| FDA ORANGE BOOK PATENTS: 1 OF 2 | |
|---|---|
| Patent | 7459561 |
| Expiration | Oct 31, 2020 |
| Applicant | ASTELLAS |
| Drug Application | N207500 (Prescription Drug: CRESEMBA. Ingredients: ISAVUCONAZONIUM SULFATE) |
VORAPAXAR SULPHATE

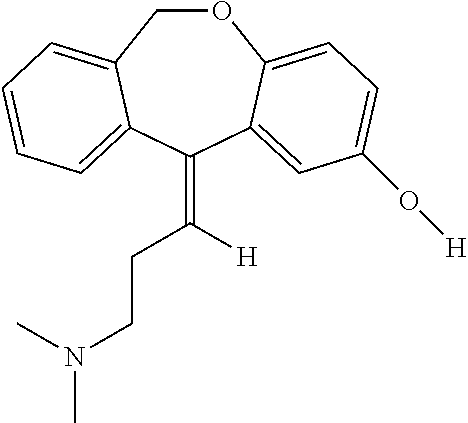
VORAPAXAR
Thrombosis, Antiplatelet Therapy, PAR1 Antagonists , MERCK ..ORIGINATOR
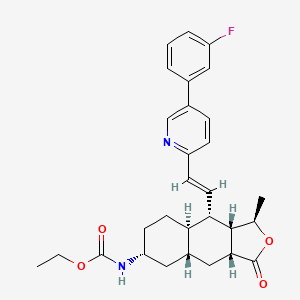
Ethyl N-[(3R,3aS,4S,4aR,7R,8aR,9aR)-4-[(E)-2-[5-(3-fluorophenyl)-2-pyridyl]vinyl]-3-methyl-1-oxo-3a,4,4a,5,6,7,8,8a,9,9a-decahydro-3H-benzo[f]isobenzofuran-7-yl]carbamate
Ethyl ((1R,3aR,4aR,6R,8aR,9S,9aS)-9-((1E)-2-(5-(3-fluorophenyl)pyridin-2-yl)ethenyl)- 1-methyl-3-oxododecahydronaphtho(2,3-c)furan-6-yl)carbamate
Carbamic acid, ((1R,3aR,4aR,6R,8aR,9S,9aS)-9-((1E)-2-(5-(3-fluorophenyl)-2- pyridinyl)ethenyl)dodecahydro-1-methyl-3-oxonaphtho(2,3-c)furan-6-yl)-, ethyl ester
618385-01-6 CAS NO FREE FORM
CAS Number: 705260-08-8 SULPHATE
Has antiplatelet activity.
- UNII-ZCE93644N2
- Zontivity
Registered – 2015 MERCK Thrombosis
Vorapaxar (formerly SCH 530348) is a thrombin receptor (protease-activated receptor, PAR-1) antagonist based on the natural product himbacine. Discovered by Schering-Plough and currently being developed by Merck & Co., it is an experimental pharmaceutical treatment for acute coronary syndrome chest pain caused by coronary artery disease.[1]
In January 2011, clinical trials being conducted by Merck were halted for patients with stroke and mild heart conditions.[2] In a randomized double-blinded trial comparing vorapaxar with placebo in addition to standard therapy in 12,944 patients who had acute coronary syndromes, there was no significant reduction in a composite end point of death from cardiovascular causes, myocardial infarction, stroke, recurrent ischemia with rehospitalization, or urgent coronary revascularization. However, there was increased risk of major bleeding.[3]
A trial published in February 2012, found no change in all cause mortality while decreasing the risk of cardiac death and increasing the risk of major bleeding.[4]
SCH-530348 is a protease-activated thrombin receptor (PAR-1) antagonist developed by Schering-Plough and waiting for approval in U.S. for the oral secondary prevention of cardiovascular events in patients with a history of heart attack and no history of stroke or transient ischemic attack. The drug candidate is being investigated to determine its potential to provide clinical benefit without the liability of increased bleeding; a tendency associated with drugs that block thromboxane or ADP pathways. In April 2006, SCH-530348 was granted fast track designation in the U.S. for the secondary prevention of cardiovascular morbidity and mortality outcomes in at-risk patients.
Vorapaxar was recommended for FDA approval on January 15, 2014.[5]
Vorapaxar is a protease-activated thrombin receptor (PAR-1) antagonist developed by Schering-Plough (now, Merck & Co.) and approved in the U.S. in 2014 for the reduction of thrombotic cardiovascular events in patients with a history of myocardial infarction or with peripheral arterial disease. However, in 2018 Aralez discontinued U.S. commercial operations. In 2015, the product was approved in the E.U. for the reduction of atherothrombotic events in adult patients with a history of myocardial infarction. In April 2006, vorapaxar was granted fast track designation in the U.S. for the secondary prevention of cardiovascular morbidity and mortality outcomes in at-risk patients. In 2016, Aralez Pharmaceuticals acquired the U.S. and Canadian rights to the product pursuant to an asset purchase agreement entered into between this company and Merck & Co.
Merck & Co (following its acquisition of Schering-Plough) has developed and launched vorapaxar (Zontivity; SCH-530348; MK-5348), an oral antagonist of the thrombin receptor (protease-activated receptor-1; PAR1); the product is marketed in the US by Aralez Pharmaceuticals
WO-03089428, published in October 2003, claims naphtho[2,3-c]furan-3-one derivatives as thrombin receptor antagonists. WO-03033501 and WO-0196330, published in April 2003 and December 2001, respectively, claim himbacine analogs as thrombin receptor antagonists. WO-9926943 published in June 1999 claims tricyclic compounds as thrombin receptor antagonists
 VORAPAXAR
VORAPAXAR17 JAN 2014
FDA advisory panel votes to approve Merck & Co’s vorapaxar REF 6
https://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/204886Orig1s000ChemR.pdf
Zontivity (vorapaxar) tablets NDA 204886



VORAPAXAR SULPHATE

CAS Number: 705260-08-8 SULPHATE
Molecular Formula: C29H33FN2O4.H2O4S
Molecular Weight: 590.7
Chemical Name: Ethyl [(1R,3aR,4aR,6R,8aR,9S,9aS)-9-[(1E)-2-[5-(3-fluorophenyl)pyridin-2- yl]ethenyl]-1-methyl-3-oxododecahydronaphtho[2,3-c]furan-6-yl]carbamate sulfate
Synonyms: Carbamic acid, [(1R,3aR,4aR,6R,8aR,9S,9aS)-9-[(1E)-2-[5-(3-fluorophenyl)-2- pyridinyl]ethenyl]dodecahydro-1-methyl-3-oxonaphtho[2,3-c]furan-6-yl]-,ethyl ester,sulfate; SCH-530348
Vorapaxar Sulfate (SCH 530348) a thrombin receptor (PAR-1) antagonist for the prevention and treatment of atherothrombosis.
POLYMORPH
U.S.Pat. No. 7,304,078 discloses Vorapaxar base. U.S.Pat. No. 7,235,567 discloses Polymorph I and II of vorapaxar sulphate
CN 106478608 provides a crystalline polymorph A
EMA
Atherosclerosis and ischemic cardiovascular (CV) diseases like coronary artery disease (CAD) are progressive systemic disorders in which clinical events are precipitated by episodes of vascular thrombosis. Patients with an established history of atherothrombotic or athero-ischemic disease are at particular risk of future cardiac or cerebral events, and vascular death. Anti-thrombotic therapy options in patients with stable atherosclerosis are not well-established. Long-term therapies to effectively modulate the key components responsible for atherothrombosis in secondary prevention of ischemic CV disease are therefore required. Vorapaxar is a first – in – class selective antagonist of the protease-activated receptor 1 (PAR-1), the primary thrombin receptor on human platelets, which mediates the downstream effects of this critical coagulation factor in hemostasis and thrombosis. Thrombin-induced platelet activation has been implicated in a variety of cardiovascular disorders including thrombosis, atherosclerosis, and restenosis following percutaneous coronary intervention (PCI). As an antagonist of PAR-1, vorapaxar blocks thrombin-mediated platelet aggregation and thereby has the potential to reduce the risk of atherothrombotic complications of coronary disease. The applicant has investigated whether a new class of antiplatelet agents, PAR-1 antagonists, can further decrease the risk of cardiovascular events in a population of established atherothrombosis when added to standard of care, in secondary prevention of ischemic diseases. The following therapeutic indication has been submitted for vorapaxar: Vorapaxar is indicated for the reduction of atherothrombotic events in patients with a history of MI. Vorapaxar has been shown to reduce the rate of a combined endpoint of cardiovascular death, MI, stroke, and urgent coronary revascularization. Vorapaxar will be contraindicated in patients with a history of stroke or TIA. The indication sought in the current application is supported by the efficacy results of the TRA 2P-TIMI, which is considered the pivotal trial for this indication. During the procedure, the applicant requested the possibility of extending the indication initially sought for, to extend it to the population of PAD patients. This request was discussed at the CHMP and not accepted by the Committee.
Introduction The finished product is presented as immediate release film-coated tablets containing 2.5 mg of vorapaxar sulfate as active substance per tablet, corresponding to 2.08 mg vorapaxar. Other ingredients are: lactose monohydrate, microcrystalline cellulose (E460), croscarmellose sodium (E468), povidone (E1201) , magnesium stearate (E572), hypromellose (E464), titanium dioxide (E171), triacetin (glycerol triacetate) (E1518), iron oxide yellow (E172), as described in section 6.1 of the SmPC. The product is available in Aluminium–Aluminium blisters (Alu-Alu) as described in section 6.5 of the SmPC.
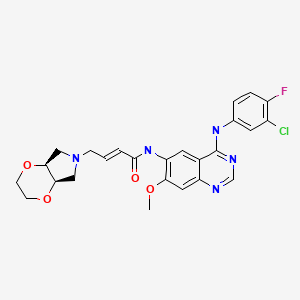
General information The chemical name of the active substance vorapaxar sulfate is ethyl[(1R,3aR,4aR,6R,8aR,9S,9aS)- -9-{(1E)-2-[5-(3-fluorophenyl)pyridin-2-yl]ethen-1-yl}-1-methyl-3-oxododecahydronaphtho[2,3-c] furan-6-yl]carbamate sulfate, corresponding to the molecular formula C29H33FN2O4 • H2SO4 and has a relative molecular mass 590.7. It has the following structure:
The structure of the active substance has been confirmed by mass spectrometry, infrared spectroscopy, 1H- and 13C-NMR spectroscopy and X-ray crystallography, all of which support the chemical structure elemental analysis. It appears as a white to off-white, slightly hygroscopic, crystalline powder. It is freely soluble in methanol and slightly soluble in ethanol and acetone but insoluble to practically insoluble in aqueous solutions at pH above 3.0. The highest solubility in aqueous solution can be achieved at pH 1.0 or in simulated gastric fluids at pH 1.4. The dissociation constant of vorapaxar sulfate was determined to be pKa = 4.7 and its partition coefficient LogP was determined to be 5.1. Vorapaxar sulfate contains seven chiral centers and a trans double bond. The seven chiral centres are defined by the manufacturing process of one of the intermediates in the vorapaxar synthesis and potential enantiomers are controlled by appropriate specifications. The cis-isomer of the double bond is controlled by a highly stereo-specific process reaction resulting in non-detectable levels of cis-isomer impurity. The cis-isomer impurity is controlled in one of the intermediates as an unspecified impurity. A single crystalline stable anhydrous form has been observed.
GENERAL INTRODUCTION
SIMILAR NATURAL PRODUCT
+ HIMBACINE


Himbacine is an alkaloid muscarinic receptor antagonist displaying more potent activity associated with M2 and M2 subtypes over M1 or M3. Observations show himbacine bound tightly to various chimeric receptors in COS-7 cells as well as possessed the ability to bind to cardiac muscarinic receptors allosterically. Recent studies have produced series of thrombin receptor (PAR1) antagonists derived from himbacine Himbacine is an inhibitor of mAChR M2 and mAChR M4.
| Physical State: | Solid |
| Derived from: | Australian pine Galbulimima baccata |
| Solubility: | Soluble in ethanol (50 mg/ml), methanol, and dichloromethane. Insoluble in water. |
| Storage: | Store at -20° C |
| Melting Point: | 132-134 °C |
| Boiling Point: | 469.65 °C at 760 mmHg |
| Density: | 1.08 g/cm3 |
| Refractive Index: | n20D 1.57 |
| Optical Activity: | α20/D +51.4º, c = 1.01 in chloroform |
| Application: | An alkaloid muscarinic receptor antagonist |
| CAS Number: | 6879-74-9 |
| Molecular Weight: | 345.5 |
| Molecular Formula: | C22H35NO2 |
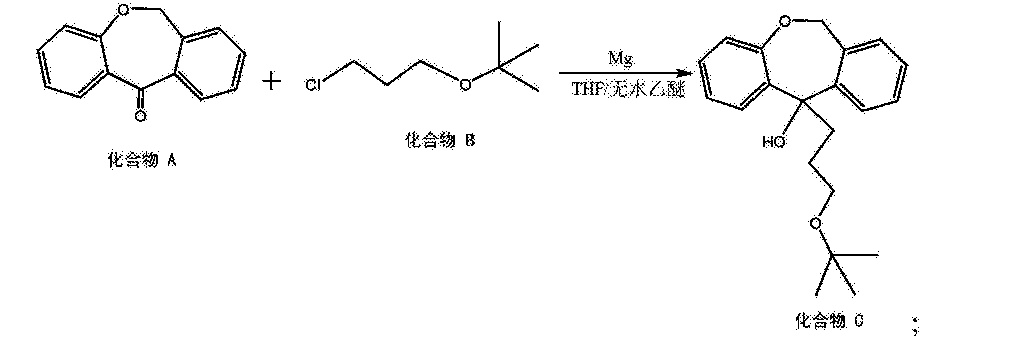
General scheme:
PATENT
WO 2006076415
WO 2006076452
WO 2003089428
US 6063847
CN 107540564
WO 2008005344
CN 106749138
PATENT
Example 1:
[0027] The steel shed amide (300mg, 7. 93mmol) and 15 blood THF was added to 100 blood Ξ jar. The starting material II (2.OOg, 5. 89mmol) was dissolved in 15mL of THF dropwise via pressure-equalizing dropping funnel to the reaction system, the process temperature will produce a large number of bubbles -2 ~ 0 ° C, in the process, Lan mix of about 0.1 until no bubbles generate. THF solution containing 13 Blood Ship (0.75 Yap, 2. 95mmol) is transferred to a pressure-equalizing dropping funnel. It was slowly added dropwise to the reaction system. After the completion of dropwise continue to embrace mix ratio. After the treatment, at 0 ° C under 0.8 blood, Imol / L 1 fat slowly dropped into the embrace mixed reaction system, after adding the right amount of water, acetic acid extraction. The combined organic phase with Imol / L of 0H (17mLX3) washing the organic phase coating. Tu brine, dried over anhydrous sulfate steel, 25 ° C under reduced pressure to spin dry to give 1. 75g light yellow oil, yield 91%.
[0028] After the content was determined using the external standard method, first prepared by a qualified reference determine its content, W this as a standard substance, measuring the external standard method to get the content of 99%.
[0029] Zan NMR: (400MHz, CD3CN):… 5 46 of r, 1H), 4 70 (td, 1H), 4 03 based 2H), 3 69-3 57 (m, 2 Η).. , 3. 45-3. 32 (based, IH), 2. 77 (br, IH), 2. 61-2. 51 (m, IH), 2. 49-2. 39 (m, 1 field, 2 30 of r IH), 2 .12-1. 92 (m, IH), 1. 87 (dt, IH), 1. 81-1. 72 (m, IH), 1. 61-1. 50 ( …. m, IH), 1 48 (d, 3H), 1 23-1 09 (m, 7H), 1. 05-0 90 (m, 2H);
[0030] MS (ES +) m / z: 326. 24 [M + + field.
[Cited 00] Example 2:
[003 cited the steel shed amide (312mg, 8. 25mmol) and 16 blood THF was added to the lOOmL Ξ jar. The starting material II (2.OOg, 5. 89mmol) was dissolved in 15mL of THF dropwise via pressure-equalizing dropping funnel to the reaction system, the process temperature will produce a large number of bubbles -2 ~ -5 ° C, in the process and takes about 45min mix until no bubbles generate. The 13 ships of blood containing 60g, 2. 36mmol) in THF solution was transferred to a pressure-equalizing dropping funnel. It was slowly added dropwise to the reaction system. After the completion of dropwise continue to embrace mix ratio. After the treatment, at 0 ° C under 0.8 blood, Imol / L 1 fat slowly dropped into the embrace mixed reaction system, after adding the right amount of water, acetic acid extraction. The combined organic phase with llmol / L of 0H (17mLX3) washing the organic phase coating. Tu brine, dried over anhydrous sulfate steel, 25 ° C under reduced pressure to spin dry to give 1. 65g light yellow oil.
[0033] Determination of Reference Example 1 in an amount of 98.7%.
[0034] MS (ES +) m / z: 326. 24 [M + + field.
[003 cited Example 3:
[0036] 50 single jar of blood, condenser. Intermediate inb (l.〇〇g, 3. 07mmol) was dissolved in 10ml of dichloromethane burn during and after the blood was added to a 50-port flask, make dioxide of 32g, 3.68mmol), the reaction of reflux. After completion of the reaction by TLC, cooled to 20 ~ 25 ° C after suction filtration, the filter cake rinsed with methylene burning (the X3 3 blood), at 30 ° CW and the filtrate was concentrated to dryness. To the residue was added 5 blood acetic acid, at 20 ~ 25 ° C after mixing 0. embrace of suction, the resulting cake was vacuum dried at 30 ° C 10 ~ 12h. Give 0. 87g of white solid.
[0037] Electric NMR: (400MHz, CD3CN):. 9 74 oriented 1H), 5 40 of r, 1H), 4 77-4.66 (m, 1H), 4 09-3 98 (m, 2H…. ), 3. 49-3. 37 (m, IH), 2. 75-2. 64 (m, 2H), 2. 55-2. 48 (m, IH), 1. 95-1. 87 (m , 2H), 1. 89-1 .77 (m, 2H), 1. 61-1. 49 (m, IH), 1. 32-1. 13 (m, 9H), 1. 08-0. 82 (m, 2H);
[0038] MS (ES +) m / z: 324. 33 [M + + field.
PATENT
CN 106478608 crystal
https://patents.google.com/patent/CN106478608A/en
The present invention provides a crystalline polymorph A one kind of the compound of formula I:
In another embodiment, the present invention provides a method of preparing a crystalline polymorph of compound A I,
Which comprising, a) the compound II is dissolved in acetonitrile and stirred to form a mixture; b) heating the mixture to 50 ° C ~ 70 ° C; c) adding sulfuric acid to the heated mixture; d) evaluating the temperature was lowered to 0 ° C ~ 20 ° C, seeded and stirred to precipitate crystals.
Preparation [0042] A crystalline polymorph of the compound of Example 1 I
Compound II (1. 0g) was dissolved in 5. 0ml of acetonitrile, stirred and heated to 50 ° C ~ 70 ° C was added and this temperature was added 1.2ml 2N H2S04 / acetonitrile solution and then lowering the temperature of the system to 15 ° C ~ 20 ° C, the system was added to the appropriate amount of seed crystals and stirred for 2h, the precipitated solid was filtered and the cake washed twice with 2. 5ml of acetonitrile to give a white solid, the white solid was placed under 40 ° C desolventizing 2 hours and then dried at 80 ° C for vacuo to give a white solid 0. 83 g, 69. 3% yield, HPLC:. 99 94%. A powder X-ray diffraction spectrum shown in Figure 1, a DSC endothermic curve shown in Figure 2, which HPLC profile shown in Fig.
PATENT
https://patents.google.com/patent/CN106478608A/en
PATENT
WO 2009093972 synthesis
https://encrypted.google.com/patents/WO2009093972A1?cl=ko&hl=en&output=html_text
Clip
Vorapaxar sulfate (Zontivity)
Merck Sharp & Dohme successfully obtained approval in the EU in 2014 for vorapaxar sulfate, marketed as Zontivity. The drug is a first-in-class thrombin receptor (also referred to as a protease-activated or PAR-1) antagonist which, when used in conjunction with antiplatelet therapy, has been shown to reduce the chance of
myocardial infarction and stroke, particularly in patients with a history of cardiac events.277
Antagonism of PAR-1 allows for thrombin-mediated fibrin deposition while blocking thrombinmediated platelet activation.277 Although a variety of papers and patents describe the synthesis of vorapaxar sulfate (XXXVII),278–282 a combination of two patents describe the largest-scale synthesis reported in the literature, and this is depicted in Scheme 52.


Retrosynthetically, the drug can be divided into olefination partners 306 and 305.283,284 Lactone 305
is further derived from synthons 300 and 299, which are readily prepared from commercially available starting materials. Dienyl acid 300 was constructed in two steps starting from commercial vinyl bromide 307, which first undergoes a Heck reaction with methacrylate (308) followed by saponification of the ester to afford the desired acid 300 in 71% over two steps (Scheme 53).
The synthesis of alcohol 299 begins with tetrahydropyranyl (THP) protection of enantioenriched alcohol 295 to afford butyne 297 (Scheme 52). Lithiation of this system followed by trapping with (benzyloxy)chloroformate and Dowex work-up to remove the protective functionality provided acetyl ester 298. Hydrogenation of the alkyne with Lindlar’s catalyst delivered cis-allylic alcohol 299 in 93% yield. Acid 300 was then esterified with alcohol 299 by way of a 1,3-dicyclohexylcarbodiimide (DCC) coupling and, upon heating in refluxing xylenes, an intramolecular Diels–
Alder reaction occurred. Subsequent subjection to DBU secured the tricyclic system 301 in 38% over three steps as a single enantiomer.
Diastereoselective hydrogenation reduced the olefin with concomitant benzyl removal to give key fragment 302. Next, acidic revelation of the ketone followed by reductive amination with ammonium formate delivered primary amines 303a/303b as a mixture of diastereomers. These amines were then converted to the corresponding carbamates, and resolution by means of recrystallization yielded 50% of 304 as the desired diastereomer. Acid 304
was treated with oxalyl chloride and the resulting acid chloride was reduced to aldehyde 305 in 66% overall yield. Finally, deprotonation of phosphonate ester 306 (whose synthesis is described in Scheme 54) followed by careful addition of 305 and acidic quench delivered vorapaxar sulfate (XXXVII) in excellent yield over the
two-step protocol.
The preparation of vorapaxar phosponate ester 306 (Scheme 54)commenced from commercial sources of 5-(3-fluorophenyl)-2-methylpyridine (310). Removal of the methyl proton with LDA followed by quench with diethyl chlorophosphonate resulted in phosponate ester 306.

277. Frampton, J. E. Drugs 2015, 75, 797.
278. Chackalamannil, S.; Wang, Y.; Greenlee, W. J.; Hu, Z.; Xia, Y.; Ahn, H.; Boykow,G.; Hsieh, Y.; Palamanda, J.; Agans-Fantuzzi, J.; Kurowski, S.; Graziano, M.;Chintala, M. J. Med. Chem. 2008, 51, 3061.
279. Sudhakar, A.; Kwok, D.; Wu, G. G.; Green, M. D. WO Patent 2006076452A2,2006.
280. Wu, G. G.; Sudhakar, A.; Wang, T.; Ji, X.; Chen, F. X.; Poirier, M.; Huang, M.;Sabesan, V.; Kwok, D.; Cui, J.; Yang, X.; Thiruvengadam, T.; Liao, J.; Zavialov, I.;Nguyen, H. N.; Lim, N. K. WO Patent 2006076415A2, 2006.
281. Yong, K. H.; Zavialov, I. A.; Yin, J.; Fu, X.; Thiruvengadam, T. K. US Patent20080004449A1, 2008.
282. Chackalamannil, S.; Clasby, M.; Greenlee, W. J.; Wang, Y.; Xia, Y.; Veltri, E.;Chelliah, M. WO Patent 03089428A1, 2003.
283. Thiruven-Gadam, T. K.; Wang, T.; Liao, J.; Chiu, J. S.; Tsai, D. J. S.; Lee, H.; Wu,W.; Xiaoyong, F. WO Patent 2006076564A1, 2006.
284. Chackalamannil, S.; Asberon, T.;Xia, Y.; Doller, D.; Clasby, M. C.; Czarniecki,M. F. US Patent 6,063,847, 2000.
PRODUCT PATENT
SYNTHESIS
Inventor Samuel ChackalamannilMartin C. ClasbyWilliam J. GreenleeYuguang WangYan XiaEnrico P. VeltriMariappan ChelliahWenxue Wu
Original Assignee Schering Corporation
Priority date 2002-04-16
THE EXACT BELOW COMPD IS 14
Example 2
Step 1 :
Phosphonate 7, described in US 6,063,847, (3.27 g, 8.1 mmol) was dissolved in THF (12 ml) and C(O)Oled to 0 °C, followed by addition of 2.5 M n- BuLi (3.2 ml, 8.1 mmol). The reaction mixture was stirred at 0 °C for 10 min and warmed up to rt. A solution of aldehyde 6, described in US 6,063,847, in THF (12 ml) was added to the reaction mixture. The reaction mixture was stirred for 30 min. Standard aqueous work-up, followed by column chromatography (30-50% EtOAc in hexane) afforded product 8. 1HNMR (CDCI3): δ 0.92-1.38 (m, 31 H), 1.41 (d, J= 6 Hz, 3H), 1.40-1.55 (m, 2H), 1.70-1.80 (m, 2H), 1.81-1.90 (m, 2H), 2.36 (m, 2H), 2.69 (m, 1 H), 3.89 (m, 4H), 4.75 (m, 1 H), 6.28-6.41 (m, 2H), 7.05-7.15 (m, 2H), 8.19 (br s, 1 H). Step 2:
Compound 8 (2.64 g, 4.8 mmol) was dissolved in THF (48 ml). The reaction mixture was C(O)Oled to 0 °C followed by addition of 1 M TBAF (4.8 ml). The reaction mixture was stirred for 5 min followed by standard aqueous work-up. Column chromatography (50% EtOAc/hexane) afforded product 9 (1.9 g, 100%). 1HNMR (CDCI3): δ 1.15-1.55 (m, 6H), 1.41 (d, J= 6 Hz, 3H), 1.70-1.82 (m, 3H), 1.85-1.90 (m, 1 H), 2.36 (m, 2H), 2.69 (m, 1 H), 3.91 (m, 4H), 4.75 (m, 1 H), 6.18- 6.45 (m, 2H), 7.19 (br s, 2H), 8.19 (br s, 1 H). Step 3:
To a solution of compound 9 (250 mg, 0.65 mmol) in pyridine (5 ml) C(O)Oled to 0 °C was added Tf2O (295 μL, 2.1 mmol). The reaction mixture was stirred overnight at rt. Standard aqueous work-up followed by column chromatography afforded product 10 (270 mg, 80%). 1HNMR (CDCI3): δ 1.15-1.55 (m, 6H), 1.41 (d, J= 6 Hz, 3H), 1.70-1.82 (m, 3H), 1.85-1.90 (m, 1 H), 2.36 (m, 2H), 2.69 (m, 1 H), 3.91 (m, 4H), 4.75 (m, 1 H), 6.42-6.68 (m, 2H), 7.25 (m, 1 H), 7.55 (m, 1 H), 8.49 (d, J= 2.8 Hz, 1 H).
Compound 10 (560 mg, 1.1 mmol), 3-fluorophenyl boronic acid (180 mg, 1.3 mmol) and K2CO3 (500 mg, 3.6 mmol) were mixed with toluene (4.4 ml), H2O (1.5 ml) and EtOH (0.7 ml) in a sealed tube. Under an atmosphere of N2, Pd(Ph3P)4 (110 mg, 0.13 mmol) was added. The reaction mixture was heated at 100 °C for 2 h under N2. The reaction mixture was C(O)Oled down to rt, poured to EtOAc (30 ml) and washed with water (2X20 ml). The EtOAc solution was dried with NaHCO3 and concentrated at reduced pressure to give a residue. Preparative TLC separation of the residue (50% EtOAc in hexane) afforded product 11 (445 mg, 89%). 1HNMR (CDCI3): δ 1.15-1.59 (m, 6H), 1.43 (d, J= 6 Hz, 3H), 1.70-1.79 (m, 2H), 1.82 (m, 1H), 1.91 (m, 2H), 2.41 (m, 2H), 2.69 (m, 1 H), 3.91 (m, 4H), 4.75 (m, 1 H), 6.52-6.68 (m, 2H), 7.15 (m, 1 H), 7.22 (m, 2H), 7.35 (m, 1 H), 7.44 (m, 1 H), 7.81 (m, 1 H), 8.77 (d, J= 1.2 Hz, 1 H). Step 5:

Compound 11 (445 mg, 0.96 mmol) was dissolved in a mixture of acetone (10 ml) and 1 N HCI (10 ml). The reaction mixture was heated at 50 °C for 1 h.
Standard aqueous work-up followed by preparative TLC separation (50% EtOAc in hexane) afforded product 12 (356 mg, 89%). 1HNMR (CDCI3): δ 1.21-1.45 (m, 2H), 1.47 (d, J= 5.6 Hz, 3H), 1.58-1.65 (m, 2H), 2.15 (m, 1 H), 2.18-2.28 (m, 2H), 2.35- 2.51 (m, 5H), 2.71 (m, 1 H), 4.79 (m, 1 H), 6.52-6.68 (m, 2H), 7.15 (m, 1 H), 7.22 (m, 2H), 7.35 (m, 1 H), 7.44 (m, 1 H), 7.81 (m, 1 H), 8.77 (d, J= 1.2 Hz, 1 H). Step 6:
Compound 12 (500 mg, 4.2 mmol) was dissolved in EtOH (40 ml) and CH2CI2 (15 ml) NH3 (g) was bubbled into the solution for 5 min. The reaction mixture was C(O)Oled to 0 °C followed by addition of Ti(O/‘Pr)4 (1.89 ml, 6.3 mmol). After stirring at 0 °C for 1 h, 1 M TiCI (6.3 ml, 6.3 mmol) was added. The reaction mixture was stirred at rt for 45 min and concentrated to dryness under reduced pressure. The residue was dissolved in CH3OH (10 ml) and NaBH3CN (510 mg, 8 mmol) was added. The reaction mixture was stirred overnight at rt. The reaction mixture was poured to 1 N NaOH (100 ml) and extracted with EtOAc (3x 100 ml). The organic layer was combined and dried with NaHC03. Removal of solvent and separation by PTLC (5% 2 M NH3 in CH3OH/ CH2CI2) afforded β-13 (spot 1 , 30 mg, 6%) and α-13 (spot 2, 98 mg, 20%). β-13: 1HNMR (CDCI3): δ 1.50-1.38 (m, 5H), 1.42 (d, J= 6 Hz, 3H), 1.51-1.75 (m, 5H), 1.84 (m, 2H), 2.38 (m, 1 H), 2.45 (m, 1 H), 3.38 (br s, 1 H), 4.78 (m, 1 H), 6.59 (m, 2H), 7.15 (m, 1 H), 7.26 (m, 2H), 7.36 (m, 1 H), 7.42 (m, 1 H), 7.82 (m, 1 H), 8.77 (d, J= 2 Hz, 1 H). α-13:1HNMR (CDCI3): δ 0.95 (m, 2H), 1.02-1.35 (m, 6H), 1.41 (d, J= 6 Hz, 3H), 1.82-1.95 (m, 4H), 2.37 (m; 2H), 2.69 (m, 2H), 4.71 (m, 1 H), 6.71 (m, 2H), 7.11 (m, 1 H), 7.25 (m, 2H), 7.38 (m, 1 H), 7.42 (m, 1 H), 7.80 (m, 1 H), 8.76 (d, J= 1.6 Hz, 1 H). Step 7:
Compound α-13 (300 mg, 0.71 mmol) was dissolved in CH2CI2 (10 ml) followed by addition of Et3N (0.9 ml). The reaction mixture was C(O)Oled to 0 °C and ethyl chloroformate (0.5 ml) was added. The reaction mixture was stirred at rt for 1 h. The reaction mixture was directly separated by preparative TLC (EtOAc/ hexane, 1 :1) to give the title compound (14) VORAPAXAR (300 mg, 86%). MS m/z 493 (M+1).
HRMS Calcd for C29H34N2O4F (M+1 ): 493.2503, found 493.2509.
PATENT
SYNTHESIS 1
http://www.google.com/patents/WO2006076564A1
VORAPAXAR= COMPD A
Example 6 – Preparation of Compound A
To a three-neck flask equipped with an agitator, thermometer and nitrogen inertion was added 7A (13.0 g), THF (30 mL). The mixture was cooled to below -200C after which lithium diisopropylamide (2M, 20 mL) was slowly added. The reaction mixture was agitated for an additional hour (Solution A). To another flask was added 6 (10.0 g) and THF (75 mL) . The mixture was stirred for about 30 minutes and then slowly transferred into the solution A while maintaining the temperature below 200C. The mixture was stirred at below -200C for an additional hour before quenching the reaction by adding 20 mL of water. The reaction mixture was warmed to 00C and the pH was adjusted to about 7 by addition of 25% HaSO4 (11 mL). The mixture was further warmed to 200C and then diluted with 100 mL of ethyl acetate and 70 mL of water. The two phases that had formed were separated and the aqueous layer was extracted with 50 mL of ethyl acetate. The solvents THF and ethyl acetate were then replaced with ethanol, and the Compound A was precipitated out as a crystalline solid from ethanol with seeding at 35 to 4O0C. After cooling to O0C, the suspension was stirred for an additional hour and then the product was filtered and washed with cold ethanol. The product was dried at 50 – 600C under vacuum to provide an off-white solid. VORAPAXAR
Yield: 12.7 g, (90%). m.p. 104.90C (DSC onset point).
1H NMR (CDCl3) δ 8.88 (d, J = 2.4 Hz, IH), 8.10 (dd, J = 8.2, 2.4 Hz, IH), 7.64 (IH), 7.61 (d, J = 8.8 Hz, IH), 7.55 (m, J = 8.2, 6.2 Hz, IH), 7.51 (d, J = 8.0 Hz, IH), 7.25 (dt, J = 9.0, 2.3 Hz, IH), 7.08 (d, J = 8.0 Hz, IH), 6.68 (dd, J = 15.4, 9.4 Hz, IH), 6.58 (d, J = 9.6 Hz, IH), 4.85 (dd, J = 14.2, 7.2 Hz, IH), 3.95 (dd, J = 14.2, 7.1 Hz, 2H), 3.29 (m, IH), 2.66 (m, J = 12.0, 6.4 Hz, IH), 2.33 (m, 2H), 1.76 (m, 4H), 1.30 (d, J = 5.6 Hz, 3H), 1.19 (m, 4H), 1.14 (t, J = 7.2 Hz, 3H), 0.98 (m, IH), 0.84 (m, IH). MS (EI) m/z: calcd. 492, found 492.
BISULPHATE SALT
Example 7 – Preparation of an Acid Salt (bisulfate) of Compound A:
Compound IA (5 g) was dissolved in about 25 mL of acetonitrile.
The solution was agitated for about 10 minutes and then heated to about 50 0C. About 6 mL of 2M sulfuric acid in acetonitrile was added into the heated reaction mixture. The solid salt of Compound A precipitated out during the addition of sulfuric acid in acetonitrile. After addition of sulfuric acid solution, the reaction mixture was agitated for 1 hour before cooling to room temperature. The precipitated solid was filtered and washed with about 30 mL of acetonitrile. The wet solid was dried under vacuum at room temperature for 1 hour and at 80 0C for about 12 hours to provide about 5 g white solid (yield 85%). m.p. 217.0 0C. 1H NMR (DMSO) 9.04 (s, IH), 8.60 (d, J = 8.1 Hz, IH), 8.10 (d, J = 8.2 Hz, IH), 7.76 (d, J = 10.4, IH), 7.71 (d, J = 7.8 Hz, IH), 7.60 (dd, J = 8.4, 1.8 Hz, IH), 7.34 (dd, 8.4, 1.8 Hz, IH), 7.08 (d, J = 8.0 Hz, IH), 7.02 (m, IH), 6.69 (d, J = 15.8 Hz, IH), 4.82 (m, IH), 3.94 (dd, J = 14.0, 7.0 Hz, 2H), 3.35 (brs, IH), 2.68 (m, IH), 2.38 (m, 2H), 1.80-1.70 (m, 4H), 1.27 (d, J = 5.8 Hz, 3H), 1.21 (m, 2H), 1.13 (t, J = 7.0 Hz, 3H), 0.95 (m, IH, 0.85 (m, IH). MS (EI) m/z calcd. 590, found 492.
INTERMEDIATE 6
Example 5- Preparation of Compound 6
To a three-neck flask equipped with an agitator, thermometer and nitrogen inert were added the crude product solution of Compound 5 (containing about 31 g. of Compound 5 in 300 mL solution) and anhydrous DMF (0.05 mL). After the mixture was agitated for 5 minutes, oxalyl chloride (12.2 mL) was added slowly while maintaining the batch temperature between 15 and 25°C. The reaction mixture was agitated for about an hour after the addition and checked by NMR for completion of reaction. After the reaction was judged complete, the mixture was concentrated under vacuum to 135 mL while maintaining the temperature of the reaction mixture below 300C. The excess oxalyl chloride was removed completely by two cycles of vacuum concentration at below 500C with replenishment of toluene (315 mL) each time, resulting in a final volume of 68 mL. The reaction mixture was then cooled to 15 to 25°C, after which THF (160 mL) and 2,6-lutidine (22 mL) were added. The mixture was agitated for 16 hours at 20 to 25°C under 100 psi hydrogen in the presence of dry 5% Pd/C (9.0 g). After the reaction was judged complete, the reaction mixture was filtered through celite to remove catalyst. More THF was added to rinse the hydrogenator and catalyst, and the reaction mixture was again filtered through celite. Combined filtrates were concentrated under vacuum at below 25°C to 315 mL. MTBE (158 mL) and 10% aqueous solution of phosphoric acid (158 mL) were added for a thorough extraction at 100C to remove 2,6- lutidine. Then phosphoric acid was removed by extracting the organic layer with very dilute aqueous sodium bicarbonate solution (about 2%), which was followed by a washing with dilute brine. The organic solution was concentrated atmospherically to a volume of 90 mL for solvent replacement. IPA (315 mL) was added to the concentrated crude product solution. The remaining residual solvent was purged to <_ 0.5% of THF (by GC) by repeated concentration under vacuum to 68 mL, with replenishment of IPA (315 mL) before each concentration. The concentrated (68 mL) IPA solution was heated to 50°C, to initiate crystallization. To this mixture n-heptane (68 mL) was added very slowly while maintaining the batch temperature at 50°C. The crystallizing mixture was cooled very slowly over 2.5 hours to 25°C. Additional n- heptane (34 mL) was added very slowly into the suspension mixture at 250C. The mixture was further cooled to 200C, and aged at that temperature for about 20 hours. The solid was filtered and washed with a solvent mixture of 25% IPA in n-heptane, and then dried to provide
19.5 g of a beige colored solid of Compound 6. (Yield: 66%) m.p. 169.30C. IH NMR (CD3CN) δ 9.74 (d, J = 3.03 Hz, IH), 5.42 (br, IH), 4.69 (m, IH), 4.03 (q, J = 7.02 Hz, 2H), 3.43 (qt, J = 3.80, 7.84 Hz, IH), 2.67 (m, 2H), 2.50 (dt, J = 3.00, 8.52 Hz, IH), 1.93 (d, J = 12.0 Hz, 2H), 1.82 (dt, J = 3.28, 9.75 Hz, 2H), 1.54 (qd, J = 3.00, 10.5 Hz, IH), 1.27 (d, J = 5.97 Hz, 3H), 1.20 (m, 6H), 1.03 – 0.92 (m, 2H). MS (ESI) m/z (M++1): calcd. 324, found 324.
INTERMEDIATE 7A
Example 4 – Preparation of Compound 7A
+ 1-Pr2NLi + (EtO)2POCI – + LiCI
![]()
7A
To a 10 L three-necked round bottomed flask equipped with an agitator, thermometer and a nitrogen inlet tube, was added 20Og of
Compound 8 (1.07 mol, from Synergetica, Philadelphia, Pennsylvania). THF (1000 mL) was added to dissolve Compound 8. After the solution was cooled to -80 0C to -50 0C, 2.0 M LDA in hexane/THF(1175 mL, 2.2 eq) was added while maintaining the batch temperature below -50 0C. After about 15 minutes of agitation at -800C to -50 0C, diethyl chlorophosphate (185 mL, 1.2 eq) was added while maintaining the batch temperature below -50 0C. The mixture was agitated at a temperature from -800C to – 50 0C for about 15 minutes and diluted with n-heptane (1000 mL). This mixture was warmed up to about -35 0C and quenched with aqueous ammonium chloride (400 g in 1400 mL water) at a temperature below -10 0C. This mixture was agitated at -150C to -10 0C for about 15 minutes followed by agitation at 150C to 25 0C for about 15 minutes. The aqueous layer was split and extracted with toluene (400 mL). The combined organic layers were extracted with 2N hydrochloric acid (700 mL) twice. The product-containing hydrochloric acid layers were combined and added slowly to a mixture of toluene (1200 mL) and aqueous potassium carbonate (300 g in 800 mL water) at a temperature below 30 0C. The aqueous layer was extracted with toluene (1200 mL). The organic layers were combined and concentrated under vacuum to about 600 ml and filtered to remove inorganic salts. To the filtrate was added n-heptane (1000 ml) at about 55 0C. The mixture was cooled slowly to 40 0C, seeded, and cooled further slowly to -10 0C. The resulting slurry was aged at about -10 0C for 1 h, filtered, washed with n- heptane, and dried under vacuum to give a light brown solid (294 g, 85% yield), m.p. 52 0C (DSC onset point).1H NMR (CDCl3) δ 8.73 (d, J = 1.5 Hz, IH), 7.85 (dd, Ji = 8.0 Hz, J2 = 1.5 Hz, IH), 7.49 (dd, Ji = 8.0 Hz, J2 = 1.3 Hz, IH), 7.42 (m, IH), 7.32 (d, J = 7.8 Hz, IH), 7.24 (m, IH), 7.08 (dt, Ji = 8.3 Hz, J2 = 2.3 Hz, IH), 4.09 (m, 4H), 3.48 (d, J = 22.0 Hz, 2H), 1.27 (t, J = 7.0 Hz, 6H). MS (ESI) for M+H calcd. 324, found 324.
Example 3 – Preparation of Compound 5:

4 5
To a three-necked round bottomed flask equipped with an agitator, thermometer and a nitrogen inlet tube was added a solution of Compound 4 in aqueous ethanol (100 g active in 2870 ml). The solution was concentrated to about 700 ml under reduced pressure at 350C to 40°C to remove ethyl alcohol. The resultant homogeneous mixture was cooled to 200C to 300C and its pH was adjusted to range from 12 to 13 with 250 ml of 25% sodium hydroxide solution while maintaining the temperature at 20-300C. Then 82 ml of ethyl chloroformate was slowly added to the batch over a period of 1 hour while maintaining the batch temperature from 200C to 300C and aged for an additional 30 minutes. After the reaction was judged complete, the batch was acidified to pH 7 to 8 with 10 ml of concentrated hydrochloric acid (37%) and 750 ml of ethyl acetate. The pH of the reaction mixture was further adjusted to pH 2 to 3 with 35% aqueous hydrochloric acid solution. The organic layer was separated and the aqueous layer was extracted again with 750 ml of ethyl acetate. The combined organic layers were washed twice with water (200 ml) . Compound 5 was isolated from the organic layer by crystallization from ethyl acetate and heptane mixture (1: 1 mixture, 1500 ml) at about 700C to 80 0C. The solid was filtered at 500C to 60 °C, washed with heptane and then dried to provide an off-white solid (yield 50%). m.p. 197.7°C. 1HNMR (CD3CN) δ 5.31 (brs, IH), 4.67 (dt, J = 16.1, 5.9 Hz, IH), 4.03 (q, J = 7.1 Hz, 2H), 3.41 (m, IH), 2.55 – 2.70 (m, 2H), 1.87 – 1.92 (m, IH), 1.32 – 1.42 (m, IH), 1.30 (d, J = 5.92 Hz, 3H), 1.30 – 1.25 (m, 6H), 0.98 (qt, J = 15.7, 3.18 Hz, 2H). MS (ESI) M+l m/z calculated 340, found 340.
Example 2 – Preparation of Compound 4;

3 4
7.4 kg of ammonium formate was dissolved in 9L of water at 15- 250C, and then cooled to 0-100C. 8.9 kg of Compound 3 was charged at 0-150C followed by an addition of 89L of 2B ethyl alcohol. The batch was cooled to 0-50C 0.9 kg of 10% Palladium on carbon (50% wet) and 9 L of water were charged. The batch was then warmed to 18-280C and agitated for 5 hours, while maintaining the temperature between 18-28 0C. After the reaction was judged complete, 7 IL of water was charged. The batch was filtered and the wet catalyst cake was then washed with 8OL of water. The pH of the filtrate was adjusted to 1-2 with 4N aqueous hydrochloric acid solution. The solution was used in the next process step without further isolation. The yield is typically quantiative. m.p. 216.40C. IH NMR (D2O+1 drop HCl) δ 3.15 (m, IH), 2.76 (m, IH), 2.62 (m, IH), 2.48 (dd,J-5.75Hz, IH), 1.94 (m, 2H), 1.78 (m, 2H), 1.38 (m, 2H), 1.20 (m, 6H), 1.18 (m, IH), 0.98 (q,J=2.99Hz, IH).
Example 1 – Preparation of Compound 3
2B 3
To a reactor equipped with an agitator, thermometer and nitrogen, were added about 10.5 kg of 2B, 68 L of acetone and 68 L of IN aqueous hydrochloric acid solution. The mixture was heated to a temperature between 50 and 600C and agitated for about 1 hour before cooling to room temperature. After the reaction was judged complete, the solution was concentrated under reduced pressure to about 42 L and then cooled to a temperature between 0 and 50C. The cooled mixture was agitated for an additional hour. The product 3 was filtered, washed with cooled water and dried to provide an off-white solid (6.9 kg, yield 76%). m.p. 2510C. Η NMR (DMSO) δ 12.8 (s, IH), 4.72 (m, J = 5.90 Hz, IH), 2.58 (m, 2H), 2.40 (m, J = 6.03 Hz, 2H), 2.21 (dd, J = 19.0, 12.8 Hz, 3H), 2.05 (m, IH), 1.87 (q, J = 8.92 Hz, IH), 1.75 (m, IH), 1.55 (m, IH), 1.35 (q, J = 12.6 Hz, IH), 1.27 (d, J = 5.88 Hz, 3H). MS (ESI) M+l m/z calcd. 267, found 267.
NOTE
Compound 7A may be prepared from Compound 8 by treating Compound 8 with diethylchlorophosphate:
Compound 8 may be obtained by the process described by Kyoku, Kagehira et al in “Preparation of (haloaryl)pyridines,” (API Corporation, Japan). Jpn. Kokai Tokkyo Koho (2004). 13pp. CODEN: JKXXAF JP
2004182713 A2 20040702. Compound 8 is subsequently reacted with a phosphate ester, such as a dialkyl halophosphate, to yield Compound 7A. Diethylchlorophosphate is preferred. The reaction is preferably conducted in the presence of a base, such as a dialkylithium amide, for example diisopropyl lithium amide.
Paper
J Med Chem 2008, 51(11): 3061
http://pubs.acs.org/doi/abs/10.1021/jm800180e
The discovery of an exceptionally potent series of thrombin receptor (PAR-1) antagonists based on the natural product himbacine is described. Optimization of this series has led to the discovery of 4 (SCH 530348), a potent, oral antiplatelet agent that is currently undergoing Phase-III clinical trials for acute coronary syndrome (unstable angina/non-ST segment elevation myocardial infarction) and secondary prevention of cardiovascular events in high-risk patients.
Ethyl [(3aR,4aR,8aR,9aS)-9(S)-[(E)-2-[5-(3-fluorophenyl)-2-
pyridinyl]ethenyl]dodecahydro-1(R)-methyl-3-oxonaphtho[2,3-c]furan-6(R)-yl]carbamate (4).
4 (300 mg, 86%). MS m/z 493 (M+1).
HRMS Calcd for C29H34N2O4F
(M+1): 493.2503, found 493.2509; mp125 °C;
[]D20 6.6 (c 0.5, MeOH).
1HNMR (CDCl3):
http://pubs.acs.org/doi/suppl/10.1021/jm800180e/suppl_file/jm800180e-file002.pdf
0.88-1.18 (m, 5 H), 1.22-1.30 (m, 3 H), 1.43 (d, J = 5.85 Hz, 3 H), 1.88-2.10 (m, 4 H), 2.33-2.42 (m, 2 H),
2.75-2.67 (m, 1 H), 3.52-3.60 (m, 1 H), 4.06-4.14 (m, 2 H), 4.54-4.80 (m, 1 H), 4.71-4.77 (m, 1 H),
6.55-6.63 (m, 2 H), 7.07-7.12 (m, 1 H), 7.26-7.29 (m, 2 H), 7.34 (d, J = 8.05 Hz, 1 H), 7.41-7.46 (m, 1 H), 7.80-7.82 (m, 1 H), 8.76-8.71 (m, 1 H).
PATENT
IN 201621010411
An improved process for preparation of Vorapaxar intermediates and a novel polymorphic form of Vorapaxar
ALEMBIC PHARMACEUTICALS LIMITED
Vorapaxar Sulfate is indicated for the reduction of thrombotic cardiovascular events in patients with a history of myocardial infarction (MI) or with peripheral arterial disease (PAD). ZONTIVITY has been shown to reduce the rate of a combined endpoint of cardiovascular death, MI, stroke, and urgent coronary revascularization (UCR).
According to present invention Vorapaxar sulfate is synthesized from compound of formula 1.
wherein R1 and R2 are each independently selected from the group consisting of H, alkyl, alkenyl, alkynyl, alkoxy, cycloalkyl, aryl, alkylaryl, arylalkyl, and heteroaryl groups. Process for the preparation of compound of formula 1 is disclosed in U.S Pat. No. 7,605,275. It disclosed preparation of compound of formula 1 via cyclization of compound 2 in presence of solvent selected from xylene, N-methylpyrrolidinone, Dimethylsulfoxide, diphenyl ether, dimethylacetamide. This cyclization step takes approximately 6-8 hrs.
There is need to develop a process which takes less time for cyclization step to prepare compound of formula 1. Therefore, our scientist works tenaciously to develop process which takes approximately 1-2 hrs for cyclization of compound 1.
5 According to present invention Vorapaxar sulfate is synthesized from intermediate compound of formula-II.
Formula-II Compound of formula-II is critical intermediate in the preparation of Vorapaxar Sulfate.
10 Patent WO2006076415 discloses the process of preparation of above Formula-II in example 7, in which purification/crystallisation step involves treating the reaction mixture having compound of Formula-II with an ethanol/water mixture followed by azeotropic distillation of the mixture. This process yielded formula-II with low yields and with low purities. WO2009055416 (page 9, second paragraph) discloses that use of various solvent systems for
15 formula-II purification such as Methyl-tert-Butyl Ether (MTBE) and various solvent/antisolvent systems, for example, ethylacetate/heptane and toluene/heptane and by using these solvent systems, compound of formula-II are obtained as oil. These oils did not yield a reduced impurity profile in synthesis of the compound of Formula II, nor provide an improvement in the quality of the product compound of Formula II.
20 The inventors surprisingly found that using the process according to the invention provides formula-II with improved yield and high purity. Further, present invention provides a process for the preparation of novel crystalline form of Vorapaxar base. The present invention also relates to novel impurity and process for its preparation.
U.S.Pat. No. 7,304,078 discloses Vorapaxar base. U.S.Pat. No. 7,235,567 discloses Polymorph I and II of vorapaxar sulphate
Example 1- Preparation of compound 1a:
Process A: 5.0 g of compound 2a was suspended in 10.0 ml silicone oil at room temperature. The reaction mixture was then heated to 125°C and stirred for 30 min. Then reaction mass was further heated up to 150°C and stirred for 30 min. After completion of reaction, the reaction mass was cooled to 50-60°C and 25 ml of cyclohexane was added to the reaction mass. The reaction mass was cooled slowly up to room temperature and stirred for 30 min.
15 The precipitated product was filtered off and washed with 5.0 ml Cyclohexane. Wet solid was suspended in mixture of 45.0 ml isopropyl alcohol and 20.0 ml denatured ethanol at 40-45°C and further epimerized with 0.17 ml DBU. The crystallized solid was filtered off with suction, washed with mixture of 1.5 ml Isopropyl alcohol and 0.67 ml denatured ethanol and dried.
20 Process B: 5.0 g of compound 2a was suspended in 10.0 ml paraffin oil at room temperature. The reaction mixture was then heated to 125°C and stirred for 30 min. Then reaction mass was further heated up to 150°C and stirred for 30 min. After completion of reaction, the reaction mass was cooled to 50-60°C and 25 ml of cyclohexane was added to the reaction mass. The reaction mass was cooled slowly up to room temperature and stirred for 30 min.
25 The precipitated product was filtered off and washed with 5.0 ml Cyclohexane. Wet solid was suspended in mixture of 45.0 ml isopropyl alcohol and 20.0 ml denatured ethanol at 40-45°C and further epimerized with 0.17 ml DBU. The crystallized solid was filtered off with suction, washed with mixture of 1.5 ml Isopropyl alcohol and 0.67 ml denatured ethanol and dried. Yield: 4.3 g
Process C: 5.0 g of compound 2a was charged in reaction vessel at room temperature. The solid was then heated to 125°C and stirred for 30 min. Then reaction mass was further heated up to 150°C and stirred for 30 min. After completion of reaction, the reaction mass was cooled to 50-60°C and was added mixture of 45.0 ml isopropyl alcohol and 20.0 ml
5 denatured ethanol at 50-60°C. This was cooled to 40-45°C and further epimerized with 0.17 ml DBU. The crystallized solid was filtered off with suction, washed with mixture of 1.5 ml Isopropyl alcohol and 0.67 ml denatured ethanol and dried. Yield: 4.5 g Example 2: Preparation of Intermediate (Formula-II) of vorapaxar
10 Example 2(a): 50.0g of 1,3,3a,4,4a,5,6,7,8,9a-Decahydro-3-methyl-7-nitro-1-oxo-N,Ndiphenylnaphtho[2,3-c]furan-4-carboxamide compound was suspended in 300.0 ml THF, 15 g 10% Pd/C (50% wet) and 200 ml Process water at room temperature. The reaction mixture was heated to 45°C and drop wise formic acid (35 ml) was added and then stirred for 15 hrs. After completion of reaction, the reaction mass was cooled to 25-30°C and 100 ml THF was
15
added and pH was made acidic with 2M sulfuric acid solution. The reaction mass was filtered and washed with 150 ml THF, 150 ml water. Organic and aqueous layer were separated and aqueous layer was extracted with THF. Organic layers were combined and washed with water. The organic layer was cooled up to 5-10°C, 20 ml of TEA and 13 ml of Ethyl chloro formate were added. The reaction mass was stirred for 30 min. After completion of reaction,
20
reaction mass was washed with 2M sulfuric acid solution and distilled out reaction mass completely under vacuum. Acetonitrile (50 ml) was added to residue and heated up to 40- 45°C. Cooled the reaction mass up to 25-30°C and filtered the solid. Purity: 94-96% Example 2(b): Crystallization with Acetonitrile Acetonitrile (50 ml) was added to above obtained solid and heated to 40-45°C. Cooled the
25 reaction mass slowly up to 25-30°C and then up to 5-10°C. The reaction mass was stirred and the solid was filtered. XRD: Fig-1 Purity: 98-99% Example 2(c): Crystallization with Ethyl acetate To the solid obtained in example-1(a) Ethyl acetate (30 ml) was added. The reaction mass was heated up to 70-75°C and stirred for 10-15 min. The reaction mass was cooled slowly up 30 to 25-30°C and then up to 5-10°C. The reaction mass was stirred for 30 min. The solid was filtered and washed with Ethyl acetate. XRD: Fig-2 Purity: 98-99%
Example 3: Preparation of Amorphous Form of Vorapaxar base Vorapaxar base (10.0 g) was dissolved in 500 ml of 40% Ethyl acetate in Cyclohexane. The solvent was then completely removed under vacuum at 45-50o C to give a solid. Yield: 9.8 g
Example 3 (a): Preparation of crystalline vorapaxar base 5 (2-{[Ethyl (ethylperoxy)phosphory]methyl}-5-(3-fluorophenyl)pyridine) (10 g) was dissolved in THF (30ml) at 25±5°C under Nitrogen. Cool the reaction mass up to -30 to – 50°C. Add drop wise LDA (2.0 M solution in THF). After 1 hr add drop wise (N- [(1R,3aR,4aR,6R,8aR,9S,9aS)-9-formyl dodecahydro-1-methyl-3-oxonaphtho[2,3-c]furan-6- yl]-ethyl ester Carbamic acid) solution (10 g dissolved in 70 ml THF). After completion of 10 reaction mass quench the reaction mass to sulphuric acid solution. Separate the layers and distilled out organic layer under vacuum get foamy residue. (purity 82%) Add MIBK (10 ml) in above residue and stir it at 40-50°C till clear solution. Add drop wise n-Heptane (10 ml) and stir the reaction mass for 30 min. Gradually cool the reaction mass up to 25-30°C. Stir the reaction mass for 24 hrs. Filter the solid and washed it with n-Heptane (5.0 ml). Dry the 15 solid. Yield: 7.0 g. XRD: Fig-3 purity 96%
Example 3(b): Preparation of crystalline vorapaxar base Vorapaxar advance intermediate (2-{[Ethyl (ethylperoxy)phosphory]methyl}-5-(3- fluorophenyl)pyridine) (10 g) was dissolved in THF (30ml) at 25±5°C under Nitrogen. Cool the reaction mass up to -30 to -50°C. Add drop wise LDA (2.0 M solution in THF). After a 1
20 hr add drop wise VORA-Aldehyde (N-[(1R,3aR,4aR,6R,8aR,9S,9aS)-9-formyl dodecahydro1-methyl-3-oxonaphtho[2,3-c]furan-6-yl]-ethyl ester Carbamic acid) solution (10 g dissolved in 70 ml THF). After completion of reaction mass quench the reaction mass to sulphuric acid solution. Separate the layers and distilled out organic layer under vacuum get foamy residue (purity 82%). Add MTBE (10 ml) in above residue and stir it at 40-50°C till clear solution.
25 Add drop wise n-Heptane (30 ml) and stir the reaction mass for 30 min. Gradually cool the reaction mass up to 25-30°C. Stir the reaction mass for 24 hrs. Filter the solid and washed it with n-Heptane (5.0 ml). Dry the solid. Yield: 8.5.0 g. XRD: Fig-4 purity 97%
References
- Samuel Chackalamannil; Wang, Yuguang; Greenlee, William J.; Hu, Zhiyong; Xia, Yan; Ahn, Ho-Sam; Boykow, George; Hsieh, Yunsheng et al. (2008). “Discovery of a Novel, Orally Active Himbacine-Based Thrombin Receptor Antagonist (SCH 530348) with Potent Antiplatelet Activity”. Journal of Medicinal Chemistry 51 (11): 3061–4.doi:10.1021/jm800180e. PMID 18447380.
- Merck Blood Thinner Studies Halted in Select Patients, Bloomberg News, January 13, 2011
- Tricoci et al. (2012). “Thrombin-Receptor Antagonist Vorapaxar in Acute Coronary Syndromes”. New England Journal of Medicine 366 (1): 20–33.doi:10.1056/NEJMoa1109719. PMID 22077816.
- Morrow, DA; Braunwald, E; Bonaca, MP; Ameriso, SF; Dalby, AJ; Fish, MP; Fox, KA; Lipka, LJ; Liu, X; Nicolau, JC; Ophuis, AJ; Paolasso, E; Scirica, BM; Spinar, J; Theroux, P; Wiviott, SD; Strony, J; Murphy, SA; TRA 2P–TIMI 50 Steering Committee and, Investigators (Apr 12, 2012). “Vorapaxar in the secondary prevention of atherothrombotic events.”. The New England Journal of Medicine 366 (15): 1404–13. doi:10.1056/NEJMoa1200933.PMID 22443427.
- “Merck Statement on FDA Advisory Committee for Vorapaxar, Merck’s Investigational Antiplatelet Medicine”. Merck. Retrieved 16 January 2014.
- http://www.forbes.com/sites/larryhusten/2014/01/15/fda-advisory-panel-votes-in-favor-of-approval-for-mercks-vorapaxar/
- SCH-530348 (Vorapaxar) is an investigational candidate for the prevention of arterial thrombosis in patients with acute coronary syndrome and peripheral arterial disease. “Convergent Synthesis of Both Enantiomers of 4-Hydroxypent-2-ynoic Acid Diphenylamide for a Thrombin Receptor Antagonist Sch530348 and Himbacine Analogues.” Alex Zaks et al.: Adv. Synth. Catal. 2009, 351: 2351-2357 Full text;
- Discovery of a novel, orally active himbacine-based thrombin receptor antagonist (SCH 530348) with potent antiplatelet activity
J Med Chem 2008, 51(11): 3061
- Stu Borman (2005). “Hopes Ride on Drug Candidates: Researchers reveal potential new medicines for thrombosis, anxiety, diabetes, and cancer”. Chemical & Engineering News 83 (16): 40–44.
PATENTS
- WO 2003089428
- WO 2006076452
- US 6063847
- WO 2006076565
- WO 2008005344
- WO2010/141525
- WO2008/5353
- US2008/26050
- WO2006/76564 mp, nmr
|
3-21-2012
|
EXO-SELECTIVE SYNTHESIS OF HIMBACINE ANALOGS
|
|
|
10-14-2011
|
EXO- AND DIASTEREO- SELECTIVE SYNTHESIS OF HIMBACINE ANALOGS
|
|
|
8-3-2011
|
Exo- and diastereo-selective syntheses of himbacine analogs
|
|
|
3-18-2011
|
COMBINATION THERAPIES COMPRISING PAR1 ANTAGONISTS WITH NAR AGONISTS
|
|
|
8-11-2010
|
Exo-selective synthesis of himbacine analogs
|
|
|
6-4-2010
|
SYNTHESIS Of DIETHYLPHOSPHONATE
|
|
|
5-12-2010
|
THROMBIN RECEPTOR ANTAGONISTS
|
|
|
3-31-2010
|
Synthesis of diethyl{[5-(3-fluorophenyl)-pyridine-2yl]methyl}phosphonate
|
|
|
12-4-2009
|
Local Delivery of PAR-1 Antagonists to Treat Vascular Complications
|
|
|
12-2-2009
|
SYNTHESIS OF HIMBACINE ANALOGS
|
|
10-21-2009
|
Exo- and diastereo- selective syntheses of himbacine analogs
|
|
|
6-31-2009
|
Synthesis of 3-(5-nitrocyclohex-1-enyl) acrylic acid and esters thereof
|
|
|
6-3-2009
|
Synthesis of himbacine analogs
|
|
|
1-23-2009
|
METHODS AND COMPOSITIONS FOR TREATING CARDIAC DYSFUNCTIONS
|
|
|
9-26-2008
|
REDUCTION OF ADVERSE EVENTS AFTER PERCUTANEOUS INTERVENTION BY USE OF A THROMBIN RECEPTOR ANTAGONIST
|
|
|
2-8-2008
|
IMMEDIATE-RELEASE TABLET FORMULATIONS OF A THROMBIN RECEPTOR ANTAGONIST
|
|
|
1-32-2008
|
SOLID DOSE FORMULATIONS OF A THROMBIN RECEPTOR ANTAGONIST
|
|
|
12-5-2007
|
Thrombin receptor antagonists
|
|
|
11-23-2007
|
THROMBIN RECEPTOR ANTAGONISTS
|
|
|
8-31-2007
|
THROMBIN RECEPTOR ANTAGONISTS AS PROPHYLAXIS TO COMPLICATIONS FROM CARDIOPULMONARY SURGERY
|
|
8-31-2007
|
CRYSTALLINE POLYMORPH OF A BISULFATE SALT OF A THROMBIN RECEPTOR ANTAGONIST
|
|
|
6-27-2007
|
Crystalline polymorph of a bisulfate salt of a thrombin receptor antagonist
|
|
|
8-4-2006
|
Preparation of chiral propargylic alcohol and ester intermediates of himbacine analogs
|
|
|
9-31-2004
|
Methods of use of thrombin receptor antagonists
|
| US6063847 * | Nov 23, 1998 | May 16, 2000 | Schering Corporation | Thrombin receptor antagonists |
| US6326380 * | Apr 7, 2000 | Dec 4, 2001 | Schering Corporation | Thrombin receptor antagonists |
| US20030216437 * | Apr 14, 2003 | Nov 20, 2003 | Schering Corporation | Thrombin receptor antagonists |
| US20040176418 * | Jan 9, 2004 | Sep 9, 2004 | Schering Corporation | Crystalline polymorph of a bisulfate salt of a thrombin receptor antagonist |
| WO2011128420A1 | Apr 14, 2011 | Oct 20, 2011 | Sanofi | Pyridyl-vinyl pyrazoloquinolines as par1 inhibitors |
//////////////fast track designation , VORAPAXAR, FDA 2014, EU 2016, Zontivity, NDA 204886, MERCK, VORAPAXAR SULPHATE
CCOC(=O)NC1CCC2C(C1)CC3C(C2C=CC4=NC=C(C=C4)C5=CC(=CC=C5)F)C(OC3=O)C
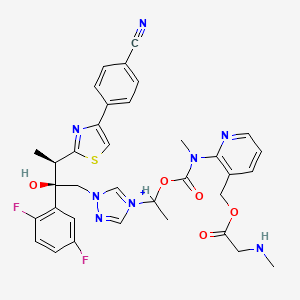
Isavuconazonium sulfate, Изавуконазониев сулфат


| MOLECULAR FORMULA: | C35H36F2N8O9S2 |
|---|---|
| MOLECULAR WEIGHT: | 814.837 g/mol |


Syn……https://newdrugapprovals.org/2013/10/02/isavuconazole-basilea-reports-positive-results-from-study/
PRODUCT PATENT
https://patents.google.com/patent/US6300353
InventorTadakatsu HayaseShigeyasu IchiharaYoshiaki IsshikiPingli LiuJun OhwadaToshiya SakaiNobuo ShimmaMasao TsukazakiIsao UmedaToshikazu Yamazaki
Current Assignee Basilea Pharmaceutica International Ltd Original
AssigneeBasilea Pharmaceutica AG Priority date 1998-03-06
https://patents.google.com/patent/WO1999045008A1/en
POLYMORPHS OF BASE
WO 2016055918
https://patents.google.com/patent/WO2016055918A1/en
PATENT
IN 2014MU03189
WOCKHARDT
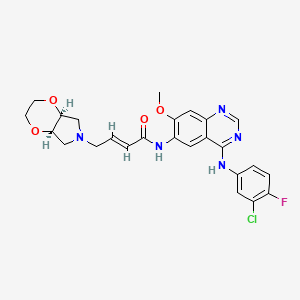
Isavuconazole, isavuconazonium, Voriconazole, and Ravuconazole are azole derivatives and known as antifungal drugs for treatment of systemic mycoses as reported in US 5,648,372, US 5,792,781, US 6,300,353 and US 6,812,238. The US patent No. 6,300,353 discloses Isavuconazole and its process. It has chemical name [(2R,3R)-3-[4-(4-cyanophenyl)thiazol-2-yl)]-1-(1H-1,2,4-triazol-1-yl)-2-(2,5- difluorophenyl)-butan-2-ol;
The Isavuconazonium iodide hydrochloride and Isavuconazonium sulfate can be prepared according to known methods, e.g. pending Indian Patent Applications IN 2424/MUM/2014 and IN 2588/MUM/2014.
Example-1: Preparation of Amorphous Isavuconazole
4-cyano Phenacyl bromide F F N N N OH N S CN Formula-I Formula-III In a round bottomed flask charged ethanol (250 ml), thioamide compound of formula-II (25.0 gm) and 4-cyano phenacyl bromide (18.4 gm) under stirring. The reaction mixture were heated to 70 0C. After completion of reaction the solvent was removed under vacuum distillation and water (250 ml) and Ethyl acetate (350 ml) were added to reaction mass. The reaction mixture was stirred and its pH was adjusted between 7 to 7.5 by 10 % solution of sodium bicarbonate. The layer aqueous layer was discarded and organic layer was washed with saturated sodium chloride solution (100 ml) and concentrated under vacuum to get residue. The residue was suspended in methyl tert-butyl ether (250 ml) and the reaction mixture was heated to at 40°C to make crystals uniform and finally reaction mass is cooled to room temperature filtered and washed with the methyl tert-butyl ether. The product was isolated dried to get pale yellowish solid product. Yield: 26.5 gm HPLC purity: 92.7%
CLIP
March 6, 2015
Release
The U.S. Food and Drug Administration today approved Cresemba (isavuconazonium sulfate), a new antifungal drug product used to treat adults with invasive aspergillosis and invasive mucormycosis, rare but serious infections.
Aspergillosis is a fungal infection caused by Aspergillus species, and mucormycosis is caused by the Mucorales fungi. These infections occur most often in people with weakened immune systems.
Cresemba belongs to a class of drugs called azole antifungal agents, which target the cell wall of a fungus. Cresemba is available in oral and intravenous formulations.
“Today’s approval provides a new treatment option for patients with serious fungal infections and underscores the importance of having available safe and effective antifungal drugs,” said Edward Cox, M.D., M.P.H, director of the Office of Antimicrobial Products in the FDA’s Center for Drug Evaluation and Research.
Cresemba is the sixth approved antibacterial or antifungal drug product designated as a Qualified Infectious Disease Product (QIDP). This designation is given to antibacterial or antifungal drug products that treat serious or life-threatening infections under the Generating Antibiotic Incentives Now (GAIN) title of the FDA Safety and Innovation Act.
As part of its QIDP designation, Cresemba was given priority review, which provides an expedited review of the drug’s application. The QIDP designation also qualifies Cresemba for an additional five years of marketing exclusivity to be added to certain exclusivity periods already provided by the Food, Drug, and Cosmetic Act. As these types of fungal infections are rare, the FDA also granted Cresemba orphan drug designations for invasive aspergillosis and invasive mucormycosis.
The approval of Cresemba to treat invasive aspergillosis was based on a clinical trial involving 516 participants randomly assigned to receive either Cresemba or voriconazole, another drug approved to treat invasive aspergillosis. Cresemba’s approval to treat invasive mucormycosis was based on a single-arm clinical trial involving 37 participants treated with Cresemba and compared with the natural disease progression associated with untreated mucormycosis. Both studies showed Cresemba was safe and effective in treating these serious fungal infections.
The most common side effects associated with Cresemba include nausea, vomiting, diarrhea, headache, abnormal liver blood tests, low potassium levels in the blood (hypokalemia), constipation, shortness of breath (dyspnea), coughing and tissue swelling (peripheral edema). Cresemba may also cause serious side effects including liver problems, infusion reactions and severe allergic and skin reactions.
Cresemba is marketed by Astellas Pharma US, Inc., based in Northbrook, Illinois.

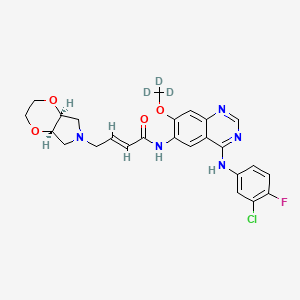
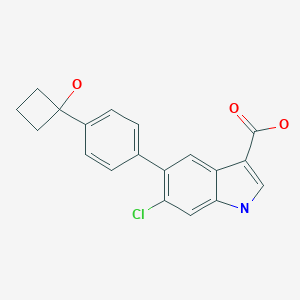
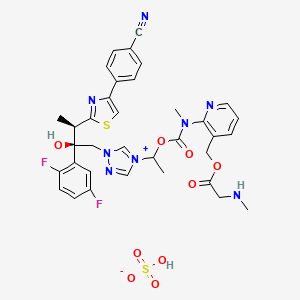
The active substance is isavuconazonium sulfate, a highly water soluble pro-drug of the active triazole isavuconazole. The chemical name of the active substance isavuconazonium sulfate is 1-{(2R,3R)-3-[4-(4-cyanophenyl)-1,3- thiazol-2-yl]-2-(2,5-difluoro-phenyl)-2-hydroxybutyl}-4-[(1RS)-1-({methyl[3-({[(methylamino)acetyl] oxy}methyl) pyridin-2-yl]carbamoyl}oxy)ethyl]-1H-1,2,4-triazol-4-ium monosulfate (IUPAC), corresponding to the molecular formula C35H35F2N8O5S·HSO4 and has a relative molecular mass of 814.84 g/mol. The relative molecular mass of isavuconazole is 437.47. The active substance has the following structure:

The structure of the active substance has been confirmed by elemental analysis, mass spectrometry, UV, IR, 1H-, 13C- and 19F-NMR spectrometry, and single crystal X-ray analysis, all of which support the chemical structure. It appears as a white, amorphous, hygroscopic powder. It is very soluble in water and over the pH range 1-7. It is also very soluble in methanol and sparingly soluble in ethanol. Two pKa values have been found and calculated to be 2.0 and 7.3. Its logPoct/wat calculated by software is 1.31.
Isavuconazonium sulfate has three chiral centres. The stereochemistry of the active substance is introduced by one of the starting materials which is controlled by appropriate specification. The two centres, C7 and C8 in the isavuconazole moiety and in an intermediate of the active substance, have R configuration. The third chiral centre, C29, is not located on isavuconazole moiety and has both the R and S configurations. The nondefined stereo centre at C29 has been found in all batches produced so far to be racemic. Erosion of stereochemical purity has not been observed in the current process. The active substance is a mixture of two epimers of C29.
An enantiomer of drug substance was identified as C7 (S), C8 (S) and C29 (R/S) structure. The control of the stereochemistry of isavuconazonium sulfate is performed by chiral HPLC on the active substance and its two precursors. Subsequent intermediates are also controlled by relevant specification in the corresponding steps. Two crystal forms have been observed by recrystallisation studies. However the manufacturing process as described yields amorphous form only.
Two different salt forms of isavuconazonuium (chloride and sulfate) were identified during development. The sulfate salt was selected for further development. A polymorph screening study was also performed. None of the investigated salts could be obtained in crystalline Form………http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/002734/WC500196130.pdf




Clip
Isavuconazonium (Cresemba ) is a water-soluble prodrug of the triazole antifungal isavuconazole (BAL4815), a 14-a-demethylase inhibitor, under development byBasilea Pharmaceutica International Ltd and Astellas Pharma Inc. Isavuconazonium, in both its intravenous and oral formulations, was approved for the treatment of invasive aspergillosis and invasive mucormycosis (formerly termed zygomycosis) in the US in March 2015. Isavuconazonium is under regulatory review in the EU for invasive aspergillosis and mucormycosis. It is also under phase III development worldwide for the treatment of invasive candidiasis and candidaemia. This article summarizes the milestones in the development of isavuconazonium leading to the first approval for invasive spergillosis and mucormycosis.
Introduction
The availability of both an intravenous (IV) and an oral formulation of isavuconazonium (Cresemba ), as a result of its water solubility, rapid hydrolysis to the active entity isavuconazole and very high oral bioavailability, provides maximum flexibility to clinicians for treating seriously ill patients with invasive fungal infections [1]. Both the IV and oral formulations have been approved by the US Food and Drug Administration (FDA) to treat adults with invasive aspergillosis and invasive mucormycosis [2]. The recommended dosages of each formulation are identical, consisting of loading doses of 372 mg (equivalent to 200 mg of isavuconazole) every eight hours for six doses, followed by maintenance therapy with 372 mg administered once daily [3]. The Qualified Infectious Disease Product (QIDP) designation of the drug with priority review status by the FDA isavuconazonium in the US provided and a five year extension of market exclusivity from launch. Owing to the rarity of the approved infections,
isavuconazonium was also granted orphan drug designation by the FDA for these indications [2]. It has also been granted orphan drug and QIDP designation in the US for the treatment of invasive candidiasis [4]. In July 2014, Basilea Pharmaceutica International Ltd submitted a Marketing Authorization Application to the European Medicines Agency (EMA) for isavuconazonium in the treatment of invasive aspergillosis and invasive mucormycosis, indications for which the EMA has granted isavuconazonium orphan designation [5, 6]. Isavuconazonium is under phase III development in many countries worldwide for the treatment of invasive candidiasis and candidaemia.
1.1 Company agreements
In 2010, Basilea Pharmaceutica International Ltd (a spinoff from Roche, founded in 2000) entered into a licence agreement with Astellas Pharma Inc in which the latter would co-develop and co-promote isavuconazonium worldwide, including an option for Japan. In return for milestone payments, Astellas Pharma was granted an exclusive right to commercialize isavuconazonium, while Basilea Pharmaceutica retained an option to co-promote the drug in the US, Canada, major European countries and China [7]. The companies amended their agreement in 2014, making Astellas Pharma responsible for all regulatory filings, commercialization and manufacturing of isavuconazonium in the US and Canada. Basilea Pharmaceutica waived its right to co-promote the product in the US and Canada, in order to assume all rights in the rest of the world [8]. However, Astellas Pharma remains as sponsor of the multinational, phase III ACTIVE trial in patients with invasive candidiasis.
2 Scientific Summary
Isavuconazonium (as the sulphate; BAL 8557) is a prodrug that is rapidly hydrolyzed by esterases (mainly butylcholinesterase) in plasma into the active moiety isavuconazole
(BAL 4815) and an inactive cleavage product (BAL 8728).
References
1. Falci DR, Pasqualotto AC. Profile of isavuconazole and its potential in the treatment of severe invasive fungal infections. Infect Drug Resist. 2013;6:163–74.
2. US Food and Drug Administration. FDA approves new antifungal drug Cresemba. 2015. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm437106.htm. Accessed 12 Mar 2015.
3. US Food and Drug Administration. Cresemba (isavuconazonium sulfate): US prescribing information. 2015. http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/207500Orig1s000lbl.pdf. Accessed 18 Mar 2015.
4. Astellas Pharma US Inc. FDA grants Astellas Qualified Infectious Disease Product designation for isavuconazole for the treatment of invasive candidiasis (media release). 2014. http://newsroom astellas.us/2014-07-16-FDA-Grants-Astellas-Qualified-Infectious-Disease-Product-Designation-for-Isavuconazole-for-the-Treatmentof-Invasive-Candidiasis.
5. European Medicines Agency. Public summary of opinion on orphan designation: isavuconazonium sulfate for the treatment of invasive aspergillosis. 2014. http://www.ema.europa.eu/docs/en_GB/document_library/Orphan_designation/2014/07/WC500169890.pdf. Accessed 18 Mar 2015.
European Medicines Agency. Public summary of opinion on orphan designation: isavuconazonium sulfate for the treatment of mucormycosis. 2014. http://www.ema.europa.eu/docs/en_GB/document_library/Orphan_designation/2014/07/WC500169714.pdf. Accessed 18 Mar 2015.
7. Basilea Pharmaceutica. Basilea announces global partnership with Astellas for its antifungal isavuconazole (media release).2010. http://www.basilea.com/News-and-Media/Basilea-announcesglobal-partnership-with-Astellas-for-its-antifungal-isavuconazole/343.
8. Basilea Pharmaceutica. Basilea swaps its isavuconazole North American co-promote rights for full isavuconazole rights outside of North America (media release). 2014. http://www.basilea.com/News-and-Media/Basilea-swaps-its-isavuconazole-North-Americanco-promote-rights-for-full-isavuconazole-rights-outside-
CLIP

http://www.jpharmsci.org/article/S0022-3549(15)00035-0/pdf
A CLIP
http://www.accessdata.fda.gov/drugsatfda_docs/nda/2015/207500Orig1207501Orig1s000ChemR.pdf
EMA
On 4 July 2014 orphan designation (EU/3/14/1284) was granted by the European Commission to Basilea Medical Ltd, United Kingdom, for isavuconazonium sulfate for the treatment of invasive aspergillosis.
Update: isavuconazonium sulfate (Cresemba) has been authorised in the EU since 15 October 2015. Cresemba is indicated in adults for the treatment of invasive aspergillosis.
Consideration should be given to official guidance on the appropriate use of antifungal agents.
The active substance is isavuconazonium sulfate, a highly water soluble pro-drug of the active triazole isavuconazole. The chemical name of the active substance isavuconazonium sulfate is 1-{(2R,3R)-3-[4-(4-cyanophenyl)-1,3- thiazol-2-yl]-2-(2,5-difluoro-phenyl)-2-hydroxybutyl}-4-[(1RS)-1-({methyl[3-({[(methylamino)acetyl] oxy}methyl) pyridin-2-yl]carbamoyl}oxy)ethyl]-1H-1,2,4-triazol-4-ium monosulfate (IUPAC), corresponding to the molecular formula C35H35F2N8O5S·HSO4 and has a relative molecular mass of 814.84 g/mol. The relative molecular mass of isavuconazole is 437.47. The active substance has the following structure
It appears as a white, amorphous, hygroscopic powder. It is very soluble in water and over the pH range 1-7. It is also very soluble in methanol and sparingly soluble in ethanol. Two pKa values have been found and calculated to be 2.0 and 7.3. Its logPoct/wat calculated by software is 1.31.
Isavuconazonium sulfate has three chiral centres. The stereochemistry of the active substance is introduced by one of the starting materials which is controlled by appropriate specification. The two centres, C7 and C8 in the isavuconazole moiety and in an intermediate of the active substance, have R configuration. The third chiral centre, C29, is not located on isavuconazole moiety and has both the R and S configurations. The nondefined stereo centre at C29 has been found in all batches produced so far to be racemic. Erosion of stereochemical purity has not been observed in the current process. The active substance is a mixture of two epimers of C29. An enantiomer of drug substance was identified as C7 (S), C8 (S) and C29 (R/S) structure. The control of the stereochemistry of isavuconazonium sulfate is performed by chiral HPLC on the active substance and its two precursors.
FDA Orange Book Patents
US 6812238
US 7459561
FREE FORM
Isavuconazonium; Isavuconazonium ion; Cresemba; BAL-8557; 742049-41-8;
[2-[1-[1-[(2R,3R)-3-[4-(4-cyanophenyl)-1,3-thiazol-2-yl]-2-(2,5-difluorophenyl)-2-hydroxybutyl]-1,2,4-triazol-4-ium-4-yl]ethoxycarbonyl-methylamino]pyridin-3-yl]methyl 2-(methylamino)acetate
| MOLECULAR FORMULA: | C35H35F2N8O5S+ |
|---|---|
| MOLECULAR WEIGHT: | 717.773 g/mol |
Patent IDDatePatent Title
US20102494262010-09-30STABILIZED PHARMACEUTICAL COMPOSITION
US74595612008-12-02N-substituted carbamoyloxyalkyl-azolium derivativesUS71898582007-03-13N-phenyl substituted carbamoyloxyalkyl-azolium derivatives
US71511822006-12-19Intermediates for N-substituted carbamoyloxyalkyl-azolium derivatives
US68122382004-11-02N-substituted carbamoyloxyalkyl-azolium derivatives
REF
http://www.drugbank.ca/drugs/DB06636
////////// BAL 8557, BAL-8557-002, CRESEMBA, ISAVUCONAZONIUM SULFATE, QIDP designation, Cresemba , priority review, FDA 2015, EU 2015, BAL8557-002, BCS CLASS I, orphan designation, invasive aspergillosis, invasive mucormycosis, RO-0098557 , AK-1820, fast track designation, QIDP, 946075-13-4
CC(C1=NC(=CS1)C2=CC=C(C=C2)C#N)C(CN3C=[N+](C=N3)C(C)OC(=O)N(C)C4=C(C=CC=N4)COC(=O)CNC)(C5=C(C=CC(=C5)F)F)O
CC(C1=NC(=CS1)C2=CC=C(C=C2)C#N)C(CN3C=[N+](C=N3)C(C)OC(=O)N(C)C4=C(C=CC=N4)COC(=O)CNC)(C5=C(C=CC(=C5)F)F)O.OS(=O)(=O)[O-]
UPDATE NEW PATENT
WOCKHARDT, WO 2016016766, ISAVUCONAZONIUM SULPHATE, NEW PATENT


(WO2016016766) A PROCESS FOR THE PREPARATION OF ISAVUCONAZONIUM OR ITS SALT THEREOF
WOCKHARDT LIMITED [IN/IN]; D-4, MIDC Area, Chikalthana, Aurangabad 431006 (IN)
KHUNT, Rupesh Chhaganbhai; (IN).
RAFEEQ, Mohammad; (IN).
MERWADE, Arvind Yekanathsa; (IN).
DEO, Keshav; (IN)
The present invention relates to a process for the preparation of stable Isavuconazonium or its salt thereof. In particular of the present invention relates to process for the preparing of isavuconazonium sulfate, Isavuconazonium iodide hydrochloride and Boc-protected isavuconazonium iodide has purity more than 90%. The process is directed to preparation of solid amorphous form of isavuconazonium sulfate, isavuconazonium iodide hydrochloride and Boc-protected isavuconazonium iodide. The present invention process of Isavuconazonium or its salt thereof is industrially feasible, simple and cost effective to manufacture of isavuconazonium sulfate with the higher purity and better yield.
Isavuconazonium sulfate is chemically known l-[[N-methyl-N-3-[(methylamino) acetoxymethyl]pyridin-2-yl] carbamoyloxy]ethyl-l-[(2R,3R)-2-(2,5-difluorophenyl)-2-hydroxy-3-[4-(4-cyanophenyl)thiazol-2-yl]butyl]-lH-[l,2,4]-triazo-4-ium Sulfate and is structurally represented by formula (I):


Formula I
Isavuconazonium sulfate (BAL8557) is indicated for the treatment of antifungal infection. Isavuconazonium sulfate is a prodrug of Isavuconazole (BAL4815), which is chemically known 4-{2-[(lR,2R)-(2,5-Difluorophenyl)-2-hydroxy-l-methyl-3-(lH-l ,2,4-triazol-l-yl)propyl]-l ,3-thiazol-4-yl}benzonitrile compound of Formula II


Formula II
US Ppatent No. 6,812,238 (referred to herein as ‘238); 7,189,858 (referred to herein as ‘858); 7,459,561 (referred to herein as ‘561) describe Isavuconazonium and its process for the preparation thereof.
The US Pat. ‘238 patent describes the process of preparation of Isavuconazonium chloride hydrochloride.
The US Pat. ‘238 described the process for the Isavuconazonium chloride hydrochloride, involves the condensation of Isavuconazole and [N-methyl-N-3((tert-butoxycarbonyl methylamino) acetoxymethyl) pyridine-2-yl]carbamic acid 1 -chloro-ethyl ester. The prior art reported process require almost 15-16 hours, whereas the present invention process requires only 8-10 hours. Inter alia prior art reported process requires too many step to prepare isavuconazonium sulfate, whereas the present invention process requires fewer steps.
Moreover, the US Pat. ‘238 describes the process for the preparation Isavuconazonium hydrochloride, which may be used as the key intermediate for the synthesis of isavuconazonium sulfate, compound of formula I. There are several drawbacks in the said process, which includes the use of anionic resin to prepare Isavuconazonium chloride hydrochloride, consequently it requires multiple time lyophilization, which makes the said prior art process industrially, not feasible.
The inventors of the present invention surprisingly found that Isavuconazonium or a pharmaceutically acceptable salt thereof in yield and purity could be prepared by using substantially pure intermediates in suitable solvent.
Thus, an object of the present invention is to provide simple, cost effective and industrially feasible processes for manufacture of isavuconazonium sulfate. Inventors of the present invention surprisingly found that isavuconazonium sulfate prepared from isavuconazonium iodide hydrochloride, provides enhanced yield as well as purity.
The process of the present invention is depicted in the following scheme:


Formula I
Formula-IA
The present invention is further illustrated by the following example, which does not limit the scope of the invention. Certain modifications and equivalents will be apparent to those skilled in the art and are intended to be included within the scope of the present application.
Examples
Example-1: Synthesis of l-[[N-methyl-N-3-[(t-butoxycarbonylmethylamino) acetoxymethyl]pyridin-2-yl]carbamoyloxy]ethyl-l-[(2R,3R)-2-(2,5-difluorophenyl)-2-hydroxy-3 – [4-(4-cyanophenyl)thiazol-2-yl]butyl] – 1 H-[ 1 ,2,4] -triazo-4-ium iodide
Isavuconazole (20 g) and [N-methyl-N-3((tert-butoxycarbonylmethylamino)acetoxy methyl)pyridine-2-yl]carbamic acid 1 -chloro-ethyl ester (24.7 g) were dissolved in acetonitrile (200ml). The reaction mixture was stirred to add potassium iodide (9.9 g). The reaction mixture was stirred at 47-50°C for 10-13 hour. The reaction mixture was cooled to room temperature. The reaction mass was filtered through celite bed and washed acetonitrile. Residue was concentrated under reduced pressure to give the crude solid product (47.7 g). The crude product was purified by column chromatography to get its pure iodide form (36.5 g).
Yield: 84.5 %
HPLC Purity: 87%
Mass: m/z 817.4 (M- 1)+
Example-2: Synthesis of l-[[N-methyl-N-3-[(methylamino)acetoxymethyl]pyridin-2-yl] carbamoyloxy]ethyl-l-[(2R,3R)-2-(2,5-difluorophenyl)-2-hydroxy-3-[4-(4-cyanophenyl) thiazol-2-yl]butyl]-lH-[l ,2,4]-triazo-4-ium iodide hydrochloride
l-[[N-methyl-N-3-[(t-butoxycarbonylmethylamino)acetoxymethyl]pyridin-2-yl] carbamoyloxy]ethyl-l-[(2R,3R)-2-(2,5-difluorophenyl)-2-hydroxy-3-[4-(4-cyanophenyl) thiazol-2-yl]butyl]-lH-[l ,2,4]-triazo-4-ium iodide (36.5 g) was dissolved in ethyl acetate (600 ml). The reaction mixture was cooled to -5 to 0 °C. The ethyl acetate hydrochloride (150 ml) solution was added to reaction mixture. The reaction mixture was stirred for 4-5 hours at room temperature. The reaction mixture was filtered and obtained solid residue washed with ethyl acetate. The solid dried under vacuum at room temperature for 20-24 hrs to give 32.0 gm solid.
Yield: 93 %
HPLC Purity: 86%
Mass: m/z 717.3 (M-HC1- 1)
Example-3: Preparation of Strong anion exchange resin (Sulfate).
Indion GS-300 was treated with aqueous sulfate anion solution and then washed with DM water. It is directly used for sulfate salt.
Example-4: Synthesis of l-[[N-methyl-N-3-[(methylamino)acetoxymethyl]pyridin-2-yl] carbamoyloxy]ethyl-l-[(2R,3R)-2-(2,5-difluorophenyl)-2-hydroxy-3-[4-(4-cyanophenyl) thiazol-2-yl]butyl]-lH-[l ,2,4]-triazo-4-ium Sulfate
Dissolved 10.0 g l-[[N-methyl-N-3-[(methylamino)acetoxymethyl]pyridin-2-yl] carbamoyloxy]ethyl-l-[(2R,3R)-2-(2,5-difluorophenyl)-2-hydroxy-3-[4-(4-cyanophenyl) thiazol-2-yl]butyl]-lH-[l ,2,4]-triazo-4-ium iodide hydrochloride in 200 ml deminerahzed water and 30 ml methanol. The solution was cooled to about 0 to 5°C. The strong anion exchange resin (sulfate) was added to the cooled solution. The reaction mixture was stirred to about 60-80 minutes. The reaction was filtered and washed with 50ml of demineralized water and methylene chloride. The aqueous layer was lyophilized to obtain
(8.0 g) white solid.
Yield: 93 %
HPLC Purity: > 90%
Mass: m/z 717.4 (M- HS04) +
PATENT
CN 105288648
PATENT
CN 106883226
https://patents.google.com/patent/CN106883226A/en
PATENT
CN 107982221
PAPER
| Title: Introduction of New Drugs Approved by the U.S. FDA in 2015 |
| Author: Ma Shuai; Wenying Ling; Zhou Weicheng; |
| Source: China Pharmaceutical Industry |
| Publisher: Tongfangzhiwang Beijing Technology Co., Ltd. |
| Year of publication: |
| DOI code: 10.16522/j.cnki.cjph.2016.01.022 |
| Registration Time: 2016-02-19 02:04:15 |
///////////////
FDA and USDA announce key step to advance collaborative efforts to streamline produce safety requirements for farmers
DRUG REGULATORY AFFAIRS INTERNATIONAL

june 5, 2018

Release
As part of the U.S. Food and Drug Administration and the U.S. Department of Agriculture’s ongoing effort…
View original post 899 more words
Penciclovir

Penciclovir
- Molecular FormulaC10H15N5O3
- Average mass253.258 Da
Cas 39809-25-1
97845-62-0 (Na salt)
Launched – 1996 PERRIGO, Herpes labialis
BRL-39123; penciclovir; BRL 39123A; penciclovir sodium; Denavir; Vectavir; Euraxvir; Fenivir
Penciclovir [USAN:INN:BAN]
- BRL 39123
- BRL-39123
- CCRIS 9213
- Denavir
- HSDB 8123
- Penciclovir
- Penciclovirum
- Penciclovirum [INN-Latin]
- UNII-359HUE8FJC
Penciclovir was approved for medical use in 1996.[2]
Developed and launched by SmithKline Beecham (SB; now GlaxoSmithKline) and now marketed in the US by Prestium Pharma and ex-US by Novartis, penciclovir (Vectavir; Fenivir; Denavir; Euraxvir) is a 1% topical cream indicated for the treatment of recurrent herpes labialis (cold sores) in adults and children 12 years of age and older
APPROVALS
THE US
In September 1996, the compound was approved by the US FDA for cold sore treatment , and was launched in the US in 1997.
EUROPE
In December 1995, SB filed for European approvals of the drug . In 1997, the drug was approved in Belgium Iceland Denmark Norway Ireland . In January 2003, the drug was launched in Sweden . In May 2007, the drug was launched in Portugal .
JAPAN
In December 1995, SB filed for Japanese approval of the drug .
CHINA
In September 1999, the compound was approved in China
FDA
Click to access 020629s016lbl.pdf
Chemically, penciclovir is known as 9-[4-hydroxy-3-(hydroxymethyl)butyl] guanine. Its molecular formula is C10H15N5O3; its molecular weight is 253.26. It is a synthetic acyclic guanine derivative
Penciclovir is a white to pale yellow solid. At 20°C it has a solubility of 0.2 mg/mL in methanol, 1.3 mg/mL in propylene glycol, and 1.7 mg/mL in water. In aqueous buffer (pH 2) the solubility is 10.0 mg/mL. Penciclovir is not hygroscopic. Its partition coefficient in n-octanol/water at pH 7.5 is 0.024 (logP = -1.62).
Medical use
In herpes labialis, the duration of healing, pain and detectable virus is reduced by up to one day,[3] compared with the total duration of 2–3 weeks of disease presentation.
Mechanism of action
Penciclovir is inactive in its initial form. Within a virally infected cell a viral thymidine kinase adds a phosphate group to the penciclovir molecule; this is the rate-limiting step in the activation of penciclovir. Cellular (human) kinases then add two more phosphate groups, producing the active penciclovir triphosphate. This activated form inhibits viral DNA polymerase, thus impairing the ability of the virus to replicate within the cell.
The selectivity of penciclovir may be attributed to two factors. First, cellular thymidine kinases phosphorylate the parent form significantly less rapidly than does the viral thymidine kinase, so the active triphosphate is present at much higher concentrations in virally infected cells than in uninfected cells. Second, the activated drug binds to viral DNA polymerase with a much higher affinity than to human DNA polymerases. As a result, penciclovir exhibits negligible cytotoxicity to healthy cells.
The structure and mode of action of penciclovir are very similar to that of other nucleoside analogues, such as the more widely used aciclovir. A difference between aciclovir and penciclovir is that the active triphosphate form of penciclovir persists within the cell for a much longer time than the activated form of aciclovir, so the concentration within the cell of penciclovir will be higher given equivalent cellular doses.
SYN
Choudary, B.M.; Geen, G.R.; Grinter, T.J.; MacBeath, F.S.; Parratt, M.J.
Influence of remote structure upon regioselectivity in the N-alkylation of 2-amino-6-chloropurine: Application to the synthesis of penciclovir
Nucleosides Nucleotides 1994, 13(4): 979
PATENT
US 6573378
PATENT
CN 102070636
PAPER
https://www.tandfonline.com/doi/abs/10.1081/SCC-120026312?journalCode=lsyc20Selective and Practical Synthesis of Penciclovir
To synthesize 3 and 4, 2-amino-6-chloropurine (ACP) is commonly used as a starting material, coupling with alkyl halide side chains (Geen et al., 1990; Geen et al., 1992; Kim et al., 1998; Brand et al., 1999; Toyokuni et al., 2003). However, considering its isomerization at N7 and N9 positions under acidic or alkaline conditions, the most challengeable issue is the selectivity of a N-alkylation at the N7 or N9 position of ACP. Normally, alkylation takes place at the N9 position as well as at the N7 position of the purine moiety, and the N9/N7 ratio is usually less than 6:1 (Kim et al., 1998). Accordingly, to improve this ratio, several approaches have been reported, mainly involving changing the structure of the side chains (Geen et al., 1992) and modification of the ACP (Brand et al., 1999). For example, as reported by Zheng et al. (2004) (Fig. 2), a side chain 6 was synthesized and separated readily at 0 °C. After coupling 6 with 2-amino-6-chloropurine 7, the ratio of the product 9-isomer purine (8a) and the 7-isomer purine (8b) could reach about 10:1. However, the reaction temperature must be strictly controlled as 6 decomposes easily even at room temperature and then an extra careful column chromatography separation procedure would be required to obtain pure 8a. Thus, finding a more practical and efficient method, which could avoid the formation of N7-alkylated compound and shorten the synthetic steps to obtain ACP, becomes attractive.
The Mitsunobu reaction might be an alternative (potential) approach (Mitsunobu, 1981; Swamy et al., 2009). This reaction has become a very popular chemical transformation due to its mildness, occurring under essentially neutral conditions, and its stereospecificity, proceeding with complete Walden inversion of stereochemistry (Mitsunobu, 1981). Moreover, it permits C-O, C-S, C-N, or C-C bonds formed by the condensation of an acidic component with a primary or a secondary alcohol. Actually, some literature has already reported successful Mitsunobu coupling of ACP and adenine with allylic and benzylic alcohol, showing a good N9 selectivity (Yang et al., 2005; Kitade et al., 2006; Yin et al., 2006). However, a poor to modest yield (20%–50%) and a limited substrate scope were observed. In order to improve these yields, Lu et al. (2007) developed a modified Mitsunobu method to couple purine with alcohols in a higher temperature (70 °C), along with two rounds of the Mitsunobu reaction; yet its long reaction procedure and poor atom economy weaken its potential. The poor solubility of ACP or its derivatives in THF, the preferred solvent for Mitsunobu reactions, is likely the primary reason for these defects being observed.
A possible process to improve the solubility of ACP is to make use of the tert-butoxycarbonyl group (Boc), which can serve as the protection of the exocylic amino groups functionality and increase the lipophilicity of the base portion of the purine. Another advantage of the Boc protection group is that its acidolytic removal is less sensitive to steric factors and can also be removed under neutral conditions (Hwu et al., 1996; Siro et al., 1998). In contrast, a few studies have recently been reported that apply the Boc group in the protection of nucleobase (Sikchi and Hultin, 2006; Porcheddu et al., 2008). As described by Porcheddu et al. (2008), solubility of nucleobases, including guanine, was increased in some organic solvents after protected by Boc groups. In addition, some results in our previous study (Yang et al., 2011) demonstrated a very good improvement in coupling purine derivatives under Mitsunobu conditions. Thus, it could be safer to presume that protecting amino groups of ACP with Boc would be an ideal way for its application in the synthesis of PCV 3 and offer similar results as shown under Mitsunobu conditions.
In this study, we firstly synthesized a bis-Boc protected ACP, namely, bis-Boc-2-amino-6-chloropurine 9 (Fig. 3) and investigated its solubility in several different Mitsunobu solvents, then coupling bis-Boc-2-amino-6-chloropurine 9 with a large scope of alcohols confirmed its good reactivity for a Mitsunobu reaction and successfully developed a new and efficient method for the preparation of PCV using Mitsunobu coupling reaction as the key step.
Synthesis of bis-Boc-6-chloropurine 9
a: 2-amino-6-chloropurine, 4,4-dimethylaminopyridine (DMAP), THF and Boc2O, 25 °C, N2; b: MeOH, NaHCO3, 55 °C
To a 250 ml N2-flushed flask with dry THF (100 ml), equipped with a magnetic stir bar, 2-amino-6-chloropurine (2.0 g, 11.8 mmol) and DMAP (0.14 g, 1.18 mmol) were added. Boc2O (10.3 g, 47.2 mmol) was added to the stirred suspension under an N2atmosphere, then the reaction mixture was stirred for 6 h at room temperature (TLC analysis indicated the disappearance of 2-mino-6-chloropurine). The excess amount of THF was removed, and the crude product was dissolved in AcOEt (400 ml), washed with HCl aqueous (2 mol/L, 1×30 ml) and brine (2×50 ml), dried with Na2SO4 and concentrated in vacuo to give a white solid (5.2 g, 94.5%). mp 51–52 °C; 1H NMR (500 MHz, CDCl3): δ=1.47 (s, 18H, C(CH3)3), 1.69 (s, 9H, C(CH3)3), 8.58 (s, 1H, CH); 13C NMR (125 MHz, CDCl3) δ=153.8, 152.0, 151.8, 150.6, 145.5, 144.7, 130.8, 88.0, 83.9, 28.0.
2. Bis-Boc-2-amino-6-chloropurine (9)
A solution of the white solid obtained above (14 g, 30 mmol) in MeOH (400 ml) was added to saturated NaHCO3 aqueous (200 ml), then the turbid solution was stirred at 55 °C for 2 h, at which point clean conversion to bis-Boc protected adenine was observed by TLC. After evaporation of MeOH, the residue mixture was cooled, added 5 mol/L hydrochloric acid to get pH=7 (approximate). A large amount of white solid formed, the reaction mixture was filtrated and then dried under a vacuum to give a white solid 9 (10.5 g, 95.5%). mp 101.3–103.3 °C; 1H NMR (500 MHz, CDCl3): δ=1.50 (s, 18H, C(CH3)3), 8.41 (s, 1H, CH); 13C NMR (125 MHz, CDCl3) δ=153.5, 151.9, 151.6, 151.3, 145.6, 128.5, 82.7, 28.5.
2.3. 5-(2-hydroxyethyl)-2,2-dimethyl-1,3-dioxane (5)
2-hydroxymethyl-1,4-butanediol 11 (8.10 g, 67.4 mmol) and 2,2-dimethoxypropane (13 ml, 105.7 mmol) were dissolved in dry THF (20 ml). The mixture was stirred and p-toluenesulfonic acid monohydrate (0.64 g, 3.4 mmol) was added, the clear solution was stirred at room temperature for 12 h, triethylamine (10 ml) was added to quench the reaction, and the solution was stirred for 30 min. Then solvents were removed to leave a colorless liquid, the residue was subject to column chromatography on silica gel eluted with 2:1 EtOAc/hexane to give a colorless liquid 5 (6.2 g, 61.5%), R f=0.46 (2:1 EtOAc/hexane). 1H NMR (500 MHz, CDCl3): δ=3.99 (dd, 2H, Heq. J 1=11.80 Hz, J 2=4.45 Hz, CH2); 3.80 (t, 2H, J=6.71 Hz, CH2), 3.34 (dd, 2H, Hax. J 1=11.80 Hz, J 2=8.11 Hz, CH2), 1.90–1.98 (m, 2H, CH and OH), 1.62 (q, 2H, J=6.85 Hz, CH2 ); 13C NMR (125 MHz, CDCl3): δ=100.5, 69.8, 60.4, 31.9, 30.3, 21.2.
2.4. Bis-Boc-2-amino-6-chloro-9-[2-(2,2-dimethyl-1,3-dioxan-5-yl)ethyl] purine (12)
Bis-Boc-2-amino-6-chloropurine 9 (1.0 equivalent) was added to a solution of the side chain 5 (1.1 equivalent) and phosphine reagent (1.1 equivalent) in anhydrous THF under N2 atmosphere at 0 °C, the resulting solution was treated with di-p-nitrobenzyl azocarboxylate (DNAD) (1.1 equivalent) dropwise and the reaction mixture was continued at room temperature for 8 h, then the solvent was evaporated and the residue dissolved in cyclohexane. The triphenylphosphane oxide precipitated and was filtered off and then the filtrate evaporated under reduced pressure. The product was purified by a column chromatography on silica gel to obtain the pure products as a white solid. mp>280 °C (dec); 1H NMR (500 MHz, CDCl3): δ=8.36 (s, 1H, CH), 4.02 (t, 2H, J=7.23 Hz, CH2), 3.79 (dd, 2H, Heq. J 1=11.57 Hz, J 2=4.46 Hz, CH2), 3.56 (dd, 2H, Hax. J 1=11.57 Hz, J 2=8.77 Hz, CH2), 1.67 (q, 2H, J=7.22 Hz, CH2), 1.53–1.61 (m, 1H, CH), 1.47 (s, 18H, C(CH3)3), 1.39 (s, 3H, CH3), 1.36 (s, 3H, CH3); 13C NMR (125 MHz, CDCl3): δ=154.3, 151.7, 151.5, 151.1, 128.0, 104.8, 81.7, 71.5, 50.8, 33.7, 28.6, 26.2, 25.7.
2.5. 2-amino-6-chloro-9-[2-(2,2-dimethyl-1,3-dioxan-5-yl) ethyl]purine (8a)
A mixture of compound 12 (2.56 g, 5.0 mmol), 2,6-dimethyl pyridine (1.18 ml, 10 mmol) and dry DCM (20 ml) was stirred at 0 °C, then TBTMS-OTf was added dropwise; after the addition, the reaction mixture was stirred at room temperature until TLC showed that compound 12 had completely disappeared. Then 30 ml saturated ammonium chloride solution was added, separated the organic layer, extracted with DCM (2×20 ml), combined and washed by saturated NaCl (2×40 ml), dried with anhydrous sodium sulfate and evaporated to give a white solid (1.21 g, 78%). mp 125–126 °C; 1H NMR (500 MHz, CDCl3): δ=8.07 (s, 1H, CH) , 6.99 (s, 2H, NH2), 4.12 (t, 2H, J=7.31 Hz, CH2), 3.82 (dd, 2H, 4′-Heq, J 1=11.79 Hz, J 2=4.50 Hz, CH2), 3.53 (dd, 2H, 4′-Hax, J 1=11.79 Hz, J 2=8.80 Hz, CH2), 1.74 (q, 2H, J=7.30 Hz, CH2), 1.53–1.65 (m, 1H, CH), 1.36 (s, 3H, CH3), 1.31 (s, 3H, CH3); 13C NMR (125 MHz, CDCl3): δ=159.94, 150.31, 150.26, 141.84, 132.11, 100.52, 68.14, 52.90, 31.32, 26.84, 26.05.
2.6. 9-[4-hydroxy-3-(hydroxymethyl)butyl] guanine (PCV 3)
Compound 12 (5.12 g, 10 mmol) was dissolved in THF (20 ml) hydrochloric acid (2 mol/L, 20 ml). The mixture was stirred for 2 h at 70 °C, and then slowly warmed to reflux for 2 h. After evaporation of the THF under reduced vacuum, 10% aqueous NaOH solution was added to neutralize the residual liquid, and a large amount of off-white solid formed, filtered, washed with acetone and then water, and dried under vacuum to give an off-white solid 3 (2.07 g, 82%). mp 274.6–276.9 °C.
Table 1
Mole fraction solubility x of bis-Boc-2-amino-6-chloropurine 9 in different Mitsunobu solvents
| T (K) (±0.05 K) | Solubility x a (%)
|
|||
| THFb | DCMb | Methylbenzeneb | Acetonitrileb | |
| 273.15 | 0.1141 | 0.0493 | 0.0213 | 0.0150 |
| 278.15 | 0.1191 | 0.0552 | 0.0253 | 0.0178 |
| 283.15 | 0.1251 | 0.0613 | 0.0303 | 0.0210 |
| 288.15 | 0.1299 | 0.0664 | 0.0349 | 0.0244 |
| 293.15 | 0.1352 | 0.0734 | 0.0405 | 0.0288 |
| 298.15 | 0.1399 | 0.0809 | 0.0470 | 0.0347 |
| 303.15 | 0.1463 | 0.0894 | 0.0544 | 0.0417 |
| 308.15 | 0.1523 | 0.0983 | 0.0634 | 0.0501 |
| 313.15 | 0.1581 | 0.1081 | 0.0734 | 0.0617 |
- a: the solubility of bis-Boc-2-amino-6-chloropurine 9 was measured by our previous method with temperature ranging from 273.15 K to 313.15 K (Wang et al., 2008) at atmospheric pressure. The laser monitoring observation technique was used to determine the disappearance of the solid phase in a solid and liquid mixture
b: all the solvents were further purified by distillation in dry agent (Na/benzophenone) and the sample bis-boc-2-amino-6-chloropurine 9 was dried in vacuum for over 2 d
As shown in Table 1, THF, which is the most common solvent in Mitsunobu reaction, has great solubility for bis-Boc-2-amino-6-chloropurine 9. Afterwards, the best solvent THF was taken for coupling 9 with a number of alcohols under normal Mitsunobu conditions to investigate its reactivity. The results were illustrated in Table 2. We clearly learned that bis-Boc-2-amino-6-chloropurine 9, as an excellent nucleophilic precursor, was able to react with a large number of alcohols, including primary alcohol, secondary alcohol, allyl alcohol, benzyl alcohol, etc., with high N9 selectivity and yields. Moreover, tert-Butyl alcohol still could not react with a protected purine as in the previous study (Yang et al., 2011), owing to its steric hindrance in tertiary carbon.
Table 2
Investigation of the reactivity of bis-Boc-2-amino-6-chloropurine 9 with different alcohols
| Entry | Alcohol | Product | Isolated yield (%) |
| 1 | 10a | 90.2 | |
| 2 | 10b | 86.6 | |
| 3 | 10c | 83.3 | |
| 4 | 10d | 84.8 | |
| 5 | 10e | 86.4 | |
| 6 | 10f | 81.2 | |
| 7 | 10g | 81.5 | |
| 8 | 10h | 80.7 | |
| 9 | 10i | 0 |
- a): a mixture of 9 (1.0 equivalent), alcohol (1.1 equivalent) and phosphine reagent (1.1 equivalent) in anhydrous THF stirring under N2 atmosphere at 0 °C, then treated with azo-reagent DNAD (1.1 equivalent) warmed to room temperature; b): the mixture of the products from procedure a, THF (20 ml) and aqueous hydrochloric acid (2 mol/L, 20 ml) was refluxed for 2 h at 70 °C
- According to the research results above, it is more reasonable and assuring to prepare PCV via a Mitsunobu reaction. This novel method for the preparation of PCV is indicated in Fig. 4. First, the side chain of 5-(2-hydroxyethyl)-2,2-dimethyl-1,3 -dioxane 5 was achieved through the commercially available starting material 2-hydroxymethyl-1,4-butanediol 11 reacting with 2,2-dimethoxypropane catalyzed by p-toluenesulfonic acid. The free –OH group of compound 5 is not necessary to be converted to the other leaving group such as chlorine, tosylate or methanesulphonate, which is always taken as a necessary step in the previous method or many other previous studies for the preparation of PVC till now (Harnden and Jarvest, 1985; Harnden et al., 1987; Zheng et al., 2004), making the synthesis of the side chain part of our method much more convenient and practical.
Synthesis of penciclovir (PCV) with new method
a: 2,2-dimethoxypropane, p-toluenesulfonic acid, THF; b: 1.1 equivalent of the side chain 5, 1.1 equivalent of PPh3, and 1.1 equivalent of azodicarboxylate reagent at rt. in THF; c: TBDMS-OTf, DCM; d: aqueous hydrochloric acid (2 mol/L), THF; e: aqueous hydrochloric acid (2 mol/L)
Our next objective was the synthesis of PCV. As was expected, bis-Boc-2-amino-6-chloropurine 9 combined with the side chain 5(1.1 equivalent) under normal Mitsunobu conditions successfully obtained the desired N9-alkylated compound 12 in 92% yield without the undesired N7 alkylation by-product being formed. Importantly, the reaction conditions were significantly milder than those reported in recent studies (Geen et al., 1990; 1992; Kim et al., 1998; Brand et al., 1999; Toyokuni et al., 2003), requiring only 1.1 equivalent of each of the alcohol, PPh3 and DNAD, and proceeding to completion within 60 min at room temperature. This is mainly due to the enhanced solubility of the compound 9 as mentioned above. By process c in Fig. 4, compound 8a was obtained under neutral conditions. It is 1H and 13C NMR spectra further indicated that no 7-isomer purine (8b) was formed. Subsequently, we could obtain PCV 3 in an acid condition as procedure e; or directly starting from 12, where hydrolytic dechlorination and deprotection step(s) were accomplished in one pot under mild acid conditions (2mol/L, hydrochloric acid in THF at room temperature) to afford the target PCV 3 in 80%–85% yield (process d). The overall yield of PCV from 11 was 44.5% higher than that in previous study (16%) (Zheng et al., 2004).
References
 [1] Ashton, W.T., Karkas, J.D., Field, A.K., Tolman, R.L., 1982. Activation by thymidine kinase and potent antiherpetic activity of 2’-nor-2’-deoxyguanosine (2’NDG). Biochemical and Biophysical Research Communications, 108(4):1716-1721.
[1] Ashton, W.T., Karkas, J.D., Field, A.K., Tolman, R.L., 1982. Activation by thymidine kinase and potent antiherpetic activity of 2’-nor-2’-deoxyguanosine (2’NDG). Biochemical and Biophysical Research Communications, 108(4):1716-1721. [2] Brand, B., Reese, C.B., Song, Q., Visintin, C., 1999. Convenient syntheses of 9-[4-hydroxy-3-(hydroxymethyl)butyl] guanine (penciclovir) and 9-[4-acetoxy-3-(acetoxymethyl) butyl]-2-amino-9H-purine (famciclovir). Tetrahedron, 55(16):5239-5252.
[2] Brand, B., Reese, C.B., Song, Q., Visintin, C., 1999. Convenient syntheses of 9-[4-hydroxy-3-(hydroxymethyl)butyl] guanine (penciclovir) and 9-[4-acetoxy-3-(acetoxymethyl) butyl]-2-amino-9H-purine (famciclovir). Tetrahedron, 55(16):5239-5252. [3] De Clercq, E., 1991. Broad-spectrum anti-DNA virus and anti-retrovirus activity of phosphonylmethoxyalkylpurines and pyrimidines. Biochemical Pharmacology, 42(5):963-972.
[3] De Clercq, E., 1991. Broad-spectrum anti-DNA virus and anti-retrovirus activity of phosphonylmethoxyalkylpurines and pyrimidines. Biochemical Pharmacology, 42(5):963-972. [4] Dey, S., Garner, P., 2000. Synthesis of tert-butoxycarbonyl (Boc)-protected purines. The Journal of Organic Chemistry, 65(22):7697-7699.
[4] Dey, S., Garner, P., 2000. Synthesis of tert-butoxycarbonyl (Boc)-protected purines. The Journal of Organic Chemistry, 65(22):7697-7699. [5] Geen, G.R., Grinter, T.J., Kincey, P.M., Jarvest, R.L., 1990. The effect of the C-6 substituent on the regioselectivity of N-alkylation of 2-aminopurines. Tetrahedron, 46(19):6903-6914.
[5] Geen, G.R., Grinter, T.J., Kincey, P.M., Jarvest, R.L., 1990. The effect of the C-6 substituent on the regioselectivity of N-alkylation of 2-aminopurines. Tetrahedron, 46(19):6903-6914. [6] Geen, G.R., Kincey, P.M., Choudary, B.M., 1992. Regiospecific Michael additions with 2-aminopurines. Tetrahedron Letters, 33(32):4609-4612.
[6] Geen, G.R., Kincey, P.M., Choudary, B.M., 1992. Regiospecific Michael additions with 2-aminopurines. Tetrahedron Letters, 33(32):4609-4612. [7] Harnden, M.R., Jarvest, R.L., 1985. An improved synthesis of the antiviral acyclonucleoside 9-(4-hydroxy-3-hydroxymethylbut-1-yl) guanine. Tetrahedron Letters, 26(35):4265-4268.
[7] Harnden, M.R., Jarvest, R.L., 1985. An improved synthesis of the antiviral acyclonucleoside 9-(4-hydroxy-3-hydroxymethylbut-1-yl) guanine. Tetrahedron Letters, 26(35):4265-4268. [8] Harnden, M.R., Jarvest, R.L., Bacon, T.H., Boyd, M.R., 1987. Synthesis and antiviral activity of 9-[4-hydroxy-3-(hydroxymethyl) but-1-yl] purines. Journal of Medicinal Chemistry, 30(9):1636-1642.
[8] Harnden, M.R., Jarvest, R.L., Bacon, T.H., Boyd, M.R., 1987. Synthesis and antiviral activity of 9-[4-hydroxy-3-(hydroxymethyl) but-1-yl] purines. Journal of Medicinal Chemistry, 30(9):1636-1642. [9] Hwu, J.R., Jain, M.L., Tsay, S.C., Hakimelahi, G.H., 1996. Ceric ammonium nitrate in the deprotection of tert-butoxycarbonyl group. Tetrahedron Letters, 37(12):2035-2038.
[9] Hwu, J.R., Jain, M.L., Tsay, S.C., Hakimelahi, G.H., 1996. Ceric ammonium nitrate in the deprotection of tert-butoxycarbonyl group. Tetrahedron Letters, 37(12):2035-2038. [10] Kim, D.K., Lee, N., Kim, Y.W., Chang, K.Y., Kim, J.S., Im, G.J., Choi, W.S., Jung, I.H., Kim, T.S., Hwang, Y.Y., 1998. Synthesis and evaluation of 2-amino-9-(3-hydroxymethyl-4-alkoxycarbonylo-xybut-1-yl) purines as potential prodrugs of penciclovir. Journal of Medicinal Chemistry, 41(18):3435-3441.
[10] Kim, D.K., Lee, N., Kim, Y.W., Chang, K.Y., Kim, J.S., Im, G.J., Choi, W.S., Jung, I.H., Kim, T.S., Hwang, Y.Y., 1998. Synthesis and evaluation of 2-amino-9-(3-hydroxymethyl-4-alkoxycarbonylo-xybut-1-yl) purines as potential prodrugs of penciclovir. Journal of Medicinal Chemistry, 41(18):3435-3441. [11] Kitade, Y., Ando, T., Yamaguchi, T., Hori, A., Nakanishi, M., Ueno, Y., 2006. 4’-fluorinated carbocyclic nucleosides: synthesis and inhibitory activity against S-adenosyl-l-homocysteine hydrolase. Bioorganic & Medicinal Chemistry, 14(16):5578-5583.
[11] Kitade, Y., Ando, T., Yamaguchi, T., Hori, A., Nakanishi, M., Ueno, Y., 2006. 4’-fluorinated carbocyclic nucleosides: synthesis and inhibitory activity against S-adenosyl-l-homocysteine hydrolase. Bioorganic & Medicinal Chemistry, 14(16):5578-5583. [12] Korba, B.E., Boyd, M.R., 1996. Penciclovir is a selective inhibitor of hepatitis B virus replication in cultured human hepatoblastoma cells. Antimicrobial Agents and Chemotherapy, 40(13):1282-1284.
[12] Korba, B.E., Boyd, M.R., 1996. Penciclovir is a selective inhibitor of hepatitis B virus replication in cultured human hepatoblastoma cells. Antimicrobial Agents and Chemotherapy, 40(13):1282-1284. [13] Lu, W., Sengupta, S., Petersen, J.L., Akhmedov, N.G., Shi, X., 2007. Mitsunobu coupling of nucleobases and alcohols: an efficient, practical synthesis for novel nonsugar carbon nucleosides. Journal of Organic Chemistry, 72(13):5012-5015.
[13] Lu, W., Sengupta, S., Petersen, J.L., Akhmedov, N.G., Shi, X., 2007. Mitsunobu coupling of nucleobases and alcohols: an efficient, practical synthesis for novel nonsugar carbon nucleosides. Journal of Organic Chemistry, 72(13):5012-5015. [14] Martin, J.C., Dvorak, C.A., Smee, D.F., Matthews, T.R., Verheyden, J.P.H., 1983. 9-(1,3-dihydroxy-2-propoxymethyl) guanine: a new potent and selective antiherpes agent. Journal of Medicinal Chemistry, 26(5):759-761.
[14] Martin, J.C., Dvorak, C.A., Smee, D.F., Matthews, T.R., Verheyden, J.P.H., 1983. 9-(1,3-dihydroxy-2-propoxymethyl) guanine: a new potent and selective antiherpes agent. Journal of Medicinal Chemistry, 26(5):759-761. [15] Mitsunobu, O., 1981. The use of diethyl azodicarboxylate and triphenylphosphine in synthesis and transformation of natural products. Synthesis, 1981(1):1-28.
[15] Mitsunobu, O., 1981. The use of diethyl azodicarboxylate and triphenylphosphine in synthesis and transformation of natural products. Synthesis, 1981(1):1-28. [16] Ogilvie, K.K., Cheriyan, U.O., Radatus, B.K., Smith, K.O., Galloway, K.S., Kennell, W.L., 1982. Biologically active acyclonucleoside analogues. II. The synthesis of 9-[[2-hydroxy-1-(hydroxymethyl)ethoxy]methyl] guanine (BIOLF-62). Canadian Journal of Chemistry, 60(24):3005-3010.
[16] Ogilvie, K.K., Cheriyan, U.O., Radatus, B.K., Smith, K.O., Galloway, K.S., Kennell, W.L., 1982. Biologically active acyclonucleoside analogues. II. The synthesis of 9-[[2-hydroxy-1-(hydroxymethyl)ethoxy]methyl] guanine (BIOLF-62). Canadian Journal of Chemistry, 60(24):3005-3010. [17] Porcheddu, A., Giacomelli, G., Piredda, I., Carta, M., Nieddu, G., 2008. A Practical and efficient approach to PNA monomers compatible with Fmoc-mediated solid-phase synthesis protocols. European Journal of Organic Chemistry, 2008(34):5786-5797.
[17] Porcheddu, A., Giacomelli, G., Piredda, I., Carta, M., Nieddu, G., 2008. A Practical and efficient approach to PNA monomers compatible with Fmoc-mediated solid-phase synthesis protocols. European Journal of Organic Chemistry, 2008(34):5786-5797. [18] Schaeffer, H.J., Beauchamp, L., Miranda, P.D., Elion, G.B., Bauer, D.J., Collins, P., 1978. 9-(2-hydroxyethoxymethyl) guanine activity against viruses of the herpes group. Nature, 272(5654):583-585.
[18] Schaeffer, H.J., Beauchamp, L., Miranda, P.D., Elion, G.B., Bauer, D.J., Collins, P., 1978. 9-(2-hydroxyethoxymethyl) guanine activity against viruses of the herpes group. Nature, 272(5654):583-585. [19] Shaw, T., Amor, P., Civitico, G., Boyd, M., Locarnini, S., 1994. In vitro antiviral activity of penciclovir, a novel purine nucleoside, against duck hepatitis B virus. Antimicrobial Agents and Chemotherapy, 38(4):719-723.
[19] Shaw, T., Amor, P., Civitico, G., Boyd, M., Locarnini, S., 1994. In vitro antiviral activity of penciclovir, a novel purine nucleoside, against duck hepatitis B virus. Antimicrobial Agents and Chemotherapy, 38(4):719-723. [20] Smith, K.O., Galloway, K.S., Kennell, W.L., Ogilvie, K.K., Radatus, B.K., 1982. A new nucleoside analog, 9-[[2-hydroxy-1-(hydroxymethyl)ethoxyl]methyl] guanine, highly active in vitro against herpes simplex virus types 1 and 2. Antimicrobial Agents and Chemotherapy, 22(1):55-61.
[20] Smith, K.O., Galloway, K.S., Kennell, W.L., Ogilvie, K.K., Radatus, B.K., 1982. A new nucleoside analog, 9-[[2-hydroxy-1-(hydroxymethyl)ethoxyl]methyl] guanine, highly active in vitro against herpes simplex virus types 1 and 2. Antimicrobial Agents and Chemotherapy, 22(1):55-61. [21] Tippie, M.A., Martin, J.C., Smee, D.F., Matthews, T.R., Verheyden, J.P.M., 1984. Antiherpes simplex virus activity of 9-[4-hydroxy-3-(hydroxymethyl)-1-butyl] guanine. Nucleosides and Nucleotides, 3(5):525-535.
[21] Tippie, M.A., Martin, J.C., Smee, D.F., Matthews, T.R., Verheyden, J.P.M., 1984. Antiherpes simplex virus activity of 9-[4-hydroxy-3-(hydroxymethyl)-1-butyl] guanine. Nucleosides and Nucleotides, 3(5):525-535. [22] Toyokuni, T., Walsh, J.C., Namavari, M., Shinde, S.S., Moore, J.R., Barrio, J.R., Satyamurthy, N., 2003. Selective and practical synthesis of penciclovir. Synthetic Communications, 33(22):3897-3905.
[22] Toyokuni, T., Walsh, J.C., Namavari, M., Shinde, S.S., Moore, J.R., Barrio, J.R., Satyamurthy, N., 2003. Selective and practical synthesis of penciclovir. Synthetic Communications, 33(22):3897-3905. [23] Sikchi, S.A., Hultin, P.G., 2006. Solventless protocol for efficient Bis-N-Boc protection of adenosine, cytidine, and guanosine derivatives. Journal of Organic Chemistry, 71(16):5888-5891.
[23] Sikchi, S.A., Hultin, P.G., 2006. Solventless protocol for efficient Bis-N-Boc protection of adenosine, cytidine, and guanosine derivatives. Journal of Organic Chemistry, 71(16):5888-5891. [24] Siro, J.G., Martin, J., Garcia-Navio, J.L., Remuinan, M.J., Vaquero, J.J., 1998. Easy microwave assisted deprotection of N-Boc derivatives. Synlett, 1998(2):147-148.
[24] Siro, J.G., Martin, J., Garcia-Navio, J.L., Remuinan, M.J., Vaquero, J.J., 1998. Easy microwave assisted deprotection of N-Boc derivatives. Synlett, 1998(2):147-148. [25] Swamy, K.C.K., Kumar, N.N.B., Balaraman, E., Kumar, K.V.P.P., 2009. Mitsunobu and related reactions: advances and applications. Chemical Reviews, 109(6):2551-2651.
[25] Swamy, K.C.K., Kumar, N.N.B., Balaraman, E., Kumar, K.V.P.P., 2009. Mitsunobu and related reactions: advances and applications. Chemical Reviews, 109(6):2551-2651. [26] Wang, L., Dai, L.Y., Lei, M., Chen, Y., 2008. Solubility of hexamethylenetetramine in a pure water, methanol, acetic acid, and ethanol+water mixture from (299.38 to 340.35) K. Journal of Chemical & Engineering Data, 53(12):2907-2909.
[26] Wang, L., Dai, L.Y., Lei, M., Chen, Y., 2008. Solubility of hexamethylenetetramine in a pure water, methanol, acetic acid, and ethanol+water mixture from (299.38 to 340.35) K. Journal of Chemical & Engineering Data, 53(12):2907-2909. [27] Yang, J., Dai, L., Wang, X., Chen, Y., 2011. Di-p-nitrobenzyl azodicarboxylate (DNAD): an alternative azo-reagent for the Mitsunobu reaction. Tetrahedron, 67(7):1456-1462.
[27] Yang, J., Dai, L., Wang, X., Chen, Y., 2011. Di-p-nitrobenzyl azodicarboxylate (DNAD): an alternative azo-reagent for the Mitsunobu reaction. Tetrahedron, 67(7):1456-1462. [28] Yang, M.M., Schneller, S.W., Korba, B., 2005. 5’-homoneplanocin a inhibits hepatitis B and hepatitis C. Journal of Medicinal Chemistry, 48(15):5043-5046.
[28] Yang, M.M., Schneller, S.W., Korba, B., 2005. 5’-homoneplanocin a inhibits hepatitis B and hepatitis C. Journal of Medicinal Chemistry, 48(15):5043-5046. [29] Yin, X.Q., Li, W.K., Schneller, S.W., 2006. An efficient Mitsunobu coupling to adenine-derived carbocyclic nucleosides. Tetrahedron Letters, 47(52):9187-9189.
[29] Yin, X.Q., Li, W.K., Schneller, S.W., 2006. An efficient Mitsunobu coupling to adenine-derived carbocyclic nucleosides. Tetrahedron Letters, 47(52):9187-9189. [30] Zheng, Q.H., Wang, J.Q., Liu, X., Fei, X.S., Mock, B.H., Glick-Wilson, B.E., Sullivan, M.L., Raikwar, S.P., Gardner, T.A., Kao, C.H., 2004. An improved total synthesis of PET HSV-tk gene reporter probe 9-(4-[18F] fluoro-3-hydroxymethylbutyl) guanine ([18F]FHBG). Synthetic Communications, 34(4):689-704.
[30] Zheng, Q.H., Wang, J.Q., Liu, X., Fei, X.S., Mock, B.H., Glick-Wilson, B.E., Sullivan, M.L., Raikwar, S.P., Gardner, T.A., Kao, C.H., 2004. An improved total synthesis of PET HSV-tk gene reporter probe 9-(4-[18F] fluoro-3-hydroxymethylbutyl) guanine ([18F]FHBG). Synthetic Communications, 34(4):689-704.
SYN

EP 0141927; ES 8602791; ES 8603887; ES 8603888; JP 1994293764; US 5075445
This compound has been obtained by two similar ways: 1) The reaction of 6-chloropurine-2-amine (I) with 6,6-dimethyl-5,7-dioxaspiro[2.5]octane-4,8-dione (II) by means of K2CO3 in DMF gives the expected condensation product (III), which is methanolized with HCl/methanol yielding 2-[2-(2-amino-6-methoxypurin-9-yl)ethyl]malonic acid dimethyl ester (IV). The reduction of (IV) with NaBH4 in tert-butanol/methanol affords the corresponding diol (V), which is finally converted into pecnciclovir by hydrolysis with 2N NaOH. 2) The reaction of purine (I) with 3-bromopropane-1,1,1-tricarboxylic acid triethyl ester (VI) by means ofK2CO3 in DMF gives the expected condensation product (VII), which is partially decarboxylated with sodium methoxide in methanol yielding 2-[2-(2-amino-6-chloropurin-9-yl)ethyl]malonic acid diethyl ester (VIII). The reduction of (VIII) with NaBH4 in tert-butanol/methanol followed by acetylation with acetic anhydride affords the corresponding diol diacetate (IX), which is finally converted into penciclovir by hydrlysis with 2N HCl.
References
- Jump up^ “Penciclovir”. Merriam-Webster Dictionary. Retrieved 2016-01-22.
- Jump up^ Long, Sarah S.; Pickering, Larry K.; Prober, Charles G. (2012). Principles and Practice of Pediatric Infectious Disease. Elsevier Health Sciences. p. 1502. ISBN 1437727026.
- Jump up^ Farmaceutiska Specialiteter i Sverige – the Swedish official drug catalog. [http://www.fass.se Fass.se –> Vectavir. Retrieved on August 12, 2009. Translated from “Tiden för läkning, smärta och påvisbart virus förkortas med upp till ett dygn.”
 |
|
| Clinical data | |
|---|---|
| Pronunciation | /ˌpɛnˈsaɪkloʊˌvɪər/[1] |
| Trade names | Denavir |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a697027 |
| Pregnancy category |
|
| Routes of administration |
Topical |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 1.5% (oral), negligible (topical) |
| Protein binding | <20% |
| Metabolism | Viral thymidine kinase |
| Elimination half-life | 2.2–2.3 hours |
| Excretion | Renal |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard | 100.189.687 |
| Chemical and physical data | |
| Formula | C10H15N5O3 |
| Molar mass | 253.258 g/mol |
| 3D model (JSmol) | |
/////////////Penciclovir, BRL-39123, BRL 39123A, penciclovir sodium, Denavir, Vectavir, Euraxvir, Fenivir,
C1=NC2=C(N1CCC(CO)CO)NC(=NC2=O)N
Carglumic acid, карглумовая кислота , حمض كاروغلوميك , カルグルミ酸 ,

Carglumic acid
N-Carbamyl-L-glutamate;
- Molecular FormulaC6H10N2O5
- Average mass190.154 Da
Carglumic acid is a Carbamoyl Phosphate Synthetase 1 Activator. The mechanism of action of carglumic acid is as a Carbamoyl Phosphate Synthetase 1 Activator.
For the treatment of acute and chronic hyperammonaemia in patients with N-acetylglutamate synthase (NAGS) deficiency. This enzyme is an important component of the urea cycle to prevent build up of neurotoxic ammonium in the blood.
EMA
Carglumic acid exists as a white powder or colourless crystals. It is soluble in boiling water, slightly soluble in cold water and practically insoluble in organic solvents (cyclohexane, dichloromethane, ether). The water solubility of carglumic acid at pH 2.0 is 21.0 g/L. It increases rapidly between the pH 3.0 (28.2 g/L) and the pH 5.0 (440.9 g/L). The solubility of carglumic acid in water is stable between pH 6.0 (555.5 g/L) and pH 8.0 (553.9 g/L). Carglumic acid is prepared from L-glutamic acid. It exhibits stereoisomerism due to the presence of one chiral centre and has one optical isomer; N-carbamoyl-D-glutamic acid.
ORIGINATOR ORPHAN EUROPE
POLA CHEMICAL
ORPHAN DRUG
EU APPROVED 2003 ORPHAN EUROPE
FDA 2010 ORPHAN EUROPE
JAPAN 2016 POLA CHEM
CARBAGLU®
(carglumic acid) Tablet for Oral Suspension
DESCRIPTION
CARBAGLU tablets for oral suspension, contain 200 mg of carglumic acid. Carglumic acid, the active substance, is a Carbamoyl Phosphate Synthetase 1 (CPS 1) activator and is soluble in boiling water, slightly soluble in cold water, and practically insoluble in organic solvents.
Chemically carglumic acid is N-carbamoyl-L-glutamic acid or (2S)-2-(carbamoylamino) pentanedioic acid, with a molecular weight of 190.16.
The structural formula is:
 |
Molecular Formula: C6H10N2O5
The inactive ingredients of CARBAGLU are croscarmellose sodium, hypromellose, microcrystalline cellulose, silica colloidal anhydrous, sodium lauryl sulfate, sodium stearyl fumarate.
Carglumic Acid is an orally active, synthetic structural analogue of N-acetylglutamate (NAG) and carbamoyl phosphate synthetase 1 (CPS 1) activator, with ammonia lowering activity. NAG, which is formed by the hepatic enzyme N-acetylglutamate synthase (NAGS), is an essential allosteric activator of the enzyme carbamoyl phosphate synthetase 1 (CPS 1). CPS 1 plays an essential role in the urea cycle and converts ammonia into urea. Upon oral administration, carglumic acid can replace NAG in NAGS deficient patients and activates CPS 1, which prevents hyperammonaemia.
Carglumic acid is an orphan drug, marketed by Orphan Europe under the trade name Carbaglu. Carglumic acid is used for the treatment of hyperammonaemia in patients with N-acetylglutamate synthase deficiency.[1][2] The initial daily dose ranges from 100 to 250 mg/kg, adjusted thereafter to maintain normal plasma levels of ammonia.
The US FDA approved it for treatment of hyperammonaemia on March 18, 2010. Orphan Drug exclusivity expired on March 18, 2017.[3]
USFDA
https://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/022562s000chemr.pdf
Carbaglu (carglumic acid) Tablets 200 mg, is a white elongated tablet with three score marks on both sides engraved C’s on one side. It is a dispersible tablet designed to be dispersed in of water and ingested or administered through a syringe via a nasogastric tube. It is indicated for treatment of acute hyperammonemia in patients with NAGS deficiency.
The drug substance, carglumic acid, is an allosteric activator of a critical urea cycle enzyme, carbamoyl phosphate synthetase (CPS). It is a close analog of the naturally occurring activator, N-acetyl glutamate (NAG). Carglumic acid is a urea-like derivative of the amino acid L-glutamate and contains one chiral center. The drug substance solid form is the neutral dicarboxylic acid and is a white crystalline powder. The water solubility of the drug substance depends on the . polymorphic solid form has been found.
The drug substance is manufactured by .
The facility was found to have acceptable cGMP status during an inspection by
the Agency in November 2009. The synthesis of carglumic acid consists of a
Regarding characterization, the drug substance structure was determined by
NMR, MS, IR and Regarding impurities, two potential
impurities are possible due to
hydantoin-5-proprionic acid (HPA) and diaza-1,3-dione-2,4-carboxy-7-
cycloheptane (Diaza). Only the has been detected at
batch release and it increases in amount during storage at elevated temperatures
but not at room temperature. This impurity also increases during drug product
storage at room temperature but not at refrigerated temperatures, see above
discussion. The starting materials, , were not
detected in several batches and therefore routine testing is not required.
Regarding drug substance specification, identity testing is by IR and HPLC.
Other tests include optical rotation, melting point, pH of 0.5% solution, loss on
drying, residue on ignition, heavy metals, assay and impurities by HPLC.
Regarding chiral purity, the observed specific optical rotation is small and
therefore not a very precise method for determination of chiral purity. Although
a chiral HPLC method was developed, since the r was not detected in
any samples (the limit of detection was 0.1%) during the development, originally
the sponsor did not propose to implement the test in the specification. However,
the Agency recommended that the chiral HPLC method be included in the
specification to assure chiral purity, and the sponsor agreed to do so with the limit
for the NMT
Batch release data were provided that justified the proposed acceptance limits. In
general, measured total impurities were low in the drug substance, about .
Appropriate in-house reference standards were established.
Stability results for 3 batches stored at 25°C/60%RH for 36 months remained
within the tight specification limits. A re-test period of for the drug
substance stored in its original packaging at room temperature is granted.
B. Description of How the Drug Product is Intended to be Used
The drug product tablets may be dispersed in a minimum amount of water
mL per tablet) and ingested immediately or administered through a syringe via a
nasogastric tube. The suspension has a slightly acidic taste.
NDA 022562
EUROPE
21 April 2017 EMA/CHMP/404487/2017 Committee for Medicinal Products for Human Use (CHMP) Assessment report Ucedane International non-proprietary name: carglumic acid Procedure No. EMEA/H/C/004019/0000
Carglumic acid (also called N-carbamyl-L-glutamate, or carbamylglutamate) is an orally active deacylaseresistant synthetic structural N-acetylglutamate (NAG) analogue. NAG, which is formed by the hepatic enzyme N-acetylglutamate synthase (NAGS), is an essential allosteric activator of the enzyme carbamoyl phosphate synthetase 1 (CPS-1). CPS-1 plays an essential role in the urea cycle and converts ammonia into urea which prevents hyperammonaemia. Despite a lower affinity of carbamoyl phosphate synthetase for carglumic acid than for N-acetylglutamate, carglumic acid has been shown in vivo to stimulate carbamoyl phosphate synthetase and to be much more effective than N-acetylglutamate in protecting against ammonia intoxication in rats.
Carglumic acid was first authorised in the EU as Carbaglu dispersible tablets in January 2003. At the time of approval Carbaglu was indicated for the treatment of hyperammonaemia associated with N-acetylglutamate synthase deficiency. Subsequently, the approved indications for Carbaglu have been extended and is now also authorised for the treatment of hyperammonaemia due to, isovaleric acidaemia, methymalonic acidaemia, or propionic acidaemia. Ucedane is indicated in treatment of hyperammonaemia due to N-acetylglutamate synthase primary deficiency. Proposed posology and method of administration for Ucedane
The chemical name of the active substance, carglumic acid, is N-Carbamyl-L-glutamic acid corresponding to the molecular formula C6H10N2O5. It has a relative molecular mass 190.16 g/mol and the following structure:
Carglumic acid exists as a white powder or colourless crystals. It is soluble in boiling water, slightly soluble in cold water and practically insoluble in organic solvents (cyclohexane, dichloromethane, ether). The water solubility of carglumic acid at pH 2.0 is 21.0 g/L. It increases rapidly between the pH 3.0 (28.2 g/L) and the pH 5.0 (440.9 g/L). The solubility of carglumic acid in water is stable between pH 6.0 (555.5 g/L) and pH 8.0 (553.9 g/L). Carglumic acid is prepared from L-glutamic acid. It exhibits stereoisomerism due to the presence of one chiral centre and has one optical isomer; N-carbamoyl-D-glutamic acid.
Adverse effects
The most common adverse effects include vomiting, abdominal pain, fever, and tonsillitis.[4]
SYNTHESIS PHARMACODIA
http://en.pharmacodia.com/web/drug/1_468.html



References
- Jump up^ Caldovic L, Morizono H, Daikhin Y, Nissim I, McCarter RJ, Yudkoff M, Tuchman M (2004). “Restoration of ureagenesis in N-acetylglutamate synthase deficiency by N-carbamylglutamate”. J Pediatr. 145 (4): 552–4. doi:10.1016/j.jpeds.2004.06.047. PMID 15480384.
- Jump up^ Elpeleg O, Shaag A, Ben-Shalom E, Schmid T, Bachmann C (2002). “N-acetylglutamate synthase deficiency and the treatment of hyperammonemic encephalopathy”. Ann Neurol. 52 (6): 845–9. doi:10.1002/ana.10406. PMID 12447942.
- Jump up^ “Patent and Exclusivity Search Results”.
- Jump up^ Drugs.com: Professional Drug Facts for Carglumic Acid.
 |
|
| Clinical data | |
|---|---|
| Synonyms | (S)-2-ureidopentanedioic acid |
| AHFS/Drugs.com | Consumer Drug Information |
| License data | |
| Pregnancy category |
|
| Routes of administration |
Oral |
| ATC code | |
| Pharmacokinetic data | |
| Bioavailability | 30% |
| Protein binding | Undetermined |
| Metabolism | Partial |
| Elimination half-life | 4.3 to 9.5 hours |
| Excretion | Fecal (60%) and renal (9%, unchanged) |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard | 100.116.323 |
| Chemical and physical data | |
| Formula | C6H10N2O5 |
| Molar mass | 190.2 g/mol |
////////////////Carglumic acid, FDA 2010, карглумовая кислота , حمض كاروغلوميك , カルグルミ酸 , ORPHAN, ORPHAN EU, JAPAN 2016, EU 2003, POLA, ORPHAN, OE 312
C(CC(=O)O)C(C(=O)O)NC(=O)N
FDA approves first biosimilar to Neulasta, Fulphila (pegfilgrastim) to help reduce the risk of infection during cancer treatment
The U.S. Food and Drug Administration today approved Fulphila (pegfilgrastim-jmdb) as the first biosimilar to Neulasta (pegfilgrastim) to decrease the chance of infection as suggested by febrile neutropenia (fever, often with other signs of infection, associated with an abnormally low number of infection-fighting white blood cells), in patients with non-myeloid (non-bone marrow) cancer who are receiving myelosuppressive chemotherapy that has a clinically significant incidence of febrile neutropenia.
June 4, 2018
Release
The U.S. Food and Drug Administration today approved Fulphila (pegfilgrastim-jmdb) as the first biosimilar to Neulasta (pegfilgrastim) to decrease the chance of infection as suggested by febrile neutropenia (fever, often with other signs of infection, associated with an abnormally low number of infection-fighting white blood cells), in patients with non-myeloid (non-bone marrow) cancer who are receiving myelosuppressive chemotherapy that has a clinically significant incidence of febrile neutropenia.
“Bringing new biosimilars to patients is a top priority for the FDA, and a key part of our efforts to help promote competition that can reduce drug costs and promote access,” said FDA Commissioner Scott Gottlieb, M.D. “We’ll continue to prioritize reviews of these products to help ensure that biosimilar medications are brought to the market efficiently and through a process that makes certain that these new medicines meet the FDA’s rigorous standard for approval. This summer, we’ll release a comprehensive new plan to advance new policy efforts that promote biosimilar product development. Biologics represent some of the most clinically important, but also costliest products that patients use to promote their health. We want to make sure that the pathway for developing biosimilar versions of approved biologics is efficient and effective, so that patients benefit from competition to existing biologics once lawful intellectual property has lapsed on these products.”
Biological products are generally derived from a living organism and can come from many sources, such as humans, animals, microorganisms or yeast. A biosimilar is a biological product that is approved based on data showing that it is highly similar to a biological product already approved by the FDA (reference product) and has no clinically meaningful differences in terms of safety, purity and potency (i.e., safety and effectiveness) from the reference product, in addition to meeting other criteria specified by law.
The FDA’s approval of Fulphila is based on review of evidence that included extensive structural and functional characterization, animal study data, human pharmacokinetic and pharmacodynamic data, clinical immunogenicity data, and other clinical safety and effectiveness data that demonstrates Fulphila is biosimilar to Neulasta. Fulphila has been approved as a biosimilar, not as an interchangeable product.
The most common side effects of Fulphila are bone pain and pain in extremities. Patients with a history of serious allergic reactions to human granulocyte colony-stimulating factors such as pegfilgrastim or filgrastim products should not take Fulphila.
Serious side effects from treatment with Fulphila include rupture of the spleen, acute respiratory distress syndrome, serious allergic reactions including anaphylaxis, acute inflammation of the kidney (glomerulonephritis), an abnormally high level of white blood cells (leukocytosis), capillary leak syndrome and the potential for tumor growth. Fatal sickle cell crises have occurred.
The FDA granted approval of Fulphila to Mylan GmbH.

//////////// pegfilgrastim, fda 2018, Fulphila, Neulasta, Mylan GmbH, biosimilars, MONOCLONAL ANTIBODY,
Doxepin, ドキセピン

Doxepin
1668-19-5
1229-29-4 (hydrochloride), 4698-39-9 ((E)-isomer); 25127-31-5 ((Z)-isomer)
Launched – 1964
| Doxepin Hydrochloride | 3U9A0FE9N5 | 1229-29-4 |
NSC-108160
P-3693A
SO-101
Aponal
Quitaxon
Silenor
Sinequan
Sinquan
Xepin
Zonalon
USP
USP32/pub/data/v32270/usp32nf27s0_m28110
N,N-Dimethyldibenz[b,e]oxepin-D11(6H),![]() -propylamine hydrochloride
-propylamine hydrochloride ![]()
![]()
![]() [1229-29-4; 4698-39-9 ((E)-isomer); 25127-31-5 ((Z)-isomer)].
[1229-29-4; 4698-39-9 ((E)-isomer); 25127-31-5 ((Z)-isomer)].
DESCRIPTION
SINEQUAN® (doxepin hydrochloride) is one of a class of psychotherapeutic agents known as dibenzoxepin tricyclic compounds. The molecular formula of the compound is C19H21NO•HCl having a molecular weight of 316. It is a white crystalline solid readily soluble in water, lower alcohols and chloroform.
Inert ingredients for the capsule formulations are: hard gelatin capsules (which may contain Blue 1, Red 3, Red 40, Yellow 10, and other inert ingredients); magnesium stearate; sodium lauryl sulfate; starch.
Inert ingredients for the oral concentrate formulation are: glycerin; methylparaben; peppermint oil; propylparaben; water.
Chemistry
SINEQUAN (doxepin HCl) is a dibenzoxepin derivative and is the first of a family of tricyclic psychotherapeutic agents. Specifically, it is an isomeric mixture of: 1-Propanamine, 3-dibenz[b,e]oxepin-11(6H)ylidene-N,N-dimethyl-, hydrochloride.
 |
For Consumers
WHAT ARE THE POSSIBLE SIDE EFFECTS OF DOXEPIN (SINEQUAN) (SINEQUAN)?
Get emergency medical help if you have any of these signs of an allergic reaction: hives; difficulty breathing; swelling of your face, lips, tongue, or throat.
Report any new or worsening symptoms to your doctor, such as: mood or behavior changes, anxiety, panic attacks, trouble sleeping, or if you feel impulsive, irritable, agitated, hostile, aggressive, restless, hyperactive (mentally or physically), more depressed, or have thoughts about suicide or hurting yourself.
Synthesis Reference
Luigi Schioppi, Brian Talmadge Dorsey, Michael Skinner, John Carter, Robert Mansbach, Philip Jochelson, Roberta L. Rogowski, Cara Casseday, Meredith Perry, Bryan Knox, “LOW-DOSE DOXEPIN FORMULATIONS AND METHODS OF MAKING AND USING THE SAME.” U.S. Patent US20090074862, issued March 19, 2009.

DOI: 10.1007/BF00904459
DOI: 10.1007/BF00901313 US 3420851
DE 1232161
SYN 2
Synth Commun 1989, 19(19): 3349, US 3438981

Condensation of dibenzo-oxepinone (I) with 3-(dimethylamino)propylmagnesium chloride (II), followed by a dehydration of the resultant tertiary alcohol with hot HCl gives the target 3-(dimethylamino)propylidene derivative.
SYN 3

Chlorination of 2-(phenoxymethyl)benzoic acid (I) with SOCl2 at 50 °C gives 2-(phenoxymethyl)benzoyl chloride (II), which undergoes cyclization in the presence of FeCl3 in toluene to furnish dibenzo[b,e]oxepin-11-one (III)
Grignard reaction of intermediate (III) with tert-butyl 3-chloropropyl ether (IV) using Mg in refluxing THF or Et2O provides 11-(3-tert-butoxypropyl)-6,11-dihydrodibenzo[b,e]oxepin-11-ol (V), which upon elimination by means of HCl in refluxing EtOH affords alkene (VI).
Treatment of tert-butyl ether (VI) with SOCl2 in refluxing toluene gives 11-(3-chloropropylidene)-6,11-dihydrodibenzo[b,e]oxepine (VII), which is then coupled with dimethylamine (VIII) in the presence of Ni(OAc)2, PPh3 and K2CO3 in DMF or in EtOH at 100 °C to furnish doxepin (VII) .
Finally, treatment of tertiary amine (VII) with HCl at 140 °C yields the target doxepin hydrochloride .
US 2014309437, CN 102924424
Doxepin is a tricyclic antidepressant (TCA) used as a pill to treat major depressive disorder, anxiety disorders, chronic hives, and for short-term help with trouble remaining asleep after going to bed (a form of insomnia).[8][7][9] As a cream it is used for short term treatment of itchiness due to atopic dermatitis or lichen simplex chronicus.[10]
At doses used to treat depression, doxepin appears to inhibit the reuptake of serotonin and norepinephrine and to have antihistamine, adrenergic and serotonin receptor antagonistic, and anticholinergic activities; at low doses used to treat insomnia it appears to be selective for the histamine H1 receptor.[11]
It was introduced under the brand names Quitaxon and Aponal by Boehringer, which discovered it, and as Sinequan by Pfizer,[12] and has subsequently been marketed under many other names worldwide.[2]
Medical uses
Doxepin is used as a pill to treat major depressive disorder, anxiety disorders, chronic hives, and for short-term help with trouble remaining asleep after going to bed (a form of insomnia).[8][7][9] As a cream it is used for short term treatment of itchiness to due atopic dermatitis or lichen simplex chronicus.[10]
In 2016 the American College of Physicians advised that insomnia be treated first by treating comorbid conditions, then with cognitive behavioral therapy and behavioral changes, and then with drugs; doxepin was among those recommended for short term help maintaining sleep, on the basis of weak evidence.[13][14] The 2017 American Academy of Sleep Medicine recommendations focused on treatment with drugs were similar.[13] A 2015 AHRQ review of treatments for insomnia had similar findings.[15]
A 2010 review found that topical doxepin is useful to treat itchiness.[16]
A 2010 review of treatments for chronic hives found that doxepin had been superseded by better drugs but was still sometimes useful as a second line treatment.[17]
Chemistry
Doxepin is a tricyclic compound, specifically a dibenzoxepin, and possesses three rings fused together with a side chain attached in its chemical structure.[38] It is the only TCA with a dibenzoxepin ring system to have been marketed.[64] Doxepin is a tertiary amine TCA, with its side chain–demethylated metabolite nordoxepin being a secondary amine.[40][41] Other tertiary amine TCAs include amitriptyline, imipramine, clomipramine, dosulepin (dothiepin), and trimipramine.[65][66] Doxepin is a mixture of (E) and (Z) stereoisomers (the latter being known as cidoxepin or cis-doxepin) and is used commercially in a ratio of approximately 85:15.[3][67] The chemical name of doxepin is (E/Z)-3-(dibenzo[b,e]oxepin-11(6H)-ylidene)-N,N-dimethylpropan-1-amine[38][68] and its free base form has a chemical formula of C19H21NO with a molecular weight of 279.376 g/mol.[68] The drug is used commercially almost exclusively as the hydrochloride salt; the free base has been used rarely.[3][69] The CAS Registry Number of the free base is 1668-19-5 and of the hydrochloride is 1229-29-4.[3][69]

clip
https://www.sciencedirect.com/science/article/pii/S0040402007016079

History
Doxepin was discovered in Germany in 1963 and was introduced in the United States as an antidepressant in 1969.[38] It was subsequently approved at very low doses in the United States for the treatment of insomnia in 2010.[44][69]
Society and culture
Generic names
Doxepin is the generic name of the drug in English and German and its INN and BAN, while doxepin hydrochloride is its USAN, USP, BANM, and JAN.[3][69][70][2] Its generic name in Spanish and Italian and its DCIT are doxepina, in French and its DCF are doxépine, and in Latin is doxepinum.[2]
The cis or (Z) stereoisomer of doxepin is known as cidoxepin, and this is its INN while cidoxepin hydrochloride is its USAN.[3]
Brand names
It was introduced under the brand names Quitaxon and Aponal by Boehringer and as Sinequan by Pfizer.[12]
As of October 2017, doxepin is marketed under many brand names worldwide: Adnor, Anten, Antidoxe, Colian, Dofu, Doneurin, Dospin, Doxal, Doxepini, Doxesom, Doxiderm, Flake, Gilex, Ichderm, Li Ke Ning, Mareen, Noctaderm, Oxpin, Patoderm, Prudoxin, Qualiquan, Quitaxon, Sagalon, Silenor, Sinepin, Sinequan, Sinequan, Sinquan, and Zonalon.[2] It is also marketed as a combination drug with levomenthol under the brand name Doxure.[2]
Approvals
The oral formulations of doxepin are FDA-approved for the treatment of depression and sleep-maintenance insomnia and its topical formulations are FDA-approved the short-term management for some itchy skin conditions.[71] Whereas in Australia and the United Kingdom, the only licensed indication(s) is/are in the treatment of major depression and pruritus in eczema, respectively.[20][72]
Research
Antihistamine
As of 2017 there was no good evidence that topical doxepin was useful to treat localized neuropathic pain.[73] Cidoxepin is under development by Elorac, Inc. for the treatment of chronic urticaria (hives).[74] As of 2017, it is in phase II clinical trials for this indication.[74] The drug was also under investigation for the treatment of allergic rhinitis, atopic dermatitis, and contact dermatitis, but development for these indications was discontinued.[74]
Headache
Doxepin was under development by Winston Pharmaceuticals in an intranasal formulation for the treatment of headache.[75] As of August 2015, it was in phase II clinical trials for this indication.[75]
PATENT
https://patents.google.com/patent/US9486437B2/en
Doxepin:
Doxepin HCl is a tricyclic compound currently approved and available for treatment of depression and anxiety. Doxepin has the following structure:
For all compounds disclosed herein, unless otherwise indicated, where a carbon-carbon double bond is depicted, both the cis and trans stereoisomers, as well as mixtures thereof are encompassed.
Doxepin belongs to a class of psychotherapeutic agents known as dibenzoxepin tricyclic compounds, and is currently approved and prescribed for use as an antidepressant to treat depression and anxiety. Doxepin has a well-established safety profile, having been prescribed for over 35 years.
Doxepin, unlike most FDA approved products for the treatment of insomnia, is not a Schedule IV controlled substance. U.S. Pat. Nos. 5,502,047 and 6,211,229, the entire contents of which are incorporated herein by reference, describe the use of doxepin for the treatment chronic and non-chronic (e.g., transient/short term) insomnias at dosages far below those used to treat depression.
It is contemplated that doxepin for use in the methods described herein can be obtained from any suitable source or made by any suitable method. As mentioned, doxepin is approved and available in higher doses (75-300 milligrams) for the treatment of depression and anxiety. Doxepin HCl is available commercially and may be obtained in capsule form from a number of sources. Doxepin is marketed under the commercial name SINEQUAN® and in generic form, and can be obtained in the United States generally from pharmacies in capsule form in amounts of 10, 25, 50, 75, 100 and 150 mg dosage, and in liquid concentrate form at 10 mg/mL. Doxepin HCl can be obtained from Plantex Ltd. Chemical Industries (Hakadar Street, Industrial Zone, P.O. Box 160, Netanya 42101, Israel), Sifavitor S.p.A. (Via Livelli 1—Frazione, Mairano, Italy), or from Dipharma S.p.A. (20021 Baranzate di Bollate, Milano, Italy). Also, doxepin is commercially available from PharmacyRx (NZ) (2820 1st Avenue, Castlegar, B.C., Canada) in capsule form in amounts of 10, 25, 50, 75, 100 and 150 mg. Furthermore, Doxepin HCl is available in capsule form in amounts of 10, 25, 50, 75, 100 and 150 mg and in a 10 mg/ml liquid concentrate from CVS Online Pharmacy Store (CVS.com).
Also, doxepin can be prepared according to the method described in U.S. Pat. No. 3,438,981, which is incorporated herein by reference in its entirety. It should be noted and understood that although many of the embodiments described herein specifically refer to “doxepin,” other doxepin-related compounds can also be used, including, for example, pharmaceutically acceptable salts, prodrugs, metabolites, in-situ salts of doxepin formed after administration, and solid state forms, including polymorphs and hydrates.
Metabolites:
In addition, doxepin metabolites can be prepared and used. By way of illustration, some examples of metabolites of doxepin can include, but are not limited to, desmethyldoxepin, hydroxydoxepin, hydroxyl-N-desmethyldoxepin, doxepin N-oxide, N-acetyl-N-desmethyldoxepin, N-desmethyl-N-formyldoxepin, quaternary ammonium-linked glucuronide, 2-O-glucuronyldoxepin, didesmethyldoxepin, 3-O-glucuronyldoxepin, or N-acetyldidesmethyldoxepin. The metabolites of doxepin can be obtained or made by any suitable method, including the methods described above for doxepin.
Desmethyldoxepin has the following structure:
Desmethyldoxepin is commercially available as a forensic standard. For example, it can be obtained from Cambridge Isotope Laboratories, Inc. (50 Frontage Road, Andover, Mass.). Desmethyldoxepin for use in the methods discussed herein can be prepared by any suitable procedure. For example, desmethyldoxepin can be prepared from 3-methylaminopropyl triphenylphosphonium bromide hydrobromide and 6,11-dihydrodibenz(b,e)oxepin-11-one according to the method taught in U.S. Pat. No. 3,509,175, which is incorporated herein by reference in its entirety.
Hydroxydoxepin has the following structure:
2-Hydroxydoxepin can be prepared by any suitable method, including as taught by Shu et al. (Drug Metabolism and Disposition (1990) 18:735-741), which is incorporated herein by reference in its entirety.
Hydroxyl-N-desmethyldoxepin has the following structure:
2-Hydroxy-N-desmethyldoxepin can be prepared any suitable method.
Doxepin N-oxide has the following structure:
Doxepin N-oxide can be prepared by any suitable method. For example, doxepin N-oxide can be prepared as taught by Hobbs (Biochem Pharmacol (1969) 18:1941-1954), which is hereby incorporated by reference in its entirety.
N-acetyl-N-desmethyldoxepin has the following structure:
N-acetyl-N-desmethyldoxepin can be prepared by any suitable means. For example, (E)-N-acetyl-N-desmethyldoxepin has been produced in filamentous fungus incubated with doxepin as taught by Moody et al. (Drug Metabolism and Disposition (1999) 27:1157-1164), hereby incorporated by reference in its entirety.
N-desmethyl-N-formyldoxepin has the following structure:
N-desmethyl-N-formyldoxepin can be prepared by any suitable means. For example, (E)-N-desmethyl-N-formyldoxepin has been produced in filamentous fungus incubated with doxepin as taught by Moody et al. (Drug Metabolism and Disposition (1999) 27:1157-1164), hereby incorporated by reference in its entirety.
N-acetyldidesmethyldoxepin has the following structure:
N-acetyldidesmethyldoxepin can be prepared by any suitable means. For example, (E)-N-acetyldidesmethyldoxepin has been produced in filamentous fungus incubated with doxepin as taught by Moody et al. (Drug Metabolism and Disposition (1999) 27:1157-1164), hereby incorporated by reference in its entirety.
Didesmethyldoxepin has the following structure:
Didesmethyldoxepin can be prepared by any suitable means. For example, (Z)- and (E)-didesmethyldoxepin have been isolated from plasma and cerebrospinal fluid of depressed patients taking doxepin, as taught by Deuschle et al. (Psychopharmacology (1997) 131:19-22), hereby incorporated by reference in its entirety.
3-O-glucuronyldoxepin has the following structure:
3-O-glucuronyldoxepin can be prepared by any suitable means. For example, (E)-3-O-glucuronyldoxepin has been isolated from the bile of rats given doxepin, as described by Shu et al. (Drug Metabolism and Disposition (1990) 18:1096-1099), hereby incorporated by reference in its entirety.
2-O-glucuronyldoxepin has the following structure:
2-O-glucuronyldoxepin can be prepared by any suitable means. For example, (E)-2-O-glucuronyldoxepin has been isolated from the bile of rats given doxepin, and also in the urine of humans given doxepin, as described by Shu et al. (Drug Metabolism and Disposition (1990) 18:1096-1099), hereby incorporated by reference in its entirety.
Quaternary ammonium-linked glucuronide of doxepin (doxepin N+-glucuronide) has the following structure:
N+-glucuronide can be obtained by any suitable means. For example, doxepin N+-glucuronide can be prepared as taught by Luo et al. (Drug Metabolism and Disposition, (1991) 19:722-724), hereby incorporated by reference in its entirety.
PATENT
https://patents.google.com/patent/CN105330638A/en
doxepin hydrochloride, the chemical name is N, N- dimethyl-3-dibenzo (b, e) _ oxepin -11 (6H) -1-propanamine salt subunit cistron iso the mixture body configuration. CAS Number 1229-29-4 thereof, of the formula
[0003]
[0004] Doxepin hydrochloride is a drug for the treatment of depression and anxiety neurosis that act to inhibit the central nervous system serotonin and norepinephrine reuptake, such that these two synaptic cleft neurotransmitter concentration increased and antidepressant effect, but also has anti-anxiety and sedative effects. Doxepin hydrochloride oral absorption, bioavailability of 13-45%, half-life (Shu 1/2) is 8-12 hours, to apparent volume of distribution (1) ^ 9-33171.Primarily metabolized in the liver to active metabolites thereof demethylation.Metabolite excretion from the kidney, elderly patients decline of metabolism and excretion ability of this product
[0005] Chinese Patent CN102924486A discloses a method for preparing a hydrochloride of doxepin. The method comprises the coupling reaction CN, i.e., the use of Ni (0Α〇) 2 / ΡΡ1 ^ φ to the amine-based compound. Although Ni catalyst the reaction step (OAc) 2 is more readily available and inexpensive, but the low yield of this step, and low product purity.
SUMMARY
[0006] Accordingly, the present invention provides a method of o-toluic acid synthesized multi doxepin hydrochloride, the higher the yield and purity of the obtained product was purified by this method.
[0007] – o-methylbenzoate method for the synthesis of doxepin hydrochloride, comprising the steps of:
[0008] (1) o-methylbenzoic acid with N- halosuccinimide benzylation halogenation reaction occurs in an acetonitrile solvent in the light conditions, to give o-halo-methylbenzoic acid (Compound J), the following reaction formula,
[0009]
[0010] (2) Compound J celite load cesium fluoride intramolecular substitution reaction, to give phthalide (Compound H) in an acetonitrile solvent and as a catalyst, the following reaction formula,
[0011]
[0012] (3) The phenol compound J with sodium methoxide in an alcohol solvent substitution reaction, to give a compound I, the following reaction formula,
[0013]
[0014] (4) The cyclization reaction of Compound I in a solvent in the catalytic DMS0 anhydrous aluminum chloride to give 6, 11-dihydro-dibenzo [b, e] oxepin -11- one (compound A), the following reaction formula,
[0015]
[0016] (5) 6, 11-dihydro-dibenzo [b, e] oxepin-11-one (Compound A) and 3-chloropropyl alkyl tert-butyl ether (compound B) is added magnesium powder and with THF and / or a nucleophilic addition of anhydrous diethyl ether under the conditions of the reaction solvent to give the hydroxy compound (compound C), the following reaction formula,
[0017]
[0018] (6) heating elimination reaction to give an olefin compound (Compound D) in a strong base in an alcoholic solvent to the hydroxy compound, the following reaction formula,
[0019]
[0020] (7) to the olefinic compound in the nucleophilic substitution reaction of a hydrogen halide acid, to give halide (Compound E), the following reaction formula,
[0022] wherein the compound E X is a C1, Br, or a a I;
[0023] (8) the halide with dimethylamine in a solvent under an organic lithium compound is added in ether to nucleophilic substitution reaction to yield doxepin (Compound F.), The following reaction formula,
[0024]
[0025] (9) the doxepin neutralization reaction with hydrochloric acid to give sulfasalazine (Compound G), the following reaction formula,
Example 1
[0043] placed in a 20L reaction vessel acetonitrile, o-methylbenzoic acid, N- bromosuccinimide, using a water bath temperature controlled at 10 ° C, under stirring for 4h. A known separation method, separation of o-bromomethyl-benzoic acid. This compound is named J.
[0044] placed in a 20L reaction container, Compound J, diatomaceous earth in an amount of 0.05 to load cesium fluoride (compound J as a mass basis), acetonitrile in an amount of 2.5 (in Compound J 1 is a mass basis), and the temperature was adjusted to 30 ° C, with stirring under reflux for 20h adjustment. Then, a known means for separating the reaction phthalide.
After [0045] placed in a 20L reaction vessel phthalide, 3 an amount of sodium methoxide in ethanol solvent (total mass of phenol phthalide and 1 meter), the reaction solution temperature adjusted to 50 ° C, was added dropwise start phenol was 1.05 mass (in mass was 1 meter phthalide), dropwise over lh. After the dropwise addition, the reaction temperature after 5h using known separation methods, to give o-methyl benzyl phenyl ether, this compound is named I.
[0046] The above compound I, in an amount of 10% anhydrous aluminum chloride (mass of Compound I was 100% basis), the amount of DMS0 3 (mass basis Compound I 1) into a reaction vessel , the temperature was adjusted to 95 ° C. The reaction time is to be 12h. Using known separation means for separating the 6, 11-dihydro-dibenzo [b, e] oxepin-11-one.
[0047] placement 6, 11-dihydro-dibenzo in a reaction vessel and 20L [b, e] oxepin-11-one, 1.1-dihydro-fold of the mole of diphenyl at 6, 11 and [ b, e] oxepin-11-one 3-chloropropyl alkyl tert-butyl ether, 2 times the mass 6, 11-dihydro-dibenzo [b, e] oxepin-11-one magnesium in , taking all of fifths THF (5 to 6 times by mass, 11-dihydro-dibenzo [b, e] THF oxepin-11-one) and heated to 35 ° C and allowed to react. After the reaction started, the remaining 3/5 of THF was added dropwise.Was added dropwise to the system to be completed into hydrogen, reflux. After a total reaction 5h, the reaction was stopped. After the system was cooled and then poured into saturated ammonium chloride solution, extracted twice with ethyl acetate was added, dried over anhydrous sodium sulfate 5h, the resulting crude product was recrystallized from acetonitrile to give hydroxy compound.
[0048] placed in a 20L reaction vessel above hydroxy compound, an ethanol solution of 1.5 times the mass of hydroxy compound class of sodium hydroxide (concentration l〇wt mass%), was heated to 65 ° C, 2h elimination reaction after the reaction was stopped, cooled, the solvent was distilled off more of the obtained crude product was crystallized from acetonitrile to give the olefinic compounds.
[0049] placed in a 20L reaction vessel of the olefin compound, in an aqueous solution plus 1 times the mass of the olefinic compound hydrochloride (concentration of 5wt%), and heated to 50 ° C, so that a nucleophilic substitution reaction . The reaction time is to be after 4h, the reaction was stopped, cooled, the solvent was distilled off more of the obtained crude product was crystallized from acetonitrile to give the halides.
[0050] placed in a 20L reaction vessel above halide, 0.1 times the mass of methyl lithium halides to 2 times the mass of the halide in diethyl ether, heated to 40 ° C, so that the nucleophilic substitution reaction. The reaction time is to be after 5h, the reaction was stopped, reaction was complete and extracted with ethylacetate three times, dried over anhydrous sodium sulfate 5h, the resulting crude product was recrystallized from acetonitrile to obtain doxepin.
[0051] 20L is placed in a pressure reactor above doxepin, 1.05 times the mass of material in the doxepin hydrochloride (concentration of 30wt%), the control pressure to 3 ~ 4MPa, and heated to 130 ° C , and among the responses. Time after to be reacted for 20 h, cooled to room temperature and should be finished by filtration, and dried to give doxepin hydrochloride. In this embodiment overall yield 37.9%, measured by HPLC obtaining 99.2% purity.
[0052] Example 2
[0053] placed in a 20L reaction vessel acetonitrile, o-methylbenzoic acid, N- bromosuccinimide, using a water bath temperature controlled at 20 ° C, under stirring for 2h. A known separation method, separation of o-toluic acid halide.
[0054] placed in a 20L reaction container, Compound J, an amount of load of cesium fluoride Celite ~ 0.05 0.15 (in mass Compound J is 1 meter), in an amount of 2.5 to 8 acetonitrile (compound J as a mass basis), and the temperature was adjusted to 30 ~ 50 ° C, 12 ~ 20h at reflux with stirring under regulation. Then, a known means for separating the reaction phthalide.
After [0055] phthalide placed in 20L reaction vessel, an amount of sodium methoxide in 10 ethanol solvent (total mass of phenol phthalide and 1 meter), adjusting the temperature of the reaction solution was 60 ° C, was added dropwise start phenol was 1.15 mass (in mass was 1 meter phthalide), dropwise over lh.After the dropwise addition, the reaction temperature after 5h using known separation methods, to give o-methyl benzyl phenyl ether, this compound is named I.
[0056] The above compound I, in an amount of 40% anhydrous aluminum chloride (mass of Compound I was 100% basis), in an amount of DMS0 8 (in compound I is a mass basis) into a reaction vessel , the temperature was adjusted to 105 ° C. The reaction time is to be for 6h. Using known separation means for separating the 6, 11-dihydro-dibenzo [b, e] oxepin-11-one.
[0057] placement 6, 11-dihydro-dibenzo in a reaction vessel and 20L [b, e] oxepin-11-one, 1.5-dihydro-fold of the mole of diphenyl at 6, 11 and [ b, e] oxepin-11-one 3-chloropropyl alkyl tert-butyl ether, 2.4 times the mass in 6, 11-dihydro-dibenzo [b, e] oxepin-11-one of magnesium, taking all fifths THF (5 to 7 times the mass in 6, 11-dihydro-dibenzo [b, e] THF oxepin-11-one) is to make, and heated to 40 ° C reaction.After the reaction started, the remaining 3/5 of THF was added dropwise. Was added dropwise to the system to be completed into hydrogen, reflux. When the total reaction 2h, the reaction was stopped. After the system was cooled and then poured into saturated ammonium chloride solution, extracted twice with ethyl acetate was added, dried over anhydrous sodium sulfate 5h, the resulting crude product was recrystallized from acetonitrile to give hydroxy compound.
[0058] placed in a 20L reaction vessel above hydroxy compound, an ethanol solution of 5 times the mass of hydroxy compound class of sodium hydroxide (concentration of 70wt%), was heated to 80 ° C, the reaction was stopped after the elimination reaction LH, cooling, the solvent was distilled off more of the obtained crude product was crystallized from acetonitrile to give the olefinic compounds.
[0059] placed in a 20L reaction vessel of the olefin compound, in an aqueous solution of 2 times the mass of the olefinic compound added hydrobromic acid (concentration of 30wt%), and heated to 60 ° C, so that nucleophilic Substitution reaction. The reaction time is to be after the 1. 5h, the reaction was stopped, cooled, the solvent was distilled off more of the obtained crude product was crystallized from acetonitrile to give the halides.
[0060] placed in a 20L reaction vessel above halide, 0.8 times the mass of phenyl lithium halide to 8 times the mass of the halide in diethyl ether, heated to 50 ° C, so that the nucleophilic substitution reaction. The reaction time is to be after 2h, the reaction was stopped, reaction was complete and extracted with ethylacetate three times, dried over anhydrous sodium sulfate 5h, the resulting crude product was recrystallized from acetonitrile to obtain doxepin.
[0061] 20L is placed in a pressure reactor above doxepin, 1.2 times the mass of material in the doxepin hydrochloride (concentration of 38wt%), the control pressure to 3 ~ 4MPa, and heated to 150 ° C , and among the responses. Time after to be reacted for 16 h, cooled to room temperature and should be finished by filtration, and dried to give doxepin hydrochloride. In this embodiment overall yield 39.7%, measured by HPLC obtaining 99.4% purity.
[0062] Example 3
[0063] placed in a 20L reaction vessel acetonitrile, o-methylbenzoic acid, N- bromosuccinimide, using a water bath temperature controlled at 15 ° C, under stirring for 3h. A known separation method, separation of o-bromomethyl-benzoic acid.
[0064] placed in a 20L reaction container, Compound J, an amount of load of cesium fluoride Celite ~ 0.05 0.15 (in mass Compound J is 1 meter), in an amount of 2.5 to 8 acetonitrile (compound J as a mass basis), and the temperature was adjusted to 30 ~ 50 ° C, 12 ~ 20h at reflux with stirring under regulation. Then, a known means for separating the reaction phthalide.
After [0065] phthalide placed in 20L reaction vessel, an amount of sodium methoxide in ethanol solvent 6 (total mass of phenol phthalide and 1 meter), adjusting the temperature of the reaction solution was 55 ° C, was added dropwise start phenol was 1.10 mass (in mass was 1 meter phthalide), dropwise over lh.After the dropwise addition, the reaction temperature after 3. 5h using known separation methods, to give o-methyl benzyl phenyl ether, this compound is named I.
[0066] Anhydrous aluminum above compound I, in an amount of 25% of the chloride (compound I mass is 100% basis), in an amount of DMS0 6. 5 (in compound I is a mass basis) into the reaction vessel temperature is adjusted to 100 ° C. The reaction time is to be 9h. Using known separation means for separating the 6, 11-dihydro-dibenzo [b, e] oxepin-11-one.
[0067] placement 6, 11-dihydro-dibenzo in a reaction vessel and 20L [b, e] oxepin-11-one, 1.3-dihydro-fold of the mole of diphenyl at 6, 11 and [ b, e] oxepin-11-one 3-chloropropyl alkyl tert-butyl ether, 2.2 times the mass in 6, 11-dihydro-dibenzo [b, e] oxepin-11-one of magnesium, taking all fifths THF (5 to 7 times the mass in 6, 11-dihydro-dibenzo [b, e] THF oxepin-11-one) is to make, and heated to 38 ° C reaction.After the reaction started, the remaining 3/5 of THF was added dropwise. Was added dropwise to the system to be completed into hydrogen, refluxed for 2h. After a total reaction 3. 5h, the reaction was stopped. After the system was cooled and then poured into saturated ammonium chloride solution, extracted twice with ethyl acetate was added, dried over anhydrous sodium sulfate 5h, the resulting crude product was recrystallized from acetonitrile to give hydroxy compound.
[0068] placed in a 20L reaction vessel above hydroxy compound, an ethanol solution of 3-hydroxysteroid times the mass of the compound of sodium hydroxide (concentration of 40wt%), and heated to 75 ° C, 1. 5h the reaction stopped after elimination the reaction was cooled, the solvent was distilled off more of the obtained crude product was crystallized from acetonitrile to give the olefinic compounds.
[0069] placed in a 20L reaction vessel of the olefin compound, an aqueous solution of 1.5-fold increase in the mass of hydroiodic olefinic compounds (concentration of 18wt%), was heated to 55 ° C, so nucleophilic substitution reaction. The reaction time is to be after 2h, the reaction was stopped, cooled, the solvent was distilled off more of the obtained crude product was crystallized from acetonitrile to give the halides.
[0070] placed in a 20L reaction vessel above halide, 0.4 times the mass of the halide in n-butyllithium, in diethyl ether five times the mass of halide and heated to 45 ° C, so that a nucleophilic substitution reaction . The reaction time is to be 3. After 5h, the reaction was stopped, reaction was complete and extracted with ethylacetate three times, dried over anhydrous sodium sulfate 5h, the resulting crude product was recrystallized from acetonitrile to obtain doxepin.
[0071] 20L is placed in a pressure reactor above doxepin, 1.12 times the mass of material in the doxepin hydrochloride (concentration of 34wt%), the control pressure to 3 ~ 4MPa, and heated to 140 ° C , and among the responses. Time after to be reacted for 18 h, cooled to room temperature and should be finished by filtration, and dried to give doxepin hydrochloride. In this embodiment overall yield 40.2%, measured by HPLC obtaining 99.5% purity.
[0072] Example 4
[0073] placed in a 20L reaction vessel acetonitrile, o-methylbenzoic acid, N- bromosuccinimide, using a water bath temperature controlled at 15 ° C, under stirring for 4h. A known separation method, separation of o-toluic acid halide.
[0074] placed in a 20L reaction container, Compound J, an amount of load of cesium fluoride Celite ~ 0.05 0.15 (in mass Compound J is 1 meter), in an amount of 2.5 to 8 acetonitrile (compound J as a mass basis), and the temperature was adjusted to 30 ~ 50 ° C, 12 ~ 20h at reflux with stirring under regulation. Then, a known means for separating the reaction phthalide.
After [0075] phthalide placed in 20L reaction vessel, 5 an amount of sodium methoxide in ethanol solvent (total mass of phenol phthalide and 1 meter), adjusting the temperature of the reaction solution was 55 ° C, was added dropwise start phenol was 1.15 mass (in mass was 1 meter phthalide), dropwise over lh.After the dropwise addition, the reaction temperature after 5h using known separation methods, to give o-methyl benzyl phenyl ether, this compound is named I.
[0076] The above compound I, in an amount of 25% anhydrous aluminum chloride (mass of Compound I was 100% basis), in an amount of DMS0 8 (in compound I is a mass basis) into a reaction vessel , the temperature was adjusted to 100 ° C. The reaction time is to be 12h. Using known separation means for separating the 6, 11-dihydro-dibenzo [b, e] oxepin-11-one.
[0077] placement 6, 11-dihydro-dibenzo in a reaction vessel and 20L [b, e] oxepin-11-one, 1.3-dihydro-fold of the mole of diphenyl at 6, 11 and [ b, e] oxepin-11-one 3-chloropropyl alkyl tert-butyl ether, 2.4 times the mass in 6, 11-dihydro-dibenzo [b, e] oxepin-11-one of magnesium, taking all fifths THF (5 to 7 times the mass in 6, 11-dihydro-dibenzo [b, e] THF oxepin-11-one) is to make, and heated to 40 ° C reaction.After the reaction started, the remaining 3/5 of THF was added dropwise. Was added dropwise to the system to be completed into hydrogen, reflux. When the total reaction 2h, the reaction was stopped. After the system was cooled and then poured into saturated ammonium chloride solution, extracted twice with ethyl acetate was added, dried over anhydrous sodium sulfate 5h, the resulting crude product was recrystallized from acetonitrile to give hydroxy compound.
[0078] placed in a 20L reaction vessel above hydroxy compound, an ethanol solution of 5 times the mass of hydroxy compound class of sodium hydroxide (concentration of 70wt%), was heated to 80 ° C, the reaction was stopped after the elimination reaction LH, cooling, the solvent was distilled off more of the obtained crude product was crystallized from acetonitrile to give the olefinic compounds.
[0079] placed in a 20L reaction vessel of the olefin compound, an aqueous solution of 1.5-fold increase in the mass of hydroiodic olefinic compounds (concentration of 30wt%), and heated to 60 ° C, so nucleophilic substitution reaction. The reaction time is to be after the 1. 5h, the reaction was stopped, cooled, the solvent was distilled off more of the obtained crude product was crystallized from acetonitrile to give the halides.
[0080] placed in a 20L reaction vessel above halide, 0.8 times in mass n-butyl lithium halide, eight times the mass of the halide in diethyl ether, heated to 50 ° C, so that a nucleophilic substitution reaction . The reaction time is to be after 2h, the reaction was stopped, reaction was complete and extracted with ethylacetate three times, dried over anhydrous sodium sulfate 5h, the resulting crude product was recrystallized from acetonitrile to obtain doxepin.
[0081] 20L is placed in a pressure reactor above doxepin, 1.2 times the mass of material in the doxepin hydrochloride (concentration of 38wt%), the control pressure to 3 ~ 4MPa, and heated to 150 ° C , and among the responses. Time after to be reacted for 16 h, cooled to room temperature and should be finished by filtration, and dried to give doxepin hydrochloride. In this embodiment overall yield 41.6%, measured by HPLC obtaining 99.7% purity.
[0082] Example 5
[0083] placed in a 20L reaction vessel acetonitrile, o-methylbenzoic acid, N- bromosuccinimide, using a water bath temperature controlled at 15 ° C, the reaction 2. 5h under stirring. A known separation method, separation of o-bromomethyl-benzoic acid.
[0084] placed in a 20L reaction vessel o-bromomethyl benzoic acid, diatomaceous earth in an amount of load of cesium fluoride 0.05 ~ 0.15 (in mass Compound J is 1 meter), in an amount of 2. 5-8 acetonitrile (compound J as a mass basis), and the temperature was adjusted to 30 ~ 50 ° C, 12 ~ 20h at reflux with stirring under regulation. Then, a known means for separating the reaction phthalide.
After [0085] phthalide placed in 20L reaction vessel, 5 an amount of sodium methoxide in ethanol solvent (total mass of phenol phthalide and 1 meter), adjusting the temperature of the reaction solution was 55 ° C, was added dropwise start was 1.08 mass of phenol (mass was phthalide 1 meter), dropwise over lh.After the dropwise addition, the reaction temperature after 3h using known separation methods, to give o-methyl benzyl phenyl ether, this compound is named I.
[0086] Anhydrous aluminum above compound I, in an amount of 25% of the chloride (compound I mass is 100% basis), in an amount of DMS0 5 (in compound I is a mass basis) into a reaction vessel , the temperature was adjusted to 100 ° C.The reaction time is to be 8h. Using known separation means for separating the 6, 11-dihydro-dibenzo [b, e] oxepin-11-one.
[0087] placement 6, 11-dihydro-dibenzo in a reaction vessel and 20L [b, e] oxepin-11-one, 1.2-dihydro-fold of the mole of diphenyl at 6, 11 and [ b, e] oxepin-11-one 3-chloropropyl alkyl tert-butyl ether, 2.2 times the mass in 6, 11-dihydro-dibenzo [b, e] oxepin-11-one of magnesium, taking all fifths THF (5 to 7 times the mass in 6, 11-dihydro-dibenzo [b, e] THF oxepin-11-one) is to make, and heated to 38 ° C reaction.After the reaction started, the remaining 3/5 of THF was added dropwise. Was added dropwise to the system to be completed into hydrogen, reflux. When the total reaction 2h, the reaction was stopped. After the system was cooled and then poured into saturated ammonium chloride solution, extracted twice with ethyl acetate was added, dried over anhydrous sodium sulfate 5h, the resulting crude product was recrystallized from acetonitrile to give hydroxy compound.
[0088] placed in a 20L reaction vessel above hydroxy compound, an ethanol solution of 2 times the mass of hydroxy compound class of sodium hydroxide (concentration of 40wt%), was heated to 70 ° C, the reaction was stopped after the elimination reaction 2h, cooling, the solvent was distilled off more of the obtained crude product was crystallized from acetonitrile to give the olefinic compounds.
[0089] placed in a 20L reaction vessel of the olefin compound, an aqueous solution of 1.5-fold increase in the mass of hydroiodic olefinic compounds (concentration of 15wt%), and heated to 50 ° C, so nucleophilic substitution reaction. The reaction time is to be after 4h, the reaction was stopped, cooled, the solvent was distilled off more of the obtained crude product was crystallized from acetonitrile to give the halides.
[0090] placed in a 20L reaction vessel above halide, 0.4 times the mass of the halide in n-butyl lithium, 2 to 8 times the mass of the halide in diethyl ether, heated to 45 ° C, so that nucleophilic Substitution reaction. The reaction time is to be after 3h, the reaction was stopped, reaction was complete and extracted with ethylacetate three times, dried over anhydrous sodium sulfate 5h, the resulting crude product was recrystallized from acetonitrile to obtain doxepin.
[0091] 20L is placed in a pressure reactor above doxepin, 1.12 times the mass of material in the doxepin hydrochloride (mass concentration 37. 6wt%), the control pressure to 3 ~ 4MPa, heated to 140 ° C, allowing the reaction among. Time after to be reacted for 20 h, cooled to room temperature and should be finished by filtration, and dried to give doxepin hydrochloride. In this embodiment overall yield 43.9%, measured by HPLC obtaining 99.9% purity.
PATENTS
 |
|
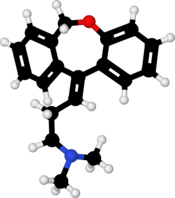 |
|
| Clinical data | |
|---|---|
| Trade names | Sinequan, many others[2] |
| Synonyms | NSC-108160[3] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682390 |
| License data | |
| Pregnancy category |
|
| Routes of administration |
By mouth, topical, intravenous, intramuscular injection[1] |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 13–45% (mean 29%)[5][6] |
| Protein binding | 76%[7] |
| Metabolism | Hepatic (CYP2D6, CYP2C19)[4][5] |
| Metabolites | Nordoxepin, glucuronide conjugates[4] |
| Elimination half-life | Doxepin: 8–24 hours (mean 17 hours)[7] Nordoxepin: 31 hours[7] |
| Excretion | Urine: ~50%[4][5] Feces: minor[5] |
| Identifiers | |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C19H21NO |
| Molar mass | 279.376 g/mol |
| 3D model (JSmol) | |
- Virtanen R, Iisalo E, Irjala K: Protein binding of doxepin and desmethyldoxepin. Acta Pharmacol Toxicol (Copenh). 1982 Aug;51(2):159-64. [PubMed:7113722]
- Virtanen R, Scheinin M, Iisalo E: Single dose pharmacokinetics of doxepin in healthy volunteers. Acta Pharmacol Toxicol (Copenh). 1980 Nov;47(5):371-6. [PubMed:7293791]
- Negro-Alvarez JM, Carreno-Rojo A, Funes-Vera E, Garcia-Canovas A, Abellan-Aleman AF, Rubio del Barrio R: Pharmacologic therapy for urticaria. Allergol Immunopathol (Madr). 1997 Jan-Feb;25(1):36-51. [PubMed:9111875]
- Sansone RA, Sansone LA: Pain, pain, go away: antidepressants and pain management. Psychiatry (Edgmont). 2008 Dec;5(12):16-9. [PubMed:19724772]
- Kirchheiner J, Meineke I, Muller G, Roots I, Brockmoller J: Contributions of CYP2D6, CYP2C9 and CYP2C19 to the biotransformation of E- and Z-doxepin in healthy volunteers. Pharmacogenetics. 2002 Oct;12(7):571-80. [PubMed:12360109]
- ZONALON® (doxepin hydrochloride) CREAM, 5% [Link]
- FDA Label: SilenorTM (doxepin) tablets for oral administration [Link]
//////////////Doxepin, ドキセピン , NSC-108160 , P-3693A , SO-101
[H]C(CCN(C)C)=C1C2=CC=CC=C2COC2=CC=CC=C12
N,N-Dimethyldibenz[b,e]oxepin-D11(6H),
USP Doxepin Hydrochloride RS.
USP Doxepin Related Compound A RS
 .
. USP Doxepin Related Compound B RS
 .
. USP Doxepin Related Compound C RS.
Identification—
Related compounds—
Chromatographic system (see Chromatography ![]() 621
621![]() )— The liquid chromatograph is equipped with a 215-nm detector and a 4.6-mm × 25-cm column that contains 5-µm packing L1. The flow rate is about 1 mL per minute. The column temperature is maintained at 30
)— The liquid chromatograph is equipped with a 215-nm detector and a 4.6-mm × 25-cm column that contains 5-µm packing L1. The flow rate is about 1 mL per minute. The column temperature is maintained at 30![]() . Chromatograph about 20 µL of the Standard solution, and record the peak areas as directed for Procedure: the resolution, R, between doxepin related compound A and doxepin related compound C is not less than 1.5; the resolution between doxepin related compound C and doxepin related compound B is not less than 1.5; and the signal-to-noise ratio for all the peaks is not less than 10. [NOTE—Use the approximate relative retention times given in Table 1 for the purpose of peak identification. The doxepin related compound C peak will be the largest peak in the Standard solution chromatogram.]
. Chromatograph about 20 µL of the Standard solution, and record the peak areas as directed for Procedure: the resolution, R, between doxepin related compound A and doxepin related compound C is not less than 1.5; the resolution between doxepin related compound C and doxepin related compound B is not less than 1.5; and the signal-to-noise ratio for all the peaks is not less than 10. [NOTE—Use the approximate relative retention times given in Table 1 for the purpose of peak identification. The doxepin related compound C peak will be the largest peak in the Standard solution chromatogram.]
| Name | Relative Retention Time (RRT) |
Limit (%) |
| Doxepin related compound A | 0.48 | 0.10 |
| Doxepin related compound C | 0.55 | 0.20 |
| Doxepin related compound B | 0.63 | 0.10 |
| Doxepin hydrochloride | 1.0 | — |
| Unknown impurity | — | 0.10 each |
Procedure— Inject a volume (about 20 µL) of the Test solution into the chromatograph, record the chromatogram for up to 2.2 times the retention time of doxepin, and measure the peak responses. Calculate the percentage of each individual doxepin related compound in the portion of Doxepin Hydrochloride taken by the formula:
in which rU is the individual peak response for each doxepin related compound obtained from the Test solution; rS is the response of the corresponding peak in theStandard solution; CS is the concentration, in mg per mL, of each doxepin related compound in the Standard solution; and CT is the concentration, in mg per mL, of Doxepin Hydrochloride in the Test solution. The related substance limits are listed in Table 1. [NOTE—Discard any peak with a relative retention time less than 0.25. This method is not intended to resolve the E- and Z-isomers of doxepin hydrochloride. Minor variations in the mobile phase composition could result in a shoulder in the trailing edge of doxepin. In cases where there may be separation, both the E- and Z-isomers should be used in the appropriate calculations.] Use the response of the doxepin peak obtained from the Standard solution and the concentration of doxepin hydrochloride in the Standard solution to calculate the percentage of unknown individual impurities.
Assay—
Procedure— Separately inject equal volumes (about 20 µL) of the Standard preparation and the Assay preparation into the chromatograph, record the chromatograms, and measure the responses for the major peaks. Calculate the quantity, in mg, of C19H21NO·HCl in the portion of Doxepin Hydrochloride taken by the formula:
in which C is the concentration, in µg per mL, of USP Doxepin Hydrochloride RS in the Standard preparation, and rU(Z) and rU(E) are the respective peak responses of the (Z)- and (E)-isomers obtained from the Assay preparation, and rS(Z) and rS(E) are the respective peak responses of the (Z)- and (E)-isomers obtained from the Standard preparation. Calculate the percentage of the (Z)-isomer in the Assay preparation taken by the formula:
in which WS is the weight, in mg, of USP Doxepin Hydrochloride RS in the Standard preparation, WT is the weight, in mg, in the portion of Doxepin Hydrochloride taken, and PZ is the labeled percentage of (Z)-isomer in USP Doxepin Hydrochloride RS. Similarly calculate the percentage of (E)-isomer in the Assay preparationtaken by the formula:
in which PE is the labeled percentage of (E)-isomer in USP Doxepin Hydrochloride RS.
Auxiliary Information— Please check for your question in the FAQs before contacting USP.
| Topic/Question | Contact | Expert Committee |
| Monograph | Ravi Ravichandran, Ph.D. Senior Scientist 1-301-816-8330 |
(MDPP05) Monograph Development-Psychiatrics and Psychoactives |
| Reference Standards | Lili Wang, Technical Services Scientist 1-301-816-8129 RSTech@usp.org |
Pharmacopeial Forum: Volume No. 32(2) Page 330
Chromatographic Column—
PF-06409577
PF-06409577
6-Chloro-5-[4-(1-hydroxycyclobutyl)phenyl]-1H-indole-3-carboxylic acid
CAS Number 1467057-23-3, C19H16ClNO3, 341.79
Biochem/physiol Actions
PF-06409577 is a potent and selective activator of 5′ adenosine monophosphate-activated protein kinase (AMPK).
PF-06409577 potently activates a1β1γ1 AMPK (5′ adenosine monophosphate-activated protein kinase) isoform, and prevents its dephosphorylation. It is similarly potent for β1 containing isoforms, but shows significantly lower potency for β2-containing isoforms of AMPK. Patch-clamp assays show that this compound does not inhibit hERG (human ether-a-go-go gene). It interacts with the allosteric drug and metabolite site (ADaM) of AMPK.
General description
PF-06409577 is a 6-chloro-indole derivative obtained from 5-bromo-6-chloro-indole.
PF-06409577 is a potent and selective activator of 5′ adenosine monophosphate-activated protein kinase (AMPK) for the Potential Treatment of diabetic nephropathy. PF-06409577 has AMPK α1β1γ1 Kd=9.0 nM. AMPK α1β1γ1 EC50 = 7.0 nM; AMPK α1β2γ1 EC50 > 40000 nM. PF-06409577 showed efficacy in a preclinical model of diabetic nephropathy. Upon the basis of its potent and selective AMPK activation, low metabolic turnover in human hepatocytes, clean off-target profile, and favorable preclinical in vivo efficacy results, PF-06409577 was profiled in regulatory toxicology studies and was subsequently advanced to clinical trials to assess human pharmacokinetics and safety/ tolerability.
Diabetes is a major public health concern because of its increasing prevalence and associated health risks. The disease is characterized by high levels of blood glucose resulting from defects in insulin production, insulin action, or both. Two major forms of diabetes are recognized, type I and type II. Type I diabetes develops when the body’s immune system destroys pancreatic beta cells, the only cells in the body that make the hormone insulin that regulates blood glucose. To survive, people with type 1 diabetes must have insulin delivered by injection or a pump. Type II diabetes accounts for about 90 to 95 percent of all diagnosed cases of diabetes. Type II diabetes usually begins as insulin resistance, a disorder in which the cells do not use insulin properly. Key target tissues, including liver, muscle, and adipose tissue, are resistant to the effects of insulin in stimulating glucose and lipid metabolism. As the need for insulin rises, the pancreas gradually loses its ability to produce insulin. Controlling type II diabetes with medication is essential; otherwise it can progress into pancreatic beta-cell failure requiring complete dependence on insulin.
Obesity increases the risk of type II diabetes as well as many other health conditions including coronary heart disease, stroke, and high blood pressure. More than one-third of U.S. adults (over 72 million people) and 17% of U.S. children are obese. During 1980-2008, obesity rates doubled for adults and tripled for children. During the past several decades, obesity rates for all population groups— regardless of age, sex, race, ethnicity, socioeconomic status, education level, or geographic region— have increased markedly.
Research has identified the enzyme 5′ adenosine monophosphate-activated protein kinase (AMPK) as a regulator of cellular and whole-body energy homeostasis. AMPK is activated by cellular stress resulting in downstream events that serve to conserve or generate ATP. AMPK is composed of three distinct subunits, each with multiple isoforms: the alpha subunit (alpha 1 or 2); the beta subunit (beta 1 or 2); and the gamma subunit (gamma 1, 2, or 3); for a total of twelve possible heterotrimeric isoforms.
In the liver, activated AMPK phosphorylates a variety of substrates including 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase (Clarke, P.R. & Hardie, D.G., EMBO J 9, 2439-2446 (1990)) and acetyl-CoA carboxylase (Carling, D. et al. FEBS Letters 223, 217-222 (1987)) which inhibits cholesterol biosynthesis and decreases fatty acid synthesis, respectively. Therefore, activation of AMPK should lead to decreases in the levels of triglycerides and cholesterol. AMPK is also thought to regulate plasma glucose levels by decreasing hepatic gluconeogenesis through downregulation of key gene products following phosphorylation of CRTC2 (Koo S.H. et. AL, Nature 437, 1109-1111 (2005)). In muscle and myocardial tissues, AMPK activates the transport activity of glucose transporter 4 (GLUT4) increasing glucose uptake into cells thereby producing an additional avenue for decreasing plasma glucose (Kurth-Kraczek, E.J. et. al., Diabetes 48, 1667-1671 (1999)). AMPK activation has also been shown to enhance mitochondrial biogenesis improving fatty acid oxidation and decreasing circulating lipids (Merrill, G.M. et. al., Am. J. Physiol. 273, E1107-E1112 (1997)). Direct activation of AMPK using AICAR (5-aminoimidazole-4-carboxamide riboside) has been shown to lead to beneficial effects on several metabolic endpoints including improved glucose disposal, decreased hepatic glucose output and decreases in plasma triglycerides and free fatty acids (Song, X.M. et. al., Diabetologia 45, 56-65 (2002); Bergeron, R. et. al., Diabetes 50, 1076-1082 (2001); Buhl, E.S.et. al., Diabetes 50, 12-17 (2001); Iglesias, M.A. et. al., Diabetes 51, 2886-2894 (2002), Fogarty, S. & Hardie, D.G., Biochim et Biophys Acta 1804, 581-591 (2010)). Because of AMPK’s pluripotent effects on carbohydrate, lipid, and cholesterol metabolism and biosynthesis, agents that activate AMPK are attractive therapeutic targets for treating metabolic syndrome disorders such as diabetes, obesity, and dyslipidemia.
Decreases in renal AMPK activation have been implicated in the etiology of diseases of the kidney, including diabetic nephropathy, acute kidney injury (AKI), and polycystic kidney disease (PKD); activation of AMPK through hormonal (adiponectin) or pharmacological (AICAR) mechanisms has been shown to be protective in rodent models of these diseases. In diabetic nephropathy decreased AMPK activation in podocytes occurs early in the disease and is associated with increased expression of the NADPH-Oxidase protein Nox4 and increased proteinuria. These effects were reduced following administration of the AMPK activators AICAR, metformin, and Adiponectin (Lee, MJ. et.al. American Journal of Physiology – Renal Physiology. 292.
F617-F627 (2007); Sharma, K. et.al. Journal of Clinical Investigation.118. 1645-1656. (2008)). In ischemia/reperfusion models of AKI the AMPK activators metformin and AICAR were shown to dose-dependently reduce subsequent proteinuria, oxidative tissue damage, and kidney macrophage infiltration (Lempiainen, J. et.al. British Journal of Pharmacology 166. 1905-1915 (2012); Seo-Mayer, P.W. et.al. American Journal of Physiology – Renal Physiology, 301, F1346-F1357 (2011)). In two rodent models of PKD the AMPK activator metformin was shown to reduce renal cyst expansion (Takiar, V. et. al. PNAS 108, 2462-2467 (2011)). These studies suggest a broad benefit of AMPK activators in multiple renal diseases.
The compounds of the present invention activate AMPK and are, therefore, useful in treating metabolic disorders such as diabetes, obesity, and dyslipidemia as well as the renal diseases chronic kidney disease, diabetic nephropathy, acute kidney injury and polycystic kidney disease.
PATENT
US 20130267493
WO 2014140704
Example 5
6-Chloro-5-(4-(3-hydroxyoxetan-3-yl)phenyl)-1H-indole-3-carboxylic acid

Step 1
6-chloro-5-(4-(3-hydroxyoxetan-3-yl)phenyl)-1H-indole-3-carbaldehyde
A mixture of 5,5,5′,5′-tetramethyl-[2,2′]bi[[1,3,2]dioxaborinanyl] (149.0 mg, 0.44 mmol), oven dried potassium acetate (173.0 mg, 1.75 mmol) and 3-(4-bromo-phenyl)-oxetan-3-ol (100.0 mg, 0.44 mmol) in 1,4-dioxane (2 mL) was degassed with N2 for 5 minutes, treated with [1,1′-bis(diphenylphosphino)ferrocene]dichloropalladium(II) (33.0 mg, 0.044 mmol) and subjected to microwave irradiation at 110 °C for 1 hour. The cooled reaction mixture was filtered through celite and concentrated in vacuo to give a black oil. To the dark oil was added 5-bromo-6-chloro-1H-indole-3-carbaldehyde (112.0 mg, 0.43 mmol), 2 N aqueous potassium carbonate (0.4 mL, 0.80 mmol), toluene (1.5 mL) and EtOH (0.5 mL). The reaction mixture was degassed with N2 for 10 minutes, treated with [1, 1′-bis(diphenylphosphino)ferrocene] dichloropalladium(II) (25.0 mg, 0.034 mmol), and heated in a pressure tube to 110 °C for 2 hours. The cooled reaction mixture was purified by flash chromatography (33-100% EtOAc/ heptanes) to give a solid. The solid was triturated in MeOH and filtered to afford the title compound (50 mg, 35%) as a yellow solid. MS (ES+) 328.0 (M+H)+. 1H NMR (400 MHz, DMSO-d6) δ 12.23 (s, 1 H), 9.92 (s, 1 H), 8.35 (s, 1 H), 8.02 (s, 1 H), 7.66 (d, J = 9.4 Hz, 2 H), 7.44 (d, J = 8.2 Hz, 2 H), 6.36 (s, 1 H), 4.80 – 4.76 (m, 2 H), 4.75 – 4.71 (m, 2 H).
Step 2
6-Chloro-5-(4-(3-hydroxyoxetan-3-yl)phenyl)-1 H-indole-3-carboxylic acid To the mixture of 6-chloro-5-[4-(3-hydroxy-oxetan-3-yl)-phenyl]-1H-indole-3-carbaldehyde (50.0 mg, 0.15 mmol) in MeCN (2 mL) was added 2-methyl-2-butene (2.0 mL, 13.7 mmol), followed by sodium chlorite (138 mg, 1.53 mmol) and sodium phosphate monobasic hydrate (211.0 mg, 1.53 mmol) in water (1 mL). The reaction mixture was stirred at room temperature for 20 hours, and concentrated in vacuo. The residue was acidified with 1 N aqueous citric acid (1 mL) and extracted with EtOAc. The organic layer was dried over MgSO4 and concentrated in vacuo. The crude material was purified by flash chromatography (34-80% EtOAc/heptanes, with 0.2% formic acid modifier) to afford the title compound (18 mg, 34%) as a brown solid. MS (ES-) 342.3 (M-H)-. 1H NMR (400 MHz, CD3OD) δ 8.02 (s, 1 H), 7.98 (s, 1 H), 7.66 (d, J = 8.20 Hz, 2 H), 7.56 (s, 1 H), 7.47 (d, J = 8.20 Hz, 2 H), 4.87 – 4.80 (m, 4 H).
Paper
Discovery and Preclinical Characterization of 6-Chloro-5-[4-(1-hydroxycyclobutyl)phenyl]-1H-indole-3-carboxylic Acid (PF-06409577), a Direct Activator of Adenosine Monophosphate-activated Protein Kinase (AMPK), for the Potential Treatment of Diabetic Nephropathy. Cameron KO et al Journal of Medicinal Chemistry 59(17), 8068-8081, (2016)
Adenosine monophosphate-activated protein kinase (AMPK) is a protein kinase involved in maintaining energy homeostasis within cells. On the basis of human genetic association data, AMPK activators were pursued for the treatment of diabetic nephropathy. Identification of an indazole amide high throughput screening (HTS) hit followed by truncation to its minimal pharmacophore provided an indazole acid lead compound. Optimization of the core and aryl appendage improved oral absorption and culminated in the identification of indole acid, PF-06409577 (7). Compound 7 was advanced to first-in-human trials for the treatment of diabetic nephropathy.
Discovery and Preclinical Characterization of 6-Chloro-5-[4-(1-hydroxycyclobutyl)phenyl]-1H-indole-3-carboxylic Acid (PF-06409577), a Direct Activator of Adenosine Monophosphate-activated Protein Kinase (AMPK), for the Potential Treatment of Diabetic Nephropathy
ACS Editors’ Choice – This is an open access article published under an ACS AuthorChoice License, which permits copying and redistribution of the article or any adaptations for non-commercial purposes.
6-Chloro-5-[4-(1-hydroxycyclobutyl)phenyl]-1H-indole-3-carboxylic Acid (7)
PAPER
Evolution of the Synthesis of AMPK Activators for the Treatment of Diabetic Nephropathy: From Three Preclinical Candidates to the Investigational New Drug PF-06409577
https://pubs.acs.org/doi/10.1021/acs.oprd.8b00059

Indole acids 1, 2, and 3 are potent 5′-adenosine monophosphate-activated protein kinase (AMPK) activators for the potential treatment of diabetic nephropathy. Compounds 1–3 were scaled to supply material for preclinical studies, and indole 3 was selected for advancement to first-in-human clinical trials and scaled to kilogram quantities. The progression of the synthesis strategy for these AMPK activators is described, as routes were selected for efficient structure–activity relationship generation and then improved for larger scales. The developed sequences employed practical isolations of intermediates and APIs, reproducible cross-coupling, hydrolysis, and other transformations, and enhanced safety and purity profiles and led to the production of 40–50 g of 1and 2 and 2.4 kg of 3. Multiple polymorphs of 3 were observed, and conditions for the reproducible formation of crystalline material suitable for clinical development were identified.
Mp: 192–194 °C. 1H NMR (400 MHz, DMSO-d6): δ 12.12 (s, 1H), 11.94 (br d, J = 2.2 Hz, 1H), 8.08 (d, J = 2.9 Hz, 1H), 7.95 (s, 1H), 7.64 (s, 1H), 7.57 (d, J = 8.3 Hz, 2H), 7.40 (d, J = 8.1 Hz, 2H), 5.52 (s, 1H), 2.48–2.40 (m, 2H), 2.35–2.26 (m, 2H), 2.00–1.89 (m, 1H), 1.74–1.63 (m, 1H). 13C NMR (101 MHz, DMSO-d6): δ 165.6, 146.6, 138.1, 136.0, 133.8, 133.0, 129.2, 125.6, 125.3, 124.6, 122.8, 112.9, 107.6, 75.1, 37.3, 12.8. MS (ES): calcd for C19H17ClNO3 ([M – H]−) 340.1; found 340.3. Anal. Calcd (%): C, 66.77; H, 4.72; N, 4.10. Found: C, 66.59; H, 4.71; N, 3.96.
///////////////////PF-06409577, PHASE 1
O=C(C1=CNC2=C1C=C(C3=CC=C(C4(O)CCC4)C=C3)C(Cl)=C2)O
Burosumab-twza, ブロスマブ
> Burosumab Heavy Chain Sequence QVQLVQSGAEVKKPGASVKVSCKASGYTFTNHYMHWVRQAPGQGLEWMGIINPISGSTSN AQKFQGRVTMTRDTSTSTVYMELSSLRSEDTAVYYCARDIVDAFDFWGQGTMVTVSSAST KGPSVFPLAPSSKSTSGGTAALGCLVKDYFPEPVTVSWNSGALTSGVHTFPAVLQSSGLY SLSSVVTVPSSSLGTQTYICNVNHKPSNTKVDKKVEPKSCDKTHTCPPCPAPELLGGPSV FLFPPKPKDTLMISRTPEVTCVVVDVSHEDPEVKFNWYVDGVEVHNAKTKPREEQYNSTY RVVSVLTVLHQDWLNGKEYKCKVSNKALPAPIEKTISKAKGQPREPQVYTLPPSRDELTK NQVSLTCLVKGFYPSDIAVEWESNGQPENNYKTTPPVLDSDGSFFLYSKLTVDKSRWQQG NVFSCSVMHEALHNHYTQKSLSLSPGK
> Burosumab Light Chain Sequence AIQLTQSPSSLSASVGDRVTITCRASQGISSALVWYQQKPGKAPKLLIYDASSLESGVPS RFSGSGSGTDFTLTISSLQPEDFATYYCQQFNDYFTFGPGTKVDIKRTVAAPSVFIFPPS DEQLKSGTASVVCLLNNFYPREAKVQWKVDNALQSGNSQESVTEQDSKDSTYSLSSTLTL SKADYEKHKVYACEVTHQGLSSPVTKSFNRGEC
ALSO
(Heavy chain)
QVQLVQSGAE VKKPGASVKV SCKASGYTFT NHYMHWVRQA PGQGLEWMGI INPISGSTSN
AQKFQGRVTM TRDTSTSTVY MELSSLRSED TAVYYCARDI VDAFDFWGQG TMVTVSSAST
KGPSVFPLAP SSKSTSGGTA ALGCLVKDYF PEPVTVSWNS GALTSGVHTF PAVLQSSGLY
SLSSVVTVPS SSLGTQTYIC NVNHKPSNTK VDKKVEPKSC DKTHTCPPCP APELLGGPSV
FLFPPKPKDT LMISRTPEVT CVVVDVSHED PEVKFNWYVD GVEVHNAKTK PREEQYNSTY
RVVSVLTVLH QDWLNGKEYK CKVSNKALPA PIEKTISKAK GQPREPQVYT LPPSRDELTK
NQVSLTCLVK GFYPSDIAVE WESNGQPENN YKTTPPVLDS DGSFFLYSKL TVDKSRWQQG
NVFSCSVMHE ALHNHYTQKS LSLSPGK
(Light chain)
AIQLTQSPSS LSASVGDRVT ITCRASQGIS SALVWYQQKP GKAPKLLIYD ASSLESGVPS
RFSGSGSGTD FTLTISSLQP EDFATYYCQQ FNDYFTFGPG TKVDIKRTVA APSVFIFPPS
DEQLKSGTAS VVCLLNNFYP REAKVQWKVD NALQSGNSQE SVTEQDSKDS TYSLSSTLTL
SKADYEKHKV YACEVTHQGL SSPVTKSFNR GEC
(dimer; disulfide bridge:H22-H96, H144-H200, H220-L213, H220-H’226, H229-H’229, H261-H321, H367-H425, H’22-H’96, H’144-H’200, H’220-L’213, H’261-H’321, H’367-H’425, L23-L88, L133-L193, L’23-L’88, L’133-L’193)
Burosumab-twza, KRN 23
ブロスマブ
CAS1610833-03-8
UNII G9WJT6RD29
Protein chemical formulaC6388H9904N1700O2006S46
Protein average weight144100.0 Da
Protein Based Therapies
Monoclonal antibody (mAb)
breakthrough therapy and orphan drug designations
Approval Status:Approved April 2018
Specific Treatments:X-linked hypophosphatemia
Crysvita (burosumab-twza) is a fibroblast growth factor 23 (FGF23) blocking antibody.
This drug is indicated for the treatment of X-linked hypophosphatemia with radiological evidence of bone disease in children of 1 year of age and older and adolescents with growing skeletons [4].

Burosumab (INN, trade name Crysvita) known as KRN23 is a human monoclonal antibody designed for the treatment of X-linked hypophosphatemia.[1][2][3] Burosumab was approved by the FDA for its intended purpose, in patients aged 1 year and older, on 17 April 2018.[4] The FDA approval fell under both the breakthrough therapy and orphan drug designations.[4]
This drug was developed by Ultragenyx and is in a collaborative license agreement with Kyowa Hakko Kirin.[5]
Burosumab (KRN23) is an entirely human monoclonal IgG1 antibody that binds excess fibroblast growth factor 23 (FGF23) and has been successfully tested in clinical trials in children with X-linked hypophosphatemic rickets [1].
The U.S. Food and Drug Administration approved Crysvita (burosumab) in April 2018. This is the first drug approved to treat adults and children ages 1 year and older with X-linked hypophosphatemia (XLH), which is a rare, inherited form of rickets. X-linked hypophosphatemia causes low circulating levels of phosphorus in the blood. It causes impaired bone growth and development in children and adolescents and issues with bone mineralization throughout a patient’s life [3].
XLH is a serious disease which affects about 3,000 children and 12,000 adults in the United States. Most children with XLH suffer from bowed or bent legs, short stature, bone pain and severe dental pain. Some adults with this condition suffer from persistent, unrelenting discomfort and complications, such as joint pain, impaired mobility, tooth abscesses and hearing loss [3]
Crysvita is specifically indicated for the treatment of X-linked hypophosphatemia (XLH) in adult and pediatric patients 1 year of age and older.
Crysvita is supplied as a subcutaneous injection. The recommended starting dose for pediatrics is 0.8 mg/kg of body weight, rounded to the nearest 10 mg, administered every two weeks. The minimum starting dose is 10 mg up to a maximum dose of 90 mg. After initiation of treatment with Crysvita, measure fasting serum phosphorus every 4 weeks for the first 3 months of treatment, and thereafter as appropriate. If serum phosphorus is above the lower limit of the reference range for age and below 5 mg/dL, continue treatment with the same dose. Follow dose adjustment schedule per the drug label. The recommended dose regimen in adults is 1 mg/kg body weight, rounded to the nearest 10 mg up to a maximum dose of 90 mg, administered every four weeks. After initiation of treatment with Crysvita, assess fasting serum phosphorus on a monthly basis, measured 2 weeks post-dose, for the first 3 months of treatment, and thereafter as appropriate. If serum phosphorus is within the normal range, continue with the same dose. See drug label for specific dose adjustments.
Mechanism of Action
Crysvita (burosumab-twza) is a fibroblast growth factor 23 (FGF23) blocking antibody. X-linked hypophosphatemia is caused by excess fibroblast growth factor 23 (FGF23) which suppresses renal tubular phosphate reabsorption and the renal production of 1,25 dihydroxy vitamin D. Burosumab-twza binds to and inhibits the biological activity of FGF23 restoring renal phosphate reabsorption and increasing the serum concentration of 1,25 dihydroxy vitamin D.
REFERENCES
1 file:///H:/761068Orig1s000ChemR.pdf
REF
- Kutilek S: Burosumab: A new drug to treat hypophosphatemic rickets. Sudan J Paediatr. 2017;17(2):71-73. doi: 10.24911/SJP.2017.2.11. [PubMed:29545670]
- Kinoshita Y, Fukumoto S: X-linked hypophosphatemia and FGF23-related hypophosphatemic diseases -Prospect for new treatment. Endocr Rev. 2018 Jan 26. pii: 4825438. doi: 10.1210/er.2017-00220. [PubMed:29381780]
- FDA approves first therapy for rare inherited form of rickets, x-linked hypophosphatemia [Link]
- Crysvita Drug Label [Link]
- Burosumab for a rare bone disease [Link]
- DRUG: Burosumab [Link]
- NHS document [Link]
- Burosumab for XLH [Link]
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Human |
| Target | FGF 23 |
| Clinical data | |
| Trade names | Crysvita |
| Synonyms | KRN23 |
| ATC code | |
| Identifiers | |
| CAS Number | |
| ChemSpider |
|
| UNII | |
| KEGG | |
| Chemical and physical data | |
| Formula | C6388H9904N1700O2006S46 |
| Molar mass | 144.1 kDa |
References
- Jump up^ Statement On A Nonproprietary Name Adopted By The USAN Council – Burosumab, American Medical Association.[permanent dead link]
- Jump up^ World Health Organization (2016). “International Nonproprietary Names for Pharmaceutical Substances (INN). Proposed INN: List 115”(PDF). WHO Drug Information. 30 (2): 255.
- Jump up^ “Burosumab (KRN23) for X-Linked Hypophosphatemia (XLH)” (PDF). n.d. Retrieved 2018-04-18.
- ^ Jump up to:a b “FDA approves first therapy for rare inherited form of rickets, x-linked hypophosphatemia” (Press release). FDA. 17 April 2018.
- Jump up^ “Collaboration with Ultragenyx to Develop and Commercialize KRN23 for X-linked Hypophosphatemia” (Press release). Kyowa Kirin. 4 September 2013. Retrieved 2018-04-17.
//////////////Burosumab-twza, Crysvita FDA 2018, BLA 761068, Protein Based Therapies, Monoclonal antibody, mAb, KRN 23, breakthrough therapy, orphan drug designations, Peptide, ブロスマブ

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO