Home » 2021 (Page 18)
Yearly Archives: 2021
BBIBP-CorV, Sinopharm COVID-19 vaccine


BBIBP-CorV, Sinopharm COVID-19 vaccine
- Inactivated novel coronavirus (2019-CoV) vaccine (Vero cells)
- Purified inactivated SARS-CoV-2 Vaccine
ref Lancet Infectious Diseases (2021), 21(1), 39-51.
BBIBP-CorV, also known as the Sinopharm COVID-19 vaccine,[1] is one of two inactivated virus COVID-19 vaccines developed by Sinopharm. In late December 2020, it was in Phase III trials in Argentina, Bahrain, Egypt, Morocco, Pakistan, Peru, and the United Arab Emirates (UAE) with over 60,000 participants.[2]
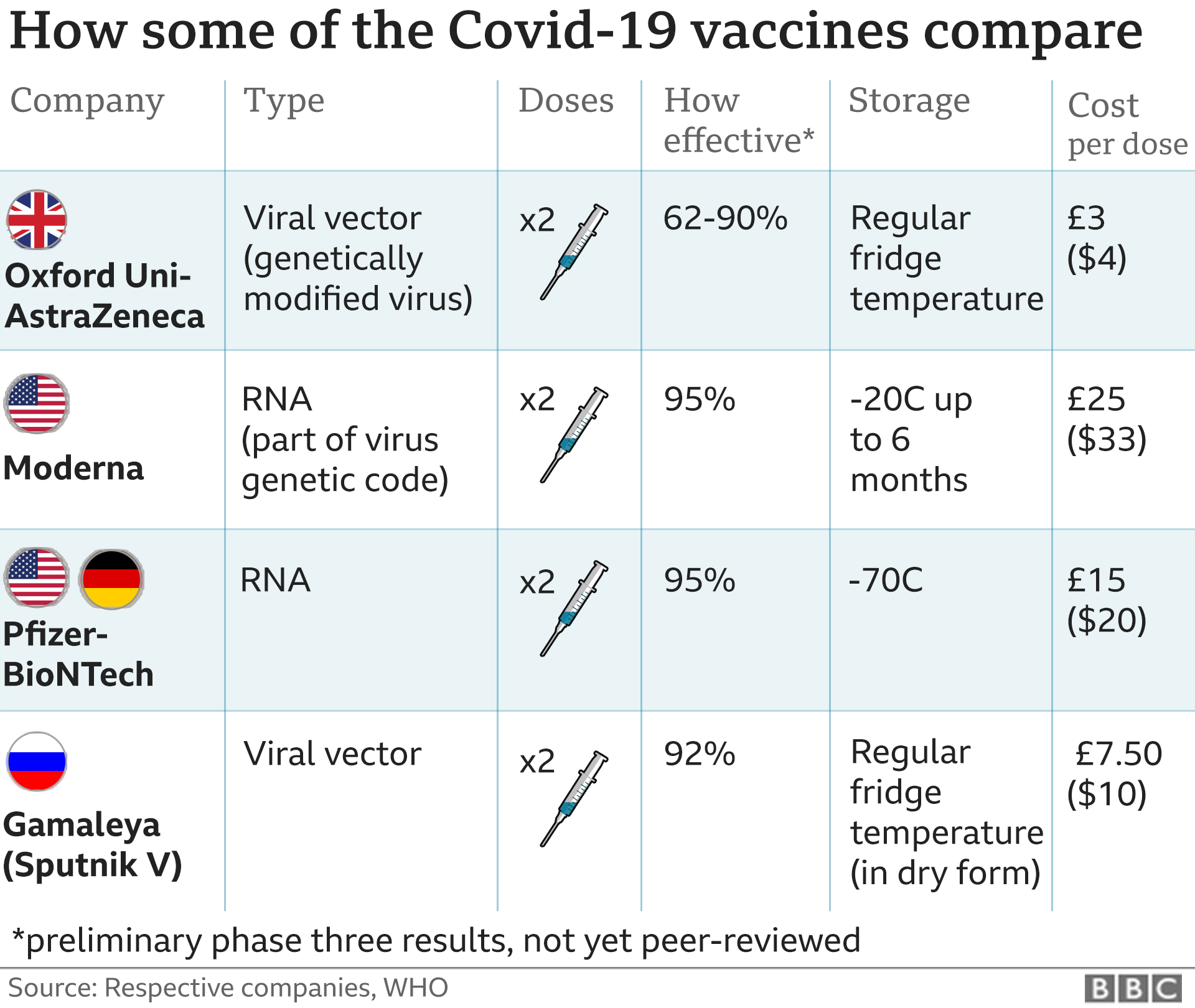
On December 9, the UAE announced interim results from Phase III trials showing BBIBP-CorV had a 86% efficacy against COVID-19 infection.[3] In late December, Sinopharm announced that its internal analysis indicated a 79% efficacy.[4] While mRNA vaccines like the Pfizer–BioNTech COVID-19 vaccine and mRNA-1273 showed higher efficacy of +90%, those present distribution challenges for some nations as they require deep-freeze facilities and trucks. BIBP-CorV could be transported and stored at normal refrigerated temperatures.[5]
BBIBP-CorV shares similar technology with CoronaVac and BBV152, other inactivated virus vaccines for COVID-19 being developed in Phase III trials.[6][7]
BBIBP-CorV is being used in vaccination campaigns by certain countries in Asia,[8][9][10] Africa,[11][12][13] South America,[14][15] and Europe.[16][17][18] Sinopharm expects to produce one billion doses of BBIBP-CorV in 2021.[19] By February 21, Sinopharm said more than 43 million doses of the vaccine had been administered in total.[20]
BBIBP-CorV vaccine contains a SARS-CoV-2 strain inactivated inside Vero Cells. Investigation shows this vaccine induces neutralizing antibodies in several mammalian species while also showing protective efficacy with SARS-CoV-2 challenge in rhesus macaques2. As of August 2020, this vaccine is being tested for prophylaxis against COVID-19 in human clinical trials.

A vaccination certificate of BBIBP-CorV (Beijing Institute of Biological Products, Sinopharm).
Clinical research
Main article: COVID-19 vaccine
Phases I and II
In April 2020, China approved clinical trials for a candidate COVID-19 vaccine developed by Sinopharm‘s Beijing Institute of Biological Products[21] and the Wuhan Institute of Biological Products.[22] Both vaccines are chemically-inactivated whole virus vaccines for COVID-19.
On October 15, the Beijing Institute of Biological Products published results of its Phase I (192 adults) and Phase II (448 adults) clinical studies for the BBIBP-CorV vaccine, showing BBIBP-CorV to be safe and well-tolerated at all tested doses in two age groups. Antibodies were elicited against SARS-CoV-2 in all vaccine recipients on day 42. These trials included individuals older than 60.[21]
On August 13, the Wuhan Institute of Biological Products published interim results of its Phase I (96 adults) and Phase II (224 adults) clinical studies. The report noted the inactivated COVID-19 vaccine had a low rate of adverse reactions and demonstrated immunogenicity, but longer-term assessment of safety and efficacy would require Phase III trials.[22]
BIBP-CorV may have characteristics favorable for vaccinating people in the developing world. While mRNA vaccines, such as the Pfizer–BioNTech COVID-19 vaccine and Moderna COVID-19 vaccine showed higher efficacy of +90%, mRNA vaccines present distribution challenges for some nations, as some may require deep-freeze facilities and trucks. By contrast, BIBP-CorV can be transported and stored at normal refrigeration temperatures.[23] While Pfizer and Moderna are among developers relying on novel mRNA technology, manufacturers have decades of experience with the inactivated virus technology Sinopharm is using.[23]
Phase III
Africa and Asia
On July 16, Sinopharm began conducting a Phase III vaccine trial of 31,000 volunteers in the UAE in collaboration with G42 Healthcare, an Abu Dhabi-based company.[24] By August, all volunteers had received their first dose and were to receive the second dose within the next few weeks.[25] On December 9, UAE’s Ministry of Health and Prevention announced the official registration of BBICP-CorV, after an interim analysis of the Phase III trial showed BBIBP-CorV to have a 86% efficacy against COVID-19 infection.[26] The vaccine had a 99% sero-conversion rate of neutralizing antibodies and 100% effectiveness in preventing moderate and severe cases of the disease.[27]
On September 2, Sinopharm began a Phase III trial in Casablanca and Rabat on 600 people.[28][29] In September, Egypt opened registration for a Phase III trial to last one year and enroll 6,000 people.[30]
In August 2020, Sinopharm began a Phase III clinical trial in Bahrain on 6,000 citizens and resident volunteers.[31][32] In a November update, 7,700 people had volunteered in the trials.[33] Also in late August, Sinopharm began a Phase III clinical trial in Jordan on 500 volunteers at Prince Hamzah Hospital.[34][35]
In Pakistan, Sinopharm began working with the University of Karachi on a trial with 3,000 volunteers.[36]
South America
On September 10, Sinopharm began a Phase III trial in Peru with the long-term goal of vaccinating a total of 6,000 people between the ages of 18 and 75.[37] In October, the trials were expanded to include an additional 6,000 volunteers.[38] On January 26, a volunteer in the placebo group of the vaccine trials had died.[39]
On September 16, Argentina began a Phase III trial with 3,000 volunteers.[40]
Manufacturing
Sinopharm’s Chariman Yang Xioyun has said the company could produce one billion doses in 2021.[19]
In October, Dubai’s G42 Healthcare reached manufacturing agreements to provide UAE and other regional states with BBIBP-CorV, with the UAE producing 75 to 100 million doses in 2021.[41]
In December, Egypt announced an agreement between Sinopharm and Egyptian Holding Company for Biological Products & Vaccines (VACSERA) for the vaccine to be manufactured locally,[42] which would also be exported to other African countries.[43]
In December, AP reported Morocco plans to produce BBIBP-CorV locally.[44]
In March, Serbia announced plans to produce 24 million doses of BBIBP-CorV annually starting in October. The production volume would be sufficient to meet the needs of Serbia and all of its neighbors, deputy prime minister Branislav Nedimović noted.[45]
In March, Belarus was looking to produce BBIBP-CorV locally.[18]
Marketing and Distribution
| show Full authorizationshow Emergency authorizationshow Received donated doses Eligible COVAX recipient (assessment in progress)[86] |
On February 21, 2021 Sinopharm said more than 43 million doses of BBIBP-CorV had been administered so far, including more than 34 million administered in China and the rest internationally.[20]
Asia
In February, Afghanistan was pledged 400,000 doses of BBIBP-CorV by China.[82]
In November 3, 2020 Bahrain granted emergency use authorization of BBIBP-CorV for frontline workers.[33] In December, Bahrain approved Sinopharm’s vaccine, citing data from Phase III clinical trials that showed an 86% efficacy rate.[87]
In February, Brunei received the first batch of Sinopharm vaccines donated by China.[84]
In January, Cambodia said China would provide a million doses.[88] Cambodia granted emergency use authorization on February 4[89] and started the vaccination campaign on February 10 with the first 600,000 doses.[90]
In China, Sinopharm obtained an EUA in July.[91] In October, it began offering the vaccine for free to students going abroad for higher studies.[92] On December 30, China‘s National Medical Products Administration approved BBIBP-CorV for general use.[93][8] In February, Macau received the first 100,000 doses of 400,000 doses.[94]
In October, Indonesia reached an agreement with Sinopharm to deliver 15 million dual-dose vaccines in 2020.[95]
In February, Iran approved emergency use of BBIBP-CorV,[96] and received the first batch of 250,000 doses on February 28.[97]
In January, Iraq approved BBIBP-CorV for emergency use[98] and has signed agreements for 2 million doses. The first doses arrived on March 2.[99]
In January, Jordan approved BBIBP-CorV for emergency use[100] and started its vaccination campaign on January 13.[101]
In March, Kyrgyzstan received a donation of 150,000 doses of the vaccine.[102]
In January, Laos began vaccinating medical workers at hospitals in Vientiane [103] and received another 300,000 doses in early February.[104]
In March, Lebanon received a donation of 50,000 doses at its request,[105] for which it granted emergency use authorization on March 2.[106]
In March, Maldives granted emergency approval for use. At the time of approval, the country had received 18,000 doses and was awaiting 200,000 additional doses.[107]
In February, Mongolia received a donation of 300,000 doses.[108] On March 10, Governor of Ulaanbaatar D. Sumiyabazar and Deputy Prime Minister S. Amarsaikhan received the first doses of BBIBP-CorV.[109]
In February, Nepal approved the vaccine for emergency use, allowing a donation of 500,000 doses to enter the country.[110]
In December, Pakistan‘s purchased 1.2 million doses,[111] which was approved for emergency use on January 18,[112] and began a vaccination campaign on February 2.[10]
In March, Palestine said it would receive 100,000 doses donated by China.[113]
In March 19, Sri Lanka approved the vaccine for emergency use, allowing a donation of 600,000 doses by China to enter the country.[114]
On 14 September 2020, the United Arab Emirates approved the vaccine for front-line workers following successful interim Phase III trials.[24] In December, the country registered BBIBP-CorV after it reviewed the results of the interim analysis.[26] In March, a small number of people who have reduced immunity against diseases, have chronic illnesses, or belong to high-risk groups have been given a 3rd booster shot.[115]
Africa
In February, Algeria received a donation of 200,000 doses.[83]
Egypt plans to buy 40 million doses of Sinpharm’s vaccine[116] which was approved for regulatory use on January 3.[116] President Abdel Fattah el-Sisi announced a vaccination campaign starting 24 January.[11]
In February, Equatorial Guinea received a donation of 100,000 doses which arrived on February 10. The country began vaccinations on February 15.[56]
In March, Gabon received a donation of 100,000 doses which was the second vaccine approved for use in the country.[117]
Morocco placed orders for 41 million vaccine doses from Sinopharm and 25 million from AstraZeneca, for a total of 66 million doses.[118] Morocco granted emergency use approval on January 23,[119] and the first 500,000 doses arrived on January 27.[12]
In February, Mozambique received a donation of 200,000 doses[120] and planned to start vaccinations on March 8.[121]
In March, Namibia received a donation of 100,000 doses and announced the start of vaccinations in the Khomas and Erongo regions.[122]
In March, Niger received a donation of 400,000 doses with vaccinations to begin on March 27.[123]
In February, Senegal received 200,000 doses in Dakar[124] and began vaccinating health workers on February 22.[125]
In February, Sierra Leone received a donation of 200,000 doses.[126] It was approved for emergency use and vaccinations began on March 15.[127]
In January, Seychelles said it would begin administering vaccinations on January 10 with 50,000 doses it had received as a gift from the UAE.[128]
In March, Republic of the Congo received 100,000 doses with vaccinations prioritizing the medically vulnerable and those over 50.[129]
In February, Zimbabwe purchased 600,000 doses on top of 200,000 doses donated by China,[130] and started vaccinations on February 18.[13] Zimbabwe later purchased an additional 1.2 million doses.[131]
North America
In February, the Dominican Republic ordered 768,000 doses of BBIBP-CorV.[132]
In March, Dominica received 20,000 doses of BBIBP-CorV which it began using in its vaccination campaign on March 4.[133]
In March, Mexico announced it would order 12 million doses of BBIBP-CorV pending approval by its health regulator.[134]
South America
In February, Argentina authorized emergency use of BBIBP-CorV[135] ahead of the arrival of 904,000 doses on February 26.[136]
In February, Bolivia purchased 400,000 doses on top of 100,000 doses donated by China,[137] and started its vaccination campaign on February 26.[15]
In March, Guyana received a donation of 20,000 doses of BBIBP-CorV.[138] Vaccinations were to start on March 7.[139]
In January, Peru purchased 38 million doses of BBIBP-CorV.[140] Peru granted emergency approval for BBIBP-CorV on January 27[141] and started vaccinations on February 9 with the first 300,000 doses.[14]
In March, Venezuela granted approval for BBIBP-CorV to be used in the country.[142] The first 500,000 doses arrived on March 2.[143]
Europe
In February, Belarus received a donation of 100,000 doses[144] and began using the vaccine on March 15.[18]
In January, Hungary became first EU member to approve BBIBP-CorV, signing a deal for 5 million doses.[145] The first 550,000 doses arrived in Budapest on February 16[146] and vaccinations started on February 24.[17] Prime Minister Viktor Orbán was vaccinated with BBIBP-CorV on February 28.[147]
In March, Moldova received 2,000 doses donated by the UAE[148] which will be used to vaccinate doctors at the State University of Mediecne and Pharmacy starting on March 22.[149]
In March 3, Montenegro received a donation of 30,000 doses of BBIBP-CorV.[85]
In February, North Macedonia signed an agreement for 200,000 doses of BBIBP-CorV, with which they hoped to launch their vaccination program later that month.[150]
In January, Serbia received one million doses, making it the first country in Europe to receive BBIBP-CorV.[151] On January 19, Serbia approved the vaccine and Health Minister Zlatibor Lončar became the first person to receive a shot.[16]
Controversies
Lack of public data
Unlike Moderna‘s MRNA-1273, Oxford–AstraZeneca‘s AZD1222, and Johnson & Johnson‘s Ad26.COV2.S, there is little public information about the Chinese vaccine’s safety or efficacy.[152] The UAE said it had reviewed Sinopharm’s interim data analysis which showed the vaccine was 100% effective to prevent moderate and severe instances of COVID-19, but did not say whether it had independently analyzed the case data in its review. It was unclear how Sinopharm drew conclusions, since the UAE announcement of the approval for BBIBP-CorV noticeably lacked details such as the number of COVID-19 cases in the placebo or active group or the volunteers ages.[153]
As of December 30, 2020, no detailed efficacy data of the vaccine has been released to the public. A Sinopharm executive said detailed data would be released later and published in scientific journals in China and internationally.[8]
Sinopharm president Wu Yonglin said the trial results exceeded the WHO’s requirements, but a director at a large pharmaceutical company in Shanghai expressed skepticism over the trials and the expectation that drug regulators in Bahrain and the UAE would not hold the same standard as the U.S. Food and Drug Administration.[154]
Unauthorized use in Asia
On December 30, Philippine Defense Secretary Delfin Lorenzana said in an interview that at least one minister and president Rodrigo Duterte‘s bodyguards were provided BBIBP-CorV which were “smuggled” but that he felt what happened was “justified”. Brigadier General Jesus Durante, head of the Presidential Security Guard (PSG), said he felt compelled and “took the risk” to have some of his men vaccinated because they provide close-in security to Duterte, who at 75 is highly vulnerable to COVID-19.[155] Ingming Aberia, an author at The Manila Times commented that FDA director-general Enrique Domingo had reason to believe Sinopharm may cause harm to the consuming public given that no COVID-19 vaccine license was issued, but out of “self-preservation”, he would not initiate charges against PSG.[156]
On January 1, Mainichi Shimbun reported that 18 wealthy people, including several owners of leading Japanese companies, have been vaccinated with Sinopharm vaccines since November 2020. The vaccines were brought in by a Chinese consultant close to a senior member of the Chinese Communist Party.[157] The Chinese embassy in Japan later expressed its dissatisfaction at the unverified claims by Japanese news media.[158]
References
- ^ https://www.nytimes.com/interactive/2020/health/sinopharm-covid-19-vaccine.html
- ^ Reuters Staff (2020-11-19). “China Sinopharm’s coronavirus vaccine taken by about a million people in emergency use”. Reuters. Retrieved 2020-12-09.
- ^ “UAE: Ministry of Health announces 86 per cent vaccine efficacy”. gulfnews.com. Retrieved 2020-12-13.
- ^ Wee, Sui-Lee; Qin, Amy (2020-12-30). “China Approves Covid-19 Vaccine as It Moves to Inoculate Millions”. The New York Times. ISSN 0362-4331. Retrieved 2021-02-12.
- ^ “China State-Backed Covid Vaccine Has 86% Efficacy, UAE Says”. Bloomberg.com. 2020-12-09. Retrieved 2020-12-09.
- ^ Cohen J (December 2020). “China’s vaccine gambit”. Science. 370 (6522): 1263–1267. Bibcode:2020Sci…370.1263C. doi:10.1126/science.370.6522.1263. PMID 33303601.
- ^ Tan Y (16 December 2020). “Covid: What do we know about China’s coronavirus vaccines?”. BBC News. Retrieved 18 December 2020.
- ^ Jump up to:a b c Liu R (2020-12-31). “China gives its first COVID-19 vaccine approval to Sinopharm”. Reuters. Retrieved 2020-12-31.
- ^ Turak, Natasha (2021-01-18). “The UAE is on track to have half its population vaccinated by the end of March”. CNBC. Retrieved 2021-01-21.
- ^ Jump up to:a b Dawn.com (2021-02-02). “PM Imran kicks off Pakistan’s Covid-19 vaccination drive”. DAWN.COM. Retrieved 2021-02-03.
- ^ Jump up to:a b Reuters Staff (2021-01-24). “Sisi says Egypt to begin COVID-19 vaccinations on Sunday”. Reuters. Retrieved 2021-01-24.
- ^ Jump up to:a b Dumpis, Toms (2021-01-27). “Morocco Receives Half a Million Doses of Chinese Sinopharm Vaccine”. Morocco World News. Retrieved 2021-01-28.
- ^ Jump up to:a b “Zimbabwe starts administering China’s Sinopharm vaccines”. thestar.com. 2021-02-18. Retrieved 2021-02-20.
- ^ Jump up to:a b Aquino, Marco (2021-02-10). “‘The best shield’: Peru launches inoculation drive with Sinopharm vaccine”. Reuters. Retrieved 2021-02-10.
- ^ Jump up to:a b “Bolivia begins inoculation with Sinopharm jabs | The Star”. http://www.thestar.com.my. Retrieved 2021-02-28.
- ^ Jump up to:a b “Serbia Becomes First European Nation To Use China’s Sinopharm Vaccine”. RadioFreeEurope/RadioLiberty. Retrieved 2021-01-21.
- ^ Jump up to:a b “Hungary first EU nation to use China’s Sinopharm vaccine against COVID”. euronews. 2021-02-24. Retrieved 2021-02-26.
- ^ Jump up to:a b c d “Belarus begins COVID-19 vaccinations with Chinese shots”. eng.belta.by. 2021-03-15. Retrieved 2021-03-16.
- ^ Jump up to:a b “Which companies will likely produce the most COVID-19 vaccine in 2021?”. Pharmaceutical Processing World. 2021-02-05. Retrieved 2021-02-28.
- ^ Jump up to:a b hermesauto (2021-02-22). “More than 43 million doses of China’s Sinopharm Covid-19 vaccines used globally”. The Straits Times. Retrieved 2021-02-22.
- ^ Jump up to:a b Xia S, Zhang Y, Wang Y, Wang H, Yang Y, Gao GF, et al. (October 2020). “Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBIBP-CorV: a randomised, double-blind, placebo-controlled, phase 1/2 trial”. The Lancet. Infectious Diseases. 21 (1): 39–51. doi:10.1016/s1473-3099(20)30831-8. PMC 7561304. PMID 33069281.
- ^ Jump up to:a b Xia S, Duan K, Zhang Y, Zhao D, Zhang H, Xie Z, et al. (September 2020). “Effect of an Inactivated Vaccine Against SARS-CoV-2 on Safety and Immunogenicity Outcomes: Interim Analysis of 2 Randomized Clinical Trials”. JAMA. 324 (10): 951–960. doi:10.1001/jama.2020.15543. PMC 7426884. PMID 32789505.
- ^ Jump up to:a b “China State-Backed Covid Vaccine Has 86% Efficacy, UAE Says”. Bloomberg.com. 2020-12-09. Retrieved 2020-12-09.
- ^ Jump up to:a b Maxwell C. “Coronavirus: UAE authorises emergency use of vaccine for frontline workers”. The National. Retrieved 14 September 2020.
- ^ “Coronavirus: 15,000 register as volunteers for Covid-19 vaccine trial in UAE”. The National. 13 August 2020. Retrieved 15 August2020.
- ^ Jump up to:a b Reuters Staff (2020-12-09). “UAE says Sinopharm vaccine has 86% efficacy against COVID-19”. Reuters. Retrieved 2020-12-09.
- ^ “UAE: Ministry of Health announces 86 per cent vaccine efficacy”. gulfnews.com. Retrieved 2020-12-09.
- ^ “Morocco orders R-Pharm Covid-19 vaccine | The North Africa Post”. northafricapost.com. Retrieved 2020-10-07.
- ^ “Chinese Clinical Trial Register (ChiCTR) – The world health organization international clinical trials registered organization registered platform”. http://www.chictr.org.cn. Retrieved 2020-10-21.
- ^ “Egypt to start receiving volunteers for COVID-19 vaccine trials”. Egypt Independent. 2020-09-12. Retrieved 2020-09-21.
- ^ “Bahrain starts Phase III trial of Sinopharm’s Covid-19 vaccine”. Clinical Trials Arena. 24 August 2020.
- ^ Manama TD. “Vaccine trial continues | THE DAILY TRIBUNE | KINGDOM OF BAHRAIN”. DT News. Retrieved 2020-10-22.
- ^ Jump up to:a b Barrington L (3 November 2020). “Bahrain allows Sinopharm COVID-19 vaccine candidate use in frontline workers”. Reuters. Retrieved 3 November 2020.
- ^ Liu R (5 September 2020). “China’s CNBG, Sinovac find more countries to test coronavirus vaccines”. Reuters. Retrieved 6 September 2020.
- ^ “Jordan starts phase 3 trial of China’s COVID-19 vaccine”. Jordan Times. 2020-08-30. Retrieved 2020-10-22.
- ^ “Coronavirus vaccine should be available in Pakistan ‘within 6-8 weeks'”. http://www.geo.tv. Retrieved 2020-11-14.
- ^ “Third Phase of Human Trials for Coronavirus Vaccine Underway in Peru | Voice of America – English”. http://www.voanews.com. Retrieved 2020-09-11.
- ^ “6,000 additional volunteers required for trials of Sinopharm’s COVID-19 vaccine” (in Spanish). Andina. Retrieved 17 October2020.
- ^ Aquino, Marco (2021-01-27). “Peru volunteer in Sinopharm vaccine trial dies of COVID-19 pneumonia, university says”. Reuters. Retrieved 2021-01-27.
- ^ “Clinical Trial to Evaluate the Efficacy, Immunogenicity and Safety of the Inactivated SARS-CoV-2 Vaccine (COVID-19) – Full Text View – ClinicalTrials.gov”. clinicaltrials.gov. Retrieved 2020-09-28.
- ^ Greaves J (2020-10-08). “UAE company nears end of Chinese Covid-19 vaccine trial”. Reuters. Retrieved 2020-10-10.
- ^ “Chinese COVID-19 vaccine effective: Egypt’s MoH”. EgyptToday. 2020-12-13. Retrieved 2020-12-15.
- ^ “Health Min: a new production line to produce Sinopharm’s Chinese vaccine in Egypt and will be exported to African countries”. EgyptToday. 2020-12-12. Retrieved 2020-12-31.
- ^ “Morocco acquires 65 million vaccine doses from China, UK”. ABC News. Retrieved 2020-12-26.
- ^ “Serbia to produce 24 mln doses of China’s Sinopharm vaccine annually – deputy PM”. seenews.com. Retrieved 2021-03-17.
- ^ “Bahrain approves China’s Sinopharm coronavirus vaccine”. Arabian Business Industries. 13 December 2020.
- ^ Kuo L. “China approves Sinopharm coronavirus vaccine, the country’s first for general use”. The Washington Post.
- ^ “President Ramkalawan and First Lady receives second dose SinoPharm Vaccine”. statehouse.gov.sc. Retrieved 5 February2021.
- ^ Wee S (9 December 2020). “Chinese Covid-19 Vaccine Gets Key Push, but Doubts Swirl”. The New York Times. Retrieved 12 December 2020.
- ^ “Coronavirus: UAE authorises emergency use of vaccine for frontline workers”. The National. Retrieved 24 November 2020.
- ^ Biannchi, Walter (21 February 2021). “Argentina approves Sinopharm COVID-19 vaccine for emergency use”. Reuters. Retrieved 23 February 2021.
- ^ “Bolivia begins inoculation with Sinopharm jabs | The Star”. The Star. Malaysia. Retrieved 28 February 2021.
- ^ Rinith T (4 February 2021). “Health Ministry grants Emergency Use Authorization to China’s Sinopharm vaccine”. Khmer Times. Retrieved 4 February 2021.
- ^ “Dominica: Melissa Skerrit receives the Sinopharm COVID-19 vaccine”. WIC News. 4 March 2021. Retrieved 7 March 2021.
- ^ “Egypt licenses China’s Sinopharm COVID-19 vaccine for emergency use: health minister – Xinhua | English.news.cn”. Xinhua News Agency.
- ^ Jump up to:a b “Equatorial Guinea President receives 1st dose of Chinese COVID-19 vaccine”. dailynewsegypt.com. Retrieved 2021-03-10.
- ^ “Gabon receives 100,000 doses of Sinopharm’s vaccine from China”. Gabon 24. 2021-03-12. Retrieved 2021-03-13.
- ^ “Sinopharm vaccine rollout starts this weekend”. Stabroek News. 6 March 2021. Retrieved 7 March 2021.
- ^ “Hungary signs deal for Chinese Sinopharm’s COVID-19 vaccine, first in EU”. National Post.
- ^ “Iran Launches Phase Two of Mass Inoculation Campaign”. Financial Tribune. 22 February 2021. Retrieved 23 February 2021.
- ^ “Iraq approves Sinopharm, AstraZeneca vaccines”. Big News Network.com. Retrieved 30 January 2021.
- ^ “First batch of Chinese Sinopharm vaccine arrives in Jordan”. Roya News. Retrieved 9 January 2021.
- ^ “Laos declares Covid-19 vaccinations safe, more to be inoculated next week | The Star”. The Star. Malaysia. Retrieved 19 February2021.
- ^ Crean, Rosabel. “China donates 50,000 doses of Sinopharm vaccine to Lebanon | News , Lebanon News | THE DAILY STAR”. Daily Star. Retrieved 2 March 2021.
- ^ “Macau receives first batch of COVID-19 vaccines”. IAG. 7 February 2021. Retrieved 24 February 2021.
- ^ “MFDA approves Pfizer, Sinopharm Covid-19 vaccines for emergency use”. raajje.mv. Retrieved 2021-03-15.
- ^ Cristina (2021-03-19). “O mie de studenți și medici-rezidenți din cadrul USMF vor fi imunizați anti-COVID cu vaccinul BBIBP-CorV, produs de către Sinopharm Beijing Institute of Biological Products”. Ziarul de Gardă (in Romanian). Retrieved 2021-03-19.
- ^ “Deputy PM and City Governor get the first dose of Sinopharm vaccine”. MONTSAME News Agency. Retrieved 2021-03-15.
- ^ “Covid-19: Morocco authorizes use of the Sinopharm vaccine”. en.yabiladi.com.
- ^ Reuters Staff (6 March 2021). “Mozambique expects to vaccinate 16 million against coronavirus by 2022”. Reuters. Retrieved 7 March 2021.
- ^ Namibian, The. “Khomas, Erongo first to get vaccinated”. The Namibian. Retrieved 2021-03-17.
- ^ Poudel, Arjun. “China’s Shinopharm vaccine gets emergency use authorisation in Nepal”. Kathmandu Post. Retrieved 19 February2021.
- ^ “Covid-19 : Le Niger réceptionne 400.000 doses de vaccin SINOPHARM, un don de la Chine | Agence Nigérienne de Presse”. http://www.anp.ne. Retrieved 2021-03-21.
- ^ Shahzad A (19 January 2021). “Pakistan approves Chinese Sinopharm COVID-19 vaccine for emergency use”. Reuters.
- ^ “Peru grants ‘exceptional’ approval for Sinopharm COVID-19 vaccine – government sources”. Reuters. 27 January 2021.
- ^ Asala, Kizzi. “Senegal Kicks Off COVID-19 Vaccination Campaign with China’s Sinopharm”. Africanews. Retrieved 23 February2021.
- ^ “Serbia Becomes First European Nation To Use China’s Sinopharm Vaccine”. RadioFreeEurope/RadioLiberty.
- ^ Thomas, Abdul Rashid (2021-03-15). “Sierra Leone’s President Bio leads the way in taking COVID-19 Vaccine”. SIERRA LEONE TELEGRAPH. Retrieved 2021-03-15.
- ^ “NMRA approves sinopharm vaccine for emergency use”. Colombo Gazette. 2021-03-19. Retrieved 2021-03-20.
- ^ Sequera, Vivian (1 March 2021). “Venezuela approves use of China’s Sinopharm coronavirus vaccine”. Reuters. Retrieved 2 March 2021.
- ^ Mutsaka, Farai (18 February 2021). “Zimbabwe starts administering China’s Sinopharm vaccines”. The Star. Retrieved 20 February 2021.
- ^ Jump up to:a b “China ‘to provide 400,000 COVID vaccine doses’ to Afghanistan”. http://www.aljazeera.com. Retrieved 2021-03-01.
- ^ Jump up to:a b Presse, AFP-Agence France. “Algeria Receives 200,000 Coronavirus Jabs From China”. http://www.barrons.com. Retrieved 2021-02-26.
- ^ Jump up to:a b “Vaccine donation from China arrives | The Star”. http://www.thestar.com.my. Retrieved 2021-02-12.
- ^ Jump up to:a b Radomir, Ralev. “Montenegro receives 30,000 doses of China’s COVID-19 vaccine”.
- ^ “Regulation and Prequalification”. World Health Organization. Retrieved 18 March 2021.
- ^ “Bahrain approves Chinese COVID-19 vaccine for use”. ABC News. Retrieved 2020-12-13.
- ^ Reuters Staff (2021-01-15). “Cambodia says China donates 1 million doses of COVID-19 vaccines”. Reuters. Retrieved 2021-01-16.
- ^ “Health Ministry grants Emergency Use Authorization to China’s Sinopharm vaccine”. Khmer Times. 2021-02-04. Retrieved 2021-02-04.
- ^ “Lt Gen Manet first to be inoculated today with the Sinopharm vaccine”. Khmer Times. 2021-02-09. Retrieved 2021-02-10.
- ^ “Sinovac’s coronavirus vaccine candidate approved for emergency use in China – source”. Reuters. 2020-08-29. Retrieved 2020-08-30.
- ^ Vivek V (15 October 2020). “China’s Sinopharm offers experimental COVID-19 vaccines to students: WSJ”. Reuters. Retrieved 15 October 2020.
- ^ “China gives conditional approval to coronavirus vaccine made by Sinopharm”. Global News. Retrieved 2020-12-31.
- ^ “First Sinopharm Covid-19 vaccines to arrive today”. Macau Business. 2021-02-06. Retrieved 2021-02-07.
- ^ Taufiqurrahman M. “Indonesia can be manufacturing hub for COVID-19 vaccine, says Chinese foreign minister”. Jakarta Post. Retrieved 13 October 2020.
- ^ “Iran Launches Phase Two of Mass Inoculation Campaign”. Financial Tribune. 2021-02-22. Retrieved 2021-02-23.
- ^ “Iran Gets Chinese Vaccine for Coronavirus – Society/Culture news”. Tasnim News Agency. Retrieved 2021-02-28.
- ^ Jangiz, Khazan. “Iraq approves the emergency use of two more COVID-19 vaccines”. http://www.rudaw.net. Retrieved 2021-01-21.
- ^ “Iraq receives first Covid vaccines, gift from China”. France 24. 3 March 2021.
- ^ “Jordan approves China’s Sinopharm Covid vaccine”. France 24. 2021-01-09. Retrieved 2021-03-07.
- ^ Omari, Raed. “Jordan begins COVID-19 vaccination drive as physician, 87, gets first jab”. Arab News.
- ^ KHARIZOV, Ruslan (2021-03-19). “150,000 doses of Sinopharm coronavirus vaccine delivered to Kyrgyzstan”. 24.kg. Retrieved 2021-03-20.
- ^ Thanabouasy, Phayboune (2021-01-27). “Laos Begins Vaccinations for Over 600 Medical Workers”. Laotian Times. Retrieved 2021-01-27.
- ^ Limited, Bangkok Post Public Company. “Laos receives 300,000 vaccine doses from China”. Bangkok Post. Retrieved 2021-02-10.
- ^ “China donates 50,000 doses of Sinopharm vaccine to Lebanon | News , Lebanon News | THE DAILY STAR”. http://www.dailystar.com.lb. Retrieved 2021-03-02.
- ^ March 2021, Naharnet Newsdesk 01; 20:39. “Lebanon Authorizes Use of Chinese Vaccine Sinopharm”. Naharnet. Retrieved 2021-03-07.
- ^ “MFDA approves Pfizer, Sinopharm Covid-19 vaccines for emergency use”. raajje.mv. Retrieved 2021-03-15.
- ^ “Mongolia receives COVID-19 vaccine donation from China – The Manila Times”. http://www.manilatimes.net. Retrieved 2021-02-28.
- ^ “Deputy PM and City Governor get the first dose of Sinopharm vaccine”. MONTSAME News Agency. Retrieved 2021-03-15.
- ^ “China’s Shinopharm vaccine gets emergency use authorisation in Nepal”. kathmandupost.com. Retrieved 2021-02-19.
- ^ Peshimam GN (2020-12-31). “Pakistan to purchase 1.2 million COVID-19 vaccine doses from China’s Sinopharm”. Reuters. Retrieved 2020-12-31.
- ^ Shahzad, Asif (2021-01-19). “Pakistan approves Chinese Sinopharm COVID-19 vaccine for emergency use”. Reuters. Retrieved 2021-01-21.
- ^ “Palestine to receive 100,000 doses of Sinopharm Covid-19 vaccine”. WAFA Agency. Retrieved 2021-03-12.
- ^ “NMRA approves sinopharm vaccine for emergency use”. Colombo Gazette. 2021-03-19. Retrieved 2021-03-20.
- ^ Sircar, Nandini. “UAE Covid vaccine: Third dose to help those with weak immunity”. Khaleej Times. Retrieved 2021-03-19.
- ^ Jump up to:a b “Egypt approves Chinese COVID vaccine, roll-out likely this month”. http://www.aljazeera.com. Retrieved 2021-01-03.
- ^ “Gabon receives 100,000 doses of Sinopharm’s vaccine from China”. Gabon 24. 2021-03-12. Retrieved 2021-03-13.
- ^ Eljechtimi, Ahmed (2021-01-26). “Morocco prepares to launch COVID-19 vaccination programme”. Reuters. Retrieved 2021-01-27.
- ^ “Moroccan health ministry grants emergency approval to Sinopharm’s Covid-19 vaccine”. wam. Retrieved 2021-01-27.
- ^ “China, Africa and the Vaccine Donations”. Modern Ghana. Retrieved 2021-03-05.
- ^ Mucari, Manuel (2021-03-06). “Mozambique expects to vaccinate 16 million against coronavirus by 2022”. Reuters. Retrieved 2021-03-07.
- ^ Namibian, The. “Khomas, Erongo first to get vaccinated”. The Namibian. Retrieved 2021-03-17.
- ^ “Covid-19 : Le Niger réceptionne 400.000 doses de vaccin SINOPHARM, un don de la Chine | Agence Nigérienne de Presse”. http://www.anp.ne. Retrieved 2021-03-21.
- ^ Staff, Reuters (2021-02-18). “Senegal takes delivery of China’s Sinopharm vaccine”. Reuters. Retrieved 2021-02-19.
- ^ AfricaNews (2021-02-23). “Senegal begins covid-19 vaccination with doses from China’s Sinopharm”. Africanews. Retrieved 2021-02-23.
- ^ AFP. “Sierra Leone to receive 200,000 virus vaccine doses”. ewn.co.za. Retrieved 2021-02-26.
- ^ Thomas, Abdul Rashid (2021-03-15). “Sierra Leone’s President Bio leads the way in taking COVID-19 Vaccine”. SIERRA LEONE TELEGRAPH. Retrieved 2021-03-15.
- ^ “Seychelles to start vaccinations with Chinese-made Sinopharm”. AP NEWS. 2021-01-08. Retrieved 2021-01-08.
- ^ “Covid-19: le Congo-Brazzaville reçoit des milliers de doses du vaccin chinois Sinopharm”. RFI (in French). 2021-03-10. Retrieved 2021-03-12.
- ^ Banya, Nelson (2021-02-11). “Zimbabwe purchases 600,000 Sinopharm COVID-19 vaccinations -information minister”. Reuters. Retrieved 2021-02-11.
- ^ Staff, Reuters (2021-02-24). “Zimbabwe to buy 1.2 million more COVID-19 vaccine doses from China”. Reuters. Retrieved 2021-02-26.
- ^ Lopez, Ezequiel Abiu (2021-02-16). “Dominican Republic launches COVID-19 vaccination campaign”. Reuters. Retrieved 2021-02-28.
- ^ “Dominica: Melissa Skerrit receives the Sinopharm COVID-19 vaccine”. WIC News. 2021-03-04. Retrieved 2021-03-05.
- ^ Jorgic, Drazen (2021-03-10). “Mexico leans on China after Biden rules out vaccines sharing in short term”. Reuters. Retrieved 2021-03-10.
- ^ Biannchi, Walter (2021-02-21). “Argentina approves Sinopharm COVID-19 vaccine for emergency use”. Reuters. Retrieved 2021-02-22.
- ^ “Buenos Aires Times | Shipment of 900,000 Sinopharm vaccine doses arrives in Argentina”. http://www.batimes.com.ar. Retrieved 2021-02-26.
- ^ Ramos, Danny (2021-02-11). “Bolivia signs deal with China´s Sinopharm for coronavirus vaccine”. Reuters. Retrieved 2021-02-11.
- ^ “China-donated Sinopharm vaccine received”. Guyana Chronicle. 2021-03-03. Retrieved 2021-03-03.
- ^ “Sinopharm vaccine rollout starts this weekend”. Stabroek News. 2021-03-06. Retrieved 2021-03-07.
- ^ Reuters Staff (2021-01-06). “Peru inks deals with Sinopharm, AstraZeneca for coronavirus vaccines -president”. Reuters. Retrieved 2021-01-07.
- ^ Aquino, Marco (2021-01-27). “Peru grants ‘exceptional’ approval for Sinopharm COVID-19 vaccine – government sources”. Reuters. Retrieved 2021-01-28.
- ^ Sequera, Vivian (2021-03-01). “Venezuela approves use of China’s Sinopharm coronavirus vaccine”. Reuters. Retrieved 2021-03-02.
- ^ Sequera, Vivian (2021-03-02). “Venezuela receives donated coronavirus vaccine from China”. Reuters. Retrieved 2021-03-02.
- ^ “China sends 100,000 coronavirus vaccines to Belarus”. eng.belta.by. 2021-02-19. Retrieved 2021-02-19.
- ^ “Hungary signs deal for Chinese Sinopharm’s COVID-19 vaccine, first in EU”. nationalpost. Retrieved 2021-01-29.
- ^ Staff, Reuters (2021-02-16). “First 550,000 doses of Chinese Sinopharm’s vaccine arrive in Hungary”. Reuters. Retrieved 2021-02-18.
- ^ “Hungary’s PM Viktor Orbán vaccinated against COVID with Chinese Sinopharm vaccine”. euronews. 2021-02-28.
- ^ “Emiratele Arabe Unite au donat Republicii Moldova un lot de vaccin împotriva COVID-19”. TV8 (in Romanian). 13 March 2021.
- ^ Cristina (2021-03-19). “O mie de studenți și medici-rezidenți din cadrul USMF vor fi imunizați anti-COVID cu vaccinul BBIBP-CorV, produs de către Sinopharm Beijing Institute of Biological Products”. Ziarul de Gardă (in Romanian). Retrieved 2021-03-19.
- ^ “Vaccine delay in North Macedonia stirs political tension”. ABC News. Retrieved 2021-02-12.
- ^ Reuters Staff (2021-01-16). “Serbia receives million doses of China’s Sinopharm COVID-19 vaccine”. Reuters. Retrieved 2021-01-16.
- ^ “Abu Dhabi starts COVID-19 vaccinations”. Arab News. 2020-12-14. Retrieved 2020-12-17.
- ^ Wee SL (9 December 2020). “Chinese Covid-19 Vaccine Gets Key Push, but Doubts Swirl”. The New York Times. Retrieved 21 December 2020.
- ^ Yu, Sun (December 31, 2020). “China approves first domestic Covid-19 vaccine for general use”. Financial Times. Retrieved January 12, 2021.
- ^ Dancel R. “Philippine officials under fire from critics, health authorities for unsanctioned Covid-19 vaccinations”. The Straits Times.
- ^ Aberia, Ingming (6 January 2021). “Did Sinopharm forget that Duque exists?”. The Manila Times. Retrieved 9 January 2021.
- ^ “水面下で出回る中国ワクチン 富裕層から永田町へ? 狙われる日本市場”. Mainichi Daily News (in Japanese). 2020-12-31. Retrieved 2021-01-02.
- ^ Elmer, Keegan (January 3, 2021). “Beijing responds to claims Japanese were given unapproved Sinopharm jabs”. South China Morning Post. Retrieved January 9, 2021.
External links
- “How the Sinopharm Covid-19 Vaccine Works”. The New York Times.
| A vial of the BBIBP-CorV COVID‑19 vaccine | |
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | Inactivated |
| Clinical data | |
| Routes of administration | Intramuscular |
| ATC code | None |
| Legal status | |
| Legal status | Authorization for use in Bahrain, China, Egypt, Iraq, Pakistan, Serbia, United Arab Emirates, Iran (emergency use) |
| Identifiers | |
| CAS Number | 2503126-65-4 |
| DrugBank | DB15807 |
| Part of a series on the |
| COVID-19 pandemic |
|---|
| SARS-CoV-2 (virus)COVID-19 (disease) |
| showTimeline |
| showLocations |
| showInternational response |
| showMedical response |
| showImpact |
| COVID-19 Portal |
| vte |
How the Sinopharm Vaccine Works
By Jonathan Corum and Carl ZimmerUpdated March 22, 2021Leer en español

In early 2020, the Beijing Institute of Biological Products created an inactivated coronavirus vaccine called BBIBP-CorV. Clinical trials run by the state-owned company Sinopharm showed that it had an efficacy rate of 79 percent. China approved the vaccine and soon began exporting it to other countries.
A Vaccine Made From Coronaviruses
BBIBP-CorV works by teaching the immune system to make antibodies against the SARS-CoV-2 coronavirus. The antibodies attach to viral proteins, such as the so-called spike proteins that stud its surface.

Spikes
Spike
protein
gene
CORONAVIRUS
To create BBIBP-CorV, the Beijing Institute researchers obtained three variants of the coronavirus from patients in Chinese hospitals. They picked one of the variants because it was able to multiply quickly in monkey kidney cells grown in bioreactor tanks.
Killing the Virus
Once the researchers produced large stocks of the coronaviruses, they doused them with a chemical called beta-propiolactone. The compound disabled the coronaviruses by bonding to their genes. The inactivated coronaviruses could no longer replicate. But their proteins, including spike, remained intact.

Beta-
propiolactone
INACTIVATED
CORONAVIRUS
Inactivated
genes
The researchers then drew off the inactivated viruses and mixed them with a tiny amount of an aluminum-based compound called an adjuvant. Adjuvants stimulate the immune system to boost its response to a vaccine.
Inactivated viruses have been used for over a century. Jonas Salk used them to create his polio vaccine in the 1950s, and they’re the bases for vaccines against other diseases including rabies and hepatitis A.
Prompting an Immune Response
Because the coronaviruses in BBIBP-CorV are dead, they can be injected into the arm without causing Covid-19. Once inside the body, some of the inactivated viruses are swallowed up by a type of immune cell called an antigen-presenting cell.

INACTIVATED
CORONAVIRUS
Engulfing
the virus
ANTIGEN-
PRESENTING
CELL
Digesting
virus proteins
Presenting
virus protein
fragments
HELPER
T CELL
The antigen-presenting cell tears the coronavirus apart and displays some of its fragments on its surface. A so-called helper T cell may detect the fragment. If the fragment fits into one of its surface proteins, the T cell becomes activated and can help recruit other immune cells to respond to the vaccine.
Making Antibodies
Another type of immune cell, called a B cell, may also encounter the inactivated coronavirus. B cells have surface proteins in a huge variety of shapes, and a few might have the right shape to latch onto the coronavirus. When a B cell locks on, it can pull part or all of the virus inside and present coronavirus fragments on its surface.
A helper T cell activated against the coronavirus can latch onto the same fragment. When that happens, the B cell gets activated, too. It proliferates and pours out antibodies that have the same shape as their surface proteins.

ACTIVATED
HELPER
T CELL
INACTIVATED
CORONAVIRUS
Activating
the B cell
Matching
surface proteins
B CELL
SECRETED
ANTIBODIES
Stopping the Virus
Once vaccinated with BBIBP-CorV, the immune system can respond to an infection of live coronaviruses. B cells produce antibodies that stick to the invaders. Antibodies that target the spike protein can prevent the virus from entering cells. Other kinds of antibodies may block the virus by other means.

ANTIBODIES
LIVE
VIRUS
Remembering the Virus
Sinopharm’s clinical trials have demonstrated that BBIBP-CorV can protect people against Covid-19. But no one can yet say how long that protection lasts. It’s possible that the level of antibodies drops over the course of months. But the immune system also contains special cells called memory B cells that might retain information about the coronavirus for years or even decades.
Vaccine Timeline
January, 2020 Sinopharm begins developing an inactivated vaccine against the coronavirus.
June Researchers report the vaccine produces promising results in monkeys. A Phase 1/2 trial shows that the vaccine doesn’t cause any serious side effects and enables people to make antibodies against the coronavirus.

A Sinopharm production plant in Beijing.Zhang Yuwei/Xinhua, via Associated Press
July A Phase 3 trial begins in the United Arab Emirates.
August Phase 3 trials begin in Morocco and Peru.

Preparing a Sinopharm dose in Lima, Peru.Ernesto Benavides/Agence France-Presse
Sept. 14 The U.A.E. gives emergency approval for Sinopharm’s vaccine to use on health care workers. Government officials and others begin to receive it.
November The chairman of Sinopharm says almost a million people in China have received Sinopharm vaccines.
Nov. 3 The ruler of Dubai, Sheikh Mohammed bin Rashid al-Maktoum, announces he received the vaccine.

Sheikh Mohammed before receiving the vaccine.Agence France-Presse
Dec. 9 The U.A.E. gives full approval to BBIBP-CorV, announcing it has an efficacy rate of 86 percent. But the government did not release any details with their announcement, leaving it unclear how they had come to their conclusions.
Dec. 13 Bahrain also approves the vaccine.

Vials of the Sinopharm vaccine at a packaging plant.Zhang Yuwei/Xinhua, via Associated Press
Dec. 30 Sinopharm announces that the vaccine has an efficacy of 79.34 percent, leading the Chinese government to approve it. The company has yet to publish detailed results of their Phase 3 trial.
Jan. 3, 2021 Egypt authorizes the vaccine for emergency use.
Sources: National Center for Biotechnology Information; Science; The Lancet; Lynda Coughlan, University of Maryland School of Medicine; Jenna Guthmiller, University of Chicago.
Data
/////////////BBIBP-CorV, Sinopharm, COVID-19 vaccine, china, covid 19, corona virus, vaccine
#BBIBP-CorV, #Sinopharm, #COVID-19 vaccine, #china, #covid 19, #corona virus, #vaccine
Sitravatinib
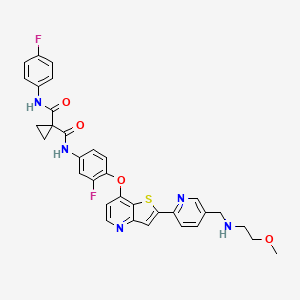
Sitravatinib
1-N‘-[3-fluoro-4-[2-[5-[(2-methoxyethylamino)methyl]pyridin-2-yl]thieno[3,2-b]pyridin-7-yl]oxyphenyl]-1-N-(4-fluorophenyl)cyclopropane-1,1-dicarboxamide
| シトラバチニブ; ситраватиниб , سيترافاتينيب , 司曲替尼 , |
| Formula | C33H29F2N5O4S |
|---|---|
| Cas | 1123837-84-2 |
| Mol weight | 629.6763 |
MGCD516
Antineoplastic, Receptor tyrosine kinase inhibitor
Sitravatinib (MGCD516) is an experimental drug for the treatment of cancer. It is a small molecule inhibitor of multiple tyrosine kinases.
Sitravatinib is being developed by Mirati Therapeutics.[1]
Ongoing phase II trials include a trial for liposcarcoma,[2] a combination trial for non-small cell lung cancer,[3] and a combination trial with nivolumab for renal cell carcinoma.[4]
Mirati Therapeutics and licensee BeiGene are developing sitravatinib, an oral multitargeted kinase inhibitor which inhibits Eph, Ret, c-Met and VEGF-1, -2 and -3, DDR, Trk, Axl kinases, CHR4q12, TYRO3 and Casitas B-lineage, in combination with immune checkpoint inhibitors, for treating advanced solid tumors.
In March 2021, sitravatinib was reported to be in phase 3 clinical development.

PDT PATENT
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2009026717
WO2009026717 , in which sitravatinib was first disclosed, claiming heterocyclic compounds as multi kinase inhibitors.
Scheme 10
Example 52
N-(3-Fluoro-4-(2-(5-((2-methoxyethylamino)methyl)pyridin-2-yl)thieno[3,2-b]pyridin-7- yloxy)phenyl)-N-(4-fluorophenyl)cyclopropane- 1 , 1 -dicarboxamide
Step 1 : tert-Butyl (6-(7-(2-Fluoro-4-(1-(4-fluorophenylcarbamoyl)-cyclopropanecarboxamido)phenoxy)thieno [3 ,2-b]pyridin-2-yl)pyridin-3 -y l)methyl(2-methoxyethyl)carbamate (146)
To aniline 126 (0.58 g, 1.1 mmol) and DIPEA (0.58 mL, 0.43 g, 3.3 mmol) in dry DMF
(20 mL) was added 1-(4-fluorophenylcarbamoyl)cyclopropanecarbpxylic acid (0.35 g, 1.5 mmol) and HATU (0.72 g, 1.9 mmol) and the mixture was stirred at r.t. for 18 h. It was then partitioned between ethyl acetate and water, the organic phase was washed with water, IM NaOH, brine, dried (MgSO4), filtered, and concentrated. Silica gel chromatography (ethyl acetate) afforded title compound Ϊ46 (0.60 g, 74 % yield). 1H NMR (400 MHz, DMSO-d6) δ (ppm): 10.40 (s, 1H), 10.01 (s, 1H), 8.52-8.49 (m, 2H), 8.33 (s, 1H), 8.27-8.24 (m, 1H), 7.92-7.88 (m, 1H), 7.78 (dd, J = 8.2, 2.1 Hz, 1H) 7.65-7.60 (m, 2H), 7.52-7.42 (m, 2H), 7.14 (t, J = 8.8 Hz, 2H), 6.65 (d, J = 5.1 Hz 1H), 4.47 (s, 2H), 3.42-3.30 (m, 4H), 3.22 (s, 3H), 1.46-1.30 (m, 13H). MS (m/z): 730.1 (M+H).
Step 2. N-(3-Fluoro-4-(2-(5-((2-methoxyethylamino)methyl)pyridin-2-yl)thieno[3,2-blpyridin-7-yloxy)phenyl)-N-(4-fluorophenyl)cyclopropane-1,1-dicarboxamide (147)
To the compound 146 (0.59 g, 0.81 mmol) in dichloromethane (50 mL) was added TFA (3 mL). The solution was stirred for 18 h then concentrated. The residue was partitioned between dichloromethane and 1 M NaOH, and filtered to remove insolubles. The organic phase was collected, washed with IM NaOH, brine, dried (MgSO4), filtered, and concentrated to afford title compound 147 (0.35 g, 69 % yield).
1H NMR (400 MHz, DMSO-d6) δ (ppm): 10.40 (s, 1H), 10.01 (s, 1H), 8.55 (d, J = 1.6 Hz, 1H), 8.51 (d, J = 5.3 Hz, 1H), 8.31 (s, 1H), 8.22 (d, J = 8.0 Hz, 1H), 7.92-7.87 (m, 2H), 7.65-7.61 (m, 2H), 7.52-7.43 (m, 2H), 7.17-7.12 (m, 2H), 6.64 (d, J = 5.5 Hz, 1H), 3.77 (s, 2H), 3.40 (t, J = 5.7 Hz, 2H), 3.23 (s, 3H), 2.64 (t, J = 5.7 Hz, 2H), 1.46 (br s, 4H). MS (m/z): 630.1 (M+H).
PATENT
WO 2009026720
https://patents.google.com/patent/WO2009026720A1
PATENT
WO-2021050580
Novel, stable crystalline polymorphic forms (form D) of sitravatinib , useful for treating a multi tyrosine kinase-associated cancer eg sarcoma, glioma, non-small cell lung, bladder, kidney, ovarian, gastric, breast or liver cancer.
International publication No. W02009/026717A disclosed compounds with the inhibition activities of multiple protein tyrosine kinases, for example, the inhibition activities of VEGF receptor kinase and HGF receptor kinase. In particular, disclosed N-(3-fluoro-4-((2-(5-(((2-methoxyethyl)amino)methyl)pyridin-2-yl)thieno[3,2-b]pyridin-7-yl)oxy)phenyl)-N-(4-fluorophenyl)cyclopropane- 1,1 -di carboxamide (Compound 1) is a multi-tyrosine kinase inhibitor with demonstrated potent inhibition of a closely related spectrum of tyrosine kinases, including RET, CBL, CHR4ql2, DDR and Trk, which are key regulators of signaling pathways that lead to cell growth, survival and tumor progression.
[003]
Compound 1
[004] Compound 1 shows tumor regression in multiple human xenograft tumor models in mice, and is presently in human clinical trials as a monotherapy as well as in combination for
treating a wide range of solid tumors. Compound 1 is presently in Phase 1 clinical trial for patients with advanced cancer, in Phase 2 studies for patients with advanced liposarcoma and non-small cell lung cancer (NSCLC).
[005] The small scale chemical synthesis of the amorphous Compound 1 had been disclosed in the Example 52 (compound 147) of W02009/026717A, however, in order to prepare the API of Compound 1 with high quality and in large quantity, crystalline forms of Compound 1 would be normally needed so the process impurities could be purged out by recrystallization.
Practically, it is difficult to predict with confidence which crystalline form of a particular compound will be stable, reproducible, and suitable for phamaceutical processing. It is even more difficult to predict whether or not a particular crystalline solid state form will be produced with the desired physical properties for pharmaceutical formulations.
[006] For all the foregoing reasons, there is a great need to produce crystalline forms of Compound 1 that provide manufacturing improvements of the pharmaceutical composition.
The present invention advantageously addresses one or more of these needs.
EXAMPLE 1
Preparation of N-(3-fluoro-4-((2-(5-(((2-methoxyethyl)amino)methyl)pyridin-2- yl)thieno[3,2-b]pyridin-7-yl)oxy)phenyl)-N-(4-fluorophenyl)cyclopropane-l,l- dicarboxamide (Compound 1)
[0085] This Example illustrates the preparation ofN-(3-fluoro-4-((2-(5-(((2-methoxyethyl)amino)methyl)pyridin-2-yl)thieno[3,2-b]pyridin-7-yl)oxy)phenyl)-N-(4-fluorophenyl)cyclopropane- 1,1 -di carboxamide (Compound 1).
[0086] Step 1: N-(Y6-bromopyridin-3-vDmethvD-2-methoxyethan-l-amine (Compound 1A)
Compound 1A
[0087] To a stirred solution of 2-Methoxyethylamine (3.0 eq) in dichloromethane (DCM) (12 vol) was added Molecular sieves (0.3 w/w) and stirred for 2 hours at 25±5°C under nitrogen atmosphere. The reaction mass water content was monitored by Karl Fischer analysis until the water content limit reached 0.5 % w/w. Once the water content limit was reached, the reaction mass cooled to 5±5°C and 6-bromonicotinaldehyde (1.0 eq) was added lot wise over period of 30 minutes to the above reaction mass at 5±5°C. The reaction mass was stirred for 30±5 minutes at 5±5°C and acetic acid (1.05 eq) was added drop wise at 5±5°C. After completion of the addition, the mass was slowly warmed to 25±5°C and stirred for 8 h to afford Compound 1 A. The imine formation was monitored by HPLC.
[0088] Step 2: tert-butyl (Y6-brom opyri din-3 -vQmethvO(2-m ethoxy ethvDcarbamate (Compound
IB)
Compound 1B
[0089] Charged Compoud 1A (1.0 eq) in THF (5.0 vol) was added and the reaction mass was stirred for 30 minutes at 25±5°C under nitrogen atmosphere. The reaction mass was cooled to temperature of about 10±5°C. Di-tert- butyl dicarbonate (1.2 eq) was added to the reaction mass at 10±5°C under nitrogen atmosphere and the reaction mass temperature was raised to 25±5°C and the reaction mass for about 2 hours. The progress of the reaction was monitored by HPLC. After IPC completion, a prepared solution of Taurine (1.5 eq) in 2M aq NaOH (3.1 vol) was charged and stirred at 10±5°C for 16 h to 18 h. The reaction mass was further diluted with 1M aq.NaOH solution (3.7 vol) and the layers were separated. The aqueous layer was extracted with DCM (2 x 4.7vol) and the extract combined with the organic layer. The combined organic layers were washed with 1M aq.NaOH solution (3.94 vol), followed by water (2×4.4 vol), and dried over sodium sulfate (2.0 w/w) . The filtrate was concentrated under reduced pressure below 40° C until no distillate was observed. Tetrahydrofuran (THF) was sequentially added (1×4 vol and lx 6vol) and concentrated under reduced pressure below 40°C until no distillate was observed to obtained Compound IB as light yellow colored syrup liquid.
[0090] Step 3: tert-butyl 7-chlorothieno[3.2-b1pyridin-2-yl)pyridin-3-yl )methyl)(2-
methoxyethvDcarbamate (Compound 1C)
Compound 1C
[0091] To a stirred solution of 7-chlorothieno[3,2-b]pyridine (1.05 eq) in tetrahydrofuran (7 vol) was added n-butyl lithium (2.5 M in hexane) drop wise at -15±10°C and stirred for 90 minutes at same temperature under nitrogen atmosphere. Zinc chloride (1.05 eq) was added to the reaction mass at -15±10°C. The reaction mass was slowly warmed to 25±5°C and stirred for 45 minutes under nitrogen atmosphere to afford Compound 1C. The progress of the reaction was monitored by HPLC.
[0092] Step 4: tert-butyl (Y6-(7-(4-amino-2-fluorophenoxy)thieno[3.2-b1pyridin-2-v0pyridin-3-vDmethvD(2-methoxyethvDcarbamate (Compound ID)
Compound 1D
[0093] 3-fluoro-4-hydroxybenzenaminium chloride (1.2 eq) in DMSO (3.9 vol) at 25±5°C was charged under nitrogen atmosphere and the reaction mass was stirred until observance of a clear solution at 25±5°C. t-BuOK was added lot wise under nitrogen atmosphere at 25±10°C. The reaction mass temperature was raised to 45±5°C and maintained for 30 minutes under nitrogen atmosphere. Compound 1C was charged lot-wise under nitrogen atmosphere at 45±5°C and stirred for 10 minutes at 45± 5°C.The reaction mixture was heated to 100± 5°C and stirred for 2 hrs. The reaction mass is monitored by HPLC.
[0094] After reaction completion, the reaction mass was cooled to 10± 5°C and quenched with chilled water (20 vol) at 10±5°C. The mass temperature was raised to 25± 5°C and stirred for 7-8 h. The resulting Compound ID crude was collected by filtration and washed with 2 vol of water. Crude Compound ID material taken in water (10 vol) and stirred for up to 20 minutes at 25±5°C. The reaction mass was heated to 45±5°C and stirred for 2-3 h at 45±5°C, filtered and vacuum-dried.
[0095] Crude Compound ID was taken in MTBE (5 vol) at 25±5°C and stirred for about 20 minutes at 25±5°C. The reaction mass temperature was raised to 45±5°C, stirred for 3-4 h at 45±5°C and then cooled to 20±5°C. The reaction mass was stirred for about 20 minutes at 20±5°C, filtered, followed by bed wash with water (0. 5 vol) and vacuum-dried.
[0096] The crude material was dissolved in acetone (10 vol) at 25±5°C and stirred for about 2h at 25±5°C. The reaction mass was filtered through a celite bed and washed with acetone (2.5 vol). The filtrate was slowly diluted with water (15 vol) at 25±5°C. The reaction mass was stirred for 2-3 h at 25±5°C, filtered and bed washed with water (2 vol) & vacuum-dried to afford Compound ID as brown solid.
[0097] Step 5 : 1 -((4-((2-(5-(((tert-butoxycarbonv0(2-methoxy ethvOaminolmethvOpyri din-2 -yl )thieno[3.2-b]pyridin-7-yl )oxy)-3 -fluorophenyl icarbamoyl level opropane-1 -carboxylic acid (Compound IE)
Compound 1E
[0098] To a solution of Compound ID (1.0 eq.) in tetrahydrofuran (7 vol.), aqueous potassium carbonate (1.0 eq.) in water (8 vol.) was added. The solution was cooled to 5±5°C, and stirred for about 60 min. While stirring, separately triethylamine (2.0 eq.) was added to a solution of 1,1-cyclopropanedicarboxylic acid (2.0 eq.) in tetrahydrofuran (8 vol.), at 5±5°C, followed by thionyl chloride (2.0 eq.) and stirred for about 60 min. The acid chloride mass was slowly added to the Compound ID solution at 5±5°C. The temperature was raised to 25±5°C and stirred for 3.0 h. The reaction was monitored by HPLC analysis.
[0099] After reaction completion, the mass was diluted with ethyl acetate (5.8 vol.), water (5.1 vol.), 10% (w/w) aqueous hydrochloric acid solution (0.8 vol.) and 25% (w/w) aqueous sodium chloride solution (2 vol.). The aqueous layer was separated and extracted with ethyl acetate (2 x 5 vol.). The combined organic layers were washed with a 0.5M aqueous sodium bicarbonate solution (7.5 vol.). The organic layer was treated with Darco activated charcoal (0.5 w/w) and sodium sulfate (0.3 w/w) at 25±5°C for 1.0 h. The organic layer was filtered through celite and washed with tetrahydofuran (5.0 vol.). The filtrate was concentrated under vacuum below 50°C to about 3 vol and co-distilled with ethyl acetate (2 x 5 vol.) under vacuum below 50°C up to ~ 3.0 vol. The organic layer was cooled to 15±5°C, stirred for about 60 min., filtered, and the solid was washed with ethyl acetate (2.0 vol.). The material was dried under vacuum at 40±5°C until water content was less than 1% to afford Compound IE as brown solid.
[00100] Step 6: tert-butyl (Y6-(7-(2-fluoro-4-(T-(Y4-fluorophenvDcarbamovDcvclopropane-l-carboxamido)phenoxy)thieno[3.2-b]pyridin-2-v0pyri din-3 – (2-
methoxyethvDcarbamate (Compound IF)
[00101] Pyridine (1.1 eq.) was added to a suspension of Compound IE (1.0 eq.) in tetrahydrofuran (10 vol.) and cooled to 5±5°C. Thionyl chloride (2.0 eq.) was added and stirred for about 60 min. The resulting acid chloride formation was confirmed by HPLC analysis after quenching the sample in methanol. Separately, aqueous potassium carbonate (2.5 eq.) solution (7.0 vol. of water) was added to a solution of 4-fluoroaniline (3.5 eq.) in tetrahydrofuran (10 vol.), cooled to 5±5°C, and stirred for about 60 min. The temperature of the acid chloride mass at 5±5°C was raised to a temperature of about 25±5°C and stirred for 3 h. The reaction monitored by HPLC analysis.
[00102] After completion of the reaction, the solution was diluted with ethyl acetate (25 vol.), the organic layer was separated and washed with a 1M aqueous sodium hydroxide solution (7.5 vol.), a 1M aqueous hydrochloric acid solution (7.5 vol.), and a 25% (w/w) aqueous sodium chloride solution (7.5 vol.). The organic layer was dried and and filtered with sodium sulfate (1.0 w/w). The filtrate was concentrated ~ 3 vol under vacuum below 50°C and co-distilled with ethyl acetate (3 x 5 vol.) under vacuum below 50°C to ~ 3.0 vol. Ethyl acetate (5 vol.) and MTBE (10 vol.) were charged, heated up to 50±5°C and stirred for 30-60 min. The mixture was cooled to 15±5°C, stirred for about 30 min., filtered, and the solid was washed with ethyl acetate (2.0 vol.). MGB3 content was analyzed by HPLC analysis. The material was dried under vacuum at 40±5°C until the water content reached about 3.0% to afford Compound IF as brown solid.
[00103] Step 7 : N-(3-fluoro-4-((2-(5-(((2-methoxyethv0amino)methv0pyridin-2-yl )thieno[3.2-b]pyridin-7-yl )oxy)phenyl)-N-(4-fluorophenyl level opropane-1. 1 -dicarboxamide (Compound 1)
Compound 1
[0100] To a mixture of Compound IF in glacial acetic acid (3.5 vol.) concentrated hydrochloric acid (0.5 vol.) was added and stirred at 25±5°C for 1.0 h. The reaction was monitored by HPLC analysis.
[0101] After reaction completion, the mass was added to water (11 vol.) and stirred for 20±5°C for 30 min. The pH was adjusted to 3.0 ± 0.5 using 10% (w/w) aqueous sodium bicarbonate solution and stirred for 20±5°C for approximately 3.0 h.. The mass was filtered, washed with water (4 x 5.0 vol.) and the pH of filtrate was checked after every wash. The material was dried under vacuum at 50±5°C until water content was about 10%.
[0102] Crude Compound 1 was taken in ethyl acetate (30 vol.), heated to 70±10°C, stirred for 1.0 h., cooled to 25±5°C, filtered, and washed with ethyl acetate (2 vol.). The material was dries under vacuum at 45±5°C for 6.0 h.
[0103] Crude Compound 1 was taken in polish filtered tetrahydrofuran (30 vol.) and pre washed Amberlyst A-21 Ion exchange resin and stirred at 25±5°C until the solution became clear. After getting the clear solution, the resin was filtered and washed with polish filtered tetrahydrofuran (15 vol.). The filtrate was concentrated by -50% under vacuum below 50°C and co-distilled with polish filtered IPA (3 x 15.0 vol.) and concentrated up to -50% under vacuum below 50°C. Charged polish filtered IPA (15 vol.) was added and the solution concentrated under vacuum below 50°C to – 20 vol. The reaction mass was heated to 80±5°C, stirred for 60 min. and cooled to 25±5°C. The resultant reaction mass was stirred for about 20 hours at 25±5°C. The reaction mass was cooled to 0±5°C, stirred for 4-5 hours, filtered, and washed with polish filtered IPA (2 vol.). The material was dried under vacuum at 45±5°C, until the water content was about 2%, to obtain the desired product Compound 1. ¾-NMR (400 MHz, DMSO- d): 510.40 (s, 1H), 10.01 (s, 1H), 8.59 – 8.55 (m, 1H), 8.53 (d, J= 5.6 Hz, 1H), 8.32 (s, 1H), 8.23 (d, J= 8.0 Hz, 1H), 7.96 – 7.86 (m, 2H), 7.70 – 7.60 (m, 2H), 7.56 – 7.43 (m, 2H), 7.20 – 7.11 (m, 2H), 6.66 (d, J= 5.6 Hz, 1H), 3.78 (s, 2H), 3.41 (t, J= 5.6 Hz, 2H), 3.25 (s, 3H), 2.66 (t, J= 5.6 Hz, 2H), 1.48 (s, 4H)ppm. MS: M/e 630 (M+l)+.
EXAMPLE 2
Preparation of Crystalline Form D of N-(3-fluoro-4-((2-(5-(((2- methoxyethyl)amino)methyl)pyridin-2-yl)thieno[3,2-b]pyridin-7-yl)oxy)phenyl)-N-(4- fluorophenyl)cyclopropane-l, 1-dicarboxamide
EXAMPLE 2A: Preparation of Compound 1 Crystalline Form D
[0104] To a 50 L reactor, 7.15 Kg of Compound 1, 40 g of Form D as crystal seed and 21 L acetone (>99%) were added. The mixture was heated to reflux ( ~56 °C) for 1~2 h. The mixture was agitated with an internal temperature of 20±5 °C for at least 24 h. Then, the suspension was filtered and washed the filter cake with 7 L acetone. The wet cake was dried under vacuum at <45 °C, to obtain 5.33 kg of Compound 1 of desired Form D
[0105] X-Ray Powder Diffraction (XRPD)
The XRPD patterns were collected with a PAN alytical X’ Pert PRO MPD diffractometer using auincident beam of Cu radiation produced using au Optix long, fine-focus source. An elliptically graded multilayer mirror was used to focus Cu Ka X -rays through the specimens and onto the detector. Prior to the analysis, a silicon specimen (NIST SRM 640e) was analyzed to verify the observed position of the Si Ill peak is consistent with the NIST-certified position. A specimen of each sample was sandwiched between 3 -pm -thick films and analyzed in transmission geometly. A beam-stop, short autiscatter extension, and an autiscatter knife edge were used to minimize the background generated by air. Sober slits for the incident aud diffracted beauls were used to minimize broadening from axial divergence. The diffraction patterns were collected using a scanning position-sensitive detector (X’Celerator) located 240 mm from the specimens and Data Collector software v. 2.2b. Pattern Match v2.3.6 was used to create XRPD patterns.
[0106] The X-ray powder diffraction (XRPD) pattern was used to characterize the Compound 1 obtained, which showed that the Compound 1 was in Crystalline Form D of Compound 1 (Compound 1 Form D), see Figure 1A. The XRPD pattern yielded is substantially the same as that shown in Figure 3C.
[0107] Differential Scanning Calorimetry (DSC)
[0108] DSC was performed using a Mettler-Toledo DSC3+ differential scanning calorimeter. Temperature calibration was performed using octane, phenyl salicylate, indium, tin, and zinc. The TAWN sensitivity was 11.9. The samples were placed into aluminum DSC pans, covered with lids, and the weights were accurately recorded. A weighed aluminum pan configured as the sample pan was placed on the reference side of the cell. The pan lids were pierced prior to sample analyses. The method name on the thermograms is an abbreviation for the start and end temperature as well as the heating rate; e.g., -30-250-10 means “from ambient to 250°C, at 10°C/min.” The nitrogen flow rate was 50.0 mL/min. This instrument does not provide gas pressure value as required by USP because it is the same as atmospheric pressure.
[0109] A broad small endotherm with a peak maximum at approximately 57°C to 62°C (onset ~20°C to 22°C) followed by a sharp endotherm with a peak maximum at approximately 180°C (onset ~178°C) were observed. These events could be due to the loss of volatiles and a melt, respectively (see Figure IB).
[0110] In an alternative embodiment Form D was prepared as follows. Designated Material O was suspended in 600 pL of acetone. Initial dissolution was observed followed by re precipitation. The amount of suspended solids was not measured because the target of the experiment was to get a suspension with enough solids to slurry isolate and collect XRPD data. Based on the solubility of Form D in acetone a very rough estimate for the scale of the experiment is about 80-100mg. The suspension was stirred at ambient temperature for approximately 2 5 weeks after which the solids were isolated by centrifugation with filtration. XRPD data appeared to be consistent with Form D The sample was then dried in vacuum oven at ~40 °C for ~2 5 hours. The XRPD pattern of the final solids was consistent with Form D EXAMPLE 2B: Preparation of Compound 1 Form D
[0111] 427.0 mg of Compound 1 was dissolved in 5 mL of THF to obtain a clear brown solution. The resulting solution was filtered, and the filtrate evaporated under flow of nitrogen. A sticky solid was obtained, which was dried under vacuum in room temperature for ~5 min, still a sticky brown solid obtained. It was dissolved in 0.2 mL of EtOAc and sonicated to dissolve. The solution obtained was stirred at room temperature for 15 min and a solid precipitated. The resulting solid was added 0.4 mL of EtOAc and stirred in room temperature for 21 h 40 min to ontian a suspension. The solid was spparated from mother liquor by centrifugation, then the resulting solid was resuspended the in 0.6 mL of EtOAc and stirred in room temperature for 2 days. The solid was isolated by centrifugation, to obtain Compound 1 of desired Form D.
[0112] The X-ray powder diffraction (XRPD) pattern was used to characterize the Compound 1 obtained, which showed that the Compound 1 was in Crystalline Form D of Compound 1 (Compound 1 Form D).
EXAMPLE 2C: Preparation of Compound 1 Form D
[0113] Single crystal X-ray diffraction data of Compound 1 was collected at 180 K on a Rigaku XtaLAB PRO 007HF(Mo) diffractometer, with Mo Ka radiation (l = 0.71073 A). Data reduction and empirical absorption correction were performed using the CrysAlisPro program. The structure was solved by a dual-space algorithm using SHELXT program. All non-hydrogen atoms could be located directly from the difference Fourier maps. Framework hydrogen atoms were placed geometrically and constrained using the riding model to the parent atoms. Final structure refinement was done using the SHELXL program by minimizing the sum of squared deviations of F2 using a full-matrix technique.
Preparation of Compound 1 Form D ( a Single Crystal )
[0114] Compound 1 Form D was dissolved in a mixture of acetone/ ACN (1/2) with the concentration of Compound 1 at ~7 mg/mL. A block single crystal was obtained, which was a single crystal.
[0115] The XRPD pattern was used to characterize the single crystal of Compound 1 Form D obtained, see Figure 2A. The crystal structural data are summarized in Table IB. The refined single crystal structure were shown in Figure 2B. The single crystal structure of Compound 1 Form D is in the P-1 space group and the triclinic crystal system. The terminal long alkyl chain is found to have large ellipsoids, indicating high mobility with disordered atoms.
[0116] The theoretical XRPD calculated from the single crystal structure and experimental XRPD are essentially similar (Figure 2A). A few small peaks are absent or shift because of orientation preference, disorder and tested temperature (180 K for single crystal data and 293 K for experimental one).
[0117] Table IB. Crystal Data and Structure Refinement for Compound 1 Form D (a Single Crystal)
References
- ^ http://www.mirati.com/go/mgcd516/
- ^ “MGCD516 in Advanced Liposarcoma and Other Soft Tissue Sarcomas – Full Text View – ClinicalTrials.gov”.
- ^ “Phase 2 Study of Glesatinib, Sitravatinib or Mocetinostat in Combination With Nivolumab in Non-Small Cell Lung Cancer – Full Text View – ClinicalTrials.gov”.
- ^ “MGCD516 Combined With Nivolumab in Renal Cell Cancer (RCC) – Full Text View – ClinicalTrials.gov”.
| Identifiers | |
|---|---|
| showIUPAC name | |
| CAS Number | 1123837-84-2 |
| ChemSpider | 52083477 |
| UNII | CWG62Q1VTB |
| KEGG | D11140 |
| Chemical and physical data | |
| Formula | C33H29F2N5O4S |
| Molar mass | 629.68 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| hideSMILESCOCCNCc1ccc(nc1)c2cc3c(s2)c(ccn3)Oc4ccc(cc4F)NC(=O)C5(CC5)C(=O)Nc6ccc(cc6)F | |
| hideInChIInChI=1S/C33H29F2N5O4S/c1-43-15-14-36-18-20-2-8-25(38-19-20)29-17-26-30(45-29)28(10-13-37-26)44-27-9-7-23(16-24(27)35)40-32(42)33(11-12-33)31(41)39-22-5-3-21(34)4-6-22/h2-10,13,16-17,19,36H,11-12,14-15,18H2,1H3,(H,39,41)(H,40,42)Key:WLAVZAAODLTUSW-UHFFFAOYSA-N |
///////////// sitravatinib, phase 3, シトラバチニブ , MGCD516, MG-516, Sitravatinib (MGCD516), UNII-CWG62Q1VTB, CWG62Q1VTB, MGCD-516, ситраватиниб , سيترافاتينيب , 司曲替尼 , Antineoplastic, MGCD 516
#sitravatinib, #phase 3, #シトラバチニブ , #MGCD516, #MG-516#Sitravatinib (MGCD516), #UNII-#CWG62Q1VTB, #CWG62Q1VTB, #MGCD-516, ситраватиниб , سيترافاتينيب , 司曲替尼 , #Antineoplastic, #MGCD516
COCCNCC1=CN=C(C=C1)C2=CC3=NC=CC(=C3S2)OC4=C(C=C(C=C4)NC(=O)C5(CC5)C(=O)NC6=CC=C(C=C6)F)F
Moderna COVID-19 vaccine, mRNA 1273


Moderna COVID-19 vaccine, mRNA 1273
CAS 2457298-05-2
An mRNA vaccine against SARS-CoV-2 expressing the prefusion-stabilized SARS-CoV-2 spike trimer
- MRNA-1273 SARS-COV-2
- CX 024414
- CX-024414
- CX024414
- mRNA-1273
| NAME | DOSAGE | STRENGTH | ROUTE | LABELLER | MARKETING START | MARKETING END | ||
|---|---|---|---|---|---|---|---|---|
| Covid-19 Vaccine Moderna | Injection | Intramuscular | Moderna Therapeutics Inc | 2020-12-23 | Not applicable | |||
| Moderna COVID-19 Vaccine | Injection, suspension | 0.2 mg/1mL | Intramuscular | Moderna US, Inc. | 2020-12-18 | Not applicable |
| FORM | ROUTE | STRENGTH |
|---|---|---|
| Injection | Intramuscular | |
| Injection, suspension | Intramuscular | 0.2 mg/1mL |
REFNature (London, United Kingdom) (2020), 586(7830), 516-527.bioRxiv (2020), 1-39Nature (London, United Kingdom) (2020), 586(7830), 567-571. Nature Biotechnology (2020), Ahead of PrintJournal of Pure and Applied Microbiology (2020), 14(Suppl.1), 831-840.Chemical & Engineering News (2020), 98(46), 12.New England Journal of Medicine (2020), 383(16), 1544-1555. Science of the Total Environment (2020), 725, 138277.JAMA, the Journal of the American Medical Association (2020), 324(12), 1125-1127.Advanced Drug Delivery Reviews (2021), 169, 137-151. bioRxiv (2021), 1-62. bioRxiv (2021), 1-51.
The Moderna COVID-19 Vaccine (mRNA-1273) is a novel mRNA-based vaccine encapsulated in a lipid nanoparticle that encodes for a full-length pre-fusion stabilized spike (S) protein of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Coronavirus disease 2019 (COVID-19) is a highly contagious infectious disease caused by the novel coronavirus, SARS-CoV-2, leading to a respiratory illness alongside other complications. COVID-19 has high interpatient variability in symptoms, ranging from mild symptoms to severe illness.5 A phase I, open-label, dose-ranging clinical trial (NCT04283461) was initiated in March 2020 in which 45 subjects received two intramuscular doses (on days 1 and 29).4 This trial was later followed by phase II and III trials, where the Moderna COVID-19 Vaccine demonstrated vaccine efficacy of 94.1%.5
On December 18, 2020, the FDA issued an emergency use authorization (EUA) for the Moderna COVID-19 Vaccine as the second vaccine for the prevention of COVID-19 caused by SARS-CoV-2 in patients aged 18 years and older, after the EUA issued for the Pfizer-BioNTech Covid-19 Vaccine on December 11, 2020. The Moderna COVID-19 Vaccine is administered as a series of two intramuscular injections, one month (28 days) apart. In clinical trials, there were no differences in the safety profiles between younger and older (65 years of age and older) study participants; however, the safety and effectiveness of the Moderna COVID-19 Vaccine have not been assessed in persons less than 18 years of age.5 On December 23, 2020, Health Canada issued an expedited authorization for the Moderna COVID-19 Vaccine.7
It is an RNA vaccine composed of nucleoside-modified mRNA (modRNA) encoding a spike protein of SARS-CoV-2, which is encapsulated in lipid nanoparticles. It is one of the two RNA vaccines developed and deployed in 2020 against COVID‑19, the other being the Pfizer–BioNTech vaccine.The Moderna COVID‑19 vaccine, codenamed mRNA-1273, is a COVID‑19 vaccine developed by the United States National Institute of Allergy and Infectious Diseases (NIAID), the Biomedical Advanced Research and Development Authority (BARDA), and Moderna. It is administered by two 0.5 mL doses given by intramuscular injection given four weeks apart.[12]
On 18 December 2020, mRNA-1273 was issued an Emergency Use Authorization by the United States Food and Drug Administration (FDA).[6][13][14][15] It was authorized for use in Canada on 23 December 2020,[2][3] in the European Union on 6 January 2021,[10][16][11] and in the United Kingdom on 8 January 2021.[17]
Design
Upon the announcement Moderna’s shares rose dramatically, and the chief executive officer (CEO) and other corporate executives began large program sales of their shareholdings.[26]In January 2020, Moderna announced development of an RNA vaccine, named mRNA-1273, to induce immunity to SARS-CoV-2.[18][19][20] Moderna’s technology uses a nucleoside-modified messenger RNA (modRNA) compound named mRNA-1273. Once the compound is inside a human cell, the mRNA links up with the cell’s endoplasmic reticulum. The mRNA-1273 is encoded to trigger the cell into making a specific protein using the cell’s normal manufacturing process. The vaccine encodes a version of the spike protein called 2P, which includes two stabilizing mutations in which the regular amino acids are replaced with prolines, developed by researchers at the University of Texas at Austin and the National Institute of Allergy and Infectious Diseases‘ Vaccine Research Center.[21][22][23][24] Once the protein is expelled from the cell, it is eventually detected by the immune system, which begins generating efficacious antibodies. The mRNA-1273 drug delivery system uses a PEGylated lipid nanoparticle drug delivery (LNP) system.[25]
Composition
The vaccine contains the following ingredients:[7][27]
- nucleoside-modified messenger RNA encoding the SARS-CoV-2 spike glycoprotein (S) stabilized in its prefusion configuration;[28]
- lipids:
- SM-102,
- polyethylene glycol [PEG] 2000-dimyristoyl glycerol [DMG],
- cholesterol,
- and 1,2-distearoyl-sn-glycero-3-phosphocholine [DSPC];
- tromethamine;
- tromethamine hydrochloride;
- acetic acid;
- sodium acetate;
- and sucrose.
Clinical trials
Phase I / II
In March 2020, the Phase I human trial of mRNA-1273 began in partnership with the U.S. National Institute of Allergy and Infectious Diseases.[29] In April, the U.S. Biomedical Advanced Research and Development Authority (BARDA) allocated up to $483 million for Moderna’s vaccine development.[30] Plans for a Phase II dosing and efficacy trial to begin in May were approved by the U.S. Food and Drug Administration (FDA).[31] Moderna signed a partnership with Swiss vaccine manufacturer Lonza Group,[32] to supply 300 million doses per annum.[33]
On 25 May 2020, Moderna began a Phase IIa clinical trial recruiting six hundred adult participants to assess safety and differences in antibody response to two doses of its candidate vaccine, mRNA-1273, a study expected to complete in 2021.[34] In June 2020, Moderna entered a partnership with Catalent in which Catalent will fill and package the vaccine candidate. Catalent will also provide storage and distribution.[35]
On 9 July, Moderna announced an in-fill manufacturing deal with Laboratorios Farmacéuticos Rovi, in the event that its vaccine is approved.[36]
On 14 July 2020, Moderna scientists published preliminary results of the Phase I dose escalation clinical trial of mRNA-1273, showing dose-dependent induction of neutralizing antibodies against S1/S2 as early as 15 days post-injection. Mild to moderate adverse reactions, such as fever, fatigue, headache, muscle ache, and pain at the injection site were observed in all dose groups, but were common with increased dosage.[37][38] The vaccine in low doses was deemed safe and effective in order to advance a Phase III clinical trial using two 100-μg doses administered 29 days apart.[37]
In July 2020, Moderna announced in a preliminary report that its Operation Warp Speed candidate had led to production of neutralizing antibodies in healthy adults in Phase I clinical testing.[37][39] “At the 100-microgram dose, the one Moderna is advancing into larger trials, all 15 patients experienced side effects, including fatigue, chills, headache, muscle pain, and pain at the site of injection.”[40] The troublesome higher doses were discarded in July from future studies.[40]
Phase III
Moderna and the National Institute of Allergy and Infectious Diseases began a Phase III trial in the United States on 27 July, with a plan to enroll and assign thirty thousand volunteers to two groups – one group receiving two 100-μg doses of mRNA-1273 vaccine and the other receiving a placebo of 0.9% sodium chloride.[41] As of 7 August, more than 4,500 volunteers had enrolled.
In September 2020, Moderna published the detailed study plan for the clinical trial.[42] On 30 September, CEO Stéphane Bancel said that, if the trial is successful, the vaccine might be available to the public as early as late March or early April 2021.[43] As of October 2020, Moderna had completed the enrollment of 30,000 participants needed for its Phase III trial.[44] The U.S. National Institutes of Health announced on 15 November 2020 that overall trial results were positive.[45]
On 30 December 2020, Moderna published results from the Phase III clinical trial, indicating 94% efficacy in preventing COVID‑19 infection.[46][47][48] Side effects included flu-like symptoms, such as pain at the injection site, fatigue, muscle pain, and headache.[47] The clinical trial is ongoing and is set to conclude in late-2022[49]
In November 2020, Nature reported that “While it’s possible that differences in LNP formulations or mRNA secondary structures could account for the thermostability differences [between Moderna and BioNtech], many experts suspect both vaccine products will ultimately prove to have similar storage requirements and shelf lives under various temperature conditions.”[50]
Since September 2020, Moderna has used Roche Diagnostics‘ Elecsys Anti-SARS-CoV-2 S test, authorized by the US Food and Drug Administration (FDA) under an Emergency Use Authorization (EUA) on 25 November 2020. According to an independent supplier of clinical assays in microbiology, “this will facilitate the quantitative measurement of SARS-CoV-2 antibodies and help to establish a correlation between vaccine-induced protection and levels of anti-receptor binding domain (RBD) antibodies.” The partnership was announced by Roche on 9 December 2020.[51]
A review by the FDA in December 2020, of interim results of the Phase III clinical trial on mRNA-1273 showed it to be safe and effective against COVID‑19 infection resulting in the issuance of an EUA by the FDA.[13]
It remains unknown whether the Moderna vaccine candidate is safe and effective in people under age 18 and how long it provides immunity.[47] Pregnant and breastfeeding women were also excluded from the initial trials used to obtain Emergency Use Authorization,[52] though trials in those populations are expected to be performed in 2021.[53]
In January 2021, Moderna announced that it would be offering a third dose of its vaccine to people who were vaccinated twice in its Phase I trial. The booster would be made available to participants six to twelve months after they got their second doses. The company said it may also study a third shot in participants from its Phase III trial, if antibody persistence data warranted it.[54][55][56]
In January 2021, Moderna started development of a new form of its vaccine, called mRNA-1273.351, that could be used as a booster shot against the 501.V2 variant of SARS-CoV-2 first detected in South Africa.[57][58] It also started testing to see if a third shot of the existing vaccine could be used to fend off the virus variants.[58] On 24 February, Moderna announced that it had manufactured and shipped sufficient amounts of mRNA-1273.351 to the National Institutes of Health to run Phase{ I clinical trials.[59] To increase the span of vaccination beyond adults, Moderna started the clinical trials of vaccines on childern age six to eleven in the U.S. and in Canada.[60]
Storage requirements
Moderna vaccine being stored in a conventional medical freezer
The Moderna news followed preliminary results from the Pfizer–BioNTech vaccine candidate, BNT162b2, with Moderna demonstrating similar efficacy, but requiring storage at the temperature of a standard medical refrigerator of 2–8 °C (36–46 °F) for up to 30 days or −20 °C (−4 °F) for up to four months, whereas the Pfizer-BioNTech candidate requires ultracold freezer storage between −80 and −60 °C (−112 and −76 °F).[61][47] Low-income countries usually have cold chain capacity for refrigerator storage.[62][63] In February 2021, the restrictions on the Pfizer vaccine were relaxed when the U.S. Food and Drug Administration (FDA) updated the emergency use authorization (EUA) to permit undiluted frozen vials of the vaccine to be transported and stored at between −25 and −15 °C (−13 and 5 °F) for up to two weeks before use.[27][64][65]
Efficacy
The interim primary efficacy analysis was based on the per-protocol set, which consisted of all participants with negative baseline SARS-CoV-2 status and who received two doses of investigational product per schedule with no major protocol deviations. The primary efficacy endpoint was vaccine efficacy (VE) in preventing protocol defined COVID-19 occurring at least 14 days after dose 2. Cases were adjudicated by a blinded committee. The primary efficacy success criterion would be met if the null hypothesis of VE ≤30% was rejected at either the interim or primary analysis. The efficacy analysis presented is based on the data at the first pre-specified interim analysis timepoint consisting of 95 adjudicated cases.[66] The data are presented below.
| Primary endpoint: COVID-19 | Cases n (%) Incidence per 1000 person-years | Vaccine efficacy (95% confidence interval) | |
|---|---|---|---|
| Vaccine group (N = 13,934) | Placebo group (N = 13,883) | ||
| All participants | 5 cases in 13,934 (<0.1%)1.840 | 90 cases in 13,883 (0.6%)33.365 | 94.5% (86.5-97.8%) |
| Participants 18–64 years of age | 5 cases in 10,407 (<0.1%)2.504 | 75 cases in 10,384 (0.7%)37.788 | 93.4% (83.7-97.3%) |
| 65 and older | 0 cases in 3,527 | 15 cases in 3,499 (0.4%) | 100% |
| Chronic lung disease | 0/661 | 6/673 | 100% |
| Significant cardiac disease | 0/686 | 3/678 | 100% |
| Severe obesity (BMI>40) | 1/901 | 11/884 | 91.2% (32-98.9%) |
| Diabetes | 0/1338 | 7/1309 | 100% |
| Liver disease | 0/93 | 0/90 | |
| Obesity (BMI>30) | 2/5269 | 46/5207 | 95.8% (82.6-99%) |
Manufacturing
An insulated shipping container with Moderna vaccine boxes ensconced by cold packs
Moderna is relying extensively on contract manufacturing organizations to scale up its vaccine manufacturing process. Moderna has contracted with Lonza Group to manufacture the vaccine at facilities in Portsmouth, New Hampshire in the United States, and in Visp in Switzerland, and is purchasing the necessary lipid excipients from CordenPharma.[67] For the tasks of filling and packaging vials, Moderna has entered into contracts with Catalent in the United States and Laboratorios Farmacéuticos Rovi in Spain.[67]
Purchase commitments
In June 2020, Singapore signed a pre-purchase agreement for Moderna, reportedly paying a price premium in order to secure early stock of vaccines, although the government declined to provide the actual price and quantity, citing commercial sensitivities and confidentiality clauses.[68][69]
On 11 August 2020, the U.S. government signed an agreement to buy one hundred million doses of Moderna’s anticipated vaccine,[70] which the Financial Times said Moderna planned to price at US$50–60 per course.[71] On November 2020, Moderna said it will charge governments who purchase its vaccine between US$25 and US$37 per dose while the E.U. is seeking a price of under US$25 per dose for the 160 million doses it plans to purchase from Moderna.[72][73]
In 2020, Moderna also obtained purchase agreements for mRNA-1273 with the European Union for 160 million doses and with Canada for up to 56 million doses.[74][75] On 17 December, a tweet by the Belgium Budget State Secretary revealed the E.U. would pay US$18 per dose, while The New York Times reported that the U.S. would pay US$15 per dose.[76]
In February 2021, Moderna said it was expecting US$18.4 billion in sales of its COVID-19 vaccine.[77]
Authorizations
| show Full authorizationshow Emergency authorization Eligible COVAX recipient (assessment in progress)[96] |
Expedited
U.S. military personnel being administered the Moderna vaccineKamala Harris, Vice President of the United States, receiving her second dose of the Moderna vaccination in January 2021.
As of December 2020, mRNA-1273 was under evaluation for emergency use authorization (EUA) by multiple countries which would enable rapid rollout of the vaccine in the United Kingdom, the European Union, Canada, and the United States.[97][98][99][100]
On 18 December 2020, mRNA-1273 was authorized by the United States Food and Drug Administration (FDA) under an EUA.[6][8][13] This is the first product from Moderna that has been authorized by the FDA.[101][14]
On 23 December 2020, mRNA-1273 was authorized by Health Canada.[2][3] Prime Minister Justin Trudeau had previously said deliveries would begin within 48 hours of approval and that 168,000 doses would be delivered by the end of December.[102]
On 5 January 2021, mRNA-1273 was authorized for use in Israel by its Ministry of Health.[103]
On 3 February 2021, mRNA-1273 was authorized for use in Singapore by its Health Sciences Authority;[104] the first shipment arrived on 17 February.[105]
Standard
On 6 January 2021, the European Medicines Agency (EMA) recommended granting conditional marketing authorization[10][106] and the recommendation was accepted by the European Commission the same day.[11][16]
On 12 January 2021, Swissmedic granted temporary authorization for the Moderna COVID-19 mRNA Vaccine in Switzerland.[107][108]
Society and culture
Controversies
In May 2020, after releasing partial and non-peer reviewed results for only eight of 45 candidates in a preliminary pre-Phase I stage human trial directly to financial markets, the CEO announced on CNBC an immediate $1.25 billion rights issue to raise funds for the company, at a $30 billion valuation,[109] while Stat said, “Vaccine experts say Moderna didn’t produce data critical to assessing COVID-19 vaccine.”[110]
On 7 July, disputes between Moderna and government scientists over the company’s unwillingness to share data from the clinical trials were revealed.[111]
Moderna also faced criticism for failing to recruit people of color in clinical trials.[112]
Patent litigation
The PEGylated lipid nanoparticle (LNP) drug delivery system of mRNA-1273 has been the subject of ongoing patent litigation with Arbutus Biopharma, from whom Moderna had previously licensed LNP technology.[25][113] On 4 September 2020, Nature Biotechnology reported that Moderna had lost a key challenge in the ongoing case.[114]
Notes
- ^ US authorization also includes the three sovereign nations in the Compact of Free Association: Palau, the Marshall Islands, and Micronesia.[93][94]
References
- ^ Moderna (23 October 2019). mRNA-3704 and Methylmalonic Acidemia (Video). YouTube. Retrieved 19 January 2021.
- ^ Jump up to:a b c “Regulatory Decision Summary – Moderna COVID-19 Vaccine”. Health Canada. 23 December 2020. Retrieved 23 December 2020.
- ^ Jump up to:a b c “Moderna COVID-19 Vaccine (mRNA-1273 SARS-CoV-2)”. COVID-19 vaccines and treatments portal. 23 December 2020. Retrieved 23 December 2020.
- ^ “Information for Healthcare Professionals on COVID-19 Vaccine Moderna”. Medicines and Healthcare products Regulatory Agency (MHRA). 8 January 2021. Retrieved 8 January 2021.
- ^ “Conditions of Authorisation for COVID-19 Vaccine Moderna”. Medicines and Healthcare products Regulatory Agency (MHRA). 8 January 2021. Retrieved 9 January 2021.
- ^ Jump up to:a b c d “FDA Takes Additional Action in Fight Against COVID-19 By Issuing Emergency Use Authorization for Second COVID-19 Vaccine”. U.S. Food and Drug Administration (FDA) (Press release). Retrieved 18 December 2020.
- ^ Jump up to:a b “Moderna COVID-19 Vaccine – cx-024414 injection, suspension”. DailyMed. Retrieved 20 December 2020.
- ^ Jump up to:a b Moderna COVID-19 Vaccine Emergency Use Authorization(PDF). U.S. Food and Drug Administration (FDA) (Report). 18 December 2020. Retrieved 20 December 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ “Moderna COVID-19 Vaccine Standing Orders for Administering Vaccine to Persons 18 Years of Age and Older” (PDF). Centers for Disease Control and Prevention (CDC).
- ^ Jump up to:a b c d “COVID-19 Vaccine Moderna EPAR”. European Medicines Agency (EMA). Retrieved 20 January 2021.
- ^ Jump up to:a b c d “European Commission authorises second safe and effective vaccine against COVID-19”. European Commission(Press release). Retrieved 6 January 2021.
- ^ “Moderna COVID-19 Vaccine”. Dosing & Administration. Infectious Diseases Society of America. 4 January 2021. Retrieved 5 January 2021.
- ^ Jump up to:a b c “Statement from NIH and BARDA on the FDA Emergency Use Authorization of the Moderna COVID-19 Vaccine”. US National Institutes of Health. 18 December 2020. Retrieved 19 December 2020.
- ^ Jump up to:a b c Oliver SE, Gargano JW, Marin M, Wallace M, Curran KG, Chamberland M, et al. (January 2021). “The Advisory Committee on Immunization Practices’ Interim Recommendation for Use of Moderna COVID-19 Vaccine – United States, December 2020”(PDF). MMWR Morbidity and Mortality Weekly Report. 69 (5152): 1653–56. doi:10.15585/mmwr.mm695152e1. PMID 33382675. S2CID 229945697.
- ^ Lovelace Jr B (19 December 2020). “FDA approves second Covid vaccine for emergency use as it clears Moderna’s for U.S. distribution”. CNBC. Retrieved 19 December 2020.
- ^ Jump up to:a b “COVID-19 Vaccine Moderna”. Union Register of medicinal products. Retrieved 14 January 2021.
- ^ “Moderna vaccine becomes third COVID-19 vaccine approved by UK regulator”. U.K. Government. 8 January 2021. Retrieved 8 January 2021.
- ^ Steenhuysen J, Kelland K (24 January 2020). “With Wuhan virus genetic code in hand, scientists begin work on a vaccine”. Reuters. Archived from the original on 25 January 2020. Retrieved 26 January 2020.
- ^ Carey K (26 February 2020). “Increasing number of biopharma drugs target COVID-19 as virus spreads”. BioWorld. Archivedfrom the original on 27 February 2020. Retrieved 1 March 2020.
- ^ Everett G (27 February 2020). “These 5 drug developers have jumped this week on hopes they can provide a coronavirus treatment”. Markets Insider. Archived from the original on 16 November 2020. Retrieved 1 March 2020.
- ^ “The tiny tweak behind COVID-19 vaccines”. Chemical & Engineering News. 29 September 2020. Retrieved 30 September2020.
- ^ “A gamble pays off in ‘spectacular success’: How the leading coronavirus vaccines made it to the finish line”. Washington Post. 6 December 2020. Retrieved 9 December 2020.
- ^ Kramer, Jillian (31 December 2020). “They spent 12 years solving a puzzle. It yielded the first COVID-19 vaccines”. National Geographic.
- ^ Corbett, Kizmekia; Edwards, Darin; Leist, Sarah (5 August 2020). “SARS-CoV-2 mRNA Vaccine Development Enabled by Prototype Pathogen Preparedness”. Nature. doi:10.1038/s41586-020-2622-0. PMC 7301911. PMID 32577634.
- ^ Jump up to:a b Auth DR, Powell MB (14 September 2020). “Patent Issues Highlight Risks of Moderna’s COVID-19 Vaccine”. New York Law Journal. Retrieved 1 December 2020.
- ^ Pendleton D, Maloney T (18 May 2020). “MIT Professor’s Moderna Stake on the Brink of Topping $1 Billion”. Bloomberg News. Retrieved 18 May 2020.
CEO Bancel, other Moderna executives have been selling shares
- ^ Jump up to:a b Fact Sheet for Healthcare Providers Administering Vaccine(PDF). U.S. Food and Drug Administration (FDA) (Report). December 2020. Retrieved 31 December 2020.
- ^ An mRNA Vaccine against SARS-CoV-2 – Preliminary Report, Lisa A. Jackson et al., New England Journal of Medicine 383 (Nov. 12, 2020), pp. 1920-1931, doi:10.1056/NEJMoa2022483.
- ^ “NIH clinical trial of investigational vaccine for COVID-19 begins”. National Institutes of Health (NIH). 16 March 2020. Archived from the original on 19 March 2020. Retrieved 18 March2020.
- ^ Kuznia R, Polglase K, Mezzofiore G (1 May 2020). “In quest for vaccine, US makes ‘big bet’ on company with unproven technology”. CNN. Archived from the original on 13 May 2020. Retrieved 2 May 2020.
- ^ Keown A (7 May 2020). “Moderna moves into Phase II testing of COVID-19 vaccine candidate”. BioSpace. Archived from the original on 16 November 2020. Retrieved 9 May 2020.
- ^ Blankenship K (1 May 2020). “Moderna aims for a billion COVID-19 shots a year with Lonza manufacturing tie-up”. FiercePharma. Archived from the original on 16 November 2020. Retrieved 9 May 2020.
- ^ “Swiss factory rushes to prepare for Moderna Covid-19 vaccine”. SWI swissinfo.ch. Archived from the original on 16 November 2020. Retrieved 7 October 2020.
- ^ Clinical trial number NCT04405076 for “Dose-Confirmation Study to Evaluate the Safety, Reactogenicity, and Immunogenicity of mRNA-1273 COVID-19 Vaccine in Adults Aged 18 Years and Older” at ClinicalTrials.gov
- ^ “Moderna eyes third quarter for first doses of potential COVID-19 vaccine with Catalent deal”. Reuters. 25 June 2020. Archivedfrom the original on 16 November 2020. Retrieved 6 November2020.
- ^ Lee J. “Moderna signs on for another COVID-19 vaccine manufacturing deal”. MarketWatch. Archived from the original on 16 November 2020. Retrieved 9 July 2020.
- ^ Jump up to:a b c Jackson LA, Anderson EJ, Rouphael NG, Roberts PC, Makhene M, Coler RN, et al. (November 2020). “An mRNA Vaccine against SARS-CoV-2 – Preliminary Report”. The New England Journal of Medicine. 383 (20): 1920–1931. doi:10.1056/NEJMoa2022483. PMC 7377258. PMID 32663912.
- ^ Jackson LA, Anderson EJ, Rouphael NG, Roberts PC, Makhene M, Coler RN, et al. (November 2020). “An mRNA Vaccine against SARS-CoV-2 – Preliminary Report”. The New England Journal of Medicine. 383 (20): 1920–31. doi:10.1056/NEJMoa2022483. PMC 7377258. PMID 32663912.
- ^ Li Y (14 July 2020). “Dow futures jump more than 200 points after Moderna says its vaccine produces antibodies to coronavirus”. CNBC. Archived from the original on 16 November 2020. Retrieved 15 July 2020.
- ^ Jump up to:a b Herper M, Garde D (14 July 2020). “First data for Moderna Covid-19 vaccine show it spurs an immune response”. Stat. Boston Globe Media. Archived from the original on 14 July 2020. Retrieved 15 July 2020.
- ^ Palca J (27 July 2020). “COVID-19 vaccine candidate heads to widespread testing in U.S.” NPR. Archived from the original on 11 October 2020. Retrieved 27 July 2020.
- ^ “Moderna, in bid for transparency, discloses detailed plan of coronavirus vaccine trial”. BioPharma Dive. Archived from the original on 16 November 2020. Retrieved 18 September 2020.
- ^ Mascarenhas L (1 October 2020). “Moderna chief says Covid-19 vaccine could be widely available by late March”. CNN. Archived from the original on 16 November 2020. Retrieved 2 October 2020.
- ^ Cohen E. “First large-scale US Covid-19 vaccine trial reaches target of 30,000 participants”. CNN. Archived from the original on 16 November 2020. Retrieved 23 October 2020.
- ^ “Promising Interim Results from Clinical Trial of NIH-Moderna COVID-19 Vaccine”. National Institutes of Health (NIH). 15 November 2020.
- ^ Baden, Lindsey R. (30 December 2020). “Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine”. New England Journal of Medicine. 384 (5): 403–416. doi:10.1056/NEJMoa2035389. PMC 7787219. PMID 33378609.
- ^ Jump up to:a b c d Lovelace Jr B, Higgins-Dunn N (16 November 2020). “Moderna says preliminary trial data shows its coronavirus vaccine is more than 94% effective, shares soar”. CNBC. Retrieved 17 November 2020.
- ^ Zimmer C (20 November 2020). “2 Companies Say Their Vaccines Are 95% Effective. What Does That Mean? You might assume that 95 out of every 100 people vaccinated will be protected from Covid-19. But that’s not how the math works”. The New York Times. Retrieved 21 November 2020.
- ^ Clinical trial number NCT04470427 for “A Study to Evaluate Efficacy, Safety, and Immunogenicity of mRNA-1273 Vaccine in Adults Aged 18 Years and Older to Prevent COVID-19” at ClinicalTrials.gov
- ^ Dolgin E (November 2020). “COVID-19 vaccines poised for launch, but impact on pandemic unclear”. Nature Biotechnology. doi:10.1038/d41587-020-00022-y. PMID 33239758. S2CID 227176634.
- ^ “Moderna Use Roche Antibody Test During Vaccine Trials”. rapidmicrobiology.com. Retrieved 13 December 2020.
- ^ Pregnant women haven’t been included in promising COVID-19 vaccine trials
- ^ FDA: Leave the door open to Covid-19 vaccination for pregnant and lactating health workers
- ^ Rio, Giulia McDonnell Nieto del (15 January 2021). “Covid-19: Over Two Million Around the World Have Died From the Virus”. The New York Times. ISSN 0362-4331. Retrieved 18 January2021.
- ^ Tirrell, Meg (14 January 2021). “Moderna looks to test Covid-19 booster shots a year after initial vaccination”. CNBC. Retrieved 18 January 2021.
- ^ “Moderna Explores Whether Third Covid-19 Vaccine Dose Adds Extra Protection”. The Wall Street Journal. Retrieved 18 January2021.
- ^ “Moderna COVID-19 Vaccine Update” (PDF). 25 January 2021.
- ^ Jump up to:a b “Is the Covid-19 Vaccine Effective Against New South African Variant?”. The New York Times. 25 January 2021. Retrieved 25 January 2021.
- ^ “Moderna Announces it has Shipped Variant-Specific Vaccine Candidate, mRNA-1273.351, to NIH for Clinical Study”. Moderna Inc. (Press release). 24 February 2021. Retrieved 24 February2021.
- ^ Loftus, Peter (16 March 2021). “Moderna Is Testing Its Covid-19 Vaccine on Young Children”. The Wall Street Journal. ISSN 0099-9660. Retrieved 16 March 2021.
- ^ “Pfizer-BioNTech COVID-19 Vaccine Vaccination Storage & Dry Ice Safety Handling”. Pfizer. Retrieved 17 December 2020.
- ^ “How China’s COVID-19 could fill the gaps left by Pfizer, Moderna, AstraZeneca”. Fortune. 5 December 2020. Archivedfrom the original on 12 December 2020. Retrieved 5 December2020.
- ^ “Pfizer’s Vaccine Is Out of the Question as Indonesia Lacks Refrigerators: State Pharma Boss”. Jakarta Globe. 22 November 2020. Archived from the original on 7 December 2020. Retrieved 5 December 2020.
- ^ “Coronavirus (COVID-19) Update: FDA Allows More Flexible Storage, Transportation Conditions for Pfizer-BioNTech COVID-19 Vaccine”. U.S. Food and Drug Administration (Press release). 25 February 2021. Retrieved 25 February 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ “Pfizer and BioNTech Submit COVID-19 Vaccine Stability Data at Standard Freezer Temperature to the U.S. FDA”. Pfizer (Press release). 19 February 2021. Retrieved 19 February 2021.
- ^ Jump up to:a b “Vaccines and Related Biological Products Advisory Committee Meeting”. U.S. Food and Drug Administration (FDA). 17 December 2020.
- ^ Jump up to:a b Mullin R (25 November 2020). “Pfizer, Moderna ready vaccine manufacturing networks”. Chemical & Engineering News. American Chemical Society. Retrieved 21 December 2020.
- ^ “Securing Singapore’s access to COVID-19 vaccines”. http://www.gov.sg. Singapore Government. 14 December 2020. Retrieved 1 February 2021.
- ^ Khalik, Salma (1 February 2021). “How Singapore picked its Covid-19 vaccines”. The Straits Times. Retrieved 1 February2021.
- ^ “Trump says U.S. inks agreement with Moderna for 100 mln doses of COVID-19 vaccine candidate”. Yahoo. Reuters. 11 August 2020. Archived from the original on 16 November 2020. Retrieved 12 August 2020.
- ^ “Moderna aims to price coronavirus vaccine at $50-$60 per course: FT”. Reuters. 28 July 2020. Retrieved 20 March 2021.
- ^ “Donald Trump appears to admit Covid is ‘running wild’ in the US”. The Guardian. 22 November 2020. ISSN 0261-3077. Retrieved 22 November 2020.
Moderna told the Germany [sic] weekly Welt am Sonntag that it will charge governments between $25 and $37 per dose of its Covid vaccine candidate, depending on the amount ordered.
- ^ Guarascio F (24 November 2020). “EU secures 160 million doses of Moderna’s COVID-19 vaccine”. Reuters. Retrieved 25 November 2020.
- ^ “Coronavirus: Commission approves contract with Moderna to ensure access to a potential vaccine”. European Commission. 25 November 2020. Retrieved 4 December 2020.
- ^ “New agreements to secure additional vaccine candidates for COVID-19”. Prime Minister’s Office, Government of Canada. 25 September 2020. Retrieved 4 December 2020.
- ^ Stevis-Gridneff M, Sanger-Katz M, Weiland N (18 December 2020). “A European Official Reveals a Secret: The U.S. Is Paying More for Coronavirus Vaccines”. The New York Times. Retrieved 19 December 2020.
- ^ “Moderna sees $18.4 billion in sales from COVID-19 vaccine in 2021”. Reuters. 25 February 2021. Retrieved 25 February 2021.
- ^ “EMA recommends COVID-19 Vaccine Moderna for authorisation in the EU” (Press release). European Medicines Agency. 6 January 2021. Retrieved 6 January 2021.
- ^ “COVID-19 Vaccine Moderna”. Union Register of medicinal products. Retrieved 14 January 2021.
- ^ Jump up to:a b “Endnu en vaccine mod COVID-19 er godkendt af EU-Kommissionen”. Lægemiddelstyrelsen (in Danish). Retrieved 7 January 2021.
- ^ “COVID-19: Bóluefninu COVID-19 Vaccine Moderna frá hefur verið veitt skilyrt íslenskt markaðsleyfi”. Lyfjastofnun (in Icelandic). Retrieved 7 January 2021.
- ^ “Status på koronavaksiner under godkjenning per 6. januar 2021”. Statens legemiddelverk (in Norwegian Bokmål). Retrieved 7 January 2021.
- ^ “Informació en relació amb la vacunació contra la COVID-19”(PDF). Govern d’Andorra. Retrieved 14 March 2021.
- ^ “Regulatory Decision Summary – Moderna COVID-19 Vaccine”. Health Canada, Government of Canada. 23 December 2020. Retrieved 23 December 2020.
- ^ “Drug and vaccine authorizations for COVID-19: List of applications received”. Health Canada, Government of Canada. 9 December 2020. Retrieved 9 December 2020.
- ^ “Israeli Ministry of Health Authorizes COVID-19 Vaccine Moderna for Use in Israel”. modernatx.com. 4 January 2021. Retrieved 4 January 2021.
- ^ “Public Health (Emergency Authorisation of COVID-19 Vaccine) Rules, 2021” (PDF). Government of Saint Vincent and the Grenadines. 11 February 2021. Retrieved 12 February 2021.
- ^ “AstraZeneca and Moderna vaccines to be administered in Saudi Arabia”. Gulf News. Retrieved 19 January 2021.
- ^ “Singapore becomes first in Asia to approve Moderna’s COVID-19 vaccine”. Reuters. 3 February 2021. Retrieved 3 February 2021.
- ^ “Swissmedic grants authorisation for the COVID-19 vaccine from Moderna” (Press release). Swiss Agency for Therapeutic Products (Swissmedic). 12 January 2020. Retrieved 12 January2020.
- ^ “Information for Healthcare Professionals on COVID-19 Vaccine Moderna”. Medicines and Healthcare products Regulatory Agency (MHRA). 8 January 2021. Retrieved 8 January 2021.
- ^ “Conditions of Authorisation for COVID-19 Vaccine Moderna”. Medicines and Healthcare products Regulatory Agency (MHRA). 8 January 2021. Retrieved 9 January 2021.
- ^ “Interior Applauds Inclusion of Insular Areas through Operation Warp Speed to Receive COVID-19 Vaccines” (Press release). United States Department of the Interior (DOI). 12 December 2020. Retrieved 13 January 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ Dorman B (6 January 2021). “Asia Minute: Palau Administers Vaccines to Keep Country Free of COVID”. Hawaii Public Radio. Retrieved 13 January 2021.
- ^ “Vietnam approves US, Russia Covid-19 vaccines for emergency use”. VnExpress. Retrieved 26 February 2021.
- ^ “Regulation and Prequalification”. World Health Organization. Retrieved 12 March 2021.
- ^ Cohen E (30 November 2020). “Moderna applies for FDA authorization for its Covid-19 vaccine”. CNN. Retrieved 4 December 2020.
- ^ Burger L (1 December 2020). “COVID-19 vaccine sprint as Pfizer-BioNTech, Moderna seek emergency EU approval”. Reuters. Retrieved 4 December 2020.
- ^ Kuchler H (30 November 2020). “Canada could be among the first to clear Moderna’s COVID-19 vaccine for use”. The Financial Post. Retrieved 4 December 2020.
- ^ Parsons L (28 October 2020). “UK’s MHRA starts rolling review of Moderna’s COVID-19 vaccine”. PharmaTimes. Retrieved 4 December 2020.
- ^ Lee J. “Moderna nears its first-ever FDA authorization, for its COVID-19 vaccine”. MarketWatch. Retrieved 19 December 2020.
- ^ Austen, Ian (23 December 2020). “Canada approves the Moderna vaccine, paving the way for inoculations in its vast Far North”. The New York Times. Retrieved 24 December 2020.
- ^ “Israel authorises use of Moderna’s COVID-19 vaccine”. Yahoo! News. Retrieved 5 January 2021.
- ^ “Singapore becomes first in Asia to approve Moderna’s COVID-19 vaccine”. Reuters. 3 February 2021. Retrieved 3 February 2021.
- ^ “First shipment of Moderna’s COVID-19 vaccine arrives in Singapore”. CNA. Retrieved 17 February 2021.
- ^ “EMA recommends COVID-19 Vaccine Moderna for authorisation in the EU” (Press release). European Medicines Agency. 6 January 2021. Retrieved 6 January 2021.
- ^ Miller, John (12 January 2021). “Swiss drugs regulator approves Moderna’s COVID-19 vaccine”. Reuters. Retrieved 17 January2021.
- ^ “Swissmedic grants authorisation for the COVID-19 vaccine from Moderna”. Swissmedic (Press release). 12 January 2020. Retrieved 12 January 2020.
- ^ Hiltzik M (19 May 2020). “Column: Moderna’s vaccine results boosted its share offering – and it’s hardly a coincidence”. The Los Angeles Times. Archived from the original on 16 November 2020. Retrieved 19 May 2020.
- ^ Branswell H (19 May 2020). “Vaccine experts say Moderna didn’t produce data critical to assessing Covid-19 vaccine”. Stat. Archived from the original on 16 November 2020. Retrieved 19 May 2020.
- ^ Taylor M, Respaut R (7 July 2020). “Exclusive: Moderna spars with U.S. scientists over COVID-19 vaccine trials”. Reuters. Archived from the original on 16 November 2020. Retrieved 10 July 2020.
- ^ “Moderna vaccine trial contractors fail to enroll enough people of color, prompting slowdown”. NBC News. Reuters. 6 October 2020. Retrieved 17 November 2020.
- ^ Vardi N (29 June 2020). “Moderna’s Mysterious Coronavirus Vaccine Delivery System”. Forbes. Retrieved 1 December 2020.
- ^ “Moderna loses key patent challenge”. Nature Biotechnology. 38 (9): 1009. September 2020. doi:10.1038/s41587-020-0674-1. PMID 32887970. S2CID 221504018.
Further reading
- World Health Organization (2021). Background document on the mRNA-1273 vaccine (Moderna) against COVID-19: background document to the WHO Interim recommendations for use of the mRNA-1273 vaccine (Moderna), 3 February 2021 (Report). World Health Organization (WHO). hdl:10665/339218. WHO/2019-nCoV/vaccines/SAGE_recommendation/mRNA-1273/background/2021.1.
External links
| Scholia has a profile for mRNA-1273 (Q87775025). |
| Wikimedia Commons has media related to Category:MRNA-1273. |
- “VRBPAC mRNA-1273 Sponsor Briefing Document” (PDF). Moderna. 17 December 2020.
- “Clinical Study Protocol mRNA-1273-P301” (PDF). Moderna.
- COVID-19 Vaccine Moderna assessment report European Medicines Agency
- “How Moderna’s Covid-19 Vaccine Works”. The New York Times.
- “Moderna COVID-19 Vaccine”. Centers for Disease Control and Prevention (CDC).
| Vials of Moderna COVID-19 vaccine | |
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | RNA |
| Clinical data | |
| Pronunciation | /məˈdɜːrnə/ mə-DUR-nə[1] |
| Trade names | Moderna COVID‑19 Vaccine, COVID‑19 Vaccine Moderna |
| Other names | mRNA-1273, CX-024414, COVID-19 mRNA Vaccine Moderna |
| AHFS/Drugs.com | Multum Consumer Information |
| MedlinePlus | a621002 |
| License data | US DailyMed: Moderna_COVID-19_Vaccine |
| Routes of administration | Intramuscular |
| ATC code | None |
| Legal status | |
| Legal status | CA: Schedule D; Authorized by interim order [2][3]UK: Conditional and temporary authorization to supply [4][5]US: Standing Order; Unapproved (Emergency Use Authorization)[6][7][8][9]EU: Conditional marketing authorization granted [10][11] |
| Identifiers | |
| DrugBank | DB15654 |
| UNII | EPK39PL4R4 |
| Part of a series on the |
| COVID-19 pandemic |
|---|
| SARS-CoV-2 (virus)COVID-19 (disease) |
| showTimeline |
| showLocations |
| showInternational response |
| showMedical response |
| showImpact |
| COVID-19 Portal |
| vte |
- Kaur SP, Gupta V: COVID-19 Vaccine: A comprehensive status report. Virus Res. 2020 Oct 15;288:198114. doi: 10.1016/j.virusres.2020.198114. Epub 2020 Aug 13. [PubMed:32800805]
- Jackson LA, Anderson EJ, Rouphael NG, Roberts PC, Makhene M, Coler RN, McCullough MP, Chappell JD, Denison MR, Stevens LJ, Pruijssers AJ, McDermott A, Flach B, Doria-Rose NA, Corbett KS, Morabito KM, O’Dell S, Schmidt SD, Swanson PA 2nd, Padilla M, Mascola JR, Neuzil KM, Bennett H, Sun W, Peters E, Makowski M, Albert J, Cross K, Buchanan W, Pikaart-Tautges R, Ledgerwood JE, Graham BS, Beigel JH: An mRNA Vaccine against SARS-CoV-2 – Preliminary Report. N Engl J Med. 2020 Jul 14. doi: 10.1056/NEJMoa2022483. [PubMed:32663912]
- Pharmaceutical Business Review: Moderna’s mRNA-1273 vaccine [Link]
- Clinical Trials: Safety and Immunogenicity Study of 2019-nCoV Vaccine (mRNA-1273) for Prophylaxis SARS CoV-2 Infection [Link]
- FDA EUA Drug Products: Moderna COVID-19 Vaccine [Link]
- FDA Press Announcements: FDA Takes Additional Action in Fight Against COVID-19 By Issuing Emergency Use Authorization for Second COVID-19 Vaccine [Link]
- Health Canada: Regulatory Decision Summary – Moderna COVID-19 Vaccine [Link]
////////CX 024414, CX-024414, CX024414, mRNA 1273, Moderna COVID-19 vaccine, COVID 19, CORONA VIRUS
CX 024414, CX-024414, CX024414, mRNA 1273, Moderna COVID-19 vaccine, COVID 19, CORONA VIRUS
#CX 024414,#CX-024414, #CX024414, #mRNA 1273, #Moderna COVID-19 vaccine, #COVID 19, #CORONA VIRUS
Anamorelin hydrochloride

Anamorelin249921-19-5[RN]
3-{(2R)-3-{(3R)-3-Benzyl-3-[(trimethylhydrazino)carbonyl]-1-piperidinyl}-2-[(2-methylalanyl)amino]-3-oxopropyl}-1H-indole
3-Piperidinecarboxylic acid, 1-[(2R)-2-[(2-amino-2-methyl-1-oxopropyl)amino]-3-(1H-indol-3-yl)-1-oxopropyl]-3-(phenylmethyl)-, 1,2,2-trimethylhydrazide, (3R)-8846анаморелинأناموريلين阿那瑞林
| Formula | C31H42N6O3 |
|---|---|
| Molar mass | 546.716 g·mol−1 |
 .HCL
.HCL
Anamorelin hydrochloride
3-Piperidinecarboxylic acid, 1-[(2R)-2-[(2-amino-2-methyl-1-oxopropyl)amino]-3-(1H-indol-3-yl)-1-oxopropyl]-3-(phenylmethyl)-, 1,2,2- trimethylhydrazide, hydrochloride (1:1), (3R)-
| Formula | C31H42N6O3. HCl |
|---|---|
| CAS | 861998-00-7 |
| Mol weight | 583.1645 |
APPROVED JAPAN PMDA Adlumiz, 22/1/2021
アナモレリン塩酸塩
ONO-7643, RC-1291, ST-1291
Antineoplastic, Growth hormone secretagogue receptor (GHSR) agonist
Anamorelin is a non-peptidic ghrelin mimetic
Treatment of cancer anorexia and cancer cachexia
Anamorelin hydrochloride has been submitted New Drug Application (NDA) for the treatment of cachexia in non-small cell lung cancer (NSCLC) patients.
It was originally developed by Novo Nordisk, then it was licensed to Ono and Helsinn Therapeutics for the treatment of cachexia and anorexia in cancer patients.
Anamorelin hydrochloride has been submitted New Drug Application (NDA) for the treatment of cachexia in non-small cell lung cancer (NSCLC) patients.
It was originally developed by Novo Nordisk, then it was licensed to Ono and Helsinn Therapeutics for the treatment of cachexia and anorexia in cancer patients.
Company:Novo Nordisk (Originator) , Helsinn,Ono
Anamorelin (INN) (developmental code names ONO-7643, RC-1291, ST-1291), also known as anamorelin hydrochloride (USAN, JAN), is a non-peptide, orally-active, centrally-penetrant, selective agonist of the ghrelin/growth hormone secretagogue receptor (GHSR) with appetite-enhancing and anabolic effects which is under development by Helsinn Healthcare SA for the treatment of cancer cachexia and anorexia.[2][3][4]
Anamorelin significantly increases plasma levels of growth hormone (GH), insulin-like growth factor 1 (IGF-1), and insulin-like growth factor-binding protein 3 (IGFBP-3) in humans, without affecting plasma levels of prolactin, cortisol, insulin, glucose, adrenocorticotropic hormone (ACTH), luteinizing hormone (LH), follicle-stimulating hormone (FSH), or thyroid-stimulating hormone (TSH).[3][5] In addition, anamorelin significantly increases appetite, overall body weight, lean body mass, and muscle strength,[4][5] with increases in body weight correlating directly with increases in plasma IGF-1 levels.[3]
As of February 2016, anamorelin has completed phase III clinical trials for the treatment of cancer cachexia and anorexia associated with non-small-cell lung carcinoma.[6][7]
On 18 May 2017, the European Medicines Agency recommended the refusal of the marketing authorisation for the medicinal product, intended for the treatment of anorexia, cachexia or unintended weight loss in patients with non-small cell lung cancer. Helsinn requested a re-examination of the initial opinion. After considering the grounds for this request, the European Medicines Agency re-examined the opinion, and confirmed the refusal of the marketing authorisation on 14 September 2017.[8] The European Medicines Agency concluded that the studies show a marginal effect of anamorelin on lean body mass and no proven effect on hand grip strength or patients’ quality of life. In addition, following an inspection at clinical study sites, the agency considered that the safety data on the medicine had not been recorded adequately. Therefore, the agency was of the opinion that the benefits of anamorelin did not outweigh its risks.[9]
EMA
The chemical name of anamorelin hydrochloride is 2-Amino-N-((R)-1-((R)-3-benzyl-3-(1,2,2-trimethylhydrazine-1-carbonyl)piperidin-1-yl)-3-(1H-indol-3-yl)-1-oxopropan-2-yl)-2-methylpropanamide hydrochloride corresponding to the molecular formula C31H42N6O3•HCl and has a relative molecular mass 583.16 g/mol and has the following structure:

The structure of the active substance was elucidated by a combination of 1 H-NMR, 13C-NMR, elemental analysis, FT-IR, UV and and mass spectrometry. Anamorelin HCl appears as a white to off-white hygroscopic solid, freely soluble in water, methanol and ethanol, sparingly soluble in acetonitrile and practically insoluble in ethyl acetate, isopropyl acetate and n-heptane. Its pka was found to be 7.79 and the partition coefficient 2.98. It has two chiral centres with the R,R absolute configuration, which is controlled in the active substance specification by chiral HPLC. Based on the presented data, neither anamorelin hydrochloride, nor any of its salts have been previously authorised in medicinal products in the European Union. Anamorelin is therefore considered as a new active substance.
SYN
OPRD

PATENT
WO 9958501
PATENT
WO 2001034593
https://patents.google.com/patent/WO2001034593A1/enExample 1A procedure for the preparation of the compound which is either 2-Amino-N-[(1 R)-2-[(3R)-3-benzyl-3-(N,N’,N’-trimethylhydrazinocarbonyl)piperidin-1-yl]-1- (1 H-indol-3-ylmethyl)-2-oxoethyl]-2-methylpropionamide

or2-Amino-N-[(1R)-2-[(3S)-3-benzyl-3-(N,N’,N’-trimethylhydrazinocarbonyl)piperidin-1-yl]-1- (1 H-indol-3-ylmethyl)-2-oxoethyl]-2-methylpropionamide

Step aPiperidine-1 ,3-dicarboxylic acid 1-tetf-butyl ester 3-ethyl ester

A one-necked round-bottom flask (1 I) equipped with a magnetic stirrer and addition funnel was charged with NaOH-pellets (15,6 g), tetrahydrofuran (400 ml) and ethylnipecotate (50 ml, 324 mmol). To the stirred mixture at room temperature was added dropwise a solution of Boc2O (84,9 g, 389 mmol) dissolved in tetrahydrofuran (150 ml) (1 hour, precipitation of white solid, NaOH-pellets dissolved, exoterm). The mixture was stirred overnight at room temperature. The mixture was added to EtOAc (500 ml) and H2O (2000 ml), and the aqueous layer was re-extracted with EtOAc (2 X 500 ml) and the combined organic layers were washed with brine (100 ml), dried over MgSO4, filtered and concentrated in vacuo to afford piperidine-1 ,3-dicarboxylic acid 1-tert-butyl ester 3-ethyl ester (82,5 g) as a thin yellow oil.1H-NMR (300 MHz, CDCI3): δ 1,25 (t, 3H, CH3); 1 ,45 (s, 9H, 3 X CH3); 2,05 (m, 1H); 2,45 (m, 1H); 2,85 (m, 1 H); 3,95 (d (broad), 1 H); 4,15 (q, 2H, CH2)Step b3-Benzylpiperidine-1 ,3-dicarboxylic acid 1-tetf-butyl ester 3-ethyl ester (racemic mixture)

A three-necked round-bottom flask (2 I) equipped with a magnetic stirrer, thermometer, nitrogen bubbler and addition funnel was evacuated, flushed with nitrogen, charged with anhydrous tetrahydrofuran (500 ml) and cooled to -70 °C. Then lithium diisopropylamine (164 ml of a 2,0 M solution in tetrahydrofuran, 327 mmol) was added. To the stirred solution at -70 °C was added dropwise over 45 min. a solution of piperidine-1 ,3-dicarboxylic acid 1- tert-butyl ester 3-ethyl ester (80 g, 311 mmol) in anhydrous tetrahydrofuran (50 ml) (temperature between -70 °C and -60 °C, clear red solution). The mixture was stirred for 20 min. and followed by dropwise addition over 40 min. of a solution of benzylbromide (37 ml, 311 mmol) in anhydrous tetrahydrofuran (250 ml) (temperature between -70 °C and -60 °C). The mixture was stirred for 1 hour at -70 °C, and then left overnight at room temperature (pale orange).The reaction mixture was concentrated in vacuo to approx. 300 ml, transferred to a separating funnel, diluted with CH2CI2 (900 ml) and washed with H2O (900 ml). Due to poor separation the aqueous layer was re-extracted with CH2CI2 (200 ml), the combined organic layers were washed with aqueous NaHSO4 (200 ml, 10%), aqueous NaHCO3 (200 ml, saturated), H2O (200 ml), brine (100 ml), dried over MgSO4> filtered and concentrated in vacuo to afford an oil, which was dissolved in EtOAc(1):heptane(10) and aged overnight. The solids formed was removed by filtration, washed with heptane and dried in vacuo to give a racemic mixture of 3-benzylpiperidine-1 ,3-dicarboxylic acid 1-ter–butyl ester 3-ethyl ester (81 ,4 g). ■ HPLC (h8): Rt = 15,79 min.LC-MS: Rt = 7,67 min. (m+1) = 348,0Step c 3-Benzylpiperidine-1 ,3-dicarboxylic acid 1-tert-butyl ester (racemic mixture)

3-Benzylpiperidine-1 ,3-dicarboxylic acid 1-tert-butyl ester 3-ethyl ester (81 g, 233 mmol) was dissolved in EtOH (400 ml) and NaOH (400 ml, 16% aqueous solution) in a one neck round- bottom flask (1 L) equipped with a condenser and a magnetic stirrer. The mixture was refluxed for 10 h under nitrogen, and cooled to room temperature, concentrated in vacuo to approx. 600 ml (precipitation of a solid), diluted with H2O (400 ml), cooled in an icebath, and under vigorous stirring acidified with 4 M H2SO4 until pH = 3 (final temperature: 28 °C). The mixture was extracted with EtOAc (2 X 700 ml), and the combined organic layers were washed with brine (200 ml), dried over MgSO4, filtered and concentrated in vacuo to afford an oil, which was dissolved in EtOAc(1):heptane(10) and aged overnight. The crystals formed were removed by filtration, washed with heptane and dried in vacuo to give a racemic mixture of 3-benzylpiperidine-1 ,3-dicarboxylic acid 1-tetf-butyl ester (66,0 g)HPLC (h8): Rt = 12,85 min.LC-MS: Rt = 5,97 min. (m+1) = 320,0Chirale HPLC (Chiracel OJ, heptane(92):iPrOH(8):TFA(0,1)): Rt = 8,29 min. 46,5 % Rt = 13,69 min. 53,5 %Step d(3R)-3-Benzylpiperidine-1 ,3-dicarboxylic acid 1-tert-butyl ester or (3S)-3-Benzylpiperidine-1,3-dicarboxylic acid 1-tert-butyl ester
(Resolution of 3-Benzylpiperidine-1 ,3-dicarboxylic acid 1-tert-butyl ester)

3-Benzylpiperidine-1 ,3-dicarboxylic acid 1-tert-butyl ester (76 g, 238 mmol) was dissolved in EtOAc (3,0 L) in a one neck flask (5L) equipped with magnetic stirring. Then H2O (30 ml), R(+)-1-phenethylamine (18,2 ml, 143 mmol) and Et3N (13,2 ml, 95 mmol) were added and the mixture was stirred overnight at room temperature resulting in precipitation of white crystals (41 ,9 g), which were removed by filtration, washed with EtOAc and dried in vacuo. The precipitate was dissolved in a mixture of aqueous NaHSO4 (300 ml, 10%) and EtOAc (600 ml), layers were separated and the aqueous layer re-extracted with EtOAc (100 ml). The combined organic layers were washed with brine (100 ml), dried over MgSO4 and filtered. The solvent was removed in vacuo to afford a colourless oil, which was dissolved in EtOAc(1):heptane(10) and aged overnight. The crystals that had been formed were removed by filtration, washed with heptane and dried in vacuo to give one compound which is either (3R)-3-benzylpiperidine-1 ,3-dicarboxylic acid 1-tert-butyl ester or (3S)-3-benzylpiperidine- 1,3-dicarboxylic acid 1-tert-butyl ester (27,8 g).Chirale HPLC (Chiracel OJ, heptane(92):iPrOH(8):TFA(0,1)):Rt = 7,96 min. 95,8 % eeStep e(3R)-3-Benzyl-3-(N,N’1N’-trimethylhvdrazinocarbonyl)piperidine-1-carboxylic acid tert-butyl ester or (3S)-3-Benzyl-3-(N,N’,N’-trimethylhvdrazinocarbonyl)piperidine-1-carboxylic acid tert-butyl ester

Trimethylhydrazine dihydrochloride (15,3 g, 104 mmol) was suspended in tetrahydrofuran (250 ml) in a one-neck round-bottom flask (1 I) equipped with a large magnetic stirrer, and an addition funnel/nitrogen bubbler. The flask was then placed in a water-bath (temp: 10- 20°C), bromo-rrts-pyrrolydino-phosphonium-hexafluorophosphate (40,4 g, 86,7 mmol) was added, and under vigorous stirring dropwise addition of diisopropylethylamine (59 ml, 347 mmol). The mixture (with heavy precipitation) was stirred for 5 min., and a solution of the product from step d which is either (3R)-3-benzylpiperidine-1 ,3-dicarboxylic acid 1-tert-butyl ester or (3S)-3-benzylpiperidine-1,3-dicarboxylic acid 1-tert-butyl ester (27,7 g, 86,7 mmol) in tetrahydrofuran (250 ml) was added slowly over 1 ,5 hour. The mixture was stirred overnight at room temperature. The reaction was diluted with EtOAc (1000 ml), washed with H2O (500 ml), aqueous NaHSO4, (200 ml, 10%), aqueous NaHCO3 (200 ml, saturated), brine (200 ml), dried over MgSO4, filtered and concentrated in vacuo to afford a thin orange oil. The mixture was dissolved in EtOAc (300 ml), added to SiO2 (150 g) and concentrated in vacuo to a dry powder which was applied onto a filter packed with SiO2 (150 g), washed with heptan (1 I) and the desired compound was liberated with EtOAc (2,5 I). After concentration in vacuo, the product which is either (3R)-3-benzyl-3-(N,N’,N’-trimethylhydrazinocarbonyl)-piperidine-1- carboxylic acid tert-butyl ester or (3S)-3-benzyl-3-(N,N’,N’-trimethylhydrazinocarbonyl)- piperidine-1-carboxylic acid tert-butyl ester (49 g) as an orange oil was obtained.HPLC (h8): Rt = 14,33 min.Ste f(3R)-3-Benzyl-piperidine-3-carboxylic acid trimethylhydrazide or (3S)-3-Benzyl-piperidine-3- carboxylic acid trimethylhydrazide

The product from step e which is either (3R)-3-Benzyl-3-(N,N’,N’- trimethylhydrazinocarbonyl)-piperidine-1 -carboxylic acid tert-butyl ester or (3S)-3-Benzyl-3- (N,N’,N’-trimethylhydrazinocarbonyl)-piperidine-1 -carboxylic acid tert-butyl ester (56,7 g, 100,9 mmol) was dissolved in EtOAc (500 ml) (clear colourless solution) in a one-neck roundbottom flask (2L) equipped with magnetic stirring. The flask was then placed in a waterbath (temp: 10-20 °C), and HCI-gas was passed through the solution for 5 min. (dust- like precipitation). After stirring for 1 hour (precipitation of large amount of white crystals), the solution was flushed with N2 to remove excess of HCI. The precipitate was removed by gentle filtration, washed with EtOAc (2 X 100 ml), and dried under vacuum at 40 °C overnight to give the product which is either (3R)-3-benzyl-piperidine-3-carboxylic acid trimethylhydrazide or (3S)-3-benzyl-piperidine-3-carboxylic acid trimethylhydrazide (37,0 g).HPLC (h8): Rt = 7,84 min.Step q r(1 R)-2-r(3R)-3-Benzyl-3-(N,N’,N’-trimethylhvdrazinocarbonyl)piperidin-1-vn-1-((1 H-indol-3- yl)methyl)-2-oxoethvncarbamic acid tert-butyl ester or .(1 R)-2-..3S)-3-Benzyl-3-(N,N’,N’- trimethylhvdrazinocarbonyl)piperidin-1-vn-1-((1 H-indol-3-yl)methyl)-2-oxoethyllcarbamic acid tert-butyl ester

Boc-D-Trp-OH (32,3 g, 106 mmol) was dissolved in dimethylacetamide (250 ml) in a one- neck roundbottom flask (500 ml) equipped with a magnetic stirrer and a nitrogen bubbler. The solution was cooled to 0-5 °C and 1-hydroxy-7-azabenzotriazole (14,4 g, 106 mmol), 1- ethyl-3-(3-dimethylaminopropyl)carbodiimid hydrochloride (20,3 g, 106 mmol), N- methylmorpholine (11 ,6 ml, 106 mmol) were added. After stirring for 20 min. at 0-5 °C the product from step f which is either (3R)-3-benzyl-piperidine-3-carboxylic acid trimethylhydrazide or (3S)-3-benzyl-piperidine-3-carboxylic acid trimethylhydrazide (37,0 g, 106 mmol) and N-methylmorpholine (24,4 ml, 223 mmol) were added. The reaction was stirred overnight at room temperature. The mixture was then added to EtOAc (750 ml) and washed with aqueous NaHSO4 (300 ml, 10 %). The layers were allowed to separate, and the aqueous layer was re-extracted with EtOAc (500 ml). The combined organic layers were washed with H2O (100 ml), aqueous NaHCO3 (300 ml, saturated), H2O (100 ml), brine (300 ml), dried over MgSO4, filtered and concentrated in vacuo to afford the product which is either [(1 R)-2-[(3R)-3-benzyl-3-(N,N’,N’-trimethylhydrazinocarbonyl)piperidin-1-yl]-1-((1H- indol-3-yl)methyl)-2-oxoethyl]carbamic acid tert-butyl ester or [(1 R)-2-[(3S)-3-benzyl-3- (N,N’,N’-trimethylhydrazinocarbonyl)piperidin-1-yl]-1-((1 H-indol-3-yl)methyl)-2- oxoethyljcarbamic acid tert-butyl ester (56,7g) as an orange oil.HPLC (h8): Rt = 14,61 min.LC-MS: Rt = 7,35 min. (m+1 ) = 562,6Step h1 -f(2R)-2-Amino-3-(1 H-indol-3-yl)propionylH3R)-3-benzylpiperidine-3-carboxylic acid trimethylhydrazide or 1-f(2R)-2-Amino-3-(1 H-indol-3-yl)propionvn-(3S)-3-benzylpiperidine-3- carboxylic acid trimethylhydrazide

The product from step g which is either [(1 R)-2-[(3R)-3-benzyl-3-(N,N’,N’- trimethylhydrazinocarbonyl)piperidin-1 -yl]-1 -((1 H-indol-3-yl)methyl)-2-oxoethyl]carbamic acid tert-butyl ester or [(1 R)-2-[(3R)-3-benzyl-3-(N,N’,N’-trimethylhydrazinocarbonyl)piperidin-1- yl]-1-((1 H-indol-3-yl)methyl)-2-oxoethyl]carbamic acid tert-butyl ester (56,7 g, 100,9 mmol) was dissolved in EtOAc (500 ml) (clear colourless solution) in a one-neck round-bottom flask (2L) equipped with magnetic stirring. The flask was then placed in a water-bath (temp: 10-20 °C), and HCI-gas was passed through the solution for 10 min. (heavy precipitation of oil). The mixture was flushed with N2 to remove excess of HCI and then separated into an oil and an EtOAc-layer. The EtOAc-layer was discarded. The oil was dissolved in H2O (500 ml), CH2CI2 (1000 ml), and solid Na2CO3 was added until pH > 7. The layers were separated, and the organic layer was washed with H2O (100 ml), brine (100 ml), dried over MgSO4, filtered and concentrated in vacuo to afford the product which is either 1-[(2R)-2-amino-3-(1 H-indol- 3-yl)propionyl]-(3R)-3-benzylpiperidine-3-carboxylic acid trimethylhydrazide or 1-[(2R)-2- amino-3-(1H-indol-3-yl)propionyl]-(3S)-3-benzylpiperidine-3-carboxylic acid trimethylhydrazide (27 g) as an orange foam.HPLC (h8): Rt = 10,03 min.Step i(1-r(1 R)-2-r(3R)-3-Benzyl-3-(N,N’,N’-trimethylhvdrazinocarbonyl)piperidin-1-vn-1-(1H-indol-3- ylmethyl)-2-oxo-ethylcarbamovπ-1 -methylethyl fcarbamic acid tert-butyl ester or1-r(1 R)-2-r(3S)-3-Benzyl-3-(N,N’.N’-trimethylhvdrazinocarbonyl)piperidin-1-vn-1-(1 H-indol-3- ylmethyl)-2-oxo-ethylcarbamovπ-1-methylethyl)carbamic acid tert-butyl ester

Boc-Aib-OH (11 ,9 g, 58,4 mmol) was dissolved in dimethylacetamide (125 ml) in a one-neck roundbottom flask (500 ml) equipped with a magnetic stirrer and nitrogen bubbler. To the stirred solution at room temperature were added 1-hydroxy-7-azabenzotriazole (7,95 g, 58,4 mmol), 1-ethyl-3-(3-dimethylaminopropyl)carbodiimid hydrochloride (11 ,2 g, 58,4 mmol), and diisopropylethylamine (13,0 ml, 75,8 mmol). After 20 min. (yellow with precipitation) a solution of the product from step h which is either 1-[(2R)-2-amino-3-(1 H-indol-3- yl)propionyl]-(3R)-3-benzylpiperidine-3:carboxylic acid trimethylhydrazide or 1-[(2R)-2- amino-3-(1 H-indol-3-yl)propionyl]-(3S)-3-benzylpiperidine-3-carboxylic acid trimethylhydrazide (27,0 g, 58,4 mmol) in dimethylacetamide (125 ml) was added. The reaction was stirred at room temperature for 3 h. The mixture was added to EtOAc (750 ml) and washed with aqueous NaHSO4 (300 ml, 10 %). The layers were allowed to separate, and the aqueous layer was re-extracted with EtOAc (500 ml). The combined organic layers were washed with H2O (100 ml), aqueous NaHCO3 (300 ml, saturated), H2O (100 ml), brine (300 ml), dried over MgSO4, filtered and concentrated in vacuo to approx. 500 ml. Then SiO2 (150 g) was added and the remaining EtOAc removed in vacuo to give a dry powder which was applied onto a filter packed with SiO2 (150 g), washed with heptan (1 L), and the desired compound was liberated with EtOAc (2,5 L). After concentration in vacuo, the product which is either {1-[(1 R)-2-[(3R)-3-benzyl-3-(N, N’, N’-trimethylhydrazinocarbonyl)piperidin-1-yl]-1- (1H-indol-3-ylmethyl)-2-oxo-ethylcarbamoyl]-1-methylethyl}carbamic acid tert-butyl ester or {1-[(1R)-2-[(3S)-3-benzyl-3-(N,N’,N’-trimethylhydrazinocarbonyl)piperidin-1-yl]-1-(1 H-indol-3- ylmethyl)-2-oxo-ethylcarbamoyl]-1-methylethyl}carbamic acid tert-butyl ester 33,9 g as an orange foam was obtained.HPLC (h8): Rt = 14,05 min.Step j2-Amino-N-r(1 R)-2-f(3R)-3-benzyl-3-(N,N’,N’-trimethylhvdrazinocarbonyl)piperidin-1-vπ-1- (1 H-indol-3-ylmethyl)-2-oxoethyll-2-methylpropionamide, fumarate or2-Amino-N-r(1 R)-2-r(3S)-3-benzyl-3-(N1N’1N’-trimethylhvdrazinocarbonyl)piperidin-1-yll-1- (1H-indol-3-ylmethyl)-2-oxoethvπ-2-methylpropionamide, fumarate

The product from step i which is either {1-[(1 R)-2-[(3R)-3-benzyl-3-(N,N’,N’- trimethylhydrazinocarbonyl)piperidin-1-yl]-1-(1H-indol-3-ylmethyl)-2-oxo-ethylcarbamoyl]-1- methylethyl}carbamic acid tert-butyl ester or {1-[(1 R)-2-[(3S)-3-benzyl-3-(N,N’,N’- trimethylhydrazinocarbonyl)piperidin-1 -yl]-1 -(1 H-indol-3-ylmethyl)-2-oxo-ethylcarbamoyl]-1 – methylethyljcarbamic acid tert-butyl ester (23,8 g, 36,8 mmol) was dissolved in of EtOAc (800 ml) (clear yellow solution) in a one neck round-bottom flask (1L) equipped with magnetic stirring. The flask was then placed in a water-bath (temp: 10-20 °C), and HCI-gas was passed through the solution for 5 min. (dust-like precipitation). After stirring for 1 hour (precipitation of large amount of yellow powder), the solution was flushed with N2 to remove excess of HCI. The precipitate was removed by gentle filtration and dried under vacuum at 40 °C overnight.The non-crystallinic precipitate was dissolved in H2O (500 ml) and washed with EtOAc (100 ml). Then CH2CI2 (1000 ml) and solid Na2CO3 was added until pH > 7. The 2 layers were separated, and the aqueous layer was e-extracted with CH2CI2 (200 ml). The combined organic layers were washed with brine (100 ml), dried over MgSO4 and filtered. The solvent was evaporated under reduced pressure and redissolved in EtOAc (500 ml) in a one neck round-bottom flask (1 L) equipped with magnetic stirring. A suspension of fumaric acid (3,67 g) in isopropanol (20 ml) and EtOAc (50 ml) was slowly added (5 min.), which resulted in precipitation of a white crystallinic salt. After 1 hour the precipitation was isolated by filtration and dried overnight in vacuum at 40 °C to give the fumarate salt of the compound which is either 2-amino-N-[(1 R)-2-[(3R)-3-benzyl-3-(N,N’,N’-trimethylhydrazinocarbonyl)piperidin-1- yl]-1-(1 H-indol-3-ylmethyl)-2-oxoethyl]-2-methylpropionamide or 2-amino-N-[(1 R)-2-[(3S)-3- benzyl-3-(N,N,,N’-trimethylhydrazinocarbonyl)piperidin-1-yl]-1-(1 H-indol-3-ylmethyl)-2- oxoethyl]-2-methylpropionamide (13,9 g) as a white powder.HPLC (A1): Rt = 33,61 min.HPLC (B1): Rt = 34,62 min. LC-MS: Rt = 5,09 min. (m+1) = 547,4
ClaimsHide Dependent
1. The compound obtainable by the procedure as described in example 1 , or a pharmaceutically acceptable salt thereof.2. The compound obtainable by the procedure as described in example 1 , and which compound is2-Amino-N-[(1 R)-2-[(3R)-3-benzyl-3-(N,N’,N’-trimethylhydrazinocarbonyl)piperidin-1-yl]-1- (1 H-indol-3-ylmethyl)-2-oxoethyl]-2-methylpropionamide

or a pharmaceutically acceptable salt thereof.3. A pharmaceutical composition comprising, as an active ingredient, a compound according to any one of claims 1-2 or a pharmaceutically acceptable salt thereof together with a pharmaceutically acceptable carrier or diluent.4. A pharmaceutical composition according to claim 3 for stimulating the release of growth hormone from the pituitary.5. A pharmaceutical composition according to claim 3 or claim 4 for administration to animals to increase their rate and extent of growth, to increase their milk and wool production, or for the treatment of ailments.6. A method of stimulating the release of growth hormone from the pituitary of a mammal, the method comprising administering to said mammal an effective amount of a compound according to any one of claims 1 or 2 or a pharmaceutically acceptable salt thereof, or of a composition according to any one of claims 3 – 5.7. A method of increasing the rate and extent of growth, the milk and wool production, or for the treatment of ailments, the method comprising administering to a subject in need thereof an effective amount of a compound according to any one of claims 1-2 or a pharmaceutically acceptable salt thereof, or of a composition according to any one of claims 3-5.8. Use of a compound according to any one of claims 1-2 or a pharmaceutically acceptable salt thereof for the preparation of a medicament.9. Use according to claim 8 wherein the medicament is for stimulating the release of growth hormone from the pituitary of a mammal.
PATENT
CN 108239141
PATENT
US 20130281701
| Growth hormone is a major participant in the control of several complex physiologic processes, including growth and metabolism. Growth hormone is known to have a number of effects on metabolic processes, e.g., stimulation of protein synthesis and free fatty acid mobilization and to cause a switch in energy metabolism from carbohydrate to fatty acid metabolism. Deficiency in growth hormone can result in a number of severe medical disorders, e.g., dwarfism. |
| The release of growth hormone from the pituitary is controlled, directly or indirectly, by number of hormones and neurotransmitters. Growth hormone release can be stimulated by growth hormone releasing hormone (GHRH) and inhibited by somatostatin. In both cases the hormones are released from the hypothalamus but their action is mediated primarily via specific receptors located in the pituitary. Other compounds which stimulate the release of growth hormone from the pituitary have also been described. For example, arginine, L-3,4-dihydroxyphenylalanine (1-Dopa), glucagon, vasopressin, PACAP (pituitary adenylyl cyclase activating peptide), muscarinic receptor agonists and a synthetic hexapeptide, GHRP (growth hormone releasing peptide) release endogenous growth hormone either by a direct effect on the pituitary or by affecting the release of GHRH and/or somatostatin from the hypothalamus. |
| The use of certain compounds for increasing the levels of growth hormone in mammals has previously been proposed. For example, U.S. Pat. Nos. 6,303,620 and 6,576,648 (the entire contents of which are incorporated herein by reference), disclose a compound: (3R)-1-(2-methylalanyl-D-tryptophyl)-3-(phenylmethyl)-3-piperidinecarboxylic acid 1,2,2-trimethylhydrazide, having the following chemical structure: |
(MOL) (CDX) which acts directly on the pituitary cells under normal experimental conditions in vitro to release growth hormone therefrom. This compound is also known under the generic name “anamorelin.” This growth hormone releasing compound can be utilized in vitro as a unique research tool for understanding, inter alia, how growth hormone secretion is regulated at the pituitary level. Moreover, this growth hormone releasing compound can also be administered in vivo to a mammal to increase endogenous growth hormone release.
Example 1
Crystallization of (3R)-1-(2-methylalanyl-D-tryptophyl)-3-(phenylmethyl)-3-piperidinecarboxylic acid 1,2,2-trimethylhydrazide form A
| 0.0103 g of (3R)-1-(2-methylalanyl-D-tryptophyl)-3-(phenylmethyl)-3-piperidinecarboxylic acid 1,2,2-trimethylhydrazide was dissolved in methanol (0.1 mL) in a glass vial. The glass vial was then covered with PARAFILM® (thermoplastic film) which was perforated with a single hole. The solvent was then allowed to evaporate under ambient conditions. An X-ray diffraction pattern showed the compound was crystalline ( FIG. 1). |
PATENT
WO 2017067438
https://patents.google.com/patent/WO2017067438A1/enAnamorelin, whose chemical name is: (3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2- Trimethylformylhydrazide is a compound that increases mammalian growth hormone levels and has a compound structure as shown in Formula I:

Cancer cachexia is a state of consumption in which patients lose a lot of weight and muscle mass. It is necessary for the treatment of cachexia because it weakens the patient, affects the quality of life and interferes with the patient’s treatment plan. The drug alamorelin produces the same effect as the so-called “starved hormone” ghrelin, which stimulates hunger. Alamolin is a mimetic of ghrelin, which is secreted by the stomach and is a ligand for growth hormone receptors. . Alamolin binds to this receptor, causing the release of growth hormone, causing a metabolic cascade that affects a variety of different factors, including fat-removing body weight, as well as blood sugar metabolism. Therefore, alamorelin can also enhance the appetite of patients and help patients stay healthy. The 2014 European Society of Medical Oncology (ESMO) in Madrid, Spain, announced that Alamolin is expected to be the first drug in history to effectively improve cancer cachexia.Alamolin is a drug developed by Helsinn Therapeutics (Switzerland) from Novo Nordisk for the development of a cachexia and anorexia for patients with cancer, including non-small cell lung cancer. It can also be used to treat hip fractures and preventive diseases. The strength of the elderly and the elderly has continued to decline. In two key, 12-week Phase III clinical trials (ROMANA 1, ROMANA 2), alamorelin can significantly increase the body fat loss, and is generally tolerated; the incidence of serious adverse drug reactions is less than 3%, mainly related to hyperglycemia and diabetes. Compared with the placebo group, alamorelin continued to increase body weight and improve cancer anorexia-cachexia-related symptoms and concerns; however, there was no significant difference in the improvement of grip strength between the alamolin group and the placebo group. Therefore, this product has excellent clinical value and market value.The polymorphic form of the drug free base and its preparation are reported as follows:Synthesis of (3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-trimethylmethyl is disclosed in the patent ZL99806010.0 A method for synthesizing hydrazide, and using [(1R)-2-[(3R)-3-benzyl-3-(N,N’,N’-trimethylmethylcarbonyl)piperidin-1-yl tert-Butyl ester of 1-((1H-indol-3-yl)methyl)-2-oxoethyl]carbamate is dissolved in dichloromethane, then trifluoroacetic acid is added to remove tert-butyl formate After the base, the mixture was concentrated to remove the solvent, and then the product was extracted with dichloromethane, and the obtained extract was concentrated to dryness to give (3R)-1-(2-methylalanyl-D-color ammonia as an amorphous powder. Acyl)-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazide.Patent ZL00815145.8 discloses the synthesis of alamorelin and its compounds as pharmaceutically acceptable salts, relating to novel diastereomeric compounds, pharmaceutically acceptable salts thereof, compositions containing them and their use in therapy Lack of use of medical conditions caused by growth hormone. Synthesis of (3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-trimethylformyl is disclosed in this patent. The synthesis method of hydrazine, and using [(1R)-2-[(3R)-3-benzyl-3-(N,N’,N’-trimethylmethylcarbonylcarbonyl)piperidin-1-yl] 1-((1H-Indol-3-yl)methyl)-2-oxoethyl]carbamic acid tert-butyl ester was dissolved in ethyl acetate, and then hydrogen chloride gas was passed to remove the tert-butyl formate protection group. , the solid is dissolved in water, and then the pH is adjusted to about 7 with sodium carbonate, and the product is extracted with dichloromethane; the extract phase is concentrated to obtain (3R)-1-(2-methylalanyl-D-tryptophan). -3-Benzyl-3-piperidine 1,2,2-trimethylformylhydrazide.Patent WO2006016995 discloses (3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-trimethylmethyl as a medicament Crystalline polymorphs of hydrazides, methods of producing and separating these polymorphs, and pharmaceutical compositions and drug therapies containing these polymorphs, the crystalline polymorphs for direct application to the pituitary Gland cells release the growth hormone. This patent discloses (4R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazone 4 Crystal form: Form A, Form B, Form C and Form D. The patent also provides the preparation of 3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazone. The method of crystal form, especially the preparation method of Form C, in which the method of removing the tert-butyl formate protecting group of methanesulfonic acid in methanol is utilized without exception. As a well-known cause in the art, clinical studies have found that mesylate is genotoxic, and its DNA alkylation leads to mutagenic effects, in which methyl methanesulfonate and ethyl methanesulfonate have been reported. (eg document EMEA/44714/2008). The invention adopts hydrochloric acid or hydrogen chloride gas to remove the tert-butyl formate protecting group, avoids the method of removing methanesulfonic acid, thereby avoiding the risk of the genotoxic impurities in the process, and increasing the risk. The safety of the drug.(3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-three prepared by the patent ZL99806010.0 and the patent ZL00815145.8 Methyl formyl hydrazide, no data on the purity of its compounds, we found that (3R)-1-(2-methylalanyl-D-tryptophan)-3 was prepared by this method. -Benzyl-3-piperidine 1,2,2-trimethylformylhydrazide does not help to remove the impurities produced, and the purity of the obtained product is not high, and it is difficult to meet the medicinal requirements. And (3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-trimethyl obtained by the preparation method of the present invention. The crystal form of the formyl hydrazide has a purity of 99.8% and a single impurity of less than 0.1%, which fully meets the requirements for medicinal purity. Moreover, the crystal form is stable to conditions such as pressure, temperature, humidity and illumination, and the preparation method is simple in operation and suitable for industrial production.Example 1:300 g of [(1R)-2-[(3R)-3-benzyl-3-(N,N’,N’-trimethylcarbamidocarbonyl)piperidin-1-yl]-1-(( 1H-Indol-3-yl)methyl)-2-oxoethyl]carbamic acid tert-butyl ester was added to the reaction flask, and then 4 L of dichloromethane was added to the reaction flask, and the raw material was completely dissolved by stirring.Then, the reaction system is cooled to 10 ° C or lower in an ice bath, hydrogen chloride gas is continuously supplied to the reaction liquid, and solids are gradually precipitated, and the reaction is further maintained at about 10 ° C for 3 to 5 hours, and the sample is detected. After the reaction of the raw materials is completed, the reaction system is completed. 1.5 L of water was added thereto, the solid was completely dissolved, and then the pH was adjusted to about 8 with a 20% aqueous sodium hydroxide solution, and the layers were separated; the aqueous phase was extracted once more with dichloromethane, and the organic phases were combined.The organic phase was dried over anhydrous sodium sulfate for 3 hrs, filtered, and then evaporated to ethylamine 3-Benzyl-3-piperidine 1,2,2-trimethylformylhydrazine crude 246 g, yield 97.2%. HPLC content (area normalization method) was 96.1%.Example 2:300 g of [(1R)-2-[(3R)-3-benzyl-3-(N,N’,N’-trimethylcarbamidocarbonyl)piperidin-1-yl]-1-(( 1H-Indol-3-yl)methyl)-2-oxoethyl]carbamic acid tert-butyl ester was added to the reaction flask, 36% concentrated hydrochloric acid was added to the reaction flask, and the reaction system was heated to 40 with stirring. The reaction was carried out at ° C to 50 for 3 hours.Then, the sample is detected. After the reaction of the raw material is completed, the reaction system is cooled to 10 or less, and 2.0 L of dichloromethane is added to the reaction system, and then the pH is adjusted to about 8 with a 20% aqueous sodium hydroxide solution, and the aqueous phase is further separated. It was extracted once with dichloromethane and the organic phases were combined.The organic phase was dried over anhydrous sodium sulfate for 3 hrs, filtered, and then evaporated to ethylamine 3-Benzyl-3-piperidine 1,2,2-trimethylformylhydrazine crude 248 g, yield 98%. HPLC content (area normalization method) was 96.2%.Preparation of (3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazone E crystal formExample 3Taking the above amorphous (3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazine crude product 10g was added to the reaction flask and 30 ml of N- was added.Methylpyrrolidone, stirred and dissolved completely. Then, 60 ml of water was added dropwise to the reaction flask at room temperature, and the reaction liquid was heated to 60 ° C. The solution became cloudy, and a white solid was gradually precipitated, and stirring was continued for 2 hours.Slowly cooled to below 20 ° C, filtered, and the filter cake was washed with a mixture of N-methylpyrrolidone / H 2 O; the cake was vacuum dried at about 55 ° C to obtain (3R)-1-(2-methylalanyl) -D-tryptophan)-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazide (white solid, 9.5 g), HPLC content (area normalization) 99.72%. The XRD pattern is shown in Fig. 1, the DSC chart is shown in Fig. 2, and the TGA pattern is shown in Fig. 3, where the crystal form is defined as the E crystal form. The DSC of the crystal form has an endotherm at 120.05, the TGA is heated at 60A, and the crystal loss of 5 is about 3.1%. Combined with the Karl Fischer method, the moisture content of the product is determined. 3.1% and 3.2% indicate that the sample is present as a monohydrate.Example 4:Taking the above amorphous (3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazine crude product 10 g was added to the reaction flask, 30 ml of N,N-dimethylformamide was added, stirred, and dissolved completely. Then, 30 ml of water was added dropwise to the reaction flask at room temperature, and the reaction solution was heated to 50 ° C. The solution became cloudy, and a white solid was gradually precipitated, and stirring was continued for 2 h.Slowly cool to below 10 ° C, filter, filter cake washed with N, N-dimethylformamide / H 2 O mixture; vacuum cake dried at around 55 ° C to obtain (3R)-1-(2-A Alanyl-D-tryptophanyl-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazide (white solid, 8.5 g), HPLC content (area normalization) ) 99.87%. Upon comparison, it was confirmed that the solid was in the E crystal form.Example 5:Taking the above amorphous (3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazine crude product 10 g was added to the reaction flask, 30 ml of dimethyl sulfoxide was added, stirred, and dissolved completely. Then, 40 ml of water was added dropwise to the reaction flask at room temperature, and the reaction liquid was heated to 60 ° C, the solution became cloudy, and a white solid was gradually precipitated, and stirring was continued for 2 hours.Slowly cooled to below 10 ° C, filtered, and the filter cake was washed with a mixture of dimethyl sulfoxide / H 2 O; the cake was vacuum dried at about 50 ° C to obtain (3R)-1-(2-methylalanyl) -D-tryptophanyl-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazide (white solid, 9.1 g), HPLC content (area normalization) 99.61%. Upon comparison, it was confirmed that the solid was in the E crystal form.Example 6Taking the above amorphous (3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazine crude product 10 g was added to the reaction flask, 40 ml of 1,4-dioxane was added, stirred, and dissolved completely. Then, 50 ml of water was added dropwise to the reaction flask at room temperature, and the reaction solution was heated to 70 ° C. The solution became cloudy, and a white solid was gradually precipitated, and stirring was continued for 2 hours.Slowly cooled to below 10 ° C, filtered, and the filter cake was washed with a mixture of 1,4-dioxane/H 2 O; the cake was vacuum dried at about 50 ° C to obtain (3R)-1-(2-methyl alanyl-D-tryptophan-3-Benzyl-3-piperidine 1,2,2-trimethylformylhydrazide (white solid, 8.7 g), HPLC content (area normalization) 99.11%. Upon comparison, it was confirmed that the solid was in the E crystal form.Example 7Taking the above amorphous (3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazine crude product 10 g was added to the reaction flask, 40 ml of N,N-dimethylacetamide was added, stirred, and dissolved completely. Then, 40 ml of water was added dropwise to the reaction flask at room temperature, and the reaction solution was heated to 70 ° C. The solution became cloudy, and was slowly cooled to about 50 ° C. Seed crystals were added thereto, and cooling was continued to gradually precipitate a solid.The reaction system was cooled to about 10 ° C, filtered, and the filter cake was washed with a mixture of N,N-dimethylacetamide/H 2 O; the cake was vacuum dried at about 50 ° C to obtain (3R)-1-(2- Methylalanyl-D-tryptophanyl-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazide (white solid, 8.1 g), HPLC content (area normalized) Law) 99.78%. Upon comparison, it was confirmed that the solid was in the E crystal form.Example 7Taking the above amorphous (3R)-1-(2-methylalanyl-D-tryptophyl)-3-benzyl-3-piperidine 1,2,2-trimethylformylhydrazine crude product 10 g was added to the reaction flask, 50 ml of acetone was added, stirred, and dissolved completely. Then, 70 ml of water was added dropwise to the reaction flask at room temperature, and the reaction liquid was heated to 45 ° C. The solution became cloudy, and a white solid was gradually precipitated, and stirring was continued for 2 hours.Slowly cool to below 10 ° C, filter, filter cake washed with acetone / H 2 O mixture; filter cake vacuum dried at around 50 ° C to obtain (3R)-1-(2-methylalanyl-D-color Aminoacyl-3-phenylmethyl-3-piperidine 1,2,2-trimethylformylhydrazide (white solid, 9.3 g), HPLC content (area normalization) 98.9%. Upon comparison, it was confirmed that the solid was in the E crystal form.
SYN
Reference:
1. Org. Process Res. Dev. 2006, 10, 339–345.

Abstract

The rapid process development of a scaleable synthesis of the pseudotripeptide RC-1291 for preclinical and clinical evaluation is described. By employing a nontraditional N-to-C coupling strategy, the peptide chain of RC-1291 was assembled in high yield, with minimal racemization and in an economical manner by introducing the most expensive component last. A one-pot deprotection/crystallization procedure was developed for the isolation of RC-1291 free base, which afforded the target compound in excellent yield and with a purity of >99.5% without chromatographic purification.
(R,R)-2-Amino-N-[2-[3-benzyl-3-(N,N′,N′-trimethyl-hydrazinocarbonyl)piperidin-1-yl]-1-(1H-indol-3-ylmethyl)- 2-oxo-ethyl]-2-methyl-propionamide (1). Crude 7 (911 g; 1.28 mol theoretical)10 was dissolved in methanol (4.12 L) in a 22-L round-bottom flask equipped with a mechanical stirrer, a temperature probe, a reflux condenser, a gas (N2) inlet, and an addition funnel. The solution was heated to 55 °C; then methanesulfonic acid (269.5 g, 2.805 mol) was added over a period of 15 min. (Caution: gas evolution!) The solution was then heated to 60 °C for a period of 1 h, after which HPLC analysis showed that no 7 remained. The temperature of the reaction mixture was increased to reflux (68-72 °C) over a period of 35 min, while simultaneously adding a solution of KOH (85%, 210.4 g, 3.187 mol) in water (4.12 L). The clear, slightly yellow solution was then allowed to cool to 20 °C at a rate of 5 °C/h. The free base of RC1291 (1) crystallized as a pale-yellow solid, which was isolated by filtration. The filter cake was washed with two portions of 50% aqueous methanol (500 mL each) and then dried under high vacuum at 20 ( 5 °C to afford 1 as an off-white, crystalline solid (595 g, 85% yield for two steps, >99.5% AUC by HPLC).
HRMS (ESI) calcd for C31H43N6O3 [M + H]+ 547.3397, found 547.3432.
1H NMR (DMSO-d6; 413 K) δ 10.30 (s, 1H), 7.85 (bs, 1H), 7.50 (d, J ) 7.8 Hz, 1H), 7.27 (d, J ) 8.1 Hz, 1H), 7.1-7.2 (m, 3H), 6.95-7.0 (m, 5H), 5.07 (t, J ) 6.3 Hz, 1H), 3.54 (d, J ) 12.3 Hz, 1H), 3.36 (bs, 1H), 3.15-3.30 (m, 1H), 3.06 (dd, J ) 7.2, 14.4 Hz, 1H), 2.96 (dd, J ) 6.0, 14.3 Hz, 2H), 2.7-2.8 (m, 6H), 2.43 (m, 6H), 2.09 (bs, 1H), 1.73 (bs, 1H), 1.45-1.55 (m, 2H), 1.3-1.40 (m, 1H), 1.18 (s, 3H), 1.15 (s, 3H).
13C NMR (DMSO-d6; 413 K) δ 175.8, 173.4, 170.3, 137.0, 135.7, 129.0, 127.2, 127.1, 125.3, 122.9, 120.1, 117.6, 110.7, 109.4, 53.6, 49.0, 47.0, 42.7, 38.5, 30.7, 28.2, 28.0, 23.2, 21.1.

PAPER
https://pubs.acs.org/doi/pdf/10.1021/acs.jmedchem.8b00322
Cachexia and muscle wasting are very common among patients suffering from cancer, chronic obstructive pulmonary disease, and other chronic diseases. Ghrelin stimulates growth hormone secretion via the ghrelin receptor, which subsequently leads to increase of IGF-1 plasma levels. The activation of the GH/IGF-1 axis leads to an increase of muscle mass and functional capacity. Ghrelin further acts on inflammation, appetite, and adipogenesis and for this reason was considered an important target to address catabolic conditions. We report the synthesis and properties of an indane based series of ghrelin receptor full agonists; they have been shown to generate a sustained increase of IGF-1 levels in dog and have been thoroughly investigated with respect to their functional activity.

Patent
https://patents.google.com/patent/EP2838892A1/enGrowth hormone is a major participant in the control of several complex physiologic processes including growth and metabolism. Growth hormone is known to have a number of effects on metabolic processes such as stimulating protein synthesis and mobilizing free fatty acids, and causing a switch in energy metabolism from carbohydrate to fatty acid metabolism. Deficiencies in growth hormone can result in dwarfism and other severe medical disorders.The release of growth hormone from the pituitary gland is controlled directly and indirectly by a number of hormones and neurotransmitters. Growth hormone release can be stimulated by growth hormone releasing hormone (GHRH) and inhibited by somatostatin.The use of certain compounds to increase levels of growth hormone in mammals has previously been proposed. Anamorelin is one such compound. Anamorelin is a synthetic orally active compound originally synthesized in the 1990s as a growth hormone secretogogue for the treatment of cancer related cachexia. The free base of anamorelin is chemically defined as:® (3R) 1 -(2-methylaIanyl~D ryptophyl)~3-(phenylraethyl)~3~piperidineearboxylie acid 1 ,2,2trimethyihydrazide,* 3-{(2R)-3-{(3R)-3-benzyi-3-| (trimethylhydrazino)carbonyi]piperidin-l»yl}-2-[(2»met hylaianyl)amino]-3-ox.opropyi}-IH-indole, or• 2-Amino-N-[(lR)-2-[(3R)-3~benzyWcarbony piperidin- 1 -yl] – 1-( 1 H-indol-3 -yl^^and has the below chemical structure;
U.S. Patent No. 6,576,648 to Artkerson reports a process of preparing anamorelin as the fumarate salt, with the hydrochloride salt produced as an intermediate in Step (j) of Example 1 . U.S. Patent No. 7,825, 138 to Lorimer describes a process for preparing crystal forms of the free base of anamorelin.There is a need to develop anamorelin monohydrochloride as an active pharmaceutical ingredient with reduced impurities and improved stability over prior art forms of anamorelin hydrochloride, such as those described in U.S. Patent No, 6,576,648, having good solubility, bioavailability and processabi!ity. There is also a need to develop methods of producing pharmaceutically acceptable forms of anamorelin monohydrochloride thai have improved yield over prior art processes, reduced residual solvents, and controlled distribution of chloride content,it has unexpectedly been discovered that the process of making the hydrochloride salt of anamorelin described in Step (j) of U.S. Patent No. 6.576,648 can result in excessive levels of chloride in the final product, and that this excess chloride leads to the long-term instability of the final product due at least, partially to an increase in the amount of the less stable dihydrochloride salt of anamorelin. Conversely, because anamorelin free base is less soluble in water than the hydrochloride salt, deficient chloride content in the final product can lead to decreased solubility of the molecule. The process described in U.S. Patent No, 6,576,648 also yields a final product that contains more than 5000 ppm (0.5%) of residual solvents, which renders the product less desirable from a pharmaceutical standpoint, as described in CH Harmonized Tripartite Guideline. See Impurities; Guideline for residual solvents Q3C(R3). in order to overcome these problems, methods have been developed which, for the first time, allow for the efficient and precise control of the reaction between anarnorehn tree base and hydrochloric acid in situ, thereby increasing the yield of anarnorehn monohydrochioride from the reaction and reducing the incidence of unwanted anamorelin dihydroeh ride. According to the method, the free base of anamorelin is dissolved in an organic solvent and combined with water and hydrochloric acid, with the molar ratio of anarnorehn and chloride tightly controlled to prevent an excess of chloride in the final product. The water and hydrochloric acid can be added either sequentially or at the same time as long as two separate phases are formed. Without wishing to be bound by any theory, it is believed thai as the anamorelin free base in the organic phase is protonated by the hydrochloric acid it migrates into the aqueous phase. The controlled ratio of anamorelin free base and hydrochloric acid and homogenous distribution in the aqueous phase allows for the controlled formation of the monohydrochioride salt over the dihydrochloride, and the controlled distribution of the resulting chloride levels within individual batches and among multiple batches of anamorelin monohydrochioride.Thus, in a fust embodiment the invention provides methods for preparing anamorelin monohydrochioride or a composition comprising anamorelin monohydrochioride comprising: (a) dissolving anamorelin free base in an organic solvent to form a solution; (b) mixing said solution with water and hydrochloric acid for a time sufficient to: (i) react said anamorelin free base with said hydrochloric acid, and (ii) form an organic phase and an aqueous phase; (c) separating the aqueous phase from the organic phase; and (d) isolating anamorelin monohydrochioride from the aqueous phase.In a particularly preferred embodiment, the molar ratio of anamorelin to hydrochloric acid used in the process is less than or equal to 1 : 1 , so as to reduce the production of anamorelin dihydrochloride and other unwanted chemical species. Thus, for example, hydrochloric acid can be added at a molar ratio of from 0,90 to 1 ,0 relative to said anamorelin, from 0.90 to 0.99, or from 0.93 to 0.97.n another particularly preferred embodiment, the anamorelin monohydrochioride or a composition comprising anamorelin monohydrochioride is isolated from the aqueous phase via spray drying, preferably preceded by distillation. This technique has proven especially useful in the manufacture of anamorelin monohydrochioride or a composition comprising anamorelin monohydrochioride because of the excellent reduction in solvent levels observed, and the production of a stable amorphous form of anamorelin monohydrochioride or a composition comprising anamorelin monohydrochioride. In other embodiments, the invention relates to the various forms of anamorelin monohvdrochloride and compositions comprising anamorelin monohvdrochloride produced by the methods of the present invention. In a first embodiment, which derives from the controlled chloride content among batches accomplished by the present methods, the invention provides anamorelin monohvdrochloride or a composition comprising anamorelin monohydrochloride having an inter-batch chloride content of from 5.8 to 6.2%, preferably from 5.8 to less than 6.2%. Alternatively, the invention provides anamorelin monohydrochloride or a composition comprising anamorelin monohydrochloride having a molar ratio of chloride to anamorelin less than or equal to 1 : 1 , such as from 0.9 to 1.0 or 0.99, in yet another embodiment the invention provides an amorphous form of anamorelin monohydrochloride or a composition comprising anamorelin monohydrochloride. Further descriptions of the anamorelin monohydrochloride and compositions comprising the anamorelin monohydrochloride are given in the detailed description which follows.EXAMPLE 1 . PREPARATION OF ANAMOREUN HYDROCHLORIDEVarious methods have been developed to prepare the hydrochloric acid salt of anarnorelin, with differing results.In a first method, which is the preferred method of the present invention, anarnorelin free base was carefully measured and dissolved in isopropyl acetate. Anarnorelin free base was prepared according to known method (e.g., U.S. Patent No, 6,576,648). A fixed volume of HCl in water containing various molar ratios (0.80, 0,95, 1.00 or 1.05) of HCl relative to the anarnorelin free base was then combined with the anamorelin/isopropyl acetate solution, to form a mixture having an organic and an aqueous phase, The aqueous phase of the mixture was separated from the organic phase and the resulting aqueous phase was concentrated by spray drying to obtain the batches of anarnorelin monohydrochloride (or a composition comprising anarnorelin monohydrochloride ) shown in Table 1 A.Approximately 150mg of the resulting spray dried sample of anarnorelin monohydrochloride (or composition comprising anarnorelin monohydrochloride) was accurately weighed out and dissolved in methanol (50mL). Acetic acid (5mL) and distilled water (5mL) were added to the mixture. The resulting mixture was potentiometricaJ ly titrated using 0,0 IN silver nitrate and the e dpoint was determined. A blank determination was also performed and correction was made, if necessary. The chloride content in the sample was calculated by the following formula. This measurement method of chloride content was performed without any cations other than proton (! ! ‘ ).Chloride content (%) = VxNx35.453x l 00x l 00/{Wx[1 00-(water content (%))-(residual solvent (%))]}V: volume at the endpoint (ml.)N; actual normality of 0.01 mol/L silver nitrate35.453 : atomic weight of ChlorineW: weight of sample (mg)TABLE 1 AHCl Chloride ContentThis data showed that anamorelin monohydrochlonde produced by a fixed volume of HCl in water containing 0.80 or 1 .05 molar equivalents of HC1 relative to anamorelin free base had levels of chloride thai were undesirable, and associated with product instability as shown in Example 3.Alternatively, a fixed volume of HCl in water containing 0.95 moles of HCl relative to anamorelin free base was used to prepare anamorelin monohydrochlonde (or composition comprising anamorelin monohydrochloride) as follows. Anamorelin free base (18.8g, 34.4mmoi) and isopropyl acetate (341.8g) were mixed in a 1000 mL flask. The mixture was heated at 40±5°C to confirm dissolution of the crystals and then cooled at 25±5°C. Distilled water (22.3g) and 3.6% diluted hydrochloric acid (33. Ig, 32.7mmoL 0.95 equivalents) were added into the flask and washed with distilled water. After 30 minutes stirring, the reaction was static for more than 15 minutes and the lower layer (aqueous layer) was transferred into a separate 250mL flask. Distilled water was added to the flask and concentrated under pressure at 50i5cC. The resulting aqueous solution was then filtered and product isolated by spray drying to afford anamorelin monohydrochlonde A (the present invention).The physical properties of anamorelin monohydrochloride A were compared to anamorelin monohydrochloride produced by a traditional comparative method (“anamorelin monohydrochloride B”) (comparative example). Anamorelin mono hydrochloride B in the comparative example was produced by bubbling HCl gas into isopropyl acetate to produce a 2M solution of HCl, and reacting 0.95 molar equivalents of the 2M HCl in isopropyl acetate with anamorelin free base. The physical properties of anamorelin monohydrochloride B are reported in Table IB. This data shows that when 0.95 equivalents of HCl is added to anamorelin free base, the chloride content (or amount of anamorelin dihydrochloride) is increased, even when a stoichiometric ratio of hydrochloride to anamorelin of less than 1 ,0 is used, possibly due to uncontrolled precipitation. In addition, this data shows that the concentration of residual solvents in anamorelin monohydrochloride B was greater than the concentration in anamorelin monohydrochloride A, TABLE I B
A similar decrease in residual solvent concentration was observed when 2-methyltetrahydrofuran was used as the dissolving solvent for anamorelin free base instead of isopropvi acetate in the process for preparing spray dried anamorelin monohydrochloride A (data not reported).The residual solvent (organic volatile impurities) concentration (specifically isopropyl acetate) of anamorelin monohydrochloride in TABLE IB was measured using gas chromatography (GC-2010, Shimadzu Corporation) according to the conditions shown in TABLE 1 C,
References
- ^ Leese PT, Trang JM, Blum RA, de Groot E (March 2015). “An open-label clinical trial of the effects of age and gender on the pharmacodynamics, pharmacokinetics and safety of the ghrelin receptor agonist anamorelin”. Clinical Pharmacology in Drug Development. 4 (2): 112–120. doi:10.1002/cpdd.175. PMC 4657463. PMID 26640742.
- ^ Currow DC, Abernethy AP (April 2014). “Anamorelin hydrochloride in the treatment of cancer anorexia-cachexia syndrome”. Future Oncology. 10 (5): 789–802. doi:10.2217/fon.14.14. PMID 24472001.
- ^ Jump up to:a b c Garcia JM, Polvino WJ (June 2009). “Pharmacodynamic hormonal effects of anamorelin, a novel oral ghrelin mimetic and growth hormone secretagogue in healthy volunteers”. Growth Hormone & IGF Research. 19 (3): 267–73. doi:10.1016/j.ghir.2008.12.003. PMID 19196529.
- ^ Jump up to:a b Garcia JM, Boccia RV, Graham CD, Yan Y, Duus EM, Allen S, Friend J (January 2015). “Anamorelin for patients with cancer cachexia: an integrated analysis of two phase 2, randomised, placebo-controlled, double-blind trials”. The Lancet. Oncology. 16 (1): 108–16. doi:10.1016/S1470-2045(14)71154-4. PMID 25524795.
- ^ Jump up to:a b Garcia JM, Friend J, Allen S (January 2013). “Therapeutic potential of anamorelin, a novel, oral ghrelin mimetic, in patients with cancer-related cachexia: a multicenter, randomized, double-blind, crossover, pilot study”. Supportive Care in Cancer. 21 (1): 129–37. doi:10.1007/s00520-012-1500-1. PMID 22699302. S2CID 22853697.
- ^ Zhang H, Garcia JM (June 2015). “Anamorelin hydrochloride for the treatment of cancer-anorexia-cachexia in NSCLC”. Expert Opinion on Pharmacotherapy. 16 (8): 1245–53. doi:10.1517/14656566.2015.1041500. PMC 4677053. PMID 25945893.
- ^ Temel JS, Abernethy AP, Currow DC, Friend J, Duus EM, Yan Y, Fearon KC (April 2016). “Anamorelin in patients with non-small-cell lung cancer and cachexia (ROMANA 1 and ROMANA 2): results from two randomised, double-blind, phase 3 trials”. The Lancet. Oncology. 17 (4): 519–531. doi:10.1016/S1470-2045(15)00558-6. PMID 26906526.
- ^ “Adlumiz”. European Medicines Agency.
- ^ “Refusal of the marketing authorisation for Adlumiz (anamorelin hydrochloride): Outcome of re-examination” (PDF). European Medicines Agency. 15 September 2017.
External links
| Clinical data | |
|---|---|
| Routes of administration | Oral |
| ATC code | None |
| Pharmacokinetic data | |
| Elimination half-life | 6–7 hours[1] |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 249921-19-5 |
| PubChem CID | 9828911 |
| ChemSpider | 8004650 |
| UNII | DD5RBA1NKF |
| CompTox Dashboard (EPA) | DTXSID20179702 |
| Chemical and physical data | |
| Formula | C31H42N6O3 |
| Molar mass | 546.716 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| hideSMILESCC(C)(C(=O)NC(CC1=CNC2=CC=CC=C21)C(=O)N3CCCC(C3)(CC4=CC=CC=C4)C(=O)N(C)N(C)C)N | |
| hideInChIInChI=1S/C31H42N6O3/c1-30(2,32)28(39)34-26(18-23-20-33-25-15-10-9-14-24(23)25)27(38)37-17-11-16-31(21-37,29(40)36(5)35(3)4)19-22-12-7-6-8-13-22/h6-10,12-15,20,26,33H,11,16-19,21,32H2,1-5H3,(H,34,39)/t26-,31-/m1/s1Key:VQPFSIRUEPQQPP-MXBOTTGLSA-N |
///////Anamorelin hydrochloride, Anamorelin, APPROVALS 2021, JAPAN 2021, PMDA, Adlumiz, 22/1/2021, アナモレリン塩酸塩, анаморелин , أناموريلين ,阿那瑞林 , ONO 7643, RC 1291, ST 1291,
#Anamorelin hydrochloride, #Anamorelin, #APPROVALS 2021, #JAPAN 2021, #PMDA, #Adlumiz, 22/1/2021, #アナモレリン塩酸塩, #анаморелин , #أناموريلين ,阿那瑞林 , #ONO 7643, #RC 1291, #ST 1291,
DASATINIB

DASATINIB
ダサチニブ水和物
BMS 354825
863127-77-9 HYDRATE, USAN, BAN INN, JAN
UNII: RBZ1571X5H
302962-49-8 FREE FORM Dasatinib anhydrous USAN, INN
Molecular Formula, C22-H26-Cl-N7-O2-S.H2-O, Molecular Weight, 506.0282T6N DNTJ A2Q D- DT6N CNJ B1 FM- BT5N CSJ DVMR BG F1[WLN]X78UG0A0RNдазатиниб [Russian] [INN]دازاتينيب [Arabic] [INN]达沙替尼 [Chinese] [INN]1132093-70-9[RN]302962-49-8[RN]5-Thiazolecarboxamide, N-(2-chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)-1-piperazinyl]-2-methyl-4-pyrimidinyl]amino]-87129966762[Beilstein]
A pyrimidine and thiazole derived ANTINEOPLASTIC AGENT and PROTEIN KINASE INHIBITOR of BCR-ABL KINASE. It is used in the treatment of patients with CHRONIC MYELOID LEUKEMIA who are resistant or intolerant to IMATINIB.
An orally bioavailable synthetic small molecule-inhibitor of SRC-family protein-tyrosine kinases. Dasatinib binds to and inhibits the growth-promoting activities of these kinases. Apparently because of its less stringent binding affinity for the BCR-ABL kinase, dasatinib has been shown to overcome the resistance to imatinib of chronic myeloid leukemia (CML) cells harboring BCR-ABL kinase domain point mutations. SRC-family protein-tyrosine kinases interact with a variety of cell-surface receptors and participate in intracellular signal transduction pathways; tumorigenic forms can occur through altered regulation or expression of the endogenous protein and by way of virally-encoded kinase genes. (NCI Thesaurus)
5-Thiazolecarboxamide, N-(2-chloro-6-methylphenyl)-2-((6-(4-(2-hydroxyethyl)-1-piperazinyl)-2-methyl-4-pyrimidinyl)amino)-, monohydrate
Synthesis ReferenceUS6596746
DASATINIB ANHYDROUS
- KIN 001-5
- NSC 759877
- Sprycel
- 302962-49-8 Dasatinib anhydrous
- 5-THIAZOLECARBOXAMIDE, N-(2-CHLORO-6-METHYLPHENYL)-2-((6-(4-(2-HYDROXYETHYL)-1-PIPERAZINYL)-2-METHYL-4-PYRIMIDINYL)AMINO)-
- BMS-354825
- DASATINIB [INN]
- DASATINIB [MI]
- DASATINIB [WHO-DD]
- DASATINIB ANHYDROUS
| No. | NDA No. | Major Technical Classification | Patent No. | Estimated Expiry Date | Drug Substance Claim | Drug Product Claim | Patent Use Code (All list) |
| 1 | N021986 | Formula | 6596746 | 2020-06-28 | Y | Y | U – 748 |
| 2 | N021986 | Formula | 6596746 | 2020-06-28 | Y | Y | U – 780 |
| 3 | N021986 | Uses(Indication) | 7125875 | 2020-04-13 | U – 779 | ||
| 4 | N021986 | Uses(Indication) | 7125875 | 2020-04-13 | U – 780 | ||
| 5 | N021986 | Uses(Indication) | 7153856 | 2020-04-28 | U – 780 | ||
| 6 | N021986 | Crystal | 7491725 | 2026-03-28 | Y | Y | |
| 7 | N021986 | Formulation | 8680103 | 2025-02-04 | Y |



SPRYCEL (dasatinib) is an inhibitor of multiple tyrosine kinases.
The chemical name for dasatinib is N-(2-chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)-1-piperazinyl]-2- methyl-4-pyrimidinyl]amino]-5-thiazolecarboxamide, monohydrate. The molecular formula is C22H26ClN7O2S • H2O, which corresponds to a formula weight of 506.02 (monohydrate).
The anhydrous free base has a molecular weight of 488.01. Dasatinib has the following chemical structure: Dasatinib is a white to off-white powder and has a melting point of 280°–286° C.
The drug substance is insoluble in water and slightly soluble in ethanol and methanol. SPRYCEL tablets are white to off-white, biconvex, film-coated tablets containing dasatinib, with the following inactive ingredients: lactose monohydrate, microcrystalline cellulose, croscarmellose sodium, hydroxypropyl cellulose, and magnesium stearate. The tablet coating consists of hypromellose, titanium dioxide, and polyethylene glycol
| DASATINIBDASATINIB (DASATINIB) | ANDA #202103 | TABLET;ORAL | Discontinued | APOTEX INC |
| SPRYCELSPRYCEL (DASATINIB) | NDA #021986 | TABLET;ORAL | Prescription | BRISTOL MYERS SQUIBBSPRYCEL (DASATINIB) | NDA #022072 | TABLET; ORAL | Prescription | BRISTOL MYERS SQUIBB |
Clip
https://www.pharmainbrief.com/files/2017/09/A-106-17-20170918-Reasons.pdfhttps://www.accessdata.fda.gov/drugsatfda_docs/appletter/2016/202103Orig1s000ltr.pdfU.S. Patent Number Expiration Date 6,596,746 (the ‘746 patent) June 28, 20207,125,875 (the ‘875 patent) April 13, 20207,153,856 (the ‘856 patent) April 28, 20207,491,725 (the ‘725 patent) March 28, 20268,680,103 (the ‘103 patent) February 4, 2025
Drug Name:Dasatinib HydrateResearch Code:BMS-354825Trade Name:Sprycel®MOA:Kinase inhibitorIndication:Acute lymphoblastic leukaemia (ALL); Chronic myeloid leukemia (CML )Status:ApprovedCompany:Bristol-Myers Squibb (Originator)Sales:$1,620 Million (Y2015);
$1,493 Million (Y2014);
$1,280 Million (Y2013);
$1,019 Million (Y2012);
$803 Million (Y2011);ATC Code:L01XE06Approved Countries or Area
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2006-06-28 | Marketing approval | Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet, Film coated | Eq. 20 mg/50 mg/70 mg/80 mg/100 mg/140 mg Dasatinib | Bristol-Myers Squibb | Priority; Orphan |
| 2006-06-28 | Additional approval | Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet, Film coated | 70 mg | Bristol-Myers Squibb | Priority |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2006-11-20 | Marketing approval | Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet, Film coated | 20 mg/50 mg/70 mg/80 mg/100 mg/140 mg | Bristol-Myers Squibb | Orphan |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2011-06-16 | Modified indication | Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet, Film coated | 20 mg/50 mg | Bristol-Myers Squibb, Otsuka | |
| 2009-01-21 | Marketing approval | Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet, Film coated | 20 mg/50 mg | Bristol-Myers Squibb, Otsuka |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2013-09-17 | Marketing approval | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 20 mg | 南京正大天晴制药 | ||
| 2013-09-17 | Marketing approval | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 50 mg | 南京正大天晴制药 | ||
| 2013-09-17 | Marketing approval | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 70 mg | 南京正大天晴制药 | ||
| 2011-09-07 | Marketing approval | 施达赛/Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 50 mg | Bristol-Myers Squibb | |
| 2011-09-07 | Marketing approval | 施达赛/Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 50 mg | Bristol-Myers Squibb | |
| 2011-09-07 | Marketing approval | 施达赛/Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 50 mg | Bristol-Myers Squibb | |
| 2011-09-07 | Marketing approval | 施达赛/Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 20 mg | Bristol-Myers Squibb | |
| 2011-09-07 | Marketing approval | 施达赛/Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 20 mg | Bristol-Myers Squibb | |
| 2011-09-07 | Marketing approval | 施达赛/Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 20 mg | Bristol-Myers Squibb | |
| 2011-09-07 | Marketing approval | 施达赛/Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 70 mg | Bristol-Myers Squibb | |
| 2011-09-07 | Marketing approval | 施达赛/Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 70 mg | Bristol-Myers Squibb | |
| 2011-09-07 | Marketing approval | 施达赛/Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 70 mg | Bristol-Myers Squibb | |
| 2011-09-07 | Marketing approval | 施达赛/Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 100 mg | Bristol-Myers Squibb | |
| 2011-09-07 | Marketing approval | 施达赛/Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 100 mg | Bristol-Myers Squibb | |
| 2011-09-07 | Marketing approval | 施达赛/Sprycel | Acute lymphoblastic leukaemia (ALL), Chronic myeloid leukemia (CML ) | Tablet | 100 mg | Bristol-Myers Squibb |
SPRYCEL (dasatinib) is a kinase inhibitor. The chemical name for dasatinib is N-(2-chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)-1-piperazinyl]-2-methyl-4-pyrimidinyl]amino]-5-thiazolecarboxamide, monohydrate. The molecular formula is C22H26ClN7O2S • H2O, which corresponds to a formula weight of 506.02 (monohydrate). The anhydrous free base has a molecular weight of 488.01. Dasatinib has the following chemical structure:
 |
Dasatinib is a white to off-white powder. The drug substance is insoluble in water and slightly soluble in ethanol and methanol.
SPRYCEL tablets are white to off-white, biconvex, film-coated tablets containing dasatinib, with the following inactive ingredients: lactose monohydrate, microcrystalline cellulose, croscarmellose sodium, hydroxypropyl cellulose, and magnesium stearate. The tablet coating consists of hypromellose, titanium dioxide, and polyethylene glycol.
Dasatinib hydrate was first approved by the U.S. Food and Drug Administration (FDA) on June 28, 2006, then approved by European Medicine Agency (EMA) on Nov 20, 2006, and approved by Pharmaceuticals and Medical Devices Agency of Japan (PMDA) on Jan 21, 2009. It was developed and marketed as Sprycel® by Bristol Myers Squibb in the US.
Dasatinibhydrate is a kinase inhibitor.It is indicated for the treatment ofchronic myeloid leukemia and acutelymphoblastic leukemia.
Sprycel® is available as film-coatedtabletfor oral use, containing 20, 50, 70, 80, 100 or 140 mg offreeDasatinib. The recommended dose is 100 mg once daily forchronic myeloid leukemia. Another dose is 140 mg once daily for accelerated phase chronic myeloid leukemia, myeloid or lymphoid blast phase chronic myeloid leukemia, or Ph+ acutelymphoblastic leukemia.
Dasatinib, also known as BMS-354825, is an orally bioavailable synthetic small molecule-inhibitor of SRC-family protein-tyrosine kinases. Dasatinib binds to and inhibits the growth-promoting activities of these kinases. Apparently because of its less stringent binding affinity for the BCR-ABL kinase, dasatinib has been shown to overcome the resistance to imatinib of chronic myeloid leukemia (CML) cells harboring BCR-ABL kinase domain point mutations.
Dasatinib, sold under the brand name Sprycel among others, is a targeted therapy medication used to treat certain cases of chronic myelogenous leukemia (CML) and acute lymphoblastic leukemia (ALL).[3] Specifically it is used to treat cases that are Philadelphia chromosome-positive (Ph+).[3] It is taken by mouth.[3]
Common adverse effects include low white blood cells, low blood platelets, anemia, swelling, rash, and diarrhea.[3] Severe adverse effects may include bleeding, pulmonary edema, heart failure, and prolonged QT syndrome.[3] Use during pregnancy may result in harm to the baby.[3] It is a tyrosine-kinase inhibitor and works by blocking a number of tyrosine kinases such as Bcr-Abl and the Src kinase family.[3]
Dasatinib was approved for medical use in the United States and in the European Union in 2006.[3][2] It is on the World Health Organization’s List of Essential Medicines.
Medical uses
Dasatinib is used to treat people with chronic myeloid leukemia and people with acute lymphoblastic leukemia who are positive for the Philadelphia chromosome.[5]
In the EU dasatinib is indicated for children with
- newly diagnosed Philadelphia chromosome-positive chronic myelogenous leukaemia in chronic phase (Ph+ CML CP) or Ph+ CML CP resistant or intolerant to prior therapy including imatinib.[2]
- newly diagnosed Ph+ acute lymphoblastic leukaemia (ALL) in combination with chemotherapy.[2]
- newly diagnosed Ph+ CML in chronic phase (Ph+ CML-CP) or Ph+ CML-CP resistant or intolerant to prior therapy including imatinib.[2]
and adults with
- newly diagnosed Philadelphia-chromosome-positive (Ph+) chronic myelogenous leukaemia (CML) in the chronic phase;[2]
- chronic, accelerated or blast phase CML with resistance or intolerance to prior therapy including imatinib mesilate;[2]
- Ph+ acute lymphoblastic leukaemia (ALL) and lymphoid blast CML with resistance or intolerance to prior therapy.[2]
Adverse effects
The most common side effects are infection, suppression of the bone marrow (decreasing numbers of leukocytes, erythrocytes, and thrombocytes),[6] headache, hemorrhage (bleeding), pleural effusion (fluid around the lungs), dyspnea (difficulty breathing), diarrhea, vomiting, nausea (feeling sick), abdominal pain (belly ache), skin rash, musculoskeletal pain, tiredness, swelling in the legs and arms and in the face, fever.[2] Neutropenia and myelosuppression were common toxic effects. Fifteen people (of 84, i.e. 18%) in the above-mentioned study developed pleural effusions, which was a suspected side effect of dasatinib. Some of these people required thoracentesis or pleurodesis to treat the effusions. Other adverse events included mild to moderate diarrhea, peripheral edema, and headache. A small number of people developed abnormal liver function tests which returned to normal without dose adjustments. Mild hypocalcemia was also noted, but did not appear to cause any significant problems. Several cases of pulmonary arterial hypertension (PAH) were found in people treated with dasatinib,[7] possibly due to pulmonary endothelial cell damage.[8]
On October 11, 2011, the U.S. Food and Drug Administration (FDA) announced that dasatinib may increase the risk of a rare but serious condition in which there is abnormally high blood pressure in the arteries of the lungs (pulmonary hypertension, PAH).[9] Symptoms of PAH may include shortness of breath, fatigue, and swelling of the body (such as the ankles and legs).[9] In reported cases, people developed PAH after starting dasatinib, including after more than one year of treatment.[9] Information about the risk was added to the Warnings and Precautions section of the Sprycel drug label.[9]
Pharmacology
Crystal structure[10] (PDB 2GQG) of Abl kinase domain (blue) in complex with dasatinib (red).
Dasatinib is an ATP-competitive protein tyrosine kinase inhibitor. The main targets of dasatinib are BCR/Abl (the “Philadelphia chromosome”), Src, c-Kit, ephrin receptors, and several other tyrosine kinases.[11] Strong inhibition of the activated BCR-ABL kinase distinguishes dasatinib from other CML treatments, such as imatinib and nilotinib.[11][12] Although dasatinib only has a plasma half-life of three to five hours, the strong binding to BCR-ABL1 results in a longer duration of action.[12]
History
See also: Discovery and development of Bcr-Abl tyrosine kinase inhibitors
Dasatinib was developed by collaboration of Bristol-Myers Squibb and Otsuka Pharmaceutical Co., Ltd,[13][14][15] and named for Bristol-Myers Squibb research fellow Jagabandhu Das, whose program leader says that the drug would not have come into existence had he not challenged some of the medicinal chemists‘ underlying assumptions at a time when progress in the development of the molecule had stalled.[16]
Society and culture
Legal status
Dasatinib was approved for used in the United States in June 2006 and in the European Union in November 2006[17][2]
In October 2010, dasatinib was approved in the United States for the treatment of newly diagnosed adults with Philadelphia chromosome positive chronic myeloid leukemia in chronic phase (CP-CML).[18]
In November 2017, dasatinib was approved in the United States for the treatment of children with Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in the chronic phase.[19]
Approval was based on data from 97 pediatric participants with chronic phase CML evaluated in two trials—a Phase I, open-label, non-randomized, dose-ranging trial and a Phase II, open-label, non-randomized trial.[19] Fifty-one participants exclusively from the Phase II trial were newly diagnosed with chronic phase CML and 46 participants (17 from the Phase I trial and 29 from the Phase II trial) were resistant or intolerant to previous treatment with imatinib.[19] The majority of participants were treated with dasatinib tablets 60 mg/m2 body surface area once daily.[19] Participants were treated until disease progression or unacceptable toxicity.[19]
Economics
The Union for Affordable Cancer Treatment objected to the price of dasatinib, in a letter to the U.S. trade representative. The average wholesale price in the U.S. is $367 per day, twice the price in other high income countries. The price in India, where the average annual per capita income is $1,570, and where most people pay out of pocket, is Rs6627 ($108) a day. Indian manufacturers offered to supply generic versions for $4 a day, but, under pressure from the U.S., the Indian Department of Industrial Policy and Promotion refused to issue a compulsory license.[20]
Bristol-Myers Squibb justified the high prices of cancer drugs with the high R&D costs, but the Union of Affordable Cancer Treatment said that most of the R&D costs came from the U.S. government, including National Institutes of Health funded research and clinical trials, and a 50% tax credit. In England and Wales, the National Institute for Health and Care Excellence recommended against dasatinib because of the high cost-benefit ratio.[20]
The Union for Affordable Cancer Treatment said that “the dasatinib dispute illustrates the shortcomings of US trade policy and its impact on cancer patients”[20]
Brand names
In Bangladesh dasatinib is available under the trade name Dasanix by Beacon Pharmaceuticals.In India, It is marketed by brand name NEXTKI by EMCURE PHARMACEUTICALS[medical citation needed]
Research
Dasatinib has been shown to eliminate senescent cells in cultured adipocyte progenitor cells.[21] Dasatinib has been shown to induce apoptosis in senescent cells by inhibiting Src kinase, whereas quercetin inhibits the anti-apoptotic protein Bcl-xL.[21] Administration of dasatinib along with quercetin to mice improved cardiovascular function and eliminated senescent cells.[22] Aged mice given dasatinib with quercetin showed improved health and survival.[22]
Giving dasatinib and quercetin to mice eliminated senescent cells and caused a long-term resolution of frailty.[23] A study of fourteen human patients suffering from idiopathic pulmonary fibrosis (a disease characterized by increased numbers of senescent cells) given dasatinib and quercetin showed improved physical function and evidence of reduced senescent cells.[21]Route 1
Reference:1. WO2005077945A2 / US2012302750A1.Route 2
Reference:1. WO0062778A1 / US6596746B1.Route 3
Reference:1. J. Med. Chem. 2004, 47, 6658-6661.
2. J. Med. Chem. 2006, 49, 6819-6832.Route 4
Reference:1. CN104292223A.Route 5
Reference:1. CN103420999A.
Syn 1

Reference
Balaji, N.; Sultana, Sayeeda. Trace level determination and quantification of potential genotoxic impurities in dasatinib drug substance by UHPLC/infinity LC. International Journal of Pharmacy and Pharmaceutical Sciences. Department of Chemistry. St. Peter’s University. Tamil Nadu, India 600054. Volume 8. Issue 10. Pages 209-216. 2016
SYN 2

Reference
Zhang, Shaoning; Wei, Hongtao; Ji, Min. Synthesis of dasatinib. Zhongguo Yiyao Gongye Zazhi. Dept. of Pharmaceutical Engineering, School of Chemistry & Chemical Engineering. Southeast University. Nanjing, Jiangsu Province, Peop. Rep. China 210096. Volume 41. Issue 3. Pages 161-163. 2010
SYN 3

Reference
Suresh, Garbapu; Nadh, Ratnakaram Venkata; Srinivasu, Navuluri; Yennity, Durgaprasad. A convenient new and efficient commercial synthetic route for dasatinib (Sprycel). Synthetic Communications. Division of Chemistry, Department of Science and Humanities. Vignan’s Foundation for Science Technology and Research University. Guntur, India. Volume 47. Issue 17. Pages 1610-1621. 2017
SYN 4

Reference
Chen, Bang-Chi; Zhao, Rulin; Wang, Bei; Droghini, Roberto; Lajeunesse, Jean; Sirard, Pierre; Endo, Masaki; Balasubramanian, Balu; Barrish, Joel C. A new and efficient preparation of 2-aminothiazole-5-carbamides: applications to the synthesis of the anticancer drug dasatinib. ARKIVOC (Gainesville, FL, United States). Discovery Chemistry. Bristol-Myers Squibb Research and Development. Princeton, USA 08543. Issue 6.Pages 32-38. 2010
SYN 5

Reference
An, Kang; Guan, Jianning; Yang, Hao; Hou, Wen; Wan, Rong. Improvement on the synthesis of Dasatinib. Jingxi Huagong Zhongjianti. College of Science. Nanjing University of Technology. Nanjing, Jiangsu Province, Peop. Rep. China 211816. Volume 41. Issue 2. Pages 42-44. 2011
PATENT
https://patents.google.com/patent/US7491725B2/en
EXAMPLESExample 1Preparation of Intermediate:
(S)-1-sec-Butylthiourea

To a solution of S— sec-butyl-amine (7.31 g, 0.1 mol) in chloroform (80 mL) at 0° C. was slowly added benzoyl isothiocyanate (13.44 mL, 0.1 mol). The mixture was allowed to warm to 10° C. and stirred for 10 min. The solvent was then removed under reduced pressure, and the residue was dissolved in MeOH (80 mL). An aqueous solution (10 mL) of NaOH (4 g, 0.1 mol) was added to this solution, and the mixture was stirred at 60° C. for another 2 h. The MeOH was then removed under reduced pressure, and the residue was stirred in water (50 mL). The precipitate was collected by vacuum filtration and dried to provide S-1-sec-butyl-thiourea (12.2 g, 92% yield). mp 133-134° C.; 1H NMR (500 MHz, DMSO-D6) δ 7.40 (s, 1H), 7.20 (br s, 1H), 6.76 (s, 1H), 4.04 (s, 1H), 1.41 (m, 2H), 1.03 (d, J=6.1 Hz, 3H), 0.81 (d, J=7.7 Hz, 3H); 13C NMR (125 MHz, DMSO-D6) δ 182.5, 50.8, 28.8, 19.9, 10.3; LRMS m/z 133.2 (M+H); Anal. Calcd for C5H12N2S: C, 45.41; H, 9.14; N, 21.18; S, 24.25. Found: C, 45.49; H, 8.88; N, 21.32; S, 24.27.
Example 2Preparation of Intermediate:
(R)-1-sec-Butylthiourea

(R)-1-sec-Butylthiourea was prepared in 92% yield according to the general method outlined for Example 1. mp 133-134° C.; 1H NMR(500 MHz, DMSO) δ 0.80(m, 3H, J=7.7), 1.02(d, 3H, J=6.1), 1.41(m, 2H), (3.40, 4.04)(s, 1H), 6.76(s, 1H), 7.20(s, br, 1H), 7.39(d, 1H, J=7.2); 13C NMR (500 MHz, DMSO) δ: 10.00, 19.56, 28.50, 50.20, 182.00; m/z 133.23 (M+H); Anal. Calcd for C5H12N2S: C, 45.41; H, 9.14; N, 21.18; S, 24.25. Found: C, 45.32; H, 9.15; N, 21.14; S, 24.38.
Example 3Preparation of:

To a solution of 3-amino-N-methyl-4-methylbenzamide hydrochloride (1.0 g, 5 mmol) in acetone (10 mL) at 0° C. was added pyridine (1.2 mL, 15 mmol) dropwise via syringe. 3-Methoxyacryloyl chloride (0.72 mL. 6.5 mmol) was added and the reaction stirred at room temperature for 1 h. The solution was cooled again to 0° C. and 1N HCl (1.5 mL) was added dropwise via pipet. The reaction mixture was stirred for 5 min, then water (8.5 mL) was added via an addition funnel. The acetone was removed in vacuo and the resulting solution stirred for 4h. Crystallization began within 15 min. After stirring for 4 h, the vessel was cooled in an ice bath for 30 min, filtered, and rinsed with ice cold water (2×3 mL) to give compound 3A (0.99 g, 78% yield) as a white solid. 1H NMR (400 MHz, CDCl3) δ 8.95 (s, 1H), 8.12 (br s, 1H), 7.76 (s, 1H), 7.29 (m, 2H), 7.05 (d, J=7.9 Hz, 1H), 5.47 (d, J=12.3 Hz, 1H), 3.48 (s, 3H), 2.54 (d, J=4.7 Hz, 3H), 2.03 (s, 3H); HPLC rt 2.28 min (Condition A).
3B. Example 3To a 50 mL RBF containing the above compound 3A (0.5 g, 2.0 mmol) was added THF (2.5 mL) and water (2 mL), followed by NBS (0.40 g, 2.22 mmol), and the solution was stirred for 90 min. R-sec-butylthiourea (Ex. 2) (267 mg), was added, and the solution was heated to 75° C. for 8 h. Conc. NH4OH was added to adjust the pH to 10 followed by the addition of EtOH (15 mL). Water (15 mL) was added and the slurry stirred for 16 h, filtered, and washed with water to give Example 3 as a light brown solid (0.48 g, 69% yield, 98% purity). MS 347.1; HPLC 2.59.
Example 4Preparation of:

Example 4 is prepared following the methods of Example 3 but using the appropriate acryl benzamide and Example 1.
Example 5Preparation of:
N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide (The Compound of Formula (IV))

5A. 1-(6-Chloro-2-methylpyrimidin-4-yl)thiourea

To a stirring slurry of 4-amino-5-chloro-2-methylpyrimidine (6.13 g, 42.7 mmol) in THF (24 mL) was added ethyl isothiocyanatoformate (7.5 mL, 63.6 mmol), and the mixture heated to reflux. After 5h, another portion of ethyl isothiocyanato formate (1.0 mL, 8.5 mmol) was added and after 10h, a final portion (1.5 mL, 12.7 mmol) was added and the mixture stirred 6h more. The slurry was evaporated under vacuum to remove most of the solvent and heptane (6 mL) added to the residue. The solid was collected by vacuum filtration and washed with heptane (2×5 mL) giving 8.01 g (68% yield) of the intermediate ethyl 6-chloro-2-methylpyrimidin-4-ylcarbamothioylcarbamate.A solution of ethyl 6-chloro-2-methylpyrimidin-4-ylcarbamothioylcarbamate (275 mg, 1.0 mmol) and 1N sodium hydroxide (3.5 eq) was heated and stirred at 50° C. for 2h. The resulting slurry was cooled to 20-22° C. The solid was collected by vacuum filtration, washed with water, and dried to give 185 mg of 1-(6-chloro-2-methylpyrimidin-4-yl)thiourea (91% yield). 1H NMR (400 MHz, DMSO-d6): δ2.51 (S, 3H), 7.05 (s, 1H), 9.35 (s,1H), 10.07 (s, 1H), 10.91 (s, 1H); 13C NMR (125 MHz, DMSO-d6) δ: 25.25, 104.56, 159.19, 159.33, 167.36, 180.91.
5B. (E)-N-(2-Chloro-6-methylphenyl)-3-ethoxyacrylamide

To a cold stirring solution of 2-chloro-6-methylaniline (59.5 g 0.42 mol) and pyridine (68 ml, 0.63 mol) in THF (600 mL) was added 3-ethoxyacryloyl chloride (84.7 g, 0.63 mol) slowly keeping the temp at 0-5° C. The mixture was then warmed and stirred for 2 h. at 20° C. Hydrochloric acid (1N, 115 mL) was added at 0-10° C. The mixture was diluted with water (310 mL) and the resulting solution was concentrated under vacuum to a thick slurry. The slurry was diluted with toluene (275 mL) and stirred for 15 min. at 20-22° C. then 1 h. at 0° C. The solid was collected by vacuum filtration, washed with water (2×75 mL) and dried to give 74.1 g (73.6% yield) of (E)-N-(2-chloro-6-methylphenyl)-3-ethoxyacrylamide). 1H NMR (400 Hz, DMSO-d6) δ 1.26 (t, 3H, J=7 Hz), 2.15 (s, 3H), 3.94 (q, 2H, J=7 Hz), 5.58 (d, 1H, J=12.4 Hz), 7.10-7.27 (m, 2H, J=7.5 Hz), 7.27-7.37 (d, 1H, J=7.5 Hz), 7.45(d, 1H, J=12.4 Hz), 9.28 (s, 1H); 13C NMR (100 MHz, CDCl3) δ: 14.57, 18.96, 67.17, 97.99, 126.80, 127.44, 129.07, 131.32, 132.89, 138.25, 161.09, 165.36.
5C. 2-Amino-N-(2-chloro-6-methylphenyl)thiazole-5-carboxamide

To a mixture of compound 5B (5.00 g, 20.86 mmol) in 1,4-dioxane (27 mL) and water (27 mL) was added NBS (4.08 g, 22.9 mmol) at −10 to 0° C. The slurry was warmed and stirred at 20-22° C. for 3h. Thiourea (1.60 g, 21 mmol) was added and the mixture heated to 80° C. After 2h, the resulting solution was cooled to 20-22° and conc. ammonium hydroxide (4.2 mL) was added dropwise. The resulting slurry was concentrated under vacuum to about half volume and cooled to 0-5° C. The solid was collected by vacuum filtration, washed with cold water (10 mL), and dried to give 5.3 g (94.9% yield) of 2-amino-N-(2-chloro-6-methylphenyl)thiazole-5-carboxamide. 1H NMR (400 MHz, DMSO-d6) δ δ 2.19 (s, 3H), 7.09-7.29 (m, 2H, J=7.5), 7.29-7.43 (d, 1H, J=7.5), 7.61 (s, 2H), 7.85 (s, 1H), 9.63 (s, 1H); 13C NMR (125 MHz, DMSO-d6) δ: 18.18, 120.63, 126.84, 127.90, 128.86, 132.41, 133.63, 138.76, 142.88, 159.45, 172.02.
5D. 2-(6-Chloro-2-methylpyrimidin-4-ylamino)-N-(2-chloro-6-methylphenyl)thiazole-5-carboxamide

To a stirring solution of compound 5C (5.00 g, 18.67 mmol) and 4,6-dichloro-2-methylpyrimidine (3.65 g 22.4/mmol) in THF (65 mL) was added a 30% wt. solution of sodium t-butoxide in THF (21.1 g, 65.36 mmol) slowly with cooling to keep the temperature at 10-20° C. The mixture was stirred at room temperature for 1.5 h and cooled to 0-5° C. Hydrochloric acid, 2N (21.5 mL) was added slowly and the mixture stirred 1.75 h at 0-5° C. The solid was collected by vacuum filtration, washed with water (15 mL) and dried to give 6.63 g (86.4% yield) of compound 5D. 1H NMR (400 MHz, DMSO-d6) δ 2.23 (s, 3H), 2.58 (s, 3H), 6.94 (s, 1H), 7.18-7.34, (m, 2H, J=7.5), 7.34-7.46 (d, 1H, J=7.5), 8.31 (s, 1H), 10.02 (s, 1H), 12.25 (s, 1H).
5E. Example 5To a mixture of compound 5D (4.00 g, 10.14 mmol) and hydroxyethylpiperazine (6.60 g, 50.69 mmol) in n-butanol (40 mL) was added DIPEA (3.53 mL, 20.26 mmol). The slurry was heated at 118° C. for 4.5 h, then cooled slowly to room temperature. The solid was collected by vacuum filtration, washed with n-butanol (5 mL), and dried. The product (5.11 g) was dissolved in hot 80% EtOH—H2O (80 mL), and the solution was clarified by filtration. The hot solution was slowly diluted with water (15 mL) and cooled slowly to room temperature. The solid was collected by vacuum filtration, washed with 50% ethanol-water (5 mL) and dried affording 4.27 g (83.2% yield) of N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide as monohydrate. 1H NMR (400 MHz, DMSO-d6) δ 2.23 (s, 3H), 2.40 (s, 3H), 2.42 (t, 2H, J=6), 2.48 (t, 4H, J=6.3), 3.50 (m, 4H), 3.53 (q, 2H, J=6), 4.45 (t, 1H, J=5.3), 6.04 (s, 1H), 7.25 (t, 1H, J=7.6), 7.27 (dd, 1H, J=7.6, 1.7), 7.40 (dd, 1H, J=7.6, 1.7), 8.21 (s, 1H), 9.87 (s, 1H), 11.47.
Example 6Preparation of:
N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide

To a slurry of (E)-N-(2-chloro-6-methylphenyl)-3-ethoxyacrylamide 5B (120 mg, 0.50 mmol) in THF (0.75 ml) and water (0.5 mL) was added NBS (98 mg, 0.55 mmol) at 0° C. The mixture was warmed and stirred at 20-22° C. for 3h. To this was added 1-(6-chloro-2-methylpyrimidin-4-yl)thiourea 5A (100 mg, 0.49 mmol), and the slurry heated and stirred at reflux for 2h. The slurry was cooled to 20-22° C. and the solid collected by vacuum filtration giving 140 mg (71% yield) of 2-(6-chloro-2-methylpyrimidin-4-ylamino)-N-(2-chloro-6-methylphenyl)thiazole-5-carboxamide 5D. 1H NMR (400 MHz, DMSO-d6) δ 2.23 (s, 3H), 2.58 (s, 3H), 6.94 (s, 1H), 7.18-7.34, (m, 2H, J=7.5), 7.34-7.46 (d, 1H, J=7.5), 8.31 (s, 1H), 10.02 (s, 1H), 12.25 (s, 1H).Compound 5D was elaborated to N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide, following Step 5E.
Example 7Preparation of:
N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide7A. 2-[4-(6-Chloro-2-methyl-pyrimidin-4-yl)-piperazin-1-yl]-ethanol
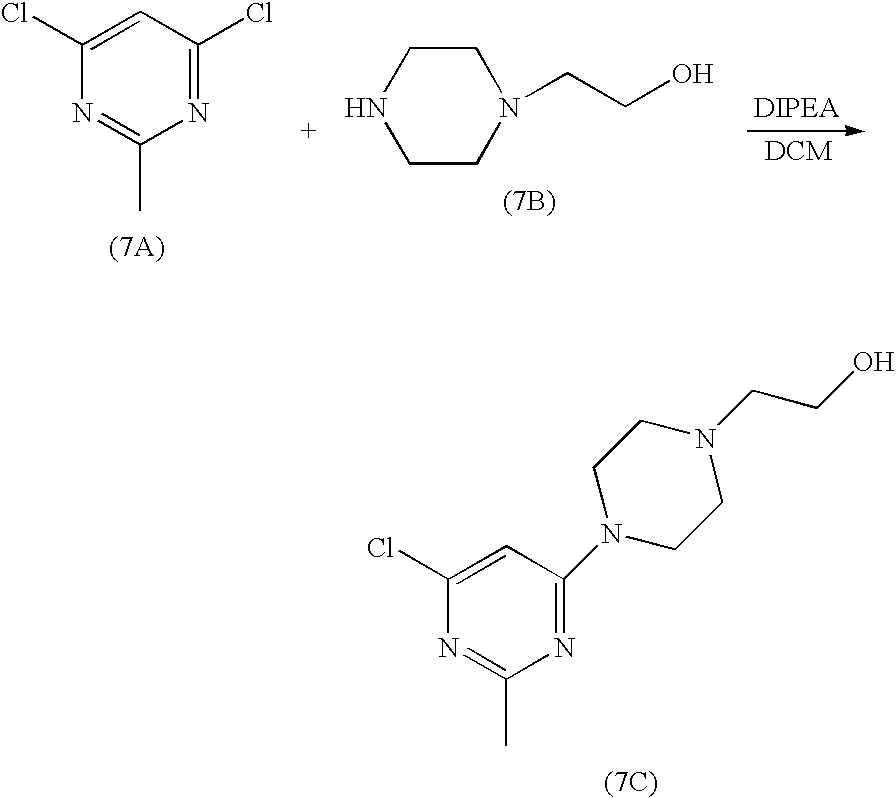
2-piperazin-1-yl-ethanol (8.2 g, 63.1 mmol) was added to a solution of 4,6-dichloro-2-methylpyrimidine (5.2 g, 31.9 mmol) in dichloromethane (80 ml) at rt. The mixture was stirred for two hours and triethylamine (0.9 ml) was added. The mixture was stirred at rt for 20h. The resultant solid was filtered. The cake was washed with dichloromethane (20 ml). The filtrate was concentrated to give an oil. This oil was dried under high vacuum for 20h to give a solid. This solid was stirred with heptane (50 ml) at rt for 5h. Filtration gave 7C (8.13 g) as a white solid
7B. Example 7

To a 250 ml of round bottom flask were charged compound 5C (1.9 g, 7.1 mmol), compound 7C (1.5 g, 5.9 mmol), K2CO3 (16 g, 115.7 mmol), Pd (OAc)2 (52 mg, 0.23 mmol) and BINAP (291 mg, 0.46 mmol). The flask was placed under vacuum and flushed with nitrogen. Toluene was added (60 ml). The suspension was heated to 100-110° C. and stirred at this temperature for 20h. After cooling to room temperature, the mixture was applied to a silica gel column. The column was first eluted with EtOAC, and then with 10% of MeOH in EtOAC. Finally, the column was washed with 10% 2M ammonia solution in MeOH/90% EtOAC. The fractions which contained the desired product were collected and concentrated to give compound IV as a yellow solid (2.3 g).
Analytical MethodsSolid State Nuclear Magnetic Resonance (SSNMR)All solid-state C-13 NMR measurements were made with a Bruker DSX-400, 400 MHz NMR spectrometer. High resolution spectra were obtained using high-power proton decoupling and the TPPM pulse sequence and ramp amplitude cross-polarization (RAMP-CP) with magic-angle spinning (MAS) at approximately 12 kHz (A. E. Bennett et al, J. Chem. Phys., 1995, 103, 6951), (G. Metz, X. Wu and S. O. Smith, J. Magn. Reson. A., 1994, 110, 219-227). Approximately 70 mg of sample, packed into a canister-design zirconia rotor was used for each experiment. Chemical shifts (δ) were referenced to external adamantane with the high frequency resonance being set to 38.56 ppm (W. L. Earl and D. L. VanderHart, J. Magn. Reson., 1982, 48, 35-54).X-Ray Powder DiffractionOne of ordinary skill in the art will appreciate that an X-ray diffraction pattern may be obtained with a measurement error that is dependent upon the measurement conditions employed. In particular, it is generally known that intensities in a X-ray diffraction pattern may fluctuate depending upon measurement conditions employed. It should be further understood that relative intensities may also vary depending upon experimental conditions and, accordingly, the exact order of intensity should not be taken into account. Additionally, a measurement error of diffraction angle for a conventional X-ray diffraction pattern is typically about 5% or less, and such degree of measurement error should be taken into account as pertaining to the aforementioned diffraction angles. Consequently, it is to be understood that the crystal forms of the instant invention are not limited to the crystal forms that provide X-ray diffraction patterns completely identical to the X-ray diffraction patterns depicted in the accompanying Figures disclosed herein. Any crystal forms that provide X-ray diffraction patterns substantially identical to those disclosed in the accompanying Figures fall within the scope of the present invention. The ability to ascertain substantial identities of X-ray diffraction patterns is within the purview of one of ordinary skill in the art.X-Ray powder diffraction data for the crystalline forms of Compound (IV) were obtained using a Bruker GADDS (BRUKER AXS, Inc., 5465 East Cheryl Parkway Madison, Wis. 53711 USA) (General Area Detector Diffraction System) manual chi platform goniometer. Powder samples were placed in thin walled glass capillaries of 1 mm or less in diameter; the capillary was rotated during data collection. The sample-detector distance was 17 cm. The radiation was Cu Kα (45 kV 111 mA, λ=1.5418 Å). Data were collected for 3<2θ<35° with a sample exposure time of at least 300 seconds.Single Crystal X-RayAll single crystal data were collected on a Bruker-Nonius (BRUKER AXS, Inc., 5465 East Cheryl Parkway Madison, Wis. 53711 USA) Kappa CCD 2000 system using Cu Kα radiation (λ=1.5418 Å) and were corrected only for the Lorentz-polarization factors. Indexing and processing of the measured intensity data were carried out with the HKL2000 software package (Otwinowski, Z. & Minor, W. (1997) in Macromolecular Crystallography, eds. Carter, W. C. Jr & Sweet, R. M. (Academic, NY), Vol. 276, pp. 307-326) in the Collect program suite (Data collection and processing user interface: Collect: Data collection software, R. Hooft, Nonius B. V., 1998).The structures were solved by direct methods and refined on the basis of observed reflections using either the SDP (SDP, Structure Determination Package, Enraf-Nonius, Bohemia NY 11716 Scattering factors, including f′ and f″, in the SDP software were taken from the “International Tables for Crystallography”, Kynoch Press, Birmingham, England, 1974; Vol IV, Tables 2.2A and 2.3.1) software package with minor local modifications or the crystallographic package, MAXUS (maXus solution and refinement software suite: S. Mackay, C. J. Gilmore, C. Edwards, M. Tremayne, N. Stewart, K. Shankland. maXus: a computer program for the solution and refinement of crystal structures from diffraction data).The derived atomic parameters (coordinates and temperature factors) were refined through full matrix least-squares. The function minimized in the refinements was Σw(|Fo|−|Fc|)2. R is defined as Σ∥Fo|−|Fc∥/Σ|Fo| while Rw=[Σw(|Fo|−|Fc|)2/Σw|Fo|2]1/2 where w is an appropriate weighting function based on errors in the observed intensities. Difference maps were examined at all stages of refinement. Hydrogens were introduced in idealized positions with isotropic temperature factors, but no hydrogen parameters were varied.The derived atomic parameters (coordinates and temperature factors) were refined through full matrix least-squares. The function minimized in the refinements was Σw(|Fo|−|Fc|)2. R is defined as Σ∥Fo|−|Fc∥/Σ|Fo| while Rw=[Σw(|Fo|−|Fc|)2/Σw|Fo|2]1/2 where w is an appropriate weighting function based on errors in the observed intensities. Difference maps were examined at all stages of refinement. Hydrogens were introduced in idealized positions with isotropic temperature factors, but no hydrogen parameters were variedDifferential Scanning CalorimetryThe DSC instrument used to test the crystalline forms was a TA Instruments® model Q1000. The DSC cell/sample chamber was purged with 100 ml/min of ultra-high purity nitrogen gas. The instrument was calibrated with high purity indium. The accuracy of the measured sample temperature with this method is within about +/−1° C., and the heat of fusion can be measured within a relative error of about +/−5%. The sample was placed into an open aluminum DSC pan and measured against an empty reference pan. At least 2 mg of sample powder was placed into the bottom of the pan and lightly tapped down to ensure good contact with the pan. The weight of the sample was measured accurately and recorded to a hundredth of a milligram. The instrument was programmed to heat at 10° C. per minute in the temperature range between 25 and 350° C.The heat flow, which was normalized by a sample weight, was plotted versus the measured sample temperature. The data were reported in units of watts/gram (“W/g”). The plot was made with the endothermic peaks pointing down. The endothermic melt peak was evaluated for extrapolated onset temperature, peak temperature, and heat of fusion in this analysis.Thermogravimetric Analysis (TGA)The TGA instrument used to test the crystalline forms was a TAInstruments® model Q500. Samples of at least 10 milligrams were analyzed at a heating rate of 10° C. per minute in the temperature range between 25° C. and about 350° C.
Example 8Preparation of:
crystalline monohydrate of N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide (IV)An example of the crystallization procedure to obtain the crystalline monohydrate form is shown here:
- Charge 48 g of the compound of formula (IV).
- Charge approximately 1056 mL (22 mL/g) of ethyl alcohol, or other suitable alcohol.
- Charge approximately 144 mL of water.
- Dissolve the suspension by heating to approximately 75° C.
- Optional: Polish filter by transfer the compound of formula (IV) solution at 75° C. through the preheated filter and into the receiver.
- Rinse the dissolution reactor and transfer lines with a mixture of 43 mL of ethanol and 5 mL of water.
Heat the contents in the receiver to 75-80° C. and maintain 75-80° C. to achieve complete dissolution.Charge approximately 384 mL of water at a rate such that the batch temperature is maintained between 75-80° C.Cool to 75° C., and, optionally, charge monohydrate seed crystals. Seed crystals are not essential to obtaining monohydrate, but provide better control of the crystallization.
- Cool to 70° C. and maintain 70° C. for ca. 1 h.
- Cool from 70 to 5 C over 2 h, and maintain the temperature between 0 at 5° C. for at least 2 h.
- Filter the crystal slurry.
- Wash the filter cake with a mixture of 96 mL of ethanol and 96 mL of water.
- Dry the material at ≦50° C. under reduced pressure until the water content is 3.4 to 4.1% by KF to afford 41 g (85 M %).
Alternately, the monohydrate can be obtained by:- 1) An aqueous solution of the acetate salt of compound IV was seeded with monohydrate and heated at 80° C. to give bulk monohydrate.
- 2) An aqueous solution of the acetate salt of compound IV was seeded with monohydrate. On standing several days at room temperature, bulk monohydrate had formed.
- 3) An aqueous suspension of compound IV was seeded with monohydrate and heated at 70° C. for 4 hours to give bulk monohydrate. In the absence of seeding, an aqueous slurry of compound IV was unchanged after 82 days at room temperature.
- 4) A solution of compound IV in a solvent such as NMP or DMA was treated with water until the solution became cloudy and was held at 75-85° C. for several hours. Monohydrate was isolated after cooling and filtering.
- 5) A solution of compound IV in ethanol, butanol, and water was heated. Seeds of monohydrate were added to the hot solution and then cooled. Monohydrate was isolated upon cooling and filtration.
One of ordinary skill in the art will appreciate that the monohydrate of the compound of formula (IV) may be represented by the XRPD as shown in FIG. 1 or by a representative sampling of peaks as shown in Table 1.Representative peaks taken from the XRPD of the monohydrate of the compound of formula (IV) are shown in Table 1.TABLE 1 2-Theta d(Å) Height 17.994 4.9257 915 18.440 4.8075 338 19.153 4.6301 644 19.599 4.5258 361 21.252 4.1774 148 24.462 3.6359 250 25.901 3.4371 133 28.052 3.1782 153The XRPD is also characterized by the following list comprising 2θ values selected from the group consisting of: 4.6±0.2, 11.2±0.2, 13.8±0.2, 15.2±0.2, 17.9±0.2, 19.1±0.2, 19.6±0.2, 23.2±0.2, 23.6±0.2. The XRPD is also characterized by the list of 2θ values selected from the group consisting of: 18.0±0.2, 18.4±0.2, 19.2±0.2, 19.6±0.2, 21.2±0.2, 24.5±0.2, 25.9±0.2, and 28.0±0.2.Single crystal x-ray data was obtained at room temperature (+25° C.). The molecular structure was confirmed as a monohydrate form of the compound of Formula (IV).The following unit cell parameters were obtained for the monohydrate of the compound of formula (IV) from the x-ray analysis at 25° C.:a(Å)=13.8632(7); b(Å)=9.3307(3); c(Å)=38.390(2);V(Å3) 4965.9(4); Z′=1; Vm=621Space group PbcaMolecules/unit cell 8Density (calculated) (g/cm3) 1.354Wherein Z′=number of drug molecules per asymmetric unit. Vm=V(unit cell)/(Z drug molecules per cell).Single crystal x-ray data was also obtained at −50° C. The monohydrate form of the compound of Formula (IV) is characterized by unit cell parameters approximately equal to the following:Cell dimensions:
- a(Å)=13.862(1);
- b(Å)=9.286(1);
- c(Å)=38.143(2);
Volume=4910(1) Å3Space group PbcaMolecules/unit cell 8Density (calculated) (g/cm3) 1.369wherein the compound is at a temperature of about −50° C.The simulated XRPD was calculated from the refined atomic parameters at room temperature.The monohydrate of the compound of formula (IV) is represented by the DSC as shown in FIG. 2. The DSC is characterized by a broad peak between approximately 95° C. and 130° C. This peak is broad and variable and corresponds to the loss of one water of hydration as seen in the TGA graph. The DSC also has a characteristic peak at approximately 287° C. which corresponds to the melt of the dehydrated form of the compound of formula (IV).The TGA for the monohydrate of the compound of Formula (IV) is shown in FIG. 2 along with the DSC. The TGA shows a 3.48% weight loss from 50° C. to 175° C. The weight loss corresponds to a loss of one water of hydration from the compound of Formula (IV).The monohydrate may also be prepared by crystallizing from alcoholic solvents, such as methanol, ethanol, propanol, i-propanol, butanol, pentanol, and water.
Example 9Preparation of:
crystalline n-butanol solvate of N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide (IV)The crystalline butanol solvate of the compound of formula (IV) is prepared by dissolving compound (IV) in 1-butanol at reflux (116-118° C.) at a concentration of approximately 1 g/25 mL of solvent. Upon cooling, the butanol solvate crystallizes out of solution. Filter, wash with butanol, and dry.The following unit cell parameters were obtained from the x-ray analysis for the crystalline butanol solvate, obtained at room temperature:a(Å)=22.8102(6); b(Å)=8.4691(3); c(Å)=15.1436(5); β=95.794(2);V(Å3) 2910.5(2); Z′=1; Vm=728Space group P21/aMolecules/unit cell 4Density (calculated) (g/cm3) 1.283Wherein Z′=number of drug molecules per asymmetric unit. Vm=V(unit cell)/(Z drug molecules per cell).One of ordinary skill in the art will appreciate that the butanol solvate of the compound of formula (IV) may be represented by the XRPD as shown in FIG. 3 or by a representative sampling of peaks. Representative peaks for the crystalline butanol solvate are 2θ values of: 5.9±0.2, 12.0±0.2, 13.0±0.2, 17.7±0.2, 24.1±0.2, and 24.6±0.2.
Example 10Preparation of:
crystalline ethanol solvate of N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide (IV)

To a 100-mL round bottom flask was charged 4.00 g (10.1 mmol) of 5D (contained 2.3 Area % 5C) 6.60 g (50.7 mmol) of 7B, 80 mL of n-butanol and 2.61 g (20.2 mmol) of DIPEA. The resulting slurry was heated to 120° C. and maintained at 120° C. for 4.5 h whereby HPLC analysis showed 0.19 relative Area % of residual 5D to compound IV. The homogeneous mixture was cooled to 20° C. and left stirring overnight. The resulting crystals were filtered. The wet cake was washed twice with 10-mL portions of n-butanol to afford a white crystalline product. HPLC analysis showed this material to contain 99.7 Area % compound IV and 0.3 Area % 5C.The resulting wet cake was returned to the 100-mL reactor, and charged with 56 mL (12 mL/g) of 200 proof ethanol. At 80° C. an additional 25 mL of ethanol was added. To this mixture was added 10 mL of water resulting in rapid dissolution. Heat was removed and crystallization was observed at 75-77° C. The crystal slurry was further cooled to 20° C. and filtered. The wet cake was washed once with 10 mL of 1:1 ethanol: water and once with 10 mL of n-heptane. The wet cake contained 1.0% water by KF and 8.10% volatiles by LOD. The material was dried at 60° C./30 in Hg for 17 h to afford 3.55 g (70 M %) of material containing only 0.19% water by KF, 99.87 Area % by HPLC. The 1H NMR spectrum, however revealed that the ethanol solvate had been formed.The following unit cell parameters were obtained from the x-ray analysis for the crystalline ethanol solvate (di-ethanolate, E2-1), obtained at −40° C.:a(Å)=22.076(1); b(Å)=8.9612(2); c(Å)=16.8764(3); β=114.783(1);V(Å3) 3031.1(1); Z′=1; Vm=758Space group P21/aMolecules/unit cell 4Density (calculated) (g/cm3) 1.271Wherein Z′=number of drug molecules per asymmetric unit. Vm=V(unit cell)/(Z drug molecules per cell).One of ordinary skill in the art will appreciate that the ethanol solvate (E2-1) of the compound of formula (IV) may be represented by the XRPD as shown in FIG. 4 or by a representative sampling of peaks. Representative peaks for the crystalline ethanol solvate are 2θ values of: 5.8±0.2, 11.3±0.2, 15.8±0.2, 17.2±0.2, 19.5±0.2, 24.1±0.2, 25.3±0.2, and 26.2±0.2.In addition, during the process to form the ethanolate (diethanolate) the formation of another ethanol solvate (½ ethanolate, T1E2-1) has been observed. To date this additional ethaonol solvate is known strictly as a partial desolvation product of the original diethanolate form E2-1, and has only been observed on occasion during crystallization of E2-1The following unit cell parameters were obtained from the x-ray analysis for the crystalline ½ ethanol solvate T1E2-1, obtained at −10° C.:a(Å)=22.03(2); b(Å)=9.20(1); c(Å)=12.31(1);β=93.49(6)V(Å3) 2491(4)); Z′=1; Vm=623;Space group P21/aMolecules/unit cell 4Density (calculated) (g/cm3) 1.363Wherein Z′=number of drug molecules per asymmetric unit. Vm=V(unit cell)/(Z drug molecules per cell).One of ordinary skill in the art will appreciate that the ethanol solvate (T1E2-1) of the compound of formula (IV) may be represented by the XRPD as shown in FIG. 7 or by a representative sampling of peaks. Representative peaks for the crystalline ethanol solvate are 2θ values of: 7.20±0.2, 12.01±0.2, 12.81±0.2, 18.06±0.2, 19.30±0.2, and 25.24±0.2.
Example 11Preparation of:
crystalline N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide (IV) (Neat form N-6)To a mixture of compound 5D (175.45 g, 0.445 mol) and hydroxyethylpiperazine (289.67 g, 2.225 mol) in NMP (1168 mL) was added DIPEA (155 mL, 0.89 mol). The suspension was heated at 110° C. (solution obtained) for 25 min., then cooled to about 90° C. The resulting hot solution was added dropwise into hot (80° C.) water (8010) mL, keeping the temperature at about 80° C. The resulting suspension was stirred 15 min at 80° C. then cooled slowly to room temperature. The solid was collected by vacuum filtration, washed with water (2×1600 mL) and dried in vacuo at 55-60° C. affording 192.45 g (88.7% yield) of N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide. 1H NMR (400 MHz, DMSO-d6): δ 2.24 (s, 3H), 2.41 (s, 3H), 2.43 (t, 2H, J=6), 2.49 (t, 4H, J=6.3), 3.51 (m, 4H), 3.54 (q, 2H, J=6), 4.46 (t, 1H, J=5.3), 6.05 (s, 1H), 7.26 (t, 1H, J=7.6), 7.28 (dd, 1H, J=7.6, 1.7), 7.41 (dd, 1H, J=7.6, 1.7), 8.23 (s, 1H), 9.89 (s, 1H), 11.48. KF0.84; DSC: 285.25° C. (onset), 286.28° C. (max).The following unit cell parameters were obtained from the x-ray analysis for the neat crystalline compound IV, obtained at 23° C.:a(Å)=22.957(1); b(Å)=8.5830(5); c(Å)=13.803(3); β=112.039(6);V(Å3)=2521.0(5); Z′=1; Vm=630Space group P21/aMolecules/unit cell 4Density (calculated) (g/cm3) 1.286Wherein Z′=number of drug molecules per asymmetric unit. Vm=V(unit cell)/(Z drug molecules per cell).One of ordinary skill in the art will appreciate that the crystalline form of the compound of formula (IV) may be represented by the XRPD as shown in FIG. 5 or by a representative sampling of peaks. Representative peaks for the crystalline neat form (N-6) are 2θ values of: 6.8±0.2, 11.1±0.2, 12.3±0.2, 13.2±0.2, 13.7±0.2, 16.7±0.2, 21.0±0.2, 24.3±0.2, and 24.8±0.2.
Example 12Preparation of:
crystalline N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide (IV) (neatform T1H1-7)The title neat form may be prepared by heating the monohydrate form of the compound of formula (IV) above the dehydration temperature.The following unit cell parameters were obtained from the x-ray analysis for the neat crystalline (T1H1-7) compound IV, obtained at 25° C.:a(Å)=13.4916; b(Å)=9.3992(2); c(Å)=38.817(1);V(Å3)=4922.4(3); Z′=1; Vm=615Space group PbcaDensity (calculated) (g/cm3) 1.317Wherein Z′=number of drug molecules per asymmetric unit. Vm=V(unit cell)/(Z drug molecules per cell).One of ordinary skill in the art will appreciate that the neat crystalline form (T1H1-7) of the compound of formula (IV) may be represented by the XRPD as shown in FIG. 6 or by a representative sampling of peaks. Representative peaks for the crystalline neat form (T1H1-7)) are 2θ values of: 8.0±0.2, 9.7±0.2, 11.2±0.2, 13.3±0.2, 17.5±0.2, 18.9±0.2, 21.0±0.2, 22.0±0.2.Obviously, numerous modifications and variations of the present invention are possible in light of the above teachings. It is therefore to be understood that within the scope of the appended claims, the invention may be practiced otherwise than as specifically described herein.PATENThttps://patents.google.com/patent/US8680103B2/enAminothiazole-aromatic amides of formula I

wherein Ar is aryl or heteroaryl, L is an optional alkylene linker, and R2, R3, R4, and R5, are as defined in the specification herein, are useful as kinase inhibitors, in particular, inhibitors of protein tyrosine kinase and p38 kinase. They are expected to be useful in the treatment of protein tyrosine kinase-associated disorders such as immunologic and oncological disorders [see, U.S. Pat. No. 6,596,746 (the ‘746 patent), assigned to the present assignee and incorporated herein by reference], and p38 kinase-associated conditions such as inflammatory and immune conditions, as described in U.S. patent application Ser. No. 10/773,790, filed Feb. 6, 2004, claiming priority to U.S. Provisional application Ser. No. 60/445,410, filed Feb. 6, 2003 (hereinafter the ‘410 application), both of which are also assigned to the present assignee and incorporated herein by reference.The compound of formula (IV), ′N-(2-Chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)-1-piperazinyl]-2-methyl-4-pyrimidinyl]amino]-5-thiazolecarboxamide, is an inhibitor of SRC/ABL and is useful in the treatment of oncological diseases.

Other approaches to preparing 2-aminothiazole-5-carboxamides are described in the ‘746 patent and in the ‘410 application. The ‘746 patent describes a process involving treatment of chlorothiazole with n-BuLi followed by reaction with phenyl isocyanates to give chlorothiazole-benzamides, which are further elaborated to aminothiazole-benzamide final products after protection, chloro-to-amino substitution, and deprotection, e.g.,

The ‘410 application describes a multi-step process involving first, converting N-unsubstituted aminothiazole carboxylic acid methyl or ethyl esters to bromothiazole carboxylic acid esters via diazotization with tert-butyl nitrite and subsequent CuBr2 treatment, e.g.,

then, hydrolyzing the resulting bromothiazole esters to the corresponding carboxylic acids and converting the acids to the corresponding acyl chlorides, e.g.,

then finally, coupling the acyl chlorides with anilines to afford bromothiazole-benzamide intermediates which were further elaborated to aminothiazole-benzamide final products, e.g.,

Other approaches for making 2-aminothiazole-5-carboxamides include coupling of 2-aminothiazole-5-carboxylic acids with amines using various coupling conditions such as DCC [Roberts et al, J. Med. Chem. (1972), 15, at p. 1310], and DPPA [Marsham et al., J. Med. Chem. (1991), 34, at p. 1594)].The above methods present drawbacks with respect to the production of side products, the use of expensive coupling reagents, less than desirable yields, and the need for multiple reaction steps to achieve the 2-aminothiazole-5-carboxamide compounds.Reaction of N,N-dimethyl-N′-(aminothiocarbonyl)-formamidines with α-haloketones and esters to give 5-carbonyl-2-aminothiazoles has been reported. See Lin, Y. et al, J. Heterocycl. Chem. (1979), 16, at 1377; Hartmann, H. et al, J. Chem. Soc. Perkin Trans. (2000), 1, at 4316; Noack, A. et al; Tetrahedron (2002), 58, at 2137; Noack, A.; et al. Angew. Chem. (2001), 113, at 3097; and Kantlehner, W. et al., J. Prakt. Chem./Chem.-Ztg. (1996), 338, at 403. Reaction of β-ethoxy acrylates and thioureas to prepare 2-aminothiazole-5-carboxylates also has been reported. See Zhao, R., et al., Tetrahedron Lett. (2001), 42, at 2101. However, electrophilic bromination of acrylanilide and crotonanilide has been known to undergo both aromatic bromination and addition to the α,β-unsaturated carbon-carbon double bonds. See Autenrieth, Chem. Ber. (1905), 38, at 2550; Eremeev et al., Chem. Heterocycl. Compd. Engl. Transl. (1984), 20, at 1102.New and efficient processes for preparing 2-aminothiazole-5-carboxamides are desired.
SUMMARY OF THE INVENTION
This invention is related to processes for the preparation of 2-aminothiazole-5-aromatic amides having the formula (I),

wherein L, Ar, R2, R3, R4, R5, and m are as defined below, comprising reacting a compound having the formula (II),

wherein Q is the group —O—P*, wherein P* is selected so that, when considered together with the oxygen atom to which P* is attached, Q is a leaving group, and Ar, L, R2, R3, and m are as defined below,
with a halogenating reagent in the presence of water followed by a thiourea compound having the formula (III),

wherein, R4 and R5 are as defined below,
to provide the compound of formula (I),

wherein,Ar is the same in formulae (I) and (II) and is aryl or heteroaryl;L is the same in formulae (I) and (II) and is optionally-substituted alkylene;R2 is the same in formulae (I) and (II), and is selected from hydrogen, alkyl, substituted alkyl, alkenyl, substituted alkenyl, alkynyl, substituted alkynyl, aryl, heteroaryl, cycloalkyl, and heterocyclo;R3 is the same in formulae (I) and (II), and is selected from hydrogen, halogen, cyano, haloalkyl, alkyl, substituted alkyl, alkenyl, substituted alkenyl, aryl, heteroaryl, cycloalkyl, and heterocyclo;R4 is (i) the same in each of formulae (I) and (III), and (ii) is independently selected from hydrogen, alkyl, substituted alkyl, alkenyl, substituted alkenyl, alkynyl, substituted alkynyl, aryl, heteroaryl, cycloalkyl, and heterocyclo, or alternatively, R4 is taken together with R5, to form heteroaryl or heterocyclo;R5 is (i) the same in each of formulae (I) and (III), and (ii) is independently selected from hydrogen, alkyl, substituted alkyl, alkenyl, substituted alkenyl, alkynyl, substituted alkynyl, aryl, heteroaryl, cycloalkyl, and heterocyclo, or alternatively, R5 is taken together with R4, to form heteroaryl or heterocyclo; andm is 0 or 1.Applicants have surprisingly discovered said process for converting β-(P*)oxy acryl aromatic amides and thioureas to 2-aminothiazole derivatives, wherein the aromatic amides are not subject to further halogenation producing other side products. Aminothiazole-aromatic amides, particularly, 2-aminothiazole-5-benzamides, can thus be efficiently prepared with this process in high yield.In another aspect, the present invention is directed to crystalline forms of the compound of formula (IV).
EXAMPLESExample 1Preparation of Intermediate:
(S)-1-sec-Butylthiourea

To a solution of S-sec-butyl-amine (7.31 g, 0.1 mol) in chloroform (80 mL) at 0° C. was slowly added benzoyl isothiocyanate (13.44 mL, 0.1 mol). The mixture was allowed to warm to 10° C. and stirred for 10 min. The solvent was then removed under reduced pressure, and the residue was dissolved in MeOH (80 mL). An aqueous solution (10 mL) of NaOH (4 g, 0.1 mol) was added to this solution, and the mixture was stirred at 60° C. for another 2 h. The MeOH was then removed under reduced pressure, and the residue was stirred in water (50 mL). The precipitate was collected by vacuum filtration and dried to provide S-1-sec-butyl-thiourea (12.2 g, 92% yield). mp 133-134° C.; 1H NMR (500 MHz, DMSO-D6) δ 7.40 (s, 1H), 7.20 (br s, 1H), 6.76 (s, 1H), 4.04 (s, 1H), 1.41 (m, 2H), 1.03 (d, J=6.1 Hz, 3H), 0.81 (d, J=7.7 Hz, 3H); 13C NMR (125 MHz, DMSO-D6) δ 182.5, 50.8, 28.8, 19.9, 10.3; LRMS m/z 133.2 (M+H); Anal. Calcd for C5H12N2S: C, 45.41; H, 9.14; N, 21.18; S, 24.25. Found: C, 45.49; H, 8.88; N, 21.32; S, 24.27.
Example 2Preparation of Intermediate:
(R)-1-sec-Butylthiourea

(R)-1-sec-Butylthiourea was prepared in 92% yield according to the general method outlined for Example 1. mp 133-134° C.; 1H NMR (500 MHz, DMSO) δ 0.80 (m, 3H, J=7.7), 1.02 (d, 3H, J=6.1), 1.41 (m, 2H), (3.40, 4.04) (s, 1H), 6.76 (s, 1H), 7.20 (s, br, 1H), 7.39 (d, 1H, J=7.2); 13C NMR (500 MHz, DMSO) δ: 10.00, 19.56, 28.50, 50.20, 182.00; m/z 133.23 (M+H); Anal. Calcd for C5H12N2S: C, 45.41; H, 9.14; N, 21.18; S, 24.25. Found: C, 45.32; H, 9.15; N, 21.14; S, 24.38.
Example 3Preparation of:

To a solution of 3-amino-N-methyl-4-methylbenzamide hydrochloride (1.0 g, 5 mmol) in acetone (10 mL) at 0° C. was added pyridine (1.2 mL, 15 mmol) dropwise via syringe. 3-Methoxyacryloyl chloride (0.72 mL 6.5 mmol) was added and the reaction stirred at room temperature for 1 h. The solution was cooled again to 0° C. and 1N HCl (1.5 mL) was added dropwise via pipette. The reaction mixture was stirred for 5 min, then water (8.5 mL) was added via an addition funnel. The acetone was removed in vacuo and the resulting solution stirred for 4 h. Crystallization began within 15 min. After stirring for 4 h, the vessel was cooled in an ice bath for 30 min, filtered, and rinsed with ice cold water (2×3 mL) to give compound 3A (0.99 g, 78% yield) as a white solid. 1H NMR (400 MHz, CDCl3) δ 8.95 (s, 1H), 8.12 (br s, 1H), 7.76 (s, 1H), 7.29 (m, 2H), 7.05 (d, J=7.9 Hz, 1H), 5.47 (d, J=12.3 Hz, 1H), 3.48 (s, 3H), 2.54 (d, J=4.7 Hz, 3H), 2.03 (s, 3H); HPLC rt 2.28 min (Condition A).
3B. Example 3To a 50 mL RBF containing the above compound 3A (0.5 g, 2.0 mmol) was added THF (2.5 mL) and water (2 mL), followed by NBS (0.40 g, 2.22 mmol), and the solution was stirred for 90 min. R-sec-butylthiourea (Ex. 2) (267 mg), was added, and the solution was heated to 75° C. for 8 h. Conc. NH4OH was added to adjust the pH to 10 followed by the addition of EtOH (15 mL). Water (15 mL) was added and the slurry stirred for 16 h, filtered, and washed with water to give Example 3 as a light brown solid (0.48 g, 69% yield, 98% purity). MS 347.1; HPLC 2.59.
Example 4Preparation of:

Example 4 is prepared following the methods of Example 3 but using the appropriate acryl benzamide and Example 1.
Example 5Preparation of:
N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide (The compound of Formula (IV))

5A. 1-(6-Chloro-2-methylpyrimidin-4-yl)thiourea

To a stirring slurry of 4-amino-5-chloro-2-methylpyrimidine (6.13 g, 42.7 mmol) in THF (24 mL) was added ethyl isothiocyanatoformate (7.5 mL, 63.6 mmol), and the mixture heated to reflux. After 5 h, another portion of ethyl isothiocyanato formate (1.0 mL, 8.5 mmol) was added and after 10 h, a final portion (1.5 mL, 12.7 mmol) was added and the mixture stirred 6 h more. The slurry was evaporated under vacuum to remove most of the solvent and heptane (6 mL) added to the residue. The solid was collected by vacuum filtration and washed with heptane (2×5 mL) giving 8.01 g (68% yield) of the intermediate ethyl 6-chloro-2-methylpyrimidin-4-ylcarbamothioylcarbamate.A solution of ethyl 6-chloro-2-methylpyrimidin-4-ylcarbamothioylcarbamate (275 mg, 1.0 mmol) and 1N sodium hydroxide (3.5 eq) was heated and stirred at 50° C. for 2 h. The resulting slurry was cooled to 20-22° C. The solid was collected by vacuum filtration, washed with water, and dried to give 185 mg of 1-(6-chloro-2-methylpyrimidin-4-yl)thiourea (91% yield). 1H NMR (400 MHz, DMSO-d6): δ2.51 (S, 3H), 7.05 (s, 1H), 9.35 (s, 1H), 10.07 (s, 1H), 10.91 (s, 1H); 13C NMR (125 MHz, DMSO-d6) δ: 25.25, 104.56, 159.19, 159.33, 167.36, 180.91.
5B. (E)-N-(2-Chloro-6-methylphenyl)-3-ethoxyacrylamide

To a cold stirring solution of 2-chloro-6-methylaniline (59.5 g 0.42 mol) and pyridine (68 ml, 0.63 mol) in THF (600 mL) was added 3-ethoxyacryloyl chloride (84.7 g, 0.63 mol) slowly keeping the temp at 0-5° C. The mixture was then warmed and stirred for 2 h. at 20° C. Hydrochloric acid (1N, 115 mL) was added at 0-10° C. The mixture was diluted with water (310 mL) and the resulting solution was concentrated under vacuum to a thick slurry. The slurry was diluted with toluene (275 mL) and stirred for 15 min. at 20-22° C. then 1 h. at 0° C. The solid was collected by vacuum filtration, washed with water (2×75 mL) and dried to give 74.1 g (73.6% yield) of (E)-N-(2-chloro-6-methylphenyl)-3-ethoxyacrylamide). 1H NMR (400 Hz, DMSO-d6) δ 1.26 (t, 3H, J=7 Hz), 2.15 (s, 3H), 3.94 (q, 2H, J=7 Hz), 5.58 (d, 1H, J=12.4 Hz), 7.10-7.27 (m, 2H, J=7.5 Hz), 7.27-7.37 (d, 1H, J=7.5 Hz), 7.45 (d, 1H, J=12.4 Hz), 9.28 (s, 1H); 13C NMR (100 MHz, CDCl3) δ: 14.57, 18.96, 67.17, 97.99, 126.80, 127.44, 129.07, 131.32, 132.89, 138.25, 161.09, 165.36.
5C. 2-Amino-N-(2-chloro-6-methylphenyl)thiazole-5-carboxamide

To a mixture of compound 5B (5.00 g, 20.86 mmol) in 1,4-dioxane (27 mL) and water (27 mL) was added NBS (4.08 g, 22.9 mmol) at −10 to 0° C. The slurry was warmed and stirred at 20-22° C. for 3 h. Thiourea (1.60 g, 21 mmol) was added and the mixture heated to 80° C. After 2 h, the resulting solution was cooled to 20-22° and conc. ammonium hydroxide (4.2 mL) was added dropwise. The resulting slurry was concentrated under vacuum to about half volume and cooled to 0-5° C. The solid was collected by vacuum filtration, washed with cold water (10 mL), and dried to give 5.3 g (94.9% yield) of 2-amino-N-(2-chloro-6-methylphenyl)thiazole-5-carboxamide. 1H NMR (400 MHz, DMSO-d6) δ δ 2.19 (s, 3H), 7.09-7.29 (m, 2H, J=7.5), 7.29-7.43 (d, 1H, J=7.5), 7.61 (s, 2H), 7.85 (s, 1H), 9.63 (s, 1H); 13C NMR (125 MHz, DMSO-d6) δ: 18.18, 120.63, 126.84, 127.90, 128.86, 132.41, 133.63, 138.76, 142.88, 159.45, 172.02.
5D. 2-(6-Chloro-2-methylpyrimidin-4-ylamino)-N-(2-chloro-6-methylphenyl)thiazole-5-carboxamide

To a stirring solution of compound 5C (5.00 g, 18.67 mmol) and 4,6-dichloro-2-methylpyrimidine (3.65 g 22.4/mmol) in THF (65 mL) was added a 30% wt. solution of sodium t-butoxide in THF (21.1 g, 65.36 mmol) slowly with cooling to keep the temperature at 10-20° C. The mixture was stirred at room temperature for 1.5 h and cooled to 0-5° C. Hydrochloric acid, 2N (21.5 mL) was added slowly and the mixture stirred 1.75 h at 0-5° C. The solid was collected by vacuum filtration, washed with water (15 mL) and dried to give 6.63 g (86.4% yield) of compound 5D. 1H NMR (400 MHz, DMSO-d6) δ 2.23 (s, 3H), 2.58 (s, 3H), 6.94 (s, 1H), 7.18-7.34, (m, 2H, J=7.5), 7.34-7.46 (d, 1H, J=7.5), 8.31 (s, 1H), 10.02 (s, 1H), 12.25 (s, 1H).
5E. Example 5To a mixture of compound 5D (4.00 g, 10.14 mmol) and hydroxyethylpiperazine (6.60 g, 50.69 mmol) in n-butanol (40 mL) was added DIPEA (3.53 mL, 20.26 mmol). The slurry was heated at 118° C. for 4.5 h, then cooled slowly to room temperature. The solid was collected by vacuum filtration, washed with n-butanol (5 mL), and dried. The product (5.11 g) was dissolved in hot 80% EtOH—H2O (80 mL), and the solution was clarified by filtration. The hot solution was slowly diluted with water (15 mL) and cooled slowly to room temperature. The solid was collected by vacuum filtration, washed with 50% ethanol-water (5 mL) and dried affording 4.27 g (83.2% yield) of N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide as monohydrate. 1H NMR (400 MHz, DMSO-d6) δ 2.23 (s, 3H), 2.40 (s, 3H), 2.42 (t, 2H, J=6), 2.48 (t, 4H, J=6.3), 3.50 (m, 4H), 3.53 (q, 2H, J=6), 4.45 (t, 1H, J=5.3), 6.04 (s, 1H), 7.25 (t, 1H, J=7.6), 7.27 (dd, 1H, J=7.6, 1.7), 7.40 (dd, 1H, J=7.6, 1.7), 8.21 (s, 1H), 9.87 (s, 1H), 11.47.
Example 6Preparation of:
N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide

To a slurry of (E)-N-(2-chloro-6-methylphenyl)-3-ethoxyacrylamide 5B (120 mg, 0.50 mmol) in THF (0.75 ml) and water (0.5 mL) was added NBS (98 mg, 0.55 mmol) at 0° C. The mixture was warmed and stirred at 20-22° C. for 3 h. To this was added 1-(6-chloro-2-methylpyrimidin-4-yl)thiourea 5A (100 mg, 0.49 mmol), and the slurry heated and stirred at reflux for 2 h. The slurry was cooled to 20-22° C. and the solid collected by vacuum filtration giving 140 mg (71% yield) of 2-(6-chloro-2-methylpyrimidin-4-ylamino)-N-(2-chloro-6-methylphenyl)thiazole-5-carboxamide 5D. 1H NMR (400 MHz, DMSO-d6) δ 2.23 (s, 3H), 2.58 (s, 3H), 6.94 (s, 1H), 7.18-7.34, (m, 2H, J=7.5), 7.34-7.46 (d, 1H, J=7.5), 8.31 (s, 1H), 10.02 (s, 1H), 12.25 (s, 1H).Compound 5D was elaborated to N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide, following Step 5E.
Example 7Preparation of:
N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide7A. 2-[4-(6-Chloro-2-methyl-pyrimidin-4-yl)-piperazin-1-yl]-ethanol

2-Piperazin-1-yl-ethanol (8.2 g, 63.1 mmol) was added to a solution of 4,6-dichloro-2-methylpyrimidine (5.2 g, 31.9 mmol) in dichloromethane (80 ml) at rt. The mixture was stirred for two hours and triethylamine (0.9 ml) was added. The mixture was stirred at rt for 20 h. The resultant solid was filtered. The cake was washed with dichloromethane (20 ml). The filtrate was concentrated to give an oil. This oil was dried under high vacuum for 20 h to give a solid. This solid was stirred with heptane (50 ml) at rt for 5 h. Filtration gave 7C (8.13 g) as a white solid
7B. Example 7

To a 250 ml of round bottom flask were charged compound 5C (1.9 g, 7.1 mmol), compound 7C (1.5 g, 5.9 mmol), K2CO3 (16 g, 115.7 mmol), Pd (OAc)2 (52 mg, 0.23 mmol) and BINAP (291 mg, 0.46 mmol). The flask was placed under vacuum and flushed with nitrogen. Toluene was added (60 ml). The suspension was heated to 100-110° C. and stirred at this temperature for 20 h. After cooling to room temperature, the mixture was applied to a silica gel column. The column was first eluted with EtOAC, and then with 10% of MeOH in EtOAC. Finally, the column was washed with 10% 2M ammonia solution in MeOH/90% EtOAC. The fractions which contained the desired product were collected and concentrated to give compound IV as a yellow solid (2.3 g).
Analytical MethodsSolid State Nuclear Magnetic Resonance (SSNMR)All solid-state C-13 NMR measurements were made with a Bruker DSX-400, 400 MHz NMR spectrometer. High resolution spectra were obtained using high-power proton decoupling and the TPPM pulse sequence and ramp amplitude cross-polarization (RAMP-CP) with magic-angle spinning (MAS) at approximately 12 kHz (A. E. Bennett et al, J. Chem. Phys., 1995, 103, 6951), (G. Metz, X. Wu and S. O, Smith, J. Magn. Reson. A, 1994, 110, 219-227). Approximately 70 mg of sample, packed into a canister-design zirconia rotor was used for each experiment. Chemical shifts (6) were referenced to external adamantane with the high frequency resonance being set to 38.56 ppm (W. L. Earl and D. L. VanderHart, J. Magn. Reson., 1982, 48, 35-54).X-Ray Powder DiffractionOne of ordinary skill in the art will appreciate that an X-ray diffraction pattern may be obtained with a measurement error that is dependent upon the measurement conditions employed. In particular, it is generally known that intensities in a X-ray diffraction pattern may fluctuate depending upon measurement conditions employed. It should be further understood that relative intensities may also vary depending upon experimental conditions and, accordingly, the exact order of intensity should not be taken into account. Additionally, a measurement error of diffraction angle for a conventional X-ray diffraction pattern is typically about 5% or less, and such degree of measurement error should be taken into account as pertaining to the aforementioned diffraction angles. Consequently, it is to be understood that the crystal forms of the instant invention are not limited to the crystal forms that provide X-ray diffraction patterns completely identical to the X-ray diffraction patterns depicted in the accompanying Figures disclosed herein. Any crystal forms that provide X-ray diffraction patterns substantially identical to those disclosed in the accompanying Figures fall within the scope of the present invention. The ability to ascertain substantial identities of X-ray diffraction patterns is within the purview of one of ordinary skill in the art.X-Ray powder diffraction data for the crystalline forms of Compound (IV) were obtained using a Bruker GADDS (BRUKER AXS, Inc., 5465 East Cheryl Parkway Madison, Wis. 53711 USA) (General Area Detector Diffraction System) manual chi platform goniometer. Powder samples were placed in thin walled glass capillaries of 1 mm or less in diameter; the capillary was rotated during data collection. The sample-detector distance was 17 cm. The radiation was Cu Kα (45 kV 111 mA, λ=1.5418 Å). Data were collected for 3<2θ<35° with a sample exposure time of at least 300 seconds.Single Crystal X-RayAll single crystal data were collected on a Bruker-Nonius (BRUKER AXS, Inc., 5465 East Cheryl Parkway Madison, Wis. 53711 USA) Kappa CCD 2000 system using Cu Kα radiation (λ=1.5418 Å) and were corrected only for the Lorentz-polarization factors. Indexing and processing of the measured intensity data were carried out with the HKL2000 software package (Otwinowski, Z. & Minor, W. (1997) in Macromolecular Crystallography, eds. Carter, W. C. Jr. & Sweet, R. M. (Academic, NY), Vol. 276, pp. 307-326) in the Collect program suite (Data collection and processing user interface: Collect: Data collection software, R. Hooft, Nonius B. V., 1998).The structures were solved by direct methods and refined on the basis of observed reflections using either the SDP (SDP, Structure Determination Package, Enraf-Nonius, Bohemia N.Y. 11716 Scattering factors, including f′ and f″, in the SDP software were taken from the “International Tables for Crystallography”, Kynoch Press, Birmingham, England, 1974; Vol IV, Tables 2.2A and 2.3.1) software package with minor local modifications or the crystallographic package, MAXUS (maXus solution and refinement software suite: S. Mackay, C. J. Gilmore, C. Edwards, M. Tremayne, N. Stewart, K. Shankland. maXus: a computer program for the solution and refinement of crystal structures from diffraction data).The derived atomic parameters (coordinates and temperature factors) were refined through full matrix least-squares. The function minimized in the refinements was Σw(|Fo|−|Fc|)2. R is defined as Σ∥Fo|−|Fc∥/Σ|Fo| while Rw=[Σw(|Fo|−|Fc|)2/Σw|Fo|2]1/2 where w is an appropriate weighting function based on errors in the observed intensities. Difference maps were examined at all stages of refinement. Hydrogens were introduced in idealized positions with isotropic temperature factors, but no hydrogen parameters were varied.The derived atomic parameters (coordinates and temperature factors) were refined through full matrix least-squares. The function minimized in the refinements was Σw(|Fo|−|Fc|)2. R is defined as Σ∥Fo|−|Fc∥/Σ|Fo| while Rw=[Σw(|Fo|−|Fc|)2/Σw|Fo|2]1/2 where w is an appropriate weighting function based on errors in the observed intensities. Difference maps were examined at all stages of refinement. Hydrogens were introduced in idealized positions with isotropic temperature factors, but no hydrogen parameters were variedDifferential Scanning CalorimetryThe DSC instrument used to test the crystalline forms was a TA INSTRUMENTS° model Q1000. The DSC cell/sample chamber was purged with 100 ml/min of ultra-high purity nitrogen gas. The instrument was calibrated with high purity indium. The accuracy of the measured sample temperature with this method is within about +/−1° C., and the heat of fusion can be measured within a relative error of about +/−5%. The sample was placed into an open aluminum DSC pan and measured against an empty reference pan. At least 2 mg of sample powder was placed into the bottom of the pan and lightly tapped down to ensure good contact with the pan. The weight of the sample was measured accurately and recorded to a hundredth of a milligram. The instrument was programmed to heat at 10° C. per minute in the temperature range between 25 and 350° C.The heat flow, which was normalized by a sample weight, was plotted versus the measured sample temperature. The data were reported in units of watts/gram (“W/g”). The plot was made with the endothermic peaks pointing down. The endothermic melt peak was evaluated for extrapolated onset temperature, peak temperature, and heat of fusion in this analysis.Thermogravimetric Analysis (TGA)The TGA instrument used to test the crystalline forms was a TA INSTRUMENTS® model Q500. Samples of at least 10 milligrams were analyzed at a heating rate of 10° C. per minute in the temperature range between 25° C. and about 350° C.
Example 8Preparation of:
Crystalline monohydrate of N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide (IV)An example of the crystallization procedure to obtain the crystalline monohydrate form is shown here:Charge 48 g of the compound of formula (IV).Charge approximately 1056 mL (22 mL/g) of ethyl alcohol, or other suitable alcohol.Charge approximately 144 mL of water.Dissolve the suspension by heating to approximately 75° C.Optional: Polish filter by transfer the compound of formula (IV) solution at 75° C. through the preheated filter and into the receiver.Rinse the dissolution reactor and transfer lines with a mixture of 43 mL of ethanol and 5 mL of water.Heat the contents in the receiver to 75-80° C. and maintain 75-80° C. to achieve complete dissolution.Charge approximately 384 mL of water at a rate such that the batch temperature is maintained between 75-80° C.Cool to 75° C., and, optionally, charge monohydrate seed crystals. Seed crystals are not essential to obtaining monohydrate, but provide better control of the crystallization.Cool to 70° C. and maintain 70° C. for ca. 1 h.Cool from 70 to 5 C over 2 h, and maintain the temperature between 0 at 5° C. for at least 2 h.Filter the crystal slurry.Wash the filter cake with a mixture of 96 mL of ethanol and 96 mL of water.Dry the material at ≦50° C. under reduced pressure until the water content is 3.4 to 4.1% by KF to afford 41 g (85 M %).Alternately, the monohydrate can be obtained by:1) An aqueous solution of the acetate salt of compound IV was seeded with monohydrate and heated at 80° C. to give bulk monohydrate.2) An aqueous solution of the acetate salt of compound IV was seeded with monohydrate. On standing several days at room temperature, bulk monohydrate had formed.3) An aqueous suspension of compound IV was seeded with monohydrate and heated at 70° C. for 4 hours to give bulk monohydrate. In the absence of seeding, an aqueous slurry of compound IV was unchanged after 82 days at room temperature.4) A solution of compound IV in a solvent such as NMP or DMA was treated with water until the solution became cloudy and was held at 75-85° C. for several hours. Monohydrate was isolated after cooling and filtering.5) A solution of compound IV in ethanol, butanol, and water was heated. Seeds of monohydrate were added to the hot solution and then cooled. Monohydrate was isolated upon cooling and filtration.One of ordinary skill in the art will appreciate that the monohydrate of the compound of formula (IV) may be represented by the XRPD as shown in FIG. 1 or by a representative sampling of peaks as shown in Table 1.Representative peaks taken from the XRPD of the monohydrate of the compound of formula (IV) are shown in Table 1.TABLE 1 2-Theta d(Å) Height 17.994 4.9257 915 18.440 4.8075 338 19.153 4.6301 644 19.599 4.5258 361 21.252 4.1774 148 24.462 3.6359 250 25.901 3.4371 133 28.052 3.1782 153The XRPD is also characterized by the following list comprising 2θ values selected from the group consisting of: 4.6±0.2, 11.2±0.2, 13.8±0.2, 15.2±0.2, 17.9±0.2, 19.1±0.2, 19.6±0.2, 23.2±0.2, 23.6±0.2. The XRPD is also characterized by the list of 2θ values selected from the group consisting of: 18.0±0.2, 18.4±0.2, 19.2±0.2, 19.6±0.2, 21.2±0.2, 24.5±0.2, 25.9±0.2, and 28.0±0.2.Single crystal x-ray data was obtained at room temperature (+25° C.). The molecular structure was confirmed as a monohydrate form of the compound of Formula (IV).The following unit cell parameters were obtained for the monohydrate of the compound of formula (IV) from the x-ray analysis at 25° C.:a(Å)=13.8632(7); b(Å)=9.3307(3); c(Å)=38.390(2);V(Å3) 4965.9(4); Z′=1; Vm=621Space group PbcaMolecules/unit cell 8Density (calculated) (g/cm3) 1.354wherein Z′=number of drug molecules per asymmetric unit. Vm=V(unit cell)/(Z drug molecules per cell).Single crystal x-ray data was also obtained at −50° C. The monohydrate form of the compound of Formula (IV) is characterized by unit cell parameters approximately equal to the following:Cell dimensions: a(Å)=13.862(1);
- b(Å)=9.286(1);
- c(Å)=38.143(2);
Volume=4910(1) Å3Space group PbcaMolecules/unit cell 8Density (calculated) (g/cm3) 1.369wherein the compound is at a temperature of about −50° C.The simulated XRPD was calculated from the refined atomic parameters at room temperature.The monohydrate of the compound of formula (IV) is represented by the DSC as shown in FIG. 2. The DSC is characterized by a broad peak between approximately 95° C. and 130° C. This peak is broad and variable and corresponds to the loss of one water of hydration as seen in the TGA graph. The DSC also has a characteristic peak at approximately 287° C. which corresponds to the melt of the dehydrated form of the compound of formula (IV).The TGA for the monohydrate of the compound of Formula (IV) is shown in FIG. 2 along with the DSC. The TGA shows a 3.48% weight loss from 50° C. to 175° C. The weight loss corresponds to a loss of one water of hydration from the compound of Formula (IV).The monohydrate may also be prepared by crystallizing from alcoholic solvents, such as methanol, ethanol, propanol, i-propanol, butanol, pentanol, and water.
Example 9Preparation of:
Crystalline n-butanol solvate of N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide (IV)The crystalline butanol solvate of the compound of formula (IV) is prepared by dissolving compound (IV) in 1-butanol at reflux (116-118° C.) at a concentration of approximately 1 g/25 mL of solvent. Upon cooling, the butanol solvate crystallizes out of solution. Filter, wash with butanol, and dry.The following unit cell parameters were obtained from the x-ray analysis for the crystalline butanol solvate, obtained at room temperature:a(Å)=22.8102(6); b(Å)=8.4691(3); c(Å)=15.1436(5); β=95.794(2);V(Å3) 2910.5(2); Z′=1; Vm=728Space group P21/aMolecules/unit cell 4Density (calculated) (g/cm3) 1.283wherein Z′=number of drug molecules per asymmetric unit. Vm=V(unit cell)/(Z drug molecules per cell).One of ordinary skill in the art will appreciate that the butanol solvate of the compound of formula (IV) may be represented by the XRPD as shown in FIG. 3 or by a representative sampling of peaks. Representative peaks for the crystalline butanol solvate are 2θ values of: 5.9±0.2, 12.0±0.2, 13.0±0.2, 17.7±0.2, 24.1±0.2, and 24.6±0.2.
Example 10Preparation of:
Crystalline ethanol solvate of N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide (IV)

To a 100-mL round bottom flask was charged 4.00 g (10.1 mmol) of 5D (contained 2.3 Area % 5C) 6.60 g (50.7 mmol) of 7B, 80 mL of n-butanol and 2.61 g (20.2 mmol) of DIPEA. The resulting slurry was heated to 120° C. and maintained at 120° C. for 4.5 h whereby HPLC analysis showed 0.19 relative Area % of residual 5D to compound IV. The homogeneous mixture was cooled to 20° C. and left stirring overnight. The resulting crystals were filtered. The wet cake was washed twice with 10-mL portions of n-butanol to afford a white crystalline product. HPLC analysis showed this material to contain 99.7 Area % compound IV and 0.3 Area % 5C.The resulting wet cake was returned to the 100-mL reactor, and charged with 56 mL (12 mL/g) of 200 proof ethanol. At 80° C. an additional 25 mL of ethanol was added. To this mixture was added 10 mL of water resulting in rapid dissolution. Heat was removed and crystallization was observed at 75-77° C. The crystal slurry was further cooled to 20° C. and filtered. The wet cake was washed once with 10 mL of 1:1 ethanol:water and once with 10 mL of n-heptane. The wet cake contained 1.0% water by KF and 8.10% volatiles by LOD. The material was dried at 60° C./30 in Hg for 17 h to afford 3.55 g (70 M %) of material containing only 0.19% water by KF, 99.87 Area % by HPLC. The 1H NMR spectrum, however revealed that the ethanol solvate had been formed.The following unit cell parameters were obtained from the x-ray analysis for the crystalline ethanol solvate (di-ethanolate, E2-1), obtained at −40° C.:a(Å)=22.076(1); b(Å)=8.9612(2); c(Å)=16.8764(3); β=114.783(1);V(Å3) 3031.1(1); Z′=1; Vm=758Space group P21/aMolecules/unit cell 4Density (calculated) (g/cm3) 1.271wherein Z′=number of drug molecules per asymmetric unit. Vm=V(unit cell)/(Z drug molecules per cell).One of ordinary skill in the art will appreciate that the ethanol solvate (E2-1) of the compound of formula (IV) may be represented by the XRPD as shown in FIG. 4 or by a representative sampling of peaks. Representative peaks for the crystalline ethanol solvate are 2θ values of: 5.8±0.2, 11.3±0.2, 15.8±0.2, 17.2±0.2, 19.5±0.2, 24.1±0.2, 25.3±0.2, and 26.2±0.2.In addition, during the process to form the ethanolate (diethanolate) the formation of another ethanol solvate (½ ethanolate, T1E2-1) has been observed. To date this additional ethanol solvate is known strictly as a partial desolvation product of the original diethanolate form E2-1, and has only been observed on occasion during crystallization of E2-1The following unit cell parameters were obtained from the x-ray analysis for the crystalline ½ ethanol solvate T1E2-1, obtained at −10° C.:a(Å)=22.03(2); b(Å)=9.20(1); c(Å)=12.31(1);β=93.49(6)V(Å3) 2491(4)); Z′=1; Vm=623;Space group P21/aMolecules/unit cell 4Density (calculated) (g/cm3) 1.363wherein Z′=number of drug molecules per asymmetric unit. Vm=V(unit cell)/(Z drug molecules per cell).One of ordinary skill in the art will appreciate that the ethanol solvate (T1E2-1) of the compound of formula (IV) may be represented by the XRPD as shown in FIG. 7 or by a representative sampling of peaks. Representative peaks for the crystalline ethanol solvate are 2θ values of: 7.20±0.2, 12.01±0.2, 12.81±0.2, 18.06±0.2, 19.30±0.2, and 25.24±0.2.
Example 11Preparation of:
Crystalline N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide (IV) (Neat form N-6)To a mixture of compound 5D (175.45 g, 0.445 mol) and hydroxyethylpiperazine (289.67 g, 2.225 mol) in NMP (1168 mL) was added DIPEA (155 mL, 0.89 mol). The suspension was heated at 110° C. (solution obtained) for 25 min., then cooled to about 90° C. The resulting hot solution was added dropwise into hot (80° C.) water (8010) mL, keeping the temperature at about 80° C. The resulting suspension was stirred 15 min at 80° C. then cooled slowly to room temperature. The solid was collected by vacuum filtration, washed with water (2×1600 mL) and dried in vacuo at 55-60° C. affording 192.45 g (88.7% yield) of N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide. 1H NMR (400 MHz, DMSO-d6): δ 2.24 (s, 3H), 2.41 (s, 3H), 2.43 (t, 2H, J=6), 2.49 (t, 4H, J=6.3), 3.51 (m, 4H), 3.54 (q, 2H, J=6), 4.46 (t, 1H, J=5.3), 6.05 (s, 1H), 7.26 (t, 1H, J=7.6), 7.28 (dd, 1H, J=7.6, 1.7), 7.41 (dd, 1H, J=7.6, 1.7), 8.23 (s, 1H), 9.89 (s, 1H), 11.48. KF0.84; DSC: 285.25° C. (onset), 286.28° C. (max).The following unit cell parameters were obtained from the x-ray analysis for the neat crystalline compound IV, obtained at 23° C.:a(Å)=22.957(1); b(Å)=8.5830(5); c(Å)=13.803(3); β=112.039(6);V(Å3)=2521.0(5); Z′=1; Vm=630Space group P21/aMolecules/unit cell 4Density (calculated) (g/cm3) 1.286wherein Z′=number of drug molecules per asymmetric unit. Vm=V(unit cell)/(Z drug molecules per cell).One of ordinary skill in the art will appreciate that the crystalline form of the compound of formula (IV) may be represented by the XRPD as shown in FIG. 5 or by a representative sampling of peaks. Representative peaks for the crystalline neat form (N-6) are 2θ values of: 6.8±0.2, 11.1±0.2, 12.3±0.2, 13.2±0.2, 13.7±0.2, 16.7±0.2, 21.0±0.2, 24.3±0.2, and 24.8±0.2.
Example 12Preparation of:
Crystalline N-(2-chloro-6-methylphenyl)-2-(6-(4-(3-hydroxyethyl)piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide (IV) (neat form T1H1-7)The title neat form may be prepared by heating the monohydrate form of the compound of formula (IV) above the dehydration temperature.The following unit cell parameters were obtained from the x-ray analysis for the neat crystalline (T1H1-7) compound IV, obtained at 25° C.:a(Å)=13.4916; b(Å)=9.3992(2); c(Å)=38.817(1);V(Å3)=4922.4(3); Z′=1; Vm=615Space group PbcaDensity (calculated) (g/cm3) 1.317wherein Z′=number of drug molecules per asymmetric unit. Vm=V(unit cell)/(Z drug molecules per cell).One of ordinary skill in the art will appreciate that the neat crystalline form (T1H1-7) of the compound of formula (IV) may be represented by the XRPD as shown in FIG. 6 or by a representative sampling of peaks. Representative peaks for the crystalline neat form (T1H1-7)) are 2θ values of: 8.0±0.2, 9.7±0.2, 11.2±0.2, 13.3±0.2, 17.5±0.2, 18.9±0.2, 21.0±0.2, 22.0±0.2.Obviously, numerous modifications and variations of the present invention are possible in light of the above teachings. It is therefore to be understood that within the scope of the appended claims, the invention may be practiced otherwise than as specifically described herein.
PAPERhttps://pubs.acs.org/doi/abs/10.1021/jm060727j
2-Aminothiazole (1) was discovered as a novel Src family kinase inhibitor template through screening of our internal compound collection. Optimization through successive structure−activity relationship iterations identified analogs 2 (Dasatinib, BMS-354825) and 12m as pan-Src inhibitors with nanomolar to subnanomolar potencies in biochemical and cellular assays. Molecular modeling was used to construct a putative binding model for Lck inhibition by this class of compounds. The framework of key hydrogen-bond interactions proposed by this model was in agreement with the subsequent, published crystal structure of 2 bound to structurally similar Abl kinase. The oral efficacy of this class of inhibitors was demonstrated with 12m in inhibiting the proinflammatory cytokine IL-2 ex vivo in mice (ED50 ∼ 5 mg/kg) and in reducing TNF levels in an acute murine model of inflammation (90% inhibition in LPS-induced TNFα production when dosed orally at 60 mg/kg, 2 h prior to LPS administration). The oral efficacy of 12m was further demonstrated in a chronic model of adjuvant arthritis in rats with established disease when administered orally at 0.3 and 3 mg/kg twice daily. Dasatinib (2) is currently in clinical trials for the treatment of chronic myelogenous leukemia.

PATENT
https://patents.google.com/patent/WO2019209908A1/enDasatinib (DAS), having the chemical designation N-(2-chloro-6-methylphenyl)-2- [[6-[4-(2-hydroxyethyl)-l-piperazinyl]-2-methyl-4-pyrimidinyl]amino]-5- thiazolecarboxamide, monohydrate, is an orally bioavailable inhibitor of the receptor tyrosine kinase (RTK) epidermal growth factor receptor (ErbB; EGFR) family, with antineoplastic activity. Dasatinib has the following structure:

Dasatinib is commercially marketed under the name SPRY CEL® and is indicated for the treatment of patients with newly diagnosed Philadelphia chromosome-positive chronic myeloid leukemia in chronic phase, for the treatment of patients chronic, accelerated, or myeloid or lymphoid blast phase Philadelphia chromosome-positive chronic myeloid leukemia with resistance or intolerance to prior therapy and for the treatment of patients with Philadelphia chromosome-positive acute lymphoblastic leukemia with resistance or intolerance to prior therapy.Solid forms of dasatinib are described in U.S. Patent Nos. 7491725 (butanol solvate, monohydrate, diethanolate, hemi-ethanolate, anhydrous), 8680103 (butanol solvate, monohydrate, diethanolate, hemi-ethanolate, anhydrous), 7973045 (anhydrous), 8067423 (isopropyl alcohol solvate), 8242270 (butanol solvate, monohydrate, diethanolate, hemi- ethanolate, anhydrous), 8884013 (monohydrates), 9249134 (amorphous), 9456992 (solid dispersion nanoparticles), 9556164 (saccharin salt crystal) and 9884857 (saccharinate, glutarate, nicotinate); in U.S. Publication Nos. 20160250153 (solid dispersion nanoparticles), 20160264565 (Form-SDI), 20160361313 (solid dispersion nanoparticles), 20170183334 (salts) and 20140031352 (anti-oxidative acid); in International Publication Nos.W02010067374 (solvated forms and Form I), W02010139980, W02010139981,W02013065063 (anhydrous), W02017103057, W02017108605 (solid dispersion),WO2017134617 (amorphous), WO2014086326 (NMP, isoamyl-OH, 1, 3-propanediol process), WO2015107545, WO2015181573, WO2017134615 (PG solvate), W02010062715 (isosorbide dimethyl ether, N,N’-dimethylethylene urea, N,N’-dimethyl-N,N’-propylene urea), WO2010139979 (DCM, DMSP, monohydrate), WO2011095588 (anhydrate, hydrochloride, hemi-ethanol), W02012014149 (N-methylformamide) and W02017002131 (propandiol, monohydrate); and in Chinese Patent Nos. CN102643275, CN103059013, CN103819469, CN104341410. None of the references describe an ethyl formate solvate of dasatinib.Dasatinib co-crystals are described in U.S. Patent No. 9,340,536 (co-crystals selected from methyl-4-hydroxybenzoate, nicotinamide, ethyl gallate, methyl gallate, propyl gallate, ethyl maltol, vanillin, menthol, and (lR,2S,5R)-(-)-menthol) and International Publication No. W02016001025 (co-crystal selected from menthol or vanillin). None of the references describe dasatinib co-crystal comprising dasatinib and a second compound, as a co-crystal former, wherein the second compound is selected from butyl paraben, propyl paraben and ethyl vanillin.Dasatinib (DAS), having the chemical designation N-(2-chloro-6-methylphenyl)-2- [[6-[4-(2-hydroxyethyl)-l-piperazinyl]-2-methyl-4-pyrimidinyl]amino]-5- thiazolecarboxamide, monohydrate, is an orally bioavailable inhibitor of the receptor tyrosine kinase (RTK) epidermal growth factor receptor (ErbB; EGFR) family, with antineoplastic activity. Dasatinib has the following structure:

Dasatinib is commercially marketed under the name SPRY CEL® and is indicated for the treatment of patients with newly diagnosed Philadelphia chromosome-positive chronic myeloid leukemia in chronic phase, for the treatment of patients chronic, accelerated, or myeloid or lymphoid blast phase Philadelphia chromosome-positive chronic myeloid leukemia with resistance or intolerance to prior therapy and for the treatment of patients with Philadelphia chromosome-positive acute lymphoblastic leukemia with resistance or intolerance to prior therapy.Solid forms of dasatinib are described in U.S. Patent Nos. 7491725 (butanol solvate, monohydrate, diethanolate, hemi-ethanolate, anhydrous), 8680103 (butanol solvate, monohydrate, diethanolate, hemi-ethanolate, anhydrous), 7973045 (anhydrous), 8067423 (isopropyl alcohol solvate), 8242270 (butanol solvate, monohydrate, diethanolate, hemi- ethanolate, anhydrous), 8884013 (monohydrates), 9249134 (amorphous), 9456992 (solid dispersion nanoparticles), 9556164 (saccharin salt crystal) and 9884857 (saccharinate, glutarate, nicotinate); in U.S. Publication Nos. 20160250153 (solid dispersion nanoparticles), 20160264565 (Form-SDI), 20160361313 (solid dispersion nanoparticles), 20170183334 (salts) and 20140031352 (anti-oxidative acid); in International Publication Nos.W02010067374 (solvated forms and Form I), W02010139980, W02010139981,W02013065063 (anhydrous), W02017103057, W02017108605 (solid dispersion),WO2017134617 (amorphous), WO2014086326 (NMP, isoamyl-OH, 1, 3-propanediol process), WO2015107545, WO2015181573, WO2017134615 (PG solvate), W02010062715 (isosorbide dimethyl ether, N,N’-dimethylethylene urea, N,N’-dimethyl-N,N’-propylene urea), WO2010139979 (DCM, DMSP, monohydrate), WO2011095588 (anhydrate, hydrochloride, hemi-ethanol), W02012014149 (N-methylformamide) and W02017002131 (propandiol, monohydrate); and in Chinese Patent Nos. CN102643275, CN103059013, CN103819469, CN104341410. None of the references describe an ethyl formate solvate of dasatinib.Dasatinib co-crystals are described in U.S. Patent No. 9,340,536 (co-crystals selected from methyl-4-hydroxybenzoate, nicotinamide, ethyl gallate, methyl gallate, propyl gallate, ethyl maltol, vanillin, menthol, and (lR,2S,5R)-(-)-menthol) and International Publication No. W02016001025 (co-crystal selected from menthol or vanillin). None of the references describe dasatinib co-crystal comprising dasatinib and a second compound, as a co-crystal former, wherein the second compound is selected from butyl paraben, propyl paraben and ethyl vanillin. hereafter. ClaimsHide Dependent What is claimed is:1. A dasatinib co-crystal comprising dasatinib and a second compound, wherein the second compound is selected from butyl paraben, propyl paraben and ethyl vanillin.2. The dasatinib co-crystal according to claim 1, wherein a molar ratio of the dasatinib to the second compound is about 1: 1.3. The dasatinib co-crystal according to claim 1, wherein the second compound is butyl paraben.4. The dasatinib co-crystal according to claim 3, wherein a molar ratio of the dasatinib to the butyl paraben is about 1 : 1.5. The dasatinib co-crystal according to claim 1, which is Form I co-crystal of dasatinib and butyl paraben.6. The dasatinib co-crystal according to claim 5, characterized by having at least 2 or more X-ray powder diffraction peaks selected from about 4.9, 9.8, 11.3, 14.9, 17.5, 20.8, 21.6, 22.6 and 25.4° 2Q degrees.7. The dasatinib co-crystal according to claim 5, characterized by a thermal event at about 287.3 °C, as measured by differential scanning calorimetry.8. The dasatinib co-crystal according to claim 5, characterized by a weight loss of 8.1% from about 70 °C through about 165 °C, as measured by thermal gravimetric analysis.9. The dasatinib co-crystal of claim 5 monoclinic, P2i/C.10. The dasatinib co-crystal d of claim 5 which has single crystal parametersa = 18.630 (2) Ab = 8.725 (1) Ac = 22.331 (2) Aa = g = 90°, b = 104.575 (8)°.11. The dasatinib co-crystal of claim 5 which has a cell volume is about 3512.9 A3.12. The dasatinib co-crystal according to claim 1, wherein the second compound is ethyl vanillin.13. The dasatinib co-crystal according to claim 9, wherein a molar ratio of the dasatinib to the ethyl vanillin is about 1 : 1.14. The dasatinib co-crystal according to claim 1, which is Form II co-crystal of dasatinib and ethyl vanillin.15. The dasatinib co-crystal according to claim 14, characterized by having at least 2 or more X-ray powder diffraction peaks selected from about 5.7, 10.9, 13.5, 17.1, 18.4, 19.4, 23.7 and 26.3° 2Q degrees.16. The dasatinib co-crystal according to claim 14, characterized by one or more thermal events selected from about 140 °C, about 181 °C, and about 293 °C, as measured by differential scanning calorimetry.17. The dasatinib co-crystal according to claim 14, characterized by a weight loss of 24.3% from about 120 through 250 °C, as measured by thermal gravimetric analysis.18. The dasatinib co-crystal of claim 14 monoclinic, P2i/n.19. The dasatinib co-crystal d of claim 14 which has single crystal parametersa = 18.452 (1) Ab = 9.441 (6) Ac = 19.377 (1) Aa = g = 90°, b = 108.78 (1)°.20. The dasatinib co-crystal of claim 5 which has a cell volume is about 3195.71 A3.21. The dasatinib co-crystal according to claim 1, wherein the second compound is propyl paraben.22. The dasatinib co-crystal according to claim 21, wherein a molar ratio of the dasatinib to the propyl paraben is about 1 : 1.23. The dasatinib co-crystal according to claim 1, which is Form III co-crystal ofdasatinib and propyl paraben.24. The dasatinib co-crystal according to claim 23, characterized by having at least 2 or more X-ray powder diffraction peaks selected from about 4.8, 9.6, 11.9, 14.8, 18.4, 22.2, 23.9 and 26.1° 2Q degrees.25. The dasatinib co-crystal of claim 23 monoclinic, P2i/n.26. The dasatinib co-crystal of claim 23 which has single crystal parametersa = 18.859 (9) Ab = 8.131 (6) Ac = 22.473 (1) Aa = g = 90°, b = 103.87(1)°.27. The dasatinib co-crystal of claim 23 which has a cell volume is about 3345.51 A3.28. An ethyl formate solvate of dasatinib.29. The ethyl formate solvate of dasatinib according to claim 28, wherein a molar ratio of the dasatinib to the ethyl formate is about 1 : 1.30. The ethyl formate solvate of dasatinib according to claim 1, which is Form I of ethyl formate solvate of dasatinib.31. The ethyl formate solvate of dasatinib according to claim 30, characterized by having at least 2 or more X-ray powder diffraction peaks selected from about 6.0, 12.1, 15.1, 18.0, 23.8 and 24.8° 2Q degrees.32. The ethyl formate solvate of dasatinib according to claim 30, characterized by athermal event at about 287.3 °C, as measured by differential scanning calorimetry.33. The ethyl formate solvate of dasatinib according to claim 30, characterized by aweight loss of 8.1% from about 70 °C through about 165 °C, as measured by thermal gravimetric analysis.34. The ethyl formate solvate of dasatinib of claim 23 orthorhombic, P2i/c.35. The ethyl formate solvate of dasatinib of claim 23 which has single crystal parameters a = 14.8928 (5) Ab = 8.3299 (3) Ac = 22.18990 (6) Aa = g =b = 90°.36. The ethyl formate solvate of dasatinib of claim 23 which has a cell volume is about 2731.9 A3.37. A pharmaceutical composition comprising a pharmaceutically effective amount of the dasatinib co-crystal according to claim 1 and pharmaceutically acceptable excipient.38. A method of treating disease in a patient comprising administering a pharmaceutical formulation according to claim 37 to the patient in need thereof.39. A method of treating disease according to claim 38, wherein the disease ismyelogenous leukemia.40. A method of treating disease according to claim 38, wherein the disease isPhiladelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase.41. A method of treating disease according to claim 38, wherein the disease Ph+ acute lymphoblastic leukemia (Ph+ ALL).42. A method of making the dasatinib co-crystal according to claim 1, comprisingdissolving dasatinib and a second compound, wherein the second compound is selected from the group consisting of butyl paraben, propyl paraben and ethyl vanillin, in heated methanol (-10: 1 – wt(mg)DAs:v(mL)MeOH and molD,\s:mohnci compound is 1 : 1.1) to form a clear solution, heating the solution under vacuum for about l8-20h to yield the dasatinib co-crystal.43. A process for the preparation Form II co-crystal of dasatinib and ethyl vanillin,according to claim 14, comprising: (g) dissolving Form I of ethyl formate solvate of dasatinib and ethyl vanillin in N-methyl-2-pyrrolidone to form a solution;(h) adding water to the solution;(i) stirring the solution for about 12-24 hours to form a slurry;(j) filtering the slurry to yield a precipitate;(k) washing the precipitate with water; and(l) drying the precipitate under vacuum with warming to yield Form II co crystal of dasatinib and ethyl vanillin.44. A process for the preparation of Form I of ethyl formate solvate of dasatinib,according to claim 30, comprising:(d) dissolving dasatinib in ethyl formate to form a solution;(e) stirring the solution for about 12-24 hours form a slurry;(f) filtering the slurry to yield Form I of ethyl formate solvate of dasatinib.45. A process for the preparation of Form I of ethyl formate solvate of dasatinib,according to claim 30, comprising:(g) dissolving dasatinib in N-Methyl-2-pyrrolidone to form a solution;(h) adding ethyl formate to the solution to form a slurry;(i) adding additional ethyl formate to the slurry;(j) stirring the slurry for about 2 hours;(k) filtering the slurry to yield a precipitate; and(l) washing the precipitate with ethyl formate to yield Form I of ethyl formate solvate of dasatinib.
ATENThttps://patents.google.com/patent/WO2013065063A1/en
Dasatinib, N-(2-chloro-6-methylphenyl)-2- [(6-[4-(2-hydroxyl)- 1 -piperazinyl]-2-methyl-4-pyrimidinyl]amino]-5- thiazolecarboxamide compound having the following chemical structure of Formula (I)

Formula IAlso known as BMS-354825, it is a drug produced by Bristol Myers Squibb and sold under the trade name Sprycel. Dasatinib is an oral dual BCR/ABL and SRC family tyrosine kinase inhibitor approved for use in patients with chronic myelogenous leukemia (CML) after Imatinib treatment has failed and Philadelphia chromosome- positive acute lymphoblastic leukemia (Ph + ALL). It is also being assessed for use in metastatic melanoma.A preparation of Dasatinib is described in US patent No. 6596746 (B l ), where the process is done by reacting compound of the following formula III with N-(2- hydroxyethyl) piperazine at 80° C.

Formula IIIThe compound of Formula (I) and its preparation is described in US Patent No. 6596746, US patent application No. 2005/0176965 Al , and US patent application No. 2006/0004067 Al .l Polymorphism is defined as “the ability of a substance to exist as two or more crystalline phases that have different arrangement and /or conformations of the molecules in the crystal Lattice. Thus, in the strict sense, polymorphs are different crystalline forms of the same pure substance in which the molecules have different arrangements and / or different configurations of the molecules”. Different polymorphs may differ in their physical properties such as melting point, solubility, X-ray diffraction patterns, 1R etc. Polymorphic forms of a compound can be distinguished in the laboratory by analytical methods such as X-ray diffraction (XRD), Differential Scanning Calorimetry (DSC) and Infrared spectrometry (IR). Solvent medium and mode of crystallization play very important role in obtaining a crystalline form.The discovery of new polymorphic forms is a continuing goal of formulators. The new polymorphs may be advantageous for dosage form development and enhancing bioavailability owing to the altered physiochemical properties. Some form may turn out to be more efficacious. Discovering novel processes to prepare known polymorphic forms is also a primary goal of the pharmaceutical development scientists. New processes can provide novel intermediates or synthetic pathways that result in product with increased chemical and polymorphic purity in addition to providing cost and other advantages. There is thus a need to provide novel synthetic routes and intermediates that can realize these goals.Several crystalline forms of Dasatinib are described in the literature; these are designated as HI -7, BU-2, E2-1 , N-6, T1 H1 -7 and TIE2-1. Crystalline Dasatinib monohydrate (H I -7) and butanol solvate (BU-2) along with the processes for their preparation are described in WO 2005077945. In addition US 2006/0004067, which is continuation of US 2005215795 also describe two ethanol solvates (E2-1 ; TIE2-1) and two anhydrous forms (N-6 and T1 H1 -7).WO 2009053854 discloses various Dasatinib solvates including their crystalline form, amorphous form and anhydrous form.US patent No. 7973045 discloses the anhydrous form of Dasatinib and process for preparation thereof. The anhydrous form disclosed therein have typical characteristic XRD peaks at about 7.2, 1 1.9, 14.4, 16.5, 17.3, 19.1 , 20.8, 22.4, 23.8, 25.3 and 29.1 on the 2- theta value. WO 2010062715 discloses isosorbide dimethyl ether solvate, Ν,Ν’- dimethylethylene urea solvate and N,N’-dimethyl-N,N’-propylene urea solvate of Dasatinib.WO 2010067374 discloses novel crystalline form I, solvates of DMF, DMSO, toluene, isopropyl acetate and processes for their preparation.WO 2010139979 discloses MDC solvate and process of preparation, for use in the manufacture of pure Dasatinib.WO 2010139980 discloses a process for the preparation of crystalline Dasatinib monohydrate.The present invention is a step forward in this direction and provides a novel anhydrous form and process for its preparation, which can be used for the preparation of pure Dasatinib, in particularly Dasatinib monohydrate.The process for preparing Dasatinib monohydrate is described in US 2006/0004067. Further studies by the inventors have shown that the preparation of Dasatinib by using the method, which is disclosed in US 2006/0004067 yields the monohydrate with ~ 90% purity. Therefore the present invention provides a novel anhydrous form which can be used to get Dasatinib monohydrate with high yield and purity.Preparing API with increased purity is always an aim of the pharmaceutical development team. The inventors of the present invention have found that preparingDasatinib monohydrate using the novel anhydrous form of the present invention resulted in a highly pure product with a good yield.Scheme 1 shows a general process for the preparation of Dasatinib as disclosed in US 2006/0004067. Intermediate 3 and N-(2-hydroxyethyl) piperazine are heated together in a solvent system comprising n-butanol as a solvent and diisopropyl ethylamine (DIPEA) as a base. On cooling of the reaction mixture, Dasatinib precipitates out which is isolated by filtration.



DasatinibScheme 1Example – 1In a reaction vessel, N-(2-chloro-6-methylphenyl)-2-[(6-chloro-2-methyl-4- pyrimidinyl) amino] -5-thiazolecarboxamide (1 gm, 2.54 mmol) and N-(2- hydroxyethyl) piperazine (5.3 gm, 40.70 mmol) was added under stirring. The reaction mixture was heated at 80 °C for 2H. Acetonitrile was added into reaction mixture at 80 °C and stirred for 30 min. Cooled the suspension to room temperature and stirred for 30 min. Filtered, washed with acetonitrile and dried at 60 °C under vacuum to get 950 mg anhydrous N-(2-chloro-6-methylphenyl)-2-[(6-[4-(2-hydroxy 1)- 1 -piperaziny l]-2- methyl-4-pyrimidinyl]amino]-5-thiazole carboxamide (76.73 % Yield).HPLC Purity 99.90 %M/C by KF 0.12 %DSC 278.17 °CTGA 2.05 %XRD as provided in Fig. 2
Patent
Publication numberPriority datePublication dateAssigneeTitleUS7491725B22004-02-062009-02-17Bristol-Myers Squibb CompanyProcess for preparing 2-aminothiazole-5-aromatic carboxamides as kinase inhibitorsWO2009147238A12008-06-062009-12-10Boehringer Ingelheim International GmbhSolid pharmaceutical formulations comprising bibw 2992WO2010062715A22008-11-032010-06-03Teva Pharmaceutical Industries Ltd.Polymorphs of dasatinib and process for preparation thereofWO2010067374A22008-12-082010-06-17Hetero Research FoundationPolymorphs of dasatinibWO2010139980A12009-06-032010-12-09Generics [Uk] LimitedProcess for preparing crystalline dasatinib monohydrateWO2010139979A22009-06-032010-12-09Generics [Uk] LimitedProcesses for preparing crystalline formsWO2010139981A22009-06-032010-12-09Generics [Uk] LimitedProcesses for preparing crystalline formsWO2011003853A22009-07-062011-01-13Boehringer Ingelheim International GmbhProcess for drying of bibw2992, of its salts and of solid pharmaceutical formulations comprising this active ingredientUS7973045B22007-10-232011-07-05Teva Pharmaceutical Industries Ltd.Anhydrous form of dasatinib and process for preparation thereofWO2011095588A12010-02-042011-08-11Ratiopharm GmbhPharmaceutical composition comprising n-(2-chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)-1-piperazinyl]-2-methyl-4-pyrimidinyl]amino]-5-thiazolecarboxamidWO2012014149A12010-07-302012-02-02Ranbaxy Laboratories LimitedN-methylformamide solvate of dasatinibCN102643275A2011-02-212012-08-22江苏先声药物研究有限公司A new preparation method for Dasatinib N-6 crystal formCN103059013A2011-10-182013-04-24北京本草天源药物研究院New crystal of Dasatinib monohydrate and preparation method thereofWO2013065063A12011-11-032013-05-10Cadila Healthcare LimitedAnhydrous form of dasatinib, process for its preparation and its useUS20140031352A12012-07-242014-01-30Laurus Labs Private LimitedSolid forms of tyrosine kinase inhibitors, process for the preparation and their pharmaceutical composition thereofCN103819469A2012-11-162014-05-28重庆医药工业研究院有限责任公司Crystal form of dasatinib and preparation method for crystal form of dasatinibWO2014086326A12012-12-062014-06-12Zentiva, K.S.A method for the preparation and purification of new and known polymorphs and solvates of dasatinibUS8884013B22010-02-082014-11-11Nan Jing Cavendish Bio-Engineering Technology Co., Ltd.Polymorphs of Dasatinib, preparation methods and pharmaceutical compositions thereofCN104341410A2013-08-092015-02-11上海科胜药物研发有限公司New Dasatinib crystal form and preparation method thereofWO2015107545A12013-12-182015-07-23Dharmesh Mahendrabhai ShahWater soluble salts of dasatinib hydrateWO2015181573A12014-05-262015-12-03Egis Gyógyszergyár Zrt.Dasatinib saltsWO2016001025A12014-06-302016-01-07Basf SeMulticomponent crystals of dasatinib with menthol or vanillinUS9249134B22013-03-262016-02-02Cadila Healthcare LimitedProcess for preparation of amorphous form of dasatinibUS9340536B22012-06-152016-05-17Basf SeMulticomponent crystals comprising dasatinib and selected co-crystal formersUS20160250153A12012-01-132016-09-01Xspray Microparticles AbNovel methodsUS20160264565A12013-11-082016-09-15Shilpa Medicare LimitedCrystalline dasatinib processWO2017002131A12015-06-292017-01-05Msn Laboratories Private LimitedCrystalline forms of n-(2-chloro-6-methy]phenvn-2-[f6-[4-(2-hvdroxvethvl)-l- piperazinvil-2-methvl-4-pvrimidinvllaminol-5-thiazolecarboxamide and their process thereofUS9556164B22013-07-252017-01-31Basf SeSalts of Dasatinib in crystalline formWO2017103057A12015-12-162017-06-22Synthon B.V.Pharmaceutical composition comprising anhydrous dasatinibWO2017108605A12015-12-222017-06-29Synthon B.V.Pharmaceutical composition comprising amorphous dasatinibWO2017134615A12016-02-032017-08-10Dr. Reddy’s Laboratories LimitedSolid state forms of dasatinib and processes for their preparationWO2017134617A12016-02-032017-08-10Dr. Reddy’s Laboratories LimitedProcess for the preparation of amorphous dasatinibUS9884857B22013-07-252018-02-06Basf SeSalts of dasatinib in amorphous form
PATENTSPublication numberPriority datePublication dateAssigneeTitleUS20060079563A1 *1999-04-152006-04-13Jagabandhu DasCyclic protein tyrosine kinase inhibitorsUS20070219370A1 *2006-03-152007-09-20Bristol-Myers Squibb CompanyProcess for preparing n-(2-chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)-1-piperazinyl]-2-methyl-4-pyrimidinyl]amino] -5-thiazolecarboxamide and related metabolites thereofUS20080275009A1 *2005-09-212008-11-06Bristol-Myers Squibb CompanyOral administration of n-(2-chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)-1-piperazinyl]-2-methyl-4-pyrimidinyl]amino]-1,3-thiazole-5-carboxamide and salts thereofUS20090030203A1 *2005-08-052009-01-29Bristol-Myers Squibb CompanyPreparation of 2-amino-thiazole-5-carboxylic-acid derivativesUS20090118297A1 *2007-10-232009-05-07Ondrej SimoPolymorphs of dasatinib and process for preparation thereofWO2012014149A12010-07-302012-02-02Ranbaxy Laboratories LimitedN-methylformamide solvate of dasatinibUS20120309968A1 *2010-02-082012-12-06Nan Jing Cavendish Bio-Engineering Technology Co., Ltd.Polymorphs of dasatinib, preparation methods and pharmaceutical compositions thereofUS8530492B22009-04-172013-09-10Nektar TherapeuticsOligomer-protein tyrosine kinase inhibitor conjugatesUS8680103B22004-02-062014-03-25Bristol-Myers Squibb CompanyProcess for preparing 2-aminothiazole-5-aromatic carboxamides as kinase inhibitorsWO2014102759A22012-12-312014-07-03Ranbaxy Laboratories LimitedProcess for the preparation of dasatinib and its intermediatesUS8816077B22009-04-172014-08-26Nektar TherapeuticsOligomer-protein tyrosine kinase inhibitor conjugatesUS20150057446A1 *2012-04-202015-02-26Shilpa Medicare LimitedProcess for preparing dasatinib monohydrateWO2016001025A12014-06-302016-01-07Basf SeMulticomponent crystals of dasatinib with menthol or vanillinUS9340536B22012-06-152016-05-17Basf SeMulticomponent crystals comprising dasatinib and selected co-crystal formersUS9556164B22013-07-252017-01-31Basf SeSalts of Dasatinib in crystalline formUS9884857B22013-07-252018-02-06Basf SeSalts of dasatinib in amorphous formWO2018078392A12016-10-292018-05-03Cipla LimitedPolymorphs of dasatinibWO2018100585A12016-12-012018-06-07Natco Pharma LimitedAn improved process for the preparation of dasatinib polymorphWO2018134189A12017-01-202018-07-26Cerbios-Pharma SaCo-crystal of an antitumoral compoundWO2018134190A12017-01-202018-07-26Cerbios-Pharma SaCo-crystals of an antitumoral compoundUS10174018B22016-12-132019-01-08Princeton Drug Discovery IncProtein kinase inhibitorsWO2019209908A12018-04-252019-10-31Johnson Matthey Public Limited CompanyCrystalline forms of dasatinibUS10722484B22016-03-092020-07-28K-Gen, Inc.Methods of cancer treatmentUS10799459B12019-05-172020-10-13Xspray Microparticles AbRapidly disintegrating solid oral dosage forms containing dasatinibFamily To Family CitationsUS7396935B22003-05-012008-07-08Bristol-Myers Squibb CompanyAryl-substituted pyrazole-amide compounds useful as kinase inhibitorsUS7652146B2 *2004-02-062010-01-26Bristol-Myers Squibb CompanyProcess for preparing 2-aminothiazole-5-carboxamides useful as kinase inhibitorsTW200600513A *2004-06-302006-01-01Squibb Bristol Myers CoA method for preparing pyrrolotriazine compoundsPE20061394A1 *2005-03-152006-12-15Squibb Bristol Myers CoMetabolites of n- (2-chloro-6-methylphenyl) -2 – [[6- [4- (2-hydroxyethyl) -1-piperazinyl] -2-methyl-4-pyrimidinyl] amino] -5-thiazolecarboxamidesUS20060235006A1 *2005-04-132006-10-19Lee Francis YCombinations, methods and compositions for treating cancerPL1885339T32005-05-052015-12-31Bristol Myers Squibb Holdings IrelandFormulations of a src/abl inhibitorWO2008076883A22006-12-152008-06-26Abraxis Bioscience, Inc.Triazine derivatives and their therapeutical applicationsWO2010139979A22009-06-032010-12-09Generics [Uk] LimitedProcesses for preparing crystalline formsWO2010139980A1 *2009-06-032010-12-09Generics [Uk] LimitedProcess for preparing crystalline dasatinib monohydrateEP2359813A12010-02-042011-08-24Ratiopharm GmbHPharmaceutical composition comprising N-(2-chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)-1-piperazinyl]-2-methyl-4-pyrimidinyl]amino]-5-thiazolecarboxamidCN102250084A *2010-02-082011-11-23南京卡文迪许生物工程技术有限公司Dasatinib polymorphic substance as well as preparation method and pharmaceutical composition thereofCN102643275B *2011-02-212016-04-20江苏先声药物研究有限公司The preparation method that a kind of Dasatinib N-6 crystal formation is newWO2013065063A12011-11-032013-05-10Cadila Healthcare LimitedAnhydrous form of dasatinib, process for its preparation and its useUS20150087687A12012-03-232015-03-26Dennis BrownCompositions and methods to improve the therapeutic benefit of indirubin and analogs thereof, including meisoindigoSG10201610869TA2012-06-262017-02-27Del Mar PharmaceuticalsMethods for treating tyrosine-kinase-inhibitor-resistant malignancies in patients with genetic polymorphisms or ahi1 dysregulations or mutations employing dianhydrogalactitol, diacetyldianhydrogalactiCN103664929B *2012-08-302016-08-03石药集团中奇制药技术(石家庄)有限公司Dasatinib polycrystalline form medicament and preparation methodCN102838595B *2012-09-132014-09-24江苏奥赛康药业股份有限公司Preparation method of high-purity dasatinib and by-product of dasatinibCN103819469A *2012-11-162014-05-28重庆医药工业研究院有限责任公司Crystal form of dasatinib and preparation method for crystal form of dasatinibCZ306598B62012-12-062017-03-22Zentiva, K.S.A method of preparation and purification of new and known polymorphs and dasatinib solvatesCN105764502A2013-07-262016-07-13现代化制药公司Combinatorial methods to improve the therapeutic benefit of bisantrene and analogs and derivatives thereofCN103408542B *2013-08-132016-06-29南京优科生物医药研究有限公司A kind of preparation method of highly purified Dasatinib anhydrideWO2015049645A2 *2013-10-042015-04-09Alembic Pharmaceuticals LimitedAn improved process for the preparation of dasatinibCZ306732B62013-12-192017-05-31Zentiva, K.S.A method of preparation of the anhydrous polymorphic form of N-6 DasatinibCN104788445B *2015-04-102017-06-23山东新时代药业有限公司A kind of synthetic method of Dasatinib intermediateCN106668022B *2015-11-052020-09-15武汉应内药业有限公司Application of aminothiazole MyD88 specific inhibitor TJM2010-5* Cited by examiner, † Cited by third party, ‡ Family to family citation
References[edit]
- ^ “Sprycel (Dasatinib)” (PDF). Therapeutic Goods Administration(TGA). Retrieved 18 July 2020.
- ^ Jump up to:a b c d e f g h i j “Sprycel EPAR”. European Medicines Agency(EMA). Retrieved 28 April 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ Jump up to:a b c d e f g h “Dasatinib”. The American Society of Health-System Pharmacists. Retrieved 8 December 2017.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ Keating GM (January 2017). “Dasatinib: A Review in Chronic Myeloid Leukaemia and Ph+ Acute Lymphoblastic Leukaemia”. Drugs. 77 (1): 85–96. doi:10.1007/s40265-016-0677-x. PMID 28032244. S2CID 207489056.
- ^ Olivieri, A.; Manzione, L. (2007). “Dasatinib: a new step in molecular target therapy”. Annals of Oncology. 18 Suppl 6: vi42–vi46. doi:10.1093/annonc/mdm223. PMID 17591830.
- ^ “NHS – Healthcare News”. nelm.nhs.uk. Archived from the original on 5 May 2013. Retrieved 27 September 2011.
- ^ Yurttaş NO, Eşkazan AE (2018). “Dasatinib-induced pulmonary arterial hypertension”. British Journal of Clinical Pharmacology. 84 (5): 835–845. doi:10.1111/bcp.13508. PMC 5903230. PMID 29334406.
- ^ Jump up to:a b c d “Sprycel (dasatinib) and risk of pulmonary arterial hypertension”. U.S. Food and Drug Administration (FDA). 23 September 2011. Retrieved 28 April 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ Tokarski JS, Newitt JA, Chang CY, Cheng JD, Wittekind M, Kiefer SE, et al. (June 2006). “The structure of Dasatinib (BMS-354825) bound to activated ABL kinase domain elucidates its inhibitory activity against imatinib-resistant ABL mutants”. Cancer Research. 66 (11): 5790–7. doi:10.1158/0008-5472.CAN-05-4187. PMID 16740718.
- ^ Jump up to:a b Piscitani L, Sirolli V, Morroni M, Bonomini M (2020). “Nephrotoxicity Associated with Novel Anticancer Agents (Aflibercept, Dasatinib, Nivolumab): Case Series and Nephrological Considerations”. International Journal of Molecular Sciences. 21(14): e4878. doi:10.3390/ijms21144878. PMC 7402330. PMID 32664269.
- ^ Jump up to:a b Braun TP, Eide CA, Druker BJ (2020). “Response and Resistance to BCR-ABL1-Targeted Therapies”. Cancer Cell. 37(4): 530–542. doi:10.1016/j.ccell.2020.03.006. PMC 7722523. PMID 32289275.
- ^ “Otsuka and Bristol-Myers Squibb Announce a Change in Contract Regarding Collaboration in Japan in the Oncology Therapy Area”.
- ^ “FDA Approves U.S. Product Labeling Update for Sprycel (dasatinib) to Include Three-Year First-Line and Five-Year Second-Line Efficacy and Safety Data in Chronic Myeloid Leukemia in Chronic Phase”. Bristol-Myers Squibb (Press release).
- ^ “Bristol-Myers Squibb Announces Extension of U.S. Agreement for ABILIFY and Establishment of an Oncology Collaboration with Otsuka”. Bristol-Myers Squibb (Press release).
- ^ Drahl C (16 January 2012). “How Jagabandhu Das made dasatinib possible”. The Safety Zone blog. Chemical & Engineering News. Retrieved 29 August 2016.
- ^ “Drug Approval Package: Sprycel (Dasatinib) NDA #021986 & 022072”. U.S. Food and Drug Administration (FDA). 6 September 2006. Retrieved 28 April 2020.
- ^ “2010 Notifications”. U.S. Food and Drug Administration (FDA). 18 November 2010. Retrieved 28 April 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ Jump up to:a b c d e “FDA approves dasatinib for pediatric patients with CML”. U.S. Food and Drug Administration (FDA). 9 November 2017. Retrieved 28 April 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ Jump up to:a b c Cohen D (November 2014). “US trade rep is pressing Indian government to forbid production of generic cancer drug, consortium says”. BMJ. 349: g6593. doi:10.1136/bmj.g6593. PMID 25370846. S2CID 206903723.
- ^ Jump up to:a b c Kirkland JL, Tchkonia T (2020). “Senolytic drugs: from discovery to translation”. Journal of Internal Medicine. 288 (5): 518–536. doi:10.1111/joim.13141. PMC 7405395. PMID 32686219.
- ^ Jump up to:a b Paez-Ribes M, González-Gualda E, Doherty GJ, Muñoz-Espín D (2019). “Targeting senescent cells in translational medicine”. EMBO Molecular Medicine. 11 (12): e10234. doi:10.15252/emmm.201810234. PMC 6895604. PMID 31746100.
- ^ Wyld L, Bellantuono I, Tchkonia T, Danson S, Kirkland JL (2020). “Senescence and Cancer: A Review of Clinical Implications of Senescence and Senotherapies”. Cancers. 12 (8): e2134. doi:10.3390/cancers12082134. PMC 7464619. PMID 32752135.
Further reading[edit]
- Lombardo LJ, Lee FY, Chen P, Norris D, Barrish JC, Behnia K, et al. (December 2004). “Discovery of N-(2-chloro-6-methyl- phenyl)-2-(6-(4-(2-hydroxyethyl)- piperazin-1-yl)-2-methylpyrimidin-4- ylamino)thiazole-5-carboxamide (BMS-354825), a dual Src/Abl kinase inhibitor with potent antitumor activity in preclinical assays”. Journal of Medicinal Chemistry. 47 (27): 6658–61. doi:10.1021/jm049486a. PMID 15615512.
External links[edit]
- “Dasatinib”. Drug Information Portal. U.S. National Library of Medicine.
/////////////DASATINIB, BMS 35482503, KIN 001-5, NSC 759877, Sprycel, BMS, APOTEX, ダサチニブ水和物 , X78UG0A0RN, дазатиниб , دازاتينيب , 达沙替尼 ,
#DASATINIB, #BMS 35482503, #KIN 001-5, #NSC 759877, #Sprycel, #BMS, #APOTEX, #ダサチニブ水和物 , #X78UG0A0RN, #дазатиниб , #دازاتينيب , #达沙替尼 ,
O.Cc1nc(Nc2ncc(s2)C(=O)Nc3c(C)cccc3Cl)cc(n1)N4CCN(CCO)CC4
PATENT
https://patents.google.com/patent/US8884013B2/enDasatinib, with the trade name SPRYCEL™, is a oral tyrosine kinase inhibitor and developed by BMS Company. It is used to cure adult chronic myelogenous leukemia (CML), acute lymphatic leukemia (ALL) with positive Philadelphia chromosome, etc. Its chemical name is N-(2-chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)-1-piperazinyl]-2-methyl-4-pyrimidyl]amino]-5-thiazolformamide and its chemical structure is as following:

Five polymorphs of Dasatinib and the preparation methods thereof were described by Bristol-Myers Squibb in the Chinese Patent Application No. CN200580011916.6 (publication date is 13 Jun. 2007). The preparation methods instructed in this document are:Monohydrate: Dasatinib (48 g) was added into ethanol (1056 mL 22 ml/g) and water (144 mL), and dissolved by heating to 75° C.; the mixture was purified, filtrated and transferred to the receiver. The solution reactor and transferring pipes were washed with the mixture of ethanol (43 mL) and water (5 mL). The solution was heated to 75˜80° C. to be soluble completely and water (384 mL) was heated and the temperature of the solution was kept between 75° C. and 80° C. The seed crystal of monohydrate (preferable) was added when cooling to 75° C., and keep the temperature at 70° C. for 1 h; cooling to 5° C. within 2 h and keeping the temperature at 0˜5° C. for 2 h. The slurry was filtrated and the filter cake was washed by the mixture of ethanol (96 mL) and water (96 mL); after being dried under vacuum≦50° C. 41 g of solid was obtained.Butanol solvate: under refluxing (116° C.˜118° C.), Dasatinib was dissolved in 1-butanol (about 1 g/25 mL) to yield crystalline butanol solvate of Dasatinib. When cooling, this butanol solvate was recrystallized from solution. The mixture was filtrated and the filter cake was dried after being washed with butanol.Ethanol solvate: 5D (4 g, 10.1 mmol), 7B (6.6 g, 50.7 mmol), n-bubanol (80 mL) and DIPEA (2.61 g, 20.2 mmol)) were added into a 100 ml round flask. The obtained slurry was heated to 120° C. and kept the temperature for 4.5 h, and then cooled to 20° C. and stirred over night. The mixture was filtrate, and the wet filter cake was washed with n-butanol (2×10 mL) to yield white crystal product. The obtained wet filter cake was put back to the 100 ml reactor and 56 mL (12 mL/g) of 200 proof ethanol was added. Then additional ethanol (25 mL) was added at 80° C., and water (10 mL) was added into the mixture to make it dissolved rapidly. Heat was removed and crystallization was observed at 75° C.˜77° C. The crystal slurry was further cooled to 20° C. and filtrated. The wet filter cake was washed with ethanol:water (1:1, 10 mL) once and then washed with n-heptane (10 mL) once. After that it was dried under the condition of 60° C./30 in Hg for 17 h to yield 3.55 g of substance only containing 0.19% water.Neat form of N-6: DIPEA (155 mL, 0.89 mmol) was added into the mixture of compound 5D (175.45 g, 0.445 mol) and hydroxyethylpiperazine (289.67 g, 2.225 mol) in NMP (1168 mL). The suspension was heated at 110° C. for 25 min to be solution, which was then cooled down to about 90° C. The obtained solution was added dropwise into hot water (80° C., 8010 mL), and the mixture was stirred at 80° C. with heat preservation for 15 min and cooled to room temperature slowly. The solid was filtrated under vacuum and collected, washed by water (2×1600 mL) and dried under vacuum at 55° C.˜60° C. to give 192.45 of compound.Neat form of T1H1-7 (neat form and pharmaceutically acceptable carrier): monohydrate of Dasatinib was heated over dehydrate temperature to yield.Because Dasatinib is practically insoluble in water or organic solvent (e.g. methanol, ethanol, propanol, isopropanol, butanol, pentanol, etc.), even in the condition of heating, a large amount (over 100 times) of solvent is needed, which is disadvantageous in industrial production; in addition, with the method described in the Patent document of CN200580011916.6, the related substances in products can not be lowed effectively during the process of crystal preparation to improve the products quality.In terms of polymorphs of drug, each polymorph has different chemical and physical characteristics, including melting point, chemical stability, apparent solubility, rate of dissolution, optical and mechanical properties, vapor pressure as well as density. Such characteristics can directly influence the work-up or manufacture of bulk drug and formulation, and also affect the stability, solubility and bioavailability of formulation. Consequently, polymorph of drug is of great importance to quality, safety and efficacy of pharmaceutical preparation. When it comes to Dasatinib, there are still needs in the art for new polymorphs suitable for industrial production and with excellent physical and chemical properties as well.Example 1Preparation of the Polymorph IA. Dasatinib (10 g) and DMSO (40 ml) were added into a flask and heated up to 60˜70° C. by stirring, after dissolving, the mixture (120 mL) of water and acetone (1:1) was added under heat preservation. When crystal was precipitated, cooled it down to 0° C. to grow the grains for 10 minutes. Filtrate it and the cake was washed by water and then by the mixture of water and acetone (1:1). After that it was dried under −0.095 MPa at about 50° C. using phosphorus pentoxide as drying aid to give 7.7 g of white solid. Yield was 77%.Contrasts Index of raw material Items before transformation Index of Polymorph I Appearance off-white powder White crystal powder Related substance 0.85% 0.07% KF moisture 0.67% 3.59% 70~150 0.72% 3.63% TGA weight loss
The following items of products prepared by Method A were detected: microscope-crystal form (See. FIG. 1); XRPD Test (See. FIG. 2), IR Test (See. FIG. 3), DSC-TGA Test (See. FIG. 4-1, 4–2), 13C Solid-state NMR Test (See. FIG. 5).B. Dasatinib (10 g) and DMSO (40 ml) were added into a flask and heated slowly up to 60˜70° C. by stirring, after dissolving, the mixture (160 mL) of ethanol and water (1:1) was added under heat preservation. When crystal was precipitated, cooled it down to 0° C. to grow the grains for 10 minutes. Filtrate it and the cake was washed by the mixture of ethanol and water (1:1) and dried under −0.095 MPa at about 50° C. using phosphorus pentoxide as drying aid to give 7.7 g of white solid. Yield was 87%.Contrasts Index of raw material Items before transformation Index of Polymorph I Appearance off-white powder White crystal powder Related substance 0.85% 0.08% KF moisture 0.67% 3.58% 70~150 0.72% 3.67% TGA weight lossHPLC.Related Substances DeterminationHPLC conditions and system applicability: octadecylsilane bonded silica as the filler; 0.05 mol/L of potassium dihydrogen phosphate (adjusted to pH 2.5 by phosphoric acid, 0.2% triethylamine)-methanol (45:55) as the mobile phase; detection wavelength was 230 nm; the number of theoretical plates should be not less than 2000, calculated according to the peak of Dasatinib. The resolution of the peak of Dasatinib from the peaks of adjacent impurities should meet requirements.Determination method: sample was dissolved in mobile phase to be the solution containing 0.5 mg per milliliter. 20 μL of such solution was injected into liquid chromatograph, and chromatogram was recorded until the sixfold retention time of major component peak. If there were impurities peaks in the chromatogram of sample solution, total impurities and any single impurity were calculated by normalization method on the basis of peak area.Stability of Polymorph in the FormulationsThe XRPD patterns of capsules and tablets respectively prepared in the Example 3 and Example 4 have been tested, and compared with XRPD characteristic peaks of Polymorph I of Dasatinib prepared by the Method A in the Example 1 in the present invention, as listed in the following table:Bulk Drug Capsules 1 Capsules 2 Tablets 2 (Polymorph (Polymorph (Polymorph Tablets 1 (Polymorph I) I) I) (Polymorph I) I) 2θ 2θ 2θ 2θ 2θ 9.060 9.080 9.070 9.060 9.070 11.100 11.120 11.110 11.100 11.110 13.640 13.670 13.650 13.640 13.650 15.100 15.120 15.110 15.100 15.110 17.820 17.840 17.830 17.820 17.820 19.380 19.400 19.390 19.380 19.390 22.940 22.970 22.950 22.950 22.950The results in the above-mentioned comparative table have shown that the crystal form had substantially no change after Polymorph I of Dasatinib in the invention were prepared into capsules or tablets by the formulation process.In addition, The relative substances of capsules and tablets respectively prepared in the Example 3 and Example 4 have been tested, and compared with those of Polymorph I of Dasatinib prepared by the Method A in the Example 1 in the present invention, as listed in the following table:Bulk Drug (Polymorph I) Capsules 1 Capsules 2 Tablets 1 Tablets 2 0.07% 0.08% 0.08% 0.07% 0.08%The results in the above-mentioned comparative table have shown that the Polymorph I of Dasatinib was stable, and there were no significantly changes in respect to the relative substances, after Polymorph I of Dasatinib in the invention were prepared into capsules or tablets by the formulation process.INDUSTRIAL APPLICATIONThe present invention provides novel polymorphs of Dasatinib, preparing methods, and pharmaceutical composition comprising them. These polymorphs have better physicochemical properties, are more stable and are more suitable for industrial scale production, furthermore, are suitable for long-term storage, and are advantageous to meet the requirements of formulation process and long-term storage of formulations. The preparation technique of this invention was simple, quite easy for operation and convenient for industrial production, and the quality of the products was controllable with paralleled yields. In addition, by the methods of polymorph preparation in this invention, the amount of organic solvent used in crystal transformation could be reduced greatly, which led to reduced cost of products; organic solvents in Class III with low toxicity could be used selectively to prepare the polymorphs of this invention, reducing the toxic effects of the organic solvents potentially on human body to some extent.PATENThttps://patents.google.com/patent/WO2010067374A2/enDasatinib are antineoplastic agents, which were disclosed in WO Patent Publication No. 00/62778 and U.S. Patent No. 6,596,746. Dasatinib, chemically N-(2-chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)-1-piperazinyl]-2-methyl-4- pyrimidinyl]amino]-5-thiazolecarboxamide, is represented by the following structure:

Polymorphism is defined as “the ability of a substance to exist as two or more crystalline phases that have different arrangement and /or conformations of the molecules in the crystal Lattice. Thus, in the strict sense, polymorphs are different crystalline forms of the same pure substance in which the molecules have different arrangements and / or different configurations of the molecules”. Different polymorphs may differ in their physical properties such as melting point, solubility, X-ray diffraction patterns, etc. Although those differences disappear once the compound is dissolved, they can appreciably influence pharmaceutically relevant properties of the solid form, such as handling properties, dissolution rate and stability. Such properties can significantly influence the processing, shelf life, and commercial acceptance of a polymorph. It is therefore important to investigate all solid forms of a drug, including all polymorphic forms, and to determine the stability, dissolution and flow properties of each polymorphic form. Polymorphic forms of a compound can be distinguished in the laboratory by analytical methods such as X-ray diffraction (XRD), Differential Scanning Calorimetry (DSC) and Infrared spectrometry (IR).Solvent medium and mode of crystallization play very important role in obtaining a crystalline form over the other. Dasatinib can exist in different polymorphic forms, which differ from each other in terms of stability, physical properties, spectral data and methods of preparation.U.S. Patent Application No. 2005/0215795 A1 (herein after referred to as the 795 patent application) described five crystalline forms of dasatinib (monohydrate, butanol solvate, ethanol solvate, neat form (N-6) and neat form (T1H1-7)), characterized by powder X-ray diffraction (P-XRD) pattern.According to the ‘795 patent application, dasatinib monohydrate is characterized by an X-ray powder diffraction pattern having peaks expressed as 2Θ at approximately 18.0, 18.4, 19.2, 19.6, 21.2, 24.5, 25.9 and 28.0 ± 0.2 degrees. As per the process exemplified in the ‘795 patent application, dasatinb monohydrate can be obtained in dasatinib, by heating and dissolving the dasatinib in an ethanol and water mixture. Crystallizing the monohydrate from the ethanol and water mixture and cooled to get dasatinib monohydrate.According to the ‘795 patent application, dasatinib crystalline butanol solvate is characterized by an X-ray powder diffraction pattern having peaks expressed as 2Θ at approximately 5.9, 12.0, 13.0, 17.7, 24.1 and 24.6 ± 0.2 degrees.According to the 795 patent application, dasatinib crystalline ethanol solvate is characterized by an X-ray powder diffraction pattern having peaks expressed as 2Θ at approximately 5.8, 11.3, 15.8, 17.2, 19.5, 24.1, 25.3 and 26.2 ± 0.2 degrees.According to the 795 patent application, dasatinib crystalline neat form (N-6) is characterized by an X-ray powder diffraction pattern having peaks expressed as 2Θ at approximately 6.8, 11.1, 12.3, 13.2, 13.7, 16.7, 21.0, 24.3 and 24.8 ± 0.2 degrees.According to the 795 patent application, dasatinib crystalline neat form (T1H1-7) is characterized by an X-ray powder diffraction pattern having peaks expressed as 2Θ at approximately 8.0, 9.7, 11.2, 13.3, 17.5, 18.9, 21.0 and 22.0 ± 0.2 degrees.U.S. Patent application No. 2006/0094728 disclosed ethanolate form (T1E2-1) of dasatinib, characterized by an X-ray powder diffraction pattern having peaks expressed as 2Θ at approximately 7.2, 12.0, 12.8, 18.0, 19.3 and 25.2 ± 0.2 degrees. We have discovered novel crystalline form of dasatinib, dasatinib dimethylformamide solvate, dasatinib dimethyl sulfoxide solvate, dasatinib toluene solvate and dasatinib isopropyl acetate solvate.Another object of the present invention is to provide process for preparing the novel crystalline form of dasatinib, dasatinib dimethylformamide solvate, dasatinib dimethyl sulfoxide solvate, dasatinib toluene solvate, dasatinib isopropyl acetate solvate and known crystalline dasatinib monohydrate.Still another object of the present invention is to provide pharmaceutical compositions containing the novel crystalline form of dasatinib.Reference Example2-(6-Cholro-2-methylpyrimidin-4-yl-amino)-N-(2-chloro-6-methylphenyl) thiazole-5-carboxamide (15 gm) was added to 1-(2-hydroxyethyl)piperazine at 250C and heated to 850C, stirred for 2 hours 30 minutes at 850C. To the solution was added water (500 ml) at 800C and slowly cooled to 250C, stirred for 1 hour at 250C. The solid was collected by filtration and the solid was washed with water (50 ml), and then dried the solid at 550C under vacuum to obtain 15 gm of dasatinib.Example 1Dasatinib (5 gm) obtained according to reference example was dissolved in ethyl acetate (300 ml) at 250C and heated to reflux temperature. To the solution was added methanol (100 ml) and stirred for 30 minutes at reflux temperature to form clear solution. The solution was slowly cooled to room temperature and then cooled to O0C, stirred for 1 hour at O0C. The solid was collected by filtration and the solid was washed with mixture of ethyl acetate and methanol (20 ml, 3:1), and then dried the solid at 500C under vacuum to obtain 3.5 gm of crystalline dasatinib form I.Example 2Dasatinib (5 gm, HPLC purity: 99.2%) was dissolved in acetone (100 ml) and methanol (250 ml) and heated to reflux temperature, stirred for 30 minutes at reflux temperature to form clear solution. The solution was cooled to room temperature and then cooled to 200C, stirred for 1 hour at 200C. The solid was collected by filtration and the solid was washed with mixture of acetone (10 ml) and methanol (25 ml), and then dried the solid at 500C under vacuum to obtain 4 gm of crystalline dasatinib form I (HPLC purity: 99.85%).Example 3Dasatinib (5 gm, HPLC purity: 99.2%) was dissolved in dimethylformamide (25 ml) at 250C and heated to 650C to form clear solution. To the solution was slowly added acetone (50 ml) at 650C and stirred for 1 hour at 650C. The solution was slowly cooled to 250C and stirred for 1 hour at 250C. The contents are filtered and the solid obtained was washed with mixture of dimethylformamide and acetone (15 ml, 1:2), and then dried the solid at 500C under vacuum to obtain 4 gm of dasatinib dimethylformamide solvate (HPLC purity: 99.94%).Example 4Dasatinib (5 gm) was dissolved in dimethylformamide (25 ml) at 250C and heated to 650C to form clear solution. Ethyl acetate (50 ml) was added slowly to the solution at 650C and stirred for 1 hour at 650C. The solution was slowly cooled to 250C, stirred for 1 hour at 250C and filtered. The solid obtained was washed with mixture of dimethylformamide and ethyl acetate (30 ml, 1:2), and then dried the solid at 500C under vacuum to obtain 4 gm of dasatinib dimethylformamide solvate.Example 5Dasatinib (5 gm, HPLC purity: 99.2%) was dissolved in dimethylformamide (25 ml) and heated to 650C to form a clear solution. The solution was cooled to 250C and then cooled to 50C, stirred for 4 hour at 50C. The solid was collected by filtration and the solid was washed with chilled dimethylformamide (10 ml), and then dried the solid at 500C under vacuum to obtain 4 gm of dasatinib dimethylformamide solvate (HPLC purity: 99.9%).Example 6Dasatinib (5 gm, HPLC purity: 99.2%) was dissolved in dimethylformamide (25 ml) and heated to 650C to form a clear solution. Water (50 ml) was added slowly to the solution at 650C and stirred for 1 hour at 650C. The solution was cooled to 250C and stirred for 30 minutes at 250C. The solid was collected by filtration and the solid was washed with mixture of dimethylformamide and water (15 ml, 1 :2), and then dried the solid at 500C under vacuum to obtain 4.7 gm of dasatinib dimethylformamide solvate (HPLC purity: 99.93%).Example 7Dasatinib dimethylformamide solvate (4.7 gm) obtained as in example 6 was dissolved in water (50 ml) and heated to 750C, stirred for 4 hours at 750C. The solution was cooled to 250C, stirred for 30 minutes at 250C and filtered. The solid obtained was washed with water (15 ml), and then dried at 500C under vacuum to obtain 4.7 gm of dasatinib monohydrate.Example 8Dasatinib (20 gm) was dissolved in dimethyl sulfoxide (100 ml) at 250C and heated to 650C to form clear solution. To the solution was slowly added water (200 ml) at 650C and stirred for 1 hour at 650C. The solution was slowly cooled to 250C and stirred for 30 minutes at 250C. The solid was collected by filtration and the solid was washed with mixture of dimethyl sulfoxide and water (30 ml, 1 :2), and then dried the solid at 500C under vacuum to obtain 19.5 gm of dasatinib monohydrate.Example 9Dasatinib (5 gm) was dissolved in isopropyl acetate (65 ml) and heated to 800C, stirred for 1 hour at 800C to form a clear solution. The solution was cooled to 250C, stirred for 1 hour at 250C and filtered. The solid obtained was washed with isopropyl acetate (15 ml) to obtain 5 gm of dasatinib isopropyl acetate solvate.Example 10Dasatinib (6 gm) was dissolved in toluene (100 ml) and heated to reflux temperature, stirred for 2 hours at reflux temperature to form a clear solution. The solution was slowly cooled to 250C. The contents are filtered and the solid obtained was washed with toluene (20 ml) to obtain 5.5 gm of dasatinib toluene solvate.Example 11Dasatinib (5 gm) was dissolved in dimethyl sulfoxide (20 ml) at 250C and heated to 650C. To the solution was slowly added ethyl acetate (200 ml) at 650C and the solution was slowly cooled to O0C, stirred for 2 hours at O0C. The solid was collected by filtration and the solid was washed with mixture of dimethyl sulfoxide and ethyl acetate (55 ml, 1 :10), and then dried the solid at 500C under vacuum to obtain 4 gm of dasatinib dimethyl sulfoxide solvate.
PATENThttps://patents.google.com/patent/WO2014086326A1/enDasatinib, N-(2-chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)- 1 -piperazinyl]-2- methyl-4-pyrimidmyl]amino]-5-thiazole carboxamide of formula I, also known as BMS- 354825, is a cancer treatment drug developed by Bristol-Myers Squibb and sold under the trade name Sprycel®. Dasatinib is a multi- BCR/ABL and Src family tyrosine kinase inhibitor and it is used for treatment of chronic myelogenous leukaemia (CML) as a secondary drug after primary treatment with imatinib (Gleevec®). It is also used for treatment of acute lymphoblastic leukaemia caused by mutation/translocation of chromosomes and development of the so-called Philadelphia chromosome (Ph+ ALL). However, its potential is so wide that the possibility of using it for treatment of other types of cancer, including advanced stages of prostate cancer, is still being investigated.

(I)In accordance with the basic patent WO2000062778A1, dasatinib is prepared by reaction of the key intermediate of formula II with l-(2-hydroxyethyl)piperazine in the presence of a base and a suitable solvent (Scheme 1). A similar preparation method was later used in a number of other process patents, only varying the corresponding base or solvent. Through the selection of a suitable solvent or procedure a great number of solvates or polymorphs can be prepared. Polymorphs have been one of the most frequently studied physical characteristics of active pharmaceutical substances (API) recently. Thus, different polymorphs of one API may have entirely different physical-chemical properties such as solubility, melting point, mechanical resistance of crystals but they may also influence the chemical and physical stability. Then, these properties may have an impact on further processes such as handling of the particular API, grinding or formulation method. These various physical-chemical characteristics of polymorphs influence the resulting bioavailability of the solid dosage form. Therefore, looking for new polymorphs and solvates is becoming an important tool for obtaining a polymorph form with the desired physical-chemical characteristics.

The process patent WO2005077945A2 describes preparation of the following solvates of dasatinib: monohydrate, butanol solvate, as well as two anhydrous forms (N-6 and T1H1- 7). A related patent also mentions two ethanol solvates, the hemi-ethanol and diethanol solvates (US 8 242 270 B2). Salts, various combinations of salts and their solvates have been described in detail in the patent application WO2007035874A1.Another process patent, WO2009053854A2, dealt with the preparation of a number of solvates or mixed solvates out of which especially the isopropanol and mixed isopropanol/dimethyl sulfoxide solvates, as well as a new solid form B, another anhydrous polymorph of dasatinib, are worth mentioning. Other patent applications have also dealt with the preparation of other solvates/mixed solvates (WO2010067374A2), or processes for the preparation and purification of the monohydrate/anhydrous form (WO2010139981A2) and its polymorphs (WO2011095059 Al).API solvates or salts are used in drug formulations in many cases. In the case of solvates the limits for individual solvents, their contents or maximum daily doses have to be strictly observed. Then, these limits can dramatically restrict their effective use. Thus, the clearly most convenient option is the use of sufficiently stable polymorphs of API that do not contain any solvents bound in the crystalline structure.Some of the above mentioned patent documents describe preparation of a stable anhydrous form of dasatinib (N-6). In accordance with individual patent documents the main disadvantages of the preparation of N-6 is the necessity of desolvation of the solvated form of the API at high temperatures (WO2009053854A2), or application of an increased temperature (50°C and more) and vacuum for a relatively long time (8-12h; WO2010139981A2 and WO2005077945A2). These procedures are very demanding from the point of view of general technology, energy and time, to say nothing of the necessity to work under an inert atmosphere to prevent possible oxidation-degradation reactions of the API. This is because dasatinib may be oxidized by atmospheric oxygen to the corresponding N-oxide (oxidation occurs in the piperazine ring), which may undergo the Cope elimination at increased temperatures. This secondary reaction may subsequently impair the purity of the prepared API.With a view to the above mentioned facts it is obvious that completely new methods and processes have to be developed even for polymorphs or solvates that are already well- known. Generally, the development of technologically and economically more efficient procedures is the main decisive parameter in their industrial utilization for the preparation of the API.Dasatinib of formula I is prepared by a reaction of the intermediate of formula II with l-(2- hydroxyethyl)piperazine in the presence of diisopropylethylamine (DIPEA) in an organic solvent from the group of dipolar aprotic solvents, higher alcohols or diols.If a dipolar aprotic solvent from the group of N-methyl-2-pyrrolidone (NMP), N^iV-dimethyl formamide (DMF), AyV-dimethyl acetamide (DMA), dimethyl sulfoxide (DMSO), formamide (FA), N,N -dimethyl propylene urea (DMPU) and l,3-dimethyl-2-imidazolidinone (DMI) is used, the reaction is carried out at 50-110°C under an inert atmosphere for 1/2-6 hours. In a preferable embodiment, NMP, DMSO, DMPU or DMI is used and the reaction is carried out at 90°C for 1-3 hours. The result of the reaction is crude dasatinib in the form of a solution in the corresponding solvent.If an alcohol from the group of isoamyl alcohol or 1,3-propanediol is used as a solvent for preparation of the crude dasatinib, the reaction mixture is heated at 120-160°C for 2-12 hours, in a preferable embodiment at 135°C for 3-6 hours.If dipolar aprotic solvents (NMP, DMF, DMA, DMSO, FA, DMPU and DMI) are used, in step a) a precipitant is added to the hot solution (90°C) under continuous stirring in an inert atmosphere in a 2- 15 fold, most preferably 4-10fold (by volume) amount with respect to the dipolar aprotic solvent. Suitable precipitants comprise especially acetonitrile, propionitrile, most preferably acetonitrile.After addition of the precipitant the obtained solution is withdrawn from the heating bath and is slowly left to cool down to 22°C under continuous stirring in an inert atmosphere. Crystallization occurs within 1-120 minutes (depending on the volume, until complete cooling). After having cooled down to 22°C (laboratory temperature), the suspension is stirred for another hour. The corresponding solvate of dasatinib is aspirated by well-known techniques in an inert atmosphere at 10-35 °C, most preferably at 22°C, and washed with the respective co-solvent.The solvate of dasatinib obtained this way can be directly used in the next step – recrystallization, without the necessity of drying. If necessary, the product may be dried at 10- 35°C, most preferably at 25°C, and at the pressure of 10-200 kPa, most preferably 50 kPa, for 6-24 hours, most preferably 12 hours.If NMP is used as the solvent in step a), the corresponding NMP solvate is isolated. The obtained dried crystalline NMP solvate (NM) of dasatinib has a characteristic XRPD pattern, which is presented in Figure no. 1. The NMP solvate (NM) has the following characteristic peaks: 5.88; 6.73; 10.73; 11.92; 13.39; 14.97; 16.72; 18.95; 20.17; 21.46; 22.81; 24.65; 25.18; 26.02 and 28.06 ± 0.2° 2-theta.If isoamyl alcohol or 1,3-propanediol are used as the solvents in step a), the reaction mixture is left to cool down to 22°C after expiration of the reaction time (3-6 h). Crystallization generally begins when the inner temperature of the reaction mixture drops to 100°C. After cooling down to 22°C (laboratory temperature), the suspension is further stirred for another 1 hour. Crystalline dasatinib is aspirated by well-known techniques in an inert atmosphere at 10-35°C, most preferably at 22°C, and washed with the corresponding solvent.The obtained product is dried at 10-35°C, most preferably at 25°C, and at the pressure of 10-200 kPa, most preferably 50 kPa, for 6-24 hours, most preferably 12 hours.The obtained crystalline isoamyl alcohol solvate (SI) of dasatinib has a characteristic XRPD pattern, which is shown in Figure no. 2. The solvate (SI) has the following characteristic peaks: 5.72; 10.35; 11.42; 12.61; 13.14; 14.27; 15.33; 17.18; 17.44; 17.97; 19.12; 19.95; 20.38; 22.05; 22.42; 23.01; 23.46; 23.68; 25.26; 26.20; 26.45; 26.62 and 27.78 ± 0.2° 2-theta.The obtained crystalline 1,3-propanediol solvate (SP) of dasatinib has a characteristic XRPD pattern, which is shown in Figure no. 3. The solvate (SP) has the following characteristic peaks: 6.04; 12.01; 15.10; 17.95; 18.35; 18.77; 21.25; 21.51; 22.96; 24.08; 24.62; 25.80; 26.16; 28.16 and 33.6578 ± 0.2° 2-theta.These solvates (or polymorph forms) are then easily converted to the desired anhydrous polymorph N-6 or another solvate in steps b) and c). All the forms prepared this way are sufficiently stable and can easily be isolated in the chemical purities of 99% and higher (in accordance with HPLC).The anhydrous polymorph form N-6 is prepared in the following way: any solvate or another polymorph is dissolved under an inert atmosphere at 90°C (reflux) in a 10-30 times, most preferably 20 times, the (weight) amount of the crystallization solvent. Suitable crystallization solvents include especially methanol, ethanol, isopropanol, most preferably methanol.A co-solvent is added in 0.1-10 times, most preferably ½-l times, the volume of the crystallization solvent used in an inert atmosphere at 90°C. The co-solvent can be, e.g., acetonitrile, propionitrile and their mixtures, most preferably acetonitrile. After addition of the co-solvent the obtained solution is withdrawn from the heating bath and is slowly left to cool down to 22°C under continuous stirring in an inert atmosphere. Crystallization occurs during 1-120 minutes (depending on the volume, until complete cooling). After having cooled down to 22°C (laboratory temperature), the suspension is stirred for another hour. Crystalline dasatinib is aspirated by well-known techniques in an inert atmosphere at 10-35°C, most preferably at 22°C, and washed with the corresponding co-solvent. The chemical purity of the obtained product is 99% (in accordance with HPLC); it is the polymorph form N-6 and its XRPD pattern is shown in Figure no. 4. The polymorph form N-6 has the following characteristic peaks: 6.77; 12.31; 13.16; 13.75; 16.70; 17.20; 18.54; 19.34; 20.25; 20.95; 21.94; 24.28; 24.82; and 27.80 ± 0.2° 2-theta.Brief Description of Drawings:Figure 1: shows an X-ray powder diffraction pattern of the crystalline solvate NM. Individual axes: independently variable: reflection angle 2Θ, dependently variable: intensity of detected radiation.Figure 2: shows an X-ray powder diffraction pattern of the isoamyl alcohol crystalline solvate SI. Individual axes: independently variable: reflection angle 2Θ, dependently variable: intensity of detected radiation. Figure 3: shows an X-ray powder diffraction pattern of the 1,3 propanediol crystalline solvate SP. Individual axes: independently variable: reflection angle 2Θ, dependently variable: intensity of detected radiation.Figure 4: shows an X-ray powder diffraction pattern of the crystalline anhydrous form N-6. Individual axes: independently variable: reflection angle 2Θ, dependently variable: intensity of detected radiation.Examples: The following working examples illustrate methods for the preparation of dasatinib of formula I, its polymorph form N-6 and its solvates NM, SI, SP.The polymorph forms and solvates of dasatinib were characterized with X-ray powder diffraction using the following methods:The diffraction patterns were measured using an X’PERT PRO MPD PANalytical diffractometer with a graphite monochromator, radiation used CuKa (λ=1.542 A), excitation voltage: 45 kV, anode current: 40 mA, measured range: 2 – 40° 2Θ, increment: 0.01° 2Θ. The measurement was carried out using a flat powder sample that was placed on a Si plate. For the primary optic setting programmable divergence diaphragms with the irradiated sample area of 10 mm, Soller diaphragms 0.02 rad and an anti-dispersion diaphragm ¼ were used. For the secondary optic setting an X’Celerator detector with the maximum opening of the detection slot, Soller diaphragms 0.02 rad and an anti-dispersion diaphragm 5.0 mm were used. HPLC method:Stock solution of samples: dissolve 5.0 mg of the sample in 10.0 ml of 50% acetonitrile R with water.Dimensions of the chromatographic HPLC column: / = 0.10 m, d= 3 mm- stationary phase: Zorbax Eclipse Plus Phenyl-Hexyl RRHD 1.8 μιη; temperature: 35 °C. Mobile phase: A: phosphate buffer (0.01 M sodium dihydrogen phosphate, pH treated by addition of sodium hydroxide to 7.00 ± 0.05); B: acetonitrile R.Gradient (A/B; flow 0.6 ml/min): 0 min 80/20; 10 min 50/50; 11 min 50/50; 12 min 80/20. Detection at the wavelength of 220 nm.Feed: 2 μΐ of the sample stock solution Example 1.Preparation of the NMP solvate (NM) of dasatinib:The intermediate of formula II (1.00 g; 2.54 mmol) and l-(2-hydroxyethyl)piperazine (1.66 g; 12.77 mmol) were dissolved in N-methylpyrrolidone (5 ml) under an inert atmosphere and diisopropylethylamine (0.9 ml, 5.18 mmol) was added to the reaction mixture. The reaction mixture was stirred and heated up to 90°C for 70 minutes and then acetonitrile (30 ml) was added to the reaction. The mixture was withdrawn from the heating bath and stirred intensively. Crystallization started after 5 minutes, the suspension was left to cool down under continuous stirring. After achieving the laboratory temperature it was stirred for another 2 hours. The crystalline substance was aspirated on frit S3, washed with acetonitrile (5 ml) and dried by suctioning under an inert nitrogen atmosphere for 15 minutes. The XRPD pattern of the sample obtained this way corresponds to the NMP solvate (NM) and can be used in the subsequent steps without the necessity of drying. Drying after 6 hours in an exsiccator at the laboratory temperature in vacuo (50 kPa) provided 1.2 g of crystalline dasatinib; 80% of the theoretical yield. HPLC purity 99.12%. The 1H NMR and 13C NMR spectra correspond to the data known from the literature. The XRPD pattern of the dried product corresponds to the NMP solvate (NM). The NM solvate is characterized by the reflections presented in Table 1 :Table 1 – NM forminterplanarpos. distance[°2Th.] [nm] rel. int. [%]5.88 1.5024 81.86.73 1.3131 100.010.73 0.8236 10.611.92 0.7420 59.213.39 0.6606 19.614.97 0.5915 38.416.72 0.5298 45.018.95 0.4679 10.920.17 0.4399 13.921.46 0.4138 13.422.81 0.3895 21.024.65 0.3608 13.325.18 0.3534 14.426.02 0.3422 11.928.06 0.3177 5.8
Norepinephrine bitartrate
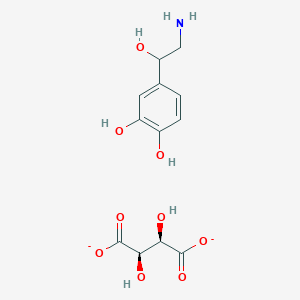
Norepinephrine bitartrate
Arterenol bitartrate
RN: 3414-63-9
FREE FORM 138-65-8
UNIIIFY5PE3ZRW
R FORM CAS Number108341-18-0,
- 1,2-Benzenediol, 4-(2-amino-1-hydroxyethyl)-, (R)-, [R-(R*,R*)]-2,3-dihydroxybutanedioate (1:1) (salt), monohydrate
- 1,2-Benzenediol, 4-[(1R)-2-amino-1-hydroxyethyl]-, (2R,3R)-2,3-dihydroxybutanedioate (1:1) (salt), monohydrate (9CI)
- Arterenol, tartrate, monohydrate (6CI)
- L-Noradrenaline bitartrate monohydrate
- Levarterenol bitartrate monohydrate
WeightAverage: 337.281
Chemical FormulaC12H19NO10
(+-)-Arterenol bitartrate
(+-)-Noradrenaline bitartrate
(+-)-Norepinephrine bitartrate
(2R,3R)-2,3-dihydroxybutanedioic acid 4-[(1R)-2-amino-1-hydroxyethyl]benzene-1,2-diol hydrate
ORD +41.3 °, water, 4% ; Wavlen: 589.3 nm; Temp: 25 °C, AND MP 163-165 °C, GB 747768 1956 NorepinephrineCAS Registry Number: 51-41-2CAS Name: 4-[(1R)-2-Amino-1-hydroxyethyl]-1,2-benzenediolAdditional Names: (-)-a-(aminomethyl)-3,4-dihydroxybenzyl alcohol; l-3,4-dihydroxyphenylethanolamine; noradrenaline; levarterenolTrademarks: Adrenor; Levophed (Winthrop)Molecular Formula: C8H11NO3Molecular Weight: 169.18Percent Composition: C 56.79%, H 6.55%, N 8.28%, O 28.37%Literature References: Demethylated precursor of epinephrine, q.v. Occurs in animals and man, and is a sympathomimetic hormone of both adrenal origin and adrenergic orthosympathetic postganglionic origin in man. Physiologic review: Malmejac, Physiol. Rev.44, 186 (1964). It has also been found in plants, e.g., Portulaca olerocea L., Portulacaceae: Fing et al.,Nature191, 1108 (1961). Synthesis of dl-form: Payne, Ind. Chem.37, 523 (1961). Historic review of synthesis: Loewe, Arzneim.-Forsch.4, 583 (1954). Resolution of dl-form: Tullar, J. Am. Chem. Soc.70, 2067 (1948); idem,US2774789 (1956 to Sterling Drug). Configuration: Pratesi et al.,J. Chem. Soc.1959, 4062. Comprehensive description: C. F. Schwender, Anal. Profiles Drug Subs.1, 149-173 (1972); T. D. Wilson, ibid.11, 555-586 (1982).Properties: Microcrystals, dec 216.5-218°. [a]D25 -37.3° (c = 5 in water with 1 equiv HCl).Optical Rotation: [a]D25 -37.3° (c = 5 in water with 1 equiv HCl)
Derivative Type: HydrochlorideCAS Registry Number: 329-56-6Trademarks: Arterenol (HMR)Molecular Formula: C8H11NO3.HClMolecular Weight: 205.64Percent Composition: C 46.73%, H 5.88%, N 6.81%, O 23.34%, Cl 17.24%Properties: Crystals, mp 145.2-146.4°. [a]D25 -40° (c = 6). Freely sol in water. Solns slowly oxidize under the influence of light and oxygen in a manner comparable to epinephrine hydrochloride.Melting point: mp 145.2-146.4°Optical Rotation: [a]D25 -40° (c = 6)
Derivative Type:d-BitartrateCAS Registry Number: 69815-49-2Additional Names: Levarterenol bitartrateTrademarks: Aktamin; BinodrenalMolecular Formula: C8H11NO3.C4H6O6Molecular Weight: 319.26Percent Composition: C 45.14%, H 5.37%, N 4.39%, O 45.10%Properties: Obtained as the monohydrate, crystals, mp 102-104°. [a]D25 -10.7° (c = 1.6 in H2O). When anhydr, mp 158-159° (some decompn). Freely sol in water.Melting point: mp 102-104°; mp 158-159° (some decompn)Optical Rotation: [a]D25 -10.7° (c = 1.6 in H2O)
Derivative Type:dl-FormProperties: Crystals, dec 191°. Sparingly sol in water; very slightly sol in alc, ether; readily sol in dilute acids, caustic.
Therap-Cat: Adrenergic (vasopressor); antihypotensive.Therap-Cat-Vet: Sympathomimetic; vasopressor in shock.Keywords: a-Adrenergic Agonist; Antihypotensive.
Precursor of epinephrine that is secreted by the adrenal medulla and is a widespread central and autonomic neurotransmitter. Norepinephrine is the principal transmitter of most postganglionic sympathetic fibers and of the diffuse projection system in the brain arising from the locus ceruleus. It is also found in plants and is used pharmacologically as a sympathomimetic.
Norepinephrine (sometimes referred to as l-arterenol/Levarterenol or l-norepinephrine) is a sympathomimetic amine which differs from epinephrine by the absence of a methyl group on the nitrogen atom.
Norepinephrine Bitartrate is (-)-α-(aminomethyl)-3,4-dihydroxybenzyl alcohol tartrate (1:1) (salt) monohydrate and has the following structural formula:
 |
LEVOPHED is supplied in sterile aqueous solution in the form of the bitartrate salt to be administered by intravenous infusion following dilution. Norepinephrine is sparingly soluble in water, very slightly soluble in alcohol and ether, and readily soluble in acids. Each mL contains the equivalent of 1 mg base of norepinephrine, sodium chloride for isotonicity, and not more than 2 mg of sodium metabisulfite as an antioxidant. It has a pH of 3 to 4.5. The air in the ampuls has been displaced by nitrogen gas.
Norepinephrine, also known as noradrenaline, is a medication used to treat people with very low blood pressure.[2] It is the typical medication used in sepsis if low blood pressure does not improve following intravenous fluids.[3] It is the same molecule as the hormone and neurotransmitter norepinephrine.[2] It is given by slow injection into a vein.[2]
Common side effects include headache, slow heart rate, and anxiety.[2] Other side effects include an irregular heartbeat.[2] If it leaks out of the vein at the site it is being given, norepinephrine can result in limb ischemia.[2] If leakage occurs the use of phentolamine in the area affected may improve outcomes.[2] Norepinephrine works by binding and activating alpha adrenergic receptors.[2]
Norepinephrine was discovered in 1946 and was approved for medical use in the United States in 1950.[2][4] It is available as a generic medication.[2]
Medical uses
Norepinephrine is used mainly as a sympathomimetic drug to treat people in vasodilatory shock states such as septic shock and neurogenic shock, while showing fewer adverse side-effects compared to dopamine treatment.[5][6]
Mechanism of action
It stimulates α1 and α2 adrenergic receptors to cause blood vessel contraction, thus increases peripheral vascular resistance and resulted in increased blood pressure. This effect also reduces the blood supply to gastrointestinal tract and kidneys. Norepinephrine acts on beta-1 adrenergic receptors, causing increase in heart rate and cardiac output.[7] However, the elevation in heart rate is only transient, as baroreceptor response to the rise in blood pressure as well as enhanced vagal tone ultimately result in a sustained decrease in heart rate.[8] Norepinephrine acts more on alpha receptors than the beta receptors.[9]
Names
Norepinephrine is the INN while noradrenaline is the BAN.
SYN
Chemical Synthesis
Norepinephrine, L-1-(3,4-dihydroxyphenyl)-2-aminoethanol (11.1.4), is synthesized by two methods starting from 3,4-dihydroxybenzaldehyde. According to the first method, the indicated aldehyde is transformed into the cyanohydrin (11.1.3) by reaction with hydrogen cyanide, which is then reduced into norepinephrine (11.1.5).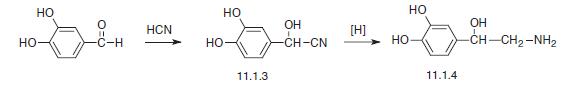
The second method consists of the condensation of diacetate of the same aldehyde with nitromethane, which forms (3,4-diacetoxyphenyl)-2-nitroethanol (11.1.5). Then the nitro group is reduced and the product (11.1.6) is hydrolyzed into the desired norepinephrine (11.1.4) [4,9,13,14].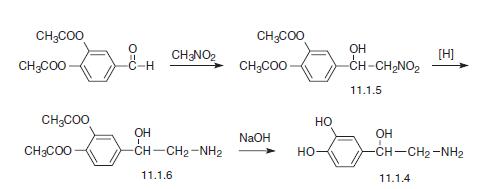
Purification Methods
Recrystallise adrenor from EtOH and store it in the dark under N2. [pKa, Lewis Brit J Pharmacol Chemother 9 488 1954, UV: Bergstr.m et al. Acta Physiol Scand 20 101 1950, Fluorescence: Bowman et al. Science NY 122 32 1955, Tullar J Am Chem Soc 70 2067 1948.] The L-tartrate salt monohydrate has m 102-104.5o, [] D -11o (c 1.6, H2O), after recrystallisation from H2O or EtOH. [Beilstein 13 III 2382.]
PATENT
https://patents.google.com/patent/WO2013008247A1/en4-[(lR)-2-amino-l-hydroxyethyl]benzene-l,2-diol, commonly known as (R)-(-)- norepinephrine or noradrenaline is a catecholamine with multiple roles including as a hormone and a neurotransmitter. As a stress hormone, norepinephrine affects parts of the brain where attention and responding actions are controlled. Along with epinephrine, norepinephrine also underlies the fight-or-flight response, directly increasing heart rate, triggering the release of glucose from energy stores, and increasing blood flow to skeletal muscle. Norepinephrine also has a neurotransmitter role when released diffusely in the brain as an antiinflammatory agent.When norepinephrine acts as a drug it increases blood pressure by increasing vascular tone through a-adrenergic receptor activation. The resulting increase in vascular resistance triggers a compensatory reflex that overcomes its direct stimulatory effects on the heart, called the baroreceptor reflex, which results in a drop in heart rate called reflex bradycardia.(R)-(-)-Norepinephrine has a following structure:

(R)-(-)-Norepinephrine was first time disclosed in the US patent US2774789, where it was obtained by resolution of dl-norepinephrine, with optically active acids such as d- tartaric acid, 1-malic acid or N-benzoyl-l-threonine. The patent does not disclose the preparation of dl-norepinephrine. The patent GB747768 describes reduction of amino ketones where 3,4-dihydroxy-a- aminoacetophenone hydrochloride was converted into its d-tartrate salt; followed by reduction of the d-tartrate salt. This process leads to formation of excessive amount of d- adrenaline d-tartrate (which is a bi-product) as it crystallized first; whereas the desired 1- adrenaline d-tartrate crystallizes after 2 days and in smaller yield. Also the patent does not disclose the source of 3,4-dihydroxy-a-aminoacetophenone hydrochloride.It has been unsuccessfully tried to treat dihydroxy-a-chloroacetophenone with hexamethylenetetramine (commonly known as hexamine) and to treat the reaction product with an acid to obtain arterenone (see Mannich, Hahn B., Berichte der deutschen chemischen Gesellschaft, volume 44, issue 2, Pages 1542 – 1552 (1911)). Mannich found that the treatment of this and similar halogen ketones with hexamine did not produce an addition compound but resulted in splitting of halogen acid which made the process impossible. Mannich also found that an addition compound of the halogen ketone and hexamine is formed only when the two phenolic hydroxyl groups are closed i.e. protected by acylation or etherification. Hence according to Mannich, the reaction is not at all possible for the compounds containing two unprotected phenolic hydroxyl groups. The US patent US 1680055 discloses the preparation of monohydroxy-a-substituted- aminoacetophenones either by reacting monohydroxy-a-bromoacetophenones with a substituted amine or by reacting protected monohydroxy-a-bromoacetophenones with a substituted amine followed by deprotection. The patent does not disclose the preparation of dihydroxy-a-aminoacetophenones (where amino group is unsubstituted).It is disclosed in the US patent US2786871 that when chloroaceto pyrocatechol is treated with ammonia, arterenone is obtained in 50% yield. However when the reaction is carried out in basic medium, darkening of the reaction mass takes place which results in coloured product. The patent also discloses preparation of amino-methyl-(monohydroxyphenyl)- ketones by reacting halogen ketone with hexamine. It is also disclosed in the patent that the process is applicable only to the halogenomethyl-monohydroxyphenyl-ketones.Following are some of the methods for preparation of 3,4-dihydroxy-a- aminoacetophenone, reported in the literature. J. Am. Pharm. Association (1946) 35, 306 – 309 discloses preparation of 3,4-dihydroxy- a-aminoacetophenone by reacting 3,4-dihydroxy-a-chloroacetophenone with dibenzyl amine followed by hydrogenation of resulting dibenzylamino ketone. The main disadvantage of this reaction is formation of derivatives of dibenzyl amines, which remain in the final product in the form of impurities.Acta Chimica Academiae Scientiarum Hungaricae (1951), 1, 395-402, discloses preparation of 3,4-dihydroxy-a-aminoacetophenone from 3,4-dihydroxyphenyloxo acetaldehyde and benzyl amine followed by reduction of benzylamino ketone intermediate. The main disadvantage of this method is that the starting acetaldehyde derivative is very expensive and not easily available.It is disclosed in Recueil des Travaux Chimiques des Pays-Bas et de la Belgique (1952), 71, 933-44, that 3,4-dihydroxy-a-aminoacetophenone hydrochloride is formed by demethylation of 3,4-dimethoxy-a-aminoacetophenone hydrochloride using 48% HBr. The reaction results in less than 10% yield of the aminoacetophenone.Monatshefte fuer Chemie (1953), 84 1021-32, discloses preparation of 3,4-dihydroxy-a- aminoacetophenone by reacting 3,4-dihydroxy-a-chloroacetophenone with sodium azide followed by hydrogenation of azide intermediate using 4% palladium on carbon as a catalyst. In the hydrogenation step, 1.6 gm of azide intermediate requires 1.4 gm of catalyst, which is not economical and industrially feasible.
Preparation of 3,4-dihydroxy-a-aminoacetophenones hydrochloride is disclosed in J. Am. Chem. Soc, 1955, volume 77, issue 10, pages 2896 – 2897. The following scheme is disclosed in the article:


It is clear from the above scheme that the process requires additional steps of protection and deprotection of hydroxyl and amino groups, and use of potassium phthalimide requires anhydrous reaction conditions. Therefore the process is time consuming and not economical.Chinese patent CN101798271A describes reduction of 3,4-dihydroxy-a- aminoacetophenone hydrochloride in water as solvent followed by neutralization with aqueous ammonia. Since dl-norepinephrine has partial solubility in aqueous basic medium result in to loss of product. Also it is necessary to maintain low volume of solvent throughout the process for better yields making the process stringent.European patent EP1930313 discloses preparation of a-amino ketones. The preparation is carried out by reacting an organic sulfide in a polar solvent with a compound containing a leaving group attached to a primary or secondary carbon atom to form a sulfonium salt, which is reacted with a ketone in presence of a base and a polar solvent. Oxiranes obtained are further converted into the corresponding aminoketone, by aminolysis followed by selective oxidation. The following scheme is disclosed in the patent.

It is clear from the above scheme that the process requires many steps and hence is time consuming. The patent does not exemplify the synthesis of dihydroxy-a- aminoacetophenones.Thus, the search for a suitable manufacturing process for (R)-norepinephrine intermediates remains undoubtedly of interest. We were surprised to find that hardly any literature discloses the process for preparation of dihydroxy-a-aminoacetophenones acid addition salts. We have found that the reaction of dihydroxy-a-haloacetophenone with hexamine is feasible and results in high yield of product although both the hydroxyl groups on the phenyl ring of acetophenone are unprotected. Object of the invention:It is therefore an object of the invention is to overcome or ameliorate at least one disadvantage of the prior art or to provide a useful alternative.Another object of the invention is to provide a novel, safe, efficient, concise, ecological, high yielding, industrially feasible and simpler process for preparation of (R)-(-)- norepinephrine intermediates.Another object of the invention is to provide a process for synthesis of 3,4-dihydroxy-a- aminoacetophenone salt, which is feasible without protecting both the hydroxyl group on the phenyl ring of acetophenone.Yet another object of the invention is to provide an improved process for hydrogenation of 3,4-dihydroxy-a-aminoacetophenone salt to prepare (dl)-norepinephrine salt.Summary of the invention:In accordance with the above objectives, the present invention provides a process for preparation of (dl)-norepinephrine intermediate of formula (III) comprising reacting 3,4- dihydroxy-a-haloacetophenone of formula (I) with hexamine to provide a quaternary ammonium salt of formula (II); followed by hydrolyzing the quaternary ammonium salt of formula (II) with an acid.In a second aspect, the present invention provides a novel quaternary ammonium salt of formula (II) and its preparation.In a third aspect, the present invention provides a novel process for hydrogenation of 3,4- dihydroxy-a-aminoacetophenone acid salt to provide (dl)-norepinephrine acid addition salt.Example 1Preparation of quaternary ammonium saltA 5000 ml four neck round bottom flask with water condenser and calcium chloride tube was charged with Hexamine (210.28 gm), chloroform (1200 ml), 3,4-dihydroxy-a- chloroacetophenone (250 gm) and isopropanol (1000 ml) at room temperature. The reaction mass was gently heated at 63°C for 4 hours. The reaction was monitored by TLC. The reaction mass was cooled to room temperature and filtered to get solid. The solid was washed with acetone and dried at 50°C for 4 hours to obtain quaternary ammonium salt which was used in the next step without purification.Yield – 410 gm (93.65%)Nature – off white solidm.p. – 180 to l82°CNMR (DMSO-d6): – δ =4.51 – 4.75 (m, 8H), 5.39 (s, 6H), 6.92 (d, 1H, J= 7.5 Hz), 7.37 – 7.42 (m, 2H), 9.67 (s, br, 1H), 10.44 (s, br, 1H)Example 2Preparation of 3,4-dihydroxy-a-aminoacetophenone hydrochlorideA 2000 ml four neck round bottom flask with water condenser and calcium chloride tube was charged with the quaternary ammonium salt obtained in the example 1 (120 gm), methanol (862.5 ml) and cone, hydrochloric acid (194.4 ml). The reaction mixture was heated to 60 to 65°C and aged at same temperature for 3 to 4 hours. The reaction was monitored by TLC. The reaction mass was cooled and neutralized using base to give 3,4- dihydroxy-a-aminoacetophenone. The solid was filtered, washed with water and dried at 50°C. This base was further converted in to its hydrochloride salt with IPA-HC1 mixture. Yield – 72 gm (96.3%)Nature – off white solidHPLC – 99.7%1H NMR(CD30D) – 5 = 3.62(s, 1H), 6.80 (d, J = 8 Hz, 1H), 7.38 (d, J = 1.3 Hz, 1H), 7.63 (d, J = 8 Hz, 1H).Example 3Preparation of (dl)-norepinephrine hydrochlorideA 500 ml hydrogenation flask was charged with 3,4-dihydroxy-a-aminoacetophenone hydrochloride obtained in the example 2 (55 gm), 10% palladium on carbon (5 gm) and methanol (300 ml). The reaction mixture was heated to 45°C with hydrogen gas pressure of 4 to 5 kg m2. The reaction mixture was stirred at 45°C for 5 hours. The catalyst was removed by filtration. The filtrate was cooled to 5 to 10 °C and ammonia gas was passed through the solvent for 2 h till the pH of the solution was around 9. The solid obtained was filtered, washed with methanol and dried in air to obtain (dl)-norepinephrine. Yield – 43.5 gm (96.7%)Nature white crystalline solidHPLC 99.6%Example 4Preparation of (dl)-norepinephrine hydrochlorideA 500 ml hydrogenation flask was charged with 3,4-dihydroxy-a-aminoacetophenone hydrochloride obtained from process similar to example 2 (55 gm), 10% palladium on carbon (5 gm) and methanol (300 ml). The reaction mixture was aged at 25 °C with hydrogen gas pressure of 4 to 3 kg/m2. The reaction mixture was stirred at 25°C for 15 hours. The reaction was monitored by TLC. The catalyst was removed by filtration. The filtrate was cooled to 5 to 10 °C and ammonia solution was added to the reaction mixture till the pH of the solution around 9. The solid obtained was filtered, washed with methanol and dried in air to obtain (dl)-norepinephrine.Yield – 41.5 gm (92.2%)Nature – white crystalline solidHPLC – 99.5%
PATENTUS-10865180https://patentscope.wipo.int/search/en/detail.jsf?docId=US283323778&_cid=P11-KMEC1N-93277-1
| Norepinephrine Bitartrate (Arterenol Bitartrate) is chemically known as (−)-α-(aminomethyl)-3, 4-dihydroxybenzyl alcohol tartrate (1:1) (salt) monohydrate is a catecholamine family that functions in the brain and body as a hormone and neurotransmitter. As a stress hormone, Norepinephrine affects parts of the brain where attention and responding actions are controlled. Along with epinephrine, Norepinephrine also underlies the fight-or-flight response, directly increasing heart rate, triggering the release of glucose from energy stores, and increasing blood flow to skeletal muscle. Norepinephrine also has a neurotransmitter role when released diffusely in the brain as an anti-inflammatory agent. |
| LEVOPHED® (l-Norepinephrine) is supplied in sterile aqueous solution in the form of the bitartrate salt to be administered by intravenous infusion following dilution. Norepinephrine is sparingly soluble in water, very slightly soluble in alcohol and ether, and readily soluble in acids. Each ml contains the equivalent of 1 mg base of Norepinephrine, sodium chloride for isotonicity, and not more than 2 mg of sodium metabisulfite as an antioxidant. |
| Norepinephrine Bitartrate is (−)-α-(amino methyl)-3,4-dihydroxybenzyl alcohol tartrate (1:1) (salt) monohydrate and has the following structural formula: |
| (l)-Norepinephrine was first disclosed in 1947 by Sterling Drugs. U.S. Pat. No. 2,774,789 discloses the resolution of dl-Norepinephrine with optically active acids such as d-tartaric acid, 1-malic acid or N-benzoyl-l-threonine. The patent does not disclose the basic synthesis of dl-Norepinephrine. |
| Journal of the American Chemical Society, Volume 70 (6), 1948 describes the resolution of dl-Norepinephrine in to d-arterenol-d-bitartrate and l-arterenol-d-bitartrate in water and aqueous methanol. Further it also describes isolation of d-arterenol and l-arterenol form above tartrate salts. |
| U.S. Pat. No. 2,786,871 discloses the process for the preparation of arterenol wherein chloroacetopyrocatechol is treated with ammonia and arterenol is obtained in 50% yield. |
| J. Am. Pharm. Association (1946) 35, 306-309 discloses preparation of 3,4-dihydroxyaminoacetophenone by reacting 3,4-dihydroxy-α-chloroacetophenone with dibenzyl amine, followed by hydrogenation of the resulting dibenzylamino ketone. The main disadvantage of this reaction is the formation of derivatives of dibenzyl amines, which carried over to final product in the form of impurities. |
| Acta Chimica Academiae Scientiarum Hungaricae (1951), 1, 395-402 discloses preparation of 3, 4-dihydroxy-α-aminoacetophenone from 3,4-dihydroxyphenyloxo acetaldehyde and benzyl amine followed by reduction of the benzylamino ketone intermediate. The main disadvantage of this method is that the starting acetaldehyde derivative is very expensive and not easily available. |
| CN101798271A describes reduction of 3,4-dihydroxy-α-aminoacetophenone hydrochloride in water as solvent followed by neutralization with aqueous ammonia. Since dl-Norepinephrine has partial solubility in aqueous basic medium, this process results in a loss of product. Also, it is necessary to maintain low volume of solvent throughout the process for better yields making the process stringent. |
| WO2009004593 describes the process for the preparation of Epinephrine wherein (−) epinephrine is obtained by chiral separation of dl-epinephrine using the chiral acid such as L-tartaric acid with an optical purity of 95.24%. |
| WO2013008247 discloses a process for preparation of (dl)-norepinephrine hydrochloride salt by reacting 3,4-dihydroxy-a-haloacetophenone with hexamethylenetetramine to provide hexamine salt; followed by hydrolysis and hydrogenation. However, this process fails to teach the resolution of (dl)-norepinephrine hydrochloride and preparation of l-Norepinephrine Bitartrate monohydrate. |
| WO2016038422 discloses a process for the preparation of optically enriched adrenaline or adrenaline tartrate comprising the steps of: (a) reacting a mixture of (−)-adrenaline and (+)-adrenaline with L(+)-tartaric acid to form adrenaline tartrate; (b) contacting the adrenaline tartrate with less than 1 equivalent of ammonium hydroxide. However, the product achieved is with purity of only 98%. |
| CN107298646 describes the process for the preparation of Norepinephrine wherein L-Norepinephrine tartrate is obtained by chiral separation of dl-Norepinephrine using the chiral acid such as L-tartaric acid. The chiral separation step using L-tartaric acid is repeated once to obtain pure Norepinephrine. However, there is no information on bitartrate salt and its optical purity. |
| In light of the above, there remains a need in the art for highly pure l-Norepinephrine Bitartrate having high enantiomeric purity i.e. greater than 99.0% so as to provide enhanced therapeutic efficacy and safety when administered. Surprisingly the present inventors have found out a process for the preparation of (l)-Norepinephrine Bitartrate having enantiomeric purity greater than 99.5%, for which protection is sought. |
Reference Example-1(U.S. Pat. No. 2,774,789, Example-A)
Preparation of l-Norepinephrine Bitartrate
| To a four necked 100 ml flask charged racemic Norepinephrine base (20 gm), d-(−) tartaric acid (18.34 gm), and water (35 ml) at room temperature. The reaction mass was stirred to obtain clear solution, cooled to 0-5° C. After 5 hours slight turbidity was observed. Turbidity increases slowly to get thick white slurry after 6 hours, reaction mass becomes very thick which was difficult to filter, washed solid wet cake by 4.0 ml water followed by two 12 ml portions of 95% ethanol. Suck dried the solid completely, dried at 45° C. to get l-Norepinephrine Bitartrate (28 gm) which is in crude form. |
| Crude l-Norepinephrine Bitartrate (20 gm) dissolved in 14 ml of water at 50° C. Clear solution was obtained. Activated charcoal was added to this solution and stirred the reaction mass for more for 30 min. Filtered through Hyflo and cooled to 0-5° C. After 2 hours, clear solution obtained gets converted to thick solid mass. Filtered and washed the solid with 1.5 ml of chilled water followed 14 ml of 95% ethanol. |
| This dry solid 8 gm (after 1 st purification) was then dissolved in 8 ml of water at 50° C. to get clear solution. This reaction mass was then cooled to 0-5° C. After 1 hour, a clear solution gets converted to a thick solid mass. Maintained the reaction mass for more than 2 hours at the same conditions. Filtered the thick solid and washed with 95% ethanol. Dried the solid at 45° C. to obtain l-Norepinephrine Bitartrate. |
| Chiral Purity by HPLC: l-Norepinephrine Bitartrate=68.45%, and d-isomer=31.55% |
| Specific Optical Rotation: −6.33° |
Reference Example-2 (JAGS, 1948, Page-2067-68, Example-a)
| To a four necked flask charged racemic Norepinephrine base (20 gm), d-(−) tartaric acid (18.34 gm), and water (35.20 ml) at room temperature. After 5 minutes reaction mass becomes clear liquid. Cooled the reaction mass to 2-3° C. After 30 minutes, reaction mass was observed to be turbid and further the reaction mass becomes very thick. This mass was, stirred for 2 hours at 0-5° C. Then filtered reaction mass at same temperature and washed solid wet cake with 3.5 ml water followed by two 11.8 ml portions of 95% ethanol. Dried the solid at air oven at 45° C. to get crude tartrate salt (15 gm). |
| Crude tartrate salt (15 gm) was dissolved in 5 ml of water at 50° C. to get clear solution. Cooled to 2-3° C. After 30 minutes, a clear solution gets converted to a thick solid mass. Filtered the solid and washed with 1.5 ml of chilled water and then 15 ml of 95% ethanol. Dried the solid at 45° C. to obtain semi pure l-Norepinephrine Bitartrate (8 gm). |
| This semi pure l-Norepinephrine Bitartrate (8 gm) was dissolved in 8 ml of water at 50° C. to get clear solution. Cooled the mass to 2-3° C. After 30 minutes clear solution gets converted to thick solid mass. Filtered the solid and washed with 8 ml of 95% ethanol. Dried the solid at 45° C. to obtain pure l-Norepinephrine Bitartrate (3 gm). |
| Chiral Purity: l-Norepinephrine Bitartrate=77.14%, d-isomer=22.86% |
| Specific Optical Rotation: −10.4° |
Example-1: Preparation of 2-Chloro-1-(3, 4-Dihydroxyacetophenone)
| In round bottom flask, charged Methylene Chloride (1000 ml), Aluminium chloride (300 gm) and cooled to 0-5° C. Pyrocatechol (100 gm) was added lot wise. Chloroacetyl chloride (108 gm) was added drop wise at 0-5° C. Then stirred the reaction mass at 25-30° C. for 20-24 hours. After completion of the reaction, reaction mass was quenched in aq. HCl, filtered the reaction mass and wet cake was charged in water containing acetic acid. Filtered the reaction mass and cooled to 15-20° C., filtered solid and washed with water. |
| Yield: 110 gm. |
| HPLC Purity: 99.5% |
Example-2: Preparation of Hexamine Salt
| In a round bottom flask charged 2-chloro-1-(3, 4-dihydroxyacetophenone) (100 gm), Hexamine (87 gm), IPA (500 ml), Chloroform (400 ml). Stirred the reaction mass at reflux temperature for 6 hours. After completion of the reaction, cooled to 25-30° C., filtered and washed the wet cake with IPA and Methanol. |
| Yield: 160 gm. |
| HPLC Purity: 99.3% |
Example-3: Preparation of 2-Amino-1-(3,4-Dihydroxyphenyl)Ethanone Hydrochloride
| In a round bottom flask charged Hexamine salt (100 gm), Methanol (600 ml), aqueous HCl and heated the reaction mass to 55-60° C. After completion of the reaction, the mass was dissolved in water, by adjusting pH with liquor ammonia. Filtered the solid and washed with water, dried the material at 45-50° C. |
| This free base was charged in 900 ml methanol and pH was adjusted to 1-1.5 by IPA.HCl and distilled off methanol completely to get white solid which was isolated by filtration. |
| Yield: 37 gm |
| HPLC Purity: 99.5% |
Example-4: Preparation of [4-(2-Amino-1-Hydroxyethyl) Benzene-1, 2-Diol] (Racemic Norepinephrine Base)
| Charged 2-amino-1-(3, 4-dihydroxyphenyl) ethanone hydrochloride (100 gm), 10% Pd/C(10 gm), methanol (700 ml) and water (300 ml) mixture in autoclave. Stirred the reaction mass at 40-45° C. After completion of reaction, Pd/C was removed by filtration. Collected filtrate and distilled off methanol. pH was adjusted by liquor ammonia. Isolated the solid by filtration and washed with water followed by methanol. Dried the solid at 40-45° C. |
| Yield: 67 gm |
| Purity: 99.2% |
Example-5: Preparation of l-Norepinephrine Base
| Charged racemic Norepinephrine base (100 gm), D-(−)-Tartaric acid (142 gm), water (100 ml) in a round bottom flask. The reaction mass was stirred to get clear solution. After some time, solid started to crystallize. Reaction mass was diluted with methanol (900 ml). Maintained the reaction mass under stirring for 24 hours at 25-30° C. Filtered and washed the wet cake with methanol to obtain Crude l-Norepinephrine tartrate salt. |
| Yield: 85 gm |
| The crude l-Norepinephrine tartrate salt was converted into its free base by dissolving this crude tartrate salt in water (500 ml) and adjusted pH to 8-8.5 by liquor ammonia and isolated the solid by filtration. Dried the material at 40-45° C. to obtain pure l-Norepinephrine free base (43 gm). |
| Yield: 43 gm (l-Norepinephrine pure base). |
| HPLC Purity: 99.7% |
| Chiral Purity: 98.0% |
Example-6: Preparation of Pure l-Norepinephrine Base
| Charged l-Norepinephrine base (100 gm) obtained from Example-5, D-(−)-Tartaric acid (142 gm), water (100 ml) in a round bottom flask. The reaction mass was stirred to get clear solution. After some time, a solid started to crystallize. Reaction mass was diluted with methanol (900 ml). Maintained the reaction mass under stirring for 24 hours at 25-30° C. Filtered and washed the wet cake with methanol to obtain l-Norepinephrine tartrate salt. |
| Yield: 88 gm |
| The l-Norepinephrine tartrate salt was converted into its free base by dissolving this crude tartrate salt in water (500 ml) and adjusted the pH to 8-8.5 by liquor ammonia and isolated the solid by filtration. Dried the material at 40-45° C. to obtain pure l-Norepinephrine free base (44 gm). |
| Yield: 44 gm (l-Norepinephrine pure base). |
| HPLC Purity: 99.7% |
| Chiral Purity: 99.1% |
Example-7: Preparation of Highly Pure Norepinephrine Bitartrate Monohydrate
| Charged Norepinephrine pure base (100 gm), L-(+) tartaric acid (100 gm), water (100 ml) and methanol (900 ml), Stirred the reaction mass to get clear solution. After some time, a solid started to crystallize then the reaction mass was diluted with methanol (900 ml). Maintained the reaction mass under stirring at 25-30° C. for 24 hours. Filtered and washed the wet cake with methanol to obtain Norepinephrine Bitartrate Monohydrate (90 gm). |
| HPLC Purity: 99.8% |
| Chiral Purity: 99.4% |
Example-8: Purification of l-Norepinephrine Bitartrate Monohydrate
| Charged 100 gm tartrate salt obtained from example-6, purified water (100 ml) and heated the reaction mass to 40-45° C. to obtain clear solution, cooled to 0-5° C. Charged IPA (100 ml) slowly and the mass was stirred for one hour. The solid was isolated by filtration and washed with IPA. Dried the material at 40-45° C. to obtain l-Norepinephrine Bitartrate Monohydrate (82 gm) having high enantiomeric purity. |
| HPLC Purity: 99.85% |
| Chiral Purity: 99.87% |
| Specific Optical rotation: −11.0° |
Example-9
| The following table sets forth the high purity of the l-Norepinephrine Bitartrate monohydrate of the invention as compared with prior art references. |
| [TABLE-US-00001] Referencel-Norepinephrine Example-2Bitartrate U.S. Pat. No.(JACS, 1948,monohydrate 2,774,789Page-2067-68,of the presentPurity CriteriaExample-AExample-a)invention Optical purity of l-68.45%77.14%99.87%NorepinephrineBitartratemonohydrateSpecific Optical−6.33°−10.4°−11.0°rotation(Limit: −10°to −12°) |
| It is evident from the above table that the compound of the present invention has substantially improved optical purity. |
PATENTCN-102525895
Publication numberPriority datePublication dateAssigneeTitleCN101053557A *2006-04-132007-10-17邵长青Noradrenaline bitartrate medicine composition frozen dried powder injectionCN102335123A *2010-07-162012-02-01上海禾丰制药有限公司Noradrenaline bitartrate injection and preparation technology thereofPublication numberPriority datePublication dateAssigneeTitleEP3110399B12014-02-272018-01-10Sintetica S.A.Process for producing a stable low concentration, injectable solution of noradrenalineFamily To Family CitationsCN109394683A *2018-12-072019-03-01远大医药(中国)有限公司A kind of preparation method of noradrenaline bitartrate injection
References
- ^ Andersen, A. M. (1975). “Structural Studies of Metabolic Products of Dopamine. IV. Crystal and Molecular Structure of (−)-Noradrenaline”. Acta Chem. Scand. 29b: 871–876. doi:10.3891/acta.chem.scand.29b-0871.
- ^ Jump up to:a b c d e f g h i j “Norepinephrine Bitartrate”. The American Society of Health-System Pharmacists. Archived from the original on 26 March 2017. Retrieved 26 March 2017.
- ^ Latifi, Rifat (2016). Surgical Decision Making: Beyond the Evidence Based Surgery. Springer. p. 67. ISBN 9783319298245. Archived from the original on 2017-03-27.
- ^ Encyclopedia of the Neurological Sciences. Academic Press. 2014. p. 224. ISBN 9780123851581. Archived from the original on 2017-03-27.
- ^ Rhodes, Andrew; Evans, Laura E (March 2017). “Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2016” (PDF). Critical Care Medicine. 45 (3): 486–552. doi:10.1097/CCM.0000000000002255. hdl:10281/267577. PMID 28098591. S2CID 52827184.
We recommend norepinephrine as the first-choice vasopressor (strong recommendation, moderate quality of evidence).
- ^ De Backer D, Biston P, Devriendt J, Madl C, Chochrad D, Aldecoa C, Brasseur A, Defrance P, Gottignies P, Vincent JL (March 2010). “Comparison of dopamine and norepinephrine in the treatment of shock”. The New England Journal of Medicine. 362 (9): 779–89. doi:10.1056/nejmoa0907118. PMID 20200382.
- ^ I Moore, Joanne (6 December 2012). Pharmacology (3 ed.). Springer Science and Business Media. p. 39. ISBN 9781468405248. Retrieved 19 November 2017.
- ^ “CV Physiology | Circulating Catecholamines”. cvphysiology.com. Retrieved 2019-02-27.
- ^ Sacha, Pollard; Stephenie, B Edwin; Cesar, Alaniz (July 2015). “Vasopressor and Inotropic Management Of Patients With Septic Shock”. Physical Therapy. 40 (7): 449–450. PMC 4495871. PMID 26185405.
External links
- “Norepinephrine”. Drug Information Portal. U.S. National Library of Medicine.
- “Norepinephrine bitartrate”. Drug Information Portal. U.S. National Library of Medicine.
////////Norepinephrine bitartrate, ARTERELOL, a-Adrenergic Agonist, Antihypotensive, levarterenol, Adrenor, Levophed,
#Norepinephrine bitartrate, #ARTERELOL, #a-Adrenergic Agonist, #Antihypotensive, #levarterenol, #Adrenor, #Levophed,
O.O[C@H]([C@@H](O)C(O)=O)C(O)=O.NC[C@H](O)C1=CC(O)=C(O)C=C1
COVAXIN, BBV 152


COVAXIN
CAS 2501889-19-4
- Whole-Virion Inactivated SARS-CoV-2 Vaccine
- UNII76JZE5DSN6
- BBV 152
- A whole virion inactivated COVID-19 vaccine candidate derived from SARS-CoV-2 strain NIV-2020-770
REF
medRxiv (2020), 1-21.
bioRxiv (2020), 1-32.
BBV152 (also known as Covaxin) is an inactivated virus-based COVID-19 vaccine being developed by Bharat Biotech in collaboration with the Indian Council of Medical Research.
BBV152 is a vaccine candidate created by the Indian Council of Medical Research (ICMR). The candidate, a whole virion inactivated SARS-CoV-2 vaccine, was developed from a well-known SARS-CoV-2 strain and a vero cell platform (CCL-81) with adjuncts of either aluminum hydroxide gel (Algel) or a novel TLR7/8 agonist adsorbed gel. The components of the vaccine include BBV152A, BBV152B, and BBV152C. Animal studies in mice, rats, and rabbits reported BBV152 immunogenicity at two separate antigen concentrations with both types of adjuvants. The formulation with the TLR7/8 adjuvant specifically induced significant Th1 biased antibody responses and increased SARS-CoV-2 lymphocyte responses. Thus, as of July 2020, BBV152 is in Phase 1/2 clinical trials assessing safety and immunogenicity in humans (NCT04471519).
Clinical research
Phase I and II trials
In May 2020, Indian Council of Medical Research’s (ICMR‘s) National Institute of Virology approved and provided the virus strains for developing a fully indigenous COVID-19 vaccine.[1][2] In June 2020, the company got permission to conduct Phase I and Phase II human trials of a developmental COVID-19 vaccine named Covaxin, from the Drugs Controller General of India (DCGI), Government of India.[3] A total of 12 sites were selected by the Indian Council for Medical Research for Phase I and II randomised, double-blind and placebo-controlled clinical trials of vaccine candidate.[4][5][6]
In December 2020, the company announced the report for Phase I trials and presented the results through medRxiv preprint;[7][8] the report was later published in the The Lancet.[9]
On March 8, 2021, Phase II results were published in The Lancet. The study showed that Phase II trials had a higher immune response and induced T-cell response due to the difference in dosing regime from Phase I. The doses in Phase II were given at 4 weeks interval as opposed to 2 weeks in Phase I. Neutralization response of the vaccine were found significantly higher in Phase II.[10]
Phase III trials[edit]
In November 2020, Covaxin received the approval to conduct Phase III human trials[11] after completion of Phase I and II.[12] The trial involves a randomised, double-blinded, placebo-controlled study among volunteers of age group 18 and above and started on 25 November.[13] The Phase III trials involved around 26,000 volunteers from across India.[14] The phase III trials covered a total of 22 sites consisting several states in the country, including Delhi, Karnataka and West Bengal.[15] Refusal rate for Phase III trials was much higher than that for Phase I and Phase II. As a result only 13,000 volunteers had been recruited by 22 December with the number increasing to 23,000 by 5 January. [16][17]
As on March 2021, the stated interim efficacy rate for phase III trial is 81%.[18][10]
B.1.1.7 (United Kingdom) variant
In December 2020, a new SARS‑CoV‑2 variant, B.1.1.7, was identified in the UK.[19] A study on this variant was carried and preliminary results presented in biorxiv have shown Covaxin to be effective in neutralizing this strain.[20]
Manufacturing
The vaccine candidate is produced with Bharat Biotech’s in-house vero cell manufacturing platform[21] that has the capacity to deliver about 300 million doses.[22] The company is in the process of setting up a second plant at its Genome Valley facility in Hyderabad to make Covaxin. The firm is in talks with other state governments like Odisha[23] for another site in the country to make the vaccine. Beside this, they are also exploring global tie-ups for Covaxin manufacturing.[24]
In December 2020, Ocugen Inc entered a partnership with Bharat Biotech to co-develop Covaxin for the U.S. market.[25][26] In January 2021, Precisa Med entered an agreement with Bharat Biotech to supply Covaxin in Brazil[27]
Emergency use authorisation
See also: COVID-19 vaccine § Trial and authorization status
Bharat Biotech has applied to the Drugs Controller General of India (DCGI), Government of India seeking an emergency use authorisation (EUA).[31] It was the third firm after Serum Institute of India and Pfizer to apply for emergency use approval.[32]
On 2 January 2021, the Central Drugs Standard Control Organisation (CDSCO) recommended permission for EUA,[33] which was granted on 3 January.[34] The emergency approval was given before Phase III trial data was published. This was criticized in some sections of the media.[35][36]
The vaccine was also approved for Emergency Use in Iran and Zimbabwe.[30][29]
References
- ^ “ICMR teams up with Bharat Biotech to develop Covid-19 vaccine”. Livemint. 9 May 2020.
- ^ Chakrabarti A (10 May 2020). “India to develop ‘fully indigenous’ Covid vaccine as ICMR partners with Bharat Biotech”. ThePrint.
- ^ “India’s First COVID-19 Vaccine Candidate Approved for Human Trials”. The New York Times. 29 June 2020.
- ^ “Human clinical trials of potential Covid-19 vaccine ‘COVAXIN’ started at AIIMS”. DD News. Prasar Bharati, Ministry of I & B, Government of India. 25 July 2020.
- ^ Press, Associated (25 July 2020). “Asia Today: Amid new surge, India tests potential vaccine”. Washington Post. Retrieved 17 December 2020.
- ^ “Delhi: 30-year-old is first to get dose of trial drug Covaxin”. The Indian Express. 25 July 2020.
- ^ Perappadan, Bindu Shajan (16 December 2020). “Coronavirus | Covaxin phase-1 trial results show promising results”. The Hindu. Retrieved 17 December 2020.
- ^ Sabarwal, Harshit (16 December 2020). “Covaxin’s phase 1 trial result shows robust immune response, mild adverse events”. Hindustan Times. Retrieved 17 December 2020.
- ^ Ella, Raches; Vadrevu, Krishna Mohan; Jogdand, Harsh; Prasad, Sai; Reddy, Siddharth; Sarangi, Vamshi; Ganneru, Brunda; Sapkal, Gajanan; Yadav, Pragya; Abraham, Priya; Panda, Samiran; Gupta, Nivedita; Reddy, Prabhakar; Verma, Savita; Rai, Sanjay Kumar; Singh, Chandramani; Redkar, Sagar Vivek; Gillurkar, Chandra Sekhar; Kushwaha, Jitendra Singh; Mohapatra, Satyajit; Rao, Venkat; Guleria, Randeep; Ella, Krishna; Bhargava, Balram (21 January 2021). “Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBV152: a double-blind, randomised, phase 1 trial”. The Lancet Infectious Diseases. doi:10.1016/S1473-3099(20)30942-7. PMC 7825810. PMID 33485468.
- ^ Jump up to:a b Ella, Raches; Reddy, Siddhart; Jogdand, Harsh; Sarangi, Vamsi; Ganneru, Brunda; Prasad, Sai; Das, Dipankar; Dugyala, Raju; Praturi, Usha; Sakpal, Gajanan; Yadav, Pragya; Reddy, Prabhakar; Verma, Savita; Singh, Chandramani; Redkar, Sagar Vivek; Singh, Chandramani; Gillurkar, Chandra Sekhar; Kushwaha, Jitendra Singh; Mohapatra, Satyajit; Mohapatra, Satyajit; Bhate, Amit; Rai, Sanjay; Panda, Samiran; Abraham, Priya; Gupta, Nivedita; Ella, Krishna; Bhargav, Balram; Vadrevu, Krishna Mohan (8 March 2021). “Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBV152: interim results from a double-blind, randomised, multicentre, phase 2 trial, and 3-month follow-up of a double-blind, randomised phase 1 trial”. The Lancet Infectious Diseases. doi:10.1016/S1473-3099(21)00070-0.
- ^ “Coronavirus | Covaxin Phase III trial from November”. The Hindu. 23 October 2020.
- ^ Ganneru B, Jogdand H, Daram VK, Molugu NR, Prasad SD, Kannappa SV, et al. (9 September 2020). “Evaluation of Safety and Immunogenicity of an Adjuvanted, TH-1 Skewed, Whole Virion InactivatedSARS-CoV-2 Vaccine – BBV152”. doi:10.1101/2020.09.09.285445. S2CID 221635203.
- ^ “An Efficacy and Safety Clinical Trial of an Investigational COVID-19 Vaccine (BBV152) in Adult Volunteers”. clinicaltrials.gov(Registry). United States National Library of Medicine. NCT04641481. Retrieved 26 November 2020.
- ^ “Bharat Biotech begins Covaxin Phase III trials”. The Indian Express. 18 November 2020.
- ^ Sen M (2 December 2020). “List of states that have started phase 3 trials of India’s first Covid vaccine”. mint.
- ^ “70%-80% Drop In Participation For Phase 3 Trials Of Covaxin: Official”. NDTV. 17 December 2020.
- ^ “Bharat Biotech’s Covaxin given conditional nod based on incomplete Phase 3 trial results data”. The Print. 3 January 2021.
- ^ Kumar, N. Ravi (3 March 2021). “Bharat Biotech says COVID-19 vaccine Covaxin shows 81% efficacy in Phase 3 clinical trials”. The Hindu.
- ^ “Inside the B.1.1.7 Coronavirus Variant”. The New York Times. 18 January 2021. Retrieved 29 January 2021.
- ^ Sapkal, Gajanan N.; Yadav, Pragya D.; Ella, Raches; Deshpande, Gururaj R.; Sahay, Rima R.; Gupta, Nivedita; Mohan, V. Krishna; Abraham, Priya; Panda, Samiran; Bhargava, Balram (27 January 2021). “Neutralization of UK-variant VUI-202012/01 with COVAXIN vaccinated human serum”. bioRxiv: 2021.01.26.426986. doi:10.1101/2021.01.26.426986. S2CID 231777157.
- ^ Hoeksema F, Karpilow J, Luitjens A, Lagerwerf F, Havenga M, Groothuizen M, et al. (April 2018). “Enhancing viral vaccine production using engineered knockout vero cell lines – A second look”. Vaccine. 36 (16): 2093–2103. doi:10.1016/j.vaccine.2018.03.010. PMC 5890396. PMID 29555218.
- ^ “Coronavirus vaccine update: Bharat Biotech’s Covaxin launch likely in Q2 of 2021, no word on pricing yet”. http://www.businesstoday.in. India Today Group. Retrieved 13 December2020.
- ^ “Odisha fast tracks coronavirus vaccine manufacturing unit”. The New Indian Express. 7 November 2020.
- ^ Raghavan P (24 September 2020). “Bharat Biotech exploring global tie-ups for Covaxin manufacturing”. The Indian Express.
- ^ Reuters Staff (22 December 2020). “Ocugen to co-develop Bharat Biotech’s COVID-19 vaccine candidate for U.S.” Reuters. Retrieved 5 January 2021.
- ^ “Bharat Biotech, Ocugen to co-develop Covaxin for US market”. The Economic Times. Retrieved 5 January 2021.
- ^ “Bharat Biotech inks pact with Precisa Med to supply Covaxin to Brazil”. mint. 12 January 2021.
- ^ Schmall E, Yasir S (3 January 2021). “India Approves Oxford-AstraZeneca Covid-19 Vaccine and 1 Other”. The New York Times. Retrieved 3 January 2021.
- ^ Jump up to:a b “Iran issues permit for emergency use for three other COVID-19 vaccines: Official”. IRNA English. 17 February 2021.
- ^ Jump up to:a b Manral, Karan (4 March 2021). “Zimbabwe approves Covaxin, first in Africa to okay India-made Covid-19 vaccine”. Hindustan Times. Retrieved 6 March 2021.
- ^ Ghosh N (7 December 2020). “Bharat Biotech seeks emergency use authorization for Covid-19 vaccine”. Hindustan Times.
- ^ “Coronavirus | After SII, Bharat Biotech seeks DCGI approval for Covaxin”. The Hindu. 7 December 2020.
- ^ “Expert panel recommends granting approval for restricted emergency use of Bharat Biotech’s Covaxin”. The Indian Express. 2 January 2021.
- ^ “Coronavirus: India approves vaccines from Bharat Biotech and Oxford/AstraZeneca”. BBC News. 3 January 2021. Retrieved 3 January 2021.
- ^ “Disputes Mount, but Heedless Govt Intent on Rolling Vaccine Candidates Out”. The Wire. 12 January 2021.
- ^ “AIPSN urges govt to reconsider emergency approval for Covaxin till Phase 3 data is published – Health News , Firstpost”. Firstpost. 8 January 2021.
External links
| Scholia has a profile for Covaxin / BBV152 (Q98703813). |
COVAXIN®, India‘s indigenous COVID-19 vaccine by Bharat Biotech is developed in collaboration with the Indian Council of Medical Research (ICMR) – National Institute of Virology (NIV).
The indigenous, inactivated vaccine is developed and manufactured in Bharat Biotech’s BSL-3 (Bio-Safety Level 3) high containment facility.
The vaccine is developed using Whole-Virion Inactivated Vero Cell derived platform technology. Inactivated vaccines do not replicate and are therefore unlikely to revert and cause pathological effects. They contain dead virus, incapable of infecting people but still able to instruct the immune system to mount a defensive reaction against an infection.
Why develop Inactivated Vaccine? Conventionally, inactivated vaccines have been around for decades. Numerous vaccines for diseases such as Seasonal Influenza, Polio, Pertussis, Rabies, and Japanese Encephalitis use the same technology to develop inactivated vaccines with a safe track record of >300 million doses of supplies to date. It is the well-established, and time-tested platform in the world of vaccine technology.
Key Attributes:
- COVAXIN® is included along with immune-potentiators, also known as vaccine adjuvants, which are added to the vaccine to increase and boost its immunogenicity.
- It is a 2-dose vaccination regimen given 28 days apart.
- It is a vaccine with no sub-zero storage, no reconstitution requirement, and ready to use liquid presentation in multi-dose vials, stable at 2-8oC.
- Pre-clinical studies: Demonstrated strong immunogenicity and protective efficacy in animal challenge studies conducted in hamsters & non-human primates. For more information about our animal study, please visit our blog page on Non-Human Primates.
- The vaccine received DCGI approval for Phase I & II Human Clinical Trials in July, 2020.
- A total of 375 subjects have been enrolled in the Phase 1 study and generated excellent safety data without any reactogenicity. Vaccine-induced neutralizing antibody titers were observed with two divergent SARS-CoV-2 strains. Percentage of all the side-effects combined was only 15% in vaccine recipients. For further information, visit our blog page on phase 1 study.
- In Phase 2 study, 380 participants of 12-65 years were enrolled. COVAXIN® led to tolerable safety outcomes and enhanced humoral and cell-mediated immune responses. Know more about our phase 2 study.

- A total of 25,800 subjects have been enrolled and randomized in a 1:1 ratio to receive the vaccine and control in a Event-Driven, randomized, double-blind, placebo-controlled, multicentre phase 3 study.
The purpose of this study is to evaluate the efficacy, safety, and immunogenicity of COVAXIN® in volunteers aged ≥18 years.
Of the 25,800 participants, >2400 volunteers were above 60 years of age and >4500 with comorbid conditions.
COVAXIN® demonstrated 81% interim efficacy in preventing COVID-19 in those without prior infection after the second dose.
COVAXIN® effective against UK variant strain:
Analysis from the National Institute of Virology indicates that vaccine-induced antibodies can neutralize the UK variant strains and other heterologous strains.
Global Acceptance of COVAXIN®:
Bharat biotech has been approached by several countries across the world for the procurement of COVAXIN®.
- Clinical trials in other countries to commence soon.
- Supplies from government to government in the following countries to take place: Mongolia, Myanmar, Sri Lanka, Philippines, Bahrain, Oman, Maldives and Mauritius.

| A person holding a vial of the Covaxin vaccine | |
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | Inactivated |
| Clinical data | |
| Trade names | Covaxin |
| Routes of administration | Intramuscular |
| ATC code | None |
| Legal status | |
| Legal status | EUA : IND, IRN, ZBW |
| Identifiers | |
| DrugBank | DB15847 |
| Part of a series on the |
| COVID-19 pandemic |
|---|
| SARS-CoV-2 (virus)COVID-19 (disease) |
| showTimeline |
| showLocations |
| showInternational response |
| showMedical response |
| showImpact |
| COVID-19 Portal |
| vte |
////////COVAXIN, BBV152, BBV 152, INDIA 2021, APPROVALS 2021, COVID 19, CORONA VIRUS, bharat biotech
#COVAXIN, #BBV152, #BBV 152, #INDIA 2021, #APPROVALS 2021, #COVID 19, #CORONA VIRUS, #bharat biotech
Lenalidomide hydrate,

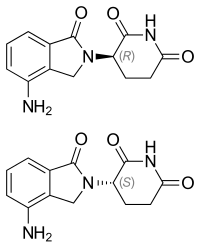
Lenalidomide hydrate
レナリドミド水和物
An immunomodulator.
CC-5013 hemihydrate
2,6-Piperidinedione, 3-(4-amino-1,3-dihydro-1-oxo-2H-isoindol-2-yl)-, hydrate (2:1)
(+/-)-2,6-Piperidinedione, 3-(4-amino-1,3-dihydro-1-oxo-2H-isoindol-2-yl)-, hydrate (2:1)
| Formula | (C13H13N3O3)2. H2O |
|---|---|
| CAS | 847871-99-2 |
| Mol weight | 536.5365 |
EMA APPROVED 2021/2/11, Lenalidomide KRKA
Research Code:CDC-501; CC-5013
Trade Name:Revlimid®
MOA:Angiogenesis inhibitor
Indication:Myelodysplastic syndrome (MDS); Mantle cell lymphoma (MCL); Multiple myeloma (MM)
Status:Approved
Company:Celgene (Originator)
Sales:$5,801.1 Million (Y2015); 
$4,980 Million (Y2014);;
$4280 Million (Y2013);;
$3766.6 Million (Y2012);;
$3208.2 Million (Y2011);ATC Code:L04AX04
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2005-12-27 | Marketing approval | Revlimid | Multiple myeloma (MM),Myelodysplastic syndrome (MDS),Mantle cell lymphoma (MCL) | Capsule | 2.5 mg/5 mg/10 mg/15 mg/20 mg/25 mg | Celgene | Priority; Orphan |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2007-06-14 | Marketing approval | Revlimid | Multiple myeloma (MM),Myelodysplastic syndrome (MDS) | Capsule | 2.5 mg/5 mg/7.5 mg/10 mg/15 mg/20 mg/25 mg | Celgene | Orphan |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2010-08-20 | New indication | Revlimid | Myelodysplastic syndrome (MDS) | Capsule | 5 mg | Celgene | |
| 2010-06-25 | Marketing approval | Revlimid | Multiple myeloma (MM) | Capsule | 5 mg | Celgene |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2013-01-23 | Marketing approval | 瑞复美/Revlimid | Multiple myeloma (MM) | Capsule | 5 mg | Celgene | |
| 2013-01-23 | Marketing approval | 瑞复美/Revlimid | Multiple myeloma (MM) | Capsule | 10 mg | Celgene | |
| 2013-01-23 | Marketing approval | 瑞复美/Revlimid | Multiple myeloma (MM) | Capsule | 15 mg | Celgene | |
| 2013-01-23 | Marketing approval | 瑞复美/Revlimid | Multiple myeloma (MM) | Capsule | 25 mg | Celgene |
| Molecular Weight | 259.26 |
| Formula | C13H13N3O3 |
| CAS No. | 191732-72-6 (Lenalidomide); |
| Chemical Name | 3(4-amino-1-oxo 1,3-dihydro-2H-isoindol-2-yl) piperidine-2,6-dione |
Lenalidomide was first approved by the U.S. Food and Drug Administration (FDA) on Dec 27, 2005, then approved by European Medicine Agency (EMA) on June 14, 2007, and approved by Pharmaceuticals and Medical Devices Agency of Japan (PMDA) on June 25, 2010. It was developed and marketed as Revlimid® by Celgene.
Lenalidomide is an analogue of thalidomide with immunomodulatory, antiangiogenic, and antineoplastic properties. In multiple myeloma cells, the combination of lenalidomide and dexamethasone synergizes the inhibition of cell proliferation and the induction of apoptosis. Revlimid® is indicated for the treatment of multiple myeloma (MM), in combination with dexamethasone, in patients who have received at least one prior therapy, transfusion-dependent anemia due to low-or intermediate-1-risk myelodysplastic syndromes (MDS) associated with a deletion 5q abnormality with or without additional cytogenetic abnormalities and mantle cell lymphoma (MCL) whose disease has relapsed or progressed after two prior therapies, one of which included bortezomib.
Revlimid® is available as capsule for oral use, containing 2.5, 5, 10, 15, 20 or 25 mg of free Lenalidomide. The recommended dose is 25 mg once daily for multiple myeloma (MM), in combination with 40 mg dexamethasone once daily, 10 mg once daily for myelodysplastic syndromes (MDS) and 25 mg once daily for mantle cell lymphoma (MCL).
Lenalidomide, sold under the trade name Revlimid among others, is a medication used to treat multiple myeloma (MM) and myelodysplastic syndromes (MDS).[2] For MM it is used after at least one other treatment and generally together with dexamethasone.[2] It is taken by mouth.[2]
Common side effects include diarrhea, itchiness, joint pain, fever, headache, and trouble sleeping.[2] Severe side effects may include low blood platelets, low white blood cells, and blood clots.[2] Use during pregnancy may harm the baby.[2] The dose may need to be adjusted in people with kidney problems.[2] It has a chemical structure similar to thalidomide but has a different mechanism of action.[3][2] How it works is not entirely clear as of 2019.[2]
Lenalidomide was approved for medical use in the United States in 2005.[2] It is on the World Health Organization’s List of Essential Medicines.[4]
Medical uses
Multiple myeloma
Lenalidomide is used to treat multiple myeloma.[5] It is a more potent molecular analog of thalidomide, which inhibits tumor angiogenesis, tumor-secreted cytokines, and tumor proliferation through induction of apoptosis.[6][7][8]
Lenalidomide is effective at inducing a complete or “very good partial” response and improves progression-free survival. Adverse events more common in people receiving lenalidomide for myeloma include neutropenia, deep vein thrombosis, infections, and an increased risk of other hematological malignancies.[9] The risk of second primary hematological malignancies does not outweigh the benefit of using lenalidomide in relapsed or refractory multiple myeloma.[10] It may be more difficult to mobilize stem cells for autograft in people who have received lenalidomide.[6]
In 2006, lenalidomide received U.S. Food and Drug Administration (FDA) clearance for use in combination with dexamethasone in people with multiple myeloma who have received at least one prior therapy.[11] In 2017, the FDA approved lenalidomide as standalone maintenance therapy (without dexamethasone) for people with multiple myeloma following autologous stem cell transplant.[12]
In 2009, The National Institute for Health and Clinical Excellence issued a final appraisal determination approving lenalidomide in combination with dexamethasone as an option to treat people with multiple myeloma who have received two or more prior therapies in England and Wales.[13]
The use of lenalidomide combined with other drugs was evaluated. It was seen that the drug combinations of lenalidomide plus dexamethasone and continuous bortezomib plus lenalidomide plus dexamethasone probably result in an increase of the overall survival.[14]
Myelodysplastic syndromes
Lenalidomide was approved by the FDA on 27 December 2005 for patients with low- or intermediate-1-risk myelodysplastic syndromes who have chromosome 5q deletion syndrome (5q- syndrome) with or without additional cytogenetic abnormalities.[15][16][17] It was approved on 17 June 2013 by the European Medicines Agency for use in patients with low- or intermediate-1-risk myelodysplastic syndromes who have 5q- deletion syndrome but no other cytogenetic abnormalities and are dependent on red blood cell transfusions, for whom other treatment options have been found to be insufficient or inadequate.[18]
Mantle cell lymphoma
Lenalidomide is approved by FDA as a specialty drug requiring a specialty pharmacy distribution for mantle cell lymphoma in patients whose disease has relapsed or progressed after at least two prior therapies, one of which must have included the medicine bortezomib.[3]
Amyloidosis
Although not specifically approved by the FDA for use in treating amyloidosis, Lenalidomide is widely used in the treatment of that condition, often in combination with dexamethasone. [19]
Adverse effects
In addition to embryo-fetal toxicity, lenalidomide carries black box warnings for hematologic toxicity (including neutropenia and thrombocytopenia) and thromboembolism.[3] Serious potential side effects include thrombosis, pulmonary embolus, hepatotoxicity, and bone marrow toxicity resulting in neutropenia and thrombocytopenia. Myelosuppression is the major dose-limiting toxicity, which is not the case with thalidomide.[20]
Lenalidomide may be associated with such adverse effects as second primary malignancy, severe cutaneous reactions, hypersensitivity reactions, tumor lysis syndrome, tumor flare reaction, hypothyroidism, and hyperthyroidism.[3]
Teratogenicity
Lenalidomide is related to thalidomide, which is known to be teratogenic. Tests in monkeys suggest that lenalidomide is likewise teratogenic.[21] It cannot be prescribed for women who are pregnant or who may become pregnant during therapy.[1] For this reason, the drug is only available in the United States through a restricted distribution system in conjunction with a risk evaluation and mitigation strategy. Females who may become pregnant must use at least two forms of reliable contraception during treatment and for at least four weeks after discontinuing treatment with lenalidomide.[3][22]
Venous thromboembolism
Lenalidomide, like its parent compound thalidomide, may cause venous thromboembolism (VTE), a potentially serious complication with their use. High rates of VTE have been found in patients with multiple myeloma who received thalidomide or lenalidomide in conjunction with dexamethasone, melphalan, or doxorubicin.[23]
Stevens-Johnson syndrome
In March 2008, the U.S. Food and Drug Administration (FDA) included lenalidomide on a list of twenty prescription drugs under investigation for potential safety problems. The drug was investigated for possibly increasing the risk of developing Stevens–Johnson syndrome, a life-threatening skin condition.[24]
FDA ongoing safety review
In 2011, the FDA initiated an ongoing review of clinical trials that found an increased risk of developing cancers such as acute myelogenous leukemia and B-cell lymphoma,[25] though it did not advise patients to discontinue treatment with lenalidomide.[26]
Mechanism of action
Lenalidomide has been used to successfully treat both inflammatory disorders and cancers in the past ten years.[when?] There are multiple mechanisms of action, and they can be simplified by organizing them as mechanisms of action in vitro and in vivo.[27] In vitro, lenalidomide has three main activities: direct anti-tumor effect, inhibition of angiogenesis, and immunomodulation. In vivo, lenalidomide induces tumor cell apoptosis directly and indirectly by inhibition of bone marrow stromal cell support, by anti-angiogenic and anti-osteoclastogenic effects, and by immunomodulatory activity. Lenalidomide has a broad range of activities that can be exploited to treat many hematologic and solid cancers.
On a molecular level, lenalidomide has been shown to interact with the ubiquitin E3 ligase cereblon[28] and target this enzyme to degrade the Ikaros transcription factors IKZF1 and IKZF3.[29] This mechanism was unexpected as it suggests that the major action of lenalidomide is to re-target the activity of an enzyme rather than block the activity of an enzyme or signaling process, and thereby represents a novel mode of drug action. A more specific implication of this mechanism is that the teratogenic and anti-neoplastic properties of lenalidomide, and perhaps other thalidomide derivatives, could be disassociated.
History
See also: Development of analogs of thalidomide
Lenalidomide was approved for medical use in the United States in 2005.[2]
Society and culture
Economics
Lenalidomide costs US$163,381 per year for the average person in the United States as of 2012.[25] Lenalidomide made almost $9.7bn for Celgene in 2018.[30]
In 2013, the UK National Institute for Health and Care Excellence (NICE) rejected lenalidomide for “use in the treatment of people with a specific type of the bone marrow disorder myelodysplastic syndrome (MDS)” in England and Scotland, arguing that Celgene “did not provide enough evidence to justify the GB£3,780 per month (US$5,746.73) price-tag of lenalidomide for use in the treatment of people with a specific type of the bone marrow disorder myelodysplastic syndrome (MDS)”.[31]
Research
Lenalidomide is undergoing clinical trial as a treatment for Hodgkin’s lymphoma,[32] as well as non-Hodgkin’s lymphoma, chronic lymphocytic leukemia and solid tumor cancers, such as carcinoma of the pancreas.[33] One Phase III clinical trial being conducted by Celgene in elderly patients with B-cell chronic lymphocytic leukemia was halted in July 2013, when a disproportionate number of cancer deaths were observed during treatment with lenalidomide versus patients treated with chlorambucil.[34]
1. WO9803502A1 / US2002173658A1.
2. Bioorg. Med. Chem. Lett. 1999, 9, 1625-1630.Route 2
Reference:
1. WO2010139266A1 / US2012077982A1.Route 3
Reference:
1. CN103497175A.Route 4
Reference:
1. WO2010139266A1 / US2012077982A1.Route 5
Reference:
1. CN103554082A.
Clip
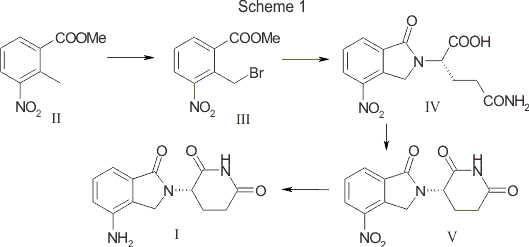
SYN

SCALABLE AND GREEN PROCESS FOR THE SYNTHESIS OF ANTICANCER DRUG LENALIDOMIDE
Yuri Ponomaryov, Valeria Krasikova, Anton Lebedev, Dmitri Chernyak, Larisa Varacheva, Alexandr Chernobroviy

Abstract
A new process for the synthesis of anticancer drug lenalidomide was developed, using platinum group metal-free and efficient reduction of nitro group with the iron powder and ammonium chloride. It was found that the bromination of the key raw material, methyl 2-methyl-3-nitrobenzoate, could be carried out in chlorine-free solvent methyl acetate without forming significant amounts of hazardous by-products. We also have compared the known synthetic methods for cyclization of methyl 2-(bromomethyl)-3-nitrobenzoate and 3-aminopiperidinedione to form lenalidomide nitro precursor.
How to Cite
Ponomaryov, Y.; Krasikova, V.; Lebedev, A.; Chernyak, D.; Varacheva, L.; Chernobroviy, A. Chem. Heterocycl. Compd. 2015, 51, 133. [Khim. Geterotsikl. Soedin. 2015, 51, 133.]
For this article in the English edition see DOI 10.1007/s10593-015-1670-0
SYN
https://link.springer.com/article/10.1007/s10593-015-1670-0

A new process for the synthesis of anticancer drug lenalidomide was developed, using platinum group metal-free and efficient reduction of nitro group with the iron powder and ammonium chloride. It was found that the bromination of the key raw material, methyl 2-methyl-3-nitrobenzoate, could be carried out in chlorine-free solvent methyl acetate without forming significant amounts of hazardous by-products. We also have compared the known synthetic methods for cyclization of methyl 2-(bromomethyl)-3-nitrobenzoate and 3-aminopiperidinedione to form lenalidomide nitro precursor.
SYN

SYN
EP 0925294; US 5635517; WO 9803502
Cyclization of N-(benzyloxycarbonyl)glutamine (I) by means of CDI in refluxing THF gives 3-(benzyloxycarbonylamino)piperidine-2,6-dione (II), which is deprotected with H2 over Pd/C in ethyl acetate/4N HCl to yield 3-aminopiperidine-2,6-dione hydrochloride (III). Bromination of 2-methyl-3-nitrobenzoic acid methyl ester (IV) with NBS in CCl4 provides 2-(bromomethyl)-3-nitrobenzoic acid methyl ester (V), which is cyclized with the aminopiperidine (III) by means of triethylamine in hot DMF to afford 3-(4-nitro-1-oxoisoindolin-2-yl)piperidine-2,6-dione (VI). Finally, the nitro group of compound (VI) is reduced with H2 over Pd/C in methanol (1, 2).
SYN
Bioorg Med Chem Lett 1999,9(11),1625
Treatment of 3-nitrophthalimide (I) with ethyl chloroformate and triethylamine produced 3-nitro-N-(ethoxycarbonyl)phthalimide (II), which was condensed with L-glutamine tert-butyl ester hydrochloride (III) to afford the phthaloyl glutamine derivative (IV). Acidic cleavage of the tert-butyl ester of (IV) provided the corresponding carboxylic acid (V). This was cyclized to the required glutarimide (VI) upon treatment with thionyl chloride and then with triethylamine. The nitro group of (VI) was finally reduced to amine by hydrogenation over Pd/C.
Lenalidomide
- Synonyms:CC-5013, CDC 501
- ATC:L04AX04
- MW:259.27 g/mol
- CAS-RN:191732-72-6
- InChI Key:GOTYRUGSSMKFNF-JTQLQIEISA-N
- InChI:InChI=1S/C13H13N3O3/c14-9-3-1-2-7-8(9)6-16(13(7)19)10-4-5-11(17)15-12(10)18/h1-3,10H,4-6,14H2,(H,15,17,18)/t10-/m0/s1
Synthesis
References
- ^ Jump up to:a b c “Lenalidomide (Revlimid) Use During Pregnancy”. Drugs.com. 13 March 2020. Retrieved 13 August 2020.
- ^ Jump up to:a b c d e f g h i j k “Lenalidomide Monograph for Professionals”. Drugs.com. Retrieved 27 October 2019.
- ^ Jump up to:a b c d e “DailyMed – Revlimid- lenalidomide capsule”. dailymed.nlm.nih.gov. Retrieved 27 October 2019.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ Armoiry X, Aulagner G, Facon T (June 2008). “Lenalidomide in the treatment of multiple myeloma: a review”. Journal of Clinical Pharmacy and Therapeutics. 33 (3): 219–26. doi:10.1111/j.1365-2710.2008.00920.x. PMID 18452408. S2CID 1228171.
- ^ Jump up to:a b Li S, Gill N, Lentzsch S (November 2010). “Recent advances of IMiDs in cancer therapy”. Current Opinion in Oncology. 22 (6): 579–85. doi:10.1097/CCO.0b013e32833d752c. PMID 20689431. S2CID 205547603.
- ^ Tageja N (March 2011). “Lenalidomide – current understanding of mechanistic properties”. Anti-Cancer Agents in Medicinal Chemistry. 11 (3): 315–26. doi:10.2174/187152011795347487. PMID 21426296.
- ^ Kotla V, Goel S, Nischal S, Heuck C, Vivek K, Das B, Verma A (August 2009). “Mechanism of action of lenalidomide in hematological malignancies”. Journal of Hematology & Oncology. 2: 36. doi:10.1186/1756-8722-2-36. PMC 2736171. PMID 19674465.
- ^ Yang B, Yu RL, Chi XH, Lu XC (2013). “Lenalidomide treatment for multiple myeloma: systematic review and meta-analysis of randomized controlled trials”. PLOS ONE. 8 (5): e64354. Bibcode:2013PLoSO…864354Y. doi:10.1371/journal.pone.0064354. PMC 3653900. PMID 23691202.
- ^ Dimopoulos MA, Richardson PG, Brandenburg N, Yu Z, Weber DM, Niesvizky R, Morgan GJ (March 2012). “A review of second primary malignancy in patients with relapsed or refractory multiple myeloma treated with lenalidomide”. Blood. 119 (12): 2764–7. doi:10.1182/blood-2011-08-373514. PMID 22323483.
- ^ “FDA approves lenalidomide oral capsules (Revlimid) for use in combination with dexamethasone in patients with multiple myeloma”. Food and Drug Administration (FDA). 29 June 2006. Retrieved 15 October 2015.[dead link]
- ^ “Lenalidomide (Revlimid)”. Food and Drug Administration(FDA). 22 February 2017.
- ^ “REVLIMID Receives Positive Final Appraisal Determination from National Institute for Health and Clinical Excellence (NICE) for Use in the National Health Service (NHS) in England and Wales”. Reuters. 23 April 2009.
- ^ Piechotta V, Jakob T, Langer P, Monsef I, Scheid C, Estcourt LJ, et al. (Cochrane Haematology Group) (November 2019). “Multiple drug combinations of bortezomib, lenalidomide, and thalidomide for first-line treatment in adults with transplant-ineligible multiple myeloma: a network meta-analysis”. The Cochrane Database of Systematic Reviews. 2019 (11). doi:10.1002/14651858.CD013487. PMC 6876545. PMID 31765002.
- ^ List A, Kurtin S, Roe DJ, Buresh A, Mahadevan D, Fuchs D, et al. (February 2005). “Efficacy of lenalidomide in myelodysplastic syndromes”. The New England Journal of Medicine. 352 (6): 549–57. doi:10.1056/NEJMoa041668. PMID 15703420.
- ^ List AF (August 2005). “Emerging data on IMiDs in the treatment of myelodysplastic syndromes (MDS)”. Seminars in Oncology. 32 (4 Suppl 5): S31-5. doi:10.1053/j.seminoncol.2005.06.020. PMID 16085015.
- ^ List A, Dewald G, Bennett J, Giagounidis A, Raza A, Feldman E, et al. (October 2006). “Lenalidomide in the myelodysplastic syndrome with chromosome 5q deletion”. The New England Journal of Medicine. 355 (14): 1456–65. doi:10.1056/NEJMoa061292. PMID 17021321.
- ^ “Revlimid Approved In Europe For Use In Myelodysplastic Syndromes”. The MDS Beacon. Retrieved 17 June 2013.
- ^ “Revlimid and Amyloidosis AL” (PDF). MyelomaUK. Retrieved 3 October 2020.
- ^ Rao KV (September 2007). “Lenalidomide in the treatment of multiple myeloma”. American Journal of Health-System Pharmacy. 64 (17): 1799–807. doi:10.2146/ajhp070029. PMID 17724360.
- ^ “Revlimid Summary of Product Characteristics. Annex I” (PDF). European Medicines Agency. 2012. p. 6.
- ^ Ness, Stacey (13 March 2014). “New Specialty Drugs”. Pharmacy Times. Retrieved 5 November 2015.
- ^ Bennett CL, Angelotta C, Yarnold PR, Evens AM, Zonder JA, Raisch DW, Richardson P (December 2006). “Thalidomide- and lenalidomide-associated thromboembolism among patients with cancer”. JAMA. 296 (21): 2558–60. doi:10.1001/jama.296.21.2558-c. PMID 17148721.
- ^ “Potential Signals of Serious Risks/New Safety Information Identified from the Adverse Event Reporting System (AERS) between January – March 2008”. Food and Drug Administration(FDA). March 2008. Archived from the original on 19 April 2014. Retrieved 16 December 2019.
- ^ Jump up to:a b Badros AZ (May 2012). “Lenalidomide in myeloma–a high-maintenance friend”. The New England Journal of Medicine. 366(19): 1836–8. doi:10.1056/NEJMe1202819. PMID 22571206.
- ^ “FDA Drug Safety Communication: Ongoing safety review of Revlimid (lenalidomide) and possible increased risk of developing new malignancies”. Food and Drug Administration (FDA). April 2011.
- ^ Vallet S, Palumbo A, Raje N, Boccadoro M, Anderson KC (July 2008). “Thalidomide and lenalidomide: Mechanism-based potential drug combinations”. Leukemia & Lymphoma. 49 (7): 1238–45. doi:10.1080/10428190802005191. PMID 18452080. S2CID 43350339.
- ^ Zhu YX, Braggio E, Shi CX, Bruins LA, Schmidt JE, Van Wier S, et al. (November 2011). “Cereblon expression is required for the antimyeloma activity of lenalidomide and pomalidomide”. Blood. 118 (18): 4771–9. doi:10.1182/blood-2011-05-356063. PMC 3208291. PMID 21860026.
- ^ Stewart AK (January 2014). “Medicine. How thalidomide works against cancer”. Science. 343 (6168): 256–7. doi:10.1126/science.1249543. PMC 4084783. PMID 24436409.
- ^ “Top 10 Best-Selling Cancer Drugs of 2018”. Genetic Engineering and Biotechnology News. 22 April 2019. Retrieved 25 April 2019.
- ^ “Revlimid faces NICE rejection for use in rare blood cancer Watchdog’s draft guidance does not recommend Celgene’s drug for NHS use in England and Wales”. Pharma News. 11 July 2013. Retrieved 5 November 2015.
- ^ “Phase II Study of Lenalidomide for the Treatment of Relapsed or Refractory Hodgkin’s Lymphoma”. ClinicalTrials.gov. US National Institutes of Health. February 2009.
- ^ “276 current clinical trials world-wide, both recruiting and fully enrolled, as of 27 February 2009”. ClinicalTrials.gov. US National Institutes of Health. February 2009.
- ^ “Celgene Discontinues Phase 3 Revlimid Study after ‘Imbalance’ of Deaths”. Nasdaq. 18 July 2013.
External links[edit]
- “Lenalidomide”. Drug Information Portal. U.S. National Library of Medicine.
//////////Lenalidomide hydrate, Lenalidomide KRKA, EU 2021, APPROVALS 2021, レナリドミド水和物 , CC-5013 hemihydrate,
#Lenalidomide hydrate, #Lenalidomide KRKA, #EU 2021, #APPROVALS 2021, #レナリドミド水和物 , #CC-5013 hemihydrate,
O.Nc1cccc2C(=O)N(Cc12)C3CCC(=O)NC3=O.Nc4cccc5C(=O)N(Cc45)C6CCC(=O)NC6=O
Lisocabtagene maraleucel
 Lisocabtagene maraleucel (liso-cel; JCAR017; Anti-CD19 CAR T-Cells) is an investigational chimeric antigen receptor (CAR) T-cell therapy designed to target CD19, [1][2] which is a surface glycoprotein expressed during normal B-cell development and maintained following malignant transformation of B cells. [3][4][5] Liso-cel CAR T-cells aim to target and CD-19 expressing cells through a CAR construct that includes an anti-CD19 single-chain variable fragment (scFv) targeting domain for antigen specificity, a transmembrane domain, a 4-1BB costimulatory domain hypothesized to increase T-cell proliferation and persistence, and a CD3-zeta T-cell activation domain. [1][2][6][7][8][9] The defined composition of liso-cel may limit product variability; however, the clinical significance of defined composition is unknown. [1][10] Image Courtesy: 2019/2020 Celgene/Juno Therapeutics / Bristol Meyers Squibb.
Lisocabtagene maraleucel (liso-cel; JCAR017; Anti-CD19 CAR T-Cells) is an investigational chimeric antigen receptor (CAR) T-cell therapy designed to target CD19, [1][2] which is a surface glycoprotein expressed during normal B-cell development and maintained following malignant transformation of B cells. [3][4][5] Liso-cel CAR T-cells aim to target and CD-19 expressing cells through a CAR construct that includes an anti-CD19 single-chain variable fragment (scFv) targeting domain for antigen specificity, a transmembrane domain, a 4-1BB costimulatory domain hypothesized to increase T-cell proliferation and persistence, and a CD3-zeta T-cell activation domain. [1][2][6][7][8][9] The defined composition of liso-cel may limit product variability; however, the clinical significance of defined composition is unknown. [1][10] Image Courtesy: 2019/2020 Celgene/Juno Therapeutics / Bristol Meyers Squibb.
Lisocabtagene maraleucel
リソカブタゲンマラルユーセル;
JCAR 017
STN# BLA 125714
- Adoptive immunotherapy agent JCAR 017
- Autologous anti-CD19 scFv/4-1BB/CD3ζ/CD28 chimeric antigen receptor-expressing CD4+/CD8+ central memory T cell JCAR 017
- CAR T-cell JCAR 017
FDA 2021, 2021/2/24, BREYANZI
Juno Therapeutics
Antineoplastic, Anti-CD19 CAR-T cell
An immunotherapeutic autologous T cell preparation expressing a chimeric antigen receptor (CAR) specific to the CD19 antigen (Juno Therapeutics, Inc., Seattle, Washington, USA – FDA Clinical Trial Data)
- For the treatment of adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified (including DLBCL arising from indolent lymphoma), high-grade B-cell lymphoma, primary mediastinal large B-cell lymphoma, and follicular lymphoma grade 3B.
Lisocabtagene maraleucel, sold under the brand name Breyanzi, is a cell-based gene therapy used to treat large B-cell lymphoma.[1][3]
Side effects of lisocabtagene maraleucel include hypersensitivity reactions, serious infections, low blood cell counts and a weakened immune system.[3]
Lisocabtagene maraleucel, a chimeric antigen receptor (CAR) T cell therapy, is the third gene therapy approved by the U.S. Food and Drug Administration (FDA) for certain types of non-Hodgkin lymphoma, including diffuse large B-cell lymphoma (DLBCL).[3] Lisocabtagene maraleucel was approved for medical use in the United States in February 2021.[1][3]
Medical uses
Lisocabtagene maraleucel is indicated for the treatment of adults with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified (including DLBCL arising from indolent lymphoma), high-grade B-cell lymphoma, primary mediastinal large B-cell lymphoma, and follicular lymphoma grade 3B.[1][3]
Lisocabtagene maraleucel is not indicated for the treatment of people with primary central nervous system lymphoma.[3]
Adverse effects
The labeling carries a boxed warning for cytokine release syndrome (CRS), which is a systemic response to the activation and proliferation of CAR T cells, causing high fever and flu-like symptoms and neurologic toxicities.[3]
History
The safety and efficacy of lisocabtagene maraleucel were established in a multicenter clinical trial of more than 250 adults with refractory or relapsed large B-cell lymphoma.[3] The complete remission rate after treatment with lisocabtagene maraleucel was 54%.[3]
The FDA granted lisocabtagene maraleucel orphan drug, regenerative medicine advanced therapy (RMAT) and breakthrough therapy designations.[3] Lisocabtagene maraleucel is the first regenerative medicine therapy with RMAT designation to be licensed by the FDA.[3] The FDA granted approval of Breyanzi to Juno Therapeutics Inc., a Bristol-Myers Squibb Company.[3]
SYN
WO 2018156680
WO 2018183366
Saishin Igaku (2018), 73(11), 1504-1512.
WO 2019148089
WO 2019220369
Leukemia & Lymphoma (2020), 61(11), 2561-2567.
WO 2020097350
WO 2020086943
Journal of Immunotherapy (2020), 43(4), 107-120.
CLIP
On February 5, 2021, the Food and Drug Administration approved lisocabtagene maraleucel (Breyanzi, Juno Therapeutics, Inc.) for the treatment of adult patients with relapsed or refractory (R/R) large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified (including DLBCL arising from indolent lymphoma), high-grade B-cell lymphoma, primary mediastinal large B-cell lymphoma, and follicular lymphoma grade 3B.
Lisocabtagene maraleucel is a CD19-directed chimeric antigen receptor (CAR) T cell immunotherapy. It consists of autologous T cells that are genetically modified to produce a CAR protein, allowing the T cells to identify and eliminate CD19-expressing normal and malignant cells.
Efficacy was evaluated in TRANSCEND (NCT02631044), a single-arm, open label, multicenter trial that evaluated lisocabtagene maraleucel, preceded by lymphodepleting chemotherapy, in adults with R/R large B-cell lymphoma after at least two lines of therapy.
Of the 192 patients evaluable for response, the overall response rate (ORR) per independent review committee assessment was 73% (95% CI: 67, 80) with a complete response (CR) rate of 54% (95% CI: 47, 61). The median time to first response was one month. Of the 104 patients who achieved CR, 65% had remission lasting at least 6 months and 62% had remission lasting at least 9 months. The estimated median duration of response (DOR) was not reached (95% CI: 16.7 months, NR) in patients who achieved a CR. The estimated median DOR among patients with partial response was 1.4 months (95% CI: 1.1, 2.2).
Cytokine release syndrome (CRS) occurred in 46% of patients (Grade 3 or higher, 4%) and neurologic toxicity occurred in 35% (Grade 3 or higher, 12%). Three patients had fatal neurologic toxicity. Other Grade 3 or higher adverse reactions included infections (19%) and prolonged cytopenias (31%). FDA approved lisocabtagene maraleucel with a Risk Evaluation and Mitigation Strategy because of the risk of fatal or life-threatening CRS and neurologic toxicities.
The recommended regimen is a single dose containing 50 to 110 x 106 CAR-positive viable T cells with a 1:1 ratio of CD4 and CD8 components, administered by IV infusion and preceded by fludarabine and cyclophosphamide for lymphodepletion. Lisocabtagene maraleucel is not indicated for the treatment of patients with primary central nervous system lymphoma.
References
- ^ Jump up to:a b c d “Lisocabtagene maraleucel”. U.S. Food and Drug Administration (FDA). 5 February 2021. Retrieved 5 February 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ https://www.fda.gov/media/145711/download
- ^ Jump up to:a b c d e f g h i j k l “FDA Approves New Treatment For Adults With Relapsed Or Refractory Large-B-Cell Lymphoma”. U.S. Food and Drug Administration (FDA) (Press release). 5 February 2021. Retrieved 5 February 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
External links
- “Lisocabtagene maraleucel”. NCI Drug Dictionary. National Cancer Institute.
- Clinical trial number NCT02631044 for “Study Evaluating the Safety and Pharmacokinetics of JCAR017 in B-cell Non-Hodgkin Lymphoma (TRANSCEND-NHL-001)” at ClinicalTrials.gov
| Clinical data | |
|---|---|
| Trade names | Breyanzi |
| Other names | JCAR017 |
| License data | US DailyMed: Lisocabtagene_maraleucel |
| Routes of administration | Intravenous |
| ATC code | None |
| Legal status | |
| Legal status | US: ℞-only [1][2] |
| Identifiers | |
| UNII | 7K2YOJ14X0 |
| KEGG | D11990 |
| ChEMBL | ChEMBL4297236 |
///////////Lisocabtagene maraleucel, BREYANZI, FDA 2021, APPROVALS 2021, リソカブタゲンマラルユーセル , Juno Therapeutics, JCAR 017, STN# BLA 125714
#Lisocabtagene maraleucel, #BREYANZI, #FDA 2021, #APPROVALS 2021, #リソカブタゲンマラルユーセル , #Juno Therapeutics, #JCAR 017, #STN# BLA 125714
Casimersen
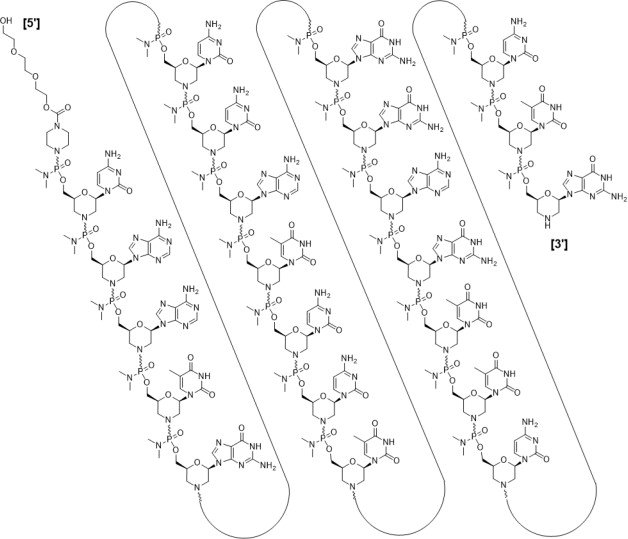
Casimersen
カシメルセン;
RNA, [P-deoxy-P-(dimethylamino)](2′,3′-dideoxy-2′,3′-imino-2′,3′-seco)(2’a→5′)(C-A-A-m5U-G-C-C-A-m5U-C-C-m5U-G-G-A-G-m5U-m5U-C-C-m5U-G), 5′-[P-[4-[[2-[2-(2-hydroxyethoxy)ethoxy]ethoxy]carbonyl]-1-piperazinyl]-N,N-dimethylphosphonamidate]
| Formula | C268H424N124O95P22 |
|---|---|
| CAS | 1422958-19-7 |
| Mol weight | 7584.4307 |
FDA 2021/2/25 , Amondys 45, Antisense oligonucleotide
Treatment of Duchenne muscular dystrophy
Nucleic Acid Sequence
Sequence Length: 224 a 7 c 5 g 6 umodified
- Exon-45: NG-12-0064
- SRP-4045
- WHO 10354
Casimersen, sold under the brand name Amondys 45, is an antisense oligonucleotide medication used for the treatment of Duchenne muscular dystrophy (DMD) in people who have a confirmed mutation of the dystrophin gene that is amenable to exon 45 skipping.[1][2][3][4] It is an antisense oligonucleotide of phosphorodiamidate morpholino oligomer (PMO).[1]
The most common side effects include upper respiratory tract infections, cough, fever, headache, joint pain and throat pain.[2]
Casimersen was approved for medical use in the United States in February 2021,[1][2] and it is the first FDA-approved targeted treatment for people who have a confirmed mutation of the DMD gene that is amenable to skipping exon 45.[2]
Duchenne muscular dystrophy (DMD) is an X-linked recessive allelic disorder characterized by a lack of functional dystrophin protein, which leads to progressive impairment of ambulatory, pulmonary, and cardiac function and is invariably fatal. A related, albeit a less severe, form of muscular dystrophy known as Becker muscular dystrophy (BMD) is characterized by shortened and partially functional dystrophin protein production. Although corticosteroids effectively slow disease progression in both DMD and BMD patients, they do not address the underlying molecular pathogenesis.1,2,3
The application of antisense oligonucleotides in DMD patients with specific mutations allows for exon skipping to produce truncated BMD-like dystrophin proteins, which restore partial muscle function and slow disease progression.1,2,4,5,7 Casimersen is a phosphorodiamidate morpholino oligonucleotide (PMO); PMOs are oligonucleotides in which the five-membered ribofuranosyl ring is replaced with a six-membered morpholino ring, and the phosphodiester links between nucleotides are replaced with a phosphorodiamidate linkage.6,7 In this manner, PMOs are much less susceptible to endo- and exonucleases and exhibit drastically reduced metabolic degradation compared to traditional synthetic oligonucleotides.6 Casimersen is the most recent in a line of approved PMOs for treating DMD, including eteplirsen and viltolarsen. However, the specific mutations, and hence the precise exon skipping, targeted by each is different.
Casimersen was granted accelerated FDA approval on February 25, 2021, based on data showing an increase in dystrophin levels in skeletal muscle of patients treated with casimersen; this approval is contingent on further verification in confirmatory trials. Casimersen is currently marketed under the tradename AMONDYS 45™ by Sarepta Therapeutics, Inc.7
Casimersen is indicated for the treatment of Duchenne muscular dystrophy (DMD) in patients confirmed to have a DMD gene mutation amenable to exon 45 skipping. This indication represents an accelerated approval based on observed efficacy; continued approval for this indication may be contingent on the verification of safety and efficacy in a confirmatory trial.7
Medical uses
Casimersen is indicated for the treatment of Duchenne muscular dystrophy (DMD) in people who have a confirmed mutation of the DMD gene that is amenable to exon 45 skipping.[1][2]
History
Casimersen was evaluated in a double-blind, placebo-controlled study in which 43 participants were randomized 2:1 to receive either intravenous casimersen or placebo.[2] All participants were male, between 7 and 20 years of age, and had a genetically confirmed mutation of the DMD gene that is amenable to exon 45 skipping.[2]
The U.S. Food and Drug Administration (FDA) granted the application for casimersen fast track, priority review, and orphan drug designations.[2][5] The FDA granted the approval of Amondys 45 to Sarepta Therapeutics, Inc.[2]
Pharmacodynamics
Casimersen is an antisense phosphorodiamidate morpholino oligonucleotide designed to bind to exon 45 of the DMD pre-mRNA, preventing its inclusion in mature mRNA and allowing the production of an internally truncated dystrophin protein in patients who would normally produce no functional dystrophin. Due to the need for continuous alteration of mRNA splicing and its relatively short half-life, casimersen is administered weekly.7 Although casimersen is associated with mostly mild adverse effects, animal studies suggest a potential for nephrotoxicity, which has also been observed after administration of some oligonucleotides.4,7 Measurement of glomerular filtration rate before starting casimersen is advised. Serum cystatin C, urine dipstick, and urine protein-to-creatinine ratio should be measured before starting therapy. They should be measured monthly (urine dipstick) or every three months (serum cystatin C and urine protein-to-creatinine ratio) during treatment. Creatinine levels are not reliable in muscular dystrophy patients and should not be used. Any persistent alteration in kidney function should be further investigated.7
Mechanism of action
Duchenne muscular dystrophy (DMD) is an X-linked recessive allelic disorder that results in the absence of functional dystrophin, a large protein comprising an N-terminal actin-binding domain, C-terminal β-dystroglycan-binding domain, and 24 internal spectrin-like repeats.1,2,3 Dystrophin is vital for normal muscle function; the absence of dystrophin leads to muscle membrane damage, extracellular leakage of creatinine kinase, calcium influx, and gradual replacement of normal muscle tissue with fibrous and adipose tissue over time.1,2 DMD shows a characteristic disease progression with early functional complaints related to abnormal gait, locomotion, and falls that remain relatively stable until around seven years of age. The disease then progresses rapidly to loss of independent ambulatory function, ventilatory insufficiency, and cardiomyopathy, with death typically occurring in the second or third decade of life.1,2,3
The human DMD gene contains 79 exons spread over approximately 2.4 million nucleotides on the X chromosome.1 DMD is associated with a variety of underlying mutations, including exon duplications or deletions, as well as point mutations leading to nonsense translation through direct production of an in-frame stop codon, frameshift production of an in-frame stop codon, or aberrant inclusion of an intronic pseudo-exon with the concomitant production of an in-frame stop codon.1,2 In all cases, no functional dystrophin protein is produced. Becker muscular dystrophy (BMD) is a related condition with in-frame mutations that result in the production of a truncated but partially functional dystrophin protein. BMD patients, therefore, have milder symptoms, delayed disease progression, and longer life expectancy compared to DMD patients.1,2,3
Casimersen is an antisense phosphorodiamidate morpholino oligonucleotide designed to bind to exon 45 of the DMD pre-mRNA and prevent its inclusion within the mature mRNA before translation.4,7 It is estimated that around 8% of DMD patients may benefit from exon 45 skipping, in which the exclusion of this exon results in the production of an internally truncated and at least partly functional dystrophin protein.4,7,5 Although fibrotic or fatty muscle tissue developed previously cannot be improved, this therapy aims to slow further disease progression through the production of partially functional dystrophin and alleviation of the pathogenic mechanism of muscle tissue necrosis.1,2
| TARGET | ACTIONS | ORGANISM |
|---|---|---|
| ADMD gene (exon 45 casimersen target site) | binder | Humans |
Absorption
DMD patients receiving IV doses of 4-30 mg/kg/week revealed exposure in proportion to dose with no accumulation of casimersen in plasma with once-weekly dosing. Following a single IV dose, casimersen Cmax was reached by the end of infusion. Inter-subject variability, as measured by the coefficient of variation, ranged from 12-34% for Cmax and 16-34% for AUC.7
Pre-clinical studies in nonhuman primates (cynomolgus monkeys) investigated the pharmacokinetics of once-weekly casimersen administered at doses of 5, 40, and 320 mg/kg. On days 1 and 78, the 5 mg/kg dose resulted in a Cmax of 19.5 ± 3.43 and 21.6 ± 5.60 μg/mL and an AUC0-t of 24.9 ± 5.17 and 26.9 ± 7.94 μg*hr/mL. The 40 mg/kg dose resulted in a Cmax of 208 ± 35.2 and 242 ± 71.1 μg/mL and an AUC0-t of 283 ± 68.5 and 320 ± 111 μg*hr/mL. Lastly, the 320 mg/kg dose resulted in a a Cmax of 1470 ± 88.1 and 1490 ± 221 μg/mL and an AUC0-t of 1960 ± 243 and 1930 ± 382 μg*hr/mL.4
Volume of distribution
Casimersen administered at 30 mg/kg had a mean steady-state volume of distribution (%CV) of 367 mL/kg (28.9%).7
Protein binding
Casimersen binding to human plasma proteins is not concentration-dependent, ranging from 8.4-31.6%.7
Metabolism
Casimersen incubated with human hepatic microsomal preparations is metabolically stables and no metabolites are detected in plasma or urine.7
Route of elimination
Casimersen is predominantly (more than 90%) excreted in the urine unchanged with negligible fecal excretion.7
Half-life
Casimersen has an elimination half-life of 3.5 ± 0.4 hours.7
Clearance
Casimersen administered at 30 mg/kg has a plasma clearance of 180 mL/hr/kg.7
| NAME | DOSAGE | STRENGTH | ROUTE | LABELLER | MARKETING START | MARKETING END | ||
|---|---|---|---|---|---|---|---|---|
| Amondys 45 | Injection | 50 mg/1mL | Intravenous | Sarepta Therapeutics, Inc. | 2021-02-25 | Not applicable |
Synthesis Reference
Diane Elizabeth Frank and Richard K. Bestwick, “Exon skipping oligomers for muscular dystrophy.” U.S. Patent US20190262375A1, issued August 29, 2019.
PATENT
https://patents.google.com/patent/WO2017205879A2/en
also
WO 2021025899
References
- ^ Jump up to:a b c d e “Amondys 45- casimersen injection”. DailyMed. Retrieved 1 March 2021.
- ^ Jump up to:a b c d e f g h i j “FDA Approves Targeted Treatment for Rare Duchenne Muscular Dystrophy Mutation”. U.S. Food and Drug Administration (FDA) (Press release). 25 February 2021. Retrieved 25 February 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ “Sarepta Therapeutics Announces FDA Approval of Amondys 45 (casimersen) Injection for the Treatment of Duchenne Muscular Dystrophy (DMD) in Patients Amenable to Skipping Exon 45” (Press release). Sarepta Therapeutics. 25 February 2021. Retrieved 25 February 2021 – via GlobeNewswire.
- ^ Rodrigues M, Yokota T (2018). “An Overview of Recent Advances and Clinical Applications of Exon Skipping and Splice Modulation for Muscular Dystrophy and Various Genetic Diseases”. Exon Skipping and Inclusion Therapies. Methods in Molecular Biology. 1828. Clifton, N.J. pp. 31–55. doi:10.1007/978-1-4939-8651-4_2. ISBN 978-1-4939-8650-7. PMID 30171533.
- ^ “Casimersen Orphan Drug Designations and Approvals”. U.S. Food and Drug Administration (FDA). 4 June 2019. Retrieved 25 February 2021.
General References
- Wein N, Alfano L, Flanigan KM: Genetics and emerging treatments for Duchenne and Becker muscular dystrophy. Pediatr Clin North Am. 2015 Jun;62(3):723-42. doi: 10.1016/j.pcl.2015.03.008. Epub 2015 Apr 20. [PubMed:26022172]
- Verhaart IEC, Aartsma-Rus A: Therapeutic developments for Duchenne muscular dystrophy. Nat Rev Neurol. 2019 Jul;15(7):373-386. doi: 10.1038/s41582-019-0203-3. [PubMed:31147635]
- Mercuri E, Bonnemann CG, Muntoni F: Muscular dystrophies. Lancet. 2019 Nov 30;394(10213):2025-2038. doi: 10.1016/S0140-6736(19)32910-1. [PubMed:31789220]
- Carver MP, Charleston JS, Shanks C, Zhang J, Mense M, Sharma AK, Kaur H, Sazani P: Toxicological Characterization of Exon Skipping Phosphorodiamidate Morpholino Oligomers (PMOs) in Non-human Primates. J Neuromuscul Dis. 2016 Aug 30;3(3):381-393. doi: 10.3233/JND-160157. [PubMed:27854228]
- Rodrigues M, Yokota T: An Overview of Recent Advances and Clinical Applications of Exon Skipping and Splice Modulation for Muscular Dystrophy and Various Genetic Diseases. Methods Mol Biol. 2018;1828:31-55. doi: 10.1007/978-1-4939-8651-4_2. [PubMed:30171533]
- Smith CIE, Zain R: Therapeutic Oligonucleotides: State of the Art. Annu Rev Pharmacol Toxicol. 2019 Jan 6;59:605-630. doi: 10.1146/annurev-pharmtox-010818-021050. Epub 2018 Oct 9. [PubMed:30285540]
- FDA Approved Drug Products: AMONDYS 45 (casimersen) injection [Link]
External links
- “Casimersen”. Drug Information Portal. U.S. National Library of Medicine.
- Clinical trial number NCT02500381 for “Study of SRP-4045 and SRP-4053 in DMD Patients (ESSENCE)” at ClinicalTrials.gov
| Clinical data | |
|---|---|
| Trade names | Amondys 45 |
| Other names | SRP-4045 |
| License data | US DailyMed: Casimersen |
| Routes of administration | Intravenous |
| Drug class | Antisense oligonucleotide |
| ATC code | None |
| Legal status | |
| Legal status | US: ℞-only [1][2] |
| Identifiers | |
| CAS Number | 1422958-19-7 |
| DrugBank | DB14984 |
| UNII | X8UHF7SX0R |
| KEGG | D11988 |
| Chemical and physical data | |
| Formula | C268H424N124O95P22 |
| Molar mass | 7584.536 g·mol−1 |
////////////Casimersen, FDA 2021, APPROVALS 2021, カシメルセン , Exon-45: NG-12-0064, SRP-4045, WHO 10354, Amondys 45, Antisense oligonucleotide, Duchenne muscular dystrophy
#Casimersen, #FDA 2021, #APPROVALS 2021, #カシメルセン , #Exon-45: NG-12-0064, #SRP-4045, #WHO 10354, #Amondys 45, #Antisense oligonucleotide, #Duchenne muscular dystrophy
Sequence:
1caaugccauc cuggaguucc ug
Sequence Modifications
| Type | Location | Description |
|---|---|---|
| modified base | c-1 | 5′-ester |
| modified base | c-1 | modified cytidine |
| modified base | a-2 | modified adenosine |
| modified base | a-3 | modified adenosine |
| modified base | u-4 | m5u |
| modified base | u-4 | modified uridine |
| modified base | g-5 | modified guanosine |
| modified base | c-6 | modified cytidine |
| modified base | c-7 | modified cytidine |
| modified base | a-8 | modified adenosine |
| modified base | u-9 | modified uridine |
| modified base | u-9 | m5u |
| modified base | c-10 | modified cytidine |
| modified base | c-11 | modified cytidine |
| modified base | u-12 | m5u |
| modified base | u-12 | modified uridine |
| modified base | g-13 | modified guanosine |
| modified base | g-14 | modified guanosine |
| modified base | a-15 | modified adenosine |
| modified base | g-16 | modified guanosine |
| modified base | u-17 | modified uridine |
| modified base | u-17 | m5u |
| modified base | u-18 | modified uridine |
| modified base | u-18 | m5u |
| modified base | c-19 | modified cytidine |
| modified base | c-20 | modified cytidine |
| modified base | u-21 | m5u |
| modified base | u-21 | modified uridine |
| modified base | g-22 | modified guanosine |
| uncommon link | c-1 – a-2 | unavailable |
| uncommon link | a-2 – a-3 | unavailable |
| uncommon link | a-3 – u-4 | unavailable |
| uncommon link | u-4 – g-5 | unavailable |
| uncommon link | g-5 – c-6 | unavailable |
| uncommon link | c-6 – c-7 | unavailable |
| uncommon link | c-7 – a-8 | unavailable |
| uncommon link | a-8 – u-9 | unavailable |
| uncommon link | u-9 – c-10 | unavailable |
| uncommon link | c-10 – c-11 | unavailable |
| uncommon link | c-11 – u-12 | unavailable |
| uncommon link | u-12 – g-13 | unavailable |
| uncommon link | g-13 – g-14 | unavailable |
| uncommon link | g-14 – a-15 | unavailable |
| uncommon link | a-15 – g-16 | unavailable |
| uncommon link | g-16 – u-17 | unavailable |
| uncommon link | u-17 – u-18 | unavailable |
| uncommon link | u-18 – c-19 | unavailable |
| uncommon link | c-19 – c-20 | unavailable |
| uncommon link | c-20 – u-21 | unavailable |
| uncommon link | u-21 – g-22 | unavailable |

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....










