Home » Uncategorized (Page 17)
Category Archives: Uncategorized
METHOCARBAMOL

Methocarbamol
- Molecular FormulaC11H15NO5
- Average mass241.240 Da
- метокарбамол , ميثوكاربامول , 美索巴莫
1,2-Propanediol, 3-(2-methoxyphenoxy)-, 1-carbamate
208-524-3[EINECS]
2-Hydroxy-3-(2-methoxyphenoxy)propyl carbamate
532-03-6[RN]
MethocarbamolCAS Registry Number: 532-03-6
CAS Name: 3-(2-Methoxyphenoxy)-1,2-propanediol 1-carbamate
Additional Names: 3-(o-methoxyphenoxy)-2-hydroxypropyl 1-carbamate; 2-hydroxy-3-(o-methoxyphenoxy)propyl 1-carbamate; guaiacol glyceryl ether carbamate
Manufacturers’ Codes: AHR-85Trademarks: Neuraxin; Miolaxene (Lepetit); Lumirelax; Etroflex; Delaxin (Ferndale); Robamol (Cenci); Traumacut (Brenner-Efeka); Tresortil; Relestrid; Robaxin (Robins)
Molecular Formula: C11H15NO5, Molecular Weight: 241.24Percent Composition: C 54.77%, H 6.27%, N 5.81%, O 33.16%
Literature References: Prepn from 3-(o-methoxyphenoxy)-2-hydroxypropyl chlorocarbonate: Murphey, US2770649 (1956 to A. H. Robins). Comprehensive description: S. Alessi-Severini et al.,Anal. Profiles Drug Subs. Excip.23, 371-399 (1994).
Properties: Crystals from benzene, mp 92-94°. uv max (water): 222, 274 nm (E1%1cm 298, 94). 1og P -0.06. Soly in water at 20°: 2.5 g/100 ml. Sol in alcohol, propylene glycol. Sparingly sol in chloroform. Practically insol in n-hexane.
Melting point: mp 92-94°
Absorption maximum: uv max (water): 222, 274 nm (E1%1cm 298, 94)
Therap-Cat: Muscle relaxant (skeletal).
Therap-Cat-Vet: Muscle relaxant (skeletal).
Keywords: Muscle Relaxant (Skeletal).
Methocarbamol, sold under the brand name Robaxin among others, is a medication used for short-term musculoskeletal pain.[3][4] It may be used together with rest, physical therapy, and pain medication.[3][5][6] It is less preferred in low back pain.[3] It has limited use for rheumatoid arthritis and cerebral palsy.[3][7] Effects generally begin within half an hour.[3] It is taken by mouth or injection into a vein.[3]
Methocarbamol is a CNS depressant indicated with rest, physical therapy and other treatments to control the discomfort associated with various acute musculoskeletal conditions.
Methocarbamol was developed in the early 1950s as a treatment for muscle spasticity and the associated pain.6,7 It is a guaiacol glyceryl ether.7
Methocarbamol tablets and intramuscular injections are prescription medicines indicated in the United States as an adjunct to rest, physical therapy, and other measures for the relief of discomforts associated with acute, painful musculoskeletal conditions.Label,9 In Canada, methocarbamol can be sold as an over the counter oral medicine at a lower dose that may be combined with acetaminophen or ibuprofen.10 A combination product with acetylsalicylic acid and codeine is available in Canada by prescription.10
Methocarbamol was FDA approved on 16 July 1957.8
Common side effect include headaches, sleepiness, and dizziness.[3][8] Serious side effects may include anaphylaxis, liver problems, confusion, and seizures.[4] Use is not recommended in pregnancy and breastfeeding.[3][4] Because of risk of injury, skeletal muscle relaxants should generally be avoided in geriatric patients.[3] Methocarbamol is a centrally acting muscle relaxant.[3] How it works is unclear, but it does not appear to affect muscles directly.[3]
Methocarbamol was approved for medical use in the United States in 1957.[3] It is available as a generic medication.[3][4] It is relatively inexpensive as of 2016.[9] In 2019, it was the 136th most commonly prescribed medication in the United States, with more than 4 million prescriptions.[10][11]
SYN
CN 109970606

SYN
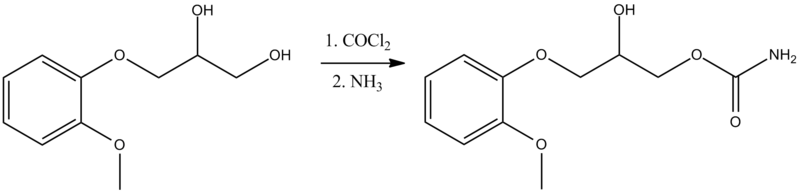
Synthesis of methocarbamol from guaifenesin. (a) methocarbamol and (b) β-isomer of methocarbamol.
SYN
https://www.sciencedirect.com/science/article/abs/pii/S0957416607003801
The muscle relaxant methocarbamol 2 and tranquilizer mephenoxalone 3, as well as intermediate cyclic carbonate 4, have been prepared in enantiopure form by starting from enantiopure guaifenesin 1 easily available by an entrainment resolution procedure. Thermal investigations reveal that 2 is probably a conglomerate forming substance, 3 forms a stable racemic compound, and 4 occupies an intermediate position. The enantiomeric excess of a binary phase eutectic point for these substances comprises 0%, 85%, and 10%, respectively.
Graphical abstract

PATENT
US 2770649
https://patents.google.com/patent/US2770649A/en
PAPER
Journal of pharmaceutical sciences (1970), 59(7), 1043-4

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Medical use
Methocarbamol is a muscle relaxant used to treat acute, painful musculoskeletal spasms in a variety of musculoskeletal conditions.[12] However, there is limited and inconsistent published research on the medication’s efficacy and safety in treating musculoskeletal conditions, primarily neck and back pain.[12]
Methocarbamol injection may have a beneficial effect in the control of the neuromuscular spasms of tetanus.[6] It does not, however, replace the current treatment regimen.[6]
It is not useful in chronic neurological disorders, such as cerebral palsy or other dyskinesias.[3]
Currently, there is some suggestion that muscle relaxants may improve the symptoms of rheumatoid arthritis; however, there is insufficient data to prove its effectiveness as well as answer concerns regarding optimal dosing, choice of muscle relaxant, adverse effects, and functional status.[7]
Comparison to similar agents
The clinical effectiveness of methocarbamol compared to other muscle relaxants is not well-known.[12] One trial of methocarbamol versus cyclobenzaprine, a well-studied muscle relaxant, in those with localized muscle spasm found there was no significant differences in their effects on improved muscle spasm, limitation of motion, or limitation of daily activities.[12]
Contraindications
There are few contraindications to methocarbamol. They include:
- Hypersensitivity to methocarbamol or to any of the injection components.[6]
- For the injectable form, suspected kidney failure or renal pathology, due to large content of polyethylene glycol 300 that can increase pre-existing acidosis and urea retention.[6]
Side effects
Methocarbamol is a centrally acting skeletal muscle relaxant that has significant adverse effects, especially on the central nervous system.[3]
Potential side effects of methocarbamol include:
- Most commonly drowsiness, blurred vision, headache, nausea, and skin rash.[8]
- Possible clumsiness (ataxia), upset stomach, flushing, mood changes, trouble urinating, itchiness, and fever.[13][14]
- Both tachycardia (fast heart rate) and bradycardia (slow heart rate) have been reported.[14]
- Hypersensitivity reactions and anaphylatic reactions are also reported.[5][6]
- May cause respiratory depression when combined with benzodiazepines, barbiturates, codeine, or other muscle relaxants.[15]
- May cause urine to turn black, blue or green.[13]
While the product label states that methocarbamol can cause jaundice, there is minimal evidence to suggest that methocarbamol causes liver damage.[8] During clinical trials of methocarbamol, there were no laboratory measurements of liver damage indicators, such as serum aminotransferase (AST/ALT) levels, to confirm hepatotoxicity.[8] Although unlikely, it is impossible to rule out that methocarbamol may cause mild liver injury with use.[8]
Elderly
Skeletal muscle relaxants are associated with an increased risk of injury among older adults.[16] Methocarbamol appeared to be less sedating than other muscle relaxants, most notably cyclobenzaprine, but had similar increased risk of injury.[15][16] Methocarbamol is cited along with “most muscle relaxants” in the 2012 Beers Criteria as being “poorly tolerated by older adults, because of anticholinergic adverse effects, sedation, increased risk of fractures,” noting that “effectiveness dosages tolerated by older adults is questionable.”[17]
Pregnancy
Methocarbamol is labeled by the FDA as a pregnancy category C medication.[6] The teratogenic effects of the medication are not known and should be given to pregnant women only when clearly indicated.[6]
Overdose
There is limited information available on the acute toxicity of methocarbamol.[5][6] Overdose is used frequently in conjunction with CNS depressants such as alcohol or benzodiazepines and will have symptoms of nausea, drowsiness, blurred vision, hypotension, seizures, and coma.[6] There are reported deaths with an overdose of methocarbamol alone or in the presence of other CNS depressants.[5][6]
Abuse
Unlike other carbamates such as meprobamate and its prodrug carisoprodol, methocarbamol has greatly reduced abuse potential.[18] Studies comparing it to the benzodiazepine lorazepam and the antihistamine diphenhydramine, along with placebo, find that methocarbamol produces increased “liking” responses and some sedative-like effects; however, at higher doses dysphoria is reported.[18] It is considered to have an abuse profile similar to, but weaker than, lorazepam.[18]
Interactions
Methocarbamol may inhibit the effects of pyridostigmine bromide.[5][6] Therefore, methocarbamol should be used with caution in those with myasthenia gravis taking anticholinesterase medications.[6]
Methocarbamol may disrupt certain screening tests as it can cause color interference in laboratory tests for 5-hydroxy-indoleacetic acid (5-HIAA) and in urinary testing for vanillylmandelic acid (VMA) using the Gitlow method.[6]
Pharmacology
Mechanism of action
The mechanism of action of methocarbamol has not currently been established.[3] Its effect is thought to be localized to the central nervous system rather than a direct effect on skeletal muscles.[3] It has no effect on the motor end plate or the peripheral nerve fiber.[6] The efficacy of the medication is likely related to its sedative effect.[3] Alternatively, methocarbamol may act via inhibition of acetylcholinesterase, similarly to carbamate.[19]
Pharmacokinetics
In healthy individuals, the plasma clearance of methocarbamol ranges between 0.20 and 0.80 L/h/kg.[6] The mean plasma elimination half-life ranges between 1 and 2 hours, and the plasma protein binding ranges between 46% and 50%.[6] The elimination half-life was longer in the elderly, those with kidney problems, and those with liver problems.[6]
Metabolism
Methocarbamol is the carbamate derivative of guaifenesin, but does not produce guaifenesin as a metabolite, because the carbamate bond is not hydrolyzed metabolically;[8][6] its metabolism is by Phase I ring hydroxylation and O-demethylation, followed by Phase II conjugation.[6] All the major metabolites are unhydrolyzed carbamates.[20][21] Small amounts of unchanged methocarbamol are also excreted in the urine.[5][6]
Society and culture
Methocarbamol was approved as a muscle relaxant for acute, painful musculoskeletal conditions in the United States in 1957.[8] Muscle relaxants are widely used to treat low back pain, one of the most frequent health problems in industrialized countries. Currently, there are more than 3 million prescriptions filled yearly.[8] Methocarbamol and orphenadrine are each used in more than 250,000 U.S. emergency department visits for lower back pain each year.[22] In the United States, low back pain is the fifth most common reason for all physician visits and the second most common symptomatic reason.[23] In 80% of primary care visits for low back pain, at least one medication was prescribed at the initial office visit and more than one third were prescribed two or more medications.[24] The most commonly prescribed drugs for low back pain included skeletal muscle relaxants.[25] Cyclobenzaprine and methocarbamol are on the U.S. Medicare formulary, which may account for the higher use of these products.[16]
Economics
The generic formulation of the medication is relatively inexpensive, costing less than the alternative metaxalone in 2016.[26][9]
Marketing

Generic methocarbamol 750mg tablet.
Methocarbamol without other ingredients is sold under the brand name Robaxin in the U.K., U.S., Canada[27] and South Africa; it is marketed as Lumirelax in France, Ortoton in Germany and many other names worldwide.[28] In combination with other active ingredients it is sold under other names: with acetaminophen (paracetamol), under trade names Robaxacet and Tylenol Body Pain Night; with ibuprofen as Robax Platinum; with acetylsalicylic acid as Robaxisal in the U.S. and Canada.[29][30] However, in Spain the tradename Robaxisal is used for the paracetamol combination instead of Robaxacet.[citation needed] These combinations are also available from independent manufacturers under generic names.[citation needed]
Research
Although opioids are a typically first line in treatment of severe pain, several trials suggest that methocarbamol may improve recovery and decrease hospital length of stay in those with muscles spasms associated with rib fractures.[31][32][33] However, methocarbamol was less useful in the treatment of acute traumatic pain in general.[34]
Long-term studies evaluating the risk of development of cancer in using methocarbamol have not been performed.[5][6] There are currently no studies evaluating the effect of methocarbamol on mutagenesis or fertility.[5][6]
The safety and efficacy of methocarbamol has not been established in pediatric individuals below the age of 16 except in tetanus.[5][6]
References
- ^ “Robaxin-750 – Summary of Product Characteristics (SmPC)”. (emc). 8 August 2017. Retrieved 19 April 2020.
- ^ Sica DA, Comstock TJ, Davis J, Manning L, Powell R, Melikian A, Wright G (1990). “Pharmacokinetics and protein binding of methocarbamol in renal insufficiency and normals”. European Journal of Clinical Pharmacology. 39 (2): 193–4. doi:10.1007/BF00280060. PMID 2253675. S2CID 626920.
- ^ Jump up to:a b c d e f g h i j k l m n o p q r “Methocarbamol Monograph for Professionals”. Drugs.com. American Society of Health-System Pharmacists.
- ^ Jump up to:a b c d British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. p. 1093. ISBN 9780857113382.
- ^ Jump up to:a b c d e f g h i “Robaxin- methocarbamol tablet, film coated”. DailyMed. 18 July 2019. Retrieved 19 April 2020.
- ^ Jump up to:a b c d e f g h i j k l m n o p q r s t u v w x “Robaxin- methocarbamol injection”. DailyMed. 10 December 2018. Retrieved 19 April 2020.
- ^ Jump up to:a b Richards, Bethan L.; Whittle, Samuel L.; Buchbinder, Rachelle (18 January 2012). “Muscle relaxants for pain management in rheumatoid arthritis”. The Cochrane Database of Systematic Reviews. 1: CD008922. doi:10.1002/14651858.CD008922.pub2. ISSN 1469-493X. PMID 22258993.
- ^ Jump up to:a b c d e f g h “Methocarbamol”. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. National Institute of Diabetes and Digestive and Kidney Diseases. 30 January 2017. PMID 31643609.
- ^ Jump up to:a b Fine, Perry G. (2016). The Hospice Companion: Best Practices for Interdisciplinary Care of Advanced Illness. Oxford University Press. p. PT146. ISBN 978-0-19-045692-4.
- ^ “The Top 300 of 2019”. ClinCalc. Retrieved 16 October 2021.
- ^ “Methocarbamol – Drug Usage Statistics”. ClinCalc. Retrieved 16 October 2021.
- ^ Jump up to:a b c d Chou, Roger; Peterson, Kim; Helfand, Mark (August 2004). “Comparative efficacy and safety of skeletal muscle relaxants for spasticity and musculoskeletal conditions: a systematic review”. Journal of Pain and Symptom Management. 28 (2): 140–175. doi:10.1016/j.jpainsymman.2004.05.002. ISSN 0885-3924. PMID 15276195.
- ^ Jump up to:a b “Methocarbamol”. MedlinePlus. Retrieved 18 April 2020.
- ^ Jump up to:a b “Methocarbamol Side Effects: Common, Severe, Long Term”. Drugs.com. Retrieved 18 April 2020.
- ^ Jump up to:a b See, Sharon; Ginzburg, Regina (1 August 2008). “Choosing a skeletal muscle relaxant”. American Family Physician. 78 (3): 365–70. ISSN 0002-838X. PMID 18711953.
- ^ Jump up to:a b c Spence, Michele M.; Shin, Patrick J.; Lee, Eric A.; Gibbs, Nancy E. (July 2013). “Risk of injury associated with skeletal muscle relaxant use in older adults”. The Annals of Pharmacotherapy. 47 (7–8): 993–8. doi:10.1345/aph.1R735. ISSN 1542-6270. PMID 23821610. S2CID 9037478.
- ^ “Beers Criteria Medication List”. DCRI. Retrieved 18 October 2020.
- ^ Jump up to:a b c Preston KL, Wolf B, Guarino JJ, Griffiths RR (1992). “Subjective and behavioral effects of diphenhydramine, lorazepam and methocarbamol: evaluation of abuse liability”. Journal of Pharmacology and Experimental Therapeutics. 262 (2): 707–20. PMID 1501118.
- ^ PubChem. “Methocarbamol”. pubchem.ncbi.nlm.nih.gov. Retrieved 6 July 2020.
- ^ Methocarbamol. In: DRUGDEX System [intranet database]. Greenwood Village, Colorado: Thomson Healthcare; c1974–2009 [cited 2009 Feb 10].
- ^ Bruce RB, Turnbull LB, Newman JH (January 1971). “Metabolism of methocarbamol in the rat, dog, and human”. J Pharm Sci. 60 (1): 104–6. doi:10.1002/jps.2600600120. PMID 5548215.
- ^ Friedman BW, Cisewski D, Irizarry E, Davitt M, Solorzano C, Nassery A, et al. (March 2018). “A Randomized, Double-Blind, Placebo-Controlled Trial of Naproxen With or Without Orphenadrine or Methocarbamol for Acute Low Back Pain”. Annals of Emergency Medicine. 71 (3): 348–356.e5. doi:10.1016/j.annemergmed.2017.09.031. ISSN 1097-6760. PMC 5820149. PMID 29089169.
- ^ Chou, Roger; Huffman, Laurie Hoyt (2 October 2007). “Medications for Acute and Chronic Low Back Pain: A Review of the Evidence for an American Pain Society/American College of Physicians Clinical Practice Guideline”. Annals of Internal Medicine. 147 (7): 505–14. doi:10.7326/0003-4819-147-7-200710020-00008. ISSN 0003-4819. PMID 17909211. S2CID 32719708.
- ^ Cherkin, D. C.; Wheeler, K. J.; Barlow, W.; Deyo, R. A. (1 March 1998). “Medication use for low back pain in primary care”. Spine. 23 (5): 607–14. doi:10.1097/00007632-199803010-00015. ISSN 0362-2436. PMID 9530793. S2CID 23664539.
- ^ Luo, Xuemei; Pietrobon, Ricardo; Curtis, Lesley H.; Hey, Lloyd A. (1 December 2004). “Prescription of nonsteroidal anti-inflammatory drugs and muscle relaxants for back pain in the United States”. Spine. 29 (23): E531–7. doi:10.1097/01.brs.0000146453.76528.7c. ISSN 1528-1159. PMID 15564901. S2CID 72742439.
- ^ Robbins, Lawrence D. (2013). Management of Headache and Headache Medications. Springer Science & Business Media. p. PT147. ISBN 978-1-4612-2124-1.
- ^ “ROBAXIN product appearance in Canada”. ctchealth.ca. Retrieved 13 December 2021.
- ^ “Methocarbamol”. Drugs.com. Retrieved 12 May 2018.
- ^ “New Drugs and Indications Reviewed at the May 2003 DEC Meeting” (PDF). ESI Canada. Archived from the original (PDF) on 10 July 2011. Retrieved 14 November 2008.
- ^ “Tylenol Body Pain Night Overview and Dosage”. Tylenol Canada. Archived from the original (website) on 31 March 2012. Retrieved 23 April 2012.
- ^ Patanwala, Asad E.; Aljuhani, Ohoud; Kopp, Brian J.; Erstad, Brian L. (October 2017). “Methocarbamol use is associated with decreased hospital length of stay in trauma patients with closed rib fractures”. The American Journal of Surgery. 214 (4): 738–42. doi:10.1016/j.amjsurg.2017.01.003. ISSN 0002-9610. PMID 28088301.
- ^ Deloney, Lindsay; Smith, Melanie; Carter, Cassandra; Privette, Alicia; Leon, Stuart; Eriksson, Evert (January 2020). “946: Methocarbamol reduces opioid use and length of stay in young adults with traumatic rib fractures”. Critical Care Medicine. 48 (1): 452. doi:10.1097/01.ccm.0000633320.62811.06. ISSN 0090-3493.
- ^ Smith, Melanie; Deloney, Lindsay; Carter, Cassandra; Leon, Stuart; Privette, Alicia; Eriksson, Evert (January 2020). “1759: Use of methocarbamol in geriatric patients with rib fractures is associated with improved outcomes”. Critical Care Medicine. 48 (1): 854. doi:10.1097/01.ccm.0000649332.10326.98. ISSN 0090-3493.
- ^ Aljuhani, Ohoud; Kopp, Brian J.; Patanwala, Asad E. (2017). “Effect of Methocarbamol on Acute Pain After Traumatic Injury”. American Journal of Therapeutics. 24 (2): e202–6. doi:10.1097/mjt.0000000000000364. ISSN 1075-2765. PMID 26469684. S2CID 24284482.
External links
- “Methocarbamol”. Drug Information Portal. U.S. National Library of Medicine.
| Clinical data | |
|---|---|
| Trade names | Robaxin, Marbaxin, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682579 |
| License data | US DailyMed: Methocarbamol |
| Pregnancy category | AU: B2 |
| Routes of administration | By mouth, intravenous |
| ATC code | M03BA03 (WHO) M03BA53 (WHO) M03BA73 (WHO) |
| Legal status | |
| Legal status | CA: OTCUK: POM (Prescription only) [1]US: ℞-only |
| Pharmacokinetic data | |
| Metabolism | Liver |
| Elimination half-life | 1.14–1.24 hours[2] |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 532-03-6 |
| PubChem CID | 4107 |
| IUPHAR/BPS | 6829 |
| DrugBank | DB00423 |
| ChemSpider | 3964 |
| UNII | 125OD7737X |
| KEGG | D00402 |
| ChEBI | CHEBI:6832 |
| ChEMBL | ChEMBL1201117 |
| CompTox Dashboard (EPA) | DTXSID6023286 |
| ECHA InfoCard | 100.007.751 |
| Chemical and physical data | |
| Formula | C11H15NO5 |
| Molar mass | 241.243 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (what is this?) (verify) |
- Sica DA, Comstock TJ, Davis J, Manning L, Powell R, Melikian A, Wright G: Pharmacokinetics and protein binding of methocarbamol in renal insufficiency and normals. Eur J Clin Pharmacol. 1990;39(2):193-4. [Article]
- Bruce RB, Turnbull LB, Newman JH: Metabolism of methocarbamol in the rat, dog, and human. J Pharm Sci. 1971 Jan;60(1):104-6. [Article]
- Witenko C, Moorman-Li R, Motycka C, Duane K, Hincapie-Castillo J, Leonard P, Valaer C: Considerations for the appropriate use of skeletal muscle relaxants for the management of acute low back pain. P T. 2014 Jun;39(6):427-35. [Article]
- Crankshaw DP, Raper C: Mephenesin, methocarbamol, chlordiazepoxide and diazepam: actions on spinal reflexes and ventral root potentials. Br J Pharmacol. 1970 Jan;38(1):148-56. doi: 10.1111/j.1476-5381.1970.tb10343.x. [Article]
- Muir WW 3rd, Sams RA, Ashcraft S: The pharmacology and pharmacokinetics of high-dose methocarbamol in horses. Equine Vet J Suppl. 1992 Feb;(11):41-4. [Article]
- Authors unspecified: Methocarbamol-A New Lissive Agent. Can Med Assoc J. 1958 Dec 15;79(12):1008-9. [Article]
- O’DOHERTY DS, SHIELDS CD: Methocarbamol; new agent in treatment of neurological and neuromuscular diseases. J Am Med Assoc. 1958 May 10;167(2):160-3. [Article]
- FDA Approved Drug Products: Robaxin [Link]
- FDA Approved Drug Products: Robaxin Intramuscular Injection [Link]
- Pfizer Canada: Robax [Link]
////////////////Methocarbamol, метокарбамол , ميثوكاربامول , 美索巴莫, AHS 85, Muscle Relaxant
COC1=C(OCC(O)COC(N)=O)C=CC=C1

NEW DRUG APPROVALS
ONE TIME
$10.00
L-CARNOSINE

L-CARNOSINE
- Molecular FormulaC9H14N4O3
- Average mass226.232 Da
(2S)-2-(3-aminopropanamido)-3-(1H-imidazol-5-yl)propanoic acid
(E)-N-(3-Amino-1-hydroxypropylidene)-L-histidine [ACD/IUPAC Name]
206-169-9[EINECS], 305-84-0[RN]
8HO6PVN24Wカルノシン , Dragosine, Ignotin, Ignotine, Karnozin, L-Carnosine, N-(β-Alanyl)-L-histidine, NSC 524045, Sevitin, β-Alanylhistidine
CarnosineCAS Registry Number: 305-84-0CAS Name: b-Alanyl-L-histidine
Additional Names: ignotine
Molecular Formula: C9H14N4O3, Molecular Weight: 226.23
Percent Composition: C 47.78%, H 6.24%, N 24.77%, O 21.22%
Literature References: Naturally occurring dipeptide found in large amounts in skeletal muscle. Also present in other tissues such as brain, cardiac muscle, kidney. Water soluble antioxidant; functions as a free-radical scavenger. Isoln: Gulewitsch, Amiradzibi, Ber.33, 1902 (1900); Wolff, Wilson, J. Biol. Chem.95, 495 (1932); 109, 565 (1935). Synthesis from histidine and b-iodo- or b-nitropropionyl chloride: Baumann, Ingvaldsen, ibid.35, 271 (1918); Barger, Tutin, Biochem. J.12, 406 (1918). Later syntheses: Sifford, du Vigneaud, J. Biol. Chem.108, 753 (1935); R. A. Turner, J. Am. Chem. Soc.75, 2388 (1953); F. J. Vinick, S. Jung, J. Org. Chem.48, 392 (1983). Crystal structure: H. Itoh et al.,Acta Crystallogr.33B, 2959 (1977). Possible role in wound healing: D. E. Fischer et al.,Proc. Soc. Exp. Biol. Med.158, 402 (1978). Review of physiological properties and therapeutic potential: S. E. Gariballa, A. J. Sinclair, Age Ageing29, 207-210 (2000).
Properties: Crystals from aqueous ethanol, mp 262° (dec) (Vinick, Jung); also reported as mp 260° (capillary tube) and as mp 308-309° (Dennis bar) (Sifford, du Vigneaud). [a]D25 +21.0° (c = 1.5 in water). pK1 2.64; pK2 6.83; pK3 9.51. Alkaline reaction. One gram dissolves in 3.1 ml water at 25°.
Melting point: mp 262° (dec) (Vinick, Jung); mp 260° (capillary tube) and as mp 308-309° (Dennis bar) (Sifford, du Vigneaud)
pKa: pK1 2.64; pK2 6.83; pK3 9.51
Optical Rotation: [a]D25 +21.0° (c = 1.5 in water)
Derivative Type: Nitrate
CAS Registry Number: 5852-98-2
Molecular Formula: C9H15N5O6, Molecular Weight: 289.25
Percent Composition: C 37.37%, H 5.23%, N 24.21%, O 33.19%
Properties: Crystals, dec 222°. [a]D20 +24.1° (c = 1.5 in water). Very sol in water.
Optical Rotation: [a]D20 +24.1° (c = 1.5 in water)
Derivative Type: Hydrochloride
CAS Registry Number: 5852-99-3
Molecular Formula: C9H15ClN4O3, Molecular Weight: 262.69
Percent Composition: C 41.15%, H 5.76%, Cl 13.50%, N 21.33%, O 18.27%
Properties: Crystals, dec 245°. Very sol in water.
Derivative Type: D-Form
CAS Registry Number: 5853-00-9
Properties: Crystals, mp 260°. [a]D28 -20.4° (c = 1.5).
Melting point: mp 260°
Optical Rotation: [a]D28 -20.4° (c = 1.5)
Carnosine (beta-alanyl-L-histidine) is a dipeptide molecule, made up of the amino acids beta-alanine and histidine. It is highly concentrated in muscle and brain tissues.[citation needed] Carnosine was discovered by Russian chemist Vladimir Gulevich.[2]
Carnosine is naturally produced by the body in the liver[3] from beta-alanine and histidine. Like carnitine, carnosine is composed of the root word carn, meaning “flesh”, alluding to its prevalence in meat.[4] There are no plant-based sources of carnosine,[5] however synthetic supplements do exist.

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT
SYN
WO2009033754 PAGE: 98 claimed protein
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2009033754
SYN
Showa Igakkai Zasshi 1974, V34(3), P271-83
Russian Journal of General Chemistry 2007, V77(9), P1576-1579
Chemische Berichte 1961, V94, P2768-78
Farmaco, Edizione Scientifica 1968, V23(9), P859-69
Paper
Journal of the American Chemical Society 1953, V75, P2388-90
| +21.9 ° |
Conc: 3.0 g/100mL;water ; Wavlenght: 589.3 nm; Temp: 20 °C
Annali di Chimica (Rome, Italy) 1968, V58(11), P1431-4
Z. physiol. Chem. 1914, V87, P1-11
PAPER
Chemistry – A European Journal (2003), 9, (8), 1714-1723.
PAPER
Journal of Magnetic Resonance (2003), 164, (2), 256-269.

SYN
WO 2001064638
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2001064638
Example 1
(S) -2- (Cyanoacetylamino) -3- (l_ * H-imidazol-4-yl) propionic acid, sodium salt
To a solution of sodium ethoxide obtained by dissolving 5.57 g (0.24 mol) of sodium in 800 ml of ethanol was added 40.0 g (0.26 mol) of L-histidine at room temperature. After 15 minutes, 44.12 g (0.39 mol) of ethyl cyanoacetate were added and the suspension was refluxed for 16 hours. After cooling to room temperature, the mixture was filtered. The yellowish filtrate was concentrated in vacuo, the residue was slurried in ethyl acetate, filtered, washed with ethyl acetate and purified by flash chromatography on silica gel (eluent: gradient ethyl acetate → methanol / ethyl acetate 3: 1).
Yield: 28.42 g (46%)
1HNMR (DMSO- ^ 6, 00 MHz): δ = 8,28 (d, 1H); 7,45 (s, 1H); 6,7 (s, 1H); 5,5 (br. s, 1H); 4,12-4,20 (m, 1H); 3,65 (s, 2H); 2,95-3,05 (m, 1H); 2,8-2,9 (m, 1H).
13C NMR (DMSO- 6, 100 MHz): δ = 174,05; 161,09; 134,25; 131,97; 119,66; 116,43; 54,83; 29,13; 25,20.
Example 2
(• S) -2- (Cyanoacetylamino) -3- (1-δ-imidazol-4-yl) propionic acid, sodium salt
9.80 g of sodium hydride (60% in mineral oil) and 50.6 g
(0.51 mol) were added at room temperature to a suspension of 40.0 g (0.26 mol) of L-histidine in 750 ml of N, N-dimethylformamide Given methyl cyanoacetate. The mixture was heated to 155 ° C. for 2 h in an open flask and the solution thus obtained was analyzed by means of HPLC.
Histidine (8 area%) and (S) -2- (cyanoacetylamino) -3- (1H-imidazol-4-yl) propionic acid sodium salt (38 area%) were identified.
Example 3
(S) -2- (Cyanoacetylamino) -3- (l-ö r -imidazol-4-yl) propionic acid
To a solution of sodium ethoxide obtained by dissolving 4.02 g (0.175 mol) of sodium in 280 ml of ethanol, 28.27 g (0.18 mol) of L-Ηistidine were added at room temperature. The mixture was heated slowly and 30.92 g (0.27 mol) of ethyl cyanoacetate were added dropwise at a temperature of 60.degree. The mixture was heated further and the ethanol was distilled off, the amount of ethanol distilled off being continuously replaced in portions by N, N-dimethylformamide. At the end of the reaction, the temperature of the solution was 130 ° C. The mixture was stirred at this temperature for a further 2 hours. The brown reaction mixture (200 g) was cooled to 50 ° C. and 30 g of concentrated hydrochloric acid were metered in. About 70 g of solvent (Η 2O / N, N-dimethylformamide mixture) distilled off. The viscous suspension was mixed with 200 g of acetone, cooled to -10 ° C. and filtered. For recrystallization, the residue was dissolved in water and the pH was adjusted to 5.0. On cooling (<5 ° C.) a white solid precipitated out, which was filtered off, washed with ethanol and dried at 40 ° C./20 mbar.
Yield: 26.39 g (66%).
IR (KBr): v = 3421, 3240, 3149, 3059, 2970, 2255, 1653, 1551, 1396, 1107, 1088, 979, 965, 826, 786, 638 cm is “1 .
1HΝMR (DMSO-c 6 , 400 MHz): δ = 11.0 (br., 2H); 8.50 (d, 1H); 7.68 (s, 1H); 6.85 (s, 1H); 4.35-4.48 ( m, 1H); 3.68 (s, 2H); 2.92-3.03 (, 1H); 2.82-2.91 (m, 1H).
13 C NMR (DMSO- 6 , 100 MHz): δ = 172.23; 161.92; 134.55; 132.70; 116.73; 115.87; 52.80; 28.68; 25.06.
LC-MS: mlz = 223 ([M + H]), 205, 177, 156, 110.
The optical purity was determined to be> 99.8% on a sample obtained according to the above procedure. The determination was carried out by hydrolysis of the amide bond (6 N hydrochloric acid, 110 ° C., 24 h), followed by derivatization of the released histidine with trifluoroacetic anhydride and isobutyl chloroformate. A D-histidine content of <0.1% was detected by gas chromatography on a chiral stationary phase.
Example 4
L-Carnosine
To a solution of 1.90 g (7.8 mmol) of (<S) -2- (cyanoacetylamino) -3- (1H-imidazol-4-yl) propionic acid sodium salt (prepared according to Example 1) in 50 ml of ethanol / conc.
Ammonia solution (V: V- 4: 1) were given 0.3 g of rhodium / activated charcoal (5% Rh). The
The mixture was hydrogenated at 110 ° C. and 45 bar for 1 hour. The catalyst was then filtered off and the filtrate was adjusted to pH 8.2 with formic acid. After the solution had been concentrated in vacuo, the residue was suspended in 200 ml of ethanol and heated to 60 ° C. for 30 minutes. The product was filtered off, washed successively with ethanol, ethyl acetate and diethyl ether and finally dried.
Yield: 1.33 g (76%)
1H NMR (D 2 O, 400 MΗz): δ = 7.70 (s, 1Η); 6.93 (s, 1Η); 4.43-4.50 (m, 1Η); 3.20-3.28 (m, 2Η); 3.11-3.19 (m, 1H); 2.95-3.03 (m, 1H); 2.61-2.71 (m, 2H).
The optical purity was determined by the method described in Example 3 to be 99.5%.
Example 5
(S) -2- (Cyanoacetylamino) -3- (1-O-imidazol-4-yl) propionic acid methyl ester
To a solution of sodium methoxide obtained by dissolving 0.94 g (40.7 mmol; 1.95 equiv.) Of sodium in 100 ml of methanol, 5.0 g (20.4 mmol) were added at room temperature
L-histidine methyl ester dihydrochloride added. After 30 minutes, 3.03 g
(30.6 mmol) of methyl cyanoacetate were added and the mixture was left on for 16 hours
Boiled under reflux. After cooling to room temperature, the mixture was filtered.
The yellowish filtrate was concentrated in vacuo and the residue was purified by means of flash chromatography on silica gel (eluent: gradient ethyl acetate – »ethyl acetate / methanol 3: 1).
Yield: 1.51 g (31%)
1H MR (OMSO-de, 400 MHz): δ = 8.65 (d, 1H); 7.52 (s. 1H); 6.8 (s, 1H); 4.45 ^ 1.55 (m,
1H); 3,69 (s, 2H); 3,62 (s, 3H); 3,3 (br., 1H); 2,82-2,98 (m, 2H).
Example 6
L-Carnosine
1.76 g of Rh / C (0.4 mol% of pure Rh based on the starting material used) in a mixture of 94.2 g of ammonia solution (25% in H 2 O) and 62.8 g of methanol were placed in a 1 liter pressure autoclave . The autoclave was closed, the contents were heated to 90 ° C. and 40 bar hydrogen was injected. A solution of 20.0 g (0.09 mol) (* S) -2- (cyanoacetylamino) -3- (1H-imidazol-4-yl) propionic acid (prepared according to Example 3) was then within one hour Mixture 94.2 g ammonia solution (25% in Η 2O) and 62.8 g of methanol are metered in. After a one hour post-reaction at 90 ° C., the reaction mixture was cooled to room temperature. The pressure in the autoclave was released and the catalyst was filtered off over activated charcoal. An HPLC in-process analysis showed that the clear greenish reaction solution (326.2 g) contained 5.74% (m / m) carnosine, which corresponds to a selectivity of 92% with complete conversion. The reaction mixture was then concentrated to approx. 60 g on a rotary evaporator. As a result of the dropwise addition of 174 g of ethanol, a white solid precipitated out, which was filtered off and dried at 50 ° C./20 mbar.
Ausbeute: 13,0 g (64%)
1H NMR (D2O, 400 MHz): δ = 7,70 (s, 1H); 6,93 (s, 1H); 4,43-4,50 (m, 1H); 3,20-3,28 (m, 2H); 3,11-3,19 (m, 1H); 2,95-3,03 (m, 1H); 2,61-2,71 (m, 2H).
I3C NMR (D20, 100 MHz): δ = 178,58; 172,39; 136,46; 133,90; 118,37; 55,99; 36,65; 33,09; 29,74.
LC-MS: m/z = 227 ([M+H]+), 210, 192, 164, 146, 136, 110.
Example 7
L-Carnosine
In a 1 liter pressure autoclave, a solution of 10.00 g (45.0 mmol) (S) -2- (cyanoacetylamino) -3 was added to 0.88 g of Rh / C (0.4 mol% of pure Rh based on the starting material used) – (1H-imidazol-4-yl) propionic acid (prepared according to Example 3) in a mixture of 157 g conc. NΗ 3/ Methanol (m / m = 3: 2) was added. The autoclave was closed and flushed twice with 40 bar nitrogen and once with hydrogen. The mixture was heated to 90 ° C. and 40 bar hydrogen was injected. After 3 h at 90 ° C., the reaction mixture was cooled to room temperature, the autoclave was depressurized and the catalyst was separated off by filtration. An in-process analysis (HPLC) showed that the reaction solution (147.2 g) contained 6.38% (m / m) carnosine, which corresponds to a selectivity of 92% when the conversion is complete. The reaction mixture was then concentrated to 41.2 g on a rotary evaporator. 124 g of ethanol were added dropwise at room temperature and the flask was placed in a refrigerator overnight. The next day the precipitate was filtered off, washed with ethanol and dried in a drying cabinet at 40 ° C./20 mbar. 7.96 g (78%) of a slightly greenish solid with a content (HPLC) of 98.0% (m / m) were obtained.
Example 8
L-Carnosine
The procedure was as described in Example 7, with the difference that 5% Rh on aluminum oxide was used as the catalyst. Under these conditions, L-carnosine was formed with 83% selectivity.
Example 9
L-Carnosine
4.5 g of Raney cobalt (doped with 0.3% iron) in 195 g of methanol were placed in a 1 liter pressure autoclave. A solution of 30.0 g (0.135 mol) (S) -2- (cyanoacetylamino) -3- (1H-imidazol-4-yl) propionic acid (prepared according to Example 3) in 375 g ammonia solution (25% in Η O) was admitted. The autoclave was closed and flushed twice with 40 bar nitrogen. Then 45 bar of hydrogen were injected and the contents were heated to 100 ° C. within half an hour. After an after-reaction of 3 hours at 100 ° C., the reaction mixture was cooled to room temperature and the pressure in the autoclave was released. An HPLC in-process analysis showed that the reaction solution (590.8 g) contained 4.68% (mim) carnosine, which corresponds to a selectivity of 91% with complete conversion.
Example 10
L-Carnosine
In a 100 ml
pressure autoclave were to a solution of 2.0 g (9.0 mmol) (ιS) -2- (cyanoacetylamino) -3- (lH-imidazol-4-yl) propionic acid (prepared according to Example 3) in a Mixture of 25 g of ammonia solution (25% in Η 2 O) and 13 g of methanol, 1.1 g of Raney nickel (doped with 1.8% molybdenum) were added. The autoclave was closed and placed in an oil bath preheated to 100.degree. After 10 minutes, 50 bar of hydrogen were injected. After 2.5 hours at 100 ° C., the reaction mixture was
cooled to room temperature and the pressure on the autoclave was released. An HPLC in-process analysis showed that the reaction solution (39.4 g) contained 4.54% (m / m) carnosine, which, with a conversion of 99%, corresponds to a selectivity of 89%.
Example 11
L-Carnosine
In a 1 liter pressure autoclave, 4.50 g of Raney cobalt (doped with 0.3% iron) in a mixture of 285 g of conc. Ammonia / methanol (mim = 1.9: 1) submitted. The autoclave was closed and flushed twice with 40 bar nitrogen. Then 45 bar of hydrogen were injected and the mixture was heated to 100.degree. A solution of 30.0 g (0.135 mol) of (S) -2- (cyanoacetylamino) -3- (1H-imidazol-4-yl) propionic acid (prepared according to Example 3) in a mixture of 285 g was then obtained within one hour conc. Ammonia / methanol (m / m = 1.9: 1) metered in. After a one hour post-reaction at 100 ° C., the reaction mixture was cooled to room temperature. The pressure in the autoclave was released and the catalyst was filtered off. A ΗPLC in-process analysis showed that the reddish brown reaction solution (310.5 g) contained 9.57% (m / m) carnosine,
Example 12
(S) -2- (Cyanoacetylamino) -3- (3-methyl-3-ö r -imidazol-4-yl) propionic acid, sodium salt
0.50 g (2.95 mmol) of 3-methyl-L-histidine were added at 40 ° C. to a solution of 0.20 g (2.94 mmol) of sodium ethoxide in 5.60 g of ethanol. The clear solution was heated to 60 ° C. and 0.50 g (4.43 mmol) ethyl cyanoacetate was added dropwise. The mixture was refluxed for 1 hour. Then 10 mg (0.15 mmol) of imidazole were added. The ethanol was then slowly distilled off and the amount of ethanol distilled off was continuously replaced in portions by N, N-dimethylformamide. After a subsequent reaction time of 2 h at 125 ° C., the reaction mixture was carefully concentrated and the residue was purified by means of flash column chromatography on silica gel (eluent: gradient ethyl acetate → ethyl acetate / methanol 2: 1). 0.49 g (64%) of a slightly yellowish solid were obtained.
DC: Rf •= 0,46 (Ethanol/H2O 3:7).
1H NMR (DMSO-öfe, 400 MHz): δ = 7,91 (d, 1H); 7,38 (s, 1H); 6,58 (s, 1H); 3,97 (q, 1H);
3,68 (s, 2H); 3,50 (s, 3H); 3,01 (dd, 1H); 2,85 (dd, 1H).
13C NMR (DMSO-^6, 100 MHz): δ = 171,54; 160,80; 136,95; 128,68; 126,91; 116,40;
54,26; 30,65; 25,97; 25,11.
LC-MS: m/z = 237 ([M+H]+), 219, 193, 191, 176, 166, 164, 150, 109.
Example 13
(S) -2- (3-aminopropionylamino) -3- (3-methyl-3Jϊ-imidazol-4-yl) propionic acid
(= anserine)
To a solution of 0.20 g (0.77 mmol) (5) -2- (cyanoacetylamino) -3- (3-methyl-3H-imidazol-4-yl) propionic acid sodium salt (prepared according to Example 12) in 2 , 4 g of methanol and 1.6 g of ammonia solution (25% in Η 2 O), 16 mg of rhodium / Al 2 O 3 (5% Rh) were added. The mixture was hydrogenated at 85 ° C. and 50 bar for 1 hour. The catalyst was then filtered off. Anserine could be clearly detected in the filtrate by means of thin-layer chromatography, HPLC (by co-injection with a commercial reference substance) and LC-MS.
Gross yield: approx. 45%.
TLC: R f = 0.25 (ethyl acetate / methanol / Ammom ‘ ak H 2 O 43: 35: 8: 10).
LC-MS: m / z = 241 ([M + H] +), 224, 206, 180, 170, 126, 109.

SYN

Synthesis of L-carnosine from two amino acids β -alanine-amide and L-histidine
SYN
https://pubs.rsc.org/en/content/articlelanding/2019/cy/c9cy01622h
L-Carnosine (L-Car, β-alanyl-L-histidine) is a bioactive dipeptide with important physiological functions. Direct coupling of unprotected β-Ala (β-alanine) with L-His (L-histidine) mediated by an enzyme is a promising method for L-Car synthesis. In this study, a new recombinant dipeptidase (SmPepD) from Serratia marcescens with a high synthetic activity toward L-Car was identified by a genome mining approach and successfully expressed in Escherichia coli. Divalent metal ions strongly promoted the synthetic activity of SmPepD, with up to 21.7-fold increase of activity in the presence of 0.1 mM MnCl2. Higher temperature, lower pH and increasing substrate loadings facilitated the L-Car synthesis. Pilot biocatalytic syntheses of L-Car were performed comparatively in batch and continuous modes. In the continuous process, an ultra-filtration membrane reactor with a working volume of 5 L was employed for catalyst retention. The dipeptidase, SmPepD, showed excellent operational stability without a significant decrease in space–time yield after 4 days. The specific yield of L-Car achieved was 105 gCar gcatalyst−1 by the continuous process and 30.1 gCar gcatalyst−1 by the batch process. A nanofiltration membrane was used to isolate the desired product L-Car from the reaction mixture by selectively removing the excess substrates, β-Ala and L-His. As a result, the final L-Car content was effectively enriched from 2.3% to above 95%, which gave L-Car in 99% purity after ethanol precipitation with a total yield of 60.2%. The recovered substrate mixture of β-Ala and L-His can be easily reused, which will enable the economically attractive and environmentally benign production of the dipeptide L-Car.



SYNhttps://patents.google.com/patent/US20170211105A1/en
- Carnosine is a dipeptide of the amino acids beta-alanine and histidine. It is highly concentrated in muscle and brain tissues.
- [0005]
β-Alanine (or beta-alanine) is a naturally occurring beta amino acid, which is an amino acid in which the amino group is at the β-position from the carboxylate group (i.e., two atoms away). - [0006]
β-Alanine is not used in the biosynthesis of any major proteins or enzymes. It is formed in vivo by the degradation of dihydrouracil and carnosine. It is a component of the naturally occurring peptides carnosine and anserine and also of pantothenic acid (vitamin B5), which itself is a component of coenzyme A. Under normal conditions, β-alanine is metabolized into acetic acid. - [0007]
β-Alanine is the rate-limiting precursor of carnosine, which is to say carnosine levels are limited by the amount of available β-alanine, not histidine. Supplementation with β-alanine has been shown to increase the concentration of carnosine in muscles, decrease fatigue in athletes and increase total muscular work done. - [0008]
Carnosine and beta-alanine are popular dietary supplements currently produced using chemical methods. Beta-alanine is also a synthetic precursor to pantothenic acid, the essential vitamin B5. Beta-alanine can also be used as a monomer for the production of a polymeric resin (U.S. Pat. No. 4,082,730). - [0009]
Naturally, carnosine is produced exclusively in animals from beta-alanine (via uracil) and histidine. In yeasts and animals, beta-alanine is typically produced by degradation of uracil. Chemically, carnosine can be synthesized from histidine and beta-alanine derivatives. For example, the coupling of an N-(thiocarboxy) anhydride of beta-alanine with histidine has been described (Vinick et al. A simple and efficient synthesis of L-carnosine. J. Org. Chem, 1983, 48(3), pp. 392-393). - [0010]
Beta-alanine can be produced synthetically by Michael addition of ammonia to ethyl- or methyl-acrylate. This requires the use of the caustic agent ammonia and high pressures. It is also natively produced in bacteria and yeasts in small quantities. In bacteria, beta-alanine is produced by decarboxylation of aspartate. Lysates of bacteria have been used in biocatalytic production from aspartate (Patent CN104531796A). - [0011]
There remains a need in the industry for a safer, more economical system for the production of carnosine and beta-alanine.
- [0105]
The present disclosure provides methods for the biosynthetic production of beta-alanine and carnosine using engineered microorganisms of the present invention. - [0106]
In one embodiment, a method of producing beta-alanine is provided. The method comprises providing a fermentation media comprising a carbon substrate, contacting said media with a recombinant yeast microorganism expressing an engineered beta-alanine biosynthetic pathway wherein said pathway comprises an aspartate to beta-alanine conversion (pathway step a), and culturing the yeast in conditions whereby beta-alanine is produced. - [0107]
In another embodiment of the present invention, a method of producing carnosine is provided. The method comprises providing a fermentation media comprising a carbon substrate, contacting said media with a recombinant yeast microorganism expressing an engineered carnosine biosynthetic pathway wherein said pathway comprises (i) an aspartate to beta-alanine conversion (pathway step a) and (ii) a beta-alanine to carnosine conversion (pathway step b), and culturing the yeast in conditions whereby carnosine is produced. - [0108]
In another embodiment of the present invention, a method of producing carnosine via biotransformation is provided. The method comprises providing a media comprising a carbon substrate and exogenously added beta-alanine, contacting said media with a recombinant yeast microorganism expressing an engineered carnosine biosynthetic pathway wherein said pathway comprises (i) a beta-alanine to carnosine conversion (pathway step b), and culturing the yeast in conditions whereby carnosine is produced. - [0109]
Some embodiments of the present invention comprise yeast strains designated ca1 and ca2 and are derived from S. cerevisiae strain S288C. Each encodes at least 2 foreign genes under inducible Gal promoters. Strain ca1 also contains an additional gene, panM. The specific proteins encoded by each strain and their sequences, source, and accession numbers are provided in Table 1. The genes for these proteins are synthesized with yeast-optimized codon usage, assembled into singular genetic cassettes, and then inserted into the HO locus of S288C under URA2 selection. Strains ca1 and ca2 served as parent strains to derivatives comprising various heterologous genes. Ca2 served as a parent strain for ca7, ca8, ca9, ca10, ca11, ca12, ca14, ca15 in which the carnosine synthase is a different ortholog. Strain ca1 served as the parent strain to strains ca19, ca20, ca21, ca22, ca23, ca24, ca27, and ca28 in which the aspartate decarboxylase is a different ortholog. The specific proteins encoded by each strain and their sequences, source, and accession numbers are provided in Table 2. - [0110]
Aspartate, histidine, and the cofactors involved in the carnosine and beta-alanine pathway are universal to all organisms, and thus the host organism could be any genetically tractable organism (plants, animals, bacteria, or fungi). Amongst yeasts, other species such as S. pombe or P. pastoris are plausible alternatives. Within the S. cerevisiae species, other strains more amenable to large-scale productions, such as CENPalpha, may be utilized. - [0111]
The Gal promoter used in embodiments of the present invention could be replaced with constitutive promoters, or other chemically-inducible, growth phase-dependent, or stress-induced promoters. Heterologous genes of the present invention may be genomically encoded or alternatively encoded on plasmids or yeast artificial chromosomes (YACs). All genes introduced could be encoded with alternate codon usage without altering the biochemical composition of the system. All enzymes used in embodiments of the present invention have extensive orthologs in the biosphere that could be encoded as alternatives. - [0112]
Aspartate, histidine, and the cofactors involved in this pathway are universal to all organisms, and thus the host organism could be any genetically tractable organism (plants, animals, bacteria, or fungi). Among yeast, other species such as S. pombe or P. pastoris are plausible alternatives. Within the S. cerevisiae species, other strains more amenable to large scale productions, such as CENPalpha, may be preferable. The panD gene can replaced with orthologs from other bacteria. Examples include Corynebacterium glutamicum Escherichia coli, Helicobacter pylori, Tribolium castaneum, Pectobacterium carotovorum, Actinoplanes sp. SE50/110, Taoultella ornithinolytica, Methanocaldococcus jannaschii DSM 2661 and Methanocaldococcus bathoardescens. This is shown in Table 2. Carnosine synthase is natively found in mammals, birds, and reptiles. Therefore, the chicken enzyme used in ca1 and ca2 could be replaced by various orthologs. Examples include Gorilla gorilla, Falco perefrinus, Allpiucator mississsippiensis, Ailuoropoda melanoleuca, Ursus maritimus, Python bivittatus, and Orcinus orca. This is shown in Table 2.
Culture Conditions
- [0113]
The growth medium used to test for production of carnosine by the engineered strains was Teknova SC Minimal Broth with Raffinose supplemented with 1% galactose. - [0114]
A variety of purification protocols including solid phase extraction and cation exchange chromatography may be employed to purify the desired products from the culture supernatant or the yeast cell pellet fraction.
SYN




| Names | |
|---|---|
| Preferred IUPAC name(2S)-2-(3-Aminopropanamido)-3-(3H-imidazol-4-yl)propanoic acid | |
| Other namesβ-Alanyl-L-histidine | |
| Identifiers | |
| CAS Number | 305-84-0 |
| 3D model (JSmol) | Interactive imageInteractive image |
| ChEBI | CHEBI:15727 |
| ChEMBL | ChEMBL242948 |
| ChemSpider | 388363 |
| ECHA InfoCard | 100.005.610 |
| IUPHAR/BPS | 4559 |
| KEGG | C00386 |
| PubChem CID | 439224 |
| UNII | 8HO6PVN24W |
| CompTox Dashboard (EPA) | DTXSID80879594 |
| showInChI | |
| showSMILES | |
| Properties | |
| Chemical formula | C9H14N4O3 |
| Molar mass | 226.236 g·mol−1 |
| Appearance | Crystalline solid |
| Melting point | 253 °C (487 °F; 526 K) (decomposition) |
| Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| Infobox references |

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Biosynthesis
Carnosine is synthesized within the body from beta-alanine and histidine. Beta-alanine is a product of pyrimidine catabolism[6] and histidine is an essential amino acid. Since beta-alanine is the limiting substrate, supplementing just beta-alanine effectively increases the intramuscular concentration of carnosine.[7][8]
Physiological effects
pH buffer
Carnosine has a pKa value of 6.83, making it a good buffer for the pH range of animal muscles.[9] Since beta-alanine is not incorporated into proteins, carnosine can be stored at relatively high concentrations (millimolar). Occurring at 17–25 mmol/kg (dry muscle),[10] carnosine (β-alanyl-L-histidine) is an important intramuscular buffer, constituting 10-20% of the total buffering capacity in type I and II muscle fibres.
Anti-oxidant
Carnosine has been proven to scavenge reactive oxygen species (ROS) as well as alpha-beta unsaturated aldehydes formed from peroxidation of cell membrane fatty acids during oxidative stress. It also buffers pH in muscle cells, and acts as a neurotransmitter in the brain. It is also a zwitterion, a neutral molecule with a positive and negative end.[citation needed]
Antiglycating
Carnosine acts as an antiglycating agent, reducing the rate of formation of advanced glycation end-products (substances that can be a factor in the development or worsening of many degenerative diseases, such as diabetes, atherosclerosis, chronic kidney failure, and Alzheimer’s disease[11]), and ultimately reducing development of atherosclerotic plaque build-up.[12][13][14]
Geroprotective
Carnosine is considered as a geroprotector.[15] Carnosine can increase the Hayflick limit in human fibroblasts,[16] as well as appearing to reduce the telomere shortening rate.[17] Carnosine may also slow aging through its anti-glycating properties (chronic glycolysis is speculated to accelerate aging).[18]
Other
Carnosine can chelate divalent metal ions.[12]
Carnosine administration has been shown to have cardioprotective properties, protecting against ischaemia-reperfusion injury, and doxorubicin-induced cardiomyopathy.[19]
Carnosine demonstrated neuroprotective effects in multiple animal studies.[20][21][22]
Research has demonstrated a positive association between muscle tissue carnosine concentration and exercise performance.[23][24][25] β-Alanine supplementation is thought to increase exercise performance by promoting carnosine production in muscle. Exercise has conversely been found to increase muscle carnosine concentrations, and muscle carnosine content is higher in athletes engaging in anaerobic exercise.[23]
Carnosine appears to protect in experimental ischemic stroke by influencing a number of mechanisms that are activated during stroke. It is a potent pH buffer and has anti matrix metalloproteinase activity, antioxidant and antiexcitotoxic properties and protects the blood brain barrier [26], [27], [28], [29], [30], [31], [32]. [33], [34], [35].
References
- ^ “C9625 L-Carnosine ~99%, crystalline”. Sigma-Aldrich.
- ^ Gulewitsch, Wl.; Amiradžibi, S. (1900). “Ueber das Carnosin, eine neue organische Base des Fleischextractes”. Berichte der Deutschen Chemischen Gesellschaft. 33 (2): 1902–1903. doi:10.1002/cber.19000330275.
- ^ Trexler, Eric T.; Smith-Ryan, Abbie E.; Stout, Jeffrey R.; Hoffman, Jay R.; Wilborn, Colin D.; Sale, Craig; Kreider, Richard B.; Jäger, Ralf; Earnest, Conrad P.; Bannock, Laurent; Campbell, Bill (2015-07-15). “International society of sports nutrition position stand: Beta-Alanine”. Journal of the International Society of Sports Nutrition. 12: 30. doi:10.1186/s12970-015-0090-y. ISSN 1550-2783. PMC 4501114. PMID 26175657.
- ^ Hipkiss, A. R. (2006). “Does chronic glycolysis accelerate aging? Could this explain how dietary restriction works?”. Annals of the New York Academy of Sciences. 1067 (1): 361–8. Bibcode:2006NYASA1067..361H. doi:10.1196/annals.1354.051. PMID 16804012. S2CID 41175541.
- ^ Alan R. Hipkiss (2009). “Chapter 3: Carnosine and Its Possible Roles in Nutrition and Health”. Advances in Food and Nutrition Research.
- ^ “beta-ureidopropionate + H2O => beta-alanine + NH4+ + CO2”. reactome. Retrieved 2020-02-08.
Cytosolic 3-ureidopropionase catalyzes the reaction of 3-ureidopropionate and water to form beta-alanine, CO2, and NH3 (van Kuilenberg et al. 2004).
- ^ Derave W, Ozdemir MS, Harris R, Pottier A, Reyngoudt H, Koppo K, Wise JA, Achten E (August 9, 2007). “Beta-alanine supplementation augments muscle carnosine content and attenuates fatigue during repeated isokinetic contraction bouts in trained sprinters”. J Appl Physiol. 103 (5): 1736–43. doi:10.1152/japplphysiol.00397.2007. PMID 17690198. S2CID 6990201.
- ^ Hill CA, Harris RC, Kim HJ, Harris BD, Sale C, Boobis LH, Kim CK, Wise JA (2007). “Influence of beta-alanine supplementation on skeletal muscle carnosine concentrations and high intensity cycling capacity”. Amino Acids. 32 (2): 225–33. doi:10.1007/s00726-006-0364-4. PMID 16868650. S2CID 23988054.
- ^ Bate-Smith, EC (1938). “The buffering of muscle in rigor: protein, phosphate and carnosine”. Journal of Physiology. 92 (3): 336–343. doi:10.1113/jphysiol.1938.sp003605. PMC 1395289. PMID 16994977.
- ^ Mannion, AF; Jakeman, PM; Dunnett, M; Harris, RC; Willan, PLT (1992). “Carnosine and anserine concentrations in the quadriceps femoris muscle of healthy humans”. Eur. J. Appl. Physiol. 64 (1): 47–50. doi:10.1007/BF00376439. PMID 1735411. S2CID 24590951.
- ^ Vistoli, G; De Maddis, D; Cipak, A; Zarkovic, N; Carini, M; Aldini, G (Aug 2013). “Advanced glycoxidation and lipoxidation end products (AGEs and ALEs): an overview of their mechanisms of formation”. Free Radic. Res. 47: Suppl 1:3–27. doi:10.3109/10715762.2013.815348. PMID 23767955. S2CID 207517855.
- ^ Jump up to:a b Reddy, V. P.; Garrett, MR; Perry, G; Smith, MA (2005). “Carnosine: A Versatile Antioxidant and Antiglycating Agent”. Science of Aging Knowledge Environment. 2005 (18): pe12. doi:10.1126/sageke.2005.18.pe12. PMID 15872311.
- ^ Rashid, Imran; Van Reyk, David M.; Davies, Michael J. (2007). “Carnosine and its constituents inhibit glycation of low-density lipoproteins that promotes foam cell formation in vitro”. FEBS Letters. 581 (5): 1067–70. doi:10.1016/j.febslet.2007.01.082. PMID 17316626. S2CID 46535145.
- ^ Hipkiss, A. R. (2005). “Glycation, ageing and carnosine: Are carnivorous diets beneficial?”. Mechanisms of Ageing and Development. 126 (10): 1034–9. doi:10.1016/j.mad.2005.05.002. PMID 15955546. S2CID 19979631.
- ^ Boldyrev, A. A.; Stvolinsky, S. L.; Fedorova, T. N.; Suslina, Z. A. (2010). “Carnosine as a natural antioxidant and geroprotector: From molecular mechanisms to clinical trials”. Rejuvenation Research. 13 (2–3): 156–8. doi:10.1089/rej.2009.0923. PMID 20017611.
- ^ McFarland, G; Holliday, R (1994). “Retardation of the Senescence of Cultured Human Diploid Fibroblasts by Carnosine”. Experimental Cell Research. 212 (2): 167–75. doi:10.1006/excr.1994.1132. PMID 8187813.
- ^ Shao, Lan; Li, Qing-Huan; Tan, Zheng (2004). “L-Carnosine reduces telomere damage and shortening rate in cultured normal fibroblasts”. Biochemical and Biophysical Research Communications. 324 (2): 931–6. doi:10.1016/j.bbrc.2004.09.136. PMID 15474517.
- ^ Hipkiss, A. R. (2006). “Does Chronic Glycolysis Accelerate Aging? Could This Explain How Dietary Restriction Works?”. Annals of the New York Academy of Sciences. 1067 (1): 361–8. Bibcode:2006NYASA1067..361H. doi:10.1196/annals.1354.051. PMID 16804012. S2CID 41175541.
- ^ McCarty, Mark F; DiNicolantonio, James J (2014-08-04). “β-Alanine and orotate as supplements for cardiac protection”. Open Heart. 1 (1): e000119. doi:10.1136/openhrt-2014-000119. ISSN 2053-3624. PMC 4189254. PMID 25332822.
- ^ Virdi, Jasleen Kaur; Bhanot, Amritansh; Jaggi, Amteshwar Singh; Agarwal, Neha (2020-10-02). “Investigation on beneficial role of l -carnosine in neuroprotective mechanism of ischemic postconditioning in mice: possible role of histidine histamine pathway”. International Journal of Neuroscience. 130 (10): 983–998. doi:10.1080/00207454.2020.1715393. ISSN 0020-7454. PMID 31951767. S2CID 210710039.
- ^ Rajanikant, G.K.; Zemke, Daniel; Senut, Marie-Claude; Frenkel, Mark B.; Chen, Alex F.; Gupta, Rishi; Majid, Arshad (November 2007). “Carnosine Is Neuroprotective Against Permanent Focal Cerebral Ischemia in Mice”. Stroke. 38 (11): 3023–3031. doi:10.1161/STROKEAHA.107.488502. ISSN 0039-2499. PMID 17916766.
- ^ Min, Jiangyong; Senut, Marie-Claude; Rajanikant, Krishnamurthy; Greenberg, Eric; Bandagi, Ram; Zemke, Daniel; Mousa, Ahmad; Kassab, Mounzer; Farooq, Muhammad U.; Gupta, Rishi; Majid, Arshad (October 2008). “Differential neuroprotective effects of carnosine, anserine, and N -acetyl carnosine against permanent focal ischemia”. Journal of Neuroscience Research. 86 (13): 2984–2991. doi:10.1002/jnr.21744. PMC 2805719. PMID 18543335.
- ^ Jump up to:a b Culbertson, Julie Y.; Kreider, Richard B.; Greenwood, Mike; Cooke, Matthew (2010-01-25). “Effects of Beta-Alanine on Muscle Carnosine and Exercise Performance:A Review of the Current Literature”. Nutrients. 2 (1): 75–98. doi:10.3390/nu2010075. ISSN 2072-6643. PMC 3257613. PMID 22253993.
- ^ Baguet, Audrey; Bourgois, Jan; Vanhee, Lander; Achten, Eric; Derave, Wim (2010-07-29). “Important role of muscle carnosine in rowing performance”. Journal of Applied Physiology. 109 (4): 1096–1101. doi:10.1152/japplphysiol.00141.2010. ISSN 8750-7587. PMID 20671038.
- ^ Varanoske, Alyssa N.; Hoffman, Jay R.; Church, David D.; Wang, Ran; Baker, Kayla M.; Dodd, Sarah J.; Coker, Nicholas A.; Oliveira, Leonardo P.; Dawson, Virgil L.; Fukuda, David H.; Stout, Jeffrey R. (2017-09-07). “Influence of Skeletal Muscle Carnosine Content on Fatigue during Repeated Resistance Exercise in Recreationally Active Women”. Nutrients. 9 (9): 988. doi:10.3390/nu9090988. ISSN 2072-6643. PMC 5622748. PMID 28880219.
26. Kim EH, Kim ES, Shin D, Kim D, Choi S, Shin YJ, Kim KA, Noh D, Caglayan AB, Rajanikant GK, Majid A, Bae ON. Carnosine Protects against Cerebral Ischemic Injury by Inhibiting Matrix-Metalloproteinases. Int J Mol Sci. 2021 Jul 13;22(14):7495. doi: 10.3390/ijms22147495. PMID: 34299128; PMCID: PMC8306548.
27. Jain S, Kim ES, Kim D, Burrows D, De Felice M, Kim M, Baek SH, Ali A, Redgrave J, Doeppner TR, Gardner I, Bae ON, Majid A. Comparative Cerebroprotective Potential of d- and l-Carnosine Following Ischemic Stroke in Mice. Int J Mol Sci. 2020 Apr 26;21(9):3053. doi: 10.3390/ijms21093053. PMID: 32357505; PMCID: PMC7246848.
28. Kim ES, Kim D, Nyberg S, Poma A, Cecchin D, Jain SA, Kim KA, Shin YJ, Kim EH, Kim M, Baek SH, Kim JK, Doeppner TR, Ali A, Redgrave J, Battaglia G, Majid A, Bae ON. LRP-1 functionalized polymersomes enhance the efficacy of carnosine in experimental stroke. Sci Rep. 2020 Jan 20;10(1):699. doi: 10.1038/s41598-020-57685-5. PMID: 31959846; PMCID: PMC6971073.
29. Schön M, Mousa A, Berk M, Chia WL, Ukropec J, Majid A, Ukropcová B, de Courten B. The Potential of Carnosine in Brain-Related Disorders: A Comprehensive Review of Current Evidence. Nutrients. 2019 May 28;11(6):1196. doi: 10.3390/nu11061196. PMID: 31141890; PMCID: PMC6627134.
30. Davis CK, Laud PJ, Bahor Z, Rajanikant GK, Majid A. Systematic review and stratified meta-analysis of the efficacy of carnosine in animal models of ischemic stroke. J Cereb Blood Flow Metab. 2016 Oct;36(10):1686-1694. doi: 10.1177/0271678X16658302. Epub 2016 Jul 8. PMID: 27401803; PMCID: PMC5046161.
31. Baek SH, Noh AR, Kim KA, Akram M, Shin YJ, Kim ES, Yu SW, Majid A, Bae ON. Modulation of mitochondrial function and autophagy mediates carnosine neuroprotection against ischemic brain damage. Stroke. 2014 Aug;45(8):2438-2443. doi: 10.1161/STROKEAHA.114.005183. Epub 2014 Jun 17. PMID: 24938837; PMCID: PMC4211270.
32. Bae ON, Majid A. Role of histidine/histamine in carnosine-induced neuroprotection during ischemic brain damage. Brain Res. 2013 Aug 21;1527:246-54. doi: 10.1016/j.brainres.2013.07.004. Epub 2013 Jul 11. PMID: 23850642.
33. Bae ON, Serfozo K, Baek SH, Lee KY, Dorrance A, Rumbeiha W, Fitzgerald SD, Farooq MU, Naravelta B, Bhatt A, Majid A. Safety and efficacy evaluation of carnosine, an endogenous neuroprotective agent for ischemic stroke. Stroke. 2013 Jan;44(1):205-12. doi: 10.1161/STROKEAHA.112.673954. Epub 2012 Dec 18. PMID: 23250994; PMCID: PMC3678096.
34. Min J, Senut MC, Rajanikant K, Greenberg E, Bandagi R, Zemke D, Mousa A, Kassab M, Farooq MU, Gupta R, Majid A. Differential neuroprotective effects of carnosine, anserine, and N-acetyl carnosine against permanent focal ischemia. J Neurosci Res. 2008 Oct;86(13):2984-91. doi: 10.1002/jnr.21744. PMID: 18543335; PMCID: PMC2805719.
35. Rajanikant GK, Zemke D, Senut MC, Frenkel MB, Chen AF, Gupta R, Majid A. Carnosine is neuroprotective against permanent focal cerebral ischemia in mice. Stroke. 2007 Nov;38(11):3023-31. doi: 10.1161/STROKEAHA.107.488502. Epub 2007 Oct 4. PMID: 17916766.
////////L-CARNOSINE, カルノシン , b-Alanyl-L-histidine, ignotine, 8HO6PVN24W, カルノシン , Dragosine, Ignotin, Ignotine, Karnozin, L-Carnosine, N-(β-Alanyl)-L-histidine, NSC 524045, Sevitin, β-Alanylhistidine

NEW DRUG APPROVALS
one time
$10.00
FOMEPIZOLE

FOMEPIZOLE
- Molecular FormulaC4H6N2
- Average mass82.104 Da
4-Methylpyrazole, 4-MP
7554-65-6[RN]
105204[Beilstein]
1H-Pyrazole, 4-methyl-
231-445-0[EINECS]фомепизол , فوميبيزول
甲吡唑
Launched – 1998 EUSA PHARMA
Fomepizole, also known as 4-methylpyrazole, is a medication used to treat methanol and ethylene glycol poisoning.[2] It may be used alone or together with hemodialysis.[2] It is given by injection into a vein.[2]
Common side effects include headache, nausea, sleepiness, and unsteadiness.[2] It is unclear if use during pregnancy is safe for the baby.[2] Fomepizole works by blocking the enzyme that converts methanol and ethylene glycol to their toxic breakdown products.[2]
Fomepizole was approved for medical use in the United States in 1997.[2] It is on the World Health Organization’s List of Essential Medicines.[3]FomepizoleCAS Registry Number: 7554-65-6
CAS Name: 4-Methyl-1H-pyrazole
Additional Names: 4-MP
Trademarks: Antizol (Orphan Med.)
Molecular Formula: C4H6N2, Molecular Weight: 82.10
Percent Composition: C 58.52%, H 7.37%, N 34.12%
Literature References: Alcohol dehydrogenase inhibitor. Prepn: H. Pechmann, E. Burkard, Ber.33, 3590 (1900); D. S. Noyce et al.,J. Org. Chem.20, 1681 (1955); T. Momose et al.,Heterocycles30, 789 (1990). Inhibition of human liver alcohol dehydrogenase: T.-K. Li, H. Theorell, Acta Chem. Scand.23, 892 (1969). Toxicity study: G. Magnusson et al.,Experientia28, 1198 (1972). GC determn in plasma and urine: R. Achari, M. Mayersohn, J. Pharm. Sci.73, 690 (1984). Clinical pharmacology: D. Jacobsen et al.,Alcohol. Clin. Exp. Res.12, 516 (1988). Pharmacokinetics: eidem,Eur. J. Clin. Pharmacol.37, 599 (1989). Clinical trial in ethylene glycol poisoning: J. Brent et al.,N. Engl. J. Med.340, 832 (1999); in methanol poisoning: idem et al., ibid.344, 424 (2001). Review: J. Likforman et al.,J. Toxicol. Clin. Exp.7, 373-382 (1987). Review of use in methanol poisoning: M. B. Mycyk, J. B. Leikin, Am. J. Therapeut.10, 68-70 (2003).
Properties: mp 15.5-18.5°. bp18mm 98.5-99.5°; bp730 204-205°. nD22 1.4913. uv max in 95% ethanol: 220 nm (log e 3.47); in 6N HCl: 226 nm (log e 3.65). Sol in water, alcohol. LD50 (7 days) in mice, rats (mmol/kg): 3.8, 3.8 i.v.; 7.8, 6.5 orally (Magnusson).
Melting point: mp 15.5-18.5°
Boiling point: bp18mm 98.5-99.5°; bp730 204-205°
Index of refraction:nD22 1.4913
Absorption maximum: uv max in 95% ethanol: 220 nm (log e 3.47); in 6N HCl: 226 nm (log e 3.65)
Toxicity data: LD50 (7 days) in mice, rats (mmol/kg): 3.8, 3.8 i.v.; 7.8, 6.5 orally (Magnusson)
Therap-Cat: Antidote to methanol and ethylene glycol poisoning.
Therap-Cat-Vet: Antidote to ethylene glycol poisoning in dogs.
Keywords: Antidote (Methanol and Ethylene Glycol Poisoning).
Fomepizole was approved by the U.S. Food and Drug Administration (FDA) on Dec 4, 1997. It was developed and marketed as Antizol® by Paladin in the US.
Fomepizole is a competitive alcohol dehydrogenase inhibitor, Alcohol dehydrogenase catalyzes the oxidation of ethanol to acetaldehyde, and it also catalyzes the initial steps in the metabolism of ethylene glycol and methanol to their toxic metabolites. Antizol® is indicated as an antidote for ethylene glycol (such as antifreeze) or methanol poisoning, or for use in suspected ethylene glycol or methanol ingestion, either alone or in combination with hemodialysis.
Antizol® is available as injection solution for intravenous use, containing 1 g/ml of free Fomepizole. The recommended dose is 15 mg/kg should be administered, followed by doses of 10 mg/kg every 12 hours for 4 doses, then 15 mg/kg every 12 hours thereafter until ethylene glycol or methanol concentrations are undetectable or have been reduced below 20 mg/dL.
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 1997-12-04 | First approval | Antizol | Methanol or ethylene glycol poisoning | Injection | 1 g/mL | Paladin | Orphan |
SYN

SYN
| CAS-RN | Formula | Chemical Name | CAS Index Name |
|---|---|---|---|
| 5920-30-9 | C4H8N2 | 4,5-dihydro-4-methylpyrazole | |
| 7803-57-8 | H6N2O | hydrazine hydrate | Hydrazine, monohydrate |
| 78-85-3 | C4H6O | methacrolein | 2-propenal, 2-methyl- |

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT
SYN
Reference:
US7553863B2.
https://patents.google.com/patent/US7553863B2/enEthylene glycol is commonly available as automobile radiator antifreeze. Because of its sweet taste, improperly stored antifreeze is a common source of ethylene glycol poisoning, particularly in children. Ethylene glycol is rapidly absorbed from the gastrointestinal tract. Toxicity can be divided into three stages:
- Stage 1—Neurological (0.5-12 hours post-ingestion)
- Stage 2—Cardiopulmonary (12-24 hours post-ingestion)
- Stage 3—Renal (24-72 hours post-ingestion)
4-Methylpyrazole, marketed as Antizol® (fomepizole) by Orphan Medical, Inc. is a specific antidote for the treatment of ethylene glycol poisoning. It works by inhibiting the enzyme alcohol dehydrogenase which is responsible for the conversion of ethylene glycol, which itself is relatively non-toxic, into its toxic metabolites that in turn cause the renal injury and metabolic acidosis. Antizol® is currently approved by the FDA as an antidote for ethylene glycol poisoning or suspected ethylene glycol poisoning and is recommended by poison control centers as first line therapy. See Antizol® (fomepizole) Injection, Product Monograph, Orphan Medical, Inc., 2001, the entire contents of which are hereby incorporated by reference.Methanol is commonly available in the home in automobile windshield washer fluid and as a gas line anti-icing additive. Methanol has a minor degree of direct toxicity. Its major toxicity follows its metabolism to formic acid. Antizol® is also a specific antidote for the treatment of methanol toxicity. It works by inhibiting the enzyme alcohol dehydrogenase which is responsible for the conversion of methanol into its toxic metabolites, formaldehyde and formic acid. Again, Antizol® is approved by the FDA for use in treating methanol poisoning or suspected methanol poisoning and is recommended by poison control centers as first line therapy.Known methods of preparing 4-methylpyrazole include the reaction of alpha, beta-unsaturated carbonyl compounds or diketones with hydrazine or hydrazine derivatives or the dehydrogenation of the corresponding 2-pyrazoline. See U.S. Pat. Nos. 3,200,128, 4,996,327, and 5,569,769. Other processes for preparing 4-methylpyrazole are disclosed in U.S. Pat. Nos. 6,229,022, 5,569,769, and 4,996,327.4-methylpyrazole prepared by synthetic routes employed heretofore may contain impurities and toxic by-products, including pyrazole, hydrazine, and nitrobenzaldehyde. Pyrazole, like 4-methylpyrazole, is also an inhibitor of alcohol dehydrogenase, but is more toxic than 4-methylpyrazole. Pyrazole is a known teratogen (Eisses, 1995) with 10 fold less potency against alcohol dehydrogenase (T. Li et al., Acta Chem. Scan. 1969, 23, 892-902). In addition, Ewen MacDonald published a paper in 1976 that showed pyrazole in contrast to 4-methylpyrazole has a detrimental effect on brain levels of noradrenaline (E. MacDonald, Acta Pharmacol. et Toxicol. 1976, 39, 513-524). Hydrazine and nitrobenzaldehyde are known mutagens and carcinogens (H. Kohno et al., Cancer Sci. 2005, 96, 69-76).These impurities and toxic by-products have been tolerated heretofore because methods of making ultrapure 4-methylpyrazole have not been available. The FDA has previously approved up to 0.5% pyrazole in Antizol®, but recently is requesting a higher level of purity of less than 0.1% pyrazole to qualify such high levels with animal and other studies. Therefore, while the purity of Antizol® is sufficiently high for its antidotal use in emergency medicine, such toxic impurities are not ideal. For example a pregnant woman who needs antidote therapy would risk exposure of a fetus to potentially toxic pyrazole of known teratogenicity and potentially high levels of known carcinogens. Therefore, a need exists for a 4-methylpyrzaole with even lower amounts of pyrazole and other impurities and for a synthesis of such an ultrapure 4-methylpyrazole.The process of the present invention is set forth in the following exemplary scheme:

EXAMPLE 1Preparation of 1,1-diethoxypropane 1Into a 2-liter flask under nitrogen were added 586 g (3.96 moles) of triethyl orthoformate, 46 g (56 ml, 1 mole) of ethanol, and 16 g of ammonium nitrate. Over the course of one hour 232 g (4 moles) of propionaldehyde were added with stirring. An ice bath was used as necessary to keep maintain the mixture at 30-36° C. The mixture turned yellow orange after one-third of the propionaldehyde had been added. The mixture was stirred overnight at room temperature and then brought to pH 7.5±0.2 with 10% aqueous sodium carbonate (about 30 ml). The aqueous layer was decanted, and the organic layer was distilled over sodium carbonate at atmospheric pressure to produce 124 g (81.6%) of 1.
EXAMPLE 2Preparation of 1-ethoxy-1-propene 2Into a 500 ml flask equipped with a 12″×¾″ packed column were added 0.25 g (0.0013 moles) of p-toluene sulfonic acid, followed by 241 g (1.82 moles) of 1. Nitrogen was bubbled into the mixture while 0.157 g (0.00065 moles) of bis(2-ethylhexyl)amine were added. The nitrogen flow was reduced, and the mixture was distilled to 160° C. to partially remove ethyl alcohol and 1-ethoxy-1-propene. The reaction mixture washed with 320 ml of water and then with 70 ml of water. The organic layer was dried over magnesium sulfate and filtered to produce 121 g (77.5%) of 2, bp 67-76° C., as a clear, colorless liquid. Gas chromatographic analysis showed less than 0.01% ethylvinyl ether.
EXAMPLE 3Preparation of 1,1,3,3-tetraethoxy-2-methylpropane 3Into a 5 liter flask equipped with a mechanical stirrer were added 790 g (5.34 moles) of triethyl orthoformate and 4.28 ml of boron trifluoride-diethyl etherate under a nitrogen atmosphere. Temperature was maintained at 25° C. with cooling as needed. To this mixture were added 230 g (2.67 moles) of 1-ethoxy-1-propene were added slowly and dropwise. The reaction mixture was exothermic; the temperature rose to about 35-38° C. The pot was cooled to 25° C. and stirring was continued for one hour. Solid anhydrous sodium carbonate (32.1 g, 0.3 moles) was added in one portion to the flask and stirring was continued for one hour. The mixture was filtered and the filtrate was fractionally distilled under reduced pressure. The light fraction was removed at a pot temperature of 55-60° C. at 10 mm pressure. The vacuum was improved to 3 mm and the pot temperature was permitted to rise to about 100-140° C. to produce 500 g (80%) of 3, bp 80-81° C. at 3 mm, as a clear, colorless to yellow-brown liquid.
EXAMPLE 4Preparation of 4-methylpyrazoleInto a 5 liter flask equipped with a mechanical stirrer were added 1750 ml of sterile USP water to which 266.7 g (2.05 moles) of hydrazine hydrosulfate were added gradually over one hour with stirring. To the above mixture was added dropwise 481 g (2.053 moles) of 3 and the reaction mixture was warmed to 80° C. Heating and stirring were maintained for 3 hours, the flask was cooled to 40° C., and the volatile components were distilled off under a reduced pressure of about 125 mm. The resulting mixture was cooled to 10° C. first with water and then with glycol; 20 ml of water were added to the flask, and cooling was continued to a temperature of 3° C. Thereafter 50% sodium hydroxide solution was added with cooling so as to maintain the temperature below 30° C. The pH of the reaction mixture should be between 4 and 6. A solution of sodium bicarbonate containing 4.9 g of sodium bicarbonate to 55 ml of water was added to the flask. Additional sodium bicarbonate solution was added until the pH reached 7.0. The flask temperature was allowed to rise to 27° C. with continued stirring. The contents of the flask were extracted with ethyl acetate and the aqueous layer was separated. The organic layer was dried over magnesium sulfate, filtered, and the extract was distilled under vacuum. The light fraction was removed at a pot temperature of 55-60° C. at 125 mm pressure. The vacuum was improved to 5 mm for the remainder of the distillation; pot temperatures were permitted to rise to 100-110° C. to produce 134.8 g (84% based on 3) of 4-methylpyrazole, bp 77-80° C. at 5 mm, as a clear, colorless to yellow liquid. Gas chromatographic analysis showed less than 0.1% pyrazole and less than 10 ppm hydrazine.
SYN
Syn
Journal of the American Chemical Society (1949), 71, 3994-4000.
SYN
Journal of Organic Chemistry (1962), 27, 2415-19.

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Fomepizole is an alcohol dehydrogenase inhibitor originally commercialized in 1998 by Orphan Medical as an antidote for ethylene glycol (such as antifreeze) or methanol poisoning, or for use in suspected ethylene glycol or methanol ingestion, either alone or in combination with hemodialysis. In January 2015, Takeda launched the product for the treatment of ethylene glycol and methanol poisoning in Japan. Raptor Pharmaceuticals (currently Horizon Therapeutics) was evaluating the compound in phase II clinical studies for the treatment of the symptoms associated with alcohol intolerance due to ALDH2 deficiency; however, no recent developments have been reported. The compound has been licensed to Paladin and Swedish Orphan Biovitrum (formerly Swedish Orphan). Prior to being acquired by Alliance Pharma in 2010, Cambridge Laboratories obtained a license to fomepizole. In 2005, Orphan Medical was acquired by Jazz Pharmaceuticals. In 2011, Takeda licensed the product from Paladin for development and commercialization rights in Japan. In 2015, orphan drug designation in Australia was assigned to the compound for the treatment of ethylene glycol and methanol poisonings. In 2015, the product was acquired by EUSA Pharma from Jazz Pharmaceuticals for the treatment of poisoning. In 2021, the compound was granted orphan drug designation in the U.S. for the treatment of acetaminophen overdose.
NMR

| Chemical structure of fomepizole | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌfoʊˈmɛpɪzoʊl/ |
| Trade names | Antizol, others |
| Other names | 4-Methylpyrazole |
| AHFS/Drugs.com | Monograph |
| License data | US DailyMed: Fomepizole |
| Routes of administration | Intravenous |
| ATC code | V03AB34 (WHO) |
| Legal status | |
| Legal status | US: ℞-only [1] |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 7554-65-6 |
| PubChem CID | 3406 |
| DrugBank | DB01213 |
| ChemSpider | 3289 |
| UNII | 83LCM6L2BY |
| KEGG | D00707 |
| ChEBI | CHEBI:5141 |
| ChEMBL | ChEMBL1308 |
| CompTox Dashboard (EPA) | DTXSID3040649 |
| ECHA InfoCard | 100.028.587 |
| Chemical and physical data | |
| Formula | C4H6N2 |
| Molar mass | 82.106 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| Density | 0.99 g/cm3 |
| Boiling point | 204 to 207 °C (399 to 405 °F) (at 97,3 kPa) |
| showSMILES | |
| show |
Medical use
Fomepizole is used to treat ethylene glycol and methanol poisoning. It acts to inhibit the breakdown of these toxins into their active toxic metabolites. Fomepizole is a competitive inhibitor of the enzyme alcohol dehydrogenase,[4] found in the liver. This enzyme plays a key role in the metabolism of ethylene glycol, and of methanol.
- Ethylene glycol is first metabolized to glycolaldehyde by alcohol dehydrogenase. Glycolaldehyde then undergoes further oxidation to glycolate, glyoxylate, and oxalate. Glycolate and oxalate are the primary toxins responsible for the metabolic acidosis, and for the renal damage, seen in ethylene glycol poisoning.
- Methanol is first metabolized to formaldehyde by alcohol dehydrogenase. Formaldehyde then undergoes further oxidation, via formaldehyde dehydrogenase, to become formic acid.[5] Formic acid is the primary toxin responsible for the metabolic acidosis, and for the visual disturbances, associated with methanol poisoning.
By competitively inhibiting the first enzyme, alcohol dehydrogenase, in the metabolism of ethylene glycol and methanol, fomepizole slows the production of the toxic metabolites. The slower rate of metabolite production allows the liver to process and excrete the metabolites as they are produced, limiting the accumulation in tissues such as the kidney and eye. As a result, much of the organ damage is avoided.[6]
Fomepizole is most effective when given soon after ingestion of ethylene glycol or methanol. Delaying its administration allows for the generation of harmful metabolites.[6]
Interaction with alcohol
Concurrent use with ethanol is contraindicated because fomepizole is known to prolong the half-life of ethanol via inhibiting its metabolism. Extending the half-life of ethanol may increase and extend the intoxicating effects of ethanol, allowing for greater (potentially dangerous) levels of intoxication at lower doses. Fomepizole slows the production of acetaldehyde by inhibiting alcohol dehydrogenase, which in turn allows more time to further convert acetaldehyde into acetic acid by acetaldehyde dehydrogenase. The result is a patient with a prolonged and deeper level of intoxication for any given dose of ethanol, and reduced “hangover” symptoms (since these adverse symptoms are largely mediated by acetaldehyde build up).
In a chronic alcoholic who has built up a tolerance to ethanol, this removes some of the disincentives to ethanol consumption (“negative reinforcement“) while allowing them to become intoxicated with a lower dose of ethanol. The danger is that the alcoholic will then overdose on ethanol (possibly fatally). If alcoholics instead very carefully reduce their doses to reflect the now slower metabolism, they may get the “rewarding” stimulus of intoxication at lower doses with less adverse “hangover” effects – leading potentially to increased psychological dependency. However, these lower doses may therefore produce less chronic toxicity and provide a harm minimization approach to chronic alcoholism.
It is, in essence, the antithesis of a disulfiram approach which tries to increase the buildup of acetaldehyde resulting in positive punishment for the patient. Compliance, and adherence, is a substantial problem in disulfiram-based approaches. Disulfiram also has a considerably longer half-life than that of fomepizole, requiring the person to not drink ethanol in order to avoid severe effects. If the person is not adequately managed on a benzodiazepine, barbiturate, acamprosate, or another GABAA receptor agonist, the alcohol withdrawal syndrome, and its attendant, life-threatening risk of delirium tremens “DT”, may occur. Disulfiram treatment should never be initiated until the risk of DT has been evaluated, and mitigated appropriately. Fomepizole treatment may be initiated while the DT de-titration sequence is still being calibrated based upon the person’s withdrawal symptoms and psychological health.[citation needed]
Adverse effects
Common side effects associated with fomepizole use include headache and nausea.[7]
Kinetics
Absorption and distribution
Fomepizole distributes rapidly into total body water. The volume of distribution is between 0.6 and 1.02 L/kg. The therapeutic concentration is from 8.2 to 24.6 mg (100 to 300 micromoles) per liter. Peak concentration following single oral doses of 7 to 50 mg/kg of body weight occurred in 1 to 2 hours. The half-life varies with dose, so has not been calculated.
Metabolism and elimination
Hepatic; the primary metabolite is 4-carboxypyrazole (about 80 to 85% of an administered dose). Other metabolites include the pyrazoles 4-hydroxymethylpyrazole and the N -glucuronide conjugates of 4-carboxypyrazole and 4-hydroxymethylpyrazole.
Following multiple doses, fomepizole rapidly induces its own metabolism via the cytochrome P450 mixed-function oxidase system.
In healthy volunteers, 1.0 to 3.5% of an administered dose was excreted unchanged in the urine. The metabolites also are excreted unchanged in the urine.
Fomepizole is dialyzable.
Other uses
Apart from medical uses, the role of 4-methylpyrazole in coordination chemistry has been studied.[8]
References
- ^ “Antizol- fomepizole injection”. DailyMed. Retrieved 24 December 2020.
- ^ Jump up to:a b c d e f g “Fomepizole”. The American Society of Health-System Pharmacists. Archived from the original on 21 December 2016. Retrieved 8 December 2016.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ Casavant MJ (January 2001). “Fomepizole in the treatment of poisoning”. Pediatrics. 107 (1): 170–171. doi:10.1542/peds.107.1.170. PMID 11134450.
- ^ “Forensic Pathology”. Archived from the original on 2008-09-17.
- ^ Jump up to:a b Brent, J (May 2009). “Fomepizole for Ethylene Glycol and Methanol Poisoning”. N. Engl. J. Med. 360 (21): 2216–23. doi:10.1056/NEJMct0806112. PMID 19458366.
- ^ Lepik, KJ; Levy, AR; Sobolev, BG; Purssell, RA; DeWitt, CR; Erhardt, GD; Kennedy, JR; Daws, DE; Brignall, JL (April 2009). “Adverse drug events associated with the antidotes for methanol and ethylene glycol poisoning: a comparison of ethanol and fomepizole”. Annals of Emergency Medicine. 53 (4): 439–450.e10. doi:10.1016/j.annemergmed.2008.05.008. PMID 18639955.
- ^ Vos, Johannes G.; Groeneveld, Willem L. (1979). “Pyrazolato and related anions. Part V. Transition metal salts of 4-methylpyrazole”. Transition Metal Chemistry. 4 (3): 137–141. doi:10.1007/BF00619054. S2CID 93580021.
External links
- “Fomepizole”. Drug Information Portal. U.S. National Library of Medicine.
/////////////FOMEPIZOLE, фомепизол , فوميبيزول ,甲吡唑 , 4 MP

NEW DRUG APPROVALS
ONE TIME
$10.00
ALLOPURINOL

ALLUPURINOL
- Molecular FormulaC5H4N4O
- Average mass136.111 Da
- аллопуринол [Russian]ألوبيرينول [Arabic]别嘌醇 [Chinese]
1H-Pyrazolo(3,4-d)pyrimidin-4-ol
2,5-Dihydro-4H-pyrazolo[3,4-d]pyrimidin-4-one
206-250-9[EINECS], 315-30-0[RN]
4H-Pyrazolo[3,4-d]pyrimidin-4-one, 1,5-dihydro-, radical ion(1+)
4H-Pyrazolo[3,4-d]pyrimidin-4-one, 1,7-dihydro-
691008-24-9[RN]
7H-Pyrazolo[3,4-d]pyrimidin-4-ol
Allopurinol is a medication used to decrease high blood uric acid levels.[2] It is specifically used to prevent gout, prevent specific types of kidney stones and for the high uric acid levels that can occur with chemotherapy.[3][4] It is taken by mouth or injected into a vein.[4]
Common side effects when used by mouth include itchiness and rash.[4] Common side effects when used by injection include vomiting and kidney problems.[4] While not recommended historically, starting allopurinol during an attack of gout appears to be safe.[5][6] In those already on the medication, it should be continued even during an acute gout attack.[5][3] While use during pregnancy does not appear to result in harm, this use has not been well studied.[1] Allopurinol is in the xanthine oxidase inhibitor family of medications.[4]
Allopurinol was approved for medical use in the United States in 1966.[4] It is on the World Health Organization’s List of Essential Medicines, the safest and most effective medicines needed in a health system.[7] Allopurinol is available as a generic medication.[4] In 2019, it was the 43rd most commonly prescribed medication in the United States, with more than 15 million prescriptions.[8][9]
ALLUPRINOLCAS Registry Number: 315-30-0
CAS Name: 1,5-Dihydro-4H-pyrazolo[3,4-d]pyrimidin-4-one
Additional Names: 1H-pyrazolo[3,4-d]pyrimidin-4-ol; 4-hydroxypyrazolo[3,4-d]pyrimidine; HPP
Manufacturers’ Codes: BW-56158
Trademarks: Adenock (Mitsubishi); Allurit (Aventis); Aloral (Lagap); Alositol (Tanabe); Allo-Puren (Isis); Allozym (Sawai); Allural (Rovi); Anoprolin (Azwell); Anzief (Nippon Chemiphar); Apulonga (Dorsch); Apurol (Siegfried); Apurin (GEA); Bleminol (Gepepharm); Caplenal (Teva); Cellidrin (Hennig); Cosuric (DDSA); Dabroson (Hoyer); Embarin (Merckle); Epidropal (Teofarma); Foligan (DESMA); Gichtex (Gerot); Hamarin (Roche); Hexanurat (Durascan); Ketanrift (Ohta); Lopurin (Abbott); Lysuron (Roche); Miniplanor (Galen); Monarch (SS Pharm.); Remid (TAD); Riball (Schering AG); Sigapurol (Siegfried); Suspendol (Merckle); Takanarumin (Takata); Uricemil (Molteni); Uripurinol (Azupharma); Urosin (Roche); Urtias (Novartis); Zyloprim (GSK); Zyloric (GSK)
Molecular Formula: C5H4N4O, Molecular Weight: 136.11
Percent Composition: C 44.12%, H 2.96%, N 41.16%, O 11.75%
Literature References: Xanthine oxidase inhibitor; decreases uric acid production. Prepn: Robins, J. Am. Chem. Soc.78, 784 (1956); Schmidt, Druey, Helv. Chim. Acta39, 986 (1956); Druey, Schmidt, US2868803 (1959 to Ciba); GB798646 (1958 to Wellcome Found.); Hitchings, Falco, US3474098 (1969 to Burroughs Wellcome). Physiological and biochemical studies: Hitchings, in Biochem. Aspects Antimetab. Drug Hydroxylation, D. Shugar, Ed. (Academic Press, London, 1969) pp 11-22, C.A.75, 3531h (1971). Clinical trial in treatment of renal calculi: M. J. V. Smith, J. Urol.117, 690 (1977); B. Ettinger et al.,N. Engl. J. Med.315, 1386 (1986). Use in hyperuricemia and gout: G. R. Boss, J. E. Seegmiller, ibid.300, 1459 (1977). Effect on renal function in treatment of gout: T. Gibson, Ann. Rheum. Dis.41, 59 (1982). Comprehensive description: S. A. Benezra, T. R. Bennett, Anal. Profiles Drug Subs.7, 1-17 (1978).
Properties: Crystals, mp above 350°. uv max (0.1N NaOH): 257 nm (e 7200); (0.1N HCl): 250 nm (e 7600); (methanol): 252 nm (e 7600). Soly in mg/ml at 25°: water 0.48; n-octanol <0.01; chloroform 0.60; ethanol 0.30; DMSO 4.6. pKa 10.2.
Melting point: mp above 350°
pKa: pKa 10.2
Absorption maximum: uv max (0.1N NaOH): 257 nm (e 7200); (0.1N HCl): 250 nm (e 7600); (methanol): 252 nm (e 7600)
Derivative Type: Sodium salt
CAS Registry Number: 17795-21-0
Trademarks: Aloprim (Nabi)
Molecular Formula: C5H3N4NaO, Molecular Weight: 158.09Percent Composition: C 37.99%, H 1.91%, N 35.44%, Na 14.54%, O 10.12%
Properties: White amorphous mass. pKa 9.31.
pKa: pKa 9.31
Therap-Cat: Treatment of hyperuricemia and chronic gout. Antiurolithic.
Keywords: Antigout; Antiurolithic; Xanthine Oxidase Inhibitor.
Synthesis ReferenceDruey, J. and Schmidt, P.; US. Patent 2868,803; January 13,1959; assigned to Ciba Pharmaceutical Products Inc. Hitchings, G.H. and Falco, EA.; U.S. Patent 3,474,098; October 21,1969; assigned to Bur- roughs Wellcome & Co. Cresswell, R.M.and Mentha, J.W.; US.Patent4,146,713; March27,1979; assigned to Bur- roughs Wellcome & Co.
SYN


AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT
SYN

http://drugsynthesis.blogspot.co.uk/2011/11/laboratory-synthesis-of-allopurinol.html
Reference(s):
- US 2 868 803 (Ciba; 13.1.1959; CH-prior. 10.2.1956).
- DAS 1 720 024 (Wellcome Found; appl. 12.7.1967; GB-prior. 14.7.1966).
Similar process:
- DAS 1 904 894 (Wellcome Found; appl. 31.1.1969; GB-prior. 2.2.1968).
- US 4 146 713 (Burroughs Wellcome; 27.3.1979; GB-prior. 2.2.1968).
Alternative syntheses:
- US 3 474 098 (Burroughs Wellcome; 21.10.1969; prior. 29.3.1956).
- DAS 2 224 382 (Henning Berlin; appl. 18.5.1972).
- DE 1 118 221 (Wellcome Found; appl. 4.8.1956; GB-prior. 10.8.1955).
- DAS 1 814 082 (Wellcome Found; appl. 11.12.1968).
- DAS 1 950 075 (Henning Berlin; appl. 3.10.1969).
SYNCondensation of hydrazine with ethoxymethylenemalononitrile (I) leads to 3-amino-4-cyanopyrazole (II), which, by hydrolysis with sulphuric acid, gives the corresponding amide (III); heating III with formamide in excess results in allopurinol (IV). The synthesis of allopurinol can be illustrated as below:

SYN
Synthesis

IR
https://www.sciencedirect.com/science/article/abs/pii/S0099542808600878
Infrared Spectrum The infrared spectrum of allopurinol is shown in Figure 1 . in KBr with a Perkin Elmer model 457 infrared spectrophotometer. with the structure of allopurinol . It was taken as a 0.2% dispersion of allopurinol Table I gives the infrareg assignments consistent Table I Infrared Spectral Assignments for Allopurinol Frequency (cm-l) Assignment
3060 CH stretching vibrations of the pyrimidine ring
1700 CO stretching vibration of the keto form of the 4-hydroxy tautomer 1
590 ring vibrations
1245 CH in-plane deformation




NMR

| Clinical data | |
|---|---|
| Trade names | Zyloprim, Caplenal, Zyloric, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682673 |
| License data | US DailyMed: Allopurinol |
| Pregnancy category | AU: B2[1] |
| Routes of administration | By mouth (tablet), intravenous |
| ATC code | M04AA01 (WHO) |
| Legal status | |
| Legal status | AU: S4 (Prescription only)UK: POM (Prescription only)US: ℞-only |
| Pharmacokinetic data | |
| Bioavailability | 78±20% |
| Protein binding | Negligible |
| Metabolism | liver (80% oxipurinol, 10% allopurinol ribosides) |
| Elimination half-life | 2 h (oxipurinol 18–30 h) |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 315-30-0 |
| PubChem CID | 135401907 |
| IUPHAR/BPS | 6795 |
| DrugBank | DB00437 |
| ChemSpider | 2010 |
| UNII | 63CZ7GJN5I |
| KEGG | D00224 |
| ChEBI | CHEBI:40279 |
| ChEMBL | ChEMBL1467 |
| CompTox Dashboard (EPA) | DTXSID4022573 |
| ECHA InfoCard | 100.005.684 |
| Chemical and physical data | |
| Formula | C5H4N4O |
| Molar mass | 136.114 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (verify) |

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Medical uses
Gout
Allopurinol is used to reduce urate formation in conditions where urate deposition has already occurred or is predictable. The specific diseases and conditions where it is used include gouty arthritis, skin tophi, kidney stones, idiopathic gout; uric acid lithiasis; acute uric acid nephropathy; neoplastic disease and myeloproliferative disease with high cell turnover rates, in which high urate levels occur either spontaneously, or after cytotoxic therapy; certain enzyme disorders which lead to overproduction of urate, for example: hypoxanthine-guanine phosphoribosyltransferase, including Lesch–Nyhan syndrome; glucose 6-phosphatase including glycogen storage disease; phosphoribosyl pyrophosphate synthetase, phosphoribosyl pyrophosphate amidotransferase; adenine phosphoribosyltransferase.
It is also used to treat kidney stones caused by deficient activity of adenine phosphoribosyltransferase.
Tumor lysis syndrome
Allopurinol was also commonly used to treat tumor lysis syndrome in chemotherapeutic treatments, as these regimens can rapidly produce severe acute hyperuricemia;[10] however, it has gradually been replaced by urate oxidase therapy.[11] Intravenous formulations are used in this indication when people cannot take medicine by mouth.[12]
Inflammatory bowel disease
Allopurinol cotherapy is used to improve outcomes for people with inflammatory bowel disease and Crohn’s disease who do not respond to thiopurine monotherapy.[13][14] Cotherapy has also been shown to greatly improve hepatoxicity side effects in treatment of IBD.[15] Cotherapy invariably requires dose reduction of the thiopurine, usually to one-third of the standard dose depending upon the patient’s genetic status for thiopurine methyltransferase.[16]
Psychiatric disorders
Allopurinol has been tested as an augmentation strategy for the treatment of mania in bipolar disorder. Meta-analytic evidence showed that adjunctive allopurinol was superior to placebo for acute mania (both with and without mixed features).[17] Its efficacy was not influenced by dosage, follow-up duration, or concurrent standard treatment.[17]
Side effects
Because allopurinol is not a uricosuric, it can be used in people with poor kidney function. However, for people with impaired kidney function, allopurinol has two disadvantages. First, its dosing is complex.[18] Second, some people are hypersensitive to the drug; therefore, its use requires careful monitoring.[19][20]
Allopurinol has rare but potentially fatal adverse effects involving the skin. The most serious adverse effect is a hypersensitivity syndrome consisting of fever, skin rash, eosinophilia, hepatitis, and worsened renal function, collectively referred to as DRESS syndrome.[19] Allopurinol is one of the drugs commonly known to cause Stevens–Johnson syndrome and toxic epidermal necrolysis, two life-threatening dermatological conditions.[19] More common is a less-serious rash that leads to discontinuing this drug.[19]
More rarely, allopurinol can also result in the depression of bone marrow elements, leading to cytopenias, as well as aplastic anemia. Moreover, allopurinol can also cause peripheral neuritis in some patients, although this is a rare side effect. Another side effect of allopurinol is interstitial nephritis.[21]
Allopurinol should not be given to people who are allergic to it.[10]
Drug interactions
Drug interactions are extensive, and are as follows:[10]
- Azathioprine and 6-mercaptopurine: Azathioprine is metabolised to 6-mercaptopurine which in turn is inactivated by the action of xanthine oxidase – the target of allopurinol. Giving allopurinol with either of these drugs at their normal dose will lead to overdose of either drug; only one-quarter of the usual dose of 6-mercaptopurine or azathioprine should be given;
- Didanosine: plasma didanosine Cmax and AUC values were approximately doubled with concomitant allopurinol treatment; it should not be co-administered with allopuroinol and if it must be, the dose of should be reduced and the person should be closely monitored.
Allopurinol may also increase the activity or half-life of the following drugs, in order of seriousness and certainty of the interaction:[10]
- Ciclosporin
- Coumarin anticoagulants, such as warfarin (reported rarely, but is serious when it occurs)
- Vidarabine
- Chlorpropamide
- Phenytoin
- Theophylline
- Cyclophosphamide, doxorubicin, bleomycin, procarbazine, mechlorethamine
Co-administration of the following drugs may make allopurinol less active or decrease its half-life:[10]
- Salicylates and medicines that increase the secretion of uric acid
- furosemide (see more on diuretics below)
Co-administration of the following drugs may cause hypersensitivity or skin rash:[10]
- Ampicillin and amoxicillin
- Diuretics, in particular thiazides, especially in renal impairment
- Angiotensin-converting-enzyme inhibitors (ACE inhibitors)
Pharmacology
A common misconception is that allopurinol is metabolized by its target, xanthine oxidase, but this action is principally carried out by aldehyde oxidase.[22] The active metabolite of allopurinol is oxipurinol, which is also an inhibitor of xanthine oxidase. Allopurinol is almost completely metabolized to oxipurinol within two hours of oral administration, whereas oxipurinol is slowly excreted by the kidneys over 18–30 hours. For this reason, oxipurinol is believed responsible for the majority of allopurinol’s effect.[23]
Mechanism of action
Allopurinol is a purine analog; it is a structural isomer of hypoxanthine (a naturally occurring purine in the body) and is an inhibitor of the enzyme xanthine oxidase.[2] Xanthine oxidase is responsible for the successive oxidation of hypoxanthine and xanthine, resulting in the production of uric acid, the product of human purine metabolism.[2] In addition to blocking uric acid production, inhibition of xanthine oxidase causes an increase in hypoxanthine and xanthine. While xanthine cannot be converted to purine ribotides, hypoxanthine can be salvaged to the purine ribotides adenosine and guanosine monophosphates. Increased levels of these ribotides may cause feedback inhibition of amidophosphoribosyl transferase, the first and rate-limiting enzyme of purine biosynthesis. Allopurinol, therefore, decreases uric acid formation and may also inhibit purine synthesis.[24]
Pharmacogenetics
The HLA-B*5801 allele is a genetic marker for allopurinol-induced severe cutaneous adverse reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN).[25][26] The frequency of the HLA-B*5801 allele varies between ethnicities: Han Chinese and Thai populations have HLA-B*5801 allele frequencies of around 8%, as compared to European and Japanese populations, who have allele frequencies of around 1.0% and 0.5%, respectively.[27] The increase in risk for developing allopurinol-induced SJS or TEN in individuals with the HLA-B*5801 allele (as compared to those who do not have this allele) is very high, ranging from a 40-fold to a 580-fold increase in risk, depending on ethnicity.[25][26] As of 2011 the FDA-approved drug label for allopurinol did not contain any information regarding the HLA-B*5801 allele, though FDA scientists did publish a study in 2011 which reported a strong, reproducible and consistent association between the allele and allopurinol-induced SJS and TEN.[28] However, the American College of Rheumatology recommends screening for HLA-B*5801 in high-risk populations (e.g. Koreans with stage 3 or worse chronic kidney disease and those of Han Chinese and Thai descent), and prescribing patients who are positive for the allele an alternative drug.[29] The Clinical Pharmacogenetics Implementation Consortium guidelines state that allopurinol is contraindicated in known carriers of the HLA-B*5801 allele.[30][31]
History
Allopurinol was first synthesized and reported in 1956 by Roland K. Robins (1926-1992), in a search for antineoplastic agents.[2][32] Because allopurinol inhibits the breakdown (catabolism) of the thiopurine drug mercaptopurine, and it was later tested by Wayne Rundles, in collaboration with Gertrude Elion‘s lab at Wellcome Research Laboratories to see if it could improve treatment of acute lymphoblastic leukemia by enhancing the action of mercaptopurine.[2][33] However, no improvement in leukemia response was noted with mercaptopurine-allopurinol co-therapy, so that work turned to other compounds and the team then started testing allopurinol as a potential for gout.[34] Allopurinol was first marketed as a treatment for gout in 1966.[33]
Society and culture

Pure allopurinol is a white powder.
Formulations
Allopurinol is sold as an injection for intravenous use[12] and as a tablet.[10]
Brands
Allopurinol has been marketed in the United States since 19 August 1966, when it was first approved by FDA under the trade name Zyloprim.[35] Allopurinol was marketed at the time by Burroughs-Wellcome. Allopurinol is a generic drug sold under a variety of brand names, including Allohexal, Allosig, Milurit, Alloril, Progout, Ürikoliz, Zyloprim, Zyloric, Zyrik, and Aluron.[36]
See also
- Lesinurad/allopurinol, a fixed-dose combination drug
- Hydroxychavicol, potent xanthine oxidase inhibitor
References
- ^ Jump up to:a b “Allopurinol Use During Pregnancy”. Drugs.com. Archived from the original on 20 August 2016. Retrieved 20 December 2016.
- ^ Jump up to:a b c d e Pacher P, Nivorozhkin A, Szabó C (March 2006). “Therapeutic effects of xanthine oxidase inhibitors: renaissance half a century after the discovery of allopurinol”. Pharmacological Reviews. 58 (1): 87–114. doi:10.1124/pr.58.1.6. PMC 2233605. PMID 16507884.
- ^ Jump up to:a b World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization. p. 39. hdl:10665/44053. ISBN 9789241547659.
- ^ Jump up to:a b c d e f g “Allopurinol”. The American Society of Health-System Pharmacists. Archived from the original on 29 April 2016. Retrieved 8 December 2016.
- ^ Jump up to:a b Robinson PC, Stamp LK (May 2016). “The management of gout: Much has changed”. Australian Family Physician. 45 (5): 299–302. PMID 27166465.
- ^ Satpanich, P; Pongsittisak, W; Manavathongchai, S (18 August 2021). “Early versus Late Allopurinol Initiation in Acute Gout Flare (ELAG): a randomized controlled trial”. Clinical Rheumatology. doi:10.1007/s10067-021-05872-8. PMID 34406530. S2CID 237156638.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ “The Top 300 of 2019”. ClinCalc. Retrieved 16 October 2021.
- ^ “Allopurinol – Drug Usage Statistics”. ClinCalc. Retrieved 16 October 2021.
- ^ Jump up to:a b c d e f g “300 mg Allopurinol tables”. UK Electronic Medicines Compendium. 7 April 2016. Archived from the original on 11 September 2016.
- ^ Jeha S (October 2001). “Tumor lysis syndrome”. Seminars in Hematology. 38 (4 Suppl 10): 4–8. doi:10.1016/S0037-1963(01)90037-X. PMID 11694945.
- ^ Jump up to:a b “Label for injectable Allopurinol”. DailyMed. June 2014. Archived from the original on 13 September 2016.
- ^ Bradford K, Shih DQ (October 2011). “Optimizing 6-mercaptopurine and azathioprine therapy in the management of inflammatory bowel disease”. World Journal of Gastroenterology. 17 (37): 4166–73. doi:10.3748/wjg.v17.i37.4166. PMC 3208360. PMID 22072847.
- ^ Sparrow MP, Hande SA, Friedman S, Cao D, Hanauer SB (February 2007). “Effect of allopurinol on clinical outcomes in inflammatory bowel disease nonresponders to azathioprine or 6-mercaptopurine”. Clinical Gastroenterology and Hepatology. 5 (2): 209–14. doi:10.1016/j.cgh.2006.11.020. PMID 17296529.
- ^ Ansari A, Patel N, Sanderson J, O’Donohue J, Duley JA, Florin TH (March 2010). “Low-dose azathioprine or mercaptopurine in combination with allopurinol can bypass many adverse drug reactions in patients with inflammatory bowel disease”. Alimentary Pharmacology & Therapeutics. 31 (6): 640–7. doi:10.1111/j.1365-2036.2009.04221.x. PMID 20015102. S2CID 6000856.
- ^ Ansari AR, Duley JA (March 2012). “Azathioprine co-therapy with allopurinol for inflammatory bowel disease: trials and tribulations” (PDF). Rev Assoc Med Bras. 58 (Suppl.1): S28–33.
- ^ Jump up to:a b Bartoli F, Cavaleri D, Bachi B, Moretti F, Riboldi I, Crocamo C, Carrà G (September 2021). “Repurposed drugs as adjunctive treatments for mania and bipolar depression: A meta-review and critical appraisal of meta-analyses of randomized placebo-controlled trials”. Journal of Psychiatric Research. 143: 230–238. doi:10.1016/j.jpsychires.2021.09.018. PMID 34509090. S2CID 237485915.
- ^ Dalbeth N, Stamp L (2007). “Allopurinol dosing in renal impairment: walking the tightrope between adequate urate lowering and adverse events”. Seminars in Dialysis. 20 (5): 391–5. doi:10.1111/j.1525-139X.2007.00270.x. PMID 17897242. S2CID 1150852.
- ^ Jump up to:a b c d Chung WH, Wang CW, Dao RL (July 2016). “Severe cutaneous adverse drug reactions”. The Journal of Dermatology. 43 (7): 758–66. doi:10.1111/1346-8138.13430. PMID 27154258. S2CID 45524211.
- ^ Tsai TF, Yeh TY (2010). “Allopurinol in dermatology”. American Journal of Clinical Dermatology. 11 (4): 225–32. doi:10.2165/11533190-000000000-00000. PMID 20509717. S2CID 36847530.
- ^ De Broe ME, Bennett WM, Porter GA (2003). Clinical Nephrotoxins: Renal Injury from Drugs and Chemicals. Springer Science+Business Media. ISBN 9781402012778.
Acute interstitial nephritis has also been reported associated with by the administration of allopurinol.
- ^ Reiter S, Simmonds HA, Zöllner N, Braun SL, Knedel M (March 1990). “Demonstration of a combined deficiency of xanthine oxidase and aldehyde oxidase in xanthinuric patients not forming oxipurinol”. Clinica Chimica Acta; International Journal of Clinical Chemistry. 187 (3): 221–34. doi:10.1016/0009-8981(90)90107-4. PMID 2323062.
- ^ Day RO, Graham GG, Hicks M, McLachlan AJ, Stocker SL, Williams KM (2007). “Clinical pharmacokinetics and pharmacodynamics of allopurinol and oxypurinol”. Clinical Pharmacokinetics. 46 (8): 623–44. doi:10.2165/00003088-200746080-00001. PMID 17655371. S2CID 20369375.
- ^ Cameron JS, Moro F, Simmonds HA (February 1993). “Gout, uric acid and purine metabolism in paediatric nephrology”. Pediatric Nephrology. 7 (1): 105–18. doi:10.1007/BF00861588. PMID 8439471. S2CID 34815040.
- ^ Jump up to:a b “Uric Acid-Lowering Drugs Pathway, Pharmacodynamics”. PharmGKB. Archived from the original on 8 August 2014.
- ^ Jump up to:a b “PharmGKB”. Archived from the original on 8 August 2014. Retrieved 1 August 2014.
- ^ “Allele Frequency Net Database”. Archived from the original on 28 August 2009.
- ^ Zineh I, Mummaneni P, Lyndly J, Amur S, La Grenade LA, Chang SH, et al. (December 2011). “Allopurinol pharmacogenetics: assessment of potential clinical usefulness”. Pharmacogenomics. 12 (12): 1741–9. doi:10.2217/pgs.11.131. PMID 22118056.
- ^ Khanna D, Fitzgerald JD, Khanna PP, Bae S, Singh MK, Neogi T, et al. (October 2012). “2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia”. Arthritis Care & Research. 64 (10): 1431–46. doi:10.1002/acr.21772. PMC 3683400. PMID 23024028.
- ^ “Annotation of CPIC Guideline for allopurinol and HLA-B”. PharmGKB. Archived from the original on 8 August 2014. Retrieved 1 August 2014.
- ^ Hershfield MS, Callaghan JT, Tassaneeyakul W, Mushiroda T, Thorn CF, Klein TE, Lee MT (February 2013). “Clinical Pharmacogenetics Implementation Consortium guidelines for human leukocyte antigen-B genotype and allopurinol dosing”. Clinical Pharmacology and Therapeutics. 93 (2): 153–8. doi:10.1038/clpt.2012.209. PMC 3564416. PMID 23232549.
- ^ Robins RK (1956). “Potential Purine Antagonists. I. Synthesis of Some 4,6-Substituted Pyrazolo \3,4-d] pyrimidines1”. J. Am. Chem. Soc. 78 (4): 784–790. doi:10.1021/ja01585a023.
- ^ Jump up to:a b Sneader W (2005). Drug Discovery: A History. John Wiley & Sons. p. 254. ISBN 9780471899792.
- ^ Elion GB (April 1989). “The purine path to chemotherapy”. Science. 244 (4900): 41–7. Bibcode:1989Sci…244…41E. doi:10.1126/science.2649979. PMID 2649979.
- ^ “FDA Approved Drug Products”. Drugs@FDA. Archived from the original on 14 August 2012. Retrieved 8 November 2013.
- ^ “Search Results for Allopurinol”. DailyMed. Archived from the original on 25 March 2012. Retrieved 27 July 2011.
Further reading
- Dean L (March 2016). “Allopurinol Therapy and HLA-B*58:01 Genotype”. In Pratt VM, McLeod HL, Rubinstein WS, et al. (eds.). Medical Genetics Summaries. National Center for Biotechnology Information (NCBI). PMID 28520356.
External links
- “Allopurinol”. Drug Information Portal. U.S. National Library of Medicine.
- “PRODUCT INFORMATION Allopurinol Tablets USP”. U.S. National Library of Medicine. Medication handout sheet (Revised: 07/2019 0603-2115)
- Allopurinol pathway on PharmGKB
/////////////////////ALLUPURINOL, BW-56158, аллопуринол , ألوبيرينول , 别嘌醇 ,

NEW DRUG APPROVALS
ONE TIME
$10.00
CITICOLINE
![[(2R,3S,4R,5R)-5-(4-amino-2-oxopyrimidin-1-yl)-3,4-dihydroxyoxolan-2-yl]methyl [hydroxy-[2-(trimethylazaniumyl)ethoxy]phosphoryl] phosphate.png](https://pubchem.ncbi.nlm.nih.gov/image/imgsrv.fcgi?cid=11583971&t=l)
CITICOLINE
- Molecular FormulaC14H26N4O11P2
- Average mass488.324 Da
5′-O-[Hydroxy({[2-(trimethylammonio)ethoxy]phosphinato}oxy)phosphoryl]cytidine
987-78-0[RN]
1-{5-O-[({Hydroxy[2-(trimethylammonio)ethoxy]phosphoryl}oxy)phosphinato]-β-D-ribofuranosyl}-4-imino-1,4-dihydro-2-pyrimidinol
213-580-7[EINECS], 2290
2-Pyrimidinol, 1,4-dihydro-1-[5-O-[hydroxy[[hydroxy[2-(trimethylammonio)ethoxy]phosphinyl]oxy]phosphinyl]-β-D-ribofuranosyl]-4-imino-, inner salt
CiticolineCAS Registry Number: 987-78-0
CAS Name: Cytidine 5¢-(trihydrogen diphosphate) P¢-[2-(trimethylammonio)ethyl] ester inner salt
Additional Names: choline cytidine 5¢-pyrophosphate (ester); cytidine diphosphate choline ester; CDP-choline
Trademarks: Difosfocin (Magis); Nicholin (Wyeth); Recognan (Asahi); Rexort (Hoechst); Somazina (Ferrer)
Molecular Formula: C14H26N4O11P2, Molecular Weight: 488.32
Percent Composition: C 34.43%, H 5.37%, N 11.47%, O 36.04%, P 12.69%
Literature References: Naturally occurring nucleotide; intermediate in the major pathway of lecithin biosynthesis. Identification: E. P. Kennedy, S. B. Weiss, J. Am. Chem. Soc.77, 250 (1955).Crystallization from yeast extract: I. Lieberman et al.,Science124, 81 (1956).Synthesis: E. P. Kennedy, J. Biol. Chem.222, 185 (1956); K. Kikugawa et al.,Chem. Pharm. Bull.19, 1011, 2466 (1971). Molecular structure: M. A. Viswamitra et al.,Nature258, 497 (1975). Series of articles on pharmacology and toxicology: Arzneim.-Forsch.33, 1009-1080 (1983). Acute toxicity: T. Grau et al.,ibid. 1033. Clinical trial in ischemic stroke: W. M. Clark et al.,Neurology49, 671 (1997).Review of biosynthesis, metabolism, pharmacology: G. B. Weiss, Life Sci.56, 637-660 (1995); and clinical experience: J. J. Secades, G. Frontera, Methods Find. Exp. Clin. Pharmacol.17, Suppl. B, 1-54 (1995).Properties: Amorphous, somewhat hygroscopic powder. [a]D25 +19.0° (c = 0.86 in H2O). uv max (pH 1): 280 nm (e 12800). Dissolves readily in water to form acidic soln. Practically insol in most organic solvents. pKa 4.4. LD50 in mice, rats (mg/kg): 4600 ±335, 4150 ±370 i.v.; both species 8 g/kg orally (Grau).
pKa: pKa 4.4Optical Rotation: [a]D25 +19.0° (c = 0.86 in H2O)
Absorption maximum: uv max (pH 1): 280 nm (e 12800)
Toxicity data: LD50 in mice, rats (mg/kg): 4600 ±335, 4150 ±370 i.v.; both species 8 g/kg orally (Grau)
Derivative Type: Sodium saltCAS Registry Number: 33818-15-4
Trademarks: Acticolin (Upsamedica); Brassel (Searle); Ceraxon (Ferrer); Neuroton (Berlin-Chemie); Sintoclar (Pulitzer)
Molecular Formula: C14H25N4NaO11P2, Molecular Weight: 510.31
Percent Composition: C 32.95%, H 4.94%, N 10.98%, Na 4.51%, O 34.49%, P 12.14%
Properties: White, crystalline, spongy, hygrosopic powder, dec 250°. [a]D20 +12.5° (c = 1.0 in H2O). Sol in water. Practically insol in alcohol.
Optical Rotation: [a]D20 +12.5° (c = 1.0 in H2O)
Therap-Cat: Neuroprotective. In treatment of ischemic stroke and head trauma.
Keywords: Neuroprotective.
Citicoline (INN), also known as cytidine diphosphate-choline (CDP-Choline) or cytidine 5′-diphosphocholine is an intermediate in the generation of phosphatidylcholine from choline, a common biochemical process in cell membranes. Citicoline is naturally occurring in the cells of human and animal tissue, in particular the organs.
Studies suggest that CDP-choline supplements increase dopamine receptor densities.[1] Intracerebroventricular administration of citicoline has also been shown to elevate ACTH independently from CRH levels and to amplify the release of other HPA axis hormones such as LH, FSH, GH and TSH in response to hypothalamic releasing factors.[2] These effects on HPA hormone levels may be beneficial for some individuals but may have undesirable effects in those with medical conditions featuring ACTH or cortisol hypersecretion including PCOS, type II diabetes and major depressive disorder.[3][4]
Citicoline was originally developed in Japan for stroke. Citicoline or its sodium salt was later introduced as a prescription drug in many European countries. In these countries it is now frequently prescribed for thinking problems related to circulation problems in the brain. In the US, citicoline is marketed as a dietary supplement. Citicoline or its sodium salt is used for Alzheimers disease and other types of dementia, head trauma, cerebrovascular disease such as stroke, age-related memory loss, Parkinsons disease, and glaucoma.
Citicoline sodium is chemically known as 5-0-[hydroxy({hydroxy[2-(trimethylammonio)ethoxy]phosphoryl}oxy)phosphoryl]cytidine sodium which is represented by formula I,
There are many process described in the art for the preparation of citicoline. Japanese patent 51028636 describes a process for the preparation of citicoline by neutralisation of Calcium salt of phosphorylcholine chloride with 98% H2SO4 to make phosphorylcholine chloride, which is further treated with cytidine-5-phosphate in presence of DCC and pyridine at 70 C to obtain citicoline hydrate. The drawback of this process is that citicoline is very unstable
in this harsh reaction condition such as formamide, 98% H2SO4 and high temperature of 70 C.
Chinese patent 1944661 describes an enzymatic process for the preparation of citicoline which involves twice pH adjustment to precipitatethe product,filtration of the solids, charcolisation, washing with pure water, eluting through chloride type ion exchange resin with water ethanol/alcohol reagents, desalting the eluate, decoloring and collecting the liquid, vacuum-concentration of the eluate by adding an alcohol solvent to get the solid to obtain the crude product and dissolving the crude product, microfiltering, ultrafiltering, adding an alcoholic solvent, to obtain the wet productand drying to obtain the final product. The primary disadvantage of this process is that the above reaction involves water and ethanol mixture for elution of ion exchange column and also vacuum concentration of water ethanol mixture which requires high energy, more time, leads to decomposition of product and also leads to the formation of more effluent hence it is not suitable for large scale production.
The primary disadvantage of this process is that the above reaction involves water and ethanol mixture for elution of ion exchange column and also vacuum concentration of water ethanol mixture which requires high energy, more time, leads to decomposition of product and also leads to the formation of more effluent hence it is not suitable for large scale production.
US20090286284 describes a microbial process for preparation of citicoline. This patent also discloses a process for purification of citicoline by passing through acidic cation exchange and anion exchange resin. The drawback of this process is that in this process citicoline is passed through cation /anion exchange resin in free form which is unstable and liable to formation of unwanted impurities. Therefore for the purification it needs very high volume of resin (200 times) and high volume (100 times) of solvent. This process further needs reconcentration of huge volume of solvents, which is time taking and energy consuming.
Chemical and Pharmaceutical Bulletin 1971, 19(5), 1011-16 describes a process for the preparation of citicoline by direct condensation of cytidine 5-
monophosphate and choline phosphate by using p-toluenesulfonyl chloride or methanesulfonyl chloride combined with DMF. After completion of reaction the mass was diluted with water, pH was adjusted with ammonia solution to 9.5 and product was purified by using Dowex-1 ion exchange resin by eluting with formic acid. Another Chemical and Pharmaceutical Bulletin 1971, 19(12), 2499-71 describes a process for the preparation of citicoline by direct condensation cytidine 5-monophosphate and choline phosphate in presence of thionyl chloride and DMF.The product obtained was further purified by using Dowex-1 ion exchange resin by eluting with formic acid.
Journal of Biological Chemistry, 1956, 185-191 describes a process for the preparation of citicoline by direct condensation5-cytidylic acid and phosphorylcholine in a mixture of water and pyridine in presence of DCC, stirred for few days by adding DCC in lots, after completion of reaction, reaction mass was diluted with water and filtered. The pH of the filtrate was adjusted 8-9 using 0.5N KOH, diluted further with water and passed through Dowex-1 formate resin by eluting with formic acid and water.
The drawbacks of these processes are that they use hazardous reagents such as p-toluenesulfonyl chloride, methanesulfonyl chloride, thionyl chloride etc. Hence they are not suitable for large scale production. Also, the prior art processes pass citicoline solution, without isolating it, to ion exchange resins for purification. During this process most of the inorganic impurities present along with citicoline or its salt pass through the column, thus making purification difficult.

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT
SYN
Journal of Chemical Research, 40(6), 358-360; 2016
An improved, three-step synthesis of cytidine diphosphate choline (CDP-choline) from cytidine was achieved in 68% overall yield. Selective phosphorylation of cytidine was accomplished by the use of morpholinophosphodichloridate to give cytidine-5′-phosphomorpholide, which was condensed with choline phosphate chloride in the presence of a catalytic amount of H2SO4 to give CDP-choline. The intermediates and products could be efficiently purified by recrystallisation, thus avoiding the use of chromatography at all stages. The reaction could be scaled up to 200 g in 64% overall yield, making this route attractive for industrial application.

Cytidine diphosphate choline (CDP-choline 1) is a nucleotide coenzyme and serves as a choline donor in the biosynthesis of lipids,1 lecithins,2 and sphingomyelin.3 It is a clinical drug for the treatment of several illnesses involving disturbance of the central nervous system, in particular, for regaining a patient’s consciousness and for treatment of neuropsychic symptoms occurring during skull traumas and brain surgery.4 Among various methods for the synthesis of CDP-choline in the literature, the current preferred method is via the condensation of cytidine-5’-phosphomorpholide (2) with choline phosphate chloride (3) under mild reaction conditions.5–7 Compound 2 was synthesised from 5’-cytidine monophosphate (4) and morpholine in the presence of DCC (N,N’-dicyclohexylcarbodiimide)8 or via the controlled hydrolysis of cytidine-5’-phosphodichloride (5) followed by P–N bond formation with morpholine (Scheme 1, route a).7 However, DCC is toxic and converted into urea which is difficult to separate from the mixture, thus leading to poor purity of product. Furthermore, phosphorylation with POCl3 always meets with side reactions from the 2’ or 3’ hydroxyls and detracts from the acceptance of this method in industry.9 In the context of ongoing projects on the synthesis of nucleoside drugs,10–14 herein we report the synthesis of CDP-choline via the selective phosphorylation of 6 wiResults and discussion Central to our approach for the synthesis of CDP-choline is the selective phosphorylation of 6 using sterically-hindered 7 as phosphorylation regent. 7 was synthesised by the direct phosphorylation of morpholine with POCl3 , a compound whose utility for the conversion of alcohols and amines into various phosphorylation derivatives.15 Due to the reactivity of three chloro atoms in POCl3 , gradually adding POCl3 to excess morpholine avoids the bifunctional reaction exclusively. After reaction, 7 could be purified by fractional distillation to yield as a colourless oil (b.p. 124–126 °C at 1.33 KPa). Due to the presence of the electron-donating morpholino group, 7 displays lower reactivity than POCl3 and could tolerate moisture and air better. Usefully, 7 could be synthesised on the 200 g scale and stored at 4 °C. The major concern of utilising 7 as phosphorylation reagent is its selectivity for the 5’ hydroxyl group. We therefore assessed the selectivity for 5’ hydroxylation using 6 and 7 in the presence of various organic bases. After phosphorylation, H2 O was added to destroy the excess of 7, and 2 was obtained in a single step. The solvent, the base, temperature and the ratio of substrates were evaluated and the results are summarised in Table 1
https://journals.sagepub.com/doi/pdf/10.3184/174751916X14628025243831


Cytidine-5’-phosphomorpholide (2): Cytidine (0.243 g, 1.0 mmol) and DMAP (0.183 g, 1.5 mmol) in MeCN (10 mL) were stirred slowly and cooled to 0 °C, and 7 (2.0 mmol) was added slowly. The mixture was heated to 50 °C and kept at this temperature for 2 h. The solvent was removed in vacuo and the residue was purified by recrystallisation from EtOH to give 2 as a white semi-solid (0.318 g); yield 81%; m.p. 62–64 °C; 1 H NMR (400 MHz, DMSO-d6 ) δ 8.43 (d, J = 7.6 Hz, 1H), 7.39 (s, 2H), 7.19 (d, J = 7.6 Hz, 1H), 5.77 (d, J = 2.8 Hz, 1H), 5.51 (d, J = 4.8 Hz, 1H), 5.18 (t, J = 5.2 Hz, 1H), 5.08 (d, J = 5.6 Hz, 1H), 3.76–3.71 (m, 1H), 3.61–3.56 (m, 1H), 3.45–3.42 (m, 4H), 3.03–2.99 (m, 4H); 13C NMR (100 MHz, DMSO-d6 ) δ 166.5, 157.8, 145.9, 141.6, 88.1, 86.2, 74.3, 70.7, 65.1, 65.0, 60.3, 60.2; HRMS calcd for C13H22N4 O8 P [M + H]+ 393.1170, found: 393.1172.
CDP-choline (1): 2 (0.392 g, 1.0 mmol) was added to MeOH (10 mL) followed by the addition of 3 (0.310 g, 1.2 mmol) and was stirred at room temperature for 10 min. Then 98% H2 SO4 (0.005 mL, 10 mol%) was added. The mixture was kept at 50 °C for 3 h. The solvent was removed in vacuo and the residue was purified by recrystallisation from EtOH to give 1 as a white solid (0.410 g); yield 85%. 1 H NMR (400 MHz, D2 O) δ 7.86 (s, 2H), 6.04 (d, J = 5.2 Hz, 1H), 5.91 (d, J = 5.2 Hz, 1H), 4.32 (brs, 2H), 4.26–4.22 (m, 2H), 4.18 (brs, 2H), 4.11 (t, J = 3.2 Hz, 1H), 3.60 (t, J = 2.4 Hz, 2H), 3.14 (s, 9H); 13C NMR (100 MHz, D2 O) δ 166.1, 157.7, 141.5, 96.6, 89.3, 82.6, 74.1, 69.3, 66.0, 65.9, 64.8, 59.9, 54.0; HRMS calcd for C14H27N4 O11P2 [M + H]+ 489.1146, found: 489.1140.
| 1H NMR | (400 MHz. D2O) δ 7.86 (s, 2H). 6.04 (d. J = 5.2 Hz, 111). 5.91 (d. J = 5.2 Hz. 1Hj, 4.32 (brs. 2H), 4.26-4.22 (m, 2H). 4.18 (brs, 2H), 4.11 (t. J = 3.2 Hz. 1H). 3.60 (t. J = 2.4 Hz. 2H), 3.14 (s, 9H) |
| 13C NMR | (100 MHz. D2O) δ 166.1. 157.7, 141.5,96.6.89.3,82.6,74.1.69.3,66.0, 65.9, 64.8. 59~9. 54.0 |
| HRMS | calcd for C14H27N4O11P2 (M + H]+ 489.1146. found: 489.1140 |
| State | white solid |
SYNKikugawa, Kiyomi; Ichino, MotonobuChemical & Pharmaceutical Bulletin (1971), 19, (5), 1011-16.https://www.jstage.jst.go.jp/article/cpb1958/19/5/19_5_1011/_pdf/-char/enCytidine diphosphate choline (CDP-choline), one of the nucleotide coenzymes, is known to be a precursor of phospholipid and play an important role in the living organisms. The coenzyme was synthesized in a fairly good yield by direct condensation of cytidine-5′ monophosphate (5′-CMP) and choline phosphate (P-choline) by the use of p-toluenesulfonyl chloride or methanesulfonyl chloride combined with dimethylformamide
Method B, with Methanesulfonyl Chloride and DMF: A mixture of 1.3g (11.5 mmole) of methanesulfonyl chloride and 3ml of DMF was added to the gummy mixture containing 10 mmole of P-choline (II). It was shaken at room temperature for 10 min, and 1.0g (3.1 mmole) of 5′-CMP (I) was added to the viscous solution. It was then stirred at room temperature for one hour. Paper chromatography and paper electrophoresis of the reaction mixture showed that CDP-choline (III) was a major reaction product. The separa tion, isolationand identification of the product (III) were same as in method A. Crystalline white powder of CDP-choline was obtained in a yield of 50.0%. Method C, with p-Toluenesulfonyl Chloride and HMPA: A mixture of 2.2g (11.5 mmole) of p-toluene sulfonyl chloride and 3ml of HMPA was added to the gummy mixture containing 10 mmole of P-choline (II). 5′-C1IP (I) (1.0g, 3.1 mmole) was reacted under the same condition as in method A, and isolation was performed similarly. Crystalline powder of CDP-choline (III) was obtained in a yield of about 10%. Method D according to the Morpholidate Method 6): 5′-CMP-Morpholidate (4-morpholine-N, N’-dicyclohexylcarboxamidinium salt) (1.28g, 2 mmole) was reacted with 8 mmole of P-choline (II) according to the method of Tanaka, et al. 6) Separation and isolation of the product were similarly performed as in method A. Crystalline powder of the authentic CDP-choline was obtained in a yield of 55%. CDP-Choline Monosodium Salt Monosodium salt of CDP-choline (III) was prepared from the product (III) obtained by method A. Thus, 200mg of CDP-choline (III) was dissolved in 1.0ml of water, and after the pH of the solution was adjusted to 6.0 with 2N NaOH, 3ml of ethanol was added. Crystallization occurred after standing at room temperature overnight to afford plates of 130 mg of CDP-choline monosodium salt. Determination of the Yield of CDP-Choline (III) in the Condensation with p-Toluenesulfonyl Chloride and DMF In the condensation reaction using p-toluenesulfonyl chloride and DMF, the effects of the amount of p-toluenesulfonyl chloride and the reaction temperature were examined. 5′-CMP (I) (1.0g, 3.1 mmole) was added to the mixture of 10 mmole of P-choline (II), 3ml of DMF and p-toluenesulfonyl chloride which were previously mixed and treated at room temperature for 10 min. The reaction mixtures were stirred at 25•‹for one hour with the varying amounts of p-toluenesulfonyl chloride of 1.5g (7.9 mmole), 1.9g (10 mmole), 2.2g (11.5 mmole), 3g (15.8 mmole), 4g (21.0 mmole) and 5g (26.3 mmole). The yields of the compound (III) estimated were 30, 50, 60, 49, 44 and 37% respectively.
SYN
Indian Pat. Appl., 2014MU00923

SYN
CN 111647636

Syn
Biotechnology and Bioengineering, 117(5), 1426-1435; 2020
https://onlinelibrary.wiley.com/doi/10.1002/bit.27291
Cytidine-5′-diphosphocholine (CDP-choline) is a widely used neuroprotective drug for multiple indications. In industry, CDP-choline is synthesized by a two-step cell culture/permeabilized cell biotransformation method because substrates often do not enter cells in an efficient manner. This study develops a novel one-step living cell fermentation method for CDP-choline production. For this purpose, the feasibility of Pichia pastoris as a chassis was demonstrated by substrate feeding and CDP-choline production. Overexpression of choline phosphate cytidylyltransferase and choline kinase enhanced the choline transformation pathway and improved the biosynthesis of CDP-choline. Furthermore, co-overexpression of ScHnm1, which is a heterologous choline transporter, highly improved the utilization of choline substrates, despite its easy degradation in cells. This strategy increased CDP-choline titer by 55-folds comparing with the wild-type (WT). Overexpression of cytidine-5′-monophosphate (CMP) kinase and CDP kinase in the CMP transformation pathway showed no positive effects. An increase in the ATP production by citrate stimulation or metabolic pathway modification further improved CDP-choline biosynthesis by 120%. Finally, the orthogonal optimization of key substrates and pH was carried out, and the resulting CDP-choline titer (6.0 g/L) at optimum conditions increased 88 times the original titer in the WT. This study provides a new paradigm for CDP-choline bioproduction by living cells.

SYN
Citicoline sodium is a chemically designate as Cytidine 5’-(trihydrogendiphosphate) P’-[2-(trimethylammonio) ethyl] ester monosodium salt, its molecular formula is C14H25N4NaO11P2 and molecular weight is 510.31(salt) and 488.32 (base- C14H26N4O11P2). It is a white crystalline, hygroscopic powder and readily soluble in water but practically insoluble in alcohol. Its melting point was 259 – 268°C and dissociation constant (Pka) was 4.4 [1]. Biopharmaceutical classification system (BCS) for Citicoline is Class – I (High solubility and High Permeability) [3]. Citicoline has a broad spectrum of therapeutic index, as a Neuroprotectant or Cerebroprotectant, in particular citicoline is useful the victims of ischemic stroke, head trauma and neurodegenerative disease. Citicoline is also used to treat unconsciousness resulting from cerebral thrombosis, hemorrhages, demyelinating diseases, cranial trauma and cerebropathies due to atherosclerosis [2]. Citicoline was originally developed in Japan for stroke. It was later introduced as a prescription drug in many European countries. In these countries it is now frequently prescribed for thinking problems related to circulation problems in the brain. In the US, citicoline is marketed as a dietary supplement [3]. Citicoline daily dosages may range from 250 mg to about 3000 mg and more preferably from 500 mg to about 2000 mg up to four or more times daily, duration of the treatment may vary from several weeks to several years, dosages may be varied over time depending on the severity of symptoms [4].

SYN
192/MUM/2012
The present invention discloses a novel, cost-effective process for preparing psychostimulant drug cytidinediphosphate-choline (CDP-Choline) commonly known as citicoline. The process comprises reacting cytidine 5-monophosphate with morpholine in presence of a coupling reagent and an organic solvent to form morpholidate compound; condensing morpholidate compound with calcium salt of phosphorylcholinehalide in presence of an acid to form citicoline calcium chloride; and purifying the citicoline calcium chlorideby passing through cationic and anionic resinsand eluting by water to form citicoline sodium of formula I.
Example:
(a) Preparation of citicoline calcium chloride:
S-Cytidine mono phosphate (1.25 kg)and morpholine (1.12 kg) were added into methanol {6.25 L) and DCC (1.50 kg) at 25 to 35 C.The reaction mixture was heated to 50 to 55 C and stirred for 7 hours. After completion of the reaction, the reaction mass was cooled to 25 to 35 C and the obtained reaction mass was added slowly to phosphoryl choline chloride calcium salt (1.9 kg) in methanol (8.75 L) solution. The pH was maintained to 3.8 to 4.2 using HC1 gas in IPA and stirred for 6 hours at 25 to 35 . The reaction mass was further heated to 45 to 5Q C. After completion of reaction the yeactkm mass was cooled and stirced for 1 hour. The product was filtered, washed with chilled methanol at 0 to 5 Cand suck dried to obtain citicoline calcium chloride.
Yield; 3.70-4.0 kg (b) Preparation of citicoline sodium:
The above obtained crude citicolinecalcium chloride was dissolved in water (6.25 L), filtered, washed with water and suck dried. Filtrate containing the product was re-filtered through Hyflo bed. The clear filtrate was eluted through column containing acidic cation exchange resins (12.5 L). The material was washed with water. The eluent was further passed through anion exchange resin (12.5 L). column and washed with water.
Complete aqueous solution after the passing through an-ion exchange resin was collected, pH of the solution was adjusted to 6.5 to 7.0 using 30 % sodium hydroxide solution (0.3Kg in 0.45L) and solution was concentrated using reverse osmosis. The solution was cooled to 25 to 35 C and charcoalated. The solution was filtered through hyflo bed at 25 to 35 C, washed with water. The solution was further filtered through ultra-filter at 25 to 35 C.
Clear filtrate and mixture of isopropanol and Methanol (1:1) (25 L) were stirred, the reaction mass was cooled to 0 to 5 C, and stirred for 2 hours. The product was filtered under nitrogen atmosphere, solid was washed with the mixture of IPA and methanol (1:1) (1.25 L) at 0 to 5 C and dried under vacuum below 95 C until moisture/LOD is less the 2.0%.
Yield: 1 to 1.2 kg

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
PATENT
https://patents.google.com/patent/CN1944661A/enEmbodiment 1:With 30 kilograms of quick-frozen yeast, 3 kilograms of phosphorylcholines, 1 kilogram 5 ‘-cytidylic acid, 10 kilograms of glucose, 2 kilograms of potassium hydroxide, 800 kg of water are mixed back temperature adjustment to 25 ℃, PH=6 carries out 65 rev/mins of stirring reactions and it was fully reacted in 6 hours; Reaction solution is warming up to 50 ℃ of deactivations, carries out liquid-solid separation; Transfer PH=8.0, part basic protein and nucleic acid precipitation are carried out liquid-solid separation, and then are transferred PH=2.5, make the acidic protein precipitation, carry out liquid-solid separation, sediment separate out; Use Activated Carbon Adsorption Separation, PH=2.5 washs with pure water; Carry out wash-out with the molten reagent of ethanol alkali, elutriant carries out desalination, decolouring is handled, and collects liquid; The elutriant vacuum concentration; Concentrated solution adds 2 times of ethanol, crystallization, liquid-solid separate crude product; Dissolving crude product, ultrafiltration behind the micro-filtration adds 2 times of ethanol, crystallization, liquid-solid separate wet product, after the drying finished product.Embodiment 2:With 80 kilograms of quick-frozen yeast, 4 kilograms of phosphorylcholines, 4 kilogram 5 ‘-cytidylic acid, 16 kilograms of glucose, 4 kilograms of potassium hydroxide, 1100 kg of water are mixed back temperature adjustment to 30 ℃, and add 0.5 kilogram of MgSO 4Solution, PH=6 carries out 120 rev/mins of stirring reactions and it was fully reacted in 8 hours; Reaction solution is warming up to 70 ℃ of deactivations, carries out liquid-solid separation; Transfer PH=10, part basic protein and nucleic acid precipitation are carried out liquid-solid separation, and then are transferred PH=4, make the acidic protein precipitation, carry out liquid-solid separation, sediment separate out; Use Activated Carbon Adsorption Separation, PH=4 washs with pure water; Carry out wash-out with the molten reagent of ethanol alkali, elutriant carries out desalination, decolouring is handled, and collects liquid; The elutriant vacuum concentration; Concentrated solution adds 2 times of methyl alcohol, crystallization, liquid-solid separate crude product; Dissolving crude product, ultrafiltration behind the micro-filtration adds 2 times of methyl alcohol, crystallization, liquid-solid separate wet product, after the drying finished product.Embodiment 3:With 100 kilograms of quick-frozen yeast, 8 kilograms of phosphorylcholines, 5 kilogram 5 ‘-cytidylic acid, 20 kilograms of glucose, 5 kilograms of potassium hydroxide, 1500 kg of water are mixed back temperature adjustment to 40 ℃, and add 6 kilograms of MgSO 4Solution, PH=8 carries out 150 rev/mins of stirring reactions and it was fully reacted in 10 hours; Reaction solution is warming up to 90 ℃ of deactivations, carries out liquid-solid separation; Transfer PH=12.0, part basic protein and nucleic acid precipitation are carried out liquid-solid separation, and then are transferred PH=5.5, make the acidic protein precipitation, carry out liquid-solid separation, sediment separate out; Use Activated Carbon Adsorption Separation, PH=5.5 washs with pure water; Carry out wash-out with the molten reagent of ethanol alkali, elutriant carries out desalination, decolouring is handled, and collects liquid; The elutriant vacuum concentration; Concentrated solution adds 2 times of first and second alcoholic solution, crystallization, liquid-solid separate crude product; Dissolving crude product, ultrafiltration behind the micro-filtration adds 2 times of first and second alcoholic solution, crystallization, liquid-solid separate wet product, after the drying finished product.
PATENThttps://patents.google.com/patent/WO2013128393A1/enCiticoline (CDP-Choline), naturally occurring nucleotide, is a neuroprotective indicated for the treatment of ischemic stroke and head trauma in patients. Citicoline (CDP-Choline) is represented by formula (I).

US patent no. 3,666,748 discloses a process for preparing Citicoline sodium by reaction of 4- morpholino-N,N’-dicyclohexylcarboxamidine chloride salt of choline phosphormorpholidate (I) with cytidine-5-monophosphate in free form or its salts with base in a solvent such as o- chlorophenol, m-cresol, acetonitrile, pyridine and the like. The Citicoline thus obtained is purified through a column chromatograph packed with activated carbon followed by elution to get ammonium salt of citicoline, which is further converted to citicoline followed by citicoline sodium.US patent no. 3,787,392 discloses a process for preparing Citicoline by adding the acidic calcium phosporyl choline chloride tetra hydrate to the solution of morpholidiate cytidine 5- monophosphate and DCC in methanol followed by isolation and purification by means of chromatography column containing anion exchanger (Dowex 1×2 type formate form; 50-100 mesh) which is further converted to its sodium salt by neutralizing with sodium hydroxide. Further, US patent no. 3,803,125 discloses a process for preparing citicoline by reacting morpholidiate cytidine 5 ‘-monophosphate with calcium phosporyl choline chloride tetra hydrate in solvent system of an aliphatic alcohol or dialkyl ketone or dimethyl formamide at pH from 1 to 6.5. The product thus obtained is further isolated; purified by means of chromatography column containing anion exchanger; concentrated; and neutralized with aqueous solution of sodium hydroxide to get citicoline sodium.Example 1To a solution of calcium phosphoryl choline chloride tetra hydrate (50.0 gm) in water, a solution of oxalic acid in RO water (19.5 gm oxalic acid in 90 ml RO water) was added at 45- 50°C. The reaction mass was filtered and distilled out to get residue followed by addition of methanol. To the above solution, solution of morpholine and DCC in methanol was added. The temperature of the reaction was raised to 50-55°C and to this, solution of cytidine 5′- monophospahte in methanol (12.2 gm in 40 ml methanolic HCl and 20 ml methanol) was added and reaction was maintained. The pH 3.5 of reaction mixture was maintained by methanolic HCl. Reaction mass was cooled and IPA was added after completion of the reaction. The precipitated product, citicoline, was filtered and dried. The crude Citicoline (16.0 gm) was dissolved in water and treated with charcoal to get the purified Citicoline acid which on reaction with aqueous sodium hydroxide gave Citicoline Sodium with purity > 99%.Example 2To the solution of cytidine 5′-monophospahate (5′-CMP) (100 gm) in methanol (750 ml), solution of morpholine (75 gm) and DCC (100 gm) in methanol was added at room temperature. The temperature of the reaction was raised to 50-55°C for a time period of 3-7 hrs followed by cooling the reaction mass and filtered to get morpholidiate cytidine 5’- monophospahate in mother liquor. To this, solution of calcium phosphoryl choline chloride (200 gm) in methanol was added and the temperature of reaction mass was raised to 50-55°C and maintained at pH of 3.5 by methanolic HCl. The reaction mass was cooled and filtered to get crude Citicoline by adding IPA. Further, morpholidiate salt of oxalic acid (138.3 gm) was added to the solution of crude citicoline in methanol at 30-35°C followed by the addition of IPA to get the precipitated Citicoline, which is further treated with activated charcoal in water followed by filtration. To filtrate containing purified Citicoline, aqueous solution of sodium hydroxide was added at room temperature followed by addition of ethanol and the temperature of reaction mass was raised to 50-55°C. The precipitated product was filtered and dried where the purity of citicoline sodium is > 99% measured by HPLC. (265 gm).
ClaimsHide Dependent
We Claim:1. A process for preparing pure Citicoline (CDP-Choline), the process comprising:reacting a cytidine 5′-monophospahte or its amide salts with calcium phosphoryl choline chloride tetra hydrate or its amide salts in presence of dicyclohexyl carbodiimide (DCC) and a solvent,wherein a dicarboxylic acid or its salt is employed in the process to obtain citicoline with a purity of more than 99% measured by HPLC.2. The process as claimed in claim 1, further comprising preparing highly pure sodium salt of citicoline by reacting the pure citicoline with sodium hydroxide.3. The process as claimed in claim 1, wherein the dicarboxylic acid is used either in the form of free acid or its base salts.4. The process as claimed in any one of the preceding claims, wherein dicarboxylic acid is selected from the group consisting of oxalic acid, malonic acid, succininc acid and glutaric acid.5. The process as claimed in any one of the preceding claims, wherein the base of dicarboxylic acid is selected from the group consisting of organic bases such as amidates, amines or inorganic base such as alkali or alkaline earth metal.6. The process as claimed in claim 1, wherein the solvent is selected from the group consisting of aliphatic alcohols from C atoms, ketones such as acetone, methyl isobutyl ketone and the like or mixture thereof.7. The process as claimed in claim 1, wherein the solvent is methanol.8. The process as claimed in any of the preceding claims, wherein the dicarboxylic acid or its salts lessen the solubility of inorganic impurities such as calcium chloride, calcium hydroxide, unreacted choline phosphate, 5-CMP.
Patent
US3666748A *1967-12-181972-05-30Takeda Chemical Industries LtdMethod for production of cytidine (or deoxycytidine)-5{40 -diphosphate choline and intermediates thereforUS3787392A *1970-12-021974-01-22Boehringer Mannheim GmbhProcess for the preparation of nucleoside diphosphate estersFamily To Family CitationsCN102010454B *2010-12-022012-03-07胡建荣Citicoline sodium compound and new method thereofPublication numberPriority datePublication dateAssigneeTitleCN104031105A *2014-06-062014-09-10浙江天冉药物研究有限公司Method for preparing citicoline sodiumCN105732752A *2016-03-182016-07-06新乡学院Citicoline and synthetic method thereofCN106146590A *2016-06-292016-11-23陈建峰A kind of preparation method of C14H25N4NaO11P2CN110684066A *2019-05-222020-01-14广东金城金素制药有限公司Cytophosphocholine medicinal preparation and new application thereof in cerebral infarction acute-stage disturbance of consciousness
| Clinical data | |
|---|---|
| Trade names | Neurocoline |
| Other names | Cytidine diphosphate choline |
| AHFS/Drugs.com | International Drug Names |
| ATC code | N06BX06 (WHO) |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 987-78-0 |
| PubChem CID | 11583971 |
| ChemSpider | 13207 |
| UNII | 536BQ2JVC7 |
| KEGG | D00057 |
| ChEBI | CHEBI:16436 |
| ChEMBL | ChEMBL1618340 |
| CompTox Dashboard (EPA) | DTXSID9048431 |
| ECHA InfoCard | 100.012.346 |
| Chemical and physical data | |
| Formula | C14H27N4O11P2+ |
| Molar mass | 489.335 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (what is this?) (verify) |
Use as a dietary supplement
Citicoline is available as a supplement in over 70 countries under a variety of brand names: Cebroton, Ceraxon, Cidilin, Citifar, Cognizin, Difosfocin, Hipercol, NeurAxon, Nicholin, Sinkron, Somazina, Synapsine, Startonyl, Trausan, Xerenoos, etc.[5] When taken as a supplement, citicoline is hydrolyzed into choline and cytidine in the intestine.[6] Once these cross the blood–brain barrier it is reformed into citicoline by the rate-limiting enzyme in phosphatidylcholine synthesis, CTP-phosphocholine cytidylyltransferase.[7][8]
Research
Memory and cognition
Studies have failed to confirm any potential benefits of citicoline for cognitive impairment.[9]
Ischemic stroke
Some preliminary research suggested that citicoline may reduce the rates of death and disability following an ischemic stroke.[10][11] However, the largest citicoline clinical trial to date (a randomised, placebo-controlled, sequential trial of 2298 patients with moderate-to-severe acute ischaemic stroke in Europe), found no benefit of administering citicoline on survival or recovery from stroke.[12] A meta-analysis of seven trials reported no statistically significant benefit for long-term survival or recovery.[13]
Vision
The effect of citicoline on visual function has been studied in patients with glaucoma, with possible positive effect for protecting vision.[14]
Mechanism of action

Enzymes involved in reactions are identified by numbers. See file description.
Neuroprotective effects
Citicoline may have neuroprotective effects due to its preservation of cardiolipin and sphingomyelin, preservation of arachidonic acid content of phosphatidylcholine and phosphatidylethanolamine, partial restoration of phosphatidylcholine levels, and stimulation of glutathione synthesis and glutathione reductase activity. Citicoline’s effects may also be explained by the reduction of phospholipase A2 activity.[15] Citicoline increases phosphatidylcholine synthesis.[16][17][18] The mechanism for this may be:
- By converting 1, 2-diacylglycerol into phosphatidylcholine
- Stimulating the synthesis of SAMe, which aids in membrane stabilization and reduces levels of arachidonic acid. This is especially important after an ischemia, when arachidonic acid levels are elevated.[19]
Neuronal membrane
The brain preferentially uses choline to synthesize acetylcholine. This limits the amount of choline available to synthesize phosphatidylcholine. When the availability of choline is low or the need for acetylcholine increases, phospholipids containing choline can be catabolized from neuronal membranes. These phospholipids include sphingomyelin and phosphatidylcholine.[15] Supplementation with citicoline can increase the amount of choline available for acetylcholine synthesis and aid in rebuilding membrane phospholipid stores after depletion.[20] Citicoline decreases phospholipase stimulation. This can lower levels of hydroxyl radicals produced after an ischemia and prevent cardiolipin from being catabolized by phospholipase A2.[21][22] It can also work to restore cardiolipin levels in the inner mitochondrial membrane.[21]
Cell signalling
Citicoline enhances cellular communication by increasing the availability of neurotransmitters, including acetylcholine, norepinephrine, and dopamine.[23] In simple terms, the choline component of citicoline is used to create acetylcholine, which is a primary executive neurotransmitter in the human brain. Clinical trials have found that citicoline supplementation improves attention, focus and learning in large part due to the increase in acetylcholine that results.[24]
Glutamate transport
Citicoline lowers increased glutamate concentrations and raises decreased ATP concentrations induced by ischemia. Citicoline also increases glutamate uptake by increasing expression of EAAT2, a glutamate transporter, in vitro in rat astrocytes. It is suggested that the neuroprotective effects of citicoline after a stroke are due in part to citicoline’s ability to decrease levels of glutamate in the brain.[25]
Pharmacokinetics
Citicoline is water-soluble, with more than 90% oral bioavailability.[20] Plasma levels peak one hour after oral ingestion, and a majority of the citicoline is excreted as CO2 in respiration, and again 24 hours after ingestion, where the remaining citicoline is excreted through urine.[26]
Side effects
Citicoline has a very low toxicity profile in animals and humans. Clinically, doses of 2000 mg per day have been observed and approved. Minor transient adverse effects are rare and most commonly include stomach pain and diarrhea.[17][unreliable medical source?] There have been suggestions that chronic citicoline use may have adverse psychiatric effects. However, a meta-analysis of the relevant literature does not support this hypothesis.[27][28] At most, citicoline may exacerbate psychotic episodes or interact with anti-psychotic medication.
Synthesis
In vivo
Phosphatidylcholine is a major phospholipid in eukaryotic cell membranes. Close regulation of its biosynthesis, degradation, and distribution is essential to proper cell function. Phosphatidylcholine is synthesized in vivo by two pathways
- The Kennedy pathway, which includes the transformation of choline to citicoline, by way of phosphorylcholine, to produce phosphatidylcholine when condensed with diacylglycerol.
- Phosphatidylcholine can also be produced by the methylation pathway, where phosphatidylethanolamine is sequentially methylated.[29]
References
- ^ Giménez R, Raïch J, Aguilar J (Nov 1991). “Changes in brain striatum dopamine and acetylcholine receptors induced by chronic CDP-choline treatment of aging mice”. British Journal of Pharmacology. 104 (3): 575–8. doi:10.1111/j.1476-5381.1991.tb12471.x. PMC 1908237. PMID 1839138.
- ^ Cavun S, Savci V (Oct 2004). “CDP-choline increases plasma ACTH and potentiates the stimulated release of GH, TSH and LH: the cholinergic involvement”. Fundamental & Clinical Pharmacology. 18 (5): 513–23. doi:10.1111/j.1472-8206.2004.00272.x. PMID 15482372. S2CID 33866107.
- ^ Benson S, Arck PC, Tan S, Hahn S, Mann K, Rifaie N, Janssen OE, Schedlowski M, Elsenbruch S (Jun 2009). “Disturbed stress responses in women with polycystic ovary syndrome”. Psychoneuroendocrinology. 34 (5): 727–35. doi:10.1016/j.psyneuen.2008.12.001. PMID 19150179. S2CID 13202703.
- ^ Florio P, Zatelli MC, Reis FM, degli Uberti EC, Petraglia F (2007). “Corticotropin releasing hormone: a diagnostic marker for behavioral and reproductive disorders?”. Frontiers in Bioscience. 12: 551–60. doi:10.2741/2081. PMID 17127316.
- ^ Single-ingredient Preparations (: Citicoline). In: Martindale: The Complete Drug Reference [ed.by Sweetman S], 35th Ed. 2007, The Pharmaceutical Press: London (UK); e-version. .
- ^ Wurtman RJ, Regan M, Ulus I, Yu L (Oct 2000). “Effect of oral CDP-choline on plasma choline and uridine levels in humans”. Biochemical Pharmacology. 60 (7): 989–92. doi:10.1016/S0006-2952(00)00436-6. PMID 10974208.
- ^ Alvarez XA, Sampedro C, Lozano R, Cacabelos R (Oct 1999). “Citicoline protects hippocampal neurons against apoptosis induced by brain beta-amyloid deposits plus cerebral hypoperfusion in rats”. Methods and Findings in Experimental and Clinical Pharmacology. 21 (8): 535–40. doi:10.1358/mf.1999.21.8.794835. PMID 10599052.
- ^ Carlezon WA, Pliakas AM, Parow AM, Detke MJ, Cohen BM, Renshaw PF (Jun 2002). “Antidepressant-like effects of cytidine in the forced swim test in rats”. Biological Psychiatry. 51 (11): 882–9. doi:10.1016/s0006-3223(01)01344-0. PMID 12022961. S2CID 21170398.
- ^ Gareri P, Castagna A, Cotroneo AM, Putignano S, De Sarro G, Bruni AC (2015). “The role of citicoline in cognitive impairment: pharmacological characteristics, possible advantages, and doubts for an old drug with new perspectives”. Clin Interv Aging. 10: 1421–9. doi:10.2147/CIA.S87886. PMC 4562749. PMID 26366063.
- ^ Warach S, Pettigrew LC, Dashe JF, Pullicino P, Lefkowitz DM, Sabounjian L, Harnett K, Schwiderski U, Gammans R (Nov 2000). “Effect of citicoline on ischemic lesions as measured by diffusion-weighted magnetic resonance imaging. Citicoline 010 Investigators”. Annals of Neurology. 48 (5): 713–22. doi:10.1002/1531-8249(200011)48:5<713::aid-ana4>3.0.co;2-#. PMID 11079534.
- ^ Saver JL (Fall 2008). “Citicoline: update on a promising and widely available agent for neuroprotection and neurorepair”. Reviews in Neurological Diseases. 5 (4): 167–77. PMID 19122569.
- ^ Dávalos A, Alvarez-Sabín J, Castillo J, Díez-Tejedor E, Ferro J, Martínez-Vila E, Serena J, Segura T, Cruz VT, Masjuan J, Cobo E, Secades JJ (Jul 2012). “Citicoline in the treatment of acute ischaemic stroke: an international, randomised, multicentre, placebo-controlled study (ICTUS trial)”. Lancet. 380 (9839): 349–57. doi:10.1016/S0140-6736(12)60813-7. hdl:10400.10/663. PMID 22691567. S2CID 134947.
- ^ Shi PY, Zhou XC, Yin XX, Xu LL, Zhang XM, Bai HY (2016). “Early application of citicoline in the treatment of acute stroke: A meta-analysis of randomized controlled trials”. J. Huazhong Univ. Sci. Technol. Med. Sci. 36 (2): 270–7. doi:10.1007/s11596-016-1579-6. PMID 27072975. S2CID 25352343.
- ^ Roberti G, Tanga L, Michelessi M, Quaranta L, Parisi V, Manni G, Oddone F (2015). “Cytidine 5′-Diphosphocholine (Citicoline) in Glaucoma: Rationale of Its Use, Current Evidence and Future Perspectives”. Int J Mol Sci. 16 (12): 28401–17. doi:10.3390/ijms161226099. PMC 4691046. PMID 26633368.
- ^ Jump up to:a b Adibhatla RM, Hatcher JF, Dempsey RJ (Jan 2002). “Citicoline: neuroprotective mechanisms in cerebral ischemia”. Journal of Neurochemistry. 80 (1): 12–23. doi:10.1046/j.0022-3042.2001.00697.x. PMID 11796739.
- ^ López-Coviella I, Agut J, Savci V, Ortiz JA, Wurtman RJ (Aug 1995). “Evidence that 5′-cytidinediphosphocholine can affect brain phospholipid composition by increasing choline and cytidine plasma levels”. Journal of Neurochemistry. 65 (2): 889–94. doi:10.1046/j.1471-4159.1995.65020889.x. PMID 7616250. S2CID 10184322.
- ^ Jump up to:a b Conant R, Schauss AG (Mar 2004). “Therapeutic applications of citicoline for stroke and cognitive dysfunction in the elderly: a review of the literature”. Alternative Medicine Review. 9 (1): 17–31. PMID 15005642.
- ^ Babb SM, Wald LL, Cohen BM, Villafuerte RA, Gruber SA, Yurgelun-Todd DA, Renshaw PF (May 2002). “Chronic citicoline increases phosphodiesters in the brains of healthy older subjects: an in vivo phosphorus magnetic resonance spectroscopy study”. Psychopharmacology. 161 (3): 248–54. doi:10.1007/s00213-002-1045-y. PMID 12021827. S2CID 28454793.
- ^ Rao AM, Hatcher JF, Dempsey RJ (Dec 1999). “CDP-choline: neuroprotection in transient forebrain ischemia of gerbils”. Journal of Neuroscience Research. 58 (5): 697–705. doi:10.1002/(sici)1097-4547(19991201)58:5<697::aid-jnr11>3.0.co;2-b. PMID 10561698.
- ^ Jump up to:a b D’Orlando KJ, Sandage BW (Aug 1995). “Citicoline (CDP-choline): mechanisms of action and effects in ischemic brain injury”. Neurological Research. 17 (4): 281–4. doi:10.1080/01616412.1995.11740327. PMID 7477743.
- ^ Jump up to:a b Rao AM, Hatcher JF, Dempsey RJ (Mar 2001). “Does CDP-choline modulate phospholipase activities after transient forebrain ischemia?”. Brain Research. 893 (1–2): 268–72. doi:10.1016/S0006-8993(00)03280-7. PMID 11223016. S2CID 37271883.
- ^ Adibhatla RM, Hatcher JF (Aug 2003). “Citicoline decreases phospholipase A2 stimulation and hydroxyl radical generation in transient cerebral ischemia”. Journal of Neuroscience Research. 73 (3): 308–15. doi:10.1002/jnr.10672. PMID 12868064. S2CID 17806057.
- ^ Secades JJ, Lorenzo JL (Sep 2006). “Citicoline: pharmacological and clinical review, 2006 update”. Methods and Findings in Experimental and Clinical Pharmacology. 28 Suppl B: 1–56. PMID 17171187.
- ^ Tardner, P. (2020-08-30). “The use of citicoline for the treatment of cognitive decline and cognitive impairment: A meta-analysis of pharmacological literature • International Journal of Environmental Science & Technology”. International Journal of Environmental Science & Technology. Retrieved 2020-08-31.
- ^ Hurtado O, Moro MA, Cárdenas A, Sánchez V, Fernández-Tomé P, Leza JC, Lorenzo P, Secades JJ, Lozano R, Dávalos A, Castillo J, Lizasoain I (Mar 2005). “Neuroprotection afforded by prior citicoline administration in experimental brain ischemia: effects on glutamate transport”. Neurobiology of Disease. 18 (2): 336–345. doi:10.1016/j.nbd.2004.10.006. PMID 15686962. S2CID 2818533.
- ^ Dinsdale JR, Griffiths GK, Rowlands C, Castelló J, Ortiz JA, Maddock J, Aylward M (1983). “Pharmacokinetics of 14C CDP-choline”. Arzneimittel-Forschung. 33 (7A): 1066–70. PMID 6412727.
- ^ Tardner, P. (2020-08-28). “Can Citicoline Cause Depression?: A review of the clinical literature • International Journal of Environmental Science & Technology”. International Journal of Environmental Science & Technology. Retrieved 2020-08-31.
- ^ Talih, Farid; Ajaltouni, Jean (2015). “Probable Nootropicinduced Psychiatric Adverse Effects: A Series of Four Cases”. Innovations in Clinical Neuroscience. 12 (11–12): 21–25. ISSN 2158-8333. PMC 4756795. PMID 27222762.
- ^ Fernández-Murray JP, McMaster CR (Nov 2005). “Glycerophosphocholine catabolism as a new route for choline formation for phosphatidylcholine synthesis by the Kennedy pathway”. The Journal of Biological Chemistry. 280 (46): 38290–6. doi:10.1074/jbc.M507700200. PMID 16172116.
//////////CITOCOLINE, CDP-choline, Neuroprotective, ischemic stroke, head trauma,
C[N+](C)(C)CCOP(=O)(O)OP(=O)([O-])OCC1C(C(C(O1)N2C=CC(=NC2=O)N)O)O

NEW DRUG APPROVALS
ONE TIME
$10.00
Povidone-iodine

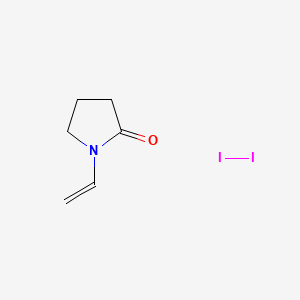
Povidone-iodine
PVP 1
UNII85H0HZU99M, BETADINE
CAS number 25655-41-8, Molecular Formula, (C6-H9-N-O)x-.x-I2, Molecular Weight, 364.9431
1-ethenylpyrrolidin-2-one;molecular iodine Povidone-Iodine
CAS Registry Number: 25655-41-8
CAS Name: 1-Ethenyl-2-pyrrolidinone homopolymer compd with iodine
Additional Names: 1-vinyl-2-pyrrolidinone polymers, iodine complex; iodine-polyvinylpyrrolidone complex; polyvinylpyrrolidone-iodine complex; PVP-I
Trademarks: Betadine (Purdue Frederick); Betaisodona (Mundipharma); Braunol (Braun Melsungen); Braunosan H (Braun Melsungen); Disadine D.P. (Stuart); Efodine (Fougera); Inadine (J & J); Isodine (Blair); Proviodine (Rougier); Traumasept (Wolff)
Literature References: An iodophor, q.v., prepd by Beller, Hosmer, US2706701; Hosmer, US2826532; Siggia, US2900305 (1955, 1958, and 1959, all to GAF). Prepn, history and use: Shelanski, Shelanski, J. Int. Coll. Surg.25, 727 (1956).
Properties: Yellowish-brown, amorphous powder with slight characteristic odor. Aq solns have a pH near 2 and may be made more neutral (but less stable) by the addition of sodium bicarbonate. Sol in alc, water. Practically insol in chloroform, carbon tetrachloride, ether, solvent hexane, acetone. Solns do not give the familiar starch test when freshly prepared.
Therap-Cat: Anti-infective (topical).
Therap-Cat-Vet: Anti-infective (topical).
Keywords: Antiseptic/Disinfectant; Halogens/Halogen Containing Compounds.
- An iodinated polyvinyl polymer used as topical antiseptic in surgery and for skin and mucous membrane infections, also as aerosol. The iodine may be radiolabeled for research purposes.
Povidone-iodine is a stable chemical complex of polyvinylpyrrolidone (povidone, PVP) and elemental iodine. It contains from 9.0% to 12.0% available iodine, calculated on a dry basis. This unique complex was discovered in 1955 at the Industrial Toxicology Laboratories in Philadelphia by H. A. Shelanski and M. V. Shelanski. During in vitro testing to demonstrate anti-bacterial activity it was found that the complex was less toxic in mice than tincture of iodine. Human clinical trials showed the product to be superior to other iodine formulations. Povidone-iodine was immediately marketed, and has since become the universally preferred iodine antiseptic.
Povidone-iodine (PVP-I), also known as iodopovidone, is an antiseptic used for skin disinfection before and after surgery.[1][2] It may be used both to disinfect the hands of healthcare providers and the skin of the person they are caring for.[2] It may also be used for minor wounds.[2] It may be applied to the skin as a liquid or a powder.[2]
Side effects include skin irritation and sometimes swelling.[1] If used on large wounds, kidney problems, high blood sodium, and metabolic acidosis may occur.[1] It is not recommended in women who are less than 32 weeks pregnant or are taking lithium.[2] Frequent use is not recommended in people with thyroid problems.[2] Povidone-iodine is a chemical complex of povidone, hydrogen iodide, and elemental iodine.[3] It contains 10% Povidone, with total iodine species equaling 10,000 ppm or 1% total titratable iodine.[3] It works by releasing iodine which results in the death of a range of microorganisms.[1]
Povidone-iodine came into commercial use in 1955.[4] It is on the World Health Organization’s List of Essential Medicines.[5] Povidone-iodine is available over the counter.[6] It is sold under a number of brand names including Betadine.[2]

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
Medical uses
Wound area covered in povidone-iodine. Gauze has also been applied.
Povidone-iodine is a broad spectrum antiseptic for topical application in the treatment and prevention of wound infection. It may be used in first aid for minor cuts, burns, abrasions and blisters. Povidone-iodine exhibits longer lasting antiseptic effects than tincture of iodine, due to its slow absorption via soft tissue, making it the choice for longer surgeries. Chlorhexidine provides superior results with equivalent adverse events.[7]
Consequently, PVP-I has found broad application in medicine as a surgical scrub; for pre- and post-operative skin cleansing; for the treatment and prevention of infections in wounds, ulcers, cuts and burns; for the treatment of infections in decubitus ulcers and stasis ulcers; in gynecology for vaginitis associated with candidal, trichomonal or mixed infections. For these purposes PVP-I has been formulated at concentrations of 7.5–10.0% in solution, spray, surgical scrub, ointment, and swab dosage forms; however, use of 10% povidone-iodine though recommended, is infrequently used, as it is poorly accepted by health care workers and is excessively slow to dry.[8][9]
Because of these critical indications, only sterile povidone-iodine should be used in most cases. Non-sterile product can be appropriate in limited circumstances in which people have intact, healthy skin that will not be compromised or cut. The non-sterile form of Povidone iodine has a long history of intrinsic contamination with Burkholderia cepacia (aka Pseudomonas cepacia), and other opportunistic pathogens. Its ability to harbor such microbes further underscores the importance of using sterile products in any clinical setting. Since these bacteria are resistant to povidone iodine, statements that bacteria do not develop resistance to PVP-I,[10] should be regarded with great caution: some bacteria are intrinsically resistant to a range of biocides including povidone-iodine.[11]
Antiseptic activity of PVP-I is because of free iodine (I2) and PVP-I only acts as carrier of I2 to the target cells. Most commonly used 10% PVP-I delivers about 1-3 ppm of I2 in a compound of more than 31,600 ppm of total iodine atoms. All the toxic and staining effects of PVP-I is due to the inactive iodine only.
Eyes
A buffered PVP-I solution of 2.5% concentration can be used for prevention of neonatal conjunctivitis, especially if it is caused by Neisseria gonorrhoeae, or Chlamydia trachomatis. It is currently unclear whether PVP-I is more effective in reducing the number of cases of conjunctivitis in neonates over other methods.[12] PVP-I appears to be very suitable for this purpose because, unlike other substances, it is also efficient against fungi and viruses (including HIV and Herpes simplex).[13]
Pleurodesis
It is used in pleurodesis (fusion of the pleura because of incessant pleural effusions). For this purpose, povidone-iodine is equally effective and safe as talc, and may be preferred because of easy availability and low cost.[14]
Alternatives
There is strong evidence that chlorhexidine and denatured alcohol used to clean skin prior to surgery is better than any formulation of povidone-iodine[7]
Contraindications
PVP-I is contraindicated in people with hyperthyroidism (overactive thyroid gland) and other diseases of the thyroid, after treatment with radioiodine, and in people with dermatitis herpetiformis[why?] (Duhring’s disease).[15]
Side effects
The sensitization rate to the product is 0.7%.[16]
Interactions
The iodine in PVP-I reacts with hydrogen peroxide, silver, taurolidine and proteins such as enzymes, rendering them (and itself) ineffective. It also reacts with many mercury compounds, giving the corrosive compound mercury iodide, as well as with many metals, making it unsuitable for disinfecting metal piercings.[15]
Iodine is absorbed into the body to various degrees, depending on application area and condition of the skin. As such, it interacts with diagnostic tests of the thyroid gland such as radioiodine diagnostics, as well as with various diagnostic agents used on the urine and stool, for example Guaiacum resin.[15]
Structure
Structure of povidone-iodine complex.
Povidone-iodine is a chemical complex of the polymer povidone (polyvinylpyrrolidone) and triiodide (I3−).[17]
It is soluble in cold and mild-warm water, ethyl alcohol, isopropyl alcohol, polyethylene glycol, and glycerol. Its stability in solution is much greater than that of tincture of iodine or Lugol’s solution.
Free iodine, slowly liberated from the povidone-iodine (PVP-I) complex in solution, kills cells through iodination of lipids and oxidation of cytoplasmic and membrane compounds. This agent exhibits a broad range of microbiocidal activity against bacteria, fungi, protozoa, and viruses. Slow release of iodine from the PVP-I complex in solution minimizes iodine toxicity towards mammalian cells.
PVP-I can be loaded into hydrogels, which can be based on carboxymethyl cellulose (CMC), poly(vinyl alcohol) (PVA), and gelatin, or on crosslinked polyacrylamide. These hydrogels can be used for wound dressing. The rate of release of the iodine in the PVP-I is heavily dependent on the hydrogel composition: it increases with more CMC/PVA and decreases with more gelatin.
History
PVP-I was discovered in 1955, at the Industrial Toxicology Laboratories in Philadelphia by H. A. Shelanski and M. V. Shelanski.[18] They carried out tests in vitro to demonstrate anti-bacterial activity, and found that the complex was less toxic in mice than tincture of iodine. Human clinical trials showed the product to be superior to other iodine formulations.[19]
Following the discovery of iodine by Bernard Courtois in 1811, it has been broadly used for the prevention and treatment of skin infections, as well as the treatment of wounds. Iodine has been recognized as an effective broad-spectrum bactericide, and is also effective against yeasts, molds, fungi, viruses, and protozoans. Drawbacks to its use in the form of aqueous solutions include irritation at the site of application, toxicity, and the staining of surrounding tissues. These deficiencies were overcome by the discovery and use of PVP-I, in which the iodine is carried in a complexed form and the concentration of free iodine is very low. The product thus serves as an iodophor.
Research
Schematic of povidone-iodine complex wrapping a single wall carbon nanotube (black).[20]
Povidone-iodine has found application in the field of nanomaterials. A wound-healing application has been developed which employs a mat of single wall carbon nanotubes (SWNTs) coated in a monolayer of povidone-iodine.[20]
Research has previously found that the polymer polyvinylpyrrolidone (PVP, povidone) can coil around individual carbon nanotubes to make them water-soluble.[21]
References
- ^ Jump up to:a b c d World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization. pp. 321–323. hdl:10665/44053. ISBN 9789241547659.
- ^ Jump up to:a b c d e f g British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. p. 840. ISBN 9780857111562.
- ^ Jump up to:a b Encyclopedia of polymer science and technology (3 ed.). John Wiley & Sons. 2013. p. 728. ISBN 9780470073698. Archived from the original on 2017-01-13.
- ^ Sneader W (2005). Drug Discovery: A History. John Wiley & Sons. p. 68. ISBN 9780470015520. Archived from the original on 2017-01-13.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06.
- ^ “Povidone/iodine solution: Indications, Side Effects, Warnings – Drugs.com”. http://www.drugs.com. Archived from the original on 13 January 2017. Retrieved 11 January 2017.
- ^ Jump up to:a b Wade RG, Burr NE, McCauley G, Bourke G, Efthimiou O (September 2020). “The Comparative Efficacy of Chlorhexidine Gluconate and Povidone-iodine Antiseptics for the Prevention of Infection in Clean Surgery: A Systematic Review and Network Meta-analysis”. Annals of Surgery. Publish Ahead of Print. doi:10.1097/SLA.0000000000004076. PMID 32773627.
- ^ Slater K, Cooke M, Fullerton F, Whitby M, Hay J, Lingard S, et al. (September 2020). “Peripheral intravenous catheter needleless connector decontamination study-Randomized controlled trial”. American Journal of Infection Control. 48 (9): 1013–1018. doi:10.1016/j.ajic.2019.11.030. PMID 31928890.
- ^ Slater K, Fullerton F, Cooke M, Snell S, Rickard CM (September 2018). “Needleless connector drying time-how long does it take?”. American Journal of Infection Control. 46 (9): 1080–1081. doi:10.1016/j.ajic.2018.05.007. PMID 29880433. S2CID 46968733.
- ^ Fleischer W, Reimer K (1997). “Povidone-iodine in antisepsis–state of the art”. Dermatology. 195 Suppl 2 (Suppl 2): 3–9. doi:10.1159/000246022. PMID 9403248.
- ^ Rose H, Baldwin A, Dowson CG, Mahenthiralingam E (March 2009). “Biocide susceptibility of the Burkholderia cepacia complex”. The Journal of Antimicrobial Chemotherapy. 63 (3): 502–10. doi:10.1093/jac/dkn540. PMC 2640157. PMID 19153076.
- ^ Martin I, Sawatzky P, Liu G, Mulvey MR (February 2015). “Neisseria gonorrhoeae in Canada: 2009-2013”. Canada Communicable Disease Report. 41 (2): 35–41. doi:10.1002/14651858.CD001862.pub3. PMC 6457593.
- ^ Najafi Bi R, Samani SM, Pishva N, Moheimani F (2003). “Formulation and Clinical Evaluation of Povidone-Iodine Ophthalmic Drop”. Iranian Journal of Pharmaceuticical Research. 2 (3): 157–160.
- ^ Agarwal R, Khan A, Aggarwal AN, Gupta D (March 2012). “Efficacy & safety of iodopovidone pleurodesis: a systematic review & meta-analysis”. The Indian Journal of Medical Research. 135: 297–304. PMC 3361864. PMID 22561614.
- ^ Jump up to:a b c Jasek W, ed. (2007). Austria-Codex (in German) (62nd ed.). Vienna: Österreichischer Apothekerverlag. pp. 983–5. ISBN 978-3-85200-181-4.
- ^ Niedner R (1997). “Cytotoxicity and sensitization of povidone-iodine and other frequently used anti-infective agents”. Dermatology. 195 Suppl 2 (Suppl 2): 89–92. doi:10.1159/000246038. PMID 9403263.
- ^ Kutscher, Bernhard (2020). “Dermatologicals (D), 4. Antiseptics and Disinfectants (D08), Anti‐Acne Preparations (D10), and Other Dermatological Preparations (D11)”. Ullmann’s Encyclopedia of Industrial Chemistry. Weinheim: Wiley-VCH. pp. 1–22. doi:10.1002/14356007.w08_w03.
- ^ U.S. Patent 2,739,922
- ^ Sneader W (2005). Drug Discovery: A History. New York: John Wiley & Sons. p. 68. ISBN 978-0-471-89979-2.
- ^ Jump up to:a b Simmons TJ, Lee SH, Park TJ, Hashim DP, Ajayan PM, Linhardt RJ (2009). “Antiseptic Single Wall Carbon Nanotube Bandages” (PDF). Carbon. 47 (6): 1561–1564. doi:10.1016/j.carbon.2009.02.005. Archived from the original (PDF) on 2010-06-21.
- ^ Simmons TJ, Hashim D, Vajtai R, Ajayan PM (August 2007). “Large area-aligned arrays from direct deposition of single-wall carbon nanotube inks”. Journal of the American Chemical Society. 129 (33): 10088–9. doi:10.1021/ja073745e. PMID 17663555.
Further reading
- Wong RH, Hung EC, Wong VW, Wan IY, Ng CS, Wan S, Underwood MJ (2009). “Povidone-iodine wound irrigation: A word of caution”. Surgical Practice. 13 (4): 123–4. doi:10.1111/j.1744-1633.2009.00461.x. S2CID 71797553.
- Wong RH, Wong VW, Hung EC, Lee PY, Ng CS, Wan IY, Underwood MJ (2011). “Topical application of povidone-iodine before wound closure is associated with significant increase in serum iodine level”. Surgical Practice. 19 (3): 79–82. doi:10.1111/j.1744-1633.2011.00547.x. S2CID 70528331.
- Wong RH, Ng CS, Underwood MJ (May 2012). “Iodine pleurodesis–a word of caution”. European Journal of Cardio-Thoracic Surgery. 41 (5): 1209. doi:10.1093/ejcts/ezr137. PMID 22219431.
External links
“Povidone-iodine”. Drug Information Portal. U.S. National Library of Medicine.
| Povidone-iodine applied to an abrasion using a cotton swab. | |
| Clinical data | |
|---|---|
| Trade names | Betadine, Wokadine, Pyodine, others |
| Other names | polyvidone iodine, iodopovidone |
| AHFS/Drugs.com | Consumer Drug Information |
| License data | US DailyMed: Povidone-iodine |
| Routes of administration | Topical |
| ATC code | D08AG02 (WHO)D09AA09 (WHO) (dressing)D11AC06 (WHO)G01AX11 (WHO)R02AA15 (WHO)S01AX18 (WHO)QG51AD01 (WHO) |
| Legal status | |
| Legal status | US: OTC / Rx-only |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 25655-41-8 |
| PubChem CID | 410087 |
| DrugBank | DB06812 |
| ChemSpider | none |
| UNII | 85H0HZU99M |
| KEGG | D00863C08043 |
| ChEBI | CHEBI:8347 |
| ChEMBL | ChEMBL1201724 |
| CompTox Dashboard (EPA) | DTXSID8035712 |
| ECHA InfoCard | 100.110.412 |
| Chemical and physical data | |
| Formula | (C6H9NO)n·xI |
| Molar mass | variable |
| (what is this?) (verify) |
///////////Povidone-iodine, PVP 1, BETADINE
C=CN1CCCC1=O.II

NEW DRUG APPROVALS
ONE TIME
$10.00
PILOCARPINE

PILOCARPINE
- Molecular FormulaC11H16N2O2
- Average mass208.257 Da
2(3H)-Furanone, 3-ethyldihydro-4-[(1-methyl-1H-imidazol-5-yl)methyl]-, (3S-cis)-
202-128-4[EINECS]92-13-7 CAS
54-71-7[RN]
(+)-pilocarpine
(3S,4R)-3-Ethyl-4-[(1-methyl-1H-imidazol-5-yl)methyl]dihydro-2(3H)-furanone
Product Ingredients
| INGREDIENT | UNII | CAS | INCHI KEY |
|---|---|---|---|
| Pilocarpine hydrochloride | 0WW6D218XJ | 54-71-7 | RNAICSBVACLLGM-GNAZCLTHSA-N |
| Pilocarpine nitrate | M20T465H6J | 148-72-1 | PRZXEPJJHQYOGF-GNAZCLTHSA-N |
PilocarpineCAS Registry Number: 92-13-7
CAS Name: (3S-cis)-3-Ethyldihydro-4-[(1-methyl-1H-imidazol-5-yl)methyl]-2(3H)-furanone
Trademarks: Ocusert Pilo (Cusi)
Molecular Formula: C11H16N2O2, Molecular Weight: 208.26
Percent Composition: C 63.44%, H 7.74%, N 13.45%, O 15.36%
Literature References: Cholinergic principle from Pilocarpus jaborandi Holmes, Rutaceae. Isoln: Petit, Polanovski, Bull. Soc. Chim. [3] 17, 557, 702 (1897). Structure: Jowett, J. Chem. Soc.77, 473, 851 (1900); 83, 438 (1903). Stereoisomeric with isopilocarpine: Polonovski, Polonovski, Bull. Soc. Chim. [4] 31, 1314 (1922). Has the cis configuration; isopilocarpine is trans: Zav’yalov, Dokl. Akad. Nauk SSSR82, 257 (1952). Absolute configuration: Hill, Barcza, Tetrahedron22, 2889 (1966). Synthesis: Preobrashenski et al.,Ber.66, 1187 (1933); Samokhvalov, Med. Prom. SSSR11, no. 2, 10 (1957); DeGraw, Tetrahedron28, 967 (1972); Link, Bernauer, Helv. Chim. Acta55, 1053 (1972). Stereoselective synthesis: A. Noordam et al.,Rec. Trav. Chim.98, 467 (1979). Review: Langenbeck, Angew. Chem.60, 297 (1948); van Rossum et al.,Experientia16, 373 (1960). Toxicity studies: Beccari, Boll. Chim. Farm.106, 8 (1967). Comprehensive description: A. A. Al-Badr, H. Y. Aboul-Enein, Anal. Profiles Drug Subs.12, 385-432 (1983). Clinical trial in Sjögren’s syndrome: F. B. Vivino et al., Arch. Intern. Med.159, 174 (1999); in radiation-induced xerostomia: J.-C. Horiot et al.,Radiother. Oncol.55, 233 (2000).
Properties: Oil or crystals, mp 34°. bp5 260° (partial conversion to isopilocarpine). [a]D18 +106° (c = 2). pK1 (20°) 7.15; pK2 (20°) 12.57. Sol in water, alcohol, chloroform; sparingly sol in ether, benzene. Almost insol in petr ether.
Melting point: mp 34°
Boiling point: bp5 260° (partial conversion to isopilocarpine)
pKa: pK1 (20°) 7.15; pK2 (20°) 12.57
Optical Rotation: [a]D18 +106° (c = 2)
Derivative Type: Hydrochloride
CAS Registry Number: 54-71-7
Trademarks: Akarpine (Akorn); Almocarpine (Ayerst); Isopto Carpine (Alcon); Pilogel (Alcon); Pilopine HS (Alcon); Pilostat (Bausch & Lomb); Salagen (MGI)
Molecular Formula: C11H16N2O2.HCl, Molecular Weight: 244.72
Percent Composition: C 53.99%, H 7.00%, N 11.45%, O 13.08%, Cl 14.49%
Properties: Hygroscopic crystals from alcohol, mp 204-205°. [a]D18 +91° (c = 2). Freely sol in water, alcohol. Practically insol in ether, chloroform. Keep well closed and protected from light.
Melting point: mp 204-205°
Optical Rotation: [a]D18 +91° (c = 2)
Derivative Type: Nitrate
CAS Registry Number: 148-72-1
Trademarks: Chibro Pilocarpine (Chibret); Licarpin (Allergan); Pilo (Novopharma); Pilofrin (Allergan); Pilagan (Allergan)
Molecular Formula: C11H16N2O2.HNO3, Molecular Weight: 271.27
Percent Composition: C 48.70%, H 6.32%, N 15.49%, O 29.49%
Properties: mp 173.5-174.0° (dec). Poisonous! [a]D +77 to +83° (c = 10). One gram dissolves in 4 ml water, 75 ml alcohol. Insol in chloroform, ether. Incompat. Silver nitrate, mercury bichloride, iodides, gold salts, tannin, calomel, KMnO4, alkalies.
Melting point: mp 173.5-174.0° (dec)
Optical Rotation: [a]D +77 to +83° (c = 10)
Derivative Type: Isopilocarpine
Additional Names: b-Pilocarpine
Properties: Hygroscopic oily liquid or prisms. bp10 261°. [a]D18 +50° (c = 2). pK1 (18°) 7.17. Miscible with water and alcohol; very sol in chloroform; less sol in benzene, ether. Almost insol in petr ether.
Boiling point: bp10 261°
pKa: pK1 (18°) 7.17
Optical Rotation: [a]D18 +50° (c = 2)
Derivative Type: Isopilocarpine hydrochloride hemihydrate
Molecular Formula: C11H16N2O2.HCl.½H2O, Molecular Weight: 253.73
Percent Composition: C 52.07%, H 7.15%, N 11.04%, O 15.76%, Cl 13.97%
Properties: Scales from alcohol + ether, mp 127°; when anhydr, mp 161°. [a]D18 +39° (c = 5). Sol in 0.27 part water; 2.1 parts alcohol.
Melting point: mp 127°; mp 161°
Optical Rotation: [a]D18 +39° (c = 5)
Derivative Type: Isopilocarpine nitrate
Molecular Formula: C11H16N2O2.HNO3, Molecular Weight: 271.27Percent Composition: C 48.70%, H 6.32%, N 15.49%, O 29.49%
Properties: Prisms from water, scales from alcohol, mp 159°. [a]D18 +39° (c = 2). Sol in 8.4 parts water, in 350 parts abs alcohol.
Melting point: mp 159°
Optical Rotation: [a]D18 +39° (c = 2)
Therap-Cat: Antiglaucoma agent; miotic; sialogogue.
Therap-Cat-Vet: Parasympathomimetic; miotic; gastric secretory stimulant.
Keywords: Antiglaucoma; Miotic; Sialagogue.
Pilocarpine is a muscarinic cholinergic agonist used on the eye to treat elevated intraocular pressure, various types of glaucoma, and to induce miosis. Also available orally to treat symptoms of dry mouth associated with Sjogren’s syndrome and radiotherapy.
Pilocarpine is a medication used to reduce pressure inside the eye and treat dry mouth.[1][3] As eye drops it is used to manage angle closure glaucoma until surgery can be performed, ocular hypertension, primary open angle glaucoma, and to bring about constriction of the pupil following its dilation.[1][4][5] However, due to its side effects it is no longer typically used in the long term management.[6] Onset of effects with the drops is typically within an hour and lasts for up to a day.[1] By mouth it is used for dry mouth as a result of Sjögren syndrome or radiation therapy.[7]
Common side effects of the eye drops include irritation of the eye, increased tearing, headache, and blurry vision.[1] Other side effects include allergic reactions and retinal detachment.[1] Use is generally not recommended during pregnancy.[8] Pilocarpine is in the miotics family of medication.[9] It works by activating cholinergic receptors of the muscarinic type which cause the trabecular meshwork to open and the aqueous humor to drain from the eye.[1]
Pilocarpine was isolated in 1874 by Hardy and Gerrard and has been used to treat glaucoma for more than 100 years.[10][11][12] It is on the World Health Organization’s List of Essential Medicines.[13] It was originally made from the South American plant Pilocarpus.[10]

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@gmail.com
////////////////////////////////////////
Pilocarpine hydrochloride, KSS-694, MGI-647, Pilobuc, Pilocar, Isopto carpine, Spersacarpin, Pilo, Isopto-pilocarpine, Pilocarpina lux, Pilogel, PilaSite(sustained release), Salagen, Pilopine HS
SYN
The alkylation of pilosine (I) with ethyl chloride (II) by means of LDA in THF gives trans-pilocarpine (III), which is isomerized with LDA in THF, yielding a mixture of cis- and trans-pilocarpine (IV). Finally, this mixture is resolved by crystallization with di-p-toluoyl tartaric acid.

SYN
Journal of Organic Chemistry, 58(1), 62-4; 1993
https://pubs.acs.org/doi/abs/10.1021/jo00053a016
SYN
Tetrahedron, 65(39), 8283-8296; 2009
SYN
Science of Synthesis, 20b, 987-1046; 2006
SYN
https://linkinghub.elsevier.com/retrieve/pii/S0040402008014002

SYN
https://www.mdpi.com/1420-3049/26/12/3676/htm
Schmidt, Theresa et alFrom Molecules, 26(12), 3676; 2021
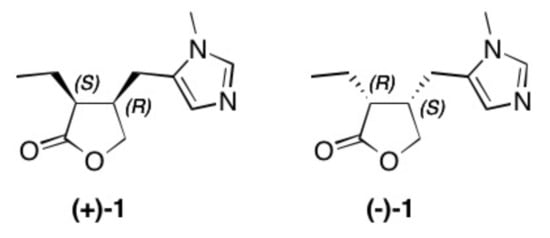
Figure 1. Structure of natural occurring pilocarpine (+)-1 and its enantiomer (–)-1.
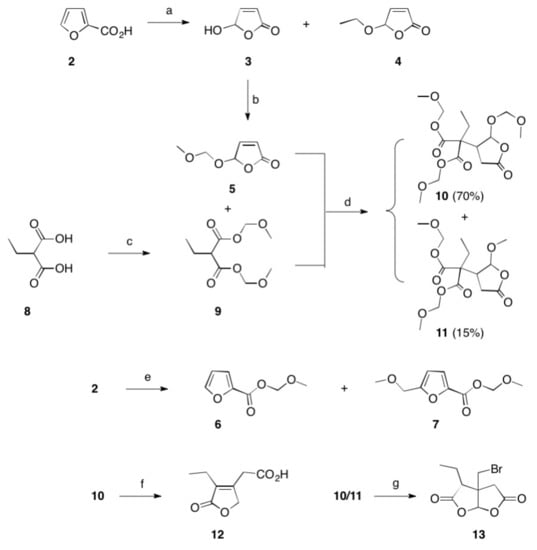
Scheme 1. Reactions and conditions: (a) hν, Bengal rosa, 8 h, 20 °C, 76% (of 3) and 5% (of 4); (b) CH2(OCH3)2, P4O10, DCM, 20 °C, 5 h, 98%; (c) CH2(OCH3)2, P4O10, DCM, 20 °C, 5 h, 99%; (d) THF, Na, 25 °C, 15 h, 72%; (e) CH2(OCH3)2, P4O10, DCM, 20 °C, 5 h, 77% (of 6) and 19% (of 7); (f) HBr, reflux, 2 d, 83%; (g) HBr, reflux, 4 d, 4%.
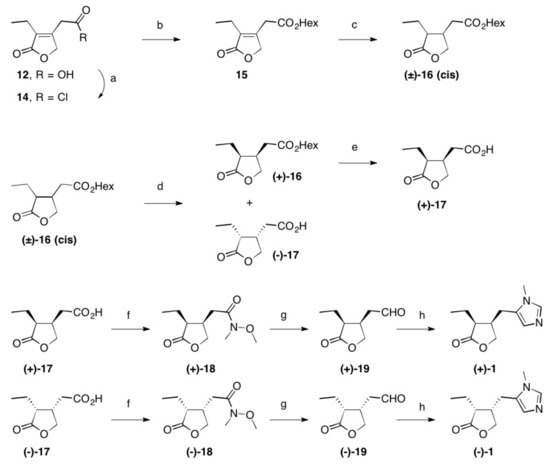
Scheme 2. Reactions and conditions: (a) SOCl2, reflux, 3 h, quant.; (b) Hex-OH, reflux, 16 h, 98%; (c) Rh/Al2O3, H2 (1 at), THF, 5 d, quant.; (d) Lipase PS, pH = 7.0, 2 d, 22 °C, 48% (of (±)-16) and 42% (of (–)-17); (e) PLE, pH = 7.0, 22 °C, 2 d, 96%; (f) N-methylmorpholine, iBu-chloroformate, N,O-dimethylhydroxylamine hydrochloride, 23 °C, 1 d, 84% (of (+)-18) and 85% of (–)-18); (g) LiAlH4, Et2O, 23 °C, 30 min, 95% (of (+)-19) and 95% of (–)-19; (h) CH3NH2, TosMic, DCM, benzene, NEt3, 7 d, 23 °C, 59% (of (+1)-1 and 60% of (–)-1; Hex stands for n-hexyl.
(+)-Pilocarpine [(+)-1]
Following the procedure given for the synthesis of its enantiomer, (+)-1 (1.92 g, 59%) was obtained as a colorless oil; Rf = 0.60 (SiO2, DCM/MeOH/aq NH4OH (25%), 95:4:1); [α]D = +115.7° (c 0.6, CHCl3), ee > 99% (by HPLC, Chiralcel OC, n-hexane/ethanol, 3:7, 0.3 mL/min, UV-detection λ = 215 nm; tR = (+)-1 47.1 min, tR = (–)-1 = 52.32 min); IR (film), 1H-NMR, 13C-NMR and MS (ESI, MeOH) were identical to the enantiomer (vide supra); analysis calcd. for C11H16N2O2 (208.26): C 63.44, H 7.74, N 13.45; found: C 63.31, H 7.98, N 13.32
PAPERBy Fuerstner, AloisFrom e-EROS Encyclopedia of Reagents for Organic Synthesis, 1-7; 2001
| Clinical data | |
|---|---|
| Trade names | Isopto Carpine, Salagen, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a608039 |
| Pregnancy category | AU: B3 |
| Routes of administration | Topical eye drops, by mouth |
| Drug class | Miotic (cholinergic)[1] |
| ATC code | N07AX01 (WHO) S01EB01 (WHO) |
| Legal status | |
| Legal status | AU: S4 (Prescription only)UK: POM (Prescription only)US: ℞-only |
| Pharmacokinetic data | |
| Elimination half-life | 0.76 hours (5 mg), 1.35 hours (10 mg)[2] |
| Excretion | urine |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 92-13-7 54-71-7 (hydrochloride) |
| PubChem CID | 5910 |
| IUPHAR/BPS | 305 |
| DrugBank | DB01085 |
| ChemSpider | 5699 |
| UNII | 01MI4Q9DI3 |
| KEGG | D00525 |
| ChEBI | CHEBI:8207 |
| ChEMBL | ChEMBL550 |
| CompTox Dashboard (EPA) | DTXSID1021162 |
| ECHA InfoCard | 100.001.936 |
| Chemical and physical data | |
| Formula | C11H16N2O2 |
| Molar mass | 208.261 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (verify) |
Medical uses
Pilocarpine stimulates the secretion of large amounts of saliva and sweat.[14] It is used to prevent or treat dry mouth, particularly in Sjögren syndrome, but also as a side effect of radiation therapy for head and neck cancer.[15]
It may be used to help differentiate Adie syndrome from other causes of unequal pupil size.[16][17][clarification needed]
It may be used to treat a form of dry eye called aqueous deficient dry eye (ADDE)[18]
Surgery
Pilocarpine is sometimes used immediately before certain types of corneal grafts and cataract surgery.[19][20] In ophthalmology, pilocarpine is also used to reduce symptomatic glare at night from lights when the patient has undergone implantation of phakic intraocular lenses; the use of pilocarpine would reduce the size of the pupils, partially relieving these symptoms.[dubious – discuss] The most common concentration for this use is pilocarpine 1%.[citation needed] Pilocarpine is shown to be just as effective as apraclonidine in preventing intraocular pressure spikes after laser trabeculoplasty.[21]
Presbyopia
In 2021, the US Food and Drug Administration approved pilocarpine hydrochloride as an eyedrop treatment for presbyopia, age-related difficulty with near-in vision. Marketed as vuity, the effect lasts for 7 to 10 hours.[22]
Other
Pilocarpine is used to stimulate sweat glands in a sweat test to measure the concentration of chloride and sodium that is excreted in sweat. It is used to diagnose cystic fibrosis.[23]
Adverse effects
Use of pilocarpine may result in a range of adverse effects, most of them related to its non-selective action as a muscarinic receptor agonist. Pilocarpine has been known to cause excessive salivation, sweating, bronchial mucus secretion, bronchospasm, bradycardia, vasodilation, and diarrhea. Eye drops can result in brow ache and chronic use in miosis.
Pharmacology
Pilocarpine is a drug that acts as a muscarinic receptor agonist. It acts on a subtype of muscarinic receptor (M3) found on the iris sphincter muscle, causing the muscle to contract – resulting in pupil constriction (miosis). Pilocarpine also acts on the ciliary muscle and causes it to contract. When the ciliary muscle contracts, it opens the trabecular meshwork through increased tension on the scleral spur. This action facilitates the rate that aqueous humor leaves the eye to decrease intraocular pressure. Paradoxically, when pilocarpine induces this ciliary muscle contraction (known as an accommodative spasm) it causes the eye’s lens to thicken and move forward within the eye. This movement causes the iris (which is located immediately in front of the lens) to also move forward, narrowing the Anterior chamber angle. Narrowing of the anterior chamber angle increases the risk of increased intraocular pressure.[24]
Society and culture
Preparation
Plants in the genus Pilocarpus are the only known sources of pilocarpine, and commercial production is derived entirely from the leaves of Pilocarpus microphyllus (Maranham Jaborandi). This genus grows only in South America, and Pilocarpus microphyllus is native to several states in northern Brazil.[25]
Pilocarpine is extracted from the powdered leaf material in a multi-step process. First the material is treated with ethanol acidified with hydrochloric acid, and the solvents removed under reduced pressure. The resultant aqueous residue is neutralized with ammonia and put aside until the resin has completely settled. It is then filtered and concentrated by sugar solution to a small volume, made alkaline with ammonia, and finally extracted with chloroform. The solvent is removed under reduced pressure.[verification needed]
Cost
Pilocarpine is one of the lowest cost medications for glaucoma.[26]
Trade names
Pilocarpine is available under several trade names such as: Diocarpine (Dioptic), Isopto Carpine (Alcon), Miocarpine (CIBA Vision), Ocusert Pilo-20 and -40 (Alza), Pilopine HS (Alcon), Salagen (MGI Pharma), Scheinpharm Pilocarpine (Schein Pharmaceutical), Timpilo (Merck Frosst) and Vuity (Abbvie).
Research
Pilocarpine is used to induce chronic epilepsy in rodents, commonly rats, as a means to study the disorder’s physiology and to examine different treatments.[27][28] Smaller doses may be used to induce salivation in order to collect samples of saliva, for instance, to obtain information about IgA antibodies.
Veterinary
Pilocarpine is given in moderate doses (about 2 mg) to induce emesis in cats that have ingested foreign plants, foods, or drugs. One feline trial determined it was effective, even though the usual choice of emetic is xylazine.
References
- ^ Jump up to:a b c d e f g “Pilocarpine”. The American Society of Health-System Pharmacists. Archived from the original on 28 December 2016. Retrieved 8 December 2016.
- ^ Gornitsky M, Shenouda G, Sultanem K, Katz H, Hier M, Black M, Velly AM (July 2004). “Double-blind randomized, placebo-controlled study of pilocarpine to salvage salivary gland function during radiotherapy of patients with head and neck cancer”. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 98 (1): 45–52. doi:10.1016/j.tripleo.2004.04.009. PMID 15243470.
- ^ Tarascon Pocket Pharmacopoeia 2019 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. 2018. p. 224. ISBN 9781284167542.
- ^ World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization. p. 439. hdl:10665/44053. ISBN 9789241547659.
- ^ “Glaucoma and ocular hypertension. NICE guideline 81”. National Institute for Health and Care Excellence. November 2017. Retrieved 19 September 2019.
Ocular hypertension… alternative options include carbonic anhydrase inhibitors such as brinzolamide or dorzolamide, a topical sympathomimetic such as apraclonidine or brimonidine tartrate, or a topical miotic such as pilocarpine, given either as monotherapy or as combination therapy.
- ^ Lusthaus J, Goldberg I (March 2019). “Current management of glaucoma” (PDF). The Medical Journal of Australia. 210 (4): 180–187. doi:10.5694/mja2.50020. PMID 30767238. S2CID 73438590.
Pilocarpine is no longer routinely used for long term IOP control due to a poor side effect profile
- ^ Hamilton R (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. p. 415. ISBN 9781284057560.
- ^ “Pilocarpine ophthalmic Use During Pregnancy | Drugs.com”. http://www.drugs.com. Archived from the original on 28 December 2016. Retrieved 28 December 2016.
- ^ British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. p. 769. ISBN 9780857111562.
- ^ Jump up to:a b Sneader W (2005). Drug Discovery: A History. John Wiley & Sons. p. 98. ISBN 978-0-471-89979-2. Archived from the original on 2016-12-29.
- ^ Rosin A (1991). “[Pilocarpine. A miotic of choice in the treatment of glaucoma has passed 110 years of use]”. Oftalmologia (in Romanian). 35 (1): 53–5. PMID 1811739.
- ^ Holmstedt, B; Wassén, SH; Schultes, RE (January 1979). “Jaborandi: an interdisciplinary appraisal”. Journal of Ethnopharmacology. 1 (1): 3–21. doi:10.1016/0378-8741(79)90014-x. PMID 397371.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ “Pilocarpine”. MedLinePlus. U.S. National Library of Medicine. Archived from the original on 2010-03-06.
- ^ Yang, WF; Liao, GQ; Hakim, SG; Ouyang, DQ; Ringash, J; Su, YX (1 March 2016). “Is Pilocarpine Effective in Preventing Radiation-Induced Xerostomia? A Systematic Review and Meta-analysis”. International Journal of Radiation Oncology, Biology, Physics. 94 (3): 503–11. doi:10.1016/j.ijrobp.2015.11.012. hdl:10722/229069. PMID 26867879.
- ^ Kanski JJ, Bowling B (2015-03-24). Kanski’s Clinical Ophthalmology E-Book: A Systematic Approach. Elsevier Health Sciences. p. 812. ISBN 9780702055744.
- ^ Bartlett JD, James SD (October 2013). “Drug Affect the Autonomous Nervous System”. Clinical Ocular Pharmacology. Elsevier. p. 118. ISBN 9781483193915.
- ^ Mannis, Mark J; Holland, Edward J (September 2016). “Chapter 33: Dry Eye”. Cornea E-Book. Elsevier Health Sciences. p. 388. ISBN 978-0-323-35758-6. OCLC 960165358.
- ^ Parker, Jack (2017). Descemet Membrane Endothelial Keratoplasty (DMEK): A Review (PDF) (Thesis). Leiden University.
- ^ Ahmed E, E A (2010). Comprehensive Manual of Ophthalmology. JP Medical Ltd. p. 345. ISBN 9789350251751.
- ^ Zhang L, Weizer JS, Musch DC (February 2017). “Perioperative medications for preventing temporarily increased intraocular pressure after laser trabeculoplasty”. The Cochrane Database of Systematic Reviews. 2 (2): CD010746. doi:10.1002/14651858.CD010746.pub2. PMC 5477062. PMID 28231380.
- ^ Bankhead, Charles (2021-11-01). “First Eye Drop Treatment for Presbyopia Wins FDA Approval”. http://www.medpagetoday.com. Retrieved 2021-11-02.
- ^ Prasad RK (2017-07-11). Chemistry and Synthesis of Medicinal Agents: (Expanding Knowledge of Drug Chemistry). BookRix. ISBN 9783743821415.
- ^ Shaarawy TM, Sherwood MB, Hitchings RA, Crowston JG (September 2014). “Lsser Peripheral Iridoplasty”. Glaucoma E-Book. Elsevier Health Sciences. p. 718. ISBN 9780702055416.
- ^ De Abreu IN, Sawaya AC, Eberlin MN, Mazzafera P (November–December 2005). “Production of Pilocarpine in Callus of Jaborandi (Pilocarpus microphyllus Stapf)”. In Vitro Cellular & Developmental Biology – Plant. Society for In Vitro Biology. 41 (6): 806–811. doi:10.1079/IVP2005711. JSTOR 4293939. S2CID 26058596.
- ^ Schwab, Larry (2007). Eye Care in Developing Nations. CRC Press. p. 110. ISBN 9781840765229.
- ^ Károly N (2018). Immunohistochemical investigations of the neuronal changes induced by chronic recurrent seizures in a pilocarpine rodent model of temporal lobe epilepsy (Thesis). University of Szeged. doi:10.14232/phd.9734.
- ^ Morimoto K, Fahnestock M, Racine RJ (May 2004). “Kindling and status epilepticus models of epilepsy: rewiring the brain”. Progress in Neurobiology. 73 (1): 1–60. doi:10.1016/j.pneurobio.2004.03.009. PMID 15193778. S2CID 36849482.
External links
- “Pilocarpine”. Drug Information Portal. U.S. National Library of Medicine.
CLIP
Firms Team Up To Sustain Natural Pilocarpine
Sustainable harvest is key to a new pharmaceutical chemicals venture
https://cen.acs.org/articles/93/i11/Firms-Team-Sustain-Natural-Pilocarpine.html
Last summer, Andrew Badrot bought a portfolio of plant-sourced pharmaceutical chemicals from Boehringer Ingelheim and acquired BI’s distribution rights for pilocarpine, a plant-derived glaucoma treatment.
For BI, the transactions were small ones. The German drugmaker had been exiting its private-label active pharmaceutical ingredients (API) business, scaling back to produce only the chemicals it uses to manufacture its own drugs.
But for Badrot the deals were potentially big. He leads the company that bought the businesses—Centroflora CMS, a joint venture between the Brazilian botanicals firm Centroflora and CMS Pharma, Badrot’s custom chemicals consultancy. Together, Centroflora and Centroflora CMS are committed to nurturing the natural source of pilocarpine, an alkaloid used medicinally for more than 100 years, and to expanding into other APIs neglected by larger firms.
Pilocarpine’s source, Pilocarpus microphyllus, better known as jaborandi, had been harvested vigorously in the wild by Merck KGaA, which in 1975 built a factory in Parnaíba in northern Brazil to extract pilocarpine. By the mid-1980s, however, jaborandi had been overharvested, and the government declared it a protected species. Merck began obtaining the leaves from a plantation in the northern Brazilian state of Maranhão.
Demand for the drug as a glaucoma treatment began to decline, and Merck eventually closed the plant. When the market for the drug revived with new indications as a dry-mouth remedy, the company saw an opportunity to sell the site and did so in 2002.
The buyer was Centroflora, which was founded in 1957 in São Paulo. The firm was interested in adding pilocarpine to its botanical extracts business, according to its chief executive, Peter Andersen, a native of Brazil whose coffee-trader father bought into Centroflora in 1983. Along with the purchase, Centroflora signed a deal for BI to distribute the drug.
The company wanted to revitalize natural harvesting of jaborandi and began working with the Brazilian government to promulgate sustainable practices in the field. Centroflora also worked closely with a German government agency, Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ), which promotes sustainable harvesting internationally and had been working in the north of Brazil for decades.
Centroflora’s distribution agreement with BI arose through connections at GIZ, according to Andersen. BI also had been Merck’s biggest customer for pilocarpine.
But ecological sustainability was only half of the problem, Andersen says. Centroflora also found itself dealing with middlemen who would collect the jaborandi from poor family farms in remote areas and pay them next to nothing. Establishing a direct supply channel was not easy.
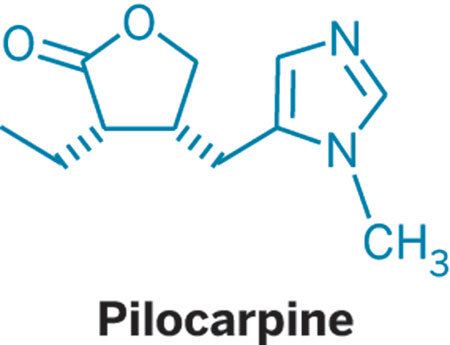
“I can spend a few days telling you about that process,” he says. “Stories of difficult relationships and difficult moments. But in some cases we managed to hire some of the middlemen to work for us on a salary basis. They made less money, but they had a job.”
Today, farmers in Brazil are paid at least twice what they were paid by intermediaries, Andersen says.
Key to the process was a program Centroflora launched in 2004 called Partnerships for a Better World to train and certify growers, establish community associations to support growers, and maintain sustainable harvesting practices.
Centroflora is the leading supplier of pilocarpine. Its only competitor, Sourcetech, with a plant near São Paulo, accesses jaborandi from the plantation that supplied Merck, now owned by U.S.-based Quercegen.
Pilocarpine accounts for only about 5% of Centroflora’s $95 million in annual sales. The company produces a long list of botanical extracts, including nutritional supplements and herbal medicines such as acai, acerola, coffee powder, and powdered fruit.The company manufactures at four facilities in Brazil, including the former Merck plant, which is dedicated to pilocarpine. But Andersen sees the partnership with CMS as a route to increase phytochemical API manufacturing at that site.
“The facility has the capacity to produce 12 metric tons per year of alkaloids,” Andersen says. It currently makes less than three metric tons. “So there is a lot of space to produce more, and the idea is that we can do some of the APIs we got from Boehringer Ingelheim.”
Those include atropine, digoxin, homatropine, and dihydroergotamine mesylate. Centroflora CMS also obtained distribution rights to BI’s scopolamine N-butyl bromide. All are derived from botanicals harvested on farms around the world.
Badrot was vice president of strategy for Lonza’s exclusive synthesis division before starting CMS in 2010 to consult on manufacturing and mergers and acquisitions in the custom chemicals business. “But for me, the dream was to return to manufacturing APIs,” he says.
The phytochemicals portfolio, including some of the oldest APIs made by BI, for which CMS has done consulting work, seemed like an ideal reentry to manufacturing, according to Badrot. “They are niche products that maybe fly a bit under the radar,” he says. “They seemed to fit us well because we can give them some attention.”
Centroflora CMS’s first order of business, he says, is to establish manufacturing for the BI products, which BI will continue to make until then. Badrot says Centroflora is well suited to manufacture at least the digoxin and atropine, but decisions have not been finalized. The partners will likely use contract manufacturers for some of the products. And Badrot says Centroflora CMS seeks to replicate the kind of deal it has with BI.
“We are looking for other companies with APIs that represent 0–1% of sales, products that lack focus,” he says. “We would take them over.”
Badrot and Andersen say they are also interested in sharing the Partnerships for a Better World program with other companies involved in harvesting natural products. And Centroflora looks for other ways to support its supply chain. Last month, it was approved as a trading member of the Union for Ethical BioTrade, a nonprofit that promotes sustainable development and biodiversity. As a member, Centroflora commits to sustainable sourcing practices and will be required to undergo periodic audits.
Last year, Centroflora received government recognition for its efforts on both the environmental and social fronts. The National Confederation of Industry in Brazil named Centroflora’s jaborandi harvesting program one of the country’s 10 most sustainable business practices. And Banco do Brasil, the national bank, recognized the firm for its work to improve conditions for farmers in the northern forest region of the country.
As the joint venture starts to work with its new portfolio of phytochemicals, both Andersen and Badrot look back at the jaborandi success as the road forward, a template for fostering a plant-based API business that may inspire other companies.
For Andersen, Partnerships for a Better World is an essential foundation of trust for the ecological and socially responsible harvesting of botanicals in Brazil. “There were a lot of problems along the way,” he says. “But we are at peace with it today.”
////////////////PILOCARPINE, Pilocarpine hydrochloride, KSS-694, MGI-647, Pilobuc, Pilocar, Isopto carpine, Spersacarpin, Pilo, Isopto-pilocarpine, Pilocarpina lux, Pilogel, PilaSite(sustained release), Salagen, Pilopine HS
CC[C@H]1[C@@H](CC2=CN=CN2C)COC1=O

NEW DRUG APPROVALS
ONE TIME
$10.00
loteprednol etabonate
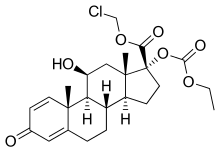
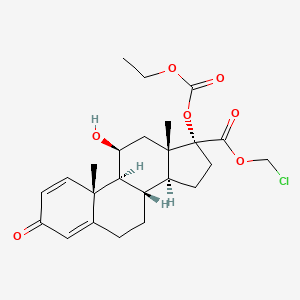
loteprednol etabonate
- Molecular FormulaC24H31ClO7
- Average mass466.952 Da
cas 82034-46-6
chloromethyl (8S,9S,10R,11S,13S,14S,17R)-17-ethoxycarbonyloxy-11-hydroxy-10,13-dimethyl-3-oxo-7,8,9,11,12,14,15,16-octahydro-6H-cyclopenta[a]phenanthrene-17-carboxylate(11b,17a)-17-[(Ethoxycarbonyl)oxy]-11-hydroxy-3-oxo-androsta-1,4-diene-17-carboxylic acid chloromethyl ester
(11b,17a)-17-[(Ethoxycarbonyl)oxy]-11-hydroxy-3-oxoandrosta-1,4-diene-17-carboxylic Acid Chloromethyl Ester
(8S,9S,10R,11S,13S,14S,17R)-17-[(éthoxycarbonyl)oxy]-11-hydroxy-10,13-diméthyl-3-oxo-6,7,8,9,10,11,12,13,14,15,16,17-dodécahydro-3H-cyclopenta[a]phénanthrène-17-carboxylate de chlorométhyle
129260-79-3[RN]
17a-Ethoxycarbonyloxy-D’-cortienic Acid Chloromethyl Ester
82034-46-6[RN]
Androsta-1,4-diene-17-carboxylic acid, 17-((ethoxycarbonyl)oxy)-11-hydroxy-3-oxo-, chloromethyl ester, (11β,17α)-
Androsta-1,4-diene-17-carboxylic acid, 17-[(ethoxycarbonyl)oxy]-11-hydroxy-3-oxo-, chloromethyl ester, (11β,17α)-
Loteprednol Etabonate
CAS Registry Number: 82034-46-6
CAS Name: (11b,17a)-17-[(Ethoxycarbonyl)oxy]-11-hydroxy-3-oxoandrosta-1,4-diene-17-carboxylic acid chloromethyl ester
Additional Names: chloromethyl 17a-ethoxycarbonyloxy-11b-hydroxyandrosta-1,4-diene-3-one-17b-carboxylate; 17a-ethoxycarbonyloxy-D¢-cortienic acid chloromethyl ester
Manufacturers’ Codes: CDDD-5604; HGP-1; P-5604
Trademarks: Alrex (Bausch & Lomb); Lotemax (Bausch & Lomb)
Molecular Formula: C24H31ClO7, Molecular Weight: 466.95
Percent Composition: C 61.73%, H 6.69%, Cl 7.59%, O 23.98%
Literature References: Ophthalmic corticosteroid. Prepn: N. S. Bodor, BE889563 (1981 to Otsuka); idem,US4996335 (1991). Physicochemical properties: M. Alberth et al.,J. Biopharm. Sci.2, 115 (1991). HPLC determn in plasma and urine: G. Hochhaus et al.,J. Pharm. Sci.81, 1210 (1992). NMR structural studies: S. Rachwal et al.,Steroids61, 524 (1996); idem et al., ibid. 63, 193 (1998). Metabolism and transdermal permeability: N. Bodor et al.,Pharm. Res.9, 1275 (1992). Evaluation of effect on intraocular pressure: J. D. Bartlett et al.,J. Ocul. Pharmacol.9, 157 (1993). Clinical trial in keratoconjunctivitis sicca: S. C. Pflugfelder et al.,Am. J. Ophthalmol.138, 444 (2004). Review of ophthalmic clinical studies: J. F. Howes, Pharmazie55, 178-183 (2000).
Properties: Crystals from THF + hexane, mp 220.5-223.5°. Soly at 25° (mg/ml): 0.0005 in water; 0.037 in 50% propylene glycol + water. Lipophilicity (log K): 3.04.
Melting point: mp 220.5-223.5°
Therap-Cat: Anti-inflammatory (topical).
Keywords: Glucocorticoid.
Research Code:HGP-1; CDDD-5604; P-5604Trade Name:Lotemax® / Alrex®MOA:CorticosteroidIndication:Acne rosacea; Superficial punctate keratitis; Postoperative inflammation and pain following ocular surgery; Iritis; Herpes zoster keratitis; Allergic conjunctivitis; CyclitisCompany:Bausch & Lomb (Originator)Sales:ATC Code:S01BA14
Loteprednol etabonate was approved by the U.S. Food and Drug Administration (FDA) on Mar 9, 1998. It was developed and marketed as Lotemax® by Bausch & Lomb.
Loteprednol etabonate is a corticosteroid used in ophthalmology. It is indicated for the treatment of steroid responsive inflammatory conditions of the palpebral and bulbar conjunctiva, cornea and anterior segment of the globe such as allergic conjunctivitis, acne rosacea, superficial punctate keratitis, herpes zoster keratitis, iritis, cyclitis, selected infective conjunctivitides.
Lotemax® is available as drops for ophthalmic use, containing 0.5% of Loteprednol etabonate. The recommended dose is one to two drops into the conjunctival sac of the affected eyes four times daily.
Loteprednol (as the ester loteprednol etabonate) is a corticosteroid used to treat inflammations of the eye. It is marketed by Bausch and Lomb as Lotemax[1] and Loterex.
It was patented in 1980 and approved for medical use in 1998.[2]
Loteprednol Etabonate is the etabonate salt form of loteprednol, an ophthalmic analog of the corticosteroid prednisolone with anti-inflammatory activity. Loteprednol etabonate exerts its effect by interacting with specific intracellular receptors and subsequently binds to DNA to modify gene expression. This results in an induction of the synthesis of certain anti-inflammatory proteins while inhibiting the synthesis of certain inflammatory mediators. Loteprednol etabonate specifically induces phospholipase A2 inhibitory proteins (collectively called lipocortins), which inhibit the release of arachidonic acid, thereby inhibiting the biosynthesis of potent mediators of inflammation, such as prostaglandins and leukotrienes.
Loteprednol etabonate is an etabonate ester, an 11beta-hydroxy steroid, a steroid ester, an organochlorine compound, a steroid acid ester and a 3-oxo-Delta(1),Delta(4)-steroid. It has a role as an anti-inflammatory drug. It derives from a loteprednol.
Loteprednol Etabonate (LE) is a topical corticoid anti-inflammatory. It is used in ophthalmic solution for the treatment of steroid responsive inflammatory conditions of the eye such as allergic conjunctivitis, uveitis, acne rosacea, superficial punctate keratitis, herpes zoster keratitis, iritis, cyclitis, and selected infective conjunctivitides. As a nasal spray, it can be used for the treatment and management of seasonal allergic rhinitis. Most prescription LE products, however, tend to be indicated for the treatment of post-operative inflammation and pain following ocular surgery. A number of such new formulations that have been approved include Kala Pharmaceutical’s Inveltys – the first twice-daily (BID) ocular corticosteroid approved for this indication, designed specifically to enhance patient compliance and simplified dosing compared to all other similar ocular steroids that are dosed four times daily. Moreover, LE was purposefully engineered to be a ‘soft drug’, one that is designed to be active locally at the site of administration and then rapidly metabolized to inactive components after eliciting its actions at the desired location, thereby subsequently minimizing the chance for adverse effects.
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2012-09-28 | New dosage form | Lotemax | Postoperative inflammation and pain following ocular surgery | Gel | 0.5% | Bausch & Lomb | |
| 2011-04-15 | New dosage form | Lotemax | Postoperative inflammation and pain following ocular surgery | Ointment | 0.5% | Bausch & Lomb | |
| 1998-03-09 | First approval | Lotemax | Allergic conjunctivitis,Acne rosacea,Superficial punctate keratitis,Herpes zoster keratitis,Iritis,Cyclitis | Suspension/ Drops | 0.5% | Bausch & Lomb |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2014-11-26 | Marketing approval | 露达舒/Lotemax | Allergic conjunctivitis,Acne rosacea,Superficial punctate keratitis,Herpes zoster keratitis,Iritis,Cyclitis,Postoperative inflammation and pain following ocular surgery | Suspension | 滴眼剂,0.5%(2.5ml:12.5mg,5ml:25mg) | Bausch & Lomb | |
| 2011-11-05 | Marketing approval | 露达舒/Lotemax | Allergic conjunctivitis,Acne rosacea,Superficial punctate keratitis,Herpes zoster keratitis,Iritis,Cyclitis,Postoperative inflammation and pain following ocular surgery | Suspension | 滴眼剂,0.5%(2.5ml:12.5mg,5ml:25mg); 滴眼剂,0.5%(10ml:50mg,15ml:75mg) | Bausch & Lomb |
Reference:1. US4710495A / US4996335A.Route 2
Reference:1. CN103183714A.
SYN
doi:10.1016/0960-0760(91)90120-T doi: 10.1016/j.steroids.2011.01.006

| Clinical data | |
|---|---|
| Trade names | Lotemax |
| Other names | 11β,17α,Dihydroxy-21-oxa-21-chloromethylpregna-1,4-diene-3,20-dione 17α-ethylcarbonate |
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| Routes of administration | Eye drops |
| Drug class | Corticosteroid; glucocorticoid |
| ATC code | S01BA14 (WHO) |
| Legal status | |
| Legal status | US: ℞-only |
| Pharmacokinetic data | |
| Bioavailability | None |
| Protein binding | 95% |
| Metabolism | Ester hydrolysis |
| Metabolites | Δ1-cortienic acid and its etabonate |
| Onset of action | ≤2 hrs (allergic conjunctivitis) |
| Elimination half-life | 2.8 hrs |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 82034-46-6 |
| PubChem CID | 444025 |
| IUPHAR/BPS | 7085 |
| DrugBank | DB14596 |
| ChemSpider | 392049 |
| UNII | YEH1EZ96K6 |
| KEGG | D01689 |
| ChEBI | CHEBI:31784 |
| ChEMBL | ChEMBL1200865 |
| CompTox Dashboard (EPA) | DTXSID2046468 |
| ECHA InfoCard | 100.167.120 |
| Chemical and physical data | |
| Formula | C24H31ClO7 |
| Molar mass | 466.96 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| Melting point | 220.5 to 223.5 °C (428.9 to 434.3 °F) |
| Solubility in water | 0.0005 mg/mL (20 °C) |
| showSMILES | |
| showInChI | |
| (what is this?) (verify) |

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@gmail.com
////////////////////////////////////////
Medical uses
Applications for this drug include the reduction of inflammation after eye surgery,[1] seasonal allergic conjunctivitis, uveitis,[3] as well as chronic forms of keratitis (e.g. adenoviral and Thygeson’s keratitis), vernal keratoconjunctivitis, pingueculitis, and episcleritis.[citation needed]
Contraindications
As corticosteroids are immunosuppressive, loteprednol is contraindicated in patients with viral, fungal or mycobacterial infections of the eye.[1][3][4]
Adverse effects
The most common adverse effects in patients being treated with the gel formulation are anterior chamber inflammation (in 5% of people), eye pain (2%), and foreign body sensation (2%).[5]
Interactions
Because long term use (more than 10 days) can cause increased intraocular pressure, loteprednol may interfere with the treatment of glaucoma. Following ocular administration, the drug is very slowly absorbed into the blood, therefore the blood level is limited to an extremely small concentration, and interactions with drugs taken by mouth or through any route other than topical ophthalmic are very unlikely.[1]
Pharmacology
Mechanism of action
Main article: Glucocorticoid § Mechanism of action
Pharmacokinetics
Neither loteprednol etabonate nor its inactive metabolites Δ1–cortienic acid and Δ1-cortienic acid etabonate are detectable in the bloodstream, even after oral administration. A study with patients receiving loteprednol eye drops over 42 days showed no adrenal suppression, which would be a sign of the drug reaching the bloodstream to a clinically relevant extent.[1]
Steroid receptor affinity was 4.3 times that of dexamethasone in animal studies.[1]
Retrometabolic drug design
Loteprednol etabonate was developed using retrometabolic drug design. It is a so-called soft drug, meaning its structure was designed so that it is predictably metabolised to inactive substances. These metabolites, Δ1-cortienic acid and its etabonate, are derivatives of cortienic acid, itself an inactive metabolite of hydrocortisone.[1][4][6]
- Cortisol, a naturally occurring corticosteroid, known as hydrocortisone when used as a drug
- Δ1-Cortienic acid, inactive metabolite of loteprednol
- Cortienic acid, inactive metabolite of hydrocortisone
Chemistry
Loteprednol etabonate is an ester of loteprednol with etabonate (ethyl carbonate). The pure chemical compound has a melting point between 220.5 °C (428.9 °F) and 223.5 °C (434.3 °F). Its solubility in water is 1:2,000,000,[4] therefore it is formulated for ophthalmic use as either an ointment, a gel, or a suspension.[7]
Loteprednol is a corticosteroid. The ketone side chain of classical corticosteroids such as hydrocortisone is replaced by a cleavable ester, which accounts for the rapid inactivation.[8] (This is not the same as the etabonate ester.)
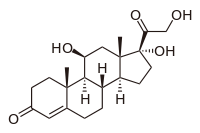

Loteprednol etabonate
Chemical synthesis
References
- ^ Jump up to:a b c d e f g Haberfeld H, ed. (2015). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 488. ISBN 9783527607495.
- ^ Jump up to:a b Loteprednol Professional Drug Facts.
- ^ Jump up to:a b c Dinnendahl V, Fricke U (2008). Arzneistoff-Profile (in German). 6 (22 ed.). Eschborn, Germany: Govi Pharmazeutischer Verlag. ISBN 978-3-7741-9846-3.
- ^ “Highlights of Prescribing Information: Lotemax” (PDF). 2012.
- ^ Bodor N, Buchwald P (2002). “Design and development of a soft corticosteroid, loteprednol etabonate”. In Schleimer RP, O’Byrne PM, Szefler SJ, Brattsand R (eds.). Inhaled Steroids in Asthma. Optimizing Effects in the Airways. Lung Biology in Health and Disease. 163. Marcel Dekker, New York. pp. 541–564.
- ^ “Loteprednol (Professional Patient Advice)”. Retrieved October 4, 2018.
- ^ Pavesio CE, Decory HH (April 2008). “Treatment of ocular inflammatory conditions with loteprednol etabonate”. The British Journal of Ophthalmology. 92 (4): 455–9. doi:10.1136/bjo.2007.132621. PMID 18245274. S2CID 25873047.
- ^ Druzgala P, Hochhaus G, Bodor N (February 1991). “Soft drugs–10. Blanching activity and receptor binding affinity of a new type of glucocorticoid: loteprednol etabonate”. The Journal of Steroid Biochemistry and Molecular Biology. 38 (2): 149–54. doi:10.1016/0960-0760(91)90120-T. PMID 2004037. S2CID 27107845.
Further reading
- Stewart R, Horwitz B, Howes J, Novack GD, Hart K (November 1998). “Double-masked, placebo-controlled evaluation of loteprednol etabonate 0.5% for postoperative inflammation. Loteprednol Etabonate Post-operative Inflammation Study Group 1”. Journal of Cataract and Refractive Surgery. 24 (11): 1480–9. doi:10.1016/s0886-3350(98)80170-3. PMID 9818338. S2CID 24423725.
////////////loteprednol etabonate
CCOC(=O)OC1(CCC2C1(CC(C3C2CCC4=CC(=O)C=CC34C)O)C)C(=O)OCCl

NEW DRUG APPROVALS
ONE TIME
$10.00
AVIPTADIL
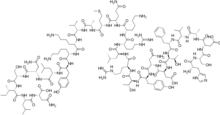

AVIPTADIL
- Molecular FormulaC147H237N43O43S
37221-79-7[RN]
6J2WVD66KR
L-Asparagine, L-histidyl-L-seryl-L-α-aspartyl-L-alanyl-L-valyl-L-phenylalanyl-L-threonyl-L-α-aspartyl-L-asparaginyl-L-tyrosyl-L-threonyl-L-arginyl-L-leucyl-L-arginyl-L-lysyl-L-glutaminyl-L-met hionyl-L-alanyl-L-valyl-L-lysyl-L-lysyl-L-tyrosyl-L-leucyl-L-asparaginyl-L-seryl-L-isoleucyl-L-leucyl-
Vasoactive intestinal octacosapeptide
Invicorp (aviptadil + phentolamine)
(2S)-4-amino-2-[[(2S)-2-[[(2S,3S)-2-[[(2S)-2-[[(2S)-4-amino-2-[[(2S)-2-[[(2S)-2-[[(2S)-6-amino-2-[[(2S)-6-amino-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S)-5-amino-2-[[(2S)-6-amino-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S,3R)-2-[[(2S)-2-[[(2S)-4-amino-2-[[(2S)-2-[[(2S,3R)-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-amino-3-(1H-imidazol-5-yl)propanoyl]amino]-3-hydroxypropanoyl]amino]-3-carboxypropanoyl]amino]propanoyl]amino]-3-methylbutanoyl]amino]-3-phenylpropanoyl]amino]-3-hydroxybutanoyl]amino]-3-carboxypropanoyl]amino]-4-oxobutanoyl]amino]-3-(4-hydroxyphenyl)propanoyl]amino]-3-hydroxybutanoyl]amino]-5-carbamimidamidopentanoyl]amino]-4-methylpentanoyl]amino]-5-carbamimidamidopentanoyl]amino]hexanoyl]amino]-5-oxopentanoyl]amino]-4-methylsulfanylbutanoyl]amino]propanoyl]amino]-3-methylbutanoyl]amino]hexanoyl]amino]hexanoyl]amino]-3-(4-hydroxyphenyl)propanoyl]amino]-4-methylpentanoyl]amino]-4-oxobutanoyl]amino]-3-hydroxypropanoyl]amino]-3-methylpentanoyl]amino]-4-methylpentanoyl]amino]-4-oxobutanoic acid

Aviptadil Acetate
CAS#: 40077-57-4 (free base)
Chemical Formula: C155H253N43O51S
Exact Mass:
Molecular Weight: 3567.039
H-His-Ser-Asp-Ala-Val-Phe-Thr-Asp-Asn-Tyr-Thr-Arg-Leu-Arg-Lys-Gln-Met-Ala-Val-Lys-Lys-Tyr-Leu-Asn-Ser-Ile-Leu-Asn-NH2 tetraacetic acid.
Aviptadil had been in phase II clinical trials for the treatment of pulmonary arterial hypertension and idiopathic pulmonary fibrosis. But these researches were discontinued in 2011.
In 2006, Orphan Drug Designations were granted in the E.U. for the treatment of pulmonary arterial hypertension, and sarcoidosis and acute lung injury in 2006, and 2008, respectively.
The compound was co-developed by Lung Rx (subsidiary of United Therapeutics) and Mondobiotech.
Aviptadil (INN) is an injectable synthetic formulation of human vasoactive intestinal peptide (VIP).[1] VIP was discovered in 1970, and has been used to treat various inflammatory conditions, such as acute respiratory distress syndrome (ARDS), asthma and chronic obstructive pulmonary disease (COPD).
| Clinical data | |
|---|---|
| Trade names | RLF-100 / Zyesamiô |
| AHFS/Drugs.com | International Drug Names |
| ATC code | none |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 40077-57-4 |
| PubChem CID | 16132300 |
| ChemSpider | 17288959 |
| UNII | A67JUW790C |
| KEGG | D12127 |
| ChEMBL | ChEMBL2106041 |
| CompTox Dashboard (EPA) | DTXSID7048584 |
| Chemical and physical data | |
| Formula | C147H237N43O43S |
| Molar mass | 3326.83 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (what is this?) (verify) |
Regulatory history
ARDS in COVID-19
Studies have found that aviptadil may be beneficial for severely ill patients with COVID-19 related ARDS.[2] ACTIV-3, a trial examining aviptadil acetate (Zyesami), is recruiting patients as of 2 July 2021.[3] A separate trial is examining inhaled aviptadil for patients with high risk for ARDS, is ongoing as of 21 May 2021.[4] A trial for intravenous aviptadil for the same indication concluded in February 2021.[5]
U.S.-Israeli NeuroRx Inc partnered with Relief Therapeutics to develop aviptadil in the United States. In June 2020, the U.S. Food and Drug Administration granted fast-track designation to aviptadil for treatment of respiratory distress in COVID-19.[6] In September 2020, NeuroRX submitted a request for an Emergency Use Authorization to the US FDA for its use in patients in intensive care.[7] May 2021: NRx Pharmaceuticals Announces Positive Results for ZYESAMI™ (Aviptadil-acetate) and Submits Emergency Use Authorization Application to USFDA to Treat Critical COVID-19 in Patients Suffering from Respiratory Failure.[8]
Jan, 2021: Zuventus healthcare Ltd seeks approval for Aviptadil from India’s drug controller for emergency use in COVID-19 treatment. Mumbai’s Zuventus healthcare Ltd. has got the nod to conduct Phase 3 clinical trials of Aviptadil injectable formulation. The SEC noted that Zuventus had presented revised Phase 3 clinical trial protocol before the committee, and after “detailed deliberation”, it recommended grant of permission of Phase 3 trials with the drug.[9] [10]
Aviptadil/phentolamine combination for Erectile Dysfunction (ED)
October 2000 UK (Invicorp): Aviptadil, an injectable formulation of vasoactive intestinal polypeptide (VIP) in combination with the adrenergic drug phentolamine is approved as an effective alternative therapy for erectile dysfunction (ED) patients. 1 dose intracavernosal injection contains 25 micrograms aviptadil and 2 mg of phentolamine mesilate for the treatment of erectile dysfunction. Aviptadil dose used for treatment of erectile dysfunction is far lesser as compared to dose used for the treatment of ARDS.[11][12]
Vasoactive intestinal peptide (VIP)
Vasoactive intestinal peptide (VIP) is a 28-residue amino acid peptide first characterized in 1970 that was initially isolated from porcine duodenum. A member of the secretin/glucagon hormone superfamily. VIP was initially discovered owing to its potent vasodilatory effects (as its name implies). VIP is widely distributed in the central and peripheral nervous system as well as in the digestive, respiratory, reproductive, and cardiovascular systems as a neurotransmitter and neuroendocrine releasing factor. These effects contribute to an extensive range of physiological and pathological processes related to development, growth, and the control of neuronal, epithelial, and endocrine cell function.[13]
VIP Receptors
VIP acts on two receptors – VPAC1 and VPAC2, which are class B of G-protein-coupled receptors (GPCRs).VPAC1 is mainly present in the lung and T-lymphocytes, whereas VPAC2 is mainly seen in the smooth muscle,mast cells and the basal parts of the lung mucosa.[14]
Expression of VIP
VIP is produced in the neurons in the central and peripheral nervous systems. VIP is mainly localized in the myenteric and submucosal neurons and nerve terminals in the GI tract. Endogenous VIP is released by numerous stimuli such as acetylcholine (ACh), ATP, serotonin (5-HT), substance P (SP), GLP-2 from at least two populations of VIP-positive nerves: cholinergic and non-cholinergic VIP-releasing nerves. In guinea pig small intestine, most VIP-positive nerves in the mucosa and submucosa are non-cholinergic secretomotor neurons and well colocalized with neuronal nitric oxide synthase (nNOS) in human colonic circular muscles. VIP is also expressed in immune cells, such as activated T cells and therefore present in lymphoid tissues including Peyer’s patches, the spleen, and lymph nodes, in addition to the VIP-ergic innervation in lymphoid tissues. Beside the neuronal source, VIP is also expressed and released from endocrine organs – Heart, Thyroid, Kidney and GI tracts.[15]
Localization of VIP
- VIP is highly localised in lungs (70%) and binds with alveolar type II (AT II) cells via VPAC1.[2] The biological (vasodilator) activity of vasoactive intestinal peptide (VIP) was discovered in the lungs before the peptide was isolated and chemical identity characterized from intestine. Although VIP levels are consideralbly high in the brain or gut:VIP is localized in key sites in the lung, has potent activities on its major functions, and appears to play an important role in pulmonary physiology and disease.[16]
- The principal localization of VIP-containing neurons in the tracheobronchial tree is in the smooth muscle layer, around submucosal mucous glands and in the walls of pulmonary and bronchial arteries. Immunoreactive VIP is also present in neuronal cell bodies forming microganglia that provide a source of intrinsic innervation of pulmonary structures.[16]
Vasoactive Intestinal Peptide (VIP) and SARS-CoV-2
VIP is highly localised in lungs and binds with alveolar type II (AT II) cells via VPAC1 receptor. AT II cells constitute only 5% of pulmonary epithelium. Angiotensin Converting Enzyme 2 (ACE 2) surface receptors arepresent in AT II cells. AT II cells produces surfactant and plays an important role in the maintenance of type 1epithelial cells. SARS-CoV-2 enters into AT II cells by binding to ACE 2 surface receptors with its spike protein. SARS CoV-2 attack mainly type II cells (not type I alveolar cells) and results in the death of alveolar type II (AT 11) cells which produces surfactant, resulting in[2]
- Profound defect in oxygenation
- Leading to hypoxia
Mechanism of action of Aviptadil
- Pulmonary alveolar type II Cells have a high concentration of ACE 2 receptors on their cell membrane
- Investigators have confirmed that the SARS-CoV family of viruses selectively attack pulmonary Alveolar Type II (ATII) cells because of their ACE2 receptors, in contrast to other pulmonary epithelial cells.
- SARS-CoV Viruses bind to ACE2 receptors in order to enter the cell. Viral replication and rupture liberates inflammatory cytokines and destroys surfactant production
- VIP binds uniquely to receptors on Alveolar Type II cells in the lung, the same cells that bind the SARS-CoV-2 virus via their ACE2 receptors
- VIP is heavily concentrated in the lung and binds specifically to VIP receptors on alveolar type II cells. VIP exerts a broad anti-cytokine effect on immune system cells
- VIP specifically upregulates surfactant production via upregulation of C-Fos protein and protects type II cells from cytokine
- Upregulating the production of surfactant, the loss of which is increasingly implicated in COVID-19 respiratory failure [17]
Aviptadil a synthetic form of VIP results in rapid clinical recovery in patients with SARS-CoV-2 infection.[2]
Effect of Aviptadil on Lungs in COVID-19
Preservation of Pulmonary Tissue
Preserving surfactant production in the lung and in protecting type 2 alveolar cells. Significantly delayed the onset of edematous lung injury, effective in preventing ischemia-reperfusion injury, Prevents NMDA-induced caspase-3 activation in the Lung.[18]
Inhibits alveolar epithelial cell Apoptosis
VIP is a proven inhibitor of activation-induced perforin, as well as of granzyme B and therefore actively contributes to the reduction of deleterious proinflammatory and cell death-inducing processes, particularly in the lungs. Aviptadil restores barrier function at the endothelial/alveolar interface and thereby protects the lung and other organs from failure.[18]
VIP Promotes synthesis of pulmonary surfactant
Studies have demonstrated that VIP binds on type II cells and increases the incorporation of methyl-choline into phosphatidylcholine – the major component of the pulmonary surfactants by enhancing the activity of the enzyme choline-phosphate cytidylyltransferase. VIP upregulates C-Fos protein expression in cultured type II alveolar cells, which is instrumental in promoting synthesis of pulmonary surfactant phospholipids (Li 2007) and induces surfactant protein A expression in ATII cells through activation of PKC/c-Fos pathway.[18]
VIP decreases Pulmonary Inflammation
Anti-cytokine effect- Inhibits IL-6,TNF-α production and inhibit NF-kB activation. Protects against HCl-induced pulmonary edema.[18]
Pharmacokinetic Properties
Half-life: Its plasma half-life of elimination is 1 to 2 minutes.[2] Metabolism/Distribution: After injection of 1 µg radioactively labelled Aviptadil as bolus to patients a very rapid tissue distribution was observed Within 30 min about 45% of the radioactivity was found in the lungs Over an observation period of 24 hrs only minimal activity was detected in the GI tract & almost no activity was found in the liver or spleen Radioactivity in the lungs decreased within four hours to 25% and within 24 hours to 10% Apparent volume of distribution: Aviptadil has a volume of distribution of 14 ml/kg.[2] Tissue Distribution:Aviptadil binds to its receptors in discrete locations within the gastrointestinal, respiratory, and genital tracts. Aviptadil is localized on respiratory epithelium, smooth muscles of the airways, blood vessels and alveolar walls. Elimination:After injection of radiolabelled Aviptadil radioactivity was almost completely eliminated by the kidneys, 35% within 4 hours, and 90% within 24 hours
Justification for Aviptadil use in the treatment of ARDS
COVID-19-related death is primarily caused by Acute Respiratory Distress Syndrome (ARDS). The trigger for ARDS is widely attributed to a cytokine storm in the lungs, in which the virus causes release of inflammatory cytokines. As a result, alveolae of the lungs fill with fluid and become impermeable to oxygen, even in the setting of mechanical ventilation. SARS-CoV-2 is known to cause respiratory failure, which is the hallmark of Acute COVID-19. Tragically, survival of patients with COVID-19 who progress to Acute Respiratory Distress is dismal. There is an urgent need for a treatment approach that goes right into the heart of the matter – the alveolar type 2 cells which are vulnerable entry points and hosts for the SARS-CoV-2 virus.[19]
Aviptadil-Evidence from Studies in ARDS
Phase III Study-Increased Recovery and Survival in Patients With COVID-19 Respiratory Failure Following Treatment with Aviptadil
A multicenter, randomized, placebo-controlled trial in 196 patients with PCR+ COVID-19 receiving intensive care at 10 U.S. hospitals – 6 tertiary care and 4 regional hospitals to determine whether intravenous aviptadil (synthetic VIP) is superior to placebo in achieving recovery from respiratory failure and survival at 60 days post treatment. Primary, prespecified endpoint was “alive and free from respiratory failure at day 60.” Across all patients and sites of care, patients treated with aviptadil were significantly more likely to be alive and free from respiratory failure at 60 days, compared to those treated with placebo (P=.02) and demonstrated improvement in survival alone (P<.001). Advantages in survival for aviptadil-treated patients were seen in both the subgroup classified as 2 on the National Institute of Allergy and Infectious Disease (NIAID) ordinal scale (58.6% vs. 0%; p=.001) and the NIAID=3 subgroup (83.1% vs. 62.8%; p=.03). Among patients who recovered successfully, those treated with Aviptadil had a median 10-day reduction in length of hospital stay compared to placebo patients (P=.025). Treatment with aviptadil demonstrates multi-dimensional efficacy in improving the likelihood of recovery from respiratory failure and survival to 60 days, and markedly reduced hospital stay in critically ill patients with respiratory failure caused by COVID-19.[20]
Case report: Rapid Clinical Recovery from Critical COVID-19 Pneumonia with Aviptadil
A 54 year old man with double lung transplant presented with headache, fever and productive cough. COVID-19 infection was confirmed by positive RT-PCR of nasopharyngeal swab. The patient required only supportive care for 3 days and was discharged home. Two weeks later he presented with worsening dyspnea, fever and severe hypoxemia requiring high flow O2 and ICU admission. Chest CT showed diffuse bilateral consolidations. He had markedly elevated inflammatory markers. He was treated with dexamethasone and tocilizumab without improvement. He was not a candidate for Remdesivir due to chronic kidney disease. Convalescent plasma was not available, Pro-BNP level was normal; echocardiogram showed preserved biventricular function. He received Aviptadil, a total of three doses, per an open label access under an emergency use approved by USFDA. Rapid improvement in oxygenation and radiologic findings were noticed. No adverse effects were recorded. Patient was transferred out of the ICU 24 hours following the third dose and discharged home on room air 15 days later. This case report of lung transplant recipient with critical COVID-19 pneumonia treated with Aviptadil demonstrates rapid clinical and radiologic improvement.This is consistent with that VIP protects ATII cells, ameliorating the inflammation and improving oxygenation in critical COVID-19 pneumonia.[21]
Posology and method of administration
Aviptadil intravenous infusion is administered by infusion pump in escalating doses for 3 successive days
- Day 1 : Aviptadil 0.166 mcg/kg/hr (equivalent to 1 vial of Aviptadil Injection)
- Day 2 : Aviptadil 0.332 mcg/kg/hr (equivalent to 2 vials of Aviptadil Injection)
- Day 3 : Aviptadil 0.498 mcg/kg/hr (equivalent to 3 vials of Aviptadil Injection)
Duration of infusion depends on the patient’s body weight
- Body weight < 60 kg – 14 hour infusions of Aviptadil at escalating doses on 3 successive days
- Body weight 60 – 90 kg – 12 hour infusions of Aviptadil at escalating doses on 3 successive days
- Body weight > 90 kg – 10 hour infusions of Aviptadil at escalating doses on 3 successive days
Undesirable Effects
Gastrointestinal Disorders – Diarrhea, Vascular disorders – Hypotension, cutaneous flushing, facial flushing & Infusion related reactions[20]

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
References
- ^ Keijzers GB (April 2001). “Aviptadil (Senatek)”. Current Opinion in Investigational Drugs. 2 (4): 545–9. PMID 11566015. Archived from the original on 2010-09-02. Retrieved 2020-04-01.
- ^ Jump up to:a b c d e f Raveendran, A; Al Dhuhli, K.; Harish Kumar, G. (2021). “Role of Aviptadil in COVID-19”. BMH Medical Journal. 8 (2): 77-83.
- ^ National Institute of Allergy and Infectious Diseases (NIAID) (2021-06-25). “A Multicenter, Adaptive, Randomized, Blinded Controlled Trial of the Safety and Efficacy of Investigational Therapeutics for Hospitalized Patients With COVID-19”. International Network for Strategic Initiatives in Global HIV Trials (INSIGHT), University of Copenhagen, Medical Research Council, Kirby Institute, Washington D.C. Veterans Affairs Medical Center, AIDS Clinical Trials Group.
- ^ Leuppi, Jörg (2021-05-20). “Inhaled Aviptadil for the Treatment of COVID-19 in Patients at High Risk for ARDS: A Randomized, Placebo Controlled, Multicenter Trial”. Clinicaltrials.gov.
- ^ NeuroRx, Inc. (2021-02-23). “ZYESAMI (Aviptadil) for the Treatment of Critical COVID-19 With Respiratory Failure”. Lavin Consulting, LLC.
- ^ “Critically ill COVID-19 patients make quick recovery with treatment RLF-100”. New York Post. 2 August 2020. Retrieved 3 August 2020.
- ^ NeuroRx. “NeuroRx submits request for Emergency Use Authorization for RLF-100™ (aviptadil) in the treatment of patients with Critical COVID-19 and Respiratory Failure who have exhausted approved therapy”. http://www.prnewswire.com. Retrieved 2020-09-24.
- ^ Pharmaceuticals, NRx. “NRx Pharmaceuticals Announces Positive Results for ZYESAMI™ (Aviptadil-acetate) and Submits Emergency Use Authorization Application to USFDA to Treat Critical COVID-19 in Patients Suffering from Respiratory Failure”. http://www.prnewswire.com.
- ^ Das, Sohini (2021-01-25). “Dr Reddy’s, Zuventus get nod to conduct Covid-19 trials on repurposed drugs”. Business Standard India.
- ^ SECmeeting, e COVID-19. “Recommendations of the SECmeeting to examine COVID-19 related proposals under accelerated approval process made in its 140thmeeting held on 18.01.2021 & 19.01.2021 at CDSCO, HQ New Delhi” (PDF). CDSCO. Retrieved 1 July 2021.
- ^ Keijzers, GB (April 2001). “Aviptadil (Senatek)”. Current Opinion in Investigational Drugs. 2 (4): 545–9. PMID 11566015.
- ^ Procivni, Aviptadil/phentolamine mesilate. “Scientific discussion” (PDF).
- ^ Iwasaki, M; Akiba, Y; Kaunitz, JD (2019). “Recent advances in vasoactive intestinal peptide physiology and pathophysiology: focus on the gastrointestinal system”. F1000Research. 8: 1629. doi:10.12688/f1000research.18039.1. PMC 6743256. PMID 31559013.
- ^ Mathioudakis, A; Chatzimavridou-Grigoriadou, V; Evangelopoulou, E; Mathioudakis, G (January 2013). “Vasoactive intestinal Peptide inhaled agonists: potential role in respiratory therapeutics”. Hippokratia. 17 (1): 12–6. PMC 3738270. PMID 23935337.
- ^ Iwasaki, M; Akiba, Y; Kaunitz, JD (2019). “Recent advances in vasoactive intestinal peptide physiology and pathophysiology: focus on the gastrointestinal system”. F1000Research. 8: 1629. doi:10.12688/f1000research.18039.1. PMC 6743256. PMID 31559013.
- ^ Jump up to:a b Said, Sami I. (June 1988). “Vasoactive Intestinal Peptide in the Lung”. Annals of the New York Academy of Sciences. 527 (1 Vasoactive In): 450–464. Bibcode:1988NYASA.527..450S. doi:10.1111/j.1749-6632.1988.tb26999.x. PMID 2898912. S2CID 26804295.
- ^ Javitt, Jonathan C (2020-07-25). “Vasoactive Intestinal Peptide treats Respiratory Failure in COVID-19 by rescuing the Alveolar Type II cell”. doi:10.22541/au.159569209.99474501. S2CID 221509046.
- ^ Jump up to:a b c d Javitt, Jonathan C (2020-05-13). “Perspective: The Potential Role of Vasoactive Intestinal Peptide in treating COVID-19”. doi:10.22541/au.158940764.42332418. S2CID 219771946.
- ^ “Relief Therapeutics and NeuroRx Announce Final Manufacturing Validation of RLF-100 for Phase 2b/3 Clinical Trial in Patients with COVID-19 Associated Acute Respiratory Distress Syndrome”. GlobeNewswire News Room. 2020-05-14.
- ^ Jump up to:a b Youssef, Jihad G.; Lee, Richard; Javitt, Jonathan; Lavin, Philip; Lenhardt, Rainer; Park, David J; Perez Fernandez, Javier; Morganroth, Melvin; Jayaweera, Dushyantha (2021). “Increased Recovery and Survival in Patients With COVID-19 Respiratory Failure Following Treatment with Aviptadil: Report #1 of the ZYESAMI COVID-19 Research Group”. SSRN 3830051.
- ^ Beshay, S.; Youssef, J.G.; Zahiruddin, F.; Al-Saadi, M.; Yau, S.; Goodarzi, A.; Huang, H.; Javitt, J. (April 2021). “Rapid Clinical Recovery from Critical COVID-19 Pneumonia with Vasoactive Intestinal Peptide Treatment”. The Journal of Heart and Lung Transplantation. 40 (4): S501. doi:10.1016/j.healun.2021.01.2036. PMC 7979412. S2CID 232282732.
//////////AVIPTADIL, RLF 100, DK 1000
CCC(C)C(C(=O)NC(CC(C)C)C(=O)NC(CC(=O)N)C(=O)O)NC(=O)C(CO)NC(=O)C(CC(=O)N)NC(=O)C(CC(C)C)NC(=O)C(CC1=CC=C(C=C1)O)NC(=O)C(CCCCN)NC(=O)C(CCCCN)NC(=O)C(C(C)C)NC(=O)C(C)NC(=O)C(CCSC)NC(=O)C(CCC(=O)N)NC(=O)C(CCCCN)NC(=O)C(CCCNC(=N)N)NC(=O)C(CC(C)C)NC(=O)C(CCCNC(=N)N)NC(=O)C(C(C)O)NC(=O)C(CC2=CC=C(C=C2)O)NC(=O)C(CC(=O)N)NC(=O)C(CC(=O)O)NC(=O)C(C(C)O)NC(=O)C(CC3=CC=CC=C3)NC(=O)C(C(C)C)NC(=O)C(C)NC(=O)C(CC(=O)O)NC(=O)C(CO)NC(=O)C(CC4=CN=CN4)N

NEW DRUG APPROVALS
ONE TIME
$10.00
Marbofloxacin

Marbofloxacin
- Molecular FormulaC17H19FN4O4
- Average mass362.356 Da
115550-35-1[RN]
2,3-Dihydro-9-fluoro-3-methyl-10-(4-methyl-1-piperazinyl)-7-oxo-7H-pyrido[3,2,1-ij][4,1,2]benzoxadiazine-6-carboxylic Acid
6807
7H-1,3,4-Oxadiazino[6,5,4-ij]quinoline-6-carboxylic acid, 9-fluoro-2,3-dihydro-3-methyl-10-(4-methyl-1-piperazinyl)-7-oxo-
8X09WU898T
марбофлоксацин
ماربوفلوكساسين
马波沙星
Marbofloxacin is a carboxylic acid derivative third generation fluoroquinolone antibiotic. It is used in veterinary medicine under the trade names Marbocyl, Forcyl, Marbo vet and Zeniquin. A formulation of marbofloxacin combined with clotrimazole and dexamethasone is available under the name Aurizon (CAS number 115550-35-1).

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
PATENT
CN 107383058,
https://patents.google.com/patent/CN107383058B/enMarbofloxacin (Marbofloxacin) is fluoroquinolone antibacterial agent for animals, the entitled fluoro- 3- methyl-1 0- of 9- of chemistry (4- methylpiperazine-1-yl) -7- oxo -2,3- dihydro -7H- pyridine [3,2,1-ij] [4,1,2] benzo oxadiazines -6- carboxylic acid, It is developed by Roche Holding Ag, and is further developed by French Vetoquinol (method national strength and prestige are grand) company earliest, in nineteen ninety-five in Europe Listing.Marbofloxacin is after Enrofloxacin (Enrofloxacin), Danofloxacin (Danofloxacin), sarafloxacin (Sarafloxacin) etc. another third generation carbostyril family antibacterial drugs after, the drug have extensive antibacterial activity simultaneously With very good dynamic characteristic, sterilizing power is strong, absorbs fastly, widely distributed in vivo, with other antimicrobials without crossing drug resistant Property, easy to use, adverse reaction is small.Pharmacokinetic is studies have shown that Marbofloxacin removes long half time in animal body, biology Availability, almost without residual in the blood of animal, excrement and tissue, is well suited for clinically to antibiosis for animals close to 100% The requirement of element, structural formula are as follows:
Structure is complicated for Marbofloxacin, not only contains methyl piperazine substituent group, but also aromatic moieties contain pyridine benzo evil two Piperazine skeleton has had many documents and patent report at present and has reviewed its synthetic method, such as patent US4801584, ZL94190968.9, EP2010/067828, CN101619068, CN102060860, CN102617595, document J.Org. Chem., 1992,57 (2), 744-766, ” chemical reagent ” 2007,29 (11), 701-703., ” Chinese Journal of Pharmaceuticals ” 2002,33 (1), 1358-1363 etc..Patent US4801584 reports fluoro- via the fluoro- 4,8- dihydroquinoline -3- carboxylic acid, ethyl ester of 6,7- bis- preparation 6,7- bis- The method of 8- hydroxyl -1- (methylamino) -4- oxo-Isosorbide-5-Nitrae-dihydroquinoline -3- carboxylic acid, ethyl ester, this method are related to using valuableness And commercialization is not easy amination reagent O- (2, the 4- dinitrophenyl) oxyammonia largely purchased in 1 upper amino, by multistep reaction After complete the preparation of fluoro- 8- hydroxyl -1- (the methylamino) -4- oxo-Isosorbide-5-Nitrae-dihydroquinoline -3- carboxylic acid, ethyl ester of 6,7- bis-, passed through after It crosses and paraformaldehyde, N methyl piperazine reacts the preparation for realizing Marbofloxacin.Correlated response formula is as follows:
The patent literature reports such as patent ZL94190968.9 are that raw material prepares Ma Bosha from 2,3,4,5 tetra fluoro benzoic acid The synthetic route of star, this method are not only related to the multisteps hazardous reactions such as carboxylic acyloxy chlorination, Grignard Reagent preparation reaction, synthesize road Wire length, and 3- (the N- methyl formyl hydrazono-) ethyl acrylate for being difficult to prepare is used, and yield is low, be not suitable for industrially putting Mass production, correlated response formula are as follows:
Patent CN101619068 is condensed using 2,3,4,5- phenyl tetrafluoride carbamoylalkyl esters and inferior amine salt, obtained N- bis- Methyl substituted enamine derivates react the enamine for preparing the substitution of N- methyl-N- acyl group under organic acid catalysis with N- methylhydrazide Derivative, then 6,7,8- tri- fluoro- 1- (methylamino) -4- oxo-Isosorbide-5-Nitrae-dihydroquinoline-are completed in cyclization and hydrolysis under alkaline condition The preparation of 3- carboxylic acid realizes Ma Bosha finally by with N methyl piperazine, dimethyl formal (or diethyl formal) reaction The preparation of star.The technique uses the dimethyl suflfate and the height hazardous reaction reagent such as sodium hydride or alkalide of severe toxicity, because And it is subject to certain restrictions in commercial process.Correlated response formula is as follows:
In conclusion there are various deficiencies, such as chemistry examinations in the synthetic route of existing synthesis Marbofloxacin The defects of agent is expensive, reaction route is too long, using the chemical reagent for being unfavorable for industrialized production, the present inventor are real after study It tests, invents a kind of new method for preparing Marbofloxacin.The preparation of embodiment 1:1,1,1- tri- chloro- 4- (4- methylpiperazine-1-yl) butyl- 3- alkene -2- ketone(E) -1,1,1- tri- chloro-4-methoxy butyl- 3- alkene -2- ketone (Formulas I, R=Me) (10.18g, 50mmol), 1- methyl The mixture of piperazine (6.0g, 60mmol) and mesitylene (50mL) is heated to reflux temperature and stirs 6 hours, and system is natural Be cooled to room temperature, remove organic solvent under high vacuum reduced pressure, residue (14.2g, crude product do not purify) without further purification, directly It connects for reacting in next step.Embodiment 2:(6,8- bis- fluoro- 7- (4- methylpiperazine-1-yl) -4- oxo -3- (2,2,2- trichloroacetyl) quinoline Quinoline -1 (4H)-yl) urethanes (Formula VII) preparationUnder nitrogen protection, the product (14.2g is not purified, is directly used) of embodiment 1 is dissolved in toluene (120mL), then body Triethylamine (72mL, 514mmol) is added in system, system is heated to reflux temperature.Under reflux temperature, slowly dripped into reaction system Add toluene (60mL) solution of 2,3,4,5- phenyl tetrafluoride formyl chloride (16g, 75.3mmol).Rear system reflux is added dropwise 30min, then system slow cooling is to 60 DEG C, heat filtering.Filtrate is transferred in 500ml reaction flask, and carbazic acid second is then added Ester (Formula V, R2=Et) (6.25g, 60mmol).System is reacted 12 hours at a temperature of 60-65 DEG C after addition.To reaction H is slowly added in system2O (150mL) quenching reaction, system are naturally cooling to room temperature.Filtering, obtains solid, and solid uses heptan Alkane/ethyl acetate system mashing processing, obtains solid (Formula VII, R2=Et) (21.2g).Embodiment 3:1- amino -6- fluoro- 8- hydroxyl -7- (4- methylpiperazine-1-yl) -4- oxo -1,4- dihydroquinoline -3- The preparation of carboxylic acid (Formula VIII)2 obtained solid of embodiment (21.2g) is placed in 200ml reaction flask, ethyl alcohol (50mL) is added into reaction system With water (50mL), system is heated to flowing back.The aqueous solution (30mL) of KOH (7.0g) is slowly added under counterflow condition to system, is dripped System maintains the reflux for state response 96 hours after adding.System is naturally cooling to room temperature, and H is added in system2O (100mL) and CH2Cl2(50ml) stands after stirring and separates organic phase, and water phase reuses CH2Cl2It is extracted twice (2 × 50mL).Water phase uses salt Sour regulation system is to acid (pH=3-4), and then water phase reuses CH2Cl2It is extracted twice (2 × 100mL), merges organic phase, subtract Pressure-off obtains solid (Formula VIII) (12.4g) after removing organic solvent.The preparation of embodiment 4:1,1,1- tri- chloro- 4- (4- methylpiperazine-1-yl) butyl- 3- alkene -2- ketoneSequentially added in reaction flask the chloro- 4- ethyoxyl butyl- 3- alkene -2- ketone (Formulas I, R=Et) of (E) -1,1,1- three (14.1g, 65mmol) and 1- methyl piperazine (7.0g, 70mmol).Then system is heated to 130-155 DEG C and is stirred to react 5 hours.System is cold But to room temperature, the complete raw material of a little unreacted of high vacuum removed under reduced pressure, residue (16.8g, crude product do not purify) is without pure Change, is directly used in and reacts in next step.Embodiment 5:(6,8- bis- fluoro- 7- (4- methylpiperazine-1-yl) -4- oxo -3- (2,2,2- trichloroacetyl) quinoline Quinoline -1 (4H)-yl) t-butyl carbamate (Formula VII, R2=tBu) preparationUnder nitrogen protection, the product (16.0g is not purified, is directly used) of embodiment 4 is dissolved in toluene (125mL), then N is added in system, N- diisopropylethylamine (104.5mL, 600mmol), system is heated to reflux temperature.Under reflux temperature, to Toluene (70mL) solution of 2,3,4,5- phenyl tetrafluoride formyl chloride (18.8g, 88mmol) is slowly added dropwise in reaction system.It is added dropwise Starting material Formula II is tracked to HPLC within system reflux 1 hour afterwards to disappear.Then system slow cooling is to 60 DEG C or so, hot mistake Filter.Filtrate is transferred in 500mL reaction flask, and tert-butyl carbazate (Formula V, R is then added2=tBu)(9.3g,70mmol).It is added After system reacted 48 hours at a temperature of 60-65 DEG C.H is slowly added into reaction system2O (150mL) quenching reaction, body System is naturally cooling to room temperature.Filtering obtains solid, and solid is handled using heptane/ethyl acetate system mashing, obtains solid (formula VII,R2=tBu) (19.3g) is directly used in next step without further purification.Embodiment 6:1- amino -6- fluoro- 8- hydroxyl -7- (4- methylpiperazine-1-yl) -4- oxo -1,4- dihydroquinoline -3- The preparation of carboxylic acid (Formula VIII)By 5 obtained solid of embodiment (19.0g) as in 200mL reaction flask, methanol (55mL) is added into reaction system With water (55mL), system is heated to flowing back.The aqueous solution (30mL) of CsOH (13.5g) is slowly added under counterflow condition to system, Rear system is added dropwise and maintains the reflux for state response 96 hours.System is naturally cooling to room temperature, and H is added in system2O (100mL) and CH2Cl2(50mL) stands after stirring and separates organic phase, and water phase reuses CH2Cl2It is extracted twice (2 × 50mL).Water phase uses salt Sour regulation system is to acid (pH=3-4), and then water phase reuses CH2Cl2It is extracted twice (2 × 100mL), merges organic phase, subtract Pressure-off obtains solid (Formula VIII) (8.8g) after removing organic solvent.Embodiment 7: the preparation of Marbofloxacin1- amino-6- fluoro- 8- hydroxyl-7- (4- methylpiperazine-1-yl) oxo-1-4- is sequentially added in 100mL reaction flask, 4- dihydroquinoline -3- carboxylic acid (Formula VIII, 6.0g), 85% formic acid (30mL) and 36.5% formalin (6.0mL). System is carefully slowly heated to 75 DEG C or so reactions 1 hour after addition.Then system is cooled to 10 DEG C hereinafter, being carefully added into 25% ammonium hydroxide (25mL), stir 0.5 hour.Then activated carbon (1g) is added into system, mistake after 1 hour is sufficiently stirred Filter, filtrate methylene chloride extract 2 times (2 × 100mL).Merge organic phase, anhydrous sodium sulfate dries, filters, organic phase high vacuum Removed under reduced pressure solvent obtains Marbofloxacin crude product (5.4g).H is added in the crude product2In O (50mL), first acid for adjusting pH value is slowly added dropwise To 3.2 (pH meter detections), 4 hours are stood, filtering, filtrate added drop-wise sodium bicarbonate aqueous solution adjusting pH value to 6.2 (pH meter detections), A large amount of solids are precipitated, and ice salt bath cooling system stirs 1 hour to 0 DEG C or so, filtering, obtain Marbofloxacin after product drying (4.72g)。

Patent
Publication numberPriority datePublication dateAssigneeTitleUS4801584A *1986-09-121989-01-31Hoffmann-La Roche Inc.Pyrido(3,2,1-IJ)-1,3,4 benzoxadiazine derivativesCN1116849A *1993-01-231996-02-14辉瑞大药厂Process for the manufacture of a tricyclic compoundCN102060860A *2011-01-072011-05-18安徽美诺华药物化学有限公司Preparation method of MarbofloxacinCN102617595A *2012-03-232012-08-01江西华士药业有限公司Preparation method of fluoroquinolone antibacterial medicament marbofloxacinCN102712598A *2009-11-192012-10-03新梅斯托克尔卡·托瓦纳·兹德拉维尔公司A process for a preparation of marbofloxacin and intermediate thereof
CN110283186A *2019-07-192019-09-27海门慧聚药业有限公司A kind of crystal form of Marbofloxacin and preparation method thereof
PATENT
CN 107522718
PATENT
CN 102617595,
PATENT
Indian Pat. Appl., 2009CH00164,


Example 2: Preparation of ethyl 6,8-difluoro-1-(N~methylfomnamido)-7-(4-methyl-1- piperazinyl)-4-oxo-4H-quinoline-3-carboxylate hydrochloride of Formula (Ilia)
STR IIIA
Water (400 ml) and the compound of Formula (IIa) (200 g) are charged into a round bottom flask at 28°C and concentrated HCI (124 ml) is added slowly at a temperature below 40°C, and the mass is heated to 95-1OO0C. 300 ml of water and ethanol are distilled under vacuum at 1004C. The mass is cooled to 25-30°C. Acetone (400 ml) Is added and the mass is cooled to 0-5°C. The mass is maintained at 0-58C for 30-60 minutes and the product is filtered. The product is washed with pre-chilled acetone (200 ml) and dried under vacuum at 70-75°C for 12-15 hours to obtain the title compound. Yield: 181.0 g (95%). Example 3: Preparation of marbofloxacin from the compound of Formula (Ilia) Ethylene glycol (100 ml) and potassium hydroxide (17.3 g) are stirred for 10- 15 minutes for dissolution. A compound of Formula (Ilia) (10 g) is added and the mass is heated to 120-130’C, and then maintained for 24 hours. The mass is cooled to 30°C and water (15 ml) is added. Hydrochloric acid (36%, 18 ml) is slowly added below 404C.rformic acid (6 ml) is slowly added below 40°C and the mass is stirred for 20-30 minutes. Formaldehyde (5 ml) is added and the mass is then heated to 70-75°C and maintained for 1-2 hours. The mass is slowly cooled to 15-20°C and stirred for 30-60 minutes. The obtained solid dihydroformate salt is filtered and the wet cake is washed with pre-chilled demineralized water (5 ml). The material is suction dried for 2-3 hours. Methanol (50 ml), demineralized water (15 ml), and the wet cake are charged into a round-bottom flask and stirred for 10-15 minutes.
Ammonia solution (25%, 7.5 ml) is added and stirred for 30-60 minutes at 25-35°C. The turbid solution is filtered and the wet cake is washed with methanol (5 ml) at 25- 35°C. The water and methanol are distilled at 60-70°C under vacuum until 20 ml remain. The mass is cooled to 0-5°C and maintained for 30-60 minutes. The solid is filtered at 0-5°C and the wet cake is washed with methanol (10 ml). The material is suction dried for 30-60 minutes and the product is dried at 60-70°C under vacuum for 18-20 hours. Yield: 6.51 g (70%). Example 4: preparation of marbofloxacin from a compound of Formula (Ilia) Ethylene glycol (150 ml) and potassium hydroxide (72.2 g) are stirred for 10- 15 minutes for dissolution. A compound of Formula (Ilia) (50 g) is added and the mass is heated to 115-1256C, and then is maintained for 10-12 hours at 115— 125°C. The mass is cooled to 25-35°C and water (150 ml) is added. Formic acid (98%, 100 m!) is slowly added below 45°C and the mass is stirred for 30-60 minutes. Formaldehyde (37-41%, 35 ml) is added to the mass, which is then heated to 70- 75°C and maintained for 1-2 hours. The mass is slowly cooled to 0-5°C and stirred for 1-2 hours. The obtained solid dihydroformate salt is filtered and the wet cake is washed with pre-chilled water (50 ml). The material is suction dried for 1 hour and washed with pre-chilled acetone (50 ml) and suction dried for 1 hour. Methanol (250 ml), water (100 ml), and the wet cake are charged into a round-bottom flask and stirred for 10-15 minutes. Ammonia solution (25%, 40 mi) is added and stirred for 30-60 minutes at 25-35°C. The turbid solution is filtered and the wet cake is washed with methanol (50 ml) at 25-35°C. The filtrate is distilled at 60-70°C under vacuum until 75-100 ml remain. The mass is cooled to 10-15’C and maintained for 30-60 minutes. The solid free base is filtered at 10-15°C and the wet cake is washed with chilled methanol (50 ml). The material is suction dried for 30-^60 minutes and the product is dried at 60-70°C under vacuum for 10-12 hours. Yield: 33.0 g (70.8%). Example 5: Preparation of marbofloxacin from a compound of Formula (Ilia) Water (350 ml) and potassium hydroxide (86.6 g) are stirred for 10 minutes. A compound of Formula (Ilia) (50 g) is added and the mass is heated to 100-104°C. The mass is maintained for 105-110 hours at 100-1040C, then is copied to 25-35°C and water (65 ml) is added. Hydrochloric acid (36%, 125 ml) is slowly added below 40°C and the mass is stirred for 30 minutes. Formaldehyde (37%, 19 ml) is added and the mass is heated to 70-756C. The mass is maintained for 1-2 hours at 70-75 0C and then is slowly cooled to 0-5°C and maintained for 30-60 minutes. The obtained solid hydrochloride salt is filtered and the bed is washed with pre-chilled water (25 ml) at 0-5°C. The material is suction dried. Ethanol (250 ml), water (75 ml), ammonia solution (25%, 38 ml) and the wet cake are charged into a round-bottom flask and stirred for 1-2 hours at 25-35° C. The turbid solution is filtered and the bed is washed with ethanol (50 ml). The filtrate is distilled at 65-70°C under vacuum until 100 ml remain. The mass is cooled to 0-5°C and maintained for 30-60 minutes. The solid free base is filtered and the wet cake is washed with pre-chilled ethanol (50 ml). The product is dried under vacuum at 60-70°C for 15-^20 hours. Yield: 23.3 g (50%).
Example 6: Preparation of marbofloxacin from a compound of Formula (IIa) Ethylene glycol (60 ml) and potassium hydroxide (28.05 g) are stirred for 10- 15 minutes for dissolution. A compound of Formula (IId) (20 g) is added. The mass is heated to 120-135°C and maintained for 4-6 hours. The mass is cooled to 30°C and water (60 ml) is added. Formic acid (98-100%, 40 ml) is slowly added below 40°C and stirred for 20-30 minutes. Formaldehyde (37-41%, 12 ml) is added to the mass, which is heated to 70-75°C and maintained for 1-2 hours. The mass is slowly cooled to O-S6C and stirred for 30-60 minutes. The obtained solid dihydroformate salt is filtered and the wet cake is washed with pre-chilled water (20 ml). The material is suction dried for 2-3 hours. Methanol (100 ml), water (30 ml), and the wet cake are charged into a round-bottom flask and stirred for 10-15 minutes. Ammonia solution (25%, 20 ml) is added and stirred for 30-60 minutes at 25-35°C. The turbid solution is filtered and the wet cake is washed with methanol (10 ml) at 25-35°C. The water and methanol are distilled at 60-70°C under vacuum until 40 ml remain. The mass is cooled to 0-5°C and maintained for 30-60 minutes. The solid free base is filtered at 0-5°C and the wet cake is washed with methanol (20 ml). The material is suction dried for 30-60 minutes and the product is dried at 60-70°C under vacuum for 18-20 hours. Yield: 12.6 g (71%)
Example 7: Purification of marbofloxacin To crude marbofloxacin (25 g) is added methanol (125 ml) and ammonia (18.75 ml). Half of the volume of the methanol and ammonia solution is removed by azeotropic distillation. The mass is slowly cooled and maintained for 1 hour. The product is filtered and washed with chilled methanol (25 ml). The product is suction dried for 30 minutes and dried under vacuum for 12 hours, to yield pure marbofloxacin of a purity 99.80%. XRD pattern, DSC thermogram, TGA1 and IR are substantially in accordance with Figs. 1, 2, 3, and 4, respectively. Yield: 22 g (88.0%),
PATENT
Indian Pat. Appl., 2009CH00163,
PATENT
WO 2011061292
PATENT
CN 102060860,
PATENT
CN 101619068,
PATENT
https://patents.google.com/patent/EP2332916A2/en
- Marbofloxacin is the common name for 9-fluoro-2,3-dihydro-3-methyl-10-(4-methyl-1-piperazinyl)-7-oxo-7H-pyridol(3,2,1-ij)(4,2,1)benzoxadiazin-6-carboxylic acid, of the formula :
- [0003]
Marbofloxacin is a potent antibiotic of the fluoroquinolone group. - [0004]
EP 259804 describes marbofloxacin as well as a synthesis for the preparation thereof by a multistep process which is unpractical for a large scale manufacture, since it requires high temperatures and reagents not suitable for large-scale production, resulting in low over-all yields. The process for the preparation is disclosed in the reaction scheme 1. - [0005]
EP 680482 discloses an alternative approach for the preparation of marbofloxacin, wherein hydroxy group is introduced into molecule by means of reaction of intermediate with alkali metal hydroxide in aqueous media. The starting material used is 2,3,4,5-tetrafluorobenzoic acid. Disadvantages of this process are relatively high excess of alkali metal hydroxide and lengthy procedure. The process for the synthesis according to this patent is shown in the reaction scheme 2. - [0006]
Research Disclosure No. 291, 1988, pages 548-551 discloses an alternative route of synthesis also starting from 2,3,4,5-tetrafluorobenzoic acid. Later steps of the process are shown in the reaction scheme 3. - [0007]
IT 1313683 relates to a process for preparation of marbofloxacin by a process via benzyl ether. Ether was debenzylated in aqueous solution by hydrogenating over 5% Pd/BaSO4 and the obtained product is cyclized using HCOOH/HCOH. - [0008]
In view of the prior art there still exists a need for an improved method for preparation of marbofloxacin and intermediates thereof suitable for a large-scale production.
Examples
- [0068]
A high resolution HPLC method is used to determine an amount and purity compounds of formula I, II and IV. The tests are carried out in X-Bridge C18, 150 x 4.6mm, 3.5µm column. The mobile phase is gradient of A) 5mM NH4COOCH3 pH=7.0 B) acetonitrile. Gradient: 0’=10%B, 10’=20%B, 25′-30’=90%B, 32’=10%B. - [0069]
The chromatograph is equipped with a UV detector set at 250 nm and 315nm, the flow rate is 1.0 ml per minute at 30°C.
Example 1a) 6,8-difluoro-1-(methylamino)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid and 6,8-difluoro-1-(methylamino)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid sodium salt
- [0070]
- [0071]
4.137g of Ethyl 6,8-difluoro-1-(N-methylformamido)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylate (10.14mmol) was put into 40mL of 10% H2SO4 and stirred at 100°C for 7 hours. Reaction mixture was cooled and crystals were formed. Mixture was cooled to 4°C and filtered with suction. Filter cake was washed with a mixture of H2O/EtOH/THF (1/1/5) and dried. 3.260g of 6,8-difluoro-1-(methylamino)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid as yellow crystals were obtained (91%). - [0072]
In case the sodium salt is desired the product obtained in previous step was put into 5mL of EtOH and 10mL of CH2Cl2 and 1.20g of NaOH dissolved in 2mL of water was added. Solution was stirred at room temperature. for 1h, dried with Na2SO4 and evaporated. 2.90g of pure title product was isolated (yellow powder, 7.71mmol, 76%).
b) 6,8-difluoro-1-(methylamino)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid
- [0073]
- [0074]
400mg of Ethyl 6,8-difluoro-1-(N-methylformamido)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylate (0, 979mmol) was put into 2mL of 10% H2SO4 and stirred at 100°C for 2 hours. Reaction mixture was cooled and crystals were formed. To this mixture 1,7mL of 25% aq. NH3 was slowly added. At first very dense suspension was formed that dissolves with further addition of ammonia solution. At the end clear solution formed with pH of 9. Ammonium sulphate was precipitated by the addition of 10mL of EtOH , filtered off and washed with 5mL of H2O/EtOH (1/2). Mother liquor was dried on the rotary evaporator and 10 mL of EtOH/H2O mixture (7/3) was added to precipitate residual inorganic salt, which was again filtered off. Remaining yellow solution was dried on a rotary evaporator to obtain 321mg of yellow powder (0.912 mmol, 93%).
Example 26-fluoro-8-hydroxy-1-(methylamino)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid
- [0075]
- [0076]
178 mg of 6,8-difluoro-1-(methylamino)-7-(4-methyl-piperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid sodium salt (0.470mmol) was mixed with 360 mg of Me4NOH.5H2O (2.00 mmol) and stirred at 100°C for 4 hours. Ammonium salt melts and dark brown oil is formed during the reaction. Reaction mixture was cooled to room temperature and 0.10mL of HCOOH was added to neutralize hydroxide. 5mL of EtOH is added to precipitate the product, which was filtered with suction and filter cake was washed with 2mL of cold EtOH. 90mg of the product was obtained.
Example 39-fluoro-3-methyl-10-(4-methylpiperazin-1-yl)-7-oxo-3,7-dihydro-2H-[1,3,4]oxadiazino[6,5,4-ij]quinoline-6-carboxylic acid formate salt
- [0077]
- [0078]
180 mg of 6,8-difluoro-1-(methylamino)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid sodium salt (0.481mmol) was mixed with 360 mg of Me4NOH.5H2O (2.00 mmol) and stirred at 100°C for 3 hours. Ammonium salt melts and dark brown oil is formed during the reaction. Reaction mixture was cooled to room temperature and 1 mL of HCOOH was added followed by addition of 0.4 mL of 37% aq. solution of HCHO and stirred at 70°C for additional hour. Reaction mixture was cooled to room temperature and 5mL of EtOH was added to precipitate the product, which was filtered with suction and filter cake was washed with 2mL of cold EtOH. 111 mg of grey powder was obtained.
Example 49-fluoro-3-methyl-10-(4-methylpiperazin-1-yl)-7-oxo-3,7-dihydro-2H-[1,3,4]oxadiazino[6,5,4-ij]quinoline-6-carboxylic acid formate salt
- [0079]
- [0080]
1.14g of 6,8-difluoro-1-(methylamino)-7-(4-methyl-piperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid (3.00mmol) was mixed with 3.06g of Me4NOH.5H2O (16.96mmol) and stirred at 100°C for 5 hours. Ammonium salt melts and dark brown oil is formed during the reaction. Reaction mixture was cooled to room temperature and 1.44 mL of HCOOH (85% aq. sol) was added followed by addition of 0.5 mL of 37o aq. solution of HCHO and the flask was cooled on the water bath at 22°C. Another 1.44mL of 85% HCOOH was added and the reaction mixture was warmed to 70°C for 30min and after cooling 20mL of EtOH was added to the reaction mixture and left in a refrigerator for 16h. Precipitate was filtered under reduced pressure and washed with cold ethanol (10mL). After drying 1.23g of grayish powder was obtained (90%) .
Example 59-fluoro-3-methyl-10-(4-methylpiperazin-1-yl)-7-oxo-3,7-dihydro-2H-[1,3,4]oxadiazino[6,5,4-ij]quinoline-6-carboxylic acid
- [0081]
- [0082]
1.145g of 6,8-difluoro-1-(methylamino)-7-(4-methyl-piperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid (3.01mmol) was mixed with 2.72g of Me4NOH.5H2O (15.00mmol) and stirred at 100°C for 8 hours. Ammonium salt melts and dark brown oil is formed during the reaction. Reaction mixture was cooled to room temperature and 3.0 mL of HCOOH was added followed by addition of 0.5 mL of 37% aq. solution of HCHO (6.0mmol) and the flask was cooled on the water bath at 22°C. Precipitate was immediately formed. The flask was warmed to 70°C, during which precipitate was dissolved. After stirring at 70°C for 30min (precipitate was formed again after 5min) reaction flask was cooled to room temperature and 20mL of EtOH was added to the reaction mixture and left in a refrigerator for 16h. Precipitate was filtered under reduced pressure and washed with cold ethanol (10mL). After drying 1.165g of grayish powder was obtained (85%), with a purity of 97.11% (HPLC). - [0083]
Crude reaction product was mixed with 0.9mL of 25% NH3 aqueous solution and crystallized in a mixture of 26mL of EtOH and 14mL H2O. 0.673g of powder was obtained (61%) with a purity of 98.75% (HPLC).
Example 69-fluoro-3-methyl-10-(4-methylpiperazin-1-yl)-7-oxo-3,7-dihydro-2H-[1,3,4]oxadiazino[6,5,4-ij]quinoline-6-carboxylic acid
- [0084]
- [0085]
1.140g of 6,8-difluoro-1-(methylamino)-7-(4-methyl-piperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid (3.00mmol) was mixed with 2.72g of Me4NOH.5H2O (15.01mmol) and stirred at 100°C for 8 hours. Ammonium salt melts and dark brown oil is formed during the reaction. Reaction mixture was cooled to room temperature and 3.0 mL of HCOOH was added followed by addition of 0.5 mL of 37% aq. solution of HCHO (6.0mmol) and the flask was cooled on the water bath at 22°C. Precipitate was immediately formed. The flask was warmed to 70°C, during which precipitate was dissolved and stirred for 30 min (after stirring for at 70°C for 5min precipitate formed again). Reaction flask was cooled to room temperature and 20mL of H2O was added to the reaction mixture and left in a refrigerator for 16h. Precipitate was filtered under reduced pressure and washed with cold ethanol (10mL). After drying 1.022g of greyish powder was obtained (75%). with a purity of 97.11% (HPLC). - [0086]
Crude reaction product was mixed with 0.9mL of 25% NH3 aqueous solution and crystallised in a mixture of 20mL of EtOH and 6mL CHCl3. 0.771g of yellow powder was obtained (71%) with a purity of 99.50% as determined by HPLC.
Example 79-fluoro-3-methyl-10-(4-methylpiperazin-1-yl)-7-oxo-3,7-dihydro-2H-[1,3,4]oxadiazino[6,5,4-ij]quinoline-6-carboxylic acid
- [0087]
- [0088]
1.142 g of 6,8-difluoro-1-(methylamino)-7-(4-methyl-piperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid (3.01mmol) was mixed with 3.26g of Me4NOH.5H2O (18.01mmol) and stirred at 100°C for 4 hours. Ammonium salt melts and dark brown oil is formed during the reaction. Reaction mixture was cooled to room temperature and 3.0 mL of HCOOH was added followed by addition of 0.5 mL of 37% aq. solution of HCHO (6.0mmol) and the flask was cooled on the water bath at 22°C. Precipitate was immediately formed. The flask was warmed to 70°C, during which precipitate was dissolved and stirred for 30 min (after stirring for at 70°C for 5min precipitate formed again). Reaction flask was cooled to room temperature and dried on the rotary evaporator. 20mL of H2O was added to the reaction mixture and cooled in a refrigerator. Precipitate was filtered under reduced pressure. After drying 1.147g of white powder was obtained (84%). - [0089]
Crude reaction product was mixed with 5mL of water and 2mL of 25% aqueous solution of NH3 and clear solution was obtained. To this solution, 7mL of EtOH was added and dried under reduced pressure. Product was crystallized in a mixture of 15mL of EtOH and 10mL CHCl3 to obtain 0.4321g of white powder (41%) with a purity of 98.63% as determined by HPLC
Example 89-fluoro-3-methyl-10-(4-methylpiperazin-1-yl)-7-oxo-3,7-dihydro-2H-[1,3,4]oxadiazino[6,5,4-ij]quinoline-6-carboxylic acid
- [0090]
- [0091]
1.136 g of 6,8-difluoro-1-(methylamino)-7-(4-methyl-piperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid (2.98mmol) was mixed with 2.73g of Me4NOH.5H2O (15.00mmol) and stirred at 100°C for 7 hours. Ammonium salt melts and dark brown oil is formed during the reaction. Reaction mixture was cooled to room temperature and 3.0 mL of HCOOH was added followed by addition of 0.5 mL of 37% aq. solution of HCHO (6.0mmol) and the flask was cooled on the water bath at 22°C. Precipitate was immediately formed. The flask was warmed to 70°C, during which precipitate was dissolved and stirred for 30 min (after stirring for at 70°C for 5min precipitate formed again). Reaction flask was cooled to room temperature and dried on the rotary evaporator. 20mL of H2O was added to the reaction mixture and cooled in a refrigerator. Precipitate was filtered under reduced pressure. After drying 1.039g of grey powder was obtained (77%). - [0092]
Crude reaction product was neutralized with 2mL of 25% aqueous solution of NH3 and clear solution was diluted with 15mL of EtOH and 9mL of H2O. Solution was partially dried under reduced pressure until the formation of precipitate. At this point mixture was cooled in a refrigerator and precipitate was isolated by filtration under reduced pressure to obtain 0.675g of powder (65%) with a purity of 98.84% as determined by HPLC.
Example 99-fluoro-3-methyl-10-(4-methylpiperazin-1-yl)-7-oxo-3,7-dihydro-2H-[1,3,4]oxadiazino[6,5,4-ij]quinoline-6-carboxylic acid
- [0093]
- [0094]
1.140g of 6,8-difluoro-1-(methylamino)-7-(4-methyl-piperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid (3.01mmol) was mixed with 3.30g of Me4NOH.5H2O (18.20mmol) and stirred at 100°C for 4 hours. Ammonium salt melts and dark brown oil is formed during the reaction. Reaction mixture was cooled to room temperature and 3.0 mL of HCOOH was added followed by addition of 0.5 mL of 37% aq. solution of HCHO (6.0mmol) and the flask was cooled on the water bath at 22°C. Precipitate was immediately formed. The flask was warmed to 70°C, during which precipitate was dissolved and stirred for 30 min (after stirring for at 70°C for 5min precipitate formed again). Reaction flask was cooled to room temperature and dried on the rotary evaporator. 20mL of H2O was added to the reaction mixture and cooled in a refrigerator. Precipitate was filtered under reduced pressure to obtain 0.847g of solid, while mother liquid was diluted with EtOH and concentrated under reduced pressure until precipitate forms, which was filtered again to obtain additional 0.208g of solid. The yield of combined solid material is 1.055g, 77%. Crude reaction product (formate salt) was crystallized in H2O/EtOH (25mL/10mL) to obtain 0.722g (53%) of yellow powder. Formate salt was put in 20mL of EtOH/CH2Cl2 mixture (1/1) and 0.5mL of 25%aq. NH3 was added to obtain clear solution. Solution was dried with Na2SO4 and solvent evaporated under reduced pressure to obtain 0.580g of yellow powder (53%).
Example 109-fluoro-3-methyl-10-(4-methylpiperazin-1-yl)-7-oxo-3,7-dihydro-2H-[1,3,4]oxadiazino[6,5,4-ij]quinoline-6-carboxylic acid
- [0095]
- [0096]
100 mL reactor with a rotary stirrer was charged with 10,16g of 6,8-difluoro-1-(methylamino)-7-(4-methyl-piperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid (28,83mmol) and 26,50g of Me4NOH˙5H2O (146,25mmol) that was previously mixed together. Temperature of the heating jacket was set to 100°C and stirring to 100s-1, while water was allowed to evaporate out of the reactor during the reaction. Reaction was stirred at specified temperature for 5 hours and homogenous dark brown oil was obtained. Temperature of reactor was cooled to 20°C, 30mL of HCOOH was added and stirred well so that all oil is transformed into brown suspension. 4,5mL of 37% aq. HCHO was added drop-wise and heated at 70°C for 30min. Reaction mixture was cooled to 20°C and 20mL of water added to precipitate the product in the form of formate complex. Suspension was cooled to 0°C and filtered under reduced pressure and washed the filter cake with additional 10mL of cold water to obtain 8,38g of white powder. Mother liquor was partially evaporated under reduced pressure and when solid started to precipitate it was filtered again to obtain additional 0.80g of powder. 50mL of EtOH was added into the mother liquor to precipitate the product and after filtration at reduced pressure further 0.80g of white powder was obtained. Product was collected and 9,98g of white powder was suspended in a mixture of 50mL of EtOH and 50mL of CH2Cl2. Into the suspension 25% aq. NH3 was added to neutralize the formate complex and after addition of 12mL of NH3 all product was dissolved and small amount of solid material is formed. 5g of anhydrous Na2SO4 was added to dry the organic solution and it was filtered off and solvent evaporated under reduced pressure. 8.99g of slightly yellow powder was obtained in 86% yield.
Example 11Crystallization from ethanol/toluene/water 2:1:1
- [0097]
8.4g of crude marbofloxacin was suspended in a mixture of 83 ml of ethanol, 41ml of toluene and 41 ml of water and heated to reflux. From the clear yellow solution formed 83 ml of solvent mixture was distilled off, whereby the temperature rose from 74 to about 79°C, and a yellow precipitate was formed. The suspension was cooled to 20° – 25°C, stirred for 1 hour, filtered, and the filter cake was washed with 3 portions of 6 ml of ethanol to yield after drying in vacuum dryer the product in more than 95% yield.
Example 12Crystallization of marbofloxacin starting from marbofloxacin formate
- [0098]
26g of marbofloxacin formate was suspended in a mixture of 65ml of ethanol and 27ml of water. Under stirring a solution of 25% ammonia in ethanol (20ml 25%NH3/10ml EtOH) is slowly (about 30 minutes) added by drops until the substance is dissolved and pH value of 7-9 is reached. The reaction was stirred for about 15 minutes and filtered. The filtrate was evaporated at 110°C until about 60ml of the solvent was distilled off and marbofloxacin started to precipitate. After distillation the suspension was cooled and stirred for 0.5 to 1 hour at 0-5°C, filtered, to yield after drying at 40°C/50mbar for 3 to 5 hours the product in 100%yield.
Example 13Crystallization from ethanol
- [0099]
1g of marbofloxacin was dissolved under heating to reflux in 160ml of ethanol, after filtration, the solution is cooled and the crystallized product is recovered in more than 90% yield.
Example 146,7,8-Trifluoro-1-methylamino-1,4-dihydro-4-oxo-3-quinoline-carboxylic acid
- [0100]
- [0101]
10mmol of 6,7,8-Trifluoro-1-(N-methylformamido)-1,4-dihydro-4-oxo-3-quinoline-carboxylic acid ethyl ester was put in the round bottomed flask. 20mL of 10% H2SO4 was added and stirred with the temperature of the sand bath of 100°C for the time periods specified in the following table. Reaction mixture was cooled down to 4°C, filtered and the cake washed with water and the conversion an yield were determined. - [0102]
The experiment was repeated but starting compound was mixed with 1.0mL of solvent (EtOH, AcOH or MeCN as specified in the following table) before adding the 10% H2SO4. - [0103]
The starting compound is insoluble in aqueous phase. By mixing the starting compound with a small amount of polar solvent (EtOH, MeCN, AcOH) a film is formed around the crystals which improves wetting of the crystals with the aqueous acid. Without addition of polar solvent prior to adding the aqueous acid solution wetting of the crystals is impaired and the reaction is slower.Exp.Reaction time (solvent)Conversion (yield)14.016h65%14.027h60%14.0324h100%14.0424h100% (94%)14.056h (0.1mL AcOH per mmol)91%14.066h (0.1mL EtOH per mmol)89%14.0721h (0.1mL MeCN per mmol)100% (97%)14.0821h (0.1mL MeCN per mmol)100% (96%)
Example 156,7,8-Trifluoro-1-methylamino-1,4-dihydro-4-oxo-3-quinoline-carboxylic acid
- [0104]
3.30g of 6,7,8-Trifluoro-1-(N-methylformamido)-1,4-dihydro-4-oxo-3-quinoline-carboxylic acid ethyl ester (10.054 mmol) was put into the round-bottomed flask equipped with the magnetic stirrer. 1mL of MeCN was added and stirred for a minute. 20mL of 10% H2SO4 was added and stirred. The flask was put into the sand bath (T = 100°C) and stirred for 21h. Suspension was cooled down to 4°C and filtered under suction. Yellow powder was washed twice with cold water and dried. 2.646g of yellow powder was obtained (9.721 mmol, 96.7%) and identified by NMR spectroscopy to be title compound.
Example 166,7,8-Trifluoro-1-methylamino-1,4-dihydro-4-oxo-3-quinoline-carboxylic acid
- [0105]
6,7,8-Trifluoro-1-(N-methylformamido)-1,4-dihydro-4-oxo-3-quinoline-carboxylic acid ethyl ester (6.868g, 20.92 mmol) was mixed with 1mL of EtOH (to decrease the hydrophobicity of the substrate). Next, 40mL of 10% aqueous H2SO4 solution was added and the mixture was stirred at the temperature of the bath of 100°C for 12h. A white suspension formed which was cooled to 0°C and filtered under reduced pressure. The white powder was washed with cold water and cold EtOH and dried. 5.135g of yellow powder was obtained and identified as title compound by 19F and 1H NMR spectroscopy. The yield of hydrolysis was 90%.
Example 176,8-Difluoro-1-(methylamino)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-quinoline-3-carboxylic acid
- [0106]
- [0107]
6,7,8-Trifluoro-1-methylamino-1,4-dihydro-4-oxo-3-quinoline-carboxylic acid (272mg, 1.0mmol, obtained as described in Example 16, and 400 mg of N-methylpiperazine (4.0mmol) were mixed with 1mL of EtOH and stirred under reflux temperature (jacket temperature Tj=100°C). After two hours of reaction clear solution formed, afterwards the product precipitated and a very dense suspension was formed. Reaction was stopped after three hours of stirring at Tj=100°C. A sample was put directly to the NMR analysis and only two signals were observed indicating reaction was quantitative. Crude reaction product was diluted with EtOH and neutralized by addition of aqueous solution of NH3 until pH of 8 was reached. Suspension was cooled to 0°C and product isolated by filtration under reduced pressure, washed further with 10mL of cool EtOH and dried. 138mg (39%) of product was obtained.
Example 186,8-Difluoro-1-(methylamino)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-quinoline-3-carboxylic acid
- [0108]
6,7,8-Trifluoro-1-methylamino-1,4-dihydro-4-oxo-3-quinoline-carboxylic acid (1.087g, 3.993mmol), 484mg of N-methylpiperazine (4.83mmol) and 484 mg of Et3N (4.78mmol) were mixed with 8mL of EtOH and stirred under reflux temperature (Tj=100°C). After 19h of reflux yellow solution and white precipitate are formed in the reaction flask. Solvent was evaporated under reduced pressure and put directly to the NMR analysis. Crude reaction product was mixed with 20mL of EtOH and suspension cooled in the refrigerator. The product (white precipitate) was isolated by filtration under reduced pressure, washed further with 10mL of cool EtOH and dried. 1.178g of white powder was obtained (3.375 mmol, 800).
Example 196,8-Difluoro-1-(methylamino)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-quinoline-3-carboxylic acid
- [0109]
In accordance with examples 17 and 18 additional experiments were carried out using different reaction conditions for the conversion of 6,7,8-trifluoro-1-methylamino-1,4-dihydro-4-oxo-3-quinoline-carboxylic acid into 6,8-difluoro-1-(methylamino)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-quinoline-3-carboxylic acid. The experiments were performed according to the following general procedure: 1.0mm of starting compound was put in the round bottomed flask and N-methylpiperazine (NMP), base and solvent were added according to the following table. Reaction mixture was stirred at the corresponding temperature. Solvent was evaporated and crude reaction mixture analyzed directly by NMR (1H and 19F).
Example 206,8-Difluoro-1-(N-methylformamido)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-quinoline-3-carboxylic acid ethyl ester
- [0111]
- [0112]
Substitution: 6,7,8-Trifluoro-1-(N-methylformamido)-4-oxo-1,4-quinoline-3-carboxylic acid ethyl ester (1.0 mmol, 324mg) was mixed with 2 equivalents of N-methylpiperazine (220mg) and 400mg Et3N stirred for three hours at 100°C. Reaction mixture liquefied in 10 minutes and solidified again within 30 minutes of the reaction (that is the reason for higher amount of TEA). After 3 hours of stirring was reaction mixture cooled to room temperature and analyzed by NMR spectroscopy. - [0113]
Substitution: The above reaction was repeated but Et3N was replaced by 1 equivalent of DABCO. - [0114]
In both cases, substitution was quantitative and analysis of the crude reaction mixtures showed that there was some hydrolysis of the ethyl ester (EE) to the free carboxylic acid (CA) group resulting in a product mixture. The results are summarized in the following table. Ethyl ester is readily soluble in water.Exp.Reaction conditionsConversion (yield)20.012.5 NMP, 1 DABCO, 100°C, 3h100% (48% EE, 52% CA)20.022.5 NMP, 4 Et3N, 100°C, 3h100% (58% EE, 42% CA)
Example 216,8-Difluoro-1-(methylamino)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-quinoline-3-carboxylic acid (one-pot reaction)
- [0115]
- [0116]
6,7,8-Trifluoro-1-(N-methylformamido)-4-oxo-1,4-quinoline-3-carboxylic acid ethyl ester (1.0 mmol, 324mg) was mixed with 2 equivalents of N-methylpiperazine (200mg) and stirred for one hour at 100°C. Reaction mixture liquefied in 10 minutes and solidified again within 30 minutes of reaction. After one hour of reaction the reaction mixture was cooled to room temperature and 10% aqueous H2SO4 (5mL) was added and stirred again at 100°C for two hours. Yellow solution was cooled to 0°C so that product precipitated. It was isolated by filtration under reduced pressure. Pure 6,8-difluoro-1-(methylamino)-7-(4-methylpiperazin-1-yl)-4-oxo-1,4-quinoline-3-carboxylic acid in the form of sulfate salt was obtained (as determined by NMR) as slightly yellow powder (279mg, 58%).
Example 22Synthesis of 9-fluoro-3-methyl-10-(4-methylpiperazin-1-yl)-7-oxo-3, 7-dihydro-2H-[1,3,4]oxadiazino[6,5,4-ij]quinoline-6-carboxylic acid (Marbofloxacin, MBX)
- [0117]
13.5 g of 6,8-Difluoro-1-(methylamino)-7-(4-methyl-piperazin-1-yl)-4-oxo-1,4-dihydroquinoline-3-carboxylic acid hydrochloride and ca. 63 g of tetramethylammonium hydroxide water solution 25 % were charged into a reactor and slowly heated to 100°C. When this temperature was reached, water was removed by distillation at reduced pressure (between 0.8 to 0.3 bar) in such a manner that ca. 25 to 32 ml of water were removed in 3 hours. The reaction mixture was stirred for another 3 hours and after completion of the conversion, the reaction mixture was cooled to 0 – 10 °C and ca. 40.5 ml of formic acid were slowly added with violent agitation. The temperature was maintained below 20°C, preferable between 0 – 10°C. Then ca. 6.1 ml of formaldehyde were slowly added. After addition the reaction mixture was heated to 70°C and maintained at this temperature for about 30 minutes. - [0118]
The reaction mixture was cooled to room temperature (20 – 30°C), ca. 27 ml of purified water were added and the mixture was stirred for 30 minutes. Then the reaction mixture was cooled to 0 – 5°C and stirred at this temperature for at least 2 hours. The product marbofloxacin formate (MBXBZ) was centrifuged and washed with 10 – 15 g of cooled (0 – 5°C) purified water. The product was spun dried and collected. - [0119]
Wet product MBXBZ was added to the mixture of 67 ml of ethanol, 67 ml of methylene chloride and 16.2 ml of ammonia solution (ca. 25 0). If phases did not separate, additional 63 ml of methylene chloride and 33 ml of purified water were added. The pH of the water phase was adjusted to be between 7 and 9.5, preferable between 7.5 and 8.5. The mixture was agitated for approximately 15 minutes to 1 hour and then the layers were separated and both phases were subjected to in process control (IPC) analysis. - [0120]
If IPC results showed that extraction was not complete, ca. 63 ml of methylene chloride were added to the water layer and the extraction was repeated until the IPC specification was met. - [0121]
The organic phases were combined and ca. 6.8 mg of sodium sulphate anhydrous and optionally 0.4 mg of activated charcoal were added. The mixture was mixed for at least 30 minutes and filtered, then organic solvent was distilled off to obtain crude marbofloxacin.
Purification of the crude Marbofloxacin
- [0122]
In an inert atmosphere 5 g of purified water, 12 g of ethanol 96 % and 4.3 g of toluene (ratio between the solvents was within the following ranges: ethanol : toluene : water : 1.8 – 2.8 : 1 : 1.1 – 1.2) were charged into a reactor and wet crude marbofloxacin (MBXCA) from the previous step was added under nitrogen. The mixture was slowly heated to reflux (70 – 80°C) until a clear solution was obtained. The solution was stirred for 0.5 hour under this temperature and then one half of the azeotrope solvent mixture (toluene : water : ethanol = 51 % : 6 % : 43 %) was evaporated. Then the remaining mixture was cooled slowly to 5°C (allowed interval is between 0 and 25 °C) with agitation (optionally 1 % mass of product of disodium-EDTA can be added). The mixture was mixed for 1 to 3 hours and the product was then isolated by centrifugation, washed with 13 g of ethanol, spun dry and collected. The product was dried at temperature 40 – 45°C, p < 100 mbar for 8 hour.
Example 23Purification of Marbofloxacin
- [0123]
Marbofloxacin was dissolved in 20 parts by weight of water by addition of acetic acid. Marbofloxacin was completely dissolved at pH of 5.3. Active charcoal was added and the mixture was stirred overnight. The mixture was then filtered using activated charcoal filter. The pH of the filtrate was adjusted to 7.2 by use of KOH, the obtained suspension was stirred for 1 hour at room temperature and then the precipitated product was recovered. Marbofloxacin with a purity of 99,9% (HPLC area) was obtained. - [0124]
HPLC analysis was performed on a pentafluorophenyl propyl (PFP) column (type Luna® PFP, 150 x 4.6mm, 3µm, Phenomenex, USA); detector: UV315 nm; flow rate: 0.8 ml/min; injection volume: 5 µl; mobile phase: A: 0.02M NaH2PO4xH2O+0,1% TEA, pH2.5; B: acetonitrile : methanol = 5:95 (v/v) ; gradient: 0’=10B, 25’=100B, 30’= 100B, 32’=10B. The HPLC chromatogram of marbofloxacin prior to purification is shown in Figure 1, the HPLC chromatogram after purification is shown in Figure 2. As evident from the chromatograms all products with retention time above 24min were successfully eliminated.
Mechanism of action
Its mechanism of action is not thoroughly understood, but it is believed to be similar to the other fluoroquinolones by impairing the bacterial DNA gyrase which results in rapid bactericidal activity.[1] The other proposed mechanisms include that it acts against nondividing bacteria and does not require protein and RNA synthesis, which block protein and RNA synthesis respectively.[2]
Activity
Marbofloxacin is a synthetic, broad spectrum bactericidal agent. The bactericidal activity of marbofloxacin is concentration dependent, with susceptible bacteria cell death occurring within 20–30 minutes of exposure. Like other fluoroquinolones, marbofloxacin has demonstrated a significant post-antibiotic effect for both gram– and + bacteria and is active in both stationary and growth phases of bacterial replication.[3]
It has good activity against many gram-negative bacilli and cocci, is effective against:
- Aeromonas
- Brucella
- Campylobacter
- Chlamydia trachomatis
- Enterobacter
- Escherichia coli
- Haemophilus
- Klebsiella spp
- Mycobacterium
- Mycoplasma
- Proteus
- Pseudomonas aeruginosa
- Salmonella
- Serratia
- Shigella
- Staphylococci (including penicillinase-producing and methicillin-resistant strains)
- Vibrio
- Yersinia
Application
Marbofloxacin can be used both orally and topically. It is particularly used for infections of the skin, respiratory system and mammary glands in dogs and cats, as well as with urinary tract infections. For dogs, a dose ranges from 2.75 – 5.5 mg/kg once a day. The duration of treatment is usually at least five days, longer if there is a concurrent fungal or yeast infection.[4] Maximum duration of treatment is 30 days.[3]
Contraindications and side effects
Marbofloxacin should usually be avoided in young animals because of potential cartilage abnormalities. In rare occasion, it can cause central nervous system (CNS) stimulation and should be used with caution in patients with seizure disorders.[3] Under certain conditions it can cause discomfort such as cramps, treatable with diazepam. Other adverse effects are usually limited to gastrointestinal tract (GI) distress (vomiting, anorexia, soft stools, diarrhoea) and decreased activity.[3]
References
- ^ Boothe, D.M. (2001) Antimicrobial drugs. In Small Animal ClinicalPharmacology and Therapeutics, pp. 150–173. W. B. Saunders Co., Philadelphia, PA.
- ^ Hunter RP, Koch DE, Coke RL, Carpenter JW, Isaza R. Identification and comparison of marbofloxacin metabolites from the plasma of ball pythons (Python regius) and blue and gold macaws (Ara ararauna). J Vet Pharmacol Ther. 2007 Jun;30(3):257-62.
- ^ Jump up to:a b c d Plumb DC (ed). Plumb’s Veterinary Handbook, 7th ed. Ames, IA: Wiley-Blackwell Publishing, 2011.
- ^ Rougier S, Borell D, Pheulpin S, Woehrlé F, Boisramé B (October 2005). “A comparative study of two antimicrobial/anti-inflammatory formulations in the treatment of canine otitis externa”. Veterinary Dermatology. 16 (5): 299–307. doi:10.1111/j.1365-3164.2005.00465.x. PMID 16238809. Archived from the original on 2013-01-05.
External links
| Clinical data | |
|---|---|
| Trade names | XeniQuin bolus & Injection (Opsonin Agrovet BD) |
| AHFS/Drugs.com | International Drug Names |
| Routes of administration | By mouth |
| ATCvet code | QJ01MA93 (WHO) |
| Legal status | |
| Legal status | Veterinary use only |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 115550-35-1 |
| ChemSpider | 54663 |
| UNII | 8X09WU898T |
| ChEMBL | ChEMBL478120 |
| CompTox Dashboard (EPA) | DTXSID4046600 |
| ECHA InfoCard | 100.168.181 |
| Chemical and physical data | |
| Formula | C17H19FN4O4 |
| Molar mass | 362.356 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (what is this?) (verify) |
///////////////Marbofloxacin, марбофлоксацин , ماربوفلوكساسين , 马波沙星 ,

NEW DRUG APPROVALS
ONE TIME
$10.00

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....










