Home » ANTIBODIES (Page 6)
Category Archives: ANTIBODIES
Stelara (ustekinumab) Receives FDA Approval to Treat Active Psoriatic Arthritis

Ustekinumab
| CAS No: | 815610-63-0 |
|---|---|
| Molecular Weight: | 145.64 g/mol |
| Chemical Formula: | C9H18N2O2 |
| IUPAC Name: | Immunoglobulin G1, anti-(human interleukin 12 p40 subunit) (human monoclonal CNTO 1275 gamma1-chain), disulfide with human monoclonal CNTO 1275 kappa-chain, dimer |
HORSHAM, Pa., Sept. 23, 2013 /PRNewswire/ — Janssen Biotech, Inc., announced today that the U.S. Food and Drug Administration (FDA) has approved Stelara (ustekinumab) alone or in combination with methotrexate for the treatment of adult patients (18 years or older) with active psoriatic arthritis. It is estimated that more than two million people in the U.S. are living with psoriatic arthritis, a chronic autoimmune disease characterized by both joint inflammation and psoriasis skin lesions
read all at
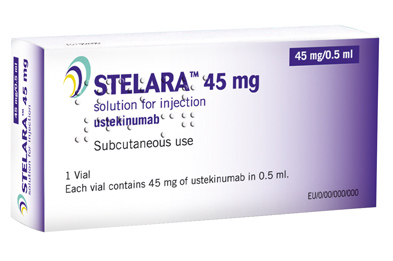
Ustekinumab (INN, experimental name CNTO 1275, proprietary commercial name Stelara, Centocor) is a human monoclonal antibody. It is directed against interleukin 12 and interleukin 23, naturally occurring proteins that regulate the immune system and immune-mediated inflammatory disorders.
Ustekinumab is a fully human monoclonal antibody (mAb) targeting the interleukin (IL)-12/23p40 subunit.
Interleukins are small soluble proteins that communicate between white blood cells (leukocytes), such as T cells. Interleukins mediate the differentiation, proliferation and many other processes of these cells. IL-12 and IL-23 are involved in the differentiation of naive T cells into T helper (Th) 1 and Th17 cells respectively.
Th1 and Th17 cells have been implicated in several autoimmune disorders, such as psoriasis. Ustekinumab targets the common p40 subunit of IL-12 and IL-23 to stop these cytokines from binding to their receptors and consequently preventing the development of Th1 and Th17 cells in an immune response.
In two Phase III trials for moderate to severe psoriasis, the longest >76 weeks, ustekinumab was safe and effective.
A third Phase III trial, ACCEPT, compared the efficacy and safety of ustekinumab with etanercept in the treatment of moderate to severe plaque psoriasis. This trial found a significantly higher clinical response with ustekinumab over the 12-week study period compared to high-dose etanercept. It also demonstrated the clinical benefit of ustekinumab among patients who failed to respond to etanercept.
Ustekinumab is approved in Canada, Europe and the United States to treat moderate to severe plaque psoriasis.
As of November 2009, the drug is being investigated for the treatment of psoriatic arthritis. It has also been tested in Phase II studies for multiple sclerosis and sarcoidosis, the latter versus golimumab (Simponi).
The US Food and Drug Administration (FDA) and European Union (EU) have approved the interleukin (IL) 12/23 inhibitor ustekinumab (Stelara, Janssen Biotech) for adults with active psoriatic arthritis who have not responded adequately to previous nonbiological disease-modifying antirheumatic drug therapy, the company announced today.
Approval of ustekinumab for psoriatic arthritis is “significant for patients and physicians as it marks the first treatment approved for this devastating and complex disease since the introduction of anti-TNF biologic medicines more than a decade ago,” Jerome A. Boscia, MD, vice president and head of immunology development, Janssen Research & Development, LLC, said in a statement.
The European Medicine Agency’s Committee for Medicinal Products for Human Use (CHMP) recommended approval of ustekinumab for active psoriatic arthritis in June, as reported by Medscape Medical News.
Ustekinumab is already approved in the US and EU for treatment of moderate to severe psoriatic plaques in adults. The drug, which can be used alone or in combination with methotrexate, is novel in that it targets both IL-12 and IL-23.
Image source: Crystal structure of human IL-12, Wikipedia, public domain

Ustekinumab binding to IL-12/23p40
FDA grants Arzerra ‘breakthrough’ designation for use with chlorambucil in CLL
The FDA today granted “breakthrough therapy” designation to ofatumumab for treatment of patients with chronic lymphocytic leukemia.
The designation applies to use of ofatumumab (Arzerra, GlaxoSmithKline) in combination with chlorambucil in patients with untreated CLL who unsuitable for fludarabine-based therapy.
Ofatumumab is a human monoclonal antibody that targets an epitope on the CD20 molecule encompassing parts of the small and large extracellular loops.
read all at
also read my post on newdrugapprovals
https://newdrugapprovals.wordpress.com/2013/07/08/gsk-tests-ofatumumab-in-rare-skin-disorder/
Ofatumumab (trade name Arzerra, also known as HuMax-CD20) is a human monoclonal antibody (for the CD20 protein) which appears to inhibit early-stage B lymphocyte activation. It is FDA approved for treating chronic lymphocytic leukemia that is refractory to fludarabine and alemtuzumab (Campath) and has also shown potential in treating Follicular non-Hodgkin’s lymphoma, Diffuse large B cell lymphoma, rheumatoid arthritis and relapsing remitting multiple sclerosis. Ofatumumab has also received conditional approval in Europe for the treatment of refractory chronic lymphocytic leukemia. This makes ofatumumab the first marketing application for an antibody produced by Genmab, as well as the first human monoclonal antibody which targets the CD20 molecule that will be available for patients with refractory CLL.Designated an orphan drug by FDA for the treatment of B-CLL
Mogamulizumab

Immunoglobulin G1, anti-(CC chemokine receptor CCR4) (human-mouse monoclonal
KW-0761 heavy chain), disulfide with human-mouse monoclonal KW-0761 κ-chain,
dimer
Immunoglobulin G1, anti-(human C-C chemokine receptor type 4 (CCR4, K5-5,
CD194)); humanized mouse monoclonal KW-0761 γ1 heavy chain (222-219′)-disulfide
with humanized mouse monoclonal KW-0761 κ light chain, dimer (228-228”:231-231”)-
bisdisulfide
MOLECULAR FORMULA C6520H10072N1736O2020S42 (peptide)
MOLECULAR WEIGHT 146.44 kDa (peptide)
SPONSOR Kyowa Hakko Kirin Co., Ltd.
CODE DESIGNATION KW-0761, KM8761
CAS REGISTRY NUMBER 1159266-37-1
THERAPEUTIC CLAIM Antineoplastic
http://www.ama-assn.org/resources/doc/usan/mogamulizumab.pdf for structure
Mogamulizumab (USAN; trade name Poteligeo) is a humanized monoclonal antibody targeting CC chemokine receptor 4(CCR4). It has been approved in Japan for the treatment of relapsed or refractory adult T-cell leukemia/lymphoma.[1]
Mogamulizumab was developed by Kyowa Hakko Kirin Co., Ltd.[2]
T-cell neoplasms, such as adult T-cell leukemia/lymphoma (ATL) and peripheral T-cell lymphoma, are particularly aggressive and, despite novel combination chemotherapy regimens, still have extremely poor prognoses. As such, there is an unmet medical need for novel therapies and the anti-chemokine CCR4 receptor antibody mogamulizumab (KW-0761) may offer such an option for the treatment of ATL. Mogamulizumab is a humanized antibody, with a defucosylated Fc region, which enhances antibody-dependent cellular cytotoxicity. As a result, mogamulizumab demonstrates potent antitumor activity at much lower doses than other therapeutic monoclonal antibodies. Clinical testing indicates that mogamulizumab is effective and well tolerated, with a predictable pharmacokinetic profile in patients with relapsed/refractory ATL. This drug was recently granted regulatory approval in Japan for this indication and continues to be evaluated in clinical trials in both the U.S. and Europe.
It has also been licensed to Amgen for development as a therapy for Asthma.[3]
- ^ Subramaniam, J; Whiteside G, McKeage K, Croxtall J (18). “Mogamulizumab: First Global Approval”. Drugs 72 (9): 1293–1298.doi:10.2165/11631090-000000000-00000. Retrieved 10 September 2012.
- ^ “Statement On A Nonproprietary Name Adopted By The USAN Council: Mogamulizumab”. American Medical Association.
- ^ “Kyowa Hakko Kirin R&D Pipeline”. Kyowa Hakko Kirin. Retrieved 10 September 2012.

old article
Tokyo, Japan, July 19, 2013 — Kyowa Hakko Kirin Co., Ltd. (Tokyo: 4151, President and CEO: Nobuo Hanai, “Kyowa Hakko Kirin”) announced today that it has been filed an application to Japan’s Ministry of Health, Labour and Welfare (“MHLW”) seeking approval for additional indication for untreated CCR4-positive adult T-cell leukemia-lymphoma (ATL), relapsed CCR4-positive peripheral T-cell lymphoma (PTCL) and cutaneous T-cell lymphoma (CTCL) of Mogamulizumab (brand name: POTELIGEO® Injection 20 mg).
Mogamulizumab is a novel, humanized monoclonal antibody directed against CC chemokine receptor 4 (CCR4), which is over-expressed on various malignant T cells, including ATL, PTCL and CTCL cells. Engineered by Kyowa Hakko Kirin’s unique POTELLIGENT® Technology, the antibody is designed to kill its target cells through potent antibody-dependent cellular cytotoxicity (ADCC). Clinical studies of Mogamulizumab in patients with untreated CCR4-positive ATL, relapsed CCR4-positive PTCL and CTCL in Japan met their primary endpoint, which allowed Kyowa Hakko Kirin to file an application. Mogamulizumab was also granted orphan drug designations for the treatment of CCR4-positive ATL in August 2010, PTCL and CTCL in March 2013 by the MHLW.
Mogamulizumab was launched in Japan with the brand name “POTELIGIO® Injection 20 mg” on May 29, 2012 for the treatment of patients with relapsed or refractory CCR4-positive ATL and is being investigated world-wide in a number of clinical studies for other potential indications.
Kyowa Hakko Kirin is committed to developing innovative therapeutics for treatment of a wide range of diseases with unmet medical needs, including lymphomas such as ATL, PTCL and CTCL, and contributing to the improvement of patients’ quality of life (QOL).
Overview of Phase II Clinical Study for untreated ATL in Japan
| Objective | Evaluate the efficacy, safety and pharmacokinetics of mLSG15 + Mogamulizumab or mLSG15 in patients with untreated CCR4-positive ATL. Mogamulizumab: 1.0 mg/kg/2wks for eight times in patients |
|---|---|
| Primary Endpoint | Efficacy (complete response rate, ORR), safety, pharmacokinetics |
| Efficacy | Efficacy was assessed in 53 patients (mLSG15 + Mogamulizumab: 29 patients, mLSG15: 24 patients) [Complete response rate] mLSG15 + Mogamulizumab: 52% (95%CI; 33-71%)(15/29) mLSG15: 33% (95%CI; 16-55%)(8/24) [ORR] mLSG15 + Mogamulizumab: 86% (95%CI; 68-96%)(25/29) mLSG15: 75% (95%CI; 53-90%)(18/24) Add-on effects of Mogamulizumab were found on mLSG15 therapy in complete response rate and ORR |
| Safety | Safety was assessed in 53 patients Common adverse events might cause by mLSG15 therapy in patients, add-on therapy of Mogamulizumab was found to be well tolerated at this dose level on mLSG15 therapy. |
Overview of Phase II Clinical Study for PTCL and CTCL in Japan
| Objective | Evaluate the efficacy, safety and pharmacokinetics of Mogamulizumab at 1.0 mg/kg weekly for eight weeks in patients with CCR4-positive relapsed PTCL and CTCL. |
|---|---|
| Primary Endpoint | Efficacy (ORR), safety, pharmacokinetics |
| Efficacy | Efficacy was assessed in 37 patients (PTCL: 29 patients, CTCL: 8 patients) [ORR] 35% (95% CI; 20-53%)(13/37) (complete response in 5 patients, partial response in 8 patients) [ORR for PTCL] 34% (95% CI; 18-54%)(10/29) (complete response in 5 patients, partial response in 5 patients) [ORR for CTCL] 38% (95% CI; 9-76%)(3/8) (partial response in 3 patients) |
| Safety | Safety was assessed in 37 patients Mogamulizumab was found to be well tolerated at this dose level. |
About CCR4 (CC chemokine receptor 4)
CCR4 is one of the chemokine receptors involved in leukocyte migration, selectively expressed in type 2 helper T (Th2) cells and regulatory T (Treg) cells. CCR4 is also shown to be over-expressed in certain hematological malignancies.
About adult T-cell leukemia-lymphoma (ATL)
ATL is a peripheral T-cell malignancy and the retrovirus HTLV-1 is thought to be involved in its onset. Estimates show that around 1,150 new cases occur every year in Japan. ATL is generally treated with combination chemotherapy, such as mLSG15, but there are currently no therapeutic methods with the potential of providing a cure for ATL, although researchers are actively looking into other methods than transplantation. For relapsed/refractory cases, various chemotherapy regimens based on malignant lymphoma therapies are currently used, but an effective treatment method has yet to be established.
About Peripheral T-Cell Lymphoma (PTCL)
Non-Hodgkin lymphomas account for the majority of malignant lymphoma cases and can be broadly divided into disease of B-cell origin and disease of T/natural killer (NK)-cell origin. Disease of T/NK-cell origin can be classified according to the main lesion site into nodal, extranodal, cutaneous, and leukemic disease. PTCL is a general term describing nodal and extranodal disease of T/NK-cell origin.
About Cutaneous T-Cell Lymphoma (CTCL)
CTCL is a rare, low grade type of non-Hodgkin’s lymphoma. CTCL is one of the most common forms of T-cell lymphoma. The two most common types of CTCL are mycosis fungoides (MF) and Sezary syndrome (SS). MF does not look the same in all patients and may present as skin patches, plaques, and tumors. SS is an advanced form of MF and includes the presence of malignant lymphocytes in the blood.
About POTELLIGENT®
POTELLIGENT® is Kyowa Hakko Kirin’s unique technology for the production of antibodies with enhanced ADCC activity. This technique enables production of antibodies with a reduced amount of fucose in their carbohydrate structure. Non-clinical studies have demonstrated that antibodies produced using this technology killed target cells more efficiently than conventional antibodies and exhibited stronger antitumor effects. For more information, please visit www.POTELLIGENT.com.
About antibody-dependent cellular cytotoxicity (ADCC)
ADCC is one of the body’s immune responses, initiated by binding of an antibody to its antigen on target cells, followed by lysis of the antibody-bound target cells by effector cells such as natural killer cells. ADCC is known to be one of the modes of action of therapeutic antibodies.
Orphan drug designation
A drug must meet the following three conditions in order to be granted an orphan drug designation in Japan.
1) The number of patients who may use the drug is less than 50,000 in Japan.
2) There are high medical needs for the drug (There is no appropriate alternative drug/treatment, or high efficacy or safety is expected compared with existing products).
3) There is high possibility of development (There should be a theoretical rationale for the use of the drug for the target disease, and the development plan should be appropriate). For designated orphan drugs, measures to support the research and development activities are taken (The orphan drug and orphan medical device research and development promotion program).
About mLSG15 therapy
The mLSG15 therapy is one of standard chemotherapies for ATL patients. The mLSG15 therapy generally consists of six courses. A course is the combination of the following three therapies, VCAP therapy (V: Vincristine Sulfate, C: Cyclophosphamide Hydrate, A: Doxorubicin Hydrochloride, P: Prednisolone), AMP therapy (A: Doxorubicin Hydrochloride, M: Ranimustine, P: Prednisolone) and VECP therapy (V: Vindesine Sulfate, E: Etoposide, C: Carboplatin, P: Prednisolone), which are administered at one week interval in turns. ATL patients are administrated cytarabine, methotrexate, and prednisolone intraspinally before the start of VCAP therapy of the 2,4,6 course (Intraspinal administration is to inject directly in and around the area of the spinal cord with anti-cancer agents to prevent relapsing cancer from these sites by distributing anti-cancer drugs to the brain and spinal cord). According to patient’s conditions, the reduction of the number of courses and doses of medicine may be done.
Marketing approval of mogamulizumab – lfb biomanufacturing
May 15, 2012 – The recent approval in Japan of mogamulizumab … Mogamulizumab is a humanized mAb derived from Kyowa Hakko Kirin’s POTELLIGENT® …
TSRI develops new technique for finding therapeutic antibodies
TSRI develops new technique for finding therapeutic antibodies
Scientists at Scripps Research Institute (TSRI) in California, US have come up with a new technique for identifying antibodies with therapeutic effects.
READ MORE AT
![]()

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....











