Home » Posts tagged 'GMP' (Page 2)
Tag Archives: GMP
Bayer, Onyx win early FDA OK for Nexavar (sorafenib) in thyroid cancer
The U.S. Food and Drug Administration said on Friday it has expanded the approved use of the cancer drug Nexavar to include late-stage differentiated thyroid cancer.
Differentiated thyroid cancer is the most common type of thyroid cancer, the FDA said. The National Cancer Institute estimates that 60,220 people in the United States will be diagnosed with it and 1,850 will die from the disease in 2013.
The drug, made by Germany’s Bayer AG and Onyx Pharmaceuticals, is already approved to treat advanced kidney cancer and liver cancer that cannot be surgically removed. Onyx was acquired by Amgen Inc earlier this year.
READ ABOUT SORAFENIB IN MY EARLIER BLOGPOST
https://newdrugapprovals.wordpress.com/2013/07/16/nexavar-sorafenib/
Daiichi Sankyo anticoagulant edoxaban succeeds in Phase III

Edoxaban, DU-176b
Daiichi Sankyo, APPROVED IN JAPAN as tosylate monohydrate salt in 2011 for the prevention of venous embolism in patients undergoing total hip replacement surgery
for synthesis see….http://www.sciencedirect.com/science/article/pii/S0968089613002642 Bioorganic & Medicinal Chemistry 21 (2013) 2795–2825, see s[pecific page 2808 for description ie 14/31 of pdf
WO 2010071121, http://www.google.com/patents/WO2010071121A1
WO 2007032498
N’-(5-chloropyridin-2-yl)-N-[(1S,2R,4S)-4-(dimethylcarbamoyl)-2-[(5-methyl-6,7-dihydro-4H-[1,3]thiazolo[5,4-c]pyridine-2-carbonyl)amino]cyclohexyl]oxamide
NOV20, 2013
Daiichi Sankyo will file edoxaban on both sides of the Atlantic shortly after the bloodthinner proved as effective and safer than warfarin in a Phase III trial of patients with atrial fibrillation.
The company has presented data on edoxaban, a once-daily oral factor Xa inhibitor, at the American Heart Association meeting in Dallas, from a study involving 21,105 patients across 46 countries. The drug, evaluated in 60mg and 30mg doses, met its primary endpoint of non-inferiority compared to warfarin for the prevention of stroke or systemic embolic events in patients with non-valvular AF.http://www.pharmatimes.com/Article/13-11-20/Daiichi_Sankyo_anticoagulant_edoxaban_succeeds_in_Phase_III.aspx
Edoxaban (INN, codenamed DU-176b, trade name Lixiana) is an anticoagulant drug which acts as a direct factor Xa inhibitor. It is being developed by Daiichi Sankyo. It was approved in July 2011 in Japan for prevention of venous thromboembolisms (VTE) following lower-limb orthopedic surgery.[1]
In animal studies, edoxaban is potent, selective for factor Xa and has good oral bioavailability.[2]
Daichi Sankyo’s edoxaban tosilate is an orally administered
coagulation factor Xa inhibitor that was approved and launched
in Japan for the preventive treatment of venous thromboembolic
events (VTE) in patients undergoing total knee arthroplasty, total
hip arthroplasty, or hip fracture surgery. Edoxaban has been
shown to have a rapid onset of anticoagulant effect due to short
Tmax (1–2 h) after dosing and sustained for up to 24 h post-dose.
Marketed under the brand name Lixiana, it is currently in phase
III studies in the US for the prevention of stroke and systemic embolic
events in patients with atrial fibrillation (AF) and venous
thromboembolism (VTE).
Several Phase II clinical trials have been conducted, for example for thromboprophylaxis after total hip replacement[3] (phase III early results compare well to enoxaparin[4]), and for stroke prevention in patients with atrial fibrillation[5][6].Those papers follow similar recent major trials showing similar results for the other new factor Xa inhibitors, rivaroxaban and apixaban.
A large phase III trial showed that edoxaban was non inferior to warfarin in preventing recurrent venous thromboembolic events with fewer episodes of major bleeding.[7]
- “First market approval in Japan for LIXIANA (Edoxaban)”. Press Release. Daiichi Sankyo Europe GmbH. 2011-04-22.
- Furugohri T, Isobe K, Honda Y, Kamisato-Matsumoto C, Sugiyama N, Nagahara T, Morishima Y, Shibano T (September 2008). “DU-176b, a potent and orally active factor Xa inhibitor: in vitro and in vivo pharmacological profiles”. J. Thromb. Haemost. 6 (9): 1542–9. doi:10.1111/j.1538-7836.2008.03064.x. PMID 18624979.
- Raskob, G.; Cohen, A. T.; Eriksson, B. I.; Puskas, D.; Shi, M.; Bocanegra, T.; Weitz, J. I. (2010). “Oral direct factor Xa inhibition with edoxaban for thromboprophylaxis after elective total hip replacement”. Thrombosis and Haemostasis 104 (3): 642–649. doi:10.1160/TH10-02-0142.PMID 20589317. edit
- “Phase III Trial Finds Edoxaban Outclasses Enoxaparin in Preventing Venous Thromboembolic Events”. 8 Dec 2010.
- Weitz JI, Connolly SJ, Patel I, Salazar D, Rohatagi S, Mendell J, Kastrissios H, Jin J, Kunitada S (September 2010). “Randomised, parallel-group, multicentre, multinational phase 2 study comparing edoxaban, an oral factor Xa inhibitor, with warfarin for stroke prevention in patients with atrial fibrillation”. Thromb. Haemost. 104 (3): 633–41. doi:10.1160/TH10-01-0066.
- Edoxaban versus Warfarin in Patients with Atrial Fibrillation Robert P. Giugliano, M.D., Christian T. Ruff, M.D., M.P.H., Eugene Braunwald, M.D., Sabina A. Murphy, M.P.H., Stephen D. Wiviott, M.D., Jonathan L. Halperin, M.D., Albert L. Waldo, M.D., Michael D. Ezekowitz, M.D., D.Phil., Jeffrey I. Weitz, M.D., Jindřich Špinar, M.D., Witold Ruzyllo, M.D., Mikhail Ruda, M.D., Yukihiro Koretsune, M.D., Joshua Betcher, Ph.D., Minggao Shi, Ph.D., Laura T. Grip, A.B., Shirali P. Patel, B.S., Indravadan Patel, M.D., James J. Hanyok, Pharm.D., Michele Mercuri, M.D., and Elliott M. Antman, M.D. for the ENGAGE AF-TIMI 48 InvestigatorsDOI: 10.1056/NEJMoa1310907
- “Edoxaban versus Warfarin for the Treatment of Symptomatic Venous Thromboembolism”. N. Engl. J. Med. August 2013. doi:10.1056/NEJMoa1306638. PMID 23991658.
- WO 03/000657 pamphlet WO 03/000680 pamphlet WO 03/016302 pamphlet WO 04/058715 pamphlet WO 05/047296 pamphlet WO 07/032498 pamphlet WO 08/129846 pamphlet WO 08/156159 pamphlet
- J Am Chem Soc 1978, 100(16): 5199
Drug formulation , lixiana, edoxaban tosylate monohydrate, CAS 912273-65-5, C24 H30 Cl N7 O4 S . C7 H8 O3 S . H2 O, 738.274
-
N1-(5-chloropyridin-2-yl)-N2-((1S,2R,4S)-4-[(dimethylamino)carbonyl]-2-{[(5-methyl-4,5,6,7-tetrahydrothiazolo[5,4-c]pyridin-2-yl)carbonyl]amino}cyclohexyl)ethanediamide p-toluenesulfonic acid monohydrate represented by the following formula (A) (hereinafter, also referred to as compound A) :
-
is known as a compound that exhibits an inhibitory effect on activated blood coagulation factor X (FXa), and is useful as a preventive and/or therapeutic drug for thrombotic diseases (Patent Literature 1 to 8).
-
For example, a method comprising mixing the free form of compound A represented by the following formula (B) (hereinafter, also referred to as compound B):
-
with p-toluenesulfonic acid or p-toluenesulfonic acid monohydrate, followed by crystallization from aqueous ethanol, is known as a method for obtaining compound A (Patent Literature 1 to 8). These literature documents do not make any mention about adding p-toluenesulfonic acid or p-toluenesulfonic acid monohydrate in a stepwise manner in the step of obtaining compound A from compound B.
Citation ListPatent Literature
-
- Patent Literature 1: International Publication No. WO 03/000657
- Patent Literature 2: International Publication No. WO 03/000680
- Patent Literature 3: International Publication No. WO 03/016302
- Patent Literature 4: International Publication No. WO 04/058715
- Patent Literature 5: International Publication No. WO 05/047296
- Patent Literature 6: International Publication No. WO 07/032498
- Patent Literature 7: International Publication No. WO 08/129846
- Patent Literature 8: International Publication No. WO 08/156159
SIMILAR

OTHER SALTS

Edoxaban hydrochloride
CAS Number: 480448-29-1
Molecular Formula: C24H30ClN7O4S · HCl
Molecular Weight: 584.52 g.mol-1
Edoxaban is reported to be a member of the so-called “Xaban-group” and as such to be a low molecular inhibitor of the enzyme factor Xa, participating in the blood coagulation system. Therefore, edoxaban is classified as an antithrombotic drug and its possible medical indications are reported to be treatment of thrombosis and thrombosis prophylaxis after orthopaedic operations, such as total hip replacement, as well as for stroke prevention in patients with atrial fibrillation, the prophylaxis of the acute coronary syndrome and the prophylaxis after thrombosis and pulmonary embolism.
The IUPAC name for edoxaban is N’-(5-chloropyridin-2-yl)-N-[(15,2^,4S)-4- (dimethylcarbamoyl)-2-[(5-methyl-6,7-dihydro-4H-[l ,3]thiazolo[5,4-c]pyridine-2- carbonyl)amino]cyclohexyl]oxamide. The chemical structure of edoxaban is shown in the formula (1) below:
formula ( 1 ) While Edoxaban is reported to be soluble in strongly acidic aqueous solutions, its solubility is considered to be very low in neutral or alkaline aqueous media. EP 2 140 867 A 1 claims an edoxaban-containing pharmaceutical composition comprising a water-swelling additive and/or a sugar alcohol. Further, it is alleged that compositions comprising lactose or cornstarch do not have good dissolution properties. The claimed pharmaceutical compositions in EP 2 140 867 Al are considered to show good dissolution properties in a neutral aqueous medium as well. Tablets comprising said composition were produced by wet granulation. However, it turned out that prior art pharmaceutical formulations comprising edoxaban being suitable for oral administration are still improvable with regards to dissolution rate and bioavailability. Further, stability and content uniformity of the known formulations could be improved. Further, due to the intolerance of many people to sugar alcohol(s), such as sorbitol, the use of sugar alcohol(s) should be avoided.
Quetiapine

Quetiapine, astrazeneca
111974-69-7 cas
US 5,948,437*PED, NDA 022047 Appr may 17 2007 sustained release formulation
NDA 020639 approved 26.9.1997
patent approved expiry
| United States | 5948437 | 1997-11-28 | 2017-11-28 |
| United States | 4879288 | 1994-09-26 | 2011-09-26 |
| Canada | 2251944 | 2007-04-10 | 2017-05-27 |
| United States | 4879288 | 1994-09-26 | 2011-09-26 |

Quetiapine (/kwɨˈtaɪ.əpiːn/ kwi-ty-ə-peen) (branded as Seroquel, Xeroquel, Ketipinor) is a short-acting atypical antipsychotic approved for the treatment of schizophrenia, bipolar disorder, and along with an antidepressant to treat major depressive disorder.
Annual sales are approximately $5.7 billion worldwide, with $2.9 billion in the United States. The U.S. patent, which expiredv in 2011, received a pediatric exclusivity extension which pushed its expiration to March 26, 2012.The patent has already expired in Canada. Quetiapine was developed by AstraZeneca from 1992-1996 as an improvement from first generation antipsychotics. It was first approved by the FDA in 1997. There are now several generic versions of quetiapine, such as Quepin, Syquel and Ketipinor
Seroquel (quetiapine) is a psychotropic medication that is used to treat schizophrenia in adults and children who are at least 13 years old. Seroquel is also used in the treatment of major depression and bipolar disorder. Side effects of Seroquel may include mood or behavior changes, constipation, drowsiness, headache, and trouble sleeping. Older adults with dementia may have a slightly increased risk of death when taking this medication.
Dosing preparations are 25, 50, 100, 200, 300, and 400 mg tablets. Seroquel may interact with a number of other drugs, including, but not limited to, antidepressant medications, antifungal drugs, steroids, cimetidine (Tagamet), thioridazine (Mellaril), and lorazepam (Ativan). During pregnancy, this medication should be used only when clearly needed. Discuss the risks and benefits with your doctor. Seroquel passes into breast milk and may have undesirable effects on a nursing infant.

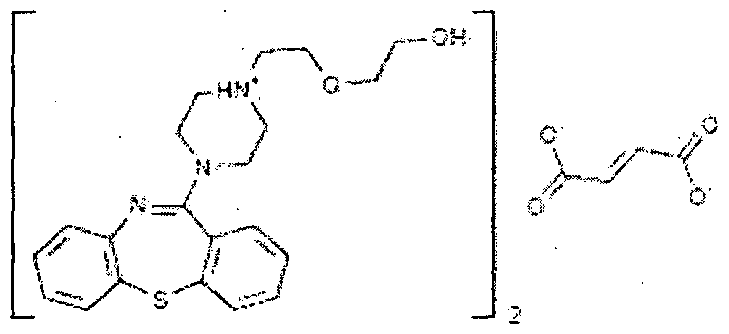
Quetiapine fumarate is a psychotropic agent belonging to a chemical class of dibenzothiazepine derivatives, designated chemically as 2-[2-(4-dibenzo [b,f] [l,4]thiazepin -1 l-yl-l-piperazinyl)ethoxy]-ethanol fumarate (2: l )(salt). Its molecular formula is C42H5oN604S2*C4H404 having a molecular weight of 883.1 1. The structural formula is:
Quetiapine is marketed as immediate release as well as extended release tablets in United States under the trade name Seroquel® and Seroquel XR® by AstraZeneca.
-
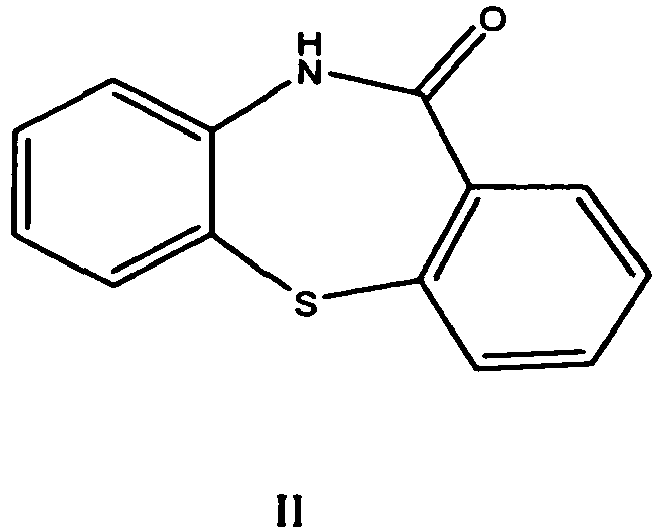
Quetiapine was first described in a patent publication EP 240228 (US 4879288 ). It is prepared starting from dibenzo[b,f][1,4]thiazepin-11-[10H]one of formula II
which is first halogenated with phosphorous oxychloride, then isolated and condensed with 1-(2-hydroxyethoxy) ethyl piperazine to obtainquetiapine. After purification by flash chromatography the yield was 77.7 %. As an alternative to halogenation a process via a thioether in the first step is presented.
-
In the process claimed in EP 282236 the piperazine ring is first condensed with 11-chloro-dibenzo[b,f][1,4] thiazepine and thereafterquetiapine is obtained by its reaction with haloethoxy ethanol. The base is further converted to the hemifumarate salt, which was isolated in 78 % yield.
-
WO 2006/117700 describes a process of EP ‘228 improved by the destruction of phosphorous oxychloride in situ to decrease the amount of hazardous waste. Phosphorous oxychloride is used only about 1 equivalent to the compound of formula II whereas in the process of EP 240228 it was used in about 15 equivalents.
-
A reaction of 11-chlorodibenzo[b,f][1,4]thiazepine with a piperazine moiety in the presence of a halide is the improvement described inWO 2006/113425 . The process is said to yield quetiapine in high purity.
-
In WO 2006/094549 there is described a process which avoids the halogenation step and the use of hazardous phosphorous halogenating agents by the reaction of 10H-dibenzo[b,f][1,4] thiazepin-11-one directly with a piperazine derivative. This is achieved by performing the reaction in the presence of titanium alkoxide. Yields of 50 – 75 % as a fumarate salt are reported. Expensive titanium alkoxide is used from about 2 to 3 fold excess to starting compound of formula II.
-
Also the process of US 2006/0063927 avoids the use of phosphorous compounds in halogenation by using oxalyl chloride as a halogenating agent. The imino chloride is obtained in 66 % yield. The reaction of 11-chloro-dibenzo[b,f][1,4] thiazepine with 1-(2-hydroxyethoxy)ethylpiperazine is performed either in the presence of a base in an organic solvent or in a two-phase system. However, the reagent used, oxalyl chloride is poisonous and requires special attention.
-
A one-pot process for the preparation of quetiapine is described inWO 2007/020011 . Phosphorous oxychloride is used in halogenation step about one equivalent to 10H-dibenzo[b,f][1,4] thiazepin-11-one.
-
WO 2007/004234 describes a process comprising the reaction of chloro ethoxy ethanol with piperazinyl-dibenzo[b,f][1,4] thiazepine dihydrocloride, which is obtained by halogenating the dibenzo[b,f][1,4] thiazepin-11-[10H]one, reacting the imino chloride obtained with piperazine, and treating the obtained compound with an alcoholic solution of hydrogen chloride.
-
All processes described above use dibenzo[b,f][1,4] thiazepin-11-[10H]one as a starting material. Its preparation requires several steps, and in most cases it has to be even halogenated to the imino chloride before the piperazine moiety can be condensed with it. Halogenating reagents, e.g. phosphorous oxychloride have been used in excess and their removal from the reaction mixture requires evaporation of large amounts.
-
A different approach using protected intermediates is used e.g. in routes described in WO 2005/014590 , WO 2005/028457 , WO 2005/028458and WO 2005/028459 . In some cases the reactions may be performed in one pot fashion and no extra purification steps are needed to get a pure product in high yield. However, protection and deprotection steps used lengthen the processes and shorter processes for the preparation of quetiapine are still needed.
-
Similar compounds are prepared in US 3, 539,573
U.S. Patent 4,879,288 discloses 1 l-[4-[2-(2-hydroxyethoxy) ethyl] -1 – piperazinyl] dibenzo [b, f] [1 , 4] thiazepine as an antipsychotic drug of dibenzothiazepine class suitable for treatment of various psychotic disorders.
US patent 5,948,437 discloses sustained release formulations of quetiapine using gelling agents such as hydroxypropyl methylcellulose and its derivatives that create a gel structure after contact with water. US patent 4,547,57 1 describes process for the preparation of carboxymethyl ethyl cellulose (CMEC) polymer.
WO 2004012699 discloses modified release dosage forms prepared by using dual – retard— technique comprising micro matrix particles containing quetiapine and hydrophobic release controlling agents, which are coated with hydrophobic release controlling agents.
WO 2005041935 discloses matrix composition comprising quetiapine and a wax material.
WO 2007086079 discloses sustained release compositions of quetiapinecomprising a channelizer and a rate controlling polymer.
WO 2008060228 discloses extended release compositions comprisingquetiapine, hydroxypropyl methyl cellulose and sodium citrate dihydrate.
WO 20091 13051 discloses sustained release compositions containingquetiapine and one or more non-gelling and/or waxy excipients.
WO 2010001413 discloses sustained release dosage forms comprisingquetiapine or its pharmaceutically acceptable salts and one or more non-gellable release controlling polymers.
WO 2010028794 discloses a matrix formulation in the form of a retard tablet comprising quetiapine, at least one matrix-forming, water-insoluble, non-swellable auxiliary agent, and at least one water-soluble binding agent.
The synthesis of quetiapine begins with a dibenzothiazepinone. The lactam is first treated with phosphoryl chloride to produce a dibenzothiazepine. A nucleophilic substitutionis used to introduce the sidechain.U.S. Patent 4,879,288.
Atypical antipsychotic quetiapine (Quetiapine, drugs used its fumarate) for the treatment of schizophrenia (schizophrenia) and dry depressive disorder (bipolar disorder), trade name Seroquel, produced by AstraZeneca. Star molecule drugs, the global sales of about $ 6 billion.
Quetiapine synthesis o-nitro-chlorobenzene ( 1 ) starting a thiophenol occurred and SNAr reaction, hydrogenation of nitro group to an amino group after reaction with phosgene isocyanate 2 , 2 ring closure in hot sulfuric acid to obtain 3 , 3 with phosphorus oxychloride isomerization chlorinated4 , 4 and 5 SNAr reaction occurs fumarate salt formation with quetiapine fumarate.
The route of the compound 4 is not stable enough, then there are improved route. 6 and the reaction of phenyl chloroformate 7

Quetiapine fumarate, Bis [2-(2-[4-(dibenzo[b,f][1,4]thiazepin-11-yl]ethoxy)ethanol] fumarate (IUPAC)2-[2-(4-dibenzo[b,f][1,4]thiazepin-11-yl-1-piperazinyl)ethoxy]-ethanol-(E)-2-butanedioate (2:1) salt), [ICI 204,636], is a novel dibenzothiazepine antipsychotic developed by Zeneca. It is marketed under the trade name ‘Seroquel’Seroquel. Quetiapine is well tolerated and clinically effective in the treatment of schizophrenia.
The initial hope of investigators was that quetiapine would have antipsychotic potential and that it might share some of the properties of clozapine without its toxicity to white blood cells.
The effective dosage range is usually 300-450 mg/day split into two doses. The dose is titrated upwards from 25 mg twice dailybd from day one to 300mg/daya fuller dosage on day 4. Elderly patients or patients with liver problems should be started on lower doses. It is both superior to placebo and, and comparable to haloperidol in reducing positive symptoms at doses ranging from 150 to 750 mg/day and is an effective treatment for in reducing negative symptoms at a dose of 300 mg/day.
Somnolence is the most common adverse event. Abnormalities of the QTqt interval on ECG appear very infrequently and there is no need for a baseline ECG or blood pressure monitoring as used to be the case with ssertindole. There is no need for haematological monitoring as with clozapine. Quetiapine, across the full dosage range, is associated with no greater extrapyramidal symptoms than placeboThere is a reduced potential for extrapyramidal symptoms compared with conventional antipsychotics.
Quetiapine’s general efficacy and side effect profile suggest that, unless there are unforeseen post-marketing complications, quetiapine deserves a major place in the initial and long term management of schizophreniform disorders.
Quetiapine fumarate, Bis [2-(2-[4-(dibenzo[b,f][1,4]thiazepin-11-yl]ethoxy)ethanol] fumarate (IUPAC) 2-[2-(4-dibenzo[b,f][1,4]thiazepin-11-yl-1-piperazinyl)ethoxy]-ethanol-(E)-2-butanedioate (2:1) salt), [ICI 204,636], is a novel dibenzothiazepine antipsychotic developed by Zeneca Pharmaceuticals. It is marketed under the trade name ‘Seroquel’. Quetiapine is well tolerated and clinically effective in the treatment of schizophrenia.

EMEDASTINE DIFUMARATE, EMADINE, 8 TH DEC 2013 PATENT EXPIRY

EMEDASTINE DIFUMARATE
Emedastine difumarate (Emadine) is a second generation antihistamine used in eye drops to treat allergic conjunctivitis. Its mechanism of action is a H1 receptor antagonist.

EMADINE
Drug Patent Expiration and Exclusivity
| Active Ingredient | Form | Dosage | Drug Type | Application | Product | |
|---|---|---|---|---|---|---|
| EMEDASTINE DIFUMARATE | SOLUTION/DROPS; OPHTHALMIC | 0.05% | RX | 020706 | 001 |
Patents
There are 1 patent(s) protecting ALCON’s EMADINE.
The last patent expires on 2013-12-08.
| Patent | Expiration | |
|---|---|---|
| US5441958 | Ophthalmic compositions comprising emedastine and methods for their use
Topical ophthalmic compositions comprising 1-(2-ethoxyethyl)-2-(4-methyl-1-homopiperazinyl)-benzimidazole and its ophthalmically acceptable acid addition salts have been found to be useful in treating allergic conjunctivitis and related ailments.
|
2013-12-8 |
Exclusivity
Exclusivity is marketing rights granted by the FDA to the ALCON.
EMADINE ® (emedastine difumarate ophthalmic solution) 0.05% is a sterile ophthalmic solution containing emedastine, a relatively selective, H1-receptorantagonist for topical administration to the eyes. Emedastine difumarate is a white, crystalline, water-soluble fine powder with a molecular weight of 534.57. The chemical structure is presented below:
Structural Formula:
 |
Chemical Name:
lH-Benzimidazole, 1-(2-ethoxyethyl)-2-(hexahydro-4-methyl-1H-1,4-diazepin-1-yl), (E)-2-butenedioate (1:2)
Each mL of EMADINE contains: Active: 0.884 mg emedastine difumarate equivalent to 0.5 mg emedastine. Preservative: benzalkonium chloride0.01%. Inactives: tromethamine; sodium chloride; hydroxypropyl methylcellulose; hydrochloric acid/sodium hydroxide (adjust pH); and purified water. It has a pH of approximately 7.4 and an osmolality of approximately 300 mOsm/kg.
l-(2- ethoxyethyl)-2-(4-methyl-l-homopiperazinyl)-benzimidazole, otherwise known asemedastine, and its ophthalmically acceptable acid addition salts and methods for their use.
Allergic conjunctivitis is frequently characterized by ocular pruritus
(itching), erythema (inflammatory redness), edema and tearing. This condition is one of the most frequently treated by ophthalmologists, optometrists and allergists. To date, treatment has been primarily through the use of topically applied histamine t antagonists in combination with α-agonists. See, for example, the following articles:
1. Miller, J. and E.H. Wolf, “Antazoline phosphate and naphazoline hydrochloride, singly and in combination for the treatment of allergic conjunctivitis – a controlled, double-blind clinical trial.” Ann. Allergy, 35:81-86 (1975). 2. Vandewalker, M.L. et al., “Efficacy of Vasocon-A and its components with conjunctival provocation testing (CPT).” j± Allergy Clin. Immunol., 83:302 (1989). 3. Abelson, M.B. et al., “Effects of topically applied ocular decongestant and antihistamine.” Am. I. Ophthalmol., 90:254- 257 (1980).
Recent studies indicate that the antihistamine levocabastine exhibits clinical activity in patients with allergic conjunctivitis without the addition of a vasoconstrictor. See, Dechant, K.L. and K.L. Goa, “Levocabastine. A review of its pharmacological properties and therapeutic potential as a topical antihistamine in allergic rhinitis and conjunctivitis/’ Drugs, 41:202-224 (1991). In addition, it has recently been demonstrated that Hα antagonists are effective in relieving conjunctival injection (hyperemia) and erythema, as well as pruritus. See, Berdy, G.J. et al., “Allergic conjunctivitis: A survey of new antihistamines.” T. Ocular Pharmacol.. 7:313-324 (1991).
Although there are many different antihistamines available for systemic treatment of allergies and related ailments, many such antihistamines are not suitable for topical ophthalmic use because of limited ocular bioavailability. For example, terfenadine (Seldane®, made by Marion Merrell Dow), astemizole (Hismanal®, made by Janssen Pharmaceutica) and loratadine (Claritin®, made by Schering) all have good systemic activity; however, terfenadine has little or no local ocular activity, and astemizole and loratadine each have greatly reduced local ocular activity (as compared to its systemic activity).
Cubist Pharmaceuticals, Inc. announced that it has submitted a NDA to the U.S. FDA for approval of its investigational antibiotic tedizolid phosphate (TR-701).
TEDIZOLID PHOSPHATE
PRONUNCIATION ted” eye zoe’ lid
THERAPEUTIC CLAIM Treatment of complicated skin and skin structure infections
CHEMICAL NAMES
1. 2-Oxazolidinone, 3-[3-fluoro-4-[6-(2-methyl-2H-tetrazol-5-yl)-3-pyridinyl]phenyl]-5- [(phosphonooxy)methyl]-, (5R)-
2. [(5R)-3-{3-fluoro-4-[6-(2-methyl-2H-tetrazol-5-yl)pyridin-3-yl]phenyl}-2-oxooxazolidin-5- yl]methyl hydrogen phosphate
http://www.ama-assn.org/resources/doc/usan/tedizolid-phosphate.pdf
MOLECULAR FORMULA C17H16FN6O6P
MOLECULAR WEIGHT 450.3
TRADEMARK None as yet
SPONSOR Trius Therapeutics
CODE DESIGNATION TR-701 FA
CAS REGISTRY NUMBER 856867-55-5
Note: This adoption statement supersedes the USAN torezolid phosphate (N09/81), which is hereby rescinded and replaced by the USAN tedizolid phosphate (N10/118).
Cubist Announces Submission of New Drug Application for Investigational Antibiotic Tedizolid for Treatment of Serious Skin Infections
LEXINGTON, Mass.–(BUSINESS WIRE)– Cubist Pharmaceuticals, Inc. today announced that it has submitted a New Drug Application (NDA) to the U.S. Food and Drug Administration (FDA) for approval of its investigational antibiotic tedizolid phosphate (TR-701). Cubist is seeking approval of tedizolid phosphate for the treatment of acute bacterial skin and skin structure infections (ABSSSI). Tedizolid phosphate is a once daily oxazolidinone being developed for both intravenous (I.V.) and oral administration for the treatment of serious Gram-positive infections, including those caused by methicillin-resistant Staphylococcus aureus (MRSA).
http://www.drugs.com/nda/tedizolid_131023.html
Emergence of bacterial resistance to known antibacterial agents is becoming a major challenge in treating bacterial infections. One way forward to treat bacterial infections, and especially those caused by resistant bacteria, is to develop newer antibacterial agents that can overcome the bacterial resistance. Coates et al. (Br. J. Pharmacol. 2007; 152(8), 1147-1154.) have reviewed novel approaches to developing new antibiotics. However, the development of new antibacterial agents is a challenging task. For example, Gwynn et al. (Annals of the New York Academy of Sciences, 2010, 1213: 5-19) have reviewed the challenges in the discovery of antibacterial agents.
Several antibacterial agents have been described in the prior art (for example, see PCT International Application Nos. PCT/US2010/060923, PCT/EP2010/067647, PCT/US2010/052109, PCT/US2010/048109, PCT/GB2009/050609, PCT/EP2009/056178 and PCT/US2009/041200). However, there remains a need for potent antibacterial agents for preventing and/or treating bacterial infections, including those caused by bacteria that are resistant to known antibacterial agents.
my old article cut paste
Tedizolid, 856866-72-3
(5R)-3-{3-fluoro-4-[6-(2-methyl-2H-tetrazol-5-yl)pyridin-3-yl]phenyl}-5-(hydroxymethyl)-1,3-oxazolidin-2-one
- Molecular Formula: C17H15FN6O3
- Average mass: 370.337799
Torezolid (also known as TR-701 and now tedizolid[1]) is an oxazolidinone drug being developed by Trius Therapeutics (originator Dong-A Pharmaceuticals) for complicated skin and skin-structure infections (cSSSI), including those caused by Methicillin-resistantStaphylococcus aureus (MRSA).[2]
As of July 2012, tedizolid had completed one phase III trial, with another one under way. [3]Both trials compare a six-day regimen of tedizolid 200mg once-daily against a ten-day regimen of Zyvox (linezolid) 600mg twice-daily.
The prodrug of tedizolid is called “TR-701″, while the active ingredient is called “TR-700″.[4][5]

March 5 2013
Trius Therapeutics will soon be reporting data from its second phase III trial (ESTABLILSH-2) and the recently announced publication of the data from its first phase III trial (ESTABLISH-1) in the Journal of the American Medical Association (JAMA)
- “Trius grows as lead antibiotic moves forward”. 31 Oct 2011.
- “Trius Completes Enrollment In Phase 2 Clinical Trial Evaluating Torezolid (TR-701) In Patients With Complicated Skin And Skin Structure Infections”. Jan 2009.
- http://clinicaltrials.gov/ct2/results?flds=Xf&flds=a&flds=b&term=tedizolid&phase=2&fund=2&show_flds=Y
- PMID 19528279 In vitro activity of TR-700, the active ingredient of the antibacterial prodrug TR-701, a novel oxazolidinone antibacterial agent.
- PMID 19218276 TR-700 in vitro activity against and resistance mutation frequencies among Gram-positive pathogens.
Iroko Pharmaceuticals Receives FDA Approval for ZORVOLEX™

Philadelphia, Pennsylvania, October 18, 2013 – Iroko Pharmaceuticals, LLC, a global specialty pharmaceutical company dedicated to advancing the science of analgesia, today announced that the U.S. Food and Drug Administration (FDA) has approved ZORVOLEX™ (diclofenac) capsules, a nonsteroidal anti-inflammatory drug (NSAID), for the treatment of mild to moderate acute pain in adults[i]. ZORVOLEX was approved at dosage strengths that are 20 percent lower than currently available diclofenac products. FDA approval of ZORVOLEX was supported by data from a Phase 3 multi-center, randomized study in which patients treated with ZORVOLEX reported significant pain relief compared with patients receiving placebo
Antifungal drugs-Antibiotics
Antifungal drugs-Antibiotics
by Parasuraman S, Senior Lecturer at AIMST University, Malaysia on Oct 20, 2013
Actelion wins crucial FDA approval for next-gen lung disease drug Opsumit

MACITENTAN
N-[5-(4-Bromophenyl)-6-[2-[(5-bromo-2-pyrimidinyl)oxy]ethoxy]-4-pyrimidinyl]-N’-propylsulfamide, CAS NO 441798-33-0
Late on Friday the FDA came through with an approval for Actelion’s pulmonary arterial hypertension (PAH) drug Opsumit (macitentan), its next-gen successor to the franchise drug Tracleer.
Read more: Actelion wins crucial FDA approval for next-gen lung disease drug Opsumit – FierceBiotech http://www.fiercebiotech.com/story/actelion-wins-crucial-fda-approval-next-gen-lung-disease-drug-opsumit/2013-10-18#ixzz2i7tDhpZT
Subscribe at FierceBiotech
Macitentan (Opsumit® )is a novel dual endothelin receptor antagonist that resulted from a tailored drug discovery process. Macitentan has a number of potentially key beneficial characteristics – i.e., increased in vivo preclinical efficacy vs. existing ERAs resulting from sustained receptor binding and tissue penetration properties. A clinical pharmacology program indicated a low propensity of macitentan for drug-drug interactions.
Macitentan is an investigational drug being studied for the treatment of pulmonary arterial hypertension. It acts as a dualendothelin receptor antagonist and is being developed by Actelion.[1] A Phase III clinical trial was successfully completed in 2012.[2]
on 22 October 2012 – Actelion (SIX: ATLN) announced that it has submitted a New Drug Application (NDA) to the US Food and Drug Administration (FDA) seeking approval for macitentan (Opsumit®) for the treatment of patients with pulmonary arterial hypertension
Actelion’s experimental lung drug macitentan prolonged overall survival by more than a third according to detailed study data, which the company hopes will convince investors it has a viable follow-up product to secure its commercial future.
Europe’s largest standalone biotech company wants the drug, which treats pulmonary arterial hypertension — a disease that causes high blood pressure in the arteries of the lungs — to replace blockbuster Tracleer.
Tracleer currently makes up 87 percent of sales but loses patent protection in 2015 and has also seen its market share eroded by Gilead’s Letairis.
Pharmacokinetics
Macitentan has an active metabolite, ACT-132577, which is an oxidative depropylation product. Both macitentan and ACT-132577 are mainly excreted in form of hydrolysis products via urine (about 2/3 of all metabolites) and faeces (1/3).[3]
Co-administration of ciclosporin has only a slight effect on the concentrations of macitentan and its active metabolite, whilerifampicin decreases the area under the curve (AUC) of the drug’s blood plasma concentration by 79%, and ketoconazoleapproximately doubles it. This corresponds to the finding that macitentan is mainly metabolised via the liver enzyme CYP3A4.[4]
- ^ Bolli, M. H.; Boss, C.; Binkert, C.; Buchmann, S.; Bur, D.; Hess, P.; Iglarz, M.; Meyer, S.; Rein, J.; Rey, M.; Treiber, A.; Clozel, M.; Fischli, W.; Weller, T. (2012). “The Discovery of N-[5-(4-Bromophenyl)-6-[2-[(5-bromo-2-pyrimidinyl)oxy]ethoxy]-4-pyrimidinyl]-N′-propylsulfamide (Macitentan), an Orally Active, Potent Dual Endothelin Receptor Antagonist”. Journal of Medicinal Chemistry 55 (17): 7849–7861. doi:10.1021/jm3009103. PMID 22862294. edit
- ^ “Macitentan”. Actelion. Retrieved 22 August 2012.
- ^ Bruderer, S.; Hopfgartner, G. R.; Seiberling, M.; Wank, J.; Sidharta, P. N.; Treiber, A.; Dingemanse, J. (2012). “Absorption, distribution, metabolism, and excretion of macitentan, a dual endothelin receptor antagonist, in humans”. Xenobiotica 42 (9): 901–910.doi:10.3109/00498254.2012.664665. PMID 22458347. edit
- ^ Bruderer, S.; Äänismaa, P. I.; Homery, M. C.; Häusler, S.; Landskroner, K.; Sidharta, P. N.; Treiber, A.; Dingemanse, J. (2011).“Effect of Cyclosporine and Rifampin on the Pharmacokinetics of Macitentan, a Tissue-Targeting Dual Endothelin Receptor Antagonist”. The AAPS Journal 14 (1): 68–78. doi:10.1208/s12248-011-9316-3. PMC 3282010. PMID 22189899. edit
External links
Actelion Ltd
Actelion Ltd is a biopharmaceutical company with its corporate headquarters in Allschwil/Basel, Switzerland. Actelion’s first drug Tracleer®, an orally available dual endothelin receptor antagonist, has been approved as a therapy for pulmonary arterial hypertension. Actelion markets Tracleer through its own subsidiaries in key markets worldwide, including the United States (based in South San Francisco), the European Union, Japan, Canada, Australia and Switzerland. Actelion, founded in late 1997, is a leading player in innovative science related to the endothelium – the single layer of cells separating every blood vessel from the blood stream. Actelion’s over 2,400 employees focus on the discovery, development and marketing of innovative drugs for significant unmet medical needs. Actelion shares are traded on the SIX Swiss Exchange (ticker symbol: ATLN) as part of the Swiss blue-chip index SMI (Swiss Market Index SMI®).
Characterization of the “hygroscopic” properties of active pharmaceutical ingredients
Characterization of the “hygroscopic” properties of active pharmaceutical ingredients.
Source
SSCI, Inc., West Lafayette, IN, USA. ann.newman@aptuit.com
http://www.ncbi.nlm.nih.gov/pubmed/17630643
Abstract
The amount of water vapor taken up by an active pharmaceutical ingredient (API) as a function of relative humidity is routinely evaluated to characterize and monitor its “hygroscopicity” throughout the drug development process. In this minireview we address the necessity of going beyond the measurement of water vapor sorption isotherms to establish the various mechanisms by which solids interact with water and the important role played by the crystalline or amorphous form of the solid. Practical approaches for choosing experimental conditions under which water vapor sorption should be measured, including the pre-treatment of samples and the time allowed to reach an equilibrium state are presented. With the assistance of a flowchart, we provide a basis for the systematic examination of samples to establish the likely mechanisms of sorption and the indicators pointing toward future problems with physical and chemical instabilities. Finally, we present strategies for managing materials that might be susceptible to the detrimental effects of water vapor sorption.
(Copyright) 2008 Wiley-Liss, Inc.

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....














 is the structure on right
is the structure on right


