Imdevimab
| (Heavy chain) QVQLVESGGG VVQPGRSLRL SCAASGFTFS NYAMYWVRQA PGKGLEWVAV ISYDGSNKYY ADSVKGRFTI SRDNSKNTLY LQMNSLRTED TAVYYCASGS DYGDYLLVYW GQGTLVTVSS ASTKGPSVFP LAPSSKSTSG GTAALGCLVK DYFPEPVTVS WNSGALTSGV HTFPAVLQSS GLYSLSSVVT VPSSSLGTQT YICNVNHKPS NTKVDKKVEP KSCDKTHTCP PCPAPELLGG PSVFLFPPKP KDTLMISRTP EVTCVVVDVS HEDPEVKFNW YVDGVEVHNA KTKPREEQYN STYRVVSVLT VLHQDWLNGK EYKCKVSNKA LPAPIEKTIS KAKGQPREPQ VYTLPPSRDE LTKNQVSLTC LVKGFYPSDI AVEWESNGQP ENNYKTTPPV LDSDGSFFLY SKLTVDKSRW QQGNVFSCSV MHEALHNHYT QKSLSLSPGK (Light chain) QSALTQPASV SGSPGQSITI SCTGTSSDVG GYNYVSWYQQ HPGKAPKLMI YDVSKRPSGV SNRFSGSKSG NTASLTISGL QSEDEADYYC NSLTSISTWV FGGGTKLTVL GQPKAAPSVT LFPPSSEELQ ANKATLVCLI SDFYPGAVTV AWKADSSPVK AGVETTTPSK QSNNKYAASS YLSLTPEQWK SHRSYSCQVT HEGSTVEKTV APTECS (Disulfide bridge: H22-H96, H147-H203, H223-L215, H229-H’229, H264-H324-H370-H428, H’22-H’96, H’147-H’203, H’223-L’215, H’264-H’324, H’370-H’428, L22-L90, L138-L197, L’22-L’90, L’138-L’197) |
イムデビマブ;
- Immunoglobulin G1, anti-(severe acute respiratory syndrome coronavirus 2 spike glycoprotein) (human monoclonal REGN10987 γ1-chain), disulfide with human monoclonal REGN10987 λ-chain, dimer
| Formula | C6396H9882N1694O2018S42 |
|---|---|
| CAS | 2415933-40-1 |
| Mol weight | 144141.7693 |
Monoclonal antibody
Treatment and prophylaxis of SARS-CoV-2 infection
ANTIVIRAL
SARS-CoV-2 spike glycoprotein
- REGN 10987
- RG 6412
Fact Sheet – US Food and Drug Administration
https://www.fda.gov › media › download
PDFBenefit of treatment with casirivimab and imdevimab has not been observed in patients hospitalized due to COVID-19. Monoclonal antibodies, such as casirivimab.
Casirivimab/imdevimab, sold under the brand name REGEN-COV,[1] is an experimental medicine developed by the American biotechnology company Regeneron Pharmaceuticals. It is an artificial “antibody cocktail” designed to produce resistance against the SARS-CoV-2 coronavirus responsible for the COVID-19 pandemic.[3][4] It consists of two monoclonal antibodies, casirivimab (REGN10933) and imdevimab (REGN10987) that must be mixed together.[1][5][6] The combination of two antibodies is intended to prevent mutational escape.[7]
Trials
In a clinical trial of people with COVID-19, casirivimab and imdevimab, administered together, were shown to reduce COVID-19-related hospitalization or emergency room visits in people at high risk for disease progression within 28 days after treatment when compared to placebo.[2] The safety and effectiveness of this investigational therapy for use in the treatment of COVID-19 continues to be evaluated.[2]
The data supporting the emergency use authorization (EUA) for casirivimab and imdevimab are based on a randomized, double-blind, placebo-controlled clinical trial in 799 non-hospitalized adults with mild to moderate COVID-19 symptoms.[2] Of these participants, 266 received a single intravenous infusion of 2,400 milligrams casirivimab and imdevimab (1,200 mg of each), 267 received 8,000 mg casirivimab and imdevimab (4,000 mg of each), and 266 received a placebo, within three days of obtaining a positive SARS-CoV-2 viral test.[2]
The prespecified primary endpoint for the trial was time-weighted average change in viral load from baseline.[2] Viral load reduction in participants treated with casirivimab and imdevimab was larger than in participants treated with placebo at day seven.[2] However, the most important evidence that casirivimab and imdevimab administered together may be effective came from the predefined secondary endpoint of medically attended visits related to COVID-19, particularly hospitalizations and emergency room visits within 28 days after treatment.[2] For participants at high risk for disease progression, hospitalizations and emergency room visits occurred in 3% of casirivimab and imdevimab-treated participants on average compared to 9% in placebo-treated participants.[2] The effects on viral load, reduction in hospitalizations and ER visits were similar in participants receiving either of the two casirivimab and imdevimab doses.[2]
As of September 2020, REGEN-COV is being evaluated as part of the RECOVERY Trial.[8]
On 12 April 2021, Roche and Regeneron announced that the Phase III clinical trial REGN-COV 2069 met both primary and secondary endpoints, reducing risk of infection by 81% for the non-infected patients, and reducing time-to-resolution of symptoms for symptomatic patients to one week vs. three weeks in the placebo group.[9]
Authorization
On 21 November 2020, the U.S. Food and Drug Administration (FDA) issued an emergency use authorization (EUA) for casirivimab and imdevimab to be administered together for the treatment of mild to moderate COVID-19 in people twelve years of age or older weighing at least 40 kilograms (88 lb) with positive results of direct SARS-CoV-2 viral testing and who are at high risk for progressing to severe COVID-19.[2][10][11] This includes those who are 65 years of age or older or who have certain chronic medical conditions.[2] Casirivimab and imdevimab must be administered together by intravenous (IV) infusion.[2]
Casirivimab and imdevimab are not authorized for people who are hospitalized due to COVID-19 or require oxygen therapy due to COVID-19.[2] A benefit of casirivimab and imdevimab treatment has not been shown in people hospitalized due to COVID-19.[2] Monoclonal antibodies, such as casirivimab and imdevimab, may be associated with worse clinical outcomes when administered to hospitalized people with COVID-19 requiring high flow oxygen or mechanical ventilation.[2]
The EUA was issued to Regeneron Pharmaceuticals Inc.[2][10][12]
On 1 February 2021, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) started a rolling review of data on the REGN‑COV2 antibody combination (casirivimab/imdevimab), which is being co-developed by Regeneron Pharmaceuticals, Inc. and F. Hoffman-La Roche, Ltd (Roche) for the treatment and prevention of COVID‑19.[13][14] In February 2021, the CHMP concluded that the combination, also known as REGN-COV2, can be used for the treatment of confirmed COVID-19 in people who do not require supplemental oxygen and who are at high risk of progressing to severe COVID-19.[15]
The Central Drugs Standards Control Organisation (CDSCO) in India, on 5 May 2021, granted an Emergency Use Authorisation to Roche (Genentech)[16] and Regeneron[17] for use of the casirivimab/imdevimab cocktail in the country. The announcement came in light of the second wave of the COVID-19 pandemic in India. Roche India maintains partnership with Cipla, thereby permitting the latter to market the drug in the country.[18]
Deployment
Although Regeneron is headquartered in Tarrytown, New York (near New York City), REGEN-COV is manufactured at the company’s primary U.S. manufacturing facility in Rensselaer, New York (near the state capital at Albany).[19] In September 2020, to free up manufacturing capacity for REGEN-COV, Regeneron began to shift production of its existing products from Rensselaer to the Irish city of Limerick.[20]
Regeneron has a deal in place with Roche (Genentech)[21]to manufacture and market REGEN-COV outside the United States.[10][22]
On 2 October 2020, Regeneron Pharmaceuticals announced that US President Donald Trump had received “a single 8 gram dose of REGN-COV2” after testing positive for SARS-CoV-2.[23][24] The drug was provided by the company in response to a “compassionate use” (temporary authorization for use) request from the president’s physicians.[23]
References
- ^ Jump up to:a b c “REGEN-COV- casirivimab and imdevimab kit”. DailyMed. Retrieved 18 March 2021.
- ^ Jump up to:a b c d e f g h i j k l m n o p q “Coronavirus (COVID-19) Update: FDA Authorizes Monoclonal Antibodies for Treatment of COVID-19”. U.S. Food and Drug Administration (FDA) (Press release). 21 November 2020. Retrieved 21 November 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ Kelland K (14 September 2020). “Regeneron’s antibody drug added to UK Recovery trial of COVID treatments”. Reuters. Retrieved 14 September 2020.
- ^ “Regeneron’s COVID-19 Response Efforts”. Regeneron Pharmaceuticals. Retrieved 14 September 2020.
- ^ Morelle R (14 September 2020). “Antibody treatment to be given to Covid patients”. BBC News Online. Retrieved 14 September2020.
- ^ “Safety, Tolerability, and Efficacy of Anti-Spike (S) SARS-CoV-2 Monoclonal Antibodies for Hospitalized Adult Patients With COVID-19”. ClinicalTrials. 3 September 2020. Retrieved 14 September2020.
- ^ Baum A, Fulton BO, Wloga E, Copin R, Pascal KE, Russo V, et al. (August 2020). “Antibody cocktail to SARS-CoV-2 spike protein prevents rapid mutational escape seen with individual antibodies”. Science. 369 (6506): 1014–1018. Bibcode:2020Sci…369.1014B. doi:10.1126/science.abd0831. PMC 7299283. PMID 32540904.
- ^ “RECOVERY COVID-19 phase 3 trial to evaluate Regeneron’s REGN-COV2 investigational antibody cocktail in the UK”. Recovery Trial. Retrieved 14 September 2020.
- ^ “Phase III prevention trial showed subcutaneous administration of investigational antibody cocktail casirivimab and imdevimab reduced risk of symptomatic COVID-19 infections by 81%”. streetinsider.com. Archived from the original on 2021-04-12. Retrieved 2021-04-12.
- ^ Jump up to:a b c “Regeneron Reports Positive Interim Data with REGEN-COV Antibody Cocktail used as Passive Vaccine to Prevent COVID-19”(Press release). Regeneron Pharmaceuticals. 26 January 2021. Retrieved 19 March 2021 – via PR Newswire.
- ^ “Fact Sheet For Health Care Providers Emergency Use Authorization (EUA) Of Casirivimab And Imdevimab” (PDF). U.S. Food and Drug Administration (FDA).
- ^ “Casirivimab and Imdevimab”. Regeneron Pharmaceuticals. Retrieved 19 March 2021.
- ^ “EMA starts rolling review of REGN‑COV2 antibody combination (casirivimab / imdevimab)” (Press release). European Medicines Agency (EMA). 1 February 2021. Retrieved 1 February 2021. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ “EMA reviewing data on monoclonal antibody use for COVID-19” (Press release). European Medicines Agency (EMA). 4 February 2021. Retrieved 4 March 2021.
- ^ “EMA issues advice on use of REGN-COV2 antibody combination (casirivimab / imdevimab)” (Press release). European Medicines Agency (EMA). 26 February 2021. Retrieved 5 March 2021. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^https://www.businesswire.com/news/home/20200818005847/en/Genentech-and-Regeneron-Collaborate-to-Significantly-Increase-Global-Supply-of-REGN-COV2-Investigational-Antibody-Combination-for-COVID-19
- ^ https://timesofindia.indiatimes.com/india/india-approves-roche/regeneron-antibody-cocktail-to-treat-covid-19/articleshow/82407551.cms
- ^ “Roche receives Emergency Use Authorisation in India for its investigational Antibody Cocktail (Casirivimab and Imdevimab) used in the treatment of Covid-19 | Cipla”. http://www.cipla.com. Retrieved 2021-05-06.
- ^ Williams, Stephen (3 October 2020). “Experimental drug given to President made locally”. The Daily Gazette.
- ^ Stanton, Dan (11 September 2020). “Manufacturing shift to Ireland frees up US capacity for Regeneron’s COVID antibodies”. BioProcess International.
- ^https://www.businesswire.com/news/home/20200818005847/en/Genentech-and-Regeneron-Collaborate-to-Significantly-Increase-Global-Supply-of-REGN-COV2-Investigational-Antibody-Combination-for-COVID-19
- ^ “Roche and Regeneron link up on a coronavirus antibody cocktail”. CNBC. 19 August 2020. Retrieved 14 September 2020.
- ^ Jump up to:a b Thomas K (2 October 2020). “President Trump Received Experimental Antibody Treatment”. The New York Times. ISSN 0362-4331. Retrieved 2 October 2020.
- ^ Hackett DW (3 October 2020). “8-Gram Dose of COVID-19 Antibody Cocktail Provided to President Trump”. http://www.precisionvaccinations.com. Archived from the original on 3 October 2020.
External links
- “Casirivimab”. Drug Information Portal. U.S. National Library of Medicine.
- “Imdevimab”. Drug Information Portal. U.S. National Library of Medicine.
- “Casirivimab and Imdevimab EUA Letter of Authorization” (PDF). U.S. Food and Drug Administration (FDA).
- “Frequently Asked Questions on the Emergency Use Authorization of Casirivimab + Imdevimab” (PDF). U.S. Food and Drug Administration (FDA).
| REGN10933 (blue) and REGN10987 (orange) bound to SARS-CoV-2 spike protein (pink). From PDB: 6VSB, 6XDG. | |
| Combination of | |
|---|---|
| Casirivimab | Monoclonal antibody against spike protein of SARS-CoV-2 |
| Imdevimab | Monoclonal antibody against spike protein of SARS-CoV-2 |
| Clinical data | |
| Trade names | REGEN-COV |
| Other names | REGN-COV2 |
| AHFS/Drugs.com | Monograph |
| License data | US DailyMed: Casirivimab |
| Routes of administration | Intravenous |
| ATC code | None |
| Legal status | |
| Legal status | US: Unapproved (Emergency Use Authorization)[1][2] |
| Identifiers | |
| DrugBank | DB15691 |
| KEGG | D11938D11939 |
////////Imdevimab, ANTI VIRAL, PEPTIDE, CORONA VIRUS, COVID19, APPROVALS 2020, FDA 2020, イムデビマブ, REGN 10987, RG 6412,

NEW DRUG APPROVALS
one time
$10.00

Casirivimab
(Heavy chain)
QVQLVESGGG LVKPGGSLRL SCAASGFTFS DYYMSWIRQA PGKGLEWVSY ITYSGSTIYY
ADSVKGRFTI SRDNAKSSLY LQMNSLRAED TAVYYCARDR GTTMVPFDYW GQGTLVTVSS
ASTKGPSVFP LAPSSKSTSG GTAALGCLVK DYFPEPVTVS WNSGALTSGV HTFPAVLQSS
GLYSLSSVVT VPSSSLGTQT YICNVNHKPS NTKVDKKVEP KSCDKTHTCP PCPAPELLGG
PSVFLFPPKP KDTLMISRTP EVTCVVVDVS HEDPEVKFNW YVDGVEVHNA KTKPREEQYN
STYRVVSVLT VLHQDWLNGK EYKCKVSNKA LPAPIEKTIS KAKGQPREPQ VYTLPPSRDE
LTKNQVSLTC LVKGFYPSDI AVEWESNGQP ENNYKTTPPV LDSDGSFFLY SKLTVDKSRW
QQGNVFSCSV MHEALHNHYT QKSLSLSPGK
(Light chain)
DIQMTQSPSS LSASVGDRVT ITCQASQDIT NYLNWYQQKP GKAPKLLIYA ASNLETGVPS
RFSGSGSGTD FTFTISGLQP EDIATYYCQQ YDNLPLTFGG GTKVEIKRTV AAPSVFIFPP
SDEQLKSGTA SVVCLLNNFY PREAKVQWKV DNALQSGNSQ ESVTEQDSKD STYSLSSTLT
LSKADYEKHK VYACEVTHQG LSSPVTKSFN RGEC
(Disulfide bridge: H22-H96, H147-H203, H223-L214, H229-H’229, H232-H’232, H264-H324, H370-H428, H’22-H’96, H’147-H’203, H’223-L’214, H’264-H’324, H’370-H’428, L23-L88, L134-L194, L’23-L’88, L’134-L’194)
Casirivimab
カシリビマブ;
- Immunoglobulin G1, anti-(severe acute respiratory syndrome coronavirus 2 spike glycoprotein) (human monoclonal REGN10933 γ1-chain), disulfide with human monoclonal REGN10933 κ-chain, dimer
| Formula | C6454H9976N1704O2024S44 |
|---|---|
| CAS | 2415933-42-3 |
| Mol weight | 145233.3296 |
Monoclonal antibody
Treatment and prophylaxis of SARS-CoV-2 infection (COVID-19)
SARS-CoV-2 spike glycoprotein
- Protein Sequence
- Sequence Length: 1328, 450, 450, 214, 214
- REGN 10933
- RG 6413
https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-monoclonal-antibodies-treatment-covid-19 November 21, 2020
Today, the U.S. Food and Drug Administration issued an emergency use authorization (EUA) for casirivimab and imdevimab to be administered together for the treatment of mild to moderate COVID-19 in adults and pediatric patients (12 years of age or older weighing at least 40 kilograms [about 88 pounds]) with positive results of direct SARS-CoV-2 viral testing and who are at high risk for progressing to severe COVID-19. This includes those who are 65 years of age or older or who have certain chronic medical conditions.
In a clinical trial of patients with COVID-19, casirivimab and imdevimab, administered together, were shown to reduce COVID-19-related hospitalization or emergency room visits in patients at high risk for disease progression within 28 days after treatment when compared to placebo. The safety and effectiveness of this investigational therapy for use in the treatment of COVID-19 continues to be evaluated.
Casirivimab and imdevimab must be administered together by intravenous (IV) infusion.
Casirivimab and imdevimab are not authorized for patients who are hospitalized due to COVID-19 or require oxygen therapy due to COVID-19. A benefit of casirivimab and imdevimab treatment has not been shown in patients hospitalized due to COVID-19. Monoclonal antibodies, such as casirivimab and imdevimab, may be associated with worse clinical outcomes when administered to hospitalized patients with COVID-19 requiring high flow oxygen or mechanical ventilation.
“The FDA remains committed to advancing the nation’s public health during this unprecedented pandemic. Authorizing these monoclonal antibody therapies may help outpatients avoid hospitalization and alleviate the burden on our health care system,” said FDA Commissioner Stephen M. Hahn, M.D. “As part of our Coronavirus Treatment Acceleration Program, the FDA uses every possible pathway to make new treatments available to patients as quickly as possible while continuing to study the safety and effectiveness of these treatments.”
Monoclonal antibodies are laboratory-made proteins that mimic the immune system’s ability to fight off harmful pathogens such as viruses. Casirivimab and imdevimab are monoclonal antibodies that are specifically directed against the spike protein of SARS-CoV-2, designed to block the virus’ attachment and entry into human cells.
“The emergency authorization of these monoclonal antibodies administered together offers health care providers another tool in combating the pandemic,” said Patrizia Cavazzoni, M.D., acting director of the FDA’s Center for Drug Evaluation and Research. “We will continue to facilitate the development, evaluation and availability of COVID-19 therapies.”
The issuance of an EUA is different than an FDA approval. In determining whether to issue an EUA, the FDA evaluates the totality of available scientific evidence and carefully balances any known or potential risks with any known or potential benefits of the product for use during an emergency. Based on the FDA’s review of the totality of the scientific evidence available, the agency has determined that it is reasonable to believe that casirivimab and imdevimab administered together may be effective in treating patients with mild or moderate COVID-19. When used to treat COVID-19 for the authorized population, the known and potential benefits of these antibodies outweigh the known and potential risks. There are no adequate, approved and available alternative treatments to casirivimab and imdevimab administered together for the authorized population.
The data supporting this EUA for casirivimab and imdevimab are based on a randomized, double-blind, placebo-controlled clinical trial in 799 non-hospitalized adults with mild to moderate COVID-19 symptoms. Of these patients, 266 received a single intravenous infusion of 2,400 milligrams casirivimab and imdevimab (1,200 mg of each), 267 received 8,000 mg casirivimab and imdevimab (4,000 mg of each), and 266 received a placebo, within three days of obtaining a positive SARS-CoV-2 viral test.
The prespecified primary endpoint for the trial was time-weighted average change in viral load from baseline. Viral load reduction in patients treated with casirivimab and imdevimab was larger than in patients treated with placebo at day seven. However, the most important evidence that casirivimab and imdevimab administered together may be effective came from the predefined secondary endpoint of medically attended visits related to COVID-19, particularly hospitalizations and emergency room visits within 28 days after treatment. For patients at high risk for disease progression, hospitalizations and emergency room visits occurred in 3% of casirivimab and imdevimab-treated patients on average compared to 9% in placebo-treated patients. The effects on viral load, reduction in hospitalizations and ER visits were similar in patients receiving either of the two casirivimab and imdevimab doses.
Under the EUA, fact sheets that provide important information about using casirivimab and imdevimab administered together in treating COVID-19 as authorized must be made available to health care providers and to patients and caregivers. These fact sheets include dosing instructions, potential side effects and drug interactions. Possible side effects of casirivimab and imdevimab include: anaphylaxis and infusion-related reactions, fever, chills, hives, itching and flushing.
The EUA was issued to Regeneron Pharmaceuticals Inc.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.
Related Information
- Casirivimab and Imdevimab EUA Letter of Authorization
- Frequently Asked Questions on the Emergency Use Authorization for Casirivimab and Imdevimab
- Emergency Use Authorization: Therapeutics
- Coronavirus Disease (COVID-19)
Casirivimab/imdevimab, sold under the brand name REGEN-COV,[1] is an experimental medicine developed by the American biotechnology company Regeneron Pharmaceuticals. It is an artificial “antibody cocktail” designed to produce resistance against the SARS-CoV-2 coronavirus responsible for the COVID-19 pandemic.[3][4] It consists of two monoclonal antibodies, casirivimab (REGN10933) and imdevimab (REGN10987) that must be mixed together.[1][5][6] The combination of two antibodies is intended to prevent mutational escape.[7]
Trials
In a clinical trial of people with COVID-19, casirivimab and imdevimab, administered together, were shown to reduce COVID-19-related hospitalization or emergency room visits in people at high risk for disease progression within 28 days after treatment when compared to placebo.[2] The safety and effectiveness of this investigational therapy for use in the treatment of COVID-19 continues to be evaluated.[2]
The data supporting the emergency use authorization (EUA) for casirivimab and imdevimab are based on a randomized, double-blind, placebo-controlled clinical trial in 799 non-hospitalized adults with mild to moderate COVID-19 symptoms.[2] Of these participants, 266 received a single intravenous infusion of 2,400 milligrams casirivimab and imdevimab (1,200 mg of each), 267 received 8,000 mg casirivimab and imdevimab (4,000 mg of each), and 266 received a placebo, within three days of obtaining a positive SARS-CoV-2 viral test.[2]
The prespecified primary endpoint for the trial was time-weighted average change in viral load from baseline.[2] Viral load reduction in participants treated with casirivimab and imdevimab was larger than in participants treated with placebo at day seven.[2] However, the most important evidence that casirivimab and imdevimab administered together may be effective came from the predefined secondary endpoint of medically attended visits related to COVID-19, particularly hospitalizations and emergency room visits within 28 days after treatment.[2] For participants at high risk for disease progression, hospitalizations and emergency room visits occurred in 3% of casirivimab and imdevimab-treated participants on average compared to 9% in placebo-treated participants.[2] The effects on viral load, reduction in hospitalizations and ER visits were similar in participants receiving either of the two casirivimab and imdevimab doses.[2]
As of September 2020, REGEN-COV is being evaluated as part of the RECOVERY Trial.[8]
On 12 April 2021, Roche and Regeneron announced that the Phase III clinical trial REGN-COV 2069 met both primary and secondary endpoints, reducing risk of infection by 81% for the non-infected patients, and reducing time-to-resolution of symptoms for symptomatic patients to one week vs. three weeks in the placebo group.[9]
Authorization
On 21 November 2020, the U.S. Food and Drug Administration (FDA) issued an emergency use authorization (EUA) for casirivimab and imdevimab to be administered together for the treatment of mild to moderate COVID-19 in people twelve years of age or older weighing at least 40 kilograms (88 lb) with positive results of direct SARS-CoV-2 viral testing and who are at high risk for progressing to severe COVID-19.[2][10][11] This includes those who are 65 years of age or older or who have certain chronic medical conditions.[2] Casirivimab and imdevimab must be administered together by intravenous (IV) infusion.[2]
Casirivimab and imdevimab are not authorized for people who are hospitalized due to COVID-19 or require oxygen therapy due to COVID-19.[2] A benefit of casirivimab and imdevimab treatment has not been shown in people hospitalized due to COVID-19.[2] Monoclonal antibodies, such as casirivimab and imdevimab, may be associated with worse clinical outcomes when administered to hospitalized people with COVID-19 requiring high flow oxygen or mechanical ventilation.[2]
The EUA was issued to Regeneron Pharmaceuticals Inc.[2][10][12]
On 1 February 2021, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) started a rolling review of data on the REGN‑COV2 antibody combination (casirivimab/imdevimab), which is being co-developed by Regeneron Pharmaceuticals, Inc. and F. Hoffman-La Roche, Ltd (Roche) for the treatment and prevention of COVID‑19.[13][14] In February 2021, the CHMP concluded that the combination, also known as REGN-COV2, can be used for the treatment of confirmed COVID-19 in people who do not require supplemental oxygen and who are at high risk of progressing to severe COVID-19.[15]
The Central Drugs Standards Control Organisation (CDSCO) in India, on 5 May 2021, granted an Emergency Use Authorisation to Roche (Genentech)[16] and Regeneron[17] for use of the casirivimab/imdevimab cocktail in the country. The announcement came in light of the second wave of the COVID-19 pandemic in India. Roche India maintains partnership with Cipla, thereby permitting the latter to market the drug in the country.[18]
Deployment
Although Regeneron is headquartered in Tarrytown, New York (near New York City), REGEN-COV is manufactured at the company’s primary U.S. manufacturing facility in Rensselaer, New York (near the state capital at Albany).[19] In September 2020, to free up manufacturing capacity for REGEN-COV, Regeneron began to shift production of its existing products from Rensselaer to the Irish city of Limerick.[20]
Regeneron has a deal in place with Roche (Genentech)[21]to manufacture and market REGEN-COV outside the United States.[10][22]
On 2 October 2020, Regeneron Pharmaceuticals announced that US President Donald Trump had received “a single 8 gram dose of REGN-COV2” after testing positive for SARS-CoV-2.[23][24] The drug was provided by the company in response to a “compassionate use” (temporary authorization for use) request from the president’s physicians.[23]
References
- ^ Jump up to:a b c “REGEN-COV- casirivimab and imdevimab kit”. DailyMed. Retrieved 18 March 2021.
- ^ Jump up to:a b c d e f g h i j k l m n o p q “Coronavirus (COVID-19) Update: FDA Authorizes Monoclonal Antibodies for Treatment of COVID-19”. U.S. Food and Drug Administration (FDA) (Press release). 21 November 2020. Retrieved 21 November 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ Kelland K (14 September 2020). “Regeneron’s antibody drug added to UK Recovery trial of COVID treatments”. Reuters. Retrieved 14 September 2020.
- ^ “Regeneron’s COVID-19 Response Efforts”. Regeneron Pharmaceuticals. Retrieved 14 September 2020.
- ^ Morelle R (14 September 2020). “Antibody treatment to be given to Covid patients”. BBC News Online. Retrieved 14 September2020.
- ^ “Safety, Tolerability, and Efficacy of Anti-Spike (S) SARS-CoV-2 Monoclonal Antibodies for Hospitalized Adult Patients With COVID-19”. ClinicalTrials. 3 September 2020. Retrieved 14 September2020.
- ^ Baum A, Fulton BO, Wloga E, Copin R, Pascal KE, Russo V, et al. (August 2020). “Antibody cocktail to SARS-CoV-2 spike protein prevents rapid mutational escape seen with individual antibodies”. Science. 369 (6506): 1014–1018. Bibcode:2020Sci…369.1014B. doi:10.1126/science.abd0831. PMC 7299283. PMID 32540904.
- ^ “RECOVERY COVID-19 phase 3 trial to evaluate Regeneron’s REGN-COV2 investigational antibody cocktail in the UK”. Recovery Trial. Retrieved 14 September 2020.
- ^ “Phase III prevention trial showed subcutaneous administration of investigational antibody cocktail casirivimab and imdevimab reduced risk of symptomatic COVID-19 infections by 81%”. streetinsider.com. Archived from the original on 2021-04-12. Retrieved 2021-04-12.
- ^ Jump up to:a b c “Regeneron Reports Positive Interim Data with REGEN-COV Antibody Cocktail used as Passive Vaccine to Prevent COVID-19”(Press release). Regeneron Pharmaceuticals. 26 January 2021. Retrieved 19 March 2021 – via PR Newswire.
- ^ “Fact Sheet For Health Care Providers Emergency Use Authorization (EUA) Of Casirivimab And Imdevimab” (PDF). U.S. Food and Drug Administration (FDA).
- ^ “Casirivimab and Imdevimab”. Regeneron Pharmaceuticals. Retrieved 19 March 2021.
- ^ “EMA starts rolling review of REGN‑COV2 antibody combination (casirivimab / imdevimab)” (Press release). European Medicines Agency (EMA). 1 February 2021. Retrieved 1 February 2021. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ “EMA reviewing data on monoclonal antibody use for COVID-19” (Press release). European Medicines Agency (EMA). 4 February 2021. Retrieved 4 March 2021.
- ^ “EMA issues advice on use of REGN-COV2 antibody combination (casirivimab / imdevimab)” (Press release). European Medicines Agency (EMA). 26 February 2021. Retrieved 5 March 2021. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^https://www.businesswire.com/news/home/20200818005847/en/Genentech-and-Regeneron-Collaborate-to-Significantly-Increase-Global-Supply-of-REGN-COV2-Investigational-Antibody-Combination-for-COVID-19
- ^ https://timesofindia.indiatimes.com/india/india-approves-roche/regeneron-antibody-cocktail-to-treat-covid-19/articleshow/82407551.cms
- ^ “Roche receives Emergency Use Authorisation in India for its investigational Antibody Cocktail (Casirivimab and Imdevimab) used in the treatment of Covid-19 | Cipla”. http://www.cipla.com. Retrieved 2021-05-06.
- ^ Williams, Stephen (3 October 2020). “Experimental drug given to President made locally”. The Daily Gazette.
- ^ Stanton, Dan (11 September 2020). “Manufacturing shift to Ireland frees up US capacity for Regeneron’s COVID antibodies”. BioProcess International.
- ^https://www.businesswire.com/news/home/20200818005847/en/Genentech-and-Regeneron-Collaborate-to-Significantly-Increase-Global-Supply-of-REGN-COV2-Investigational-Antibody-Combination-for-COVID-19
- ^ “Roche and Regeneron link up on a coronavirus antibody cocktail”. CNBC. 19 August 2020. Retrieved 14 September 2020.
- ^ Jump up to:a b Thomas K (2 October 2020). “President Trump Received Experimental Antibody Treatment”. The New York Times. ISSN 0362-4331. Retrieved 2 October 2020.
- ^ Hackett DW (3 October 2020). “8-Gram Dose of COVID-19 Antibody Cocktail Provided to President Trump”. http://www.precisionvaccinations.com. Archived from the original on 3 October 2020.
External links
- “Casirivimab”. Drug Information Portal. U.S. National Library of Medicine.
- “Imdevimab”. Drug Information Portal. U.S. National Library of Medicine.
- “Casirivimab and Imdevimab EUA Letter of Authorization” (PDF). U.S. Food and Drug Administration (FDA).
- “Frequently Asked Questions on the Emergency Use Authorization of Casirivimab + Imdevimab” (PDF). U.S. Food and Drug Administration (FDA).
| REGN10933 (blue) and REGN10987 (orange) bound to SARS-CoV-2 spike protein (pink). From PDB: 6VSB, 6XDG. | |
| Combination of | |
|---|---|
| Casirivimab | Monoclonal antibody against spike protein of SARS-CoV-2 |
| Imdevimab | Monoclonal antibody against spike protein of SARS-CoV-2 |
| Clinical data | |
| Trade names | REGEN-COV |
| Other names | REGN-COV2 |
| AHFS/Drugs.com | Monograph |
| License data | US DailyMed: Casirivimab |
| Routes of administration | Intravenous |
| ATC code | None |
| Legal status | |
| Legal status | US: Unapproved (Emergency Use Authorization)[1][2] |
| Identifiers | |
| DrugBank | DB15691 |
| KEGG | D11938 |
//////////// Casirivimab, ANTI VIRAL, PEPTIDE, SARS-CoV-2, MONOCLONAL ANTIBODY, FDA 2020, 2020APPROVALS, CORONA VIRUS, COVID 19, カシリビマブ, REGN-COV2, REGN10933+REGN10987 combination therapy, REGN 10933, RG 6413

NEW DRUG APPROVALS
ONE TIME
$10.00

Idecabtagene vicleucel
Idecabtagene vicleucel
CAS 2306267-75-2
STN: BLA 125736
An autologous T lymphocyte-enriched cell transduced ex vivo with an anti-BCMA CAR lentiviral vector encoding a chimeric antigen receptor CAR, comprising a CD8 hinge and TM domain, 4-1BB costimulatory domain and CD3ζ signaling domain, targeting human B cell maturation antigen for cancer immunotherapy (Celgene Corp., NJ)
- Bb2121
| Name | Idecabtagene vicleucel (USAN); Abecma (TN) |
|---|---|
| Product | ABECMA (Celgene Corporation) |
| CAS | 2306267-75-2 |
| Efficacy | Antineoplastic, Anti-BCMA CAR-T cell |
| Disease | Multiple myeloma [DS:H00010] |
| Comment | Cellular therapy product |
USFDA 2021/4/21 APPROVED
Dendritic cells (DCs) are antigen-presenting cells (APCs) that process antigens and display them to other cells of the immune system. Specifically, dendritic cells are capable of capturing and presenting antigens on their surfaces to activate T cells such as cytotoxic T cells (CTLs). Further, activated dendritic cells are capable of recruiting additional immune cells such as macrophages, eosinophils, natural killer cells, and T cells such as natural killer T cells.
Despite major advances in cancer treatment, cancer remains one of the leading causes of death globally. Hurdles in designing effective therapies include cancer immune evasion, in which cancer cells escape destructive immunity, as well as the toxicity of many conventional cancer treatments such as radiation therapy and chemotherapy, which significantly impacts a patient’s ability to tolerate the therapy and/or impacts the efficacy of the treatment.
Given the important role of dendritic cells in immunity, derailed dendritic cell functions have been implicated in diseases such as cancer and autoimmune diseases. For example, cancer cells may evade immune detection and destruction by crippling dendritic cell functionality through prevention of dendritic cell recruitment and activation. In addition, dendritic cells have been found in the brain during central nervous system inflammation and may be involved in the pathogenesis of autoimmune diseases in the brain.
One mechanism by which cancers evade immune detection and destruction is by crippling dendritic cell functionality through prevention of dendritic cell (DC) recruitment and activation. Accordingly, there remains a need for cancer therapies that can effectively derail tumor evasion and enhance anti-tumor immunity as mediated, for example, by dendritic cells.

NEW DRUG APPROVALS
ONE TIME
$10.00
DESCRIPTION
ABECMA is a BCMA-directed genetically modified autologous T cell immunotherapy product consisting of a patient’s own T cells that are harvested and genetically modified ex vivo through transduction with an anti-BCMA02 chimeric antigen receptor (CAR) lentiviral vector (LVV). Autologous T cells transduced with the anti-BCMA02 CAR LVV express the anti-BCMA CAR on the T cell surface. The CAR is comprised of a murine extracellular single-chain variable fragment (scFv) specific for recognizing B cell maturation antigen (BCMA) followed by a human CD8α hinge and transmembrane domain fused to the T cell cytoplasmic signaling domains of CD137 (4-1BB) and CD3ζ chain, in tandem. Binding of ABECMA to BCMA-expressing target cells leads to signaling initiated by CD3ζ and 4-1BB domains, and subsequent CAR-positive T cell activation. Antigen-specific activation of ABECMA results in CAR-positive T cell proliferation, cytokine secretion, and subsequent cytolytic killing of BCMA-expressing cells.
ABECMA is prepared from the patient’s peripheral blood mononuclear cells (PBMCs), which are obtained via a standard leukapheresis procedure. The mononuclear cells are enriched for T cells, through activation with anti-CD3 and anti-CD28 antibodies in the presence of IL-2, which are then transduced with the replication-incompetent lentiviral vector containing the anti-BCMA CAR transgene. The transduced T cells are expanded in cell culture, washed, formulated into a suspension, and cryopreserved. The product must pass a sterility test before release for shipping as a frozen suspension in one or more patient-specific infusion bag(s). The product is thawed prior to infusion back into the patient [see DOSAGE AND ADMINISTRATION and HOW SUPPLIED/Storage And Handling].
The ABECMA formulation contains 50% Plasma-Lyte A and 50% CryoStor® CS10, resulting in a final DMSO concentration of 5%.
FDA approves idecabtagene vicleucel for multiple myeloma
On March 26, 2021, the Food and Drug Administration approved idecabtagene vicleucel (Abecma, Bristol Myers Squibb) for the treatment of adult patients with relapsed or refractory multiple myeloma after four or more prior lines of therapy, including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody. This is the first FDA-approved cell-based gene therapy for multiple myeloma.
Idecabtagene vicleucel is a B-cell maturation antigen (BCMA)-directed genetically modified autologous chimeric antigen receptor (CAR) T-cell therapy. Each dose is customized using a patient’s own T-cells, which are collected and genetically modified, and infused back into the patient.
Safety and efficacy were evaluated in a multicenter study of 127 patients with relapsed and refractory multiple myeloma who received at least three prior lines of antimyeloma therapies; 88% had received four or more prior lines of therapies. Efficacy was evaluated in 100 patients who received idecabtagene vicleucel in the dose range of 300 to 460 x 106 CAR-positive T cells. Efficacy was established based on overall response rate (ORR), complete response (CR) rate, and duration of response (DOR), as evaluated by an Independent Response committee using the International Myeloma Working Group Uniform Response Criteria for Multiple Myeloma.
The ORR was 72% (95% CI: 62%, 81%) and CR rate was 28% (95% CI 19%, 38%). An estimated 65% of patients who achieved CR remained in CR for at least 12 months.
The idecabtagene vicleucel label carries a boxed warning for cytokine release syndrome (CRS), neurologic toxicities, hemophagocytic lymphohistiocytosis/ macrophage activation syndrome, and prolonged cytopenias. The most common side effects of idecabtagene vicleucel include CRS, infections, fatigue, musculoskeletal pain, and hypogammaglobulinemia.
Idecabtagene vicleucel is approved with a risk evaluation and mitigation strategy requiring that healthcare facilities that dispense the therapy must be specially certified to recognize and manage CRS and nervous system toxicities. To evaluate long-term safety, the FDA is requiring the manufacturer to conduct a post-marketing observational study involving patients treated with idecabtagene vicleucel.
The recommended dose range for idecabtagene vicleucel is 300 to 460 × 106 CAR-positive T cells. View full prescribing information for Abecma.
This application was granted breakthrough therapy designation and orphan drug designation. A description of FDA expedited programs is in the Guidance for Industry: Expedited Programs for Serious Conditions-Drugs and Biologics.
FDA D.I.S.C.O. Burst Edition: FDA approval of ABECMA (idecabtagene vicleucel) the first FDA approved cell-based gene therapy for the treatment of adult patients with relapsed or refractory multiple myeloma
Welcome back to the D.I.S.C.O., FDA’s Drug Information Soundcast in Clinical Oncology, Burst Edition, brought to you by FDA’s Division of Drug Information in partnership with FDA’s Oncology Center of Excellence. Today we have another quick update on a recent FDA cancer therapeutic approval.
On March 26, 2021, the FDA approved idecabtagene vicleucel (brand name Abecma) for the treatment of adult patients with relapsed or refractory multiple myeloma after four or more prior lines of therapy, including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody. This is the first FDA-approved cell-based gene therapy for multiple myeloma.
Idecabtagene vicleucel is a B-cell maturation antigen-directed genetically modified autologous chimeric antigen receptor T-cell therapy. Each dose is customized using a patient’s own T-cells, which are collected and genetically modified, and infused back into the patient.
Safety and efficacy were evaluated in a multicenter study of 127 patients with relapsed and refractory multiple myeloma who received at least three prior lines of antimyeloma therapies, 88% of whom had received four or more prior lines of therapies. Efficacy was evaluated in 100 patients who received idecabtagene vicleucel and was established based on overall response rate, complete response rate, and duration of response, as evaluated by an Independent Response committee using the International Myeloma Working Group Uniform Response Criteria for Multiple Myeloma.
The overall response rate was 72% and complete response rate was 28%. An estimated 65% of patients who achieved complete response remained in complete response for at least 12 months.
The idecabtagene vicleucel label carries a boxed warning for cytokine release syndrome, neurologic toxicities, hemophagocytic lymphohistiocytosis/ macrophage activation syndrome, and prolonged cytopenias. Idecabtagene vicleucel is approved with a risk evaluation and mitigation strategy requiring that healthcare facilities dispensing the therapy must be specially certified to recognize and manage cytokine release syndrome and nervous system toxicities. To evaluate long-term safety, the FDA is requiring the manufacturer to conduct a post-marketing observational study involving patients treated with idecabtagene vicleucel.
Full prescribing information for this approval can be found on the web at www.fda.gov, with key word search “Approved Cellular and Gene Therapy Products”.
Health care professionals should report serious adverse events to FDA’s MedWatch Reporting System at www.fda.gov/medwatch.
Follow the Division of Drug Information on Twitter @FDA_Drug_InfoExternal Link Disclaimer and the Oncology Center of Excellence @FDAOncologyExternal Link Disclaimer. Send your feedback via email to FDAOncology@fda.hhs.gov. Thanks for tuning in today to the DISCO Burst Edition.
PAT
WO 2019148089
In various aspects, the present invention relates to XCR1 binding agents having at least one targeting moiety that specifically binds to XCR1. In various embodiments, these XCR1 binding agents bind to, but do not functionally modulate ( e.g . partially or fully neutralize) XCR1. Therefore, in various embodiments, the present XCR1 binding agents have use in, for instance, directly or indirectly recruiting a XCR1-expressing cell to a site of interest while still allowing the XCR1-expressing cell to signal via XCR1 (i.e. the binding of the XCR1 binding agent does not reduce or eliminate XCR1 signaling at the site of interest). In various embodiments, the XCR-1 binding agent functionally modulates XCR1. In an embodiment, the targeting moiety is a single domain antibody (e.g. VHH, HUMABODY, scFv, on antibody). In various embodiments, the XCR1 binding agent further comprises a signaling agent, e.g., without limitation, an interferon, an interleukin, and a tumor necrosis factor, that may be modified to attenuate activity. In various embodiments, the XCR1 binding agent comprises additional targeting moieties that bind to other targets (e.g. antigens, receptor) of interest. In an embodiment, the other targets (e.g. antigens, receptor) of interest are present on tumor cells. In another embodiment, the other targets (e.g. antigens, receptor) of interest are present on immune cells. In some embodiments, the present XCR1 binding agent may directly or indirectly recruit an immune cell (e.g. a dendritic cell) to a site of action (such as, by way of non-limiting example, the tumor microenvironment). In some embodiments, the present XCR1 binding agent facilitates the presentation of antigens (e.g., tumor antigens) by dendritic cells.
In various embodiments, the present XCR binding agent or targeting moiety of the present chimeric proteins comprises the heavy chain of SEQ ID NO: 223 and/or the light chain of SEQ ID NO: 224, or a variant thereof (e.g. an amino acid sequence having at least about 90%, or at least about 93%, at least about 95%, at least about 97%, at least about 98%, at least about 99%, identity with SEQ ID NO: 223 and/or SEQ ID NO: 224).
In various embodiments, the present XCR binding agent or targeting moiety of the present chimeric proteins comprises a heavy chain CDR 1 of SHNLH (SEQ ID NO: 225), heavy chain CDR 2 of AIYPGNGNTAYNQKFKG (SEQ ID NO: 226), and heavy chain CDR 3 of WGSVVGDWYFDV (SEQ ID NO: 227) and/or a light chain CDR 1 of RSSLGLVHRNGNTYLH (SEQ ID NO: 228), light chain CDR 2 of KVSHRFS (SEQ ID NO: 229), and light chain CDR 3 of SQSTFIVPWT (SEQ ID NO: 230), or a variant thereof (e.g. with four or fewer amino acid substitutions, or with three or fewer amino acid substitutions, or with two or fewer amino acid substitutions, or with one amino acid substitution).
In various embodiments, the present XCR binding agent or targeting moiety of the present chimeric proteins comprises a heavy chain CDR 1 of SHNLH (SEQ ID NO: 225), heavy chain CDR 2 of AIYPGNGNTAYNQKFKG (SEQ ID NO: 226), and heavy chain CDR 3 of WGSVVGDWYFDV (SEQ ID NO: 227).
Illustrative Disease Modifying Therapies
EXAMPLES
Example 1. Identification and Characterization of Human XCR1 Ab AFNs
As used in this Example and associated figures,“AFN” is a chimera of the anti-Xcr1 5G7 antibody and human IFNa2 with an R149A mutation.
AFNs were made based on the 5G7 anti-hXcr1 Ab using the intact (full) Ab or a scFv format.
The 5G7 heavy chain is:
QAYLQQSGAELVRPGASVKMSCKASGYTFTSHNLHWVKQTPRQGLQWIGAIYPGNGNTAYNQKFKGKATLTVD
KSSSTAYMQLSSLTSDDSAVYFCARWGSVVGDWYFDVWGTGTTVTVSSASTKGPSVFPLAPCSRSTSESTAAL
GCLVKDYFPEPVTVSWNSGALTSGVHTFPAVLQSSGLYSLSSWTVPSSNFGTQTYTCNVDHKPSNTKVDKTVE
RKCCVECPPCPAPPAAAPSVFLFPPKPKDTLMISRTPEVTCVWDVSHEDPEVQFNWYVDGVEVHNAKTKPREE
QFNSTFRVVSVLTWHQDWLNGKEYKCKVSNKGLPAPIEKTISKTKGQPREPQVYTLPPSREEMTKNQVSLTCLV
KGFYPSDIAVEWESNGQPENNYKTTPPMLDSDGSFFLYSKLTVDKSRWQQGNVFSCSVMHEALHNHYTQKSLS
LSPGK (SEQ ID NO: 223)
The 5G7 light chain is:
DWMTQTPLSLPVTLGNQASIFCRSSLGLVHRNGNTYLHWYLQKPGQSPKLLIYKVSHRFSGVPDRFSGSGSGT DFTLKISRVEAEDLGVYFCSQSTHVPWTFGGGTKLEIKRTVAAPSVFIFPPSDEQLKSGTASWCLLNNFYPREAK VQWKVDNALQSGNSQESVTEQDSKDSTYSLSSTLTLSKADYEKHKVYACEVTHQGLSSPVTKSFNRGEC (SEQ ID NO: 224)
5G7 Heavy chain CDR 1 is SHNLH (SEQ ID NO: 225), Heavy chain CDR 2 is AIYPGNGNTAYNQKFKG (SEQ ID NO: 226), Heavy chain CDR 3 is WGSVVGDWYFDV (SEQ ID NO: 227). 5G7 Light chain CDR 1 is RSSLGLVHRNGNTYLH (SEQ ID NO: 228), Light chain CDR 2 is KVSHRFS (SEQ ID NO: 229), and Light chain CDR 3 is SQSTHVPWT (SEQ ID NO: 230).
The sequence of hulFNa2(R149A) is:
CDLPQTHSLGSRRTLMLLAQMRKISLFSCLKDRHDFGFPQEEFGNQFQKAETIPVLHEMIQQIFNLFSTKDSSAA WDETLLDKFYTELYQQLNDLEACVIQGVGVTETPLMKEDSILAVRKYFQRITLYLKEKKYSPCAWEVVRAEIMASF SLSTNLQESLRSKE (SEQ ID NO: 231).
In case of the intact Ab AFN, the 5G7 Ab heavy chain was fused to h I FN a2_R149A (human IFNal with a R149A mutation) via a flexible (GGS)2oG-linker and co-expressed with the 5G7 Ab light chain (sequences shown below). 5G7 scFv-AFN was constructed by linking the Ab VL and VH domains via a (GGGS)4 linker and followed by a (GGS)2o-linker and the sequence encoding hlFNa2_R149A. Recombinant proteins, cloned in the pcDNA3.4 expression-vector, were produced in ExpiCHO cells (Thermo Fisher Scientific) and purified on HisPUR spin plates (Thermo Fisher Scientific) according to the manufacturer’s instructions.
To test binding of the AFNs, parental HL1 16 and HL1 16 cells stably expressing hXcrl (HL116-hXcr1) were incubated with a serial dilution AFN for two hours at 4°C. Binding was detected using THE™ HIS antibody-FITC (GenScript) and measured on a MACSQuant X instrument (Miltenyi Biotec) and analysed using the FlowLogic software (Miltenyi Biotec). Data in Figures 1A and 1 B clearly show that both 5G7 Ab-AFN and 5G7 scFv bind specifically to hXcrl expressing cells.
Biological activity was measured on parental HL1 16 cells (an IFN responsive cell-line stably transfected with a p6-16 luciferase reporter) and the derived HL116-hXcr1 cells. Cells were seeded overnight and stimulated for 6 hours with a serial dilution 5G7 AFNs. Luciferase activity was measured on an EnSight Multimode Plate Reader (Perkin Elmer). Data in Figures 2A and 2B clearly illustrate that 5G7 AFNs, in the intact Ab format or as scFv, are clearly more active on cells expressing hXcrl compared to parental cells, illustrating that it is possible to restore signaling of an IFNa2 mutant by specific targeting to hXcrl .
Example 2. Identification and Characterization of Mouse Xcr1 Ab AFNs
As used in this Example and associated figures,“AFN” is a chimera of the anti-Xcr1 MAARX10 antibody and human IFNa2 with Q124R mutation.
Similar to the anti-human Xcr1 Ab, AFNs based on the MARX10 anti-mouse Xcr1 Ab were made, as intact Ab or as scFv. In case of the intact Ab AFN, the MARX10 Ab heavy chain was fused to hlFNa2_Q124R (human IFNa2 with Q124R mutation) via a flexible (GGS)2oG-linker and co-expressed with the MARX10 Ab light chain. scFv-AFN was constructed by linking the Ab VL and VH domains, in VH-VL (scFv(1 )) or VL-VH (scFv(2)) orientation, via a (GGGS)4 linker and followed by a (GGS)2o-linker and h I FN a2_Q 124R.
Selectivity of AFNs (produced and purified as described above for the human Xcr1 Ab AFNs) was tested by comparing binding at 2.5 pg/ml to MOCK or mouse Xcr1 transfected Hek293T cells. Binding was detected using THE™ HIS antibody-FITC (GenScript) and measured on a MACSQuant X instrument (Miltenyi Biotec) and analysed using the FlowLogic software (Miltenyi Biotec). Data in Figure 3 clearly show that all three specifically bind to mXcrl expressing cells.
REF
New England Journal of Medicine (2021), 384(8), 705-716
https://www.rxlist.com/abecma-drug.htm#indications
///////////Idecabtagene vicleucel, breakthrough therapy designation, orphan drug designation, FDA 2021, APPROVALS 2021, Bb2121, Bb , ABECMA
Manufacturer: Celgene Corporation, a Bristol-Myers Squibb Company
Indications:
- Treatment of adult patients with relapsed or refractory multiple myeloma after four or more prior lines of therapy including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody.
Product Information
- Package Insert – ABECMA
- Demographic Subgroup Information – idecabtagene vicleucel [ABECMA]
Refer to Section 1.1 of the Clinical Review Memo for information about participation in the clinical trials and any analysis of demographic subgroup outcomes that is notable.
Supporting Documents
Loncastuximab tesirine


Loncastuximab tesirine
ZYNLONTA FDA APPROVED 2021/4/23
| Formula | C6544H10048N1718O2064S52 |
|---|---|
| Exact mass | 147387.9585 |
| CAS | 1879918-31-6 |
| Efficacy | Antineoplasitc, Anti-CD19 antibody |
| Disease | Diffuse large B-cell lymphoma not otherwise specified [DS:H02434] |
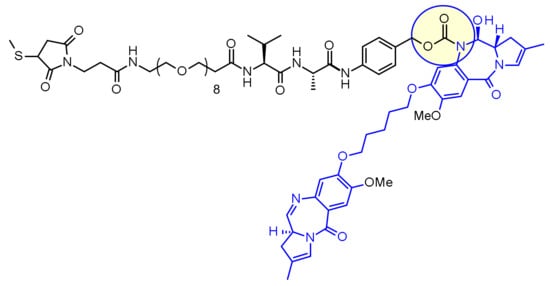
| Comment | Antibody-drug conjugate Treatment of hematological cancers |
ロンカスツキシマブテシリン; ADCT-402, ADCX 19
Immunoglobulin G1, anti-(human CD19 antigen) (human-Mus musculus monoclonal RB4v1.2 γ1-chain), disulfide with human-Mus musculus monoclonal RB4v1.2 κ-chain, dimer, bis(thioether) with N-[31-(3-mercapt-2,5-dioxo-1-pyrrolidinyl)-1,29-dioxo-4,7,10,13,16,19,22,25-octaoxa-28-azahentriacont-1-yl]-L-valyl-N-[4-[[[[(11S,11aS)-8-[[5-[[(11aS)-5,11a-dihydro-7-methoxy-2-methyl-5-oxo-1H-pyrrolo[2,1-c][1,4]benzodiazepin-8-yl]oxy]pentyl]oxy]-11,11a-dihydro-11-hydroxy-7-methoxy-2-methyl-5-oxo-1H-pyrrolo[2,1-c][1,4]benzodiazepin-10(5H)-yl]carbonyl]oxy]methyl]phenyl]-L-alaninamide

NEW DRUG APPROVALS
ONETIME
$10.00
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Humanized |
| Target | CD19 |
| Clinical data | |
| Trade names | Zynlonta |
| Other names | ADCT-402, loncastuximab tesirine-lpyl |
| License data | US DailyMed: Loncastuximab_tesirine |
| ATC code | None |
| Legal status | |
| Legal status | US: ℞-only [1] |
| Identifiers | |
| CAS Number | 1879918-31-6 |
| DrugBank | DB16222 |
| ChemSpider | none |
| UNII | 7K5O7P6QIU |
| KEGG | D11338 |
| Chemical and physical data | |
| Formula | C6544H10048N1718O2064S52 |
| Molar mass | 147481.45 g·mol−1 |
| NAME | DOSAGE | STRENGTH | ROUTE | LABELLER | MARKETING START | MARKETING END | ||
|---|---|---|---|---|---|---|---|---|
| Zynlonta | Injection, powder, lyophilized, for solution | 5 mg/1mL | Intravenous | ADC Therapeutics America, Inc. | 2021-04-30 | Not applicable |
Loncastuximab tesirine-lpyl is a CD19-directed antibody and alkylating agent conjugate, consisting of a humanized IgG1 kappa monoclonal antibody conjugated to SG3199, a pyrrolobenzodiazepine (PBD) dimer cytotoxic alkylating agent, through a protease-cleavable valine–alanine linker. SG3199 attached to the linker is designated as SG3249, also known as tesirine.
 |
Loncastuximab tesirine-lpyl has an approximate molecular weight of 151 kDa. An average of 2.3 molecules of SG3249 are attached to each antibody molecule. Loncastuximab tesirine-lpyl is produced by chemical conjugation of the antibody and small molecule components. The antibody is produced by mammalian (Chinese hamster ovary) cells, and the small molecule components are produced by chemical synthesis.
ZYNLONTA (loncastuximab tesirine-lpyl) for injection is supplied as a sterile, white to off-white, preservative-free, lyophilized powder, which has a cake-like appearance, for intravenous infusion after reconstitution and dilution. Each single-dose vial delivers 10 mg of loncastuximab tesirine-lpyl, L-histidine (2.8 mg), L-histidine monohydrochloride (4.6 mg), polysorbate 20 (0.4 mg), and sucrose (119.8 mg). After reconstitution with 2.2 mL Sterile Water for Injection, USP, the final concentration is 5 mg/mL with a pH of approximately 6.0.
Loncastuximab tesirine , sold under the brand name Zynlonta, is used for the treatment of large B-cell lymphoma. It is an antibody-drug conjugate (ADC) composed of a humanized antibody targeting the protein CD19, which is expressed in a wide range of B cell hematological tumors.[2] The experimental drug, developed by ADC Therapeutics is being tested in clinical trials for the treatment of B-cell non-Hodgkin lymphoma (NHL) and B-cell acute lymphoblastic leukemia (ALL).
On April 23, 2021, the Food and Drug Administration granted accelerated approval to loncastuximab tesirine-lpyl (Zynlonta, ADC Therapeutics SA), a CD19-directed antibody and alkylating agent conjugate, for adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, DLBCL arising from low grade lymphoma, and high-grade B-cell lymphoma.
Approval was based on LOTIS-2 (NCT03589469), an open-label, single-arm trial in 145 adult patients with relapsed or refractory DLBCL or high-grade B-cell lymphoma after at least two prior systemic regimens. Patients received loncastuximab tesirine-lpyl 0.15 mg/kg every 3 weeks for 2 cycles, then 0.075 mg/kg every 3 weeks for subsequent cycles. Patients received treatment until progressive disease or unacceptable toxicity.
The main efficacy outcome measure was overall response rate (ORR), as assessed by an independent review committee using Lugano 2014 criteria. The ORR was 48.3% (95% CI: 39.9, 56.7) with a complete response rate of 24.1% (95% CI: 17.4, 31.9). After a median follow-up of 7.3 months, median response duration was 10.3 months (95% CI: 6.9, NE). Of the 70 patients who achieved objective responses, 36% were censored for response duration prior to 3 months.
Most common (≥20%) adverse reactions in patients receiving loncastuximab tesirine-lpyl, including laboratory abnormalities, are thrombocytopenia, increased gamma-glutamyltransferase, neutropenia, anemia, hyperglycemia, transaminase elevation, fatigue, hypoalbuminemia, rash, edema, nausea, and musculoskeletal pain.
The prescribing information provides warnings and precautions for adverse reactions including edema and effusions, myelosuppression, infections, and cutaneous reactions.
The recommended loncastuximab tesirine-lpyl dosage is 0.15 mg/kg every 3 weeks for 2 cycles, then 0.075 mg/kg every 3 weeks for subsequent cycles, by intravenous infusion over 30 minutes on day 1 of each cycle (every 3 weeks). Patients should be premedicated with dexamethasone 4 mg orally or intravenously twice daily for 3 days beginning the day before loncastuximab tesirine-lpyl.
Technology
The humanized monoclonal antibody is stochastically conjugated via a valine-alanine cleavable, maleimide linker to a cytotoxic (anticancer) pyrrolobenzodiazepine (PBD) dimer. The antibody binds to CD19, a protein which is highly expressed on the surface of B-cell hematological tumors[3] including certain forms of lymphomas and leukemias. After binding to the tumor cells the antibody is internalized, the cytotoxic drug PBD is released and the cancer cells are killed. PBD dimers are generated out of PBD monomers, a class of natural products produced by various actinomycetes. PBD dimers work by crosslinking specific sites of the DNA, blocking the cancer cells’ division that cause the cells to die. As a class of DNA-crosslinking agents they are significantly more potent than systemic chemotherapeutic drugs.[4]
Clinical trials
Two phase I trials are evaluating the drug in patients with relapsed or refractory B-cell non-Hodgkin’s lymphoma and relapsed or refractory B-cell acute lymphoblastic leukemia.[5] At the 14th International Conference on Malignant Lymphoma interim results from a Phase I, open-label, dose-escalating study designed to evaluate the treatment of loncastuximab tesirine in relapsed or refractory non-Hodgkin’s lymphoma were presented.[6] Among the patients enrolled at the time of the data cutoff the overall response rate was 61% in the total patient population (42% complete response and 19% partial response) and in patients with relapsing or refractory diffuse large B-cell lymphoma (DLBCL) the overall response rate was 57% (43% complete response and 14% partial response).[7][8]
Orphan drug designation
Loncastuximab tesirine was granted Orphan Drug Designation by the U.S. Food and Drug Administration (FDA) for the treatment of diffuse large B-cell lymphoma and mantle cell lymphoma.[9]
References
- ^ https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/761196s000lbl.pdf
- ^ WHO Drug Information: International Nonproprietary Names for Pharmaceutical Substances
- ^ Wang K, Wei G, Liu D (November 2012). “CD19: a biomarker for B cell development, lymphoma diagnosis and therapy”. Experimental Hematology & Oncology. 1 (1): 36. doi:10.1186/2162-3619-1-36. PMC 3520838. PMID 23210908.
- ^ “Pyrrolobenzodiazepine”. ADC Review.
- ^ Clinical trial number NCT02669017 for “ADCT-402 in B-NHL” at ClinicalTrials.gov
- ^ Kahl B, Hamadani M, Caimi PF, Reid EG, Havenith K, He S, Feingold JM, O’Connor O (June 2017). “First clinical results of ADCT‐402, a novel pyrrolobenzodiazepine-based antibody drug conjugate (ADC), in relapsed/refractory B‐cell linage NHL” (PDF). Hematol Oncol. 35 (S2): 49–51. doi:10.1002/hon.2437_33.
- ^ “First clinical results of ADCT-402”. ADC Review.
- ^ Bainbridge K. “Grandfather fighting deadly cancer reveals scans of tumors after testing new drug”. Mirror.
- ^ “ADCT-402 Orphan Drug Designation” (PDF). ADC Therapeutics press release.
External links
- “Loncastuximab tesirine”. Drug Information Portal. U.S. National Library of Medicine.
/////////Loncastuximab tesirine, FDA 2021, APPROVALS 2021, ZYNLONTA, ロンカスツキシマブテシリン, ORPHAN DRUG, ADCT-402, priority review, ADCX 19
ZyCoV-D

ZyCoV-D
CAS 2541524-47-2
DNA vaccine construct encoding a spike protein antigen of SARS-CoV-2 virus (Zydus-Cadila)
UPDATE. APPROVED IN INDIA AUG 2021
http://ctri.nic.in/Clinicaltrials/showallp.php?mid1=51254&EncHid=&userName=ZyCoV-D
bioRxiv (2021), 1-26.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7423510/
| ZyCoV-D | (CTRI/2020/07/026352, 2020, CTRI/2020/07/026352, 2020; Myupchar, 2020) | ZYDUS CADILA |
ZyCoV-D is a genetically engineered DNA plasmid based vaccine encoding for the membrane proteins of the virus. The clinical trials to study the immunogenicity, and safety of the vaccine, will administer three doses at an interval of 28 days in 1048 individuals.
Phase 1/2: CTRI/2020/07/026352
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | DNA |
| Clinical data | |
| Routes of administration |
Intradermal |
| ATC code | None |
| Identifiers | |
| DrugBank | DB15892 |
| Part of a series on the |
| COVID-19 pandemic |
|---|
| SARS-CoV-2 (virus)COVID-19 (disease) |
| showTimeline |
| showLocations |
| showInternational response |
| showMedical response |
| showImpact |
| COVID-19 portal |
ZyCoV-D is a DNA plasmid based COVID-19 vaccine being developed by Cadila Healthcare with support from the Biotechnology Industry Research Assistance Council.
The ZYCOV-D vaccine candidate was developed by Cadila Healthcare Ltd. based in India1. The vaccine was developed using a DNA vaccine platform with a non-replicating and non-integrating plasmid carrying the gene of interest3. Once the plasmid DNA is introduced into host cells and the viral protein is translated, it elicits a strong immune response, stimulating the humoral and cellular components of the immune system3. The DNA vaccine platform offers minimal biosafety requirements, more improved vaccine stability, and lower cold chain requirements3. Phase I clinical trials of this vaccine candidate were completed in July 2020, with the company reporting successful dosing and tolerance1,2. As of August, 2020 the candidate is in Phase II clinical trials1.

NEW DRUG APPROVALS
ONE TIME
$10.00
Clinical research
Phase I and II trials
In February 2020, Cadila Healthcare decided to develop a DNA plasmid based COVID-19 vaccine at their Vaccine Technology Centre (VTC) in Ahmedabad.[1] The vaccine candidate was able to pass the pre-clinical trials on animal models successfully. A report of the study was made available via bioRxiv.[2] Thereafter, human trials for Phase I and II were approved by the regulator.[3]
The Phase II trials of the vaccine candidate were conducted in over 1,000 volunteers as part of the adaptive Phase I/II multi-centric, dose escalation, randomised, double-blind placebo controlled method.[4][5]
Phase III trials
In November 2020, the company announced it would test the vaccine candidate on 30,000 patients in Phase III trials.[6] The vaccine would be given out in three doses at five sites across four cities of India.[7] In January 2021, the Drugs Controller General of India (DCGI) granted permission to conduct the Phase III clinical trials for 28,216 Indian participants.[8][9]
In April 2021, the company reported that they expected to have initial data for the Phase III trials by May 2021.[10]
Production
On 23 April 2021, production of the ZyCoV-D vaccine was started, with a yearly capacity of 240 million doses. It is expected to get emergency use authorization in May or June.[11]
References
- ^ “Zydus Cadila launches a fast tracked programme to develop vaccine for the novel coronavirus, 2019-nCoV (COVID-19)”(PDF). http://www.zyduscadila.com. Cadila Healthcare.
- ^ Dey A, Rajanathan C, Chandra H, Pericherla HP, Kumar S, Choonia HS, et al. (26 January 2021). “Immunogenic Potential of DNA Vaccine candidate, ZyCoV-D against SARS-CoV-2 in Animal Models”. bioRxiv: 2021.01.26.428240. doi:10.1101/2021.01.26.428240. S2CID 231777527.
- ^ “A prospective, randomized, adaptive, phase I/II clinical study to evaluate the safety and immunogenicity of Novel Corona Virus −2019-nCov vaccine candidate of M/s Cadila Healthcare Limited by intradermal route in healthy subjects”. ctri.nic.in. Clinical Trials Registry India. 15 December 2020. CTRI/2020/07/026352. Archived from the original on 22 November 2020.
- ^ “Zydus Cadila’s ZyCov-D vaccine found to be ‘safe and immunogenic'”. @businessline. The Hindu. 24 December 2020.
- ^ Rawat K, Kumari P, Saha L (February 2021). “COVID-19 vaccine: A recent update in pipeline vaccines, their design and development strategies”. European Journal of Pharmacology. 892: 173751. doi:10.1016/j.ejphar.2020.173751. PMC 7685956. PMID 33245898.
- ^ Thacker T (7 November 2020). “Zydus Cadila to test ZyCoV-D on 30,000 patients in Phase-3 trials”. The Economic Times.
- ^ “Covid 19 vaccine in India: Zydus Cadila begins enrolment for Phase 3 trial of ZyCoV-D in 4 cities”. The Financial Express. 22 January 2021.
- ^ “DBT-BIRAC supported indigenously developed DNA Vaccine Candidate by Zydus Cadila, approved for Phase III clinical trials”. pib.gov.in. Press Information Bureau. 3 January 2021.
- ^ “Novel Corona Virus-2019-nCov vaccine by intradermal route in healthy subjects”. ctri.nic.in. Clinical Trials Registry – India. Retrieved 10 April 2021.
- ^ Das, Sohini (22 April 2021). “Cadila Healthcare testing two-shot regimen for ZyCoV-D, data likely by May”. Business Standard India.
- ^ Writer, Staff (24 April 2021). “Cadila Healthcare starts production of Covid vaccine candidate”. mint. Retrieved 27 April 2021.
Zydus Cadila Covid vaccine close to getting approved in India, says MD Sharvil Patel
In an exclusive interview with India Today TV, Managing Director of Zydus Cadila Dr Sharvil Patel said the company’s Covid vaccine candidate ZyCoV-D against the Covid-19 infection is very close to getting approved in India. They are likely to apply for emergency use authorisation this month.
Ahmedabad-based pharmaceutical company Zydus Cadila is likely to submit the application for emergency use authorisation of its Covid-19 vaccine candidate ‘ZyCoV-D’ in India this month. The company is confident that the vaccine will be approved in May itself. The company plants to produce one crore doses of its ‘painless’ Covid-19 vaccine per month.
If approved, ZyCoV-D will be the fourth vaccine to be used in India’s Covid-19 vaccination drive. Made in India, the company plans to ramp up the vaccine’s production to 3-4 crore doses per month and is already in talks with two other manufacturing companies for the same
Although the vaccine should ideally be stored between 2 and 8 degrees Celsius, it remains stable even at room temperature conditions at 25 degrees Celsius. It is easy to administer, the developers said, and will be administered via intradermal injection.
If approved for emergency use, ZyCoV-D could help India fill the vacuum of vaccine doses currently being experienced in the country’s immunisation drive.
Earlier in April, Zydus Cadila announced that its drug Virafin had received restricted emergency use approval from the Drug Controller General of India for the treatment of mild cases of Covid-19.
In an exclusive interview with India Today TV, Sharvil Patel sheds details on all aspects of the Covid-19 vaccine ZyCoV-D.
When asked the status of Covid vaccine candidate ZyCoV-D and when exactly Zydus Cadila would apply for emergency use authorisation in India, Dr Sharvil Patel said the vaccine was getting very close to getting approved in the country.
“I am very happy to say that India’s first indigenously developed DNA vaccine candidate against Covid, which is our ZyCoV-D, is getting very close to approval,” he said.
“We have almost completed all our recruitment for the clinical trials. We have, by far, recruited the largest number of patients for a Covid vaccine trial in India. The number of volunteers who have been vaccinated as a part of the trial is 28,000,” Sharvil Patel said.
Sharvil Patel also said that his company has also included children in the 12-17 age group for the vaccine trials.
He said, “The recruitment holds very important milestones in terms of cohorts because not only have we included the elderly and those with co-morbidities, but also children in the age group of 12 to 17 years.”
Sharvil Patel said as soon as the efficacy data is obtained, Sydus Cadila will file for emergency use authorisation. As soon as the approval is granted, Zydus Cadila will start production of Covid-19 vaccines from July, he said.
“We hope to see our efficacy data in the middle of May. As soon as we see strong efficacy which correlates to the vaccine’s strong immunogenicity in Phase 2, we will file for emergency use authorization. We hope to produce a good quantity of the vaccine from July onwards to make sure it is available to the people. That is the need of the hour right now,” Sharvil Patel said.
He said by May the company will be in a position to talk to the regulators about the restricted use of the Covid-19 vaccine. “The regulatory process is a rolling one. I believe the regulators look at the data in a short period of time,” Sharvil Patel said.
“We have submitted a lot of data already so that it will aid the regulators once we provide them with the efficacy results. We are, hence, expecting to get the approval in May itself,” Sharvil Patel said.
///////////ZyCoV-D, COVID 19, CORONA VIRUS, VACCINE, INDIA 2021, APPROVALS 2021, SARS-CoV-2
Dostarlimab
(Heavy chain)
EVQLLESGGG LVQPGGSLRL SCAASGFTFS SYDMSWVRQA PGKGLEWVST ISGGGSYTYY
QDSVKGRFTI SRDNSKNTLY LQMNSLRAED TAVYYCASPY YAMDYWGQGT TVTVSSASTK
GPSVFPLAPC SRSTSESTAA LGCLVKDYFP EPVTVSWNSG ALTSGVHTFP AVLQSSGLYS
LSSVVTVPSS SLGTKTYTCN VDHKPSNTKV DKRVESKYGP PCPPCPAPEF LGGPSVFLFP
PKPKDTLMIS RTPEVTCVVV DVSQEDPEVQ FNWYVDGVEV HNAKTKPREE QFNSTYRVVS
VLTVLHQDWL NGKEYKCKVS NKGLPSSIEK TISKAKGQPR EPQVYTLPPS QEEMTKNQVS
LTCLVKGFYP SDIAVEWESN GQPENNYKTT PPVLDSDGSF FLYSRLTVDK SRWQEGNVFS
CSVMHEALHN HYTQKSLSLS LGK
(Light chain)
DIQLTQSPSF LSAYVGDRVT ITCKASQDVG TAVAWYQQKP GKAPKLLIYW ASTLHTGVPS
RFSGSGSGTE FTLTISSLQP EDFATYYCQH YSSYPWTFGQ GTKLEIKRTV AAPSVFIFPP
SDEQLKSGTA SVVCLLNNFY PREAKVQWKV DNALQSGNSQ ESVTEQDSKD STYSLSSTLT
LSKADYEKHK VYACEVTHQG LSSPVTKSFN RGEC
(Disulfide bridge: H22-H96, H130-L214, H143-H199, H222-H’222, H225-H’225, H257-H317, H363-H421, H’22-H’96, H’130-L’214, H’143-H’199, H’257-H’317, H’363-H’421, L23-L88, L134-L194, L’23-L’88, L’194-L’134)
>Heavy Chain EVQLLESGGGLVQPGGSLRLSCAASGFTFSSYDMSWVRQAPGKGLEWVSTISGGGSYTYY QDSVKGRFTISRDNSKNTLYLQMNSLRAEDTAVYYCASPYYAMDYWGQGTTVTVSSASTK GPSVFPLAPCSRSTSESTAALGCLVKDYFPEPVTVSWNSGALTSGVHTFPAVLQSSGLYS LSSVVTVPSSSLGTKTYTCNVDHKPSNTKVDKRVESKYGPPCPPCPAPEFLGGPSVFLFP PKPKDTLMISRTPEVTCVVVDVSQEDPEVQFNWYVDGVEVHNAKTKPREEQFNSTYRVVS VLTVLHQDWLNGKEYKCKVSNKGLPSSIEKTISKAKGQPREPQVYTLPPSQEEMTKNQVS LTCLVKGFYPSDIAVEWESNGQPENNYKTTPPVLDSDGSFFLYSRLTVDKSRWQEGNVFS CSVMHEALHNHYTQKSLSLSLGK
>Light Chain DIQLTQSPSFLSAYVGDRVTITCKASQDVGTAVAWYQQKPGKAPKLLIYWASTLHTGVPS RFSGSGSGTEFTLTISSLQPEDFATYYCQHYSSYPWTFGQGTKLEIKRTVAAPSVFIFPP SDEQLKSGTASVVCLLNNFYPREAKVQWKVDNALQSGNSQESVTEQDSKDSTYSLSSTLT LSKADYEKHKVYACEVTHQGLSSPVTKSFNRGEC
References:
- Statement on a Nonproprietary Name Adopted by the USAN Council: Dostarlimab [Link]
Dostarlimab
Immunoglobulin G4, anti-(programmed cell death protein 1 (PDCD1)) (humanized clone ABT1 γ4-chain), disulfide with humanized clone ABT1 κ-chain, dimer
Protein Sequence
Sequence Length: 1314, 443, 443, 214, 214multichain; modified (modifications unspecified)
- GSK-4057190
- GSK4057190
- TSR 042
- TSR-042
- WBP-285
- ANB 011
| Formula | C6420H9832N1680O2014S44 |
|---|---|
| CAS | 2022215-59-2 |
| Mol weight | 144183.6677 |
Jemperli FDA 2021/4/22 AND EMA 2021/4/21

NEW DRUG APPROVALS
ONE TIME
$10.00
Dostarlimab, sold under the brand name Jemperli, is a monoclonal antibody medication used for the treatment of endometrial cancer.[1][2][3][4]
The most common adverse reactions (≥20%) were fatigue/asthenia, nausea, diarrhea, anemia, and constipation.[1][2] The most common grade 3 or 4 adverse reactions (≥2%) were anemia and transaminases increased.[1][2]
Dostarlimab is a programmed death receptor-1 (PD-1)–blocking antibody.[1][2]
Dostarlimab was approved for medical use in the United States in April 2021.[1][2][5]
| NAME | DOSAGE | STRENGTH | ROUTE | LABELLER | MARKETING START | MARKETING END | ||
|---|---|---|---|---|---|---|---|---|
| Jemperli | Injection | 50 mg/1mL | Intravenous | GlaxoSmithKline LLC | 2021-04-22 | Not applicable |
Medical uses
Dostarlimab is indicated for the treatment of adults with mismatch repair deficient (dMMR) recurrent or advanced endometrial cancer, as determined by an FDA-approved test, that has progressed on or following prior treatment with a platinum-containing regimen.[1][2]
On April 22, 2021, the Food and Drug Administration granted accelerated approval to dostarlimab-gxly (Jemperli, GlaxoSmithKline LLC) for adult patients with mismatch repair deficient (dMMR) recurrent or advanced endometrial cancer, as determined by an FDA-approved test, that has progressed on or following a prior platinum-containing regimen.
Efficacy was evaluated based on cohort (A1) in GARNET Trial (NCT02715284), a multicenter, multicohort, open-label trial in patients with advanced solid tumors. The efficacy population consisted of 71 patients with dMMR recurrent or advanced endometrial cancer who progressed on or after a platinum-containing regimen. Patients received dostarlimab-gxly, 500 mg intravenously, every 3 weeks for 4 doses followed by 1,000 mg intravenously every 6 weeks.
The main efficacy endpoints were overall response rate (ORR) and duration of response (DOR), as assessed by blinded independent central review (BICR) according to RECIST 1.1. Confirmed ORR was 42.3% (95% CI: 30.6%, 54.6%). The complete response rate was 12.7% and partial response rate was 29.6%. Median DOR was not reached, with 93.3% of patients having durations ≥6 months (range: 2.6 to 22.4 months, ongoing at last assessment).
Serious adverse reactions occurred in 34% of patients receiving dostarlimab-gxly. Serious adverse reactions in >2% of patients included sepsis , acute kidney injury , urinary tract infection , abdominal pain , and pyrexia . The most common adverse reactions (≥20%) were fatigue/asthenia, nausea, diarrhea, anemia, and constipation. The most common grade 3 or 4 adverse reactions (≥2%) were anemia and transaminases increased. Immune-mediated adverse reactions can occur including pneumonitis, colitis, hepatitis, endocrinopathies, and nephritis.
The recommended dostarlimab-gxly dose and schedule (doses 1 through 4) is 500 mg every 3 weeks. Subsequent dosing, beginning 3 weeks after dose 4, is 1,000 mg every 6 weeks until disease progression or unacceptable toxicity. Dostarlimab-gxly should be administered as an intravenous infusion over 30 minutes.
View full prescribing information for Jemperli.
This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial(s).
FDA also approved the VENTANA MMR RxDx Panel as a companion diagnostic device for selecting endometrial cancer patients for treatment with dostarlimab-gxly.
This review used the Real-Time Oncology Review (RTOR) pilot program, which streamlined data submission prior to the filing of the entire clinical application, and the Assessment Aid, a voluntary submission from the applicant to facilitate the FDA’s assessment.
This application was granted priority review, and breakthrough therapy designation. A description of FDA expedited programs is in the Guidance for Industry: Expedited Programs for Serious Conditions-Drugs and Biologics.
Side effects
Serious adverse reactions in >2% of patients included sepsis, acute kidney injury, urinary tract infection, abdominal pain, and pyrexia.[1][2]
Immune-mediated adverse reactions can occur including pneumonitis, colitis, hepatitis, endocrinopathies, and nephritis.[1][2]
History
Like several other available and experimental monoclonal antibodies, it is a PD-1 inhibitor. As of 2020, it is undergoing Phase I/II and Phase III clinical trials.[6][7][8] The manufacturer, Tesaro, announced prelimary successful results from the Phase I/II GARNET study.[6][9][10]
In 2020, the GARNET study announced that Dostarlimab was demonstrating potential to treat a subset of women with recurrent or advanced endometrial cancer.[11]
April 2021, Dostarlimab is approved for the treatment of recurrent or advanced endometrial cancer with deficient mismatch repair (dMMR), which are genetic anomalies abnormalities that disrupt DNA repair.[12]
On April 22, 2021, the Food and Drug Administration granted accelerated approval to dostarlimab-gxly (Jemperli, GlaxoSmithKline LLC).[1] Efficacy was evaluated based on cohort (A1) in GARNET Trial (NCT02715284), a multicenter, multicohort, open-label trial in patients with advanced solid tumors.[1]
Society and culture
Legal status
On 25 February 2021, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) adopted a positive opinion, recommending the granting of a conditional marketing authorization for the medicinal product Jemperli, intended for the treatment of certain types of recurrent or advanced endometrial cancer.[13] The applicant for this medicinal product is GlaxoSmithKline (Ireland) Limited.[13]
References[
- ^ Jump up to:a b c d e f g h i j k “FDA grants accelerated approval to dostarlimab-gxly for dMMR endometri”. U.S. Food and Drug Administration(FDA) (Press release). 22 April 2021. Retrieved 22 April 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ Jump up to:a b c d e f g h i “Jemperli- dostarlimab injection”. DailyMed. Retrieved 28 April 2021.
- ^ Statement On A Nonproprietary Name Adopted By The USAN Council – Dostarlimab, American Medical Association.
- ^ World Health Organization (2018). “International Nonproprietary Names for Pharmaceutical Substances (INN). Proposed INN: List 119” (PDF). WHO Drug Information. 32 (2).
- ^ “FDA grants accelerated approval for GSK’s Jemperli (dostarlimab-gxly) for women with recurrent or advanced dMMR endometrial cancer” (Press release). GlaxoSmithKline. 22 April 2021. Retrieved 22 April 2021 – via PR Newswire.
- ^ Jump up to:a b Clinical trial number NCT02715284 for “A Phase 1 Dose Escalation and Cohort Expansion Study of TSR-042, an Anti-PD-1 Monoclonal Antibody, in Patients With Advanced Solid Tumors (GARNET)” at ClinicalTrials.gov
- ^ Clinical trial number NCT03981796 for “A Study of Dostarlimab (TSR-042) Plus Carboplatin-paclitaxel Versus Placebo Plus Carboplatin-paclitaxel in Patients With Recurrent or Primary Advanced Endometrial Cancer (RUBY)” at ClinicalTrials.gov
- ^ Clinical trial number NCT03602859 for “A Phase 3 Comparison of Platinum-Based Therapy With TSR-042 and Niraparib Versus Standard of Care Platinum-Based Therapy as First-Line Treatment of Stage III or IV Nonmucinous Epithelial Ovarian Cancer (FIRST)” at ClinicalTrials.gov
- ^ “Data from GARNET study indicates robust activity of dostarlimab in patients with advanced or recurrent endometrial cancer”. Tesaro (Press release). Retrieved 1 January 2020.
- ^ Scalea B (28 May 2019). “Dostarlimab Effective in Endometrial Cancer Regardless of MSI Status”. Targeted Oncology. Retrieved 1 January 2020.
- ^ “GSK Presents New Data from the GARNET Study Demonstrating Potential of Dostarlimab to Treat a Subset of Women with Recurrent or Advanced Endometrial Cancer – Drugs.com MedNews”. Drugs.com. Retrieved 29 April 2020.
- ^ “FDA Approves New Immunotherapy for Endometrial Cancer”. Medscape. Retrieved 23 April 2021.
- ^ Jump up to:a b “Jemperli: Pending EC decision”. European Medicines Agency (EMA) (Press release). 25 February 2021. Retrieved 22 April 2021.
External links
- “Dostarlimab”. Drug Information Portal. U.S. National Library of Medicine.
- Clinical trial number NCT02715284 for “Study of TSR-042, an Anti-programmed Cell Death-1 Receptor (PD-1) Monoclonal Antibody, in Participants With Advanced Solid Tumors (GARNET)” at ClinicalTrials.gov
- Kaplon H, Muralidharan M, Schneider Z, Reichert JM: Antibodies to watch in 2020. MAbs. 2020 Jan-Dec;12(1):1703531. doi: 10.1080/19420862.2019.1703531. [Article]
- Temrikar ZH, Suryawanshi S, Meibohm B: Pharmacokinetics and Clinical Pharmacology of Monoclonal Antibodies in Pediatric Patients. Paediatr Drugs. 2020 Apr;22(2):199-216. doi: 10.1007/s40272-020-00382-7. [Article]
- Green AK, Feinberg J, Makker V: A Review of Immune Checkpoint Blockade Therapy in Endometrial Cancer. Am Soc Clin Oncol Educ Book. 2020 Mar;40:1-7. doi: 10.1200/EDBK_280503. [Article]
- Deshpande M, Romanski PA, Rosenwaks Z, Gerhardt J: Gynecological Cancers Caused by Deficient Mismatch Repair and Microsatellite Instability. Cancers (Basel). 2020 Nov 10;12(11). pii: cancers12113319. doi: 10.3390/cancers12113319. [Article]
- FDA Approved Drug Products: Jemperli (dostarlimab-gxly) for intravenous injection [Link]
- FDA News Release: FDA grants accelerated approval to dostarlimab-gxly for dMMR endometrial cancer [Link]
- Statement on a Nonproprietary Name Adopted by the USAN Council: Dostarlimab [Link]
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Humanized |
| Target | PCDP1 |
| Clinical data | |
| Trade names | Jemperli |
| Other names | TSR-042, WBP-285, dostarlimab-gxly |
| License data | US DailyMed: Dostarlimab |
| Routes of administration | Intravenous |
| Drug class | Antineoplastic |
| ATC code | L01XC40 (WHO) |
| Legal status | |
| Legal status | US: ℞-only [1][2] |
| Identifiers | |
| CAS Number | 2022215-59-2 |
| PubChem SID | 384585344 |
| DrugBank | DB15627 |
| UNII | P0GVQ9A4S5 |
| KEGG | D11366 |
| Chemical and physical data | |
| Formula | C6420H9832N1690O2014S44 |
| Molar mass | 144325.73 g·mol−1 |
/////////Dostarlimab, PEPTIDE, ANTINEOPLASTIC, CANCER, ドスタルリマブ , GSK 4057190, GSK4057190, TSR 042, TSR-042, WBP-285, FDA 2021, EU 2021
2-Deoxy-D-glucose

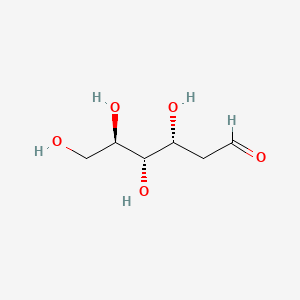
2-Deoxy-D-glucose
- Molecular FormulaC6H12O5
- Average mass164.156 Da
2-Deoxy-D-glucose
(4R,5S,6R)-6-(Hydroxymethyl)tetrahydro-2H-pyran-2,4,5-triol(4R,5S,6R)-6-(Hydroxyméthyl)tétrahydro-2H-pyran-2,4,5-triol
154-17-6[RN]
- 2-Deoxy-D-arabino-hexose
- 2 DG
- 2-Deoxy-D-glucose
- 2-Deoxy-D-mannose
- 2-Deoxyglucose
- 2-Desoxy-D-glucose
- Ba 2758
- D-Glucose, 2-deoxy-
- NSC 15193
2-Deoxy-D-arabino-hexopyranose2-deoxy-D-glucopyranose2-deoxyglucose
2-DGD-arabino-2-DesoxyhexoseD-arabino-Hexopyranose, 2-deoxy- [(4R,5S,6R)-6-(Hydroxymethyl)oxane-2,4,5-triol2-deoxyglucopyranose2-deoxymannopyranose2-dGlc
D-arabino-2-Deoxyhexoseglucitol, 2,5-anhydro-
2-Deoxy-D-glucose
CAS Registry Number: 154-17-6
CAS Name: 2-Deoxy-D-arabino-hexose
Additional Names: D-arabino-2-desoxyhexose; 2-deoxyglucose; 2-DGManufacturers’ Codes: Ba-2758Molecular Formula: C6H12O5Molecular Weight: 164.16Percent Composition: C 43.90%, H 7.37%, O 48.73%Literature References: Antimetabolite of glucose, q.v., with antiviral activity.
Synthesis: M. Bergmann et al.,Ber.55, 158 (1922); 56, 1052 (1923); J. C. Sowden, H. O. L. Fischer, J. Am. Chem. Soc.69, 1048 (1947); H. R. Bolliger, Helv. Chim. Acta34, 989 (1954); H. R. Bolliger, M. D. Schmid, ibid. 1597, 1671; H. R. Bolliger, “2-Deoxy-D-arabino-hexose (2-Deoxy-D-glucose)” in Methods in Carbohydrate Chemistryvol. I, R. L. Whistler, M. L. Wolfrom, Eds. (Academic Press, New York, 1962) pp 186-189.
Inhibition of influenza virus multiplication: E. D. Kilbourne, Nature183, 271 (1959).
Effects on herpes simplex virus: R. J. Courtney et al.,Virology52, 447 (1973). Mechanism of action studies: M. R. Steiner et al.,Biochem. Biophys. Res. Commun.61, 745 (1974); E. K. Ray et al.,Virology58, 118 (1978). Use in human genital herpes infections: H. A. Blough, R. L. Giuntoli, J. Am. Med. Assoc.241, 2798 (1979); L. Corey, K. K. Holmes, ibid.243, 29 (1980). Effect vs respiratory syncytial viral infections in calves: S. B. Mohanty et al.,Am. J. Vet. Res.42, 336 (1981).
Properties: Cryst from acetone or butanone, mp 142-144°. [a]D17.5 +38.3° (35 min) ®+45.9° (c = 0.52 in water); +22.8° (24 hrs) ® +80.8° (c = 0.57 in pyridine).
Melting point: mp 142-144°
Optical Rotation: [a]D17.5 +38.3° (35 min) ®+45.9° (c = 0.52 in water); +22.8° (24 hrs) ® +80.8° (c = 0.57 in pyridine) Derivative Type: a-Form
Properties: Cryst from isopropanol, mp 134-136°. [a]D26 +156° ® +103° (c = 0.9 in pyridine).Melting point: mp 134-136°Optical Rotation: [a]D26 +156° ® +103° (c = 0.9 in pyridine) Use: Exptlly as an antiviral agent.


Source Temperature: 210 °C Sample Temperature: 150 °C Direct, 75 eV
14.0 2.2
15.0 11.5
17.0 3.9
18.0 19.4
19.0 13.7
26.0 2.5
27.0 12.1
28.0 21.9
29.0 31.2
30.0 4.6
31.0 41.3
32.0 12.4
39.0 5.9
40.0 2.1
41.0 10.9
42.0 12.4
43.0 46.3
44.0 31.5
45.0 34.3
46.0 2.8
47.0 4.1
53.0 1.5
54.0 2.0
55.0 14.4
56.0 35.3
57.0 55.7
58.0 11.4
59.0 2.0
60.0 100.0
61.0 31.1
62.0 2.3
68.0 4.6
69.0 12.2
70.0 3.0
71.0 34.9
72.0 7.0
73.0 25.3
74.0 46.6
75.0 5.1
81.0 1.5
82.0 2.4
83.0 1.3
84.0 1.3
85.0 18.1
86.0 55.3
87.0 4.6
89.0 1.2
91.0 1.5
97.0 3.6
98.0 2.9
99.0 1.7
100.0 3.5
102.0 1.1
103.0 19.8
104.0 1.4
111.0 1.6
115.0 25.2
116.0 3.0
117.0 2.1
120.0 3.3
128.0 1.0
129.0 2.5
133.0 1.8
147.0 2.2
1H NMR DMSO D6


1H NMR D20


IR NUJOL MULL

IR KBR

PAPERCollection of Czechoslovak Chemical Communications (1955), 20, 42-5. http://cccc.uochb.cas.cz/20/1/0042/
Preparation of 2-deoxy-D-glucose
By: Stanek, Jaroslav; Schwarz, Vladimir
Triacetyl-D-glucal (I) adds (BzO)2IAg and (BzO)2BrAg, to give 1-benzoyl-3,4,6-triacetyl-2-deoxy-2-iodo-α-D-glucopyranose (II) and 1-benzoyl-3,4,6-triacetyl-2-deoxy-2-bromo-α-D-glucopyranose (III), resp. Both halogen derivs. give 2-deoxy-D-glucose (IV) by reduction. Adding a C6H6 soln. of 16.7 g. iodine into a suspension of 33.6 g. dry BzOAg in 200 ml. C6H6, treating the mixt. with a soln. of 20 g. I in 200 ml. C6H6, heating the mixt. 7 hrs. on the steam bath, removing the AgI, evapg. the solvent, and crystg. the residue from EtOH gave 20.8 g. (54.7%) II, m. 129-30°, [α]21D 21.7°. Analogous procedure with 13.4 g. BzOAg, 4.6 g. Br, and 8 g. I gave 3.9 g. (33%) III, m. 139-40°, [α]17D 33.5°. The same compd. (3 g.), m. 140°, [α]18D 33.6°, was obtained by adding 3.2 g. Br to a soln. of 5.44 g. I in 50 ml. CCl4, by refluxing the mixt. 2 hrs. with 6 g. BzOAg, filtering off the AgBr, and evapg. the solvent. Reducing 8 g. II or an equiv. III in 150 ml. MeOH with 60 g. Zn activated by 1 hr. immersion in a soln. of 60 g. CuSO4 in 1500 ml. H2O, removing Zn after 8 hrs., evapg. the MeOH, and sapong. the residue with Ba(OH)2 yielded 0.42 g. (20%) IV, m. 145°, [α]18D 46.1°.
Wavlen: 589.3 nm; Temp: 18 °C, +46.1 ° ORD
PATENT
https://patents.google.com/patent/WO2004058786A1/enThe present invention relates to a process for the synthesis of 2-deoxy-D-glucose. Background of the invention 2-deoxy-D-glucose is useful in control of respiratory infections and for application as an antiviral agent for treatment of human genital herpes.Prior art for preparation of 2-deoxy-D-glucose while operable, tend to be expensive and time consuming. Reference may be made to Bergmann, M., Schotte, H., Lechinsky, W., Ber, 55, 158 (1922) and Bergmann, M., Schotte, H., Lechinsky, W., Ber 56, 1052 (1923) which disclose the preparation of 2-deoxy-D-glucose in low yield by mineral acid catalyzed addition of water to D-glucal. Another method of producing 2-deoxy-D-glucose is from diethyldithioacetal derivative of D-glucose (Bolliger, H.R. Schmid, M.D., Helv. Chim. Ada 34, 989 (1951); Bolliger, H.R., Schmid, M.D., Helv. Chim. A a 34, 1597 (1951); Bolliger, H.R. Schmid, M.D., Helv. Chim. Ada 34, 1671 (1951) and from D-arabhiose by reaction with nitromethane followed by acetylation, reduction and hydrolysis (Sowden, J.C, Fisher, H.O.L., J. Am. Chem., 69, 1048 (1947). However these methods result in the formation of 2- deoxy-D-glucose in low yield and of inferior purity due to the formation of several byproducts and involve use of toxic reagents such as ethanethiol and nitromethane. As a result purification of 2-deoxy-D-glucose has to be done by recrystallisation which is tedious, time consuming and difficult.Accordingly it is important to develop a process for synthesis of 2-deoxy-D-glucose which obviates the drawbacks as detailed above and results in good yield and good purity. Objects of the inventionThe main object of the present invention is to provide a process for the synthesis of 2- deoxy-D-glucose resulting in good yield and with good purity.Another object of the invention is to provide an economical process for the synthesis of 2-deoxy-D-glucose. Summary of the inventionA process that would produce 2-deoxy-D-glucose economically and with desired purity, is a welcome contribution to the art. This invention fulfills this need efficiently.Accordingly the present invention relates to a process for the synthesis of 2-deoxy- D-glucose comprising haloalkoxylation of R-D-Glucal wherein R is selected from H and 3, 4, 6-tri-O-benzyl, to obtain alkyl 2-deoxy-2-halo-R-α/ -D-gluco/mannopyranoside, converting alkyl 2-deoxy-2-halo-R-α/β-D-gluco/mannopyranoside by reduction to alkyl 2- deoxy-α/β-D-glucopyranoside, hydrolysing alkyl 2-deoxy-α/β-D-glucopyranoside to 2- deoxy-D-glucose.In one embodiment of the invention, the alkyl 2-deoxy-α/β-D-glucopyranoside is obtained by (a) haloalkoxylating 3,4,6,-tri-O-benzyl-D-glucal to alkyl 2-deoxy-2-halo-3,4,6-tri-O- benzyl-α/β-D-gluco-/mannopyranoside; (b) subjecting alkyl 2-deoxy-2-halo-3,4,6-tri-O-benzyl-α/β-D-gluco/mannopyranoside to reductive dehalogenation and debenzylation to obtain alkyl 2-deoxy -α/β-D- glucopyranoside. In another embodiment of the invention, in step (a) haloalkoxylation of 3,4,6-tri-O- benzyl-D-glucal is carried out by reaction with a haloalkoxylating agent selected from a N- halosuccinimide and a N-haloacetamide, and alcohol.The reaction scheme for the reactions involved in the process of the invention are also given below:

in R’=CH3I R=C6H5CH2 H R=C6H5CH2, X=Br, R’=CH3 IV R=H V R=CH3, C2HSJ C6H5CH3, iPr, X=Br

Such overall synthesis may be depicted as follows where R=H, CH3, C2H5, (CH3)2CH, C6H5CH ; RX-CH3; X-CL, Br.Example 1 To a solution of 3,4,6-tri-O-benzyl-D-glucal (39 g, 0.09 mol) in dichloromethane (20ml) and methanol (100 ml) was added N-bromosuccinimide (18.7 g, 0.09 mil) during 10 min. at room temperature and stirred for 4 h. After completion of the reaction solvent was distilled off. The resultant residue extracted into carbon tetrachloride (2×100 ml) and organic phase concentrated to obtain methyl 2-bromo 2-deoxy-3,4,6-tri-O-benzyl-α/β-D-gluco- /mannopyranoside as a syrup. Quantity obtained 50 g. 1H NMR (200 MHz, CDC13) 3.40-4.00 (m, 7H, H-2,5,6,6′ and OCH3) 4.30-5.10 (m, 9H, H-1,3,4 and 3xPhCH2O), 7.10-7.60 (m, 15H, Ar-H). A solution of methyl 2-bromo-2-deoxy-3,4,6-tri-O-benzyl-α/β-D-gluco- /mannopyranoside (50 g) in methanol (300) was charged into one litre autoclave along with Raney nickel (10 ml) Et3N (135 ml) and subjected to hydrogenation at 120 psi pressure at 50°C for 8 h. After completion of the reaction the catalyst was filtered off and the residue washed with methanol (25 ml). The filtrate was concentrate to obtain methyl 2-deoxy-3,4,6- tri-O-benzyl-α/β-D-glucopyranoside as a syrup (37.9 g, 89%). 1H NMR (200 MHz, CDC13): δ 1.50-2.40 (m,2H,H-2,2′)5 3.32, 3.51 (2s, 3H, OCH3) 3.55-4.00 (m, 5H, H-3,4,5,6,6′), 4.30-5.00 (m, 7H, 3xPhCH2, H-l), 7.10-7.45 (m, 15H, Ar-H). The syrup of methyl 2-deoxy-3,4,6- tri-O-benzyl-α/β-D-glucopyranoside (37.9g) was dissolved in methanol (200 ml). 1 g of 5%Pd/C was added and hydrogenated at 150 psi pressure at room temperature. After 5 hours catalyst was filtered off and solvent evaporated. Quantity of the methyl 2-deoxy-α/β-D- glucopyranoside obtained 10.5 g (70%). [ ]D + 25.7° (c 1.0, MeOH), 1H NMR (200 MHz, D2O); δ 1.45-2.40 (m, 2H, H-2,2′) 3.20-4.80, (m 9H, H- 1,3,4,5,6,6′ – OCH3).Example 2 To a solution of D-glucal (64.6g, 0.44 mol) in methanol (325 ml) at 10°C was addedN-bromosuccinimide (78.7 g, 0.44 mol) during 40 min. maintaining the temperature between 10-15°C during the addition. The reaction mixture was stirred at room temperature. After 5 hours solvent was evaporated to obtain a residue which was refluxed in ethyl acetate (100 ml). Ethyl acetate layer was discarded to leave a residue of methyl 2-bromo-2-deoxy-α/β-D- gluco/mannopyranoside (105 g) as a syrup. [α]D + 36° (c 1.0, MeOH). 1H NMR (200 MHz, D2O): δ 3.47, 3.67 (2s, 3H, OCH3), 3.70-4.05 (m, 6h, H-23,4,5,6,6′), 4.48-5.13 (2s, 1H, H-l). The syrupy methyl 2-bromo-2-deoxy-α/β-D-gluco-/mannopyranoside was dissolved in methanol (400 ml), a slurry of 80 g Raney nickel (a 50% slurry in methanol), Et3N (30 ml) and hydrogenated in a Parr apparatus at 120 psi. After 8-9 hours, the reaction mixture was filtered through a Celite filter pad and washed with MeOH. The washings and filtrate were combined and triturated with hexane to separate and remove by filtration insoluble triethylamine hydrobromide and traces of succinimide. The filtrate was concentrated to a residue. The isolated yield of methyl 2-deoxy-α/β-D-glucopyranoside was 89%. Ethyl 2-bromo-2deoxy-α/β-D-gluco-/mannopyranoside: When solvent was ethanol instead of methanol the compound obtained was ethyl 2- bromo-2-deoxy-α/β-D-gluco-/mannopyranoside. 1HNMR (200 MHz, D2O): δ 1.10-1.32 (m, 3H, CH3), 2.80 (s, 4H, -CO(CH2)2CO-NH-), 3.40-4.10 (m, 8H, H-2,3,4,5,6,6′, CH2), 4.40, 5.20 (2s 1H, H-l α/β).Isopropyl 2-bromo-2-deoxy- /β-D-gluco-/mannopyranoside: When isopropanol instead of methanol was used as a solvent the compound obtained was isopropyl 2-bromo-2-deoxy-α/β-D-gluco/mannopyranoside. 1H NMR (200 MHz, D2O): δ 1.10-1.30 (m, 6H, 2xCH3) 2.80 (s, 4H, -CO(CH2)2CO-NH-), 3.60-4.60 (m 8H,H- 2,3,4,5,6,6′, CH2) 4.40, 5.30 (2s, 1H, H-l, α/β).Example 3 A mixture of D-glucal (64.6 g), methanol (400 ml), N-bromosuccinimide (79 g) were stirred at 15 C for 6 h. The reaction mixture was hydrogenated in a Parr apparatus in presence of 60 g of Raney nickel catalyst (a 50% slurry in methanol) and triethylamine (62 ml). After 8-9 h, the reaction mixture was filtered on a Celite filter pad. The Celite pad was washed with methanol. The washings and filtrate were combined, concentrated to a thick heavy syrup, dissolve in chloroform (500 ml), pyridine (400 ml) and acetic anhydride (251 ml) was added while stirring, maintaining the temperature between 5-10°C. After 12 hours, the reaction mixture was diluted with CHC13 (500 ml) transferred to a separating funnel and organic phase was washed with water. The organic phase was separated, dried (Na2SO4) and concentrated to obtain methyl 2-deoxy-3,4,6-tri-O-acetyl-2 deoxy-α/β-D-glucopyranoside as a syrup (163.43 g, 87%). [α]D + 65.0° (c 1.0, CHC13) 1H NMR (200 MHz, CDC13): δ 1.55-1.90 (m, 2H, H-2,2′), 2.01, 2.04,2.11, 2.15, (4s, 9H, 3xOCOCH3), 2.18,3.40 (2s, 3H, OCH3), 3.45-50 (m, 3H, H-5, 6,6′) 4.80-5.40 (m, 3H,H-1,3,4). The syrup was dissolved in methanol (600 ml) IN NaOMe in methanol (25ml) was added and left at room temperature. After 6-10 h, dry CO2 gas was passed into the reaction mixture, solvent was evaporated to obtain a syrupy residue. The residue was once again extracted into dry methanol and concentrated to obtain methyl 2-deoxy-α/β-D-glucopyranoside as syrup. Quantity obtained 81 g (92%).Example 4 A 500 ml round bottom flask equipped with magnetic stir bar was charged with a solution of D-glucal (32.3 g) in methanol (175 ml), cooled to 15°C, N-bromosucci-t imide (NBS) (39.4 g) was added and stirred for 6 hours at 15°C. The reaction mixture was concentrated to half the volume, cooled to 0°C and separated succinimide was removed by filtration. To the filtrate was added a slurry of 30 g Raney nickel (a 50% slurry in methanol) Et3N (32 ml) and hydrogenated in a Parr apparatus at 120 psi. After 7-8 hours, the reaction mixture was filtered through a Celite filter pad, and washed with MeOH. The washings and filtrate were combined and triturate with hexane to separate and remove by filtration insoluble triethylamine hydrobromide and succinimide. The filtrate was concentrated to a residue, dissolved in methanol and triturated with hexane to remove most of the triethylamine hydrobromide and succinimide. The filtrate was concentrated to obtain methyl 2-deoxy-α/β- D-glucopyranoside (85%).Example 5 To a stirred solution of methyl 3,4,6-tri-O-acetyl-2-deoxy-α/β-D-glucopyranoside (47 g) (from example 3) in acetic acid (40 ml) and acetic anhydride (110 ml) was added concentrated sulphuric acid (0.94 ml) at 0°. The reaction mixture was brought to room temperature and stirred. After 2 hours the reaction mixture was diluted with water (50 ml) and extracted into CH2C12 (3×150 ml). The organic phase was separated, washed with saturated NaHCO3 solution, H2O dried over Na2SO and concentrated to obtain 2-deoxy- 1,3,4,6-tetra-O-acetyl-α/β-D-glucopyranoside as a crystalline compound, mp. 115-118°C. Quantity obtained 44.5 g (86%). [α]D + 21.5° (c 1.0, CHC13). 1H NMR (200 MHz, CDC13): δ 1.50-2.45 (m, 14H, H-2,2′, 4xOCOCH3), 3.85-5.40, (m, 5H, H-3,4,5,6,6′), 5.75-6.20 (m, 1H, H-l,α/ β). To a heterogeneous mixture of l,3,4,6-tetra-O-acetyl-2-deoxy-α/β-D- glucopyranoside (10 g) in water (100 ml) was added acetyl chloride (10 ml) and heated to 80°C. After 6 hours the reaction mixture was cooled to room temperature, neutralised with saturated aq. Ba(OH)2, concentrated to half the volume and filtered on a Celite pad. Filtrate was concentrated on a rotary evaporator and dried over anhydrous P2O5 to obtain a residue which was dissolved in hot isopropyl alcohol and filtered on a pad of Celite to obtain a clear filtrate. The filtrate was concentrated to a residue, dissolved in hot isopropyl alcohol (50 ml), acetone (75 ml) and seeded with a few crystals of 2-deoxy-D-glucose. After 15-18 hours at 5°C crystalline title product was filtered. Quantity obtained 3.21 g (64.9%) m.p. 148-149°C.Example 6 A heterogeneous mixture of l,3,4,6-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (9 g) (from example 5), water (30 ml) and 11% aq. H2SO (0.3 ml) was stirred at 85°C for 7 h to obtain a homogenous solution. The reaction mixture was cooled, neutralised with aq. Ba(OH)2 solution and filtered. The filtrate obtained was concentrated to half the volume and solids separated were filtered. To the filtrate was added activated carbon (1 g) and filtered. The filtrate was concentrated on a rotary evaporator and dried over P2O5 to obtain 2-deoxy- D-glucose that was crystallized from methyl alcohol (27 ml) and acetone (54 ml). Quantity obtained 2.4 g. mp. 146-149°C.Example 7A heterogeneous mixture of l,3,4,6-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside(25g) (from example 5), H2O (250 ml), toluene (250 ml) and glacial acetic acid (1.25 ml) was heated to reflux for 10-12 hours, while it was connected to a Dean- Stark azeotropic distillation apparatus. An azeotropic mixture of acetic acid, toluene was collected to remove acetic acid and every one hour fresh toluene (50 ml) was introduced. After completion of the reaction, toluene was removed by distillation from the reaction mixture to obtain a residue that was dissolved in methanol, treated with charcoal and filtered. The filtrate was separated, concentrated to a residue and crystallized from isopropyl alcohol and acetone to obtain 2- deoxy-D-glucose (7.33 g, 59%). mp. 148-151°C.Example 8 A heterogeneous mixture of l,3,4,5-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (lOg) (from example 5), H2O (200 ml) cone. HC1 (0.3 ml) and glacial acetic acid (0.5 ml) was heated to 85°C. After 6 hours the reaction mixture was cooled to room temperature, neutralized with aq. Ba(OH)2 and filtered on a pad of Celite. Filtrate was separated, treated with charcoal and filtered. The filtrate was concentrated to a residue and crystallized from MeOH, acetone to obtain the product. Quantity obtained 2.75 g. mp. 147-148°C.Example 9 A heterogeneous mixture of l,3,4,5-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside(lOg) (from example 3) water (100 ml) and cone. HCI (0.5ml) was heated to 80°C. After 2-5 hours the reaction mixture was cooled to room temperature, neutralized with aq. Ba(OH)2 and filtered on a pad of Celite. The filtrate was concentrated to a residue, dissolved in ethanol, treated with charcoal and filtered. The filtrate was concentrated to a solid residue andcrystallized from methanol-acetone to obtain the title product. Quantity obtained 3.15g mp. 148-151°C.Example 10A solution of methyl 2-deoxy-α/β-D-glucopyranoside (30g) (from example 2) water(15 ml) and cone. HCI (1.5 ml) was heated to 80-85°C. After 3-5 hours the reaction mixture was cooled to room temperature, neutralized with aq. Ba(OH)2 and filtered to remove insoluble salts. The filtrate was concentrated to a residue, crystallized from MeOH, acetone and hexane to obtain 2-deoxy-D-glucose (11.77 g) mp. 149-151°C.Example 11A solution of methyl 2-deoxy-α/β-D-glucopyranoside (30g) (from example 2) water (195 ml) and cone. H2SO (5.9 ml) was heated to 80°C. After 2-3 hours the reaction mixture was cooled, neutralized with aq. Ba(OH)2 and filtered. The filtrate was separated, treated with charcoal and filtrate. The Filtrate was concentrated to a residue and crystallized from isopropyl alcohol to obtain the title product. Quantity obtained 5.2 g. mp. 152-154°C.Example 12 A mixture of methyl 2-deoxy-α/β-D-glucopyranoside (24g) (from example 2) water(125 ml) and IR 120 H+ resin (7.5 ml) was heated to 90-95°C for 2h. The reaction mixture was cooled to room temperature, filtered and the resin was washed with water (20 ml). The filtrate was concentrated to residue and crystallized from ethanol to obtain 2-deoxy-D- glucose (8.8 g), mp. 150-152°C. The main advantages of the present invention are:-1). It does not involve the use of toxic mercaptans like ethane thiol. 2). This process does not involve reaction of D-glucal with mineral acid, thereby avoiding the formation of Ferrier by-products.
2-Deoxy-d-glucose is a glucose molecule which has the 2-hydroxyl group replaced by hydrogen, so that it cannot undergo further glycolysis. As such; it acts to competitively inhibit the production of glucose-6-phosphate from glucose at the phosphoglucoisomerase level (step 2 of glycolysis).[2] In most cells, glucose hexokinase phosphorylates 2-deoxyglucose, trapping the product 2-deoxyglucose-6-phosphate intracellularly (with exception of liver and kidney)[; thus, labelled forms of 2-deoxyglucose serve as a good marker for tissue glucose uptake and hexokinase activity. Many cancers have elevated glucose uptake and hexokinase levels. 2-Deoxyglucose labeled with tritium or carbon-14 has been a popular ligand for laboratory research in animal models, where distribution is assessed by tissue-slicing followed by autoradiography, sometimes in tandem with either conventional or electron microscopy.
2-DG is uptaken by the glucose transporters of the cell. Therefore, cells with higher glucose uptake, for example tumor cells, have also a higher uptake of 2-DG. Since 2-DG hampers cell growth, its use as a tumor therapeutic has been suggested, and in fact, 2-DG is in clinical trials. [3] A recent clinical trial showed 2-DG can be tolerated at a dose of 63 mg/kg/day, however the observed cardiac side-effects (prolongation of the Q-T interval) at this dose and the fact that a majority of patients’ (66%) cancer progressed casts doubt on the feasibility of this reagent for further clinical use.[4] However, it is not completely clear how 2-DG inhibits cell growth. The fact that glycolysis is inhibited by 2-DG, seems not to be sufficient to explain why 2-DG treated cells stop growing.[5] Because of its structural similarity to mannose, 2DG has the potential to inhibit N-glycosylation in mammalian cells and other systems, and as such induces ER stress and the Unfolded Protein Response (UPR) pathway.[6][7][8]
Clinicians have noted that 2-DG is metabolised in the pentose phosphate pathway in red blood cells at least, although the significance of this for other cell types and for cancer treatment in general is unclear.
Work on the ketogenic diet as a treatment for epilepsy have investigated the role of glycolysis in the disease. 2-Deoxyglucose has been proposed by Garriga-Canut et al. as a mimic for the ketogenic diet, and shows great promise as a new anti-epileptic drug.[9][10] The authors suggest that 2-DG works, in part, by increasing the expression of Brain-derived neurotrophic factor (BDNF), Nerve growth factor (NGF), Arc (protein) (ARC), and Basic fibroblast growth factor (FGF2).[11] Such uses are complicated by the fact that 2-deoxyglucose does have some toxicity.
A study found that by combining the sugar 2-deoxy-D-glucose (2-DG) with fenofibrate, a compound that has been safely used in humans for more than 40 years to lower cholesterol and triglycerides, an entire tumor could effectively be targeted without the use of toxic chemotherapy.[12][13]
2-DG has been used as a targeted optical imaging agent for fluorescent in vivo imaging.[14][15] In clinical medical imaging (PET scanning), fluorodeoxyglucose is used, where one of the 2-hydrogens of 2-deoxy-D-glucose is replaced with the positron-emitting isotope fluorine-18, which emits paired gamma rays, allowing distribution of the tracer to be imaged by external gamma camera(s). This is increasingly done in tandem with a CT function which is part of the same PET/CT machine, to allow better localization of small-volume tissue glucose-uptake differences.
Resistance to 2-DG has been reported in HeLa cells [16] and in yeast;[17][8] in the latter, it involves the detoxification of a metabolite derived from 2-DG (2DG-6-phosphate) by a phosphatase. Despite the existence of such a phosphatase in human (named HDHD1A) However it is unclear whether it contributes to the resistance of human cells to 2DG or affects FDG-based imaging.
SYN
Indian Pat. Appl., 2004DE02075,

SYN
CN 106496288,
STARTING MATERIAL CAS 69515-91-9
C14 H20 O9, 332.30
D-arabino-Hexopyranose, 2-deoxy-, 1,3,4,6-tetraacetate
SYN
Bioorganic & Medicinal Chemistry Letters, 22(10), 3540-3543; 2012
https://www.sciencedirect.com/science/article/abs/pii/S0960894X12004258
PATENT
https://patents.google.com/patent/US6933382B2/en2-deoxy-D-glucose is useful in control of respiratory infections and for application as an antiviral agent for treatment of human genital herpes.Prior art for preparation of 2-deoxy-D-glucose while operable, tend to be expensive and time consuming. Reference may be made to Bergmann M., Schotte, H., Lechinsky, W., Ber, 55, 158 (1922) and Bergmann, M., Schotte, H., Lechinsky, W., Ber 56, 1052 (1923) which disclose the preparation of 2-deoxy-D-glucose in low yield by mineral acid catalyzed addition of water to D-glucal. Another method of producing 2-deoxy-D-glucose is from diethyldithioacetal derivative of D-glucose (Bolliger, H. R. Schmid, M. D., Helv. Chim. Acta 34, 989 (1951); Bolliger, H. R., Schmid, M. D., Helv, Chim. Acta 34, 1597 (1951); Bolliger, H. R Schmid, M. D., Helv. Chim. Acta 34, 1671 (1951) and from D-arabinose by reaction with nitromethane followed by acetylation, reduction and hydrolysis (Sowden, J. C., Fisher, H. O. L., J. Am. Chem., 69, 1048 (1947). However these methods result in the formation of 2-deoxy-D-glucose in low yield and of inferior purity due to the formation of several by-products and involve use of toxic reagents such as ethanethiol and nitromethane. As a result purification of 2-deoxy-D-glucose has to be done by recrystallisation which is tedious, time consuming and difficult.

EXAMPLE 1To a solution of 3,4,6-tri-O-benzyl-D-glucal (39 g, 0.09 mmol) in dichloromethane (20 ml) and methanol (100 ml) was added N-bromosuccinimide (18.7 g, 0.09 mil) during 10 min. at room temperature and stirred for 4 h. After completion of the reaction solvent was distilled off. The resultant residue extracted into carbon tetrachloride (2×100 ml) and organic phase concentrated to obtain methyl 2-bromo 2-deoxy-3,4,6-tri-O-benzyl-α/β-D-gluco-/mannopyranoside as a syrup. Quantity obtained 50 g. 1H NMR (200 MHz, CDCl3) 3.40-4.00 (m, 7H, H-2,5,6,6′ and OCH3) 4.30-5.10 (m, 9H, H-1,3,4 and 3×PhCH2O), 7.10-7.60 (m 15H, Ar—H). A solution of methyl 2-bromo-2-deoxy-3,4,6-tri-O-benzyl/α/β-D-gluco-/mannopyranoside (50 g) in methanol (300) was charged into one liter autoclave along with Raney nickel (10 ml) Et3N (135 ml) and subjected to hydrogenation at 120 psi pressure at 50° C. for 8 h. After completion of the reaction the catalyst was filtered off and the residue washed with methanol (25 ml). The filtrate was concentrate to obtain methyl 2-deoxy-3,4,6-tri-O-benzyl-α/β-D-glucopyranoside as a syrup (37.9 g, 89%). 1H NMR (200 MHz CDCl3): δ 1.50-2.40 (m,2H,H-2,2′), 3.32, 3.51 (2s, 3H, OCH3) 3.55-4.00 (m, 5, H-3,4,5,6,6′) 4.30-5.00 (M 7H, 3×PhCH2, H-1), 7.10-7.45 (m, 15H, Ar—H). The syrup of methyl 2-deoxy-3,4, 6-tri-O-benzyl-α/β-D-glucopyranoside (37.9 g) was dissolved in methanol (200 ml). 1 g of 5% Pd/C was added and hydrogenated at 150 psi pressure at room temperature. After 5 hours catalyst was filtered off and solvent evaporated. Quantity of the methyl 2-deoxy-α/β-D-glucopyranoside obtained 10.5 g (70%). [α]D+25.7° (c 1.0, MeOH), 1H NMR (200 MHz, D2O); δ 1.45-2.40 (m, 2H, H-2,2′) 3.20-4.80, (m 9H, H-1,3,4,5,6,6′—OCH3).EXAMPLE 2To a solution of D-glucal (64.6 g, 0.44 mmol) in methanol (325 ml) at 10° C. was added N-bromosuccinimide (78.7 g, 0.44 mol) during 40 min. maintaining the temperature between 10-15° C. during the addition. The reaction mixture was stirred at room temperature. After 5 hours solvent was evaporated to obtain a residue which was refluxed in ethyl acetate (100 ml). Ethyl acetate layer was discarded to leave a residue of methyl 2-bromo-2-deoxy-α/β-D-gluco/mannopyranoside (105 g) as a syrup. [α]D+36° (c 1.0, MeOH). 1H NMR (200 MHz, D2O): δ 3.47, 3.67 (2s, 3H, OCH3), 3.70-4.05 (m, 6h, H-2,3,4,5,6,6′), 4.48-5.13 (28, 1H, 1H, H-1). The syrupy methyl 2-bromo-2-deoxy-α/β-D-gluco-/mannopyranoside was dissolved in methanol (400 ml), a slurry of 80 g Raney nickel (a 50% slurry in methanol), Et3N (30 ml) and hydrogenated in a Parr apparatus at 120 psi. After 8-9 hours, the reaction mixture was filtered through a Celite filter pad and washed with MeOH. The washings and filtrate were combined and triturated with hexane to separate and remove by filtration insoluble triethylamine hydrobromide and traces of succinimide. The filtrate was concentrated to a residue. The isolated yield of methyl 2-deoxy-α/β-D-glucopyranoside was 89%.Ethyl 2-bromo-2deoxy-α/β-D-gluco-/mannopyranoside:When solvent was ethanol instead of methanol the compound obtained was ethyl 2-bromo-2deoxy-α/β-D-gluco-/mannopyranoside. 1H NMR (200 MHz, D2O): δ 1.10-1.32 (m, 3H, CH3), 2.80 (s, 4H, —CO(CH2)2CO—NH—), 3.40-4.10 (m, 8H, H-2,3,4,5,6,6′, CH2), 4.40, 5.20 (2s 1H, H-1, α/β).Isopropyl 2-bromo-2-deoxy-α/β-D-gluco-/mannopyranoside:When isopropanol instead of methanol was used as a solvent the compound obtained was isopropyl 2-bromo-2-deoxy-α/β-D-gluco/mannopyranoside, 1H NMR (200 MHz, D2O): δ 1.10-1.30 (m, 6H, 2×CH3) 2.80 (s, 4H, —CO(CH2)2CO—NH—), 3.60-4.60 (m 8H,H-2,3,4,5,6,6′, CH2) 4.40, 5,30 (2s, 1H, H-1, α/β.EXAMPLE 3A mixture of D-glucal (64.6 g), methanol (400 ml), N-bromosuccinimide (79 g) were stirred at 15° C. for 6 h. The reaction mixture was hydrogenated in a Parr apparatus in presence of 60 g of Raney nickel catalyst (a 50% slurry in methanol) and triethylamine (62 ml). After 8-9 h, the reaction mixture was filtered on a Celite filter pad. The Celite pad was washed with methanol. The washings and filtrate were combined, concentrated to a thick heavy syrup, dissolve in chloroform (500 ml), pyridine (400 ml) and acetic anhydride (251 ml) was added while stirring, maintaining the temperature between 5-10° C. After 12 hours, the reaction mixture was diluted with CHCl3 (500 ml) transferred to a separating funnel and organic phase was washed with water. The organic phase was separated, dried (Na2SO4) and concentrated to obtain methyl 2-deoxy-3,4,6-tri-O-acetyl-2 deoxy-α/β-D-glucopyranoside as a syrup (163.43 g, 87%). [α]D+65.0° (c 1.0, CHCl3) 1H NMR (200 MHz, CDCl3): δ 1.55-1.90 (m, 2H, H-22′), 2.01, 2.04, 2.11, 2.15, (4s, 9H, 3×OCOCH3), 2.18, 3.40 (2s, 3H, OCH3), 3.45-50 (m, 3H, H-5, 6,6′) 4.80-5.40 (m, 3H,H-1,3,4). The syrup was dissolved in methanol (600 ml) 1N NaOMe in methanol (25 ml) was added and left at room temperature. After 6-10 h, dry CO2 gas was passed into the reaction mixture, solvent was evaporated to obtain a syrupy residue. The residue was once again extracted into dry methanol and concentrated to obtain methyl 2-deoxy-α/β-D-glucopyranoside as syrup. Quantity obtained 81 g (92%).EXAMPLE 4A 500 ml round bottom flask equipped with magnetic stir bar was charged with a solution of D-glucal (323 g) in methanol (175 ml), cooled to 15° C., N-bromosuccinimide (NIBS) (39.4 g) was added and stirred or 6 hours at 15° C., The reaction mixture was concentrated to half the volume, cooled to 0° C. and separated succinimide, was removed by filtration. To the filtrate was added a slurry of 30 g Raney nickel (a 50% slurry in Methanol) Et3N (32 ml) and hydrogenated in a Parr apparatus at 120 psi. After 7-8 hours, the reaction mixture was filtered through a Celite filter pad, and washed with MeOH. The washings and filtrate were combined and triturate with hexane to separate and remove by filtration insoluble triethylamine hydrobromide and succinimide. The filtrate was concentrated to a residue, dissolved in methanol and triturated with hexane to remove most of the triethylamine hydrobromide and succinimide. The filtrate was concentrated to obtain methyl 2-deoxy-α/β-D-glucopyranoside (85%).EXAMPLE 5To a stirred solution of methyl 3,4,6-tri-O-acetyl-2-deoxy-α/β-D-glucopyranoside (47 g) (from example 3) in acetic acid (40 ml) and acetic anhydride (110 ml) was added concentrated sulphuric acid (0.94 ml) at 0°. The reaction mixture was brought to room temperature and stirred. After 2 hours the reaction mixture was diluted with water (50 ml) and extracted into CH2Cl2 (3×150 ml). The organic phase was separated, washed with saturated NaHCO3 solution H2O dried over Na2SO4 and concentrated to obtain 2-deoxy-1,3,4,6-tetra-O-acetyl-α/β-D-glucopyranoside as a crystalline compound. mp. 115-118° C. Quantity obtained 44.5 g (86%). [α]D+21.5° (c 1.0, CHCl3). 1H NMR (200 MHz, CDCl3): δ 1.50-2.45 (m, 14H, H-2,2′, 4×OCOCH3), 3.85-5.40, (m, 5H, H-3,4,5,6,6′), 5.75-6.20 (m, 1H, H-1, α/β). To a heterogeneous mixture of 1,3,4,6-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (10 g) in water (100 ml) was added acetyl chloride (10 ml) and heated to 80° C. After 6 hours the reaction mixture was cooled to room temperature, neutralised with saturated aq. Ba(OH)2, concentrated to half the volume and filtered on a Celite pad, Filtrate was concentrated on a rotary evaporator and dried over anhydrous P2O5 to obtain a residue which was dissolved in hot isopropyl alcohol and filtered on a pad of Celite to obtain a clear filtrate. The filtrate was concentrated to a residue, dissolved in hot isopropyl alcohol (50 ml), acetone (75 ml) and seeded with a few crystals of 2-deoxy-D-glucose. After 15-18 hours at 5° C. crystalline title product was filtered. Quantity obtained 3.21 g (64.9%) m.p. 148-149° C.EXAMPLE 6A heterogeneous mixture of 1,3,4,6-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (9 g) (from example 5), water (30 ml) and 11% aq. H2SO4 (0.3 ml) was stirred at 85° C. for 7 h to obtain a homogenous solution. The reaction mixture was cooled, neutralised with aq. Ba(OH)2 solution and filtered. The filtrate obtained was concentrated to half the volume and solids separated were filtered. To the filtrate was added activated carbon (1 g) and filtered. The filtrate was concentrated on a rotary evaporator and dried over P2O5 to obtain 2-deoxy-D-glucose that was crystallized from methyl alcohol (27 ml) and acetone (54 ml). Quantity obtained 2.4 g. mp. 146-149° C.,EXAMPLE 7A heterogeneous mixture of 1,3,4,tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (25 g) (from example 5), H2O (250 ml), toluene (250 ml) and glacial acetic acid (1.25 ml) was heated to reflux for 10-12 hours, while it was connected to a Dean-Stark azeotropic distillation apparatus. An azeotropic mixture of acetic acid, toluene was collected to remove acetic acid and every one hour fresh toluene (50 ml) was introduced. After completion of the reaction, toluene was removed by distillation from the reaction mixture to obtain a residue that was dissolved in methanol, treated with charcoal and filtered. Be filtrate was separated, concentrated to a residue and crystallized from isopropyl alcohol and acetone to obtain 2-deoxy-D-glucose (7.33 g, 59%). mp. 148-151° C.EXAMPLE 8A heterogeneous mixture of 1,3,4,5-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (10 g) (tom example 5), H2O (200 ml) conc. HCl (0.3 ml) and glacial acetic acid (0.5 ml) was heated to 85° C. After 6 hours the reaction mixture was cooled to room temperature, neutralized with aq. Ba(OH)2 and filtered on a pad of Celite. Filtrate was separated, treated with charcoal and filtered. The filtrate was concentrated to a residue and crystallized from MeOH, acetone to obtain the product. Quantity obtained 275 g. mp. 147-148° C.EXAMPLE 9A heterogeneous mixture of 1,3,4,5-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (10 g) (from example 3) water (100 ml) and conc. HCl (0.5 ml) was heated to 80° C. After 2-5 hours the reaction mixture was cooled to room temperature, neutralized with aq. Ba(OH)2 and filtered on a pad of Celite. The filtrate was concentrated to a residue, dissolved in ethanol, treated with charcoal and filtered. The filtrate was concentrated to a solid residue and crystallized from methanol-acetone to obtain the title product. Quantity obtained 3.15 g mp. 148-151° C.,EXAMPLE 10A solution of methyl 2-deoxy-α/β-D-glucopyranoside (30 g) (from example 2) water (15 ml) and conc. HCl (1.5 ml) was heated to 80-85° C. After 3-5 hours the reaction mixture was cooled to room temperature, neutralize with aq. Ba(OH)2 and filtered to remove insoluble salts. The filtrate was concentrated to a residue, crystallized from MeOH, acetone and hexane to obtain 2-deoxy-D-glucose (11.77 g) mp. 149-151° C.EXAMPLE 11A solution of methyl 2-deoxy-α/β-D-glucopyranoside (30 g) (form example 2) water (195 ml) and conc. H2SO4 (5.9 ml) was heated to 80° C. After 2-3 hours the reaction mixture was cooled, neutralized with aq. Ba(OH)2 and filtered. The filtrate was separated, treated with charcoal and filtrate. The Filtrate was concentrated to a residue and crystallized from isopropyl alcohol to obtain the title product. Quantity obtained 5.2 g. mp. 152-154° C.EXAMPLE 12A mixture of methyl 2-deoxy-α/β-D-glucopyranoside (24 g) (from example 2) water (125 ml) and IR 120H+resin (7.5 ml) was heated to 90-95° C. for 2 h. The reaction mixture was cooled to room temperature, filtered and the resin was washed with water (20 ml). The filtrate was concentrated to residue and crystallized from ethanol to obtain 2-deoxy-D-glucose (8.8 g), mp. 150-152° C.CLIP
References
- ^ Merck Index, 11th Edition, 2886.
- ^ Wick, AN; Drury, DR; Nakada, HI; Wolfe, JB (1957). “Localization of the primary metabolic block produced by 2-deoxyglucose”(PDF). J Biol Chem. 224 (2): 963–969. doi:10.1016/S0021-9258(18)64988-9. PMID 13405925.
- ^ Pelicano, H; Martin, DS; Xu, RH; Huang, P (2006). “Glycolysis inhibition for anticancer treatment”. Oncogene. 25 (34): 4633–4646. doi:10.1038/sj.onc.1209597. PMID 16892078.
- ^ Raez, LE; Papadopoulos, K; Ricart, AD; Chiorean, EG; Dipaola, RS; Stein, MN; Rocha Lima, CM; Schlesselman, JJ; Tolba, K; Langmuir, VK; Kroll, S; Jung, DT; Kurtoglu, M; Rosenblatt, J; Lampidis, TJ (2013). “A phase I dose-escalation trial of 2-deoxy-D-glucose alone or combined with docetaxel in patients with advanced solid tumors”. Cancer Chemother. Pharmacol. 71 (2): 523–30. doi:10.1007/s00280-012-2045-1. PMID 23228990. S2CID 2990078.
- ^ Ralser, M.; Wamelink, M. M.; Struys, E. A.; Joppich, C.; Krobitsch, S.; Jakobs, C.; Lehrach, H. (2008). “A catabolic block does not sufficiently explain how 2-deoxy-D-glucose inhibits cell growth”. Proceedings of the National Academy of Sciences. 105 (46): 17807–17811. Bibcode:2008PNAS..10517807R. doi:10.1073/pnas.0803090105. PMC 2584745. PMID 19004802.
- ^ Kurtoglu, M.; Gao, N.; Shang, J.; Maher, J. C.; Lehrman, M. A.; Wangpaichitr, M.; Savaraj, N.; Lane, A. N.; Lampidis, T. J. (2007-11-07). “Under normoxia, 2-deoxy-D-glucose elicits cell death in select tumor types not by inhibition of glycolysis but by interfering with N-linked glycosylation”. Molecular Cancer Therapeutics. 6 (11): 3049–3058. doi:10.1158/1535-7163.mct-07-0310. ISSN 1535-7163. PMID 18025288.
- ^ Xi, Haibin; Kurtoglu, Metin; Liu, Huaping; Wangpaichitr, Medhi; You, Min; Liu, Xiongfei; Savaraj, Niramol; Lampidis, Theodore J. (2010-07-01). “2-Deoxy-d-glucose activates autophagy via endoplasmic reticulum stress rather than ATP depletion”. Cancer Chemotherapy and Pharmacology. 67 (4): 899–910. doi:10.1007/s00280-010-1391-0. ISSN 0344-5704. PMC 3093301. PMID 20593179.
- ^ Jump up to:a b Defenouillère, Quentin; Verraes, Agathe; Laussel, Clotilde; Friedrich, Anne; Schacherer, Joseph; Léon, Sébastien (2019-09-03). “The induction of HAD-like phosphatases by multiple signaling pathways confers resistance to the metabolic inhibitor 2-deoxyglucose”. Science Signaling. 12 (597): eaaw8000. doi:10.1126/scisignal.aaw8000. ISSN 1945-0877. PMID 31481524. S2CID 201829818.
- ^ Garriga-Canut, Mireia; Schoenike, Barry; Qazi, Romena; Bergendahl, Karen; Daley, Timothy J.; Pfender, Rebecca M.; Morrison, John F.; Ockuly, Jeffrey; Stafstrom, Carl; Sutula, Thomas; Roopra, Avtar (2006). “2-Deoxy-D-glucose reduces epilepsy progression by NRSF-CTBP–dependent metabolic regulation of chromatin structure”. Nature Neuroscience. 9 (11): 1382–1387. doi:10.1038/nn1791. PMID 17041593. S2CID 10175791.
- ^ Garriga-Canut, M.; Schoenike, B.; Qazi, R.; Bergendahl, K.; Daley, T. J.; Pfender, R. M.; Morrison, J. F.; Ockuly, J.; Stafstrom, C.; Sutula, T.; Roopra, A. (2006). “2-Deoxy-D-glucose reduces epilepsy progression by NRSF-CtBP–dependent metabolic regulation of chromatin structure”. Nature Neuroscience. 9 (11): 1382–1387. doi:10.1038/nn1791. PMID 17041593. S2CID 10175791.
- ^ Jia Yao, Shuhua Chen, Zisu Mao, Enrique Cadenas, Roberta Diaz Brinton “2-Deoxy-D-Glucose Treatment Induces Ketogenesis, Sustains Mitochondrial Function, and Reduces Pathology in Female Mouse Model of Alzheimer’s Disease”, PLOS ONE
- ^ Researchers develop novel, non-toxic approach to treating variety of cancers. ScienceDaily
- ^ Liu, Huaping; Kurtoglu, Metin; León-Annicchiarico, Clara Lucia; Munoz-Pinedo, Cristina; Barredo, Julio; Leclerc, Guy; Merchan, Jaime; Liu, Xiongfei; Lampidis, Theodore J. (2016). “Combining 2-deoxy-D-glucose with fenofibrate leads to tumor cell death mediated by simultaneous induction of energy and ER stress”. Oncotarget. 7 (24): 36461–36473. doi:10.18632/oncotarget.9263. PMC 5095013. PMID 27183907.
- ^ Kovar, Joy L.; Volcheck, William; Sevick-Muraca, Eva; Simpson, Melanie A.; Olive, D. Michael (2009). “Characterization and performance of a near-infrared 2-deoxyglucose optical imaging agent for mouse cancer models”. Analytical Biochemistry. 384(2): 254–262. doi:10.1016/j.ab.2008.09.050. PMC 2720560. PMID 18938129.
- ^ Cheng, Z., Levi, J., Xiong, Z., Gheysens, O., Keren, S., Chen, X., and Gambhir, S., Bioconjugate Chemistry, 17(3), (2006), 662-669
- ^ Barban, Stanley (December 1962). “Induced resistance to 2-deoxy-d-glucose in cell cultures”. Biochimica et Biophysica Acta. 65(2): 376–377. doi:10.1016/0006-3002(62)91065-x. ISSN 0006-3002. PMID 13966473.
- ^ Sanz, Pascual; Randez-Gil, Francisca; Prieto, José Antonio (September 1994). “Molecular characterization of a gene that confers 2-deoxyglucose resistance in yeast”. Yeast. 10 (9): 1195–1202. doi:10.1002/yea.320100907. ISSN 0749-503X. PMID 7754708. S2CID 9497505.
The Drugs Controller General of India (DCGI) has given permission for the emergency use of drug 2-deoxy-D-glucose (2-DG) as an adjunct therapy in moderate to severe Covid-19 cases, said Defence Research and Development Organisation on Saturday.
“Being a generic molecule and analogue of glucose, it can be easily produced and made available in plenty,” said the DRDO in a statement.
An adjunct therapy refers to an alternative treatment that is used together with the primary treatment. Its purpose is to assist the primary treatment.
“The drug has been developed by DRDO lab Institute of Nuclear Medicine and Allied Sciences in collaboration with Dr Reddy’s Laboratories. Clinical trial have shown that this molecule helps in faster recovery of hospitalized patients and reduces supplemental oxygen dependence,” the statement read.
According to DRDO, the patients treated with 2-DG showed faster symptomatic cure than Standard of Care (SoC) on various endpoints in the efficacy trends.
“A significantly favourable trend (2.5 days difference) was seen in terms of the median time to achieving normalization of specific vital signs parameters when compared to SOC,” it said.
The drug comes in powder form in sachets, which is taken orally by dissolving it in water.
“It accumulates in the virus-infected cells and prevents virus growth by stopping viral synthesis and energy production,” said the DRDO.
In April 2020, during the first wave of the Covid-19 pandemic, INMAS-DRDO scientists conducted laboratory experiments of 2-DG with the help of the Centre for Cellular and Molecular Biology (CCMB), Hyderabad.
They found that this molecule works effectively against the SARS-CoV-2 virus and inhibits viral growth.
Based on the results, the DCGI had in May 2020 permitted Phase-II clinical trial of 2-DG in Covid-19 patients.
In Phase-II trials (including dose-ranging) conducted from May to October 2020, the drug was found to be safe and showed significant improvement in the patients’ recovery.
“Phase IIa was conducted in 6 hospitals and Phase IIb (dose-ranging) clinical trial was conducted at 11 hospitals all over the country. Phase-II trial was conducted on 110 patients,” said the DRDO.

NEW DRUG APPROVALS
ONE TIME
$10.00
| Names | |
|---|---|
| IUPAC name(4R,5S,6R)-6-(hydroxymethyl)oxane-2,4,5-triol | |
| Other names2-Deoxyglucose 2-Deoxy-d-mannose 2-Deoxy-d-arabino-hexose 2-DG | |
| Identifiers | |
| CAS Number | 154-17-6 |
| 3D model (JSmol) | Interactive image |
| ChEMBL | ChEMBL2074932 |
| ChemSpider | 388402 |
| EC Number | 205-823-0 |
| IUPHAR/BPS | 4643 |
| PubChem CID | 108223 |
| UNII | 9G2MP84A8W |
| showInChI | |
| showSMILES | |
| Properties | |
| Chemical formula | C6H12O5 |
| Molar mass | 164.16 g/mol |
| Melting point | 142 to 144 °C (288 to 291 °F; 415 to 417 K) |
| Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). |
////////////2-Deoxy-D-glucose, 2 dg, 2-dg, 2 DEOXY D GLUCOSE, COVID 19, CORONA VIRUS, INDIA 2021, DCGI, DRDO, DR REDDYS
C(C=O)C(C(C(CO)O)O)O
Pegylated Interferon alpha-2b, (PegIFN), Virafin
DB00022 sequence CDLPQTHSLGSRRTLMLLAQMRRISLFSCLKDRHDFGFPQEEFGNQFQKAETIPVLHEMI QQIFNLFSTKDSSAAWDETLLDKFYTELYQQLNDLEACVIQGVGVTETPLMKEDSILAVR KYFQRITLYLKEKKYSPCAWEVVRAEIMRSFSLSTNLQESLRSKE
CDLPQTHSLG SRRTLMLLAQ MRRISLFSCL KDRHDFGFPQ EEFGNQFQKA ETIPVLHEMI
QQIFNLFSTK DSSAAWDETL LDKFYTELYQ QLNDLEACVI QGVGVTETPL MKEDSILAVR
KYFQRITLYL KEKKYSPCAW EVVRAEIMRS FSLSTNLQES LRSKE

Chemical structure of peginterferon α-2a and α-2b. Abbreviations: PeG-IFN, peginterferon; IFN, interferon; Lys, lysine; His, histidine; Cys, cysteine; Ser, serine.
Pegylated Interferon alpha-2b
(PegIFN), Virafin

| Formula | C860H1353N229O255S9 |
|---|---|
| CAS | 99210-65-8, 98530-12-2, 215647-85-1 |
| Mol weight | 19268.9111 |
- Interferon α2b, pegylated
- PegIFN a-2b
- PegIFN a-2b (biologics)
- PegIFN α-2b
- PegIntron
- Pegaferon
- PegiHep
- Peginterferon alfa-2b
- Peginterferon α-2b
- Pegylated interferon alfa-2b
- Pegylated interferon α-2b
- Pegylated interferons, PegIFN a-2b
- Proteinaceous biopharmaceuticals, PegIFN a-2b
- Sch 54031
- Sylatron
- ViraferonPeg
Active Moieties
| NAME | KIND | UNII | CAS | INCHI KEY |
|---|---|---|---|---|
| Interferon alfa-2b | unknown | 43K1W2T1M6 | 98530-12-2 | Not applicable |
| Clinical data | |
|---|---|
| Trade names | PegIntron, Sylatron, ViraferonPeg, others |
| AHFS/Drugs.com | Professional Drug Facts |
| MedlinePlus | a605030 |
| License data | EU EMA: by INN |
| Routes of administration | Subcutaneous injection |
| ATC code | L03AB10 (WHO) |
| Legal status | |
| Legal status | US: ℞-only [1][2]EU: Rx-only |
| Pharmacokinetic data | |
| Elimination half-life | 22–60 hrs |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 215647-85-1 |
| IUPHAR/BPS | 7462 |
| DrugBank | DB00022 |
| ChemSpider | none |
| UNII | G8RGG88B68 |
| KEGG | D02745 |
| ChEMBL | ChEMBL1201561 |
| ECHA InfoCard | 100.208.164 |
| Chemical and physical data | |
| Formula | C860H1353N229O255S9 |
| Molar mass | 19269.17 g·mol−1 |

NEW DRUG APPROVALS
ONE TIME
$10.00
New Delhi: ,,,,,,https://www.ndtv.com/india-news/zydus-virafin-gets-emergency-use-approval-for-treating-moderate-covid-19-cases-2420358
Zydus Cadila received emergency use approval from the Drugs Controller General of India (DGCI) on Friday for the use of “Virafin”, Pegylated Interferon alpha-2b (PegIFN) in treating moderate COVID-19 infection in adults.
A single-dose subcutaneous regimen of the antiviral Virafin will make the treatment more convenient for the patients. When administered early on during COVID-19, Virafin will help patients recover faster and avoid much of the complications, the company said.
In a release, Cadila Health highlighted that “the drug has also shown efficacy against other viral infections.”
Speaking on the development, Dr Sharvil Patel, Managing Director, Cadila Healthcare Limited said, “The fact that we are able to offer a therapy which significantly reduces the viral load when given early on can help in better disease management. It comes at a much-needed time for patients and we will continue to provide them access to critical therapies in this battle against COVID-19.”
In its Phase III clinical trials, the therapy had shown better clinical improvement in the patients suffering from COVID-19. During the trials, a higher proportion of patients administered with PegIFN arm were RT-PCR negative by day 7. The drug ensures faster viral clearance and has several add-on advantages compared to other anti-viral agents, the release further reads.
The development and the nod from DGCI come at a time when India is combating the second wave of coronavirus.
The central government in one of its major announcements decided to administer COVID-19 vaccines to all age above 18 years.
India recorded 3,32,730 new COVID-19 cases in the last 24 hours, the highest single-day spike since the pandemic broke out last year. India has crossed the mark of 3 lakh COVID-19 cases for two consecutive days now. This has taken the cumulative count of the COVID infection in the country to 1,62,63,695.
2CommentsThe country has recorded 2,263 new deaths due to COVID-19 in the last 24 hours. As many as 1,86,920 people have succumbed to the viral infection in India so far. There are 24,28,616 active COVID-19 cases in the country now.
PATENT
https://patents.google.com/patent/EP1562634B1/en
- Interferon alpha-2a plays an important role for the treatment of chronic hepatitis C, but it is limited in its efficacy by the short in vivo half-life. To improve the half-life and efficacy, interferon alpha-2a was conjugated with a polyethylene glycol moiety. Pegylation changes physicochemical and biological properties of the protein. One effect is the decrease of the proteolytic degradation and the renal clearance. This increases the half-life of the pegylated protein in blood. Another effect is the altered distribution in the body, depending on the size of the PEG moiety of the protein. Interferon alpha 2a pegylated with a large polyethylene glycol moiety (PEG moiety) such as a 40 kDa branched polyethylene moietywherein R and R’ are independently lower alkyl; n and n’ are integers having a sum of from 600 to 1500; and the average molecular weight of the polyethylene glycol units in said conjugate is from about 26,000 daltons to about 66,000 daltons;
has an improved biological activity and exhibits sustained adsorption and reduced renal clearance, resulting in a strong antiviral pressure throughout a once-weekly dosing schedule, see Perry M. C., et al. Drugs, 2001,15,2263-2288 and Lamb M. W., et al. The Annals of Pharmacotherapy, 2002, 36, 933-938. - [0003]See also Monkarsh et al. Analytical Biochemistry, 1997, 247, 434- 440 (Positional Isomers of Mono-pegylated Interferon α-2a) and Bailon et al. Bioconjugate Chemistry, 2001, 12, 195-202 (Rational Design of a Potent, Long-Lasting Form of interferon).
- [0004]The method for the pegylation of interferon alpha-2a is described in EP A 809 996. Since this pegylation is performed by reaction of PEG2-NHS of formulawith primary amino groups on for example lysine or to the N-terminus of the interferon alpha.one or more PEG moieties may be attached and form a mixture of unpegylated, mono- and multiple-pegylated interferon. Monopegylated interferon alpha can be isolated from the mixture by methods known in the art. Furthermore, since interferon alpha-2a molecule exhibits 12 sites for pegylation (11 lysines and the N-terminus) it is a mixture of positional isomers. From these possible twelve isomers, nine were isolated and characterized, each of these being conjugated to the branched polyethylene glycol chain at a specific lysine, namely,
at Lys(31) to form interferon alpha 2a pegylated at Lys(31) [referred to as PEG-Lys(31)],
at Lys(49) to form interferon.alpha 2a pegylated at Lys(49) [referred to as PEG-Lys(49)],
at Lys(70) to form interferon alpha 2a pegylated at Lys(70) [referred to as PEG-Lys(70)],
at Lys(83) to form interferon alpha 2a pegylated at Lys(83) [referred to as PEG-Lys(83)],
at Lys(112) to form interferon alpha 2a pegylated at Lys(112) [referred to as PEG-Lys(112)],
at Lys(121) to form interferon alpha 2a pegylated at Lys(121) [referred to as PEG-Lys(121)],
at Lys(131) to form interferon alpha 2a pegylated at Lys(131) [referred to as PEG-Lys(131)],
at Lys(134) to form interferon alpha 2a pegylated at Lys(134) [referred to as PEG-Lys(134)],
at Lys(164) to form interferon alpha 2a pegylated at Lys(164) [referred to as PEG-Lys(164)]. - [0005]It has been found that PEG-Lys(31) and PEG-Lys(134) have higher activities in an antiviral assay than the mixture, the activity of PEG-Lys(164) was equal to the mixture, whereas the activities of PEG-Lys(49), PEG-Lys(70), PEG-Lys(83), PEG-Lys(112), PEG-Lys(121) and PEG-Lys(131) were lower.
- The following examples will further illustrate the invention
Example 1A Separation of the positional isomers
- [0035]A two-step isolation and purification scheme was used to prepare the monopegylated isoforms of PEG-interferon alpha 2a.
- a) The first step was a separation of the positional isomers on a preparative low pressure liquid chromatography column with a weak-cation exchange matrix (TOSOH-BIOSEP, Toyopearl CM-650S, e.g. Resin Batch no. 82A the diameter of the column being 16 mm, the length 120 cm). A linear pH-gradient of increasing sodium acetate concentration (25 mM, pH 4.0 up 75 mM to pH 7.8) was applied at a flow rate of 0.7 mL/min. Detection was at 280 nm. With this chromatographic step species 1, 2, 5,6 and a mixture of 3, 4, 4a, 7 and 8 could be collected, see Table 1.
- b) The fractions were further separated and purified in the second preparation step. A preparative column with the same matrix as the analytical strong-cation exchange column (Resin Batch no. 82A having a ion exchange capacity of 123 mEq/ml) as described above but larger dimensions (30 mm i.d. and 70 mm length), further a higher flow rate and an extended run time was used. As for the analytical method the column was pre-equilibrated with 3.4 mM sodium acetate, 10% ethanol and 1% diethylene glycol, adjusted to pH 4.4 (buffer A). After loading the PEG-IFN samples, the column was washed with buffer A, followed by an ascending linear gradient to 10 mM dibasic potassium phosphate, 10% ethanol and 1% diethylene glycol, adjusted to pH 6.6 (buffer B). The flow rate was 1.0 mL/min and the detection at 218 nm.
- [0036]The protein concentration of the PEG-IFN alpha 2a isomer was determined by spectrophotometry, based on the 280 nm absorption of the.protein moiety of the PEG-IFN alpha 2a.
- [0037]An analytical elution profile of 180 µg of PEG-IFN alpha 2a is shown in Figure 1. The result of this method is a separation into 8 peaks, 2 peaks with baseline separation and 6 with partial separation. The decrease of the baseline absorption towards the end of the chromatogram suggests that there were no other monopegylated species of IFN alpha 2a eluting at higher retention time.
- [0038]In addition, looking carefully at the IEC-chromatogram a further peak close to the detection limit is visible between peaks 2 and 3 indicating the presence of additional positional isomers that should also contribute to the specific activity of the PEG-IFN alpha 2a mixture. Additional species were expected as the interferon alpha-2a molecule exhibits 12 sites for pegylation (11 lysines and the N-terminus). However, given the low abundance of the these species, they were not isolated and characterised.
- [0039]Isomer samples derived from IEC optimisation runs were investigated directly after the isolation (t = 0) and after 2 of weeks of storage at 5°C (data not shown). No significant differences were observed for the protein derived from IEC-peaks with regard to the protein content as determined by spectrometric methods; nor were any changes to be detected in the monopegylation site, the content of oligo-PEG-IFN alpha 2a, the amount of aggregates and the bioassay activity. Taking into account the relative abundance of the individual isomers – as determined by the IEC method – as well as the specific activities – as determined in the anti-viral assay – almost the total specific bioactivity of the PEG-IFN alpha 2a mixture used for their isolation is recovered (approximately 93%).
- [0040]The analytical IE-HPLC was used to check the purity of the individual isomers with respect to contamination with other positional isomers in the IEC fractions. The peaks 2, 3, 4, 4a, 5 and 7 had more than 98%, the peaks 1 and 8 had 93% and peak 6 had 88 % purity. Table 1:PEG-peptides identified by comparison of the Lys-C digest spectra of the isomers and the reference standard.Identified PEG Sites in the separated PEG-IFN SpeciesPeakmissing peaks in peptide mapPEG-IFNPEG siteMr (DA)SequencePeak 1K31A,E24-49Peak 2K134I, I’134-164Peak 3K131C122-131aPeak 4K121B, C113-131Peak 4aK164b134-164a,bPeak 5K70D, F50-83Peak 6K83D, H71-112Peak 7K49E, F32-70Peak 8K112B, H84-121a132-133 too small to detect.a,b RP-HPLC.
- [0041]The fractions were characterised by the methods described in examples 2 to 6.
Example 1B Analytical separation of positional isomers of mono-pegylated interferon alpha 2a
- [0042]HPLC Equipment:HP1100Column:SP-NPR, TosoH Bioscience, Particle size: 2.5µm, nonporous, Order#: 13076Injection:5-10 µg monopegylated IFNmobile Phase:Buffer A: 10% v/vEthanol 1% v/vDiethylenglycol 2.3 mMNa-Acetat 5.2 mMAcetic acid, in purified water, no pH adjustment Buffer B: 10% v/vEthanol 1% v/vDiethylenglycol 16.4 mMKH2PO4 4.4 mMK2HPO4, in purified water, no pH adjustmentGradient:0 Min40 %B 2 Min40 %B 2.1 Min48 %B 25 Min68 %B 27 Min75 %B 30 Min75 %B 34 Min40 %B 40 Min40 %BFlow:1.0 ml/min Column Temperature:25°C Detection:218 nm a typical Chromatogram is given in Figure 8.
Example 2 Analysis of the fractions by mass spectrometry peptide mapping
- [0043]Mass spectra were recorded on a MALDI-TOF MS instrument (PerSeptive Biosystems Voyager-DE STR with delayed extraction). Each IEC fraction (Ion Exchange Chromatography) was desalted by dialysis, reduced with 0.02 M 1,4-dithio-DL-threitol (DTT) and alkylated with 0.2 M 4-vinyl pyridine. Then the proteins were digested with endoproteinase Lys-C (Wako Biochemicals) in 0.25 M Tris (tris(hydroxymethyl)-aminoethane) at pH 8.5 with an approximate enzyme to protein ratio of 1:30. The reaction was carried out over night at 37 °C.
- [0044]A solution of 20 mg/ml α-cyano-4-hydroxycinnamic acid and 12 mg/ml nitrocellulose in acetone/isopropanol 40/60 (v/v) was used as matrix (thick-layer application). First, 0.5 µL of matrix was placed on the target and allowed to dry. Then, 1.0 µL of sample was added. The spectra were obtained in linear positive ionisation mode with an accelerating voltage of 20.000 V and a grid voltage of 95 %. At least 190 laser shots covering the complete spot were accumulated for each spectrum. Des-Arg1-bradykinin and bovine insulin were used for internal calibration.
Example 3 high-performance liquid chromatography (RP-HPLC) Peptide Mapping
- [0045]The peptides were characterized by reverse-phase high-performance liquid chromatography (RP-HPLC) Peptide Mapping. The IEC fractions were reduced, alkylated and digested with endoproteinase Lys-C as described for the MALDI-TOF MS peptide mapping. The analysis of the digested isomers was carried out on a Waters Alliance HPLC system with a Vydac RP-C18 analytical column (5 µm, 2.1 × 250 mm) and a precolumn with the same packing material. Elution was performed with an acetonitrile gradient from 1 % to 95 % for 105 min in water with a flow rate of 0.2 mL/min. Both solvents contained 0.1 % (v/v) TFA. 100 µL of each digested sample were injected and monitored at 215 nm.
Example 4 MALDI-TOF spectra of undigested protein
- [0046]An 18 mg/ml solution of trans-3-indoleacrylic acid in acetonitrile/0.1 % trifluoroacetic acid 70/30 (v/v) was premixed with the same volume of sample solution. Then 1.0 µL of the mixture was applied to the target surface. Typically 150 – 200 laser shots were averaged in linear positive ionisation mode. The accelerating voltage was set to 25.000 V and the grid voltage to 90 %. Bovine albumin M+ and M2+ were used for external calibration.
Example 5 SE-HPLC (size exclusion HPLC)
- [0047]SE-HPLC was performed with a Waters Alliance 2690 HPLC system equipped with a TosoHaas TSK gel G 4000 SWXL column (7.8 × 300 mm). Proteins were eluted using a mobile phase containing 0.02 M NaH2PO4, 0.15 M NaCl, 1% (v/v) diethylene glycol and 10 % (v/v) ethanol (pH 6.8) at a flow rate of 0.4 mL/min and detected at 210 nm. The injection amounts were 20 µg of each isomers.
- [0048]Size Exclusion HPLC and SDS-PAGE were used to determine the amount of oligo-PEG-IFN alpha 2a forms and aggregates in the different IEC fractions. The reference material contains 2.3 % aggregates and 2.2 % oligomers (Figure 4).
- [0049]Peaks 1, 4, 4a, 5, 6 and 8 contain < 0.7 % of the oligopegylated IFN alpha 2a forms, whereas in,peaks 2, 3, and 7 the percentage of the oligopegylated IFN alpha 2a forms are under the detection limit (< 0.2 %). In the case of the aggregates a different trend could be seen. In all peaks the amount of aggregates is below 0.9 %.
Example 6 SDS-PAGE
- [0050]SDS-PAGE was carried out both under non-reducing and under reducing conditions using Tris-Glycine gels of 16 % (1.5 mm, 10 well). Novex Mark 12 molecular weight markers with a mass range from 2.5 to 200 kDa were used for calibration, bovine serum albumin (BSA) was used as sensitivity standard (2 ng). Approximately 1 µg of all the samples and 0.5 µg of standard were applied to the gel. The running conditions were 125 V and 6 W for 120 min. The proteins were fixed and stained using the silver staining kit SilverXpress from Novex.
- [0051]The gels that were recorded under non-reducing conditions for the IEC fractions 1- 8 (Figure 2) show a pattern that is comparable to that of the PEG-IFN alpha 2a reference standard.
- [0052]Under reducing conditions, the gels show an increase in intensity of the minor bands at about 90 kDa as compared to the standard. Between 6 and 10 kDa protein fragments appear for peaks 6, 7 and 8 (Figure 3). Both bands together correspond to approximately 1 % of clipped material. In the lanes of isomer 1, 5, 6, 7, 8 additional bands with more than 100 kDa can be seen which are also present in the standard. These can be assigned to oligomers. Thus SDS-PAGE confirms the results of the SE-HPLC analysis.
- [0053]Overall, RP-HPLC and SDS-PAGE experiments indicate that the purity of the IEC fractions can be considered comparable to the PEG-IFN alpha 2a reference standard.
- [0054]The structure of the PEG-IFN alpha 2a species derived from the 9 IEC-fractions were identified based on the results of the methods described above using the strategy mentioned above.
Example 7 The antiviral activity (AVA)
- [0055]The antiviral activity was estimated by its protective effect on Madin-Darby bovine kidney (MDBK) cells against the infection by vesticular stomatitis virus (VSV) and compared with a PEG-IFN alpha 2a standard. Samples and reference standard were diluted in Eagle’s Minimum Essential Medium (MEM) containing 10 % fetal bovine serum to a final concentration of 10 ng/mL (assay starting concentration). Each sample was assayed in quadruplicate.
- [0056]The antiviral protection of Madin-Darby bovine kidney cells (MDBK) with vesicular stomatitis virus was tested according to the method described in Virol. 1981, 37, 755-758. All isomers induced an activity in the anti-viral assay as presented in Table 2. The activities range between 1061 and 339 U/µg, indicating that the difference in specific activities of the protein in the positional isomers is significant. The know-how and the results generated so far will allow the initiation of further investigations to establish this structure-function relationship between the positional isomers and the IFN alpha receptors. Table 2:In Vitro Antiviral Activities of PEG-IFN alpha 2a and individual PEG-IFN alpha 2a isomers. The Antiviral activity was determined in MDBK cells infected with vesicular stomatitis virus. The results present the averages of three assays performed independently.Antiviral Assay of PEG-IFNPeakU/µgPEG-IFN1061 ± 50Peak 11818 ± 127Peak 21358 ± 46Peak 3761197Peak 4339 ± 33Peak 4a966 ± 107Peak 5600 ± 27Peak 6463 ± 25Peak7513 ± 20Peak 8468 ± 23
- [0057]The results are further illustrated by the following figures
- Figure 1: Analytical IEC-HPLC of 180µg of PEG-IFN alpha 2a. An analytical strong-cation exchange column was used to check the purity of the separated positional isomers from each purification step (TOSOH-BIOSEP, SP-SPW,10 µm particle size, 7.5 mm diameter, 7.5 cm length).
- Figure 2: A/B: SDS-PAGE analysis with Tris-glycine (16%), the samples were electrophoresed under non-reduced conditions. The gels were stained for protein with Silver Stain. Lanes: M, molecular weight marker proteins/ 2, Peak 1/ 3, Peak 2/ 4, Peak 3/ 5, Peak 4/ 6, Peak 4a/ 7, Peak 5/ 8, Peak 6/ 9, Peak 7/10, Peak 8/ 11, Ix PEG-IFN standard/ 12, 1.5x PEG-IFN standard/ C1, IFN standard.
- Figure 3: A/B: SDS-PAGE analysis with Tris-glycine (16%), the samples were electrophoresed under reduced conditions. The gels were stained for protein with Silver Stain. Lanes: M, molecular weight marker proteins/ 2, Peak 1/ 3, Peak 2/ 4, Peak 3/ 5, Peak 4/ 6, Peak 4a/ 7, Peak 5/ 8, Peak 6/ 9, Peak 7/ 10, Peak 8/ 11, 1x PEG-IFN standard/ 12, 1.5x PEG-IFN standard/ C1, IFN standard.
- Figure 4: Size Exclusion (SE-) HPLC was used to determine the amount of oligo PEG-IFN forms and aggregates in the different IEC fractions. SE-HPLC was performed with a TosoHaas TSK gel G 4000 SWXL column (7.8 × 300 mm).
- Figure 5: MALDI-TOF spectrometry was used to determine the molecular weight of each isomer in order to ensure that the PEG-IFN molecules were still intact after IEC chromatography and to confirm the monopegylation.
- Figure 6: MALDI-TOF Lys-C peptide maps of the PEG-IFN reference standard and the peaks 1, 2, 3, 4, 4a, 5, 6, 7, 8. Missing peaks compared to the standard are indicated by arrows.
- Figure 7: RP-HPLC chromatograms of the Lys-C digests of the PEG-IFN reference and peak 4a
- Figure 8: Analytical HPLC of 5-10µg of PEG-IFN alpha 2a mixture of positional isomers on a column charged with SP-NPR, TosoH Bioscience, Particle size: 2.5µm, nonporous as described in Example 1B..
- Figure 9: Ribbon structure of interferon alpha-2a showing the pegylation sites. This is the high resolution structure of human interferon alpha-2a determined with NMR spectroscopy see J. Mol. Biol. 1997, 274, 661-675. The pegylation sites of pegylated interferon alpha-2a are coloured red and labelled with residue type and residue number.
Pegylated interferon alfa-2b, sold under the brand name PegIntron among others, is a medication used to treat hepatitis C and melanoma.[3] For hepatitis C it is typically used with ribavirin and cure rates are between 33 and 82%.[3][4] For melanoma it is used in addition to surgery.[3] It is given by injection under the skin.[3]
Side effects are common.[5] They may include headache, feeling tired, mood changes, trouble sleeping, hair loss, nausea, pain at the site of injection, and fever.[3] Severe side effects may include psychosis, liver problems, blood clots, infections, or an irregular heartbeat.[3] Use with ribavirin is not recommended during pregnancy.[3] Pegylated interferon alfa-2b is in the alpha interferon family of medications.[3] It is pegylated to protect the molecule from breakdown.[5]
Pegylated interferon alfa-2b was approved for medical use in the United States in 2001.[3] It is on the World Health Organization’s List of Essential Medicines.[6]
Peginterferon alfa-2b is a form of recombinant interferon used as part of combination therapy to treat chronic Hepatitis C, an infectious liver disease caused by infection with Hepatitis C Virus (HCV). HCV is a single-stranded RNA virus that is categorized into nine distinct genotypes, with genotype 1 being the most common in the United States, and affecting 72% of all chronic HCV patients 3. Treatment options for chronic Hepatitis C have advanced significantly since 2011, with the development of Direct Acting Antivirals (DAAs) resulting in less use of Peginterferon alfa-2b. Peginterferon alfa-2b is derived from the alfa-2b moeity of recombinant human interferon and acts by binding to human type 1 interferon receptors. Activation and dimerization of this receptor induces the body’s innate antiviral response by activating the janus kinase/signal transducer and activator of transcription (JAK/STAT) pathway. Use of Peginterferon alfa-2b is associated with a wide range of severe adverse effects including the aggravation and development of endocrine and autoimmune disorders, retinopathies, cardiovascular and neuropsychiatric complications, and increased risk of hepatic decompensation in patients with cirrhosis. The use of Peginterferon alfa-2b has largely declined since newer interferon-free antiviral therapies have been developed.
In a joint recommendation published in 2016, the American Association for the Study of Liver Diseases (AASLD) and the Infectious Diseases Society of America (IDSA) no longer recommend Peginterferon alfa-2b for the treatment of Hepatitis C 2. Peginterferon alfa-2b was used alongside Ribavirin(https://go.drugbank.com/drugs/DB00811) with the intent to cure, or achieve a sustained virologic response (SVR), after 48 weeks of therapy. SVR and eradication of HCV infection is associated with significant long-term health benefits including reduced liver-related damage, improved quality of life, reduced incidence of Hepatocellular Carcinoma, and reduced all-cause mortality 1.
Peginterferon alfa-2b is available as a variable dose injectable product (tradename Pegintron) used for the treatment of chronic Hepatitis C. Approved in 2001 by the FDA, Pegintron is indicated for the treatment of HCV with Ribavirin or other antiviral drugs Label. When combined together, Peginterferon alfa-2b and Ribavirin have been shown to achieve a SVR between 41% for genotype 1 and 75% for genotypes 2-6 after 48 weeks of treatment.
Medical uses
It is used to treat hepatitis C and melanoma. For hepatitis C it is typically used with ribavirin. For melanoma it is used in addition to surgery.[3]
For hepatitis C it may also be used with boceprevir, telaprevir, simeprevir, or sofosbuvir.[5]
In India, in 2021, DGCI approved emergency use of Zydus Cadila‘s Virafin in treating moderate COVID-19 infection.[7]
Host genetic factors
For genotype 1 hepatitis C treated with pegylated interferon-alfa-2a or pegylated interferon-alfa-2b combined with ribavirin, it has been shown that genetic polymorphisms near the human IL28B gene, encoding interferon lambda 3, are associated with significant differences in response to the treatment. This finding, originally reported in Nature,[8] showed that genotype 1 hepatitis C patients carrying certain genetic variant alleles near the IL28B gene are more likely to achieve sustained virological response after the treatment than others. A later report from Nature[9] demonstrated that the same genetic variants are also associated with the natural clearance of the genotype 1 hepatitis C virus.
Side effects
Common side effects include headache, feeling tired, mood changes, trouble sleeping, hair loss, nausea, pain at the site of injection, and fever. Severe side effects may include psychosis, liver problems, blood clots, infections, or an irregular heartbeat.[3] Use with ribavirin is not recommended during pregnancy.[3]
Mechanism of action
One of the major mechanisms of PEG-interferon alpha-2b utilizes the JAK-STAT signaling pathway. The basic mechanism works such that PEG-interferon alpha-2b will bind to its receptor, interferon-alpha receptor 1 and 2 (IFNAR1/2). Upon ligand binding the Tyk2 protein associated with IFNAR1 is phosphorylated which in turn phosphorylates Jak1 associated with IFNAR2. This kinase continues its signal transduction by phosphorylation of signal transducer and activator of transcription (STAT) 1 and 2 via Jak 1 and Tyk2 respectively. The phosphorylated STATs then dissociate from the receptor heterodimer and form an interferon transcription factor with p48 and IRF9 to form the interferon stimulate transcription factor-3 (ISGF3). This transcription factor then translocates to the nucleus where it will transcribe several genes involved in cell cycle control, cell differentiation, apoptosis, and immune response.[10][11]
PEG-interferon alpha-2b acts as a multifunctional immunoregulatory cytokine by transcribing several genes, including interleukin 4 (IL4). This cytokine is responsible for inducing T helper cells to become type 2 helper T cells. This ultimately results in the stimulation of B cells to proliferate and increase their antibody production. This ultimately allows for an immune response, as the B cells will help to signal the immune system that a foreign antigen is present.[12]
Another major mechanism of type I interferon alpha (IFNα) is to stimulate apoptosis in malignant cell lines. Previous studies have shown that IFNα can cause cell cycle arrest in U266, Daudi, and Rhek-1 cell lines.[13]
A follow-up study researched to determine if the caspases were involved in the apoptosis seen in the previous study as well as to determine the role of mitochondrial cytochrome c release. The study confirmed that there was cleavage of caspase-3, -8, and -9. All three of these cysteine proteases play an important role in the initiation and activation of the apoptotic cascade. Furthermore, it was shown that IFNα induced a loss in the mitochondrial membrane potential which resulted in the release of cytochrome c from the mitochondria. Follow-up research is currently being conducted to determine the upstream activators of the apoptotic pathway that are induced by IFNα.[14]
History
It was developed by Schering-Plough. Merck studied it for melanoma under the brand name Sylatron. It was approved for this use in April 2011.
References
- ^ “PegIntron- peginterferon alfa-2b injection, powder, lyophilized, for solution PegIntron- peginterferon alfa-2b kit”. DailyMed. Retrieved 28 September 2020.
- ^ “Sylatron- peginterferon alfa-2b kit”. DailyMed. 28 August 2019. Retrieved 28 September 2020.
- ^ Jump up to:a b c d e f g h i j k l “Peginterferon Alfa-2b (Professional Patient Advice) – Drugs.com”. http://www.drugs.com. Archived from the original on 16 January 2017. Retrieved 12 January 2017.
- ^ “ViraferonPeg Pen 50, 80, 100, 120 or 150 micrograms powder and solvent for solution for injection in pre-filled pen CLEAR CLICK – Summary of Product Characteristics (SPC) – (eMC)”. http://www.medicines.org.uk. Archived from the original on 13 January 2017. Retrieved 12 January 2017.
- ^ Jump up to:a b c “Peginterferon alfa-2b (PegIntron)”. Hepatitis C Online. Archived from the original on 23 December 2016. Retrieved 12 January 2017.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ https://www.aninews.in/news/national/general-news/dgci-approves-emergency-use-of-zyduss-virafin-in-treating-moderate-covid-19-infection20210423163622/
- ^ Ge D, Fellay J, Thompson AJ, et al. (2009). “Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance”. Nature. 461 (7262): 399–401. Bibcode:2009Natur.461..399G. doi:10.1038/nature08309. PMID 19684573. S2CID 1707096.
- ^ Thomas DL, Thio CL, Martin MP, et al. (2009). “Genetic variation in IL28B and spontaneous clearance of hepatitis C virus”. Nature. 461 (7265): 798–801. Bibcode:2009Natur.461..798T. doi:10.1038/nature08463. PMC 3172006. PMID 19759533.
- ^ Ward AC, Touw I, Yoshimura A (January 2000). “The JAK-STAT pathway in normal and perturbed hematopoiesis”. Blood. 95 (1): 19–29. doi:10.1182/blood.V95.1.19. PMID 10607680. Archived from the original on 2014-04-26.
- ^ PATHWAYS :: IFN alpha[permanent dead link]
- ^ Thomas H, Foster G, Platis D (February 2004). “Corrigendum toMechanisms of action of interferon and nucleoside analogues J Hepatol 39 (2003) S93–8″. J Hepatol. 40 (2): 364. doi:10.1016/j.jhep.2003.12.003.
- ^ Sangfelt O, Erickson S, Castro J, Heiden T, Einhorn S, Grandér D (March 1997). “Induction of apoptosis and inhibition of cell growth are independent responses to interferon-alpha in hematopoietic cell lines”. Cell Growth Differ. 8 (3): 343–52. PMID 9056677. Archived from the original on 2014-04-26.
- ^ Thyrell L, Erickson S, Zhivotovsky B, et al. (February 2002). “Mechanisms of Interferon-alpha induced apoptosis in malignant cells”. Oncogene. 21 (8): 1251–62. doi:10.1038/sj.onc.1205179. PMID 11850845.
External links
- Peginterferon alfa-2b in the U.S. National Library of Medicine’s Drug Information Portal
- Medicines patent loophole ‘found’ at the BBC, 2007
- PEG-Intron (Peginterferon Alfa-2B) — Platelet Count Decreased from DrugLib.com
///////////Pegylated Interferon alpha-2b, PegIFN, Virafin, COVID 19, CORONA VIRUS, INDIA 2021, APPROVALS 2021
DEXMETHYLPHENIDATE
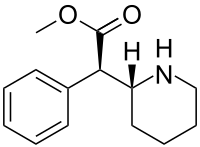
DEXMETHYLPHENIDATE
SynonymsDexmethylphenidate HCl, UNII1678OK0E08, CAS Number19262-68-1, WeightAverage: 269.77
Chemical FormulaC14H20ClNO2
methyl (2R)-2-phenyl-2-[(2R)-piperidin-2-yl]acetate hydrochloride
| CAS Number | 40431-64-9 as HCl: 19262-68-1 |
|---|---|
| PubChem CID | 154101as HCl: 154100 |
| IUPHAR/BPS | 7554 |
| DrugBank | DB06701 as HCl: DBSALT001458 |
| ChemSpider | 135807 as HCl: 135806 |
| UNII | M32RH9MFGPas HCl: 1678OK0E08 |
Trade Name:Focalin® / Attenade®MOA:Norepinephrine-dopamine reuptake inhibitorIndication:Attention deficit hyperactivity disorder (ADHD)Status:ApprovedCompany:Novartis (Originator) , CelgeneSales:$365 Million (Y2015); 
$492 Million (Y2014);
$594 Million (Y2013);
$554 Million (Y2012);
$550 Million (Y2011);ATC Code:N06BA11
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2005-05-26 | New dosage form | Focalin XR | Attention deficit hyperactivity disorder (ADHD) | Capsule, Extended release | 5 mg/10 mg/15 mg/20 mg/25 mg/30 mg/35 mg/40 mg | Novartis | |
| 2001-11-13 | Marketing approval | Focalin | Attention deficit hyperactivity disorder (ADHD) | Tablet | 2.5 mg/5 mg/10 mg | Novartis |
Dexmethylphenidate hydrochloride was approved by the U.S. Food and Drug Administration (FDA) on Nov 13, 2001. It was developed and marketed as Focalin® by Novartis in the US.
Dexmethylphenidate hydrochloride is a norepinephrine-dopamine reuptake inhibitor (NDRI). It is indicated for the treatment of attention deficit hyperactivity disorder (ADHD).
Focalin® is available as tablet for oral use, containing 2.5 mg, 5 mg or 10 mg of Dexmethylphenidate hydrochloride. The recommended dose is 10 mg twice daily, at least 4 hours apart.

NEW DRUG APPROVALS
ONE TIME
$10.00
NDA 212994, AZSTARYS
FDA APPROVE 2021

Drug Product Name Serdexmethylphenidate and Dexmethylphenidate (SDX/d-MPH)
Dosage Form capsule Strength 26.1/5.2 mg SDX/d-MPH 39.2/7.8 mg SDX/d-MPH 52.3/10.4 mg SDX/d-MPH
Route of Administration oral
Rx/OTC Dispensed Rx
Maximum Daily Dose 52.3 mg serdexmethylphenidate /10.4 mg dmethylphenidate as free base or 56 mg serdexmethylphenidate Chlorid
Dexmethylphenidate, sold under the brand name Focalin among others, is a medication used to treat attention deficit hyperactivity disorder (ADHD) in those over the age of five years.[3] If no benefit is seen after four weeks it is reasonable to discontinue its use.[3] It is taken by mouth.[3] The immediate release formulation lasts up to five hours while the extended release formulation lasts up to twelve hours.[4]
Common side effects include abdominal pain, loss of appetite, and fever.[3] Serious side effects may include abuse, psychosis, sudden cardiac death, mania, anaphylaxis, seizures, and dangerously prolonged erection.[3] Safety during pregnancy and breastfeeding is unclear.[5] Dexmethylphenidate is a central nervous system (CNS) stimulant.[6][3] How it works in ADHD is unclear.[3] It is the more active enantiomer of methylphenidate.[3]
Dexmethylphenidate was approved for medical use in the United States in 2001.[1] It is available as a generic medication.[3] In 2018, it was the 156th most commonly prescribed medication in the United States, with more than 3 million prescriptions.[7][8] It is also available in Switzerland.[9]
Reference:1. US6528530B2.
2. J. Org. Chem. 1998, 63, 9628-9629.Route 2
Reference:1. J. Am. Chem. Soc. 1999, 121,6509-6510.Route 3
Reference:1. Org. Process Res. Dev. 2010, 14, 1473–1475.Route 4
Reference:1. J. Med. Chem. 1998, 41,591-601.Route 5
Reference:1. Org. Lett. 1999, 1, 175-178.
2. Organic Syntheses 1985, 63, 206-212.
Four isomers of methylphenidate are possible, since the molecule has two chiral centers. One pair of threo isomers and one pair of erythro are distinguished, from which primarily d-threo-methylphenidate exhibits the pharmacologically desired effects.[102][124] The erythro diastereomers are pressor amines, a property not shared with the threo diastereomers. When the drug was first introduced it was sold as a 4:1 mixture of erythro:threo diastereomers, but it was later reformulated to contain only the threo diastereomers. “TMP” refers to a threo product that does not contain any erythro diastereomers, i.e. (±)-threo-methylphenidate. Since the threo isomers are energetically favored, it is easy to epimerize out any of the undesired erythro isomers. The drug that contains only dextrorotatory methylphenidate is sometimes called d-TMP, although this name is only rarely used and it is much more commonly referred to as dexmethylphenidate, d-MPH, or d-threo-methylphenidate. A review on the synthesis of enantiomerically pure (2R,2′R)-(+)-threo-methylphenidate hydrochloride has been published.[125]Methylphenidate synthesis

Method 1: Methylphenidate preparation elucidated by Axten et al. (1998)[126] via Bamford-Stevens reaction.
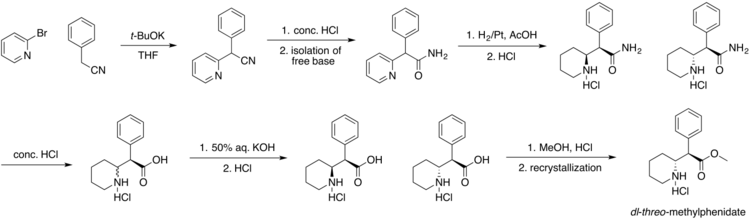
Method 2: Classic methylphenidate synthesis[127]
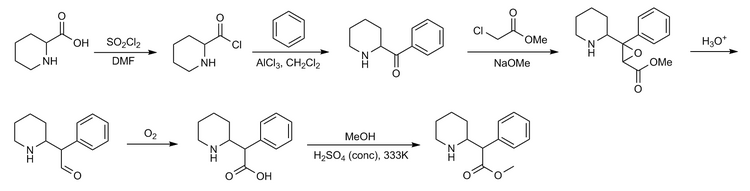
Method 3: Another synthesis route of methylphenidate which applies Darzens reaction to obtain aldehyde as an intermediate. This route is significant for its selectivity.SYNhttps://onlinelibrary.wiley.com/doi/abs/10.1002/jhet.2705SUN
1.9 Synthesis of (R, R), (R, S), (S, S) and (S, R) methyl 2-piperidin-2-yl-phenylacetate hydrochloride (1a, 1b, 1c and 1d)
Compound 8a, 8b, 8c or 8d (400 mg, 1.3 mmol) was dissolved into methanol solution (15 mL), and then thionyl chloride (1 mL) was added drop-wise. The reaction mixture was stirred for 12 hours and concentrated in vacuum; a white solid was precipitated and filtered to afford the final product. (1a. 0.28 g, 82% yield; 1b. 0.30 g, 84% yield; 1c. 0.31 g, 85% yield; 1d. 0.30 g, 84% yield). The characterization data of the four final products had been reported [2] by us in 2016.
SYN
https://patents.google.com/patent/US20040180928A1/en
- Dexmethylphenidate, also known as d-threo-methylphenidate, (R,R)-methylphenidate or (R,R)-α-phenyl-2-piperidineacetic acid methyl ester, having the formula:
- [0029]
is CNS (central nervous system) stimulant that is chemically and pharmacologically similar to the amphetamines. Dexmethylphenidate’s CNS actions is milder than those of the amphetamines and have more noticeable effects on mental activities than on motor activities. - [0030]
It has been reported by Sporzny (1961) that among racemic mixtures of threo and erythro diastereomers of methylphenidate, only threo-isomer displays stimulant properties. Dexmethylphenidate hydrochloride (i.e. the d-threo enantiomer of methylphenidate hydrochloride) has been reported to be 5 to 38 times more active than the corresponding (S,S)-methylphenidate hydrochloride (Prashad 2000). - [0031]
A commercially available drug is sold under the name Focalin™ (Novartis) and it consists of dexmethylphenidate in the form of the hydrochloride salt. This product is orally administered and clinically used in the treatment of narcolepsy and as adjunctive treatment in children with attention deficit disorder (ADD) and attention-deficit hyperactivity disorder (ADHD). - [0032]
A synthesis of dexmethylphenidate hydrochloride was firstly described in U.S. Pat. No. 2,838,519 and include resolution of erythro-α-phenyl-2-piperidineacetamide to obtain enantiopure (2R,2′S)-α-phenyl-2-piperidineacetamide, which was subjected to epimerization, hydrolysis, and esterification as shown in Scheme 1: - [0033]
Related example of preparation of dexmethylphenidate from erythro-α-phenyl-2-piperidineacetamide was described in U.S. Pat. No. 5,936,091. - [0034]
Preparation of dexmethylphenidate through optical resolution of threo-α-phenyl-2-piperidineacetamide was described in U.S. Pat. No. 5,965,734, as shown in Scheme 2: - [0035]
Synthetic methods for the preparation of racemic mixture of threo- and erythro-α-phenyl-2-piperidineacetamides as raw materials for the preparation of dexmethylphenidate were described by Panizzon (1944) and Patric (1982) and in U.S. Pat. Nos. 2,507,631, 2,838,519, 2,957,880 and 5,936,091, and in WO 01/27070. These methods include using sodium amide as base in the nucleophilic substitution of chlorine in 2-chloropyridine with phenylacetonitrile followed by hydrolysis of the formed nitrile and reduction of a pyridine ring to a piperidine one by hydrogenation on PtO 2 catalyst, as shown in Scheme 3: - [0036]
Alternatively, 2-bromopyridine was used instead of 2-chloropyridine by Deutsch (1996). - [0037]
In some other methods threo-methylphenidate was used as the raw material for the preparation of dexmethylphenidate. Threo-methylphenidate may be prepared by a several routes, inter alia by the following two processes: - [0038]
i) by esterification of threo-ritalinic acid which may be prepared from erythro-enriched and threo-α-phenyl-2-piperidineacetamides as shown in Scheme 4: - [0039]
ii) by cyclization of easily available 1-(phenylglyoxylyl)piperidine arenesulfonylhydrazone to (R*,R*)-enriched 7-phenyl-1-azabicyclo[4.2.0]octan-8-one and further converting the β-lactam to threo-methylphenidate hydrochloride, as described by Axten (1998), Corey (1965) and Earle (1969) and in WO 99/36403 and shown in Scheme 5: - [0040]
The resolution of threo-methylphenidate to afford dexmethylphenidate was first reported by Patric (1987) which used (R)-(−)-binaphthyl-2,2′-diyl hydrogen phosphate as the resolving agent. Several new resolutions of threo-methylphenidate have been reported recently by Prashad (1999) and in U.S. Pat. Nos. 6,100,401, 6,121,453, 6,162,919 and 6,242,464 as described in Scheme 6: - [0041]
wherein the chiral acid is one of the following: (R)-(−)-binaphthyl-2,2′-diyl hydrogen phosphate, (−)-menthoxyacetic acid, ditoluoyl-D-tartaric acid or dibenzoyl-D-tartaric acid. - [0042]
Resolution of threo-methylphenidate may be also achieved by enzymatic hydrolysis methods as proposed by Prashad (1998) and in WO 98/25902. Such resolution is described in Scheme 7: - [0043]
Resolution of threo-ritalinic acid hydrochloride with (S)-1-phenylethylamine give complex salt (R,R)-enriched threo-ritalinic acid.HCl.(S)-1-phenylethylamine with 77% ee optical purity of ritalinic acid (U.S. Ser. No. 2002/0019535), Scheme 8:
- [0119]
- [0120]
Gaseous hydrogen chloride was passed through a boiling solution of (R,R)-N-Boc-ritalinic acid (95.4 g, 299 mmol) in methanol (1.5 L). The mixture was stirred for 12 hours under reflux conditions and concentrated to the volume of 250 mL. Toluene (750 mL) was added to the stirred residue, then methanol lo was removed from boiling suspension under normal pressure. The obtained mixture was stirred overnight at 0-5° C. The precipitated solids were filtered off, washed on the filter with toluene (3×50 mL) and dried under reduced pressure to give 78.4 g (97.2% yield) of dexmethylphenidate hydrochloride as white crystals with mp 222-224° C. and [α]D 25 87.0° (c=1, MeOH).
- [0117]
- [0118]
A mixture of crystalline salt of (R,R)-N-Boc-ritalinic acid and (S)-1-phenylamine with [α]D 20 −28.6° (c=1, MeOH) (133.0 g, 302 mmol), ethyl acetate (1.3 L) and solution of citric acid (164.0 g, 845 mmol) in water (1.3 L) was stirred at 15-25° C. for 1.5 hours. The organic layer was separated, washed lo with brine (20 mL), dried over sodium sulfate, filtered and evaporated under reduced pressure to give 95.4 g (99%) of (R,R)-N-B
- [0115]
- [0116]
(S)-1-Phenylethylamine (113.8 g, 0.94 mol, 0.6 eq) was added dropwise to a stirred solution of N-Boc-threo-ritalinic acid (500 g, 1.57 mol, 1 eq) in ethyl acetate (5 L) for 1 hour at 20-40° C. The mixture was stirred for 1 hour at 40° C. and overnight at 5° C. The precipitated solids were filtered off, washed on the lo filter with cold ethyl acetate (2×500 mL) and dried under reduced pressure to give 380 g of white crystals with [α]D 20−23.3° (c=1, MeOH). The salt was twice recrystallized from aqueous methanol. The precipitated crystals were filtered off, washed on the filter with cold aqueous methanol and dried under reduced pressure to a constant weight to give 265 g (33.5% yield) of salt of (R,R)-N-Boc-ritalinic acid and (S)
- [0113]
- [0114]
A mixture of solution of N-Boc-threo-ritalinic acid sodium salt (1700 g, 4.98 mmol), citric acid (1150 g, 5.98 mmol) and water (5 mL) was stirred at 15-25° C. for 0.5 hour and extracted with ethyl acetate (3×4 L). Combined organic extracts were washed with brine (2×3 L), dried over sodium sulfate, filtered and evaporated under reduced pressure to constant weight to give 1560 g (98.1% yield) of N-Boc-threo-ritalinic acid with mp 133-134° C. (EtOAc/hexane) and 99.8% purity by HPLC.
Medical uses
Dexmethylphenidate is used as a treatment for ADHD, usually along with psychological, educational, behavioral or other forms of treatment. It is proposed that stimulants help ameliorate the symptoms of ADHD by making it easier for the user to concentrate, avoid distraction, and control behavior. Placebo-controlled trials have shown that once-daily dexmethylphenidate XR was effective and generally well tolerated.[6]
Improvements in ADHD symptoms in children were significantly greater for dexmethylphenidate XR versus placebo.[6] It also showed greater efficacy than osmotic controlled-release oral delivery system (OROS) methylphenidate over the first half of the laboratory classroom day but assessments late in the day favoured OROS methylphenidate.[6]
CLIP
An Improved and Efficient Process for the Production of Highly Pure Dexmethylphenidate Hydrochloride
Long-Xuan Xing, Cheng-Wu Shen, Yuan-Yuan Sun, Lei Huang, Yong-Yong Zheng,* Jian-Qi Li*
https://onlinelibrary.wiley.com/doi/abs/10.1002/jhet.2705
The present work describes an efficient and commercially viable process for the synthesis of dexmethylphenidate hydrochloride (1), a mild nervous system stimulant. The overall yield is 23% with ~99.9% purity (including seven chemical steps). Formation and control of possible impurities are also described in this report.

(R)-methyl 2-phenyl-2-((R)-piperidin-2-yl)acetate hydrochloride (1). ………… afford 1 as a white solid (107.6 g, 87.3% yield) with 99.50% purity and 99.70% ee. The crude product (107.6 g, 0.4 mol) was further purified by recrystallization from pure water (100 mL) to obtain the qualified product 1 (98.3 g, 91.4% yield) with 99.92 purity and 99.98% ee.
[α] 25 D +85.6 (MeOH, c 1) (lit [4b]. [α] 25 D +84 (MeOH, c 1));
Mp 222-223 C (lit [4b]. Mp 222– 224°C); MS m/z 234 [M + H]+ .
1 H NMR (400Hz, DMSO-d6) δ 1 H NMR (400 MHz, DMSO-d6) δ 9.64 (br, 1H), 8.97 (br, 1H), 7.41-7.26 (m, 5H), 4.18-4.16 (d, J = 9.2Hz, 1H), 3.77-3.75 (m, 1H), 3.66 (s, 3H), 3.25 (m, 1H), 2.94 (m, 1H), 1.67-1.64 (m, 3H), 1.41-1.25 (m, 3H).
13C NMR (100.6 MHz, DMSO-d6) δ 171.3, 134.2, 129.1, 128.6, 128.2, 56.8, 53.3, 52.6, 44.5, 25.7, 21.5, 21.4.
1H-NMR, and 13C-NMR of compound 1………………………………….. 10-11


DEPT,

COSY, NOESY, GHMBC, and HMQC of compound 1……………… 12-14

COSY

NOESY

GHMBC

HMQC
Contraindications
This section is transcluded from Methylphenidate. (edit | history)
Methylphenidate is contraindicated for individuals using monoamine oxidase inhibitors (e.g., phenelzine, and tranylcypromine), or individuals with agitation, tics, glaucoma, or a hypersensitivity to any ingredients contained in methylphenidate pharmaceuticals.[10]
The US Food and Drug Administration (FDA) gives methylphenidate a pregnancy category of C, and women are advised to only use the drug if the benefits outweigh the potential risks.[11] Not enough human studies have been conducted to conclusively demonstrate an effect of methylphenidate on fetal development.[12] In 2018, a review concluded that it has not been teratogenic in rats and rabbits, and that it “is not a major human teratogen”.[13]
Adverse effects
Part of this section is transcluded from Methylphenidate. (edit | history)
Products containing dexmethylphenidate have a side effect profile comparable to those containing methylphenidate.[14]

Addiction experts in psychiatry, chemistry, pharmacology, forensic science, epidemiology, and the police and legal services engaged in delphic analysis regarding 20 popular recreational drugs. Methylphenidate was ranked 13th in dependence, 12th in physical harm, and 18th in social harm.[15]
The most common adverse effects include appetite loss, dry mouth, anxiety/nervousness, nausea, and insomnia. Gastrointestinal adverse effects may include abdominal pain and weight loss. Nervous system adverse effects may include akathisia (agitation/restlessness), irritability, dyskinesia (tics), lethargy (drowsiness/fatigue), and dizziness. Cardiac adverse effects may include palpitations, changes in blood pressure and heart rate (typically mild), and tachycardia (rapid heart rate).[16] Smokers with ADHD who take methylphenidate may increase their nicotine dependence, and smoke more often than before they began using methylphenidate, with increased nicotine cravings and an average increase of 1.3 cigarettes per day.[17] Ophthalmologic adverse effects may include blurred vision and dry eyes, with less frequent reports of diplopia and mydriasis.[18]
There is some evidence of mild reductions in height with prolonged treatment in children.[19] This has been estimated at 1 centimetre (0.4 in) or less per year during the first three years with a total decrease of 3 centimetres (1.2 in) over 10 years.[20][21]
Hypersensitivity (including skin rash, urticaria, and fever) is sometimes reported when using transdermal methylphenidate. The Daytrana patch has a much higher rate of skin reactions than oral methylphenidate.[22]
Methylphenidate can worsen psychosis in people who are psychotic, and in very rare cases it has been associated with the emergence of new psychotic symptoms.[23] It should be used with extreme caution in people with bipolar disorder due to the potential induction of mania or hypomania.[24] There have been very rare reports of suicidal ideation, but some authors claim that evidence does not support a link.[19] Logorrhea is occasionally reported. Libido disorders, disorientation, and hallucinations are very rarely reported. Priapism is a very rare adverse event that can be potentially serious.[25]
USFDA-commissioned studies from 2011 indicate that in children, young adults, and adults there is no association between serious adverse cardiovascular events (sudden death, heart attack, and stroke) and the medical use of methylphenidate or other ADHD stimulants.[26]
Because some adverse effects may only emerge during chronic use of methylphenidate, a constant watch for adverse effects is recommended.[27]
A 2018 Cochrane review found that methylphenidate might be associated with serious side effects such as heart problems, psychosis, and death; the certainty of the evidence was stated as very low and the actual risk might be higher.[28]
Overdose
The symptoms of a moderate acute overdose on methylphenidate primarily arise from central nervous system overstimulation; these symptoms include: vomiting, nausea, agitation, tremors, hyperreflexia, muscle twitching, euphoria, confusion, hallucinations, delirium, hyperthermia, sweating, flushing, headache, tachycardia, heart palpitations, cardiac arrhythmias, hypertension, mydriasis, and dryness of mucous membranes.[29][30] A severe overdose may involve symptoms such as hyperpyrexia, sympathomimetic toxidrome, convulsions, paranoia, stereotypy (a repetitive movement disorder), rapid muscle breakdown, coma, and circulatory collapse.[29][30][31] A methylphenidate overdose is rarely fatal with appropriate care.[31] Following injection of methylphenidate tablets into an artery, severe toxic reactions involving abscess formation and necrosis have been reported.[32]
Treatment of a methylphenidate overdose typically involves the administration of benzodiazepines, with antipsychotics, α-adrenoceptor agonists and propofol serving as second-line therapies.[31]
Addiction and dependence[edit]
| ΔFosB accumulation from excessive drug use Top: this depicts the initial effects of high dose exposure to an addictive drug on gene expression in the nucleus accumbens for various Fos family proteins (i.e., c-Fos, FosB, ΔFosB, Fra1, and Fra2). Bottom: this illustrates the progressive increase in ΔFosB expression in the nucleus accumbens following repeated twice daily drug binges, where these phosphorylated (35–37 kilodalton) ΔFosB isoforms persist in the D1-type medium spiny neurons of the nucleus accumbens for up to 2 months.[33][34] |
Methylphenidate is a stimulant with an addiction liability and dependence liability similar to amphetamine. It has moderate liability among addictive drugs;[35][36] accordingly, addiction and psychological dependence are possible and likely when methylphenidate is used at high doses as a recreational drug.[36][37] When used above the medical dose range, stimulants are associated with the development of stimulant psychosis.[38] As with all addictive drugs, the overexpression of ΔFosB in D1-type medium spiny neurons in the nucleus accumbens is implicated in methylphenidate addiction.[37][39]
Methylphenidate has shown some benefits as a replacement therapy for individuals who are addicted to and dependent upon methamphetamine.[40] Methylphenidate and amphetamine have been investigated as a chemical replacement for the treatment of cocaine addiction[41][42][43][44] in the same way that methadone is used as a replacement drug for physical dependence upon heroin. Its effectiveness in treatment of cocaine or psychostimulant addiction, or psychological dependence has not been proven and further research is needed.[45]
Biomolecular mechanisms
Further information: Addiction § Biomolecular mechanisms
Methylphenidate has the potential to induce euphoria due to its pharmacodynamic effect (i.e., dopamine reuptake inhibition) in the brain’s reward system.[39] At therapeutic doses, ADHD stimulants do not sufficiently activate the reward system, or the reward pathway in particular, to the extent necessary to cause persistent increases in ΔFosB gene expression in the D1-type medium spiny neurons of the nucleus accumbens;[36][39][46] consequently, when taken as directed in doses that are commonly prescribed for the treatment of ADHD, methylphenidate use lacks the capacity to cause an addiction.[36][39][46] However, when methylphenidate is used at sufficiently high recreational doses through a bioavailable route of administration (e.g., insufflation or intravenous administration), particularly for use of the drug as a euphoriant, ΔFosB accumulates in the nucleus accumbens.[36][39] Hence, like any other addictive drug, regular recreational use of methylphenidate at high doses eventually gives rise to ΔFosB overexpression in D1-type neurons which subsequently triggers a series of gene transcription-mediated signaling cascades that induce an addiction.[39][46][47]
Overdose
This section is transcluded from Methylphenidate. (edit | history)
The symptoms of a moderate acute overdose on methylphenidate primarily arise from central nervous system overstimulation; these symptoms include: vomiting, nausea, agitation, tremors, hyperreflexia, muscle twitching, euphoria, confusion, hallucinations, delirium, hyperthermia, sweating, flushing, headache, tachycardia, heart palpitations, cardiac arrhythmias, hypertension, mydriasis, and dryness of mucous membranes.[29][30] A severe overdose may involve symptoms such as hyperpyrexia, sympathomimetic toxidrome, convulsions, paranoia, stereotypy (a repetitive movement disorder), rapid muscle breakdown, coma, and circulatory collapse.[29][30][31] A methylphenidate overdose is rarely fatal with appropriate care.[31] Following injection of methylphenidate tablets into an artery, severe toxic reactions involving abscess formation and necrosis have been reported.[32]
Treatment of a methylphenidate overdose typically involves the administration of benzodiazepines, with antipsychotics, α-adrenoceptor agonists and propofol serving as second-line therapies.[31]
Interactions
This section is transcluded from Methylphenidate. (edit | history)
Methylphenidate may inhibit the metabolism of vitamin K anticoagulants, certain anticonvulsants, and some antidepressants (tricyclic antidepressants, and selective serotonin reuptake inhibitors). Concomitant administration may require dose adjustments, possibly assisted by monitoring of plasma drug concentrations.[48] There are several case reports of methylphenidate inducing serotonin syndrome with concomitant administration of antidepressants.[49][50][51][52]
When methylphenidate is coingested with ethanol, a metabolite called ethylphenidate is formed via hepatic transesterification,[53][54] not unlike the hepatic formation of cocaethylene from cocaine and ethanol. The reduced potency of ethylphenidate and its minor formation means it does not contribute to the pharmacological profile at therapeutic doses and even in overdose cases ethylphenidate concentrations remain negligible.[55][54]
Coingestion of alcohol (ethanol) also increases the blood plasma levels of d-methylphenidate by up to 40%.[56]
Liver toxicity from methylphenidate is extremely rare, but limited evidence suggests that intake of β-adrenergic agonists with methylphenidate may increase the risk of liver toxicity.[57]
Mode of activity
Methylphenidate is a catecholamine reuptake inhibitor that indirectly increases catecholaminergic neurotransmission by inhibiting the dopamine transporter (DAT) and norepinephrine transporter (NET),[58] which are responsible for clearing catecholamines from the synapse, particularly in the striatum and meso-limbic system.[59] Moreover, it is thought to “increase the release of these monoamines into the extraneuronal space.”[2]
Although four stereoisomers of methylphenidate (MPH) are possible, only the threo diastereoisomers are used in modern practice. There is a high eudysmic ratio between the SS and RR enantiomers of MPH. Dexmethylphenidate (d-threo-methylphenidate) is a preparation of the RR enantiomer of methylphenidate.[60][61] In theory, D-TMP (d-threo-methylphenidate) can be anticipated to be twice the strength of the racemic product.[58][62]
| Compd[63] | DAT (Ki) | DA (IC50) | NET (Ki) | NE (IC50) |
|---|---|---|---|---|
| D-TMP | 161 | 23 | 206 | 39 |
| L-TMP | 2250 | 1600 | >10K | 980 |
| DL-TMP | 121 | 20 | 788 | 51 |
Pharmacology
Main article: Methylphenidate § Pharmacology
Dexmethylphenidate has a 4–6 hour duration of effect (a long-acting formulation, Focalin XR, which spans 12 hours is also available and has been shown to be as effective as DL (dextro-, levo-)-TMP (threo-methylphenidate) XR (extended release) (Concerta, Ritalin LA), with flexible dosing and good tolerability.[64][65]) It has also been demonstrated to reduce ADHD symptoms in both children[66] and adults.[67] d-MPH has a similar side-effect profile to MPH[14] and can be administered without regard to food intake.[68]
References
- ^ Jump up to:a b “Focalin- dexmethylphenidate hydrochloride tablet”. DailyMed. 24 June 2020. Retrieved 15 November 2020.
- ^ Jump up to:a b “Focalin XR- dexmethylphenidate hydrochloride capsule, extended release”. DailyMed. 27 June 2020. Retrieved 15 November 2020.
- ^ Jump up to:a b c d e f g h i “Dexmethylphenidate Hydrochloride Monograph for Professionals”. Drugs.com. American Society of Health-System Pharmacists. Retrieved 15 April 2019.
- ^ Mosby’s Drug Reference for Health Professions – E-Book. Elsevier Health Sciences. 2013. p. 455. ISBN 9780323187602.
- ^ “Dexmethylphenidate Use During Pregnancy”. Drugs.com. Retrieved 15 April 2019.
- ^ Jump up to:a b c d Moen MD, Keam SJ (December 2009). “Dexmethylphenidate extended release: a review of its use in the treatment of attention-deficit hyperactivity disorder”. CNS Drugs. 23(12): 1057–83. doi:10.2165/11201140-000000000-00000. PMID 19958043. S2CID 24975170.
- ^ “The Top 300 of 2021”. ClinCalc. Retrieved 18 February 2021.
- ^ “Dexmethylphenidate Hydrochloride – Drug Usage Statistics”. ClinCalc. Retrieved 18 February 2021.
- ^ “Focalin XR”. Drugs.com. Retrieved 15 April 2019.
- ^ “DAYTRANA” (PDF). United States Food and Drug Administration. Noven Pharmaceuticals, Inc. October 2013. Archived (PDF) from the original on 14 July 2014. Retrieved 13 June 2014.
- ^ “Methylphenidate: Use During Pregnancy and Breastfeeding”. Drugs.com. Archived from the original on 2 January 2018.
- ^ Humphreys C, Garcia-Bournissen F, Ito S, Koren G (2007). “Exposure to attention deficit hyperactivity disorder medications during pregnancy”. Canadian Family Physician. 53 (7): 1153–5. PMC 1949295. PMID 17872810.
- ^ Ornoy, Asher (6 February 2018). “Pharmacological Treatment of Attention Deficit Hyperactivity Disorder During Pregnancy and Lactation”. Pharmaceutical Research. 35 (3): 46. doi:10.1007/s11095-017-2323-z. PMID 29411149. S2CID 3663423.
- ^ Jump up to:a b Keating GM, Figgitt DP (2002). “Dexmethylphenidate”. Drugs. 62 (13): 1899–904, discussion 1905–8. doi:10.2165/00003495-200262130-00009. PMID 12215063.
- ^ Nutt D, King LA, Saulsbury W, Blakemore C (March 2007). “Development of a rational scale to assess the harm of drugs of potential misuse”. Lancet. 369 (9566): 1047–53. doi:10.1016/S0140-6736(07)60464-4. PMID 17382831. S2CID 5903121.
- ^ “Ritalin LA® (methylphenidate hydrochloride) extended-release capsules” (PDF). Novartis. Archived from the original (PDF)on 20 July 2011.
- ^ Bron TI, Bijlenga D, Kasander MV, Spuijbroek AT, Beekman AT, Kooij JJ (2013). “Long-term relationship between methylphenidate and tobacco consumption and nicotine craving in adults with ADHD in a prospective cohort study”. European Neuropsychopharmacology. 23 (6): 542–554. doi:10.1016/j.euroneuro.2012.06.004. PMID 22809706. S2CID 23148548.
- ^ Jaanus SD (1992). “Ocular side effects of selected systemic drugs”. Optometry Clinics. 2 (4): 73–96. PMID 1363080.
- ^ Jump up to:a b Cortese S, Holtmann M, Banaschewski T, Buitelaar J, Coghill D, Danckaerts M, et al. (March 2013). “Practitioner review: current best practice in the management of adverse events during treatment with ADHD medications in children and adolescents”. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 54 (3): 227–46. doi:10.1111/jcpp.12036. PMID 23294014.
- ^ Poulton A (August 2005). “Growth on stimulant medication; clarifying the confusion: a review”. Archives of Disease in Childhood. 90 (8): 801–6. doi:10.1136/adc.2004.056952. PMC 1720538. PMID 16040876.
- ^ Hinshaw SP, Arnold LE (January 2015). “ADHD, Multimodal Treatment, and Longitudinal Outcome: Evidence, Paradox, and Challenge”. Wiley Interdisciplinary Reviews. Cognitive Science. 6(1): 39–52. doi:10.1002/wcs.1324. PMC 4280855. PMID 25558298.
- ^ Findling RL, Dinh S (March 2014). “Transdermal therapy for attention-deficit hyperactivity disorder with the methylphenidate patch (MTS)”. CNS Drugs. 28 (3): 217–28. doi:10.1007/s40263-014-0141-y. PMC 3933749. PMID 24532028.
- ^ Kraemer M, Uekermann J, Wiltfang J, Kis B (July 2010). “Methylphenidate-induced psychosis in adult attention-deficit/hyperactivity disorder: report of 3 new cases and review of the literature”. Clinical Neuropharmacology. 33 (4): 204–6. doi:10.1097/WNF.0b013e3181e29174. PMID 20571380. S2CID 34956456.
- ^ Wingo AP, Ghaemi SN (2008). “Frequency of stimulant treatment and of stimulant-associated mania/hypomania in bipolar disorder patients”. Psychopharmacology Bulletin. 41 (4): 37–47. PMID 19015628.
- ^ “Methylphenidate ADHD Medications: Drug Safety Communication – Risk of Long-lasting Erections”. U.S. Food and Drug Administration. 17 December 2013. Archived from the original on 17 December 2013. Retrieved 17 December 2013.
- ^ “FDA Drug Safety Communication: Safety Review Update of Medications used to treat Attention-Deficit/Hyperactivity Disorder (ADHD) in children and young adults”. United States Food and Drug Administration. 20 December 2011. Archived from the original on 30 October 2013. Retrieved 4 November 2013.
• Cooper WO, Habel LA, Sox CM, Chan KA, Arbogast PG, Cheetham TC, Murray KT, Quinn VP, Stein CM, Callahan ST, Fireman BH, Fish FA, Kirshner HS, O’Duffy A, Connell FA, Ray WA (November 2011). “ADHD drugs and serious cardiovascular events in children and young adults”. N. Engl. J. Med. 365 (20): 1896–1904. doi:10.1056/NEJMoa1110212. PMC 4943074. PMID 22043968.
• “FDA Drug Safety Communication: Safety Review Update of Medications used to treat Attention-Deficit/Hyperactivity Disorder (ADHD) in adults”. United States Food and Drug Administration. 15 December 2011. Archived from the original on 30 October 2013. Retrieved 4 November 2013.
• Habel LA, Cooper WO, Sox CM, Chan KA, Fireman BH, Arbogast PG, Cheetham TC, Quinn VP, Dublin S, Boudreau DM, Andrade SE, Pawloski PA, Raebel MA, Smith DH, Achacoso N, Uratsu C, Go AS, Sidney S, Nguyen-Huynh MN, Ray WA, Selby JV (December 2011). “ADHD medications and risk of serious cardiovascular events in young and middle-aged adults”. JAMA. 306 (24): 2673–2683. doi:10.1001/jama.2011.1830. PMC 3350308. PMID 22161946. - ^ Gordon N (1999). “Attention deficit hyperactivity disorder: possible causes and treatment”. International Journal of Clinical Practice. 53(7): 524–8. PMID 10692738.
- ^ Storebø OJ, Pedersen N, Ramstad E, Kielsholm ML, Nielsen SS, Krogh HB, et al. (May 2018). “Methylphenidate for attention deficit hyperactivity disorder (ADHD) in children and adolescents – assessment of adverse events in non-randomised studies”. The Cochrane Database of Systematic Reviews. 5: CD012069. doi:10.1002/14651858.CD012069.pub2. PMC 6494554. PMID 29744873.
- ^ Jump up to:a b c d Noven Pharmaceuticals, Inc. (17 April 2015). “Daytrana Prescribing Information” (PDF). United States Food and Drug Administration. pp. 1–33. Archived (PDF) from the original on 23 June 2015. Retrieved 23 June 2015.
- ^ Jump up to:a b c d Heedes G, Ailakis J. “Methylphenidate hydrochloride (PIM 344)”. INCHEM. International Programme on Chemical Safety. Archived from the original on 23 June 2015. Retrieved 23 June2015.
- ^ Jump up to:a b c d e f Spiller HA, Hays HL, Aleguas A (June 2013). “Overdose of drugs for attention-deficit hyperactivity disorder: clinical presentation, mechanisms of toxicity, and management”. CNS Drugs. 27 (7): 531–543. doi:10.1007/s40263-013-0084-8. PMID 23757186. S2CID 40931380.
The management of amphetamine, dextroamphetamine, and methylphenidate overdose is largely supportive, with a focus on interruption of the sympathomimetic syndrome with judicious use of benzodiazepines. In cases where agitation, delirium, and movement disorders are unresponsive to benzodiazepines, second-line therapies include antipsychotics such as ziprasidone or haloperidol, central alpha-adrenoreceptor agonists such as dexmedetomidine, or propofol. … However, fatalities are rare with appropriate care
- ^ Jump up to:a b Bruggisser M, Bodmer M, Liechti ME (2011). “Severe toxicity due to injected but not oral or nasal abuse of methylphenidate tablets”. Swiss Med Wkly. 141: w13267. doi:10.4414/smw.2011.13267. PMID 21984207.
- ^ Nestler EJ, Barrot M, Self DW (September 2001). “DeltaFosB: a sustained molecular switch for addiction”. Proceedings of the National Academy of Sciences of the United States of America. 98(20): 11042–6. Bibcode:2001PNAS…9811042N. doi:10.1073/pnas.191352698. PMC 58680. PMID 11572966.
Although the ΔFosB signal is relatively long-lived, it is not permanent. ΔFosB degrades gradually and can no longer be detected in brain after 1–2 months of drug withdrawal … Indeed, ΔFosB is the longest-lived adaptation known to occur in adult brain, not only in response to drugs of abuse, but to any other perturbation (that does not involve lesions) as well.
- ^ Nestler EJ (December 2012). “Transcriptional mechanisms of drug addiction”. Clinical Psychopharmacology and Neuroscience. 10 (3): 136–43. doi:10.9758/cpn.2012.10.3.136. PMC 3569166. PMID 23430970.
The 35–37 kD ΔFosB isoforms accumulate with chronic drug exposure due to their extraordinarily long half-lives. … As a result of its stability, the ΔFosB protein persists in neurons for at least several weeks after cessation of drug exposure. … ΔFosB overexpression in nucleus accumbens induces NFκB
- ^ Morton WA, Stockton GG (2000). “Methylphenidate Abuse and Psychiatric Side Effects”. Prim Care Companion J Clin Psychiatry. 2 (5): 159–164. doi:10.4088/PCC.v02n0502. PMC 181133. PMID 15014637.
- ^ Jump up to:a b c d e Malenka RC, Nestler EJ, Hyman SE (2009). “Chapter 15: Reinforcement and Addictive Disorders”. In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. 368. ISBN 9780071481274.
Cocaine, [amphetamine], and methamphetamine are the major psychostimulants of abuse. The related drug methylphenidate is also abused, although it is far less potent. These drugs elicit similar initial subjective effects ; differences generally reflect the route of administration and other pharmacokinetic factors. Such agents also have important therapeutic uses; cocaine, for example, is used as a local anesthetic (Chapter 2), and amphetamines and methylphenidate are used in low doses to treat attention deficit hyperactivity disorder and in higher doses to treat narcolepsy (Chapter 12). Despite their clinical uses, these drugs are strongly reinforcing, and their long-term use at high doses is linked with potential addiction, especially when they are rapidly administered or when high-potency forms are given.
- ^ Jump up to:a b Steiner H, Van Waes V (January 2013). “Addiction-related gene regulation: risks of exposure to cognitive enhancers vs. other psychostimulants”. Prog. Neurobiol. 100: 60–80. doi:10.1016/j.pneurobio.2012.10.001. PMC 3525776. PMID 23085425.
- ^ Auger RR, Goodman SH, Silber MH, Krahn LE, Pankratz VS, Slocumb NL (2005). “Risks of high-dose stimulants in the treatment of disorders of excessive somnolence: a case-control study”. Sleep. 28 (6): 667–72. doi:10.1093/sleep/28.6.667. PMID 16477952.
- ^ Jump up to:a b c d e f Kim Y, Teylan MA, Baron M, Sands A, Nairn AC, Greengard P (2009). “Methylphenidate-induced dendritic spine formation and DeltaFosB expression in nucleus accumbens”. Proc. Natl. Acad. Sci. U.S.A. 106 (8): 2915–20. Bibcode:2009PNAS..106.2915K. doi:10.1073/pnas.0813179106. PMC 2650365. PMID 19202072.
Despite decades of clinical use of methylphenidate for ADHD, concerns have been raised that long-term treatment of children with this medication may result in subsequent drug abuse and addiction. However, meta analysis of available data suggests that treatment of ADHD with stimulant drugs may have a significant protective effect, reducing the risk for addictive substance use (36, 37). Studies with juvenile rats have also indicated that repeated exposure to methylphenidate does not necessarily lead to enhanced drug-seeking behavior in adulthood (38). However, the recent increase of methylphenidate use as a cognitive enhancer by the general public has again raised concerns because of its potential for abuse and addiction (3, 6–10). Thus, although oral administration of clinical doses of methylphenidate is not associated with euphoria or with abuse problems, nontherapeutic use of high doses or i.v. administration may lead to addiction (39, 40).
- ^ Elkashef A, Vocci F, Hanson G, White J, Wickes W, Tiihonen J (2008). “Pharmacotherapy of methamphetamine addiction: an update”. Substance Abuse. 29 (3): 31–49. doi:10.1080/08897070802218554. PMC 2597382. PMID 19042205.
- ^ Grabowski J, Roache JD, Schmitz JM, Rhoades H, Creson D, Korszun A (December 1997). “Replacement medication for cocaine dependence: methylphenidate”. Journal of Clinical Psychopharmacology. 17 (6): 485–8. doi:10.1097/00004714-199712000-00008. PMID 9408812.
- ^ Gorelick DA, Gardner EL, Xi ZX (2004). “Agents in development for the management of cocaine abuse”. Drugs. 64 (14): 1547–73. doi:10.2165/00003495-200464140-00004. PMID 15233592. S2CID 5421657. Archived from the original on 1 July 2019. Retrieved 1 July 2019.
- ^ Karila L, Gorelick D, Weinstein A, Noble F, Benyamina A, Coscas S, et al. (May 2008). “New treatments for cocaine dependence: a focused review”. The International Journal of Neuropsychopharmacology. 11 (3): 425–38. doi:10.1017/S1461145707008097. PMID 17927843.
- ^ “NIDA InfoFacts: Understanding Drug Abuse and Addiction”(PDF). 2008. Archived from the original (PDF) on 15 December 2010.
- ^ Shearer J (May 2008). “The principles of agonist pharmacotherapy for psychostimulant dependence”. Drug and Alcohol Review. 27 (3): 301–8. doi:10.1080/09595230801927372. PMID 18368612.
- ^ Jump up to:a b c Nestler EJ (December 2013). “Cellular basis of memory for addiction”. Dialogues in Clinical Neuroscience. 15 (4): 431–43. doi:10.31887/DCNS.2013.15.4/enestler. PMC 3898681. PMID 24459410.
Despite the importance of numerous psychosocial factors, at its core, drug addiction involves a biological process: the ability of repeated exposure to a drug of abuse to induce changes in a vulnerable brain that drive the compulsive seeking and taking of drugs, and loss of control over drug use, that define a state of addiction. … A large body of literature has demonstrated that such ΔFosB induction in D1-type NAc neurons increases an animal’s sensitivity to drug as well as natural rewards and promotes drug self-administration, presumably through a process of positive reinforcement … Another ΔFosB target is cFos: as ΔFosB accumulates with repeated drug exposure it represses c-Fos and contributes to the molecular switch whereby ΔFosB is selectively induced in the chronic drug-treated state.41. … Moreover, there is increasing evidence that, despite a range of genetic risks for addiction across the population, exposure to sufficiently high doses of a drug for long periods of time can transform someone who has relatively lower genetic loading into an addict.4
- ^ Ruffle JK (November 2014). “Molecular neurobiology of addiction: what’s all the (Δ)FosB about?”. The American Journal of Drug and Alcohol Abuse. 40 (6): 428–37. doi:10.3109/00952990.2014.933840. PMID 25083822. S2CID 19157711.
The strong correlation between chronic drug exposure and ΔFosB provides novel opportunities for targeted therapies in addiction (118), and suggests methods to analyze their efficacy (119). Over the past two decades, research has progressed from identifying ΔFosB induction to investigating its subsequent action (38). It is likely that ΔFosB research will now progress into a new era – the use of ΔFosB as a biomarker. …
Conclusions
ΔFosB is an essential transcription factor implicated in the molecular and behavioral pathways of addiction following repeated drug exposure. The formation of ΔFosB in multiple brain regions, and the molecular pathway leading to the formation of AP-1 complexes is well understood. The establishment of a functional purpose for ΔFosB has allowed further determination as to some of the key aspects of its molecular cascades, involving effectors such as GluR2 (87,88), Cdk5 (93) and NFkB (100). Moreover, many of these molecular changes identified are now directly linked to the structural, physiological and behavioral changes observed following chronic drug exposure (60,95,97,102). New frontiers of research investigating the molecular roles of ΔFosB have been opened by epigenetic studies, and recent advances have illustrated the role of ΔFosB acting on DNA and histones, truly as a molecular switch(34). As a consequence of our improved understanding of ΔFosB in addiction, it is possible to evaluate the addictive potential of current medications (119), as well as use it as a biomarker for assessing the efficacy of therapeutic interventions (121,122,124). Some of these proposed interventions have limitations (125) or are in their infancy (75). However, it is hoped that some of these preliminary findings may lead to innovative treatments, which are much needed in addiction.
• Biliński P, Wojtyła A, Kapka-Skrzypczak L, Chwedorowicz R, Cyranka M, Studziński T (2012). “Epigenetic regulation in drug addiction”. Annals of Agricultural and Environmental Medicine. 19(3): 491–6. PMID 23020045.For these reasons, ΔFosB is considered a primary and causative transcription factor in creating new neural connections in the reward centre, prefrontal cortex, and other regions of the limbic system. This is reflected in the increased, stable and long-lasting level of sensitivity to cocaine and other drugs, and tendency to relapse even after long periods of abstinence. These newly constructed networks function very efficiently via new pathways as soon as drugs of abuse are further taken … In this way, the induction of CDK5 gene expression occurs together with suppression of the G9A gene coding for dimethyltransferase acting on the histone H3. A feedback mechanism can be observed in the regulation of these 2 crucial factors that determine the adaptive epigenetic response to cocaine. This depends on ΔFosB inhibiting G9a gene expression, i.e. H3K9me2 synthesis which in turn inhibits transcription factors for ΔFosB. For this reason, the observed hyper-expression of G9a, which ensures high levels of the dimethylated form of histone H3, eliminates the neuronal structural and plasticity effects caused by cocaine by means of this feedback which blocks ΔFosB transcription
• Robison AJ, Nestler EJ (October 2011). “Transcriptional and epigenetic mechanisms of addiction”. Nature Reviews. Neuroscience. 12 (11): 623–37. doi:10.1038/nrn3111. PMC 3272277. PMID 21989194.ΔFosB has been linked directly to several addiction-related behaviors … Importantly, genetic or viral overexpression of ΔJunD, a dominant negative mutant of JunD which antagonizes ΔFosB- and other AP-1-mediated transcriptional activity, in the NAc or OFC blocks these key effects of drug exposure14,22–24. This indicates that ΔFosB is both necessary and sufficient for many of the changes wrought in the brain by chronic drug exposure. ΔFosB is also induced in D1-type NAc MSNs by chronic consumption of several natural rewards, including sucrose, high fat food, sex, wheel running, where it promotes that consumption14,26–30. This implicates ΔFosB in the regulation of natural rewards under normal conditions and perhaps during pathological addictive-like states.
- ^ “Concerta product monograph” (PDF). Janssen Pharmaceuticals. Archived (PDF) from the original on 28 January 2017. Retrieved 4 December 2016.
- ^ Ishii M, Tatsuzawa Y, Yoshino A, Nomura S (April 2008). “Serotonin syndrome induced by augmentation of SSRI with methylphenidate”. Psychiatry and Clinical Neurosciences. 62 (2): 246. doi:10.1111/j.1440-1819.2008.01767.x. PMID 18412855. S2CID 5659107.
- ^ Türkoğlu S (2015). “Serotonin syndrome with sertraline and methylphenidate in an adolescent”. Clinical Neuropharmacology. 38(2): 65–6. doi:10.1097/WNF.0000000000000075. PMID 25768857.
- ^ Park YM, Jung YK (May 2010). “Manic switch and serotonin syndrome induced by augmentation of paroxetine with methylphenidate in a patient with major depression”. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 34 (4): 719–20. doi:10.1016/j.pnpbp.2010.03.016. PMID 20298736. S2CID 31984813.
- ^ Bodner RA, Lynch T, Lewis L, Kahn D (February 1995). “Serotonin syndrome”. Neurology. 45 (2): 219–23. doi:10.1212/wnl.45.2.219. PMID 7854515. S2CID 35190429.
- ^ Patrick KS, González MA, Straughn AB, Markowitz JS (2005). “New methylphenidate formulations for the treatment of attention-deficit/hyperactivity disorder”. Expert Opinion on Drug Delivery. 2(1): 121–43. doi:10.1517/17425247.2.1.121. PMID 16296740. S2CID 25026467.
- ^ Jump up to:a b Markowitz JS, DeVane CL, Boulton DW, Nahas Z, Risch SC, Diamond F, Patrick KS (2000). “Ethylphenidate formation in human subjects after the administration of a single dose of methylphenidate and ethanol”. Drug Metabolism and Disposition. 28 (6): 620–4. PMID 10820132.
- ^ Markowitz JS, Logan BK, Diamond F, Patrick KS (1999). “Detection of the novel metabolite ethylphenidate after methylphenidate overdose with alcohol coingestion”. Journal of Clinical Psychopharmacology. 19 (4): 362–6. doi:10.1097/00004714-199908000-00013. PMID 10440465.
- ^ Patrick KS, Straughn AB, Minhinnett RR, Yeatts SD, Herrin AE, DeVane CL, Malcolm R, Janis GC, Markowitz JS (March 2007). “Influence of ethanol and gender on methylphenidate pharmacokinetics and pharmacodynamics”. Clinical Pharmacology and Therapeutics. 81 (3): 346–53. doi:10.1038/sj.clpt.6100082. PMC 3188424. PMID 17339864.
- ^ Roberts SM, DeMott RP, James RC (1997). “Adrenergic modulation of hepatotoxicity”. Drug Metab. Rev. 29 (1–2): 329–53. doi:10.3109/03602539709037587. PMID 9187524.
- ^ Jump up to:a b Markowitz JS, Patrick KS (June 2008). “Differential pharmacokinetics and pharmacodynamics of methylphenidate enantiomers: does chirality matter?”. Journal of Clinical Psychopharmacology. 28 (3 Suppl 2): S54-61. doi:10.1097/JCP.0b013e3181733560. PMID 18480678.
- ^ Schweri MM, Skolnick P, Rafferty MF, Rice KC, Janowsky AJ, Paul SM (October 1985). “[3H]Threo-(+/-)-methylphenidate binding to 3,4-dihydroxyphenylethylamine uptake sites in corpus striatum: correlation with the stimulant properties of ritalinic acid esters”. Journal of Neurochemistry. 45 (4): 1062–70. doi:10.1111/j.1471-4159.1985.tb05524.x. PMID 4031878. S2CID 28720285.
- ^ Ding YS, Fowler JS, Volkow ND, Dewey SL, Wang GJ, Logan J, et al. (May 1997). “Chiral drugs: comparison of the pharmacokinetics of [11C]d-threo and L-threo-methylphenidate in the human and baboon brain”. Psychopharmacology. 131 (1): 71–8. doi:10.1007/s002130050267. PMID 9181638. S2CID 26046917.
- ^ Ding YS, Gatley SJ, Thanos PK, Shea C, Garza V, Xu Y, et al. (September 2004). “Brain kinetics of methylphenidate (Ritalin) enantiomers after oral administration”. Synapse. 53 (3): 168–75. CiteSeerX 10.1.1.514.7833. doi:10.1002/syn.20046. PMID 15236349. S2CID 11664668.
- ^ Davids E, Zhang K, Tarazi FI, Baldessarini RJ (February 2002). “Stereoselective effects of methylphenidate on motor hyperactivity in juvenile rats induced by neonatal 6-hydroxydopamine lesioning”. Psychopharmacology. 160 (1): 92–8. doi:10.1007/s00213-001-0962-5. PMID 11862378. S2CID 8037050.
- ^ Williard RL, Middaugh LD, Zhu HJ, Patrick KS (February 2007). “Methylphenidate and its ethanol transesterification metabolite ethylphenidate: brain disposition, monoamine transporters and motor activity”. Behavioural Pharmacology. 18 (1): 39–51. doi:10.1097/FBP.0b013e3280143226. PMID 17218796. S2CID 20232871.
- ^ McGough JJ, Pataki CS, Suddath R (July 2005). “Dexmethylphenidate extended-release capsules for attention deficit hyperactivity disorder”. Expert Review of Neurotherapeutics. 5 (4): 437–41. doi:10.1586/14737175.5.4.437. PMID 16026226. S2CID 6561452.
- ^ Silva R, Tilker HA, Cecil JT, Kowalik S, Khetani V, Faleck H, Patin J (2004). “Open-label study of dexmethylphenidate hydrochloride in children and adolescents with attention deficit hyperactivity disorder”. Journal of Child and Adolescent Psychopharmacology. 14(4): 555–63. doi:10.1089/cap.2004.14.555. PMID 15662147.
- ^ Arnold LE, Lindsay RL, Conners CK, Wigal SB, Levine AJ, Johnson DE, et al. (Winter 2004). “A double-blind, placebo-controlled withdrawal trial of dexmethylphenidate hydrochloride in children with attention deficit hyperactivity disorder”. Journal of Child and Adolescent Psychopharmacology. 14 (4): 542–54. doi:10.1089/cap.2004.14.542. PMID 15662146.
- ^ Spencer TJ, Adler LA, McGough JJ, Muniz R, Jiang H, Pestreich L (June 2007). “Efficacy and safety of dexmethylphenidate extended-release capsules in adults with attention-deficit/hyperactivity disorder”. Biological Psychiatry. 61 (12): 1380–7. doi:10.1016/j.biopsych.2006.07.032. PMID 17137560. S2CID 45976373.
- ^ Teo SK, Scheffler MR, Wu A, Stirling DI, Thomas SD, Stypinski D, Khetani VD (February 2004). “A single-dose, two-way crossover, bioequivalence study of dexmethylphenidate HCl with and without food in healthy subjects”. Journal of Clinical Pharmacology. 44 (2): 173–8. doi:10.1177/0091270003261899. PMID 14747426. S2CID 20694072.
External links
- “Dexmethylphenidate”. Drug Information Portal. U.S. National Library of Medicine.
- “Dexmethylphenidate hydrochloride”. Drug Information Portal. U.S. National Library of Medicine.
///////////DEXMETHYLPHENIDATE, FDA 2021, APPROVALS 2021
Cl.[H][C@@](C(=O)OC)(C1=CC=CC=C1)[C@@]1([H])CCCCN1

NEW DRUG APPROVALS
ONE TIME
$10.00

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO