| FDA Orange Book Patents: 1 of 1 (FDA Orange Book Patent ID) | |
|---|---|
| Patent | 9549999 |
| Expiration | Mar 10, 2030 |
| Applicant | GE HEALTHCARE |
| Drug Application |
|
Home » Uncategorized (Page 29)
Category Archives: Uncategorized
Pirlindole

Pirlindole
- Molecular FormulaC15H18N2
- Average mass226.317 Da
Pirlindole (Lifril, Pyrazidol) is a reversible inhibitor of monoamine oxidase A (RIMA) which was developed and is used in Russia as an antidepressant.[1]:337 It is structurally and pharmacologically related to metralindole.
Biovista is investigating BVA-201, a repurposed oral formulation of pirlindole mesylate, for the potential treatment of multiple sclerosis
SYN 1

SYN 2

PAPER
Khimiko-Farmatsevticheskii Zhurnal (1986), 20(3), 300-3.
PATENT
U.S.S.R. (1986), SU 276060
PAPER
Sudebno-meditsinskaia ekspertiza (1989), 32(4), 49-50
PAPER
Journal of Pharmaceutical and Biomedical Analysis
https://www.sciencedirect.com/science/article/abs/pii/S0731708598002131
PATENT
claiming method for resolving racemic mixture of pirlindole hydrochloride into enantiomerically pure (S)-pirlindole and/or (R)-pirlindole,
Pirlindole, 2, 3, 3a, 4, 5, 6-hexahydro-lH-8-methyl-pyrazine
[3, 2, 1-j , k] carbazole, is a tetracyclic compound of the formula I
(I)
Pirlindole is a reversible monoamine oxidase A inhibitor being up to date useful as a medicament in the treatment of depression.
Pirlindole has an asymmetric carbon atom which implies that there are two enantiomers, (S) -pirlindole and (R) -pirlindole .
The state of the art teaches several methods for the enantiomeric separation of pirlindole. For example, The Journal of Pharmaceutical and Biomedical Analysis, 18(1998) 605- 614, “Enantiomeric separation of pirlindole by liquid chromatography using different types of chiral stationary phases”, Ceccato et al, discloses the enantiomeric separation of pirlindole by liquid chromatography (LC) using three different chiral stationary phases.
Further, The Journal of Pharmaceutical and Biomedical Analysis 27(2002) 447-455, “Automated determination of pirlindole enantiomers in plasma by on-line coupling of a pre-column packed with restricted access material to a chiral liquid chromatographic column”, Chiap et al., discloses the use of a pre-column packed with restricted access material for sample clean up coupled to a column containing a cellulose based chiral stationary phase for separation and quantitative analysis of the enantiomers .
According to the prior art, Chirality 11:261-266 (1999) all attempts to obtain the enantiomers of pirlindole by selective crystallization with optically active acids failed, and it was only possible to obtain at laboratory scale (few grams) as hydrochloride salt, using derivatization technique in conjunction with preparative chromatography.
The characteristics of the process disclosed in the state of the art limit in a definitive way, its implementation on an industrial or semi-industrial scale due to the necessity to use a separation by chromatography on a large scale which makes the process very costly, difficult to implement and with poor reproducibility. .
EXAMPLE 7
(R) -Pirlindole mesylate
Starting from 10 g of (R) -pirlindole (S) -mandelate obtained in Example 1 and following the procedure described in Example 5 using methanesulfonic acid as pharmaceutical acceptable acid, ,
7.4 g (0.023 mole) of (R) -pirlindole mesylate were obtained (yield = 85.2% ). Chiral HPLC (enantiomeric purity = 98.0%).
XAMPLE 9
(S) -pirlindole mesylate
Starting from 10 g of (S) -pirlindole (R) -mandelate obtained in Example 2 and following the procedure described in Example 6 using methanesulfonic acid as pharmaceutical acceptable acid, 6.8 g (0.021 mole) of (S) -pirlindole mesylate were obtained (yield = 77.8%). Chiral HPLC (enantiomeric purity = 98.0%).
PATENT
Process for the preparation of pirlindole . useful for treating depression.
Pirlindole (8-methyl-2,3,3a,4,5,6-hexahydro-lH-pyrazino[3,2,l-jk]carbazole) of formula I
Compound Formula I
also described as Pyrazidole™ represents a new class of original tetracyclic antidepressants, the pyrazinocarbazole derivatives. The drug was synthesized and characterized at the end of the 1960s and was marketed as an anti-depressant in 1975. Current clinical trials have demonstrated to be a highly effective short-acting and safe drug.
[0003] Pirlindole is a selective, reversible inhibitor of MAO-A. In-vitro evidence suggest the catalytic oxidation of Pirlindole into dehydro-pirlindole by MAO-A. Dehydro-pirlindole may be a more potent slowly reversible inhibitor of MAO-A and this might explain the persistence of MAO-A inhibition in-vivo (MAO-The mother of all amine oxidases, John P.M. Finberg et al. 1998, Springer).
[0004] Pirlindole chemical structure is composed of one stereogenic centre which indicates the existence of two enantiomers, the ( ?)-Pirlindole and the (S)-Pirlindole.
[0005] Although Pirlindole pharmacological data and the clinical use were performed on the racemate, recently there have been increasing interest in the pharmacological profile of each enantiomer (WO 2015/171005 Al).
[0006] International patent publication WO 2015/171003A1 filed 9th May 2014 discloses a resolution of racemic pirlindole into optically active pirlindole. The Resolution-Racemization-Recycle (RRR) synthesis described involves derivatization by preparation of pairs of diastereomers in the form of salts from an optically active organic acid. These diastereomers can be separated by conventional techniques such as crystallisation. Although it is a very efficient procedure to prepare laboratorial scale or pre-clinical batch of (/?)- or (S)-Pirlindole, it is not economically convenient at an industrial scale because the process relies on Pirlindole racemate as the starting material.
[0007] Andreeva et al. (Pharmaceutical Chemistry 1992, 26., 365-369) discloses the first isolation of Pirlindole enantiomers in isolated form. ( ?)-Pirlindole of formula II
was isolated as an hydrochloride salt from a racemic base by the fractional crystallization of racemic pirlindole salt with (+)-camphor-10-sulfonic acid. (S)-Pirlindole formula III
was also isolated as an hydrochloride salt although via asymmetric synthesis from the 6-methyl-2,3,4,9-tetrahydro-lH-carbazol-l-one IV
[0008] Compound of formula IV was reacted with chiral auxiliary (S)-(-)-a-methylbenzylamine to afford asymmetric (S)-6-methyl-N-(l-phenylethyl)-2,3,4,9-tetrahydro-lH-carbazol-l-imine V
[0009] Compound of formula V was subjected to stereoselective reduction with sodium borohydride in ethanol. According to Andreeva et al. the reaction might occur through directed intramolecular hydride transfer after formation of a complex between compound of formula V and reducing agent to afford (S)-6-methyl-N-((S)-l-phenylethyl)-2,3,4,9-tetrahydro-lH-carbazol-l-amine VI
[0010] Compound of formula VI is reacted with ethylene glycol ditosylate by ethylene bridge formation under alkaline conditions to yield (S)-8-methyl-3-((S)-l-phenylethyl)-2,3,3a,4,5,6-hexahydro-lH-pyrazino[3,2,l-jk]carbazole VII.
[0011] Alkaline agent is sodium hydride (NaH), in the presence of dimethyl sulfoxide (DMSO) or dimethylformamide (DMF).
[0012] The ratio between alkaline agent, compound of formula VI and ethylene glycol ditosylate is 1.2:1:1.
[0013] The cyclization reaction occurs at room temperature for a period of 4.5 hours. [0014] Compound of formula VII was subjected to catalytic hydrogenolysis conditions to afford the desired hydrochloride salt of compound of formula III.
[0015] The hydrogenolysis reaction was catalysed by Palladium on charcoal (Pd content 0.1 g, 9 mol%) and was conducted in methanol. The conversion of compound of formula VII into compound of formula III was performed under a hydrogen pressure of 1.8-2.0 MPa at 22 °C for a period of 17h.
[0016] The work-up conditions for the hydrogenolysis reaction involved neutralization with ammonia solution followed by benzene recrystallization. The hydrochloride salt of compound of formula III was formed from addition of hydrochloric acid to a solution of free base in ethanol.
[0017] The process yielded (S)-Pirlindole hydrochloride with a final yield of 10% with respect to the intermediate VI.
[0018] The mixture of sodium hydride with DMSO generates dimsyl anion. This anion is very often used in laboratory scale, but because it is unstable its use on large scale should be under specific precautions. Dimsyl anion decomposition is exotermic. It is reported that dimsyl anion decomposition starts even at 20 °C, and above 40 °C it decomposes at an appreciable rate (Lyness, W. I. et ai, U.S. 3,288,860 1966, CI. 260-607).
[0019] The mixture of DMF and sodium hydride is reported in ‘Sax & Lewis’s Dangerous Properties of Industrial Materials’ to give a violent reaction with ignition above 50 °C. Buckey, J. et ai, Chem. Eng. News 1982, 60(28), 5, describes the thermal runaway of a pilot plant reactor containing sodium hydride and DMF from 50 °C. Accelerated Rate Calorimetry (ARC) tests showed exothermic activity as low as 26 °C. Similar behaviour was also seen with DMA. De Wall, G. et ai, Chem. Eng. News 1982, 60(37), 5, reports a similar incident, wherein runaway started at 40 °C, and rose 100 °C in less than 10 minutes, boiling off most of the DMF.
[0020] There exists a need for safe, industrial- and eco-friendly processes for the preparation of Pirlindole enantiomers. These facts are disclosed in order to illustrate the technical problem addressed by the present disclosure.
[0068] In an embodiment, the preparation of (S)-8-methyl-3-((S)-l-phenylethyl)-2,3,3a,4,5,6-hexahydro-lH-pyrazino[3,2,l-jk]carbazole, compound of formula VII was carried out as follow.
[0069] In an embodiment, in a 2 L three necked round bottomed flask equipped with magnetic stirrer, ethylene glycol ditosylate (73 g, 197 mmol) and DMI (240 mL) were loaded. To the resulting clear solution, NaH (60% suspension in mineral oil, 15.8 g, 394 mmol) was added carefully. To the resulting suspension a solution of VI ((S)-6-methyl-N-((S)-l-phenylethyl)-2,3,4,9-tetrahydro-lH-carbazol-l-amine) (30 g, 98.5 mmol) in DMI (60 mL) was added dropwise at 60 °C. The mixture was stirred for 1 h at 60 °C. The mixture was cooled down to room temperature, then MeOH was added slowly with ice-water cooling. A white precipitation appeared, and the resulting suspension was stirred and then filtered. The filtered product was washed with water-MeOH. The product was dried under vacuum to give 24.9 g of compound of formula VII (75.2 mmol, yield: 76%). Purity >99.9area% (HPLC).
[0070] In an embodiment, the preparation of hydrochloride salt of (S)-Pirlindole, compound of formula III, was performed as follow.
[0071] In an embodiment, the free amine VII ((S)-8-methyl-3-((S)-l-phenylethyl)-2,3,3a,4,5,6-hexahydro-lH-pyrazino[3,2,l-jk]carbazole) (8,32 g, 25 mmol) was dissolved in DCM (42 mL) and excess of HCI in MeOH (42 mL) was added. The solvents were evaporated under reduced pressure to dryness to give a yellow oil. The residue was dissolved in MeOH (120 mL) and was added to the dispersion of Pd/C (1,74 g, -50% water) in MeOH (20 mL). The reaction mixture was stirred at 50 °C under a 750 KPa (7.5 bar) pressure of hydrogen for 5h. After completion (HPLC) the suspension was filtered through a celite pad, and the filter cake was washed with MeOH. The pH of the resulting solution was checked (<3) and it was evaporated to give the crude hydrochloride salt of compound of formula III. To the crude material iPrOH was added and the suspension was allowed to stir at reflux. The suspensions were filtered, and the product was dried under vacuum to give the hydrochloride salt of (S)-Pirlindole, compound of formula III (5.11 g, 19.5 mmol, yield: 77%). Purity > 99.5% (HPLC). Enantiomeric purity 99.5% (Chiral HPLC). MS (ESI): m/z 227.2 (M+H)+.
PATENT
Process for the preparation of piperazine ring for the synthesis of pyrazinocarbazole derivatives, such as the antidepressant pirlindole .
Pirlindole hydrochloride is the compound represented in formula I
[0003] It is the common name of 8-methyl-2,3,3a,4,5,6-hexahydro-lH-pyrazino[3,2,l-jk]carbazole hydrochloride which is an active pharmaceutical ingredient marketed with the name Pyrazidol™. The compound is effective as an anti-depressant agent.
[0004] Pirlindole chemical structure belongs to the pyrazinocarbazole group. It is composed of one stereogenic centre which anticipate the existence of two enantiomers, the ( ?)-Pirlindole of formula II and the (S)-Pirlindole of formula III.
[0005] Although Pirlindole pharmacological data and the clinical use were performed on the racemate, recently there have been increasing interest in the pharmacological profile of each enantiomer (WO 2015/171005 Al).
[0006] The document WO 2015/171003Al(Tecnimede group) filed 9th May 2014 discloses a resolution of racemic pirlindole into optically active pirlindole. The Resolution-Racemization-Recycle (RRR) synthesis described involves derivatization by preparation of pairs of diastereomers in the form of salts from an optically active organic acid. These diastereomers can be separated by conventional techniques such as crystallisation. Although it is a very efficient procedure to prepare laboratorial scale or pre-clinical batch of (/?)- or (S)-Pirlindole, it is not economically convenient at an industrial scale because the process relies on Pirlindole racemate as the starting material.
[0007] Processes to prepare Pirlindole involve the formation of a piperazine ring. The state of the art discloses different processes for piperazine ring formation but they are generally a multistep approach, and they are hampered by low yields, expensive reagents, or are reported as unsuccessful (Roderick et al. Journal of Medicinal Chemistry 1966, 9, 181-185).
[0008] The first asymmetric synthesis of Pirlindole enantiomers described by Andreeva et al. (Pharmaceutical Chemistry 1992, 26, 365-369) discloses a one-step process to prepare pyrazinocarbazole piperazine ring system from a tetrahydrocarbazole-amine. The process discloses a very low yield (23.8 %) and employs the use of sodium hydride (NaH) in the presence of dimethyl sulfoxide (DMSO) or dimethyl formamide (DMF), both conditions described as generating exothermic decomposition that can cause reaction ignition or reaction thermal runaway.
[0009] The mixture of sodium hydride with DMSO generates dimsyl anion. This anion is very often used in laboratory scale, but because it is unstable its use on large scale should be under specific precautions. The dimsyl anion decomposition is exothermic. It is reported that dimsyl anion decomposition starts even at 20 °C, and above 40 °C it decomposes at an appreciable rate (Lyness et al. US 3288860).
[0010] The mixture of DMF and sodium hydride is reported in Sax & Lewis’s Dangerous Properties of Industrial Materials to give a violent reaction with ignition above 50 °C. Buckey et al., (Chemical & Engineering News, 1982, 60(28), 5) describes the thermal runaway of a pilot plant reactor containing sodium hydride and DMF from 50 °C. Accelerated Rate Calorimetry (ARC) tests showed exothermic activity as low as 26 °C.
Similar behaviour was also seen with DMA. De Wall et al. (Chem. Eng. News, 1982, 60(37), 5) reports a similar incident, wherein runaway started at 40 °C, and rose 100 °C in less than 10 minutes, boiling off most of the DMF.
[0011] An alternative process for the preparation of a piperazine ring system of a pyrazinocarbazole derivative can involve the formation of a lactam ring in a three steps approach:
1. N-acylation reaction;
2. intramolecular indole acetamide cyclisation to afford a lactam ring;
3. lactam reduction.
[0012] Intramolecular indole chloroacetamide cyclization to yield a lactam ring has been described by Bokanov et al. (Pharmaceutical Chemistry Journal 1988, 23, 12, 1311-1315) particularly in the non-enantioselective synthesis of pyrazinocarbazolone derivatives. Bokanov et al. did not describe the lactam reduction into a piperazine ring.
[0013] Intramolecular indole chloroacetamide cyclization to yield a lactam ring has also been described both by Rubiralta et al. (Journal of Organic Chemistry 54, 23, 5591-5597) and Bennasar, et al. (Journal of Organic Chemistry 1996., 61, 4, 1239-1251), as an unexpected outcome of a photocyclization reaction. The lactam conversion was low (<11% yield).
[0014] Lactam reduction of a pyrazinone into piperazine ring systems is disclosed both by Aubry et al. (Biorganic Medicinal Chemistry Letters 2007, 17, 2598-2602) and Saito et al. (Tetrahedron 1995, 51, 30, 8213-8230) in the total synthesis of alkaloid natural products.
[0015] There exists the need for improved processes for the preparation of piperazine ring derivatives in particular enantioselective processes for the preparation of pyrazinocarbazole intermediates precursors of Pirlindole enantiomers compounds of formula II and III.
Example 1 – Preparation of (S)-8-methyl-3-((S)-l-phenylethyl)-3a,4,5,6-tetrahydro-lH-pyrazino[3,2,l-jk]carbazol-2(3H)-one – Formula IV
[00106] In an embodiment, the preparation of (S)-8-methyl-3-((S)-l-phenylethyl)-3a,4,5,6-tetrahydro-lH-pyrazino[3,2,l-jk]carbazol-2(3H)-one (Formula IV) was carried out as follows. To the solution of VI (S)-6-methyl-N-((S)-l-phenylethyl)-2,3,4,9-tetrahydro-lH-carbazol-l-amine (30 g, 98.5 mmol) in toluene (300 mL), 50 % (w/v) aqueous NaOH (79 g) was added dropwise at 0-5 °C, then the solution of chloroacetyl
chloride (12 mL, 148 mmol, 1.5 equiv.) in toluene (15 mL) was added dropwise at 0-5 °C. The mixture was stirred at 0-5 °C for approximately 2.5 h, and additional chloroacetyl chloride (12 mL, 148 mmol, 1.5 equiv.) in toluene (15 mL) was added dropwise at 0-5 °C. The mixture was stirred at 0-5 °C for approximately 1.5 h. Water was added to the reaction mixture keeping the temperature below 5 °C. The phases were separated, and the aqueous phase was extracted with toluene. The organic phase was treated with 2M aqueous HCI. The resulting suspension was filtered. The filtered solid was identified as the HCI salt of VI, which can be liberated and driven back to the chloroacetylation step. The phases of the mother liquor were separated, and the aqueous phase was extracted with toluene. The organic phase was dried over Na2S04, filtered and concentrated under reduced pressure to about 350 mL as a solution in toluene. The toluene solution of the crude product compound of formula X was reacted in the next step.
[00107] In an embodiment, in the same reaction vessel to the toluene solution of crude intermediate obtained in previous step were added TBAB (0.394 g, 1.22 mmol, 1 w/w% for the theoretical yield of prev. step) and 50 % (w/v) aqueous NaOH (8.1 g, 10 equiv.). The reaction mixture was stirred for 1 h at 65 °C, while the reaction was complete. Water was added to the mixture at 0 °C, and the phases were separated, the organic phase was washed with aqueous HCI, and with water, then dried over Na2S04, filtered and evaporated to give 32.87 g of compound IV (S)-8-methyl-3-((S)-l-phenylethyl)-3a,4,5,6-tetrahydro-lH-pyrazino[3,2,l-jk]carbazol-2(3H)-one (yield: 97% for the two steps) as a brown solid. The crude product was reacted in the next step without further purification.
Example 2 – Preparation of (S)-8-methyl-3-((S)-l-phenylethyl)-2,3,3a,4,5,6-hexahydro-lH-pyrazino[3,2,l-jk]carbazole _ Formula V
[00108] In an embodiment, the preparation of (S)-8-methyl-3-((S)-l-phenylethyl)-2,3,3a,4,5,6-hexahydro-lH-pyrazino[3,2,l-jk]carbazole (Formula V) was performed as follows. To the stirred solution of 32.87 g of IV, (S)-8-methyl-3-((S)-l-phenylethyl)-3a,4,5,6-tetrahydro-lH-pyrazino[3,2,l-jk]carbazol-2(3H)-one (95.4 mmol) in dry THF (170 mL) 66 mL solution of sodium bis(2-methoxyethoxy)aluminium hydride in toluene (70 w/w%, 237 mmol, 2.5 equiv.) was added dropwise. The reaction mixture was warmed to 40 °C, and the end of the addition the mixture was stirred at 50 °C until the total consumption of the starting material. Additional 22 mL of sodium bis(2-methoxyethoxy)aluminium hydride solution (70 w/w%, 79 mmol, 0.8 equiv.) was added dropwise. After completion the mixture was cooled to room temperature and 5% aqueous NaOH was added carefully. Water and DCM were added to the mixture, the phases were separated, and the aqueous phase was extracted with DCM. The organic phase was dried over Na2S04, filtered and the solvent was evaporated to get a brown solid (28.8 g). This crude product was dissolved in DCM and MeOH was added. White solid precipitated. The solid was filtered and washed with MeOH to give V (S)-8-methyl-3-((S)-l-phenylethyl)-2,3,3a,4,5,6-hexahydro-lH-pyrazino[3,2,l-j‘k]carbazole 14.6 g (yield: 46%) as an off-white cotton-like solid.
Example 3 – Preparation of (S)-Pirlindole Hydrochloride – Formula III
[00109] In an embodiment, the preparation of (S)-Pirlindole hydrochloride III was carried out as follows. The free amine V ((S)-8-methyl-3-((S)-l-phenylethyl)-2,3,3a, 4,5,6-hexahydro-lH-pyrazino[3,2,l-jk]carbazole) (8.32 g, 25 mmol) was dissolved in DCM (42 mL) and excess of HCI in MeOH (42 mL) was added. The solvents were evaporated under reduced pressure to dryness to give a yellow oil. The residue was dissolved in MeOH (120 mL) and was added to the dispersion of Pd/C (1.74 g, -50% water) in MeOH (20 mL). The reaction mixture was stirred at 50 °C under 750 KPa (7.5 bar) pressure of hydrogen for 5h. After completion (HPLC) the suspension was filtered through a celite pad, and the filter cake was washed with MeOH. The pH of the resulting solution was checked (<3) and it was evaporated to give the crude hydrochloride salt of compound of formula III. To the crude material iPrOH was added and the suspension was allowed to stir at reflux. The suspensions were filtered, and the product was dried under vacuum to give the hydrochloride salt of (S)-Pirlindole, compound of formula III (5.11 g, 19.5 mmol, yield: 77%). Purity > 99.5% (HPLC). Enantiomeric purity 99.5% (Chiral HPLC). MS (ESI): m/z 227.2 (M+H)+.
[00110] Table 1. Comparative yields
Synthesis Reference
http://www.biomedsearch.com/nih/Pirlindole-in-treatment-depression-meta/21053988.html
General References
- Branco JC, Tome AM, Cruz MR, Filipe A: Pirlindole in the treatment of depression and fibromyalgia syndrome. Clin Drug Investig. 2011 Oct 1;31(10):675-89. doi: 10.2165/11595410-000000000-00000. [PubMed:21877764]
- Bruhwyler J, Liegeois JF, Geczy J: Pirlindole: a selective reversible inhibitor of monoamine oxidase A. A review of its preclinical properties. Pharmacol Res. 1997 Jul;36(1):23-33. doi: 10.1006/phrs.1997.0196. [PubMed:9368911]
- Psychiatry: The State of the Art Volume 3 Pharmacopsychiatry [Link]
- Chemistry Dashboard- Pirlindole [Link]
- Pirlindole in the Treatment of Depression and Fibromyalgia Syndrome [Link]
- Hypertensive effect and cheese [Link]
- Monamine oxide inhibitors [Link]
References
- Jump up^ Medvedev AE, et al. The influence of the antidepressant pirlindole and its dehydro-derivative on the activity of monoamine oxidase A and GABAA receptor binding. Chapter 36 in MAO – The Mother of all Amine Oxidases (Journal of Neural Transmission. Supplementa). Eds Finberg JPM, Youdim MBH, Riederer P, Tipton KF. Special edition of Journal of Neural Transmission, Suppl. 52 1st ed. 1998 ISBN 978-3211830376
 |
|
| Clinical data | |
|---|---|
| Trade names | Pirazidol |
| Routes of administration |
Oral |
| ATC code |
|
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 20–30% |
| Protein binding | 95% |
| Metabolism | hepatic |
| Onset of action | 2 to 8 hours |
| Elimination half-life | 185 hours |
| Excretion | urine (50–70%), feces (25–45%) |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C15H18N2 |
| Molar mass | 226.32 g/mol |
| 3D model (JSmol) | |
//////////////Pirlindole, Lifril, Pyrazidol, 60762-57-4, DEPRESSION
CC1=CC2=C(C=C1)N3CCNC4C3=C2CCC4
A call to (green) arms: a rallying cry for green chemistry and engineering for CO2 capture, utilisation and storage
A call to (green) arms: a rallying cry for green chemistry and engineering for CO2 capture, utilisation and storage
Abstract
Chemists, engineers, scientists, lend us your ears… Carbon capture, utilisation, and storage (CCUS) is among the largest challenges on the horizon and we need your help. In this perspective, we focus on identifying the critical research needs to make CCUS a reality, with an emphasis on how the principles of green chemistry (GC) and green engineering can be used to help address this challenge. We identify areas where GC principles can readily improve the energy or atom efficiency of processes or reduce the environmental impact. Conversely, we also identify dilemmas where the…
View original post 115 more words
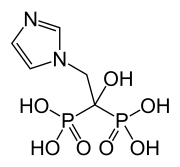
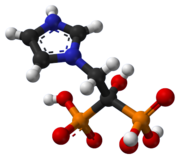
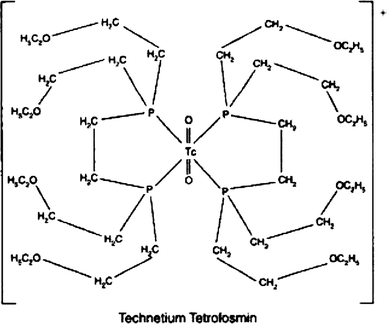
Technetium (99mTc) tetrofosmin, テトロホスミンテクネチウム (99mTc)

Technetium (99mTc) tetrofosmin, 99mTc-Tetrofosmin
テトロホスミンテクネチウム (99mTc)
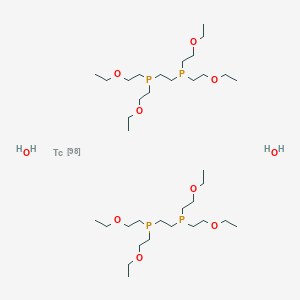
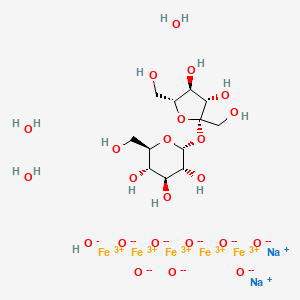
| Formula | C36H80O10P4Tc |
|---|---|
| Molar mass | 895.813 g/mol |
| CAS Number |
|
|---|
UNII42FOP1YX93
2-[bis(2-ethoxyethyl)phosphanyl]ethyl-bis(2-ethoxyethyl)phosphane;technetium-98;dihydrate
Technetium Tc 99m tetrofosmin; Technetium Tc-99m tetrofosmin; TECHNETIUM TC-99M TETROFOSMIN KIT; Tc-99m tetrofosmin; Technetium-99 tetrofosmin; Technetium (99mTc) tetrofosmin
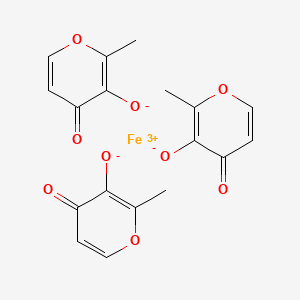
Technetium Tc-99m Tetrofosmin is a radiopharmaceutical consisting of tetrofosmin, composed of two bidentate diphosphine ligands chelating the metastable radioisotope technetium Tc-99 (99mTc), with potential imaging activity upon SPECT (single photon emission computed tomography). Upon administration, technetium Tc 99m tetrofosmin is preferentially taken up by, and accumulates in, myocardial cells. Upon imaging, myocardial cells can be visualized and changes in ischemia and/or perfusion can be detected.
Technetium Tc-99m tetrofosmin is a drug used in nuclear myocardial perfusion imaging. The radioisotope, technetium-99m, is chelated by two 1,2-bis[di-(2-ethoxyethyl)phosphino]ethane ligands which belong to the group of diphosphines and which are referred to as tetrofosmin. It is a lipophilic technetium phosphine dioxo cation that was formulated into a freeze-dried kit which yields an injection.[A31592] Technetium Tc-99m tetrofosmin was developed by GE Healthcare and FDA approved on February 9, 1996.
Technetium Tc-99m tetrofosmin is a drug used in nuclear myocardial perfusion imaging. The radioisotope, technetium-99m, is chelated by two 1,2-bis[di-(2-ethoxyethyl)phosphino]ethane ligands which belong to the group of diphosphines and which are referred to as tetrofosmin. It is a lipophilic technetium phosphine dioxo cation that was formulated into a freeze-dried kit which yields an injection.[1] Technetium Tc-99m tetrofosmin was developed by GE Healthcare and FDA approved on February 9, 1996.
Technetium (99mTc) tetrofosmin is a drug used in nuclear medicine cardiac imaging. It is sold under the brand name Myoview (GE Healthcare). The radioisotope, technetium-99m, is chelated by two 1,2-bis[di-(2-ethoxyethyl)phosphino]ethane ligands which belong to the group of diphosphines and which are referred to as tetrofosmin.[1][2]
Tc-99m tetrofosmin is rapidly taken up by myocardial tissue and reaches its maximum level in approximately 5 minutes. About 66% of the total injected dose is excreted within 48 hours after injection (40% urine, 26% feces). Tc-99m tetrofosmin is indicated for use in scintigraphic imaging of the myocardium under stress and rest conditions. It is used to determine areas of reversible ischemia and infarcted tissue in the heart. It is also indicated to detect changes in perfusion induced by pharmacologic stress (adenosine, lexiscan, dobutamine or persantine) in patients with coronary artery disease. Its third indication is to assess left ventricular function (ejection fraction) in patients thought to have heart disease. No contraindications are known for use of Tc-99m tetrofosmin, but care should be taken to constantly monitor the cardiac function in patients with known or suspected coronary artery disease. Patients should be encouraged to void their bladders as soon as the images are gathered, and as often as possible after the tests to decrease their radiation doses, since the majority of elimination is renal. The recommended dose of Tc-99m tetrofosmin is between 5 and 33 millicuries (185-1221 megabecquerels). For a two-dose stress/rest dosing, the typical dose is normally a 10 mCi dose, followed one to four hours later by a dose of 30 mCi. Imaging normally begins 15 minutes following injection.[3]

Amersham (formerly Nycomed Amersham , now GE Healthcare ) has developed and launched 99mTc-tetrofosmin (Myoview) as an injectable nuclear imaging agent for ischemic heart disease in several major territories and for use in detecting breast tumors
Technetium (99mTc) tetrofosmin is a drug used in nuclear medicine cardiac imaging. It is sold under the brand name Myoview (GE Healthcare). The radioisotope, technetium-99m, is chelated by two 1, 2-bis-[bis-(2-ethoxyethyl)phosphino] ethane ligands, which belong to the group of diphosphines and which are referred to as tetrofosmin and has the structural Formula 1 :
Formula 1
99mTc -based radiopharmaceuticals are commonly used in diagnostic nuclear medicine, especially for in vivo imaging (e.g. via immunoscintigraphy or radiolabeling). Usually cold kits are manufactured in advance in accordance with strict requirements of Good Manufacturing Practice (GMP) Guidelines, containing the chemical ingredients (e.g. 99mTc -coordinating ligands, preservatives) in lyophilized form. The radioactive isotope 99mTc (ti/2 = 6h) is added to those kits shortly before application to the patient via intravenous or subcutaneous injection.
Tc-99m tetrofosmin is rapidly taken up by myocardial tissue and reaches its maximum level in approximately 5 minutes. About 66% of the total injected dose is excreted within 48 hours after injection (40% urine, 26% feces). Tc-99m tetrofosmin is indicated for use in scintigraphic imaging of the myocardium under stress and rest conditions. It is used to determine areas of reversible ischemia and infarcted tissue in the heart. It is also indicated to detect changes in perfusion induced by pharmacologic stress (adenosine, lexiscan, dobutamine or persantine) in patients with coronary artery disease. Its third indication is to assess left ventricular function (ejection fraction) in patients thought to have heart disease. No contraindications are known for use of Tc-99m tetrofosmin, but care should be taken to constantly monitor the cardiac function in patients with known or suspected coronary artery disease. Patients should be encouraged to void their bladders as soon as the images are gathered, and as often as possible after the tests to decrease their radiation doses, since the majority of elimination is renal. The recommended dose of Tc-99m tetrofosmin is between 5 and 33 millicuries (185-1221 megabecquerels). For a two-dose stress/rest dosing, the typical dose is normally a 10 mCi dose, followed one to four hours later by a dose of 30 mCi. Imaging normally begins 15 minutes following injection.
99mTc -Tetrofosmin is also described to be useful for tumor diagnostics, in particular of breast cancer and parathyroid gland cancer, and for multidrug resistance (MDR) research.
US5045302 discloses 99mTc-coordinating diphosphine ligands (L), wherein one preferred example thereof is the ether functionalized diphosphine ligand l,2-bis[bis(2-ethoxy- ethyl)phosphino]ethane according to Formula 1, called tetrofosmin (“P53”), that forms a dimeric cationic technetium (V) dioxo phosphine complex, [TCO2L2] with 99mTc, useful as myocardial imaging agent. Example 1 of said patent described the process for preparing tetrofosmin by reacting ethyl vinyl ether, bis(diphosphino)ethane in the presence of a-azo-isobutyronitrile (AIBN) in a fischer pressure-bottle equipped with a teflon stirring bar followed by removal of volatile materials and non-distillable material obtained, as per below mentioned Scheme 1.
Scheme 1
Formula 2 Formula 3 Formula 1
CN 1184225 C discloses tetrofosmin salts containing chloride or bromide or aryl sulfonates as negatively charged counter ions, which can be used for the preparation of a 99mTc- Tetrofosmin radiopharmaceutical composition. According to this patent tetrofosmin hydrochloride is a viscous liquid. Own experiments of the inventors of the present invention revealed that the halide salts of tetrofosmin are hygroscopic oils, which are complicated to handle, e.g. when weighed. The oily and hygrospcopic
properties of tetrofosmin hydrochloride hampers its use in pharmaceutical preparations. Attempts to synthesize the subsalicylate salt of tetrofosmin failed because the starting material sulfosalicylic acid was not soluble in ether in the concentration specified in the patent (3.4 g in 15 ml).
WO2006/064175A1 discloses tetrofosmin was converted to tetrofosmin subsalicylate by reaction with 2.3 to 2.5 molar equivalents of 5-sulfosalicyclic acid at room temperature in ethanol, followed by recrystallisation from ethanol/ether.
WO2015/114002A1 relates to tetrafluoroborate salt of tetrafosmin and its process for the preparation thereof. Further this application also discloses one-vial and two vial kit formulation with tetrafluoroborate salt of tetrafosmin.
The article Proceedings of the International Symposium, 7th, Dresden, Germany, June 18-22, 2000 by Amersham Pharmacia Biotech UK Limited titled “The synthesis of [14C]tetrofosmin, a compound vital to the development of Myoview, Synthesis and Applications of Isotopically Labelled Compounds” disclosed a process for the preparation of tetrofosmin as per below mentioned Scheme 2:
Scheme 2
Formula 1A Formula 7
The starting material was bis(2- ethoxyethyl)benzylphosphine of Formula 4 . This was prepared from benzyl phosphonate, PhCH2P(0)(OEt)2 by reduction with lithium aluminium hydride to give the intermediate benzylphosphine, PhCH2PH2, followed by a photolysis reaction in the presence of ethyl vinyl ether to give compound of Formula 4. The compound of Formula 4 in acetonitrile was treated with dibromo[U-14C]ethane to give compound of Formula 6, further it was treated with excess of 30% aqueous sodium hydroxide in ethanol. The mixture was stirred at room temperature for 24 hours. The solvent was removed and the residue was treated with excess concentrated hydrochloric acid at 0°C. Aqueous work up gave compound of Formula 7. Then compound of Formula 7 in dry benzene was treated with hexachlorodisilane and hydrolysed with excess 30% aqueous sodium hydroxide at 0°C. Aqueous work up followed by flash column chromatography on silica gave [bisphosphinoethane- 1,2-14C]tetrofosmin of formula 1A.
The article Polyhedron (1995), 14(8), 1057-65, titled “Synthesis and characterization of Group 10 metal complexes with a new trifunctional ether phosphine. The X-ray crystal structures of bis[bis(2-ethoxyethyl)benzylphosphine]dichloronickel(II) and bis[bis(2-ethoxyethyl)benzylphosphine]chlorophenylnickel(II)” disclosed the process for the preparation of bis(2-ethoxyethyl)benzylphosphine as per below mentioned Scheme 3:
Scheme 3
Formula 8 Formula 9 Formula 4
The compound bis(2-ethoxyethyl)benzylphosphine of Formula 4 was prepared by first reduction of diethylbenzylphosphonate of Formula 8 using lithium aluminium hydride to obtain benzyl phosphine of Formula 9 followed by radical catalysed coupling reaction with ethyl vinyl ether carried out by using UV photolysis.
Tetrofosmin is extremely sensitive to atmospheric oxygen, which makes synthesis of the substance, as well as manufacturing and handling of the kit complicated as the substance has constantly to be handled in an oxygen free atmosphere.
High purity and stability under dry and controlled conditions are pivotal requirements for chemical compounds used as active ingredients in pharmaceuticals.
The processes disclosed in prior art for the preparation of compound of Formula 4 involves that coupling reaction of benzyl phosphine of Formula 9 with ethyl vinyl ether carried out by using photolytic conditions. Such technology is expensive as it requires separate instruments including isolated facility (to avoid the UV radiation exposure etc.), also it is not suitable for commercial scale production.
PATENT
WO-2018162964
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2018162964&tab=PCTDESCRIPTION&maxRec=1000
Example 1
Preparation of benzyl phosphine:
A mixture of lithium aluminium hydride (25 g) in methyl tertiary butyl ether (MTBE) (800 ml) was cooled to 0 to 5°C and added a solution of diethylbenzylphosphonate in methyl tertiary butyl ether (100 g in 200ml). The temperature of reaction mixture was raised to 25 to 30 °C and stirred for 14 to 16 hour. After completion of the reaction, the reaction mixture was cooled to 0 to 5°C and 6N hydrochloric acid was added slowly. Further raised the temperature of reaction mixture to 25 to 30 °C and stirred for 30-45 minutes. The layers were separated, the aqueous layer was extracted with MTBE (250ml) and the combined organic layer was washed with deoxygenated water. The organic layer was dried over sodium sulfate and concentrated to obtain the title compound as non-distillable liquid.
Example 2
Preparation of benzylbis(2-ethoxyethyl)phosphane:
To a mixture of benzyl phosphine (obtained from example 1) and vinyl ethyl ether (250 ml) in pressure RB flask was added a-azo-isobutyronitrile (AIBN) (1.5g). The resulting reaction mixture was maintained at 80 to 90°C for 14 to 16 hours. The mixture was cooled to 20 to 30°C and AIBN (0.5g) added, then continued to heat the reaction mixture at 80 to 90°C for 6 to 7 hours. After completion of the reaction, the reaction mixture was allowed to cool to room temperature and distilled under vacuum to obtain title compound as an oil (107 g).
Example 3
Preparation of Ethane- 1,2-diylbis (benzylbis(2-ethoxyethyl) phosphonium) bromide:
To a mixture of benzylbis(2-ethoxyethyl)phosphane 107.g) in acetonitrile (100ml) in pressure bottle was added 1, 2-dibromoethane (30.5 g). The reaction mixture was maintained at 80 to 90°C for 20 to 25 hours. After completion of the reaction, the reaction mass was cooled to room temperature and stirred for 45 to 60 minutes to obtain the solid. To the solid obtained was added methyl tertiary butyl ether (MTBE) (500ml) and stirred at room temperature for 2 to 3 hour. The reaction mass was filtered, washed with MTBE and suck dried. Further the filtered solid was heated in acetone (400ml) at 50 to 55°C for 2 to 3 hour. Then cooled the reaction mixture to room temperature, stirred, filtered and washed with acetone to obtain the title compound as white solid. (85g)
Example 4
Preparation of Ethane- 1, 2-diylbis (bis (2-ethoxy ethyl) phosphine oxide):
To a mixture of Ethane- 1,2-diylbis (benzylbis(2-ethoxyethyl) phosphonium) bromide (80g) in ethanol (480 ml) was added an aq. solution of sodium hydroxide ( 48g in 160 ml water) at room temperature. The reaction mass was maintained at 25 to 35°C for 10 to 12 hour. After completion of the reaction, the reaction mass was cone, under vacuum to obtained the residue. The residue was dissolved in deoxygenated water (400 ml) and washed with MTBE (400 ml x 2). The layers were separated, the aqueous layer was cooled to 10 to 20°C and 6N hydrochloric acid (200 ml) was added slowly. Then extracted the aqueous layer with dichloromethane (2000 ml), washed the organic layer with deoxygenated water (160 ml), dried the organic layer using sodium sulfate, filtered, and distilled under vacuum to obtain the residue. Further MTBE (160 ml x 2) was added to the residue and continued distillation under vacuum, degassed to obtain the solid. To the obtained solid, MTBE (400 ml) was added and heated at 45 to 50°C for 1-2 hour, further slowly cooled the reaction mass to 25 to 30°C, filtered the solid product. Again MTBE (400 ml) was added to the solid product and heated at 45 to 50°C for 1-2 hour, further slowly cooled the reaction mass to 25 to 30°C, filtered, washed with MTBE and dried under vacuum to obtain the title compound as white solid (32g).
Example 5
Preparation of tetrofosmin free base:
To a mixture of ethane- 1, 2-diylbis (bis (2-ethoxyethyl) phosphine oxide (18g) in toluene (180ml) in pressure RB flask argon/nitrogen gas was purged for 5 minute and hexachlorodisilane (30g) was added. The reaction mixture was heated to 80 to 90°C, stirred for 10 to 12 hour, further slowly cooled to -5 to 0°C and slowly added 30% aqueous sodium hydroxide solution (45g sodium hydroxide in 150 ml deoxygenated water) the temperature of reaction mixture was raised to 25 to 30°C and stirred for 1 to 2 hour. The layers were separated and the aq. layer was extracted with Toluene (180 ml). The combined organic layer was washed with deoxygenated water (180 ml). Further dried the organic layer using sodium sulfate, distilled under vacuum to obtain the residue of tetrofosmin free base (15.5g).
Example 6
Preparation of tetrofosmin disulfosalicylate salt:
To the residue of tetrofosmin free base (15.5g) was added an aq. solution of 5-sulfosalicylic acid dihydrate (21.6g in 75ml deoxygenated water) and stirred at 25 to 30°C for 25 to 30 minutes. Further heated the reaction mass to 55 to 60°C, stirred for 15 to 30 minute, slowly cooled the reaction mass to 10 to 15°C and stirred for 1-2 hour. Filtered, washed with chilled deoxygenated water, and dried under vacuum to obtain the title compound as white solid. (30g).
Example 7
Preparation of Form J of tetrofosmin disulfosalicylate salt:
An aq. solution of 5-sulfosalicylic acid dihydrate (21.6g in 75ml deoxygenated water) was added slowly into tetrofosmin free base (15.5g) and stirred at room temperature for 30 to 40 minutes. The temperature of reaction mixture was further raised to 50 to 60°C, stirred for 20 to 30 minute, cooled the reaction mass to 10 to 15°C and stirred for 1-2 hour. Filtered, washed with chilled deoxygenated water, and dried under vacuum to obtain the title compound.
PATENT
EP337654 ,
PATENT
US9549999
FDA Orange Book Patents
References
- Jump up^ Kelly JD, Alan M. Forster AM, Higley B, et al. (February 1993). “Technetium-99m-Tetrofosmin as a new radiopharmaceutical for myocardial perfusion imaging”. Journal of Nuclear Medicine. 34 (2): 222–227. PMID 8429340.
- Jump up^ Elhendy A, Schinkel AF, et al. (December 2005). “Risk stratification of patients with angina pectoris by stress 99mTc-tetrofosmin myocardial perfusion imaging”. Journal of Nuclear Medicine. 46 (12): 2003–2008. PMID 16330563.
- Jump up^ Myoview package insert. Arlington Heights, IL: GE Healthcare, 2006, Aug.
 |
|
| Clinical data | |
|---|---|
| Routes of administration |
Intravenous |
| ATC code | |
| Pharmacokinetic data | |
| Bioavailability | N/A |
| Identifiers | |
| CAS Number |
|
| Chemical and physical data | |
| Formula | C36H80O10P4Tc |
| Molar mass | 895.813 g/mol |
External links
Myoview Prescribing Information Page
//////////99mTc-Tetrofosmin, Technetium (99mTc) tetrofosmin, テトロホスミンテクネチウム (99mTc)
CCOCCP(CCOCC)CCP(CCOCC)CCOCC.CCOCCP(CCOCC)CCP(CCOCC)CCOCC.O.O.[Tc]
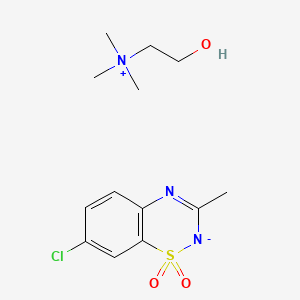
Diazoxide choline
Diazoxide choline,
RN: 1098065-76-9
UNII: 2U8NRZ7P8L
Diazoxide choline; UNII-2U8NRZ7P8L; 2U8NRZ7P8L; YLLWQNAEYILHLV-UHFFFAOYSA-N
| Molecular Formula: | C13H20ClN3O3S |
|---|---|
| Molecular Weight: | 333.831 g/mol |
Ethanaminium, 2-hydroxy-N,N,N-trimethyl-, compd. with 7-chloro-3-methyl-2H-1,2,4-benzothiadiazine dioxide (1:1)
7-chloro-3-methyl-1$l^{6},2,4-benzothiadiazin-2-ide 1,1-dioxide;2-hydroxyethyl(trimethyl)azanium
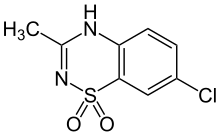
 Diazoxide
Diazoxide
CAS: 364-98-7 FREE FORM
2H-1,2,4-Benzothiadiazine, 7-chloro-3-methyl-, 1,1-dioxide
- 4H-1,2,4-Benzothiadiazine, 7-chloro-3-methyl-, 1,1-dioxide (7CI)
- 3-Methyl-7-chloro-1,2,4-benzothiadiazine 1,1-dioxide
- 7-Chloro-3-methyl-2H-1,2,4-benzothiadiazine 1,1-dioxide
- Diazoxide
- Dizoxide
- Eudemine injection
- Hyperstat
- Hypertonalum
- Mutabase
- NSC 64198
- NSC 76130
- Proglicem
- Proglycem
- SRG 95213
- Sch 6783
Diazoxide (INN; brand name Proglycem[1]) is a potassium channel activator, which causes local relaxation in smooth muscle by increasing membrane permeability to potassium ions. This switches off voltage-gated calcium ion channels, preventing calcium flux across the sarcolemma and activation of the contractile apparatus.
In the United States, this agent is only available in the oral form and is typically given in hospital settings.[2]
Medical uses
Diazoxide is used as a vasodilator in the treatment of acute hypertension or malignant hypertension.[3]
Diazoxide also inhibits the secretion of insulin by opening ATP-sensitive potassium channel of beta cells of the pancreas, thus it is used to counter hypoglycemia in disease states such as insulinoma (a tumor producing insulin)[4] or congenital hyperinsulinism.
Diazoxide acts as a positive allosteric modulator of the AMPA and kainate receptors, suggesting potential application as a cognitive enhancer.[5]
Side effects
The Food and Drug Administration published a Safety Announcement in July 2015 highlighting the potential for development of pulmonary hypertension in newborns and infants treated with this drug.[2]Diazoxide interferes with insulin release through its action on potassium channels.[6] Diazoxide is one of the most potent openers of the K+ ATP channels present on the insulin producing beta cells of the pancreas. Opening these channels leads to hyperpolarization of cell membrane, a decrease in calcium influx, and a subsequently reduced release of insulin.[7] This mechanism of action is the mirror opposite of that of sulfonylureas, a class of medications used to increase insulin release in Type 2 Diabetics. Therefore, this medicine is not given to non-insulin dependent diabetic patients.
SYN
Medicinal Chemistry Research, 12(9), 457-470; 2004

PATENT
WO 2009006483
https://patents.google.com/patent/WO2009006483A1/enIt
PATENT
US 20120238554
PATENT
WO 2013130411
able 16. Characterization of Forms A and B of Diazoxide Choline Salt In
Screening Study
Experiment Form A Form B
*Maj or peaks (2-Θ):
Form A (9.8, 10.5, 14.9, 17.8, 17.9, 18.5, 19.5, 22.1, 22.6, 26.2, 29.6, 31.2);
Form B (8.9, 10.3, 12.0, 18.3, 20.6, 24.1, 24.5, 26.3, 27.1, 28.9).
** Unique FTIR (ATR) absorbances (cm 1):
Form A (2926, 2654, 1592, 1449, 1248);
Form B (3256, 2174, 2890, 1605, 1463, 1235).
6.1.5.1. Solubility Screen in organic solvents.
[00725] Diazoxide choline, prepared in MEK using choline hydroxide as 50 wt % solution in water (see above) displayed some solubility in the following solvents:
acetonitrile, acetone, ethanol, IPA, MEK, DMF, and methanol. These solvents were chosen due to differences in functionality, polarity, and boiling points and their ability to dissolve diazoxide. Other solvents which showed poor ability to dissolve salts were used as antisolvents and in slurry experiments where some solubility was observed: dioxane, MTBE, EtOAc, IP Ac, THF, water, cyclohexane, heptane, CH2C12, and toluene.
[00726] Solvents for crystallizations during screening were chosen based on the solubility screen summarized in Table 17. Crystallizations of diazoxide choline from all conditions afforded a total of two forms, A and B. Forms A and B were found to be anhydrous polymorphs of diazoxide choline. Form B was observed to be generated from most solvents used. It was difficult to isolate pure Form A on large scales (>50 mg) as conditions observed to produce Form A on a smaller scale (approximately 50 mg or less) were found to result in Form B or mixtures of both forms on larger scales. Based on room-temperature slurry experiments, anhydrous Form B was found to be the most thermodynamically stable form in this study. Form A readily converted to Form B in all slurry solvents utilized.
Table 17. Solubility Screen for Diazoxide Choline Salt
Solvent Cmpd Solvent Cone. Temp. Soluble
(mg) (mL) (mg/niL) (°C)
CH2CI2 1.3 5.00 0.26 55 Partially
Toluene 1.4 5.00 0.28 55 No
.1.5.2. Single-Solvent Crystallizations
[00727] Fast cooling procedure: Diazoxide (approximately 20 mg) was weighed out into vials and enough solvent (starting with 0.25 mL) was added until the material completely dissolved at elevated temperature. After hot filtration the vials were placed in a refrigerator (4 °C) for 16 hours. After the cooling-process the samples were observed for precipitates which were isolated by filtration. Vials not demonstrating precipitates were evaporated down to dryness using a gentle stream of nitrogen. All solids were dried in vacuo at ambient temperature and 30 in. Hg.
[00728] Slow cooling procedure: Diazoxide (approximately 30 mg of choline salt) was weighed out into vials and enough solvent was added until the material went into solution at elevated temperature. After hot filtration the vials were then slowly cooled to room temperature at the rate of 20 °C/h and stirred at room temperature for 1-2 hours. All solids were dried in vacuo at ambient temperature and 30 in. Hg.
[00729] Based on the initial solubility study, seven solvents were selected for the fast-cooling crystallization: acetonitrile, acetone, ethanol, IPA, MEK, DMF, and methanol. Table 18 shows a list of the solvents that were used and the amount of solvent needed to dissolve the material. After the cooling-process precipitates were noticed in samples # 2, 3, 5, and 6, the solids were isolated by filtration. The other samples (# 1, 4, and 7) were evaporated down to dryness using a gentle stream of nitrogen. The diazoxide choline salts were found to be consistent with Form A by XRPD analysis for all solids with the exception of sample #2 (consistent with the freeform) and sample #5 (consistent with Form B with preferred orientation observed).
Table 18. Single- Solvent Crystallization of Diazoxide Choline Salt Using Fast- Cooling Procedure
[00730] In accordance with the data obtained from fast-cooling experiments, four solvents which showed precipitation of solids were chosen for the slow-cooling experiments: MeOH, EtOH, MeCN, and IPA (Table 19). All obtained analyzable solids of the choline salt were found to be consistent with Form B by XRPD with the exception of Entry #1 which was consistent with diazoxide freeform and Entry #2 which was not analyzable. Mother liquor of Entry #2 was concentrated to dryness and the residual solids were analyzed by XRPD and found to be Form B material. As a result of obtaining freeform material from the single- solvent crystallizations in methanol, three more alcohols were tested for the single- solvent crystallizations using fast- and slow-cooling procedures. Tables 20 and 21 provide a list of the solvents that were used and the amount of solvent needed to dissolve the material. XRPD patterns of the fast-cooling procedure showed freeform of diazoxide from isobutanol, Form B from isoamyl alcohol, and Form A from tert-amyl alcohol compared to the slow-cooling procedure, which afforded Form B material from all three solvents.
Table 19. Single-Solvent Crystallization of Diazoxide Choline Salt Using Slow- Cooling Procedure
Table 20. Single- Solvent Crystallization of Diazoxide Choline Salt Using Fast- Cooling Procedure
Table 21. Single-Solvent Crystallization of Diazoxide Choline Salt Using Slow- Cooling Procedure
[00731] The results of the choline salt single- solvent fast- and slow-cooling crystallizations (see Tables 19 to 21) indicated that Form A was more likely to be isolated with fast-cooling profiles and Form B with slow-cooling profiles.
6.1.5.3. Binary Solvent Crystallizations
[00732] Binary- solvent crystallizations of the choline salt were performed using four primary solvents (MeOH, EtOH, IPA, and MeCN) and nine cosolvents (MTBE, EtOAc, IPAc, THF, c-hexane, heptane, toluene, CH2CI2, and dioxane) with a fast-cooling profile (supra). XRPD patterns showed that Form B was obtained from mixtures of MeOH with MTBE, EtOAc, IPAc, toluene, and dioxane. As shown in Table 22, Form A was obtained from mixtures of MeOH with THF and with CH2CI2 after evaporating the solvent to dryness. The mixtures of MeOH with cyclohexane and heptane provided the freeform of diazoxide. All solids obtained from fast-cooling procedures with EtOH, IPA, and MeCN as primary solvents provided Form B material.
Table 22. Binary-Solvent Crystallizations of Choline Salt of Diazoxide Using Fast- Cooling Procedure and MeOH as a Primary Solvent
* Solids were dissolved at 62 °C.
** Freeform of diazoxide.
[00733] Binary- solvent recrystallizations of the choline salt with the slow-cooling procedure were performed using two primary solvents (IPA and MeCN) and nine cosolvents (MTBE, EtOAc, IPAc, THF, c-hexane, heptane, toluene, CH2C12, and dioxane). All solids obtained from a slow-cooling procedure with IPA and MeCN as primary solvents provided Form B material based on XRPD analysis. The results of
binary- solvent crystallizations indicated that Form B was the most thermodynamic ally stable form of diazoxide choline.
6.1.5.4. Binary Solvent Crystallizations Using Water as a Cosolvent
[00734] In an attempt to investigate the formation of hydrates of the choline salt, experiments was performed using fast- and slow-cooling procedures and water as a cosolvent.
[00735] The fast cooling procedure (supra) was used with the exception of using different primary solvents which were miscible with water: acetone, acetonitrile, DMF, IPA, i-BuOH, i-AmOH, and t-AmOH. Water was utilized in these crystallizations as a cosolvent. All solids obtained from the fast-cooling procedure with water as the cosolvent provided diazoxide freeform material by XRPD analysis.
[00736] To compare the results obtained from the fast-cooling procedure a set of experiments was performed using a slow-cooling procedure and water as a cosolvent. All obtained solids were analyzed by XRPD and afforded patterns consistent with diazoxide freeform. Without wishing to be bound by theory, these results suggest that the conditions used for crystallization caused dissociation of the choline salt. A small amount of a second crop was obtained in each sample, but only two samples were analyzable by XRPD and indicated that the samples were freeform material. All mother liquors were evaporated to dryness and the residual solids were also analyzed by XRPD to afford patterns consistent with Form B of the choline salt.
6.1.5.5. Metastable Zone Width Estimation
[00737] Form B: To produce a robust process, an understanding of the solubility profiles of the various solid forms under consideration is required. From a practical standpoint, this involves the measurement of the metastable zone width (MSZW) of pure forms, whereby the saturation and supersaturation curves of the different forms are generated over a well defined concentration and temperature range. This knowledge can then be used to design a crystallization protocol that should ideally favor a selective crystal growth of the desired form.
[00738] Form B of diazoxide choline salt showed moderate solubility in a solvent mixture made of MeCN/MeOH/MtBE (10: 1: 12, volume ratios). The wide width of the metastable zone as shown in Table 23 gives many seeding options. During the MSZW measurement, aliquots from the crystallizing material were withdrawn and analyzed by XRPD to ensure that no form conversion occurred during the experiment. Indeed, the material remained unchanged during the test.
Table 23. Meta-Stable Zone Width For Form B Diazoxide Choline Salt in
MeCN/MeOH/MtBE (10:1:12) (v/v).
[00739] Form A: The metastable zone width for Form could not be estimated because this polymorphic form converted during the experiment to Form B.
6.1.5.6. Crystallization of Form A of Diazoxide Choline Salt
[00740] The choline salt of diazoxide (160.3 mg) was dissolved in 1 mL of IPA at 55 °C which was then passed through a Millipore 0.45 μΜ filter into a clean vial. This vial was placed in freezer a -20 °C overnight. Solids were not noticed and the flask was scratched with a micro- spatula. The vial was placed back in the freezer and nucleation was noticed after ten minutes. The solids were collected by vacuum filtration and washed with 1 mL of MtBE. The solids were dried in vacuo at 40 °C and 30 in. Hg to afford 70 mg (43.6% recovery) of Form A as determined by XRPD.
6.1.5.7. 500-mg Scale Crystallization of Form B of Diazoxide Choline Salt
[00741] The choline salt of diazoxide (524.3 mg) was dissolved in 3 mL of IPA at 78 °C and this solution was then cooled to 55 °C for the addition of MtBE. The MtBE (4 mL) was added until nucleation was observed. After nucleation the batch was allowed to cool to room temperature at a rate of 20 °C /h. The solids were collected by vacuum filtration and washed with 1 mL of MtBE. The solids were dried in vacuo at 40 °C and 30 in. of Hg to afford 426.7 mg (81.3% recovery) of Form B as determined by XRPD.
6.1.5.8. 2-g Scale Crystallization of Form B of Diazoxide Choline Salt
[00742] The choline salt of diazoxide (2.0015 g) was dissolved in 5.5 mL of IPA at 78 °C to afford a clear solution. This solution was passed through a Millipore Millex FH 0.45 μΜ filter. This solution was then cooled to 55 °C. MtBE was added in 1 mL portions, with a two minute interval between portions. Nucleation was noted after the second addition of MtBE. This suspension was allowed to cool to room temperature at a rate of 20 °C /h and stirred at this temperature for 16 hours. The solids were collected by vacuum filtration and washed with 1 mL of MtBE. The solids were dried in vacuo at 40 °C and 30 in. of Hg to afford 1.6091 g (80.4% recovery) of Form B as determined by XRPD.
6.1.5.9. Detection of Form Impurities
[00743] Mixtures of diazoxide choline Forms A and B were prepared by adding a minor amount of Form A to Form B. Samples were lightly ground by hands with a mortar and pestle for approximately one minute. Samples were then analyzed by XRPD analysis. XRPD analysis was found to be suitable for detecting 5% of Form A in Form B.
References
- Jump up^ Diazoxide, drugs.com
- ^ Jump up to:a b “FDA Drug Safety Communication: FDA warns about a serious lung condition in infants and newborns treated with Proglycem (diazoxide)” (Press release). Food and Drug Administration. July 16, 2015. Retrieved 2015-07-19.
- Jump up^ van Hamersvelt HW, Kloke HJ, de Jong DJ, Koene RA, Huysmans FT (August 1996). “Oedema formation with the vasodilators nifedipine and diazoxide: direct local effect or sodium retention?”. Journal of Hypertension. 14 (8): 1041–5. doi:10.1097/00004872-199608000-00016. PMID 8884561.

- Jump up^ Huang Q, Bu S, Yu Y, et al. (January 2007). “Diazoxide prevents diabetes through inhibiting pancreatic beta-cells from apoptosis via Bcl-2/Bax rate and p38-beta mitogen-activated protein kinase”. Endocrinology. 148 (1): 81–91. doi:10.1210/en.2006-0738. PMID 17053028.

- Jump up^ Randle, John C.R.; Biton, Catherine; Lepagnol, Jean M. (15 November 1993). “Allosteric potentiation by diazoxide of AMPA receptor currents and synaptic potentials”. European Journal of Pharmacology. 247 (3): 257–65. doi:10.1016/0922-4106(93)90193-D. PMID 8307099.

- Jump up^ Panten, Uwe; Burgfeld, Johanna; Goerke, Frank; Rennicke, Michael; Schwanstecher, Mathias; Wallasch, Andreas; Zünkler, Bernd J.; Lenzen, Sigurd (1989-04-15). “Control of insulin secretion by sulfonylureas, meglitinide and diazoxide in relation to their binding to the sulfonylurea receptor in pancreatic islets”. Biochemical Pharmacology. 38 (8): 1217–1229. doi:10.1016/0006-2952(89)90327-4.
- Jump up^ Doyle, Máire E.; Egan, Josephine M. (2003-03-01). “Pharmacological Agents That Directly Modulate Insulin Secretion”. Pharmacological Reviews. 55 (1): 105–131. doi:10.1124/pr.55.1.7. ISSN 1521-0081. PMID 12615955.
 |
|
| Clinical data | |
|---|---|
| Trade names | Proglycem |
| AHFS/Drugs.com | Monograph |
| Pregnancy category |
|
| Routes of administration |
Oral, intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | 90% |
| Metabolism | Hepatic oxidation and sulfate conjugation |
| Elimination half-life | 21-45 hours |
| Excretion | Renal |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard | 100.006.063 |
| Chemical and physical data | |
| Formula | C8H7ClN2O2S |
| Molar mass | 230.672 g/mol |
| 3D model (JSmol) | |
//////////////Diazoxide choline
CC1=NC2=C(C=C(C=C2)Cl)S(=O)(=O)[N-]1.C[N+](C)(C)CCO
CC1=NC2=C(C=C(C=C2)Cl)S(=O)(=O)[N-]1.C[N+](C)(C)CCO
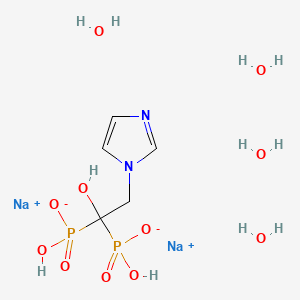
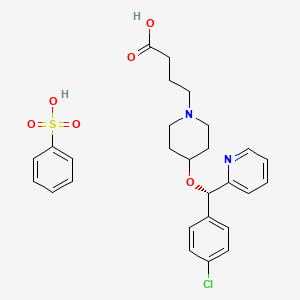
Bepotastine Besilate, ベポタスチンベシル酸塩
Bepotastine Besilate
ベポタスチンベシル酸塩
- Molecular FormulaC27H31ClN2O6S
- Average mass547.063 Da
HL-151
-
- Use:antiallergic, antihistaminic
| 10 mg Tablets | For the treatment of allergic rhinitis | 27.03.2017 CDSCO
APPROVED |
USFDA
NDA 22-288 Bepotastine Besilate 1.5% Ophthalmic Solution ISTA Pharmaceuticals, Inc.
https://www.accessdata.fda.gov/drugsatfda_docs/nda/2009/02228s000_ChemR.pdf
Drug Substance Bepotastine besilate is manufactured by Ube Industries and the information for the NDA is submitted through DMF #19966. Bepotastine besilate is a white crystalline powder with no odor and bitter taste. It is very soluble in but sparingly soluble in . It is stable when exposed to light, and optically active. The S-isomer is the active drug and is controlled as an impurity through synthesis. The distribution coefficient in 1-octanol is higher than in aqueous buffer in the pH 5-9 range. There are 10 potential impurities but only one impurity is above 0.1%. Two potential genotoxic impurities are controlled below . Residual is controlled below Bepotastine besilate is stable under long term storage conditions for (25ºC/60% RH) over 5 years
Bepotastine besilate was originally developed as an oral tablet dosage form and got approval in Japan in 2000 for allergic rhinitis. It is a non-sedating anti-allergic drug. The proposed NDA is an ophthalmic solution indicated for allergic conjunctivitis. Bepotastine besilate ophthalmic solution 1.5% is a sterile solution. It is an aqueous solution to be administered as drops at or near physiological pH range of tears. The formulation contains sodium chloride, monobasic sodium phosphate as dihydrate, benzalkonium chloride, sodium hydroxide and purified water; typically these components are used for , preservative action, pH adjustment,
INTRO
Bepotastine is a non-sedating, selective antagonist of the histamine 1 (H1) receptor. Bepotastine was approved in Japan for use in the treatment of allergic rhinitis and uriticaria/puritus in July 2000 and January 2002, respectively, and is marketed by Tanabe Seiyaku Co., Ltd. under the brand name Talion. It is available in oral and opthalmic dosage forms in Japan. The opthalmic solution is FDA approved since Sept 8, 2009 and is under the brand name Bepreve.
Tae Hee Ha, Chang Hee Park, Won Jeoung Kim, Soohwa Cho, Han Kyong Kim, Kwee Hyun Suh, “PROCESS FOR PREPARING BEPOTASTINE AND INTERMEDIATES USED THEREIN.” U.S. Patent US20100168433, issued July 01, 2010., US20100168433
BEPREVE® (bepotastine besilate ophthalmic solution) 1.5% is a sterile, topically administered drug for ophthalmic use. Each mL of BEPREVE contains 15 mg bepotastine besilate.
Bepotastine besilate is designated chemically as (+) -4-[[(S)-p-chloro-alpha -2pyridylbenzyl] oxy]-1-piperidine butyric acid monobenzenesulfonate. The chemical structure for bepotastine besilate is:
 |
Bepotastine besilate is a white or pale yellowish crystalline powder. The molecular weight of bepotastine besilate is 547.06 daltons. BEPREVE ophthalmic solution is supplied as a sterile, aqueous 1.5% solution, with a pH of 6.8.
The osmolality of BEPREVE (bepotastine besilate ophthalmic solution) 1.5% is approximately 290 mOsm/kg.
ベポタスチンベシル酸塩 JP17
Bepotastine Besilate

C21H25ClN2O3▪C6H6O3S : 547.07
[190786-44-8]
Bepotastine (Talion, Bepreve) is a 2nd generation antihistamine.[1] It was approved in Japan for use in the treatment of allergic rhinitisand urticaria/pruritus in July 2000 and January 2002, respectively. It is currently marketed in the United States under the brand-name Bepreve, by ISTA Pharmaceuticals.
Bepotastine besilate is a second-generation antihistamine that was launched in a tablet formulation under a collaboration between Tanabe Seiyaku and Ube in 2000 and in 2002 for the treatment of allergic rhinitis including sneeze, mucus discharge and solidified mucus, and for the treatment of urticaria, respectively. An orally disintegrating tablet was made available in Japan in 2006, while a dry syrup formulation for the treatment of allergic rhinitis was studied in clinical trials at Tanabe Seiyaku for the treatment of allergic rhinitis
Originally developed at Ube, bepotastine besilate was later licensed to Tanabe Seiyaku as part of a collaboration agreement. In 2010, rights were licensed to Dong-A and Mitsubishi Tanabe Pharma in Korea for the treatment of eye disorders.
Pharmacology
Bepotastine is available as an ophthalmic solution and oral tablet. It is a direct H1-receptor antagonist that inhibits the release of histamine from mast cells.[2] The ophthalmic formulation has shown minimal systemic absorption, between 1 and 1.5% in healthy adults.[3] Common side effects are eye irritation, headache, unpleasant taste, and nasopharyngitis.[3] The main route of elimination is urinary excretion, 75-90% excreted unchanged.[3]
Marketing history
It is marketed in Japan by Tanabe Seiyaku under the brand name Talion. Talion was co-developed by Tanabe Seiyaku and Ube Industries, the latter of which discovered bepotastine. In 2001, Tanabe Seiyaku granted Senju, now owned by Allergan, exclusive worldwide rights, with the exception of certain Asian countries, to develop, manufacture and market bepotastine for ophthalmic use. Senju, in turn, has granted the United States rights for the ophthalmic preparation to ISTA Pharmaceuticals.
Sales and patents
In 2011, ISTA pharmaceuticals experienced a 2.4% increase in net revenues from 2010, which was driven by the sales of Bepreve. Their net revenue for 2011 was $160.3 million.[4] ISTA Pharmaceuticals was acquired by Bausch & Lomb in March 2012 for $500 million.[5] Bausch & Lomb hold the patent for bepotastine besilate (https://www.accessdata.fda.gov/scripts/cder/ob/docs/temptn.cfm. On November 26, 2014, Bausch & Lomb sue Micro Labs USA for patent infringement.[6] Bausch & Lomb was recently bought out by Valeant Pharmaceuticals in May 2013 for $8.57 billion, Valeant’s largest acquisition to date, causing the company’s stock to rise 25% when the deal was announced.[7]
Clinical trials
A Phase III clinical trial was carried out in 2010 to evaluate the effectiveness of bepotastine besilate ophthalmic solutions 1.0% and 1.5%.[8] These solutions were compared to a placebo and evaluated for their ability to reduce ocular itchiness. The study was carried out with 130 individuals and evaluated after 15 minutes, 8 hours, or 16 hours. There was a reduction in itchiness at all-time points for both ophthalmic solutions. The study concluded that bepotastine besilate ophthalmic formulations reduced ocular itchiness for at least 8 hours after dosing compared to placebo. Phase I and II trials were carried out in Japan.
Studies have been performed in animals and bepotastine besilate was not found to be teratogenic in rats during fetal development, even at 3,300 times more that typical use in humans.[3] Evidence of infertility was seen in rats at 33,000 times the typical ocular does in humans.[3] The safety and efficacy has not been established in patients under 2 years of age and has been extrapolated from adults for patients under 10 years of age.[3]
SYN
EP 0335586; JP 1989242574; JP 1990025465; JP 1993294929; US 4929618
The reaction of 4-[1-(4-chlorophenyl)-1-(2-pyridyl)methoxy]piperidine (I) with ethyl 4-bromobutyrate (II) by means of K2CO3 in refluxing acetone gives the corresponding condensation product (III), which is then hydrolyzed with NaOH in ethanol/water yielding compound (IV).
SYN 2
JP 1998237070; JP 2000198784; WO 9829409
A new synthesis of betotastine has been developed: The racemic 4-[1-(4-chlorophenyl)-1-(2-pyridyl)methoxy]piperidine (I) is submitted to optical resolution with N-acyl amino acids such as N-acetyl-L-phenylalanine (preferred), N-acetyl-L-leucine, N-(benzyloxycarbonyl)-L-phenylalanine, N-(benzyloxycarbonyl)-L-valine, N-(benzyloxycarbonyl)-L-threonine, N-(benzyloxycarbonyl)-L-serine or with (2R,3R)-3-(5-chloro-2-nitrophenylsulfanyl)-2-hydroxy-3-(4-methoxyphenyl)propionic acid (preferred) or (2R,3R)-2-hydroxy-3-(4-methoxyphenyl)-3-(2-nitrophenylsulfanyl)propionic acid as chiral intermediates, yielding the (S)-isomer (II). The condensation of (II) with ethyl 4-bromobutyrate (III) by means of a base such as Na2CO3, NaHCO3, K2CO3 or KHCO3 gives the expected 4-(1-piperidinyl)butyric acid ester (IV), which is finally hydrolyzed with NaOH or KOH in aqueous ethanol or methanol.
SYN 3
A new synthesis of betotastine has been developed: The racemic 4-[1-(4-chlorophenyl)-1-(2-pyridyl)methoxy]piperidine (I) is submitted to optical resolution with N-acyl amino acids such as N-acetyl-L-phenylalanine (preferred), N-acetyl-L-leucine, N-(benzyloxycarbonyl)-L-phenylalanine, N-(benzyloxycarbonyl)-L-valine, N-(benzyloxycarbonyl)-L-threonine, N-(benzyloxycarbonyl)-L-serine or with (2R,3R)-3-(5-chloro-2-nitrophenylsulfanyl)-2-hydroxy-3-(4-methoxyphenyl)propionic acid (preferred) or (2R,3R)-2-hydroxy-3-(4-methoxyphenyl)-3-(2-nitrophenylsulfanyl)propionic acid as chiral intermediates, yielding the (S)-isomer (II). The condensation of (II) with ethyl 4-bromobutyrate (III) by means of a base such as Na2CO3, NaHCO3, K2CO3 or KHCO3 gives the expected 4-(1-piperidinyl)butyric acid ester (IV), which is finally hydrolyzed with NaOH or KOH in aqueous ethanol or methanol.
CLIP
A Novel Synthetic Method for Bepotastine, a Histamine H1 Receptor …
file:///C:/Users/91200291/Downloads/B130241_549.pdf


Scheme 1. Synthesis of bepotastine l-menthyl ester N-benzyloxycarbonyl-L-aspartic acid complex (3), bepotastine besilate (4) and bepotastine calcium (5). Reagents and conditions; i) 4-bromobutanoic acid l-menthyl ester, K2CO3, acetone, reflux, 7 h, 95-99%; ii) N-benzyloxycarbonyl-L-aspartic acid (NCbzLAA), ethyl acetate, rt, 12 h, 71-73%; iii) Ethyl acetate/H2O, NaHCO3, 97-99%; iv) EtOH:H2O = 1:1, NaOH, rt, 12 h, 3.0 N-HCl Neutralization, 92- 95%; v) AcOH, reflux, 12 h, racemization 97-100%; vi) Bezensulfonic acid, acetonitrile, rt, 12 h, 64-67%; vii) NaOH, H2O, CaCl2, rt, 12 h, 86-89%.
Synthesis of (S)-Bepotastine Besilate (4). Bepotastine (50 g, 0.13 mol) was dissolved in 500 mL of acetonitrile, and benzenesulfonic acid monohydrate (20 g, 0.11 mol) was added to the reaction mixture. Bepotastine besilate (0.5 g, 1.28 mmol) was seeded in the reaction mixture and stirred at rt for 12 h. The solid precipitate was filtered and dried. The product was obtained 38 g (yield: 64%, optical purity: 99.5% ee) as a pale white crystalline powder. Melting point: 161- 163 o C. Water: 0.2% (Karl-Fischer water determination). MS: m/z 389.1 [M+H]; 1 H-NMR (300 MHz, DMSO-d6) δ 9.2 (br s, 1H), 8.5 (d, J = 4.1 Hz, 1H), 7.8 (t, J = 7.7 Hz, 1H), 7.6 (m, 3H), 7.4 (m, 4H), 7.3 (m, 4H), 5.7 (s, 1H), 3.7 (br s, 2H), 3.3 (br s, 3H), 3.1 (br s, 2H), 2.3 (t, J = 14.1 Hz, 2H), 2.2 (m, 1H), 2.0 (m, 1H), 1.8 (m, 3H), 1.7 (m, 1H); IR (KBr, cm−1 ): 3422, 2996, 2909, 2735, 2690, 2628, 1719, 1592, 1572, 1488, 1470, 1436, 1411, 1320, 1274, 1221, 1160, 1123, 1066, 1031, 1014, 996, 849, 830, 771, 759, 727, 693, 612, 564
Synthesis
FDA Orange Book Patents
| FDA Orange Book Patents: 1 of 3 (FDA Orange Book Patent ID) | |
|---|---|
| Patent | 8784789 |
| Expiration | Sep 5, 2024 |
| Applicant | BAUSCH AND LOMB INC |
| Drug Application | N022288 (Prescription Drug: BEPREVE. Ingredients: BEPOTASTINE BESILATE) |
| FDA Orange Book Patents: 2 of 3 (FDA Orange Book Patent ID) | |
|---|---|
| Patent | 6780877 |
| Expiration | Sep 19, 2019 |
| Applicant | BAUSCH AND LOMB INC |
| Drug Application | N022288 (Prescription Drug: BEPREVE. Ingredients: BEPOTASTINE BESILATE) |
| FDA Orange Book Patents: 3 of 3 (FDA Orange Book Patent ID) | |
|---|---|
| Patent | 8877168 |
| Expiration | Jul 30, 2023 |
| Applicant | BAUSCH AND LOMB INC |
| Drug Application | N022288 (Prescription Drug: BEPREVE. Ingredients: BEPOTASTINE BESILATE) |
 |
|
| Clinical data | |
|---|---|
| Trade names | Bepreve |
| AHFS/Drugs.com | International Drug Names |
| MedlinePlus | a610012 |
| Pregnancy category |
|
| Routes of administration |
Oral, topical (eye drops) |
| ATC code |
|
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | High (oral) Minimal (topical) |
| Protein binding | ~55% |
| Excretion | Renal (75–90%) |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C21H25ClN2O3 |
| Molar mass | 388.88 g/mol |
| 3D model (JSmol) | |
References
-
- EP 335 586 (Ube Ind.; appl. 22.3.1989; J-prior. 25.3.1988).
- EP 485 984 (Ube Ind.; appl. 13.11.1991; J-prior. 15.11.1990).
- WO 9 829 409 (Ube Ind.; appl. 25.12.1997; J-prior. 26.12.1996).
-
racemization :
- JP 10 237 069 (Ube Ind.; appl. 21.2.1997).
References
- Jump up^ H. Takahashi; A. Ishida-Yamamoto; H. Iizuka (September 2004). “Effects of bepotastine, cetirizine, fexofenadine, and olopatadine on histamine-induced wheal-and flare-response, sedation, and psychomotor performance”. Clinical and Experimental Dermatology. 29: 526–532. doi:10.1111/j.1365-2230.2004.01618.x.
- Jump up^ “Bepotastine Monograph”. LexiComp.
- ^ Jump up to:a b c d e f “Bepreve prescribing Information” (PDF).
- Jump up^ [phx.corporate-ir.net/External.File?item…t=1 “2011 Net Revenues Increase to $160.3 Million On an Adjusted Cash Net Income Basis, ISTA Posts Second Year of Profitability Company Reaffirms 2012 Financial Guidance”] Check
|url=value (help). - Jump up^ “Bausch & Lomb to Buy ISTA Pharmaceuticals for $500 Million”. DealBook. Retrieved 2015-12-05.
- Jump up^ “Bausch & Lomb Inc. et al. v. Micro Labs USA, Inc. et al.”
- Jump up^ “Valenant pharmaceuticals eyes China with Bausch deal”.
- Jump up^ Macejko, Thomas T.; Bergmann, Mark T.; Williams, Jon I.; Gow, James A.; Gomes, Paul J.; McNamara, Timothy R.; Abelson, Mark B. (2010-07-01). “Multicenter Clinical Evaluation of Bepotastine Besilate Ophthalmic Solutions 1.0% and 1.5% to Treat Allergic Conjunctivitis”. American Journal of Ophthalmology. 150 (1): 122–127.e5. doi:10.1016/j.ajo.2010.02.007.
////////////Bepotastine Besilate, ベポタスチンベシル酸塩 ,Talion , tau284, TAU-284DS, TAU-284, DA-5206
HL-151 , SNJ-1773
C1CN(CCC1OC(C2=CC=C(C=C2)Cl)C3=CC=CC=N3)CCCC(=O)O.C1=CC=C(C=C1)S(=O)(=O)O
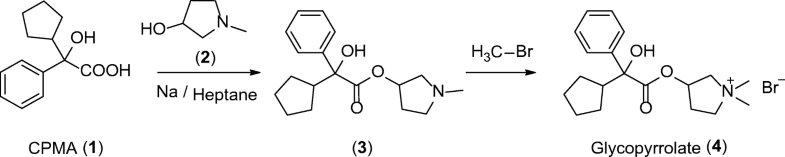
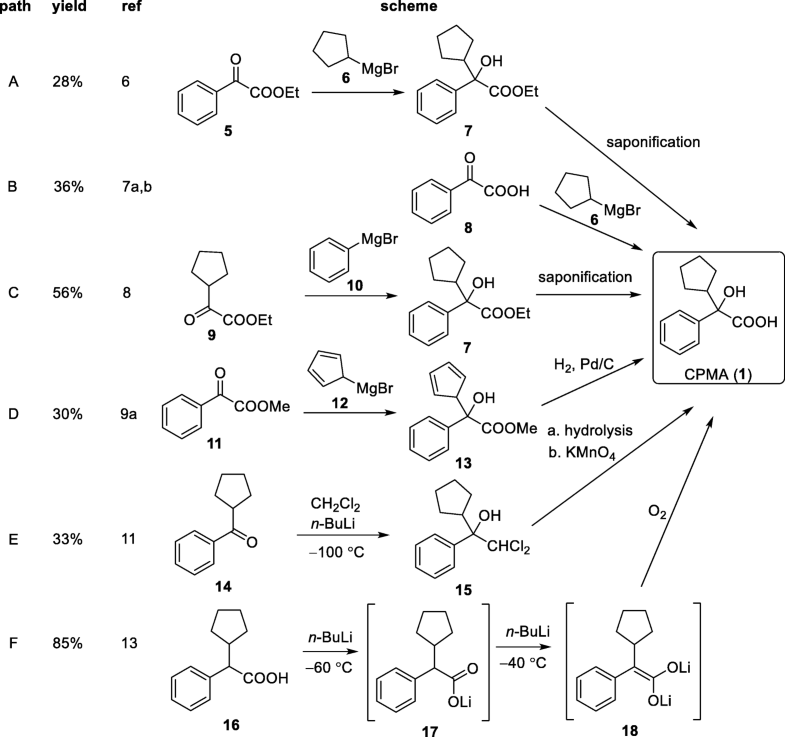
Glycopyrronium bromide, гликопиррония бромид , بروميد غليكوبيرونيوم , 格隆溴铵 , グリコピロニウム臭化物

Glycopyrronium bromide
Cas 596-51-0,
- 3-Hydroxy-1,1-dimethylpyrrolidinium bromide α-cyclopentylmandelate (6CI,7CI)
- Pyrrolidinium, 3-[(cyclopentylhydroxyphenylacetyl)oxy]-1,1-dimethyl-, bromide (9CI)
- Pyrrolidinium, 3-hydroxy-1,1-dimethyl-, bromide, α-cyclopentylmandelate (8CI)
- 1,1-Dimethyl-3-hydroxypyrrolidinium bromide α-cyclopentylmandelate
- AHR-504
- Asecryl
- Copyrrolate
- Gastrodyn
- Glycopyrrolate
- Glycopyrrolate bromide
- Glycopyrrone bromide
- Glycopyrronium bromide
- NSC 250836
- NSC 251251
- NSC 251252
- NVA 237
- Nodapton
- Robanul
- Robinul
- Seebri
- Tarodyl
- Tarodyn
- β-1-Methyl-3-pyrrolidyl-α-cyclopentylmandelate methobromide
CAS FREE FORM OF ABOVE 13283-82-4
Glycopyrrolate, ATC:A03AB02
- Use:anticholinergic, antispasmodic
- Chemical name:3-[(cyclopentylhydroxyphenylacetyl)oxy]-1,1-dimethylpyrrolidinium bromide
- Formula:C19H28BrNO3, MW:398.34 g/mol
- EINECS:209-887-0
- LD50:15 mg/kg (M, i.v.); 570 mg/kg (M, p.o.);
709 mg/kg (R, p.o.)
- Pyrrolidinium, 3-[(cyclopentylhydroxyphenylacetyl)oxy]-1,1-dimethyl-, bromide, (R*,S*)-(±)-
- Pyrrolidinium, 3-[[(2R)-cyclopentylhydroxyphenylacetyl]oxy]-1,1-dimethyl-, bromide, (3S)-rel- (9CI)
- erythro-Glycopyrronium bromide
FREE FORM OF ABOVE 740028-90-4
NMR analysis of the diastereomers of glycopyrronium bromide
Finnish Chemical Letters (1975), (3-4), 94-6
Michael Woehrmann, Lara Terstegen, Stefan Biel, Thomas Raschke, Svenja-Kathrin Cerv, Werner Zilz, Sven Untiedt, Thomas Nuebel, Uwe Schoenrock, Heiner Max, Helga Biergiesser, Yvonne Eckhard, Heike Miertsch, Heike Foelster, Cornelia Meier-Zimmerer, Bernd Traupe, Inge Kruse, “GLYCOPYRROLATE IN COSMETIC PREPARATIONS.” U.S. Patent US20090208437, issued August 20, 2009.US20090208437

Glycopyrrolate is a muscarinic antagonist used as an antispasmodic, in some disorders of the gastrointestinal tract, and to reduce salivation with some anesthetics.
Glycopyrronium (as the bromide salt glycopyrrolate) is a synthetic anticholinergic agent with a quaternary ammonium structure. A muscarinic competitive antagonist used as an antispasmodic, in some disorders of the gastrointestinal tract, and to reduce salivation with some anesthetics. In October 2015, glycopyrrolate was approved by the FDA for use as a standalone treatment for Chronic obstructive pulmonary disease (COPD), as Seebri Neohaler.
Medical uses
In anesthesia, glycopyrronium injection can be used as a before surgery in order to reduce salivary, tracheobronchial, and pharyngealsecretions, as well as decreasing the acidity of gastric secretion. It is also used in conjunction with neostigmine, a neuromuscular blocking reversal agent, to prevent neostigmine’s muscarinic effects such as bradycardia.
It is also used to reduce excessive saliva (sialorrhea),[3][4][5] and Ménière’s disease.[6]
It decreases acid secretion in the stomach and so may be used for treating stomach ulcers, in combination with other medications.
It has been used topically and orally to treat hyperhidrosis, in particular, gustatory hyperhidrosis.[7][8]
In inhalable form it is used to treat chronic obstructive pulmonary disease (COPD). Doses for inhalation are much lower than oral ones, so that swallowing a dose will not have an effect.[9][10]
Side effects
Since glycopyrronium reduces the body’s sweating ability, it can even cause hyperthermia and heat stroke in hot environments. Dry mouth, difficulty urinating, headaches, diarrhea and constipation are also observed side effects of the medication. The medication also induces drowsiness or blurred vision, an effect exacerbated by the consumption of alcohol.
Pharmacology
Mechanism of action
Glycopyrronium blocks muscarinic receptors,[11] thus inhibiting cholinergic transmission.
Pharmacokinetics
Glycopyrronium bromide affects the gastrointestinal tracts, liver and kidney but has a very limited effect on the brain and the central nervous system. In horse studies, after a single intravenous infusion, the observed tendencies of glycopyrronium followed a tri-exponential equation, by rapid disappearance from the blood followed by a prolonged terminal phase. Excretion was mainly in urine and in the form of an unchanged drug. Glycopyrronium has a relatively slow diffusion rate, and in a standard comparison to atropine, is more resistant to penetration through the blood-brain barrier and placenta.[12]
Research
It has been studied in asthma.[13][14]

Synthesis
PATENT
https://patents.google.com/patent/CN103819384A/en


PAtent
https://patents.google.com/patent/CN103159659A/en

glycopyrrolate (I)
Methyl ethyl ketone (20mL) IOOmL three-necked flask was added 8 (4.6g, 15mmol) was, at (Γ5 ° C was added dropwise dibromomethane (2.9g, 30mmol) in butanone (5 mL) was added dropwise completed, continued The reaction was stirred for 15min, and a white solid precipitated, was allowed to stand 36h at room temperature, filtered off with suction, the filter cake was sufficiently dried to give crude ketone was recrystallized twice to give a white powdery crystals I (3.9g, 66%) mp 191~193 ° C chromatographic purity 99.8% [HPLC method, mobile phase: lmol / L triethylamine acetate – acetonitrile – water (1: 150: 49); detection wavelength: 230nm, a measurement of the area normalization method] .MS m / z: 318 ( m-BrO 1HNMR (CD3OD) δ:! 1.33~1.38 (m, 2H), 1.55~1.70 (m, 6H), 2.11~2.21 (m, 1H), 2.67~2.80 (m, 1H), 3.02 (m, 1H), 3.06 (s, 3H), 3.23 (s, 3H), 3.59~3.71 (m, 3H), 3.90 (dd, /=13.8,1H), 5.47 (m, 1H), 7.27 (t, 1H) , 7.35 (t, 2H), 7.62 (dd, 2H) .13C bandit R (DMSO) δ: 27.0, 27.4, 28.0, 31.3, 47.8, 53.8, 54.3, 66.0, 71.3, 74.6, 81.1, 126.9,128.7,129.3 , 143.2 17 5.00
Patent
https://patents.google.com/patent/WO2016204998A1/en

PATENT
https://patents.google.com/patent/EP2417106B1/en
-
Glycopyrronium bromide, also known as 3-[(cyclopentylhydroxyphenylacetyl)oxy]-1,1-dimethylpyrrolidinium bromide or glycopyrrolate, is an antimuscarinic agent that is currently administered by injection to reduce secretions during anaesthesia and or taken orally to treat gastric ulcers.
- [0003]
- [0004]
United States patent US 2,956,062 discloses that 1-methyl-3-pyrrolidyl alpha-cyclopentyl mandelate and can be prepared from methyl alpha cyclopentylmandelate and that the methyl bromide quaternary salt can be prepared by saturating a solution of 1-methyl-3-pyrrolidyl alpha-cyclopentyl mandelate in dry ethyl acetate with methyl bromide and filtering the crystalline solid that appears on standing.
- [0005]
The process of US 2,956,062 for preparing 1-methyl-3-pyrrolidyl alpha-cyclopentyl mandelate involves transesterifying methyl glycolate with an amino alcohol under the influence of metallic sodium to give a glycolate intermediate. Metallic sodium is highly reactive, which poses health and safety risks that make its use undesirable on an industrial scale for commercial manufacture.
- [0006]
The process of US 2,956,062 requires preparing the methylester in a previous step and alkylating the amino esters in a later step to form the desired quaternary ammonium salts.
- [0007]
The process of US 2,956,062 provides a mixture of diastereoisomers. The relative proportions of the diastereoisomers can vary widely between batches. This variation can give rise to surprising differences when preparing dry powder formulations from glycopyrronium bromide, which can cause problems when formulating such dry powders for pharmaceutical use.
- [0008]
United States patent application US 2007/0123557 discloses 1-(alkoxycarbonylmethyl)-1-methylpyrrolidyl anticholinergic esters. It describes coupling (R)-cyclopentylmandelic acid with (R,S)-1-methyl-pyrrolidin-3-ol under Mitsunobu conditions to give pure (R)-stereoisomeric compounds that are reacted with a bromoacetate to give the desired esters. It should be noted however that the chemicals used in Mitsunobu reactions, typically dialkyl azodicarboxylates and triphenylphosphine, pose health, safety and ecological risks that make their use undesirable on an industrial scale for commercial manufacture. They are also generally too expensive to source and too laborious to use in commercial manufacture.
- [0009]
United States patent application US 2006/0167275 discloses a process for the enrichment of the R, R- or S, S-configured glycopyrronium isomers and their thienyl analogues having R, S or S, R configuration.
- [0010]
WO 03/087094 A2 discloses new therapeutically useful pyrrolidinium derivatives, processes for their preparation and pharmaceutical compositions containing them.

EXAMPLE Example 1 Preparation of (3S,2’R)- and (3R,2’S)-3-[(cyclopentyl-hydroxyphenylacetyl)-oxy]-1,1-dimethylpyrrolidinium bromide
- [0071]
30 g of cyclopentyl mandelic acid, dissolved in 135 g dimethylformamide (DMF), were treated with 27 g carbonyldiimidazole at 18°C (in portions) to form the “active amide”. After the addition of 16.9 g of 1-methyl-pyrrolidin-3-ol, the mixture was heated to 60°C within 1 hour and stirred for 18 hours at this temperature. After checking for complete conversion, the mixture was cooled and 200 g water was added. The mixture was extracted with 200 g toluene and the extract was washed with water three times. The organic phase was concentrated to obtain cyclopentyl-hydroxy-phenyl-acetic acid 1-methyl-pyrrolidin-3-yl ester as an about 50% solution in toluene, ready to use for the next step.
- [0072]
This solution was diluted with 120 g of n-propanol and cooled to 0°C. 16.8 g methyl bromide was introduced and the mixture was stirred for 2 hours and then gradually heated to 60°C to evaporate the excess methyl bromide into a scrubber. The mixture was then cooled to 50°C and seed crystals were added to facilitate crystallisation. The temperature was then slowly reduced over 18 hours to 15°C. The solid was then isolated by filtration to obtain 22.7 g after drying. It was composed mainly of one pair of enantiomers, a racemic mixture of (3S,2’R)- and (3R,2’S)-3-[(cyclopentyl-hydroxyphenylacetyl)-oxy]-1,1-dimethylpyrrolidinium bromide, with a purity greater than 90% (by HPLC). The other pair of diastereoisomers ((3R,2’R)- and (3S,2’S)-3-[(cyclopentyl-hydroxyphenyl-acetyl)-oxyl-1,1-dimethylpyrrolidinium bromide) remains mainly in the filtrate as those compounds are significantly more soluble in n-propanol than the other stereoisomers.
- [0073]
The solid obtained is further recrystallised in n-propanol (1:10 wt) to give pure (3S,2’R)- and (3R,2’S)-3-[(cyclopentyl-hydroxyphenylacetyl)-oxy]-1,1-dimethylpyrrolidinium bromide i.e. purity > 99.9% as determined by high performance liquid chromatography (HPLC).
- [0074]
Reference Example 2 Preparation of cyclopentyl-hydroxy-phenyl-acetic acid 1-methyl-pyrrolidin-3yl-ester in toluene
- [0075]
1 g of cyclopentyl mandelic acid was suspended in 4.7 g of toluene and 1.5 g of carbonyldiimidazole were added as a solid. After 30 minutes 0.69 g of 1-methyl-pyrrolidin-3-ol and 20 mg of sodium tert-butylate were added. The mixture was stirred at room temperature for 18 hours then water was added. After stirring the phases were separated and the organic phase was washed with water twice and evaporated to obtain an approximately 50% solution of cyclopentyl-hydroxy-phenyl-acetic acid 1-methyl-pyrrolidin-3yl-ester in toluene.
Example 3 Preparation of 2-cyclopentyl-2-hydroxy-1-imidazol-1-yl-2-phenyl-ethanone, the active intermediate
- [0076]
The imidazolidyl derivative of cyclopentylmandelic acid was prepared and isolated as a solid by the following method:
- [0077]
10 g of cyclopentylmandelic acid were suspended in 30 ml of acetonitrile and the mixture was cooled to 0°C. 10.3 g of carbonyldiimidazole were added as a solid and the mixture was warmed to room temperature for 2 hours. Carbon dioxide evolved as a gas as a precipitate formed. The mixture was then cooled to 5°C and the solid was filtered, washed with acetonitrile and dried in vacuum at 40°C to obtain 7.3 g of pure 2-cyclopentyl-2-hydroxy-1-imidazol-1-yl-2-phenyl-ethanone.
- [0078]
- [0079]
High resolution MS-spectroscopy revealed the molecular formula of the compound (as M+H) to be C16H19O2N2 with an exact mass of 271.14414 (0.14575ppm deviation from the calculated value).
1H-NMR-spectroscopy (600MHz, DMSO-d6): 1.03-1.07 (m, 1H), 1.25-1.30 (m, 1H), 1.35-1.40 (m, 1H), 1.40-1.50 (m, 1H), 1.53-1.56 (m, 2H), 1-60-1.67 (m, 1H), 1.75-1.84 (m, 1H), 1.03 – 1.85 (8H, 8 secondary CH2-protons in the cyclopentylring, H-C11, H-C12, H-C13, H-C14); 2.7-2.9 (m, 1H, H-C10); 6.76 (1H, H-C5); 6.91 (1H, H-C4); 7.29 (1H, H-C18); 7.39 (2H, H-C17, H-C19); 7.49 (2H, H-C16, H-C20); 7.65 (1H, H-C2). - [0080]
The compound was characterised by IR-spectroscopy (measured as a solid film on a BRUKER TENSOR 27 FT-IR spectrometer over a wave number range of 4000-600 cm-1 with a resolution of 4 cm-1). An assignment of the most important bands is given below:
Wavenumber (cm-1) Assignments 3300 ∼ 2500 O-H stretching 3167, 3151, 3120 Imidazole CH stretching 2956, 2868 Cyclopentyl CH stretching 1727 C=O stretching 1600, 1538, 1469 Aromatic rings stretching 735 Mono-subst. benzene CH o.o.p. bending 704 Mono-subst. benzene ring o.o.p. bending
SYN
PAPER
https://link.springer.com/article/10.1007/s41981-018-0015-4
Journal of Flow Chemistry, pp 1–8| Cite as
Sequential α-lithiation and aerobic oxidation of an arylacetic acid – continuous-flow synthesis of cyclopentyl mandelic acid
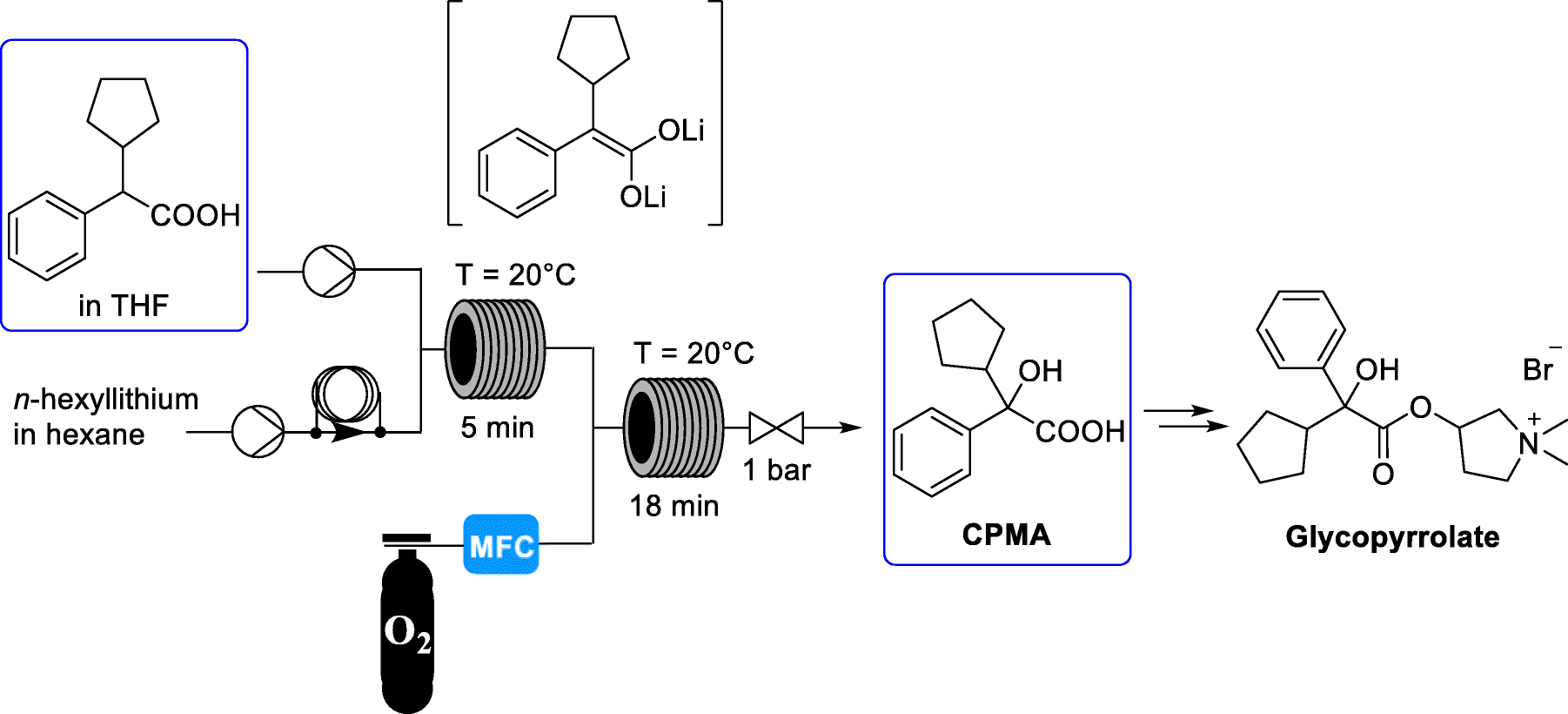
The medicinal properties of glycopyrronium bromide (glycopyrrolate, 4) were first identified in the late 1950s [1]. Glycopyrrolate is an antagonist of muscarinic cholinergic receptors and is used for the treatment of drooling or excessive salivation (sialorrhea) [2], excess sweating (hyperhidrosis) [3], and overactive bladder and for presurgery treatment. In addition, it has recently been introduced as an effective bronchodilator for the treatment of chronic obstructive pulmonary disease (COPD) for asthma patients [4]. Glycopyrrolate displays few side effects because it does not pass through the blood brain barrier. Cyclopentyl mandelic acid (CPMA, 1), or its corresponding ester derivatives, are key intermediates in the synthetic routes to 4. CPMA (1) reacts with 1-methyl-pyrrolidin-3-ol (2) to form tertiary amine 3. N-Methylation of 3 by methyl bromide gives quaternary ammonium salt glycopyrrolate 4 as a racemate (Scheme 1) [5].
Scheme 1
Synthesis of glycopyrrolate 4 from CPMA (1)
CPMA (1) is a synthetically challenging intermediate to prepare (Scheme 2). Routes A to D are most likely to be the commercially applied methods because these procedures are described in patents [5]. The published descriptions for the yields of 1 range from 28 to 56% for routes A to D. Ethyl phenylglyoxylate is reacted with cyclopentyl magnesium bromide to form an ester which is then hydrolyzed (route A) [6]. Phenylglyoxylic acid can be reacted in a similar manner with cyclopentyl magnesium bromide to directly form 1 (route B) [7]. Alternatively, the inverse addition of phenyl-Grignard reagent to cyclopentyl glyoxylic acid ester is reported (route C) [8]. Cyclopentyl glyoxylic acid ester can also be reacted with cyclopentadienyl magnesium bromide which is followed by an additional hydrogenation step with Pd/C and H2 to afford 1 (route D) [9, 10].
Scheme 2
Existing synthetic pathways to CPMA (1)
PATENT
EXA M PL E S
EXAM PL E 1
Scheme 1
ST E P I
To a stirred solution of N-methyl pyrrol i din- 3-ol (2, 1 equiv) and Et3N (1.2 equiv) in dichloromethane was added a solution of 2-cyclopentyl-2-oxoacetyl chloride (1, 1.1 equiv) in DCM at O °C under nitrogen atmosphere for 20 min. The resulting solution was allowed to stir at room temperature over 10h. After completion, the mixture was quenched with water and extracted with diethyl ether to afford the pure product (3A).
Similarly, the product 3A is also obtained by reaction of 2 with other reagents, phenyl oxalic acid, methyl phenyl oxalate, and phenyl hemi-oxaldehyde respectively as shown in Scheme 1.
ST E P II
3A
To a mixture of bromobenzene (2.2 equiv) and Mg metal (2.2 equiv) in TH F (15 mL) was stirred over a period of 30 min at 0 · C. To this mixture, a solution of 1 -methyl pyrrol idin-3-yl 2-cyclopentyl-2-oxoacetate (3, 1 equiv) in T HF was added in portions over a period of 30 min. Up on completion, the reaction mixture was poured into ice water and extracted with ethyl acetate. The organic layer was separated and concentrated in vacuo. The resulting residue was purified by column chromatography to afford the pure product (5).
ST E P III
To a solution of compound 5 (1 equiv) in acetonitrile and chloroform mixture (10 mL, 2:3) was added methyl bromide (4 equiv). The mixture was stirred at room temperature for 72h. The solvents were evaporated, and the resulting residue was washed with diethyl ether to afford the pure product (6) as a white solid.
EXAM PL E 2
Scheme 2
ST E P I
To a stirred solution of N-methyl pyrrol i din- 3-ol (2, 1 equiv) and Et3N (1.2 equiv) in dichloromethane was added a solution of 2- oxo-2- phenyl acetyl chloride (1.1 equiv) in dichloromethane at 0 °C under nitrogen atmosphere for 15 min. The resulting solution was allowed to stir at room temperature over 12h. After completion, the mixture was quenched with water and extracted with diethyl ether to afford the pure product (3B).
Similarly, the product 3B is also obtained by reaction of 2 with other reagents, phenyl oxalic acid, methyl phenyl oxalate, and phenyl hemi-oxaldehyde respectively as shown in Scheme 2.
ST E P II
To a mixture of cyclopentyl bromide (4, 2.2 equiv) and Mg metal (2.2 equiv) in THF (15 mL) was stirred over a period of 30 min at 0 – C. To this mixture, a solution of 1-methylpyrrolidin-3-yl-2-oxo-2-phenylacetate (3B, 1 equiv) in TH F was added in portions over a period of 30 min. Up on completion, the reaction mixture was poured into ice water and extracted with ethyl acetate. The organic layer was separated and concentrated in vacuo. The resulting residue was purified by column chromatography to afford the pure product (5).
ST E P III
To a solution of compound 5 (1 equiv) in acetonitrile and chloroform mixture (10 mL, 2:3) was added methyl bromide (4 equiv). The mixture was stirred at room temperature for 75h. The solvents were evaporated, and the resulting residue was washed with diethyl ether to afford the pure product (6) as a white solid.
The invention has been described in detail with reference to preferred embodiments thereof. However, it will be appreciated by those skilled in the art that changes may be made in these embodiments without departing from the principles and nature of the invention, the scope of which is defined in the appended claims and their equivalents.
References
- Jump up^ Bajaj V, Langtry JA (July 2007). “Use of oral glycopyrronium bromide in hyperhidrosis”. Br. J. Dermatol. 157 (1): 118–21. doi:10.1111/j.1365-2133.2007.07884.x. PMID 17459043.
- Jump up^ “FDA OKs first drug made to reduce excessive sweating”. AP News. Retrieved 2018-07-02.
- Jump up^ Mier RJ, Bachrach SJ, Lakin RC, Barker T, Childs J, Moran M (December 2000). “Treatment of sialorrhea with glycopyrrolate: A double-blind, dose-ranging study”. Arch Pediatr Adolesc Med. 154 (12): 1214–8. doi:10.1001/archpedi.154.12.1214. PMID 11115305.
- Jump up^ Tscheng DZ (November 2002). “Sialorrhea – therapeutic drug options”. Ann Pharmacother. 36 (11): 1785–90. doi:10.1345/aph.1C019. PMID 12398577.[permanent dead link]
- Jump up^ Olsen AK, Sjøgren P (October 1999). “Oral glycopyrrolate alleviates drooling in a patient with tongue cancer”. J Pain Symptom Manage. 18 (4): 300–2. doi:10.1016/S0885-3924(99)00080-9. PMID 10534970.
- Jump up^ Maria, Sammartano Azia; Claudia, Cassandro; Pamela, Giordano; Andrea, Canale; Roberto, Albera (1 December 2012). “Medical therapy in Ménière’s disease”. Audiological Medicine. 10 (4): 171–177. doi:10.3109/1651386X.2012.718413 – via Taylor and Francis+NEJM.
- Jump up^ Kim WO, Kil HK, Yoon DM, Cho MJ (August 2003). “Treatment of compensatory gustatory hyperhidrosis with topical glycopyrrolate”. Yonsei Med. J. 44 (4): 579–82. doi:10.3349/ymj.2003.44.4.579. PMID 12950111.
- Jump up^ Kim WO, Kil HK, Yoon KB, Yoon DM (May 2008). “Topical glycopyrrolate for patients with facial hyperhidrosis”. Br. J. Dermatol. 158 (5): 1094–7. doi:10.1111/j.1365-2133.2008.08476.x. PMID 18294315.
- Jump up^ “EPAR – Product information for Seebri Breezhaler” (PDF). European Medicines Agency. 28 September 2012.
- Jump up^ Tzelepis G, Komanapolli S, Tyler D, Vega D, Fulambarker A (January 1996). “Comparison of nebulized glycopyrrolate and metaproterenol in chronic obstructive pulmonary disease”. Eur. Respir. J. 9 (1): 100–3. doi:10.1183/09031936.96.09010100. PMID 8834341.
- Jump up^ Haddad EB, Patel H, Keeling JE, Yacoub MH, Barnes PJ, Belvisi MG (May 1999). “Pharmacological characterization of the muscarinic receptor antagonist, glycopyrrolate, in human and guinea-pig airways”. Br. J. Pharmacol. 127 (2): 413–20. doi:10.1038/sj.bjp.0702573. PMC 1566042
 . PMID 10385241.
. PMID 10385241. - Jump up^ Rumpler, M.J.; Colahan, P.; Sams, R.A. (2014). “The pharmacokinetics of glycopyrrolate in Standardbred horses”. J. Vet Pharmacol Ther. 37 (3): 260–8. doi:10.1111/jvp.12085. PMID 24325462.
- Jump up^ Hansel TT, Neighbour H, Erin EM, et al. (October 2005). “Glycopyrrolate causes prolonged bronchoprotection and bronchodilatation in patients with asthma”. Chest. 128 (4): 1974–9. doi:10.1378/chest.128.4.1974. PMID 16236844.
- Jump up^ Gilman MJ, Meyer L, Carter J, Slovis C (November 1990). “Comparison of aerosolized glycopyrrolate and metaproterenol in acute asthma”. Chest. 98 (5): 1095–8. doi:10.1378/chest.98.5.1095. PMID 2225951.
 |
|
| Clinical data | |
|---|---|
| Trade names | Robinul, Cuvposa, Seebri, Qbrexza, others |
| License data | |
| Pregnancy category |
|
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| CAS Number | |
| PubChemCID | |
| ChemSpider | |
| UNII | |
| ECHA InfoCard | 100.008.990 |
| Chemical and physical data | |
| Formula | C19H28BrNO3 |
| Molar mass | 398.335 g/mol |
| 3D model (JSmol) | |
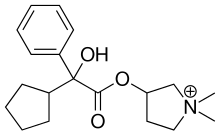 |
|
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a602014 |
| Pregnancy category |
|
| Routes of administration |
By mouth, intravenous, inhalation |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Elimination half-life | 0.6–1.2 hours |
| Excretion | 85% renal, unknown amount in the bile |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| ECHA InfoCard | 100.008.990 |
| Chemical and physical data | |
| Formula | C19H28NO3+ |
| Molar mass | 318.431 g/mol |
| 3D model (JSmol) | |
Sucroferric oxyhydroxide, 含糖酸化鉄, スクロオキシ水酸化鉄


Sucroferric oxyhydroxide
Iron sucrose (USP);
Ferric oxide, saccharated;
Sucroferric oxyhydroxide;
Venofer (TN)
含糖酸化鉄;
スクロオキシ水酸化鉄
| Molecular Formula: | C12H29Fe5Na2O23 |
|---|---|
| Molecular Weight: | 866.546 g/mol |
|
CAS REGISTRY NUMBER 12134-57-5, 8047-67-4
disodium;(2R,3R,4S,5S,6R)-2-[(2S,3S,4S,5R)-3,4-dihydroxy-2,5-bis(hydroxymethyl)oxolan-2-yl]oxy-6-(hydroxymethyl)oxane-3,4,5-triol;iron(3+);oxygen(2-);hydroxide;trihydrate
Iron sugar; Saccharated iron; Sucroferric oxyhydroxide; Saccharated iron oxide; Saccharated ferric oxide; Ferrivenin
Ferric oxyhydroxide; Ferrihydrite; Iron oxyhydroxide; P-TOL; PA-21; PA21-1; Phosphate binder – Vifor Pharma; suroferric oxyhydroxide tablets; Velphoro
NDC 49230-645-51
Iron saccharate (Sucroferric oxyhydroxide or Iron Sucrose) is used as a source of iron in patients with iron deficiency anemia with chronic kidney disease (CKD), including those who are undergoing dialysis (hemodialysis or peritoneal) and those who do not require dialysis. Due to less side effects than iron dextran, iron saccharate is more preferred in chronic kidney disease patients.
Mixture of polynuclear iron(III)-oxyhydroxide, starch and sucrose
VIFOR FRESENIUS MEDICAL CARE RENAL PHARMA FRANCE
Approved in US
Indicated for the control of serum phosphorus levels in patients with chronic kidney disease on dialysis.
THERAPEUTIC CLAIM Oral phosphate binder, treatement of elevated
phosphate levels in patients undergoing dialysis
CHEMICAL DESCRIPTIONS
1. Ferric hydroxide oxide
2. Mixture of iron(III) oxyhydroxide, sucrose, starches
3. Polynuclear iron(III) oxyhydroxide stabilized with sucrose and starches
structure
O =Fe -OH
MOLECULAR FORMULA FeHO2•xC12H22O11•y(C6H10O5)n
SPONSOR Vifor (International) Inc.
CODE DESIGNATIONS PA21
CAS REGISTRY NUMBER 12134-57-5
- ClassFerric compounds; Hyperphosphataemia therapies
- Mechanism of ActionPhosphate binding modulators
- MarketedHyperphosphataemia
- 24 Jun 2018Biomarkers information updated
- 19 Jun 2018Kissei Pharmaceutical completes a phase III trial in Hyperphosphataemia (Treatment-experienced) in Japan (PO) (UMIN000023657)
- 09 Jun 2017Phase-II clinical trials in Hyperphosphataemia in Austria (PO) (NCT03010072)
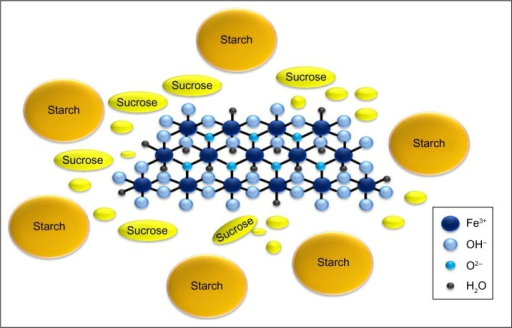
Sucroferric oxyhydroxide is a brown, amorphous powder. The drug substance is relatively poorly defined, so that the manufacturing process is particularly important. Sucroferric oxyhydroxide is prepared by basifying a ferric chloride solution, giving a polynuclear iron(III)-oxyhydroxide suspension which is mixed with potato and maize starches and sucrose. Vifor states that the sucrose stabilises the iron core and thus maintain the high phosphate adsorption capacity while the starches function as processing aids, but they are added simultaneously and the drug substance is probably a complex mixture of species.
The solubility of the active moiety, polynuclear iron oxyhydroxide, is evidently low in the gastrointestinal (GI) tract so that iron absorption is low. Aqueous solubility at different pH has been very poorly quantified. Vifor states that the “sucrose part is soluble in water, iron(III)-oxyhydroxide/starch mixture is practically insoluble in water.” While the iron oxide particle size is important in determining the phosphate binding, it is relatively difficult to directly measure. The sucrose/starch “wrapped” drug substance particle size is established and the process is controlled, but it does not correlate well with phosphate adsorption. Sucroferric oxyhydroxide cannot be controlled in the manner of a well-defined molecular drug and some variability between batches is likely. The drug substance specification includes a phosphate adsorption test. Vifor has tested the adsorption of a range of other in vivo chemical species to sucroferric oxyhydroxide and not identified any likely to be strongly bound, or affect phosphate binding, except for oxalate. Some drugs, however, do interact, for example alendronate is strongly absorbed (and the PI warnings in that context should be generalised to all bisphosphonates, not just identify the single drug in class studied)….https://www.tga.gov.au/sites/default/files/auspar-sucroferric-oxyhydroxide-150219.pdf
EMA
| Name | Active substance | Therapeutic area | Date of authorisation / refusal | Has current safety alert | Status | ||||
|---|---|---|---|---|---|---|---|---|---|
| Velphoro | mixture of polynuclear iron(III)-oxyhydroxide, sucrose and starches | HyperphosphatemiaRenal Dialysis | 26/08/2014 | Authorised |
Product details
| Name | Velphoro |
|---|---|
| Agency product number | EMEA/H/C/002705 |
| Active substance | mixture of polynuclear iron(III)-oxyhydroxide, sucrose and starches |
| International non-proprietary name(INN) or common name | mixture of polynuclear iron(III)-oxyhydroxide, sucrose and starches |
| Therapeutic area | HyperphosphatemiaRenal Dialysis |
| Anatomical therapeutic chemical (ATC) code | V03AE05 |
| Additional monitoring | This medicine is under additional monitoring. This means that it is being monitored even more intensively than other medicines. For more information, see medicines under additional monitoring. |
Publication details
| Marketing-authorisation holder | Vifor Fresenius Medical Care Renal Pharma France |
|---|---|
| Revision | 5 |
| Date of issue of marketing authorisation valid throughout the European Union | 26/08/2014 |
Contact address:
Vifor Fresenius Medical Care Renal Pharma France
100-101 Terrasse Boieldieu
Tour Franklin- La Défense 8
92042 Paris la Défense Cedex
France
Sucroferric oxyhydroxide (INN; trade name Velphoro, by Vifor Fresenius Medical Care Renal Pharma) is a non-calcium, iron-based phosphate binder used for the control of serum phosphorus levels in adult patients with chronic kidney disease (CKD) on haemodialysis(HD) or peritoneal dialysis (PD).[1] It is used in form of chewable tablets.
Hyperphosphatemia
In a healthy person, normal serum phosphate levels are maintained by the regulation of dietary absorption, bone formation and resorption, equilibration with intracellular stores, and renal excretion.[2] When kidney function is impaired, phosphate excretion declines. Without specific treatment, hyperphosphataemia occurs almost universally, despite dietary phosphate restriction and conventional dialysis treatment.[2][3] In patients on dialysis, hyperphosphataemia is an independent risk factor for fractures, cardiovascular disease and mortality.[4][5] Abnormalities in phosphate metabolism such as hyperphosphatemia are included in the definition of the new chronic kidney disease–mineral and bone disorder (CKD-MBD).[5]
Structure and mechanism of action
Sucroferric oxyhydroxide comprises a polynuclear iron(III)-oxyhydroxide core that is stabilised with a carbohydrate shell composed of sucrose and starch.[6][7] The carbohydrate shell stabilises the iron(III)-oxyhydroxide core to preserve the phosphate adsorption capacity.
Dietary phosphate binds strongly to sucroferric oxyhydroxide in the gastrointestinal (GI) tract. The bound phosphate is eliminated in the faeces and thereby prevented from absorption into the blood. As a consequence of the decreased dietary phosphate absorption, serum phosphorus concentrations are reduced.
Medical uses
Sucroferric oxyhydroxide is approved by the United States Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for the control of serum phosphorus levels in patients with chronic kidney disease (CKD) on dialysis.[1][8]
Adverse effects
The most frequently reported adverse drug reactions reported from trials were diarrhoea and discoloured faeces.[1][8] The vast majority of gastrointestinal adverse events occurred early during treatment and abated with time under continued dosing.[1]
Interactions
Drug-interaction studies and post hoc analyses of Phase 3 studies showed no clinically relevant interaction of sucroferric oxyhydroxide with the systemic exposures to losartan, furosemide, omeprazole, digoxin, and warfarin,[9] the lipid-lowering effects of statins,[10] and oral vitamin D receptor agonists.[11] According to the European label (Summary of Product Characteristics), medicinal products that are known to interact with iron (e.g. doxycycline) or have the potential to interact with Velphoro should be administered at least one hour before or two hours after Velphoro.[1] This allows sucroferric oxyhydroxide to bind phosphate as intended and be excreted without coming into contact with medications in the gut that it might interact with. According to the US prescribing information, Velphoro should not be prescribed with oral levothyroxine.[8] The combination of sucroferric oxyhydroxide and levothyroxine is contraindicated because sucroferric oxyhydroxide contains iron, which may cause levothyroxine to become insoluble in the gut, thereby preventing the intestinal absorption of levothyroxine.[12]
Chewability
The chewability of sucroferric oxyhydroxide compares well with that of Calcimagon, a calcium containing tablet used as a standard for very good chewability.[13] Tablets of sucroferric oxyhydroxide easily disintegrated in artificial saliva.
Effectiveness and phosphate binding
Clinical Phase 3 studies showed that sucroferric oxyhydroxide achieves and maintains phosphate levels in compliance with the KDOQI guidelines.[14][15] The reduction in serum phosphate levels of sucroferric oxyhydroxide-treated patients was non-inferior to that in sevelamer-treated patients. The required daily pill burden was lower with sucroferric oxyhydroxide.[14]
Sucroferric oxyhydroxide binds phosphate under empty and full stomach conditions and across the physiologically relevant pH range of the GI tract.[7]
In a retrospective, real-world study, hyperphosphatemic peritoneal dialysis patients who were prescribed to switch to sucroferric oxyhydroxide from sevelamer, lanthanum carbonate, or calcium acetate had significant reductions in serum phosphorus levels, along with a 53% decrease in the prescribed daily pill burden.[16]
Sucroferric oxyhydroxide nonproprietary drug name
1. February 27, 2013. N13/36. STATEMENT ON A NONPROPRIETARY NAME ADOPTED BY THE USAN COUNCIL. USAN (ZZ-19). SUCROFERRIC …
The US Food and Drug Administration has given the green light to Vifor Fresenius Medical Care Renal Pharma’s hyperphosphatemia drug Velphoro.
The approval for Velphoro (sucroferric oxyhydroxide), formerly known as PA21, is based on Phase III data demonstrated that the drug successfully controls the accumulation of phosphorus in the blood with the advantage of a much lower pill burden than the current standard of care in patients with chronic kidney disease on dialysis, namely Sanofi’s Renvela (sevelamer carbonate). read this at
http://www.pharmatimes.com/Article/13-11-28/FDA_okays_Vifor_Fresenius_phosphate_binder_Velphoro.aspx
Velphoro (PA21) receives US FDA approval for the treatment of hyperphosphatemia in Chronic Kidney Disease Patients on dialysis
Velphoro (sucroferric oxyhydroxide) has received US Food and Drug Administration (FDA) approval for the control of serum phosphorus levels in patients with Chronic Kidney Disease (CKD) on dialysis. Velphoro will be launched in the US by Fresenius Medical Care North America in 2014.
Velphoro (previously known as PA21) is an iron-based, calcium-free, chewable phosphate binder. US approval was based on a pivotal Phase III study, which met its primary and secondary endpoints. The study demonstrated that Velphoro® successfully controls hyperphosphatemia with fewer pills than sevelamer carbonate, the current standard of care in patients with CKD on dialysis. The average daily dose to control hyperphosphatemia was 3.3 pills per day after 52 weeks.
Velphoro was developed by Vifor Pharma. In 2011, all rights were transferred to Vifor Fresenius Medical Care Renal Pharma, a common company of Galenica and Fresenius Medical Care. In the US, Velphorowill be marketed by Fresenius Medical Care North America, a company with a strong marketing and sales organization, and expertise in dialysis care. The active ingredient of Velphoro is produced by Vifor Pharma in Switzerland.
Hyperphosphatemia, an abnormal elevation of phosphorus levels in the blood, is a common and serious condition in CKD patients on dialysis. Most dialysis patients are treated with phosphate binders. However, despite the availability of a number of different phosphate binders, up to 50% of patients depending on the region are still unable to achieve and maintain their target serum phosphorus levels. In some patients, noncompliance due to the high pill burden and poor tolerability appear to be key factors in the lack of control of serum phosphorus levels. On average, dialysis patients take approximately 19 pills per day with phosphate binders comprising approximately 50% of the total daily pill burden. The recommended starting dose of Velphoro is 3 tablets per day (1 tablet per meal).
Full results from the pivotal Phase III study involving more than 1,000 patients were presented at both the 50th ERA-EDTA (European Renal Association European Dialysis and Transplant Association) Congress in Istanbul, Turkey, in May 2013, and the American Society of Nephrology (ASN) Kidney Week in Atlanta, Georgia, in November 2013. Velphorowas shown to be a potent phosphate binder, with lower pill burden and a good safety profile.
Based on these data, Vifor Fresenius Medical Care Renal Pharma believes that Velphoro offers a new and effective therapeutic option for the control of serum phosphorus levels in patients with chronic kidney disease on dialysis.
The regulatory processes in Europe, Switzerland and Singapore are ongoing and decisions are expected in the first half 2014. Further submissions for approval are being prepared.
PATENT
https://patents.google.com/patent/WO2016038541A1/en
Hyperphosphatemia is associated with significant increase in morbidity and mortality, and may induce severe complications, such as hypocalcemia, decreasing of vitamin-D production and metastatic calcification. Hyperphosphatemia is also contributing to the increased incidence of cardiovascular disease among dialysis-dependent patients. The phosphate binding capacity of iron oxide hydroxides is known in the art. The possible medical application of iron hydroxides and iron oxide hydroxides as phosphate adsorbents is also described.
US 4,970,079 patent discloses a method of controlling serum phosphate level in patients by iron oxy-hydroxides which bind to ingested phosphate. US 5,514,281 patent also discloses a process for the selective elimination of inorganic phosphate from body fluids by using a polynuclear metal oxyhydroxide preferably iron (III) oxyhydroxide.
US 6,174,442 patent describes an adsorbent for phosphate and a process for the preparation thereof, which contains polynuclear β-iron hydroxide stabilized by carbohydrates and/or humic acid.
In order to obtain an iron-based compound which can be used as a pharmaceutical, it is necessary to have an iron-based compound which is stable. It is known that iron oxide- hydroxide is not a stable compound with time ageing occurs. Ageing usually not only involves crystallization but also particle enlargement. Such ageing may alter the phosphate binding of an iron oxide -hydroxide based phosphate adsorbent. Accordingly, there exists a need for a process for manufacturing of an iron containing phosphate adsorbent. The process needs to be scalable, robust and consistently producing an iron containing phosphate adsorbent of the required pharmaceutical grade.
Examples
In examples which are intended to illustrate embodiments of the invention but which are not intended to limit the scope of the invention: ) Method of Making an Iron Containing Phosphate Adsorbent
To a solution of 1.96 kg sodium carbonate dissolved in 12.5 liter water, solution of 2.5 kg iron (III) chloride hexahydrate dissolved in 17.5 liter water was added at a temperature of 5 – 10°C. The resulting mixture was stirred for 90 to 120 minutes at 5 – 10°C. (25.0×3) liter water was added to the reaction mass and raised the temperature at 15 – 20°C with stirring. Stopped the stirring, settled precipitate and the supernatant water was removed. The precipitate was filtered and washed with 1.25 liter water. A suspension of the precipitate was prepared in water. To this, 875.0 gm sucrose and 695.0 gm potato starch were added and stirred for 120 minutes at 25 – 35°C. Cooled the reaction mass at 10 – 15°C and stirred for 90 to 120 minutes. 25.0 liters cold acetone was added to the reaction mass at 10 – 15°C and stirred for 90 to 120 minutes. The final product was filtered and washed with 1.25 liter cold acetone and further dried under vacuum at 30-35°C.
Yield: 2.08 kg ) Large-scale Method of Making an Iron Containing Phosphate Adsorbent
An aqueous solution of sodium carbonate and an aqueous solution of iron (III) chloride hexahydrate were mixed at a temperature of 5 – 10°C, optionally in the presence of solvent- 1. A volume of aqueous solution of sodium carbonate necessary to maintain the pH at about 7.0 to form a colloidal suspension of ferric hydroxide. The resulting mixture was stirred for 90 to 120 minutes at 5 – 10°C. Water was added to the reaction mass with stirring. Stopped the stirring, settled precipitated product and the water was decanted or siphoned. The precipitated product was further filtered and washed with using water. Suspension of the precipitated product was prepared in the water. Subsequently, sucrose and starch were added in to the suspension and stirred for 120 minutes at 25 – 35°C. Cooled the reaction mixture at 10 – 15°C and stirred for 90 to 120 minutes. Solvent-2 was added to the reaction mixture at 10 – 15°C and stirred for 90 to 120 minutes. The product was filtered and washed with the solvent-2 and further dried under vacuum at 30-35°C. Few illustrative examples provided in Table- 1, wherein the iron containing phosphate adsorbents were prepared according to the process of example-2 using the respective combination of Solvent- 1 and Solvent-2 as given in the table:
Table-1
3) Physical Properties of an Iron Containing Phosphate Adsorbents prepared as per above example-2.
> BET active Surface Area:
· Instrument : Surface area analyzer
• Condition : Surface area (m2/gm) at N2.P/P0 = 10%
Table-2
> Phosphate Binding Capacity at pH 3.0:
· Method : Ion Chromatography Instrument : Metrohm IC equipped with pump, Injector, conductivity detector and recorder.
Column Dionex Ion Pac AS-11 (4.0 x 250mm), 13μπι
Guard column Dionex Ion Pac AG-11 (4.0 x 50mm), 13μπι
Buffer preparation Weigh accurately about 2.118g of Sodium carbonate and 180mg of Sodium hydroxide in 1700mL water.
Mobile phase preparation : Buffer and acetonitrile (1700:300).
Results: Phosphate binding of an iron containing phosphate adsorbents obtained by following the process of the present invention found in the range of 30 mg/gm to 60 mg/gm. Particle Size Distribution:
Instrument Model : Malvern Mastersizer 2000 Particle size analyzer
Sampling Unit : Hydro 2000S
Analysis Model : General Purpose
Dispersant : 0.1% Span 85 in n-Hexane
Dispersant RI : 1.380
Stirrer Speed : 2200 RPM
Absorption : 1
Particle RI : 1.5
Obscuration : 10% to 20%
Sample Measurement time : 12 seconds
Background Measurement time : 12 seconds Table-3
Particle size distribution
Example no.
d(0.9) (μηι)
3d 43.67
3e 65.37
3f 37.75

References
- ^ Jump up to:a b c d e “Velphoro (sucroferric oxyhydroxide). Summary of Product Characteristics”(PDF). EMA. Archived from the original on October 21, 2014. Retrieved 24 October 2014.
- ^ Jump up to:a b Jha V, Garcia-Garcia G, Iseki K, Li Z, Naicker S, Plattner B, Saran R, Wang AY, Yang CW (July 2013). “Chronic kidney disease: global dimension and perspectives”. Lancet. 382(9888): 260–72. doi:10.1016/S0140-6736(13)60687-X. PMID 23727169.
- Jump up^ Hutchison AJ, Smith CP, Brenchley PE (September 2011). “Pharmacology, efficacy and safety of oral phosphate binders”. Nature Reviews. Nephrology. 7 (10): 578–89. doi:10.1038/nrneph.2011.112. PMID 21894188.
- Jump up^ Isakova T, Gutiérrez OM, Chang Y, Shah A, Tamez H, Smith K, Thadhani R, Wolf M (February 2009). “Phosphorus binders and survival on hemodialysis”. Journal of the American Society of Nephrology. 20 (2): 388–96. doi:10.1681/ASN.2008060609. PMC 2637053
 . PMID 19092121.
. PMID 19092121. - ^ Jump up to:a b “KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD)”. Kidney International Supplement. 76 (113): S1–130. August 2009. doi:10.1038/ki.2009.188. PMID 19644521.
- Jump up^ Vifor Fresenius Medical Care Renal Pharma. Product Monograph 2015.
- ^ Jump up to:a b Wilhelm M, Gaillard S, Rakov V, Funk F (April 2014). “The iron-based phosphate binder PA21 has potent phosphate binding capacity and minimal iron release across a physiological pH range in vitro”. Clinical Nephrology. 81 (4): 251–8. doi:10.5414/cn108119. PMID 24656315.
- ^ Jump up to:a b c “Highlights of Prescribing information for Velphoro”. Fresenius. September 2014.
- Jump up^ Chong E, Kalia V, Willsie S, Winkle P (December 2014). “Drug-drug interactions between sucroferric oxyhydroxide and losartan, furosemide, omeprazole, digoxin and warfarin in healthy subjects”. Journal of Nephrology. 27 (6): 659–66. doi:10.1007/s40620-014-0080-1. PMC 4242982
 . PMID 24699894.
. PMID 24699894. - Jump up^ Levesque V, Chong EMF, Moneuse P (2013). “Post-hoc analysis of pharmacodynamic interaction of PA21 with statins in a Phase 3 study of PA21 in dialysis patients with hyperphosphatemia”. J Am Soc Nephrol. 24: 758A.
- Jump up^ Floege J, Botha J, Chong E et al. (31 May 2014). PA21 does not interact with oral vitamin D receptor agonists: a post hoc analysis of a Phase 3 study. ERA-EDTA congress. Amsterdam, The Netherlands. Abstract no. SP257.
- Jump up^ Prescribing Information. Synthroid (levothyroxine). Chicago, IL: Abbott Laboratories. March 1, 2008.
- Jump up^ Lanz M, Baldischweiler J, Kriwet B, Schill J, Stafford J, Imanidis G (December 2014). “Chewability testing in the development of a chewable tablet for hyperphosphatemia”. Drug Development and Industrial Pharmacy. 40 (12): 1623–31. doi:10.3109/03639045.2013.838583. PMID 24010939.
- ^ Jump up to:a b Floege J, Covic AC, Ketteler M, Rastogi A, Chong EM, Gaillard S, Lisk LJ, Sprague SM (September 2014). “A phase III study of the efficacy and safety of a novel iron-based phosphate binder in dialysis patients”. Kidney International. 86 (3): 638–47. doi:10.1038/ki.2014.58. PMC 4150998
 . PMID 24646861.
. PMID 24646861. - Jump up^ Floege J, Covic AC, Ketteler M, Mann JF, Rastogi A, Spinowitz B, Chong EM, Gaillard S, Lisk LJ, Sprague SM (June 2015). “Long-term effects of the iron-based phosphate binder, sucroferric oxyhydroxide, in dialysis patients”. Nephrology, Dialysis, Transplantation. 30(6): 1037–46. doi:10.1093/ndt/gfv006. PMC 4438742
 . PMID 25691681.
. PMID 25691681. - Jump up^ Kalantar-Zadeh K, Parameswaran V, Ficociello LH, Anderson L, Ofsthun NJ, Kwoh C, Mullon C, Kossmann RJ, Coyne DW (2018). “Real-World Scenario Improvements in Serum Phosphorus Levels and Pill Burden in Peritoneal Dialysis Patients Treated with Sucroferric Oxyhydroxide”. American Journal of Nephrology. 47 (3): 153–161. doi:10.1159/000487856. PMC 5906196
 . PMID 29514139.
. PMID 29514139.
| Clinical data | |
|---|---|
| Trade names | Velphoro |
| AHFS/Drugs.com | Consumer Drug Information |
| License data | |
| Pregnancy category |
|
| Routes of administration |
Oral (chewable tablets) |
| ATC code | |
| Legal status | |
| Legal status |
|
| Chemical and physical data | |
| Formula | Varies |
FDA Orange Book Patents
| FDA Orange Book Patents: 1 of 2 (FDA Orange Book Patent ID) | |
|---|---|
| Patent | 6174442 |
| Expiration | Dec 19, 2018 |
| Applicant | VIFOR FRESENIUS |
| Drug Application | N205109 (Prescription Drug: VELPHORO. Ingredients: SUCROFERRIC OXYHYDROXIDE) |
/////////////Sucroferric oxyhydroxide, EU 2014, Iron sugar, Saccharated iron, Sucroferric oxyhydroxide, Saccharated iron oxide, Saccharated ferric oxide, Ferrivenin, 含糖酸化鉄, スクロオキシ水酸化鉄 , NDC 49230-645-51
C(C1C(C(C(C(O1)OC2(C(C(C(O2)CO)O)O)CO)O)O)O)O.O.O.O.[OH-].[O-2].[O-2].[O-2].[O-2].[O-2].[O-2].[O-2].[O-2].[Na+].[Na+].[Fe+3].[Fe+3].[Fe+3].[Fe+3].[Fe+3]
Ferric Maltol, マルトール第二鉄
Ferric Maltol
Iron, tris(3-hydroxy-2-methyl-4H-pyran-4-onato-O3,O4)-
| Molecular Formula: | C18H15FeO9 |
|---|---|
| Molecular Weight: | 431.154 g/mol |
iron(3+);2-methyl-4-oxopyran-3-olate
RN: 33725-54-1
UNII: MA10QYF1Z0
Feraccru
Ferric maltol; UNII-MA10QYF1Z0; MA10QYF1Z0; Ferric maltol (INN); Ferric maltol [INN]; 33725-54-1
Shield Therapeutics, under license from Vitra Pharmaceuticals
UPDATE
- Originator University of Cambridge; University of London
- Developer Shield Therapeutics
- Class Antianaemics; Ferric compounds; Pyrones; Small molecules
- Mechanism of Action Iron replacements
- Marketed Iron deficiency anaemia
Most Recent Events
- 26 Jul 2019 Registered for Iron deficiency anaemia (In adults) in USA (PO)
- 24 Apr 2019 Swissmedic approves a extension of the approved indication for ferric maltol to include treatment of all adults with iron deficiency (ID) with or without anaemia
- 14 Mar 2019 The European Patent Office decides in favour of Shield Therapeutics in relation to the group’s patent No. 2 668 175
The US Food and Drug Administration (FDA) has approved oral ferric maltol(Accrufer, Shield Therapeutics) AUG 2019 for the treatment of iron deficiency in adults.
The product is already approved in the European Union and Switzerland for the treatment of iron deficiency in adults, where it is sold as Feraccru.
OLD DATA NDA filing expected in US in 2H 2018, Ph 3 trial is planned in 2018/19 for treatment of iron deficiency anemia (IDA) in children., Expected dose form: Oral Capsule; 30 mg
Treatment of iron deficiency anemia (IDA) associated with inflammatory bowel disease (IBD) and Chronic Kidney disease.
Iron deficiency anaemia (IDA) occurs when iron levels are insufficient to support red blood cell production and is defined – according to the WHO – as haemoglobin levels below 13 g/dL in men over 15 years, below 12 g/dL in non-pregnant women over 15 years, and below 11 g/dL in pregnant women. Iron is absorbed at the apical surface of enterocytes to be transported by ferroportin, the only known iron exporter, across the basolateral surface of the enterocyte into circulation. Inflammation from IBD interferes with iron absorption by causing an increase in hepcidin, a peptide hormone synthesized in the liver that inhibits ferroportin activity. Anaemia is the most common extra-intestinal complication of inflammatory bowel disease (IBD) and although it often involves a combination of IDA and anaemia of chronic disease, IDA remains an important contributor in this condition due to chronic intestinal bleeding and decreased iron intake (from avoidance of foods that may exacerbate symptoms of IBD). In a variety of populations with IBD, the prevalence of iron deficiency anaemia ranges from 36%-76%. The serum markers of iron deficiency are low ferritin, low iron, raised total iron binding capacity, raised red cell protoporhyrin and increased transferrin binding receptor (sTfR). Serum ferritin is the most powerful test for iron deficiency. The cut-off level of ferritin which is diagnostic varies between 12-15 µg/L. Higher levels of serum ferritin do not exclude the possibility of iron deficiency, and a serum ferritin level of <100 μg/L may still be consistent with iron deficiency in patients with IBD. A transferrin saturation of <16% is indicative of iron deficiency, either absolute or functional. Other findings on a complete blood count panel that are suggestive of iron deficiency anaemia, but are not considered diagnostic, include microcytosis, hypochromia, and elevation of red cell distribution width.
A deficiency of iron can have a significant impact on a patient’s quality of life. Appropriate diagnosis and treatment of iron deficiency anaemia are important to improve or maintain the quality of life of patients. The goals of treatment are to treat the underlying cause, limit further blood loss or malabsorption, avoid blood transfusions in haemodynamically stable patients, relieve symptoms, and improve quality of life. More specifically, therapeutic goals of treatment include normalizing haemoglobin levels within 4 weeks (or achieving an increase of >2 g/dL) and replenishing iron stores (transferrin saturation >30%). Oral iron supplementation has been considered standard treatment because of an established safety profile, lower cost, and ease of administration. It has been shown to be effective in correcting anaemia and repleting iron stores. One concern with higher doses of daily oral iron is intolerance due to GI side effects. Symptoms include nausea, vomiting, diarrhea, abdominal pain, constipation, and melena-like stools. Guidelines on the Diagnosis and Management of Iron Deficiency and Anaemia in Inflammatory Bowel Diseases recommend IV iron therapy over oral iron supplementation in the treatment of iron deficiency anaemia in patients with IBD, citing faster and prolonged response to treatment, decreased irritation of existing GI inflammation, improved patient tolerance, and improved quality of life. Patients with severe anaemia (haemoglobin level of <10 g/dL), failure to respond or intolerance to oral iron therapy, severe intestinal disease or patients receiving concomitant erythropoietin are recommended indications for IV iron therapy. Other conditions where patients should be considered for first-line IV therapy over oral therapy include congestive heart failure, upper GI bleeding, and in situations where rapid correction of anaemia may be required.
Across EU there are several iron (Fe+2) oral preparations as ferrous fumarate, ferrous gluconate, ferrous sulphate and ferrous glycine sulfate, formulated as tablet, solution or gastroresistent capsules. All ferrous compounds are oxidised in the lumen of the gut or within the mucosa with release of activated hydroxyl radicals, which may attack the gut wall and can effect a range of gastrointestinal symptoms and discomfort. Ferric preparations also exist but with less bioavailability. Across EU there are also several IV products on the market: iron (III) hydroxide dextran complex, iron sucrose, ferric carboxymaltose, iron isomaltoside. IV iron therapy, however, is inconvenient, invasive and associated with the risk of rare but serious hypersensitivityreactions; it is used in those situations when oral preparations cannot be used or when there is a need to deliver iron rapidly. Feraccru is a trivalent iron, oral iron replacement preparation. The active substance of Feraccru is ferric maltol (also known as 3-hydroxy-2-methyl-4H-pyrane-4-one iron (III) complex, or ST10, or ferric trimaltol or ferric maltol) an oral ferric iron/maltol complex. It is presented as red hard gelatine capsules containing 30 mg iron (ferric iron). Maltol is a sugar derivative that strongly chelates iron in the ferric form (FeIII) rendering the iron stable and available for absorption. Upon dissociation of the ferric maltol complex, the maltol molecules are absorbed and glucuronidated in the intestinal wall, and within the liver during first pass metabolism, and subsequently eliminated from the body in the urine. The iron is absorbed via the endogenous dietary iron uptake system. The indication finally agreed with the CHMP was: Feraccru is indicated in adults for the treatment of iron deficiency anaemia (IDA) in patients with inflammatory bowel disease (IBD) (see section 5.1). The proposed dosage is one 30 mg capsule twice daily on an empty stomach, corresponding to 60 mg ferric iron per day. There was agreement in the paediatric investigation plan to grant a deferral and a waiver for iron as iron (III)-maltol complex (EMEA-001195-PIP01-11).The PDCO granted a waiver in infants under 6 months of age and a referral for the completion of the planned paediatric studies (ST10-021 PK-PED/ST10-01-102, an open label, randomised, multiple-dose, parallel PK study and ST10-01-303, a randomised, open label comparative safety and efficacy study of ST10 and oral ferrous sulphate as comparator) until the adult studies are completed.

SYN
Patent
https://patents.google.com/patent/WO2017167963A1/en
The sugar derivative maltol is a hydroxypyrone (IUPAC name: 3- hydroxy-2-methyl-4£f-pyran-4-one) and it strongly chelates iron and the resulting complex (ferric trimaltol) is well absorbed, unlike many other ferric iron therapies. Ferric trimaltol appears well tolerated even in populations highly susceptible to gastrointestinal side-effects, such as IBD patients (Harvey et al . , 1998), and as such it provides a valuable alternative to patients who are intolerant of oral ferrous iron products, notably in place of intravenous iron. Clinical trials using ferric trimaltol have been carried out, see for example, Gasche et al., 2015.
However, despite the evidence of bioavailability and tolerability for ferric trimaltol, its clinical development has been limited by the absence of adequate synthetic routes. In particular, most manufacturing processes require the use of organic solvents, which increase manufacturing costs, for example to deal with post-synthesis solvent removal, and require additional safety measures, for example to deal with flammability . Critically, solvent-based syntheses are not robust and often generate ferric hydroxide, described in the prior art to be an unwanted impurity of the synthesis.
WO 03/097627 (Vitra Pharmaceuticals Limited) describes the synthesis of ferric trimaltol from iron salts of carboxylic acids in aqueous solution at a pH greater than 7. In a first
synthesis, ferric citrate is added to a solution of sodium hydroxide at room temperature and maltol is added to a second solution of sodium hydroxide at pH 11.6. The ferric citrate solution is added to the maltol solution, leading to the
production of a deep red precipitate. This composition is then evaporated until dryness and the material is powdered and dried. Alternative syntheses are described using ferrous fumarate or ferrous gluconate as the iron carboxylate salt starting material, and by dissolving maltol in sodium carbonate solution in place of sodium hydroxide. However, despite the fact that this process is fully aqueous, several of the iron carboxylate salts employed are expensive, especially as they need to be pharmaceutical grade if the ferric trimaltol is to be suitable for human administration. More importantly, this process introduces high levels of
carboxylates (equimolar to iron or greater) to the synthesis that are not easily removed by filtration or centrifugation of the ferric trimaltol cake. Instead these water soluble contaminants must be washed off (e.g. water washed), but this would result in considerable losses of the product due to the amphipathic nature of ferric trimaltol.
WO 2012/101442 (Iron Therapeutic Holdings AG) describes the synthesis of ferric trimaltol by reacting maltol and a non- carboxylate iron salt in an aqueous solution at alkaline pH .
However, despite the lower cost of non-carboxylate iron salts, pharmaceutically appropriate grades are still required if the ferric trimaltol is to be suitable for human administration and hence are comparatively expensive starting materials.
Importantly, the use of non-carboxylate iron salts (e.g. ferric chloride) results in the addition of considerable levels of the respective counter-anion (e.g. three moles of chloride per every mole of iron) of which a significant part is retained in the filtration (or centrifugation) cake and thus must be washed off. As such, WO 2012/101442 does not address the problem of product losses in WO 03/097627. Furthermore, the addition of a non- carboxylate iron salt (e.g. ferric chloride) to a very alkaline solution, as described in WO 2012/101442, promotes the formation of stable iron oxides, which is an unwanted contaminant in ferric trimaltol . As a consequence, further costly and time-consuming processing of the material would be required for manufacturing .
Overall, the cost of the current aqueous syntheses is driven by regulatory demands for low levels of toxic heavy metals and residual reagents in the final pharmaceutical formulation, which force the use of highly purified, and thus expensive, iron salts as well as thorough washing of the final product (resulting in significant losses of product) . This will impact on the final price of ferric trimaltol and potentially limits patient access to this therapy. As such, there is a need for a process that can use lower iron grades and limited wash cycles, whilst producing ferric trimaltol of adequate purity.
Ferric maltols are a class of compounds that include ferric trimaltol, a chemical complex formed between ferric iron (Fe3+) and the hydroxypyrone, maltol (IUPAC name: 3-Hydroxy-2-methyl-4£f- pyran-4-one) , in a molar ratio of ferric iron to maltol of 3:1. Maltol strongly chelates the ferric iron and the resulting complex (ferric trimaltol which may also be written as ferric tri-maltol) is well absorbed, in contrast to some other ferric iron supplements, fortificants and therapies. Maltol binds metal cations mainly in the form of a dioxobidentate ligand in a similar manner proposed for other 4 ( 1H) -pyranones :
Structure of maltol (3-hydroxy-2-methyl-4 (H) -pyran-4-one) and dioxo-chelation to metal cations (M) such as iron. For ferric trimaltol three maltol groups surround one iron.
Examples
Example 1: Ferric trimaltol from L-lyslne coated ferric hydroxide
Synthesis of lysine-coated ferric hydroxide colloid
14.87g FeCl3. 6H20 was added to 25 mL UHP water and stirred until dissolved. 14.9g NaOH 5M was then added drop-wise to this solution with constant stirring, during which a ferric hydroxide colloid was gradually produced. This colloidal suspension was then added to a L-Lysine suspension (5.02g in 25mL ddH2<D) .
Ferric trimaltol synthesis
7 g NaOH pellets was added to 25 mL UHP water and stirred until dissolved. Next, 24.5g maltol was added and stirred until dissolved. Then, the suspension of lysine-coated ferric
hydroxide colloids was gradually added to the maltol with vigorous stirring, producing a dark red precipitate (with a significant brown hue) . This suspension was incubated overnight during which time it became lighter and the brown hue
disappeared. This precipitate was then recovered by
centrifugation (4500 rpm x 5min) and dried overnight (50°C) .
Example 2: Ferric trimaltol from L-lysine modified ferric hydroxide
Synthesis of lysine-modified ferric hydroxide gel
14.87g FeCl3.6H20 and 5.02g L-Lysine were added to 25 mL UHP water and stirred until dissolved. 32 mL NaOH 5M was then gradually added to this solution producing a ferric hydroxide gel .
Ferric trimaltol synthesis
7 g NaOH pellets was added to 25 mL UHP water and stirred until dissolved. Next, 24.5g maltol was added and stirred until dissolved. Next, the lysine-modified ferric hydroxide gel was gradually added to this solution with vigorous stirring. A 1.2 M HC1 solution was then used to drop the pH of the solution to 10, which was then incubated for 70 min. Finally, a dark red precipitate (i.e., ferric trimaltol) was recovered by
centrifugation (4500 rpmx5min) and dried overnight (45°C) .
Example 3: Absence of ferric hydroxide in ferric trimaltol
Ferric trimaltol is soluble in ethanol whereas ferric hydroxide (a potential contaminant) is not. As such ferric trimaltol powders produced as per Examples 1 and 2 were dissolved in ethanol. The material from Example 2 dissolved completely confirming the absence of iron hydroxides whereas the material from Example 1 did not. This supported the preference in the present invention for ligand modification, rather just surface coating, to ensure full conversion to ferric trimaltol .
Example 4: Ferric trimaltol from tartrate-modified ferric hydroxide
Synthesis of tartrate-modified ferric hydroxide gel
14.87g FeCl3.6H20 (0.055 mol) was added to 25 mL UHP water and stirred until dissolved. 4.12 g tartaric acid (0.0275 mol) was added to this solution and stirred until dissolved. 38 mL NaOH 5M was then gradually added to this solution producing a ferric hydroxide gel .
Ferric trimaltol synthesis
2 g NaOH pellets was added to 25 mL UHP water and stirred until dissolved. Next, 24.5g maltol was added and stirred. This produced a slurry in which most of the maltol remained
undissolved. Next, the tartrate-modified ferric hydroxide gel was gradually added to this solution with vigorous stirring during which the remainder of maltol dissolved. After 15 min a dark red precipitate (i.e. ferric trimaltol) had been formed and pH had stabilised at 8.5. The material was then washed by (1)
centrifuging, (2) disposing of the supernatant and (3)
resuspending in water back to its original volume. Finally, the material was recovered by centrifugation (4500 rpm x 5min) and dried overnight (50°C) . Previously disclosed synthetic processes for the production of ferric trimaltol under aqueous conditions require the addition of NaOH (or other suitable bases) for conversion of maltol from its protonated form to its deprotonated form prior to complexation of iron. However this results in the formation of unwanted sodium ions which must be washed off. In contrast, the use of ferric hydroxides according to the methods of the present invention reduces the requirements for base and associated counter cation (e.g. sodium), which is a favourable feature. Note that ferric hydroxides are represented above as Fe (OH) 3 for illustrative purposes only. Different iron hydroxides possess different structures and elemental compositions (see Cornell & Schwertmann, The Iron Oxides Structure, Properties, Reactions, Occurrence and Uses. 2nd edition, 1996, VCH Publishers, New York) . Example 5: Ferric trimaltol from tartrate-modified ferric hydroxide (with removal of contaminants from ferric hydroxide)
Material prepared as in Example 4, except excess reactants and reaction products (e.g. unbound tartaric acid, sodium chloride) were removed from the ferric hydroxide gel. This was achieved by centrifuging the ferric hydroxide gel after its synthesis and discarding the supernatant, which contained unwanted soluble species. Finally, the ferric hydroxide gel was re-suspended in water back to its original volume prior to being added to a maltol slurry.
Example 6: Ethanolic clean up for ferric trimaltol produced from ligand coated ferric hydroxide
Ferric trimaltol precipitate was purified as it contained an unwanted iron oxide fraction. Part of the wet pellet recovered by centrifugation (4.5 g) was dissolved in 1L ethanol. The iron oxide fraction (which remained undissolved) was then removed by filtration, producing a turbidity-free solution. Next, ethanol was evaporated (40°C in a rotavapor under vacuum) producing a concentrated ferric trimaltol slurry. This was then recovered and oven dried overnight at 50°C.
PATENT
https://patents.google.com/patent/WO2012101442A1/en
Comparative Example 1
Preparation of Iron Trimaltol from Pure Maltol Maltol was dissolved in an aqueous solution of ferric chloride and ferric trimaltol was precipitated upon the addition of sodium hydroxide.
An accurate mass of ferric chloride hexahydrate granules (330g) was dissolved in distilled water to yield a pH of 0.6. To this solution, an equimolar amount of maltol was added (490g in total, initially 250g) and allowed to dissolve with continuous stirring. The pH of this solution was found to be zero and the colour of this solution was deep- purple. Spectroscopy showed that the initial solution was mainly a 1 :1 Fe/maltol mixture with some 1 :2 component. The remaining maltol was added. After an hour of stirring, sodium hydroxide (147g NaOH in 750 ml water) was added dropwise to the solution until a pH of 8.3 was achieved. The solution and precipitate were red. The precipitate was collected using a Buchner funnel under vacuum. The precipitate was dried at 40°C under vacuum.
Maltol is only slightly soluble in an aqueous acidic reaction medium. After an hour of stirring, traces of undissolved maltol were visible on the surface of the ferric chloride/maltol solution, on the walls of the reaction vessel and on the stirrer. Upon addition of sodium hydroxide, there appeared to be lumps of a brownish-black substance on the walls of the reaction vessel and on the stirrer which seemed to add to the impurities in the desired product.
An attempt to heat the ferric chloride/maltol solution so as to assist the maltol to dissolve in the ferric chloride solution resulted in a burnt, off spec, colour iron maltol sample. This method also produces two by-products which consume expensive maltol namely Fe(OH)2 (Maltol) and Fe (OH) (Maltol)2.
The sodium hydroxide solution has to be added extremely slowly to prevent “gumming up” and formation of undesirable lumps at the bottom of the reaction vessel. A yield of about 78% ferric trimaltol was obtained using this method of preparation.
When maltol is added to a ferric chloride solution at a low pH, no ferric trimaltol is formed and ferric hydroxide is generated with ferric monomaltol and a small percentage of ferric dimaltol species. The charge neutralisation of these complexes is either the hydroxy! functional group or the chloride anion. This addition also results in the formation of black deposits and gums consisting of ferric chloride/ferric hydroxide polymers. These black deposits are also produced if the solutions are heated. Therefore it is not possible to obtain the correct stoichiometry for the formation of ferric trimaltol and manufacture a pharmaceutically acceptable product using this method.
The addition of maltol to an aqueous solution of ferric or ferrous chloride was deemed impractical for scale up and manufacturing purposes and Examples 2 to 4 investigate the addition of the iron chlorides to maltol in solution.
The problem of working in an aqueous environment
Ferric chloride as a hydrated ion in aqueous solution is a strong Lewis acid with a Ka of 7x 103 and ferrous chloride as a hydrated ion in aqueous solution is also a strong Lewis acid with a Ka of 5 x 10“9. Over the desired range for using iron chlorides as starting materials for the synthesis of ferric trimaltol, ferric chloride in aqueous solution has a pH value in the range of 1-3 and ferrous chloride has a pH in the range of 3-5. Furthermore, commercial solutions of iron chlorides have a pH circa 1 because they are stabilised by the addition of hydrochloric acid to prevent the precipitation of ferric hydroxide species.
The present invention recognises that maltol is virtually insoluble at these low pH values and has limited solubility when dissolved in water in the pH range 6-8. The maximum aqueous solubility is 1g/100m! at 20°C. However, the solubility of maltol can be increased to 10g/100ml by heating to near boiling temperatures. Maltol is stable in aqueous solution at these temperatures and this property has been employed in Example 4 to synthesise ferric trimaltol. At low pH values ferric trimaltol is not the preferred species due to disproportionation. In order to obtain significant amounts of ferric trimaltol using a stoichiometric ratio of iron salt to hydroxypyrone of 1 :3, the eventual pH of the solution must exceed 7 since below that pH ferric dimaltol and monomaltol species will exist. Therefore two methods of increasing the pH were researched 1) using sodium carbonate and 2) using sodium hydroxide. Other alkali hydroxides could be used such as potassium hydroxide. The sodium carbonate neutralisation was found to be less preferable due to C02 generation. This research lead to an improved synthesis of ferric trimaltol.
Example 2
Maltol was dissolved in an aqueous solution of sodium hydroxide and iron maltol was precipitated upon the addition of ferric chloride.
In view of some of the difficulties experienced in Example 1 , and the fact that maltol is very soluble in aqueous alkali hydroxide solutions, it was decided to change the manufacturing procedure.
The initial work using this method of preparation showed that a 90% yield was achieved. Various operating parameters were then optimised and the following procedure outlines the final method chosen. A yield of 95% was then achieved. An accurate mass of sodium hydroxide pellets (20g) was dissolved in distilled water to yield a pH of 13.50. An equimolar amount of maltol (63g) was added to this aqueous solution of NaOH to give a clear yellow coloured solution with a pH of 11.6. Almost immediately a stoichiometric amount of ferric chloride (45g) was added slowly to this solution to give a pH of 7.1 and a red precipitate formed, which was then collected using a Buchner funnel under vacuum. The precipitate was then dried at 40°C under vacuum.
Adding the maltol solution in sodium hydroxide to ferric chloride as in method 1 is not preferred since it gives an off spec product and gums and a black precipitate.
Maltol is very soluble in aqueous alkali hydroxide solutions giving a yellow solution. The concentration of the hydroxide solution preferably does not exceed 20%.
This method is advantageous since it has the potential to produce only one by-product viz, ferric hydroxide Fe(OH)3 which consumes some of the iron intended to complex with the maltol. This is not easily measurable in the presence of iron maltol and so the following method was used to measure the ferric hydroxide. Fe(OH)3 is insoluble in ethanol and so the iron maltol product was dissolved in ethanol. It was found that small amounts of Fe(OH)3 may be present in the batches of iron maltol synthesized according to Example 2.
Taking the extremes of the specification, in one embodiment, the amount of Fe(OH)3 present in the active material may not exceed 2 wt. % Fe(OH)3 based on the total weight of the composition. In view of its well known inert characteristics the level of this compound is adequately controlled and a final specification including controlled ferric hydroxide should be acceptable.
The mass balance for maltol and iron was closed at 99%.
A yield of 95% iron maltol was obtained using this method of preparation.
Example 3
Maltol was dissolved in an aqueous solution of Sodium Carbonate and Iron Maltol was precipitated upon the addition of Ferric Chloride.
An accurate mass of sodium carbonate (Na2C03) (53g) was dissolved in distilled water to give a solution having pH = 11.5. An equimolar amount of maltol (65g) was added to this aqueous alkali solution to give a murky creme coloured solution of pH = 9.9. A stoichiometric amount of a ferric chloride solution was added drop wise to this solution to a pH of 8.00. A further 15 grams of Na2C03 was added to this solution to increase the pH to 9.00. The remainder of the ferric chloride solution was then added to give a solution pH = 8.77 and a red coloured precipitate appeared.
The precipitate was collected using a Buchner funnel under vacuum. The precipitate was then dried at 40°C under vacuum. The release of C02 during the reaction tends to make this process less desirable due to foaming on the surface. The final product is a gellike solid when wet and the removal of moisture during drying can therefore be time consuming. The process may not be preferred but the ferric trimaltol produced could be acceptable.
Example 4 Maltol was dissolved in water and heated to a near boiling temperature and ferric or ferrous chloride was added to form a 1 :1/1:2 mixture of ferric maltol. The solution was allowed to cool and was added to maltol dissolved in sodium hydroxide. Stage 1
Depending on the batch size required, the ferric chloride was added slowly to a maltol solution in water at a pH of 6-7. The solubility of maltol is greatly enhanced up to 10g/100ml by heating to temperatures above 60°C. Addition of ferric chloride or ferrous chloride and monitoring the pH of the solution and maintaining the pH> 3 mainly produces ferric dimaltol species but very little ferric trimaltol. Above pH 3, no ferric hydroxide appeared to be generated. Ferric monomaltol and dimaltol species either with hydroxy or chloride giving the charge neutralisation are very soluble and a concentrated solution in excess of 30g/100ml can be generated. In order to obtain the correct stoichiometry for the formation of ferric trimaltol, further maltol is required and the pH needs to be corrected to values higher than 7.
As anhydrous ferrous or ferric chloride either 126g or 162g in 200ml of water can be added to a litre of water containing 120g of maltol. This ratio of iron to maltol does not provide sufficient maltol to produce any significant amounts of ferric trimaltol which does not precipitate at this stage.
Stage 2 Maltol in alkaline solution has been described as set out above. Conveniently, because maltol solutions up to 20% in sodium hydroxide have a pH circa 11.6, mixing of this solution with the ferric mono/dimaltol solutions from stage 1 yields a precipitate of ferric trimaltol with a deep characteristic burgundy red colour of high purity as determined by UV-vis spectroscopy. The filtrate yields product which is suitable for a GMP (good manufacturing process). The sodium chloride which is generated by this process is found in the supernatant since it has a much higher solubility at 35g/100ml than ferric trimaltol. The small amounts of sodium chloride in the ferric trimaltol can be reduced, if required, by washing in water. A further, surprising feature of the research resulted from work on ferrous chloride. Ferrous chloride may be substituted in stage 1 to form ferric dimaltol since the maltol was found to auto-oxidise the ferrous to ferric during the process of chelation. One aspect of this work which was considered to be potentially very useful if larger batch sizes were required arose from the finding that being a weaker Lewis acid than ferric chloride the pH of the starting solution was in excess of 3. Therefore the risk of generating ferric hydroxide was lower than with the use of ferric chloride at higher concentrations.
Ferrous and ferric chloride in solution or as a solid may be added to an alkaline solution of maltol in sodium hydroxide, combining stages 1 & 2. Providing a small excess of maltol up to about 10% is added then a precipitate of ferric trimaltol with a small amount of maltol is obtained. Such a preparation would be satisfactory as a GMP ferric trimaltol product.
PATENT
https://patents.google.com/patent/WO2017167963A1/en
AMPLE 1
Synthesis of ferric trimaltol using ferric citrate
NaOH (12g, 0.3 moles) is dissolved in water (50 ml) to form a sodium hydroxide solution. 20 ml of the sodium hydroxide solution is placed in a separate vessel.
Ferric citrate (30g, 0.11 moles) is slowly added to the sodium hydroxide solution in the separate vessel at room temperature with gentle stirring. Further portions of the sodium hydroxide solution are added to the solution of ferric citrate, as necessary, in order to ensure that all of the ferric citrate is dissolved.
Maltol (49g, 0.39 moles) is added to the remaining volume of sodium hydroxide solution and dissolved. The pH of the maltol solution is 11.6.
The ferric citrate solution is slowly added to the maltol solution with gentle stirring. A deep red precipitate forms; the supernatant is a deep red colour.
The solution is slowly evaporated to dryness at 60 to 80° C until the material is suitable for powdering. The material is powdered and the powder is then dried to a constant weight.
The yield of the final product is 87g. The final product comprises ferric trimaltol and sodium citrate. The product was assayed, using elemental analysis, for iron and sodium content. The iron content is 7.89% (theoretical 7.8%) and the sodium content is 13.45%.
The pH of a solution of the final product in water was measured. The pH of a 1% solution of the product by total weight of aqueous solution is 9.9 at 20°C.
EXAMPLE 2
Synthesis of ferric trimaltol using ferrous fumarate
NaOH (40g, 1 mole) is dissolved in water (100 ml) to form a sodium hydroxide solution. The pH of the solution is approximately 13.0.
Ferrous fumarate (170g, 1 mole) is slowly added to the sodium hydroxide solution at room temperature with gentle stirring.
Maltol (408g, 3.23 moles) is added to a separate volume of sodium hydroxide (40g, 1 mole) dissolved in water (100 ml) and dissolved. The pH of the solution is approximately 11.
The ferrous fumarate solution is slowly added to the maltol solution with gentle stirring. A deep red precipitate forms; the supernatant is a deep red colour.
The solution is slowly evaporated to dryness at 60 to 80° C until the material is suitable for powdering. The material is powdered and the powder is then dried to a constant weight. The yield of the final product is 615g.
The final product comprises ferric trimaltol and sodium fumarate.
EXAMPLE 3
Synthesis of ferric trimaltol using sodium carbonate to vary pH
Sodium carbonate (2.5g) is dissolved in 10ml of distilled water at room temperature. The pH of the solution is 11.6. Maltol (9.6g – three molar equivalents of sodium carbonate) is added to the sodium carbonate solution to give a cream coloured solution having a pH of 10.0.
A stoichiometric amount of ferric citrate (5g, allowing for a small excess of maltol) in an aqueous solution of sodium hydroxide (lg in 5ml of distilled water) is added slowly to the solution of maltol. The pH of the combined solutions is about 9. A red precipitate appears which is separated by decantation and dried at 80°C in an oven.
The red precipitate is ferric trimaltol, as confirmed by UV-Vis spectrometry.
EXAMPLE 4
Synthesis of ferric trimaltol using ferrous gluconate
Potassium hydroxide (5.5g) is dissolved in 50ml of distilled water at room temperature. To 25ml of this solution, maltol (16.5g, 0.13 moles) is added and gently heated to form a clear solution. To the other 25ml aliquot of the potassium hydroxide solution ferrous gluconate (22.5g) is added. This is gently heated to form a dark green saturated solution. The ferrous gluconate solution is added to the maltol solution and immediately a colour change to dark brown is noted.
On cooling, a deep brown precipitate forms (which is ferric trimaltol). The supernatant is a deep brown solution containing ferric trimaltol and potassium gluconate. The precipitate and the supernatant are dried separately at 80°C in an oven. The ferric trimaltol is a deep red brown powder with a characteristic caramel odour and UV-vis spectrum in aqueous solution.
EXAMPLE 5
Synthesis of ferric trimaltol using solid ferrous gluconate
Example 4 was repeated with the modification that the maltol is added to all of the 50 ml solution of potassium hydroxide and then solid ferrous gluconate is added directly to the maltol solution. This method gives similar end products to Example 4.
EXAMPLE 6
Synthesis of ferric trimaltol using sodium ferrous citrate
A 20% solution w/v of sodium ferrous citrate in distilled water is prepared from 7.5g of sodium ferrous citrate in 37.5ml of water. The solution of sodium ferrous citrate is dark green with an iron content of about 20%. A solution of maltol (containing 10g/50ml) in 20% sodium hydroxide is added to the solution of sodium ferrous citrate. A characteristic deep red/brown iron complex of ferric trimaltol is formed.
EXAMPLE 7
Synthesis of ferric trimaltol using solid sodium ferrous citrate
Example 6 was repeated using the same amounts and concentrations of components but the method is varied in that solid sodium ferrous citrate (7.5g) is added directly to the maltol solution (containing lOg of maltol in 50ml). Ferric trimaltol is formed using this alternative method.
EXAMPLE 8
Synthesis of ferric trimaltol using sodium ferric citrate
A 20% solution w/v of sodium ferric citrate in distilled water is prepared from 7.5g of sodium ferric citrate in 37.5ml of water. The solution of sodium ferric citrate is dark brown with an iron content of about 20%.
A solution of maltol (containing 10g/50ml) in 20% sodium hydroxide is added to the solution of sodium ferric citrate. A characteristic deep red/brown iron complex of ferric trimaltol is formed. EXAMPLE 9
Example 8 was repeated using the same amounts and concentrations of components but the method is varied in that solid sodium ferric citrate (7.5g) is added directly to the maltol solution (containing lOg of maltol in 50ml). Ferric trimaltol is formed using this alternative method.
If any of Examples 3 to 9 are repeated using maltol in a neutral or acidic aqueous medium, such as for example in buffered citric acid, brown/black impurities appear and insoluble fractions are formed (probably of ferric hydroxide) and the UN-vis spectra of the solutions are not correct. In particular, there is a peak shift towards 510nm indicating the formation of mono or dimaltol complexes or compounds.
PATENT
WO 2017167970
POLYMORPH
GB 2531742
PATENT
WO 2016066555
https://patents.google.com/patent/WO2016066555A1/en
An adequate supply of iron to the body is an essential requirement for tissue growth and the maintenance of good health in both man and animals. Moreover, in certain pathological conditions where there is an insidious blood loss, or where there is a mal-distribution of iron in the body, there may be a state of low iron stores in the body leading to an iron deficiency and a concomitant chronic anaemia. This is seen in inflammatory diseases of the gastrointestinal tract, such as gastric and peptic ulcers, reflux oesophagitis, ulcerative colitis and Crohn’s disease.
Anaemia can also follow operations that result in serious blood loss and can be associated with gastrointestinal infections, such as those caused by Helicobacter pylori.
Ferric maltol comprises a complex of one ferric iron and three maltol anions and has the following molecular formula: (C6H503)3Fe. Maltol is also known as 3-hydroxy-2-methyl-4- pyrone.
Polymorphic forms occur where the same composition of matter crystallises in a different lattice arrangement, resulting in different thermodynamic properties and stabilities specific to the particular polymorphic form. WO 03/097627 A1 discloses a method of forming iron hydroxypyrone compounds.
EP 0 159 917 A3 describes a pharmaceutical composition containing a hydroxypyrone-iron complex. WO 2012/101442 A1 discloses a method of forming iron hydroxypyrone compounds.
Schlindwein et al (Dalton Transactions, 2006, Vol. 10, pages 1313-1321) describes lipophilic 3-hydroxy-4-pyridinonate iron(lll) complexes. Ferric maltol has been known for about 100 years but no polymorphs have been identified or studied prior to this invention.
We have now found that it is possible to produce different polymorphs of ferric maltol, which crystalline forms may be referred to herein as the “compounds of the invention”. One polymorph form can be preferable in some circumstances when certain aspects, such as ease of preparation and stability, such as thermodynamic stability are required. In other situations, a different polymorph may be preferred for greater solubility and/or superior pharmacokinetics. The polymorphs of the invention can provide advantages in terms of improved or better bioavailability or improved or better stability or solubility.
The term “ferric maltol” as used herein refers to both ferric trimaltol and the designation INN ferric maltol. In one aspect of the invention there is provided a Form I polymorph of ferric maltol characterized by a powder X-ray diffraction pattern comprising characteristic crystalline peaks expressed in degrees 2-theta at each of 15.6 and 22.5 ± 0.25 or 0.2 degrees, optionally wherein the Form I polymorph comprises greater than about 92 wt.% ferric maltol based on the weight of the polymorph, such as greater than about 95 wt.%, preferably greater than about 96 wt.%, or about 98 wt.%, or about 99 wt.% such as about 99.8 wt.%.
In a further aspect of the invention there is provided a Form II polymorph of ferric maltol characterized by a powder X-ray diffraction pattern comprising a peak expressed in degrees 2-theta at 8.3 ± 0.25 degrees.
In a yet further aspect of the invention there is provided a Form III polymorph of ferric maltol characterized by a powder X-ray diffraction pattern comprising a peak expressed in degrees 2-theta at 7.4 ± 0.25 degrees. In a still further aspect of the invention there is provided a Form IV polymorph of ferric maltol characterized by a powder X-ray diffraction pattern comprising peaks expressed in degrees 2-theta at 9.5 and 14.5 ± 0.2 degrees.
The measurements of degrees 2-theta generally refer to measurements at ambient temperature, such as from about 5 to about 40°C, preferably about 10 to about 30°C. The relative intensities of the peaks can vary, depending on the sample preparation technique, the sample mounting procedure, the particular instrument employed, and the morphology of the sample. Moreover, instrument variation and other factors can affect the 2-theta values. Therefore, XRPD peak assignments for the polymorphs of the invention, as defined herein in any embodiment, can vary by, for example, ± 0.2, such as ±0.1 or ±0.05. The term “about” in relation to XRPD peak values may include for example, ±0.25 or ± 0.2, such as ±0.1 or ±0.05. These ranges may apply to any of the peak values in degrees referred to herein.
In another embodiment of the invention, there is provided a process for the preparation of a ferric maltol polymorph, such as Form I or Form II polymorph, which comprises combining ferric citrate with maltol anions to form a mixture comprising ferric maltol and wherein the process comprises the use of a ferric maltol seed crystal. The seed crystal may comprise a Form I and/or Form II polymorph as described herein and these polymorphs may be prepared using the methods described herein.
In another aspect of the invention, there is provided a process for the preparation of Form I polymorph, which comprises combining ferric citrate with maltol anions to form a mixture comprising ferric maltol polymorph Form I wherein the process comprises the use of a ferric maltol seed crystal comprising Form I and/or Form II polymorph and preferably wherein the polymorph formed is washed (typically with water) prior to drying.
In a further aspect of the invention, there is provided a process for the preparation of Form II polymorph, which comprises combining ferric citrate with maltol anions in solution to form a mixture comprising ferric maltol polymorph Form II, wherein the process preferably comprises the use of a ferric maltol seed crystal comprising Form I and/or Form II polymorph and preferably wherein the polymorph formed is washed (typically with water) prior to drying.
The invention also provides a pharmaceutical composition comprising a polymorph according to the invention, or mixtures thereof, and a pharmaceutically acceptable adjuvant, diluent or carrier. In addition, the invention provides a composition comprising Form I and Form II polymorphs as defined herein.
In an aspect of the invention, the polymorph of the invention is for use in the prevention or treatment of iron deficiency with or without anaemia in a subject. The anaemia is preferably iron deficiency anaemia.
In a further aspect of the invention there is provided the use of a polymorph of the invention for the manufacture of a medicament for the prevention or treatment of iron deficiency with or without anaemia in a subject. The anaemia is preferably iron deficiency anaemia.
The invention further provides a method for the prevention or treatment of iron deficiency with or without anaemia which method comprises the administration of a polymorph according to the invention to a subject in need of such treatment. The anaemia is preferably iron deficiency anaemia.
Preferably the polymorphs of the invention are obtained in forms that are greater than about 90%, such as greater than about 95%, crystalline (e.g. greater than about 98% crystalline and, particularly, 100%, or nearly 100%, crystalline). By “substantially crystalline” we include greater than about 60%, preferably greater than about 75%, and more preferably greater than about 80% (such as about 90%) crystalline. The degree (%) of crystallinity may be determined by the skilled person using X-ray powder diffraction (XRPD). Other techniques, such as solid state NMR, FT-IR, Raman spectroscopy, differential scanning calorimetry (DSC) microcalorimetry and calculations of the true density may also be used.
The polymorphs of the invention may be characterised by an X-ray powder diffraction pattern comprising the following characteristic crystalline peaks with approximate 2-Theta values (in degrees) as well as an indication of the relative intensity of those peaks in brackets, where a percentage relative intensity of approximately 25- 00% is termed “vs” (very strong), approximately 10-25% is termed “s” (strong), approximately 3-10% is termed “m” (medium) and approximately 1-3% is termed “w” (weak).
Form I: The Form I polymorph preferably comprises characteristic crystalline peaks with 2-Theta values (in degrees) of around (i.e. at about or at approximately) 15.6 and 22.5 ± 0.25, or 0.2 degrees. The diffraction pattern typically does not comprise peaks at one or more, or all, or each of, about 6.9, 7.4, 8.3, 9.3, 10.5, or about 11.8 degrees, such as 8.3 or 11.8 ± 0.25, or ± 0.2, or ±0.1 such as about ±0.05 degrees.
Form II:
The form II polymorph preferably comprises a characteristic crystalline peak with 2-Theta value (in degrees) of around (i.e. at about or at approximately) 8.3 ± 0.25, or ± 0.2, or +0.1 such as about ±0.05 degrees. The diffraction pattern typically does not comprise peaks at one or more, or all, or each of, about 6.9, 7.4, 9.3, 9.5, 10.5, 11.4 or about 13.7 degrees, such as 11.4 or 13.8 ±0.25, or ±0.2, or ±0.1 such as about ±0.05 degrees.
The Form III polymorph preferably comprises a characteristic crystalline peak with 2-Theta value (in degrees) of around (i.e. at about or at approximately) 7.4 ±0.3, ±0.25, or 0.2, or ±0.1 such as about ±0.05 degrees. The diffraction pattern typically does not comprise peaks at one or more, or two or more, or three or more or each of, about 6.9, 8.3, 9.5, 11.3, 12.0, 12.5, 12.9, 14.5, or about 15.8 degrees, such as 6.9, 9.5, 11.3 ±0.25, or ±0.2, or ±0.1 such as about ±0.05 degrees.
The form IV polymorph preferably comprises a characteristic crystalline peaks with 2-Theta values (in degrees) of around (i.e. at about or at approximately) 9.5 and 14.5 +0.2, or ±0.1 such as about ±0.05 degrees. The diffraction pattern typically does not comprise peaks at one or more, or two or more, or three or more or each of, about 6.9, 8.3, 10.5, 11.7, 12.0, 12.2, 12.5, 13.0, 13.4, and about 15.8 degrees, such as 6.9, 8.3, 11.7 ±0.25, or ±0.2, or ±0.1 such as about ±0.05 degrees.
Example 1 : Form I 9.04 kg ferric citrate was combined with 29 litres of purified water. Separately, 12.2 kg of maltol was combined with 15.2 litres of sodium hydroxide solution (20 % w/w). The ferric citrate and sodium hydroxide were charged into a vessel with the addition of 4 litres of water and then stirred at 20 to 25°C. A seed was then added. The seed was 65g of ferric maltol polymorph in 12 litres of water. The seed crystal was prepared by the same process as described in Example 1 but without the use of a seed crystal. The seed was added to the vessel to aid a consistent crystallisation/precipitation. The mixture was held in the vessel, as a suspension, to allow crystal growth and then filtered and washed three times, each time with 13 litres of water. The resulting solid was dried at less than 80°C and produced 13.25 kg of dried ferric maltol.
The ferric maltol in Example 1 was produced on a scale of 12 to 15 kg in different batches. The analysis of the ferric maltol produced showed the % w/w of iron present was about 12.8 to 13.0 and the % w/w of maltol present was about 87.6 to 89.3.
Patent
//////////////Ferric Maltol, マルトール第二鉄 , Feraccru, FDA 2019
CC1=C(C(=O)C=CO1)[O-].CC1=C(C(=O)C=CO1)[O-].CC1=C(C(=O)C=CO1)[O-].[Fe+3]
CC1=C(C(=O)C=CO1)[O-].CC1=C(C(=O)C=CO1)[O-].CC1=C(C(=O)C=CO1)[O-].[Fe+3]
LAFUTIDINE, ラフチジン
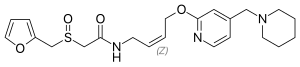

LAFUTIDINE
N-[4-[4-(Piperidin-1-ylmethyl)pyridin-2-yloxy]-(Z)-but-2-en-1-yl]-2-(furfurylsulfinyl)acetamide
-
- FRG-8813
- ATC:A02B
- Use:antisecretory, gastric H2-antagonist
- (+)-2-[(2-furanylmethyl)sulfinyl]-N-[(2Z)-4-[[4-(1-piperidinylmethyl)-2-pyridinyl]oxy]-2-butenyl]acetamide
- Formula:C22H29N3O4S
- MW:431.56 g/mol
- CAS-RN:118288-08-7
-
(±)-2-(Furfurylsulfinyl)-N-(4-(4-(piperidinomethyl)-2-pyridyl)oxy-(Z)-2-butenyl)acetamide
-
(Z)-2-((2-Furanylmethyl)sulfinyl)-N-(4-((4-(1-piperidinylmethyl)-2-pyridinyl)oxy)-2-butenyl)acetamide
-
118288-08-7
FRG‐8813、2‐(Furfurylsulfinyl)‐N‐[(Z)‐4‐[[4‐(piperidinomethyl)‐2‐pyridinyl]oxy]‐2‐butenyl]acetamide、ロクチジン、Loctidine、ラフチジン・・・
Lafutidine , also named N-[4-[4-(piperidin-1-ylmethyl)pyridin-2-yloxy]-(Z)-but-2-en-1-yl]-2-(furfurylsulfinyl)acetamide, is a histamine H2 receptor antagonist that was first produced in Japan by Taiho and UCB Japan for the oral treatment of peptic ulcers in 2000. In 2010 it was approved for the treatment of mild gastroesophageal reflux disease, and in 2012 it was approved to help improve symptoms of gastric mucosal lesions due to gastritis
Lafutidine (INN) is a second generation histamine H2 receptor antagonist having multimodal mechanism of action and used to treat gastrointestinal disorders. It is marketed in Japan and India.
Medical use
Lafutidine is used to treat gastric ulcers, duodenal ulcers, as well as wounds in the lining of the stomach associated with acute gastritis and acute exacerbation of chronic gastritis.[1][2]
Adverse effects
Adverse events observed during clinical trials included constipation, diarrhea, drug rash, nausea, vomiting and dizziness.[2]
Mechanism of action
Like other H2 receptor antagonists it prevents the secretion of gastric acid.[2] It also activates calcitonin gene-related peptide, resulting in the stimulation of nitric oxide (NO) and regulation of gastric mucosal blood flow, increases somatostatin levels also resulting in less gastric acid secretion, causes the stomach lining to generate more mucin, inhibits neutrophil activation thus preventing injury from inflammation, and blocks the attachment of Helicobacter pylori to gastric cells.[2]

Trade names
It is marketed in Japan as Stogar by UCB[1] and in India as Lafaxid by Zuventus Healthcare.[2]





N-[4-[4-(Piperidin-1-ylmethyl)pyridin-2-yloxy]-(Z)-but-2-en-1-yl]-2-(furfurylsulfinyl)acetamide 1 as a white solid (15.8 kg, 91.3%).(2,3)
1H NMR (600 MHz, CDCl3): δ 1.43 (m, 2H), 1.56–1.60 (m, 4H), 2.36 (m, 4H), 3.34 (d, 1H, J = 14.4 Hz), 3.40 (s, 2H), 3.59 (d, 1H, J = 14.4 Hz), 4.10 (t, 2H, J = 6.6 Hz), 4.17 (d, 1H, J = 13.8 Hz), 4.31 (d, 1H, J = 13.8 Hz), 4.93 (d, 2H, J = 6.6 Hz), 5.67–5.69 (m, 1H), 5.83–5.87 (m, 1H), 6.39 (dd, 1H, J = 1.8, 3.0 Hz), 6.47 (d, 1H, J = 3.0 Hz), 6.72 (s, 1H), 6.87 (d, 1H, J = 5.4 Hz), 7.19 (s, 1H), 7.43 (d, 1H, J = 1.8 Hz), 8.03 (d, 1H, J = 5.4 Hz).
13C NMR (150 MHz, CDCl3): δ 24.2, 26.0, 26.0, 37.2, 50.2, 53.4, 54.6, 54.6, 61.4, 62.4, 110.8, 111.3, 112.2, 117.7, 128.4, 128.9, 143.3, 143.9, 146.3, 151.5, 163.6, 163.6.
IR (KBr): 3325, 2935, 1638, 1613, 1041 cm–1.
ESI-MS: m/z 431.1.
Increasing the Purity of Lafutidine Using a “Suicide Substrate”
Chengjun Wu, Zhen Li, Chunchao Wang, Yanan Zhou, and Tiemin Sun*
https://pubs.acs.org/doi/suppl/10.1021/acs.oprd.8b00070/suppl_file/op8b00070_si_001.pdf
CLIP
http://www.drugfuture.com/synth/syndata.aspx?ID=145925

EP 0282077; JP 1988225371; JP 1989230556; JP 1989230576; US 4912101
1) The reaction of 2-bromo-4-(piperidin-1-ylmethyl)pyridine (I) with 4-amino-2(Z)-buten-1-ol (II) by means of NaH in THF gives 4-[4-(piperidin-1-ylmethyl)pyridin-2-yloxy]-2(Z)-buten-1-amine (III), which is then condensed with 2-(2-furylmethylsulfinyl)acetic acid (IV) by means of 1-ethyl-3-[3-(dimethylamino)propyl]carbodiimide (EDCD) in dichloromethane.
 EP 0582304; JP 1994192195
EP 0582304; JP 1994192195
The condensation of 2-chloro-4-(piperidin-1-ylmethyl)pyridine (V) with 4-(tetrahydropyranyloxy)-2(Z)-buten-1-ol (VI) by means of NaH in THF gives 4-(piperidin-1-ylmethyl)-2-[4-(tetrahydropyranyloxy)-2(Z)-butenyloxy)pyridine (VII), which is deprotected with 4-methylbenzenesulfonic acid in methanol, yielding the free butenol (VIII). The acylation of (VIII) with methanesulfonyl chloride in toluene affords the corresponding mesylate (IX), which is finally condensed with 2-(2-furylmethylsulfonyl)acetamide (X) (obtained from the corresponding 4-nitrophenyl ester (XI) with ammonia) by means of potassium tert-butoxide in toluene.
 Chem Pharm Bull 1998,46(4),616
Chem Pharm Bull 1998,46(4),616
A new synthesis of lafutidine has been described: The condensation of 2-bromopyridine-4-carbaldehyde ethylene ketal (I) with 4-(tetrahydropyranyloxy)-2(Z)-buten-1-ol (II) by means of NaOH, K2CO3 and tetrabutylammonium bisulfate in refluxing toluene gives the corresponding substitution product (III), which by treatment with pyridinium p-toluenesulfonate (PPTS) in hot ethanol yields the 2(Z)-butenol (IV). The reaction of (IV) with SOCl2 and then with potassium phthalimide (V) affords the substituted phthalimide (VI), which by treatment with hydrazine hydrate in refluxing methanol gives the 2(Z)-butenamine (VII). The condensation of (VII) with 2-(2-furylmethylsulfinyl)acetic acid 4-nitrophenyl ester (VIII) in THF yields the expected amide (IX), which is treated with p-toluenesulfonic acid in refluxing acetone/water to eliminate the ethylene ketal protecting group yilding the aldehyde (X). Finally, this compound is reductocondensed with piperidine (XI) by means of NaBH4 in ethanol.
CLIP
Synthesis Path
References
References
- ^ Jump up to:a b UCB Japan Revised: April 2005 Stogar tablets
- ^ Jump up to:a b c d e Zuventus Healthcare Ltd. India Lafaxid tablets
-
- a EP 582 304 (Fujirebio; 5.8.1993; J-prior. 7.8.1992).
-
preparation of 2-benzenesulfonyl-4-methylpyridine:
- EP 931 790 (Kuraray; 26.1.1999; J-prior. 26.1.1998).
-
chlorination of 2-benzenesulfonyl-4-methylpyridine:
- JP 10 231 288 (Kuraray; 2.9.1998; J-prior. 21.2.1997).
- WO 9 626 188 (Sagami Res. Center; 21.2.1996; J-prior. 22.2.1995).
- b EP 282 077 (Fujirebio; 11.3.1988; J-prior. 13.3.1987).
- US 4 912 101 (Fujirebio; 27.3.1990; J-prior. 13.3.1987).
-
preparation of I:
- JP 10 231 288 (Kuraray; 2.9.1998; J-prior. 21.2.1997).
-
chlorination of 2-chloromethylpyridines forming 2-chloro-4-trichloromethylpyridine:
- EP 557 967 (Central Glass Co.; 1.9.1993; J-prior. 24.2.1993).
-
treatment of I with (Z)-4-(tetrahydro-2H-pyran-2-yloxy)-2-buten-1-ol:
- US 5 382 589 (Fujirebio; 17.1.1995; J-prior. 27.1.1992).
-
preparation of furfuryl acetate and derivatives:
- JP 8 198 844 (Fujirebio; 6.8.1996; J-prior. 23.1.1995).
- JP 8 198 843 (Fujirebio; 6.8.1996; J-prior. 23.1.1995).
- JP 07 010 860 (Central Glass Co.; 13.1.1995; J-prior. 25.6.1993).
- JP 07 010 864 (Central Glass Co.; 13.1.1995; J-prior. 25.6.1993).
-
2-(furfurylsulfinyl)acetic acid nitrophenyl ester:
- JP 07 010 862 (Central Glass Co.; 13.1.1995; J-prior. 25.6.1993).
-
4-(tetrahydro-2-pyranyloxy)-2(Z)-buten-1-ol from 2(Z)-butene-1,4-diol:
- Nishiguchi, T. et al.: J. Org. Chem. (JOCEAH) 63, 23, 8183 (1998).
- Davis, K. J. et al.: Synth. Commun. (SYNCAV) 29, 10, 1679 (1999).
- Nishiguchi, T. et al.: J. Chem. Soc., Perkin Trans. 1 (JCPRB4) 1995, 24, 2491.
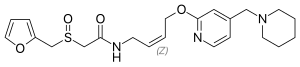 |
|
| Clinical data | |
|---|---|
| AHFS/Drugs.com | International Drug Names |
| Routes of administration |
Oral |
| ATC code | |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ECHA InfoCard | 100.118.935 |
| Chemical and physical data | |
| Formula | C22H29N3O4S |
| Molar mass | 431.54 g/mol |
| 3D model (JSmol) | |
/////////////////LAFUTIDINE, ラフチジン , FRG-8813, ATC:A02B
C1CCN(CC1)CC2=CC(=NC=C2)OCC=CCNC(=O)CS(=O)CC3=CC=CO3

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....