QazCovid-in

QazCovid-in
 QazCovid-in
QazCovid-in Vaccine
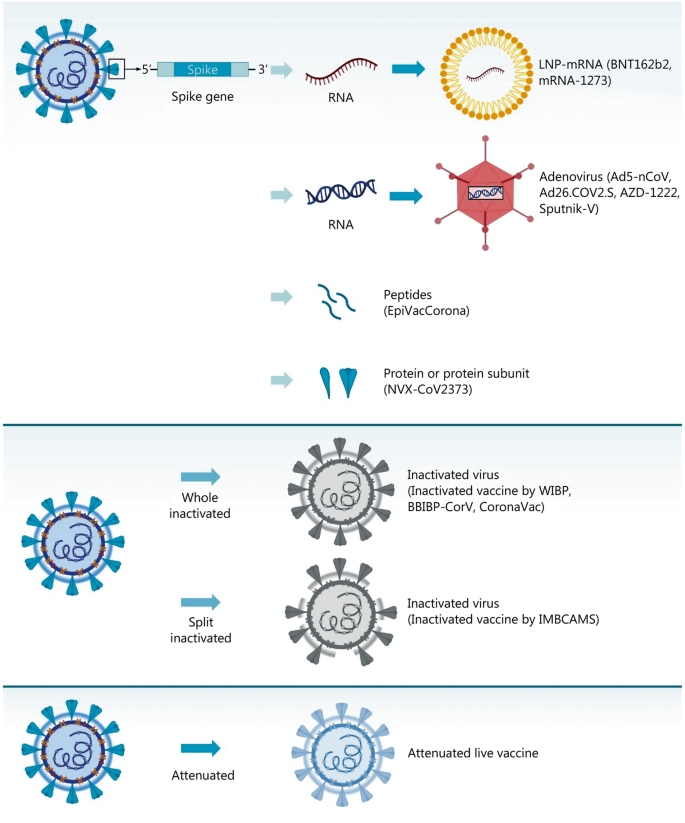
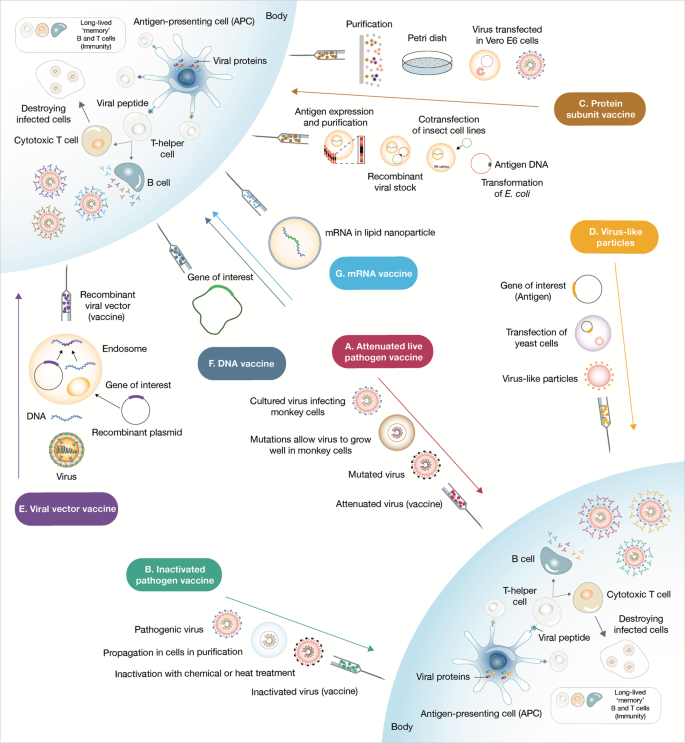
Vaccine Phase I/II/IIIThe QazCovid-in vaccine is an inactivated vaccine. Inactive viral vaccines are created by propagating viruses in cell culture (such as in Vero cells) and/or by inactivation using a chemical reagent (such as beta-propiolactone or formaldehyde). Upon vaccination, this allows the body to generate a diverse immune response against numerous viral antigens while having no threat of actually being infected because the virus is inactive.NEWS FEED December 31, 2020The Republic of Khazakstan’s QazCovid-in COVID19 vaccine enters phase 3 with an expected 3000 participants. August 28, 2020QazCovid-in, an inactive viral vaccine manufactured by Research Institute for Biological Safety Problems Republic of Kazakhstan enters Phase 1/2 clinical trials.ORGANIZATIONSResearch Institute for Biological Safety Problems, National Scientific Center for Phthisiopulmonology of the Republic of Kazakhstan, City polyclinic No. 4 of the UZO of Almaty, Clinic of the International Institute of Postgraduate Education, City Multidisciplinary Hospital of the Health Department of the Akimat of Zhambyl RegionCOUNTRIES INVOLVED TRIAL PARTICIPANTS
Phase I/II/IIIThe QazCovid-in vaccine is an inactivated vaccine. Inactive viral vaccines are created by propagating viruses in cell culture (such as in Vero cells) and/or by inactivation using a chemical reagent (such as beta-propiolactone or formaldehyde). Upon vaccination, this allows the body to generate a diverse immune response against numerous viral antigens while having no threat of actually being infected because the virus is inactive.NEWS FEED December 31, 2020The Republic of Khazakstan’s QazCovid-in COVID19 vaccine enters phase 3 with an expected 3000 participants. August 28, 2020QazCovid-in, an inactive viral vaccine manufactured by Research Institute for Biological Safety Problems Republic of Kazakhstan enters Phase 1/2 clinical trials.ORGANIZATIONSResearch Institute for Biological Safety Problems, National Scientific Center for Phthisiopulmonology of the Republic of Kazakhstan, City polyclinic No. 4 of the UZO of Almaty, Clinic of the International Institute of Postgraduate Education, City Multidisciplinary Hospital of the Health Department of the Akimat of Zhambyl RegionCOUNTRIES INVOLVED TRIAL PARTICIPANTS
Phase 1: 44
Phase 2: 200
Phase 3: 3000CLINICAL TRIAL NUMBERNCT04530357NCT04691908
QazCovid-in, also known as QazVac, is an inactivated virus vaccine developed by the Research Institute for Biological Safety Problems in Kazakhstan.[499]
Kazakhstan[499]
https://fortune.com/2021/04/26/new-covid-19-vaccine-kazakhstan-qazvac/
A new vaccine on the scene: Kazakhstan begins rollout of homegrown QazVac
The world’s approved COVID-19 vaccines have all come from large economies such as the U.S., China, the U.K., Russia, and India. Until today.
On Monday, Kazakhstan started rolling out its homegrown vaccine, now known as QazVac. Before a rebranding at the end of last month, it was called QazCovid-in, but the central Asian country’s government decided that name might be a turnoff for the public.
The vaccine was developed by Kazakhstan’s Research Institute for Biological Safety Problems, which claimed 96% efficacy in the second stage of clinical trials. The final phase is still ongoing, with a conclusion expected in July, but Kazakh health authorities decided it was fine to begin the rollout as long as the 3,000-participant Phase III trial was at least halfway finished.
This isn’t an adenovirus vector vaccine like those from Johnson & Johnson and AstraZeneca—though it does share their relatively mild refrigeration requirements—nor is it an mRNA-based jab like the BioNTech/Pfizer and Moderna vaccines. Instead, it uses an inactivated form of the SARS-CoV-2 virus itself, much like China’s CoronaVac and India’s Covaxin, which are both in use, and Valneva’s vaccine, which isn’t there yet. The QazVac regimen comprises two doses, to be administered three weeks apart.
‘Turn the tide’
Health Minister Alexei Tsoi was one of the first QazVac recipients on Monday morning. Tsoi was at the start of this month on the receiving end of a public dressing-down by President Kassym-Jomart Tokayev, who was furious about the sluggish start to the country’s inoculation campaign amid rising case numbers.
“You must turn the tide, otherwise a personnel decision that is going to be very disappointing for you will follow,” Tokayev told Tsoi. The vaccination campaign, which had previously focused on frontline workers, then reportedly sprang to life for others too in the oil-rich country.
Thus far, Kazakhstan’s vaccination drive has been powered by Russia’s Sputnik V, which has been produced locally for the past couple of months (Tokayev opted for the Russian shot, rather than waiting for QazVac). By late last week, just over 800,000 people had received their first dose. Kazakhstan has a population of 18.8 million people; the government plans to inoculate 2 million each month.
Tokayev tweeted Friday that domestic production would provide vaccine availability to all citizens. If so, that would be a remarkable turnaround—Almaty health officials said five weeks ago that the largest Kazakh city had run out of vaccines, and mass vaccination would not be realistic in the near future.
QazVac may have given Tokayev the opportunity to praise Kazakhstan’s scientific prowess, but production remains a bottleneck. The first batch to be distributed runs to only 50,000 doses, and the next tranche, to be produced in May, will be of the same volume.
Tsoi said Monday that the Kazakh government was talking to Turkish manufacturers about increasing production capacity.
QazCovid-in, commercially known as QazVac,[1][2] is a COVID-19 vaccine developed by the Research Institute for Biological Safety Problems in Kazakhstan.[3][4][5] QazCoVac-P is a second COVID-19 vaccine developed by the Kazakh Biosafety Research Institute and in clinical trials.[6]
Clinical research
QazVac is currently in Phase 3 (III) of the Clinical Trial, which is expected to be fully completed by 9 July 2021.[7][8] It is unclear when the first preliminary results will be published.[9][10]
The administration of the vaccine for the general population began at the end of April 2021.[11] The Research Institute Kunsulu Zakarya’s Director General’s justification is that the trial is almost 50% completed and “people who have received [the] vaccine feel well; there have been no side-effects and the effectiveness of the vaccine is high”.[12]
Production
The vaccine was first manufactured by Kazakhstan’s Research Institute of Biological Safety Problems. Production capacity has been capped at 50,000 doses per month.
Beginning in June 2021, the vaccine is slated[13] to be packaged in large bulk to be bottled in Turkey by a major Turkish company.[14][15] This will allow for a production capacity of 500,000-600,000 doses per month.[16] The contract is still being negotiated,[17] despite earlier claims that suggesting the deal had already been finalized.[18][19]
Vaccine innoculation
The first batch of 50,000 doses was delivered on 26 April 2021, and vaccination began shortly after.[20] In June 2021, the capacity will increase to 100,000 doses per month, regardless of the contract for bottling in Turkey.[21]
Authorization
| Full authorization Emergency authorization |
See also: List of COVID-19 vaccine authorizations § QazCovid-in
Characteristics
The vaccine can be stored at standard refrigeration temperatures (2°C-8°C) and is a two-dose régime with the doses administered twenty-one days apart.[22]
References
- ^ “Kazakhstan: Officials under fire over vaccination failures | Eurasianet”. eurasianet.org. Retrieved 11 April 2021.
- ^ INFORM.KZ (31 March 2021). “Vaccination with homegrown QazVac vaccine likely to start in late April”. http://www.inform.kz. Retrieved 11 April 2021.
- ^ Yergaliyeva A (20 December 2020). “Kazakhstan Begins Vaccinating 3,000 Volunteers With Self-Made QazCovid-in”. The Astana Times. Retrieved 2 March2021.
- ^ Clinical trial number NCT04691908 for “Immunogenicity, Efficacy and Safety of QazCovid-in® COVID-19 Vaccine” at ClinicalTrials.gov
- ^ “Reactogenicity, Safety and Immunogenicity of QazCovid-in® COVID-19 Vaccine – Full Text View – ClinicalTrials.gov”. clinicaltrials.gov.
- ^ “Kazakh Biosafety Research Institute Begins Clinical Trials of Another Vaccine Against COVID-19”. The Astana Times.
- ^ INFORM.KZ (31 March 2021). “Vaccination with homegrown QazVac vaccine likely to start in late April”. http://www.inform.kz. Retrieved 11 April 2021.
- ^ “QazVac готова и уже на подходе”. Время (in Russian). Retrieved 11 April2021.
- ^ INFORM.KZ (9 April 2021). “3rd stage of clinical trials of QazCovid-in vaccine to be 50% complete by Apr 15”. http://www.inform.kz. Retrieved 11 April 2021.
- ^ “Kazakhstan’s COVID-19 vaccine to be bottled in Turkey”. http://www.aa.com.tr. Retrieved 11 April 2021.
- ^ tengrinews.kz (9 April 2021). “Как правильно применять казахстанскую вакцину QazVac, рассказал ученый”. Главные новости Казахстана – Tengrinews.kz (in Russian). Retrieved 11 April 2021.
- ^ “QazVac готова и уже на подходе”. Время (in Russian). Retrieved 11 April2021.
- ^ It’s unclear at which level of preparation the vaccine will be send to Turkey.
- ^ MENAFN. “Kazakh COVID-19 vaccine to be bottled in Turkey”. menafn.com. Retrieved 11 April 2021.
- ^ “QazVac готова и уже на подходе”. Время (in Russian). Retrieved 11 April2021.
- ^ “Kazakhstan Launches Production of First Homegrown Vaccine, ‘QazVac'”. caspiannews.com. Retrieved 26 April 2021.
- ^ INFORM.KZ (21 April 2021). “Healthcare Ministry comments on production of QazVac vaccine”. http://www.inform.kz. Retrieved 22 April 2021.
- ^ “К концу апреля в Казахстане будет выпущено 50000 доз собственной вакцины”. “СНГ СЕГОДНЯ” – последние новости стран СНГ читайте на SNG.TODAY. Retrieved 12 April 2021.
- ^ “Kazakhstan’s COVID-19 vaccine to be bottled in Turkey”. http://www.aa.com.tr. Retrieved 12 April 2021.
- ^ contributor, Guest (26 April 2021). “Kazakhstan launches QazVac, its own COVID-19 vaccine”. EU Reporter. Retrieved 26 April 2021.
- ^ “Казахстанскую вакцину QazVac будут разливать в Турции”. informburo.kz(in Russian). 9 April 2021. Retrieved 12 April 2021.
- ^ INFORM.KZ (26 April 2021). “Health Minister Alexei Tsoi to be one of the first to get homegrown QazCovid-in vaccine”. http://www.inform.kz. Retrieved 26 April 2021.
External links
| Scholia has a profile for QazCovid-in (Q99518269). |
The QazCovid-in vaccine, an inactivated vaccine, was developed and tested in the Kazakh Research Institute for Biological Safety Problems1. It demonstrated high efficacy, safety, and immunogenicity at 96% in initial Phase I and II trials (NCT04530357), and will now be undergoing upcoming Phase III trials2,3.
- The Astana Times: Kazakhstan Begins Vaccinating 3,000 Volunteers With Self-Made QazCovid-in [Link]
- The Lancet: COVID-19 response in central Asia [Link]
- Economic Research Institute: QazCovid-in [Link]
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | Inactivated |
| Clinical data | |
| Routes of administration | Intramuscular |
| Identifiers | |
| DrugBank | DB16441 |
| Part of a series on the |
| COVID-19 pandemic |
|---|
| COVID-19 (disease)SARS-CoV-2 virus (variants) |
| showTimeline |
| showLocations |
| showInternational response |
| showMedical response |
| showImpact |
| COVID-19 portal |
///////////QazVac, COVID 19, vaccine, QazCovid-in, kazakhastan, SARS-CoV-2, corona virus

NEW DRUG APPROVALS
one time
$10.00
Convidicea (Ad5-nCoV)
| A vial of Convidecia vaccine | |
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | Viral vector |
| Clinical data | |
| Trade names | Convidecia |
| Routes of administration | Intramuscular, Intranasal |
| ATC code | None |
| Legal status | |
| Legal status | Full and Emergency authorizations |
| Identifiers | |
| DrugBank | DB15655 |
Convidicea (Ad5-nCoV)
Recombinant vaccine (adenovirus type 5 vector)
Recombinant Novel Coronavirus Vaccine (Adenovirus Type 5 Vector)
CanSino Biologics, china
see https://covid19.trackvaccines.org/vaccines/2/
AD5-nCOV, trade-named Convidecia, is a single-dose[1] viral vector vaccine for COVID-19 developed by CanSino Biologics. It conducted its Phase III trials in Argentina,[2] Chile,[3] Mexico,[4] Pakistan,[5] Russia,[6] and Saudi Arabia[7] with 40,000 participants.
In February 2021, global data from Phase III trials and 101 COVID cases showed that the vaccine had a 65.7% efficacy in preventing moderate symptoms of COVID-19, and 91% efficacy in preventing severe disease.[8] It has similar efficacy to Johnson & Johnson’s Ad26.COV2.S, another one-shot adenovirus vector vaccine with 66% efficacy in a global trial.[9][1] Convidecia is similar to other viral vector vaccines like AZD1222, Gam-COVID-Vac, and Ad26.COV2.S.[10] Its single-dose regimen and normal refrigerator storage requirement (2°to 8 °C) could make it a favorable vaccine option for many countries.[9]
Convidecia is approved for use by some countries in Asia,[11][12][13] Europe,[14][15] and Latin America.[16][17][18] Production capacity for Ad5-NCov should reach 500 million doses in 2021. Manufacturing will take place in China,[19] Malaysia,[13] Mexico,[20] and Pakistan.[21]
Ad5-nCoV is a recombinant adenovirus type-5 vector (Ad5) vaccine currently being investigated for prophylaxis against SARS-CoV-2.1,2 It is being developed by CanSino Biologics Inc., in partnership with the Beijing Institute of Biotechnology, who in March 2020 announced the approval of a phase I clinical trial (ChiCTR2000030906)1 with an expected completion in December 2020. The study will evaluate antibody response in healthy patients between the ages of 18 and 60 who will receive one of three study doses, with follow-up taking place at weeks 2 and 4 and months 3 and 6 post-vaccination.2
- Chinese Clinical Trial Register: A phase I clinical trial for recombinant novel coronavirus (2019-COV) vaccine (adenoviral vector) [Link]
- Antibody Society: COVID-19 Archives [Link]
Technology
Convidecia is a viral vector vaccine similar to AstraZeneca‘s AZD1222 and Gamaleya‘s Gam-COVID-Vac.[10] Ad5-nCOV can be stored in less extreme cold conditions compared to mRNA vaccines.[22][9]
Efficacy
In February 2021, data released from an interim analysis of Phase III trials with 30,000 participants and 101 COVID cases showed that globally, the vaccine had an efficacy of 65.7% at preventing moderate cases of COVID-19 and 90.98% efficacy at preventing severe cases. In the Pakistan trial subset, the vaccine had an efficacy of 74.8% at preventing symptomatic cases 100% for preventing severe disease.[8]
While the efficacy rates were lower than the Pfizer–BioNTech and Moderna vaccines, its single-dose regimen and normal refrigerator storage requirement (2 to 8 °C) could make it a favorable option for many countries. It has similar efficacy to Johnson & Johnson’s Ad26.COV2.S, another one-shot adenovirus vaccine found to be 66% effective in a global trial.[9][1]
Clinical trials
Phase I-II
In early 2020, Chen Wei led a joint team of the Institute of Biotechnology, the Academy of Military Medical Sciences and CanSino Biologics to develop AD5-nCOV. According to the Chinese state media, the team registered an experimental COVID-19 vaccine for Phase I trial in China on 17 March 2020 to test its safety. The trial was conducted on 108 healthy adults aged 18 to 60 in two medical facilities in Wuhan, Hubei province.[23]
In April, Ad5-nCoV became the first COVID-19 vaccine candidate in the world to begin Phase II trials.[24] The Phase II trial results were published in the peer-reviewed journal The Lancet in August 2020, and noted neutralizing antibody and T cell responses based on statistical analyses of data involving 508 eligible participants.[25] In September, Zeng Guang, chief scientist of the Chinese Center for Disease Control and Prevention said the amount of COVID-19 antibodies in subjects from the Phase I trials remained high six months after the first shot. Zeng said the high levels of antibodies suggested the shots may provide immunity for an extended period of time, although Phase III results were still required.[26] On September 24, CanSino began Phase IIb trials on 481 participants to evaluate the safety and immunogenicity of Ad5-nCoV for children ages 6–17 and elderly individuals ages 56 and above.[27]
In August, China’s National Intellectual Property Administration issued the country’s first COVID-19 vaccine patent to CanSino.[28]
On 16 May 2020, Canadian Prime Minister Justin Trudeau announced Health Canada had approved Phase II trials to be conducted by the Canadian Center for Vaccinology (CCfV) on the COVID-19 vaccine produced by CanSino. Scott Halperin, director of the CCfV said the vaccine would not be the only one going into clinical trials in Canada, and any potential vaccine would not be publicly available until after Phase 3 is complete.[29][30] If the vaccine trials were successful, then the National Research Council would work with CanSino to produce and distribute the vaccine in Canada.[30] In August 2020, the National Research Council disclosed the vaccine had not been approved by Chinese customs to ship to Canada, after which the collaboration between CanSino and the Canadian Center for Vaccinology was abandoned.[31]
Nasal spray trials
In September, CanSino began a Phase I trial in China with 144 adults to determine the safety and immunogenicity of the vaccine to be administered as a nasal spray, in contrast with most COVID-19 vaccine candidates which require intramuscular injection.[32] On June 3, 2021, Chen Wei announced the expansion of clinical trials was approved by the NMPA, in the meantime, they are applying for Emergency Use Listing for the nasal spray.[33]
Phase III
In August, Saudi Arabia confirmed it would begin Phase III trials on 5,000 people for Ad5-nCoV in the cities of Riyadh, Dammam, and Mecca.[7]
In October, Mexico began Phase III trials on 15,000 volunteers.[34][4]
In September, Russia began Phase III trials on 500 volunteers,[35] which Petrovax later received approval from the government to expand to 8,000 more volunteers.[36][6]
In September, Pakistan began Phase III trials on 40,000 volunteers as part of a global multi-center study.[5] As of December, about 13,000 volunteers have participated in trials of Ad5-nCoV.[22]
In November, Chile began Phase III trials on 5,200 volunteers to be managed by University of La Frontera.[37][3]
In December, Argentina’s Fundación Huésped began Phase III trials in 11 health centers in the metropolitan area of Buenos Aires and Mar del Plata.[2]
Combination trials
In April 2021, a new trial was registered in Jiangsu involving one dose of Convidecia followed by a dose of ZF2001 28 or 56 days later using different technologies as a way to further boost efficacy.[38]
Manufacturing
In February, Chen Wei who lead the development of the vaccine, said annual production capacity for Ad5-NCov could reach 500 million doses in 2021.[19]
In February, Mexico received the first batch of active ingredients for Convidecia, which is being packaged in Querétaro by Drugmex.[20]
In Malaysia, final filling and packaging of the vaccine for distribution would be completed by Solution Biologics.[13]
In May, Pakistan began filling and finishing 3 million doses a month at the National Institute of Health, which would be branded as PakVac for domestic distribution.[39]
If the vaccine is approved in Russia, Petrovax said it would produce 10 million doses per month in 2021.[40]
Marketing and deployment
See also: List of COVID-19 vaccine authorizations § Convidecia
Asia
On 25 June 2020, China approved the vaccine for limited use by the military.[42] In February 2021, China approved the vaccine for general use.[11]
In February, Malaysia‘s Solution Biologics agreed to supply 3.5 million doses to the government.[43] The doses would be delivered starting in April with 500,000 complete doses, with the rest in bulk to be finished by Solution Biologics.[13]
In October, Indonesia reached an agreement with CanSino to deliver 100,000 doses in November 2020, with the expectation that an additional 15 to 20 million doses would be delivered in 2021.[44]
In February, Pakistan approved the vaccine for emergency use.[45] The country purchased 20 million doses of the vaccine[12] of which the first 3 million doses are to arrive in May.[12]
Europe
In March, Hungary granted emergency use approval for the vaccine.[14]
In March, Moldova authorized use of the vaccine.[46]
North America
In December 2020, Mexico‘s Foreign Minister Marcelo Ebrard signed an agreement for 35 million doses.[47] In February, Mexico approved the vaccine for emergency use.[48] Mexico received active ingredients for 2 million doses with a total of 6 million doses expected to arrive in February.[16]
South America
In June, Argentina approved emergency use of the vaccine and ordered 5.4 million doses.[17]
In June, Brazil announced plans to purchase 60 million doses.[49] In May, Brazil began reviewing the vaccine for emergency use.[50]
In March, Chile signed a deal for 1.8 million doses for delivery between May and June,[51] for which emergency use approval was granted in April.[18]
In June, Ecuador approved emergency use and ordered 6 million doses for delivery between June and August 2021.[52]
References
- ^ Jump up to:a b c “It’s not just Johnson & Johnson: China has a single-dose COVID-19 vaccine that has 65% efficacy”. Fortune. Retrieved 2021-02-11.
- ^ Jump up to:a b “Comenzará en la Argentina un nuevo estudio de vacuna recombinante contra el SARS-CoV-2”. infobae (in Spanish). 14 December 2020. Retrieved 2020-12-15.
- ^ Jump up to:a b “Gob.cl – Article: Science Minister: “We Work With Maximum Rigor So That Science And Technology Benefit People’S Health””. Government of Chile. Retrieved 2020-11-21.
- ^ Jump up to:a b “Chinese Covid vaccine trials to be expanded to five more states”. Mexico News Daily. 2020-11-10. Retrieved 2020-11-11.
- ^ Jump up to:a b “Phase III Trial of A COVID-19 Vaccine of Adenovirus Vector in Adults 18 Years Old and Above – Full Text View – ClinicalTrials.gov”. clinicaltrials.gov. Retrieved 2020-10-21.
- ^ Jump up to:a b Reuters Staff (2020-12-07). “Russia approves clinical trials for Chinese COVID-19 vaccine Ad5-Ncov: Ifax”. Reuters. Retrieved 2020-12-07.
- ^ Jump up to:a b Eltahir N (9 August 2020). “CanSino to start Phase III trial of COVID-19 vaccine in Saudi”. Reuters. Retrieved 9 August 2020.
- ^ Jump up to:a b “CanSinoBIO’s COVID-19 vaccine 65.7% effective in global trials, Pakistan official says”. Reuters. 8 February 2021. Retrieved 2021-02-08.
- ^ Jump up to:a b c d “China’s CanSino Covid Vaccine Shows 65.7% Efficacy”. Bloomberg.com. 2021-02-08. Retrieved 2021-02-10.
- ^ Jump up to:a b Zimmer C, Corum J, Wee SL (2020-06-10). “Coronavirus Vaccine Tracker”. The New York Times. ISSN 0362-4331. Retrieved 2020-12-12.
- ^ Jump up to:a b Liu R (2021-02-25). “China approves two more domestic COVID-19 vaccines for public use”. Reuters. Retrieved 2021-02-26.
- ^ Jump up to:a b c “Pakistan purchases over 30 million COVID doses from China: sources”. ARY NEWS. 2021-04-25. Retrieved 2021-04-26.
- ^ Jump up to:a b c d “Malaysia to receive CanSino vaccine this month | The Malaysian Insight”. http://www.themalaysianinsight.com. Retrieved 2021-04-03.
- ^ Jump up to:a b Ashok R (2021-03-22). “UPDATE 2-China’s CanSino Biologics COVID-19 vaccine receives emergency use approval in Hungary”. Reuters. Retrieved 2021-03-22.
- ^ “Membrii NITAG au venit cu recomandări privind utilizarea vaccinurilor împotriva COVID-19 în Republica Moldova”. Ministerul Sănătății, Muncii și Protecţiei Sociale. 2021-03-03. Retrieved 2021-05-21.
- ^ Jump up to:a b “‘Our gratitude always’: From China’s CanSino, Mexico welcomes biggest vaccine shipment yet”. Reuters. 2021-02-11. Retrieved 2021-02-11.
- ^ Jump up to:a b “Argentina issues emergency approval to China’s single-dose Cansino COVID-19 vaccine”. Reuters. 2021-06-11. Retrieved 2021-06-11.
- ^ Jump up to:a b “ISP Approves Emergency Use And Importation Of Cansino Vaccine To Fight COVID-19”. Institute of Public Health of Chile. Retrieved 2021-04-08.
- ^ Jump up to:a b “China can hit 500-mln-dose annual capacity of CanSinoBIO COVID-19 vaccine this year”. finance.yahoo.com. Retrieved 2021-02-28.
- ^ Jump up to:a b Solomon DB (2021-02-28). “China’s CanSino says first vaccines packaged in Mexico will be ready in March”. Reuters. Retrieved 2021-03-12.
- ^ “Pakistan develops homemade anti-Covid vaccine ‘PakVac'”. The Express Tribune. 2021-05-24. Retrieved 2021-05-25.
- ^ Jump up to:a b Constable P, Hussain S. “Defying fears and skepticism, thousands in Pakistan volunteer for Chinese vaccine trials”. The Washington Post. ISSN 0190-8286. Retrieved 2021-01-01.
- ^ Cui J (23 March 2020). “Human vaccine trial gets underway”. China Daily. Retrieved 18 April 2020.
- ^ Xie J (15 April 2020). “China Announces Phase 2 of Clinical Trials of COVID-19 Vaccine”. Voice of America. Retrieved 18 April2020.
- ^ Zhu FC, Guan XH, Li YH, Huang JY, Jiang T, Hou LH, et al. (August 2020). “Immunogenicity and safety of a recombinant adenovirus type-5-vectored COVID-19 vaccine in healthy adults aged 18 years or older: a randomised, double-blind, placebo-controlled, phase 2 trial”. Lancet. 396 (10249): 479–488. doi:10.1016/S0140-6736(20)31605-6. PMC 7836858. PMID 32702299.
- ^ O’Brien E (2020-09-25). “Covid Antibodies Endure Over Six Months in China Trial Subjects”. http://www.bloomberg.com. Retrieved 2020-09-29.
- ^ “Phase IIb Clinical Trial of A COVID-19 Vaccine Named Recombinant Novel Coronavirus Vaccine (Adenovirus Type 5 Vector) – Full Text View – ClinicalTrials.gov”. clinicaltrials.gov. Retrieved 2020-10-21.
- ^ Yu S (17 August 2020). “China grants country’s first COVID-19 vaccine patent to CanSino: state media”. Reuters. Retrieved 17 August 2020.
- ^ Bogart N (16 May 2020). “Health Canada approves first clinical trial for potential COVID-19 vaccine”. CTV News. Retrieved 7 September 2020.
- ^ Jump up to:a b Ryan H (May 16, 2020). “Canada’s first COVID-19 vaccine trials approved for Halifax university”. CBC News. Retrieved January 4, 2021.
- ^ Cooke A (26 August 2020). “Canadian COVID-19 clinical trial scrapped after China wouldn’t ship potential vaccine”. CBC News. Retrieved 7 September 2020.
- ^ “A Clinical Trial of a Recombinant Adenovirus 5 Vectored COVID-19 Vaccine (Ad5-nCoV) With Two Doses in Healthy Adults – Full Text View – ClinicalTrials.gov”. clinicaltrials.gov. Retrieved 25 September 2020.
- ^ Cao X, Liu Y (2021-06-04). “陈薇院士:雾化吸入式新冠疫苗正在申请紧急使用”. Sci Tech Daily. Chinanews.com. Retrieved 2021-06-04.
- ^ “México recibe el primer lote de la vacuna candidata de CanSino Biologics; alistan pruebas”. EL CEO (in Spanish). 2020-11-03. Retrieved 2020-11-03.
- ^ “Clinical Trial of Recombinant Novel Coronavirus Vaccine (Adenovirus Type 5 Vector) Against COVID-19 – Full Text View – ClinicalTrials.gov”. clinicaltrials.gov. Retrieved 2020-10-21.
- ^ Bloomberg News (2020-11-25). “Russia’s Richest Man Seeks Global Market for Local Covid-19 Drug – BNN Bloomberg”. BNN. Retrieved 2020-11-28.
- ^ Yáñez PL (2020-11-15). “Así funcionan las cuatro vacunas que se probarán en Chile”. La Tercera. Retrieved 2020-11-17.
- ^ “China trials mixing of CanSinoBIO’s and Zhifei Longcom’s COVID-19 vaccines -data”. Reuters. 2021-04-19. Retrieved 2021-06-16.
- ^ “Covid vaccine: Pakistan starts production of CanSino, China’s single-dose jab”. Khaleej Times. Retrieved 2021-05-28.
- ^ “Russian Recruits Show ‘No Side Effects’ in Chinese Coronavirus Vaccine Trials”. The Moscow Times. 2020-09-21. Retrieved 2020-09-22.
- ^ “Status of COVID-19 Vaccines within WHO EUL/PQ evaluation process”. World Health Organization (WHO).
- ^ Reuters Staff (2020-06-29). “CanSino’s COVID-19 vaccine candidate approved for military use in China”. Reuters. Retrieved 2020-12-13.
- ^ Reuters Staff (2021-02-04). “Malaysia’s Solution Group to supply 3.5 million doses of CanSino vaccine to government”. Reuters. Retrieved 2021-02-04.
- ^ Taufiqurrahman M. “Indonesia can be manufacutring hub for COVID-19 vaccine, says Chinese foreign minister”. Jakarta Post. Retrieved 13 October 2020.
- ^ Shahzad A (2021-02-12). “Pakistan approves Chinese CanSinoBIO COVID vaccine for emergency use”. Reuters. Retrieved 2021-02-12.
- ^ “Membrii NITAG au venit cu recomandări privind utilizarea vaccinurilor împotriva COVID-19 în Republica Moldova”. Ministerul Sănătății, Muncii și Protecţiei Sociale. 2021-03-03. Retrieved 2021-05-21.
- ^ Reuters Staff (2020-12-10). “Mexico agrees to buy 35 million doses of CanSino COVID vaccine”. Reuters. Retrieved 2020-12-10.
- ^ “Mexico approves China’s CanSino and Sinovac COVID-19 vaccines”. Reuters. 10 February 2021.
- ^ “Brazil to buy single-shot Chinese COVID-19 vaccine”. Reuters. 2021-06-15. Retrieved 2021-06-16.
- ^ “Brazil in vaccine talks with Moderna, reviewing CanSino shot”. Reuters. 2021-05-19. Retrieved 2021-05-21.
- ^ Sherwood D (2021-03-30). “Chile inks deal for 1.8 million doses of CanSino COVID-19 vaccine as inoculation drive plows ahead”. Reuters. Retrieved 2021-03-30.
- ^ Valencia A. “Ecuador authorizes use of China’s CanSino vaccine against COVID-19”. Reuters. Retrieved 2021-06-16.
Further reading
- Zhu FC, Li YH, Guan XH, Hou LH, Wang WJ, Li JX, et al. (June 2020). “Safety, tolerability, and immunogenicity of a recombinant adenovirus type-5 vectored COVID-19 vaccine: a dose-escalation, open-label, non-randomised, first-in-human trial”. Lancet. 395 (10240): 1845–1854. doi:10.1016/S0140-6736(20)31208-3. PMC 7255193. PMID 32450106.
External links
| Scholia has a profile for Ad5-nCoV (Q96695265). |
/////////Convidicea, Ad5-nCoV, Recombinant vaccine, adenovirus type 5 vector, CanSino Biologics, china, SARS-CoV-2, corona virus, vaccine, covid 19
Convidecia
Convidecia is a viral vector vaccine[478] produced by the Chinese company CanSino Biologics and the Beijing Institute of Biotechnology of the Academy of Military Medical Sciences.Full (1)
- China[479]
Emergency (8)
- Argentina[480]
- Chile[481]
- Ecuador[482]
- Hungary[483][272]
- Malaysia[484]
- Mexico[436]
- Moldova[229]
- Pakistan[485]

NEW DRUG APPROVALS
one time
$10.00
EpiVacCorona


Origin of EpiVacCorona antigenes
- MKIEEGKLVIWINGDKGYNGLAEVGKKFEKDTGIKVTVEHPDKLEEKFPQVAATGDGPDIIFWAHDRFGGYAQSGLLAEITPDKAFQDKLYPFTWDAVRYNGKLIAYPIAVEALSLIYNKDLLPNPPKTWEEIPALDKELKAKGKSALMFNLQEPYFTWPLIAADGGYAFKYENGKYDIKDVGVDNAGAKAGLTFLVDLIKNKHMNADTDYSIAEAAFNKGETAMTINGPWAWSNIDTSKVNYGVTVLPTFKGQPSKPFVGVLSAGINAASPNKELAKEFLENYLLTDEGLEAVNKDKPLGAVALKSYEEELAKDPRIAATMENAQKGEIMPNIPQMSAFWYAVRTAVINAASGRQTVDEALKDAQTNSSSNNNNNNNNNNLGDNGPQNQRNAPRITFGGPSDSTGSNQNGERSGARSKQRRPQGLPNNTASWFTALTQHGKEDLKFPRGQGVPINTNSSPDDQIGYYRRATRRIRGGDGKMKDLSPRWYFYYLGTGPEAGLPYGANKDGIIWVATEGALNTPKDHIGTRNPANNAAIVLQLPQGTTLPKGFYAEGSRGGSQASSRSSSRSRNSSRNSTPGSSRGTSPARMAGNGGDAALALLLLDRLNQLESKMSGKGQQQQGQTVTKKSAAEASKKPRQKRTATKAYNVTQAFGRRGPEQTQGNFGDQELIRQGTDYKHWPQIAQFAPSASAFFGMSRIGMEVTPSGTWLTYTGAIKLDDKDPNFKDQVILLNKHIDAYKTFPPTEPKKDKKKKADETQALPQRQKKQQTVTLLPAADLDDLSKQLQQSMSSADSTQA. “Carrier protein sequence”.
EpiVacCorona
Federal Budgetary Research Institution State Research Center of Virology and Biotechnology
peptide, russia
PATENT https://www.fips.ru/registers-doc-view/fips_servlet?DB=RUPAT&DocNumber=2743594&TypeFile=htmlRU 2 743 594 RU 2 743 593RU 2 743 595 RU 2 738 081 Science (Washington, DC, United States) (2021), 372(6538), 116-117.
EpiVacCorona (Russian: ЭпиВакКорона, tr. EpiVakKorona) is a peptide-based vaccine against COVID-19 developed by the VECTOR center of Virology.[1][2][3] It consists of three chemically synthesized peptides (short fragments of a viral spike protein) that are conjugated to a large carrier protein. This protein is a fusion product of a viral nucleocapsid protein and a bacterial MBP protein.The third phase of a clinical trial, which should show whether the vaccine is able to protect people from COVID-19 or not, was launched in November 2020 with more than three thousand participants.[2] It is assumed it will be completed in August 2021.[2] According to the vaccine developers, the peptides and the viral part of the chimeric protein should immunize people who received this vaccine against SARS-CoV-2 and trigger the production of protective antibodies. However, some experts in the field have expressed concerns about the selection of peptides for use as vaccine antigens.[3][4] In addition, there are also serious concerns about the vaccine immunogenicity data, which have fueled independent civic research efforts[5][6][7] and criticism by some experts.[3][8][4][9][10] Meanwhile, the EpiVacCorona has received vaccine emergency authorization in a form of government registration and is available for vaccination outside the clinical trials.[11] The vaccine delivered via intramuscular route and aluminum hydroxide serves as an immunological adjuvant.
Description[edit]

Origin of EpiVacCorona antigenes
Composition
The vaccine includes three chemically synthesized short fragments of the viral spike protein – peptides, which, according to the developers of EpiVacCorona represent the protein regions containing B-cell epitopes that should be recognized by the human immune system.
These peptides are represented by following amino acid sequences:
1) CRLFRKSNLKPFERDISTEIYQAGS, 2) CKEIDRLNEVAKNLNESLIDLQE, 3) CKNLNESLIDLQELGKYEQYIK.[1][12][13]
In the vaccine all peptides are conjugated to a carrier protein, which is an expression product of the chimeric gene. This chimeric gene was created by fusion of two genes originating from different organisms, namely a gene encoding a viral nucleocapsid protein and a gene encoding a bacterial maltose-binding protein (MBP). The fusion chimeric gene expressed in Escherichia coli. The sequence of the chimeric protein is available from the patent.[4] The genetic construct of the chimeric gene also includes a short genetic fragment encoding a polyhistidine-tag, which is used to purify the chimeric protein from E. coli lysate. After the purification, the protein is conjugated with three peptides in a way that only one variant of the peptide molecule is attached to each protein molecule. As a result, three types of conjugated molecules are created: chimeric protein with attached peptide number 1, the same protein with peptide number 2, and finally the same protein with peptide number 3. All three types of conjugated molecules are included in the vaccine.[citation needed]

EpiVacCorona: antigens origin and composition
Vaccine antigens and antibodies
According to the developers’ publications,[14][5][6] vaccine antigens are three peptides of the spike protein and a chimeric protein consisting of two parts (viral nucleocapsid protein and bacterial maltose-binding protein). In addition, the polyhistidine-tag – a short peptide that is introduced into a vaccine composition to purify a chimeric protein from a bacterial lysate – is also a vaccine antigen against which antibodies can form in those who have received the vaccine. A person vaccinated with EpiVacCorona can develop antibodies not only to the peptides of the spike protein, but also to other antigens present in the vaccine. According to Anna Popova who is a head of the Federal Service for Supervision of Consumer Rights Protection and Human Welfare, it takes 42 days for those vaccinated with EpiVacCorona to develop immunity.[15]
Development

Immunogenic peptide screening in rabbits for EpiVacCorona design
Preclinical studies
The primary screening of peptides for the search for the most immunogenic ones was carried out in animals. The level of antibodies that was triggered by each tested peptide after administration to rabbits was measured. In the test, hemocyanin protein was used as a carrier protein for the studied peptides. Further, on six species of animals (mice, rats, rabbits, African green monkeys, rhesus monkeys, guinea pigs), the vaccine was shown to be harmless in terms of such parameters as general toxicity, allergic properties, and mutagenic activity. In four species of animals (hamsters, ferrets, African green monkeys, rhesus monkeys), specific activity was shown: immunogenicity and protective properties against SARS-CoV-2. The main results of preclinical studies are published in the “Bulletin of the Russian Academy of Medical Sciences”.[12][13]
Clinical studies
The studies development timeline was reported in Russian media in January 2021.[16] There are currently two clinical trials of EpiVacCorona registered in the ClinicalTrials.gov database.[17][18][2]
Phase I-II
The trial “Study of the Safety, Reactogenicity and Immunogenicity of “EpiVacCorona” Vaccine for the Prevention of COVID-19 (EpiVacCorona)”[18] was registered in clinical trial database with ClinicalTrials.gov identifier: NCT04780035. Another trial with the same title was registered with ClinicalTrials.gov Identifier: NCT04527575. Results of the trial that included data on 86 participants were published in Russian Journal of Infection and Immunity, indicating preliminary evidence of safety and an immune response.[1] The publication reports preliminary results of the first two phases of clinical trials of the vaccine in volunteers, of which 14 people aged 18-30 years participated in the first phase, and 86 volunteers aged 18-60 years in the second phase. It is claimed that antibodies were formed in 100% of the volunteers, and the vaccine is also claimed to be safe.[1]

EpiVacCorona Vaccine Development Timeline
Phase III
The third phase of a clinical trial, which should show whether the vaccine is able to protect people from COVID-19 or not, was launched in November 2020 with more than three thousand participants planned. It is expected to be completed in September 2021.[2] In the clinical trials database the phase III trial etitled “Study of the Tolerability, Safety, Immunogenicity and Preventive Efficacy of the EpiVacCorona Vaccine for the Prevention of COVID-19[2]” was registered only in March 2021 with ClinicalTrials.gov Identifier: NCT04780035. Phase 3-4 trial was registered in Russia at 18.11.2020 with 4991 participants planned.[19]
Intellectual property
The following patents of the Russian Federation for invention have been published, which protect the EpiVacCorona vaccine:
“Peptide immunogens and vaccine composition against coronavirus infection COVID-19 using peptide immunogens” (No. 2738081). There are 7 peptides in patented vaccine compositions.
“Peptide immunogens and vaccine composition against coronavirus infection COVID-19 using peptide immunogens” (No. 2743593). The patented vaccine composition contains 2 peptides.
“Peptide immunogens used as a component of a vaccine composition against coronavirus infection COVID-19″ (No. 2743594). The patented vaccine composition contains 3 peptides.
“Vaccine composition against coronavirus infection COVID-19″ (No. 2743595). The patented vaccine composition contains 3 peptides.
In all of these patents, the carrier protein is referred to as a chimeric fusion protein with an amino acid sequence derived from two parts, a bacterial maltose binding protein and a viral nucleocapsid protein.[20]

EpiVacCorona vaccine registration certificate
Authorization
| Full authorization Emergency authorization |
See also: List of COVID-19 vaccine authorizations § EpiVacCorona
The VECTOR has received vaccine emergency authorization in a form of government registration in October 2020.[21]
In Russia phase III clinical study is called post-registration study. Therefore, government registration of the vaccine means permission to perform phase III clinical research and public vaccination outside of clinical trials as well.[21] Since December 2020, the vaccine has been released for public vaccination in Russia.[22]
As of March 2021, Turkmenistan is the only foreign state to register EpiVacCorona with full authorization.[23][24]
Russia’s Chief Health Officer Anna Popova said: “In December 2020 the EpiVacCorona documents were presented to the World Health Organization, and we are expecting a decision from WHO.”[25] However, Deutsche Welle reports “As of March 1, the WHO had yet to receive an Expression of Interest (EOI) from EpiVacCorona’s developers, “VECTOR,” to enable WHO experts to evaluate their vaccine.”[26]
Export
The Deputy Director-General of the World Health Organization (WHO) Dr. Soumya Swaminathan during news conference in Geneva that took place in October 2020, told: “We will only be able to have a position on a vaccine when we see results of the phase III clinical trials.”[27] According to the center’s director Rinat Maksyutov, many government and non-government organizations want to test or be involved in the production of the vaccine.[28] As of March 30, Venezuela obtained 1000 doses of the Russian EpiVacCorona vaccine for a trial.[29] Venezuela also has reached a deal to purchase doses of the vaccine, as well as manufacture it locally, Vice President Delcy Rodriguez provided this information on June 4, 2021.[30] Turkmenistan expects to receive EpiVacCorona, as the vaccine has already been approved for use in that country.[31]
Controversy
Independent study of clinical trial participants

Ministry of Health’s response to a request from trial participants to perform independent antibody screening tests

English translation of Ministry of Health’s response to a request from trial participants to perform independent antibody screening tests.
At the start of the Phase III, trial participants and those vaccinated outside the trial began to form a community through the Telegram messenger network. On January 18, 2021, the members of the community turned to the Ministry of Health of the Russian Federation with an open letter, in which they stated that the production of antibodies after vaccination among them is much lower than declared by vaccine developers. Study participants claimed that antibodies were not found in more than 50% of those who documented their participation in the study, although only 25% of the participants should have had a placebo according to the study design. The trial participants also claimed that negative results were obtained using the a special ELISA test developed and recommended by VECTOR for EpiVacCorona detection.[5][6][4] More questions about the quality and protectiveness of antibodies induced by EpiVacCorona appeared along with the first results of a special antibody VECTOR’s test, when, with a positive special test, negative results of all other commercially available tests were otained: LIAISON SARS-CoV-2 S1 / S2 IgG – DiaSorin, IgM / IgG – Mindray, SARS-CoV-2 IgG – Abbott Architect, Anti-SARS-CoV-2 ELISA (IgG) – Euroimmun, Access SARS-CoV-2 IgG (RBD) – Beckman Coulter, “SARS-CoV-2-IgG-ELISA -BEST “-” Vector-Best “,” Anti-RBD IgG “- Gamaleya Research Center.[5][6][4][8] Clinical trial participants conducted their own antibody mini-study that was performed in independent Russian laboratory. The study participants asked Dr. Alexander Chepurnov, the former head of the infectious diseases department at VECTOR, who now works at another medical institute, to check neutralizing antibodies presence in their serum samples.[3] They also sent to Dr. Chepurnov control serum samples from former COVID-19 patients or people vaccinated with another Russian vaccine, Sputnik V, which is known to trigger the production of neutralizing antibodies.[32] All serum samples were blinded before antibody tests. On 23 March 2021, the participants reported the results of their mini-study in an open letter to the Ministry of Health of the Russian Federation.[6][7] According to the letter, even with the help of the VECTOR antibody detection system, antibodies were detected only in 70-75% of those vaccinated with EpiVacCorona. However, the level of antibodies was very low. Moreover, according to the letter, virus-neutralizing antibodies were not detected in the independent research Dr. Alexander Chepurnov laboratory at all.[3][6][7] The trial participants asked Ministry of Health in their open letter to perform independent study for the verification of their findings.[3][6][7] In addition, the letter reports 18 cases of COVID-19 cases as of March 22, 2021 among those who received the vaccine and became ill (sometimes severe) three weeks or later after the second dose of EpiVacCorona.[33][6][7] April 20, 2021 the study participants got a reply, with refusal of performing any additional verification antibody tests or investigation of sever COVID-19 cases among vaccinated individuals. The reply include the following text: “Considering that the listed immunobiological preparations (vaccines) for the prevention of COVID-19 are registered in the prescribed manner, their effectiveness and safety have been confirmed.”
Vaccine criticism by independent experts
Some independent experts criticized the vaccine design[3][4] and clinical data presentation in the publication.[8][9][10] The experts are saying that peptide selection is “crucial” for the innovative peptide approach, which VECTOR uses for EpiVacCorona design. However, some researchers are not convinced that the viral spike protein peptides selected for the vaccine are actually “visible” by human immune system.[3][4][34] They stated that these peptides do not overlap[35] with peptides that have been shown in several publications to contain human linear B cell epitopes in spike protein of SARS-CoV-2.[36][37][38][39][40] Moreover, the study was criticized for the lack of positive control of convalescent plasma samples in reports related to neutralizing antibody titers in vaccinated individuals.[1][10] The same study was also criticized for presence of detectable antibodies in negative controls samples that were not discussed by authors.[1][10] In addition, vaccine developers have been criticized for aggressively advertising their vaccine efficacy prior to the completion of phase III clinical trial. The most substantial criticism came from Dr. Konstantin Chumakov, who currently serves as the Associate Director for Research at the FDA Office of Vaccines Research and Review. Dr. Chumakov said: “I would not be in a hurry to call this peptide formulation a vaccine yet, because its effectiveness has not yet been proven…For the introduction of such a vaccine, the level of evidence must be much higher, and therefore the developers of EpiVacCorona, before launching their vaccine on the market, had to conduct clinical trials and prove that their vaccine actually protects against the disease. However, such tests were not carried out, which is absolutely unacceptable.”[41]

The title page of the “EpiVacCorona” patent with Anna’s Popova name among inventors
Conflict of interest
The vaccine design was protected by several already issued patents (see section above). In each patent one of its co-authors is a namesake of Anna Popova who is a head of the Federal Service for Supervision of Consumer Rights Protection and Human Welfare. This patent authorship represents an issue as far as Anna Popova is a head of the Russian agency that is charged with overseeing vaccine safety and efficacy. As a co-author of these patents, she might have an interest in promoting the vaccine despite its shortcomings.
References
- ^ Jump up to:a b c d e f Ryzhikov AB, Ryzhikov EA, Bogryantseva MP, Usova SV, Danilenko ED, Nechaeva EA, Pyankov OV, Pyankova OG, Gudymo AS, Bodnev SA, Onkhonova GS, Sleptsova ES, Kuzubov VI, Ryndyuk NN, Ginko ZI, Petrov VN, Moiseeva AA, Torzhkova PY, Pyankov SA, Tregubchak TV, Antonec DV, Gavrilova EV, Maksyutov RA (2021). “A single blind, placebo-controlled randomized study of the safety, reactogenicity and immunogenicity of the “EpiVacCorona” Vaccine for the prevention of COVID-19, in volunteers aged 18–60 years (phase I–II)”. Russian Journal of Infection and Immunity. 11 (2): 283–296. doi:10.15789/2220-7619-ASB-1699.
- ^ Jump up to:a b c d e Federal Budgetary Research Institution State Research Center of Virology and Biotechnology “Vector” (2 March 2021). “Multicenter Double-blind Placebo-controlled Comparative Randomized Study of the Tolerability, Safety, Immunogenicity and Prophylactic Efficacy of the EpiVacCorona Peptide Antigen-based Vaccine for the Prevention of COVID-19, With the Participation of 3000 Volunteers Aged 18 Years and Above (Phase III-IV)”.
- ^ Jump up to:a b c d e f g DobrovidovaApr. 6, Olga; 2021; Am, 11:05 (6 April 2021). “Russia’s COVID-19 defense may depend on mystery vaccine from former bioweapons lab—but does it work?”. Science | AAAS. Retrieved 24 April 2021.
- ^ Jump up to:a b c d e f Dobrovidova, Olga (9 April 2021). “Latest Russian vaccine comes with a big dose of mystery”. Science. 372 (6538): 116–117. doi:10.1126/science.372.6538.116. ISSN 0036-8075. PMID 33833104. S2CID 233191522.
- ^ Jump up to:a b c Staff, Reuters (26 March 2021). “Volunteers break rank to raise doubts in trial of Russia’s second COVID-19 vaccine”. Reuters. Retrieved 23 April 2021.
- ^ Jump up to:a b c d e f g “”ЭпиВакКорона” глазами участников клинических испытаний и ученых-биологов”. Троицкий вариант — Наука (in Russian). 23 March 2021. Retrieved 23 April 2021.
- ^ Jump up to:a b c d e https://epivakorona.com/openletter.htm
- ^ Jump up to:a b c “EpiVacCorona’s race to the finish line Meduza speaks to the developer and manufacturer about concerns surrounding Russia’s latest coronavirus vaccine”. meduza.io. Retrieved 23 April2021.
- ^ Jump up to:a b “Нет антител, вопросы к составу, непрозрачность данных. Что не так с вакциной “ЭпиВакКорона””. BBC News Русская служба (in Russian). Retrieved 23 April 2021.
- ^ Jump up to:a b c d “Sputnik V’s ugly cousin Clinical results for Russia’s EpiVacCorona vaccine are finally here, but developers published in an obscure local journal, raising questions and concerns”. meduza.io. Retrieved 23 April 2021.
- ^ “About 200,000 EpiVacCorona vaccine doses go into civil circulation in Russia”. TASS. Retrieved 25 April 2021.
- ^ Jump up to:a bhttps://www.researchgate.net/publication/350822775_Immunogenicity_and_protectivity_of_the_peptide_candidate_vaccine_against_SARS-CoV-2
- ^ Jump up to:a b Ryzhikov AB, Ryzhikov EA, Bogryantseva MP, Usova SV, Danilenko ED, Imatdinov IR, Nechaeva EA, Pyankov OV, Pyankova OG, Gudymo AS, Bodnev SA, Onkhonova GS, Sleptsova ES, Kuzubov VI, Ryndyuk NN, Ginko ZI, Petrov VN, Moiseeva AA, Torzhkova PY, Pyankov SA, Tregubchak TV, Antonec DV, Sleptsova ES, Gavrilova EV, Maksyutov RA (2021). “Immunogenicity and Protectivityof the Peptide Vaccine againstSARS-CoV-2”. Annals of the Russian Academy of Medical Sciences. 76 (1): 5–19. doi:10.15690/vramn1528.
- ^ Ryzhikov, A. B.; Ryzhikov, Е. А.; Bogryantseva, M. P.; Usova, S. V.; Danilenko, E. D.; Nechaeva, E. A.; Pyankov, O. V.; Pyankova, O. G.; Gudymo, A. S. (24 March 2021). “A single blind, placebo-controlled randomized study of the safety, reactogenicity and immunogenicity of the “EpiVacCorona” Vaccine for the prevention of COVID-19, in volunteers aged 18–60 years (phase I–II)”. Russian Journal of Infection and Immunity. Retrieved 23 April 2021.
- ^ “People vaccinated with Russia’s EpiVacCorona need 42 days to develop immunity – watchdog”. TASS. Retrieved 25 April 2021.
- ^ “Что ждать от “ЭпиВакКороны”. Все о пептидной вакцине против COVID-19″. РИА Новости(in Russian). 1 January 2021. Retrieved 24 April 2021.
- ^ s.r.o, Direct Impact. “AIM database substance – EpiVacCorona”. AIM. Retrieved 25 April 2021.
- ^ Jump up to:a b Federal Budgetary Research Institution State Research Center of Virology and Biotechnology “Vector” (20 February 2021). “Simple, Blind, Placebo-controlled, Randomized Study of the Safety, Reactogenicity and Immunogenicity of Vaccine Based on Peptide Antigens for the Prevention of COVID-19 (EpiVacCorona), in Volunteers Aged 18-60 Years (I-II Phase)”.
- ^ Реестр Клинических исследований COV/pept-03/20; [1]
- ^MKIEEGKLVIWINGDKGYNGLAEVGKKFEKDTGIKVTVEHPDKLEEKFPQVAATGDGPDIIFWAHDRFGGYAQSGLLAEITPDKAFQDKLYPFTWDAVRYNGKLIAYPIAVEALSLIYNKDLLPNPPKTWEEIPALDKELKAKGKSALMFNLQEPYFTWPLIAADGGYAFKYENGKYDIKDVGVDNAGAKAGLTFLVDLIKNKHMNADTDYSIAEAAFNKGETAMTINGPWAWSNIDTSKVNYGVTVLPTFKGQPSKPFVGVLSAGINAASPNKELAKEFLENYLLTDEGLEAVNKDKPLGAVALKSYEEELAKDPRIAATMENAQKGEIMPNIPQMSAFWYAVRTAVINAASGRQTVDEALKDAQTNSSSNNNNNNNNNNLGDNGPQNQRNAPRITFGGPSDSTGSNQNGERSGARSKQRRPQGLPNNTASWFTALTQHGKEDLKFPRGQGVPINTNSSPDDQIGYYRRATRRIRGGDGKMKDLSPRWYFYYLGTGPEAGLPYGANKDGIIWVATEGALNTPKDHIGTRNPANNAAIVLQLPQGTTLPKGFYAEGSRGGSQASSRSSSRSRNSSRNSTPGSSRGTSPARMAGNGGDAALALLLLDRLNQLESKMSGKGQQQQGQTVTKKSAAEASKKPRQKRTATKAYNVTQAFGRRGPEQTQGNFGDQELIRQGTDYKHWPQIAQFAPSASAFFGMSRIGMEVTPSGTWLTYTGAIKLDDKDPNFKDQVILLNKHIDAYKTFPPTEPKKDKKKKADETQALPQRQKKQQTVTLLPAADLDDLSKQLQQSMSSADSTQA. “Carrier protein sequence”.
- ^ Jump up to:a b “Russia begins post-registration trials of EpiVacCorona Covid-19 vaccine”. http://www.clinicaltrialsarena.com. Retrieved 25 April 2021.
- ^ “Вакцина “ЭпиВакКорона” поступила в гражданский оборот”. РИА Новости (in Russian). 11 December 2020. Retrieved 23 April 2021.
- ^ “Turkmenistan registers vaccines for the prevention of infectious diseases”. Turkmenistan Today. 29 January 2021.
- ^ “Turkmenistan: Master Berdymukhamedov goes to Moscow | Eurasianet”. eurasianet.org. Retrieved 25 April 2021.
- ^ “Russia submits EpiVacCorona vaccine documents to WHO – Rospotrebnadzor head Popova”. interfax.com. Retrieved 23 April 2021.
- ^ Welle (www.dw.com), Deutsche. “Two more Russian vaccines: What we do and don’t know | DW | 09.03.2021”. DW.COM. Retrieved 23 April 2021.
- ^ “COVID-19 vaccine: WHO in talks with Russia on its second vaccine EpiVacCorona”. mint. 16 October 2020. Retrieved 9 June 2021.
- ^ “Vector Center says has over 45 inquiries from abroad about its EpiVacCorona vaccine”. TASS. Retrieved 25 April 2021.
- ^ Foundation, Thomson Reuters. “Venezuela receives doses of Russian EpiVacCorona vaccine for trials”. news.trust.org. Retrieved 25 April 2021.
- ^ “Venezuela to purchase and manufacture Russia’s EpiVacCorona vaccine”. Reuters. 5 June 2021. Retrieved 13 June 2021.
- ^ turkmenportal. “Turkmenistan Approves Use of Russia’s EpiVacCorona Vaccine | Society”. Business Turkmenistan Information Center. Retrieved 25 April 2021.
- ^ Jones, Ian; Roy, Polly (20 February 2021). “Sputnik V COVID-19 vaccine candidate appears safe and effective”. The Lancet. 397 (10275): 642–643. doi:10.1016/S0140-6736(21)00191-4. ISSN 0140-6736. PMC 7906719. PMID 33545098.
- ^ “Участники КИ “ЭпиВакКороны” продолжают исследовать эффективность вакцины”. pcr.news. Retrieved 24 April 2021.
- ^ Li, Yang; Ma, Ming-Liang; Lei, Qing; Wang, Feng; Hong, Wei; Lai, Dan-Yun; Hou, Hongyan; Xu, Zhao-Wei; Zhang, Bo; Chen, Hong; Yu, Caizheng (30 March 2021). “Linear epitope landscape of the SARS-CoV-2 Spike protein constructed from 1,051 COVID-19 patients”. Cell Reports. 34 (13): 108915. doi:10.1016/j.celrep.2021.108915. ISSN 2211-1247. PMC 7953450. PMID 33761319.
- ^ “Вакцина “ЭпиВакКорона” в иллюстрациях”. Троицкий вариант — Наука (in Russian). 23 March 2021. Retrieved 24 April 2021.
- ^ Yi, Zhigang; Ling, Yun; Zhang, Xiaonan; Chen, Jieliang; Hu, Kongying; Wang, Yuyan; Song, Wuhui; Ying, Tianlei; Zhang, Rong; Lu, HongZhou; Yuan, Zhenghong (December 2020). “Functional mapping of B-cell linear epitopes of SARS-CoV-2 in COVID-19 convalescent population”. Emerging Microbes & Infections. 9 (1): 1988–1996. doi:10.1080/22221751.2020.1815591. ISSN 2222-1751. PMC 7534331. PMID 32844713.
- ^ Poh, Chek Meng; Carissimo, Guillaume; Wang, Bei; Amrun, Siti Naqiah; Lee, Cheryl Yi-Pin; Chee, Rhonda Sin-Ling; Fong, Siew-Wai; Yeo, Nicholas Kim-Wah; Lee, Wen-Hsin; Torres-Ruesta, Anthony; Leo, Yee-Sin (1 June 2020). “Two linear epitopes on the SARS-CoV-2 spike protein that elicit neutralising antibodies in COVID-19 patients”. Nature Communications. 11 (1): 2806. doi:10.1038/s41467-020-16638-2. ISSN 2041-1723. PMC 7264175. PMID 32483236.
- ^ Li, Yang; Lai, Dan-Yun; Zhang, Hai-Nan; Jiang, He-Wei; Tian, Xiaolong; Ma, Ming-Liang; Qi, Huan; Meng, Qing-Feng; Guo, Shu-Juan; Wu, Yanling; Wang, Wei (October 2020). “Linear epitopes of SARS-CoV-2 spike protein elicit neutralizing antibodies in COVID-19 patients”. Cellular & Molecular Immunology. 17 (10): 1095–1097. doi:10.1038/s41423-020-00523-5. ISSN 2042-0226. PMC 7475724. PMID 32895485.
- ^ Farrera-Soler, Lluc; Daguer, Jean-Pierre; Barluenga, Sofia; Vadas, Oscar; Cohen, Patrick; Pagano, Sabrina; Yerly, Sabine; Kaiser, Laurent; Vuilleumier, Nicolas; Winssinger, Nicolas (2020). “Identification of immunodominant linear epitopes from SARS-CoV-2 patient plasma”. PLOS ONE. 15 (9): e0238089. doi:10.1371/journal.pone.0238089. ISSN 1932-6203. PMC 7480855. PMID 32903266.
- ^ Shrock, Ellen; Fujimura, Eric; Kula, Tomasz; Timms, Richard T.; Lee, I.-Hsiu; Leng, Yumei; Robinson, Matthew L.; Sie, Brandon M.; Li, Mamie Z.; Chen, Yuezhou; Logue, Jennifer (27 November 2020). “Viral epitope profiling of COVID-19 patients reveals cross-reactivity and correlates of severity”. Science. 370 (6520): eabd4250. doi:10.1126/science.abd4250. ISSN 1095-9203. PMC 7857405. PMID 32994364.
- ^ “Константин Чумаков: “Даже если человек переболел COVID-19, ему все равно нужно привиться. Иммунный ответ на прививку лучше и долговечнее, чем на саму болезнь””. republic.ru (in Russian). Retrieved 24 April 2021.
External links
- Margarita Romanenko’s Lecture about Russian Covid-vaccines
- Meduza – Interview with EpiVacCorona developers, 23 March 2021
- Infection and Immunity – Study of the safety, reactogenicity and immunogenecity of the “EpiVacCorona” vaccine (PHASE I–II)
| EpiVacCorona vaccine | |
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | Peptide subunit |
| Clinical data | |
| Trade names | EpiVacCorona |
| Routes of administration | Intramuscular |
| ATC code | None |
| Legal status | |
| Legal status | Registered in Russia on 14 October 2020 RU Registered.TU approved.Full list : List of EpiVacCorona COVID-19 vaccine authorizations |
| Identifiers | |
| DrugBank | DB16439 |
| Part of a series on the |
| COVID-19 pandemic |
|---|
| COVID-19 (disease)SARS-CoV-2 (virus) |
| showTimeline |
| showLocations |
| showInternational response |
| showMedical response |
| showImpact |
| COVID-19 portal |
EpiVacCorona Vaccine, developed by the Vektor State Research Center of Virology and Biotechnology in Russia, is based on peptide-antigens that facilitate immunity to the SARS-CoV-2 virus1. It is currently being tested in Phase I/II clinical trials for safety and immunogenicity (NCT04527575)1,2.
- Precision Vaccinations: VACCINE INFO EpiVacCorona Vaccine [Link]
- The Pharma Letter: Russia’s EpiVacCorona vaccine post-registration trials started [Link]
//////EpiVacCorona, SARS-CoV-2, RUSSIA, CORONA VIRUS, COVID 19, VACCINE, PEPTIDE

NEW DRUG APPROVALS
ONE TIME
$10.00
ZF2001, ZIFIVAX
| Republic of Uzbekistan Oʻzbekiston Respublikasi (Uzbek) |
|---|
| FlagState emblem |
ZF2001
ZIFIVAX
CAS 2609662-31-7
A COVID-19 vaccine comprising a dimeric form of SARS-CoV-2 receptor-binding domain (RBD) produced in China hamster ovary (CHO) cells and adjuvanted with aluminum hydroxide (Anhui Zhifei Longcom/Institute of Microbiol. China Academy of Sciences)
Recombinant vaccine
Anhui Zhifei Longcom Biopharmaceutical, Institute of Microbiology of the Chinese Academy of Sciences
China, Uzbekistan
CHO Cells Recombinant Vaccine
- ZF-2001
- ZF-UZ-VAC2001
- Chinese Academy of Sciences (Originator)
- Zhifei Longcom (Originator)
Human SARS-CoV-2 (Covid-19 coronavirus) vaccine consisting of recombinant dimer comprising two RBD domains (R319-K527) of the spike glycoprotein of SARS-CoV-2 fused via a disulfide link; expressed in CHO cells
ZF-2001 is a recombinant coronavirus vaccine jointly developed by the Institute of Microbiology of the Chinese Academy of Sciences and Zhifei Longcom. The vaccine became available in 2021 in Uzbekistan under an emergency use authorization for the prevention of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (COVID-19). The vaccine is currently evaluated in phase III clinical trials.
This vaccine candidate, developed in China, uses SARS-CoV-2 protein subunits that are entirely engineered, created, and secreted by Chinese Hamster Ovary (CHO) cells1. The vaccine candidate is sponsored by Anhui Zhifei Longcom Biologic Pharmacy Co., Ltd. and is undergoing phase I clinical trials to evaluate safety and tolerability.
ZF2001, trade-named ZIFIVAX, is an adjuvanted protein subunit COVID-19 vaccine developed by Anhui Zhifei Longcom in collaboration with the Institute of Microbiology at the Chinese Academy of Sciences.[1][2] As of December 2020, the vaccine candidate was in Phase III trials with 29,000 participants in China, Ecuador, Malaysia, Pakistan, and Uzbekistan.[3][4]
ZF2001 employs technology similar to other protein-based vaccines in Phase III trials from Novavax, Vector Institute, and Medicago.[5] It is administered in 3 doses over a period of 2 months.[6]
ZF2001 was first approved for use in Uzbekistan and later China.[7][8] Production capacity is expected to be one billion doses a year.[6] Phase II results published in The Lancet on the three dose administration showed seroconversion rates of neutralizing antibodies of between 92% to 97%.[9]
Anhui Zhifei Longcom Biopharmaceuticals began a phase 3 clinical trial for its recombinant protein vaccine candidate in December, according to the WHO. State-run China Global Television Network in November reported that a one-year trial would take place in Uzbekistan and aim to recruit 5,000 volunteers. Anhui Zhifei is a unit of private firm Chongqing Zhifei Biological Products. It is co-developing the vaccine with the Chinese Academy of Sciences, a government institution.
Emergency Use Authorization received in UZ by Zhifei Longcom for the prevention of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (COVID-19)
Description
As described in Cell, the CoV spike receptor-binding domain (RBD) is an attractive vaccine target for coronaviruses but is constrained by limited immunogenicity, however a dimeric form of MERS-CoV RBD offers greater protection. The RBD-dimer significantly increases neutralizing antibodies compared to a conventional monomeric form and protected mice against MERS-CoV infection. CoV RBD-dimer have been produced at high yields in pilot scale production.[10]
Rather than injecting a whole virus, subunit vaccines contains virus particles specially selected to stimulate an immune response. Because the fragments are incapable of causing disease, subunit vaccines are considered very safe.[11] Subunit vaccines in widespread use include the Hepatitis B vaccine and Pertussis vaccine. However, as only a few viral components are included in the vaccine which does not display the full complexity of the virus, their efficacy may be limited.[12] Subunit vaccines are delivered alongside adjuvants and booster doses may be required.[11]
According to industry experts, production for this kind of vaccine is stable and reliable, and easier to achieve large-scale industrial production at home and overseas. However it was noted it can be very inconvenient for people to come back for a second and third dose.[6]
ZF2001 (Anhui Zhifei Longcom Biopharmaceutical/Chinese Academy of Medical Sciences)
The latest subunit vaccine candidate to enter Phase 3 clinical studies is the adjuvanted RBD-dimeric antigen designed by Anhui Zhifei Longcom Biopharmaceutical and the Institute of Microbiology of the Chinese Academy of Medical Sciences. Phase 3 clinical study was launched on December104 and will be initially carried out in China and Uzbekistan while Indonesia, Pakistan and Ecuador will follow as study sites (Clinical Trial Identifier: NCT04646590 and Registration Number: ChiCTR2000040153). The design of the study involves recruitment of 22,000 volunteers from China and 7000 subjects outside China for a total of 29,000 volunteers. There are still no published results on this candidate, however data from its Phase 2 placebo-controlled clinical trial (Clinical Trial Identifier: NCT04466085) conducted on a total of 900 participants ranging from 18 to 59 years old suggest that a 2 or 3 dose regimen is evaluated. Each immunization will be separated by the next by 4 weeks.
Development
Phase I and II trials and results
In June, Longcom began a double-blind, randomized, placebo parallel controlled Phase I trial with 50 participants aged 18–59 in Chongqing divided into low-dose, high-dose, and placebo groups.[13]
In July, Longcom began a randomized, double-blind, placebo-controlled Phase II trial with 900 participants aged 18–59 in Changsha, Hunan divided into low-dose, high-dose, and placebo groups.[14] In August, an additional Phase II trial was launched with 50 participants aged 60 and above.[15][1]
In Phase II results published in The Lancet, on the two-dose schedule, seroconversion rates of neutralizing antibodies after the second dose were 76% (114 of 150 participants) in a 25 μg group and 72% (108 of 150) in a 50 μg group. On the three-dose schedule, seroconversion rate of neutralizing antibodies after the third dose were 97% (143 of 148 participants) in the 25 μg group and 93% (138 of 148) in the 50 μg group. 7 to 14 days after the administration of the third dose, the GMTs of neutralizing antibodies reached levels that were significantly higher than observed in human convalescent serum of recovering COVID-19 patients, especially in the 25 μg group.[9]
Phase III trials
In December, Longcom began enrollment of a Phase III randomized, double-blind, placebo-controlled clinical trial for 29,000 participants, including 750 participants between 18-59 and 250 participants 60 and older in China and 21,000 participants between 18-59 and 7,000 participants 60 and older outside China.[16][17]
In December, Malaysia‘s MyEG announced it would conduct Phase III trials. If the trials were successful, MyEG would be the sole distributor of ZF2001 in Malaysia for 3 years.[4]
In December, Uzbekistan began a year-long Phase III trial of ZF2001 with 5,000 volunteers between 18 and 59.[18][19]
In December, Ecuador‘s Minister of Health, Juan Carlos Zevallos announced Phase III trials would involve between 5,000 and 8,000 volunteers.[20]
In February, Pakistan‘s Drug Regulatory Authority (DRAP) approved Phase III trials with approximately 10,000 participants to be conducted at UHS Lahore, National Defense Hospital, and Agha Khan Hospital.[21]
Discussions to begin Phase III trials are also underway in Indonesia.[17][22]
COVID-19 Variants
In February, lab studies of twelve serum samples taken from recipients of BBIBP-CorV and ZF2001 retained neutralizing activity against the Beta variant although with weaker activity than against the original virus.[23] For ZF-2001, geometric mean titers declined by 1.6-fold, from 106.1 to 66.6, which was less than antisera from mRNA vaccine recipients with a 6-folds decrease.[24] Preliminary clinical data from Novavax and Johnson & Johnson also showed they were less effective in preventing COVID-19 in South Africa, where the new variant is widespread.[23]
Manufacturing
The company’s vaccine manufacturing facility was put into use in September.[17] In February 2021, Pu Jiang, General Manager of Zhifei Longcom, said the company had an annual production capacity of 1 billion doses.[6]
Marketing and deployment
| Full authorization Emergency authorization |
See also: List of COVID-19 vaccine authorizations § RBD-Dimer
On March 1, Uzbekistan granted approval for ZF2001 (under tradename ZF-UZ-VAC 2001) after having taken part in the Phase III trials.[8] In March, Uzbekistan received 1 million doses and started vaccinations in April.[25] By May, a total of 3 million doses had been delivered.[26]
On March 15, China approve of ZF2001 for emergency use after being approved by Uzbekistan earlier in the month.[7]
References
- ^ Jump up to:a b “Anhui Zhifei Longcom: RBD-Dimer – COVID19 Vaccine Tracker”. covid19.trackvaccines.org. Retrieved 27 December2020.
- ^ “COVID-19 Vaccine: ZIFIVAX by Anhui Zhifei Longcom Biopharma, Institute of Microbiology Chinese Academy of Sciences”. covidvax.org. Retrieved 27 December 2020.
- ^ “Fifth Chinese Covid-19 vaccine candidate ready to enter phase 3 trials”. South China Morning Post. 20 November 2020. Retrieved 27 December 2020.
- ^ Jump up to:a b Ying TP (7 December 2020). “MYEG to conduct phase 3 clinical trial for China’s Covid-19 vaccine in Msia | New Straits Times”. NST Online. Retrieved 27 December 2020.
- ^ Zimmer C, Corum J, Wee SL (10 June 2020). “Coronavirus Vaccine Tracker”. The New York Times. ISSN 0362-4331. Retrieved 27 December 2020.
- ^ Jump up to:a b c d “China’s production bottleneck ‘could be eased with latest Covid-19 vaccine'”. South China Morning Post. 17 March 2021. Retrieved 18 March 2021.
- ^ Jump up to:a b Liu, Roxanne (15 March 2021). “China IMCAS’s COVID-19 vaccine obtained emergency use approval in China”. Reuters. Retrieved 15 March 2021.
- ^ Jump up to:a b Mamatkulov, Mukhammadsharif (1 March 2021). “Uzbekistan approves Chinese-developed COVID-19 vaccine”. Reuters. Retrieved 2 March 2021.
- ^ Jump up to:a b Yang, Shilong; Li, Yan; Dai, Lianpan; Wang, Jianfeng; He, Peng; Li, Changgui; Fang, Xin; Wang, Chenfei; Zhao, Xiang; Huang, Enqi; Wu, Changwei (24 March 2021). “Safety and immunogenicity of a recombinant tandem-repeat dimeric RBD-based protein subunit vaccine (ZF2001) against COVID-19 in adults: two randomised, double-blind, placebo-controlled, phase 1 and 2 trials”. The Lancet Infectious Diseases. 0. doi:10.1016/S1473-3099(21)00127-4. ISSN 1473-3099. PMC 7990482. PMID 33773111.
- ^ Dai L, Zheng T, Xu K, Han Y, Xu L, Huang E, et al. (August 2020). “A Universal Design of Betacoronavirus Vaccines against COVID-19, MERS, and SARS”. Cell. 182 (3): 722–733.e11. doi:10.1016/j.cell.2020.06.035. PMC 7321023. PMID 32645327.
- ^ Jump up to:a b “What are protein subunit vaccines and how could they be used against COVID-19?”. http://www.gavi.org. Retrieved 27 December2020.
- ^ Dong Y, Dai T, Wei Y, Zhang L, Zheng M, Zhou F (October 2020). “A systematic review of SARS-CoV-2 vaccine candidates”. Signal Transduction and Targeted Therapy. 5 (1): 237. doi:10.1038/s41392-020-00352-y. PMC 7551521. PMID 33051445.
- ^ Clinical trial number NCT04445194 for “Phase I Clinical Study of Recombinant Novel Coronavirus Vaccine” at ClinicalTrials.gov
- ^ Clinical trial number NCT04466085 for “A Randomized, Blinded, Placebo-controlled Trial to Evaluate the Immunogenicity and Safety of a Recombinant New Coronavirus Vaccine (CHO Cell) With Different Doses and Different Immunization Procedures in Healthy People Aged 18 to 59 Years” at ClinicalTrials.gov
- ^ Clinical trial number NCT04550351 for “A Randomized, Double-blind, Placebo-controlled Phase I Clinical Trial to Evaluate the Safety and Tolerability of Recombinant New Coronavirus Vaccines (CHO Cells) in Healthy People Aged 60 Years and Above” at ClinicalTrials.gov
- ^ Clinical trial number NCT04646590 for “A Phase III Randomized, Double-blind, Placebo-controlled Clinical Trial in 18 Years of Age and Above to Determine the Safety and Efficacy of ZF2001, a Recombinant Novel Coronavirus Vaccine (CHO Cell) for Prevention of COVID-19” at ClinicalTrials.gov
- ^ Jump up to:a b c “Another Chinese Covid-19 vaccine enters late-stage human trials with a plan to produce 300 million doses annually”. Business Insider. Retrieved 27 December 2020.
- ^ Reuters Staff (11 November 2020). “Uzbekistan to carry out late-stage trial of Chinese COVID-19 vaccine candidate”. Reuters. Retrieved 27 December 2020.
- ^ “Uzbekistan poised to start trials on Chinese COVID-19 vaccine | Eurasianet”. eurasianet.org. Retrieved 27 December 2020.
- ^ “Ecuador participará en ensayos de una vacuna china contra el covid-19”. CNN (in Spanish). 29 December 2020. Retrieved 23 January 2021.
- ^ “China’s third vaccine enters Pakistan”. The Nation. 15 February 2021. Retrieved 28 February 2021.
- ^ “Covid vaccine tracker: How do the leading jabs compare?”. http://www.ft.com. 23 December 2020. Retrieved 27 December 2020.
- ^ Jump up to:a b Liu, Roxanne (3 February 2021). “Sinopharm’s COVID-19 vaccine remained active against S.Africa variant, effect reduced – lab study”. Reuters. Retrieved 29 March 2021.
- ^ Huang, Baoying; Dai, Lianpan; Wang, Hui; Hu, Zhongyu; Yang, Xiaoming; Tan, Wenjie; Gao, George F. (2 February 2021). “Neutralization of SARS-CoV-2 VOC 501Y.V2 by human antisera elicited by both inactivated BBIBP-CorV and recombinant dimeric RBD ZF2001 vaccines”. bioRxiv: 2021.02.01.429069. doi:10.1101/2021.02.01.429069.
- ^ uz, Kun. “Uzbekistan receives 1 million doses of ZF-UZ-VAC 2001 vaccine”. Kun.uz. Retrieved 28 March 2021.
- ^ Romakayeva, Klavdiya (18 May 2021). “Uzbekistan receives third batch of Chinese-Uzbek COVID-19 vaccine”. Trend.Az. Retrieved 19 May 2021.
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | Protein subunit |
| Clinical data | |
| Trade names | ZIFIVAX |
| Routes of administration | Intramuscular |
| ATC code | None |
| Identifiers | |
| DrugBank | DB15893 |
| Part of a series on the |
| COVID-19 pandemic |
|---|
| COVID-19 (disease)SARS-CoV-2 (virus) |
| showTimeline |
| showLocations |
| showInternational response |
| showMedical response |
| showImpact |
| COVID-19 portal |
////////ZF2001, ZIFIVAX, corona virus, covid 19, SARS-CoV-2, ZF 2001, ZF-UZ-VAC2001, Uzbekistan, approvals 2021

NEW DRUG APPROVALS
one time
$10.00
Estetrol

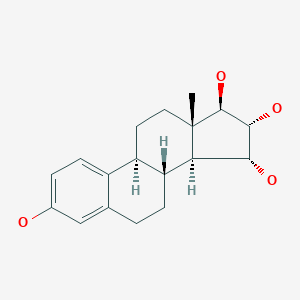
Estetrol
エステトロール;
| Formula | C18H24O4 |
|---|---|
| CAS | 15183-37-6 |
| Mol weight | 304.3808 |
FDA 4/15/2021, To prevent pregnancy, Nextstellis
New Drug Application (NDA): 214154
Company: MAYNE PHARMA
PATENT
https://patents.google.com/patent/EP1562976B1/en
Estrogenic substances are commonly used in methods of Hormone Replacement Therapy (HRT) and methods of female contraception. These estrogenic substances can be divided in natural estrogens and synthetic estrogens. Examples of natural estrogens that have found pharmaceutical application include estradiol, estrone, estriol and conjugated equine estrogens. Examples of synthetic estrogens, which offer the advantage of high oral bioavailability include ethinyl estradiol and mestranol.Recently, estetrol has been found effective as an estrogenic substance for use in HRT, disclosure of which is given in the Applicant’s co-pending application WO 02/094276 . Estetrol is a biogenic estrogen that is endogeneously produced by the fetal liver during human pregnancy. Other important applications of estetrol are in the fields of contraception, therapy of auto-immune diseases, prevention and therapy of breast and colon tumors, enhancement of libido, skin care, and wound healing as described in the Applicant’s co-pending applications WO 02/094276 , WO 02/094279 , WO 02/094278 , WO 02/094275 , EP 1511496 A1 , EP 1511498 A1 , WO 03/041718 , WO 03/018026 , EP 1526856 A1 and WO 04/0278032 .[0004]The synthesis of estetrol and derivatives thereof on a laboratory scale basis is known in the art: Fishman J., Guzik H., J. Org. Chem. 33, 3133 – 3135 (1968); Nambara T. et al., Steroids 27, 111 – 121 (1976); or Suzuki E. et al., Steroids 60, 277 – 284(1995).[0005]
Fishman J., Guzik H., J. Org. Chem. 33, 3133 – 3135 (1968) discloses a successful synthesis of estetrol from an estrone derivative (compound (III); cf. for a synthesis of compound (III) Cantrall, E.W., Littell, R., Bernstein, S. J. Org. Chem 29, 214 – 217 (1964)). In a first step, the carbonyl group at C17 of compound (III) was reduced with LiAlH4 to estra-1,3,5(10),15-tetraene-3,17-diol (compound VIa) that was isolated as the diacetate (compound VIb). Compound VIb was subjected to cis-hydroxylation of the double bond of ring D by using OsO4 which resulted into the formation of estra-1,3,5(10)-triene-3,15α,16α,17β-tetraol-3,17-diacetate (compound Ib) that under heating with K2CO3 in methanol produces estetrol (Scheme 1).

[0006]
The overall yield of this three step process is, starting from estrone derivative III, only about 7%. It is worth noting that the protected derivative 17,17-ethylenedioxyestra-1,3,5(10),15-tetraene-3-ol-3-acetate (compound IV) could be cis-hydroxylated to its 15α,16α-diol derivative (compound Va), but that thereafter the dioxolane group could not be removed (p-toluene sulfonic acid in acetone at room temperature) or that the hydrolysis (aqueous sulfuric acid in warm dioxane) of the dioxolane group resulted in a mixture containing a multitude of products (Scheme 2).

[0007]Nambara T. et al., Steroids 27, 111 – 121 (1976) discloses another synthesis of estetrol wherein estrone is the starting material. The carbonyl group of estrone is first protected by treatment with ethylene glycol and pyridine hydrochloride followed by acetylation of the hydroxy group at C3. The next sequence of steps involved a bromination/base catalyzed dehydrobromination resulting into the formation of 17,17-ethylenedioxyestra-1,3,5(10),15-tetraene-3-ol (compound IVa). This compound IVa was subsequently acetylated which produced 17,17-ethylenedioxyestra-1,3,5(10),15-tetraene-3-ol-3-acetate (compound IVb). In a next step, the dioxolane group of compound IVb was hydrolysed by using p-toluene sulfonic acid to compound Vb, followed subsequently by reduction of the carbonyl group at C17 (compound Vc) and oxidation of the double bond of ring D thereby forming estra-1,3,5(10)-triene-3,15α,16α,17β-tetraol-3,17-diacetate (compound VIb). See Scheme 3.[0008]
Suzuki E. et al., Steroids 60, 277 – 284 (1995) also discloses the synthesis of estetrol by using compound Vb of Nambara T. et al. as starting material. The carbonyl group at C17 of this compound was first reduced followed by acetylation yielding estra-1,3,5(10),15-tetraene-3,17-diol-3,17-diacetate (compound 2b). The latter was subjected to oxidation with OsO4 which provided estra-1,3,5(10)-triene-3,15α,16α,17β-tetraol-3,17-diacetate (compound 3b) in 46% yield.

[0009]According to the Nambara T. et al. and Suzuki E. et al., the synthesis of estetrol can be performed with a yield of approximately 8%, starting from estrone.0010]
Poirier D., et al., Tetrahedron 47, 7751 – 7766 (1991) discloses the following compounds which were prepared according to methods that have been used to prepare similar compounds:

[0011]Dionne, P. et al., Steriods 62, 674 – 681 (1997) discloses the compound shown above wherein R is either methyl or t-butyldimethylsilyl.[0012]Magnus, P. et al., J. Am. Chem. Soc. 120, 12486 -12499 (1998) discloses that the main methods for the synthesis of α,β-unsaturated ketones from saturated ketones are (a) halogenation followed by dehydrohalogenation, (b) utilising sulphur or selenium derivatives, (c) DDQ and (d) utilizing palladium(II) complexes.[0013]Furthermore, it has also been found that by following the prior art methods mentioned above, estetrol of high purity was obtained only in low yield when using an acetyl group as a protecting group for the 3-hydroxy group of estra-1,3,5(10),15-tetraen-3-ol-17-one, in particular because its sensitivity to hydrolysis and solvolysis. In particular, the lability of the acetyl group lead not only to an increased formation of byproducts during the reactions, but also during chromatography and crystallisation for purification of intermediate products when protic solvents such as methanol were used. Therefore, it is difficult to isolate purified estetrol and intermediates thereof in good yield.
Example 7 3-Benzyloxy-estra-1,3,5 (10),15-tetraen-17-ol (compound 5; A = benzyl)
[0088]To a solution of 3-benzyl-dehydroestrone (compound 6; A = benzyl; 58 g, 162 mmol) in a mixture of MeOH (900 mL) and THF (200 mL) at room temperature was added CeCl3 heptahydrate (66.4 g, 178 mmol). After stirring for 1 h the mixture was cooled to 0-5°C using an ice/water bath. Then NaBH4 (12.2 g, 324 mmol) was added in small portions maintaining a temperature below 8°C. After stirring for 2 h at 0-5°C (TLC showed the reaction to be complete) 1 N NaOH (300 mL) and DCM (1 L) were added and the mixture was stirred for ½ h at room temperature. The layers were separated and the aqueous layer was extracted with DCM (200 mL). The organic layers were combined, dried (Na2SO4) and concentrated in vacuo to give an off-white solid (55.0 g, 152.8 mmol, 94%) TLC: Rf = 0.25 (heptanes/ethyl acetate = 4:1); HPLC-MS: 93% β-isomer, 2% α-isomer; DSC: Mp. 149.7°C, purity 96.6%; 1H-NMR (200 MHz, CDCl3) δ 7.48 (m, 5H), 7.27 (d, 1H, J = 8.4 Hz), 6.85 (dd, 1H, J1 = 2.8 Hz, J2 = 8.6 Hz), 6.81 (d, 1H, J = 2.4 Hz), 6.10 (d, 1H, J = 5.8 Hz), 5.79 (dd, 1H, J1 = 1.8 Hz, J2 = 3.4 Hz), 5.11 (s, 2H), 4.48 (d, 1H, J = 7.6), 2.96 (m, 2H), 2.46 – 1.64 (m, 9H), 0.93 (s, 3H) ppm.
Example 8 17-Acetyloxy-3-benzyloxy-estra-1,3,5 (10),15-tetraene (compound 4; A = benzyl, C = acetyl)
[0089]A solution of 3-Benzyloxy-estra-1,3,5 (10),15-tetraen-17-ol (compound 5; A = benzyl; 55.0 g, max. 153 mmol) in pyridine (400 mL) was treated with Ac2O (50 mL, 0.53 mol) and 4-dimethylaminopyridine (1.5 g, 12.3 mmol). The mixture was stirred for 2 h at room temperature (TLC showed the reaction to be complete). It was concentrated in vacuo. The residue was dissolved in EtOAc (400 mL), washed with water (200 mL) and brine (150 mL), dried (Na2SO4) and concentrated in vacuo to yield a yellow solid (54.0 g, 49.8 mmol, 88%). The product was purified by recrystallization from heptanes/ EtOAc/ EtOH (1:0.5:1) to afford a white solid (45.0 g, 112 mmol, 73%) TLC: Rf = 0.6 (heptanes/ethyl acetate = 4/1); HPLC-MS: 98% β-isomer, 1% α-isomer, 1.3% ß-estradiol; DSC: Mp. 122.8°C, purity 99.8%; 1H-NMR (200 MHz, CDCl3) δ 7.44 (m, 5H), 7.27 (d, 1H, J = 8.4 Hz), 6.86 (dd, 1H, J1 = 2.6 Hz, J2 = 8.4 Hz), 6.80 (d, 1H, J = 2.6 Hz), 6.17 (d, 1H, J = 5.8 Hz), 5.78 (dd, 1H, J1 = 1.4 Hz, J2 = 3.2 Hz), 5.45 (m, 1H), 5.11 (s, 2H), 2.96 (m, 2H), 2.40 – 1.54 (m, 10H), 2.18 (s, 3H), 0.93 (s, 3H) ppm.
Example 9 17-Acetyl-3-Benzyl estetrol (compound 3; A = benzyl, C = acetyl)
[0090]OsO4 on PVP (9 g, ~5% w/w OsO4 on PVP, prepared according to Cainelli et al. Synthesis, 45 – 47 (1989) was added to a solution of 17-Acetyloxy-3-benzyloxy-estra-1,3,5 (10),15-tetraene (compound 4; A = benzyl, C = acetyl; 45 g, 112 mmol) in THF (450 mL) and the mixture was heated to 50°C. Trimethylamine-N-oxide dihydrate (24.9 g, 224 mmol) was added portion-wise over 2 h. After stirring for 36 h at 50°C (TLC showed the reaction to be complete) the reaction mixture was cooled to room temperature. The solids were filtered off, washed with THF (100 mL) and the filtrate was concentrated. The residue was taken up in EtOAc (250 mL) and water (250 mL) was added. The aqueous layer was acidified with 1 N HCl (ca. 10 mL). The layers were separated and the aqueous layer was extracted with EtOAc (150 mL). The organic layers were combined, dried (Na2SO4) and concentrated in vacuo. The residue was triturated with heptanes/EtOAc (1:1, 100 mL), stirred for 2 h and the resulting white precipitate was filtered off to give the product as a white solid (41 g, 94 mmol, 84%). The product was purified by recrystallization from heptanes/ ethyl acetate/ EtOH (2:1:1) three times to afford a white solid (21 g, 48.2 mmol, 43%). HPLC-MS: 99.5% βαα-isomer; DSC: Mp. 159.3°C, purity 98.7%; 1H-NMR (200 MHz, CDCl3) δ 7.49 (m, 5H), 7.27 (d, 1H, J = 8.4 Hz), 6.84 (dd, 1H, J1 = 2.6 Hz, J2 = 8.4 Hz), 6.81 (d, 1H, J = 2.4 Hz), 5.11 (s, 2H), 4.45 (d, 1H, J = 4.4), 4.11 (m, 3H), 3.12 (m, 1H) 2.95 (m, 2H), 2.46 -1.64 (m, 10H), 2.24 (s, 3H), 0.93 (s, 3H) ppm.
Example 10 17-Acetyl estetrol (compound 2; C = acetyl)
[0091]To a solution of 17-acetyl-3-benzyl estetrol (compound 3; A = benzyl, C = acetyl; 21 g, 48.2 mmol) in MeOH (600 mL, HPLC-grade) was added a preformed suspension of 10% Palladium on activated carbon (2 g) in methanol (50 mL). The mixture was placed under an atmosphere of H2 at 1 atm and stirred for 24 h (TLC showed the reaction to be completed) at room temperature. It was filtered over Celite® and the filter cake was washed with MeOH (200 mL). The filtrate was concentrated in vacuo to give 17-acetyl estetrol as a white solid (15 g, 43.4 mmol, 90%). TLC: Rf = 0.2 (heptanes/ethyl acetate = 1/1); HPLC-MS: 99.2%, DSC: Mp. 212.2°C, purity 98.9%; 1H-NMR (200 MHz, CD3OD) δ 7.14 (d, 1H, J = 8.0 Hz), 6.60 (dd, 1H, J1 = 2.6 Hz, J2 = 8.8 Hz), 6.56 (d, 1H, J = 2.4 Hz), 4.81 (dd, 1H, J1 = 3.4 Hz, J2 = 6.4 Hz), 4.07 (m, 3H), 3.12 (m, 1H), 2.85 (m, 2H), 2.37 – 1.37 (m, 10H), 2.18 (s, 3H), 0.91 (s, 3H) ppm.
Example 11 Estetrol
[0092]17-Acetyl-estetrol (compound 2; C = acetyl; 15 g, 43.4 mmol) and K2CO3 (6 g, 43.4 mmol) were suspended in MeOH (500 mL, HPLC-grade) and stirred for 4 h at room temperature (TLC showed the reaction to be complete). The solvents were evaporated in vacuo. Water (200 mL) and CHCl3 (70 mL) were added and the mixture was stirred and neutralized with 0.1 N HCl (50 mL). The product was collected by filtration, washed with water (100 mL) and CHCl3 (100 mL) to give estetrol as a white solid (12.2 g, 40.1 mmol, 92.5%, overall yield from estrone 10.8%) after drying at 40°C in an air-ventilated oven. TLC: Rf = 0.05 (heptanes/ethyl acetate = 1/1); HPLC-MS: 99.1%, DSC: Mp. 243.7°C, purity 99.5%; 1H-NMR (200 MHz, CD3OD) δ 7.14 (d, 1H, J = 8.6 Hz), 6.61 (dd, 1H, J1 = 2.6 Hz, J2 = 8.4 Hz), 6.56 (d, 1H, J = 2.4 Hz), 4.83 (m, 1H), 3.93 (m, 3H), 3.50 (d, 1H, J = 5.2), 3.38 (m, 2H), 2.84 (m, 2H), 2.32 (m, 3H), 1.97 (m, 1H), 1.68 – 1.24 (m, 5H), 0.86 (s, 3H) ppm.
SYN
https://www.tandfonline.com/doi/abs/10.1080/13697130802054078?journalCode=icmt20
Estetrol (E4), or oestetrol, is a weak estrogen steroid hormone, which is found in detectable levels only during pregnancy in humans.[1][2] It is produced exclusively by the fetal liver.[1] Estetrol is closely related to estriol (E3), which is also a weak estrogen that is found in high quantities only during pregnancy.[1][2] Along with estradiol (E2), estrone (E1), and E3, estetrol (E4) is a major estrogen in the body, although only during pregnancy.[1]
In addition to its role as a natural hormone, estetrol is under clinical development for use as a medication, for instance in hormonal contraception (in combination with drospirenone) and as menopausal hormone therapy; for information on estetrol as a medication, see the estetrol (medication) article.
Biological function
Estetrol is an estrogen and has estrogenic effects in various tissues.[1] Estetrol interacts with nuclear Estrogen Receptor (ERα) in a manner identical to that of the other estrogens and distinct from that observed with Selective Estrogen Receptor Modulators (SERMs).[3][4] So far the physiological function of estetrol is unknown. The possible use of estetrol as a marker for fetal well-being has been studied quite extensively. However, due to the large intra- and inter-individual variation of maternal estetrol plasma levels during pregnancy this appeared not to be feasible.[5][6][7][8][9]
Biological activity
Estetrol is an agonist of the estrogen receptors (ERs), and hence is an estrogen.[10][11] It has moderate affinity for ERα and ERβ, with Ki values of 4.9 nM and 19 nM, respectively.[10][12] As such, estetrol has 4- to 5-fold preference for the ERα over the ERβ.[10][12] The estrogen has low affinity for the ERs relative to estradiol, and both estetrol and the related estrogen estriol require substantially higher concentrations than estradiol to produce similar effects to estradiol.[10] The affinity of estetrol for the ERs is about 0.3% (rat) to 6.25% (human) of that of estradiol, and its in vivo potency in animals is about 2 to 3% of that of estradiol.[10] Estetrol shows high selectivity for the ERs.[10][12]
Biochemistry
Biosynthesis
Estetrol is synthesized during pregnancy only in the fetal liver from estradiol (E2) and estriol (E3) by the two enzymes 15α- and 16α-hydroxylase.[13][14][15] Alternatively, estetrol is synthesized with 15α-hydroxylation of 16α-hydroxy-DHEA sulfate as an intermediate step.[16] It appears in maternal urine at around week 9 of pregnancy.[2] After birth the neonatal liver rapidly loses its capacity to synthesize estetrol because these two enzymes are no longer expressed.
Estetrol reaches the maternal circulation through the placenta and was already detected at nine weeks of pregnancy in maternal urine.[17][18] During the second trimester of pregnancy high levels were found in maternal plasma, with steadily rising concentrations of unconjugated estetrol to about 1 ng/mL (>3 nM) towards the end of pregnancy.[1]
Distribution
In terms of plasma protein binding, estetrol is moderately bound to albumin, and is not bound to sex hormone-binding globulin (SHBG).[19][20]
Metabolism
Estetrol undergoes no phase I metabolism by CYP P450 enzymes.[10] It is conjugated via glucuronidation and to a lesser extent sulfation and then excreted.[10][21]
Excretion
Estetrol is excreted mostly or completely in urine.[21][10]
Chemistry
See also: List of estrogens
vteStructures of major endogenous estrogens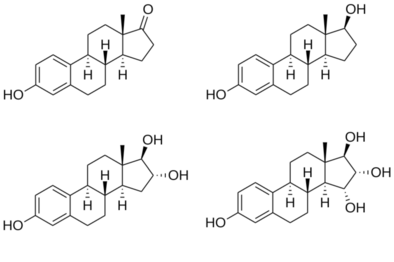 Estrone (E1)Estradiol (E2)Estriol (E3)Estetrol (E4) Estrone (E1)Estradiol (E2)Estriol (E3)Estetrol (E4) |
Estetrol, also known as 15α-hydroxyestriol or as estra-1,3,5(10)-triene-3,15α,16α,17β-tetrol, is a naturally occurring estrane steroid and derivative of estrin (estratriene).[10][11] It has four hydroxyl groups, which explains the abbreviation E4.[10][11]
Synthesis
Chemical syntheses of estetrol have been published.[22]
History
Estetrol was discovered in 1965 by Egon Diczfalusy and coworkers at the Karolinska Institute in Stockholm, Sweden, via isolation from the urine of pregnant women.[10][23]
References
- ^ Jump up to:a b c d e f Holinka CF, Diczfalusy E, Coelingh Bennink HJ (May 2008). “Estetrol: a unique steroid in human pregnancy”. J. Steroid Biochem. Mol. Biol. 110 (1–2): 138–43. doi:10.1016/j.jsbmb.2008.03.027. PMID 18462934.
- ^ Jump up to:a b c Reproductive Endocrinology: Physiology, Pathophysiology, and Clinical Management, 3rd ed., SSC Yen and RB Jaffe (eds.), pp. 936–981, Copyright Elsevier/Saunders 1991
- ^ Abot, Anne; Fontaine, Coralie; Buscato, Mélissa; Solinhac, Romain; Flouriot, Gilles; Fabre, Aurélie; Drougard, Anne; Rajan, Shyamala; Laine, Muriel; Milon, Alain; Muller, Isabelle (2014). “The uterine and vascular actions of estetrol delineate a distinctive profile of estrogen receptor α modulation, uncoupling nuclear and membrane activation”. EMBO Molecular Medicine. 6 (10): 1328–1346. doi:10.15252/emmm.201404112. ISSN 1757-4676. PMC 4287935. PMID 25214462.
- ^ Foidart, JM; et al. (2019). “30th Annual Meeting of The North America Menopause Society September 25 – 28, 2019, Chicago, IL”. Menopause. 26 (12): 1445–1481. doi:10.1097/GME.0000000000001456. ISSN 1530-0374.
- ^ J. Heikkilä, T. Luukkainen, Urinary excretion of estriol and 15a-hydroxyestriol in complicated pregnancies, Am. J. Obstet. Gynecol. 110 (1971) 509-521.
- ^ D. Tulchinsky, F.D. Frigoletto, K.J. Ryan, J. Fishman, Plasma estetrol as an index of fetal well-being, J. Clin. Endocrinol. Metab. 40 (1975) 560-567
- ^ A.D. Notation, G.E. Tagatz, Unconjugated estriol and 15a-hydroxyestriol in complicated pregnancies, Am. J. Obstet. Gynecol. 128 (1977) 747-756.
- ^ N. Kundu, M. Grant, Radioimmunoassay of 15a-hydroxyestriol (estetrol) in pregnancy serum, Steroids 27 (1976) 785-796.
- ^ N. Kundu, M. Wachs, G.B. Iverson, L.P. Petersen, Comparison of serum unconjugated estriol and estetrol in normal and complicated pregnancies, Obstet. Gynecol. 58 (1981) 276-281.
- ^ Jump up to:a b c d e f g h i j k l Coelingh Bennink HJ, Holinka CF, Diczfalusy E (2008). “Estetrol review: profile and potential clinical applications”. Climacteric. 11 Suppl 1: 47–58. doi:10.1080/13697130802073425. PMID 18464023.
- ^ Jump up to:a b c Visser M, Coelingh Bennink HJ (March 2009). “Clinical applications for estetrol” (PDF). J. Steroid Biochem. Mol. Biol. 114(1–2): 85–9. doi:10.1016/j.jsbmb.2008.12.013. PMID 19167495.
- ^ Jump up to:a b c Visser M, Foidart JM, Coelingh Bennink HJ (2008). “In vitro effects of estetrol on receptor binding, drug targets and human liver cell metabolism”. Climacteric. 11 Suppl 1: 64–8. doi:10.1080/13697130802050340. PMID 18464025.
- ^ J. Schwers, G. Eriksson, N. Wiqvist, E. Diczfalusy, 15a-hydroxylation: A new pathway of estrogen metabolism in the human fetus and newborn, Biochim. Biophys. Acta. 100 (1965) 313-316
- ^ J. Schwers, M. Govaerts-Videtsky, N. Wiqvist, E. Diczfalusy, Metabolism of oestrone sulphate by the previable human foetus, Acta Endocrinol. 50 (1965) 597-610.
- ^ S. Mancuso, G. Benagiano, S. Dell’Acqua, M. Shapiro, N. Wiqvist, E. Diczfalusy, Studies on the metabolism of C-19 steroids in the human foeto-placental unit, Acta Endocrinol. 57 (1968) 208-227.
- ^ Jerome Frank Strauss; Robert L. Barbieri (2009). Yen and Jaffe’s Reproductive Endocrinology: Physiology, Pathophysiology, and Clinical Management. Elsevier Health Sciences. pp. 262–. ISBN 1-4160-4907-X.
- ^ J. Heikkilä, H. Adlercreutz, A method for the determination of urinary 15α-hydroxyestriol and estriol, J. Steroid Biochem. 1 (1970) 243-253
- ^ J. Heikkilä, Excretion of 15α-hydroxyestriol and estriol in maternal urine during normal pregnancy, J. Steroid Biochem. 2 (1971) 83-93.
- ^ Visser M, Holinka CF, Coelingh Bennink HJ (2008). “First human exposure to exogenous single-dose oral estetrol in early postmenopausal women”. Climacteric. 11 Suppl 1: 31–40. doi:10.1080/13697130802056511. PMID 18464021.
- ^ Hammond GL, Hogeveen KN, Visser M, Coelingh Bennink HJ (2008). “Estetrol does not bind sex hormone binding globulin or increase its production by human HepG2 cells”. Climacteric. 11 Suppl 1: 41–6. doi:10.1080/13697130701851814. PMID 18464022.
- ^ Jump up to:a b Mawet M, Maillard C, Klipping C, Zimmerman Y, Foidart JM, Coelingh Bennink HJ (2015). “Unique effects on hepatic function, lipid metabolism, bone and growth endocrine parameters of estetrol in combined oral contraceptives”. Eur J Contracept Reprod Health Care. 20 (6): 463–75. doi:10.3109/13625187.2015.1068934. PMC 4699469. PMID 26212489.
- ^ Warmerdam EG, Visser M, Coelingh Bennink HJ, Groen M (2008). “A new route of synthesis of estetrol”. Climacteric. 11 Suppl 1: 59–63. doi:10.1080/13697130802054078. PMID 18464024.
- ^ Hagen AA, Barr M, Diczfalusy E (June 1965). “Metabolism of 17-beta-oestradiol-4-14-C in early infancy”. Acta Endocrinol. 49: 207–20. doi:10.1530/acta.0.0490207. PMID 14303250.
| Names | |
|---|---|
| Preferred IUPAC name(1R,2R,3R,3aS,3bR,9bS,11aS)-11a-Methyl-2,3,3a,3b,4,5,9b,10,11,11a-decahydro-1H-cyclopenta[a]phenanthrene-1,2,3,7-tetrol | |
| Other namesOestetrol; E4; 15α-Hydroxyestriol; Estra-1,3,5(10)-triene-3,15α,16α,17β-tetrol | |
| Identifiers | |
| CAS Number | 15183-37-6 |
| 3D model (JSmol) | Interactive image |
| ChEBI | CHEBI:142773 |
| ECHA InfoCard | 100.276.707 |
| KEGG | D11513 |
| PubChem CID | 27125 |
| UNII | ENB39R14VF |
| CompTox Dashboard (EPA) | DTXSID50164888 |
| showSMILES | |
| Properties | |
| Chemical formula | C18H24O4 |
| Molar mass | 304.386 g/mol |
| Solubility in water | 1.38 mg/mL |
| Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| Infobox references |
//////////estetrol, Nextstellis, fda 2021, approvals 2021

NEW DRUG APPROVALS
one time
$10.00
Nanatinostat
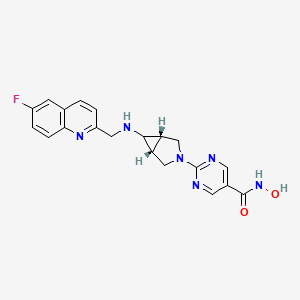
Nanatinostat
Tractinostat
CHR-3996, CHR 3996, VRx 3996,
C20H19FN6O2, 394.41
CAS 1256448-47-1
2-[(1α,5α,6α)-6-[[(6-Fluoro-2-q
2-[(1R,5S,6R)-6-{[(6-fluoroquinolin-2-yl)methyl]amino}-3-azabicyclo[3.1.0]hexan-3-yl]-N-hydroxypyrimidine-5-carboxamide2-[(1R,5S,6s)-6-{[(6-Fluoro-2-quinolinyl)methyl]amino}-3-azabicyclo[3.1.0]hex-3-yl]-N-hydroxy-5-pyrimidinecarboxamide5-Pyrimidinecarboxamide, 2-[(1R,5S)-6-[[(6-fluoro-2-quinolinyl)methyl]amino]-3-azabicyclo[3.1.0]hex-3-yl]-N-hydroxy-Chroma Therapeutics Ltd. (Originator)
- OriginatorChroma Therapeutics
- DeveloperChroma Therapeutics; Viracta Therapeutics
- ClassAmides; Antineoplastics; Pyrimidines; Quinolines; Small molecules
- Mechanism of ActionHistone deacetylase inhibitors
- Orphan Drug StatusYes – Post-transplant lymphoproliferative disorder; Plasmablastic lymphoma; T-cell lymphoma
- Phase IILymphoma
- Phase I/IIMultiple myeloma
- Phase ISolid tumours
- No development reportedGastric cancer; Nasopharyngeal cancer; Post-transplant lymphoproliferative disorder
- 01 Jun 2021Phase-II clinical trials in Lymphoma (Combination therapy, Second-line therapy or greater) in North America, Europe, Asia (PO)
- 18 May 2021Ninatinostat is still in phase I trials for Solid tumour in United Kingdom and Netherlands (Viracta Therapeutics pipeline, May 2021)
- 18 May 2021Virata Therapeutics has patent protection for dose regimen in NAVAL-1 trial in USA
Nanatinostat is under investigation in clinical trial NCT00697879 (Safety Study of the Histone Deacetylase Inhibitor, CHR-3996, in Patients With Advanced Solid Tumours).
Nanatinostat is an orally bioavailable, second-generation hydroxamic acid-based inhibitor of histone deacetylase (HDAC), with potential antineoplastic activity. Nanatinostat targets and inhibits HDAC, resulting in an accumulation of highly acetylated histones, the induction of chromatin remodeling, and the selective transcription of tumor suppressor genes; these events result in the inhibition of tumor cell division and the induction of tumor cell apoptosis. This agent may upregulate HSP70 and downregulate anti-apoptotic Bcl-2 proteins more substantially than some first-generation HDAC inhibitors. HDACs, upregulated in many tumor cell types, are a family of metalloenzymes responsible for the deacetylation of chromatin histone proteins.

Patent
WO2006123121
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2006123121
Example 44: N-Hvdroxy 2-(6-fr(6-fluoroαuinolin-2-yl)methvnamino)-3-azabicvclorS.I.OIhex-S-vDpyrimidine-δ-carboxamide
LCMS purity >98%, m/z 395 [M+H]+, 1H NMR (300 MHz, c/6-DMSO) δ: 2.30 (2H, s), 2.75 (1 H, s), 3.60 (2H, dm, J = 11.7 Hz), 3.88 (2H, d, J = 11.7 Hz), 4.69 (2H, br s), 7.66 (1 H, d, J = 8.4 Hz), 7.75 (1 H, td, J = 8.7, 3.0 Hz), 7.88 (1 H, dd, J = 9.3, 2.7 Hz), 8.48 (1 H, d, J = 8.4 Hz), 8.67 (2H, s), 9.01 (1 H, br s), 9.61 (1 H, br s), 11.09 (1 H, br s).
PATENT
WO-2021113694
Crystalline hydrate form A of N-hydroxy 2-{6-[(6-fluoro-quinolin-2-ylmethyl)-amino]-3-aza-bicyclo[3.1.0]hex-3-yl}pyrimidine-5-carboxamide ( nanatinostat ) .
Compound 1 is also known as nanatinostat, VRx-3996, or CHR-3996. It has been previously described in patents and patent applications, e.g. US patent 7,932,246 and US patent application 15/959,482, each of which is incorporated by reference in their entirety.
Compound 1
PATENT
WO2021071809 , claiming dosages for HDAC treatment with reduced side effects.
/////////Nanatinostat, CHR-3996, CHR 3996, VRx 3996, CHROMA, ORPHAN DRUG, Tractinostat, PHASE 2
| FC1=CC=C2N=C(CN[C@H]3[C@]4([H])CN(C5=NC=CC(C(NO)=O)=N5)C[C@]34[H])C=CC2=C1 |

NEW DRUG APPROVALS
ONE TIME
$10.00
Drospirenone
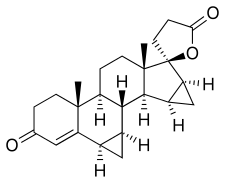
Drospirenone
FDA APPROVED 4/15/2021, To prevent pregnancy Nextstellis
New Drug Application (NDA): 214154
Company: MAYNE PHARMALabel (PDF)
Letter (PDF)
ReviewLabel (PDF)DrospirenoneCAS Registry Number: 67392-87-4
CAS Name: (2¢S,6R,7R,8R,9S,10R,13S,14S,15S,16S)-1,3¢,4¢,6,7,8,9,10,11,12,13,14,15,16,20,21-Hexadecahydro-10,13-dimethylspiro[17H-dicyclopropa[6,7:15,16]cyclopenta[a]phenanthrene-17,2¢(5¢H)-furan]-3,5¢(2H)-dione
Additional Names: 6b,7b,15b,16b-dimethylene-3-oxo-4-androstene-[17(b-1¢)-spiro-5¢]perhydrofuran-2¢-one; 6b,7b,15b,16b-dimethylen-3-oxo-17a-pregn-4-ene-21,17-carbolactone; dihydrospirorenone
Manufacturers’ Codes: ZK-30595
Molecular Formula: C24H30O3Molecular Weight: 366.49Percent Composition: C 78.65%, H 8.25%, O 13.10%
Literature References: Synthetic progestogen exhibiting antimineralocorticoid and antiandrogenic activity. Prepn: R. Wiechert et al.,DE2652761; eidem,US4129564 (both 1978 to Schering AG); D. Bittler et al.,Angew. Chem.94, 718 (1982). HPLC determn in human plasma: W. Krause, U. Jakobs, J. Chromatogr.230, 37 (1982). Pharmacological profile: P. Muhn et al.,Contraception51, 99 (1995). Review of synthesis: H. Laurent et al.,J. Steroid Biochem.19, 771-776 (1983); of pharmacology and clinical experience: W. Oelkers, Mol. Cell. Endocrinol.217, 255-261 (2004).
Properties: mp 201.3°. [a]D22 -182° (c = 0.5 in chloroform). uv (methanol): 265 nm (e 19000).
Melting point: mp 201.3°
Optical Rotation: [a]D22 -182° (c = 0.5 in chloroform)
Derivative Type: Mixture with ethinyl estradiolTrademarks: Angeliq (Schering AG); Yasmin (Schering AG)Literature References: Clinical trial as oral contraceptive: K. S. Parsey, A. Pong, Contraception61, 105 (2000); in treatment of menopausal symptoms: R. Schürmann et al., Climacteric7, 189 (2004).
Therap-Cat: Progestogen. In combination with estrogen as oral contaceptive and in treatment of menopausal symptoms.Keywords: Progestogen; Contraceptive (Oral).SYNhttps://www.sciencedirect.com/science/article/abs/pii/S0039128X15002135
Abstract
A general methodology for the synthesis of different steroidal 17-spirolactones is described. This method uses lithium acetylide of ethyl propiolate as the three carbon synthon and the method was successfully applied for the process development of drospirenone.
Graphical abstract

SYN
Steroid Hormones
Ruben Vardanyan, Victor Hruby, in Synthesis of Best-Seller Drugs, 2016
Drospirenone–Yaz
The synthesis of drospirenone (27.4.12) is believed to have been described for the first time in Wiechert et al [79], with a total yield of approximately 2 to 3% via the pathway presented in Scheme 27.4.

Each compound produced after each reaction step was purified by column chromatography.
Androsta-5,15-diene-3-ol-17-one was methylenated at the 15,16-position (27.4.13) and reacted with organometallic reagent (3,3-dimethoxypropyl)lithium prepared from 3-bromo-1,1-dimethoxypropane (27.4.14) and lithium in THF to produce the tertiary alcohol (27.4.15), which on short-term reflux with toluenesulfonic acid in acetone transformed to cyclic 21,17-hemiacetal (27.4.16). Oppenanuer oxidation with aluminium isopropoxide in excess of cyclohexanone in toluene was brought to mild oxidation of both secondary alcohol groups, and the simultaneous isomerization of the 5,6 double bond to the 4,5 position produced the compound (27.4.17). The last was oxidized with Jones reagent—chromic trioxide in diluted sulfuric acid—producing conjugated diene-one (27.4.18). Corey methylenation of the obtained product with dimethyloxosulfonium methylide in DMSO containing sodium hydride produced the final compound, the desired drospirenone (27.4.12).
The following patents and publications [80-83], which differ slightly from one another, disclose similar processes for preparing drospirenone and are presented in Scheme 27.5.

In Scheme 27.5, drospirenone (27.4.12) is prepared by converting the key starting compound (27.4.19) into the corresponding chloride (27.4.20) via reaction with triphenylphosphine and tetrachloromethane under mild conditions. Reductive dechlorination with Zn in acetic acid in THF tetrahydrofuran produced 5-hydroxy-15β,16β-methylene-3β-pivaloyloxy-5β-androst-6-en-17-one (27.4.21). The pivaloyl protecting group of the last was removed with the mixture of potassium hydroxide and sodium perchlorate in THF/methanol mixture to produce the diol (27.4.22). Simmons–Smith cyclopropanation reaction was applied to this compound. For that purpose, solution of (27.4.22) in dimethyl Cellosolve was stirred at 80°C with zinc-copper couple and methylene iodide, which produced the desired compound (27.4.23). The compound (27.4.23) underwent ethinylation with propargyl alcohol using potassium methylate in THF as a base to produce the 1,4-butindiol derivative (27.4.24). The triple bond of the 1,4-butindiol derivative (27.4.24) was hydrogenated in aTHF/methanol/pyridine mixture in the presence of palladium on carbon to produce the 1,4-butanediol derivative (27.4.25). The obtained compound underwent oxidation–lactonization at 50°C using a solution of CrO3 in water and pyridine to produce the desired drospirenone (27.4.12).
Several other synthetic routes for the production of drospirenone have been proposed [84-96], one of which [96] is presented in Scheme 27.6.

According to Scheme 27.6, a mixture of the key starting ketodiol (27.4.26), synthesis of which was described previously [84], with ethyl propiolate in THF was added to a solution of lithium hexamethyldisilylamide to produce, after quenching with acetic acid and saturated ammonium chloride solution, ethinyl alcohol (27.4.27). This product was hydrogenated on H2-Pd/C catalyst to produce ethyl 4-hydroxybutanoate (27.4.28). The 3-hydroxy group in the obtained product was oxidized to the keto group with (2,2,6,6-tetramethyl-piperidin-1-yl)oxyl, resulting in the compound (27.4.29). Treatment of the last with potassium hydroxide in a methanol–water mixture affects both hydrolysis of the ester group and dehydration of 5-hydroxy substituent. Acidification of the resulting intermediate results in drospirenone (27.4.12).
Drospirenone is a unique synthetic progestogen derived from 17α-spirolactone; it has a pharmacological profile very similar to that of endogenous progesterone. Drospirenone prevents ovulation and is used in contraceptive pills; it is also used as a postmenopausal hormone replacement. Drospirenone provides reliable and well-tolerated contraception and effective treatment of menopause. It has progestational, antialdosterone, and antiandrogenic properties, but is devoid of any estrogenic, androgenic, glucocorticoid, antiglucocorticoid, and mineralocorticoid activities. The affinity of drospirenone for the mineralocorticoid receptor makes it an antagonist of aldosterone, which is not only important in the renin–angiotensin–aldosterone system, but also means it acts directly on the cardiovascular system. It is progestin with antimineralocorticoid property that acts to suppress gonadotropins. It is thus able to prevent excessive sodium loss and regulate blood pressure. Drospirenone slightly decreases body weight and blood pressure and shares many pharmacodynamic properties with progesterone [97-110].
PATENT
https://patents.google.com/patent/US8334375B2/enDrospirenone is a synthetic steroid with progestin, anti-mineral corticoid and anti androgen activity. Drospirenone is currently being used as a synthetic progestin in oral contraceptive formulations. A regioselective synthesis for drospirenone has been described (see e.g., Angew. Chem. 94, 1982, 718) that uses the 17 keto derivative (1) as a key intermediate.

The synthesis of intermediate (1) and the transformation of intermediate (1) into drospirenone has been described in, for example, U.S. Published Patent Application Nos. 2009/0023914; 20080207575; 2008/0200668; 2008/0076915, 20070049747, and 20050192450; U.S. Pat. Nos. 6,933,395; 6,121,465, and 4,129,564, European Patent No. 0 075 189 and PCT Publication No. WO 2006/061309, all of which are incorporated herein by reference. Many of these routes introduce the required C3 side chain in the 17 position of intermediate (1). These conversions are usually carried out with carbanions, such as propargylalcohol, trimethylsulfoxonium iodide, or the use of the anion generated from a suitably protected derivative of 1-bromopropionaldehyde. After oxidation of the 3-hydroxy substituent to a 3-keto group, and the oxidative formation of the 17-spirolactone, the 3-keto-5-hydroxy-17-spirolactone is transformed via acid catalysis into drospireneone. If the oxidation is performed under acidic conditions at elevated temperatures, the oxidation and elimination can be run without isolation of the intermediate products.Most of these procedures rely on the acid-catalyzed elimination of the 5-hydroxy group in the last step of the synthesis. It has been documented that 15,16-methylene-17-spirolactones are prone to undergo rearrangement to generate the inverted 17-spirolactone under mild acidic conditions (see, for example, Tetrahedron Letters, Vol. 27, No 45, 5463-5466) in considerable amounts. This isomer has very similar physical chemical properties, and typically requires chromatographic separation or repeated fractional recrystallizations to purify the product. This isomerization can make these approaches less desirable from an economical point of view.FIG. 1Experimental Example

A solution of compound (1) (5 g; 15.2 mmol) and tert-butyldimethyl (2-propynyloxy)silane (2.83 g, 16.7 mmol) in 75 ml of dry THF was added dropwise through an addition funnel to a precooled slurry of potassium tert-butoxide (8.49 g, 75.7 mmol) at −10 C. A thick white precipitate is formed during the addition and the resulting mixture was stirred for an hour at 0 C. TLC analysis (70% EtOAc/Hexanes) showed completion of the reaction and showed a less polar product. The reaction was quenched by the addition of ice water (100 ml) and neutralized by adding acetic acid (4.3 ml). The THF layer was separated and the aqueous layer was extracted with EtOAc (2×50 ml). The combined organic layers were washed with water (2×100 ml), brine (100 ml) and dried over anhydrous sodium sulfate. The solvent was removed under vacuum to afford compound (2a) (7.5 g, 99.2%) as a solid which was used in the next step without any purification.NMR (CDCl3) δ 0.139 (s, 6H, S1—CH3), 0.385 (m, 1H), 0.628 (m, 1H), 0.857 (s, 18-Me), 0.896 (s, 19-Me), 0.918 (s, 3H, Si—CH3), 0.927 (s, 6H, Si—CH3), 4.05 (s, 1H), 4.428 (s, 2H, —O—CH2) FTIR (ATR): 3311, 3017, 2929, 2858, 2270, 1058 cm−1

Compound (2a) (5 g, 9.98 mmol) was dissolved in 100 ml of ethyl acetate in a Parr hydrogenation bottle and was mixed with 10% palladium on charcoal (1 g, 0.09 mmol). This mixture was hydrogenated on a Parr apparatus at a pressure of 20 psi for 90 minutes. The catalyst was filtered and washed with ethyl acetate. The solvent was removed in vacuo to afford compound (3a) as a colorless foam (5.01 g, 99%).NMR (CDCl3) δ 0.0758 (s, 6H, Si—CH3), 0.283 (m, 1H), 0.628 (m, 1H), 0.856 (s, 18-Me), 0.893 (s, 19-Me), 0.918 (s, 9H, Si—CH3), 3.69 (m, 2H), 4.05 (s, 1H). FTIR (ATR): 3374, 3017, 2929, 2858, 1259, 1091, 1049, 835 cm−1

Chromium trioxide (4.95 g, 49.5 mmol) was added to a solution of pyridine (7.83 g, 99.05 mmol) in anhydrous dichloromethane (100 ml). The resulting mixture was stirred for 15 minutes during which time the color changed to burgundy. A solution of compound (1a) (5 g, 9.90 mmol) in 50 ml of dichloromethane was added and the mixture was stirred at room temperature for 6 h. The excess oxidizing agent was quenched by adding isopropanol. The reaction mixture was diluted with MTBE (50 ml) and was passed through a short pad of Celite. The solid was washed again with 2:1 MTBE-CH2Cl2 (50 ml x2). The solvent was removed in vacuo to give a residue which was dissolved in 100 ml of EtOAc, was washed with water, and dried over anhydrous sodium sulfate. The solvent was removed in vacuo to afford compound (4a) as a pale yellow foam (4.5 g, 90.3%).NMR (CDCl3) δ 0.08 (s, 6H, Si—CH3), 0.31 (m, 1H), 0.914 (s, 9H, Si—CH3), 0.931 (s, 6H, 18-Me, 19-Me) 3.70 (m, 2H). FTIR (ATR): 3399, 3022, 2950, 2929, 2862, 1708, 1649, 1259, 1041 cm−1

A solution of compound (4a) (5 g, 9.94 mmol) in 50 ml of MeOH was refluxed with NaOH (397 mg, 9.94 mmol) for 3 h. When the reaction was over, as shown by TLC, the reaction mixture was cooled to room temperature and added to ice cold water (150 ml). The mixture was extracted with ethyl acetate (3×50 mL). The combined EtOAc layers were washed with water (100 ml) brine (50 ml) and dried over sodium sulfate. The solvent was removed in vacuo to afford compound (5) as a colorless amorphous solid (4.5 g, 92%).NMR (CDCl3) δ 0.05 (s, 6H, Si—CH3), 0.296 (m, 1H), 0.886 (s, 9H, Si—CH3), 0.908 (s, 3H, 18-Me), 1.07 (s, 3H, 19-Me), 3.68 (m, 2-H), 5.95 (s, 1H). FTIR (ATR): 3450, 3009, 2950, 2858, 1653, 1603, 1095 cm−1

A solution of compound (5a) (5 g, 9.94 mmol) in 30 ml of acetone was cooled to −15 C as a 2.7M solution of Jones reagent (3.68 ml, 9.94 mmol) was added drop wise. The reaction mixture was stirred at 0 C for 2 h, during this time TLC showed completion of the reaction. The reaction was quenched by adding isopropanol and diluted with water. The reaction mixture was extracted with EtOAc. The combined EtOAc layers were washed with water, sat. NaHCO3 and brine. The EtOAc layers were dried over sodium sulfate and solvent was removed by vacuum to afford crude drospirenone as a pale yellow foam (3 g, 82%) Recrystallization from acetone-hexane gave 1.5 g of pure drospirenone as white solid.NMR (CDCl3) δ 0.0548 (m, 1H), 0.88 (m, 1H), 1.008 (s, 3H, 18-Me), 1.11 (s, 3H, 18-Me), 6.03 (s, 1H). FTIR (ATR): 3025, 2971, 2942, 1763, 1654, 1590, 1186 cm−1FIG. 2Experimental Example

Lithium hexamethyldisilylamide (LiHMDS) 1.0 M/THF (75.7 mL, 75.7 mmol) was introduced into a 500 mL, 3-neck flask equipped with an addition funnel and a pierced septa for the introduction of a thermocouple probe. The mixture was diluted with THF (25 mL). The solution was stirred (Teflon paddle) and chilled to an internal temperature of −72° C. A THF (75 mL) solution of ketodiol (5 g, 15.13 mmol) containing ethyl propiolate (3.07 mL, 30.26 mmol) was added dropwise over 1 hour while not allowing the temperature to rise above −65° C. Upon completion of the addition the mixture was stirred for 3 hrs while allowing the temperature to warm slowly to −60° C. Finally, the mixture was warned to −40° C. over 1 hour.The mixture was quenched through the addition of acetic acid (4.25 mL)/water (5.0 mL) followed by the addition of saturated ammonium chloride solution (100 mL). The mixture was stirred for 3 min and then transferred to a separatory funnel. The layers were separated and the upper, THF layer was diluted with ethyl acetate (75 mL). The organic phase was washed with water (3×100 mL) and brine (1×100 mL). All the aqueous washes were extracted with ethyl acetate (2×30 mL). The combined organic extract was dried over sodium sulfate, filtered, and evaporated in vacuo (45° C.) to afford a thick oil. Dichloromethane (ca. 35 mL) was added and evaporated in vacuo. The flask was cooled slightly and dichloromethane (33 ml) was added to give a solid mass. The solid was broken up and stirred until a homogeneous slurry was obtained. Hexanes (35 mL) was added slowly to the stirred mixture and the mixture was stored at 2-4 C overnight. The solid was filtered, washed with 30% dichloromethane/hexanes, and dried in vacuo at ambient temperature for 4 hours to give (2b) 5.86 g (90.4%) of a white powder.
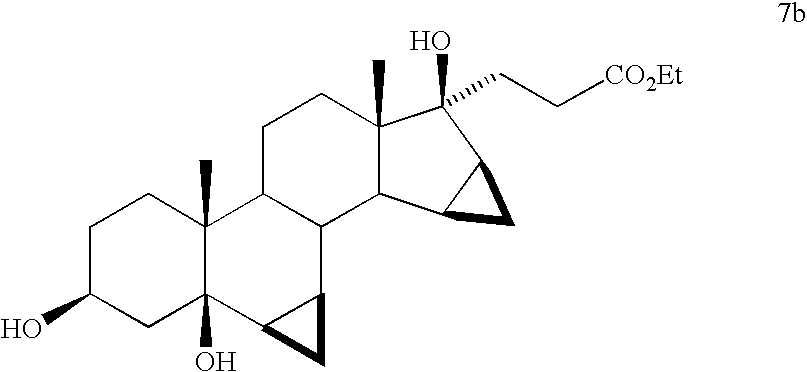
Compound (2b) (5.0 g, 11.67 mmol) was dissolved in THF (50 mL) and 5% Pd/C (622 mg, 0.29 mmol Pd) was added and the mixture was shaken at 15 psi H2 for 2 hours. The mixture was diluted with ethyl acetate (25 mL) and filtered through a pad of Celite. The filter pad was washed with ethyl acetate (3×25 mL) and the filtrate was evaporated to dryness to afford 5.0 g (99.1%) of triol (7b) as a stable foam.

Compound (7a) (5.0 g, 11.56 mmol) was dissolved in dichloromethane (50 mL) and the solution was stirred vigorously and chilled to −15° C. (NaCl/ice) and TEMPO (45.16 mg, 0.29 mmol, 2.5 mol %) was added. The mixture was treated dropwise over about 15-20 min. with a mixture of sodium hypochlorite (12.5%) (11.17 mL, 23.12 mmol) in water (8.0 mL) containing potassium bicarbonate (833 mg, 8.32 mmol). The mixture was allowed to warm to 0 C for 1.25 hrs. Analysis of the reaction by TLC (60% EtOAc/hex) shows the appearance of a slightly less polar product (ΔRf=0.8 cm). The mixture was chilled to −5 C and was quenched through the dropwise addition (ca 10-15 min) of a water (15.0 mL) solution of sodium phosphate (1.27 g, 7.75 mmol) and sodium metabisulfite (1.10 g, 5.78 mmol). The layers were separated and the dichloromethane solution was washed with water (2×) and brine. All aqueous washes were extracted with additional dichloromethane (2×15 mL). The combined dichloromethane extract was dried over sodium sulfate, filtered, and evaporated to give 4.88 g (98.08%) of ketone (8b) as a stable foam.

Compound (8b) was added to a methanol (10 mL) solution containing 8.0 M KOH solution (6.3 mL, 50.36 mmol) preheated to 60 C. The solution was heated at reflux for 2.5 hours. The mixture was chilled in an ice bath and treated with acetic acid (36 mL) and water (5.0 mL). The solution was stirred at 50-60 C for 15 hours. The volatiles were evaporated in vacuo and the acetic acid solution was poured into cold water (150 mL) to give a white precipitate. The aqueous mixture was extracted with ethyl acetate (2×100 mL). The ethyl acetate extracts were washed with water (2×), saturated sodium bicarbonate solution, and brine. The combined ethyl acetate extract was dried over sodium sulfate. Evaporation of the solvent gave a yellow foam. Trituration of the foam with acetone/hexane followed by evaporation gave 4.27 g (92.62%) of a light yellow solid. Recrystallization of the solid from acetone/hexanes gave 3.07 g of drospirenone with an HPLC purity of 99.66%. Evaporation of the mother liquor and recrystallization of the residue affords an additional 0.54 g of slightly impure drospirenone.FIG. 3Experimental Example

Lithium hexamethyldisilylamide (LiHMDS) 1.0 M/THF (75.7 mL, 75.7 mmol) was introduced into a 500 mL, 3-neck flask equipped with an addition funnel and a pierced septa for the introduction of a thermocouple probe. The mixture was diluted with THF (25 mL). The solution was stirred (Teflon paddle) and chilled to an internal temperature of −72° C. A THF (75 mL) solution of ketodiol (5 g, 15.13 mmol) containing ethyl propiolate (3.07 mL, 30.26 mmol) was added dropwise over 1 hour while not allowing the temperature to rise above −65° C. Upon completion of the addition the mixture was stirred for 3 hrs while allowing the temperature to warm slowly to −60° C. Finally, the mixture was warmed to −40° C. over 1 hour.The mixture was quenched through the addition of acetic acid (4.25 mL)/water (5.0 mL) followed by the addition of saturated ammonium chloride solution (100 mL). The mixture was stirred for 3 min and then transferred to a separatory funnel. The layers were separated and the upper, THF layer was diluted with ethyl acetate (75 mL). The organic phase was washed with water (3×100 mL) and brine (1×100 mL). All the aqueous washes were extracted with ethyl acetate (2×30 mL). The combined organic extract was dried over sodium sulfate, filtered, and evaporated in vacuo (45° C.) to afford a thick oil. Dichloromethane (ca. 35 mL) was added and evaporated in vacuo. The flask was cooled slightly and dichloromethane (33 ml) was added to give a solid mass. The solid was broken up and stirred until a homogeneous slurry was obtained. Hexanes (35 mL) was added slowly to the stirred mixture and the mixture was stored at 2-4 C overnight. The solid was filtered, washed with 30% dichloromethane/hexanes, and dried in vacuo at ambient temperature for 4 hours to give (2c) 5.86 g (90.4%) of a white powder.

Propiolate adduct (2c) (5.86 g, 13.67 mmol) was suspended in dichloromethane (60 mL). The mixture was stirred vigorously and chilled to −15° C. (NaCl/ice) and TEMPO (54 mg, 0.35 mmol, 2.5 mol %) was added. The mixture was treated dropwise over about 15-20 min. with a mixture of sodium hypochlorite (12.5%) (13.2 mL, 27.34 mmol) in water (8.0 mL) containing potassium bicarbonate (985 mg, 9.84 mmol). During the addition of the hypochlorite solution, a 5-8 C temperature rise was observed and the mixture became yellow. The mixture was allowed to warm to at 0 C for 2 hrs. Analysis of the reaction by TLC (60% EtOAc/hex) shows the appearance of a slightly less polar product (ΔRf=0.8 cm). The mixture was chilled to −5 C and was quenched through the dropwise addition (ca 10-15 min) of a water (150 mL) solution of sodium phosphate (1.50 g, 9.16 mmol) and sodium metabisulfite (1.30 g, 6.84 mmol). Once again, a temperature rise of 5-8 C was observed and the yellow color was quenched. The layers were separated and the dichloromethane solution was washed with water (2×) and brine. All aqueous washes were extracted with additional dichloromethane (2×15 mL). The combined dichloromethane extract was dried over sodium sulfate and the bulk of the solvent was evaporated in vacuo. Upon the observation of solids in the mixture during the evaporation, the evaporation was discontinued and the residue in the flask diluted with MTBE (35 mL). While stirring, the mixture was slowly diluted with hexanes (35 mL). The mixture was then chilled in an ice bath for 30 min. The solid was filtered, washed with 25% MTBE/hexane, and dried to give intermediate (9c) (4.98 g, 85.31%) as a white solid.NMR (CDCl3) δ 0.462 (q, 1H), 0.699 (m, 1H), 0.924 (s, 18-Me), 0.952 (s, 19-Me), 1.338 (t, J=7 Hz, OCH2CH 3), 2.517 (d, 1H), 3.021 (d, 1H), 4.269 (t, OCH 2CH3) ppm. FTIR (ATR): 3493, 3252, 2948, 2226, 1697, 1241 cm−1.
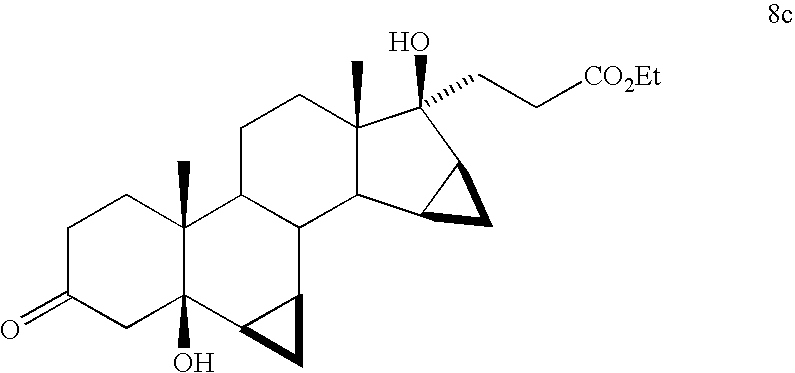
Alkynyl ketone (9c) (5.37 g, 12.59 mmol) was dissolved in THF (27 mL) in a 250 mL shaker bottle. 5% Pd/C (670 mg, 2.5 mol %) was added to the solution and the mixture was shaken under a hydrogen pressure of 15 psi. Over approximately 30 min, there was observed a rapid up take of hydrogen. The pressure was continually adjusted to 15 psi until the uptake of hydrogen ceased and was shaken for a total of 1.5 hrs. The mixture was diluted with a small amount of methanol and filtered through Celite. The filter pad was washed with methanol (ca. 3×25 mL).NMR (CDCl3) δ 0.353 (q, 1H), 0.704 (m, 2H), 0.930 (s, 18-Me), 0.933 (s, 19-Me), 1.279 (t, J=7 Hz, OCH2CH 3), 2.480 (d, 1H), 2.672 (m, 2H), 3.981 (d, 1H), 4.162 (t, OCH 2CH3) ppm. FTIR (ATR): 3465, 2946, 1712, cm−1.

The filtrate containing compound (8c) described above, was added in one portion to a methanol (10 mL) solution containing 8.0 M KOH solution (6.3 mL, 50.36 mmol) preheated to 60 C. The solution was heated at reflux for 2.5 hours. The mixture was chilled in an ice bath and treated with acetic acid (36 mL) and water (5.0 mL). The solution was stirred at 50-60 C for 15 hours. The volatiles were evaporated in vacuo and the acetic acid solution was poured into cold water (150 mL) to give a white precipitate. The aqueous mixture was extracted with ethyl acetate (2×100 mL). The ethyl acetate extracts were washed with water (2×), saturated sodium bicarbonate solution, and brine. The combined ethyl acetate extract was dried over sodium sulfate. Evaporation of the solvent gave a yellow foam. Trituration of the foam with acetone/hexane followed by evaporation gave 4.27 g (92.62%) of a light yellow solid. Recrystallization of the solid from acetone/hexanes gave 3.07 g of drospirenone with an HPLC purity of 99.66%. Evaporation of the mother liquor and recrystallization of the residue affords an additional 0.54 g of slightly impure drospirenone.FIG. 4Experimental Example

Lithium hexamethyldisilylamide (LiHMDS) 1.0 M/THF (75.7 mL, 75.7 mmol) was introduced into a 500 mL, 3-neck flask equipped with an addition funnel and a pierced septa for the introduction of a theiniocouple probe. The mixture was diluted with THF (25 mL). The solution was stirred (Teflon paddle) and chilled to an internal temperature of −72° C. A THF (75 mL) solution of ketodiol (5 g, 15.13 mmol) containing ethyl propiolate (3.07 mL, 30.26 mmol) was added dropwise over 1 hour while not allowing the temperature to rise above −65° C. Upon completion of the addition the mixture was stirred for 3 hrs while allowing the temperature to warm slowly to −60° C. Finally, the mixture was warmed to −40° C. over 1 hour.The mixture was quenched through the addition of acetic acid (4.25 mL)/water (5.0 mL) followed by the addition of saturated ammonium chloride solution (100 mL). The mixture was stirred for 3 min and then transferred to a separatory funnel. The layers were separated and the upper, THF layer was diluted with ethyl acetate (75 mL). The organic phase was washed with water (3×100 mL) and brine (1×100 mL). All the aqueous washes were extracted with ethyl acetate (2×30 mL). The combined organic extract was dried over sodium sulfate, filtered, and evaporated in vacuo (45° C.) to afford a thick oil. Dichloromethane (ca. 35 mL) was added and evaporated in vacuo. The flask was cooled slightly and dichloromethane (33 ml) was added to give a solid mass. The solid was broken up and stirred until a homogeneous slurry was obtained. Hexanes (35 mL) was added slowly to the stirred mixture and the mixture was stored at 2-4 C overnight. The solid was filtered, washed with 30% dichloromethane/hexanes, and dried in vacuo at ambient temperature for 4 hours to give (2d) 5.86 g (90.4%) of a white powder.

Propiolate adduct (2d) (5.86 g, 13.67 mmol) was suspended in dichloromethane (60 mL). The mixture was stirred vigorously and chilled to −15° C. (NaCl/ice) and TEMPO (54 mg, 0.35 mmol, 2.5 mol %) was added. The mixture was treated dropwise over about 15-20 min. with a mixture of sodium hypochlorite (12.5%) (13.2 mL, 27.34 mmol) in water (8.0 mL) containing potassium bicarbonate (985 mg, 9.84 mmol). During the addition of the hypochlorite solution, a 5-8 C temperature rise was observed and the mixture became yellow. The mixture was allowed to warm to at 0 C for 2 hrs. Analysis of the reaction by TLC (60% EtOAc/hex) shows the appearance of a slightly less polar product (ΔRf=0.8 cm). The mixture was chilled to −5 C and was quenched through the dropwise addition (ca 10-15 min) of a water (15.0 mL) solution of sodium phosphate (1.50 g, 9.16 mmol) and sodium metabisulfite (1.30 g, 6.84 mmol). Once again, a temperature rise of 5-8 C was observed and the yellow color was quenched. The layers were separated and the dichloromethane solution was washed with water (2×) and brine. All aqueous washes were extracted with additional dichloromethane (2×15 mL). The combined dichloromethane extract was dried over sodium sulfate and the bulk of the solvent was evaporated in vacuo. Upon the observation of solids in the mixture during the evaporation, the evaporation was discontinued and the residue in the flask diluted with MTBE (35 mL). While stirring, the mixture was slowly diluted with hexanes (35 mL). The mixture was then chilled in an ice bath for 30 min. The solid was filtered, washed with 25% MTBE/hexane, and dried to give intermediate (9d) (4.98 g, 85.31%) as a white solid.NMR (CDCl3) δ 0.462 (q, 1H), 0.699 (m, 1H), 0.924 (s, 18-Me), 0.952 (s, 19-Me), 1.338 (t, J=7 Hz, OCH2CH 3), 2.517 (d, 1H), 3.021 (d, 1H), 4.269 (t, OCH 2CH3) ppm. FTIR (ATR): 3493, 3252, 2948, 2226, 1697, 1241 cm−1.

Compound (9d) (5.0 g) was dissolved in methanol (50 mL) and treated with 1.0 N sulfuric acid (10 mL). The mixture was heated to reflux for 3 hours, cooled, and neutralized through the addition of saturated sodium bicarbonate solution. Most of the methanol was evaporated in vacuo at ambient temperature and diluted with water. The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water and brine, dried over sodium sulfate, filtered, and evaporated to give 4.95 g of unsaturated ketone (10d) as a stable foam.

Compound (10d) (5.0 g, 12.24 mmol) was dissolved in degassed benzene (50 mL) and treated with chlorotris(triphenylphosphine)rhodium (I) (283.1 mg, 0.31 mmol and the resulting mixture was stirred in a hydrogen atmosphere for 10 hours. The solution was evaporated, reconstituted in 50% ethyl acetate/hexanes, and passed through a short column of neutral alumina. Evaporation of the solvent gave 4.95 g of (11d) as a stable foam.

Compound (11d) (4.95 g, 12.01 mmol) was dissolved in 10% aqueous methanol (50 mL) and solid potassium carbonate (4.98 g, 36.04 mmol) was added. The mixture was stirred at room temperature for 30 min and the bicarbonate was neutralized through the addition of acetic acid (2.06 mL, 36.04 mmol). The methanol was evaporated in vacuo at ambient temperature and diluted with water. The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water and brine, dried over sodium sulfate, filtered, and evaporated to give 4.10 g (93%) of a semi solid. The material was dissolved in dichloromethane and evaporated in vacuo to give a stable foam. The foam was dissolved in ethyl acetate (5 mL) and allowed to stand overnight. The resulting solid was filtered, washed with cold ethyl acetate, and dried in vacuo to afford 2.86 g (66%) of pure drospirenone.FIG. 5Experimental Example 1

A dichloromethane (50 mL) solution of ketodiol (1) (5.0 g, 15.13 mmol) was treated with ethyl vinyl ether (7.24 mL, 75.65 mmol), followed by the addition of pyridinium tosylate (380 mg, 1.15 mmol). The solution was stirred at room temperature for 30 min. The dichloromethane solution was washed with water (2×), brine, and dried over sodium sulfate. Following filtration, evaporation of the solvent gave 6.14 g of the 3-protected compound (1e) as a stable foam.
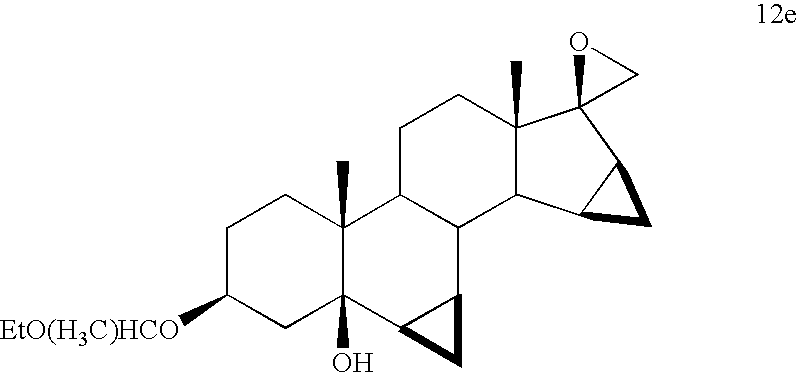
Compound (1e) (6.14 g, 15.13 mmol) was dissolved in DMSO/THF (15 mL/15 mL), treated with trimethylsulfonium iodide (4.63 g, 22.70 mmol) and the mixture was chilled to −15 C. The mixture was treated portion wise with potassium t-butoxide (3.23 g, 28.82 mmol). The mixture was stirred at −15 C for 45 min and then poured into ice/water (200 mL). The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (2×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 6.21 g (98.42%) of oxirane (12e) as a stable foam.

A THF (30 mL) solution of di-isopropyl amine (12.02 mL, 85.03 mmol) was chilled to −40 C and treated with butyl lithium (2.5 M/hexanes, 34.01 mL, 85.03 mmol) and the mixture was stirred for 15 min. A THF (5 mL) solution of acetonitrile (4.7 mL, 90.79 mmol) was added dropwise to the in situ generated lithium di-isopropylamide (LDA) solution to give a slurry of the acetonitrile anion. After stirring for 15 min at −40° C., compound (12e) (6.21 g, 14.91 mmol) as a THF (25 mL) solution was added dropwise over 10 min. The mixture was stirred for 30 min and then quenched through the addition of saturated ammonium chloride solution (210 mL). The mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (3×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 7.07 g of the addition product (13e) as a tacky foam.

Compound 13e (5.0 g, 10.93 mmol) was dissolved in acetone (25 mL) and chilled to 0 C. The stirred solution was treated dropwise with 2.7M chromic acid (Jones Reagent) (7.0 mL, 18.91 mmol). After 1.5 hrs, the excess Cr (VI) was quenched through the addition of 2-propanol until the green color of Cr (IV) was evident. Water (300 mL) was added and the mixture was stirred until all the chromium salts were dissolved. The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (2×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 3.83 g (96%) of ketone (14e) as a stable foam.

Compound (14e) (3.83 g, 10.48 mmol) was dissolved in methanol (38 mL) and treated with 8.0 M KOH solution (7.0 mL, 56 mmol) and the mixture was heated at reflux for 5 hours. The mixture was cooled to 0 C and treated with acetic acid (15 mL) and water (6 mL) and the mixture was stirred at 50 C for 6 hours. The solvents were evaporated in vacuo and the residue was diluted with water (200 mL). The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (2×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 3.76 g (94%) of crude drospirenone as a stable foam. The crude drospirenone was dissolved in 60% ethyl acetate/hexanes and passed through a short column of neutral alumina (10× w/w) and the column was eluted with the same solvent. Following evaporation of the solvent, 2.58 g (65%) of crystalline drospirenone was obtained. Recrystallization from acetone/hexanes afforded pure drospirenone.FIG. 5Experimental Example 2

Intermediate (1) (5 g, 15.13 mmol) was dissolved in DMSO/THF (50 mL/50 mL), treated with trimethylsulfonium iodide (4.63 g, 22.70 mmol), and the mixture was chilled to −15 C. The mixture was treated portion wise with potassium t-butoxide (5.03 g, 43.88 mmol). The mixture was stirred at −15 C for 45 min and then poured into ice/water (200 mL). The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (2×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 5.11 g (98%) of oxirane (12f) as a stable foam.

A THF (30 mL) solution of di-isopropyl amine (12.02 mL, 85.03 mmol) was chilled to −40 C and treated with butyl lithium (2.5 M/hexanes, 34.01 mL, 85.03 mmol) and the mixture was stirred for 15 min. A THF (5 mL) solution of acetonitrile (4.7 mL, 90.79 mmol) was added dropwise to the above lithium di-isopropylamide (LDA) solution to give a slurry of the acetonitrile anion. After stirring for 15 min at −40 C, compound (12f) (5.11 g, 14.83 mmol) as a THF (75 mL) solution was added dropwise over 10 min. The mixture was stirred for 30 min and then quenched through the addition of saturated ammonium chloride solution (300 mL). The mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (3×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 5.75 g of addition product (13f) as a tacky foam.

Compound 13f (5.75 g, 14.95 mmol) was dissolved in acetone (25 mL) and chilled to 0 C. The stirred solution was treated dropwise with 2.7M chromic acid (Jones Reagent) until the orange color of Cr (VI) persisted. After 1.5 hrs, the excess Cr (VI) was quenched through the addition of 2-propanol until the green color of Cr (IV) was evident. Water (300 mL) was added and the mixture was stirred until all the chromium salts were dissolved. The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (2×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 5.5 g (96%) of ketone (14f) as a stable foam.
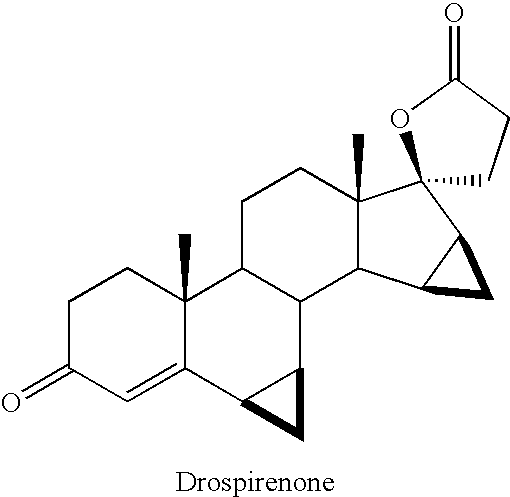
Compound (14f) (5.5 g, 14.38 mmol) was dissolved in methanol (50 mL) and treated with 8.0 M KOH solution (9.35 mL, 74.77 mmol) and the mixture was heated at reflux for 5 hours. The mixture was cooled to 0 C and treated with acetic acid (25 mL) and water (10 mL) and the mixture was stirred at 50 C for 6 hours. The solvents were evaporated in vacuo and the residue was diluted with water (300 mL). The aqueous mixture was extracted with ethyl acetate. The ethyl acetate extract was washed with water (2×) and brine, dried over sodium sulfate, and filtered. Evaporation of the solvent gave 4.95 g (94%) of crude drospirenone as a stable foam. The crude drospirenone was dissolved in 60% ethyl acetate/hexanes and passed through a short column of neutral alumina (10× w/w) and the column was eluted with the same solvent. Following evaporation of the solvent, 3.43 g (65%) of crystalline drospirenone was obtained. Recrystallization from acetone/hexanes afforded pure drospirenone.
Drospirenone is a progestin medication which is used in birth control pills to prevent pregnancy and in menopausal hormone therapy, among other uses.[1][7] It is available both alone under the brand name Slynd and in combination with an estrogen under the brand name Yasmin among others.[7][2] The medication is taken by mouth.[2][1]
Common side effects include acne, headache, breast tenderness, weight increase, and menstrual changes.[2] Rare side effects may include high potassium levels and blood clots, among others.[2][8] Drospirenone is a progestin, or a synthetic progestogen, and hence is an agonist of the progesterone receptor, the biological target of progestogens like progesterone.[1] It has additional antimineralocorticoid and antiandrogenic activity and no other important hormonal activity.[1] Because of its antimineralocorticoid activity and lack of undesirable off-target activity, drospirenone is said to more closely resemble bioidentical progesterone than other progestins.[9][10]
Drospirenone was patented in 1976 and introduced for medical use in 2000.[11][12] It is available widely throughout the world.[7] The medication is sometimes referred to as a “fourth-generation” progestin.[13][14] It is available as a generic medication.[15] In 2018, a formulation of drospirenone with ethinylestradiol was the 167th most commonly prescribed medication in the United States, with more than 3 million prescriptions.[16][17]
Medical uses
Drospirenone (DRSP) is used by itself as a progestogen-only birth control pill, in combination with the estrogens ethinylestradiol (EE) or estetrol (E4), with or without supplemental folic acid (vitamin B9), as a combined birth control pill, and in combination with the estrogen estradiol (E2) for use in menopausal hormone therapy.[2] A birth control pill with low-dose ethinylestradiol is also indicated for the treatment of moderate acne, premenstrual syndrome (PMS), premenstrual dysphoric disorder (PMDD), and dysmenorrhea (painful menstruation).[18][19] For use in menopausal hormone therapy, E2/DRSP is specifically approved to treat moderate to severe vasomotor symptoms (hot flashes), vaginal atrophy, and postmenopausal osteoporosis.[20][21][22] The drospirenone component in this formulation is included specifically to prevent estrogen-induced endometrial hyperplasia.[23] Drospirenone has also been used in combination with an estrogen as a component of hormone therapy for transgender women.[24][25]
Studies have found that EE/DRSP is superior to placebo in reducing premenstrual emotional and physical symptoms while also improving quality of life.[26][27] E2/DRSP has been found to increase bone mineral density and to reduce the occurrence of bone fractures in postmenopausal women.[28][23][29][30] In addition, E2/DRSP has a favorable influence on cholesterol and triglyceride levels and decreases blood pressure in women with high blood pressure.[29][30] Due to its antimineralocorticoid activity, drospirenone opposes estrogen-induced salt and water retention and maintains or slightly reduces body weight.[31]
Available forms
Drospirenone is available in the following formulations, brand names, and indications:[32][33]
- Drospirenone 4 mg (Slynd) – progestogen-only birth control pill[2]
- Drospirenone 3 mg and estetrol 14.2 mg (Nextstellis (US)) – combined birth control pill[34][35][36]
- Ethinylestradiol 30 μg and drospirenone 3 mg (Ocella, Syeda, Yasmin, Zarah, Zumandimine) – combined birth control pill[37][38][39][40]
- Ethinylestradiol 20 μg and drospirenone 3 mg (Gianvi, Jasmiel, Loryna, Lo-Zumandimine, Nikki, Vestura, Yaz) – combined birth control pill, acne, PMS, PMDD, dysmenorrhea[18]
- Ethinylestradiol 30 μg, drospirenone 3 mg, and levomefolate calcium 0.451 mg (Beyaz, Tydemy) – combined birth control pill with vitamin B9 supplementation, acne, PMS[41][42]
- Estetrol 15 mg and drospirenone 3 mg (Nextstellis (CA)) – combined birth control pill[43][44]
- Estradiol 0.5 or 1 mg and drospirenone 0.25 or 0.5 mg (Angeliq) – menopausal hormone therapy (menopausal syndrome, postmenopausal osteoporosis)[20]
Contraindications
Contraindications of drospirenone include renal impairment or chronic kidney disease, adrenal insufficiency, presence or history of cervical cancer or other progestogen-sensitive cancers, benign or malignant liver tumors or hepatic impairment, undiagnosed abnormal uterine bleeding, and hyperkalemia (high potassium levels).[2][45][46] Renal impairment, hepatic impairment, and adrenal insufficiency are contraindicated because they increase exposure to drospirenone and/or increase the risk of hyperkalemia with drospirenone.[2]
Side effects
Adverse effects of drospirenone alone occurring in more than 1% of women may include unscheduled menstrual bleeding (breakthrough or intracyclic) (40.3–64.4%), acne (3.8%), metrorrhagia (2.8%), headache (2.7%), breast pain (2.2%), weight gain (1.9%), dysmenorrhea (1.9%), nausea (1.8%), vaginal hemorrhage (1.7%), decreased libido (1.3%), breast tenderness (1.2%), and irregular menstruation (1.2%).[2]
High potassium levels
Drospirenone is an antimineralocorticoid with potassium-sparing properties, though in most cases no increase of potassium levels is to be expected.[45] In women with mild or moderate chronic kidney disease, or in combination with chronic daily use of other potassium-sparing medications (ACE inhibitors, angiotensin II receptor antagonists, potassium-sparing diuretics, heparin, antimineralocorticoids, or nonsteroidal anti-inflammatory drugs), a potassium level should be checked after two weeks of use to test for hyperkalemia.[45][47] Persistent hyperkalemia that required discontinuation occurred in 2 out of around 1,000 women (0.2%) with 4 mg/day drospirenone alone in clinical trials.[2]
Blood clots
Birth control pills containing ethinylestradiol and a progestin are associated with an increased risk of venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE).[48] The incidence is about 4-fold higher on average than in women not taking a birth control pill.[48] The absolute risk of VTE with ethinylestradiol-containing birth control pills is small, in the area of 3 to 10 out of 10,000 women per year, relative to 1 to 5 out of 10,000 women per year not taking a birth control pill.[49][50] The risk of VTE during pregnancy is 5 to 20 in 10,000 women per year and during the postpartum period is 40 to 65 per 10,000 women per year.[50] The higher risk of VTE with combined birth control pills is thought to be due to the ethinylestradiol component, as ethinylestradiol has estrogenic effects on liver synthesis of coagulation factors which result in a procoagulatory state.[8] In contrast to ethinylestradiol-containing birth control pills, neither progestogen-only birth control nor the combination of transdermal estradiol and an oral progestin in menopausal hormone therapy is associated with an increased risk of VTE.[8][51]
Different progestins in ethinylestradiol-containing birth control pills have been associated with different risks of VTE.[8] Birth control pills containing progestins such as desogestrel, gestodene, drospirenone, and cyproterone acetate have been found to have 2- to 3-fold the risk of VTE of birth control pills containing levonorgestrel in retrospective cohort and nested case–control observational studies.[8][49] However, this area of research is controversial, and confounding factors may have been present in these studies.[8][49][52] Other observational studies, specifically prospective cohort and case control studies, have found no differences in risk between different progestins, including between birth control pills containing drospirenone and birth control pills containing levonorgestrel.[8][49][52][53] These kinds of observational studies have certain advantages over the aforementioned types of studies, like better ability to control for confounding factors.[53] Systematic reviews and meta-analyses of all of the data in the mid-to-late 2010s found that birth control pills containing cyproterone acetate, desogestrel, drospirenone, or gestodene overall were associated with a risk of VTE of about 1.3- to 2.0-fold compared to that of levonorgestrel-containing birth control pills.[54][55][49]
Androgenic progestins have been found to antagonize to some degree the effects of ethinylestradiol on coagulation.[56][57][58][59] As a result, more androgenic progestins, like levonorgestrel and norethisterone, may oppose the procoagulatory effects of ethinylestradiol and result in a lower increase in risk of VTE.[8][60] Conversely, this would be the case less or not at all with progestins that are less androgenic, like desogestrel and gestodene, as well as progestins that are antiandrogenic, like drospirenone and cyproterone acetate.[8][60]
In the early 2010s, the FDA updated the label for birth control pills containing drospirenone and other progestins to include warnings for stopping use prior to and after surgery, and to warn that such birth control pills may have a higher risk of blood clots.[46]
Breast cancer
Drospirenone has been found to stimulate the proliferation and migration of breast cancer cells in preclinical research, similarly to certain other progestins.[61][62] However, some evidence suggests that drospirenone may do this more weakly than certain other progestins, like medroxyprogesterone acetate.[61][62] The combination of estradiol and drospirenone has been found to increase breast density, an established risk factor for breast cancer, in postmenopausal women.[63][64][65]
Data on risk of breast cancer in women with newer progestins like drospirenone are lacking at present.[66] Progestogen-only birth control is not generally associated with a higher risk of breast cancer.[66] Conversely, combined birth control and menopausal hormone therapy with an estrogen and a progestogen are associated with higher risks of breast cancer.[67][66][68]
Overdose
These have been no reports of serious adverse effects with overdose of drospirenone.[2] Symptoms that may occur in the event of an overdose may include nausea, vomiting, and vaginal bleeding.[2] There is no antidote for overdose of drospirenone and treatment of overdose should be based on symptoms.[2] Since drospirenone has antimineralocorticoid activity, levels of potassium and sodium should be measured and signs of metabolic acidosis should be monitored.[2]
Interactions
Inhibitors and inducers of the cytochrome P450 enzyme CYP3A4 may influence the levels and efficacy of drospirenone.[2] Treatment for 10 days with 200 mg twice daily ketoconazole, a strong CYP3A4 inhibitor among other actions, has been found to result in a moderate 2.0- to 2.7-fold increase in exposure to drospirenone.[2] Drospirenone does not appear to influence the metabolism of omeprazole (metabolized via CYP2C19), simvastatin (metabolized via CYP3A4), or midazolam (metabolized via CYP3A4), and likely does not influence the metabolism of other medications that are metabolized via these pathways.[2] Drospirenone may interact with potassium-sparing medications such as ACE inhibitors, angiotensin II receptor antagonists, potassium-sparing diuretics, potassium supplements, heparin, antimineralocorticoids, and nonsteroidal anti-inflammatory drugs to further increase potassium levels.[2] This may increase the risk of hyperkalemia (high potassium levels).[2]
Pharmacology
Pharmacodynamics
Drospirenone binds with high affinity to the progesterone receptor (PR) and mineralocorticoid receptor (MR), with lower affinity to the androgen receptor (AR), and with very low affinity to the glucocorticoid receptor (GR).[1][69][70][4] It is an agonist of the PR and an antagonist of the MR and AR, and hence is a progestogen, antimineralocorticoid, and antiandrogen.[1][69][4][62] Drospirenone has no estrogenic activity and no appreciable glucocorticoid or antiglucocorticoid activity.[1][69][4][62]
Progestogenic activity
Drospirenone is an agonist of the PR, the biological target of progestogens like progesterone.[1][69] It has about 35% of the affinity of promegestone for the PR and about 19 to 70% of the affinity of progesterone for the PR.[1][3][62] Drospirenone has antigonadotropic and functional antiestrogenic effects as a result of PR activation.[1][69] The ovulation-inhibiting dosage of drospirenone is 2 to 3 mg/day.[72][73][1][74] Inhibition of ovulation occurred in about 90% of women at a dose of 0.5 to 2 mg/day and in 100% of women at a dose of 3 mg/day.[75] The total endometrial transformation dose of drospirenone is about 50 mg per cycle, whereas its daily dose is 2 mg for partial transformation and 4 to 6 mg for full transformation.[1][76][75] The medication acts as a contraceptive by activating the PR, which suppresses the secretion of luteinizing hormone, inhibits ovulation, and alters the cervical membrane and endometrium.[77][2]
Due to its antigonadotropic effects, drospirenone inhibits the secretion of the gonadotropins, luteinizing hormone (LH) and follicle-stimulating hormone (FSH), and suppresses gonadal sex hormone production, including of estradiol, progesterone, and testosterone.[1][78][3] Drospirenone alone at 4 mg/day has been found to suppress estradiol levels in premenopausal women to about 40 to 80 pg/mL depending on the time of the cycle.[78] No studies of the antigonadotropic effects of drospirenone or its influence on hormone levels appear to have been conducted in men.[79][80][81] In male cynomolgus monkeys however, 4 mg/kg/day oral drospirenone strongly suppressed testosterone levels.[69]
Antimineralocorticoid activity
Drospirenone is an antagonist of the MR, the biological target of mineralocorticoids like aldosterone, and hence is an antimineralocorticoid.[69] It has about 100 to 500% of the affinity of aldosterone for the MR and about 50 to 230% of the affinity of progesterone for the MR.[1][3][71][62] Drospirenone is about 5.5 to 11 times more potent as an antimineralocorticoid than spironolactone in animals.[69][75][82] Accordingly, 3 to 4 mg drospirenone is said to be equivalent to about 20 to 25 mg spironolactone in terms of antimineralocorticoid activity.[83][2] It has been said that the pharmacological profile of drospirenone more closely resembles that of progesterone than other progestins due to its antimineralocorticoid activity.[69] Drospirenone is the only clinically used progestogen with prominent antimineralocorticoid activity besides progesterone.[1] For comparison to progesterone, a 200 mg dose of oral progesterone is considered to be approximately equivalent in antimineralocorticoid effect to a 25 to 50 mg dose of spironolactone.[84] Both drospirenone and progesterone are actually weak partial agonists of the MR in the absence of mineralocorticoids.[4][3][62]
Due to its antimineralocorticoid activity, drospirenone increases natriuresis, decreases water retention and blood pressure, and produces compensatory increases in plasma renin activity as well as circulating levels and urinary excretion of aldosterone.[3][85][1] This has been shown to occur at doses of 2 to 4 mg/day.[3] Similar effects occur during the luteal phase of the menstrual cycle due to increased progesterone levels and the resulting antagonism of the MR.[3] Estrogens, particularly ethinylestradiol, activate liver production of angiotensinogen and increase levels of angiotensinogen and angiotensin II, thereby activating the renin–angiotensin–aldosterone system.[3][1] As a result, they can produce undesirable side effects including increased sodium excretion, water retention, weight gain, and increased blood pressure.[3] Progesterone and drospirenone counteract these undesirable effects via their antimineralocorticoid activity.[3] Accumulating research indicates that antimineralocorticoids like drospirenone and spironolactone may also have positive effects on adipose tissue and metabolic health.[86][87]
Antiandrogenic activity
Drospirenone is an antagonist of the AR, the biological target of androgens like testosterone and dihydrotestosterone (DHT).[1][3] It has about 1 to 65% of the affinity of the synthetic anabolic steroid metribolone for the AR.[1][3][4][62] The medication is more potent as an antiandrogen than spironolactone, but is less potent than cyproterone acetate, with about 30% of its antiandrogenic activity in animals.[1][88][69][75] Progesterone displays antiandrogenic activity in some assays similarly to drospirenone,[3] although this issue is controversial and many researchers regard progesterone as having no significant antiandrogenic activity.[89][1][4]
Drospirenone shows antiandrogenic effects on the serum lipid profile, including higher HDL cholesterol and triglyceride levels and lower LDL cholesterol levels, at a dose of 3 mg/day in women.[3] The medication does not inhibit the effects of ethinylestradiol on sex hormone-binding globulin (SHBG) and serum lipids, in contrast to androgenic progestins like levonorgestrel but similarly to other antiandrogenic progestins like cyproterone acetate.[3][1][74] SHBG levels are significantly higher with ethinylestradiol and cyproterone acetate than with ethinylestradiol and drospirenone, owing to the more potent antiandrogenic activity of cyproterone acetate relative to drospirenone.[90] Androgenic progestins like levonorgestrel have been found to inhibit the procoagulatory effects of estrogens like ethinylestradiol on hepatic synthesis of coagulation factors, whereas this may occur less or not at all with weakly androgenic progestins like desogestrel and antiandrogenic progestins like drospirenone.[8][60][56][57][58][59]
Other activity
Drospirenone stimulates the proliferation of MCF-7 breast cancer cells in vitro, an action that is independent of the classical PRs and is instead mediated via the progesterone receptor membrane component-1 (PGRMC1).[91] Certain other progestins act similarly in this assay, whereas progesterone acts neutrally.[91] It is unclear if these findings may explain the different risks of breast cancer observed with progesterone and progestins in clinical studies.[66]
Pharmacokinetics
Absorption
The oral bioavailability of drospirenone is between 66 and 85%.[1][3][4] Peak levels occur 1 to 6 hours after an oral dose.[1][3][2][82] Levels are about 27 ng/mL after a single 4 mg dose.[2] There is 1.5- to 2-fold accumulation in drospirenone levels with continuous administration, with steady-state levels of drospirenone achieved after 7 to 10 days of administration.[1][2][3] Peak levels of drospirenone at steady state with 4 mg/day drospirenone are about 41 ng/mL.[2] With the combination of 30 μg/day ethinylestradiol and 3 mg/day drospirenone, peak levels of drospirenone after a single dose are 35 ng/mL, and levels at steady state are 60 to 87 ng/mL at peak and 20 to 25 ng/mL at trough.[3][1] The pharmacokinetics of oral drospirenone are linear with a single dose across a dose range of 1 to 10 mg.[2][3] Intake of drospirenone with food does not influence the absorption of drospirenone.[2]
Distribution
The distribution half-life of drospirenone is about 1.6 to 2 hours.[3][1] The apparent volume of distribution of drospirenone is approximately 4 L/kg.[2] The plasma protein binding of drospirenone is 95 to 97%.[2][1] It is bound to albumin and 3 to 5% circulates freely or unbound.[2][1] Drospirenone has no affinity for sex hormone-binding globulin (SHBG) or corticosteroid-binding globulin (CBG), and hence is not bound by these plasma proteins in the circulation.[1]
Metabolism
The metabolism of drospirenone is extensive.[3] It is metabolized into the acid form of drospirenone by opening of its lactone ring.[1][2] The medication is also metabolized by reduction of its double bond between the C4 and C5 positions and subsequent sulfation.[1][2] The two major metabolites of drospirenone are drospirenone acid and 4,5-dihydrodrospirenone 3-sulfate, and are both formed independently of the cytochrome P450 system.[2][3] Neither of these metabolites are known to be pharmacologically active.[2] Drospirenone also undergoes oxidative metabolism by CYP3A4.[2][3][5][6]
Elimination
Drospirenone is excreted in urine and feces, with slightly more excreted in feces than in urine.[2] Only trace amounts of unchanged drospirenone can be found in urine and feces.[2] At least 20 different metabolites can be identified in urine and feces.[3] Drospirenone and its metabolites are excreted in urine about 38% as glucuronide conjugates, 47% as sulfate conjugates, and less than 10% in unconjugated form.[3] In feces, excretion is about 17% glucuronide conjugates, 20% sulfate conjugates, and 33% unconjugated.[3]
The elimination half-life of drospirenone is between 25 and 33 hours.[2][3][1] The half-life of drospirenone is unchanged with repeated administration.[2] Elimination of drospirenone is virtually complete 10 days after the last dose.[3][2]
Chemistry
See also: Spirolactone, List of progestogens § Spirolactone derivatives, and List of steroidal antiandrogens § Spirolactone derivatives
vteChemical structures of spirolactones ProgesteroneSpirolactoneCanrenoneSpironolactoneDrospirenoneSpirorenone ProgesteroneSpirolactoneCanrenoneSpironolactoneDrospirenoneSpirorenone |
Drospirenone, also known as 1,2-dihydrospirorenone or as 17β-hydroxy-6β,7β:15β,16β-dimethylene-3-oxo-17α-pregn-4-ene-21-carboxylic acid, γ-lactone, is a synthetic steroidal 17α-spirolactone, or more simply a spirolactone.[7][92] It is an analogue of other spirolactones like spironolactone, canrenone, and spirorenone.[7][92] Drospirenone differs structurally from spironolactone only in that the C7α acetylthio substitution of spironolactone has been removed and two methylene groups have been substituted in at the C6β–7β and C15β–16β positions.[93]
Spirolactones like drospirenone and spironolactone are derivatives of progesterone, which likewise has progestogenic and antimineralocorticoid activity.[94][95][96] The loss of the C7α acetylthio group of spironolactone, a compound with negligible progestogenic activity,[97][98] appears to be involved in the restoration of progestogenic activity in drospirenone, as SC-5233, the analogue of spironolactone without a C7α substitution, has potent progestogenic activity similarly to drospirenone.[99]
History
Drospirenone was patented in 1976 and introduced for medical use in 2000.[11][12] Schering AG of Germany has been granted several patents on the production of drospirenone, including WIPO and US patents, granted in 1998 and 2000, respectively.[100][101] It was introduced for medical use in combination with ethinylestradiol as a combined birth control pill in 2000.[11] Drospirenone is sometimes described as a “fourth-generation” progestin based on its time of introduction.[13][14] The medication was approved for use in menopausal hormone therapy in combination with estradiol in 2005.[20] Drospirenone was introduced for use as a progestogen-only birth control pill in 2019.[2] A combined birth control pill containing estetrol and drospirenone was approved in 2021.[102]
Society and culture
Generic names
Drospirenone is the generic name of the drug and its INN, USAN, BAN, and JAN, while drospirénone is its DCF.[7] Its name is a shortened form of the name 1,2-dihydrospirorenone or dihydrospirenone.[7][92] Drospirenone is also known by its developmental code names SH-470 and ZK-30595 (alone), BAY 86-5300, BAY 98-7071, and SH-T-00186D (in combination with ethinylestradiol), BAY 86-4891 (in combination with estradiol), and FSN-013 (in combination with estetrol).[7][92][103][104][105][106][102]
Brand names
Drospirenone is marketed in combination with an estrogen under a variety of brand names throughout the world.[7] Among others, it is marketed in combination with ethinylestradiol under the brand names Yasmin and Yaz, in combination with estetrol under the brand name Nextstellis, and in combination with estradiol under the brand name Angeliq.[7][102]
Availability
See also: List of progestogens available in the United States
Drospirenone is marketed widely throughout the world.[7]
Generation
Drospirenone has been categorized as a “fourth-generation” progestin.[62]
Litigation
Many lawsuits have been filed against Bayer, the manufacturer of drospirenone, due to the higher risk of venous thromboembolism (VTE) that has been observed with combined birth control pills containing drospirenone and certain other progestins relative to the risk with levonorgestrel-containing combined birth control pills.[52]
In July 2012, Bayer notified its stockholders that there were more than 12,000 such lawsuits against the company involving Yaz, Yasmin, and other birth control pills with drospirenone.[107] They also noted that the company by then had settled 1,977 cases for US$402.6 million, for an average of US$212,000 per case, while setting aside US$610.5 million to settle the others.[107]
As of July 17, 2015, there have been at least 4,000 lawsuits and claims still pending regarding VTE related to drospirenone.[108] This is in addition to around 10,000 claims that Bayer has already settled without admitting liability.[108] These claims of VTE have amounted to US$1.97 billion.[108] Bayer also reached a settlement for arterial thromboembolic events, including stroke and heart attacks, for US$56.9 million.[108]
Research
See also: Estetrol/drospirenone and Ethinylestradiol/drospirenone/prasterone
A combination of ethinylestradiol, drospirenone, and prasterone is under development by Pantarhei Bioscience as a combined birth control pill for prevention of pregnancy in women.[109] It includes prasterone (dehydroepiandrosterone; DHEA), an oral androgen prohormone, to replace testosterone and avoid testosterone deficiency caused by suppression of testosterone by ethinylestradiol and drospirenone.[109] As of August 2018, the formulation is in phase II/III clinical trials.[109]
Drospirenone has been suggested for potential use as a progestin in male hormonal contraception.[79]
Drospirenone has been studied in forms for parenteral administration.[110][111][112][113]
References
- ^ Jump up to:a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai ajak al Kuhl, H (2005). “Pharmacology of estrogens and progestogens: influence of different routes of administration”. Climacteric. 8 (sup1): 3–63. doi:10.1080/13697130500148875. ISSN 1369-7137. PMID 16112947. S2CID 24616324.
- ^ Jump up to:a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai ajak al am an ao ap aq ar as at au “Slynd- drospirenone tablet, film coated”. DailyMed. Retrieved 17 April 2021.
- ^ Jump up to:a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ahKrattenmacher, Rolf (2000). “Drospirenone: pharmacology and pharmacokinetics of a unique progestogen”. Contraception. 62 (1): 29–38. doi:10.1016/S0010-7824(00)00133-5. ISSN 0010-7824. PMID 11024226.
- ^ Jump up to:a b c d e f g h i Stanczyk FZ, Hapgood JP, Winer S, Mishell DR (April 2013). “Progestogens used in postmenopausal hormone therapy: differences in their pharmacological properties, intracellular actions, and clinical effects”. Endocr. Rev. 34 (2): 171–208. doi:10.1210/er.2012-1008. PMC 3610676. PMID 23238854.
- ^ Jump up to:a b Bachmann, Gloria (2009). “Drospirenone/ethinyl estradiol 3 mg/20 μg (24/4 day regimen): hormonal contraceptive choices – use of a fourth-generation progestin”. Patient Preference and Adherence. 3: 259–64. doi:10.2147/PPA.S3901. ISSN 1177-889X. PMC 2778416. PMID 19936169.
- ^ Jump up to:a b Wiesinger, Herbert; Berse, Matthias; Klein, Stefan; Gschwend, Simone; Höchel, Joachim; Zollmann, Frank S.; Schütt, Barbara (2015). “Pharmacokinetic interaction between the CYP3A4 inhibitor ketoconazole and the hormone drospirenone in combination with ethinylestradiol or estradiol”. British Journal of Clinical Pharmacology. 80 (6): 1399–1410. doi:10.1111/bcp.12745. ISSN 0306-5251. PMC 4693482. PMID 26271371.
- ^ Jump up to:a b c d e f g h i j k “Drospirenone”.
- ^ Jump up to:a b c d e f g h i j Han L, Jensen JT (December 2015). “Does the Progestogen Used in Combined Hormonal Contraception Affect Venous Thrombosis Risk?”. Obstet. Gynecol. Clin. North Am. 42(4): 683–98. doi:10.1016/j.ogc.2015.07.007. PMID 26598309.
- ^ Oelkers W (December 2000). “Drospirenone–a new progestogen with antimineralocorticoid activity, resembling natural progesterone”. Eur J Contracept Reprod Health Care. 5 Suppl 3: 17–24. PMID 11246598.
- ^ Oelkers W (December 2002). “Antimineralocorticoid activity of a novel oral contraceptive containing drospirenone, a unique progestogen resembling natural progesterone”. Eur J Contracept Reprod Health Care. 7 Suppl 3: 19–26, discussion 42–3. PMID 12659403.
- ^ Jump up to:a b c Enrique Ravina (11 January 2011). The Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs. John Wiley & Sons. pp. 193–. ISBN 978-3-527-32669-3.
- ^ Jump up to:a b Fischer, Jnos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 459. ISBN 9783527607495.
- ^ Jump up to:a b Robert Anthony Hatcher; Anita L. Nelson, M.D. (2007). Contraceptive Technology. Ardent Media. pp. 196–. ISBN 978-1-59708-001-9.
- ^ Jump up to:a b James Q. Del Rosso; Joshua A. Zeichner (20 April 2016). Advances in Acne Management, An Issue of Dermatologic Clinics, E-Book. Elsevier Health Sciences. pp. 160–. ISBN 978-0-323-41753-2.
- ^ “Generic Yasmin Availability”.
- ^ “The Top 300 of 2021”. ClinCalc. Retrieved 18 February 2021.
- ^ “Drospirenone; Ethinyl Estradiol – Drug Usage Statistics”. ClinCalc. Retrieved 18 February 2021.
- ^ Jump up to:a b “Yaz- drospirenone and ethinyl estradiol kit”. DailyMed. Retrieved 17 April 2021.
- ^ Cerner Multum, Inc. (June 11, 2012). “drospirenone and ethinyl estradiol”. Auckland, New Zealand: Drugs.com. Retrieved October 24, 2011.
- ^ Jump up to:a b c “Angeliq- drospirenone and estradiol tablet, film coated”. DailyMed. Retrieved 17 April 2021.
- ^ Maclennan, A. H.; Broadbent, J. L.; Lester, S.; Moore, V. (18 October 2004). “Oral oestrogen and combined oestrogen/progestogen therapy versus placebo for hot flushes”. The Cochrane Database of Systematic Reviews (4): CD002978. doi:10.1002/14651858.CD002978.pub2. ISSN 1469-493X. PMC 7004247. PMID 15495039.
- ^ Torgerson, D. J.; Bell-Syer, S. E. (13 June 2001). “Hormone replacement therapy and prevention of nonvertebral fractures: a meta-analysis of randomized trials”. JAMA. 285 (22): 2891–2897. doi:10.1001/jama.285.22.2891. ISSN 0098-7484. PMID 11401611. S2CID 25078579.
- ^ Jump up to:a b Whitehead M (March 2006). “Hormone replacement therapy with estradiol and drospirenone: an overview of the clinical data”. J Br Menopause Soc. 12 Suppl 1: 4–7. doi:10.1258/136218006775992185. PMID 16513012. S2CID 38095916.
- ^ Majumder A, Sanyal D (2017). “Outcome and preferences in male-to-female subjects with gender dysphoria: Experience from Eastern India”. Indian J Endocrinol Metab. 21 (1): 21–25. doi:10.4103/2230-8210.196000. PMC 5240066. PMID 28217493.
- ^ Majumder, Anirban; Chatterjee, Sudip; Maji, Debasis; Roychaudhuri, Soumyabrata; Ghosh, Sujoy; Selvan, Chitra; George, Belinda; Kalra, Pramila; Maisnam, Indira; Sanyal, Debmalya (2020). “IDEA group consensus statement on medical management of adult gender incongruent individuals seeking gender reaffirmation as female”. Indian Journal of Endocrinology and Metabolism. 24 (2): 128–135. doi:10.4103/ijem.IJEM_593_19. ISSN 2230-8210. PMC 7333765. PMID 32699777.
- ^ Lanza di Scalea, Teresa (June 2017). “Premenstrual Dysphoric Disorder”. Psychiatric Clinics of North America. 40 (2): 201–206. doi:10.1016/j.psc.2017.01.002. PMID 28477648.
- ^ Lopez LM, Kaptein AA, Helmerhorst FM (February 2012). “Oral contraceptives containing drospirenone for premenstrual syndrome”. Cochrane Database Syst Rev (2): CD006586. doi:10.1002/14651858.CD006586.pub4. PMID 22336820.
- ^ Christiansen C (October 2005). “Effects of drospirenone/estrogen combinations on bone metabolism”. Climacteric. 8 Suppl 3: 35–41. doi:10.1080/13697130500330283. PMID 16203654. S2CID 42803561.
- ^ Jump up to:a b Archer DF (February 2007). “Drospirenone and estradiol: a new option for the postmenopausal woman”. Climacteric. 10 Suppl 1: 3–10. doi:10.1080/13697130601114859. PMID 17364592. S2CID 9221524.
- ^ Jump up to:a b “Drospirenone in HRT?”. Drug Ther Bull. 47 (4): 41–4. April 2009. doi:10.1136/dtb.2009.03.0011. PMID 19357298. S2CID 1909717.
- ^ Foidart JM, Faustmann T (December 2007). “Advances in hormone replacement therapy: weight benefits of drospirenone, a 17alpha-spirolactone-derived progestogen”. Gynecol. Endocrinol. 23 (12): 692–9. doi:10.1080/09513590701582323. PMID 18075844. S2CID 12572825.
- ^ “Drugs@FDA: FDA Approved Drug Products”. United States Food and Drug Administration. Retrieved 23 December 2019.
- ^ Research, Center for Drug Evaluation and. “Drug Safety and Availability – FDA Drug Safety Communication: Updated information about the risk of blood clots in women taking birth control pills containing drospirenone”. http://www.fda.gov. Retrieved 2017-11-07.
- ^https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/214154s000lbl.pdf
- ^https://www.maynepharma.com/media/2507/mayne_pharma_drsp-e4_news_release_041421.pdf
- ^ https://www.maynepharma.com/media/2506/fda-approval-of-novel-oral-contraceptive-nextstellis.pdf
- ^ “Ocella- drospirenone and ethinyl estradiol kit”. DailyMed. Retrieved 17 April 2021.
- ^ “Syeda- drospirenone and ethinyl estradiol kit”. DailyMed. Retrieved 17 April 2021.
- ^ “Yasmin- drospirenone and ethinyl estradiol kit”. DailyMed. Retrieved 17 April 2021.
- ^ “Zarah- drospirenone and ethinyl estradiol kit”. DailyMed. Retrieved 17 April 2021.
- ^ “Beyaz- drospirenone/ethinyl estradiol/levomefolate calcium and levomefolate calcium kit”. DailyMed. Retrieved 17 April 2021.
- ^ “Tydemy- drospirenone, ethinyl estradiol and levomefolate calcium and levomefolate calcium kit”. DailyMed. Retrieved 17 April 2021.
- ^https://web.archive.org/web/20210413054728/https://pdf.hres.ca/dpd_pm/00060352.PDF
- ^ “Mithra and Searchlight Pharma Announce Nextstellis Approval in Canada”. Searchlight Pharma (Press release). 8 March 2021. Retrieved 17 April 2021.
- ^ Jump up to:a b c Bayer (March 25, 2013). “Summary of Product Characteristics (SPC): Yasmin”. London: electronic Medicines Compendium (eMC), Datapharm. Retrieved April 24, 2014.
4.3. Contraindications: • Severe chronic kidney disease or acute kidney failure. • Presence or history of severe hepatic disease as long as liver function values have not returned to normal.
- ^ Jump up to:a b Bayer (April 10, 2012). “Yasmin full prescribing information”(PDF). Silver Spring, Md.: Food and Drug Administration (FDA). Retrieved April 14, 2012.
4. Contraindications: • Renal impairment. • Adrenal insufficiency. • Liver disease.
- ^ Nelson, Anita L.; Cwiak, Carrie (2011). “Combined oral contraceptives (COCs)”. In Hatcher, Robert A.; Trussell, James; Nelson, Anita L.; Cates, Willard Jr.; Kowal, Deborah; Policar, Michael S. (eds.). Contraceptive Technology (20th revised ed.). New York: Ardent Media. pp. 249–341. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734.
- ^ Jump up to:a b Heit JA, Spencer FA, White RH (2016). “The epidemiology of venous thromboembolism”. J. Thromb. Thrombolysis. 41 (1): 3–14. doi:10.1007/s11239-015-1311-6. PMC 4715842. PMID 26780736.
- ^ Jump up to:a b c d e Bateson D, Butcher BE, Donovan C, Farrell L, Kovacs G, Mezzini T, Raynes-Greenow C, Pecoraro G, Read C, Baber R (2016). “Risk of venous thromboembolism in women taking the combined oral contraceptive: A systematic review and meta-analysis”. Aust Fam Physician. 45 (1): 59–64. PMID 27051991.
- ^ Jump up to:a b “FDA Drug Safety Communication: Updated information about the risk of blood clots in women taking birth control pills containing drospirenone”. April 27, 2019. Archived from the original on 2019-04-27.
- ^ Vinogradova Y, Coupland C, Hippisley-Cox J (January 2019). “Use of hormone replacement therapy and risk of venous thromboembolism: nested case-control studies using the QResearch and CPRD databases”. BMJ. 364: k4810. doi:10.1136/bmj.k4810. PMC 6326068. PMID 30626577.
- ^ Jump up to:a b c Batur P, Casey PM (February 2017). “Drospirenone Litigation: Does the Punishment Fit the Crime?”. J Womens Health (Larchmt). 26 (2): 99–102. doi:10.1089/jwh.2016.6092. PMID 27854556.
- ^ Jump up to:a b Sitruk-Ware R (November 2016). “Hormonal contraception and thrombosis”. Fertil. Steril. 106 (6): 1289–1294. doi:10.1016/j.fertnstert.2016.08.039. PMID 27678035.
- ^ Oedingen C, Scholz S, Razum O (May 2018). “Systematic review and meta-analysis of the association of combined oral contraceptives on the risk of venous thromboembolism: The role of the progestogen type and estrogen dose”. Thromb. Res. 165: 68–78. doi:10.1016/j.thromres.2018.03.005. PMID 29573722.
- ^ Dragoman MV, Tepper NK, Fu R, Curtis KM, Chou R, Gaffield ME (June 2018). “A systematic review and meta-analysis of venous thrombosis risk among users of combined oral contraception”. Int J Gynaecol Obstet. 141 (3): 287–294. doi:10.1002/ijgo.12455. PMC 5969307. PMID 29388678.
- ^ Jump up to:a b Wiegratz I, Kuhl H (September 2006). “Metabolic and clinical effects of progestogens”. Eur J Contracept Reprod Health Care. 11(3): 153–61. doi:10.1080/13625180600772741. PMID 17056444. S2CID 27088428.
- ^ Jump up to:a b Kuhl H (May 1996). “Effects of progestogens on haemostasis”. Maturitas. 24 (1–2): 1–19. doi:10.1016/0378-5122(96)00994-2. PMID 8794429.
- ^ Jump up to:a b Sitruk-Ware R, Nath A (February 2013). “Characteristics and metabolic effects of estrogen and progestins contained in oral contraceptive pills”. Best Pract. Res. Clin. Endocrinol. Metab. 27 (1): 13–24. doi:10.1016/j.beem.2012.09.004. PMID 23384742.
- ^ Jump up to:a b Nelson AL (2015). “An update on new orally administered contraceptives for women”. Expert Opin Pharmacother. 16 (18): 2759–72. doi:10.1517/14656566.2015.1100173. PMID 26512437. S2CID 207481206.
- ^ Jump up to:a b c Farris M, Bastianelli C, Rosato E, Brosens I, Benagiano G (October 2017). “Pharmacodynamics of combined estrogen-progestin oral contraceptives: 2. effects on hemostasis”. Expert Rev Clin Pharmacol. 10 (10): 1129–1144. doi:10.1080/17512433.2017.1356718. PMID 28712325. S2CID 205931204.
- ^ Jump up to:a b Simoncini T, Genazzani AR (February 2010). “A review of the cardiovascular and breast actions of drospirenone in preclinical studies”. Climacteric. 13 (1): 22–33. doi:10.3109/13697130903437375. PMID 19938948. S2CID 4306359.
- ^ Jump up to:a b c d e f g h i j Africander D, Verhoog N, Hapgood JP (June 2011). “Molecular mechanisms of steroid receptor-mediated actions by synthetic progestins used in HRT and contraception”. Steroids. 76 (7): 636–52. doi:10.1016/j.steroids.2011.03.001. PMID 21414337. S2CID 23630452.
- ^ Palacios S, Mejía A (November 2016). “Progestogen safety and tolerance in hormonal replacement therapy”. Expert Opin Drug Saf. 15 (11): 1515–1525. doi:10.1080/14740338.2016.1223041. PMID 27548404. S2CID 31497860.
- ^ Caglayan EK, Caglayan K, Alkis I, Arslan E, Okur A, Banli O, Engin-Ustün Y (August 2015). “Factors Associated with Mammographic Density in Postmenopausal Women”. J Menopausal Med. 21 (2): 82–8. doi:10.6118/jmm.2015.21.2.82. PMC 4561745. PMID 26357645.
- ^ Hirschberg AL, Tani E, Brismar K, Lundström E (August 2019). “Effects of drospirenone and norethisterone acetate combined with estradiol on mammographic density and proliferation of breast epithelial cells-A prospective randomized trial”. Maturitas. 126: 18–24. doi:10.1016/j.maturitas.2019.04.205. PMID 31239112.
- ^ Jump up to:a b c d Trabert B, Sherman ME, Kannan N, Stanczyk FZ (September 2019). “Progesterone and breast cancer”. Endocr. Rev. 41 (2): 320–344. doi:10.1210/endrev/bnz001. PMC 7156851. PMID 31512725.
- ^ Collaborative Group on Hormonal Factors in Breast Cancer (September 2019). “Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence”. Lancet. 394 (10204): 1159–1168. doi:10.1016/S0140-6736(19)31709-X. PMC 6891893. PMID 31474332.
- ^ Sturdee DW (2013). “Are progestins really necessary as part of a combined HRT regimen?”. Climacteric. 16 Suppl 1: 79–84. doi:10.3109/13697137.2013.803311. PMID 23651281. S2CID 21894200.
- ^ Jump up to:a b c d e f g h i j Muhn P, Fuhrmann U, Fritzemeier KH, Krattenmacher R, Schillinger E (1995). “Drospirenone: a novel progestogen with antimineralocorticoid and antiandrogenic activity”. Ann. N. Y. Acad. Sci. 761 (3): 311–35. Bibcode:1995NYASA.761..311M. doi:10.1111/j.1749-6632.1995.tb31386.x. PMID 7625729. S2CID 36861309.
- ^ Fuhrmann, Ulrike; Krattenmacher, Rolf; Slater, Emily P.; Fritzemeier, Karl-Heinrich (1996). “The novel progestin drospirenone and its natural counterpart progesterone: Biochemical profile and antiandrogenic potential”. Contraception. 54 (4): 243–251. doi:10.1016/S0010-7824(96)00195-3. ISSN 0010-7824. PMID 8922878.
- ^ Jump up to:a b Hapgood JP, Africander D, Louw R, Ray RM, Rohwer JM (July 2014). “Potency of progestogens used in hormonal therapy: toward understanding differential actions”. J. Steroid Biochem. Mol. Biol. 142: 39–47. doi:10.1016/j.jsbmb.2013.08.001. PMID 23954501. S2CID 12142015.
- ^ Bastianelli C, Farris M, Rosato E, Brosens I, Benagiano G (November 2018). “Pharmacodynamics of combined estrogen-progestin oral contraceptives 3. Inhibition of ovulation”. Expert Rev Clin Pharmacol. 11 (11): 1085–1098. doi:10.1080/17512433.2018.1536544. PMID 30325245. S2CID 53246678.
- ^ Endrikat J, Gerlinger C, Richard S, Rosenbaum P, Düsterberg B (December 2011). “Ovulation inhibition doses of progestins: a systematic review of the available literature and of marketed preparations worldwide”. Contraception. 84 (6): 549–57. doi:10.1016/j.contraception.2011.04.009. PMID 22078182.
- ^ Jump up to:a b Kuhl H (2011). “Pharmacology of Progestogens” (PDF). J Reproduktionsmed Endokrinol. 8 (1): 157–177.
- ^ Jump up to:a b c d Elger W, Beier S, Pollow K, Garfield R, Shi SQ, Hillisch A (November 2003). “Conception and pharmacodynamic profile of drospirenone”. Steroids. 68 (10–13): 891–905. doi:10.1016/j.steroids.2003.08.008. PMID 14667981. S2CID 41756726.
- ^ Schindler AE, Campagnoli C, Druckmann R, Huber J, Pasqualini JR, Schweppe KW, Thijssen JH (December 2003). “Classification and pharmacology of progestins”. Maturitas. 46 Suppl 1: S7–S16. doi:10.1016/j.maturitas.2003.09.014. PMID 14670641.
- ^ “Drospirenone”. pubchem.ncbi.nlm.nih.gov.
- ^ Jump up to:a b Hadji P, Colli E, Regidor PA (December 2019). “Bone health in estrogen-free contraception”. Osteoporos Int. 30 (12): 2391–2400. doi:10.1007/s00198-019-05103-6. PMC 7203087. PMID 31446440.
- ^ Jump up to:a b Cornia, Paul B; Anawalt, Bradley D (2005). “Male hormonal contraceptives: a potentially patentable and profitable product”. Expert Opinion on Therapeutic Patents. 15 (12): 1727–1737. doi:10.1517/13543776.15.12.1727. ISSN 1354-3776. S2CID 83941717.
- ^ Nieschlag E (2010). “Clinical trials in male hormonal contraception” (PDF). Contraception. 82 (5): 457–70. doi:10.1016/j.contraception.2010.03.020. PMID 20933120.
- ^ Nieschlag, Eberhard; Behre, Hermann M.; Nieschlag, Eberhard; Behre, Hermann M.; Nieschlag, Susan (2012). “The essential role of testosterone in hormonal male contraception”. In Nieschlag, Eberhard; Behre, Hermann M; Nieschlag, Susan (eds.). Testosterone. pp. 470–493. doi:10.1017/CBO9781139003353.023. ISBN 9781139003353.
- ^ Jump up to:a b Stanczyk, Frank Z. (2007). “Structure –Function Relationships, Pharmacokinetics, and Potency of Orally and Parenterally Administered Progestogens”. Treatment of the Postmenopausal Woman. pp. 779–798. doi:10.1016/B978-012369443-0/50067-3. ISBN 9780123694430.
- ^ Hermann P.G. Schneider; Frederick Naftolin (22 September 2004). Climacteric Medicine – Where Do We Go?: Proceedings of the 4th Workshop of the International Menopause Society. CRC Press. pp. 133–. ISBN 978-0-203-02496-6.
- ^ Simon JA (December 1995). “Micronized progesterone: vaginal and oral uses”. Clinical Obstetrics and Gynecology. 38 (4): 902–14. doi:10.1097/00003081-199538040-00024. PMID 8616985.
- ^ Genazzani, Andrea R.; Mannella, Paolo; Simoncini, Tommaso (February 2007). “Drospirenone and its antialdosterone properties”. Climacteric. 10 (Supplement 1): 11–18. doi:10.1080/13697130601114891. PMID 17364593. S2CID 24872884. Retrieved November 26, 2011.
- ^ Infante, Marco; Armani, Andrea; Marzolla, Vincenzo; Fabbri, Andrea; Caprio, Massimiliano (2019). “Adipocyte Mineralocorticoid Receptor”. Vitamins and Hormones. Elsevier. 109: 189–209. doi:10.1016/bs.vh.2018.10.005. ISBN 9780128177822. ISSN 0083-6729. PMID 30678856.
- ^ Giordano A, Frontini A, Cinti S (June 2016). “Convertible visceral fat as a therapeutic target to curb obesity”. Nat Rev Drug Discov. 15(6): 405–24. doi:10.1038/nrd.2016.31. PMID 26965204. S2CID 2632187.
- ^ Sitruk-Ware R, Husmann F, Thijssen JH, Skouby SO, Fruzzetti F, Hanker J, Huber J, Druckmann R (September 2004). “Role of progestins with partial antiandrogenic effects”. Climacteric. 7 (3): 238–54. doi:10.1080/13697130400001307. PMID 15669548. S2CID 23112620.
- ^ Yeh YT, Chang CW, Wei RJ, Wang SN (2013). “Progesterone and related compounds in hepatocellular carcinoma: basic and clinical aspects”. Biomed Res Int. 2013: 290575. doi:10.1155/2013/290575. PMC 3581253. PMID 23484104.
- ^ Schindler, Adolf E. (2015). “Hormonal Contraceptives: Progestogen and Thrombotic Risk”. Frontiers in Gynecological Endocrinology. ISGE Series. pp. 69–75. doi:10.1007/978-3-319-09662-9_8. ISBN 978-3-319-09661-2. ISSN 2197-8735.
- ^ Jump up to:a b Neubauer H, Ma Q, Zhou J, Yu Q, Ruan X, Seeger H, Fehm T, Mueck AO (October 2013). “Possible role of PGRMC1 in breast cancer development”. Climacteric. 16 (5): 509–13. doi:10.3109/13697137.2013.800038. PMID 23758160. S2CID 29808177.
- ^ Jump up to:a b c d Martin Negwer; Hans-Georg Scharnow (4 October 2001). Organic-chemical drugs and their synonyms: (an international survey). Wiley-VCH. p. 2539. ISBN 978-3-527-30247-5.
- ^ Howard J.A. Carp (9 April 2015). Progestogens in Obstetrics and Gynecology. Springer. pp. 115–. ISBN 978-3-319-14385-9.
- ^ Ménard J (2004). “The 45-year story of the development of an anti-aldosterone more specific than spironolactone”. Mol. Cell. Endocrinol. 217 (1–2): 45–52. doi:10.1016/j.mce.2003.10.008. PMID 15134800. S2CID 19701784.
[Spironolactone] was synthesized after the demonstration of the natriuretic effect of progesterone (Landau et al., 1955).
- ^ J. Larry Jameson; Leslie J. De Groot (18 May 2010). Endocrinology – E-Book: Adult and Pediatric. Elsevier Health Sciences. pp. 2401–. ISBN 978-1-4557-1126-0.
[Spironolactone] is a potent antimineralocorticoid which was developed as a progestational analog […]
- ^ Aldosterone. Elsevier Science. 23 January 2019. p. 46. ISBN 978-0-12-817783-9.
In addition to spironolactone, which is a derivative of progesterone […]
- ^ Hu X, Li S, McMahon EG, Lala DS, Rudolph AE (2005). “Molecular mechanisms of mineralocorticoid receptor antagonism by eplerenone”. Mini Rev Med Chem. 5 (8): 709–18. doi:10.2174/1389557054553811. PMID 16101407.
- ^ Nakajima ST, Brumsted JR, Riddick DH, Gibson M (1989). “Absence of progestational activity of oral spironolactone”. Fertil. Steril. 52 (1): 155–8. doi:10.1016/s0015-0282(16)60807-5. PMID 2744183.
- ^ Hertz R, Tullner WW (1958). “Progestational activity of certain steroid-17-spirolactones”. Proc. Soc. Exp. Biol. Med. 99 (2): 451–2. doi:10.3181/00379727-99-24380. PMID 13601900. S2CID 20150966.
- ^ WO patent 9806738, Mohr, Jörg-Thorsten & Klaus Nickisch, “PROCESS FOR PRODUCING DROSPIRENONE (6ss,7ss;15ss,16ss-DIMETHYLENE-3-OXO-17 alpha -PREGN-4-EN-21,17-CARBOLACTONE, DRSP), AS WELL AS 7 alpha -(3-HYDROXY-1-PROPYL)-6ss,7ss;15ss,16ss-DIMETHYLENE-5ss-ANDROSTANE-3ss,5,17ss-TRIOL (ZK 92836) AND 6ss,7ss;15ss,16ss-DIMETHYLENE-5ss HYDROXY-5-OXO-17 alpha -ANDROSTANE-21, 17-CARBOLACTONE”, issued 1998-02-19, assigned to Shering AG
- ^ US patent 6121465, Mohr, Joerg-Thorston & Klaus Nickisch, “Process for production drospirenone and intermediate products of the process”, issued 2000-09-19, assigned to Scheiring AG and Bayer Schering Pharma
- ^ Jump up to:a b c “Drospirenone/Estetrol – Mithra Pharmaceuticals – AdisInsight”.
- ^ “Ethinylestradiol/drospirenone – AdisInsight”.
- ^ “Ethinylestradiol/drospirenone/folic acid – AdisInsight”.
- ^ “Drospirenone/ethinylestradiol low-dose – Bayer HealthCare Pharmaceuticals – AdisInsight”.
- ^ “Estradiol/drospirenone – Bayer HealthCare Pharmaceuticals – AdisInsight”.
- ^ Jump up to:a b Feeley, Jef; Kresge, Naomi (July 31, 2012). “Bayer’s Yasmin lawsuit settlements rise to $402.6 million”. Bloomberg News. New York. Retrieved November 11, 2012.
- ^ Jump up to:a b c d AG, Bayer. “Quarterly Reports of Bayer”. http://www.bayer.com.
- ^ Jump up to:a b c “Drospirenone/estradiol/prasterone – ANI Pharmaceuticals/Pantarhei Bioscience – AdisInsight”. adisinsight.springer.com.
- ^ Nippe S, General S (September 2011). “Parenteral oil-based drospirenone microcrystal suspensions-evaluation of physicochemical stability and influence of stabilising agents”. Int J Pharm. 416 (1): 181–8. doi:10.1016/j.ijpharm.2011.06.036. PMID 21729745.
- ^ Nippe S, General S (November 2012). “Combination of injectable ethinyl estradiol and drospirenone drug-delivery systems and characterization of their in vitro release”. Eur J Pharm Sci. 47 (4): 790–800. doi:10.1016/j.ejps.2012.08.009. PMID 22940138.
- ^ Nippe S, Preuße C, General S (February 2013). “Evaluation of the in vitro release and pharmacokinetics of parenteral injectable formulations for steroids”. Eur J Pharm Biopharm. 83 (2): 253–65. doi:10.1016/j.ejpb.2012.09.006. PMID 23116659.
- ^ Nippe S, General S (April 2015). “Investigation of injectable drospirenone organogels with regard to their rheology and comparison to non-stabilized oil-based drospirenone suspensions”. Drug Dev Ind Pharm. 41 (4): 681–91. doi:10.3109/03639045.2014.895375. PMID 24621345. S2CID 42932558.
Further reading
- Archer DF (February 2007). “Drospirenone and estradiol: a new option for the postmenopausal woman”. Climacteric. 10 Suppl 1: 3–10. doi:10.1080/13697130601114859. PMID 17364592. S2CID 9221524.
- Archer DF (February 2007). “Drospirenone-containing hormone therapy for postmenopausal women. Perspective on current data”. J Reprod Med. 52 (2 Suppl): 159–64. PMID 17477110.
- Archer DF (2007). “Drospirenone, a progestin with added value for hypertensive postmenopausal women”. Menopause. 14 (3 Pt 1): 352–4. doi:10.1097/gme.0b013e31804d440b. PMID 17414576.
- Batur P, Casey PM (February 2017). “Drospirenone Litigation: Does the Punishment Fit the Crime?”. J Womens Health (Larchmt). 26 (2): 99–102. doi:10.1089/jwh.2016.6092. PMID 27854556.
- Bitzer J, Paoletti AM (2009). “Added benefits and user satisfaction with a low-dose oral contraceptive containing drospirenone: results of three multicentre trials”. Clin Drug Investig. 29 (2): 73–8. doi:10.2165/0044011-200929020-00001. PMID 19133702. S2CID 10356578.
- Carranza-Lira S (2009). “Safety, efficacy and patient acceptability of drospirenone and estradiol in the treatment of menopausal vasomotor symptoms: a review”. Clin Interv Aging. 4: 59–62. doi:10.2147/CIA.S4117. PMC 2685225. PMID 19503766.
- Christiansen C (October 2005). “Effects of drospirenone/estrogen combinations on bone metabolism”. Climacteric. 8 Suppl 3: 35–41. doi:10.1080/13697130500330283. PMID 16203654. S2CID 42803561.
- Dickerson V (November 2002). “Quality of life issues. Potential role for an oral contraceptive containing ethinyl estradiol and drospirenone”. J Reprod Med. 47 (11 Suppl): 985–93. PMID 12497673.
- Fenton C, Wellington K, Moen MD, Robinson DM (2007). “Drospirenone/ethinylestradiol 3mg/20microg (24/4 day regimen): a review of its use in contraception, premenstrual dysphoric disorder and moderate acne vulgaris”. Drugs. 67 (12): 1749–65. doi:10.2165/00003495-200767120-00007. PMID 17683173. S2CID 46976925.
- Foidart JM (October 2005). “Added benefits of drospirenone for compliance”. Climacteric. 8 Suppl 3: 28–34. doi:10.1080/13697130500330309. PMID 16203653. S2CID 31883491.
- Foidart JM, Faustmann T (December 2007). “Advances in hormone replacement therapy: weight benefits of drospirenone, a 17alpha-spirolactone-derived progestogen”. Gynecol. Endocrinol. 23 (12): 692–9. doi:10.1080/09513590701582323. PMID 18075844. S2CID 12572825.
- Genazzani AR, Mannella P, Simoncini T (February 2007). “Drospirenone and its antialdosterone properties”. Climacteric. 10 Suppl 1: 11–8. doi:10.1080/13697130601114891. PMID 17364593. S2CID 24872884.
- Han L, Jensen JT (October 2014). “Expert opinion on a flexible extended regimen of drospirenone/ethinyl estradiol contraceptive”. Expert Opin Pharmacother. 15 (14): 2071–9. doi:10.1517/14656566.2014.949237. PMID 25186109. S2CID 25338932.
- Heinemann LA, Dinger J (2004). “Safety of a new oral contraceptive containing drospirenone”. Drug Saf. 27 (13): 1001–18. doi:10.2165/00002018-200427130-00003. PMID 15471507. S2CID 1773936.
- Idota N, Kobayashi M, Miyamori D, Kakiuchi Y, Ikegaya H (March 2015). “Drospirenone detected in postmortem blood of a young woman with pulmonary thromboembolism: A case report and review of the literature”. Leg Med (Tokyo). 17 (2): 109–15. doi:10.1016/j.legalmed.2014.10.001. PMID 25454533.
- Keam SJ, Wagstaff AJ (2003). “Ethinylestradiol/drospirenone: a review of its use as an oral contraceptive”. Treat Endocrinol. 2 (1): 49–70. doi:10.2165/00024677-200302010-00005. PMID 15871554. S2CID 209144694.
- Krattenmacher R (July 2000). “Drospirenone: pharmacology and pharmacokinetics of a unique progestogen”. Contraception. 62 (1): 29–38. doi:10.1016/S0010-7824(00)00133-5. PMID 11024226.
- Larivée N, Suissa S, Khosrow-Khavar F, Tagalakis V, Filion KB (September 2017). “Drospirenone-containing oral contraceptive pills and the risk of venous thromboembolism: a systematic review of observational studies”. BJOG. 124 (10): 1490–1499. doi:10.1111/1471-0528.14623. PMID 28276140.
- Lete I, Chabbert-Buffet N, Jamin C, Lello S, Lobo P, Nappi RE, Pintiaux A (2015). “Haemostatic and metabolic impact of estradiol pills and drospirenone-containing ethinylestradiol pills vs. levonorgestrel-containing ethinylestradiol pills: A literature review”. Eur J Contracept Reprod Health Care. 20 (5): 329–43. doi:10.3109/13625187.2015.1050091. PMID 26007631. S2CID 41601833.
- Li J, Ren J, Sun W (March 2017). “A comparative systematic review of Yasmin (drospirenone pill) versus standard treatment options for symptoms of polycystic ovary syndrome”. Eur. J. Obstet. Gynecol. Reprod. Biol. 210: 13–21. doi:10.1016/j.ejogrb.2016.11.013. PMID 27923166.
- Lopez LM, Kaptein AA, Helmerhorst FM (February 2012). “Oral contraceptives containing drospirenone for premenstrual syndrome”. Cochrane Database Syst Rev (2): CD006586. doi:10.1002/14651858.CD006586.pub4. PMID 22336820.
- Machado RB, Pompei Lde M, Giribela AG, Giribela CG (January 2011). “Drospirenone/ethinylestradiol: a review on efficacy and noncontraceptive benefits”. Womens Health (Lond). 7 (1): 19–30. doi:10.2217/whe.10.84. PMID 21175386.
- Mallareddy M, Hanes V, White WB (2007). “Drospirenone, a new progestogen, for postmenopausal women with hypertension”. Drugs Aging. 24 (6): 453–66. doi:10.2165/00002512-200724060-00002. PMID 17571911. S2CID 39236155.
- Motivala A, Pitt B (2007). “Drospirenone for oral contraception and hormone replacement therapy: are its cardiovascular risks and benefits the same as other progestogens?”. Drugs. 67 (5): 647–55. doi:10.2165/00003495-200767050-00001. PMID 17385938. S2CID 22985078.
- Oelkers W (December 2002). “Antimineralocorticoid activity of a novel oral contraceptive containing drospirenone, a unique progestogen resembling natural progesterone”. Eur J Contracept Reprod Health Care. 7 Suppl 3: 19–26, discussion 42–3. PMID 12659403.
- Oelkers W (December 2000). “Drospirenone–a new progestogen with antimineralocorticoid activity, resembling natural progesterone”. Eur J Contracept Reprod Health Care. 5 Suppl 3: 17–24. PMID 11246598.
- Oelkers W (March 2004). “Drospirenone, a progestogen with antimineralocorticoid properties: a short review”. Mol. Cell. Endocrinol. 217 (1–2): 255–61. doi:10.1016/j.mce.2003.10.030. PMID 15134826. S2CID 19936032.
- Oelkers W (February 2002). “The renin-aldosterone system and drospirenone”. Gynecol. Endocrinol. 16 (1): 83–7. doi:10.1080/gye.16.1.83.87. PMID 11915587. S2CID 32410408.
- Oelkers WH (October 2005). “Drospirenone in combination with estrogens: for contraception and hormone replacement therapy”. Climacteric. 8 Suppl 3: 19–27. doi:10.1080/13697130500330341. PMID 16203652. S2CID 42837148.
- Palacios S, Foidart JM, Genazzani AR (November 2006). “Advances in hormone replacement therapy with drospirenone, a unique progestogen with aldosterone receptor antagonism” (PDF). Maturitas. 55 (4): 297–307. doi:10.1016/j.maturitas.2006.07.009. hdl:2268/9932. PMID 16949774.
- Pérez-López FR (June 2008). “Clinical experiences with drospirenone: from reproductive to postmenopausal years”. Maturitas. 60 (2): 78–91. doi:10.1016/j.maturitas.2008.03.009. PMID 18468818.
- Rapkin AJ, Sorger SN, Winer SA (February 2008). “Drospirenone/ethinyl estradiol”. Drugs Today. 44 (2): 133–45. doi:10.1358/dot.2008.44.2.1191057. PMID 18389090. S2CID 32413831.
- Rapkin AJ, Winer SA (May 2007). “Drospirenone: a novel progestin”. Expert Opin Pharmacother. 8 (7): 989–99. doi:10.1517/14656566.8.7.989. PMID 17472544. S2CID 6954183.
- Rapkin RB, Creinin MD (October 2011). “The combined oral contraceptive pill containing drospirenone and ethinyl estradiol plus levomefolate calcium”. Expert Opin Pharmacother. 12 (15): 2403–10. doi:10.1517/14656566.2011.610791. PMID 21877996. S2CID 40231903.
- Rübig A (October 2003). “Drospirenone: a new cardiovascular-active progestin with antialdosterone and antiandrogenic properties”. Climacteric. 6 Suppl 3: 49–54. PMID 15018248.
- Scheinfeld NS (2007). “Yaz (3 mg drospirenone/20 microg ethinyl estradiol)”. Skinmed. 6 (6): 289. doi:10.1111/j.1540-9740.2007.07338.x. PMID 17975349.
- Sehovic N, Smith KP (May 2010). “Risk of venous thromboembolism with drospirenone in combined oral contraceptive products”. Ann Pharmacother. 44 (5): 898–903. doi:10.1345/aph.1M649. PMID 20371756. S2CID 8248469.
- Shulman LP (June 2006). “A review of drospirenone for safety and tolerability and effects on endometrial safety and lipid parameters contrasted with medroxyprogesterone acetate, levonorgestrel, and micronized progesterone”. J Womens Health (Larchmt). 15 (5): 584–90. doi:10.1089/jwh.2006.15.584. PMID 16796485.
- Simoncini T, Genazzani AR (February 2010). “A review of the cardiovascular and breast actions of drospirenone in preclinical studies”. Climacteric. 13 (1): 22–33. doi:10.3109/13697130903437375. PMID 19938948. S2CID 4306359.
- Sitruk-Ware R (October 2005). “Pharmacology of different progestogens: the special case of drospirenone”. Climacteric. 8 Suppl 3: 4–12. doi:10.1080/13697130500330382. PMID 16203650. S2CID 24205704.
- Thorneycroft IH (November 2002). “Evolution of progestins. Focus on the novel progestin drospirenone”. J Reprod Med. 47 (11 Suppl): 975–80. PMID 12497671.
- Toni I, Neubert A, Botzenhardt S, Gratzki N, Rascher W (September 2013). “Venous thromboembolism in adolescents associated with drospirenone-containing oral contraceptives – two case reports”. Klin Padiatr. 225 (5): 266–7. doi:10.1055/s-0033-1353169. PMID 23975850.
- White WB (February 2007). “Drospirenone with 17beta-estradiol in the postmenopausal woman with hypertension”. Climacteric. 10 Suppl 1: 25–31. doi:10.1080/13697130601114933. PMID 17364595. S2CID 9451771.
- Whitehead M (March 2006). “Hormone replacement therapy with estradiol and drospirenone: an overview of the clinical data”. J Br Menopause Soc. 12 Suppl 1: 4–7. doi:10.1258/136218006775992185. PMID 16513012. S2CID 38095916.
- Wu CQ, Grandi SM, Filion KB, Abenhaim HA, Joseph L, Eisenberg MJ (June 2013). “Drospirenone-containing oral contraceptive pills and the risk of venous and arterial thrombosis: a systematic review”. BJOG. 120 (7): 801–10. doi:10.1111/1471-0528.12210. PMID 23530659. S2CID 206904730.
- Zhao X, Zhang XF, Zhao Y, Lin X, Li NY, Paudel G, Wang QY, Zhang XW, Li XL, Yu J (September 2016). “Effect of combined drospirenone with estradiol for hypertensive postmenopausal women: a systemic review and meta-analysis”. Gynecol. Endocrinol. 32 (9): 685–689. doi:10.1080/09513590.2016.1183629. PMID 27176003. S2CID 9116138.
- “Drospirenone in HRT?”. Drug Ther Bull. 47 (4): 41–4. April 2009. doi:10.1136/dtb.2009.03.0011 (inactive 2021-05-06). PMID 19357298. S2CID 1909717.
External links
- “Drospirenone”. Drug Information Portal. U.S. National Library of Medicine.
//////////drospirenone, Nextstellis, ZK 30595, FDA 2021, APPROVALS 2021

NEW DRUG APPROVALS
ONE TIME
$10.00
Samidorphan
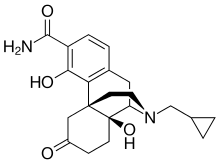
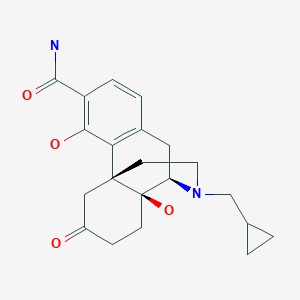
Samidorphan
サミドルファン;
| Formula | C21H26N2O4 |
|---|---|
| CAS | 852626-89-2 |
| Mol weight | 370.4421 |
FDA APPROVED 5/28/2021 Lybalvi
- ALKS 33
- ALKS-33
- RDC-0313
- RDC-0313-00
Product Ingredients
UNII0AJQ5N56E0
CAS Number1204592-75-5
WeightAverage: 504.536
Monoisotopic: 504.210780618
Chemical FormulaC25H32N2O9
| INGREDIENT | UNII | CAS | INCHI KEY |
|---|---|---|---|
| Samidorphan L-malate | 0AJQ5N56E0 | 1204592-75-5 | RARHXUAUPNYAJF-QSYGGRRVSA-N |
IUPAC Name(1R,9R,10S)-17-(cyclopropylmethyl)-3,10-dihydroxy-13-oxo-17-azatetracyclo[7.5.3.0^{1,10}.0^{2,7}]heptadeca-2,4,6-triene-4-carboxamide; (2S)-2-hydroxybutanedioic acid
MOA:mu-Opioid antagonist; delta-Opioid partial agonist; kappa-Opioid partial agonistsIndication:Alcohol dependence
New Drug Application (NDA): 213378
Company: ALKERMES INChttps://www.accessdata.fda.gov/drugsatfda_docs/label/2021/213378s000lbl.pdfhttps://www.accessdata.fda.gov/drugsatfda_docs/appletter/2021/213378Orig1s000,%20Orig2s000ltr.pdf
To treat schizophrenia in adults and certain aspects of bipolar I disorder in adults
LYBALVI is a combination of olanzapine, an atypical antipsychotic, and samidorphan (as samidorphan L-malate), an opioid antagonist.
Olanzapine is 2-methyl-4-(4-methyl-1-piperazinyl)-10H-thieno[2,3-b][1,5]benzodiazepine. The molecular formula of olanzapine is: C17H20N4S and the molecular weight is 312.44 g/mol. It is a yellow crystalline powder and has pKa values of 7.80 and 5.44. The chemical structure is:
 |
Samidorphan L-malate is morphinan-3-carboxamide, 17-(cyclopropylmethyl)-4, 14-dihydroxy-6-oxo-, (2S)-2-hydroxybutanedioate. The molecular formula of samidorphan L-malate is C21H26N2O4 • C4H6O5 and the molecular weight is 504.54 g/mol. It is a white to off-white crystalline powder and has pKa values of 8.3 (amine) and 10.1 (phenol). The chemical structure is:
 |
LYBALVI is intended for oral administration and is available as film-coated, bilayer tablets in the following strengths: 5 mg/10 mg, 10 mg/10 mg, 15 mg/10 mg, and 20 mg/10 mg of olanzapine and samidorphan (equivalent to 13.6 mg of samidorphan L-malate).
Inactive ingredients include colloidal silicon dioxide, crospovidone, lactose monohydrate, magnesium stearate, and microcrystalline cellulose. The film coating ingredients include hypromellose, titanium dioxide, triacetin, and color additives [iron oxide yellow (5 mg/10 mg); iron oxide yellow and iron oxide red (10 mg/10 mg); FD&C Blue No. 2/ indigo carmine aluminum lake (15 mg/10 mg); iron oxide red (20 mg/10 mg)].
- to treat schizophrenia
- alone for short-term (acute) or maintenance treatment of manic or mixed episodes that happen with bipolar I disorder
- in combination with valproate or lithium to treat manic or mixed episodes that happen with bipolar I disorder
Olanzapine is an effective atypical antipsychotic that, like other antipsychotics, is associated with weight gain, metabolic dysfunction, and increased risk of type II diabetes.5,6 Samidorphan is a novel opioid antagonist structurally related to naltrexone, with a higher affinity for opioid receptors, more potent μ-opioid receptor antagonism, higher oral bioavailability, and a longer half-life, making it an attractive candidate for oral dosing.1,5,11 Although antipsychotic-induced weight gain is incompletely understood, it is thought that the opioid system plays a key role in feeding and metabolism, such that opioid antagonism may be expected to ameliorate these negative effects. Samidorphan has been shown in animal models and clinical trials to ameliorate olanzapine-induced weight gain and metabolic dysfunction.5,6
Samidorphan was first approved as a variety of fixed-dose combination tablets with olanzapine by the FDA on May 28, 2021, and is currently marketed under the trademark LYBALVI™ by Alkermes Inc.11
Samidorphan (INN, USAN) (developmental code names ALKS-33, RDC-0313), also known as 3-carboxamido-4-hydroxynaltrexone,[2] is an opioid antagonist that preferentially acts as an antagonist of the μ-opioid receptor (MOR). It is under development by Alkermes for the treatment of major depressive disorder and possibly other psychiatric conditions.[3]
Development
Samidorphan has been investigated for the treatment of alcoholism and cocaine addiction by its developer, Alkermes,[4][5] showing similar efficacy to naltrexone but possibly with reduced side effects.
However, it has attracted much more attention as part of the combination product ALKS-5461 (buprenorphine/samidorphan), where samidorphan is combined with the mixed MOR weak partial agonist and κ-opioid receptor (KOR) antagonist buprenorphine, as an antidepressant. Buprenorphine has shown antidepressant effects in some human studies, thought to be because of its antagonist effects at the KOR, but has not been further developed for this application because of its MOR agonist effects and consequent abuse potential. By combining buprenorphine with samidorphan to block the MOR agonist effects, the combination acts more like a selective KOR antagonist, and produces only antidepressant effects, without typical MOR effects such as euphoria or substance dependence being evident.[6][7]
Samidorphan is also being studied in combination with olanzapine, as ALKS-3831 (olanzapine/samidorphan), for use in schizophrenia.[8] A Phase 3 study found that the addition of samidorphan to olanzapine significantly reduced weight gain compared to olanzapine alone.[9] The combination is now under review for approval by the US Food and Drug Administration.[10]
Pharmacology
Pharmacodynamics
The known activity profile of samidorphan at the opioid receptors is as follows:[11][12]
- μ-Opioid receptor (Ki = 0.052 nM; EC50 = N/A; Emax = 3.8%; IC50 = 0.88 nM; Imax = 92%)
- κ-Opioid receptor (Ki = 0.23 nM; EC50 = 3.3 nM; Emax = 36%; IC50 = 38 nM; Imax = 57%)
- δ-Opioid receptor (Ki = 2.6 nM; EC50 = 1.5 nM; Emax = 35%; IC50 = 6.9 nM; Imax = 56%)
As such, samidorphan is primarily an antagonist, or extremely weak partial agonist of the MOR.[11][12] In accordance with its in vitro profile, samidorphan has been observed to produce some side effects that are potentially consistent with activation of the KOR such as somnolence, sedation, dizziness, and hallucinations in some patients in clinical trials at the doses tested.[13]
SYNPATENT
WO2006052710A1.
https://patents.google.com/patent/WO2006052710A1/enExample 1 -Synthesis of 3-Carboxyamido-4-hvdroxy-naltrexone derivative 3

(A) Synthesis of 3-Carboxyamido-naltrexone 2[029] The triflate 11 of naltrexone was prepared according to the method of Wentland et al. (Bioorg. Med. Chem. Lett. 9, 183-187 (2000)), and the carboxamide 2 was prepared by the method described by Wentland et al. [(Bioorg. Med. Chem. Lett. ϋ, 623-626 (2001); and Bioorg. Med. Chem. Lett. 11, 1717-1721 (2001)] involving Pd-catalyzed carbonylation of the triflate 11 in the presence of ammonia and the Pd(O) ligand, DPPF ([l,l’-bis(diphenylρhosphino)ferrocene]) and DMSO.(B) Synthesis of 3-Carboxyamido-4-hydroxy-naltrexone derivative 3[030] Zinc dust (26 mg, 0.40 mmol) was added in portions to a solution of 2 (50 mg, 0.14 mmol) in HCl (37%, 0.2 mL) and AcOH (2 mL) at reflux. After heating at reflux for a further 15 min, the reaction was cooled by the addition of ice/water (10 mL) and basified (pH=9) with NH3/H2O, and the solution was extracted with EtOAc (3×10 mL). The organic extracts were washed with brine, dried, and concentrated. The residue was purified by column chromatography (SiO2, CH2Cl2, CH3OH : NH3/H2O = 15:1:0.01) to give compound 3 as a foam (25 mg, 50%). 1H NMR (CDC13) δl3.28(s, IH, 4-OH), 7.15(d, IH, J=8.1, H-2), 6.47(d, IH, J=8.4, H- 1), 6.10(br, IH, N-H), 4.35(br, IH, N-H), 4.04(dd,lH, J=I.8, 13.5, H-5), 3.11( d, IH, J=6), 2.99( d, IH, J=5.7), 2.94( s, IH), 2.86( d, IH, J= 6), 2.84-2.75(m, 2H), 2.65-2.61(m, 2H), 2.17-2.05(m, IH), 1.89-1.84(m, 2H), 0.85(m, IH), 0.56-0.50(m, 2H), 0.13-0.09(m, 2H). [α]D25= -98.4° (c=0.6, CH2Cl2). MS m/z (ESI) 371(MH+).
Paper
Bioorg. Med. Chem. Lett. 2000, 10, 183-187.
https://www.sciencedirect.com/science/article/abs/pii/S0960894X99006708
Abstract
Opioid binding affinities were assessed for a series of cyclazocine analogues where the prototypic 8-OH substituent of cyclazocine was replaced by amino and substituted-amino groups. For μ and κ opioid receptors, secondary amine derivatives having the (2R,6R,11R)-configuration had the highest affinity. Most targets were efficiently synthesized from the triflate of cyclazocine or its enantiomers using Pd-catalyzed amination procedures.
PAPER
Bioorg. Med. Chem. Lett. 2001, 11, 1717-1721.
https://www.sciencedirect.com/science/article/abs/pii/S0960894X01002785
Abstract
In response to the unexpectedly high affinity for opioid receptors observed in a novel series of cyclazocine analogues where the prototypic 8-OH was replaced by a carboxamido group, we have prepared the corresponding 3-CONH2 analogues of morphine and naltrexone. High affinity (Ki=34 and 1.7 nM) for μ opioid receptors was seen, however, the new targets were 39- and 11-fold less potent than morphine and naltrexone, respectively.
Abstract
High-affinity binding to μ opioid receptors has been identified in a series of novel 3-carboxamido analogues of morphine and naltrexone.

References
- ^ Turncliff R, DiPetrillo L, Silverman B, Ehrich E (February 2015). “Single- and multiple-dose pharmacokinetics of samidorphan, a novel opioid antagonist, in healthy volunteers”. Clinical Therapeutics. 37 (2): 338–48. doi:10.1016/j.clinthera.2014.10.001. PMID 25456560.
- ^ Wentland MP, Lu Q, Lou R, Bu Y, Knapp BI, Bidlack, JM (April 2005). “Synthesis and opioid receptor binding properties of a highly potent 4-hydroxy analogue of naltrexone”. Bioorganic & Medicinal Chemistry Letters. 15 (8): 2107–10. doi:10.1016/j.bmcl.2005.02.032. PMID 15808478.
- ^ “Samidorphan”. Adis Insight. Springer Nature Switzerland AG.
- ^ Hillemacher T, Heberlein A, Muschler MA, Bleich S, Frieling H (August 2011). “Opioid modulators for alcohol dependence”. Expert Opinion on Investigational Drugs. 20 (8): 1073–86. doi:10.1517/13543784.2011.592139. PMID 21651459.
- ^ Clinical trial number NCT01366001 for “ALK33BUP-101: Safety and Pharmacodynamic Effects of ALKS 33-BUP Administered Alone and When Co-administered With Cocaine” at ClinicalTrials.gov
- ^ “ALKS 5461 drug found to reduce depressive symptoms in Phase 1/2 study”.
- ^ “Investigational ALKS 5461 Channels ‘Opium Cure’ for Depression”.
- ^ LaMattina J (15 January 2013). “Will Alkermes’ Antipsychotic ALKS-3831 Become Another Tredaptive?”. Forbes.
- ^ Correll, Christoph U.; Newcomer, John W.; Silverman, Bernard; DiPetrillo, Lauren; Graham, Christine; Jiang, Ying; Du, Yangchun; Simmons, Adam; Hopkinson, Craig; McDonnell, David; Kahn, René S. (2020-08-14). “Effects of Olanzapine Combined With Samidorphan on Weight Gain in Schizophrenia: A 24-Week Phase 3 Study”. American Journal of Psychiatry. 177 (12): 1168–1178. doi:10.1176/appi.ajp.2020.19121279. ISSN 0002-953X.
- ^ “FDA Panel: Some Risk OK for Olanzapine Combo With Less Weight Gain”. http://www.medpagetoday.com. 2020-10-09. Retrieved 2021-01-23.
- ^ Jump up to:a b Linda P. Dwoskin (29 January 2014). Emerging Targets & Therapeutics in the Treatment of Psychostimulant Abuse. Elsevier Science. pp. 398–399, 402–403. ISBN 978-0-12-420177-4.
- ^ Jump up to:a b Wentland MP, Lou R, Lu Q, Bu Y, Denhardt C, Jin J, et al. (April 2009). “Syntheses of novel high affinity ligands for opioid receptors”. Bioorganic & Medicinal Chemistry Letters. 19 (8): 2289–94. doi:10.1016/j.bmcl.2009.02.078. PMC 2791460. PMID 19282177.
- ^ McElroy SL, Guerdjikova AI, Blom TJ, Crow SJ, Memisoglu A, Silverman BL, Ehrich EW (April 2013). “A placebo-controlled pilot study of the novel opioid receptor antagonist ALKS-33 in binge eating disorder”. The International Journal of Eating Disorders. 46(3): 239–45. doi:10.1002/eat.22114. PMID 23381803.
External links
| Clinical data | |
|---|---|
| Other names | ALKS-33, RDC-0313; 3-Carboxamido-4-hydroxynaltrexone |
| Routes of administration | Oral |
| Pharmacokinetic data | |
| Elimination half-life | 7–9 hours[1] |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 852626-89-2 |
| PubChem CID | 11667832 |
| ChemSpider | 23259667 |
| UNII | 7W2581Z5L8 |
| KEGG | D10162 |
| Chemical and physical data | |
| Formula | C21H26N2O4 |
| Molar mass | 370.449 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI |
/////////samidorphan, サミドルファン, ALKS 33, ALKS-33, RDC-0313, RDC-0313-00, APPROVALS 2021, FDA 2021, Lybalvi
SMILESO[C@@H](CC(O)=O)C(O)=O.NC(=O)C1=CC=C2C[C@H]3N(CC4CC4)CC[C@@]4(CC(=O)CC[C@@]34O)C2=C1O

NEW DRUG APPROVALS
one time
$10.00
Colchicine

Colchicine
CAS Registry Number: 64-86-8CAS Name:N-[(7S)-5,6,7,9-Tetrahydro-1,2,3,10-tetramethoxy-9-oxobenzo[a]heptalen-7-yl]acetamideMolecular Formula: C22H25NO6Molecular Weight: 399.44
CSIR-Laxai Life Sciences get DCGI nod for clinical trials Colchicine on Covid patients


It is an important therapeutic intervention for Covid-19 patients with cardiac co-morbidities and also for reducing proinflammatory cytokines
The Council of Scientific & Industrial Research (CSIR), and Laxai Life Sciences Pvt. Ltd. Hyderabad, have obtained approval from the Drug Controller General of India (DCGI) to undertake a two-arm phase-II clinical trial of the drug Colchicine for Covid-19 treatment.
The partner CSIR institutes in this important clinical trial are the CSIR-Indian Institute of Chemical Technology (IICT), Hyderabad and CSIR-Indian Institute of Integrative Medicine (IIIM), Jammu.
According to Ram Vishwakarma, advisor to DG-CSIR, colchicine, in combination with standard of care, will be an important therapeutic intervention for Covid-19 patients with cardiac co-morbidities and also for reducing proinflammatory cytokines, leading to faster recovery.
A number of global studies have confirmed now that cardiac complications during the course of Covid-19 infections and post-covid syndrome are leading to the loss of many lives, and it is essential to look for new or repurposed drugs.

VAMI MADDIPATLA
CHAIRMAN AND MD, LAXAI
A visionary & an entrepreneur with 17 years of experience in technology and bio-pharma industries. Founder and ex-CEO of LAXAI Pharma Ltd – a clinical data services company based in NJ, USA. Past employment: Pfizer, Wyeth Pharmaceuticals, Johnson & Johnson and Deloitte.
Vamsi provides a unique blend of operational and financial experience – along with a strong and expansive network of key influencers, industry experts and financial partners. He delivers a visionary understanding of client challenges and opportunities, and the instinctive ability to facilitate collaboration between the right people to turn strategic concepts into actionable plans – and, ultimately, into business results.
Dr S Chandrasekhar (Director CSIR-IICT, Hyderabad) and Dr. DS Reddy (Director, CSIR-IIIM, Jammu), the two partner institutes from CSIR said that they were looking forward to the outcome of this Phase II clinical efficacy trial on Colchicine, which may lead to life-saving intervention in the management of hospitalised patients.

Dr S Chandrasekhar (Director CSIR-IICT, Hyderabad)

Dr. DS Reddy (Director, CSIR-IIIM, Jammu)
India is one of the largest producers of this key drug and if successful, it will be made available to the patients at an affordable cost.
According to Ram Upadhayay, CEO, Laxai the enrollment of patients has already begun at multiple sites across India and the trial is likely to be completed in the next 8-10 weeks.
The drug can be made available to the large population of India based on the results of this trial and regulatory approval, he added.
Recent clinical studies have reported in leading medical journals about colchicine being associated with a significant reduction in the rates of recurrent pericarditis, post-pericardiotomy syndrome, and peri-procedural atrial fibrillation following cardiac surgery and atrial fibrillation ablation, according to a release.

Ram Upadhayaya, PhD
Chief Executive Officer, LAXAI
Ram Upadhayaya, CEO of Laxai Life Sciences, brings with him more than two decades of R&D experience spanning both academia and industry. A Ph. D in synthetic organic Chemistry, Ram has held key positions with leading international drug discovery organizations such as Bioimics AB Sweden, and Lupin India. Apart from his industrial background, Ram has been deeply associated with academic research. He was associated with Institute of Molecular Medicine, India as Principal Scientist as well as Uppsala University, Sweden in the capacity of Assistant Professor (Forskare). During these stints he significantly contributed to the development of novel therapeutics against infectious diseases such as AIDS and TB.
Ram has 10 international patents to his credit and has authored 25 peer reviewed publications. He is concurrently a consultant to the scientific advisory committee of the Principal Scientific Advisor, Government of India.

Raghava Reddy Kethiri, PhD, LAXAI
Chief Scientific Officer
25+ years of experience at various leadership positions in Biotech, CRO and Universities; Ex Karlsruhe Institute of Technology (KIT), Technical University of Dresden (TUD), JADO Technologies , Dresden, Germany, Jubilant Biosys, India
Delivered several leads, optimised leads and PCCs/DCs across Oncology, Pain, CNS, MD and Antibacterial therapeutics areas for global pharmaceutical companies. Co-Inventor of two clinical candidates ASN-001 ( NCT 02349139) for Metastatic Castration Resistant Prostrate Cancer & ASN-007 (NCT 03415126) for metastatic KRAS, NRAS & HRAS mutated solid tumors. Co-authored over 60 publications/patents (US/EU/Indian)
Colchicine
CAS Registry Number: 64-86-8
CAS Name:N-[(7S)-5,6,7,9-Tetrahydro-1,2,3,10-tetramethoxy-9-oxobenzo[a]heptalen-7-yl]acetamideMolecular Formula: C22H25NO6Molecular Weight: 399.44Percent Composition: C 66.15%, H 6.31%, N 3.51%, O 24.03%
Literature References: A major alkaloid of Colchicum autumnale L., Liliaceae. Extraction procedure: Chemnitius, J. Prakt. Chem. [II] 118, 29 (1928); F. E. Hamerslag, Technology and Chemistry of Alkaloids (New York, 1950) pp 66-80. Structure: Dewar, Nature155, 141 (1945); King et al.,Acta Crystallogr.5, 437 (1952); Horowitz, Ullyot, J. Am. Chem. Soc.74, 487 (1952). Crystal structure: L. Lessinger, T. N. Margulis, Acta Crystallogr.B34, 578 (1978).
Total synthesis: Schreiber et al.,Helv. Chim. Acta44, 540 (1961); Van Tamelen et al.,Tetrahedron14, 8 (1961); Nakamura, Chem. Pharm. Bull.8, 843 (1960); Sunagawa et al.,ibid.9, 81 (1961); 10, 281 (1962); Scott et al.,Tetrahedron21, 3605 (1965); Woodward, Harvey Lectures, Ser. 59 (Academic Press, New York, 1965) p 31; Kotani et al.,Chem. Commun.1974, 300; D. A. Evans et al.,J. Am. Chem. Soc.103, 5813 (1981).
Biosynthesis: Leete, Tetrahedron Lett.1965, 333; Battersby et al.,J. Chem. Soc.1964, 4257; Hill, Unrau, Can. J. Chem.43, 709 (1965). Tubulin-binding activity: J. M. Andreu, S. N. Timasheff, Proc. Natl. Acad. Sci. USA79, 6753 (1982). Toxicity: S. J. Rosenbloom, F. C. Ferguson, Toxicol. Appl. Pharmacol.13, 50 (1968); R. P. Beliles, ibid.23, 537 (1972). Clinical evaluations in cirrhosis of the liver: M. M. Kaplan et al.,N. Engl. J. Med.315, 1448 (1986); D. Kershenobich et al.,ibid.318, 1709 (1988). Bibliography of early literature: Eigsti, Lloydia10, 65 (1947).
Monograph: O. J. Eigsti, P. Dustin, Jr., Colchicine in Agriculture, Medicine, Biology and Chemistry (Iowa State College Press, Ames, Iowa, 1955). Reviews: Fleming, Selected Organic Syntheses (John Wiley, London, 1973) pp 183-207; G. Lagrue et al.,Ann. Med. Interne132, 496-500 (1981); F. D. Malkinson, Arch. Dermatol.118, 453-457 (1982). Comprehensive description: D. K. Wyatt et al.,Anal. Profiles Drug Subs.10, 139-182 (1981).
Properties: Pale yellow scales or powder, mp 142-150°. Darkens on exposure to light. Has been crystallized from ethyl acetate, pale yellow needles, mp 157°. [a]D17 -429° (c = 1.72). [a]D17 -121° (c = 0.9 in chloroform). pK at 20°: 12.35; pH of 0.5% soln: 5.9. uv max (95% ethanol): 350.5, 243 nm (log e 4.22; 4.47). One gram dissolves in 22 ml water, 220 ml ether, 100 ml benzene; freely sol in alcohol or chloroform. Practically insol in petr ether. Forms two cryst compds with chloroform, B.CHCl3 or B.2CHCl3, which do not give up their chloroform unless heated between 60 and 70° for considerable time. LD50 in rats (mg/kg): 1.6 i.v. (Rosenbloom, Ferguson); in mice (mg/kg): 4.13 i.v. (Beliles).
Melting point: mp 142-150°; mp 157°pKa: pK at 20°: 12.35; pH of 0.5% soln: 5.9Optical Rotation: [a]D17 -429° (c = 1.72); [a]D17 -121° (c = 0.9 in chloroform)Absorption maximum: uv max (95% ethanol): 350.5, 243 nm (log e 4.22; 4.47)
Toxicity data: LD50 in rats (mg/kg): 1.6 i.v. (Rosenbloom, Ferguson); in mice (mg/kg): 4.13 i.v. (Beliles)Use: In research in plant genetics (for doubling chromosomes).Therap-Cat: Gout suppressant. Treatment of Familial Mediterranean Fever.Therap-Cat-Vet: Has been used as an antineoplastic.Keywords: Antigout.
SYN
DOI: 10.1039/C39740000300
DOI: 10.1002/hlca.19610440225 DOI: 10.1021/ja00409a032
http://www.druglead.com/cds/Colchicine.html

SYN
https://pubs.rsc.org/en/content/articlelanding/2017/sc/c7sc01341h#!divAbstract
Here, we describe a concise, enantioselective, and scalable synthesis of (−)-colchicine (9.2% overall yield, >99% ee). Moreover, we have also achieved the first syntheses of (+)-demecolcinone and metacolchicine, and determined their absolute configurations. The challenging tricyclic 6-7-7 core of colchicinoids was efficiently introduced using an intramolecular oxidopyrylium-mediated [5 + 2] cycloaddition reaction. Notably, the synthesized colchicinoid 23 exhibited potent inhibitory activity toward the cell growth of human cancer cell lines (IC50 = ∼3.0 nM), and greater inhibitory activity towards microtubule assembly than colchicine, making it a promising lead in the search for novel anticancer agents.
Enantioselective total synthesis of (−)- and (+)-colchicine
The synthesis began with the transition-metal-catalyzed C–H bond functionalization of 7 with 14 (Scheme 1). Inspired by Li’s seminal work,18 we applied the strategy to compound 7. Pleasingly, after optimization, we successfully generated the N-sulfonyl imine in situ by reaction of 7 with TsNH2 (15) in the presence of anhydrous CuSO4 in THF. Furthermore, subsequent treatment of this imine with [RhCp*Cl2]2 (1 mol%), AgSbF6 (4 mol%), NaOAc (2.0 equiv.), and 14 (2.0 equiv.) at 80 °C afforded ortho-olefinated benzaldehyde 16 in good yield (90% on a 0.5 g scale; 70% on a 5.0 g scale). This modified catalytic C–H bond activation involved a transient directing group.19

SYN
https://chemistry.stackexchange.com/questions/67473/synthesis-of-colchicine
Recently one of my relatives have fallen ill and was prescribed with some colchicine. Looking at the structure of the molecule, and with nothing much to do, I decided to put my retrosynthetic skills to the test. Here is a picture of my thought process:
Is there a better way to design a synthesis for this compound using the disconnection method.
From 11b, a Birch reduction is carried out to give the qunione 10b. A rearrangement of the ketone with methanediazonium gives 9b. A dihydroxylation with a peroxy acid and subsequent addition of water gives 8b. A double dehydration reaction with sulfuric acid, coupled with the protection of the ketone with propan-1,3-diol gives the seven-membered quinone 7b. A Heck reaction (or Ullmann reaction) with 7a with a palladium catalyst yields 6. (The protection group is thereafter labelled “PG”) Friedel-Crafts acylation with ethanoyl chloride yields 5 (although on second thoughts, I should have done the acylation from 7a from the start). A Michael addition is then carried out with BuLiBuLi to lithiate the ketone to give the terminal imine 4. Since this terminal imine is unstable, a mild reducing agent converts the imine to the amine 3. The ketone is then removed by addition of dithiol and subsequently reduced by Raney nickel to form 2. Finally, a simple condensation reaction between the amine and acetic anhydride, followed by deprotection of the ketone using an acid, yields the final product colchicine, 1.
Colchicine is a medication used to treat gout[1][2] and Behçet’s disease.[3] In gout, it is less preferred to NSAIDs or steroids.[1] Other uses for colchicine include the management of pericarditis and familial Mediterranean fever.[1][4] Colchicine is taken by mouth.[1]
Colchicine has a narrow therapeutic index and overdosing is therefore a significant risk. Common side effects of colchicine include gastrointestinal upset, particularly at high doses.[5] Severe side effects may include low blood cells and rhabdomyolysis, and the medication can be deadly in overdose.[1] It is not clear whether colchicine is safe for use during pregnancy, but its use during breastfeeding appears to be safe.[1][6] Colchicine works by decreasing inflammation via multiple mechanisms.[7]
Colchicine, in the form of the autumn crocus (Colchicum autumnale), has been used as early as 1500 BC to treat joint swelling.[8] It was approved for medical use in the United States in 1961.[9] It is available as a generic medication in the United Kingdom.[6] In 2017, it was the 201st-most commonly prescribed medication in the United States, with more than two million prescriptions.[10][11]
Medical uses
Gout
Colchicine is an alternative for those unable to tolerate NSAIDs in gout.[12] At high doses, side effects (primarily gastrointestinal upset) limit its use.[13][14] At lower doses, it is well tolerated.[13][15][16][17] One review found low-quality evidence that low-dose colchicine (1.8 mg in one hour or 1.2 mg per day) reduced gout symptoms and pain, whereas high-dose colchicine (4.8 mg over 6 hours) was effective against pain, but caused more severe side effects, such as diarrhea, nausea or vomiting.[16]
For treating gout symptoms, colchicine is used orally with or without food, as symptoms first appear.[18] Subsequent doses may be needed if symptoms worsen.[18][16] There is preliminary evidence that daily colchicine (0.6 mg twice daily) was effective as a long-term prophylaxis when used with allopurinol to reduce the risk of increased uric acid levels and acute gout flares,[2] although adverse gastrointestinal effects may occur.[19]
Other conditions
Colchicine is also used as an anti-inflammatory agent for long-term treatment of Behçet’s disease.[20] It appears to have limited effect in relapsing polychondritis, as it may only be useful for the treatment of chondritis and mild skin symptoms.[21] It is a component of therapy for several other conditions, including pericarditis, pulmonary fibrosis, biliary cirrhosis, various vasculitides, pseudogout, spondyloarthropathies, calcinosis, scleroderma, and amyloidosis.[20][22][23] Research regarding the efficacy of colchicine in many of these diseases has not been performed.[23] It is also used in the treatment of familial Mediterranean fever,[20] in which it reduces attacks and the long-term risk of amyloidosis.[24]
Colchicine is effective for prevention of atrial fibrillation after cardiac surgery.[25] Potential applications for the anti-inflammatory effect of colchicine have been studied with regard to atherosclerosis and chronic coronary disease (e.g., stable ischemic heart disease).[26] In people with recent myocardial infarction (recent heart attack), it has been found to reduce risk of future cardiovascular events. Its clinical use may grow to include this indication.[27][28]
Colchicine is also being studied in clinical trials for possible effects on COVID-19.[29][30]
Contraindications
Long-term (prophylactic) regimens of oral colchicine are absolutely contraindicated in people with advanced kidney failure (including those on dialysis).[18] About 10-20 percent of a colchicine dose is excreted unchanged by the kidneys; it is not removed by hemodialysis. Cumulative toxicity is a high probability in this clinical setting, and a severe neuromyopathy may result. The presentation includes a progressive onset of proximal weakness, elevated creatine kinase, and sensorimotor polyneuropathy. Colchicine toxicity can be potentiated by the concomitant use of cholesterol-lowering drugs.[18]
Adverse effects
Deaths – both accidental and intentional – have resulted from overdose of colchicine.[18] Typical side effects of moderate doses may include gastrointestinal upset, diarrhea, and neutropenia.[13] High doses can also damage bone marrow, lead to anemia, and cause hair loss. All of these side effects can result from inhibition of mitosis,[31] which may include neuromuscular toxicity and rhabdomyolysis.[18]
Toxicity
According to one review, colchicine poisoning by overdose (range of acute doses of 7 to 26 mg) begins with a gastrointestinal phase occurring 10–24 hours after ingestion, followed by multiple organ dysfunction occurring 24 hours to 7 days after ingestion, after which the affected person either declines into multi-organ failure or recovers over several weeks.[32]
Colchicine can be toxic when ingested, inhaled, or absorbed in the eyes.[13] Colchicine can cause a temporary clouding of the cornea and be absorbed into the body, causing systemic toxicity. Symptoms of colchicine overdose start 2 to 24 hours after the toxic dose has been ingested and include burning in the mouth and throat, fever, vomiting, diarrhea, and abdominal pain.[18] This can cause hypovolemic shock due to extreme vascular damage and fluid loss through the gastrointestinal tract, which can be fatal.[32][33]
If the affected person survives the gastrointestinal phase of toxicity, they may experience multiple organ failure and critical illness. This includes kidney damage, which causes low urine output and bloody urine; low white blood cell counts that can last for several days; anemia; muscular weakness; liver failure; hepatomegaly; bone marrow suppression; thrombocytopenia; and ascending paralysis leading to potentially fatal respiratory failure. Neurologic symptoms are also evident, including seizures, confusion, and delirium; children may experience hallucinations. Recovery may begin within six to eight days and begins with rebound leukocytosis and alopecia as organ functions return to normal.[32][31]
Long-term exposure to colchicine can lead to toxicity, particularly of the bone marrow, kidney, and nerves. Effects of long-term colchicine toxicity include agranulocytosis, thrombocytopenia, low white blood cell counts, aplastic anemia, alopecia, rash, purpura, vesicular dermatitis, kidney damage, anuria, peripheral neuropathy, and myopathy.[31]
No specific antidote for colchicine is known, but supportive care is used in cases of overdose. In the immediate period after an overdose, monitoring for gastrointestinal symptoms, cardiac dysrhythmias, and respiratory depression is appropriate,[31] and may require gastrointestinal decontamination with activated charcoal or gastric lavage.[32][33]
Mechanism of toxicity
With overdoses, colchicine becomes toxic as an extension of its cellular mechanism of action via binding to tubulin.[32] Cells so affected undergo impaired protein assembly with reduced endocytosis, exocytosis, cellular motility, and interrupted function of heart cells, culminating in multi-organ failure.[7][32]
Epidemiology
In the United States, there are several hundred recorded cases of colchicine toxicity annually; approximately 10% of which end with serious morbidity or mortality. Many of these cases are intentional overdoses, but others were accidental; for example, if the drug was not dosed appropriately for kidney function. Most cases of colchicine toxicity occur in adults. Many of these adverse events resulted from the use of intravenous colchicine.[23]
Drug interactions
Colchicine interacts with the P-glycoprotein transporter, and the CYP3A4 enzyme involved in drug and toxin metabolism.[18][32] Fatal drug interactions have occurred when colchicine was taken with other drugs that inhibit P-glycoprotein and CYP3A4, such as erythromycin or clarithromycin.[18]
People taking macrolide antibiotics, ketoconazole or cyclosporine, or those who have liver or kidney disease, should not take colchicine, as these drugs and conditions may interfere with colchicine metabolism and raise its blood levels, potentially increasing its toxicity abruptly.[18][32] Symptoms of toxicity include gastrointestinal upset, fever, muscle pain, low blood cell counts, and organ failure.[13][18] People with HIV/AIDS taking atazanavir, darunavir, fosamprenavir, indinavir, lopinavir, nelfinavir, ritonavir, or saquinavir may experience colchicine toxicity.[18] Grapefruit juice and statins can also increase colchicine concentrations.[18]
In gout, inflammation in joints results from the precipitation of circulating uric acid, exceeding its solubility in blood and depositing as crystals of monosodium urate in and around synovial fluid and soft tissues of joints.[7] These crystal deposits cause inflammatory arthritis, which is initiated and sustained by mechanisms involving various proinflammatory mediators, such as cytokines.[7] Colchicine accumulates in white blood cells and affects them in a variety of ways: decreasing motility, mobilization (especially chemotaxis) and adhesion.[23]
Under preliminary research are various mechanisms by which colchicine may interfere with gout inflammation:
- inhibits microtubule polymerization by binding to its constitutive protein, tubulin[7]
- as availability of tubulin is essential to mitosis, colchicine may inhibit mitosis[7]
- inhibits activation and migration of neutrophils to sites of inflammation[18]
- interferes with the inflammasome complex found in neutrophils and monocytes that mediate interleukin-1β activation, a component of inflammation[18]
- inhibits superoxide anion production in response to urate crystals[7]
- interrupts mast cell and lysosome degranulation[7][23]
- inhibits release of glycoproteins that promote chemotaxis from synovial cells and neutrophils[23]
Generally, colchicine appears to inhibit multiple proinflammatory mechanisms, while enabling increased levels of anti-inflammatory mediators.[7] Apart from inhibiting mitosis, colchicine inhibits neutrophil motility and activity, leading to a net anti-inflammatory effect, which has efficacy for inhibiting or preventing gout inflammation.[7][18]
The plant source of colchicine, the autumn crocus (Colchicum autumnale), was described for treatment of rheumatism and swelling in the Ebers Papyrus (circa 1500 BC), an Egyptian medical papyrus.[34] It is a toxic alkaloid and secondary metabolite.[13][35][18] Colchicum extract was first described as a treatment for gout in De Materia Medica by Pedanius Dioscorides, in the first century AD. Use of the bulb-like corms of Colchicum to treat gout probably dates to around 550 AD, as the “hermodactyl” recommended by Alexander of Tralles. Colchicum corms were used by the Persian physician Avicenna, and were recommended by Ambroise Paré in the 16th century, and appeared in the London Pharmacopoeia of 1618.[36][23] Colchicum use waned over time, likely due to the severe gastrointestinal side effects preparations caused. In 1763, Colchicum was recorded as a remedy for dropsy (now called edema) among other illnesses.[23] Colchicum plants were brought to North America by Benjamin Franklin, who had gout himself and had written humorous doggerel about the disease during his stint as United States Ambassador to France.[37]
Colchicine was first isolated in 1820 by the French chemists P. S. Pelletier and J. B.Caventou.[38] In 1833, P. L. Geiger purified an active ingredient, which he named colchicine.[39] It quickly became a popular remedy for gout.[23] The determination of colchicine’s structure required decades, although in 1945, Michael Dewar made an important contribution when he suggested that, among the molecule’s three rings, two were seven-member rings.[40] Its pain-relieving and anti-inflammatory effects for gout were linked to its ability to bind with tubulin.
An unintended consequence of the 2006 U.S. Food and Drug Administration (FDA) safety program called the Unapproved Drugs Initiative—through which the FDA sought more rigorous testing of efficacy and safety of colchicine and other unapproved drugs[41]—was a price increase of 2000 percent [42] for “a gout remedy so old that the ancient Greeks knew about its effects.”[42] Under Unapproved Drugs Initiative small companies like URL Pharma, a Philadelphia drugmaker, were rewarded with licenses for testing of medicines like colchicine. In 2009, the FDA reviewed a New Drug Application for colchicine submitted by URL Pharma. URL Pharma did the testing, gained FDA formal approval, and was granted rights over colchicine. With this monopoly pricing power, the price of colchicine increased.
In 2012 Asia’s biggest drugmaker, Takeda Pharmaceutical Co., acquired URL Pharma for $800 million including the rights to colchicine (brand name Colcrys) earning $1.2 billion in revenue by raising the price even more.[42]
Oral colchicine had been used for many years as an unapproved drug with no FDA-approved prescribing information, dosage recommendations, or drug interaction warnings.[43] On July 30, 2009, the FDA approved colchicine as a monotherapy for the treatment of three different indications (familial Mediterranean fever, acute gout flares, and for the prophylaxis of gout flares[43]), and gave URL Pharma a three-year marketing exclusivity agreement[44] in exchange for URL Pharma doing 17 new studies and investing $100 million into the product, of which $45 million went to the FDA for the application fee. URL Pharma raised the price from $0.09 per tablet to $4.85, and the FDA removed the older unapproved colchicine from the market in October 2010, both in oral and intravenous forms, but allowed pharmacies to buy up the older unapproved colchicine.[45] Colchicine in combination with probenecid has been FDA-approved before 1982.[44]
July 29, 2009, colchicine won FDA approval in the United States as a stand-alone drug for the treatment of acute flares of gout and familial Mediterranean fever.[46][47] It had previously been approved as an ingredient in an FDA-approved combination product for gout. The approval was based on a study in which two doses (1.2 mg and 0.6 mg) an hour apart were as effective as higher doses in combating the acute flare of gout.[17]
As a drug antedating the FDA, colchicine was sold in the United States for many years without having been reviewed by the FDA for safety and efficacy. The FDA reviewed approved colchicine for gout flares, awarding Colcrys a three-year term of market exclusivity, prohibiting generic sales, and increasing the price of the drug from $0.09 to $4.85 per tablet.[48][49][50]
Numerous consensus guidelines, and previous randomized controlled trials, had concluded that colchicine is effective for acute flares of gouty arthritis. However, as of 2006, the drug was not formally approved by the FDA, owing to the lack of a conclusive randomized control trial (RCT). Through the Unapproved Drugs Initiative, the FDA sought more rigorous testing of the efficacy and safety of colchicine and other unapproved drugs.[41] In exchange for paying for the costly testing, the FDA gave URL Pharma three years of market exclusivity for its Colcrys brand,[51] under the Hatch-Waxman Act, based in part on URL-funded research in 2007, including pharmacokinetic studies and a randomized control trial with 185 patients with acute gout.
In April 2010, an editorial in the New England Journal of Medicine said that the rewards of this legislation are not calibrated to the quality or value of the information produced, that no evidence of meaningful improvement to public health was seen, and that it would be less expensive for the FDA, the National Institutes of Health or large insurers to pay for trials themselves. Furthermore, the cost burden of this subsidy falls primarily on patients or their insurers.[52] In September 2010, the FDA ordered a halt to marketing unapproved single-ingredient oral colchicine.[53]
Colchicine patents expire on February 10, 2029.[54]
URL Pharma also received seven years of market exclusivity for Colcrys in the treatment of familial Mediterranean fever, under the Orphan Drug Law. URL Pharma then raised the price per tablet from $0.09 to $4.85 and sued to remove other versions from the market, increasing annual costs for the drug to U.S. state Medicaid programs from $1 million to $50 million. Medicare also paid significantly higher costs, making this a direct money-loser for the government. (In a similar case, thalidomide was approved in 1998 as an orphan drug for leprosy and in 2006 for multiple myeloma.)[52]
Regulation
It is classified as an extremely hazardous substance in the United States as defined in Section 302 of the U.S. Emergency Planning and Community Right-to-Know Act (42 U.S.C. 11002) and is subject to strict reporting requirements by facilities which produce, store, or use it in significant quantities.[55]
Formulations and dosing
Trade names for colchicine are Colcrys or Mitigare which are manufactured as a dark– and light-blue capsule having a dose of 0.6 mg.[18][56] Colchicine is also prepared as a white, yellow, or purple pill (tablet) having a dose of 0.6 mg.[56]
Colchicine is typically prescribed to mitigate or prevent the onset of gout, or its continuing symptoms and pain, using a low-dose prescription of 0.6 to 1.2 mg per day, or a high-dose amount of up to 4.8 mg in the first 6 hours of a gout episode.[5][18][16] With an oral dose of 0.6 mg, peak blood levels occur within one to two hours.[35] For treating gout, the initial effects of colchicine occur in a window of 12 to 24 hours, with a peak within 48 to 72 hours.[18] It has a narrow therapeutic window, requiring monitoring of the subject for potential toxicity.[18] Colchicine is not a general pain relief drug, and is not used to treat pain in other disorders.[18]
Biosynthesis
According to laboratory research, the biosynthesis of colchicine involves the amino acids phenylalanine and tyrosine as precursors. Giving radioactive phenylalanine-2-14C to C. byzantinum, another plant of the family Colchicaceae, resulted in its incorporation into colchicine.[57] However, the tropolone ring of colchicine resulted from the expansion of the tyrosine ring. Radioactive feeding experiments of C. autumnale revealed that colchicine can be synthesized biosynthetically from (S)-autumnaline. That biosynthesic pathway occurs primarily through a phenolic coupling reaction involving the intermediate isoandrocymbine. The resulting molecule undergoes O-methylation directed by S-adenosylmethionine. Two oxidation steps followed by the cleavage of the cyclopropane ring leads to the formation of the tropolone ring contained by N-formyldemecolcine. N-formyldemecolcine hydrolyzes then to generate the molecule demecolcine, which also goes through an oxidative demethylation that generates deacetylcolchicine. The molecule of colchicine appears finally after addition of acetyl-coenzyme A to deacetylcolchicine.[58][59]

Purification
Colchicine may be purified from Colchicum autumnale (autumn crocus) or Gloriosa superba (glory lily). Concentrations of colchicine in C. autumnale peak in the summer, and range from 0.1% in the flower to 0.8% in the bulb and seeds.[23]
Colchicine is widely used in plant breeding by inducing polyploidy in plant cells to produce new or improved varieties, strains and cultivars.[60] When used to induce polyploidy in plants, colchicine cream is usually applied to a growth point of the plant, such as an apical tip, shoot, or sucker. Seeds can be presoaked in a colchicine solution before planting. Since chromosome segregation is driven by microtubules, colchicine alters cellular division by inhibiting chromosome segregation during meiosis; half the resulting gametes, therefore, contain no chromosomes, while the other half contains double the usual number of chromosomes (i.e., diploid instead of haploid, as gametes usually are), and lead to embryos with double the usual number of chromosomes (i.e., tetraploid instead of diploid).[60] While this would be fatal in most higher animal cells, in plant cells it is not only usually well-tolerated, but also frequently results in larger, hardier, faster-growing, and in general more desirable plants than the normally diploid parents. For this reason, this type of genetic manipulation is frequently used in breeding plants commercially.[60]
When such a tetraploid plant is crossed with a diploid plant, the triploid offspring are usually sterile (unable to produce fertile seeds or spores), although many triploids can be propagated vegetatively. Growers of annual triploid plants not readily propagated vegetatively cannot produce a second-generation crop from the seeds (if any) of the triploid crop and need to buy triploid seed from a supplier each year. Many sterile triploid plants, including some trees, and shrubs, are becoming increasingly valued in horticulture and landscaping because they do not become invasive species and will not drop undesirable fruit and seed litter. In certain species, colchicine-induced triploidy has been used to create “seedless” fruit, such as seedless watermelons (Citrullus lanatus). Since most triploids do not produce pollen themselves, such plants usually require cross-pollination with a diploid parent to induce seedless fruit production.
The ability of colchicine to induce polyploidy can be also exploited to render infertile hybrids fertile, for example in breeding triticale (× Triticosecale) from wheat (Triticum spp.) and rye (Secale cereale). Wheat is typically tetraploid and rye diploid, with their triploid hybrid infertile; treatment of triploid triticale with colchicine gives fertile hexaploid triticale.[61]
References
- ^ Jump up to:a b c d e f “Colchicine Monograph for Professionals”. Drugs.com. American Society of Health-System Pharmacists. Retrieved 27 March 2019.
- ^ Jump up to:a b Shekelle PG, Newberry SJ, FitzGerald JD, Motala A, O’Hanlon CE, Tariq A, et al. (January 2017). “Management of Gout: A Systematic Review in Support of an American College of Physicians Clinical Practice Guideline”. Annals of Internal Medicine. 166 (1): 37–51. doi:10.7326/M16-0461. PMID 27802478.
- ^ Schachner LA, Hansen RC (2011). Pediatric Dermatology E-Book. Elsevier Health Sciences. p. 177. ISBN 9780723436652.
- ^ Hutchison, Stuart J. (2009). Pericardial Diseases: Clinical Diagnostic Imaging Atlas with DVD. Elsevier Health Sciences. p. 58. ISBN 9781416052746.
- ^ Jump up to:a b “Colchicine for acute gout: updated information about dosing and drug interactions”. National Prescribing Service, Australia. 14 May 2010. Archived from the original on 30 June 2012. Retrieved 14 May 2010.
- ^ Jump up to:a b British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 1085–1086. ISBN 9780857113382.
- ^ Jump up to:a b c d e f g h i j Dalbeth N, Lauterio TJ, Wolfe HR (October 2014). “Mechanism of action of colchicine in the treatment of gout”. Clinical Therapeutics. 36 (10): 1465–79. doi:10.1016/j.clinthera.2014.07.017. PMID 25151572.
- ^ Wall, Wilson John (2015). The Search for Human Chromosomes: A History of Discovery. Springer. p. 88. ISBN 9783319263366.
- ^ “Colchicine capsule”. DailyMed. Retrieved 27 March 2019.
- ^ “The Top 300 of 2020”. ClinCalc. Retrieved 11 April 2020.
- ^ “Colchicine – Drug Usage Statistics”. ClinCalc. Retrieved 11 April 2020.
- ^ Chen LX, Schumacher HR (October 2008). “Gout: an evidence-based review”. Journal of Clinical Rheumatology. 14 (5 Suppl): S55-62. doi:10.1097/RHU.0b013e3181896921. PMID 18830092.
- ^ Jump up to:a b c d e f “Colcrys (colchicine, USP) tablets 0.6 mg. Drug Approval Package”. US Food and Drug Administration. 17 February 2010. Retrieved 19 August 2018.
- ^ “Information for Healthcare Professionals: New Safety Information for Colchicine (marketed as Colcrys)”. U.S. Food and Drug Administration.
- ^ Laubscher T, Dumont Z, Regier L, Jensen B (December 2009). “Taking the stress out of managing gout”. Canadian Family Physician. 55 (12): 1209–12. PMC 2793228. PMID 20008601.
- ^ Jump up to:a b c d van Echteld I, Wechalekar MD, Schlesinger N, Buchbinder R, Aletaha D (August 2014). “Colchicine for acute gout”. The Cochrane Database of Systematic Reviews. 8 (8): CD006190. doi:10.1002/14651858.CD006190.pub2. PMID 25123076.
- ^ Jump up to:a b Terkeltaub RA, Furst DE, Bennett K, Kook KA, Crockett RS, Davis MW (April 2010). “High versus low dosing of oral colchicine for early acute gout flare: Twenty-four-hour outcome of the first multicenter, randomized, double-blind, placebo-controlled, parallel-group, dose-comparison colchicine study”. Arthritis and Rheumatism. 62 (4): 1060–8. doi:10.1002/art.27327. PMID 20131255.
- ^ Jump up to:a b c d e f g h i j k l m n o p q r s t u v “Colchicine”. Drugs.com. 1 January 2017. Retrieved 19 August 2018.
- ^ Qaseem A, Harris RP, Forciea MA (January 2017). “Management of Acute and Recurrent Gout: A Clinical Practice Guideline From the American College of Physicians”. Annals of Internal Medicine. 166 (1): 58–68. doi:10.7326/M16-0570. PMID 27802508.
- ^ Jump up to:a b c Cocco G, Chu DC, Pandolfi S (December 2010). “Colchicine in clinical medicine. A guide for internists”. European Journal of Internal Medicine. 21 (6): 503–8. doi:10.1016/j.ejim.2010.09.010. PMID 21111934.
- ^ Puéchal X, Terrier B, Mouthon L, Costedoat-Chalumeau N, Guillevin L, Le Jeunne C (March 2014). “Relapsing polychondritis”. Joint Bone Spine. 81 (2): 118–24. doi:10.1016/j.jbspin.2014.01.001. PMID 24556284.
- ^ Alabed S, Cabello JB, Irving GJ, Qintar M, Burls A (August 2014). “Colchicine for pericarditis” (PDF). The Cochrane Database of Systematic Reviews. 8 (8): CD010652. doi:10.1002/14651858.CD010652.pub2. PMID 25164988.
- ^ Jump up to:a b c d e f g h i j Goldfrank’s toxicologic emergencies. Nelson, Lewis, 1963- (Eleventh ed.). New York. 2019-04-11. ISBN 978-1-259-85961-8. OCLC 1020416505.
- ^ Portincasa P (2016). “Colchicine, Biologic Agents and More for the Treatment of Familial Mediterranean Fever. The Old, the New, and the Rare”. Current Medicinal Chemistry. 23 (1): 60–86. doi:10.2174/0929867323666151117121706. PMID 26572612.
- ^ Lennerz C, Barman M, Tantawy M, Sopher M, Whittaker P (December 2017). “Colchicine for primary prevention of atrial fibrillation after open-heart surgery: Systematic review and meta-analysis” (PDF). International Journal of Cardiology. 249: 127–137. doi:10.1016/j.ijcard.2017.08.039. PMID 28918897.
- ^ Malik, Jahanzeb; Javed, Nismat; Ishaq, Uzma; Khan, Umar; Laique, Talha (17 May 2020). “Is There a Role for Colchicine in Acute Coronary Syndromes? A Literature Review”. Cureus. 12(5): e8166. doi:10.7759/cureus.8166. PMC 7296886. PMID 32550081.
- ^ Imazio M, Andreis A, Brucato A, Adler Y, De Ferrari GM (July 2020). “Colchicine for acute and chronic coronary syndromes”. Heart. 106 (20): heartjnl–2020–317108. doi:10.1136/heartjnl-2020-317108. PMID 32611559. S2CID 220305546.
- ^ Nidorf SM, Fiolet AT, Mosterd A, Eikelboom JW, Schut A, Opstal TS, et al. (August 2020). “Colchicine in Patients with Chronic Coronary Disease”. The New England Journal of Medicine. 383(19): 1838–1847. doi:10.1056/NEJMoa2021372. PMID 32865380.
- ^ Kaul S, Gupta M, Bandyopadhyay D, Hajra A, Deedwania P, Roddy E, et al. (December 2020). “Gout Pharmacotherapy in Cardiovascular Diseases: A Review of Utility and Outcomes”. American Journal of Cardiovascular Drugs : Drugs, Devices, and Other Interventions. doi:10.1007/s40256-020-00459-1. PMC 7768268. PMID 33369719.
- ^ Reyes, Aaron Z; Hu, Kelly A; Teperman, Jacob; Wampler Muskardin, Theresa L; Tardif, Jean-Claude; Shah, Binita; Pillinger, Michael H (2020-12-08). “Anti-inflammatory therapy for COVID-19 infection: the case for colchicine”. Annals of the Rheumatic Diseases: annrheumdis–2020–219174. doi:10.1136/annrheumdis-2020-219174. ISSN 0003-4967. PMID 33293273.
- ^ Jump up to:a b c d “CDC – The Emergency Response Safety and Health Database: Biotoxin: Cochicine”. Centers for Disease Control and Prevention, US Department of Health and Human Services. Retrieved 31 December 2015.
- ^ Jump up to:a b c d e f g h Finkelstein Y, Aks SE, Hutson JR, Juurlink DN, Nguyen P, Dubnov-Raz G, et al. (June 2010). “Colchicine poisoning: the dark side of an ancient drug”. Clinical Toxicology. 48 (5): 407–14. doi:10.3109/15563650.2010.495348. PMID 20586571. S2CID 33905426.
- ^ Jump up to:a b Matt Doogue (2014). “Colchicine – extremely toxic in overdose” (PDF). Christchurch and Canterbury District Health Board, New Zealand. Retrieved 23 August 2018.
- ^ Graham W, Roberts JB (March 1953). “Intravenous colchicine in the management of gouty arthritis”. Annals of the Rheumatic Diseases. 12 (1): 16–9. doi:10.1136/ard.12.1.16. PMC 1030428. PMID 13031443.
- ^ Jump up to:a b “Colcrys (colchicine). Summary review for regulatory action”(PDF). Center for Drug Evaluation and Research, US Food and Drug Administration. 30 July 2009. Retrieved 19 August 2018.
- ^ Hartung EF (September 1954). “History of the use of colchicum and related medicaments in gout; with suggestions for further research”. Annals of the Rheumatic Diseases. 13 (3): 190–200. doi:10.1136/ard.13.3.190. PMC 1006735. PMID 13198053.(free BMJ registration required)
- ^ Ebadi MS (2007). Pharmacodynamic basis of herbal medicine. ISBN 978-0-8493-7050-2.
- ^ Pelletier and Caventou (1820) “Examen chimique des plusieurs végétaux de la famille des colchicées, et du principe actif qu’ils renferment. [Cévadille (veratrum sabadilla); hellébore blanc (veratrum album); colchique commun (colchicum autumnale)]”(Chemical examination of several plants of the meadow saffron family, and of the active principle that they contain.) Annales de Chimie et de Physique, 14 : 69-81.
- ^ Geiger, Ph. L. (1833) “Ueber einige neue giftige organische Alkalien” (On some new poisonous organic alkalis) Annalen der Pharmacie, 7 (3) : 269-280; colchicine is discussed on pages 274-276.
- ^ Dewar MJ (February 3, 1945). “Structure of colchicine”. Letters to Editor. Nature. 155 (3927): 141–142. Bibcode:1945Natur.155..141D. doi:10.1038/155141d0. S2CID 4074312. Dewar did not prove the structure of colchicine; he merely suggested that it contained two seven-membered rings. Colchicine’s structure was determined by X-ray crystallography in 1952 King MV, de Vries JL, Pepinsky R (July 1952). “An x-ray diffraction determination of the chemical structure of colchicine”. Acta Crystallographica. 5 (4): 437–440. doi:10.1107/S0365110X52001313. Its total synthesis was first accomplished in 1959 Eschenmoser A (1959). “Synthese des Colchicins”. Angewandte Chemie. 71 (20): 637–640. doi:10.1002/ange.19590712002.
- ^ Jump up to:a b “FDA Unapproved Drugs Initiative”.
- ^ Jump up to:a b c Langreth R, Koons C (6 October 2015). “2,000% Drug Price Surge Is a Side Effect of FDA Safety Program”. Bloomberg. Retrieved 27 October 2015.
- ^ Jump up to:a b “FDA Approves Colchicine With Drug Interaction and Dose Warnings”. July 2009.
- ^ Jump up to:a b “Orange Book: Approved Drug Products with Therapeutic Equivalence Evaluations”. fda.gov.
- ^ “Questions and Answers for Patients and Healthcare Providers Regarding Single-ingredient Oral Colchicine Products”. fda.gov.
- ^ “FDA Approves Gout Treatment After Long Years of Use”. medpagetoday.com. 3 August 2009. Archived from the original on 5 August 2009. Retrieved 3 August 2009.
- ^ Cerquaglia C, Diaco M, Nucera G, La Regina M, Montalto M, Manna R (February 2005). “Pharmacological and clinical basis of treatment of Familial Mediterranean Fever (FMF) with colchicine or analogues: an update”. Current Drug Targets. Inflammation and Allergy. 4 (1): 117–24. doi:10.2174/1568010053622984. PMID 15720245. Archived from the original on 2008-12-11. Retrieved 2019-07-06.
- ^ Karst KR (21 October 2009). “California Court Denies Preliminary Injunction in Lanham Act Case Concerning Unapproved Colchicine Drugs”.
- ^ Meyer H (29 December 2009). “The High Price of FDA Approval”. The Philadelphia Inquirer – via Kaiser Health News.
- ^ Colcrys vs. Unapproved Colchicine Statement from URL Pharma
- ^ “About Colcrys”. Colcrys. URL Pharma. Retrieved 11 September 2011.
- ^ Jump up to:a b Kesselheim AS, Solomon DH (June 2010). “Incentives for drug development–the curious case of colchicine”. The New England Journal of Medicine. 362 (22): 2045–7. doi:10.1056/NEJMp1003126. PMID 20393164.
- ^ “FDA orders halt to marketing of unapproved single-ingredient oral colchicine”. 30 September 2010.
- ^ “Generic Colcrys Availability”. drugs.com.
- ^ “40 CFR Appendix A to Part 355, The List of Extremely Hazardous Substances and Their Threshold Planning Quantities”. LII / Legal Information Institute. Retrieved 2018-03-11.
- ^ Jump up to:a b “Colchicine images”. Drugs.com. 6 August 2018. Retrieved 21 August 2018.
- ^ Leete E (1963). “The biosynthesis of the alkaloids of Colchicum: The incorporation of phenylalaline-2-C14 into colchicine and demecolcine”. J. Am. Chem. Soc. 85 (22): 3666–3669. doi:10.1021/ja00905a030.
- ^ Herbert, Richard B. (2001). “The biosynthesis of plant alkaloids and nitrogenous microbial metabolites”. Nat. Prod. Rep. 18 (1): 50–65. doi:10.1039/A809393H. PMID 11245400.
- ^ Dewick PM (2009). Medicinal natural products: A biosynthetic approach. Wiley. pp. 360–362.
- ^ Jump up to:a b c Griffiths AJF, Gelbart WM, Miller JH (1999). Modern Genetic Analysis: Changes in Chromosome Number. W. H. Freeman, New York.
- ^ Derman H, Emsweller SL. “The use of colchicine in plant breeding”. archive.org. Retrieved 26 April 2016.
Further reading
- Dowd, Matthew J. (April 30, 1998). “Colchicine”. Virginia Commonwealth University. Archived from the original on 2010-06-10.
- EXT LINKS
- “Colchicine”. Drug Information Portal. U.S. National Library of Medicine.
- “Colchicine : Biotoxin”. Emergency Response Safety and Health Database. 8 November 2017.
| Clinical data | |
|---|---|
| Trade names | Colcrys, Mitigare, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682711 |
| License data | US DailyMed: Colchicine |
| Pregnancy category | AU: D |
| Routes of administration | By mouth |
| ATC code | M04AC01 (WHO) |
| Legal status | |
| Legal status | AU: S4 (Prescription only)CA: ℞-onlyUK: POM (Prescription only)US: ℞-only |
| Pharmacokinetic data | |
| Bioavailability | 45% |
| Protein binding | 35-44% |
| Metabolism | Metabolism, partly by CYP3A4 |
| Elimination half-life | 26.6-31.2 hours |
| Excretion | Faeces (65%) |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 64-86-8 |
| PubChem CID | 6167 |
| IUPHAR/BPS | 2367 |
| DrugBank | DB01394 |
| ChemSpider | 5933 |
| UNII | SML2Y3J35T |
| KEGG | D00570 |
| ChEBI | CHEBI:27882 |
| ChEMBL | ChEMBL107 |
| CompTox Dashboard (EPA) | DTXSID5024845 DTXSID20274387, DTXSID5024845 |
| ECHA InfoCard | 100.000.544 |
| Chemical and physical data | |
| Formula | C22H25NO6 |
| Molar mass | 399.437 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (verify) |
///////////Colchicine, CSIR, Laxai Life Sciences, DCGI, clinical trials, Covid patients, covid 19, corona virus

NEW DRUG APPROVALS
ONE TIME
$10.00

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....












