Home » Monoclonal antibody (Page 9)
Category Archives: Monoclonal antibody
Stelara (ustekinumab) Receives FDA Approval to Treat Active Psoriatic Arthritis

Ustekinumab
| CAS No: | 815610-63-0 |
|---|---|
| Molecular Weight: | 145.64 g/mol |
| Chemical Formula: | C9H18N2O2 |
| IUPAC Name: | Immunoglobulin G1, anti-(human interleukin 12 p40 subunit) (human monoclonal CNTO 1275 gamma1-chain), disulfide with human monoclonal CNTO 1275 kappa-chain, dimer |
HORSHAM, Pa., Sept. 23, 2013 /PRNewswire/ — Janssen Biotech, Inc., announced today that the U.S. Food and Drug Administration (FDA) has approved Stelara (ustekinumab) alone or in combination with methotrexate for the treatment of adult patients (18 years or older) with active psoriatic arthritis. It is estimated that more than two million people in the U.S. are living with psoriatic arthritis, a chronic autoimmune disease characterized by both joint inflammation and psoriasis skin lesions
read all at
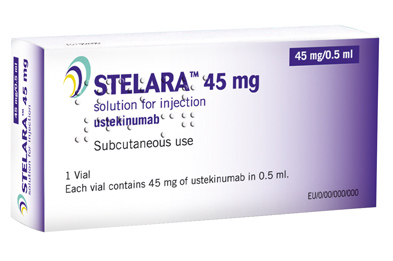
Ustekinumab (INN, experimental name CNTO 1275, proprietary commercial name Stelara, Centocor) is a human monoclonal antibody. It is directed against interleukin 12 and interleukin 23, naturally occurring proteins that regulate the immune system and immune-mediated inflammatory disorders.
Ustekinumab is a fully human monoclonal antibody (mAb) targeting the interleukin (IL)-12/23p40 subunit.
Interleukins are small soluble proteins that communicate between white blood cells (leukocytes), such as T cells. Interleukins mediate the differentiation, proliferation and many other processes of these cells. IL-12 and IL-23 are involved in the differentiation of naive T cells into T helper (Th) 1 and Th17 cells respectively.
Th1 and Th17 cells have been implicated in several autoimmune disorders, such as psoriasis. Ustekinumab targets the common p40 subunit of IL-12 and IL-23 to stop these cytokines from binding to their receptors and consequently preventing the development of Th1 and Th17 cells in an immune response.
In two Phase III trials for moderate to severe psoriasis, the longest >76 weeks, ustekinumab was safe and effective.
A third Phase III trial, ACCEPT, compared the efficacy and safety of ustekinumab with etanercept in the treatment of moderate to severe plaque psoriasis. This trial found a significantly higher clinical response with ustekinumab over the 12-week study period compared to high-dose etanercept. It also demonstrated the clinical benefit of ustekinumab among patients who failed to respond to etanercept.
Ustekinumab is approved in Canada, Europe and the United States to treat moderate to severe plaque psoriasis.
As of November 2009, the drug is being investigated for the treatment of psoriatic arthritis. It has also been tested in Phase II studies for multiple sclerosis and sarcoidosis, the latter versus golimumab (Simponi).
The US Food and Drug Administration (FDA) and European Union (EU) have approved the interleukin (IL) 12/23 inhibitor ustekinumab (Stelara, Janssen Biotech) for adults with active psoriatic arthritis who have not responded adequately to previous nonbiological disease-modifying antirheumatic drug therapy, the company announced today.
Approval of ustekinumab for psoriatic arthritis is “significant for patients and physicians as it marks the first treatment approved for this devastating and complex disease since the introduction of anti-TNF biologic medicines more than a decade ago,” Jerome A. Boscia, MD, vice president and head of immunology development, Janssen Research & Development, LLC, said in a statement.
The European Medicine Agency’s Committee for Medicinal Products for Human Use (CHMP) recommended approval of ustekinumab for active psoriatic arthritis in June, as reported by Medscape Medical News.
Ustekinumab is already approved in the US and EU for treatment of moderate to severe psoriatic plaques in adults. The drug, which can be used alone or in combination with methotrexate, is novel in that it targets both IL-12 and IL-23.
Image source: Crystal structure of human IL-12, Wikipedia, public domain

Ustekinumab binding to IL-12/23p40
FDA grants Arzerra ‘breakthrough’ designation for use with chlorambucil in CLL
The FDA today granted “breakthrough therapy” designation to ofatumumab for treatment of patients with chronic lymphocytic leukemia.
The designation applies to use of ofatumumab (Arzerra, GlaxoSmithKline) in combination with chlorambucil in patients with untreated CLL who unsuitable for fludarabine-based therapy.
Ofatumumab is a human monoclonal antibody that targets an epitope on the CD20 molecule encompassing parts of the small and large extracellular loops.
read all at
also read my post on newdrugapprovals
https://newdrugapprovals.wordpress.com/2013/07/08/gsk-tests-ofatumumab-in-rare-skin-disorder/
Ofatumumab (trade name Arzerra, also known as HuMax-CD20) is a human monoclonal antibody (for the CD20 protein) which appears to inhibit early-stage B lymphocyte activation. It is FDA approved for treating chronic lymphocytic leukemia that is refractory to fludarabine and alemtuzumab (Campath) and has also shown potential in treating Follicular non-Hodgkin’s lymphoma, Diffuse large B cell lymphoma, rheumatoid arthritis and relapsing remitting multiple sclerosis. Ofatumumab has also received conditional approval in Europe for the treatment of refractory chronic lymphocytic leukemia. This makes ofatumumab the first marketing application for an antibody produced by Genmab, as well as the first human monoclonal antibody which targets the CD20 molecule that will be available for patients with refractory CLL.Designated an orphan drug by FDA for the treatment of B-CLL
Niche play, alliances hold promise for Biocon

DR KIRAN SHAW MAXUMDAR
MD BIOCON
Niche play, alliances hold promise for Biocon
While biosimilar opportunity in the regulated markets is likely to play out in the medium term, its existing biopharma and branded portfolio will ensure growth in the short term
Niche play, alliances hold promise for Biocon
Business Standard
Innovator sales for these two drugs are pegged at $10 billion which is slightly over half of the worldwide insulin market of $19 billion.On the monoclonal antibody front, the company is in phase III for the cancer drug Trastuzumab which has a market …
READ ALL THIS AT
FDA has approved a new use of Avastin® (bevacizumab) in combination with fluoropyrimidine-based irinotecan or oxaliplatin chemotherapy for people with metastatic colorectal cancer (mCRC).
Bevacizumab, CAS NO 216974-75-3
A MONOCLONAL ANTIBODY
January 23, 2013
Avastin (bevacizumab) is a recombinant humanized monoclonal IgG1 antibody that binds to and inhibits the biologic activity of human vascular endothelial growth factor (VEGF) in in vitro and in vivo assay systems. Bevacizumab contains human framework regions and the complementarity-determining regions of a murine antibody that binds to VEGF. Avastin has an approximate molecular weight of 149 kD. Bevacizumab is produced in a mammalian cell (Chinese Hamster Ovary) expression system in a nutrient medium containing the antibiotic gentamicin. Gentamicin is not detectable in the final product.
FDA has approved a new use of Avastin® (bevacizumab) in combination with fluoropyrimidine-based irinotecan or oxaliplatin chemotherapy for people with metastatic colorectal cancer (mCRC).
On January 23, 2013, the FDA has approved a new use of Avastin® (bevacizumab) in combination with fluoropyrimidine-based irinotecan or oxaliplatin chemotherapy for people with metastatic colorectal cancer (mCRC). The new indication will allow people who received Avastin plus an irinotecan or oxaliplatin containing chemotherapy as an initial treatment (first-line) for mCRC to continue to receive Avastin plus a different irinotecan or oxaliplatin containing chemotherapy after their cancer worsens (second-line treatment).
People who start on Avastin for mCRC can now stay on Avastin after their cancer worsens.
Bevacizumab (trade name Avastin, Genentech/Roche) is an angiogenesis inhibitor, a drug that slows the growth of new blood vessels. It is licensed to treat various cancers, including colorectal, lung, breast (outside the USA), glioblastoma (USA only), kidney and ovarian.
Bevacizumab is a humanized monoclonal antibody that inhibits vascular endothelial growth factor A (VEGF-A).[1] VEGF-A is a chemical signal that stimulates angiogenesis in a variety of diseases, especially in cancer. Bevacizumab was the first clinically available angiogenesis inhibitor in the United States.[citation needed]
Bevacizumab was approved by the U.S. Food and Drug Administration (FDA) for certain metastatic cancers. It received its first approval in 2004, for combination use with standard chemotherapy for metastatic colon cancer.[2] It has since been approved for use in certain lung cancers, renal cancers, and glioblastoma multiforme of the brain.
At one point bevacizumab was approved for breast cancer by the FDA, but the approval was revoked on 18 November 2011.[3][4]
- Los, M.; Roodhart, J. M. L.; Voest, E. E. (2007). “Target Practice: Lessons from Phase III Trials with Bevacizumab and Vatalanib in the Treatment of Advanced Colorectal Cancer”. The Oncologist 12 (4): 443–50. doi:10.1634/theoncologist.12-4-443. PMID 17470687.
- http://www.gene.com/gene/products/information/pdf/avastin-prescribing.pdf
- Pollack, Andrew (18 November 2011). “F.D.A. Revokes Approval of Avastin for Breast Cancer”. New York Times.
- “Cancer drug Avastin loses US approval”. BBC. November 18, 2011.
SEQUENCE
>1bj1_H|Fab-12, F(ab)-12, 12-IgG1, rhuMAb-VEGF|||VH-CH1 (VH(1-123)+CH1(124-215))|||||||231||||MW 24867.8|MW 24867.8| EVQLVESGGGLVQPGGSLRLSCAASGYTFTNYGMNWVRQAPGKGLEWVGWINTYTGEPTY AADFKRRFTFSLDTSKSTAYLQMNSLRAEDTAVYYCAKYPHYYGSSHWYFDVWGQGTLVT VSSASTKGPSVFPLAPSSKSTSGGTAALGCLVKDYFPEPVTVSWNSGALTSGVHTFPAVL QSSGLYSLSSVVTVPSSSLGTQTYICNVNHKPSNTKVDKKVEPKSCDKTHT >1bj1_L|Fab-12, F(ab)-12, 12-IgG1, rhuMAb-VEGF|||L-KAPPA (V-KAPPA(1-107)+C-KAPPA(108-213))|||||||214||||MW 23451.0|MW 23451.0| DIQMTQSPSSLSASVGDRVTITCSASQDISNYLNWYQQKPGKAPKVLIYFTSSLHSGVPS RFSGSGSGTDFTLTISSLQPEDFATYYCQQYSTVPWTFGQGTKVEIKRTVAAPSVFIFPP SDEQLKSGTASVVCLLNNFYPREAKVQWKVDNALQSGNSQESVTEQDSKDSTYSLSSTLT LSKADYEKHKVYACEVTHQGLSSPVTKSFNRGEC >1bj1_J|Fab-12, F(ab)-12, 12-IgG1, rhuMAb-VEGF|||L-KAPPA (V-KAPPA(1-107)+C-KAPPA(108-213))|||||||214||||MW 23451.0|MW 23451.0| DIQMTQSPSSLSASVGDRVTITCSASQDISNYLNWYQQKPGKAPKVLIYFTSSLHSGVPS RFSGSGSGTDFTLTISSLQPEDFATYYCQQYSTVPWTFGQGTKVEIKRTVAAPSVFIFPP SDEQLKSGTASVVCLLNNFYPREAKVQWKVDNALQSGNSQESVTEQDSKDSTYSLSSTLT LSKADYEKHKVYACEVTHQGLSSPVTKSFNRGEC >1bj1_K|Fab-12, F(ab)-12, 12-IgG1, rhuMAb-VEGF|||VH-CH1 (VH(1-123)+CH1(124-215))|||||||231||||MW 24867.8|MW 24867.8| EVQLVESGGGLVQPGGSLRLSCAASGYTFTNYGMNWVRQAPGKGLEWVGWINTYTGEPTY AADFKRRFTFSLDTSKSTAYLQMNSLRAEDTAVYYCAKYPHYYGSSHWYFDVWGQGTLVT VSSASTKGPSVFPLAPSSKSTSGGTAALGCLVKDYFPEPVTVSWNSGALTSGVHTFPAVL QSSGLYSLSSVVTVPSSSLGTQTYICNVNHKPSNTKVDKKVEPKSCDKTHT
Peregrine Pharmaceuticals Announces Results From Phase II Clinical Trial of Bavituximab in Stage IV Pancreatic Cancer
TUSTIN, CA 02/13/13 — Peregrine Pharmaceuticals announced results from its 70 patient open-label, randomized Phase II clinical trial of bavituximab used in combination with gemcitabine in patients with previously untreated, advanced Stage IV pancreatic cancer. The trial included the enrollment of patients with advanced metastatic disease including significant liver involvement and poor performance status associated with rapid disease progression. Results showed that the combination of bavituximab and gemcitabine resulted in more than a doubling of overall response rates (ORR) and an improvement in overall survival (OS) when compared with gemcitabine alone (control arm). In the trial, patients treated with a combination of bavituximab and gemcitabine had a 28% tumor response rate as compared to 13% in the control arm. Median OS, the primary endpoint of the trial, was 5.6 months for the bavituximab plus gemcitabine arm and 5.2 months for the control arm (hazard ratio = 0.75).
Bavituximab binds to phosphatidylserine which is exposed on the surface of certain atypical animal cells, including tumour cells and cells infected with any of six different families of virus. These viral families contain the viruses hepatitis C, influenza A and B, HIV 1 and 2, measles, respiratory syncytial virus and pichinde virus, which is a model for the deadly Lassa virus.[2] Other cells are not affected since phosphatidylserine normally is only intracellular.[3]

Bavituximab binds to various aminophospholipids and is dependent on interaction with plasma protein beta-2 glycoprotein I to mediate binding.
These target aminophospholipids, usually residing only on the inner leaflet of the plasma membrane of cells, become exposed in virally infected, damaged or malignant cells, and more generally in most cells undergoing the process of apoptosis.
The antibody’s binding to phospholipids alerts the body’s immune system to attack the tumor endothelial cells, thrombosing the tumor’s vascular network and/or attacking free floating virally infected and metastatic cells while potentially minimizing side effects in healthy tissues.
- Statement on a nonproprietary name adopted by the USAN council
- Nature Medicine 14, 1357 – 1362 (2008)
- He, J.; Yin, Y.; Luster, T. A.; Watkins, L.; Thorpe, P. E. (2009). “Antiphosphatidylserine Antibody Combined with Irradiation Damages Tumor Blood Vessels and Induces Tumor Immunity in a Rat Model of Glioblastoma”. Clinical Cancer Research 15 (22): 6871–6880. doi:10.1158/1078-0432.CCR-09-1499. PMID 19887482. edit
- New Progression-Free Survival Data From Peregrine’s Bavituximab in Phase II Refractory Breast Cancer
- Phase II Advanced Breast Cancer Data to Be Presented at ASCO Highlight Promising Tumor Response and Progression-Free Survival Data With Peregrine’s Bavituximab
- Pharma company completes humanization of 3G4 antibody
- He, J.; Luster, T. A.; Thorpe, P. E. (2007). “Radiation-Enhanced Vascular Targeting of Human Lung Cancers in Mice with a Monoclonal Antibody That Binds Anionic Phospholipids”. Clinical Cancer Research 13 (17): 5211–5218. doi:10.1158/1078-0432.CCR-07-0793. PMID 17785577. edit
- Ran; Downes, A.; Thorpe, P. E. (2002). “Increased exposure of anionic phospholipids on the surface of tumor blood vessels”. Cancer Research 62 (21): 6132–6140. PMID 12414638.
<a href=”http://www.bloglovin.com/blog/4758019/?claim=ukqfxgh6tk3″>Follow my blog with Bloglovin</a>
Chugai files Herceptin for post surgical Adjuvant treatment of HER2+ve breast cancer in Japan

Trastuzumab, monoclonal antibody
Thursday, 7 February 2013
Trastuzumab (INN; trade names Herclon, Herceptin) is a monoclonal antibody that interferes with the HER2/neu receptor. Its main use is to treat certain breast cancers.
The HER receptors are proteins that are embedded in the cell membrane and communicate molecular signals from outside the cell (molecules called EGFs) to inside the cell, and turn genes on and off. The HER proteins stimulate cell proliferation. In some cancers, notably certain types of breast cancer, HER2 is over-expressed, and causes cancer cells to reproduce uncontrollably.[1]
The original studies of trastuzumab showed that it improved overall survival in late-stage (metastatic) breast cancer from 20.3 to 25.1 months,[1] but there is controversy over whether trastuzumab is effective in earlier stage cancer.[2]Trastuzumab is also controversial because of its cost, as much as $100,000 per year,[3] and while certain private insurance companies in the U.S. and government health care systems in Canada, England and elsewhere have refused to pay for trastuzumab for certain patients, some companies have since accepted trastuzumab treatment as a covered preventative treatment.[4]
Trastuzumab is also being studied for the treatment of other cancers.[5] It has been used with some success in women with uterine papillary serous carcinomas that overexpress HER2/neu.[6]
References
- Hudis, CA (2007). “Trastuzumab–mechanism of action and use in clinical practice”. N Engl J Med. 357 (1): 39–51.doi:10.1056/NEJMra043186. PMID 17611206. Jul 5;357(1):39-51. Review /article
- 129 Herceptin and early breast cancer: a moment for caution [Editorial]. Lancet 2005;366:1673.
- “Herceptin or Trastuzumab: Efficacy, Side Effects”. Health and Life.
- “At last, Axa pays for Herceptin”. 2006.
- Vecchione L. Novel investigational drugs for gastric cancer.Expert Opin Investig Drugs. 2009 May 26. [Epub ahead of publication]. Review /article.
- Santin AD, Bellone S, Roman JJ, McKenney JK, Pecorelli S. (2008). “Trastuzumab treatment in patients with advanced or recurrent endometrial carcinoma overexpressing HER2/neu”.Int J Gynaecol Obstet 102 (2): 128–31.doi:10.1016/j.ijgo.2008.04.008. PMID 18555254.
ZALTRAP Approved in the EU for Patients with Previously Treated Metastatic Colorectal Cancer

Ziv-aflibercept is a recombinant fusion protein consisting of Vascular Endothelial Growth Factor (VEGF)-binding portions from the extracellular domains of human VEGF Receptors 1 and 2 fused to the Fc portion of the human IgG1. Ziv-aflibercept is produced by recombinant DNA technology in a Chinese hamster ovary (CHO) K-1 mammalian expression system. Ziv-aflibercept is a dimeric glycoprotein with a protein molecular weight of 97 kilodaltons (kDa) and contains glycosylation, constituting an additional 15% of the total molecular mass, resulting in a total molecular weight of 115 kDa.
ZALTRAP is a sterile, clear, colorless to pale yellow, non-pyrogenic, preservative-free, solution for administration by intravenous infusion. ZALTRAP is supplied in single-use vials of 100 mg per 4 ml and 200 mg per 8 ml formulated as 25 mg/mL ziv-aflibercept in polysorbate 20 (0.1%), sodium chloride (100 mM), sodium citrate (5 mM), sodium phosphate (5 mM), and sucrose (20%), in Water for Injection USP, at a pH of 6.2.
5th feb 2013
Sanofi and Regeneron Pharmaceuticals, Inc. today announced that the European Commission (EC) has granted marketing authorization in the European Union for ZALTRAP 25mg/ml concentrate for solution for infusion in combination with irinotecan/5-fluorouracil/folinic acid (FOLFIRI) chemotherapy in adults with metastatic colorectal cancer (mCRC) that is resistant to or has progressed after an oxaliplatin-containing regimen. This decision was based on the efficacy and safety results of the VELOUR Phase 3 trial
“ZALTRAP is an important addition to the metastatic colorectal cancer treatment landscape and helps to fill a critical treatment gap,” said Eric Van Cutsem, M.D., Ph.D., University Hospitals Leuven, Belgium and lead investigator of the VELOUR study. “ZALTRAP is the first and only agent to demonstrate a survival improvement in a Phase 3 trial in patients previously treated with an oxaliplatin-based regimen who are being treated with FOLFIRI for their metastatic disease.” “I would like to thank the physicians, patients, and their families for their support in moving ZALTRAP through the clinical trial process leading to approval in Europe,” said Debasish Roychowdhury, M.D., Senior Vice President and Head, Sanofi Oncology. “We are thrilled to provide a new therapy that further extends the lives of patients with metastatic colorectal cancer and look forward to working with European health authorities to ensure patients have access to ZALTRAP.” In Europe, colorectal cancer is the most common cancer in both men and women and is the second leading cause of cancer death. In 2008, there were 436,000 new cases diagnosed and 212,000 deaths from colorectal cancer.[1] Commenting on the marketing authorization, George D. Yancopoulos, M.D., Ph.D., Chief Scientific Officer of Regeneron and President of Regeneron Laboratories, added: “The European approval of ZALTRAP provides a new option to address the unmet medical need in this patient population. There continues to be a need to develop new cancer therapies and Regeneron and Sanofi are committed to finding novel investigational treatments and combinations.” ZALTRAP received approval from the U.S. Food and Drug Administration (FDA) in August 2012 after a Priority Review, and marketing authorization applications for ZALTRAP are under review with other regulatory agencies worldwide
Roche’s Phase III leukemia drug Obinutuzumab (GA101) yields positive results
- GA101 is the first glycoengineered, type II anti-CD20 mAb.

Roche’s Phase III leukemia drug Obinutuzumab (GA101) yields positive results
Obinutuzumab (GA101)
| Formula | C6512H10060N1712O2020S44 |
|---|
GA101 is the first glycoengineered, type II anti-CD20 monoclonal antibody (mAb) that has been designed for increased antibody-dependent cellular cytotoxicity (ADCC) and Direct CellDeath.1 This agent is being investigated in collaboration with Biogen Idec.
Swiss pharmaceutical company Roche has announced that its early Phase III trial of Leukemia drug obinutuzumab (GA101) demonstrated significantly improved progression-free survival in people with chronic lymphocytic leukemia (CLL).
The positive results yield from stage 1 of a three-arm study called CLL11, designed to investigate the efficacy and safety profile of obinutuzumab (GA101) plus chlorambucil, a chemotherapy, compared with chlorambucil alone in people with previously untreated chronic lymphocytic leukemia (CLL).
This phase of the study met its primary endpoint and an improvement in progression-free survival was achieved; obinutuzumab plus chlorambucil significantly reduced the risk of disease worsening or death compared to chlorambucil alone.
Roche chief medical officer and global product development head Hal Barron said; “the improvement in progression-free survival seen with GA101 is encouraging for people with CLL, a chronic illness of older people for which new treatment options are needed.”
“GA101 demonstrates our ongoing commitment to the research and development of new medicines for this disease.”
Obinutuzumab is Roche’s most advanced drug in development for the treatment of hematological malignancies.
It has been specifically designed as the first glycoengineered, type 2 anti-CD20 monoclonal antibody in development for B cell malignancies.
Afutuzumab is a monoclonal antibody being developed by Hoffmann-La Roche Inc. for the treatment of lymphoma.[1] It acts as an immunomodulator.[2][3] It was renamed obinutuzumab in 2009.[4]
References
- Robak, T (2009). “GA-101, a third-generation, humanized and glyco-engineered anti-CD20 mAb for the treatment of B-cell lymphoid malignancies”. Current opinion in investigational drugs (London, England : 2000) 10 (6): 588–96. PMID 19513948.
- Statement On A Nonproprietary Name Adopted By The Usan Council – Afutuzumab,American Medical Association.
- International Nonproprietary Names for Pharmaceutical Substances (INN), World Health Organization.
- International Nonproprietary Names for Pharmaceutical Substances (INN), World Health Organization.
-
obinutuzumab isMonoclonal antibody Type Whole antibody Source Humanized (from mouse) Target CD20
Health Canada Approves ADCETRIS® (Brentuximab Vedotin) for the Treatment of Relapsed or Refractory Hodgkin Lymphoma (HL) and Systemic Anaplastic Large Cell Lymphoma (sALCL)

Structure of brentuximab vedotin
Brentuximab vedotin on track for BLA filing with FDA during first half of 2011. [© Sebastian Kaulitzki – Fotolia.com]
Brentuximab is a human antibody. The antibody portion of Brentuximab vedotin has the sequence of two copies of:
>Brentuximab vedotin - heavy chain QIQLQQSGPEVVKPGASVKISCKASGYTFTDYYITWVKQKPGQGLEWIGWIYPGSGNTKY NEKFKGKATLTVDTSSSTAFMQLSSLTSEDTAVYFCANYGNYWFAYWGQGTQVTVSAAST KGPSVFPLAPSSKSTSGGTAALGCLVKDYFPEPVTVSWNSGALTSGVHTFPAVLQSSGLY SLSSVVTVPSSSLGTQTYICNVNHKPSNTKVDKKVEPKSCDKTHTCPPCPAPELLGGPSV FLFPPKPKDTLMISRTPEVTCVVVDVSHEDPEVKFNWYVDGVEVHNAKTKPREEQYNSTY RVVSVLTVLHQDWLNGKEYKCKVSNKALPAPIEKTISKAKGQPREPQVYTLPPSRDELTK NQVSLTCLVKGFYPSDIAVEWESNGQPENNYKTTPPVLDSDGSFFLYSKLTVDKSRWQQG NVFSCSVMHEALHNHYTQKSLSLSPG >Brentuximab vedotin - light chain DIVLTQSPASLAVSLGQRATISCKASQSVDFDGDSYMNWYQQKPGQPPKVLIYAASNLES GIPARFSGSGSGTDFTLNIHPVEEEDAATYYCQQSNEDPWTFGGGTKLEIKRTVAAPSVF IFPPSDEQLKSGTASVVCLLNNFYPREAKVQWKVDNALQSGNSQESVTEQDSKDSTYSLS STLTLSKADYEKHKVYACEVTHQGLSSPVTKSFNRGEC
February 01, 2013
Seattle Genetics, Inc. today announced that Health Canada has issued a Notice of Compliance with conditions (NOC/c), authorizing marketing of ADCETRIS for two lymphoma indications: (1) the treatment of patients with Hodgkin lymphoma (HL) after failure of autologous stem cell transplant (ASCT) or after failure of at least two multi-agent chemotherapy regimens in patients who are not ASCT candidates, and (2) the treatment of patients with systemic anaplastic large cell lymphoma (sALCL) after failure of at least one multi-agent chemotherapy regimen. The indications for ADCETRIS were authorized based on promising response rates demonstrated in single-arm trials. No data demonstrate increased survival with ADCETRIS.
“they are focused on making ADCETRIS available globally to all eligible patients with relapsed HL and sALCL. The approval of ADCETRIS in Canada, as well as the recent approval in the European Union, are important milestones to accomplish this goal,” said Clay B. Siegall, Ph.D., President and Chief Executive Officer of Seattle Genetics. “Now that Health Canada has approved ADCETRIS, we are committed to working closely with public and private insurers to secure reimbursement coverage for patients in Canada.”
“The approval of ADCETRIS in Canada marks a significant milestone for patients with relapsed HL or sALCL who have had few new treatment options in several decades,” Joseph M. Connors, M.D., FRCPC, Clinical Director, Center for Lymphoid Cancer at BC Cancer Agency in Vancouver, Canada.
Health Canada grants NOC/c, a form of market approval, on the basis of promising evidence of clinical effectiveness, for products intended for the treatment of serious, life-threatening or severely debilitating illnesses that meet a serious unmet medical need or demonstrate a significant improvement in the benefit/risk profile over existing therapies. Conditions associated with market authorization under the NOC/c policy include a requirement that Seattle Genetics conduct clinical trials designed to confirm the anticipated clinical benefit of ADCETRIS in these patients. Two confirmatory phase III clinical trials evaluating ADCETRIS in the front-line treatment setting of HL and mature T-cell lymphoma (MTCL), including sALCL, are currently underway and enrolling patients.
ADCETRIS (brentuximab vedotin) was issued marketing authorization under the NOC/c policy based on results from a single-arm, phase II pivotal trial in HL patients with relapsed or refractory disease following an ASCT and a single-arm, phase II pivotal trial in relapsed or refractory sALCL patients. ADCETRIS is administered in hospitals through IV infusion over 30 minutes every three weeks and patients who achieve stable disease or better should receive a minimum of 8 cycles and up to a maximum of 16 cycles (approximately one year).
ADCETRIS is the first in a new class of antibody-drug conjugates (ADCs) to be approved in Canada. Using Seattle Genetics’ proprietary technology, the ADC consists of a monoclonal antibody directed to an antigen called CD30. The monoclonal antibody is connected to a cell-killing agent by a linker system that is designed to be stable in the bloodstream but to release the cell-killing agent into CD30-expressing cells, resulting in target cell death. The CD30 antigen is known to be expressed on the Reed-Sternberg cells of HL and on sALCL, an aggressive type of T-cell non-Hodgkin lymphoma.
“Health Canada’s approval of ADCETRIS is the first step in getting patients access to this important therapy,” said Sue Robson, Executive Director of Lymphoma Foundation Canada. “The Lymphoma Foundation is committed to working with Canada provincial governments to ensure that appropriate patients have access to this new therapy.”
About Lymphoma
Lymphoma is a general term for a group of cancers that originate in the lymphatic system. There are two major categories of lymphoma: Hodgkin lymphoma and non-Hodgkin lymphoma. Hodgkin lymphoma is distinguished from other types of lymphoma by the presence of one characteristic type of cell, known as the Reed-Sternberg cell. The Reed-Sternberg cell generally expresses CD30. Systemic ALCL is an aggressive type of T-cell non-Hodgkin lymphoma that also expresses CD30.
Brentuximab vedotin (INN, codenamed SGN-35 and previously cAC10-vcMMAE) is an antibody-drug conjugate approved to treat anaplastic large cell lymphoma (ALCL) and Hodgkin lymphoma. The U.S. Food and Drug Administration granted the agent an accelerated approval on August 19, 2011 for use against these two diseases.[1] It is marketed as Adcetris.[2]
The compound consists of the chimeric monoclonal antibody brentuximab (which targets the cell-membrane protein CD30) linked to three to five units of the antimitotic agent monomethyl auristatin E (MMAE, reflected by the ‘vedotin’ in the drug’s name). The antibody portion of the drug attaches to CD30 on the surface of malignant cells, delivering MMAE which is responsible for the anti-tumour activity.[3][4] Hence it is an antibody-drug conjugate.
In a 2010 clinical trial,[5] 34% of patients with refractory Hodgkin Lymphoma achieved complete remission and another 40% had partial remission.[6] Tumor reductions were achieved in 94% of patients. In ALCL, 87% of patients had tumors shrink at least 50% and 97% of patients had some tumors shrinkage.[7]
On 28 February 2011 a Biologics License Application (BLA) was submitted to the U.S. Food and Drug Administration (FDA) for the use of brentuximab vedotin in relapsed or refractory Hodgkin’s lymphoma and relapsed or refractory systemic anaplastic large cell lymphoma.[8] Both indications were approved by the FDA in Aug 2011.[9]
For these same indications brentuximab vedotin received a conditional Marketing authorization from the European Medicines Agency in october 2012.[10]
- FDA: Brentuximab Vedotin
- Seattle Genetics to Present Brentuximab Vedotin and SGN-75 Clinical Data at the American Society of Clinical Oncology Annual Meeting
- Seattle Genetics: Brentuximab vedotin (SGN-35)
- Francisco, Joseph A; et al. (2003). “cAC10-vcMMAE, an anti-CD30–monomethyl auristatin E conjugate with potent and selective antitumor activity”. Blood 102 (4): 1458–1465. doi:10.1182/blood-2003-01-0039. PMID 12714494.
- ClinicalTrials.gov NCT00848926 A Pivotal Open-Label Trial of SGN-35 for Hodgkin Lymphoma
- “Seattle Genetics and Millennium Report Positive Data from Pivotal Trial of Brentuximab Vedotin (SGN-35) in Relapsed or Refractory Hodgkin Lymphoma at ASH Annual Meeting”. Dec 2010.
- “Is Seattle Genetics the Next Big Thing?”. 2 Dec 2010.
- “Seattle Genetics Submits BLA to FDA for Brentuximab Vedotin in Relapsed or Refractory Hodgkin Lymphoma and Systemic ALCL”. 28 Feb 2011.
- Genetic Engineering & Biotechnology News: Seattle Genetics’ Antibody-Drug Conjugate Receives FDA Okay to Treat Lymphomas
- http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/002455/WC500135004.pdf

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....














