- Unpleasant metallic taste
- This could be avoided by “taste-masked and controlled release” formulations such as multiple emulsions.[21]
- Chloroquine retinopathy
- Electrocardiographic changes[22]
- This manifests itself as either conduction disturbances (bundle-branch block, atrioventricular block) or Cardiomyopathy – often with hypertrophy, restrictive physiology, and congestive heart failure. The changes may be irreversible. Only two cases have been reported requiring heart transplantation, suggesting this particular risk is very low. Electron microscopy of cardiac biopsies show pathognomonic cytoplasmic inclusion bodies.
- Pancytopenia, aplastic anemia, reversible agranulocytosis, low blood platelets, neutropenia.[23]
Pregnancy
Chloroquine has not been shown to have any harmful effects on the fetus when used for malarial prophylaxis.[24] Small amounts of chloroquine are excreted in the breast milk of lactating women. However, this drug can be safely prescribed to infants, the effects are not harmful. Studies with mice show that radioactively tagged chloroquine passed through the placenta rapidly and accumulated in the fetal eyes which remained present five months after the drug was cleared from the rest of the body.[23][25] Women who are pregnant or planning on getting pregnant are still advised against traveling to malaria-risk regions.[24]
Elderly
There is not enough evidence to determine whether chloroquine is safe to be given to people aged 65 and older. Since it is cleared by the kidneys, toxicity should be monitored carefully in people with poor kidney functions.[23]
Drug interactions
Chloroquine has a number of drug-drug interactions that might be of clinical concern:[citation needed]
- Ampicillin– levels may be reduced by chloroquine;[23]
- Antacids– may reduce absorption of chloroquine;[23]
- Cimetidine– may inhibit metabolism of chloroquine; increasing levels of chloroquine in the body;[23]
- Cyclosporine– levels may be increased by chloroquine;[23] and
- Mefloquine– may increase risk of convulsions.[23]
Overdose
Chloroquine is very dangerous in overdose. It is rapidly absorbed from the gut. In 1961, a published compilation of case reports contained accounts of three children who took overdoses and died within 2.5 hours of taking the drug. While the amount of the overdose was not stated, the therapeutic index for chloroquine is known to be small.[26] One of the children died after taking 0.75 or 1 gram, or twice a single therapeutic amount for children. Symptoms of overdose include headache, drowsiness, visual disturbances, nausea and vomiting, cardiovascular collapse, seizures, and sudden respiratory and cardiac arrest.[23]
An analog of chloroquine – hydroxychloroquine – has a long half-life (32–56 days) in blood and a large volume of distribution (580–815 L/kg).[27] The therapeutic, toxic and lethal ranges are usually considered to be 0.03 to 15 mg/l, 3.0 to 26 mg/l and 20 to 104 mg/l, respectively. However, nontoxic cases have been reported up to 39 mg/l, suggesting individual tolerance to this agent may be more variable than previously recognised.[27]
Pharmacology
Chloroquine’s absorption of the drug is rapid. It is widely distributed in body tissues. It’s protein binding is 55%.[ It’s metabolism is partially hepatic, giving rise to its main metabolite, desethylchloroquine. It’s excretion os ≥50% as unchanged drug in urine, where acidification of urine increases its elimination It has a very high volume of distribution, as it diffuses into the body’s adipose tissue.
Accumulation of the drug may result in deposits that can lead to blurred vision and blindness. It and related quinines have been associated with cases of retinal toxicity, particularly when provided at higher doses for longer times. With long-term doses, routine visits to an ophthalmologist are recommended.
Chloroquine is also a lysosomotropic agent, meaning it accumulates preferentially in the lysosomes of cells in the body. The pKa for the quinoline nitrogen of chloroquine is 8.5, meaning—in simplified terms, considering only this basic site—it is about 10% deprotonated at physiological pH (per the Henderson-Hasselbalch equation) This decreases to about 0.2% at a lysosomal pH of 4.6.Because the deprotonated form is more membrane-permeable than the protonated form, a quantitative “trapping” of the compound in lysosomes results.
Mechanism of action
Malaria
Hemozoin formation in P. falciparum: many antimalarials are strong inhibitors of hemozoin crystal growth.
The lysosomotropic character of chloroquine is believed to account for much of its antimalarial activity; the drug concentrates in the acidic food vacuole of the parasite and interferes with essential processes. Its lysosomotropic properties further allow for its use for in vitro experiments pertaining to intracellular lipid related diseases,[28][29] autophagy, and apoptosis.[30]
Inside red blood cells, the malarial parasite, which is then in its asexual lifecycle stage, must degrade hemoglobin to acquire essential amino acids, which the parasite requires to construct its own protein and for energy metabolism. Digestion is carried out in a vacuole of the parasitic cell.[citation needed]
Hemoglobin is composed of a protein unit (digested by the parasite) and a heme unit (not used by the parasite). During this process, the parasite releases the toxic and soluble molecule heme. The heme moiety consists of a porphyrin ring called Fe(II)-protoporphyrin IX (FP). To avoid destruction by this molecule, the parasite biocrystallizes heme to form hemozoin, a nontoxic molecule. Hemozoin collects in the digestive vacuole as insoluble crystals.[citation needed]
Chloroquine enters the red blood cell by simple diffusion, inhibiting the parasite cell and digestive vacuole. Chloroquine then becomes protonated (to CQ2+), as the digestive vacuole is known to be acidic (pH 4.7); chloroquine then cannot leave by diffusion. Chloroquine caps hemozoin molecules to prevent further biocrystallization of heme, thus leading to heme buildup. Chloroquine binds to heme (or FP) to form the FP-chloroquine complex; this complex is highly toxic to the cell and disrupts membrane function. Action of the toxic FP-chloroquine and FP results in cell lysis and ultimately parasite cell autodigestion. [31] Parasites that do not form hemozoin are therefore resistant to chloroquine.[32]
Resistance in malaria[edit source]
Since the first documentation of P. falciparum chloroquine resistance in the 1950s, resistant strains have appeared throughout East and West Africa, Southeast Asia, and South America. The effectiveness of chloroquine against P. falciparum has declined as resistant strains of the parasite evolved. They effectively neutralize the drug via a mechanism that drains chloroquine away from the digestive vacuole. Chloroquine-resistant cells efflux chloroquine at 40 times the rate of chloroquine-sensitive cells; the related mutations trace back to transmembrane proteins of the digestive vacuole, including sets of critical mutations in the P. falciparum chloroquine resistance transporter (PfCRT) gene. The mutated protein, but not the wild-type transporter, transports chloroquine when expressed in Xenopus oocytes (frog’s eggs) and is thought to mediate chloroquine leak from its site of action in the digestive vacuole.[33] Resistant parasites also frequently have mutated products of the ABC transporter P. falciparum multidrug resistance (PfMDR1) gene, although these mutations are thought to be of secondary importance compared to Pfcrt. Verapamil, a Ca2+ channel blocker, has been found to restore both the chloroquine concentration ability and sensitivity to this drug. Recently, an altered chloroquine-transporter protein CG2 of the parasite has been related to chloroquine resistance, but other mechanisms of resistance also appear to be involved.[34] Research on the mechanism of chloroquine and how the parasite has acquired chloroquine resistance is still ongoing, as other mechanisms of resistance are likely.[citation needed]
Other agents which have been shown to reverse chloroquine resistance in malaria are chlorpheniramine, gefitinib, imatinib, tariquidar and zosuquidar.[35]
Chloroquine has antiviral effects.[36] It increases late endosomal or lysosomal pH, resulting in impaired release of the virus from the endosome or lysosome – release requires a low pH. The virus is therefore unable to release its genetic material into the cell and replicate.[37][38]
Chloroquine also seems to act as a zinc ionophore, that allows extracellular zinc to enter the cell and inhibit viral RNA-dependent RNA polymerase.[39][40]
Other
Chloroquine inhibits thiamine uptake.[41] It acts specifically on the transporter SLC19A3.
Against rheumatoid arthritis, it operates by inhibiting lymphocyte proliferation, phospholipase A2, antigen presentation in dendritic cells, release of enzymes from lysosomes, release of reactive oxygen species from macrophages, and production of IL-1.
History
In Peru the indigenous people extracted the bark of the Cinchona plant[42] trees and used the extract (Chinchona officinalis) to fight chills and fever in the seventeenth century. In 1633 this herbal medicine was introduced in Europe, where it was given the same use and also began to be used against malaria.[43] The quinoline antimalarial drug quinine was isolated from the extract in 1820, and chloroquine is an analogue of this.
Chloroquine was discovered in 1934, by Hans Andersag and coworkers at the Bayer laboratories, who named it “Resochin”.[44] It was ignored for a decade, because it was considered too toxic for human use. During World War II, United States government-sponsored clinical trials for antimalarial drug development showed unequivocally that chloroquine has a significant therapeutic value as an antimalarial drug. It was introduced into clinical practice in 1947 for the prophylactic treatment of malaria.[45]
Society and culture
Resochin tablet package
Formulations
Chloroquine comes in tablet form as the phosphate, sulfate, and hydrochloride salts. Chloroquine is usually dispensed as the phosphate.[46]
Names
Brand names include Chloroquine FNA, Resochin, Dawaquin, and Lariago.[47]
Other animals
Chloroquine is used to control the aquarium fish parasite Amyloodinium ocellatum.[48]
Research
COVID-19
In late January 2020 during the 2019–20 coronavirus outbreak, Chinese medical researchers stated that exploratory research into chloroquine and two other medications, remdesivir and lopinavir/ritonavir, seemed to have “fairly good inhibitory effects” on the SARS-CoV-2 virus, which is the virus that causes COVID-19. Requests to start clinical testing were submitted.[49] Chloroquine had been also proposed as a treatment for SARS, with in vitro tests inhibiting the SARS-CoV virus.[50][51]
Chloroquine has been recommended by Chinese, South Korean and Italian health authorities for the treatment of COVID-19.[52][53] These agencies noted contraindications for people with heart disease or diabetes.[54] Both chloroquine and hydroxychloroquine were shown to inhibit SARS-CoV-2 in vitro, but a further study concluded that hydroxychloroquine was more potent than chloroquine, with a more tolerable safety profile.[55] Preliminary results from a trial suggested that chloroquine is effective and safe in COVID-19 pneumonia, “improving lung imaging findings, promoting a virus-negative conversion, and shortening the disease course.”[56] Self-medication with chloroquine has caused one known fatality.[57]
On 24 March 2020, NBC News reported[58] a fatality due to misuse of a chloroquine product used to control fish parasites.[59]
Other viruses
In October 2004, a group of researchers at the Rega Institute for Medical Research published a report on chloroquine, stating that chloroquine acts as an effective inhibitor of the replication of the severe acute respiratory syndrome coronavirus (SARS-CoV) in vitro.[60]
Chloroquine was being considered in 2003, in pre-clinical models as a potential agent against chikungunya fever.[61]
Other
The radiosensitizing and chemosensitizing properties of chloroquine are beginning to be exploited in anticancer strategies in humans.[62][63] In biomedicinal science, chloroquine is used for in vitro experiments to inhibit lysosomal degradation of protein products.
SYN


CLIP
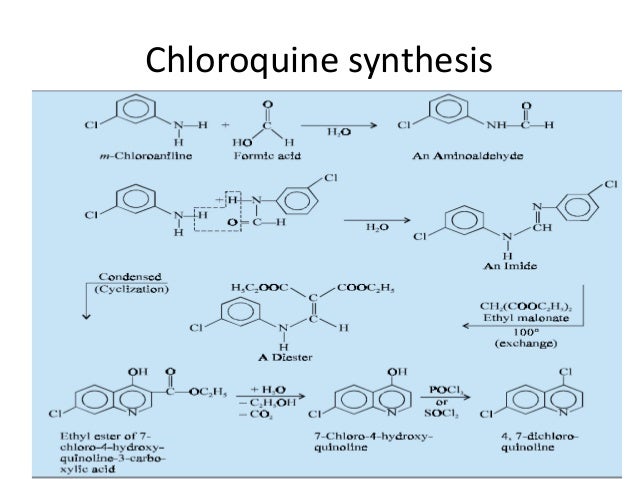
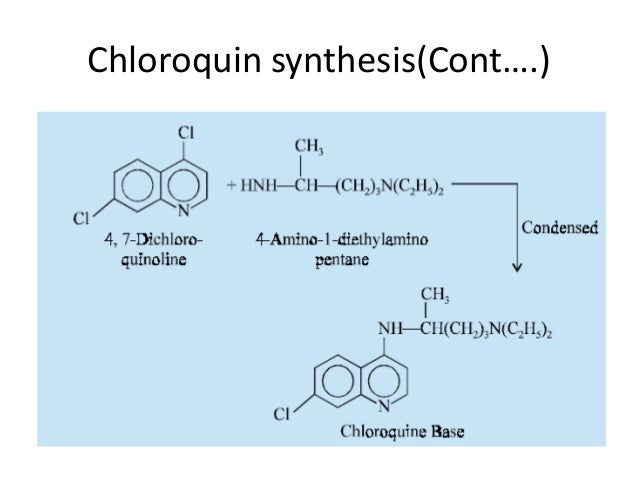
CLIP

CLIP
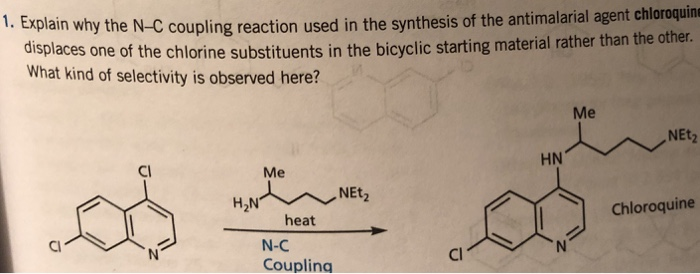
CLIP

References
- ^ Jump up to:a b c d e f g h i j k l m n “Aralen Phosphate”. The American Society of Health-System Pharmacists. Archived from the original on 8 December 2015. Retrieved 2 December 2015.
- ^ “Chloroquine Use During Pregnancy”. Drugs.com. Archivedfrom the original on 16 April 2019. Retrieved 16 April 2019.
There are no controlled data in human pregnancies.
- ^ Mittra, Robert A.; Mieler, William F. (1 January 2013). Ryan, Stephen J.; Sadda, SriniVas R.; Hinton, David R.; Schachat, Andrew P.; Sadda, SriniVas R.; Wilkinson, C. P.; Wiedemann, Peter; Schachat, Andrew P. (eds.). Retina (Fifth Edition). W.B. Saunders. pp. 1532–1554 – via ScienceDirect.
- ^ Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S (March 2020). “A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19”. Journal of Critical Care. doi:10.1016/j.jcrc.2020.03.005. PMID 32173110.
- ^https://www.sciencedirect.com/science/article/pii/S0924857920300881
- ^https://www.sciencedirect.com/science/article/pii/B9781455707379000898
- ^ Manson P, Cooke G, Zumla A, eds. (2009). Manson’s tropical diseases (22nd ed.). [Edinburgh]: Saunders. p. 1240. ISBN 9781416044703. Archived from the original on 2 November 2018. Retrieved 9 September 2017.
- ^ Bhattacharjee M (2016). Chemistry of Antibiotics and Related Drugs. Springer. p. 184. ISBN 9783319407463. Archived from the original on 1 November 2018. Retrieved 9 September 2017.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ “Chloroquine (Base)”. International Drug Price Indicator Guide. Archived from the original on 27 August 2018. Retrieved 4 December 2015.
- ^ “Frequently Asked Questions (FAQs): If I get malaria, will I have it for the rest of my life?”. US Centers for Disease Control and Prevention. 8 February 2010. Archived from the original on 13 May 2012. Retrieved 14 May 2012.
- ^ Plowe CV (2005). “Antimalarial drug resistance in Africa: strategies for monitoring and deterrence”. Malaria: Drugs, Disease and Post-genomic Biology. Current Topics in Microbiology and Immunology. 295. pp. 55–79. doi:10.1007/3-540-29088-5_3. ISBN 3-540-25363-7. PMID 16265887.
- ^ Uhlemann AC, Krishna S (2005). “Antimalarial multi-drug resistance in Asia: mechanisms and assessment”. Malaria: Drugs, Disease and Post-genomic Biology. Current Topics in Microbiology and Immunology. 295. pp. 39–53. doi:10.1007/3-540-29088-5_2. ISBN 3-540-25363-7. PMID 16265886.
- ^ “Chloroquine phosphate tablet – chloroquine phosphate tablet, coated”. dailymed.nlm.nih.gov. Archived from the original on 8 December 2015. Retrieved 4 November 2015.
- ^ CDC. Health information for international travel 2001–2002. Atlanta, Georgia: U.S. Department of Health and Human Services, Public Health Service, 2001.
- ^ Amebic Hepatic Abscesses~treatment at eMedicine
- ^ Jump up to:a b c d e f “Drugs & Medications”. http://www.webmd.com. Retrieved 22 March 2020.
- ^ Jump up to:a b c d “Chloroquine Side Effects: Common, Severe, Long Term”. Drugs.com. Retrieved 22 March 2020.
- ^ “Chloroquine: MedlinePlus Drug Information”. medlineplus.gov. Retrieved 22 March 2020.
- ^ Ajayi AA (September 2000). “Mechanisms of chloroquine-induced pruritus”. Clinical Pharmacology and Therapeutics. 68 (3): 336. PMID 11014416.
- ^ Vaziri A, Warburton B (1994). “Slow release of chloroquine phosphate from multiple taste-masked W/O/W multiple emulsions”. Journal of Microencapsulation. 11 (6): 641–8. doi:10.3109/02652049409051114. PMID 7884629.
- ^ Tönnesmann E, Kandolf R, Lewalter T (June 2013). “Chloroquine cardiomyopathy – a review of the literature”. Immunopharmacology and Immunotoxicology. 35 (3): 434–42. doi:10.3109/08923973.2013.780078. PMID 23635029.
- ^ Jump up to:a b c d e f g h i “Aralen Chloroquine Phosphate, USP” (PDF). Archived (PDF) from the original on 25 March 2020. Retrieved 24 March 2020.
- ^ Jump up to:a b “Malaria – Chapter 3 – 2016 Yellow Book”. wwwnc.cdc.gov. Archived from the original on 14 January 2016. Retrieved 11 November 2015.
- ^ Ullberg S, Lindquist NG, Sjòstrand SE (September 1970). “Accumulation of chorio-retinotoxic drugs in the foetal eye”. Nature. 227 (5264): 1257–8. Bibcode:1970Natur.227.1257U. doi:10.1038/2271257a0. PMID 5452818.
- ^ Cann HM, Verhulst HL (January 1961). “Fatal acute chloroquine poisoning in children”. Pediatrics. 27: 95–102. PMID 13690445.
- ^ Jump up to:a b Molina DK (March 2012). “Postmortem hydroxychloroquine concentrations in nontoxic cases”. The American Journal of Forensic Medicine and Pathology. 33 (1): 41–2. doi:10.1097/PAF.0b013e3182186f99. PMID 21464694.
- ^ Chen PM, Gombart ZJ, Chen JW (March 2011). “Chloroquine treatment of ARPE-19 cells leads to lysosome dilation and intracellular lipid accumulation: possible implications of lysosomal dysfunction in macular degeneration”. Cell & Bioscience. 1 (1): 10. doi:10.1186/2045-3701-1-10. PMC 3125200. PMID 21711726.
- ^ Kurup P, Zhang Y, Xu J, Venkitaramani DV, Haroutunian V, Greengard P, et al. (April 2010). “Abeta-mediated NMDA receptor endocytosis in Alzheimer’s disease involves ubiquitination of the tyrosine phosphatase STEP61”. The Journal of Neuroscience. 30(17): 5948–57. doi:10.1523/JNEUROSCI.0157-10.2010. PMC 2868326. PMID 20427654.
- ^ Kim EL, Wüstenberg R, Rübsam A, Schmitz-Salue C, Warnecke G, Bücker EM, et al. (April 2010). “Chloroquine activates the p53 pathway and induces apoptosis in human glioma cells”. Neuro-Oncology. 12 (4): 389–400. doi:10.1093/neuonc/nop046. PMC 2940600. PMID 20308316.
- ^ Hempelmann E (March 2007). “Hemozoin biocrystallization in Plasmodium falciparum and the antimalarial activity of crystallization inhibitors”. Parasitology Research. 100 (4): 671–6. doi:10.1007/s00436-006-0313-x. PMID 17111179.
- ^ Lin JW, Spaccapelo R, Schwarzer E, Sajid M, Annoura T, Deroost K, et al. (June 2015). “Replication of Plasmodium in reticulocytes can occur without hemozoin formation, resulting in chloroquine resistance” (PDF). The Journal of Experimental Medicine. 212(6): 893–903. doi:10.1084/jem.20141731. PMC 4451122. PMID 25941254. Archived (PDF) from the original on 22 September 2017. Retrieved 4 November 2018.
- ^ Martin RE, Marchetti RV, Cowan AI, Howitt SM, Bröer S, Kirk K (September 2009). “Chloroquine transport via the malaria parasite’s chloroquine resistance transporter”. Science. 325 (5948): 1680–2. Bibcode:2009Sci…325.1680M. doi:10.1126/science.1175667. PMID 19779197.
- ^ Essentials of medical pharmacology fifth edition 2003, reprint 2004, published by-Jaypee Brothers Medical Publisher Ltd, 2003, KD Tripathi, pages 739,740.
- ^ Alcantara LM, Kim J, Moraes CB, Franco CH, Franzoi KD, Lee S, et al. (June 2013). “Chemosensitization potential of P-glycoprotein inhibitors in malaria parasites”. Experimental Parasitology. 134 (2): 235–43. doi:10.1016/j.exppara.2013.03.022. PMID 23541983.
- ^ Savarino A, Boelaert JR, Cassone A, Majori G, Cauda R (November 2003). “Effects of chloroquine on viral infections: an old drug against today’s diseases?”. The Lancet. Infectious Diseases. 3(11): 722–7. doi:10.1016/s1473-3099(03)00806-5. PMID 14592603.
- ^ Al-Bari MA (February 2017). “Targeting endosomal acidification by chloroquine analogs as a promising strategy for the treatment of emerging viral diseases”. Pharmacology Research & Perspectives. 5 (1): e00293. doi:10.1002/prp2.293. PMC 5461643. PMID 28596841.
- ^ Fredericksen BL, Wei BL, Yao J, Luo T, Garcia JV (November 2002). “Inhibition of endosomal/lysosomal degradation increases the infectivity of human immunodeficiency virus”. Journal of Virology. 76 (22): 11440–6. doi:10.1128/JVI.76.22.11440-11446.2002. PMC 136743. PMID 12388705.
- ^ Xue J, Moyer A, Peng B, Wu J, Hannafon BN, Ding WQ (1 October 2014). “Chloroquine is a zinc ionophore”. PloS One. 9(10): e109180. doi:10.1371/journal.pone.0109180. PMC 4182877. PMID 25271834.
- ^ te Velthuis AJ, van den Worm SH, Sims AC, Baric RS, Snijder EJ, van Hemert MJ (November 2010). “Zn(2+) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture”. PLoS Pathogens. 6 (11): e1001176. doi:10.1371/journal.ppat.1001176. PMC 2973827. PMID 21079686.
- ^ Huang Z, Srinivasan S, Zhang J, Chen K, Li Y, Li W, et al. (2012). “Discovering thiamine transporters as targets of chloroquine using a novel functional genomics strategy”. PLOS Genetics. 8 (11): e1003083. doi:10.1371/journal.pgen.1003083. PMC 3510038. PMID 23209439.
- ^ Fern, Ken (2010–2020). “Cinchona officinalis – L.” Plans for a Future. Archived from the original on 25 August 2017. Retrieved 2 February 2020.
- ^ V. Kouznetsov, Vladímir (2008). “Antimalarials: construction of molecular hybrids based on chloroquine” (PDF). Universitas Scientiarum: 1. Archived (PDF) from the original on 22 February 2020. Retrieved 22 February 2020 – via scielo.
- ^ Krafts K, Hempelmann E, Skórska-Stania A (July 2012). “From methylene blue to chloroquine: a brief review of the development of an antimalarial therapy”. Parasitology Research. 111 (1): 1–6. doi:10.1007/s00436-012-2886-x. PMID 22411634.
- ^ “The History of Malaria, an Ancient Disease”. Centers for Disease Control. 29 July 2019. Archived from the original on 28 August 2010.
- ^ “Chloroquine”. nih.gov. National Institutes of Health. Retrieved 24 March 2020.
- ^ “Ipca Laboratories: Formulations – Branded”. Archived from the original on 6 April 2019. Retrieved 14 March 2020.
- ^ Francis-Floyd, Ruth; Floyd, Maxine R. “Amyloodinium ocellatum, an Important Parasite of Cultured Marine Fish” (PDF). agrilife.org.
- ^ “Could an old malaria drug help fight the new coronavirus?”. asbmb.org. Archived from the original on 6 February 2020. Retrieved 6 February 2020.
- ^ Keyaerts E, Vijgen L, Maes P, Neyts J, Van Ranst M (October 2004). “In vitro inhibition of severe acute respiratory syndrome coronavirus by chloroquine”. Biochemical and Biophysical Research Communications. 323 (1): 264–8. doi:10.1016/j.bbrc.2004.08.085. PMID 15351731.
- ^ Devaux CA, Rolain JM, Colson P, Raoult D. New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19? Int J Antimicrob Agents. 2020 Mar 11:105938. doi:10.1016/j.ijantimicag.2020.105938 PMID 32171740
- ^ “Physicians work out treatment guidelines for coronavirus”. m.koreabiomed.com (in Korean). 13 February 2020. Archivedfrom the original on 17 March 2020. Retrieved 18 March 2020.
- ^ “Azioni intraprese per favorire la ricerca e l’accesso ai nuovi farmaci per il trattamento del COVID-19”. aifa.gov.it (in Italian). Retrieved 18 March 2020.
- ^ “Plaquenil (hydroxychloroquine sulfate) dose, indications, adverse effects, interactions… from PDR.net”. http://www.pdr.net. Archivedfrom the original on 18 March 2020. Retrieved 19 March 2020.
- ^ Yao X, Ye F, Zhang M, Cui C, Huang B, Niu P, et al. (March 2020). “In Vitro Antiviral Activity and Projection of Optimized Dosing Design of Hydroxychloroquine for the Treatment of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)”. Clinical Infectious Diseases. doi:10.1093/cid/ciaa237. PMID 32150618.
- ^ Gao J, Tian Z, Yang X (February 2020). “Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies”. Bioscience Trends. 14: 72–73. doi:10.5582/bst.2020.01047. PMID 32074550. Archived from the original on 19 March 2020. Retrieved 19 March 2020.
- ^ Edwards, Erika; Hillyard, Vaughn (23 March 2020). “Man dies after ingesting chloroquine in an attempt to prevent coronavirus”. NBC News. Retrieved 24 March 2020.
- ^ “A man died after ingesting a substance he thought would protect him from coronavirus”. NBC News. Retrieved 25 March 2020.
- ^ “Banner Health experts warn against self-medicating to prevent or treat COVID-19”. Banner Health (Press release). 23 March 2020. Retrieved 25 March 2020.
- ^ Keyaerts E, Vijgen L, Maes P, Neyts J, Van Ranst M (October 2004). “In vitro inhibition of severe acute respiratory syndrome coronavirus by chloroquine”. Biochemical and Biophysical Research Communications. 323 (1): 264–8. doi:10.1016/j.bbrc.2004.08.085. PMID 15351731.
- ^ Savarino A, Boelaert JR, Cassone A, Majori G, Cauda R (November 2003). “Effects of chloroquine on viral infections: an old drug against today’s diseases?”. The Lancet. Infectious Diseases. 3(11): 722–7. doi:10.1016/S1473-3099(03)00806-5. PMID 14592603.
- ^ Savarino A, Lucia MB, Giordano F, Cauda R (October 2006). “Risks and benefits of chloroquine use in anticancer strategies”. The Lancet. Oncology. 7 (10): 792–3. doi:10.1016/S1470-2045(06)70875-0. PMID 17012039.
- ^ Sotelo J, Briceño E, López-González MA (March 2006). “Adding chloroquine to conventional treatment for glioblastoma multiforme: a randomized, double-blind, placebo-controlled trial”. Annals of Internal Medicine. 144 (5): 337–43. doi:10.7326/0003-4819-144-5-200603070-00008. PMID 16520474.
“Summaries for patients. Adding chloroquine to conventional chemotherapy and radiotherapy for glioblastoma multiforme”. Annals of Internal Medicine. 144 (5): I31. March 2006. doi:10.7326/0003-4819-144-5-200603070-00004. PMID 16520470.
External links
“Chloroquine”. Drug Information Portal. U.S. National Library of Medicine.
- “Medicines for the Prevention of Malaria While Traveling – Chloroquine (Aralen)” (PDF) (Fact sheet). U.S. Centers for Disease Control and Prevention (CDC).
 The dictionary definition of chloroquine at Wiktionary
The dictionary definition of chloroquine at Wiktionary
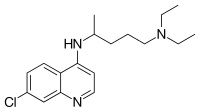 |
|
 |
|
| Clinical data | |
|---|---|
| Pronunciation | /ˈklɔːrəkwɪn/ |
| Trade names | Aralen, other |
| Other names | Chloroquine phosphate |
| AHFS/Drugs.com | Monograph |
| License data |
|
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Metabolism | Liver |
| Elimination half-life | 1-2 months |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| NIAID ChemDB | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.175 |
| Chemical and physical data | |
| Formula | C18H26ClN3 |
| Molar mass | 319.872 g·mol−1 |
| 3D model (JSmol) | |
//////////////CHLOROQUINE,, クロロキン, ANTIMALARIAL, COVID 19, CORONA VIRUS, Хлорохин , クロロキン , كلوروكين
Niclosamide, ニクロサミド , никлосамид , نيكلوساميد , 氯硝柳胺 ,

Niclosamide
ニクロサミド;
| Formula |
C13H8Cl2N2O4
|
|---|---|
| cas |
50-65-7
|
| Mol weight |
327.1196
|
CAS Registry Number: 50-65-7
Niclosamide, sold under the brand name Niclocide among others, is a medication used to treat tapeworm infestations.[2] This includes diphyllobothriasis, hymenolepiasis, and taeniasis.[2] It is not effective against other worms such as pinworms or roundworms.[3] It is taken by mouth.[2]
Side effects include nausea, vomiting, abdominal pain, and itchiness.[2] It may be used during pregnancy and appears to be safe for the baby.[2] Niclosamide is in the anthelmintic family of medications.[3] It works by blocking the uptake of sugar by the worm.[4]
Niclosamide was discovered in 1958.[5] It is on the World Health Organization’s List of Essential Medicines, the safest and most effective medicines needed in a health system.[6] The wholesale cost in the developing world is about 0.24 USD for a course of treatment.[7] It is not commercially available in the United States.[3] It is effective in a number of other animals.[4]
Side effects
Side effects include nausea, vomiting, abdominal pain, constipation, and itchiness.[2] Rarely, dizziness, skin rash, drowsiness, perianal itching, or an unpleasant taste occur. For some of these reasons, praziquantel is a preferable and equally effective treatment for tapeworm infestation.[citation needed]
Mechanism of action
Niclosamide inhibits glucose uptake, oxidative phosphorylation, and anaerobic metabolism in the tapeworm.[8]
Other applications
Niclosamide’s metabolic effects are relevant to wide ranges of organisms, and accordingly it has been applied as a control measure to organisms other than tapeworms. For example, it is an active ingredient in some formulations such as Bayluscide for killing lamprey larvae,[9][10] as a molluscide,[11] and as a general purpose piscicide in aquaculture. Niclosamide has a short half-life in water in field conditions; this makes it valuable in ridding commercial fish ponds of unwanted fish; it loses its activity soon enough to permit re-stocking within a few days of eradicating the previous population.[11] Researchers have found that niclosamide is effective in killing invasive zebra mussels in cool waters.[12]
Research
Niclosamide is being studied in a number of types of cancer.[13] Niclosamide along with oxyclozanide, another anti-tapeworm drug, was found in a 2015 study to display “strong in vivo and in vitro activity against methicillin-resistant Staphylococcus aureus (MRSA)”.[14]
syn
https://www.sciencedirect.com/science/article/pii/S0099542805320028

References
- ^ Jump up to:a b c d e f World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization. pp. 81, 87, 591. hdl:10665/44053. ISBN 9789241547659.
- ^ Jump up to:a b c “Niclosamide Advanced Patient Information – Drugs.com”. http://www.drugs.com. Archived from the original on 20 December 2016. Retrieved 8 December 2016.
- ^ Jump up to:a b Jim E. Riviere; Mark G. Papich (13 May 2013). Veterinary Pharmacology and Therapeutics. John Wiley & Sons. p. 1096. ISBN 978-1-118-68590-7. Archived from the original on 10 September 2017.
- ^ Mehlhorn, Heinz (2008). Encyclopedia of Parasitology: A-M. Springer Science & Business Media. p. 483. ISBN 9783540489948. Archived from the original on 2016-12-20.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ “Niclosamide”. International Drug Price Indicator Guide. Archived from the original on 10 May 2017. Retrieved 1 December 2016.
- ^ Weinbach EC, Garbus J (1969). “Mechanism of action of reagents that uncouple oxidative phosphorylation”. Nature. 221 (5185): 1016–8. doi:10.1038/2211016a0. PMID 4180173.
- ^ Boogaard, Michael A. Delivery Systems of Piscicides “Request Rejected”(PDF). Archived (PDF) from the original on 2017-06-01. Retrieved 2017-05-30.
- ^ Verdel K.Dawson (2003). “Environmental Fate and Effects of the Lampricide Bayluscide: a Review”. Journal of Great Lakes Research. 29 (Supplement 1): 475–492. doi:10.1016/S0380-1330(03)70509-7.
- ^ Jump up to:a b “WHO Specifications And Evaluations. For Public Health Pesticides. Niclosamide” (PDF).[dead link]
- ^ “Researchers find new methods to combat invasive zebra mussels”. The Minnesota Daily. Retrieved 2018-11-19.
- ^ “Clinical Trials Using Niclosamide”. NCI. Retrieved 20 March 2019.
- ^ Rajamuthiah R, Fuchs BB, Conery AL, Kim W, Jayamani E, Kwon B, Ausubel FM, Mylonakis E (April 2015). Planet PJ (ed.). “Repurposing Salicylanilide Anthelmintic Drugs to Combat Drug Resistant Staphylococcus aureus”. PLoS ONE. 10 (4): e0124595. doi:10.1371/journal.pone.0124595. ISSN 1932-6203. PMC 4405337. PMID 25897961.
External links
- “Niclosamide”. Drug Information Portal. U.S. National Library of Medicine.
- Taber, Clarence Wilbur; Venes, Donald; Thomas, Clayton L. (2001). Taber’s cyclopedic medical dictionary. Philadelphia: F.A.Davis Co.
- Niclosamide in the Pesticide Properties DataBase (PPDB)
- “MedlinePlus Drug Information: Niclosamide (Oral)”. MedlinePlus. U.S. National Library of Medicine. 1995-06-23. Archived from the original on 2006-12-16.
- World Health Organization (1995). “Helminths: Cestode (tapeworm) infection: Niclosamide”. WHO model prescribing information : drugs used in parasitic diseases (2nd ed.). World Health Organization (WHO). hdl:10665/41765.
Niclosamide
 |
|
| Clinical data | |
|---|---|
| Trade names | Niclocide, Fenasal, Phenasal, others[1] |
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| Routes of administration |
By mouth |
| ATC code | |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.052 |
| Chemical and physical data | |
| Formula | C13H8Cl2N2O4 |
| Molar mass | 327.119 g/mol g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 225 to 230 °C (437 to 446 °F) |
//////////Niclosamide ニクロサミド , никлосамид , نيكلوساميد , 氯硝柳胺 , covid 19, corona virus
Nitazoxanide ニタゾキサニド;


Nitazoxanide
| Formula |
C12H9N3O5S
|
|---|---|
| Exact mass |
307.0263
|
| Mol weight |
307.282
|
Nitazoxanide is a broad-spectrum antiparasitic and broad-spectrum antiviral drug that is used in medicine for the treatment of various helminthic, protozoal, and viral infections.[4][5][6] It is indicated for the treatment of infection by Cryptosporidium parvum and Giardia lamblia in immunocompetent individuals and has been repurposed for the treatment of influenza.[1][6] Nitazoxanide has also been shown to have in vitro antiparasitic activity and clinical treatment efficacy for infections caused by other protozoa and helminths;[4][7] emerging evidence suggests that it possesses efficacy in treating a number of viral infections as well.[6]
Chemically, nitazoxanide is the prototype member of the thiazolides, a class of drugs which are synthetic nitrothiazolyl-salicylamide derivatives with antiparasitic and antiviral activity.[4][6][8] Tizoxanide, an active metabolite of nitazoxanide in humans, is also an antiparasitic drug of the thiazolide class.[4][9]
Uses
Nitazoxanide is an effective first-line treatment for infection by Blastocystis species[10][11] and is indicated for the treatment of infection by Cryptosporidium parvum or Giardia lamblia in immunocompetent adults and children.[1] It is also an effective treatment option for infections caused by other protozoa and helminths (e.g., Entamoeba histolytica,[12] Hymenolepis nana,[13] Ascaris lumbricoides,[14] and Cyclospora cayetanensis[15]).[7]
As of September 2015, it is in phase 3 clinical trials for the treatment influenza due to its inhibitory effect on a broad range of influenza virus subtypes and efficacy against influenza viruses that are resistant to neuraminidase inhibitors like oseltamivir.[6][16] Nitazoxanide is also being researched as a potential treatment for chronic hepatitis B, chronic hepatitis C, rotavirus and norovirus gastroenteritis.[6]
Chronic hepatitis B
Nitazoxanide alone has shown preliminary evidence of efficacy in the treatment of chronic hepatitis B over a one-year course of therapy.[17] Nitazoxanide 500 mg twice daily resulted in a decrease in serum HBV DNA in all of 4 HBeAg-positive patients, with undetectable HBV DNA in 2 of 4 patients, loss of HBeAg in 3 patients, and loss of HBsAg in one patient. Seven of 8 HBeAg-negative patients treated with nitazoxanide 500 mg twice daily had undetectable HBV DNA and 2 had loss of HBsAg. Additionally, nitazoxanide monotherapy in one case and nitazoxanide plus adefovir in another case resulted in undetectable HBV DNA, loss of HBeAg and loss of HBsAg.[18] These preliminary studies showed a higher rate of HBsAg loss than any currently licensed therapy for chronic hepatitis B. The similar mechanism of action of interferon and nitazoxanide suggest that stand-alone nitazoxanide therapy or nitazoxanide in concert with nucleos(t)ide analogs have the potential to increase loss of HBsAg, which is the ultimate end-point of therapy. A formal phase Ⅱ study is being planned for 2009.[19]
Chronic hepatitis C
Romark initially decided to focus on the possibility of treating chronic hepatitis C with nitazoxanide.[20] The drug garnered interest from the hepatology community after three phase II clinical trials involving the treatment of hepatitis C with nitazoxanide produced positive results for treatment efficacy and similar tolerability to placebo without any signs of toxicity.[20] A meta-analysis from 2014 concluded that the previous held trials were of low-quality and with held with a risk of bias. The authors concluded that more randomized trials with low risk of bias are needed to give any determine if Nitazoxanide can be used as an effective treatment for chronic hepatitis C patients.[21]
Clinical trials
Nitazoxanide has gone through Phase II clinical trials for the treatment of hepatitis C, in combination with peginterferon alfa-2a and ribavirin.[22][23]Romark Laboratories has announced encouraging results from international Phase I and II clinical trials evaluating a controlled release version of nitazoxanide in the treatment of chronic hepatitis C virus infection. The company used 675 mg and 1,350 mg twice daily doses of controlled release nitazoxanide showed favorable safety and tolerability throughout the course of the study, with mild to moderate adverse events. Primarily GI-related adverse events were reported.
A randomised double-blind placebo-controlled study published in 2006, with a group of 38 young children (Lancet, vol 368, page 124-129)[24] concluded that a 3-day course of nitazoxanide significantly reduced the duration of rotavirus disease in hospitalized pediatric patients. Dose given was “7.5 mg/kg twice daily” and the time of resolution was “31 hours for those given nitazoxanide compared with 75 hours for those in the placebo group.” Rotavirus is the most common infectious agent associated with diarrhea in the pediatric age group worldwide.
Teran et al.. conducted a study at the Pediatric Center Albina Patinö, a reference hospital in the city of Cochabamba, Bolivia, from August 2007 to February 2008. The study compared nitazoxanide and probiotics in the treatment of acute rotavirus diarrhea. They found Small differences in favor of nitazoxanide in comparison with probiotics and concluded that nitazoxanide is an important treatment option for rotavirus diarrhea.[17]
Lateef et al.. conducted a study in India that evaluated the effectiveness of nitazoxanide in the treatment of beef tapeworm (Taenia saginata) infection. They concluded that nitazoxanide is a safe, effective, inexpensive, and well-tolerated drug for the treatment of niclosamide- and praziquantel-resistant beef tapeworm (Taenia saginata) infection.[18]
A retrospective review of charts of patients treated with nitazoxanide for trichomoniasis by Michael Dan and Jack D. Sobel demonstrated negative result. They reported three case studies; two of which with metronidazole-resistant infections. In Case 3, they reported the patient to be cured with high divided dose tinidazole therapy. They used a high dosage of the drug (total dose, 14–56 g) than the recommended standard dosage (total dose, 3 g) and observed a significant adverse reaction (poorly tolerated nausea) only with the very high dose (total dose, 56 g). While confirming the safety of the drug, they showed nitazoxanide is ineffective for the treatment of trichomoniasis.[25]
Contraindications
Nitazoxanide is contraindicated only in individuals who have experienced a hypersensitivity reaction to nitazoxanide or the inactive ingredients of a nitazoxanide formulation.[1]
Adverse effects
The side effects of nitazoxanide do not significantly differ from a placebo treatment for giardiasis;[1] these symptoms include stomach pain, headache, upset stomach, vomiting, discolored urine, excessive urinating, skin rash, itching, fever, flu syndrome, and others.[1][26] Nitazoxanide does not appear to cause any significant adverse effects when taken by healthy adults.[1][2]
Overdose
Information on nitazoxanide overdose is limited. Oral doses of 4 grams in healthy adults do not appear to cause any significant adverse effects.[1][2] In various animals, the oral LD50 is higher than 10 g/kg.[1]
Interactions
Due to the exceptionally high plasma protein binding (>99.9%) of nitazoxanide’s metabolite, tizoxanide, the concurrent use of nitazoxanide with other highly plasma protein-bound drugs with narrow therapeutic indices (e.g., warfarin) increases the risk of drug toxicity.[1] In vitro evidence suggests that nitazoxanide does not affect the CYP450 system.[1]
Pharmacology
Pharmacodynamics
The anti-protozoal activity of nitazoxanide is believed to be due to interference with the pyruvate:ferredoxin oxidoreductase (PFOR) enzyme-dependent electron transfer reaction which is essential to anaerobic energy metabolism.[1][8] PFOR inhibition may also contribute to its activity against anaerobic bacteria.[27]
It has also been shown to have activity against influenza A virus in vitro.[28] The mechanism appears to be by selectively blocking the maturation of the viral hemagglutinin at a stage preceding resistance to endoglycosidase H digestion. This impairs hemagglutinin intracellular trafficking and insertion of the protein into the host plasma membrane.
Nitazoxanide modulates a variety of other pathways in vitro, including glutathione-S-transferase and glutamate-gated chloride ion channels in nematodes, respiration and other pathways in bacteria and cancer cells, and viral and host transcriptional factors.[27]
Pharmacokinetics
Following oral administration, nitazoxanide is rapidly hydrolyzed to the pharmacologically active metabolite, tizoxanide, which is 99% protein bound.[1][9] Tizoxanide is then glucuronide conjugated into the active metabolite, tizoxanide glucuronide.[1] Peak plasma concentrations of the metabolites tizoxanide and tizoxanide glucuronide are observed 1–4 hours after oral administration of nitazoxanide, whereas nitazoxanide itself is not detected in blood plasma.[1]
Roughly 2⁄3 of an oral dose of nitazoxanide is excreted as its metabolites in feces, while the remainder of the dose excreted in urine.[1] Tizoxanide is excreted in the urine, bile and feces.[1] Tizoxanide glucuronide is excreted in urine and bile.[1]
Chemistry
History
Nitazoxanide is the prototype member of the thiazolides, which is a drug class of structurally-related broad-spectrum antiparasitic compounds.[4] Nitazoxanide is a light yellow crystalline powder. It is poorly soluble in ethanol and practically insoluble in water.
Nitazoxanide was originally discovered in the 1980s by Jean-François Rossignol at the Pasteur Institute. Initial studies demonstrated activity versus tapeworms. In vitro studies demonstrated much broader activity. Dr. Rossignol co-founded Romark Laboratories, with the goal of bringing nitazoxanide to market as an anti-parasitic drug. Initial studies in the USA were conducted in collaboration with Unimed Pharmaceuticals, Inc. (Marietta, GA) and focused on development of the drug for treatment of cryptosporidiosis in AIDS. Controlled trials began shortly after the advent of effective anti-retroviral therapies. The trials were abandoned due to poor enrollment and the FDA rejected an application based on uncontrolled studies.
Subsequently, Romark launched a series of controlled trials. A placebo-controlled study of nitazoxanide in cryptosporidiosis demonstrated significant clinical improvement in adults and children with mild illness. Among malnourished children in Zambia with chronic cryptosporidiosis, a three-day course of therapy led to clinical and parasitologic improvement and improved survival. In Zambia and in a study conducted in Mexico, nitazoxanide was not successful in the treatment of cryptosporidiosis in advanced infection with human immunodeficiency virus at the doses used. However, it was effective in patients with higher CD4 counts. In treatment of giardiasis, nitazoxanide was superior to placebo and comparable to metronidazole. Nitazoxanide was successful in the treatment of metronidazole-resistant giardiasis. Studies have suggested efficacy in the treatment of cyclosporiasis, isosporiasis, and amebiasis.[29] Recent studies have also found it to be effective against beef tapeworm(Taenia saginata).[30]
Research
Nitazoxanide is also under investigation for the treatment of COVID-19.[31]
Pharmaceutical products
Dosage forms
Nitazoxanide is currently available in two oral dosage forms: a tablet (500 mg) and an oral suspension (100 mg per 5 ml when reconstituted).[1]
An extended release tablet (675 mg) has been used in clinical trials for chronic hepatitis C; however, this form is not currently marketed and available for prescription.[20]
Brand names
Nitazoxanide is sold under the brand names Adonid, Alinia, Allpar, Annita, Celectan, Colufase, Daxon, Dexidex, Diatazox, Kidonax, Mitafar, Nanazoxid, Parazoxanide, Netazox, Niazid, Nitamax, Nitax, Nitaxide, Nitaz, Nizonide, NT-TOX, Pacovanton, Paramix, Toza, and Zox.
SYN


https://www.sciencedirect.com/science/article/pii/S0960894X11002848
CLIP


CLIP
PATENT

https://patents.google.com/patent/CN105175352A/zh
References
- ^ Jump up to:a b c d e f g h i j k l m n o p q r s t u v w “Nitazoxanide Prescribing Information” (PDF). Romark Pharmaceuticals. August 2013. pp. 1–5. Archived from the original (PDF) on 16 January 2016. Retrieved 3 January 2016.
- ^ Jump up to:a b c d e Stockis A, Allemon AM, De Bruyn S, Gengler C (May 2002). “Nitazoxanide pharmacokinetics and tolerability in man using single ascending oral doses”. Int J Clin Pharmacol Ther. 40 (5): 213–220. doi:10.5414/cpp40213. PMID 12051573.
- ^ “Nitazoxanide”. PubChem Compound. National Center for Biotechnology Information. Retrieved 3 January 2016.
- ^ Jump up to:a b c d e Di Santo N, Ehrisman J (2013). “Research perspective: potential role of nitazoxanide in ovarian cancer treatment. Old drug, new purpose?”. Cancers (Basel). 5 (3): 1163–1176. doi:10.3390/cancers5031163. PMC 3795384. PMID 24202339.
Nitazoxanide [NTZ: 2-acetyloxy-N-(5-nitro-2-thiazolyl)benzamide] is a thiazolide antiparasitic agent with excellent activity against a wide variety of protozoa and helminths. … Nitazoxanide (NTZ) is a main compound of a class of broad-spectrum anti-parasitic compounds named thiazolides. It is composed of a nitrothiazole-ring and a salicylic acid moiety which are linked together by an amide bond … NTZ is generally well tolerated, and no significant adverse events have been noted in human trials [13]. … In vitro, NTZ and tizoxanide function against a wide range of organisms, including the protozoal species Blastocystis hominis, C. parvum, Entamoeba histolytica, G. lamblia and Trichomonas vaginalis [13]
- ^ White CA (2004). “Nitazoxanide: a new broad spectrum antiparasitic agent”. Expert Rev Anti Infect Ther. 2 (1): 43–9. doi:10.1586/14787210.2.1.43. PMID 15482170.
- ^ Jump up to:a b Anderson, V. R.; Curran, M. P. (2007). “Nitazoxanide: A review of its use in the treatment of gastrointestinal infections”. Drugs. 67(13): 1947–1967. doi:10.2165/00003495-200767130-00015. PMID 17722965.
Nitazoxanide is effective in the treatment of protozoal and helminthic infections … Nitazoxanide is a first-line choice for the treatment of illness caused by C. parvum or G. lamblia infection in immunocompetent adults and children, and is an option to be considered in the treatment of illnesses caused by other protozoa and/or helminths.
- ^ Jump up to:a b Sisson G1, Goodwin A, Raudonikiene A, Hughes NJ, Mukhopadhyay AK, Berg DE, Hoffman PS. (July 2002). “Enzymes associated with reductive activation and action of nitazoxanide, nitrofurans, and metronidazole in Helicobacter pylori”. Antimicrob. Agents Chemother. 46 (7): 2116–23. doi:10.1128/aac.46.7.2116-2123.2002. PMC 127316. PMID 12069963.
Nitazoxanide (NTZ) is a redox-active nitrothiazolyl-salicylamide
- ^ Jump up to:a b Korba BE, Montero AB, Farrar K, et al. (January 2008). “Nitazoxanide, tizoxanide and other thiazolides are potent inhibitors of hepatitis B virus and hepatitis C virus replication”. Antiviral Res. 77 (1): 56–63. doi:10.1016/j.antiviral.2007.08.005. PMID 17888524.
- ^ “Blastocystis: Resources for Health Professionals”. United States Centers for Disease Control and Prevention. 2017-05-02. Retrieved 4 January 2016.
- ^ Roberts T, Stark D, Harkness J, Ellis J (May 2014). “Update on the pathogenic potential and treatment options for Blastocystis sp”. Gut Pathog. 6: 17. doi:10.1186/1757-4749-6-17. PMC 4039988. PMID 24883113.
Blastocystis is one of the most common intestinal protists of humans. … A recent study showed that 100% of people from low socio-economic villages in Senegal were infected with Blastocystis sp. suggesting that transmission was increased due to poor hygiene sanitation, close contact with domestic animals and livestock, and water supply directly from well and river [10]. …
Table 2: Summary of treatments and efficacy for Blastocystis infection - ^ Muñoz P, Valerio M, Eworo A, Bouza E (2011). “Parasitic infections in solid-organ transplant recipients”. Curr Opin Organ Transplant. 16 (6): 565–575. doi:10.1097/MOT.0b013e32834cdbb0. PMID 22027588. Retrieved 7 January 2016.
Nitazoxanide: intestinal amoebiasis: 500 mg po bid x 3 days
- ^ “Hymenolepiasis: Resources for Health Professionals”. United States Centers for Disease Control and Prevention. 2017-05-02. Retrieved 4 January 2016.
- ^ Hagel I, Giusti T (October 2010). “Ascaris lumbricoides: an overview of therapeutic targets”. Infectious Disorders – Drug Targets. 10 (5): 349–67. doi:10.2174/187152610793180876. PMID 20701574.
new anthelmintic alternatives such as tribendimidine and Nitazoxanide have proved to be safe and effective against A. lumbricoides and other soil-transmitted helminthiases in human trials.
- ^ Shoff WH (5 October 2015). Chandrasekar PH, Talavera F, King JW (eds.). “Cyclospora Medication”. Medscape. WebMD. Retrieved 11 January 2016.
Nitazoxanide, a 5-nitrothiazole derivative with broad-spectrum activity against helminths and protozoans, has been shown to be effective against C cayetanensis, with an efficacy 87% by the third dose (first, 71%; second 75%). Three percent of patients had minor side effects.
- ^ Li TC, Chan MC, Lee N (September 2015). “Clinical Implications of Antiviral Resistance in Influenza”. Viruses. 7 (9): 4929–4944. doi:10.3390/v7092850. PMC 4584294. PMID 26389935.
Oral nitazoxanide is an available, approved antiparasitic agent (e.g., against cryptosporidium, giardia) with established safety profiles. Recently, it has been shown (together with its active metabolite tizoxanide) to possess anti-influenza activity by blocking haemagglutinin maturation/trafficking, and acting as an interferon-inducer [97]. … A large, multicenter, Phase 3 randomized-controlled trial comparing nitazoxanide, oseltamivir, and their combination in uncomplicated influenza is currently underway (NCT01610245).
Figure 1: Molecular targets and potential antiviral treatments against influenza virus infection - ^ Jump up to:a b Teran, C. G.; Teran-Escalera, C. N.; Villarroel, P. (2009). “Nitazoxanide vs. Probiotics for the treatment of acute rotavirus diarrhea in children: A randomized, single-blind, controlled trial in Bolivian children”. International Journal of Infectious Diseases. 13(4): 518–523. doi:10.1016/j.ijid.2008.09.014. PMID 19070525.
- ^ Jump up to:a b Lateef, M.; Zargar, S. A.; Khan, A. R.; Nazir, M.; Shoukat, A. (2008). “Successful treatment of niclosamide- and praziquantel-resistant beef tapeworm infection with nitazoxanide”. International Journal of Infectious Diseases. 12 (1): 80–82. doi:10.1016/j.ijid.2007.04.017. PMID 17962058.
- ^ World Journal of Gastroenterology 2009 April 21, Emmet B Keeffe MD, Professor, Jean-François Rossignol The Romark Institute for Medical Research, Tampa
- ^ Jump up to:a b c Keeffe, E. B.; Rossignol, J. F. (2009). “Treatment of chronic viral hepatitis with nitazoxanide and second generation thiazolides”. World Journal of Gastroenterology. 15 (15): 1805–1808. doi:10.3748/wjg.15.1805. PMC 2670405. PMID 19370775.
- ^ Nikolova, Kristiana; Gluud, Christian; Grevstad, Berit; Jakobsen, Janus C (2014). “Nitazoxanide for chronic hepatitis C”. Cochrane Database of Systematic Reviews (4): CD009182. doi:10.1002/14651858.CD009182.pub2. ISSN 1465-1858. PMID 24706397.
- ^ “Romark Initiates Clinical Trial Of Alinia For Chronic Hepatitis C In The United States” (Press release). Medical News Today. August 16, 2007. Retrieved 2007-10-11.
- ^ Franciscus, Alan (October 2, 2007). “Hepatitis C Treatments in Current Clinical Development”. HCV Advocate. Archived from the original on September 6, 2003. Retrieved 2007-10-11.
- ^ Rossignol, Jean-François; Abu-Zekry, Mona; Hussein, Abeer; Santoro, M Gabriella (2006). “Effect of nitazoxanide for treatment of severe rotavirus diarrhoea: randomised double-blind placebo-controlled trial”. The Lancet. 368 (9530): 124–9. CiteSeerX 10.1.1.458.1597. doi:10.1016/S0140-6736(06)68852-1. PMID 16829296.
- ^ Dan, M.; Sobel, J. D. (2007). “Failure of Nitazoxanide to Cure Trichomoniasis in Three Women”. Sexually Transmitted Diseases. 34 (10): 813–4. doi:10.1097/NMD.0b013e31802f5d9a. PMID 17551415.
- ^ “Nitazoxanide”. MedlinePlus. Retrieved 9 April 2014.
- ^ Jump up to:a b Shakya, A; Bhat, HR; Ghosh, SK (2018). “Update on Nitazoxanide: A Multifunctional Chemotherapeutic Agent”. Current Drug Discovery Technologies. 15 (3): 201–213. doi:10.2174/1570163814666170727130003. PMID 28748751.
- ^ Rossignol, J. F.; La Frazia, S.; Chiappa, L.; Ciucci, A.; Santoro, M. G. (2009). “Thiazolides, a New Class of Anti-influenza Molecules Targeting Viral Hemagglutinin at the Post-translational Level”. Journal of Biological Chemistry. 284 (43): 29798–29808. doi:10.1074/jbc.M109.029470. PMC 2785610. PMID 19638339.
- ^ White Jr, AC (2003). “Nitazoxanide: An important advance in anti-parasitic therapy”. Am. J. Trop. Med. Hyg. 68 (4): 382–383. doi:10.4269/ajtmh.2003.68.382. PMID 12875283.
- ^ Lateef, M.; Zargar, S. A.; Khan, A. R.; Nazir, M.; Shoukat, A. (2008). “Successful treatment of niclosamide- and praziquantel-resistant beef tapeworm infection with nitazoxanide”. International Journal of Infectious Diseases. 12 (1): 80–2. doi:10.1016/j.ijid.2007.04.017. PMID 17962058.
- ^ Cynthia Liu, Qiongqiong Zhou, Yingzhu Li, Linda V. Garner, Steve P. Watkins, Linda J. Carter, Jeffrey Smoot, Anne C. Gregg, Angela D. Daniels, Susan Jervey, Dana Albaiu. Research and Development on Therapeutic Agents and Vaccines for COVID-19 and Related Human Coronavirus Diseases. ACS Central Science 2020; doi:10.1021/acscentsci.0c00272
External links
- “Nitazoxanide”. MedlinePlus Drug Information. U.S. National Library of Medicine. 28 July 2010. Retrieved 2010-08-19.
- “Parasitic infections”. Am J Transplant. 4 (Suppl 10): 142–55. 2004. doi:10.1111/j.1600-6135.2004.00677.x. PMID 15504227.
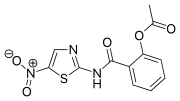 |
|
| Clinical data | |
|---|---|
| Trade names | Alinia, Nizonide, and others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a603017 |
| License data |
|
| Pregnancy category |
|
| Routes of administration |
Oral |
| Drug class | Antiprotozoal Broad-spectrum antiparasitic Broad-spectrum antiviral |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Protein binding | Nitazoxanide: ? Tizoxanide: over 99%[1][2] |
| Metabolism | Rapidly hydrolyzed to tizoxanide[1] |
| Metabolites | tizoxanide[1][2] tizoxanide glucuronide[1][2] |
| Elimination half-life | 3.5 hours[3] |
| Excretion | Renal, biliary, and fecal[1] |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| NIAID ChemDB | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.054.465 |
| Chemical and physical data | |
| Formula | C12H9N3O5S |
| Molar mass | 307.283 g/mol g·mol−1 |
| 3D model (JSmol) | |
//////////////nitazoxanide, corona virus, covid 19
Galidesivir

Galidesivir
- Molecular FormulaC11H15N5O3
- Average mass265.268 Da
Galidesivir
249503-25-1
222631-44-9, BCX-4430 (HCL salt form of galidesivir)
Galidesivir (BCX4430, Immucillin-A) is an antiviral drug, an adenosine analog[1] (a type of nucleoside analog).[2] It is developed by BioCryst Pharmaceuticals with funding from NIAID, originally intended as a treatment for hepatitis C, but subsequently developed as a potential treatment for deadly filovirus infections such as Ebola virus disease and Marburg virus disease.
It also shows broad-spectrum antiviral effectiveness against a range of other RNA virus families, including bunyaviruses, arenaviruses, paramyxoviruses, coronaviruses, flaviviruses and phleboviruses.[3] BCX4430 has been demonstrated to protect against both Ebola and Marburg viruses in both rodents and monkeys, even when administered up to 48 hours after infection,[1] and development for use in humans was then being fast-tracked due to concerns about the lack of treatment options for the 2013-2016 Ebola virus epidemic in West Africa.[4]
BCX4430 later showed efficacy against Zika virus in a mouse model, though there are no plans for human trials at this stage.[5]
Galidesivir is one of several antiviral drugs being tested for coronavirus disease 2019.[6]

CLIP
https://www.sciencedirect.com/science/article/pii/S0040402017305926

CLIP

When any new virus emerges, drug and vaccine developers spring into action, searching for products to stop it in its tracks. Drug discovery campaigns launch, vaccine development efforts ramp up, and everyone mobilizes to get it all into the clinic as quickly as possible.
The current pandemic, driven by a coronavirus known as SARS-CoV-2, is no different. Already, a Phase I study of an mRNA-based vaccine developed by Moderna has begun, and major pharma companies and small biotechs are working on other types of vaccines. But even if they work, the most optimistic timelines put a vaccine a year to 18 months away.
The more immediate approach to an outbreak is to scour the medicine cabinet for existing molecules that could be repurposed against a new virus. The most advanced potential treatment is Gilead Sciences’ remdesivir, an antiviral discovered during the 2014 Ebola epidemic. The compound is already being tested in four, Phase III trials—two in China and two in the US—against the respiratory disease COVID-19. Gilead expects the first dataset from those studies to come out in April.
A new paper from CAS explored remdesivir and other possible options the cabinet might contain (ACS Cent. Sci. 2020, DOI: 10.1021/acscentsci.0c00272). CAS, a division of the American Chemical Society, which publishes C&EN, looked at the landscape of patent and journal articles covering small molecules, antibodies, and other therapeutic classes to identify therapies with potential activity against COVID-19.
SARS-CoV-2, belongs to the same family as two coronaviruses responsible for earlier outbreaks, Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS). Because all three feature structurally similar proteins that allow entry into and replication inside host cells, CAS searched for patent data related to those more well-studied coronaviruses.
C&EN has assembled the relevant small molecules identified by CAS, which can be explored by the stage in the viral life cycle they aim to disrupt.
Patents
| Patent ID | Title | Submitted Date | Granted Date |
|---|---|---|---|
| US7390890 | Inhibitors of nucleoside metabolism | 2007-08-23 | 2008-06-24 |
| US7211653 | Inhibitors of nucleoside metabolism | 2005-02-03 | 2007-05-01 |
| US6803455 | Inhibitors of nucleoside metabolism | 2003-05-22 | 2004-10-12 |
| US6492347 | Inhibitors of nucleoside metabolism | 2002-05-23 | 2002-12-10 |
| US6228847 | Inhibitors of nucleoside metabolism | 2001-05-08 |
| Patent ID | Title | Submitted Date | Granted Date |
|---|---|---|---|
| EP1023308 | INHIBITORS OF NUCLEOSIDE METABOLISM | 2000-08-02 | 2005-09-07 |
| US6066722 | Inhibitors of nucleoside metabolism | 2000-05-23 |
References
- ^ Jump up to:a b Warren TK, Wells J, Panchal RG, Stuthman KS, Garza NL, Van Tongeren SA, et al. (April 2014). “Protection against filovirus diseases by a novel broad-spectrum nucleoside analogue BCX4430” (PDF). Nature. 508 (7496): 402–5. Bibcode:2014Natur.508..402W. doi:10.1038/nature13027. PMID 24590073.
- ^ Kamat SS, Burgos ES, Raushel FM (October 2013). “Potent inhibition of the C-P lyase nucleosidase PhnI by Immucillin-A triphosphate”. Biochemistry. 52 (42): 7366–8. doi:10.1021/bi4013287. PMC 3838859. PMID 24111876.
- ^ Westover JB, et al. Galidesivir limits Rift Valley fever virus infection and disease in Syrian golden hamsters. Antiviral Res. 2018 Aug;156:38-45. Westover, J. B.; Mathis, A.; Taylor, R.; Wandersee, L.; Bailey, K. W.; Sefing, E. J.; Hickerson, B. T.; Jung, K. H.; Sheridan, W. P.; Gowen, B. B. (2018). “Galidesivir limits Rift Valley fever virus infection and disease in Syrian golden hamsters”. Antiviral Research. 156: 38–45. doi:10.1016/j.antiviral.2018.05.013. PMC 6035881. PMID 29864447.
- ^ Rodgers P (8 April 2014). “BioWar Lab Helping To Develop Treatment For Ebola”. Forbes Magazine.
- ^ Julander JG, Siddharthan V, Evans J, Taylor R, Tolbert K, Apuli C, et al. (January 2017). “Efficacy of the broad-spectrum antiviral compound BCX4430 against Zika virus in cell culture and in a mouse model”. Antiviral Research. 137: 14–22. doi:10.1016/j.antiviral.2016.11.003. PMC 5215849. PMID 27838352.
- ^ Praveen Duddu. Coronavirus outbreak: Vaccines/drugs in the pipeline for Covid-19. clinicaltrialsarena.com 19 February 2020.
 |
|
| Legal status | |
|---|---|
| Legal status | |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| Chemical and physical data | |
| Formula | C11H15N5O3 |
| Molar mass | 265.268 g·mol−1 |
| 3D model (JSmol) | |
//////////////Galidesivir, Immucillin-A, OLF97F86A7, UNII:OLF97F86A7, галидесивир , غاليديسيفير , 加利司韦 , BCX4430, BCX 4430, CORONAVIRUS, COVID 19
nitazoxanide

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....