Home » COVID-19 (Page 3)
Category Archives: COVID-19
Casirivimab
(Heavy chain)
QVQLVESGGG LVKPGGSLRL SCAASGFTFS DYYMSWIRQA PGKGLEWVSY ITYSGSTIYY
ADSVKGRFTI SRDNAKSSLY LQMNSLRAED TAVYYCARDR GTTMVPFDYW GQGTLVTVSS
ASTKGPSVFP LAPSSKSTSG GTAALGCLVK DYFPEPVTVS WNSGALTSGV HTFPAVLQSS
GLYSLSSVVT VPSSSLGTQT YICNVNHKPS NTKVDKKVEP KSCDKTHTCP PCPAPELLGG
PSVFLFPPKP KDTLMISRTP EVTCVVVDVS HEDPEVKFNW YVDGVEVHNA KTKPREEQYN
STYRVVSVLT VLHQDWLNGK EYKCKVSNKA LPAPIEKTIS KAKGQPREPQ VYTLPPSRDE
LTKNQVSLTC LVKGFYPSDI AVEWESNGQP ENNYKTTPPV LDSDGSFFLY SKLTVDKSRW
QQGNVFSCSV MHEALHNHYT QKSLSLSPGK
(Light chain)
DIQMTQSPSS LSASVGDRVT ITCQASQDIT NYLNWYQQKP GKAPKLLIYA ASNLETGVPS
RFSGSGSGTD FTFTISGLQP EDIATYYCQQ YDNLPLTFGG GTKVEIKRTV AAPSVFIFPP
SDEQLKSGTA SVVCLLNNFY PREAKVQWKV DNALQSGNSQ ESVTEQDSKD STYSLSSTLT
LSKADYEKHK VYACEVTHQG LSSPVTKSFN RGEC
(Disulfide bridge: H22-H96, H147-H203, H223-L214, H229-H’229, H232-H’232, H264-H324, H370-H428, H’22-H’96, H’147-H’203, H’223-L’214, H’264-H’324, H’370-H’428, L23-L88, L134-L194, L’23-L’88, L’134-L’194)
Casirivimab
カシリビマブ;
- Immunoglobulin G1, anti-(severe acute respiratory syndrome coronavirus 2 spike glycoprotein) (human monoclonal REGN10933 γ1-chain), disulfide with human monoclonal REGN10933 κ-chain, dimer
| Formula | C6454H9976N1704O2024S44 |
|---|---|
| CAS | 2415933-42-3 |
| Mol weight | 145233.3296 |
Monoclonal antibody
Treatment and prophylaxis of SARS-CoV-2 infection (COVID-19)
SARS-CoV-2 spike glycoprotein
- Protein Sequence
- Sequence Length: 1328, 450, 450, 214, 214
- REGN 10933
- RG 6413
https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-monoclonal-antibodies-treatment-covid-19 November 21, 2020
Today, the U.S. Food and Drug Administration issued an emergency use authorization (EUA) for casirivimab and imdevimab to be administered together for the treatment of mild to moderate COVID-19 in adults and pediatric patients (12 years of age or older weighing at least 40 kilograms [about 88 pounds]) with positive results of direct SARS-CoV-2 viral testing and who are at high risk for progressing to severe COVID-19. This includes those who are 65 years of age or older or who have certain chronic medical conditions.
In a clinical trial of patients with COVID-19, casirivimab and imdevimab, administered together, were shown to reduce COVID-19-related hospitalization or emergency room visits in patients at high risk for disease progression within 28 days after treatment when compared to placebo. The safety and effectiveness of this investigational therapy for use in the treatment of COVID-19 continues to be evaluated.
Casirivimab and imdevimab must be administered together by intravenous (IV) infusion.
Casirivimab and imdevimab are not authorized for patients who are hospitalized due to COVID-19 or require oxygen therapy due to COVID-19. A benefit of casirivimab and imdevimab treatment has not been shown in patients hospitalized due to COVID-19. Monoclonal antibodies, such as casirivimab and imdevimab, may be associated with worse clinical outcomes when administered to hospitalized patients with COVID-19 requiring high flow oxygen or mechanical ventilation.
“The FDA remains committed to advancing the nation’s public health during this unprecedented pandemic. Authorizing these monoclonal antibody therapies may help outpatients avoid hospitalization and alleviate the burden on our health care system,” said FDA Commissioner Stephen M. Hahn, M.D. “As part of our Coronavirus Treatment Acceleration Program, the FDA uses every possible pathway to make new treatments available to patients as quickly as possible while continuing to study the safety and effectiveness of these treatments.”
Monoclonal antibodies are laboratory-made proteins that mimic the immune system’s ability to fight off harmful pathogens such as viruses. Casirivimab and imdevimab are monoclonal antibodies that are specifically directed against the spike protein of SARS-CoV-2, designed to block the virus’ attachment and entry into human cells.
“The emergency authorization of these monoclonal antibodies administered together offers health care providers another tool in combating the pandemic,” said Patrizia Cavazzoni, M.D., acting director of the FDA’s Center for Drug Evaluation and Research. “We will continue to facilitate the development, evaluation and availability of COVID-19 therapies.”
The issuance of an EUA is different than an FDA approval. In determining whether to issue an EUA, the FDA evaluates the totality of available scientific evidence and carefully balances any known or potential risks with any known or potential benefits of the product for use during an emergency. Based on the FDA’s review of the totality of the scientific evidence available, the agency has determined that it is reasonable to believe that casirivimab and imdevimab administered together may be effective in treating patients with mild or moderate COVID-19. When used to treat COVID-19 for the authorized population, the known and potential benefits of these antibodies outweigh the known and potential risks. There are no adequate, approved and available alternative treatments to casirivimab and imdevimab administered together for the authorized population.
The data supporting this EUA for casirivimab and imdevimab are based on a randomized, double-blind, placebo-controlled clinical trial in 799 non-hospitalized adults with mild to moderate COVID-19 symptoms. Of these patients, 266 received a single intravenous infusion of 2,400 milligrams casirivimab and imdevimab (1,200 mg of each), 267 received 8,000 mg casirivimab and imdevimab (4,000 mg of each), and 266 received a placebo, within three days of obtaining a positive SARS-CoV-2 viral test.
The prespecified primary endpoint for the trial was time-weighted average change in viral load from baseline. Viral load reduction in patients treated with casirivimab and imdevimab was larger than in patients treated with placebo at day seven. However, the most important evidence that casirivimab and imdevimab administered together may be effective came from the predefined secondary endpoint of medically attended visits related to COVID-19, particularly hospitalizations and emergency room visits within 28 days after treatment. For patients at high risk for disease progression, hospitalizations and emergency room visits occurred in 3% of casirivimab and imdevimab-treated patients on average compared to 9% in placebo-treated patients. The effects on viral load, reduction in hospitalizations and ER visits were similar in patients receiving either of the two casirivimab and imdevimab doses.
Under the EUA, fact sheets that provide important information about using casirivimab and imdevimab administered together in treating COVID-19 as authorized must be made available to health care providers and to patients and caregivers. These fact sheets include dosing instructions, potential side effects and drug interactions. Possible side effects of casirivimab and imdevimab include: anaphylaxis and infusion-related reactions, fever, chills, hives, itching and flushing.
The EUA was issued to Regeneron Pharmaceuticals Inc.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.
Related Information
- Casirivimab and Imdevimab EUA Letter of Authorization
- Frequently Asked Questions on the Emergency Use Authorization for Casirivimab and Imdevimab
- Emergency Use Authorization: Therapeutics
- Coronavirus Disease (COVID-19)
Casirivimab/imdevimab, sold under the brand name REGEN-COV,[1] is an experimental medicine developed by the American biotechnology company Regeneron Pharmaceuticals. It is an artificial “antibody cocktail” designed to produce resistance against the SARS-CoV-2 coronavirus responsible for the COVID-19 pandemic.[3][4] It consists of two monoclonal antibodies, casirivimab (REGN10933) and imdevimab (REGN10987) that must be mixed together.[1][5][6] The combination of two antibodies is intended to prevent mutational escape.[7]
Trials
In a clinical trial of people with COVID-19, casirivimab and imdevimab, administered together, were shown to reduce COVID-19-related hospitalization or emergency room visits in people at high risk for disease progression within 28 days after treatment when compared to placebo.[2] The safety and effectiveness of this investigational therapy for use in the treatment of COVID-19 continues to be evaluated.[2]
The data supporting the emergency use authorization (EUA) for casirivimab and imdevimab are based on a randomized, double-blind, placebo-controlled clinical trial in 799 non-hospitalized adults with mild to moderate COVID-19 symptoms.[2] Of these participants, 266 received a single intravenous infusion of 2,400 milligrams casirivimab and imdevimab (1,200 mg of each), 267 received 8,000 mg casirivimab and imdevimab (4,000 mg of each), and 266 received a placebo, within three days of obtaining a positive SARS-CoV-2 viral test.[2]
The prespecified primary endpoint for the trial was time-weighted average change in viral load from baseline.[2] Viral load reduction in participants treated with casirivimab and imdevimab was larger than in participants treated with placebo at day seven.[2] However, the most important evidence that casirivimab and imdevimab administered together may be effective came from the predefined secondary endpoint of medically attended visits related to COVID-19, particularly hospitalizations and emergency room visits within 28 days after treatment.[2] For participants at high risk for disease progression, hospitalizations and emergency room visits occurred in 3% of casirivimab and imdevimab-treated participants on average compared to 9% in placebo-treated participants.[2] The effects on viral load, reduction in hospitalizations and ER visits were similar in participants receiving either of the two casirivimab and imdevimab doses.[2]
As of September 2020, REGEN-COV is being evaluated as part of the RECOVERY Trial.[8]
On 12 April 2021, Roche and Regeneron announced that the Phase III clinical trial REGN-COV 2069 met both primary and secondary endpoints, reducing risk of infection by 81% for the non-infected patients, and reducing time-to-resolution of symptoms for symptomatic patients to one week vs. three weeks in the placebo group.[9]
Authorization
On 21 November 2020, the U.S. Food and Drug Administration (FDA) issued an emergency use authorization (EUA) for casirivimab and imdevimab to be administered together for the treatment of mild to moderate COVID-19 in people twelve years of age or older weighing at least 40 kilograms (88 lb) with positive results of direct SARS-CoV-2 viral testing and who are at high risk for progressing to severe COVID-19.[2][10][11] This includes those who are 65 years of age or older or who have certain chronic medical conditions.[2] Casirivimab and imdevimab must be administered together by intravenous (IV) infusion.[2]
Casirivimab and imdevimab are not authorized for people who are hospitalized due to COVID-19 or require oxygen therapy due to COVID-19.[2] A benefit of casirivimab and imdevimab treatment has not been shown in people hospitalized due to COVID-19.[2] Monoclonal antibodies, such as casirivimab and imdevimab, may be associated with worse clinical outcomes when administered to hospitalized people with COVID-19 requiring high flow oxygen or mechanical ventilation.[2]
The EUA was issued to Regeneron Pharmaceuticals Inc.[2][10][12]
On 1 February 2021, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) started a rolling review of data on the REGN‑COV2 antibody combination (casirivimab/imdevimab), which is being co-developed by Regeneron Pharmaceuticals, Inc. and F. Hoffman-La Roche, Ltd (Roche) for the treatment and prevention of COVID‑19.[13][14] In February 2021, the CHMP concluded that the combination, also known as REGN-COV2, can be used for the treatment of confirmed COVID-19 in people who do not require supplemental oxygen and who are at high risk of progressing to severe COVID-19.[15]
The Central Drugs Standards Control Organisation (CDSCO) in India, on 5 May 2021, granted an Emergency Use Authorisation to Roche (Genentech)[16] and Regeneron[17] for use of the casirivimab/imdevimab cocktail in the country. The announcement came in light of the second wave of the COVID-19 pandemic in India. Roche India maintains partnership with Cipla, thereby permitting the latter to market the drug in the country.[18]
Deployment
Although Regeneron is headquartered in Tarrytown, New York (near New York City), REGEN-COV is manufactured at the company’s primary U.S. manufacturing facility in Rensselaer, New York (near the state capital at Albany).[19] In September 2020, to free up manufacturing capacity for REGEN-COV, Regeneron began to shift production of its existing products from Rensselaer to the Irish city of Limerick.[20]
Regeneron has a deal in place with Roche (Genentech)[21]to manufacture and market REGEN-COV outside the United States.[10][22]
On 2 October 2020, Regeneron Pharmaceuticals announced that US President Donald Trump had received “a single 8 gram dose of REGN-COV2” after testing positive for SARS-CoV-2.[23][24] The drug was provided by the company in response to a “compassionate use” (temporary authorization for use) request from the president’s physicians.[23]
References
- ^ Jump up to:a b c “REGEN-COV- casirivimab and imdevimab kit”. DailyMed. Retrieved 18 March 2021.
- ^ Jump up to:a b c d e f g h i j k l m n o p q “Coronavirus (COVID-19) Update: FDA Authorizes Monoclonal Antibodies for Treatment of COVID-19”. U.S. Food and Drug Administration (FDA) (Press release). 21 November 2020. Retrieved 21 November 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ Kelland K (14 September 2020). “Regeneron’s antibody drug added to UK Recovery trial of COVID treatments”. Reuters. Retrieved 14 September 2020.
- ^ “Regeneron’s COVID-19 Response Efforts”. Regeneron Pharmaceuticals. Retrieved 14 September 2020.
- ^ Morelle R (14 September 2020). “Antibody treatment to be given to Covid patients”. BBC News Online. Retrieved 14 September2020.
- ^ “Safety, Tolerability, and Efficacy of Anti-Spike (S) SARS-CoV-2 Monoclonal Antibodies for Hospitalized Adult Patients With COVID-19”. ClinicalTrials. 3 September 2020. Retrieved 14 September2020.
- ^ Baum A, Fulton BO, Wloga E, Copin R, Pascal KE, Russo V, et al. (August 2020). “Antibody cocktail to SARS-CoV-2 spike protein prevents rapid mutational escape seen with individual antibodies”. Science. 369 (6506): 1014–1018. Bibcode:2020Sci…369.1014B. doi:10.1126/science.abd0831. PMC 7299283. PMID 32540904.
- ^ “RECOVERY COVID-19 phase 3 trial to evaluate Regeneron’s REGN-COV2 investigational antibody cocktail in the UK”. Recovery Trial. Retrieved 14 September 2020.
- ^ “Phase III prevention trial showed subcutaneous administration of investigational antibody cocktail casirivimab and imdevimab reduced risk of symptomatic COVID-19 infections by 81%”. streetinsider.com. Archived from the original on 2021-04-12. Retrieved 2021-04-12.
- ^ Jump up to:a b c “Regeneron Reports Positive Interim Data with REGEN-COV Antibody Cocktail used as Passive Vaccine to Prevent COVID-19”(Press release). Regeneron Pharmaceuticals. 26 January 2021. Retrieved 19 March 2021 – via PR Newswire.
- ^ “Fact Sheet For Health Care Providers Emergency Use Authorization (EUA) Of Casirivimab And Imdevimab” (PDF). U.S. Food and Drug Administration (FDA).
- ^ “Casirivimab and Imdevimab”. Regeneron Pharmaceuticals. Retrieved 19 March 2021.
- ^ “EMA starts rolling review of REGN‑COV2 antibody combination (casirivimab / imdevimab)” (Press release). European Medicines Agency (EMA). 1 February 2021. Retrieved 1 February 2021. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ “EMA reviewing data on monoclonal antibody use for COVID-19” (Press release). European Medicines Agency (EMA). 4 February 2021. Retrieved 4 March 2021.
- ^ “EMA issues advice on use of REGN-COV2 antibody combination (casirivimab / imdevimab)” (Press release). European Medicines Agency (EMA). 26 February 2021. Retrieved 5 March 2021. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^https://www.businesswire.com/news/home/20200818005847/en/Genentech-and-Regeneron-Collaborate-to-Significantly-Increase-Global-Supply-of-REGN-COV2-Investigational-Antibody-Combination-for-COVID-19
- ^ https://timesofindia.indiatimes.com/india/india-approves-roche/regeneron-antibody-cocktail-to-treat-covid-19/articleshow/82407551.cms
- ^ “Roche receives Emergency Use Authorisation in India for its investigational Antibody Cocktail (Casirivimab and Imdevimab) used in the treatment of Covid-19 | Cipla”. http://www.cipla.com. Retrieved 2021-05-06.
- ^ Williams, Stephen (3 October 2020). “Experimental drug given to President made locally”. The Daily Gazette.
- ^ Stanton, Dan (11 September 2020). “Manufacturing shift to Ireland frees up US capacity for Regeneron’s COVID antibodies”. BioProcess International.
- ^https://www.businesswire.com/news/home/20200818005847/en/Genentech-and-Regeneron-Collaborate-to-Significantly-Increase-Global-Supply-of-REGN-COV2-Investigational-Antibody-Combination-for-COVID-19
- ^ “Roche and Regeneron link up on a coronavirus antibody cocktail”. CNBC. 19 August 2020. Retrieved 14 September 2020.
- ^ Jump up to:a b Thomas K (2 October 2020). “President Trump Received Experimental Antibody Treatment”. The New York Times. ISSN 0362-4331. Retrieved 2 October 2020.
- ^ Hackett DW (3 October 2020). “8-Gram Dose of COVID-19 Antibody Cocktail Provided to President Trump”. http://www.precisionvaccinations.com. Archived from the original on 3 October 2020.
External links
- “Casirivimab”. Drug Information Portal. U.S. National Library of Medicine.
- “Imdevimab”. Drug Information Portal. U.S. National Library of Medicine.
- “Casirivimab and Imdevimab EUA Letter of Authorization” (PDF). U.S. Food and Drug Administration (FDA).
- “Frequently Asked Questions on the Emergency Use Authorization of Casirivimab + Imdevimab” (PDF). U.S. Food and Drug Administration (FDA).
| REGN10933 (blue) and REGN10987 (orange) bound to SARS-CoV-2 spike protein (pink). From PDB: 6VSB, 6XDG. | |
| Combination of | |
|---|---|
| Casirivimab | Monoclonal antibody against spike protein of SARS-CoV-2 |
| Imdevimab | Monoclonal antibody against spike protein of SARS-CoV-2 |
| Clinical data | |
| Trade names | REGEN-COV |
| Other names | REGN-COV2 |
| AHFS/Drugs.com | Monograph |
| License data | US DailyMed: Casirivimab |
| Routes of administration | Intravenous |
| ATC code | None |
| Legal status | |
| Legal status | US: Unapproved (Emergency Use Authorization)[1][2] |
| Identifiers | |
| DrugBank | DB15691 |
| KEGG | D11938 |
//////////// Casirivimab, ANTI VIRAL, PEPTIDE, SARS-CoV-2, MONOCLONAL ANTIBODY, FDA 2020, 2020APPROVALS, CORONA VIRUS, COVID 19, カシリビマブ, REGN-COV2, REGN10933+REGN10987 combination therapy, REGN 10933, RG 6413

NEW DRUG APPROVALS
ONE TIME
$10.00

ZyCoV-D

ZyCoV-D
CAS 2541524-47-2
DNA vaccine construct encoding a spike protein antigen of SARS-CoV-2 virus (Zydus-Cadila)
UPDATE. APPROVED IN INDIA AUG 2021
http://ctri.nic.in/Clinicaltrials/showallp.php?mid1=51254&EncHid=&userName=ZyCoV-D
bioRxiv (2021), 1-26.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7423510/
| ZyCoV-D | (CTRI/2020/07/026352, 2020, CTRI/2020/07/026352, 2020; Myupchar, 2020) | ZYDUS CADILA |
ZyCoV-D is a genetically engineered DNA plasmid based vaccine encoding for the membrane proteins of the virus. The clinical trials to study the immunogenicity, and safety of the vaccine, will administer three doses at an interval of 28 days in 1048 individuals.
Phase 1/2: CTRI/2020/07/026352
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | DNA |
| Clinical data | |
| Routes of administration |
Intradermal |
| ATC code | None |
| Identifiers | |
| DrugBank | DB15892 |
| Part of a series on the |
| COVID-19 pandemic |
|---|
| SARS-CoV-2 (virus)COVID-19 (disease) |
| showTimeline |
| showLocations |
| showInternational response |
| showMedical response |
| showImpact |
| COVID-19 portal |
ZyCoV-D is a DNA plasmid based COVID-19 vaccine being developed by Cadila Healthcare with support from the Biotechnology Industry Research Assistance Council.
The ZYCOV-D vaccine candidate was developed by Cadila Healthcare Ltd. based in India1. The vaccine was developed using a DNA vaccine platform with a non-replicating and non-integrating plasmid carrying the gene of interest3. Once the plasmid DNA is introduced into host cells and the viral protein is translated, it elicits a strong immune response, stimulating the humoral and cellular components of the immune system3. The DNA vaccine platform offers minimal biosafety requirements, more improved vaccine stability, and lower cold chain requirements3. Phase I clinical trials of this vaccine candidate were completed in July 2020, with the company reporting successful dosing and tolerance1,2. As of August, 2020 the candidate is in Phase II clinical trials1.

NEW DRUG APPROVALS
ONE TIME
$10.00
Clinical research
Phase I and II trials
In February 2020, Cadila Healthcare decided to develop a DNA plasmid based COVID-19 vaccine at their Vaccine Technology Centre (VTC) in Ahmedabad.[1] The vaccine candidate was able to pass the pre-clinical trials on animal models successfully. A report of the study was made available via bioRxiv.[2] Thereafter, human trials for Phase I and II were approved by the regulator.[3]
The Phase II trials of the vaccine candidate were conducted in over 1,000 volunteers as part of the adaptive Phase I/II multi-centric, dose escalation, randomised, double-blind placebo controlled method.[4][5]
Phase III trials
In November 2020, the company announced it would test the vaccine candidate on 30,000 patients in Phase III trials.[6] The vaccine would be given out in three doses at five sites across four cities of India.[7] In January 2021, the Drugs Controller General of India (DCGI) granted permission to conduct the Phase III clinical trials for 28,216 Indian participants.[8][9]
In April 2021, the company reported that they expected to have initial data for the Phase III trials by May 2021.[10]
Production
On 23 April 2021, production of the ZyCoV-D vaccine was started, with a yearly capacity of 240 million doses. It is expected to get emergency use authorization in May or June.[11]
References
- ^ “Zydus Cadila launches a fast tracked programme to develop vaccine for the novel coronavirus, 2019-nCoV (COVID-19)”(PDF). http://www.zyduscadila.com. Cadila Healthcare.
- ^ Dey A, Rajanathan C, Chandra H, Pericherla HP, Kumar S, Choonia HS, et al. (26 January 2021). “Immunogenic Potential of DNA Vaccine candidate, ZyCoV-D against SARS-CoV-2 in Animal Models”. bioRxiv: 2021.01.26.428240. doi:10.1101/2021.01.26.428240. S2CID 231777527.
- ^ “A prospective, randomized, adaptive, phase I/II clinical study to evaluate the safety and immunogenicity of Novel Corona Virus −2019-nCov vaccine candidate of M/s Cadila Healthcare Limited by intradermal route in healthy subjects”. ctri.nic.in. Clinical Trials Registry India. 15 December 2020. CTRI/2020/07/026352. Archived from the original on 22 November 2020.
- ^ “Zydus Cadila’s ZyCov-D vaccine found to be ‘safe and immunogenic'”. @businessline. The Hindu. 24 December 2020.
- ^ Rawat K, Kumari P, Saha L (February 2021). “COVID-19 vaccine: A recent update in pipeline vaccines, their design and development strategies”. European Journal of Pharmacology. 892: 173751. doi:10.1016/j.ejphar.2020.173751. PMC 7685956. PMID 33245898.
- ^ Thacker T (7 November 2020). “Zydus Cadila to test ZyCoV-D on 30,000 patients in Phase-3 trials”. The Economic Times.
- ^ “Covid 19 vaccine in India: Zydus Cadila begins enrolment for Phase 3 trial of ZyCoV-D in 4 cities”. The Financial Express. 22 January 2021.
- ^ “DBT-BIRAC supported indigenously developed DNA Vaccine Candidate by Zydus Cadila, approved for Phase III clinical trials”. pib.gov.in. Press Information Bureau. 3 January 2021.
- ^ “Novel Corona Virus-2019-nCov vaccine by intradermal route in healthy subjects”. ctri.nic.in. Clinical Trials Registry – India. Retrieved 10 April 2021.
- ^ Das, Sohini (22 April 2021). “Cadila Healthcare testing two-shot regimen for ZyCoV-D, data likely by May”. Business Standard India.
- ^ Writer, Staff (24 April 2021). “Cadila Healthcare starts production of Covid vaccine candidate”. mint. Retrieved 27 April 2021.
Zydus Cadila Covid vaccine close to getting approved in India, says MD Sharvil Patel
In an exclusive interview with India Today TV, Managing Director of Zydus Cadila Dr Sharvil Patel said the company’s Covid vaccine candidate ZyCoV-D against the Covid-19 infection is very close to getting approved in India. They are likely to apply for emergency use authorisation this month.
Ahmedabad-based pharmaceutical company Zydus Cadila is likely to submit the application for emergency use authorisation of its Covid-19 vaccine candidate ‘ZyCoV-D’ in India this month. The company is confident that the vaccine will be approved in May itself. The company plants to produce one crore doses of its ‘painless’ Covid-19 vaccine per month.
If approved, ZyCoV-D will be the fourth vaccine to be used in India’s Covid-19 vaccination drive. Made in India, the company plans to ramp up the vaccine’s production to 3-4 crore doses per month and is already in talks with two other manufacturing companies for the same
Although the vaccine should ideally be stored between 2 and 8 degrees Celsius, it remains stable even at room temperature conditions at 25 degrees Celsius. It is easy to administer, the developers said, and will be administered via intradermal injection.
If approved for emergency use, ZyCoV-D could help India fill the vacuum of vaccine doses currently being experienced in the country’s immunisation drive.
Earlier in April, Zydus Cadila announced that its drug Virafin had received restricted emergency use approval from the Drug Controller General of India for the treatment of mild cases of Covid-19.
In an exclusive interview with India Today TV, Sharvil Patel sheds details on all aspects of the Covid-19 vaccine ZyCoV-D.
When asked the status of Covid vaccine candidate ZyCoV-D and when exactly Zydus Cadila would apply for emergency use authorisation in India, Dr Sharvil Patel said the vaccine was getting very close to getting approved in the country.
“I am very happy to say that India’s first indigenously developed DNA vaccine candidate against Covid, which is our ZyCoV-D, is getting very close to approval,” he said.
“We have almost completed all our recruitment for the clinical trials. We have, by far, recruited the largest number of patients for a Covid vaccine trial in India. The number of volunteers who have been vaccinated as a part of the trial is 28,000,” Sharvil Patel said.
Sharvil Patel also said that his company has also included children in the 12-17 age group for the vaccine trials.
He said, “The recruitment holds very important milestones in terms of cohorts because not only have we included the elderly and those with co-morbidities, but also children in the age group of 12 to 17 years.”
Sharvil Patel said as soon as the efficacy data is obtained, Sydus Cadila will file for emergency use authorisation. As soon as the approval is granted, Zydus Cadila will start production of Covid-19 vaccines from July, he said.
“We hope to see our efficacy data in the middle of May. As soon as we see strong efficacy which correlates to the vaccine’s strong immunogenicity in Phase 2, we will file for emergency use authorization. We hope to produce a good quantity of the vaccine from July onwards to make sure it is available to the people. That is the need of the hour right now,” Sharvil Patel said.
He said by May the company will be in a position to talk to the regulators about the restricted use of the Covid-19 vaccine. “The regulatory process is a rolling one. I believe the regulators look at the data in a short period of time,” Sharvil Patel said.
“We have submitted a lot of data already so that it will aid the regulators once we provide them with the efficacy results. We are, hence, expecting to get the approval in May itself,” Sharvil Patel said.
///////////ZyCoV-D, COVID 19, CORONA VIRUS, VACCINE, INDIA 2021, APPROVALS 2021, SARS-CoV-2
2-Deoxy-D-glucose

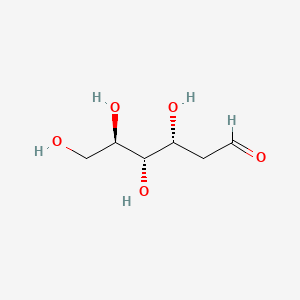
2-Deoxy-D-glucose
- Molecular FormulaC6H12O5
- Average mass164.156 Da
2-Deoxy-D-glucose
(4R,5S,6R)-6-(Hydroxymethyl)tetrahydro-2H-pyran-2,4,5-triol(4R,5S,6R)-6-(Hydroxyméthyl)tétrahydro-2H-pyran-2,4,5-triol
154-17-6[RN]
- 2-Deoxy-D-arabino-hexose
- 2 DG
- 2-Deoxy-D-glucose
- 2-Deoxy-D-mannose
- 2-Deoxyglucose
- 2-Desoxy-D-glucose
- Ba 2758
- D-Glucose, 2-deoxy-
- NSC 15193
2-Deoxy-D-arabino-hexopyranose2-deoxy-D-glucopyranose2-deoxyglucose
2-DGD-arabino-2-DesoxyhexoseD-arabino-Hexopyranose, 2-deoxy- [(4R,5S,6R)-6-(Hydroxymethyl)oxane-2,4,5-triol2-deoxyglucopyranose2-deoxymannopyranose2-dGlc
D-arabino-2-Deoxyhexoseglucitol, 2,5-anhydro-
2-Deoxy-D-glucose
CAS Registry Number: 154-17-6
CAS Name: 2-Deoxy-D-arabino-hexose
Additional Names: D-arabino-2-desoxyhexose; 2-deoxyglucose; 2-DGManufacturers’ Codes: Ba-2758Molecular Formula: C6H12O5Molecular Weight: 164.16Percent Composition: C 43.90%, H 7.37%, O 48.73%Literature References: Antimetabolite of glucose, q.v., with antiviral activity.
Synthesis: M. Bergmann et al.,Ber.55, 158 (1922); 56, 1052 (1923); J. C. Sowden, H. O. L. Fischer, J. Am. Chem. Soc.69, 1048 (1947); H. R. Bolliger, Helv. Chim. Acta34, 989 (1954); H. R. Bolliger, M. D. Schmid, ibid. 1597, 1671; H. R. Bolliger, “2-Deoxy-D-arabino-hexose (2-Deoxy-D-glucose)” in Methods in Carbohydrate Chemistryvol. I, R. L. Whistler, M. L. Wolfrom, Eds. (Academic Press, New York, 1962) pp 186-189.
Inhibition of influenza virus multiplication: E. D. Kilbourne, Nature183, 271 (1959).
Effects on herpes simplex virus: R. J. Courtney et al.,Virology52, 447 (1973). Mechanism of action studies: M. R. Steiner et al.,Biochem. Biophys. Res. Commun.61, 745 (1974); E. K. Ray et al.,Virology58, 118 (1978). Use in human genital herpes infections: H. A. Blough, R. L. Giuntoli, J. Am. Med. Assoc.241, 2798 (1979); L. Corey, K. K. Holmes, ibid.243, 29 (1980). Effect vs respiratory syncytial viral infections in calves: S. B. Mohanty et al.,Am. J. Vet. Res.42, 336 (1981).
Properties: Cryst from acetone or butanone, mp 142-144°. [a]D17.5 +38.3° (35 min) ®+45.9° (c = 0.52 in water); +22.8° (24 hrs) ® +80.8° (c = 0.57 in pyridine).
Melting point: mp 142-144°
Optical Rotation: [a]D17.5 +38.3° (35 min) ®+45.9° (c = 0.52 in water); +22.8° (24 hrs) ® +80.8° (c = 0.57 in pyridine) Derivative Type: a-Form
Properties: Cryst from isopropanol, mp 134-136°. [a]D26 +156° ® +103° (c = 0.9 in pyridine).Melting point: mp 134-136°Optical Rotation: [a]D26 +156° ® +103° (c = 0.9 in pyridine) Use: Exptlly as an antiviral agent.


Source Temperature: 210 °C Sample Temperature: 150 °C Direct, 75 eV
14.0 2.2
15.0 11.5
17.0 3.9
18.0 19.4
19.0 13.7
26.0 2.5
27.0 12.1
28.0 21.9
29.0 31.2
30.0 4.6
31.0 41.3
32.0 12.4
39.0 5.9
40.0 2.1
41.0 10.9
42.0 12.4
43.0 46.3
44.0 31.5
45.0 34.3
46.0 2.8
47.0 4.1
53.0 1.5
54.0 2.0
55.0 14.4
56.0 35.3
57.0 55.7
58.0 11.4
59.0 2.0
60.0 100.0
61.0 31.1
62.0 2.3
68.0 4.6
69.0 12.2
70.0 3.0
71.0 34.9
72.0 7.0
73.0 25.3
74.0 46.6
75.0 5.1
81.0 1.5
82.0 2.4
83.0 1.3
84.0 1.3
85.0 18.1
86.0 55.3
87.0 4.6
89.0 1.2
91.0 1.5
97.0 3.6
98.0 2.9
99.0 1.7
100.0 3.5
102.0 1.1
103.0 19.8
104.0 1.4
111.0 1.6
115.0 25.2
116.0 3.0
117.0 2.1
120.0 3.3
128.0 1.0
129.0 2.5
133.0 1.8
147.0 2.2
1H NMR DMSO D6


1H NMR D20


IR NUJOL MULL

IR KBR

PAPERCollection of Czechoslovak Chemical Communications (1955), 20, 42-5. http://cccc.uochb.cas.cz/20/1/0042/
Preparation of 2-deoxy-D-glucose
By: Stanek, Jaroslav; Schwarz, Vladimir
Triacetyl-D-glucal (I) adds (BzO)2IAg and (BzO)2BrAg, to give 1-benzoyl-3,4,6-triacetyl-2-deoxy-2-iodo-α-D-glucopyranose (II) and 1-benzoyl-3,4,6-triacetyl-2-deoxy-2-bromo-α-D-glucopyranose (III), resp. Both halogen derivs. give 2-deoxy-D-glucose (IV) by reduction. Adding a C6H6 soln. of 16.7 g. iodine into a suspension of 33.6 g. dry BzOAg in 200 ml. C6H6, treating the mixt. with a soln. of 20 g. I in 200 ml. C6H6, heating the mixt. 7 hrs. on the steam bath, removing the AgI, evapg. the solvent, and crystg. the residue from EtOH gave 20.8 g. (54.7%) II, m. 129-30°, [α]21D 21.7°. Analogous procedure with 13.4 g. BzOAg, 4.6 g. Br, and 8 g. I gave 3.9 g. (33%) III, m. 139-40°, [α]17D 33.5°. The same compd. (3 g.), m. 140°, [α]18D 33.6°, was obtained by adding 3.2 g. Br to a soln. of 5.44 g. I in 50 ml. CCl4, by refluxing the mixt. 2 hrs. with 6 g. BzOAg, filtering off the AgBr, and evapg. the solvent. Reducing 8 g. II or an equiv. III in 150 ml. MeOH with 60 g. Zn activated by 1 hr. immersion in a soln. of 60 g. CuSO4 in 1500 ml. H2O, removing Zn after 8 hrs., evapg. the MeOH, and sapong. the residue with Ba(OH)2 yielded 0.42 g. (20%) IV, m. 145°, [α]18D 46.1°.
Wavlen: 589.3 nm; Temp: 18 °C, +46.1 ° ORD
PATENT
https://patents.google.com/patent/WO2004058786A1/enThe present invention relates to a process for the synthesis of 2-deoxy-D-glucose. Background of the invention 2-deoxy-D-glucose is useful in control of respiratory infections and for application as an antiviral agent for treatment of human genital herpes.Prior art for preparation of 2-deoxy-D-glucose while operable, tend to be expensive and time consuming. Reference may be made to Bergmann, M., Schotte, H., Lechinsky, W., Ber, 55, 158 (1922) and Bergmann, M., Schotte, H., Lechinsky, W., Ber 56, 1052 (1923) which disclose the preparation of 2-deoxy-D-glucose in low yield by mineral acid catalyzed addition of water to D-glucal. Another method of producing 2-deoxy-D-glucose is from diethyldithioacetal derivative of D-glucose (Bolliger, H.R. Schmid, M.D., Helv. Chim. Ada 34, 989 (1951); Bolliger, H.R., Schmid, M.D., Helv. Chim. A a 34, 1597 (1951); Bolliger, H.R. Schmid, M.D., Helv. Chim. Ada 34, 1671 (1951) and from D-arabhiose by reaction with nitromethane followed by acetylation, reduction and hydrolysis (Sowden, J.C, Fisher, H.O.L., J. Am. Chem., 69, 1048 (1947). However these methods result in the formation of 2- deoxy-D-glucose in low yield and of inferior purity due to the formation of several byproducts and involve use of toxic reagents such as ethanethiol and nitromethane. As a result purification of 2-deoxy-D-glucose has to be done by recrystallisation which is tedious, time consuming and difficult.Accordingly it is important to develop a process for synthesis of 2-deoxy-D-glucose which obviates the drawbacks as detailed above and results in good yield and good purity. Objects of the inventionThe main object of the present invention is to provide a process for the synthesis of 2- deoxy-D-glucose resulting in good yield and with good purity.Another object of the invention is to provide an economical process for the synthesis of 2-deoxy-D-glucose. Summary of the inventionA process that would produce 2-deoxy-D-glucose economically and with desired purity, is a welcome contribution to the art. This invention fulfills this need efficiently.Accordingly the present invention relates to a process for the synthesis of 2-deoxy- D-glucose comprising haloalkoxylation of R-D-Glucal wherein R is selected from H and 3, 4, 6-tri-O-benzyl, to obtain alkyl 2-deoxy-2-halo-R-α/ -D-gluco/mannopyranoside, converting alkyl 2-deoxy-2-halo-R-α/β-D-gluco/mannopyranoside by reduction to alkyl 2- deoxy-α/β-D-glucopyranoside, hydrolysing alkyl 2-deoxy-α/β-D-glucopyranoside to 2- deoxy-D-glucose.In one embodiment of the invention, the alkyl 2-deoxy-α/β-D-glucopyranoside is obtained by (a) haloalkoxylating 3,4,6,-tri-O-benzyl-D-glucal to alkyl 2-deoxy-2-halo-3,4,6-tri-O- benzyl-α/β-D-gluco-/mannopyranoside; (b) subjecting alkyl 2-deoxy-2-halo-3,4,6-tri-O-benzyl-α/β-D-gluco/mannopyranoside to reductive dehalogenation and debenzylation to obtain alkyl 2-deoxy -α/β-D- glucopyranoside. In another embodiment of the invention, in step (a) haloalkoxylation of 3,4,6-tri-O- benzyl-D-glucal is carried out by reaction with a haloalkoxylating agent selected from a N- halosuccinimide and a N-haloacetamide, and alcohol.The reaction scheme for the reactions involved in the process of the invention are also given below:

in R’=CH3I R=C6H5CH2 H R=C6H5CH2, X=Br, R’=CH3 IV R=H V R=CH3, C2HSJ C6H5CH3, iPr, X=Br

Such overall synthesis may be depicted as follows where R=H, CH3, C2H5, (CH3)2CH, C6H5CH ; RX-CH3; X-CL, Br.Example 1 To a solution of 3,4,6-tri-O-benzyl-D-glucal (39 g, 0.09 mol) in dichloromethane (20ml) and methanol (100 ml) was added N-bromosuccinimide (18.7 g, 0.09 mil) during 10 min. at room temperature and stirred for 4 h. After completion of the reaction solvent was distilled off. The resultant residue extracted into carbon tetrachloride (2×100 ml) and organic phase concentrated to obtain methyl 2-bromo 2-deoxy-3,4,6-tri-O-benzyl-α/β-D-gluco- /mannopyranoside as a syrup. Quantity obtained 50 g. 1H NMR (200 MHz, CDC13) 3.40-4.00 (m, 7H, H-2,5,6,6′ and OCH3) 4.30-5.10 (m, 9H, H-1,3,4 and 3xPhCH2O), 7.10-7.60 (m, 15H, Ar-H). A solution of methyl 2-bromo-2-deoxy-3,4,6-tri-O-benzyl-α/β-D-gluco- /mannopyranoside (50 g) in methanol (300) was charged into one litre autoclave along with Raney nickel (10 ml) Et3N (135 ml) and subjected to hydrogenation at 120 psi pressure at 50°C for 8 h. After completion of the reaction the catalyst was filtered off and the residue washed with methanol (25 ml). The filtrate was concentrate to obtain methyl 2-deoxy-3,4,6- tri-O-benzyl-α/β-D-glucopyranoside as a syrup (37.9 g, 89%). 1H NMR (200 MHz, CDC13): δ 1.50-2.40 (m,2H,H-2,2′)5 3.32, 3.51 (2s, 3H, OCH3) 3.55-4.00 (m, 5H, H-3,4,5,6,6′), 4.30-5.00 (m, 7H, 3xPhCH2, H-l), 7.10-7.45 (m, 15H, Ar-H). The syrup of methyl 2-deoxy-3,4,6- tri-O-benzyl-α/β-D-glucopyranoside (37.9g) was dissolved in methanol (200 ml). 1 g of 5%Pd/C was added and hydrogenated at 150 psi pressure at room temperature. After 5 hours catalyst was filtered off and solvent evaporated. Quantity of the methyl 2-deoxy-α/β-D- glucopyranoside obtained 10.5 g (70%). [ ]D + 25.7° (c 1.0, MeOH), 1H NMR (200 MHz, D2O); δ 1.45-2.40 (m, 2H, H-2,2′) 3.20-4.80, (m 9H, H- 1,3,4,5,6,6′ – OCH3).Example 2 To a solution of D-glucal (64.6g, 0.44 mol) in methanol (325 ml) at 10°C was addedN-bromosuccinimide (78.7 g, 0.44 mol) during 40 min. maintaining the temperature between 10-15°C during the addition. The reaction mixture was stirred at room temperature. After 5 hours solvent was evaporated to obtain a residue which was refluxed in ethyl acetate (100 ml). Ethyl acetate layer was discarded to leave a residue of methyl 2-bromo-2-deoxy-α/β-D- gluco/mannopyranoside (105 g) as a syrup. [α]D + 36° (c 1.0, MeOH). 1H NMR (200 MHz, D2O): δ 3.47, 3.67 (2s, 3H, OCH3), 3.70-4.05 (m, 6h, H-23,4,5,6,6′), 4.48-5.13 (2s, 1H, H-l). The syrupy methyl 2-bromo-2-deoxy-α/β-D-gluco-/mannopyranoside was dissolved in methanol (400 ml), a slurry of 80 g Raney nickel (a 50% slurry in methanol), Et3N (30 ml) and hydrogenated in a Parr apparatus at 120 psi. After 8-9 hours, the reaction mixture was filtered through a Celite filter pad and washed with MeOH. The washings and filtrate were combined and triturated with hexane to separate and remove by filtration insoluble triethylamine hydrobromide and traces of succinimide. The filtrate was concentrated to a residue. The isolated yield of methyl 2-deoxy-α/β-D-glucopyranoside was 89%. Ethyl 2-bromo-2deoxy-α/β-D-gluco-/mannopyranoside: When solvent was ethanol instead of methanol the compound obtained was ethyl 2- bromo-2-deoxy-α/β-D-gluco-/mannopyranoside. 1HNMR (200 MHz, D2O): δ 1.10-1.32 (m, 3H, CH3), 2.80 (s, 4H, -CO(CH2)2CO-NH-), 3.40-4.10 (m, 8H, H-2,3,4,5,6,6′, CH2), 4.40, 5.20 (2s 1H, H-l α/β).Isopropyl 2-bromo-2-deoxy- /β-D-gluco-/mannopyranoside: When isopropanol instead of methanol was used as a solvent the compound obtained was isopropyl 2-bromo-2-deoxy-α/β-D-gluco/mannopyranoside. 1H NMR (200 MHz, D2O): δ 1.10-1.30 (m, 6H, 2xCH3) 2.80 (s, 4H, -CO(CH2)2CO-NH-), 3.60-4.60 (m 8H,H- 2,3,4,5,6,6′, CH2) 4.40, 5.30 (2s, 1H, H-l, α/β).Example 3 A mixture of D-glucal (64.6 g), methanol (400 ml), N-bromosuccinimide (79 g) were stirred at 15 C for 6 h. The reaction mixture was hydrogenated in a Parr apparatus in presence of 60 g of Raney nickel catalyst (a 50% slurry in methanol) and triethylamine (62 ml). After 8-9 h, the reaction mixture was filtered on a Celite filter pad. The Celite pad was washed with methanol. The washings and filtrate were combined, concentrated to a thick heavy syrup, dissolve in chloroform (500 ml), pyridine (400 ml) and acetic anhydride (251 ml) was added while stirring, maintaining the temperature between 5-10°C. After 12 hours, the reaction mixture was diluted with CHC13 (500 ml) transferred to a separating funnel and organic phase was washed with water. The organic phase was separated, dried (Na2SO4) and concentrated to obtain methyl 2-deoxy-3,4,6-tri-O-acetyl-2 deoxy-α/β-D-glucopyranoside as a syrup (163.43 g, 87%). [α]D + 65.0° (c 1.0, CHC13) 1H NMR (200 MHz, CDC13): δ 1.55-1.90 (m, 2H, H-2,2′), 2.01, 2.04,2.11, 2.15, (4s, 9H, 3xOCOCH3), 2.18,3.40 (2s, 3H, OCH3), 3.45-50 (m, 3H, H-5, 6,6′) 4.80-5.40 (m, 3H,H-1,3,4). The syrup was dissolved in methanol (600 ml) IN NaOMe in methanol (25ml) was added and left at room temperature. After 6-10 h, dry CO2 gas was passed into the reaction mixture, solvent was evaporated to obtain a syrupy residue. The residue was once again extracted into dry methanol and concentrated to obtain methyl 2-deoxy-α/β-D-glucopyranoside as syrup. Quantity obtained 81 g (92%).Example 4 A 500 ml round bottom flask equipped with magnetic stir bar was charged with a solution of D-glucal (32.3 g) in methanol (175 ml), cooled to 15°C, N-bromosucci-t imide (NBS) (39.4 g) was added and stirred for 6 hours at 15°C. The reaction mixture was concentrated to half the volume, cooled to 0°C and separated succinimide was removed by filtration. To the filtrate was added a slurry of 30 g Raney nickel (a 50% slurry in methanol) Et3N (32 ml) and hydrogenated in a Parr apparatus at 120 psi. After 7-8 hours, the reaction mixture was filtered through a Celite filter pad, and washed with MeOH. The washings and filtrate were combined and triturate with hexane to separate and remove by filtration insoluble triethylamine hydrobromide and succinimide. The filtrate was concentrated to a residue, dissolved in methanol and triturated with hexane to remove most of the triethylamine hydrobromide and succinimide. The filtrate was concentrated to obtain methyl 2-deoxy-α/β- D-glucopyranoside (85%).Example 5 To a stirred solution of methyl 3,4,6-tri-O-acetyl-2-deoxy-α/β-D-glucopyranoside (47 g) (from example 3) in acetic acid (40 ml) and acetic anhydride (110 ml) was added concentrated sulphuric acid (0.94 ml) at 0°. The reaction mixture was brought to room temperature and stirred. After 2 hours the reaction mixture was diluted with water (50 ml) and extracted into CH2C12 (3×150 ml). The organic phase was separated, washed with saturated NaHCO3 solution, H2O dried over Na2SO and concentrated to obtain 2-deoxy- 1,3,4,6-tetra-O-acetyl-α/β-D-glucopyranoside as a crystalline compound, mp. 115-118°C. Quantity obtained 44.5 g (86%). [α]D + 21.5° (c 1.0, CHC13). 1H NMR (200 MHz, CDC13): δ 1.50-2.45 (m, 14H, H-2,2′, 4xOCOCH3), 3.85-5.40, (m, 5H, H-3,4,5,6,6′), 5.75-6.20 (m, 1H, H-l,α/ β). To a heterogeneous mixture of l,3,4,6-tetra-O-acetyl-2-deoxy-α/β-D- glucopyranoside (10 g) in water (100 ml) was added acetyl chloride (10 ml) and heated to 80°C. After 6 hours the reaction mixture was cooled to room temperature, neutralised with saturated aq. Ba(OH)2, concentrated to half the volume and filtered on a Celite pad. Filtrate was concentrated on a rotary evaporator and dried over anhydrous P2O5 to obtain a residue which was dissolved in hot isopropyl alcohol and filtered on a pad of Celite to obtain a clear filtrate. The filtrate was concentrated to a residue, dissolved in hot isopropyl alcohol (50 ml), acetone (75 ml) and seeded with a few crystals of 2-deoxy-D-glucose. After 15-18 hours at 5°C crystalline title product was filtered. Quantity obtained 3.21 g (64.9%) m.p. 148-149°C.Example 6 A heterogeneous mixture of l,3,4,6-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (9 g) (from example 5), water (30 ml) and 11% aq. H2SO (0.3 ml) was stirred at 85°C for 7 h to obtain a homogenous solution. The reaction mixture was cooled, neutralised with aq. Ba(OH)2 solution and filtered. The filtrate obtained was concentrated to half the volume and solids separated were filtered. To the filtrate was added activated carbon (1 g) and filtered. The filtrate was concentrated on a rotary evaporator and dried over P2O5 to obtain 2-deoxy- D-glucose that was crystallized from methyl alcohol (27 ml) and acetone (54 ml). Quantity obtained 2.4 g. mp. 146-149°C.Example 7A heterogeneous mixture of l,3,4,6-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside(25g) (from example 5), H2O (250 ml), toluene (250 ml) and glacial acetic acid (1.25 ml) was heated to reflux for 10-12 hours, while it was connected to a Dean- Stark azeotropic distillation apparatus. An azeotropic mixture of acetic acid, toluene was collected to remove acetic acid and every one hour fresh toluene (50 ml) was introduced. After completion of the reaction, toluene was removed by distillation from the reaction mixture to obtain a residue that was dissolved in methanol, treated with charcoal and filtered. The filtrate was separated, concentrated to a residue and crystallized from isopropyl alcohol and acetone to obtain 2- deoxy-D-glucose (7.33 g, 59%). mp. 148-151°C.Example 8 A heterogeneous mixture of l,3,4,5-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (lOg) (from example 5), H2O (200 ml) cone. HC1 (0.3 ml) and glacial acetic acid (0.5 ml) was heated to 85°C. After 6 hours the reaction mixture was cooled to room temperature, neutralized with aq. Ba(OH)2 and filtered on a pad of Celite. Filtrate was separated, treated with charcoal and filtered. The filtrate was concentrated to a residue and crystallized from MeOH, acetone to obtain the product. Quantity obtained 2.75 g. mp. 147-148°C.Example 9 A heterogeneous mixture of l,3,4,5-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside(lOg) (from example 3) water (100 ml) and cone. HCI (0.5ml) was heated to 80°C. After 2-5 hours the reaction mixture was cooled to room temperature, neutralized with aq. Ba(OH)2 and filtered on a pad of Celite. The filtrate was concentrated to a residue, dissolved in ethanol, treated with charcoal and filtered. The filtrate was concentrated to a solid residue andcrystallized from methanol-acetone to obtain the title product. Quantity obtained 3.15g mp. 148-151°C.Example 10A solution of methyl 2-deoxy-α/β-D-glucopyranoside (30g) (from example 2) water(15 ml) and cone. HCI (1.5 ml) was heated to 80-85°C. After 3-5 hours the reaction mixture was cooled to room temperature, neutralized with aq. Ba(OH)2 and filtered to remove insoluble salts. The filtrate was concentrated to a residue, crystallized from MeOH, acetone and hexane to obtain 2-deoxy-D-glucose (11.77 g) mp. 149-151°C.Example 11A solution of methyl 2-deoxy-α/β-D-glucopyranoside (30g) (from example 2) water (195 ml) and cone. H2SO (5.9 ml) was heated to 80°C. After 2-3 hours the reaction mixture was cooled, neutralized with aq. Ba(OH)2 and filtered. The filtrate was separated, treated with charcoal and filtrate. The Filtrate was concentrated to a residue and crystallized from isopropyl alcohol to obtain the title product. Quantity obtained 5.2 g. mp. 152-154°C.Example 12 A mixture of methyl 2-deoxy-α/β-D-glucopyranoside (24g) (from example 2) water(125 ml) and IR 120 H+ resin (7.5 ml) was heated to 90-95°C for 2h. The reaction mixture was cooled to room temperature, filtered and the resin was washed with water (20 ml). The filtrate was concentrated to residue and crystallized from ethanol to obtain 2-deoxy-D- glucose (8.8 g), mp. 150-152°C. The main advantages of the present invention are:-1). It does not involve the use of toxic mercaptans like ethane thiol. 2). This process does not involve reaction of D-glucal with mineral acid, thereby avoiding the formation of Ferrier by-products.
2-Deoxy-d-glucose is a glucose molecule which has the 2-hydroxyl group replaced by hydrogen, so that it cannot undergo further glycolysis. As such; it acts to competitively inhibit the production of glucose-6-phosphate from glucose at the phosphoglucoisomerase level (step 2 of glycolysis).[2] In most cells, glucose hexokinase phosphorylates 2-deoxyglucose, trapping the product 2-deoxyglucose-6-phosphate intracellularly (with exception of liver and kidney)[; thus, labelled forms of 2-deoxyglucose serve as a good marker for tissue glucose uptake and hexokinase activity. Many cancers have elevated glucose uptake and hexokinase levels. 2-Deoxyglucose labeled with tritium or carbon-14 has been a popular ligand for laboratory research in animal models, where distribution is assessed by tissue-slicing followed by autoradiography, sometimes in tandem with either conventional or electron microscopy.
2-DG is uptaken by the glucose transporters of the cell. Therefore, cells with higher glucose uptake, for example tumor cells, have also a higher uptake of 2-DG. Since 2-DG hampers cell growth, its use as a tumor therapeutic has been suggested, and in fact, 2-DG is in clinical trials. [3] A recent clinical trial showed 2-DG can be tolerated at a dose of 63 mg/kg/day, however the observed cardiac side-effects (prolongation of the Q-T interval) at this dose and the fact that a majority of patients’ (66%) cancer progressed casts doubt on the feasibility of this reagent for further clinical use.[4] However, it is not completely clear how 2-DG inhibits cell growth. The fact that glycolysis is inhibited by 2-DG, seems not to be sufficient to explain why 2-DG treated cells stop growing.[5] Because of its structural similarity to mannose, 2DG has the potential to inhibit N-glycosylation in mammalian cells and other systems, and as such induces ER stress and the Unfolded Protein Response (UPR) pathway.[6][7][8]
Clinicians have noted that 2-DG is metabolised in the pentose phosphate pathway in red blood cells at least, although the significance of this for other cell types and for cancer treatment in general is unclear.
Work on the ketogenic diet as a treatment for epilepsy have investigated the role of glycolysis in the disease. 2-Deoxyglucose has been proposed by Garriga-Canut et al. as a mimic for the ketogenic diet, and shows great promise as a new anti-epileptic drug.[9][10] The authors suggest that 2-DG works, in part, by increasing the expression of Brain-derived neurotrophic factor (BDNF), Nerve growth factor (NGF), Arc (protein) (ARC), and Basic fibroblast growth factor (FGF2).[11] Such uses are complicated by the fact that 2-deoxyglucose does have some toxicity.
A study found that by combining the sugar 2-deoxy-D-glucose (2-DG) with fenofibrate, a compound that has been safely used in humans for more than 40 years to lower cholesterol and triglycerides, an entire tumor could effectively be targeted without the use of toxic chemotherapy.[12][13]
2-DG has been used as a targeted optical imaging agent for fluorescent in vivo imaging.[14][15] In clinical medical imaging (PET scanning), fluorodeoxyglucose is used, where one of the 2-hydrogens of 2-deoxy-D-glucose is replaced with the positron-emitting isotope fluorine-18, which emits paired gamma rays, allowing distribution of the tracer to be imaged by external gamma camera(s). This is increasingly done in tandem with a CT function which is part of the same PET/CT machine, to allow better localization of small-volume tissue glucose-uptake differences.
Resistance to 2-DG has been reported in HeLa cells [16] and in yeast;[17][8] in the latter, it involves the detoxification of a metabolite derived from 2-DG (2DG-6-phosphate) by a phosphatase. Despite the existence of such a phosphatase in human (named HDHD1A) However it is unclear whether it contributes to the resistance of human cells to 2DG or affects FDG-based imaging.
SYN
Indian Pat. Appl., 2004DE02075,

SYN
CN 106496288,
STARTING MATERIAL CAS 69515-91-9
C14 H20 O9, 332.30
D-arabino-Hexopyranose, 2-deoxy-, 1,3,4,6-tetraacetate
SYN
Bioorganic & Medicinal Chemistry Letters, 22(10), 3540-3543; 2012
https://www.sciencedirect.com/science/article/abs/pii/S0960894X12004258
PATENT
https://patents.google.com/patent/US6933382B2/en2-deoxy-D-glucose is useful in control of respiratory infections and for application as an antiviral agent for treatment of human genital herpes.Prior art for preparation of 2-deoxy-D-glucose while operable, tend to be expensive and time consuming. Reference may be made to Bergmann M., Schotte, H., Lechinsky, W., Ber, 55, 158 (1922) and Bergmann, M., Schotte, H., Lechinsky, W., Ber 56, 1052 (1923) which disclose the preparation of 2-deoxy-D-glucose in low yield by mineral acid catalyzed addition of water to D-glucal. Another method of producing 2-deoxy-D-glucose is from diethyldithioacetal derivative of D-glucose (Bolliger, H. R. Schmid, M. D., Helv. Chim. Acta 34, 989 (1951); Bolliger, H. R., Schmid, M. D., Helv, Chim. Acta 34, 1597 (1951); Bolliger, H. R Schmid, M. D., Helv. Chim. Acta 34, 1671 (1951) and from D-arabinose by reaction with nitromethane followed by acetylation, reduction and hydrolysis (Sowden, J. C., Fisher, H. O. L., J. Am. Chem., 69, 1048 (1947). However these methods result in the formation of 2-deoxy-D-glucose in low yield and of inferior purity due to the formation of several by-products and involve use of toxic reagents such as ethanethiol and nitromethane. As a result purification of 2-deoxy-D-glucose has to be done by recrystallisation which is tedious, time consuming and difficult.

EXAMPLE 1To a solution of 3,4,6-tri-O-benzyl-D-glucal (39 g, 0.09 mmol) in dichloromethane (20 ml) and methanol (100 ml) was added N-bromosuccinimide (18.7 g, 0.09 mil) during 10 min. at room temperature and stirred for 4 h. After completion of the reaction solvent was distilled off. The resultant residue extracted into carbon tetrachloride (2×100 ml) and organic phase concentrated to obtain methyl 2-bromo 2-deoxy-3,4,6-tri-O-benzyl-α/β-D-gluco-/mannopyranoside as a syrup. Quantity obtained 50 g. 1H NMR (200 MHz, CDCl3) 3.40-4.00 (m, 7H, H-2,5,6,6′ and OCH3) 4.30-5.10 (m, 9H, H-1,3,4 and 3×PhCH2O), 7.10-7.60 (m 15H, Ar—H). A solution of methyl 2-bromo-2-deoxy-3,4,6-tri-O-benzyl/α/β-D-gluco-/mannopyranoside (50 g) in methanol (300) was charged into one liter autoclave along with Raney nickel (10 ml) Et3N (135 ml) and subjected to hydrogenation at 120 psi pressure at 50° C. for 8 h. After completion of the reaction the catalyst was filtered off and the residue washed with methanol (25 ml). The filtrate was concentrate to obtain methyl 2-deoxy-3,4,6-tri-O-benzyl-α/β-D-glucopyranoside as a syrup (37.9 g, 89%). 1H NMR (200 MHz CDCl3): δ 1.50-2.40 (m,2H,H-2,2′), 3.32, 3.51 (2s, 3H, OCH3) 3.55-4.00 (m, 5, H-3,4,5,6,6′) 4.30-5.00 (M 7H, 3×PhCH2, H-1), 7.10-7.45 (m, 15H, Ar—H). The syrup of methyl 2-deoxy-3,4, 6-tri-O-benzyl-α/β-D-glucopyranoside (37.9 g) was dissolved in methanol (200 ml). 1 g of 5% Pd/C was added and hydrogenated at 150 psi pressure at room temperature. After 5 hours catalyst was filtered off and solvent evaporated. Quantity of the methyl 2-deoxy-α/β-D-glucopyranoside obtained 10.5 g (70%). [α]D+25.7° (c 1.0, MeOH), 1H NMR (200 MHz, D2O); δ 1.45-2.40 (m, 2H, H-2,2′) 3.20-4.80, (m 9H, H-1,3,4,5,6,6′—OCH3).EXAMPLE 2To a solution of D-glucal (64.6 g, 0.44 mmol) in methanol (325 ml) at 10° C. was added N-bromosuccinimide (78.7 g, 0.44 mol) during 40 min. maintaining the temperature between 10-15° C. during the addition. The reaction mixture was stirred at room temperature. After 5 hours solvent was evaporated to obtain a residue which was refluxed in ethyl acetate (100 ml). Ethyl acetate layer was discarded to leave a residue of methyl 2-bromo-2-deoxy-α/β-D-gluco/mannopyranoside (105 g) as a syrup. [α]D+36° (c 1.0, MeOH). 1H NMR (200 MHz, D2O): δ 3.47, 3.67 (2s, 3H, OCH3), 3.70-4.05 (m, 6h, H-2,3,4,5,6,6′), 4.48-5.13 (28, 1H, 1H, H-1). The syrupy methyl 2-bromo-2-deoxy-α/β-D-gluco-/mannopyranoside was dissolved in methanol (400 ml), a slurry of 80 g Raney nickel (a 50% slurry in methanol), Et3N (30 ml) and hydrogenated in a Parr apparatus at 120 psi. After 8-9 hours, the reaction mixture was filtered through a Celite filter pad and washed with MeOH. The washings and filtrate were combined and triturated with hexane to separate and remove by filtration insoluble triethylamine hydrobromide and traces of succinimide. The filtrate was concentrated to a residue. The isolated yield of methyl 2-deoxy-α/β-D-glucopyranoside was 89%.Ethyl 2-bromo-2deoxy-α/β-D-gluco-/mannopyranoside:When solvent was ethanol instead of methanol the compound obtained was ethyl 2-bromo-2deoxy-α/β-D-gluco-/mannopyranoside. 1H NMR (200 MHz, D2O): δ 1.10-1.32 (m, 3H, CH3), 2.80 (s, 4H, —CO(CH2)2CO—NH—), 3.40-4.10 (m, 8H, H-2,3,4,5,6,6′, CH2), 4.40, 5.20 (2s 1H, H-1, α/β).Isopropyl 2-bromo-2-deoxy-α/β-D-gluco-/mannopyranoside:When isopropanol instead of methanol was used as a solvent the compound obtained was isopropyl 2-bromo-2-deoxy-α/β-D-gluco/mannopyranoside, 1H NMR (200 MHz, D2O): δ 1.10-1.30 (m, 6H, 2×CH3) 2.80 (s, 4H, —CO(CH2)2CO—NH—), 3.60-4.60 (m 8H,H-2,3,4,5,6,6′, CH2) 4.40, 5,30 (2s, 1H, H-1, α/β.EXAMPLE 3A mixture of D-glucal (64.6 g), methanol (400 ml), N-bromosuccinimide (79 g) were stirred at 15° C. for 6 h. The reaction mixture was hydrogenated in a Parr apparatus in presence of 60 g of Raney nickel catalyst (a 50% slurry in methanol) and triethylamine (62 ml). After 8-9 h, the reaction mixture was filtered on a Celite filter pad. The Celite pad was washed with methanol. The washings and filtrate were combined, concentrated to a thick heavy syrup, dissolve in chloroform (500 ml), pyridine (400 ml) and acetic anhydride (251 ml) was added while stirring, maintaining the temperature between 5-10° C. After 12 hours, the reaction mixture was diluted with CHCl3 (500 ml) transferred to a separating funnel and organic phase was washed with water. The organic phase was separated, dried (Na2SO4) and concentrated to obtain methyl 2-deoxy-3,4,6-tri-O-acetyl-2 deoxy-α/β-D-glucopyranoside as a syrup (163.43 g, 87%). [α]D+65.0° (c 1.0, CHCl3) 1H NMR (200 MHz, CDCl3): δ 1.55-1.90 (m, 2H, H-22′), 2.01, 2.04, 2.11, 2.15, (4s, 9H, 3×OCOCH3), 2.18, 3.40 (2s, 3H, OCH3), 3.45-50 (m, 3H, H-5, 6,6′) 4.80-5.40 (m, 3H,H-1,3,4). The syrup was dissolved in methanol (600 ml) 1N NaOMe in methanol (25 ml) was added and left at room temperature. After 6-10 h, dry CO2 gas was passed into the reaction mixture, solvent was evaporated to obtain a syrupy residue. The residue was once again extracted into dry methanol and concentrated to obtain methyl 2-deoxy-α/β-D-glucopyranoside as syrup. Quantity obtained 81 g (92%).EXAMPLE 4A 500 ml round bottom flask equipped with magnetic stir bar was charged with a solution of D-glucal (323 g) in methanol (175 ml), cooled to 15° C., N-bromosuccinimide (NIBS) (39.4 g) was added and stirred or 6 hours at 15° C., The reaction mixture was concentrated to half the volume, cooled to 0° C. and separated succinimide, was removed by filtration. To the filtrate was added a slurry of 30 g Raney nickel (a 50% slurry in Methanol) Et3N (32 ml) and hydrogenated in a Parr apparatus at 120 psi. After 7-8 hours, the reaction mixture was filtered through a Celite filter pad, and washed with MeOH. The washings and filtrate were combined and triturate with hexane to separate and remove by filtration insoluble triethylamine hydrobromide and succinimide. The filtrate was concentrated to a residue, dissolved in methanol and triturated with hexane to remove most of the triethylamine hydrobromide and succinimide. The filtrate was concentrated to obtain methyl 2-deoxy-α/β-D-glucopyranoside (85%).EXAMPLE 5To a stirred solution of methyl 3,4,6-tri-O-acetyl-2-deoxy-α/β-D-glucopyranoside (47 g) (from example 3) in acetic acid (40 ml) and acetic anhydride (110 ml) was added concentrated sulphuric acid (0.94 ml) at 0°. The reaction mixture was brought to room temperature and stirred. After 2 hours the reaction mixture was diluted with water (50 ml) and extracted into CH2Cl2 (3×150 ml). The organic phase was separated, washed with saturated NaHCO3 solution H2O dried over Na2SO4 and concentrated to obtain 2-deoxy-1,3,4,6-tetra-O-acetyl-α/β-D-glucopyranoside as a crystalline compound. mp. 115-118° C. Quantity obtained 44.5 g (86%). [α]D+21.5° (c 1.0, CHCl3). 1H NMR (200 MHz, CDCl3): δ 1.50-2.45 (m, 14H, H-2,2′, 4×OCOCH3), 3.85-5.40, (m, 5H, H-3,4,5,6,6′), 5.75-6.20 (m, 1H, H-1, α/β). To a heterogeneous mixture of 1,3,4,6-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (10 g) in water (100 ml) was added acetyl chloride (10 ml) and heated to 80° C. After 6 hours the reaction mixture was cooled to room temperature, neutralised with saturated aq. Ba(OH)2, concentrated to half the volume and filtered on a Celite pad, Filtrate was concentrated on a rotary evaporator and dried over anhydrous P2O5 to obtain a residue which was dissolved in hot isopropyl alcohol and filtered on a pad of Celite to obtain a clear filtrate. The filtrate was concentrated to a residue, dissolved in hot isopropyl alcohol (50 ml), acetone (75 ml) and seeded with a few crystals of 2-deoxy-D-glucose. After 15-18 hours at 5° C. crystalline title product was filtered. Quantity obtained 3.21 g (64.9%) m.p. 148-149° C.EXAMPLE 6A heterogeneous mixture of 1,3,4,6-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (9 g) (from example 5), water (30 ml) and 11% aq. H2SO4 (0.3 ml) was stirred at 85° C. for 7 h to obtain a homogenous solution. The reaction mixture was cooled, neutralised with aq. Ba(OH)2 solution and filtered. The filtrate obtained was concentrated to half the volume and solids separated were filtered. To the filtrate was added activated carbon (1 g) and filtered. The filtrate was concentrated on a rotary evaporator and dried over P2O5 to obtain 2-deoxy-D-glucose that was crystallized from methyl alcohol (27 ml) and acetone (54 ml). Quantity obtained 2.4 g. mp. 146-149° C.,EXAMPLE 7A heterogeneous mixture of 1,3,4,tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (25 g) (from example 5), H2O (250 ml), toluene (250 ml) and glacial acetic acid (1.25 ml) was heated to reflux for 10-12 hours, while it was connected to a Dean-Stark azeotropic distillation apparatus. An azeotropic mixture of acetic acid, toluene was collected to remove acetic acid and every one hour fresh toluene (50 ml) was introduced. After completion of the reaction, toluene was removed by distillation from the reaction mixture to obtain a residue that was dissolved in methanol, treated with charcoal and filtered. Be filtrate was separated, concentrated to a residue and crystallized from isopropyl alcohol and acetone to obtain 2-deoxy-D-glucose (7.33 g, 59%). mp. 148-151° C.EXAMPLE 8A heterogeneous mixture of 1,3,4,5-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (10 g) (tom example 5), H2O (200 ml) conc. HCl (0.3 ml) and glacial acetic acid (0.5 ml) was heated to 85° C. After 6 hours the reaction mixture was cooled to room temperature, neutralized with aq. Ba(OH)2 and filtered on a pad of Celite. Filtrate was separated, treated with charcoal and filtered. The filtrate was concentrated to a residue and crystallized from MeOH, acetone to obtain the product. Quantity obtained 275 g. mp. 147-148° C.EXAMPLE 9A heterogeneous mixture of 1,3,4,5-tetra-O-acetyl-2-deoxy-α/β-D-glucopyranoside (10 g) (from example 3) water (100 ml) and conc. HCl (0.5 ml) was heated to 80° C. After 2-5 hours the reaction mixture was cooled to room temperature, neutralized with aq. Ba(OH)2 and filtered on a pad of Celite. The filtrate was concentrated to a residue, dissolved in ethanol, treated with charcoal and filtered. The filtrate was concentrated to a solid residue and crystallized from methanol-acetone to obtain the title product. Quantity obtained 3.15 g mp. 148-151° C.,EXAMPLE 10A solution of methyl 2-deoxy-α/β-D-glucopyranoside (30 g) (from example 2) water (15 ml) and conc. HCl (1.5 ml) was heated to 80-85° C. After 3-5 hours the reaction mixture was cooled to room temperature, neutralize with aq. Ba(OH)2 and filtered to remove insoluble salts. The filtrate was concentrated to a residue, crystallized from MeOH, acetone and hexane to obtain 2-deoxy-D-glucose (11.77 g) mp. 149-151° C.EXAMPLE 11A solution of methyl 2-deoxy-α/β-D-glucopyranoside (30 g) (form example 2) water (195 ml) and conc. H2SO4 (5.9 ml) was heated to 80° C. After 2-3 hours the reaction mixture was cooled, neutralized with aq. Ba(OH)2 and filtered. The filtrate was separated, treated with charcoal and filtrate. The Filtrate was concentrated to a residue and crystallized from isopropyl alcohol to obtain the title product. Quantity obtained 5.2 g. mp. 152-154° C.EXAMPLE 12A mixture of methyl 2-deoxy-α/β-D-glucopyranoside (24 g) (from example 2) water (125 ml) and IR 120H+resin (7.5 ml) was heated to 90-95° C. for 2 h. The reaction mixture was cooled to room temperature, filtered and the resin was washed with water (20 ml). The filtrate was concentrated to residue and crystallized from ethanol to obtain 2-deoxy-D-glucose (8.8 g), mp. 150-152° C.CLIP
References
- ^ Merck Index, 11th Edition, 2886.
- ^ Wick, AN; Drury, DR; Nakada, HI; Wolfe, JB (1957). “Localization of the primary metabolic block produced by 2-deoxyglucose”(PDF). J Biol Chem. 224 (2): 963–969. doi:10.1016/S0021-9258(18)64988-9. PMID 13405925.
- ^ Pelicano, H; Martin, DS; Xu, RH; Huang, P (2006). “Glycolysis inhibition for anticancer treatment”. Oncogene. 25 (34): 4633–4646. doi:10.1038/sj.onc.1209597. PMID 16892078.
- ^ Raez, LE; Papadopoulos, K; Ricart, AD; Chiorean, EG; Dipaola, RS; Stein, MN; Rocha Lima, CM; Schlesselman, JJ; Tolba, K; Langmuir, VK; Kroll, S; Jung, DT; Kurtoglu, M; Rosenblatt, J; Lampidis, TJ (2013). “A phase I dose-escalation trial of 2-deoxy-D-glucose alone or combined with docetaxel in patients with advanced solid tumors”. Cancer Chemother. Pharmacol. 71 (2): 523–30. doi:10.1007/s00280-012-2045-1. PMID 23228990. S2CID 2990078.
- ^ Ralser, M.; Wamelink, M. M.; Struys, E. A.; Joppich, C.; Krobitsch, S.; Jakobs, C.; Lehrach, H. (2008). “A catabolic block does not sufficiently explain how 2-deoxy-D-glucose inhibits cell growth”. Proceedings of the National Academy of Sciences. 105 (46): 17807–17811. Bibcode:2008PNAS..10517807R. doi:10.1073/pnas.0803090105. PMC 2584745. PMID 19004802.
- ^ Kurtoglu, M.; Gao, N.; Shang, J.; Maher, J. C.; Lehrman, M. A.; Wangpaichitr, M.; Savaraj, N.; Lane, A. N.; Lampidis, T. J. (2007-11-07). “Under normoxia, 2-deoxy-D-glucose elicits cell death in select tumor types not by inhibition of glycolysis but by interfering with N-linked glycosylation”. Molecular Cancer Therapeutics. 6 (11): 3049–3058. doi:10.1158/1535-7163.mct-07-0310. ISSN 1535-7163. PMID 18025288.
- ^ Xi, Haibin; Kurtoglu, Metin; Liu, Huaping; Wangpaichitr, Medhi; You, Min; Liu, Xiongfei; Savaraj, Niramol; Lampidis, Theodore J. (2010-07-01). “2-Deoxy-d-glucose activates autophagy via endoplasmic reticulum stress rather than ATP depletion”. Cancer Chemotherapy and Pharmacology. 67 (4): 899–910. doi:10.1007/s00280-010-1391-0. ISSN 0344-5704. PMC 3093301. PMID 20593179.
- ^ Jump up to:a b Defenouillère, Quentin; Verraes, Agathe; Laussel, Clotilde; Friedrich, Anne; Schacherer, Joseph; Léon, Sébastien (2019-09-03). “The induction of HAD-like phosphatases by multiple signaling pathways confers resistance to the metabolic inhibitor 2-deoxyglucose”. Science Signaling. 12 (597): eaaw8000. doi:10.1126/scisignal.aaw8000. ISSN 1945-0877. PMID 31481524. S2CID 201829818.
- ^ Garriga-Canut, Mireia; Schoenike, Barry; Qazi, Romena; Bergendahl, Karen; Daley, Timothy J.; Pfender, Rebecca M.; Morrison, John F.; Ockuly, Jeffrey; Stafstrom, Carl; Sutula, Thomas; Roopra, Avtar (2006). “2-Deoxy-D-glucose reduces epilepsy progression by NRSF-CTBP–dependent metabolic regulation of chromatin structure”. Nature Neuroscience. 9 (11): 1382–1387. doi:10.1038/nn1791. PMID 17041593. S2CID 10175791.
- ^ Garriga-Canut, M.; Schoenike, B.; Qazi, R.; Bergendahl, K.; Daley, T. J.; Pfender, R. M.; Morrison, J. F.; Ockuly, J.; Stafstrom, C.; Sutula, T.; Roopra, A. (2006). “2-Deoxy-D-glucose reduces epilepsy progression by NRSF-CtBP–dependent metabolic regulation of chromatin structure”. Nature Neuroscience. 9 (11): 1382–1387. doi:10.1038/nn1791. PMID 17041593. S2CID 10175791.
- ^ Jia Yao, Shuhua Chen, Zisu Mao, Enrique Cadenas, Roberta Diaz Brinton “2-Deoxy-D-Glucose Treatment Induces Ketogenesis, Sustains Mitochondrial Function, and Reduces Pathology in Female Mouse Model of Alzheimer’s Disease”, PLOS ONE
- ^ Researchers develop novel, non-toxic approach to treating variety of cancers. ScienceDaily
- ^ Liu, Huaping; Kurtoglu, Metin; León-Annicchiarico, Clara Lucia; Munoz-Pinedo, Cristina; Barredo, Julio; Leclerc, Guy; Merchan, Jaime; Liu, Xiongfei; Lampidis, Theodore J. (2016). “Combining 2-deoxy-D-glucose with fenofibrate leads to tumor cell death mediated by simultaneous induction of energy and ER stress”. Oncotarget. 7 (24): 36461–36473. doi:10.18632/oncotarget.9263. PMC 5095013. PMID 27183907.
- ^ Kovar, Joy L.; Volcheck, William; Sevick-Muraca, Eva; Simpson, Melanie A.; Olive, D. Michael (2009). “Characterization and performance of a near-infrared 2-deoxyglucose optical imaging agent for mouse cancer models”. Analytical Biochemistry. 384(2): 254–262. doi:10.1016/j.ab.2008.09.050. PMC 2720560. PMID 18938129.
- ^ Cheng, Z., Levi, J., Xiong, Z., Gheysens, O., Keren, S., Chen, X., and Gambhir, S., Bioconjugate Chemistry, 17(3), (2006), 662-669
- ^ Barban, Stanley (December 1962). “Induced resistance to 2-deoxy-d-glucose in cell cultures”. Biochimica et Biophysica Acta. 65(2): 376–377. doi:10.1016/0006-3002(62)91065-x. ISSN 0006-3002. PMID 13966473.
- ^ Sanz, Pascual; Randez-Gil, Francisca; Prieto, José Antonio (September 1994). “Molecular characterization of a gene that confers 2-deoxyglucose resistance in yeast”. Yeast. 10 (9): 1195–1202. doi:10.1002/yea.320100907. ISSN 0749-503X. PMID 7754708. S2CID 9497505.
The Drugs Controller General of India (DCGI) has given permission for the emergency use of drug 2-deoxy-D-glucose (2-DG) as an adjunct therapy in moderate to severe Covid-19 cases, said Defence Research and Development Organisation on Saturday.
“Being a generic molecule and analogue of glucose, it can be easily produced and made available in plenty,” said the DRDO in a statement.
An adjunct therapy refers to an alternative treatment that is used together with the primary treatment. Its purpose is to assist the primary treatment.
“The drug has been developed by DRDO lab Institute of Nuclear Medicine and Allied Sciences in collaboration with Dr Reddy’s Laboratories. Clinical trial have shown that this molecule helps in faster recovery of hospitalized patients and reduces supplemental oxygen dependence,” the statement read.
According to DRDO, the patients treated with 2-DG showed faster symptomatic cure than Standard of Care (SoC) on various endpoints in the efficacy trends.
“A significantly favourable trend (2.5 days difference) was seen in terms of the median time to achieving normalization of specific vital signs parameters when compared to SOC,” it said.
The drug comes in powder form in sachets, which is taken orally by dissolving it in water.
“It accumulates in the virus-infected cells and prevents virus growth by stopping viral synthesis and energy production,” said the DRDO.
In April 2020, during the first wave of the Covid-19 pandemic, INMAS-DRDO scientists conducted laboratory experiments of 2-DG with the help of the Centre for Cellular and Molecular Biology (CCMB), Hyderabad.
They found that this molecule works effectively against the SARS-CoV-2 virus and inhibits viral growth.
Based on the results, the DCGI had in May 2020 permitted Phase-II clinical trial of 2-DG in Covid-19 patients.
In Phase-II trials (including dose-ranging) conducted from May to October 2020, the drug was found to be safe and showed significant improvement in the patients’ recovery.
“Phase IIa was conducted in 6 hospitals and Phase IIb (dose-ranging) clinical trial was conducted at 11 hospitals all over the country. Phase-II trial was conducted on 110 patients,” said the DRDO.

NEW DRUG APPROVALS
ONE TIME
$10.00
| Names | |
|---|---|
| IUPAC name(4R,5S,6R)-6-(hydroxymethyl)oxane-2,4,5-triol | |
| Other names2-Deoxyglucose 2-Deoxy-d-mannose 2-Deoxy-d-arabino-hexose 2-DG | |
| Identifiers | |
| CAS Number | 154-17-6 |
| 3D model (JSmol) | Interactive image |
| ChEMBL | ChEMBL2074932 |
| ChemSpider | 388402 |
| EC Number | 205-823-0 |
| IUPHAR/BPS | 4643 |
| PubChem CID | 108223 |
| UNII | 9G2MP84A8W |
| showInChI | |
| showSMILES | |
| Properties | |
| Chemical formula | C6H12O5 |
| Molar mass | 164.16 g/mol |
| Melting point | 142 to 144 °C (288 to 291 °F; 415 to 417 K) |
| Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). |
////////////2-Deoxy-D-glucose, 2 dg, 2-dg, 2 DEOXY D GLUCOSE, COVID 19, CORONA VIRUS, INDIA 2021, DCGI, DRDO, DR REDDYS
C(C=O)C(C(C(CO)O)O)O
Pegylated Interferon alpha-2b, (PegIFN), Virafin
DB00022 sequence CDLPQTHSLGSRRTLMLLAQMRRISLFSCLKDRHDFGFPQEEFGNQFQKAETIPVLHEMI QQIFNLFSTKDSSAAWDETLLDKFYTELYQQLNDLEACVIQGVGVTETPLMKEDSILAVR KYFQRITLYLKEKKYSPCAWEVVRAEIMRSFSLSTNLQESLRSKE
CDLPQTHSLG SRRTLMLLAQ MRRISLFSCL KDRHDFGFPQ EEFGNQFQKA ETIPVLHEMI
QQIFNLFSTK DSSAAWDETL LDKFYTELYQ QLNDLEACVI QGVGVTETPL MKEDSILAVR
KYFQRITLYL KEKKYSPCAW EVVRAEIMRS FSLSTNLQES LRSKE

Chemical structure of peginterferon α-2a and α-2b. Abbreviations: PeG-IFN, peginterferon; IFN, interferon; Lys, lysine; His, histidine; Cys, cysteine; Ser, serine.
Pegylated Interferon alpha-2b
(PegIFN), Virafin

| Formula | C860H1353N229O255S9 |
|---|---|
| CAS | 99210-65-8, 98530-12-2, 215647-85-1 |
| Mol weight | 19268.9111 |
- Interferon α2b, pegylated
- PegIFN a-2b
- PegIFN a-2b (biologics)
- PegIFN α-2b
- PegIntron
- Pegaferon
- PegiHep
- Peginterferon alfa-2b
- Peginterferon α-2b
- Pegylated interferon alfa-2b
- Pegylated interferon α-2b
- Pegylated interferons, PegIFN a-2b
- Proteinaceous biopharmaceuticals, PegIFN a-2b
- Sch 54031
- Sylatron
- ViraferonPeg
Active Moieties
| NAME | KIND | UNII | CAS | INCHI KEY |
|---|---|---|---|---|
| Interferon alfa-2b | unknown | 43K1W2T1M6 | 98530-12-2 | Not applicable |
| Clinical data | |
|---|---|
| Trade names | PegIntron, Sylatron, ViraferonPeg, others |
| AHFS/Drugs.com | Professional Drug Facts |
| MedlinePlus | a605030 |
| License data | EU EMA: by INN |
| Routes of administration | Subcutaneous injection |
| ATC code | L03AB10 (WHO) |
| Legal status | |
| Legal status | US: ℞-only [1][2]EU: Rx-only |
| Pharmacokinetic data | |
| Elimination half-life | 22–60 hrs |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 215647-85-1 |
| IUPHAR/BPS | 7462 |
| DrugBank | DB00022 |
| ChemSpider | none |
| UNII | G8RGG88B68 |
| KEGG | D02745 |
| ChEMBL | ChEMBL1201561 |
| ECHA InfoCard | 100.208.164 |
| Chemical and physical data | |
| Formula | C860H1353N229O255S9 |
| Molar mass | 19269.17 g·mol−1 |

NEW DRUG APPROVALS
ONE TIME
$10.00
New Delhi: ,,,,,,https://www.ndtv.com/india-news/zydus-virafin-gets-emergency-use-approval-for-treating-moderate-covid-19-cases-2420358
Zydus Cadila received emergency use approval from the Drugs Controller General of India (DGCI) on Friday for the use of “Virafin”, Pegylated Interferon alpha-2b (PegIFN) in treating moderate COVID-19 infection in adults.
A single-dose subcutaneous regimen of the antiviral Virafin will make the treatment more convenient for the patients. When administered early on during COVID-19, Virafin will help patients recover faster and avoid much of the complications, the company said.
In a release, Cadila Health highlighted that “the drug has also shown efficacy against other viral infections.”
Speaking on the development, Dr Sharvil Patel, Managing Director, Cadila Healthcare Limited said, “The fact that we are able to offer a therapy which significantly reduces the viral load when given early on can help in better disease management. It comes at a much-needed time for patients and we will continue to provide them access to critical therapies in this battle against COVID-19.”
In its Phase III clinical trials, the therapy had shown better clinical improvement in the patients suffering from COVID-19. During the trials, a higher proportion of patients administered with PegIFN arm were RT-PCR negative by day 7. The drug ensures faster viral clearance and has several add-on advantages compared to other anti-viral agents, the release further reads.
The development and the nod from DGCI come at a time when India is combating the second wave of coronavirus.
The central government in one of its major announcements decided to administer COVID-19 vaccines to all age above 18 years.
India recorded 3,32,730 new COVID-19 cases in the last 24 hours, the highest single-day spike since the pandemic broke out last year. India has crossed the mark of 3 lakh COVID-19 cases for two consecutive days now. This has taken the cumulative count of the COVID infection in the country to 1,62,63,695.
2CommentsThe country has recorded 2,263 new deaths due to COVID-19 in the last 24 hours. As many as 1,86,920 people have succumbed to the viral infection in India so far. There are 24,28,616 active COVID-19 cases in the country now.
PATENT
https://patents.google.com/patent/EP1562634B1/en
- Interferon alpha-2a plays an important role for the treatment of chronic hepatitis C, but it is limited in its efficacy by the short in vivo half-life. To improve the half-life and efficacy, interferon alpha-2a was conjugated with a polyethylene glycol moiety. Pegylation changes physicochemical and biological properties of the protein. One effect is the decrease of the proteolytic degradation and the renal clearance. This increases the half-life of the pegylated protein in blood. Another effect is the altered distribution in the body, depending on the size of the PEG moiety of the protein. Interferon alpha 2a pegylated with a large polyethylene glycol moiety (PEG moiety) such as a 40 kDa branched polyethylene moietywherein R and R’ are independently lower alkyl; n and n’ are integers having a sum of from 600 to 1500; and the average molecular weight of the polyethylene glycol units in said conjugate is from about 26,000 daltons to about 66,000 daltons;
has an improved biological activity and exhibits sustained adsorption and reduced renal clearance, resulting in a strong antiviral pressure throughout a once-weekly dosing schedule, see Perry M. C., et al. Drugs, 2001,15,2263-2288 and Lamb M. W., et al. The Annals of Pharmacotherapy, 2002, 36, 933-938. - [0003]See also Monkarsh et al. Analytical Biochemistry, 1997, 247, 434- 440 (Positional Isomers of Mono-pegylated Interferon α-2a) and Bailon et al. Bioconjugate Chemistry, 2001, 12, 195-202 (Rational Design of a Potent, Long-Lasting Form of interferon).
- [0004]The method for the pegylation of interferon alpha-2a is described in EP A 809 996. Since this pegylation is performed by reaction of PEG2-NHS of formulawith primary amino groups on for example lysine or to the N-terminus of the interferon alpha.one or more PEG moieties may be attached and form a mixture of unpegylated, mono- and multiple-pegylated interferon. Monopegylated interferon alpha can be isolated from the mixture by methods known in the art. Furthermore, since interferon alpha-2a molecule exhibits 12 sites for pegylation (11 lysines and the N-terminus) it is a mixture of positional isomers. From these possible twelve isomers, nine were isolated and characterized, each of these being conjugated to the branched polyethylene glycol chain at a specific lysine, namely,
at Lys(31) to form interferon alpha 2a pegylated at Lys(31) [referred to as PEG-Lys(31)],
at Lys(49) to form interferon.alpha 2a pegylated at Lys(49) [referred to as PEG-Lys(49)],
at Lys(70) to form interferon alpha 2a pegylated at Lys(70) [referred to as PEG-Lys(70)],
at Lys(83) to form interferon alpha 2a pegylated at Lys(83) [referred to as PEG-Lys(83)],
at Lys(112) to form interferon alpha 2a pegylated at Lys(112) [referred to as PEG-Lys(112)],
at Lys(121) to form interferon alpha 2a pegylated at Lys(121) [referred to as PEG-Lys(121)],
at Lys(131) to form interferon alpha 2a pegylated at Lys(131) [referred to as PEG-Lys(131)],
at Lys(134) to form interferon alpha 2a pegylated at Lys(134) [referred to as PEG-Lys(134)],
at Lys(164) to form interferon alpha 2a pegylated at Lys(164) [referred to as PEG-Lys(164)]. - [0005]It has been found that PEG-Lys(31) and PEG-Lys(134) have higher activities in an antiviral assay than the mixture, the activity of PEG-Lys(164) was equal to the mixture, whereas the activities of PEG-Lys(49), PEG-Lys(70), PEG-Lys(83), PEG-Lys(112), PEG-Lys(121) and PEG-Lys(131) were lower.
- The following examples will further illustrate the invention
Example 1A Separation of the positional isomers
- [0035]A two-step isolation and purification scheme was used to prepare the monopegylated isoforms of PEG-interferon alpha 2a.
- a) The first step was a separation of the positional isomers on a preparative low pressure liquid chromatography column with a weak-cation exchange matrix (TOSOH-BIOSEP, Toyopearl CM-650S, e.g. Resin Batch no. 82A the diameter of the column being 16 mm, the length 120 cm). A linear pH-gradient of increasing sodium acetate concentration (25 mM, pH 4.0 up 75 mM to pH 7.8) was applied at a flow rate of 0.7 mL/min. Detection was at 280 nm. With this chromatographic step species 1, 2, 5,6 and a mixture of 3, 4, 4a, 7 and 8 could be collected, see Table 1.
- b) The fractions were further separated and purified in the second preparation step. A preparative column with the same matrix as the analytical strong-cation exchange column (Resin Batch no. 82A having a ion exchange capacity of 123 mEq/ml) as described above but larger dimensions (30 mm i.d. and 70 mm length), further a higher flow rate and an extended run time was used. As for the analytical method the column was pre-equilibrated with 3.4 mM sodium acetate, 10% ethanol and 1% diethylene glycol, adjusted to pH 4.4 (buffer A). After loading the PEG-IFN samples, the column was washed with buffer A, followed by an ascending linear gradient to 10 mM dibasic potassium phosphate, 10% ethanol and 1% diethylene glycol, adjusted to pH 6.6 (buffer B). The flow rate was 1.0 mL/min and the detection at 218 nm.
- [0036]The protein concentration of the PEG-IFN alpha 2a isomer was determined by spectrophotometry, based on the 280 nm absorption of the.protein moiety of the PEG-IFN alpha 2a.
- [0037]An analytical elution profile of 180 µg of PEG-IFN alpha 2a is shown in Figure 1. The result of this method is a separation into 8 peaks, 2 peaks with baseline separation and 6 with partial separation. The decrease of the baseline absorption towards the end of the chromatogram suggests that there were no other monopegylated species of IFN alpha 2a eluting at higher retention time.
- [0038]In addition, looking carefully at the IEC-chromatogram a further peak close to the detection limit is visible between peaks 2 and 3 indicating the presence of additional positional isomers that should also contribute to the specific activity of the PEG-IFN alpha 2a mixture. Additional species were expected as the interferon alpha-2a molecule exhibits 12 sites for pegylation (11 lysines and the N-terminus). However, given the low abundance of the these species, they were not isolated and characterised.
- [0039]Isomer samples derived from IEC optimisation runs were investigated directly after the isolation (t = 0) and after 2 of weeks of storage at 5°C (data not shown). No significant differences were observed for the protein derived from IEC-peaks with regard to the protein content as determined by spectrometric methods; nor were any changes to be detected in the monopegylation site, the content of oligo-PEG-IFN alpha 2a, the amount of aggregates and the bioassay activity. Taking into account the relative abundance of the individual isomers – as determined by the IEC method – as well as the specific activities – as determined in the anti-viral assay – almost the total specific bioactivity of the PEG-IFN alpha 2a mixture used for their isolation is recovered (approximately 93%).
- [0040]The analytical IE-HPLC was used to check the purity of the individual isomers with respect to contamination with other positional isomers in the IEC fractions. The peaks 2, 3, 4, 4a, 5 and 7 had more than 98%, the peaks 1 and 8 had 93% and peak 6 had 88 % purity. Table 1:PEG-peptides identified by comparison of the Lys-C digest spectra of the isomers and the reference standard.Identified PEG Sites in the separated PEG-IFN SpeciesPeakmissing peaks in peptide mapPEG-IFNPEG siteMr (DA)SequencePeak 1K31A,E24-49Peak 2K134I, I’134-164Peak 3K131C122-131aPeak 4K121B, C113-131Peak 4aK164b134-164a,bPeak 5K70D, F50-83Peak 6K83D, H71-112Peak 7K49E, F32-70Peak 8K112B, H84-121a132-133 too small to detect.a,b RP-HPLC.
- [0041]The fractions were characterised by the methods described in examples 2 to 6.
Example 1B Analytical separation of positional isomers of mono-pegylated interferon alpha 2a
- [0042]HPLC Equipment:HP1100Column:SP-NPR, TosoH Bioscience, Particle size: 2.5µm, nonporous, Order#: 13076Injection:5-10 µg monopegylated IFNmobile Phase:Buffer A: 10% v/vEthanol 1% v/vDiethylenglycol 2.3 mMNa-Acetat 5.2 mMAcetic acid, in purified water, no pH adjustment Buffer B: 10% v/vEthanol 1% v/vDiethylenglycol 16.4 mMKH2PO4 4.4 mMK2HPO4, in purified water, no pH adjustmentGradient:0 Min40 %B 2 Min40 %B 2.1 Min48 %B 25 Min68 %B 27 Min75 %B 30 Min75 %B 34 Min40 %B 40 Min40 %BFlow:1.0 ml/min Column Temperature:25°C Detection:218 nm a typical Chromatogram is given in Figure 8.
Example 2 Analysis of the fractions by mass spectrometry peptide mapping
- [0043]Mass spectra were recorded on a MALDI-TOF MS instrument (PerSeptive Biosystems Voyager-DE STR with delayed extraction). Each IEC fraction (Ion Exchange Chromatography) was desalted by dialysis, reduced with 0.02 M 1,4-dithio-DL-threitol (DTT) and alkylated with 0.2 M 4-vinyl pyridine. Then the proteins were digested with endoproteinase Lys-C (Wako Biochemicals) in 0.25 M Tris (tris(hydroxymethyl)-aminoethane) at pH 8.5 with an approximate enzyme to protein ratio of 1:30. The reaction was carried out over night at 37 °C.
- [0044]A solution of 20 mg/ml α-cyano-4-hydroxycinnamic acid and 12 mg/ml nitrocellulose in acetone/isopropanol 40/60 (v/v) was used as matrix (thick-layer application). First, 0.5 µL of matrix was placed on the target and allowed to dry. Then, 1.0 µL of sample was added. The spectra were obtained in linear positive ionisation mode with an accelerating voltage of 20.000 V and a grid voltage of 95 %. At least 190 laser shots covering the complete spot were accumulated for each spectrum. Des-Arg1-bradykinin and bovine insulin were used for internal calibration.
Example 3 high-performance liquid chromatography (RP-HPLC) Peptide Mapping
- [0045]The peptides were characterized by reverse-phase high-performance liquid chromatography (RP-HPLC) Peptide Mapping. The IEC fractions were reduced, alkylated and digested with endoproteinase Lys-C as described for the MALDI-TOF MS peptide mapping. The analysis of the digested isomers was carried out on a Waters Alliance HPLC system with a Vydac RP-C18 analytical column (5 µm, 2.1 × 250 mm) and a precolumn with the same packing material. Elution was performed with an acetonitrile gradient from 1 % to 95 % for 105 min in water with a flow rate of 0.2 mL/min. Both solvents contained 0.1 % (v/v) TFA. 100 µL of each digested sample were injected and monitored at 215 nm.
Example 4 MALDI-TOF spectra of undigested protein
- [0046]An 18 mg/ml solution of trans-3-indoleacrylic acid in acetonitrile/0.1 % trifluoroacetic acid 70/30 (v/v) was premixed with the same volume of sample solution. Then 1.0 µL of the mixture was applied to the target surface. Typically 150 – 200 laser shots were averaged in linear positive ionisation mode. The accelerating voltage was set to 25.000 V and the grid voltage to 90 %. Bovine albumin M+ and M2+ were used for external calibration.
Example 5 SE-HPLC (size exclusion HPLC)
- [0047]SE-HPLC was performed with a Waters Alliance 2690 HPLC system equipped with a TosoHaas TSK gel G 4000 SWXL column (7.8 × 300 mm). Proteins were eluted using a mobile phase containing 0.02 M NaH2PO4, 0.15 M NaCl, 1% (v/v) diethylene glycol and 10 % (v/v) ethanol (pH 6.8) at a flow rate of 0.4 mL/min and detected at 210 nm. The injection amounts were 20 µg of each isomers.
- [0048]Size Exclusion HPLC and SDS-PAGE were used to determine the amount of oligo-PEG-IFN alpha 2a forms and aggregates in the different IEC fractions. The reference material contains 2.3 % aggregates and 2.2 % oligomers (Figure 4).
- [0049]Peaks 1, 4, 4a, 5, 6 and 8 contain < 0.7 % of the oligopegylated IFN alpha 2a forms, whereas in,peaks 2, 3, and 7 the percentage of the oligopegylated IFN alpha 2a forms are under the detection limit (< 0.2 %). In the case of the aggregates a different trend could be seen. In all peaks the amount of aggregates is below 0.9 %.
Example 6 SDS-PAGE
- [0050]SDS-PAGE was carried out both under non-reducing and under reducing conditions using Tris-Glycine gels of 16 % (1.5 mm, 10 well). Novex Mark 12 molecular weight markers with a mass range from 2.5 to 200 kDa were used for calibration, bovine serum albumin (BSA) was used as sensitivity standard (2 ng). Approximately 1 µg of all the samples and 0.5 µg of standard were applied to the gel. The running conditions were 125 V and 6 W for 120 min. The proteins were fixed and stained using the silver staining kit SilverXpress from Novex.
- [0051]The gels that were recorded under non-reducing conditions for the IEC fractions 1- 8 (Figure 2) show a pattern that is comparable to that of the PEG-IFN alpha 2a reference standard.
- [0052]Under reducing conditions, the gels show an increase in intensity of the minor bands at about 90 kDa as compared to the standard. Between 6 and 10 kDa protein fragments appear for peaks 6, 7 and 8 (Figure 3). Both bands together correspond to approximately 1 % of clipped material. In the lanes of isomer 1, 5, 6, 7, 8 additional bands with more than 100 kDa can be seen which are also present in the standard. These can be assigned to oligomers. Thus SDS-PAGE confirms the results of the SE-HPLC analysis.
- [0053]Overall, RP-HPLC and SDS-PAGE experiments indicate that the purity of the IEC fractions can be considered comparable to the PEG-IFN alpha 2a reference standard.
- [0054]The structure of the PEG-IFN alpha 2a species derived from the 9 IEC-fractions were identified based on the results of the methods described above using the strategy mentioned above.
Example 7 The antiviral activity (AVA)
- [0055]The antiviral activity was estimated by its protective effect on Madin-Darby bovine kidney (MDBK) cells against the infection by vesticular stomatitis virus (VSV) and compared with a PEG-IFN alpha 2a standard. Samples and reference standard were diluted in Eagle’s Minimum Essential Medium (MEM) containing 10 % fetal bovine serum to a final concentration of 10 ng/mL (assay starting concentration). Each sample was assayed in quadruplicate.
- [0056]The antiviral protection of Madin-Darby bovine kidney cells (MDBK) with vesicular stomatitis virus was tested according to the method described in Virol. 1981, 37, 755-758. All isomers induced an activity in the anti-viral assay as presented in Table 2. The activities range between 1061 and 339 U/µg, indicating that the difference in specific activities of the protein in the positional isomers is significant. The know-how and the results generated so far will allow the initiation of further investigations to establish this structure-function relationship between the positional isomers and the IFN alpha receptors. Table 2:In Vitro Antiviral Activities of PEG-IFN alpha 2a and individual PEG-IFN alpha 2a isomers. The Antiviral activity was determined in MDBK cells infected with vesicular stomatitis virus. The results present the averages of three assays performed independently.Antiviral Assay of PEG-IFNPeakU/µgPEG-IFN1061 ± 50Peak 11818 ± 127Peak 21358 ± 46Peak 3761197Peak 4339 ± 33Peak 4a966 ± 107Peak 5600 ± 27Peak 6463 ± 25Peak7513 ± 20Peak 8468 ± 23
- [0057]The results are further illustrated by the following figures
- Figure 1: Analytical IEC-HPLC of 180µg of PEG-IFN alpha 2a. An analytical strong-cation exchange column was used to check the purity of the separated positional isomers from each purification step (TOSOH-BIOSEP, SP-SPW,10 µm particle size, 7.5 mm diameter, 7.5 cm length).
- Figure 2: A/B: SDS-PAGE analysis with Tris-glycine (16%), the samples were electrophoresed under non-reduced conditions. The gels were stained for protein with Silver Stain. Lanes: M, molecular weight marker proteins/ 2, Peak 1/ 3, Peak 2/ 4, Peak 3/ 5, Peak 4/ 6, Peak 4a/ 7, Peak 5/ 8, Peak 6/ 9, Peak 7/10, Peak 8/ 11, Ix PEG-IFN standard/ 12, 1.5x PEG-IFN standard/ C1, IFN standard.
- Figure 3: A/B: SDS-PAGE analysis with Tris-glycine (16%), the samples were electrophoresed under reduced conditions. The gels were stained for protein with Silver Stain. Lanes: M, molecular weight marker proteins/ 2, Peak 1/ 3, Peak 2/ 4, Peak 3/ 5, Peak 4/ 6, Peak 4a/ 7, Peak 5/ 8, Peak 6/ 9, Peak 7/ 10, Peak 8/ 11, 1x PEG-IFN standard/ 12, 1.5x PEG-IFN standard/ C1, IFN standard.
- Figure 4: Size Exclusion (SE-) HPLC was used to determine the amount of oligo PEG-IFN forms and aggregates in the different IEC fractions. SE-HPLC was performed with a TosoHaas TSK gel G 4000 SWXL column (7.8 × 300 mm).
- Figure 5: MALDI-TOF spectrometry was used to determine the molecular weight of each isomer in order to ensure that the PEG-IFN molecules were still intact after IEC chromatography and to confirm the monopegylation.
- Figure 6: MALDI-TOF Lys-C peptide maps of the PEG-IFN reference standard and the peaks 1, 2, 3, 4, 4a, 5, 6, 7, 8. Missing peaks compared to the standard are indicated by arrows.
- Figure 7: RP-HPLC chromatograms of the Lys-C digests of the PEG-IFN reference and peak 4a
- Figure 8: Analytical HPLC of 5-10µg of PEG-IFN alpha 2a mixture of positional isomers on a column charged with SP-NPR, TosoH Bioscience, Particle size: 2.5µm, nonporous as described in Example 1B..
- Figure 9: Ribbon structure of interferon alpha-2a showing the pegylation sites. This is the high resolution structure of human interferon alpha-2a determined with NMR spectroscopy see J. Mol. Biol. 1997, 274, 661-675. The pegylation sites of pegylated interferon alpha-2a are coloured red and labelled with residue type and residue number.
Pegylated interferon alfa-2b, sold under the brand name PegIntron among others, is a medication used to treat hepatitis C and melanoma.[3] For hepatitis C it is typically used with ribavirin and cure rates are between 33 and 82%.[3][4] For melanoma it is used in addition to surgery.[3] It is given by injection under the skin.[3]
Side effects are common.[5] They may include headache, feeling tired, mood changes, trouble sleeping, hair loss, nausea, pain at the site of injection, and fever.[3] Severe side effects may include psychosis, liver problems, blood clots, infections, or an irregular heartbeat.[3] Use with ribavirin is not recommended during pregnancy.[3] Pegylated interferon alfa-2b is in the alpha interferon family of medications.[3] It is pegylated to protect the molecule from breakdown.[5]
Pegylated interferon alfa-2b was approved for medical use in the United States in 2001.[3] It is on the World Health Organization’s List of Essential Medicines.[6]
Peginterferon alfa-2b is a form of recombinant interferon used as part of combination therapy to treat chronic Hepatitis C, an infectious liver disease caused by infection with Hepatitis C Virus (HCV). HCV is a single-stranded RNA virus that is categorized into nine distinct genotypes, with genotype 1 being the most common in the United States, and affecting 72% of all chronic HCV patients 3. Treatment options for chronic Hepatitis C have advanced significantly since 2011, with the development of Direct Acting Antivirals (DAAs) resulting in less use of Peginterferon alfa-2b. Peginterferon alfa-2b is derived from the alfa-2b moeity of recombinant human interferon and acts by binding to human type 1 interferon receptors. Activation and dimerization of this receptor induces the body’s innate antiviral response by activating the janus kinase/signal transducer and activator of transcription (JAK/STAT) pathway. Use of Peginterferon alfa-2b is associated with a wide range of severe adverse effects including the aggravation and development of endocrine and autoimmune disorders, retinopathies, cardiovascular and neuropsychiatric complications, and increased risk of hepatic decompensation in patients with cirrhosis. The use of Peginterferon alfa-2b has largely declined since newer interferon-free antiviral therapies have been developed.
In a joint recommendation published in 2016, the American Association for the Study of Liver Diseases (AASLD) and the Infectious Diseases Society of America (IDSA) no longer recommend Peginterferon alfa-2b for the treatment of Hepatitis C 2. Peginterferon alfa-2b was used alongside Ribavirin(https://go.drugbank.com/drugs/DB00811) with the intent to cure, or achieve a sustained virologic response (SVR), after 48 weeks of therapy. SVR and eradication of HCV infection is associated with significant long-term health benefits including reduced liver-related damage, improved quality of life, reduced incidence of Hepatocellular Carcinoma, and reduced all-cause mortality 1.
Peginterferon alfa-2b is available as a variable dose injectable product (tradename Pegintron) used for the treatment of chronic Hepatitis C. Approved in 2001 by the FDA, Pegintron is indicated for the treatment of HCV with Ribavirin or other antiviral drugs Label. When combined together, Peginterferon alfa-2b and Ribavirin have been shown to achieve a SVR between 41% for genotype 1 and 75% for genotypes 2-6 after 48 weeks of treatment.
Medical uses
It is used to treat hepatitis C and melanoma. For hepatitis C it is typically used with ribavirin. For melanoma it is used in addition to surgery.[3]
For hepatitis C it may also be used with boceprevir, telaprevir, simeprevir, or sofosbuvir.[5]
In India, in 2021, DGCI approved emergency use of Zydus Cadila‘s Virafin in treating moderate COVID-19 infection.[7]
Host genetic factors
For genotype 1 hepatitis C treated with pegylated interferon-alfa-2a or pegylated interferon-alfa-2b combined with ribavirin, it has been shown that genetic polymorphisms near the human IL28B gene, encoding interferon lambda 3, are associated with significant differences in response to the treatment. This finding, originally reported in Nature,[8] showed that genotype 1 hepatitis C patients carrying certain genetic variant alleles near the IL28B gene are more likely to achieve sustained virological response after the treatment than others. A later report from Nature[9] demonstrated that the same genetic variants are also associated with the natural clearance of the genotype 1 hepatitis C virus.
Side effects
Common side effects include headache, feeling tired, mood changes, trouble sleeping, hair loss, nausea, pain at the site of injection, and fever. Severe side effects may include psychosis, liver problems, blood clots, infections, or an irregular heartbeat.[3] Use with ribavirin is not recommended during pregnancy.[3]
Mechanism of action
One of the major mechanisms of PEG-interferon alpha-2b utilizes the JAK-STAT signaling pathway. The basic mechanism works such that PEG-interferon alpha-2b will bind to its receptor, interferon-alpha receptor 1 and 2 (IFNAR1/2). Upon ligand binding the Tyk2 protein associated with IFNAR1 is phosphorylated which in turn phosphorylates Jak1 associated with IFNAR2. This kinase continues its signal transduction by phosphorylation of signal transducer and activator of transcription (STAT) 1 and 2 via Jak 1 and Tyk2 respectively. The phosphorylated STATs then dissociate from the receptor heterodimer and form an interferon transcription factor with p48 and IRF9 to form the interferon stimulate transcription factor-3 (ISGF3). This transcription factor then translocates to the nucleus where it will transcribe several genes involved in cell cycle control, cell differentiation, apoptosis, and immune response.[10][11]
PEG-interferon alpha-2b acts as a multifunctional immunoregulatory cytokine by transcribing several genes, including interleukin 4 (IL4). This cytokine is responsible for inducing T helper cells to become type 2 helper T cells. This ultimately results in the stimulation of B cells to proliferate and increase their antibody production. This ultimately allows for an immune response, as the B cells will help to signal the immune system that a foreign antigen is present.[12]
Another major mechanism of type I interferon alpha (IFNα) is to stimulate apoptosis in malignant cell lines. Previous studies have shown that IFNα can cause cell cycle arrest in U266, Daudi, and Rhek-1 cell lines.[13]
A follow-up study researched to determine if the caspases were involved in the apoptosis seen in the previous study as well as to determine the role of mitochondrial cytochrome c release. The study confirmed that there was cleavage of caspase-3, -8, and -9. All three of these cysteine proteases play an important role in the initiation and activation of the apoptotic cascade. Furthermore, it was shown that IFNα induced a loss in the mitochondrial membrane potential which resulted in the release of cytochrome c from the mitochondria. Follow-up research is currently being conducted to determine the upstream activators of the apoptotic pathway that are induced by IFNα.[14]
History
It was developed by Schering-Plough. Merck studied it for melanoma under the brand name Sylatron. It was approved for this use in April 2011.
References
- ^ “PegIntron- peginterferon alfa-2b injection, powder, lyophilized, for solution PegIntron- peginterferon alfa-2b kit”. DailyMed. Retrieved 28 September 2020.
- ^ “Sylatron- peginterferon alfa-2b kit”. DailyMed. 28 August 2019. Retrieved 28 September 2020.
- ^ Jump up to:a b c d e f g h i j k l “Peginterferon Alfa-2b (Professional Patient Advice) – Drugs.com”. http://www.drugs.com. Archived from the original on 16 January 2017. Retrieved 12 January 2017.
- ^ “ViraferonPeg Pen 50, 80, 100, 120 or 150 micrograms powder and solvent for solution for injection in pre-filled pen CLEAR CLICK – Summary of Product Characteristics (SPC) – (eMC)”. http://www.medicines.org.uk. Archived from the original on 13 January 2017. Retrieved 12 January 2017.
- ^ Jump up to:a b c “Peginterferon alfa-2b (PegIntron)”. Hepatitis C Online. Archived from the original on 23 December 2016. Retrieved 12 January 2017.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ https://www.aninews.in/news/national/general-news/dgci-approves-emergency-use-of-zyduss-virafin-in-treating-moderate-covid-19-infection20210423163622/
- ^ Ge D, Fellay J, Thompson AJ, et al. (2009). “Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance”. Nature. 461 (7262): 399–401. Bibcode:2009Natur.461..399G. doi:10.1038/nature08309. PMID 19684573. S2CID 1707096.
- ^ Thomas DL, Thio CL, Martin MP, et al. (2009). “Genetic variation in IL28B and spontaneous clearance of hepatitis C virus”. Nature. 461 (7265): 798–801. Bibcode:2009Natur.461..798T. doi:10.1038/nature08463. PMC 3172006. PMID 19759533.
- ^ Ward AC, Touw I, Yoshimura A (January 2000). “The JAK-STAT pathway in normal and perturbed hematopoiesis”. Blood. 95 (1): 19–29. doi:10.1182/blood.V95.1.19. PMID 10607680. Archived from the original on 2014-04-26.
- ^ PATHWAYS :: IFN alpha[permanent dead link]
- ^ Thomas H, Foster G, Platis D (February 2004). “Corrigendum toMechanisms of action of interferon and nucleoside analogues J Hepatol 39 (2003) S93–8″. J Hepatol. 40 (2): 364. doi:10.1016/j.jhep.2003.12.003.
- ^ Sangfelt O, Erickson S, Castro J, Heiden T, Einhorn S, Grandér D (March 1997). “Induction of apoptosis and inhibition of cell growth are independent responses to interferon-alpha in hematopoietic cell lines”. Cell Growth Differ. 8 (3): 343–52. PMID 9056677. Archived from the original on 2014-04-26.
- ^ Thyrell L, Erickson S, Zhivotovsky B, et al. (February 2002). “Mechanisms of Interferon-alpha induced apoptosis in malignant cells”. Oncogene. 21 (8): 1251–62. doi:10.1038/sj.onc.1205179. PMID 11850845.
External links
- Peginterferon alfa-2b in the U.S. National Library of Medicine’s Drug Information Portal
- Medicines patent loophole ‘found’ at the BBC, 2007
- PEG-Intron (Peginterferon Alfa-2B) — Platelet Count Decreased from DrugLib.com
///////////Pegylated Interferon alpha-2b, PegIFN, Virafin, COVID 19, CORONA VIRUS, INDIA 2021, APPROVALS 2021
PF-07321332, Nirmatrelvir


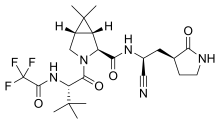
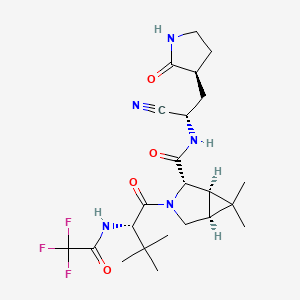
PF-07321332
Nirmatrelvir
UNII-7R9A5P7H32
7R9A5P7H32
PF07321332
CAS 2628280-40-8
C23H32F3N5O4, 499.5
(1R,2S,5S)-N-[(1S)-1-cyano-2-[(3S)-2-oxopyrrolidin-3-yl]ethyl]-3-[(2S)-3,3-dimethyl-2-[(2,2,2-trifluoroacetyl)amino]butanoyl]-6,6-dimethyl-3-azabicyclo[3.1.0]hexane-2-carboxamide
https://clinicaltrials.gov/ct2/show/NCT04756531

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT
SYN
https://pubmed.ncbi.nlm.nih.gov/34726479/
https://www.science.org/doi/10.1126/science.abl4784
Science. 2021 Dec 24;374(6575):1586-1593. doi: 10.1126/science.abl4784. Epub 2021 Nov 2.
An oral SARS-CoV-2 M pro inhibitor clinical candidate for the treatment of COVID-19
file:///C:/Users/Inspiron/Downloads/science.abl4784_sm.pdf
The worldwide outbreak of COVID-19 caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has become a global pandemic. Alongside vaccines, antiviral therapeutics are an important part of the healthcare response to countering the ongoing threat presented by COVID-19. Here, we report the discovery and characterization of PF-07321332, an orally bioavailable SARS-CoV-2 main protease inhibitor with in vitro pan-human coronavirus antiviral activity and excellent off-target selectivity and in vivo safety profiles. PF-07321332 has demonstrated oral activity in a mouse-adapted SARS-CoV-2 model and has achieved oral plasma concentrations exceeding the in vitro antiviral cell potency in a phase 1 clinical trial in healthy human participants.
Synthesis of PF-07321332 (Compound 6): Anhydrous, MTBE solvate form
(1R,2S,5S)-N-{(1S)-1-Cyano-2-[(3S)-2-oxopyrrolidin-3-yl]ethyl}-6,6-dimethyl-3-[3-methyl-N- (trifluoroacetyl)-L-valyl]-3-azabicyclo[3.1.0]hexane-2-carboxamide (1 eq tert-butyl methyl ether solvate) (6, MTBE solvate). This experiment was carried out in 2 parallel batches. Methyl N- (triethylammoniosulfonyl)carbamate, inner salt (Burgess reagent; 69.3 g, 276 mmol) was added to a solution of T18 (61 g, 111 mmol) in dichloromethane (550 ml). After the reaction mixture had been stirred at 25 °C for 1 h. The reaction mixture was quenched by a mixture of saturated aqueous sodium bicarbonate solution (200 ml) and saturated aqueous sodium chloride solution (100 ml). The separated organic phase was concentrated. The resulting residue was dissolved in 50% ethyl acetate/ tert-butyl methyl ether (600 ml), washed by a mixture of saturated aqueous sodium bicarbonate solution (200 ml) and saturated aqueous sodium chloride solution (100 ml) twice, saturated aqueous sodium chloride solution (200 ml), a mixture of HCl (1 M; 200 ml) and saturated aqueous sodium chloride solution (100 ml) twice. The organic layer was then dried over magnesium sulfate, filtered, and concentrated. The residue was treated with a mixture of ethyl acetate and tert-butyl methyl ether (1:10, 400 ml) and heated to 50 °C; after stirring for 1 hour at 50 °C, it was cooled to 25 °C and stirred overnight. The solid was collected via filtration, dissolved in dichloromethane (100 ml) and filtered through silica gel (200 g); the silica gel was then washed with ethyl acetate (1 Liter), 10% methanol in ethyl acetate (2 Liters). The combined eluates were concentrated. The 2 batches were combined, taken up in a mixture of ethyl acetate and tert-butyl methyl ether (5:95, 550 ml). This mixture was heated to 50 °C for 1 h, cooled to 25 °C, and stirred overnight. Filtration afforded 6, MTBE solvate, as a white solid. Yield: 104 g, 75 %. 1H NMR (600 MHz, DMSO-d6) δ 9.43 (d, J = 8.4 Hz, 1H), 9.03 (d, J = 8.6 Hz, 1H), 7.68 (s, 1H), 4.97 (ddd, J = 10.9, 8.6, 5.1 Hz, 1H), 4.41 (d, J = 8.4 Hz, 1H), 4.15 (s, 1H), 3.91 (dd, J = 10.4, 5.5 Hz, 1H), 3.69 (d, J = 10.4 Hz, 1H), 3.17 – 3.11 (m, 1H), 3.07 (s, 3H, MTBE), 3.04 (td, J = 9.4, 7.1 Hz, 1H), 2.40 (tdd, J = 10.4, 8.4, 4.4 Hz, 1H), 2.14 (ddd, J = 13.4, 10.9, 4.4 Hz,
1H), 2.11 – 2.03 (m, 1H), 1.76 – 1.65 (m, 2H), 1.57 (dd, J = 7.6, 5.5 Hz, 1H), 1.32 (d, J = 7.6 Hz, 1H), 1.10 (s, 9H, MTBE), 1.03 (s, 3H), 0.98 (s, 9H), 0.85 (s, 3H). Anal. Calcd for C23H32F3N5O4 .C5H12O: C, 57.23; H, 7.55; N, 11.92. Found: C, 57.08; H, 7.55; N, 11.85. mp = 118.8 oC

cry

Compound 6 (anhydrous MTBE solvate, 200 g, 332.8 mmol, 83.11 mass%) was charged into a reactor with overhead half-moon stirring at 350 rpm. Heptane (1000 ml) was charged, followed by isopropyl acetate (1000 ml) and the stirring was continued at 20 oC overnight. Additional heptane (1000 ml) was charged over 120 minutes. The reaction vessel was then cooled to 10 oC over 30 min and stirred at that temp for 3 days. The solid was filtered, washing with a mixture of isopropyl acetate (80 ml) and heptane (320 ml). It was then dried under vacuum at 50 °C to provide 6, anhydrous ‘Form 1’, as a white crystalline solid. Yield: 160.93 g, 322 mmol, 97%. 1H NMR (600 MHz, DMSO-d6) δ 9.43 (d, J = 8.4 Hz, 1H), 9.03 (d, J = 8.6 Hz, 1H), 7.68 (s, 1H), 4.97 (ddd, J = 10.9, 8.6, 5.1 Hz, 1H), 4.41 (d, J = 8.4 Hz, 1H), 4.15 (s, 1H), 3.91 (dd, J = 10.4, 5.5 Hz, 1H), 3.69 (d, J = 10.4 Hz, 1H), 3.17 – 3.11 (m, 1H), 3.04 (td, J = 9.4, 7.1 Hz, 1H), 2.40 (tdd, J = 10.4, 8.4, 4.4 Hz, 1H), 2.14 (ddd, J = 13.4, 10.9, 4.4 Hz, 1H), 2.11 – 2.03 (m, 1H), 1.76 – 1.65 (m, 2H), 1.57 (dd, J = 7.6, 5.5 Hz, 1H), 1.32 (d, J = 7.6 Hz, 1H), 1.03 (s, 3H), 0.98 (s, 9H), 0.85 (s, 3H). 13C NMR (151 MHz, DMSO-d6) δ 177.50, 170.72, 167.45, 156.95 (q, J = 37.0 Hz), 119.65, 115.84 (q, J = 286.9 Hz), 60.08, 58.19, 47.63, 37.77, 36.72, 34.60, 34.15, 30.28, 27.34, 26.86, 26.26, 25.72, 18.86, 12.34. 19F NMR (376 MHz, DMSO-d6) δ -72.94. HRMS (ESI-TOF) m/z calcd. for C23H33F3N5O4 [M + H]+ 500.2474, found 500.2472. Anal. Calcd for C23H32F3N5O4: C, 55.30; H, 6.46; N, 14.02. Found: C, 55.30; H, 6.49; N, 13.96. mp = 192.9 oC









SYN
Bioorganic & medicinal chemistry letters (2021), 50, 128333.
https://www.sciencedirect.com/science/article/pii/S0960894X21005606
https://pubmed.ncbi.nlm.nih.gov/34418570/
pecific anti-coronaviral drugs complementing available vaccines are urgently needed to fight the COVID-19 pandemic. Given its high conservation across the betacoronavirus genus and dissimilarity to human proteases, the SARS-CoV-2 main protease (Mpro) is an attractive drug target. SARS-CoV-2 Mpro inhibitors have been developed at unprecedented speed, most of them being substrate-derived peptidomimetics with cysteine-modifying warheads. In this study, Mpro has proven resistant towards the identification of high-affinity short substrate-derived peptides and peptidomimetics without warheads. 20 cyclic and linear substrate analogues bearing natural and unnatural residues, which were predicted by computational modelling to bind with high affinity and designed to establish structure-activity relationships, displayed no inhibitory activity at concentrations as high as 100 μM. Only a long linear peptide covering residues P6 to P5‘ displayed moderate inhibition (Ki = 57 µM). Our detailed findings will inform current and future drug discovery campaigns targeting Mpro.
SYN
https://pubmed.ncbi.nlm.nih.gov/34498651/
Chemical communications (Cambridge, England) (2021), 57(72), 9096-9099We present a detailed computational analysis of the binding mode and reactivity of the novel oral inhibitor PF-07321332 developed against the SARS-CoV-2 3CL protease. Alchemical free energy calculations suggest that positions P3 and P4 could be susceptible to improvement in order to get a larger binding strength. QM/MM simulations unveil the reaction mechanism for covalent inhibition, showing that the nitrile warhead facilitates the recruitment of a water molecule for the proton transfer step.
PATENT
WO 2021234668
SYNOral inhibitors of the SARS-CoV-2 main protease for the treatment of COVID-19Owen, D., 261st Am Chem Soc (ACS) Natl Meet · 2021-04-05 Abst 243Synthesis of intermediate : Aminolysis of methyl N-Boc-3-[2-oxopyrrolidin-3(S)-yl]-L-alaninate in the presence of NH3 and subsequent N-deprotection using HCl leads to 2(S)-amino-3-[2-oxopyrrolidin-3(S)-yl]propenamide hydrochloride

Condensation of Boc-L-tert-leucine with methyl (1R,2S,5S)-6,6-dimethyl-3-azabicyclo[3.1.0]hexane-2-carboxylate using HATU gives the corresponding amide, which upon hydrolysis of methyl ester moiety in the presence of LiOH and subsequent N-deprotection by means of HCl affords intermediate,. N-Acylation of amine with ethyl trifluoroacetate yields diamide derivative, which upon condensation with 2(S)-amino-3-[2-oxopyrrolidin-3(S)-yl]propenamide hydrochloride using EDC and HOPO generates compound N-1 STEP. Burgess dehydration of amide derivative furnishes PF-7321332 .
In about November to December 2019 a novel coronavirus was identified as the cause of pneumonia cases in Wuhan (China). It spread, resulting in an epidemic throughout China, and thereafter in other countries throughout the world. In February 2020, the World Health Organization designated the disease COVTD-19, which stands for coronavirus disease 2019. The virus is also known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (1)
COVID-19 is a betacoronavirus in the same subgenus as the severe acute respiratory syndrome (SARS) virus (as well as several bat coronaviruses), but in a different clade. The structure of the receptor- binding gene region is very similar to that of the SARS coronavirus, and the virus has been shown to use the same receptor, the angiotensin converting enzyme 2 (ACE2), for cell entry (2).
In the situation of rapidly increasing cases, inappropriate management of mild cases could increase the burden of healthcare system and medical costs. Viral clearance is a major standard in the assessment of recovery and discharge from medical care, but early results illustrated that the persistence of viral RNA is heterogeneous despite the rapid remission of symptoms and can last over three weeks even in very mild cases. In addition, long hospitalization stays may increase the risk for hospital-associated mental health problems and unexpected hospital-acquired infections. (9)
At the beginning, the outbreak identified an initial association with a seafood market that sold live animals in Wuhan, China. However, as the outbreak progressed, person-to-person spread became the main mode of transmission.
Person to person transmission is thought to occur mainly via respiratory droplets, resembling the spread of influenza. With droplet transmission, the virus is released in respiratory secretions when an infected person breathes, coughs, sneezes, or talks, and can infect another person if such secretions make direct contact with the mucous membranes. Infection can also occur if a person touches an infected surface and then touches his or her eyes, nose, or mouth. Droplets typically do not travel more than six feet (about two meters) and do not linger in the air. There is still controversy about this topic.
Whether SARS-CoV-2 can be transmitted through the airborne route (through particles smaller than droplets that remain in the air over time and distance) under natural conditions has been controversial.
Reflecting the current uncertainty regarding transmission mechanisms, recommendations on airborne precautions in the health care setting vary by location; airborne precautions are universally recommended when aerosol-generating procedures are performed.
It appears that SARS-CoV-2 can be transmitted prior to the development of symptoms and throughout the course of illness. However, most data informing this issue is from studies evaluating viral RNA detection from respiratory and other specimens, and detection of viral RNA does not necessarily indicate the presence of infectious virus.
A study suggested infectiousness started 2.3 days prior to symptom onset, peaked 0.7 days before symptom onset, and declined within seven days; however, most patients were isolated following symptom onset, which would reduce the risk of transmission later in illness regardless of infectiousness. These findings raise the possibility that patients might be more infectious in the earlier stage of infection, but additional data is needed to confirm this hypothesis (3).
How long a person remains infectious is also uncertain. The duration of viral shedding is variable; there appears to be a wide range, which may depend on severity of the illness. In one study of 21 patients with mild illness (no hypoxia), 90 percent had repeated negative viral RNA tests on nasopharyngeal swabs by 10 days after the onset of symptoms; tests were positive for longer in patients with more severe illness (4). In contrast, in another study of 56 patients with mild to moderate illness (none required intensive care), the median duration of viral RNA shedding from nasal or oropharyngeal specimens was 24 days, and the longest was 42 days (5). However, as mentioned above, detectable viral RNA does not always correlate with isolation of infectious virus, and there may be a threshold of viral RNA level below which infectivity is unlikely. In the study of nine patients with mild COVID-19 described above, infectious virus was not detected from respiratory specimens when the viral RNA level was <106 copies/mL (6).
Risk of transmission from an individual with SARS-CoV-2 infection varies by the type and duration of exposure, use of preventive measures, and likely individual factors (e.g., the amount of virus in respiratory secretions).
Antibodies against the virus are induced in those who have become infected. Preliminary evidence suggests that some of these antibodies are protective, but this remains to be definitively established. It is unknown whether all infected patients develop a protective immune response and how long any protective effect will last.
Diagnosis of COVID-19 is made by detection of SARS-CoV-2 RNA by reverse transcription polymerase chain reaction (RT-PCR). Various RT-PCR assays are used around the world; different assays amplify and detect different regions of the SARSCoV-2 genome. Common gene targets include nucleocapsid (N), envelope (E), spike (S), and RNA-dependent RNA polymerase (RdRp), as well as regions in the first open reading frame (7).
Serologic tests detect antibodies to SARS-CoV-2 in the blood, and those that have been adequately validated can help identify patients who have had COVID-19. However, sensitivity and specificity are still not well defined. Detectable antibodies generally take several days to weeks to develop, for example, up to 12 days for IgM and 14 days for IgG(Si-
………………………………..
PF-07321332 (or nirmatrelvir) is an antiviral drug developed by Pfizer which acts as an orally active 3CLprotease inhibitor. The combination of PF-07321332 with ritonavir has been in phase III trials for the treatment of COVID-19 since September 2021[2][3][4] and is expected to be sold under the brand name Paxlovid.[5] After promising results preventing hospitalization and death if given within the first 3 days of symptoms, Pfizer submitted an application to the U.S. Food and Drug Administration (FDA) for emergency authorization for PF-07321332 in combination with ritonavir in November 2021.[6]
PF-07321332 is an azabicyclohexane that is (1R,5S)-3-azabicyclo[3.1.0]hexane substituted by {(1S)-1-cyano-2-[(3S)-2-oxopyrrolidin-3-yl]ethyl}aminoacyl, 3-methyl-N-(trifluoroacetyl)-L-valinamide, methyl and methyl groups at positions 2S, 3, 6 and 6, respectively. It is an inhibitor of SARS-CoV-2 main protease which is currently under clinical development for the treatment of COVID-19. It has a role as an EC 3.4.22.69 (SARS coronavirus main proteinase) inhibitor and an anticoronaviral agent. It is a nitrile, a member of pyrrolidin-2-ones, a secondary carboxamide, a pyrrolidinecarboxamide, a tertiary carboxamide, an organofluorine compound and an azabicyclohexane.
Development
Pharmaceutical
Coronaviral proteases cleave multiple sites in the viral polyprotein, usually after glutamine residues. Early work on related human rhinoviruses showed that the flexible glutamine side chain could be replaced by a rigid pyrrolidone.[7][8] These drugs had been further developed prior to the SARS CoV2 pandemic for other diseases including SARS.[9] The utility of targeting the 3CL protease in a real world setting was first demonstrated in 2018 when GC376 (a prodrug of GC373) was used to treat the previously 100% lethal cat coronavirus disease, feline infectious peritonitis, caused by Feline coronavirus.[10]
The Pfizer drug is an analog of GC373, where the aldehyde covalent cysteine acceptor has been replaced by a nitrile.[11][12]
PF-07321332 was developed by modification of an earlier clinical candidate lufotrelvir,[13][14] which is also a covalent inhibitor but its warhead is a phosphate prodrug of a hydroxyketone. However, lufotrelvir needs to be administered intravenously limiting its use to a hospital setting. Stepwise modification of the tripeptide protein mimetic led to PF-0732133, which is suitable for oral administration.[1] Key changes include a reduction in the number of hydrogen bond donors, and the number of rotatable bonds by introducing the rigid bicyclic non-canonical amino acid, which mimics the leucine residue found in earlier inhibitors. This residue had previously been used in the synthesis of boceprevir.[15]
Clinical
In April 2021, Pfizer began phase I trials.[16] In September 2021, Pfizer began a phase II/III trial.[17] In November 2021, Pfizer announced 89% reduction in hospitalizations of high risk patients studied when given within three days after symptom onset.[5]
On December 14, Pfizer announced that Paxlovid, when given within three days of symptom onset, reduced risk of hospitalization or death by 89% compared to placebo in 2,246 high risk patients studied.[18]
Chemistry and pharmacology
Full details of the synthesis of PF-07321332 were first published by scientists from Pfizer.[1]
In the penultimate step, a synthetic homochiral amino acid is coupled with a homochiral amino amide using the water-soluble carbodiimide EDCI as coupling agent. The resulting intermediate is then treated with Burgess reagent, which dehydrates the amide group to the nitrile of the product.
PF-07321332 is a covalent inhibitor, binding directly to the catalytic cysteine (Cys145) residue of the cysteine protease enzyme.[19]
In the drug combination, ritonavir serves to slow down metabolism of PF-07321332 by cytochrome enzymes to maintain higher circulating concentrations of the main drug.[20]
Public health system reactions to development
Despite not being approved yet in any country, the UK placed an order for 250,000 courses after Pfizer´s press release in October 2021,[21][22] and Australia pre-ordered 500,000 courses of the drug.[23]
As of November 2021, the US government was expected to sign a contract to buy around 10 million courses of the combination treatment.[24][25]
Legal status
In November 2021, Pfizer signed a license agreement with the United Nations–backed Medicines Patent Pool to allow PF-07321332 to be manufactured and sold in 95 countries.[26] Pfizer stated that the agreement will allow local medicine manufacturers to produce the pill “with the goal of facilitating greater access to the global population”. However, the deal excludes several countries with major COVID-19 outbreaks including Brazil, China, Russia, Argentina, and Thailand.[27][28]
On 16 November 2021, Pfizer submitted an application to the U.S. Food and Drug Administration (FDA) for emergency authorization for PF-07321332 in combination with ritonavir.[29][30][31]
Misleading comparison with ivermectin
Conspiracy theorists on the internet have claimed that Paxlovid is merely a “repackaged” version of the antiparasitic drug ivermectin, which has been erroneously promoted as a COVID-19 “miracle cure”. Their claims, sometimes using the nickname “Pfizermectin”,[32] are based on a narrative that Pfizer is suppressing the true benefits of ivermectin and rely on superficial correspondences between the drugs and a misunderstanding of their respective pharmacokinetics.[33] Paxlovid is not structurally related or similar to ivermectin, and while both are 3C-like protease inhibitors, Paxlovid is much more potent with an IC50 around 10,000 times lower, allowing for effective oral dosing within the therapeutic margin.[34]
References
- ^ Jump up to:a b c Owen DR, Allerton CM, Anderson AS, Aschenbrenner L, Avery M, Berritt S, et al. (November 2021). “An oral SARS-CoV-2 Mpro inhibitor clinical candidate for the treatment of COVID-19″. Science: eabl4784. doi:10.1126/science.abl4784. PMID 34726479. S2CID 240422219.
- ^ Vandyck K, Deval J (August 2021). “Considerations for the discovery and development of 3-chymotrypsin-like cysteine protease inhibitors targeting SARS-CoV-2 infection”. Current Opinion in Virology. 49: 36–40. doi:10.1016/j.coviro.2021.04.006. PMC 8075814. PMID 34029993.
- ^ Şimşek-Yavuz S, Komsuoğlu Çelikyurt FI (August 2021). “Antiviral treatment of COVID-19: An update”. Turkish Journal of Medical Sciences. doi:10.3906/sag-2106-250. PMID 34391321. S2CID 237054672.
- ^ Ahmad B, Batool M, Ain QU, Kim MS, Choi S (August 2021). “Exploring the Binding Mechanism of PF-07321332 SARS-CoV-2 Protease Inhibitor through Molecular Dynamics and Binding Free Energy Simulations”. International Journal of Molecular Sciences. 22 (17): 9124. doi:10.3390/ijms22179124. PMC 8430524. PMID 34502033.
- ^ Jump up to:a b “Pfizer’s Novel COVID-19 Oral Antiviral Treatment Candidate Reduced Risk Of Hospitalization Or Death By 89% In Interim Analysis Of Phase 2/3 EPIC-HR Study”. Pfizer Inc. 5 November 2021.
- ^ Mahase E (November 2021). “Covid-19: Pfizer’s paxlovid is 89% effective in patients at risk of serious illness, company reports”. BMJ. 375: n2713. doi:10.1136/bmj.n2713. PMID 34750163. S2CID 243834203.
- ^ Anand K, Ziebuhr J, Wadhwani P, Mesters JR, Hilgenfeld R (June 2003). “Coronavirus Main Proteinase (3CLpro) Structure: Basis for Design of Anti-SARS Drugs”. Science. 300 (5626): 1763–1767. Bibcode:2003Sci…300.1763A. doi:10.1126/science.1085658. PMID 12746549. S2CID 13031405.
- ^ Dragovich PS, Prins TJ, Zhou R, Webber SE, Marakovits JT, Fuhrman SA, et al. (April 1999). “Structure-based design, synthesis, and biological evaluation of irreversible human rhinovirus 3C protease inhibitors. 4. Incorporation of P1 lactam moieties as L-glutamine replacements”. Journal of Medicinal Chemistry. 42 (7): 1213–1224. doi:10.1021/jm9805384. PMID 10197965.
- ^ Pillaiyar T, Manickam M, Namasivayam V, Hayashi Y, Jung SH (July 2016). “An Overview of Severe Acute Respiratory Syndrome-Coronavirus (SARS-CoV) 3CL Protease Inhibitors: Peptidomimetics and Small Molecule Chemotherapy”. Journal of Medicinal Chemistry. 59 (14): 6595–6628. doi:10.1021/acs.jmedchem.5b01461. PMC 7075650. PMID 26878082.
- ^ Pedersen NC, Kim Y, Liu H, Galasiti Kankanamalage AC, Eckstrand C, Groutas WC, et al. (April 2018). “Efficacy of a 3C-like protease inhibitor in treating various forms of acquired feline infectious peritonitis”. Journal of Feline Medicine and Surgery. 20 (4): 378–392. doi:10.1177/1098612X17729626. PMC 5871025. PMID 28901812.
- ^ Halford B (7 April 2021). “Pfizer unveils its oral SARS-CoV-2 inhibitor”. Chemical & Engineering News. 99 (13): 7. doi:10.47287/cen-09913-scicon3. S2CID 234887434.
- ^ Vuong W, Khan MB, Fischer C, Arutyunova E, Lamer T, Shields J, et al. (August 2020). “Feline coronavirus drug inhibits the main protease of SARS-CoV-2 and blocks virus replication”. Nature Communications. 11 (1): 4282. doi:10.1038/s41467-020-18096-2. PMC 7453019. PMID 32855413.
- ^ Clinical trial number NCT04535167 for “First-In-Human Study To Evaluate Safety, Tolerability, And Pharmacokinetics Following Single Ascending And Multiple Ascending Doses of PF-07304814 In Hospitalized Participants With COVID-19 ” at ClinicalTrials.gov
- ^ Boras B, Jones RM, Anson BJ, Arenson D, Aschenbrenner L, Bakowski MA, et al. (February 2021). “Discovery of a Novel Inhibitor of Coronavirus 3CL Protease for the Potential Treatment of COVID-19”. bioRxiv: 2020.09.12.293498. doi:10.1101/2020.09.12.293498. PMC 7491518. PMID 32935104.
- ^ Njoroge FG, Chen KX, Shih NY, Piwinski JJ (January 2008). “Challenges in modern drug discovery: a case study of boceprevir, an HCV protease inhibitor for the treatment of hepatitis C virus infection”. Accounts of Chemical Research. 41 (1): 50–59. doi:10.1021/ar700109k. PMID 18193821. S2CID 2629035.
- ^ Nuki P (26 April 2021). “Pfizer is testing a pill that, if successful, could become first-ever home cure for COVID-19”. National Post. Archived from the original on 27 April 2021.
- ^ “Pfizer begins dosing in Phase II/III trial of antiviral drug for Covid-19”. Clinical Trials Arena. 2 September 2021.
- ^ Press release (14 December 2021). “Pfizer Announces Additional Phase 2/3 Study Results Confirming Robust Efficacy of Novel COVID-19 Oral Antiviral Treatment Candidate in Reducing Risk of Hospitalization or Death”.
- ^ Pavan M, Bolcato G, Bassani D, Sturlese M, Moro S (December 2021). “Supervised Molecular Dynamics (SuMD) Insights into the mechanism of action of SARS-CoV-2 main protease inhibitor PF-07321332”. J Enzyme Inhib Med Chem. 36 (1): 1646–1650. doi:10.1080/14756366.2021.1954919. PMC 8300928. PMID 34289752.
- ^ Woodley M (19 October 2021). “What is Australia’s potential new COVID treatment?”. The Royal Australian College of General Practitioners (RACGP). Retrieved 6 November 2021.
- ^ “Pfizer Covid pill ‘can cut hospitalisations and deaths by nearly 90%'”. The Guardian. 5 November 2021. Retrieved 17 November 2021.
- ^ Mahase E (October 2021). “Covid-19: UK stockpiles two unapproved antiviral drugs for treatment at home”. BMJ. 375: n2602. doi:10.1136/bmj.n2602. PMID 34697079. S2CID 239770104.
- ^ “What are the two new COVID-19 treatments Australia has gained access to?”. ABC News (Australia). 17 October 2021. Retrieved 5 November 2021.
- ^ “U.S. to Buy Enough of Pfizer’s Covid Antiviral Pills for 10 Million People”. The New York Times. 17 November 2021. Retrieved 17 November 2021.
- ^ Pager T, McGinley L, Johnson CY, Taylor A, Parker C. “Biden administration to buy Pfizer antiviral pills for 10 million people, hoping to transform pandemic”. The Washington Post. Retrieved 16 November 2021.
- ^ “Pfizer and The Medicines Patent Pool (MPP) Sign Licensing Agreement for COVID-19 Oral Antiviral Treatment Candidate to Expand Access in Low- and Middle-Income Countries” (Press release). Pfizer. 16 November 2021. Retrieved 17 November 2021 – via Business Wire.
- ^ “Covid-19: Pfizer to allow developing nations to make its treatment pill”. BBC News. 16 November 2021. Archived from the original on 16 November 2021. Retrieved 17 November 2021.
- ^ “Pfizer Will Allow Its Covid Pill to Be Made and Sold Cheaply in Poor Countries”. The New York Times. 16 November 2021. Retrieved 17 November 2021.
- ^ “Pfizer Seeks Emergency Use Authorization for Novel COVID-19 Oral Antiviral Candidate”. Business Wire (Press release). 16 November 2021. Retrieved 17 November 2021.
- ^ Kimball S (16 November 2021). “Pfizer submits FDA application for emergency approval of Covid treatment pill”. CNBC. Retrieved 17 November 2021.
- ^ Robbins R (5 November 2021). “Pfizer Says Its Antiviral Pill Is Highly Effective in Treating Covid”. The New York Times. ISSN 0362-4331. Archived from the original on 8 November 2021. Retrieved 9 November 2021.
- ^ Bloom J (2 December 2021). “How Does Pfizer’s Pavloxid Compare With Ivermectin?”. American Council on Science and Health. Retrieved 12 December 2021.
- ^ Gorski D (15 November 2021). “Pfizer’s new COVID-19 protease inhibitor drug is not just ‘repackaged ivermectin'”. Science-Based Medicine.
- ^ von Csefalvay C (27 November 2021). “Why Paxlovid is not Pfizermectin”. Bits and Bugs. Chris von Csefalvay. Retrieved 28 November 2021.
External links
- “PF-07321332”. Drug Information Portal. U.S. National Library of Medicine.
- “Early Data Suggest Pfizer Pill May Prevent Severe COVID-19”. National Institutes of Health. 16 November 2021.
Pfizer to make COVID-19 pill available in low- and middle-income nations
If authorized by global health authorities, the drug promises to reduce deaths and hospitalizations linked to
the novel coronavirus.
By Brian Buntz | November 16, 2021FacebookTwitterLinkedInShare
In late October, Merck (NYSE:MRK) and its partner Ridgeback Biotherapeutics agreed to make the COVID-19 antiviral molnupiravir available in the developing world.
Now, Pfizer (NYSE:PFE) is taking a similar approach for its investigational antiviral cocktail Paxlovid, which contains PF-07321332 and ritonavir.
Pfizer, like Merck, struck an agreement with the Medicines Patent Pool (MPP) related to Paxlovid.
MPP’s mission is to expand low- and middle-income countries’ access to vital medicines. The United Nations supports the organization.
Pfizer announced earlier this month that Paxlovid was 89% effective in reducing the risk of hospitalization or death in an interim analysis of the Phase 2/3 EPIC-HR trial.
The collaboration with MPP will enable generic drug makers internationally with sub-licenses to produce Paxlovid for use in 95 countries, which comprise more than half of the world’s population.
“This license is so important because, if authorized or approved, this oral drug is particularly well-suited for low- and middle-income countries and could play a critical role in saving lives, contributing to global efforts to fight the current pandemic,” said Charles Gore, executive director of MPP, in a press release. “PF-07321332 is to be taken together with ritonavir, an HIV medicine we know well, as we have had a license on it for many years, and we will be working with generic companies to ensure there is enough supply for both COVID-19 and HIV.”
At present, MPP has signed agreements with ten patient holders for 13 HIV antiretrovirals and several other drugs.
Filed Under: clinical trials, Drug Discovery, Infectious Disease
Tagged With: Medicines Patent Pool, Merck, PF-07321332, Pfizer, Ridgeback Biotherapeutics, ritonavir
PFIZER INITIATES PHASE 1 STUDY OF NOVEL ORAL ANTIVIRAL THERAPEUTIC AGENT AGAINST SARS-COV-2
Tuesday, March 23, 2021 – 11:00am
- In-vitro studies conducted to date show that the clinical candidate PF-07321332 is a potent protease inhibitor with potent anti-viral activity against SARS-CoV-2
- This is the first orally administered coronavirus-specific investigational protease inhibitor to be evaluated in clinical studies, and follows Pfizer’s intravenously administered investigational protease inhibitor, which is currently being evaluated in a Phase 1b multi-dose study in hospitalized clinical trial participants with COVID-19
NEW YORK–(BUSINESS WIRE)– Pfizer Inc. (NYSE: PFE) announced today that it is progressing to multiple ascending doses after completing the dosing of single ascending doses in a Phase 1 study in healthy adults to evaluate the safety and tolerability of an investigational, novel oral antiviral therapeutic for SARS-CoV-2, the virus that causes COVID-19. This Phase 1 trial is being conducted in the United States. The oral antiviral clinical candidate PF-07321332, a SARS-CoV2-3CL protease inhibitor, has demonstrated potent in vitro anti-viral activity against SARS-CoV-2, as well as activity against other coronaviruses, suggesting potential for use in the treatment of COVID-19 as well as potential use to address future coronavirus threats.
“Tackling the COVID-19 pandemic requires both prevention via vaccine and targeted treatment for those who contract the virus. Given the way that SARS-CoV-2 is mutating and the continued global impact of COVID-19, it appears likely that it will be critical to have access to therapeutic options both now and beyond the pandemic,” said Mikael Dolsten, MD, PhD., Chief Scientific Officer and President, Worldwide Research, Development and Medical of Pfizer. “We have designed PF-07321332 as a potential oral therapy that could be prescribed at the first sign of infection, without requiring that patients are hospitalized or in critical care. At the same time, Pfizer’s intravenous antiviral candidate is a potential novel treatment option for hospitalized patients. Together, the two have the potential to create an end to end treatment paradigm that complements vaccination in cases where disease still occurs.”
Protease inhibitors bind to a viral enzyme (called a protease), preventing the virus from replicating in the cell. Protease inhibitors have been effective at treating other viral pathogens such as HIV and hepatitis C virus, both alone and in combination with other antivirals. Currently marketed therapeutics that target viral proteases are not generally associated with toxicity and as such, this class of molecules may potentially provide well-tolerated treatments against COVID-19.
The Phase 1 trial is a randomized, double-blind, sponsor-open, placebo-controlled, single- and multiple-dose escalation study in healthy adults evaluating the safety, tolerability and pharmacokinetics of PF-07321332.
Initiation of this study is supported by preclinical studies that demonstrated the antiviral activity of this potential first-in-class SARS-CoV-2 therapeutic designed specifically to inhibit replication of the SARS-CoV2 virus. The structure of PF-07321332, together with the pre-clinical data, will be shared in a COVID-19 session of the Spring American Chemical Society meeting on April 6.
Pfizer is also investigating an intravenously administered investigational protease inhibitor, PF-07304814, which is currently in a Phase 1b multi-dose trial in hospitalized clinical trial participants with COVID-19.
About Pfizer: Breakthroughs That Change Patients’ Lives
At Pfizer, we apply science and our global resources to bring therapies to people that extend and significantly improve their lives. We strive to set the standard for quality, safety and value in the discovery, development and manufacture of health care products, including innovative medicines and vaccines. Every day, Pfizer colleagues work across developed and emerging markets to advance wellness, prevention, treatments and cures that challenge the most feared diseases of our time. Consistent with our responsibility as one of the world’s premier innovative biopharmaceutical companies, we collaborate with health care providers, governments and local communities to support and expand access to reliable, affordable health care around the world. For more than 170 years, we have worked to make a difference for all who rely on us. We routinely post information that may be important to investors on our website at www.Pfizer.com. In addition, to learn more, please visit us on www.Pfizer.com and follow us on Twitter at @Pfizer and @Pfizer News, LinkedIn, YouTube and like us on Facebook at Facebook.com/Pfizer.
.CLIP
https://cen.acs.org/content/cen/articles/99/i13/Pfizer-unveils-oral-SARS-CoV.html

Drugmaker Pfizer revealed its oral COVID-19 antiviral clinical candidate PF-07321332 on Tuesday at the American Chemical Society Spring 2021 meeting. The compound, which is currently in Phase 1 clinical trials, is the first orally administered compound in the clinic that targets the main protease (also called the 3CL protease) of SARS-CoV-2, the virus that causes COVID-19. By inhibiting the main protease, PF-07321332 prevents the virus from cleaving long protein chains into the parts it needs to reproduce itself. Dafydd Owen, director of medicinal chemistry at Pfizer, presented the compound in a symposium of the Division of Medicinal Chemistry.
Last year, Pfizer reported PF-07304814, a different small molecule inhibitor of SARS-CoV-2’s main protease. The work to develop that compound began during the 2002-2003 outbreak of SARS-CoV, severe acute respiratory syndrome. But that molecule can only be given intravenously, which limits its use to hospital settings.
Because PF-07321332 can be taken orally, as a pill or capsule, it could be given outside of hospitals if it proves to be safe and effective. People who have been exposed to SARS-CoV-2 could take it as a preventative measure, for example.
“For the foreseeable future, we will expect to see continued outbreaks from COVID-19. And therefore, as with all viral pandemics, it’s important we have a full toolbox on how to address it,” Charlotte Allerton, Pfizer’s head of medicine design, told C&EN.
PF-07321332 was developed from scratch during the current pandemic. It’s a reversible covalent inhibitor that reacts with one of the main protease’s cysteine residues. Owen also discussed the chemistry involved in scaling up the compound. The first 7 mg of the compound were synthesized in late July 2020. Encouraged by the early biological data, the Pfizer team aimed to scale up the synthesis. By late October, they’d made 100 g of the compound. Just two weeks later, the chemists had scaled up the synthesis to more than 1 kg. Owen said 210 researchers had worked on the project. Ana Martinez, who studies COVID-19 treatments at the Spanish National Research Council CSIC and also presented during the symposium, told C&EN that having a COVID-19 antiviral is of critical importance. She eagerly anticipates the safety and efficacy data from the trials of PF-07321332. “Hopefully we will have a new drug to fight against COVID-19,” Martinez said. And because the molecule targets the main protease, she said that it might be useful for fighting other coronaviruses and preventing future pandemics.Chemical & Engineering News
| Clinical data | |
|---|---|
| ATC code | None |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 2628280-40-8 |
| PubChem CID | 155903259 |
| UNII | 7R9A5P7H32 |
| KEGG | D12244 |
| ChEBI | CHEBI:170007 |
| Chemical and physical data | |
| Formula | C23H32F3N5O4 |
| Molar mass | 499.535 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| Melting point | 192.9[1] °C (379.2 °F) |
| showSMILES | |
| showInChI |
Xray crystal structure (PDB:7SI9 and 7VH8) of the SARS-CoV-2 protease inhibitor PF-07321332 bound to the viral 3CLpro (Mpro) protease enzyme. Ribbon diagram of the protein with the drug shown as sticks. The catalytic residues (His41, Cys145) are shown as yellow sticks.
./////////////////PF-07321332, PF 07321332, COVID 19, CORONA VIRUS, SARS-CoV-2 inhibitor, PHASE 1, nirmatrelvir, PAXLOVID, CORONA VIRUS, COVID 19
C1N(C([C@@H]2C1[C@]2(C)C)C(=O)N[C@@H](CC3C(NCC3)=O)C#N)C(C([C@@](C)(C)C)NC(=O)C(F)(F)F)=O
C1N(C(C2C1C2(C)C)C(=O)N[C@@H](CC3C(NCC3)=O)C#N)C(C([C@@](C)(C)C)NC(=O)C(F)(F)F)=O

NEW DRUG APPROVALS
ONE TIME
$10.00
Sinovac COVID-19 vaccine, CoronaVac,


Sinovac COVID-19 vaccine, CoronaVac,
- PiCoVacc
CoronaVac, also known as the Sinovac COVID-19 vaccine,[1] is an inactivated virus COVID-19 vaccine developed by the Chinese company Sinovac Biotech.[2] It has been in Phase III clinical trials in Brazil,[3] Chile,[4] Indonesia,[5] the Philippines,[6] and Turkey.[7]
It relies on traditional technology similar to BBIBP-CorV and BBV152, other inactivated-virus COVID-19 vaccines in Phase III trials.[8] CoronaVac does not need to be frozen, and both the vaccine and raw material for formulating the new doses could be transported and refrigerated at 2–8 °C (36–46 °F), temperatures at which flu vaccines are kept.[9]
Brazil announced results on 13 January 2021 showing 50.4% effective at preventing symptomatic infections, 78% effective in preventing mild cases needing treatment, and 100% effective in preventing severe cases.[10] Final Phase III results from Turkey announced on 3 March 2021 showed an efficacy of 83.5%.[11] Interim results in Indonesia were announced on 11 January 2021 with an efficacy of 65.3%.[12] A detailed report containing confidence intervals, efficacy by age and side effects has not yet been released.
CoronaVac is being used in vaccination campaigns by certain countries in Asia,[13][14][15] South America,[16][17][18] North America,[19][20] and Europe.[21] In March, a Sinovac spokesman told Reuters production capacity for CoronaVac could reach 2 billion doses a year by June 2021.[22] As of March 21, 70 million doses of CoronaVac had been administered worldwide.[23
Technology
CoronaVac is an inactivated vaccine. It uses a similar, more traditional technology as in BBIBP-CorV and BBV152, other inactivated-virus vaccines for COVID-19 in Phase III trials.[24][25] CoronaVac does not need to be frozen, and both the vaccine and raw material for formulating the new doses could be transported and refrigerated at 2–8 °C (36–46 °F), temperatures at which flu vaccines are kept.[26] CoronaVac could remain stable for up to three years in storage, which might offer some advantage in vaccine distribution to regions where cold chains are not developed.[27]

NEW DRUG APPROVALS
one time
$10.00
Efficacy

Empty bottle of CoronaVac
On 7 January 2021, results from Phase III trials in Brazil among 13,000 volunteers revealed the vaccine was 78% effective in preventing symptomatic cases of COVID-19 requiring medical assistance (grade 3 on the WHO Clinical Progression Scale[28]) and 100% effective against moderate and severe infections.[29] After mounting pressure from scientists, Butantan said on 12 January that these rates only included volunteers who had mild to severe cases of COVID-19.[30] The overall efficacy, including asymptomatic cases and symptomatic cases not requiring medical assistance (WHO grade 2), was 50.38%.[31] Of the 220 participants infected, 160 cases were in the placebo group and 60 cases in the group that received CoronaVac.[32]
On 3 March 2021, final Phase III results from Turkey showed an efficacy of 83.5%. The final efficacy rate was based on 41 infections, 32 of which had received a placebo, said Murat Akova, head of the Phase III trials in Turkey. He added the vaccine prevented hospitalization and severe illness in 100% of cases, saying six people who were hospitalized were all in the placebo group. The final results were based on a 10,216 participants, 6,648 of whom received the vaccine as part of the Phase III study that began mid-September. Turkey had announced an interim result with 29 infections in December, which placed the efficacy at 91.25%.[33][34]
On 11 January, Indonesia released Phase III results from an interim analysis of 25 cases which showed an efficacy rate of 65.3% based on data of 1,600 participants in the trial.[35] The trial was conducted in the city of Bandung, and it was not clear how Indonesian scientists made their calculations.[30]
Variability in results
Officials said the lowered figure of 50.4% included “very light” cases of COVID-19 among participants omitted in the earlier analysis. Ricardo Palácios, Medical Director of Instituto Butantan said Sinovac’s relatively low efficacy rate of 50% was due to more rigorous standards for what counts as an infection among trial participants. The Institute included six types of cases in its results: asymptomatic, very mild, mild, two levels of moderate, and severe, while western vaccine makers generally included only mild, moderate, and severe categories. Brazil’s trial was also largely made up of frontline health care workers. “They are more exposed to the virus and may explain the relatively low efficacy rate,” said Yanzhong Huang, a senior fellow for global health at the Council on Foreign Relations.[36]
The release of more definitive data on CoronaVac’s efficacy was delayed because Sinovac needed to reconcile results from different trials using varying protocols.[32] According to Instituto Butantan director Dimas Covas, the Brazilian group was considered more vulnerable to infection and exposure to higher viral loads. In Turkish and Indonesian Phase III trials, the composition of volunteers was similar to that of the general population.[37]
COVID-19 variants
On March 10, Instituto Butantan Director Dimas Covas said CoronaVac was efficient against three variants of COVID-19 in the country; British B.1.1.7, South African 501.V2, and Brazil’s P.1, of which are derived variants P.1 from Manaus state, and P.2 from Rio de Janeiro.[38]
CoronaVac and other inactivated virus vaccines have all parts of the virus. Butantan said this may generate a more comprehensive immune response compared to other vaccines using only a part of the spike protein used by COVID-19 to infect cells. Tests run by Butantan used the serum of vaccinated people, which are placed in a cell culture and subsequently infected with the variants. The neutralization consists of determining whether antibodies generated from the vaccine will neutralize the virus in the culture.[38]
Clinical trials
For broader coverage of this topic, see COVID-19 vaccine.
Phase I–II
In a Phase II clinical trial completed in July 2020 and published in The Lancet, CoronaVac showed seroconversion of neutralising antibodies for 109 (92%) of 118 participants in the 3 μg group, 117 (98%) of 119 in the 6 μg group, after the days 0 and 14 schedule; whereas at day 28 after the days 0 and 28 schedule, seroconversion was seen in 114 (97%) of 117 in the 3 μg group, 118 (100%) of 118 in the 6 μg group.[39]
In May, CoronaVac began Phase I–II trials in China on adults over the age 60, and in September CoronaVac began Phase I–II trials in China on children ages 3–17.[40] Phase II results for older adults published in The Lancet showed CoronaVac was safe and well tolerated in older adults, with neutralising antibody induced by a 3 μg dose were similar to those of a 6 μg dose.[41]
Phase III
Latin America
In late July 2020, Sinovac began conducting a Phase III vaccine trial to evaluate efficacy and safety on 9,000 volunteer healthcare professionals in Brazil, collaborating with Butantan Institute.[42][43] On 19 October, São Paulo Governor João Doria said the first results of the clinical study conducted in Brazil proved that among the vaccines being tested in the country, CoronaVac is the safest, the one with the best and most promising immunization rates.[44] On 23 October, São Paulo announced the creation of six new centers for trials of CoronaVac, increasing the number of volunteers in the trials to 13,000.[45]
Brazil briefly paused Phase III trials on 10 November after the suicide of a volunteer before resuming on 11 November. Instituto Butantan said the suicide had no relation to the vaccine trial.[46][47]
In August, a Phase III trial was started in Chile, headed by Pontifical Catholic University of Chile, which was expected to include 3,000 volunteers between the ages of 18 and 65.[48]
Europe
In September, Turkey began Phase III trials with 13,000 volunteers on a two-dose 14-day interval.[49] The monitoring process for CoronaVac is underway at 25 centers in 12 cities across the country.[50]

The Governor of West Java Ridwan Kamil participating in phase 3 trial of the Sinovac COVID-19 vaccine in Indonesia.
Asia
In August, Sinovac began Phase III trials in Indonesia with Bio Farma in Bandung involving 1,620 volunteers.[51] In November, Padjadjaran University Medical School provided an update that the trials were running smoothly and that “at most, they found a slight body fever which disappeared within two days”.[52]
In October, Saudi Arabia signed an agreement with Sinovac to distribute CoronaVac to 7,000 healthcare workers, after conducting Phase III trials with the Saudi Arabian National Guard.[53]
Manufacturing

Brazilian version of CoronaVac, manufactured by Butantan
In March, a Sinovac spokesman told Reuters production capacity for CoronaVac could reach 2 billion doses a year by June. The figure is double the capacity of 1 billion doses in bulk ingredients the firm said it could reach by February.[22]
After Indonesia’s Phase III trials, Bio Farma plans to ramp up production to 250 million doses a year.[54]
On 9 November, São Paulo began building a facility to produce 100 million doses a year.[55] On 10 December, João Doria said Butantan aimed to fill and finish 1 million doses per day on its production line for a vaccination campaign starting 25 January. Doria said 11 Brazilian states have contacted Butantan seeking doses of CoronaVac.[56]
In Malaysia, Pharmaniaga will manufacture, fill, and finish CoronaVac. Pharmaniaga signed a deal to obtain bulk supply of the vaccine as well as technology transfer from Sinovac.[57]
In Egypt, the government was in “advanced stage” discussions with Sinovac to manufacture CoronaVac for local use and export to African countries.[58]
Market and deployment
As of March 21, 70 million doses of CoronaVac had been administered worldwide.[23]
| show Full authorizationshow Emergency authorization Eligible COVAX recipient (assessment in progress)[80] |
South America

São Paulo State Secretary of Health Jean Gorinchteyn (left) and Instituto Butantan chairman Dimas Covas (right) holding single-dose prefilled syringes of CoronaVac, part of the fourth shipment of Sinovac-manufactured vaccine to arrive in Brazil
In Brazil, São Paulo governor João Doria signed a $90 million contract with Sinovac in September to receive the initial 46 million doses of CoronaVac.[81] The price for CoronaVac was announced to be US$10.3 (about R$59).[82] In January, Brazil announced it would obtain 100 million total doses.[83] On 17 January, ANVISA approved emergency use of CoronaVac, with a 54-year-old nurse in São Paulo being the first to receive a vaccine outside of clinical trials in the country.[16] In early February, Brazil said it intends to buy an additional 30 million doses to be produced locally on top of the existing 100 million doses.[84]
In January, Bolivia authorized use of CoronaVac. Butantan Institute had opened negotiations with South American countries to sell the vaccine, which would be produced in São Paulo.[85]
In October, Chile signed an agreement to purchase 20 million doses of CoronaVac[86] which was approved for emergency use on 20 January.[87] By early March, the country had received 10 million doses of CoronaVac and had vaccinated 4.1 million people.[88]
In February, Colombia had purchased 5 million doses of CoronaVac and was in talks for an additional 5 million doses,[89] which had been approved for emergency use on February 5.[90]
In February, Ecuador signed a deal for 2 million doses of CoronaVac which had been approved for emergency use.[91] Chile donated 20,000 doses of CoronaVac to Ecuador on March 6.[92]
In March, Paraguay received a donation of 20,000 doses of CoronaVac from Chile.[92] Paraguay began vaccinations with CoronaVac on March 10.[93]
In January, Uruguay announced the purchased of 1.75 million doses of CoronaVac.[94] The first 192,000 doses arrived on 25 February and vaccinations started on 1 March.[18]
Europe
In March, Albania received 192,000 doses of a first batch of 1 million doses purchased through Turkey.[95]
In November, Turkey signed a contract to buy 50 million doses of CoronaVac.[96] Turkey approved emergency use on 13 January[97] and President Recep Tayyip Erdoğan received his first dose at Ankara City Hospital.[98] In February, Turkey signed a deal for another 50 million doses for a total of 100 million doses.[21] By March 10.7 million doses had been administered, and 852 of the 1.3 million people who had received both doses were later diagnosed with the disease. 53 were hospitalized, but none of those hospitalized were intubated or died.[99]
In December, Ukraine signed a contract to purchase 1.8 million doses of CoronaVac. One dose of CoronaVac would cost 504 hryvnias (around $18).[100] On March 9, Ukraine granted approval for use of CoronaVac.[101]
Asia
On 19 January, Azerbaijan launched its vaccination campaign with CoronaVac. Azerbaijan plans to receive 4 million doses of the vaccine and aims to vaccinate 40% of the population.[102]
In February, Cambodia approved Coronavac[103] for emergency use and later ordered 1.5 million doses to arrive on March 26.[104]
In late August, China approved CoronaVac for emergency use to vaccinate high-risk groups such as medical staff.[105] In early February, China approved CoronaVac for general use.[15]
In December, Hong Kong ordered 7.5 million doses of CoronaVac.[106] The vaccination campaign with CoronaVac began on 26 February.[107]
In August, Indonesia’s Foreign Minister Retno Marsudi said an agreement was signed with Sinovac for 50 million doses,[108] which later increased to 140 million doses.[109] Indonesia approved emergency use authorization on 11 January and[35] President Joko Widodo received the first shot of the vaccine, which would be free for all Indonesian citizens.[13] By March, Indonesia had received 53.5 million doses of CoronaVac.[110]
On 26 January, Malaysia ordered 12 million doses.[57] CoronaVac was approved for emergency use on 2 March.[111] Malaysian Science, Technology and Innovation Minister Khairy Jamaluddin received the first dose with CoronaVac on 18 March as part of the vaccination campaign.[112]
In January, the Philippine’s announced the country had secured 25 million doses.[113] The vaccine was approved on 22 February but not for all health workers as it had lower efficacy when used with health workers compared to healthy individuals aged 18-59. The first 600,000 doses of CoronaVac arrived on 28 February.[114]
Singapore has signed advance purchase agreements for CoronaVac.[115] In February, the first doses arrived in the country.[116]
In early January, Thailand’s Ministry of Public Health announced an order for 2 million doses of CoronaVac,[117] which was approved for emergency use on 22 February.[118] Thailand started its vaccination program on 27 February.[14] In March, Thailand was in talks to purchase an additional 5 million doses.[119]
North America
By March 8, Dominican Republic had vaccinated 400,000 people and had reserved delivery for 10 million additional doses of CoronaVac.[19]
In February, Mexico approved emergency use of CoronaVac.[120] The country has ordered 20 million doses,[121] of which the first 200,000 doses arrived on 20 February.[122] It is currently used as part of the national vaccination campaign.[20]
Africa
In March, Benin received 203,000 doses of CoronaVac with vaccinations to start with health workers and the medically vulnerable.[123]
In March, South Africa’s drug regulator began assessing CoronaVac for use in the country.[124] South African firm Numolux said it could supply 5 million doses once it secured regulatory clearances.[125]
In March, Tunisia’s Ministry of Health approved marketing authorization of CoronaVac in the country.[126]
In March, Zimbabwe approved CoronaVac for emergency use.[127]
Oceania
In March, Fiji said it would be receiving a donation of CoronaVac.[128]
Controversies
Politicization
CoronaVac has been championed by the governor of São Paulo, João Doria, who many believe will challenge Jair Bolsonaro for the presidency in 2022.[129] A political showdown began in October 2020, when Bolsonaro vetoed a deal between the Brazilian health ministry and the São Paulo government for the purchase of 46 million doses of the vaccine.[130] After Instituto Butantan announced CoronaVac’s efficacy rate, Bolsonaro mocked the vaccine’s effectiveness against COVID-19.[131] Critics against the politicization of vaccines have warned that failure to follow international testing and safety protocols risks undermining public trust and can increase people’s hesitancy to inoculation.[129] Doctors in São Paulo said they were struggling to convince patients that CoronaVac would be safe.[132]
In March 2021, the Paraná Pesquisas opinion polling institute found that the vaccines preferred by Brazilians are CoronaVac and the Oxford–AstraZeneca vaccine, chosen by 23.6% and 21.2% of Brazilians interviewed, respectively, against 11.3% of those who would prefer the Pfizer–BioNTech vaccine.[133]
Delays in releasing results
On 23 December 2020, researchers in Brazil said the vaccine was more than 50% effective, but withheld full results at Sinovac’s request, raising questions again about transparency as it was the third delay in releasing results from the trials.[134] São Paulo Health Secretary Jean Gorinchteyn later said the vaccine didn’t reach 90% efficacy. Turkey said its trial showed an estimated efficacy rate of 91.25%, though that was based on only 29 infected cases.[32] When São Paulo state officials announced the protection rate, they declined to provide a more detailed breakdown of the trial, such as information about age groups and side effects of the vaccine.[32] Scientists said the lack of transparency about the data ran the risk of damaging CoronaVac’s credibility, with Brazilians and others world-wide already reluctant to take it.[30] Nikolai Petrovsky, a professor at the College of Medicine and Public Health at Flinders University said, “There is enormous financial and prestige pressure for these trials to massively overstate their results.”[135]
References
- ^ Corum, Jonathan; Zimmer, Carl. “How the Sinovac Vaccine Works”. The New York Times. ISSN 0362-4331. Retrieved 1 March 2021.
- ^ Nidhi Parekh (22 July 2020). “CoronaVac: A COVID-19 Vaccine Made From Inactivated SARS-CoV-2 Virus”. Retrieved 25 July2020.
- ^ “New coronavirus vaccine trials start in Brazil”. AP News. 21 July 2020. Retrieved 7 October 2020.
- ^ “Chile initiates clinical study for COVID-19 vaccine”. Chile Reports. 4 August 2020. Retrieved 7 October 2020.
- ^ “248 volunteers have received Sinovac vaccine injections in Bandung”. Antara News. 30 August 2020. Retrieved 7 October2020.
- ^ “DOH eyes 5 hospitals for Sinovac vaccine Phase 3 clinical trial”. PTV News. 16 September 2020. Retrieved 7 October 2020.
- ^ “Turkey begins phase three trials of Chinese Covid-19 vaccine”. TRT World News. 1 September 2020. Retrieved 7 October 2020.
- ^ Zimmer, Carl; Corum, Jonathan; Wee, Sui-Lee. “Coronavirus Vaccine Tracker”. The New York Times. ISSN 0362-4331. Retrieved 12 February 2021.
- ^ “CoronaVac: Doses will come from China on nine flights and can…” AlKhaleej Today (in Arabic). 1 November 2020. Retrieved 12 February 2021.
- ^ “Sinovac: Brazil results show Chinese vaccine 50.4% effective”. BBC News. 13 January 2021. Retrieved 12 February 2021.
- ^ AGENCIES, DAILY SABAH WITH (25 December 2020). “Turkey set to receive ‘effective’ COVID-19 vaccine amid calls for inoculation”. Daily Sabah. Retrieved 12 February 2021.
- ^ hermesauto (11 January 2021). “Indonesia grants emergency use approval to Sinovac’s vaccine, local trials show 65% efficacy”. The Straits Times. Retrieved 12 February 2021.
- ^ Jump up to:a b TARIGAN, EDNA; MILKO, VICTORIA (13 January 2021). “Indonesia starts mass COVID vaccinations over vast territory”. Associated Press. Retrieved 15 January 2021.
- ^ Jump up to:a b “Thailand Kicks Off Covid-19 Vaccine Program With Sinovac Shots”. Bloomberg.com. Retrieved 28 February 2021.
- ^ Jump up to:a b “China approves Sinovac vaccines for general public use”. South China Morning Post. 6 February 2021. Retrieved 6 February2021.
- ^ Jump up to:a b Fonseca, Jamie McGeever, Pedro (17 January 2021). “Brazil clears emergency use of Sinovac, AstraZeneca vaccines, shots begin”. Reuters. Retrieved 17 January 2021.
- ^ Miranda, Natalia A. Ramos (28 January 2021). “Chile receives two million-dose first delivery of Sinovac COVID-19 vaccine”. Reuters. Retrieved 30 January 2021.
- ^ Jump up to:a b “BNamericas – Uruguay prepares to launch COVID-19 vaccinat…” BNamericas.com. Retrieved 1 March 2021.
- ^ Jump up to:a b “Anticovid vaccines run out as Dominican Republic awaits arrival of more doses”. Dominican Today. Retrieved 10 March2021.
- ^ Jump up to:a b “Venustiano Carranza next up for Covid vaccination in Mexico City”. Mexico News Daily. 15 March 2021. Retrieved 16 March2021.
- ^ Jump up to:a b “Turkey aims to vaccinate 60 percent of population: Minister – Turkey News”. Hürriyet Daily News. Retrieved 12 February 2021.
- ^ Jump up to:a b Liu, Roxanne (3 March 2021). “Sinovac eyes two billion doses in annual capacity of virus vaccine by June”. Reuters. Retrieved 3 March 2021.
- ^ Jump up to:a b Liu, Roxanne (21 March 2021). “China steps up COVID-19 vaccination, considers differentiated visa policies”. Reuters. Retrieved 21 March 2021.
- ^ Tan Y (16 December 2020). “Covid: What do we know about China’s coronavirus vaccines?”. BBC News. Retrieved 18 December 2020.
- ^ Zimmer C, Corum J, Wee SL (10 June 2020). “Coronavirus Vaccine Tracker”. The New York Times. ISSN 0362-4331. Retrieved 27 December 2020.
- ^ “CoronaVac: Doses will come from China on nine flights and can…” AlKhaleej Today (in Arabic). 1 November 2020. Archivedfrom the original on 16 December 2020. Retrieved 1 November2020.
- ^ Staff (7 September 2020). “China’s Sinovac coronavirus vaccine candidate appears safe, slightly weaker in elderly”. Reuters. Archived from the original on 7 October 2020. Retrieved 6 October 2020.
- ^ WHO Working Group on the Clinical Characterisation and Management of COVID-19 infection (2020). “A minimal common outcome measure set for COVID-19 clinical research”. The Lancet Infectious Diseases. 20 (8): e192–e197. doi:10.1016/S1473-3099(20)30483-7. PMC 7292605. PMID 32539990.
- ^ Mariz, Fabiana; Caires, Luiza (7 January 2021). “Eficaz em prevenir doença grave e morte por covid, Coronavac deve ter impacto em frear pandemia”. Jornal da USP (in Portuguese). Retrieved 7 January 2021.
- ^ Jump up to:a b c Pearson, Samantha; Magalhaes, Luciana (12 January 2021). “Chinese Covid-19 Vaccine Is Far Less Effective Than Initially Touted in Brazil”. The Wall Street Journal. Retrieved 12 January2021.
- ^ Gielow, Igor; Lopes Batista, Everton; Bottallo, Ana (12 January 2021). “Coronavac tem eficácia geral de 50,38% no estudo feito pelo Butantan”. Folha de S. Paulo (in Portuguese). Retrieved 12 January 2021.
- ^ Jump up to:a b c d “Sinovac’s Covid Shot Proves 78% Effective in Brazil Trial”. Bloomberg L.P. 7 January 2021. Retrieved 7 January 2021.
- ^ Kucukgocmen, Ali (3 March 2021). “Turkish study revises down Sinovac COVID-19 vaccine efficacy to 83.5%”. Reuters. Retrieved 7 March 2021.
- ^ “China’s Sinovac vaccine efficacy 83.5 percent: Turkish researchers – Turkey News”. Hürriyet Daily News. Retrieved 7 March 2021.
- ^ Jump up to:a b hermesauto (11 January 2021). “Indonesia grants emergency use approval to Sinovac’s vaccine, local trials show 65% efficacy”. The Straits Times. Retrieved 11 January 2021.
- ^ “Why did the efficacy of China’s top vaccine drop from 78% to 50%?”. Fortune. Retrieved 14 January 2021.
- ^ “Coronavac tem eficácia de 78% contra a Covid-19 em estudo no Brasil”. Folha de S.Paulo (in Portuguese). 7 January 2021. Retrieved 7 January 2021.
- ^ Jump up to:a b “Estudos mostram eficácia da CoronaVac contra três variantes do vírus”. Agência Brasil (in Portuguese). 10 March 2021. Retrieved 18 March 2021.
- ^ Zhang Y, Zeng G, Pan H, Li C, Hu Y, Chu K, et al. (November 2020). “Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18–59 years: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial”. The Lancet. Infectious Diseases. 21 (2): 181–192. doi:10.1016/S1473-3099(20)30843-4. PMC 7832443. PMID 33217362. S2CID 227099817. Archived from the original on 16 December 2020. Retrieved 18 November 2020.
- ^ Clinical trial number NCT04551547 for “A Randomized, Double-Blinded, Placebo-Controlled, Phase I/II Clinical Trial, to Evaluate the Safety and Immunogenicity of the SARS-CoV-2 Inactivated Vaccine (Vero Cell) in Healthy Population Aged 3–17 Years” at ClinicalTrials.gov
- ^ Wu, Zhiwei; Hu, Yaling; Xu, Miao; Chen, Zhen; Yang, Wanqi; Jiang, Zhiwei; Li, Minjie; Jin, Hui; Cui, Guoliang; Chen, Panpan; Wang, Lei (3 February 2021). “Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine (CoronaVac) in healthy adults aged 60 years and older: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial”. The Lancet Infectious Diseases. 0. doi:10.1016/S1473-3099(20)30987-7. ISSN 1473-3099. PMC 7906628. PMID 33548194.
- ^ Savarese M (21 July 2020). “New coronavirus vaccine trials start in Brazil”. Associated Press. Archived from the original on 13 August 2020. Retrieved 15 August 2020.
- ^ Palacios R, Patiño EG, de Oliveira Piorelli R, Conde MT, Batista AP, Zeng G, et al. (October 2020). “Double-Blind, Randomized, Placebo-Controlled Phase III Clinical Trial to Evaluate the Efficacy and Safety of treating Healthcare Professionals with the Adsorbed COVID-19 (Inactivated) Vaccine Manufactured by Sinovac – PROFISCOV: A structured summary of a study protocol for a randomised controlled trial”. Trials. 21 (1): 853. doi:10.1186/s13063-020-04775-4. PMC 7558252. PMID 33059771. Archived from the original on 16 December 2020. Retrieved 28 October 2020.
- ^ “World’s vaccine testing ground deems Chinese COVID candidate ‘the safest, most promising'”. Fortune. Archived from the original on 31 October 2020. Retrieved 9 November 2020.
- ^ “Doria says it guarantees purchase of 100 million doses of CoronaVac…” AlKhaleej Today (in Arabic). 29 October 2020. Archived from the original on 1 November 2020. Retrieved 30 October 2020.
- ^ “Brazil Clears Sinovac Trial to Resume Two Days After Halting It”. Bloomberg L.P. 11 November 2020. Archived from the original on 11 November 2020. Retrieved 11 November 2020.
- ^ “Brazil’s health regulator says China’s Sinovac can resume Covid-19 vaccine trial after suspension”. CNBC. 12 November 2020. Archived from the original on 13 November 2020. Retrieved 17 November 2020.
- ^ “Chile initiates clinical study for COVID-19 vaccine”. Government of Chile. 4 August 2020. Archived from the original on 11 October 2020. Retrieved 28 August 2020.
- ^ Health Institutes of Turkey (8 October 2020). “Randomized, Double-Blind, Placebo-Controlled Phase III Clinical Trial For Evaluation of Efficacy and Safety of SARS-CoV-2 Vaccine (Vero Cell), Inactivated”. ClinicalTrials. Archived from the original on 20 October 2020. Retrieved 21 October 2020.
- ^ “Chinese COVID-19 vaccine to be free, 1st doses to be delivered soon: Turkey’s health minister”. Daily Sabah. 23 November 2020. Archived from the original on 23 November 2020. Retrieved 23 November 2020.
- ^ “248 volunteers have received Sinovac vaccine injections in Bandung”. Antara News. Archived from the original on 30 September 2020. Retrieved 22 September 2020.
- ^ antaranews.com. “Phase 3 Sinovac clinical trial running smoothly: research team”. Antara News. Archived from the original on 3 November 2020. Retrieved 3 November 2020.
- ^ “Virus vaccine waiting on Saudi ‘green light'”. Arab News. 31 October 2020. Archived from the original on 16 December 2020. Retrieved 1 November 2020.
- ^ hermesauto (12 October 2020). “Indonesia aims to start administering coronavirus vaccines in early November”. The Straits Times. Archived from the original on 13 October 2020. Retrieved 12 October 2020.
- ^ “Sao Paulo starts building production plant for China’s Sinovac vaccine – governor”. Financial Post. Archived from the original on 29 November 2020. Retrieved 9 November 2020.
- ^ Mano A, Simões (10 December 2020). “Chinese vaccine draws demand across Latin America, say Brazilian officials”. Reuters. Archived from the original on 10 December 2020. Retrieved 10 December 2020.
- ^ Jump up to:a b Choong, Jerry (26 January 2021). “Health Ministry: Malaysia secures 18.4 million doses of Russian, Chinese Covid-19 vaccines”. The Malay Mail. Retrieved 26 January 2021.
- ^ Mourad, Mahmoud (22 March 2021). “Egypt aims for deal to produce Sinovac COVID-19 vaccines”. Reuters. Retrieved 22 March 2021.
- ^ Jump up to:a b c Liu R (6 February 2021). “China approves Sinovac Biotech COVID-19 vaccine for general public use”. Reuters. Retrieved 7 February 2021.
- ^ Sipalan, Joseph; Donovan, Kirsten (3 March 2021). “Malaysia approves Sinovac, AstraZeneca COVID-19 vaccines for use”. Reuters. Retrieved 7 March 2021.
- ^ Aliyev J. “Azerbaijan kicks off COVID-19 vaccination”. Anadolu Agency. Retrieved 7 February 2021.
- ^ “Bolívia autoriza uso de vacinas Sputnik V e CoronaVac contra covid-19”. noticias.uol.com.br (in Portuguese). Retrieved 6 January 2021.
- ^ McGeever J, Fonseca P (17 January 2021). “Brazil clears emergency use of Sinovac, AstraZeneca vaccines, shots begin”. Reuters. Retrieved 17 January 2021.
- ^ Chanritheara, Torn. “Cambodia Approves AstraZeneca and Sinovac Vaccines for COVID-19 Emergency Use”. Cambodianess. Retrieved 12 February 2021.
- ^ “Chile aprueba el uso de emergencia de la vacuna china de Sinovac contra covid-19”. France 24. 20 January 2021. Retrieved 30 January 2021.
- ^ Aliyev J. “Colombia approves emergency use of CoronaVac vaccine”. Anadolu Agency. Retrieved 7 February 2021.
- ^ “Anticovid vaccines run out as Dominican Republic awaits arrival of more doses”. DominicanToday. Retrieved 10 March 2021.
- ^ “Ecuador signs agreement with Sinovac for 2 million COVID-19 vaccine: minister”. National Post. Retrieved 26 February 2021.
- ^ “Use of Sinovac vaccine authorised”. Government of Hong Kong. 18 February 2021. Retrieved 19 February 2021.
- ^ Soeriaatmadja W (11 January 2021). “Indonesia grants emergency use approval to Sinovac’s vaccine, local trials show 65% efficacy”. The Straits Times. Retrieved 11 January 2021.
- ^ “BPOM Grants Emergency Use Authorization for Sinovac Vaccine”. Tempo. 11 January 2021. Retrieved 11 January 2021.
- ^ Barrera, Adriana (11 February 2021). “Mexico approves China’s CanSino and Sinovac COVID-19 vaccines”. Reuters. Retrieved 11 February 2021.
- ^ “CoronaVac, vacuna de alta eficacia”. Ministerio de Salud Publica Y Bienestar Social.
- ^ “Philippines approves Sinovac’s COVID-19 vaccine for emergency use”. Reuters. 22 February 2021.
- ^ Thepgumpanat, Panarat (22 February 2021). “Thailand allows emergency use of Sinovac’s COVID-19 vaccine”. Reuters. Retrieved 23 February 2021.
- ^ “Tunisia approva vaccino cinese Sinovac” (in Italian). Agenzia Nazionale Stampa Associata (in Italian). 5 March 2021. Retrieved 7 March 2021.
- ^ “Turkey to begin COVID-19 vaccine jabs by this weekend”. Anadolu. 11 January 2021. Retrieved 11 January 2021.
- ^ Zinets, Natalia (9 March 2021). “Ukraine approves China’s Sinovac COVID-19 vaccine”. Reuters. Retrieved 10 March 2021.
- ^ “Covid-19: Zimbabwe authorises Sputnik V, Sinovac vaccines for emergency use”. news24.com. 9 March 2021.
- ^ “Regulation and Prequalification”. World Health Organization. Retrieved 12 March 2021.
- ^ Simoes E (30 September 2020). “Brazil’s Sao Paulo signs agreement with Sinovac for COVID vaccine doses”. Reuters. Archived from the original on 1 October 2020. Retrieved 1 October 2020.
- ^ Fonseca I (30 October 2020). “CoronaVac May Be Four Times More Costly Than Flu Vaccine”. The Rio Times. Archived from the original on 3 November 2020. Retrieved 30 October 2020.
- ^ “Em meio a críticas por atrasos, Pazuello diz que Brasil está preparado para iniciar vacinação em janeiro”. Folha de S.Paulo(in Portuguese). 6 January 2021. Retrieved 7 January 2021.
- ^ Rochabrun, Marcelo. “Brazil health ministry says plans to order 30 million more Coronavac doses | The Chronicle Herald”. http://www.thechronicleherald.ca. Retrieved 26 February 2021.
- ^ “Bolívia autoriza uso de vacinas Sputnik V e CoronaVac contra covid-19”. noticias.uol.com.br (in Portuguese). Retrieved 7 January 2021.
- ^ “Government meets with Sinovac for first COVID-19 vaccine clinical trial in Chile”. Government of Chile. 13 October 2020. Archived from the original on 17 October 2020. Retrieved 8 November 2020.
- ^ Presse, AFP-Agence France. “Chile Approves Chinese Coronavirus Vaccine”. barrons.com. Retrieved 21 January 2021.
- ^ “Fifth shipment with over two million Sinovac vaccines arrives to Chile”. Chile Reports. Retrieved 12 March 2021.
- ^ “Colombia extends health state of emergency, seeks more Sinovac vaccines”. Reuters. Retrieved 26 February 2021.
- ^ MENAFN. “Colombia declares emergency use of Sinovac vaccines”. menafn.com. Retrieved 4 February 2021.
- ^ “Ecuador signs agreement with Sinovac for 2 million COVID-19 vaccine: minister”. nationalpost. Retrieved 26 February 2021.
- ^ Jump up to:a b Valencia, Alexandra (7 March 2021). “Chile donates 40,000 doses of Sinovac vaccine to Ecuador and Paraguay”. Reuters. Retrieved 7 March 2021.
- ^ “CoronaVac, vacuna de alta eficacia”. Ministerio de Salud Publica Y Bienestar Social.
- ^ “Uruguay will receive first batches of Pfizer and Sinovac vaccines late February or early March: US$ 120 million investment”. MercoPress. Retrieved 24 January 2021.
- ^ “Albania gets 192,000 doses of Chinese Sinovac vaccine”. CNA. Retrieved 25 March 2021.
- ^ “Turkey signs 50 million dose COVID-19 vaccine deal, health minister says”. Reuters. 25 November 2020. Archived from the original on 1 December 2020. Retrieved 27 November 2020.
- ^ “Turkey grants emergency authorization to Sinovac’s CoronaVac: Anadolu”. Reuters. 13 January 2021. Retrieved 15 January 2021.
- ^ “Turkish president gets COVID-19 vaccine”. Anadolu Agency. 14 January 2021. Retrieved 20 January 2021.
- ^ SABAH, DAILY (12 March 2021). “Few virus infections reported among vaccinated people in Turkey”. Daily Sabah. Retrieved 12 March 2021.
- ^ “Ukraine signs up for China’s Sinovac vaccine, with doses expected soon”. Reuters. 30 December 2020. Retrieved 30 December 2020.
- ^ Zinets, Natalia (9 March 2021). “Ukraine approves China’s Sinovac COVID-19 vaccine”. Reuters. Retrieved 9 March 2021.
- ^ Aliyev, Jeyhun (19 January 2021). “Azerbaijan kicks off COVID-19 vaccination”. Anadolu Agency.
- ^ “Cambodian PM okays two more Covid-19 vaccines – Sinovac and AstraZeneca – for emergency use | The Star”. http://www.thestar.com.my. Retrieved 19 March 2021.
- ^ “Have no fear about shortage of vaccines, 1.5 million doses of Sinovac arriving on March 26”. Khmer Times. 19 March 2021. Retrieved 19 March 2021.
- ^ “Sinovac’s coronavirus vaccine candidate approved for emergency use in China – source”. Reuters. 29 August 2020. Archived from the original on 31 August 2020. Retrieved 30 August 2020.
- ^ “Government announces latest development of COVID-19 vaccine procurement” Archived 11 December 2020 at the Wayback Machine (Hong Kong Government Press Releases, 12 December 2020)
- ^ “Hong Kong kicks off COVID-19 vaccinations with Sinovac jab”. AP NEWS. 26 February 2021. Retrieved 7 March 2021.
- ^ “Indonesia books 50 million coronavirus vaccine doses from Sinovac”. Reuters. 21 August 2020. Archived from the original on 29 August 2020. Retrieved 21 August 2020.
- ^ “Sinovac vaccine has no critical side effects, BPOM says”. The Jakarta Post. Retrieved 21 December 2020.
- ^ Arkyasa, Mahinda (25 March 2021). “16 Million Sinovac Vaccines Material Arrives in Indonesia”. Tempo. Retrieved 25 March 2021.
- ^ “Malaysia’s NPRA Approves AstraZeneca, Sinovac Covid-19 Vaccines”. CodeBlue. 2 March 2021. Retrieved 2 March 2021.
- ^ Babulal, Veena (18 March 2021). “KJ gets first dose of Sinovac vaccine [NSTTV] | New Straits Times”. NST Online. Retrieved 19 March 2021.
- ^ “Duque says deal sealed for 25M doses of Sinovac COVID-19 vaccine”. GMA News Online. Retrieved 10 January 2021.
- ^ “Philippines receives COVID-19 vaccine after delays”. AP NEWS. 28 February 2021. Retrieved 28 February 2021.
- ^ Chen F (24 December 2020). “Brazil joins ranks of Chinese vaccine backers”. Asia Times Online. Retrieved 30 December2020.
- ^ “Singapore receives China’s Sinovac vaccine ahead of approval”. The Star. 25 February 2021. Retrieved 26 February2021.
- ^ “Thailand to get 2 million shots of China’s Sinovac”. Bangkok Post. Bangkok Post Public Company. Retrieved 4 January 2021.
- ^ “Thailand gives emergency use authorisation for Sinovac’s COVID-19 vaccine – official”. Reuters. 22 February 2021. Retrieved 23 February 2021.
- ^ Limited, Bangkok Post Public Company. “Thailand in talks to buy another 5m Sinovac shots”. Bangkok Post. Retrieved 20 March2021.
- ^ “Mexico approves China’s CanSino and Sinovac COVID-19 vaccines”. Reuters. 11 February 2021. Retrieved 11 February2021.
- ^ Jorgic, Drazen (10 March 2021). “Mexico leans on China after Biden rules out vaccines sharing in short term”. Reuters. Retrieved 10 March 2021.
- ^ Exteriores, Secretaría de Relaciones. “The Mexican Government receives 200,000 Sinovac COVID-19 vaccines”. gob.mx (in Spanish). Retrieved 7 March 2021.
- ^ “Lutte contre la Covid-19 : 203.000 doses de vaccins s dont 100.000 offertes par la Chine au Bénin”. Concentrées d’informations sur le Bénin et le monde à votre service depuis 2009(in French). 23 March 2021. Retrieved 25 March 2021.
- ^ Winning, Alexander. “South Africa’s drugs regulator to start assessing Sinovac COVID-19 vaccine”. U.S. Retrieved 12 March2021.
- ^ Nijini, Felix (18 March 2021). “Sinovac May Supply South Africa With 5 Million Vaccines: Report – BNN Bloomberg”. BNN. Retrieved 19 March 2021.
- ^ “Covid: Tunisia approva vaccino cinese Sinovac”. Agenzia Nazionale Stampa Associata (in Italian). 5 March 2021. Retrieved 7 March 2021.
- ^ Dzirutwe, MacDonald (10 March 2021). “Zimbabwe authorises Sputnik V, Sinovac coronavirus vaccines for emergency use”. Reuters. Retrieved 13 March 2021.
- ^ “China to donate Sinovac Vaccine to Fiji”. Fiji Broadcasting Corporation. Retrieved 17 March 2021.
- ^ Jump up to:a b Phillips, Tom (10 November 2020). “Jair Bolsonaro claims ‘victory’ after suspension of Chinese vaccine trial”. The Guardian. Retrieved 18 January 2021.
- ^ Baptista, Eduardo (11 December 2020). “China-made coronavirus vaccine at heart of political showdown in Brazil”. South China Morning Post. Retrieved 18 January 2021.
- ^ Carvalho, Daniel (14 January 2021). “‘Is 50% Good?’, Asks Bolsonaro, Mocking Coronavac’s Effectiveness”. Folha de S.Paulo. Retrieved 18 January 2021.
- ^ Pearson, Samantha; Magalhaes, Luciana (10 November 2020). “Brazil’s Medical Experts Worry Politics Is Hampering Covid-19 Vaccine Progress”. The Wall Street Journal. Retrieved 18 January 2021.
- ^ “Covid: 70% dos brasileiros não fazem questão de escolher vacina” [Covid: 70% of Brazilians do not make a point of choosing vaccine]. R7.com (in Portuguese). 3 March 2021. Retrieved 9 March2021.
- ^ Fonseca P. “Brazil institute says CoronaVac efficacy above 50%, but delays full results”. Reuters. Retrieved 25 December 2020.
- ^ Hong, Jinshan (12 January 2021). “How Effective Is China’s Sinovac Vaccine? Data Confuse Experts”. Bloomberg News. Retrieved 12 January 2021.
External links
- Clinical Research Protocol for CoronaVac Phase III Trials in Brazil
- Clinical Research Protocol for CoronaVac Phase III Trials in Chile
- “How the Sinovac Covid-19 Vaccine Works”. The New York Times.
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | Inactivated |
| Clinical data | |
| Routes of administration | Intramuscular injection |
| ATC code | None |
| Legal status | |
| Legal status | Emergency authorization for use in China, Indonesia, Brazil and Turkey |
| Identifiers | |
| DrugBank | DB15806 |
| Part of a series on the |
| COVID-19 pandemic |
|---|
| SARS-CoV-2 (virus)COVID-19 (disease) |
| showTimeline |
| showLocations |
| showInternational response |
| showMedical response |
| showImpact |
| COVID-19 Portal |
| vte |
Sinovac Biotech Ltd. (Chinese: 北京科兴生物制品有限公司, Nasdaq: SVA) is a Chinese biopharmaceutical company that focuses on the research, development, manufacture and commercialization of vaccines that protect against human infectious diseases. The company is based in Haidian District, Beijing.[2] The company is listed on the NASDAQ but the exchange halted Sinovac’s trading in February 2019 due to a proxy fight.[3][4]
Vaccines
Sinovac’s commercialized vaccines include Healive (hepatitis A), Bilive (combined hepatitis A and B), Anflu (influenza), Panflu (H5N1) and PANFLU.1 (H1N1). Sinovac is currently developing a Universal Pandemic Influenza vaccine and a Japanese encephalitis vaccine.[5][better source needed]
Sinovac is also developing vaccines for enterovirus 71 and human rabies. Its wholly owned subsidiary, Tangshan Yian, is conducting field trials for independently developed inactivated animal rabies vaccines.[citation needed]
COVID-19 vaccine development
Main article: CoronaVac
CoronaVac is an inactivated virus COVID-19 vaccine developed by Sinovac.[6] It has been in Phase III clinical trials in Brazil,[7] Chile,[8] Indonesia,[9] Malaysia,[10] Philippines,[11] and Turkey.[12]
It relies on traditional technology similar to BBIBP-CorV and BBV152, other inactivated-virus COVID-19 vaccines in Phase III trials.[13] CoronaVac does not need to be frozen, and both the vaccine and raw material for formulating the new doses could be transported and refrigerated at 2–8 °C (36–46 °F), temperatures at which flu vaccines are kept.[14]
Brazil announced results on January 13, 2021 showing 50.4% effective at preventing symptomatic infections, 78% effective in preventing mild cases needing treatment, and 100% effective in preventing severe cases.[15] Final Phase III results from Turkey announced on 3 March 2021 showed an efficacy of 83.5%.[16] Interim results in Indonesia were announced on 11 January 2021 with an efficacy of 65.3%.[17]
CoronaVac is being used in vaccination campaigns by certain countries in Asia,[18][19][20] South America,[21][22] and Europe.[23] In March, a Sinovac spokesman told Reuters production capacity for CoronaVac could reach 2 billion doses a year by June 2021.[24] As of 27 February 36 million doses had been administered in total.[25]
See also
References
- ^ “China’s Vaccine Front-Runner Aims to Beat Covid the Old-Fashioned Way”. Bloomberg. 24 August 2020.
- ^ “Home (English)”. Sinovac. Retrieved 2021-03-06.
Add: No. 39 Shangdi Xi Road, Haidian District, Beijing, P.R.C. 100085
– Chinese address: “地址:中国· 北京 海淀区上地西路39号北大生物城(100085)” - ^ Dou, Eva (December 4, 2020). “As China nears a coronavirus vaccine, bribery cloud hangs over drugmaker Sinovac”. The Washington Post. ISSN 0190-8286. Archived from the original on December 4, 2020. Retrieved 2020-12-06.
- ^ Levine, Matt (May 22, 2020). “A Vaccine With a Poison Pill”. Bloomberg News. Archived from the original on June 21, 2020. Retrieved December 6, 2020.
- ^ Google Finance, url=https://www.google.com/finance?q=Sinovac
- ^ Nidhi Parekh (22 July 2020). “CoronaVac: A COVID-19 Vaccine Made From Inactivated SARS-CoV-2 Virus”. Retrieved 25 July2020.
- ^ “New coronavirus vaccine trials start in Brazil”. AP News. 21 July 2020. Retrieved 2020-10-07.
- ^ “Chile initiates clinical study for COVID-19 vaccine”. Chile Reports. 4 August 2020. Retrieved 2020-10-07.
- ^ “248 volunteers have received Sinovac vaccine injections in Bandung”. Antara News. 30 August 2020. Retrieved 2020-10-07.
- ^ “Malaysia Receives China’s Sinovac Vaccine For Regulatory Testing”. Bloomberg.com. 2021-02-27. Retrieved 2021-03-02.
- ^ “DOH eyes 5 hospitals for Sinovac vaccine Phase 3 clinical trial”. PTV News. 16 September 2020. Retrieved 2020-10-07.
- ^ “Turkey begins phase three trials of Chinese Covid-19 vaccine”. TRT World News. 1 September 2020. Retrieved 2020-10-07.
- ^ Zimmer, Carl; Corum, Jonathan; Wee, Sui-Lee. “Coronavirus Vaccine Tracker”. The New York Times. ISSN 0362-4331. Retrieved 2021-02-12.
- ^ “CoronaVac: Doses will come from China on nine flights and can…” AlKhaleej Today (in Arabic). 2020-11-01. Retrieved 2021-02-12.
- ^ “Sinovac: Brazil results show Chinese vaccine 50.4% effective”. BBC News. 2021-01-13. Retrieved 2021-02-12.
- ^ AGENCIES, DAILY SABAH WITH (25 December 2020). “Turkey set to receive ‘effective’ COVID-19 vaccine amid calls for inoculation”. Daily Sabah. Retrieved 12 February 2021.
- ^ hermesauto (11 January 2021). “Indonesia grants emergency use approval to Sinovac’s vaccine, local trials show 65% efficacy”. The Straits Times. Retrieved 12 February 2021.
- ^ TARIGAN, EDNA; MILKO, VICTORIA (13 January 2021). “Indonesia starts mass COVID vaccinations over vast territory”. Associated Press. Retrieved 15 January 2021.
- ^ Aliyev, Jeyhun (19 January 2021). “Azerbaijan kicks off COVID-19 vaccination”. Anadolu Agency.
- ^ “China approves Sinovac vaccines for general public use”. South China Morning Post. 6 February 2021. Retrieved 6 February2021.
- ^ Fonseca, Jamie McGeever, Pedro (17 January 2021). “Brazil clears emergency use of Sinovac, AstraZeneca vaccines, shots begin”. Reuters. Retrieved 17 January 2021.
- ^ Miranda, Natalia A. Ramos (28 January 2021). “Chile receives two million-dose first delivery of Sinovac COVID-19 vaccine”. Reuters. Retrieved 30 January 2021.
- ^ “Turkey aims to vaccinate 60 percent of population: Minister – Turkey News”. Hürriyet Daily News. Retrieved 12 February 2021.
- ^ Liu, Roxanne (2021-03-03). “Sinovac eyes two billion doses in annual capacity of virus vaccine by June”. Reuters. Retrieved 2021-03-03.
- ^ “Malaysia receives first batch of Sinovac Covid-19 vaccine today”. Bernama. 27 February 2021. Retrieved 27 February 2021– via The Malay Mail.
External links
- Official website
- Business data for Sinovac Biotech:
| Type | Public |
|---|---|
| Traded as | Nasdaq: SVA (American Depository Receipts) |
| Founded | 1999; 22 years ago |
| Founder | Yin Weidong[1] |
| Headquarters | Beijing,China |
| Website | http://www.sinovac.com/ |
| Sinovac Biotech | |
|---|---|
| Simplified Chinese | 北京科兴生物制品有限公司 |
| Traditional Chinese | 北京科興生物製品有限公司 |
| hideTranscriptionsStandard MandarinHanyu PinyinBěijīng Kē Xìng Shēngwù Zhìpǐn Yǒuxiàn Gōngsī |
/////////Sinovac COVID-19 vaccine, CoronaVac, corona virus, covid 19, vaccine, china, Sinovac Biotech, PiCoVacc
#Sinovac COVID-19 vaccine, #CoronaVac, #corona virus, #covid 19, #vaccine, #china, #Sinovac Biotech, #PiCoVacc
Sputnik V, Gam-COVID-Vac, Gamaleya

Sputnik V
Gam-COVID-Vac
Gamaleya
- Gam-COVID-Vac Lyo

Gam-COVID-Vac was created by Gamaleya Research Institute of Epidemiology and MIcrobiology in Russia. The vaccine candidate is a heterologous COVID-19 vaccine containing two components, recombinant adenovirus type 26 (rAd26) vector and recombinant adenovirus type 5 (rAd5) vector which both carry the SARS-CoV-2 spike glycoprotein. The vaccine is offered in both a frozen (Gam-COVID-Vac) and freeze-dried formulation (lyophilizate; Gam-COVID-Vac Lyo). Phase 1/2 human trials with 76 participants evaluated the safety, tolerability, and immunogenicity of both frozen (Gam-COVID-Vac;NCT04436471) and freeze-dried (Gam-COVID-Vac Lyo;NCT04437875) vaccine candidates in June 2020, and were completed in early August 2020. Preliminary results suggested that all participants developed antibodies to the SARS-CoV-2 glycoproteins with a good safety profile in both trials.
Sputnik V (Russian: Спутник V, literally Traveler V) is a COVID-19 vaccine developed by the Gamaleya Research Institute of Epidemiology and Microbiology. Registered on 11 August 2020 by the Russian Ministry of Health as Gam-COVID-Vac (Russian: Гам-КОВИД-Вак, romanized: Gam-KOVID-Vak),[2][3] Sputnik V is an adenovirus viral vector vaccine. The “V” in the name is the letter V, not the Roman numeral for five.[4]
Gam-COVID-Vac was initially approved for distribution in Russia on the preliminary results of Phase I–II studies eventually published on 4 September 2020.[5] The quick approval in early August of Gam-COVID-Vac was met with criticism in mass media and precipitated discussions in the scientific community whether this decision was justified in the absence of robust scientific research confirming the safety and efficacy of the vaccine.[2][3][6][7][8] On 2 February 2021, an interim analysis from the trial was published in The Lancet, indicating 91.6% efficacy without unusual side effects.[9]
Emergency mass-distribution of the vaccine began in December 2020 in multiple countries including Russia, Argentina, Belarus, Hungary, Serbia and the United Arab Emirates. As of February 2021, over a billion doses of the vaccine were ordered for immediate distribution globally.[10]


NEW DRUG APPROVALS
ONE TIME
$10.00
Technology
President Putin‘s meeting with government members, on 11 August 2020 via videoconference, at which he announced a conditionally registered vaccine against COVID-19.[2][3] Medical worker in Moscow with the vaccineSee also: COVID-19 vaccine
Gam-COVID-Vac is a viral two-vector vaccine based on two human adenoviruses – a common cold virus – containing the gene that encodes the full-length spike protein (S) of SARS-CoV-2 to stimulate an immune response.[5][11][12] The Gam-COVID-Vac vaccine was developed by a cellular microbiologists team of the government-backed Gamaleya Research Institute of Epidemiology and Microbiology. The group was led by MD and RAS associate member Denis Logunov, who also worked on vaccines for the Ebolavirus and the MERS-coronavirus.[13]
The recombinant adenovirus types 26 and 5 are both used as vectors in the vaccine. They were biotechnology-derived and contain the SARS-CoV-2 S protein cDNA. Both of them are administered into the deltoid muscle: the Ad26-based vaccine is used on the first day and the Ad5 vaccine is used on the 21st day to boost immune response.[11][14][15]
The vaccine can be formulated as frozen (storage temperature must be −18 °C or 0 °F or lower) and freeze-dried (“Gam-COVID-Vac-Lyo”, storage temperature is 2–8 °C or 36–46 °F) dosage forms.[16] The first formulation was developed for large-scale use, it is cheaper and easier to manufacture. The production of a lyophilized formulation takes much more time and resources, although it is more convenient for storage and transportation. Gam-COVID-Vac-Lyo was developed especially for vaccine delivery to hard-to-reach regions of Russia.[17] The head of the Gamaleya Research Institute Alexander Ginzburg estimates that it will take 9–12 months to vaccinate the vast majority of the Russian population, assuming in-country resources are adequate.[18][19] A single-dose version is also being developed to speed up vaccination outside Russia. It will offer less protection than the two-dose versions, but it is still expected to reach an efficacy of 85%.[20][21]
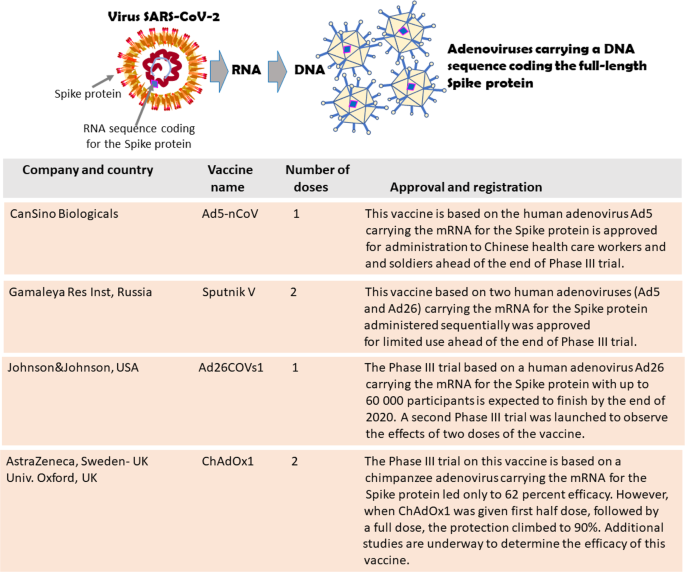
Clinical research
Phase I–II
A phase I safety trial began on 18 June.[2] On 4 September, data on 76 participants in a phase I–II trial were published, indicating preliminary evidence of safety and an immune response.[5] The results were challenged by international vaccine scientists as being incomplete, suspicious, and unreliable when identical data were reported for many of the trial participants,[22] but the authors responded that there was a small sample size of nine, and the measured results of titration could only take discrete values (800, 1600, 3200, 6400). Coupled with the observation that values tended to reach a plateau after three to four weeks, they contend that it is not unlikely that several participants would show identical results for days 21 to 28.[23]
Phase III
Sputnik V, efficacy for different conditions. The error bars indicate the confidence interval containing the efficacy with 95% probability
In early November 2020, Israel Hadassah Medical Center director-general Prof. Zeev Rotstein stated that Hadassah’s branch in Moscow’s Skolkovo Innovation Center was collaborating on a phase III clinical trial.[24]
The ongoing phase III study is a randomised, double-blind, placebo-controlled, multi-centre clinical trial involving 40,000 volunteers in Moscow, and is scheduled to run until May 2021.[25] In 2020–2021, phase III clinical studies were also being conducted in Belarus,[26] UAE,[27] India[28] and Venezuela.[29]
On 2 February 2021, an interim analysis from the Moscow trial was published in The Lancet, indicating 91.6% efficacy (95% CI 85.6–95.2) after the second vaccination, without unusual side effects.[30] The trial started on 7 September 2020 using the frozen liquid form of the vaccine, and data was analysed up to the second database lock on 24 November 2020. The over-60-years-old group in the trial (oldest participant was 87) had essentially the same efficacy (91.8%) as for all ages. The lowest age participants were 18 years old.[9][31]
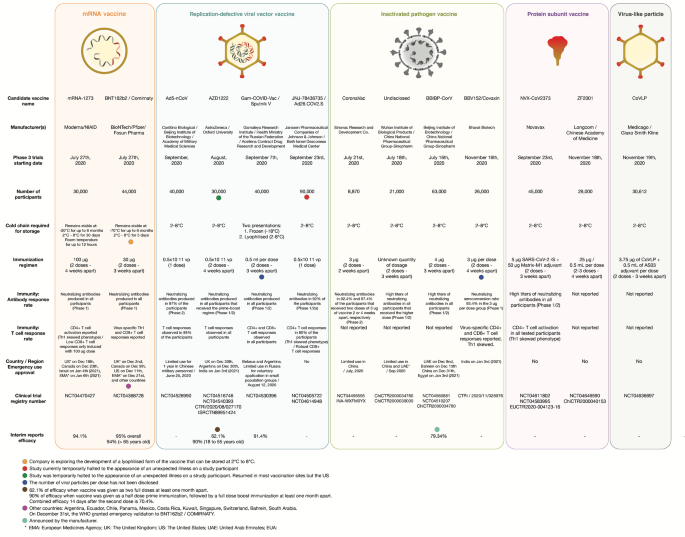
Sputnik–AstraZeneca COVID-19 vaccine trials
On 21 December 2020 the Russian Direct Investment Fund (RDIF), the Gamaleya National Center, AstraZeneca and R-Pharm have signed an agreement aimed at the development and implementation of a clinical research program to assess the immunogenicity and safety of the combined use of one of the components of the Sputnik V vaccine developed by the Gamaleya Center, and one of the components of the AZD1222 vaccine, developed by AstraZeneca and the University of Oxford.[32] The study program will last 6 months in several countries, and it is planned to involve 100 volunteers in each study program. On 9 February 2021, the Ministry of Health of the Republic of Azerbaijan allowed clinical studies in the country for the combined use of the Sputnik V vaccine and the vaccine developed by AstraZeneca, stating that the trials would begin before the end of February 2021.[33][34]
Composition
The Gam-COVID-Vac is a two-vector vaccine.[1] The active component for both vectors is a modified (recombinant) replication-defective adenovirus of a different serotype (Serotype 26 for the first vaccination and serotype 5 for the second vaccination), which has been modified to include the protein S-expressing gene of SARS-CoV-2.[1]
The other ingredients (excipients) are the same, both quantitatively and qualitatively, in the two components.[35]
- Tris(hydroxymethyl)aminomethane
- Sodium chloride
- Sucrose
- Magnesium chloride hexahydrate
- Disodium EDTA dihydrate (buffer)
- Polysorbate 80
- Ethanol 95%
- Water
As per the official datasheet, no further components or ingredients, including other adjuvants, should be included in the vaccine.[1]
History
In May 2020, the Gamaleya Research Institute of Epidemiology and Microbiology announced that it had developed the vaccine without serious side effects. By August 2020, phases I and II of two clinical trials (involving 38 patients each) were completed. Only one of them used the formulation which later obtained marketing authorization under limited conditions.[36][37] This vaccine was given the trade name “Sputnik V”, after the world’s first artificial satellite.[3][7][38]
During preclinical and clinical trials, 38 participants who received one or two doses of the Gam-COVID-Vac vaccine had produced antibodies against SARS-CoV-2’s spike protein, including potent neutralizing antibodies that inactivate viral particles.[2] On 11 August 2020, the Russian minister of Health Mikhail Murashko announced at a government briefing with the participation of President Vladimir Putin regulatory approval of the vaccine for widespread use. The state registration of the vaccine was carried out “conditionally” with post-marketing measures according to the decree of the Government of the Russian Federation. The registration certificate for the vaccine stated that it could not be used widely in Russia until 1 January 2021, and before that, it may be provided to “a small number of citizens from vulnerable groups”, such as medical staff and the elderly, according to a Ministry of Health spokesperson.[3] The license under register number No. ЛП-006395 (LP-006395) was issued on 11 August by the Russian Ministry of Health. Although the announcement was made even before the vaccine candidate had been entered into Phase III trials, the practice of marketing authorization “on conditions” also exists in other countries.[39][40] On 26 August, certificate No. ЛП-006423 (LP-006423) was issued for the lyophilized formulation “Gam-COVID-Vac-Lyo”.[2][3][7][41][5]
The commercial release of the Gam-COVID-Vac was first scheduled for September 2020. In October, Mikhail Murashko said that the Gam-COVID-Vac will be free for all Russian citizens after the launching of mass production.[42][43] Later on, Russian Ministry of Health registered maximum ex-factory price equal to 1,942 rubles for two components and included them into The National List of Essential medicines.[44] There were also suggestions to include the vaccine in the National Immunisation Calendar of Russia.[44]
According to Russian media, the mass production of the Gam-COVID-Vac was launched by 15 August. By that moment, the Russian Federation has already received applications from 20 countries for the supply of 1 billion doses of vaccine. Three facilities were able to produce about a million doses per month at each with a potential doubling of capacity by winter. By the end of 2020, Gamaleya Research Institute’s production, according to an interview with the organization’s spokesperson, was planned to produce 3–5 million doses.[45][46]
On 9 March 2021, an agreement was signed by the RDIF sovereign wealth fund and Swiss-based pharmaceutical company Adienne to produce the vaccine in Italy. Kirill Dmitriev, RDIF’s head, told Russian state TV his fund had also struck deals with production facilities in Spain, France and Germany for local manufacturing of the vaccine.[47]
Scientific assessment
Balram Bhargava, director of the Indian Council of Medical Research, said that Russia had managed to fast-track a COVID-19 vaccine candidate through its early phases.[48]
On 11 August 2020, a World Health Organization (WHO) spokesperson said, “… prequalification of any vaccine includes the rigorous review and assessment of all required safety and efficacy data”.[8]
- A WHO assistant director said, “You cannot use a vaccine or drugs or medicines without following through all of these stages, having complied with all of these stages”.[49]
- Francois Balloux, a geneticist at University College London, called the Russian government’s approval of Gam-COVID-Vac a “reckless and foolish decision”.[2] Professor Paul Offit, the director of the Vaccine Education Center at Children’s Hospital of Philadelphia, characterized the announcement was a “political stunt”, and stated that the untested vaccine could be very harmful.[8]
Stephen Griffin, Associate Professor in the School of Medicine, University of Leeds, said “that we can be cautiously optimistic that SARS-CoV2 vaccines targeting the spike protein are effective.” Moreover, as the Sputnik antigen is delivered via a different modality, namely using a disabled Adenovirus rather than formulated RNA, this provides flexibility in terms of perhaps one or other method providing better responses in certain age-groups, ethnicities, etc., plus the storage of this vaccine ought to be more straightforward.[50][failed verification][51]
Stephen Evans, professor of pharmacoepidemiology at the London School of Hygiene and Tropical Medicine, said “the data [is] compatible with the vaccine being reasonably effective … These results are consistent with what we see with other vaccines, because the really big message for global health scientists is that this disease [COVID-19] is able to be addressed by vaccines.”[50]
Julian Tang, clinical virologist at the University of Leicester, said: “Despite the earlier misgivings about the way this Russian Sputnik V vaccine was rolled out more widely – ahead of sufficient Phase 3 trial data – this approach has been justified to some extent now.”[52]
Ian Jones, a professor of virology at the University of Reading, and Polly Roy, professor and Chair of Virology at The London School of Hygiene and Tropical Medicine, commenting on phase III results published in the Lancet in February 2021, said “The development of the Sputnik V vaccine has been criticised for unseemly haste, corner cutting, and an absence of transparency. But the outcome reported here is clear and the scientific principle of vaccination is demonstrated, which means another vaccine can now join the fight to reduce the incidence of COVID-19.”[53]
Hildegund C. J. Ertl, a vaccine scientist at the Wistar Institute, called the phase-III results published on 2 February 2021 “great”: “Good safety profile, more than 90% efficacy across all age groups, 100% efficacy against severe disease or death, can be stored in the fridge and low cost. What more would we want?”[54]
According to preliminary review by experts,[who?] the lyophilized formulation of Gam-COVID-Vac is similar to the smallpox vaccine, circumventing the need for continuous “colder chain” or cold-chain storage – as required for the Pfizer–BioNTech and Moderna vaccines respectively – and allowing transportation to remote locations with reduced risk of vaccine spoilage.[55][56]
On 6 March 2021, Director of the U.S. National Institute of Allergy and Infectious Diseases (NIAID), Anthony Fauci, said that the data from Sputnik V “looked pretty good” to him.[57]
Distribution, vaccination and public perception
Early perception
An opinion poll of Canadians conducted by Léger in August 2020 found that a majority (68%) would not take the Russian vaccine if offered a free dose, compared to 14% who said they would take it. When Americans were asked the same question, 59% would not take the Russian vaccine if offered a free dose, compared to 24% who said they would take it.[58][59]
- At that time, British and American officials stated that the Gam-COVID-Vac vaccine would likely be rejected due to concerns that the normally rigorous process of vaccine clinical testing was not followed.[60] One public health expert said the quick approval of Gam-COVID-Vac by the Russian government was “cutting corners”, and may harm public confidence if the vaccine proves to be unsafe or ineffective.[7] “There is a huge risk that confidence in vaccines would be damaged by a vaccine that received approval and was then shown to be harmful”, said immunologist Peter Openshaw.[7]
As for early September 2020, according to public opinion polls, only half of the Russian population would take the vaccine voluntarily.[61]
In Russia
Vaccination of military personnel and civilian specialists of the Northern Fleet with the second component of the drug “Gam-COVID-Vac” (“Sputnik V”).
In the beginning of December 2020, Russian authorities announced the start of a large-scale free of charge vaccination with Gam-COVID-Vac for Russian citizens: the “immunization” program was launched on 5 December 2020 (with 70 Moscow-based medical centers providing vaccinations).[62]
Doctors and other medical workers, teachers, and social workers were given priority due to their highest risk of exposure to the disease.[63] The age for those receiving shots was initially capped at 60, later this restriction was lifted.[64]
Potential recipients were notified via text messaging, which says “You are working at an educational institution and have top-priority for the COVID-19 vaccine, free of charge”. Patients are asked a few general health questions before getting the vaccine. Program’s leaflet is handed to the patient, which warns of possible side effects, suggesting those are most likely to be mild and last a couple of days at most.[65][66][67] People with certain underlying health conditions, pregnant women, and those who have had a respiratory illness for the past two weeks are barred from vaccination.[63] Vaccine vial is removed from medical centre’s freezer about 15 minutes before use.
In early December 2020, the Minister of Health, Mikhail Murashko, said that Russia had already vaccinated more than 100,000 high-risk people.[68] Forty thousand of those are volunteers in Sputnik V’s Phase 3 trials, another 60,000 medics and doctors have also taken the vaccine.[69] The head of the Russian Direct Investment Fund, Kirill Dmitriev, said in an interview with the BBC that Russian medics expect to give about 2 million people coronavirus vaccinations in December.[70]
Up to the beginning of December 2020, Generium (which is supervised by Pharmstandard) and Binnopharm (which is supervised by AFK Sistema) companies produced Gam-COVID-Vac on a large scale.
On 10 December, Deputy Prime Minister Tatyana Golikova announced that approximately 6.9 million doses of the Sputnik V vaccine will enter civilian circulation in Russia before the end of February 2021.[71] Moscow Mayor Sergei Sobyanin announced that the newly-opened Moscow-based “R-Pharm” will become a leading manufacturer of Russia’s Sputnik V coronavirus vaccine. Working at full capacity, the factory will produce up to 10 million doses a month.[72]
Outside of Russia
In dark green are the countries that ordered (Russian or licensed domestic production; China also plans to produce Sputnik V on its territory.) or approved Sputnik V vaccine against COVID-19 (w/disputed Crimea). In light green are the countries that have shown interest in obtaining the vaccine.
According to the Russian Direct Investment Fund, they had received orders for more than 1.2 billion doses of the vaccine as of December 2020. Over 50 countries had made requests for doses, with supplies for the global market being produced by partners in India, Brazil, China, South Korea, Hungary, and other countries.[73][74] In August 2020, according to the Russian authorities, there were at least 20 countries that wanted to obtain the vaccine.[75]
While free in Russia, the cost per dose would be less than US$10 (or less than US$20 for the two doses needed to vaccinate one person) on international markets, which makes it much more affordable compared to mRNA vaccines from other manufacturers. Kirill Dmitriev, head of the fund, told reporters that over 1 billion doses of the vaccine are expected to be produced in 2021 outside of Russia.[76][77]
The Israeli Hadassah Medical Center has signed a commercial memorandum of understanding to obtain 1.5–3 million doses.[78]
- According to The New York Times’ sources,[79] to secure the release of an Israeli civilian held in Syria, Israel agreed to finance a supply of Russian-made Covid-19 vaccines for Damascus.
Argentina had agreed to buy 25 million doses of Russia’s Covid-19 vaccine.[80] The vaccine was registered and approved in Argentina in late December 2020.[81] The Brazilian state of Bahia has also signed an agreement to conduct Phase III clinical trials of the Sputnik V vaccine and plans to buy 50 million doses to market in northeastern Brazil.[82]
On 21 January 2021, the Argentine president Alberto Fernández became the first Latin American leader to be inoculated against the disease via the then recently approved Sputnik V.[83][84]
Due to the delay in shipping of doses from Italy and the European Union, San Marino imported doses of the Sputnik V vaccine (not approved by the E.M.A.) and started a mass vaccination on 28 February of its healthcare workers.[85]
EMA’s human medicines committee (CHMP) has started a rolling review of Sputnik V (Gam-COVID-Vac), a COVID-19 vaccine developed by Russia’s Gamaleya National Centre of Epidemiology and Microbiology. [86] Asked about the prospect of Austria taking the same step (as some other European countries chose to do), EMA management board chair Christa Wirthumer-Hoche told Austria’s ORF broadcaster: “It’s somewhat comparable to Russian roulette. I would strongly advise against a national emergency authorisation,” she said, pointing to the fact that there was not yet sufficient safety data about those who had already been given the vaccine. “We could have Sputnik V on the market in future, when we’ve examined the necessary data,” she said, adding that the vaccine needed to match up to European criteria on quality control and efficacy.[87]
Although vaccination rates in Russia are below those of other developed nations (as of March 2021),[88] Russia is pursuing deals to supply its vaccine abroad.[89]
Emergency use authorization
| show Full authorizationshow Emergency authorizationshow Ordered doses Eligible COVAX recipient (assessment in progress)[143] EMA review in progress[144] |
As of December 2020, Belarus and Argentina granted emergency use authorization for the vector-based vaccine.[145] On 21 January 2021, Hungary became the first European Union country to register the shot for emergency use, as well as the United Arab Emirates in the Gulf region.[146][147][148][149][150]
On 19 January 2021, the Russian authorities applied for the registration of Sputnik V in the European Union, according to the RDIF.[151] On 10 February, the European Medicines Agency (EMA) said that they had “not received an application for a rolling review or a marketing authorisation for the vaccine”. The developers have only expressed their interest that the vaccine be considered for a rolling review, but EMA’s Human Medicines Committee (CHMP) and the COVID-19 EMA pandemic Task Force (COVID-ETF) need to give their agreement first before developers can submit their application for initiation of the rolling review process.[152] On 4 March 2021, the Committee for Medicinal Products for Human Use (CHMP) of the EMA started a rolling review of Sputnik V.[153] The EU applicant is R-Pharm Germany GmbH.[153]
Emergency use has also been authorized in Algeria, Bolivia, Serbia, the Palestinian territories,[154] and Mexico.[155]
On 25 January 2021, Iran approved the vaccine, with Foreign Minister Mohammad Javad Zarif saying the country hopes to begin purchases and start joint production of the shot “in the near future”, after Supreme Leader Ayatollah Ali Khamenei banned the government from importing vaccines from the United States and United Kingdom.[156][157]
On 1 March 2021, Slovakia bought two million Sputnik V vaccines. Slovakia received the first batch of 200,000 vaccines, and expects to receive another 800,000 doses in March and April. Another 1 million vaccines are set to arrive in May and June.[158] The Czech Republic is also considering buying Sputnik V.[159]
On 18 March 2021, German regional leaders including State Premiers and the major of Berlin called for the swift approval of the Russian vaccine by the European Medicines Agency to counteract the acute shortages of effective vaccines in Europe. German medical experts have recommended its approval also, and consider the Sputnik Vaccine “clever” and “highly safe”.[160]
On 19 March 2021, the Philippine Food and Drug Administration granted emergency use authorization for Sputnik V, the fourth COVID-19 vaccine to be given authorization. The Philippine government is planning to buy 20 million doses of the vaccine.[161][162]
As of March 23, 2021, 56 countries have granted Sputnik V emergency use authorization.[163]
Production
As of March 2021, RDIF has licensed production in India, China, South Korea and Brazil. In the EU, RDIF has signed production agreements, subject to European Medicines Agency approval, with companies in Germany, Spain and France, and is in negotiations with a Swiss/Italian company. By the end of March 2021 RDIF anticipates 33 million doses will have been manufactured in Russia, less than 5% of which will have been exported.[164]
An agreement for the production of over 100 million doses of vaccine in India has been made with Dr. Reddy’s Laboratories, who on 11 January 2021 submitted mid-stage trial data to the Indian regulator and recommended moving onto late-stage trials.[154] The RDIF announced plans to sell 100 million doses to India, 35 million to Uzbekistan, and 32 million to Mexico, as well as 25 million each to Nepal and Egypt.[165]
In March 2021, the Italian-Russian Chamber of Commerce announced that Italy would be the first EU country to manufacture the two-dose COVID-19 vaccine under license. From July to the end of 2021, the Italian-Swiss pharmaceutical company Adienne in Caponago will manufacture 10 million doses. The announcement came in a time of acute vaccine shortages in Europe while the Sputnik V vaccine was still under review by the European Medicines Agency. Russian authorities said they would be able to provide a total of 50 million doses to European countries beginning in June 2021.[166]
The Sputnik V doses to be manufactured in South Korea are not for domestic use. The vaccine is to be exported to Russia, Algeria, Argentina, Hungary, Iran and the United Arab Emirates.[167]
References
- ^ Jump up to:a b c d “Sputnik V”. Russian drug reference. Medum.ru.
- ^ Jump up to:a b c d e f g Callaway E (August 2020). “Russia’s fast-track coronavirus vaccine draws outrage over safety”. Nature. 584(7821): 334–335. doi:10.1038/d41586-020-02386-2. PMID 32782400.
- ^ Jump up to:a b c d e f Cohen J (11 August 2020). “Russia’s approval of a COVID-19 vaccine is less than meets the press release”. Science. Retrieved 13 August 2020.
- ^ How Sputnik V works, Gamaleya Research Institute of Epidemiology and Microbiology, 11 January 2021, retrieved 18 March 2021
- ^ Jump up to:a b c d Logunov DY, Dolzhikova IV, Zubkova OV, Tukhvatullin AI, Shcheblyakov DV, Dzharullaeva AS, et al. (September 2020). “Safety and immunogenicity of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine in two formulations: two open, non-randomised phase 1/2 studies from Russia”. Lancet. 396 (10255): 887–897. doi:10.1016/S0140-6736(20)31866-3. PMC 7471804. PMID 32896291.
- ^ Mahase E (August 2020). “Covid-19: Russia approves vaccine without large scale testing or published results”. BMJ. 370: m3205. doi:10.1136/bmj.m3205. PMID 32816758.
- ^ Jump up to:a b c d e Burki TK (November 2020). “The Russian vaccine for COVID-19”. The Lancet. Respiratory Medicine. 8 (11): e85–e86. doi:10.1016/S2213-2600(20)30402-1. PMC 7837053. PMID 32896274.
- ^ Jump up to:a b c Berkeley Jr L (11 August 2020). “Scientists worry whether Russia’s Sputnik V’ coronavirus vaccine is safe and effective”. CNBC. Retrieved 11 August 2020.
- ^ Jump up to:a b Logunov DY, Dolzhikova IV, Shcheblyakov DV, Tukhvatulin AI, Zubkova OV, Dzharullaeva AS, et al. (2 February 2021). “Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: an interim analysis of a randomised controlled phase 3 trial in Russia”. The Lancet. 397 (10275): 671–681. doi:10.1016/s0140-6736(21)00234-8. PMC 7852454. PMID 33545094.
- ^ Kramer, Andrew. “Russia is offering to export hundreds of millions of vaccine doses, but can it deliver?”. nytimes.com. Retrieved 20 February 2021.
- ^ Jump up to:a b “An Open Study of the Safety, Tolerability and Immunogenicity of the Drug ‘Gam-COVID-Vac’ Vaccine Against COVID-19”. ClinicalTrials.gov. 22 June 2020.
- ^ “Coronavirus Vaccine Trials Advance in Race for Covid-19 Protection”. Bloomberg. Retrieved 10 August 2020.
- ^ “Russia’s RDIF & Prominent Government Lab Progress COVID-19 Vaccine: Production Facility Readied in the Moscow Region”. trialsitenews.com. 10 June 2020. Retrieved 11 August 2020.
- ^ Sokolov A (12 December 2020). “Сколько хотят заработать на прививках от коронавируса”. Vedomosti. Archived from the original on 12 August 2020. Retrieved 20 December 2020.
- ^ “Нормативная документация ЛП-006395-110820” (PDF) (in Russian). Russian Ministry of Health. 2020. Retrieved 21 September 2020.
- ^ Rinat, Sagdiev; Ivanova, Polina (17 November 2020). “Russia focuses on freeze-dried vaccine doses as transport fix”. Reuters. Moscow. Retrieved 16 March 2021.
- ^ Logunov DY, Dolzhikova IV, Zubkova OV, Tukhvatullin AI, Shcheblyakov DV, Dzharullaeva AS, et al. (September 2020). “Safety and immunogenicity of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine in two formulations: two open, non-randomised phase 1/2 studies from Russia”. Lancet. 396 (10255): 887–897. doi:10.1016/S0140-6736(20)31866-3. PMC 7471804. PMID 32896291.
- ^ “Центр Гамалеи назвал сроки вакцинации большей части населения России”. RBK. 4 September 2020. Retrieved 6 September 2020.
- ^ Sagdiev R, Ivanova P, Nikolskaya P, Swift R, Smout A (17 November 2020). Mason J, Macfie N (eds.). “Russia focuses on freeze-dried vaccine doses as transport fix”. Reuters. Moscow. Retrieved 20 November 2020.
- ^ “Russia to try out ‘Sputnik-Light’ COVID vaccine to make it go further”. Reuters. Moscow. 11 January 2021. Retrieved 20 March2021.
- ^ “Study to Evaluate Efficacy, Immunogenicity and Safety of the Sputnik-Light (SPUTNIK-LIGHT)”. ClinicalTrials.gov. National Institutes of Health. 19 February 2021. Retrieved 20 March 2021.
- ^ Ellyatt H (10 September 2020). “Scientists question ‘strange’ data in Russian coronavirus vaccine trial after ‘unlikely’ patterns”. CNBC. Retrieved 10 September 2020.
- ^ Logunov DY, Dolzhikova IV, Tukhvatullin AI, Shcheblyakov DV (October 2020). “Safety and efficacy of the Russian COVID-19 vaccine: more information needed – Authors’ reply”. Lancet. 396(10256): e54–e55. doi:10.1016/S0140-6736(20)31970-X. PMC 7503057. PMID 32971043. S2CID 221805026.
- ^ “Hadassah bringing 1.5 million doses of Russian COVID-19 vaccine to Israel”. The Jerusalem Post | JPost.com. Retrieved 19 November 2020.
- ^ “Clinical Trial of Efficacy, Safety, and Immunogenicity of Gam-COVID-Vac Vaccine Against COVID-19”. National Library of Medicine. Retrieved 28 September 2020.
- ^ “Clinical Trial of Efficacy, Safety, and Immunogenicity of Gam-COVID-Vac Vaccine Against COVID-19 in Belarus”. clinicaltrials.gov. Retrieved 14 January 2021.
- ^ “UAE volunteers receive Russian Covid-19 vaccine”. Khaleej Times. 10 January 2021.
- ^ Bharadwaj S (15 January 2021). “Dr Reddy’s gets DCGI nod for Covid-19 vaccine Sputnik V Phase III trials”. The Times Of India.
- ^ Clinical trial number NCT04642339 for “Clinical Trial of the Immunogenicity, Safety, and Efficacy of the Gam-COVID-Vac Vaccine Against COVID-19 in Venezuela” at ClinicalTrials.gov
- ^ Logunov, Denis (2 February 2021). “Sputnik V COVID-19 vaccine candidate appears safe and effective”. The Lancet. doi:10.1016/S0140-6736(21)00234-8.
- ^ The Guardian: Sputnik V vaccine has 91.6% efficacy against symptomatic Covid, Russian trial suggests
- ^ “RDIF, The Gamaleya National Center, AstraZeneca and R-Pharm sign an agreement to cooperate on COVID-19 vaccine development”. The Russian Direct Investment Fund. 21 December 2020.
- ^ “Azerbaijan allowed for the first in the world to study a combination of “Sputnik V” vaccine and COVID-19 vaccine developed by “AstraZeneca” Company”. MoH of Azerbaijan. 9 February 2021.
- ^ “Study in Adults to Determine the Safety and Immunogenicity of AZD1222, a Non-replicating ChAdOx1 Vector Vaccine, Given in Combination With rAd26-S, Recombinant Adenovirus Type 26 Component of Gam-COVID-Vac Vaccine, for the Prevention of COVID-19”. ClinicalTrials.gov. U.S. National Library of Medicine. 14 January 2021. NCT04686773. Retrieved 9 February 2021.
- ^ “ИНСТРУКЦИЯ ПО МЕДИЦИНСКОМУ ПРИМЕНЕНИЮ ЛЕКАРСТВЕННОГО ПРЕПАРАТА Гам-КОВИД-Вак, Комбинированная векторная вакцина для профилактики коронавирусной инфекции, вызываемой вирусом SARS-CoV-2” (PDF). МИНИСТЕРСТВО ЗДРАВООХРАНЕНИЯ РОССИЙСКОЙ ФЕДЕРАЦИИ.
- ^ “Russia plans to start producing coronavirus vaccine in September”. Daily Sabah. 13 June 2020. Retrieved 10 August2020.
- ^ Ermakov A (11 August 2020). “Вакцина от COVID-19 – в словах чиновников и документах разработчика” [Vaccine for COVID-19 – in the words of officials and developer documents] (in Russian). Fontanka.ru. Retrieved 21 September 2020.
- ^ Tétrault-Farber G, Soldatkin V (11 August 2020). “Russia becomes first country to approve a COVID-19 vaccine, says Putin”. Reuters. Moscow. Retrieved 11 August 2020.
- ^ “About the vaccine to prevent the novel coronavirus infection COVID-19, “Gam-COVID-Vac”, developed by the National Research Centre for Epidemiology and Microbiology named after academician N. F. Gamalei of the Ministry of Health of the Russian Federation”. Federal Service for Surveillance in Healthcare. 12 August 2020. Retrieved 18 August 2020.
- ^ “Ministry of Health of the Russian Federation has issued a registration certification № ЛП-006395 dated 11 August 2020 for a vaccine to prevent the novel coronavirus infection COVID-19”. Federal Service for Surveillance in Healthcare. 11 August 2020. Retrieved 21 September 2020.
- ^ “Coronavirus: Putin says vaccine has been approved for use”. BBC. 11 August 2020. Retrieved 11 August 2020.
- ^ “Минздрав пообещал россиянам бесплатную вакцинацию от COVID-19” [Ministry of Health promised Russians free vaccination against COVID-19]. RBC.ru (in Russian). Retrieved 23 October 2020.
- ^ “В будущем вакцинация от COVID-19 будет проходить бесплатно” [In the future, vaccination against COVID-19 will be free of charge]. Russian Newspaper (in Russian). Retrieved 23 October 2020.
- ^ Jump up to:a b “Минздрав зарегистрировал предельную отпускную цену на вакцину “Спутник V”” [The Ministry of Health registered the maximum selling price for the Sputnik V vaccine] (in Russian). RIA. 5 December 2020. Retrieved 21 September 2020.
- ^ “Голикова назвала сроки выпуска первых партий вакцин НИЦ Гамалеи и “Вектора”” [Golikova announced the timing of the release of the first batches of vaccines of the Research Center of Gamaleya and “Vector”] (in Russian). Interfax. 29 July 2020.
- ^ “Запущено производство российской антикоронавирусной вакцины” [Production of Russian anti-coronavirus vaccine launched] (in Russian). Vesti. 15 August 2020. Retrieved 21 September 2020.
- ^ Osborn A, Tétrault-Farber G (9 March 2021). “Russia’s Sputnik V COVID-19 vaccine could be produced in western Europe for first time after reported deals”. The Globe and Mail. Retrieved 9 March 2021.
- ^ “Russia has successfully fast tracked Covid-19 vaccine development, says India”. Mint. 14 July 2020. Retrieved 11 August 2020.
- ^ Nebehay S (11 August 2020). Shields M (ed.). “WHO says discussing new COVID-19 vaccine with Russia”. Reuters. Geneva. Retrieved 11 August 2020.
- ^ Jump up to:a b Brown C (28 November 2020). “Russia says its COVID vaccine is 95% effective. So why is there still Western resistance to it?”. http://www.cbc.ca. Retrieved 3 December 2020.
- ^ Reuters Staff (2020-11-11). “Instant view-Russia says its Sputnik V COVID-19 vaccine is 92% effective”
- ^ Zamira Rahim. “Russia’s Sputnik V vaccine is 91.6% effective against symptomatic Covid-19, interim trial results suggest”. CNN. Retrieved 9 February 2021.
- ^ Jones, Ian; Roy, Polly (2 February 2021). “Sputnik V COVID-19 vaccine candidate appears safe and effective”. The Lancet. 397(10275): 642–643. doi:10.1016/S0140-6736(21)00191-4. ISSN 0140-6736. PMC 7906719. PMID 33545098.
- ^ Taylor, Adam; Johnson, Carolyn Y. “Russian vaccine Sputnik V more than 90% effective in interim trial”. Washington Post. ISSN 0190-8286. Retrieved 9 February 2021.
- ^ Balakrishnan VS (1 October 2020). “The arrival of Sputnik V”. The Lancet Infectious Diseases. 20 (10): 1128. doi:10.1016/S1473-3099(20)30709-X. PMC 7511201. PMID 32979327.
- ^ Irfan U (11 December 2020). “Why staying cold is so important to a Covid-19 vaccine. The Moderna and Pfizer vaccines need to be stored at low temperatures. Are global health systems prepared?”. Vox. Retrieved 27 December 2020.
- ^ “US’ top infectious disease official commends Russia’s Sputnik”. United News of India. 6 March 2021.
- ^ Cyr E (24 August 2020). “Leger’s Weekly Survey” (PDF). leger360.com. Archived from the original (PDF) on 5 September 2020. Retrieved 5 September 2020.
- ^ Leger’s Weekly Survey on Russian vaccine; saved copy on 5 38.com
- ^ Mullin J, Malnick E (1 August 2020). “Britain unlikely to use Russia’s ‘untrustworthy’ Covid vaccine”. The Telegraph. Archived from the original on 19 August 2020. Retrieved 6 September 2020.
- ^ Ullah Z, Chernova A (6 September 2020). “Putin’s vaccine meets opposition from frontline workers in Russia”. CNN. Retrieved 6 September 2020.
- ^ “Covid: Russia begins vaccinations in Moscow”. BBC. 5 December 2020. Retrieved 11 December 2020.
- ^ Jump up to:a b Soldatkin V, Oziel C (5 December 2020). Char P (ed.). “Moscow rolls out Sputnik V COVID-19 vaccine to most exposed groups”. Reuters.
- ^ “Russia approves Sputnik V COVID-19 vaccine for people over 60: media”. Reuters. 26 December 2020.
- ^ “Covid: Russia begins vaccinations in Moscow”. BBC News. 5 December 2020.
- ^ “Moscow delivers Russia’s Sputnik V coronavirus vaccine to clinics”. The Guardian. Reuters. 5 December 2020.
- ^ “Coronavirus: Russia rolls out COVID vaccination in Moscow”. Deutsche Welle. 5 December 2020.
- ^ Marrow A, Ostroukh A (2 December 2020). “Putin orders Russia to begin a large-scale voluntary COVID-19 vaccination program next week”. The Globe and Mail. Retrieved 3 December 2020.
- ^ “COVID-19: Moscow opens Sputnik V clinics – but 100,000 have already had it”. Sky News.
- ^ “Russia to vaccinate two million against COVID-19 in Dec – RDIF head to BBC”. Reuters. 4 December 2020. Retrieved 21 September 2020.
- ^ “About 6.9 mln doses of Sputnik V vaccine to enter circulation in Russia by end of February”. TASS. 10 December 2020. Retrieved 21 September 2020.
- ^ “Coronavirus in Russia: The Latest News”. The Moscow Times. 22 December 2020. Retrieved 21 September 2020.
- ^ Rodgers J. “Facing Record COVID-19 Case Rise, Russia Rolls Out Sputnik V Vaccine”. Forbes.
- ^ Arkhipov I, Kravchenko S (2 December 2020). “Putin Orders Start of Mass Covid-19 Shots Hours After U.K. News”. Bloomberg News.
- ^ Meyer H, Arkhipov I. “Russia Defends First Covid-19 Vaccine as Safe Amid Skepticism”. Bloomberg News. Retrieved 12 August2020.
- ^ Litvinova D (24 November 2020). “Russian virus vaccine to cost less than $10 per dose abroad”. Associated Press.
- ^ Osborn A, Nikolskaya P (24 November 2020). “Russia’s Sputnik COVID-19 vaccine to cost less than $20 per person internationally”. The Globe and Mail. Retrieved 28 November2020.
- ^ Jaffe-Hoffman M (12 November 2020). “Israel to receive Russia’s 92% effective COVID vaccine”. The Jerusalem Post. Retrieved 19 November 2020.
- ^ Kingsley, Patrick; Bergman, Ronen; Kramer, Andrew E. (21 February 2021). “Israel Secretly Agrees to Fund Vaccines for Syria as Part of Prisoner Swap”. The New York Times. ISSN 0362-4331. Retrieved 3 March 2021.
- ^ “Argentina agrees to buy 25 million doses of Russia’s Covid-19 vaccine”. http://www.batimes.com.ar. 30 November 2020.
- ^ “Argentina Approves Russian Vaccine With Plane Waiting in Moscow”. Bloomberg.com. 23 December 2020.
- ^ Boadle A (24 October 2020). Wallis D (ed.). “Second Brazilian company to produce Russia’s Sputnik V COVID-19 vaccine”. Reuters.
- ^ “Argentina’s president sits for Russian Covid jab”. France 24. 21 January 2021.
- ^ Centenera M (21 January 2021). “Alberto Fernández, primer presidente de América Latina en vacunarse contra la covid-19 (in Spanish)”. EL PAÍS (in Spanish).
- ^ Camparsi, Maria Letizia. “Vaccino Sputnik, a San Marino 400 dosi al giorno dal 1 marzo: “Sicurezza? Confortati dagli studi. Per ora lo diamo solo ai nostri cittadini” (in Italian). Il Fatto Quotidiano. Retrieved 1 March 2021.
- ^ “EMA starts rolling review of the Sputnik V COVID-19 vaccine”.
- ^ “EU medical official warns of Sputnik jab ‘Russian roulette'”.
- ^ “Coronavirus (COVID-19) Vaccinations – Statistics and Research”. Our World in Data. Retrieved 3 March 2021.
- ^ “Putin Battles to Sell Russia’s Vaccine in New Rift With West”. Bloomberg.com. 31 December 2020. Retrieved 3 March 2021.
- ^ Jump up to:a b c “Angola, Congo Republic and Djibouti approve Russia’s Sputnik V vaccine”. Reuters. 3 March 2021.
- ^ “Hungarian drug regulator approves Sputnik V vaccine: website”. The Moscow Times. 7 February 2021.
- ^ Jump up to:a b c “Sputnik V vaccine registered in Bosnia and Herzegovina’s Republika Srpska”. TASS. 5 February 2021. Retrieved 8 February2021.
- ^ “Sputnik V registered in Kyrgyzstan”. Gamaleya Center (Press release). 23 February 2021.
- ^ “Syria authorizes use of Sputnik-V”. Roya. 22 February 2021.
- ^ “Turkmenistan is the first in Central Asia to have registered “Sputnik V” vaccine”. Orient. 18 January 2021.
- ^ “Uzbekistan Certifies Russia’s Sputnik Vaccine For Mass Use”. Agence France-Presse (Barron’s). 17 February 2021.
- ^ “Covid19: National Pharmaceuticals Agency registers Sputnik V vaccine”. Algeria Press service. 10 January 2021.
- ^ “Argentina has registered the Sputnik V vaccine based on Russian clinical trial data” (Press release). Gamaleya Center. Retrieved 1 January 2021.
- ^ “Armenia approves Russia’s Sputnik V coronavirus vaccine -Russia’s RDIF”. Reuters. 1 February 2021. Retrieved 1 February2021.
- ^ “Bahrain authorises Sputnik V COVID-19 vaccine for emergency use – Bahrain TV”. Reuters. 10 February 2021. Retrieved 19 February 2021.
- ^ “Belarus registers Sputnik V vaccine, in first outside Russia – RDIF”. Reuters. 21 December 2020. Retrieved 22 December2020.
- ^ “Ministerio de Salud de Bolivia – Bolivia y Rusia firman contrato para adquirir 5,2 millones de dosis de la vacuna Sputnik-V contra la COVID-19”. minsalud.gob.bo. Retrieved 1 January 2021.
- ^ “COVID-19: Egypt authorises Sputnik V, AstraZeneca virus jabs”. Gulf News. Retrieved 24 February 2021.
- ^ “Sputnik V authorised in Gabon” (Press release). Gamaleya Center. Retrieved 17 February 2021.
- ^ “Ghana approves Russia’s Sputnik V vaccine for emergency use – RDIF”. Reuters. 20 February 2021.
- ^ “Guatemala to receive Russia’s Sputnik vaccine in coming weeks”. Reuters. 24 February 2021.
- ^ “Guinea Begins Administering Russia’s Sputnik V Covid-19 Vaccine”. Africa news. 31 December 2020.
- ^ “Russia’s Sputnik V vaccine expands its reach in Latin America”. CNN. 3 March 2021.
- ^ “Honduras approves use of Sputnik V vaccine against COVID-19”. Xinhua News Agency. 25 February 2021.
- ^ “Iran approves Russian coronavirus vaccine Sputnik V”. Reuters. 26 January 2021.
- ^ “Sputnik V authorized in Iraq” (Press release). PharmiWeb.com. 4 March 2021.
- ^ “Jordan approves Russia’s Sputnik V vaccine for use against COVID-19” (Press release). Reuters. 10 March 2021.
- ^ “Kazakhstan begins mass vaccination by Russian Sputnik V”. 1 February 2021. Retrieved 19 February 2021.
- ^ “Morocco, Kenya approve Russian coronavirus vaccine for use – RDIF”. 10 March 2021. Retrieved 12 March 2021.
- ^ “Laos declares Covid-19 vaccinations safe, more to be inoculated next week | The Star”. The Star. Malaysia. Retrieved 19 February2021.
- ^ “Lebanon authorises emergency use of Russia’s Sputnik V vaccine”. Reuters. 5 February 2021.
- ^ “Mexico, Germany warm to Russia’s Sputnik V virus vaccine”. The Jakarta Post. 3 February 2021.
- ^ “Mongolia Approves Russia’s Sputnik V Coronavirus Vaccine – RDIF”. Urdu Point. 9 February 2021.
- ^ “Montenegro and St. Vincent approve Russia’s Sputnik V vaccine – RDIF”. Reuters. 12 February 2021.
- ^ “Morocco orders one million doses of Russia’s Sputnik V vaccine”. Yabiladi. 11 March 2021.
- ^ “Myanmar registers Russia’s Sputnik V COVID-19 vaccine”. TASS. Retrieved 19 February 2021.
- ^ “Namibia becomes the 50th country to authorize Sputnik V”(Press release). Moscow: Gamaleya Research Institute of Epidemiology and Microbiology. 11 March 2021. Retrieved 15 March 2021.
- ^ “Nicaragua approves Russian COVID-19 vaccine”. wsoctv. 3 February 2021.
- ^ “NRussia’s Sputnik V COVID 19 vaccine registered in North Macedonia”. TASS. 7 March 2021.
- ^ “Govt okays Russian vaccine for ’emergency use'”. Dawn. 24 January 2021.
- ^ “Palestine has become the first country in the Middle East to register Sputnik V vaccine”. RFID. 11 January 2021.
- ^ “Paraguay approves Russia’s Sputnik V vaccine: RDIF”. Reuters. 15 January 2021. Retrieved 15 January 2021.
- ^ “Russia’s Sputnik V approved for emergency use in PH”. CNN Philippines. 19 March 2021. Retrieved 19 March 2021.
- ^ Burki TK (November 2020). “The Russian vaccine for COVID-19”. The Lancet. Respiratory Medicine. 8 (11): e85–e86. doi:10.1016/S2213-2600(20)30402-1. PMC 7837053. PMID 32896274.
- ^ “Public Health (Emergency Authorisation of COVID-19 Vaccine) Rules, 2021” (PDF). Government of Saint Vincent and the Grenadines. 11 February 2021. Retrieved 12 February 2021.
- ^ “San Marino buys the Sputnik vaccine: “First doses already in the next few days””. Unioneonline. 20 February 2021.
- ^ “Agencija odobrila uvoz ruske vakcine Sputnjik V u Srbiju”. N1(in Serbian). 31 December 2020.
- ^ “Sputnik V approved for use in Slovakia”. rdif.ru. Retrieved 1 March 2021.
- ^ “Sri Lanka approves Russia’s Sputnik V vaccine”. The Hindu. 4 March 2021.
- ^ “Sputnik V vaccine authorized in Tunisia” (Press release). Gamaleya Center. Retrieved 30 January 2021.
- ^ “UAE approves Russia’s Sputnik vaccine for emergency use”. Khaleej Times. 21 January 2021. Retrieved 21 January 2021.
- ^ “Venezuela firma contrato para la adquisición de la vacuna rusa Sputnik V” (in Spanish). Reuters. 29 December 2020.
- ^ “Vietnam approves US, Russia Covid-19 vaccines for emergency use”. VnExpress. Retrieved 26 February 2021.
- ^ “Covid-19: Zimbabwe authorises Sputnik V, Sinovac vaccines for emergency use”. news24.com. 9 March 2021.
- ^ McCluskey, Mitchell; Pozzebon, Stefano; Arias, Tatiana; Lister, Tim (3 March 2021). “Russia’s Sputnik V vaccine expands its reach in Latin America”. CNN. Retrieved 15 March 2021.
- ^ “COVID vaccine: Italy to be first EU country to make RussiaN Sputnik V jab”. Euronews. Agence France-Presse. 9 March 2021. Retrieved 15 March 2021.
- ^ “RDIF inks contract with Malaysia to supply Sputnik V vaccine”. TASS. 26 January 2021. Retrieved 21 March 2021.
- ^ “Regulation and Prequalification”. World Health Organization. Retrieved 12 March 2021.
- ^ “EMA starts rolling review of the Sputnik V COVID-19 vaccine”. European Medicines Agency. 4 March 2021. Retrieved 12 March2021.
- ^ “Belarus registers Sputnik V vaccine, in first outside Russia – RDIF”. Reuters. 21 December 2020. Retrieved 22 December2020.
- ^ Turak N (21 January 2021). “Russia’s Sputnik vaccine gets its first approval in the EU, greenlight from UAE amid ongoing trials”. CNBC.
- ^ “Coronavirus: Hungary first in EU to approve Russian vaccine”. BBC News. 21 January 2021.
- ^ Walker S (21 January 2021). “Hungary breaks ranks with EU to license Russian vaccine”. The Guardian.
- ^ “Hungary Becomes First in EU to Approve Russian Covid Vaccine”. Bloomberg.com. 21 January 2021.
- ^ “COVID: Hungary fast-tracks Russian vaccine with EU approval in the works | DW | 21.01.2021”. DW.COM.
- ^ “Russia files for Sputnik vaccine registration in EU”. Euractiv.com. 20 January 2021.
- ^ “Clarification on Sputnik V vaccine in the EU approval process”(Press release). European Medicines Agency (EMA). 10 February 2021.
- ^ Jump up to:a b “EMA starts rolling review of the Sputnik V COVID-19 vaccine” (Press release). European Medicines Agency (EMA). 4 March 2021. Retrieved 4 March 2021.
- ^ Jump up to:a b Ahmed A, Kumar AM (11 January 2021). “Russia’s Sputnik V vaccine found safe in India mid-stage trial – Dr.Reddy’s”. Reuters. Retrieved 26 January 2021.
- ^ “Da la Cofepris autorización para que la vacuna Sputnik V se aplique en México”. Diario de Yucatán (in Spanish). 2 February 2021.
- ^ “Iran approves Russia’s Sputnik V COVID-19 vaccine”. Al Jazeera.
- ^ Reuters Staff (26 January 2021). “Iran approves Russian coronavirus vaccine Sputnik V”. Reuters.
- ^ “Sputnik V vaccines landed in Slovakia”. The Slovak Spectator. 1 March 2021. Retrieved 2 March 2021.
- ^ “Czech Republic turns to Russian vaccine amid soaring COVID cases”. Al Jazeera. 28 February 2021. Retrieved 1 March 2021.
- ^ “German leaders urge quick EU approval of Russia’s Sputnik V jab” thelocal.de. Retrieved 20 March 2021.
- ^ “Philippines grants emergency authorization for Russia’s Sputnik V vaccine”. ABS-CBN News. 19 March 2021. Retrieved 19 March2021.
- ^ “Russia’s Sputnik V approved for emergency use in PH”. CNN Philippines. 19 March 2021. Retrieved 19 March 2021.
- ^ “SPUTNIK V APPROVED IN VIETNAM”. sputnikvaccine.com. 23 March 2021. Retrieved 23 March 2021.
- ^ Foy, Henry; Seddon, Max; Sciorilli, Silvia Borrelli (10 March 2021). “Russia seeks to make Sputnik V in Italy as overseas demand surges”. Financial Times. Retrieved 10 March 2021.
- ^ “More Countries Line Up for Russia’s Sputnik V Coronavirus Vaccine”. The Moscow Times. 13 November 2020.
- ^ COVID vaccine: Italy to be first EU country to make Russian Sputnik V jab Euronews. Retrieved 11 March 2021.
- ^ Shim, Elizabeth (25 February 2021). “South Korean consortium to make 500 million doses of Sputnik V vaccine”. UPI. Retrieved 1 March 2021.
External links
| Scholia has a profile for Gam-COVID-Vac (Q98270627). |
| Russian Ministry of Health image of Gam-COVID-Vac vials | |
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | Viral vector |
| Clinical data | |
| Trade names | Sputnik V[1]Спутник V |
| Other names | Gam-COVID-VacГам-КОВИД-Вак |
| Routes of administration | Intramuscular |
| ATC code | None |
| Legal status | |
| Legal status | Registered in Russia on 11 August 2020 AE, AG, DZ, BO, BY, HU, IR, PS, RS: EUA only |
| Identifiers | |
| DrugBank | DB15848 |
////////SARS-CoV-2, corona virus, covid 19, Gam-COVID-Vac Lyo, Sputnik V, Gam-COVID-Vac, Gamaleya, russia
#SARS-CoV-2, #corona virus, #covid 19, #Gam-COVID-Vac Lyo, #Sputnik V, #Gam-COVID-Vac, #Gamaleya, #russia, #vaccine
Johnson & Johnson COVID-19 vaccine, JNJ 78436735

Johnson & Johnson COVID-19 vaccine, JNJ 78436735
- Ad26.COV2.S
- JNJ-78436735
- Ad26COVS1
- VAC31518
- UNII: JT2NS6183B
| NAME | DOSAGE | STRENGTH | ROUTE | LABELLER | MARKETING START | MARKETING END | ||
|---|---|---|---|---|---|---|---|---|
| Covid-19 Vaccine Janssen | Injection, suspension | 0.95 Inf. U | Intramuscular | Janssen Cilag International Nv | 2021-03-17 | Not applicable | ||
| Janssen COVID-19 Vaccine | Injection, suspension | 50000000000 {VP}/0.5mL | Intramuscular | Janssen Products, LP | 2021-01-04 | Not applicable |
| NAME | INGREDIENTS | DOSAGE | ROUTE | LABELLER | MARKETING START | MARKETING END | ||
|---|---|---|---|---|---|---|---|---|
| Janssen COVID-19 Vaccine | Ad26.COV2.S (50000000000 {VP}/0.5mL) | Injection, suspension | Intramuscular | Janssen Products, LP | 2021-01-04 | Not applicable |
| FORM | ROUTE | STRENGTH |
|---|---|---|
| Injection, suspension | Intramuscular | 0.95 Inf. U |
| Injection, suspension | Intramuscular | 50000000000 {VP}/0.5mL |
The Johnson & Johnson COVID-19 vaccine is a human adenovirus viral vector COVID-19 vaccine[12] developed by Janssen Vaccines in Leiden in The Netherlands,[13] and its Belgian parent company Janssen Pharmaceuticals,[14] subsidiary of American company Johnson & Johnson (J&J).[15][16]
The vaccine is based on a human adenovirus that has been modified to contain the gene for making the spike protein of the SARS-CoV-2 virus that causes COVID-19.[3] The vaccine requires only one dose and does not need to be stored frozen.[17]
The vaccine started clinical trials in June 2020, with Phase III trials involving around 43,000 people.[18] On 29 January 2021, Janssen announced that the vaccine was 66% effective in a one-dose regimen in preventing symptomatic COVID-19, with an 85% efficacy in preventing severe COVID-19.[19][20][21] The most common side effects were pain at the injection site, headache, fatigue, muscle aches and nausea.[22] Most of these side effects were mild to moderate in severity and lasted one or two days.
The vaccine has been granted an Emergency Use Authorization by the US Food and Drug Administration[23] and a conditional marketing authorisation by the European Medicines Agency.[11][24][25]
Ad26.COV2.S is a lead recombinant vaccine candidate that contains an adenovirus serotype 26 (Ad26) vector expressing a stabilized SARS-CoV-2 spike protein. The vaccine was created in collaboration with Johnson and Johnson (J&J), Janssen Pharmaceutical, and the Beth Israel Deaconess Medical Center. This vaccine lead candidate uses Janssen’s AdVac® and PER.C6® technologies. A preclinical study in hamsters infected with SARS-COV-2 infection1 showed a single immunization with the vaccine elicited neutralizing responses and protected against SARS-CoV-2 induced pneumonia and mortality, providing protection against the disease progression. Follow up preclinical studies in rhesus monkeys2 showed that the Ad26 vaccine produced a robust response and provided near perfect protection in nasal swabs and bronchoalveolar lavage following SARS-COV-2 challenge. As of June 2020, a Phase 1/2 clinical trial in adult humans was announced to evaluate the safety, immunogenicity, and efficacy of the ad26.COV.S vaccine in 1045 healthy adults between the ages of 18-55 (NCT04436276).

NEW DRUG APPROVALS
one time
$10.00
Description
The Johnson & Johnson COVID-19 vaccine consists of a replication-incompetent recombinant adenovirus type 26 (Ad26) vector expressing the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike (S) protein in a stabilized conformation.[26][4] The stabilized version of the spike protein – that includes two mutations in which the regular amino acids are replaced with prolines – was developed by researchers at the National Institute of Allergy and Infectious Diseases‘ Vaccine Research Center and the University of Texas at Austin.[27][28][29] The vaccine also contains the following inactive ingredients: citric acid monohydrate, trisodium citrate dihydrate, ethanol (alcohol), 2-hydroxypropyl-β-cyclodextrin (HBCD) (hydroxypropyl betadex), polysorbate 80, sodium chloride, sodium hydroxide, and hydrochloric acid.[26][1]
Characteristics
The Johnson & Johnson COVID-19 vaccine can remain viable for months in a standard refrigerator.[30][31][32] Unlike the Pfizer–BioNTech COVID-19 vaccine and the Moderna COVID-19 vaccine, the Johnson & Johnson COVID-19 vaccine is administered as a single dose instead of two separate doses and it is not shipped frozen.[33][17]
The storage and handling information in the Fact Sheet supersedes the storage and handling information on the carton and vial labels.[17] The vaccine should not be stored frozen.[17] Unpunctured vials may be stored between 9 to 25 °C (48 to 77 °F) for up to twelve hours.[26][17]
Development
During the COVID-19 pandemic, Johnson & Johnson committed over US$1 billion toward the development of a not-for-profit COVID-19 vaccine in partnership with the Biomedical Advanced Research and Development Authority (BARDA) Office of the Assistant Secretary for Preparedness and Response (ASPR) at the U.S. Department of Health and Human Services (HHS).[34][35] Johnson & Johnson stated that its vaccine project would be “at a not-for-profit level” as the company viewed it as “the fastest and the best way to find all the collaborations in the world to make this happen”.[36]

Inside of an Emergent BioSolutions facility where, in collaboration with Johnson & Johnson, vaccines are produced.
Janssen Vaccines, in partnership with Beth Israel Deaconess Medical Center (BIDMC), is responsible for developing the vaccine candidate, based on the same technology used to make its Ebola vaccine.[16][37][38]
Clinical trials
Phase I-II
In June 2020, Johnson & Johnson and the National Institute of Allergy and Infectious Diseases (NIAID) confirmed its intention to start a clinical trials of the Ad26.COV2.S vaccine in September 2020, with the possibility of Phase I/IIa human clinical trials starting at an accelerated pace in the second half of July.[39][40][41]
A Phase I/IIa clinical trial started with the recruitment of the first subject on 15 July 2020, and enrolled study participants in Belgium and the US.[42] Interim results from the Phase I/IIa trial established the safety, reactogenicity, and immunogenicity of Ad26.COV2.S.[43][44]
Phase III
A Phase III clinical trial called ENSEMBLE started enrollment in September 2020, and completed enrollment on 17 December 2020. It was designed as a randomized, double-blind, placebo-controlled clinical trial designed to evaluate the safety and efficacy of a single-dose vaccine versus placebo in adults aged 18 years and older. Study participants received a single intramuscular injection of Ad26.COV2.S at a dose level of 5×1010 virus particles on day one.[45] The trial was paused on 12 October 2020, because a volunteer became ill,[46] but the company said it found no evidence that the vaccine had caused the illness and announced on 23 October 2020, that it would resume the trial.[47][48] On 29 January 2021, Janssen announced safety and efficacy data from an interim analysis of ENSEMBLE trial data, which demonstrated the vaccine was 66% effective at preventing the combined endpoints of moderate and severe COVID-19 at 28 days post-vaccination among all volunteers. The interim analysis was based on 468 cases of symptomatic COVID-19 among 43,783 adult volunteers in Argentina, Brazil, Chile, Colombia, Mexico, Peru, South Africa, and the United States. No deaths related to COVID-19 were reported in the vaccine group, while five deaths in the placebo group were related to COVID-19.[49] During the trial, no anaphylaxis was observed in participants.[49]
A second Phase III clinical trial called ENSEMBLE 2 started enrollment on 12 November 2020. ENSEMBLE 2 differs from ENSEMBLE in that its study participants will receive two intramuscular (IM) injections of Ad26.COV2.S, one on day 1 and the next on day 57.[50]
Manufacturing
In April 2020, Johnson & Johnson entered a partnership with Catalent who will provide large-scale manufacturing of the Johnson & Johnson vaccine at Catalent’s Bloomington, Indiana facility.[51] In July 2020, the partnership was expanded to include Catalent’s Anagni, Italy facility.[52]
In July 2020, Johnson & Johnson pledged to deliver up to 300 million doses of its vaccine to the U.S., with 100 million upfront and an option for 200 million more. The deal, worth more than $1 billion, will be funded by the Biomedical Advanced Research and Development Authority (BARDA) and the U.S. Defense Department.[53][54] The deal was confirmed on 5 August.[55]
In September 2020, Grand River Aseptic Manufacturing agreed with Johnson & Johnson to support the manufacture of the vaccine, including technology transfer and fill and finish manufacture, at its Grand Rapids, Michigan facility.[56]
In December 2020, Johnson & Johnson and Reig Jofre, a Spanish pharmaceutical company, entered into an agreement to manufacture the vaccine at Reig Jofre’s Barcelona facility.[57] If the European Medicines Agency (EMA) grants approval to the vaccine by March 2021, a European Union regulator said that Johnson & Johnson could start supplying vaccines to EU states starting on April 2021.[58][59]
In August 2020, Johnson & Johnson signed a contract with the U.S. federal government for US$1 billion, agreeing to deliver 100 million doses of the vaccine to the U.S. following the U.S. Food and Drug Administration (FDA) grant of approval or emergency use authorization (EUA) for the vaccine.[54] Under its agreement with the U.S. government, Johnson & Johnson was targeted to produce 12 million doses by the end of February 2021, more than 60 million doses by the end of April 2021, and more than 100 million doses by the end of June 2021. However, in January 2021, Johnson & Johnson acknowledged manufacturing delays would likely prevent it from meeting its contract of 12 million doses delivered to the U.S. by the end of February.[60] In late February 2021 congressional testimony by a company executive, however, Johnson & Johnson indicated that the company could deliver 20 million doses to the U.S. government by the end of March, and 100 million doses in the first half of 2021.[61]
In February 2021, Sanofi and Johnson & Johnson struck a deal for Sanofi to provide support and infrastructure at Sanofi’s Marcy-l’Étoile, France facility to manufacture approximately 12 million doses of the Johnson & Johnson vaccine per month once authorized.[62]
In March 2021, Merck & Co and Johnson & Johnson struck a deal for Merck to manufacture the Johnson & Johnson vaccine at two facilities in the United States to help expand the manufacturing capacity of the vaccine using provisions of the Defense Production Act.[63]
Regulatory approval process
Europe
Beginning on 1 December 2020, clinical trial of the vaccine candidate has been undergoing a “rolling review” process by the Committee for Medicinal Products for Human Use of the European Medicines Agency (EMA), a step to expedite EMA consideration of an expected conditional Marketing Authorisation Application.[58][78] On 16 February 2021, Janssen applied to the EMA for conditional marketing authorization of the vaccine.[3][79] The Committee for Medicinal Products for Human Use (CHMP) approved the COVID-19 Vaccine Janssen on 11 March.[11][25] Shipments of the vaccine are scheduled to start in the second half of April, with a commitment to deliver at least 200 million doses to the EU in 2021.[80]
United States
On 4 February 2021, Janssen Biotech applied to the U.S. Food and Drug Administration (FDA) for an EUA, and the FDA announced that its Vaccines and Related Biological Products Advisory Committee (VRBPAC) would meet on 26 February to consider the application.[30][33][81][82] Johnson & Johnson announced that it planned to ship the vaccine immediately following authorization.[49] On 24 February, ahead of the VRBPAC meeting, briefing documents from Janssen and the FDA were issued; the FDA document recommends granting the EUA, concluding that the results of the clinical trials and safety data are consistent with FDA EUA guidance for COVID-19 vaccines.[83][84][26][85] At the 26 February meeting, VRBPAC voted unanimously (22–0) to recommend that a EUA for the vaccine be issued.[86] The FDA granted the EUA for the vaccine the following day.[9][10][87] On 28 February, the CDC Advisory Committee on Immunization Practices (ACIP) recommended the use of the vaccine for those aged 18 and older.[88][23]
Elsewhere
On 11 February 2021, Saint Vincent and the Grenadines issued an EUA for the Johnson & Johnson vaccine, as well as the Moderna vaccine, the Pfizer–BioNTech vaccine, the Sputnik V vaccine, and the Oxford–AstraZeneca vaccine.[89]
In December 2020, Johnson & Johnson entered into an agreement in principle with Gavi, the Vaccine Alliance to support the COVAX Facility. On 19 February 2021, Johnson & Johnson submitted its formal request and data package to the World Health Organization for an Emergency Use Listing (EUL); an EUL is a requirement for participation in COVAX. Johnson & Johnson anticipates providing up to 500 million doses through 2022 for COVAX.[90][31][91]
On 25 February 2021, Bahrain authorized the vaccine for emergency use.[92][93]
On 26 February 2021, the South Korean Ministry of Food and Drug Safety began a review of Johnson & Johnson’s application for approval of its vaccine.[94]
In late November 2020, Johnson & Johnson submitted a rolling review application to Health Canada for approval of its vaccine.[95] The Canadian government has placed an order with Johnson & Johnson for 10 million doses, with an option to purchase up to 28 million additional doses; on 5 March, the vaccine became the fourth to receive Health Canada approval.[96]
In February 2021, the vaccine received emergency authorization in South Africa.[97][98][99]
Deployment and impact
Given the Johnson & Johnson vaccine is a single dose and has a lower cost, it is expected that it will play an important role in low and middle-income countries.[100] With lower costs and lower requirements of storage and distribution in comparison to the COVID-19 vaccines by Pfizer and Moderna, the Johnson & Johnson vaccine will be more easily transported, stored, and administered.[101] South African health minister Zweli Mkhize announced on 9 February 2021 that the country would sell or swap its one million doses of AstraZeneca vaccine.[102] Once it did so, South Africa began vaccination using the Johnson & Johnson vaccine on 17 February 2021,[99] marking the vaccine’s first use outside of a clinical trial.[103]
Ethical concerns
The United States Conference of Catholic Bishops has expressed ethical concerns about the vaccine due to the use of tissue from aborted fetuses in the 1980s.[104]
See also
Notes
- ^ US authorization also includes the three sovereign nations in the Compact of Free Association: Palau, the Marshall Islands, and Micronesia.[75][76]
References
- ^ Jump up to:a b c “Janssen COVID-19 Vaccine- ad26.cov2.s injection, suspension”. DailyMed. Retrieved 27 February 2021.
- ^ “Janssen COVID-19 Emergency Use Authorization (EUA) Official Website”. Janssen. 28 February 2021. Retrieved 28 February2021.
- ^ Jump up to:a b c “EMA receives application for conditional marketing authorisation of COVID-19 Vaccine Janssen” (Press release). European Medicines Agency (EMA). 16 February 2021. Retrieved 16 February 2021.
- ^ Jump up to:a b c d e “A Randomized, Double-blind, Placebo-controlled Phase 3 Study to Assess the Efficacy and Safety of Ad26.COV2.S for the Prevention of SARS-CoV-2-mediated COVID-19 in Adults Aged 18 Years and Older ENSEMBLE Protocol VAC31518COV3001; Phase 3” (PDF). Janssen Vaccines & Prevention.
- ^ Jump up to:a b c d “A Randomized, Double-blind, Placebo-controlled Phase 3 Study to Assess the Efficacy and Safety of Ad26.COV2.S for the Prevention of SARS-CoV-2-mediated COVID-19 in Adults Aged 18 Years and Older ENSEMBLE 2 Protocol VAC31518COV3009; Phase 3” (PDF). Janssen Vaccines & Prevention.
- ^ Jump up to:a b “Johnson & Johnson Initiates Pivotal Global Phase 3 Clinical Trial of Janssen’s COVID-19 Vaccine Candidate”. Johnson & Johnson (Press release). Retrieved 23 September 2020.
- ^ “Regulatory Decision Summary – Janssen COVID-19 Vaccine – Health Canada”. Health Canada. 5 March 2021. Retrieved 5 March 2021.
- ^ “Janssen COVID-19 Vaccine monograph” (PDF). Janssen. 5 March 2021.
- ^ Jump up to:a b c “FDA Issues Emergency Use Authorization for Third COVID-19 Vaccine”. U.S. Food and Drug Administration (FDA) (Press release). 27 February 2021. Retrieved 27 February 2021.
- ^ Jump up to:a b c https://www.fda.gov/media/146303/download
- ^ Jump up to:a b c “COVID-19 Vaccine Janssen EPAR”. European Medicines Agency (EMA). 5 March 2021. Retrieved 16 March 2021.
- ^ “A Study of Ad26.COV2.S for the Prevention of SARS-CoV-2-Mediated COVID-19 in Adult Participants (ENSEMBLE)”. ClinicalTrials.gov. Retrieved 30 January 2021.
- ^ “Leiden developed Covid-19 vaccine submitted to EMA for approval”. 16 February 2021.
- ^ “Clinical trial COVID-19 vaccine candidate underway”. Janssen Belgium. Retrieved 13 March 2021.
- ^ “EMA recommends Johnson & Johnson Covid vaccine for approval; Developed in Leiden”. NL Times.
- ^ Jump up to:a b Saltzman J (12 March 2020). “Beth Israel is working with Johnson & Johnson on a coronavirus vaccine”. The Boston Globe.
- ^ Jump up to:a b c d e “Fact Sheet for Vaccine Providers & full EUA PI”(PDF). Janssen. Retrieved 28 February 2021.
- ^ Commissioner, Office of the (2 March 2021). “FDA Issues Emergency Use Authorization for Third COVID-19 Vaccine”. FDA. Retrieved 7 March 2021.
- ^ Salzman S (29 January 2021). “Johnson & Johnson single-shot vaccine 85% effective against severe COVID-19 disease”. ABC News.
- ^ Gallagher J (29 January 2021). “Covid vaccine: Single dose Covid vaccine 66% effective”. BBC News. Retrieved 29 January 2021.
- ^ Sohn R (29 January 2021). “J&J’s Covid vaccine is 66% effective, a weapon but not a knockout punch”. Stat. Retrieved 29 January2021.
- ^ Commissioner, Office of the (2 March 2021). “FDA Issues Emergency Use Authorization for Third COVID-19 Vaccine”. FDA. Retrieved 7 March 2021.
- ^ Jump up to:a b “Media Statement from CDC Director Rochelle P. Walensky, MD, MPH, on Signing the Advisory Committee on Immunization Practices’ Recommendation to Use Janssen’s COVID-19 Vaccine in People 18 and Older”. Centers for Disease Control and Prevention (CDC) (Press release). 28 February 2021. Retrieved 1 March 2021.
- ^ “EMA recommends COVID-19 Vaccine Janssen for authorisation in the EU” (Press release). European Medicines Agency (EMA). 11 March 2021. Retrieved 11 March 2021.
- ^ Jump up to:a b “COVID-19 Vaccine Janssen”. Union Register of medicinal products. Retrieved 16 March 2021.
- ^ Jump up to:a b c d FDA Briefing Document Janssen Ad26.COV2.S Vaccine for the Prevention of COVID-19 (PDF) (Report). U.S. Food and Drug Administration (FDA). Lay summary.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ “The tiny tweak behind COVID-19 vaccines”. Chemical & Engineering News. 29 September 2020. Retrieved 1 March 2021.
- ^ Kramer, Jillian (31 December 2020). “They spent 12 years solving a puzzle. It yielded the first COVID-19 vaccines”. National Geographic.
- ^ Mercado NB, Zahn R, Wegmann F, Loos C, Chandrashekar A, Yu J, et al. (October 2020). “Single-shot Ad26 vaccine protects against SARS-CoV-2 in rhesus macaques”. Nature. 586 (7830): 583–88. Bibcode:2020Natur.586..583M. doi:10.1038/s41586-020-2607-z. PMC 7581548. PMID 32731257. S2CID 220893461.
- ^ Jump up to:a b Johnson CY, McGinley L (4 February 2021). “Johnson & Johnson seeks emergency FDA authorization for single-shot coronavirus vaccine”. The Washington Post.
- ^ Jump up to:a b Weintraub K. “One-dose J&J COVID-19 vaccine meets criteria as safe and effective, FDA report finds”. USA Today. Retrieved 25 February 2021.
- ^ Mole B (29 January 2021). “COVID variants throw J&J vaccine a curveball, lowering efficacy to 66%”. Ars Technica. Retrieved 26 February 2021.
- ^ Jump up to:a b Chander V (4 February 2021). “J&J files COVID-19 vaccine application with U.S. FDA”. Reuters. Retrieved 4 February 2021.
- ^ Vecchione A (13 March 2020). “J&J collaborates to accelerate COVID-19 vaccine development”. NJBIZ. Retrieved 22 April2020.
- ^ “Prisma Health collaborates with Ethicon Inc. to make, distribute VESper Ventilator Expansion Splitter Device”. WSPA 7News. 6 April 2020. Retrieved 22 April 2020.
- ^ “Coronavirus: Johnson & Johnson vows to make ‘not-for-profit’ vaccine”. Sky News. Retrieved 22 April 2020.
- ^ “A Beth Israel researcher helped create a COVID-19 vaccine that awaits approval. It could be a ‘game changer'”. The Boston Globe. 16 January 2021. Retrieved 28 February 2021.
- ^ “FDA grants third COVID-19 vaccine, developed in part at BIDMC, emergency use authorization”. Beth Israel Deaconess Medical Center (BIDMC). 27 February 2021. Retrieved 28 February 2021.
- ^ Coleman J (10 June 2020). “Final testing stage for potential coronavirus vaccine set to begin in July”. TheHill. Retrieved 11 June 2020.
- ^ “Moderna, AstraZeneca and J&J coronavirus shots rev up for NIH tests beginning in July: WSJ”. FiercePharma. Retrieved 11 June2020.
- ^ “Johnson & Johnson to start human testing of COVID-19 vaccine next week”. FiercePharma. Retrieved 20 July 2020.
- ^ “A Study of Ad26.COV2.S in Adults (COVID-19)”. ClinicalTrials.gov. Retrieved 19 February 2021.
- ^ Sadoff J, Le Gars M, Shukarev G, Heerwegh D, Truyers C, de Groot AM, et al. (January 2021). “Interim Results of a Phase 1-2a Trial of Ad26.COV2.S Covid-19 Vaccine”. New England Journal of Medicine. doi:10.1056/NEJMoa2034201. PMC 7821985. PMID 33440088.
- ^ “Johnson & Johnson COVID-19 Vaccine Candidate Interim Phase 1/2a Data Published in New England Journal of Medicine”. Johnson & Johnson (Press release). Retrieved 16 January 2021.
- ^ “Fourth large-scale COVID-19 vaccine trial begins in the United States”. National Institutes of Health. Retrieved 30 January 2021.
- ^ Hughes V, Thomas K, Zimmer C, Wu KJ (12 October 2020). “Johnson & Johnson halts coronavirus vaccine trial because of sick volunteer”. The New York Times. ISSN 0362-4331. Retrieved 12 October 2020.
- ^ “Johnson & Johnson Prepares to Resume Phase 3 ENSEMBLE Trial of its Janssen COVID-19 Vaccine Candidate in the U.S.”Johnson & Johnson (Press release). 23 October 2020. Retrieved 28 October 2020.
- ^ Edwards E, Miller SG (23 October 2020). “AstraZeneca, Johnson & Johnson resume late-stage Covid-19 vaccine trials”. NBC News. Retrieved 28 October 2020.
- ^ Jump up to:a b c “Johnson & Johnson Announces Single-Shot Janssen COVID-19 Vaccine Candidate Met Primary Endpoints in Interim Analysis of its Phase 3 ENSEMBLE Trial”. Johnson & Johnson(Press release). Retrieved 1 February 2021.
- ^ “A Study of Ad26.COV2.S for the Prevention of SARS-CoV-2-mediated COVID-19 in Adults (ENSEMBLE 2)”. ClinicalTrials.gov. Retrieved 30 January 2021.
- ^ Vecchione A (29 April 2020). “Catalent to lead US manufacturing for J&J’s lead COVID-19 vaccine candidate”. NJBIZ. Retrieved 13 November 2020.
- ^ “J&J expands COVID-19 vaccine pact with Catalent for finishing work at Italian facility”. FiercePharma. Retrieved 13 November2020.
- ^ “HHS, DOD Collaborate With Johnson & Johnson to Produce Millions of COVID-19 Investigational Vaccine Doses”. HHS.gov(Press release). 5 August 2020. Retrieved 6 August 2020.
- ^ Jump up to:a b “Johnson & Johnson Announces Agreement with U.S. Government for 100 Million Doses of Investigational COVID-19 Vaccine”. Johnson & Johnson (Press release). Retrieved 6 August 2020.
- ^ “US to Pay Johnson and Johnson $1 Billion for COVID-19 Vaccine”. Voice of America. Retrieved 5 August 2020.
- ^ “Ramping Up COVID-19 Vaccine Fill and Finish Capacity”. Contract Pharma. 3 November 2020.
- ^ Allen JF (15 December 2020). “Spain’s Reig Jofre to manufacture J&J’s COVID-19 vaccine, shares soar”. Reuters.
- ^ Jump up to:a b Guarascio F (13 January 2021). “J&J COVID-19 vaccine could be available in Europe in April: source”. Reuters.
- ^ “EMA expected to approve Johnson & Johnson vaccine by March – CEO of Janssen Italy to paper”. Reuters. 10 February 2021. Retrieved 13 February 2021.
- ^ Zimmer C, LaFraniere S, Weiland N (13 January 2021). “Johnson & Johnson Expects Vaccine Results Soon but Lags in Production”. The New York Times.
- ^ Sarah Owermohle, Johnson & Johnson says it can provide 20M vaccine doses by late March, Politico (22 February 2021).
- ^ France’s Sanofi to help Johnson & Johnson manufacture COVID-19 vaccine, Reuters (22 February 2021).
- ^ “Biden Administration Announces Historic Manufacturing Collaboration Between Merck and Johnson & Johnson to Expand Production of COVID-19 Vaccines”. HHS (Press release). 2 March 2021. Retrieved 4 March 2021.
- ^ “European Commission authorises fourth safe and effective vaccine against COVID-19”. European Commission (Press release). 11 March 2021.
- ^ Jump up to:a b “EU-Kommissionen har i dag udstedt en betinget markedsføringstilladelse til Johnson & Johnsons COVID-19- vaccine. Tilladelsen gælder i Danmark”. Lægemiddelstyrelsen (in Danish). Retrieved 12 March 2021.
- ^ “The Icelandic Medicines Agency have issued a conditional marketing authorisation”. covid.is. Retrieved 12 March 2021.
- ^ “The European Commission has now approved the Johnson & Johnson vaccine. This means that the vaccine is approved for use in the EU and Norway”. vg. Retrieved 12 March 2021.
- ^ “Informació en relació amb la vacunació contra la COVID-19”(PDF). Govern d’Andorra. Retrieved 14 March 2021.
- ^ “Bahrain first to approve Johnson & Johnson COVID-19 vaccine for emergency use”. Reuters. 25 February 2021. Retrieved 25 February 2021.
- ^ “Bahrain becomes 1st nation to grant J&J shot emergency use”. ABC News. 25 February 2021. Retrieved 25 February 2021.
- ^ “Johnson & Johnson COVID-19 vaccine becomes 4th to receive Health Canada approval | CBC News”. Canadian Broadcasting Corporation. Retrieved 5 March 2021.
- ^ https://www.jnj.com/johnson-johnson-single-shot-covid-19-vaccine-granted-conditional-marketing-authorization-by-european-commission
- ^ “Public Health (Emergency Authorisation of COVID-19 Vaccine) Rules, 2021” (PDF). Government of Saint Vincent and the Grenadines. 11 February 2021. Retrieved 12 February 2021.
- ^ “Coronavirus: South Africa rolls out vaccination programme”. BBC News. 17 February 2021. Retrieved 19 February 2021.
- ^ “Interior Applauds Inclusion of Insular Areas through Operation Warp Speed to Receive COVID-19 Vaccines” (Press release). United States Department of the Interior (DOI). 12 December 2020. Retrieved 13 January 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ Dorman B (6 January 2021). “Asia Minute: Palau Administers Vaccines to Keep Country Free of COVID”. Hawaii Public Radio. Retrieved 13 January 2021.
- ^ “WHO approves J&J’s COVID-19 vaccine for emergency listing”. Channel News Asia. 13 March 2021. Retrieved 13 March2021.
- ^ “Johnson & Johnson Announces Initiation of Rolling Submission for its Single-dose Janssen COVID-19 Vaccine Candidate with the European Medicines Agency” (Press release). Johnson & Johnson. 1 December 2020.
- ^ Johnson & Johnson Announces Submission of European Conditional Marketing Authorisation Application to the EMA for its Investigational Janssen COVID-19 Vaccine Candidate
- ^ M, Muvija; Aripaka, Pushkala (11 March 2021). “Europe clears J&J’s single-shot COVID-19 vaccine as roll-out falters”. Reuters. Retrieved 16 March 2021.
- ^ “FDA Announces Advisory Committee Meeting to Discuss Janssen Biotech Inc.’s COVID-19 Vaccine Candidate” (Press release). U.S. Food and Drug Administration. 4 February 2021. Retrieved 4 February 2021.
- ^ “VRBPAC February 26, 2021 Meeting Announcement”. U.S. Food and Drug Administration. Retrieved 19 February 2021.
- ^ Janssen Biotech, Inc. COVID-19 Vaccine Ad26.COV2.S VRBPAC Briefing Document (PDF) (Report). Janssen Biotech.
- ^ Janssen Biotech, Inc. COVID-19 Vaccine Ad26.COV2.S VRBPAC Briefing Document Addendum (PDF) (Report). Janssen Biotech.
- ^ Christensen J (24 February 2021). “FDA says Johnson & Johnson Covid-19 vaccine meets requirements for emergency use authorization”. CNN.
- ^ Lovelace Jr B (26 February 2021). “FDA panel unanimously recommends third Covid vaccine as J&J wins key vote in path to emergency use”.
- ^ McGinley L, Johnson CY (27 February 2021). “FDA authorizes Johnson & Johnson’s single-shot coronavirus vaccine, adding to the nation’s arsenal against the pandemic”. The Washington Post.
- ^ Feuer W (28 February 2021). “CDC panel recommends use of J&J’s single-shot Covid vaccine, clearing way for distribution”. CNBC. Retrieved 28 February 2021.
- ^ “Public Health (Emergency Authorisation of COVID-19 Vaccine) Rules, 2021” (PDF). Government of Saint Vincent and the Grenadines. 11 February 2021. Retrieved 12 February 2021.
- ^ Johnson & Johnson Announces Submission to World Health Organization for Emergency Use Listing of Investigational Single-Shot Janssen COVID-19 Vaccine Candidate, Johnson & Johnson (19 February 2021).
- ^ Heeb G. “Johnson & Johnson Applies For Emergency Use Vaccine Approval At W.H.O.” Forbes. Retrieved 25 February2021.
- ^ “Bahrain first to approve Johnson & Johnson COVID-19 vaccine for emergency use”. Reuters. 25 February 2021. Retrieved 25 February 2021.
- ^ “Bahrain becomes 1st nation to grant J&J shot emergency use”. ABC News. 25 February 2021. Retrieved 25 February 2021.
- ^ South Korea launches review of Johnson & Johnson’s COVID-19 vaccine, Reuters (26 February 2021).
- ^ Terry Haig, Novavax submits its vaccine for Health Canada approval, Radio Canada International (1 February 2021).
- ^ “Johnson & Johnson COVID-19 vaccine becomes 4th to receive Health Canada approval”. CBC.
- ^ “SA is the first country to roll out Johnson & Johnson vaccine – what you need to know about the jab”. BusinessInsider. 17 February 2021. Retrieved 4 March 2021.
- ^ Browdie, Brian (20 February 2021). “South Africa to be first to use Johnson Johnson Covid-19 vaccine”. Quartz. Retrieved 4 March2021.
- ^ Jump up to:a b Steinhauser G (17 February 2021). “South Africa Rolls Out J&J Covid-19 Vaccine to Healthcare Workers”. The Wall Street Journal.
- ^ Grady D (29 January 2021). “Which Covid Vaccine Should You Get? Experts Cite the Effect Against Severe Disease”. The New York Times. Retrieved 9 February 2021.
- ^ Brueck H. “Moderna vaccine creator calls Johnson & Johnson’s competing shot a ‘darn good’ tool to fight the pandemic”. Business Insider. Retrieved 9 February 2021.
- ^ Winning A, Roelf W (9 February 2021). “South Africa may sell AstraZeneca shots as it switches to J&J vaccine to fight variant”. Yahoo!. Reuters. Retrieved 11 February 2021.
- ^ “Johnson & Johnson applies to WHO for emergency use listing of COVID-19 vaccine”. Reuters. 19 February 2021. Retrieved 19 March 2021.
- ^ “Some US bishops discourage Catholics from getting Johnson & Johnson vaccine if others are available”. CNN. 3 March 2021. Retrieved 20 March 2021.
External links
| Scholia has a profile for Ad26.COV2.S (Q98655215). |
- “How the Johnson & Johnson Covid-19 Vaccine Works”. The New York Times.
- “Janssen COVID-19 Vaccine (Johnson & Johnson)”. Centers for Disease Control and Prevention (CDC).
| A vial of Janssen COVID-19 Vaccine | |
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | Viral vector |
| Clinical data | |
| Trade names | Janssen COVID-19 Vaccine,[1][2] COVID-19 Vaccine Janssen[3] |
| Other names | Ad26.COV2.S[4][5][6]JNJ-78436735[4][5][6]Ad26COVS1[4][5]VAC31518[4][5] |
| License data | US DailyMed: Janssen_COVID-19_Vaccine |
| Routes of administration | Intramuscular |
| ATC code | None |
| Legal status | |
| Legal status | CA: Schedule D; Authorized by interim order [7][8]US: Unapproved (Emergency Use Authorization)[9][1][10]EU: Conditional marketing authorization granted [11] |
| Identifiers | |
| DrugBank | DB15857 |
| UNII | JT2NS6183B |
| Part of a series on the |
| COVID-19 pandemic |
|---|
| SARS-CoV-2 (virus)COVID-19 (disease) |
| showTimeline |
| showLocations |
| showInternational response |
| showMedical response |
| showImpact |
| COVID-19 Portal |
| vte |
////////////////Johnson & Johnson, COVID-19 vaccine, JNJ 78436735, Ad26.COV2.S, JNJ-78436735, Ad26COVS1, VAC31518, vaccine, corona virus, covid 19
#Johnson & Johnson, #COVID-19 vaccine, #JNJ 78436735, #Ad26.COV2.S, #JNJ-78436735, #Ad26COVS1, VAC31518, #vaccine, #corona virus, #covid 19
NOVAWAX, NVX-CoV2373,

NOVAWAX
SARS-CoV-2 rS Nanoparticle Vaccine
MCDC OTA agreement number W15QKN-16-9-1002
Novavax COVID-19 vaccine, Coronavirus disease 19 infection
SARS-CoV-2 rS, TAK 019
Novavax, Inc. is an American vaccine development company headquartered in Gaithersburg, Maryland, with additional facilities in Rockville, Maryland and Uppsala, Sweden. As of 2020, it had an ongoing Phase III clinical trial in older adults for its candidate vaccine for seasonal influenza, NanoFlu and a candidate vaccine (NVX-CoV2373) for prevention of COVID-19.
NVX-CoV2373 is a SARS-CoV-2 rS vaccine candidate and was shown to have high immunogenicity in studies. The vaccine is created from the genetic sequence of COVID-19 and the antigen derived from the virus spike protein is generated using recombinant nanoparticle technology. The vaccine was developed and tested by Novavax. As of May 2020, the company is pursuing a Phase 1 clinical trial (NCT04368988) to test the vaccine.
History
Novavax was founded in 1987. It focused principally on experimental vaccine development, but did not achieve a successful launch up to 2021.[4]
In June 2013, Novavax acquired the Matrix-M adjuvant platform with the purchase of Swedish company Isconova AB and renamed its new subsidiary Novavax AB.[5]
In 2015, the company received an $89 million grant from the Bill & Melinda Gates Foundation to support the development of a vaccine against human respiratory syncytial virus for infants via maternal immunization.[6][7][8][9]
In March 2015 the company completed a Phase I trial for its Ebola vaccine candidate,[10] as well as a phase II study in adults for its RSV vaccine, which would become ResVax.[11] The ResVax trial was encouraging as it showed significant efficacy against RSV infection.[11]
2016 saw the company’s first phase III trial, the 12,000 adult Resolve trial,[11] for its respiratory syncytial virus vaccine, which would come to be known as ResVax, fail in September.[3] This triggered an eighty-five percent dive in the company’s stock price.[3] Phase II adult trial results also released in 2016 showed a stimulation of antigencity, but failure in efficacy.[11] Evaluation of these results suggested that an alternative dosing strategy might lead to success, leading to plans to run new phase II trials.[3] The company’s difficulties in 2016 led to a three part strategy for 2017: cost reduction through restructuring and the termination of 30% of their workforce; pouring more effort into getting ResVax to market; and beginning clinical trials on a Zika virus vaccine.[3]
Alongside the adult studies of ResVax, the vaccine was also in 2016 being tested against infant RSV infection through the route of maternal immunization.[11]
In 2019, late-stage clinical testing of ResVax, failed for a second time, which resulted in a major downturn in investor confidence and a seventy percent reduction in capital value for the firm.[12][13] As a secondary result, the company was forced to conduct a reverse stock split in order to maintain Nasdaq minimum qualification, meaning it was in risk of being delisted.[13]
The company positions NanoFlu for the unmet need for a more effective vaccine against influenza, particularly in the elderly who often experience serious and sometimes life-threatening complications. In January 2020, it was granted fast track status by the U.S. Food and Drug Administration (FDA) for NanoFlu.
External sponsorships
In 2018, Novavax received a US$89 million research grant from the Bill and Melinda Gates Foundation for development of vaccines for maternal immunization.[14]
In May 2020, Novavax received US$384 million from the Coalition for Epidemic Preparedness Innovations to fund early-stage evaluation in healthy adults of the company’s COVID-19 vaccine candidate NVX-CoV2373 and to develop resources in preparation for large-scale manufacturing, if the vaccine proves successful.[15] CEPI had already invested $4 million in March.[15]
Drugs in development
ResVax is a nanoparticle-based treatment using a recombinant F lipoprotein or saponin, “extracted from the Quillaja saponaria [or?] Molina bark together with cholesterol and phospholipid.”[16] It is aimed at stimulating resistance to respiratory syncytial virus infection, targeting both adult and infant populations.[11]
In January 2020, Novavax was given Fast Track status by the FDA to expedite the review process for NanoFlu, a candidate influenze vaccine undergoing a Phase III clinical trial scheduled for completion by mid-2020.[17]
COVID-19 vaccine candidate
See also: NVX-CoV2373 and COVID-19 vaccine
In January 2020, Novavax announced development of a vaccine candidate, named NVX-CoV2373, to establish immunity to SARS-CoV-2.[18] NVX-CoV2373 is a protein subunit vaccine that contains the spike protein of the SARS-CoV-2 virus.[19] Novavax’s work is in competition for vaccine development among dozens of other companies.
In January 2021, the company released phase 3 trials showing that it has 89% efficacy against Covid-19, and also provides strong immunity against new variants.[20] It has applied for emergency use in the US and UK but will be distributed in the UK first.Novavax COVID-19 Vaccine Demonstrates 89.3% Efficacy in UK Phase 3 TrialJan 28, 2021 at 4:05 PM ESTDownload PDF
First to Demonstrate Clinical Efficacy Against COVID-19 and Both UK and South Africa Variants
- Strong efficacy in Phase 3 UK trial with over 50% of cases attributable to the now-predominant UK variant and the remainder attributable to COVID-19 virus
- Clinical efficacy demonstrated in Phase 2b South Africa trial with over 90% of sequenced cases attributable to prevalent South Africa escape variant
- Company to host investor conference call today at 4:30pm ET
GAITHERSBURG, Md., Jan. 28, 2021 (GLOBE NEWSWIRE) — Novavax, Inc. (Nasdaq: NVAX), a biotechnology company developing next-generation vaccines for serious infectious diseases, today announced that NVX-CoV2373, its protein-based COVID-19 vaccine candidate, met the primary endpoint, with a vaccine efficacy of 89.3%, in its Phase 3 clinical trial conducted in the United Kingdom (UK). The study assessed efficacy during a period with high transmission and with a new UK variant strain of the virus emerging and circulating widely. It was conducted in partnership with the UK Government’s Vaccines Taskforce. Novavax also announced successful results of its Phase 2b study conducted in South Africa.
“With today’s results from our UK Phase 3 and South Africa Phase 2b clinical trials, we have now reported data on our COVID-19 vaccine from Phase 1, 2 and 3 trials involving over 20,000 participants. In addition, our PREVENT-19 US and Mexico clinical trial has randomized over 16,000 participants toward our enrollment goal of 30,000. NVX-CoV2373 is the first vaccine to demonstrate not only high clinical efficacy against COVID-19 but also significant clinical efficacy against both the rapidly emerging UK and South Africa variants,” said Stanley C. Erck, President and Chief Executive Officer, Novavax. “NVX-CoV2373 has the potential to play an important role in solving this global public health crisis. We look forward to continuing to work with our partners, collaborators, investigators and regulators around the world to make the vaccine available as quickly as possible.”
NVX-CoV2373 contains a full-length, prefusion spike protein made using Novavax’ recombinant nanoparticle technology and the company’s proprietary saponin-based Matrix-M™ adjuvant. The purified protein is encoded by the genetic sequence of the SARS-CoV-2 spike (S) protein and is produced in insect cells. It can neither cause COVID-19 nor can it replicate, is stable at 2°C to 8°C (refrigerated) and is shipped in a ready-to-use liquid formulation that permits distribution using existing vaccine supply chain channels.
UK Phase 3 Results: 89.3% Efficacy
The study enrolled more than 15,000 participants between 18-84 years of age, including 27% over the age of 65. The primary endpoint of the UK Phase 3 clinical trial is based on the first occurrence of PCR-confirmed symptomatic (mild, moderate or severe) COVID-19 with onset at least 7 days after the second study vaccination in serologically negative (to SARS-CoV-2) adult participants at baseline.
The first interim analysis is based on 62 cases, of which 56 cases of COVID-19 were observed in the placebo group versus 6 cases observed in the NVX-CoV2373 group, resulting in a point estimate of vaccine efficacy of 89.3% (95% CI: 75.2 – 95.4). Of the 62 cases, 61 were mild or moderate, and 1 was severe (in placebo group).
Preliminary analysis indicates that the UK variant strain that was increasingly prevalent was detected in over 50% of the PCR-confirmed symptomatic cases (32 UK variant, 24 non-variant, 6 unknown). Based on PCR performed on strains from 56 of the 62 cases, efficacy by strain was calculated to be 95.6% against the original COVID-19 strain and 85.6% against the UK variant strain [post hoc].
The interim analysis included a preliminary review of the safety database, which showed that severe, serious, and medically attended adverse events occurred at low levels and were balanced between vaccine and placebo groups.
“These are spectacular results, and we are very pleased to have helped Novavax with the development of this vaccine. The efficacy shown against the emerging variants is also extremely encouraging. This is an incredible achievement that will ensure we can protect individuals in the UK and the rest of the world from this virus,” said Clive Dix, Chair, UK Vaccine Taskforce.
Novavax expects to share further details of the UK trial results as additional data become available. Additional analysis on both trials is ongoing and will be shared via prepublication servers as well as submitted to a peer-reviewed journal for publication. The company initiated a rolling submission to the United Kingdom’s regulatory agency, the MHRA, in mid-January.
South Africa Results: Approximately 90% of COVID-19 cases attributed to South Africa escape variant
In the South Africa Phase 2b clinical trial, 60% efficacy (95% CI: 19.9 – 80.1) for the prevention of mild, moderate and severe COVID-19 disease was observed in the 94% of the study population that was HIV-negative. Twenty-nine cases were observed in the placebo group and 15 in the vaccine group. One severe case occurred in the placebo group and all other cases were mild or moderate. The clinical trial also achieved its primary efficacy endpoint in the overall trial population, including HIV-positive and HIV-negative subjects (efficacy of 49.4%; 95% CI: 6.1 – 72.8).
This study enrolled over 4,400 patients beginning in August 2020, with COVID-19 cases counted from September through mid-January. During this time, the triple mutant variant, which contains three critical mutations in the receptor binding domain (RBD) and multiple mutations outside the RBD, was widely circulating in South Africa. Preliminary sequencing data is available for 27 of 44 COVID-19 events; of these, 92.6% (25 out of 27 cases) were the South Africa escape variant.
Importantly in this trial, approximately 1/3 of the patients enrolled (but not included in the primary analyses described above) were seropositive, demonstrating prior COVID-19 infection at baseline. Based on temporal epidemiology data in the region, the pre-trial infections are thought to have been caused by the original COVID-19 strain (i.e., non-variant), while the subsequent infections during the study were largely variant virus. These data suggest that prior infection with COVID-19 may not completely protect against subsequent infection by the South Africa escape variant, however, vaccination with NVX-CoV2373 provided significant protection.
“The 60% reduced risk against COVID-19 illness in vaccinated individuals in South Africans underscores the value of this vaccine to prevent illness from the highly worrisome variant currently circulating in South Africa, and which is spreading globally. This is the first COVID-19 vaccine for which we now have objective evidence that it protects against the variant dominating in South Africa,” says Professor Shabir Maddi, Executive Director of the Vaccines and Infectious Diseases Analytics Research Unit (VIDA) at Wits, and principal investigator in the Novavax COVID-19 vaccine trial in South Africa. “I am encouraged to see that Novavax plans to immediately begin clinical development on a vaccine specifically targeted to the variant, which together with the current vaccine is likely to form the cornerstone of the fight against COVID-19.”
Novavax initiated development of new constructs against the emerging strains in early January and expects to select ideal candidates for a booster and/or combination bivalent vaccine for the new strains in the coming days. The company plans to initiate clinical testing of these new vaccines in the second quarter of this year.
“A primary benefit of our adjuvanted platform is that it uses a very small amount of antigen, enabling the rapid creation and large-scale production of combination vaccine candidates that could potentially address multiple circulating strains of COVID-19,” said Gregory M. Glenn, M.D., President of Research and Development, Novavax. “Combined with the safety profile that has been observed in our studies to-date with our COVID-19 vaccine, as well as prior studies in influenza, we are optimistic about our ability to rapidly adapt to evolving conditions.”
The Coalition for Epidemic Preparedness Innovations (CEPI) funded the manufacturing of doses of NVX-CoV2373 for this Phase 2b clinical trial, which was supported in part by a $15 million grant from the Bill & Melinda Gates Foundation.
Significant progress on PREVENT-19 Clinical Trial in US and Mexico
To date, PREVENT-19 has randomized over 16,000 participants and expects to complete our targeted enrollment of 30,000 patients in the first half of February. PREVENT-19 is being conducted with support from the U.S. government partnership formerly known as Operation Warp Speed, which includes the Department of Defense, the Biomedical Advanced Research and Development Authority (BARDA), part of the U.S. Department of Health and Human Services (HHS) Office of the Assistant Secretary for Preparedness and Response, and the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH) at HHS. BARDA is also providing up to $1.75 billion under a Department of Defense agreement.
PREVENT-19 (the PRE-fusion protein subunit Vaccine Efficacy Novavax Trial | COVID-19) is a Phase 3, randomized, placebo-controlled, observer-blinded study in the US and Mexico to evaluate the efficacy, safety and immunogenicity of NVX-CoV2373 with Matrix-M in up to 30,000 subjects 18 years of age and older compared with placebo. The trial design has been harmonized to align with other Phase 3 trials conducted under the auspices of Operation Warp Speed, including the use of a single external independent Data and Safety Monitoring Board to evaluate safety and conduct an unblinded review when predetermined interim analysis events are reached.
The trial’s primary endpoint is the prevention of PCR-confirmed, symptomatic COVID-19. The key secondary endpoint is the prevention of PCR-confirmed, symptomatic moderate or severe COVID-19. Both endpoints will be assessed at least seven days after the second study vaccination in volunteers who have not been previously infected with SARS-CoV-2.
Conference Call
Novavax will host a conference call today at 4:30pm ET. The dial-in numbers for the conference call are (877) 212-6076 (Domestic) or (707) 287-9331 (International), passcode 7470222. A replay of the conference call will be available starting at 7:30 p.m. ET on January 28, 2021 until 7:30 p.m. ET on February 4, 2021. To access the replay by telephone, dial (855) 859-2056 (Domestic) or (404) 537-3406 (International) and use passcode 7470222.
A webcast of the conference call can also be accessed on the Novavax website at novavax.com/events. A replay of the webcast will be available on the Novavax website until April 28, 2021.
About NVX-CoV2373
NVX-CoV2373 is a protein-based vaccine candidate engineered from the genetic sequence of SARS-CoV-2, the virus that causes COVID-19 disease. NVX-CoV2373 was created using Novavax’ recombinant nanoparticle technology to generate antigen derived from the coronavirus spike (S) protein and is adjuvanted with Novavax’ patented saponin-based Matrix-M™ to enhance the immune response and stimulate high levels of neutralizing antibodies. NVX-CoV2373 contains purified protein antigen and can neither replicate, nor can it cause COVID-19. Over 37,000 participants have participated to date across four different clinical studies in five countries. NVX-CoV2373 is currently being evaluated in two pivotal Phase 3 trials: a trial in the U.K that completed enrollment in November and the PREVENT-19 trial in the U.S. and Mexico that began in December.
About Matrix-M™
Novavax’ patented saponin-based Matrix-M™ adjuvant has demonstrated a potent and well-tolerated effect by stimulating the entry of antigen presenting cells into the injection site and enhancing antigen presentation in local lymph nodes, boosting immune response.
About Novavax
Novavax, Inc. (Nasdaq: NVAX) is a biotechnology company that promotes improved health globally through the discovery, development and commercialization of innovative vaccines to prevent serious infectious diseases. The company’s proprietary recombinant technology platform combines the power and speed of genetic engineering to efficiently produce highly immunogenic nanoparticles designed to address urgent global health needs. Novavax is conducting late-stage clinical trials for NVX-CoV2373, its vaccine candidate against SARS-CoV-2, the virus that causes COVID-19. NanoFlu™, its quadrivalent influenza nanoparticle vaccine, met all primary objectives in its pivotal Phase 3 clinical trial in older adults and will be advanced for regulatory submission. Both vaccine candidates incorporate Novavax’ proprietary saponin-based Matrix-M™ adjuvant to enhance the immune response and stimulate high levels of neutralizing antibodies.
For more information, visit www.novavax.com and connect with us on Twitter and LinkedIn.
Candidate: NVX-CoV2373
Category: VAX
Type: Stable, prefusion protein made using Novavax’ proprietary nanoparticle technology, and incorporating its proprietary saponin-based Matrix-M™ adjuvant.
2021 Status: Novavax on March 11 announced final efficacy of 96.4% against mild, moderate and severe disease caused by the original COVID-19 strain in a pivotal Phase III trial in the U.K. of NVX–CoV2373. The study enrolled more than 15,000 participants between 18-84 years of age, including 27% over the age of 65.
The company also announced the complete analysis of its Phase IIb trial in South Africa, showing the vaccine had an efficacy of 55.4% among a cohort of HIV-negative trial participants, and an overall efficacy of 48.6% against predominantly variant strains of SARS-CoV-2 among 147 PCR-positive cases (51 cases in the vaccine group and 96 in the placebo group). Across both trials, NVX-CoV2373 demonstrated 100% protection against severe disease, including all hospitalization and death.
Philippines officials said March 10 that they secured 30 million doses of NVX-CoV2373 through an agreement with the Serum Institute of India, the second vaccine deal signed by the national government, according to Agence France-Presse. The first was with AstraZeneca for 2.6 million doses of its vaccine, developed with Oxford University.
The Novavax vaccine will be available from the third quarter, at a price that has yet to be finalized. The government hopes to secure 148 million doses this year from seven companies—enough for around 70% of its population.
In announcing fourth quarter and full-year 2020 results on March 1, Novavax said it could file for an emergency use authorization with the FDA in the second quarter of 2021. Novavax hopes it can use data from its Phase III U.K. clinical trial in its FDA submission, and expects the FDA to examine data in May, a month after they are reviewed by regulators in the U.K., President and CEO Stanley C. Erck said on CNBC. Should the FDA insist on waiting for U.S. data, the agency may push the review timeline by one or two months, he added.
The company also said that NVX-CoV2373 showed 95.6% efficacy against the original strain of COVID-19 and 85.6% against the UK variant strain, and re-stated an earlier finding that its vaccine met the Phase III trial’s primary endpoint met with an efficacy rate of 89.3%.
Novavax said February 26 that it signed an exclusive license agreement with Takeda Pharmaceutical for Takeda to develop, manufacture, and commercialize NVX-CoV2373 in Japan.
Novavax agreed to transfer the technology for manufacturing of the vaccine antigen and will supply its Matrix-M™ adjuvant to Takeda. Takeda anticipated the capacity to manufacture over 250 million doses of the COVID-19 vaccine per year. Takeda agreed in return to pay Novavax undisclosed payments tied to achieving development and commercial milestones, plus a portion of proceeds from the vaccine.
Takeda also disclosed that it dosed the first participants in a Phase II clinical trial to test the immunogenicity and safety of Novavax’ vaccine candidate in Japanese participants.
Novavax on February 18 announced a memorandum of understanding with Gavi, the Vaccine Alliance (Gavi), to provide 1.1 billion cumulative doses of NVX-CoV2373 for the COVAX Facility. Gavi leads the design and implementation of the COVAX Facility, created to supply vaccines globally, and has committed to working with Novavax to finalize an advance purchase agreement for vaccine supply and global distribution allocation via the COVAX Facility and its partners.
The doses will be manufactured and distributed globally by Novavax and Serum Institute of India (SII), the latter under an existing agreement between Gavi and SII.
Novavax and SK Bioscience said February 15 that they expanded their collaboration and license agreement, with SK finalizing an agreement to supply 40 million doses of NVX-CoV2373 to the government of South Korea beginning in 2021, for an undisclosed price. SK also obtained a license to manufacture and commercialize NVX-CoV2373 for sale to South Korea, as a result of which SK said it will add significant production capacity.
The agreement also calls on Novavax to facilitate technology transfer related to the manufacturing of its protein antigen, its Matrix M adjuvant, and support to SK Bioscience as needed to secure regulatory approval.
Rolling review begins—On February 4, Novavax announced it had begun a rolling review process for authorization of NVX-CoV2373 with several regulatory agencies worldwide, including the FDA, the European Medicines Agency, the U.K. Medicines and Healthcare products Regulatory Agency (MHRA), and Health Canada. The reviews will continue while the company completes its pivotal Phase III trials in the U.S. and U.K., and through initial authorization for emergency use granted under country-specific regulations, and through initial authorization for emergency use.
A day earlier, Novavax executed a binding Heads of Terms agreement with the government of Switzerland to supply 6 million doses of NVX-CoV2373, to the country. Novavax and Switzerland plan to negotiate a final agreement, with initial delivery of vaccine doses slated to ship following successful clinical development and regulatory review.
On January 28, Novavax electrified investors by announcing that its COVID-19 vaccine NVX-CoV2373 showed efficacy of 89.3% in the company’s first analysis of data from a Phase III trial in the U.K., where a variant strain (B.1.1.7) accounted for about half of all positive cases.
However, NVX-CoV2373 achieved only 60% efficacy in a Phase IIb trial in South Africa, where that country’s escape variant of the virus (B.1.351, also known as 20H/501Y.V2) was seen in 90% of cases, Novavax said.
Novavax said January 7 it executed an Advance Purchase Agreement with the Commonwealth of Australia for 51 million doses of NVX-CoV2373 for an undisclosed price, with an option to purchase an additional 10 million doses—finalizing an agreement in principle announced in November 2020. Novavax said it will work with Australia’s Therapeutics Goods Administration (TGA), to obtain approvals upon showing efficacy in clinical studies. The company aims to deliver initial doses by mid-2021.
2020 Status: Phase III trial launched—Novavax said December 28 that it launched the pivotal Phase III PREVENT-19 trial (NCT04611802) in the U.S. and Mexico to evaluate the efficacy, safety and immunogenicity of NVX-CoV2373. The randomized, placebo-controlled, observer-blinded study will assess the efficacy, safety and immunogenicity of NVX-CoV2373 in up to 30,000 participants 18 years of age and older compared with placebo. The trial’s primary endpoint is the prevention of PCR-confirmed, symptomatic COVID-19. The key secondary endpoint is the prevention of PCR-confirmed, symptomatic moderate or severe COVID-19. Both endpoints will be assessed at least seven days after the second study vaccination in volunteers who have not been previously infected with SARS-CoV-2.
Two thirds of the participants will be assigned to randomly receive two intramuscular injections of the vaccine, administered 21 days apart, while one third of the trial participants will receive placebo. Trial sites were selected in locations where transmission rates are currently high, to accelerate the accumulation of positive cases that could show efficacy. Participants will be followed for 24 months following the second injection
PREVENT-19 is being conducted with support from federal agencies involved in Operation Warp Speed, the Trump administration’s effort to promote development and distribution of COVID-19 vaccines and drugs. Those agencies include the Department of Defense (DoD), the NIH’s National Institute of Allergy and Infectious Diseases (NIAID), and the Biomedical Advanced Research and Development Authority (BARDA)—which has committed up to $1.6 billion to Novavax under a DoD agreement (identifier MCDC OTA agreement number W15QKN-16-9-1002).
Novavax is also conducting a pivotal Phase III study in the United Kingdom, a Phase IIb safety and efficacy study in South Africa, and an ongoing Phase I/II trial in the U.S. and Australia. Data from these trials are expected as soon as early first quarter 2021, though timing will depend on transmission rates in the regions, the company said.
Novavax said November 9 that the FDA granted its Fast Track designation for NVX-CoV2373. By the end of November, the company expected to finish enrollment in its Phase III U.K. trial, with interim data in that study expected as soon as early first quarter 2021.
Five days earlier, Novavax signed a non-binding Heads of Terms document with the Australian government to supply 40 million doses of NVX-CoV2373 to Australia starting as early as the first half of 2021, subject to the successful completion of Phase III clinical development and approval of the vaccine by Australia’s Therapeutic Goods Administration (TGA). The vaccine regimen is expected to require two doses per individual, administered 21 days apart.
Australia joins the U.S., the U.K., and Canada in signing direct supply agreements with Novavax. The company is supplying doses in Japan, South Korea, and India through partnerships. Australian clinical researchers led the global Phase I clinical trial in August, which involved 131 Australians across two trial sites (Melbourne and Brisbane). Also, approximately 690 Australians have participated in the Phase II arm of the clinical trial, which has been conducted across up to 40 sites in Australia and the U.S.
Novavax joined officials in its headquarters city of Gaithersburg, MD, on November 2 to announce expansion plans. The company plans to take 122,000 square feet of space at 700 Quince Orchard Road, and has committed to adding at least 400 local jobs, nearly doubling its current workforce of 450 worldwide. Most of the new jobs are expected to be added b March 2021.
Maryland’s Department of Commerce—which has prioritized assistance to life sciences companies—approved a $2 million conditional loan tied to job creation and capital investment. The state has also approved a $200,000 Partnership for Workforce Quality training grant, and the company is eligible for several tax credits, including the Job Creation Tax Credit and More Jobs for Marylanders.
Additionally, Montgomery County has approved a $500,000 grant tied to job creation and capital investment, while the City of Gaithersburg said it will approve a grant of up to $50,000 from its Economic Development Opportunity Fund. The city accelerated its planning approval process to accommodate Novavax’ timeline, given the company’s role in fighting COVID-19 and resulting assistance from Operation Warp Speed, the Trump administration’s effort to accelerate development of COVID-19 vaccines.
On October 27, Novavax said that it had enrolled 5,500 volunteers in the Phase III U.K. trial, which has been expanded from 10,000 to 15,000 volunteers. The increased enrollment “is likely to facilitate assessment of safety and efficacy in a shorter time period,” according to the company.
The trial, which is being conducted with the U.K. Government’s Vaccines Taskforce, was launched in September and is expected to be fully enrolled by the end of November, with interim data expected by early first quarter 2021, depending on the overall COVID-19 attack rate. Novavax has posted the protocol for the Phase III U.K. trial online. The protocol calls for unblinding of data once 152 participants have achieved mild, moderate or severe endpoints. Two interim analyses are planned upon occurrence of 66 and 110 endpoints.
Novavax also said it expects to launch a second Phase III trial designed to enroll up to 30,000 participants in the U.S. and Mexico by the end of November—a study funded through the U.S. government’s Operation Warp Speed program. The patient population will reflect proportional representation of diverse populations most vulnerable to COVID-19, across race/ethnicity, age, and co-morbidities.
The company cited progress toward large-scale manufacturing while acknowledging delays from original timeframe estimates. Novavax said it will use its contract manufacturing site at FUJIFILM Diosynth Biotechnologies’ Morrisville, NC facility to produce material for the U.S. trial.
On September 25, Novavax entered into a non-exclusive agreement with Endo International subsidiary Par Sterile Products to provide fill-finish manufacturing services at its plant in Rochester, MI, for NVX-CoV2373. Under the agreement, whose value was not disclosed, the Rochester facility has begun production of NVX-CoV2373 final drug product, with initial batches to be used in Novavax’ Phase III clinical trial in the U.S. Par Sterile will also fill-finish NVX-CoV2373 vaccine intended for commercial distribution in the U.S.
A day earlier, Novavax launched the U.K. trial. The randomized, placebo-controlled, observer-blinded study to evaluate the efficacy, safety and immunogenicity of NVX-CoV2373 with Matrix-M in up to 10,000 subjects 18-84 years of age, with and without “relevant” comorbidities, over the following four to six weeks, Novavax said. Half the participants will receive two intramuscular injections of vaccine comprising 5 µg of protein antigen with 50 µg Matrix‑M adjuvant, 21 days apart, while half of the trial participants will receive placebo. At least 25% of the study population will be over age 65.
The trial’s first primary endpoint is first occurrence of PCR-confirmed symptomatic COVID-19 with onset at least seven days after the second study vaccination in volunteers who have not been previously infected with SARS-CoV-2. The second primary endpoint is first occurrence of PCR-confirmed symptomatic moderate or severe COVID-19 with onset at least seven days after the second study vaccination in volunteers who have not been previously infected with SARS-CoV-2
“The data from this trial is expected to support regulatory submissions for licensure in the UK, EU and other countries,” stated Gregory M. Glenn, M.D., President, Research and Development at Novavax.
Maryland Gov. Larry Hogan joined state Secretary of Commerce Kelly M. Schulz and local officials in marking the launch of Phase III studies with a tour of the company’s facilities in Gaithersburg: “The coronavirus vaccine candidate that’s been developed by Novavax is one of the most promising in the country, if not the world.”
On August 31, Novavax reached an agreement in principle with the government of Canada to supply up to 76 million doses of NVX-CoV2373. The value was not disclosed. Novavax and Canada did say that they expect to finalize an advance purchase agreement under which Novavax will agree to supply doses of NVX-CoV2373 to Canada beginning as early as the second quarter of 2021.
The purchase arrangement will be subject to licensure of the NVX-CoV2373 by Health Canada, Novavax said. The vaccine is in multiple Phase II clinical trials: On August 24, Novavax said the first volunteers had been enrolled in the Phase II portion of its ongoing Phase I/II clinical trial (NCT04368988), designed to evaluate the immunogenicity and safety of two doses of of NVX-CoV2373 (5 and 25 µg) with and without 50 µg of Matrix‑M™ adjuvant in up to 1,500 volunteers ages 18-84.
The randomized, placebo-controlled, observer-blinded study is designed to assess two dose sizes (5 and 25 µg) of NVX-CoV2373, each with 50 µg of Matrix‑M. Unlike the Phase I portion, the Phase II portion will include older adults 60-84 years of age as approximately half of the trial’s population. Secondary objectives include preliminary evaluation of efficacy. The trial will be conducted at up to 40 sites in the U.S. and Australia, Novovax said.
NVX-CoV2373 is in a pair of Phase II trials launched in August—including a Phase IIb study in South Africa to assess efficacy, and a Phase II safety and immunogenicity study in the U.S. and Australia.
On August 14, the U.K. government agreed to purchase 60 million doses of NVX-CoV2373 from the company, and support its planned Phase III clinical trial in the U.K., through an agreement whose value was not disclosed. The doses are set to be manufactured as early as the first quarter of 2021.
The trial will be designed to evaluate the ability of NVX-CoV2373 to protect against symptomatic COVID-19 disease as well as evaluate antibody and T-cell responses. The randomized, double-blind, placebo-controlled efficacy study will enroll approximately 9,000 adults 18-85 years of age in the U.K., and is expected to start in the third quarter.
Novavax also said it will expand its collaboration with FUJIFILM Diosynth Biotechnologies (FDB), which will manufacture the antigen component of NVX-CoV2373 from its Billingham, Stockton-on-Tees site in the U.K., as well as at U.S. sites in Morrisville, NC, and College Station, TX. FDB’s U.K. sitevis expected to produce up to 180 million doses annually.
On August 13, Novavax said it signed a development and supply agreement for the antigen component of NVX-CoV2373 with Seoul-based SK bioscience, a vaccine business subsidiary of SK Group. The agreement calls for supply to global markets that include the COVAX Facility, co-led by Gavi, the Coalition for Epidemic Preparedness Innovations (CEPI) and the World Health Organization.
Novavax and SK signed a letter of intent with South Korea’s Ministry of Health and Welfare to work toward broad and equitable access to NVX-CoV2373 worldwide, as well as to make the vaccine available in South Korea. SK bioscience agreed to manufacture the vaccine antigen component for use in the final drug product globally during the pandemic, at its vaccine facility in Andong L-house, South Korea, beginning in August. The value of the agreement was not disclosed.
On August 7, Novavax licensed its COVID-19 vaccine technology to Takeda Pharmaceutical through a partnership by which Takeda will develop, manufacture, and commercialize NVX‑CoV2373 in Japan, using Matrix-M adjuvant to be supplied by Novavax. Takeda will also be responsible for regulatory submission to Japan’s Ministry of Health, Labour and Welfare (MHLW).
MHLW agreed to provide funding to Takeda—the amount was not disclosed in the companies’ announcement—for technology transfer, establishment of infrastructure, and scale-up of manufacturing. Takeda said it anticipated the capacity to manufacture over 250 million doses of NVX‑CoV2373 per year.
Five days earlier, Serum Institute of India agreed to license rights from Novavax to NVX‑CoV2373 for development and commercialization in India as well as low- and middle-income countries (LMIC), through an agreement whose value was not disclosed. Novavax retains rights to NVX-CoV2373 elsewhere in the world.
Novavax and Serum Institute of India agreed to partner on clinical development, co-formulation, filling and finishing and commercialization of NVX-CoV2373. Serum Institute will oversee regulatory submissions and marketing authorizations in regions covered by the collaboration. Novavax agreed to provide both vaccine antigen and Matrix‑M adjuvant, while the partners said they were in talks to have the Serum Institute manufacture vaccine antigen in India. Novavax and Seerum Institute plan to split the revenue from the sale of product, net of agreed costs.
A day earlier, Novavax announced positive results from the Phase I portion of its Phase I/II clinical trial (NCT04368988), designed to evaluate two doses of NVX-CoV2373 (5 and 25 µg) with and without Matrix‑M™ adjuvant in 131 healthy adults ages 18-59. NVX-CoV2373, adjuvanted with Matrix-M, elicited robust antibody responses numerically superior to human convalescent sera, according to data submitted for peer-review to a scientific journal.
All participants developed anti-spike IgG antibodies after a single dose of vaccine, Novavax said, many also developing wild-type virus neutralizing antibody responses. After the second dose, all participants developed wild-type virus neutralizing antibody responses. Both anti-spike IgG and viral neutralization responses compared favorably to responses from patients with clinically significant COVID‑19 disease, the company said—adding that IgG antibody response was highly correlated with neutralization titers, showing that a significant proportion of antibodies were functional.
For both dosages of NVX‑CoV2373 with adjuvant, the 5 µg dose performed “comparably” with the 25 µg dose, Novavax said. NVX‑CoV2373 also induced antigen-specific polyfunctional CD4+ T cell responses with a strong bias toward the Th1 phenotype (IFN-g, IL-2, and TNF-a).
Based on an interim analysis of Phase I safety and immunogenicity data, the trial was expanded to Phase II clinical trials in multiple countries, including the U.S. The trial—which began in Australia in May—is being funded by up-to $388 million in funding from the Coalition for Epidemic Preparedness Innovations (CEPI). If the Phase I/II trial is successful, CEPI said, it anticipates supporting further clinical development that would advance NVX-CoV2373 through to licensure.
On July 23, Novavax joined FDB to announce that FDB will manufacture bulk drug substance for NVX-CoV2373, under an agreement whose value was not disclosed. FDB’s site in Morrisville, NC has begun production of the first batch of NVX-CoV2373. Batches produced at FDB’s Morrisville site will be used in Novavax’s planned pivotal Phase III clinical trial, designed to assess NVX-CoV2373 in up to 30,000 participants, and set to start this fall.
The Phase III trial is among R&D efforts to be funded through the $1.6 billion awarded in July to Novavax through President Donald Trump’s “Operation Warp Speed” program toward late-stage clinical trials and large-scale manufacturing to produce 100 million doses of its COVID-19 vaccine by year’s end. Novavax said the funding will enable it to complete late-stage clinical studies aimed at evaluating the safety and efficacy of NVX-CoV2373.
In June, Novavax said biotech investor and executive David Mott was joining its board as an independent director, after recently acquiring nearly 65,000 shares of the company’s common stock. Also, Novavax was awarded a $60 million contract by the U.S. Department of Defense (DoD) for the manufacturing of NVX‑CoV2373. Through the Defense Health Program, the Joint Program Executive Office for Chemical, Biological, Radiological and Nuclear Defense Enabling Biotechnologies (JPEO-CBRND-EB) agreed to support production of several vaccine components to be manufactured in the U.S. Novavax plans to deliver this year for DoD 10 million doses of NVX‑CoV2373 that could be used in Phase II/III trials, or under an Emergency Use Authorization (EUA) if approved by the FDA.
Also in June, AGC Biologics said it will partner with Novavax on large-scale GMP production of Matrix-M– significantly increasing Novavax’ capacity to deliver doses in 2020 and 2021—through an agreement whose value was not disclosed. And Novavax joined The PolyPeptide Group to announce large-scale GMP production by the global CDMO of two unspecified key intermediate components used in the production of Matrix-M.
In May, Novavax acquired Praha Vaccines from the India-based Cyrus Poonawalla Group for $167 million cash, in a deal designed to ramp up Novavax’s manufacturing capacity for NVX-CoV2373. Praha Vaccines’ assets include a 150,000-square foot vaccine and biologics manufacturing facility and other support buildings in Bohumil, Czech Republic. Novavax said the Bohumil facility is expected to deliver an annual capacity of over 1 billion doses of antigen starting in 2021 for the COVID-19 vaccine.
The Bohumil facility is completing renovations that include the addition of Biosafety Level-3 (BSL-3) capabilities. The site’s approximately 150 employees with “significant experience” in vaccine manufacturing and support have joined Novavax, the company said.
On May 11, Novavax joined CEPI in announcing up to $384 million in additional funding for the company toward clinical development and large-scale manufacturing of NVX-CoV2373. CEPI agreed to fund preclinical as well as Phase I and Phase II studies of NVX-CoV2373. The funding multiplied CEPI’s initial $4 million investment in the vaccine candidate, made two months earlier. Novavax’s total $388 million in CEPI funding accounted for 87% of the total $446 million awarded by the Coalition toward COVID-19 vaccine R&D as of that date.
Novavax identified its COVID-19 vaccine candidate in April. The company said NVX-CoV2373 was shown to be highly immunogenic in animal models measuring spike protein-specific antibodies, antibodies that block the binding of the spike protein to the receptor, and wild-type virus neutralizing antibodies. High levels of spike protein-specific antibodies with ACE-2 human receptor binding domain blocking activity and SARS-CoV-2 wild-type virus neutralizing antibodies were also seen after a single immunization.
In March, Emergent Biosolutions disclosed it retained an option to allocate manufacturing capacity for an expanded COVID-19 program under an agreement with Novavax to provide “molecule-to-market” contract development and manufacturing (CDMO) services to produce Novavax’s NanoFlu™, its recombinant quadrivalent seasonal influenza vaccine candidate.
Earlier in March, Emergent announced similar services to support clinical development of Novavax’s COVID-19 vaccine candidate, saying March 10 it agreed to produce the vaccine candidate and had initiated work, anticipating the vaccine candidate will be used in a Phase I study within the next four months. In February, Novavax said it had produced and was assessing multiple nanoparticle vaccine candidates in animal models prior to identifying an optimal candidate for human testing.
References
- ^ “Company Overview of Novavax, Inc”. Bloomberg.com. Archived from the original on 24 February 2017. Retrieved 2 June2019.
- ^ https://www.globenewswire.com/news-release/2021/03/01/2184674/0/en/Novavax-Reports-Fourth-Quarter-and-Full-Year-2020-Financial-Results-and-Operational-Highlights.html
- ^ Jump up to:a b c d e Bell, Jacob (November 14, 2016). “Novavax aims to rebound with restructuring, more trials”. BioPharma Dive. Washington, D.C.: Industry Dive. Archived from the original on 2017-03-29. Retrieved 2017-03-28.
- ^ Thomas, Katie; Twohey, Megan (2020-07-16). “How a Struggling Company Won $1.6 Billion to Make a Coronavirus Vaccine”. The New York Times. ISSN 0362-4331. Retrieved 2021-01-29.
- ^ Taylor, Nick Paul (3 June 2013). “Novavax makes $30M bid for adjuvant business”. FiercePharma. Archived from the original on 14 September 2016. Retrieved 9 September 2016.
- ^ “Gaithersburg Biotech Receives Grant Worth up to $89 million”. Bizjournals.com. Archived from the original on 2017-04-01. Retrieved 2017-03-28.
- ^ “With promising RSV data in hand, Novavax wins $89M Gates grant for PhIII | FierceBiotech”. Fiercebiotech.com. Archivedfrom the original on 2017-04-14. Retrieved 2017-03-28.
- ^ “Novavax RSV vaccine found safe for pregnant women, fetus”. Reuters. 2016-09-29. Archived from the original on 2016-10-07. Retrieved 2017-03-28.
- ^ Herper, Matthew. “Gates Foundation Backs New Shot To Prevent Babies From Dying Of Pneumonia”. Forbes. Archived from the original on 2016-09-21. Retrieved 2017-03-28.
- ^ “Novavax’s Ebola vaccine shows promise in early-stage trial”. Reuters. 2017-07-21. Archived from the original on 2016-10-02. Retrieved 2017-03-28.
- ^ Jump up to:a b c d e f Adams, Ben (September 16, 2016). “Novavax craters after Phase III RSV F vaccine failure; seeks path forward”. FierceBiotech. Questex. Archived from the original on 18 August 2020. Retrieved 25 Jan 2020.
- ^ Shtrubel, Marty (December 12, 2019). “3 Biotech Stocks That Offer the Highest Upside on Wall Street”. Biotech. Nasdaq. Archived from the original on 2020-01-26. Retrieved 25 Jan 2020.
- ^ Jump up to:a b Budwell, George (January 20, 2020). “3 Top Biotech Picks for 2020”. Markets. Nasdaq. Novavax: A catalyst awaits. Archivedfrom the original on 2020-01-25. Retrieved 25 Jan 2020.
- ^ Mark Terry (February 16, 2018). “Why Novavax Could be a Millionaire-Maker Stock”. BioSpace. Archived from the original on 22 November 2020. Retrieved 6 March 2020.
- ^ Jump up to:a b Eric Sagonowsky (2020-05-11). “Novavax scores $384M deal, CEPI’s largest ever, to fund coronavirus vaccine work”. FiercePharma. Archived from the original on 2020-05-16. Retrieved 2020-05-12.
- ^ “Novavax addresses urgent global public health needs with innovative technology”. novavax.com. Archived from the original on 10 September 2020. Retrieved 30 August 2020.
- ^ Sara Gilgore (January 15, 2020). “Novavax earns key FDA status for its flu vaccine. Wall Street took it well”. Washington Business Journal. Archived from the original on 10 November 2020. Retrieved 6 March 2020.
- ^ Sara Gilgore (February 26, 2020). “Novavax is working to advance a potential coronavirus vaccine. So are competitors”. Washington Business Journal. Archived from the original on March 16, 2020. Retrieved March 6, 2020.
- ^ Nidhi Parekh (July 24, 2020). “Novavax: A SARS-CoV-2 Protein Factory to Beat COVID-19”. Archived from the original on November 22, 2020. Retrieved July 24, 2020.
- ^ “Covid-19: Novavax vaccine shows 89% efficacy in UK trials”. BBC news. Retrieved 1 February 2021.
Further reading
- “Novavax, Inc. Common Stock (NVAX) News Headlines”. Market Activity. Nasdaq. Retrieved 25 Jan 2020. Continuously updated listing of Nasdaq publications related to Novavax, newest items first.
External links
- Official website
- Business data for Novavax, Inc.:
General References
| Type | Public |
|---|---|
| Traded as | Nasdaq: NVAX Russell 2000 Component |
| Industry | Biotechnology |
| Founded | 1987; 34 years ago [1] |
| Headquarters | Gaithersburg, Maryland,United States |
| Area served | Worldwide |
| Key people | Stanley Erck (CEO) |
| Products | Vaccines |
| Revenue | |
| Number of employees | 500+[3] |
| Website | www.novavax.com |
The Novavax COVID-19 vaccine, codenamed NVX-CoV2373, and also called SARS-CoV-2 rS (recombinant spike) protein nanoparticle with Matrix-M1 adjuvant, is a COVID-19 vaccine candidate developed by Novavax and Coalition for Epidemic Preparedness Innovations (CEPI). It requires two doses[1] and is stable at 2 to 8 °C (36 to 46 °F) (refrigerated).[2]
Description
NVX-CoV2373 has been described as both a protein subunit vaccine[3][4][5] and a virus-like particle vaccine,[6][7] though the producers call it a “recombinant nanoparticle vaccine”.[8]
The vaccine is produced by creating an engineered baculovirus containing a gene for a modified SARS-CoV-2 spike protein. The baculovirus then infects a culture of Sf9 moth cells, which create the spike protein and display it on their cell membranes. The spike proteins are then harvested and assembled onto a synthetic lipid nanoparticle about 50 nanometers across, each displaying up to 14 spike proteins.[3][4][8]
The formulation includes a saponin-based adjuvant.[3][4][8]
Development
In January 2020, Novavax announced development of a vaccine candidate, codenamed NVX-CoV2373, to establish immunity to SARS-CoV-2.[9] Novavax’s work is in competition for vaccine development among dozens of other companies.[10]
In March 2020, Novavax announced a collaboration with Emergent BioSolutions for preclinical and early-stage human research on the vaccine candidate.[11] Under the partnership, Emergent BioSolutions will manufacture the vaccine at large scale at their Baltimore facility.[12] Trials have also taken place in the United Kingdom, and subject to regulatory approval, at least 60 million doses will be manufactured by Fujifilm Diosynth Biotechnologies in Billingham for purchase by the UK government.[13][14] They also signed an agreement with Serum Institute of India for mass scale production for developing and low-income countries.[15] It has also been reported, that the vaccine will be manufactured in Spain.[16] The first human safety studies of the candidate, codenamed NVX-CoV2373, started in May 2020 in Australia.[17][18]
In July, the company announced it might receive $1.6 billion from Operation Warp Speed to expedite development of its coronavirus vaccine candidate by 2021—if clinical trials show the vaccine to be effective.[19][20] A spokesperson for Novavax stated that the $1.6 billion was coming from a “collaboration” between the Department of Health and Human Services and Department of Defense,[19][20] where Gen. Gustave F. Perna has been selected as COO for Warp Speed. In late September, Novavax entered the final stages of testing its coronavirus vaccine in the UK. Another large trial was announced to start by October in the US.[21]
In December 2020, Novavax started the PREVENT-19 (NCT04611802) Phase III trial in the US and Mexico.[22][full citation needed][23]
On 28 January 2021, Novavax reported that preliminary results from the United Kingdom trial showed that its vaccine candidate was more than 89% effective.[24][2] However, interim results from a trial in South Africa showed a lower effectiveness rate against the 501.V2 variant of the virus, at around 50-60%.[1][25]
On 12 March 2021, they announced their vaccine candidate was 96.4% effective in preventing the original strain of COVID-19 and 86% effective against the U.K variant. It proved 55% effective against the South African variant in people without HIV/AIDS. It was also 100% effective at preventing severe illness.[citation needed]
Deployment
On 2 February 2021, the Canadian Prime Minister Justin Trudeau announced that Canada has signed a tentative agreement for Novavax to produce millions of doses of its COVID-19 vaccine in Montreal, Canada, once it’s approved for use by Health Canada, making it the first COVID-19 vaccine to be produced domestically.[26]
References
- ^ Jump up to:a b Wadman M, Jon C (28 January 2021). “Novavax vaccine delivers 89% efficacy against COVID-19 in UK—but is less potent in South Africa”. Science. doi:10.1126/science.abg8101.
- ^ Jump up to:a b “New Covid vaccine shows 89% efficacy in UK trials”. BBC News. 28 January 2021. Retrieved 28 January 2021.
- ^ Jump up to:a b c Wadman M (November 2020). “The long shot”. Science. 370 (6517): 649–653. Bibcode:2020Sci…370..649W. doi:10.1126/science.370.6517.649. PMID 33154120.
- ^ Jump up to:a b c Wadman M (28 December 2020). “Novavax launches pivotal U.S. trial of dark horse COVID-19 vaccine after manufacturing delays”. Science. doi:10.1126/science.abg3441.
- ^ Parekh N (24 July 2020). “Novavax: A SARS-CoV-2 Protein Factory to Beat COVID-19”. Archived from the original on 22 November 2020. Retrieved 24 July 2020.
- ^ Chung YH, Beiss V, Fiering SN, Steinmetz NF (October 2020). “COVID-19 Vaccine Frontrunners and Their Nanotechnology Design”. ACS Nano. 14 (10): 12522–12537. doi:10.1021/acsnano.0c07197. PMC 7553041. PMID 33034449.
- ^ Medhi R, Srinoi P, Ngo N, Tran HV, Lee TR (25 September 2020). “Nanoparticle-Based Strategies to Combat COVID-19”. ACS Applied Nano Materials. 3 (9): 8557–8580. doi:10.1021/acsanm.0c01978. PMC 7482545.
- ^ Jump up to:a b c “Urgent global health needs addressed by Novavax”. Novavax. Retrieved 30 January 2021.
- ^ Gilgore S (26 February 2020). “Novavax is working to advance a potential coronavirus vaccine. So are competitors”. Washington Business Journal. Archived from the original on 16 March 2020. Retrieved 6 March 2020.
- ^ “COVID-19 vaccine tracker (click on ‘Vaccines’ tab)”. Milken Institute. 11 May 2020. Archived from the original on 6 June 2020. Retrieved 12 May 2020. Lay summary.
- ^ Gilgore S (10 March 2020). “Novavax’s coronavirus vaccine program is getting some help from Emergent BioSolutions”. Washington Business Journal. Archived from the original on 9 April 2020. Retrieved 10 March 2020.
- ^ McCartney R. “Maryland plays an outsized role in worldwide hunt for a coronavirus vaccine”. Washington Post. Archived from the original on 7 May 2020. Retrieved 8 May 2020.
- ^ Boseley S, Davis N (28 January 2021). “Novavax Covid vaccine shown to be nearly 90% effective in UK trial”. The Guardian. Retrieved 29 January 2021.
- ^ Brown M (14 August 2020). “60m doses of new covid-19 vaccine could be made in Billingham – and be ready for mid-2021”. TeesideLive. Reach. Retrieved 29 January 2021.
- ^ “Novavax signs COVID-19 vaccine supply deal with India’s Serum Institute”. Reuters. 5 August 2020.
- ^ “Spain, again chosen to produce the vaccine to combat COVID-19”. This is the Real Spain. 18 September 2020.
- ^ Sagonowsky E (11 May 2020). “Novavax scores $384M deal, CEPI’s largest ever, to fund coronavirus vaccine work”. FiercePharma. Archived from the original on 16 May 2020. Retrieved 12 May 2020.
- ^ “Novavax starts clinical trial of its coronavirus vaccine candidate”. CNBC. 25 May 2020. Archived from the original on 26 May 2020. Retrieved 26 May 2020.
- ^ Jump up to:a b Thomas K (7 July 2020). “U.S. Will Pay $1.6 Billion to Novavax for Coronavirus Vaccine”. The New York Times. Archived from the original on 7 July 2020. Retrieved 7 July 2020.
- ^ Jump up to:a b Steenhuysen J (7 July 2020). “U.S. government awards Novavax $1.6 billion for coronavirus vaccine”. Reuters. Archived from the original on 14 September 2020. Retrieved 15 September 2020.
- ^ Thomas K, Zimmer C (24 September 2020). “Novavax Enters Final Stage of Coronavirus Vaccine Trials”. The New York Times. ISSN 0362-4331. Archived from the original on 28 September 2020. Retrieved 28 September 2020.
- ^ Clinical trial number NCT04611802 for “A Study Looking at the Efficacy, Immune Response, and Safety of a COVID-19 Vaccine in Adults at Risk for SARS-CoV-2” at ClinicalTrials.gov
- ^ “Phase 3 trial of Novavax investigational COVID-19 vaccine opens”. National Institutes of Health (NIH). 28 December 2020. Retrieved 28 December 2020.
- ^ Lovelace B (28 January 2020). “Novavax says Covid vaccine is more than 89% effective”. CNBC.
- ^ Facher L, Joseph A (28 January 2021). “Novavax says its Covid-19 vaccine is 90% effective in late-stage trial”. Stat. Retrieved 29 January 2021.
- ^ “Canada signs deal to produce Novavax COVID-19 vaccine at Montreal plant”. CP24. 2 February 2021. Retrieved 2 February2021.
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | Subunit |
| Clinical data | |
| Other names | NVX-CoV2373 |
| Routes of administration | Intramuscular |
| ATC code | None |
| Identifiers | |
| DrugBank | DB15810 |
| Part of a series on the |
| COVID-19 pandemic |
|---|
| SARS-CoV-2 (virus)COVID-19 (disease) |
| showTimeline |
| showLocations |
| showInternational response |
| showMedical response |
| showImpact |
| COVID-19 Portal |
| vte |
////////////// Novavax, COVID-19, vaccine, CORONA VIRUS, NVX-CoV2373, SARS-CoV-2 rS, TAK 019
#Novavax, #COVID-19, #vaccine, #CORONA VIRUS, #NVX-CoV2373, #SARS-CoV-2 rS, #TAK 019
UPDATE
SARS-CoV-2 Spike glycoprotein vaccine antigen nvx-cov2373
SARS-CoV-2 rS;
Novavax Covid-19 vaccine (TN);
Nuvaxovid (TN)
SARS-CoV-2 rS;
組換えコロナウイルス (SARS-CoV-2) ワクチン;
コロナウイルス(SARS-CoV-2)スパイク糖タンパク質抗原nvx-cov2373ワクチン;
SARS-CoV-2 Spike glycoprotein vaccine antigen nvx-cov2373;
SARS-CoV-2 rS
APPROVED JAPAN Nuvaxovid, 2022/4/19
//////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE
join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
/////////SARS-CoV-2 Spike glycoprotein vaccine antigen nvx-cov2373, JAPAN 2022, APPROVALS 2022, VACCINE, COVID 19. CORONA VACCINE, SARS-CoV-2
BBIBP-CorV, Sinopharm COVID-19 vaccine


BBIBP-CorV, Sinopharm COVID-19 vaccine
- Inactivated novel coronavirus (2019-CoV) vaccine (Vero cells)
- Purified inactivated SARS-CoV-2 Vaccine
ref Lancet Infectious Diseases (2021), 21(1), 39-51.
BBIBP-CorV, also known as the Sinopharm COVID-19 vaccine,[1] is one of two inactivated virus COVID-19 vaccines developed by Sinopharm. In late December 2020, it was in Phase III trials in Argentina, Bahrain, Egypt, Morocco, Pakistan, Peru, and the United Arab Emirates (UAE) with over 60,000 participants.[2]
On December 9, the UAE announced interim results from Phase III trials showing BBIBP-CorV had a 86% efficacy against COVID-19 infection.[3] In late December, Sinopharm announced that its internal analysis indicated a 79% efficacy.[4] While mRNA vaccines like the Pfizer–BioNTech COVID-19 vaccine and mRNA-1273 showed higher efficacy of +90%, those present distribution challenges for some nations as they require deep-freeze facilities and trucks. BIBP-CorV could be transported and stored at normal refrigerated temperatures.[5]
BBIBP-CorV shares similar technology with CoronaVac and BBV152, other inactivated virus vaccines for COVID-19 being developed in Phase III trials.[6][7]
BBIBP-CorV is being used in vaccination campaigns by certain countries in Asia,[8][9][10] Africa,[11][12][13] South America,[14][15] and Europe.[16][17][18] Sinopharm expects to produce one billion doses of BBIBP-CorV in 2021.[19] By February 21, Sinopharm said more than 43 million doses of the vaccine had been administered in total.[20]
BBIBP-CorV vaccine contains a SARS-CoV-2 strain inactivated inside Vero Cells. Investigation shows this vaccine induces neutralizing antibodies in several mammalian species while also showing protective efficacy with SARS-CoV-2 challenge in rhesus macaques2. As of August 2020, this vaccine is being tested for prophylaxis against COVID-19 in human clinical trials.

A vaccination certificate of BBIBP-CorV (Beijing Institute of Biological Products, Sinopharm).
Clinical research
Main article: COVID-19 vaccine
Phases I and II
In April 2020, China approved clinical trials for a candidate COVID-19 vaccine developed by Sinopharm‘s Beijing Institute of Biological Products[21] and the Wuhan Institute of Biological Products.[22] Both vaccines are chemically-inactivated whole virus vaccines for COVID-19.
On October 15, the Beijing Institute of Biological Products published results of its Phase I (192 adults) and Phase II (448 adults) clinical studies for the BBIBP-CorV vaccine, showing BBIBP-CorV to be safe and well-tolerated at all tested doses in two age groups. Antibodies were elicited against SARS-CoV-2 in all vaccine recipients on day 42. These trials included individuals older than 60.[21]
On August 13, the Wuhan Institute of Biological Products published interim results of its Phase I (96 adults) and Phase II (224 adults) clinical studies. The report noted the inactivated COVID-19 vaccine had a low rate of adverse reactions and demonstrated immunogenicity, but longer-term assessment of safety and efficacy would require Phase III trials.[22]
BIBP-CorV may have characteristics favorable for vaccinating people in the developing world. While mRNA vaccines, such as the Pfizer–BioNTech COVID-19 vaccine and Moderna COVID-19 vaccine showed higher efficacy of +90%, mRNA vaccines present distribution challenges for some nations, as some may require deep-freeze facilities and trucks. By contrast, BIBP-CorV can be transported and stored at normal refrigeration temperatures.[23] While Pfizer and Moderna are among developers relying on novel mRNA technology, manufacturers have decades of experience with the inactivated virus technology Sinopharm is using.[23]
Phase III
Africa and Asia
On July 16, Sinopharm began conducting a Phase III vaccine trial of 31,000 volunteers in the UAE in collaboration with G42 Healthcare, an Abu Dhabi-based company.[24] By August, all volunteers had received their first dose and were to receive the second dose within the next few weeks.[25] On December 9, UAE’s Ministry of Health and Prevention announced the official registration of BBICP-CorV, after an interim analysis of the Phase III trial showed BBIBP-CorV to have a 86% efficacy against COVID-19 infection.[26] The vaccine had a 99% sero-conversion rate of neutralizing antibodies and 100% effectiveness in preventing moderate and severe cases of the disease.[27]
On September 2, Sinopharm began a Phase III trial in Casablanca and Rabat on 600 people.[28][29] In September, Egypt opened registration for a Phase III trial to last one year and enroll 6,000 people.[30]
In August 2020, Sinopharm began a Phase III clinical trial in Bahrain on 6,000 citizens and resident volunteers.[31][32] In a November update, 7,700 people had volunteered in the trials.[33] Also in late August, Sinopharm began a Phase III clinical trial in Jordan on 500 volunteers at Prince Hamzah Hospital.[34][35]
In Pakistan, Sinopharm began working with the University of Karachi on a trial with 3,000 volunteers.[36]
South America
On September 10, Sinopharm began a Phase III trial in Peru with the long-term goal of vaccinating a total of 6,000 people between the ages of 18 and 75.[37] In October, the trials were expanded to include an additional 6,000 volunteers.[38] On January 26, a volunteer in the placebo group of the vaccine trials had died.[39]
On September 16, Argentina began a Phase III trial with 3,000 volunteers.[40]
Manufacturing
Sinopharm’s Chariman Yang Xioyun has said the company could produce one billion doses in 2021.[19]
In October, Dubai’s G42 Healthcare reached manufacturing agreements to provide UAE and other regional states with BBIBP-CorV, with the UAE producing 75 to 100 million doses in 2021.[41]
In December, Egypt announced an agreement between Sinopharm and Egyptian Holding Company for Biological Products & Vaccines (VACSERA) for the vaccine to be manufactured locally,[42] which would also be exported to other African countries.[43]
In December, AP reported Morocco plans to produce BBIBP-CorV locally.[44]
In March, Serbia announced plans to produce 24 million doses of BBIBP-CorV annually starting in October. The production volume would be sufficient to meet the needs of Serbia and all of its neighbors, deputy prime minister Branislav Nedimović noted.[45]
In March, Belarus was looking to produce BBIBP-CorV locally.[18]
Marketing and Distribution
| show Full authorizationshow Emergency authorizationshow Received donated doses Eligible COVAX recipient (assessment in progress)[86] |
On February 21, 2021 Sinopharm said more than 43 million doses of BBIBP-CorV had been administered so far, including more than 34 million administered in China and the rest internationally.[20]
Asia
In February, Afghanistan was pledged 400,000 doses of BBIBP-CorV by China.[82]
In November 3, 2020 Bahrain granted emergency use authorization of BBIBP-CorV for frontline workers.[33] In December, Bahrain approved Sinopharm’s vaccine, citing data from Phase III clinical trials that showed an 86% efficacy rate.[87]
In February, Brunei received the first batch of Sinopharm vaccines donated by China.[84]
In January, Cambodia said China would provide a million doses.[88] Cambodia granted emergency use authorization on February 4[89] and started the vaccination campaign on February 10 with the first 600,000 doses.[90]
In China, Sinopharm obtained an EUA in July.[91] In October, it began offering the vaccine for free to students going abroad for higher studies.[92] On December 30, China‘s National Medical Products Administration approved BBIBP-CorV for general use.[93][8] In February, Macau received the first 100,000 doses of 400,000 doses.[94]
In October, Indonesia reached an agreement with Sinopharm to deliver 15 million dual-dose vaccines in 2020.[95]
In February, Iran approved emergency use of BBIBP-CorV,[96] and received the first batch of 250,000 doses on February 28.[97]
In January, Iraq approved BBIBP-CorV for emergency use[98] and has signed agreements for 2 million doses. The first doses arrived on March 2.[99]
In January, Jordan approved BBIBP-CorV for emergency use[100] and started its vaccination campaign on January 13.[101]
In March, Kyrgyzstan received a donation of 150,000 doses of the vaccine.[102]
In January, Laos began vaccinating medical workers at hospitals in Vientiane [103] and received another 300,000 doses in early February.[104]
In March, Lebanon received a donation of 50,000 doses at its request,[105] for which it granted emergency use authorization on March 2.[106]
In March, Maldives granted emergency approval for use. At the time of approval, the country had received 18,000 doses and was awaiting 200,000 additional doses.[107]
In February, Mongolia received a donation of 300,000 doses.[108] On March 10, Governor of Ulaanbaatar D. Sumiyabazar and Deputy Prime Minister S. Amarsaikhan received the first doses of BBIBP-CorV.[109]
In February, Nepal approved the vaccine for emergency use, allowing a donation of 500,000 doses to enter the country.[110]
In December, Pakistan‘s purchased 1.2 million doses,[111] which was approved for emergency use on January 18,[112] and began a vaccination campaign on February 2.[10]
In March, Palestine said it would receive 100,000 doses donated by China.[113]
In March 19, Sri Lanka approved the vaccine for emergency use, allowing a donation of 600,000 doses by China to enter the country.[114]
On 14 September 2020, the United Arab Emirates approved the vaccine for front-line workers following successful interim Phase III trials.[24] In December, the country registered BBIBP-CorV after it reviewed the results of the interim analysis.[26] In March, a small number of people who have reduced immunity against diseases, have chronic illnesses, or belong to high-risk groups have been given a 3rd booster shot.[115]
Africa
In February, Algeria received a donation of 200,000 doses.[83]
Egypt plans to buy 40 million doses of Sinpharm’s vaccine[116] which was approved for regulatory use on January 3.[116] President Abdel Fattah el-Sisi announced a vaccination campaign starting 24 January.[11]
In February, Equatorial Guinea received a donation of 100,000 doses which arrived on February 10. The country began vaccinations on February 15.[56]
In March, Gabon received a donation of 100,000 doses which was the second vaccine approved for use in the country.[117]
Morocco placed orders for 41 million vaccine doses from Sinopharm and 25 million from AstraZeneca, for a total of 66 million doses.[118] Morocco granted emergency use approval on January 23,[119] and the first 500,000 doses arrived on January 27.[12]
In February, Mozambique received a donation of 200,000 doses[120] and planned to start vaccinations on March 8.[121]
In March, Namibia received a donation of 100,000 doses and announced the start of vaccinations in the Khomas and Erongo regions.[122]
In March, Niger received a donation of 400,000 doses with vaccinations to begin on March 27.[123]
In February, Senegal received 200,000 doses in Dakar[124] and began vaccinating health workers on February 22.[125]
In February, Sierra Leone received a donation of 200,000 doses.[126] It was approved for emergency use and vaccinations began on March 15.[127]
In January, Seychelles said it would begin administering vaccinations on January 10 with 50,000 doses it had received as a gift from the UAE.[128]
In March, Republic of the Congo received 100,000 doses with vaccinations prioritizing the medically vulnerable and those over 50.[129]
In February, Zimbabwe purchased 600,000 doses on top of 200,000 doses donated by China,[130] and started vaccinations on February 18.[13] Zimbabwe later purchased an additional 1.2 million doses.[131]
North America
In February, the Dominican Republic ordered 768,000 doses of BBIBP-CorV.[132]
In March, Dominica received 20,000 doses of BBIBP-CorV which it began using in its vaccination campaign on March 4.[133]
In March, Mexico announced it would order 12 million doses of BBIBP-CorV pending approval by its health regulator.[134]
South America
In February, Argentina authorized emergency use of BBIBP-CorV[135] ahead of the arrival of 904,000 doses on February 26.[136]
In February, Bolivia purchased 400,000 doses on top of 100,000 doses donated by China,[137] and started its vaccination campaign on February 26.[15]
In March, Guyana received a donation of 20,000 doses of BBIBP-CorV.[138] Vaccinations were to start on March 7.[139]
In January, Peru purchased 38 million doses of BBIBP-CorV.[140] Peru granted emergency approval for BBIBP-CorV on January 27[141] and started vaccinations on February 9 with the first 300,000 doses.[14]
In March, Venezuela granted approval for BBIBP-CorV to be used in the country.[142] The first 500,000 doses arrived on March 2.[143]
Europe
In February, Belarus received a donation of 100,000 doses[144] and began using the vaccine on March 15.[18]
In January, Hungary became first EU member to approve BBIBP-CorV, signing a deal for 5 million doses.[145] The first 550,000 doses arrived in Budapest on February 16[146] and vaccinations started on February 24.[17] Prime Minister Viktor Orbán was vaccinated with BBIBP-CorV on February 28.[147]
In March, Moldova received 2,000 doses donated by the UAE[148] which will be used to vaccinate doctors at the State University of Mediecne and Pharmacy starting on March 22.[149]
In March 3, Montenegro received a donation of 30,000 doses of BBIBP-CorV.[85]
In February, North Macedonia signed an agreement for 200,000 doses of BBIBP-CorV, with which they hoped to launch their vaccination program later that month.[150]
In January, Serbia received one million doses, making it the first country in Europe to receive BBIBP-CorV.[151] On January 19, Serbia approved the vaccine and Health Minister Zlatibor Lončar became the first person to receive a shot.[16]
Controversies
Lack of public data
Unlike Moderna‘s MRNA-1273, Oxford–AstraZeneca‘s AZD1222, and Johnson & Johnson‘s Ad26.COV2.S, there is little public information about the Chinese vaccine’s safety or efficacy.[152] The UAE said it had reviewed Sinopharm’s interim data analysis which showed the vaccine was 100% effective to prevent moderate and severe instances of COVID-19, but did not say whether it had independently analyzed the case data in its review. It was unclear how Sinopharm drew conclusions, since the UAE announcement of the approval for BBIBP-CorV noticeably lacked details such as the number of COVID-19 cases in the placebo or active group or the volunteers ages.[153]
As of December 30, 2020, no detailed efficacy data of the vaccine has been released to the public. A Sinopharm executive said detailed data would be released later and published in scientific journals in China and internationally.[8]
Sinopharm president Wu Yonglin said the trial results exceeded the WHO’s requirements, but a director at a large pharmaceutical company in Shanghai expressed skepticism over the trials and the expectation that drug regulators in Bahrain and the UAE would not hold the same standard as the U.S. Food and Drug Administration.[154]
Unauthorized use in Asia
On December 30, Philippine Defense Secretary Delfin Lorenzana said in an interview that at least one minister and president Rodrigo Duterte‘s bodyguards were provided BBIBP-CorV which were “smuggled” but that he felt what happened was “justified”. Brigadier General Jesus Durante, head of the Presidential Security Guard (PSG), said he felt compelled and “took the risk” to have some of his men vaccinated because they provide close-in security to Duterte, who at 75 is highly vulnerable to COVID-19.[155] Ingming Aberia, an author at The Manila Times commented that FDA director-general Enrique Domingo had reason to believe Sinopharm may cause harm to the consuming public given that no COVID-19 vaccine license was issued, but out of “self-preservation”, he would not initiate charges against PSG.[156]
On January 1, Mainichi Shimbun reported that 18 wealthy people, including several owners of leading Japanese companies, have been vaccinated with Sinopharm vaccines since November 2020. The vaccines were brought in by a Chinese consultant close to a senior member of the Chinese Communist Party.[157] The Chinese embassy in Japan later expressed its dissatisfaction at the unverified claims by Japanese news media.[158]
References
- ^ https://www.nytimes.com/interactive/2020/health/sinopharm-covid-19-vaccine.html
- ^ Reuters Staff (2020-11-19). “China Sinopharm’s coronavirus vaccine taken by about a million people in emergency use”. Reuters. Retrieved 2020-12-09.
- ^ “UAE: Ministry of Health announces 86 per cent vaccine efficacy”. gulfnews.com. Retrieved 2020-12-13.
- ^ Wee, Sui-Lee; Qin, Amy (2020-12-30). “China Approves Covid-19 Vaccine as It Moves to Inoculate Millions”. The New York Times. ISSN 0362-4331. Retrieved 2021-02-12.
- ^ “China State-Backed Covid Vaccine Has 86% Efficacy, UAE Says”. Bloomberg.com. 2020-12-09. Retrieved 2020-12-09.
- ^ Cohen J (December 2020). “China’s vaccine gambit”. Science. 370 (6522): 1263–1267. Bibcode:2020Sci…370.1263C. doi:10.1126/science.370.6522.1263. PMID 33303601.
- ^ Tan Y (16 December 2020). “Covid: What do we know about China’s coronavirus vaccines?”. BBC News. Retrieved 18 December 2020.
- ^ Jump up to:a b c Liu R (2020-12-31). “China gives its first COVID-19 vaccine approval to Sinopharm”. Reuters. Retrieved 2020-12-31.
- ^ Turak, Natasha (2021-01-18). “The UAE is on track to have half its population vaccinated by the end of March”. CNBC. Retrieved 2021-01-21.
- ^ Jump up to:a b Dawn.com (2021-02-02). “PM Imran kicks off Pakistan’s Covid-19 vaccination drive”. DAWN.COM. Retrieved 2021-02-03.
- ^ Jump up to:a b Reuters Staff (2021-01-24). “Sisi says Egypt to begin COVID-19 vaccinations on Sunday”. Reuters. Retrieved 2021-01-24.
- ^ Jump up to:a b Dumpis, Toms (2021-01-27). “Morocco Receives Half a Million Doses of Chinese Sinopharm Vaccine”. Morocco World News. Retrieved 2021-01-28.
- ^ Jump up to:a b “Zimbabwe starts administering China’s Sinopharm vaccines”. thestar.com. 2021-02-18. Retrieved 2021-02-20.
- ^ Jump up to:a b Aquino, Marco (2021-02-10). “‘The best shield’: Peru launches inoculation drive with Sinopharm vaccine”. Reuters. Retrieved 2021-02-10.
- ^ Jump up to:a b “Bolivia begins inoculation with Sinopharm jabs | The Star”. http://www.thestar.com.my. Retrieved 2021-02-28.
- ^ Jump up to:a b “Serbia Becomes First European Nation To Use China’s Sinopharm Vaccine”. RadioFreeEurope/RadioLiberty. Retrieved 2021-01-21.
- ^ Jump up to:a b “Hungary first EU nation to use China’s Sinopharm vaccine against COVID”. euronews. 2021-02-24. Retrieved 2021-02-26.
- ^ Jump up to:a b c d “Belarus begins COVID-19 vaccinations with Chinese shots”. eng.belta.by. 2021-03-15. Retrieved 2021-03-16.
- ^ Jump up to:a b “Which companies will likely produce the most COVID-19 vaccine in 2021?”. Pharmaceutical Processing World. 2021-02-05. Retrieved 2021-02-28.
- ^ Jump up to:a b hermesauto (2021-02-22). “More than 43 million doses of China’s Sinopharm Covid-19 vaccines used globally”. The Straits Times. Retrieved 2021-02-22.
- ^ Jump up to:a b Xia S, Zhang Y, Wang Y, Wang H, Yang Y, Gao GF, et al. (October 2020). “Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBIBP-CorV: a randomised, double-blind, placebo-controlled, phase 1/2 trial”. The Lancet. Infectious Diseases. 21 (1): 39–51. doi:10.1016/s1473-3099(20)30831-8. PMC 7561304. PMID 33069281.
- ^ Jump up to:a b Xia S, Duan K, Zhang Y, Zhao D, Zhang H, Xie Z, et al. (September 2020). “Effect of an Inactivated Vaccine Against SARS-CoV-2 on Safety and Immunogenicity Outcomes: Interim Analysis of 2 Randomized Clinical Trials”. JAMA. 324 (10): 951–960. doi:10.1001/jama.2020.15543. PMC 7426884. PMID 32789505.
- ^ Jump up to:a b “China State-Backed Covid Vaccine Has 86% Efficacy, UAE Says”. Bloomberg.com. 2020-12-09. Retrieved 2020-12-09.
- ^ Jump up to:a b Maxwell C. “Coronavirus: UAE authorises emergency use of vaccine for frontline workers”. The National. Retrieved 14 September 2020.
- ^ “Coronavirus: 15,000 register as volunteers for Covid-19 vaccine trial in UAE”. The National. 13 August 2020. Retrieved 15 August2020.
- ^ Jump up to:a b Reuters Staff (2020-12-09). “UAE says Sinopharm vaccine has 86% efficacy against COVID-19”. Reuters. Retrieved 2020-12-09.
- ^ “UAE: Ministry of Health announces 86 per cent vaccine efficacy”. gulfnews.com. Retrieved 2020-12-09.
- ^ “Morocco orders R-Pharm Covid-19 vaccine | The North Africa Post”. northafricapost.com. Retrieved 2020-10-07.
- ^ “Chinese Clinical Trial Register (ChiCTR) – The world health organization international clinical trials registered organization registered platform”. http://www.chictr.org.cn. Retrieved 2020-10-21.
- ^ “Egypt to start receiving volunteers for COVID-19 vaccine trials”. Egypt Independent. 2020-09-12. Retrieved 2020-09-21.
- ^ “Bahrain starts Phase III trial of Sinopharm’s Covid-19 vaccine”. Clinical Trials Arena. 24 August 2020.
- ^ Manama TD. “Vaccine trial continues | THE DAILY TRIBUNE | KINGDOM OF BAHRAIN”. DT News. Retrieved 2020-10-22.
- ^ Jump up to:a b Barrington L (3 November 2020). “Bahrain allows Sinopharm COVID-19 vaccine candidate use in frontline workers”. Reuters. Retrieved 3 November 2020.
- ^ Liu R (5 September 2020). “China’s CNBG, Sinovac find more countries to test coronavirus vaccines”. Reuters. Retrieved 6 September 2020.
- ^ “Jordan starts phase 3 trial of China’s COVID-19 vaccine”. Jordan Times. 2020-08-30. Retrieved 2020-10-22.
- ^ “Coronavirus vaccine should be available in Pakistan ‘within 6-8 weeks'”. http://www.geo.tv. Retrieved 2020-11-14.
- ^ “Third Phase of Human Trials for Coronavirus Vaccine Underway in Peru | Voice of America – English”. http://www.voanews.com. Retrieved 2020-09-11.
- ^ “6,000 additional volunteers required for trials of Sinopharm’s COVID-19 vaccine” (in Spanish). Andina. Retrieved 17 October2020.
- ^ Aquino, Marco (2021-01-27). “Peru volunteer in Sinopharm vaccine trial dies of COVID-19 pneumonia, university says”. Reuters. Retrieved 2021-01-27.
- ^ “Clinical Trial to Evaluate the Efficacy, Immunogenicity and Safety of the Inactivated SARS-CoV-2 Vaccine (COVID-19) – Full Text View – ClinicalTrials.gov”. clinicaltrials.gov. Retrieved 2020-09-28.
- ^ Greaves J (2020-10-08). “UAE company nears end of Chinese Covid-19 vaccine trial”. Reuters. Retrieved 2020-10-10.
- ^ “Chinese COVID-19 vaccine effective: Egypt’s MoH”. EgyptToday. 2020-12-13. Retrieved 2020-12-15.
- ^ “Health Min: a new production line to produce Sinopharm’s Chinese vaccine in Egypt and will be exported to African countries”. EgyptToday. 2020-12-12. Retrieved 2020-12-31.
- ^ “Morocco acquires 65 million vaccine doses from China, UK”. ABC News. Retrieved 2020-12-26.
- ^ “Serbia to produce 24 mln doses of China’s Sinopharm vaccine annually – deputy PM”. seenews.com. Retrieved 2021-03-17.
- ^ “Bahrain approves China’s Sinopharm coronavirus vaccine”. Arabian Business Industries. 13 December 2020.
- ^ Kuo L. “China approves Sinopharm coronavirus vaccine, the country’s first for general use”. The Washington Post.
- ^ “President Ramkalawan and First Lady receives second dose SinoPharm Vaccine”. statehouse.gov.sc. Retrieved 5 February2021.
- ^ Wee S (9 December 2020). “Chinese Covid-19 Vaccine Gets Key Push, but Doubts Swirl”. The New York Times. Retrieved 12 December 2020.
- ^ “Coronavirus: UAE authorises emergency use of vaccine for frontline workers”. The National. Retrieved 24 November 2020.
- ^ Biannchi, Walter (21 February 2021). “Argentina approves Sinopharm COVID-19 vaccine for emergency use”. Reuters. Retrieved 23 February 2021.
- ^ “Bolivia begins inoculation with Sinopharm jabs | The Star”. The Star. Malaysia. Retrieved 28 February 2021.
- ^ Rinith T (4 February 2021). “Health Ministry grants Emergency Use Authorization to China’s Sinopharm vaccine”. Khmer Times. Retrieved 4 February 2021.
- ^ “Dominica: Melissa Skerrit receives the Sinopharm COVID-19 vaccine”. WIC News. 4 March 2021. Retrieved 7 March 2021.
- ^ “Egypt licenses China’s Sinopharm COVID-19 vaccine for emergency use: health minister – Xinhua | English.news.cn”. Xinhua News Agency.
- ^ Jump up to:a b “Equatorial Guinea President receives 1st dose of Chinese COVID-19 vaccine”. dailynewsegypt.com. Retrieved 2021-03-10.
- ^ “Gabon receives 100,000 doses of Sinopharm’s vaccine from China”. Gabon 24. 2021-03-12. Retrieved 2021-03-13.
- ^ “Sinopharm vaccine rollout starts this weekend”. Stabroek News. 6 March 2021. Retrieved 7 March 2021.
- ^ “Hungary signs deal for Chinese Sinopharm’s COVID-19 vaccine, first in EU”. National Post.
- ^ “Iran Launches Phase Two of Mass Inoculation Campaign”. Financial Tribune. 22 February 2021. Retrieved 23 February 2021.
- ^ “Iraq approves Sinopharm, AstraZeneca vaccines”. Big News Network.com. Retrieved 30 January 2021.
- ^ “First batch of Chinese Sinopharm vaccine arrives in Jordan”. Roya News. Retrieved 9 January 2021.
- ^ “Laos declares Covid-19 vaccinations safe, more to be inoculated next week | The Star”. The Star. Malaysia. Retrieved 19 February2021.
- ^ Crean, Rosabel. “China donates 50,000 doses of Sinopharm vaccine to Lebanon | News , Lebanon News | THE DAILY STAR”. Daily Star. Retrieved 2 March 2021.
- ^ “Macau receives first batch of COVID-19 vaccines”. IAG. 7 February 2021. Retrieved 24 February 2021.
- ^ “MFDA approves Pfizer, Sinopharm Covid-19 vaccines for emergency use”. raajje.mv. Retrieved 2021-03-15.
- ^ Cristina (2021-03-19). “O mie de studenți și medici-rezidenți din cadrul USMF vor fi imunizați anti-COVID cu vaccinul BBIBP-CorV, produs de către Sinopharm Beijing Institute of Biological Products”. Ziarul de Gardă (in Romanian). Retrieved 2021-03-19.
- ^ “Deputy PM and City Governor get the first dose of Sinopharm vaccine”. MONTSAME News Agency. Retrieved 2021-03-15.
- ^ “Covid-19: Morocco authorizes use of the Sinopharm vaccine”. en.yabiladi.com.
- ^ Reuters Staff (6 March 2021). “Mozambique expects to vaccinate 16 million against coronavirus by 2022”. Reuters. Retrieved 7 March 2021.
- ^ Namibian, The. “Khomas, Erongo first to get vaccinated”. The Namibian. Retrieved 2021-03-17.
- ^ Poudel, Arjun. “China’s Shinopharm vaccine gets emergency use authorisation in Nepal”. Kathmandu Post. Retrieved 19 February2021.
- ^ “Covid-19 : Le Niger réceptionne 400.000 doses de vaccin SINOPHARM, un don de la Chine | Agence Nigérienne de Presse”. http://www.anp.ne. Retrieved 2021-03-21.
- ^ Shahzad A (19 January 2021). “Pakistan approves Chinese Sinopharm COVID-19 vaccine for emergency use”. Reuters.
- ^ “Peru grants ‘exceptional’ approval for Sinopharm COVID-19 vaccine – government sources”. Reuters. 27 January 2021.
- ^ Asala, Kizzi. “Senegal Kicks Off COVID-19 Vaccination Campaign with China’s Sinopharm”. Africanews. Retrieved 23 February2021.
- ^ “Serbia Becomes First European Nation To Use China’s Sinopharm Vaccine”. RadioFreeEurope/RadioLiberty.
- ^ Thomas, Abdul Rashid (2021-03-15). “Sierra Leone’s President Bio leads the way in taking COVID-19 Vaccine”. SIERRA LEONE TELEGRAPH. Retrieved 2021-03-15.
- ^ “NMRA approves sinopharm vaccine for emergency use”. Colombo Gazette. 2021-03-19. Retrieved 2021-03-20.
- ^ Sequera, Vivian (1 March 2021). “Venezuela approves use of China’s Sinopharm coronavirus vaccine”. Reuters. Retrieved 2 March 2021.
- ^ Mutsaka, Farai (18 February 2021). “Zimbabwe starts administering China’s Sinopharm vaccines”. The Star. Retrieved 20 February 2021.
- ^ Jump up to:a b “China ‘to provide 400,000 COVID vaccine doses’ to Afghanistan”. http://www.aljazeera.com. Retrieved 2021-03-01.
- ^ Jump up to:a b Presse, AFP-Agence France. “Algeria Receives 200,000 Coronavirus Jabs From China”. http://www.barrons.com. Retrieved 2021-02-26.
- ^ Jump up to:a b “Vaccine donation from China arrives | The Star”. http://www.thestar.com.my. Retrieved 2021-02-12.
- ^ Jump up to:a b Radomir, Ralev. “Montenegro receives 30,000 doses of China’s COVID-19 vaccine”.
- ^ “Regulation and Prequalification”. World Health Organization. Retrieved 18 March 2021.
- ^ “Bahrain approves Chinese COVID-19 vaccine for use”. ABC News. Retrieved 2020-12-13.
- ^ Reuters Staff (2021-01-15). “Cambodia says China donates 1 million doses of COVID-19 vaccines”. Reuters. Retrieved 2021-01-16.
- ^ “Health Ministry grants Emergency Use Authorization to China’s Sinopharm vaccine”. Khmer Times. 2021-02-04. Retrieved 2021-02-04.
- ^ “Lt Gen Manet first to be inoculated today with the Sinopharm vaccine”. Khmer Times. 2021-02-09. Retrieved 2021-02-10.
- ^ “Sinovac’s coronavirus vaccine candidate approved for emergency use in China – source”. Reuters. 2020-08-29. Retrieved 2020-08-30.
- ^ Vivek V (15 October 2020). “China’s Sinopharm offers experimental COVID-19 vaccines to students: WSJ”. Reuters. Retrieved 15 October 2020.
- ^ “China gives conditional approval to coronavirus vaccine made by Sinopharm”. Global News. Retrieved 2020-12-31.
- ^ “First Sinopharm Covid-19 vaccines to arrive today”. Macau Business. 2021-02-06. Retrieved 2021-02-07.
- ^ Taufiqurrahman M. “Indonesia can be manufacturing hub for COVID-19 vaccine, says Chinese foreign minister”. Jakarta Post. Retrieved 13 October 2020.
- ^ “Iran Launches Phase Two of Mass Inoculation Campaign”. Financial Tribune. 2021-02-22. Retrieved 2021-02-23.
- ^ “Iran Gets Chinese Vaccine for Coronavirus – Society/Culture news”. Tasnim News Agency. Retrieved 2021-02-28.
- ^ Jangiz, Khazan. “Iraq approves the emergency use of two more COVID-19 vaccines”. http://www.rudaw.net. Retrieved 2021-01-21.
- ^ “Iraq receives first Covid vaccines, gift from China”. France 24. 3 March 2021.
- ^ “Jordan approves China’s Sinopharm Covid vaccine”. France 24. 2021-01-09. Retrieved 2021-03-07.
- ^ Omari, Raed. “Jordan begins COVID-19 vaccination drive as physician, 87, gets first jab”. Arab News.
- ^ KHARIZOV, Ruslan (2021-03-19). “150,000 doses of Sinopharm coronavirus vaccine delivered to Kyrgyzstan”. 24.kg. Retrieved 2021-03-20.
- ^ Thanabouasy, Phayboune (2021-01-27). “Laos Begins Vaccinations for Over 600 Medical Workers”. Laotian Times. Retrieved 2021-01-27.
- ^ Limited, Bangkok Post Public Company. “Laos receives 300,000 vaccine doses from China”. Bangkok Post. Retrieved 2021-02-10.
- ^ “China donates 50,000 doses of Sinopharm vaccine to Lebanon | News , Lebanon News | THE DAILY STAR”. http://www.dailystar.com.lb. Retrieved 2021-03-02.
- ^ March 2021, Naharnet Newsdesk 01; 20:39. “Lebanon Authorizes Use of Chinese Vaccine Sinopharm”. Naharnet. Retrieved 2021-03-07.
- ^ “MFDA approves Pfizer, Sinopharm Covid-19 vaccines for emergency use”. raajje.mv. Retrieved 2021-03-15.
- ^ “Mongolia receives COVID-19 vaccine donation from China – The Manila Times”. http://www.manilatimes.net. Retrieved 2021-02-28.
- ^ “Deputy PM and City Governor get the first dose of Sinopharm vaccine”. MONTSAME News Agency. Retrieved 2021-03-15.
- ^ “China’s Shinopharm vaccine gets emergency use authorisation in Nepal”. kathmandupost.com. Retrieved 2021-02-19.
- ^ Peshimam GN (2020-12-31). “Pakistan to purchase 1.2 million COVID-19 vaccine doses from China’s Sinopharm”. Reuters. Retrieved 2020-12-31.
- ^ Shahzad, Asif (2021-01-19). “Pakistan approves Chinese Sinopharm COVID-19 vaccine for emergency use”. Reuters. Retrieved 2021-01-21.
- ^ “Palestine to receive 100,000 doses of Sinopharm Covid-19 vaccine”. WAFA Agency. Retrieved 2021-03-12.
- ^ “NMRA approves sinopharm vaccine for emergency use”. Colombo Gazette. 2021-03-19. Retrieved 2021-03-20.
- ^ Sircar, Nandini. “UAE Covid vaccine: Third dose to help those with weak immunity”. Khaleej Times. Retrieved 2021-03-19.
- ^ Jump up to:a b “Egypt approves Chinese COVID vaccine, roll-out likely this month”. http://www.aljazeera.com. Retrieved 2021-01-03.
- ^ “Gabon receives 100,000 doses of Sinopharm’s vaccine from China”. Gabon 24. 2021-03-12. Retrieved 2021-03-13.
- ^ Eljechtimi, Ahmed (2021-01-26). “Morocco prepares to launch COVID-19 vaccination programme”. Reuters. Retrieved 2021-01-27.
- ^ “Moroccan health ministry grants emergency approval to Sinopharm’s Covid-19 vaccine”. wam. Retrieved 2021-01-27.
- ^ “China, Africa and the Vaccine Donations”. Modern Ghana. Retrieved 2021-03-05.
- ^ Mucari, Manuel (2021-03-06). “Mozambique expects to vaccinate 16 million against coronavirus by 2022”. Reuters. Retrieved 2021-03-07.
- ^ Namibian, The. “Khomas, Erongo first to get vaccinated”. The Namibian. Retrieved 2021-03-17.
- ^ “Covid-19 : Le Niger réceptionne 400.000 doses de vaccin SINOPHARM, un don de la Chine | Agence Nigérienne de Presse”. http://www.anp.ne. Retrieved 2021-03-21.
- ^ Staff, Reuters (2021-02-18). “Senegal takes delivery of China’s Sinopharm vaccine”. Reuters. Retrieved 2021-02-19.
- ^ AfricaNews (2021-02-23). “Senegal begins covid-19 vaccination with doses from China’s Sinopharm”. Africanews. Retrieved 2021-02-23.
- ^ AFP. “Sierra Leone to receive 200,000 virus vaccine doses”. ewn.co.za. Retrieved 2021-02-26.
- ^ Thomas, Abdul Rashid (2021-03-15). “Sierra Leone’s President Bio leads the way in taking COVID-19 Vaccine”. SIERRA LEONE TELEGRAPH. Retrieved 2021-03-15.
- ^ “Seychelles to start vaccinations with Chinese-made Sinopharm”. AP NEWS. 2021-01-08. Retrieved 2021-01-08.
- ^ “Covid-19: le Congo-Brazzaville reçoit des milliers de doses du vaccin chinois Sinopharm”. RFI (in French). 2021-03-10. Retrieved 2021-03-12.
- ^ Banya, Nelson (2021-02-11). “Zimbabwe purchases 600,000 Sinopharm COVID-19 vaccinations -information minister”. Reuters. Retrieved 2021-02-11.
- ^ Staff, Reuters (2021-02-24). “Zimbabwe to buy 1.2 million more COVID-19 vaccine doses from China”. Reuters. Retrieved 2021-02-26.
- ^ Lopez, Ezequiel Abiu (2021-02-16). “Dominican Republic launches COVID-19 vaccination campaign”. Reuters. Retrieved 2021-02-28.
- ^ “Dominica: Melissa Skerrit receives the Sinopharm COVID-19 vaccine”. WIC News. 2021-03-04. Retrieved 2021-03-05.
- ^ Jorgic, Drazen (2021-03-10). “Mexico leans on China after Biden rules out vaccines sharing in short term”. Reuters. Retrieved 2021-03-10.
- ^ Biannchi, Walter (2021-02-21). “Argentina approves Sinopharm COVID-19 vaccine for emergency use”. Reuters. Retrieved 2021-02-22.
- ^ “Buenos Aires Times | Shipment of 900,000 Sinopharm vaccine doses arrives in Argentina”. http://www.batimes.com.ar. Retrieved 2021-02-26.
- ^ Ramos, Danny (2021-02-11). “Bolivia signs deal with China´s Sinopharm for coronavirus vaccine”. Reuters. Retrieved 2021-02-11.
- ^ “China-donated Sinopharm vaccine received”. Guyana Chronicle. 2021-03-03. Retrieved 2021-03-03.
- ^ “Sinopharm vaccine rollout starts this weekend”. Stabroek News. 2021-03-06. Retrieved 2021-03-07.
- ^ Reuters Staff (2021-01-06). “Peru inks deals with Sinopharm, AstraZeneca for coronavirus vaccines -president”. Reuters. Retrieved 2021-01-07.
- ^ Aquino, Marco (2021-01-27). “Peru grants ‘exceptional’ approval for Sinopharm COVID-19 vaccine – government sources”. Reuters. Retrieved 2021-01-28.
- ^ Sequera, Vivian (2021-03-01). “Venezuela approves use of China’s Sinopharm coronavirus vaccine”. Reuters. Retrieved 2021-03-02.
- ^ Sequera, Vivian (2021-03-02). “Venezuela receives donated coronavirus vaccine from China”. Reuters. Retrieved 2021-03-02.
- ^ “China sends 100,000 coronavirus vaccines to Belarus”. eng.belta.by. 2021-02-19. Retrieved 2021-02-19.
- ^ “Hungary signs deal for Chinese Sinopharm’s COVID-19 vaccine, first in EU”. nationalpost. Retrieved 2021-01-29.
- ^ Staff, Reuters (2021-02-16). “First 550,000 doses of Chinese Sinopharm’s vaccine arrive in Hungary”. Reuters. Retrieved 2021-02-18.
- ^ “Hungary’s PM Viktor Orbán vaccinated against COVID with Chinese Sinopharm vaccine”. euronews. 2021-02-28.
- ^ “Emiratele Arabe Unite au donat Republicii Moldova un lot de vaccin împotriva COVID-19”. TV8 (in Romanian). 13 March 2021.
- ^ Cristina (2021-03-19). “O mie de studenți și medici-rezidenți din cadrul USMF vor fi imunizați anti-COVID cu vaccinul BBIBP-CorV, produs de către Sinopharm Beijing Institute of Biological Products”. Ziarul de Gardă (in Romanian). Retrieved 2021-03-19.
- ^ “Vaccine delay in North Macedonia stirs political tension”. ABC News. Retrieved 2021-02-12.
- ^ Reuters Staff (2021-01-16). “Serbia receives million doses of China’s Sinopharm COVID-19 vaccine”. Reuters. Retrieved 2021-01-16.
- ^ “Abu Dhabi starts COVID-19 vaccinations”. Arab News. 2020-12-14. Retrieved 2020-12-17.
- ^ Wee SL (9 December 2020). “Chinese Covid-19 Vaccine Gets Key Push, but Doubts Swirl”. The New York Times. Retrieved 21 December 2020.
- ^ Yu, Sun (December 31, 2020). “China approves first domestic Covid-19 vaccine for general use”. Financial Times. Retrieved January 12, 2021.
- ^ Dancel R. “Philippine officials under fire from critics, health authorities for unsanctioned Covid-19 vaccinations”. The Straits Times.
- ^ Aberia, Ingming (6 January 2021). “Did Sinopharm forget that Duque exists?”. The Manila Times. Retrieved 9 January 2021.
- ^ “水面下で出回る中国ワクチン 富裕層から永田町へ? 狙われる日本市場”. Mainichi Daily News (in Japanese). 2020-12-31. Retrieved 2021-01-02.
- ^ Elmer, Keegan (January 3, 2021). “Beijing responds to claims Japanese were given unapproved Sinopharm jabs”. South China Morning Post. Retrieved January 9, 2021.
External links
- “How the Sinopharm Covid-19 Vaccine Works”. The New York Times.
| A vial of the BBIBP-CorV COVID‑19 vaccine | |
| Vaccine description | |
|---|---|
| Target | SARS-CoV-2 |
| Vaccine type | Inactivated |
| Clinical data | |
| Routes of administration | Intramuscular |
| ATC code | None |
| Legal status | |
| Legal status | Authorization for use in Bahrain, China, Egypt, Iraq, Pakistan, Serbia, United Arab Emirates, Iran (emergency use) |
| Identifiers | |
| CAS Number | 2503126-65-4 |
| DrugBank | DB15807 |
| Part of a series on the |
| COVID-19 pandemic |
|---|
| SARS-CoV-2 (virus)COVID-19 (disease) |
| showTimeline |
| showLocations |
| showInternational response |
| showMedical response |
| showImpact |
| COVID-19 Portal |
| vte |
How the Sinopharm Vaccine Works
By Jonathan Corum and Carl ZimmerUpdated March 22, 2021Leer en español

In early 2020, the Beijing Institute of Biological Products created an inactivated coronavirus vaccine called BBIBP-CorV. Clinical trials run by the state-owned company Sinopharm showed that it had an efficacy rate of 79 percent. China approved the vaccine and soon began exporting it to other countries.
A Vaccine Made From Coronaviruses
BBIBP-CorV works by teaching the immune system to make antibodies against the SARS-CoV-2 coronavirus. The antibodies attach to viral proteins, such as the so-called spike proteins that stud its surface.

Spikes
Spike
protein
gene
CORONAVIRUS
To create BBIBP-CorV, the Beijing Institute researchers obtained three variants of the coronavirus from patients in Chinese hospitals. They picked one of the variants because it was able to multiply quickly in monkey kidney cells grown in bioreactor tanks.
Killing the Virus
Once the researchers produced large stocks of the coronaviruses, they doused them with a chemical called beta-propiolactone. The compound disabled the coronaviruses by bonding to their genes. The inactivated coronaviruses could no longer replicate. But their proteins, including spike, remained intact.

Beta-
propiolactone
INACTIVATED
CORONAVIRUS
Inactivated
genes
The researchers then drew off the inactivated viruses and mixed them with a tiny amount of an aluminum-based compound called an adjuvant. Adjuvants stimulate the immune system to boost its response to a vaccine.
Inactivated viruses have been used for over a century. Jonas Salk used them to create his polio vaccine in the 1950s, and they’re the bases for vaccines against other diseases including rabies and hepatitis A.
Prompting an Immune Response
Because the coronaviruses in BBIBP-CorV are dead, they can be injected into the arm without causing Covid-19. Once inside the body, some of the inactivated viruses are swallowed up by a type of immune cell called an antigen-presenting cell.

INACTIVATED
CORONAVIRUS
Engulfing
the virus
ANTIGEN-
PRESENTING
CELL
Digesting
virus proteins
Presenting
virus protein
fragments
HELPER
T CELL
The antigen-presenting cell tears the coronavirus apart and displays some of its fragments on its surface. A so-called helper T cell may detect the fragment. If the fragment fits into one of its surface proteins, the T cell becomes activated and can help recruit other immune cells to respond to the vaccine.
Making Antibodies
Another type of immune cell, called a B cell, may also encounter the inactivated coronavirus. B cells have surface proteins in a huge variety of shapes, and a few might have the right shape to latch onto the coronavirus. When a B cell locks on, it can pull part or all of the virus inside and present coronavirus fragments on its surface.
A helper T cell activated against the coronavirus can latch onto the same fragment. When that happens, the B cell gets activated, too. It proliferates and pours out antibodies that have the same shape as their surface proteins.

ACTIVATED
HELPER
T CELL
INACTIVATED
CORONAVIRUS
Activating
the B cell
Matching
surface proteins
B CELL
SECRETED
ANTIBODIES
Stopping the Virus
Once vaccinated with BBIBP-CorV, the immune system can respond to an infection of live coronaviruses. B cells produce antibodies that stick to the invaders. Antibodies that target the spike protein can prevent the virus from entering cells. Other kinds of antibodies may block the virus by other means.

ANTIBODIES
LIVE
VIRUS
Remembering the Virus
Sinopharm’s clinical trials have demonstrated that BBIBP-CorV can protect people against Covid-19. But no one can yet say how long that protection lasts. It’s possible that the level of antibodies drops over the course of months. But the immune system also contains special cells called memory B cells that might retain information about the coronavirus for years or even decades.
Vaccine Timeline
January, 2020 Sinopharm begins developing an inactivated vaccine against the coronavirus.
June Researchers report the vaccine produces promising results in monkeys. A Phase 1/2 trial shows that the vaccine doesn’t cause any serious side effects and enables people to make antibodies against the coronavirus.

A Sinopharm production plant in Beijing.Zhang Yuwei/Xinhua, via Associated Press
July A Phase 3 trial begins in the United Arab Emirates.
August Phase 3 trials begin in Morocco and Peru.

Preparing a Sinopharm dose in Lima, Peru.Ernesto Benavides/Agence France-Presse
Sept. 14 The U.A.E. gives emergency approval for Sinopharm’s vaccine to use on health care workers. Government officials and others begin to receive it.
November The chairman of Sinopharm says almost a million people in China have received Sinopharm vaccines.
Nov. 3 The ruler of Dubai, Sheikh Mohammed bin Rashid al-Maktoum, announces he received the vaccine.

Sheikh Mohammed before receiving the vaccine.Agence France-Presse
Dec. 9 The U.A.E. gives full approval to BBIBP-CorV, announcing it has an efficacy rate of 86 percent. But the government did not release any details with their announcement, leaving it unclear how they had come to their conclusions.
Dec. 13 Bahrain also approves the vaccine.

Vials of the Sinopharm vaccine at a packaging plant.Zhang Yuwei/Xinhua, via Associated Press
Dec. 30 Sinopharm announces that the vaccine has an efficacy of 79.34 percent, leading the Chinese government to approve it. The company has yet to publish detailed results of their Phase 3 trial.
Jan. 3, 2021 Egypt authorizes the vaccine for emergency use.
Sources: National Center for Biotechnology Information; Science; The Lancet; Lynda Coughlan, University of Maryland School of Medicine; Jenna Guthmiller, University of Chicago.
Data
/////////////BBIBP-CorV, Sinopharm, COVID-19 vaccine, china, covid 19, corona virus, vaccine
#BBIBP-CorV, #Sinopharm, #COVID-19 vaccine, #china, #covid 19, #corona virus, #vaccine

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....











