Home » Uncategorized (Page 11)
Category Archives: Uncategorized
ATUZAGINSTAT


ATUZAGINSTAT, COR388
cas 2211981-76-7
Cyclopentanecarboxamide, N-[(1S)-5-amino-1-[2-(2,3,6-trifluorophenoxy)acetyl]pentyl]-
Cyclopentanecarboxamide, n-((1s)-5-amino-1-(2-(2,3,6-trifluorophenoxy)acetyl)pentyl)-N-((3s)-7-amino-2-oxo-1-(2,3,6- trifluorophenoxy)heptan-3-yl)cyclopentanecarboxamide
C19H25F3N2O3
386.415
UNII-DGN7ROZ8EN
- OriginatorCortexyme
- DeveloperQuince Therapeutics
- ClassAnti-inflammatories; Antibacterials; Antidementias; Antineoplastics; Antiparkinsonians; Neuroprotectants; Small molecules
- Mechanism of ActionPeptide hydrolase inhibitors
- Phase II/IIIAlzheimer’s disease
- Phase IIPeriodontal disorders
- PreclinicalParkinson’s disease; Squamous cell cancer
- 27 Jan 2023COR 388 licensed to Lighthouse Pharmaceuticals in the US
- 01 Aug 2022Atuzaginstat is available for licensing as of 01 Aug 2022. http://www.quincetx.com
- 01 Aug 2022Cortexyme is now called Quince Therapeutics
You need to be a logged in or subscribed to view this content
This small molecule is an orally available protease inhibitor targeting the lysine proteases of the periodontal pathogen Porphyromonas gingivalis. Known as gingipains, these proteases penetrate gingival tissue and cause inflammation at the site of periodontitis (O’Brien-Simpson et al., 2009). Periodontitis has been linked epidemiologically to cognitive impairment, and P. gingivalis bacterial lipopolysaccharide has been detected in postmortem brain tissue of people with AD (Poole et al., 2013). Oral P. gingivalis has been called a risk factor for Alzheimer’s disease (Kanagasingam et al., 2020).
Cortexyme’s approach is based on the theory that P. gingivalis invades the brain, where gingipains contribute to Alzheimer’s pathology (see Sabbagh and Decourt, 2022). The company reported elevated gingipain in brain tissue from people with AD, and a correlation between levels of gingipain and tau proteins in postmortem middle temporal gyrus from AD and healthy control tissue. P. gingivalis DNA was detected in postmortem cortices from people with AD and healthy controls, and in CSF of AD patients (Jan 2019 news on Dominy et al., 2019). In the same study, they show that in mice, oral P. gingivalis infection led to the appearance of bacterial DNA in the brain, increased brain Aβ42 production, neuroinflammation, and hippocampal degeneration. The first three findings were reported to be reduced by atuzaginstat; results for hippocampal cell death were not reported.
In preclinical work from other labs, infection with P. gingivalis was reported to worsen AD pathology and cognitive impairment in AD transgenic mice, and to cause neuroinflammation, memory impairment, neurodegeneration, micro- and astrogliosis, increased brain Aβ and phospho-tau, and neurofibrillary tangles in wild-type C57Bl6 mice (Ishida et al., 2017; Ilievski et al., 2018; Ding et al., 2018). For a review of the preclinical literature, see Costa et al., 2021.
In human neurons grown in culture, P. gingivalis infection led to tau phosphorylation and degradation, synapse loss, and cell death (Haditsch et al., 2020).
P. gingivalis is associated with cardiovascular disease. In rabbits, oral infection was reported to increase arterial plaque and levels of the inflammatory marker CRP. Both were reversed by treatment with COR388 (2020 AAIC abstract). In aged dogs with periodontal disease, ninety days of COR388 reduced oral bacterial load and gum pathology (Arastu-Kapur et al., 2020). In addition, older dogs had bacterial antigens and ribosomal RNA in their brains, consistent with systemic infection seen in humans.
Findings
Two Phase 1 trials of atuzaginstat were completed by June 2019. In a single-dose study of 5 to 250 mg capsules in 34 healthy adults, the compound was safe and well-tolerated. A multiple-dose study assessed safety and tolerability in 24 healthy older adults (mean age of 60 years) and nine with AD (mean age 72). According to a company press release and a poster presentation at the 2018 CTAD conference, healthy adults received 25, 50, or 100 mg COR388 or placebo every 12 hours for 10 days; AD patients took 50 mg or placebo every 12 hours for 28 days. The pharmacokinetic profiles of COR388 in AD and controls were reported to be similar. All volunteers with AD had P. gingivalis DNA fragments in their CSF at baseline. COR388 caused no serious adverse reactions, and no one withdrew. Gingipains also were reported to degrade ApoE, and 28 days of treatment with COR388 was claimed to reduce CSF ApoE fragments (2020 AAIC abstract).
A Phase 2/3 trial (GAIN) evaluating a 48-week course of COR388 in 643 people with mild to moderate AD began in April 2019. Participants took either 40 mg, 80 mg, or placebo twice daily. The primary endpoint was to be ADAS-Cog11 score, and the ADCS-ADL was added later as a co-primary functional endpoint. Further outcomes included CDR-SB, MMSE, NPI, the Winterlight Speech Assessment, MRI brain scans, and change in periodontal disease status. Investigators assessed CSF Aβ and tau, plus P. gingivalis DNA and gingipains in CSF, blood, and saliva, before and after treatment. A dental substudy of 228 participants is assessing effects of COR388 on periodontal disease. This trial involves 93 sites in the U.S. and Europe. The U.S. sites are offering a 48-week open-label extension.
According to a presentation at the 2020 CTAD, GAIN was fully enrolled. At baseline, more than 80 percent of participants had CSF Aβ and tau levels consistent with amyloid positivity or an AD diagnosis. All had detectable antibodies to P. gingivalis in their blood. In the dental substudy, 90 percent had periodontal disease. In December 2020, an independent data-monitoring committee recommended continuing the trial after a planned futility analysis of 300 patients treated for six months (press release).
In February 2021, the FDA placed a partial clinical hold on GAIN because of liver abnormalities in some participants (press release). Dosing in the open-label extension was stopped, but the placebo-controlled portion of GAIN continued. Cortexyme characterized the liver effects as reversible and showing no risk of long-term effects.
In October 2021, Cortexyme announced top-line results indicating the trial had missed its co-primary endpoints of ADAS-Cog11 and ADCS-ADL (press release). The company reported a statistically significant 57 percent slowing of decline on the ADAS-Cog11 in a subgroup with detectable saliva P. gingivalis DNA at baseline who took the higher dose; a 42 percent slowing on the lower dose did not reach statistical significance. This prespecified subgroup analysis included 242 participants; it found no effect on the ADCS-ADL. Improvements in ADAS-Cog and other cognitive endpoints correlated with reductions in saliva P. gingivalis DNA, according to data presented at CTAD 2021 in November. The most common treatment-related adverse events were gastrointestinal, occurring in 12 to 15 percent of treated participants. The treatment groups had dose-related liver enzyme elevations greater than three times the upper limit of normal, in 7 and 15 percent of participants on low and high doses, respectively, with bilirubin elevation reported in two participants on the high dose. The elevations occurred mainly in the first six weeks of treatment, and all resolved without long-term effects. Discontinuations due to transaminase elevations numbered one on placebo, and five and 17 in the 40 mg and 80 mg groups, respectively. The overall dropout rate was 25 percent in the placebo group, and 40 percent in atuzaginstat groups. There were five deaths in the high dose arm, and one in the low dose. All were deemed unrelated to drug. There was no evidence of ARIA or other imaging abnormalities.
At CTAD, the company announced plans for a confirmatory trial, pending discussions with regulators. The plan was to test atuzaginstat in people with mild to moderate AD and evidence of P. gingivalis infection, at the lower dose of 40 mg twice daily, reached by titration to minimize liver effects. The company was also planning a trial in Parkinson’s disease to begin in 2022. These trials were never registered.
In September 2021, Cortexyme began a Phase 1 trial of a second-generation lysin-gingipain inhibitor, COR588 (press release). This compound is expected to require only once-daily dosing. Results were expected in May 2022.
In January 2022, the company announced that the FDA had placed a full clinical hold on atuzaginstat due to concerns about liver toxicity (press release). The company said it intended to develop its backup compound, COR588, for Alzheimer’s disease, pending Phase 1 results. In July 2022, Cortexyme announced that COR588 had met safety and tolerability endpoints in a single- and multiple-ascending dose study in healthy adults (press release).
In August 2022, Cortexyme discontinued the gingipain inhibitor program, and offered it for external licensing (press release). The company changed its name to Quince, and its focus to bone disease. In January 2023, Quince put out word that it had sold Cortexyme’s legacy small molecule protease inhibitor portfolio to Lighthouse Pharmaceuticals, a company co-founded by a former Cortexyme CEO (press release).
For all trials of atuzaginstat, see clinicaltrials.gov.
SCHEME

Patent
- US10730826, Compound 1a-racemic
- US10730826, Compound 1a-non-racemic
- Ketone inhibitors of lysine gingipainPublication Number: EP-3512846-A1Priority Date: 2016-09-16
- Ketone inhibitors of lysine gingipainPublication Number: US-2019210960-A1Priority Date: 2016-09-16
- Ketone inhibitors of lysine gingipainPublication Number: WO-2018053353-A1Priority Date: 2016-09-16
- Ketone inhibitors of lysine gingipainPublication Number: US-10730826-B2Priority Date: 2016-09-16Grant Date: 2020-08-04
- Ketone inhibitors of lysine gingipainPublication Number: US-2021053908-A1Priority Date: 2016-09-16
PATENT
WO2018053353
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2018053353&_cid=P10-M1OFBK-46119-1



VIII. Examples
Example 1. Preparation of (S)-N-(7-amino-2-oxo-1-(2,3,6-trifluorophenoxy)heptan-3- yl)cyclopentanecarboxamide(1)hydrochloride
[0224] To a mixture of compound 1.4 (23.0 g, 67.2 mmol, 1.00 eq) in THF (200 mL) was added NMM (6.79 g, 67.2 mmol, 7.38 mL, 1.00 eq), isobutyl carbonochloridate (9.17 g, 67.2 mmol, 8.82 mL, 1.00 eq), and diazomethane (5.65 g, 134 mmol, 2.00 eq) at -40 °C under N2 (15 psi). The mixture was stirred at 0 °C for 30 min. LCMS showed the reaction was completed. FLO (200 mL) was added to the reaction and extracted with two 300-mL portions of ethyl acetate. The combined organic phase was washed with two 200-mL portions of brine (200, dried with anhydrous Na2SO4, filtered and concentrated under vacuum to provide crude compound 1.3 (30.0 g, crude) as a yellow oil.
[0225] To a mixture of compound 1.3 (20.0 g, 54.6 mmol, 1.00 eq) in EtOAc (300 mL) was
added hydrogen bromide(29.8 g, 121.7 mmol, 20.0 mL, 33% purity, 2.23 eq) at -20 °C under
N2 (15 psi). The mixture was stirred at -20 °C for 10 min. TLC (petroleum ether : ethyl
acetate = 0:1) showed the reaction was completed. The reaction was basified by addition of
saturated NaHCO3 until the pH of the mixture reached 8, and the mixture was extracted with
three 500-mL portions of EtOAc. The combined organic phase was washed with two 200-mL portions of brine, dried over anhydrous Na2SO4, filtered and concentrated under vacuum
to afford crude compound 1.2 (15.0 g, crude) as a yellow solid.
[0226] To a mixture of compound 1.2 (4.00 g, 9.54 mmol, 1.00 eq) in DMF (40.0 mL) was
added 2,6-difluorophenol (1.49 g, 11.4 mmol, 1.20 eq) and KF (1.66 g, 28.6 mmol, 670 μL,
3.00 eq) at 25 °C. The mixture was stirred at 25 °C for 3 h. TLC (petroleum ether: ethyl
acetate = 1:1) showed the reaction was completed. H2O (150 mL) was added to the mixture
and extracted with two 200-mL portions of ethyl acetate. The combined organic phase was
washed with two 100-mL portions of brine, dried with anhydrous Na2SO4, filtered, and
concentrated under vacuum. The residue was purified by silica gel chromatography
(petroleum ether: ethyl acetate = 100:1, 5:1) to afford compound 1.1 (2.50 g, 5.35 mmol,
56.1 % yield) as a yellow solid.
[0227] To a mixture of compound 1.1 (4.00 g, 8.22 mmol, 1.00 eq) in EtOAc (3.00 mL) was added HCl/EtOAc (40.0 mL) at 25 °C. The mixture was stirred at 25 °C for 2 h. TLC (petroleum ether : ethyl acetate=2:1) showed the reaction was completed. The mixture was concentrated in reduced pressure to provide (.S)-N-(7-amino-2-oxo-1-(2,3,6-trifluorophenoxy)heptan-3-yl)cyclopentanecarboxamide 1 hydrochloride salt (1.34 g, 3.16 mmol) as a light yellow solid. LCMS (ESI): m/z: [M + H] calcd for C19H25N2F3O3: 387.2; found 387.1; RT=2.508 min. 1HNMR (400 MHz, DMSO-d6) δ ppm 1.21 – 1.83 (m, 15 H) 2.60 – 2.81 (m, 3 H) 4.30 (ddd, J=9.70, 7.17, 4.52 Hz, 1 H) 5.02 – 5.22 (m, 2 H) 7.12 – 7.24 (m, 2 H) 7.98 (br s, 3 H) 8.32 (d, J=7.28 Hz, 1 H).
Paper Citations
- Raha D, Broce S, Haditsch U, Rodriguez L, Ermini F, Detke M, Kapur S, Hennings D, Roth T, Nguyen M, Holsinger LJ, Lynch CC, Dominy S. COR388, a novel gingipain inhibitor, decreases fragmentation of APOE in the central nervous system of Alzheimer’s disease patients: Abstract. Alzheimer’s & Dementia, 07 December 2020
- O’Brien-Simpson NM, Pathirana RD, Walker GD, Reynolds EC. Porphyromonas gingivalis RgpA-Kgp proteinase-adhesin complexes penetrate gingival tissue and induce proinflammatory cytokines or apoptosis in a concentration-dependent manner. Infect Immun. 2009 Mar;77(3):1246-61. Epub 2008 Dec 29 PubMed.
- Poole S, Singhrao SK, Kesavalu L, Curtis MA, Crean S. Determining the presence of periodontopathic virulence factors in short-term postmortem Alzheimer’s disease brain tissue. J Alzheimers Dis. 2013 Jan 1;36(4):665-77. PubMed.
- Kanagasingam S, Chukkapalli SS, Welbury R, Singhrao SK. Porphyromonas gingivalis is a Strong Risk Factor for Alzheimer’s Disease. J Alzheimers Dis Rep. 2020 Dec 14;4(1):501-511. PubMed.
- Sabbagh MN, Decourt B. COR388 (atuzaginstat): an investigational gingipain inhibitor for the treatment of Alzheimer disease. Expert Opin Investig Drugs. 2022 Oct;31(10):987-993. Epub 2022 Sep 1 PubMed.
- Dominy SS, Lynch C, Ermini F, Benedyk M, Marczyk A, Konradi A, Nguyen M, Haditsch U, Raha D, Griffin C, Holsinger LJ, Arastu-Kapur S, Kaba S, Lee A, Ryder MI, Potempa B, Mydel P, Hellvard A, Adamowicz K, Hasturk H, Walker GD, Reynolds EC, Faull RL, Curtis MA, Dragunow M, Potempa J. Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv. 2019 Jan;5(1):eaau3333. Epub 2019 Jan 23 PubMed.
- Ishida N, Ishihara Y, Ishida K, Tada H, Funaki-Kato Y, Hagiwara M, Ferdous T, Abdullah M, Mitani A, Michikawa M, Matsushita K. Periodontitis induced by bacterial infection exacerbates features of Alzheimer’s disease in transgenic mice. NPJ Aging Mech Dis. 2017;3:15. Epub 2017 Nov 6 PubMed.
- Ilievski V, Zuchowska PK, Green SJ, Toth PT, Ragozzino ME, Le K, Aljewari HW, O’Brien-Simpson NM, Reynolds EC, Watanabe K. Chronic oral application of a periodontal pathogen results in brain inflammation, neurodegeneration and amyloid beta production in wild type mice. PLoS One. 2018;13(10):e0204941. Epub 2018 Oct 3 PubMed.
- Ding Y, Ren J, Yu H, Yu W, Zhou Y. Porphyromonas gingivalis , a periodontitis causing bacterium, induces memory impairment and age-dependent neuroinflammation in mice. Immun Ageing. 2018;15:6. Epub 2018 Jan 30 PubMed.
- Costa MJ, de Araújo ID, da Rocha Alves L, da Silva RL, Dos Santos Calderon P, Borges BC, de Aquino Martins AR, de Vasconcelos Gurgel BC, Lins RD. Relationship of Porphyromonas gingivalis and Alzheimer’s disease: a systematic review of pre-clinical studies. Clin Oral Investig. 2021 Mar;25(3):797-806. Epub 2021 Jan 20 PubMed.
- Haditsch U, Roth T, Rodriguez L, Hancock S, Cecere T, Nguyen M, Arastu-Kapur S, Broce S, Raha D, Lynch CC, Holsinger LJ, Dominy SS, Ermini F. Alzheimer’s Disease-Like Neurodegeneration in Porphyromonas gingivalis Infected Neurons with Persistent Expression of Active Gingipains. J Alzheimers Dis. 2020;75(4):1361-1376. PubMed.
- Ermini F, Rojas P, Dean A, Stephens D, Patel M, Haditsch U, Roth T, Rodriguez L, Broce S, Raha D, Nguyen M, Kapur S, Lynch CC, Dominy SS, Holsinger LJ, Hasturk H. Targeting porphyromonas gingivalis to treat Alzheimer’s disease and comorbid cardiovascular disease: abstract. Alzheimer’s & Dementia, 07 December 2020
- Arastu-Kapur S, Nguyen M, Raha D, Ermini F, Haditsch U, Araujo J, De Lannoy IA, Ryder MI, Dominy SS, Lynch C, Holsinger LJ. Treatment of Porphyromonas gulae infection and downstream pathology in the aged dog by lysine-gingipain inhibitor COR388. Pharmacol Res Perspect. 2020 Feb;8(1):e00562. PubMed.
///////ATUZAGINSTAT, COR388, COR 388, Cortexyme, Quince Therapeutics
Votoplam



Votoplam
CAS 2407849-89-0
| Molecular Formula | C21H25N9O |
| Molecular Weight | 419.4829 |
2-[3-(2,2,6,6-tetramethylpiperidin-4-yl)triazolo[4,5-c]pyridazin-6-yl]-5-(triazol-2-yl)phenol
UNII D7EZ7B585X
Votoplam is a gene splicing modulator, used to inhibit Huntington’s disease.
Target: DNA/RNA Synthesis
Pathway: Cell Cycle/DNA Damage
Huntington’s disease (HD) is a progressive, autosomal dominant neurodegenerative disorder of the brain, having symptoms characterized by involuntary movements, cognitive impairment, and mental deterioration. Death, typically caused by pneumonia or coronary artery disease, usually occurs 13 to 15 years after the onset of symptoms. The prevalence of HD is between three and seven individuals per 100,000 in populations of western European descent. In North America, an estimated 30,000 people have HD, while an additional 200,000 people are at risk of inheriting the disease from an affected parent. The disease is caused by an expansion of uninterrupted trinucleotide CAG repeats in the “mutant” huntingtin (Htt) gene, leading to production of HTT (Htt protein) with an expanded poly-glutamine (polyQ) stretch, also known as a “CAG repeat” sequence. There are no current small molecule therapies targeting the underlying cause of the disease, leaving a high unmet need for medications that can be used for treating or ameliorating HD. Consequently, there remains a need to identify and provide small molecule compounds for treating or ameliorating HD.
SCHEME

PATENT
PTC Therapeutics Inc., WO2022104058
WO2022103980’
PATENT
WO2020005873
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2020005873&_cid=P20-M1EWD1-90833-1
Example 37
Preparation of Compound 163


- Novel rna transcriptPublication Number: US-2022162610-A1Priority Date: 2020-11-12
- Novel rna transcriptPublication Number: WO-2022103980-A1Priority Date: 2020-11-12
- Novel rna transcriptPublication Number: WO-2022103980-A9Priority Date: 2020-11-12
- Heterocyclic and heteroaryl compounds for treating Huntington’s diseasePublication Number: JP-2021528467-APriority Date: 2018-06-27
- Heterocyclic and heteroaryl compounds for treating huntington’s diseasePublication Number: US-2021238186-A1Priority Date: 2018-06-27
References
REFERENCES
[1]. Sydorenko, et al. Preparation of heterocyclic and heteroaryl compounds for treating Huntington’s disease. World Intellectual Property Organization, WO2020005873 A1.
2020-01-02.
20240216369THE USE OF A SPLICING MODULATOR FOR A TREATMENT SLOWING PROGRESSION OF HUNTINGTON’S DISEASE
20240132509HETEROCYCLIC AND HETEROARYL COMPOUNDS FOR TREATING HUNTINGTON’S DISEASE
20230405000TABLET FOR USE IN TREATING HUNTINGTON’S DISEASE AND METHOD OF MAKING THE SAME
20220162610NOVEL RNA TRANSCRIPT
20210238186Heterocyclic and heteroaryl compounds for treating Huntington’s disease
3814357HETEROCYCLIC AND HETEROARYL COMPOUNDS FOR TREATING HUNTINGTON’S DISEASE
112654625HETEROCYCLIC AND HETEROARYL COMPOUNDS FOR TREATING HUNTINGTON’S DISEASE
WO/2020/005873HETEROCYCLIC AND HETEROARYL COMPOUNDS FOR TREATING HUNTINGTON’S DISEASE
/////////PTC Therapeutics, Votoplam
Atilotrelvir


Atilotrelvir, BDBM622370, GST-HG171
2850365-55-6, ALIGOS THERAPEUTICS, INC
511.5 C24H32F3N5O4
(1S,3S,4R)-N-[(1S)-1-cyano-2-[(3S)-2-oxopyrrolidin-3-yl]ethyl]-2-[(2S)-3,3-dimethyl-2-[(2,2,2-trifluoroacetyl)amino]butanoyl]spiro[2-azabicyclo[2.2.1]heptane-5,1′-cyclopropane]-3-carboxamide
Atilotrelvir (GST-HG171) is antiviral agent, can inhibit coronavirus, picornavirus and norovirus infection.
SCHEME

SYNTHESIS
Patents are available for this chemical structure:
https://patentscope.wipo.int/search/en/result.jsf?inchikey=GTRJFXDJASEGSW-KBCNZALWSA-N
PATENT
US20230312571, Embodiment 11
PATENT
WO2023043816 EX 50

[0312] To a stirred mixture of (1R,4S,6S)-5-(tert-butoxycarbonyl)-5-azaspiro[bicyclo[2.2.1]heptane-2,1′-cyclopropane]-6-carboxylic acid (120 mg, 0.449 mmol, 1.0 eq.) and o-(7-Azabenzotriazol-1-yl)-N,N,N’,N’-tetramethyluronium hexafluorophosphate (204 mg, 0.539 mmol, 1.2 eq.) in DMF (2 mL) was added N-ethyl-N-isopropylpropan-2-amine (348 mg, 2.69 mmol, 6.0 eq.). The mixture was stirred for 10 min at 0 °C, and then (2S)-2-amino-3-[(3S)-2-oxopyrrolidin-3-yl]propanamide hydrochloride (102 mg, 0.494 mmol, 1.1 eq.) was added. The mixture was stirred for 1 h at rt. The crude product was purified by C18 column with CH3CN:Water (0.05% FA). The desired fractions were concentrated under reduced pressure to provide tert-butyl (1R,4S,6S)-6-{[(1S)-1-carbamoyl-2-[(3S)-2-oxopyrrolidin-3-yl]ethyl]carbamoyl}-5-azaspiro[bicyclo[2.2.1]heptane-2,1′-cyclopropane]-5-carboxylate (120 mg, 60 %) as a white solid. LC-MS (ESI, m/z): 421 [M+H]+.
[0313] To a stirred mixture of tert-butyl (1R,4S,6S)-6-{[(1S)-1-carbamoyl-2-[(3S)-2-oxopyrrolidin-3-yl]ethyl]carbamoyl}-5-azaspiro[bicyclo[2.2.1]heptane-2,1′-cyclopropane]-5-carboxylate (140 mg, 0.333 mmol, 1.0 eq.) in DCM (1 mL) was added hydrogen chloride (3 mL, 2M in Et2O). The mixture was stirred for 1 h at rt, and then concentrated under reduced pressure to afford (2S)-2-[(1R,4S,6S)-5-azaspiro[bicyclo[2.2.1]heptane-2,1′-cyclopropan]-6-ylformamido]-3-[(3S)-2-oxopyrrolidin-3-yl]propanamide hydrochloride (110 mg, crude) as a white solid. LC-MS (ESI, m/z): 321 [M+H]+.
[0314] To a stirred mixture of (2S)-3,3-dimethyl-2-(2,2,2-trifluoroacetamido)butanoic acid (70.7 mg, 0.311 mmol, 1.1 eq.) and o-(7-Azabenzotriazol-1-yl)-N,N,N’,N’-tetramethyluronium hexafluorophosphate (129 mg, 0.340 mmol, 1.2 eq.) in DMF (2 mL) were added N-ethyl-N-isopropylpropan-2-amine (219 mg, 1.69 mmol, 6.0 eq.). The mixture was stirred for 10 min at 0 °C, and then (2S)-2-[(1R,4S,6S)-5-azaspiro[bicyclo[2.2.1]heptane-2,1′-cyclopropan]-6-ylformamido]-3-[(3S)-2-oxopyrrolidin-3-yl]propanamide hydrochloride (101 mg, 0.283 mmol, 1.0 eq.) was added. The mixture was stirred for 1 h at rt and purified by C18 column with CH3CN/Water (0.05% FA). The desired fractions were concentrated under reduced pressure to provide (2S)-2-[(1R,4S,6S)-5-[(2S)-3,3-dimethyl-2-(2,2,2-trifluoroacetamido)butanoyl]-5-azaspiro[bicyclo[2.2.1]heptane-2,1′-cyclopropan]-6-ylformamido]-3-[(3S)-2-oxopyrrolidin-3-yl]propanamide (90.0 mg, 57 %) as a white solid. LC-MS (ESI, m/z): 530 [M+H]+.
[0315] To a stirred mixture of (2S)-2-[(1R,4S,6S)-5-[(2S)-3,3-dimethyl-2-(2,2,2- trifluoroacetamido)butanoyl]-5-azaspiro[bicyclo[2.2.1]heptane-2,1′-cyclopropan]-6- ylformamido]-3-[(3S)-2-oxopyrrolidin-3-yl]propanamide (90.0 mg, 0.170 mmol, 1.0 eq.) and pyridine (53.7 mg, 0.680 mmol, 4.0 eq.) in DCM (2 mL) was added trifluoroacetic anhydride (64.2 mg, 0.306 mmol, 1.8 eq.). The mixture was stirred for 1 h at rt. The reaction was quenched with water (10 mL). The mixture was extracted with dichloromethane (3 x 10 mL). The organic layers were combined, washed with brine (2 x 10 mL), dried over anhydrous sodium sulfate, filtered and concentrated under reduced pressure to afford the crude product. The crude product was purified by prep-HPLC with the following conditions (Column: Mobile Phase B: ACN; Flow rate: 25 mL/min; Gradient: 38% B to 68% B in 7 min, 68% B; Wave Length: 254 nm; RT1(min): 5.07) to afford (1R,4S,6S)-N-[(1S)-1-cyano-2-[(3S)-2- oxopyrrolidin-3-yl]ethyl]-5-[(2S)-3,3-dimethyl-2-(2,2,2-trifluoroacetamido)butanoyl]-5- azaspiro[bicyclo[2.2.1]heptane-2,1′-cyclopropane]-6-carboxamide (18.2 mg, 20%) as a white solid. 1H NMR (400 MHz,
8.45-9.03 (m, 1H), 7.30- 7.65 (m, 1H), 4.80-4.98 (m, 1H), 4.42-4.76 (m, 2H), 4.02-4.18 (m, 1H), 3.10-3.30 (m, 2H), 2.30-2.44 (m, 1H), 1.97-2.25 (m, 3H), 1.59-1.97 (m, 5H), 1.40-1.58 (m, 1H), 0.90-1.06 (m, 9H), 0.61-0.83 (m, 2H), 0.21-0.54 (m, 2H). LC-MS (ESI, m/z): 512 [M+H]+.
REF
//////////Atilotrelvir, BDBM622370, 2850365-55-6, ALIGOS THERAPEUTICS, GST-HG171, GST HG171, GSTHG-171, GSTHG 171,
Zelatriazin


Zelatriazin,
C18H15F3N4O3, 392.3 g/mol
1929519-13-0
NBI-1065846 or TAK-041
Phase 2
(S)-2-(4-oxobenzo[d][1,2,3]triazin-3(4H)-yl)-N-(1-(4-(trifluoromethoxy)phenyl)ethyl)acetamide
Zelatriazin (NBI-1065846 or TAK-041) is a small-molecule agonist of GPR139. It was developed for schizophrenia and anhedonia in depression but trials were unsuccessful and its development was discontinued in 2023.[1][2][3][4][5][6][7]
SCHEME

SYN
WO2016081736
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2016081736&_cid=P21-M0X9BK-38013-1
Example 2: (S)-2-(4-oxobenzo[d][l,2,3]triazin-3(4H)-yl)-N-(l-(4-(trifluoromethoxy)phenyl)ethyl)acetamide
[0166] To a vial containing 2-(4-oxobenzo[d][l,2,3]triazin-3(4H)-yl)acetic acid (15 mg, 0.073 mmol), HOBT (15 mg, 0.095 mmol) and EDC (21 mg, 0.110 mmol) was added DMF (244 μΕ). After stirring at RT for 5 min, (S)- 1 -(4-(trifluoromethoxy)phenyl)ethanamine (18 mg, 0.088 mmol) and DIPEA (64, 0.366 mmol) were added. The reaction mixture was
allowed to stir at RT for 1 h then water was added (5 mL). The solid was filtered off and washed with water to yield the title compound as a white solid (20 mg, 71 % yield). XH NMR
(500 MHz, DMSO-i¾) δ ppm 1.40 (d, J=6.8 Hz, 3 H), 4.98 (quin, J=7.1 Hz, 1 H), 5.09 (s, 2
H), 7.33 (d, J=7.8 Hz, 2 H), 7.44 – 7.49 (m, 2 H), 7.93 – 7.98 (m, 1 H), 8.09 – 8.15 (m, 1 H),
8.21 – 8.29 (m, 2 H), 8.85 (d, J=7.8 Hz, 1 H); ESI-MS m/z [M+H]+ 393.9.
REF
Takeda Pharmaceutical Company Limited, WO2016081736
WO2022058791
Journal of Medicinal Chemistry (2021), 64(15), 11527-11542
Publication Name: Journal of Medicinal Chemistry, Publication Date: 2023-10-13, PMID: 37830160
DOI: 10.1021/acs.jmedchem.3c01034
PATENT
https://patents.google.com/patent/US9556130B2/en
Example 2(S)-2-(4-oxobenzo[d][1,2,3]triazin-3(4H)-yl)-N-(1-(4-(trifluoromethoxy)phenyl)ethyl)acetamide

To a vial containing 2-(4-oxobenzo[d][1,2,3]triazin-3(4H)-yl)acetic acid (15 mg, 0.073 mmol), HOBT (15 mg, 0.095 mmol) and EDC (21 mg, 0.110 mmol) was added DMF (244 μL). After stirring at RT for 5 min, (S)-1-(4-(trifluoromethoxy)phenyl)ethanamine (18 mg, 0.088 mmol) and DIPEA (64, 0.366 mmol) were added. The reaction mixture was allowed to stir at RT for 1 h then water was added (5 mL). The solid was filtered off and washed with water to yield the title compound as a white solid (20 mg, 71% yield). 1H NMR (500 MHz, DMSO-d6) δ ppm 1.40 (d, J=6.8 Hz, 3H), 4.98 (quin, J=7.1 Hz, 1H), 5.09 (s, 2H), 7.33 (d, J=7.8 Hz, 2H), 7.44-7.49 (m, 2H), 7.93-7.98 (m, 1H), 8.09-8.15 (m, 1H), 8.21-8.29 (m, 2H), 8.85 (d, J=7.8 Hz, 1H); ESI-MS m/z [M+H]+ 393.9.
PATENT
| Clinical data | |
|---|---|
| Other names | NBI-1065846; TAK-041 |
| Legal status | |
| Legal status | Investigational |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 1929519-13-0 |
| PubChem CID | 121349608 |
| Chemical and physical data | |
| Formula | C18H15F3N4O3 |
| Molar mass | 392.338 g·mol−1 |
References
- ^ Kamel, Amin; Bowlin, Steve; Hosea, Natalie; Arkilo, Dimitrios; Laurenza, Antonio (February 2021). “In Vitro Metabolism of Slowly Cleared G Protein–Coupled Receptor 139 Agonist TAK-041 Using Rat, Dog, Monkey, and Human Hepatocyte Models (HepatoPac): Correlation with In Vivo Metabolism”. Drug Metabolism and Disposition. 49 (2): 121–132. doi:10.1124/dmd.120.000246. PMID 33273044. S2CID 227282766.
- ^ Schiffer, Hans; Atienza, Josephine; Reichard, Holly; Mulligan, Victoria; Cilia, Jackie; Monenschein, Holger; Collia, Deanna; Ray, Jim; Kilpatrick, Gavin; Brice, Nicola; Carlton, Mark; Hitchcock, Steve; Corbett, Ged; Hodgson, Robert (18 May 2020). “S180. The Selective Gpr139 Agonist Tak-041 Reverses Anhedonia and Social Interaction Deficits in Rodent Models Related to Negative Symptoms in Schizophrenia”. Schizophrenia Bulletin. 46 (Supplement_1): S106–S107. doi:10.1093/schbul/sbaa031.246. PMC 7234360.
- ^ Yin, Wei; Han, David; Khudyakov, Polyna; Behrje, Rhett; Posener, Joel; Laurenza, Antonio; Arkilo, Dimitrios (August 2022). “A phase 1 study to evaluate the safety, tolerability and pharmacokinetics of TAK-041 in healthy participants and patients with stable schizophrenia”. British Journal of Clinical Pharmacology. 88 (8): 3872–3882. doi:10.1111/bcp.15305. PMC 9544063. PMID 35277995. S2CID 247407736.
- ^ Rabiner, Eugenii A.; Uz, Tolga; Mansur, Ayla; Brown, Terry; Chen, Grace; Wu, Jingtao; Atienza, Joy; Schwarz, Adam J.; Yin, Wei; Lewis, Yvonne; Searle, Graham E.; Dennison, Jeremy M. T. J.; Passchier, Jan; Gunn, Roger N.; Tauscher, Johannes (June 2022). “Endogenous dopamine release in the human brain as a pharmacodynamic biomarker: evaluation of the new GPR139 agonist TAK-041 with [11C]PHNO PET”. Neuropsychopharmacology. 47 (7): 1405–1412. doi:10.1038/s41386-021-01204-1. PMC 9117280. PMID 34675381.
- ^ Reichard, Holly A.; Schiffer, Hans H.; Monenschein, Holger; Atienza, Josephine M.; Corbett, Gerard; Skaggs, Alton W.; Collia, Deanna R.; Ray, William J.; Serrats, Jordi; Bliesath, Joshua; Kaushal, Nidhi; Lam, Betty P.; Amador-Arjona, Alejandro; Rahbaek, Lisa; McConn, Donavon J.; Mulligan, Victoria J.; Brice, Nicola; Gaskin, Philip L. R.; Cilia, Jackie; Hitchcock, Stephen (12 August 2021). “Discovery of TAK-041: a Potent and Selective GPR139 Agonist Explored for the Treatment of Negative Symptoms Associated with Schizophrenia”. Journal of Medicinal Chemistry. 64 (15): 11527–11542. doi:10.1021/acs.jmedchem.1c00820. PMID 34260228. S2CID 235908256.
- ^ Münster, Alexandra; Sommer, Susanne; Kúkeľová, Diana; Sigrist, Hannes; Koros, Eliza; Deiana, Serena; Klinder, Klaus; Baader-Pagler, Tamara; Mayer-Wrangowski, Svenja; Ferger, Boris; Bretschneider, Tom; Pryce, Christopher R.; Hauber, Wolfgang; von Heimendahl, Moritz (August 2022). “Effects of GPR139 agonism on effort expenditure for food reward in rodent models: Evidence for pro-motivational actions”. Neuropharmacology. 213: 109078. doi:10.1016/j.neuropharm.2022.109078. PMID 35561791. S2CID 248574904.
- ^ Taylor, Nick Paul (10 November 2023). “Neurocrine hit with one-two punch as Takeda and Xenon pacts deliver midphase flops”. Fierce Biotech. Retrieved 4 December 2023.
//////Zelatriazin, 1929519-13-0, NBI-1065846, TAK-041, Phase 2
Arbemnifosbuvir, AT-752, PD160572


Arbemnifosbuvir, AT-752, 1998705-63-7, PD160572
E9V7VHK36U INN 12706
C24H33FN7O7P 581.5 g/mol

SYN
propan-2-yl (2S)-2-[[[(2R,3R,4R,5R)-5-[2-amino-6-(methylamino)purin-9-yl]-4-fluoro-3-hydroxy-4-methyloxolan-2-yl]methoxy-phenoxyphosphoryl]amino]propanoate
L-ALANINE, N-((P(R),2’R)-2-AMINO-2′-DEOXY-2′-FLUORO-N,2′-DIMETHYL-P-PHENYL-5′ -ADENYLYL)-, 1-METHYLETHYL ESTER
N-((P(R),2’R)-2-AMINO-2′-DEOXY-2′-FLUORO-N,2′-DIMETHYL-P-PHENYL-5′ -ADENYLYL)-L-ALANINE 1-METHYLETHYL ESTER
WO2022040473 Atea Pharmaceuticals, Inc.
CN113784721
US20160257706
WO2022076903 US10874687
PATENT
US20160257706
https://patentscope.wipo.int/search/en/detail.jsf?docId=US177601863&_cid=P11-M0VTE4-38538-1


Example 1. Preparation of isopropyl ((((R,S)-(2R,3R,4R,5R)-5-(2-amino-6-(methylamino)-9H-purin-9-yl)-4-fluoro-3-hydroxy-4-methyltetrahydrofuran-2-yl)methoxy)-phenoxy-phosphoryl)-L-alaninate
Step 1. Preparation of ((2R,3R,4R,5R)-3-(benzoyloxy)-5-bromo-4-fluoro-4-methyltetrahydrofuran-2-yl)methyl benzoate (2)
Step 2. Preparation of (2R,3R,4R,5R)-5-(2-amino-6-chloro-9H-purin-9-yl)-2-(benzoyloxymethyl)-4-fluoro-4-methyltetrahydrofuran-3-yl benzoate (3)
Step 3. Preparation of (2R,3R,4R,5R)-5-(2-amino-6-(methylamino)-9H-purin-9-yl)-4-fluoro-2-(hydroxymethyl)-4-methyltetrahydrofuran-3-ol (4)
Step 4. Preparation of isopropyl ((((R,S)-(2R,3R,4R,5R)-5-(2-amino-6-(methylamino)-9H-purin-9-yl)-4-fluoro-3-hydroxy-4-methyltetrahydrofuran-2-yl)methoxy)-phenoxy-phosphoryl)-L-alaninate (5)
PATENT
/////Arbemnifosbuvir, AT-752, 1998705-63-7, PD160572, E9V7VHK36U INN 12706
Zelicapavir


Zelicapavir, Enanta Pharmaceuticals
Alternative Names: EDP-938; EP 023938
cas 2070852-76-3
RSV-IN-7
549.5 g/mol, C27H22F3N7O3
UNII U4OI721DMD
(3S)-3-[[5-[3-morpholin-4-yl-5-(trifluoromethyl)pyridin-2-yl]-1,3,4-oxadiazol-2-yl]amino]-5-phenyl-1,3-dihydro-1,4-benzodiazepin-2-one
SYN
New England Journal of Medicine (2022), 386(7), 655-666
WO2022157327
WO2018152413
WO2019067864
WO2017015449
PATENT
WO2018152413
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2018152413&_cid=P20-M0V26A-30323-1
Step 5 : (<Sf)-3-((5-(3-morpholino-5-(trifluoromethyl)pyridin-2-yl)-1.3.4-oxadiazol-2-

To a mixture of (5)-2-(3-morpholino-5-(trifluoromethyl)picolinoyl)-N-2-oxo-5-phenyl-2,3-dihydro-lH-benzo[e] [l,4]diazepin-3-yl)hydrazine-l-carboxamide (1.4 kg, 1 eq.) in DCM (11.2 L) in a flask was charged with 4A-MS (1.4 kg) and stirred at 20±5 °C for 2hrs. Then, it was cooled to 0°C, charged with triethylamine (0.62 Kg, 2.5 eq.) and stirred for 10 min. /^-Toluenesulfonyl chloride (0.7 kg, 1.5 eq.) in DCM (1.4 L) solution was dropwise added to the reaction mixture with maintaining below 5°C and stirred at at 0±5 °C for 5 hrs. The reaction mixture was filtered and washed with DCM (2 X 4.2 L). The filtrate was treated with water (4.2 L) at 0°C and stirred between 0 and 10°C for 5 min. After separation, the organic phase was washed with 5% aqueous NaHCC solution (7 L), water (7 L) and brine (7 L) successively and separated. The DCM layer was concentrated in vacuo at below 30°C to leave ~7L of organic layer. MTBE (7 L) was added to organic layer and concentrated in vacuo to leave ~ 7 L of organic layer (This step was repeated once). The organic layer was charged with water (7 L) and stirred at 20±5 °C for 4 hrs. The solid was filtered and washed with MTBE (3 X 2.1 L) and purified water (2.8 L). The wet cake was stirred with ethyl acetate (7 L) for 12 hrs, charged with n-heptane (14 L) and stirred at 20±5 °C for 5 hrs. The solid was filtered, washed with n-heptane (2 X 2.8 L) and dried under vacuum at ambient temperature to provide the title compound (0.776 kg, 99.6% purity by HPLC, 97.8%
chiral purity by chiral HPLC) as a pale yellowish solid. LC-MS(ESI, m/z): 550.17 [M+H]+;
¾ NMR: ( DMSO-c 6400 MHz): δ 10.98 (br-s, 1H), 9.40 (d, J=8.0 Hz, 1H), 8.69 (br-d, J=4.0 Hz, 1H), 7.89 (d, J=4.0 Hz, 1H), 7.68 (dt, J=8.0 and 4.0 Hz, 1H), 7.56-7.51 (m, 3H), 7.49-7.45 (m, 2H), 7.38-7.35 (m, 2H), 7.29 (br-t, J=8.0 Hz, 1H)
5.22 (d, J=8.0 Hz, 1H), 3.75-3.72 (m, 4H), 3.09-3.07 (m, 4H); 13C (DMSO-c¾, 100 MHz): δ 167.3, 167.0, 162.8, 156.4, 147.2, 139.2, 138.7, 138.4, 138.3, 138.0, 132.30, 130.7, 130.5, 129.5, 128.4, 126.2, 124.5, 123.4, 121.5, 71.8, 65.9, 51.0.
SCHEME

PATENT
https://patentscope.wipo.int/search/en/detail.jsf?docId=US368999603&_cid=P20-M0V2BF-36596-1
Example 253
Example 160 was prepared using a procedure similar to that used to prepare Example 152 where methyl 5-cyano-3-morpholinopicolinate was used in place of ethyl 2-morpholino-4-(trifluoromethyl)benzoate. ESI-MS m/z: 507.2 [M+H] +. 1H NMR (400 MHz, DMSO-d 6) δ 3.02-3.04 (m, 4H), 3.71-3.73 (m, 4H), 5.19-5.21 (d, J=8.0 Hz, 1H), 7.26-7.30 (m, 1H), 7.34-7.36 (m, 2H), 7.44-7.55 (m, 5H), 7.65-7.70 (m, 1H), 8.13 (s, 1H), 8.72 (s, 1H), 9.42-9.45 (m, 1H), 10.98 (s, 1H).
//////////////Zelicapavir, EDP-938, EP 023938, EDP 938, RSV-IN-7, ENANTA
Palopegteriparatide

Palopegteriparatide
Yorvipath , FDA 2024, 8/9/2024, To treat hypoparathyroidism
- G2N64C3385
- 2222514-07-8
- Palopegteriparatide
- UNII-G2N64C3385
- ACP-014
- Mpeg 40000-teriparatide
- Palopegteriparatide [INN]
- Transcon parathyroid hormone (1-34)
- Transcon pth (1-34)
- Palopegteriparatide [USAN]
- TransCon PTH
- WHO 11060


Palopegteriparatide, sold under the brand name Yorvipath, is a hormone replacement therapy used for the treatment of hypoparathyroidism.[1][2] It is a transiently pegylated parathyroid hormone.[4] It is a parathyroid hormone analog.[1]
Palopegteriparatide was approved for medical use in the European Union in November 2023,[2] and in the United States in August 2024.[1][5]
Medical uses
Palopegteriparatide is indicated for the treatment of adults with hypoparathyroidism.[1][2]
Adverse effects
The US Food and Drug Administration (FDA) prescription label for palopegteriparatide includes warnings for a potential risk of risk of unintended changes in serum calcium levels related to number of daily injections and total delivered dose, serious hypocalcemia and hypercalcemia (blood calcium levels that are too high), osteosarcoma (a rare bone cancer) based on findings in rats, orthostatic hypotension (dizziness when standing), and a risk of a drug interaction with digoxin (a medicine for certain heart conditions).[5]
History
The effectiveness of palopegteriparatide was evaluated in a 26-week, randomized, double-blind, placebo-controlled trial that enrolled 82 adults with hypoparathyroidism.[5] Prior to randomization, all participants underwent an approximate four-week screening period in which calcium and active vitamin D supplements were adjusted to achieve an albumin-corrected serum calcium concentration between 7.8 and 10.6 mg/dL, a magnesium concentration ≥1.3 mg/dL and below the upper limit of the reference range, and a 25(OH) vitamin D concentration between 20 to 80 ng/mL.[5] During the double-blind period, participants were randomized to either palopegteriparatide (N = 61) or placebo (N= 21), at a starting dose of 18 mcg/day, co-administered with conventional therapy (calcium and active vitamin D).[5] Study drug and conventional therapy were subsequently adjusted according to the albumin-corrected serum calcium levels.[5] At the end of the trial, 69% of the participants in the palopegteriparatide group compared to 5% of the participants in the placebo group were able to maintain their calcium level in the normal range, without needing active vitamin D and high doses of calcium (calcium dose ≤ 600 mg/day).[5]
The FDA granted the application for palopegteriparatide orphan drug and priority review designations.[5]
Society and culture
Legal status
In September 2023, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) adopted a positive opinion, recommending the granting of a marketing authorization for the medicinal product Yorvipath, intended for the treatment of chronic hypoparathyroidism in adults.[4][6] The applicant for this medicinal product is Ascendis Pharma Bone Diseases A/S.[4] Palopegteriparatide was approved for medical use in the European Union in November 2023.[2]
Palopegteriparatide was granted an orphan drug designation by the US Food and Drug Administration (FDA) in 2018,[7] and by the EMA in 2020.[8]
Brand names
Palopegteriparatide is the international nonproprietary name.[9][10]
Palopegteriparatide is sold under the brand name Yorvipath.[2]
References
- ^ Jump up to:a b c d e “Yorvipath injection, solution”. DailyMed. 14 August 2024. Retrieved 5 September 2024.
- ^ Jump up to:a b c d e f “Yorvipath EPAR”. European Medicines Agency. 19 October 2020. Archived from the original on 10 December 2023. Retrieved 11 December 2023. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ “Yorvipath Product information”. Union Register of medicinal products. 20 November 2023. Archived from the original on 26 November 2023. Retrieved 11 December 2023.
- ^ Jump up to:a b c “Yorvipath: Pending EC decision”. European Medicines Agency. 15 September 2023. Archived from the original on 24 September 2023. Retrieved 24 September 2023. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ Jump up to:a b c d e f g h “FDA approves new drug for hypoparathyroidism, a rare disorder”. U.S. Food and Drug Administration (FDA) (Press release). 9 August 2024. Archived from the original on 13 August 2024. Retrieved 13 August 2024.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ “Ascendis Pharma Receives Positive CHMP Opinion for TransCon PTH (palopegteriparatide) for Adults with Chronic Hypoparathyroidism”. Ascendis Pharma (Press release). 14 September 2023. Archived from the original on 24 September 2023. Retrieved 24 September 2023.
- ^ “TransCon Parathyroid Hormone (mPEG conjugated parathyroid hormone 1-34) Orphan Drug Designations and Approvals”. U.S. Food and Drug Administration (FDA). Archived from the original on 24 September 2023. Retrieved 24 September 2023.
- ^ “EU/3/20/2350”. European Medicines Agency. 15 September 2023. Archived from the original on 24 September 2023. Retrieved 24 September 2023.
- ^ World Health Organization (2021). “International nonproprietary names for pharmaceutical substances (INN): recommended INN: list 86”. WHO Drug Information. 35 (3). hdl:10665/346562.
- ^ World Health Organization (2023). “International nonproprietary names for pharmaceutical substances (INN): recommended INN: list 89”. WHO Drug Information. 37 (1). hdl:10665/366661.
External links
- Palopegteriparatide Global Substance Registration System
- Palopegteriparatide NCI Thesaurus
- Clinical trial number NCT04701203 for “A Trial Investigating the Safety, Tolerability and Efficacy of TransCon PTH Administered Daily in Adults With Hypoparathyroidism (PaTHway)” at ClinicalTrials.gov
| Clinical data | |
|---|---|
| Trade names | Yorvipath |
| Other names | ACP-014, TransCon PTH |
| License data | US DailyMed: Palopegteriparatide |
| Routes of administration | Subcutaneous |
| Drug class | Hormonal agent |
| ATC code | H05AA05 (WHO) |
| Legal status | |
| Legal status | US: ℞-only[1]EU: Rx-only[2][3] |
| Identifiers | |
| CAS Number | 2222514-07-8 |
| UNII | G2N64C3385 |
| KEGG | D12395 |
//////Palopegteriparatide, APPRoVALS 2024, FDA 2024, Yorvipath, hypoparathyroidism, UNII-G2N64C3385, ACP-014, TransCon PTH, WHO 11060
Aneratrigine


Aneratrigine
2097163-74-9
5-chloro-2-fluoro-4-[4-fluoro-2-[methyl-[2-(methylamino)ethyl]amino]anilino]-N-(1,3-thiazol-4-yl)benzenesulfonamide
5-chloro-2-fluoro-4-((4-fluoro-2-(3-(methylamino)pyridin-1-yl)phenyl)amino)-N-(thiazol-4-yl)benzenesulfonamide hydrochloride
| Benzenesulfonamide, 5-chloro-2-fluoro-4-[[4-fluoro-2-[methyl[2-(methylamino)ethyl]amino]phenyl]amino]-N-4-thiazolyl- |
C19H20ClF2N5O2S2 488.0 g/mol
UNII 6A5ZY5LT78
WHO
SYN

Assignee: Daewoong Pharmaceutical Co., Ltd.
World Intellectual Property Organization, WO2017082688
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2017082688&_cid=P11-M0UEPF-95506-1
Preparation of 5-chloro-2-fluoro-4-((4-fluoro-2-(3-(methylamino)pyridin-1-yl)phenyl)amino)-N-(thiazol-4-yl)benzenesulfonamide hydrochloride
Step 1) Preparation of tert-butyl (1-(2-amino-5-fluorophenyl)pyridin-3-yl)(methyl)carbamate
2,4-Difluoro-1-nitrobenzene (2.0 g, 12.6 ng/mol) and tert-butyl methyl (pyridin-3-yl)carbamate (2.5 g, 1.0 eq.) were dissolved in DMF (20 mL), and K2C03 ( 2.6 g , 1.5 eq .) was added. The internal temperature was maintained at 60–70 ° C and the mixture was stirred for 2 hours. The completion of the reaction was confirmed by TLC when the reaction solution turned deep yellow. After cooling to room temperature, ethyl acetate (EA)/H20 was added, stirred, and the layers were separated. MgS04 was added to the separated organic layer, stirred, dried, and filtered. After concentrating the filtrate under reduced pressure, the residue was dissolved in EtOH (10 mL) and distilled water (10 mL), and then Na 2 S 2 0 4 (13.0 g, 6 eq.) was added. After stirring for 2 hours while maintaining the internal temperature at 60 to 70 ° C, the completion of the reaction was confirmed by TLC when the yellow color of the reaction solution lightened and became almost colorless. After cooling to room temperature, distilled water (50 mL) was added and extracted twice with EA (100 mL). MgS0 4 was added to the organic layer, stirred, dried, and filtered. The filtrate was concentrated under reduced pressure, and the obtained residue was separated by column chromatography (n-Hexane/EA = 3/1) to obtain the title compound (2.0 g, 51. ).
1H NMR (MeOD): 6.73(m, 1H), 6.57(t, 1H), 3.23(m, 1H), 3.10(m, 2H), 2.94(m, 1H), 2.91(s, 3H), 2.25( m, 1H), 1.99(m, 1H)
Step 2) Preparation of tert-butyl thiazol-4-ylcarbamate
Thiazole-4-carboxylic acid (5.0 g, 38.8 vol) was dissolved in t-Bu0H (100 mL), and then TEA (8.1 mL, 1.5 eq.) and DPPA (7.1 mL, 1.5 eq.) were added. The internal temperature was maintained at 90–100 ° C, and the mixture was stirred for 3 days. The completion of the reaction was confirmed by TLC. The product was concentrated under reduced pressure, distilled water (50 mL) was added, and the solution was washed with EA (100 mL).
It was extracted twice. MgSQ 4 was added to the organic layer, stirred, dried, and filtered.
After concentrating the filtrate under reduced pressure, the residue was added to a small amount of EA, slurried, and the resulting solid was filtered to obtain the white title compound (4.0 g, 51.5%).
1H NMR (MeOD): 8.73(s, 1H), 7.24(s, 1H), 1.52(s, 9H)
Step 3) Preparation of tert-butyl ((4-bromo-5-chloro-2-fluorophenyl)sulfonyl)(thiazol-4-yl)carbamate
Step 2) The tert-Butyl thiazol-4-ylcarbamate (4.0 g, 20.0 ng ol) prepared in the reaction vessel was placed in a reaction vessel and the interior was replaced with nitrogen gas. After dissolving in THF (32 mL), it was cooled to _78 ° C using dry ice— acetone. After cooling, LiHMDS (22.4 mL, 1.5 eq.) was slowly added and the reaction mass was stirred for 30 minutes. 4-Bromo-5-chloro-2-fluorobenzenesulfonyl chloride (6.0 g, 1.0 eq.) was dissolved in THF (10 mL) and slowly added to the reaction mixture. The reaction mass was stirred overnight and the completion of the reaction was confirmed by TLC. Distilled water (50 mL) was added and extracted twice with EA (100 mL). MgS0 4 was added to the organic layer, stirred, dried, and filtered. After concentrating the filtrate under reduced pressure, the residue was crystallized from THF/n-hexane to obtain the title compound (4.4 g, 59.0%).
1H NMR (MeOD): 9.00(s, 1H), 8.22(d, 1H), 7.90(d, 1H), 7.78(s, 1H), 1.35(s, 9H)
Step 4) Preparation of tert-butyl (l-(2-((4-(N-(tert-butyloxycarbonyl)-N-(thiazol-4-yl)sulfamoyl)-2-chloro-5-fluorophenyl)amino)-5-fluorophenyl)pyrlidin-3-yl)(methyl)carbamate
Tert-butyl (1-(2-amino-5-fluorophenyl)pyrlidin-3-yl)(methyl)carbamate (0.5 g, 1.1 ng ol) prepared in Step 1) and tert-butyl ((4-bromo-5-chloro-2-fluorophenyl)sulfonyl)(thiazol-4-yl)carbamate (0.9 g, 1.2 eq.) prepared in Step 3) were dissolved in 1,4-dioxane (10 mL). Pd(OAc) 2 (0.03 g, 0.1 eq), rac-BINAP (0.19 g, 0.2 eq.), Cs 2 C0 3 (1.5 g, 3.0 eq.) were added to the reaction solution. After reacting at 120 ° C for 30 minutes using a microwave initiator, the completion of the reaction was confirmed by TLC. Distilled water (50 mL) was added and extracted twice with EA (100 mL).
MgS0 4 was added to the organic layer, stirred, filtered and dried. The filtrate was concentrated under reduced pressure, and the residue was separated by column chromatography (EA/n-Hexane = 1/1). This was repeated twice to obtain the title compound (2.0 g, 88.2%).
1H NMR (MeOD): 8.95(s, 1H), 7.94(d, 1H), 7.65(s, 1H), 7.14(t, 1H), 6.70(d, 1H), 6.64(t, 1H), 6.07( d, 1H)ᅳ 3.40(m, 1H), 3.28(m, 2H), 3.16(m, 1H), 2.64(s, 3H), 2.06(m, 1H), 1.89(m, 1H), 1.41(s , 9H), 1.36(s, 9H)
Step 5) Preparation of 5-chloro-2-fluoro-4-((4-fluoro-2-(3-(methylamino)pyridin-1-yl)phenyl)amino)-N-(thiazol-4-yl)benzenesulfonamide hydrochloride
Step 4) was prepared by adding 1.25 M HCl in MeOH (15 mL) to tert-butyl (1-(2-((4-(Ν-(tert-butoxycarbonyl)-N-(thiazol-4-yl)sulfamoyl)—2-chloro-5-fluorophenyl)amino)-5-fluorophenyl)pyrlidin-3-yl) (methyl)carbamate (2.0 g, 2.9 µl). The mixture was heated to 40–50 ° C and stirred overnight, and the completion of the reaction was confirmed by TLC. The product was concentrated, and methylene chloride (15 mL) was added to the residue, which was stirred for 1 hour, and the resulting solid was filtered to obtain the title compound (0.9 g, 58.8%).
1H 證 (MeOD): 8.73(s, 1H), 7.75(d, 1H), 7.12(t, 1H), 7.00(s, 1H), 6.69(d, 1H), 6.67(t, 1H), 6.05( d, 1H), 3.73(m, 1H) , 3.54(m, 1H), 3.45(m, 1H), 3.38(m, 1H), 3.26(m, 1H), 2.63(s, 3H) , 2.31(m , 1H), 1.96(m, 1H)
PATENTS
0002705578SODIUM CHANNEL BLOCKER
20180346459Substituted benzenesulfonamides as sodium channel blockers
2018533606ナトリウムチャネル遮断剤
3375782SODIUM CHANNEL BLOCKER
108349963SODIUM CHANNEL BLOCKER
1020170056461SODIUM CHANNEL BLOCKER

////////////Aneratrigine, DAEWOONG
Zevotrelvir, EDP 235
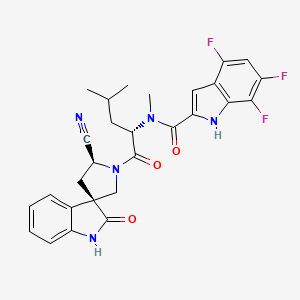
Zevotrelvir, EDP 235
cas 2773516-53-1
N-[(2S)-1-[(2′S,3R)-2′-cyano-2-oxospiro[1H-indole-3,4′-pyrrolidine]-1′-yl]-4-methyl-1-oxopentan-2-yl]-4,6,7-trifluoro-N-methyl-1H-indole-2-carboxamide
C28H26F3N5O3, 537.5
Zevotrelvir (Compound 52) is a coronavirus inhibitor with IC50 ranges of <0.1 μM and <0.1mM for 229E hCoV and SARS-CoV-23C-like (3CL) proteases, respectively. Zevotrelvir has the potential to study viral infections.
Coronaviruses are enveloped, positive-sense, single-stranded RNA viruses. The genomic RNA of CoVs has a 5′-cap structure and 3′-poly-A tail and contains at least 6 open reading frames (ORFs). The first ORF (ORF 1a/b) directly translates two polyproteins: pp1a and pp1ab. These polyproteins are processed by a 3C-Like protease (3CLpro), also known as the main protease (Mpro), into 16 non-structural proteins. These non-structural proteins engage in the production of subgenomic RNAs that encode four structural proteins, namely envelope, membrane, spike, and nucleocapsid proteins, among other accessory proteins. As a result, it is understood that 3C-Like protease has a critical role in the coronavirus life cycle.
3CLpro is a cysteine protease involved in most cleavage events within the precursor polyprotein. Active 3CLpro is a homodimer containing two protomers and features a Cys-His dyad located in between domains I and II.3CLpro is conserved among coronaviruses and several common features are shared among the substrates of 3CLpro in different coronaviruses. As there is no human homolog of 3CLpro, it is an ideal antiviral target. Although compounds have been reported to inhibit 3CLpro activity, they have not been approved as coronavirus therapies. (Refer to
WO 2004101742 A2, US 2005/0143320 Al, US 2006/0014821 Al, US 2009/0137818
Al, WO 2013049382 A2, WO 2013166319 A1, WO2018042343, WO2018023054, WO 2022013684, WO 2021252644, WO2022020711, WO 2022020242, US 11,174,231 B1, US 11,124,497 B1, WO 2005113580, and WO2006061714).
There is a need in the art for novel therapeutic agents that treat, ameliorate or prevent SARS-CoV-2 infection. The present invention provides the process of novel compounds which act in inhibiting or preventing SARS-CoV-2 viral replication and thus are used in the treatment of COVID-19 (see PCT/US21/60247).
Synthesis of substituted spirooxindole and its intermediate has been previously published (Refer to PCT/US21/60247, WO2019086142, WO 2020221811, WO2020221826, J. Med. Chem.2012, 55, 9069). However, the scale-up using previous process is very challenging due to the safety concern associated with certain intermediates, instability of certain intermediates as well as lack of purification process other than column chromatograph. Thus, there is a strong need for developing a safe and efficient processes for the large-scale preparation of these novel substituted spirooxindole derivatives.
SYNTHESIS

https://patents.google.com/patent/US11352363B1/en

PATENT
SYN
[1]. Guoqiang Wang, et al. Novel spiropyrrolidine derived antiviral drugs. Patent CN114524821A.
1.20230295175PROCESSES FOR THE PREPARATION OF SUBSTITUTED SPIROOXINDOLE DERIVATIVES
2.WO/2023/177854PROCESSES FOR THE PREPARATION OF SUBSTITUTED SPIROOXINDOLE DERIVATIVES
3.WO/2022/109363NOVEL SPIROPYRROLIDINE DERIVED ANTIVIRAL AGENTS
Enanta Pharmaceuticals, Inc.
WO2023177854




Example 15. Preparation of Preparation of (3R,5’S)-1′-(N-methyl-N-(4,6,7-trifluoro-1H-indole-2-carbonyl)-L-leucyl)-2-oxospiro[indoline-3,3′-pyrrolidine]-5′-carboxamide (Compound (n))

DMF (760 kg, 8V) was added into the reaction at 0 °C (-5~5 °C) followed by compound (j) (63 kg, 1.05 eq) and N-Methylmorpholine (56 kg, 2 eq), HATU
(106 kg, 1.0 eq) and Compound (m-1) (100 kg, 1.0 eq). The reactor was rinsed with DMF (190 kg, 2V) under and warmed up to 25 °C (20~30 °C) and stirred for 5 h (3~6 h) at 25 °C (20~30 °C). After that, additional HATU (0.1 eq) was added and the reaction mixture was stirred for 16-24 h.25% Ammonium hydroxide (38 kg) was added to the reaction mixture at 25 °C (20~30 °C) and stirred for 2 h (1~3 h) at 25 °C (20~30 °C). The reaction mixture was then added to water (5000 kg, 50V) at 20-30°C over 2 h and the resulting slurry was stirred for 2 h (1~5 h) at 25 °C (20~30 °C). The mixture was filtered and the cake was rinsed with water (500 kg, 5 V). The cake was dissolved in ethyl acetate (1350 kg, 15 V) and washed with 10% sodium chloride solution (500 kg) for three times. The organic layer was separated to 1.5-2.5V at not more than 45℃ under vacuum. The solution was cooled to 25 °C (20~30 °C) and Dichloromethane (660 kg, 5V) was added. The mixture was stirred for 2 h (2~5 h) at 25 °C (20~30 °C) and a slurry was formed. n-Heptane (137 kg, 2V) was added dropwise over 0.5 h (0.5~2 h) at 25 °C (20~30 °C) and stirred for additional 2 h (1~3 h) at 25 °C (20~30 °C). The reaction mixture was filtered and the wet cake was rinsed with DCM/heptane (5/2). The wet cake was dried at 50 °C (45~55 °C) for 20 h (15~25 h) to provide Compound (n) as the white solid in 80-85% yield.
1H NMR (300 MHz, DMSO-d6) δ 12.46 (s, 1H), 10.68 (s, 1H), 7.56 (s, 1H), 7.15 – 7.00 (m, 3H), 6.91 (t, J = 4.4 Hz, 2H), 6.84 (d, J = 7.7 Hz, 1H), 6.55 (d, J = 2.8 Hz, 1H), 5.34 (t, J = 7.3 Hz, 1H), 4.63 (dd, J = 9.8, 8.0 Hz, 1H), 3.83 (q, J = 10.3 Hz, 2H), 3.45 (qd, J = 7.0, 5.1 Hz, 1H), 3.16 (s, 3H), 2.35 – 2.13 (m, 2H), 1.69 (t, J = 7.1 Hz, 2H), 1.56 (dq, J = 13.1, 6.5 Hz, 1H), 0.93 (dd, J = 12.2, 6.3 Hz, 6H).
Example 16. Preparation of (3R,5’S)-1′-(N-methyl-N-(4,6,7-trifluoro-1H-indole-2-carbonyl)-L-leucyl)-2-oxospiro[indoline-3,3′-pyrrolidine]-5′-carboxamide (Compound (n))
DMF solution of Compound (m-2) (1 kg, 1.0 eq.) was added to a reactor at around 0-10oC. Compound (l) (600 g, 1.0 eq.), NMM (3.00 eq., 850 g) and HATU (1.00 eq., 1.06 kg) was added to the reactor while maintaining the temperature at 0-10oC; The reaction was warmed to 20±5oC, and stirred for at least 6 hours at 20±5oC. HATU (0.20 eq., 210 g) was added to the reactor at 20±5oC and stirred for at least 6 hours at 20±5oC.25% Ammonium hydroxide (390 g, 1.0 eq) was added to the reaction mixture at 20 °C and stirred for 2 h (1~3 h) at 20 °C. EtOAc (14.0 V) and water (14 V) was added at around 25oC over 20 minutes, and the
solution was stirred for at least 30 min. Aqueous phase was extracted with EtOAc for three times and the organic phase was combined, and washed with 10% aq. NaCl for three times at 20±5oC. The organic phase was concentrated to 6 V then EtOH (7.0 V) was charged. The EtOAc-EtOH solvent swap was repeated for three times and concentrated to 5 V before water (7.0 v) was added at 20±5oC. The mixture was cooled to 0-10oC and stirred for 1 h before being filtered. The filter cake was dissolved in ethyl acetate (15 V) and washed with 10% sodium chloride solution for three times. The organic layer was concentrated to 2-3V at not more than 45℃ under vacuum. The solution was cooled to 25 °C (20~30 °C) and Dichloromethane (5V) was added. The mixture was stirred for 2 h (2~5 h) at 25 °C (20~30 °C) and a slurry was formed. n-Heptane (2V) was added dropwise over 0.5 h (0.5~2 h) at 25 °C (20~30 °C) and stirred for additional 2 h (1~3 h) at 25 °C (20~30 °C). The reaction mixture was filtered and wet cake was rinsed with DCM/heptane (5/2). The wet cake was dried at 50 °C (45~55 °C) for 20 h (15~25 h) to provide Compound (n) as the white solid in about 70-75% yield over two steps.
1H NMR (300 MHz, DMSO-d6) δ 12.46 (s, 1H), 10.68 (s, 1H), 7.56 (s, 1H), 7.15 – 7.00 (m, 3H), 6.91 (t, J = 4.4 Hz, 2H), 6.84 (d, J = 7.7 Hz, 1H), 6.55 (d, J = 2.8 Hz, 1H), 5.34 (t, J = 7.3 Hz, 1H), 4.63 (dd, J = 9.8, 8.0 Hz, 1H), 3.83 (q, J = 10.3 Hz, 2H), 3.45 (qd, J = 7.0, 5.1 Hz, 1H), 3.16 (s, 3H), 2.35 – 2.13 (m, 2H), 1.69 (t, J = 7.1 Hz, 2H), 1.56 (dq, J = 13.1, 6.5 Hz, 1H), 0.93 (dd, J = 12.2, 6.3 Hz, 6H).
Example 17. Preparation of (3R,5’S)-1′-(N-methyl-N-(4,6,7-trifluoro-1H-indole-2-carbonyl)-L-leucyl)-2-oxospiro[indoline-3,3′-pyrrolidine]-5′-carboxamide (Compound (n))
DMF (10.0 v) was added to a reactor at 25 °C followed by Compound (l) (4.4 kg, 1.0 eq.), NMM (3.0 eq.) Compound (m-3) (1.0 eq.) and HATU (1.0 eq) at 20-25oC. The reaction mixture was stirred for at least 12 hours at 20-25 °C. Once reaction was complete, aqueous ammonium hydroxide (1.0 eq.) was to the reaction system at 20-25 °C, then stirred for at least 2 hours at 20-25oC. The reaction mixture was then added to water (220 kg, 50V) at 20-30°C over 2 h and the resulting slurry was stirred for 2 h (1~5 h) at 25 °C (20~30 °C). The mixture was filtered and the cake was rinsed with water (22 kg, 5 V). The cake was dissolved in ethyl acetate (135 g, 15 V) and washed with 10% sodium chloride solution (22 kg) for three times. The organic layer was separated to 1.5-2.5V at not more than 45 ℃ under vacuum. The solution was cooled to 25 °C (20~30 °C) and Dichloromethane (5V) was added. The mixture was stirred for 2 h (2~5 h) at 25 °C (20~30 °C) and a slurry was formed. n-Heptane (2V) was added dropwise over 0.5 h (0.5~2 h) at 25 °C (20~30 °C) and stirred for additional 2 h (1~3 h) at 25 °C (20~30 °C). The reaction mixture was filtered and wet cake was rinsed with DCM/heptane (5/2). The wet cake was dried at 50 °C (45~55 °C) for 20 h (15~25 h) to provide Compound (n) as the white solid in 80-85% yield.
1H NMR (300 MHz, DMSO-d6) δ 12.46 (s, 1H), 10.68 (s, 1H), 7.56 (s, 1H), 7.15 – 7.00 (m, 3H), 6.91 (t, J = 4.4 Hz, 2H), 6.84 (d, J = 7.7 Hz, 1H), 6.55 (d, J = 2.8 Hz, 1H), 5.34 (t, J = 7.3 Hz, 1H), 4.63 (dd, J = 9.8, 8.0 Hz, 1H), 3.83 (q, J = 10.3 Hz, 2H), 3.45 (qd, J = 7.0, 5.1 Hz, 1H), 3.16 (s, 3H), 2.35 – 2.13 (m, 2H), 1.69 (t, J = 7.1 Hz, 2H), 1.56 (dq, J = 13.1, 6.5 Hz, 1H), 0.93 (dd, J = 12.2, 6.3 Hz, 6H). Example 18. Preparation of N-((S)-1-((3R,5’S)-5′-cyano-2-oxospiro[indoline-3,3′-pyrrolidin]-1′-yl)-4-methyl-1-oxopentan-2-yl)-4,6,7-trifluoro-N-methyl-1H-indole-2-carboxamide toluene solvate (Compound (I))
(I))

Ethyl acetate (630 kg, 10 V) was added into reactor (R1) followed by Compound (n) (70 kg). Make sure the water content was less than 0.20% (w/w). The reaction was cooled to 0 °C (-5 – 5°C) and then triethylamine (89.6 kg) was added followed by trifluoroacetic anhydride (92.4 kg) at 0 °C (-5 – 5°C). The reaction was stirred for 1 h (0.5~2 h) at 0 °C (-5 – 5°C). Once the reaction was complete, the reaction mixture was added slowly to 0.2 N aqueous HCl solution (700 kg) over 1 h at 0 °C (-5~5 °C). The resulting solution was stirred for 30 min at 0 °C (-5~5 °C) and the organic layer was separated.1% aqueous ammonium hydroxide (700 kg) was added to the organic layer and stirred at 20 °C for 30 min (15~25 °C). The organic layer was separated and washed with 10% brine for four times. Then the organic layer was separated and distilled to 2-3 V. Toluene-EtOAc swap was performed until precipitate was observed at 3-4 V. Then Toluene (5-6 V) was added and the slurry was stirred at 50 oC for 2 h. Then the solution was cooled down to 20 oC over 1-2 h and stirred for 10 hr (6~14 hr) at 20 °C (15~25 °C). The reaction mixture was filtered and the wet cake was rinsed with toluene (120 kg, 2V). The wet cake was then dried at 50˚C (45~55 °C) for 48 hr to provide desired compound (o) as a white solid in 80-85% yield.
1H NMR (400 MHz, Acetone-d6) δ 11.17 (s, 1H), 9.65 (s, 1H), 7.02 (dd, J = 13.7, 7.3 Hz, 2H), 6.94 (dd, J = 6.0, 3.5 Hz, 1H), 6.92 – 6.85 (m, 2H), 6.81 (t, J = 7.5 Hz, 1H), 5.56 (dd, J = 9.4, 5.6 Hz, 1H), 5.21 (t, J = 8.3 Hz, 1H), 4.25 (d, J = 10.7 Hz, 1H), 3.99 (d, J = 10.6 Hz, 1H), 3.43 (s, 3H), 2.79 – 2.61 (m, 2H), 1.93 (ddd, J = 14.4, 9.5, 5.1 Hz, 1H), 1.79 (ddd, J = 14.2, 8.7, 5.6 Hz, 1H), 1.64 (dpd, J = 8.7, 6.6, 5.1 Hz, 1H), 0.98 (dd, J = 18.5, 6.6 Hz, 6H).
US20230103494
CN114524821
SCHEME

MAIN

////////Zevotrelvir, EDP 235
O=C1[C@@]2(CN([C@@H](C2)C#N)C([C@H](CC(C)C)N(C)C(C3=CC4=C(F)C=C(F)C(F)=C4N3)=O)=O)C5=CC=CC=C5N1
Afimetoran
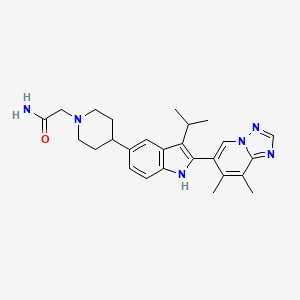

Afimetoran BMS-986256, WHO 11516
cas 2171019-55-7
2-[4-[2-(7,8-dimethyl-[1,2,4]triazolo[1,5-a]pyridin-6-yl)-3-propan-2-yl-1H-indol-5-yl]piperidin-1-yl]acetamide
C26H32N6O,444.583, phase 1
Afimetoran is an immunomodulator and an antagonist of toll-like receptors 7 and 8.1,2 It is also is under investigation in clinical trial NCT04269356 (Study to Assess the Way the Body Absorbs, Distributes, Breaks Down and Eliminates Radioactive BMS-986256 in Healthy Male Participants).

Ref
WO2018005586
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2018005586&_cid=P20-M0RQ0D-09010-1
The invention further pertains to pharmaceutical compositions containing at least one compound according to the invention that are useful for the treatment of conditions related to TLR modulation, such as inflammatory and autoimmune diseases, and methods of inhibiting the activity of TLRs in a mammal.
Toll/IL-1 receptor family members are important regulators of inflammation and host resistance. The Toll-like receptor family recognizes molecular patterns derived from infectious organisms including bacteria, fungi, parasites, and viruses (reviewed in Kawai, T. et al., Nature Immunol., 11:373-384 (2010)). Ligand binding to the receptor induces dimerization and recruitment of adaptor molecules to a conserved cytoplasmic motif in the receptor termed the Toll/IL-1 receptor (TIR) domain. With the exception of TLR3, all TLRs recruit the adaptor molecule MyD88. The IL-1 receptor family also contains a cytoplasmic TIR motif and recruits MyD88 upon ligand binding (reviewed in Sims, J.E. et al., Nature Rev. Immunol., 10:89-102 (2010)).
Toll-like receptors (TLRs) are a family of evolutionarily conserved, transmembrane innate immune receptors that participate in the first-line defense. As pattern recognition receptors, the TLRs protect against foreign molecules, activated by pathogen associated molecular patterns (PAMPs), or from damaged tissue, activated by danger associated molecular patterns (DAMPs). A total of 13 TLR family members have been identified, 10 in human, that span either the cell surface or the endosomal compartment. TLR7-9 are among the set that are endosomally located and respond to single-stranded RNA (TLR7and TLR8) or unmethylated single-stranded DNA containing cytosine-phosphate-guanine (CpG) motifs (TLR9).
Activation of TLR7/8/9 can initiate a variety of inflammatory responses (cytokine production, B cell activation and IgG production, Type I interferon response). In the case of autoimmune disorders, the aberrant sustained activation of TLR7/8/9 leads to worsening of disease states. Whereas overexpression of TLR7 in mice has been shown to exacerbate autoimmune disease, knockout of TLR7 in mice was found to be protective against disease in lupus-prone MRL/lpr mice. Dual knockout of TLR7 and 9 showed further enhanced protection.
As numerous conditions may benefit by treatment involving modulation of cytokines, IFN production and B cell activity, it is immediately apparent that new compounds capable of modulating TLR7 and/or TLR8 and/or TLR9 and methods of using these compounds could provide substantial therapeutic benefits to a wide variety of patients.
The present invention relates to a new class of [1,2,4]triazolo[1,5-a]pyridinyl substituted indole compounds found to be effective inhibitors of signaling through TLR7/8/9. These compounds are provided to be useful as pharmaceuticals with desirable stability, bioavailability, therapeutic index, and toxicity values that are important to their drugability.
EXAMPLE 15
2-(4-(2-(7,8-dimethyl-[1,2,4]triazolo[1,5-a]pyridin-6-yl)-3-isopropyl-1H-indol-5-yl) piperidin-1-yl)acetamide

To a reaction flask were added
6-(3-isopropyl-5-(piperidin-4-yl)-1H-indol-2-yl)-7,8-dimethyl-[1,2,4]triazolo[1,5-a]pyrid ine, 2 HCl (47.66 g, 104 mmol), DCE (220 mL), DBU (62.4 mL, 414 mmol), and 2-bromoacetamide (17.14 g, 124 mmol). The reaction flask was capped. The reaction mixture was stirred overnight at room temperature. The reaction mixture was concentrated, diluted with water, and stirred for 30 minutes then filtered. The solid was recrystallized using ethanol to afford 2-(4-(2-(7,8-dimethyl-[1,2,4]triazolo[1,5-a] pyridin-6-yl)-3-isopropyl-1H-indol-5-yl)piperidin-1-yl)acetamide (42.3 g, 93 mmol,
90% yield) as a white solid. LCMS MH+: 445. HPLC Ret. Time 1.20 min. Method QC-ACN-TFA-XB. 1HNMR (400 MHz, DMSO-d6) δ 10.97-10.86 (m, 1H), 8.78-8.69 (m, 1H), 8.54-8.40 (m, 1H), 7.64-7.49 (m, 1H), 7.30-7.21 (m, 2H), 7.17-7.09 (m, 1H), 7.06-6.93 (m, 1H), 2.99-2.82 (m, 5H), 2.62-2.54 (m, 4H), 2.24-2.12 (m, 5H), 1.92-1.72 (m, 4H), 1.37-1.29 (m, 6H).
ACS Medicinal Chemistry Letters (2022), 13(5), 812-818 83%
References
- Bristol-Myers Squibb: Investor Series [Link]
- Bristol-Myers Squibb: Investor Series [Link]
- MedKoo Biosciences: Afimetoran [Link]
//////////////Afimetoran, BMS-986256, BMS 986256, WHO 11516, phase 1

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....










