IC50 value: 16 nM
Target: androgen receptor
WORLD RECORD VIEWS holder on THIS BLOG, ………live, by DR ANTHONY MELVIN CRASTO, Worldpeaceambassador, Worlddrugtracker, Helping millions, 100 million hits on google, pushing boundaries,2.5 lakh plus connections worldwide, 45 lakh plus VIEWS on this blog in 227 countries, 7 CONTINENTS ……A 90 % paralysed man in action for you, I am suffering from transverse mylitis and bound to a wheel chair, [THIS BLOG HOLDS WORLD RECORD VIEWS ]

Trioxacarcin A, DC-45A
CAS No. 81552-36-5
Trioxacarcin B; Antibiotic DC 45B1; DC-45-B1; Trioxacarcin A, 14,17-deepoxy-14,17-dihydroxy-; AC1MJ5N1; 81534-36-3;
| Molecular Formula: | C42H54O21 |
|---|---|
| Molecular Weight: | 894.86556 g/mol |
(CAS NO.81781-28-4):C42H54O20
Molecular Weight: 878.8662 g/mol
Structure of Trioxacarcin C :


The trioxacarcins are polyoxygenated, structurally complex natural products that potently inhibit the growth of cultured human cancer cells
Natural products that bind and often covalently modify duplex DNA figure prominently in chemotherapy for human cancers. The trioxacarcins are a new class of DNA- modifying natural products with antiproliferative effects. The trioxacarcins were first described in 1981 by Tomita and coworkers (Tomita et al. , J. Antibiotics, 34( 12): 1520- 1524, 1981 ; Tamaoki et al., J. Antibiotics 34( 12): 1525- 1530, 1981 ; Fujimoto et al. , J. Antibiotics 36(9): 1216- 1221 , 1983). Trioxacarcin A, B, and C were isolated by Tomita and coworkers from the culture broth of Streptomyces bottropensis DO-45 and shown to possess anti-tumor activity in murine models as well as gram-positive antibiotic activity. Subsequent work led to the discovery of other members of this family. Trioxacarcin A is a powerful anticancer agent with subnanmolar IC70 values against lung (LXFL 529L, H-460), mammary (MCF-7), and CNS (SF-268) cancer cell lines. The trioxacarcins have also been shown to have antimicrobial activity {e.g., anti-bacterial and anti-malarial activity) (see, e.g. , Maskey et al., J. Antibiotics (2004) 57:771 -779).
trioxacarcin A
An X-ray crystal structure of trioxacarcin A bound to N-7 of a guanidylate residue in a duplex DNA oligonucleotide substrate has provided compelling evidence for a proposed pathyway of DNA modification that proceeds by duplex intercalation and alkylation (Pfoh et al, Nucleic Acids Research 36( 10):3508-3514, 2008).
All trioxacarcins appear to be derivatives of the aglycone, which is itself a bacterial isolate referred to in the patent literature as DC-45-A2. U.S. Patent 4,459,291 , issued July 10, 1984, describes the preparation of DC-45-A2 by fermentation. DC-45-A2 is the algycone of trioxacarcins A, B, and C and is prepared by the acid hydrolysis of the fermentation products trioxacarcins A and C or the direct isolation from the fermentation broth of Streptomyces bottropensis.
Based on the biological activity of the trioxacarcins, a fully synthetic route to these compounds would be useful in exploring the biological and chemical activity of known trioxacarcin compounds and intermediates thereto, as well as aid in the development of new trioxacarcin compounds with improved biological and/or chemical properties.
PAPER
Component-Based Syntheses of Trioxacarcin A, DC-45-A1, and Structural Analogs
T. Magauer, D. Smaltz, A. G. Myers, Nat. Chem. 2013, 5, 886–893. (Link)

PAPER

A schematic shows a trioxacarcin C molecule, whose structure was revealed for the first time through a new process developed by the Rice lab of synthetic organic chemist K.C. Nicolaou. Trioxacarcins are found in bacteria but synthetic versions are needed to study them for their potential as medications. Trioxacarcins have anti-cancer properties. Source: Nicolaou Group/Rice University
A team led by Rice University synthetic organic chemist K.C. Nicolaou has developed a new process for the synthesis of a series of potent anti-cancer agents originally found in bacteria.
The Nicolaou lab finds ways to replicate rare, naturally occurring compounds in larger amounts so they can be studied by biologists and clinicians as potential new medications. It also seeks to fine-tune the molecular structures of these compounds through analog design and synthesis to improve their disease-fighting properties and lessen their side effects.
Such is the case with their synthesis of trioxacarcins, reported this month in the Journal of the American Chemical Society.
PAPER

PATENT
http://www.google.com/patents/EP2550285A1?cl=en

(S)-9-Hvdrox v- 10-methoxy-5-(4-methoxybenzylox v)- 1 -(methoxymethox y)-3- methyl-8-oxo-5,6.7.8-tetrahvdroanthracene-2-carbaldehvde. Potassium osmate dihydrate (29 mg, 0.079 mmol, 0.05 equiv) was added to an ice -cooled mixture of (S,£)-9-hydroxy- 10- methoxy-4-(4-methoxybenzyloxy)-8-(methoxymethoxy)-6-methyl-7-(prop- l -enyl)-3,4- dihydroanthracen-l -one (780 mg, 1.58 mmol, 1 equiv), 2,6-lutidine (369 μί, 3.17 mmol, 2.0 equiv), and sodium periodate ( 1.36 g, 6.33 mmol, 4.0 equiv) in a mixture of tetrahydrofuran (20 mL) and water ( 10 mL). After 10 min, the cooling bath was removed and the reaction flask was allowed to warm to 23 °C. After 1.5 h, the reaction mixture was partitioned between water ( 100 mL) and ethyl acetate (150 mL). The layers were separated. The organic layer was washed with aqueous sodium chloride solution (50 mL) and the washed solution was dried over sodium sulfate. The dried solution was filtered and the filtrate was concentrated. The residue was purified by flash-column chromatography (20% ethyl acetate- hexanes) to provide 498 mg of the product, (5)-9-hydroxy- 10-methoxy-5-(4- methoxybenzyloxy)- l -(methoxymethoxy)-3-methyl-8-oxo-5,6,7,8-tetrahydroanthracene-2- carbaldehyde, as an orange foam (65%). Ή NMR (500 MHz, CDC13): 15.17 (s, 1 H), 10.74 (s, 1 H), 7.66 (s, 1 H), 7.27 (d, 2H, 7 = 8.5 Hz), 6.86 (d, 2H, 7 = 8.6 Hz), 5.30-5.18 (m, 3H), 4.63 (d, 1H,7= 11.1 Hz), 4.52 (d, 1H,7 = 12.0 Hz), 3.86 (s, 3H), 3.79 (s, 3H), 3.62 (s, 3H), 3.22 (m, 1H), 2.75 (s, 3H), 2.63 (m, 1H), 2.54 (m, 1H), 2.08 (m, 1H). I3C NMR (125 MHz, CDC13): 204.9, 193.2, 163.2, 161.7, 159.2, 144.4, 141.7, 137.0, 130.1, 129.4, 120.7, 117.9, 113.8, 110.0, 102.8, 70.4, 67.2, 62.9, 58.3, 55.2, 32.3, 26.3, 22.2. FTIR, cm-1 (thin film): 2936 (m), 2907 (m), 1684 (s), 1611 (s), 1377 (s), 1246 (s). HRMS (ESI): Calcd for
(C27H2808+K)+: 519.1416; Found 519.1368. TLC (20% ethyl acetate-hexanes): R,= 0.17 (CAM).
86% yield
[00457] (S)-l,9-Dihvdroxy-10-methoxy-5-(4-methoxybenzyloxy)-3-methyl-8-oxo-5,6,7,8- tetrahydroanthracene-2-carbaldehyde. A solution of B-bromocatecholborane (418 mg, 2.10 mmol, 2.0 equiv) in dichloromethane (15 mL) was added to a solution of (S)-9-hydroxy-10- methoxy-5-(4-methoxybenzyloxy)-l-(methoxymethoxy)-3-methyl-8-oxo-5,6,7,8- tetrahydroanthracene-2-carbaldehyde (490 mg, 1.05 mmol, 1 equiv) in dichloromethane (15 mL) at -78 °C. After 50 min, the reaction mixture was diluted with saturated aqueous sodium bicarbonate solution (25 mL) and dichloromethane (100 mL). The cooling bath was removed, and the partially frozen mixture was allowed to warm to 23 °C. The biphasic mixture was diluted with 0.2 M aqueous sodium hydroxide solution (100 mL). The layers were separated. The aqueous layer was extracted with dichloromethane (100 mL). The organic layers were combined. The combined solution was washed sequentially with 0.1 M aqueous hydrochloric acid solution (100 mL), water (2 x 100 mL), then saturated aqueous sodium chloride solution (100 mL) and the washed solution was dried over sodium sulfate. The dried solution was filtered and the filtrate was concentrated to provide 380 mg of the product, (S)-\ ,9- dihydroxy-10-methoxy-5-(4-methoxybenzyloxy)-3-methyl-8-oxo-5,6,7,8- tetrahydroanthracene-2-carbaldehyde, as a yellow foam (86%). Ή NMR (500 MHz, CDCI3):
15.89 (brs, 1H), 12.81 (br s, 1H), 10.51 (s, 1H), 7.27-7.26 (m, 3H), 6.86 (d, 2H, J = 9.2 Hz), 5.14 (app s, 1H),4.62 (d, \H,J= 11.0 Hz), 4.51 (d, 1H,7= 11.0 Hz), 3.85 (s, 3H), 3.80 (s, 3H), 3.21 (m, 1H), 2.73 (s, 3H), 2.62 (m, 1H), 2.54 (m, 1H), 2.07 (m, 1H). I3C NMR (125 MHz, CDCI3): 204.4, 192.7, 166.6, 164.3, 159.3, 144.4, 142.7, 137.9, 130.4, 130.2, 129.4, 114.9, 114.2, 113.9, 113.8, 109.4, 70.4, 67.1,62.8, 55.3, 31.8, 26.5. FTIR, cm-1 (thin film): 3316 (brw), 2938 (m), 1678 (m), 1610 (s), 1514 (m), 1393 (m), 1246 (s). HRMS (ESI): Calcd for (C25H2407+Na)+ 459.1414; Found 459.1354. TLC (50% ethyl acetate-hexanes): R = 0.30 (CAM).
[00458] (5)-2,2-Di-/erf-butyl-7-methoxy-8-(4-methoxybenzyloxy)-5-methyl- 1 1 -oxo- 8,9, 10, 1 1 -tetrahydroanthra[9, 1 -de \ 1 ,3,21dioxasiline-4-carbaldehyde. Όι‘-tert- butyldichlorosilane (342 μL·, 1.62 mmol, 1.8 equiv) was added to a solution of (5)-l ,9- dihydroxy- 10-methoxy-5-(4-methoxybenzyloxy)-3-methyl-8-oxo-5,6,7,8- tetrahydroanthracene-2-carbaldehyde (380 mg, 0.90 mmol, 1 equiv), hydroxybenzotriazole (60.8 mg, 0.45 mmol, 0.50 equiv) and diisopropylethylamine (786 μί, 4.50 mmol, 5.0 equiv) in dimethylformamide (30 mL). The reaction flask was heated in an oil bath at 55 °C. After 2 h, the reaction flask was allowed to cool to 23 °C. The reaction mixture was partitioned between saturated aqueous sodium bicarbonate solution (100 mL) and ethyl acetate (150 mL). The layers were separated. The organic layer was washed sequentially with water (2 x 100 mL) then saturated aqueous sodium chloride solution (100 mL) and the washed solution was dried over sodium sulfate. The dried solution was filtered and the filtrate was concentrated. The residue was purified by flash-column chromatography (10% ethyl acetate- hexanes) to provide 285 mg of the product, (S)-2,2-di-/<?ri-butyl-7-methoxy-8-(4- methoxybenzyloxy)-5-methyl- 1 1 -oxo-8,9, 10, 1 1 -tetrahydroanthra[9, 1 -de] [ 1 ,3,2]dioxasiline-4- carbaldehyde, as a yellow foam (56%). The enantiomeric compound (/?)-2,2-di-½ri-butyl-7- methoxy-8-(4-methoxybenzyloxy)-5-methyl- l 1 -oxo-8,9, 10, 1 1 -tetrahydroanthra[9, 1 – i/e][ l ,3,2]dioxasiline-4-carbaldehyde has been prepared using the same route by utilizing R- (4-methoxybenzyloxy)cyclohex-2-enone as starting material. Ή NMR (500 MHz, CDCI3): 10.84 (s, 1 H), 7.37 (s, 1 H), 7.25 (d, 2H, J = 8.8 Hz), 6.85 (d, 2H, = 8.7 Hz), 5.20 (app s, 1 H), 4.62 (d, 1 H, 7 = 10.0 Hz), 4.51 (d, 1H, J = 1 1.4 Hz), 3.88 (s, 3H), 3.78 (s, 3H), 3.03 (m, 1H), 2.73 (s, 3H), 2.57-2.53 (m, 2H), 2.07 (m, 1H), 1.16 (s, 9H), 1.14 (s, 9H). 13C NMR (125 MHz, CDCl3): 195.6, 190.9, 160.5, 159.2, 150.4, 145.7, 140.4, 134.0, 133.9, 130.3, 129.4, 1 19.5, 1 16.6, 1 15.8, 1 15.3, 1 13.8, 70.4, 67.8, 62.9, 55.2, 34.0, 26.0, 26.0, 22.5, 21.3, 21.1. FTIR, cm“1 (thin film): 2936 (m), 2862 (m), 1682 (s), 1607 (s), 1371 (s), 1244 (s) 1057 (s). HRMS (ESI): Calcd for (C33H4o07Si+H)+ 577.2616; Found 577.2584. TLC (10% ethyl acetate-hexanes): R/ = 0.19 (CAM). Alternative Routes to (4S,6S)-6-(½rt-Butyldimethylsilyloxy)-4-(4-methoxybenzyloxy) cyclohex-2-enone.
Alternative Route 1.
[00459] (25,45,55)-2,4-Bis(ferf-butyldimethylsilyloxy)-5-hvdroxycvclohexanone. Dess- Martin periodinane (6.1 1 g, 14.4 mmol, 1.1 equiv) was added to a solution of diol (5.00 g, 13.3 mmol, 1 equiv) in tetrahydrofuran (120 mL) at 23 °C (Lim, S. M.; Hill, N.; Myers, A. G. J. Am. Chem. Soc. 2009, 131, 5763-5765). After 40 min, the reaction mixture was diluted with ether (300 mL). The diluted solution was filtered through a short plug of silica gel (-5 cm) and eluted with ether (300 mL). The filtrate was concentrated. The bulk of the product was transformed as outlined in the following paragraph, without purification. Independently,
s
an analytically pure sample of the product was obtained by flash-column chromatography (20% ethyl acetate-hexanes) and was characterized by Ή NMR, l 3C NMR, IR, and HRMS. TLC: (17% ethyl acetate-hexanes) R = 0.14 (CAM); Ή NMR (500 MHz, CDCI3) δ: 4.41 (dd, 1 H, 7 = 9.8, 5.5 Hz), 4.05 (m, l H), 4.00 (m, 1H), 2.81 (ddd, 1 H, 7 = 14.0, 3.7, 0.9 Hz), 2.52 (ddd, 1 H, 7 = 14.0, 5.3, 0.9 Hz), 2.29 (br s, 1 H), 2.18 (m, 1H), 1.98 (m, 1 H), 0.91 (s, 9H), 0.89 (s, 9H), 0.13 (s, 3H), 0.1 1 (s, 3H), 0.09 (s, 3H), 0.04 (s, 3H); l 3C NMR (125 MHz, CDCI3) δ: 207.9, 73.9, 73.3, 70.5, 43.3, 39.0, 25.7, 25.6, 18.3, 17.9, -4.7, -4.8, -4.9, -5.4; FTIR (neat), cm“‘ : 3356 (br), 2954 (m), 2930 (m), 2857 (m), 1723 (m), 1472 (m). 1253 (s), 1 162 (m), 1 105 (s), 1090 (s), 1059 (s), 908 (s), 834 (s), 776 (s), 731 (s); HRMS (ESI): Calcd for (C|8H3804Si2+H)+ 375. 2381 , found 375.2381.
[00460] (4 ,6 )-4.6-Bis(fcr/-butyldimethylsilyloxy)cvclohex-2-enone. Trifluoroacetic anhydride (6.06 mL, 43.6 mmol, 3.3 equiv) was added to an ice-cooled solution of the alcohol ( 1 equiv, see paragraph above) and triethylamine ( 18.2 mL, 131 mmol, 9.9 equiv) in dichloromethane (250 mL) at 0 °C. After 20 min, the cooling bath was removed and the reaction flask was allowed to warm to 23 °C. After 18 h, the reaction flask was cooled in an ice bath at 0 °C, and the product solution was diluted with water ( 100 mL). The cooling bath was removed and the reaction flask was allowed to warm to 23 °C. The layers were separated. The aqueous layer was extracted with dichloromethane (2 x 200 mL). The organic layers were combined. The combined solution was washed with saturated aqueous sodium chloride solution ( 100 mL) and the washed solution was dried over sodium sulfate. The dried solution was filtered and the filtrate was concentrated. The residue was purified by flash- column chromatography (6% ethyl acetate-hexanes) to provide 3.02 g of the product, (4S,65)-4,6-bis(/eri-butyldimethylsilyloxy)cyclohex-2-enone, as a colorless oil (64% over two steps). TLC: (20% ethyl acetate-hexanes) R = 0.56 (CAM); Ή NMR (500 MHz, CDC13) δ: 6.76 (dd, 1 Η, / = 10.1 , 3.6 Hz), 5.88 (d, 1 H, 7 = 10.1 Hz), 4.66 (ddd, 1 H, 7 = 5.6, 4.1 , 3.6 Hz), 4.40 (dd, 1 H, 7 = 8.1 , 3.7 Hz), 2.26 (ddd, 1 H, / = 13.3, 8.0, 4.1 Hz), 2.1 1 (ddd, 1 H, J = 13.2, 5.6, 3.8 Hz), 0.91 (s, 9H), 0.89 (s, 9H), 0.12 (s, 3H), 0. 1 1 (s, 3H), 0. 10 (s, 3H), 0.10 (s, 3H); 13C NMR ( 125 MHz, CDC13) δ: 197.5, 150.3, 127.0, 71 .0, 64.8, 41.6, 25.7, 25.7, 18.3, 18.1 , -4.7, -4.8, -4.8, -5.4; FTIR (neat), cm-1 : 3038 (w), 2955 (m), 2930 (m), 1705 (m), 1472 (m), 1254 (m), 1084 (m), 835 (s), 777 (s), 675 (s); HRMS (ESI): Calcd for (C,8H3602Si2+Na)+ 379. 2095, found 379. 2080.
[00461] (4S,6S)-6-(/er/-Butyldimethylsilyloxy)-4-hydroxycvclohex-2-enone. Tetra- j- butylammonium fluoride ( 1 .0 M solution in tetrahydrofuran, 8.00 mL, 8.00 mmol, 1 .0 equiv) was added to an ice-cooled solution of the enone (2.85 g, 8.00 mmol, 1 equiv) and acetic acid (485 ί, 8.00 mmol, 1 .0 equiv) in tetrahydrofuran (80 mL) at 0 °C. After 2 h, the cooling bath was removed and the reaction flask was allowed to warm to 23 °C. After 22 h, the reaction mixture was partitioned between water ( 100 mL) and ethyl acetate (300 mL). The layers were separated. The aqueous layer was extracted with ethyl acetate (2 x 300 mL). The organic layers were combined. The combined solution was washed sequentially with saturated aqueous sodium bicarbonate solution ( 100 mL) then saturated aqueous sodium chloride solution ( 100 mL) and the washed solution was dried over sodium sulfate. The dried solution was filtered and the filtrate was concentrated. The residue was purified by flash- column chromatography (25% ethyl acetate-hexanes) to provide 760 mg of the product, (4S,6S)-6-(ferNbutyldimethylsilyloxy)-4-hydroxycyclohex-2-enone, as a white solid (39%). TLC: (20% ethyl acetate-hexanes) R/ = 0.20 (CAM); Ή NMR (500 MHz, CDC13) δ: 6.87 (dd, 1 Η, 7 = 10.2, 3.2 Hz), 5.95 (dd, 1H, J = 10.3, 0.9 Hz), 4.73 (m, 1 H), 4.35 (dd, 1 H, 7 = 7.6, 3.7 Hz), 2.39 (m, 1 H), 2. 13 (ddd, 1 H, J = 13.3, 6.2, 3.4 Hz), 1.83 (d, 1 H, J = 6.2), 0.89 (s, 9H), 0.10 (s, 3H), 0. 10 (s, 3H); 13C NMR ( 125 MHz, CDCb) δ: 197.3, 150.0, 127.5, 70.9, 64.2, 41 .0, 25.7, 18.2, -4.8, -5.4; FTIR (neat), cm“1 : 2956 (w), 293 1 (w), 2858 (w), 1694 (m); HRMS (ESI): Calcd for (C |2H2203Si+H)+ 243.141 1 , found 243. 1412.
82″:.
[00462] (45.6S)-6-(fgrf-Butyldimethylsilyloxy)-4-(4-methoxybenzyloxy)cvclohex-2- enone. Triphenylmethyl tetrafluoroborate ( 16 mg, 50 μπιοΐ, 0.050 equiv) was added to a solution of 4-methoxybenzyl-2,2,2-trichloroacetimidate (445 μΙ_, 2.5 mmol, 2.5 equiv) and alcohol (242 mg, 1 .0 mmol, 1 equiv) in ether ( 10 mL) at 23 °C. After 4 h, the reaction mixture was partitioned between saturated aqueous sodium bicarbonate solution ( 15 mL) and ethyl acetate (50 mL). The layers were separated. The aqueous layer was extracted with ethyl acetate (50 mL). The organic layers were combined. The combined solution was washed with water (2 x 20 mL) and the washed solution was dried over sodium sulfate. The dried solution was filtered and the filtrate was concentrated. The residue was purified by flash column chromatography (5% ethyl acetate-hexanes initially, grading to 10% ethyl acetate-hexanes) to provide 297 mg of the product, (4S,6S)-6-(im-butyldimethylsilyloxy)-4-(4- methoxybenzyloxy)cyclohex-2-enone, as a colorless oil (82%).
Alternative Route 2.
[00463] (5)-?erf-Butyl(4-(4-methoxybenzyloxy)cvclohexa- 1.5-dienyloxy)dimethylsilane. rerr-Butyldimethylsilyl trifluoromethanesulfonate (202 iL, 0.94 mmol, 2.0 equiv) was added to an ice-cooled solution of triethylamine (262 μί, 1.88 mmol, 4.0 equiv) and enone ( 109 mg, 0.47 mmol, 1 equiv) in dichloromethane (5.0 mL). After 30 min, the reaction mixture was partitioned between saturated aqueous sodium bicarbonate solution ( 10 mL), water (30 mL), and dichloromethane (40 mL). The layers were separated. The organic layer was washed sequentially with saturated aqueous ammonium chloride solution (20 mL) then saturated aqueous sodium chloride solution (20 mL) and the washed solution was dried over sodium sulfate. The dried solution was filtered and the filtrate was concentrated. The residue was purified by flash-column chromatography with triethylamine-treated silica gel (5% ethyl acetate-hexanes), to provide 130 mg of the product, (5)-ierr-butyl(4-(4- methoxybenzyloxy)cyclohexa- l ,5-dienyloxy)dimethylsilane, as a colorless oil (80%). Ή
NMR (500 MHz, CDC13): 7.27 (d, 2H, J = 8.7 Hz), 6.88 (d, 2H, J = 8.6 Hz), 5.96 (dd, 1 H, J = 9.9, 3.5 Hz), 5.87 (d, 1 H, 7 = 9.6 Hz), 4.94 (m, l H), 4.46 (s, 2H), 4.14 (m, 1 H), 3.81 (s, 3H), 2.49 (m, 2H), 0.93 (s, 9H), 0. 16 (s, 3H), 0.15 (s, 3H). , 3C NMR ( 125 MHz, CDC13): 159.1 , 147.5, 130.9, 129.2, 128.6, 128.1 , 1 13.8, 101.4, 70.2, 69.0, 55.3, 28.5, 25.7, 18.0, ^1.5, -4.5. FTIR, cm-1 (thin film): 2957 (m), 2931 (m), 2859 (m), 1655 (w), 1613 (w), 1515 (s), 1248 (s), 1229 (s), 1037 (m), 910 (s). HRMS (ESI): Calcd for (C2oH3o03Si+H)+ 347.2037; Found 347.1912. TLC (20% ethyl acetate-hexanes): R = 0.74 (CAM).
OP B OPMB DM 00 ,,Α,,
c Ύ’“ -ietone ii ·η- ) ‘”OH
OTBS 82 Q
[00464] (4S,6S)-6-Hvdroxy-4-(4-methoxybenzyloxy)cvclohex-2-enone. A solution of dimethyldioxirane (0.06 M solution in acetone, 2.89 mL, 0.17 mmol, 1.2 equiv) was added to an ice-cooled solution of (S)-ieri-butyl(4-(4-methoxybenzyloxy)cyclohexa- l ,5- dienyloxy)dimethylsilane (50 mg, 0.14 mmol, 1 equiv). After 10 min, the reaction mixture was partitioned between dichloromethane ( 15 mL) and 0.5 M aqueous hydrochloric acid ( 10 mL). The layers were separated. The organic layer was washed sequentially with saturated aqueous sodium bicarbonate solution ( 10 mL) then water ( 10 mL) and the washed solution was dried over sodium sulfate. The dried solution was filtered and the filtrate was concentrated. The residue was purified by flash-column chromatography to provide 30 mg of the product, (4S,6S)-6-hydroxy-4-(4-methoxybenzyloxy)cyclohex-2-enone, as a colorless oil (82%). Ή NMR (500 MHz, CDC13): 7.28 (d, 2H, J = 8.2 Hz), 6.89 (m, 3H), 6.09 (d, 1 H, J = 10.1 Hz), 4.64 (m, 2H), 4.53 (d, 1 H, 7 = 1 1 .4 Hz), 4.24 (m, 1 H), 3.81 (s, 3H), 3.39 (d, 1 H, 7 = 1.4 Hz), 2.67 (m, 1 H), 1 .95 (ddd, 1 H, 7 = 12.8, 12.8, 3.6 Hz). I 3C NMR ( 125 MHz, CDC13): 200.4, 159.5, 146.6, 129.7, 129.4, 127.8, 1 14.0, 71.6, 69.8, 68.9, 55.3, 35.1 . FTIR, cm-1 (thin film): 3474 (br), 2934 (m), 2864 (m), 1692 (s), 1613 (m), 1512 (s), 1246 (s), 1059 (s), 1032 (s). HRMS (ESI): Calcd for (C,4Hl6O4+Na)+ 271.0941 ; Found 271.0834. TLC (50% ethyl acetate-hexanes): R/ = 0.57 (CAM).
[00465] (45,65)-6-(½rt-Butyldimethylsilyloxy)-4-(4-methoxybenzyloxy)cvclohex-2- enone. rerr-Butyldimethychlorosilane (26 mg, 0.18 mmol, 1.5 equiv) was added to an ice- cooled solution of (45,65)-6-hydroxy-4-(4-methoxybenzyloxy)cyclohex-2-enone (29 mg, 0.12 mmol, 1 equiv) and imidazole (24 mg, 0.35 mmol, 3 equiv) in dimethylformamide (0.5 mL). After 45 min, the reaction mixture was partitioned between water (15 mL), saturated aqueous sodium chloride solution (15 mL), and ethyl acetate (20 mL). The layers were separated. The organic layer was washed with water (2 x 20 mL) and the washed solution was dried over sodium sulfate. The dried solution was filtered and the filtrate was concentrated. The residue was purified by flash-column chromatography to provide 29 mg of the product, (4S,6S)-6-(rm-butyldimethylsilyloxy)-4-(4-methoxybenzyloxy)cyclohex-2- enone, as a colorless oil (87%).
Glycosylation experiments
[00466] Glycosylation experiments demonstrate that the chemical process developed allows for the preparation of synthetic, glycosylated trioxacarcins. Specifically, the C4 or CI 3 hydroxyl group may be selectively glycosylated with a glycosyl donor (for example, a glycosyl acetate) and an activating agent (for example, TMSOTf), which enables preparation of a wide array of trioxacarcin analogues.
Selective Glycosylation of the C4 Hydroxyl Group
[00467] 2,3-Dichloro-5,6-dicyanobenzoquinone ( 19.9 mg, 88 μιτιοΐ, 1.1 equiv) was added to a vigorously stirring, biphasic solution of differentially protected trioxacarcin precursor (60 mg, 80 μιτιοΐ, 1 equiv) in dichloromethane ( 1.1 mL) and pH 7 phosphate buffer (220 μί) at 23 °C. The reaction flask was covered with aluminum foil to exclude light. Over the course of 3 h, the reaction mixture was observed to change from myrtle green to lemon yellow. The product solution was partitioned between water (5 mL) and dichloromethane (50 mL). The layers were separated. The organic layer was dried over sodium sulfate. The dried solution was filtered and the filtrate was concentrated. The residue was purified by preparatory HPLC (Agilent Prep-C 18 column, 10 μιτι, 30 x 150 mm, UV detection at 270 nm, gradient elution with 40→90% acetonitrile in water, flow rate: 15 mL/min) to provide 33 mg of the product as a yellow-green powder (65%).
[00468] Trimethylsilyl triflate ( 10% in dichloromethane, 28.3 μί, 16 μπιοΐ, 0.3 equiv) was added to a suspension of deprotected trioxacarcin precursor (33 mg, 52 μπιοΐ, 1 equiv), 1 -0- acetyltrioxacarcinose A ( 14.1 mg, 57 μιτιοΐ, 1.1 equiv), and powdered 4- A molecular sieves (-50 mg) in dichloromethane (1 .0 mL) at -78 °C. After 5 min, the mixture was diluted with dichloromethane containing 10% triethylamine and 10% methanol (3 mL). The reaction flask was allowed to warm to 23 °C. The mixture was filtered and partitioned between
dichloromethane (40 mL) and saturated aqueous sodium chloride solution (5 mL). The layers were separated. The organic layer was dried over sodium sulfate. The dried solution was filtered and the filtrate was concentrated. The residue was purified by preparatory HPLC (Agilent Prep-C 18 column, 10 μπι, 30 x 150 mm, UV detection at 270 nm, gradient elution with 40→90% acetonitrile in water, flow rate: 15 mL/min) to provide 20 mg of the product as a yellow-green powder (47%). TLC: (5% methanol-dichloromethane) R = 0.40 (CAM); Ή NMR (500 MHz, CDC13) δ: 7.47 (s, 1H), 5.38 (d, 1H, J = 3.6 Hz), 5.35 (app s, 1 H), 5.26 ppm (d, 1 H, 7 = 4.0 Hz), 4.84 (d, 1 H, J = 4.0 Hz), 4.78 (dd, 1 H, 7 = 12.3, 5.2 Hz), 4.75 (s, 1H), 4.71 (s, 1 H), 4.52 (q, 1H, J = 6.6 Hz), 3.86 (s, 1 H), 3.83 (s, 3H), 3.62 (s, 3H), 3.47 (s, 3H), 3.15 (d, l H, y = 5.3 Hz), 3.05 (d, 1 H, 7 = 5.3 Hz), 2.60 (s, 3H), 2.58 (m, 1H), 2.35 (m, 1 H), 2.14 (s, 3H), 1.96 (dd, 1 H, 7 = 14.6, 4.1 Hz), 1.62 (d, 1 H, 7 = 14.6 Hz), 1.26 (s, 1 H), 1.23 (d, 3H, J = 6.6 Hz), 1.08 (s, 3H), 0.95 (s, 9H), 0.24 (s, 3H), 0.16 (s, 3H); ‘3C NMR ( 125 MHz, CDC13) 6: 202.8, 170.5, 163.2, 151.8, 144.4, 142.4, 135.2, 126.6, 1 16.8, 1 15.2, 1 15.1 , 108.3, 104.0, 100.3, 98.6, 98.3, 74.6, 73.4, 69.8, 69.5, 69.5, 68.9, 69.5, 69.5, 68.9, 68.4, 62.9, 62.7, 57.2, 56.8, 50.7, 38.8, 36.8, 26.0, 25.9, 21.1 , 20.6, 18.6, 17.0, -4.2, -5.3; FTIR (neat), cm“‘ : 2953 (w), 2934 (w), 2857 (w), 1749 (w), 1622 (m), 1570 (w), 1447 (w), 1391 (m), 1321 (w), 1294 (w), 1229 (m), 1 159 (m), 1 121 (s), 1084 (s), 1071 (m), 1020 (m), 995 (s), 943 (s), 868 (m), 837 (m), 779 (m); HRMS (ESI): Calcd for (C4oH540i6Si+Na)+ 841.3073, found
841.3064.
Glycosylation of a Cycloaddition Coupling Partner
[00469] 2,3-Dichloro-5,6-dicyanobenzoquinone ( 14.3 mg, 63 μπιοΐ, 1.2 equiv) was added to a vigorously stirring, biphasic solution of differentially protected aldehyde (37 mg, 52 μιτιοΐ, 1 equiv) in dichloromethane (870 μί) and water (175 μί) at 23 °C. The reaction flask was covered with aluminum foil to exclude light. Over the course of 2 h, the reaction mixture was observed to change from myrtle green to lemon yellow. The product solution was partitioned between water (5 mL) and dichloromethane (40 mL). The layers were separated. The organic layer was dried over sodium sulfate. The dried solution was filtered and the filtrate was concentrated. The residue was purified by flash-column chromatography (5% ethyl acetate-hexanes initially, grading to 10% ethyl acetate-hexanes) to provide 28 mg of the product as a yellow powder (91 %). TLC: (20% ethyl acetate-hexanes) R/ = 0.37 (CAM); Ή NMR (500 MHz, CDC13) δ: 10.83 (s, 1H), 7.30 (s, 1 H), 5.45 (m, 1H), 4.68 (dd, 1H, / = 10.3, 4.2 Hz), 3.97 (s, 3H), 3.31 (brs, 1H), 2.72 (s, 3H), 2.51-2.45 (m, 1H), 2.41-2.37 (m, 1H), 1.15 (s, 9H), 1 , 13 (s, 9H), 0.88 (s, 9H), 0.15 (s, 3H), 0.1 1 (s, 3H); l 3C NMR (125 MHz, CDCI3) δ: 194.6, 191 , 160.5, 150.2, 146, 140.8, 135.8, 134, 1 19.6, 1 16.2, 1 15.4, 1 14.7, 72.7, 63.7, 62.4, 38.8, 29.9, 62.4, 38.8, 63.7, 62.4, 38.8, 63.7, 62.4, 38.8, 29.9, 26.2, 26.1 , 26, 22.7, 21.4; FTIR (neat), cm“1 : 3470 (br, w), 2934 (w), 2888 (w), 1684 (s), 1607 (s), 1560 (w), 1472 (m), 1445 (w), 1392 (m), 1373 (s), 1242 (s), 1 153 (s), 1 1 19 (w), 1074 (m), 1044 (s), 1013 (s), 982 (w), 934 (m), 907 (w), 870 (m), 827 (s), 795 (s), 779 (s), 733 (s), 664 (s); HRMS (ESI): Calcd for (C3iH4607Si2+H)+ 587.2855, found 587.2867.
[00470] Trimethylsilyl triflate (10% in dichloromethane, 25.9 μί, 14 μπιοΐ, 0.3 equiv) was added to a suspension of deprotected aldehyde (28 mg, 48 μηιοΐ, 1 equiv), 1-0- acetyltrioxacarcinose A (12.9 mg, 52 μπιοΐ, 1.1 equiv), and powdered 4-A molecular sieves (-50 mg) in dichloromethane ( 1.0 mL) at -78 °C. After 5 min, the mixture was diluted with dichloromethane containing 10% triethylamine and 10% methanol (3 mL). The reaction flask was allowed to warm to 23 °C. The mixture was filtered and partitioned between dichloromethane (40 mL) and saturated aqueous sodium chloride solution (5 mL). The layers were separated. The organic layer was dried over sodium sulfate. The dried solution was filtered and the filtrate was concentrated. The residue was purified by preparatory HPLC (Agilent Prep-C 18 column, 10 μπι, 30 x 150 mm, UV detection at 270 nm, gradient elution with 80→98% acetonitrile in water, flow rate: 15 mL/min) to provide 15 mg of the product as a yellow powder (41 %). TLC: (20% ethyl acetate-hexanes) R/ = 0.29 (CAM); Ή NMR (500 MHz, CDC13) δ: 10.83 (s, 1 H), 7.32 (s, 1 H), 5.43 (d, 1 H, J = 3.9 Hz), 5.32 (m, 1H), 4.74 (s, 1 H), 4.67 (dd, 1 H, J = 12.3, 5.0 Hz), 4.54 (q, 1H, J = 6.6 Hz), 3.91 (s, 1H), 3.88 (s, 3H), 2.72 (s, 3H), 2.59 (ddd, 1 H, J = 13.8, 5.0, 3.2 Hz), 2.34 (m, 1H), 2.14 (s, 3H), 1.97 (dd, 1H, J = 14.2, 4.2 Hz), 1.71 (d, 1 Η, / = 14.6 Hz), 1.22 (d, 3H, J = 6.3 Hz), 1.15 (s, 9H), 1.15 (s, 9H), 1.08 (s, 3H), 0.93 (s, 9H), 0.23 (s, 3H), 0.13 (s, 3H); 13C NMR (125 MHz, CDC13) δ: 193.9, 191.0, 170.5, 146.4, 140.9, 134.0, 132.4, 1 19.8, 1 16.8, 1 15.8, 1 15.0, 1 10.8, 99.6, 74.6, 71.5, 70.4, 68.9, 62.9, 62.7, 39.1 , 36.9, 26.2, 26.1 , 26.1 , 25.9, 24.1 , 22.7, 21.5, 21.3, 21.1 , 18.7, 16.9, -4.1 , -5.3; FTIR (neat), cm-1 : 3524 (br, w), 2934 (m), 2861 (m), 1749 (m), 1686 (s), 1607 (s), 1560 (m), 1474 (m), 1447 (m), 1424 (w), 1375 (s), 1233 (s), 1 159 (s), 1 1 17 (m), 1080 (m), 1049 (s), 1015 (s), 997 (s), 937 (m), 883 (m), 872 (m), 827 (s), 797 (m), 781 (m), 737 (w), 677 (w), 667 (m); HRMS (ESI): Calcd for (C40H60O, ,Si2+H)+773.3747, found 773.3741.
General Glycosylation Procedure of the C13 Hydroxyl Group
[00471] Crushed 4-A molecular sieves (-570 mg / 1 mmol sugar donor) was added to a stirring solution of the sugar acceptor (1 equiv.) and the sugar donor (30.0 equiv.) in dichloromethane ( 1.6 mL / 1 mmol sugar donor) and diethylether (0.228 mL / 1 mmol sugar donor) at 23 °C. The bright yellow mixture was stirred for 90 min at 23 °C and finally cooled to -78 °C. TMSOTf (10.0 equiv.) was added over the course of 10 min at -78 °C. After 4 h, a second portion of TMSOTf (5.0 equiv.) was added at -78 °C and stirring was continued for 1 h. The last portion of TMSOTf (5 equiv.) was added. After 1 h, triethylamine (20 equiv.) was added and the reaction the product mixture was filtered through a short column of silica gel deactivated with triethylamine (30% ethyl acetate-hexanes initially, grading to 50% ethyl acetate-hexanes). H NMR analysis of the residue showed minor sugar donor remainings and that the sugar acceptor had been glycosylated. The residue was purified by preparatory HPLC (Agilent Prep-C 18 column, 10 μπι, 30 x 150 mm, UV detection at 270 nm, gradient elution with 40→100% acetonitrile in water, flow rate: 15 mL/min) to provide the glycosylation product as a bright yellow oil
Three Specific Compounds Prepared by the General Glycosylation Procedure for the CI 3 Hydroxyl Group:
[00472] 10% yield; TLC: (50% ethyl acetate-hexane) R = 0.58 (UV, CAM); Ή NMR (600 MHz, CDC13) δ: 7.43 (s, 1 H), 5.84 (t, J = 3.6 Hz, 1 H), 5.29 (d, J = 4.2 Hz, 1 H), 5.19 (d, J = 4.2 Hz, 1 H), 5.01 (q, J = 6.6 Hz, 1 H), 4.75 (t, J = 3.6 Hz, 1 H), 4.73 (s, 1 H), 3.88 (s, OH), 3.77 (s, 3H), 3.63 (s, 3H), 3.47 (s, 3H), 3.03 (app q, J = 5.4 Hz, 2H), 2.84 (d, J = 6.0 Hz, 1 H), 2.77 (d, J = 6.0 Hz, 1 H), 2.72 (t, J = 6.6 Hz, 2H), 2.58 (s, 3H), 2.36 (s, 3H), 2.33 (t, J = 3.0 Hz, 2H), 2.23 (s, 3H), 2.1 1 -2.06 (m, 2H), 1.08 (d, J = 6.0 Hz, 3H). ‘
[00473] 81 % yield, TLC: (50% ethyl acetate-hexane) R = 0.30 (UV, CAM); Ή NMR (600 MHz, CDCI3) δ: 7.46 (s, 1 H), 7.28 (d, J = 9 Hz, 2H), 6.87 (d, J = 8.4 Hz, 2 H), 5.83 (dd, J = 3.6, 1.8 Hz, 1 H), 5.30 (d, J = 4.2 Hz, 1 H), 5.19 (d, J = 4.2 Hz, 1 H), 5.19 (m, 1 H), 5.00 (q, J = 6.0 Hz, 1 H), 4.96 (dd, J = 12.0, 4.8 Hz, 1 H), 4.75 (t, J = 3.6 Hz, 1 H), 4.74 (s, l H), 4.70 (d, y = 10.8 Hz, 1 H), 4.59 (d, J = 10.8 Hz, 1 H), 3.86 (s, OH), 3.83 (s, 3H), 3.80 (s, 3H), 3.63 (s, 3H), 3.47 (s, 3H), 2.81 (d, J = 6.0 Hz, 1 H), 2.73-2.68 (m, 1 H), 2.70 (d, J = 6.0 Hz, 1 H), 2.59 (s, 3H), 2.35 (s, 3H), 2.33-2.28 (m, 2H), 2.22 (s, 3H), 2.19- 2.1 3 (m, 1 H), 1 .08 (d, J = 6.0 Hz, 3H), 0.97 (s, 9H), 0.25 (s, 3H), 0.17 (s, 3H); HRMS (ESI): Calcd for (C49H62018Si+H)+ 967.3778, found 967.3795; HRMS (ESI): Calcd for (C ¾20,8Si+Na)+ 989.3598, found 989.3585.
[00474] Compound Detected by ESI Mass Spectrometry: Calculated Mass for
[C52H7| N302i Si-Hrl = 1 100.4277, Measured Mass = 1 100.4253.
PATENT
US 4511560
https://www.google.com/patents/US4511560
The physico-chemical characteristics of DC-45-A and DC-4-5-B2 according to this invention are as follows:
(1) DC-45-A
(1) Elemental analysis: H:5.74%, C:55.11%
(2) Molecular weight: 877
(3) Molecular formula: C42 H52 O20
(4) Melting point: 180° C.±3° C. (decomposed)
(5) Ultraviolet absorption spectrum: As shown in FIG. 1 (in 50% methanol)
(6) Infrared absorption spectrum: As shown in FIG. 2 (KBr tablet method)
(7) Specific rotation: [α]D 25 =-15.3° (c=1.0, ethanol)
(8) PMR spectrum (in CDC]3 ; ppm): 1.07 (3H,s); 1.10 (3H, d, J=6.8); 1.24 (3H,d, J=6.5); many peaks between 1.40-2.30; 2.14 (3H,s); 2.49 (3H,s); 2.63 (3H,s); many peaks between 2.30-2.80; 2.91 (1H,d, J=5.6); 3.00 (1H,d, J=5.6); 3.49 (3H,s); 3.63 (3H,s); 3.85 (3H, s); many peaks between 3.60-4.00; 4.18 (1H,s); 4.55 (1H,q, J=6.8); many peaks between 4.70-4.90; 5.03 (1H, q, J=6.5); 5.25 (1H,d, J=4.0); 5.39 (1H, d, J=4.0); 5.87 (1H, m); 7.52 (1H,s); 14.1 (1H,s)
(9) CMR spectrum (in CDCl3 ; ppm): 210.9; 203.8; 170.3; 162.1; 152.5; 145.2; 142.3; 135.3; 126.7; 117.0; 114.2; 108.3; 105.3; 99.7; 97.2; 93.7; 85.1; 79.0; 74.6; 71.1; 69.6; 69.3; 68.8; 67.9; 66.3; 64.0; 62.8; 57.3; 55.9; 36.5; 32.2; 28.0; 25.7; 20.9; 20.2; 17.0; 14.7
(10) Solubility: Soluble in methanol, ethanol, water and chloroform; slightly soluble in acetone and ethyl acetate, and insoluble in ether and n-hexane
(2) DC-45-B2
(1) Elemental analysis: H: 6.03%, C: 54.34%
(2) Molecular weight: 879
(3) Molecular formula: C42 H54 O20
(4) Melting point: 181°-182° C. (decomposed)
(5) Ultraviolet absorption spectrum: As shown in FIG. 5 (in 95% ethanol)
(6) Infrared absorption spectrum: As shown in FIG. 6 (KBr tablet method)
(7) Specific rotation: [α]D 25 =-10° (c=0.2, ethanol)
(8) PMR spectrum (in CDCl3 ; ppm): 1.07 (3H,s); many peaks between 1.07-1.5; many peaks between 1.50-2.80; 2.14 (3H,s); 2.61 (3H, broad s); 2.86 (1H, d, J=5.7); 2.96 (1H, d, J=5.7); 3.46 (3H,s); 3.63 (3H, s); 3.84 (3H, s); many peaks between 3.65-4.20; many peaks between 4.40-5.00; many peaks between 5.10-5.50; 5.80 (1H, broad s); 7.49 (1H, d, J=1.0); 14.1 (1H, s)
(9) CMR spectrum (in CDCl3 ; ppm): 202.8; 170.2; 163.1; 151.8; 144.8; 142.9; 135.4; 126.5; 116.8; 114.9; 107.3; 104.6; 101.5; 99.6; 98.0; 94.4; 74.4; 72.5; 71.4; 70.4; 69.1; 68.8; 68.3; 67.9; 67.5; 66.4; 62.9; 62.7; 56.8; 56.5; 48.0; 36.7; 32.3; 25.7; 20.8; 20.3; 18.2; 16.9; 15.5
(10) Solubility: Soluble in methanol, ethanol, acetone, ethyl acetate and chloroform; slightly soluble in benzene, ether and water; and insoluble in n-hexane.
//////
CC1C(C(CC(O1)OC2CC(C(=O)C3=C(C4=C5C(=C(C=C4C(=C23)OC)C)C6C7C(O5)(C8(CO8)C(O6)(O7)C(OC)OC)OC9CC(C(C(O9)C)(C(=O)C)O)O)O)O)(C)O)OC(=O)C
DRUG REGULATORY AFFAIRS INTERNATIONAL
Since 1st October 2012, special regulations have been applying to the US Type II Drug Master Files. This year in February, the FDA published a new Guidance for Industry. Read here what the DMF holder has to consider when submitting data about the API Drug Master File.
Since the coming into force of the “Generic Drug User Fee Act” (GDUFA) on 1st October 2012, special regulations have been applying to the submission to the FDA of a Drug Master Files for a pharmaceutical API (Type II DMF). The DMF holder must pay a one-time fee when authorising the reference of his/ her DMF in an application for a generic drug (Abbreviated New Drug Application, ANDA). Moreover, the DMF will undergo a completeness assessment through the FDA.
This year in February, the FDA published a Guidance for Industry entitled “Completeness Assessments for Type II API DMFs under GDUFA”…
View original post 350 more words

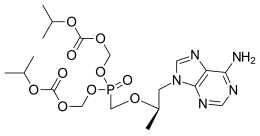
Tenofovir Disoproxil Fumarate
For full details see end of page


The current three-step manufacturing route for the preparation of tenofovir disoproxil fumarate (1) was assessed and optimized leading to a higher yielding, simpler, and greener process. Key improvements in the process route include the refinement of the second stage through the replacement of the problematic magnesium tert-butoxide (MTB) with a 1:1 ratio of a Grignard reagent and tert-butanol. The development of a virtually solvent-free approach and the establishment of a workup and purification protocol which allows the isolation of a pure diethyl phosphonate ester (8) was achieved
see………….http://pubs.acs.org/doi/abs/10.1021/acs.oprd.5b00364

Department of Chemistry, Natural and Agricultural Sciences, University of Pretoria, 2 Lynnwood Road, Hatfield, 0002, Gauteng, South Africa

///////

5-[[(1R)-2-(6-Amino-9H-purin-9-yl)-1-methylethoxy]methyl]-2,4,6,8-tetraoxa-5-phosphanonanedioic Acid 1,9-Bis(1-methylethyl) Ester 5-Oxide (2E)-2-Butenedioate; GS 4331-05; PMPA Prodrug; Tenofovir DF; Virea; Viread;
GILEAD-4331-300
201341-05-1 – free base, (Tenofovir Disoproxil
Fumarate |
202138-50-9 |
| 113-115°C (dec.) |
| CAS No.: | 202138-50-9 |
|---|---|
| Name: | Tenofovir disoproxil fumarate |
| Molecular Structure: | |
 |
|
| Formula: | C19H30N5O10P.C4H4O4 |
| Molecular Weight: | 635.51 |
| Synonyms: | TDF;PMPA prodrug;Tenofovir Disoproxil Fumarate [USAN];9-((R)-2-((Bis(((isopropoxycarbonyl)oxy)methoxy)phosphinyl)methoxy)propyl)adenine, fumarate;201341-05-1;Bis(NeopentylOC)PMPA;Viread;GS 4331-05 (*1:1 Fumarate salt*);Viread (*1:1 Fumarate salt*);Truvada;Tenofovir DF;[[(2R)-1-(6-aminopurin-9-yl)propan-2-yl]oxymethyl-(propan-2-yloxycarbonyloxymethoxy)phosphoryl]oxymethyl propan-2-yl carbonate; |
|
|
|
|
|
Tenofovir disoproxil is an antiretroviral medication used to prevent and treat HIV/AIDS and to treat chronic hepatitis B.[1] The active substance is tenofovir, while tenofovir disoproxil is a prodrug that is used because of its better absorption in the gut.
The drug is on the World Health Organization’s List of Essential Medicines, the most important medications needed in a basic health system.[2] It is marketed by Gilead Sciences under the trade name Viread (as the fumarate, TDF).[3] As of 2015 the cost for a typical month of medication in the United States is more than 200 USD.[4]
A Cochrane review examined the use of tenofovir for prevention of HIV before exposure. It found that both tenofovir alone and the tenofovir/emtricitabine combination decreased the risk of contracting HIV.[7]
The U. S. Centers for Disease Control and Prevention (CDC) conducted a study in partnership with the Thailand Ministry of Public Health to ascertain the effectiveness of providing people who inject drugs illicitly with daily doses of the antiretroviral drug tenofovir as a prevention measure. The results of the study were released in mid-June 2013 and revealed a 48.9%-reduced incidence of the virus among the group of subjects who received the drug, in comparison to the control group who received a placebo. The principal investigator of the study stated: “We now know that pre-exposure prophylaxis can be a potentially vital option for HIV prevention in people at very high risk for infection, whether through sexual transmission or injecting drug use.”[8]
The most common side effects associated with tenofovir include nausea, vomiting, diarrhea, and asthenia. Less frequent side effects include hepatotoxicity, abdominal pain, and flatulence.[9] Tenofovir has also been implicated in causing renal toxicity, particularly at elevated concentrations.[10]
Tenofovir can cause acute renal failure, Fanconi syndrome, proteinuria, or tubular necrosis.[citation needed] These side effects are due to accumulation of the drug in proximal tubules.[citation needed] Tenofovir can interact with didanosine by increasing didanosine’s concentration.[citation needed] It also decreases the concentration of atazanavir sulfate.[citation needed]
Tenofovir is a defective adenosine nucleotide that selectively interferes with the action of reverse transcriptase, but only weakly interferes with mammalian DNA polymerases α, β, and mitochondrial DNA polymerase γ.[11] Tenofovir prevents the formation of the 5′ to 3′ phosphodiester linkage essential for DNA chain elongation. A phosphodiester bond cannot be formed because the tenofovir molecule lacks an —OH group on the 3′ carbon of its deoxyribose sugar.[11] Once incorporated into a growing DNA strand, tenofovir causes premature termination of DNA transcription. The drug is classified as a nucleotide analogue reverse transcriptase inhibitor (NRTI), that inhibits reverse transcriptase.[11] Reverse transcriptase is a crucial viral enzyme in retroviruses such as human immunodeficiency virus (HIV) and in hepatitis B virus infections.[5]
Tenofovir was initially synthesized by Antonín Holý at the Institute of Organic Chemistry and Biochemistry, Academy of Sciences of the Czech Republic in Prague. The patent[12] filed by Holý in 1984 makes no mention of the potential use of the compound for the treatment of HIV infection, which had only been discovered one year earlier.
In 1985, De Clercq and Holý described the activity of PMPA against HIV in cell culture.[13] Shortly thereafter, a collaboration with the biotechnology company Gilead Sciences led to the investigation of PMPA’s potential as a treatment for HIV infected patients. In 1997 researchers from Gilead and the University of California, San Francisco demonstrated that tenofovir exhibits anti-HIV effects in humans when dosed by subcutaneous injection.[14]
The initial form of tenofovir used in these studies had limited potential for widespread use because it was not absorbed when administered orally. A medicinal chemistry team at Gilead developed a modified version of tenofovir, tenofovir disoproxil.[15] This version of tenofovir is often referred to simply as “tenofovir”. In this version of the drug, the two negative charges of the tenofovir phosphonic acid group are masked, thus enhancing oral absorption.
Tenofovir disoproxil was approved by the U.S. FDA on October 26, 2001, for the treatment of HIV, and on August 11, 2008, for the treatment of chronic hepatitis B.[16][17]
Tenofovir disoproxil is a prodrug form of tenofovir. It is also marketed under the brand name Reviro by Dr. Reddy’s Laboratories. Tenofovir is also available in a fixed-dose combination with emtricitabine in a product with the brand name Truvada for once-a-day dosing. Efavirenz/emtricitabine/tenofovir disoproxil (brand name Atripla) — a fixed-dose triple combination of tenofovir, emtricitabine, and efavirenz, was approved by the FDA on 12 July 2006 and is now available, providing a single daily dose for the treatment of HIV.
Tenofovir may be measured in plasma by liquid chromatography. Such testing is useful for monitoring therapy and to prevent drug accumulation and toxicity in people with kidney or liver problems.[18][19][20]
PATENT
http://www.google.com/patents/EP2545063A2?cl=en
Tenofovir Disoproxil is chemically known as 9-[-2-(R)-[[bis [[(isopropoxycarbonyl) oxy]methoxy] phosphinoyl]methoxy]propyl]-adenine, having the following structural formula-I.
Formula-I
Tenofovir is a highly potent antiviral agent, particularly for the therapy or prophylaxis of retroviral infections and belongs to a class of drugs called Nucleotide Reverse Transcriptase Inhibitors (NRTI) which blocks reverse transcriptase an enzyme crucial to viral production in HIV-infected people.
Tenofovir Disoproxil and its pharmaceutically acceptable salts were first disclosed in US 5,922,695. This patent discloses the preparation of Tenofovir Disoproxil by the esterification of Tenofovir with chloromethyl isopropyl carbonate using l-methyl-2- pyrrolidinone and triethylamine. In this patent Tenofovir Disoproxil is converted into its Fumarate salt without isolation. PCT Publication WO 2008007392 discloses process for the preparation of Tenofovir Disoproxil fumarate, wherein the isolated crystalline Tenofovir Disoproxil is converted into fumarate salt.
Tenofovir Disoproxil processes in the prior art are similar to process disclosed in product patent US 5,922,695. According to the prior art processes, Tenofovir Disoproxil fumarate obtained is having low yields and also show the presence of impurities such as dimers.
scheme- 1.
Tenofovir disoproxil chloromethyl isopropyl carbonate
Tenofovir disoproxil fumarate
Example 1 : Process for the preparation of Tenofovir Disoproxil fumarate
Toluene (500 ml) was added to the Tenofovir (100 gm) and stirred at room temperature. To this triethylamine (66.31 gm) was added, temperature was raised to 90° C and water was collected by azeotropic distillation at 110°C. Toluene was completely distilled under vacuum at same temperature. The reaction mixture was cooled to room temperature and to this a mixture of N-methyl pyrrolidine (300 gm), triethylamine (66.31 gm), Tetrabutyl ammonium bromide (52.8 gm) and trimethyl silyl chloride (17.8 gm) were added. The above reaction mixture was heated to 50-55 °C and was added slowly chloromethyl. isopropyl carbonate (CMIC) and maintained the reaction mixture at 50-55°C for 5 hrs. (Qualitative HPLC analysis shows about 85% product formation). The above reaction mixture was cooled to room temperature and filtered. The filtrate was added to DM water at 5-10°C and extract with dichloromethane. The combined dichloromethane layer was concentrated under vacuum and the crude was Co-distilled with cyclohexane and this crude was taken into isopropyl alcohol (1000 ml). To this fumaric acid (38 gm) was added and temperature was raised to 50° C. The reaction mixture was filtered and filtrate was cooled to 5-10° C. The obtained solid was filtered and washed with isopropyl alcohol. The compound was dried under vacuum to yield Tenofovir Disoproxil fumarate (140 gm).
Example-2 : Preparation of Tenofovir
N-methyl-2-pyrrolidone (25 gm) was taken along with toluene (150 gm) into a reaction vessel. l-(6-amino-purin-9-yl)-propan-2-ol (100 gm); toluene-4-sulfonic acid diethoxy phosphoryl methyl ester (200 gm) and magnesium ter-butoxide (71.2 gm) were also taken at’ 25-35°C. Temperature was raised to 74-75 °C and maintained for 5-6hrs. After completion of reaction, acetic acid (60 gm) was added and maintained for 1 hr. Later aq.HBr (332 gm) was taken and heated to 90-95 °C. After reaction completion, salts were filtered and filtrate was subjected to washings with water and extracted into methylene dichloride. Later pH was adjusted using CS lye below 10 °C. Tenofovir product was isolated using acetone.
Yield: 110 gm.
Example 3 : Preparation of Tenofovir disoproxil
(R)-9-[2-(phosphonomethoxy)propyl]adenine (25 gm), triethyl amine (25 ml) and cyclohexane (200 ml) were combined and heated to remove water and the solvent was distilled off under vacuum. The reaction mass was cooled to room temperature N-methyl pyrrolidinone (55 ml), triethyl amine (25 ml) and tetra butyl ammonium bromide(54 gms) were added to the reaction mixture. The reaction mass was heated to 50-60°C and chloromethyl isopropyl carbonate (65 gm) was added and maintained for 4-8 hrs at 50- 60°C and then cooled to 0°C. The reaction mass was diluted with chilled water or ice and precipitated solid product was filtered. The mother liquor was extracted with methylene chloride (150 ml). The methylene chloride layer was washed with water (200 ml). The filtered solid and the methylene chloride layer were combined and washed with water and the solvent was distilled under vacuum. Ethyl acetate was charged to the precipitated solid. The reaction mass was then cooled to 0-5 °C and maintained for 6 hrs. The solid was filtered and dried to produce Tenofovir disoproxil (45 gm).
CLIPS
The reaction of chloromethyl chloroformate (I) with isopropyl alcohol (II) by means of pyridine or triethylamine in ether gives the mixed carbonate (III), which is then condensed with (R)-PMPA (IV) by means of diisopropyl ethyl-amine in DMF.
| US 5922695; WO 9804569 |

1) The protection of isobutyl D-(+)-lactate (I) with dihydropyran (DHP)/HCl in DMF gives the tetrahydropyranyloxy derivative (II), which is reduced with bis(2-methoxyethoxy)aluminum hydride in refluxing ether/ toluene yielding 2(R)-(tetrahydropyranyloxy)-1-propanol (III). The tosylation of (III) with tosyl chloride as usual affords the expected tosylate (VI), which is condensed with adenine (V) by means of Cs2CO3 in hot DMF, affording 9-[2(R)-(tetrahydropyranyloxy)propyl]adenine (VI). The deprotection of (VI) with sulfuric acid affords 9-[2(R)-hydroxypropyl]adenine (VII), which is N-benzoylated with benzoyl chloride/chlorotrimethylsilane in pyridine to give the benzamide (VIII), which is condensed with tosyl-oxymethylphosphonic acid diisopropyl ester (IX) by means of NaH in DMF to yield 9-[2(R)-(diisopropoxyphosphorylmethoxy)propyl]adenine (X). Finally, this compound is hydrolyzed by means of bromotrimethylsilane in acetonotrile.

2) The reaction of the previously described (R)-2-(2-tetrahydropyranyloxy)-1-propanol (III) with benzyl bromide (XI) by means of NaH in DMF, followed by a treatment with Dowex 50X, gives 1-benzyloxy-2(R)-propanol (XII), which is condensed with tosyloxymethylphosphonic acid diisopropyl ester (IX) by means of NaH in THF, yielding 2-benzyloxy-1(R)-methylethoxymethylphosphonic acid diisopropyl ester (XIII). The hydrogenolysis of (XIII) over Pd/C in methanol affords 2-hydroxy-1(R)-methylethoxymethylphosphonic acid diisopropyl ester (XIV), which is tosylated with tosyl chloride/dimethyl-aminopyridine in pyridine to give the expected tosylate (XV). The condensation of (XV) with adenine (VI) by means of Cs2CO3 in hot DMF yields 9-[2(R)-(diisopropoxyphosphorylmethoxy)propyl]adenine (X), which is finally hydrolyzed as before.

3) The catalytic hydrogenation of (S)-glycidol (XVI) over Pd/C gives the (R)-1,2-propanediol (XVII), which is esterified with diethyl carbonate (XVIII)/NaOEt, yielding the cyclic carbonate (XIX). The reaction of (XIX) with adenine (V) by means of NaOH in DMF affords 9-[2(R)-hydroxypropyl]adenine (VII), which is condensed with tosyloxymethylphosphonic acid diethyl ester (XX) by means of lithium tert-butoxide in THF, giving 9-[2(R)-(diethoxyphosphorylmethoxy)propyl]adenine (XXI). Finally, this compound is hydrolyzed with bromotrimethylsilane as before. Compound (XX) is obtained by reaction of diethyl phosphite (XXII) with paraformaldehyde, yielding hydroxy- methylphosphonic acid diethyl ester (XXIII), which is finally tosylated as usual.

| WO2008007392A2 | Jul 11, 2007 | Jan 17, 2008 | Matrix Lab Ltd | Process for the preparation of tenofovir |
| US5922695 | Jul 25, 1997 | Jul 13, 1999 | Gilead Sciences, Inc. | Antiviral phosphonomethyoxy nucleotide analogs having increased oral bioavarilability |
| WO2015051874A1 | Sep 22, 2014 | Apr 16, 2015 | Zentiva, K.S. | An improved process for the preparation of tenofovir disoproxil and pharmaceutically acceptable salts thereof |
| CN103360425A * | Apr 1, 2012 | Oct 23, 2013 | 安徽贝克联合制药有限公司 | Synthesis method of tenofovir disoproxil and fumarate thereof |
| CN103374038A * | Apr 11, 2012 | Oct 30, 2013 | 广州白云山制药股份有限公司广州白云山制药总厂 | Preparation method of antiviral medicine |
| CN103848868A * | Dec 4, 2012 | Jun 11, 2014 | 蚌埠丰原涂山制药有限公司 | Method for preparing tenofovir |
| CN103848869A * | Dec 4, 2012 | Jun 11, 2014 | 上海医药工业研究院 | Method for preparing tenofovir |
| CN103980319A * | Apr 24, 2014 | Aug 13, 2014 | 浙江外国语学院 | Preparation method of tenofovir |
| CN103980319B * | Apr 24, 2014 | Dec 2, 2015 | 浙江外国语学院 | 一种泰诺福韦的制备方法 |
| EP2860185A1 | Oct 9, 2013 | Apr 15, 2015 | Zentiva, k.s. | An improved process for the preparation of Tenofovir disoproxil and pharmaceutically acceptable salts thereof |
The chemical name of tenofovir disoproxil fumarate is 9-[(R)-2[[bis[[(isopropoxycarbonyl)oxy]methoxy]phosphinyl]methoxy]propyl]adenine fumarate (1:1). It has a molecular formula of C19H30N5O10P • C4H4O4 and a molecular weight of 635.52. It has the following structural formula:
 |
Tenofovir disoproxil fumarate is a white to off-white crystalline powder with a solubility of 13.4 mg/mL in distilled water at 25 °C. It has an octanol/phosphate buffer (pH 6.5) partition coefficient (log p) of 1.25 at 25 °C.
VIREAD is available as tablets or as an oral powder.
VIREAD tablets are for oral administration in strengths of 150, 200, 250, and 300 mg of tenofovir disoproxil fumarate, which are equivalent to 123, 163, 204 and 245 mg of tenofovir disoproxil, respectively. Each tablet contains the following inactive ingredients: croscarmellose sodium, lactose monohydrate, magnesium stearate, microcrystalline cellulose, and pregelatinized starch. The 300 mg tablets are coated with Opadry II Y-3010671-A, which contains FD&C blue #2 aluminum lake, hypromellose 2910, lactose monohydrate, titanium dioxide, and triacetin. The 150, 200, and 250 mg tablets are coated with Opadry II 32K-18425, which contains hypromellose 2910, lactose monohydrate, titanium dioxide, and triacetin.
VIREAD oral powder is available for oral administration as white, taste-masked, coated granules containing 40 mg of tenofovir disoproxil fumarate per gram of oral powder, which is equivalent to 33 mg of tenofovir disoproxil. The oral powder contains the following inactive ingredients: mannitol, hydroxypropyl cellulose, ethylcellulose, and silicon dioxide.
 |
|
| Systematic (IUPAC) name | |
|---|---|
|
Bis{[(isopropoxycarbonyl)oxy]methyl} ({[(2R)-1-(6-amino-9H-purin-9-yl)-2-propanyl]oxy}methyl)phosphonate
|
|
| Clinical data | |
| Trade names | Viread |
| AHFS/Drugs.com | monograph |
| Pregnancy category |
|
| Routes of administration |
Oral (tablets) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 25% |
| Identifiers | |
| CAS Number | 201341-05-1 |
| ATC code | J05AF07 (WHO) |
| PubChem | CID 5481350 |
| ChemSpider | 4587262 |
| UNII | F4YU4LON7I |
| ChEBI | CHEBI:63717 |
| NIAID ChemDB | 080741 |
| Chemical data | |
| Formula | C19H30N5O10P |
| Molar mass | 519.443 g/mol |
 |
|
| Systematic (IUPAC) name | |
|---|---|
|
({[(2R)-1-(6-amino-9H-purin-9-yl)propan-2-yl]oxy}methyl)phosphonic acid
|
|
| Clinical data | |
| MedlinePlus | a602018 |
| Routes of administration |
In form of prodrugs |
| Pharmacokinetic data | |
| Protein binding | < 1% |
| Biological half-life | 17 hours |
| Excretion | Renal |
| Identifiers | |
| CAS Number | 147127-20-6 |
| ATC code | None |
| PubChem | CID 464205 |
| DrugBank | DB00300 |
| ChemSpider | 408154 |
| UNII | 99YXE507IL |
| KEGG | D06074 |
| ChEBI | CHEBI:63625 |
| ChEMBL | CHEMBL483 |
| Synonyms | 9-(2-Phosphonyl-methoxypropyly)adenine (PMPA) |
| Chemical data | |
| Formula | C9H14N5O4P |
| Molar mass | 287.213 g/mol |
///////


Liarozole fumarate is prepared as shown in Scheme 20970301a. Anisol is reacted with 3-chlorobenzoyl chloride (I) under Friedel-Craft conditions to give (3-chlorophenyl)(4-methoxyphenyl)methanone (II). Nitration of (II) is carried out in dichloromethane at 10 C to yield (III). The methoxy group in (III) is replaced by the amino group by means of NH3 in 2-propanol at 100 C under pressure, giving (IV). By reduction of the keto function of (IV) with sodium borohydride in 2-propanol, the corresponding alcohol (V) is obtained, which upon treatment with 1,1′-carbonyldiimidazole in refluxing dichloromethane yields the imidazolyl compound (VI). Hydrogenation of the nitro group in (VI), followed by cyclization of (VII) in a refluxing mixture of formic acid and 4N hydrochloric acid, gives the benzimidazole derivative (VIII). Finally, the treatment of (VIII) with fumaric acid in ethanol yields liarozole fumarate (IX).
http://www.google.com/patents/WO1995022540A1?cl=en
Liarozole is a racemic mixture, i.e. a mixture of its optical isomers, and is specifically mentioned as compound 28 in EP-0,371,559. Said patent application mentions the use of compounds like liarozole in the treatment of epithelial disorders. EP-0,260,744 describes the use of compounds like liarozole for inhibiting or lowering androgen formation. Whereas EP-0,371,559 and EP-0,260,744 recognize that compounds like liarozole have stereochemically isomeric forms, no example of an enantiomerically pure form is given of liarozole.
Chemically liarozole is (±)-5-[3-chlorophenyl]-lH-imidazol-l-ylmethyl]-lH-benz- imidazole, and is represented by formula (I). As can be seen from the chemical structure, liarozole has one stereogenic center (indicated with an asterisk in formula (I)).
The subject of this invention is the enantiomerically pure dextrorotatory isomer or (+)-isomer of liarozole. Said isomer will hereinafter be referred to as (+)-liarozole. Many organic compounds exist in optically active forms, i.e. they have the ability to rotate the plane of plane-polarized light. In describing an optically active compound, the prefixes D and L or R and S are used to denote the absolute configuration of the molecule about its chiral center(s). The prefixes (+) and (-) or d and 1 are employed to designate the sign of rotation of plane-polarized light by the compound, with (-) or 1 meaning that the compound is iaevorotatory and with (+) or d meaning that the compound is dextrorotatory. For a given chemical structure the optically active isomers having an opposite sign of optical rotation are called enantiomers. Said enantiomers are identical except that they are mirror images of one another. A 1: 1 -mixture of such enantiomers is called a racemic mixture.
General preparation of structures including liarozole have been extensively described in EP-0,371,559 and EP-0,260,744.
Enantiomerically pure (+)-liarozole may be prepared by reacting an enantiomerically pure intermediate diamine of formula (B)-(II) with formic acid or a functional derivative thereof.
Said functional derivative of formic acid is meant to comprise the halide, anhydride, amide and ester, including the ortho and imino ester form thereof. Also methanimidamide or an acid addition salt thereof can be used as cyclizing agent.
The general reaction conditions, work-up procedures and conventional isolation techniques for carrying out the above and following reactions are described in the prior art. When more specific conditions are required they are mentioned hereinunder. The enantiomerically pure intermediate diamine of formula (B)-(II) may be prepared by reducing an intermediate of formula (B)-(iπ) by a standard nitro-to-amine reduction reaction.
The desired enantiomer of the intermediate of formula (B)-(]H) can be prepared by fractional crystallization of a racemic mixture of the intermediate of formula (HI) with an enantiomerically pure chiral acid. Preferred chiral acid for the above fractional crystallization is 7,7-dimethyl-2-oxobicyclo[2.2.1]heptane-l-methanesulfonic acid (i.e. 10-camphorsulfonic acid).
Appropriate solvents for carrying out said fractional crystallization are water, ketones, e.g. 2-propane, 2-butanone; alcohols, e.g. methanol, ethanol, 2-propanol. Mixtures of ketones and water are very suitable for the above fractional crystallization. Preferably a mixture of 2-propanone and water is used.
The ratio of water/2-propanone by volume may vary from 1/10 to 1/2. Preferred range of said ratio is 1/5 to 1/3.
The fractional crystallizations are suitably carried out below room temperature, preferably below 5°C.
It was also found that the subsequent reaction step can be carried out without any appreciable racemization.
Alternatively the (+)-isomer of the compound of formula (I) may be prepared by cyclizing an intermediate of formula (B)-(IV) following procedures as described above for the cyclization of intermediates of formula (B)-(II) and desulfurating the thus obtained intermediate of formula (B)-(V). In formulas (B)-(TV) and (B)-(V) R represents Ci^alkyl, wherein Ci-^alkyl means a straight or branch chained saturated hydrocarbon radicals having 1 to 6 carbon atoms such as, for example, methyl, ethyl, propyl, butyl, pentyl, hexyl. Preferably R is methyl.
The intermediates of formula (B)-(IV) may be prepared by reacting an intermediate of formula (B)-(VI) with a reagent of formula (VII), alkylating the thus formed thiourea derivative of formula (B)-(VIII) subsequently cyclizing the intermediate of formula
(B)-(D ), and reducing the nitro group of the intermediate (B)-(X). In the formulas
(Vπ), (B)-(Vm), (B)-(IX) and (B)-(X) R represents Ci^alkyl as defined hereinabove.
S OR
(B)-(IV)
Experimental part
A. Preparation of the intermediates
Example 1 a) A heterogeneous mixture of (±)-4-[(3-chlorophenyl)-lH-imidazol-l-ylmethyl]-2- nitrobenzenamine (the preparation of which is described in EP-371,559) (500 g) in
2-propanone (2000 ml) and water (100 ml) was stirred at 22°C. (-)-(lR)-7,7-dimethyl- 2-oxo-bicyclo[2.2.1]heptane-l-methanesulfonic acid (353.2 g) was added and the mixture became homogeneous after 10 minutes. The mixture was first stirred for 18 hours at 20°C and then for 3 hours at 0-5°C. The precipitate was filtered off, washed with 2-propanone/water 95/5 (150 ml) and dried, yielding 308.9 g (36.2%) of product A sample (306.7 g) was partitioned between dichloromethane (500 ml) and water (750 ml). Ammonium hydroxide (100 ml) was added. This mixture was stirred for 15 minutes. The aqueous layer was separated and extracted twice with dichloromethane (250 ml each time). The separated organic layer was washed with water (250 ml), dried, filtered and the solvent was evaporated, yielding 179.7 g of (-)-(B)-4-[(3-chlorophenyl)-
20 lH-imidazol-l-ylmethyl]-2-nitrobenzenamine; mp. 89.8°C; [α]D = -19.80° (c = 0.5% in methanol) (interm. 1). b) A mixture of intermediate (1)(179.7 g) in methanol (656 ml) and a solution of ammonia in methanol (32.7 ml) was hydrogenated at 20-25 °C with platinum on activated carbon (13.1 g) as a catalyst in the presence of thiophene (0.27 g). After uptake of hydrogen (3 eq.) the catalyst was filtered off and washed with 2-propanol (30 ml). A solution of hydrochloric acid in 2-propanol (522 ml) was added to the filtrate at <30°C. The mixture was stirred for 3 hours at 20 °C, then for 3 hours at 0-5 °C. The resulting precipitate was slowly filtered off, washed with methanol (100 ml) and dried
(50 °C), yielding 185.60 g (83.2%) (+)-(B)-4-[(3-chlorophenyl)-lH-imidazol-l-yl-
20 methyl]- 1,2-benzenediamine trihydrochloride; mp. 172.5°C; [α^ = +23.73° (c = 1% in methanol) (interm. 2).
Example 2 a) A mixture of (4-amino-3-nitrophenyl) (3-chlorophenyl)methanone (50 g), formamide (375 ml) and formic acid (63 ml) was stiιτed and refluxed for 17 hours. After cooling, the mixture was poured on ice. The precipitate was filtered off and dried, yielding 55 g (99.4%) of (±)-N-[(4-amino-3-nitrophenyl) (3-chlorophenyl)methyl]formamide (interm. 3). b) A mixture of intermediate (3) (50.7 g), hydrochloric acid 6N (350 ml) and 2-propanol (70 ml) was stirred and refluxed for 17 hours. The yellow precipitate was filtered off and dried in vacuo, yielding 51 g (97.8%) of (±)-4-amino-α-(3-chloro- phenyl)-3-nitrobenzenemethanamine monohydrochloride; mp. 263°C (interm.4). c) To a solution of intermediate (4) (43 g) in tetrahydrofuran (400 ml) at room temperature was added succesively N,N-diethylethanamine (13.8 g) and (R)-(-)-α- hydroxybenzeneacetic acid (20.8 g). Then a solution of 1-hydroxybenzotriazole monohydrate (22.2 g) in tetrahydrofuran (200 ml) was added. After complete addition a solution of N,N’-dicyclohexylcarbodiimide (33.9 g) in dichloromethane (300 ml) was introduced to the mixture. After stirring for 2 hours at room temperature N,N’- dicyclohexylurea was filtered off. The filtrate was washed with a solution of potassium carbonate (10%) and the organic layer was dried to give a mixture of diastereomers (60g) (fraction 1). The same experiment with intermediate (4) (16 g) as starting material resulted in a yield of 26 g of a mixture of diastereomers (fraction 2). Fraction 1 and 2 were combined and purified by HPLC (eluent : CH2θ2/ethyl acetate 90:10), yielding 30g (32.3%) of (±)-(R,B)-N-[(4-amino-3-nitrophenyl)(3-chlorophenyl)methyl]-α- hydroxybenzeneacetamide (interm.5). d) A mixture of intermediate (5) (30 g), hydrochloric acid 12N (300 ml) and 1-propanol (100 ml) was stirred and refluxed for 17 hours and poured on ice. The mixture was extracted with ethyl acetate. The aqueous phase was basified with ammonium hydroxide and extracted with dichloromethane. The dichloromethane extracts were dried, filtered and evaporated, yielding 7.3 g (36.0%) of (+)-(B)-4-amino-α-(3-chlorophenyl)-3- nitrobenzenemethanamine (interm. 6). e) A mixture of intermediate (6) (7.3 g), 2-isothiocyanato-l,l-dimethoxyethane (4.8 g) and methanol (75 ml) was stirred and refluxed for 2 hours. The mixture was evaporated to an oily residue, yielding 11 g (100%) of (+)-(B)-N-[(4-amino-3-nitrophenyl)(3- chlorophenyl)methyl]-N’-(2,2-dimethoxyethyl)thiourea (interm.7). f) A mixture of intermediate (7) (11 g), iodomethane (2 ml) and potassium carbonate (4.97 g) was stirred at room temperature for 48 hours. The solvent was evaporated and the residue was taken off with dichloromethane and washed with water. The organic layer was dried, filtered and evaporated, yielding 11.4 g of (+)-(S)-methyl (B)-N- [(4-amino-3-nitrophenyl)(3-chlorophenyl)methyl]-N’-(2,2-dimethoxyethyl)carbam- imidothioate as an oily residue (interm. 8). g) To intermediate (8) (11.4 g) at 0°C was added sulfuric acid (100ml) (precooled to 5°C). The mixture was stirred at 5°C until complete dissolution and then was warmed to room temperature. After stirring for 2 hours, the solution was poured on ice and basified with ammonium hydroxide. The aqueous solution was extracted with ethyl acetate. The organic layer was dried, filtered and evaporated. The residue was purified by column chromatography (eluent : CH2CI2/CH3OH 98:2). The eluent of the desired fraction was evaporated, yielding 3.7 g (38.0%) of (+)-(B)-4-[(3-chlorophenyl)[2-(methylthio)-lH- imidazol-l-yl]methyl]-2-nitrobenzenamine (interm.9). h) A mixture of intermediate (9) (6.2 g), Raney nickel (6 g) and methanol (100 ml) was hydrogenated for 2 hours at 2 bar and at room temperature. After the calculated amount of hydrogen was taken up, the catalyst was filtered off. The filtrate, (+)-(B)-4-[(3- chlorophenyl)[2-(methylthio)-lH-imidazol-l-yl]methyl]-l,2-benzenediamine (interm. 10), was used for the next step. i) A mixture of intermediate (10) (5.7 g), methanimidamide monoacetate (5.2 g) and methanol (100 ml) was stirred and refluxed for 3 hours. The reaction mixture was evaporated and the residue was taken off in dichloromethane and washed with sodium hydrogen carbonate (10%). The organic layer was dried, filtered and evaporated. The oily residue was purified by column chromatography (eluent : CH2CI2/CH3OH 95:5). The eluent of the desired fraction was evaporated, yielding 4.9 g (83.7%) of (+)-(B)-5-[(3-cWorophenyl)[2-(methylthio)-lH-imidazol-l-yl]methyl]-lH-benzimidazole (interm. 11).
B. Preparation of the final compounds Example 3
A mixture of intermediate (2) (185 g) in water (512 ml) was stirred at 20 °C. Hydrochloric acid (289 ml) was added. Formic acid (85%) (61.17 ml) was added and this mixture was heated to 55°C. The reaction mixture was stirred for 3 hours at 55 °C and then cooled to 20°C. Dichloromethane (1223 ml) was added. Ammonium hydroxide (730 ml) was added dropwise at < 25°C. The separated organic layer was washed with water (500 ml), dried, filtered and the solvent was evaporated, yielding 152.88 g (108.5%) of product. A sample was dried (18 hours at 55 °C), yielding 3.18 g of (+)-(B)-5-[(3-chlorophenyl)-lH-imidazol-l-ylmethyl]-lH-benzimidazole; mp.
20 113.7°C; [αjj = +43.46° (c = 1% in methanol) (comp. 1).
Example 4
A mixture of intermediate (11) (4.9 g), Raney nickel (2 g) and ethanol (100ml) was stirred and refluxed for 5 days, while every day an additional amount of Raney nickel (2 g) was added. The catalyst was filtered off and rinsed with dichloromethane. The filtrate was evaporated and the residue was purified twice by column chromatography (silica gel; CH2CI2/CH3OH 95:5 ; CH2CI2/CH3OH NH4OH 80:20:3). The eluent of the desired fraction was evaporated and the residue was converted into the hydrochloride salt in 2-propanol and ethanol. The salt was recrystallized from 2-butanone, yielding 1.8 g (37.2%) of (+)-(B)-5-[(3-chlorophenyl)(lH-imidazol-l-yl)methyl]-lH-benzimidazole
20 monohydrochloride; mp. 212.1°C; [α]D = +42.43° (c = 1% in ethanol) (comp. 2)
Example 5
Compound (1) (149.7 g) was dissolved in 2-butanone (2424 ml). A mixture of hydrochloric acid in 2-propanol (82.6 ml) in 2-butanone (727 ml) was added over a 2 hour period at 20 °C. The reaction mixture was stirred for 16 hours at 20 °C. The precipitate was filtered off, washed with 2-butanone (242 ml) and dried (vacuum; 80°C); yielding 147.5 g (99.3%) of (+)-(B)-5-[(3-chlorophenyl)-lH-imidazol-l-ylmethyl]-lH-
20 benzimidazole monohydrochloride; mp. 214.5°C; [α] j = +36.20° (c = 1% in methanol) (comp. 2). Example 6
A mixture of compound (1) (0.72 g) in ethanol (5.1 ml; denaturated) was stirred at 20 °C until it became homogeneous. (E)-2-butenedioic acid (0.54 g) was added The mixture was stirred for 18 hours at 20 °C and then cooled 0-5 °C and precipitation resulted. More denaturated ethanol (2 ml) was added and the mixture was stirred for 2 hours at 20 °C. The precipitate was filtered off, washed with ethanol (3 ml; denaturated) and dried (vacuum; 50 °C), yielding 0.26 g (23.4%) (B)-5-[(3-chlorophenyl)-lH-imidazol-l-yl- methyl]-lH-benzimidazole (E)-2-butenedioate (2:3).ethanolate (2:1); mp. 111.2°C (comp. 3).
PAPER


Paper
1 Vahlquist, A; Blockhuys, S; Steijlen, P; Van Rossem, K; Didona, B; Blanco, D; Traupe, H (2013). “Oral liarozole in the treatment of patients with moderate/severe lamellar ichthyosis: Results of a randomized, double-blind, multinational, placebo-controlled phase II/III trial”. The British journal of dermatology 170 (1): n/a. doi:10.1111/bjd.12626. PMID 24102348.
Literature References: Inhibits cytochrome P450-dependent enzymes involved in steroid biosynthesis and retinoic acid catabolism. Prepn: A. H. M. Raeymaekers et al., EP 260744; eidem, US 4859684 (1988, 1989 both to Janssen). In vivo antitumor activity: R. Van Ginckel et al., Prostate 16, 313 (1990). Pharmacology and effect on steroid synthesis: J. Bruynseels et al., ibid., 345; and effect on retinoic acid: R. De Coster et al., J. Steroid Biochem. Mol. Biol. 43, 197 (1992). Clinical evaluation in prostate cancer: C. Mahler et al., Cancer 71, 1068 (1993); in psoriasis: P. Dockx et al., Br. J. Dermatol. 133, 426 (1995); in combination therapy for malignant brain tumors: M. E. Westarp et al., Onkologie 16, 22 (1993).
 |
|
| Names | |
|---|---|
| IUPAC name
6-[(3-Chlorophenyl)-imidazol-1-ylmethyl]-1H-benzimidazole
|
|
| Identifiers | |
| 115575-11-6 | |
| ChemSpider | 54664 |
| 5210 | |
| Jmol interactive 3D | Image |
| PubChem | 60652 |
| Properties | |
| C17H13ClN4 | |
| Molar mass | 308.77 g·mol−1 |
///////
C1=CC(=CC(=C1)Cl)C(C2=CC3=C(C=C2)N=CN3)N4C=CN=C4

ODM 201, BAY 1841788; ODM-201
N-((S)-1-(3-(3-chloro-4-cyanophenyl)-1H-pyrazol-1-yl)propan-2-yl)-5-(1-hydroxyethyl)-1H-pyrazole-3-carboxamide
CAS 1297538-32-9
Chemical Formula: C19H19ClN6O2
Exact Mass: 398.1258
SYNTHESIS SEE BELOW
Phase III Prostate cancer


ODM-201 (also known as BAY-1841788) is a non-steroidal antiandrogen, specifically, a full and high-affinity antagonist of the androgen receptor (AR), that is under development by Orion and Bayer HealthCare[1] for the treatment of advanced, castration-resistant prostate cancer (CRPC).[2][3]
Relative to enzalutamide (MDV3100 or Xtandi) and apalutamide (ARN-509), two other recent non-steroidal antiandrogens, ODM-201 shows some advantages.[3] ODM-201 appears to negligibly cross the blood-brain-barrier.[3] This is beneficial due to the reduced risk of seizures and other central side effects from off-target GABAA receptor inhibition that tends to occur in non-steroidal antiandrogens that are structurally similar to enzalutamide.[3] Moreover, in accordance with its lack of central penetration, ODM-201 does not seem to increase testosterone levels in mice or humans, unlike other non-steroidal antiandrogens.[3] Another advantage is that ODM-201 has been found to block the activity of all tested/well-known mutant ARs in prostate cancer, including the recently-identified clinically-relevant F876L mutation that produces resistance to enzalutamide and ARN-509.[3] Finally, ODM-201 shows higher affinity and inhibitory efficacy at the AR (Ki = 11 nM relative to 86 nM for enzalutamide and 93 nM for ARN-509; IC50 = 26 nM relative to 219 nM for enzalutamide and 200 nM for ARN-509) and greater potency/efficaciousness in non-clinical models of prostate cancer.[3]
ODM-201 has been studied in phase I and phase II clinical trials and has thus far been found to be effective and well-tolerated,[4] with the most commonly reported side effects including fatigue, nausea, and diarrhea.[5][6] No seizures have been observed.[6][7] As of July 2015, ODM-201 is in phase III trials for CRPC.[3]
ORM-15341 is the main active metabolite of ODM-201.[3] It, similarly, is a full antagonist of the AR, with an affinity (Ki) of 8 nM and an IC50 of 38 nM.[3]

ODM-201 is a new-generation, potent and selective androgen receptor (AR) inhibitor which is potential useful for treatment of castration-resistant prostate cancer (CRPC). ODM-201 is a full and high-affinity AR antagonist that, similar to second-generation antiandrogens enzalutamide and ARN-509, inhibits testosterone-induced nuclear translocation of AR. Importantly, ODM-201 also blocks the activity of the tested mutant ARs arising in response to antiandrogen therapies, including the F876L mutation that confers resistance to enzalutamide and ARN-509. In addition, ODM-201 reduces the growth of AR-overexpressing VCaP prostate cancer cells both in vitro and in a castration-resistant VCaP xenograft model. ODM-201 overcomes resistance to AR-targeted therapies by antagonizing both overexpressed and mutated ARs. ODM-201 is currently in a phase 3 trial in CRPC
Figure 1: The structures of ODM-201 (A) and its main metabolite ORM-15341 (B).
Representative binding affinities of ODM-201, ORM-15341, enzalutamide, and ARN-509 measured in competition with [3H]mibolerone using wtAR isolated from rat ventral prostates (C). All data points are means of quadruplicates ±SEM. Ki values are presented in parentheses. D. Antagonism to wtAR was determined using AR-HEK293 cells treated with ODM-201, ORM-15341, enzalutamide, or ARN-509 together with 0.45 nM testosterone in steroid-depleted medium for 24 hours before luciferase activity measurements. All data points are means of triplicates ±SEM. IC50 values are presented in parentheses.
WHIPPANY, N.J., Sept. 16, 2014 /PRNewswire/ — Bayer HealthCare and Orion Corporation, a pharmaceutical company based in Espoo, Finland, have begun to enroll patients in a Phase III trial with ODM-201, an investigational oral androgen receptor inhibitor in clinical development. The study, called ARAMIS, evaluates ODM-201 in men with castration-resistant prostate cancer who have rising Prostate Specific Antigen (PSA) levels and no detectable metastases. The trial is designed to determine the effects of the treatment on metastasis-free survival (MFS).
“The field of treatment options for prostate cancer patients is evolving rapidly. However, once prostate cancer becomes resistant to conventional anti-hormonal therapy, many patients will eventually develop metastatic disease,” said Dr. Joerg Moeller, Member of the Bayer HealthCare Executive Committee and Head of Global Development. “The initiation of a Phase III clinical trial for ODM-201 marks the starting point for a potential new treatment option for patients whose cancer has not yet spread. This is an important milestone for Bayer in our ongoing effort to meet the unmet needs of men affected by prostate cancer.”
Earlier this year, Bayer and Orion entered into a global agreement under which the companies will jointly develop ODM-201, with Bayer contributing a major share of the costs of future development. Bayer will commercialize ODM-201 globally, and Orion has the option to co-promote ODM-201 in Europe. Orion will be responsible for the manufacturing of the product.
About the ARAMIS Study
The ARAMIS trial is a randomized, Phase III, multicenter, double-blind, placebo-controlled trial evaluating the safety and efficacy of oral ODM-201 in patients with non-metastatic CRPC who are at high risk for developing metastatic disease. About 1,500 patients are planned to be randomized in a 2:1 ratio to receive 600 mg of ODM-201 twice a day or matching placebo. Randomisation will be stratified by PSA doubling time (PSADT less than or equal to 6 months vs. > 6 months) and use of osteoclast-targeted therapy (yes vs. no).
The primary endpoint of this study is metastasis-free survival (MFS), defined as time between randomization and evidence of metastasis or death from any cause. The secondary objectives of this study are overall survival (OS), time to first symptomatic skeletal event (SSE), time to initiation of first cytotoxic chemotherapy, time to pain progression, and characterization of the safety and tolerability of ODM-201.
About ODM-201
ODM-201 is an investigational androgen receptor (AR) inhibitor that is thought to block the growth of prostate cancer cells. ODM-201 binds to the AR and inhibits receptor function by blocking its cellular function.
About Oncology at Bayer
Bayer is committed to science for a better life by advancing a portfolio of innovative treatments. The oncology franchise at Bayer now includes three oncology products and several other compounds in various stages of clinical development. Together, these products reflect the company’s approach to research, which prioritizes targets and pathways with the potential to impact the way that cancer is treated.
About Bayer HealthCare Pharmaceuticals Inc.
Bayer HealthCare Pharmaceuticals Inc. is the U.S.-based pharmaceuticals business of Bayer HealthCare LLC, a subsidiary of Bayer AG. Bayer HealthCare is one of the world’s leading, innovative companies in the healthcare and medical products industry, and combines the activities of the Animal Health, Consumer Care, Medical Care, and Pharmaceuticals divisions. As a specialty pharmaceutical company, Bayer HealthCare provides products for General Medicine, Hematology, Neurology, Oncology and Women’s Healthcare. The company’s aim is to discover and manufacture products that will improve human health worldwide by diagnosing, preventing and treating diseases.
Bayer® and the Bayer Cross® are registered trademarks of Bayer.

PATENT
US 2015203479
http://www.google.com/patents/WO2011051540A1?cl=en
PATENT
WO 2012143599
http://www.google.com/patents/US20140094474?cl=de
Fenner A. Prostate cancer: ODM-201 tablets complete phase I. Nat Rev Urol. 2015 Dec;12(12):654. doi: 10.1038/nrurol.2015.268. Epub 2015 Nov 3. PubMed PMID: 26526759.
2: Massard C, Penttinen HM, Vjaters E, Bono P, Lietuvietis V, Tammela TL, Vuorela A, Nykänen P, Pohjanjousi P, Snapir A, Fizazi K. Pharmacokinetics, Antitumor Activity, and Safety of ODM-201 in Patients with Chemotherapy-naive Metastatic Castration-resistant Prostate Cancer: An Open-label Phase 1 Study. Eur Urol. 2015 Oct 10. pii: S0302-2838(15)00964-1. doi: 10.1016/j.eururo.2015.09.046. [Epub ahead of print] PubMed PMID: 26463318.
3: Fizazi K, Albiges L, Loriot Y, Massard C. ODM-201: a new-generation androgen receptor inhibitor in castration-resistant prostate cancer. Expert Rev Anticancer Ther. 2015;15(9):1007-17. doi: 10.1586/14737140.2015.1081566. PubMed PMID: 26313416; PubMed Central PMCID: PMC4673554.
4: Bambury RM, Rathkopf DE. Novel and next-generation androgen receptor-directed therapies for prostate cancer: Beyond abiraterone and enzalutamide. Urol Oncol. 2015 Jul 7. pii: S1078-1439(15)00269-0. doi: 10.1016/j.urolonc.2015.05.025. [Epub ahead of print] Review. PubMed PMID: 26162486.
5: Moilanen AM, Riikonen R, Oksala R, Ravanti L, Aho E, Wohlfahrt G, Nykänen PS, Törmäkangas OP, Palvimo JJ, Kallio PJ. Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies. Sci Rep. 2015 Jul 3;5:12007. doi: 10.1038/srep12007. PubMed PMID: 26137992; PubMed Central PMCID: PMC4490394.
6: Thibault C, Massard C. [New therapies in metastatic castration resistant prostate cancer]. Bull Cancer. 2015 Jun;102(6):501-8. doi: 10.1016/j.bulcan.2015.04.016. Epub 2015 May 26. Review. French. PubMed PMID: 26022286.
7: Bjartell A. Re: activity and safety of ODM-201 in patients with progressive metastatic castration-resistant prostate cancer (ARADES): an open-label phase 1 dose-escalation and randomised phase 2 dose expansion trial. Eur Urol. 2015 Feb;67(2):348-9. doi: 10.1016/j.eururo.2014.11.019. PubMed PMID: 25760250.
8: De Maeseneer DJ, Van Praet C, Lumen N, Rottey S. Battling resistance mechanisms in antihormonal prostate cancer treatment: Novel agents and combinations. Urol Oncol. 2015 Jul;33(7):310-21. doi: 10.1016/j.urolonc.2015.01.008. Epub 2015 Feb 21. Review. PubMed PMID: 25708954.
9: Boegemann M, Schrader AJ, Krabbe LM, Herrmann E. Present, Emerging and Possible Future Biomarkers in Castration Resistant Prostate Cancer (CRPC). Curr Cancer Drug Targets. 2015;15(3):243-55. PubMed PMID: 25654638.
10: ODM-201 is safe and active in metastatic castration-resistant prostate cancer. Cancer Discov. 2014 Sep;4(9):OF10. doi: 10.1158/2159-8290.CD-RW2014-150. Epub 2014 Jul 9. PubMed PMID: 25185192.
11: Fizazi K, Massard C, Bono P, Jones R, Kataja V, James N, Garcia JA, Protheroe A, Tammela TL, Elliott T, Mattila L, Aspegren J, Vuorela A, Langmuir P, Mustonen M; ARADES study group. Activity and safety of ODM-201 in patients with progressive metastatic castration-resistant prostate cancer (ARADES): an open-label phase 1 dose-escalation and randomised phase 2 dose expansion trial. Lancet Oncol. 2014 Aug;15(9):975-85. doi: 10.1016/S1470-2045(14)70240-2. Epub 2014 Jun 25. PubMed PMID: 24974051.
12: Agarwal N, Di Lorenzo G, Sonpavde G, Bellmunt J. New agents for prostate cancer. Ann Oncol. 2014 Sep;25(9):1700-9. doi: 10.1093/annonc/mdu038. Epub 2014 Mar 20. Review. PubMed PMID: 24658665.
13: Pinto Á. Beyond abiraterone: new hormonal therapies for metastatic castration-resistant prostate cancer. Cancer Biol Ther. 2014 Feb;15(2):149-55. doi: 10.4161/cbt.26724. Epub 2013 Nov 1. Review. PubMed PMID: 24100689; PubMed Central PMCID: PMC3928129.
14: Yin L, Hu Q, Hartmann RW. Recent progress in pharmaceutical therapies for castration-resistant prostate cancer. Int J Mol Sci. 2013 Jul 4;14(7):13958-78. doi: 10.3390/ijms140713958. Review. PubMed PMID: 23880851; PubMed Central PMCID: PMC3742227.
15: Leibowitz-Amit R, Joshua AM. Targeting the androgen receptor in the management of castration-resistant prostate cancer: rationale, progress, and future directions. Curr Oncol. 2012 Dec;19(Suppl 3):S22-31. doi: 10.3747/co.19.1281. PubMed PMID: 23355790; PubMed Central PMCID: PMC3553559.
 |
|
| Systematic (IUPAC) name | |
|---|---|
|
N((R)-1-(3-(4-Cyano-3-(trifluoromethyl)phenyl)-1H-pyrazol-1-yl)propan-2-yl)-5-(1-hydroxyethyl)-1H-pyrazole-3-carboxamide[1]
|
|
| Identifiers | |
| ChemSpider | 38772320 |
| Chemical data | |
| Formula | C19H19ClN6O2 |
| Molar mass | 398.85 g·mol−1 |
/////
O=C(C1=NNC(C(O)C)=C1)N[C@@H](C)CN2N=C(C3=CC=C(C#N)C(Cl)=C3)C=C2

ARN-509; cas 956104-40-8; ARN 509; UNII-4T36H88UA7;
ARN-509; JNJ-56021927; JNJ-927\
Phase III Prostate cancer
4-(7-(6-CYANO-5-(TRIFLUOROMETHYL)PYRIDIN-3-YL)-8-OXO-6-THIOXO-5,7-DIAZASPIRO[3.4]OCTAN-5-YL)-2-FLUORO-N-METHYLBENZAMIDE;
4-(7-(6-cyano-5-(trifluoroMethyl)pyridin-3-yl)-8-oxo-6-thioxo-5,7-diazaspirooctan-5-yl)-2-fluoro-N-MethylbenzaMide;
| Molecular Formula: | C21H15F4N5O2S |
|---|---|
| Molecular Weight: | 477.434713 g/mol |
| Product Name | Sponsor Only | Condition | Start Date | End Date | Phase | Last Change Date |
|---|---|---|---|---|---|---|
| ARN-509 | Aragon Pharmaceuticals Inc | Hormone refractory prostate cancer | 31-JUL-10 | 30-JUN-13 | Phase 2 | 17-SEP-13 |
| Aragon Pharmaceuticals Inc | 31-MAR-13 | 30-JUN-13 | Phase 1 | 17-SEP-13 | ||
| Aragon Pharmaceuticals Inc | Hormone refractory prostate cancer | 31-OCT-13 | 31-DEC-16 | Phase 3 | 05-NOV-13 | |
| Aragon Pharmaceuticals Inc; Johnson & Johnson | Hormone refractory prostate cancer | 28-FEB-13 | 01-FEB-14 | Phase 1 | 07-OCT-13 | |
| Aragon Pharmaceuticals Inc | Hormone dependent prostate cancer | 28-FEB-13 | 28-FEB-18 | Phase 2 | 18-OCT-13 |
Apalutamide, also known as ARN-509 and JNJ-56021927 , is an androgen receptor antagonist with potential antineoplastic activity. ARN-509 binds to AR in target tissues thereby preventing androgen-induced receptor activation and facilitating the formation of inactive complexes that cannot be translocated to the nucleus. This prevents binding to and transcription of AR-responsive genes. This ultimately inhibits the expression of genes that regulate prostate cancer cell proliferation and may lead to an inhibition of cell growth in AR-expressing tumor cells.
Apalutamide (INN) (developmental code name ARN-509, also JNJ-56021927) is a non-steroidal antiandrogen that is under development for the treatment of prostate cancer.[1] It is similar to enzalutamide both structurally and pharmacologically,[2] acting as a selective competitive antagonist of the androgen receptor (AR), but shows some advantages, including greater potency and reduced central nervous system permeation.[1][3][4] Apalutamide binds weakly to the GABAA receptor similarly to enzalutamide, but due to its relatively lower central concentrations, may have a lower risk of seizures in comparison.[1][3][5] The drug has been found to be effective and well-tolerated in clinical trials thus far,[2][4] with the most common side effects reported including fatigue, nausea, abdominal pain, and diarrhea.[6][3][5] Apalutamide is currently in phase III clinical trials for castration-resistant prostate cancer.[7]
Recently, the acquired F876L mutation of the AR identified in advanced prostate cancer cells was found to confer resistance to both enzalutamide and apalutamide.[8][9] A newer antiandrogen, ODM-201, is not affected by this mutation, nor has it been found to be affected by any other tested/well-known AR mutations.[10]
Apalutamide may be effective in a subset of prostate cancer patients with acquired resistance to abiraterone acetate.[2]
The chemical structure of ARN-509 is very similar structure to that of Enzalutamide (MDV3100) with two minor modifications: (a) two methyl groups in the 5-member ring of MDV3100 is linked by a CH2 group in ARN-509; (b) the carbon atom in the benzene ring of MDV3100 is replaced by a nitrogen atom in ARN-509. ARN-509 is considered as a Me-Too drug of Enzalutamide (MDV3100). ARN-509 was claimed to be more active than Enzalutamide (MDV3100).
ARN-509 is a novel 2nd Generation anti-androgen that is targeted to treat castration resistant prostate cancers where 1st generation anti-androgens fail. ARN-509 is unique in its action in that it inhibits both AR nuclear translocation and AR binding to androgen response elements in DNA. Importantly, and in contrast to the first-generation anti-androgen bicalutamide, it exhibits no agonist activity in prostate cancer cells that over-express AR. ARN-509 is easily synthesized, and its oral bioavailability and long half-life allow for once-daily oral dosing. In addition, its excellent preclinical safety profile makes it well suited as either a mono- or a combination therapy across the entire spectrum of prostate cancer disease states. (source: http://www.aragonpharm.com/programs/arn509.htm).
ARN-509 is a competitive AR inhibitor, which is fully antagonistic to AR overexpression, a common and important feature of CRPC. ARN-509 was optimized for inhibition of AR transcriptional activity and prostate cancer cell proliferation, pharmacokinetics and in vivo efficacy. In contrast to bicalutamide, ARN-509 lacked significant agonist activity in preclinical models of CRPC. Moreover, ARN-509 lacked inducing activity for AR nuclear localization or DNA binding. In a clinically valid murine xenograft model of human CRPC, ARN-509 showed greater efficacy than MDV3100. Maximal therapeutic response in this model was achieved at 30 mg/kg/day of ARN-509 , whereas the same response required 100 mg/kg/day of MDV3100 and higher steady-state plasma concentrations. Thus, ARN-509 exhibits characteristics predicting a higher therapeutic index with a greater potential to reach maximally efficacious doses in man than current AR antagonists. Our findings offer preclinical proof of principle for ARN-509 as a promising therapeutic in both castration-sensitive and castration-resistant forms of prostate cancer. (source: Cancer Res. 2012 Jan 20. [Epub ahead of print] )
(source: Cancer Res. 2012 Jan 20. [Epub ahead of print] )
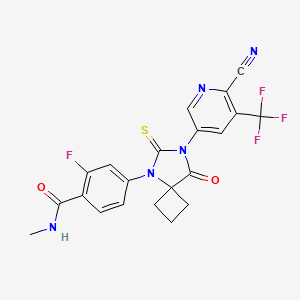 SYNTHESISS
SYNTHESISS

WO 2008119015
WO2011103202
WO2014190895
WO2011103202
http://www.google.com/patents/WO2011103202A2?cl=en


 Prostate cancer is one of the most common forms of cancer found in Western men and the second leading cause of cancer death in Western men. When prostate cancer is confined locally, the disease can usually be treated by surgery and/or radiation. Advanced disease is frequently treated with anti-androgen therapy, also known as androgen deprivation therapy. Administration of anti-androgens blocks androgen receptor (AR) function by competing for androgen binding; and therefore, anti-androgen therapy reduces AR activity. Frequently, such therapy fails after a time, and the cancer becomes hormone refractory, that is, the prostate cancer no longer responds to hormone therapy and the cancer does not require androgens to progress.
Prostate cancer is one of the most common forms of cancer found in Western men and the second leading cause of cancer death in Western men. When prostate cancer is confined locally, the disease can usually be treated by surgery and/or radiation. Advanced disease is frequently treated with anti-androgen therapy, also known as androgen deprivation therapy. Administration of anti-androgens blocks androgen receptor (AR) function by competing for androgen binding; and therefore, anti-androgen therapy reduces AR activity. Frequently, such therapy fails after a time, and the cancer becomes hormone refractory, that is, the prostate cancer no longer responds to hormone therapy and the cancer does not require androgens to progress.
Overexpression of AR has been identified as a cause of hormone refractory prostate cancer (Nat. Med., 10:33-39, 2004; incorporated herein by reference). Overexpression of AR is sufficient to cause progression from hormone sensitive to hormone refractory prostate cancer, suggesting that better AR antagonists than the current drugs may be able to slow the progression of prostate cancer. It has been demonstrated that overexpression of AR converts anti-androgens from antagonists to agonists in hormone refractory prostate cancer. This work explains why anti-androgen therapy fails to prevent the progression of prostate cancer.
The identification of compounds that have a high potency to anatgonize AR activity would overcome the hormone refractory prostate cancer and slowdown the progression of hormone sensitive prostate cancer. Such compounds have been identified by Sayers et al. (WO 2007/126765, published Nov. 8, 2007; which is incorporated herein by reference). One compound is known as A52, a biarylthiohydantoin, and has the chemical structure
Moilanen AM, Riikonen R, Oksala R, Ravanti L, Aho E, Wohlfahrt G, Nykänen PS, Törmäkangas OP, Palvimo JJ, Kallio PJ (2015). “Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies”. Sci Rep 5: 12007. doi:10.1038/srep12007. PMC 4490394. PMID 26137992
11Clegg NJ, Wongvipat J, Tran C, Ouk S, Dilhas A, Joseph J, Chen Y, Grillot K, Bischoff ED, Cai L, Aparicio A, Dorow S, Arora V, Shao G, Qian J, Zhao H, Yang G, Cao C, Sensintaffar J, Wasielewska T, Herbert MR, Bonnefous C, Darimont B, Scher HI, Smith-Jones PM, Klang M, Smith ND, de Stanchina E, Wu N, Ouerfelli O, Rix P, Heyman R, Jung ME, Sawyers CL, Hager JH. ARN-509: a novel anti-androgen for prostate cancer treatment. Cancer Res. 2012 Mar 15;72(6):1494-1503. Epub 2012 Jan 20.PubMed PMID: 22266222.
| Patent ID | Date | Patent Title |
|---|---|---|
| US2014309262 | 2014-10-16 | ANDROGEN RECEPTOR MODULATOR FOR THE TREATMENT OF PROSTATE CANCER AND ANDROGEN RECEPTOR-ASSOCIATED DISEASES |
| US2014296312 | 2014-10-02 | TREATMENT OF BREAST CANCER |
| US2014243416 | 2014-08-28 | Topical Antiandrogen Therapy for the Treatment of Becker’s Nevus |
| US8802689 | 2014-08-12 | Androgen receptor modulator for the treatment of prostate cancer and androgen receptor-associated diseases |
| US2014107085 | 2014-04-17 | Bifunctional AKR1C3 Inhibitors/Androgen Receptor Modulators and Methods of Use Thereof |
| US2014088129 | 2014-03-27 | ANTI-ANDROGENS FOR THE TREATMENT OF NON-METASTATIC CASTRATE-RESISTANT PROSTATE CANCER |
| US2013225821 | 2013-08-29 | SYNTHESIS OF THIOHYDANTOINS |
| US2013116258 | 2013-05-09 | ANDROGEN RECEPTOR MODULATORS AND USES THEREOF |
| US2011003839 | 2011-01-06 | ANDROGEN RECEPTOR MODULATOR FOR THE TREATMENT OF PROSTATE CANCER AND ANDROGEN RECEPTOR-ASSOCIATED DISEASES |
| US2010190991 | 2010-07-29 | SYNTHESIS OF THIOHYDANTOINS |
 |
|
| Systematic (IUPAC) name | |
|---|---|
|
4-[7-[6-Cyano-5-(trifluoromethyl)pyridin-3-yl]-8-oxo-6-sulfanylidene-5,7-diazaspiro[3.4]octan-5-yl]-2-fluoro-N-methylbenzamide
|
|
| Clinical data | |
| Pregnancy category |
|
| Routes of administration |
Oral |
| Identifiers | |
| CAS Number | 956104-40-8 |
| ATC code | None |
| PubChem | CID 24872560 |
| ChemSpider | 28424131 |
| Chemical data | |
| Formula | C21H15F4N5O2S |
| Molar mass | 477.434713 g/mol |
////////
CNC(=O)C1=C(C=C(C=C1)N2C(=S)N(C(=O)C23CCC3)C4=CN=C(C(=C4)C(F)(F)F)C#N)F
CNC(=O)C1=C(C=C(C=C1)N2C(=S)N(C(=O)C23CCC3)C4=CN=C(C(=C4)C(F)(F)F)C#N)F
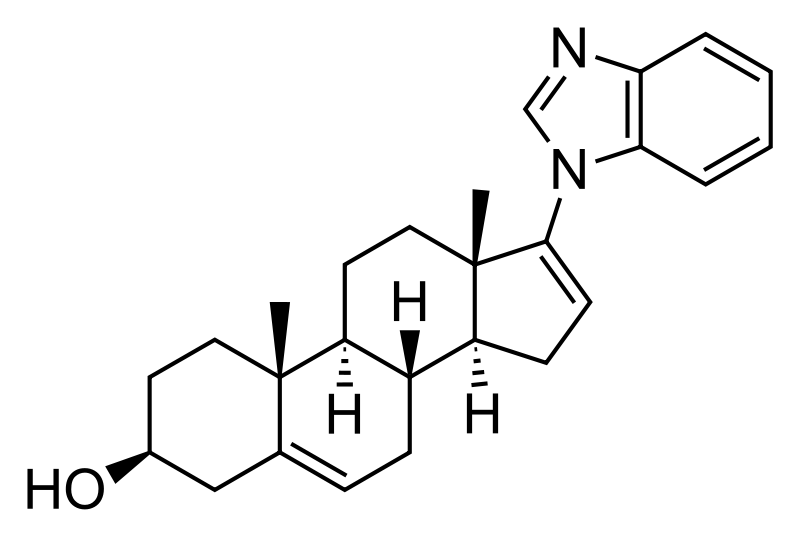
Galeterone
SYNTHESIS SEE BELOW
A SARM potentially for the treatment of prostate cancer.
Research Code, TOK-001; VN; 124; 124-1; 1241
TOK-001; Galeterone; 851983-85-2; VN/124; UNII-WA33E149SW; VN/124-1;
CAS No. 851983-85-2(Galeterone)
(3S,8R,9S,10R,13S,14S)-17-(benzimidazol-1-yl)-10,13-dimethyl-2,3,4,7,8,9,11,12,14,15-decahydro-1H-cyclopenta[a]phenanthren-3-ol
Fast track 2012 f
| Molecular Formula: | C26H32N2O |
|---|---|
| Molecular Weight: | 388.54508 g/mol |

Galeterone (TOK-001 or VN/124-1) is a novel steroidal antiandrogen under development by Tokai Pharmaceuticals for the treatment of prostate cancer. It possesses a unique dual mechanism of action, acting as both an androgen receptor antagonist and an inhibitor of CYP17A1, an enzyme required for the biosynthesis of the androgens.[1] It shows selectivity for 17,20-lyase over 17-hydroxylase.[2]
As of 2016, galeterone is being compared to enzalutamide in a phase III clinical trial (ARMOR3-SV) for AR-V7-expressing metastatic castration-resistant prostate cancer.[3][4]
Specific Androgen Receptor Modulator CYP17 Inhibitor TOK-001 is an orally bioavailable small-molecule androgen receptor modulator and CYP17 lyase inhibitor with potential antiandrogen activity. Galeterone exhibits three distinct mechanisms of action: 1) as an androgen receptor antagonist, 2) as a CYP17 lyase inhibitor and 3) by decreasing overall androgen receptor levels in prostate cancer tumors, all of which may result in a decrease in androgen-dependent growth signaling. Localized to the endoplasmic reticulum (ER), the cytochrome P450 enzyme CYP17 (P450C17 or CYP17A1) exhibits both 17alpha-hydroxylase and 17,20-lyase activities, and plays a key role in the steroidogenic pathway that produces progestins, mineralocorticoids, glucocorticoids, androgens, and estrogens.
Tokai’s lead product candidate is galeterone, a highly-selective, oral small molecule with the potential to transform the treatment of prostate cancer. We are focusing our late-stage development of galeterone on the treatment of men with metastatic, castration-resistant prostate cancer, or CRPC, whose prostate tumor cells express the AR-V7 splice variant.
We are conducting ARMOR3-SV, a Phase 3 clinical trial of galeterone evaluating whether administration of galeterone results in a statistically significant increase in radiographic progression-free survival as compared to Xtandi® (enzalutamide), an oral therapy currently approved for the treatment of CRPC, in AR-V7 positive metastatic CRPC patients. ARMOR3-SV is the first pivotal trial in prostate cancer to employ a precision medicine approach for patient selection. For more information regarding ARMOR3-SV, click here.
Galeterone has been studied in over 250 subjects in Phase 1 and Phase 2 clinical trials, including in CRPC patients with and without the AR-V7 splice variant. In these trials, galeterone demonstrated good tolerability and showed clinically meaningful reductions in levels of prostate specific antigen, or PSA, a biochemincal marker used to evaluate prostate cancer patients for signs of response to therapy.
We are currently focusing our late-stage development of galeterone on AR-V7 positive metastatic CRPC patients because it represents an unmet need in prostate cancer and our precision medicine approach provides an efficient development path. Based on the data we and our collaborators have produced to date, we also believe there is rationale for the broader clinical exploration of galeterone in the future.
Galeterone acts by disrupting the androgen receptor signaling pathway. This pathway is activated by the binding of male hormones (also known as androgens), such as testosterone and dihydrotestosterone (DHT) to androgen receptors in prostate cancer cells.
Galeterone disrupts the activation of the androgen receptor pathway in three ways:
Tokai retains global rights to galeterone. We intend to commercialize galeterone in the United States on our own, and to seek a partner to further develop and commercialize galeterone outside of the United States.
Galeterone has been granted Fast Track designation by U.S. Food and Drug Administration for the treatment of CRPC. Fast Track designation is designed to facilitate the development and expedite review of drugs intended to treat serious or life-threatening conditions and that demonstrate the potential to address unmet medical needs.


DETAILED DESCRIPTION
1J loss reaction.
(1) raw material specifications to match.
acetate pregnancy dehydropregnenolone: toluene + ethanol: Batch steep: hydrochloric acid amine light = 1: 3: 0 4: 0.213, which pregnenolone acetate pregnancy 160kg, toluene + ethanol 320kg + 160kg, approved Steep 64kg, hydrochloric acid amine light 34kg.
(2) process operation.
In the first input 1000L tank oximation with hydroxylamine hydrochloride in pyridine, and then pumped into a mixed solvent of toluene and ethanol, the reaction solution was stirred and heated to complete dissolution, pregnancy-dehydropregnenolone acetate was added and heated under reflux for 3 hours, cooling and crystallization, The Department conducted into the centrifuge centrifugal drying, apply a recovery from the mother liquor, rinse with warm water mixture to no foam, centrifugal drying, drying to a moisture at 0.2% or less, that acetic acid in pregnancy dehydropregnenolone oxime (oxime compounds) 163kg, content of 99%, a melting point of 202-204 ° C, a yield of about 102% (for pregnenolone acetate pregnancy weight ratio).
2, heavy drain hydrolysis reaction.
(1) raw material specifications to match.
acetate pregnancy dehydropregnenolone waning: Benzene: Batch steep: phosphorus oxychloride and toluene: HCl + water = 1: 6 5: 0 4: 1: 3.5, which acetate pregnancy alcohol one hand 163kg, benzene 1060kg, batch steep 64kg, phosphorus oxychloride and toluene 80kg + 80kg, hydrochloric acid + water 245kg + 325kg.
(2) process operation.
The first drying 2000L rearrangement reaction tank, then pumped to the reaction tank benzene, alcohol into acetate pregnancy oxime, pulls out into benzene, stirring heated to reflux until the reaction mixture is completely dissolved, cooling to 1 (TC When, pyridine, of the reaction liquid at temperatures down to 6 ° C, start dropping a mixed solution of previously prepared phosphorus oxychloride and toluene (1: 1 mass ratio), slowly dropping, dropping control, first After slow fast reaction when dropping liquid temperature control in 4-8 ° C, the addition was complete, the reaction solution at 9-12 ° C for 3 hours the first time under.
After incubation, a solution has been a mixed solution of hydrochloric acid and water, good preparation, while dropping the reaction liquid temperature is controlled at 15-25 ° C, the addition was complete, the reaction solution at 15-25 ° C under a second Insulation 1. 5-2 hours. After incubation, stand 40 minutes, then points to lower acidic water layer, the remaining upper layer was added 0.3 times the amount of 30-35 ° C in the brine and let stand 20 minutes, a second watershed, sub lower aqueous layer was then allowed to stand for 30 minutes, a third water diversion, to give the final weight of the upper layer reaction solution was drained.
3, the red Dingding steam distillate process.
The rearrangement reaction liquid was pumped to punch distillate tank, conduct atmospheric distillate punch, has been rushed to the reaction mixture was distilled benzene mixed solvent only, at the start of the steam valve not to open too much, so as not to rush material, distillation after cooling discharge, centrifugal drying, washing with tap water to neutral, and then into the oven dried to a moisture in the square. 5% acetic acid in dehydroepiandrosterone (rearrangement thereof) The crude product is about 142kg, content of about 97.5%, a melting point of 160 ° C _165 ° C or so, yield about 88% (for acetate pregnancy dehydropregnenolone weight ratio).
4, refining processes.
The drying in acetic acid Dehydroepiandrosterone crude into refined tin, adding 8 times the weight of the crude methanol and 0.10 times the weight of activated carbon, heat, stirring to dissolve, reflux billion. 5 hours, filtered , concentrated, cooled to about 5 ° C, the discharge


| Patent ID | Date | Patent Title |
|---|---|---|
| US2011034428 | 2011-02-10 | Treatment of Prostate Cancer |
| US7875599 | 2011-01-25 | C-17-heteroaryl steroidal CYP17 inhibitors/antiandrogens, in vitro biological activities, pharmacokinetics and antitumor activity |
| US2010137269 | 2010-06-03 | Novel C-17-Heteroaryl Steroidal Cyp17 Inhibitors/Antiandrogens: Synehesis, In Vitro Biological Activities, Pharmacokinetics and Antitumor Activity |
| US2010048914 | 2010-02-25 | Novel C-17-Heteroaryl Steroidal Cyp17 Inhibitors/Antiandrogens, In Vitro Biological Activities, Pharmacokinetics and Antitumor Activity |
| US2010048913 | 2010-02-25 | Novel C-17-Heteroaryl Steroidal CYP17 Inhibitors/Antiandrogens Synthesis In Vitro Biological Activities, Pharmacokinetics and Antitumor Activity |
| US2010048912 | 2010-02-25 | Novel C-17-Heteroaryl Steroidal CYP17 Inhibitors/Antiandrogens, In Vitro Biological Activities, Pharmacokinetics and Antitumor Activity |
| US2010048524 | 2010-02-25 | Novel C-17-Heteroaryl Steroidal CYP17 Inhibitors/Antiandrogens Synthesis In Vitro Biological Activities, Pharmacokinetics and Antitumor Activity |
| US2010047338 | 2010-02-25 | Novel C-17-Heteroaryl Steroidal CYP17 Inhibitors/Antiandrogens, In Vitro Biological Activities, Pharmacokinetics and Antitumor Activity |
| Patent ID | Date | Patent Title |
|---|---|---|
| US2013336962 | 2013-12-19 | AZIRIDINE BISPHENOL ETHERS AND RELATED COMPOUNDS AND METHODS FOR THEIR USE |
| US8569393 | 2013-10-29 | UV-LED curable compositions and inks |
| US2013203615 | 2013-08-08 | ANTIANDROGEN THERAPY MONITORING METHODS AND COMPOSITIONS |
| US2012309861 | 2012-12-06 | PHOTOINITIATORS FOR UV-LED CURABLE COMPOSITIONS AND INKS |
| US2012237502 | 2012-09-20 | METHOD FOR TREATING BREAST CANCER AND OVARIAN CANCER |
| US2011319369 | 2011-12-29 | COMBINATION OF A 17 ALPHA-HYDROXYLASE/C17, 20-LYASE INHIBITOR WITH AN ADDITIONAL THERAPEUTIC AGENT |
| US2011312924 | 2011-12-22 | NOVEL STEROIDAL CYP17 INHIBITORS/ANTIANDROGENS |
| US2011312916 | 2011-12-22 | NOVEL PRODRUGS OF STEROIDAL CYP17 INHIBITORS/ANTIANDROGENS |
| US2011118219 | 2011-05-19 | NOVEL PRODRUGS OF C-17-HETEROARYL STEROIDAL CYP17 INHIBITORS/ANTIANDROGENS: SYNTHESIS, IN VITRO BIOLOGICAL ACTIVITIES, PHARMACOKINETICS AND ANTITUMOR ACTIVITY |
| US2011105445 | 2011-05-05 | ANDROGEN RECEPTOR INACTIVATION CONTRIBUTES TO ANTITUMOR EFFICACY OF CYP17 INHIBITORS IN PROSTATE CANCER |
| Patent ID | Date | Patent Title |
|---|---|---|
| US2015051179 | 2015-02-19 | NOVEL STEROIDAL CYP17 INHIBITORS/ANTIANDROGENS |
| US2015005265 | 2015-01-01 | METHODS AND COMPOSITIONS FOR COMBINATION THERAPY USING P13K/MTOR INHIBITORES |
| US2014371261 | 2014-12-18 | INDOMETHACIN ANALOGS FOR THE TREATMENT OF CASTRATE-RESISTANT PROSTATE CANCER |
| US2014371181 | 2014-12-18 | NOVEL PRODRUGS OF STEROIDAL CYP17 INHIBITORS/ANTIANDROGENS |
| US2014343024 | 2014-11-20 | TREATMENT OF PROSTATE CANCER |
| US2014288037 | 2014-09-25 | NOVEL COMPOSITIONS AND METHODS FOR TREATING PROSTATE CANCER |
| US2014288036 | 2014-09-25 | NOVEL C-17-HETEROARYL STEROIDAL CYP17 INHIBITORS/ANTIANDROGENS, IN VITRO BIOLOGICAL ACTIVITIES, PHARMACOKINETICS AND ANTITUMOR ACTIVITY |
| US2014274983 | 2014-09-18 | NOVEL PRODRUGS OF C-17-HETEROARYL STEROIDAL CYP17 INHIBITORS/ANTIANDROGENS: SYNTHESIS, IN VITRO BIOLOGICAL ACTIVITIES, PHARMACOKINETICS AND ANTITUMOR ACTIVITY |
| US2014107085 | 2014-04-17 | Bifunctional AKR1C3 Inhibitors/Androgen Receptor Modulators and Methods of Use Thereof |
| US2013336962 | 2013-12-19 | AZIRIDINE BISPHENOL ETHERS AND RELATED COMPOUNDS AND METHODS FOR THEIR USE |


| CN101691392A * | Sep 17, 2009 | Apr 7, 2010 | 扬州市天平化工厂有限公司 | Method for preparing 3beta-acetoxyl group-5androstene-17ketone |
| CN102212099A * | Apr 2, 2011 | Oct 12, 2011 | 邵阳市科瑞化学品有限公司 | Synthesis method for dehydroepiandrosterone |
| CN102603839A * | Jan 13, 2012 | Jul 25, 2012 | 宜城市共同药业有限公司 | Preparation method of dehydroepiandrosterone |
| CN102746356A * | Jul 17, 2012 | Oct 24, 2012 | 湖北芳通药业股份有限公司 | Process for producing dehydroepiandrosterone acetate through homogeneous phase method |
| Reference | ||||
|---|---|---|---|---|
| 1 | * | 石诚等: “5-雄甾烯-3β-醇-17-酮-3-醋酸酯的工艺研究“, 《山东化工》, vol. 41, no. 1, 31 December 2012 (2012-12-31) | ||
| 2 | * | 石诚等: “醋酸妊娠双烯醇酮肟的工艺研究“, 《广州化工》, vol. 39, no. 23, 31 December 2011 (2011-12-31), pages 78 – 79 | ||
Silberstein, John L.; Taylor, Maritza N.; Antonarakis, Emmanuel S. (2016-04-01). “Novel Insights into Molecular Indicators of Response and Resistance to Modern Androgen-Axis Therapies in Prostate Cancer”. Current Urology Reports 17 (4): 29. doi:10.1007/s11934-016-0584-4. ISSN 1534-6285. PMID 26902623.
 |
|
| Systematic (IUPAC) name | |
|---|---|
|
17-(1H-benzimidazol-1-yl)androsta-5,16-dien-3β-ol
|
|
| Clinical data | |
| Routes of administration |
Oral |
| Identifiers | |
| CAS Number | 851983-85-2 |
| PubChem | CID 11188409 |
| ChemSpider | 9363493 |
| KEGG | D10125 |
| Chemical data | |
| Formula | C26H32N2O |
| Molar mass | 388.25 |
///////
C[C@]12CC[C@@H](CC1=CC[C@@H]3[C@@H]2CC[C@]4([C@H]3CC=C4N5C=NC6=CC=CC=C65)C)O
CC12CCC(CC1=CCC3C2CCC4(C3CC=C4N5C=NC6=CC=CC=C65)C)O

IC200214; ITI-214
(6aR,9aS)-2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-3-(phenylamino)-5,6a,7,8,9,9a-hexahydrocyclopenta[4,5]imidazo[1,2-a]pyrazolo[4,3-e]pyrimidin-4-(2H)-one phosphate
(6aR,9aS)-5-methyl-3-(phenylamino)-2-(4-(6-fluoropyridin-2-yl)-benzyl)-5,6a,7,8,9,9a-hexahydrocyclopent[4,5]imidazo[1,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one…BASE
CAS: 1642303-38-5 (phosphate);
1160521-50-5 (free base).
Chemical Formula: C29H29FN7O5P
Molecular Weight: 605.5672
Takeda Pharmaceutical Company Limited,Intra-Cellular Therapies, Inc.
ITI-214 is an orally active, potent and Selective Inhibitors of Phosphodiesterase 1 for the Treatment of Cognitive Impairment Associated with Neurodegenerative and Neuropsychiatric Diseases. ITI-214 exhibited picomolar inhibitory potency for PDE1, demonstrated excellent selectivity against all other PDE families, and showed good efficacy in vivo. Currently, this investigational new drug is in Phase I clinical development and being considered for the treatment of several indications including cognitive deficits associated with schizophrenia and Alzheimer’s disease, movement disorders, attention deficit and hyperactivity disorders, and other CNS and non-CNS disorders.
Phosphodiesterase-1 (PDE-1) inhibitor
which is a picomolar PDE1 inhibitor with excellent selectivity against other PDE family members and against a panel of enzymes, receptors, transporters, and ion channels.
It is disclosed in WO 2009/075784 (U.S. Pub. No. 2010/0273754). This compound has been found to be a potent and selective phosphodiesterase 1 (PDE 1) inhibitor useful for the treatment or prophylaxis of disorders characterized by low levels of cAMP and/or cGMP in cells expressing PDE1, and/or reduced dopamine Dl receptor signaling activity (e.g., Parkinson’s disease, Tourette’s Syndrome, Autism, fragile X syndrome, ADHD, restless leg syndrome, depression, cognitive impairment of schizophrenia, narcolepsy); and/or any disease or condition that may be ameliorated by the enhancement of progesterone signaling. This list of disorders is exemplary and not intended to be exhaustive.

PATENT
WO 2013192556
http://www.google.com/patents/WO2013192556A2?cl=en
The method of making the Compound (ea^^a^-S^a ^^^a-hexahydro-S- methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)- cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one is generally described in WO 2009/075784, the contents of which are incorporated by reference in their entirety. This compound can also be prepared as summarized or similarly summarized in the following
CMU PCU PHU PPU (SM2)
In particular, (6aR,9aS)-3-chloro-2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl- 5,6a,7,8,9,9a-hexahydrocyclopenta[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)- one may be prepared as described or similarly described below.
PATENT
http://www.google.com/patents/WO2009075784A1?cl=en
EXAMPLE 14
(6aJ?,9aS)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6- fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]iinidazo[l,2-fl]pyrazolo[4,3- e]pyrimidin-4(2//)-one
This compound may be made using similar method as in example 13 wherein 2-(4-(bromomethyl)phenyl)-6-fluoropyridine may be used instead of 2-(4- (dibromomethyl)phenyl)-5-fluoropyridine.
PATENT
WO 2014205354
https://www.google.co.in/patents/WO2014205354A2?cl=en

EXAMPLES
The method of making the Compound (ea^^a^-S^a ^^^a-hexahydro-S-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one is generally described in WO 2009/075784, the contents of which are incorporated by reference in their entirety. This compound can also be prepared as summarized or similarly summarized in the following

CMU PCU PHU PPU (SM2)
![]()

In particular, (6aR,9aS)-3-chloro-2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-5,6a,7,8,9,9a-hexahydrocyclopenta[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one (Int-5) may be prepared as described or similarly described below. The free base crystals and the mono-phosphate salt crystals of the invention may be prepared by using the methods described or similarly described in Examples 1-14 below.
Preparation of (6aR,9aS)-3-chloro-2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-5,6a,7,8,9,9a-hexahydrocyclopenta[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one
(4-(6-fluoropyridin-2-yl)phenyl)methanol

The mixture of Na2C03 (121 g), water (500 mL), THF (650 mL), PdCl2(PPh3)2 (997 mg), 2-bromo-6-fluoropyridine (100 g) and 4-(hydroxymethyl)phenylboronic acid (90.7 g) is stirred at 65°C for 4 h under the nitrogen atmosphere. After cooling to room temperature, THF (200 mL) is added. The organic layer is separated and washed with 5% NaCl solution twice. The organic layer is concentrated to 400 mL. After the addition of toluene (100 mL), heptane (500 mL) is added at 55°C. The mixture is cooled to room temperature. The crystals are isolated by filtration, washed with the mixture of toluene (100 mL) and heptane (100 mL) and dried to give (4-(6-fluoropyridin-2-yl)phenyl)methanol (103 g). ]H NMR (500 MHz, CDC13) δ 1.71-1.78 (m, 1H), 4.74-4.79 (m, 2H), 6.84-6.88 (m, 1H), 7.44-7.50 (m, 2H), 7.61-7.65 (m, 1H), 7.80-7.88 (m, 1H), 7.98-8.04 (m, 2H).
2-(4-(chloromethyl)phenyl)-6-fluoropyridine

The solution of thionylchloride (43.1 mL) in AcOEt (200 mL) is added to the mixture of (4-(6-fluoropyridin-2-yl)phenyl)methanol (100 g), DMF (10 mL) and AcOEt (600 mL) at room temperature. The mixture is stirred at room temperature for 1 h. After cooling to 10°C, 15% Na2C03 solution is added. The organic layer is separated and washed with water (500 mL) and 5% NaCl solution (500 mL) twice. The organic layer is concentrated to 500 mL. After the addition of EtOH (500 mL), the mixture is concentrated to 500 mL. After addition of EtOH (500 mL), the mixture is concentrated to 500 mL. After the addition of EtOH (500 mL), the mixture is concentrated to 500 mL. After addition of EtOH (200 mL), water (700 mL) is added at 40°C. The mixture is stirred at room temperature. The crystals are isolated by filtration and dried to give 2-(4-(chloromethyl)phenyl)-6-fluoropyridine (89.5 g). ]H NMR (500 MHz, CDC13) δ 4.64 (s, 2H), 6.86-6.90 (m, 1H), 7.47-7.52 (m, 2H), 7.60-7.65 (m, 1H), 7.82-7.88 (m, 1H), 7.98-8.03 (m, 2H).
6-chloro-l-(4-methoxybenzyl)-3-methylpyrimidine-2,4(lH,3H)-dione

The mixture of 6-chloro-3-methyluracil (100 g), p-methoxybenzylchloride (107 g), K2CO3 (86.1 g) and DMAc (600 mL) is stirred at 75°C for 4 h. Water (400 mL) is added at 45°C and the mixture is cooled to room temperature. Water (800 mL) is added and the mixture is stirred at room temperature. The crystals are isolated by filtration, washed with the mixture of DMAc and water (1:2, 200mL) and dried to give 6-chloro-l-(4-methoxybenzyl)-3-methylpyrimidine-2,4(lH,3H)-dione (167 g). ]H NMR (500 MHz, CDC13) δ 3.35 (s, 3H), 3.80 (s, 3H), 5.21 (s, 2H), 5.93 (s, 1H), 6.85-6.89 (m, 2H), 7.26-7.32 (m, 2H).
izinyl-l-(4-methoxybenzyl)-3-methylpyrimidine-2,4(lH,3H)-dione

The mixture of 6-chloro-l-(4-methoxybenzyl)-3-methylpyrimidine-2,4(lH,3H)-dione (165 g), IPA (990 mL), water (124 mL) and hydrazine hydrate (62.9 mL) is stirred at room temperature for 1 h. The mixture is warmed to 60°C and stirred at the same temperature for 4 h. Isopropyl acetate (1485 mL) is added at 45°C and the mixture is stirred at the same temperature for 0.5 h. The mixture is cooled at 10°C and stirred for lh. The crystals are isolated by filtration, washed with the mixture of IPA and isopropyl acetate (1:2, 330 mL) and dried to give 6-hydrazinyl-l-(4-methoxybenzyl)-3-methylpyrimidine-2,4(lH,3H)-dione (153 g). ]H NMR (500 MHz, DMSO-i¾) δ 3.12 (s, 3H), 3.71 (s, 3H), 4.36 (s, 2H), 5.01 (s, 2H), 5.14 (s, 1H), 6.87-6.89 (m, 2H), 7.12-7.17 (m, 2H), 8.04 (s, 1H).
7-(4-methoxybenzyl)-5-methyl-2H-pyrazolo[3,4-d]pyrimidine-4,6(5H,7H)-dione

To the mixture of DMF (725 mL) and 6-hydrazinyl-l-(4-methoxybenzyl)-3-methylpyrimidine-2,4(lH,3H)-dione (145 g) is added POCI3 (58.5 mL) at 5°C. The mixture is stirred at room temperature for 1 h. Water (725 mL) is added at 50°C and the mixture is stirred at room temperature for 1 h. The crystals are isolated by filtration, washed with the mixture of DMF and water (1:1, 290 mL) and dried to give 7-(4-methoxybenzyl)-5-methyl-
2H-pyrazolo[3,4-d]pyrimidine-4,6(5H,7H)-dione (145 g). ]H NMR (500 MHz, DMSO-i¾) δ 3.23 (s, 3H), 3.71 (s, 3H), 5.05 (s, 2H), 6.82-6.90 (m, 2H), 7.28-7.36 (m, 2H), 8.48 (s, IH), 13.51 (br, IH).
2-(4-(6-fluoropyridin-2-yl)benzyl)-7-(4-methoxybenzyl)-5-methyl-2H-pyrazolo[3,4-d]pyrimidine-4,6(5H,7H)-dione

The mixture of 2-(4-(chloromethyl)phenyl)-6-fluoropyridine (100 g), 7-(4-methoxybenzyl)-5-methyl-2H-pyrazolo[3,4-d]pyrimidine-4,6(5H,7H)-dione (129 g), K2CO3(62.3 g) and DMAc (1500 mL) is stirred at 45°C for 5 h. Water (1500 mL) is added at 40°C and the mixture is stirred at room temperature for 1 h. The crystals are isolated by filtration, washed with the mixture of DMAc and water (1:1, 500 mL) and dried to give 2-(4-(6-fluoropyridin-2-yl)benzyl)-7-(4-methoxybenzyl)-5-methyl-2H-pyrazolo[3,4-d]pyrimidine-4,6(5H,7H)-dione (207 g). ]H NMR (500 MHz, DMSO- ) δ 3.21 (s, 3H), 3.66 (s, 3H), 4.98 (s, 2H), 5.45 (s, 2H), 6.77-6.82 (m, 2H), 7.13-7.16 (m, IH), 7.25-7.30 (m, 2H), 7.41-7.44 (m, 2H), 7.92-7.96 (m, IH), 8.04-8.11 (m, 3H), 8.68 (s, IH).
2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-2H-pyrazolo[3,4-d]pyrimidine-4,6(5H,7H)-dione

The mixture of 2-(4-(6-fluoropyridin-2-yl)benzyl)-7-(4-methoxybenzyl)-5-methyl-2H-pyrazolo[3,4-d]pyrimidine-4,6(5H,7H)-dione (105 g), CF3COOH (300 mL) and
CF3SO3H (100 g) is stirred at room temperature for 10 h. Acetonitrile (1000 mL) is added. The mixture is added to the mixture of 25% N¾ (1000 mL) and acetonitrile (500 mL) at 10°C. The mixture is stirred at room temperature for 1 h. The crystals are isolated by filtration, washed with the mixture of acetonitirile and water (1:1, 500 mL) and dried to give the crude product. The mixture of the crude product and AcOEt (1200 mL) is stirred at room temperature for 1 h. The crystals are isolated by filtration, washed with AcOEt (250 mL) and dried to give 2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-2H-pyrazolo[3,4-d]pyrimidine-4,6(5H,7H)-dione (75.3 g). ]H NMR (500 MHz, DMSO-rf6) δ 3.16 (s, 3H), 3.50-4.00 (br, 1H), 5.40 (s, 2H), 7.13-7.16 (m, 1H), 7.41-7.44 (m, 2H), 7.91-7.94 (m, 1H), 8.04-8.10 (m, 3H), 8.60 (s, 1H).
2-(4-(6-fluoropyridin-2-yl)benzyl)-6-(((lR,2R)-2-hydroxycyclopentyl)amino)-5-methyl-2H-pyrazolo[3,4-d]pyrimidin-4(5H)-one

The mixture of BOP reagent (126 g), 2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-2H-pyrazolo[3,4-d]pyrimidine-4,6(5H,7H)-dione (80 g), DBU (136 mL) and THF (1120 mL) is stirred at room temperature for 1 h. (lR,2R)-2-Aminocyclopentanol hydrochloride (37.6 g) and THF (80 mL) are added and the mixture is stirred at room temperature for 5 h. After the addition of 5% NaCl (400 mL) and AcOEt (800 mL), the organic layer is separated. The organic layer is washed with 10% NaCl (400 mL), 1M HC1 15% NaCl (400 mL), 5% NaCl (400 mL), 5% NaHC03 (400 mL) and 5%NaCl (400 mL) successively. After treatment with active charcoal, the organic layer is concentrated to 400 mL. After the addition of acetonitrile (800 mL), the mixture is concentrated to 400 mL. After the addition of acetonitrile (800 mL), seed crystals are added at 40°C. The mixture is concentrated to 400 mL. Water (800 mL) is added at room temperature and the mixture is stirred for 2 h. The crystals are isolated by filtration, washed with the mixture of acetonitrile and water (1:2, 400 mL) and dried to give 2-(4-(6-fluoropyridin-2-yl)benzyl)-6-(((lR,2R)-2-
hydroxycyclopentyl)amino)-5-methyl-2H-pyrazolo[3,4-d]pyrimidin-4(5H)-one (81.7 g). ]H NMR (500 MHz, CDC13) δ 1.47-1.59 (m, 1H), 1.68-1.93 (m, 3H), 2.02-2.12 (m, 1H), 2.24-2.34 (m, 1H), 3.42 (s, 3H), 3.98-4.12 (m, 2H), 4.68-4.70 (m, 1H), 5.37 (s, 2H), 6.86-6.90 (m, 1H), 7.36-7.42 (m, 2H), 7.58-7.63 (m, 1H), 7.81-7.88 (m, 1H), 7.89 (s, 1H), 7.97-8.01 (m, 2H).
(6aR,9aS)-2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-5,6a,7,8,9,9a-hexahydrocyclopenta[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one

The mixture of 2-(4-(6-fluoropyridin-2-yl)benzyl)-6-(((lR,2R)-2-hydroxycyclopentyl)amino)-5-methyl-2H-pyrazolo[3,4-d]pyrimidin-4(5H)-one (80 g), p-toluenesulfonylchloride (38.6 g), Et3N (28.2 mL), N,N-dimethylaminopyridine (24.7 g) and THF (800 mL) is stirred at 50°C for 10 h. To the mixture is added 8M NaOH (11.5 mL) at room temperature and the mixture is stirred for 2 h. After the addition of 5% NaCl (400 mL) and AcOEt (800 mL), the organic layer is separated. The organic layer is washed with 5 NaCl (400 mL) twice. The organic layer is concentrated to 240 mL. After the addition of MeOH (800 mL), the mixture is concentrated to 240 mL. After the addition of MeOH (800 mL), the mixture is concentrated to 240 mL. After the addition of MeOH (160 mL), the mixture is stirred at room temperature for 1 h and at 0°C for 1 h. The crystals are isolated by filtration, washed with cold MeOH (160 mL) and dried to give (6aR,9aS)-2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-5,6a,7,8,9,9a-hexahydrocyclopenta[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one (55.7 g). ]H NMR (500 MHz, CDC13) δ 1.39-1.54 (m, 1H), 1.58-1.81 (m, 3H), 1.81-1.92 (m, 1H), 2.12-2.22 (m, 1H), 3.28 (s, 3H), 4.61-4.70 (m, 2H), 5.20 (s, 2H), 6.79-6.85 (m, 1H), 7.25-7.32 (m, 2H), 7.53-7.58 (m, 1H), 7.68 (s, 1H), 7.75-7.83 (m, 1H), 7.92-7.98 (m, 2H).
(6aR,9aS)-3-chloro-2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-5,6a,7,8,9,9a-
hexahydrocyclopenta[4,5]imi ]pyrimidin-4(2H)-one

The mixture of (6aR,9aS)-2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-5,6a,7,8,9,9a-hexahydrocyclopenta[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one (50 g) and toluene (1000 mL) is concentrated to 750 mL under the nitrogen atmosphere. Toluene (250 mL) and NCS (24 g) is added. To the mixture is added LiHMDS (1M THF solution, 204 mL) at 0°C and the mixture is stirred for 0.5 h. To the mixture is added 20% NH4C1 (50 mL) at 5°C. The mixture is concentrated to 250 mL. After the addition of EtOH (250 mL), the mixture is concentrated to 150 mL. After the addition of EtOH (250 mL), the mixture is concentrated to 200 mL. After the addition of EtOH (200 mL), the mixture is warmed to 50°C. Water (300 mL) is added and the mixture is stirred at 50°C for 0.5 h. After stirring at room temperature for 1 h, the crystals are isolated by filtration, washed with the mixture of EtOH and water (1:1, 150 mL) and dried to give (6aR,9aS)-3-chloro-2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-5,6a,7,8,9,9a-hexahydrocyclopenta[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one (51.1 g). ]H NMR (500 MHz, CDC13) δ 1.46-1.61 (m, 1H), 1.67-1.90 (m, 3H), 1.92-2.00 (m, 1H), 2.19-2.27 (m, 1H), 3.37 (s, 3H), 4.66-4.77 (m, 2H), 5.34 (s, 2H), 6.87-6.93 (m, 1H), 7.35-7.41 (m, 2H), 7.59-7.65 (m, 1H), 7.82-7.91 (m, 1H), 7.97-8.05 (m, 2H).
EXAMPLE 1
Crystals of (6a/f,9a5)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one free base mono-ethanol solvate

The mixture of (6a/?,9a5′)-3-chloro-2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-5,6a,7,8,9,9a-hexahydrocyclopenta[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one (2.5 g), K2C03 (1.53 g), Pd(OAc)2 (12.5 mg), Xantphos (32 mg), aniline (0.76 mL), and xylene (12.5 mL) is stirred at 125°C for 7 h under nitrogen atmosphere. After addition of water (12.5 mL), the organic layer is separated. The organic layer is washed with water (12.5 mL) twice. The organic layer is extracted with the mixture of DMAc (6.25 mL) and 0.5N HCl (12.5 mL). The organic layer is extracted with the mixture of DMAc (3.2 mL) and 0.5N HCl (6.25 mL). After addition of DMAc (6.25 mL), xylene (12.5 mL) and 25 wt % aqueous NH3 solution to the combined aqueous layer, the organic layer is separated. The aqueous layer is extracted with xylene (6.25 mL). The combined organic layer is washed with water (12.5 mL), 2.5 wt % aqueous 1 ,2-cyclohexanediamine solution (12.5 mL) twice and water (12.5 mL) successively. After treatment with active charcoal, the organic layer is concentrated. After addition of EtOH (12.5 mL), the mixture is concentrated. After addition of EtOH (12.5 mL), the mixture is concentrated. After addition of EtOH (12.5 mL), n-heptane (25 mL) is added at 70°C. The mixture is cooled to 5°C and stirred at same temperature. The crystals are isolated by filtration and dried to give (ea^^a^-S^a ^^^a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one free base mono-ethanol solvate (2.56 g) as crystals.
]H NMR (500 MHz, DMSO-d6) δ 0.98-1.13 (m, 3H), 1.34-1.52 (m, 1H), 1.54-1.83 (m, 4H), 2.03-2.17 (m, 1H), 3.11 (s, 3H), 3.39-3.54 (m, 2H), 4.29-4.43 (m, 1H), 4.51-4.60 (m, 1H), 4.60-4.70 (m, 1H), 5.15-5.35 (m, 2H), 6.71-6.88 (m, 3H), 7.05-7.29 (m, 5H), 7.81-7.93 (m, 1H), 7.94-8.11 (m, 3H), 8.67 (s, 1H).
EXAMPLE 4
Crystals of (6a/f,9a5)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one free

Crystals of (6a«,9a5′)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one free base mono-n-propanol solvate (2.0 g) is dissolved with ethanol (10 mL) at 70°C. Isopropyl ether (20 mL) is added and the mixture is cooled to 45°C. Isopropyl ether (10 mL) is added and the mixture is stirred at 40°C. The mixture is cooled to 5°C and stirred at same temperature. The crystals are isolated by filtration and dried to give (ea/^^a^)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one free base non-solvate (1.7 g) as crystals.
[0082] ]H NMR (500 MHz, DMSO-d6) δ 1.32-1.51 (m, 1H), 1.53-1.83 (m, 4H), 1.97-2.20 (m, 1H), 3.11 (s, 3H), 4.49-4.60 (m, 1H), 4.60-4.69 (m, 1H), 5.13-5.37 (m, 2H), 6.70-6.90 (m, 3H), 7.04-7.31 (m, 5H), 7.82-7.93 (m, 1H), 7.93-8.12 (m, 3H), 8.67 (s, 1H).
EXAMPLE 5
Crystals of (6a/f,9a5)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one free base non-solvate

The mixture of (6a/?,9a5′)-3-chloro-2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-5,6a,7,8,9,9a-hexahydrocyclopenta[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one (25 g), K2C03 (15.4 g), Pd(OAc)2 (125 mg), Xantphos (321 mg), aniline (7.6 mL), DMAc (6.25 mL) and xylene (125 mL) is stirred at 125°C for 6.5 h under nitrogen atmosphere. After addition of water (125 mL) and DMAc (50 mL), the organic layer is separated. The organic layer is washed with the mixture of DMAc (50 mL) and water (125 mL) twice. The organic layer is extracted with the mixture of DMAc (50 mL) and 0.5N HCl (125 mL). The organic layer is extracted with the mixture of DMAc (50 mL) and 0.5N HCl (62.5 mL). After addition of DMAc (50 mL), xylene (125 mL) and 25 wt % aqueous NH3 solution (25 mL) to the combined aqueous layer, the organic layer is separated. The aqueous layer is extracted with xylene (62.5 mL). The combined organic layer is washed with the mixture of DMAc (50 mL) and water (125 mL), the mixture of DMAc (50 mL) and 2.5 wt % aqueous 1,2-cyclohexanediamine solution (125 mL) twice and the mixture of DMAc (50 mL) and water (125 mL) successively. After treatment with active charcoal (1.25 g), the organic layer is concentrated to 75 mL. After addition of EtOH (125 mL), the mixture is concentrated to 75 mL. After addition of EtOH (125 mL), the mixture is concentrated to 75 mL. After addition of EtOH (125 mL), n-heptane (250 mL) is added at 70°C. After addition of seed crystals of (6a/?,9a5′)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one non-solvate, the mixture is cooled to room temperature and stirred at room temperature. The crystals are isolated by filtration and dried to give (ea^^a^-S^a ^^^a-hexahydro-S-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo-[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one free base non-solvate (23.8 g) as crystals.
EXAMPLE 8
(6a/f,9a5)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one mono-phosphate salt

[0094] Crystals of (6a«,9a5′)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one free base non-solvate (20 g) are dissolved in acetonitrile (60 mL) at 50°C. After addition of the active charcoal (1 g), the mixture is stirred at same temperature for 0.5 h. The active charcoal is removed by filtration and washed with acetonitrile (40 mL). The filtrate and the washing are combined and warmed to 50°C. A solution of 85 wt. % phosphoric acid (2.64 mL) in acetonitrile (100 mL) is added. After addition of water (20 mL), the mixture is stirred at 50°C for lh. The crystals are isolated by filtration, washed with acetonitrile (60 mL x 3) and dried to give (6a/?,9a5′)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one mono-phosphate salt (20.5 g).
EXAMPLE 9
(6a/f,9a5)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one mono-phosphate salt

[0095] Crystals of (6a«,9a5′)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one free base mono-ethanol solvate (4 g) are dissolved in acetonitrile (12 mL) at 50°C. After addition of active charcoal (0.2 g), the mixture is stirred at same temperature for 0.5 h. Active charcoal is removed by filtration and washed with acetonitrile (8 mL). The filtrate and the washing are combined and warmed to 50°C. A solution of 85 wt. % phosphoric acid (0.528 mL) in acetonitrile (20 mL) is added. After addition of water (4 mL), the mixture is stirred at 50°C for lh. The crystals are isolated by filtration, washed with acetonitrile (12 mL x 3) and dried to give (6a/?,9a5′)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one mono-phosphate salt (4.01 g).
EXAMPLE 10
(6a/f,9a5)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one mono-phosphate salt

Crystals of (6a«,9a5′)-5,6a,7,8,9,9a-Hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one free base non-solvate (20 g) are dissolved in acetone (60 mL) at 32°C. After addition of active charcoal (1 g), the mixture is stirred at same temperature for 0.5 h. Active charcoal is removed by filtration and washed with acetone (40 mL). The filtrate and the washing are combined and warmed to 39°C. A solution of 85 wt. % phosphoric acid (2.64 mL) in acetone (100 mL) is added. After addition of water (20 mL), the mixture is stirred at 40°C for lh. The crystals are isolated by filtration, washed with acetone (60 mL x 3) and dried to give (6a/?,9a5′)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one mono-phosphate salt (22.86 g).
EXAMPLE 11
(6a/f,9a5)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one mono-phosphate salt

Crystals of (6a«,9a5′)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one free base mono-ethanol solvate (20 g) are dissolved in acetone (60 mL) at 38°C. After addition of active charcoal (1 g), the mixture is stirred at same temperature for 0.5 h. Active charcoal is removed by filtration and washed with acetone (40 mL). The filtrate and the washing are combined and warmed to 38°C. A solution of 85 wt. % phosphoric acid (2.64 mL) in acetone (100 mL) is added. After addition of water (20 mL), the mixture is stirred at 40°C for lh. The crystals are isolated by filtration, washed with acetone (60 mL x 3) and dried to give (6a/?,9a5′)-5,6a,7,8,9,9a-hexahydro-5-methyl-3-(phenylamino)-2-((4-(6-fluoropyridin-2-yl)phenyl)methyl)-cyclopent[4,5]imidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one mono-phosphate salt (23.2 g).
PAPER
A diverse set of 3-aminopyrazolo[3,4-d]pyrimidinones was designed and synthesized. The structure–activity relationships of these polycyclic compounds as phosphodiesterase 1 (PDE1) inhibitors were studied along with their physicochemical and pharmacokinetic properties. Systematic optimizations of this novel scaffold culminated in the identification of a clinical candidate, (6aR,9aS)-2-(4-(6-fluoropyridin-2-yl)benzyl)-5-methyl-3-(phenylamino)-5,6a,7,8,9,9a-hexahydrocyclopenta[4,5]imidazo[1,2-a]pyrazolo[4,3-e]pyrimidin-4-(2H)-one phosphate (ITI-214), which exhibited picomolar inhibitory potency for PDE1, demonstrated excellent selectivity against all other PDE families and showed good efficacy in vivo. Currently, this investigational new drug is in Phase I clinical development and being considered for the treatment of several indications including cognitive deficits associated with schizophrenia and Alzheimer’s disease, movement disorders, attention deficit and hyperactivity disorders, and other central nervous system (CNS) and non-CNS disorders
The synthetic methods disclosed in WO 2009/075784 and WO 2013/192556 are particularly applicable, as they include the methods to prepare the compound of Formula I-B. Those skilled in the art will readily see how those methods are applicable to the synthesis of the compounds of the present invention.

Formula I-B
For example, Compounds of the Invention wherein any one or more of R1 through R8 are D, can be prepared from the corresponding aminocyclopentanol, according to the method described in WO 2009/075784 or WO 2013/192556. For example, by reacting said aminocyclopentanol, optionally as its acid salt, with Intermediate A in the presence of a coupling agent, e.g., benzotriazol-1-yloxy)tris(dimethylamino)phosphonium hexafluorophosphate (BOP reagent), and a base, e.g., l,8-diazabicyclo[5.4.0]undec-7-ene (DBU), in a solvent such as tetrahydrofuran (THF). The intermediate alcohol is then cyclized by treatment with toluenesulfonyl chloride (TsCl) in the presence of one or more bases, such as dimethylaminopyridine (DMAP) and triethylamine (TEA) in a solvent, such as THF. The reaction is summarized in the following scheme:

The required aminocyclopentanols can be prepared by methods known to those skilled in the art. For example, the aminocyclopentanol wherein R1 is D can be prepared via a reductive amination procedure that uses a reducing agent such as sodium triacetoxyborodeuteride or sodium borodeuteride as the reducing agent. For example, an optionally protected (R)-2-hydroxycyclopentanone can be reacted with 4-methoxybenzylamine in the presence of sodium triacetoxyborodeuteride to yield the desired deuterated secondary amine, wherein P is the protecting group. Reaction of the resulting amine with a strong acid such as trifluoromethanesulfonic acid (TMFSA) will result in removal of the 4-methoxybenzyl group and the protecting group to yield the desired aminocyclopentanol. Those skilled in the art will know how to choose a suitable protecting group for the secondary alcohol such that deprotection can take place during the acid treatment step (e.g., a tert-butyldimethylsilyl group or a tert-butoxycarbonyl group). Alternatively, those skilled in the art could choose a protecting group that would survive this step. If desired, the protected intermediate can be purified by chiral HPLC in order to enhance the optical purity of the final

As another example, Compounds of the Invention wherein any one or more of R9 to R15 or R21 to R22 are D can be prepared from the corresponding benzyl halide, according to the method described in WO 2009/075784 or WO 2013/192556. For example, by reacting said benzyl halide with the Intermediate B in the presence of suitable base, such as cesium carbonate or potassium carbonate, in a suitable solvent, such as dimethylformamide or dimethylacetamide. The corresponding benzyl halide can be prepared by methods well known to those skilled in the art. The reaction is summarized in the following scheme:

As another example, compounds of the invention wherein any one or more of R16 to R20 are D can be prepared from the corresponding phenyl
isothiocyanate, according to the method described in WO 2009/075784 or WO
2013/192556. For example, by reacting said phenyl isothiocyanate with Intermediate C in a suitable solvent, such as dimethylformamide. The corresponding phenyl isothiocyanate can be prepared by methods well known to those skilled in the art. The reaction is summarized in the following scheme:

Alternatively, compounds of the invention wherein any one or more of R16 to R20 are D can be prepared from the corresponding aniline, according to the method described in WO 2009/075784 or WO 2013/192556. For example, by reacting said aniline with Intermediate D and a strong base, such as lithium
hexamethyldisilylazide (LiHMDS), in a suitable solvent, such as THF at elevated temperature. Such a reaction can also be achieved by catalytic amination using a catalyst, such as tris(dibenzylideneacetone)dipalladium (Pd2(dba)3), and a ligand, such as Xantphos. The corresponding aniline can be prepared by methods well known to those skil

EXAMPLE 1. (6aR,9a5)-5-Methyl-3-(2,3,4,5,6-pentadeuterophenylamino)-2-(4-(6-fluoropyridin-2-yl)-benzyl)-5,6fl,7,8,9,9fl-hexahydrocyclopent[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one

To a solution of (6a/?,9a5′)-5,6a,7,8,9,9a-hexahydro-3-chloro-5-methyl-2-(4-(6-fluoropyridin-2-yl)-benzyl)-cyclopent[4,5]irnidazo[l,2-fl]pyrazolo[4,3-e]pyrimidin-4(2H)-one (200 mg, 0.444 mmol) and 2,3,4,5,6-pentadeuteroaniline (162 μΐ,, 1.8 mmol) in anhydrous 2-methyltetrahydrofuran (3 mL) is added LiHMDS (1.0 M in THF, 0.89 mL) dropwise at room temperature under argon atmosphere. The reaction mixture is gradually heated to 75 °C over a period of 90 min, and then heated at 75 °C for an hour. The mixture is cooled with an ice bath and then quenched by adding 0.2 mL of water. After solvent evaporation, the residue is dissolved in DMF and then filter with a 0.45 m microfilter. The collected filtrated is purified with a semi-preparative HPLC system using a gradient of 0 – 70% acetonitrile in water containing 0.1% formic acid over 16 min to give (6a/?,9a5′)-5-methyl-3-(2,3,4,5,6-pentadeuterophenylamino)-2-(4-(6-fluoropyridin-2-yl)-benzyl)-5,6fl,7,8,9,9fl-hexahydrocyclopent[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one as a formate salt, which is dissolved in ethyl acetate, basified with 12.5 mL of 5% sodium carbonate, and then extracted with ethyl acetate three times. The combined organic phase is evaporated to dryness. The residue is dissolved in 4.5 mL of THF and then filter through a 0.45 m microfilter. The filtrate is evaporated to dryness and further dried under vacuum to give (6a/?,9a5′)-5-methyl-3-(2,3,4,5,6-pentadeuterophenylamino)-2-(4-(6-fluoropyridin-2-yl)-benzyl)-5,6fl,7,8,9,9fl-hexahydrocyclopent[4,5]imidazo[l,2-a]pyrazolo[4,3-e]pyrimidin-4(2H)-one as a white solid (185.8 mg, 81.6% yield). ¾ NMR (400 MHz, CDCb) δ 7.88 (d, / = 8.4 Hz, 2H), 7.88 – 7.77 (m, 1H), 7.58 (dd, J = 7.5, 2.4 Hz, 1H), 7.05 (d, J = 8.3 Hz, 2H), 6.90 – 6.80 (m, 2H), 4.94 (s, 2H), 4.82 – 4.68 (m, 2H), 3.34 (s, 3H), 2.27 (dd, / = 12.4, 5.7 Hz, 1H), 2.09 – 1.91 (m, 1H), 1.91 – 1.67 (m, 3H), 1.67 – 1.49 (m, 1H).MS (ESI) m/z 513.3 [M+H]+.
NEW YORK and OSAKA, Japan, Nov. 3, 2014 (GLOBE NEWSWIRE) — Intra-Cellular Therapies, Inc. (Nasdaq:ITCI) and Takeda Pharmaceutical Company Limited announced today that they have entered into an agreement to mutually terminate the February 2011 license agreement covering Intra-Cellular Therapies’ proprietary compound ITI-214 and related PDE1 inhibitors and to return the rights for these compounds to Intra-Cellular Therapies.
|
||||||
Under the terms of the agreement, Intra-Cellular Therapies has regained all worldwide development and commercialization rights for the compounds previously licensed to Takeda. Takeda will be responsible for transitioning the compounds back toIntra-Cellular Therapies and will not participate in future development or commercialization activities. After transition of the program, Intra-Cellular Therapies plans to continue the clinical development of PDE1 inhibitors for the treatment of central nervous system, cardiovascular and other disorders.
“We are grateful for Takeda’s substantial efforts in advancing this program into clinical development,” said Dr. Sharon Mates, Chairman and CEO of Intra-Cellular Therapies. “This provides us with the opportunity to unify our PDE1 platform and we look forward to continuing the development of ITI-214 and our other PDE1 inhibitors.”
Intra-Cellular Therapies will discuss the PDE1 program in its previously announced earnings call on Monday, November 3, 2014 at 8:30 a.m. Eastern Time. To participate in the conference call, please dial 844-835-6563 (U.S.) or 970-315-3916 (International) five to ten minutes prior to the start of the call. The participant passcode is 25568442.
About PDE1 Inhibitors
PDE1 inhibitors are unique, orally available, investigational drug candidates being developed for the treatment of cognitive impairments accompanying schizophrenia, Alzheimer’s disease and other neuropsychiatric disorders and neurological diseases and may also treat patients with Attention Deficit Hyperactivity Disorder and Parkinson’s disease. These compounds may also have the potential to improve motor dysfunction associated with these conditions and may also have the potential to treat patients with multiple sclerosis and other autoimmune diseases and pulmonary arterial hypertension. These compounds are very selective for the PDE1 subfamily relative to other PDE subfamilies. They have no known significant off target activities at other enzymes, receptors or ion channels.
About Intra-Cellular Therapies
Intra-Cellular Therapies, Inc. (the “Company”) is developing novel drugs for the treatment of neuropsychiatric and neurodegenerative disease and other disorders of the central nervous system (“CNS”). The Company is developing its lead drug candidate, ITI-007, for the treatment of schizophrenia, behavioral disturbances in dementia, bipolar disorder and other neuropsychiatric and neurological disorders. The Company is also utilizing its phosphodiesterase platform and other proprietary chemistry platforms to develop drugs for the treatment of CNS disorders.
About Takeda Pharmaceutical Company Limited
Located in Osaka, Japan, Takeda is a research-based global company with its main focus on pharmaceuticals. As the largest pharmaceutical company in Japan and one of the global leaders of the industry, Takeda is committed to strive towards better health for people worldwide through leading innovation in medicine. Additional information about Takeda is available through its corporate website, www.Takeda.com.
Source: Intra-Cellular Therapies, Inc.; Takeda Pharmaceutical Company Limited
| US20080188492 * | Jun 6, 2006 | Aug 7, 2008 | Intra-Cellular Therapies, Inc | Organic Compounds |
| US20100273754 * | Dec 6, 2008 | Oct 28, 2010 | Peng Li | Organic compounds |
| US20110237561 * | Dec 7, 2009 | Sep 29, 2011 | Peng Li | Organic compounds |
| US20120071450 * | Dec 7, 2009 | Mar 22, 2012 | Peng Li | Organic compounds |
| US20120238589 * | Sep 20, 2012 | Peng Li | Organic compounds |
| WO2014205354A3 * | Jun 20, 2014 | May 28, 2015 | Takeda Pharmaceutical Company Limited | Free base crystals |
| WO2015196186A1 * | Jun 22, 2015 | Dec 23, 2015 | Intra-Cellular Therapies, Inc. | Organic compounds |
| US8829008 | Jun 1, 2012 | Sep 9, 2014 | Takeda Pharmaceutical Company Limited | Organic compounds |
| US9000001 | Jul 18, 2012 | Apr 7, 2015 | Intra-Cellular Therapies, Inc. | Organic compounds |
| US9006258 | Dec 5, 2007 | Apr 14, 2015 | Intra-Cellular Therapies, Inc. | Method of treating female sexual dysfunction with a PDE1 inhibitor |
| US9073936 | Mar 13, 2014 | Jul 7, 2015 | Intra-Cellular Therapies, Inc. | Organic compounds |
| WO2009075784A1 * | Dec 6, 2008 | Jun 18, 2009 | Intra Cellular Therapies Inc | Organic compounds |
| WO2010065151A1 * | Dec 7, 2009 | Jun 10, 2010 | Intra-Cellular Therapies, Inc. | Organic compounds |
| WO2013192556A2 * | Jun 21, 2013 | Dec 27, 2013 | Intra-Cellular Therapies, Inc. | Salt crystal |
//////
O=C(C1=C(NC2=CC=CC=C2)N(CC3=CC=C(C4=NC(F)=CC=C4)C=C3)N=C1N56)N(C)C5=N[C@@]7([H])[C@]6([H])CCC7.O=P(O)(O)O
OR
Fc1cccc(n1)c2ccc(cc2)Cn7nc5N3C(=N[C@@H]4CCC[C@H]34)N(C)C(=O)c5c7Nc6ccccc6
DRUG REGULATORY AFFAIRS INTERNATIONAL
The FDA has presented the draft of a revised guideline on dissolution testing for immediate release. Under certain conditions, the tests can now be standardised. Read on to get more information about FDA’s Guideline on Dissolution Testing.
http://www.gmp-compliance.org/enews_05230_FDA-Guideline-on-Dissolution-Testing_15398,Z-QCM_n.html
In August 2015, the FDA published the draft of a guideline on dissolution testing for immediate release solid oral dosage forms. It is planned that after its finalisation, a part of this guideline will replace the current guideline from August 1997.
The Biopharmaceutics Classification System (BCS) distinguishes 4 different classes of APIs depending on their solubility and permeability.
On the basis of this classification, a decision can be taken for determining when bioavailability or bioequivalence studies are required, or when a successful in vitro-in vivo correlation (IVIVC) is likely.
The BCS proposes that, for certain medicinal products which contain a high soluble API, dissolution testing can be standardised. Due to their high solubility…
View original post 121 more words