Home » Posts tagged 'Phase3 drugs' (Page 3)
Tag Archives: Phase3 drugs
Phase III Study of Oral Laquinimod for Relapsing-Remitting Multiple Sclerosis
Laquinimod
5-chloro-N-ethyl-4-hydroxy-1-methyl-2-oxo-
N-phenyl-1,2-dihydroquinoline-3-carboxamide
Laquinimod is an experimental immunomodulator developed by Active Biotech and Teva. It is currently being investigated as an oral treatment for multiple sclerosis (MS).
Laquinimod is the successor of Active Biotech’s failed experimental immunomodulator linomide.[1]
The compound has been investigated in two Phase II trials using successive magnetic resonance scans (MRI). Laquinimod seems to be able to reduce the MS disease activity on MRI.[2][3] However, the response to a given dose was discrepant between both studies.[4]
Phase III studies for MS started in December 2007.[5] In 2011, Teva announced its clinical trials involving laquinimod had failed, being unable to significantly reduce relapses into MS among patients beyond a placebo.[6] However, the final results of above mentioned phase III trial proved oral laquinimod administered once daily slowed the progression of disability and reduced the rate of relapse in patients with relapsing–remitting multiple sclerosis [7]
Mar 6, 2013 –
CONCERTO Study Enrolling Patients Globally to Evaluate Impact of Laquinimod on Disability Progression
Teva Pharmaceutical Industries Ltd. and Active Biotech announced today enrollment of the first patient in the CONCERTO study – the third Phase III placebo-controlled study designed to evaluate the efficacy, safety and tolerability of once-daily oral laquinimod in patients with relapsing-remitting multiple sclerosis (RRMS). The primary outcome measure of CONCERTO will be confirmed disability progression as measured by the Expanded Disability Status Scale (EDSS).
“Previous Phase III studies in more than 2,400 people with RRMS suggest a unique profile of laquinimod, directly affecting the neurodegenerative processes that lead to disability progression, the main concern in the treatment of RRMS,” said CONCERTO principal investigator, Dr. Timothy Vollmer, Professor of Neurology, University of Colorado Denver, Medical Director of the Rocky Mountain Multiple Sclerosis Center, and Co-Director of the RMMSC at Anschutz. “We are currently enrolling patients in this third pivotal study to further examine the clinical benefits of laquinimod on disability progression, the primary endpoint of the CONCERTO trial, and brain atrophy, at both the previously studied 0.6 mg dose, and now a higher 1.2 mg dose.”
The multinational, randomized, double blind placebo-controlled study will aim to enroll approximately 1,800 patients at more than 300 sites globally (http://clinicaltrials.gov/show/NCT01707992). Along with the primary endpoint of time to confirmed disability progression, the study will also examine the impact of laquinimod on endpoints such as percent change in brain volume and other clinical and MRI markers of disease activity.
“For nearly 30 years, Teva has been focused on improving the lives of people with multiple sclerosis by delivering innovative treatment options that address this complex disease,” said Dr. Michael Hayden, President of Global R&D and Chief Scientific Officer at Teva Pharmaceutical Industries Ltd. “The CONCERTO study demonstrates our commitment to collaborating with MS communities worldwide to further develop laquinimod and address unmet patient needs.”
ABOUT LAQUINIMOD
Laquinimod is an oral, once-daily CNS-active immunomodulator with a novel mechanism of action being developed for the treatment of MS. In animal models laquinimod crosses the blood brain barrier to potentially have a direct effect on resident CNS inflammation and neurodegeneration. The global Phase III clinical development program evaluating oral laquinimod in MS includes two pivotal studies, ALLEGRO and BRAVO.
In addition to the MS clinical studies, laquinimod is currently in clinical development for Crohn’s disease and Lupus.
ABOUT CONCERTO
CONCERTO is a multinational, multicenter, randomized, double-blind, parallel-group, placebo-controlled study followed by an active treatment phase, to evaluate the efficacy, safety and tolerability of two doses of oral administration of laquinimod 0.6 mg/day or 1.2 mg/day in subjects with RRMS. This third Phase III laquinimod study will evaluate laquinimod in approximately 1,800 patients for up to 24 months, after which patients will continue to an active treatment period with laquinimod for an additional 24 months. The primary outcome measure will be time to confirmed disability progression as measured by the Expanded Disability Status Scale (EDSS). The study will also examine the impact of laquinimod on endpoints such as percent change in brain volume, as well as other clinical and MRI markers of disease activity.
ABOUT MULTIPLE SCLEROSIS
MS is the leading cause of neurological disability in young adults. It is estimated that more than 400,000 people in the United States are affected by the disease and that two million people may be affected worldwide. Multiple sclerosis is a degenerative disease of the central nervous system in which inflammation and axonal damage and loss result in the development of progressive disability.
ABOUT TEVA
Teva Pharmaceutical Industries Ltd. (NYSE: TEVA) is a leading global pharmaceutical company, committed to increasing access to high-quality healthcare by developing, producing and marketing affordable generic drugs as well as innovative and specialty pharmaceuticals and active pharmaceutical ingredients. Headquartered in Israel, Teva is the world’s leading generic drug maker, with a global product portfolio of more than 1,000 molecules and a direct presence in about 60 countries. Teva’s branded businesses focus on CNS, oncology, pain, respiratory and women’s health therapeutic areas as well as biologics. Teva currently employs approximately 46,000 people around the world and reached $20.3 billion in net revenues in 2012.
ABOUT ACTIVE BIOTECH
Active Biotech AB is a biotechnology company with focus on autoimmune/inflammatory diseases and cancer. Projects in or entering pivotal phase are laquinimod, an orally administered small molecule with unique immunomodulatory properties for the treatment of multiple sclerosis, TASQ for prostate cancer as well as ANYARA for use in cancer targeted therapy, primarily of renal cell cancer. In addition, laquinimod is in Phase II development for Crohn’s and Lupus. Further projects in clinical development comprise the two orally administered compounds, 57-57 for SLE & Systemic Sclerosis and RhuDex(TM) for RA. Please visit http://www.activebiotech.com for more information.
- Tan IL, Lycklama à Nijeholt GJ, Polman CH et al. (April 2000). “Linomide in the treatment of multiple sclerosis: MRI results from prematurely terminated phase-III trials”. Mult Scler 6 (2): 99–104. PMID 10773855.
- Comi G, Pulizzi A, Rovaris M et al. (June 2008). “Effect of laquinimod on MRI-monitored disease activity in patients with relapsing-remitting multiple sclerosis: a multicentre, randomised, double-blind, placebo-controlled phase IIb study”. Lancet 371 (9630): 2085–2092. doi:10.1016/S0140-6736(08)60918-6. PMID 18572078.
- Polman C, Barkhof F, Sandberg-Wollheim M et al. (March 2005). “Treatment with laquinimod reduces development of active MRI lesions in relapsing MS”. Neurology 64 (6): 987–91. doi:10.1212/01.WNL.0000154520.48391.69. PMID 15781813.
- Keegan BM, Weinshenker BG (June 2008). “Laquinimod, a new oral drug for multiple sclerosis”. Lancet 371 (9630): 2059–2060. doi:10.1016/S0140-6736(08)60894-6. PMID 18572062.
- ClinicalTrials.gov NCT00509145 Safety and Efficacy of Orally Administered Laquinimod Versus Placebo for Treatment of Relapsing Remitting Multiple Sclerosis (RRMS) (ALLEGRO)
- Kresege, Naomi (1 August 2011). “Teva’s Copaxone Successor Fails in Latest Clinical Trial”. Bloomberg. http://www.bloomberg.com/news/2011-08-01/teva-s-oral-multiple-sclerosis-drug-fails-to-meet-goal-of-clinical-trial.html. Retrieved 2 August 2011. “Teva Pharmaceutical Industries Ltd. (TEVA)’s experimental multiple sclerosis pill failed to reduce relapses more than placebo in a clinical trial, dealing a blow to the company’s effort to find a successor to an older drug.”
- (Comi et al. N Engl J Med 2012;366:1000).

EP 1073639; JP 2002513006; US 6077851; WO 9955678
5-Chloroisatoic anhydride (I) is alkylated with iodomethane and NaH to afford (II). Subsequent condensation of anhydride (II) with the malonic monoamide (III) in the presence of NaH in hot DMA furnishes the target quinoline carboxamide.
…

Reaction of 2-amino-6-chlorobenzoic acid (I) with phosgene and NaHCO3 in dioxane gives 5-chloroisatoic anhydride (II), which is methylated by means of iodomethane and NaH in DMF to yield 5-chloro-1-methylisatoic anhydride (III). Finally, anhydride (III) is condensed with the malonic monoamide (IV) by means of NaH in hot dimethylacetamide. Alternatively, condensation of anhydride (III) with ethoxy malonyl chloride (V) by means of NaOMe and triethylamine in dichloromethane affords 5-chloro-4-hydroxy-1-methyl-2-oxo-1,2-dihydroquinoline-3- carboxylic acid ethyl ester (VI), which is finally condensed with N-ethylaniline (VII) in refluxing toluene. Alternatively, ester (VI) is hydrolyzed by means of concentrated HCl in hot Ac2O to give the carboxylic acid (VIII), which is finally condensed with N-ethylaniline (VII) by means of SOCl2 and TEA in dichloromethane
Ziopharm Oncology will be releasing its Phase III results for its drug Palifofsamide towards the end of March 2013

(Zymafos; ZIO-201) is a cytotoxic, active metabolite of the alkylating agent ifosfamide, which causes irreparable DNA interstrand cross-linking in cancer cells. This prevents DNA replication and cell division, leading to cell death.
In contrast to ifosfamide, palifosfamide is not metabolised to the toxins acrolein and chloracetaldehyde, which are associated with haemorrhagic cystitis, and neuro- and nephro-toxicities respectively. Also, palifosfamide is not a substrate for aldehyde dehydrogenase (ALDH), an important mediator of drug resistance

Cyclophosphamide and ifosfamide are nitrogen mustard alkylating agents that act by crosslinking DNA strands at the guanine N-7 position, resulting in cell death. Both of these are prodrugs that are metabolised in the liver to phosphoramide mustard active metabolites, but their use is limited by toxic side-effects. They are also prone to tumour resistance, which results from numerous mechanisms, including DNA repair.
In an attempt to overcome some of these problems, Ziopharm Oncology has developed palifosfamide tromethamine, which is a salt formulation of isophosphoramide mustard, the active metabolite of isofosfamide.1

isofosamide

palifosfamide
In a Phase I trial, it was given in combination with doxorubicin to 13 patients with advanced refractory tumours – eight with soft tissue sarcoma and the remainder with small cell lung cancer – for whom there was no available standard therapy.2 It was given on the first three days of a three-week cycle, with a starting dose of 150mg/m2, and doxorubicin given on the first day at a starting dose of 60mg/m2. The doses were escalated to a maximum tolerated dose of 150mg/m2 for palifosfamide and 75mg/m2 for doxorubicin. It was well tolerated, and three of the 12 assessable patients had a partial response, two of whom were from the sarcoma group, and the median progression free survival was 20 weeks.
references
1. S. Jung and B. Kasper, IDrugs 2010, 13, 38
2. L.J. Camacho et al. J. Clin. Oncol. 2009, 27 (Suppl.), Abst. 10577
3. C.F. Verschraegen et al. J. Clin. Oncol. 2010, 28 (Suppl.), A
Palifosfamide, A Novel Molecule for the Treatment of Soft Tissue Sarcoma
Palifosfamide (Zymafos™ or ZIO-201) references a novel composition (tris formulation) that is the functional active metabolite of ifosfamide (IFOS), a bi-functional DNA alkylator being investigated as a potential therapy for the treatment of soft tissue sarcoma (STS). Palifosfamide is formulated by combining the tris (hydroxymethyl) amino methane (tris) salt of palifosfamide and a number of excipients to create the final drug product. Preclinical development of palifosfamide has included in vitro and in vivo studies demonstrating activity against various sarcomas, breast cancers, other solid tumors and leukemias, including several that are resistant to IFOS. Several clinical studies have been initiated in a variety of cancer types. A Phase I study in advanced cancers, using the original lysine formulation, has been completed. A two-stage Phase I/II Study in advanced sarcomas, introducing the tris salt formulation, has completed enrollment and data retrieval is ongoing. A Phase I study in combination with doxorubicin evaluating patients with advanced, refractory solid tumors for whom treatment with doxorubicin is considered medically acceptable, has completed enrollment and data retrieval is ongoing. Based on the result of the Phase I combination study, an international randomized Phase II study comparing palifosfamide in combination with doxorubicin versus doxorubicin alone in 1st and 2nd line patients with advanced STS has been completed. phase 3 on now also
What is Soft Tissue Sarcoma, and what are the currently available treatments?
Soft-tissue sarcomas (STS) represent a rare and diverse group of tumors that are not very well understood. Although soft-tissue sarcomas account for <1% of all cancers, they represent a high percentage of cancer-related deaths worldwide (Ref. 3, Ref. 4, Ref. 5). STS tumors can occur anywhere within the body, originating in various soft tissues including fat, smooth or striated muscle, nerve/nerve sheath, vascular tissue, and other connective tissues; the extremities are the most common site of origin, accounting for approximately 50% of cases
Phase 3 , breast cancer, Ridaforolimus (MK-8669; AP23573; formerly Deforolimus) Merck, license,Ariad Pharmaceuticals
Ridaforolimus
572924-54-0
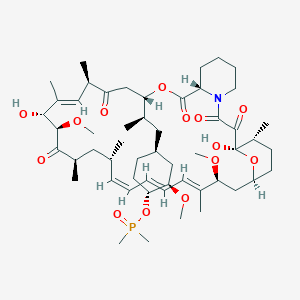
(1R,2R,4S)-4-[(2R)-2-[(1R,9S,12S,15R,16E,18R,19R,21R,23S,24E,26E,28Z,30S,32S,35R)-1,18-dihydroxy-19,30-dimethoxy-15,17,21,23,29,35-hexamethyl-2,3,10,14,20-pentaoxo-11,36-dioxa-4-azatricyclo[30.3.1.04,9]hexatriaconta-16,24,26,28-tetraen-12-yl]propyl]-2-methoxycyclohexyl dimethylphosphinate
Dimethyl-phosphinic Acid C-43 Rapamycin Ester
42-(dimethylphosphinate) Rapamycin
Deforolimus, MK-8669, AP-23573, S1022_Selleck, AP23573, AP23573, MK-8669, Ridaforolimus, Deforolimus, 572924-54-0, MK 8669
- AP 23573
- AP23573
- Deforolimus
- MK 8669
- MK-8669
- MK8669
- Ridaforolimus
- Taltorvic
- UNII-48Z35KB15K
Molecular Formula: C53H84NO14P Molecular Weight: 990.206122
An mTOR inhibitor for the treatment of cancer.
Ridaforolimus (MK-8669; AP23573; formerly Deforolimus)
Merck, under exclusive worldwide license agreement with Ariad Pharmaceuticals
Method of Action: Oral inhibitor of mammalian target of rapamycin inhibitor (mTOR)
Indications/Phase of Trial: Maintenance therapy for metastatic soft-tissue sarcoma and bone sarcomas after at least four chemotherapy cycles (under review after receiving Complete Response letter from FDA in June; NME)
Ridaforolimus is an investigational small-molecule inhibitor of the protein mTOR, a protein that acts as a central regulator of protein synthesis, cell proliferation, cell cycle progression and cell survival, integrating signals from proteins, such as PI3K, AKT and PTEN, known to be important to malignancy.
TARGET- mTOR
Ridaforolimus (also known as AP23573 and MK-8669; formerly known as Deforolimus[1]) is an investigational targeted and small-molecule inhibitor of the protein mTOR, a protein that acts as a central regulator of protein synthesis, cell proliferation, cell cycle progression and cell survival, integrating signals from proteins, such as PI3K, AKT and PTEN known to be important to malignancy. Blocking mTOR creates a starvation-like effect in cancer cells by interfering with cell growth, division, metabolism, and angiogenesis.
It has had promising results in a clinical trial for advanced soft tissue and bone sarcoma.
RIDAFOROLIMUS
NMR….http://file.selleckchem.com/downloads/nmr/S102201-Deforolimus-HNMR-Selleck.pdf
HPLC . http://file.selleckchem.com/downloads/hplc/S102201-Deforolimus-HPLC-Selleck.pdf
MSDS..http://www.selleckchem.com/msds/Deforolimus-MSDS.html
| Commercial arrangements |
Ridaforolimus is being co-developed by Merck and ARIAD Pharmaceuticals. On May 5, 2010, Ariad Pharmaceuticals and Merck & Company announced a clinical development and marketing agreement. With this agreement, Ariad received $125 million in upfront payments from Merck and $53 million in milestone payments. Future payments are triggered upon acceptance of the NDA by the FDA with another payment when the drug receives marketing approval. There are similar milestones for acceptance and approval in both Europe and Japan. Other milestone payments are tied to revenue goals for the drug.[2] ARIAD has opted to co-promote ridaforolimus in the U.S. Merck plans to submit a New Drug Application (NDA) for ridaforolimus to the U.S. Food and Drug Administration (FDA) and a marketing application in the European Union in 2011.[3]
Clinical trials
Phase III SUCCEED
On June 6, 2011, Ariad and Merck announced detailed results from the largest randomized study ever in the soft tissue and bone sarcoma population, the Phase III SUCCEED clinical trial. SUCCEED evaluated oral ridaforolimus, in patients with metastatic soft-tissue or bone sarcomas who previously had a favorable response to chemotherapy. In this patient population, ridaforolimus improved progression-free survival (PFS) compared to placebo, the primary endpoint of the study. The complete study results were presented by Sant P. Chawla, M.D., director, Sarcoma Oncology Center, Santa Monica, CA, during the 2011 American Society of Clinical Oncology (ASCO) annual meeting.
The SUCCEED (Sarcoma Multi-Center Clinical Evaluation of the Efficacy of Ridaforolimus) trial was a randomized (1:1), placebo-controlled, double-blind study of oral ridaforolimus administered at 40 mg/day (five of seven days per week) in patients with metastatic soft-tissue or bone sarcomas who previously had a favorable response to chemotherapy. Oral ridaforolimus was granted a Special Protocol Assessment (SPA) by the FDA for the SUCCEED trial.
Based on 552 progression-free survival (PFS) events in 711 patients, (ridaforolimus (N=347), placebo (N=364) determined by an independent radiological review committee, the study achieved its primary endpoint of improvement in PFS, with a statistically significant (p=0.0001) 28 percent reduction in the risk of progression or death observed in those treated with ridaforolimus compared to placebo (hazard ratio=0.72).
Median PFS was 17.7 weeks for those treated with ridaforolimus compared to 14.6 weeks in the placebo group. Furthermore, based on the full analysis of PFS determined by investigator assessment, there was a statistically significant (p<0.0001) 31 percent reduction by ridaforolimus in the risk of progression or death compared to placebo (hazard ratio=0.69). In the investigator assessment analysis, median PFS was 22.4 weeks for those treated with ridaforolimus compared to 14.7 weeks in the placebo group [4
EU WITHDRAWAL IN NOV 2012
Merck, known as MSD outside the U.S. and Canada, announced today that it has formally notified the European Medicines Agency (EMA) of Merck’s decision to withdraw the Marketing Authorisation Application (MAA) for ridaforolimus.
The application for Marketing Authorisation for ridaforolimus was accepted by the EMA in August 2011. At the time of the withdrawal it was under review by the Agency’s Committee for Medicinal Products for Human Use (CHMP). In its letter to the EMA, Merck said that the withdrawal of ridaforolimus was based on the provisional view of the CHMP that the data available to date and provided in the Marketing Authorisation Application were not sufficient to permit licensure of ridaforolimus in the European Union for the maintenance treatment of patients with soft tissue sarcoma or primary malignant bone tumor.
Although the application for these uses was withdrawn, Merck is studying ridaforolimus in combination with other drugs in other tumor types. The withdrawal of the European application of ridaforolimus for the maintenance treatment of patients with soft tissue sarcoma or primary malignant bone tumor does not change Merck’s commitment to the ongoing clinical trials with ridaforolimus.
Description
42-(dimethylphosphinate) Rapamycin (Ridaforolimus) represented by the following formula I:
2. Description of RelatedArt
The mammalian target of Rapamycin (mTOR) is known as a mechanistic target of Rapamycin (H), which is found in the studies of Rapamycin. On the other hand, 42-(dimethylphosphinate) Rapamycin (Ridaforolimus) (I) is a derivative of Rapamycin (II), which is also a kind of mTOR inhibitor. Ridaforolimus (I) can inhibit cell division and possibly lead to tumor cell death. Hence, there are many studies related to solid tumor treatments and blood cancer treatments using Ridaforolimus (I). In addition, in 2011, Merck also applied a certification of this compound against soft tissue and bone cancer.
U.S. Pat. No. 7,091,213 discloses a process for preparing 42-(dimethylphosphinate) Rapamycin (Ridaforolimus) (I), and the process thereof is shown in the following Scheme I.
In this process, a solution of Rapamycin (II) in dichloromethane (DCM) was respectively added with 2,6-di-tert-butyl-4-methylpyridine or 3,5-lutidine as a base, and followed by the addition of a solution of dimethylphosphinic chloride (DMP-Cl) to perform a phosphorylation reaction at 0° C., under a stream of N2(g). The crude product was purified by flash chromatography (eluted with MeOH/DCM/EtOAc/hexane=1:10:3:3) to provide 42-(dimethyl- phosphinate) Rapamycin (Ridaforolimus) (I), which is a phosphorylated compound at 42-hydroxyl position of Rapamycin (II). In addition, this patent also disclosed a side product of 31,42-bis(dimethyl phosphinate) Rapamycin (III), which is a phosphorylated compound at both 31- hydroxyl position and 42- hydroxyl position of Rapamycin (II).
…………………..
SYNTHESIS
Some additional transformations of potential interest to the practitioner are shown below, including the preparation of reagents for generating the described C-43 phosphorus-containing rapalogs:
Preparation of Diakyl/diaryl Chlorophoshates
Preparation of Alkyl Halide Phosphonates
Illustrative routes for using the foregoing sorts of reagents to prepare certain rapalogs of this invention are shown below.
The synthesis of compounds of this invention often involves preparation of an activated form of the desired moiety “J”, such as a phosphoryl chloride as shown above (e.g. (R)(RO)P—Cl or RR′P(═O)—Cl, etc), and reaction of that reagent with rapamycin (or the appropriate rapalog) under conditions yielding the desired product, which may then be recovered from residual reactants and any undesired side products. Protecting groups may be chosen, added and removed as appropriate using conventional methods and materials.
Purification of Compounds of the Invention
A variety of materials and methods for purifying rapamycin and various rapalogs have been reported in the scientific and patent literatures and may be adapted to purification of the rapalogs disclosed herein. Flash chromatography using a BIOTAGE prepacked cartridge system has been particularly effective. A typical protocol is disclosed in the Examples which follow.
Physicochemical Characterization of Compounds of the Invention
The identity, purity and chemical/physical properties of the rapalogs may be determined or confirmed using known methods and materials, including HPLC, mass spectral analysis, X ray crystallography and NMR spectroscopy. High resolution 1D 1H and 31P NMR spectra acquired using a typical relaxation delay of 3 seconds have proved useful, as has reverse phase HPLC analysis (analytical column, 3 micron particle size, 120 ansgstrom pore size, thermostatted to 50° C. with a mobile phase of 50% acetonitrile, 5% methanol and 45% water (all % s by volume), for example, in an isocratic elution system, with elution of product and impurity peaks followed by UV detection at 280 nanometers). Normal phase HPLC may also be used, especially to evaluate the level of residual rapamycin or rapalog by-products. The presence of residual solvent, heavy metals, moisture and bioburden may be assessed using conventional methods.
Example 9
Dimethyl-phosphinic Acid C-43 Rapamycin Ester
Dimethyl-phosphinic Acid C-43 Rapamycin Ester
To a cooled (0° C.) solution of rapamycin (0.1 g, 0.109 mmol) in 1.8 mL of dichloromethane was added 0.168 g (0.82 mmol) of 2,6-di-t-butyl-4-methyl pyridine, under a stream of N2, followed immediately by a solution of dimethylphosphinic chloride (0.062 g, 0.547 mmol) in 0.2 mL of dichloromethane. The slightly yellow reaction solution was stirred at 0° C., under an atmosphere of N2, for 3.5 h (reaction monitored by TLC). The cold (0° C.) reaction solution was diluted with ˜20 mL EtOAc then transferred to a separatory funnel containing EtOAc (150 mL) and saturated NaHCO3 (100 mL). Upon removing the aqueous layer, the organic layer was washed successively with ice cold 1N HCl (1×100 mL), saturated NaHCO3 (1×100 mL), and brine (1×100 mL), then dried over MgSO4 and concentrated. The crude product was purified by silica gel flash chromatography (eluted with 1:10:3:3 MeOH/DCM/EtOAc/hexane) to provide 0.092 g of a white solid:
1H NMR (300 MHz, CDCl3) d 4.18 (m, 1H), 4.10 (m, 1H), 3.05 (m, 1H), 1.51 (m, 6H);
31P NMR (121 MHz, CDCl3) d 53.6; 1013 m/z (M+Na).
Example 9
Alternative Synthesis
Rapamycin and dichloromethane are charged into a nitrogen-purged reaction flask. The stirred solution is cooled to approximately 0° C. (an external temperature of −5±5° C. is maintained throughout the reaction). A solution of dimethylphosphinic chloride (2.0 molar equivalents) in dichloromethane is then added over a period of approximately 8–13 minutes.
This is followed immediately by the addition of a solution of 3,5-lutidine (2.2 molar equivalents) in dichloromethane over a period of approximately 15–20 minutes. Throughout both additions, the internal temperature of the reaction sssstays below 0° C. The cooled reaction solution is stirred for 1 hour and then transferred, while still cold, to an extractor containing saturated aqueous NaHCO3 and methyl-t-butyl ether (MTBE), ethyl acetate or diethyl ether. In-process samples are removed at 30 and 60 minute time points.
Samples are prepared in a similar fashion to that described for the reaction workup. Reaction progress is monitored by TLC (1:10:3:3 MeOH/DCM/EtOAc/hexanes) and reverse-phase HPLC analyses. The isolated organic layer is successively washed with ice cold 1N HCl, saturated aqueous NaHCO3 (2×), saturated aqueous NaCl, and dried over sodium sulfate. Upon filtration and solvent removal, the residue undergoes solvent exchange with acetone followed by concentration in vacuo to provide crude product, which may be analyzed for purity by normal- and reversed-phase HPLC.
…………………….
SYNTHESIS
The process of the present invention is shown in the following Scheme II.
EXAMPLE 7
Preparation of 42-(dimethylphosphinate) Rapamycin (Ridaforolimus) (I)
42-(dimethylphosphinate)-31-triethylsilylether Rapamycin (VI-b) (2.312 g, available from 1.945 mmole of Rapamycin -28-triethylsilylether) and tetrahydrofuran (60 mL) was placed into a flask, and the resulting solution was cooled to 0˜−5° C. Next, a sulthric acid solution (2 N, 6 mL) was slowly added into the resulting solution dropwise. When the 42-(dimethylphosphinate)-31-triethylsilylether Rapamycin (VI-b) was less than 2%, ethyl acetate (1000 mL) was added into the resulting solution. Then, the organic layer was successively washed with a NaCl saturated solution (300 mL), a NaHCO3saturated solution (200 mL) and a NaCl saturated solution (200 mL), dried over anhydrous sodium sulfate and concentrated to obtain a crude product of 42-(dimethylphosphinate) Rapamycin (Ridaforolimus) (I) (2.341 g). The crude product was then purified by Licrhoprep RP-18 silica gel chromatography (eluted with acetonitrile: 0.02 M ammonium formate solution=6:4, wherein the pH of the ammonium formate solution was adjusted to 4.0 with formic acid), extracted with ethyl acetate, concentrated and dried to obtain a white foam solid 42-(dimethylphosphinate) Rapamycin (Ridaforolimus) (I) (1.840 g, purity=99.48%). The yield thereof was 95.55% based on 2.0 g of 31-triethylsilyl ether Rapamycin.
1H-NMR(400 MHz, CDCl3)d 4.18(m, 1H), 4.10(m, 1H), 3.05(m, 1H),1.51(m, 6H); 31P-NMR(161 MHz, CDCl3)d 53.33; 1012.6 m/z [M+Na]+.
- “ARIAD Reports First Quarter 2009 Development Progress and Financial Results- Ridaforolimus New USAN Name to Replace Deforolimus”. ARIAD Pharmaceuticals. 2009. Retrieved 2009-05-07.
- “ARIAD – News release”. Phx.corporate-ir.net. Retrieved 2012-10-07.
- “ARIAD – News release”. Phx.corporate-ir.net. 2011-03-17. Retrieved 2012-10-07.
- “ARIAD – News release”. Phx.corporate-ir.net. 2011-06-06. Retrieved 2012-10-07.
|
7-11-2012
|
FULLY HUMAN ANTI-VEGF ANTIBODIES AND METHODS OF USING
|
|
|
10-28-2011
|
METHODS OF TREATMENT
|
|
|
1-21-2011
|
ANTI-IGF1R
|
|
|
1-5-2007
|
Methods for treating neurofibromatosis 1
|
|
|
4-16-2004
|
Phosphorus-containing compounds and uses thereof
|
Phase 3 Boehringer Ingelheim Announces Interim Results Evaluating Virologic Response Rates in HCV/HIV Co-Infected Patients Treated with Faldaprevir

Faldaprevir
BI 201335
http://clinicaltrials.gov/ct2/show/NCT01343888
CAS Number: 801283-95-4
Molecular Formula: C40H49BrN6O9S
Molecular Weight: 869.82 g.mol
RIDGEFIELD, Conn., March 4, 2013
Boehringer Ingelheim Pharmaceuticals, Inc. announced the first interim results in HCV/HIV co-infected patients from the company’s ongoing hepatitis C (HCV) clinical trial program, HCVerso™. These results, from the Phase 3 trial STARTVerso™ 4, were presented today at the 20th annual Conference on Retroviruses and Opportunistic Infections (CROI) in Atlanta, GA.
The interim results showed that 80% of HCV/HIV co-infected patients achieved early treatment success (ETS)*, as defined by the study protocol, when given an investigational HCV regimen that included faldaprevir (BI 201335). Results were consistent across patients regardless of HIV therapy or prior HCV treatment status, including patients who were HCV treatment-naive or had previously relapsed during HCV treatment with pegylated interferon and ribavirin (PegIFN/RBV). Patients who achieved ETS were eligible for randomization to a shortened duration of treatment (24 weeks versus 48 weeks). Investigators also reported on-treatment virologic response at week 12, which showed that 84% of all study patients had undetectable levels of hepatitis C virus.
For more information, please visit http://us.boehringer-ingelheim.com

Faldaprevir, also known as BI 201335, is an investigational, oral protease inhibitor that is specifically designed to target viral replication in the liver. The ongoing multi-study Phase 3 STARTVerso™ trial program, evaluating faldaprevir combined with PegIFN/RBV in treatment-naive, treatment-experienced and HIV co-infected patients with chronic genotype-1 HCV, is near clinical completion. BI 207127 is an investigational NS5B non-nucleoside polymerase inhibitor that has shown the potential to eliminate interferon from HCV treatment when combined in a regimen with faldaprevir and RBV. Phase 2 trials of this interferon-free regimen have been completed and Phase 3 HCVerso™ trials investigating this regimen are now underway.
Faldaprevir and BI 207127 are investigational compounds and not approved by the FDA. Their safety and efficacy have not been established.
Hepatitis C is a blood-born infectious disease and a leading cause of chronic liver disease,transplant and failure that affects as many as 150 million people globally. In the United States, an estimated 4.1 million Americans have been infected with HCV, of which approximately 3.2 million have chronic HCV infection. Since 1999 there has been a significant increase in deaths due to chronic HCV, accounting for 15,000 deaths in the United States in 2007.
Phase III Study of Teva’s Milprosa (Progesterone) Vaginal Ring Published in Fertility and Sterility

Progesterone
Data Demonstrated Once-Weekly Milprosa™ Provides Similar Pregnancy Rates to Daily 8 Percent Progesterone Vaginal Gel
Mar 4, 2013 –
Teva Pharmaceutical Industries Ltd. today announced the publication of results of the Phase III clinical trial of Milprosa™ (progesterone) vaginal ring in Fertility and Sterility. The study compared the efficacy and safety of once-weekly Milprosa™ to daily 8 percent progesterone vaginal gel for luteal phase support in in vitro fertilization (IVF) and found that clinical pregnancy rates per retrieval at eight and 12 weeks were comparable between patient groups. Adverse event (AE) profiles were similar between the two treatment groups and consistent with known AEs associated with progesterone.
“The study results demonstrate that Milprosa™ may be an effective and safe option for progesterone supplementation during the luteal phase among women undergoing IVF,” said Laurel Stadtmauer, M.D., Ph.D., professor of Obstetrics and Gynecology at Jones Institute for Reproductive Medicine at Eastern Virginia Medical School and study author. “Since normal luteal function may be compromised among women undergoing IVF, progesterone supplementation is essential and the more options patients have, the better. If approved, the once-weekly dosing of Milprosa™ may offer convenience for patients.”
The Phase III randomized, single-blinded, multicenter, noninferiority study was conducted at 22 clinical sites in the U.S. and included 1,297 patients between the ages of 18 and 42. Of enrolled patients, 646 were randomized to Milprosa™ and 651 to the 8 percent progesterone vaginal gel.
“The Fertility and Sterility publication of the Milprosa™ Phase III data is a significant milestone for Teva, especially because fertility is a meaningful new area of specialization for the company and one in which significant unmet need exists,” said Jill DeSimone, senior vice president & general manager, Global Teva Women’s Health. “We look forward to continuing to share important updates about Milprosa™ and demonstrating our investment in and commitment to women’s health.”
About the Study
The Phase III study randomized patients into two treatment groups: one group received once-weekly Milprosa™ and the other received daily 8 percent progesterone vaginal gel. Milprosa™ and the vaginal gel were initiated on the day following egg retrieval and continued through 12 weeks’ gestation. Efficacy was evaluated by comparing clinical pregnancy rates of patients at eight and 12 weeks gestation.
- At week eight, clinical pregnancy rates per retrieval were 48.0 percent for the Milprosa™ group and 47.2 percent for the vaginal gel group (between-group difference, 0.8%; 95% CI, -4.6%, 6.3%).
- At week 12, clinical pregnancy rates per retrieval for Milprosa™ and the vaginal gel were 46.4 percent and 45.2 percent respectively (between-group difference, 1.3%; 95% CI, -4.1%, 6.7%).
A secondary efficacy endpoint was the rate of live birth.
- The overall live birth rate per retrieval for women using Milprosa™ was 45.2 percent; among women using the vaginal gel, the rate was 43.3 percent.
- The majority of patients pregnant at week 12, when progesterone treatment ended, went on to have a live birth: 97.4 percent for the Milprosa™ group and 96.5 percent for the vaginal gel group.
The most commonly reported adverse events (those greater than or equal to 10% in the Milprosa™ treatment group) were nausea, headache, abdominal pain, post-procedural discomfort, abdominal distension, back pain, fatigue, vomiting and constipation. Serious adverse events (SAEs) occurred in approximately 12 percent of all patients, with no significant difference in the rate between treatment groups. The majority of SAEs that occurred were mild to moderate in severity and not related to treatment. Rates of discontinuation of treatment due to AEs were low and similar between both groups (approximately 6%).
About Milprosa™ (Progesterone) Vaginal Ring
Milprosa™ is an investigational, once-weekly progesterone ring inserted in the vagina. It is flexible and designed to continuously release a steady dose of micronized progesterone. Milprosa™ is in development to support embryo transplantation and early pregnancy (up to 10 weeks post-embryo transfer) by supplementation of corpus luteal function as part of an Assisted Reproductive Technology (ART) treatment program for infertile women.
About Supplementation of Corpus Luteal Function
The corpus luteum is a temporary endocrine gland that develops during the luteal phase of a woman’s menstrual cycle. It is an important contributor of progesterone and is critical for the maintenance of early pregnancy. During in vitro fertilization, progesterone supplementation is needed because natural levels of the hormone may be insufficient. This supplementation improves implantation rates and thus pregnancy rates. Additionally, progesterone supplementation supports early pregnancy.
About Teva
Teva Pharmaceutical Industries Ltd. (NYSE: TEVA) is a leading global pharmaceutical company, committed to increasing access to high-quality healthcare by developing, producing and marketing affordable generic drugs as well as innovative and specialty pharmaceuticals and active pharmaceutical ingredients. Headquartered in Israel, Teva is the world’s leading generic drug maker, with a global product portfolio of more than 1,000 molecules and a direct presence in about 60 countries. Teva’s branded businesses focus on CNS, oncology, pain, respiratory and women’s health therapeutic areas as well as biologics. Teva currently employs approximately 46,000 people around the world and reached $20.3 billion in net revenues in 2012.
Phase3 Rindopepimut ,CDX-110 Celldex Therapeutics’ brain cancer vaccine

http://clinicaltrials.gov/ct2/show/NCT01480479
MAR 2013
Rindopepimut
Immunotherapeutic vaccine called Rindopepimut showed positive results in prolonging survival in patients with newly diagnosed EGFRvIII-positive glioblastoma (GB), one of the most aggressive forms of brain cancer
Celldex Therapeutics’ brain cancer vaccine, rindopepimut, also known as CDX-110, targets EGFRvIII, an activated mutation of the epidermal growth factor receptor (EGFR). This mutation is found in about 31% of cases of glioblastoma multiforme, a form of fast-growing brain cancer and the most common type of primary brain tumor. It can contribute to tumor growth, and is linked with poor long-term survival. It is not seen in normal tissue.
In the ACT III Phase II trial, which involved people with newly diagnosed EGFRvIII-positive glioblastoma, 65 patients were given rindopepimut in combination with standard-of-care treatment (temozolomide), after having undergone surgery and standard chemotherapy and radiation therapy.
focus on is Rindopepimut, an immunotherapy treatment that targets EGFRvIII. As it’s not found at significant levels in normal tissues but expressed in 30ish% of primary glioblastoma, it’s an ideal target that has produced promising results to date. The drug candidate has shown consistent benefit for patients across three phase 2 studies- that’s no fluke! It’s currently in a global phase 3 trial in patients with newly diagnosed glioblastoma with results due in a couple years
| Phase 3 Study of Rindopepimut in Patients With Newly Diagnosed Glioblastoma (ACT IV) | |
 |
|
| Design: | Phase 3, double-blind, study of rindopepimut compared with KLH control |
| Status: | Currently enrolling at multiple centers in the US; additional centers outside the US planned to be activated in 2012 |
ABOUT THE CLINICAL TRIAL
This 2-arm, randomized, Phase 3 study will investigate the efficacy and safety of the addition of rindopepimut to the current standard of care, temozolomide, in patients with recently diagnosed EGFRvIII positive glioblastoma. All patients will be administered temozolomide. Half the patients will be randomly assigned to receive rindopepimut (given along with GM-CSF as a vaccine adjuvant) and half the patients will be randomly assigned to receive a keyhole limpet hemocyanin (KLH). Patients will be treated in a blinded fashion (neither the patient nor the doctor will know which arm of the study the patient is on). Patients will be treated until disease progression or intolerance to therapy and all patients will be followed for survival.
All patients enrolled in the study will be closely monitored to determine if their cancer is responding to treatment and for any side effects that may occur.
KYTHERA Biopharmaceuticals, Inc. Announces Positive Interim Results from Open-Label Study of ATX-101 in the Reduction of Unwanted Submental Fat (SMF) or “Double Chin”
http://clinicaltrials.gov/ct2/show/NCT01426373
synthesis………..https://newdrugapprovals.org/2014/07/14/some-thing-for-your-chin-fda-accepts-kytheras-atx-101-new-drug-application/
The drug is sodium deoxycholate for injection, code-named ATX-101 was developed for the treatment of lipomas – benign tumors of subcutaneous adipose tissue, as well as other unwanted fatty growths, such as a double chin. This substance, which is a salt of one of the bile acids, emulsifies fats, destroying their excess deposits


ATX-101 (a first-in-class injectable drug being studied for the reduction of localized fat. ATX-101 is a proprietary formulation of deoxycholate a well-studied endogenous compound that is present in the body), a facial injectable drug for the reduction of unwanted fat under the chin, or submental fat. V. Leroy Young, MD, FACS, presented the initial results at the American Society for Aesthetic Plastic Surgery (ASAPS) 45th Annual Aesthetic Meeting in Vancouver, British Columbia, on May 4, 2012.
In August 2010 Bayer Consumer Care AG signed a licensing and development collaboration agreement with KYTHERA, thereby obtaining commercialization rights to ATX-101 outside the US and Canada. KYTHERA and Bayer are collaborating on the development of ATX-101 in Europe.
KYTHERA Biopharmaceuticals Inc. 02 MAR 3013, announced positive interim results from a Phase IIIb multi-center open-label study (ATX-101-11-26) to evaluate the safety and efficacy of ATX-101 an investigational injectable drug for the reduction of unwanted submental fat (SMF) commonly known as double chin. The results presented at the Late Breaking Research Symposium at the 71st American Academy of Dermatology (AAD) Annual Meeting in Miami Beach Fla. found that ATX-101 is well-tolerated and may be effective in reducing SMF by both clinician and patient reported outcome measures. The ATX-101 global clinical development program has enrolled more than 2500 total patients of which more than 1500 have been treated with ATX-101.
“In my practice patients often request a non-surgical way to treat their submental fat or undesirable double chin” said investigator Susan Weinkle MD FAAD a board certified dermatologist and affiliate clinical professor at the University of South Florida. “For these patients double chin is often resistant to diet and exercise. The results of this study suggest that microinjections of ATX-101 can reduce submental fat without worsening skin laxity.”
ATX-101 is a proprietary synthetically-derived formulation of deoxycholic acid (DCA) a naturally-occurring molecule found in the body that aids in fat metabolism. In this open-label Phase IIIb study interim results three months after the last ATX-101 treatment found:
- Reduction of submental fat
- 87 percent of patients achieved at least a one-grade improvement from baseline on the Clinician-Reported Submental Fat Rating Scale (CR-SMFRS)
- Similarly 83 percent of patients achieved at least a one-grade improvement on the Patient-Reported Submental Fat Rating Scale (PR-SMFRS)
- 96 percent of patients had unchanged or improved skin laxity based on the clinician rated Submental Skin Laxity Grading Scale (SMSLG)
- 95 percent of patients were satisfied with treatment based on the Global Post Treatment Satisfaction Scale
- Adverse events were of mild to moderate intensity transient and primarily associated with the treatment area

Topline results from this study were announced in November 2012. As previously announced 71.3 percent of subjects had at least a one-grade improvement on the CR-SMFRS / PR-SMFRS composite and 14.0 percent had at least a two-grade improvement on the same composite measure.
These results are based on a multicenter 12-month open-label Phase IIIb study conducted at 21 sites across the United States evaluating 165 adults who received injections of ATX-101 for up to six treatments at four-week intervals. Patients received ATX-101 (2 mg/cm2) by subcutaneous microinjections directly into their SMF and were evaluated three months after their last treatment. The study population includes females (77.6 percent) and males (22.4 percent) with a mean age of 47 who report at least moderate SMF and dissatisfaction with the appearance of their chin. All Fitzpatrick Skin Types an industry standard scale to categorize skin tone are represented.
“We are pleased with these ATX-101 study results” said Patricia S. Walker M.D. Ph.D. chief medical officer KYTHERA Biopharmaceuticals Inc. “These results along with efficacy analyses in double-blind placebo-controlled studies support ATX-101 entering the market as potentially the first medical aesthetic drug approved for the reduction of submental fat.”
About ATX-101
ATX-101 is a potential first-in-class injectable drug candidate under clinical investigation for the reduction of unwanted submental fat. ATX-101 is a proprietary formulation of synthetic deoxycholic acid a well-characterized endogenous compound that is present in the body to promote the natural breakdown of dietary fat. ATX-101 is designed to be a locally-injected drug that causes proximal preferential destruction of adipocytes or fat cells with minimal effect on surrounding tissue. Based on clinical trials conducted to date ATX-101 has exhibited significant meaningful and durable results in the reduction of submental fat which commonly presents as an undesirable “double chin.” These results correspond with subject satisfaction measures demonstrating meaningful improvement in perceived chin appearance.
In August 2010 Bayer signed a licensing and collaboration development agreement with KYTHERA thereby obtaining development and commercialization rights to ATX-101 outside of the U.S. and Canada. Bayer recently completed two pivotal Phase III trials of ATX-101 in Europe for the reduction of submental fat. Topline results from these trials were reported in the second quarter of 2012. KYTHERA completed enrollment in its pivotal Phase III clinical program for ATX-101 in more than 1000 subjects randomized to ATX-101 or placebo in 70 centers across the United States and Canada in August 2012. The Company expects to release topline results in mid-2013.
About KYTHERA Biopharmaceuticals Inc.
KYTHERA Biopharmaceuticals Inc. is a clinical-stage biopharmaceutical company focused on the discovery development and commercialization of novel prescription products for the aesthetic medicine market. KYTHERA initiated its pivotal Phase III clinical program for ATX-101 in March 2012 and completed enrollment of more than 1000 patients randomized to ATX-101 or placebo in 70 centers across the U.S. and Canada in August 2012. KYTHERA also maintains an active research interest in hair and fat biology. Find more information at www.kytherabiopharma.com.
Celgene phase 3 – Oral Apremilast Achieves Statistical Significance for the Primary Endpoint of PASI-75 in the First Phase III Study in Patients with Psoriasis

APREMILAST, N-{2-[(1S)-1-(3-Ethoxy-4-methoxyphenyl)-2-(methylsulfonyl)ethyl]-1,3-dioxo-2,3-dihydro-1H-isoindol-4-yl}acetamide
mar02,2013
Celgene International Sàrl, a subsidiary of Celgene Corporation (NASDAQ: CELG) today presented the results from ESTEEM 1, the Company’s first phase III study in psoriasis, at the American Academy of Dermatology annual meeting in Miami, Florida.
“I see this as a prime candidate for future management of psoriasis that allows us to treat a range of patients, including more moderate cases earlier on”
The company previously announced statistical significance for the primary and major secondary endpoint of PASI-75 at Week 16 and the Static Physician Global Assessment for patients receiving apremilast in the ESTEEM 1&2 phase III studies. ESTEEM 1&2 are the phase III registrational randomized, placebo-controlled studies evaluating the Company’s oral small-molecule inhibitor of phosphodiesterase-4 (PDE4) in patients with moderate-to-severe chronic plaque psoriasis.
ESTEEM 1, presented today, evaluated efficacy and safety in a range of patients. Approximately one-third of the study population was systemic and/or phototherapy treatment-naïve. Nearly 30 percent of the overall study population had prior biologic therapy, which included biologic-failures.
In the ESTEEM 1 study, a significantly higher percentage of apremilast-treated patients demonstrated PASI-75 at week 16 than did placebo patients (33.1% vs. 5.3%; P<0.0001). Significantly higher PASI-75 scores at week 16 were demonstrated across all patient segments enrolled in this study, including systemic-naïve and biologic-naïve patients receiving apremilast 30 mg BID compared with placebo (38.7% vs. 7.6%; P<0.0001 and 35.8% vs. 5.9%; P<0.0001 respectively). Apremilast demonstrated maintenance of effect over time, as measured by the Mean Percent Change from Baseline in PASI score over 32 weeks, with apremilast demonstrating a 54.9% reduction at week 16 and a 61.9% reduction at week 32.
Statistical significance at week 16 was also demonstrated in the major secondary endpoint, Static Physician Global Assessment (sPGA) of clear or almost clear (P<0.0001), and other key secondary endpoints (change in BSA, Pruritus VAS, DLQI), as well as in assessments of difficult to treat areas (nail and scalp psoriasis).
“I see this as a prime candidate for future management of psoriasis that allows us to treat a range of patients, including more moderate cases earlier on,” said Kristian Reich, M.D., SCIderm Research Institute and Dermatologikum Hamburg, Germany.
The overall safety and tolerability profile was consistent with results from previously reported phase III psoriatic arthritis trials. No cases of tuberculosis or lymphoma were observed through week 16, and there was no increased risk of cardiovascular events or serious opportunistic infection. Apremilast was generally well tolerated. The most common adverse events (AEs) greater than placebo were diarrhea, nausea and headache. Greater than 96% of patients in the study reported no AEs or mild to moderate AEs. A similar percentage of patients reported both serious AEs and severe AEs in the apremilast 30 mg BID treatment group compared to placebo (2.1% vs. 2.8% and 3.6% vs. 3.2%, respectively).
An NDA submission to the U.S. Food and Drug Administration, based on the combined ESTEEM 1&2 studies for psoriasis, is expected in the second half of 2013. The Company previously announced it expects to file a separate NDA for psoriatic arthritis in the first quarter of 2013. A combined PsA/psoriasis MAA submission in Europe is also planned for the second half of 2013.
Top-line positive results from the two pivotal, randomized, placebo-controlled phase III studies of apremilast in psoriasis (ESTEEM 1&2) were released in January 2013. The studies included more than 1,200 patients with moderate-to-severe psoriasis and are ongoing. Results from PSOR-005, a phase IIb dose-range study, were recently published in The Lancet (http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(12)60642-4/fulltext).
About ESTEEM 1 & 2
ESTEEM 1 & 2 are two pivotal phase III randomized, placebo-controlled studies evaluating apremilast in subjects with a diagnosis of moderate-to-severe chronic plaque psoriasis for at least 12 months prior to the screening, and at baseline, and who were also candidates for phototherapy and/or systemic therapy. Approximately 1,250 patients were randomized 2:1 to receive either apremilast 30 mg BID or placebo for the first 16 weeks, followed by a maintenance phase from weeks 16-32 in which placebo subjects were switched to apremilast 30 mg BID through week 32, and a randomized withdrawal phase for responders from Week 32-Week 52 based on their initial apremilast randomization and PASI response.
Apremilast, an oral small-molecule inhibitor of phosphodiesterase 4 (PDE4), works intracellularly to modulate a network of pro-inflammatory and anti-inflammatory mediators. PDE4 is a cyclic adenosine monophosphate (cAMP)-specific PDE and the dominant PDE in inflammatory cells (see http://discoverpde4.com/). PDE4 inhibition elevates intracellular cAMP levels, which in turn down-regulates the inflammatory response by modulating the expression of TNF-α, IL-23, and other inflammatory cytokines. Elevation of cAMP also increases anti-inflammatory cytokines such as IL-10. To learn more go to www.discoverpde4.com/.
Top-line positive results from three pivotal randomized, placebo-controlled phase III studies of apremilast in PsA (PALACE 1, 2 & 3) were released in September 2012. PALACE 1 was also presented as an oral presentation at the ACR annual meeting in November 2012. Taken together, the PALACE program comprises the most comprehensive psoriatic arthritis studies to date intended for regulatory submission.
Results from PSA-001, the phase II study of apremilast in psoriatic arthritis, were recently published online in the journal Arthritis & Rheumatism (http://onlinelibrary.wiley.com/doi/10.1002/art.34627/abstract).
A randomized, placebo-controlled phase III study (POSTURE) of apremilast in ankylosing spondylitis (AS) began enrolling patients in April 2012. AS, a debilitating disease, which may cause fusion of the spine, arthritis, inflammation of the eye and damage to the heart, affects approximately 1.5 million people in the U.S. and Europe. The trial will randomize approximately 450 patients to receive 20 mg or 30 mg apremilast BID, or placebo BID.
Psoriasis is an immune-mediated, non-contagious chronic inflammatory skin disorder of unknown cause. The disorder is a chronic recurring condition that varies in severity from minor localized patches to complete body coverage. Plaque psoriasis is the most common type of psoriasis. About 80 percent of people who develop psoriasis have plaque psoriasis, which appears as patches of raised, reddish skin covered by silvery-white scales. These patches, or plaques, frequently form on the elbows, knees, lower back, and scalp. Psoriasis occurs nearly equally in males and females. Recent studies show that there may be an ethnic link. Psoriasis is believed to be most common in Caucasians and slightly less common in other ethnic groups. Worldwide, psoriasis is most common in Scandinavia and other parts of northern Europe. About 10 percent to 30 percent of patients with psoriasis also develop a condition called psoriatic arthritis, which causes pain, stiffness and swelling in and around the joints.
Celgene International Sàrl, located in Boudry, in the Canton of Neuchâtel, Switzerland, is a wholly owned subsidiary and international headquarters of Celgene Corporation. Celgene Corporation, headquartered in Summit, New Jersey, is an integrated global pharmaceutical company engaged primarily in the discovery, development and commercialization of innovative therapies for the treatment of cancer and inflammatory diseases through gene and protein regulation. For more information, please visit the Company’s website at www.celgene.com.
Apremilast is an orally available small molecule inhibitor of PDE4 being developed by Celgene for ankylosing spondylitis, psoriasis, and psoriatic arthritis.[1][2] The drug is currently in phase III trials for the three indications. Apremilast, an anti-inflammatory drug, specifically inhibits phosphodiesterase 4. In general the drug works on an intra-cellular basis to moderate proinflammatory and anti-inflammatory mediator production.
Apremilast is being tested for its efficacy in treating “psoriasis, psoriatic arthritis and other chronic inflammatory diseases such as ankylosing spondylitis, Behcet’s disease, and rheutmatoid arthritis.”
- “Apremilast Palace Program Demonstrates Robust and Consistent Statistically Significant Clinical Benefit Across Three Pivotal Phase III Studies (PALACE-1, 2 & 3) in Psoriatic Arthritis” (Press release). Celgene Corporation. 6 September 2012. Retrieved 2012-09-10.
- “US HOT STOCKS: OCZ, VeriFone, Men’s Wearhouse, AK Steel, Celgene”. The Wall Street Journal. 6 September 2012. Retrieved 2012-09-06
Phase 3 Amicus in collaboration with GlaxoSmithKline (GSK) is developing the investigational pharmacological chaperone migalastat HCl for the treatment of Fabry disease
 CAS Number:75172-81-5
CAS Number:75172-81-5-
3,4,5-Piperidinetriol,2-(hydroxymethyl)-, hydrochloride (1:1), (2R,3S,4R,5S)-
- Molecular Structure:

- Formula:C6H14ClNO4
- Molecular Weight:199.63
- Synonyms:3,4,5-Piperidinetriol,2-(hydroxymethyl)-, hydrochloride, (2R,3S,4R,5S)- (9CI);3,4,5-Piperidinetriol,2-(hydroxymethyl)-, hydrochloride, [2R-(2a,3a,4a,5b)]-;Migalastat hydrochloride;Galactostatin hydrochloride;(2S,3R,4S,5S)-2-(hydroxymethyl)piperidine-3,4,5-triol hydrochloride;
- Melting Point:260 °C
- Boiling Point:382.7 °C at 760 mmHg
- Flash Point:185.2 °C
end feb 2013
About Amicus Therapeutics
Amicus Therapeutics is a biopharmaceutical company at the forefront of therapies for rare and orphan diseases. The Company is developing orally-administered, small molecule drugs called pharmacological chaperones, a novel, first-in-class approach to treating a broad range of human genetic diseases. Amicus’ late-stage programs for lysosomal storage disorders include migalastat HCl monotherapy in Phase 3 for Fabry disease; migalastat HCl co-administered with enzyme replacement therapy (ERT) in Phase 2 for Fabry disease; and AT2220 co-administered with ERT in Phase 2 for Pompe disease.
About Migalastat HCl
Amicus in collaboration with GlaxoSmithKline (GSK) is developing the investigational pharmacological chaperone migalastat HCl for the treatment of Fabry disease. Amicus has commercial rights to all Fabry products in the United States and GSK has commercial rights to all of these products in the rest of world.
As a monotherapy, migalastat HCl is designed to bind to and stabilize, or “chaperone” a patient’s own alpha-galactosidase A (alpha-Gal A) enzyme in patients with genetic mutations that are amenable to this chaperone in a cell-based assay. Migalastat HCl monotherapy is in Phase 3 development (Study 011 and Study 012) for Fabry patients with genetic mutations that are amenable to this chaperone monotherapy in a cell-based assay. Study 011 is a placebo-controlled study intended primarily to support U.S. registration, and Study 012 compares migalastat HCl to ERT to primarily support global registration.
For patients currently receiving ERT for Fabry disease, migalastat HCl in combination with ERT may improve ERT outcomes by keeping the infused alpha-Gal A enzyme in its properly folded and active form thereby allowing more active enzyme to reach tissues.2 Migalastat HCl co-administered with ERT is in Phase 2 (Study 013) and migalastat HCl co-formulated with JCR Pharmaceutical Co. Ltd’s proprietary investigational ERT (JR-051, recombinant human alpha-Gal A enzyme) is in preclinical development.
About Fabry Disease
Fabry disease is an inherited lysosomal storage disorder caused by deficiency of an enzyme called alpha-galactosidase A (alpha-Gal A). The role of alpha-Gal A within the body is to break down specific lipids in lysosomes, including globotriaosylceramide (GL-3, also known as Gb3). Lipids that can be degraded by the action of α-Gal are called “substrates” of the enzyme. Reduced or absent levels of alpha-Gal A activity leads to the accumulation of GL-3 in the affected tissues, including the kidneys, heart, central nervous system, and skin. This accumulation of GL-3 is believed to cause the various symptoms of Fabry disease, including pain, kidney failure, and increased risk of heart attack and stroke.
It is currently estimated that Fabry disease affects approximately 5,000 to 10,000 people worldwide. However, several literature reports suggest that Fabry disease may be significantly under diagnosed, and the prevalence of the disease may be much higher.
2. Benjamin, et al., Molecular Therapy: April 2012, Vol. 20, No. 4, pp. 717–726.
http://clinicaltrials.gov/show/NCT01458119
http://www.docstoc.com/docs/129812511/migalastat-hcl
| Chemical Name: | DEOXYGALACTONOJIRIMYCIN, HYDROCHLORIDE |
| Synonyms: | DGJ;Amigal;Unii-cly7m0xd20;GALACTOSTATIN HCL;DGJ, HYDROCHLORIDE;Migalastat hydrochloride;Galactostatin hydrochloride;DEOXYGALACTONOJIRIMYCIN HCL;1-DEOXYGALACTONOJIRIMYCIN HCL;1,5-dideoxy-1,5-imino-d-galactitol |

Phase 3 FDA -Acorafloxacin (Avarofloxacin) Granted QIDP and Fast Track Designation

Avarofloxacin Granted QIDP and Fast Track Designation
JNJ-Q2, JNJ-32729463-AAA
CAS NO 878592-87-1 of base
7-[3-[2-Amino-1(E)-fluoroethylidene]piperidin-1-yl]-1-cyclopropyl-6-fluoro-8-methoxy-4-oxo-1,4-dihydroquinoline-3-carboxylic acid

Furiex Pharmaceuticals Inc. announced that the FDA has granted Qualified Infectious Disease Product (QIDP) and Fast Track designation for avarofloxacin (JNJ-Q2). Avarofloxacin is a Phase 3-ready broad-spectrum fluoroquinolone antibiotic for the treatment of acute bacterial skin and skin-structure (ABSSSI) infections, community-acquired pneumonia and has proven to be effective in treating methicillin-resistant Staphylococcus aureus (MRSA) infections.
Avarofloxacin is an investigational novel fluoroquinolone antibiotic that has been shown to be effective in a Phase 2 study of ABSSSI infections. In this study, avarofloxacin demonstrated favorable efficacy for both early clinical response endpoints as well as all clinical cure endpoints for the intent to treat population.

Avarofloxacin has a low tendency for development of drug resistance and exhibits a broad range of antibacterial activities in vitro, including MRSA, fluoroquinolone-resistant Staphylococcus aureus, Streptococcus pneumoniae (including multi-drug resistant strains), gram positive, gram negative, atypical respiratory pathogens (such as legionella and mycoplasma) and anaerobic bacteria, which are often associated with abscesses of the skin and other organs.
The availability of IV and oral formulations for avarofloxacin differentiates it from a number of other products for MRSA infections which are only available for intravenous administration.
For more information call (919) 456-7800or visit http://www.furiex.com/
About Methicillin-Resistant Staphylococcus aureus (MRSA)
MRSA is a strain of the bacteria Staphylococcus aureus (staph) which commonly causes skin and soft tissue infections and is resistant to many antibiotics. Although MRSA had previously been primarily a hospital-acquired pathogen, its incidence has been rising in the community, and it has become the most frequent cause of skin and soft tissue infections presenting to emergency departments in the United States. There are a limited number of antibiotics approved to treat MRSA, and their frequent usage has led to emergence of multi-drug resistant bacteria. Thus, we believe there is significant unmet medical need for new antibiotics such as avarofloxacin that provide flexible (hospital and outpatient) treatment options for MRSA.

WO-2006/101603 describes 7-amino alkylidenyl- heterocyclic quinolones as antimicrobial compounds and the synthesis of 7-[(3E)-3-(2-amino-l-fluoroethylidene)-l- piperidinyl]- 1 -cyclopropyl-6-fluoro- 1 ,4-dihydro-8-methoxy-4-oxo 3-quinolinecarboxylic acid is disclosed as compound (303) in Table 1 on page 20. This compound is conveniently referred to as compound ‘A’ hereafter.
compound ‘A’
7-[(3E)-3-(2-amino-1 -fluoroethylidene)-1 -piperidinyl]-1 -cyclopropyl-6-fluoro- 1 ,4-dihydro-8-methoxy-4-oxo 3-quinolinecarboxylic acid
The in vitro antibacterial properties of compound ‘A’ are described by Morrow B.J. et al. in Antimicrobial Agents and Chemotherapy, vol. 54, pp. 1995 – 1964 (2010).
WO-2008/005670 discloses one-pot methods for the production of substituted allylic alcohols as well as extractive methods for the separation of certain isomeric alcohol products which are useful for preparing quinolones such as the antimicrobial compound 7-[(3E)-3-(2-amino- 1 -fluoroethylidene)- 1 -piperidinyl]- 1 -cyclopropyl-6-fluoro- 1 ,4- dihydro-8-methoxy-4-oxo 3-quinolinecarboxylic acid (i.e. compound ‘Α’). An important intermediate in the overall synthesis route of said antimicrobial compound ‘A’ is 2-[(2E)-2-fluoro-2-(3-piperidinylidene)ethyl]-lH-isoindole-l,3(2H)- dione and its hydrochloric acid salt thereof : compound (1 )
2-[(2E)-2-fluoro-2-(3-piperidinylidene)ethyl]-1 H-isoindole-1 ,3(2H)-dione compound (1 ) .HCI
Compound (1) introduces the desired E- stereochemistry into the overall synthesis route for the antimicrobial compound ‘Α’.
WO-2008/005670 discloses a synthesis route for compound (1) on page 38 as depicted below :
– highly enriched (E)
(Step 3a) O
The detailed reaction procedure for compound (1) is disclosed in WO-2008/005670 in Example 1 on pages 37 to 44 affording compound (1) in Method A with a E:Z ratio of 97:3 in an approximate overall yield of 18 % in Method A (step 1 for the first 3 heptane layers has a yield of 34 % with a ratio E:Z of 71 :29, step 2a has a yield of 53.4% with a ratio E:Z of 97:3, and step 3 has quantitave yield), or affording compound (1) in Method B with an approximate overall yield of 15% with a ratio E:Z of 94.4 : 5.6. WO-2008/005670 discloses a synthesis route for the hydrochloric acid addition salt of compound (1) on page 15 in Scheme 2 as depicted below :
into n-butanol,
1 ) 5/6 N HCl in IPA
2) heat to distill
3) add IPA
enriched E-isomer
compound (1 ) .HCl
The detailed reaction procedure to prepare the HCl salt of compound (1) is disclosed in WO-2008/005670 in Example 4 on pages 49 to 52 affording >95% of desired E-isomer with an overall yield of 18 – 22% starting from N-boc-3-piperidone.
The reaction procedures described in WO-2008/005670 for the preparation of compound (1) or its HCl salt are characterized by lack of selectivity of the Wadsworth- Emmons-Horner reaction which produces the undesired Z-isomer in large quantities. This undesired Z-isomer requires additional time consuming separation steps.
Hence there is a need for a more efficient and less waste-producing procedure for the preparation of compound (1) or its HCl salt. WO-2010/056633 discloses a synthesis scheme XIV on page 87 to prepare tert-butyl 4- (2-ethoxy-2-oxoethylidene)piperidinyl-l-carboxylate and a synthesis scheme XXVI on page 111 to prepare (l-benzyl-piperidin-4-ylidene)bromoacetic acid ethyl ester.
In a first embodiment the present invention relates to an improved process for preparing compounds of formula (III) having an improved ratio of the desired (E)-isomer over the undesired (Z)-isomer.
(I)
In a further embodiment the compound (E)-(III) is then converted in to compound (1) or its hydrochloric acid addition salt thereof.

…………………………..
WO 2008005670
http://www.google.com/patents/WO2008005670A2?cl=en
Scheme 1
3 eq NaBH4 OH
30 – 4O0C
2a 2b 2a
2b shows the preparation of alcohol 2
Scheme 2
1 ) HCI (5 eq )
aqueous layer to enriched E isomer pH 9-10 then extract into n-Butanol, discard aqueous layer
Preparation of
7-[3-(2-Amino-l-fluoroethylidene)piperidin-l-yl]-l-cyclopropyl- 6-fluoro-8-methoxy-4-oxo-l,4-dihydroquinoline-3-carboxylic acid (10) and its HCl salt (12)
7-[3-(2-Amino-1-fluoro-ethyhdene)-piperidin-1-yl]-1-cyclopropyl–fluoro-8-mΘthoxy-4-oxo-1 ,4-dιhydro-quιnolιne-3-carboxylιc acid (10)
Step 1: Preparation of 3-(l-fluoro-2-hydroxyethylidene)piperidine-l-carboxylic acid tert-butyl ester (2a)
A 22-L 4-neck round bottom flask, equipped with a thermocouple controller, overhead mechanical stirrer, condenser, nitrogen inlet adapter, and stopper, was charged with N-Boc-3-piperidone (663.36 g, 3.34 mol), 2-methoxyethanol (6.0 L) and 2-fluorotriethylphosphonoacetate (843.54 g, 3.49 mol). The mixture was stirred to obtain a homogeneous solution and then CS2CO3 was added in portions over 1.5 h. After the CS2CO3 addition was complete, NaBH4 was added in portions over 6 h; during most of this addition the reaction temperature was maintained between 35 0C to 40 0C. After the addition was complete, the reaction was allowed to stir overnight after which time HPLC analysis indicated that the reaction was complete. This run was combined with two additional runs of equal size and transferred to a stirred 100-L Hastalloy® reactor containing water (90 L). The aqueous mixture was extracted with heptane (4 x 20 L) followed by extraction with MTBE (methyl tert-butyl ether) (20 L). The first three heptane extracts provided 842 g of the allylic alcohol as 71:29 (E: Z) mixture (HPLC and NMR). The product mixture from the first three heptane extractions was carried on to the next step without any additional purification. The fourth heptane extract gave 114 g of product that was a 67:33 mixture of is: Z alcohols (NMR). MTBE extraction and concentration gave 1.1 Kg of product as a 33:67 mixture of E:Z alcohols (HPLC). The total overall yield for both isomers was 2.06 Kg (83%). 1H NMR of 2a (400 MHz, CDCl3): £ 1.45 (s, 9 H), 1.52 (m, 2 H), 2.40 (m, 2 H), 3.45 (m, 2 H), 3.90 (s, 2 H), 4.25 (d, 2 H). 1H NMR of 2b (400 MHz, CDCl3): δ 1.46 (s, 9 H), 1.65 (m, 2 H), 2.27 (m, 2 H), 3.45 (m, 2 H), 4.1 (s, 2 H), 4.25 (d, 2 H).
Step 2, Method A: Preparation of 3-is-[2-(l,3-dioxo-l,3-dihydroisoindol-2-yl)-l- fluoroethylidene]-piperidine-l-carboxylic acid tert-butyl ester (3-ϋ)
A 22-L 4-neck round bottom flask, equipped with a thermocouple controller, overhead mechanical stirrer, condenser, pressure-equalizing addition funnel, nitrogen inlet adapter, and stopper, was charged with E:Z alcohol mixture 2a and 2b (377.5 g, 1.296 mol corrected), 2-MeTHF (3.31 L), phthalimide (232.8 g, 1.581 mol), and Ph3P (411.3 g, 1.568 mol). The white suspension was stirred under N2 and cooled to -12 0C in an acetone/Dry-Ice bath, DIAD (309 mL, 1.49 mol) was added via the addition funnel over a 36-min period, while the reaction temperature was maintained at -15 0C to -10 0C. After the addition, the reaction was warmed to 20 0C in a water bath and stirred for 2 h. The reaction was cooled to 0 0C in an ice/water bath and quenched with cold 1.0 M HCl (950 mL). The aqueous phase was separated and EtOAc (1.70 L) was added to the organic phase. This phase was washed with cold 1.0 M HCl (0.95 L) (the aqueous phase was pH < 2) and then separated. The organic phase was next washed with cold 4 NNaOH (1.70 L), the alkaline aqueous phase (pH > 13) was separated and the EtOAc layer washed with brine (1.70 L). Concentration of the organic phase at 60 0C under house vacuum (-120 mm Hg) afforded 1,442.0 g of crude 3. This run was repeated on the same scale to provide an additional 1,431.0 g of crude material for a combined yield of 2,873 g (159%). HPLC analysis (area%) indicated crude 3 was a mixture of 3-E (29.4%), 3-Z (10.4 %), Ph3PO (51.0 %), and phthalimide (1.1 %). This was purified by recrystallization as described in step 2a.
Step 2a, Method A: Purification of 3-is-[2-(l,3-dioxo-l,3-dihydroisoindol-2-yl)-l- fluoroethylidene]-piperidine-l-carboxylic acid tert-butyl ester
A 22-L 4-neck round bottom flask equipped with a thermocouple controller, overhead mechanical stirrer, condenser, pressure-equalizing addition funnel, nitrogen inlet adapter and stopper was charged with the combined crude 3 (2,873 g) and MeOH (9.0 L). The solution was stirred under nitrogen and heated to 65 0C, while hot (60 0C) D.I. water (7.8 L) was added over a 15-min period. The solution was stirred at 65 0C for 5 min, and then the heating mantle was replaced with a water bath, and the mixture was gradually cooled to 0 0C over a 4-h period, and continued stirring for 1 h at 0 0C. The off-white solid was collected by filtration, and dried by air-suction at 60 0C for 20 h, this provided 1,172.6 g of a mixture of 3-E and 3-Z.
The partially purified product above was recrystallized a second time in the same manner using hot MeOH (7.2 L) and hot water (5.0 L) except that the water was added over a 10-min period to afford 515.6 g (53.4%) of 3-E as a 97:3 mixture of E:Z geometric isomers. This material was used in the next step without additional purification. . 1H NMR of 3-E (400 MHz, CDCl3): δ 1.48 (s, 9 H), 1.52-1.66 (m, 2 H), 2.28-2.38 (m, 2 H), 3.40-3.51 (m, 2 H), 4.18 (s, 2 H), 4.55 (d, J= 21.0 Hz, 2 H), 7.68- 7.77 (m, 2 H), 7.80-7.89 (m, 2 H). MS: 397 (M+Na)+, 771 (2M+Na)+.
3 -E-[2-( 1 ,3 -dioxo- 1 ,3-dihydroisoindol-2-yl)- 1 -fluoroethylidene]-piperidine- 1 – carboxylic acid tert-butyl ester was also prepared with Method B below: Step 2, Method B: Preparation of 3-£-[2-(l,3-dioxo-l,3-dihydroisoindol-2-yl)-l- fluoroethylidene]-piperidine-l-carboxylic acid tert-butyl ester (3-E)
Preparation of the methanesulfonate and chloride derivatives
2a
A 12-L 4-neck round bottom flask equipped with an overhead stirrer, thermocouple, pressure-equalizing addition funnel, and a nitrogen inlet adapter was charged with 2a (297.0 g, 1.21 mol) and CH2Cl2 (3.9 L). The solution was cooled to 0 0C under N2 and EtsN (320 mL, 2.30 mol) was added via the addition funnel over a 10- min period. This was followed by methanesulfonyl chloride (115 mL, 1.49 mol) added over a 60-min period then the reaction was stirred for an additional 60-min at 0 0C. The mixture was poured into a mixture of deionized water (4.4 L) and saturated NaHCθ3 (0.78 L), the layers were separated, the aqueous layer was extracted with CH2Cl2 (2 x 2 L). All the CH2Cl2 layers were combined and washed with saturated NaHCθ3 (2 L). The CH2Cl2 was removed under vacuum at 40 0C to afford a mixture of the mesylate and chloride (342.3 g). This mixture was taken on to the next step without any purification.
Conversion of the methanesulfonate/chloride to phthalimide 3
A 5-L 4-neck round bottom flask equipped with an overhead stirrer, thermocouple, pressure-equalizing addition funnel, and a nitrogen inlet adapter was charged with the mixture of the mesylate and chloride from above (342.2 g, 1.21 mol) and DMF (2.0 L) followed by potassium phthalimide (224.9 g, 1.21 mol). The mixture was stirred at 60 0C for 1-h then at 20 0C for 18 h. The mixture was poured into ice- water, allowed to stand for 30-min and filtered. The liquors from the filtration were allowed to stand at 0 0C over the weekend and filtered again. The combined solids were dissolved in acetone (4 L) and concentrated on the rotary evaporator, this process was repeated a second time to give the phthalimide derivative 3 as a mixture oiEIZ (79/31) isomers (263.2 g, 58.1 %).
Step 2a, Method B: Purification of 3-£-[2-(l,3-dioxo-l,3-dihydroisoindol-2-yl)-l- fluoroethylidene]-piperidine-l-carboxylic acid tert-butyl ester
A 12-L 4-neck round bottom flask equipped with an overhead stirrer, thermocouple, pressure-equalizing addition funnel, and a nitrogen inlet adapter was charged with the crude phthalimide derivative 3 (263.1 g) and MeOH (2.74 L). The mixture was heated to 66 – 68 0C while water (2.1 L) was added over 20-min, the mixture was stirred at 68 0C for 5-min, then gradually cooled to 20 0C for 18-h. While the crystallization mixture was cooling it was seeded at 60 0C, 56 0C and 530C. This crystallization gave a white solid that was filtered and dried under vacuum at 50 0C to afford 3-E (118.8 g, 45.2%) as a mixture containing 94.4% E and 5.6% Z isomers (NMR analysis).
Step 3: Preparation of 2-[2-fluoro-2-(3-piperidinylidene)ethyl]-lH-isoindole-l,3)- dione (4)
A 12-L 4-neck round bottom flask equipped with an overhead stirrer, thermocouple, pressure-equalizing addition funnel, and a nitrogen inlet adapter was charged with 3-E (578.0 g, 1.544 mol) and CH2Cl2 (4.5 L). The solution was stirred at 200C under N2 and TFA (476 mL, 6.18 mol) was added via the addition funnel over a 10-min period. The mixture was gently heated to 38 0C and stirred for 3 h. The solvent was removed under vacuum to give the TFA salt of 4 (962.6 g). This material was dissolved in CH2Cl2 (4.0 L) and washed with 2.5 NNa2CO3 (4.6 L)-followed by saturated NaHCO3 (4.6 L). The organic phase was dried (MgSO4), filtered, and condensed in vacuo. The off-white solid was dried at 40 0C under vacuum (20 mm Hg) for 20 h to afford 464.3 g of the free base of 4 as slightly yellowish foamy substance. 1H NMR of 4 TFA salt (400 MHz, CDCl3): δ 1.87-1.98 (m, 2 H), 2.42-2.55 (m, 2 H), 3.38-3.50 (m, 2 H), 4.08-4.18 (br s, 2 H), 4.50 (d, J= 21.0 Hz, 2 H), 7.69-7.78 (m, 2 H), 7.79-7.87 (m, 2 H), 7.98-8.23 (br s, 1 H), 12.48 (s, 1 H). MS: 275 (MH)+, 549 (2M+H)+.
Step 4: Preparation of l-Cyclopropyl-ό^-difluoro-S-methoxy^-oxo-l^- dihydroquinoline-3-carboxylic acid difluoroborate ester (6)
A 22-L 4-neck round bottom flask equipped with an overhead stirrer, thermocouple, condenser, pressure equalizing addition funnel, and a nitrogen inlet adapter was charged with quinoline-3-carboxylic acid 5 (450.0 g, 1.524 mol), THF (5.40 L) and K2CO3 (247.2 g, 1.753 mol). This suspension was first stirred at 20 0C under N2 for 5 min, and BF3 »Et20 (259 mL, 2.04 mol) was added dropwise via the addition funnel to the stirred mixture over a 5-min period. After the addition, the mixture was heated to reflux (66 0C) for 6 h. The reaction was cooled to 10 0C, diluted with Et2O (9.0 L) and stirred for 10 min. The solid was filtered and washed with Et2O (200 mL x 2) and then dried at 50 0C under house vacuum (-160 mm Hg) for 20 h to afford 771.O g of crude difluoroborate ester 6. After this, the crude material was suspended in MeCN (8.0 L) and stirred at 20 0C for 20 min; the solid was collected by filtration. The filter cake was re-suspended and stirred in MeCN four more times (2.0 L x 4), and all filtrates were combined and concentrated at 60 0C under hi-vac (~10 mmHg). The resulting off- white solid was dried at 50 0C under house vacuum (-160 mmHg) for 20 h to afford 508.66 g (97.2% isolated yield, HPLC = 99.2% by area) of pure difluoroborate ester 6. 1H NMR of 6 (400 MHz, CD3CN): «51.17-1.28 (m, 2 H), 1.29-1.40 (m, 2 H), 4.19 (s, 3 H), 4.40-4.52 (m, 1 H), 8.16 (dd, J= 6.9, 7.0 Hz, 1 H), 9.17 (s, 1 H). MS: 344 (MH)+, 667 (2M-F)+.
Step 5: Preparation of intermediate 8
A 5-L 4-neck round bottom flask equipped with an overhead stirrer, thermocouple, condenser, pressure-equalizing addition funnel and a nitrogen inlet adapter was charged with difluoroborate ester 6 (320.0 g, 0.933 mol), DMF (1.10 L) and piperidine 4 (289.0 g, 1.053 mole). This suspension was stirred at 20 0C under N2 for 5 min, EtsN (299 mL, 2.15 mol) was added to the stirred mixture via the addition funnel over an additional 5-min period. After this addition, the mixture was heated to 60 0C and stirred for 3 h, to give crude intermediate 7. HPLC analysis (area%) indicated crude 7 is a mixture of 7 (40.5%), 8 (1.7 %), 6 (24.1%), and the rest of unknowns (33.7%). MS: 598 (MH)+. The coupled crude product 7 was carried on to the next step without isolation.
Removal of the Fluoroborate Ester The above stirred reaction mixture containing 7 was treated in the same flask with EtOH (6.80 L) and Et3N (299 mL, 2.147 mol) under N2 at 60 0C. The amber solution was heated to reflux at 72 0C for 2 h and cooled to 20 0C. The reaction mixture was poured into a rapidly stirred 22-L 4-neck round bottom flask containing a 1 : 1 (v/v) ice-water mixture (8.0 L) over a 10-min period; stirring was continued for -10 min. Cold 1 NHCl (4.0 L) was added to the solution over 20 min to adjust the pH from 9-10 to 3; stirring was continued for an additional 20 min at 0 0C. The yellow solid was isolated by filtration and dried in a filter funnel by air-suction using house vacuum (-160 mm Hg) at 20 0C for 20 h to afford 1,889.0 g of crude 8 as a damp solid (HPLC = 33.6%, area%).
Purification of Intermediate 8
To a 22-L 4-neck round bottom flask equipped with an overhead stirrer, thermocouple, pressure-equalizing addition funnel, and a nitrogen inlet adapter was charged with crude 8 (1889.0 g), MeCN (3.6 L) and EtOH (3.2 L). The suspension was heated to reflux (76 0C), while D.I. H2O (500 mL) was added over 10 min. The solution was stirred at 76 0C for 5 min, and then gradually cooled to 10 0C over 1 h; stirred for an additional hour. The yellow solid was collected by filtration, dried in a vacuum oven under house vacuum (-160 mm Hg) at 60 0C for 20 h to afford 229. Ig (45%) of 8, which was used in next step without further purification. 1H ΝMR of 8 (400 MHz, DMSO-d6): £ 1.02-1.10 (m, 2 H), 1.11-1.19 (m, 2 H), 1.67-1.79 (m, 2 H), 2.34-2.45 (m, 2 H), 3.38-3.49 (m, 2 H), 3.78 (s, 3 H), 4.10 (s, 2 H), 4.15-4.26 (m, 1 H), 4.54 (d, J= 21.0 Hz, 1 H), 7.72 (d, J= 9.1 Hz, 1 H), 7.81 (s, 4 H), 8.71 (s, I H), 14.98 (s, 1 H). MS: 550 (MH)+.
Step 6: Preparation of 7-[3-(2-amino-l-fluoro-ethylidene)-piperidin-l-yl]-l- cyclopropyl-6-fluoro-8-methoxy-4-oxo-l,4-dihydro-quinoline-3-carboxylic acid (10)
8 10 A
22-L 4-neck round bottom flask equipped with an overhead stirrer, thermocouple, condenser, pressure-equalizing addition funnel and a nitrogen inlet adapter was charged with 8 (253.6 g, 0.462 mol) and MeOH (5.10 L). This suspension was stirred at 20 0C under N2 and H2NNH2 (86.9 mL, 2.796 mol) was added over a 5-min period. The yellow suspension was heated to 65 0C and refluxed for 1 h. The reaction was cooled to 60 0C and MeCN (3.84 L) was added. The mixture was heated to reflux for 5 min, and then cooled to 20 0C in a water bath. The light-yellow solid was collected by filtration and the filter cake was washed with MeCN (150 mL x 2). The combined filtrate was concentrated at 60 0C affording 322.0 g of crude product 10. This product was recrystallized from a mixture of MeOH (1.0 L) and water (1.195 L) to give 176.6 g (91.2%) of pure product 10 as a light yellow solid.
BASE FORM
1H NMR of 10 (400 MHz, DMSO- d6): £ 1.0-1.09 (m, 2 H), 1.10-1.19 (m, 2 H), 1.66-1.78 (m, 2 H), 2.30-2.41 (m, 2 H), 3.17 (s, 2 H), 3.35 (s, 1 H), 3.36-3. 47 (m, 2 H), 3.74 (s, 3 H), 3.89 (s, 2 H), 4.13-4.22 (m, 1 H), 5.35-6.18 (br, 2 H), 7.74 (d, J= 8.9 Hz, 1 H), 8.69 (s, 1 H).
MS: 420 (MH)+.
Example 3
Preparation of7-[3-(2-Amino-l-fluoro-ethylidene)-piperidin-l-yl]-l-cyclopropyl-
6-fluoro-8-methoxy-4-oxo-l,4-dihydro-quinoline-3-carboxylic acid hydrogen chloride salt (12)
7-[3-(2-amino-l-fluoro-ethylidene)-piperidin-l-yl]-l-cyclopropyl-6-fluoro-8- methoxy-4-oxo-l,4-dihydro-quinoline-3-carboxylic acid (10) was prepared as described in Step 6 of Example 1.
A 5-L 4-neck round bottom flask equipped with an overhead stirrer, thermocouple, condenser, pressure-equalizing addition funnel, and a nitrogen inlet adapter was charged with compound 10 (176.0 g, 0.4196 mol) and EtOH (2.40 L). The suspension was stirred under N2 and cooled to 10 0C with an ice/water bath. A solution of HCl in EtOH (1.25 M, 350 mL) was added via the addition funnel over a 20-min period. After the addition, the reaction was stirred at 10 0C for 5 min. The water bath was replaced with a heating mantle and the solution was heated to 76 0C and stirred for 5 min. The heating mantle was replaced with the water bath, the solution was cooled to 0 0C over 1 h and stirred at this temperature for an additional 1 h. The solid was collected by filtration, washed with ice-cold EtOH (100 mL x 2) and dried at 60 0C under vacuum (~4 mmHg) for 60 h. There was obtained 88.9 g (82%) of HCl salt 12 as an off-white to very light-yellow solid.
HCl SALT
1H NMR of HCl salt 12 (400 MHz, CD3CO2D): £ 1.10-1.19 (m, 2 H), 1.29-1.38 (m, 2 H), 1.81-1.93 (m, 2 H), 2.51-2.60 (m, 2 H), 3.48- 3.60 (m, 2 H), 3.86 (s, 3 H), 4.08 (s, 2 H), 4.18 (s, 1 H), 4.19-4.30 (m, 2 H), 7.92 (d, J= 8.6 Hz, 1 H), 8.98 (s, 1 H) 11.65 (s, 1 H).
MS: 420 (MH)+

………………………………………
http://www.google.com/patents/WO2013045599A1?cl=en
Experiment 6
(VI) compound (1 ) .HCI
Compound (1) .HCI salt from Compound (Via) :
9.8 ml (90.6 mmol) of 1-chloroethyl chloro formate are added slowly to a solution of 30 g (82.3 mmol) of compound (E)-(Va) in 165 ml of toluene kept at 0°C. The reaction mixture is stirred 1 hour at room temperature than 1 hour at 80°C and filtered. 24 ml of ethanol and 15.35 ml (90.6 mmol) of 6M HCI solution in isopropanol are added to the filtrate and the resulting mixture is refluxed for 4 hours then cooled to 0°C. The precipitate is filtered, washed with 16 ml of acetone and 16 ml of toluene and dried under vacuum to give 21.94 g of compound (1) . HCI salt. Yield: 86%>.
NMR and MS data are identical to those of the literature.
-
Avarofloxacin nonproprietary drug name
http://www.ama-assn.org/resources/doc/usan/avarofloxacin.pdf
November 28, 2012. N12/130. STATEMENT ON A NONPROPRIETARY NAME ADOPTED BY THE USAN COUNCIL. USAN (ZZ-145). AVAROFLOXACIN.
- [PDF]
Avarofloxacin hydrochloride nonproprietary drug name
http://www.ama-assn.org/resources/doc/usan/avarofloxacin-hydrochloride.pdf

WO2006101603A1 Feb 2, 2006 Sep 28, 2006 Janssen Pharmaceutica Nv 7-amino alkylidenyl-heterocyclic quinolones and naphthyridones WO2008005670A2 Jun 14, 2007 Jan 10, 2008 Janssen Pharmaceutica Nv One-pot condensation reduction methods for preparing substituted allylic alcohols WO2010056633A2 Nov 10, 2009 May 20, 2010 Janssen Pharmaceutica Nv 7-amino alkylidenyl-heterocyclic quinolones and naphthyridones

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
















































