Home » Articles posted by DR ANTHONY MELVIN CRASTO Ph.D (Page 427)
Author Archives: DR ANTHONY MELVIN CRASTO Ph.D
Health Canada approval-aHUS Canada applauds approval of Soliris® (eculizumab) first treatment for fatal, ultra-rare disease affecting children and adults


CAS number 219685-50-4
Soliris is a formulation of eculizumab which is a recombinant humanized monoclonal IgG2/4;κ antibody produced by murine myeloma cell culture and purified by standard bioprocess technology. Eculizumab contains human constant regions from human IgG2 sequences and human IgG4 sequences and murine complementarity-determining regions grafted onto the human framework light- and heavy-chain variable regions. Eculizumab is composed of two 448 amino acid heavy chains and two 214 amino acid light chains and has a molecular weight of approximately 148 kDa.
TORONTO, March 7, 2013
Atypical Hemolytic Uremic Syndrome (aHUS) Canada is thrilled by Health Canada’s recent approval of Soliris® (eculizumab) for the treatment of patients with atypical Hemolytic Uremic Syndrome (aHUS), 1 a very rare, chronic and life-threatening genetic condition affecting fewer than 60 patients in Canada.
aHUS leaves a part of the immune system (known as the complement system) uncontrolled and always active. As a result, the immune system attacks the body’s unhealthy and healthy cells which can cause blood vessel damage, abnormal blood clotting 2,3 and progressive damage to the body’s major organs, leading to heart attack, stroke, kidney failure and death.4
The management of aHUS has relied on plasma infusion and plasma exchange therapies with variable results.5 These lifelong therapies are costly, painful and time-consuming, and have not been studied or approved for the treatment of aHUS.6 If kidney failure has already occurred as a result of aHUS, dialysis is required, though it is not a curative treatment.7 Within a year of diagnosis, over half of patients will need dialysis, will have irreversible kidney damage, or will not survive.6 The majority of patients progress to end-stage kidney failure within three years of diagnosis.8,9
With the approval of Soliris, aHUS patients and their families finally have a reason for hope.
Sonia DeBortoli knows all too well the destructive force of the disease. Sonia’s 11-year-old son Joshua was diagnosed with aHUS in March 2012 and experienced kidney failure, internal bleeding and a blood clot in his groin as a result. He endured several painful hours of daily dialysis and plasma therapy, and was on prednisone and oxygen. Then, a chance to join a clinical trial for Soliris restored Joshua’s health so that he no longer needed the other therapies.
“Our whole world changed when Joshua was given Soliris – we now believe he has a long and healthy future. He is back at school, taking karate lessons and playing soccer,” Sonia says. “We got our little boy back, he got his life back, and we want the same for anyone who has to deal with this rare and devastating disease.”
A groundbreaking treatment advance for aHUS patients
Soliris (eculizumab) is the first and only pharmaceutical treatment for aHUS, and is being hailed by experts worldwide as a critical breakthrough in treating the disease. It has been shown to significantly improve patients’ health and quality of life.10 In clinical trials, Soliris has been proven effective in preventing blood vessel damage and abnormal blood clotting,11,12 leading to remission and significant improvement in kidney function.5,4 Soliris has also allowed patients to discontinue dialysis and plasma exchange therapies.10
Soliris is also indicated, and proven safe and effective, for the treatment of another rare and life-threatening disorder called paroxysmal nocturnal hemoglobinuria (PNH).13 Canadians living with PNH already have access to Soliris through private health insurance and provincial drug plans.
Immediate and sustained access to treatment urgently needed
Now that this new treatment option has been approved for the small number of Canadians living with the devastating symptoms of aHUS, Soliris must be made immediately accessible to all aHUS patients whose lives depend on this treatment.
“We are so hopeful that the Common Drug Review will recognize the urgent need for access to Soliris, and that provincial governments will act swiftly to provide reimbursement to patients who are in urgent need of this life-saving treatment,” says Tracy MacIntyre, a founder of aHUS Canada whose daughter is living with aHUS. “Immediate access to the drug would have a profoundly positive impact on the few Canadians living with aHUS, while any delay in funding treatment could lead to devastating consequences.”
About aHUS Canada
aHUS Canada was formed in November 2012 to support Canadian patients and families living with aHUS. In addition to establishing a Canadian aHUS community, the group is committed to building public awareness and understanding of aHUS and advocating for the best possible care and treatment for patients. For more information, please visit http://www.ahuscanada.org.
Eculizumab (INN and USAN; trade name Soliris®) is a humanized monoclonal antibody that is a first-in-class terminal complement inhibitor and the first therapy approved for the treatment of paroxysmal nocturnal hemoglobinuria (PNH), a rare, progressive, and sometimes life-threatening disease characterized by excessive destruction of red blood cells (hemolysis).[1] It costs £400,000 ($US 600,000) per year per patient.[1]
Eculizumab also is the first agent approved for the treatment of atypical hemolytic uremic syndrome (aHUS), an ultra-rare genetic disease that causes abnormal blood clots to form in small blood vessels throughout the body, leading to kidney failure, damage to other vital organs and premature death.[2][3]
In clinical trials in patients with PNH, eculizumab was associated with reductions in chronic hemolysis, thromboembolic events, and transfusion requirements, as well as improvements in PNH symptoms, quality of life, and survival.[1][4][5][6] Clinical trials in patients with aHUS demonstrated inhibition of thrombotic microangiopathy (TMA),[7] the formation of blood clots in small blood vessels throughout the body,[1][3][4] including normalization of platelets and lactate dehydrogenase (LDH), as well as maintenance or improvement in renal function.[7]
Eculizumab was discovered and developed by Alexion Pharmaceuticals and is manufactured by Alexion. It was approved by the United States Food and Drug Administration (FDA) on March 16, 2007 for the treatment of PNH, and on September 23, 2011 for the treatment of aHUS. It was approved by the European Medicines Agency for the treatment of PNH on June 20, 2007, and on November 24, 2011 for the treatment of aHUS. Eculizumab is currently being investigated as a potential treatment for other severe, ultra-rare disorders
- Hillmen, Young, Schubert, P, N, J, et al (2006). “The complement inhibitor eculizumab in paroxysmal nocturnal hemoglobinuria”. N Engl J Med 355 (12): 1233–1243. doi:10.1056/NEJMMoa061648. PMID 16990386.
- Noris, Caprioli, Bresin, M, J, E, et al. (2010). “Relative role of genetic complement abnormalities in sporadic and familial aHUS and their impact on clinical phenotype”. Clin J Am Soc Nephrol 5: 1844–1859.
- Caprioli, Noris, Brioschi, J, M, S, et al (2006). “Genetics of HUS: the impact of MPC, CFH, and IF mutations on clinical presentation, response to treatment, and outcome”. Blood 108: 1267–1279.
- Hillman, Hall, Marsh, P, C, JC, et al (2004). “Effect of eculizumab on hemolysis and transfusion requirements in patients with paroxysmal nocturnal hemoglobinuria”. N Eng J Med 350: 552–559.
- Ray, Burrows, Ginsberg, Burrows, JG, RF, JS, EA (2000). “Paroxysmal nocturnal hemoglobinuria and the risk of venous thrombosis: review and recommendations for management of the pregnant and nonpregnant patient”. Haemostasis 30: 103–107.
- Kelly, Hill, Arnold, RJ, A, LM, et al (2011). “Long-term treatment with eculizumab in paroxysmal nocturnal hemoglobinuria: sustained efficacy and improved survival”. Blood 117: 6786–6792.
- .Soliris® (eculizumab) prescribing information (2011). Cheshire, CT: Alexion Pharmaceuticals. http://www.soliris.net/sites/default/files/assets/soliris)pi.pdf.
Phase 2, Sarepta Therapeutics, Efficacy, Safety, and Tolerability Rollover Study of Eteplirsen in Subjects With Duchenne Muscular Dystrophy
Eteplirsen, also called AVI-4658, is an experimental drug, currently in clinical trials. It is designed for treatment of some mutations which cause Duchenne muscular dystrophy (DMD), a genetic degenerative muscle disease. Eteplirsen is a product of Sarepta Therapeutics Inc.
s excision of exon 51 during pre-mRNA splicing of the dystrophin RNA transcript. Skipping exon 51 changes the downstream reading frame of dystrophin;[1] giving eteplirsen to a healthy person would result in production of dystrophin mRNA which would not code for functional dystrophin protein but, for DMD patients with particular frameshifting mutations, giving eteplirsen can restore the reading frame of the dystrophin mRNA and result in production of functional (though internally-truncated) dystrophin.[2] Eteplirsen is given by intravenous infusion for systemic treatment of DMD.
Clinical studies
Several clinical trials have been conducted to test eteplirsen, one in the UK involving local injection to the foot,[3][4] one in the UK involving systemic injection at low doses[5][6] and one in the USA at higher systemic doses[7] that progressed to a rollover extension study.[8]
References
- “Exon Skipping Quantification by qRT-PCR in Duchenne Muscular Dystrophy Patients Treated with the Antisense Oligomer Eteplirsen”. Hum Gene Ther Methods.. 17 Oct 2012.
- “Morpholinos and Their Peptide Conjugates: Therapeutic Promise and Challenge for Duchenne Muscular Dystrophy.”. Biochim Biophys Acta. 1798 (12): 2296–303.. 17 Feb 2010.
- Gary Roper/Manager Clinical Research Governance Organisation, Imperial College London. “Safety and Efficacy Study of Antisense Oligonucleotides in Duchenne Muscular Dystrophy”. ClinicalTrials.gov. US Government, NIH. Retrieved 30 October 2012.
- Lancet Neurol. 8 (10): 918–28. 25 Aug 2009.
- Professor Francesco Muntoni, University College of London Institute of Child Health. “Dose-Ranging Study of AVI-4658 to Induce Dystrophin Expression in Selected Duchenne Muscular Dystrophy (DMD) Patients”. ClinicalTrials.gov. US Government, NIH. Retrieved 30 October 2012.
- “Exon skipping and dystrophin restoration in patients with Duchenne muscular dystrophy after systemic phosphorodiamidate morpholino oligomer treatment: an open-label, phase 2, dose-escalation study.”. Lancet. 378 (9791): 595–605. 23 Jul 2011.
- Sarepta Therapeutics. “Efficacy Study of AVI-4658 to Induce Dystrophin Expression in Selected Duchenne Muscular Dystrophy Patients”. ClinicalTrials.gov. US Government, NIH. Retrieved 30 October 2012.
- Sarepta Therapeutics. “Efficacy, Safety, and Tolerability Rollover Study of Eteplirsen in Subjects With Duchenne Muscular Dystrophy”. ClinicalTrials.gov. US Government, NIH. Retrieved 30 October 2012.
Phase 2 Drug: Ustekinumab A monoclonal antibody against the p40 subunit of IL-12/23 Other Name: Stelara
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Human |
| Target | IL-12 and IL-23
|

Ustekinumab, CAS number 815610-63-0, is also known by it’s brand name Stelara, which is marketed by Janssen Biotech, Inc. Developed as a treatment for adults with moderate to severe plaque psoriasis
Rockefeller University, MAR 2013
http://clinicaltrials.gov/ct2/show/NCT01806662
Atopic dermatitis (AD) is a chronic disease associated with intense itching, which affects most aspects of everyday life in the majority of patients. Acute inflammation and extensor/facial involvement is common in infants, whereas chronic inflammation increases in prevalence with age, as do localization to flexures. AD has a complex background characterized by immune activation, increased epidermal thickness in chronic diseased skin, and defective barrier function. In normal, healthy skin, the outer layer of the epidermis, the stratum corneum is made up flattened dead cells called corneocytes held together by a mixture of lipids and proteins. The stratum corneum and, in particular, the lipid layer are vital in providing a natural barrier function that locks water inside the skin and keeps allergens and irritants out. In people with AD, the barrier function is defective, which leads to dry skin. As the skin dries out, it cracks allowing allergens and irritants to penetrate.
Mild AD can be controlled with emollients and topical medications. However, moderate to severe AD is extremely difficult to control and requires systemic treatment that is often unsatisfactory due to impracticality and lack of effectiveness. Only three therapeutic options exist for moderate to severe AD, including: 1) oral steroids 2) cyclosporine A (CsA), that is not widely used in the US as it is not FDA approved for AD and 3) ultraviolet phototherapy. Oral steroids and CsA treatments have major side effects and UV radiation therapy is highly inconvenient for patients. Several biologic medications, such as TNF-alpha inhibitors, are effective, convenient, and relatively safe therapies for psoriasis, but have thus far not shown efficacy in AD. Ustekinumab is a unique biologic medication that may specifically target AD.
The investigators study will determine whether there is a reversal of the skin thickness and the immune pathways involved in the disease during treatment with Ustekinimab and what specific immune cells are involved. The investigators are also interested to understand how the clinical reversal of the disease will correlate with tissue reversal of the disease.
Detailed Description:
In psoriasis, epidermal hyperplasia is driven by underlying immune activation, whether as a direct response to IL-20 family cytokines that induces hyperplasia and inhibits keratinocyte terminal differentiation or as an indirect response to immune-mediated injury to keratinocytes. The epidermal reaction in psoriasis is largely restored to normal with selective immune suppression. Hence, one might hypothesize that similar epidermal responses should occur in the presence of “generalized” cellular immune activation, in diseases with similar inflammatory infiltrate and epidermal hyperplasia, such as AD. In fact, psoriasis and AD share features of dense T-cells and dentritic cell infiltrates, as well as over-expression of IL-22 in skin lesions. These diseases also share similar epidermal hyperplasia in their chronic phases.
Work from the investigators group showed that IL-22 is a key cytokine in the pathogenesis of both AD and psoriasis. The investigators have demonstrated that in psoriasis, ustekinumab suppresses the production of IL-12, IL-23, and IL-22. Additionally, by RT-PCR the investigators demonstrated that the mRNA expression of p40 cytokine and the IL23R is up-regulated in AD as compared to both normal skin and psoriasis. The investigators therefore hypothesize that ustekinumab will suppress IL-22 and possibly also p40 production in AD lesions and reverse both the epidermal growth/differentiation defects and the underlying immune activation, and hence will suppress disease activity. Interestingly, p40 was also found to be significantly up-regulated in non-lesional AD skin as compared with normal skin.
Although AD is thought to be predominately a disease of Th2-type cells, in the chronic stage, there is large Th1 component. To date, the precise mechanism by which sequential activation of Th2 and Th1 cells in AD is achieved remains unknown. IL-12 induces the differentiation and maturation of human Th cells into Th1-type cells. Recent circumstantial evidence suggests that in AD patients IL-12 may facilitate a change from the Th2-type to a Th1 cytokine profile. IL-12 was recently shown to be highly elevated in pediatric AD and its levels were strongly associated with disease severity.
Expression of IL-12 p40 mRNA is significantly enhanced in lesional skin from AD, suggesting that the enhanced local production of IL-12 in dendritic cells and macrophages may be responsible for the increased production of IFN-γ in chronic lesions potentially suggesting that IL-12 may have a pivotal role in promoting inflammation in atopic dermatitis. Topical steroids which constitute a mainstay of therapy in AD are known to strongly down-regulate IL-12 expression, possibly also indicating that targeted anti IL-12 therapy might important role in treating AD.
Recently, the Th1/Th2 paradigm in autoimmunity and allergy has been revisited to include a role for a new population of IL-17-producing Th cells known as Th17. Th17 cells are characterized by the production of inflammatory cytokines such as IL-17A, IL-17F, IL-22, and IL-26. One of the key factors involved in naive Th-cell commitment to a Th17 phenotype is IL-23.
Patients with acute AD were found to have increased Th17 T-cells in peripheral blood by flow cytometry and intracellular cytokine staining 26 as well as by immunohistochemistry (IHC) in lesions. Since IL-23 is the major inducer of Th17 T-cells, as well as “T22” T-cells, neutralization of IL-23 could potentially result in both decreased Th17 signal in acute AD as well as decreased “T22/IL22″ signal. Therefore the investigators postulate that ustekinumab in AD will act both inhibiting the IL-12-dependent Th1 shift in chronic AD stage as well as the pathogenic IL-22/”T22” axis in this disease.
Ustekinumab [1] (INN, experimental name CNTO 1275, proprietary commercial name Stelara,[2] Centocor) is a human monoclonal antibody. It is directed against interleukin 12 and interleukin 23, naturally occurring proteins that regulate the immune system and immune-mediated inflammatory disorders.[3]
In two Phase III trials for moderate to severe psoriasis, the longest >76 weeks, ustekinumab was safe and effective.[4][5]
A third Phase III trial, ACCEPT, compared the efficacy and safety of ustekinumab with etanercept in the treatment of moderate to severe plaque psoriasis.[6] This trial found a significantly higher clinical response with ustekinumab over the 12-week study period compared to high-dose etanercept.[6] It also demonstrated the clinical benefit of ustekinumab among patients who failed to respond to etanercept.[6]
Ustekinumab is approved in Canada, Europe and the United States to treat moderate to severe plaque psoriasis.[7]
As of November 2009, the drug is being investigated for the treatment of psoriatic arthritis.[8][9] It has also been tested in Phase II studies for multiple sclerosis[10] and sarcoidosis, the latter versus golimumab (Simponi).[11]
- Cingoz, Oya (2009). “Ustekinumab”. MAbs 1 (3): 216–221. doi:10.4161/mabs.1.3.8593. PMC 2726595. PMID 20069753.
- ^ European Medicines Agency, 20 November 2008, http://www.emea.europa.eu/pdfs/human/opinion/Stelara_58227008en.pdf
- ^ Reddy M, Davis C, Wong J, Marsters P, Pendley C, Prabhakar U (May 2007). “Modulation of CLA, IL-12R, CD40L, and IL-2Ralpha expression and inhibition of IL-12- and IL-23-induced cytokine secretion by CNTO 1275”. Cell. Immunol. 247 (1): 1–11. doi:10.1016/j.cellimm.2007.06.006. PMID 17761156.
- ^ Leonardi CL, Kimball AB, Papp KA, et al. (May 2008). “Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 76-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 1)”. Lancet 371 (9625): 1665–74. doi:10.1016/S0140-6736(08)60725-4. PMID 18486739.
- ^ Papp KA, Langley RG, Lebwohl M, et al. (May 2008). “Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 52-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 2)”. Lancet 371 (9625): 1675–84. doi:10.1016/S0140-6736(08)60726-6. PMID 18486740.
- ^ a b c Griffiths C, Strober B, van de Kerkhof P et al. (2010). “Comparison of Ustekinumab and Etanercept for Moderate-to-Severe Psoriasis”. N Engl J Med 362 (2): 118–28. doi:10.1056/NEJMoa0810652. PMID 20071701.
- ^ Medarex to Receive Milestone Payment for Approval of STELARA(TM) (Ustekinumab) for the Treatment of Moderate to Severe Plaque Psoriasis
- ^ ClinicalTrials.gov NCT00267956 A Study of the Safety and Efficacy of CNTO 1275 in Patients With Active Psoriatic Arthritis
- ^ ClinicalTrials.gov NCT01009086 A Study of the Safety and Efficacy of Ustekinumab in Patients With Psoriatic Arthritis
- ^ ClinicalTrials.gov NCT00207727 A Safety and Efficacy Study of CNTO1275 in Patients With Multiple Sclerosis
- ^ ClinicalTrials.gov NCT00955279 A Study to Evaluate the Safety and Effectiveness of Ustekinumab or Golimumab Administered Subcutaneously (SC) in Patients With Sarcoidosis
- ^ http://www.empr.com/stelara-approved-for-moderate-to-severe-psoriasis/article/149760/
- ^ a b Centocor 12/19/08 Press Release, http://www.centocor.com/centocor/i/press_releases/FDA_ISSUES_COMPLETE_RESPONSE_LETTER_TO_CENTOCOR_FOR_USTEKINUMAB_BIOLOGIC_LICENSE_APPLICATION_
- ^ Johnson LL. “Study: Drug for serious psoriasis tops competition” The Associated Press. 18 Sept 2008.[dead link]
- ^ Wild, David (November 2011), “Novel IL-12/23 Antagonist Shows Potential in Severe Crohn’s”, Gastroenterology & Endoscopy News 62 (11), retrieved 2011-12-04
- ^ a b c Weber J, Keam SJ (2009). “Ustekinumab”. BioDrugs 23 (1): 53–61. doi:10.2165/00063030-200923010-00006. PMID 19344192.
- ^ Segal BM, Constantinescu CS, Raychaudhuri A, Kim L, Fidelus-Gort R, Kasper LH (September 2008). “Repeated subcutaneous injections of IL12/23 p40 neutralising antibody, ustekinumab, in patients with relapsing-remitting multiple sclerosis: a phase II, double-blind, placebo-controlled, randomised, dose-ranging study”. Lancet Neurol 7 (9): 796–804. doi:10.1016/S1474-4422(08)70173-X. PMID 18703004.
- ^ “Important Safety Information”. STELARA® (ustekinumab). Janssen Biotech.
External links
- Centocor Ortho Biotech official site
- CNTO 1275 research studies registered with U.S. National Institutes of Health:
- ClinicalTrials.gov NCT00207727 Phase II Study on Multiple Sclerosis
- ClinicalTrials.gov NCT00320216 Phase II Study on Psoriasis
- ClinicalTrials.gov NCT00267969 Phase III Study on Psoriasis
- ClinicalTrials.gov NCT00307437 Phase III Study on Psoriasis
- ClinicalTrials.gov NCT00267956 Phase II Study on Psoriatic Arthritis
- Sylvester, Bruce (2006-03-06). “CNTO 1275 Shows Efficacy for Psoriasis: Presented at AAD”. Doctor’s Guide Publishing. Retrieved 2007-01-25.
10 MAR 2013, MAA EU SUBMITTED, APPROVED US, CANADA, LURASIDONE, LATUDA, SCHIZOPRENIA, DAINIPPON SUMITOMO
LURASIDONE
(3aR,4S,7R,7aS)-2-[((1R,2R)-2-{[4-(1,2-benzisothiazol-3-yl)-piperazin-1-yl]methyl}cyclohexyl)methyl]hexahydro-1H-4,7-methanisoindol-1,3-dione
STATUS AS ON 10 MARCH 2012
Lurasidone (trade name Latuda) is an atypical antipsychotic developed by Dainippon Sumitomo Pharma.[1] It was approved by the U.S. Food and Drug Administration (FDA) for treatment of schizophrenia on October 28, 2010[2] after a review that found that two of the four Phase III clinical trials supported efficacy, while one showed only marginal efficacy and one was not interpretable because of high drop-out rates.[3] It is currently pending approval for the treatment of bipolar disorder in the United States.
Clinical effects
In clinical studies, lurasidone alleviates positive symptoms (e.g., hallucinations, delusions) without inducing extrapyramidal side effects except for akathisia,[4] despite its potent D2 antagonistic actions. Effectiveness against negative symptoms of schizophrenia has yet to be established.
Lurasidone may be useful for treating the cognitive and memory deficits seen in schizophrenia. In animal studies, it reversed dizocilpine-induced learning and memory impairment and was found to be superior in doing this to all of the other antipsychotics examined, including risperidone, olanzapine, quetiapine, clozapine, aripiprazole, and haloperidol.[5][6] Lurasidone has activity at several serotonin receptors that are involved in learning and memory, and unlike most other antipsychotics, lacks any anticholinergic effects (which are known to impair cognitive processes and memory).[5] These properties may underlie its improved effectiveness in treating these symptoms relative to older agents.[5]
References
- Meyer JM, Loebel AD, Schweizer E (September 2009). “Lurasidone: a new drug in development for schizophrenia”. Expert Opinion on Investigational Drugs 18 (11): 1715–26. doi:10.1517/13543780903286388. PMID 19780705.
- “FDA approves Latuda to treat schizophrenia in adults” (Press release). USFDA. 2010-10-28. Retrieved October 29, 2010.
- FDA Clinical Review of lurasidone for the treatment of schizophrenia Nakamura M, Ogasa M, Guarino J, et al. (June 2009).
- “Lurasidone in the treatment of acute schizophrenia: a double-blind, placebo-controlled trial”. The Journal of Clinical Psychiatry 70 (6): 829–36. doi:10.4088/JCP.08m04905. PMID 19497249.
- Ishiyama T, Tokuda K, Ishibashi T, Ito A, Toma S, Ohno Y (October 2007). “Lurasidone (SM-13496), a novel atypical antipsychotic drug, reverses MK-801-induced impairment of learning and memory in the rat passive-avoidance test”. European Journal of Pharmacology 572 (2-3): 160–70. doi:10.1016/j.ejphar.2007.06.058. PMID 17662268.
- Enomoto T, Ishibashi T, Tokuda K, Ishiyama T, Toma S, Ito A (January 2008). “Lurasidone reverses MK-801-induced impairment of learning and memory in the Morris water maze and radial-arm maze tests in rats”. Behavioural Brain Research 186 (2): 197–207. doi:10.1016/j.bbr.2007.08.012. PMID 17881065.
- Dainippon Sumitomo Pharma (August 26, 2009). “Lurasidone Demonstrated Efficacy in Treating Patients with Schizophrenia in Pivotal Phase III Study”.
- “Latuda: Prescribing Information”. Psychotherapeutic Drugs. Retrieved 2010-12-17.
- “Latuda”. Drugs.com. Retrieved 2010-12-17.
- “Atypical antipsychotics and risk of cerebrovascular accidents”. Retrieved 28 July 2012.
LATUDA® (lurasidone hydrochloride) Schizophrenia,Bipolar disorder
- Developed in-house
- LATUDA® (lurasidone hydrochloride) is an atypical antipsychotic agent which is believed to have an affinity for dopamine D2, serotonin 5-HT2A and serotonin 5-HT7 receptors where it has antagonist effects. In addition, LATUDA is a partial agonist at the serotonin 5-HT1A receptor and has no appreciable affinity for histamine or muscarinic receptors. In the clinical trials supporting the U.S. FDA approval, the efficacy of LATUDA for the treatment of schizophrenia was established in four, short-term (6-week), placebo-controlled clinical studies in adult patients who met DSM-IV criteria for schizophrenia. In these studies, LATUDA demonstrated significantly greater improvement versus placebo on the primary efficacy measures [the Positive and Negative Syndrome Scale (PANSS) total score and the Brief Psychiatric Rating Scale-derived from PANSS (BPRSd)] at study endpoint. A total of five short-term placebo controlled clinical trials contributed to the understanding of the tolerability and safety profile of LATUDA. LATUDA was approved for the treatment of schizophrenia by the U.S. Food and Drug Administration (FDA) in October 2010, and launched by Sunovion in February 2011 in the U.S. Launched in Canada for the treatment of schizophrenia in September 2012.
- Development stage:
Schizophrenia: Submitted MAA (Europe: Co-development with Takeda Pharmaceutical)
Phase III in Japan
In addition, Phase III study is ongoing in the U.S., Europe, etc. to test the hypothesis that LATUDA is effective in the long term maintenance treatment of schizophrenia.Bipolar I Depression: Submitted in the U.S. and Canada.
In addition, plans to submit an MAA in Europe through Co-development with Takeda Pharmaceutical. (Phase III in Europe).Bipolar Maintenance: Phase III in the U.S. and Europe, etc. MDD with mixed features: Phase III in the U.S
Phase 2- Cylene Pharmaceuticals and TetraGene Enter Agreement for Quarfloxin and Anticancer Quadruplex Technologies

Quarfloxin, CX-3543
Molecular Formula: C35H33FN6O3
cas no 865311-47-3
Molecular Formula: 604.67
SAN DIEGO, March 6, 2013
Cylene Pharmaceuticals, Inc. announced today that it has entered into an exclusive, worldwide Option and License Agreement that will allow TetraGene LLC to advance the development of Quarfloxin and Cylene’s associated anticancer quadruplex-targeting technologies. Cylene will receive an upfront fee, as well as potential milestone payments and royalties on product sales for the exclusive license.
TetraGene is developing small molecule drugs aimed at highly validated cancer-causing genes, by directly targeting G-quadruplex structures in genomic DNA. TetraGene has the option to acquire worldwide rights to the technologies licensed from Cylene, which include the Phase II compound Quarfloxin and several registered patents. Quarfloxin has been demonstrated to be safe and well-tolerated in Phase I clinical trials.
“This agreement is a clear win for both organizations,” stated William G. Rice, PhD, President and CEO of Cylene Pharmaceuticals. “TetraGene is well placed to advance Quarfloxin through the clinic and to capture exclusive worldwide rights to the quadruplex-targeting technologies. Cylene will receive standard industry payments as the quadruplex program progresses and we will continue to focus our in-house development efforts on CX-5461, Cylene’s clinical stage Pol I inhibitor that activates the p53 tumor suppressor selectively in cancer cells and not normal cells.”
“The agreement between TetraGene and Cylene immediately provides us with access to a clinical stage drug,” commented Laurence H. Hurley, PhD, CSO of TetraGene and a pioneer of G-quadruplex targeted therapeutics. “The validity of drug targeting G-quadruplex DNA and modulating expression of cancer genes has dramatically increased in the last few years and our team is uniquely positioned to take advantage of these new insights.”
About Cylene Pharmaceuticals
Cylene Pharmaceuticals is a clinical-stage private company developing small molecule drugs against newly validated targets in essential cancer pathways. The Company’s Pol I program provides a non-genotoxic mechanism for activating p53 to kill cancer cells. Cylene’s leadership in exploiting CK2 pathways enables rational drug combinations for improved treatment outcomes against many cancer indications. Cylene’s unique approaches deliver innovative cancer agents that can enable pharmaceutical companies to expand their portfolios and extend the efficacy, lifecycle and reach of current cancer therapeutics. For more information on Cylene and its programs, please visit www.cylenepharma.com.
About TetraGene
TetraGene leverages a novel platform technology to develop cancer drugs that target well-validated cancer-causing oncogenes previously considered as undruggable by the pharmaceutical industry. This technology exploits a gene regulatory mechanism where the expression of a gene is controlled by folded DNA structures (called G-quadruplex DNA). By targeting gene transcription, TetraGene has carved out a niche where its technology platform can be directly applied to inhibit these undruggable cancer targets. For more information about TetraGene please visit www.tetragene.com.
…………………………………….
DR ANTHONY MELVIN CRASTO Ph.D , Born in Mumbai in 1964 and graduated from Mumbai University, Completed his PhD from ICT ,1991, Mumbai, India in Organic chemistry, The thesis topic was Synthesis of Novel Pyrethroid Analogues,
Currently he is working with GLENMARK- GENERICS LTD, Research centre as Principal Scientist, Process Research (bulk actives) at Mahape, Navi Mumbai, India.
Prior to joining Glenmark, he worked with major multinationals like Hoechst Marion Roussel, now Sanofi Aventis, & Searle India ltd, now Rpg lifesciences, etc. He has worked in Basic research, Neutraceuticals, Natural products, Flavors, Fragrances, Pheromones, Vet Drugs, Drugs, formulation, GMP etc. He has total 25 yrs exp in this field, he is now helping millions, has million hits on google on all organic chemistry websites.
His New Drug Approvals , Green Chemistry International, Eurekamoments in Organic Chemistry , Organic Chemistry by Dr Anthony, WIX BLOG , are some most read chemistry blogs
He has hands on experience in initiation and developing novel routes for drug molecules and implementation them on commercial scale over a 25 year tenure, good knowledge of IPM, GMP, Regulatory aspects, he has several international drug patents published worldwide .
He has good proficiency in Technology Transfer, Spectroscopy , Stereochemistry , Synthesis, Reactions in Org Chem , Polymorphism, Pharmaceuticals , Medicinal chemistry , Organic chemistry literature , Patent related site , Green chemistry , Reagents , R & D , Molecules , Heterocyclic chem , Sourcing etc
He suffered a paralytic stroke in dec 2006 and is bound to a wheelchair, this seems to have injected feul in him to help chemists around the world, he is more active than before and is pushing boundaries, he has one lakh connections on all networking sites, He makes himself available to all, contact him on +91 9323115463, amcrasto@gmail.com

Phase 3-Gilead’s newly-acquired Sofosbuvir, GS-7977 shines in Hepatitis C trial
Sofosbuvir
Isopropyl (2S)-2-[[[(2R,3R,4R,5R)-5-(2,4-dioxopyrimidin-1-yl)-4-fluoro-3-hydroxy-4-methyl-tetrahydrofuran-2-yl]methoxy-phenoxy-phosphoryl]amino]propanoate
The Foster City, CA-based Gilead said that its experimental drug GS-7977, originally known as PSI-7977 before the acquisition, when combined with ribavirin, cured a group of genotype 1 hepatitis C patients after four weeks of treatment. The clinical study involved hepatitis C patients who either failed to respond to previous therapies or had not been treated before. The genotype 1 is the most common form of HCV in the United States. It affects 70 to 90 percent of the people in this country who have hepatitis C.
Norbert Bischofberger, chief scientific officer at Gilead said patients with genotype 1 hepatitis C had no detectable signs of the virus after treated with GS-7977 combination therapy for a course of close to a month. Previous study showed the drug candidate could also cure patients with genotype 2 and 3 HCV.
Gilead gained rights to GS-7977 through the $11 billion Pharmasset acquisition deal, which enable the company to be in an advanced position to compete with a few pharma companies seeking to develop an all-oral regimen for hepatitis C. The 100 percent cure rate data suggested that GS-7977 may be one of the most promising therapies for hepatitis C.
Last year, GS-7977, an oral uridine nucleotide analog polymerase inhibitor of HCV, received fast track designation from the U.S. FDA for the treatment of HCV infection.
The World Health Organization estimated that 3–4 million people are infected with HCV each year. Some 130–170 million people are chronically infected with HCV and at risk of developing liver cirrhosis and/or liver cancer, and more than 350,000 people die yearly from hepatitis C-related diseases.
Sofosbuvir (formerly PSI-7977 or GS-7977) is an experimental drug candidate for the treatment of hepatitis C.[1] It was discovered at Pharmasset and then acquired for development by Gilead Sciences. It is currently in Phase III clinical trials.[2]
Sofosbuvir is a prodrug that is metabolized to the active antiviral agent 2′-deoxy-2′-α-fluoro-β-C-methyluridine-5′-monophosphate.[3]
Sofosbuvir is a nucleotide analogue inhibitor of the hepatitis C virus (HCV) polymerase.[4] The HCV polymerase or NS5B protein is a RNA-dependent RNA polymerase critical for the viral cycle.
Sofosbuvir is being studied in combination with pegylated interferon and ribavirin, with ribavirin alone, and with other direct-acting antiviral agents.[5] It has shown excellent clinical efficacy when used either with pegylated interferon/ribavirin or in interferon-free combinations. In particular, combinations of sofosbuvir with NS5A inhibitors, such as daclatasvir or GS-5885, have shown sustained virological response rates of up to 100% in people infected with HCV.[6]
- Sofia, M. J.; Bao, D.; Chang, W.; Du, J.; Nagarathnam, D.; Rachakonda, S.; Reddy, P. G.; Ross, B. S. et al. (2010). “Discovery of a β-d-2′-Deoxy-2′-α-fluoro-2′-β-C-methyluridine Nucleotide Prodrug (PSI-7977) for the Treatment of Hepatitis C Virus”. Journal of Medicinal Chemistry 53 (19): 7202–7218. doi:10.1021/jm100863x. PMID 20845908. edit
- “PSI-7977”. Gilead Sciences.
- Murakami, E.; Tolstykh, T.; Bao, H.; Niu, C.; Steuer, H. M. M.; Bao, D.; Chang, W.; Espiritu, C. et al. (2010). “Mechanism of Activation of PSI-7851 and Its Diastereoisomer PSI-7977”. Journal of Biological Chemistry 285 (45): 34337–34347. doi:10.1074/jbc.M110.161802. PMC 2966047. PMID 20801890. edit
- Alejandro Soza (November 11, 2012). “Sofosbuvir”. Hepaton.
- Tom Murphy (November 21, 2011). “Gilead Sciences to buy Pharmasset for $11 billion”. Bloomberg Businessweek.
- http://www.gilead.com/pr_1757156
- AASLD: PSI-7977 plus Ribavirin Can Cure Hepatitis C in 12 Weeks without Interferon. Highleyman, L. HIVandHepatitis.com. 8 November 2011.
- Nucleotide Polymerase Inhibitor Sofosbuvir plus Ribavirin for Hepatitis C. Gane, E et al. New England Journal of Medicine 368:3444. January 3, 2013.
- CROI 2013: Sofosbuvir + Ledipasvir + Ribavirin Combo for HCV Produces 100% Sustained Response. Highleyman, L. HIVandHepatitis.com. 4 March 2013.
MAA EU -GSK submits diabetes drug Eperzan, albiglutide in EU

MAA EU =marketing authorisation application EU
MAR 08 2013
GlaxoSmithKline has announced the submission of a marketing authorisation application for albiglutide, which will have the brand name Eperzan, to the European Medicines Agency.
The filing of albiglutide, a once-weekly treatment for type 2 diabetes, comes almost two months after it was filed in the USA. The drug is a GLP-1 receptor agonist, the same class of injectable treatments dominated by Novo Nordisk’s once-a-day Victoza (liraglutide), twice-daily Byetta (exenatide) and an extended-release formulation of the latter, Bydureon. They were developed and sold by Amylin, which was then acquired by Bristol-Myers Squibb and AstraZeneca.
The filing is based in part on a study which assessed albiglutide against Merck & Co’s DPP-4 inhibitor Januvia (sitagliptin) which showed that GSK’s drug showed clinically and statistically significant reductions in HbA1c from baseline and superiority versus the US firm’s diabetes blockbuster. However in data from a late-stage study released in November 2011, albiglutide failed to show non-inferiority to Victoza and a number of analysts believe GSK will have its work cut out to grab a decent share of the GLP-1 market.
Albiglutide is a glucagon-like peptide-1 agonist (GLP-1 agonist) drug under investigation by GlaxoSmithKline for treatment of type 2 diabetes. It is a dipeptidyl peptidase-4-resistant glucagon-like peptide-1 dimer fused to human albumin.
Albiglutide has a half-life of four to seven days, which is considerably longer than the other two GLP-1 analogs approved for market use, exenatide (Byetta) and liraglutide (Victoza).[1] [2] GLP-1 drugs are currently only available for subcutaneous administration on a daily basis, so a GLP-1 drug with a longer half-life is desirable. Such a drug would only need to be injected biweekly or weekly instead of daily, reducing the discomfort and inconvenience of GLP-1 administration considerably.
It has not yet been determined whether albiglutide is as effective an antidiabetic agent as GLP-1 drugs currently on the market, and final data remain to be published regarding the incidence of adverse effects related to the drug. To evaluate the efficacy and safety of the drug, albiglutide is undergoing eight Phase III clinical trials. Four of these trials should report useful data by end 2010.[3]
- Matthews JE, Stewart MW, De Boever EH, et al. (December 2008). “Pharmacodynamics, Pharmacokinetics, Safety, and Tolerability of Albiglutide, a Long-Acting Glucagon-Like Peptide-1 Mimetic, in Patients with Type 2 Diabetes”. J. Clin. Endocrinol. Metab. 93 (12): 4810–4817. doi:10.1210/jc.2008-1518. PMID 18812476.
- Baggio et al. (2008). “Glucagon-like Peptide-1 Analogs Other Than Exenatide”.
- “Phase III clinical trials of Albiglutide”.
Phase 2 SMP-986(afacifenacin fumarate) Overactive bladder/ Dainippon Sumitomo Pharma and Nippon Shinyaku conclude a license agreement for SMP-986, a therapeutic agent for urology
877606-63-8 cas no of afacifenacin
any str error, mail to amcrasto@gmail.com
SMP-986 (afacifenacin fumarate)
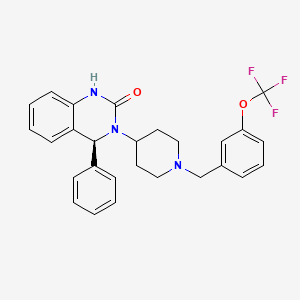
(4S)-4-phenyl-3-(1-{[3-(trifluoromethoxy)phenyl]methyl}piperidin- 4-yl)-3,4-dihydroquinazolin-2(1H)-one muscarinic receptor antagonist

- Developed in-house
- SMP-986 possesses the dual pharmacological actions of muscarinic receptor antagonism (non-selective) and inhibition of the bladder afferent pathway through Na+-channel blockade. This compound is being evaluated for its ability to ease urinary urgency and reduce the frequency of both urination and incontinence. The compound has also exhibited the potential to have lower incidence of side effects related to muscarinic receptor antagonism, such as dry mouth.
- Development stage: Phase II in the U.S. and Europe. Phase II in Japan
7 mar 2013
Dainippon Sumitomo Pharma Co., Ltd. (DSP) and Nippon Shinyaku Co., Ltd. Announce they have concluded a license agreement for exclusive rights to develop, manufacture and commercialize SMP-986 in Japan, a new therapeutic agent for overactive bladder created by DSP.
DCVax®-Direct Phase I/II Trial For All Inoperable Solid Tumors Is Expected To Produce Ongoing Results In 2013

BETHESDA, Md., \
March 5, 2013 Northwest Biotherapeutics (NW Bio), a biotechnology company developing DCVax® personalized immune therapies for solid tumor cancers, announced today that its Phase I/II DCVax-Direct clinical trial for all inoperable solid tumor cancers is planned to begin within approximately the next sixty days. As a Phase I/II trial, this trial is not blinded and the results will be seen as the trial proceeds. With an efficacy endpoint of tumor regression (i.e., tumor shrinkage or elimination), this innovative trial is expected to yield meaningful ongoing results by the second half of 2013.
This clinical trial is approved by the FDA for all types of solid tumor cancers (i.e., cancers in any tissues of the body), and is configured to provide rapid results. In the Phase I portion, it will test both safety and a variety of dosing regimes, and will do so in multiple different cancers – avoiding the need to conduct separate Phase I studies in each such cancer, as is usually the case. Then, the trial will go directly into the Phase II portion, testing for efficacy, without the need for another FDA review.
DCVax®
All immune responses start in the same way that involves initially a single cell type, the dendritic cell (DC). This cell functions like the General of an army, in that it directs all ensuing activities of the immune response. The immune system is like an army with many divisions, and multiple soldiers with various types of weapons. When an invader, which could be a virus, bacteria, or a cancer cell, encounters a DC the result is that the DC consumes or eats the invader and chops it into small pieces. In the process, the DC becomes activated and starts traveling to the lymph node. In the lymph nodes the DC elicits a cascade of events eventually involving the entire army that leads to a full-blown immune response. Importantly, the nature of the invader and the nature of the DC activation dictate the type of immune response: the DC is the general of the army who directs all the soldiers to work in synchrony, and who determines which weapons to use to best defeat the enemy. We believe that preparing the DC outside the body, as done for DCVax® products, allows the greatest degree of control and begins the immune response in the natural fashion leading to the most complete attack on the foreign invader.
Different Approaches
We believe that the optimal way to arrive at the most effective immune response is through the control of the DC. Most traditional immunization approaches, including traditional virus, specific antigen or peptide vaccines as well as some that are used for immunotherapy of cancer, try to control the already existing DC in the body, or they try to modulate only one arm of the immune system. The immunogen, i.e. the virus, specific antigen, peptide or the cancer cells used to prepare the vaccine, is in those cases injected into the body in a formulation that aims at targeting and activating local DC. Examples are viral, specific antigen or peptide vaccines formulated with adjuvant, or killed tumor cells alone or modified to produce the DC mobilizing protein GM-CSF. In these instances, it is left to chance as to whether the immunogen arrives at the DC, whether the DC are properly activated, and effectively migrate to lymph nodes to produce an effective immune response. We believe that the failure of several recent clinical trials may be the result of the inability of these other approaches to effectively mount a natural and robust immune response.
Treatments that use only a single division of the immune system may employ only large amounts of T cells, or a single (monoclonal) antibody. DCVax® products are being developed to activate all aspects of the immune response, both cellular and antibody, thus potentially providing a broader and longer lasting immune and clinical response. Northwest Biotherapeutics’ products are deigned as pure, activated DC loaded with the immunogen as would naturally occur, and that are capable of migrating to lymph nodes. The intended result is a very robust, and full immune response consisting of both a specific cellular T cell response and a specific antibody response against the cancer associated antigen. Data obtained in our Phase I and Phase II clinical trials suggest that such response may occur and may translate into a clinical benefit.
Cancer and the Immune System
Cancer cells produce many substances that shut down the immune response, as well as substances that paralyze the DC that are resident in the body. We believe therefore that the optimal time for controlling cancer growth by activating the immune system is at the time when tumor burden is low. Northwest Biotherapeutics targets patients with brain cancer following surgery, radiation and chemotherapy, and hormone independent prostate cancer patients with no detectable tumor growth. This approach aims at inducing powerful immune responses to control progression of the disease.
Manufacturing
Northwest Biotherapeutics has focused on solving many of the challenges that are typically associated with producing personalized products that consist of living cells. The Company’s new automated cell processing system allows high-throughput production of products for a fraction of the historical cost.
- DCVax® products contain pure DC
- The DC in DCVax® are prepared outside the body, which eliminates many uncontrollable variables, and are subjected to a potency test designed to ensure that the DC administered to the patient are capable of eliciting an immune response
- DCVax® is used in patients with low tumor burden
- DCVax® products can be manufactured in a cost-efficient manner
ViiV Healthcare presents phase III SAILING study data of dolutegravir vs raltegravir in treatment-experienced adults with HIV-1

Dolutegravir
| Identifiers | |
|---|---|
| CAS number | 1051375-16-6 |
8 TH MATCH 2013
ViiV Healthcare, a global specialist HIV company established in November 2009 by GSK and Pfizer dedicated to delivering advances in treatment and care for people living with HIV, has announced 24-week data from the phase III SAILING (ING111762) study evaluating the investigational integrase inhibitor dolutegravir in patients with HIV-1 who are failing on current therapy, but had not been treated with an integrase inhibitor.
At 24 weeks, 79% of study participants receiving the once-daily dolutegravir regimen were virologically suppressed (HIV-1 RNA <50 c/mL) vs. 70% of participants on the twice-daily raltegravir regimen. This difference in response was statistically significant with a 95% confidence interval for the difference of 3.4% to 15.9% (p=0.003).
The SAILING study was designed to demonstrate non-inferiority of a regimen containing dolutegravir versus raltegravir (both with up to two background agents) and the analysis met this criterion; statistical superiority was concluded as part of a pre-specified testing procedure. These data were presented at the 20th Conference on Retroviruses and Opportunistic Infections (CROI) in Atlanta, Georgia.
Differences in treatment outcome in favour of the dolutegravir arm were driven by greater virologic response: at Week 24, 15% of patients receiving the dolutegravir regimen had virologic non-response vs. 24% of patients receiving the raltegravir regimen. In addition, fewer subjects failed therapy with integrase inhibitor resistance on dolutegravir (n=2) than on raltegravir (n=10, p=0.016).
Overall, the tolerability of dolutegravir (DTG) was similar to that of raltegravir (RAL). At 24 weeks, 2% of subjects on the dolutegravir regimen discontinued due to adverse events (AEs) vs. 4% of subjects on the raltegravir regimen. The rate of drug-related AEs was similar for both arms (DTG 20%, RAL 23%) and commonly reported AEs (defined as events that occurred in more than 10% of subjects) were similar on both arms, namely diarrhoea (20% DTG, 17% RAL) and upper respiratory tract infection (11% DTG, 8% RAL).
“People living with HIV who have developed resistance to more than one antiretroviral drug class face increasingly narrow treatment options and clinical decisions become increasingly complex. We welcome these initial results supporting the efficacy and tolerability of dolutegravir as a potentially useful addition in the management of HIV in treatment-experienced patients.” said John Pottage, chief scientific and medical officer, ViiV Healthcare. “These encouraging data were included as part of the comprehensive clinical data package supporting recent regulatory submissions for dolutegravir and we look forward to receiving the primary analysis at 48 weeks in due course.”
The primary objective of the ongoing double-blind, double-dummy phase III SAILING study is to demonstrate the antiviral activity of once-daily dolutegravir 50mg compared to twice-daily raltegravir 400mg over 48 weeks in HIV-1 infected, antiretroviral-experienced, integrase inhibitor-naïve adults. At baseline, 715 study participants were randomised 1:1 to receive either dolutegravir or raltegravir plus investigator-selected background regimen of no more than 2 agents, one of which was fully active. All subjects had documented genotypic or phenotypic resistance to agents from at least two antiretroviral therapy drug classes, and ongoing virologic replication. Median baseline HIV-1 RNA levels were 4.18 log10 c/mL and median baseline CD4+ cell counts were 200 cells/mm3. The study population included 32% women, 42% were of African American/African heritage, and 46% of study participants were classified as CDC Class C (patients who have one or more AIDS-defining illness). The 48-week primary analysis of this study will be presented at a future scientific meeting.
S/GSK1349572 (dolutegravir, DTG) is an investigational integrase inhibitor currently in development for the treatment of HIV; it does not require an additional pharmacokinetic boosting drug to be added to the regimen. Integrase inhibitors block HIV replication by preventing the viral DNA from integrating into the genetic material of human immune cells (T-cells). This step is essential in the HIV replication cycle and is also responsible for establishing chronic infection.
SAILING is the fourth phase III dolutegravir study reporting in 2012 and 2013. Data from the two studies in treatment-naïve populations, SPRING-2 (ING113086) and SINGLE (ING114467), were announced in April and July of 2012 respectively. Data from VIKING-3 (ING112574) in integrase inhibitor-resistant patients were announced in November 2012. Dolutegravir is not yet approved as a treatment for HIV or any other indication anywhere in the world.
Dolutegravir[1] is an experimental new drug under investigation for the treatment of HIV infection. Dolutegravir is an integrase inhibitor. Also known as S/GSK1349572 or just “572”, the drug is under development by GlaxoSmithKline (GSK). Studies have shown dolutegravir to be effective in patients with resistance to the integrase inhibitor, raltegravir.[2] Clinical trials are underway to support dolutegravir in combination with abacavir and lamivudine, in a new new fixed dose combination called 572-Trii.[3] In February, 2013 the Food and Drug Administration announced that it would fast track dolutegravir’s approval process.[4]
Results from the 96-week comparison with efavirenz, SPRING-1, showed dolutegravir 50mg orally to be effective at reducing HIV viral load and raising CD4 counts in integrase-naive patients. [5]
References
- [1] American Medical Association (AMA), STATEMENT ON A NONPROPRIETARY NAME ADOPTED BY THE USAN COUNCIL (Dolutegravir) Accessed 3 December 2011.
- Dolutegravir (“572”) Holds Up in Heavily Raltegravir-Resistant Patients, Phase 2B Study Finds Nelson Vergel. The Body PRO. Accessed 23 April 2011.
- Shionogi-ViiV Healthcare Starts Phase 3 Trial for “572-Trii” Test positive airwave. The Body PRO. Accessed 23 April 2011.
- “GSK wins priority status for new HIV drug in U.S”. Reuters. 16 February 2013. Retrieved 18 February 2013.
- Horn, Tim. ViiV’s Dolutegravir Continues to Show Well After 96 Weeks, Versus Sustiva, for First-Time Treatment. AIDSmeds.com 7 Mar 2012. Accessed 14 Mar 2012.

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....













