Home » Posts tagged 'Bayer HealthCare'
Tag Archives: Bayer HealthCare
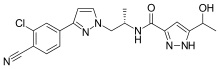
DAROLUTAMIDE даролутамид , دارولوتاميد , 达罗他胺 , ダロルタミド
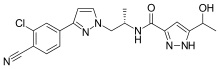

Darolutamide
N-((S)-1-(3-(3-Chloro-4-cyanophenyl)-1H-pyrazol-1-yl)-propan-2-yl)-5-(1-hydroxyethyl)-1H-pyrazole-3-carboxamide
N-((S)- 1 -(3-(3-chloro-4-cyanophenyl)- lH-pyrazol- 1 -yl)-propan-2-yl)-5-(l-hydroxyethyl)-lH-pyrazole-3-carboxamide
- MF C19H19ClN6O2
- MW 398.846
BAY 1841788; ODM-201

Orion and licensee Bayer are codeveloping darolutamide (ODM-201, BAY-1841788), an androgen receptor antagonist, for the potential treatment of castration-resistant prostate cancer (CRPC) and metastatic hormone-sensitive prostate cancer (HSPC) .
In September 2014, a phase III trial (ARAMIS) was initiated for non-metastatic CRPC; in April 2018, the trial was ongoing . In November 2016, a phase III trial in metatstic HSPC (ARASENS) was initiated .
PRODUCT PATENT
US-09657003 provides patent protection until May 2032.
Priority date 2009-10-27
InventorGerd WohlfahrtOlli TörmäkangasHarri SaloIisa HöglundArja KarjalainenPia KoivikkoPatrik HolmSirpa RaskuAnniina Vesalainen Current Assignee Orion Corp Original AssigneeOrion Corp
05-May-2011 WO-2011051540-A1, Priority date 2009-10-27
| Patent ID | Patent Title | Submitted Date | Granted Date |
|---|---|---|---|
| US8921378 | Androgen receptor modulating carboxamides |
2012-04-20
|
2014-12-30
|
| US8975254 | ANDROGEN RECEPTOR MODULATING COMPOUNDS |
2010-10-27
|
2012-09-06
|
| US2017260206 | ANDROGEN RECEPTOR MODULATING COMPOUNDS |
2017-04-13
|
|
| US9657003 | ANDROGEN RECEPTOR MODULATING COMPOUNDS |
2015-01-16
|
2015-07-23
|
PHASE III
In September 2014, the double-blind, randomized, placebo-controlled, phase III trial (NCT02200614; ; ARAMIS) began to evaluate the safety and efficacy of darolutamide in patients (expected n = 1500, Taiwanese n = 20) in the US, Argentina, Australia, Brazil, Canada, Europe, Israel, Japan, Peru, South Korea, Russian Federation, South Africa, Taiwan and Turkey with non-metastatic CRPC. The primary endpoint was metastasis-free survival (MFS), defined as time between randomization and evidence of metastasis or death from any cause . In April 2018, the trial was expected to complete in September 2018

- Originator Orion
- Developer Bayer HealthCare; Orion
- Class Antineoplastics
- Mechanism of Action Androgen receptor antagonists
- Phase III Prostate cancer
-
Most Recent Events
- 03 Jun 2016 Bayer and Orion plan the phase III ARASENS trial for Prostate cancer
- 03 Jun 2016 Bayer and Orion expand the licensing agreement to include joint development of ODM 201 for Metastatic hormone-sensitive prostate cancer (mHSPC)
- 06 May 2016 Long-term combined adverse events data from the the ARADES (phase I/II) and the ARAFOR (phase I) trials in Prostate cancer presented at the 111th Annual Meeting of the American Urological Association (AUA -2016)
Darolutamide (INN) (developmental code names ODM-201, BAY-1841788) is a non-steroidal antiandrogen, specifically, a full and high-affinity antagonist of the androgen receptor (AR), that is under development by Orion and Bayer HealthCare[1] for the treatment of advanced, castration-resistant prostate cancer (CRPC).[2][3]
Orion and licensee Bayer are co-developing darolutamide, an androgen receptor antagonist, for treating castration-resistant prostate cancer and metastatic hormone-sensitive prostate cancer. In August 2016, darolutamide was reported to be in phase 3 clinical development. The drug appears to be first disclosed in WO2011051540, claiming novel heterocyclic derivatives as tissue-selective androgen receptor modulators, useful for the treatment of prostate cancer.

Mode of action
Relative to enzalutamide (MDV3100 or Xtandi) and apalutamide (ARN-509), two other recent non-steroidal antiandrogens, darolutamide shows some advantages.[3] Darolutamide appears to negligibly cross the blood-brain-barrier.[3] This is beneficial due to the reduced risk of seizures and other central side effects from off-target GABAA receptor inhibition that tends to occur in non-steroidal antiandrogens that are structurally similar to enzalutamide.[3] Moreover, in accordance with its lack of central penetration, darolutamide does not seem to increase testosterone levels in mice or humans, unlike other non-steroidal antiandrogens.[3] Another advantage is that darolutamide has been found to block the activity of all tested/well-known mutant ARs in prostate cancer, including the recently-identified clinically-relevant F876L mutation that produces resistance to enzalutamide and apalutamide.[3] Finally, darolutamide shows higher affinity and inhibitory efficacy at the AR (Ki = 11 nM relative to 86 nM for enzalutamide and 93 nM for apalutamide; IC50 = 26 nM relative to 219 nM for enzalutamide and 200 nM for apalutamide) and greater potency/efficaciousness in non-clinical models of prostate cancer.[3]
ORM-15341 is the main active metabolite of darolutamide.[3] It, similarly, is a full antagonist of the AR, with an affinity (Ki) of 8 nM and an IC50 of 38 nM.[3]

Clinical trials
Darolutamide has been studied in phase I and phase II clinical trials and has thus far been found to be effective and well-tolerated,[4] with the most commonly reported side effects including fatigue, nausea, and diarrhea.[5][6] No seizures have been observed.[6][7] As of July 2015, darolutamide is in phase III trials for CRPC.[3]
Representative binding affinities of ODM-201, ORM-15341, enzalutamide, and ARN-509 measured in competition with [3H]mibolerone using wtAR isolated from rat ventral prostates (C). All data points are means of quadruplicates ±SEM. Ki values are presented in parentheses. D. Antagonism to wtAR was determined using AR-HEK293 cells treated with ODM-201, ORM-15341, enzalutamide, or ARN-509 together with 0.45 nM testosterone in steroid-depleted medium for 24 hours before luciferase activity measurements. All data points are means of triplicates ±SEM. IC50 values are presented in parentheses.
WHIPPANY, N.J., Sept. 16, 2014 /PRNewswire/ — Bayer HealthCare and Orion Corporation, a pharmaceutical company based in Espoo, Finland, have begun to enroll patients in a Phase III trial with ODM-201, an investigational oral androgen receptor inhibitor in clinical development. The study, called ARAMIS, evaluates ODM-201 in men with castration-resistant prostate cancer who have rising Prostate Specific Antigen (PSA) levels and no detectable metastases. The trial is designed to determine the effects of the treatment on metastasis-free survival (MFS).
“The field of treatment options for prostate cancer patients is evolving rapidly. However, once prostate cancer becomes resistant to conventional anti-hormonal therapy, many patients will eventually develop metastatic disease,” said Dr. Joerg Moeller, Member of the Bayer HealthCare Executive Committee and Head of Global Development. “The initiation of a Phase III clinical trial for ODM-201 marks the starting point for a potential new treatment option for patients whose cancer has not yet spread. This is an important milestone for Bayer in our ongoing effort to meet the unmet needs of men affected by prostate cancer.”
Earlier this year, Bayer and Orion entered into a global agreement under which the companies will jointly develop ODM-201, with Bayer contributing a major share of the costs of future development. Bayer will commercialize ODM-201 globally, and Orion has the option to co-promote ODM-201 in Europe. Orion will be responsible for the manufacturing of the product.
About the ARAMIS Study
The ARAMIS trial is a randomized, Phase III, multicenter, double-blind, placebo-controlled trial evaluating the safety and efficacy of oral ODM-201 in patients with non-metastatic CRPC who are at high risk for developing metastatic disease. About 1,500 patients are planned to be randomized in a 2:1 ratio to receive 600 mg of ODM-201 twice a day or matching placebo. Randomisation will be stratified by PSA doubling time (PSADT less than or equal to 6 months vs. > 6 months) and use of osteoclast-targeted therapy (yes vs. no).
The primary endpoint of this study is metastasis-free survival (MFS), defined as time between randomization and evidence of metastasis or death from any cause. The secondary objectives of this study are overall survival (OS), time to first symptomatic skeletal event (SSE), time to initiation of first cytotoxic chemotherapy, time to pain progression, and characterization of the safety and tolerability of ODM-201.
About ODM-201
ODM-201 is an investigational androgen receptor (AR) inhibitor that is thought to block the growth of prostate cancer cells. ODM-201 binds to the AR and inhibits receptor function by blocking its cellular function.
About Oncology at Bayer
Bayer is committed to science for a better life by advancing a portfolio of innovative treatments. The oncology franchise at Bayer now includes three oncology products and several other compounds in various stages of clinical development. Together, these products reflect the company’s approach to research, which prioritizes targets and pathways with the potential to impact the way that cancer is treated.
About Bayer HealthCare Pharmaceuticals Inc.
Bayer HealthCare Pharmaceuticals Inc. is the U.S.-based pharmaceuticals business of Bayer HealthCare LLC, a subsidiary of Bayer AG. Bayer HealthCare is one of the world’s leading, innovative companies in the healthcare and medical products industry, and combines the activities of the Animal Health, Consumer Care, Medical Care, and Pharmaceuticals divisions. As a specialty pharmaceutical company, Bayer HealthCare provides products for General Medicine, Hematology, Neurology, Oncology and Women’s Healthcare. The company’s aim is to discover and manufacture products that will improve human health worldwide by diagnosing, preventing and treating diseases.
Bayer® and the Bayer Cross® are registered trademarks of Bayer.
SYNTHESIS

cas 1297538-32-9
Synthesis
WO 2016162604

POLYMORPH
CRYSTALLINE FORM I, I’, I” IN WO-2016120530

PATENTS
WO2011051540
https://www.google.com/patents/WO2011051540A1?cl=en
PATENT
US 2015203479
http://www.google.com/patents/WO2011051540A1?cl=en
PATENT
WO 2012143599
http://www.google.com/patents/US20140094474?cl=de
PATENT
IN 2011KO00570
PATENT
Compound of (I) (5 g) was dissolved in an acetonitrile and distilled water. The reaction mixture was heated at 75 °C and then slowly cooled down at RT and stirred at RT for 3 days. The solid obtained was filtered, washed twice with the acetonitrile: water and dried under vacuum at 40 °C and 60 °C to yield crystalline form of (I) (4.42 g) with 88% of yield (example 1, page 10).
Compound (I) can be synthetized using the procedures described in WO
201 1/051540.

Pure diastereomers (la) and (lb) can be suitably synthetized, for example, using ketoreductase enzymes (KREDs) for both S- and R-selective reduction of compound 1 to compound 2 as shown in Scheme 1, wherein R is H or Ci_6 alkyl.


Scheme 1.
For example, Codexis KRED-130 and KRED -NADH-110 enzymes are useful for obtaining excellent stereoselectivity, even stereospecificity. In Scheme 1 the starting material 1 is preferably an ester (R= Ci_6 alkyl), for example ethyl ester (R=ethyl), such as to facilitate extraction of the product into the organic phase as the compound where R=H has a tendency to remain in the water phase. Intermediate 2 can be protected, preferably with silyl derivatives such as tert-butyldiphenylsilyl, in order to avoid esterification in amidation step. In the case of R=Ci_6 alkyl, ester hydrolysis is typically performed before amidation step, preferably in the presence of LiOH, NaOH or KOH. Amidation from compound 3 to compound 5_is suitably carried out using EDCI HBTU, DIPEA system but using other typical amidation methods is also possible. Deprotection of 5 give pure diastereomers (la) and (lb).
Pyrazole ring without NH substitution is known tautomerizable functionality and is described here only as single tautomer but every intermediate and end product here can exist in both tautomeric forms at the same time.
The stereochemistry of the compounds can be confirmed by using optically pure starting materials with known absolute configuration as demonstrated in Scheme 2, wherein R=H or Ci_6 alkyl, preferably alkyl, for example ethyl. The end products of Scheme 2 are typically obtained as a mixture of tautomers at +300K 1H-NMR analyses in DMSO.


Scheme 2. Synthesis pathway to stereoisomers by using starting materials with known absolute configuration
The crystalline forms I, Γ and Γ ‘ of compounds (I), (la) and (lb), respectively, can be prepared, for example, by dissolving the compound in question in an
acetonitrile: water mixture having volume ratio from about 85: 15 to about 99: 1, such as from about 90: 10 to about 98:2, for example about 95:5, under heating and slowly cooling the solution until the crystalline form precipitates from the solution. The concentration of the compound in the acetonitrile: water solvent mixture is suitably about 1 kg of the compound in 5-25 liters of acetonitrile: water solvent mixture, for example 1 kg of the compound in 10-20 liters of acetonitrile: water solvent mixture. The compound is suitably dissolved in the acetonitrile: water solvent mixture by heating the solution, for example near to the reflux temperature, for example to about 60-80 °C, for example to about 75 °C, under stirring and filtering if necessary. The solution is suitably then cooled to about 0-50 °C, for example to about 5-35 °C, for example to about RT, over about 5 to about 24 hours, for example over about 6 to 12 hours, and stirred at this temperature for about 3 to 72 hours, for example for about 5 to 12 hours. The obtained crystalline product can then be filtered, washed, and dried. The drying is suitably carried out in vacuum at about 40 to 60 °C, for example at 55 °C, for about 1 to 24 hours, such as for about 2 to 12 hours, for example 2 to 6 hours.
The crystalline forms I, Γ and I” of compounds (I), (la) and (lb), respectively, are useful as medicaments and can be formulated into pharmaceutical dosage forms, such as tablets and capsules for oral administration, by mixing with pharmaceutical excipients known in the art.
The disclosure is further illustrated by the following examples.
Example 1. Crystallization of N-((S)- 1 -(3 -(3 -chloro-4-cyanophenyl)- 1 H-pyrazol- 1 -yl)-propan-2-yl)-5 -( 1 -hydroxyethyl)- 1 H-pyrazole-3 -carboxamide (I)
N-((iS)- 1 -(3 -(3 -chloro-4-cyanophenyl)- 1 H-pyrazol- 1 -yl)-propan-2-yl)-5 -( 1 -hydroxyethyl)-! H-pyrazole-3 -carboxamide (I) (5 g), 71.25 ml of acetonitrile, and 3.75 ml of distilled water were charged to a flask, and the mixture was heated up to 75 °C. The mixture was slowly cooled down to RT and stirred at RT for 3 days. The solid obtained was filtered and washed twice with acetonitrile: water (9.5 ml:0.5 ml). The product was dried under vacuum at 40 °C and finally at 60°C to obtain 4.42 g of crystalline title compound (yield of 88 %) which was used in X-ray diffraction study.
Example 3. Synthesis of N-((S)- 1 -(3-(3-chloro-4-cyanophenyl)- lH-pyrazol- 1 -yl)-propan-2-yl)-5-((S)- 1 -hy droxy ethyl)- lH-pyrazole-3-carboxamide (la)
a) Ethyl-5 -((S) 1 -hydroxy ethyl)- 1 H-pyrazole-3 -carboxylate


HO
MgS04 x7H20 (341 mg), NADP monosodium salt (596 mg), D(+)-glucose (9.26 g) and optimized enzyme CDX-901 lyophilized powder (142 mg) were added to 0.2 mM of KH2P04 buffer (pH 7.0, 709 ml) to prepare solution I. To this solution I was added solution II which contained ethyl-5 -acetyl- 1 H-pyrazole-3 -carboxylate (8.509 g; 46.70 mmol), EtOH (28 ml) and K ED-130 (NADPH ketoreductase, 474 mg). The mixture was agitated at 30-32°C for 5.5 h (monitoring by HPLC) and allowed to cool to RT. The mixture was evaporated to smaller volume and the residue was agitated with diatomaceous earth and filtered. The mother liquid was extracted with 3×210 ml of EtOAc and dried. The solution was filtered through silica (83 g) and evaporated to dryness to give 7.40 g of the title compound. The optical purity was 100 % ee.
b) Ethyl 5-((S)-l -((tert-butyldiphenylsilyl)oxy)ethyl)- 1 H-pyrazole-3 -carboxylate


Diphenyl-tert-butyl chlorosilane (7.48 g, 27.21 mmol) was added in 26 ml of DMF to a mixture of compound of Example 3(a) (5.00 g, 27.15 mmol) and imidazole (2.81 g, 41.27 mmol) in DMF (50 ml) at RT. The mixture was stirred at RT for 24 h.
Saturated aqueous NaHC03 (56 ml) and water (56 ml) were added and the mixture was stirred at RT for 20 min. The mixture was extracted with 2×100 ml of EtOAc. Combined organic phases were washed with water (1×100 ml, 1×50 ml), dried (Na2S04), filtered and concentrated to give 10.92 g of crude title compound.
c) 5-((S)-l -((tert-Butyldiphenylsilyl)oxy)ethyl)- 1 H-pyrazole-3 -carboxylic acid


2 M NaOH (aq) (38.8 ml; 77.5 mmol) was added to a solution of the compound of Example 3(b) (10.9 g, 25.8 mmol) in 66 ml of THF. The mixture was heated up to reflux temperature. Heating was continued for 2.5 h and THF was removed in vacuum. Water (40 ml) and EtOAc (110 ml) were added. Clear solution was obtained after addition of more water (10 ml). Layers were separated and aqueous phase was extracted with 100 ml of EtOAc. Combined organic phases were dried (Na2S04), filtered and concentrated to give 9.8 g of the title compound.
d) 5-((S)- 1 -((tert-Butyldiphenylsilyl)oxy)ethyl)-N-((S)- 1 -(3-(3-chloro-4-cyano-phenyl)- 1 H-pyrazol- 1 -yl)propan-2-yl)- 1 H-pyrazole-3 -carboxamide


Under nitrogen atmosphere HBTU (0.84 g; 2.22 mmol), EDCIxHCl (3.26 g; 17.02 mmol) and (S)-4-(l-(2-aminopropyl)-lH-pyrazol-3-yl)-2-chlorobenzonitrile (3.86 g; 14.80 mmol) were added to a mixture of crude compound of Example 3(c) (8.68g; purity 77.4 area-%) and DIPEA (2.20 g; 17.02 mmol) in DCM (50 ml). The mixture was stirred at RT for 46 h (6 ml of DCM was added after 20 h). The mixture was washed with 3×20 ml of water, dried (Na2S04), filtered and concentrated to give 13.7 g of crude title compound.
e) N-((S)- 1 -(3-(3-chloro-4-cyanophenyl)- lH-pyrazol- 1 -yl)propan-2-yl)-5-((S)- 1 -hydroxy ethyl)- 1 H-pyrazole-3 -carboxamide (la)
TBAF hydrate (Bu4NF x 3H20; 2.34 g; 7.40 mmol) in 10 ml of THF was added to the solution of the compound of Example 3(d) (9.43 g; 14.79 mmol) in THF (94 ml) at 0 °C under nitrogen atmosphere. Stirring was continued at RT for 21.5 h and the mixture was concentrated. DCM (94 ml) was added to the residue and the solution was washed with 3×50 ml of water, dried (Na2S04), filtered and concentrated. Crude product was purified by flash chromatography (EtOAc/n-heptane) to give 2.1 g of the title compound. 1H-NMR (400MHz; d6-DMSO; 300K): Major tautomer (-85 %): δ 1.11 (d, 3H), 1.39 (d, 3H), 4.24-4.40 (m, 2H), 4.40-4.50 (m, 1H), 6.41(s, 1H), 6.93 (d, 1H), 7.77-7.82 (m, 1H), 7.88-8.01 (m, 2H), 8.08 (s, 1H), 8.19 (d, 1H), 13.02 (broad s, 1H). Minor tautomer (-15 %) δ 1.07-1.19 (m, 3H), 1.32-1.41 (m, 3H), 4.24-4.40 (m, 2H), 4.40-4.50 (m, 1H), 6.80 (broad s, 1H), 6.91-6-94 (m, 1H), 7.77-7.82 (m, 1H), 7.88-8.01 (m, 2H), 8.05-8.09 (m, 1H), 8.31 (d, 1H), 13.10 (broad s, 1H).
Example 4. Crystallization of N-((S)- 1 -(3-(3-chloro-4-cyanophenyl)- lH-pyrazol- 1 -yl)propan-2-yl)-5-((S)- 1 -hy droxy ethyl)- lH-pyrazole-3-carboxamide (la)
N-((S)- 1 -(3-(3-chloro-4-cyanophenyl)- lH-pyrazol- 1 -yl)propan-2-yl)-5-((S)- 1 -hydroxyethyl)-lH-pyrazole-3-carboxamide (la) (5.00 g; 12.54 mmol) was mixed with 47.5 ml of ACN and 2.5 ml of water. The mixture was heated until compound (la) was fully dissolved. The solution was allowed to cool slowly to RT to form a precipitate. The mixture was then further cooled to 0 °C and kept in this temperature for 30 min. The mixture was filtered and the precipitate was dried under vacuum to obtain 4.50 g of crystalline title compound which was used in the X-ray diffraction study.
Example 6. Synthesis of N-((S)- 1 -(3-(3-chloro-4-cyanophenyl)- lH-pyrazol- 1 -yl)-propan-2-yl)-5-((R)- 1 -hy droxy ethyl)- lH-pyrazole-3-carboxamide (lb)
a) Ethyl-5 -((R)- 1 -hydroxy ethyl)- 1 H-pyrazole-3 -carboxylate


Potassium dihydrogen phosphate buffer (Solution I) was prepared by dissolving potassium dihydrogen phosphate (11.350 g, 54.89 mmol) to water (333 ml) and adjusting pH of the solution to 7.0 by addition of 5 M solution of NaOH. MgS04 x 7 H20 (1.650 g), NAD monosodium salt (0.500 g), D(+)-glucose (10.880 g) and optimised enzyme CDX-901 lyophilised powder (0.200 g) were added to Solution I. To this solution (Solution II) were added KRED-NADH- 110 (0.467 g), ethyl-5-acetyl-1 H-pyrazole-3 -carboxylate (10.00 g; 54.89 mmol) and 2-methyltetrahydro-furan (16 ml). The mixture was agitated at 30° C for 11 h and allowed to cool to RT overnight. The pH of the mixture was kept at 7 by addition of 5 M solution of NaOH. The mixture was evaporated to a smaller volume. The evaporation residue was agitated for 10 min with diatomaceous earth (40 g) and activated charcoal (0.54 g), and filtered. Material on the filter was washed with water (40 ml) and the washings were combined with the filtrate. Layers were separated and aqueous phase was extracted with EtOAc (450 ml and 2×270 ml). Combined organic phases were dried over Na2S04, filtered and evaporated to dryness to give 9.85 g of the title compound (100 % ee).
b) Ethyl-5 -((R)- 1 -((tert-butyldiphenylsilyl)oxy)ethyl)- 1 H-pyrazole-3 -carboxylate


Imidazole (5.32 g; 78.08 mmol) was added to a DCM (67 ml) solution of the compound of Example 6(a) (9.85 g; 53.48). The mixture was stirred until all reagent was dissolved and tert-butyldiphenyl chlorosilane (13.21 ml; 50.80 mmol) was added to the mixture. The mixture was stirred for 1.5 h, 70 ml of water was added and stirring was continued for 15 min. Layers were separated and organic phase was washed with 2×70 ml of water and dried over Na2S04, filtered and concentrated to give 22.07 g of crude title compound.
c) 5 -((R)- 1 -((tert-Butyldiphenylsilyl)oxy)ethyl)- 1 H-pyrazole-3 -carboxylic acid


Compound of Example 6(b) (11.3 g; 26.74 mmol; theoretical yield from the previous step) was dissolved in 34 ml of THF and 50 ml of 2 M NaOH (aq.) was added. The mixture was heated under reflux temperature for 70 min. The mixture was extracted with 2×55 ml of EtOAc and combined organic phases were washed with brine, dried over Na2S04, filtered and concentrated. Evaporation residue was triturated in 250 ml of n-heptane, filtered and dried to give 17.58 g of crude title compound.
d) 5-((R)- 1 -((tert-Butyldiphenylsilyl)oxy)ethyl)-N-((S)- 1 -(3-(3-chloro-4-cyano-phenyl)- 1 H-pyrazol- 1 -yl)propan-2-yl)- 1 H-pyrazole-3 -carboxamide


A mixture of the compound of Example 6(c) (11.14 g; 26.75 mmol; theoretical yield from the previous step), 91 ml of DCM, HBTU (1.52 g; 4.01 mmol), EDCIxHCl
(5.90 g; 30.76 mmol), (S)-4-(l-(2-aminopropyl)-lH-pyrazol-3-yl)-2-chlorobenzo-nitrile (6.97 g; 26.75 mmol) and DIPEA (3.98 g; 30.76 mmol) was stirred at RT for 3 h and at 30° C for 22 h. The mixture was washed with 2×90 ml of 0.5 M HC1 and 4×90 ml of water, dried over Na2S04, filtered and concentrated. Crude product was purified by flash column chromatography (n-heptane-EtOAc) to give 16.97 g of title compound.
e) N-((S)- 1 -(3-(3-chloro-4-cyanophenyl)- lH-pyrazol- 1 -yl)propan-2-yl)-5-((R)- 1 -hydroxy ethyl)- 1 H-pyrazole-3 -carboxamide (lb)
A mixture of the compound of Example 6(d) (6.09 g; 9.56 mmol), 61 ml of THF and TBAF was stirred at 40 °C for 6.5 h. The mixture was concentrated and 61 ml of EtOAc was added to the evaporation residue. Solution was washed with 2×50 ml of 0.5 M HC1 and 4×50 ml of water, dried over Na2S04, filtered and concentrated. Crude product was purified by flash column chromatography (n-heptane-EtOAc) to give 1.71 g of the title compound. 1H-NMR (400MHz; d6-DMSO; 300K): Major tautomer (~85%): 5 1.10 (d, 3H), 1.38 (d, 3H), 4.14-4.57 (m, 2H), 5.42 (d, 1H),
6.39(s, 1H), 6.86-6.98 (m, 1H), 7.74-7.84 (m, 1H), 7.86-8.02 (m, 2H), 8.08 (s, 1H), 8.21 (d, 1H), 13.04 (broad s, 1H). Minor tautomer (-15%) δ 0.95-1.24 (m, 3H), 1.25-1.50 (m, 3H), 4.14-4.57 (m, 2H), 4.60-4.90 (m, 1H), 5.08 (d, 1H), 6.78 (broad s, 1H), 6.86-6.98 (m, 1H), 7.77-7.84 (m, 1H), 7.86-8.02 (m, 2H), 8.02-8.12 (m, 1H), 8.32 (d, 1H), 13.1 1 (broad s, 1H).
Example 7. Crystallization of N-((S)- 1 -(3-(3-chloro-4-cyanophenyl)- lH-pyrazol- 1 -yl)propan-2-yl)-5-((R)- 1 -hy droxy ethyl)- 1 H-pyrazole-3 -carboxamide (lb)
N-((S)- 1 -(3-(3-chloro-4-cyanophenyl)- lH-pyrazol- 1 -yl)propan-2-yl)-5-((R)- 1 -hydroxyethyl)-l H-pyrazole-3 -carboxamide (lb) (3.7 g; 9.28 mmol) was mixed with 70 ml of ACN and 3.5 ml of water. The mixture was heated to reflux temperature until compound (lb) was fully dissolved. The solution was allowed to cool slowly. The mixture was filtered at 50 °C to obtain 6.3 mg of the precipitate. Mother liquid was cooled to 41 °C and filtered again to obtain 20.7 mg of the precipitate. Obtained mother liquid was then cooled to 36 °C and filtered to obtain 173 mg of the precipitate. The final mother liquid was cooled to RT, stirred overnight, cooled to 0 °C, filtered, washed with cold ACN: water (1 : 1) and dried to obtain 2.71 g of the precipitate. The precipitates were checked for optical purity and the last precipitate of crystalline title compound (optical purity 100 %) was used in the X-ray diffraction study.
Example 9. Synthesis of Ethyl-5 -((S) 1 -hydroxy ethyl)- 1 H-pyrazole-3 -carboxylate


HO
Zinc trifluoromethanesulfonate (0.259 g; 0.713 mmol) and (S)-(-)-3-butyn-2-ol (0.25 g; 3.57 mmol) were added to 0.75 ml (5.35 mmol) of Et3N under nitrogen
atmosphere. Ethyldiazoacetate (0.45 ml; 4.28 mmol) was added slowly and the
mixture was heated at 100 °C for 2 h. The mixture was cooled to RT and 5 ml of water was added. The mixture was washed with 15 ml of DCM, 5 ml of water was added and phases were separated. Water phase was washed twice with DCM, all organic layers were combined, dried with phase separator filtration and evaporated to dryness to give 0.523 g of crude material. The product was purified by normal phase column chromatography (0-5 % MeOH:DCM) to give 0.165 mg of the title compound. 1H-NMR (400MHz; d6-DMSO; temp +300 K): Tautomer 1 (major 77%): δ 1.28 (t, 3H), 1.39 (d, 3H), 4.20-4.28 (m, 2H), (d, 1H), 4.75-4.85 (m, 1H) 5.43 (broad d, 1H), 6.54 (broad s, 1H), 13.28 (broad s, 1H). Tautomer 2 (minor 23%): δ 1.28 (t, 3H), 1.39 (d, 3H), 4.20-4.28 (m, 2H), 4.66-4.85 (m, 1H), 5.04-5.15 (broad s, 1H), 6.71 (broad s, 1H), 13.60 (broad s, 1H).
Exam le 10. Ethyl-5 -((R)- 1 -hydroxy ethyl)- 1 H-pyrazole-3 -carboxylate

Zinc trifluoromethanesulfonate (1.037 g; 2.85 mmol) and (R)-(+)-3-butyn-2-ol (1.00 g; 14.27 mmol) were added to 2.98 ml (21.40 mmol) of Et3N under nitrogen atmosphere. Ethyldiazoacetate (1.80 ml; 21.40 mmol) was added slowly and then refluxed for 3 h. The mixture was cooled to RT and 45 ml of water was added. The mixture was extracted with 3×50 ml of DCM, organic layers were combined, dried with phase separator filtration and evaporated to dryness to give 2.503 g of crude material which was purified by normal phase column chromatography (0-10 % MeOH:DCM) to give 0.67 lmg of the title compound. 1H-NMR (400MHz; d6-DMSO; temp +300 K): Tautomer 1 (major 78%): δ 1.28 (t, 3H), 1.39 (d, 3H), 4.18-4.35 (m, 2H), (d, 1H), 4.75-4.85 (m, 1H) 5.42 (broad d, 1H), 6.54 (s, 1H), 13.29 (broad s, 1H). Tautomer 2 (minor 22%): δ 1.28 (t, 3H), 1.39 (d, 3H), 4.18-4.35 (m, 2H), 4.66-4.85 (m, 1H), 5.09 (broad s, 1H), 6.71 (broad s, 1H), 13.61 (broad s, 1H).
References
- “Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies.”. Sci Rep. 5: 12007. 2015. doi:10.1038/srep12007. PMC 4490394
 . PMID 26137992.
. PMID 26137992. - Fizazi K, Albiges L, Loriot Y, Massard C (2015). “ODM-201: a new-generation androgen receptor inhibitor in castration-resistant prostate cancer”. Expert Rev Anticancer Ther. 15(9): 1007–17. doi:10.1586/14737140.2015.1081566. PMID 26313416.
- Moilanen AM, Riikonen R, Oksala R, Ravanti L, Aho E, Wohlfahrt G, Nykänen PS, Törmäkangas OP, Palvimo JJ, Kallio PJ (2015). “Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies”. Sci Rep. 5: 12007.doi:10.1038/srep12007. PMC 4490394
 . PMID 26137992.
. PMID 26137992. - “ODM-201 is safe and active in metastatic castration-resistant prostate cancer”. Cancer Discov. 4 (9): OF10. 2014. doi:10.1158/2159-8290.CD-RW2014-150. PMID 25185192.
- Pinto Á (2014). “Beyond abiraterone: new hormonal therapies for metastatic castration-resistant prostate cancer”. Cancer Biol. Ther. 15 (2): 149–55. doi:10.4161/cbt.26724.PMC 3928129
 . PMID 24100689.
. PMID 24100689. - Fizazi K, Massard C, Bono P, Jones R, Kataja V, James N, Garcia JA, Protheroe A, Tammela TL, Elliott T, Mattila L, Aspegren J, Vuorela A, Langmuir P, Mustonen M (2014). “Activity and safety of ODM-201 in patients with progressive metastatic castration-resistant prostate cancer (ARADES): an open-label phase 1 dose-escalation and randomised phase 2 dose expansion trial”. Lancet Oncol. 15 (9): 975–85. doi:10.1016/S1470-2045(14)70240-2. PMID 24974051.
- Agarwal N, Di Lorenzo G, Sonpavde G, Bellmunt J (2014). “New agents for prostate cancer”. Ann. Oncol. 25 (9): 1700–9. doi:10.1093/annonc/mdu038. PMID 24658665.
External links
Fenner A. Prostate cancer: ODM-201 tablets complete phase I. Nat Rev Urol. 2015 Dec;12(12):654. doi: 10.1038/nrurol.2015.268. Epub 2015 Nov 3. PubMed PMID: 26526759.
2: Massard C, Penttinen HM, Vjaters E, Bono P, Lietuvietis V, Tammela TL, Vuorela A, Nykänen P, Pohjanjousi P, Snapir A, Fizazi K. Pharmacokinetics, Antitumor Activity, and Safety of ODM-201 in Patients with Chemotherapy-naive Metastatic Castration-resistant Prostate Cancer: An Open-label Phase 1 Study. Eur Urol. 2015 Oct 10. pii: S0302-2838(15)00964-1. doi: 10.1016/j.eururo.2015.09.046. [Epub ahead of print] PubMed PMID: 26463318.
3: Fizazi K, Albiges L, Loriot Y, Massard C. ODM-201: a new-generation androgen receptor inhibitor in castration-resistant prostate cancer. Expert Rev Anticancer Ther. 2015;15(9):1007-17. doi: 10.1586/14737140.2015.1081566. PubMed PMID: 26313416; PubMed Central PMCID: PMC4673554.
4: Bambury RM, Rathkopf DE. Novel and next-generation androgen receptor-directed therapies for prostate cancer: Beyond abiraterone and enzalutamide. Urol Oncol. 2015 Jul 7. pii: S1078-1439(15)00269-0. doi: 10.1016/j.urolonc.2015.05.025. [Epub ahead of print] Review. PubMed PMID: 26162486.
5: Moilanen AM, Riikonen R, Oksala R, Ravanti L, Aho E, Wohlfahrt G, Nykänen PS, Törmäkangas OP, Palvimo JJ, Kallio PJ. Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies. Sci Rep. 2015 Jul 3;5:12007. doi: 10.1038/srep12007. PubMed PMID: 26137992; PubMed Central PMCID: PMC4490394.
6: Thibault C, Massard C. [New therapies in metastatic castration resistant prostate cancer]. Bull Cancer. 2015 Jun;102(6):501-8. doi: 10.1016/j.bulcan.2015.04.016. Epub 2015 May 26. Review. French. PubMed PMID: 26022286.
7: Bjartell A. Re: activity and safety of ODM-201 in patients with progressive metastatic castration-resistant prostate cancer (ARADES): an open-label phase 1 dose-escalation and randomised phase 2 dose expansion trial. Eur Urol. 2015 Feb;67(2):348-9. doi: 10.1016/j.eururo.2014.11.019. PubMed PMID: 25760250.
8: De Maeseneer DJ, Van Praet C, Lumen N, Rottey S. Battling resistance mechanisms in antihormonal prostate cancer treatment: Novel agents and combinations. Urol Oncol. 2015 Jul;33(7):310-21. doi: 10.1016/j.urolonc.2015.01.008. Epub 2015 Feb 21. Review. PubMed PMID: 25708954.
9: Boegemann M, Schrader AJ, Krabbe LM, Herrmann E. Present, Emerging and Possible Future Biomarkers in Castration Resistant Prostate Cancer (CRPC). Curr Cancer Drug Targets. 2015;15(3):243-55. PubMed PMID: 25654638.
10: ODM-201 is safe and active in metastatic castration-resistant prostate cancer. Cancer Discov. 2014 Sep;4(9):OF10. doi: 10.1158/2159-8290.CD-RW2014-150. Epub 2014 Jul 9. PubMed PMID: 25185192.
11: Fizazi K, Massard C, Bono P, Jones R, Kataja V, James N, Garcia JA, Protheroe A, Tammela TL, Elliott T, Mattila L, Aspegren J, Vuorela A, Langmuir P, Mustonen M; ARADES study group. Activity and safety of ODM-201 in patients with progressive metastatic castration-resistant prostate cancer (ARADES): an open-label phase 1 dose-escalation and randomised phase 2 dose expansion trial. Lancet Oncol. 2014 Aug;15(9):975-85. doi: 10.1016/S1470-2045(14)70240-2. Epub 2014 Jun 25. PubMed PMID: 24974051.
12: Agarwal N, Di Lorenzo G, Sonpavde G, Bellmunt J. New agents for prostate cancer. Ann Oncol. 2014 Sep;25(9):1700-9. doi: 10.1093/annonc/mdu038. Epub 2014 Mar 20. Review. PubMed PMID: 24658665.
13: Pinto Á. Beyond abiraterone: new hormonal therapies for metastatic castration-resistant prostate cancer. Cancer Biol Ther. 2014 Feb;15(2):149-55. doi: 10.4161/cbt.26724. Epub 2013 Nov 1. Review. PubMed PMID: 24100689; PubMed Central PMCID: PMC3928129.
14: Yin L, Hu Q, Hartmann RW. Recent progress in pharmaceutical therapies for castration-resistant prostate cancer. Int J Mol Sci. 2013 Jul 4;14(7):13958-78. doi: 10.3390/ijms140713958. Review. PubMed PMID: 23880851; PubMed Central PMCID: PMC3742227.
15: Leibowitz-Amit R, Joshua AM. Targeting the androgen receptor in the management of castration-resistant prostate cancer: rationale, progress, and future directions. Curr Oncol. 2012 Dec;19(Suppl 3):S22-31. doi: 10.3747/co.19.1281. PubMed PMID: 23355790; PubMed Central PMCID: PMC3553559.
 |
|
| Systematic (IUPAC) name | |
|---|---|
|
N-((S)-1-(3-(3-chloro-4-cyanophenyl)-1H-pyrazol-1-yl)propan-2-yl)-5-(1-hydroxyethyl)-1H-pyrazole-3-carboxamide[1]
|
|
| Identifiers | |
| ChemSpider | 38772320 |
| UNII | X05U0N2RCO |
| Chemical data | |
| Formula | C19H19ClN6O2 |
| Molar mass | 398.85 g·mol−1 |
//////////// Bayer HealthCare, Orion, Antineoplastics, Androgen receptor antagonists, Phase III, Prostate cancer, BAY 1841788, ODM-201, даролутамид , دارولوتاميد , 达罗他胺 , دارولوتاميد , ダロルタミド
O=C(N[C@@H](C)Cn1ccc(n1)c2ccc(C#N)c(Cl)c2)c3cc(nn3)C(O)C

Bayer HealthCare has obtained approval from the Japanese Ministry of Health, Labour and Welfare (MHLW) for its Nexavar (sorafenib) for treatment of patients with unresectable differentiated thyroid carcinoma.

Sorafenib
(4-(4-(3-(4-chloro-3-(trifluoromethyl)phenyl)ureido)phenoxy)-N-methylpicolinamide)
BAY 43-9006

Bayer HealthCare has obtained approval from the Japanese Ministry of Health, Labour and Welfare (MHLW) for its Nexavar (sorafenib) for treatment of patients with unresectable differentiated thyroid carcinoma.
Bayer HealthCare has obtained approval from the Japanese Ministry of Health, Labour and Welfare (MHLW) for its Nexavar (sorafenib) for treatment of patients with unresectable differentiated thyroid carcinoma.
Nexavar’s approval in Japan is supported by data from the multicentre, placebo-controlled Phase III DECISION (‘stuDy of sorafEnib in loCally advanced or metastatIc patientS with radioactive Iodine refractory thyrOid caNcer’) study.
The international Phase III DECISION study, which randomised a total of 417 patients, met its primary endpoint of extended progression-free survival. Safety and tolerability profile of sorafenib was generally consistent with the known profile of sorafenib.
The most common treatment-emergent adverse events in the sorafenib arm were hand-foot skin reaction, diarrhea, alopecia, weight loss, fatigue, hypertension and rash.
Nexavar was awarded orphan drug status by the MHLW for thyroid carcinoma in September 2013.
Sorafenib (co-developed and co-marketed by Bayer and Onyx Pharmaceuticals as Nexavar),[1] is a drug approved for the treatment of primary kidney cancer (advanced renal cell carcinoma), advanced primary liver cancer (hepatocellular carcinoma), and radioactive iodine resistant advanced thyroid carcinoma.
Medical uses
At the current time sorafenib is indicated as a treatment for advanced renal cell carcinoma (RCC), unresectable hepatocellular carcinomas (HCC) and thyroid cancer.[2][3][4][5]
Kidney cancer
An article in The New England Journal of Medicine, published January 2007, showed compared with placebo, treatment with sorafenib prolongs progression-free survival in patients with advanced clear cell renal cell carcinoma in whom previous therapy has failed. The median progression-free survival was 5.5 months in the sorafenib group and 2.8 months in the placebo group (hazard ratio for disease progression in the sorafenib group, 0.44; 95% confidence interval [CI], 0.35 to 0.55; P<0.01).[6] A few reports described patients with stage IV renal cell carcinomas that were successfully treated with a multimodal approach including neurosurgical, radiation, and sorafenib.[7] This is one of two TGA-labelled indications for sorafenib, although it is not listed on the Pharmaceutical Benefits Scheme for this indication.[5][8]
Liver cancer
At ASCO 2007, results from the SHARP trial[9] were presented, which showed efficacy of sorafenib in hepatocellular carcinoma. The primary endpoint was median overall survival, which showed a 44% improvement in patients who received sorafenib compared to placebo (hazard ratio 0.69; 95% CI, 0.55 to 0.87; p=0.0001). Both median survival and time to progression showed 3-month improvements. There was no difference in quality of life measures, possibly attributable to toxicity of sorafenib or symptoms related to underlying progression of liver disease. Of note, this trial only included patients with Child-Pugh Class A (i.e. mildest) cirrhosis. The results of the study appear in the July 24, 2008, edition of The New England Journal of Medicine. Because of this trial Sorafenib obtained FDA approval for the treatment of advanced hepatocellular carcinoma in November 2007.[10]
In a randomized, double-blind, phase II trial combining sorafenib with doxorubicin, the median time to progression was not significantly delayed compared with doxorubicin alone in patients with advanced hepatocellular carcinoma. Median durations of overall survival and progression-free survival were significantly longer in patients receiving sorafenib plus doxorubicin than in those receiving doxorubicin alone.[10] A prospective single-centre phase II study which included the patients with unresectable hepatocellular carcinoma (HCC)concluding that the combination of sorafenib and DEB-TACE in patients with unresectable HCC is well tolerated and safe, with most toxicities related to sorafenib.[11] This is the only indication for which sorafenib is listed on the PBS and hence the only Government-subsidised indication for sorafenib in Australia.[8] Along with renal cell carcinoma, hepatocellular carcinoma is one of the TGA-labelled indications for sorafenib.[5]
Thyroid cancer
A phase 3 clinical trial has started recruiting (November 2009) to use sorafenib for non-responsive thyroid cancer.[12] The results were presented at the ASCO 13th Annual Meeting and are the base for FDA approval. The Sorafenib in locally advanced or metastatic patients with radioactive iodine-refractory differentiated thyroid cancer: The Phase 3 DECISION trial showed significant improvement in progression-free survival but not in overall survival. However, as is known, the side effects were very frequent, specially hand and foot skin reaction.[13]
Adverse effects
Adverse effects by frequency
Note: Potentially serious side effects are in bold.
Very common (>10% frequency)
- Lymphopenia
- Hypophosphataemia[Note 1]
- Haemorrhage[Note 2]
- Hypertension[Note 3]
- Diarrhea
- Rash
- Alopecia (hair loss; occurs in roughly 30% of patients receiving sorafenib)
- Hand-foot syndrome
- Pruritus (itchiness)
- Erythema
- Increased amylase
- Increased lipase
- Fatigue
- Pain[Note 4]
- Nausea
- Vomiting[Note 5][14]
Common (1-10% frequency)
- Leucopoenia[Note 6]
- Neutropoenia[Note 7]
- Anaemia[Note 8]
- Thrombocytopenia[Note 9]
- Anorexia (weight loss)
- Hypocalcaemia[Note 10]
- Hypokalaemia[Note 11]
- Depression
- Peripheral sensory neuropathy
- Tinnitus[Note 12]
- Congestive heart failure
- Myocardial infarction[Note 13]
- Myocardial ischaemia[Note 14]
- Hoarseness
- Constipation
- Stomatitis[Note 15]
- Dyspepsia[Note 16]
- Dysphagia[Note 17]
- Dry skin
- Exfoliative dermatitis
- Acne
- Skin desquamation
- Arthralgia[Note 18]
- Myalgia[Note 19]
- Renal failure[Note 20]
- Proteinuria[Note 21]
- Erectile dysfunction
- Asthenia (weakness)
- Fever
- Influenza-like illness
- Transient increase in transaminase
Uncommon (0.1-1% frequency)
- Folliculitis
- Infection
- Hypersensitivity reactions[Note 22]
- Hypothyroidism[Note 23]
- Hyperthyroidism[Note 24]
- Hyponatraemia[Note 25]
- Dehydration
- Reversible posterior leukoencephalopathy
- Hypertensive crisis
- Rhinorrhoea[Note 26]
- Interstitial lung disease-like events[Note 27]
- Gastro-oesophageal reflux disease (GORD)
- Pancreatitis[Note 28]
- Gastritis[Note 29]
- Gastrointestinal perforations[Note 30]
- Increase in bilirubin leading, potentially, to jaundice[Note 31]
- Cholecystitis[Note 32]
- Cholangitis[Note 33]
- Eczema
- Erythema multiforme[Note 34]
- Keratoacanthoma[Note 35]
- Squamous cell carcinoma
- Gynaecomastia (swelling of the breast tissue in men)
- Transient increase in blood alkaline phosphatase
- INR abnormal
- Prothrombin level abnormal
- bulbous skin reaction[15]
Rare (0.01-0.1% frequency)
Mechanism of action
Sorafenib is a small molecular inhibitor of several tyrosine protein kinases (VEGFR and PDGFR) and Raf kinases (more avidly C-Raf than B-Raf).[16][17] Sorafenib also inhibits some intracellular serine/threonine kinases (e.g. C-Raf, wild-type B-Raf and mutant B-Raf).[10] Sorafenib treatment induces autophagy,[18] which may suppress tumor growth. However, autophagy can also cause drug resistance.[19]
History
Renal cancer
Sorafenib was approved by the U.S. Food and Drug Administration (FDA) in December 2005,[20] and received European Commission marketing authorization in July 2006,[21] both for use in the treatment of advanced renal cancer.
Liver cancer
The European Commission granted marketing authorization to the drug for the treatment of patients with hepatocellular carcinoma(HCC), the most common form of liver cancer, in October 2007,[22] and FDA approval for this indication followed in November 2007.[23]
In November 2009, the UK’s National Institute of Clinical Excellence declined to approve the drug for use within the NHS in England, Wales and Northern Ireland, stating that its effectiveness (increasing survival in primary liver cancer by 6 months) did not justify its high price, at up to £3000 per patient per month.[24] In Scotland the drug had already been refused authorization by the Scottish Medicines Consortium for use within NHS Scotland, for the same reason.[24]
In March 2012, the Indian Patent Office granted a domestic company, Natco Pharma, a license to manufacture generic Sorafenib, bringing its price down by 97%. Bayer sells a month’s supply, 120 tablets, of Nexavar for![]() 280000 (US$4,700). Natco Pharma will sell 120 tablets for
280000 (US$4,700). Natco Pharma will sell 120 tablets for ![]() 8800 (US$150), while still paying a 6% royalty to Bayer.[25][26] Under Indian Patents Act, 2005 and the World Trade Organisation TRIPS Agreement, the government can issue a compulsory license when a drug is not available at an affordable price.[27]
8800 (US$150), while still paying a 6% royalty to Bayer.[25][26] Under Indian Patents Act, 2005 and the World Trade Organisation TRIPS Agreement, the government can issue a compulsory license when a drug is not available at an affordable price.[27]
Thyroid Cancer
As of November 22, 2013, sorafenib has been approved by the FDA for the treatment of locally recurrent or metastatic, progressive differentiated thyroid carcinoma (DTC) refractory to radioactive iodine treatment.[28]
Research
Lung
In some kinds of lung cancer (with squamous-cell histology) sorafenib administered in addition to paclitaxel and carboplatin may be detrimental to patients.[29]
Brain (Recurrent Glioblastoma)
There is a phase I/II study at the Mayo Clinic[30] of sorafenib and CCI-779 (temsirolimus) for recurrent glioblastoma.
Desmoid Tumor (Aggressive Fibromatosis)
A study performed in 2011 showed that Sorafenib is active against Aggressive fibromatosis. This study is being used as justification for using Sorafenib as an initial course of treatment in some patients with Aggressive fibromatosis.[31]
Nexavar Controversy
In January 2014, Bayer’s CEO stated that Nexavar was developed for “western patients who [could] afford it”. At the prevailing prices, a kidney cancer patient would pay $96,000 (£58,000) for a year’s course of the Bayer-made drug. However, the cost of the Indian version of the generic drug would be around $2,800 (£1,700).[32]
Notes
- Low blood phosphate levels
- Bleeding; including serious bleeds such as intracranial and intrapulmonary bleeds
- High blood pressure
- Including abdominal pain, headache, tumour pain, etc.
- Considered a low (~10-30%) risk chemotherapeutic agent for causing emesis)
- Low level of white blood cells in the blood
- Low level of neutrophils in the blood
- Low level of red blood cells in the blood
- Low level of plasma cells in the blood
- Low blood calcium
- Low blood potassium
- Hearing ringing in the ears
- Heart attack
- Lack of blood supply for the heart muscle
- Mouth swelling, also dry mouth and glossodynia
- Indigestion
- Not being able to swallow
- Sore joints
- Muscle aches
- Kidney failure
- Excreting protein [usually plasma proteins] in the urine. Not dangerous in itself but it is indicative kidney damage
- Including skin reactions and urticaria (hives)
- Underactive thyroid
- Overactive thyroid
- Low blood sodium
- Runny nose
- Pneumonitis, radiation pneumonitis, acute respiratory distress, etc.
- Swelling of the pancreas
- Swelling of the stomach
- Formation of a hole in the gastrointestinal tract, leading to potentially fatal bleeds
- Yellowing of the skin and eyes due to a failure of the liver to adequately cope with the amount of bilirubin produced by the day-to-day actions of the body
- Swelling of the gallbladder
- Swelling of the bile duct
- A potentially fatal skin reaction
- A fairly benign form of skin cancer
- A potentially fatal abnormality in the electrical activity of the heart
- Swelling of the skin and mucous membranes
- A potentially fatal allergic reaction
- Swelling of the liver
- A potentially fatal skin reaction
- A potentially fatal skin reaction
- The rapid breakdown of muscle tissue leading to the build-up of myoglobin in the blood and resulting in damage to the kidneys
 |
|
 |
|
| Systematic (IUPAC) name | |
|---|---|
| 4-[4-[[4-chloro-3-(trifluoromethyl)phenyl]carbamoylamino] phenoxy]-N-methyl-pyridine-2-carboxamide |
|
| Clinical data | |
| Trade names | Nexavar |
| AHFS/Drugs.com | monograph |
| MedlinePlus | a607051 |
| Licence data | EMA:Link, US FDA:link |
| Pregnancy cat. | D (AU) D (US) |
| Legal status | Prescription Only (S4) (AU) ℞-only (CA) POM (UK) ℞-only (US) |
| Routes | Oral |
| Pharmacokinetic data | |
| Bioavailability | 38–49% |
| Protein binding | 99.5% |
| Metabolism | Hepatic oxidation and glucuronidation (CYP3A4 & UGT1A9-mediated) |
| Half-life | 25–48 hours |
| Excretion | Faeces (77%) and urine (19%) |
| Identifiers | |
| CAS number | 284461-73-0 |
| ATC code | L01XE05 |
| PubChem | CID 216239 |
| DrugBank | DB00398 |
| ChemSpider | 187440 |
| UNII | 9ZOQ3TZI87 |
| KEGG | D08524 |
| ChEBI | CHEBI:50924 |
| ChEMBL | CHEMBL1336 |
| Synonyms | Nexavar Sorafenib tosylate |
| PDB ligand ID | BAX (PDBe, RCSB PDB) |
| Chemical data | |
| Formula | C21H16ClF3N4O3 |
| Mol. mass | 464.825 g/mol |
4-(4-{3-[4-chloro-3-(trifluoromethyl)phenyl]ureido}phenoxy)-Λ/2-methylpyridine-2- carboxamide is commonly known as sorafenib (I). Sorafenib is prepared as its tosylate salt. Sorafenib blocks the enzyme RAF kinase, a critical component of the RAF/MEK/ERK signaling pathway that controls cell division and proliferation; in addition, sorafenib inhibits the VEGFR-2/PDGFR-beta signaling cascade, thereby blocking tumor angiogenesis.
Sorafenib, marketed as Nexavar by Bayer, is a drug approved for the treatment of advanced renal cell carcinoma (primary kidney cancer). It has also received “Fast Track” designation by the FDA for the treatment of advanced hepatocellular carcinoma (primary liver cancer). It is a small molecular inhibitor of Raf kinase, PDGF (platelet-derived growth factor), VEGF receptor 2 & 3 kinases and c Kit the receptor for Stem cell factor.
Sorafenib and pharmaceutically acceptable salts thereof is disclosed in WO0042012. Sorafenib is also disclosed in WO0041698. Both these patents disclose processes for the preparation of sorafenib.
WO0042012 and WO0041698 describe the process as given in scheme I which comprises reacting picolinic acid (II) with thionyl chloride in dimethyl formamide (DMF) to form acid chloride salt (III). This salt is then reacted with methylamine dissolved in tetrahydrofuran (THF) to give carboxamide (IV). This carboxamide when further reacted with 4- aminophenol in anhydrous DMF and potassium tert-butoxide 4-(2-(N-methylcarbamoyl)-4- pyridyloxy)aniline (V) is formed. Subsequent reaction of this aniline with 4-chloro-3- (trifluoromethyl) phenyl isocyanate (Vl) in methylene chloride yields sorafenib (I). The reaction is represented by Scheme I as given below.
Scheme I
Picolini
Sorafenib (I)
WO2006034796 also discloses a process for the preparation of sorafenib and its tosylate salt. The process comprises reacting 2-picolinic acid (II) with thionyl chloride in a solvent inert toward thionyl chloride without using dimethyl formamide to form acid chloride salt (III). This acid salt on further reaction with aqueous solution methylamine or gaseous methylamine gives compound (IV). Compound (IV) is then reacted with 4-aminophenol with addition of a carbonate salt in the presence of a base to yield compound (V).
Compound (V) can also be obtained by reacting compound (IV) with 4-aminophenol in the presence of water with addition of a phase transfer catalyst. Compound (V) when reacted with 4-chloro-3-(trifluoromethyl) phenyl isocyanate (Vl) in a non-chlorinated organic solvent, inert towards isocyanate gives sorafenib (I). Sorafenib by admixing with p- toluenesulfonic acid in a polar solvent gives sorafenib tosylate (VII). The reaction is represented by Scheme Il as given below.
Scheme Il
P
A key step in the synthesis of sorafenib is the formation of the urea bond. The processes disclosed in the prior art involve reactions of an isocyanate with an amine. These isocyanate compounds though commercially available are very expensive. Further synthesis of isocyanate is very difficult which requires careful and skillful handling of reagents.
Isocyanate is prepared by reaction of an amine with phosgene or a phosgene equivalent, such as bis(trichloromethyl) carbonate (triphosgene) or trichloromethyl chloroformate (diphosgene). Isocyanate can also be prepared by using a hazardous reagent such as an azide. Also, the process for preparation of an isocyanate requires harsh reaction conditions such as strong acid, higher temperature etc. Further, this isocyanate is reacted with an amine to give urea.
Reactions of isocyanates suffer from one or more disadvantages. For example phosgene or phosgene equivalents are hazardous and dangerous to use and handle on a large scale. These reagents are also not environment friendly. Isocyanates themselves are thermally unstable compounds and undergo decomposition on storage and they are incompatible with a number of organic compounds. Thus, the use of isocyanate is not well suited for industrial scale application.
Sorafenib and its pharmaceutically acceptable salts and solvates are reported for the first time in WO0041698 (corresponding US 03139605) by Bayer. In the literature only one route is disclosed for the preparation of sorafenib. According to this route (Scheme-I), picolinic acid of formula III is reacted with thionyl chloride to give the 4-chloro derivative which on treatment
VII
Scheme-I with methanol gave the methyl ester of formula V. Compound of formula V is reacted with methylamine to get the corresponding amide of formula VL Compound of formula VI is reacted with 4-aminophenol to get the ether derivative of formula VII. Compound of formula VII is reacted with 4-chloro-3-trifluoromethylphenylisocyante to get sorafenib base of formula I. Overall yield of sorafenib in this process is 10% from commercially available 2-picolinic acid of formula II. Main drawback in this process is chromatographic purification of the intermediates involved in the process and low yield at every step.
Donald Bankston’s (Org. Proc. Res. Dev., 2002, 6, 777-781) development of an improved synthesis of the above basic route afforded sorafenib in an overall yield of 63% without involving any chromatographic purification. Process improvements like reduction of time in thionyl chloride reaction; avoid the isolation of intermediates of formulae IV and V5 reduction of base quantity in p-aminophenol reaction, etc lead to the simplification of process and improvement in yield of final compound of formula I.
Above mentioned improvements could not reduce the number of steps in making sorafenib of formula-I. In the first step all the raw materials are charged and heated to target temperature (72°C). Such a process on commercial scale will lead to sudden evolution of gas emissions such as sulfur dioxide and hydrogen chloride. Also, in the aminophenol reaction two bases (potassium carbonate and potassium t-butoxide) were used in large excess to accomplish the required transformation.
A scalable process for the preparation of sorafenib is disclosed in WO2006034796. In this process also above mentioned chemistry is used in making sorafenib of formula I. In the first step, catalytic quantity. of DMF used in the prior art process is replaced with reagents like hydrogen bromide, thionyl bromide and sodium bromide. Yield of required product remained same without any advantages from newly introduced corrosive reagents. Process improvements like change of solvents, reagents, etc were applied in subsequent steps making the process scalable. Overall yield of sorafenib is increased to 74% from the prior art 63% yield. Purity of sorafenib is only 95% and was obtained as light brown colored solid.
Main drawbacks in this process are production of low quality sorafenib and requirement of corrosive and difficult to handle reagents such as thionyl bromide and hydrogen bromide. Also, there is no major improvement in the yield of sorafenib.
Sorafenib tosylate ( Brand name: Nexavar ®, BAY 43-9006 other name, Chinese name: Nexavar, sorafenib, Leisha Wa) was Approved by U.S. FDA for the treatment of advanced kidney cancer in 2005 and liver cancer in 2007 .
Sorafenib, co-Developed and co-marketed by Germany-based Bayer AG and South San Francisco-based Onyx Pharmaceuticals , is an Oral Multi-kinase inhibitor for VEGFR1, VEGFR2, VEGFR3, PDGFRbeta, Kit, RET and Raf-1.
In March 2012 Indian drugmaker Natco Pharma received the first compulsory license ever from Indian Patent Office to make a generic Version of Bayer’s Nexavar despite the FACT that Nexavar is still on Patent. This Decision was based on the Bayer Drug being too expensive to most patients. The Nexavar price is expected to drop from $ 5,500 per person each month to $ 175, a 97 percent decline. The drug generated $ 934 million in global sales in 2010, according to India’s Patent Office.
Sorafenib tosylate
Chemical Name: 4-Methyl-3-((4 – (3-pyridinyl)-2-pyrimidinyl) amino)-N-(5 – (4-methyl-1H-imidazol-1-yl) -3 – (trifluoromethyl) phenyl) benzamide monomethanesulfonate, Sorafenib tosylate
CAS Number 475207-59-1 (Sorafenib tosylate ) , 284461-73-0 (Sorafenib)
References for the Preparation of Sorafenib References
1) Bernd Riedl, Jacques Dumas, Uday Khire, Timothy B. Lowinger, William J. Scott, Roger A. Smith, Jill E. Wood, Mary-Katherine Monahan, Reina Natero, Joel Renick, Robert N. Sibley; Omega-carboxyaryl Substituted diphenyl Ureas as RAF kinase inhibitors ; U.S. Patent numberUS7235576
2) Rossetto, Pierluigi; Macdonald, Peter, Lindsay; Canavesi, Augusto; Process for preparation of sorafenib and Intermediates thereof , PCT Int. Appl., WO2009111061
3) Lögers, Michael; gehring, Reinhold; Kuhn, Oliver; Matthäus, Mike; Mohrs, Klaus; müller-gliemann, Matthias; Stiehl, jürgen; berwe, Mathias; Lenz, Jana; Heilmann, Werner; Process for the preparation of 4 – {4 – [( {[4-chloro-3-(TRIFLUOROMETHYL) phenyl] amino} carbonyl) amino] phenoxy}-N-methylpyridine-2-carboxamide , PCT Int. Appl., WO2006034796
4) Shikai Xiang, Liu Qingwei, Xieyou Rong, sorafenib preparation methods, invention patent application Publication No. CN102311384 , Application No. CN201010212039
5) Zhao multiply there, Chenlin Jie, Xu Xu, MASS MEDIA Ji Yafei; sorafenib tosylate synthesis ,Chinese Journal of Pharmaceuticals , 2007 (9): 614 -616
Preparation of Sorafenib Tosylate (Nexavar) Nexavar, sorafenib Preparation of methyl sulfonate
Sorafenib (Sorafenib) chemical name 4 – {4 – [({[4 – chloro -3 – (trifluoromethyl) phenyl] amino} carbonyl) amino] phenoxy}-N-methyl-pyridine -2 – formamide by Bayer (Bayer) research and development, in 2005 the U.S. Food and Drug Administration (FDA) approval. Trade name Nexavar (Nexavar). This product is an oral multi-kinase inhibitor, for the treatment of liver cancer and kidney cancer.
Indian Patent Office in March this year for Bayer’s Nexavar in liver and kidney cancer drugs (Nexavar) has released a landmark “compulsory licensing” (compulsory license). Indian Patent Office that due to the high price Nexavar in India, the vast majority of patients can not afford the drug locally, thus requiring local Indian pharmaceutical company Natco cheap Nexavar sales. Nexavar in 2017 before patent expiry, Natco pay only Bayer’s pharmaceutical sales to 6% royalties. The move to make Nexavar patent drug prices, the supply price from $ 5,500 per month dropped to $ 175, the price reduction of 97%. Compulsory licensing in India for other life-saving drugs and patent medicines overpriced open a road, the Indian Patent Office through this decision made it clear that the patent monopoly does not guarantee that the price is too high. Nexavar is a fight against advanced renal cell carcinoma, liver cancer cure. In China, a box of 60 capsules of Nexavar price of more than 25,000 yuan. In accordance with the recommended dose, which barely enough to eat half of patients with advanced cancer. In September this year India a patent court rejected Bayer Group in India cheap drugmaker emergency appeal. Indian government to refuse patent medicine overpriced undo “compulsory licensing rules,” allowing the production of generic drugs Nexavar.
Sorafenat by Natco – Sorafenib – Nexavar – India natco Nexavar
Chemical Synthesis of Sorafenib Tosylate (Nexavar)
Sorafenib tosylate (brand name :Nexavar®, other name BAY 43-9006, was approved by US FDA for the treatment of kidney cancer in 2005 and advanced liver cancer in 2007.
US Patent US7235576, WO2006034796, WO2009111061 and Faming Zhuanli Shenqing(CN102311384) disclosed processes for preparation of sorafenib base and its salt sorafenib tosylate.
References
1)Bernd Riedl, Jacques Dumas, Uday Khire, Timothy B. Lowinger, William J. Scott, Roger A. Smith, Jill E. Wood, Mary-Katherine Monahan, Reina Natero, Joel Renick, Robert N. Sibley; Omega-carboxyaryl substituted diphenyl ureas as raf kinase inhibitors; US patent numberUS7235576
2)Rossetto, pierluigi; Macdonald, peter, lindsay; Canavesi, augusto; Process for preparation of sorafenib and intermediates thereof, PCT Int. Appl., WO2009111061
3)Lögers, michael; gehring, reinhold; kuhn, oliver; matthäus, mike; mohrs, klaus; müller-gliemann, matthias; stiehl, jürgen; berwe, mathias; lenz, jana; heilmann, werner; Process for the preparation of 4-{4-[({[4-chloro-3-(trifluoromethyl)phenyl]amino}carbonyl)amino]phenoxy}-n-methylpyridine-2-carboxamide, PCT Int. Appl., WO2006034796CN102311384, CN201010212039
Full Experimental Details for the preparation of Sorafenib Tosylate (Nexavar)
Synthesis of 4-(2-(N-methylcarbamoyl)-4-pyridyloxy)aniline.
A solution of 4-aminophenol (9.60 g, 88.0 mmol) in anh. DMF (150 mL) was treated with potassium tert-butoxide (10.29 g, 91.7 mmol), and the reddish-brown mixture was stirred at room temp. for 2 h. The contents were treated with 4-chloro- N -methyl-2-pyridinecarboxamide (15.0 g, 87.9mmol) and K2CO3 (6.50 g, 47.0 mmol) and then heated at 80°C. for 8 h. The mixture was cooled to room temp. and separated between EtOAc (500 mL) and a saturated NaCl solution (500 mL). The aqueous phase was back-extracted with EtOAc (300 mL). The combined organic layers were washed with a saturated NaCl solution (4×1000 mL), dried (Na2SO4) and concentrated under reduced pressure. The resulting solids were dried under reduced pressure at 35°C. for 3 h to afford 4-(2-(N-methylcarbamoyl)-4-pyridyloxy)aniline as a light-brown solid 17.9 g, 84%):. 1H-NMR (DMSO-d6) δ 2.77 (d, J = 4.8 Hz, 3H), 5.17 (br s, 2H), 6.64, 6.86 (AA’BB’ quartet, J = 8.4 Hz, 4H), 7.06 (dd, J = 5.5, 2.5 Hz, 1H), 7.33 (d, J = 2.5 Hz, 1H), 8.44 (d, J = 5.5 Hz; 1H), 8.73 (br d, 1H); HPLC ES-MS m/z 244 ((M+H)+).
Synthesis of 4-{4-[({[4-Chloro-3-(trifluoromethyl)phenyl]amino}carbonyl)amino]phenoxy}-N-methylpyridine-2-carboxamide (sorafenib)
4-(4-Aminophenoxy)-N-methyl-2-pyridinecarboxamide (52.3 kg, 215 mol) is suspended in ethyl acetate (146 kg) and the suspension is heated to approx. 40° C. 4-Chloro-3-trifluoromethylphenyl isocyanate (50 kg, 226 mol), dissolved in ethyl acetate (58 kg), is then added to such a degree that the temperature is kept below 60° C. After cooling to 20° C. within 1 h, the mixture is stirred for a further 30 min and the product is filtered off. After washing with ethyl acetate (30 kg), the product is dried under reduced pressure (50° C., 80 mbar). 93 kg (93% of theory) of the title compound are obtained as colorless to slightly brownish crystals. m.p. 206-208° C. 1H-NMR (DMSO-d6, 500 MHz): δ =2.79 (d, J=4.4 Hz, 3H, NCH3); 7.16 (dd, J=2.5, 5.6 Hz, 1H, 5-H); 7.18 (d, J=8.8 Hz, 2H, 3′-H, 5′-H); 7.38 (d, J=2.4 Hz, 1H, 3-H); 7.60-7.68 (m, 4H, 2′-H, 6′-H, 5″-H, 6″-H); 8.13 (d, J=1.9 Hz, 1H, 2″-H); 8.51 (d, J=5.6 Hz, 1H, 6-H); 8.81 (d, J=4.5 Hz, 1H, NHCH3); 9.05 (br. s, 1H, NHCO); 9.25 (br. s, 1H, NHCO) MS (ESI, CH3CN/H2O): m/e=465 [M+H]+.
Synthesis of Sorafenib Tosylate (Nexavar)
4-(4-{3-[4-chloro-3-(trifluoromethyl)phenyl]ureido}phenoxy)-N2-methylpyridine-2-carboxamide (sorafenib) (50g, 0.1076 mol) is suspended in ethyl acetate (500 g) and water (10g). The mixture is heated to 69°C within 0.5 h, and a filtered solution of p-toluenesulfonic acid monohydrate (3.26 g, 0.017 mol) in a mixture of water (0.65 g) and ethyl acetate (7.2 g) is added. After filtration a filtered solution of p-toluenesulfonic acid monohydrate (22g, 0.11 mol) in a mixture of ethyl acetate (48 g) and water (4.34 g) is added. The mixture is cooled to 23°C within 2 h. The product is filtered off, washed twice with ethyl acetate (92.5 g each time) and dried under reduced pressure. The sorafenib tosylate (65.5 g, 96% of theory) is obtained as colorless to slightly brownish crystals.
…………………..
http://www.google.com/patents/EP2195286A2?cl=en
Example 22: Synthesis of Sorafenib
Phenyl 4-chloro-3-(trifluoromethyl)phenylcarbamate (100 g, 0.3174 mol) and 4-(4- aminophenoxy)-N-methylpicolinamide (77.14 g, 0.3174 mol) were dissolved in N1N- dimethyl formamide (300 ml) to obtain a clear reaction mass. The reaction mass was agitated at 40-450C for 2-3 hours, cooled to room temperature and diluted with ethyl acetate (1000 ml). The organic layer was washed with water (250 ml) followed by 1N HCI (250ml) and finally with brine (250 ml). The organic layer was separated, dried over sodium sulfate and degassed to obtain solid. This solid was stripped with ethyl acetate and finally slurried in ethyl acetate (1000 ml) at room temperature. It was then filtered and vacuum dried to give (118 g) of 4-(4-(3-(4-chloro-3- (trifluoromethyl)phenyl)ureido)phenoxy)-N-methylpicolinamide (sorafenib base).
Example 23: Synthesis of 1-(4-chloro-3-(trifluoromethyl)phenyl)urea (Compound 4)
Sodium cyanate (1.7 g, 0.02mol) was dissolved in water (17ml) at room temperature to obtain a clear solution. This solution was then charged drop wise to the clear solution of 3- trifluoromethyl-4-chloroaniline (5 g, 0.025 mol) in acetic acid (25 ml) at 40°C-45°C within 1- 2 hours. The reaction mass was agitated for whole day and cooled gradually to room temperature. The obtained solid was filtered washed with water and vacuum dried at 500C to afford the desired product (5.8 g) i.e. 1-(4-chloro-3-(trifluoromethyl)phenyl)urea.
Example 24: Synthesis of Sorafenib
1-(4-chloro-3-(trifluoromethyl) phenyl)urea (15 g, 0.0628 mol), 1 ,8- diazabicyclo[5.4.0]undec-7-ene (11.75 ml, 0.078 mol) and 4-(4-aminophenoxy)-N- methylpicolinamide (15.27 g, 0.0628 mol) were mixed with dimethyl sulfoxide (45 ml) and the reaction mass was then heated to 110-1200C for 12-18 hours. The reaction mass was cooled to room temperature and quenched in water (250 ml). The quenched mass was extracted repeatedly with ethyl acetate and the combined ethyl acetate layer was then back washed with water. It was dried over sodium sulfate and evaporated under vacuum to obtain solid. The obtained solid was slurried in acetonitrile (150 ml) at ambient temperature and filtered to give 4-(4-(3-(4-chloro-3-(trifluoromethyl) phenyl) ureido) phenoxy)-N-methylpicolinamide (sorafenib base) (17.5 g).
………………………..
http://www.google.com/patents/WO2009054004A2?cl=en

EXAMPLES
Example 1
Preparation of l-(4-chloro-3-(trifluoromethyl)phenyI)-3-(4-hydroxyphenyl)urea Into a 250 ml, four-necked RB flask was charged 1O g of 4-aminophenol and 100 ml of toluene. A solution of 4-chloro-3-(trifluoromethyl)phenyl isocyante (20.4 g) in toluene (50 ml) was added to the reaction mass at 25-300C. The reaction mass was stirred at room temperature for 16 h. The reaction mass was filtered and washed the. solid with 50 ml of toluene. The wet material was dried in the oven at 50-60°C to get 29.8 g of title compound as white solid. M.P. is 218-222°C. IR (KBr): 3306, 1673, 1625, 1590, 1560, 1517, 1482, 1435, 1404, 1328, 1261, 1182, 1160, 1146, 1125, 1095, 1032, 884, 849, 832, 812, 766, 746, 724, 683, 539 and 434 cm“1.
Example 2 Preparation of sorafenib tosylate
Into a 100 ml, three-necked RB flask was charged 2.0 g of l-(4-chloro-3- (trifluoromethyl)-phenyl)-3-(4-hydroxyphenyl)urea and 10 ml of DMF. Potassium tert- butoxide (2.3 g) was added to the reaction mass and stirred for 45 min at RT. 4-Chlro-N- methylpicolinamide (1.14 g) and potassium carbonate (0.42 g) were added to the reaction mass and heated to 80°C. The reaction mass was maintained at 80-85°C for 8 h and cooled to 30°C. The reaction mass was poured into water and extracted with ethyl acetate. Ethyl acetate layer was washed with water, brine and dried over sodium sulphate. Solvent was distilled of under reduced pressure.
The crude compound (4.7 g) was dissolved in 10 ml of IPA and added 1.9 g of p- toluenesulfonic acid. The reaction mass was stirred at RT for 15 h and filtered. The wet solid was washed with 10 ml of IPA and dried at 50-60°C to get 3.4 g of title compound as off-white crystalline solid.
…………………..
A Scaleable Synthesis of BAY 43-9006: A Potent Raf Kinase Inhibitor for the Treatment of Cancer
http://pubs.acs.org/doi/abs/10.1021/op020205n

Urea 3 (BAY 43–9006), a potent Raf kinase inhibitor, was prepared in four steps with an overall yield of 63%. Significant process research enabled isolation of each intermediate and target without chromatographic purification, and overall yield increases >50% were observed compared to those from previous methods. This report focuses on improved synthetic strategies for production of scaled quantities of 3 for preclinical, toxicological studies. These improvements may be useful to assemble other urea targets as potential therapeutic agents to combat cancer.
References
- “FDA Approves Nexavar for Patients with Inoperable Liver Cancer” (Press release). FDA. November 19, 2007. Retrieved November 10, 2012.
- “Nexavar (sorafenib) dosing, indications, interactions, adverse effects, and more”. Medscape Reference. WebMD. Retrieved 26 December 2013.
- “NEXAVAR (sorafenib) tablet, film coated [Bayer HealthCare Pharmaceuticals Inc.]”. DailyMed. Bayer HealthCare Pharmaceuticals Inc. November 2013. Retrieved 26 December 2013.
- “Nexavar 200mg film-coated tablets – Summary of Product Characteristics (SPC) – (eMC)”. electronic Medicines Compendium. Bayer plc. 27 March 2013. Retrieved 26 December 2013.
- “PRODUCT INFORMATION NEXAVAR® (sorafenib tosylate)” (PDF). TGA eBusiness Services. Bayer Australia Ltd. 12 December 2012. Retrieved 26 December 2013.
- Escudier, B; Eisen, T; Stadler, WM; Szczylik, C; Oudard, S; Siebels, M; Negrier, S; Chevreau, C; Solska, E; Desai, AA; Rolland, F; Demkow, T; Hutson, TE; Gore, M; Freeman, S; Schwartz, B; Shan, M; Simantov, R; Bukowski, RM (January 2007). “Sorafenib in advanced clear-cell renal-cell carcinoma”. New England Journal of Medicine 356 (2): 125–34. doi:10.1056/NEJMoa060655. PMID 17215530.
- Walid, MS; Johnston, KW (October 2009). “Successful treatment of a brain-metastasized renal cell carcinoma”. German Medical Science 7: Doc28. doi:10.3205/000087. PMC 2775194. PMID 19911072.
- “Pharmaceutical Benefits Scheme (PBS) -SORAFENIB”. Pharmaceutical Benefits Scheme. Australian Government Department of Health. Retrieved 27 December 2013.
- Llovet, et al. (2008). “Sorafenib in Advanced Hepatocellular Carcinoma” (PDF). New England Journal of Medicine 359 (4): 378–90.
- Keating GM, Santoro A (2009). “Sorafenib: a review of its use in advanced hepatocellular carcinoma”. Drugs 69 (2): 223–40. doi:10.2165/00003495-200969020-00006. PMID 19228077.
- Pawlik TM, Reyes DK, Cosgrove D, Kamel IR, Bhagat N, Geschwind JF (October 2011). “Phase II trial of sorafenib combined with concurrent transarterial chemoembolization with drug-eluting beads for hepatocellular carcinoma”. J. Clin. Oncol. 29 (30): 3960–7. doi:10.1200/JCO.2011.37.1021. PMID 21911714.
- “Phase 3 Trial of Nexavar in Patients With Non-Responsive Thyroid Cancer”[dead link]
- [1]
- “Chemotherapy-Induced Nausea and Vomiting Treatment & Management”. Medscape Reference. WebMD. 3 July 2012. Retrieved 26 December 2013.
- Hagopian, Benjamin (August 2010). “Unusually Severe Bullous Skin Reaction to Sorafenib: A Case Report”. Journal of Medical Cases 1 (1): 1–3. doi:10.4021/jmc112e. Retrieved 11 February 2014.
- Smalley KS, Xiao M, Villanueva J, Nguyen TK, Flaherty KT, Letrero R, Van Belle P, Elder DE, Wang Y, Nathanson KL, Herlyn M (January 2009). “CRAF inhibition induces apoptosis in melanoma cells with non-V600E BRAF mutations”. Oncogene 28 (1): 85–94. doi:10.1038/onc.2008.362. PMC 2898184. PMID 18794803.
- Wilhelm SM, Adnane L, Newell P, Villanueva A, Llovet JM, Lynch M (October 2008). “Preclinical overview of sorafenib, a multikinase inhibitor that targets both Raf and VEGF and PDGF receptor tyrosine kinase signaling”. Mol. Cancer Ther. 7 (10): 3129–40. doi:10.1158/1535-7163.MCT-08-0013. PMID 18852116.
- Zhang Y (Jan 2014). “Screening of kinase inhibitors targeting BRAF for regulating autophagy based on kinase pathways.”. J Mol Med Rep 9 (1): 83–90. PMID 24213221.
- Gauthier A (Feb 2013). “Role of sorafenib in the treatment of advanced hepatocellular carcinoma: An update..”. Hepatol Res 43 (2): 147–154. doi:10.1111/j.1872-034x.2012.01113.x. PMID 23145926.
- FDA Approval letter for use of sorafenib in advanced renal cancer
- European Commission – Enterprise and industry. Nexavar. Retrieved April 24, 2007.
- “Nexavar® (Sorafenib) Approved for Hepatocellular Carcinoma in Europe” (Press release). Bayer HealthCare Pharmaceuticals and Onyx Pharmaceuticals. October 30, 2007. Retrieved November 10, 2012.
- FDA Approval letter for use of sorafenib in inoperable hepatocellular carcinoma
- “Liver drug ‘too expensive‘“. BBC News. November 19, 2009. Retrieved November 10, 2012.
- http://www.ipindia.nic.in/ipoNew/compulsory_License_12032012.pdf
- “Seven days: 9–15 March 2012”. Nature 483 (7389): 250–1. 2012. doi:10.1038/483250a.
- “India Patents (Amendment) Act, 2005”. WIPO. Retrieved 16 January 2013.
- [2]
- “Addition of Sorafenib May Be Detrimental in Some Lung Cancer Patients”
- ClinicalTrials.gov NCT00329719 Sorafenib and Temsirolimus in Treating Patients With Recurrent Glioblastoma
- “Activity of sorafenib against desmoid tumor/deep fibromatosis”
- “‘We didn’t make this medicine for Indians… we made it for western patients who can afford it‘“. Daily Mail Reporter. 24 Jan 2014.
External links
- Nexavar.com – Manufacturer’s website
- Prescribing Information – includes data from the key studies justifying the use of sorafenib for the treatment of kidney cancer (particularly clear cell renal cell carcinoma, which is associated with the von Hippel-Lindau gene)
- Patient Information from FDA
- Sorafenib in Treating Patients With Soft Tissue Sarcomas
- Sorafenib Sunitinib differences – diagram
- ClinicalTrials.gov NCT00217399 – Sorafenib and Anastrozole in Treating Postmenopausal Women With Metastatic Breast Cancer
- Cipla launches Nexavar generic at 1/10 of Bayer’s price
| Reference | ||
|---|---|---|
| 1 | * | D. BANKSTON ET AL.: “A Scalable Synthesis of BAY 43-9006: A Potent Raf Kinase Inhibitor for the Treatment of Cancer” ORGANIC PROCESS RESEARCH & DEVELOPMENT, vol. 6, no. 6, 2002, pages 777-781, XP002523918 cited in the application |
| 2 | * | PAN W ET AL: “Pyrimido-oxazepine as a versatile template for the development of inhibitors of specific kinases” BIOORGANIC & MEDICINAL CHEMISTRY LETTERS, PERGAMON, ELSEVIER SCIENCE, GB, vol. 15, no. 24, 15 December 2005 (2005-12-15), pages 5474-5477, XP025314229 ISSN: 0960-894X [retrieved on 2005-12-15] |
| Citing Patent | Filing date | Publication date | Applicant | Title |
|---|---|---|---|---|
| WO2011036647A1 | Sep 24, 2010 | Mar 31, 2011 | Ranbaxy Laboratories Limited | Process for the preparation of sorafenib tosylate |
| WO2011036648A1 | Sep 24, 2010 | Mar 31, 2011 | Ranbaxy Laboratories Limited | Polymorphs of sorafenib acid addition salts |
| WO2011058522A1 | Nov 12, 2010 | May 19, 2011 | Ranbaxy Laboratories Limited | Sorafenib ethylsulfonate salt, process for preparation and use |
| WO2011092663A2 | Jan 28, 2011 | Aug 4, 2011 | Ranbaxy Laboratories Limited | 4-(4-{3-[4-chloro-3-(trifluoromethyl)phenyl]ureido}phenoxy)-n2-methylpyridine-2-carboxamide dimethyl sulphoxide solvate |
| WO2011113367A1 * | Mar 17, 2011 | Sep 22, 2011 | Suzhou Zelgen Biopharmaceutical Co., Ltd. | Method and process for preparation and production of deuterated ω-diphenylurea |
| US8552197 | Nov 12, 2010 | Oct 8, 2013 | Ranbaxy Laboratories Limited | Sorafenib ethylsulfonate salt, process for preparation and use |
| US8604208 | Sep 24, 2010 | Dec 10, 2013 | Ranbaxy Laboratories Limited | Polymorphs of sorafenib acid addition salts |
| US8609854 | Sep 24, 2010 | Dec 17, 2013 | Ranbaxy Laboratories Limited | Process for the preparation of sorafenib tosylate |
| US8618305 | Jan 28, 2011 | Dec 31, 2013 | Ranbaxy Laboratories Limited | Sorafenib dimethyl sulphoxide solvate |
| US8669369 | Mar 17, 2011 | Mar 11, 2014 | Suzhou Zelgen Biopharmaceutical Co., Ltd. | Method and process for preparation and production of deuterated Ω-diphenylurea |

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....

























