Home » Posts tagged 'GENERIC DRUG' (Page 6)
Tag Archives: GENERIC DRUG
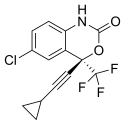
EFAVIRENZ – Huahai Pharma China-Approved to Produce AIDS Treatment

Efavirenz
DMP 266
- Sustiva (USA, Bristol-Myers Squibb)
- Stocrin (EU, MSD)
- Aspen Efavirenz (Sub-Saharan Africa, Aspen Pharmacare)
- E.F (McNeil & Argus)
- Efavir (Cipla)
- Efcure (Emcure Pharmaceuticals)
- Efferven (Ranbaxy Laboratories)
- Estiva (Hetero)
- Evirenz (Alkem Laboratories)
- Viranz (Aurobindo Pharma)
Zhejiang Huahai Pharma received CFDA approval to produce efavirenz, an oral non-nucleoside reverse transcriptase inhibitor (NNRTI) used to control the symptoms of AIDS. Huahai is the first China drugmaker approved to make the drug. Huahai produced efavirenz API for Merck, which marketed the drug under the name Stocrin
read at
http://www.sinocast.com/readbeatarticle.do?id=99634
Efavirenz (EFV), sold under the brand names Sustiva among others, is a non-nucleoside reverse transcriptase inhibitor (NNRTI). It is used as part of highly active antiretroviral therapy (HAART) for the treatment of a human immunodeficiency virus (HIV) type 1. For HIV infection that has not previously been treated, the United States Department of Health and Human Services Panel on Antiretroviral Guidelines currently recommends the use of efavirenz in combination with tenofovir/emtricitabine (Truvada) as one of the preferred NNRTI-based regimens in adults and adolescents.[1] Efavirenz is also used in combination with other antiretroviral agents as part of an expanded postexposure prophylaxis regimen to reduce the risk of HIV infection in people exposed to a significant risk (e.g. needlestick injuries, certain types of unprotected sex etc.).
It is usually taken on an empty stomach at bedtime to reduce neurological and psychiatric adverse effects.
Efavirenz was combined with the HIV medications tenofovir and emtricitabine, all of which are reverse transcriptase inhibitors. This combination of three medications under the brand name Atripla, provides HAART in a single tablet taken once a day.
Efavirenz was discovered at Merck Research Laboratories. It is on the WHO Model List of Essential Medicines, the most important medication needed in a basic health system.[2] As of 2015 the cost for a typical month of medication in the United States is more than 200 USD.[3]
Efavirenz (EFV, brand names Sustiva, Stocrin, Efavir etc.) is a non-nucleoside reverse transcriptase inhibitor (NNRTI) and is used as part of highly active antiretroviral therapy(HAART) for the treatment of a human immunodeficiency virus (HIV) type 1.
For HIV infection that has not previously been treated, the United States Department of Health and Human Services Panel on Antiretroviral Guidelines currently recommends the use of efavirenz in combination with tenofovir/emtricitabine (Truvada) as one of the preferred NNRTI-based regimens in adults and adolescents.
Efavirenz is also used in combination with other antiretroviral agents as part of an expanded postexposure prophylaxis regimen to reduce the risk of HIV infection in people exposed to a significant risk (e.g. needlestick injuries, certain types of unprotected sex etc.).
The usual adult dose is 600 mg once a day. It is usually taken on an empty stomach at bedtime to reduce neurological and psychiatric adverse effects.
Efavirenz was combined with the popular HIV medication Truvada, which consists oftenofovir and emtricitabine, all of which are reverse transcriptase inhibitors. This combination of three medications approved by the U.S. Food and Drug Administration(FDA) in July 2006 under the brand name Atripla, provides HAART in a single tablet taken once a day. It results in a simplified drug regimen for many patients.

doi:10.1016/0040-4039(95)01955-H
Merck synthesis of Efavirenz
History
Efavirenz was approved by the FDA on September 21, 1998, making it the 14th approved antiretroviral drug.
-
Efavirenz is a non-nucleoside reverse trancriptase inhibitor being studied clinically for use in the treatment of HIV infections and AIDS.
- Efavirenz chemically known as (-) 6-Chloro-4-cyclopropylethynyl-4-trifluoromethyl- 1 , 4- dihydro-2H-3, 1-benzoxa zin-2-one, is a highly potent non-nucleoside reverse transcriptase inhibitor (NNRTI).A number of compounds are effective in the treatment of the human immunodeficiency virus (HIV) which is the retrovirus that causes progressive destruction of the human immune system. Effective treatment through inhibition of HIV reverse transcriptase is known for non- nucleoside based inhibitors. Benzoxazinones have been found to be useful non-nucleoside based inhibitors of HIV reverse transcriptase.(-) β-chloro^-cyclopropylethynyM-trifluoromethyl-l ,4-dihydro-2H-3,l -ben zoxazin-2-one (Efavirenz) is efficacious against HIV reverse transcriptase resistance. Due to the importance of (-)6-chloro-4-cyclopropylethynyl-4-trifluoromethyl-l,4-dihydro-2H-3,l-ben zoxazin-2- one, economical and efficient synthetic processes for its production needs to be developed.The product patent US5519021. discloses the preparation of Efavirenz, in Example-6, column-29, involving cyclisation of racemic mixture of 2-(2-amino-5-chlorophenyl)-4- cyclopropyl-l,l,l-trifluoro-3-butyn-2-ol using l ,l ‘-carbonyldiimidazole as carbonyl delivering agent to give racemic Efavirenz. Further, resolution of the racemic Efavirenz is carried out using (-) camphanic acid chloride to yield optically pure Efavirenz. However, research article published in the Drugs of the future, 1998, 23(2), 133-141 discloses process for manufacture of optically pure Efavirenz. The process involves cyclisation of racemic 2-(2-amino-5-chlorophenyl)-4-cyclopropyl-l, 1, l-trifluoro-3-butyn-2- ol using 1, 1-carbonyldiimidazole as carbonyl delivering agent to give racemic Efavirenz and further resolution by (-) camphanic acid chloride.Similarly research article published in Synthesis 2000, No. 4, 479-495 discloses stereoselective synthesis of Efavirenz (95%yield, 99.5%ee), as shown below
Even though many prior art processes report method for the preparation of Efavirenz, each process has some limitations with respect to yield, purity, plant feasibility etc. Hence in view of the commercial importance of Efavirenz there remains need for an improved process.
- US 6 028 237 discloses a process for the manufacture of optically pure Efavirenz.
-
The synthesis of efavirenz and structurally similar reverse transcriptase inhibitors are disclosed in US Patents 5,519,021, 5,663,169, 5,665,720 and the corresponding PCT International Patent Application WO 95/20389, which published on August 3, 1995. Additionally, the asymmetric synthesis of an enantiomeric benzoxazinone by a highly enantioselective acetylide addition and cyclization sequence has been described by Thompson, et al., Tetrahedron Letters 1995, 36, 8937-8940, as well as the PCT publication, WO 96/37457, which published on November 28, 1996.
-
Additionally, several applications have been filed which disclose various aspects of the synthesis of(-)-6-chloro-4-cyclopropylethynyl-4-trifluoromethyl-1,4-dihydro-2H-3,1-benzoxazin-2-one including: 1) a process for making the chiral alcohol, U.S.S.N. 60/035,462, filed 14 January 1997; 2) the chiral additive, U.S.S.N. 60/034,926, filed 10 January 1997; 3) the cyclization reaction, U.S.S.N. 60/037,059, filed 12 February 1997; and the anti-solvent crystallization procedure, U.S.S.N. 60/037,385 filed 5 February 1997 and U.S.S.N. 60/042,807 filed 8 April 1997.




Syntheses of EFV API; different routes of manufacturingAPI, active pharmaceutical ingredient; EFV efavirenz. BELOW
Related substances and degradants (partial listing) in EFVAPI, active pharmaceutical ingredient; CPA, cyclopropylacetylene; EFV, efavirenz
Syntheses of EFV API; different routes of manufacturingAPI, active pharmaceutical ingredient; EFV efavirenz.
Chemical properties
Efavirenz is chemically described as (S)-6-chloro-(cyclopropylethynyl)-1,4-dihydro-4-(trifluoromethyl)-2H-3,1-benzoxazin-2-one. Its empirical formula is C14H9ClF3NO2. Efavirenz is a white to slightly pink crystalline powder with a molecular mass of 315.68 g/mol. It is practically insoluble in water (<10 µg/mL).
History
Efavirenz was approved by the FDA on September 21, 1998, making it the 14th approved antiretroviral drug.
Society and culture
Pricing information
A one-month supply of 600 mg tablets cost approximately $550 in April 2008.[16] Merck provides efavirenz in certain developing countries at cost, currently about $0.65 per day.[17] Some emerging countries have opted to purchase Indian generics[18] such as Efavir by Cipla Ltd.[19] In Thailand, one month supply of efavirenz + truvada, as of June 2012, costs THB 2900 ($90), there’s also a social program for poorer patients who can’t afford even this price. In South Africa, a license has been granted to generics giant Aspen Pharmacare to manufacture, and distribute to Sub-Saharan Africa, a cost-effective antiretroviral drug.[20]
PATENT
http://www.google.com/patents/WO1999061026A1?cl=en
EXAMPLE 1
Cl
1a
To a solution of trifluoroethanol and (IR, 2S)-N-pyrrolidinyl norephedrine in THF (9 L) under nitrogen is added a solution of diethylzinc in hexane at 0 °C slowly enough to keep the temperature below 30 °C. The mixture is stirred at room temperature for 0.5 ~ 1 h. In another dry flask a solution of chloromagnesium cyclopropyl acetylide is prepared as follows: To neat cyclopropyl acetylene at 0 °C is added a solution of rc-butylmagnesium chloride slowly enough to keep the internal temperature < 30 °C. The solution is stirred at 0 °C for ~ 40 min and transfered to the zinc reagent via cannula with 0.36 L of THF as a wash. The mixture is cooled to -10 °C and ketoaniline la is added. The mixture is stirred at -2 to -8 °C for 35 h, warmed to room temperature, stirred for 3 h, and quenched with 30% potassium carbonate over 1.5 h. The mixture is stirred for 4 h and the solid is removed by filtration and washed with THF (2 cake volume). The wet solid still contains -18 wt% of pyrrolidinyl norephedrine and is saved for further study. The filtrate and wash are combined and treated with 30% citric acid. The two layers are separated. The organic layer is washed with water (1.5 L). The combined aqueous layers are extracted with 2.5 L of toluene and saved for norephedrine recovery. The toluene extract is combined with the organic solution and is concentrated to ~ 2.5 L. Toluene is continuously feeded and distilled till THF is not detectable by GC. The final volume is controlled at 3.9 L. Heptane (5.2 L) is added over 1 h. The slurry is cooled to 0 °C, aged for 1 h, and filtered. The solid is washed with heptane (2 cake volume) and dried to give 1.234 Kg (95.2% yield) of amino alcohol 3 as a white crystalline. The material is 99.8 A% pure and 99.3% ee.
EXAMPLE 2
To a three necked round bottom flask, equipped with a mechanical stirrer, nitrogen line, and thermocouple, was charged the solid amino alcohol 3, MTBE (500 L), and aqueous KHCO3 (45 g in 654 mL H2O). Solid 4-nitrophenyl chloroformate was added, in 4 batches, at 25°C. During the addition the solution pH was monitored. The pH was maintained between 8.5 and 4 during the reaction and ended up at 8.0. The mixture was stirred at 20-25°C for two hours. Aqueous KOH (2N) was added over 20 minutes, until the pH of the aqueous layer reached 11.0.
The layers were separated and 500 mL brine was added to the MTBE layer. 0.1 N Acetic acid was added until the pH was 6-7. The layers were separated and the organic phase was washed with brine (500 mL). At this point the mixture was solvent switched to EtOH/IPA and crystallized as recited in Examples 5 and 6.
EXAMPLE 3
To a three necked round bottom flask, equipped with a mechanical stirrer, nitrogen line, and thermocouple, was charged the solid amino alcohol 3a, toulene (500 mL), and aqueous KHCO3 (86.5 g in 500 L H2O). Phosgene solution in toulene was added at 25°C, and the mixture was stirred at 20-25°C for two hours.
The layers were separated and the organic phase was washed with brine (500 mL). At this point the mixture was solvent switched to EtOH/IPA and crystallized as recited in Examples 5 and 6.
EXAMPLE 4
To a three necked round bottom flask, equipped with a mechanical stirrer, nitrogen line, and thermocouple, was charged the solid amino alcohol 3a, MTBE (500 mL), and aqueous KHCO3 (86.5 g in 500 mL H2O). Phosgene gas was slowly passed into the solution at 25°C, until the reaction was complete.
The layers were separated and the organic phase was washed with brine (500 mL). At this point the mixture was solvent switched to EtOH/IPA and crystallized as recited in Examples 5 and 6.
EXAMPLE 5
Crystallization of efavirenz from 30% 2-Propanol in Water using a ratio of 15 ml solvent per gram efavirenz Using Controlled Anti-Solvent Addition on a 400 g Scale.
400 g. of efavirenz starting material is dissolved in 1.8 L of 2- propanol. The solution is filtered to remove extraneous matter. 1.95 L of deionized (DI) water is added to the solution over 30 to 60 minutes. 10 g. to 20 g. of efavirenz seed (Form II wetcake) is added to the solution. The seed bed is aged for 1 hour. The use of Intermig agitators is preferred to mix the slurry. If required (by the presence of extremely long crystals or a thick slurry), the slurry is wet-milled for 15 – 60 seconds. 2.25 L of DI water is added to the slurry over 4 to 6 hours. If required (by the presence of extremely long crystals or a thick slurry), the slurry is wet- milled for 15 – 60 seconds during the addition. The slurry is aged for 2 to 16 hours until the product concentration in the supernatant remains constant. The slurry is filtered to isolate a crystalline wet cake. The wet cake is washed with 1 to 2 bed volumes of 30 % 2-propanol in water and then twice with 1 bed volume of DI water each. The washed wet cake is dried under vacuum at 50°C.
EXAMPLE 6
Crystallization of efavirenz from 30% 2-Propanol in Water using a ratio of 15 ml solvent per gram efavirenz Using a Semi-Continuous Process on a 400 g Scale.
400 g. of efavirenz starting material is dissolved in 1.8 L of 2- propanol. A heel slurry is produced by mixing 20 g. of Form II efavirenz in 0.3 L of 30 % (v/v) 2-propanol in water or retaining part of a slurry froma previous crystallization in the crystallizer. The dissolved batch and 4.2 L of DI water are simultaneously charged to the heel slurry at constant rates over 6 hours to maintain a constant solvent composition in the crystallizer. Use of Intermig agitators during the crystallization is preferred. During this addition the slurry is wet-milled when the crystal lengths become excessively long or the slurry becomes too thick. The slurry is aged for 2 to 16 hours until the product concentration in the supernatant remains constant. The slurry is filtered to isolate a crystalline wet cake. The wet cake is washed with 1 to 2 bed volumes of 30 % 2-propanol in water and then twice with 1 bed volume of DI water each. The washed wet cake is dried under vacuum at 50°C.
EXAMPLE 7 Preparation of Amino Alcohol 3 and ee Upgrading— Through Process
1a
A solution of diethyl zinc in hexane was added to a solution of trifluoroethanol (429.5 g, 4.29’mol) and (IR, 2S)-N-pyrrolidinyl norephedrine (1.35 kg, 6.58 mol) in THF (9 L), under nitrogen, at 0 °C. The resulting mixture was stirred at room temperature for approx. 30 min. In another dry flask a solution of chloromagnesium- cyclopropylacetylide was prepared as follows. To a solution of n- butylmagnesium chloride in THF (2 M, 2.68 L, 5.37 mol) was added neat cyclopropylacetylene at 0 °C keeping the temperature < 25 °C. The solution was stirred at 0 °C for 1 ~ 2 h. The solution of chloromagnesiumcyclopropylacetylide was then warmed to room temperature and was transferred into the zinc reagent via cannula over 5 min followed by vessel rinse with 0.36 L of THF. The resulting mixture was aged at ~ 30 °C for 0.5 h and was then cooled to 20 °C. The ketoaniline 1 (1.00 kg, 4.47 mol) was added in one portion as a solid, and the resulting mixture was stirred at 20-28 °C for 3 h.
The reaction was quenched with 30% aq. potassium carbonate (1.2 L) and aged for 1 h. The solid waste was filtered and the cake was washed with THF (3 cake volumes). The filtrate and wash were combined and solvent switched to IP Ac.
The IPAc solution of product 3 and pyrrolidinyl norephedrine was washed with citric acid (3.5 L) and with water (1.5 L). The combined aqueous layers were extracted with IPAc (2 L) and saved for norephedrine recovery. To the combined organic layers was added
12N HC1 (405 mL, 4.88 mol), to form a thin slurry of the amino alcohol-
HC1 salt. The mixture was aged for 30 min at 25 °C and was then dried azeotropically. The slurry was aged at 25 °C for 30 min and filtered. The cake was washed with 2.5 L of IPAc and dried at 25 °C under vacuum/nitrogen for 24 h to give 1.76 kg of the wet HC1 salt.
The salt was dissolved in a mixture of MTBE (6 L) and aq Na2Cθ3 (1.18 kg in 6.25 L water). The layers were separated and the organic layer was washed with 1.25 L of water. The organic layer was then solvent switched into toluene.
Heptane (5 L) was added over 1 h at 25 °C. The slurry was cooled to 0 °C, aged for 1 h, and filtered. The solid was washed with heptane (2 cake volumes) and was dried to give 1.166 kg (90% overall yield) of amino alcohol 3 as a white crystalline solid. Norephedrine recovery
The aqueous solution was basified to pH13 using 50% aq NaOH, and extracted with heptane (2 L). The heptane solution was washed with water (1 L) and concentrated to remove residual IPAc and water. The final volume was adjusted to about 3 L. The heptane solution was cooled to -20 °C, aged for 2 h, and filtered. The solid was washed with cold heptane (1 cake volume) and dried to give 1.269 kg solid (94% recovery)




CLIPS
http://www.mdpi.com/1420-3049/21/2/221/htm



| WO2007013047A2 * | Jul 31, 2006 | Feb 1, 2007 | Ranbaxy Lab Ltd | Water-dispersible anti-retroviral pharmaceutical compositions |
| WO2007013047A3 * | Jul 31, 2006 | May 31, 2007 | Ranbaxy Lab Ltd | Water-dispersible anti-retroviral pharmaceutical compositions |
| WO2007052289A2 * | Jul 24, 2006 | May 10, 2007 | Rubicon Res Pvt Ltd | Novel dispersible tablet composition |
| WO2007052289A3 * | Jul 24, 2006 | Dec 27, 2007 | Rubicon Res Pvt Ltd | Novel dispersible tablet composition |
| WO2011131943A2 | Apr 20, 2011 | Oct 27, 2011 | Cipla Limited | Pharmaceutical compositions |
| WO2012048884A1 | Oct 14, 2011 | Apr 19, 2012 | Lonza Ltd | Process for the synthesis of cyclic carbamates |
| WO2012048886A1 | Oct 14, 2011 | Apr 19, 2012 | Lonza Ltd | Process for the synthesis of cyclic carbamates |
| WO2015059466A1 | Oct 22, 2014 | Apr 30, 2015 | Cipla Limited | Pharmaceutical compositions comprising efavirenz |
| EP1448170A2 * | Nov 26, 2002 | Aug 25, 2004 | Bristol-Myers Squibb Company | Efavirenz tablet formulation having unique biopharmaceutical characteristics |
| EP2441759A1 | Oct 14, 2010 | Apr 18, 2012 | Lonza Ltd. | Process for the synthesis of cyclic carbamates |
| EP2447255A1 | Oct 14, 2010 | May 2, 2012 | Lonza Ltd. | Process for the synthesis of cyclic carbamates |
| US6238695 | Apr 6, 1999 | May 29, 2001 | Dupont Pharmaceuticals Company | Formulation of fast-dissolving efavirenz capsules or tablets using super-disintegrants |
| US6555133 | Apr 2, 2001 | Apr 29, 2003 | Bristol-Myers Squibb Company | Formulation of fast-dissolving efavirenz capsules or tablets using super-disintegrants |
| US8871271 | Jul 29, 2013 | Oct 28, 2014 | Gilead Sciences, Inc. | Method and composition for pharmaceutical product |
| US8957204 | Oct 14, 2011 | Feb 17, 2015 | Lonza Ltd. | Process for the synthesis of cyclic carbamates |
| US8969550 | Oct 14, 2011 | Mar 3, 2015 | Lonza Ltd. | Process for the synthesis of cyclic carbamates |
| US9018192 | Oct 10, 2013 | Apr 28, 2015 | Bristol-Myers Squibb & Gilead Sciences, Inc. | Unitary pharmaceutical dosage form |
| US9198862 | Jul 24, 2006 | Dec 1, 2015 | Rubicon Research Private Limited | Dispersible tablet composition |
| WO1995020389A1 * | Jan 24, 1995 | Aug 3, 1995 | Merck & Co Inc | Benzoxazinones as inhibitors of hiv reverse transcriptase |
| WO1996037457A1 * | May 21, 1996 | Nov 28, 1996 | Merck & Co Inc | Asymmetric synthesis of (-) 6-chloro-4-cyclopropyl-ethynyl-4-trifluoromethyl-1,4-dihydro-2h-3,1-benzoxazin-2-one |
| WO1998052570A1 * | May 14, 1998 | Nov 26, 1998 | David Walter Barry | Antiviral combinations containing the carbocyclic nucleoside 1592u89 |
References
- 1 “Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents”. Retrieved 10 May 2013.
- 2
- “WHO Model List of EssentialMedicines” (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- 3
- Hamilton, Richart (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. p. 62. ISBN 9781284057560.
- 4
- Cespedes, MS; Aberg, JA (2006). “Neuropsychiatric complications of antiretroviral therapy.”. Drug safety : an international journal of medical toxicology and drug experience 29 (10): 865–74. doi:10.2165/00002018-200629100-00004. PMID 16970510.
- 5
- “www.accessdata.fda.gov” (PDF).
- 6
- DHHS panel. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents (October 10, 2006). (Available for download from AIDSInfo)
- 7
- Ford, N.; Mofenson, L.; Kranzer, K.; Medu, L.; Frigati, L.; Mills, E. J.; Calmy, A. (2010). “Safety of efavirenz in first-trimester of pregnancy: A systematic review and meta-analysis of outcomes from observational cohorts”. AIDS 24 (10): 1461–1470. doi:10.1097/QAD.0b013e32833a2a14. PMID 20479637.
- 8
- Rossi, S; Yaksh, T; Bentley, H; Van Den Brande, G; Grant, I; Ellis, R (2006). “Characterization of interference with 6 commercial delta9-tetrahydrocannabinol immunoassays by efavirenz (glucuronide) in urine”. Clinical Chemistry 52 (5): 896–7. doi:10.1373/clinchem.2006.067058. PMID 16638958.
- 9
- Röder, CS; Heinrich, T; Gehrig, AK; Mikus, G (2007). “Misleading results of screening for illicit drugs during efavirenz treatment”. AIDS (London, England) 21 (10): 1390–1. doi:10.1097/QAD.0b013e32814e6b3e. PMID 17545727.
- 10
- Ren J, Bird LE, Chamberlain PP; et al. (2002). “Structure of HIV-2 reverse transcriptase at 2.35-A resolution and the mechanism of resistance to non-nucleoside inhibitors”. Proc Natl Acad Sci USA 99 (22): 14410–15. doi:10.1073/pnas.222366699. PMC 137897. PMID 12386343.
- 11
- Sustiva (efavirenz) capsules and tablets. Product information (April 2005)
- 12
- Simen AA, Ma J, Svetnik V, Mayleben D, Maynard J, Roth A, Mixson L, Mogg R, Shera D, George L, Mast TC, Beals C, Stoch A, Struyk A, Shire N, Fraser I (2014). “Efavirenz modulation of sleep spindles and sleep spectral profile”. J Sleep Res 24: 66–73. doi:10.1111/jsr.12196. PMID 25113527.
- 13
- Gatch MB, Kozlenkov A, Huang RQ, Yang W, Nguyen JD, González-Maeso J, Rice KC, France CP, Dillon GH, Forster MJ, Schetz JA (2013). “The HIV antiretroviral drug efavirenz has LSD-like properties”. Neuropsychopharmacology 38 (12): 2373–84. doi:10.1038/npp.2013.135. PMC 3799056. PMID 23702798.
- 14
- Dabaghzadeh F, Ghaeli P, Khalili H, Alimadadi A, Jafari S, Akhondzadeh S, Khazaeipour Z (2013). “Cyproheptadine for prevention of neuropsychiatric adverse effects of efavirenz: a randomized clinical trial”. AIDS Patient Care STDS 27 (3): 146–54. doi:10.1089/apc.2012.0410. PMID 23442031.
- 15
- Dabaghzadeh F, Khalili H, Ghaeli P, Dashti-Khavidaki S (2012). “Potential benefits of cyproheptadine in HIV-positive patients under treatment with antiretroviral drugs including efavirenz”. Expert Opin Pharmacother 13 (18): 2613–24. doi:10.1517/14656566.2012.742887. PMID 23140169.
- 16
- Price listed on http://drugstore.com website, 4/20/2008
- 17
- “Merck & Co., Inc., Again Reduces Price of Stocrin (efavirenz) for Patients in Least Developed Countries and Countries Hardest Hit by Epidemic – Drugs.com MedNews”.
- 18
- IndiaDaily – A new trend in emerging nations – Brazil opts for Indian generic drug ignoring US pharmaceutical giant Merck’s patent on AIDS drug Efavirenz
- 19
- http://www.cipla.com
- 20
- Patrick Lumumba Osewe; Yvonne Korkoi Nkrumah; Emmanuel K. Sackey (15 June 2008). Improving Access to HIV/AIDS Medicines in Africa: Trade-Related Aspects of Intellectual Property Rights (TRIPS) Flexibilities Utilization. World Bank Publications. pp. 35–39. ISBN 978-0-8213-7544-0. Retrieved 30 June 2012.
- 21
- http://www.sustiva.com/
- 22
- http://www.medsafe.govt.nz/consumers/cmi/s/stocrin.pdf
- 23
- Drugsupdate.com generic brands list: http://www.drugsupdate.com/brand/generic/Efavirenz/87
- 24
- http://mcneilargusindia.com/
- 25
- http://www.alkemlabs.com/
- 26
- “Regast® (efavirenz) film-coated tablets.”. http://www.pharmasyntez.com (in Russian). Pharmasyntez, 2011. Retrieved 28 June 2015. External link in
|website=(help) - 27
- IOL: Thugs get high on stolen Aids drugs IOL News May 12, 2007
- 28
- Getting high on HIV drugs in S Africa. BBC News, 8 December 2008.
- 29
- ‘No Turning Back’: Teens Abuse HIV Drugs. ABC News, April 6, 2009.
- 30
- Getting High On HIV Medication Vice 7.04.2014.
- 31
- Gatch, M. B.; Kozlenkov, A.; Huang, R. Q.; Yang, W.; Nguyen, J. D.; González-Maeso, J.; Rice, K. C.; France, C. P.; Dillon, G. H.; Forster, M. J.; Schetz, J. A. (2013). “The HIV Antiretroviral Drug Efavirenz has LSD-Like Properties”. Neuropsychopharmacology 38 (12): 2373–84. doi:10.1038/npp.2013.135. PMC 3799056. PMID 23702798.
- Sütterlin, S.; Vögele, C.; Gauggel, S. (2010). “Neuropsychiatric complications of Efavirenz therapy: suggestions for a new research paradigm”. The Journal of Neuropsychiatry and Clinical Neurosciences 22 (4): 361–369. doi:10.1176/jnp.2010.22.4.361.
External links

|
|
 |
|
| Systematic (IUPAC) name | |
|---|---|
|
(4S)-6-chloro-4-(2-cyclopropylethynyl)-4-(trifluoromethyl)-2,4-dihydro-1H-3,1-benzoxazin-2-one
|
|
| Clinical data | |
| Trade names | Sustiva, Stocrin, others |
| AHFS/Drugs.com | monograph |
| MedlinePlus | a699004 |
| Pregnancy category |
|
| Routes of administration |
By mouth (capsules, tablets) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 40–45% (under fasting conditions) |
| Protein binding | 99.5–99.75% |
| Metabolism | Hepatic (CYP2A6 and CYP2B6-mediated) |
| Onset of action | 3–5 hours |
| Biological half-life | 40–55 hours |
| Excretion | Urine (14–34%) and feces (16–61%) |
| Identifiers | |
| CAS Number | 154598-52-4 |
| ATC code | J05AG03 (WHO) |
| PubChem | CID 64139 |
| DrugBank | DB00625 |
| ChemSpider | 57715 |
| UNII | JE6H2O27P8 |
| KEGG | D00896 |
| ChEBI | CHEBI:119486 |
| ChEMBL | CHEMBL223228 |
| NIAID ChemDB | 032934 |
| PDB ligand ID | EFZ (PDBe, RCSB PDB) |
| Chemical data | |
| Formula | C14H9ClF3NO2 |
| Molar mass | 315.675 g/mol |

Glaxo, Theravance Asthma Drug Elvar Ellipta OK’d in Japan
umeclidinium
vilanterol
ELVAR™ ELLIPTA™ Gains Approval in Japan for the Treatment of Asthma
LONDON, UNITED KINGDOM and SOUTH SAN FRANCISCO, CA–(Marketwired – Sep 20, 2013) – GlaxoSmithKline plc (LSE: GSK) (NYSE: GSK) and Theravance, Inc. (NASDAQ: THRX) today announced that the Japanese Ministry of Health, Labour and Welfare (MHLW) has approved RELVAR™ ELLIPTA™ for the treatment of bronchial asthma (in cases where concurrent use of inhaled corticosteroid and long-acting inhaled beta2 agonist is required). Relvar Ellipta is not indicated for the treatment of chronic obstructive pulmonary disease (COPD) in Japan.
Relvar is a combination of the inhaled corticosteroid (ICS), fluticasone furoate “FF”, and the long-acting beta2 agonist (LABA), vilanterol “VI”. The MHLW has approved two doses of FF/VI – 100/25 mcg and 200/25 mcg. Both strengths will be administered once-daily using the Ellipta, a new dry powder inhaler (DPI).
Anoro Ellipta is the proposed proprietary name for UMEC/VI, a combination of two investigational bronchodilator molecules — GSK573719 or umeclidinium bromide (UMEC), a long-acting muscarinic antagonist (LAMA) and vilanterol (VI), a long-acting beta2 agonist (LABA), administered using the Ellipta inhaler.
The FDA Advisory Committee also voted that the safety of the investigational medicine has been adequately demonstrated at the 62.5/25mcg dose for the proposed indication (10 yes, 3 no), and the efficacy data provided substantial evidence of a clinically meaningful benefit for UMEC/VI 62.5/25mcg once daily for the long-term, maintenance treatment of airflow obstruction in COPD (13 yes, 0 no).
Patrick Vallance, GSK’s President of Pharmaceuticals R&D, said: “Today’s recommendation is good news and a reflection of our commitment to giving an alternative treatment option for patients living with COPD — a disease that affects millions of Americans. If approved, Anoro Ellipta will be the first, once-daily dual bronchodilator available in the US, marking another significant milestone for GSK’s portfolio of medicines to treat respiratory disease. We will continue to work with the FDA as they complete their review.”
“We are pleased with the Advisory Committee’s support of UMEC/VI,” said Rick E Winningham, Chief Executive Officer of Theravance. “This is a transformative year for Theravance and today’s positive recommendation brings the second major respiratory medicine in our GSK collaboration closer to approval and becoming an important therapeutic option for COPD patients.”
In December 2012, a New Drug Application (NDA) was submitted to the FDA for the use of UMEC/VI administered by the Ellipta™ inhaler for the long-term once-daily maintenance bronchodilator treatment of airflow obstruction in patients with COPD, including chronic bronchitis and/or emphysema. UMEC/VI is not proposed for the relief of acute bronchospasm or for the treatment of asthma in any of the regulatory applications.
The FDA Advisory Committee provides non-binding recommendations for consideration by the FDA, with the final decision on approval made by the FDA. The Prescription Drug User Fee Act (PDUFA) goal date for UMEC/VI is 18 December 2013.
UMEC/VI is an investigational medicine and is not currently approved anywhere in the world.
Safety Information
Across the four pivotal COPD studies for UMEC/VI, the most frequently reported adverse events across all treatment arms, including placebo, were headache, nasopharyngitis, cough, upper respiratory tract infection, and back pain. COPD exacerbation was the most common serious adverse event reported. In addition, in the four pivotal COPD studies, a small imbalance was observed in cardiac ischemia which was not observed in the long term safety study.
The UMEC/VI clinical development programme involved over 6,000 COPD patients.
About COPD
Chronic obstructive pulmonary disease (COPD) is a term referring to two lung diseases, chronic bronchitis and emphysema, that are characterized by obstruction to airflow that interferes with normal breathing. COPD is the third most common cause of death in the US and The National Heart, Lung and Blood Institute (NHLBI) estimates that nearly 15 million US adults have COPD and another 12 million are undiagnosed or developing COPD(1).
According to the NHLI, long-term exposure to lung irritants that damage the lungs and the airways are usually the cause of COPD and in the United States, the most common irritant that causes COPD is cigarette smoke. Breathing in second hand smoke, air pollution, or chemical fumes or dust from the environment or workplace also can contribute to COPD. Most people who have COPD are at least 40 years old when symptoms begin.
EMA approves biosimilar Somatropin from Biopartners Gmbh
![OMNITROPE® (somatropin [rDNA origin] injection) Structural Formula Illustration](https://i0.wp.com/images.rxlist.com/images/rxlist/omnitrope1.gif)
SOMATROPIN
The European Medicine agency has approved a biosimilar somatropin from Biopartners GMBH. Somatropin biopartner would be the third biosimilar version of somatropin the European market. Other players selling somatropin inlcude Sandoz and Roche. Sandoz sells under the brand Omnitrope, while Roche which is the innovator of somatropin sells it under the brand name NutropinAq.
READ AT
DETAILS OF OMNITROPE
Omnitrope® (somatropin-[rDNA] origin) is a polypeptide hormone of recombinant DNA origin. It has 191 amino acid residues and a molecular weight of 22,125 daltons. The amino acid sequence of the product is identical to that of human growth hormone of pituitary origin (somatropin). Omnitrope® is synthesized in a strain of. Escherichia coli that has been modified by the addition of the gene for human growth hormone. Omnitrope® Cartridge is a clear, colorless, sterile solution for subcutaneous injection. Omnitrope® for Injection is a lyophilized powder that is reconstituted for subcutaneous injection.
Figure 1: Schematic amino acid sequence of human growth hormone including the disulfide bonds
![OMNITROPE® (somatropin [rDNA origin] injection) Structural Formula Illustration](https://i0.wp.com/images.rxlist.com/images/rxlist/omnitrope1.gif) |
Each Omnitrope® Cartridge or vial contains the following (see Table 4):
Table 4. Contents of Omnitrope® Cartridges and Vial
| Product | Cartridge 5 mg/1.5 mL | Cartridge 10 mg/1.5 mL | For Injection 5.8 mg/vial |
| Component | |||
| Somatropin | 5 mg | 10 mg | 5.8 mg |
| Disodium hydrogen phosphate heptahydrate | 1.3 mg | 1.70 mg | 2.09 mg |
| Sodium dihydrogen phosphate dihydrate | 1.6 mg | 1.35 mg | 0.56 mg |
| Poloxamer 188 | 3.0 mg | 3.0 mg | – |
| Mannitol | 52.5 mg | – | – |
| Glycine | – | 27.75 mg | 27.6 mg |
| Benzyl alcohol | 13.5 mg | – | – |
| Phenol | – | 4.50 mg | – |
| Water for Injection | to make 1.5 mL | to make 1.5 mL | – |
| Diluent (vials only) | Bacteriostatic Water for Injection | ||
| Water for injection | to make 1.14 mL | ||
| Benzyl alcohol | 17 mg | ||
Genzyme’s multiple sclerosis treatment approved by European Commission

Alemtuzumab
Sanofi and its subsidiary Genzyme have been given marketing approval by the European Commission for Lemtrada (alemtuzumab), a treatment for multiple sclerosis. read all at
click on title below
Genzyme’s multiple sclerosis treatment approved by European Commission
Generic versions of high cholesterol drug Lovaza can be developed, rules judge
LOVAZA, a lipid-regulating agent, is supplied as a liquid-filled gel capsule for oral administration. Each 1-gram capsule of LOVAZA (omega-3-acid ethyl esters) contains at least 900 mg of the ethyl esters of omega-3 fatty acids. These are predominantly a combination of ethyl esters of eicosapentaenoic acid (EPA – approximately 465 mg) and docosahexaenoic acid (DHA – approximately 375 mg).
The structural formula of EPA ethyl ester is:

The empirical formula of EPA ethyl ester is C22H34O2, and the molecular weight of EPA ethyl ester is 330.51.
The structural formula of DHA ethyl ester is:

The empirical formula of DHA ethyl ester is C24H36O2, and the molecular weight of DHA ethyl ester is 356.55.
LOVAZA capsules also contain the following inactive ingredients: 4 mg α-tocopherol (in a carrier of partially hydrogenated vegetable oils including soybean oil), and gelatin, glycerol, and purified water (components of the capsule shell).
Lovaza
A US appeals court ruled on this week that drug companies can develop generic versions of fish oil-derived, high-cholesterol drug Lovaza.
read all at

Lovaza is a brand name prescription drug. The capsule sold by GlaxoSmithKline but developed by Reliant Pharmaceuticals, contains esterified fish oils and is approved by the U.S. Food and Drug Administration to lower very high triglyceride levels. It is metabolized intoOmega-3 fatty acids. It is a dietary supplement that has been purified, chemically altered, branded, and been put through the approval process of the U.S. Food and Drug Administration (FDA); in these respects it is considered a pharmaceutical. Due to the esterification process during manufacturing there is no risk of contamination[citation needed] by methyl mercury, arsenic,[1] or other pollutants that are often seen in the world’s oceans. Each 1-gram capsule is 38% DHA, 47% EPA, and 17% other fish oils in the form of the ethyl ester.
Lovaza is named Omacor in Europe (and this name was once used in the US).[2]
Effectiveness
Lovaza is approved in the U.S. for treatment of patients with very high triglycerides (hypertriglyceridemia).[3]
In the European markets and other major markets outside the US Lovaza is known as Omacor, and is indicated for:
- Hypertriglyceridemia. Used as monotherapy, or in combination with a statin for patients with mixed dyslipidemia.
- Secondary prevention after myocardial infarction (heart attack)
in addition to other standard therapy (e.g. statins, antiplatelets medicinal products, beta-blockers, and ACE-I).
Lovaza has been demonstrated to reduce triglycerides in patients with high or very high triglycerides. [3]
Lovaza has also been demonstrated to reduce VLDL-cholesterol and non-HDL-cholesterol, and increase HDL-cholesterol. But, it can raise LDL-cholesterol up to 45%.[4] The LDL raising activity correlates with a reduction in ApoB levels, though. Lovaza, through the stimulation of Lipoprotein Lipase, seems to stimulate the production of less atherogenic LDL species. In some patients, it can elevatealanine transaminase levels, so liver enzymes should be checked, periodically.[4]
Effects on significant patient outcomes such as acute myocardial infarction, stroke, cardiovascular and all-cause mortality have been studied in patients who have suffered a myocardial infarction (this is in the US; however, data from GISSI-P showed a combined end-point of all-cause death, non-fatal MI, and non-fatal stroke was significantly reduced by 15%). Lovaza has not been shown to lower the rates of all cause mortality and cardiovascular mortality, or the combination of mortality and non-fatal cardiovascular events.[3]
GlaxoSmithKline‘s patent expired in September 2012. Generic versions may be made available at that time. Other DHA/EPA products containing similar amounts of Omega-3 fatty acids are currently sold over the counter in the United States as dietary supplements.
Competitors
In July 2012, Amarin Corporation received U.S. FDA marketing approval for Vascepa, also referred to as AMR-101.[5] Vascepa will undoubtedly become a major competitor for Lovaza.[6] In clinicial trials, Vascepa was shown to lower triglycerides; while Lovaza also lowers the triglyceride concentration, Vascepa also lowers LDL-C; Lovaza does not. Lovaza was approved to treat people with very high triglyceride levels (>500 mg/dl), Vascepa is also approved for this market; however the company has also demonstrated that the drug can impact levels in people with high triglyceride (> 200 mg/dl and < 500 mg/dl) levels and will file an sNDA for this indication late in 2012.[7]
In 2011, Ariix started selling an almost identical FDA-Certified Omega3 Ethyl Ester 1000 mg capsule ‘OmegaQ’ fish oil through direct marketing and online auto-ship at a discounted price, creating another major competitor for Lovaza and Amarin’s Vascepa. One capsule contains 295 mg EPA, and 235 mg DHA, but it is unique in that it is combined with 20 mg of the coenzyme CoQ-10, with reported ‘anti-aging’ effects on the cell’s telomeres, which are still under study.
Forms of Lovaza
Lovaza is available as 1-gram soft-gelatin capsules.[8]
Active Ingredient: Omega-3-acid ethyl esters
Inactive Ingredients: Gelatin, glycerol, purified water, alpha-tocopherol (in soybean oil)
References
- NIFES (Nasjonalt institutt for ernærings- og sjømatforskning – Norwegian National Institute for Nutrition and Seafood Research)
- University of Utah Pharmacy Services (August 15, 2007) “Omega-3-acid Ethyl Esters Brand Name Changed from Omacor to Lovaza”
- GSK Information for Medical Professionals
- Pharmacy & Therapeutics (May, 2008) “Omega-3-acid Ethyl Esters (Lovaza) For Severe Hypertriglyceridemia”
- “Amarin Prescription Fish-Oil Pill Approved – TheStreet”. Retrieved 26 July 2012.
- “http://www.reuters.com/article/2012/07/26/us-amarin-fda-vascepa-idUSBRE86P1SX20120726”. Reuters. 26 July 2012. Retrieved 27 July 2012.
- “Amarin’s AMR101 Phase 3 ANCHOR Trial Meets all Primary and Secondary Endpoints with Statistically Significant Reductions in Triglycerides at Both 4 Gram and 2 Gram Doses and Statistically Significant Decrease in LDL-C (NASDAQ:AMRN)”. Amarin. 18 April 2011. Retrieved 26 July 2012.
- http://www.rxwiki.com/lovaza
External links
The first generic version of the oral chemotherapy drug Xeloda (capecitabine) has been approved by the U.S. Food and Drug Administration to treat cancers of the colon/rectum or breast,
capecitabine
- R-340, Ro-09-1978, Xeloda
pentyl [1-(3,4-dihydroxy-5-methyltetrahydrofuran-2-yl)-5-fluoro-2-oxo-1H-pyrimidin-4-yl]carbamate

MONDAY Sept. 16, 2013 — The first generic version of the oral chemotherapy drug Xeloda (capecitabine) has been approved by the U.S. Food and Drug Administration to treat cancers of the colon/rectum or breast, the agency said Monday in a news release.
This year, an estimated 142,820 people will be diagnosed with cancer of the colon/rectum, and 50,830 are predicted to die from the disease, the FDA said, citing the U.S. National Cancer Institute. An estimated 232,340 women will be diagnosed with cancer of the breast this year, and some 39,620 will die from it.
The most common side effects of the drug are diarrhea, vomiting; pain, redness, swelling or sores in the mouth; fever and infection, the FDA said.
The agency stressed that approved generics have the same high quality and strength as their brand-name counterparts.
License to produce the generic drug was given to Israel-based Teva Pharmaceuticals. The brand name drug is produced by the Swiss pharma firm Roche.
Capecitabine (INN) /keɪpˈsaɪtəbiːn/ (Xeloda, Roche) is an orally-administered chemotherapeutic agent used in the treatment of metastatic breast and colorectal cancers. Capecitabine is a prodrug, that is enzymatically converted to 5-fluorouracil in the tumor, where it inhibits DNA synthesis and slows growth of tumor tissue. The activation of capecitabine follows a pathway with three enzymatic steps and two intermediary metabolites, 5′-deoxy-5-fluorocytidine (5′-DFCR) and 5′-deoxy-5-fluorouridine (5′-DFUR), to form 5-fluorouracil

Indications
Capecitabine is FDA-approved for:
- Adjuvant in colorectal cancer Stage III Dukes’ C – used as first-line monotherapy.
- Metastatic colorectal cancer – used as first-line monotherapy, if appropriate.
- Metastatic breast cancer – used in combination with docetaxel, after failure of anthracycline-based treatment. Also as monotherapy, if the patient has failed paclitaxel-based treatment, and if anthracycline-based treatment has either failed or cannot be continued for other reasons (i.e., the patient has already received the maximum lifetime dose of an anthracycline).
In the UK, capecitabine is approved by the National Institute for Health and Clinical Excellence (NICE) for colon and colorectal cancer, and locally advanced or metastatic breast cancer.[1] On March 29, 2007, the European Commission approved Capecitabine, in combination with platinum-based therapy (with or without epirubicin), for the first-line treatment of advanced stomach cancer.
Capecitabine is a cancer chemotherapeutic agent that interferes with the growth of cancer cells and slows their distribution in the body. Capecitabine is used to treat breast cancer and colon or rectum cancer that has spread to other parts of the body.
Formulation
Capecitabine (as brand-name Xeloda) is available in light peach 150 mg tablets and peach 500 mg tablets.
- Lacy, Charles F; Armstrong, Lora L; Goldman, Morton P; Lance, Leonard L (2004). Lexi-Comp’s Drug Information Handbook (12th Edition). Lexi-Comp Inc. ISBN 1-59195-083-X
- Fischer, David S; Knobf, M Tish; Durivage, Henry J; Beaulieu, Nancy J (2003). The Cancer Chemotherapy Handbook (6th Edition). Mosby. ISBN 0-323-01890-4
- Thomson Centerwatch: Drugs Approved by the FDA (Xeloda) Retrieved 6/05
- Mercier C, Ciccolini J (2007). “Severe or lethal toxicities upon capecitabine intake: is DPYD genetic polymorphism the ideal culprit?”. Trends in pharmacological sciences 28 (12): 597–598. doi:10.1016/j.tips.2007.09.009. PMID 18001850.
- “Subtopics”. Nice.org.uk. Retrieved 2012-08-15.
- Fingerprints May Vanish With Cancer Drug – US News and World Report
- Cancer Drug Erases Man’s Fingerprints – CNN
- “Stritch School of Medicine”. Stritch.luc.edu. Retrieved 2012-08-15.
- Xeloda.com (patient information, tools, and resources)
- OralChemo Advisor (patient information)

Capecitabine is an orally-administered anticancer agent widely used in the treatment of metastatic breast and colorectal cancers. Capecitabine is a ribofuranose-based nucleoside, and has the sterochemical structure of a ribofuranose having an β-oriented 5-fluorocytosine moiety at C-I position.
US Patent Nos. 5,472,949 and 5,453,497 disclose a method for preparing capecitabine by glycosylating tri-O-acetyl-5-deoxy-β-D-ribofuranose of formula I using 5-fluorocytosine to obtain cytidine of formula II; and carbamoylating and hydrolyzing the resulting compound, as shown in Reaction Scheme 1 :
Reaction Scheme 1
1
The compound of formula I employed as an intermediate in Reaction
Scheme 1 is the isomer having a β-oriented acetyl group at the 1 -position, for the reason that 5-fluorocytosine is more reactive toward the β-isomer than the α-isomer in the glycosylation reaction due to the occurrence of a significant neighboring group participation effect which takes place when the protecting group of the 2-hydroxy group is acyl.
Accordingly, β-oriented tri-O-acetyl-5-deoxy-β-D-ribofuranose (formula
I) has been regarded in the conventional art to the essential intermediate for the preparation of capecitabine. However, such a reaction gives a mixture of β- and α-isomers from which cytidine (formula II) must be isolated by an uneconomical step.
Meanwhile, US Patent No. 4,340,729 teaches a method for obtaining capecitabine by the procedure shown in Reaction Scheme 2, which comprises hydrolyzing 1-methyl-acetonide of formula III to obtain a triol of formula IV; acetylating the compound of formula IV using anhydrous acetic anhydride in pyridine to obtain a β-/α-anomeric mixture of tri-O-acetyl-5-deoxy-D-ribofuranose of formula V; conducting vacuum distillation to purify the β-/α-anomeric mixture; and isolating the β-anomer of formula I therefrom:
Reaction Scheme 2
III IV
However, the above method is also hampered by the requirement to perform an uneconomical and complicated recrystallization steps for isolating the β-anomer from the mixture of β-/α-anomers of formula V, which leads to a low yield of only about 35% to 40% (Guangyi Wang et al., J. Med. Chem., 2000, vol. 43, 2566-2574; Pothukuchi Sairam et al., Carbohydrate Research, 2003, vol. 338, 303-306; Xiangshu Fei et al., Nuclear Medicine and Biology, 2004, vol. 31, 1033-1041; and Henry M. Kissman et al., J. Am. Chem. Soc, 1957, vol. 79, 5534-5540).
Further, US Patent No. 5,476,932 discloses a method for preparing capecitabine by subjecting 5′-deoxy-5-fluorocytidine of formula VI to a reaction with pentylchloroformate to obtain the compound of formula VII having the amino group and the 2-,3-hydroxy groups protected with C5Hi1CO2 groups; and removing the hydroxy-protecting groups from the resulting compound, as shown in Reaction Scheme 3 :
Reaction Scheme 3
Vl VII 1
However, this method suffers from a high manufacturing cost and also requires several complicated steps for preparing the 5′-deoxy-5-fluorocytidine of formula VI: protecting the 2-,3-hydroxy groups; conducting a reaction thereof with 5-fluorocytosine; and deprotecting the 2-,3-hydroxy groups.
Accordingly, the present inventors have endeavored to develop an efficient method for preparing capecitabine, and have unexpectedly found an efficient, novel method for preparing highly pure capecitabine using a trialkyl carbonate intermediate, which does not require the uneconomical β-anomer isolation steps.
synthesis

more info and description
Aspects of the present invention relate to capecitabine and processes for the preparation thereof.
The drug compound having the adopted name “capecitabine” has a chemical name 5′-deoxy-5-fluoro-N-[(pentyloxy) carbonyl] cytidine and has structural formula I.
H
OH OH I
This compound is a fluoropyrimidine carbamate with antineoplastic activity. The commercial product XELODA™ tablets from Roche Pharmaceuticals contains either 150 or 500 mg of capecitabine as the active ingredient.
U.S. Patent No. 4,966,891 describes capecitabine generically and a process for the preparation thereof. It also describes pharmaceutical compositions, and methods of treating of sarcoma and fibrosarcoma. This patent also discloses the use of ethyl acetate for recrystallization of capecitabine. The overall process is summarized in Scheme I.
Scheme I
U.S. Patent No. 5,453,497 discloses a process for producing capecitabine that comprises: coupling of th-O-acetyl-5-deoxy-β-D-hbofuranose with 5- fluorocytosine to obtain 2′,3′-di-O-acetyl-5′-deoxy-5-fluorocytidine; acylating a 2′, 3′- di-O-acetyl-5′-deoxy-5-fluorocytidine with n-pentyl chloroformate to form 5′-deoxy- 2′,3′-di-O-alkylcarbonyl-5-fluoro-N-alkyloxycarbonyl cytidine, and deacylating the 2′ and 3′ positions of the carbohydrate moiety to form capecitabine. The overall process is summarized in Scheme II.
Capecitabine
Scheme Il
The preparation of capecitabine is also disclosed by N. Shimma et al., “The Design and Synthesis of a New Tumor-Selective Fluoropyrimidine Carbamate, Capecitabine,” Bioorganic & Medicinal Chemistry, Vol. 8, pp. 1697-1706 (2000). U.S. Patent No. 7,365,188 discloses a process for the production of capecitabine, comprising reacting 5-fluorocytosine with a first silylating agent in the presence of an acid catalyst under conditions sufficient to produce a first silylated compound; reacting the first silylated compound with 2,3-diprotected-5- deoxy-furanoside to produce a coupled product; reacting the coupled product with a second silylating agent to produce a second silylated product; acylating the second silylated product to produce an acylated product; and selectively removing the silyl moiety and hydroxyl protecting groups to produce capecitabine. The overall process is summarized in Scheme III. te
R: hydrocarbyl
Scheme III
Further, this patent discloses crystallization of capecitabine, using a solvent mixture of ethyl acetate and n-heptane. International Application Publication No. WO 2005/080351 A1 describes a process for the preparation of capecitabine that involves the refluxing N4– pentyloxycarbonyl-5-fluorocytosine with trimethylsiloxane, hexamethyl disilazanyl, or sodium iodide with trimethyl chlorosilane in anhydrous acetonitrile, dichloromethane, or toluene, and 5-deoxy-1 ,2,3-tri-O-acetyl-D-ribofuranose, followed by hydrolysis using ammonia/methanol to give capecitabine. The overall process is summarized in Scheme IV.
Scheme IV
International Application Publication No. WO 2007/009303 A1 discloses a method of synthesis for capecitabine, comprising reacting 5′-deoxy-5- fluorocytidine using double (trichloromethyl) carbonate in an inert organic solvent and organic alkali to introduce a protective lactone ring to the hydroxyl of the saccharide moiety; reacting the obtained compound with chloroformate in organic alkali; followed by selective hydrolysis of the sugar component hydrolytic group using an inorganic base to give capecitabine. The overall process is summarized in Scheme V.
Scheme V
Even though all the above documents collectively disclose various processes for the preparation of capecitabine, removal of process-related impurities in the final product has not been adequately addressed. Impurities in any active pharmaceutical ingredient (API) are undesirable, and, in extreme cases, might even be harmful to a patient. Furthermore, the existence of undesired as well as unknown impurities reduces the bioavailability of the API in pharmaceutical products and often decreases the stability and shelf life of a pharmaceutical dosage form.
nmr
1H NMR(CD3OD) δ 0.91(3H5 t), 1.36~1.40(4H, m), 1.41(3H, d), 1.68~1.73(2H, m), 3.72(1H, dd), 4.08(1H, dd), 4.13~4.21(3H, m), 5.7O(1H, s), 7.96(1H, d)

- The acetylation of 5′-deoxy-5-fluorocytidine (I) with acetic anhydride in dry pyridine gives 2′,3′-di-O-acetyl-5′-deoxy-5-fluorocytidine (II), which is condensed with pentyl chloroformate (III) by means of pyridine in dichromethane yielding 2′,3′-di-O-acetyl-5′-deoxy-5-fluoro-N4-(pentyloxycarbonyl)cytidine (IV). Finally, this compound is deacetylated with NaOH in dichloromethane/water. The diacetylated cytidine (II) can also be obtained by condensation of 5-fluorocytosine (V) with 1,2,3-tri-O-acetyl-5-deoxy-beta-D-ribofuranose (VI) by means of trimethylchlorosilane in acetonitrile or HMDS and SnCl4 in dichloromethane..
-
- EP 602454, JP 94211891, US 5472949.
- Capecitabine. Drugs Fut 1996, 21, 4, 358,
- Bioorg Med Chem Lett2000,8,(7):1697,
- Capecitabine. Drugs Fut 1996, 21, 4, 358,
- EP 602454, JP 94211891, US 5472949.
Paclitaxel Against Cancer: A Short Review
| Priyadarshini K1* and 2Department of Biotechnology, Loyola Academy Degree & PG College, Secunderabad, IndiaKeerthi Aparajitha U2 | ||||||
| http://www.omicsonline.org/paclitaxel-against-cancer-a-short-review-2161-0444.1000130.php?aid=9996 | ||||||
| Corresponding Author : | Priyadarshini K Department of Biotechnology JSS College for Arts Commerce & Science Mysore, India E-mail: prits_bhargav88@yahoo.com |
|||||
| Received November 16, 2012; Accepted November 28, 2012; Published November 30, 2012 | ||||||
| Citation: Priyadarshini K, Keerthi Aparajitha U (2012) Paclitaxel Against Cancer: A Short Review. Med chem 2:139-141. doi:10.4172/2161-0444.1000130 | ||||||
| Copyright: © 2012 Priyadarshini K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | ||||||
|
||||||
How Long Is A Drug Patent Good For?
 Patents are good for 20 years after the invention of a drug–not after the drug comes to market. It can easily take eight years for the pharmaceutical companies to gather enough data to get approval for their new invention from the U.S. Food and Drug Administration. Meanwhile the FDA can send the drug company back for more clinical studies (experiments using humans as subjects to test the drugs’ efficacy and side effects) and more data, and all the while the patent clock is ticking.
Patents are good for 20 years after the invention of a drug–not after the drug comes to market. It can easily take eight years for the pharmaceutical companies to gather enough data to get approval for their new invention from the U.S. Food and Drug Administration. Meanwhile the FDA can send the drug company back for more clinical studies (experiments using humans as subjects to test the drugs’ efficacy and side effects) and more data, and all the while the patent clock is ticking.
That’s why the name of the game for pharmaceutical companies is working to extend those patents for a top-selling drug
read all at
How Long Is A Drug Patent Good For? – Drugsdb.com http://www.drugsdb.com/blog/how-long-is-a-drug-patent-good-for.html#ixzz2evb9L5rn
BENAZEPRIL HYDROCHLORIDE SYNTHESIS AND REVIEW

BENAZEPRIL HYDROCHLORIDE, CAS NO 86541-74-4
Benazepril, brand name Lotensin (Novartis), is a medication used to treat high blood pressure (hypertension), congestive heart failure, and chronic renal failure. Upon cleavage of its ester group by the liver, benazepril is converted into its active form benazeprilat, a non-sulfhydryl angiotensin-converting enzyme (ACE) inhibitor.
Dosage forms
Benazepril is available as oral tablets, in 5-, 10-, 20-, and 40-mg doses.
Benazepril is also available in combination with hydrochlorothiazide, under the trade name Lotensin HCT, and with amlodipine(trade name Lotrel).

Side effects
Most commonly, headaches and cough can occur with its use. Anaphylaxis, angioedema and hyperkalemia, the elevation of potassium levels, can also occur.
Benazepril may cause harm to the fetus during pregnancy.
According to coverage of the study on WebMD:
| “ | ACE inhibitors can pose a potential threat to kidneys as well. The key question was whether damaged kidneys would worsen if patients took ACE inhibitors. In a nutshell, concerns centered on blood levels of potassium andcreatinine, waste products that are excreted by the kidneys. Testing creatinine levels in the blood is used as a way to monitor kidney function (…) kidney problems worsened more slowly in those taking Lotensin. Overall, there were no major differences in side effects between patients taking Lotensin or the placebo.[2] | ” |
This study marks the first indication that benazepril, and perhaps other ACE inhibitors, may actually be beneficial in the treatment of hypertension in patients with kidney disease.
The Benazepril hydrochloride, with the CAS registry number 86541-74-4, is also known as (3S)-3-(((1S)-1-Carboxy-3-phenylpropyl)amino)-2,3,4,5-tetrahydro-2-oxo-1H-1-benzazepine-1-acetic acid, 3-ethyl ester, monohydrochloride; Benazepril HCl; Cibacen; Cibacen CHF; Labopol. It belongs to the product categories of Intermediates & Fine Chemicals; Pharmaceuticals; Amines; Aromatics; Heterocycles. This chemical’s molecular formula is C24H29ClN2O5 and molecular weight is 460.96. What’s more, its IUPAC name 2-[(3S)-3-[[(2S)-1-ethoxy-1-oxo-4-phenylbutan-2-yl]amino]-2-oxo-4,5-dihydro-3H-1-benzazepin-1-yl]acetic acid hydrochloride. In addition, Benazepril hydrochloride (CAS 86541-74-4) is crystalline solid which is soluble in DMSO. It is used in high blood pressure and congestive heart failure. When you are using this chemical, you should not breathe dust and avoid contact with skin and eyes.
Veterinary use
Under the brand names Fortekor (Novartis) and VetACE (Jurox Animal Health), benazepril hydrochloride is used to treat congestive heart failure in dogs and chronic renal failure in dogs and cats.
- ^ Hou F, Zhang X, Zhang G, Xie D, Chen P, Zhang W, Jiang J, Liang M, Wang G, Liu Z, Geng R (2006). “Efficacy and safety of benazepril for advanced chronic renal insufficiency”. N Engl J Med 354 (2): 131–40. doi:10.1056/NEJMoa053107. PMID 16407508.
- ^ a b Hitti, Miranda; Chang, Louise (January 11, 2006). “Drug May Treat Advanced Kidney Disease”. WebMD. Retrieved 2006-09-07.

| Benazepril hydrochloride, TWT-8154, CGS-14824A, Cibacene, Briem, Cibacen, Lotensin | |
| 1-Carboxymethyl-3(S)-[1(S)-ethoxycarbonyl-3-phenylpropylamino]-2,3,4,5-tetrahydro-1H-1-benzazepin-2-one monohydrochloride; 3(S)-[1(S)-Ethoxycarbonyl-3-phenylpropylamino]-2-oxo-2,3,4,5-tetrahydro-1-benzazepine-1-acetic acid monohydrochloride | |
| 【CAS】 | 86541-74-4, 86541-75-5 (free base) |
| MF | C24-H28-N2-O5.Cl-H |
| MW | 460.9551rot–[Alpha] 20 D -141.0 °. (C = 0.9, ethanol) |
| Cardiovascular Drugs, Hypertension, Treatment of, Angiotensin-I Converting Enzyme (ACE) Inhibitors | |
| Launched-1990 | |
| Novartis (Originator), Pierre Fabre (Licensee), Andrx (Generic), Eon Labs (Generic), KV Pharmaceutical (Generic), Mylan (Generic) |

Above Preparation of Benazepril hydrochloride (CAS 86541-74-4): The reaction of 2(R)-hydroxy-4-phenyl butyric acid ethyl ester (I) with trifluoromethanesulfonic anhydride in dichloromethane gives the corresponding triflate (II), which is then condensed with the amino benzazepinone (III) by means of NMM in the same solvent to provide the target benazepril.

ABOVE SCHEME-EP 1891014 B1
BACKGROUND
-
Benazepril (CAS REGISTRY No. 86541-75-5) first disclosed inUS 4,410,520 is one of the well-known ACE inhibitors and is used for the treatment of hypertension.
-
Chemically, Benazepril, is (3S)-1-(carboxymethyl-[[(1(S)-1-(ethoxycarbonyl)-3-phenylpropyl]amino]-2,3,4,5-tetrahydro-1H-[1]benzazepine-2-one.
-
The preparation of benazepril disclosed in US 4,410,520 , J. Med. Chem. 1985, 28, 1511-1516, and Helvetica Chimica Acta (1988) 71, 337-342, as given in scheme 1, involves reductive amination of ethyl 2-oxo-4-phenyl butyrate (IV) with sodium salt of (3S)-3-amino-1-carboxymethyl-2,3,4,5-tetrahydro-1 H-benzazepin-2-one (III).
-
In example 12 of US 4,410,520 , the crude benazepril (II) obtained in a diastereomeric ratio of SS: SR=70:30 was dissolved in dichloromethane and treated with HCl gas to obtain benazepril hydrochloride. The benazepril hydrochloride of formula (I) obtained as a foam was crystallized from methyl ethyl ketone to obtain in a SS: SR=95:5 diastereomeric ratio. Benazepril hydrochloride was further purified by recrystallization from a mixture of 3-pentanone/methanol (10:1), melting point: 188-190 °C.
-
Alternatively, in example 27 of US 4,410,520 , benazepril hydrochloride was purified by refluxing in chloroform, filtering, and washing first with chloroform and then with diethyl ether. The melting point of benazepril hydrochloride obtained as per this example is 184-186 °C.
-
An alternative process disclosed in US 4,785,089 involves nucleophilic substitution of (3S)-3-amino-1-t-butoxycarbonylmethyl-2,3,4,5-tetrahydro-1H-benzazepine-2-one (V), using the chiral substrate ethyl (2R)-2-(4-nitrobenzenesulfonyl)-4-phenyl butyrate (VI) in presence of N-methylmorpholine (scheme 2). The benazepril t-butyl ester (IIa) obtained in a diastereomeric ratio of SS: SR=96:4 was hydrolyzed to benazepril (II) and converted to hydrochloride salt by treating with HCl gas in ethyl acetate. The crystalline suspension of benazepril hydrochloride in ethyl acetate was diluted with acetone and filtered to obtain in a diastereomeric ratio of SS: SR=99.1:0.9. Further purification by refluxing in ethyl acetate afforded benazepril hydrochloride in a diastereomeric ratio of SS: SR=99.7:0.3, melting point of 181 °C.
-
The above documents do not disclose the crystalline form of benazepril hydrochloride obtained by following the purification processes disclosed in the examples.
-
The Merck Index., 12th edition reports benazepril hydrochloride crystals obtained from 3-pentanone+methanol (10:1), melting point 188-190 °C
-
The crystallization methods taught in the prior art does not consistently produce a constant diastereomeric composition of SS:SR diastereomer. This is evident from the variation in the melting points of the benazepril hydrochloride reported in three different working examples, which varies between 181 to 190°C.
-
The variation in diastereomeric composition of a pharmaceutical substance is not desirable as it would affect its efficacy. Hence there is a need for a crystallization process that consistently produce a constant diastereomeric composition of SS diastereomer in greater than 99.8%.
-
Coming to the crystalline form, it is well known in the art that the solid form of a pharmaceutical substance affect the dissolution rate, solubility and bioavailability. The solid form may be controlled by process employed for the manufacture of the pharmaceutical substance. In particular the process of purification of the solid substance by crystallization is used to control the solid form (Organic Process Research & Development, 2003, 7, 958-1027).
-
It has been found that the crystalline form of benazepril hydrochloride obtained from processes of prior art documents is designated as crystalline Form A as evident from the following documents.
-
In a monograph published by Al-badar et al in Profiles of Drug Substances, Excipients, and Related Methodology, Vol. 31, 2004, p117-161; benazepril hydrochloride prepared by the process disclosed in US 4,410,520 , and J. Med. Chem. 1985, 28, 1511-1516, has been characterized by powder X-ray diffraction pattern having 2θ peaks at 6.6, 9.9, 11.9, 13.7, 14.0, 14.9, 15.3, 16.4, 17.3, 18.9, 19.6, 20.2, 20.9, 21.5, 22.2, 25.2, 25.5, 26.4, 26.6, 27.1, 27.9, 29.8, 30.4, 31.0, 32.6, 33.3, 33.8, 34.4, 35.5, 38.2, 39.9, 43.9, 48.9.
-
The major peaks are at 6.6, 9.9, 11.9, 13.7, 14.9, 16.4, 17.3, 18.9, 19.6, 20.2, 20.9, 21.5, 25.2, 25.5, 26.4, 26.6, 27.9, 31.0, and 32.6.
-
WO 2004/013105 A1 also discloses that by following the processes of the prior art mentioned above, crystalline benazepril hydrochloride is isolated in a form designated as Form A having a powder X-ray diffraction pattern with 2θ values at 6.7, 10.1, 12.0, 13.8, 15.1, 16.4, 17.4, 19.0, 19.6, 20.2, 20.9, 21.0, 25.3, 25.5, 26.4, 26.6, 27.6, 28.0, 31.0, 32.7.
-
WO 2004/013105 A1 discloses that benazepril hydrochloride Form A may be prepared from a concentrated solution of the benazepril hydrochloride in a solvent selected from C1-C10 alcohol, N,N-dimethylformamide, N-methylpyrrolidone by adding an anti-solvent selected from C4-C12 alkane or C1-C10 acetate, preferably, hexane or ethyl acetate.
-
WO 2004/013105 A1 in Example 5 describes a process of making crystalline form A of benazepril hydrochloride by passing HCl gas into a solution of benazepril free base in diethyl ether and filtering the resulting suspension.
-
Similarly, in Example 6, the benazepril hydrochloride was dissolved in water free ethanol and the resulting solution was added to heptane at 20° C to obtain the crystalline Form A.
-
Further, WO 2004/013105 A1 , mentions a list of solvents and anti-solvents that can be used to make benazepril hydrochloride crystalline Form A. However, there is no enabling disclosure and the document is silent on the diastereomeric purity of the crystalline form A obtainable by the process disclosed.
-
The processes of crystallization and/or recrystallization disclosed in the prior art do not consistently produce benazepril hydrochloride with constant diasteromeric content as evident from the variation in the melting point of the crystalline benazepril hydrochloride obtained from crystallization from various solvents.
SYNTHETIC SCHEMES
| Benzazepin-2-ones, process for their preparation, pharmaceutical preparations containing these compounds and the compounds for therapeutical use | |
| Watthey, J.W.H. (Novartis AG) | |
| EP 0072352; GB 2103614; JP 8338260 | |
 |
|
| The reaction of 2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (I) with PCl5 in hot xylene gives 3,3-dichloro-2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (II), which is treated with sodium acetate and reduced with H2 over Pd/C in acetic acid yielding 3-chloro-2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (III). The reaction of (III) with sodium azide in DMSO affords 3-azido-2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (IV), which is condensed with benzyl bromoacetate (V) by means of NaH in DMF giving 3-azido-1-(benzyloxycarbonylmethyl)-2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (VI). The treatment of (VI) with Raney-Ni in ethanol-water yields 3-amino-1-(benzyloxycarbonylmethyl)-2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (VII), which is debenzylated by hydrogenation with H2 over Pd/C in ethanol affording 3-amino-1-(carboxymethyl)-2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (VIII). Finally, this compound is condensed with ethyl 3-benzylpyruvate (IX) by means of sodium cyanoborohydride in methanol acetic acid. | |
| Process for the preparation of benazepril | |
| Kumar, Y.; De, S.; Thaper, R.K.; Kumar, D.S.M. (Ranbaxy Laboratories Ltd.) | |
| WO 0276375 | |
 |
|
| The reaction of 2(R)-hydroxy-4-phenyl butyric acid ethyl ester (I) with trifluoromethanesulfonic anhydride in dichloromethane gives the corresponding triflate (II), which is then condensed with the amino benzazepinone (III) by means of NMM in the same solvent to provide the target benazepril. | |
| CGS-14824 A | |
| Casta馿r, J.; Serradell, M.N. | |
| Drugs Fut 1984,9(5),317 | |
 |
|
| The reaction of 2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (I) with PCl5 in hot xylene gives 3,3-dichloro-2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (II), which is treated with sodium acetate and reduced with H2 over Pd/C in acetic acid yielding 3-chloro-2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (III). The reaction of (III) with sodium azide in DMSO affords 3-azido-2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (IV), which is condensed with benzyl bromoacetate (V) by means of NaH in DMF giving 3-azido-1-(benzyloxycarbonylmethyl)-2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (VI). The treatment of (VI) with Raney-Ni in ethanol-water yields 3-amino-1-(benzyloxycarbonylmethyl)-2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (VII), which is debenzylated by hydrogenation with H2 over Pd/C in ethanol affording 3-amino-1-(carboxymethyl)-2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (VIII). Finally, this compound is condensed with ethyl 3-benzylpyruvate (IX) by means of sodium cyanoborohydride in methanol acetic acid. | |
| Synthesis of 14C-labeled 3-([1-ethoxycarbonyl-3-phenyl-(1S)-propyl]amino)-2,3,4,5-tetrahydro-2-oxo-1H-1-(3S)-benzazepine-1-acetic acid hydrochloride ([14C]CGS 14824A) | |
| Chaudhuri, N.K.; Patera, R.; Markus, B.; Sung, M.-S. | |
| J Label Compd Radiopharm 1987,24(10),1177-84 | |
 |
|
| A new synthesis of CGS-14824A is given: The reaction of 3-bromo-1-phenylpropane (I) with KCN gives 4-phenylbutyronitrile (II), which is hydrolyzed to the corresponding butyric acid (III). The cyclization of (III) with polyphosphoric acid affords 1-tetralone (IV), which is brominated to 2-bromo-1-tetralone (V) and treated with hydroxylamine to give the oxime (VI). The Beckman rearrangement of (VI) yields 3-bromo-2,3,4,5-tetrahydro-1H-(1)benzazepin-2-one (VII), which is treated with sodium azide to afford the azide derivative (VIII). The N-alkylation of (VIII) with ethyl bromoacetate (IX) by means of KOH and tetrabutylammonium bromide in THF gives the N-alkylated azide (X), which is reduced by catalytic hydrogenation to the corresponding amine (XI). The hydrolysis of the ester group of (XI) with NaOH yields the free acetic acid derivative (XII), which is finally reductocondensed with ethyl 2-oxo-4-phenylbutyrate (XIII) by means of sodium cyanoborohydride. | |

US 6548665 B2– above

see translated vesrsion————-First, 2,3,4,5 – tetrahydro-1H-[1] azepin-2 phenyl – one (2) Preparation of
the dry reaction flask, add α- tetralone 20g (0.137mol), stacked acid 7.36g (0.171mol) and chloroform 140ml, was stirred at 40 ℃ in 1h concentrated sulfuric acid was slowly added dropwise 36ml, acid layer was separated and poured into 900ml water to give a creamy solid. Recrystallization with hot water to give white crystals (2) 15.5g (70%), mp141 ℃. (Acidic filtrate and after a small amount of product can be obtained.)
Second, 3,3 – dichloro-2, 3,4,5 – tetrahydro-1H-[1] benzene azepin-2 – one (3) of the prepared
in a dry reaction flask, (2) 48.3g (0.3mol) and xylene solution of 1300ml, phosphorus pentachloride 188g (0.9mol), stirred and gradually heated to at 0.5h 90 ℃, (Caution! When phosphorus pentachloride dissolved hydrogen chloride gas had severe.) 90 ℃ the reaction was continued for 0.5h, filtered to remove a small amount of suspended solids, solvent recovery under reduced pressure, to the residue was added saturated sodium bicarbonate solution, 100ml, stirred until a solid precipitate complete, filtered and the cake washed with ethanol (100ml × 2), diethyl ether (50ml) and dried to give (3) 69.0g (90%), mp185 ~ 187 ℃.
III.3 – chloro-2 ,3,4,5 – tetrahydro-1H-[1] benzene azepin-2 – one (4) Preparation of
the reaction flask (3) 10g (0.087mol), Sodium acetate 77g (0.11mol), acetic acid 460ml and 5% Pd-C 0.86g, under atmospheric pressure at room temperature to a hydrogen-absorbing up total of 950ml (about 0.5h). Filtration, recycling the catalyst recovered solvent, the residue was dried under reduced pressure, and then added 900ml of 10% sodium bicarbonate solution and dichloromethane 300ml, stirring, standing, the organic layer was separated and the aqueous layer extracted with dichloromethane (300ml × 3) extracted organic layers were combined, dried over anhydrous sodium sulfate, the solvent recovered under reduced pressure. Diethyl ether was added to the cured 350ml, and mashed, filtered and dried to give (4) 8.19g (95%), mp163 ~ 167 ℃.
4 (3) – azido-2, 3,4,5 – tetrahydro-1H-[1] benzene azepin-2 – one (5) Preparation of
the dry reaction flask (4) 15.9g ( 0.08mol), sodium azide 6.4g (0.10mol) and 320ml solution of dimethyl sulfate, the reaction was stirred at 80 ℃ 3h, cooled to room temperature, poured into ice-water (1L) to precipitate a pale yellow solid , filtered and dried under reduced pressure at 75 ℃ to give (5) 14.7g (90%), mp142 ~ 145 ℃.
V.3 – azido-2 ,3,4,5 – tetrahydro-1H-[1] benzene azepin-2 – one-1 – acetate (6) Preparation of
the dry reaction flask, (5) 3.0g (0.015mol), tetrabutylammonium bromide, 0.5g (0.0015 mol), powdered potassium hydroxide 1.1g (0.016mol) and 30ml of tetrahydrofuran solution of ethyl bromoacetate was added 1.9ml ( 0.016mol), stirred rapidly at room temperature for 1.5h (nitrogen). Water was added: dichloromethane (50:100 ml), stirred, allowed to stand, the organic layer separated. Washed with water, dried over anhydrous sodium sulfate, the solvent recovered under reduced pressure to give a pale yellow oil (6) 4.1g (96%) (can be used directly in the next step).
VI.3 – amino-2 ,3,4,5 – tetrahydro-1H-[1] benzene azepin-2 – one-1 – acetate (7) Preparation of
the dry reaction flask, (6 ) 20.0g (0.070mol), ethanol 100ml, 10% Pd-C 1.0g stirring, at room temperature, 303.9kPa hydrogenated under a hydrogen pressure 1.5h, intermittent deflated to remove the generated nitrogen gas, after the reaction was collected by filtration Pd / C, recovery of solvents under reduced pressure to give a yellow oil, add ether l00ml, mashed, filtered and dried to give a white solid (7) 17.0g (93%) mp101 ~ 102 ℃.
Seven, (3S) -3 – amino-2 ,3,4,5 – tetrahydro-1H-[1] benzene azepin-2 – one-1 – acetate (8) Preparation of
the reaction flask, adding (7) 25.1g (0.096mol), L – tartaric acid 14.4g (0.096mol) and hot ethanol 200ml, stirring to dissolve, cooled at room temperature overnight, filtered and dried under reduced pressure to give a white powder 30.7g, with ethanol Recrystallization twice (each 200ml), to give (8) tartaric acid salt of 13.6g (34%), mp168 ~ 169 ℃, with 10% ammonium hydroxide, to give a white solid (8) 8.0g (95%) mp104 ~ 106 ℃.
Eight, (3S) -3 – amino-2 ,3,4,5 – tetrahydro-1H-[1] benzene azepin-2 – one-1 – acetate (9) Preparation of
the reaction flask, (8) 4.0g (0.056mol) and 150ml of methanol solution of sodium hydroxide 2.1g (0.056moI) and a solution of 5ml of water, stirred at room temperature for 2h, the solvent recovered under reduced pressure, the residue was dried and diethyl ether was added 100ml, trace broken, filtered, and dried to give (9) 12.9g (89%) (used directly in the next step).
IX benazepril (1) Synthesis of
the reaction flask (9) 12.9g (0.050mol), 2 – oxo-4 – phenylbutyrate 31.0g (0.15mol), acetic acid and 100ml methanol 75ml, the reaction was stirred at room temperature for 1h (nitrogen). Of sodium borohydride cyanide was slowly added dropwise 3.8g (0.062mol) and 30ml of methanol solution of (4h was completed within), stirred overnight, heat. Concentrated hydrochloric acid 10ml, 1h stirring at room temperature, the solvent was recovered under reduced pressure, water was added to the residue and diethyl ether 400ml l00ml, dissolved with concentrated ammonium hydroxide and the pH adjusted to 9.3, the organic layer was separated and the aqueous layer acidified with concentrated hydrochloric to pH 4.3, extracted with ethyl acetate (100ml × 3) extracted organic layers were combined, dried over anhydrous magnesium sulfate, the solvent recovered under reduced pressure, to the residue was added methylene chloride (150ml) to dissolve. And pass into dry hydrogen chloride after 5min recovered solvent under reduced pressure, to the residue was added hot ethyl ketone 100ml, stirring to dissolve, cooled and precipitated solid was filtered to give crude product (1). A 3 – amyl ketone / methanol (volume ratio 10:1) (110ml) was recrystallized (1) 5.8 g, mp 188 ~ 190 ℃, [alpha] D 20 -141.0 (C = 0.9, C 2 H 5 OH )
[Spectral Data] (free base) [2]
MS: m / Z (%) 424 (M + , 2), 351 (100), 190 (22), 91 (65)
] [other synthetic routes
described in the reference literature.
[References]
[1] Briggs LH et al. J Chem Soc, 1937, 456
[2] Watthey WH et al. J Med Clmm, 1985, 28:1511
[3] EP 1986, 206933 (CA, 1987, 107: 77434e)
[4] EP 1983, 72352 (CA, 1983, 99:53621 d)
[5] package insert: Lotensin
[6] property protection case I: Lotensin
[7] property protection case II: Lotensin
[8] Drug Monograph information: BENAZEPRIL
more info
Partition Coefficient.
Gas Chromatography.
High Performance Liquid Chromatography.
Ultraviolet Spectrum.
Clarke’s Analysis of Drugs and Poisons
Watthey, J.W.H. et al.: J. Med. Chem. (JMCMAR) 28, 1511 (1985).
US 4 410 520 (Ciba-Geigy; 18.10.1983; prior. 11.8.1981, 9.11.1981, 19.7.1982).
EP 72 352 (Ciba-Geigy; appl. 5.8.1982; USA-prior. 11.8.1981, 9.11.1981).
FDA Approves Botox Cosmetic to Improve the Appearance of Crow’s Feet Lines
WEDNESDAY, September 11, 2013 — The U.S. Food and Drug Administration today approved a new use for Botox Cosmetic (onabotulinumtoxinA) for the temporary improvement in the appearance of moderate to severe lateral canthal lines, known as crow’s feet, in adults. Botox Cosmetic is the only FDA approved drug treatment option for lateral canthal lines.
The FDA approved Botox Cosmetic in 2002 for the temporary improvement of glabellar lines (wrinkles between the eyebrows, known as frown lines), in adults. Botox Cosmetic works by keeping muscles from tightening so wrinkles are less prominent
READ ALL AT

BOTOX Cosmetic (onabotulinum toxin A) For Injection, is a sterile, vacuum-dried purifiedbotulinum toxin type A, produced from fermentation of Hall strain Clostridium botulinumtype A grown in a medium containing casein hydrolysate, glucose, and yeast extract, intended for intramuscular use. It is purified from the culture solution by dialysis and a series of acid precipitations to a complex consisting of the neurotoxin, and several accessory proteins. The complex is dissolved in sterile sodium chloride solution containing Albumin Human and is sterile filtered (0.2 microns) prior to filling and vacuum-drying.
The primary release procedure for BOTOX Cosmetic uses a cell-based potency assay to determine the potency relative to a reference standard. The assay is specific to Allergan’s products BOTOX and BOTOX Cosmetic. One Unit of BOTOX Cosmetic corresponds to the calculated median intraperitoneal lethal dose (LD50) in mice. Due to specific details of this assay such as the vehicle, dilution scheme and laboratory protocols, Units of biological activity of BOTOX Cosmetic cannot be compared to nor converted into Units of any other botulinum toxin or any toxin assessed with any other specific assay method. The specific activity of BOTOX Cosmetic is approximately 20 Units/nanogram of neurotoxin protein complex.
Each vial of BOTOX Cosmetic contains either 50 Units of Clostridium botulinum type A neurotoxin complex, 0.25 mg of Albumin Human, and 0.45 mg of sodium chloride; or 100 Units of Clostridium botulinum type A neurotoxin complex, 0.5 mg of Albumin Human, and 0.9 mg of sodium chloride in a sterile, vacuum-dried form without a preservative.
Since the approval of BOTOX® Cosmetic by the U.S. Food and Drug Administration in 2002, Allergan has virtually changed the face of medical aesthetics. Men and women between the ages of 18 to 65 now have the ability to choose science-based, non-invasive medical aesthetic solutions, including BOTOX® Cosmetic and the JUVÉDERM® family of dermal fillers, to achieve their own results. Over the last seven years, there have been nearly 11.8 million BOTOX® Cosmetic treatments recorded in the United States.1 More importantly, its 97 percent satisfaction rating (survey of 117 patients)2,3 is just one indication of the trust consumers have placed in Allergan.
BOTOX® Cosmetic is a simple, non-surgical procedure for temporarily reducing the appearance of moderate to severe glabellar lines – the vertical frown lines between the eyebrows that look like an “11” – in adult women and men aged 18 to 65. BOTOX® Cosmetic reduces the activity of the muscles that cause the “11s” to form by blocking nerve impulses that trigger wrinkle-causing muscle contractions, creating an improved appearance between the brows. Results can last up to four months and may vary with each patient. Ask your doctor if BOTOX® Cosmetic is right for you.

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....



































