Home » Articles posted by DR ANTHONY MELVIN CRASTO Ph.D (Page 411)
Author Archives: DR ANTHONY MELVIN CRASTO Ph.D
GSK announces regulatory submission for umeclidinium monotherapy in European Union
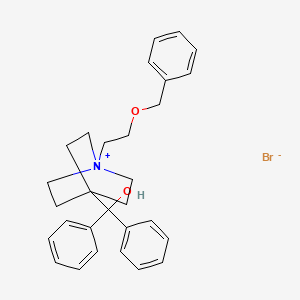
Umeclidinium bromide
http://www.ama-assn.org/resources/doc/usan/umeclidinium-bromide.pdf
26 April 2013
GlaxoSmithKline plc today announced the submission of a regulatory application in the European Union for the investigational once-daily medicine, umeclidinium bromide (UMEC), for patients with chronic obstructive pulmonary disease (COPD).
UMEC is an investigational bronchodilator molecule (formerly known as GSK573719), a long-acting muscarinic antagonist (LAMA), administered using the ELLIPTA™ inhaler.
A Marketing Authorisation Application (MAA) for UMEC monotherapy (55 mcg delivered dose) has been submitted to the European Medicines Agency (EMA), for a maintenance bronchodilator treatment to relieve symptoms in adult patients with COPD.
Regulatory filings for UMEC monotherapy are imminent in the US and planned in other countries during the course of 2013.
Daiichi Sankyo enrolls first patient in Nimotuzumab Phase 3 clinical trials

Nimotuzumab
25 April 2013
Daiichi Sankyo Company, Limited announced today that the first patient has been enrolled in two pivotal phase 3 clinical trials of nimotuzumab (DE-766), a recombinant humanized monoclonal antibody targeting the Epidermal Growth Factor Receptor (EGFR), which is being evaluated for the treatment of patients diagnosed with lung cancer and with gastric cancer.
About Phase 3 Clinical Trials for Lung Cancer
The phase 3 clinical trial is a multicenter, randomized, double-blind, placebo-controlled study investigating nimotuzumab for the first-line therapy in patients with unresectable and locally advanced squamous cell lung cancer. The patients will receive either nimotuzumab in combination with concurrent chemoradiotherapy or placebo in combination with concurrent chemoradiotherapy. The primary endpoint is overall survival (OS), and the secondary endpoints are progression free survival (PFS) and safety. Approximately 420 patients are planned to be enrolled at approximately 60 clinical centers in Japan. Additional details of the trial are available onwww.clinicaltrials.jp/user/cteSearch.jsp.
About Phase 3 Clinical Trials for Gastric Cancer (ENRICH study)
The ENRICH study is a randomized, open-label, Japan-Korea collaborative study of previously treated patients with EGFR overexpressed advanced gastric and gastroesophageal junction cancer who will receive either nimotuzumab and irinotecan hydrochloride hydrate (hereafter, irinotecan) combination therapy or irinotecan monotherapy. The primary endpoint is overall survival (OS), and the secondary endpoints are progression free survival (PFS) and safety. Approximately 400 patients are planned to be enrolled at approximately 40 clinical centers in Japan and South Korea. In Korea, Kuhnil Pharmaceutical Company, Limited (hereafter, Kuhnil) is implementing this trial. Additional details of the trial are available on www.clinicaltrials.gov.
About Unresectable and Locally Advanced Squamous Cell Lung Cancer
In Japan, lung cancer is the first leading cause of cancer death, with about 70,000 deaths in 2011.i Non-small cell lung cancer (adenocarcinoma, squamous cell carcinoma, and large cell carcinoma) occupies more than 80 percent of lung cancer. Concurrent chemoradiotherapy for a radical cure is currently used as the standard treatment for patients with stage III locally advanced non-small cell lung cancer, in which radical surgery is not possible but radiotherapy is.ii Of these cases, between 30 and 40 percent are squamous cell carcinoma and EGFR is known to be overexpressed.iii
About Gastric Cancer
Half of the total number of gastric cancer cases worldwide occurs in Eastern Asia.iv In Japan, gastric cancer is the second leading cause of cancer death, with an estimated about 50,000 deaths. i In South Korea, about 10,000 gastric cancer deaths in 2011 were reported.v Numerous improvements have occurred in the management of gastric cancer; however, gastric cancer still has a poor prognosis. For patients with earlier stages of disease, more than 50% undergo surgery, but even after a curative resection, 60% of these patients eventually relapse locally or with distant metastases. vi
About Nimotuzumab and EGFR
Nimotuzumab is an intravenously administered recombinant humanized monoclonal antibody directed against human EGFR and is produced by CIMAB S.A. (Cuba). Nimotuzumab blocks the binding of EGF to its receptor interfering with the cell signaling pathway. Nimotuzumab has been approved for head and neck cancer, glioma, and esophageal cancer in several countries. EGFR is known to be overexpressed in a wide variety of human tumors.vii Overexpression of EGFR in tumors correlates with increased metastasis, decreased survival, and a poor prognosis. It is known that EGFR is activated by exposure to radiation.
In 2006, Daiichi Sankyo introduced nimotuzumab from CIMAB S.A. and CIMYM BioSciences Inc. (Canada) and has the rights to develop and commercialize in Japan. In Korea, Kuhnil has the rights to develop and commercialize.
15 top blockbuster drug contenders, compiled:Fiercebiotech, by John Carroll and Ryan McBride
15 top blockbuster drug contenders, compiled fiercebiotech, by John Carroll and Ryan McBride
read all this at
http://www.fiercebiotech.com/special-reports/top-15-blockbuster-contenders

Top 20 Best-Selling Drugs Approved and Launched During 2012
Biotechnology from bench to business
Top 20 Best-Selling Drugs Approved and Launched During 2012
What new medicines are shaking things up?
read all this at http://www.genengnews.com/insight-and-intelligence/top-20-best-selling-drugs-approved-and-launched-during-2012/77899791/
have a good reading
Biosimilars: 10 Drugs to Watch
Biotechnology from bench to business
Biosimilars: 10 Drugs to Watch
Which innovator drugs are companies scrambling to copy?
read at
http://www.genengnews.com/insight-and-intelligence/biosimilars-10-drugs-to-watch/77899804/
http://www.genengnews.com/insight-and-intelligence
have a great reading
Researchers at Northeastern University in Boston have developed a gene therapy approach that may one day stop Parkinson’s disease (PD) in it tracks, preventing disease progression and reversing its symptoms
Glial cell derived neurotrophic factor structure (credit: Wikimedia Commons)
http://experimentalbiology.org/EB/pages/default.aspx?splashpage=1
A noninvasive avenue for Parkinson’s disease gene therapy
April 26, 2013
Researchers at Northeastern University in Boston have developed a gene therapy approach that may one day stop Parkinson’s disease (PD) in it tracks, preventing disease progression and reversing its symptoms.
The novelty of the approach lies in the nasal route of administration and nanoparticles containing a gene capable of rescuing dying neurons in the brain.
Parkinson’s is a devastating neurodegenerative disorder caused by the death of dopamine neurons in a key motor area of the brain, the substantia nigra (SN). Loss of these neurons leads to the characteristic tremor and slowed movements of PD, which get increasingly worse with time.
Currently, more than 1% of the population over age 60 has PD and approximately 60,000 Americans are newly diagnosed every year. The available drugs on the market for PD mimic or replace the lost dopamine but do not get to the heart of the problem, which is the progressive loss of the dopamine neurons.
The focus of Dr. Barbara Waszczak‘s lab at Northeastern University in Boston is to find a way to harvest the potential of glial cell line-derived neurotrophic factor (GDNF) as a treatment for PD. GDNF is a protein known to nourish dopamine neurons by activating survival and growth-promoting pathways inside the cells.
Bypassing the blood-brain barrier
Not surprisingly, GDNF is able to protect dopamine neurons from injury and restore the function of damaged and dying neurons in many animal models of PD. However, the action of GDNF is limited by its inability to cross the blood-brain barrier (BBB), thus requiring direct surgical injection into the brain.
To circumvent this problem, Waszczak’s lab is investigating intranasal delivery as a way to bypass the BBB. Their previous work showed that intranasal delivery of GDNF protects dopamine neurons from damage by the neurotoxin, 6-hydroxydopamine (6-OHDA), a standard rat model of PD.
Taking this work a step further, Brendan Harmon, working in Waszczak’s lab, has adapted the intranasal approach so that cells in the brain can continuously produce GDNF. His work utilized nanoparticles, developed by Copernicus Therapeutics, Inc., which are able to transfect brain cells with an expression plasmid carrying the gene for GDNF (pGDNF).
When given intranasally to rats, these pGDNF nanoparticles increase GDNF production throughout the brain for long periods, avoiding the need for frequent re-dosing.
Now, in new research presented at Experimental Biology 2013 in Boston, Harmon reported that intranasal administration of Copernicus’ pGDNF nanoparticles results in GDNF expression sufficient to protect SN dopamine neurons in the 6-OHDA model of PD.
Waszczak and Harmon believe that intranasal delivery of Copernicus’ nanoparticles may provide an effective and non-invasive means of GDNF gene therapy for PD, and an avenue for transporting other gene therapy vectors to the brain.
This work, which was funded in part by the Michael J. Fox Foundation for Parkinson’s Research and Northeastern University, has the potential to greatly expand treatment options for PD and many other central nervous system disorders.
Potential diabetes breakthrough Harvard researchers discover hormone that spurs beta cell production
Betatrophin causes a specific increase in pancreatic β cell replication. Betatrophin is a secreted protein expressed in liver and fat. The increase in β cell replication and mass improves glycemic control. (Credit: Peng Yi, Ji-Sun Park, Douglas A. Melton/Cell)
Potential diabetes breakthrough
Researchers at the Harvard Stem Cell Institute (HSCI) have discovered a hormone that holds promise for a dramatically more effective treatment of type 2 diabetes, a metabolic illness afflicting an estimated 26 million Americans.
The researchers believe that the hormone might also have a role in treating type 1, or juvenile, diabetes.
The work was published by the journal Cell.
The hormone, called betatrophin, causes mice to produce insulin-secreting pancreatic beta cells at up to 30 times the normal rate. The new beta cells only produce insulin when called for by the body, offering the potential for the natural regulation of insulin and a great reduction in the complications associated with diabetes, the leading medical cause of amputations and non-genetic loss of vision.
The researchers who discovered betatrophin, HSCI co-director Doug Melton and postdoctoral fellow Peng Yi, caution that much work remains to be done before it could be used as a treatment in humans. But the results of their work, which was supported in large part by a federal research grant, already have attracted the attention of drug manufacturers.
“If this could be used in people,” said Melton, Harvard’s Xander University Professor and co-chair of the University’s Department of Stem Cell and Regenerative Biology, “it could eventually mean that instead of taking insulin injections three times a day, you might take an injection of this hormone once a week or once a month, or in the best case maybe even once a year.”
Type 2 diabetes, a disease associated with the national obesity epidemic, is usually caused by a combination of excess weight and lack of exercise. It causes patients to slowly lose beta cells and the ability to produce adequate insulin. One recent study has estimated that diabetes treatment and complications cost the United States $218 billion annually, or about 10 percent of the nation’s entire health bill.
“Our idea here is relatively simple,” Melton said. “We would provide this hormone, the type 2 diabetic will make more of their own insulin-producing cells, and this will slow down, if not stop, the progression of their diabetes. I’ve never seen any treatment that causes such an enormous leap in beta cell replication.”
CHINA MARKET-Takeda and Sanofi Sign Co-promotion Agreement to Expand Reach of Diabetes Treatment Alogliptin in China

ALOGLIPTIN
22.04.2013
• Alogliptin is a DPP-4 inhibitor that is designed to slow the inactivation of incretin hormones GLP-1 and GIP
• Agreement is part of Takeda’s strategy to complement capabilities through partnerships
• Agreement complements Sanofi’s diabetes portfolio and expand its offer of innovative diabetes treatment to Chinese patients
• The regulatory approval of alogliptin in China is expected in 2013
Shanghai, China, April 22, 2013 – Takeda and Sanofi today announced that they have entered into an agreement for the co-promotion of alogliptin in China for the treatment of type 2 diabetes. Alogliptin is Takeda’s new type 2 diabetes therapy, which has been filed for marketing authorization in China. It is a dipeptidyl peptidase-4 inhibitor (DPP-4i) that is designed to slow the inactivation of incretin hormones GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic peptide).
Under the terms of the agreement, Takeda will grant Sanofi the exclusive right to co-promote alogliptin in China. Sanofi will utilize its commercial capabilities and experience to promote the product in defined territories in China. The commercial terms of the agreement were not disclosed.
“Diabetes has become a major public health problem in China with a rapid increase in the prevalence over recent years. China is now the country with the largest number of people with diabetes,” said Haruhiko Hirate, Corporate Officer and Head of North Asia of Takeda. “The collaboration will expand our reach to Chinese physicians treating patients with type 2 diabetes. Both Takeda and Sanofi have a long history and significant experience in diabetes and this makes for a win-win partnership, as we work together to advance patient care and help to meet the needs of this growing patient population.”
“We are pleased to announce the collaboration with Takeda,” said Fabrice Baschiera, General Manager, Pharmaceutical Operations, Sanofi China. “Alogliptin reinforces the strategic focus of Sanofi in the diabetes field. The new addition of alogliptin strengthens our offer of innovative diabetes treatment to Chinese patients, which includes best-in-class oral and insulin drugs. We look forward to working with Takeda to make alogliptin more widely available to patients with type 2 diabetes in China,” added Mr. Baschiera.
Alogliptin was approved and marketed in Japan in 2010 under the brand name of Nesina®, where it is currently the best-selling DPP-4i for type 2 diabetes. It was approved by the U.S. FDA as a monotherapy and also in fixed-dose combination with pioglitazone (Oseni®) and metformin (Kazano®) in January 2013 for the treatment of type 2 diabetes in adults as adjuncts to diet and exercise.
In China, the rapid economic development has brought mass urbanization, changing diets and increasingly sedentary lifestyles. These factors greatly increase the risk of developing type 2 diabetes. China has the largest number of people with diabetes1, with approximately 92.4 million adults suffering from the disease, 60.7% of which are undiagnosed2. Over the next 20 years, an additional 40 million Chinese adults are expected to develop type 2 diabetes, surpassing the overall prevalence rate of the United States3.
Alogliptin is under registration review in China. Takeda is expecting to obtain the regulatory approval in 2013.
Notes
1 International Diabetes Federation. New diabetes figures in China: IDF press statement
2 Diabetes: Wenying Yang et al, N ENGL J MED, March 25, 2010;
3 Kantar Health. The Burden of the Complicated Type 2 Diabetes Patient in China.
About Alogliptin
Alogliptin is a DPP-4i for the treatment of type 2 diabetes as an adjunct to diet and exercise. DPP-4 is designed to slow the inactivation of incretin hormones GLP-1 and GIP. As a result, an increased amount of active incretins enables the pancreas to secrete insulin in a glucose-dependent manner, thereby assisting in the management of blood glucose levels. A New Drug Application (NDA) for NESINA (alogliptin) was approved in April 2010 by the Japanese Ministry of Health, Labour and Welfare for the treatment of type 2 diabetes, and the therapy is available under the same brand name in Japan. NESINA (alogliptin) was approved by the U.S. FDA as a monotherapy and also in fixed-dose combination with pioglitazone (OSENI) and metformin (KAZANO) in January 2013 for the treatment of type 2 diabetes in adults as adjuncts to diet and exercise.
About Type 2 Diabetes
Type 2 diabetes is the most common form of diabetes affecting millions of people globally. Type 2 diabetes is a progressive and chronic condition and patients should work with a health care professional to manage and monitor their disease. In addition to diet and exercise, patients often need to take multiple medications in order to help them manage their blood glucose levels. According to the International Diabetes Federation, the global health care expenditures for diabetes (both type 1 and 2) were estimated at $471.6 billion in 2012. By 2030, this number is projected to exceed $595 billion. China is now the country with the largest number of people with diabetes and 92.4 million adults are suffering from the disease.
About Takeda
Located in Osaka, Japan, Takeda is a research-based global company with its main focus on pharmaceuticals. As the largest pharmaceutical company in Japan and one of the global leaders of the industry, Takeda is committed to strive towards better health for patients worldwide through leading innovation in medicine. Additional information about Takeda is available through its corporate website,www.takeda.com.
About Sanofi
Sanofi, a global and diversified healthcare leader, discovers, develops and distributes therapeutic solutions focused on patients’ needs. Sanofi has core strengths in the field of healthcare with seven growth platforms: diabetes solutions, human vaccines, innovative drugs, consumer healthcare, emerging markets, animal health and the new Genzyme. Sanofi is listed in Paris (EURONEXT: SAN) and in New York (NYSE: SNY).
From a structural point has uracil (Uracil) structure, synthesis of these compounds are usually replaced with urea or urea and 1,3 – parents Electric reagent directly related ring, and substituted ureas from amines and isocyanate obtained. Compound 1 and methyl isocyanate urea derivatives obtained by reacting 2 , 2 and 1,3 – diethyl reaction 3 , 3 chlorination with phosphorus oxychloride to obtain 4 , 4 with a secondary amine 5 reaction of 6 , 6 de-Boc protected with acid reaction and generate benzoate Alogliptin benzoate.
EMA- Committee for Medicinal Products for Human Use (CHMP) adopted a positive opinion, recommending the granting of a marketing authorisation for Spedra, for the treatment of erectile dysfunction in adult men.
AVANAFIL, SPEDRA
On 25 April 2013, the Committee for Medicinal Products for Human Use (CHMP) adopted a positive opinion, recommending the granting of a marketing authorisation for the medicinal product Spedra, 50 mg, 100 mg, 200 mg, tablet intended for the treatment of erectile dysfunction in adult men.
The applicant for this medicinal product is VIVUS BV.
They may request a re-examination of any CHMP opinion, provided they notify the European Medicines Agency in writing of their intention within 15 days of receipt of the opinion. The active substance of Spedra is avanafil, a selective phosphodiesterase (PDE) type 5 inhibitor that leads to higher cyclic guanosine monophosphate (cGMP)-specific PDE5 levels. This enhances smooth muscle relaxation, which results in an inflow of blood into the penile tissues, thereby producing an erection. The benefit with Spedra is its effect on the ability of men with erectile dysfunction to achieve and maintain an erection sufficient for satisfactory sexual activity. It was observed in clinical trials that Spedra increased the percentage of sexual attempts resulting in successful intercourse by roughly 20-30% over placebo in the general population of adult men with erectile dysfunction. The most common side effects are headache, flushing, nasal and sinus congestion, dyspepsia and back pain. A pharmacovigilance plan for Spedra will be implemented as part of the marketing authorisation. The approved indication is: “Treatment of erectile dysfunction in adult men. In order for Spedra to be effective, sexual stimulation is required.” Detailed recommendations for the use of this product will be described in the summary of product characteristics (SmPC), which will be published in the European public assessment report (EPAR) and made available in all official European Union languages after the marketing authorisation has been granted by the European Commission. The CHMP, on the basis of quality, safety and efficacy data submitted, considers there to be a favourable benefit-to-risk balance for Spedra and therefore recommends the granting of the marketing authorisation.
Avanafil is a PDE5 inhibitor approved for erectile dysfunction on April 27, 2012.[1] Avanafil is known by the trademark name Stendra and was developed by Vivus Inc. It acts by inhibiting a specific phosphodiesterase type 5 enzyme which is found in various body tissues, but primarily in the corpus cavernosum penis, as well as the retina. Other similar drugs are sildenafil, tadalafil and vardenafil. The advantage of avanafil is that it has very fast onset of action compared with other PDE5 inhibitors.
Avanafil can be synthesized from a benzylamine derivative and a pyrimidine derivative:
“FDA approves Stendra for erectile dysfunction” (Press release). Food and Drug Administration (FDA). April 27, 2012.
Yamada, K.; Matsuki, K.; Omori, K.; Kikkawa, K.; 2004, U.S. Patent 6,797,709
A cutting that phenanthrene by a methylthio urea ( a ) and ethoxy methylene malonate ( 2 ) cyclization of 3 , chloride, phosphorus oxychloride get 4 , 4 with benzyl amine 5 occurred SNAr the reaction product after oxidation with mCPBA 6 . In pyrimidine, if the 2 – and 4 – positions are active simultaneously the same leaving group in the case, SNAr reaction occurs preferentially at 4 – position, but does not guarantee the 2 – side reaction does not occur. Here is an activity of the poor leaving group sulfide spans 2 – bit, and a good leaving group active chlorine occupy four – position, thus ensuring a high regioselectivity of the reaction. 4 – position after completion of the reaction, then the 2 – position of the group activation, where sulfide sulfoxide better than the leaving group. Amino alcohols 7 and 6 recurrence SNAr reaction 8 , 8 after alkaline hydrolysis and acid alpha amidation get that phenanthrene.
European Medicines Agency recommends approval of first treatment for pseudobulbar affect
26/04/2013
Dextromethorphan

Quinidine
European Medicines Agency recommends approval of first treatment for pseudobulbar affect
Medicine to help curb bouts of uncontrolled emotional expression in patients with certain neurological disorders
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended the granting of a marketing authorisation for Nuedexta, a medicine for the treatment of pseudobulbar affect in adults.
Pseudobulbar affect is a medical condition in which patients experience sudden and uncontrollable bouts of laughing or crying unrelated or disproportionate to their emotional state. It occurs when certain neurological disorders, such as multiple sclerosis (MS) and amyotrophic lateral sclerosis (ALS) or a stroke, damage areas of the brain that are involved in the control of normal expression of emotion. This damage can disrupt brain signalling, resulting in the alteration or loss of control of emotional expression.
Although pseudobulbar affect is a non-life-threatening condition, it can have a significant impact on an individual’s ability to interact normally in society and on their relationships with others. There is currently no treatment approved for pseudobulbar affect in the European Union.
Nuedexta is a combination of two known active substances, dextromethorphan hydrobromide and quinidine sulphate. In studies, treatment with these medicines significantly decreased episodes of involuntary, uncontrollable laughing or crying.
Pseudobulbar affect is observed in a number of neurological conditions. Nuedexta has currently only been studied in patients with MS and ALS. Nuedexta is not suitable for treating episodes of laughing or crying brought on by mood swings and not due to pseudobulbar affect.
The CHMP’s opinion on Nuedexta will now be sent to the European Commission for the adoption of a marketing authorisation.
Note
- The marketing authorisation holder for Nuedexta is Jenson Pharmaceutical Services Ltd.
Dextromethorphan/quinidine (trade name Nuedexta) is a combination drug containing the active ingredients dextromethorphan and quinidine. It was the first FDA-approved drug for the treatment of pseudobulbar affect (PBA).
In a 12 week randomized, double-blind trial, amyotrophic lateral sclerosis and multiple sclerosis patients with significant PBA were given either Nudexta 30/10 mg or placebo. In 326 randomized patients, the PBA-episode daily rate was 46.9% (p < 0.0001) lower for Nudexta than for placebo.
Nuedexta was approved in February 2011 and is marketed in the United States by Avanir Pharmaceuticals.

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....