Home » Posts tagged 'GENERIC DRUG' (Page 2)
Tag Archives: GENERIC DRUG
EPROSARTAN MESYLATE

TEVETEN® (eprosartan mesylate) is a non-biphenyl non-tetrazole angiotensin II receptor (AT1) antagonist. A selective non-peptide molecule, TEVETEN® is chemically described as the monomethanesulfonate of (E)-2-butyl-1 -(p-carboxybenzyl)-α-2-thienylmethylimid-azole-5 -acrylic acid.
Its empirical formula is C23H24N2O4S•CH4O3S and molecular weight is 520.625. Its structural formula is:
 |
EPROSARTAN MESYLATE
tevetenEprosartan mesilate, SK&F-108566-J(?, SK&F-108566, Teveten SB, Navixen, Regulaten, Tevetenz, Teveten
| US 5656650 | exp Aug 12, 2014 |
CAS EPROSARTAN
144143-96-4
133040-01-4
| Chemical Name: | Eprosartan mesylate |
| Synonyms: | EPROSARTAN MESYLATE;Eprosartan Methanesulfonate;4-[[2-butyl-5-(2-carboxy-3-thiophen-2-yl-prop-1-enyl)-imidazol-1-yl]methyl]benzoic acid mesylate;4-({2-butyl-5-[(1E)-2-carboxy-2-(thiophen-2-ylMethyl)eth-1-en-1-yl]-1H-iMidazol-1-yl}Methyl)benzoic acid;(E)-α-[[2-Butyl-1-[(4-carboxyphenyl)Methyl]-1H-iMidazol-5-yl]Methylene]-2-thiophenepropanoic Acid Methanesulfonate;(αE)-α-[[2-Butyl-1-[(4-carboxyphenyl)Methyl]-1H-iMidazol-5-yl]Methylene]-2-thiophenepropanoic Acid MonoMethanesulfonate |
| CBNumber: | CB4842192 |
| Molecular Formula: | C24H28N2O7S2 |
| Formula Weight: | 520.61832 |
Eprosartan is an angiotensin II receptor antagonist used for the treatment of high blood pressure. It is marketed as Teveten byAbbott Laboratories in the United States.It is marketed as Eprozar by INTAS Pharmaceuticals in India and by Abbott Laboratorieselsewhere. It is sometimes paired with hydrochlorothiazide, marketed in the US as Teveten HCT and elsewhere as TevetenPlus.
The drug acts on the renin-angiotensin system in two ways to decrease total peripheral resistance. First, it blocks the binding ofangiotensin II to AT1 receptors in vascular smooth muscle, causing vascular dilatation. Second, it inhibits sympatheticnorepinephrine production, further reducing blood pressure.
As with other angiotensin II receptor antagonists, eprosartan is generally better tolerated than enalapril (an ACE inhibitor), especially among the elderly.[1]
- Ruilope L, Jäger B, Prichard B (2001). “Eprosartan versus enalapril in elderly patients with hypertension: a double-blind, randomized trial”. Blood Press. 10 (4): 223–9. doi:10.1080/08037050152669747. PMID 11800061.
PAT APR EXP
| Canada | 2250395 | 2005-09-06 | 2017-03-26 |
| Canada | 2115170 | 2004-05-25 | 2012-08-12 |
| United States | 5656650 | 1994-08-12 | 2014-08-12 |
| United States | 5185351 | 1993-02-09 | 2010-02-09 |
| Canada | 2115170 | 2004-05-25 | 2012-08-12 |
| United States | 5656650 | 1994-08-12 | 2014-08-12 |
| Canada | 2250395 | 2005-09-06 | 2017-03-26 |
J Med Chem1991,34,(4):1514-7
J Med Chem1993,36,(13):1880-92
Synth Commun1993,23,(22):3231-48
AU 9056901, EP 403159, JP 91115278, US 5185351.
Drugs Fut1997,22,(10):1079

Eprosartan mesylate was developed successfully by SmithKline Beecham Corporation in 1997, and marketed in Germany in 1998 under the trade-name Teveten and in the United States later in 1999. Eprosartan mesylate, as an angiotensin II receptor blocker, is an antihypertensive drug of the latest generation. Eprosartan mesylate is potent to lower systolic and diastolic pressures in mild, moderate and severe hypertensive patients, and is safe and tolerable. Eprosartan mesylate is rapidly absorbed when administrated orally, with a bioavailability of 13% and a protein binding rate of 98%. The blood peak concentration and AUC (Area Under Curve) can be elevated by about 50% in patients with liver and kidney dysfunction, or fullness after administration, and can be elevated by 2 to 3 folds in elderly patients. Eprosartan mesylate has a structure shown as follows:
U.S. Pat. No. 5,185,351 discloses a method for preparing eprosartan mesylate using Eprosartan and methanesulfonic acid in isopropanol (U.S. Pat. No. 5,185,351, Example 41 (ii)). However, it is found when following this method for preparing eprosartan mesylate in industry, an esterification reaction can occur between eprosartan and isopropanol and the following two impurities can be generated:
In addition to the above two esterification impurities, the salifying method provided by the above patent is prone to produce isopropyl mesylate. Considering currently known potential risk of gene toxicity of methylsulfonic acid ester on human as well as the stringent requirements of methylsulfonic acid ester from the Europe and the America authorities, it is important to produce eprosartan mesylate in a non-alcohol solvent during the process of producing eprosartan mesylate, since it avoids the formation of methylsulfonic acid ester and the residue thereof in the final product. Since the dosage of eprosartan mesylate is high, it is particularly important to strictly control methylsulfonic acid ester in eprosartan mesylate.
In addition, for the above salifying method, solid eprosartan is suspended in propanol at a low temperature, then methanesulfonic acid is added, about ten seconds later a great deal of eprosartan mesylate precipitate is obtained. Therefore, solid eprosartan may be embedded by the precipitated eprosartan mesylate. Since isopropyl alcohol has a high viscosity at low temperature, a heavy filtering operation burden is needed to obtain solid from isopropanol, and the obtained solid contains quite an amount of isopropanol.

Eprosartan has been obtained by several different ways: 1) The iodination of 2-butylimidazole (I) with I2 and Na2CO3 in dioxane/water gives 2-butyl-4,5-diiodoimidazole (II), which is treated with benzyl chloromethyl ether (III) and K2CO3 in DMF yielding the imidazole derivative (IV). The condensation of (IV) with N-methyl-N-(2-pyridyl)formamide (V) by means of butyllithium in THF affords 1-(benzyloxymethyl)-2-butyl-4-iodoimidazole-5-carbaldehyde (VI), which is deprotected with concentrated HCl ethanol to give 2-butyl-4-iodoimidazole-5-carbaldehyde (VII). The acylation of (VII) with methyl 4-(bromomethyl)benzoate (VIII) by means of K2CO3 in hot DMF yields 4-(2-butyl-5-formyl-4-iodoimidazol-1 ylmethyl)benzoic acid methyl ester (IX), which is deiodinated by hydrogenation with H2 over Pd/C in methanol affording compound (X). The condensation of (X) with methyl 3-(2-thienyl)propionate (XI) by means of lithium diisopropylamide (LDA) in THF gives (XII), which is acylated with acetic anhydride and dimethylaminopyridine (DMAP) in dichloromethane yielding the corresponding acetate (XIII). Elimination of acetic acid from (XIII) with 1,8-diazabicyclo[5.4.0]undec-7-ene (DBU) in hot toluene affords the expected propenoic ester (XIV), which is finally saponified with NaOH or KOH in ethanol/water.
…………………………………………………………………………………………………….
WO 1998035962 A1

…………………………………………………………………………………………..



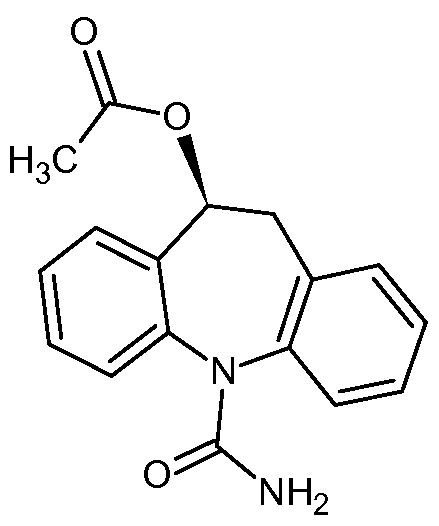
Aptiom (eslicarbazepine acetate) has been approved by the U.S. Food and Drug Administration as an add-on drug to help treat adults with partial epileptic seizures.
Eslicarbazepine acetate, 236395-14-5 cas no
(S)-10-Acetoxy- 10,11-dihydro- 5H-dibenz[b,f]azepine- 5-carboxamide
Sunovion Pharmaceuticals Inc. A US-based subsidiary of Japanese drugmaker Dainippon Sumitomo Pharma Announces FDA Approval of Aptiom® (eslicarbazepine acetate) as Once-Daily Adjunctive Treatment of Partial-Onset Seizures
MONDAY Nov. 11, 2013 — Aptiom (eslicarbazepine acetate) has been approved by the U.S. Food and Drug Administration as an add-on drug to help treat adults with partial epileptic seizures.
Epilepsy, caused by abnormal activity in the brain’s nerve cells, is diagnosed in some 200,000 people annually in the United States, the agency said in a news release. So-called “partial” seizures are the most common type of seizure among people with epilepsy, triggering possible symptoms including repetitive movement of limbs, unusual behavior and convulsions.http://www.drugs.com/news/aptiom-approved-seizures-48845.html
The FDA has determined that APTIOM will not be classified as a controlled substance. Sunovion expects APTIOM to be available in U.S. pharmacies in the second quarter (April – June) of 2014
APTIOM, a voltage-gated sodium channel inhibitor, is a prescription medicine approved for use as adjunctive treatment of partial-onset seizures. Treatment with APTIOM should be initiated at 400 mg once daily. After one week, dosage may be increased to the recommended maintenance dosage of 800 mg once daily. Some patients may benefit from the maximum recommended maintenance dosage of 1,200 mg once daily, although this dosage is associated with an increase in adverse reactions. The maximum dose of 1,200 mg daily should only be initiated after the patient has tolerated 800 mg daily for at least a week. For some patients, treatment may be initiated at 800 mg once daily if the need for additional seizure reduction outweighs an increased risk of adverse reactions during initiation.
The initial research and development of eslicarbazepine acetate was performed by BIAL, a privately held Portuguese research-based pharmaceutical company. Subsequently, Sunovion acquired the rights under an exclusive license to further develop and commercialize eslicarbazepine acetate in the U.S. and Canadian markets from BIAL. In February 2009, Eisai Europe Limited, a European subsidiary of Eisai Co., Ltd. (Eisai), entered into a license and co-promotion agreement with BIAL, which gave the rights to Eisai to sell eslicarbazepine acetate under the trade name Zebinix® in Europe. Zebinix was approved by the European Commission on April 21, 2009 as adjunctive therapy in adult patients with partial-onset seizures with or without secondary generalization and is currently marketed in Europe under the agreement.
Eslicarbazepine acetate (BIA 2-093) is an antiepileptic drug. It is a prodrug which is activated to eslicarbazepine (S–licarbazepine), an active metabolite of oxcarbazepine.[1]
It is being developed by Bial[2] and will be marketed as Zebinix or Exalief by Eisai Co. in Europe and as Stedesa by Sepracor[3] in America.
The European Medicines Agency (EMA) has recommended granting marketing authorization in 2009 for adjunctive therapy for partial-onset seizures, with or without secondary generalisation, in adults with epilepsy.[1] The U.S. Food and Drug Administration (FDA) announced on 2 June 2009 that the drug has been accepted for filing.[3]
Eslicarbazepine acetate is a prodrug for S(+)-licarbazepine, the major active metabolite of oxcarbazepine.[4] Its mechanism of action is therefore identical to that of oxcarbazepine. [5] There may, however, be pharmacokinetic differences. Eslicarbazepine acetate may not produce as high peak levels of (S)-(+)-licarbazepine immediately after dosing as does oxcarbazepine which could theoretically improve tolerability.
Like oxcarbazepine, eslicarbazepine may be used to treat bipolar disorder and trigeminal neuralgia.
The first European patent to protect this drug is EP 0751129 . The priority of this European patent is the Portuguese patent application PT 101732 .
- Dulsat, C., Mealy, N., Castaner, R., Bolos, J. (2009). “Eslicarbazepine acetate”. Drugs of the Future 34 (3): 189. doi:10.1358/dof.2009.034.03.1352675.
- Community register of medicinal products for human use: Exalief
- Medical News Today: Sepracor’s STEDESA (Eslicarbazepine Acetate) New Drug Application Formally Accepted For Review By The FDA
- Rogawski, MA (Jun 2006). “Diverse Mechanisms of Antiepileptic Drugs in the Development Pipeline”. Epilepsy Res 69 (3): 273–294. doi:10.1016/j.eplepsyres.2006.02.004. PMC 1562526. PMID 16621450.
- Rogawski MA, Löscher W (July 2004). “The neurobiology of antiepileptic drugs”. Nature Reviews Neuroscience 5 (7): 553–64. doi:10.1038/nrn1430. PMID 15208697.
- https://newdrugapprovals.wordpress.com/2013/03/11/sunovion-announces-fda-acceptance-for-review-of-new-drug-application-resubmission-for-stedesa-eslicarbazepine-acetate/
Eslicarbazepine acetate of Formula A, chemically known as (10S)-5-carbamoyl- 10,1 l-dihydro-5H-dibenzo[Z?,/]azepin- 10-yl acetate is indicated as adjunctive therapy in adults with partial-onset seizures with or without secondary generalisation.
Formula A
lO-oxo-10,1 l-dihydro-5H-dibenzo[Z?/]azepine-5-carboxamide of Formula 1, commonly known as oxcarbazepine, is an antiepileptic drug marketed under the trade name Trileptal®and is indicated for use as monotherapy or adjunctive therapy in the treatment of partial seizures in adults and as monotherapy in the treatment of partial seizures in children aged 4 years and above with epilepsy, and as adjunctive therapy in children aged 2 years and above with epilepsy. Oxcarbazepine is an intermediate for the preparation of eslicarbazepine.
Formula 1
Several processes are known in the literature for making and purifying eslicarbazepine acetate, for example, U.S. Patent No 5,753,646; and PCT Publications WO 2006/005951 ; WO 2007/1 17166; and WO 2010/1 13179.
U.S. Patent No. 5,753,646 provides a process for the preparation of eslicarbazepine acetate which involves adding dropwise a solution of acetyl chloride in dichloromethane to a suspension of (-)- 10-hydroxy-10,l l-dihydro-5H-dibenz/b,f/azepine-5-carboxamide in dichloromethane and pyridine at a temperature of less than 10°C under stirring. The residue obtained after workup was crystallized from a mixture of dichloromethane and ethyl acetate to give the eslicarbazepine acetate as white crystals.
U.S Publication No. 2009/0203902 provides preparation of eslicarbazepine acetate which involves the acylation of (S)-(+)-10,l l-dihydro-10-hydroxy-5H-dibenz/b,f/azepine- 5-carboxamide with acetic anhydride in presence of 4-(N,N-dimethylamino)pyridine and pyridine in dichloromethane at reflux temperature. The resulting solid obtained after work-up was slurried with isopropanol at reflux to obtain a solution. The solution was cooled to 1°C to 5°C and eslicarbazepine acetate was isolated from the reaction mass by filtration followed by washing with isopropanol.
PCT Publication No. WO 2010/1 13179 provides various purification methods of eslicarbazepine acetate which involve the use of acetonitrile/methyl tertiary butyl ether, tetrahydrofuran/n-hexane, tetrahydrofuran/methyl tertiary butyl methyl ether;
tetrahydrofuran, methyl ethyl ketone/n-hexane.
Several processes are known in the literature for making oxcarbazepine, for example, U.S. Patent Nos. 4,452,738 and 7,459,553; PCT Publication Nos. WO
2010/000196; WO 2008/012837; WO 2007/141798; WO 2006/075925; WO 2005/122671 ; WO 2005/1 18550; WO 2005/096709; WO 2005/092862; WO
2005/066133; WO 02/096881 ; WO 00/55138; and WO 96/21649.
PCT Publication No. WO 02/096881 provides a process for the preparation of oxcarbazepine which involves oxidation of 10,1 1 -dihydro- 10-hydroxy-5H- dibenz/b,f/azepine-5-carboxamide with peroxyacetic acid in presence of potassium dichromate adsorbed on silica gel at room temperature.
Japanese Patent Publication No. JP 2004- 175761 provides a process for the preparation of oxcarbazepine which involves oxidation of 10, 1 1 -dihydro- 10-hydroxy-5H- dibenzo[b,f]azepine-5-carboxamide with dimethyl sulfoxide and an activator such as sulfur trioxide-pyridine complex.
Chinese Publication No. CN 101302198 provides a process for the preparation of oxcarbazepine which involves oxidation of 10-hydroxy- 10, l 1 -dihydro-5H- dibenzo[Z?/]azepine-5-carbonitrile with TEMPO and sodium hypochlorite to provide 10- oxo- 10,1 l-dihydro-5H-dibenzo[Z?/]azepine-5-carbonitrile which was further hydrolysed with sulfuric acid to obtain oxcarbazepine.
-
Eslicarbazepine acetate, (S)-(-)-10-acetoxy-10,11-dihydro-5H-dibenz/b,f/azepine-5-carboxamide (“BIA 2-093”), is a new drug currently being developed which is useful for the treatment of various conditions, such as, for example, epilepsy and affective brain disorders, as well as pain conditions and nervous function alterations in degenerative and post-ischemic diseases. Although chemically related to carbamazepine and oxcarbazepine, eslicarbazepine acetate is believed to avoid the production of certain toxic metabolites (such as, for example, epoxides) and to avoid the unnecessary production of enantiomers or diastereoisomers of metabolites and conjugates, without losing pharmacological activity. See Benes et al., “Anticonvulsant and Sodium Channel-Blocking Properties of Novel 10,11-Dihydro-5H-dibenz[b,f]azepine-5-carboxamide Derivatives,” J. Med. Chem., 42, 2582-2587 (1999).
-
Like carbamazepine and oxcarbazepine, eslicarbazepine acetate is believed to be a voltage-gated sodium channel (VGSC) blocker that competitively interacts with site 2 of the inactivated state of the sodium channel. The affinity for this state of the channel is similar to that of carbamazepine, while the affinity for the resting state of the channel is about 3-fold lower than that of carbamazepine. This profile may suggest an enhanced inhibitory selectivity of eslicarbazepine acetate for rapidly firing neurons over those displaying normal activity. See Bonifacio et al., “Interaction of the Novel Anticonvulsant, BIA 2-093, with Voltage-Gated Sodium Channels: Comparison with Carbamazepine,” Epilepsia, 42, 600-608(2001).
-
Evaluation of the metabolic profile of eslicarbazepine acetate, following chiral analysis, in liver microsomes from rats, dogs, monkeys and humans was found to give the S(+) enantiomer of licarbazepine, (S)-(+)-10,11-dihydro-10-hydroxy-5H dibenz/b,f/azepine-5-carboxamide (also known as “eslicarbazepine”), and not the R(-) form of licarbazepine, (R)-(-)-10,11-dihydro-10-hydroxy-5H dibenz/b,f/azepine-5-carboxamide (also known as “R-licarbazepine”).
-
Studies in humans have shown that, after oral administration, eslicarbazepine acetate appears to be rapidly and extensively metabolized to the active metabolite eslicarbazepine and, in a minor extent, to R-licarbazepine. See Silveira et al., “BIA 2-093 Pharmacokinetics in Healthy Elderly Subjects,” Epilepsia, 45 (suppl. 3), 157 (2004). For example, the plasma concentrations of the parent drug (eslicarbazepine acetate) have been systematically found below the limit of quantification (LOQ) of the assay (10 ng/mL). See Almeida I; Almeida, L. & Soares-da-Silva, P., “Safety, Tolerability and Pharmacokinetic Profile of BIA 2-093, a Novel Putative Antiepileptic Agent, during First Administration to Humans,” Drugs R&D, 4, 269-284 (2003) (herein referred to as “Almeida II“). When a non-chiral method is used, the assay does not distinguish between eslicarbazepine and the R-enantiomer, and the mixture was reported as “BIA 2-005” or “racemic licarbazepine.”
-
The inventors performed entry-into-man studies in healthy subjects, the results of which they described in the Almeida I and Almeida II articles, both of which are hereby incorporated by reference. In these studies, the healthy subjects received a single oral dose of eslicarbazepine acetate wherein the dose ranged from 20 mg to 1200 mg (see Almeida II), and multiple daily-doses of eslicarbazepine acetate ranging from 200 mg twice-daily to 1200 mg once-daily (see Almeida I). Further studies (not yet published) by the inventors have investigated higher doses of eslicarbazepine acetate, including, for example, doses ranging up to 2400 mg once-daily. The studies showed that BIA 2-005 maximum observed plasma concentration (Cmax) was attained at about 1 hour to about 4 hours post-dose (tmax), the extent of systemic exposure to BIA 2-005 was approximately dose-proportional, and steady-state of BIA 2-005 plasma concentrations was attained at about 4 to 5 days. The mean renal clearance of BIA 2-005 from plasma was about 20-30 mL/min, and the total amount of BIA 2-005 recovered in the urine was approximately 20% and 40% within 12 hours and 24 hours post-dose, respectively.
-
The studies also showed that the apparent terminal half-life of BIA 2-005 ranged from about 8 hours to about 17 hours. See, e.g., Almeida II.
-
U.S. Patent No. 6,296,873 discloses a sustained release delivery system for carbamazepine, which has a half-life ranging from 25 hours to 85 hours. To avoid adverse effects, U.S. Patent No. 6,296,873 teaches that the carbamazepine should be administered in tablet form up to two or more times daily to slowly release the compound to maintain concentration levels between 4-12 µg/mL. Such a delivery system requires a form that is capable of delivering the compound over an extended period of time, such as a tablet form.

http://www.sciencedirect.com/science/article/pii/S0040403913005030

ESLICARBAZEPINE ACETATE
Physiochemical Pr operties:
| Molecular weight | : | 296.32 |
| Category | : | Anti-epileptic |
| Molecular formula | : | C17H16N2O5 |
| Chemical Name | : | (S)-(-)-10-acetoxy-10,11-dihydro-5H-dibenz [b, f] |
| azepine-5-carboxamide. | ||
| Description | : | White to off-White, odourless, non-hygroscopic, |
| crystalline powder. | ||
| Solubility | : | Freely soluble in dichloromethane, sparingly soluble |
| in acetone, acetonitrile, methanol, tetrahydrofuran and | ||
| slightly soluble in ethanol and 2-propanol, insoluble in | ||
| water | ||
| Melting Point | : | 184-187°C |
| Storage | : | Can be easily stored at temperatures up to 30°C |
HPLC, NMR

NMR NUMBERING

http://www.sciencedirect.com/science/article/pii/S0731708511006753
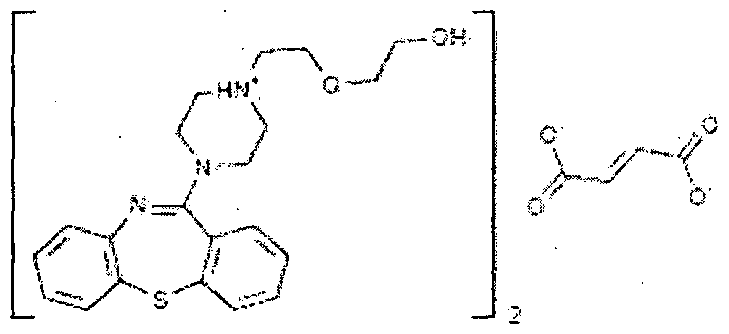
Quetiapine

Quetiapine, astrazeneca
111974-69-7 cas
US 5,948,437*PED, NDA 022047 Appr may 17 2007 sustained release formulation
NDA 020639 approved 26.9.1997
patent approved expiry
| United States | 5948437 | 1997-11-28 | 2017-11-28 |
| United States | 4879288 | 1994-09-26 | 2011-09-26 |
| Canada | 2251944 | 2007-04-10 | 2017-05-27 |
| United States | 4879288 | 1994-09-26 | 2011-09-26 |

Quetiapine (/kwɨˈtaɪ.əpiːn/ kwi-ty-ə-peen) (branded as Seroquel, Xeroquel, Ketipinor) is a short-acting atypical antipsychotic approved for the treatment of schizophrenia, bipolar disorder, and along with an antidepressant to treat major depressive disorder.
Annual sales are approximately $5.7 billion worldwide, with $2.9 billion in the United States. The U.S. patent, which expiredv in 2011, received a pediatric exclusivity extension which pushed its expiration to March 26, 2012.The patent has already expired in Canada. Quetiapine was developed by AstraZeneca from 1992-1996 as an improvement from first generation antipsychotics. It was first approved by the FDA in 1997. There are now several generic versions of quetiapine, such as Quepin, Syquel and Ketipinor
Seroquel (quetiapine) is a psychotropic medication that is used to treat schizophrenia in adults and children who are at least 13 years old. Seroquel is also used in the treatment of major depression and bipolar disorder. Side effects of Seroquel may include mood or behavior changes, constipation, drowsiness, headache, and trouble sleeping. Older adults with dementia may have a slightly increased risk of death when taking this medication.
Dosing preparations are 25, 50, 100, 200, 300, and 400 mg tablets. Seroquel may interact with a number of other drugs, including, but not limited to, antidepressant medications, antifungal drugs, steroids, cimetidine (Tagamet), thioridazine (Mellaril), and lorazepam (Ativan). During pregnancy, this medication should be used only when clearly needed. Discuss the risks and benefits with your doctor. Seroquel passes into breast milk and may have undesirable effects on a nursing infant.

Quetiapine fumarate is a psychotropic agent belonging to a chemical class of dibenzothiazepine derivatives, designated chemically as 2-[2-(4-dibenzo [b,f] [l,4]thiazepin -1 l-yl-l-piperazinyl)ethoxy]-ethanol fumarate (2: l )(salt). Its molecular formula is C42H5oN604S2*C4H404 having a molecular weight of 883.1 1. The structural formula is:
Quetiapine is marketed as immediate release as well as extended release tablets in United States under the trade name Seroquel® and Seroquel XR® by AstraZeneca.
-
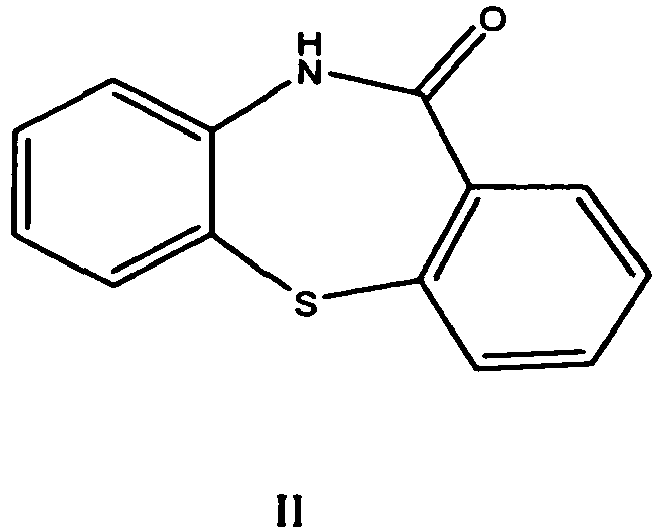
Quetiapine was first described in a patent publication EP 240228 (US 4879288 ). It is prepared starting from dibenzo[b,f][1,4]thiazepin-11-[10H]one of formula II
which is first halogenated with phosphorous oxychloride, then isolated and condensed with 1-(2-hydroxyethoxy) ethyl piperazine to obtainquetiapine. After purification by flash chromatography the yield was 77.7 %. As an alternative to halogenation a process via a thioether in the first step is presented.
-
In the process claimed in EP 282236 the piperazine ring is first condensed with 11-chloro-dibenzo[b,f][1,4] thiazepine and thereafterquetiapine is obtained by its reaction with haloethoxy ethanol. The base is further converted to the hemifumarate salt, which was isolated in 78 % yield.
-
WO 2006/117700 describes a process of EP ‘228 improved by the destruction of phosphorous oxychloride in situ to decrease the amount of hazardous waste. Phosphorous oxychloride is used only about 1 equivalent to the compound of formula II whereas in the process of EP 240228 it was used in about 15 equivalents.
-
A reaction of 11-chlorodibenzo[b,f][1,4]thiazepine with a piperazine moiety in the presence of a halide is the improvement described inWO 2006/113425 . The process is said to yield quetiapine in high purity.
-
In WO 2006/094549 there is described a process which avoids the halogenation step and the use of hazardous phosphorous halogenating agents by the reaction of 10H-dibenzo[b,f][1,4] thiazepin-11-one directly with a piperazine derivative. This is achieved by performing the reaction in the presence of titanium alkoxide. Yields of 50 – 75 % as a fumarate salt are reported. Expensive titanium alkoxide is used from about 2 to 3 fold excess to starting compound of formula II.
-
Also the process of US 2006/0063927 avoids the use of phosphorous compounds in halogenation by using oxalyl chloride as a halogenating agent. The imino chloride is obtained in 66 % yield. The reaction of 11-chloro-dibenzo[b,f][1,4] thiazepine with 1-(2-hydroxyethoxy)ethylpiperazine is performed either in the presence of a base in an organic solvent or in a two-phase system. However, the reagent used, oxalyl chloride is poisonous and requires special attention.
-
A one-pot process for the preparation of quetiapine is described inWO 2007/020011 . Phosphorous oxychloride is used in halogenation step about one equivalent to 10H-dibenzo[b,f][1,4] thiazepin-11-one.
-
WO 2007/004234 describes a process comprising the reaction of chloro ethoxy ethanol with piperazinyl-dibenzo[b,f][1,4] thiazepine dihydrocloride, which is obtained by halogenating the dibenzo[b,f][1,4] thiazepin-11-[10H]one, reacting the imino chloride obtained with piperazine, and treating the obtained compound with an alcoholic solution of hydrogen chloride.
-
All processes described above use dibenzo[b,f][1,4] thiazepin-11-[10H]one as a starting material. Its preparation requires several steps, and in most cases it has to be even halogenated to the imino chloride before the piperazine moiety can be condensed with it. Halogenating reagents, e.g. phosphorous oxychloride have been used in excess and their removal from the reaction mixture requires evaporation of large amounts.
-
A different approach using protected intermediates is used e.g. in routes described in WO 2005/014590 , WO 2005/028457 , WO 2005/028458and WO 2005/028459 . In some cases the reactions may be performed in one pot fashion and no extra purification steps are needed to get a pure product in high yield. However, protection and deprotection steps used lengthen the processes and shorter processes for the preparation of quetiapine are still needed.
-
Similar compounds are prepared in US 3, 539,573
U.S. Patent 4,879,288 discloses 1 l-[4-[2-(2-hydroxyethoxy) ethyl] -1 – piperazinyl] dibenzo [b, f] [1 , 4] thiazepine as an antipsychotic drug of dibenzothiazepine class suitable for treatment of various psychotic disorders.
US patent 5,948,437 discloses sustained release formulations of quetiapine using gelling agents such as hydroxypropyl methylcellulose and its derivatives that create a gel structure after contact with water. US patent 4,547,57 1 describes process for the preparation of carboxymethyl ethyl cellulose (CMEC) polymer.
WO 2004012699 discloses modified release dosage forms prepared by using dual – retard— technique comprising micro matrix particles containing quetiapine and hydrophobic release controlling agents, which are coated with hydrophobic release controlling agents.
WO 2005041935 discloses matrix composition comprising quetiapine and a wax material.
WO 2007086079 discloses sustained release compositions of quetiapinecomprising a channelizer and a rate controlling polymer.
WO 2008060228 discloses extended release compositions comprisingquetiapine, hydroxypropyl methyl cellulose and sodium citrate dihydrate.
WO 20091 13051 discloses sustained release compositions containingquetiapine and one or more non-gelling and/or waxy excipients.
WO 2010001413 discloses sustained release dosage forms comprisingquetiapine or its pharmaceutically acceptable salts and one or more non-gellable release controlling polymers.
WO 2010028794 discloses a matrix formulation in the form of a retard tablet comprising quetiapine, at least one matrix-forming, water-insoluble, non-swellable auxiliary agent, and at least one water-soluble binding agent.
The synthesis of quetiapine begins with a dibenzothiazepinone. The lactam is first treated with phosphoryl chloride to produce a dibenzothiazepine. A nucleophilic substitutionis used to introduce the sidechain.U.S. Patent 4,879,288.
Atypical antipsychotic quetiapine (Quetiapine, drugs used its fumarate) for the treatment of schizophrenia (schizophrenia) and dry depressive disorder (bipolar disorder), trade name Seroquel, produced by AstraZeneca. Star molecule drugs, the global sales of about $ 6 billion.
Quetiapine synthesis o-nitro-chlorobenzene ( 1 ) starting a thiophenol occurred and SNAr reaction, hydrogenation of nitro group to an amino group after reaction with phosgene isocyanate 2 , 2 ring closure in hot sulfuric acid to obtain 3 , 3 with phosphorus oxychloride isomerization chlorinated4 , 4 and 5 SNAr reaction occurs fumarate salt formation with quetiapine fumarate.
The route of the compound 4 is not stable enough, then there are improved route. 6 and the reaction of phenyl chloroformate 7

Quetiapine fumarate, Bis [2-(2-[4-(dibenzo[b,f][1,4]thiazepin-11-yl]ethoxy)ethanol] fumarate (IUPAC)2-[2-(4-dibenzo[b,f][1,4]thiazepin-11-yl-1-piperazinyl)ethoxy]-ethanol-(E)-2-butanedioate (2:1) salt), [ICI 204,636], is a novel dibenzothiazepine antipsychotic developed by Zeneca. It is marketed under the trade name ‘Seroquel’Seroquel. Quetiapine is well tolerated and clinically effective in the treatment of schizophrenia.
The initial hope of investigators was that quetiapine would have antipsychotic potential and that it might share some of the properties of clozapine without its toxicity to white blood cells.
The effective dosage range is usually 300-450 mg/day split into two doses. The dose is titrated upwards from 25 mg twice dailybd from day one to 300mg/daya fuller dosage on day 4. Elderly patients or patients with liver problems should be started on lower doses. It is both superior to placebo and, and comparable to haloperidol in reducing positive symptoms at doses ranging from 150 to 750 mg/day and is an effective treatment for in reducing negative symptoms at a dose of 300 mg/day.
Somnolence is the most common adverse event. Abnormalities of the QTqt interval on ECG appear very infrequently and there is no need for a baseline ECG or blood pressure monitoring as used to be the case with ssertindole. There is no need for haematological monitoring as with clozapine. Quetiapine, across the full dosage range, is associated with no greater extrapyramidal symptoms than placeboThere is a reduced potential for extrapyramidal symptoms compared with conventional antipsychotics.
Quetiapine’s general efficacy and side effect profile suggest that, unless there are unforeseen post-marketing complications, quetiapine deserves a major place in the initial and long term management of schizophreniform disorders.
Quetiapine fumarate, Bis [2-(2-[4-(dibenzo[b,f][1,4]thiazepin-11-yl]ethoxy)ethanol] fumarate (IUPAC) 2-[2-(4-dibenzo[b,f][1,4]thiazepin-11-yl-1-piperazinyl)ethoxy]-ethanol-(E)-2-butanedioate (2:1) salt), [ICI 204,636], is a novel dibenzothiazepine antipsychotic developed by Zeneca Pharmaceuticals. It is marketed under the trade name ‘Seroquel’. Quetiapine is well tolerated and clinically effective in the treatment of schizophrenia.

Aeterna Zentaris Submits New Drug Application to FDA for Macimorelin Acetate (AEZS-130) for Evaluation of AGHD

Macimorelin
CAS 381231-18-1
Chemical Formula: C26H30N6O3
Exact Mass: 474.23794
Molecular Weight: 474.55480
Elemental Analysis: C, 65.80; H, 6.37; N, 17.71; O, 10.11
945212-59-9 (Macimorelin acetate)
AEZS-130
ARD-07
D-87875
EP-01572
EP-1572
JMV-1843
USAN (ab-26)
MACIMORELIN ACETATE
THERAPEUTIC CLAIM
Diagnostic agent for adult growth hormone deficiency (AGHD)
CHEMICAL NAMES
1. D-Tryptophanamide, 2-methylalanyl-N-[(1R)-1-(formylamino)-2-(1H-indol-3-yl)ethyl]-, acetate (1:1)
2. N2-(2-amino-2-methylpropanoyl-N1-[(1R)-1-formamido-2-(1H-indol-3-yl)ethyl]- D-tryptophanamide acetate
MOLECULAR FORMULA
C26H30N6O3.C2H4O2
MOLECULAR WEIGHT
534.6
SPONSOR
Aeterna Zentaris GmbH
CODE DESIGNATIONS
D-87575, EP 1572, ARD 07
CAS REGISTRY NUMBER
945212-59-9
Macimorelin (also known as AEZS-130, EP-1572) is a novel synthetic small molecule, acting as a ghrelin agonist, that is orally active and stimulates the secretion of growth hormone (GH). Based on results of Phase 1 studies, AEZS-130 has potential applications for the treatment of cachexia, a condition frequently associated with severe chronic diseases such as cancer, chronic obstructive pulmonary disease and AIDS. In addition to the therapeutic application, a Phase 3 trial with AEZS-130 as a diagnostic test for growth hormone deficiencies in adults has been completed.
http://www.ama-assn.org/resources/doc/usan/macimorelin-acetate.pdf
QUEBEC, Nov. 5, 2013 /PRNewswire/ – Aeterna Zentaris Inc. (the “Company”) today announced that it has submitted a New Drug Application (“NDA”) to the U.S. Food and Drug Administration (“FDA”) for its ghrelin agonist, macimorelin acetate (AEZS-130). Phase 3 data have demonstrated that the compound has the potential to become the first orally-approved product that induces growth hormone release to evaluate adult growth hormone deficiency (“AGHD”), with accuracy comparable to available intravenous and intramuscular testing procedures. read at
http://www.drugs.com/nda/macimorelin_acetate_131105.html
http://www.ama-assn.org/resources/doc/usan/macimorelin-acetate.pdf
macimorelin (JMV 1843), a ghrelin-mimetic growth hormone secretagogue in Phase III for adult growth hormone deficiency (AGHD)
Macimorelin, a growth hormone modulator, is currently awaiting registration in the U.S. by AEterna Zentaris as an oral diagnostic test of adult growth hormone deficit disorder. The company is also developing the compound in phase II clinical trials for the treatment of cancer related cachexia. The compound was being codeveloped by AEterna Zentaris and Ardana Bioscience; however, the trials underway at Ardana were suspended in 2008 based on a company strategic decision. AEterna Zentaris owns the worldwide rights of the compound. In 2007, orphan drug designation was assigned by the FDA for the treatment of growth hormone deficit in adults.
New active series of growth hormone secretagogues
J Med Chem 2003, 46(7): 1191
WO 2001096300
WO 2007093820
…………………………
J Med Chem 2003, 46(7): 1191
http://pubs.acs.org/doi/full/10.1021/jm020985q


Synthetic Pathway for JMV 1843 and Analoguesa
a Reagents and conditions: (a) IBCF, NMM, DME, 0 °C; (b) NH4OH; (c) H2, Pd/C, EtOH, HCl; (d) BOP, NMM, DMF, Boc-(d)-Trp-OH; (e) Boc2O, DMAP cat., anhydrous CH3CN; (f) BTIB, pyridine, DMF/H2O; (g) 2,4,5-trichlorophenylformate, DIEA, DMF; (h) TFA/anisole/thioanisole (8:1:1), 0 °C; (i) BOP, NMM, DMF, Boc-Aib-OH; (j) TFA/anisole/thioanisole (8:1:1), 0 °C; (k) RP preparative HPLC.
TFA, H-Aib-(d)-Trp-(d)-gTrp-CHO (7). 6 (1 g, 1.7 mmol) was dissolved in a mixture of trifluoroacetic acid (8 mL), anisole (1 mL), and thioanisole (1 mL) for 30 min at 0 °C. The solvents were removed in vacuo, the residue was stirred in ether, and the precipitated TFA, H-Aib-(d)-Trp-(d)-gTrp-CHO was filtered. 7 was purified by preparative HPLC and obtained in 52% yield. 1H NMR (400 MHz, DMSO-d6) + correlation 1H−1H: δ 1.21 (s, 3H, CH3 (Aib)), 1.43 (s, 3H, CH3 (Aib)), 2.97 (m, 2H, (CH2)β), 3.1 (m, 2H, (CH2)β‘), 4.62 (m, 1H, (CH)αA and (CH)αB), 5.32 (q, 0.4H, (CH)α‘B), 5.71 (q, 0.6H, (CH)α‘A), 7.3 (m, 4H, H5 and H6 (2 indoles)), 7.06−7.2 (4d, 2H, H2A and H2B (2 indoles)), 7.3 (m, 2H, H4 or H7 (2 indoles)), 7.6−7.8 (4d, 2H, H4A and H4B or H7A and H7B), 7.97 (s, 3H, NH2 (Aib) and CHO (formyl)), 8.2 (d, 0.4H, NH1B (diamino)), 8.3 (m,1H, NHA and NHB), 8.5 (d, 0.6H, NH1A (diamino)), 8.69 (d, 0.6H, NH2A (diamino)), 8.96 (d, 0.4H, NH2B (diamino)), 10.8 (s, 0.6H, N1H1A (indole)), 10.82 (s, 0.4H, N1H1B (indole)), 10.86 (s, 0.6H, N1H2A (indole)), 10.91 (s, 0,4H, N1H2B (indole)). MS (ES), m/z: 475 [M + H]+, 949 [2M + H]+. HPLC tR: 16.26 min (conditions A).
…………………………..
http://www.google.com/patents/US8192719
The inventors have now found that the oral administration of growth hormone secretagogues (GHSs) EP 1572 and EP 1573 can be used effectively and reliably to diagnose GHD.
EP 1572 (Formula I) or EP 1573 (Formula II) are GHSs (see WO 01/96300, Example 1 and Example 58 which are EP 1572 and EP 1573, respectively) that may be given orally.
EP 1572 and EP 1573 can also be defined as H-Aib-D-Trp-D-gTrp-CHO and H-Aib-D-Trp-D-gTrp-C(O)NHCH2CH3. Wherein, His hydrogen, Aib is aminoisobutyl, D is the dextro isomer, Trp is tryptophan and gTrp is a group of Formula III:
…………………………….
http://www.google.com/patents/US6861409
Example 1 H-Aib-D-Trp-D-gTrp-CHO
Total synthesis (percentages represent yields obtained in the synthesis as described below):
Z-D-Tr-NH2
Z-D-Trp-OH (8.9 g; 26 mmol; 1 eq.) was dissolved in DME (25 ml) and placed in an ice water bath to 0° C. NMM (3.5 ml; 1.2 eq.), IBCF (4.1 ml; 1.2 eq.) and ammonia solution 28% (8.9 ml; 5 eq.) were added successively. The mixture was diluted with water (100 ml), and the product Z-D-Trp-NH2 precipitated. It was filtered and dried in vacuo to afford 8.58 g of a white solid.
Yield=98%.
C19H19N3O3, 337 g.mol−1.
Rf=0.46 {Chloroform/Methanol/Acetic Acid (180/10/5)}.
1H NMR (250 MHZ, DMSO-d6): δ 2.9 (dd, 1H, Hβ, Jββ′=14.5 Hz; Jβα=9.8 Hz); 3.1 (dd, 1H, Hβ′, Jβ′β=14.5 Hz; Jβ′α=4.3 Hz); 4.2 (sextuplet, 1H, Hα); 4.95 (s, 2H, CH2 (Z); 6.9-7.4 (m, 11H); 7.5 (s, 1H, H2); 7.65 (d, 1H, J=7.7 Hz); 10.8 (s, 1H, N1H).
Mass Spectrometry (Electrospray), m/z 338 [M+H]+, 360 [M+Na]+, 675 [2M+H]+, 697 [2M+Na]+.
Boc-D-Trp-D-Trp-NH2
Z-D-Trp-NH2 (3 g; 8.9 mmol; 1 eq.) was dissolved in DMF (100 ml). HCl 36% (845 μl; 1.1 eq.), water (2 ml) and palladium on activated charcoal (95 mg, 0.1 eq.) were added to the stirred mixture. The solution was bubbled under hydrogen for 24 hr. When the reaction went to completion, the palladium was filtered on celite. The solvent was removed in vacuo to afford HCl, H-D-Trp-NH2 as a colorless oil.
In 10 ml of DMF, HCl, H-D-Trp-NH2 (8.9 mmol; 1 eq.), Boc-D-Trp-OH (2.98 g; 9.8 mmol; 1.1 eq.), NMM (2.26 ml; 2.1 eq.) and BOP (4.33 g; 1.1 eq.) were added successively. After 1 hr, the mixture was diluted with ethyl acetate (100 ml) and washed with saturated aqueous sodium hydrogen carbonate (200 ml), aqueous potassium hydrogen sulfate (200 ml, 1M), and saturated aqueous sodium chloride (100 ml). The organic layer was dried over sodium sulfate, filtered and the solvent removed in vacuo to afford 4.35 g of Boc-D-Trp-D-Trp-NH2 as a white solid.
Yield=85%.
C27H31N5O4, 489 g.mol−1.
Rf=0.48 {Chloroform/Methanol/Acetic Acid (85/10/5)}.
1H NMR (200 MHZ, DMSO-d6): δ 1.28 (s, 9H, Boc); 2.75-3.36 (m, 4H, 2 (CH2)β; 4.14 (m, 1H, CHα); 4.52 (m, 1H, CHα′); 6.83-7.84 (m, 14H, 2 indoles (10H), NH2, NH (urethane) and NH (amide)); 10.82 (d, 1H, J=2 Hz, N1H); 10.85 (d, 1H, J=2 Hz, N1H).
Mass Spectrometry (Electrospray), m/z 490 [M+H]+, 512 [M+Na]+, 979 [2M+H]+.
Boc-D-(NiBoc)Trp-D-(NiBoc)Trp-NH2
Boc-D-Trp-D-Trp-NH2 (3 g; 6.13 mmol; 1 eq.) was dissolved in acetonitrile (25 ml).
To this solution, di-tert-butyl-dicarbonate (3.4 g; 2.5 eq.) and 4-dimethylaminopyridine (150 mg; 0.2 eq.) were successively added. After 1 hr, the mixture was diluted with ethyl acetate (100 ml) and washed with saturated aqueous sodium hydrogen carbonate (200 ml), aqueous potassium hydrogen sulfate (200 ml, 1M), and saturated aqueous sodium chloride (200 ml). The organic layer was dried over sodium sulfate, filtered and the solvent removed in vacuo. The residue was purified by flash chromatography on silica gel eluting with ethyl acetate/hexane {5/5} to afford 2.53 g of Boc-D-(NiBoc)Trp-D-(NiBoc)Trp-NH2 as a white solid.
Yield=60%.
C37H47N5O8, 689 g.mol−1.
Rf=0.23 {ethyl acetate/hexane (5/5)}.
1H NMR (200 MHZ, DMSO-d6): δ 1.25 (s, 9H, Boc); 1.58 (s, 9H, Boc); 1.61 (s, 9H, Boc); 2.75-3.4 (m, 4H, 2 (CH2)β); 4.2 (m, 1H, CHα′); 4.6 (m, 1H, CHα); 7.06-8 (m, 14H, 2 indoles (10H), NH (urethane), NH and NH2 (amides)).
Mass Spectrometry (Electrospray), m/z 690 [M+H]+, 712 [M+Na]+, 1379 [2M+H]+, 1401 [2M+Na]+.
Boc-D-(NiBoc)Trp-D-g(NiBoc)Trp-H
Boc-D-(NiBoc)Trp-D-(NiBoc)Trp-NH2 (3 g; 4.3 mmol; 1 eq.) was dissolved in the mixture DMF/water (18 ml/7 ml). Then, pyridine (772 μl; 2.2 eq.) and Bis(Trifluoroacetoxy)IodoBenzene (2.1 g; 1.1 eq.) were added. After 1 hr, the mixture was diluted with ethyl acetate (100 ml) and washed with saturated aqueous sodium hydrogen carbonate (200 ml), aqueous potassium hydrogen sulfate (200 ml, 1M), and aqueous saturated sodium chloride (200 ml). The organic layer was dried over sodium sulfate, filtered and the solvent removed in vacuo. Boc-D-NiBoc)Trp-D-g(NiBoc)Trp-H was used immediately for the next reaction of formylation.
Rf=0.14 {ethyl acetate/hexane (7/3)}.
C36H47N5O7, 661 g.mol−1.
1H NMR (200 MHZ, DMSO-d6): δ 1.29 (s, 9H, Boc); 1.61 (s, 18H, 2 Boc); 2.13 (s, 2H, NH2 (amine)); 3.1-2.8 (m, 4H, 2 (CH2)β); 4.2 (m, 1H, CHα′); 4.85 (m, 1H, CHα); 6.9-8 (m, 12H, 2 indoles (10H), NH (urethane), NH (amide)).
Mass Spectrometry (Electrospray), m/z 662 [M+H]+, 684 [M+Na]+.
Boc-D-(NiBoc)Trp-D-g(NiBoc)Trp-CHO
Boc-D-(NiBoc)Trp-D-g(NiBoc)Trp-H (4.3 mmol; 1 eq.) was dissolved in DMF (20 ml). Then, N,N-diisopropylethylamine (815 μl; 1.1 eq.) and 2,4,5-trichlorophenylformate (1.08 g; 1.1 eq.) were added. After 30 minutes, the mixture was diluted with ethyl acetate (100 ml) and washed with saturated aqueous sodium hydrogen carbonate (200 ml), aqueous potassium hydrogen sulfate (200 ml, 1M), and saturated aqueous sodium chloride (200 ml). The organic layer was dried over sodium sulfate, filtered and the solvent removed in vacuo. The residue was purified by flash chromatography on silica gel eluting with ethyl acetate/hexane {5/5} to afford 2.07 g of Boc-D-(NiBoc)Trp-D-g(NiBoc)Trp-CHO as a white solid.
Yield=70%.
C37H47N5O8, 689 g.mol−1.
Rf=0.27 {ethyl acetate/hexane (5/5)}.
1H NMR (200 MHZ, DMSO-d6): δ 1.28 (s, 9H, Boc); 1.6 (s, 9H, Boc); 1.61 (s, 9H, Boc); 2.75-3.1 (m, 4H, 2 (CH2)β); 4.25 (m, 1H, (CH)αA&B); 5.39 (m, 0.4H, (CH)α′B); 5.72 (m, 0.6H, (CH)α′A); 6.95-8.55 (m, 14H, 2 indoles (10H), NH (urethane), 2 NH (amides), CHO (formyl)).
Mass Spectrometry (Electrospray), m/z 690 [M+H]+, 712 [M+Na]+, 1379 [2M+H]+.
Boc-Aib-D-Trp-D-gTrp-CHO
Boc-D-(NiBoc)Trp-D-g(NiBoc)Trp-CHO (1.98 g; 2.9 mmol; 1 eq.) was dissolved in a -mixture of trifluoroacetic acid (16 ml), anisole (2 ml) and thioanisole (2 ml) for 30 minutes at 0° C. The solvents were removed in vacuo, the residue was stirred with ether and the precipitated TFA, H-D-Trp-D-gTrp-CHO was filtered.
TFA, H-D-Trp-D-gTrp-CHO (2.9 mmol; 1 eq.), Boc-Aib-OH (700 mg; 1 eq.), NMM (2.4 ml; 4.2 eq.) and BOP (1.53 g; 1.2 eq.) were successively added in 10 ml of DMF. After 1 hr, the mixture was diluted with ethyl acetate (100 ml) and washed with saturated aqueous sodium hydrogen carbonate (200 ml), aqueous potassium hydrogen sulfate (200 ml, 1M), and saturated aqueous sodium chloride (200 ml). The organic layer was dried over sodium sulfate, filtered and the solvent removed in vacuo. The residue was purified by flash chromatography on silica gel eluting with ethyl acetate to afford 1.16 g of Boc-Aib-D-Trp-D-gTrp-CHO as a white solid.
Yield=70%.
C31H38N6O5, 574 g.mol−1.
Rf=0.26 {Chloroform/Methanol/Acetic Acid (180/10/5)}.
1H NMR (200 MHZ, DMSO-d6): δ 1.21 (s, 6H, 2 CH3(Aib)); 1.31 (s, 9H, Boc); 2.98-3.12 (m, 4H, 2 (CH2)β); 4.47 (m, 1H, (CH)αA&B); 5.2 (m, 0.4H, (CH)α′B); 5.7 (m, 0.6H, (CH)α′A); 6.95-8.37 (m, 15H, 2 indoles (10H), 3 NH (amides), 1 NH (urethane) CHO (formyl)); 10.89 (m, 2H, 2 N1H (indoles)).
Mass Spectrometry (Electrospray), ml/z 575 [M+H]+, 597 [M+Na]+, 1149 [2M+H]+, 1171 [2M+Na]+.
H-Aib-D-Trp-D-gTrT-CHO
Boc-Aib-D-Trp-D-gTrp-CHO (1 g; 1.7 nmmol) was dissolved in a mixture of trifluoroacetic acid (8 ml), anisole (1 ml) and thioanisole (1 ml) for 30 minutes at 0° C. The solvents were removed in vacuo, the residue was stirred with ether and the precipitated TFA, H-Aib-D-Trp-D-gTrp-CHO was filtered.
The product TFA, H-Aib-D-Trp-D-gTrp-CHO was purified by preparative HPLC (Waters, delta pak, C18, 40×100 mm, 5 μm, 100 A).
Yield=52%.
C26H30N6O3, 474 g.mol−1.
1H NMR (400 MHZ, DMSO-d6)+1H/1H correlation: δ 1.21 (s, 3H, CH3 (Aib)); 1.43 (s, 3H, CH3 (Aib)); 2.97 (m, 2H, (CH2)β); 3.1 (m, 2H, (CH2)β′); 4.62 (m, 1H, (CH)αA&B); 5.32 (q, 0.4H, (CH)α′B); 5.71 (q, 0.6H, (CH)α′A); 7.3 (m, 4H5 and H6 (2 indoles)); 7.06-7.2 (4d, 2H, H2A et H2B (2 indoles)); 7.3 (m, 2H, H4 or H7 (2 indoles)); 7.6-7.8 (4d, 2H, H4A and H4B or H7A et H7B); 7.97 (s, 3H, NH2 (Aib) and CHO (Formyl));8.2 (d, 0.4H, NH1B (diamino)); 8.3 (m,1H, NHA&B); 8.5 (d, 0.6H, NH1A (diamino)); 8.69 (d, 0.6H, NH2A (diamino)); 8.96 (d, 0.4H, NH2B (diamino)); 10.8 (s, 0.6H, N1H1A (indole)); 10.82 (s, 0.4H, N1H1B (indole)); 10.86 (s, 0.6H, N1H2A (indole)); 10.91 (s, 0.4, N1H2B (indole)).
Mass Spectrometry (Electrospray), m/z 475 [M+H]+, 949 [2M+H]+.
………………………………
UPDATED INFO AS ON JAN 6 2014
Aeterna Zentaris NDA for Macimorelin Acetate in AGHD Accepted for Filing by the FDA
Quebec City, Canada, January 6, 2014 – Aeterna Zentaris Inc. (NASDAQ: AEZS) (TSX: AEZS) (the “Company”) today announced that the U.S. Food and Drug Administration (“FDA”) has accepted for filing the Company’s New Drug Application (“NDA”) for its ghrelin agonist, macimorelin acetate, in Adult Growth Hormone Deficiency (“AGHD”). The acceptance for filing of the NDA indicates the FDA has determined that the application is sufficiently complete to permit a substantive review.
The Company’s NDA, submitted on November 5, 2013, seeks approval for the commercialization of macimorelin acetate as the first orally-administered product that induces growth hormone release to evaluate AGHD. Phase 3 data have demonstrated the compound to be well tolerated, with accuracy comparable to available intravenous and intramuscular testing procedures. The application will be subject to a standard review and will have a Prescription Drug User Fee Act (“PDUFA”) date of November 5, 2014. The PDUFA date is the goal date for the FDA to complete its review of the NDA.
David Dodd, President and CEO of Aeterna Zentaris, commented, “The FDA’s acceptance of this NDA submission is another significant milestone in our strategy to commercialize macimorelin acetate as the first approved oral product for AGHD evaluation. We are finalizing our commercial plan for this exciting new product. We are also looking to broaden the commercial application of macimorelin acetate in AGHD for use related to traumatic brain injury victims and other developmental areas, which would represent significant benefit to the evaluation of growth hormone deficiency, while presenting further potential revenue growth opportunities for the Company.”
About Macimorelin Acetate
Macimorelin acetate, a ghrelin agonist, is a novel orally-active small molecule that stimulates the secretion of growth hormone. The Company has completed a Phase 3 trial for use in evaluating AGHD, and has filed an NDA to the FDA in this indication. Macimorelin acetate has been granted orphan drug designation by the FDA for use in AGHD. Furthermore, macimorelin acetate is in a Phase 2 trial as a treatment for cancer-induced cachexia. Aeterna Zentaris owns the worldwide rights to this novel patented compound.
About AGHD
AGHD affects about 75,000 adults across the U.S., Canada and Europe. Growth hormone not only plays an important role in growth from childhood to adulthood, but also helps promote a hormonally-balanced health status. AGHD mostly results from damage to the pituitary gland. It is usually characterized by a reduction in bone mineral density, lean mass, exercise capacity, and overall quality of life.
About Aeterna Zentaris
Aeterna Zentaris is a specialty biopharmaceutical company engaged in developing novel treatments in oncology and endocrinology. The Company’s pipeline encompasses compounds from drug discovery to regulatory approval.

back to home for more updates
![]()

DR ANTHONY MELVIN CRASTO Ph.D
Pfizer Receives FDA Approval for a Prior Approval Supplement for EMBEDA® (morphine sulfate and naltrexone hydrochloride) Extended Release Capsules CII
NEW YORK, November 04, 2013–(BUSINESS WIRE)–Pfizer Inc. (NYSE: PFE) announced today that the U.S. Food and Drug Administration (FDA) has approved a Prior Approval Supplement for EMBEDA® (morphine sulfate and naltrexone hydrochloride) Extended Release Capsules CII.
The Prior Approval Supplement included an update to the EMBEDA manufacturing process that addressed the pre-specified stability requirement that led to the voluntary recall of EMBEDA from the market in March 2011. Pfizer anticipates product availability in the second quarter of 2014.
http://www.pharmalive.com/fda-oks-prior-approval-supplement-for-embeda

back to home for more updates
Cempra’s Taksta secures FDA orphan drug status for prosthetic joint infections treatment

FUSIDIC ACID, 6990-06-3
2-[(1S,2S,5R,6S,7S,10S,11S,13S,14Z,15R,17R)-13-(acetyloxy)-5,17-dihydroxy-2,6,10,11-tetramethyltetracyclo[8.7.0.02,7.011,15]heptadecan-14-ylidene]-6-methylhept-5-enoic acid
Taksta (CEM-102)
Clinical-stage pharmaceutical firm Cempra has secured orphan drug status from the US Food and Drug Administration (FDA) for its drug candidate Taksta (CEM-102) to treat patients with prosthetic joint infections (PJI).
Cempra’s Taksta secures FDA orphan drug status for prosthetic joint infections treatment
TAKSTATM (CEM-102)
Fusidic acid is a bacteriostatic antibiotic that is often used topically in creams and eyedrops, but may also be given systemically as tablets or injections. The global problem of advancing antimicrobial resistance has led to a renewed interest in its use recently.
Fusidic acid acts as a bacterial protein synthesis inhibitor by preventing the turnover ofelongation factor G (EF-G) from the ribosome. Fusidic acid is effective primarily ongram-positive bacteria such as Staphylococcus species, Streptococcus species, and Corynebacterium species. Fusidic acid inhibits bacterial replication and does not kill the bacteria, and is therefore termed bacteriostatic.
Fusidic acid is a true antibiotic, derived from the fungus Fusidium coccineum and was developed by Leo Laboratories in Ballerup, Denmark and released for clinical use in the 1960s. It has also been isolated from Mucor ramannianus and Isaria kogana. The drug is licensed for use as its sodium salt sodium fusidate, and it is approved for use under prescription in South Korea, Japan, UK, Canada, Europe, Australia, New Zealand, Thailand, India and Taiwan. A different oral dosing regimen, based on the compound’s Pharmacokinetic/pharmacodynamic (PK-PD) profile is in clinical development in the U.S. as Taksta.
Fusidic acid (TAKSTATM, CEM-102) is an antibiotic with a long history of safety and efficacy outside the United States. Cempra has exclusive rights to the supply of the compound for the U.S. market. Fusidic acid is orally active against gram-positive bacteria, including all S. aureus strains such as HA-MRSA and CA-MRSA. A novel dosing regimen has been successfully evaluated in a Phase II trial in patients with acute bacterial skin and skin structure infections (aBSSSI). Cempra is conducting a Phase II trial of TAKSTA for patients with prosthetic joint infections.
Profile of TAKSTA (CEM-102)
Prosthetic joint infections (PJI) occur in about 1% of hip replacements and 2% of knee replacements, translating to an incidence rate of about 10,000 per year in the U.S. at current hip and knee arthroplasty rates. There are few good options to treat these serious staphylococcal, often MRSA infections, which require long-term antibiotic treatment. Current therapy in the U.S. is with intravenous antibiotics such as vancomycin. An oral drug that can be safely administered for a long period of time could improve care and quality of life for these patients.
TAKSTA has shown potent activity against a large number of S. aureus strains, including CA-MRSA, HA-MRSA and linezolid-resistant strains, isolated in the U.S over a 10 year period. Its broad S. aureus coverage makes it useful for a broad range of clinical applications. Because of its safety and tolerability profile, TAKSTA could be ideal for patients suffering from staphylococcal infections that require long-term therapy such as patients with PJIs.
Cempra has developed a unique oral loading dose regimen to optimize key pathogen coverage and minimize drug resistance development. This regimen is incorporated in our Phase II trial to treat PJIs with TAKSTA in combination with rifampin, which is commonly used with injectible antibiotics such as vancomycin to treat PJIs.
Research on TAKSTA
Publications
The links for the articles go to subscription-based sites and may require a fee to view the article.
In Vitro Activity of CEM-102 (Fusidic Acid) Against Prevalent Clones and Resistant Phenotypes of Staphylococcus aureus
DF Sahm, J Deane, CM Pillar, P Fernandes
Antimicrobial Agents and Chemotherapy. June 2013 57: 4535-4346
http://aac.asm.org/content/57/9/4535
Efforts to Support the Development of Fusidic Acid in the United States
P Fernandes, D Pereira
Clinical Infectious Disease. June 2011 52:S542-6
http://www.ncbi.nlm.nih.gov/pubmed/21546632
Case report: Treatment of Chronic Osteomyelitis
CR Wolfe
Clinical Infectious Disease. June 2011 52:S538-41
http://cid.oxfordjournals.org/content/52/suppl_7/S538.long
The Safety Record of Fusidic Acid in Non-US markets: A Focus on Skin Infections
CN Kraus, BW Burnstead
Clinical Infectious Disease. June 2011 52:S527-37
http://cid.oxfordjournals.org/content/52/suppl_7/S527.long
A Randomized, Double-Blind Phase 2 Study Comparing the Efficacy and Safety of an Oral Fusidic Acid Loading-Dose Regimen to Oral Linezolid in the Treatment of Acute Bacterial Skin and Skin Structure Infections
JC Craft, SR Moriarty, K Clark, D Scott, TP Degenhardt, JG Still, GR Corey, A Das, P Fernandes
Clinical Infectious Disease. June 2011 52:S520-26
http://cid.oxfordjournals.org/content/52/suppl_7/S520.long
Application of Pharmacokinetic-Pharmacodynamic Modeling and the Justification of a Novel Fusidic Acid Dosing Regimen: Raising Lazarus from the Dead
BT Tsuji, OO Okusanya, JB Bulitta, A Forrest, SM Bhavnani, P Fernandes, PG Ambrose
Clinical Infectious Disease. June 2011 52:S513-19
http://cid.oxfordjournals.org/content/52/suppl_7/S513.long
Pharmacokinetics and Safety of Single, Multiple, and Loading Doses of Fusidic Acid in Healthy Subjects
JG Still, K Clark, TP Degenhardt, D. Scott, P. Fernandes, M. J. Gutierrez
Clinical Infectious Disease. June 2011 52:S504-12
http://cid.oxfordjournals.org/content/52/suppl_7/S504.long
Activity of Fusidic Acid Against Extracellular and Intracellular Staphylococcus aureus: Influence of pH and Comparison with Linezolid and Clindamycin
S Lemaire, F Van Bambeke, D Pierard, PC Appelbaum, PM Tulkens
Clinical Infectious Disease. June 2011 52:S493-503
http://cid.oxfordjournals.org/content/52/suppl_7/S493.long
Characterization of Global Patterns and the Genetics of Fusidic Acid Resistance
DJ Farrell, M Castanheira, I Chopra
Clinical Infectious Disease. June 2011 52:S487-92
http://cid.oxfordjournals.org/content/52/suppl_7/S493.long
In Vitro Antimicrobial Findings for Fusidic Acid Tested Against Contemporary (2008-2009) Gram-Positive Organisms Collected in the United States
RN Jones, RE Mendes, HS Sader, M Castanheira
Clinical Infectious Disease. June 2011 52:S477-86
http://cid.oxfordjournals.org/content/52/suppl_7/S477.long
New Rules for Clinical Trials in Patients with Acute Bacterial Skin and Skin Structure Iinfections: Do not Let the Perfect be the Enemy of the Good
GR Corey, ME Stryjewski
Clinical Infectious Disease. June 2011 52:S469-76
http://cid.oxfordjournals.org/content/52/suppl_7/S469.long
Introduction: Fusidic Acid Enters the United States
RC Moellering, GR Corey, ML Grayson
Clinical Infectious Disease. June 2011 52:S467-8
http://cid.oxfordjournals.org/content/52/suppl_7/S467.long
Evaluation of the Pharmacokinetics-Pharmacodynamics of Fusidic Acid Against Staphylococcus aureus and Streptococcus pyogenes Using In Vitro Infection Models: Implications for Dose Selection
OO Okusanya, BT Tsuji, JB Bulitta, A Forrest, CC Bulik, SM Bhavnani, P Fernandes, PG Ambrose
Diagnostic Microbiology & Infectious Disease. June 2011 70:101-11
http://www.ncbi.nlm.nih.gov/pubmed/21513848
In Vitro Activity of Fusidic Acid (CEM-102, Sodium Fusidate) Against Staphylococcus aureus Isolated from Cystic Fibrosis Patients and its Effect on the Activities of Tobramycin and Amikacin against Pseudomonas aeruginosa and Burkholderia cepacia
P McGhee, K Credito, L Beachel, PC Appelbaum, K Kosowaska-Shick
Antimicrobial Agents and Chemotherapy. June 2011 55:2417-19
http://www.ncbi.nlm.nih.gov/pubmed/21513848
Occurrence and Molecular Characterization of Fusidic Acid Resistance Mechanisms Among Staphylococcus spp. From European Countries (2008)
Castanheira, M., AA Watters, RE Mendes, DJ Farrell, RN Jones
Antimicrobial Agents and Chemotherapy. April 2010 65:1353-8
http://jac.oxfordjournals.org/content/65/7/1353.long
Update on Fusidic Acid (CEM-102) Tested Against Neisseria gonorrhoeae and Chlamydia trachomatis
R Jones, D Biedenbach, P Roblin, S Kohlhoff, M Hammerschlag
Antimicrobial Agents and Chemotherapy. October 2010 54: 4518-4519
http://aac.asm.org/cgi/content/citation/54/10/4518
Fusidic Acid Resistance Rates and Prevalence of Resistance Mechanisms Among Staphylococcus spp. Isolated in North America and Australia, 2007-2008
M Castanheira, AA Watters, JM Bell, JD Turnidge, RN Jones
Antimicrobial Agents and Chemotherapy. September 2010 54: 3614-3617
http://www.ncbi.nlm.nih.gov/pubmed/20566766
Spectrum of Activity, Mutation Rates, Synergistic Interactions, and the Effects of pH and Serum Proteins for Fusidic Acid (CEM-102)
D Biedenbach, P Rhomberg, R Mendes, R Jones
Diagnostic Microbiology & Infectious Disease. March 2010 66: 301-307
http://www.dmidjournal.com/article/S0732-8893(09)00424-6/abstract
Performance of Fusidic Acid (CEM-102) Susceptibility Testing Reagents: Broth Microdilution, Disk Diffusion, and Etest Methods as Applied to Staphylococcus aureus
R Jones, M Castanheira, P Rhomberg, L Woosley, M Pfaller
Journal of Clinical Microbiology. March 2010 48: 972-976
http://jcm.asm.org/cgi/content/abstract/48/3/972
Evaluation of the Activity of Fusidic Acid Tested Against Contemporary Gram-Positive Clinical Isolates From the USA and Canada
M Pfaller, M Castaneira, H Sader, R Jones
International Journal of Antimicrobial Agents. March 2010 35: 282-287
http://www.ijaaonline.com/article/S0924-8579(09)00510-X/abstract
Quantitative and qualitative assessment of antibiotic activity against Staphylococcus aureus biofilm.
Siala, W., M. P. Mingeot-Leclercq, P. M. Tulkens, and F. Van Bambeke.
Abstr. 6th Am. Soc. Microbiol. Conf. Biofilms, abstr A-179.
Download Poster 
Activity of Fusidic Acid Against Methicillin-resistant Staphylococcus Aureus (MRSA) Isolated from CF Patients
Prabhavathi Fernandes, Donald Anderson, K. Kosowska-Shick, P. McGhee, L. Beachel and P.C. Appelbaum
Download Abstract  | Download Poster
| Download Poster 
Evaluation of L6 Ribosomal Protein Alterations in Fusidic Acid-Resistant Staphylococcus aureus: Fitness Cost and Time Kill Analysis
M Castanheira, RN Jones, LN Woosley, RE Mendes, GJ Moet, DJ Farrell
Download Abstract 
Fusidic Acid Activity and Coverage of Gram-positive Pathogens Associated with Acute Bacterial Skin and Skin Structure Infections (ABSSSI) in the USA (2008-2010)
RN Jones, DJ Farrell, HS Sader, M Castanheira
Download Abstract  | Download Poster
| Download Poster 
Activity of Fusidic Acid Tested Against Contemporary Staphylococcus aureus Collected from United States Hospitals
M. Castanheira, R.E. Mendes, P.R. Rhomberg, R.N. Jones
Download Abstract  | Download Poster
| Download Poster 
Pharmacokinetics-Pharmacodynamics (PK-PD) of CEM- 102 (Sodium Fusidate) Against Streptococcus pyogenes Using In Vitro Pharmacodynamic Models (IVPM)
B. T. Tsuji, A. Forrest, P. A. Kelchlin, T. Brown, P. N. Holden, O. O. Okusanya, S. M. Bhavnani, P. Fernandes, P. G. Ambrose
Download Abstract  | Download Poster
| Download Poster 
Activity of CEM-102 (sodium fusidate) against 40 MRSA from Cystic Fibrosis Patients
Cynthia Todd, Pamela Mcghee, and Peter Appelbaum
Download Abstract  | Download Poster
| Download Poster 
Ability of CEM-102 (Fusidic Acid), Linezolid, Daptomycin to Select Resistant S.aureus Mutants at Steady-state Serum Levels
K. Kosowska-Shick, P. Mcghee, L. Beachel, P. C. Appelbaum;
Download Abstract  | Download Poster
| Download Poster 
CEM-102 (Fusidic Acid) Maintains Potency against Resistant MRSA and Prevalent Hospital Acquired, Community Acquired,and Epidemic MRSA Clones
C.M. Pillar, M.K. Torres, D.F. Sahm and P. Fernandes
Download Abstract  | Download Poster
| Download Poster 
In Vitro Activity Of Fusicic Acid (CEM-102) Against Resistant Strains Of Staphylococcus aureus
J. dubois, P. Fernandes
Download Abstract  | Download Poster
| Download Poster 
Trade names and preparations
- Fucidin (of Leo in Canada and the US)
- Fucidin H (topical cream with corticosteroid – Leo)
- Fucidin (of Leo in UK/ Leo-Ranbaxy-Croslands in India)
- Fucidine (of Leo in France)
- Fucidin (of Leo in Norway)
- Fucidin (of Adcock Ingram, licenced from Leo, in South Africa)
- Fucithalmic (of Leo in the UK, the Netherlands, Denmark and Portugal)
- Fucicort (topical mixture with hydrocortisone)
- Fucibet (topical mixture with betamethasone)
- Ezaderm (topical mixture with betamethasone)(of United Pharmaceutical “UPM” in Jordan)
- Fuci (of pharopharm in Egypt)
- Fucizon (topical mixture with hydrocortisone of pharopharm in Egypt)
- Foban (topical cream in New Zealand)
- Betafusin (cream mixture with betamethasone valerate in Greece)
- Fusimax (of Schwartz in India)
- Fusiderm (topical cream and ointment by indi pharma in India)
- Fusid (in Nepal)
- Fudic (topical cream in India)
- Fucidin (후시딘, of Dong Wha Pharm in South Korea)
- Stanicid (in Serbia)
- Dermy (Topical cream of W.Woodwards in Pakistan)
- Fugen Cream (膚即淨軟膏 in Taiwan)
- Phudicin Cream (in China; 夫西地酸[24])
- Dermofucin cream ,ointment and gel (in Jordan)
- Optifucin viscous eye drops (of API in Jordan)
- Verutex (of Roche in Brazil)
- TAKSTA (of Cempra in U.S.)
- Futasole (of Julphar in Gulf and north Africa)
- Stanicid (2% ointment of Hemofarm in Serbia)
- Fuzidin (tablets of Biosintez in Russia)
- Fuzimet (ointment with methyluracil of Biosintez in Russia)
- Axcel Fusidic Acid(2% cream and ointment of Kotra Pharma, Malaysia)
MORE INFO

Fusidic acid (FA) is a tetracyclic triterpenoid or fusidane (steroidal) antibiotic derived from the fungus Fusidium coccineum that inhibits bacterial protein synthesis. FA is effective against gram-positive bacteria such as Staphylococcusspecies and Corynebacterium species (L. Verbist, J. Antimicro. Chemo. 25, Suppl. B, 1-5 (1990); A. Bryskier, Fusidic Acid, Chapter 23, in Antimicrobial Agents: Antibacterials and Antifungals (Andre Bryskier, Ed., ASM Press, Washington, USA, 2005)). FA also has moderate activity against Group A beta-hemolytic streptococci, or Streptococcus pyogenes (L. Verbist, J. Antimicro. Chemo. 25, Suppl. B, 1-5 (1990); A. Bryskier, Fusidic Acid, Chapter 23, inAntimicrobial Agents: Antibacterials and Antifungals (Andre Bryskier, Ed., ASM Press, Washington, USA, 2005); Skov et al., Diag. Micro. Infect. Dis. 40:111-116 (2001)).
-
Fusidic acid, chemically (3α, 4α, 8α, 9α, 11α, 13α, 14α, 16α, 17Z)-16-(Acetyloxy)-3,11-dihydroxy-29-nordammara-17(20), 24-dien-21-oic acid, is an antibacterial agent. It is a well-known antibiotic with a unique steroid-like tetracyclic ring system structure, and it is the most potent of a small family of steroidal antibiotics, the fusidanes. It is produced by fermentation under controlled conditions of the fungus Fusidium Coccineum.
-
The excellent distribution in various tissues, low degree of toxicity and allergic reactions and the absence cross-resistance with other clinically used antibiotics has made fusidic acid a highly valuable antibiotic,especially for skin and eye infections. The drug is used clinically both in its acid form, and as the sodium salt (Fusidin®), however Fusidin® is more favored one because of its better solubility in water, enabling a fast absorption from gastro-intestinal tract. As a result, it is more preferable to use sodium salt of fusidin in oral solid forms.
-
Fusidin® has the actions and uses of fusidic acid, and it has been shown that it ameliorates the course of several organ-specific immuno-inflammatory diseases such as chronic uveitis, Behcet’s disease, type I diabetes mellitus, Guillain-Barre syndrome, hepatitis, sepsis, pancreatitis, formalin-induced edema, multiple sclerosis, and scleroderma, whereby fucidin formulations have a great importance in pharmaceutical production.
-
Fusidin® can be presented in various formulations that differ significantly in their pharmacokinetic behaviors such as oral tablets, oral suspensions, intravenous formulations and topical preparation. Considering oral tablets, many of the early clinical studies were performed with capsule containing sodium fusidate. This was also the formulation marketed for many years in several countries. It is currently available as an oral tablet containing the sodium salt. Originally the sodium salt was available as an enteric-coated form but later it was reformulated as a film-coated tablet that appears to be better tolerated and gives higher blood levels.
-
Fusidic acid sodium salt was used in capsules as well as in tablets which were coated enterically. However by this enteric coating, the active fusidic acid sodium salt was not released before the tablets reached the part of the gastrointestinal tract in which the enteric coating would be dissolved. Depending on the time of passage through the stomach together with the food and the pH in the gastrointestinal tract, this led to unpredictable variations in the blood concentration of the patient undergoing treatment. Because of these adverse differences in blood concentration, the tablets without enteric coating were produced. Now, sodium fusidate is available in tablet, oral solution and injection form
-
PCT/WO9603128 A (LEO PHARMACEUTICALS PRODUCTS LTD. ET.AL.) describes the preparation of fusidic acid sodium salt tablets without an enteric coating by using dry granulation method in which a roller compactor was used. The compacted material so produced was size reduced to form a granulate having a bulk density in the range 0.45 to 0.9 g/m3 which was then formed into tablets.
FA was developed for clinical use in the 1960s and it is approved for human use outside of the United States, such as in the UK, Canada, Europe, Israel, Australia and New Zealand. It is typically prescribed at doses of 500 mg TID for treating skin and skin structure infections caused by Staphylococcus aureus (A. Bryskier,Fusidic Acid, Chapter 23, in Antimicrobial Agents: Antibacterials and Antifungals(Andre Bryskier, Ed., ASM Press, Washington, USA, 2005); Collignon et al., Int’l J. Antimicrobial Agents 12:S45-S58 (1999); D. Spelman, Int’l J. Antimicrobial Agents 12:S59-S66 (1999)), although some physicians have routinely prescribed the compound at 500 mg BID for treating skin and skin structure infections due to the long half-life of the compound (Fusidic Acid, in Principles and Practice of Infectious Diseases, 6th ed. (Mandell et al. eds., Elsevier, 2006)).
Treatment using FA has been well studied and it is generally regarded as safe when administered to humans, as evidenced by the fact that the drug has been in continuous use for more than 40 years. There are, however, several characteristics of FA that have prevented use of the drug against a wider spectrum of bacteria and in the treatment in additional types of infection. For example, approved dosing regimens have been shown to select for bacterial resistance, such as in S. aureus. Approved dosing regimens provide low multiples of the MIC and as a result, S. aureus resistant mutants can be selected after the first day of dosing. Once resistance has developed, FA is not effective against the resistant strains. Resistance is reported to occur if FA is used as a single drug as the resistance frequency at 4 and 8 times the MIC is in the range of 10−6 or 10−8 (Evans et al., J. Clin. Path. 19:555-560 (1966); Hansson et al., J. Mol. Biol.348:939-949 (2005), Jensen et al., Acta Pathol Microbiol Scand. 60:271-284 (1964); Besier et al., Antimicrob. Agents Chemo., 49(4):1426-1431 (2005); Gemmell et al., J. Antimicrobial Chemo. 57:589-608 (2006)).
The dosage of the drug cannot be simply increased as a means of avoiding development of resistance. It is difficult to achieve high concentrations of FA in the blood due to the substantial protein binding of the drug (approximately 95-97%) (K. Christiansen, International Journal of Antimicrobial Agents 12:S3-S9 (1999); Coutant et al., Diagn Microbiol Infect Dis 25:9-13 (1996); D. Reeves, J. Antimicrob. Chemo. 20:467-476 (1987); J. Turnidge, Int’l J. Antimicrobial Agents12:S23-S34 (1999); Rieutord et al., Int’l J. Pharmaceutics 119:57-64 (1995)). Moreover, high dosages of FA are not well-tolerated by patients receiving the drug. High doses of FA (e.g., 1 gram TID) are required if the drug is to be used in the treatment of bone and joint infections, less susceptible bacteria and other serious infections. However, treatment regimens using high doses of the drug induce nausea and vomiting and are rejected by patients (Fusidic Acid, inPrinciples and Practice of Infectious Diseases, 6th ed. (Mandell et al. eds., Elsevier, 2006); K. Christiansen, International Journal of Antimicrobial Agents 12:S3-S9 (1999); Nordin et al., Eur. J. Clin. Res. 5:97-106 (1994)).
In view of the tremendous costs associated with the de novo development of new anti-bacterials, expanding the indications for drugs that have already been demonstrated to be safe and effective is strongly needed. Overcoming the limitations on the uses of FA would broaden the population of bacterial infections against which it could be used and thus meet this need.
In a specific commercial pharmaceutical formulation, fusidic acid is presently marketed [see Monographs in the European Pharmacopeia 5.0] as a hemihydrate, which is the only hemihydrate form which has been described.
Patent GB 930,786 discloses salts of fusidic acid with organic and inorganic bases, solvates of fusidic acid, namely a benzene solvate and a methanol solvate. This patent further discloses an unspecified fusidic acid form with IR absorption bands (KBr) at 1265, 1385, 1695, 1730 and 3450 cm“1 and having a specific rotation [α]D 22 of minus 9 degrees (1% solution in CHCI3) obtainable by crystallisation of the methanol solvate of fusidic acid from ether. However, this form is distinct from the form of the present invention evident from the depicted IR spectrum in GB 930,786 which indicates that this form actually corresponds to the presently marketed hemihydrate form.
Solvates and salts of fusidic acid have also been disclosed in British patent GB 999,794. Patent ES 2208110 discloses two solvent free crystalline forms offusidic acid called Form I and Form II, and a crystalline hemihydrate called Form III which is identical to the presently marketed hemihydrate, respectively. The crystalline forms were identified and characterised by IR spectroscopy, differential scanning calorimetry, X-ray diffraction and melting points.
Patent WO 96/03128 discloses tablets containing a sodium salt form of fusidicacid and WO 86/03966 describes an ophthalmic gel composition comprising an undefined form of suspended fusidic acid.
GADODIAMIDE, OMNISCAN Drug Patent Expiration, 1 st oct 2013
GADODIAMIDE
GE HEALTHCARE, OMNISCAN
Drug Patent Expiration
1 st oct 2013, US5560903, CAS 122795-43-1
| GADODIAMIDE | INJECTABLE; INJECTION | 287MG/ML | RX | NDA 020123 |
Gadodiamide is a gadolinium-based MRI contrast agent, used in MR imaging procedures to assist in the visualization of blood vessels. It is commonly marketed under the trade name Omniscan.
For intravenous use in MRI to visualize lesions with abnormal vascularity (or those thought to cause abnormalities in the blood-brain barrier) in the brain (intracranial lesions), spine, and associated tissues.
Gadodiamide is a contrast medium for cranial and spinal magnetic resonance imaging (MRI) and for general MRI of the body after intravenous administration. The product provides contrast enhancement and facilitates visualisation of abnormal structures or lesions in various parts of the body including the central nervous system (CNS). It does not cross an intactblood brain barrier but might give enhancement in pathological conditions.
Based on the behavior of protons when placed in a strong magnetic field, which is interpreted and transformed into images by magnetic resonance (MR) instruments. Paramagnetic agents have unpaired electrons that generate a magnetic field about 700 times larger than the proton’s field, thus disturbing the proton’s local magnetic field. When the local magnetic field around a proton is disturbed, its relaxation process is altered. MR images are based on proton density and proton relaxation dynamics. MR instruments can record 2 different relaxation processes, the T1 (spin-lattice or longitudinal relaxation time) and the T2 (spin-spin or transverse relaxation time). In magnetic resonance imaging (MRI), visualization of normal and pathological brain tissue depends in part on variations in the radiofrequency signal intensity that occur with changes in proton density, alteration of the T1, and variation in the T2. When placed in a magnetic field, gadodiamide shortens both the T1 and the T2 relaxation times in tissues where it accumulates. At clinical doses, gadodiamide primarily affects the T1 relaxation time, thus producing an increase in signal intensity. Gadodiamide does not cross the intact blood-brain barrier; therefore, it does not accumulate in normal brain tissue or in central nervous system (CNS) lesions that have not caused an abnormal blood-brain barrier (e.g., cysts, mature post-operative scars). Abnormal vascularity or disruption of the blood-brain barrier allows accumulation of gadodiamide in lesions such as neoplasms, abscesses, and subacute infarcts.

1.Schenker MP, Solomon JA, Roberts DA. (2001). Gadolinium Arteriography Complicated by Acute Pancreatitis and Acute Renal Failure, Journal of vascular and interventional radiology 12(3):393.[1]
2 Unal O, Arslan H. (1999). Cardiac arrest caused by IV gadopentetate dimeglumine. AJR Am J Roentgenol 172:1141.[2]
3 Cacheris WP, Quay SC, Rocklage SM. (1990). The relationship between thermodynamics and the toxicity of gadolinium complexes, Magn Reson Imaging 8(6):467-81. doi:10.1016/0730-725X(90)90055-7
4 Canavese, C; Mereu, MC; Aime, S; Lazzarich, E; Fenoglio, R; Quaglia, M; Stratta, P (2008). “Gadolinium-associated nephrogenic systemic fibrosis: the need for nephrologists’ awareness”. Journal of nephrology 21 (3): 324–36. PMID 18587720.
COUNTRY PATENT APPROVED, EXPIRY
| United States | 5560903 | 1993-10-01 | 2013-10-01 |
| Canada | 1335819 | 1995-06-06 | 2012-06-06 |
| United States | 5362475 | 1994-11-08 | 2011-11-08 |
| Canada | 1335819 | 1995-06-06 | 2012-06-06 |
| United States | 5560903 | 1993-10-01 | 2013-10-01 |
Gadolinium contrast agents are used as contrast media to enhance magnetic resonance imaging as they are paramagnetic. This compound has a low incidence of adverse side effects, although there is a rare association with nephrogenic systemic fibrosis (NSF) when given to people with severe renal impairment (ie, GFRglomerular filtration rate <30mL/min/1·73m2).It seems to be related to the liberation of free gadolinium ions, and UK CHM advice is against using the least stable of the agents – Omniscan (gadodiamide) – in patients with severe renal impairment, and carefully considering whether to use others where renal function is impaired.
OMNISCAN (gadodiamide) Injection is the formulation of the gadolinium complex of diethylenetriamine pentaacetic acid bismethylamide, and is an injectable, nonionic extracellular enhancing agent for magnetic resonance imaging. OMNISCAN is administered by intravenous injection. OMNISCAN is provided as a sterile, clear, colorless to slightly yellow, aqueous solution. Each 1 mL contains 287 mg gadodiamide and 12 mg caldiamide sodium in Water for Injection.
The pH is adjusted between 5.5 and 7.0 with hydrochloric acid and/or sodium hydroxide. OMNISCAN contains no antimicrobial preservative. OMNISCAN is a 0.5 mol/L solution of aqua[5,8-bis(carboxymethyl)11-[2-(methylamino)-2-oxoethyl]-3-oxo-2,5,8,11-tetraazatridecan-13-oato (3-)-N5, N8, N11, O3, O5, O8, O11, O13] gadolinium hydrate, with a molecular weight of 573.66 (anhydrous), an empirical formula of C16H28GdN5O9•xH2O, and the following structural formula:
 |
Pertinent physicochemical data for OMNISCAN are noted below:
PARAMETER
| Osmolality (mOsmol/kg water) | @ 37°C | 789 |
| Viscosity (cP) | @ 20°C | 2 |
| @ 37°C | 1.4 | |
| Density (g/mL) | @ 25°C | 1.14 |
| Specific gravity | @ 25°C | 1.15 |
OMNISCAN has an osmolality approximately 2.8 times that of plasma at 37°C and is hypertonic under conditions of use.
gadodiamide, chemical name: [5,8 _ bis (carboxymethyl) -11 – [2_ (methylamino)-2_ ethyl] -3 – O 2 ,5,8, 11 – tetraazacyclododecane-decane -13 – oxo-(3 -)] gadolinium trihydrate. Its structure is shown in formula one.
[0003] Structural Formula:
[0004]
[0005] Magnetic resonance contrast agent gadodiamide resonance than ionic contrast agents safer generation of products, it is non-ionic structure significantly reduces the number of particles in solution, osmotic balance of body fluids is very small.Meanwhile, gadodiamide relatively low viscosity to bring the convenience of nursing staff, making it easier to bolus. In addition, gadodiamide pioneered the use of amide-substituted carboxyl part, not only reduces the toxicity of carboxyl groups and ensure the non-ionic nature of the product solution.
[0006] reported in the literature and their intermediates gadodiamide synthetic route is as follows:
[0007] 1. Compound III synthetic routes for its preparation in U.S. Patent No. US5508388 described as: In the synthesis process, the inventors using acetonitrile as solvent, acetic anhydride as dehydrating agent, pyridine as acid-binding agent, at 55 ~ 60 ° C, the reaction 18h. Anti-
See the reaction should be a process. The disadvantage of this synthesis are acetonitrile toxicity, not widely used.
[0008]
[0009] Reaction a
[0010] (2) Synthesis of Compound III in many articles are reported in the patent and its implementation method similar to the patent US5508388.
[0011] In US3660388, the diethylenetriamine pentaacetic acid (Compound II), pyridine, acetic anhydride, the mixture was reacted at 65 ° C or 20h at 125 ° C the reaction 5min, to give compound III.
[0012] In US4822594, the compounds II, pyridine, acetic anhydride mixture was reacted at 65 ° C 20h, to give compound III.
[0013] In US4698263, the compounds II, pyridine, acetic anhydride heated in a nitrogen or argon atmosphere under reflux for 18h, to give compound III. [0014] In the EPO183760B1, the compounds II, pyridine, acetic anhydride mixture was reacted at 55 ° C 24h, to give compound III.
[0015] In CN1894223A, the compounds II, pyridine, acetic anhydride, the mixture above 65 ° C the reaction mixture, and the pyridine of DTPA feed ratio is: 1: (0.5 to 3).
[0016] The above patents do not provide for the compound III is post-processing method.
[0017] 3 Synthesis of Compound IV.
[0018] In U.S. Patent US4859451, the diethylenetriamine pentaacetic acid dianhydride (compound III) and ammonia, methanol and the reaction of compounds IV, see Reaction Scheme II.
[0019]
[0020] Reaction two
[0021] In the patent US5087439, the compound III with methylamine in aqueous solution for several hours, or overnight reactions, see reaction formula III.
[0022]
[0023] Reactive three
[0024] These two patents using ammonia and methylamine, which can form explosive mixtures with air, in case of fire or high pressure can cause an explosion in the production process of great insecurity. Although raw material prices are lower, but higher production conditions (such as requiring sealed, low temperature, etc.). Compared to this synthesis process,
[0025] 4, gadodiamide (Compound I) synthesis.
[0026] In the patent US4859451, the use of gadolinium chloride with the compound IV is carried out under acidic conditions, complexing. Finally, tune
Section PH neutral, see reaction IV.
[0027]
[0028] Reaction formula tetrakis [0029] in the patent US5087439, the chlorides are used as reactants, and details of the post-processing method of Compound I.
[0030] In the patent US5508388, the use of gadolinium oxide with compound IV in acetonitrile, water with stirring, the resulting compound I.
[0032] The synthetic route is as follows:
[0033]
[0034] 1) Compound II (diethylenetriamine pentaacetic acid) in pyridine, acetic anhydride in the presence of a dehydration reaction into the acid anhydride, and the product was stirred with cold DMF, leaving the solid filtered, washed with ether reagents, drying , to obtain a white powdery solid compound III (diethylenetriamine pentaacetic acid anhydride);
[0035] 2) Compound III in DMF with methylamine hydrochloride, the reaction of the compound IV (5,8 _ bis carboxymethyl methyl-11 – [2 – (dimethylamino) -2 – oxoethyl] – 3 – oxo -2,5,8,11 – tetraazacyclododecane _13_ tridecyl acid); and the control compound III: MeNH2 · HCl molar ratio = 1: (1 to 4), control the temperature between 20 ~ 80 ° C, the reaction time is 4 ~ 6h, after the treatment, the method of distillation under reduced pressure to remove DMF, the product is dissolved in a polar solvent, methanol, and then adding a solvent polarity modulation, so that the target Compound IV from system completely precipitated;
[0036] 3) Compound IV with gadolinium oxide formed in the presence of hydrochloric acid of the complex, after the reaction, filtration and drying, to obtain a white powdery compound I, i.e. gadodiamide.
[0037] Existing gadodiamide Synthesis basically from the synthesis of Compound IV as a starting material, the present invention is first introduced to the compound II as a starting material to synthesize gadodiamide. Synthesis of the conventional method of gadodiamide, the present invention has the advantage of inexpensive starting materials, convenient and easy to get. In addition, the synthetic pathway intermediates are involved in the post-processing is simple, enabling continuous reaction, saving time and cost savings, the reaction becomes controlled step by step, and try to avoid the use of toxic reagents, reducing the possibility of operator injury , while also greatly reducing damage to the environment.
Biosimilars-in-India
http://www.ibef.org/download/Biosimilars-in-India-30312.pdf
-
Biosimilars – India Brand Equity Foundation
www.ibef.org/download/Biosimilars-in-India-30312.pdfpatented/registered biotech products, but are manufactured by new companies after the patent expiry of the originator product. The global. Biosimilars market is …
Founder of leading Indian pharmaceutical company, Sun Pharmaceuticals has been named India’s third richest man

This is the first time Mr Dilip Shanghvi, founder of Sun Pharmaceutical has been named in the top three with a 66 percent surge in his wealth –
25 oct 2013
Singapore: For the first time, founder of leading Indian drugmaker Sun Pharmaceuticals, Mr Dilip Shanghvi has been named in the top three of India’s richest men. Mr Shanghvi has made an appearance in the list prepared by China based ‘Hurun India Rich List’ as the third richest Indian man with a 66 percent surge in his wealth. Energy tycoon and Reliance Industries chairman Mr Mukesh Ambani has topped the list as India’s richest man with personal assets of $18.9 billion, news reports mentioned. The report pointed out that Mr Ambani has retained the top position for the second year even after a wealth decrease of two percent. London-based steel baron Mr Lakshmi Narayan Mittal has been named the second richest, with assets of $15.9 billion. – See more at: http://www.biospectrumasia.com/biospectrum/news/199210/sun-pharma-s-founder-named-india-s-3rd-richest#.Umzu4fmnqls
Read more at: http://www.biospectrumasia.com/biospectrum/news/199210/sun-pharma-s-founder-named-india-s-3rd-richest#.Umzu4fmnql
s
Potential of US pipeline continues to be under appreciated
SUNP’s US pipeline is shaping up well, with an interesting mix of complex products, branded generics and me-too products. Motilal Oswal believe that SUNP’s strong pipeline in the US is well placed to deliver revenue CAGR of 25% to USD1.8b. While a meaningful contribution to this growth is being led by Doxil and recently acquired URL Pharma, we estimate that SUNP’s own pipeline is set to witness revenue CAGR of 40% to USD6 20m. They build flat sales growth for Taro as they expect incremental competition to impact the market share for key Taro products. If competition is delayed, their estimates may have room for positive surprise.
Even after a 50-plus per cent return in one year, Sun Pharma’s stock continues to hold promise. While domestic revenues are growing well, US sales growth has been phenomenal, driven by a strong product pipeline and the acquisitions of Taro, DUSA, URL generics and Caraco.
-
[PDF]
NCE & NDDS Development Pipeline – Sun Pharma
www.sunpharma.com/pressdownload.php?download_file=329.pdfNCE & NDDS Development Pipeline / 2. Disclaimer. Except for the historical information contained herein, statements in this presentation and the subsequent …
-
[PDF]
Pipeline of Potential Ocular Therapies to Help Millions … – Sun Pharma
www.sunpharma.com/pressdownload.php?…Press%20Release%20SunPh…Oct 1, 2013 – 1. For Immediate Release. Sun Pharma and Intrexon Form Joint Venture to Develop. New Class of Therapeutics for Ocular Diseases. Pipeline …
pipeline
Sun Pharma Advanced Research (SPARC, US$345
mn market cap), a proprietary product research
company, detailed its NDDS and NCE product pipelines
in its latest filing with the SEBI, pursuant to its proposed
rights issue. Overall, there has been modest
clinical/regulatory progression in the NDDS pipeline
since the last disclosure six-seven months back. See
Exhibits 1 and 4 inside.
Key highlights: Big picture – New Drug Delivery
System (NDDS) – Overall SPARC is developing a
diverse collection of seven technology platforms for oral,
injectable and topical delivery systems (including nano
particulate, bio-degradable depot, DPI, SMM, GFR).
SPARC has 19 NDDS products under development.
New Chemical Entity (NCE) – The company has a
pipeline of five compounds that are pro-drugs of existing
molecules (such as baclofen, gabapentin etc). The NCE
pipeline appears to be in its early stages, with market
launch a few years away.
Update on key products (NDDS) – Three lead drugs:
1) levetiracetam XR 1000/1500 mg (505(b)(2) filing with
USFDA is now targeted for F1Q13), 2) baclofen GRS
(Special Protocol Assessment, SPA, agreement has
been received from FDA and patient enrollment for
Phase 3 studies is targeted in F4Q12) and 3) BAK-free
latanoprost (Phase III patient enrollment over in US).
These timelines imply that the first product launch in the
US is likely in 2H13. SPARC continues to validate its
underlying technology platforms by launching drugs in
the domestic market (six proprietary launches, seven
generic launches so far).
Other milestones for CY12: IND filing with USFDA for
two drugs – Octreotide Depot Inj (1 month) and Dry
Powder Inhaler (Salmeterol and Fluticasone
combination); paclitaxel (with carboplatin) Phase I
results in US and clinical progress of second WRAP
based drug, cardiovascular agent (and its combination)NDDS
LATANOPROST
LATANOPROST+TIMOLOLOL
BACLOFEN VENLAFAXINE
LEVETIRACETAM
PICN, PACLITAXEL
NCE
SUN597,
SUN L731
SUN K706
OTHERS
DRY POWDER INHALER
DOCETAXEL NANODISPERSION
OCTEOTIDE

MAY 2013
mn market cap), a proprietary product research
company, detailed its NDDS and NCE product pipelines
in its latest filing with the SEBI, pursuant to its proposed
rights issue. Overall, there has been modest
clinical/regulatory progression in the NDDS pipeline
since the last disclosure six-seven months back. See
Exhibits 1 and 4 inside.
Key highlights: Big picture – New Drug Delivery
System (NDDS) – Overall SPARC is developing a
diverse collection of seven technology platforms for oral,
injectable and topical delivery systems (including nano
particulate, bio-degradable depot, DPI, SMM, GFR).
SPARC has 19 NDDS products under development.
New Chemical Entity (NCE) – The company has a
pipeline of five compounds that are pro-drugs of existing
molecules (such as baclofen, gabapentin etc). The NCE
pipeline appears to be in its early stages, with market
launch a few years away.
Update on key products (NDDS) – Three lead drugs:
1) levetiracetam XR 1000/1500 mg (505(b)(2) filing with
USFDA is now targeted for F1Q13), 2) baclofen GRS
(Special Protocol Assessment, SPA, agreement has
been received from FDA and patient enrollment for
Phase 3 studies is targeted in F4Q12) and 3) BAK-free
latanoprost (Phase III patient enrollment over in US).
These timelines imply that the first product launch in the
US is likely in 2H13. SPARC continues to validate its
underlying technology platforms by launching drugs in
the domestic market (six proprietary launches, seven
generic launches so far).
Other milestones for CY12: IND filing with USFDA for
two drugs – Octreotide Depot Inj (1 month) and Dry
Powder Inhaler (Salmeterol and Fluticasone
combination); paclitaxel (with carboplatin) Phase I
results in US and clinical progress of second WRAP
based drug, cardiovascular agent (and its combination)
ATACAND, CANDESARTAN CILEXETIL, ASTRAZENECA.Drug Patent Expiration on 9 th Jan 2014
Candesartan cilexetil Candesartan cilexetil, Candesartan hexetil, H212/91, TCV-116, Kenzen, Blopress 16 mg Plus, Parapres, Ratacand, Blopress, Amias, Atacand
ATACAND
ATACAND (candesartan cilexetil), a prodrug, is hydrolyzed to candesartan during absorption from the gastrointestinal tract. Candesartan is a selective AT1 subtype angiotensin II receptor antagonist. Candesartan cilexetil, a nonpeptide, is chemically described as (±)-1-Hydroxyethyl 2-ethoxy-1-[p-(o-1H-tetrazol-5ylphenyl)benzyl]-7-benzimidazolecarboxylate, cyclohexyl carbonate (ester). Its empirical formula is C33H34N6O6, and its structural formula is:
 |
Candesartan cilexetil is a white to off-white powder with a molecular weight of 610.67. It is practically insoluble in water and sparingly soluble in methanol. Candesartan cilexetil is a racemic mixture containing one chiral center at the cyclohexyloxycarbonyloxy ethyl ester group. Following oral administration, candesartan cilexetil undergoes hydrolysis at the ester link to form the active drug, candesartan, which is achiral. ATACAND is available for oral use as tablets containing either 4 mg, 8 mg, 16 mg, or 32 mg of candesartan cilexetil and the following inactive ingredients: hydroxypropyl cellulose, polyethylene glycol, lactose, corn starch, carboxymethylcellulose calcium, and magnesium stearate. Ferric oxide (reddish brown) is added to the 8-mg, 16-mg, and 32-mg tablets as a colorant.
Drug Patent Expiration and Exclusivity
| Active Ingredient | Form | Dosage | Drug Type | Application | Product | |
|---|---|---|---|---|---|---|
| CANDESARTAN CILEXETIL | TABLET; ORAL | 4MG | RX | 020838 | 001 | |
| CANDESARTAN CILEXETIL | TABLET; ORAL | 8MG | RX | 020838 | 002 | |
| CANDESARTAN CILEXETIL | TABLET; ORAL | 16MG | RX | 020838 | 003 | |
| CANDESARTAN CILEXETIL | TABLET; ORAL | 32MG | RX | 020838 | 004 |
Patents
There are 6 patent(s) protecting ASTRAZENECA’s ATACAND. The last patent 5534534*PED expires on 2014-01-09.View patent at USPTO
| Patent US | US | Expiration |
|---|---|---|
| 5534534*PED | 2014-1-9 | |
| 5534534 | Pharmaceutical compositions for oral use and method of preparing them
A pharmaceutical composition for oral use comprising an effective amount of a compound of the formula (I) having antagonistic action to angiotensin II ##STR1## (wherein the ring W is an optionally substituted N-containing heterocyclic residue; R.sup.3 is a group capable of forming an anion or a group convertible thereinto; X is a direct bond or a spacer having an atomic length of two or less between the phenylene group and the phenyl group; and n is an integer of 1 or 2) and an oily substance having a lower melting point, and a method for preparing a pharmaceutical composition for oral use comprising an effective amount of a compound of the formula (I) and an oily substance having a lower melting point, which comprises admixing the compound of the formula (I) with an oily substance having a lower melting point and then subjecting the mixture to molding.
|
2013-7-9(expired) |
| 5196444*PED | 2012-12-4(expired) | |
| 5196444 | 1-(cyclohexyloxycarbonyloxy)ethyl 2-ethoxy-1-[[2′-(1H-tetrazol-5-yl)biphenyl-4-yl]methyl]benzimidazole-7-c arboxylate and compositions and methods of pharmaceutical use thereof
1-(Cyclohexyloxycarbonyloxy)ethyl 2-ethoxy-1-[[2′-(1H-tetrazol-5-yl)biphenyl-4-yl]methyl]benzimidazole-7-car boxylate or a pharmaceutically acceptable salt thereof has potent angiotensin II antihypertensive activity, thus being useful as therapeutic agents for treating circulatory system diseases such as hypertensive diseases, heart diseases (e.g. hypercardia, heart failure, cardiac infarction, etc.), strokes, cerebral apoplexy, nephritis, etc.
|
2012-6-4(expired) |
| 7538133*PED | 2011-10-18(expired) | |
| 5705517*PED | 2011-10-18(expired) |
Exclusivity
Exclusivity is marketing rights granted by the FDA to the ASTRAZENECA.
| Date | Supplement No. | Action | Documents |
|---|---|---|---|
| 2013-04-26 | 038 | Labeling Revision | |
| 2012-04-27 | 035 | Labeling Revision | |
| 2012-04-13 | 032 | Labeling Revision | |
| 1998-06-04 | 000 | Approval | |
| 2011-06-24 | 033 | Labeling Revision | |
| 2009-10-22 | 031 | Patient Population Altered | |
| 2006-08-17 | 026 | Labeling Revision | |
| 2005-05-18 | 022 | New or Modified Indication | |
| 2005-02-22 | 024 | New or Modified Indication | |
| 2004-12-16 | 023 | Labeling Revision | |
| 2000-06-14 | 008 | Labeling Revision | |
| 2002-09-13 | 015 | Comparative Efficacy Claim | |
| 2003-01-22 | 017 | Labeling Revision | |
| 2003-04-23 | 019 | Labeling Revision | |
| 2013-02-21 | 037 | Manufacturing Change or Addition | |
| 1999-08-11 | 005 | Package Change | |
| 2000-12-27 | 009 | Manufacturing Change or Addition | |
| 2001-05-24 | 012 | Manufacturing Change or Addition | |
| 2001-11-28 | 016 | Labeling Revision | |
| 1999-07-28 | 004 | Control Supplement | |
| 2001-04-02 | 011 | Manufacturing Change or Addition | |
| 2001-10-04 | 014 | Control Supplement | |
| 1998-11-16 | 002 | Manufacturing Change or Addition | |
| 1999-12-08 | 006 | Package Change | |
| 2001-06-07 | 010 | Manufacturing Change or Addition | |
| 2001-03-29 | 013 | Package Change | |
| 1998-12-07 | 001 | Manufacturing Change or Addition |
 Candesartan is marketed as the cyclohexyl 1-hydroxyethyl carbonate (cilexetil) ester, known ascandesartan cilexetil. Candesartan cilexetil is metabolised completely by esterases in theintestinal wall during absorption to the active candesartan moieity. The use of a prodrug form increases the bioavailability of candesartan. Despite this, absolute bioavailability is relatively poor at 15% (candesartan cilexetil tablets) to 40% (candesartan cilexetil solution). Its IC50 is 15 µg/kg. U.S. Patent Nos. 5,196,444 and 5,578,733 describe the removal of a trityl protecting group of the N-protected tetrazolyl compounds using methanol in the presence of a mineral acid, such as hydrochloric acid, which requires complex extractions or chromatographic purification to produce pure candesartan cilexetil. U.S. Patent No. 7,345,072 describes the deprotection of tetrazolyl compounds, including candesartan cilexetil, in the presence of an anhydrous mineral acid or aqueous mineral acid at a concentration higher than 20% w/w. The strong acidic conditions produce more decomposition products and thereby reduces the overall purity of the final product. WO 05/021535 discloses the preparation of candesartan cilexetil by the deprotection of trityl moiety at a reflux temperature in the presence of anhydrous Ci to C5 alcohol under neutral or slightly basic conditions involving longer reaction time (for e.g. stirring for several hours, such as 18-24 hours); this is followed by removal of the triphenylmethylether moiety precipitated as a solid, and thereby increases the number of reaction steps. WO 05/037821 describes the deprotection of the trityl candesartan cilexetil by the use of methane sulphonic acid, p-toluene sulphonic acid, formic and trifluoroacetic acid in solvent mixture or by refluxing candesartan cilexetil in mixture of toluene, water, and methanol. The initial product obtained by these procedures is mostly a viscous oil or a semi solid, which is difficult to handle. WO 07/074399 and WO 07/042161 disclose the preparation of candesartancilexetil from trityl candesartan cilexetil involving Lewis acids such as boron trifluoride, zinc chloride, aluminium trihalide, or titanium tetrachloride which are costly and thus are not commercially viable.
Candesartan is marketed as the cyclohexyl 1-hydroxyethyl carbonate (cilexetil) ester, known ascandesartan cilexetil. Candesartan cilexetil is metabolised completely by esterases in theintestinal wall during absorption to the active candesartan moieity. The use of a prodrug form increases the bioavailability of candesartan. Despite this, absolute bioavailability is relatively poor at 15% (candesartan cilexetil tablets) to 40% (candesartan cilexetil solution). Its IC50 is 15 µg/kg. U.S. Patent Nos. 5,196,444 and 5,578,733 describe the removal of a trityl protecting group of the N-protected tetrazolyl compounds using methanol in the presence of a mineral acid, such as hydrochloric acid, which requires complex extractions or chromatographic purification to produce pure candesartan cilexetil. U.S. Patent No. 7,345,072 describes the deprotection of tetrazolyl compounds, including candesartan cilexetil, in the presence of an anhydrous mineral acid or aqueous mineral acid at a concentration higher than 20% w/w. The strong acidic conditions produce more decomposition products and thereby reduces the overall purity of the final product. WO 05/021535 discloses the preparation of candesartan cilexetil by the deprotection of trityl moiety at a reflux temperature in the presence of anhydrous Ci to C5 alcohol under neutral or slightly basic conditions involving longer reaction time (for e.g. stirring for several hours, such as 18-24 hours); this is followed by removal of the triphenylmethylether moiety precipitated as a solid, and thereby increases the number of reaction steps. WO 05/037821 describes the deprotection of the trityl candesartan cilexetil by the use of methane sulphonic acid, p-toluene sulphonic acid, formic and trifluoroacetic acid in solvent mixture or by refluxing candesartan cilexetil in mixture of toluene, water, and methanol. The initial product obtained by these procedures is mostly a viscous oil or a semi solid, which is difficult to handle. WO 07/074399 and WO 07/042161 disclose the preparation of candesartancilexetil from trityl candesartan cilexetil involving Lewis acids such as boron trifluoride, zinc chloride, aluminium trihalide, or titanium tetrachloride which are costly and thus are not commercially viable.
Synthesis
Candesartan is synthesised as follows:  kubo, K.; Kohara, Y.; Imamiya, E.; Sugiura, Y.; Inada, Y.; Furukawa, Y.; Nishikawa, K.; Naka, T. (1993). “Nonpeptide angiotensin II receptor antagonists. Synthesis and biological activity of benzimidazolecarboxylic acids”. Journal of Medicinal Chemistry 36 (15): 2182–2195. doi:10.1021/jm00067a016. PMID 8340921. Candesartan, a blocking agent against angiotensin II receptor, has been used for years for treating high blood pressure and heart failure. Candesartan cilexetil, a prodrug of candesartan is commercially available from AstraZeneca and Takeda Pharmaceuticals Ltd. European Patent No. 0459136B1 of Takeda Chemical Industries discloses that methods for preparing candesartan cilexetil schematically represented by the following Reaction Scheme 1: Reaction Scheme 1
kubo, K.; Kohara, Y.; Imamiya, E.; Sugiura, Y.; Inada, Y.; Furukawa, Y.; Nishikawa, K.; Naka, T. (1993). “Nonpeptide angiotensin II receptor antagonists. Synthesis and biological activity of benzimidazolecarboxylic acids”. Journal of Medicinal Chemistry 36 (15): 2182–2195. doi:10.1021/jm00067a016. PMID 8340921. Candesartan, a blocking agent against angiotensin II receptor, has been used for years for treating high blood pressure and heart failure. Candesartan cilexetil, a prodrug of candesartan is commercially available from AstraZeneca and Takeda Pharmaceuticals Ltd. European Patent No. 0459136B1 of Takeda Chemical Industries discloses that methods for preparing candesartan cilexetil schematically represented by the following Reaction Scheme 1: Reaction Scheme 1
The method has technical problems as follows: a) the starting material is obtained by a minor reaction, b) its yield is relatively low and its industrial applicability is poor (due to N2 gas formation) because the Curtius rearrangement reaction is involved, and c) materials industrially hard to handle such as SOCI2 or NaH are used. In addition, methods for preparing an intermediate of candesartan cilexetil are disclosed in Organic Process Research & Development 11:490-493(2007), as represented by the following Reaction Scheme 2: Reaction Scheme 2
3:1 s
However, the preparation process has also shortcomings of a) undesired byproducts formed by nitrogenation at ortho- or para-position, b) safety problems from strong acids (sulfuric acid and nitric acid) used twice when introducing and rearranging nitrogen groups, and c) utilization of high-flammable Raney Ni.
cut paste
Novel and Practical Synthesis of Candesartan Cilexetil
Yongjun Mao, Ruisheng Xiong, Zheng Liu, Haihong Li, Jingkang Shen, and Jingshan Shen* *Chinese Academy of Sciences, Shanghai Institute of Materia Medica, 555 Zuchongzhi Rd., Zhangjiang Hi-Tech Park, Shanghai, 201203, China
Abstract
A novel and convergent synthetic route of candesartan cilexetil (API of Atacand), an effective angiotensin II receptor blocker, is described. Cleavage of the N-Boc and N-trityl protective group are implemented simultaneously and formation of the benzimidazole ring is conducted at the last step of this route, which gives candesartan cilexetil in 55% yield over six steps with 99.1% purity (HPLC). Full Text HTMLPDF (567KB)PDF with Links (932KB)
 This compound can be obtained by two related ways: 1) The partial esterification of 3-nitrophthalic acid (I) with ethanol and H2SO4 gives 3-nitrophthalic acid 1-monoethyl ester (II), which is treated with SOCl2 in refluxing benzene to yield the corresponding acyl chloride (III). The reaction of (III) first with sodium azide in DMF and then with refluxing tert-butanol affords 2-(tert-butoxycarbonylamino)-3-nitrobenzoic acid ethyl ester (IV), which is condensed with 4-(2-cyanophenyl)benzyl bromide (V) by means of NaH in THF giving 2-(2′-cyanobiphenyl-4-ylmethylamino)-3-nitrobenzoic acid ethyl ester (VI). The reduction of (VI) with SnCl2.2H2O in ethanol yields the corresponding 3-amino derivative (VII), which is cyclocondensed with ethyl orthocarbonate and acetic acid affording 1-(2′-cyanobiphenyl-4-ylmethyl)-2-ethoxybenzimidazole-7-carboxylic acid ethyl ester (VIII). The reaction of (VIII) with trimethyltin azide in refluxing toluene gives the 2′-(1H-tetrazol-5-yl) derivative (IX), which is saponified with NaOH in ethanol to the corresponding free acid (X). Protection of (X) with trityl chloride and triethylamine in dichloromethane gives the protected compound (XI), which is finally esterified with cyclohexyl 1-iodoethyl carbonate (XII) by means of K2CO3 in DMF. 2) Compound (VIII) can also be obtained by reaction of 2-chloro-1-(2′-cyanobiphenyl-4-ylmethyl)benzimidazole-7-carboxylic acid ethyl ester (XIII) with sodium ethoxide in refluxing ethanol.
This compound can be obtained by two related ways: 1) The partial esterification of 3-nitrophthalic acid (I) with ethanol and H2SO4 gives 3-nitrophthalic acid 1-monoethyl ester (II), which is treated with SOCl2 in refluxing benzene to yield the corresponding acyl chloride (III). The reaction of (III) first with sodium azide in DMF and then with refluxing tert-butanol affords 2-(tert-butoxycarbonylamino)-3-nitrobenzoic acid ethyl ester (IV), which is condensed with 4-(2-cyanophenyl)benzyl bromide (V) by means of NaH in THF giving 2-(2′-cyanobiphenyl-4-ylmethylamino)-3-nitrobenzoic acid ethyl ester (VI). The reduction of (VI) with SnCl2.2H2O in ethanol yields the corresponding 3-amino derivative (VII), which is cyclocondensed with ethyl orthocarbonate and acetic acid affording 1-(2′-cyanobiphenyl-4-ylmethyl)-2-ethoxybenzimidazole-7-carboxylic acid ethyl ester (VIII). The reaction of (VIII) with trimethyltin azide in refluxing toluene gives the 2′-(1H-tetrazol-5-yl) derivative (IX), which is saponified with NaOH in ethanol to the corresponding free acid (X). Protection of (X) with trityl chloride and triethylamine in dichloromethane gives the protected compound (XI), which is finally esterified with cyclohexyl 1-iodoethyl carbonate (XII) by means of K2CO3 in DMF. 2) Compound (VIII) can also be obtained by reaction of 2-chloro-1-(2′-cyanobiphenyl-4-ylmethyl)benzimidazole-7-carboxylic acid ethyl ester (XIII) with sodium ethoxide in refluxing ethanol.
| Benzimidazole derivs., their production and use | |
| Naka, T.; Nishikawa, K.; Kato, T. (Takeda Chemical Industries, Ltd.) | |
| EP 0459136; EP 0720982; JP 1992364171; JP 1996099960; US 5196444; US 5328919; US 5401764; US 5703110; US 5705517; US 5962491; US 6004989 |
more info Candesartan cilexetil of Formula I, disclosed in U.S. Patent No. 5,196,444 as crystalline form, i.e., Form-I (C-type crystals), is chemically described as 1- cyclohexyloxycarbonyloxyethyl 2-ethoxy-3-[[4-[2-(2H-tetrazol-5- yl)phenyl]phenyl]methyl]benzimidazole-4-carboxylate.
H Formula I It is useful in the treatment of cardiovascular complaints such as hypertension and heart failure. Candesartan cilexetil is poorly soluble in water, which is attributed to its hydrophobic nature. Solubility plays an important role in achieving the desired concentration of a drug in systemic circulation for accomplishing the pharmacological response. Various techniques are known in literature to increase the solubility of poorly-soluble drugs, including decreasing the particle size, complexation, changing the surface characteristics of the particles, and incorporation of drug particles into colloidal systems like nanoparticles and liposomes. Among these, the most commonly used technique to increase the solubility is particle size reduction. Sometimes the rate of dissolution of a poorly-soluble drug is the rate limiting factor in its rate of absorption by the body. These drugs may be more readily bioavailable if administered in a finely divided state. Particle size reduction increases the surface area causing an increase in the dissolution rate of the compound, and hence, its bioavailability. There are certain techniques reported in literature to reduce the particle size of such poorly-soluble drugs. PCT Publication No. WO 2006/122254 discloses stable candesartan cilexetil of fine particle size, wherein the stable micronized candesartan cilexetil is prepared by slurrying a sample of candesartan cilexetil of fine particle size in a suitable solvent for a suitable amount of time. In this application, candesartan cilexetil of fine particle size is obtained directly from the synthesis of candesartan cilexetil or by comminuting candesartan cilexetil using milling. PCT Publication No. WO 2005/123720 describes fine particles of candesartan cilexetil having improved pharmacokinetic profile and a process for their production, wherein fine particle size is obtained by a) dissolving candesartan cilexetil in an organic solvent; b) cooling the solution obtained in step a) under stirring to crystallize candesartan cilexetil from the solution; and c) isolating candesartan cilexetil having a particle size of with d90 not more than about 25 μ. U.S. Patent Application No. 2006/0165806 describes compositions comprising a candesartan, such as candesartan cilexitil. The candesartan particles of the composition have an effective average particle size of less than about 2000 nm. U.S. Patent Application No. 2008/0038359 describes a nanoparticle pharmaceutical formulation comprising a poorly soluble drug substance having an average particle size of less than about 1000 nm, a solid or semisolid dispersion vehicle, and optionally a non-surface modifying excipient. U.S. Patent No. 7,828,996 discloses the methods for forming nanoparticles of a material of narrow polydispersity with ultrasonic waves using a partially submersed sonicator that does not touch any part of the apparatus and the point of addition of organic solvent is in the wave funnel produced by sonication and within the selected distance from the wave-source depending on the desired particle size. U.S. Patent No. 7,780,989 discloses the preparation of a dispersion of nanocrystalline particles in an aqueous medium using ultrasound. U.S. Patent No. 5,314,506 describes a crystallization process in which a jet of a solution containing a substance is impinged with a second jet containing an anti-solvent for the substance. The rapid mixing produced by the impinging jets results in a reduction of the crystals so formed compared to conventional slow crystallization processes. The smallest crystals disclosed are about 3 μ and the majority are in the range of from about 3 μ to about 20 μ. PCT Publication No. WO 00/44468 describes a modification to the apparatus described in U.S. Patent No. 5,314,506, wherein ultrasound energy is applied at the point of impingement of the two jets to further enhance localized mixing and is stated to give direct formation of small crystals with a diameter of less than 1 μ. Generally, the crystalline particles described have an average size of 0.5 μ. Conventional particle size reduction methods such as high energy milling may result in loss of yield, noise and dusting, as well as unwanted exposure to highly potent pharmaceutical compounds. Also, in the case of crystalline compounds, stress generated on crystal surfaces during milling can adversely affect labile compounds. Therefore, there is a need for a process for particle size reduction of candesartan cilexetil, which is industrially advantageous, easy to handle and is cost effective.
-
Candesartan is a potent, selective AT1 subtype angiotensin II receptor antagonist and used for treatment of hypertension. Due to poor absorption of Candesartan in body, the prodrug candesartan cilexetilwas developed. The candesartan cilexetil is rapidly and completely hydrolyzed to candesartan in gastrointestinal tract.
-
[0004]U.S. Pat. No. 5,196,444 discloses Candesartan cilexetil and a process for its preparation by the reaction of 2-ethoxy-[[2′-(1H-tetrazol-5-yl)biphenyl-4-yl]methyl]benzimidazole-7-carboxylic acid with trityl chloride in presence of triethyl amine in methylene chloride and purification by column chromatography gives 2-ethoxy-1-[[2′-(N-triphenylmethyltetrazol-5-yl)-biphenyl-4-yl]methyl] benzimidazole -7-carboxylic acid, which upon condensation with cyclohexyl 1-iodoethyl carbonate in presence of potassium carbonate in DMF followed by purification with column chromatography gives a colorless powder which is recrystallized in ethanol yields ‘C’ type crystals of Candesartancilexitil.
-
[0005]U.S. Pat. Application No. 2005/131027 discloses a process for preparation of candesartan cilexetil by reaction of trityl candesartanwith cilexetil halide and at least one base in a low boiling solvent in presence of phase transfer catalyst to give Trityl candesartan cilexetil, which upon deprotection with at least one organic acid in at least one organic solvent. U.S. Pat. Application 2005/131027 further discloses the deprotection of Trityl candesartan cilexetil in methanol without an acid.
-
[0006]The PCT publication WO 2005/021535 discloses the deprotection of Trityl candesartan cilexetil with neutral or slightly basic medium in alcohol.
-
[0007]Chem.Pharm.Bull. 47(2), 182-186 (1999) discloses two novel crystalline forms of Candesartan cilexetil, form-I and form-II.
-
[0008]PCT publication WO 04/085426 discloses Candesartan cilexetil 1,4-Dioxane solvate and two more crystalline forms, designated as form-III and form-IV. The disclosed process for preparation of form-III involves crystallization of Candesartan cilexetil in toluene and for form-IV involves crystallization in a mixture of methyl tert-butyl ether and methanol.
-
[0009]PCT publication WO 2005/077941 discloses several crystalline forms, solvates of Candesartan cilexetil along with a process for preparation of form-I (type-C).
-
[0010]The prior art disclosed methods for preparation of Candesartan cilexetilinvolves purification of Trityl candesartan and Candesartan cilexetil by column chromatography or involves the use of strong acids like IN HCl or the use of organic acids or without an acid in methanol for detrytilation of Trityl candesartan cilexetil.
-
[0011]There is a requirement of a process for preparation of Candesartancilexetil which yields a pure Candesartan cilexetil without involving the purification by column chromatography and the usage of strong acids for deprotection.
Candesartan cilexetil of formula (I) shown beiow is chemicaily described as (+/-)-1- [[(cyclohexyloxy)carbonyl]oxy]ethyl-2-ethoxy-1 -[[2′-(1 H-tetrazol-5-yl)-1 , 1 ‘-biphenyl- 4-yl]methyl]-1 H-benzimidazoie-7-carboxylate. An alternative designation is (+-)-1- hydroxyethyf 2~Ethoxy-1 -{p-(o-1 H-tetrazo!-5-yIphenyi)benzyJ)-7-benzϊmidazoie~ carboxyiic acid cyclohexyl carbonate (ester), with candesartan being the underlying carboxylic acid, i.e. 2-Ethoxy-1 -(p-(o-1 H-tetrazol-5-ylphenyl)benzy!)-7-benz- imidazolecarboxylic acid.
Because of its ability to inhibit the angiotensin-converting enzyme it is widely used for the treatment of hypertension and related diseases and conditions. As an angiotensin Ii receptor antagonist, candesartan ciiexetil avoids the side-effects of calcium antagonists, and shows high stability and obvious curative effects. Currently candesartan ciiexetil is soid as racemic mixture, it is produced according to published patents, e.g. EP 0 720 982 B1 and EP 0 459 136. in Chem. Pharm. Bull. 47(2), 182-186 (1999) two crystalline forms (Form I and II), together with an amorphous form, are disclosed and characterized by their DSC thermograms, X-ray diffraction patterns and IR spectra. US 5,196,444 disclosed the C-type crystal (Form I) of candesartan cilexetif, and processes for producing it under acidic conditions. WO 04/085426 discloses the dioxane solvate of candesartan ciiexetil, together with two additional crystalline forms. WO 2005/077941 discloses hydrates and solvates of candesartan ciiexetil, together with processes for their preparation. WO 2006/048237 also describes the preparation of new polymorphic forms ofcandesartan ciiexetil, together with processes for their preparation, including the preparation of amorphous candesartan ciiexetil by precipitating it with a liquid cyclic hydrocarbon from a solution of candesartan ciiexetil in a chlorinated solvent. in WO 2005/123721 processes for the preparation of amorphous candesartanciiexetil are provided, comprised of spray-drying and precipitation. HPLC CUT PASTE , READER TO PICK ONLY REQUIRED INFO Candesartan cilexetil (60 g) is dissolved in isopropanol (900 m!_) at 60-65 0C. Solution is hot filtered into reactor and quickly cooled to 35 0C. At this temperature nucleation is provoked with 300 mg of candesartan cilexetil form I and stirring is enforced. Suspension is cooled to 3O0C in 1 hour and rigorous stirring is continued at this temperature for additional 5 hours. Then stirring power is reduced and the suspension is cooled to 2O0C in 8 hours. The product is filtered, washed with isopropanoi and dried for 2 hours at 38°C. Yield: 48.7 g of candesartan cilexetil form I. Area % HPLC: candesartan cilexetil: 99.73%, alky ester of candesartan cilexetil 0.08%, candesartan cilexetii pyran below 0.05%, tritylcandesartan cϋexetil 0.09% Average particle size: 19 /vm, no agglomerates present (see Figure 2) B) Detection of impurities in candesartan cilexetil Example 6 Detection of candesartan cϊlexetil pyran in candesartan cilexetii by HPLC HPLC (external standard method) was performed using the following specifications : Column: Zorbax Eclipse XDB-C18, 50 mm x 4.6 mm i.d.τ 1.8 μm particles Eluent A: 0.01 M NaH2PO4, pH 2.5 Eluent B: acetonitriie Gradient of Eluent:
Flow rate: about 1.2 ml/min Diluent: acetonitriie : water = 70 : 30 (V/V). Detection: UV, wavelength 225 nm injection volume: 5 μl Column temperature : 500C Autosampler temperature: 7°C Example 7 Detection of cilexetil pyran in 1 -chloroethyl cyclohexylcarbonate by GC GC/FID (area percent method) was performed using the following specifications: Column: capillary (fused-silica) AT-WAX or adequate Length: 30 m ID: 0.32 mm Film thickness: 0.25 μm Carrier gas: helium Carrier gas flow rate: 2.0 ml/mi n Split ratio: 10 : 1 Air flow rate: 400 ml/min Hydrogen flow rate: 40 ml/min Make up gas flow ISb rate: 25 ml/min Column temperature 100°C (0 min) → 10°C/min → 2000C (10 min or prolonged if necessary) Injector temperature: 21 O0C Detector temperature: 250OC Injection volume : 1 μl Diluent: Acetonithle: chromatography grade. Chromatographic system suitability Signal/noise of 1 -chloroethyl cyclohexyl carbonate: not less than 10
………………
Seki M * Mitsubishi Tanabe Pharma Corporation, Osaka, Japan An Efficient C–H Arylation of a 5-Phenyl-1H-tetrazole Derivative: A Practical Synthesis of an Angiotensin II Receptor Blocker. Synthesis 2012; 44: 3231-3237 
Significance
Candesartan cilexetil (Atacand®) is an angiotensin II receptor antagonist that is prescribed for the treatment of hypertension. It is a prodrug that is hydrolyzed to candesartan in the gut. The synthesis depicted, features an efficient protocol for ruthenium-catalyzed C–H arylation of the tetrazole A. Comment A significant challenge in this small-scale synthesis was the final removal of the benzyl protecting group from the tetrazole unit using transfer hydrogenation. Best results were obtained using a ‘thickshell’ Pd/C catalyst from Evonik

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....