Home » Posts tagged 'Antisense oligonucleotide'
Tag Archives: Antisense oligonucleotide
Casimersen
Casimersen
カシメルセン;
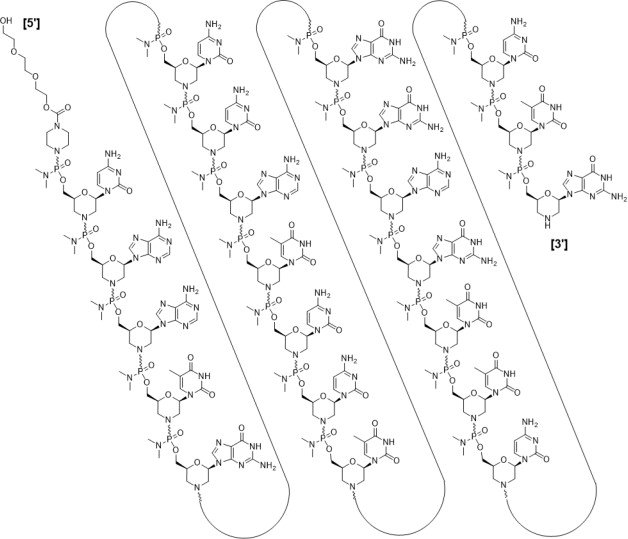
RNA, [P-deoxy-P-(dimethylamino)](2′,3′-dideoxy-2′,3′-imino-2′,3′-seco)(2’a→5′)(C-A-A-m5U-G-C-C-A-m5U-C-C-m5U-G-G-A-G-m5U-m5U-C-C-m5U-G), 5′-[P-[4-[[2-[2-(2-hydroxyethoxy)ethoxy]ethoxy]carbonyl]-1-piperazinyl]-N,N-dimethylphosphonamidate]
| Formula | C268H424N124O95P22 |
|---|---|
| CAS | 1422958-19-7 |
| Mol weight | 7584.4307 |
FDA 2021/2/25 , Amondys 45, Antisense oligonucleotide
Treatment of Duchenne muscular dystrophy
Nucleic Acid Sequence
Sequence Length: 224 a 7 c 5 g 6 umodified
- Exon-45: NG-12-0064
- SRP-4045
- WHO 10354
Casimersen, sold under the brand name Amondys 45, is an antisense oligonucleotide medication used for the treatment of Duchenne muscular dystrophy (DMD) in people who have a confirmed mutation of the dystrophin gene that is amenable to exon 45 skipping.[1][2][3][4] It is an antisense oligonucleotide of phosphorodiamidate morpholino oligomer (PMO).[1]
The most common side effects include upper respiratory tract infections, cough, fever, headache, joint pain and throat pain.[2]
Casimersen was approved for medical use in the United States in February 2021,[1][2] and it is the first FDA-approved targeted treatment for people who have a confirmed mutation of the DMD gene that is amenable to skipping exon 45.[2]
Duchenne muscular dystrophy (DMD) is an X-linked recessive allelic disorder characterized by a lack of functional dystrophin protein, which leads to progressive impairment of ambulatory, pulmonary, and cardiac function and is invariably fatal. A related, albeit a less severe, form of muscular dystrophy known as Becker muscular dystrophy (BMD) is characterized by shortened and partially functional dystrophin protein production. Although corticosteroids effectively slow disease progression in both DMD and BMD patients, they do not address the underlying molecular pathogenesis.1,2,3
The application of antisense oligonucleotides in DMD patients with specific mutations allows for exon skipping to produce truncated BMD-like dystrophin proteins, which restore partial muscle function and slow disease progression.1,2,4,5,7 Casimersen is a phosphorodiamidate morpholino oligonucleotide (PMO); PMOs are oligonucleotides in which the five-membered ribofuranosyl ring is replaced with a six-membered morpholino ring, and the phosphodiester links between nucleotides are replaced with a phosphorodiamidate linkage.6,7 In this manner, PMOs are much less susceptible to endo- and exonucleases and exhibit drastically reduced metabolic degradation compared to traditional synthetic oligonucleotides.6 Casimersen is the most recent in a line of approved PMOs for treating DMD, including eteplirsen and viltolarsen. However, the specific mutations, and hence the precise exon skipping, targeted by each is different.
Casimersen was granted accelerated FDA approval on February 25, 2021, based on data showing an increase in dystrophin levels in skeletal muscle of patients treated with casimersen; this approval is contingent on further verification in confirmatory trials. Casimersen is currently marketed under the tradename AMONDYS 45™ by Sarepta Therapeutics, Inc.7
Casimersen is indicated for the treatment of Duchenne muscular dystrophy (DMD) in patients confirmed to have a DMD gene mutation amenable to exon 45 skipping. This indication represents an accelerated approval based on observed efficacy; continued approval for this indication may be contingent on the verification of safety and efficacy in a confirmatory trial.7
Medical uses
Casimersen is indicated for the treatment of Duchenne muscular dystrophy (DMD) in people who have a confirmed mutation of the DMD gene that is amenable to exon 45 skipping.[1][2]
History
Casimersen was evaluated in a double-blind, placebo-controlled study in which 43 participants were randomized 2:1 to receive either intravenous casimersen or placebo.[2] All participants were male, between 7 and 20 years of age, and had a genetically confirmed mutation of the DMD gene that is amenable to exon 45 skipping.[2]
The U.S. Food and Drug Administration (FDA) granted the application for casimersen fast track, priority review, and orphan drug designations.[2][5] The FDA granted the approval of Amondys 45 to Sarepta Therapeutics, Inc.[2]
Pharmacodynamics
Casimersen is an antisense phosphorodiamidate morpholino oligonucleotide designed to bind to exon 45 of the DMD pre-mRNA, preventing its inclusion in mature mRNA and allowing the production of an internally truncated dystrophin protein in patients who would normally produce no functional dystrophin. Due to the need for continuous alteration of mRNA splicing and its relatively short half-life, casimersen is administered weekly.7 Although casimersen is associated with mostly mild adverse effects, animal studies suggest a potential for nephrotoxicity, which has also been observed after administration of some oligonucleotides.4,7 Measurement of glomerular filtration rate before starting casimersen is advised. Serum cystatin C, urine dipstick, and urine protein-to-creatinine ratio should be measured before starting therapy. They should be measured monthly (urine dipstick) or every three months (serum cystatin C and urine protein-to-creatinine ratio) during treatment. Creatinine levels are not reliable in muscular dystrophy patients and should not be used. Any persistent alteration in kidney function should be further investigated.7
Mechanism of action
Duchenne muscular dystrophy (DMD) is an X-linked recessive allelic disorder that results in the absence of functional dystrophin, a large protein comprising an N-terminal actin-binding domain, C-terminal β-dystroglycan-binding domain, and 24 internal spectrin-like repeats.1,2,3 Dystrophin is vital for normal muscle function; the absence of dystrophin leads to muscle membrane damage, extracellular leakage of creatinine kinase, calcium influx, and gradual replacement of normal muscle tissue with fibrous and adipose tissue over time.1,2 DMD shows a characteristic disease progression with early functional complaints related to abnormal gait, locomotion, and falls that remain relatively stable until around seven years of age. The disease then progresses rapidly to loss of independent ambulatory function, ventilatory insufficiency, and cardiomyopathy, with death typically occurring in the second or third decade of life.1,2,3
The human DMD gene contains 79 exons spread over approximately 2.4 million nucleotides on the X chromosome.1 DMD is associated with a variety of underlying mutations, including exon duplications or deletions, as well as point mutations leading to nonsense translation through direct production of an in-frame stop codon, frameshift production of an in-frame stop codon, or aberrant inclusion of an intronic pseudo-exon with the concomitant production of an in-frame stop codon.1,2 In all cases, no functional dystrophin protein is produced. Becker muscular dystrophy (BMD) is a related condition with in-frame mutations that result in the production of a truncated but partially functional dystrophin protein. BMD patients, therefore, have milder symptoms, delayed disease progression, and longer life expectancy compared to DMD patients.1,2,3
Casimersen is an antisense phosphorodiamidate morpholino oligonucleotide designed to bind to exon 45 of the DMD pre-mRNA and prevent its inclusion within the mature mRNA before translation.4,7 It is estimated that around 8% of DMD patients may benefit from exon 45 skipping, in which the exclusion of this exon results in the production of an internally truncated and at least partly functional dystrophin protein.4,7,5 Although fibrotic or fatty muscle tissue developed previously cannot be improved, this therapy aims to slow further disease progression through the production of partially functional dystrophin and alleviation of the pathogenic mechanism of muscle tissue necrosis.1,2
| TARGET | ACTIONS | ORGANISM |
|---|---|---|
| ADMD gene (exon 45 casimersen target site) | binder | Humans |
Absorption
DMD patients receiving IV doses of 4-30 mg/kg/week revealed exposure in proportion to dose with no accumulation of casimersen in plasma with once-weekly dosing. Following a single IV dose, casimersen Cmax was reached by the end of infusion. Inter-subject variability, as measured by the coefficient of variation, ranged from 12-34% for Cmax and 16-34% for AUC.7
Pre-clinical studies in nonhuman primates (cynomolgus monkeys) investigated the pharmacokinetics of once-weekly casimersen administered at doses of 5, 40, and 320 mg/kg. On days 1 and 78, the 5 mg/kg dose resulted in a Cmax of 19.5 ± 3.43 and 21.6 ± 5.60 μg/mL and an AUC0-t of 24.9 ± 5.17 and 26.9 ± 7.94 μg*hr/mL. The 40 mg/kg dose resulted in a Cmax of 208 ± 35.2 and 242 ± 71.1 μg/mL and an AUC0-t of 283 ± 68.5 and 320 ± 111 μg*hr/mL. Lastly, the 320 mg/kg dose resulted in a a Cmax of 1470 ± 88.1 and 1490 ± 221 μg/mL and an AUC0-t of 1960 ± 243 and 1930 ± 382 μg*hr/mL.4
Volume of distribution
Casimersen administered at 30 mg/kg had a mean steady-state volume of distribution (%CV) of 367 mL/kg (28.9%).7
Protein binding
Casimersen binding to human plasma proteins is not concentration-dependent, ranging from 8.4-31.6%.7
Metabolism
Casimersen incubated with human hepatic microsomal preparations is metabolically stables and no metabolites are detected in plasma or urine.7
Route of elimination
Casimersen is predominantly (more than 90%) excreted in the urine unchanged with negligible fecal excretion.7
Half-life
Casimersen has an elimination half-life of 3.5 ± 0.4 hours.7
Clearance
Casimersen administered at 30 mg/kg has a plasma clearance of 180 mL/hr/kg.7
| NAME | DOSAGE | STRENGTH | ROUTE | LABELLER | MARKETING START | MARKETING END | ||
|---|---|---|---|---|---|---|---|---|
| Amondys 45 | Injection | 50 mg/1mL | Intravenous | Sarepta Therapeutics, Inc. | 2021-02-25 | Not applicable |
Synthesis Reference
Diane Elizabeth Frank and Richard K. Bestwick, “Exon skipping oligomers for muscular dystrophy.” U.S. Patent US20190262375A1, issued August 29, 2019.
PATENT
https://patents.google.com/patent/WO2017205879A2/en
also
WO 2021025899
References
- ^ Jump up to:a b c d e “Amondys 45- casimersen injection”. DailyMed. Retrieved 1 March 2021.
- ^ Jump up to:a b c d e f g h i j “FDA Approves Targeted Treatment for Rare Duchenne Muscular Dystrophy Mutation”. U.S. Food and Drug Administration (FDA) (Press release). 25 February 2021. Retrieved 25 February 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ “Sarepta Therapeutics Announces FDA Approval of Amondys 45 (casimersen) Injection for the Treatment of Duchenne Muscular Dystrophy (DMD) in Patients Amenable to Skipping Exon 45” (Press release). Sarepta Therapeutics. 25 February 2021. Retrieved 25 February 2021 – via GlobeNewswire.
- ^ Rodrigues M, Yokota T (2018). “An Overview of Recent Advances and Clinical Applications of Exon Skipping and Splice Modulation for Muscular Dystrophy and Various Genetic Diseases”. Exon Skipping and Inclusion Therapies. Methods in Molecular Biology. 1828. Clifton, N.J. pp. 31–55. doi:10.1007/978-1-4939-8651-4_2. ISBN 978-1-4939-8650-7. PMID 30171533.
- ^ “Casimersen Orphan Drug Designations and Approvals”. U.S. Food and Drug Administration (FDA). 4 June 2019. Retrieved 25 February 2021.
General References
- Wein N, Alfano L, Flanigan KM: Genetics and emerging treatments for Duchenne and Becker muscular dystrophy. Pediatr Clin North Am. 2015 Jun;62(3):723-42. doi: 10.1016/j.pcl.2015.03.008. Epub 2015 Apr 20. [PubMed:26022172]
- Verhaart IEC, Aartsma-Rus A: Therapeutic developments for Duchenne muscular dystrophy. Nat Rev Neurol. 2019 Jul;15(7):373-386. doi: 10.1038/s41582-019-0203-3. [PubMed:31147635]
- Mercuri E, Bonnemann CG, Muntoni F: Muscular dystrophies. Lancet. 2019 Nov 30;394(10213):2025-2038. doi: 10.1016/S0140-6736(19)32910-1. [PubMed:31789220]
- Carver MP, Charleston JS, Shanks C, Zhang J, Mense M, Sharma AK, Kaur H, Sazani P: Toxicological Characterization of Exon Skipping Phosphorodiamidate Morpholino Oligomers (PMOs) in Non-human Primates. J Neuromuscul Dis. 2016 Aug 30;3(3):381-393. doi: 10.3233/JND-160157. [PubMed:27854228]
- Rodrigues M, Yokota T: An Overview of Recent Advances and Clinical Applications of Exon Skipping and Splice Modulation for Muscular Dystrophy and Various Genetic Diseases. Methods Mol Biol. 2018;1828:31-55. doi: 10.1007/978-1-4939-8651-4_2. [PubMed:30171533]
- Smith CIE, Zain R: Therapeutic Oligonucleotides: State of the Art. Annu Rev Pharmacol Toxicol. 2019 Jan 6;59:605-630. doi: 10.1146/annurev-pharmtox-010818-021050. Epub 2018 Oct 9. [PubMed:30285540]
- FDA Approved Drug Products: AMONDYS 45 (casimersen) injection [Link]
External links
- “Casimersen”. Drug Information Portal. U.S. National Library of Medicine.
- Clinical trial number NCT02500381 for “Study of SRP-4045 and SRP-4053 in DMD Patients (ESSENCE)” at ClinicalTrials.gov
| Clinical data | |
|---|---|
| Trade names | Amondys 45 |
| Other names | SRP-4045 |
| License data | US DailyMed: Casimersen |
| Routes of administration | Intravenous |
| Drug class | Antisense oligonucleotide |
| ATC code | None |
| Legal status | |
| Legal status | US: ℞-only [1][2] |
| Identifiers | |
| CAS Number | 1422958-19-7 |
| DrugBank | DB14984 |
| UNII | X8UHF7SX0R |
| KEGG | D11988 |
| Chemical and physical data | |
| Formula | C268H424N124O95P22 |
| Molar mass | 7584.536 g·mol−1 |
////////////Casimersen, FDA 2021, APPROVALS 2021, カシメルセン , Exon-45: NG-12-0064, SRP-4045, WHO 10354, Amondys 45, Antisense oligonucleotide, Duchenne muscular dystrophy
#Casimersen, #FDA 2021, #APPROVALS 2021, #カシメルセン , #Exon-45: NG-12-0064, #SRP-4045, #WHO 10354, #Amondys 45, #Antisense oligonucleotide, #Duchenne muscular dystrophy
Sequence:
1caaugccauc cuggaguucc ug
Sequence Modifications
| Type | Location | Description |
|---|---|---|
| modified base | c-1 | 5′-ester |
| modified base | c-1 | modified cytidine |
| modified base | a-2 | modified adenosine |
| modified base | a-3 | modified adenosine |
| modified base | u-4 | m5u |
| modified base | u-4 | modified uridine |
| modified base | g-5 | modified guanosine |
| modified base | c-6 | modified cytidine |
| modified base | c-7 | modified cytidine |
| modified base | a-8 | modified adenosine |
| modified base | u-9 | modified uridine |
| modified base | u-9 | m5u |
| modified base | c-10 | modified cytidine |
| modified base | c-11 | modified cytidine |
| modified base | u-12 | m5u |
| modified base | u-12 | modified uridine |
| modified base | g-13 | modified guanosine |
| modified base | g-14 | modified guanosine |
| modified base | a-15 | modified adenosine |
| modified base | g-16 | modified guanosine |
| modified base | u-17 | modified uridine |
| modified base | u-17 | m5u |
| modified base | u-18 | modified uridine |
| modified base | u-18 | m5u |
| modified base | c-19 | modified cytidine |
| modified base | c-20 | modified cytidine |
| modified base | u-21 | m5u |
| modified base | u-21 | modified uridine |
| modified base | g-22 | modified guanosine |
| uncommon link | c-1 – a-2 | unavailable |
| uncommon link | a-2 – a-3 | unavailable |
| uncommon link | a-3 – u-4 | unavailable |
| uncommon link | u-4 – g-5 | unavailable |
| uncommon link | g-5 – c-6 | unavailable |
| uncommon link | c-6 – c-7 | unavailable |
| uncommon link | c-7 – a-8 | unavailable |
| uncommon link | a-8 – u-9 | unavailable |
| uncommon link | u-9 – c-10 | unavailable |
| uncommon link | c-10 – c-11 | unavailable |
| uncommon link | c-11 – u-12 | unavailable |
| uncommon link | u-12 – g-13 | unavailable |
| uncommon link | g-13 – g-14 | unavailable |
| uncommon link | g-14 – a-15 | unavailable |
| uncommon link | a-15 – g-16 | unavailable |
| uncommon link | g-16 – u-17 | unavailable |
| uncommon link | u-17 – u-18 | unavailable |
| uncommon link | u-18 – c-19 | unavailable |
| uncommon link | c-19 – c-20 | unavailable |
| uncommon link | c-20 – u-21 | unavailable |
| uncommon link | u-21 – g-22 | unavailable |
Celgene oral Crohn’s drug GED-0301, Mongersen impresses in Phase II

Nogra制药,Celgene
公司寡核苷酸(Oligonucleotides)
克罗恩病(Crohn’s disease)
Shares in Celgene Corp have risen steadily following promising mid-stage data of its closely-watched Crohn’s disease drug mongersen.
| Company | Nogra Pharma Ltd. |
| Description | Antisense oligonucleotide targeting SMAD family member 7 (MADH7; SMAD7) |
| Molecular Target | SMAD family member 7 (MADH7) (SMAD7) |
| Mechanism of Action | |
| Therapeutic Modality | Nucleic acid: Linear RNA: Antisense |
| Latest Stage of Development | Phase II |
| Standard Indication | Crohn’s disease |
| Indication Details | Treat moderate to severe Crohn’s disease |
| Regulatory Designation | |
| Partner |
Mongersen (GED-0301) from Celgene Corp. (NASDAQ:CELG) produced clinical remission rates as high as 65.1% in a Phase II trial in 166 patients with moderate to severe Crohn’s disease, according to an abstract published in advance of the United European Gastroenterology’s meeting in Vienna.
In the trial, 55% of patients receiving 40 mg/day of mongersen and 65.1% of those receiving 160 mg/day achieved clinical remission compared with 9.5% of placebo patients (p<0.0001 for both). A cohort receiving 10 mg/day achieved a clinical remission rate of 12.2%, which was not significantly better than placebo.
The study’s primary outcomes were clinical remission, defined by a CDAI score less than 150 at day 15 and maintained for more than two weeks, and safety. Mongersen was well-tolerated, and toxicities associated with systemically active antisense therapies were not observed.
The study’s secondary endpoint is clinical response, defined as a CDAI score reduction of 100 points at day 28. Those rates were dose-dependent: 36.6%, 57.5% and 72.1% for the low, medium and high doses compared with 16.7% for placebo.
Celgene said it plans to start Phase III testing of mongersen shortly. The company paid $710 million up front to obtain exclusive, worldwide rights to the antisense oligonucleotide targeting SMAD family member 7 (MADH7; SMAD7) from Nogra Pharma Ltd. (Dublin, Ireland) in April. Nogra is eligible for $1.9 billion in milestones, plus tiered single-digit royalties.
GED-0301, an antisense oligonucleotide targeting the SMAD7 gene, is in phase II clinical trials at Nogra Pharma for the oral treatment of moderate to severe Crohn’s disease.
生物技术公司新基(Celgene)从爱尔兰制药商Nogra制药手中获得了一种处于后期临床开发的克罗恩病(Crohn’s disease)药物GED-0301。GED-0301是一种口服反义药物,靶向于Smad7信使RNA(mRNA),该药开发用于中度至重度克罗恩病 的治疗。反义药物是一种合成的核酸拷贝,旨在结合导致疾病的基因的mRNA,关闭基因的表达;口服;【Celgene签署$26亿协议获克罗恩病反义药物 GED-0301】http://www.hfoom.com/product/20140425/8311.html
Inflammatory bowel disease (IBD) is a chronic inflammatory disorder of the gastrointestinal tract suffered by approximately one million patients in the United States. The two most common forms of IBD are Crohn’s disease (CD) and ulcerative colitis (UC). Although CD can affect the entire gastrointestinal tract, it primarily affects the ilieum (the distal or lower portion of the small intestine) and the large intestine. UC primarily affects the colon and the rectum. Current treatment for both CD and UC include aminosalicylates (e.g., 5- aminosalicylic acid, sulfasalazine and mesalamine), antibiotics (e.g., ciprofloxacin and metronidazole), corticosteroids (e.g., budesonide or prednisone), immunosuppressants (e.g., azathioprine or methotrexate) and tumor necrosis factor (TNF) antagonists (e.g., infliximab (Remicade®)). Patient response to these therapies varies with disease severity and it can vary over cycles of active inflammation and remission. Moreover, many of the current therapies for IBD are associated with undesirable side effects.
Although the etiologies of CD and UC are unknown, both are considered inflammatory diseases of the intestinal mucosa. Recent studies have demonstrated that TGF-β 1 acts as a potent immunoregulator able to control mucosal intestinal inflammation. TGF-βΙ binds a heterodimeric transmembrane serine/threonine kinase receptor containing two subunits, TGF-βΙ Rl and TGF-βΙ R2. Upon ligand binding, the TGF-βΙ Rl receptor is phosphorylated by the constitutively active TGF-βΙ R2 receptor and signal is propagated to the nucleus by proteins belonging to the SMAD family. Activated TGF-β Ι Rl directly phosphorylates SMAD2 and SMAD3 proteins, which then interact with SMAD4. The complex of SMAD2/SMAD3/SMAD4 translocates to the nucleus and modulates the transcription of certain genes.
Additional studies have demonstrated that another SMAD protein, SMAD7, also plays a role in inflammation. SMAD7, an intracellular protein, has been shown to interfere with binding of SMAD2/SMAD3 to the TGF-βΙ Rl preventing phosphorylation and activation of these proteins. Further, increased expression of SMAD7 protein is associated with an inhibition of TGF-βΙ mediated-signaling. Mucosal samples from IBD patients are characterized by high levels of SMAD7 and reduced levels of phosphorylated-SMAD3 indicating that TGF-βΙ -mediated signaling is compromised in these patients.
Recent studies have focused on SMAD7 as a target for treating patients suffering from IBD.
Such therapies include anti-SMAD7 antisense therapies. As such, there is a need for methods based on predictive biomarkers that can be used to identify patients that are likely (or unlikely) to respond to treatment with anti- SMAD7 therapies.
GTCGCCCCTTCTCCCCGCAGC
GED-0301, Mongersen
Phosphorothioate antisense oligonucleotide targeting human mothers against decapentaplegic homolog 7 (SMAD7) gene, whose sequence is 5′-GTCGCCCCTTCTCCCCGCAGC-3′, wherein ‘C’ at postions 3 and 16 is 5-methyl 2′-deoxycytidine 5′-monophosphate
WO 2004087920
http://www.google.com/patents/WO2004087920A1?cl=en
…………………………
WO 2013037970
http://www.google.com/patents/WO2013037970A1?cl=en
…………………
WO 2013158868
http://www.google.com/patents/WO2013158868A1?cl=en
……………………………………………
http://www.google.com/patents/WO2014140333A1?cl=en
5*-GTCGCCCCTTCTCCCCGCAGC-3* (SEQ ID NO: 3).
| Reference | ||
|---|---|---|
| 1 | BADARU, A.; PIHOKER, C.: ‘Type 2 diabetes in childhood: clinical characteristics and role of beta-cell autoimmunity‘ CURR. DIAB. REP. vol. 12, 2012, pages 75 – 81 | |
| 2 | * | BHAT ET AL: “Antisense inhibition of 11betahydroxysteroid dehydrogenase type 1 improves diabetes in a novel cortisone-induced diabetic KK mouse model“, BIOCHEMICAL AND BIOPHYSICAL RESEARCH COMMUNICATIONS, ACADEMIC PRESS INC. ORLANDO, FL, US, vol. 365, no. 4, 20 November 2007 (2007-11-20), pages 740-745, XP022384861, ISSN: 0006-291X, DOI: 10.1016/J.BBRC.2007.11.032 |
| 3 | * | GUTIERREZ-AGUILAR ET AL: “Minor contribution of SMAD7 and KLF10 variants to genetic susceptibility of type 2 diabetes“, DIABETES & METABOLISM, PARIS, AMSTERDAM, NL, vol. 33, no. 5, 10 October 2007 (2007-10-10), pages 372-378, XP022327080, ISSN: 1262-3636, DOI: 10.1016/J.DIABET.2007.06.002 |
| 4 | * | H. Y. CHEN ET AL: “The Protective Role of Smad7 in Diabetic Kidney Disease: Mechanism and Therapeutic Potential“, DIABETES, vol. 60, no. 2, 27 October 2010 (2010-10-27), pages 590-601, XP55071874, ISSN: 0012-1797, DOI: 10.2337/db10-0403 |
| 5 | HONG, S. ET AL.: ‘Smad7 sensitizes tumor necrosis factor induced apoptosis through the inhibition of antiapoptotic gene expression by suppressing activation of the nuclear factor-kappaB pathway‘ CANCER RES. vol. 67, 2007, pages 9577 – 9583 | |
| 6 | HOOK, S. M. ET AL.: ‘Smad2: A candidate gene for the murine autoimmune diabetes locus Idd21.1‘ 1. CLIN. ENDOCRINOL. METAB. vol. 96, 2011, pages E2072 – E2077 | |
| 7 | KAWAMOTO, K. ET AL.: ‘Transforming growth factor beta 1 (TGF-?1) and rapamycin synergize to effectively suppress human T cell responses via upregulation of FoxP3+ Tregs‘ TRANSPL. IMMUNOL. vol. 23, 2010, pages 28 – 33 | |
| 8 | LI, M. O.; FLAVELL, R. A.: ‘TGF-beta: a master of all T cell trades‘ CELL vol. 134, 2008, pages 392 – 404 | |
| 9 | * | LIANG Y ET AL: “Reduction in Glucagon Receptor Expression by an Antisense Oligonucleotide Ameliorates Diabetic Syndrome in db/db Mice“, DIABETES, AMERICAN DIABETES ASSOCIATION, US, vol. 53, February 2004 (2004-02), pages 410-417, XP002995165, ISSN: 0012-1797, DOI: 10.2337/DIABETES.53.2.410 |
| 10 | * | LU ZHU ET AL: “Unraveling the biological functions of Smad7 with mouse models“, CELL & BIOSCIENCE, BIOMED CENTRAL LTD, LONDON, UK, vol. 1, no. 1, 28 December 2011 (2011-12-28), page 44, XP021132085, ISSN: 2045-3701, DOI: 10.1186/2045-3701-1-44 |
| 11 | LUO, X. ET AL.: ‘Systemic transforming growth factor-?1 gene therapy induces Foxp3+ regulatory cells, restores self-tolerance, and facilitates regeneration of beta cell function in overtly diabetic nonobese diabetic mice‘ TRANSPLANTATION vol. 79, 2005, pages 1091 – 1096 | |
| 12 | MARGOLLES-CLARK, E. ET AL.: ‘Small molecule costimulatory blockade: organic dye inhibitors of the CD40-CD154 interaction‘ J. MOL. MED. vol. 87, 2009, pages 1133 – 1143 | |
| 13 | * | MIZOBUCHI TERUAKI ET AL: “Differential expression of Smad7 transcripts identifies the CD4+CD45RChigh regulatory T cells that mediate type V collagen-induced tolerance to lung allografts“, THE JOURNAL OF IMMUNOLOGY, THE AMERICAN ASSOCIATION OF IMMUNOLOGISTS, US, vol. 171, no. 3, 1 August 2003 (2003-08-01), pages 1140-1147, XP002430371, ISSN: 0022-1767 |
| 14 | MONTELEONE, G. ET AL.: ‘A failure of transforming growth factor-?1 negative regulation maintains sustained NF-KB activation in gut inflammation‘ J. BIOL. CHEM. vol. 279, 2004, pages 3925 – 3932 | |
| 15 | MORITANI, M. ET AL.: ‘Abrogation of autoimmune diabetes in nonobese diabetic mice and protection against effector lymphocytes by transgenic paracrine TGF-?1‘ J. CLIN. INVEST. vol. 102, 1998, pages 499 – 506 | |
| 16 | * | NORA G. SMART ET AL: “Conditional Expression of Smad7 in Pancreatic [beta] Cells Disrupts TGF-[beta] Signaling and Induces Reversible Diabetes Mellitus“, CELL, vol. 88, no. 2, 31 January 2006 (2006-01-31), page 561, XP55071875, ISSN: 0092-8674, DOI: 10.1371/journal.pbio.0040039 |
| 17 | OLIVIERI, A. ET AL.: ‘Serum transforming growth factor ?1 during diabetes development in non-obese diabetic mice and humans‘ CLIN. EXP. IMMUNOL. vol. 162, 2010, pages 407 – 414 | |
| 18 | ‘Remington’s Pharmaceutical Sciences‘, 1990, MACK PUBLISHING COMPANY | |
| 19 | ROEP, B. O. ET AL.: ‘Satisfaction (not) guaranteed: re-evaluating the use of animal models of type 1 diabetes‘ NAT. REV. IMMUNOL. vol. 4, 2004, pages 989 – 997 | |
| 20 | * | S. M. HOOK ET AL: “Smad2: A Candidate Gene for the Murine Autoimmune Diabetes Locus Idd21.1“, JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM, vol. 96, no. 12, 5 October 2011 (2011-10-05), pages E2072-E2077, XP55071877, ISSN: 0021-972X, DOI: 10.1210/jc.2011-0463 |
| 21 | SHODA, L. K. ET AL.: ‘A comprehensive review of interventions in the NOD mouse and implications for translation‘ IMMUNITY vol. 23, 2005, pages 115 – 126 | |
| 22 | SMART, N. G. ET AL.: ‘Conditional expression of Smad7 in pancreatic beta cells disrupts TGF-beta signaling and induces reversible diabetes mellitus‘ PLOS BIOL. vol. 4, 2006, page E39 | |
| 23 | WALLBERG, M. ET AL.: ‘An islet-specific pulse of TGF-? abrogates CTL function and promotes ? cell survival independent of Foxp3+ T cells‘ J. IMMUNOL. vol. 186, 2011, pages 2543 – 2551 | |
| 24 | YAN, X.; CHEN, Y. G.: ‘Smad7: not only a regulator, but also a cross-talk mediator of TGF-beta signalling‘ BIOCHEM. J. vol. 434, 2011, pages 1 – 10 | |
| WO2003037368A2 * | Oct 31, 2002 | May 8, 2003 | Andreas Steinbrecher | Smad7 inhibitors for the treatment of cns diseases |
| WO2009129544A1 * | Apr 20, 2009 | Oct 22, 2009 | Baxter International Inc. | Microsphere-based composition for preventing and/or reversing new-onset autoimmune diabetes |
| WO2010054826A1 | Nov 13, 2009 | May 20, 2010 | Giuliani International Limited | Antisense compositions and methods of making and using same |

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....










