Home » Articles posted by DR ANTHONY MELVIN CRASTO Ph.D (Page 413)
Author Archives: DR ANTHONY MELVIN CRASTO Ph.D
DURECT Announces Submission of New Drug Application for POSIDUR™ (SABER®-Bupivacaine)

Bupivacaine
DURECT Announces Submission of New Drug Application for POSIDUR™ (SABER®-Bupivacaine)
“We’re extremely pleased to submit this NDA for POSIDUR to the FDA. If approved by the FDA, POSIDUR will provide a non-opioid alternative treatment option for post-surgical pain,” James E. Brown, D.V.M., President and CEO of DURECT, stated, “Treating post-surgical pain with a true long-acting local anesthetic has the potential benefit of reducing the need for opioids and their associated systemic side effects that can prolong the time to recovery and result in extended hospital stays.”
We expect that the FDA will notify us whether our NDA submission has been accepted for filing within 74 days of submission, which the FDA bases on their initial 60-day review of the completeness of our application. If accepted for filing, the FDA would be expected to assign a PDUFA date of 10 months after the submission.
About POSIDUR
POSIDUR is a post-operative pain relief depot that utilizes DURECT’s patented SABER®technology to deliver bupivacaine to provide up to three days of pain relief after surgery. We are in discussions with potential partners regarding licensing development and commercialization rights to POSIDUR, for which we hold worldwide rights.
About DURECT Corporation
DURECT is a specialty pharmaceutical company developing innovative drugs for pain and other chronic diseases, with late-stage development programs including REMOXY®, POSIDUR™, ELADUR®, and TRANSDUR®-Sufentanil. DURECT’s proprietary oral, transdermal and injectable depot delivery technologies enable new indications and superior clinical/commercial attributes such as abuse deterrence, improved convenience, compliance, efficacy and safety for small molecule and biologic drugs. For more information, please visit www.durect.com.
DRUG SPOTLIGHT- Pemetrexed

Pemetrexed
(2S)-2-{[4-[2-(2-amino-4-oxo-1,7-dihydro
pyrrolo[2,3-d]pyrimidin-5-yl)ethyl]benzoyl]amino}
pentanedioic acid
N-[4-[2-(2-amino-4,7-dihydro-4-oxo-3H-pyrrolo[2,3-d]-pyrimidin-5-yl)ethyl] benzoyl]-L-glutamic acid or N-[4-[2-(2-amino-4,7-dihydro-4-oxo-1 H-pyrrolo [2,3-d]-pyrimidin-5-yl)ethyl] benzoyl]-L-glutamic acid
GENERIC LICENSING NEWSLETTER TODAY 23 APRIL 2013 REPORTED, SEE LINK BELOW
http://www.leadformix.com/ef1/preview_campaign.php?lf1=775434470d357512625317e6516156
 |
PEMETREXED
Pemetrexed is a chemotherapy drug used in the treatment of pleural mesothelioma as well as non-small cell lung cancer.Used in combination with cisplatin for the treatment of malignant pleural mesothelioma in adults whose disease is unresectable or who otherwise are not candidates for potentially curative surgery. Also used as a monotherapy for the treatment of locally advanced or metastatic non-small cell lung cancer (NSCLC) after prior chemotherapy.Click here to contact Logenex about this product.
|
Pemetrexed (brand name Alimta) is a chemotherapy drug manufactured and marketed by Eli Lilly and Company. Its indications are the treatment of pleural mesothelioma andnon-small cell lung cancer.
The molecular structure of pemetrexed was developed by Edward C. Taylor at Princeton University and clinically developed by Indianapolis based drug maker, Eli Lilly and Company in 2004.
 PEMETREXED
PEMETREXED
Pemetrexed is chemically similar to folic acid and is in the class of chemotherapy drugs called folate antimetabolites. It works by inhibiting three enzymes used in purine andpyrimidine synthesis—thymidylate synthase (TS), dihydrofolate reductase (DHFR), andglycinamide ribonucleotide formyltransferase[1][2] (GARFT). By inhibiting the formation of precursor purine and pyrimidine nucleotides, pemetrexed prevents the formation of DNAand RNA, which are required for the growth and survival of both normal cells and cancer cells.
Pemetrexed disodium is chemically described as L-Glutamic acid, N-[4-[2- (2-amino-4,7-dihydro-4-oxo-1 H-pyrrolo[2,3-d]pyrimidin-5-yl)ethyl]benzoyl]- disodium salt heptahydrate, represented by the chemical structure of Formula (I).
Formula I
Pemetrexed is an anti-folate anti-neoplastic agent that exerts its action by disrupting folate-dependent metabolic processes essential for cell replication. It is believed to work by inhibiting three enzymes that are required in purine and pyrimidine biosynthesis — thymidylate synthase (TS), dihydrofolate reductase (DHFR), and glycinamide ribonucleotide formyl transferase (GARFT). Pemetrexed is available in the market under the brand name ALIMTA®.
Taylor et al., in describe pemetrexed, its related compounds and pharmaceutically acceptable cation. Chelius et al., in WO 01/14379 A2 disclose pemetrexed disodium crystalline hydrate Form I and process for preparation thereof.
Chelius et al., in WO 01/62760 disclose pemetrexed disodium heptahydrate crystalline Form Il and process for the preparation thereof.
Journal of Organic Process Research & Development, Volume 3, 1999, page 184 describes a process for the preparation of pemetrexed diacid. Busolli et al., in WO200802141 1 disclose process for preparation of pharmaceutically acceptable salt of pemetrexed diacid.
Busolli et al., in WO2008021405A1 disclose seven crystalline forms of pemetrexed diacid designated as Form A, B, C, D, E, F, & G and processes for preparation thereof.
In February 2004, the Food and Drug Administration approved pemetrexed for treatment of malignant Pleural Mesothelioma, a type of tumor of the lining of the lung, in combination with cisplatin[3] for patients whose disease is either unresectable or who are not otherwise candidates for curative surgery.[4] In September 2008, the FDA granted approval as a first-line treatment, in combination with cisplatin, against locally-advanced and metastatic non-small cell lung cancer (NSCLC) in patients with non-squamous histology. A Phase III study showed benefits of maintenance use of pemetrexed for non-squamous NSCLC.Activity has been shown in malignant peritoneal mesothelioma.Trials are currently testing it against esophagus and other cancers.
MECHANISM

Pemetrexed is also recommended in combination with carboplatin for the first-line treatment of advanced non-small cell lung cancer.However, the relative efficacy or toxicity of pemetrexed-cisplatin versus pemetrexed-carboplatin has not been established beyond what is generally thought about cisplatin or carboplatin doublet drug therapy
In addition to the brand name Alimta, this drug is also marketed in India by Abbott Healthcare as Pleumet and by Cadila Healthcare asPemecad.
-
Pemetrexed disodium is a multitargeted antifolate agent approved as a single agent for the treatment of non-small cell lung cancer, and in combination with cisplatin for the treatment of patient with malignant pleural mesothelioma, under the trade name Alimta®.
Pemetrexed disodium is available in a number of crystalline forms. -
Barnett et al, Organic Process Research & Development, 1999, 3, 184-188 discloses synthesis and crystallization of pemetrexed disodium from water-ethanol. The product obtained by the process disclosed herein is the 2.5 hydrate of pemetrexed disodium.
-
United States patent number 7,138,521 discloses a crystalline heptahydrate form of pemetrexed disodium, which has enhanced stability when compared to the known 2.5 hydrate.
-
To date workers have concentrated on producing stable crystalline forms of pemetrexed disodium and there has been no disclosure of any non-crystalline form of this active.
-
We have now found a new form of pemetrexed disodium, which is an amorphous form, as characterized by powder X-ray diffraction. Surprisingly, we have found that it is possible to prepare an amorphous form of pemetrexed disodium and that this form is stable. The amorphous form of the invention is stable contrary to expectations. The amorphous form of pemetrexed disodium of the present invention is stable as it retains it’s amorphous character under a variety of storage conditions. The amorphous form of the present invention is particularly advantageously characterized by a bulk density in the range of 0.15 to 0.35 gm/ml.
N-[4-[2-(2-amino-4,7-dihydro-4-oxo-3H-pyrrolo[2,3-d]-pyrimidin-5-yl)ethyl] benzoyl]-L-glutamic acid or N-[4-[2-(2-amino-4,7-dihydro-4-oxo-1 H-pyrrolo [2,3-d]-pyrimidin-5-yl)ethyl] benzoyl]-L-glutamic acid (also known as
“Pemetrexed”)
R = H: Pemetrexed; I
R = Na: Pemetrexed Disodium; II is a known compound. Pemetrexed Disodium is an known anticancer agent. It is clinically active in several solid tumors and approved for treatment of malignant pleural mesothelioma (MPM) and metastatic non-small cell lung cancer (NSCLC). Pemetrexed Disodium is supplied as a sterile lyophilized powder for intravenous administration.
The compound of formula I including pharmaceutically salts thereof as well as a process for its preparation is at first and specifically disclosed in EP patent no. 0432677 B1. The preparation and isolation of Pemetrexed (compound of formula I) as its Disodium salt (compound of formula II) was described for the first time in WO patent no. 9916742 A1 and in Drugs of the future 1998, 23(5), 498-507 as well as by Charles J. Barnett et al. in Organic Process Research & Development, 1999, 3, 184-188 and by Peter Norman in Current Opinion in Investigational Drugs 2001 , 2(11 ), 1611-1622.
Detailed information about the crystalline form of Pemetrexed Disodium prepared according to the process as described above were not provided but it is reported by Charles J. Barnett et al. in Organic Process Research & Development, 1999, 3, 184-188 that the disodium salt II was obtained as a hygroscopic solid.
The first crystalline form of Pemetrexed Disodium has been described in WO patent no. 0114379 designated Disodium MTA Hydrate Form I (MTA = multi- targeted antifolate, disodium N-[4-[2-(2-amino-4,7-dihydro-4-oxo-3H- pyrrolo[2,3-d]-pyrimidin-5-yl)ethyl]benzoyl]-L-glutamic acid salt). The Disodium MTA Hydrate Form I obtained according to the Examples 2, 3 and 4 contained different amounts of water (Example 2: water = 9.1%; Example 3: water = 17.7%; Example 4: water = 11.7%). The Disodium MTA Hydrate Form I has a typical XRD pattern as shown in Figure 4 (the corresponding 2theta values have been calculated from the provided d-spacing values).
An improved crystalline form of Pemetrexed Disodium has been disclosed in WO patent no. 0162760. It is teached that Pemetrexed Disodium can exist in the form of a heptahydrate (Form II; theoretical amount of water: approx 21%) which is much more stable than the previously known 2.5 hydrate (Form I; theoretical amount of water: 8.7%). The Pemetrexed Disodium Heptahydrate Form (Form II) has a typical XRD pattern as shown in Figure 5 (the corresponding 2theta values have been calculated from the provided d- spacing values).
The Chinese patent no. 1778802 describes a hydrate or trihydrate form of Pemetrexed Disodium. The preparation of Pemetrexed Disodium hydrate or trihydrate includes crystallization from water and water soluble solvent. An overview of the X ray powder diffraction data for Pemetrexed Disodium Hydrate provided in Chinese patent no. 1778802 is shown in Figure 6.
The WO patent no. 2008124485 disclose besides crystalline Forms of the diacid Pemetrexed also amorphous Pemetrexed Disodium as well as a crystalline Form III thereof including a composition containing a major amount of amorphous Form and a minor amount of crystalline Form III of Pemetrexed Disodium. An overview of the X ray powder diffraction data for Pemetrexed Disodium crystalline Form 3 is shown in Figure 7.
EP patent application no. 2072518 disclose a stable amorphous form of Pemetrexed Disodium.
-
According to the more recent US 5,416,211 , which is incorporated herein by reference, pemetrexed can be synthesized from 4-[2-(2-amino-4,7-dihydro-4-oxo-1H-pyrrolo[2,3-d]pyrimidin-5-yl)ethyl]benzoic acid of formula 1, obtained from simple precursors, in accordance with the following Scheme 1:
-
This second method seems to be used also for the industrial preparation of the active ingredient. In fact, the same type of synthesis scheme is also described in C. J. Barnett, T. W. Wilson and M. E. Kobierski, Org. Proc. Res. & Develop., 1999, 3, 184-188, in which the experimental examples refer to a scale of the order of tens of kgs.



……………………….
Example 1 Preparation of crude pemetrexed disodium
[0023] N-[4-2-(2-Amino-4, 7-dihydro-4-oxo-
1 H-pyrrolo[2,3-d]pyrimidin-5-yl)ethyl]benzoyl]-L-glutamic Acid Diethyl Ester
4-Methylbenzenesulfonic Acid Salt and purified process water (PPW) (about 10 kg) are charged to a suitable vessel under nitrogen. The reactor is cooled to NMT 10Ό under nitrogen. Pre-cooled sodium hydroxide solution (about 1.5 kg )/PPW (about 11.4 kg) are added and the temperature is maintained at NMT 10Ό. The mixture is stirred at NMT 0 until the solid is dissolved. Pre-cooled isopropanol (about 62.8 kg) is added and the mixture temperature is maintained at NMT 5 . Pre-cooled 1 N hydrochloric acid in isopropanol is added to adjust the pH to 6.5 to 9.5, preferably between pH 7.5 to pH 8.5, at NMT 5 . The mixture is warmed to a room temperature (i.e., 15-30Ό, preferably 20-25″C) and stirred. The solids are filtered and washed with isopropanol/PPW. The wet cake is vacuum dried to provide crude pemetrexed disodium (about 2.30 kg).
Example 2 Purification of crude pemetrexed disodium to pemetrexed disodium
[0024] Crude pemetrexed disodium (about 2.1 kg) and PPW (about 23.3 kg) are charged under nitrogen to a suitable vessel at 15 to 30 . Isopropanol (about 28.3 kg) is added slowly to cloud point and stirred. Isopropanol (up to about 55 kg) is charged and stirred. The solids are filtered arid washed with isopropanol/PPW. The wet cake is vacuum dried to provide pemetrexed disodium (about 1.9 kg) (90% Yiled). 1 H NMR (D20): δ 7.51 (2H, d, J=8.0 Hz), 6.98 (2H, d, J=8.0 Hz), 6.12 (1 H, s), 4.26-4.23 (H, m), 3.60-3.54 (4H, m), 2.27-2.23 (2H, m), 2.13-2.08 (1 H, m), 2.00-1.94 (1 H, m)
HPLC
Example 7
HPLC Analysis method
-
Reagent: Water :milliQ,
Sodium perchlorate :AR Grade
Perchloric acid :AR Grade
Acetonitrile :J.T.Baker gradient
Trifluroacetic acid :AR Grade
Buffer solution: 6.1 g of sodium perchlorate into a 1000ml water. Adjust the pH to 3.0 (± 0.1) with perchloric acid.
Mobile phase A:
mixture of buffer and acetonitrile in the proportion of (90:10).
Mobile phase B:
mixture of buffer and acetonitrile in the proportion of (10 : 90).
Diluent -1 : mixture of water and acetonitrile in the ratio of 50 : 50.
Diluent -2: mixture of water and acetonitrile in the ratio of 90 : 10.
Standard Stock Solution:
Transfer accurately weighed 1.5 mg impurity-E RS and into a 200 ml volumetric flask. Dissolve in and dilute upto mark with diluent-1.
Blank solution
-
Add 10 ml diluent-2 and 50µl of 3% trifluro acetic acid to a 50 ml volumetric flask, and dilute upto mark with diluent-2.
System suitability solution
-
Transfer about 25 mg accurately weighed pemetrexed disodium sample in to a 50 ml volumetric flask. First add 10ml of diluent-2 and sonicate to dissolve the contents.Then add 50µl of 3% trifluro acetic acid (prepared in water) and add 5 ml of standard stock solution and dilute up to mark with diluent-2.
Sample preparation
-
Transfer about 25 mg accurately weighed pemetrexed disodium sample in to a 50 ml volumetric flask. First add 10ml of diluent-2 and sonicate to dissolve the contents.Then add 50µl of 3% trifluro acetic acid (prepared in water) and dilute up to mark with diluent-2 (500 µg/ml).
Chromatographic system :
-
Use a suitable high pressure liquid chromatography system equipped with Column: 250 mm x 4.6mm containing 5µ packing material (suggested column – Inertsil ODS 3V)
Detector: UV detector set to 240 nm
Cooler temp: 5°C.
Flow rate: about 1.5 ml/min. -
The system is also equipped to deliver the two phases in a programmed manner as shown in the following table :
Gradient programme :
-
[0082]
0 92 8 15 85 15 30 65 35 35 65 35 36 92 8 40 92 8
Procedure:
-
Inject 20µl of blank and system suitability solution into the chromatograph set to above conditions and record the chromatograms up to 40 min.
Calculate the resolution between pemetrexed disodium and impurity-E. The resolution should not be less than 3.0. Calculate the Number of theoretical plate and tailing factor for pemetrexed peak. Number of theoretical plate is NLT 4000 and tailing factor is NMT 2.0. -
Inject 20µl of test solution and calculate the chromatographic purity by area normalisation method.
……………………..
Synthetic Route for the Preparation of Pemetrexed Disodium
Starting from commercially available materials a novel synthetic route for the synthesis of Pemetrexed-IM8 (the dimethyl ester of Pemetrexed) was developed which was then used for the preparation of Pemetrexed Disodium (Scheme 1).
The current synthetic route for the preparation of Pemetrexed IM8 starts with an aldol-condensation reaction of Methyl-4-formylbenzoate (SM1) with 1,1-Dimethoxyacetone (SM2) to give Pemetrexed IM1a. As Pemetrexed IM1a irreversibly converts to its aldol-addition product Pemetrexed IM1b under reaction conditions the reaction mixture is directly submitted to hydrogenation (i.e. without isolation of Pemetrexed IM1a) over Pd/C to give Pemetrexed IM2. As under the hydrogenation conditions not only the double-bond of IM1a is hydrogenated but also some amount of Pemetrexed IM2 is converted to Pemetrexed IM3 (hydrogenation of the carbonyl function to the corresponding secondary alcohol) a solution of NaBH4 is added to the reaction mixture to ensure complete conversion to Pemetrexed IM3. The Pd-catalyst is removed by filtration and the reaction mixture is extracted with toluene. The combined organic layers are evaporated to give crude Pemetrexed IM3 as oil. This oil is dissolved in THF and the alcohol functionality is converted to a mesylate using MsCl and NEt3. The salts are removed by filtration, glacial acetic acid is added and THF is removed by distillation. Upon addition of water Pemetrexed IM4 crystallizes and is isolated by filtration. The dried Pemetrexed IM4 is dissolved in glacial acetic acid and gaseous HCl is added to cleave the dimethoxy acetale and liberate the aldehyde functionality of Pemetrexed IM5. Upon complete deprotection a solution of 2,6-diamino-4-hydroxypyrimidine in aq. NaOH and acetonitrile is added. Upon complete conversion the crystallized Pemetrexed IM6 is isolated by filtration. The saponification of the methyl ester of Pemetrexed IM6 to Pemetrexed IM7 is done using aqueous NaOH. Upon addition of aq. HCl first the Na-salt of Pemetrexed IM7 crystallizes from the reaction mixture. The salt is isolated by filtration, purified by slurry in a mixture of MeOH and water and then converted to Pemetrexed IM7 by pH adjustment in water using aq. HCl. Dried Pemetrexed IM7 (water content not more than 6.0%) is dissolved in DMF, activated using 1,1-carbonyldiimidazolide (CDI) and then reacted with dimethyl-L-glutamate hydrochlorid to give, upon addition of water and filtration, crude Pemetrexed IM8. This intermediate is purified by tosylate salt formation, followed by recrystallization and liberation to give pure Pemetrexed IM8. Starting with the saponification of Pemetrexed IM8 the preparation of different solid forms of Pemetrexed Disodium can be achieved.
Methods For Preparing Pemetrexed Disodium Form IV and Investigation of its Stability
An overview on the possible transformations of Pemetrexed IM8 to Pemetrexed Disodium Form IV is shown in FIG. 20.
Description of Possible Routes for the Preparation of Pemetrexed Disodium Form IV Starting from Pemetrexed IM8
All routes start with saponification of Pemetrexed IM8 in water at IT=20° C. to 30° C. using 3.25 eq of NaOH. Upon complete conversion an aqueous solution of Pemetrexed Disodium with a pH of 13.0 to 13.5 is obtained. Starting from this mixture the desired route can be accessed by addition of HCl to adjust the pH to a certain value (depending on the route, FIG. 20).
Structures of Pemetrexed (Compound I), Pemetrexed Disodium (Compound II) and Pemetrexed Monosodium (Compound IV)
Surprisingly we found that the crucial feature of all successful transformations to Pemetrexed Disodium Form IV is the presence of Pemetrexed Monosodium during the transformation. Routes starting from pure Pemetrexed Disodium Heptahydrate, Pemetrexed Disodium 2.5 hydrate or Pemetrexed Disodium Form A in the presence of seeding crystals of Pemetrexed Disodium Form IV were not successful and resulted in isolation of Pemetrexed Disodium Form A. The same transformations, if carried out in the presence of 0.15 eq of Pemetrexed Monosodium were successful and after addition of 0.15 eq NaOH allowed the isolation of pure Pemetrexed Disodium Form IV. The use of 0.15 eq HCl instead of 0.15 eq Pemetrexed Monosodium under the same conditions resulted in isolation of Pemetrexed Disodium Form A without any Pemetrexed Disodium Form IV. Transformations via isolated Pemetrexed Monosodium gave complete transformation to Pemetrexed Disodium Form IV if either 1.0 eq NaOH were added slowly (over a period of several hours) to Pemetrexed Monosodium or if initially only 0.85 eq of NaOH (based on Pemetrexed Monosodium) were added, followed by 0.15 eq once the transformation to Pemetrexed Disodium Form IV was complete. Very fast addition (<1 min) of 1.0 eq NaOH resulted in formation of Pemetrexed Disodium Form A containing traces of Pemetrexed Disodium Heptahydrate.
Starting from Pemetrexed (compound I) the transformation to Pemetrexed Disodium Form IV would be possible if initially 1.85 eq of NaOH were added followed by 0.15 eq once the transformation was complete. Alternatively, 2.0 eq of NaOH could be added over a long period of time (i.e several hours) to achieve formation of Pemetrexed Form IV. Fast addition (<1 min) of 2.0 eq of NaOH is assumed to result in formation of Pemetrexed Disodium Form A. All these experiments show the presence of Pemetrexed Monosodium to be crucial during the transformations. This presence can be achieved by either addition of catalytic amounts of Pemetrexed Monosodium to Pemetrexed Disodium, by slow addition over several hours of NaOH to Pemetrexed Monosodium or by portionwise addition of NaOH to Pemetrexed Monosodium. Addition of catalytic amounts of HCl to Pemetrexed Disodium (in situ preparation of Pemetrexed Monosodium) failed to give Pemetrexed Disodium Form IV.
Fast addition of NaOH to Pemetrexed Monosodium results in fast formation of Pemetrexed Disodium, thereby lacking the necessary catalytic amounts of Pemetrexed Monosodium to catalyze the transformation to Pemetrexed Disodium Form IV. EtOH as solvent and water content of EtOH were found to be crucial parameters for the transformation to Pemetrexed Disodium Form IV. So far the transformation has only been observed in EtOH containing 0-4% water (v/v). A water content>4% (v/v) results in formation of Pemetrexed Disodium Heptahydrate. Under the conditions used (EtOH containing 0-4% water (v/v)) both Pemetrexed Disodium Heptahydrate and Pemetrexed Disodium 2.5 hydrate are transformed to Pemetrexed Form A. Therefore the mechanism of the transformation to Pemetrexed Disodium Form IV is assumed to proceed via Pemetrexed Disodium Form A with Pemetrexed Monosodium acting as catalyst for the transformation.
Preparation of Pemetrexed Disodium Heptahydrate
a) Preparation of Pemetrexed Disodium Heptahydrate Starting from Pemetrexed IM8
Pemetrexed Disodium Heptahydrate was prepared by adjustment of the pH of the Pemetrexed Disodium solution after saponification from pH=13 to pH=8 using HCl followed by addition of EtOH (3 times the volume of water) to achieve crystallization. Precipitated Pemetrexed Disodium Heptahydrate was isolated by filtration, washed with a mixture of EtOH and water (4:1 v/v) followed by EtOH. The wet product was dried in vacuo at 200 mbar at 20° C. to 30° C. until water content of the dried product was 20.1% to 22.1%.
b) Conversion of Pemetrexed Disodium Form A to Pemetrexed Disodium Heptahydrate
To a suspension of Pemetrexed Disodium Form A in EtOH was added water until a mixture of EtOH containing 25% water (v/v) was obtained. The resulting suspension was stirred at 20° C. to 30° C. until conversion was complete according to PXRD. Pemetrexed Disodium Heptahydrate was isolated by filtration, washed with EtOH and dried in vacuo at 200 mbar at 20° C. to 30° C. until water content of the dried product was 20.1% to 22.1%.
………………………..

- REFERENCES
- McLeod, Howard L.; James Cassidy, Robert H. Powrie, David G. Priest, Mark A. Zorbas, Timothy W. Synold, Stephen Shibata, Darcy Spicer, Donald Bissett, Yazdi K. Pithavala, Mary A. Collier, Linda J. Paradiso, John D. Roberts (Jul-2000).“Pharmacokinetic and Pharmacodynamic Evaluation of the Glycinamide Ribonucleotide Formyltransferase Inhibitor AG2034”. Clinical Cancer Research 6 (7): 2677–84.PMID 10914709. More than one of
|work=and|journal=specified (help) - Avendano, Carmen; Menendez, J. Carlos (April 2008).Medicinal Chemistry of Anticancer Drugs. Amsterdam:Elsevier. p. 37. ISBN 0-444-52824-5.
- Manegold C (August 2003). “Pemetrexed (Alimta, MTA, multitargeted antifolate, LY231514) for malignant pleural mesothelioma”. Semin. Oncol. 30 (4 Suppl 10): 32–6.doi:10.1016/S0093-7754(03)00283-5. PMID 12917819.
- National Cancer Institute: FDA Approval for Pemetrexed Disodium
| US6090168 * | Oct 6, 1999 | Jul 18, 2000 | Eli Lilly And Company | Processes and intermediates useful to make antifolates |
| US7138521 | Feb 12, 2001 | Nov 21, 2006 | Eli Lilly And Company | Crystalline of N-[4-[2-(2-Amino-4,7-dihydro-4oxo-3H-pyrrolo[2,3-D]pyrimidin-5-YL)ethyl]benzoyl]-L-glutamic acid and process therefor |
| US20030216416 * | Feb 12, 2001 | Nov 20, 2003 | Chelius Erik Christopher | Novel crystalline of n-[4-[2-(2-amino-4,7-dihydro-4oxo-3h-pyrrolo[2,3-d]pyrimidin-5-yl)ethyl]benzoyl]-l-glutamic acid and process therefor |
| WO2001014379A2 * | Aug 15, 2000 | Mar 1, 2001 | Erik Christopher Chelius | A novel crystalline form of disodium n-[4-[2-(2-amino-4,7-dihydro-4-oxo-3h-pyrrolo[2,3-d]-pyrimidin-5-yl)ethyl]benzoyl]-l-glutamic acid salt and processes therefor |
| WO2008021405A1 * | Aug 14, 2007 | Feb 21, 2008 | Sicor Inc | Crystalline forms of pemetrexed diacid and processes for the preparation thereof |
| WO2008124485A2 * | Apr 3, 2008 | Oct 16, 2008 | Reddys Lab Ltd Dr | Solid forms of pemetrexed |
FDA Approves Amitiza [lubiprostone] for Opioid-Induced Constipation

7-[(1R,3R,6R,7R)-3-(1,1-difluoropentyl)-3-hydroxy-
8-oxo-2-oxabicyclo[4.3.0]non-7-yl]heptanoic acid
Lubiprostone
136790-76-6 cas no
- FDA Approves Supplemental New Drug Application for AMITIZA® (lubiprostone), the First Oral Treatment for Opioid-induced Constipation in Adults with Chronic Non-Cancer Pain
Apr. 23, 2013– Sucampo Pharmaceuticals, Inc. and Takeda Pharmaceuticals U.S.A., Inc. announced today that the United States (U.S.) Food and Drug Administration (FDA) has approved Sucampo’s supplemental new drug application (sNDA) for Amitiza (lubiprostone) (24 mcg twice daily) as the first and only oral medication for the treatment of opioid-induced constipation (OIC) in adult patients with chronic, non-cancer pain. The effectiveness of Amitiza in the treatment of opioid-induced constipation in patients taking diphenylheptane opioids (e.g., methadone) has not been established.
This is the third indication for Amitiza, which is also approved in the U.S. for the treatment of chronic idiopathic constipation (CIC) in adults (24 mcg twice daily) and irritable bowel syndrome with constipation (IBS-C) in adult women (8 mcg twice daily). There are more than 200 million prescriptions for opioid use in the U.S. annually, and a substantial number of these prescriptions are for non-cancer chronic pain. Scientific literature indicates that approximately 40-80% of patients taking opioids chronically for non-cancer pain report constipation.
Opioid-based medicines are widely used in the management of chronic pain, with OIC being a common adverse effect of chronic opioid use. Some patients may discontinue opioid therapy and thereby endure pain rather than suffer from the constipation the opioids cause.
Amitiza is a specific activator of ClC-2 chloride channels in the intestinal epithelium. Amitiza, via activation of apical ClC-2 channels in the intestinal epithelium, bypasses the antisecretory action of opiates.
This approval is based on results from Phase 3, well-controlled studies of 12 weeks’ duration in patients taking opioids (among them morphine, oxycodone, and fentanyl) chronically for non-cancer pain, as well as a long-term, open-label safety study, which provides additional support for use in this population. Two of the Phase 3 studies met their overall efficacy endpoint, while a third Phase 3 study did not.
OIC is a common adverse effect of chronic opioid use. Binding of opioids to peripheral opioid receptors in the gastrointestinal tract results in absorption of electrolytes, such as chloride, and subsequent reduction in small intestinal fluid. In addition, activation of enteric opioid receptors results in abnormal GI motility. Together, these processes result in OIC, which is characterized by infrequent and incomplete evacuation of stool, hard stool consistency, and straining associated with bowel movements.
|
Amitiza (lubiprostone) capsules are indicated for the treatment of chronic idiopathic constipation (CIC) in adults and opioid-induced constipation (OIC) in adults with chronic, non-cancer pain (24 mcg twice daily). The effectiveness in patients with OIC taking diphenylheptane opioids (e.g., methadone) has not been established. Amitiza is also indicated for irritable bowel syndrome with constipation (IBS-C) in women > 18 years old (8 mcg twice daily).
Lubiprostone (rINN, marketed under the trade name Amitiza) is a medicationused in the management of chronic idiopathic constipation and irritable bowel syndrome. It was approved by the U.S. Food and Drug Administration (FDA) for this purpose on 31 January 2006.
Lubiprostone is used for the treatment of chronic constipation of unknown cause and irritable bowel syndrome associated with constipation.
As of 20 July 2006, Lubiprostone had not been studied in children. There is current research underway to determine the efficacy in postoperative bowel dysfunction, and opioid-induced bowel dysfunction

- “amitiza”. The American Society of Health-System Pharmacists. Retrieved 3 April 2011.
- Sobrera, L. A.; Castaner, J. (2004). Drugs of the Future 29 (4): 336.
PHASE 2 -TetraLogic’s BIRINAPANT for treatment of acute myeloid leukemia, pancreatic cancer, or ovarian cancer
BIRINAPANT, Apoptosis inhibitor
(2S,2’S)-N,N’-((2S,2’S)-((3S,3’S,5R,5’R)-5,5′-((6,6′-difluoro-1H,1’H-[2,2′-biindole]-3,3′-diyl)bis(methylene))bis(3-hydroxypyrrolidine-5,1-diyl))bis(1-oxobutane-2,1-diyl))bis(2-(methylamino)propanamide)
1260251-31-7 cas no
Birinapant is an antagonist of XIAP and cIAP1 with Kd value of 45 nM and <1 nM, respectively.
US20110003877,WO 2013049350 A1
| Molecular Weight: | 806.94 |
| Birinapant Formula: | C42H56F2N8O6 |
Birinapant, also known as TL32711, is a synthetic small molecule and peptido mimetic of second mitochondrial-derived activator of caspases (SMAC) and inhibitor of IAP (Inhibitor of Apoptosis Protein) family proteins, with potential antineoplastic activity. As a SMAC mimetic and IAP antagonist, TL32711 binds to and inhibits the activity of IAPs, such as X chromosome-linked IAP (XIAP) and cellular IAPs 1 and 2. Since IAPs shield cancer cells from the apoptosis process, this agent may restore and promote the induction of apoptosis through apoptotic signaling pathways in cancer cells. IAPs are overexpressed by many cancer cell types and suppress apoptosis by binding and inhibiting active caspases-3, -7 and -9 via their baculoviral lAP repeat (BIR) domains
Birinapant is currently in Phase II clinical trials in patients with acute myeloid leukemia, pancreatic cancer, or ovarian cancer. Although these trials don’t have a control group, the emerging data are promising, TetraLogic chief executive officer John M. Gill told C&EN. (Early-stage cancer clinical trials are commonly run without placebo groups.) The birinapant trials show preliminary evidence both that the drug is having the desired effect and that this effect is associated with signs of clinical activity. Given these results, the company plans to launch randomized Phase II studies early in 2014
Birinapant, also called TL32711, is a potent antagonist for XIAP with Kd value of 45 nM and cIAP1 with Kd value <1 nM [1].
Birinapant not only binds to the isolated BIR3 domains of cIAP1, cIAP2, XIAP but the single BIR domain of ML-IAP with high affinity and degrades TRAF2-bound cIAP1 and cIAP2 rapidly accordingly inhibiting the activation of TNF-mediated NF- kB. Additionally, birinapantcan promote the formation of caspase-8: RIPK1 complex in response to TNF stimulation, which result in downstream caspasesactivation [4].
In the inorganic SUM149- and SUM190-derived cells, which with differential XIAP expression (SUM149 wtXIAP, SUM190 shXIAP) and other high cIAP1/2 but low XIAP binding affinity bivalent Smac mimetic GT13402, XIAP inhibition are needed for increasing TRAIL potency. Opposite, single agent efficacy of Birinapant is owing to pan-IAP antagonism. Rapid cIAP1 degradation was caused by birinapant, as well as NF-κB activation, PARP cleavage andcaspase activation. While combined withTNF-α, showing strong combination activity, the combination was more effective than individual. The response in spheroid models was conserved, whereas in vivo birinapant inhibited tumor growth without adding TNF-α in vitro to resistant cell lines. In a parental cell line, TNF-αcombined withbirinapantinhibited the growth of a melanoma cell line with acquired resistance to the same extent of BRAF inhibition [1, 2].
Drug treatment increased the mean [18F]ICMT-11 tumor uptake with a peak at 24 hours for CPA (40 mg/kg; AUC40-60: 8.04 ± 1.33 and 16.05 ± 3.35 %ID/mL × min at baseline and 24 hours, respectively) and 6 hours for birinapant (15 mg/kg; AUC40-60: 20.29 ± 0.82 and 31.07 ± 5.66 %ID/mL × min, at baseline and 6 hours, respectively). Voxel-based spatiotemporal analysis of tumor-intrinsic heterogeneity showed that [18F] ICMT-11 could detect the discrete pockets of caspase-3 activation. Caspase-3 activation that measured ex vivo associated with the increased tumor [18F] ICMT-11, and early radiotracer uptake predicted apoptosis, distinct from the glucose metabolism with [18F] fluorodeoxyglucose-PET, which depicted the continuous loss of cell viability [3].


Birinapant was designed to reinstate cancer cells’ ability to die. Many cancers that are resistant to conventional chemotherapy drugs have defects in the cell death pathway known as apoptosis. The human body uses apoptosis every day to clear away abnormal or unwanted cells.
Apoptosis is a tightly regulated process, Condon explains, with a network of proteins that activate or block the process. TetraLogic’s target is a family of proteins called the Inhibitor of Apoptosis proteins. As their name suggests, these proteins block apoptosis. They interfere with protease enzymes that carry out cellular dismantling.
TetraLogic’s aim is to lift that blockade to restart apoptosis in tumors. Many tumors have excesses of the apoptosis inhibitor proteins relative to normal cells, so targeting this process has the potential to be less toxic to normal cells compared with conventional chemotherapy.
It turns out nature has a way of negating the inhibitor proteins’ actions—a protein known as Smac. TetraLogic’s founders demonstrated that only a tiny portion of Smac is necessary to keep the inhibitor proteins at bay—the four amino acids at the protein’s N-terminus. “Once you can get a protein down to a tetrapeptide,” about the size of a small-molecule drug, “you start getting a lot of interest from the pharma community,” Condon told C&EN.
Peptides fall apart in the body too quickly to be drugs, so Condon’s team worked with molecular mimics of the Smac tetrapeptide. Their biggest advance was realizing that combining two copies of their tetrapeptide mimics into one molecule made their compounds highly effective at reinstating apoptosis in cancer cell lines. Many proteins in the apoptosis pathway function as dimers, so using these so-called bivalent mimics against them makes sense, Condon said.
However, several of the bivalent compounds were associated with pronounced body weight loss in mice. Condon’s team eventually learned that replacing a branched side chain on their peptide mimics and adding a hydroxyl group to a proline residue improved the tolerability for the animals without impacting the antitumor effect. With that, birinapant was born.
In mice, birinapant shrank tumors. The compound has been in clinical trials since 2009, both on its own and in combination with other chemotherapy drugs such as irinotecan and gemcitabine. On the basis of other biochemical work on the apoptosis pathway, TetraLogic thinks these drugs could act in synergy with birinapant to treat cancer, Condon said.
Birinapant is currently in Phase II clinical trials in patients with acute myeloid leukemia, pancreatic cancer, or ovarian cancer. Although these trials don’t have a control group, the emerging data are promising, TetraLogic chief executive officer John M. Gill told C&EN. (Early-stage cancer clinical trials are commonly run without placebo groups.) The birinapant trials show preliminary evidence both that the drug is having the desired effect and that this effect is associated with signs of clinical activity. Given these results, the company plans to launch randomized Phase II studies early in 2014.
1H NMR













spectral data
1H NMR (300 MHz, CDC13): 511.74 (s, 2H), 8.27 (d, J= 8.7 Hz, 2H), 7.71 (dd, J= 5.4, 8.4 Hz, 2H), 7.55 (dd, J =2.4, 9.6 Hz, 2H), 6.88 (ddd, J= 2.4, 9.3, 9.3 Hz, 2H), 4.62-4.78 (m, 4H), 4.43 (dd, J= 9.3, 9.9 Hz, 2H), 4.03 (dd, J= 4.8, 11.4 Hz, 2H), 3.80 (d, J = 11.4 Hz, 2H), 3.66 (dd, J= 2.7, 14.4 Hz, 2H), 3.53 (dd, J = 11.4, 14.4 Hz, 2H), 3.11 (q, J = 6.9 Hz, 2H), 2.56 (s, 6H), 2.45 (m, 2H), 2.19 (d, J= 14.4 Hz, 2H), 1.76-2.10 (m, 6H), 1.59 (br s, 2H), 1.39 (d, J= 6.9 Hz, 6H), 1.22-1.38 (m, 2H), 1.07 (t, J = 7.2 Hz, 6H) ppm;
13C NMR (75 MHz, d6– DMSO): 5175.2, 172.8, 161.6, 158.5, 137.3, 137.2, 128.4, 128.3, 126.4, 120.8, 120.6, 109.4, 108.7, 108.4, 98.4, 98.0, 70.8, 60.2, 59.9, 56.6, 51.8, 36.4, 35.3, 28.3, 25.6, 20.0, 10.6 ppm.
Mass spectrum (ESI), m/z 807.5 [(M)+; calcd for C42H56F2N806: 806.9].
Paper
Click to access op5b00390_si_001.pdf
Click to access op5b00390_si_001.pdf
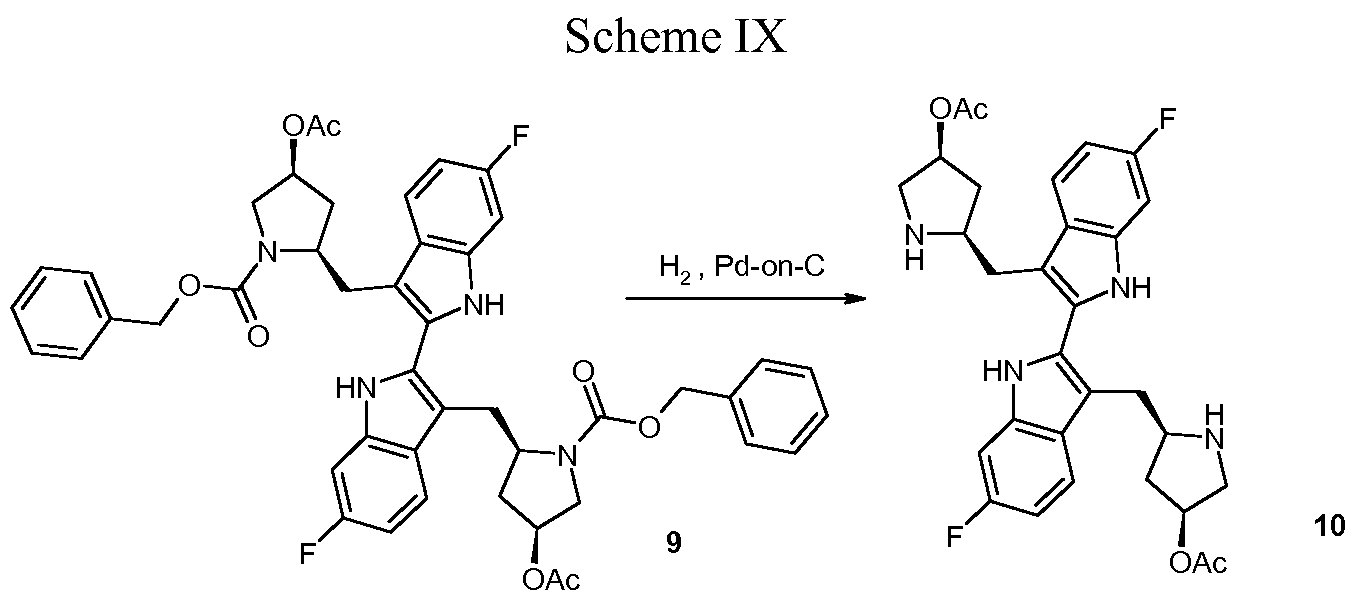
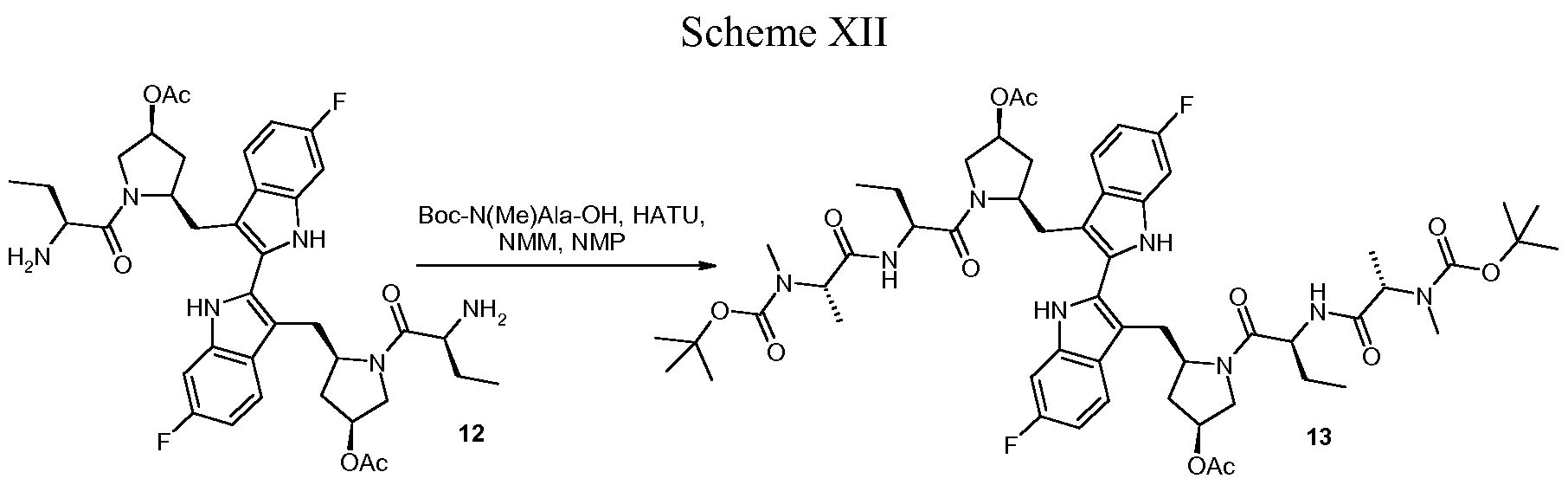
Process Development and Synthesis of Birinapant: Large Scale Preparation and Acid-Mediated Dimerization of the Key Indole Intermediate

Birinapant/TL32711 (1) is a novel bivalent antagonist of the inhibitor of apoptosis (IAP) family of proteins which is currently in clinical development for the treatment of cancer and hepatitis B virus (HBV) infection. In this report, we present a detailed description of the 1 drug substance synthesis used to support our ongoing clinical studies. Key transformations in this process included the development of a scalable, high-yielding route to acyl indole 14 as well as a two-step dimerization/oxidation of indole 19 that afforded biindole 21 in excellent yield and purity (70% yield, 2 steps; >95 area% purity by HPLC analysis). In addition, partial defluorination of 21 was observed following hydrogen-mediated benzyloxycarbonyl (Cbz) protective group removal which was obviated by the use of HBr/HOAc for this transformation. The use of commercially available amino acid derivatives afforded related impurities which proved difficult to purge in subsequent steps. Thus, defining the impurity specification for these reagents was critical to providing 1 drug substance of >99 area% chemical purity. Using this process, we have successfully prepared 1 drug substance multiple times on >500-g-scale in support of our clinical development program.
References:
1.Allensworth JL, Sauer S, Lyerly HK, et al. Smac mimetic Birinapant induces apoptosis and enhances TRAIL potency in inflammatory breast cancer cells in an IAP-dependent and TNF-a-independent mechanism. Breast Cancer Research, 2013, 137:359-371.
2.Krepler C, Chunduru SK, Halloran MB, et al. The novel SMAC mimetic birinapant exhibits potent activity against human melanoma cells. Clinical Cancer Research, 2013, 19 (7): 1784-1794.
3.Nguyen QD, Lavdas I, Gubbins J, et al. Temporal and Spatial Evolution of Therapy-Induced Tumor Apoptosis Detected by Caspase-3–Selective Molecular Imaging. Clinical Cancer Research, 2013, 19 (14): 3914-3924.
4.Benetatos CA, Mitsuuchi Y, Burns JM, et al. Birinapant (TL32711), a Bivalent SMAC Mimetic, Targets TRAF2-Associated cIAPs, Abrogates TNF-Induced NF-kB Activation, and Is Active in Patient-Derived Xenograft Models. 2014, 13(4):867-879.

PHASE 1- MGL-3196 (VIA-3196)Madrigal Pharmaceuticals, to treat high cholesterol/high triglycerides
MGL-3196 (VIA-3196) photo credit The haystack http://cenblog.org/the-haystack/tag/mgl-3196/
Madrigal Pharmaceuticals, acquired from VIA Pharmaceuticals, licensed from Roche to treat high cholesterol/high triglycerides , it mimics thyroid hormone, targeted to thyroid hormone receptor beta in the liver
Specifically, MGL-3196 is a thyroid hormone analog, designed to target a thyroid hormone receptor in the liver. These receptors regulate genes involved in cholesterol regulation and metabolism.
MGL-3196 is an orally administered, small-molecule liver-directed ß-selective THR agonist designed to specifically target receptors in the liver involved in metabolism and cholesterol regulation, and avoid side effects associated with thyroid hormone receptor activation outside the liver, including those mediated by THR-α receptors. MGL-3196 has currently completed Phase I single and multiple dose trials in healthy volunteers. MGL-3196 is being developed for dyslipidemia/hypercholesterolemia to lower LDL cholesterol, triglyceride levels and Lp(a), and was inlicensed from Roche Pharmaceuticals. MGL-3196 has excellent safety in comparative studies with other THR agonists tested previously because of MGL-3196’s high liver uptake and high ß-selectivity and nearly complete lack of THR-α activity.

MGL-3196 has completed a single ascending dose study in healthy volunteers in which the compound appeared safe at all doses tested. The multiple ascending dose study in healthy volunteers with mildly elevated LDL cholesterol was completed in October 2012 and provided additional safety and pharmacodynamic information. The Phase I multiple dose, proof of concept study enrolled 48 healthy volunteers with mildly elevated LDL cholesterol to evaluate the safety, pharmacokinetics and pharmacodynamics of MGL-3196 after two weeks of daily dosing. Results showed that MGL-3196 was well tolerated and appeared safe at all doses tested. Daily doses of 50-200 mg showed highly statistically significant reductions relative to placebo of up to 30% LDL-cholesterol (p=.05-<.0001; 28%, non-HDL cholesterol (p=.027-.0001); 24% Apolipoprotein B (p=.008-.0004); and strong trends and up to 60% reduction of triglycerides (range, p=.13-.016).

phase 2-LGX818, Novartis Research Foundation to treat melanoma with a specific mutation in B-RAF kinase V600E

LGX818
Methyl [(2S)-1-{[4-(3-{5-chloro-2-fluoro-3-[(methylsulfonyl)amino]phenyl}-1-isopropyl-1H-pyrazol-4-yl)-2-pyrimidinyl]amino}-2-propanyl]carbamate
Novartis Institutes for Biomedical Research and Genomics Institute of the Novartis Research Foundation to treat melanoma with a specific mutation in B-RAF kinase V600E, selective mutant B-RAF kinase inhibitor
LGX818 is currently in Phase Ib/II clinical trials. Patients with colon cancer or melanoma with the BRAF mutation, including patients resistant to other BRAF-targeted drugs, are receiving LGX818 pills alone or as part of drug cocktails to determine whether the drug is safe and efficacious
A phase Ib/II drug structure by Novartis disclosed at the spring 2013 American Chemical Society meeting in New Orleans to treat melanoma with a V600E mutation in the B-RAF kinase which it inhibits.[1][2][3]
Several clinical trials of LGX818 , either alone or in combinations with the MEK inhibitorMEK162[4], CDK4 inhibitor LEE011[5] are being run. The initial results are encouraging [6].
- C. Drahl, Liveblogging First-Time Disclosures of Drug Structures from #ACSNOLA, 2013, http://cenblog.org/the-haystack/2013/04/liveblogging-first-time-disclosures-of-drug-structures-from-acsnola/
- http://patentscope.wipo.int/search/en/detail.jsf?docId=WO2011023773
- http://patentscope.wipo.int/search/en/detail.jsf?docId=WO2011025927
- http://www.cancer.gov/clinicaltrials/search/view?cdrid=728588&version=HealthProfessional&protocolsearchid=11645832
- http://www.cancer.gov/clinicaltrials/search/view?cdrid=745927&version=HealthProfessional&protocolsearchid=11645832
- http://www.novartis.com/downloads/investors/event-calendar/2012/6-bridging-science-and-patients.pdf
PHASE 1-BMS-906024 by Bristol-Myers Squibb to treat breast, lung, and colon cancers and leukemia

BMS-906024 is in Phase I clinical trials, both alone and in combination with other agents. Patients with colon, lung, breast, and other cancers are receiving intravenous doses of the compound to determine its safety and optimum dose ranges
New Phase I drug structure by Bristol-Myers Squibb disclosed at the spring 2013American Chemical Society meeting in New Orleans to treat breast, lung, and colon cancers and leukemia.[1] The drug works as an pan-Notch inhibitor. The structure is one of a set patented in 2012,[2] and it currently being studied in clinical trials.[3][4]
- C. Drahl, Liveblogging First-Time Disclosures of Drug Structures from #ACSNOLA, 2013, http://cenblog.org/the-haystack/2013/04/liveblogging-first-time-disclosures-of-drug-structures-from-acsnola/
- http://patentscope.wipo.int/search/en/detail.jsf?docId=WO2012129353
- http://clinicaltrials.gov/show/NCT01653470
- http://clinicaltrials.gov/show/NCT01292655
Phase 2, AZD5423 BY ASTRAZENECA FOR COPD

AZD5423
The compound is now in a Phase II study in patients with COPD, where its efficacy and safety are being measured against that of a typical steroid or a placebo
A phase II drug structure by AstraZeneca disclosed at the spring 2013 American Chemical Society meeting in New Orleans to treat respiratory diseases and in particular the chronic obstructive pulmonary disease.[1][2][3][4]
- C. Drahl, Liveblogging First-Time Disclosures of Drug Structures from #ACSNOLA, 2013, http://cenblog.org/the-haystack/2013/04/liveblogging-first-time-disclosures-of-drug-structures-from-acsnola/
- GB2010051905 COMBINATIONS COMPRISING A GLUCOCORTICOID RECEPTOR MODULATOR FOR THE TREATMENT OF RESPIRATORY DISEASES
- SE2009050900 A COMBINATION OF (A) GLUCOCORTICOID RECEPTOR MODULATOR AND (B) A MUSCARINIC ANTAGONIST
- SE2009000264 COMBINATION OF (A) GLUCOCORTICOID RECEPTOR MODULATOR AND (B) A B2-AGONIST
EU OKs Sanofi’s 6 in 1 Pediatric Vaccine
Hexyon/ Hexyon/Hexyon/Hexyon/ Hexacima Hexacima Hexacima 6-in -1 Pediatric Vaccine 1 Pediatric Vaccine 1 Pediatric Vaccine1 Pediatric Vaccine 1 Pediatric Vaccine Approved in Europe
Hexyon/Hexacima is the only fully liquid, ready-to-use, 6-in-1 pediatric vaccine –
Lyon, France – April 22, 2013 – Sanofi Pasteur, the vaccines division of Sanofi (EURONEXT: SAN and NYSE: SNY), announced today that the European Commission approved Sanofi Pasteur’s 6-in-1 pediatric vaccine HexyonTM/Hexacima® (DTaP-IPV-Hib-HepB vaccine) for primary and booster vaccination of infants from six weeks of age.
HexyonTM/Hexacima® is the only fully liquid, ready-to-use, 6-in-1 vaccine to protect infants against diphtheria, tetanus, pertussis (whooping cough), Hepatitis B, poliomyelitis and invasive infections caused by Haemophilus influenzae type b…………………….read more at pharmalive
http://www.pharmalive.com/eu-oks-sanofis-6-in-1-pediatric-vaccine
also read at
AstraZeneca inks cancer deals with Bind and Horizon
AstraZeneca has signed a nanomedicines pact with Bind Therapeutics in a deal which could be worth $200 million to the privately-held US biopharma firm.
The firms will work together to develop what Bind calls an “Accurin”, a targeted and programmable cancer nanomedicine, based on a kinase inhibitor owned by the Anglo-Swedish drugmaker……………………..READ MORE AT PHARMATIMES
http://www.pharmatimes.com/Article/13-04-22/AstraZeneca_inks_cancer_deals_with_Bind_and_Horizon.aspx

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....





















