Home » 2014 (Page 65)
Yearly Archives: 2014
Stem cell therapy regenerates heart muscle damaged from heart attacks in primates
Heart cells created from human embryonic stem cells successfully restored damaged heart muscles in monkeys. The results of the experiment appear in the April 30 advanced online edition of the journal Nature in a paper titled, “Human embryonic-stem cell derived cardiomyocytes regenerate non-human primate hearts.”
The findings suggest that the approach should be feasible in humans, the researchers said.
“Before this study, it was not known if it is possible to produce sufficient numbers of these cells and successfully use them to remuscularize damaged hearts in a large animal whose heart size and physiology is similar to that of the human heart,” said Dr. Charles Murry, UW professor of pathology and bioengineering, who led the research team that conducted the experiment.
A physician/scientist, Murry directs the UW Center for Cardiovascular Biology and is a UW Medicine pathologist.
Murry said he expected the approach could be ready for clinical trials in…
View original post 611 more words
Sanfilippo Syndrome: FDA Orphan Designations For Gene Therapy
SF is a genetic metabolism disorder that prohibits the proper breakdown of the body’s sugar molecules. There are 4 types of MPS III (MPS III A, MPS III B, MPS III C, and MPS III D), each with a deficiency in one of four lysosomal enzymes. The disease first affects the central nervous system, causing severe brain damage, and typically results in hearing loss, vision loss…
View original post 226 more words
Bulaquine a CDRI India Antimalarial

Bulaquine
CAS NO.: 79781-00-3
2(3H)-Furanone, dihydro-3-(1-((4-((6-methoxy-8-quinolinyl)amino)pentyl)amino)ethylidene)-,
3-[l-[[4-[(6-methoxy-8-quinolinyl)amino]pentyl]amino]- ethyMene]-dihydro-2(3H)furanone
N1– (3-ethylidinotetrahydrofuran-2-one)-N4– (6-methoxy-8-quinolinyl)-1,4-pentanediamine
BULAQUINE
https://www.ncbi.nlm.nih.gov/pubmed?cmd=search&term=%22bulaquine%22%5BNM%5D
………………….

http://www.cdriindia.org/Bulaquin.htm
|
|
|
It is being increasingly felt that the eroding efficacy of commonly used antimalarials has contributed substantially to the resurgence of malaria during last three decades. Although new antimalarials have appeared in the market during this time, none has yet supplemented chloroquine. There are no drugs in the market or in advanced stages of development that appear to be as well tolerated as chloroquine. Combinations of existing antimalarials especially those now available in rural clinics and market hold great potential for effective, self-administered therapies for uncomplicated malaria, particularly where relapses are frequently encountered. Applying combined therapies to the problem should demand a high standard of proof of safety and efficacy in randomised double blind, placebo controlled trials. Bulaquin is without any side effects that have been observed with primaquine. A comparative data analysis on initial (0 day pre-drug) and final (+7 day post-drug) values of haemoglobin, methaemoglobin, prothrombin time, partial thromboplastin time and fibrinogen in healthy human subjects treated with primaquine (15 mg OD x7 days) and Bulaquin (25 mg OD x7 days) have been carried out. The study has shown that one week primaquine treatment leads to rise in methaemoglobin levels from 3.97% to 16.32%, which is highly significant in comparison to the 2.29% and 3.02% levels of methaemoglobin before and after 7 days treatment with Bulaquin respectively. Thus, it is evident that primaquine treatment produces rise in methaemoglobin contrary to Bulaquine does not produce rise in methaemoglobin levels. This result manifests a clear superiority of Bulaquin over Primaquine. Bulaquin has been licenced to Nicholas Piramal India Ltd., Mumbai for marketing. Nicholas Piramal has introduced Bulaquin alongwith chloroquine into the market as a combination pack under the trade name Aablaquine. The objective of the combined therapy is to control P.vivax malaria more effectively by providing initial cure and thereafter preventing relapses by use of this combination pack. It is hoped that the introduction of this combination pack of Bulaquin should contribute substantially to the ongoing National Malaria action programme advocated by Government of India. |
|
http://www.google.com/patents/EP1292306A2?cl=en
Malaria, caused by a parasitic protozoan called Plasmodium, is one of the most serious and complex tropical parasitic diseases. Generally human malaria is caused by four species of malarial parasites which are Plasmodium falciparwn, Plasmodium vivax, Plasmodium ovale and Plasmodium malariae. Of these P. falciparum and P. vivαx are most widespread and cause most of the mortality and morbidity associated with these types of infections.
It is known that the malarial parasites undergo complex life cycle in humans, which is initiated through the bite of an infected female Anopheles mosquito. When the mosquito bites a host, some of the sporozoites are injected into the bloodstream of the host and through the circulation they reach the liver where they multiply and liberate merozoites into the bloodstream which then invade the erythrocytes. In case of infections caused by P. vivαx, most of the time the parasites remain dormant in the liver which stage is termed hypnozoites. Hypnozoites are reactivated and reinitiate blood stage parasitemias causing relapse. It has often been observed that people infected with P. vivax do not experience any symptoms for a very long period after their initial illness but become symptomatic after certain period (Korean J. Intern Med, 1999 Juk 14(2): 86-9).
A number of drugs ranging from those of natural origin to synthetic ones have been developed for the treatment of malaria. Quinine and artemisinin are the commonly known drugs of natural origin, which are mostly used for the treatment of malaria. A number of synthetic anti- malarial drugs such as chloroquine, mefloquine, primaquine, halofantrine, ainodiaquine, proguanil, maloprim are known in the literature. Of all the synthetic anti-malarial agents chloroquine has been the most widely prescribed drug for the treatment of malaria of all the types, for more than last 60 years.
Chloroquine has been the effective treatment so far for the P. vivax malarial infections, however, some strains of P. vivax have shown resistance to this well known drug {Ann. Trop. Med. ParasitoL, 1999 Apr; 93(3): 225-230). In recent years drug resistant malaria has become one of the most serious problems in malaria control. Drug resistance necessitates the use of drugs which are more expensive and may have dangerous side effects. To overcome the problems associated with drug resistance, treatments comprising combinations of anti-malarial agents are on the rise. A number of anti-malarial combinations are already known in the malarial chemotherapy. For example, a combination of amodiaquine and tetracycline, a combination of sulfadoxine and pyrimethamine known as fansidar, are known therapies for the treatment of P. falάparum. Also fansimef, a combination of mefloquine with sulfadoxine and pyrimetha min e is used against multidrug resistant strains of P. faldparum.
United States Patent No. 5 998 449 describes a method for the treatment of malaria wherein combination of atovaquone and proguanil is used for the treatment of malaria. In US Patent No. 5 834 505, combination of fenozan with another anti-malarial agent selected from artemisinin, sodium artesunate, chloroquine, mefloquine is described for the prophylactic and curative treatment of malaria.
All the aforementioned anti-malarial combinations reported heretofore are generally used for the treatment of P. faldparum. None of the standard anti-malarial combination treatment regimens have been found to be favourable for the treatment of P. vivax malaria which is the most relapsing type of malaria. For a very long time chloroquine was used for the treatment of infections caused by P. vivax, however, chloroquine eradicates only the asexual erythrocytic stages of P. vivax and does not eliminate the hypnozoites. Until recently primaquine has been the drug of choice for the treatment of malarial relapse. Generally the standard therapy for the P. vivax malarial infection comprises of a sequential chloroquine-primaquine combination treatment regimen wherein primaquine is administered for 14 days following the 3 days course of chloroquine. WHO (World Health Organisation) also recommends a 14 days primaquine treatment for P. vivax malarial infection. A shorter duration of cMoroquine-primaquine treatment regimen was also tried out wherein primaquine was administered only for 5 days following the chloroquine course. However, the outcome of the treatment was not encouraging, since the percentage relapse was more than the standard 14 days primaquine treatment regimen (Trans. R. Soc. Trop. Med. Hyg., 93(6), 641-643). Also primaquine is known to cause hemolytic anemia in persons deficient in the enzyme glucose-6-phosphate dehydrogenase (G6PD) (Pharmacol Rev. 21: 73-103 (1969); Rev. Cubana Med trop, 1997; 49 (2): 136-8 ). Moreover, methemoglobin toxicity is another predictable dose-related adverse effect associated with primaquine. Needless to say that in the case of sequential combination therapy the patient may not complete the course once the symptoms of malaria are diminished, hence this may increase the chances of relapse. Thus, the chloroquine- primaquine treatment regimen is not safe with respect to toxicity of primaquine and has a further limitation from the standpoint of patient compliance due to longer duration of treatment.
Another anti-relapse agent namely tafenoquine is disclosed in United States Patent 4 617 394. Though more effective than primaquine, the drug was found to cause methemoglobin toxicity almost three times more than that of primaqu ie (Fundam. Appl. Toxicol. 1988, 10(2), 270-275), hence has drawbacks in terms of safety.
The compound, 3-[l-[[4-[(6-nιethoxy-8-quinolinyl)aιnino]pentyl)am.ino]- ethylidene]-dihydro-2(3H)furanone is a derivative of primaquine. It was described in Indian Patent Specification No. 158111 as 6-methoxy-8-(4-
N-(3′-aceto-4^5′-dihydro-2-furanylamino)- l-methylbutylamino)quinoline , the structure of which was revised to that represented by the following formula I. As per the revised structure, the compound is named 3-[l-[[4-
[(6-metJhoxy-8-quinolmyl)amino]pentyl]amino]ethylidene]-dihydro-2(3H)- furanone (hereinafter referred to as compound I). The revised structure is described in WHO Drug Information Vol. 13, No. 4, pg. 268 (1999).
The compound of formula (I) has been found to be safer and less toxic than the parent compound primaquine (Am. J. Trop. Med. Hyg, 1989 Dec; 41(6): 635-637). Its anti-relapse activity has been found to be comparable to primaquine.
Over the years primaquine was the only drug used for the radical cure of malaria caused by P. vivax. Primaquine is associated with a number of severe adverse effects, therefore there is a need to develop agents which are more effective and/ or less toxic than primaquine. The compound I has been found to exhibit anti-relapse activity comparable to Primaquine (Am. J. Trop. Med. Hyg., 41(6): 633-637 (1989)). However, this compound has been shown to cause less methemoglobin formation (Am. J. Trop Hyg., 41(6): 638-642 (1989) ) and also has less effect on anti-oxidant defence enzymes than primaquine (Biochem Pharmacol. 46(10): 1859- 1860 (1993) ). Thus, this primaquine derivative (I) is found to be less toxic as compared to the parent drug, primaquine.
Therefore, there is a longfelt need for a more practical, effective, patient compliant and safe remedy for the radical cure of P. vivax malarial infection.
The inventors have found that the longfelt need may be fulfilled by providing a treatment regimen consisting of regulated use of chloroquine and 3-[l-[[4-[(6-methoxy-8-quinolinyl)aιnino]pentyl]amino]ethylidene]- dihydro-2(3H)furanone of formula I over a period of between 5 to 8 days.
It has also been found that the treatment regimen may be executed most effectively and in a user friendly manner by providing a combination kit which comprises two anti-malarial agents, namely chloroquine and 3-[l- [[4-[(6-meth.oxy-8-qumolmyl)am^
…………………

The title enamine derivative is prepared by condensation of primaquine (I) with acetyl butyrolactone (II) by means of piperidine.
……………….
http://www.google.com/patents/EP1055427B1?cl=en
-
manufacture fo a medicament for the treatment of malaria of primaquine derivative N1-(3-ethylidinotetrahydrofuran-2-one)-N4-(6-methoxy-8-quinolinyl)-1,4-pentanediamine as a gametocytocidal agent. More particularly, this invention relates to the use of primaquine derivative N1– (3-ethylidinotetrahydrofuran-2-one)-N4– (6-methoxy-8-quinolinyl)-1,4-pentanediamine of formula 1 shown below useful for controlling the spread of malaria by virtue of its high therapeutic value as a gametocytocidal agent.
-
The primaquine derivative of the present invention does not damage either normal or G-6PD deficient erythrocytes to the extent it is observed with the use of primaquine.
The following example illustrates the details of the process of this invention:
N1– (3-ethylidinotetrahydrofuran-2-one)-N4– (6-methoxy-8-quinolinyl)-1,4-pentanediamine
-
A mixture of primaquine base (0.97g, 3.7 mmole) freshly distilled 3-acetyl-r-butyrolactone (1.0g, 7.8 mmole) and a base like piperidine (2-3 drops) were stirred under magnetic stirrer at room temperature. In an hour or so the reaction mixture solidified. The product was titrated in ether and filtered to get the product. It was crystallised from alcoholic solvent like propanol. Yield 0.89g, m.p. 118-120°C.
…………..
BELL A.: “Recent developments in the chemotherapy of malaria.” CURRENT OPINION IN ANTI-INFECTIVE INVESTIGATIONAL DRUGS, (2000) 2/1 (63-70). , XP001038054 |
||
| 2 | * | DUTTA, G. P. ET AL: “Radical curative activity of a new 8-aminoquinoline derivative ( CDRI 80/53) against Plasmodium cynomolgi B in monkeys” AM. J. TROP. MED. HYG. (1989), 41(6), 635-7 , 1989, XP001037488 cited in the application |
| 3 | * | KAR, K. ET AL: “Pharmacology of compound CDRI 80/53;a potential new antirelapse antimalarial agent” INDIAN J. PARASITOL. (1988), 12, 259-62 , 1988, XP001034143 |
| 4 | * | NEWTON P. ET AL: “Malaria: New developments in treatment and prevention.” ANNUAL REVIEW OF MEDICINE, (1999) 50/- (179-192). , XP001036946 |
| 5 | * | PALIWAL, JYOTI KUMAR ET AL: “Simultaneous determination of a new antimalarial agent, CDRI compound 80/53, and its metabolite primaquine in serum by high-performance liquid chromatography” J. CHROMATOGR., BIOMED. APPL. (1993), 616(1), 155-60 , 1993, XP000955186 |
| 6 | * | PURI, S. K. ET AL: “Methemoglobin toxicity and hematological studies on malaria anti-relapse compound CDRI 80/53 in dogs” AM. J. TROP. MED. HYG. (1989), 41(6), 638-42 , 1989, XP001037486 cited in the application |
| 7 | * | SETHI, N. ET AL: “Long term toxicity studies with a synthetic anti-relapse antimalarial compound 80/53 in rats and monkeys” INDIAN J. PARASITOL. (1993), 17(1), 15-26 , 1993, XP001034142 |
| 8 | * | VALECHA, NEENA ET AL: “Comparative antirelapse efficacy of CDRI compound 80/53 (Bulaquine) vs. primaquine in double blind clinical trial” CURR. SCI. (2001), 80(4), 561-563 , 2001, XP001037095 |
Whey beneficially affects diabetes and cardiovascular disease risk factors in obese adults
View original post 296 more words
Merimepodib; VX-497 selective IMPDH inhibitor and immunosuppressive agent


Merimepodib; VX-497; VX497; VX 497; MMP, VI21497; VI-21497; VI 21497.
198821-22-6
(S)-tetrahydrofuran-3-yl 3-(3-(3-methoxy-4-(oxazol-5-yl)phenyl)ureido)benzylcarbamate
N-[3-[3-[3-Methoxy-4-(5-oxazolyl)phenyl]ureido]benzyl]carbamic acid tetrahydrofuran-3(S)-yl ester
S) -tetrahydrofuran-3-yl 3- (3- (3-methoxy-4- (oxazol-5-yl)phenyl)ureido)benzylcarbamate
C23H24N4O6
Molecular Weight: 452.46
Vertex Pharmaceuticals innovator
selective IMPDH inhibitor and immunosuppressive agent
Merimepodib, an orally administered small molecule inhibitor of the enzyme inosine 5′-monophosphate dehydrogenase (IMPDH), has completed a phase II clinical trial at Vertex in combination with pegylated interferon and ribavirin for the treatment of hepatitis C viral (HCV).
Merimepodib, also known as VX-497, is orally bioavailable IMPDH inhibitor, which inhibits the proliferation of primary human, mouse, rat, and dog lymphocytes at concentrations of approximately 100 nM. In vivo, oral administration of VX-497 inhibits the primary IgM antibody response in a dose-dependent manner, with an ED(50) value of approximately 30-35 mg/kg in mice. Single daily dosing of VX-497 is observed to be as effective as twice-daily dosing in this model of immune activation. These studies demonstrate that VX-497 is a potent, specific, and reversible IMPDH inhibitor that selectively inhibits lymphocyte proliferation.
IMPDH inhibition leads to a reduction in intracellular guanosine triphosphate (GTP), a cellular molecule required by viruses for replication. Reports indicate that IMPDH inhibitors may enhance the antiviral activity of ribavirin in vitro by depleting GTP and increasing the rate of incorporation of ribavirin into viral RNA, rendering the virus nonfunctional.
EP 0902782; US 5807876; US 6054472; WO 9740028

The oxidation of 3-methoxy-4-methylnitrobenzene (I) with CrO3, H2SO4 and AC2O in acetic acid gives the gem-diacetate (II), which is hydrolyzed with HCl in refluxing dioxane to yield 2-methoxy-4-nitrobenzaldehyde (III). Cyclization of (III) with tosylmethyl isocyanide and K2CO3 in refluxing methanol affords 3-methoxy-4-(5-oxazolyl)nitrobenzene (IV), which is reduced with H2 over Pd/C in ethyl acetate to provide the corresponding aniline (V). The activation of (V) with carbonyldiimidazole (CDI) in THF gives the carboxamide (VI), which is condensed with 3-(tert-butoxycarbonylaminomethyl)aniline (VII), obtained by reaction of 3-aminobenzylamine with Boc2O, and DMAP in refluxing THF to yield the urea (IX). Deprotection of (IX) with TFA in dichloromethane affords the free benzylamine (X), which is finally condensed with the 3-furyl ester of the succinimidyl-activated carbonate (XI) by means of TEA in dichloromethane/DMF.
…………………
http://www.google.com/patents/EP0902782A1?cl=en
Example 13
(168)
A suspension of 113 (from Example 5) (250mg, 5.76mmol) in CH2CI2 (lrtiL) was treated in a dropwise fashion at ambient temperature with several equivalents of trifluoroacetic acid and stirred for 90mm. The resulting solution was stripped m vacuo and tritrated with CH2CI2 and methanol. Pure product 168 was isolated by filtration in a yield of 258mg (99%) . The -H NMR was consistent with that of the desired product,
(120)
A suspension of 168 (250mg, 0.55mmol) in 21mL of CH2CI2/DMF (20:1 by volume) was treated with tπethyl amme (193μL, 1.38mmol) and stirred at ambient temperature until homogeneity was reached. The solution was cooled to 0 C, treated with (S) 3- tetrahydrofuranyl-N-oxysuccιnιmιdyl carbonate (635mg, 0.608mmol) and allowed to stir overnight with warming to ambient temperature. The mixture was poured into ethyl acetate (500mL), washed with NaHC0 (aq) ( 2x) , water (2x) , and brme(lx), dried over Na2S04 and stripped m vacuo . Pure product 120 was isolated by tπtration (30mL CH2C12, lOO L ether) in a yield of
212mg (85%) . The *H NMR was consistent with that of the desired product.
Org Process Res Dev 2002,6(5),677
http://pubs.acs.org/doi/full/10.1021/op025546f

The desired intermediate 5-(2-methoxy-4-nitrophenyl)oxazole (IV) has been obtained as follows. The carbonylation of 2-methoxy-4-nitrophenyldiazonium tetrafluoroborate (I) by means of carbon monoxide catalyzed by Pd(OAc)2 and Tes-H in ethyl ether/acetonitrile gives 2-methoxy-4-nitrobenzaldehyde (II), which is cyclized with tosylmethyl isocyanate (III) by means of K2CO3 in refluxing methanol to afford the target intermediate 5-(2-methoxy-4-nitrophenyl)oxazole (IV) (see scheme no. 24362801a, intermediate (IV)).

…………
WO 2006122072
http://www.google.com/patents/WO2006122072A2?cl=en
Scheme 2:
-*0-C
2a
2d 2e
2f 2g
2e 2h
Scheme 2A:
2d 2e
2f 2g
2e 2h
Scheme 2A:
2d 2e
2f 2g
2e 2h
Experimental Procedures :
2a toluene/H2O, 5O0C
(S)-tetrahydrofuran-3-yl 3-nitrobenzylcarbamate (2c)
Added 13.84 g Na2CO3 to a 500 ml three neck round bottom flask equipped with a mechanical stirrer, addition funnel, and thermocouple. Then added 86 ml water and stirred until full dissolution at room temperature. 20 g 3-nitrobenzylamine HCl 2b was then added, followed by 154 ml toluene. The mixture was heated to 500C wherein a clear biphasic solution results. Added a 20% w/w solution of (S) -tetrahydrofuran-3-yl chloroformate, 2a (16 g) in toluene (80 ml) dropwise over 45 minutes wherein very little exotherm was noted. The reaction mixture was stirred for an additional 1 hour before the layers were separated at 500C. The mixture was concentrated to ~85 ml, cooled to 00C and stirred for 1 hour at 00C. Precipitated product was collected by filtration and dried for 18 hours at 53°C to give 26.64 g (94.4% yield, 99.90% a/a) of (S)- tetrahydrofuran-3-yl 3-nitrobenzylcarbamate (2c) as a white crystalline solid with consistent 1H NMR (500 MHz, dβ-DMSO) : 8.10 (m, 2H) ; 7.90 (m, IH) ; 7.70 (d, IH) ; 7.62 (t, IH) ; 5.10 (br, IH) ; 4.30 (d, 2H) ; 3.72 (m, 4H) ; 2.10 (m, IH) ; 1.87 (m,
IH) ppm.
£3- [ ( (S) -tetrahydro-furan-S-yloscycarbonylamino) – methyl] -phenyl}-carbamic acid phenyl ester (2e)
2c 2d
2e
Charged 15 g of (S) -tetrahydrofuran-3-yl 3- nitrobenzylcarbamate 2c in 120 ml EtOAc to a IL Parr bomb at room temperature under a blanket of N2. The agitator was started and the vessel pressurized with N2 to 0.75 bar, then the pressure was released. This procedure was repeated 3 times, then the agitator was stopped before adding 0.225 g of 5% Pd/C. The agitator was started, the vessel pressurized with N2 to 0.75 bar, then the pressure was released. This procedure was repeated 3 times, then the agitator was stopped. The vessel was pressurized with H2 to 2 bar, then the pressure was released. This procedure was repeated 3 times, then the vessel was pressurized with H2 to 6.75 bar. The agitator was started and the suspension stirred until complete conversion was evident by HPLC. The H2 pressure was released, the vessel re-pressurized with N2 to 0.75 bar, then the pressure was released. This procedure was repeated 3 times then, the agitator was stopped, the reaction mixture filtered through celite and the filter cake rinsed with 30 ml EtOAc to give crude (S) -tetrahydrofuran-3-yl 3-aminobenzylcarbamate 2d as a solution in EtOAc that was used as is immediately in the next step.
Dissolved 17.6 g of Na2SO4 in 105 ml water at 200C in a separate container. Charged the EtOAc solution of aniline 2d and the aqueous solution of Na2SO4 into a 250 ml glass jacketed vessel purged with N2. The agitator was started to blend the phases and the mixture heated to 500C. Phenyl chloroformate (7.72 ml) was added dropwise to the solution over 1 hour while maintaining the temperature at 500C. The reaction was monitored by HPLC for consumption of 2d and phenyl chloroformate. Once the reaction was complete the agitator was stopped, the phases separated and the agitator restarted. Added 60 ml water at 500C, stirred the contents for 30 minutes at 500C, then stopped the agitator, separated the layers and restarted the agitator.
The reaction mixture was concentrated to 4 volumes, treated with isopropyl acetate (150 ml) , concentrated to 4 volumes, treated with isopropyl acetate (150 ml) , concentrated to 4 volumes, then cooled to 15-200C and stirred for 30 minutes. The slurry was filtered, then dried under house vacuum at 45°C until a constant weight to give 17.72 g (88% yield, 99.86% a/a) of {3- [ ( (S) -tetrahydro-furan-3- yloxycarbonylamino) -methyl] -phenyl} -carbamic acid phenyl ester 2e as a colorless crystalline solid with consistent 1H NMR (500 MHz, de-DMSO) : 10.20 (br, IH); 7.85 (br, IH); 7.40 (m, 4H); 7.25 (t, 2H); 7.20 (d, IH); 6.95 (m, IH); 6.75 (m, IH); 5.15 (m, IH); 4.15 (d, 2H); 3.75 (m, 2H); 3.70 (m, 2H); 2.10(m, IH) ; 1.90 (m, IH) ppm.
{3- [ ( (S) -tβtrahydro-furan-3-yloxycarbonylamino) – methyl] -phenyl}-carbamic acid phenyl ester (2e)
2c
2e
A mixture of 2c (50 g, 1.00 equivalent), 5% Pd/C (0.75 g, 50% water, 0.75 wt %) and isopropyl acetate (400 ml, 8 volumes) was added to a hydrogenation vessel under nitrogen and heated to 60 0C. The vessel was pressurized with hydrogen (1.00 bar overpressure) and the mixture stirred at 60 0C. The reaction was complete within 3 hours. The pressure was released and the vessel purged with nitrogen. The mixture was filtered through a pad of Celite® and then the hydrogenation vessel and pad were rinsed with isopropyl acetate (100 ml, 2 volumes) . The solution of 2d in isopropyl acetate was then combined with a solution of sodium sulfate (29.3 g, 1.10 equivalents) in water (150 ml, 3 vol) and then the mixture was heated to 70 0C. Phenyl chloroformate (25.7 ml, 1.10 equivalents) was then added to the mixture while maintaining a temp, of 70 0C. The reaction was stirred for 30 min after the end of addition and then the stirring was stopped. The phases were allowed to separate and the aqueous phase was removed. Water (150 ml, 3 vol) was then added and the mixture stirred for an additional 30 min before the stirring was stopped. The phases were allowed to separate and the aqueous phase removed. The mixture was then distilled at atmospheric pressure to azeotropically remove water from the organic phase. Compound 2β precipitated from solution when all of the water was removed. Distillation continued until there were 4 volumes of solvent remaining. The mixture was cooled to 20 0C over 5 hours then filtered to isolate the solid. The reactor and filter cake were washed with isopropyl acetate (2 vol) then the cake was dried under vacuum at 50 0C to afford 61. Ig (91%) of 2e. [0112] 3-metho2£y-4-(oxazol-5-yl)benzenainine (2g)
2f 2g
Added 10 g of 5- (2-methoxy-4-nitrophenyl) oxazole 2f to a 500 ml 3-neck flask then added 1.0 g of Nuchar SA.20 charcoal. Next added 200 ml of isopropyl acetate, heated the reaction vessel to 400C under nitrogen, stirred for 2 hours at 400C then heated to 800C and hot filtered to remove the charcoal. The filtrate was concentrated to 1/2 volume on a rotary evaporator before adding the solution to a 500 ml Parr bomb containing 600 mg of 5% Pd/C (50% wet) . The suspension was purged with nitrogen for 20 minutes, then the system was sealed the agitator started. The mixture was heated to 400C while continuing the flow of nitrogen, then the bomb was pressurized to 40 psi with hydrogen. The pressure was released, then the vessel re-pressurized with Hydrogen to 40 psi and the process repeated 3 more times. Finally, 40 psi of hydrogen was maintained until intermediate pressure chromatography showed a complete conversion to 3-methoxy-4- (oxazol-5-yl)benzenamine 2g.
Nitrogen was passed through the reaction, the mixture was cooled to room temperature, filtered through CeIite, rinsed with 20 ml of isopropyl acetate, then the filtrate volume reduced to 1/3 volume on a rotary evaporator under reduced pressure at 47°C. The mixture was cooled to room temperature, charged with 100 ml n-Heptane, the filtrate volume reduced to 1/3 on a rotary evaporator under reduced pressure at 47°C and this process was repeated one more time. The mixture was cooled to room temperature, filtered and dried at 45°C in a house vacuum oven to give 7.91 g of 3-methoxy-4- (oxazol-5- yl)benzenamine 2g (91% yield, 99.7% a/a) as a yellow solid with consistent 1H NMR (500 MHz, d6-DMSO) : 8.20 (s, IH); -7.32
(d, IH); 7.15 (s, IH); 6.31 (s, IH); 6.25 (d, IH); 5.50 (s, 2H) ; 3.80 (s, 3H) ppm.
[0114] 3-methoxy-4- (oxazol-5-yl) benzenamine (2g)
[0115] Compound 2f (50 g, 1.0 eq. , Nippon Soda) and 1% Pt, 2% V on C (2.78 g, 64% wet, 2.0 wt % on a dry basis, Degussa Type CF1082) were charged to a hydrogenation vessel under nitrogen. Ethyl acetate (500 ml, 10 vol) was added and the mixture was heated to 60 0C. The vessel was pressurized with hydrogen (1.00 bar overpressure) and the mixture was stirred at 60 0C. The reaction was complete within 3 hours. The pressure was released and nitrogen was bubbled through the reaction mixture. The reaction mixture was filtered through Celite® and washed with EtOAc (100 ml, 2 vol) . The solvent level was reduced to 4 vol by distillation at reduced pressure and toluene (500 ml, 10 vol) was charged into the vessel. The solvent level was reduced to 4 vol by distillation at reduced pressure and a second portion of toluene (500 ml, 10 vol) was charged into the vessel. The solvent level was reduced to 5 vol under reduced pressure then the mixture was heated to 90 0C at atmospheric pressure to dissolve any solids. The solution was then cooled slowly to 20 0C to induce crystallization. The resulting yellow solid was filtered and washed with toluene (100 ml, 2 vol) to give compound 2g which was dried in a vacuum oven at 50 0C with a nitrogen bleed until a constant weight of 39.4 g (91%) was achieved.
[0116] (S)-tβtrahydrofuran-3-yl 3- (3- (3-methoxy-4- (oκazol- 5-yl)phenyl)ureido)benzylcarbamatβ (2h)
Added 15 g of {3- [ ( (S) -tetrahydro-furan-3- yloxycarbonylamino) -methyl] -phenyl} -carbamic acid phenyl ester 2e and 8.58 g of 3-methoxy-4- (oxazol-5-yl)benzenamine 2g into a 500 ml 3-necked flask and then purged the system with nitrogen before adding 225 ml of ethyl acetate. Next added 5.43 g of diisopropylethylamine over 1 minute, then heated at reflux for 24 hours. Once the reaction was complete, the mixture was cooled to room temperature and stired for an additional 1 hour. Precipitated solid was filtered, washed with 45 ml of EtOAc 2 times, then dried at 58°C for 18 hours (until a LOD is achieved of less than 1%) to give 17.46 g of crude (S) -tetrahydrofuran-3-yl 3- (3- (3-methoxy-4- (oxazol-5- yl) phenyl) ureido)benzylcarbamate 2h (90.4% yield, 98.46% a/a) as a white crystalline solid.
Crude 2h was recrystallized in a 500 ml 3-neck flask by the following procedure. 15 g of 2h was dissolved in 84 ml of NMP and stirred for 10 minutes at 200C. The mixture was heated to 48°C, then MeOH (67.5 ml) was added dropwise over 20 minutes using a syringe pump and the mixture seeded with 0.15 g of crude 2h. The mixture was stirred at 480C for 10 minutes, during which time a thin slurry results. Additional MeOH (88.5 ml) was added dropwise using a syringe pump over 90 minutes at 48°C. After completed addition, the reactor was cooled to 00C over 5 hours and further stirred at 00C for 1 hour. The suspension was filtered, washed 2 times with MeOH (150 ml each) wherein each wash was stirred for 1 hour at ambient temperature and then pressed dry using nitrogen. The solid was dried at 500C in a house vacuum oven for 5 hours to give 11.7 g of
S) -tetrahydrofuran-3-yl 3- (3- (3-methoxy-4- (oxazol-5-yl)phenyl)ureido)benzylcarbamate 2h (78% recovery, 99.93% a/a) as a white crystalline solid with consistent
1H NMR (500 MHz, de-DMSO) : 8.90 (br, IH); 8.75 (br, IH); 8.35 (s, IH); 7.75 (t, IH); 7.60 (d, IH); 7.50 (d, IH); 7.41 (s, IH); 7.38 (m, IH); 7.33 (m, IH); 7.25 (t, IH); 7.05 (d, IH); 6.85 (d, IH); 5.15 (m, IH); 4.15 (d, 2H); 3.90 (s, 3H); 3.77 (m, 2H); 3.70 (m, 2H); 2.10 (m, IH); 1.90 (m, IH) ppm.
(S) -tetrahydrofuran-3-yl 3- (3- (3-methoxy-4- (oxazol- 5-yl)phenyl)ureido)benzylcarbamate (2h)
Added 2e (15 g, 1.0 eq) and 2g (8.58 g, 1.07 eq) into a jacketed reactor of suitable size before adding ethyl acetate (225 ml, 15 vol) and diisopropylethylamine (5.43 g, 1.0 eq) , then heated the mixture to reflux (75-85°C) for 24 hours. Once the reaction was complete, the mixture was cooled to room temperature and stired for an additional 1 hour. Precipitated solid was filtered, washed with EtOAc 2 times (45 ml, 3 vol each wash) , then dried at 580C for 18 hours (until a LOD is achieved of less than 1%) to give 17.46 g of crude 2h
(90.4% yield, 98.46% a/a) as a white crystalline solid. Crude 2h was recrystallized in a 500 ml 3-neck flask by the following procedure. 15 g of 2h was dissolved in 84 ml of NMP and stirred for 10 minutes at 200C. The mixture was heated to 48°C, then MeOH (67.5 ml) was added dropwise over 20 minutes using a syringe pump and the mixture seeded with 0.15 g of crude 2h. The mixture was stirred at 48°C for 10 minutes, during which time a thin slurry results. Additional MeOH (88.5 ml) was added dropwise using a syringe pump over 90 minutes at 48°C. After completed addition, the reactor was cooled to 00C over 5 hours and further stirred at 00C for 1 hour. The suspension was filtered, washed 2 times with MeOH (150 ml each) wherein each wash was stirred for 1 hour at ambient temperature and then pressed dry using nitrogen. The solid was dried at 500C in a house vacuum oven for 5 hours to give 11.7 g of S) -tetrahydrofuran-3-yl 3- (3- (3-methoxy-4- (oxazol-5-yl)phenyl)ureido)benzylcarbamate 2h (78% recovery, 99.93% a/a) as a white crystalline solid with consistent
1H NMR (500 MHz, d6-DMSO) : 8.90 (br, IH); 8.75 (br, IH); 8.35 (s, IH); 7.75 (t, IH); 7.60 (d, IH); 7.50 (d, IH); 7.41 (s, IH); 7.38 (m, IH); 7.33 (m, IH); 7.25 (t, IH); 7.05 (d, IH); 6.85 (d, IH); 5.15 (m, IH); 4.15 (d, 2H); 3.90 (s, 3H); 3.77 (m, 2H); 3.70 (m, 2H); 2.10 (m, IH); 1.90 (m, IH) ppm.
References
1 McHutchison JG, Shiffman ML, Cheung RC, Gordon SC, Wright TL, Pottage JC Jr, McNair L, Ette E, Moseley S, Alam J. A randomized, double-blind, placebo-controlled dose-escalation trial of merimepodib (VX-497) and interferon-alpha in previously untreated patients with chronic hepatitis C. Antivir Ther. 2005;10(5):635-43. PubMed PMID: 16152757.
2: Decker CJ, Heiser AD, Chaturvedi PR, Faust TJ, Ku G, Moseley S, Nimmesgern E. The novel IMPDH inhibitor VX-497 prolongs skin graft survival and improves graft versus host disease in mice. Drugs Exp Clin Res. 2001;27(3):89-95. PubMed PMID: 11447770.
3: Phase II clinical trial of VX-497 for HCV infection begins. AIDS Patient Care STDS. 1998 Dec;12(12):944. PubMed PMID: 11362074.
4: Jain J, Almquist SJ, Shlyakhter D, Harding MW. VX-497: a novel, selective IMPDH inhibitor and immunosuppressive agent. J Pharm Sci. 2001 May;90(5):625-37. PubMed PMID: 11288107.
5: Markland W, McQuaid TJ, Jain J, Kwong AD. Broad-spectrum antiviral activity of the IMP dehydrogenase inhibitor VX-497: a comparison with ribavirin and demonstration of antiviral additivity with alpha interferon. Antimicrob Agents Chemother. 2000 Apr;44(4):859-66. PubMed PMID: 10722482; PubMed Central PMCID: PMC89783
|
11-23-2005
|
Inhibitors of IMPDH enzyme
|
|
|
6-3-2005
|
Inhibitors of serine proteases, particularly HCV NS3-NS4A protease
|
|
|
5-27-2005
|
Combination therapy for HCV infection
|
|
|
4-2-2003
|
Inhibitors of IMPDH enzyme
|
|
|
2-6-2002
|
Inhibitors of IMPDH enzyme
|
|
|
4-26-2000
|
Inhibitors of IMPDH enzyme
|
|
9-24-2008
|
Inosine monophosphate dehydrogenase inhibitory phosphonate compounds
|
|
|
7-4-2008
|
Compositions and methods for treatment of viral diseases
|
|
|
5-28-2008
|
Inhibitors of serine proteases, particularly HCV NS3-NS4A protease
|
|
|
2-13-2008
|
Inhibitors of IMPDH enzyme
|
|
|
9-21-2007
|
Pharmaceutical Compositions
|
|
|
5-11-2007
|
Inhibitors of serine proteases
|
|
|
4-25-2007
|
Inhibitors of serine proteases, particularly HCV NS3-NS4A proteases
|
|
|
11-31-2006
|
Interferon-IgG fusion
|
|
|
9-8-2006
|
Anti-inflammatory phosphonate compounds
|
|
|
4-28-2006
|
Pharmaceutical compositions
|
|
10-2-2009
|
ANTI-INFLAMMATORY PHOSPHONATE COMPOUNDS
|
|
|
9-23-2009
|
Peptide viral entry inhibitors
|
|
|
9-11-2009
|
PHOSPHONATE COMPOUNDS HAVING IMMUNO-MODULATORY ACTIVITY
|
|
|
6-10-2009
|
Processes for preparing biaryl ureas and analogs thereof
|
|
|
4-29-2009
|
Treatments for flaviviridae virus infection
|
|
|
12-31-2008
|
Phosphonate compounds having immuno-modulatory activity
|
|
|
11-19-2008
|
Anti-cancer phosphonate analogs
|
|
|
10-31-2008
|
Hcv Ns3-Ns4a Protease Inhibition
|
|
|
10-8-2008
|
Anti-inflammatory phosphonate compounds
|
|
|
9-31-2008
|
Antiviral phosphonate analogs
|
|
5-14-2010
|
PEPTIDE VIRAL ENTRY INHIBITORS
|
|
|
4-16-2010
|
Compositions and methods for treatment of viral diseases
|
|
|
3-24-2010
|
Inhibitors of serine proteases, particularly HCV NS3-NS4A protease
|
|
|
2-5-2010
|
HEPATITIS C VIRUS INFECTION BIOMARKERS
|
|
|
1-29-2010
|
ANTI-CANCER PHOSPHONATE ANALOGS
|
|
|
1-22-2010
|
FLUIDIZED SPRAY DRYING
|
|
|
1-15-2010
|
COMPOSITIONS AND METHODS FOR TREATMENT OF VIRAL DISEASES
|
|
|
1-13-2010
|
Therapeutic phosphonate compounds
|
|
|
11-27-2009
|
INHIBITORS OF SERINE PROTEASES, PARTICULARLY HCV NS3-NS4A PROTEASE
|
|
|
10-21-2009
|
Polymorphic forms of (S)-1-tetrahydrofuran-3-yl-3-(3-(3-methoxy-4-(oxazol-5-yl)phenyl)ureido)benzyl carbamate
|
| WO1997040028A1 * | Apr 21, 1997 | Oct 30, 1997 | Vertex Pharma | Urea derivatives as inhibitors of impdh enzyme |
| US5807876 * | Apr 23, 1996 | Sep 15, 1998 | Vertex Pharmaceuticals Incorporated | Inhibitors of IMPDH enzyme |
| US6054472 * | Apr 2, 1997 | Apr 25, 2000 | Vertex Pharmaceuticals, Incorporated | Inhibitors of IMPDH enzyme |
| US20020011378 * | Jun 20, 2001 | Jan 31, 2002 | Bailey Jeffrey R. | Acoustic receiver |
|
10-19-2011
|
Inhibitors of serine proteases, particularly HCV NS3-NS4A protease
|
|
|
9-21-2011
|
ANTIVIRAL PHOSPHONATE ANALOGS
|
|
|
7-27-2011
|
Inhibitors of serine proteases
|
|
|
12-31-2010
|
INHIBITORS OF SERINE PROTEASES, PARTICULARLY HCV NS3-NS4A PROTEASE
|
|
|
10-29-2010
|
Inhibitors of Serine Proteases
|
|
|
10-22-2010
|
Pharmaceutical Compositions
|
|
|
10-20-2010
|
TREATMENTS FOR FLAVIVIRIDAE VIRUS INFECTION
|
|
|
8-18-2010
|
PROCESSES FOR PREPARING BIARYL UREAS AND ANALOGS THEREOF
|
|
|
7-9-2010
|
Combination Therapy for the Treatment of HCV Infection
|
|
|
6-30-2010
|
Inhibitors of serine proteases, particularly HCV NS3-NS4A protease
|
Glenmark Kicks Off Monoclonal Antibody Pain Studies
Glenmark Pharmaceuticals S.A., a wholly owned Swiss subsidiary of Glenmark Pharmaceuticals Ltd., announced that GBR 900, a novel monoclonal antibody is entering human trials. GBR 900 targets TrkA, a receptor for nerve growth factor (NGF) involved in chronic pain signaling.
In 2010, Glenmark gained an exclusive worldwide license from Lay Line Genomics S.p.A. (Italy) for anti-TrkA antibodies and their entire intellectual property portfolio in the TrkA field. GBR 900 is the optimized anti-TrkA antibody emerging from this exclusive worldwide license.
read all at
http://www.dddmag.com/news/2014/04/glenmark-kicks-monoclonal-antibody-pain-studies
Glenmark Kicks Off Monoclonal Antibody Pain Studies
Glenmark Pharmaceuticals today said its novel monoclonal antibody for potential treatment of chronic pain is entering human trials.
Tafenoquine…..GSK Launches Phase 3 Malaria Drug Trials

Tafenoquine
N-[2,6-dimethoxy-4-methyl-5-[3-(trifluoromethyl)phenoxy]quinolin-8-yl]pentane-1,4-diamine
Medicines for Malaria Venture
Walter Reed Army Institute (Originator)
April 28, 2014
GlaxoSmithKline (GSK) and Medicines for Malaria Venture (MMV) announced the start of a Phase 3 global program to evaluate the efficacy and safety of tafenoquine, an investigational medicine which is being developed for the treatment and relapse prevention (radical cure) of Plasmodium vivax (P. vivax) malaria.
P. vivax malaria, a form of the disease caused by one of several species of Plasmodium parasites known to infect humans, occurs primarily in South and South East Asia, Latin America and the horn of Africa. Severe anemia, malnutrition and respiratory distress are among the most serious consequences described to be caused by the infection.
The Phase 3 program includes two randomized, double-blind treatment studies to investigate tafenoquine in adult patients with P. vivax malaria. The DETECTIVE study (TAF112582) aims to evaluate the efficacy, safety and tolerability of tafenoquine as a radical cure for P. vivax malaria, co-administered with chloroquine, a blood stage anti-malarial treatment. The GATHER study (TAF116564) aims to assess the incidence of hemolysis and safety and efficacy of tafenoquine compared to primaquine, the only approved treatment currently available for the radical cure of P. vivax malaria.
Tafenoquine is not yet approved or licensed for use anywhere in the world.
“P. vivax malaria can affect people of all ages and is particularly insidious because it has the potential to remain dormant within the body in excess of a year, and causes some patients to experience repeated episodes of illness after the first mosquito bite,” said Nicholas Cammack, head, Tres Cantos Medicines Development Center for Diseases of the Developing World. “Our investigation of tafenoquine for the treatment of P. vivax malaria is part of GSK’s efforts to tackle the global burden of malaria. Working with our partners, including MMV, we are determined to stop malaria in all its forms.”
“One of the big challenges we face in tackling malaria is to have new medicines to prevent relapse, caused by dormant forms of P. vivax,” said Dr. Timothy Wells, MMV’s chief scientific officer. “The Phase 3 program is designed to build upon the promising results of the Phase 2b study which showed that treatment with tafenoquine prevented relapses. If successful, tafenoquine has the potential to become a major contributor to malaria elimination. It’s a great privilege to be working with GSK on this project; they have a clear commitment to changing the face of public health in the countries in which we are working.”

Tafenoquine succinate, Etaquine, SB-252263, WR-238605
in phase 2
Medicines for Malaria Venture
Walter Reed Army Institute (Originator)
Tafenoquine is an 8-aminoquinoline drug manufactured by GlaxoSmithKline that is being investigated as a potential treatment for malaria, as well as for malaria prevention.[1][2]
The proposed indication for tafenoquine is for treatment of the hypnozoite stages of Plasmodium vivax (and also Plasmodium ovale) that are responsible for relapse of these malaria species even when the blood stages are successfully cleared. This is only now achieved by administration of daily primaquine for 14 days. The main advantage of tafenoquine is that it has a long half-life (2–3 weeks) and therefore a single treatment may be sufficient to clear hypnozoites. The shorter regimen has been described as an advantage.[3]
Like primaquine, tafenoquine causes haemolysis in people with G-6-P deficiency.[1] Indeed the long half-life of tafenoquine suggests that particular care should be taken to ensure that individuals with severe deficiency do not receive the drug.
The dose of tafenoquine has not been firmly established, but for the treatment of Plasmodium vivax malaria, a dose of 800 mg over three days has been used.[4]
Synonyms
………………..
US 4431807

Nitration of 1,2-dimethoxybenzene (XXIX) with HNO3/AcOH gives 4,5-dimethoxy-1,2-dinitrobenzene (XXX), which is treated with ammonia in hot methanol to yield 4,5-dimethoxy-2-nitroaniline (XXXI). Cyclization of compound (XXXI) with buten-2-one (XXXII) by means of H3PO4 and H3AsO4 affords 5,6-dimethoxy-4-methyl-8-nitroquinoline (XXXIII), which is selectively mono-demethylated by means of HCl in ethanol to provide 5-hydroxy-6-methoxy-4-methyl-8-nitroquinoline (XXXIV). Reaction of quinoline (XXXIV) with POCl3 gives the corresponding 5-chloro derivative (XXXV), which is condensed with 3-(trifluoromethyl)phenol (IV) by means of KOH to yield the diaryl ether (XXXVI). Finally, the nitro group of (XXXVI) is reduced by means of H2 over PtO2 in THF or H2 over Raney nickel.

Nitration of 2-fluoroanisole (XXXVII) with HNO3/Ac2O gives 3-fluoro-4-methoxynitrobenzene (XXXVIII), which is reduced to the corresponding aniline (XXXIX) with SnCl2/HCl. Reaction of compound (XXXIX) with Ac2O yields the acetanilide (XL), which is nitrated with HNO3 to afford 5-fluoro-4-methoxy-2-nitroacetanilide (XLI). Hydrolysis of (XLI) with NaOH provides 5-fluoro-4-methoxy-2-nitroaniline (XLII), which is cyclized with buten-2-one (XXXII) by means of As2O5 and H3PO4 to furnish 5-fluoro-6-methoxy-4-methyl-8-nitroquinoline (XLIII). Condensation of quinoline (XLIII) with 3-(trifluoromethyl)phenol (IV) by means of K2CO3 gives the diaryl ether (XXXIV), which is finally reduced by means of H2 over PtO2 in THF.
………………..
US 4617394

Reaction of 8-amino-6-methoxy-4-methyl-5-[3-(trifluoromethyl)phenoxy]quinoline (XIV) with phthalic anhydride (XV) affords the phthalimido derivative (XVI), which is oxidized with MCPBA to yield the quinoline N-oxide (XVII). Treatment of compound (XVII) with neutral alumina gives the quinolone derivative (XVIII), which by reaction with POCl3 in refluxing CHCl3 provides the 2-chloroquinoline derivative (XIX). Alternatively, reaction of the quinoline N-oxide (XVII) with POCl3 as before also gives the 2-chloroquinoline derivative (XIX) The removal of the phthalimido group of compound (XIX) by means of hydrazine in refluxing ethanol gives the chlorinated aminoquinoline (XX), which is finally treated with MeONa in hot DMF.
……………….
US 6479660; WO 9713753

Chlorination of 6-methoxy-4-methylquinolin-2(1H)-one (I) with SO2Cl2 in hot acetic acid gives the 5-chloro derivative (II), which is nitrated with HNO3 in H2SO4 to yield the 8-nitroquinolinone (III). Condensation of compound (III) with 3-(trifluoromethyl)phenol (IV) by means of KOH in NMP provides the diaryl ether (V), which is treated with refluxing POCl3 to afford the 2-chloroquinoline (VI). Reaction of compound (VI) with MeONa in refluxing methanol results in the 2,6-dimethoxyquinoline derivative (VII), which is reduced with hydrazine over Pd/C to give the 8-aminoquinoline derivative (VIII). Condensation of aminoquinoline (VIII) with N-(4-iodopentyl)phthalimide (IX) by means of diisopropylamine in hot NMP yields the phthalimido precursor (X), which is finally cleaved with hydrazine in refluxing ethanol.

Reaction of 1,4-dibromopentane (XI) with potassium phthalimide (XII) gives N-(4-bromopentyl)phthalimide (XIII), which is then treated with NaI in refluxing acetone.

Reaction of 4-methoxyaniline (XXI) with ethyl acetoacetate (XXII) by means of triethanolamine in refluxing xylene gives the acetoacetanilide (XXIII), which is cyclized by means of hot triethanolamine and H2SO4 to yield 6-methoxy-4-methylquinolin-2(1H)-one (I), which is treated with refluxing POCl3 to provide 2-chloro-6-methoxy-4-methylquinoline (XXIV). Reaction of compound (XXIV) with SO2Cl2 in hot AcOH affords 2,5-dichloro-6-methoxy-4-methylquinoline (XXV), which is treated with MeONa in refluxing methanol to furnish 5-chloro-2,6-dimethoxy-4-methylquinoline (XXVI). Alternatively, the reaction of compound (XXIV) with MeONa as before gives 2,6-dimethoxy-4-methylquinoline (XXVII), which is treated with SO2Cl2 in hot AcOH to give the already described 5-chloro-2,6-dimethoxy-4-methylquinoline (XXVI). Nitration of compound (XXVI) with KNO3 and P2O5 gives the 8-nitroquinoline derivative (XXVIII), which is condensed with 3-(trifluoromethyl)phenol (IV) by means of KOH in hot NMP to yield the diaryl ether (VII). Finally, the nitro group of compound (VII) is reduced with hydrazine over Pd/C.
//////////////////////
J Med Chem 1989,32(8),1728-32

Synthesis of the intermediate diazepinone (IV) is accomplished by a one-pot synthesis. Condensation of 2-chloro-3-aminopyridine (I) with the anthranilic ester (II) is effected in the presence of potassium tert-butoxide as a catalyst. The resulting anthranilic amide (III) is cyclized under the influence of catalytic amounts of sulfuric acid. Treatment of (IV) with chloroacetylchloride in toluene yields the corresponding choroacetamide (V). The side chain of AQ-RA 741 is prepared starting from 4-picoline, which is alkylated by reaction with 3-(diethylamino)propylchloride in the presence of n-butyllithium. Hydrogenation of (VIII) using platinum dioxide as a catalyst furnishes the diamine (IX), which is coupled with (V) in the presence of catalytic amounts of sodium iodide in acetone leading to AQ-RA 741 as its free base.
- Shanks GD, Oloo AJ, Aleman GM et al. (2001). “A New Primaquine Analogue, Tafenoquine (WR 238605), for prophylaxis against Plasmodium falciparum malaria”. Clin Infect Dis 33 (12): 1968–74. doi:10.1086/324081. JSTOR 4482936.PMID 11700577.
- Lell B, Faucher JF, Missinou MA et al. (2000). “Malaria chemoprophylaxis with tafenoquine: a randomised study”.Lancet 355 (9220): 2041–5. doi:10.1016/S0140-6736(00)02352-7. PMID 10885356.
- Elmes NJ, Nasveld PE, Kitchener SJ, Kocisko DA, Edstein MD (November 2008). “The efficacy and tolerability of three different regimens of tafenoquine versus primaquine for post-exposure prophylaxis of Plasmodium vivax malaria in the Southwest Pacific”. Transactions of the Royal Society of Tropical Medicine and Hygiene 102 (11): 1095–101.doi:10.1016/j.trstmh.2008.04.024. PMID 18541280.
- Nasvelda P, Kitchener S. (2005). “Treatment of acute vivax malaria with tafenoquine”. Trans R Soc Trop Med Hyg 99 (1): 2–5. doi:10.1016/j.trstmh.2004.01.013. PMID 15550254.
- Peters W (1999). “The evolution of tafenoquine–antimalarial for a new millennium?”. J R Soc Med 92 (7): 345–352.PMID 10615272.
- J Med Chem 1982,25(9),1094
|
8-3-2007
|
Methods and compositions for treating diseases associated with pathogenic proteins
|
|
|
12-6-2006
|
Process for the preparation of quinoline derivatives
|
|
|
3-14-2002
|
PROCESS FOR THE PREPARATION OF ANTI-MALARIAL DRUGS
|
|
|
4-2-1998
|
MULTIDENTATE METAL COMPLEXES AND METHODS OF MAKING AND USING THEREOF
|
|
|
4-18-1997
|
PROCESS FOR THE PREPARATION OF ANTI-MALARIAL DRUGS
|
|
|
12-20-1996
|
MULTIDENTATE METAL COMPLEXES AND METHODS OF MAKING AND USING THEREOF
|
|
|
12-15-1993
|
Use of interferon and a substance with an antimalarial activity for the treatment of malaria infections
|
|
|
10-15-1986
|
4-methyl-5-(unsubstituted and substituted phenoxy)-2,6-dimethoxy-8-(aminoalkylamino) quinolines
|
FDA Approves Zykadia, Ceritinib, LDK378 for ALK-Positive NSCLC


Acting 4 months ahead of schedule, the FDA has granted an accelerated approval to ceritinib (Zykadia; LDK378) as a treatment for patients with ALK-positive metastatic non-small cell lung cancer (NSCLC) following treatment with crizotinib (Xalkori), based on a single-arm clinical trial demonstrating a durable improvement in overall response rates (ORR).
The approval for the second-generation ALK inhibitor was supported by results from an analysis of 163 patients treated with single-agent ceritinib at 750 mg daily following progression on crizotinib. In these select patients, the ORR was 54.6% with a 7.4-month median duration of response, according to data submitted to the FDA by Novartis, the company developing the drug. Based on these findings, the FDA granted ceritinib a Breakthrough Therapy designation, Priority Review, and orphan product designation.
“Today’s approval illustrates how a greater understanding of the underlying molecular pathways of a disease can lead to the development of specific therapies aimed at these pathways,” Richard Pazdur, MD, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, said in a statement. “It also demonstrates the FDA’s commitment to working cooperatively with companies to expedite a drug’s development, review and approval, reflecting the promise of the breakthrough therapy designation program.”
In the study that was the basis for the approval, the primary endpoint was ORR by RECIST criteria with a secondary outcome measure of duration of response. Treatment with ceritinib resulted in an ORR of 54.6% by investigator assessment with a median duration of response of 7.4 months. By blinded independent central review, the ORR was 43.6% and the duration of response was 7.1 months.
Earlier this year, results from a dose escalation study that examined ceritinib in 130 patients who were untreated or refractory to crizotinib were published in the New England Journal of Medicine. In this analysis for patients who received doses of at least 400 mg (n = 114), the ORR was 58%. Patients who had progressed on crizotinib (n = 80) experienced an ORR of 56% and those who were crizotinib-naïve (n =34) had an ORR of 62%.
The median progression-free survival was 7.0 months and the median duration of response was 8.2 months (95% CI; 6.9-11.4). Additionally, responses were seen in patients with untreated metastatic brain lesions who progressed on prior therapy with crizotinib, the authors of the study noted.
The most frequent adverse events were nausea (82%), diarrhea (75%), vomiting (65%), fatigue (47%) and increased alanine aminotransferase levels (35%). These adverse events were generally mild and resolved when treatment stopped or the dose was reduced.
The most common grade 3 or 4 drug-related adverse events were increased alanine aminotransferase levels (21%), increased aspartate aminotransferase levels (11%), diarrhea (7%) and increased lipase levels (7%), all of which were reversible upon treatment discontinuation.
“Zykadia represents an important treatment option for ALK-positive NSCLC patients who relapse after starting initial therapy with crizotinib,” Alice Shaw, MD, PhD, of the Massachusetts General Hospital (MGH) Cancer Center, lead author of the report, said in a statement. “This approval will affect the way we manage and monitor patients with this type of lung cancer, as we will now be able to offer them the opportunity for continued treatment response with a new ALK inhibitor.”
Two phase III studies are enrolling patients to further explore the efficacy and safety of ceritinib in patients with ALK-positive NSCLC. These studies will likely act as confirmation for the accelerated approval. In the first, ceritinib will be compared with chemotherapy in untreated patients with ALK-rearranged NSCLC (NCT01828099). The second will compare ceritinib to chemotherapy in ALK-positive patients with NSCLC following progression on chemotherapy and crizotinib (NCT01828112).
“The approval of Zykadia less than three and a half years after the first patient entered our clinical trial exemplifies what is possible with a highly focused approach to drug development and strong collaboration,” Alessandro Riva, MD, president of Novartis Oncology ad interim and global head of Oncology Development and Medical Affairs, said in a statement. “The dedication of clinical investigators, patients, the FDA and others has enabled us to bring this medicine to patients in need as swiftly as possible.”


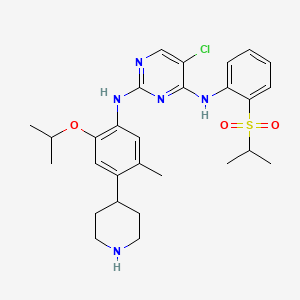
Nitration of 2-chloro-4-fluoro-1-methylbenzene with KNO3 in the presence of H2SO4 gives 1-chloro-5-fluoro-2-methyl-4-nitrobenzene , which upon condensation with isopropyl alcohol in the presence of Cs2CO3 in 2-PrOH at 60 °C yields 5-isopropoxy-2-methyl-4-nitrobenzene .
Suzuki coupling of chloride with 4-pyridineboronic acid in the presence of Pd2dba3, K3PO4 and SPhos in dioxane/water at 150 °C (microwave irradiation) provides 4-(5-isopropoxy-2-methyl-4-nitrophenyl)pyridine , which is then subjected to global reduction using H2 over PtO2 in the presence of TFA in AcOH to afford 2-isopropoxy-5-methyl-4-piperidin-4-ylaniline .
N-Protection of piperidine with Boc2O in the presence of Et3N in CH2Cl2 furnishes the corresponding carbamate (VIII), which upon Buchwald-Hartwig cross coupling with 2,5-dichloropyrimidine derivative (prepared by condensation of 2-(isopropylsulfonyl)aniline and 2,4,5-trichloropyrimidine in the presence of NaH in DMSO/DMF) in the presence of Pd(OAc)2, Xantphos and Cs2CO3 in THF affords Boc-protected ceritinib . Finally, removal of Boc-group in compound using TFA in CH2Cl2 furnishes the target compound ceritinib
/////////////////

Anaplastic lymphoma kinase (ALK), a member of the insulin receptor superfamily of receptor tyrosine kinases, has been implicated in oncogenesis in hematopoietic and non- hematopoietic tumors. The aberrant expression of full-length ALK receptor proteins has been reported in neuroblastomas and glioblastomas; and ALK fusion proteins have occurred in anaplastic large cell lymphoma. The study of ALK fusion proteins has also raised the possibility of new therapeutic treatments for patients with ALK-positive malignancies. (Pulford et al., Cell. MoI. Life Sci. 61:2939-2953 (2004)).
Focal Adhesion Kinase (FAK) is a key enzyme in the integrin-mediated outside-in signal cascade (D. Schlaepfer et al., Prog Biophys MoI Biol 1999, 71, 43578). The trigger in the signal transduction cascade is the autophosphorylation of Y397. Phosphorylated Y397 is a SH2 docking site for Src family tyrosine kinases; the bound c-Src kinase phosphorylates other tyrosine residues in FAK. Among them, phsophorylated Y925 becomes a binding site for the SH2 site of Grb2 small adaptor protein. This direct binding of Grb2 to FAK is one of the key steps for the activation of down stream targets such as the Ras-ERK2/MAP kinase cascade.
Zeta-chain-associated protein kinase 70 (ZAP-70), a member of the protein tyrosine kinase family, is of potential prognostic importance in chronic lymphocytic leukemia (CLL). ZAP-70, known to be of importance in T and NK cell signaling but absent in normal peripheral B cells, is expressed in the majority of the poorer prognosis unmutated CLL and absent in most cases with mutated IgVH genes. ZAP-70 is also expressed in a minority of other B cell tumors. (Orchard et al., Leuk. Lymphoma 46:1689-98 (2005)). [0006] Insulin- like growth factor (IGF-I) signaling is highly implicated in cancer, with the IGF-I receptor (IGF-IR) as the predominating factor. IGR-IR is important for tumor transformation and survival of malignant cells, but is only partially involved in normal cell growth. Targeting of IGF-IR has been suggested to be a promising option for cancer therapy. (Larsson et al., Br. J. Cancer 92:2097-2101 (2005)).
Because of the emerging disease-related roles of ALK, FAK, ZAP-70 and IGF-IR, there is a continuing need for compounds which may be useful for treating and preventing a disease which responds to inhibition of ALK, FAK, ZAP-70 and/or IGF-IR
The compound 5-Chloro-N2-(2-isopropoxy-5-methyl-4-piperidin-4-yl-phenyl)-N4-[2- (propane-2-sulfonyl)-phenyl]-pyrimidine-2, 4-diamine, in the form of a free base, of formula
(I)
is an anaplastic lymphoma kinase (ALK) inhibitor, a member of the insulin receptor super family of receptor tyrosine kinases. Compound I was originally described in WO 2008/073687 Al as Example 7, compound 66. WO 2008/073687 Al , however, provides no information about crystalline forms of 5-
Chloro-N2-(2-isopropoxy-5-methyl-4-piperidin-4-yl-phenyl)-N4-[2-(propane-2-sulfonyl)- phenyl]-pyriniidine-2, 4-diamine or its corresponding salts. Crystalline forms of 5-Chloro-N2- (2-isopropoxy-5-methyl-4-piperidin-4-yl-phenyl)-N4-[2-(propane-2-sulfonyl)-phenyl]- pyrimidine-2, 4-diamine have been discovered, which are useful in treating diseases which respond to inhibition of anaplastic lymphoma kinase activity, focal adhesion kinase (FAK), zeta- chain-associated protein kinase 70 (ZAP-70) insulin-like growth factor (IGF-1 or a
combination thereof. The crystalline forms exhibit new physical properties that may be exploited in order to obtain new pharmacological properties, and that may be utilized in the drug product development of 5-Chloro-N2-(2-isopropoxy-5-methyl-4-piperidin-4-yl-phenyl)-N4-[2- (propane-2-sulfonyl)-phenyl]-pyrimidine-2, 4-diamine.
…………………….
WO 2008073687
http://www.google.com/patents/WO2008073687A2?cl=en
Example 7
5-Chloro-N2-(2-isopropoxy-5-methyl-4-piperidin-4-yl-phenyl)-N4-r2-(propane-2-sulfonyl)- phenvH-pyrimidine-2,4-diamine (66)
1 : 4-(5-Isopropoxv-2-methvl-4-nitro-phenyl)-pvridine
[0111] 4-Pyridineboronic acid (147 mg, 1.20 mmol, 1.1 equiv.) is dissolved in a 2:1 v/v mixture of dioxane and H2O (15 mL) and N2 is bubbled through for 5 minutes. Tris(dibenzylidene acetone)dipalladium (0) (100 mg, 0.109 mmol, 0.1 equiv.), 2- dicyclohexylphosphine-2′-6′-dimethoxy biphenyl (112 mg, 0.272 mmol, 0.25 equiv.), 1-chloro- 5-isopropoxy-2-methyl-4-nitro-benzene (Intermediate 4, 250 mg, 1.09 mmol, 1.0 equiv.) and K3PO4 (462 mg, 2.18 mmol, 2.0 equiv.) are added under a N2 blanket. The reaction vessel is sealed and heated with microwave irradiation to 150 0C for 20 min. After cooling to room temperature, the reaction is diluted with ethyl acetate and washed with 1 N aqueous NaOH (2x), the organic layer is then dried over Na2SO4 and filtered. After concentration, the crude product is purified by silica gel chromatography (gradient from hexanes to 30% ethyl acetate in hexanes) to give 4-(5-Isopropoxy-2-methyl-4-nitro-phenyl)-pyridine as a brown solid: ESMS m/z 273.1 (M + H+).
Steps 2 and 3 : 4-(4-Amino-5-isopropoxy-2-methyl-phenyl)-piperidine-l-carboxylic acid tert- butyl ester
[0112] 4-(5-Isopropoxy-2-methyl-4-nitro-phenyl)-pyridine from the previous step(438 mg, 1.61 mmol) dissolved in acetic acid (30 mL) is treated with TFA (0.24 mL, 3.22 mmol) and PtO2 (176 mg, 40% w/w). The reaction mixture is vigorously stirred under 1 atm. H2 for 36 hours. The reaction mixture is filtered and the filtrate is concentrated under vacuum. The resulting residue is diluted with ethyl acetate and washed with 1 N aqueous NaOH (2x), the organic layer is then dried over Na2SO4 and filtered. After concentration, the crude product (391 mg) is dissolved in anhydrous CH2Cl2 (30 mL). TEA is added (0.44 mL, 3.15, 2 equiv.) followed by Boc2O (344 mg, 1.57 equiv, 1 equiv.). The reaction is stirred at room temperature for 30 min. The reaction is concentrated under vacuum. The resulting residue is purified by silica gel chromatography (gradient from hexanes to 30% ethyl acetate in hexanes) to give 4-(4-amino-5- isopropoxy-2-methyl-phenyl)-piperidine-l-carboxylic acid tert-butyl ester as a sticky foam: ESMS m/z 293.1 (M-?Bu+H)+.
Steps 4 and 5
[0113] 4-(4-Amino-5-isopropoxy-2-methyl-phenyl)-piperidine-l-carboxylic acid tert-butyl ester (170 mg, 0.488 mmol) from the previous step, (2,5-Dichloro-pyrimidin-4-yl)-[2-(propane- 2-sulfonyl)-phenyl]-amine (Intermediate 2, 169 mg, 0.488 mmol, 1 equiv.), xantphos (28 mg, 0.049 mmol, 0.1 equiv.), palladium acetate (5.5 mg, 0.024 mmol, 0.05 equiv.), and Cs2CO3 (477 mg, 1.46 mmol, 3 equiv.) are dissolved in anhydrous THF (6 mL). N2 is bubbled through the reaction mixture for 5 minutes and then the reaction vessel is sealed and heated with microwave irradiation to 150 0C for 20 min. The reaction is filtered and the filtrate concentrated under vacuum. After concentration, the crude product is purified by silica gel chromatography (gradient from hexanes to 30% ethyl acetate in hexanes) to give 4-(4-{5-chloro-4-[2-(propane-2- sulfonyl)-phenylamino]-pyrimidin-2-ylamino}-5-isopropoxy-2-methyl-phenyl)-piperidine-l- carboxylic acid tert-butyl ester as a yellow film: ESMS m/z 658.3 (M + H+). This product (105 mg, 0.160 mmol) is dissolved in CH2Cl2 (3 mL) and treated with TFA (3 mL). After 45 min., the reaction is concentrated under vacuum. 1 N HCl in Et2O (5 mL x 2) is added causing the product HCl salt to precipitate. The solvent is removed by decantation. The resulting 5- Chloro-N2-(2-isopropoxy-5-methyl-4-piperidin-4-yl-phenyl)-N4-[2-(propane-2-sulfonyl)- phenyl]-pyrimidine-2,4-diamine (66) is dried under high vacuum, generating an off-white powder: 1H NMR (400 MHz, DMSO-J6+ trace D2O) δ 8.32 (s, IH), 8.27 (d, IH), 7.88 (d, IH), 7.67 (dd, IH), 7.45 (dd, IH), 7.42 (s, IH), 6.79 (s, IH), 4.56-4.48 (m, IH), 3.49-3.32 (m, 3H), 3.10-2.91 (m, 3H), 2.09 (s, 3H), 1.89-1.77 (m, 4H), 1.22 (d, 6H), 1.13 (d, 6H); ESMS m/z 558.1 (M + H+).
 66
66
……………………..
WO 2012082972
http://www.google.com/patents/WO2012082972A1
EXAMPLE 1
Preparation of Form A of 5-chloro-N-(2-isopropoxy-5-methyl-4-(piperidin-4-ylphenyl)-N-2- (isopropylsulfonyl phenyl)-2^-diamine
5-chloro-N-(2-isopropoxy-5-methyl-4-(piperidin-4-ylphenyl)-N-2-(isopropylsulfonyl)phenyl)- 2,4-diamine di-hydrochloride salt
The compound 2-isopropoxy-5-methyl-4-(piperdin-4-yl) aniline dihydrochloride (33.00 g, 85.25 mmol) and 2,5-dichloro-N-(2-(isopropyl sulfonyl )phenyl)pyrimidin-4-amine (32.53 g) was added to a 3 -necked 500-mL round-bottomed flask equipped with mechanical stirring, thermocouple, reflux condenser and N2 inlet-outlet. A solvent, 2-propanol (255.0 g, 325 mL), was added and the mixture to heated to reflux at 82±2 °C and stirred for at least 14 hours. The mixture was cooled to 22±3 °C over 1 hour and stirred at 22±3 °C for 3 hours. The resulting solids were filtered and rinsed with 3 x 40 g (3 x 51 mL) of 2-propanol. The solids were dried at 50±5 °C/10 mbar for 16 hours to yield 44.63 g of 5-chloro-N-(2-isopropoxy-5-methyl-4- (piperidin-4-ylphenyl)-N-2-(isopropylsulfonyl)phenyl)-2,4-diamine di-hydrochloride salt. Chemical Purity (as determined by HPLC): 97.3%. Corrected yield: 71.6%. LOD = 11.60%. The dihydrochloride salt was recrystallized using acetone:water (10:l,v/v). Chemical Purity (as determined by HPLC): 98.8%.
…………….
J Med Chem 2013, 56(14): 5675
http://pubs.acs.org/doi/abs/10.1021/jm400402q

Synthesis of 5-Chloro-N2-(2-isopropoxy-5-methyl-4-piperidin-4-ylphenyl)-N4-[2-(propane-2-sulfonyl)phenyl]pyrimidine-2,4-diamine 15b
|
10-21-2011
|
COMPOUNDS AND COMPOSITIONS AS PROTEIN KINASE INHIBITORS
|
|
|
10-21-2011
|
COMPOUNDS AND COMPOSITIONS AS PROTEIN KINASE INHIBITORS
|
|
|
10-19-2011
|
COMPOUNDS AND COMPOSITIONS AS PROTEIN KINASE INHIBITORS
|
|
|
8-5-2011
|
COMPOUNDS AND COMPOSITIONS AS PROTEIN KINASE INHIBITORS
|
Water molecules control inactivation and recovery of potassium channels

Depiction of simulated potassium channel and surrounding environment. Potassium ions (green) are unable to pass through because water molecules (red and white) are present inside the protein, locking the channel into an inactivated state. Credit: Benoit Roux, University of Chicago
Just 12 molecules of water cause the long post-activation recovery period required by potassium ion channels before they can function again. Using molecular simulations that modeled a potassium channel and its immediate cellular environment, atom for atom, University of Chicago scientists have revealed this new mechanism in the function of a nearly universal biological structure, with implications ranging from fundamental biology to the design of pharmaceuticals. Their findings were published online July 28 in Nature.
“Our research clarifies the nature of this previously mysterious inactivation state. This gives us better understanding of fundamental biology and should improve the rational design of drugs, which often target the inactivated state of…
View original post 339 more words

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....