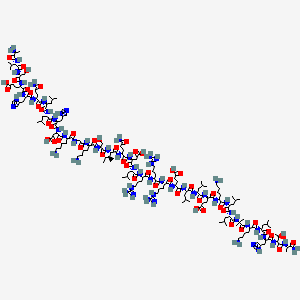
(3S)-N-[(3S,5S,6R)-6-methyl-2-oxo-1-(2,2,2-trifluoroethyl)-5-(2,3,6-trifluorophenyl)piperidin-3-yl]-2-oxospiro[1H-pyrrolo[2,3-b]pyridine-3,6′-5,7-dihydrocyclopenta[b]pyridine]-3′-carboxamide
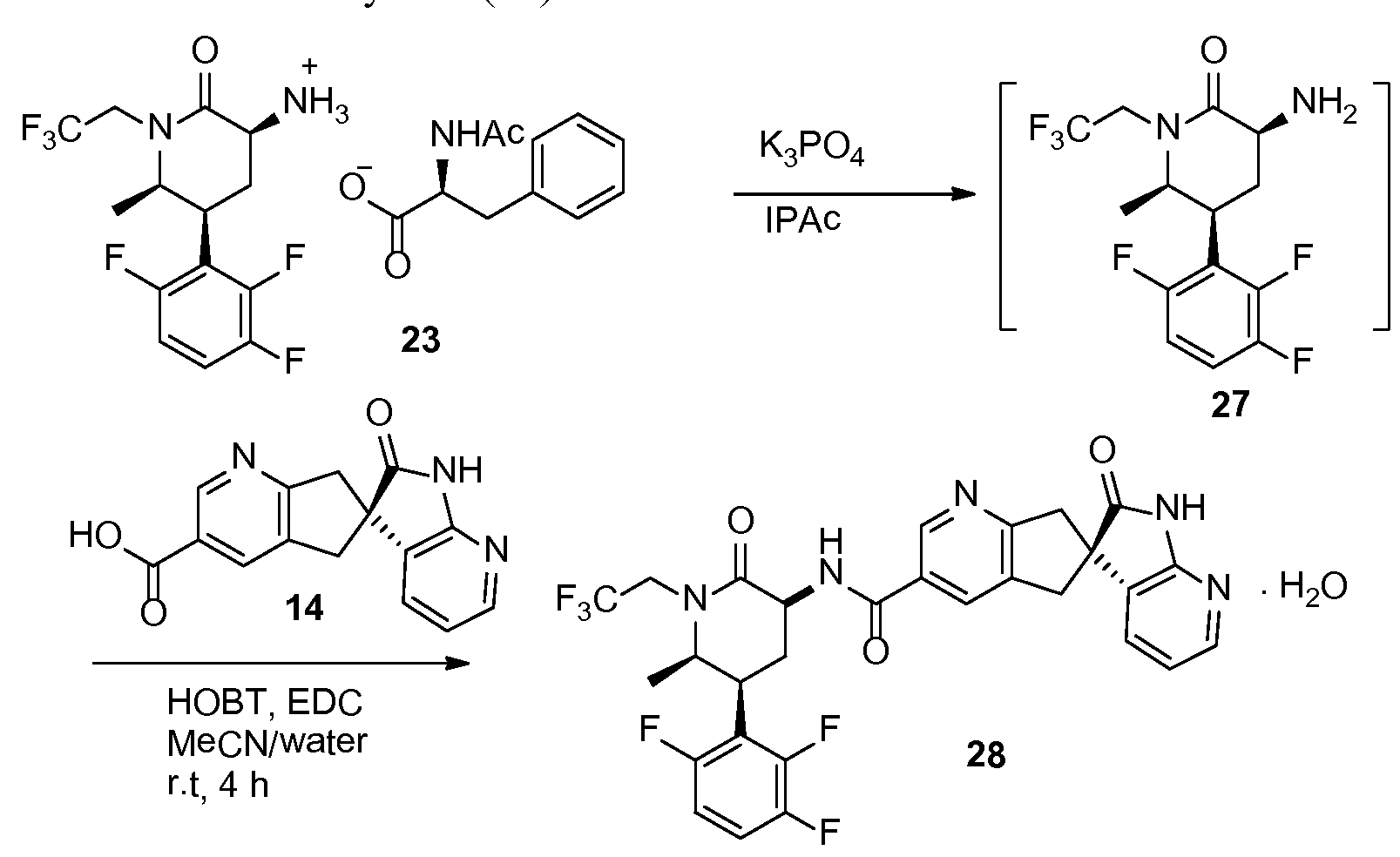
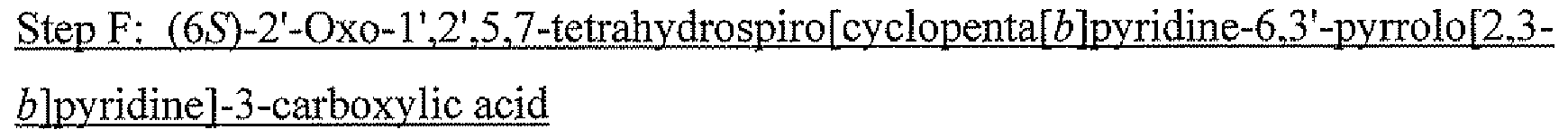
INTERMEDIATE 1
carboxylic acid
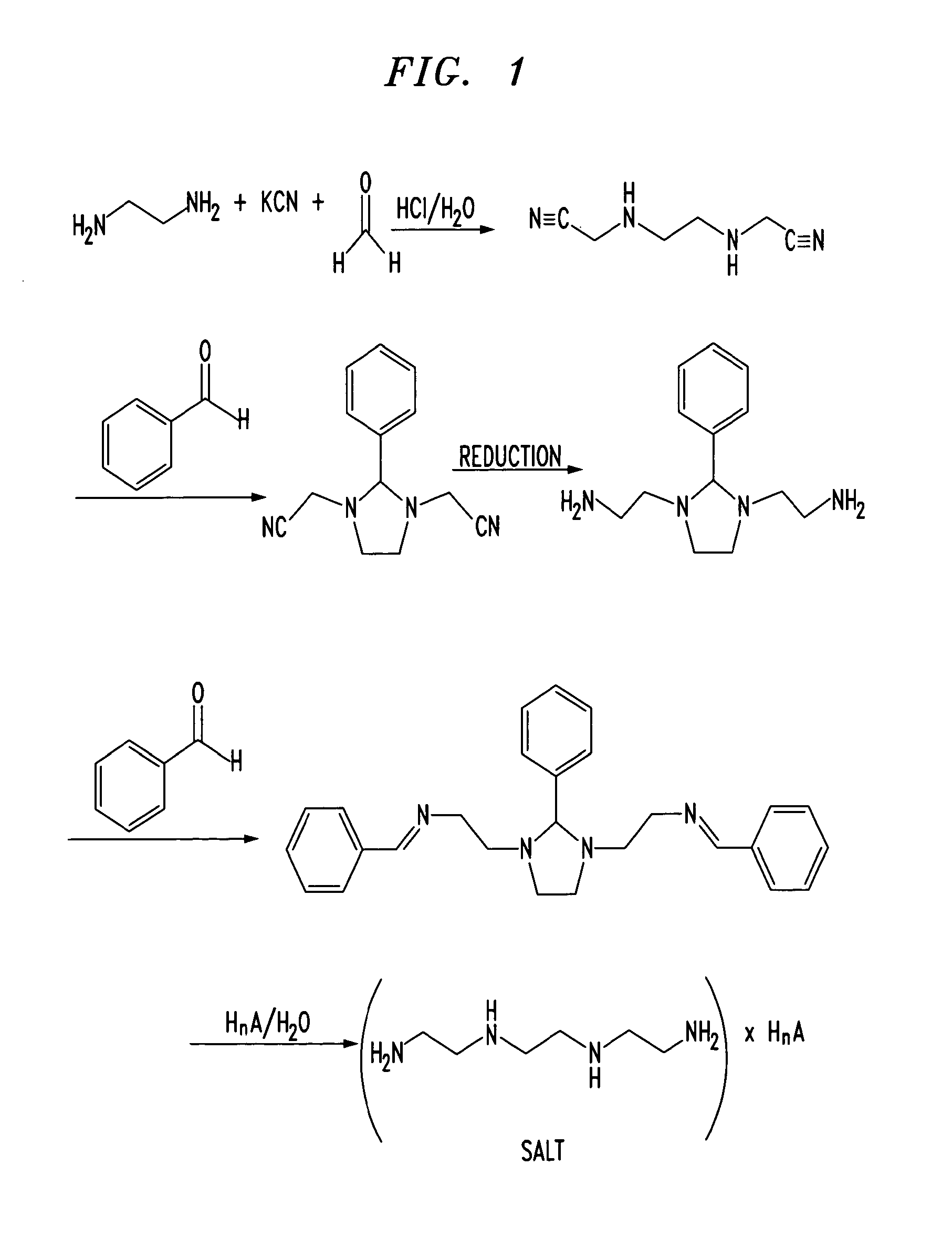
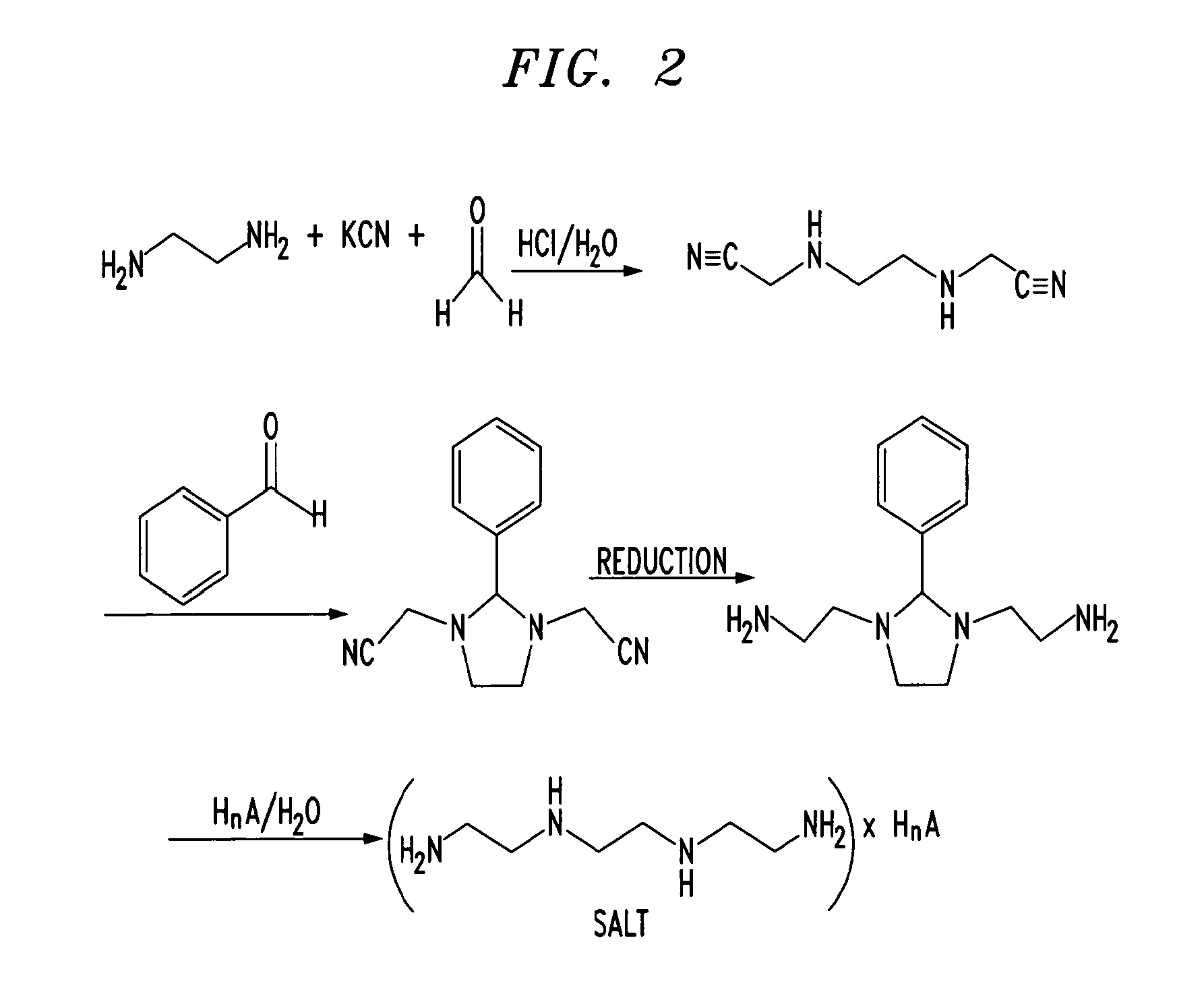
The title compound can be prepared by either Method I or Method II as described below.
Method I:
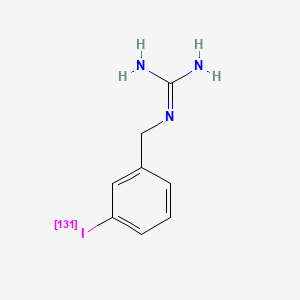
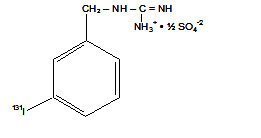
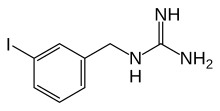
Step A: (6S)-3-Iodo-5 J-dihyc ospiro cyclopentar¾1pyrid e-6 ‘-py
one
A solution of sodium nitrite (36.1 g, 523 mmol) in water (20 mL) was added dropwise over 5 min to a solution of (6S -3-amino-5,7-dihydros iro[cyclopenta[ί)]pyridi e-6,3,– pyrrolo[2,3-0]pyridin]-2′(rH)-one (prepared according to the procedures described in
WO2008/020902, 66.0 g, 262 mmol) and -toluenesulfonic acid (149 g, 785 mmol) in acetonitrile (650 mL) at 23 °C. After stirring for 30 min, a solution of potassium iodide (109 g, 654 mmol) in water (20 mL) was added over 5 min. The resulting mixture was stirred at 23 °C for 40 min, then diluted with water (1 L) and basified by the addition of solid NaOH (33.0 g, 824 mmol) with stirring. Iodine by-product was reduced by the addition of 10% aqueous sodium thio sulfate solution and stirring for an additional 30 min. The solids were collected by filtration, washed with water, and dried under nitrogen atmosphere to give the title compound, which was used without further purification. MS: mlz = 363.9 (M + 1).
Step B: Methyl (65V2′-oxo-lΛ2 5J-tetrahydrospiroicvclopenta[6]p ridine-6.3′-pyrlΌlo[‘2. – 6]py ridine] – 3 -car boxy late
A solution of (65)-3-iodo~5 ,7-dihydrospiro[cyclopenta[&]pyridine-6,3′- pyrrolo[2,3-&]pyridin]-2′(rH)-one (51.0 g, 140 mmol), sodium acetate (23.0 g, 281 mmol) and dichloro l,l’~bis(diphenylphosphino)ferrocene palladium(II) dichloromethane adduct (2.9 g, 3.5 mmol) in MeOH (560 mL) was pressurized to 120 psi of CO at 23 °C and then heated at 80 °C for 12 h with stirring. The reaction mixture was diluted with water (1 L), and the precipitate collected by filtration, washed with water, and dried under nitrogen atmosphere to give the title compound, which was used without further purification. MS: mlz = 296.1 (M + 1).
3 -carboxylic acid
A mixture of methyl (6S)-2′-oxo-r,2′,5,7-tetrahydrospiro[cyclopenta[i)]pyridine- 6,3′-pyrrolo[2,3-&]pyridine]-3-carboxylate (30.0 g, 102 mmol) and aqueous 6 N sodium hydroxide solution (50.8 mL, 305 mmol) in MeOH (920 mL) was heated at reflux for 1 h. The mixture was allowed to cool to 23 °C before it was acidified to pH ~6 with aqueous 1 N hydrochloric acid solution, resulting in a black precipitate which was removed by filtration. The filtrate was concentrated under reduced pressure to a volume of ~100 mL and then partitioned between water (500 mL) and 2-methyltetrahydrofuran (2- eTHF, 250 mL). The aqueous layer was extracted with 2-MeTHF (5 χ 250 mL), and the combined organic layers were dried over sodium sulfate and concentrated to provide the title compound. MS: mlz ~ 282.0 (M + 1).
Method II:
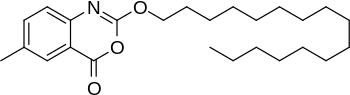
Step A: Dimethyl 5-bromopyridine-2,3-dicarboxylate
Concentrated sulfuric acid (1 L, 18.7 mol) was added slowly over 10 min to a . suspension of pyridine-2,3-dicarboxylic acid (5.00 kg, 29.9 mol) in methanol (50 L), dissolving the suspension. The resulting mixture was heated at reflux for 48 h then cooled to 40 °C.
Bromine (8.0 kg, 50 mol) was added slowly over 2 h in 1-kg portions, keeping the temperature below 55 °C. The reaction mixture was then heated at 55 °C for 24 h, cooled to 50 °C and additional Br2 (4.0 kg, 25 mol) was added slowly over 1 h in 1-kg portions, keeping temperature below 55 °C. The reaction mixture was heated at 55 °C for 24 h, concentrated to a minimum volume (internal temp -30 °C, solution may occasionally foam), then diluted with isopropyl acetate (50 L) and washed with a saturated aqueous sodium sulfite solution (3 x 20 L) (final extract is ~pH 8) followed by water (20 L). The organic layer was concentrated to
approximately 15 L then diluted with heptane (40 L). The resulting slurry was stirred for 24 h at 23 °C. The solids were filtered, washed with heptane (10 L), and dried to give the title compound. Step B: (5-Bromopyridine-23-diyl)dimcthanol
Sodium borohydride (15.9g, 420 mmol) was added portionwise over 30 min to a solution of dimethyl 5-bromopyridine-2,3-dicarboxylate (20 g, 73 mmol) in ethanol (460 mL) precooled to 0 °C. A solution of calcium chloride (23.3 g, 209 mmol) in 150 mL was added slowly at 0 °C, and the reaction mixture was warmed to 23 °C and stirred overnight. Excess sodium borohydride was quenched by slow addition of aqueous 2 N HCl solution (230 mL, 460 mmol), followed by a stirring at 23 °C for 2 h. The mixture was concentrated to dryness.
Saturated aqueous sodium bicarbonate solution was added to the residue until a pH of approximately 7 was reached. The aqueous mixture was extracted with 2-methyltetrahydrofuran (4 x 200 mL). The combined organic layers were dried over sodium sulfate then treated with a solution of 4 N HC1 in dioxane (25 mL, 100 mmol). The resulting solid was filtered, washed with 2-methyltetrahydrofuran, and dried to give the title compound as a hydrochloride salt. MS: m!z = 218.1 (M + 1). Step C: (5-Bromopyridine-2,3-diyI)dimethanediyl dimethanesulfonate
A slurry of (5-bromopyridine-2,3-diyl)dimethanol hydrochloride (12.9g, 59.2 mmol) in tetrahydrofuran (400 mL) at 0 °C was treated with triethylamine (37.1 mL, 266 mmol). To the resulting mixture was added portionwise methanesulfonic anhydride (30.9 g, 177 mmol), keeping temperature below 5 °C. The reaction mixture was stirred at 0 °C for 1 h, then partitioned between saturated aqueous sodium bicarbonate solution (500 mL) and ethyl acetate (500 mL). The organic layer was washed saturated aqueous sodium bicarbonate solution, dried over magnesium sulfate, and concentrated to give the title compound. MS: m/z – 376.0 (M + 1).
Step D: 3-Bromo-r-{[2-(trimethylsilyl)ethoxy]methyl}-5,7- dihyjirpspiro [cyclop
(5-Bromopyridine-2,3-diyI)dimethanediyl dimethanesulfonate (17.0 g, 45.4 mmol) was added to a mixture of l-{[2-(trimetliylsilyl)ethoxy]methyl}-l}3-dihydro-2H- pyrrolo[2,3-&]pyridin-2-one (prepared according to the procedures described in
WO2008/020902, 14.0 g, 53.0 mmol) and cesium carbonate (49.0 g, 150 mmol) in ethanol (500 mL) 23 °C, and the resulting mixture was stirred for 20 h. The reaction mixture was
concentrated then partitioned between ethyl acetate (500 mL) and water (500 mL). The organic layer was dried over magnesium sulfate and concentrated. The residue was purified via silica gel chromatography (heptane initially, grading to 100% EtOAc) to give the title compound. MS: m/z = 448.1 (M + 1).
Step E: Methyl (6<Sf)-2′-oxo-r-{r2-(trimethylsilyl ethoxylmethyli-r,2′,5 J- tetrahydrospiro [cy clopenta[6] pyridine-6 ,3 ‘-pyrrolo [2, 3 -b]py ridinel -3 -carboxy late
A mixture of 3-bromo-r-{[2-(trimethylsilyl)ethoxy]methyl}-5,7- dihydrospiro[cyclopenta[¾]pyridine-6,3′-pyrrolo[2,3-¾pyridin]-2′(rH)-one (22.0 g, 49.3 mmol), PdCl2(dppf)»CH Cl2 (2.012g, 2.46 mmol), and sodium acetate (8.1g, 99 mmol) in in methanol (150 mL) was pressurized to 300 psi of carbon monoxide and then heated at 85 °C for 72 h. The reaction mixture was allowed to cool then concentrated. The residue was purified via silica gel chromatography (heptane initially, grading to 100% EtOAc) to give the title compound as a racemic mixture. MS: m/z – 426.1 (M +1). Resolution of the enantiomers by supercritical fluid chromatography (SFC) using a ChiralPak AD-H column and eluting with 40% ethanol in C02 (0.05% diethylamine as modifier) provided the title compound as the second enantiomer to elute.
A solution of methyl (65)-2′-oxo- -{[2-(trimethylsilyl)ethoxy]methyl}-r!2′f5,7- tetrahydrospiro[cyclopenta[&]pyridine-6,3′-pyrrolo[2,3-&]pyridine]-3-carboxylate (238 g, 559 mmol) in methanol (2 L) was saturated with HCI gas, allowing temperature to increase to 55 °C. The reaction mixture was cooled to 23 °C, stirred for 20 h, then concentrated. Aqueous 10 N sodium hydroxide (400 mL, 4 mol) was added to a solution of the residue in methanol (2 L), and the resulting mixture was heated at reflux for 2 h. The solution was cooled to 23 °C and the pH was adjusted to 3 with concentrated HCI. The resulting solid was filtered, washed with water then heptane, and dried to give the title compound. MS: m!z = 282.2 (M + 1).
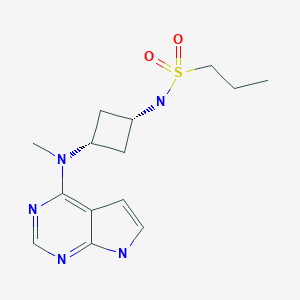
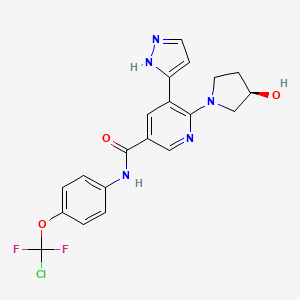
INTERMEDIATE 15
hydrochloride
Step A: (5SSR & 5j?,6y)-6-Methvi-l-r2.2.2-trifluoroethvn-5-(2,3.6-trifluorophenvnpiperidin-2- one
Essentially following the procedures described in Intermediate 14, but using 2,3,6-trifluorophenylboronic acid in place of 2,3,5-trifluorophenylboronic acid, the title compound was obtained. MS: m/z = 326.0 (M + 1).
Step B: GS.5S.6R & 3i?,5J?.6 ‘ -3-Azido-6-methyl-i-r2.2.2 rifluoroethyl)-5-(2.3.6- trifluorophenyl)piperidin-2-one
To a stirred solution of lithium 6w(trimethylsilyl)amide (1.0 M in THF, 4.80 mL,
4.80 mmol) in THF (20 mL) at -78 °C was added a cold (-78 °C) solution of (5S,6R & 5i?,6,S)-6- methyl-l-(2,2,2-trifluoroethyl)-5-(2,3,6-trifluorophenyl)piperidin-2-one (1.30 g, 4,00 mmol) in THF (10 mL) dropwise, keeping the internal temperature of the reaction mixture below -65 °C. The resulting mixture was stirred at -78 °C for 30 min, then a cold (-78 °C) solution of 2,4,6- triisopropylbenzenesulfonyl azide (Harmon et l. (1973) J Org. Chem. 38, 11-16) (1.61 g, 5.20 mmol) in THF (10 mL) was added dropwise, keeping the internal temperature of the reaction mixture below -65 °C. The reaction mixture was stirred at -78 °C for 30 min, then AcOH (1.05 mL, 18.4 mmol) was added. The resulting mixture was allowed to warm slowly to ambient temperature and was poured into saturated aqueous sodium bicarbonate (50 mL) and the mixture was extracted with EtOAc (2 χ 75 mL). The combined organic layers were washed with brine, then dried over sodium sulfate, filtered, and concentrated to dryness in vacuo. The crude product was purified by silica gel chromatography, eluting with a gradient of hexanes:EtOAc – 100:0 to 20:80, to give the diastereomeric azide products (3R,5Sf6R & 3S, ;5i?,65)-3-azido-6- methyl-l-(2,2,2-trifluoroethyl)-5-(2f3,5-trifluorophenyl)piperidin-2-one, which eluted second, and the title compound, which eluted first. MS: mlz = 367.1 (M+ 1).
Step C: ferf-Butyl [(3&5^6^ν6^Φν1-2-οχο-1-(2.2,2-ΐπΑηοΓθ£υΐν1 -5-ί2.3,6- trifluorophenyl)piperidin-3-yl“|carbamate
To a solution of ( S,5S,6R & 3JR,5if,6S)-3-azido-6-methyl-l-(2,2,2- trifiuoroethyl)-5-(2,3,5-trifluorophenyl)piperidin-2-one (280 mg, 0.764 mmol) and di-tert-butyl dicarbonate (217 mg, 0.994 mmol) in EtOH (5 mL) was added 10% palladium on carbon (25 mg, 0.024 mmol) and the resulting mixture was stirred vigorously under an atmosphere of hydrogen (ca. 1 atm) for 1 h. The reaction mixture was filtered through a pad of Celite® washing with EtOH, and the filtrate was concentrated in vacuo to give a crude solid. The crude product was purified by silica gel chromatography, eluting with a gradient of hexanes:EtOAc – 100:0 to 30:70, to give the racemic title compound. Separation of the enantiomers was achieved by SFC on a ChiralTech IC column, eluting with C02:MeOH:CH CN – 90:6.6:3.3, to give tert- butyl [(3i?,5i?,65)-6-methyl-2-oxo-l-(2J2,2-trifluoroemyl)-5-(2,3J6-tri¾orophenyl)piperidin-3- yl]carbamate as the first major peak, and fert-butyl [(3Sf5S,6R)-6-methyl-2-oxo-l -(2,2,2- trifluoroethyl)-5-(2,3,6-trifiuorophenyl)piperidin-3-yl]carbamate, the title compound, as the second major peak. MS: mlz = 463.2 (M + Na).
Step D: (3&5^6i?)-3-Amino-6-methyi-l-(2,2.2-trifluoroethyl)-5-(2,3,6- trifluorophenyl)piperidin-2-one hydrochloride
A solution of tert-butyl [(35′,55′,6ii)-6-methyl-2-oxo-l-(2J2,2-trifluoroethyl)-5-
(2s3,6-trifluorophenyl)piperidin-3-yl]carbamate (122 mg, 0.277 mmol) in EtOAc (10 mL) was saturated with HCl (g) and aged for 30 min. The resulting mixture was concentrated in vacuo to give the title compound. MS: mlz = 341.1 (M + 1); lH NM (500 MHz, CD3OD) δ 7.33 (qd, 1H, J- 9.3, 4.9 Hz), 7.05 (tdd, 1H, J= 9.8, 3.7, 2.2 Hz), 4.78 (dq, 1H, J= 15.4, 9.3 Hz), 4.22 (dd, 1H, J = 12.2, 6.6 Hz ), 4.06 (ddd, 1H, J- 13.3, 4.5, 2.7 Hz ), 3.97 (m, 1H), 3.73 (dq, 1H, J = 15.4, 8.8 Hz), 2.91 (qt, 1H, J- 12.7, 3.1 Hz), 2.36 (ddd, 1H, J= 12.7, 6.4, 2.0 Hz), 1.22 (d, 3H, J = 6.6 Hz).
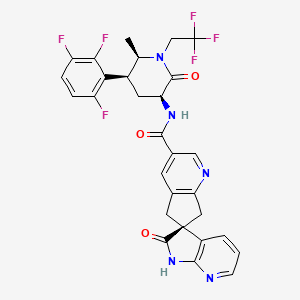
EXAMPLE 4
f6SyN-[f3£5£6iO-6-Methyl-2-QXO-i-(2,2,,2-trifl^yl]-2′-oxo-l\2 5J~tetrahydrospiro[cyciopen^
carboxamide dihvdrochloride
To a stirred mixture of (6>$)-2′-οχο-Γ,2′,5,7- tetrahydrospirotcyclopenta[6]pyridine-6,3′-pyrroio[2,3-6]pyridine]-3-carboxylic acid (described in Intermediate 1) (264 mg, 0.939 mmol), (35′,5S’36J?)-3-amino-6-methyl-l-(2,2,2-trifluoroethyl)- 5-(2f3s6-trifluorophenyl)piperidin-2-one hydrochloride (described in Intermediate 15) (295 mg, 0.782 mmol), HOBT (144 mg, 0.939 mmol), and EDC (180 mg, 0.939 mmol) in DMF (8 mL) was added 7V,N-diisopropylethylamine (0.34 mL, 1.96 mmol), and the resulting mixture was stirred at ambient temperature for 3 h. The reaction mixture was then poured into saturated aqueous sodium bicarbonate (30 mL) and extracted with EtOAc (2 χ 40 mL). The combined organic layers were washed with brine, dried over sodium sulfate, and concentrated in vacuo. The residue was purified by silica gel chromatography, eluting with a gradient of
CH2Cl2:MeOH:NH40H – 100:0:0 to 90:10:0.1, to give the product, which was treated with HC1 in EtOAc at 0 °C to afford the title compound. HRMS: m/z = 604.1783 (M + 1), calculated m/z = 604.1778 for C29H24F6N5O3. iH NMR (500 MHz, CD3OD) δ 9.09 (s, 1H), 8.69 (s, 1H), 8.18 (dd, 1H, J = 5.9, 1.5 Hz), 7.89 (dd5 1H, J= 7.3, 1.5 Hz), 7.30 (m, 1H), 7.23 (dd, 1H, J= 7.3, 5.9 Hz), 7.03 (m, 1H), 4.78 (m, 1H), 4.61 (dd, 1H, J = 11.5, 6.6 Hz), 4.05 (dd, 1H, J= 13.8, 2.8 Hz), 3.96 (m, 1H), 3.84 (d, 1H, J= 18.6 Hz), 3.76 (d, 1H, J = 18.6 Hz), 3.73 (d, 1H, J= 17.3 Hz), (m, 1H), 3.61 (d, 1H, J = 17.3 Hz), 3.22 (m, 1H), 2.38 (m, 1H), 1.34 (d, 3H, J= 6.6 Hz).
This invention relates to a process for making piperidinone carboxamide indane and azainane derivatives, which are CGRP receptor antagonists useful for the treatment of migraine. This class of compounds is described in U.S. Patent Application Nos. 13/293,166 filed November 10, 2011, 13/293,177 filed November 10, 2011 and 13/293,186 filed November 10, 2011, and PCT International Application Nos. PCT/US11/60081 filed November 10, 2011 and PCT/US 11/60083 filed November 10, 2011.
CGRP (Calcitonin Gene -Related Peptide) is a naturally occurring 37-amino acid peptide that is generated by tissue-specific alternate processing of calcitonin messenger RNA and is widely distributed in the central and peripheral nervous system. CGRP is localized
predominantly in sensory afferent and central neurons and mediates several biological actions, including vasodilation. CGRP is expressed in alpha- and beta-forms that vary by one and three amino acids in the rat and human, respectively. CGRP-alpha and CGRP -beta display similar biological properties. When released from the cell, CGRP initiates its biological responses by binding to specific cell surface receptors that are predominantly coupled to the activation of adenylyl cyclase. CGRP receptors have been identified and pharmacologically evaluated in several tissues and cells, including those of brain, cardiovascular, endothelial, and smooth muscle origin.
Based on pharmacological properties, these receptors are divided into at least two subtypes, denoted CGRPi and CGRP2- Human a-CGRP-(8-37), a fragment of CGRP that lacks seven N-terminal amino acid residues, is a selective antagonist of CGRPi, whereas the linear analogue of CGRP, diacetoamido methyl cysteine CGRP ([Cys(ACM)2,7]CGRP), is a selective agonist of CGRP2- CGRP is a potent neuromodulator that has been implicated in the pathology of cerebrovascular disorders such as migraine and cluster headache. In clinical studies, elevated levels of CGRP in the jugular vein were found to occur during migraine attacks (Goadsby et al, Ann. Neurol, 1990, 28, 183-187), salivary levels of CGRP are elevated in migraine subjects between attacks (Bellamy et al., Headache, 2006, 46, 24-33), and CGRP itself has been shown to trigger migrainous headache (Lassen et al., Cephalalgia, 2002, 22, 54-61). In clinical trials, the CGRP antagonist BIBN4096BS has been shown to be effective in treating acute attacks of migraine (Olesen et al, New Engl. J. Med., 2004, 350, 1104-1110) and was able to prevent headache induced by CGRP infusion in a control group (Petersen et al., Clin. Pharmacol. Ther., 2005, 77, 202-213).
CGRP -mediated activation of the trigeminovascular system may play a key role in migraine pathogenesis. Additionally, CGRP activates receptors on the smooth muscle of intracranial vessels, leading to increased vasodilation, which is thought to contribute to headache pain during migraine attacks (Lance, Headache Pathogenesis: Monoamines, Neuropeptides, Purines and Nitric Oxide, Lippincott-Raven Publishers, 1997, 3-9). The middle meningeal artery, the principle artery in the dura mater, is innervated by sensory fibers from the trigeminal ganglion which contain several neuropeptides, including CGRP. Trigeminal ganglion stimulation in the cat resulted in increased levels of CGRP, and in humans, activation of the trigeminal system caused facial flushing and increased levels of CGRP in the external jugular vein (Goadsby et al., Ann. Neurol., 1988, 23, 193-196). Electrical stimulation of the dura mater in rats increased the diameter of the middle meningeal artery, an effect that was blocked by prior administration of CGRP(8-37), a peptide CGRP antagonist (Williamson et al., Cephalalgia, 1997, 17, 525-531). Trigeminal ganglion stimulation increased facial blood flow in the rat, which was inhibited by CGRP(8-37) (Escott et al, Brain Res. 1995, 669, 93-99). Electrical stimulation of the trigeminal ganglion in marmoset produced an increase in facial blood flow that could be blocked by the non-peptide CGRP antagonist BIBN4096BS (Doods et al, Br. J.
Pharmacol., 2000, 129, 420-423). Thus the vascular effects of CGRP may be attenuated, prevented or reversed by a CGRP antagonist.
CGRP -mediated vasodilation of rat middle meningeal artery was shown to sensitize neurons of the trigeminal nucleus caudalis (Williamson et al., The CGRP Family:
Calcitonin Gene -Related Peptide (CGRP), Amylin, and Adrenomedullin, Landes Bioscience, 2000, 245-247). Similarly, distention of dural blood vessels during migraine headache may sensitize trigeminal neurons. Some of the associated symptoms of migraine, including extracranial pain and facial allodynia, may be the result of sensitized trigeminal neurons (Burstein et al, Ann. Neurol. 2000, 47, 614-624). A CGRP antagonist may be beneficial in attenuating, preventing or reversing the effects of neuronal sensitization.
The ability of the compounds to act as CGRP antagonists makes them useful pharmacological agents for disorders that involve CGRP in humans and animals, but particularly in humans. Such disorders include migraine and cluster headache (Doods, Curr Opin Inves Drugs, 2001, 2 (9), 1261-1268; Edvinsson et al, Cephalalgia, 1994, 14, 320-327); chronic tension type headache (Ashina et al, Neurology, 2000, 14, 1335-1340); pain (Yu et al, Eur. J. Pharm., 1998, 347, 275-282); chronic pain (Hulsebosch et al, Pain, 2000, 86, 163-175);
neurogenic inflammation and inflammatory pain (Holzer, Neurosci., 1988, 24, 739-768; Delay- Goyet et al, Acta Physiol. Scanda. 1992, 146, 537-538; Salmon et al, Nature Neurosci., 2001, 4(4), 357-358); eye pain (May et al. Cephalalgia, 2002, 22, 195-196), tooth pain (Awawdeh et al, Int. Endocrin. J., 2002, 35, 30-36), non-insulin dependent diabetes mellitus (Molina et al, Diabetes, 1990, 39, 260-265); vascular disorders; inflammation (Zhang et al, Pain, 2001, 89, 265), arthritis, bronchial hyperreactivity, asthma, (Foster et al, Ann. NY Acad. Sci., 1992, 657, 397-404; Schini et al, Am. J. Physiol, 1994, 267, H2483-H2490; Zheng et al, J. Virol, 1993, 67, 5786-5791); shock, sepsis (Beer et al, Crit. Care Med., 2002, 30 (8), 1794-1798); opiate withdrawal syndrome (Salmon et al, Nature Neurosci., 2001, 4(4), 357-358); morphine tolerance (Menard et al, J. Neurosci., 1996, 16 (7), 2342-2351); hot flashes in men and women (Chen et al, Lancet, 1993, 342, 49; Spetz et al, J. Urology, 2001, 166, 1720-1723); allergic dermatitis (Wallengren, Contact Dermatitis, 2000, 43 (3), 137-143); psoriasis; encephalitis, brain trauma, ischaemia, stroke, epilepsy, and neurodegenerative diseases (Rohrenbeck et al, Neurobiol. of Disease 1999, 6, 15-34); skin diseases (Geppetti and Holzer, Eds., Neurogenic Inflammation, 1996, CRC Press, Boca Raton, FL), neurogenic cutaneous redness, skin rosaceousness and erythema; tinnitus (Herzog et al, J. Membrane Biology, 2002, 189(3), 225); inflammatory bowel disease, irritable bowel syndrome, (Hoffman et al. Scandinavian Journal of Gastroenterology, 2002, 37(4) 414-422) and cystitis. Of particular importance is the acute or prophylactic treatment of headache, including migraine and cluster headache.
The present invention describes a novel process for making piperidinone carboxamide indane and azainane derivatives, which are CGRP receptor antagonists, having less steps and improved yields as compared to previous synthetic methods for making these compounds.
Another embodiment of the invention encompasses crystalline monohydrate free base of the compound having the structure
and having the following chemical name: (S)-N-((3S,5S,6R)-6-mQthyl-2-oxo-l -(2,2,2- trifluoroethyl)-5-(2,3,6-trifluorophenyl)piperidin-3-yl)-2′-oxo- ,2′,5,7- tetrahydrospiro [cyclopenta[b]pyridine-6,3 ‘-pyrrolo [2,3 -b]pyridine] -3 -carboxamide monohydrate
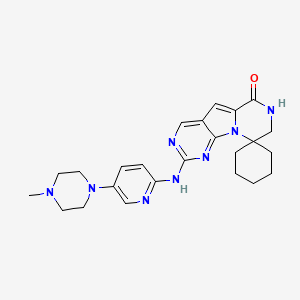
EXAMPLE 2 acetamide (17)
K2C03, water
To a solution of DMF (58.1 mL, 750 mmol) in iPAc (951 mL) was added POCl3 (55.9 mL, 600 mmol) under ice-cooling. After aged for 1 h under ice-bath, acid 16 (95 g, 500 mmol) was added under ice-cooling. The solution was stirred under ice-cooling for 30 min. The solution was added over 30 min into a solution of K2CO3 (254 g, 1.835 mol) and
NHMe(OMe)HCl (73.2 g, 750 mmol) in water (951 mL) below 8 °C. After aged for 30 min below 8 °C, the organic layer was separated, washed with water (500 mL) twice and sat. NaCl aq (100 mL) once, and concentrated in vacuo to afford 17 as an oil (117.9 g, 97.7 wt%, 99% yield). ‘H NMR (CDCI3, 400 MHz); δ 7.05 (m, 1H), 6.82 (m, 1H), 3.86 (s, 2H), 3.76 (s, 3H), 3.22 (s,
3H); 19F NMR (CDCI3, 376.6 MHz); δ -120.4 (dd, J= 15.1, 2.7 Hz), -137.9 (dd, J= 20.8, 2.7 Hz), -143.5 (dd, J= 20.8, 15.1 Hz); 13C NMR (CDC13, 100 MHz); δ 169.4, 156.9 (ddd, J= 244, 6.2, 2.7 Hz), 149.3 (ddd, J= 249, 14.4, 8.4 Hz), 147.1 (ddd, J= 244, 13.1, 3.5 Hz), 115.5 (ddd, J = 19.4, 9.9, 1.5 Hz), 133.4 (dd, J= 22.3, 16.4 Hz), 110.2 (ddd, J= 24.8, 6.7, 4.1 Hz), 32.4 (broad), 26.6 (m); HRMS m/z calcd for C10H10F3NO2 234.0736 (M+H); found 234.0746 l-(2,3,6-Trifluorophenyl)propan-2-one (18)

A mixture of CeCl3 (438 g, 1779 mmol) and THF (12 L) was heated at 40 °C for about 2 h then cooled to 5 °C. Methylmagensium chloride in THF (3 M, 3.4 L) was charged at 5- 9 °C and then it was warmed up to 16 °C and held for 1 h. The suspension was re-cooled to -10 to -15 °C. A solution of 17 (1.19 kg) in THF (2.4 L) was charged into the suspension over 15 min. After confirmation of completion of the reaction, the reaction mixture was transferred to a cold solution of hydrochloric acid (2 N, 8.4 L) and MTBE (5 L) in 5-10°C. The aqueous phase was separated and the organic layer was washed with aqueous 5%> K2CO3 (6 L) and then 10%> aqueous NaCl (5 L). The organic layer was dried over Na2S04, concentrated to give crude 18 (917g, >99wt%>) in 95% yield. The crude 18 was used in the next step without further purification. Analytically pure 18 was obtained by silica gel column.
!H NMR (CDCI3, 400 MHz); δ 7.07 (m, 1H), 6.84 (m, 1H), 3.82 (s, 2H), 2.28 (s, 3H); 19F NMR (CDCI3, 376.6 MHz); δ -120.3 (dd, J= 15.3, 2.5 Hz), -137.8 (dd, J= 21.2, 2.5 Hz), -143.0 (dd, J = 20.2, 15.3 Hz); 13C NMR (CDCI3, 100 MHz); δ 202.2, 156.5 (ddd, J= 244, 6.3, 2.9 Hz), 148.9 (ddd, J= 249, 14.4, 8.6 Hz), 147.0 (ddd, J = 244, 13.1, 3.5 Hz), 115.7 (ddd, J = 19.4, 10.5, 1.2 Hz), 112.8 (dd, J= 22.7, 17.0 Hz), 110.3 (ddd, J = 24.8, 6.7, 4.1 Hz), 37.2 (d, J=1.2 Hz), 29.3. Isopropyl 2-((tert-butoxycarbonyl)amino)-5-oxo-4-(2,3,6-trifluorophenyl)hexanoate (19)

To a solution of 18 (195 g, 1.03 mol) in MTBE (1.8 L) was added zinc bromide (67 g, 0.30 mol) followed by 2 (390 g, 1.2 mol). tert-BuOLi (290 g, 3.6 mol) was then added in several portions while maintaining the reaction temperature below 40 °C. The resulting mixture was stirred at 35 °C for 24 h and quenched into a mixture of 2 N HC1 (5.6 L) and heptane (5 L) at 0 °C. The organic layer was separated and washed with 5% aqueous NaHC03 (5 L) twice. The resulting organic solution was concentrated under vacuum. The residue was dissolved in heptane (2 L) and the solution was concentrated again under vacuum. The resulting oil was dissolved in DMSO (2.5 L) and the solution was used in the next step without further purification. HPLC analysis indicated that the solution contained the desired product 19 (290 g, 67% yield) as the major component along with 5% of starting material 18. The analytically pure product 19 as one pair of diastereomers was isolated by chromatography on silica gel with ethyl acetate and heptane mixture as an eluant. HRMS: m/z calcd for C2oH26F3N05 418.1836 (M+H); found 418.1849. tert- Butyl ((55,,6i?)-6-methyl-2-oxo-5-(2,3,6-trifluorophenyl)piperidin-3-yl)carbamate (20)

To a 0.5 L cylindrical Sixfors reactor with an overhead stirring, a temperature control, a pH probe and a base addition line, was added sodiumtetraborate decahydrate (3.12 g) and DI water (163 mL). After all solids were dissolved, isopropylamine (9.63 g) was added. The pH of the buffer was adjusted to pH 10.5 using 6 N HC1. The buffer was cooled to room temperature. Then, pyridoxal-5 -phosphate (0.33 g) and SEQ ID NO: 1 (8.15 g) were added and slowly dissolved at room temperature. Crude keto ester 19 (23.6 g, 69 wt%, 16.3 g assay, 39 mmol) was dissolved in DMSO (163 mL) and the solution was added to the reactor over 5-10 min. Then the reaction was heated to 55 °C. The pH was adjusted to 10.5 according to a handheld pH meter and controlled overnight with an automated pH controller using 8 M aqueous isopropylamine. The reaction was aged for 27.5 hours.
After confirmation of >95A% conversion by HPLC, the reaction was extracted by first adding a mixture of iPA: iPAc (3:4, 350 mL) and stirring for 20 min. The phases were separated and the aqueous layer was back extracted with a mixture of iPA: iPAc (2:8, 350 mL). The phases were separated. The organic layers were combined and washed with DI water (90 mL). The HPLC based assay yield in the organic layer was 20 (9.86 g, 70.5 % assay yield) with >60:1 dr at the positions C5 and C6. tert- utyl ((35′,55′,6i?)-6-methyl-2-oxo-5-(2,3,6-trifiuorophenyl)piperidin-3-yl)carbamate (21)

A solution of crude cis and trans mixture 20 in a mixture of iPAc and iPA (1.83 wt%, 9.9 kg; 181 g assay as a mixture) was concentrated in vacuo and dissolved in 2-Me-THF (3.6 L). To the solution was added tert-BuOK (66.6 g, 0.594 mol) at room temperature. The suspension was stirred at room temperature for 2 h. The mixture was poured into water (3.5 L) and the organic layer was separated, washed with 15 wt% of aqueous NaCl (3.5 L), dried over Na2S04, and concentrated to dryness. The residue was suspended with iPAc (275 mL) and heptane (900 mL) at 60 °C. The suspension was slowly cooled down to 1 °C. The solid was filtered and rinsed with iPAc and heptane (1 :3), dried to afford 21 (166 g, 93 wt%; 85 %) as crystals. Mp 176-179 °C; 1H NMR (CDC13, 500 MHz): δ 7.06 (m, 1H), 6.84 (m, 1H), 5.83 (broad s, 1H), 5.58 (broad s, 1H), 4.22 (m, 1H), 3.88-3.79 (m, 2H), 2.77 (m, 1H), 2.25 (m, 1H), 1.46 (s, 9H), 1.08 (d, J= 6.4 Hz, 3H); 19F NMR (CDCI3, 376 MHz): δ -117 (d, J= 14 Hz), -135 (d, J= 20 Hz), -142 (dd, J= 20, 14 Hz); 13C NMR (CDC13, 100 MHz): δ 171.1, 156.6 (ddd, J = 245, 6.4, 2.8 Hz), 155.8, 149.3 (ddd, J= 248, 14.4, 8.8 Hz), 147.4 (ddd, J= 245, 14.2, 3.8 Hz), 118.0 (dd, J= 19.3, 14.5 Hz), 115.9 (dd, J= 19.2, 10.4 Hz), 111.0 (ddd, J = 26.4, 6.0, 4.3 Hz), 79.8, 51.4, 49.5, 34.1, 29.3, 28.3, 18.0; HRMS: m/z calcd for Ci7H2iF3N203 381.1396 (M+ Na); found 381.1410. tert-Butyl ((55′,6i?)-6-methyl-2-oxo-l-(2,2,2-trifluoroethyl)-5-(2,3,6-trifluorophenyl)piperidin-3- yl)carbamate (22)

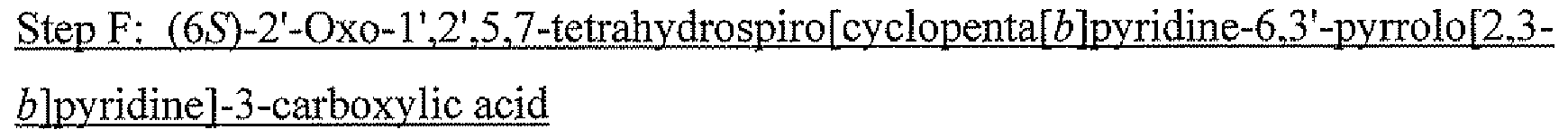
To a solution of 21 (10 g, 87% purity, 24.3 mmol) in THF (70 ml) was added tert- BuOLi (2.5 g, 31.2 mmol) at 5 °C in one portion. The solution was cooled to between 0 and 5 °C and trifluoroethyl trifluoromethanesulfonate (10.0 g, 43 mmol) was added in one portion. DMPU (7 mL) was added slowly over 15 min while maintaining the the reaction temperature below 5 °C. After the mixture was stirred at 0 °C for 3 h, additional tert-BuOLi (0.9 g, 11.2 mmol) was added. The mixture was aged for an additional 90 min. The mixture was quenched with 0.2 N HC1 (70 ml), followed by addition of heptane (80 ml). The organic layer was separated and aqueous layer extracted with heptane (30 ml). The combined organic layers were washed with 15%) aquoeus citric acid (50 mL) and 5% aqueous NaHC03 (50 mL). The solution was concentrated under vacuum at 40 °C and the resulting oil was dissolved in iPAc (30 mL). The solution was used directly in the next step without further purification. The HPLC analysis indicated that the solution contained 22 (9.8 g, 92% as cis and trans mixture in a ratio of 6.5 to 1) along with 4% of starting material 21 and 8% of a N,N’-alkylated compound. Analytically pure 22 (cis isomer) was isolated by chromatography on silica gel with ethyl acetate and heptane as an eluant. 1H NMR (CDC13, 500 MHz): δ 7.15 (m, 1H), 6.85 (m, 1H), 5.45 (broad, s, 1H), 4.90 (m, H), 4.20 (m, 1H), 3.92 (m, 2H), 3.28 (m, 1H), 2.70 (m, 2H), 1.48 (s, 9H), 1.20 (d, J= 5.9 Hz, 3H); 13C NMR (CDC13, 100 MHz): δ 170.2, 156.9 (ddd, J= 245, 6.3,2.7 Hz), 156.0, 149.6 (ddd, J= 251, 14.8, 8.8 Hz), 147.6 (ddd, J= 246, 13.9,3.6 Hz), 124.5 (q, J= 281 Hz), 117.6 (dd, J = 19.2, 3.7 Hz), 116.4 (dd, J= 19.1, 10.4 Hz), 111.4 (ddd, J= 25.8, 6.4,4.1Hz), 56.6, 52.8, 45.3 (q, J= 34.2 Hz), 35.2, 28.7, 28.3 (br t, J= 4 Hz), 14.6; HRMS: m/z calcd for Ci9H22F6N203 (M+H): 441.1607; found 441.1617. (35′,55′,6i?)-6-Methyl-2-oxo-l-(2,2,2-trifluoroethyl)-5-(2,3,6-trifluorophenyl)piperi (S)-2-acetamido-3 -phenylpropanoate (23)

iPAc solution of 22 (529 g assayed, 1.2 mol), obtained from previous step, was diluted to 6 L with iPAc, /?-toluenesulfonic acid monohydride (343 g, 1.8 mol) was added and the solution was heated to 55 °C. After 4 h, the reaction completed (>99% conversion). Aqueous K2CO3 (530 g in 3 L of water) was charged into the solution after cooled to 15-25 °C. The aqueous layer was separated and was back-extracted with iPAc (2 L). The iPAc solutions were combined and the total volume was adjudted to 10 L by adding iPAc. The solution was heated to 50-60 °C. About 20 g of N-acetyl L-phenylalanine was added and the solution was agitated for 15 min or until solids precipitated out. The remaining N-acetyl L-phenylalanine (total 250 g, 1.2 mol) was charged slowly and 2-hydroxy-5-nitrobenzaldehyde (2 g) was charged. The suspension was agitated for 12 h at 20 °C and then cooled to 0 °C for 3 h. The suspension was filtrated, washed with iPAc three times and dried to give 23 (583g, 89% yield) as crystals. Mp 188 – 190 °C; 1H NMR (DMSO-de, 400 MHz): δ 7.96 (d, J= 8.0 Hz, 1H) , 7.48 (m, 1H), 7.15-7.25 (m, 6H), 4.65 (ddd, J= 19.4, 15.3, 9.6 Hz, 1H), 4.33 (ddd, J= 8.7, 8.4, 4.9 Hz, 1H), 3.70-3.87 (m, 3H), 3.57 (dd, J= 11.5, 6.6 Hz, 1H), 3.04 (dd, J= 13.7, 4.9 Hz, 1H), 2.82 (dd, J= 13.7, 8.9 Hz,lH), 2.59 (m, 1H), 2.24 (m, 1H), 2.95 (s, 3H), 1.10 (d, J= 6.4 Hz, 1H); 19F NMR (DMSO-d6, 376 MHz): δ -69 (s) , -118 (d, J= 15 Hz), -137 (d, J = 21 Hz), -142 (dd, J= 21, 15 Hz); 13C NMR (DMSO-d6, 100 MHz): δ 173.6, 171,. l, 168.7, 156.3 (ddd, J= 243.5, 7.0, 3.1 Hz), 148.7 (ddd, J= 249, 14.4, 9.1 Hz), 146.8 (ddd, J = 245, 13.7, 3.1 Hz), 138.5, 129.2, 128.0, 126.1, 124.9 (q, J= 280.9 Hz), 117.4.0 (dd, J= 19.3, 13.8 Hz), 116.7 (dd, J= 19.3, 10.6 Hz), 111.8 (ddd, J= 26.0, 6.7, 3.6 Hz), 56.6, 54.3, 51,2, 44.3 (q, J= 32.5 Hz), 37.2, 34.8, 26.9 (br t, J= 4 Hz), 22.5, 14.1.
(35′,55′,6i?)-6-methyl-2-oxo-l-(2,2,2-trifluoroethyl)-5-(2,3,6-trifluorophenyl)piperidin-3- aminium 2,2-diphenylacetate (25)

To a mixture of crude material containing (55′,6i?)-3-amino-6-methyl-l -(2,2,2- trifluoroethyl)-5-(2,3,6-trifluorophenyl)piperidin-2-one (24, 2.00 g, 5.88 mmol), prepared according to the same method as the previous example, and 3,5-dichloro-2-hydroxybenzaldehyde (0.011 g, 0.059 mmol) in isopropyl acetate (15.0 ml) at 55-60 °C under nitrogen was slowly added a solution of diphenylacetic acid (1.26 g, 5.88 mmol) in THF (10.0 ml) over 2 h. Upon completion of acid addition, a thick salt suspension was agitated at 55-60 °C for another 18 h and then was allowed to cool to ambient temperature. The salt was filtered and washed with isopropyl acetate. After drying at 60 °C in a vacuum oven with nitrogen purge for 8 hours, 25 (2.97 g, 91.4%) was obtained as crystals. 1H NMR (500 MHz, DMSO-d6): δ 7.48 (qd, J= 9.4, 4.9 Hz, 1 H), 7.32 (d, J= 7.7 Hz, 4 H), 7.25-7.26 (m, 4 H), 7.19-7.17 (m, 3 H), 6.79 (br, 3H), 4.95 (s, 1 H), 4.67 (dq, J= 15.3, 9.7 Hz, 1 H), 3.81-3.79 (m, 3 H), 3.62 (dd, J= 11.6, 6.5 Hz, 1 H), 2.66-2.62 (m, 1 H), 2.25 (dd, J= 12.9, 6.4 Hz, 1 H), 1.11 (d, J= 6.5 Hz, 3 H); 13C NMR (100 MHz, DMSO-de): δ 174.4, 171.8, 156.9 (ddd, J= 244, 7.0, 2.5 Hz), 149.1 (ddd, J= 249, 14.4, 8.5 Hz), 147.2 (ddd, J= 246, 13.9, 3.2 Hz), 141.4, 129.0, 128.5, 126.7, 125.5 (q, J= 281 Hz), 118.0 (dd, J= 19.8, 13.8 Hz), 117.1 (dd, J= 19.2, 10.6 Hz), 112.3 (ddd, J= 26.1, 6.7, 3.3 Hz), 58.5, 57.1, 51.7, 44.8 (q, J= 32.7 Hz), 35.3, 27.5 (br t, J= 4.6 Hz), 14.5.
(35′,55′,6i?)-6-methyl-2-oxo-l-(2,2,2-trifluoroethyl)-5-(2,3,6-trifluorophenyl)piperidin-3-amM lH-indole-2-carboxylate (26)

To a mixture of crude material containing 24 (2.00 g, 5.88 mmol) and 3,5-dichloro-2- hydroxybenzaldehyde (0.011 g, 0.059 mmol) in isopropyl acetate (15.0 ml) at 55-60 °C under nitrogen was slowly added a solution of lH-indole-2-carboxylic acid (0.96 g, 5.88 mmol) in THF (10.0 ml) over 2 hours. Upon completion of acid addition, a thick salt suspension was agitated at 55-60 °C for another 18 h and then was allowed to cool to ambient temperature. The salt was filtered and washed with isopropyl acetate. After drying at 60 °C in a vacuum oven with nitrogen purge for 8 h, 26 (2.33 g, 79.0%) was isolated as crystals. 1H NMR (500 MHz, DMSO): δ 11.40 (s, 1 H), 7.56 (d, J= 8.0 Hz, 1 H), 7.45 (br, 3 H), 7.47 (ddd, J= 14.8, 10.1, 8.3 Hz, 1 H), 7.41- 7.40 (m, 1 H), 7.16-7.14 (m, 2 H), 6.98-6.97 (m, 1 H), 6.87 (s, 1 H), 4.69 (dq, J= 15.3, 9.6 Hz, 1 H), 3.84-3.81 (m, 4 H), 2.76-2.71 (m, 1 H), 2.34 (dd, J= 12.7, 6.3 Hz, 1 H), 1.13 (d, J= 6.5 Hz, 3 H); 13C NMR (100 MHz, DMSO-d6): δ 170.9, 164.8, 156.8 (ddd, J= 244, 7.0, 2.5 Hz), 149.1 (ddd, J= 249, 14.4, 8.5 Hz), 147.2 (ddd, J = 246, 13.9, 3.2 Hz), 137.0, 133.5, 127.8, 125.4 (q, J = 282 Hz), 123.3, 121.8, 119.7, 117.8 (dd, J= 19.8, 13.8 Hz), 117.2 (dd, J= 19.2, 10.6 Hz), 112.7, 112.3 (ddd, J= 26.1, 6.7, 3.3 Hz), 105.1, 57.1, 51.3, 44.8 (q, J= 32.7 Hz), 35.2, 26.9, 14.5.

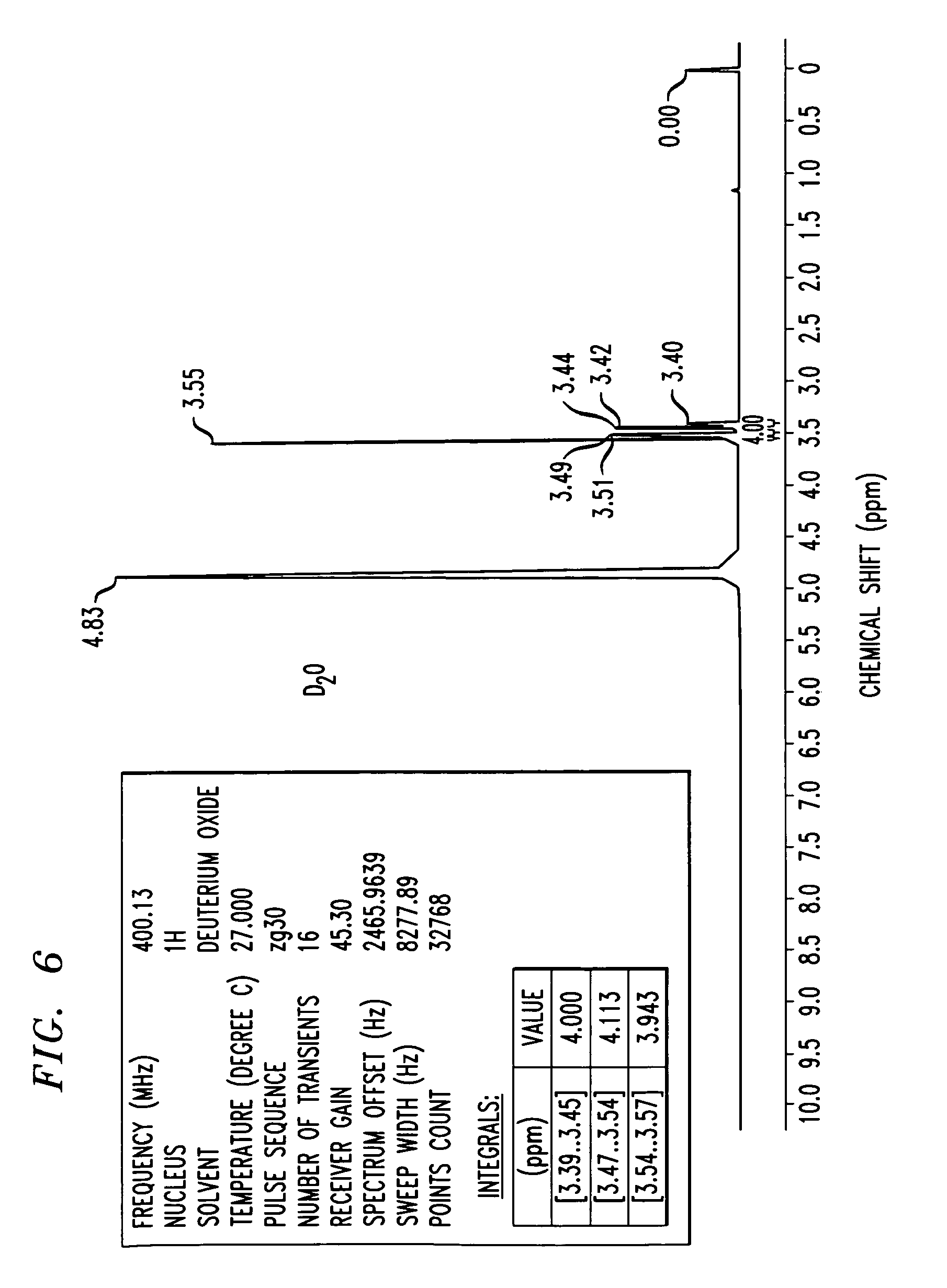
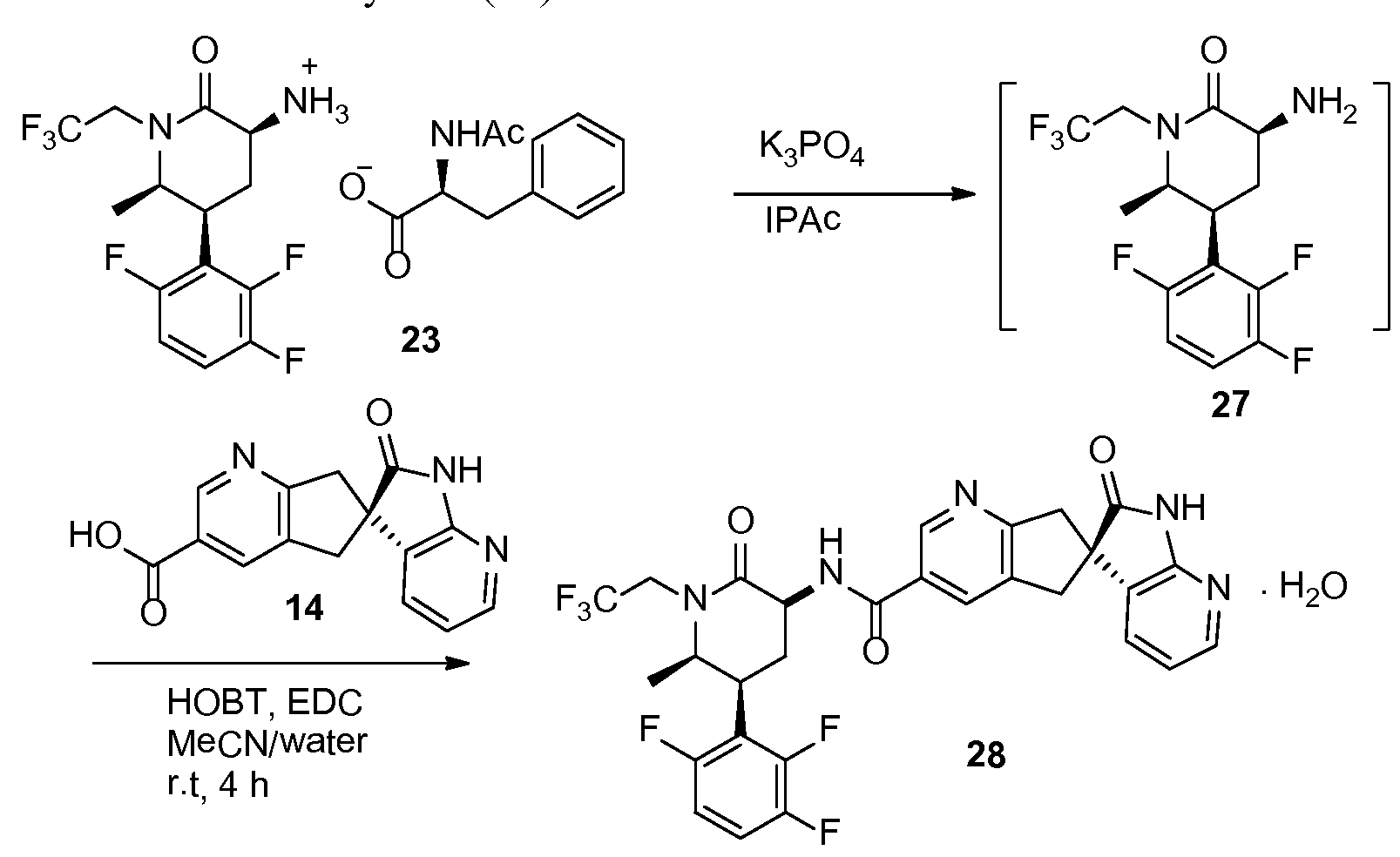
2′-oxo-l\2 5,7-tetrahydrospiro[cyclopenta[¾]pyridine-6,3′-pyrrolo[2,3-¾]pyridine]-3- carboxamide monohydrate (28)
To a suspension of 23 (5.0 g, 9.1 mmol) in isopropyl acetate (50 mL) was added 5% aqueous K3PO4 (50 mL). The mixture was stirred for 5 min. The organic layer was separated and washed with aqueous K3PO4 (50 mL). Solvent removed under vacuum and resulting oil (27) was dissolved in acetonitrile (20 mL). To another flask was added 14 (2.57 g), acetonitrile (40 mL), water (20 mL) and NaOH solution (10N, 0.9 mL). The solution of 27 in acetonitrile was charged to the mixture followed by HOBT monohydrate (1.5 g) and EDC hydrochloride (2.6 g). The mixture was agitated at room temperature for 4 h and HPLC analysis indicated a complete conversion. The reaction mixture was stirred with isopropyl acetate (60 mL) and the aqueous layer was removed. The organic layer was washed with 5% aquoues NaHC03 (40 mL) followed by a mixture of 15% aqueous citric acid (40 mL) and saturated aqueous NaCl (10 mL). The resulting organic layer was finally washed with 5% aquous NaHC03 (40 mL). The solvent was removed under vacuum and the residue was dissolved in methanol (20 mL). The methanol solution was slowly charged into a mixture of water (50 mL) and methanol (5 mL) over 30 min with good agitation, followed by addition of water (50 mL) over 30 min. The suspension was stirred over night at room temperature. The mixture was filtered and crystals were dried in a vacuum oven for 5 h at 50 °C to give 28 (5.4 g, 95%) as monohydrate. Ή NMR (500 MHz, CD3OD): δ 8.88 (t, J= 1.2 Hz, 1 H), 8.15 (t, J = 1.2 Hz, 1 H), 8.09 (dd, J= 5.3, 1.5 Hz, 1 H), 7.36 (dd, J= 7.4, 1.5 Hz, 1 H), 7.28 (qd, J= 9.3, 4.7 Hz, 1 H), 7.01 (tdd, J= 9.7, 3.6, 1.9 Hz, 1 H), 6.96 (dd, J= 7.4, 5.3 Hz, 1 H), 4.80 (dq, J= 15.2, 9.2 Hz, 1 H), 4.56 (dd, J= 11.7, 6.8 Hz, 1 H), 4.03 (ddd, J= 13.6, 4.2, 2.6 Hz, 1 H), 3.97-3.90 (m, 1 H), 3.68 (dq, J= 15.3, 8.8 Hz, 1 H), 3.59 (t, J= 16.2 Hz, 2 H), 3.35 (d, J= 4.4 Hz, 1 H), 3.32 (d, J= 3.5 Hz, 1 H), 3.21 (qt, J= 12.7, 3.1 Hz, 1 H), 2.38-2.32 (m, 1 H), 1.34 (d, J= 6.5 Hz, 3 H); 13C NMR (126 MHz, CD3OD): δ 182.79, 171.48, 168.03, 166.71, 159.37 (ddd, J= 244.1, 6.5, 2.1 Hz), 157.43, 150.88 (ddd, J = 249.4, 14.4, 8.7 Hz), 148.96 (ddd, J= 243.8, 13.7, 3.1 Hz), 148.67, 148.15, 136.84, 133.43, 131.63, 130.83, 130.48, 126.41 (q, J = 280.0 Hz), 119.85, 118.89 (dd, J= 19.0, 13.5 Hz), 117.77 (dd, J= 19.8, 10.8 Hz), 112.80 (ddd, J= 26.5, 6.5, 4.2 Hz), 58.86, 53.67, 52.87, 46.56 (q, J = 33.3 Hz), 45.18, 42.06, 36.95, 27.76 (t, J= 4.8 Hz), 14.11.
EXAMPLE 3
3-Hydroxy-3-(2,3,6-trifluorophenyl)butan-2-one (30)

To a solution of 1,2,4-trifluorobenzene (29, 49.00 g, 371 mmol) and diisopropylamine (4.23 mL, 29.7 mmol) in THF (750 mL) at -70 °C was slowly added 2.5 M of ft-BuLi (156.0 ml, 390 mmol) to maintain temperature between -45 to -40 °C. The batch was agitated for 30 min. To another flask, a solution of 2,3-butadione (37.7 mL, 427 mmol) in THF (150 mL) was prepared and cooled to -70 °C. The previously prepared lithium trifluorobenzene solution was transferred to the second flask between -70 to -45 °C. The reaction was agitated for 1 hour at -55 to -45 and then quenched by adding AcOH (25.7 mL, 445 mmol) and then water (150 mL). After warmed to room temperature, the aqueous layer was seperated. The aqueous solution was extracted with MTBE (200 mL x 1) and the combined organic layers were washed with brine (100 mL x 1). The organic layer was concentrated at 25-35 °C. The residue was flashed with heptane (100 mL x 1) and concentrated to dryness and give 30 (87.94 g, 90.2 wt%, 98% yield, and >99% HPLC purity) as an oil. H NMR (CDCI3, 400 MHz): δ 7.16 (m, 1H), 6.86 (m, 1H), 6.88 (s, 1H), 4.59 (s, 1H), 2.22 (s, 3H), 1.84 (dd, J= 4.0, 2.8 Hz, 3H); 19F NMR (CDCI3, 376.6 MHz): δ -114.6 (dd, J= 14.5, 1.4 Hz), -133.6 (d, J= 19.9 Hz), -141.3 (dd, J =
19.9, 14.5 Hz); 13C NMR (CDCI3, 100 MHz): δ 207.4, 156.4 (ddd, J= 247, 6.2, 2.9 Hz), 149.4 (ddd, J= 253, 15.0, 9.0 Hz), 147.5 (ddd, J= 245, 14.4, 3.3 Hz), 119.4 (dd, J=17.3, 11.7 Hz), 117.0 (ddd, J=19.3, 11.1, 1.4 Hz), 116.6 (ddd, J= 26.6, 6.5, 4.1 Hz), 77.9, 25.0 (dd, J= 6.5, 4.9 Hz), 23.3. -(2,3,6-Trifluorophenyl)but-3-en-2-one (31)

The hydroxy ketone 30 (7.69 g, 35.2 mmol) and 95% H2S04 (26.2 mL, 492.8 mmol) were pumped at 2.3 and 9.2 mL/min respectively into the flow reactor. The temperature on mixing was controlled at 22-25 °C by placing the reactor in a water bath (21 °C). The effluent was quenched into a a mixture of cold water ( 106 g) and heptane/IP Ac ( 1 : 1 , 92 mL) in a j acketed reactor cooled at 0 °C; the internal temperature of the quench solution was ~ 7 °C during the reaction. The layers in the quench reactor were separated and the organic layer was washed with 10% NaH2P04/Na2HP04 (1 :1, 50 mL). The pH of the final wash was 5-6. Solka flock (3.85 g, 50 wt%>) was added to the organic solution. The resulting slurry was concentrated and solvent- switched to heptanes at 25-30 °C. The mixture was filtered, rinsed with heptanes (50 mL x 1). The combined filtrates were concentrated under vacuum to give 31 as an light yellow oil (6.86 g, 90 wt%, 87% yield), which solidified in a freezer. *H NMR (CDC13, 400 MHz): δ 7.13 (m, 1H), 6.86 (m, 1H), 6.60 (s, 1H), 6.15 (s, 1H), 2.46 (s, 3H); 19F NMR (CDC13, 376.6 MHz): δ -117.7 (dd, J= 15.0, 1.4 Hz), -135.4 (dd, J= 21.4, 1.4 Hz), -42.7 (dd, J= 21.4, 15.0 Hz); 13C NMR (CDCls, 100 MHz): δ 196.3, 155.3 (ddd, J= 245, 5.1, 2.9 Hz), 147.9 (ddd, J= 250, 14.5, 7.8 Hz), 147.0 (ddd, J = 245, 13.4, 3.7 Hz), 137.5 (d, J=1.3 Hz), 131.7, 116.6 (ddd, J= 19.9, 9.7, 1.2 Hz), 116.2 (dd, J= 22.6, 16.5 Hz), 110.6 (ddd, J= 24.8, 6.5, 4.1 Hz), 25.8.
Alternative synthesis of 3-(2,3,6-trifluorophenyl)but-3-en-2-one (31)
A solution of 18 (3.5 g, 18.6 mmol), acetic acid (0.34 ml, 5.58 mmol), piperidine (0.37 ml, 3.72 mmol), formaldehyde (6.0 g, 37%> aqueous solution) in MeCN (20 mL) was heated over weekend. The conversion was about 60%. Reaction was heated to 70 °C overnight. The mixtrure was concentrated and extracted with MTBE and HC1 (0.5N). The organic layer was washed with aqueous K2CO3 (0.5N) and water, in turns. The organic layer was concentrated. The product was isolated by chromatography column (hexane and EtOAc), yielding 31 (2.29 g, 61.5%).
Isopropyl 2-((diphenylmethylene)amino)-5-oxo-4-(2,3,6-trifluorophenyl)hexanoate (32)
Diphenylidene isopropyl glycinate (2.0 g, 7.0 mmol) and 31 (1.4 g, 7.0 mmole) were dissolved in THF (10 ml). The solution was cooled to -10 °C. tert- uOLi (0.56 g, 7.0 mmole) was charged into the solution in several portions. The reaction was warmed up to room temperature slowly and stirred overnight. After quenched by addition of aqueous NH4CI, the solvents were removed by distillation under vacuum. The residue was subjected to silica chromatography column eluted by hexane and EtOAc yielding 32 (3.0 g, 89 %) as an oil, which was directly used in the next step.
Isopropyl 2-((tert-butoxycarbonyl)amino)-5-oxo-4-(2,3,6-trifluorophenyl)hexanoate (19)
Compound 32 (100 mg, 0.21 mmol) was dissolved in THF (2 ml) and the solution was cooled to -10 °C. Hydrochloric acid (2N, 1 ml) was added and stirred until all starting material disappeared by TLC. The pH of the reaction was adjusted (pH.>10) by addition of aqueous K2CO3. Boc20 (68 mg, 0.31 mmole) was added into the mixture and stirred overnight. The reaction was completed checked by TLC and the product was identical to the one prepared from the iodo coupling route.
Isopropyl 2-((tert-butoxycarbonyl)amino)-5-oxo-4-(2,3,6-trifluorophenyl)hexanoate (19)
To a 100 mL round bottom was charged 2-methyl THF (43.7 mL) and diisopropyl amine (4.92 mL, 34.2 mmol) and the solution was cooled to -70 °C. n-BuLi (13.08 mL, 32.7 mmol) was charged dropwise during which the temperature was controlled below -45 °C. The mixture was stirred at -45 °C for 0.5 h. N-Boc-glycine ester (3.58 g) was added dropwise keeping temperature between -45 to -40 °C and aged at the same temperature for 1 h.
The solution of 31 (2.91 g, 14.5 mmol) in 2-methyl THF (2.9 mL) was then added dropwise in the same manner at -45 to -40 °C. After a 0.5-1 h age, LC analysis showed nearly complete reaction. The reaction was quenched by addition of HO Ac (3.83 mL) and the mixture was warmed to -10 °C and water (1 1.6 mL, 4 vol) was charged at < 20 °C. The phase was separated, and the organic layer was washed with 16% NaCl aqueous solution (11.6 mL). Assay desired product 19 as a mixture of diastereomers in the organic solution was 5.40 g (89% yield). The organic layer was concentrated to give crude product 19, which was directly used in the next step reaction. For characterization purposes, a small sample was purified by flash chromatography (silica gel, EtOAc/hexanes = 1 : 10) to give two diastereomers 19A and 19B. 19A as a colorless oil, 1H NMR (CD3CN, 400 MHz) δ: 7.29 (m, 1 H), 7.02 (m, 1 H), 5.58 (d, J = 6.1 Hz, 1 H), 4.91 (m, 1 H), 4.19-4.05 (m, 2 H), 2.79 (m, 1 H), 2.05 (s, 3 H), 1.84 (m, 1 H), 1.41 (s, 9 H), 1.23 (d, J = 6.7 Hz, 3 H), 1.22 (d, J = 6.7 Hz, 3 H); 13C NMR (CD3CN, 100 MHz) δ: 204.7, 172.4, 158.6 (ddd, J = 244, 6, 3 Hz), 156.3, 149.8 (ddd, J = 248, 15, 9 Hz), 148.5 (ddd, J = 242, 14, 3 Hz), 118.3 (dd, J = 21, 16 Hz), 117.7 (ddd, J = 19, 10, 2 Hz), 112.6 (ddd, J = 26, 7, 4 Hz), 80.2, 70.0, 53.5, 46.0, 32.0, 28.5, 22.0, 21.9. 19B as colorless crystals, MP 91.5-92.0 °C, 1H NMR (CD3CN, 400 MHz) δ: 7.31 (m, 1 H), 7.03 (m, 1 H), 5.61 (d, J = 8.2 Hz, 1 H), 4.95 (m, 1 H), 4.19 (dd, J = 10.2, 5.1 Hz, 1 H), 3.72 (m, 1 H), 2.45-2.29 (m, 2 H), 2.09 (s, 3 H), 1.41 (s, 9 H), 1.21 (d, J = 6.3 Hz, 3 H), 1.20 (d, J = 6.3 Hz, 3 H); 13C NMR (CD3CN, 100 MHz) δ: 205.0, 172.8, 157.9 (ddd, J= 244, 7, 3 Hz), 156.5, 150.3 (ddd, J= 248, 149, 9 Hz), 148.5 (ddd, J = 242, 13, 4 Hz), 117.9 (dd, J = 19, 10 Hz), 115.9 (dd, J = 21, 15 Hz), 111.5 (ddd, J = 25, 8, 4 Hz), 80.1, 69.9, 52.9, 46.5, 31.1, 28.5, 22.0, 21.9.
CC1C(CC(C(=O)N1CC(F)(F)F)NC(=O)C2=CC3=C(CC4(C3)C5=C(NC4=O)N=CC=C5)N=C2)C6=C(C=CC(=C6F)F)F

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....



























































































































































































 2HCl : 219.16
2HCl : 219.16