FDA Approves BMS Drug for Rare Fat Disorder
1. Leptin (human), N-methionyl-
2. N-methionylleptin (human)
STRUCTURAL FORMULA
MVPIQKVQDD TKTLIKTIVT RINDISHTQS VSSKQKVTGL DFIPGLHPIL 50
TLSKMDQTLA VYQQILTSMP SRNVIQISND LENLRDLLHV LAFSKSCHLP 100
WASGLETLDS LGGVLEASGY STEVVALSRL QGSLQDMLWQ LDLSPGC 147
Disulfide bridge location
97-147
http://www.ama-assn.org/resources/doc/usan/metreleptin.pdf
MOLECULAR FORMULA C714H1167N191O221S6
MOLECULAR WEIGHT 16.16 kDa
MANUFACTURER Amylin Pharmaceuticals, Inc.
CODE DESIGNATION r-metHuLeptin
An analog of human leptin, metreleptin, has been approved in Japan and is currently under review by the FDA in the US for the treatment of diabetes and/or hypertriglyceridemia, in patients with rare forms of lipodystrophy, syndromes characterized by abnormalities in adipose tissue distribution, and severe metabolic abnormalities. Bristol-Myers Squibb has submitted a New Drug Approval (NDA) for metreleptin to the US Food and Drug Administration (FDA) Office of Orphan Products Development. In a three-year study of metreleptin in patients with lipodystrophy organized by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health, metreleptin treatment was associated with a significant decrease in blood glucose (A1c decreased from 9.4% at baseline to 7.0% at study end) and triglyceride concentration (from 500 mg/dl at baseline to 200 mg/dl at study end). The Juvenile Diabetes Research Foundation has also partnered with Amylin Pharmaceuticals and researchers at the University of Texas Southwestern Medical Center to study whether metreleptin can be used to improve the treatment of type 1 diabetes.
N-Methionylleptin (human)
Recombinant human OB protein, purified to homogenicity as a 16-kDa monomer
Treatment of obesity and related disorders (metabolic homeostasis regulator)
- Brand name: Myalept
- Generic name: metreleptin
- Company: Amylin Pharmaceuticals, Inc.
- Treatment for: Lipodystrophy
| Feb 25, 2014 | FDA Approves Myalept to Treat Generalized Lipodystrophy |
| Dec 12, 2013 | FDA Advisory Committee Votes on Investigational Medicine Metreleptin |
| Apr 3, 2012 | Amylin Completes Biologics License Application for Metreleptin to Treat Diabetes and/or Hypertriglyceridemia in Patients With Rare Forms of Lipodystrophy |
| Dec 20, 2010 | Amylin Submits Clinical and Nonclinical Sections of Rolling Biologics License Application for Metreleptin to Treat Rare Forms of Lipodystrophy |
| Leptin | |
|---|---|

Structure of the obese protein leptin-E100.
|
“Myalept is the first approved therapy indicated for treating the complications associated with congenital or acquired generalized lipodystrophy and provides a needed treatment option for patients with this orphan disease,” said Mary Parks, M.D., deputy director of the Office of Drug Evaluation II in the FDA’s Center for Drug Evaluation and Research.
The safety and effectiveness of Myalept, an analog of leptin made through recombinant DNA technology, were evaluated in an open-label, single-arm study that included 48 patients with congenital or acquired generalized lipodystrophy who also had diabetes mellitus, hypertriglyceridemia, and/or elevated levels of fasting insulin. The trial showed reductions in HbA1c (a measure of blood sugar control), fasting glucose, and triglycerides.
Anti-drug antibodies with neutralizing activity to leptin and/or Myalept may develop, which could result in severe infections or loss of treatment effectiveness. T-cell lymphoma has been reported in patients with acquired generalized lipodystrophy, both treated and not treated with Myalept, so healthcare professionals should carefully consider the benefits and risks of treatment with Myalept in patients with significant hematologic abnormalities and/or acquired generalized lipodystrophy. Myalept is contraindicated in patients with general obesity. Myalept is not approved for use in patients with HIV-related lipodystrophy or in patients with metabolic disease, including diabetes mellitus and hypertriglyceridemia, without concurrent evidence of generalized lipodystrophy.
Because of the risks associated with the development of neutralizing antibodies and lymphoma, Myalept is available only through the Myalept Risk Evaluation and Mitigation Strategy (REMS) Program. Under this REMS program, prescribers must be certified with the program by enrolling in and completing training. Pharmacies must be certified with the program and only dispense Myalept after receipt of the Myalept REMS Prescription Authorization Form for each new prescription.
Myalept is also approved with a Medication Guide and instructions for use that provides patients with important information about the medication. The guide will be distributed each time a patient fills a prescription.
The FDA is requiring seven studies (post-marketing requirements) for Myalept, including a long-term prospective observational study (product exposure registry) of patients treated with Myalept, a study to assess for the immunogenicity (antibody formation) of Myalept, and an assessment and analysis of spontaneous reports of potential serious risks related to the use of Myalept. Eight additional studies are being requested as post-marketing commitments.
In clinical trials, the most common side effects observed in patients treated with Myalept were low blood sugar (hypoglycemia), headache, decreased weight, and abdominal pain.
Myalept is marketed by San Diego-based Amylin Pharmaceuticals, L.L.C.
For more information:
Metreleptin is an analogue of the human hormone leptin being developed by Amylin Pharmaceuticals (a subsidiary of Bristol-Myers Squibb) for the subcutaneous treatment of metabolic disorders including lipodystrophy. The compound is expected to improve insulin sensitivity, hypertriglyceridaemia and hyperglycaemia in patients with lipodystrophy who are unresponsive to conventional treatment.
Metreleptin has been approved in Japan as a leptin therapy for the treatment of lipodystrophy. Amylin has also completed a submission for regulatory approval to the US FDA for metreleptin in the treatment of diabetes mellitus and/or hypertriglyceridaemia in patients with rare forms of lipodystrophy.
Clinical development of the drug is also underway in the USA for the treatment of type 1 diabetes. Amgen was previously assessing the use of metreleptin as a treatment for amenorrhoea; however, it appears that development in this indication has been discontinued. This article summarizes the milestones in the development of metreleptin leading to this first approval for lipodystrophy.
Metreleptin is a leptin replacement therapy first launched in Japan in 2013 for the treatment of congenital lipodystrophy. Amylin filed for approval in the U.S. in 2010 for the treatment of diabetes and/or hypertriglyceridemia in patients with rare forms of lipodystrophy. In 2013, the Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) recommended the approval for the treatment of pediatric and adult patients with generalized lipodystrophy , but not for partial lipodystrophy.
Phase II clinical studies are also under way at Beth Israel Deaconess Medical Center for the treatment of lipodystrophy syndrome associated with AIDS. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) is conducting phase II clinical trials for the treatment of nonalcoholic steatohepatitis. Phase II are ongoing at the National Institute for Diabetes and Digestive and Kidney Diseases for the treatment of non-alcoholic fatty liver disease (NAFLD) associated with lipodystropy. Early clinical studies had also been ongoing for the treatment of leptin deficiencies.
The University Texas Southwestern Medical Center at Dallas is evaluating metreleptin for the treatment of type 1 diabetes. Beth Israel Deaconess Medical Center is conducting phase II clinical trials for the treatment of amenorrhea. Amgen had been conducting clinical trials for this indication and for the treatment of type 1 diabetes and depression; however no recent development has been reported for this research.
In 2011, Amylin and Takeda put on hold their clinical trials with metreleptin in combination with pramlintide for the treatment of obesity in order to investigate an antibody-related laboratory finding. Amylin is currently evaluating the compound as monotherapy for the treatment of obesity. The companies had been conducting phase II clinical trials of metreleptin not in combination with pramlintide for the treatment of obesity; however, no recent development has been reported for this research.
Originally developed at the Rockefeller University, an exclusive license to metreleptin was granted to Amgen in 1995. In 2009, the drug candidate was licensed to Takeda by Amylin worldwide for the treatment of obesity. In 2010, orphan drug designation was assigned in the U.S. for the treatment of metabolic disorders secondary to lipodystrophy and for the treatment of leptin deficiency secondary to generalized lipodystrophy and partial familial lipodystrophy.
In 2012, orphan drug designation was assigned in Japan for the treatment of diabetes or hyperlipidemia due to lipoatrophy. In 2012, orphan drug designation was assigned in the E.U. for the treatment of Barraquer-Simons syndrome, Berardinelli-Seip syndrome, familial partial lipodystrophy and Lawrence syndrome. In 2014, AstraZeneca acquired the global rigths for development, manufacture and commercialization of the product.
……………
Other exemplary leptins for use in the methods and compositions described herein include, but are not limited to, the amino acid sequence for mature, recombinant methionyl human leptin (herein called rmetHu-Leptin 1-146 or Metreleptin) having the amino acid sequence:
MVPIQKVQDDTKTLIKTΓVTRINDISHTQSVSSKQKVTGLDFIPGLHPILTLSKMDQTLA VYQQILTSMPSRNVIQISNDLENLRDLLHVLAFSKSCHLPWASGLETLDSLGGVLEASG YSTEWALSRLQGSLQDMLWQLDLSPGC (SEQ ID NO:274).
Regulatory Considerations for Biosimilars

Biological medicines are already becoming an increasingly important part of health care. With patent expiries on originator biological products, biosimilars are also increasingly become a part of this future. In fact, by 2020 twelve of the top-selling biologicals will have lost patent protection, opening up an estimated US$24 billion in EU sales and US$30 billion in US sales.
Biologicals have potential to reach up to 50% share in global pharmaceutical market in the next few years.
India is one of the leading contributors in the world biosimilar market and is the third-largest in the Asia-Pacific region, after Australia and China. India has demonstrated high acceptance of biosimilars, which is reflected in the 40 biologicals marketed in India, of which 25 are biosimilars The Indian biotechnology industry is also gaining momentum, with revenues of over US$4 billion in 2011, and which are projected to reach up to US$580 million by 2012.
While small molecule drugs are ideal for generics replication, biological drugs are not so simple. Biological drugs are usually large, complex molecular structures derived from or produced through a living organism, making them very difficult to replicate
Currently there is considerable interest in the legislative debate around generic biological drugs or “biosimilars” in the EU and US due to the large, lucrative market that it offers to the industry. While some countries have issued a few regulatory guidelines as well as product specific requirements, there is no general consensus as to a single, simple mechanism similar to the bioequivalence determination that leads to approval of generic small molecules all over the world. The inherent complex nature of the molecules, along with complicated manufacturing and analytical techniques to characterize them make it difficult to rely on a single human pharmacokinetic study for assurance of safety and efficacy.
In general, the concept of comparability has been used for evaluation of the currently approved “similar” biological where a step by step assessment on the quality, preclinical and clinical aspects is made. In India, the focus is primarily on the availability and affordability of life-saving drugs. In this context every product needs to be evaluated on its own merit irrespective of the innovator brand. The formation of the National Biotechnology Regulatory Authority may provide a step in the right direction for regulation of these complex molecules. However, in order to have an efficient machinery for initial approval and ongoing oversight with a country-specific focus, cooperation with international authorities for granting approvals and continuous risk-benefit review is essential. Several steps are still needed for India to be perceived as a country that leads the world in providing quality biological products.

We are now in the twenty-fifth anniversary year of the Drug Price Competition and Patent Term Restoration Act of 1984 (better known as the Hatch Waxman Act), the landmark US regulation that jump-started the generic pharmaceutical industry. The legislation provided the required impetus to make not just cheaper price alternative medicines available to US consumers but stimulated the emergence of the Indian pharmaceutical industry which is now the dominant supplier of generic drugs to the USA.
The regulatory pathway for bringing generic drugs to market is the abbreviated new drug application (ANDA) process which relies on proving bioequivalence to the listed reference product and showing equivalent product quality. Since duplication of proof of safety and efficacy in the preclinical and clinical setting is not required, there are significant cost savings in bringing a copy of a small chemical molecule to market. This model has been so successful in economic terms that almost 7 out of 10 prescriptions in the US are now generic and for the vast majority of products there is no concern in substitution of a generic equivalent for a brand-name prescription.1

The success story of generic small molecule drugs has stimulated interest in the pharmaceutical and biotech industry for applying an analogous approach towards the highly lucrative biologics business. But biologic drugs are very different from small molecules both in their final form and in the process required to produce and control their quality. It is therefore difficult to find a simple, precise “regulatory” definition of biologics. However, biologics are generally understood to be drugs derived from an organic source. Thus, biologics may be obtained or created from living organisms, either naturally or via genetic manipulation or are manufactured from building blocks of living organisms. They demonstrate considerable molecular complexity and may comprise a diversity of molecular forms. Their larger size and heterogeneity make it difficult for complete characterization via physicochemical analysis which is possible for synthetic chemical entities. In general, biologic drugs are more expensive and the cost of a yearly treatment may run into thousands of dollars for some. They are therefore ideal targets for developing cheaper alternatives.
US FDA definition – A “biological product” means a virus, therapeutic serum, toxin, antitoxin, vaccine, blood, blood component or derivative, allergenic product, or analogous product, or arsphenamine or derivative of arsphenamine (or any other trivalent organic arsenic compound), applicable to the prevention, treatment, or cure of a disease or condition of human beings (Public Health Service Act Sec. 351(i)).
Given the complexity of the final biologic product, it is clear that the nature of the manufacturing process is also complicated. In addition to aspects that are disclosed in regulatory applications, there may still be several aspects which might be held as trade secrets, thereby making it practically impossible for another company to make an identical copy of a biologic drug. While changing a host cell line or vector will definitely impact the product, effects of minor changes like temperature used in the manufacturing process may have an effect on the final characteristics of the biologic drug, including its safety and efficacy. It has been stated often that for a biologic, “the process defines the product”. Thus, while it may be possible to make a similar product, it may not be truly bioequivalent. As a result, even the term used to describe these similar biologic drugs has not been standardized globally. While the parallel term for a biologic generic may intuitively be “biogeneric”, the accepted term in Europe and Canada is “biosimilar” and the preferred term in the US is “follow-on biologic”.
Given these differences among innovator biologics and their “similar” counterparts, there is considerable hesitation on the part of the regulatory agencies to follow an abbreviated approval path similar to one widely used for generic small molecules.
Status of biosimilar regulation in Europe
EMEA Guidelines for Similar Biological Medical Products ( CHMP/437/04, 30 October 2005).2
EMEA’s Guideline on Similar Biological Medicinal Products Containing Biotechnology-derived Proteins as Active Substance: Nonclinical and Clinical Issues (EMEA/ CHMP/BMWP/42832/2005).3
EMEA’s Guideline on Similar Biological Medicinal Products Containing Biotechnology-derived Proteins as Active Substance: Quality Issues, EMEA/CHMP/49348/05.4
In Europe, the Committee for Medicinal Products for Human Use (CHMP), the European Medicines Agency (EMEA) led the way for biosimilars, by issuing its first specific regulatory guidance in October 2005. Two general guidance documents addressing quality and nonclinical and clinical perspectives (June 2006), five product-specific annexes on nonclinical and clinical issues (June-July 2006) and a manufacturing change comparability guideline (November 2007) are now available.
Biosimilars
Testing the bioequivalence of biosimilars differs from that of standard generics. Bioequivalence testing procedures for biosimilars are to be performed against the originator product as a control (reference) and include preclinical and clinical testing [2].
In the Biologics Price Competition and Innovation (BPCI) Act, a biosimilar product is defined as a product that is ‘highly similar’ to the reference product, notwithstanding minor differences in clinically inactive components and there are no clinically meaningful differences in terms of safety, purity and potency. However, little or no discussion regarding how similar is considered ‘highly similar’ is given in the BPCI Act.
For biosimilars, most of which have long half-lives, crossover study would be ineffective and unethical. This is due to the fact that a crossover study requires a wash-out period (which would be long for biosimilars with long half-lives) where the patient is not allowed to take the drug and therefore will have no treatment for their condition. On the other hand, parallel-group studies are required, but these studies do not provide an estimate of within-subject variation. For a parallel-group study, each drug is administered to a different group of subjects. Thus, we can only estimate total variance (between and within-subject variances), not individual variance components. This makes an evaluation of interchangeability difficult.
Statistical tests that may be used to asses biosimilarity are Shuirmann’s two one-sided tests procedure or the confidence interval approach.
Status of Biosimilar Regulation in US
In US, in March 2009, Representative Henry Waxman introduced H.R. 1427 to the Congress “Promoting Innovation and Access to Life-saving Medicines Act”, which authorizes FDA to approve follow-on biologics in an abbreviated manner. It has market exclusivity clauses with time frames similar to ones used currently for drugs. Other bills are expected to follow in the 2009 legislative agenda in order to establish a pathway for approval of these follow-on biologics. The contentious issues as expected, are focused around the duration of exclusivity benefits granted to innovators. The issue of substitutability of followon biologics for reimbursement is also an important one as the legislators debate the merits of each bill.
Korea and Singapore have released draft guidelines on biosimilars in 2009. The Singapore guideline is derived mainly from the EMEA guidelines and defines a similar biological/ biosimilar product as “a biological medicinal product referring to an existing registered product, submitted for medicinal product registration by an independent applicant, and is subject to all applicable data protection periods and/or intellectual property rights for the original product”. In addition to specifying the requirements for biosimilars, the guidance requires that the product have prior approval in countries such as Australia, Canada, EMEA or US.
Indian scenario
The Indian biotech industry is a thriving industry which got its start from vaccine manufacturing. In addition to meeting domestic demands, the Indian vaccine industry also fulfils export requirements to a large extent. Therefore it is evident that manufacturing expertise in producing biologic products of required export quality already exists in the country. What is not readily evident is whether these products can prove to be “comparable” to innovator products when we look into all categories of biologics.
The evolution of regulations governing pharmaceuticals in India has historically been driven by the need to make essential medicines accessible to patients. Access encompasses availability and affordability. It applies to medicines for all indications, acute and chronic illness, small molecules and biologics alike. The absence of product patent regulations for drugs marked a period in the country’s history where it was imperative to make inexpensive medicinal products available to the masses – it did not matter whether these products were innovator-made or copies thereof. In the post-TRIPS era however, there is need to offer and enforce adequate protections for patentable drugs, particularly biologics that inherently involve huge investments in R & D, manufacture and clinical development.

Today, several biologics have been approved in India , including recombinant human insulin, recombinant human erythropoietin (EPO), interferon (IFN), granulocyte colony stimulating factor (GCSF). The versions of biologics available in India are typically products whose patents have expired or do not exist in India. Therefore, from a technical standpoint, there is no concern about patent infringement regarding these (there are no patents in India for these products). If a biosimilar results in a price drop of 30%, it is a significant improvement to patients who may now be able to afford this generic version of a life-saving drug. In many ways, the debate about biosimilars that rages across the developed world and regulated markets is irrelevant to India where the central concern revolves around access.
Partly due to the dearth of appropriate resources and experience, Indian regulators have sought to mimic regulations already in use in the developed world without much customization. A host of agencies have been created to address the issues brought forth by biologics.
Basic facts about biosimilars.
Biotechnological drugs have become an essential part of modern pharmacotherapy and are expected to reach a 50% share in the pharmaceutical market in the next few years. The expiry of patent protection for many original biotechnological medicines has led to the development of what are called biosimilars or follow-on biologics. Biosimilars attempt to copy the original technology leading to the production of innovative biotechnological medicines to obtain a product which is similar to the original one. The first two biosimilars have recently been approved in the European Union and one application was rejected. Many more biosimilars will likely see approval in the near future. Our experience with biosimilars has been very limited to date and long-term safety data including immunogenicity are not available. Although biosimilars will likely lower the cost of modern therapies there are issues which have to be discussed at this stage among physicians regarding in particular the differences between biosimilars and generics of the classical chemical drugs, need for appropriate regulations as well as identification of potential problems with biosimilars. Other specific problems which will also be addressed in this review are safety of biosimilars, pharmacovigilance, automatic substitution, naming and labeling/prescription rules. 7
List of agencies
- Indian Council for Medical Research (ICMR)
- Central Drugs Standard Control Organisation (CDSCO)
- Department of Biotechnology (DBT)
- Genetic Engineering Approval Committee (GEAC)
- Recombinant DNA advisory Committee (RDAC)
- Review Committee on Genetic Manipulation (RCGM)
- Institutional Biosafety Committee (IBSC)
- National Centre for Biological Sciences
- National Control Laboratory for Biologicals
Notwithstanding the above, there is clarity on the fact that biologics and drugs need to be scrutinized differently. With this in mind, the DBT has been given the mandate to set up the National Biotechnology Regulatory Authority (NBRA). This is envisaged as an independent, autonomous and professionally led body to provide a single window mechanism for biosafety clearance of genetically modified products and processes.
Before such an organization can be effectively implemented, it will be necessary to put in place appropriate new legislation, namely the “National Biotechnology Regulatory Act” or the NBR Act. Draft establishment plan and “Draft National Biotechnology Regulatory Bill, 2008” are currently available on the DBT website for comments. The responsibility of consolidating the feedback has been entrusted to Biotech Consortium India Limited (BCIL). The draft bill envisions the scope of this authority to encompass research, manufacture, import and use of genetically engineered organisms and products derived thereof.
Biosimilars: how similar or dissimilar are they?
The imminent expiry of patents on biological medicinal products, such as epoetin alfa in 2006, has significant implications for nephrology in Australia. The purpose of this review is to examine the differences between biosimilars (similar biological medicinal products) and generic low molecular weight (chemical) drugs. The approach that regulatory agencies, including the European Medicines Agency (EMEA) and the Therapeutic Goods Administration (TGA), are taking towards biosimilars is also discussed. Biosimilars differ from generic chemical drugs in many important ways, including the size and complexity of the active substance, the nature of the starting materials (cell banks, tissues and other biological products), and the complexity of the manufacturing processes. Therefore, it has been acknowledged by the EMEA that established legal and regulatory principles of ‘essential similarity’ that are applied to standard chemical generics cannot be readily applied to biosimilars. One of the key areas of concern with the introduction of biosimilars into the field of nephrology will be guaranteeing the safety and efficacy of biosimilars. New manufacturers will need to ensure that their biopharmaceutical has a similar efficacy and safety profile to the innovator product through more extensive clinical trials than the limited testing done for generic versions of low molecular weight chemical medicines. 6
Safety
The primary importance of the manufacturing process was highlighted when a slight change in the production process of an originator recombinant erythropoietin resulted in patients developing pure red cell aplasia.
To try to address this possible safety issue, guidelines from EMA on comparability of biosimilars state that preclinical data must be insufficient to demonstrate the immunological safety of some biosimilars. This means that safety must be demonstrated in cohorts of patients enrolled in clinical trials and using post marketing surveillance.
-
The challenge of biosimilars.
The purpose of this report was to review issues associated with the introduction of alternative versions of biosimilars used in the oncology setting.
Data were obtained by searches of MEDLINE, PubMed, references from relevant English-language articles, and guidelines from the European Medicines Agency.
When biosimilars are approved in EU, they will be considered ‘comparable’ to the reference product, but this does not ensure therapeutic equivalence. Inherent differences between biosimilars may produce dissimilarities in clinical efficacy, safety, and immunogenicity. Switching biosimilars should be considered a change in clinical management. Regulatory guidelines have been established for some biosimilar categories but, because of the limited clinical experience with biosimilars at approval, pharmacovigilance programs will be important to establish clinical databases. Guidelines also provide a mechanism for the extrapolation of clinical indications (approved indications for which the biosimilar has not been studied). This may be of concern where differences in biological activity can result in adverse outcomes or when safety is paramount (e.g. stem cell mobilization in healthy donors). These issues should be addressed in biosimilar labeling.
Biosimilars should provide cost savings and greater accessibility to biopharmaceuticals. A thorough knowledge surrounding biosimilars will ensure the appropriate use of biopharmaceuticals.
Pharmacovigilance
Due to the limited clinical database at the time of approval of a biosimilar, vigorous pharmacovigilance is required. EMA guidelines require pharmacovigilance programmes to monitor the safety of biosimilar products post-approval.Substitution
For small molecule generics the issue of substitution is easy, since they are considered identical to the originator molecule. This, however, is not the case for biosimilars, which are large complex molecules prone to heterogeneity.In the US, the BPCI Act gives FDA the authority to designate a biosimilar as interchangeable with its reference product. This means that the biosimilar may be substituted for the originator product by the pharmacist without reference to the prescribing physician. This is not the case, however, in the EU, where decisions on interchangeability are not made by EMA, but at a national level.
Global concerns regarding product safety and quality
Every drug/biologic manufacturer needs to own the responsibility for putting a high quality, safe drug on the market, after appropriate review and approval by the concerned regulatory authority. While the safety of original biologics products is assured by the innovator by adherence to rigorous standards required for approval, the resistance towards biosimilars on the part of regulators, stems from the concern that an abbreviated approval process may not be adequate to ensure safe performance of the product in the market. For a manufacturer looking to get into the biosimilar market, he needs to overcome major challenges in making a complex product, getting regulatory approval by satisfying stringent criteria and then selling it in the market. Typically, facilities required for manufacture of biologicals are very expensive and the kind of infrastructure required to meet high regulatory expectations is limited to only a few companies. Clinical trial expenditure and ongoing analysis requires compliance to pharmacopoeial monographs when available and access to reference standards, which are not always available.
The cornerstone of generic drug approvals has been the concept of bioequivalence, using equivalence of pharmacokinetic parameters as surrogates for clinical efficacy. But in the context of biosimilars, the concept of comparability is the one used to make such an evaluation. Comparability protocols are used for chemistry, manufacturing and controls (CMC) sections to make the case on the quality aspects of the product. Preclinical testing requires knowledge of study designs used by innovator in order to truly compare performance of the biosimilar. For clinical evaluation, at least one clinical comparability trial is required to demonstrate comparability (non-inferiority in terms of efficacy to innovator and comparable safety profile). But long term safety issues remain unaddressed for biosimilars, requiring thorough postmarketing studies and pharmacovigilance and adequate risk management plans.
In terms of preclinical studies, for biologics, pharmacodynamic endpoints are more relevant than pharmacokinetics, which is the key measure with small molecules. For animal safety studies, choice of appropriate animal species and duration of studies are important criteria for proving comparability. Clinically, comparative PK/PD study is required to compare the reference and biosimilar product. However, clinical trial design selection and a thorough understanding and a priori statement of margins chosen for comparability must be stated for meaningful evaluation of data.
Follow-on biologics: challenges of the “next generation”.
The imminent patent expiration of many biopharmaceutical products will produce the possibility for generic versions of these therapeutic agents (i.e. biosimilars). However, there are a number of issues that will make approval of biosimilars much more complicated than the approval of generic equivalents of conventional pharmaceuticals. These issues centre on the intrinsic complexity of biopharmaceutical agents, which are recombinant proteins in most cases, and the heterogeneity of proteins produced by different manufacturing processes (i.e. differences in host cells, purification and processing, formulation and packaging). The increased occurrence of antibody (Ab)-mediated pure red cell aplasia (PRCA) associated with a change in the formulation of one particular epoetin-alpha product highlights the potential for increased immunogenicity of recombinant proteins with different formulations, or those manufactured by different processes. Thus, verification of the similarity to or substitutability of biosimilars with reference innovator biopharmaceutical products will require much more than a demonstration of pharmacokinetic similarity, which is sufficient for conventional, small molecule generic agents. Regulatory requirements for the approval of biosimilars have not yet been fully established, but preliminary guidelines from the European Agency for the Evaluation of Medicinal Products (EMEA) state that the complexity of the product, the types of changes in the manufacturing process, and differences in quality, safety and efficacy must be taken into account when evaluating biosimilars. For most products, results of clinical trials demonstrating safety and efficacy are likely to be required. In addition, because of the unpredictability of the onset and incidence of immunogenicity, extended post-marketing surveillance is also important and may be required. 10
Statistical assessment of biosimilar products.
Biological products or medicines are therapeutic agents that are produced using a living system or organism. Access to these life-saving biological products is limited because of their expensive costs. Patents on the early biological products will soon expire in the next few years. This allows other biopharmaceutical/biotech companies to manufacture the generic versions of the biological products, which are referred to as follow-on biological products by the U.S. Food and Drug Administration (FDA) or as biosimilar medicinal products by the European Medicine Agency (EMEA) of the European Union (EU). Competition of cost-effective follow-on biological products with equivalent efficacy and safety can cut down the costs and hence increase patients’ access to the much-needed biological pharmaceuticals. Unlike for the conventional pharmaceuticals of small molecules, the complexity and heterogeneity of the molecular structure, complicated manufacturing process, different analytical methods, and possibility of severe immunogenicity reactions make evaluation of equivalence (similarity) between the biosimilar products and their corresponding innovator product a great challenge for both the scientific community and regulatory agencies. In this paper, we provide an overview of the current regulatory requirements for approval of biosimilar products. A review of current criteria for evaluation of bioequivalence for the traditional chemical generic products is provided. A detailed description of the differences between the biosimilar and chemical generic products is given with respect to size and structure, immunogenicity, product quality attributed, and manufacturing processes. In addition, statistical considerations including design criteria, fundamental biosimilar assumptions, and statistical methods are proposed. The possibility of using genomic data in evaluation of biosimilar products is also explored.15
A way forward for India
In today’s scenario, India needs to focus on quality of each biological product per se, whether that is demonstrated through comparability or by its own merit; and assurance of safety through appropriate regulatory review and approval of available data.
Irrespective of the authority entrusted to oversight of biologics, the debate on appropriate level of regulatory scrutiny for biologics will continue to focus on requiring adequate characterization while balancing cost, with the overall goal of having a much needed product on the market with reasonable assurance of efficacy and safety. Intense discussion on publication of appropriate monographs in the Indian Pharmacopeia and availability of reference standards continues amidst regulatory circles. Indian manufacturers have always sought to enter new markets and have voluntarily raised the bar in order to secure approvals for their products in the regulated markets where profit margins are high. From a facility infrastructure and systems point of view, most companies eyeing the regulated markets for their products will most likely fulfil expectations. State-of-the art analytical techniques are available within the industry. Therefore from a quality standpoint, biologic products made in India should not have any trouble in meeting market expectations. However, physicochemical characterization of a biologic product and compliant facilities form only one part of the evaluation required to demonstrate product comparability.
The practical way forward for approval of biosimilar products in India would have to be unique to the Indian context while staying rooted to scientific basics and keeping in mind the needs and limitations of the country. The large majority of biosimilars introduced in India would be products whose patents have expired and where the “original innovator” product may not be approved in the country. It is also possible that no patent exists in India for some products and therefore , originator and similars coexist. For all products, the question of available reference standards and monographs would continue to remain. The next wave of biologics of commercial interest to the industry will become a burning issue where the regulator cannot expect to wait to see how the legislation is crafted in the US or elsewhere before making a move.
In my opinion, it seems that India, having the benefit of in-house (in-country) expertise in the area, should utilize the various agencies currently entrusted with splintered tasks and responsibilities to come up with working group or taskforce whose goal is to develop product-specific guidelines for approval. These can be developed using available worldwide regulatory knowledge by signing appropriate MOUs if necessary, studying the scientific literature and current industry standards and practice with respect to characterization, focusing on specific areas of unique concern for each product and proposing an approval path. These guidelines can be widely disseminated in the community. There will still be grey areas that need clarification and in such cases, a system for formal meeting with members of the working group/taskforce can be instituted, similar to the scientific advice that is currently available through the EMEA or individual European country competent authorities.
As a nation that takes pride in being the “exporter to the world” in the arena of pharmaceuticals, it behooves not just the regulators but all those in the regulatory affairs profession in India to support such initiatives to make life-saving products available to our countrymen that are unquestionably of the highest standards in terms of quality, safety and efficacy such that we become the supplier of choice when it comes to exporting biosimilars to markets in every corner of the world.
Biosimilar therapeutics-what do we need to consider?
Patents for the first generation of approved biopharmaceuticals have either expired or are about to expire. Thus the market is opening for generic versions, referred to as ‘biosimilars’ (European Union) or ‘follow-on protein products’ (United States). Healthcare professionals need to understand the critical issues surrounding the use of biosimilars to make informed treatment decisions.The complex high-molecular-weight three-dimensional structures of biopharmaceuticals, their heterogeneity and dependence on production in living cells makes them different from classical chemical drugs. Current analytical methods cannot characterize these complex molecules sufficiently to confirm structural equivalence with reference molecules. Verification of the similarity of biosimilars to innovator biopharmaceuticals remains a key challenge. Furthermore, a critical safety issue, the immunogenicity of biopharmaceuticals, has been highlighted in recent years, confirming a need for comprehensive immunogenicity testing prior to approval and extended post-marketing surveillance.Biosimilars present a new set of challenges for regulatory authorities when compared with conventional generics. While the demonstration of a pharmacokinetic similarity is sufficient for conventional, small-molecule generic agents, a number of issues will make the approval of biosimilars more complicated. Documents recently published by the European Medicines Agency (EMEA) outlining requirements for the market approval of biosimilars provide much-needed guidance. The EMEA has approved a number of biosimilar products in a scientifically rigorous and balanced process. Outstanding issues include the interchangeability of biosimilars and innovator products, the possible need for unique naming to differentiate the various biopharmaceutical products, and more comprehensive labelling for biosimilars to include relevant clinical data. 5
Biosimilars: policy, clinical, and regulatory considerations.
The regulatory background surrounding biosimilars (biopharmaceuticals that are considered similar in composition to an innovator product, but not necessarily clinically interchangeable); equivalence, interchangeability, and unique considerations associated with biopharmaceuticals; the biopharmaceutical protein production process; scientific facts for use in the policy discussion about biosimilars; the European Union system for biosimilars; and the current status of biosimilars legislation in the United States are described.
An abbreviated regulatory pathway for the approval of biosimilars, and a process for safely demonstrating the therapeutic interchangeability of these proteins, has the potential to provide meaningful cost savings. This economic advantage to patients can translate into important public health benefits. But to date, no formal regulatory process exists in the United States for bringing these drugs to market. In addition, the current tools for fully characterizing biopharmaceuticals are not–in certain cases–well developed, especially for proteins that have complex structures or are heavily glycosylated. In addition, using “similar” but not completely “identical” proteins interchangeably raises concerns about potentiating immunogenicity. The bottom line is that demonstrating therapeutic equivalence and interchangeability for biosimilars is not a straightforward matter–it cannot be based on the same criteria as for conventional small-molecule drugs. The science, while obtainable, is more complex. For example, it is assumed that showing that a biosimilar protein can be safely used interchangeably with an innovator protein would require, at the least, some limited clinical data and interchangeability studies. Notwithstanding the more complex scientific and clinical issues particular to protein products, most believe that a process for enabling the approval of safe and effective biosimilar proteins is not only possible, but an important public health goal. The European Union system for biosimilars may provide a model for anticipating and resolving the scientific and policy issues related to biosimilars in the U.S.
The legal and regulatory status of biosimilars remains to be resolved in the United States as policymakers address the scientific and policy issues surrounding product manufacturing, patent terms, and clinical use.
Biosimilars: it’s not as simple as cost alone.
Biosimilars or follow-on biologics (FoB) are biopharmaceuticals that, unlike small molecule generic products, are copies of larger, much more complex proteins. As such, data generated from one biopharmaceutical cannot be extrapolated to another. Unlike small molecule generics, FoB require a full developmental programme, albeit smaller than for an originator product. This has been recognized by European regulatory authorities and it is becoming clear that accelerated processes for FoB marketing approval are not feasible.
To determine the balance between costs surrounding FoB (including relatively extensive developmental programmes and subsequent price to the market) and the necessity to ensure efficacy and safety.
It is important that FoB are sufficiently tested to ensure patient safety is not compromised. Conducting such a development programme followed by sound pharmacovigilance is very challenging and costly.
Cost-savings associated with FoB may be limited. 10
Recommendations regarding technical standards for follow-on biologics: comparability, similarity, interchangeability.
Policy makers around the world are currently considering the creation of a regulatory pathway for follow-on biologics (FOB), which will have to account for the substantial technical challenges associated with FOB development. These challenges will likely involve more complexity than comparability assessments of process changes made by the same manufacturer. The history of industry-regulator comparability discussions helps explain why the same degree of testing and flexibility now applied to change-control within a manufacturer’s own process, at this time, cannot be extrapolated to the observed and possibly unknown differences between two manufacturing processes that are independently developed by different (non-collaborating) parties.
This commentary provides recommendations on the technical aspects that should be considered in the creation of an approval pathway for FOB products.
In the authors’ view, analytical methodology in its current state cannot alone provide full assurance that the FOB is sufficiently similar to the innovator product. Moreover, the FOB manufacturer will not have access to the extensive knowledge accumulated by the innovator manufacturer from early development through marketing. Thus, extensive clinical evaluation will likely be necessary to provide assurance that the FOB is safe and efficacious. If such testing demonstrates the FOB is safe and efficacious per existing regulatory standards, the product should receive marketing approval as a ‘similar’ product. Since ‘similarity’ is a fundamentally different determination than establishing interchangeability between the two products, an interchangeability determination must be based on additional testing and market experience to ensure patient safety. Post-marketing surveillance of the FOB should be conducted to ensure that the approved molecule has similar clinical safety and efficacy as the innovator product, prior to any consideration of interchangeability 11
European regulatory guidelines for biosimilars.
The impending arrival en masse of biosimilars on Western markets is placing drug regulatory agencies under pressure to realign their policies. Biosimilars require more rigorous assessments than traditional chemical generics. This is because of the molecular complexity of recombinant proteins, and the complexity of biological manufacturing processes. Small differences can arise in a recombinant protein product which are hard or impossible to detect with even state-of-the-art analytical techniques. Yet, these differences can have significant impact on the safety and efficacy of the drug. The European Medicines Agency (EMEA) has taken the lead in issuing guidelines, most of which are still under review. The guidelines advocate pre-clinical and clinical testing of biosimilars prior to market authorization, complemented by tailored pharmacovigilance plans. These guidelines provide a valuable base from which to develop in this evolving regulatory environment.12
Legislative initiatives in Europe, Canada and the US for market authorization of follow-on biologics.
The formulation and application of legal and regulatory requirements for the market authorization of follow-on versions of biological drugs present challenges. This review discusses relevant regulatory guidelines and legislative initiatives related to market authorization for follow-on biologics in Europe, Canada and the US. The respective positions of these three markets is analyzed with regard to several factors: criteria for the choice of reference products; requirements for the comparability exercise between a candidate follow-on biologic and the selected reference product, with an emphasis on considerations of quality, safety and efficacy data; the interchangeability of a reference product with related follow-on drugs; data exclusivity provisions; and the application of specialized patent enforcement mechanisms to follow-on biologics.13
Quality, safety and efficacy of follow-on biologics in Japan.
Recently, WHO, EU, Japan and Canada have published guidelines on biosimilar/follow-on biologics. While there seems to be no significant difference in the general concept in these guidelines, the data to be submitted for product approval are partially different. Differences have been noted in the requirements for comparability studies on stability, prerequisites for reference product, or for the need of comparability exercise for determination of process-related impurities. In Japan, there have been many discussions about the amount and extent of data for approval of follow-on biologics. We try to clarify the scientific background and rational for regulatory pathway of biosimilar/follow-on biologics in Japan in comparison with the guidelines available from WHO, EU and Canada. In this article, we address and discuss the scientific background underlying these differences to facilitate the harmonization of follow-on biologic principles in the guidelines in future.14
References
RAMELTEON, TAK 375 ..Melatonin MT1/MT2 receptor agonist

RAMELTEON
- HSDB 7787
- Ramelteon
- Rozerem
- TAK-375
- UNII-901AS54I69
| CAS number | 196597-26-9 |
|---|
| (S)-N-[2-(1,6,7,8-tetrahydro-2H-indeno-[5,4-b]furan-8-yl)ethyl]propionamide |
(5)-N-[2-(l,6,7,8-tetrahydro-2H-indeno-[5,4-ό]furan-8- yl)ethyl]propionamide
| United States | US 6034239 | 1999-07-22 | expiry 2019-07-22 |
EP885210B1 , EP1792899A1 and J. Med Chem. 2002, 45, 4222-4239
read all at
http://www.allfordrugs.com/2014/02/23/ramelteon-tak-375-melatonin-mt1mt2-receptor-agonist/
Vertex Pharmaceuticals: Another Step Forward For Kalydeco
.
On February 21st, Vertex Pharmaceuticals announces that the FDA approves a supplemental New Drug Application (sNDA) for orphan drug Kalydeco (Ivacaftor) for people with Cystic Fibrosis (CF), ages 6 and older, who have one of the 8 additional mutations in the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) gene :
• G178R
• S549N
• S549R
• G551S
• G1244E
• S1251N
• S1255P
• G1349D.
Kalydeco receives approval from the FDA in January 2012 for CF patients, ages 6 and older who have at least one copy of the G551D mutation. Thus, Kalydeco is currently approved for 9 mutations. The new approval affects approximately 150 in the United States.
The sNDA approval is based on previously announced data from a Phase III, 2-part, randomized, double-blind, placebo-controlled, cross-over study of 39 CF patients who have one of the above listed 8 mutations + the G970R mutation. Based on this…
View original post 262 more words
Immune cells regulate blood stem cells

Blood stem cell cultures: Blood stem cells from colonies (cell clusters) in vitro consisting of different blood cells. Nine blood stem cell colonies are illustrated in the image, which have developed into differentiated cell types, particularly into white blood cells (leukocytes).Credit: Department of Clinical Research of the University of Bern, Tumor-Immunology research group
Researchers in Bern, Switzerland have discovered that, during a viral infection, immune cells control the blood stem cells in the bone marrow and therefore also the body’s own defences. The findings could allow for new forms of therapy, such as for bone marrow diseases like leukaemia.
During a viral infection, the body needs various defence mechanisms – amongst other things, a large number of white blood cells (leukocytes) must be produced in the bone marrow within a short period of time. In the bone marrow, stem cells are responsible for this task: the blood stem cells. In…
View original post 390 more words
KW-4490 A PDE4 inhibitor from Kyowa Hakko Kirin
 KW 4490
KW 4490- cis-4-Cyano-4-(2,3-dihydro-8-methoxy-1,4-benzodioxin-5-yl)cyclohexanecarboxylic Acid
- Cyclohexanecarboxylic acid, 4-cyano-4-(2,3-dihydro-8-methoxy-1,4-benzodioxin-5-yl)-, cis–
- cis-4-Cyano-4-(2,3-dihydro-8-methoxy-1,4-benzodioxin-5-yl)cyclohexane-1-carboxylic acid;
- cis-4-Cyano-4-(8-methoxy-1,4-benzodioxan-5-yl)cyclohexanecarboxylic acid
KF 66490; KW 4490;
MF C17 H19 N O5
A phosphodiesterase type 4 inhibitor, commonly referred to as a PDE4 inhibitor, is a drug used to block the degradative action ofphosphodiesterase 4 (PDE4) on cyclic adenosine monophosphate (cAMP). It is a member of the larger family of PDE inhibitors. The PDE4 family of enzymes are the most prevalent PDE in immune cells. They are predominantly responsible for hydrolyzing cAMP within both immune cells and cells in the central nervous system
PDE4 hydrolyzes cyclic adenosine monophosphate (cAMP) to inactive adenosine monophosphate (AMP). Inhibition of PDE4 blocks hydrolysis of cAMP, thereby increasing levels of cAMP within cells.
Practical synthesis of the PDE4 inhibitor, KW-4490
ORGN 699 |
|
Arata Yanagisawa, arata.yanagisawa@kyowa.co.jp1, Koichiro Nishimura2, Tetsuya Nezu2, Kyoji Ando2, Ayako Maki2, Eiichiro Imai2, and Shin-ichiro Mohri2. (1) Pharmaceutical Research Center, Medicinal Chemistry Research Laboratories, Kyowa Hakko Kogyo Co., Ltd, 1188 Shimotogari, Nagaizumi-cho, Sunto-gun, Shizuoka, Japan, (2) Pharmaceutical Research Center, Sakai Research Laboratories, Kyowa Hakko Kogyo Co., Ltd, 1-1-53 Takasu-cyo, Sakai-ku, Sakai, Osaka, Japan
|
A practical and scaleable synthesis of the PDE4 inhibitor, KW-4490 (1), was developed for the multi-kilogram preparation. This improved synthesis features construction of the 1-arylcyclohexene by Diels-Alder reaction, followed by a newly established acid-mediated hydrocyanation. The synthesis was achieved in 7 steps in 38% overall yield. Efforts toward increasing the regioselectivity in the Diels-Alder reaction, optimization of crystallization-induced dynamic resolution of the hydrocyanation product, and investigation of other synthetic routes will be presented. |
|
New Reactions and Methodology, Metal-Mediated Reactions, Physical Organic Chemistry, Molecular Recognition and Self-Assembly
7:00 PM-9:00 PM, Wednesday, August 20, 2008 Pennsylvania Convention Center — Blrm A/B, PosterDivision of Organic ChemistryThe 236th ACS National Meeting, Philadelphia, PA, August 17-21, 2008 |
A team at Kyowa Hakko Kirin in Japan has used a crystallisation-induced dynamic resolution in the synthesis of KW-4490, a PDE-4 inhibitor being developed for asthma and chronic obstructive pulmonary disease.6 Towards the end of the synthesis, they were faced with a mixture of cis and trans diastereomers of an intermediate derived from a hydrocyanation reaction, which was about 62:38 cis:trans; altering the conditions of the reaction did not give a selective process. The desired isomer was the cis, so they wanted to convert the unwanted trans isomer to cis to improve the yield (Scheme 2).
They first tried using a base-induced isomerisation using a base such as potassium t-butoxide, but although this worked to a degree the best ratio of products obtained was 75:25. The same result was obtained when they tested the system on both pure cis and trans isomers, indicating that this ratio represented the thermodynamic equilibrium. However, they realised that the cis isomer was less soluble in ethanol, so they thought the answer might lie in crystallisation-induced dynamic resolution.
They therefore suspended a crude mixture of the two isomers in ethanol and added a catalytic amount of potassium t-butoxide to effect the isomerisation. It was stirred and warmed, and hexane added portion-wise to crash the cis isomer out of solution. The group managed to increase the ratio of isomers to 99:1 by continuous isomerisation, with a 90% isolated yield.
 Scheme 2: Kyowa Hakko Kirin found a way to improve the yield of the cis isomer
Scheme 2: Kyowa Hakko Kirin found a way to improve the yield of the cis isomerA Practical Synthesis of the PDE4 Inhibitor, KW-4490
http://pubs.acs.org/doi/abs/10.1021/op1001287?prevSearch=KW%2B4490&searchHistoryKey=



Compound (XIII) is disclosed in WO00/14085 as being useful as a PDE-IV inhibitor. A method for the preparation of a typical compound among compounds (XIII) disclosed in WO00/14085 is as follows:
However, this method is not practically satisfactory as a industrially applicable preparation method, because of (1) requiring multiple steps, (2) low overall yield, (3) requiring purification by silica-gel column chromatography, and the like.
REFERENCE EXAMPLE 1
Synthesis of cis-4-cyano-4-(2,3-dihydro-8-methoxy-1,4-benzodioxine-5-yl)cyclohexanecarboxylic acid
(1) Synthesis of cis-4-cyano-4-(2,3-dihydro-8-methoxy-1,4-benzodioxine-5-yl)cyclohexanecarboxylic acid ethyl ester
Under a nitrogen atmosphere, trifluoromethanesulfonic acid (2.25 g) and trimethylsilylcyanide (1.57 mL) were dissolved in benzotrifluoride (10 mL), and a solution of 4-(2,3-dihydro-8-methoxy-1,4-benzodioxine-5-yl)-3-cyclohexenecarboxylic acid ethyl ester (0.79 g) prepared according to the method described in EXAMPLE 1 in benzotrifluoride (10 mL) was added dropwise at −25° C. After being stirred for for one hour at −20° C., an aqueous saturated sodium hydrogen carbonate was added and the mixture was extracted with ethyl acetate. The organic layer was washed with brine and dried over anhydrous magnesium sulfate, and the solvent was evaporated under reduced pressure. The residue was crystallized from ethanol (1 mL) to give a solid substance (0.64 g). The solid substance (0.030 g) was crystallized from a mixed solvent of diisopropyl ether and ethyl acetate (0.36 mL, diisopropyl ether/ethyl acetate=4/1) to give cis-4-cyano-4-(2,3-dihydro-8-methoxy-1,4-benzodioxine-5-yl)cyclohexanecarboxylic acid ethyl ester (0.019 g, 47.3%) as a solid.
Melting point 131° C.
1H-NMR (CDCl3, δ ppm) 6.84 (d, J=8.9 Hz, 1H), 6.49 (d, J=8.9 Hz, 1H), 4.39−4.33 (m, 4H), 4.17 (q, J=7.1 Hz, 2H), 3.88 (s, 3H), 2.44 (brd, J=12.6 Hz, 2H), 2.32 (tt, J=11.8, 3.8 Hz, 1H), 2.18−1.95 (m, 4H), 1.86 (dt, J=3.6, 12.6 Hz, 2H), 1.28 (t, J=7.1 Hz, 3H).
[0184] IR (KBr, cm−1) 2953, 2228, 1722, 1607, 1504, 1460, 1381, 1325, 1281, 1117, 1043, 953, 787.
MS (m/z) 346(M+H)+.
(2) Synthesis of cis-4-cyano-4-(2,3-dihydro-8-methoxy-1,4-benzodioxine-5-yl)cyclohexanecarboxylic acid
To a suspension of cis-4-cyano-4-(2,3-dihydro-8-methoxy-1,4-benzodioxine-5-yl)cyclohexanecarboxylic acid ethyl ester (397 g) prepared according to the method described (1) of REFERENCE EXAMPLE 1 in ethanol (1.99 L) was added a 6 ml/L aqueous potassium hydroxide (377 mL), and the mixture was stirred for 4 hours at room temperature. After water (2.03 L) was added to the reaction mixture, a 6 mol/L aqueous hydrochloric acid (576 mL) was added to crystallize and to give cis-4-cyano-4-(2,3-dihydro-8-methoxy-1,4-benzodioxine-5-yl)cyclohexanecarboxylic acid (366 g, 98.1%) as a solid.
Melting point 245° C.
1H-NMR (DMSO-d6, δ ppm) 12.26 (brs, 1H), 6.79 (d, J=8.9 Hz, 1H), 6.59 (d, J=8.9 Hz, 1H), 4.27 (dd, J=11.9, 5.0 Hz, 4H), 3.75 (s, 3H), 2.34−2.26 (m, 3H), 2.05−2.00 (m, 2H), 1.86−1.63 (m, 4H).
IR (KBr, cm−1) 3287, 2932,1728, 1609, 1508, 1454, 1285, 1119, 953, 802, 764.
MS (m/z) 318(M+H)+.
-
To a solution of 12 g (62 mmol) of 8-methoxy-1,4-benzodioxane-5-carbaldehyde in 140 ml of acetonitrile was added 12 g (110 mmol) of lithium bromide, and then 12 ml (95 mmol) of trimethylsilyl chloride was dropwise added thereto. After 15 minutes, the mixture was ice-cooled, and 19 ml (110 mmol) of 1,1,3,3-tetramethyldisiloxane was dropwise added thereto, followed by stirring at room temperature for 2 hours. The mixture was diluted with methylene chloride, and then was filtered through Celite. The solvent was evaporated in vacuo from the filtrate to give a pale yellow oily substance. To a solution of the obtained crude 5-bromomethyl-8-methoxy-1,4-benzodioxane in 180 ml of DMF was added 9.2 g (190 mmol) of sodium cyanide, followed by stirring at room temperature for 60 hours. To the mixture was added water under ice-cooling, and a solid separated out therefrom was collected by filtration to give 6.8 g (53%) of Compound 1a as an ash-colored solid.Melting Point: 121 – 125 °C
1H-NMR (CDCl3, δ, ppm) 3.60 (s, 2H), 3.88 (s, 3H), 4.33 (s, 4H), 6.50 (d, J = 8 Hz, 1H), 6.86 (d, J = 8 Hz, 1H).
MASS (m/z) 205 (M+).
- Example 1.
- 4-Cyano-4-(8-methoxy-1,4-benzodioxan-5-yl) cyclohexanone (Compound 1)(Step A)
- Synthesis of 2-(8-methoxy-1,4-benzodioxan-5-yl)acetonitrile (Compound 1a)
-
To a solution of 6.2 g (30 mmol) of Compound 1a obtained in Step A in 94 ml of acetonitrile were added 1.4 ml (3.0 mmol) of a 40% methanolic solution of Triton B and 27 ml (300 mmol) of methyl acrylate, followed by heating under reflux for 5 hours. The mixture was allowed to stand for cooling, and then poured into water, followed by extraction with ethyl acetate. The organic layer was washed with brine and dried over sodium sulfate, and the solvent was evaporated in vacuo. The residue was purified by silica gel column chromatography (eluted with hexane/ethyl acetate = 2/1) to give 6.4 g (56%) of Compound 1b as a pale yellow oily substance.
1H-NMR (CDCl3, δ, ppm) 2.05-2.37 (m, 4H), 2.39-2.59 (m, 2H), 2.62-2.82 (m, 2H), 3.60 (s, 6H), 3.87 (s, 3H), 4.20-4.40 (m, 4H), 6.48 (d, J = 9 Hz, 1H), 7.01 (d, J = 9 Hz, 1H).
MASS (m/z) 377 (M+).
- (Step B) Synthesis of dimethyl 4-cyano-4-(8-methoxy-1,4-benzodioxan-5-yl)pimelate (Compound 1b)
-
To a solution of 6.4 g (17 mmol) of Compound 1b obtained in Step B in 96 ml of 1,2-dimethoxyethane was added 2.0 g (50 mmol) of 60% sodium hydride. After heating under reflux for 3 hours, the mixture was allowed to stand for cooling, poured into ice water, acidified with a 6 mol/liter aqueous hydrochloric acid and extracted with ethyl acetate. The organic layer was washed with brine and dried over sodium sulfate, and the solvent was evaporated. The residue was purified by silica gel column chromatography (eluted with hexane/ethyl acetate = 2/1) to give 5.0 g (86%) of Compound 1c as a white solid.
Melting Point: 129 – 132 °C
1H-NMR (CDCl3, δ, ppm) 2.21-2.50 (m, 3H), 2.61-2.89 (m, 2H), 3.11(d, J = 15 Hz, 1H), 3.79 (s, 3H), 3.89 (s, 3H), 4.37 (s, 4H), 6.49 (d, J = 9 Hz, 1H), 6.84 (d, J = 9 Hz, 1H), 12.2 (s, 1H).
MASS (m/z) 345 (M+).
- (Step C) Synthesis of 4-cyano-4-(8-methoxy-1,4-benzodioxan-5-yl)-2-methoxycarbonylcyclohexanone (Compound 1c)
-
A mixture of 5.0 g (15 mmol) of Compound 1c obtained in Step C, 50 ml of DMSO, 5 ml of water, and 5.0 g of sodium chloride was stirred at 150°C for 5 hours. The mixture was allowed to stand for cooling, and water was added thereto, followed by extraction with ethyl acetate. The organic layer was washed with brine and dried over sodium sulfate, and the solvent was evaporated in vacuo. The residue was purified by silica gel column chromatography (eluted with hexane/ethyl acetate = 3/1) to give 3.6 g (86%) of Compound 1 as a white solid.
Melting Point: 157 – 161 °C
1H-NMR (CDCl3, δ, ppm) 2.21-2.41 (m, 2H), 2.45-2.72 (m, 4H), 2.81-3.00 (m, 2H), 3.89 (s, 3H), 4.37 (s, 4H), 6.51 (d, J = 9 Hz, 1H), 6.88 (d, J = 9 Hz, 1H).
MASS (m/z) 287 (M+).
- (Step D) Synthesis of Compound 1
-
In 65 ml of THF was dissolved 10 g (41 mmol) of 5-bromo-8-methoxy-1,4-benzodioxane, and 28 ml (45 mmol) of a 1.59 mol/liter solution of n-butyl lithium in hexane was dropwise added thereto at -78°C. After 15 minutes, a solution of 9.6 g (61 mmol) of 1,4-cyclohexadione monoethyleneketal in 50 ml of THF was dropwise added thereto. The mixture was stirred for 1 hour, followed by stirring at room temperature for 20 minutes. Water was added thereto, the mixture was extracted with ethyl acetate, and the extract was washed with brine and dried over sodium sulfate. The solvent was evaporated therefrom, and the residue was purified by silica gel column chromatography (eluted with hexane/ethyl acetate = 1/1) to give 9.0 g (68%) of Compound 2a as a white solid.
Melting Point: 94 – 96 °C
1H-NMR (CDCl3, δ, ppm) 1.58-1.72 (m, 2H), 1.88-2.28 (m, 6H), 3.57 (s, 1H), 3.86 (s, 3H), 3.90-4.07 (m, 4H), 4.35 (s, 4H), 6.46 (d, J = 9 Hz, 1H), 6.82 (d, J = 9 Hz, 1H).
MASS (m/z) 322 (M+). -
- (Step B) Synthesis of Compound 2
-
In 4.9 ml of methylene chloride was dissolved 0.49 g (1.5 mmol) of Compound 2a obtained in Step A, 0.26 ml (1.9 mmol) of trimethylsilyl cyanide was added thereto at -78°C, then 0.20 ml (1.6 mmol) of a boron trifluoride-ethyl ether complex was dropwise added thereto, and the mixture was stirred for 10 minutes, followed by stirring at room temperature for 10 minutes. A saturated aqueous solution of sodium bicarbonate was added thereto and the mixture was extracted with ethyl acetate. The extract was washed with brine and dried over sodium sulfate, and the solvent was evaporated. The residue was purified by silica gel column chromatography (eluted with hexane/ethyl acetate = 2/1) to give 0.30 g (61%) of Compound 2 as a colorless oily substance.
1H-NMR (CDCl3, δ, ppm) 1.79-1.95 (m, 2H), 2.06-2.20 (m, 4H), 2.30-2.46 (m, 2H), 3.87 (s, 3H), 3.90-4.07 (m, 4H), 4.36 (s, 4H), 6.48 (d, J = 9 Hz, 1H), 6.82 (d, J = 9 Hz, 1H).
MASS (m/z) 331 (M+).
-
- Example 2. 4-Cyano-4-(8-methoxy-1,4-benzodioxan-5-yl)cyclohexanone ethyleneketal (Compound 2)
- (Step A)Synthesis of 4-hydroxy-4-(8-methoxy-1,4-benzodioxan-5-yl)cyclohexanone ethyleneketal (Compound 2a)
-
In 2.9 ml of acetone was dissolved 0.29 g (0.87 mmol) of Compound 2 obtained in Example 2, 1.2 ml (7.2 mmol) of a 6 mol/liter aqueous hydrochloric acid was added thereto, and the mixture was heated under reflux for 3 hours. The mixture was allowed to stand for cooling and poured into a saturated aqueous solution of sodium bicarbonate, the mixture was extracted with ethyl acetate, and the extract was washed with brine. The mixture was dried over sodium sulfate, and the solvent was evaporated to give 0.23 g (92%) of Compound 1 as a white solid.
- Example 3. Compound 1
- Example 4. Methyl
cis-4-cyano-4-(8-methoxy-1,4-benzodioxan-5-yl)cyclohexanecarboxylate (Compound 3) and methyltrans-4-cyano-4-(8-methoxy-1,4-benzodioxan-5-yl)cyclohexanecarboxylate (Compound 4)(Step A) Synthesis of 2-[4-cyano-4-(8-methoxy-1,4-benzodioxan-5-yl)cyclohexylidene]-1,3-dithiane (Compound 3a)
-
To a solution of 5.0 ml (26 mmol) of 2-trimethylsilyl-1,3-dithiane in 50 ml of THF was added dropwise 17 ml (26 mmol) of a 1.54 mol/liter solution of n-butyl lithium in hexane under ice-cooling. After 10 minutes, the mixture was cooled to -78°C, and a solution of 3.6 g (13 mmol) of Compound 1 obtained in Example 1 in 40 ml of THF was dropwise added thereto. After 10 minutes, to the mixture was added brine, followed by addition of water at room temperature. The mixture was extracted with ethyl acetate, the extract was dried over sodium sulfate, and the solvent was evaporated. The residue was purified by silica gel column chromatography (eluted with hexane/ethyl acetate = 4/1) to give 3.9 g (79%) of Compound 3a as a white solid.
Melting Point: 164 – 166 °C
1H-NMR (CDCl3, δ, ppm) 1.70-1.92 (m, 2H), 2.05-2.24 (m, 2H), 2.28-2.53 (m, 4H), 2.89 (t, J = 6 Hz, 4H), 3.18-3.38 (m, 2H), 3.87 (s, 3H), 4.36 (s, 4H), 6.47 (d, J = 9 Hz, 1H), 6.79 (d, J = 9 Hz, 1H).
MASS (m/z) 389 (M+).
-
In 120 ml of methanol was suspended 3.9 g (10 mmol) of Compound 3a obtained in Step A, 1.7 ml (20 mmol) of 70% perchloric acid, and 4.3 g (16 mmol) of mercury chloride (HgCl2) were added thereto, and the mixture was stirred for 4 hours. The mixture was diluted with methylene chloride and was filtered through Celite, the filtrate was poured into a saturated aqueous solution of sodium bicarbonate, and the mixture was extracted with methylene chloride. The organic layer was washed with brine and dried over sodium sulfate, and the solvent was evaporated. The residue was purified by silica gel column chromatography (eluted with hexane/ethyl acetate = 1/1) to give the crude Compound 3 as a white solid and also to give 0.18 g (5.5%) of Compound 4 as a colorless transparent oily substance. Compound 3 was further recrystallized from ethyl acetate to give 0.57 g (17%) of white crystals.
Compound 3
Melting Point: 123 – 124 °C
1H-NMR (CDCl3, δ, ppm) 1.75-2.22 (m, 6H), 2.27-2.51 (m, 3H), 3.71 (s, 3H), 3.88 (s, 3H), 4.36 (s, 4H), 6.48 (d, J = 9 Hz, 1H), 6.84 (d, J = 9 Hz, 1H).
MASS (m/z) 331 (M+).
Compound 4
1H-NMR (CDCl3, δ, ppm) 1.92-2.38 (m, 8H), 2.70-2.88 (m, 1H), 3.69 (s, 3H), 3.87 (s, 3H), 4.36 (s, 4H), 6.48 (d, J = 9 Hz, 1H), 6.81 (d, J = 9 Hz, 1H).
MASS (m/z) 331 (M+).
- (Step B) Synthesis of Compound 3 and Compound 4
Example 5.
cis-4-Cyano-4-(8-methoxy-1,4-benzodioxan-5-yl)cyclohexanecarboxylic acid (Compound 5)
-
To a mixture of 0.55 g (1.7 mmol) of Compound 3 obtained in Example 4 and 3.3 ml of methanol was added 3.3 ml of THF to dissolve them. To the mixture was dropwise added 2.6 ml of a 1.3 mol/liter aqueous solution of potassium hydroxide, followed by stirring at room temperature for 1 hour. The mixture was poured into water, ethyl acetate was added thereto, and an aqueous layer was extracted. The aqueous layer was acidified with a 1 mol/liter aqueous hydrochloric acid, and the precipitated solid was collected by filtration and re-slurried with ethanol to give 0.45 g (86%) of Compound 5 as a white solid.
Melting Point: 228 – 230 °C
1H-NMR (DMSO-d6 , δ, ppm) 1.59-1.90 (m, 4H), 1.94-2.10 (m, 2H), 2.20-2.45 (m, 3H), 3.75 (s, 3H), 4.27 (dd, J = 5, 12 Hz, 4H), 6.60 (d, J = 9 Hz, 1H), 6.79 (d, J = 9 Hz, 1H), 12.2 (br s, 1H).
MASS (m/z) 317 (M+).Elemental analysis: C17H19NO5 Found (%) C 64.09, H : 6.01, N : 4.51 Calcd. (%) C 64.34, H : 6.03, N : 4.41
-
Teixeira, M. M.; Gristwood, R. W.; Cooper, N.; Hellewell, P. G. Trends Pharmacol. Sci.1997, 18, 164– 170, [PubMed],
-
Dyke, H. J.; Montana, J. G. Exp. Opin. Investig. Drugs 2002, 11, 1– 13Lipworth, B. J. Lancet 2005, 365 ( 9454) 167– 175Kroegel, C.; Foerster, M. Exp. Opin. Investig. Drugs 2007, 16, 109– 124
-
Yanagawa, K. The 26th Medicinal Chemistry Symposium, 2007, 2P-29.Ohshima, E.;Yanagawa, K.; Manabe, H.; Miki, I.; Masuda, Y. PCT Int. Appl. WO0164666 A1, 2001.
-
Christensen, S. B.; Guider, A.; Forster, C. J.; Gleason, J. G.; Bender, P. E.; Karpinski, J. M.; DeWolf, W. E., Jr.; Barnette, M. S.; Underwood, D. C.; Griswold, D. E.; Cieslinski, L. B.; Burman, M.; Bochnowicz, S.; Osborn, R. R.; Manning, C. D.; Grous, M.; Hillegas, L. M.; O’Leary-Bartus, J.; Ryan, M. D.; Eggleston, D. S.; Haltiwanger, R. C.; Torphy, T. J. J. Med. Chem. 1998, 41, 821– 835
-
Caron, S.; Vazquez, E.; Wojcik, J. M. J. Am. Chem. Soc. 2000, 122, 712– 713Culkin, D. A.; Hartwig, J. F. Acc. Chem. Res. 2003, 36, 234– 245You, J.; Verkade, J. G. Angew. Chem., Int. Ed. 2003, 42, 5051–5053
-
Muratake, H.; Natsume, M. Tetrahedron 1990, 46, 6331– 6342Caron, S.; Vazquez, E. Org. Process Res. Dev. 2001, 5, 587– 592
-
North, M. In Comprehensive Organic Functional Group Transformations; Katritzky, A. R.;Meth-Cohn, O.; Rees, C. W., Eds.; Pergamon: Oxford, 1995; Vol. 3, p 614.
-
Lemaire, M.; Doussot, J.; Guy, A. Chem. Lett. 1988, 1581– 1584Guy, A.; Doussot, J.; Guette, J.-P.; Garreau, R.; Lemaire, M. Synlett 1992, 821– 822Kurti, L.; Czako, B.; Corey, E. J. Org. Lett. 2008, 10, 5247– 5250
-
Yanagisawa, A.; Nezu, T.; Mohri, S. Org. Lett. 2009, 11, 5286– 5289
-
Brown, H. C.; Cole, T. E. Organometallics 1983, 2, 1316– 1319
-
Kuivila, H. G.; Nahabedian, K. V. J. Am. Chem. Soc. 1961, 83, 2159– 2163Kuivila, H. G.; Nahabedian, K. V. J. Am. Chem. Soc. 1961, 83, 2164– 2166Nahabedian, K. V.; Kuivila, H. G. J. Am. Chem. Soc. 1961, 83, 2167–2174
-
Stang, P. J.; Fisk, T. E. Synthesis 1979, 438– 440Stang, P. J.; Treptow,W. Synthesis 1980, 283– 284Saulnier, M. G.; Kadow, J. F.; Tun, M. M.; Langley, D. R.; Vyas, D. M. J. Am. Chem. Soc. 1989, 111, 8320– 8321
-
Kato, S.; Chujo, I.; Suzuki, K. PCT Int. Appl. WO04000795 A1, 2004.
-
Miyaura, N.; Suzuki, A. Chem. Rev. 1995, 95, 2457– 2483O’Keefe,D. F.; Dannock, M. C.; Marcuccio, S. M. Tetrahedron Lett. 1992, 33, 6679– 6680Segelstein, B. E.; Bulter, T. W.; Chenard, B. L. J. Org. Chem. 1995, 60, 12– 13Kong, K.-C.; Cheng, C.-H. J. Am. Chem. Soc. 1991, 113, 6313– 6315
-
Brands, K. M. J.; Davies, A. J. Chem. Rev. 2006, 106, 2711– 2733
-
Baker, W.; Jukes, E. H. T.; Subrahmanyam, C. A. J. Chem. Soc. 1934, 1681–1684Dallacker, F.; Van Wersh, J. Chem. Ber. 1972, 105, 3301–3305
- Yanagisawa, Arata; Organic Process Research & Development 2010, 14(5), P1182-1187
- Yanagisawa, Arata; Organic Letters 2009, 11(22), P5286-5289
- US 20010056117
- WO 2002059105
- WO 2000014085
| WO1998022455A1 * | Nov 19, 1997 | May 28, 1998 | Michio Ichimura | Oxygenic heterocyclic compounds |
| JP10147585A * | Title not available |
| WO2001064666A1 * | Mar 2, 2001 | Sep 7, 2001 | Kyowa Hakko Kogyo Kk | Oxygen-containing heterocyclic compounds |
| WO2002059105A1 * | Jan 25, 2002 | Aug 1, 2002 | Kyowa Hakko Kogyo Kk | Styrene derivatives and process for production thereof |
| WO2006041120A1 * | Oct 13, 2005 | Apr 20, 2006 | Daisuke Harada | Pharmaceutical composition |
| WO2006041121A1 * | Oct 13, 2005 | Apr 20, 2006 | Daisuke Harada | Remedies/preventives for chronic skin disease |
| WO2006123726A1 * | May 18, 2006 | Nov 23, 2006 | Daisuke Harada | Pharmaceutical composition |
| WO2011134468A1 | Apr 28, 2011 | Nov 3, 2011 | Leo Pharma A/S | Biaryl phosphodiesterase inhibitors |
| EP1362853A1 * | Jan 25, 2002 | Nov 19, 2003 | Kyowa Hakko Kogyo Co., Ltd | Styrene derivatives and process for production thereof |
FDA Accepts Filing of NDA for IV Antibiotic Oritavancin with Priority Review

Oritavancin
(4R)-22-O-(3-Amino-2,3,6-trideoxy-3-C-methyl-alpha-L-arabinohexopyranosyl)-N3-(p-(p-chlorophenyl)benzyl)vancomycin
(3S, 6R, 7R, 22R, 23S, 26S, 36R, 38aR) -22 – (3-Amino-2 ,3,6-trideoxy-3-C-methyl-alpha-L-mannopyranosyloxy) -3 – (carbamoylmethyl ) -10,19-dichloro-44-[2-O-[3 – (4′-chlorobiphenyl-4-ylmethylamino) -2,3,6-trideoxy-3-C-methyl-alpha-L-mannopyranosyl] – beta-D-glucopyranosyloxy] –
| CAS No. | 171099-57-3 |
| CBNumber: | CB92451283 |
| Molecular Formula: | C86H97Cl3N10O26 |
| Formula Weight: | 1793.12 |
Also known as NDISACC-(4-(4-chlorophenyl)benzyl)A82846B and LY333328,N-(4-(4-chlorophenyl)benzyl)A82846B
Abbott (Supplier), Lilly (Originator), InterMune (Licensee)
The medicines company—
-
the Oritavancin Program Results.pdf
 phx.corporate-ir.net/External.File?item…t=1
phx.corporate-ir.net/External.File?item…t=1Jul 2, 2013 – Inhibits two key steps of cell wall synthesis: – Transglycosylation. – Transpeptidation. • Disrupts bacterial membrane integrity. Differentiated from …

FDA Accepts Filing of NDA for IV Antibiotic Oritavancin with Priority Review
PARSIPPANY, NJ — (Marketwired) — 02/19/14 — The Medicines Company (NASDAQ: MDCO) today announced that the U.S. Food and Drug Administration (FDA) has accepted the filing of a new drug application (NDA) for oritavancin, an investigational intravenous antibiotic, with priority review. The Medicines Company is seeking approval of oritavancin for the treatment of acute bacterial skin and skin structure infections (ABSSSI) caused by susceptible gram-positive bacteria, including methicillin-resistant Staphylococcus aureus (MRSA), administered as a single dose.
In December 2013, the FDA designated oritavancin as a Qualified Infectious Disease Product (QIDP). The QIDP designation provides oritavancin priority review, and an additional five years of exclusivity upon approval of the product for the treatment of ABSSSI. Priority review means the FDA’s goal is to take action on the application within six months, compared to 10 months under standard review. The FDA action date (PDUFA date) for oritavancin is August 6, 2014.
Oritavancin (INN, also known as LY333328) is a novel semi-synthetic glycopeptide antibiotic being developed for the treatment of serious Gram-positive infections. Originally discovered and developed by Eli Lilly, oritavancin was acquired by InterMune in 2001 and then by Targanta Therapeuticsin late 2005.[1]
In Dec 2008 the FDA declined to approve it, and an EU application was withdrawn.
In 2009 the development rights were acquired by The Medicine Co. who are running clinical trials for a possible new FDA application in 2013.[2]
Its structure is similar to vancomycin[3] It is a lipoglycopeptide

About Oritavancin
Oritavancin is an investigational intravenous antibiotic for which The Medicines Company is seeking approval in the treatment of ABSSSI caused by susceptible gram-positive bacteria, including MRSA. In clinical trials, the most frequently reported adverse events associated with oritavancin were nausea, headache, vomiting and diarrhea. Hypersensitivity reactions have been reported with the use of antibacterial agents including oritavancin.
Oritavancin shares certain properties with other members of the glycopeptide class of antibiotics, which includes vancomycin, the current standard of care for serious Gram-positive infections in the United States and Europe.[4] Data presented at the 47th Annual Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC) in September 2007 demonstrated that oritavancin possesses potent and rapid bactericidal activity in vitro against a broad spectrum of both resistant and susceptible Gram positive bacteria, including Staphylococcus aureus, methicillin-resistant Staphylococcus aureus, Enterococci, and Streptococci.[5] Two posters presented at the meeting also demonstrated that oritavancin was more active than either metronidazole or vancomycin against strains of Clostridium difficile tested.[6]
Anthrax : Research presented at the American Society for Microbiology (ASM) 107th Annual General Meeting in May 2007, suggested oritavancin’s potential utility as a therapy for exposure to Bacillus anthracis, the gram-positive bacterium that causes anthrax, having demonstrated efficacy in a mouse model both pre- and post-exposure to the bacterium[7]
 oritavancin
oritavancin
The 4′-chlorobiphenylmethyl group disrupts the cell membrane of gram positive bacteria.[8] It also acts by inhibition of transglycosylation and inhibition of transpeptidation.[9]
Results have been presented (in 2003) but possibly not yet published from two pivotal Phase 3 clinical trials testing the efficacy of daily intravenous oritavancin for the treatment of complicated skin and skin-structure infections (cSSSI) caused by Gram-positive bacteria. The primary endpoints of both studies were successfully met, with oritavancin achieving efficacy with fewer days of therapy than the comparator agents (vancomycin followed by cephalexin). In addition, oritavancin showed a significantly improved safety profile with a 19.2 percent relative reduction in the overall incidence of adverse events versus vancomycin/cephalexin (p<0.001) in the second and larger pivotal trial.[10]
A Phase 2 clinical study was planned to run until May 2008 entitled “Single or Infrequent Doses for the Treatment of Complicated Skin and Skin Structure Infections (SIMPLIFI),” evaluating the efficacy and safety of either a single dose of oritavancin or an infrequent dose of oritavancin compared to the previously studied dosing regimen of 200 mg oritavancin given once daily for 3 to 7 days.[11] Results published May 2011.[12]
Regulatory submissions
USA
On February 11, 2008, Targanta submitted a New Drug Application (NDA) to the US FDA seeking approval of oritavancin;[13] in April 2008, the FDA accepted the NDA submission for standard review.[14] On 9 Dec 2008 the FDA said insufficient data for approval of oritavancin had been provided and they requested a further phase 3 clinical study to include more patients with MRSA.[15]
Europe
June 2008, Targanta’s Marketing Authorization Application (MAA) for oritavancin was submitted and accepted for review by the European Medicines Agency (EMEA),[16] but the company later withdrew the application in Aug 2009.[17]
About The Medicines Company
The Medicines Company’s purpose is to save lives, alleviate suffering, and contribute to the economics of healthcare by focusing on 3,000 leading acute/intensive care hospitals worldwide. Its vision is to be a leading provider of solutions in three areas: acute cardiovascular care, surgery and perioperative care, and serious infectious disease care. The company operates in the Americas, Europe and the Middle East, and Asia Pacific regions with global centers today in Parsippany, NJ, USA and Zurich, Switzerland.
“We look forward to working with the FDA during the review process, and sharing the knowledge we have gained in our studies of oritavancin,” said Matthew Wikler, MD, Vice President and Medical Director, Infectious Disease Care for The Medicines Company. “We believe that upon approval, oritavancin, administered as a single dose for the treatment of ABSSSI, will offer new options for both physicians and their patients for the treatment of these infections.”
The oritavancin NDA is based on data from two Phase 3 clinical trials, SOLO I and SOLO II, which were conducted under a Special Protocol Assessment (SPA) agreement with the FDA. These Phase 3 trials evaluated the efficacy and safety of a single 1200mg dose of oritavancin compared to 7 to 10 days of twice-daily vancomycin in adults with ABSSSI, including infections caused by MRSA. The combined SOLO studies were conducted in 1,959 patients (modified intent-to -treat population, or mITT), with 405 of the patients suffering from an ABSSSI with a documented MRSA infection.
 oritavancin
oritavancin
Drug substance
Oritavancin diphosphate
CLINICAL TRIALS..http://clinicaltrials.gov/search/intervention=oritavancin
- LY 333328 diphosphate
- LY333328 diphosphate
- Oritavancin diphosphate
- UNII-VL1P93MKZN
- 192564-14-0 CAS NO
INTRODUCTION
Oritavancin
Oritavancin inhibits cell wall synthesis by complexing with the terminal D-Ala-D-Ala of a nascent peptidoglycan chain and also to the pentaglycine bridge, thus inhibiting transglyco- sylation and transpeptidation. Unlike other glycopeptides, oritavancin is able to bind to depsipeptides including D-Ala-D-Lac, which fa- cilitates its inhibition of cell wall synthesis even in organisms exhibiting VanA-type resistance. Oritavancin forms homodimers prior to binding to D-Ala-D-Ala or D-Ala-D-Lac, which increases its binding affinity for the target site.The p-chloro-phenylbenzyl side chain of oritavancin interacts with the cell membrane, exerting two beneficial effects. This binding acts to main- tain the antibacterial in a prime position for peptidoglycan interactions and it also imparts oritavancin with the ability to disrupt the bac- terial membrane potential and thus increase membrane permeability.[22,23] Oritavancin has been shown to dissipate membrane potential in both stationary and exponential phase growing bacteria, which is rare and may carry clinical implications in terms of its activity against slowly growing organisms and biofilms. The dual mechanism of action could also theoretically increase effectiveness and reduce the risk of resist- ance selection. In addition to the aforemen- tioned mechanisms, it has also been hypothesized that oritavancin inhibits RNA synthesis.


vancomycin, desmethylvancomycin, eremomycin, teicoplanin (complex of five compounds), dalbavancin, oritavancin, telavancin, and A82846B (LY264826) having structures A, B, C, D, E, F, G and H:
R = B-2-Acetylamido-glucopyraπosyl- Attorney Docket No 33746-704 602
Dalbavancin, oritavancin and telavancin are semisynthetic lipoglycopeptides that demonstrate promise for the treatment of patients with infections caused by multi-drug-resistant Gram-positive pathogens. Each of these agents contains a heptapeptide core, common to all glycopeptides, which enables them to inhibit transglycosylation and transpeptidation (cell wall synthesis). Modifications to the heptapeptide core result in different in vitro activities for the three semisynthetic lipoglycopeptides. All three lipoglycopeptides contain lipophilic side chains, which prolong their half-life, help to anchor the agents to the cell membrane and increase their activity against Gram-positive cocci. In addition to inhibiting cell wall synthesis, telavancin and oritavancin are also able to disrupt bacterial membrane integrity and increase membrane permeability; oritavancin also inhibits RNA synthesis. Enterococci exhibiting the VanA phenotype (resistance to both vancomycin and teicoplanin) are resistant to both dalbavancin and telavancin, whileoritavancin retains activity. Dalbavancin, oritavancin and telavancin exhibit activity against VanB vancomycin-resistant enterococci.
All three lipoglycopeptides demonstrate potent in vitro activity against Staphylococcus aureus and Staphylococcus epidermidis regardless of their susceptibility to meticillin, as well as Streptococcus spp. Both dalbavancin and telavancin are active against vancomycin-intermediate S. aureus (VISA), but display poor activity versus vancomycin-resistant S. aureus (VRSA). Oritavancin is active against both VISA and VRSA. Telavancin displays greater activity against Clostridium spp. than dalbavancin, oritavancin or vancomycin. The half-life of dalbavancin ranges from 147 to 258 hours, which allows for once-weekly dosing, the half-life of oritavancin of 393 hours may allow for one dose per treatment course, while telavancin requires daily administration. Dalbavancin and telavancin exhibit concentration-dependent activity and AUC/MIC (area under the concentration-time curve to minimum inhibitory concentration ratio) is the pharmacodynamic parameter that best describes their activities.
Oritavancin’s activity is also considered concentration-dependent in vitro, while in vivo its activity has been described by both concentration and time-dependent models; however, AUC/MIC is the pharmacodynamic parameter that best describes its activity. Clinical trials involving patients with complicated skin and skin structure infections (cSSSIs) have demonstrated that all three agents are as efficacious as comparators. The most common adverse effects reported with dalbavancin use included nausea, diarrhoea and constipation, while injection site reactions, fever and diarrhoea were commonly observed withoritavancin therapy. Patients administered telavancin frequently reported nausea, taste disturbance and insomnia. To date, no drug-drug interactions have been identified for dalbavancin, oritavancin or telavancin. All three of these agents are promising alternatives for the treatment of cSSSIs in cases where more economical options such as vancomycin have been ineffective, in cases of reduced vancomycin susceptibility or resistance, or where vancomycin use has been associated with adverse events.
Oritavancin diphosphate (oritavancin) is a semi-synthetic lipoglycopeptide derivative of a naturally occurring glycopeptide. Its structure confers potent antibacterial activity against gram-positive bacteria, including vancomycin-resistant enterococci (VRE), methicillin- and vancomycin-resistant staphylococci, and penicillin-resistant streptococci. The rapidity of its bactericidal activity against exponentially-growing S. aureus (≧3-log reduction within 15 minutes to 2 hours against MSSA, MRSA, and VRSA) is one of the features that distinguishes it from the prototypic glycopeptide vancomycin (McKay et al., J Antimicrob Chemother. 63(6):1191-9 (2009), Epub 2009 Apr. 15).
Oritavancin inhibits the synthesis of peptidoglycan, the major structural component of the bacterial cell wall by a mechanism that is shared with glycopeptides, such as vancomycin (Allen et al., Antimicrob Agents Chemother 41(1):66-71 (1997); Cegelski et al., J Mol Biol 357:1253-1262 (2006); Arhin et al., Poster C1-1471: Mechanisms of action of oritavancin in Staphylococcus aureus [poster]. 47th Intersci Conf Antimicro Agents Chemo, Sep. 17-20, 2007; Chicago, Ill.). Oritavancin, like vancomycin, binds to the Acyl-D-Alanyl-D-Alanine terminus of the peptidoglycan precursor, lipid-bound N-acetyl-glucosamine-N-acetyl-muramic acid-pentapeptide (Reynolds, Eur J Clin Microbiol Infect Dis 8(11):943-950 (1989); Nicas and Allen, Resistance and mechanism of action.
In: Nagarajan R, editor. Glycopeptide antibiotics. New York: Marcel Dekker 195-215 (1994); Allen et al., Antimicrob Agents Chemother 40(10):2356-2362 (1996); Allen and Nicas, FEMS Microbiology Reviews 26:511-532 (2003); Kim et al., Biochemistry 45:5235-5250 (2006)). However, oritavancin inhibits cell wall biosynthesis even when the substrate is the altered peptidoglycan precursor that is present in VRE and vancomycin-resistant S. aureus (VRSA). Thus, the spectrum of oritavancin antibacterial activity extends beyond that of vancomycin to include glycopeptide-resistant enterococci and staphylococci (Ward et al., Expert Opin Investig Drugs 15:417-429 (2006); Scheinfeld, J Drugs Dermatol 6:97-103 (2007)). Oritavancin may inhibit resistant bacteria by interacting directly with bacterial proteins in the transglycosylation step of cell wall biosynthesis (Goldman and Gange, Curr Med Chem 7(8):801-820 (2000); Halliday et al., Biochem Pharmacol 71(7):957-967 (2006); Wang et al., Poster C1-1474: Probing the mechanism of inhibition of bacterial peptidoglycan glycotransferases by glycopeptide analogs. 47th Intersci Conf Antimicro Agents Chemo, Sep. 17-20, 2007). Oritavancin also collapses transmembrane potential in gram positive bacteria, leading to rapid killing (McKay et al., Poster C1-682: Oritavancin disrupts transmembrane potential and membrane integrity concomitantly with cell killing in Staphylococcus aureus and vancomycin-resistant Enterococci. 46th Intersci Conf Antimicro Agents Chemo, San Francisco, Calif., Sep. 27-30, 2006). These multiple effects contribute to the rapid bactericidal activity of oritavancin.
Vancomycin (U.S. Patent 3,067,099); A82846A, A82846B, and A82846C (U.S. Patent 5,312,738, European Patent Publication 256,071 A1); PA-42867 factors A, C, and D (U.S. Patent4,946,941 and European Patent Publication 231,111 A2); A83850 (U.S. Patent No. 5,187,082); avoparcm (U.S. Patent 3,338,786 and U.S. Patent 4,322,343); actmoidin, also known as K288 (J. Antibiotics Series A 14:141 (1961); helevecardin (Chem. Abstracts 110:17188 (1989) and Japanese Patent Application 86/157,397); galacardin (Chem. Abstracts 110:17188 (1989) and Japanese Patent Application 89/221,320); and M47767 (European Patent Publication 339,982).
Oritavancin is in clinical development against serious gram-positive infections, where administration of the drug is via intravenous infusion using several dosages administered over a series of days. The development of alternative dosing regimens for the drug could expand treatment options available to physicians. The present invention is directed to novel dosing regimens.
Means for the preparation of the glycopeptide antibiotics, including oritavancin and analogs thereof, may be found, for example, in U.S. Pat. No. 5,840,684,
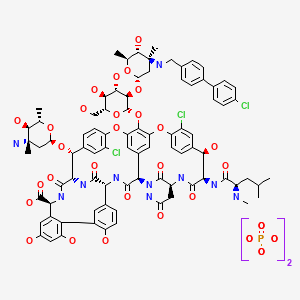
 SYNTHESIS
SYNTHESIS

LY-333328 was synthesized by reductocondensation of the glycopeptide antibiotic A82846B (I) with 4′-chlorobiphenyl-4-carboxaldehyde (II) by means of sodium cyanoborohydride in refluxing methanol.
J Antibiot1996, 49, (6) :575-81
(3S,6R,7R,22R,23S,26S,36R,38aR)-3-(Carbamoylmethyl)-10,19-dichloro-7,28,30,32-tetrahydroxy-6-(N-methyl-D-leucylamido)-2,5,24,38,39-pentaoxo-22-(L-vancosaminyloxy)-44-[2-O-(L-vancosaminyl)-beta-D-glucopyranosyloxy]-2,3,4,5,6,7,23,24,25,26,36,37,38,38a-tetradecahydro-1H,22H-8,11:18,21-dietheno-23,36-(iminomethano)-13,16:31,36-dimetheno-[1,6,9]oxadiazacyclohexadecino[4,5-m][10,2,16]benzoxadiazacyclotetracosine-26-carboxylic acid; A82846B (I)
4′-chloro[1,1′-biphenyl]-4-carbaldehyde (II)
LY-333328 was synthesized by reductocondensation of the glycopeptide antibiotic A82846B (I) with 4′-chlorobiphenyl-4-carboxaldehyde (II) by means of sodium cyanoborohydride in refluxing methanol.
…………………..
EXAMPLE 4
Preparation of Compound 229
A three liter 3-necked flask was fitted with a
condenser, nitrogen inlet and overhead mechanical stirring apparatus. The flask was charged with pulverized A82846B acetate salt (20.0 g, 1.21 × 10-3 mol) and methanol (1000 mL) under a nitrogen atmosphere. 4′-chlorobiphenylcarboxaldehyde (2.88 g, 1.33 × 10-2 mol, 1.1 eq.) was added to this stirred mixture, followed by methanol (500 mL). Finally, sodium cyanoborohydride (0.84 g, 1.33 × 10-2 mol, 1.1 eq.) was added followed by methanol (500 mL). The resulting mixture was heated to reflux (about 65°C).
After 1 hour at reflux, the reaction mixture attained homogeneity. After 25 hours ac reflux, the heat source was removed and the clear reaction mixture was measured with a pH meter (6.97 at 58.0°C). 1 N NaOH (22.8 mL) was added
dropwise to adjust the pH to 9.0 (at 54.7°C). The flask was equipped with a distillation head and the mixture was concentrated under partial vacuum to a weight of 322.3 grams while maintaining the pot temperature between 40-45°C.
The distillation head was replaced with an addition funnel containing 500 mL of isopropanol (IPA). The IPA was added dropwise to the room temperature solution over 1 hour. After approximately 1/3 of the IPA was added, a granular precipitate formed. The remaining IPA was added at a faster rate after precipitation had commenced. The flask was weighed and found to hold 714.4 grams of the IPA/methanol slurry.
The flask was re-equipped with a still-head and
distilled under partial vacuum to remove the remaining methanol. The resulting slurry (377.8 g) was allowed to chill in the freezer overnight. The crude product was filtered through a polypropylene pad and rinsed twice with 25 mL of cold IPA. After pulling dry on the funnel for 5 minutes, the material was placed in the vacuum oven to dry at 40°C. A light pink solid (22.87 g (theory = 22.43 g) ) was recovered. HPLC analysis versus a standard indicated 68.0% weight percent of Compound 229 (4- [4-chlorophenyl] benzyl-A82846B] in the crude solid, which translated into a
corrected crude yield of 69.3%.
The products of the reaction were analyzed by reverse-phase HPLC utilizing a Zorbax SB-C18 column with ultraviolet light (UV; 230 nm) detection. A 20 minute gradient solvent system consisting of 95% aqueous buffer/5% CH3CN at time=0 minutes to 40% aqueous buffer/60% CH3CN at time=20 minutes was used, where the aqueous buffer was TEAP (5 ml CH3CN, 3 ml phosphoric acid in 1000 ml water).
………………….
Oritavancin (also termed N-(4-(4-chlorophenyl)benzyl)A82846B and LY333328) has the following Formula III:

References
- Targanta Revives Oritavancin: Next Weapon Against cSSSI? BioWorld Today, November 26, 2007
- “Biotechs pick up slack in antibiotics development”. 17 May 2011.
- http://www.farm.ucl.ac.be/Full-texts-FARM/Domenech-2009-1.pdf “Interactions of oritavancin, a new lipoglycopeptide derived from vancomycin, with phospholipid bilayers: Effect on membrane permeability and nanoscale lipid membrane organization” 2009
- Scheinfeld, N (2007). “A comparison of available and investigational antibiotics for complicated skin infections and treatment-resistant Staphylococcus aureus and enterococcus“.J Drugs Dermatol. 6 (4): 97–103. PMID 17373167.
- 2007 ICAAC Posters: E-1612 “In Vitro Activity Profile of Oritavancin against a Broad Spectrum of Aerobic and Anaerobic Bacterial Pathogens”/E -1613 “In Vitro Activity Profile of Oritavancin (ORI) Against Organisms Demonstrating Key Resistance Profiles to Other Antimicrobial Agents”/E-1614 “In vitro Time Kill Studies of Oritavancin against Drug-resistant Isolates ofStaphylococcus aureus and Enterococci”/E-1615 “Anti-Enterococcal Activity Profile of Oritavancin, a Potent Lipoglycopeptide under Development for Use Against Gram-Positive Infections”/E-1616 “Anti-Streptococcal Activity Profile of Oritavancin, a Potent Lipoglycopeptide under Development for Use Against Gram-Positive Infections”/E-1617 “In Vitro Activity Profile of Oritavancin (ORI) Against Resistant Staphylococcal Populations From a Recent Surveillance Initiative”/E-1620 “Pharmacokinetic Concentrations of Oritavancin Kill Stationary-Phase and Biofilm Staphylococcus aureus In Vitro.” / Targanta Press Release September 19, 2007
- ICAAC 2007 Posters: “In Vitro Susceptibility of Genotypically Distinct Clostridium difficileStrains to Oritavancin” and “Activity of Metronidazole, Vancomycin and Oritavancin Against Epidemic Clostridium difficile Spores” / Targanta Press Release September 19, 2007
- ASM 2007 Poster: “Efficacy of Oritavancin in a Murine Model of Bacillus anthracis Spore Inhalation Anthrax” / Targanta Press Release May 24, 2007
- Belley; McKay, GA; Arhin, FF; Sarmiento, I; Beaulieu, S; Fadhil, I; Parr Jr, TR; Moeck, G (2010).“Oritavancin Disrupts Membrane Integrity of Staphylococcus aureus and Vancomycin-Resistant Enterococci To Effect Rapid Bacterial Killing”. Antimicrobial agents and chemotherapy 54(12): 5369–71. doi:10.1128/AAC.00760-10. PMC 2981232. PMID 20876372.
- Zhanel et al. (2012). “Oritavancin: Mechanism of Action”. Clin Infect Dis.doi:10.1093/cid/cir920.
- ICAAC 2003 Late-breaker poster: “Phase III Trial Comparing 3-7 days of Oritavancin vs. 10-14 days of Vancomycin/Cephalexin in the Treatment of Patients with Complicated Skin and Skin Structure Infections (cSSSI)” / InterMune Press Release September 15, 2003
- ClinicalTrials.gov NCT00514527
- Comparison of the Efficacy and Safety of Oritavancin Front-Loaded Dosing Regimens to Daily Dosing: An Analysis of the SIMPLIFI Trial. May 2011. doi:10.1128/AAC.00029-11.
- “Drugs.com, Targanta Submits Oritavancin New Drug Application”. Retrieved 2008-02-12.
- “FDA News, Targanta to Get FDA Decision by December”. Retrieved 2008-04-10.
- http://www.fiercebiotech.com/press-releases/fda-issues-complete-response-letter-oritavancin Dec 2008.
- “Pharmaceutical Business Review, EMEA accepts Targanta’s oritavancin MAA for review”. Retrieved 2008-06-26.
- http://www.nelm.nhs.uk/en/NeLM-Area/News/2009—August/24/European-application-for-investigational-antibiotic-oritavancin-withdrawn-/
- http://onlinelibrary.wiley.com/doi/10.1111/j.1574-6976.2003.tb00628.x/pdf

- http://www.pjps.pk/wp-content/uploads/pdfs/26/5/Paper-30.pdf

- Antimicrobial Agents and Chemotherapy, 2003 , vol. 47, 5 p. 1700 – 1706
- Antimicrobial Agents and Chemotherapy, 1999 , vol. 43, 1 p. 115 – 120
- Antimicrobial Agents and Chemotherapy, 1997 , vol. 41, 10 p. 2165 – 2172
- Tetrahedron, 2004 , vol. 60, 47 p. 10611 – 10618………… NMRhttp://www.sciencedirect.com/science/article/pii/S0040402004015108
 Cooper, R.D.G.; Snyder, N.J.; Zweifel, M.J.; et al.; Reductive alkylation of glycopeptide antibiotics: Synthesis and antibacterial activity. J Antibiot 1996, 49, 6, 575-81.
Cooper, R.D.G.; Snyder, N.J.; Zweifel, M.J.; et al.; Reductive alkylation of glycopeptide antibiotics: Synthesis and antibacterial activity. J Antibiot 1996, 49, 6, 575-81.
Cooper, R.D.G.; Huff, B.E.; Nicas, T.I.; Quatroche, J.T.; Rodriguez, M.J.; Snyder, N.J.; Staszak, M.A.; Thompson, R.C.; Wilkie, S.C.; Zweifel, M.J. (Eli Lilly and Company); Glycopeptide antibiotic derivs. EP 0667353; EP 1016670; EP 1031576 .

| EP0435503A1 * | Dec 11, 1990 | Jul 3, 1991 | Eli Lilly And Company | Improvements in or relating to gylcopeptide derivatives |
| US4639433 * | Aug 14, 1985 | Jan 27, 1987 | Eli Lilly And Company | Glycopeptide derivatives |
| US4698327 * | Apr 18, 1986 | Oct 6, 1987 | Eli Lilly And Company | Novel glycopeptide derivatives |
| US20040106590 * | Aug 29, 2003 | Jun 3, 2004 | Barry Eisenstein | Methods and reagents for treating infections of clostridium difficile and diseases associated therewith |
| US20050197333 | Dec 22, 2004 | Sep 8, 2005 | Van Duzer John H. | Rifamycin analogs and uses thereof |
| US20070014849 | Sep 20, 2006 | Jan 18, 2007 | Daniela Jabes | Use of ramoplanin to treat diseases associated with the use of antibiotics |
| US20030176327 * | Oct 18, 2002 | Sep 18, 2003 | Cassell Gail Houston | Antibiotics for treating biohazardous bacterial agents |
| US20040147441 | Aug 25, 2003 | Jul 29, 2004 | Leach Timothy S. | Methods and reagents for preventing bacteremias |
| WO1999010006A1 | Aug 18, 1998 | Mar 4, 1999 | Lilly Co Eli | Therapy for staphylococcus aureus |
| WO2000066144A2 | Apr 19, 2000 | Nov 9, 2000 | Lilly Co Eli | Monthly doses of glycopeptide antibiotics for treatment of streptococcus pneumoniae infections |
| WO2008097364A2 | Sep 24, 2007 | Aug 14, 2008 | Targanta Therapeutics Corp | Use of oritavancin for prevention and treatment of anthrax |
| WO1998052592A1 * | May 5, 1998 | Nov 26, 1998 | Lilly Co Eli | Urea and thiourea derivatives of glycopeptides |
| WO2002036612A1 * | Nov 2, 2001 | May 10, 2002 | Univ Cambridge Tech | Antibacterial agents comprising conjugates of glycopeptides and peptidic membrane-associating elements |
| WO2007138999A1 | May 25, 2007 | Dec 6, 2007 | Shionogi & Co | Glycopeptide antibiotic derivative |
| WO2009081958A1 | Dec 25, 2008 | Jul 2, 2009 | Shionogi & Co | Glycosylated glycopeptide antibiotic derivative |
| EP2314599A1 | Nov 24, 2005 | Apr 27, 2011 | National University Corporation Nagoya University | Glycopeptide antibiotic monomer derivatives |
| US5919756 * | May 1, 1997 | Jul 6, 1999 | Eli Lilly And Company | Amides |
| US5919771 * | Apr 30, 1998 | Jul 6, 1999 | Eli Lilly And Company | Urea and thiourea derivatives of glycopeptides |
| US7078380 | Nov 2, 2001 | Jul 18, 2006 | Cambridge University Technical Services Limited | Antibacterial agents comprising conjugates of glycopeptides and peptidic membrane associating elements |
| US8481696 | Dec 25, 2008 | Jul 9, 2013 | Shionogi & Co., Ltd. | Glycosylated glycopeptide antibiotic derivatives |



Cinnamon cuts blood glucose levels in diabetes patients
Consumption of cinnamon is associated with favorable reductions in plasma glucose and lipid levels, according to research published in the September/October issue of the Annals of Family Medicine.
Robert W. Allen, Pharm.D., of the Western University of Health Sciences in Pomona, Calif., and colleagues used data from 10 randomized, controlled trials involving 543 patients with type 2 diabetes to conduct an update of a previous systematic review and meta-analysis examining the effect of cinnamon consumption on glucose and lipid levels.
The researchers found that cinnamon, in daily doses of 120 mg/d to 6 g/d for four to 18 weeks, was associated with a significant reduction in levels of fasting plasma glucose (?24.59 mg/dL), but no significant effect on glycosylated hemoglobin. Cinnamon intake also was linked to significant changes in lipid levels, including decreases in levels of total cholesterol (?15.60 mg/dL), low-density lipoprotein cholesterol (LDL-C) (?9.42 mg/dL), and triglycerides…
View original post 89 more words
Sonidegib/Erismodegib..Novartis Cancer Drug LDE225 Meets Primary Endpoint in Phase 2


Sonidegib/Erismodegib
CODE DESIGNATION ..LDE225, NVP-LDE-225
Treatment of medulloblastoma PHASE3 2014 FDA FILING
Treatment of advanced basal cell carcinoma PHASE3 2014 FDA FILING
Treatment of SOLID TUMORS..PHASE1 2017 FDA FILING
READMalignant Solid Tumors of Childhood
THERAPEUTIC CLAIM Oncology, Antineoplastics & Adjunctive Therapies

CHEMICAL NAMES
1. [1,1′-Biphenyl]-3-carboxamide, N-[6-[(2R,6S)-2,6-dimethyl-4-morpholinyl]-3-pyridinyl]-2-
methyl-4′-(trifluoromethoxy)-, rel-
2. N-{6-[(2R,6S)-2,6-dimethylmorpholin-4-yl]pyridin-3-yl}-2-methyl-4′-
(trifluoromethoxy)biphenyl-3-carboxamide
N-[6-[(2S,6R)-2,6-dimethylmorpholin-4-yl]pyridin-3-yl]-2-methyl-3-[4-(trifluoromethoxy)phenyl]benzamide
N-(6-((2S,6R)-2,6-dimethylmorpholino)pyridin-3-yl)-2-methyl-4′-(trifluoromethoxy)biphenyl-3-carboxamide
MOLECULAR FORMULA C26H26F3N3O3
MOLECULAR WEIGHT 485.5
SPONSOR Novartis Pharma AG
CAS REGISTRY NUMBER 956697-53-3 free form
NOTE… DIPHOSPHATE SALT IS THE DRUG WITH CAS 1218778-77-8
sonidegib – European Medicines Agency READ THIS..
Summary EudraCT Number: 2012-004022-21 Sponsor’s Protocol … READ THIS


About the Study
The Phase II, randomized, double-blind BOLT (Basal cell carcinoma Outcomes in LDE225 Trial) study was designed to assess the safety and efficacy of two oral dose levels of LDE225 (200 mg and 800 mg) in patients with locally advanced or metastatic basal cell carcinoma[4], which are subtypes of advanced basal cell carcinoma.
The primary endpoint was the proportion of patients achieving an objective response rate, defined as a confirmed complete response and partial response as their best overall response per modified RECIST criteria, within six months of starting treatment with LDE225. Key secondary endpoints of the study included assessing the duration of tumor responseand the rate of complete response. Other secondary endpoints included progression-free survival, time to tumor response and overall surviva

Sonidegib (INN) or Erismodegib (USAN), also known as LDE225 is a Hedgehog signalling pathway inhibitor (via smoothened antagonism) being developed as an anticancer agent by Novartis.[1][2] It has been investigated as a potential treatment for:
- Pancreatic cancer[3][4][5][6]
- Breast cancer[7][8]
- Basal cell carcinoma of the skin[9][10][11]
- Small cell lung cancer[12]
- Medulloblastoma[13][14]
- Advanced solid tumours (including ovarian, breast, pancreatic, stomach, oesophageal cancers and glioblastoma multiforme)[15][16][17]
- Acute leukaemia[18]
- Chronic myeloid leukaemia[19]
- Myelofibrosis and Essential thrombocythaemia[20]
NVP-LDE-225, a product candidate developed by Novartis, is in phase III clinical trials for the treatment of medulloblastoma and basal cell carcinoma. Phase II trials are in progress for the treatment of adult patients with relapsed or refractory or untreated elderly patients with acute leukemia.
Early clinical trials are ongoing for the oral treatment of advanced solid tumors, for the treatment of myelofibrosis in combination with ruxolitinib and for the treatment of small cell lung cancer. A phase II clinical trial for the treatment of basal cell carcinomas in Gorlin’s syndrome patients with a cream formulation of NVP-LDE-225 was discontinued in 2011 since the formulation did not demonstrate tumor clearance rate sufficient to support further development.
Dana-Farber Cancer Institute and the Massachusetts General Hospital are conducting phase I clinical trials for the treatment of locally advanced or metastatic pancreatic cancer in combination with chemotherapy. In 2009, orphan drug designation was assigned in the E.U. for the treatment of Gorlin syndrome.
It has demonstrated significant efficacy against melanoma in vitro and in vivo.[21] It also demonstrated efficacy in a mouse model of pancreatic cancer.[22]

NVP-LDE225 Diphosphate salt (Erismodegib, Sonidegib)

- Synonym:Erismodegib, Sonidegib
- CAS Number:1218778-77-8
- Mol. Formula:C26H26F3N3O3 ∙ 2H3PO4
- MW:681.5
- nmr.http://www.chemietek.com/Files/Line2/Chemietek,%20NVP-LDE225%20[02],%20NMR.pdf
- hplc–http://www.chemietek.com/Files/Line3/Chemietek,%20NVP-LDE225%20[02],%20HPLC.pdf
Brief Description:
About LDE225
LDE225 (sonidegib) is an oral, investigational, selective smoothened inhibitor being studied in a variety of cancers. Smoothened (SMO) is a molecule that regulates the hedgehog (Hh) signaling pathway, which plays a critical role in stem cell maintenance and tissue repair. LDE225 is currently in clinical development for a variety of diseases including myelofibrosis, leukemia and solid tumors.
Given that LDE225 is an investigational compound, the safety and efficacy profile has not yet been fully established. Access to this investigational compound is available only through carefully controlled and monitored clinical trials. These trials are designed to better understand the potential benefits and risks of the compound. Given the uncertainty of clinical trials, there is no guarantee that LDE225 will ever be commercially available anywhere in the world.
Possibility (LDE225) is effective in medulloblastoma relapsed or refractory hedgehog pathway inhibitor sonidegib has been revealed. That the anti-tumor effect was observed in some patients and tolerability in 1/2 test phase.
4th Quadrennial Meeting of the World Federation of Neuro-Oncology in conjunction with the 18th Annual Meeting of the Society for Neuro-Oncology, which was held in San Francisco November 21 to 24 in (WFNO-SNO2013), rice Dana-Farber It was announced by Mark Kieran Mr. Children’s Hospital Cancer Center.
The research group, announced the final results of the Phase 1 trial that target advanced solid cancer in children of sonidegib. 1 dose increased multi-test phase, was initiated from 372mg/m2 once-daily dosing to target children under the age of 18 more than 12 months. (233mg/m2 group 11 people, 16 people 372mg/m2 group, 11 people group 425mg/m2, 680mg/m2 group 21 women) who participated 59 people, including medulloblastoma 38 patients. 12 median age was (2-17).
Creatine phosphokinase elevation of grade 4 only were seen at 372mg/m2 as dose-limiting toxicity only, and became two recommended dose phase and 680mg/m2. Nausea muscle pain creatine kinase rise malaise (22.0%) (15.3%) (15.3%), (13.6%), vomiting side effects were many, was (13.6%). Hypersensitivity vomiting creatine kinase increased (3.4%) (1.7%) (1.7%), rhabdomyolysis side effects of grade 3/4 was (1.7%). (One group 372mg/m2, 425mg/m2 group one) complete response was obtained in two people, a strong correlation was found between the activation of the hedgehog pathway and effect.
Phase III clinical trials that target medulloblastoma the activated hedgehog pathway currently are underway.
About Novartis
Novartis provides innovative healthcare solutions that address the evolving needs of patients and societies. Headquartered in Basel, Switzerland, Novartis offers a diversified portfolio to best meet these needs: innovative medicines, eye care, cost-saving generic pharmaceuticals, preventive vaccines and diagnostic tools, over-the-counter and animal health products. Novartis is the only global company with leading positions in these areas. In 2013, the Group achieved net sales of USD 57.9 billion, while R&D throughout the Group amounted to approximately USD 9.9 billion (USD 9.6 billion excluding impairment and amortization charges). Novartis Group companies employ approximately 136,000 full-time-equivalent associates and operate in more than 140 countries around the world.



The following Examples serve to illustrate the invention without limiting the scope thereof, it is understood that the invention is not limited to the embodiments set forth herein, but embraces ali such forms thereof as come within the scope of the disclosure,
Step 1:
To a solution of 2-chloro-5-nitro-pyridine 1 (5.58 g, 35.2 mmoL) and c/s-2,6- dimethylmorpholine (4.05 g, 35.2 mmoL) in anhydrous DMF (30 mi.) was added K2CO3 (9.71 g, 70.4 mnrtoL). The mixture was heated at 50ºC overnight. After concentration, the residue is partitioned between EtOAc and water. The EtOAc layer is dried over anhydrous Na2SO4 and concentrated to give crude product 3 as a yellow solid, after purification by silica gel chromatography, obtained pure product (7.80 g, 93.2%). LC-MS m/z: 238.2 (M+ 1).
Step 2:
The above material 3 (7.3Og. 30.8 mmoL) was hydrogenated in the presence of 10% Pd-C (1.0 g) in MeOH (120 ml) under hydrogen overnight. The suspension was filtered through celite and the filtrate was concentrated to give the crude product 4 (5.92 g) as a dark brown oil which was used directly in the next step without further purification. LC-MS m/z. 208.2 (M+1).
Step 3:
To a solution of 3-bromo-2-methyl benzoic acid (2.71 g, 12.6 mmoL), 6-((2S,6R)-2,6- dimethylmorpholino)pyridin-3-arnine 4 (2.61 g, 12.6 mmoL), and HATU (4.80 g, 12.6 mmoL) in anhydrous DMF (30 mL) was added diisopropylethylamine (6.58 mL, 37.8 mmoL) dropwise. The resulting mixture was stirred overnight at room temperature. The reaction mixture was diluted with water (50 mL), and then extracted with EtOAc (3×120 mL). The organic layer was dried and concentrated to give the crude product. This crude product was then purified by flash column chromatography using 30% EtOAc in hexane as eiuent to give 5 as a white solid (4.23 g, 83.0%). LC-MS m/z: 404.1 (M+1).
Step 4:
A mixture of 4-(trif!uoromethoxy)phenylboronic acid (254 mg, 1.24 mmol), 3-bromo- N-[6-(2,6-dimethyl-morpholin-4-yl)-pyridin-3-ylJ-4-methyl-benzamide 5 (250 mg, 0.62mmol), Pd(PPh3)4 (36 mg, 0.03 mmol), Na2CO3 (2.0M aqueous solution, 1.23 mL, 2.4 mmol) and DME (4.5 mL) in a sealed tube was heated at 130ºC overnight. The reaction mixture was diluted with EtOAc and water. The aqueous layer was extracted with EtOAc. The combined organic layer was washed with brine and concentrated to give the crude product which was then purified by preparative mass triggered HPLC (C18 column, etuted with CH3CN-H2O containing 0.05% TFA) to give N-(6-((2S,6R)-2,6-dimethyfmorpholino)pyridin-3-yl)-2-rnethyl- 4′-(trifluoromethoxy)biphenyi-3-carboxamide (183.5 mg, 61.1% yield). LC-MS m/z: 486.2 (M+1).
The resultant crystalline product (Form A) was converted to the amorphous form by dissolving in 3% w/w aqueous ethanol, and the resultant solution spray dried at about 150ºC.
Form B was prepared by heating the amorphous form in an oven at 110ºC for 2 hours. In a further embodiment, the invention relates to a process step or steps, or an intermediate as described herein.


…………………………..

SYNTHESIS

| LC-MS m/z 486.2 (M + 1) |
Step 1: To a solution of 3-iodo-4-methyl-benzoic acid (10.0 g, 38.2 mmol) in methanol (70 ml) is added concentrated sulfuric acid (0.5 ml). The reaction mixture is heated at 70° C. for 48 hours, cooled to room ambient temperature and then concentrated. After that, ethyl acetate (100 ml) and aqueous NaHCO3 (saturated, 100 ml) solution are added to the residue. The organic layer is separated and washed again with aqueous NaHCO3 (saturated, 100 ml) solution. The organic layer is separated, dried over anhydrous Na2SO4 and concentrated to yield 3-iodo-4-methyl-benzoic acid methyl ester 1. It is used without further purification in the next step. 1H NMR (400 MHz, DMSO-d6) δ 8.31 (s, 1H), 7.87 (d, 1H, J=8.4 Hz), 7.48 (d, 1H, J=8.4 Hz), 3.85 (s, 3H), 3.35 (s, 3H); LC-MS m/z: 277.0 (M+1).
Step 2: To a round-bottom flask containing 3-iodo-4-methyl-benzoic acid methyl ester (1.38 g, 5.00 mmol), 4-cyanophenylboronic acid (1.10 g, 7.48 mmol), palladium acetate (168 mg, 0.748 mmol), 2-(dicyclohexylphosphino)biphenyl (0.526 g, 1.50 mmol) and potassium fluoride (0.870 g, 15.0 mmol) is added anhydrous 1,4-dioxane (15 ml). The flask is purged with argon and sealed. The mixture is stirred at 130° C. for 18 hours, cooled to ambient temperature and then water (20 ml) and ethyl acetate (20 ml) are added. Solid is removed under vacuum filtration. The filtrate is extracted with EtOAc (20 ml×2). The organic layers are combined, washed with aqueous HCl (5%, 20 ml) and saturated NaHCO3 (20 ml). It is dried over MgSO4, and concentrated. The residue is purified by silica gel column chromatography (EtOAc/Hexane, gradient) to give 4′-cyano-6-methyl-biphenyl-3-carboxylic acid methyl ester 2; LC-MS m/z: 252.1 (M+1).
Step 3: To a solution of 4′-cyano-6-methyl-biphenyl-3-carboxylic acid methyl ester 2 (2.56 g, 10.3 mmol) in 1,4-dioxane-H2O (1:1 mixture, 20 ml) is added NaOH (1.22 g, 30.2 mmol)). The reaction is stirred at ambient temperature for 24 hours. To this mixture is added aqueous HCl (1 N, 36 ml) and it is then extracted with ethyl acetate (40 ml×3). The organic layers are combined, dried over anhydrous Na2SO4. The solver is removed. The solid obtained is washed with small amount of acetonitrile and air dried to give 4′-cyano-6-methyl-biphenyl-3-carboxylic acid 3: 1H NMR (DMSO-d6) δ 7.94 (d, 2H, J=8.0 Hz), 7.84 (dd, 1H, J1=8.4 Hz, J2=1.2 Hz), 7.75 (d, 1H, J=1.2 Hz), 7.61 (d, 2H, J=8.0 Hz), 7.48 (d, 1H, J=8.4 Hz), 2.29 (s, 3 H); LC-MS m/z 238.1 (M+1).
Step 4: To a suspension of 4′-cyano-6-methyl-biphenyl-3-carboxylic acid 3 (40 mg, 0.17 mmol) in anhydrous methylene chloride (5 ml) is added 2 drops of DMF. Then oxalyl chloride (32 mg, 22 μl, 0.25 mmol) is added. The mixture is stirred at ambient temperature until it turns clear. After that, it is concentrated, re-dissolved in anhydrous methylene chloride (3 ml), and added to a solution of 4-(morpholine-4-sulfonyl)-phenylamine (61 mg, 0.25 mmol) and triethylamine (34 mg, 47 μl, 0.33 mmol) in methylene chloride (2 ml). The mixture is stirred for 2 hours, concentrated and the residue is purified by preparative mass triggered HPLC (C18 column, eluted with CH3CN—H2O containing 0.05% TFA) to give 4′-cyano-6-methyl-biphenyl-3-carboxylic acid [4-(morpholine-4-sulfonyl)-phenyl]-amide: 1H NMR (DMSO-d6) δ 10.64 (s, 1H), 8.07 (d, 2H, J=8.8 Hz), 7.97 (d, 2H, J=8.4 Hz), 7.95 (d, 1H, J=8.8 Hz), 7.89 (s, 1H), 7.43 (d, 2H, J=8.4 Hz), 7.67 (d, 2H, J=8.8 Hz), 7.53 (d, 2H, J=8.8 Hz), 3.63 (m, 4H), 2.84 (m, 4H) 2.32 (s, 3H); LC-MS m/z: 462.1 (M+1).
Example 2 4′-cyano-6-methyl-biphenyl-3-carboxylic acid [6-(2,6-dimethyl-morpholin-4-yl)-pyridin-3-yl]-amide
Step 1: To a solution of 2-chloro-5-nitro-pyridine 4 (2.38 g, 15 mmol.) and cis-2,6-dimethylmorpholine (1.73 g, 15 mmol.) is added K2CO3 (4.14 g, 30 mmol.). The mixture was heated at 50° C. overnight. After concentration, the residue is partitioned between EtOAc and water. The EtOAc layer is dried over anhydrous Na2SO4 and concentrated to give crude product 6 as a yellow solid. The crude product is used directly in next step without further purification. LC-MS m/z: 238.1 (M+1).
Step 2: The above crude material 6 is hydrogenated in the presence of Pd—C (0.2 g) in MeOH (100 mL) under hydrogen over 10 h. The suspension is filtered through celite and the filtrate is concentrated to give the crude product 7 as a dark brown oil which is used directly in the next step without further purification. LC-MS m/z: 208.1 (M+1).
Step 3: To a solution of 3-bromo-4-methyl benzoic acid (108 mg, 0.5 mmol.), 6-(2,6-Dimethyl-morpholin-4-yl)-pyridin-3-ylamine 7 (104 mg, 0.5 mmol.), amd HATU (190 mg, 0.5 mmol.) in dry DMF (5 mL) is added triethylamine (139 uL, 1.0 mmol.) dropwise. The resulting mixture is stirred at room temperature for 2 h. After concentration, the residue is partitioned between EtOAc and water. The organic layer is dried and concentrated to give the crude product. The final compound is purified by flash column chromatography using 50% EtOAc in hexane as eluent to give 8 as a white solid. LC-MS m/z: 404.1 (M+1).
Step 4: A mixture of 4-cyanophenyl boronic acid (18 mg, 0.12 mmol), 3-bromo-N-[6-(2,6-dimethyl-morpholin-4-yl)-pyridin-3-yl]-4-methyl-benzamide 8 (40 mg, 0.1 mmol), Pd(PPh3)4 (11 mg, 0.01 mmol), and Na2CO3 (42 mg, 0.4 mmol) in a combined solvent system of toluene (0.2 mL) and water (0.2 mL) and ethanol (0.05 mL) is heated at 140° C. under microwave irradiation for 30 min. The reaction mixture is diluted with EtOAc and water. The aqueous layer is extracted with EtOAc. The combined organic layer is washed with brine and concentrated to give the crude product which is purified by preparative mass triggered HPLC (C18 column, eluted with CH3CN—H2O containing 0.05% TFA) to give 4′-cyano-6-methyl-biphenyl-3-carboxylic acid [6-(2,6-dimethyl-morpholin-4-yl)-pyridin-3-yl]-amide. LC-MS m/z: 427.2 (M+1).

4-(Trifluoromethoxy)phenylboronic acid
- CAS Number 139301-27-2
- Linear Formula CF3OC6H4B(OH)2
- Molecular Weight 205.93
CONDENSE WITH …3-bromo-N-[6-(2,6-dimethyl-morpholin-4-yl)-pyridin-3-yl]-4-methyl-benzamideACS Medicinal Chemistry Letters, 2010 , vol. 1, 3 p. 130 – 134


A mixture of 4-(trifluoromethoxy)phenylboronic acid (254 mg, 1.24 mmol), 3-bromo-N-[6-(2,6-
dimethyl-morpholin-4-yl)-pyridin-3-yl]-4-methyl-benzamide E (250 mg, 0.62mmol), Pd(PPh3)4
(36 mg, 0.03 mmol), Na2CO3 (2.0M aqueous solution, 1.23 mL, 2.4 mmol) and DME (4.5 mL)
in a sealed tube was heated at 1300C overnight. The reaction mixture was diluted with EtOAc
and water. The aqueous layer was extracted with EtOAc. The combined organic layer was
washed with brine and concentrated to give the crude product which was then purified by
preparative mass triggered HPLC (C18 column, eluted with CH3CN-H2O containing 0.05% TFA)
to give N-(6-((2S,6R)-2,6-dimethylmorpholino)pyridin-3-yl)-2-methyl-4′-
(trifluoromethoxy)biphenyl-3-carboxamide (5m, 183.5 mg, 61.1% yield). LC-MS m/z: 486.2 (M+1).
HRMS (m/z): [M+H]+
calcd for C26H27N3O3F3 486.2005; found 486.1986,
1H-NMR (500 MHz, DMSO-d6): δ (ppm) 10.15 (s, 1H), 8.43 (d, 1H), 7.94 (dd, 1H), 7.52-7.43
(m, 5H), 7.38 (m, 1H), 7.33 (m, 1H), 6.86 (d, 1H), 4.06 (d, 2H), 3.62 (m, 2H), 2,34 (m, 2H), 2.22
(s, 3H), 1.16 (d, 6H).
http://pubs.acs.org/doi/suppl/10.1021/ml1000307/suppl_file/ml1000307_si_001.pdf

Reference
- “LDE225 – PubChem”. PubChem. National Institutes of Health. Retrieved 16 February 2014.
- Pan, S; Wu, X; Jiang, J; Gao, W; Wan, Y; Cheng, D; Han, D; Liu, J; Englund, NP; Wang, Y; Peukert, S; Miller-Moslin, K; Yuan, J; Guo, R; Matsumoto, M; Vattay, A; Jiang, Y; Tsao, J; Sun, F; Pferdekamper, AC; Dodd, S; Tuntland, T; Maniara, W; Kelleher, JF; Yao, Y; Warmuth, M; Williams, J; Dorsch, M (10 June 2010). “Discovery of NVP-LDE225, a Potent and Selective Smoothened Antagonist”. ACS Medicinal Chemistry Letters 1 (3): 130–134. doi:10.1021/ml1000307.
- “A Biomarker Study to Identify Predictive Signatures of Response to LDE225 (Hedgehog Inhibitor) In Patients With Resectable Pancreatic Cancer”. ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “Gemcitabine + Nab-paclitaxel With LDE-225 (Hedgehog Inhibitor) as Neoadjuvant Therapy for Pancreatic Adenocarcinoma”.ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “Dose-escalation, and Safety Study of LDE225 and Gemcitabine in Locally Advanced or Metastatic Pancreatic Cancer Patients”.ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “A Pilot Study of a Hedgehog Pathway Inhibitor (LDE-225) in Surgically Resectable Pancreas Cancer”. ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “Study With LDE225 in Combination With Docetaxel in Triple Negative (TN) Advanced Breast Cancer (ABC) Patients (EDALINE)”.ClinicalTrials.gov. National Institutes of Health. 13 February 2014.
- “LDE225 in Treating Patients With Stage II-III Estrogen Receptor- and HER2-Negative Breast Cancer”. ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “A Phase II Study of Efficacy and Safety in Patients With Locally Advanced or Metastatic Basal Cell Carcinoma (BOLT)”.ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “To Evaluate the Safety, Local Tolerability, PK and PD of LDE225 on Sporadic Superficial and Nodular Skin Basal Cell Carcinomas(sBCC)”. ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “A Trial to Evaluate the Safety, Local Tolerability, Pharmacokinetics and Pharmacodynamics of LDE225 on Skin Basal Cell Carcinomas in Gorlin Syndrome Patients”. ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “Combination of the Hedgehog Inhibitor, LDE225, With Etoposide and Cisplatin in the First-Line Treatment of Patients With Extensive Stage Small Cell Lung Cancer (ES-SCLC)”. ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “A Phase III Study of Oral LDE225 Versus (vs) Temozolomide (TMZ) in Patients With Hedge-Hog (Hh)-Pathway Activated Relapsed Medulloblastoma (MB)”. ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “A Phase I Dose Finding and Safety Study of Oral LDE225 in Children and a Phase II Portion to Assess Preliminary Efficacy in Recurrent or Refractory MB”. ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “Phase Ib, Dose Escalation Study of Oral LDE225 in Combination With BKM120 in Patients With Advanced Solid Tumors”.ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “Dose Finding and Safety of Oral LDE225 in Patients With Advanced Solid Tumors”. ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “LDE225 and Paclitaxel in Solid Tumors”. ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “Study of Efficacy and Safety of LDE225 in Adult Patients With Relapsed/Refractory Acute Leukemia”. ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “Nilotinib and LDE225 in the Treatment of Chronic or Accelerated Phase Myeloid Leukemia in Patients Who Developed Resistance to Prior Therapy”. ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- “A Phase Ib/II Dose-finding Study to Assess the Safety and Efficacy of LDE225 + INC424 in Patients With MF”. ClinicalTrials.gov. National Institutes of Health. 13 February 2014. Retrieved 16 February 2014.
- Jalili, A; Mertz, KD; Romanov, J; Wagner, C; Kalthoff, F; Stuetz, A; Pathria, G; Gschaider, M; Stingl, G; Wagner, SN (30 July 2013). “NVP-LDE225, a potent and selective SMOOTHENED antagonist reduces melanoma growth in vitro and in vivo.” (PDF). PloS one 8 (7): e69064. doi:10.1371/journal.pone.0069064. PMC 3728309.PMID 23935925.
- Fendrich, V; Wiese, D; Waldmann, J; Lauth, M; Heverhagen, AE; Rehm, J; Bartsch, DK (November 2011). “Hedgehog inhibition with the orally bioavailable Smo antagonist LDE225 represses tumor growth and prolongs survival in a transgenic mouse model of islet cell neoplasms.”. Annals of Surgery 254 (5): 818–23.doi:10.1097/SLA.0b013e318236bc0f. PMID 22042473.
- ChemMedChem, 2013 , vol. 8, 8 p. 1261 – 1265
- ACS Med. Chem. Lett., 2010, 1 (3), pp 130–134.
- MORE REF
 sonidegib
sonidegib
Skin Cancer Foundation. “Skin Cancer Facts.” Available at:http://www.skincancer.org/skin-cancer-information/skin-cancer-facts . Accessed on February 14, 2014.
Rubin AI, Chen EH, Ratner D (2005). Current Concepts: Basal-Cell Carcinoma. N Engl J Med; 353:2262-9.
ClinicalTrials.gov. “A Phase II Study of Efficacy and Safety in Patients With Locally Advanced or Metastatic Basal Cell Carcinoma (BOLT)” Available at:http://clinicaltrials.gov/ct2/show/NCT01327053?term=%22LDE225%22+and+%22BOLT%22&rank=1. Accessed on February 14, 2014.
National Cancer Institute Dictionary of Cancer Terms. “Complete Response.” Available at: http://www.cancer.gov/dictionary?CdrID=45652 . Accessed on February 14, 2014.
National Cancer Institute Dictionary of Cancer Terms. “Partial Response.” Available at: http://www.cancer.gov/dictionary?CdrID=45819 . Accessed on February 14, 2014.
Wong C S M, Strange R C, Lear J T (2003). Basal cell carcinoma. BMJ; 327:794-798.
Copcu E, Aktas A. Simultaneous two organ metastases of the giant basal cell carcinoma of the skin. Int Semin Surg Oncol. 2005;2:1-6. Available at:http://www.ncbi.nlm.nih.gov/pmc/articles/PMC544837/ . Accessed on February 14, 2014.
Skin Cancer Foundation. “Basal Cell Carcinoma Treatment Options.” Available athttp://www.skincancer.org/skin-cancer-information/basal-cell-carcinoma/bcc-treatment-options . Accessed on February 14, 2014.
Stuetz A, et al. LDE225, a specific smoothened inhibitor, for the topical treatment of nevoid basal cell carcinoma syndrome (Gorlin’s syndrome). Melanoma Research. 2010; 20:e40. Available at:http://journals.lww.com/melanomaresearch/Fulltext/2010/06001/FC24_LDE225,_a_specific_smoothened_inhibitor,_for.87.aspx#FC24_LDE225%2C_a_specific_smoothened_inhibitor%2C_for.87.aspx?s=2&_suid=139234380607909969110518506816.
Novartis.com. “The Pipeline of Novartis Oncology: LDE225.” Available at:http://www.novartisoncology.com/research-innovation/pipeline.jsp #. Accessed on February 14, 2014.
Children’s Medical Research Center, Children’s Memorial Hospital/Northwestern University Feinberg School of Medicine. “The Sonic hedgehog/patched/gli signal transduction pathway.” Available at http://www.childrensmrc.org/iannaccone/gli/ . Accessed on February 14, 2014.
Gupta S, Takebe N, LoRusso P. Targeting the Hedgehog pathway in cancer. Ther Adv Med Oncol. 2010 July; 2(4): 237-250. Available at:http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3126020/ . Accessed on February 14, 2014.
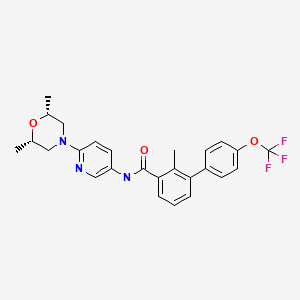

| WO2004078163A2 | Feb 26, 2004 | Sep 16, 2004 | Oern Almarsson | Pharmaceutical co-crystal compositions of drugs such as carbamazepine, celecoxib, olanzapine, itraconazole, topiramate, modafinil, 5-fluorouracil, hydrochlorothiazide, acetaminophen, aspirin, flurbiprofen, phenytoin and ibuprofen |
| WO2007113120A1 | Mar 22, 2007 | Oct 11, 2007 | Frank Hoffmann | Stamping apparatus with feed device |
| WO2007131201A2 * | May 4, 2007 | Nov 15, 2007 | Irm Llc | Compounds and compositions as hedgehog pathway modulators |
| WO2008154259A1 | Jun 4, 2008 | Dec 18, 2008 | Irm Llc | Biphenylcarboxamide derivatives as hedgehog pathway modulators |

THANKS AND REGARD’S
DR ANTHONY MELVIN CRASTO Ph.D
web link
blogs are

MY BLOG ON MED CHEM
ALL FOR DRUGS ON WEB
http://scholar.google.co.uk/citations?user=bxm3kYkAAAAJ

![]()
FDA Breakthrough Therapy Designation: Fourth Drug Receives FDA Approval
.
The FDA approves on February 12, the fourth drug to have the coveted Breakthrough Therapy Designation (BTD). The approval is for orphan drug Imbruvica (Ibrutinib) as a single agent for the treatment of patients with Chronic Lymphocytic Leukemia (CLL) who have received at least one prior therapy. Imbruvica, a once-daily, oral kinase inhibitor, is developed and commercialized by Pharmacyclics and Janssen Biotech. Imbruvica is the :
• 1st FDA BTD drug to receive approval in 2014
• 1st FDA BTD drug to receive approval for a 2nd indication – Mantle Cell Lymphoma (MCL) on 11.13.13
• 2nd FDA BTD drug to receive approval for the same indication, Chronic Lymphocytic Leukemia (CLL) – Genentech’s Gazyva (Obinutuzumab) receives approval for CLL on 11.01.13
• 3rd FDA BTD drug to receive approval for an oncology indication
• 4th FDA BTD drug to receive approval.
The media, investors, patients, regulatory agencies, and the pharmaceutical industry…
View original post 194 more words

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
























