Home » Articles posted by DR ANTHONY MELVIN CRASTO Ph.D (Page 265)
Author Archives: DR ANTHONY MELVIN CRASTO Ph.D
Scientists reveal molecular ‘yin-yang’ of blood vessel growth
Biologists at The Scripps Research Institute (TSRI) have discovered a crucial process that regulates the development of blood vessels. The finding could lead to new treatments for disorders involving abnormal blood vessel growth, including common disorders such as diabetic retinopathy and cancer.
“Essentially we’ve shown how the protein SerRS acts as a brake on new blood vessel growth and pairs with the growth-promoting transcription factor c-Myc to bring about proper vascular development,” said TSRI Professor Xiang-Lei Yang. “They act as the yin and yang of transcriptional regulation.”
Yang and her colleagues reported the new findings this week in the biology journaleLife.
Multitasking Enzymes
SerRS (seryl tRNA synthetase) belongs to a family of enzymes that have fundamental, evolutionarily ancient roles in the protein-making machinery of cells. But as Yang’s and other laboratories have been finding in recent years, some of these protein-maker enzymes seem to have evolved extra functions.
View original post 582 more words
BMS-791325, Beclabuvir In Phase 2 for Hepatitis C (HCV)
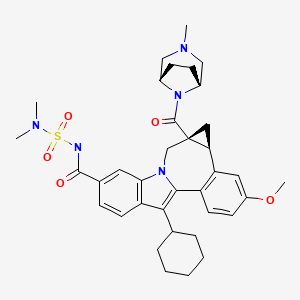
BMS-791325, Beclabuvir
IN PHASE 2 for Hepatitis C (HCV)
An NS5B inhibitor.

BMS-791325 preferably is

958002-33-0
958002-36-3 (as hydrochloride)
C36 H45 N5 O5 S, 659.838
Cycloprop(d)indolo(2,1-a)(2)benzazepine-9-carboxamide, 12-cyclohexyl-N-((dimethylamino)sulfonyl)-4b,5,5a,6-tetrahydro-3-methoxy-5a-((3-methyl-3,8-diazabicyclo(3.2.1)oct-8-yl)carbonyl)-, (4bS,5aR)-
(4bS,5aR)-12-Cyclohexyl-N-(dimethylsulfamoyl)-3-methoxy-5a-((3-methyl-3,8-diazabicyclo(3.2.1)oct-8-yl)carbonyl)-4b,5,5a,6-tetrahydrocyclopropa(d)indolo(2,1-a)(2)benzazepine-9-carboxamide
(4bS,5aR)-12-Cyclohexyl-N-(dimethylsulfamoyl)-3-methoxy-5a-((3-methyl-3,8-diazabicyclo(3.2.1)oct-8-yl)carbonyl)-4b,5,5a,6-tetrahydrocyclopropa(d)indolo(2,1-a)(2)benzazepine-9-carboxamide
(1aR,12bS)-8-Cyclohexyl-N-(dimethylsulfamoyl)-11-methoxy-1a-[(3-methyl-3,8-diazabicyclo[3.2.1]oct-8-yl)carbonyl]-1,1a,2,12b-tetrahydrocyclopropa[d]indolo[2,1-a][2]benzazepine-5-carboxamide
Cycloprop [d] indolo [2, 1 -a] [2]benzazepine-5-carboxamide, 8-cyclohexyl-N- [(dimethylamino)sulfonyl]-l,la,2,12b-tetrahydro-ll-methoxy-la-[(3-methyl-3,8- diazabicyclo[3.2.1]oct-8-yl)carbonyl]-, (laR,12bS)-
Bristol-Myers Squibb (Originator)
RNA-Directed RNA Polymerase (NS5B) Inhibitors
UNII-MYW1X5CO9S
BMS-791325 is in phase II clinical studies at Bristol-Myers Squibb for the treatment of chronic hepatitis C. In 2013, the company received breakthrough therapy designation in the U.S. for the treatment of chronic hepatitis C in combination with daclatasvir and asunaprevir.
| Patent | WO 2007136982 |
Want to know everything on vir series
click
http://drugsynthesisint.blogspot.in/p/vir-series-hep-c-virus-22.html
AND
http://medcheminternational.blogspot.in/p/vir-series-hep-c-virus.html
http://www.google.com/patents/WO2007136982A1?cl=en
Scheme 1.
N-protected piperazines can also be coupled to the intermediate indolobenzazepine acids and the resultant piperazine carboxamides can be deprotected using methods known in the art and derivatized using a variety of synthetic protocols, some illustrative examples of which are shown below (See Scheme 2).
Scheme 2.
An intermediate useful for the synthesis of some compounds of the invention involves the preparation of the tert-butyl ester indolobenzazepine shown in Scheme 3. Scheme 3.
t-Butylation either:
This methodology involves base catalyzed hydrolysis of the indole methyl ester shown, followed by its reaction with either thionyl chloride and potassium tertiary butoxide, or alkylation with silver carbonate and tertiary butyl bromides. The resultant compound can be transformed using chemistry analogous to that outlined previously to provide the mixed ester indolobenzazepines shown above.
Scheme 4.
Some examples exist as stereoisomeric mixtures. The invention encompasses all stereoisomers of the compounds. Methods of fractionating stereoisomeric mixtures are well known in the art, and include but are not limited to; preparative chiral supercritical fluid chromatography (SFC) and chiral high performance liquid chromatography (HPLC). An example using this approach is shown in scheme 5. Scheme 5.
An additional method to achieve such separations involves the preparation of mixtures of diastereomers which can be separated using a variety of methods known in the art. One example of this approach is shown below (Scheme 6).
Scheme 6.
Diastereomers separated by reverse phase HPLC
Some diastereomeric amides can be separated using reverse phase HPLC. After hydroysis, the resultant optically active acids can be coupled with bridged piperazine derivatives (Scheme 6). For example, O-(lH-benzotriazol-l-yl)-N,N, N’,N’-tetramethyluronium tetrafluoroborate and diisopropyl ethyl amine in DMSO can be used to give the alkyl bridged piperazine carboxamides. Other standard acid amine coupling methods can also be used to give optically active carboxamides.
Schemes 7-9 illustrate other methods of making intermediates and compounds.
Scheme 8.
Scheme 9.
Biological Methods
The compounds demonstrated activity against HCV NS5B as determined in the following HCV RdRp assays.
DESCRIPTION OF SPECIFIC EMBODIMENTS
Unless otherwise specified, analytical LCMS data on the following intermediates and examples were acquired using the following columns and conditions. Stop time: Gradient time + 1 minute; Starting cone: 0% B unless otherwise noted; Eluent A: 5% CH3CN / 95% H2O with 10 mM NH4OAc (for columns A, D and E); 10 % MeOH / 90 % H2O with 0.1% TFA (for columns B and C); Eluent B: 95% CH3CN / 5% H2O with 10 mM NH4OAc (for columns A, D and E); 90 % MeOH / 10 % H2O with 0.1% TFA (for columns B and C); Column A:
Phenomenex lOμ 4.6 x 50 mm C18; Column B: Phenomenex C18 lOμ 3.0 x 50 mm; Column C: Phenomenex 4.6 x 50 mm C18 lOμ; Column D: Phenomenex Lina C18 5μ 3.0 x 50 mm; Column E: Phenomenex 5μ 4.6 x 50 mm Cl 8.
Intermediate 1
lH-Indole-6-carboxylic acid, 2-bromo-3-cyclohexyl-, methyl ester. Freshly recrystallized pyridinium tribromide (recrystallization from hot AcOH (5 mL per 1 g), rinsed with cold AcOH and dried under high vacuum over KOH) was added in portions (over 10 min.) to a stirring solution of methyl 3-cyclohexyl-lH-indole-6- carboxylate (60 g, 233 mmol) (prepared using procedures describe in WO2004/065367) in CHC1/THF (1: 1, 1.25 L) at 2o C. The reaction solution was stirred at 0-5 °C for 2.5h, and washed with sat. aq. NaHSO3 (1 L), 1 N HCl (1 L) and brine (1 L). The organic layer was dried (MgSO4) and concentrated. The resulting red oil was diluted with Et2θ and concentrated. The resulting pink solid was dissolved into Et2θ (200 mL) treated with hexanes (300 mL) and partially concentrated. The solids were collected by filtration and rinsed with hexanes. The mother liquor was concentrated to dryness and the procedure repeated. The solids were combined to yield lH-indole-6-carboxylic acid, 2-bromo-3-cyclohexyl-, methyl ester (64 g, 190 mmol, 82%) as a fluffy pink solid, which was used without further purification. IHNMR (300 MHz, CDCl3) δ 8.47 (br s, IH), 8.03 (d, J = 1.4 Hz, IH), 7.74 (dd, J = 1.4, 8.8 Hz, IH), 7.69 (d, J = 8.8 Hz, IH), 3.92 (s, 3H), 2.82 (tt, J = 3.7, 11.7 Hz, IH), 1.98 – 1.72 (m, 7H), 1.50 – 1.27 (m, 3H). 13CNMR (75 MHz, CDC13) δ 168.2, 135.6, 130.2, 123.1, 120.8, 120.3, 118.7, 112.8, 110.7, 52.1, 37.0, 32.2(2), 27.0(2), 26.1. LCMS: m/e 334 (M-H)“, ret time 3.34 min, column A, 4 minute gradient.
Intermediate 2
lH-Indole-6-carboxylic acid, 2-bromo-3-cyclohexyl-. A solution of methyl 2- bromo-S-cyclohexyl-lH-indole-ό-carboxylate (20 g, 60 mmol) and LiOH (3.8 g, 160 mmol) in MeOΗ/TΗF/Η2O ( 1 : 1 : 1 , 300 mL) was heated at 90 °C for 2h. The reaction mixture was cooled in an ice/H2O bath, neutralized with IM HCl (-160 mL) diluted with H2O (250 mL) and stirred for Ih at rt. The precipitates were collected by filtration rinse with H2O and dried to yield lH-indole-6-carboxylic acid, 2-bromo-3- cyclohexyl- (quant.) which was used without further purification.
An alternative procedure that can by used to provide lH-indole-6-carboxylic acid, 2-bromo-3-cyclohexyl- is described below: A solution of methyl 2-bromo-3-cyclohexyl-lH-indole-6-carboxylate (117 g, 349 mmol) and LiOKH2O (26.4 g, 629 mmol) in MeOH/THF/H2O (1: 1: 1, 1.8 L) was heated at reflux for 3h. The reaction mixture was cooled in an ice/H2O bath to ~2 °C, neutralized with IM HCl (-650 mL) (added at such a rate that temperature did not exceed 5 °C), diluted with H2O (1 L) and stirred while warming to ambient temperature. The precipitates were collected by filtration rinsed with H2O and dried to yield the mono THF solvate of lH-indole-6-carboxylic acid, 2-bromo-3- cyclohexyl- (135.5 g, 345 mmol, 99%) as a yellow solid, which was used without further purification. IHNMR (300 MHz, CDCl3) δ 11.01 (br s, IH), 8.77 (s, IH), 8.07 (d, J = 1.5 Hz, IH), 7.82 (dd, J = 1.5, 8.8 Hz, IH), 7.72 (d, J = 8.8 Hz, IH), 3.84 – 3.74 (m, 4H), 2.89 (m, IH), 1.98 – 1.72 (m, HH), 1.50 – 1.24 (m, 3H). 13CNMR (75 MHz, CDC13) δ 172.7, 135.5, 130.7, 122.3, 120.9(2), 118.8, 113.3, 111.1, 67.9(2), 37.0, 32.2(2), 27.0(2), 26.1, 25.5(2). LCMS: m/e 320 (M-H)“, ret time 2.21 min, column A, 4 minute gradient.
Intermediate 3
lH-Indole-6-carboxamide, 2-bromo-3-cyclohexyl-N-
[(dimethylamino)sulfonyl]-. l,l’-Carbonyldiimidazole (1.17 g, 7.2 mmol) was added to a stirred solution of 2-bromo-3-cyclohexyl-lH-indole-6-carboxylic acid (2.03 g, 6.3 mmol) in THF (6 mL) at 22 °C. The evolution of CO2 was instantaneous and when it slowed the solution was heated at 50°C for 1 hr and then cooled to 220C. N,N-Dimethylsulfamide (0.94 g, 7.56 mmol) was added followed by the dropwise addition of a solution of DBU (1.34 g ,8.8 mmol) in THF (4 mL). Stirring was continued for 24 hr. The mixture was partitioned between ethyl acetate and dilute HCl. The ethyl acetate layer was washed with water followed by brine and dried over Na2SO4. The extract was concentrated to dryness to leave the title product as a pale yellow friable foam, (2.0 g, 74 %, >90 % purity , estimated from NMR). 1H NMR (300 MHz, DMSO-D6) δ ppm 1.28 – 1.49 (m, 3 H) 1.59 – 2.04 (m, 7 H) 2.74 – 2.82 (m, 1 H) 2.88 (s, 6 H) 7.57 (dd, J=8.42, 1.46 Hz, 1 H) 7.74 (d, J=8.78 Hz, 1 H) 7.91 (s, 1 H) 11.71 (s, 1 H) 12.08 (s, 1 H).
An alternative method for the preparation of lH-indole-6-carboxamide, 2- bromo-3-cyclohexyl-N-[(dimethylamino)sulfonyl]- is described below.
To a 1 L four necked round bottom flask equipped with a mechanical stirrer, a temperature controller, a N2 inlet , and a condenser, under N2, was added 2-bromo-3- cyclohexyl-lH-indole-6-carboxylic acid (102.0 g, 0.259 mol) and dry TΗF (300 mL). After stirring for 10 min, CDI (50.3 g, 0.31 mol) was added portion wise. The reaction mixture was then heated to 50 oC for 2 h. After cooling to 30 oC, N,N- dimethylaminosulfonamide (41.7 g, 0.336 mol) was added in one portion followed by addition of DBU (54.1 mL, 0.362 mol) drop wise over a period of 1 h. The reaction mixture was then stirred at rt for 20 h. The solvent was removed in vacuo and the residue was partitioned between EtOAc and 1 Ν HCl (1 : 1, 2 L). The organic layer was separated and the aqueous layer was extracted with EtOAc (500 mL). The combined organic layers were washed with brine (1.5 L) and dried over MgSO4. The solution was filtered and concentrated in vacuo to give the crude product (111.0 g). The crude product was suspended in EtOAc (400 mL) at 60 oC. To the suspension was added heptane (2 L) slowly. The resulting suspension was stirred and cooled to 0 oC. It was then filtered. The filter cake was rinsed with small amount of heptane and house vacuum air dried for 2 days. The product was collected as a white solid (92.0 g, 83%). 1H ΝMR (MeOD, 300 MHz) δ 7.89 (s, H), 7.77 (d, J= 8.4 Hz, IH), 7.55 (dd, J= 8.4 and 1.8 Hz, IH), 3.01 (s, 6H), 2.73-2.95 (m, IH), 1.81-2.05 (m, 8H), 1.39-1.50 (m, 2H); m/z 429 (M +H)+. Intermediate 4
lH-Indole-6-carboxamide, 3-cyclohexyl-N-[(dimethylamino)sulfonyl]-2-(2- formyl-4-methoxyphenyl)-. A mixture of the 2-Bromo-3-cyclohexyl- N- [(dimethylamino)sulfonyl]-lH-indole-6-carboxamide (4.28g, 0.01 mol), 4-methoxy- 2-formylphenyl boronic acid (2.1%, 0.015 mol), 2-dicyclohexylphosphino-2′,6′- dimethoxy-biphenyl (41 mg, 0.0001 mol), palladium acetate (11.2 mg), and finely ground potassium carbonate (4.24g, 0.02 mol) in toluene (30 mL) was stirred under reflux and under nitrogen for 30 min, at which time LC/MS analysis showed the reaction to be complete. The reaction mixture was then diluted with ethyl acetate and water, and then acidified with an excess of dilute HCl. The ethyl acetate layer was then collected and washed with dilute HCl, water and brine. The organic solution was then dried (magnesium sulfate), filtered and concentrated to give a gum. The gum was diluted with hexanes (250 ml) and ethyl acetate (25 mL), and the mixture was stirred for 20 hr at 22° C during which time the product was transformed into a bright yellow granular solid (4.8 g) which was used directly without further purification.
An alternative procedure for the preparation of lH-indole-6-carboxamide, 3- cyclohexyl-N-[(dimethylamino)sulfonyl]-2-(2-formyl-4-methoxyphenyl)- is provided below:
To a slurried solution of 2-bromo-3-cyclohexyl-N-[(dimethylamino)sulfonyl]- indole-6-carboxamide (54.0 g, 126 mmol), 4-methoxy-2-formylphenylboronic acid (29.5 g, 164 mmol) and LiCl (13.3 g, 315 mmol) in EtOH/toluene (1 : 1, 1 L) was added a solution of Na2CO3 (40.1 g, 379 mmol) in water (380 mL). The reaction mixture was stirred 10 min. and then Pd(PPh3)4 (11.3 g, 10.0 mmol) was added. The reaction solution was flushed with nitrogen and heated at 70 °C (internal monitoring) overnight and then cooled to rt. The reaction was diluted with EtOAc (1 L) and EtOH (100 mL), washed carefully with IN aqueous HCl (1 L) and brine (500 mL), dried (MgSO4), filtered and concentrated. The residual solids were stirred with Et20 (600 mL) for Ih and collected by filtration to yield lH-indole-6-carboxamide, 3- cyclohexyl-N-[(dimethylamino)sulfonyl]-2-(2-formyl-4-methoxyphenyl)- (52.8g, 109 mmol, 87%) as a yellow powder which was used without further purification. IHNMR (300 MHz, d6-DMSO) δ 11.66 (s, IH), 8.17 (s, IH), 7.75 (d, J = 8.4 Hz, IH), 7.74 (d, J = 8.4 Hz, IH), 7.59 (dd, J = 1.4, 8.4 Hz, IH), 7.23 – 7.16 (m, 2H), 7.08 (dd, J = 2.6, 8.4 Hz, IH), 6.54 (d, J = 8.8 Hz, IH), 3.86 (s, 3H), 3.22 – 3.08 (m, IH), 2.91 (s, 6H), 2.00 – 1.74 (m, 7H), 1.60 – 1.38 (m, 3H). 13CNMR (75 MHz, CDC13) δ 165.7, 158.8, 147.2, 139.1, 134.3, 132.0, 123.4, 122.0, 119.2, 118.2, 114.8, 112.3, 110.4, 109.8, 79.6, 45.9, 37.2(2), 34.7, 32.0(2), 25.9(2), 24.9. LCMS: m/e 482 (M- H)“, ret time 2.56 min, column A, 4 minute gradient.
Intermediate 5
6H-Isoindolo[2,l-a]indole-3-carboxamide, 11-cyclohexyl-N-
[(dimethylamino)sulfonyl]-6-ethoxy-8-methoxy-. To a 5 L four necked round bottom flask equipped with a temperature controller, a condenser, a N2 inlet and a mechanical stirrer, was charged toluene (900 mL), EtOH (900 mL), 2-bromo-3- cyclohexyl-N^NjN-dimethylsulfamoyiyiH-indole-ό-carboxamide (90 g, 0.21 mol), 2-formyl-4-methoxyphenylboronic acid (49.2 g, 0.273 mol) and LiCl (22.1 g, 0.525 mol). The resulting solution was bubbled with Ν2 for 15 mins. A solution of Na2CO3 (66.8 g, 0.63 mol) in Η2O (675 mL) was added and the reaction mixture was bubbled with N2 for another (10 mins). Pd(PPh3)4 (7.0 g, 6.3 mmol) was added and the reaction mixture was heated to 70 °C for 20 h. After cooling to 35 °C, a solution of 1 N HCl (1.5 L) was added slowly. The resulting mixture was transferred to a 6 L separatory funnel and extracted with EtOAc (2 X 1.5 L). The combined organic extracts were washed with brine (2 L), dried over MgSO4, filtered and concentrated in vacuo to give a yellow solid, which was triturated with 20% EtOAc in hexane (450 mL, 50 °C to 0 °C) to give 3-cyclohexyl-N-(N,N-dimethylsulfamoyl)-2-(2-formyl-4- methoxyphenyl)-lH-indole-6-carboxamide(65.9 g) as a yellow solid. HPLC purity, 98%.
The mother liquid from the trituration was concentrated in vacuo. The residue was refluxed with EtOH (50 mL) for 3 h. The solution was then cooled to 0 °C. The precipitates were filtered and washed with cooled TBME (5 °C) (20 mL). The filter cake was house vacuum air dried to give a further quantity of the title compound as a white solid (16.0 g). HPLC purity, 99%. 1H NMR (CDC13, 300 MHz) δ 8.75 (s, IH), 7.96 (s, IH), 7.73 (d, J= 8.4 Hz, IH), 7.67 (d, J= 8.4 Hz, IH), 7.45 (dd, J= 8.4 and 1.4 Hz, IH), 7.09 (d, J= 2.2 Hz, IH), 6.98 (dd, J= 8.4 and 2.2 Hz, IH), 6.50 (s, IH), 3.86 (s, 3H), 3.05 (s, 6H), 2.92-3.13 (m, 3H), 1.85-1.93 (m, 7 H), 1.40-1.42 (m, 3H), 1.05 (t, J= 7.1 Hz, 3H). m/z 512 (M + H)+.
Intermediate 6
lH-indole-6-carboxamide, 3-cyclohexyl-N-[(dimethylamino)sulfonyl]-2-(2- formyl-4-methoxyphenyl)-. 1 l-cyclohexyl-N-(N,N-dimethylsulfamoyl)-6-ethoxy-8- methoxy-6H-isoindolo[2,l-a]indole-3-carboxamide was dissolved in THF (75 mL). To the solution was added a solution of 2 N HCl (300 mL). The mixture was vigorously stirred under N2 at rt for 16 h. The resulting suspension was filtered and washed with cooled TBME (2 X 30 mL). the filer cake was vacuum air dried overnight to give the title compound as a yellow solid. HPLC purity, 99% 1H NMR (DMSO-d6, 300 MHz) δ 11.65 (s, IH), 8.16 (s, IH), 7.76 (d, J= 5.9 Hz, IH), 7.73 (d, J= 5.9 Hz, IH), 7.58 (dd, J= 8.5 and 1.5 Hz, IH), 7.17-7.20 (m, 2H), 7.08 (dd, J = 8.5 and 1.4 Hz, IH), 6.55 (d, J= 8.6 Hz, IH), 3.86 (s, 3H), 3.14-3.18 (m, IH), 2.91 (s, 6H), 1.75-1.99 (m, 7H), 1.48-1.60 (m, 3H); m/z 484 (M + H)+.
Intermediate 7
7H-Indolo[2, 1-a] ‘ [2] benzazepine-6-carboxylic acid, 13-cyclohexyl-10- [[[(dimethylamino)sulfonyl] amino] carbonyl]-3-methoxy-, methyl ester. A mixture of the 3-cyclohexyl-N-(N,N-dimethylsulfamoyl)-2-(2-formyl-4-methoxyphenyl)-lH- indole-6-carboxamide (4.8g, 0.01 mol), methyl 2-(dimethoxyphosphoryl)acrylate (9.7 g, 0.02 mol) and cesium carbonate (7.1g, 0.02 mol) in DMF (28mL) was stirred for 20 hr at an oil bath temperature of 55 ° C. The mixture was poured into ice-water and acidified with dilute HCl to precipitate the crude product. The solid was collected, dried and flash chromatographed on Siθ2 (11Og) using an ethyl acetate and methylene chloride (1: 10) solution containing 2% acetic acid. Homogeneous fractions were combined and evaporated to afford the title compound as a pale yellow solid (3.9g, 71 % yield). MS: 552 (M=H+).
An alternate procedure for the preparation of 7H-indolo[2,l- a] [2]benzazepine-6-carboxylic acid, 13-cyclohexyl-10- [[[(dimethylamino)sulfonyl]amino]carbonyl]-3-methoxy-, methyl ester is provided below. A solution of l l-cyclohexyl-N-[(dimethylamino)sulfonyl]-6-hydroxy-8- methoxy-6H-isoindolo[2,l-a]indole-3-carboxamide (cyclic hemiaminal) (63.0 g, 130 mmol), methyl 2-(dimethoxyphosphoryl)acrylate (60 g, 261 mmol), cesium carbonate (106 g, 326 mmol) in DMF (400 mL) was heated at 60 °C (bath temp) for 4.5h. Additional methyl 2-(dimethoxyphosphoryl)acrylate (15 g, 65 mmol) and cesium carbonate (21.2 g, 65 mmol) were added and the reaction was heated at 60 °C overnight then and cooled to rt. The stirring reaction mixture was diluted with H2O (1 L), slowly neutralized with IN aqueous HCl (800 mL), stirred 3h, and then the precipitates were collected by filtration. The solids were triturated with Et20 (800 mL) and dried to yield methyl 7H-indolo[2,l-a][2]benzazepine-6-carboxylic acid, 13- cyclohexyl-10-[[[(dimethylamino)sulfonyl]amino]carbonyl]-3-methoxy-, methyl ester (70.2 g, 127 mmol, 98%) as a yellow solid which was used without further purification. IHNMR (300 MHz, CDC13) δ 8.67 (s, IH), 8.09 (s, IH), 7.86 (d, J = 8.4 Hz, IH), 7.80 (s, IH), 7.50 (d, J = 8.4 Hz, IH), 7.42 (d, J = 8.8 Hz, IH), 7.08 (dd, J = 2.6, 8.8 Hz, IH), 6.98 (d, J = 2.6 Hz, IH), 5.75 – 5.51 (m, IH), 4.29 – 4.01 (m, IH), 3.89 (s, 3H), 3.82 (s, 3H), 3.05 (s, 6H), 2.87 – 2.73 (m, IH), 2.11 – 1.12 (m, 10H). LCMS: m/e 550 (M-H)-, ret time 3.21 min, column A, 4 minute gradient.
Example 1
Cycloprop[d]indolo[2,l-a] [2]benzazepine-5-carboxamide, 8-cyclohexyl-N- [(dimethylamino)sulfonyl]-l,la,2,12b-tetrahydro-ll-methoxy-la-[(3-methyl-3,8- diazabicyclo[3.2.1]oct-8-yl)carbonyl]-, (+/-)-. TBTU (43.7 mg, 0.136mmol) and DIPEA (0.095 mL, 0.544 mmol) were added to a solution of (+/-) cycloprop[d]indolo[2,l-a][2]benzazepine-la(2H)-carboxylic acid, 8-cyclohexyl-5- [[[(dimethylamino)sulfonyl]amino]carbonyl]-l,12b-dihydro-l 1-methoxy- (50 mg, 0.0906 mmol) in DMSO (2.0 mL). The reaction mixture was stirred at rt for 15 min. 3-Methyl-3,8-diaza-bicyclo[3.2. l]octane dihydrochloride {J & W PharmLab, LLC Morrisville, PA 19067-3620}. (27.1 mg, 0. 136 mmol) was then added and the reaction mixture was stirred at rt for 3 hr. It was then concentrated and the residue was purified by preparative reverse phase HPLC to give the final product as a yellow solid, (32 mg, 46% yield). MS m/z 660(MH+), Retention time: 2.445 min IH NMR (300 MHz, MeOD) δ ppm 0.20 (m, 0.23 H) 1.11 – 2.25 (m, 15.77 H) 2.58 (m, 0.23 H) 2.69 (m, 0.77 H) 2.75 – 3.11 (m, 10 H) 3.28 – 3.75 (m, 5 H) 3.91 (s, 2.31 H) 3.92 (s, 0.69 H) 4.15 – 4.37 (m, 1 H) 4.68 (m ,br, 1 H) 4.94 – 5.00 (m, 0.23 H) 5.16 (d, J=15.00 Hz, 0.77 H) 7.00 – 7.09 (m, 1 H) 7.18 (d, J=2.56 Hz, 0.23 H) 7.21 (d, J=2.56 Hz, 0.77 H) 7.33 (d, J=8.41 Hz, 0.77 H) 7.35 (d, J=8.42 Hz, 0.23 H) 7.57 (dd, J=8.42, 1.46 Hz, 0.77 H) 7.62 (dd, J=8.78, 1.46 Hz, 0.23 H) 7.91 (d, J=8.42 Hz, 0.77 H) 7.93 (d, J=8.42 Hz, 0.23 H) 8.00 (s, 0.77 H) 8.07 (s, 0.23 H).
Example 4
Cycloprop[d]indolo[2,l-a] [2]benzazepine-5-carboxamide, 8-cyclohexyl-N- [(dimethylamino)sulfonylj ‘- 1 , Ia, 2, 12b-tetrahydro-ll-methoxy-la-[(8-methyl-3, 8- diazabicyclo[3.2.1]oct-3-yl)carbonyl]-, (+/-)-. To a solution of (+/-) cycloprop[d]indolo[2,l-a][2]benzazepine-5-carboxamide, 8-cyclohexyl-la-(3,8- diazabicyclo[3.2.1]oct-3-ylcarbonyl)-N-[(dimethylamino)sulfonyl]-l,la,2,12b- tetrahydro-11-methoxy- (54 mg, 0.071 mmol) in methanol (3 mL), paraformaldehyde (6.4 mg, 0.213 mmol), ZnCl2 (29 mg, 0.213 mmol) and
Na(CN)BH3 (13.4 mg, 0.213 mmol) were added. The resultant mixture was heated at 60°C for 2hr, and then cooled to rt. The solid present was removed by filtration, and the filtrate was concentrated under vacuum and the residue purified by preparative reverse phase HPLC to give the title compound as a light yellow colored solid, (37 mg, 67% yield). MS ml 660(MH+), Retention time: 2.495 min. IH NMR (500 MHz, MeOD) δ ppm 0.21 (m, 0.3 H) 1.13 (m, 0.3 H) 1.18 – 2.22 (m, 15.4 H) 2.58 (m, 0.3 H) 2.68 (m, 0.7 H) 2.76 – 3.11 (m, 11 H) 3.32 – 3.37 (m, 1 H) 3.63 (d, J=15.56 Hz, 0.7 H) 3.82 – 4.32 (m, 7.3 H) 4.88 – 4.92 (m, 0.3 H) 5.08 (d, J=15.56 Hz, 0.7 H) 7.00 – 7.08 (m, 1 H) 7.18 (d, J=2.14 Hz, 0.3 H) 7.21 (d, J=2.14 Hz, 0.7 H) 7.32 (d, J=8.55 Hz, 0.7 H) 7.35 (d, J=8.55 Hz, 0.3H) 7.57 (d, J=7.93 Hz, 0.7 H) 7.62 (dd, J=8.39, 1.37 Hz, 0.3 H) 7.91 (d, J=8.55 Hz, 0.7 H) 7.93 – 7.99 (m, 1 H) 8.09 (s, 0.3 H).
Example 6
Cycloprop [d] indolo [2, 1 -a] [2]benzazepine-5-carboxamide, 8-cyclohexyl-N- [(dimethylamino)sulfonyl]-l,la,2,12b-tetrahydro-ll-methoxy-la-[(3-methyl-3,8- diazabicyclo[3.2.1]oct-8-yl)carbonyl]-, (laR,12bS)-. To a solution of (-) cycloprop[d]indolo[2,l-a][2]benzazepine-la(2H)-carboxylic acid, 8-cyclohexyl-5- [[[(dimethylamino)sulfonyl]amino]carbonyl]-l,12b-dihydro-l 1-methoxy- (204 mg, 0.37 mmol) in DMSO (8.0 mL), TBTU (178 mg, 0.555 mmol) and DIPEA (0.39 mL, 2.22 mmol) were added. The reaction mixture was stirred at rt for 15 min. Then 3- methyl-3,8-diaza-bicyclo[3.2.1]octane dihydrochloride (111 mg, 0. 555 mmol) was added and the reaction mixture was stirred at rt for 2 hr. It was then concentrated and the residue was purified by preparative reverse phase HPLC to give a yellow solid as final TFA salt. (265 mg, 92% yield). Average Specific Rotation: -53.56° Solvent, MeOH.; Wavelength 589 nm; 50 cm cell. MS m/z 660(MH+), Retention time: 3.035 min. 1H NMR (300 MHz, MeOD) δ ppm 0.20 (m, 0.23 H) 1.11 – 2.25 (m, 15.77 H) 2.58 (m, 0.23 H) 2.69 (m, 0.77 H) 2.75 – 3.11 (m, 10 H) 3.28 – 3.75 (m, 5 H) 3.91 (s, 2.31 H) 3.92 (s, 0.69 H) 4.15 – 4.37 (m, 1 H) 4.68 (m ,br, 1 H) 4.94 – 5.00 (m, 0.23 H) 5.16 (d, J=15.00 Hz, 0.77 H) 7.00 – 7.09 (m, 1 H) 7.18 (d, J=2.56 Hz, 0.23 H) 7.21 (d, J=2.56 Hz, 0.77 H) 7.33 (d, J=8.41 Hz, 0.77 H) 7.35 (d, J=8.42 Hz, 0.23 H) 7.57 (dd, J=8.42, 1.46 Hz, 0.77 H) 7.62 (dd, J=8.78, 1.46 Hz, 0.23 H) 7.91 (d, J=8.42 Hz, 0.77 H) 7.93 (d, J=8.42 Hz, 0.23 H) 8.00 (s, 0.77 H) 8.07 (s, 0.23 H). An alternate procedure for the synthesis of cycloprop[d]indolo[2,l- a][2]benzazepine-5-carboxamide, 8-cyclohexyl-N-[(dimethylamino)sulfonyl]- l,la,2,12b-tetrahydro-l l-methoxy-la-[(3-methyl-3,8-diazabicyclo[3.2.1]oct-8- yl)carbonyl]-, (laR,12bS)-rel-(-)-is provided below. To a mixture of (-) cycloprop[<i]indolo[2,l-α][2]benzazepine-la(2H)-carboxylic acid, 8-cyclohexyl-5- [[[(dimethylamino)sulfonyl]amino]carbonyl]-l,12b-dihydro-l 1-methoxy- (25.2 g, 45.68 mmol) and 3-methyl-3,8-diazabicyclo-[3.2.1]octane dihydrochloride (10.0 g, 50.22 mmol) in anhydrous MeCN (300 mL) was added DIPEA (23.62 g, 182.72 mmol) under N2. After 15 min, TBTU (16.12 g, 50.22 mmol) was added. The reaction solution was stirred for 30 min under N2. The ΗPLC indicated the disappearance of starting material. The solvent in the solution was evaporated to give a foam. This was dissolved in EtOAc (2.5 L), washed with H2O (1.5 L), H2O/brine (8:2) (1.5 L), brine (1.5 L), dried over Na2SO4 and evaporated to give 28.8 g of crude product. This solid was pooled with 45.4 g of material obtained from five separated reactions to afford a total of 74.2 g of crude product. This was passed through a pad of silica gel (E. Merck 230-400 mesh, 1 kg), eluting with MeOH/CH2Cl2 (2.5:97.5). After evaporation, it gave a foam, which was treated with EtOAc and hexane to turn into a solid. After drying at 50 °C under vacuum for 7 h, the GC analysis indicated it has 1.4% each of EtOAc and hexane. After further drying at 61-64 °C, the GC analysis indicated it still has 1.0% of hexane and 1.4% of EtOAc. The product was dissolved in Et2O and slowly evaporated in vacuum three times, dried at 60 °C under vacuum for 3 h to give 68.3 g. This was washed with H2O (900 mL) and redried at 68 °C under vacuum for 7 h to give 67.1 g (77% yield) of the compound of example 6. The GC analysis indicated it has 0.97% Of Et2O. HPLC conditions column: Cadenza CD-C18 3 x 250 mm; UV: 257 and 220 nm; 25 °C; flow rate: 0.5 mL/min; gradient time: 38 min, 0 – 80% B (0 – 35 min) and 80% B (35 – 38 min); solvent A: 25 nM CH3COONH4 at pH 4.7 in water, solvent B: MeCN. HPLC purity 99.7% (Rt 26.54 min); Chiral HPLC conditions column: Regis (S5S) Whelk-Ol 250 x 4.6 mm; UV 258nm; 35 °C; flow rate 2.0 mL/min; mobile phase C02/Me0H; gradient time 20 min, 30% MeOH (0 – 1 min), 30 – 48% MeOH (1 – 19 min), 48% MeOH (19 – 20 min). Chiral HPLC purity > 99.8% (Rt 16.60 min); LC/MS (ES+) 660.36 (M+H, 100); HRMS: calcd. 660.3220, found 660.3197; [α]D 25 C – 79.66 ° (c 1.06, MeOH); Anal. Calcd for C36H45N5O5S-O-O H2O»0.09 Et2O: C, 64.53; H, 7.00; N, 10.35; S, 4.74; H2O, 1.51; Et2O, 0.97. Found: C, 64.50; H, 7.12; N, 10.41; S, 5.14; H2O, 1.52; Et2O, 0.97. The absolute stereochemistry of cycloprop[d]indolo[2,l- a][2]benzazepine-5-carboxamide, 8-cyclohexyl-N-[(dimethylamino)sulfonyl]- l,la,2,12b-tetrahydro-l l-methoxy-la-[(3-methyl-3,8-diazabicyclo[3.2.1]oct-8- yl)carbonyl]-, (laR,12bS)-rel-(-)- is as drawn above, and was determined from an x- ray crystal structure obtained on the (R)-camphorsulfonic acid salt.
Additionally, the following salts were prepared: hydrochloride, phosphate, acetate, sulfate, camsylate, sodium, calcium, and magnesium. The hydrochloride salt had the following characteristics. DSC: small, broad endotherm from 25°C to 75°C, and potential melt/degradation endotherm with peak at temperatures ranging between 253 °C and 258 °C; TGA: Early weight loss from 25°C to 75°C ranging between 0.003% and 1.5%, and degradation weight loss starting at approximately 200°C.
Want to know everything on vir series
click
http://drugsynthesisint.blogspot.in/p/vir-series-hep-c-virus-22.html
AND
http://medcheminternational.blogspot.in/p/vir-series-hep-c-virus.html
| WO2006020082A1 * | Jul 15, 2005 | Feb 23, 2006 | Squibb Bristol Myers Co | Inhibitors of hcv replication |
| WO2006046030A2 * | Oct 25, 2005 | May 4, 2006 | Angeletti P Ist Richerche Bio | Tetracyclic indole derivatives as antiviral agents |
| Citing Patent | Filing date | Publication date | Applicant | Title |
|---|---|---|---|---|
| WO2008111978A1 | Mar 13, 2007 | Sep 18, 2008 | Squibb Bristol Myers Co | Cyclopropyl fused indolobenzazepine hcv ns5b inhibitors |
| WO2008112473A1 * | Mar 5, 2008 | Sep 18, 2008 | Squibb Bristol Myers Co | Compounds for the treatment of hepatitis c |
| WO2008112841A1 * | Mar 13, 2008 | Sep 18, 2008 | Squibb Bristol Myers Co | Compounds for the treatment of hepatitis c |
| WO2008112848A1 * | Mar 13, 2008 | Sep 18, 2008 | Squibb Bristol Myers Co | Compounds for the treatment of hepatitis c |
| WO2008112851A1 * | Mar 13, 2008 | Sep 18, 2008 | Squibb Bristol Myers Co | Cyclopropyl fused indolobenzazepine hcv inhibitors |
| WO2008112863A1 * | Mar 13, 2008 | Sep 18, 2008 | Squibb Bristol Myers Co | Compounds for the treatment of hepatitis c |
| WO2009067108A1 * | Nov 20, 2007 | May 28, 2009 | Squibb Bristol Myers Co | Cyclopropyl fused indolobenzazepine hcv ns5b inhibitors |
| WO2009067392A1 * | Nov 17, 2008 | May 28, 2009 | Squibb Bristol Myers Co | Cyclopropyl fused indolobenzazepine derivatives for the treatment of hepatitis c |
| WO2009067481A1 * | Nov 19, 2008 | May 28, 2009 | Squibb Bristol Myers Co | Compounds for the treatment of hepatitis c |
| WO2010080874A1 | Jan 7, 2010 | Jul 15, 2010 | Scynexis, Inc. | Cyclosporine derivative for use in the treatment of hcv and hiv infection |
| WO2013059265A1 * | Oct 17, 2012 | Apr 25, 2013 | Bristol-Myers Squibb Company | A compound for the treatment of hepatitis c |
| WO2014014885A1 * | Jul 16, 2013 | Jan 23, 2014 | Bristol-Myers Squibb Company | Novel methods and intermediates for the preparation of (4bs,5ar)-12-cyclohexyl-n-(n,n-dimethylsulfamoyl)-3-methoxy-5a-((1 r,5s) -3-methyl-3,8-diazabicyclo[3.2.1]octane-8-carbonyl)-4b,5,5a,6-tetrahydrobenzo [3,4]cyclopropa[5,6]azepino[1,2-a]indole-9-carboxamide |
| CN101679442B | Mar 13, 2008 | Feb 20, 2013 | 百时美施贵宝公司 | Compounds for the treatment of hepatitis c |
| EP2518073A1 * | Nov 19, 2008 | Oct 31, 2012 | Bristol-Myers Squibb Company | Compounds for the treatment of Hepatitis C |
The First Kilogram Synthesis of Beclabuvir, an HCV NS5B Polymerase Inhibitor
The process development and kilogram-scale synthesis of beclabuvir (BMS-791325, 1) is described. The convergent synthesis features the use of asymmetric catalysis to generate a chiral cyclopropane fragment and coupling with an indole fragment via an alkylation. Subsequent palladium-catalyzed intramolecular direct arylation efficiently builds the central seven-membered ring. The target was prepared in 12 linear steps with five isolations in an overall yield of 8%.
Preparation of (4bS,5aR)-12-Cyclohexyl-N-(N,N-dimethylsulfamoyl)-3-methoxy-5a-((1R,5S)-3-methyl-3,8-diazabicyclo[3.2.1]octane-8-carbonyl)-4b,5,5a,6-tetrahydrobenzo[3,4]cyclopropa[5,6]azepino[1,2-a]indole-9-carboxamide Hydrochloride (1·HCl)
BMS-791325·HCl (1·HCl) was isolated in 89.5% yield.
1H NMR (600 MHz, 10:1 v/v CD3CN/D2O): major rotamer: 7.91 (br s, 1H), 7.90 (d, J = 8.5 Hz, 1H), 7.55 (br d, J = 8.5 Hz, 1H), 7.29 (d, J = 8.5 Hz, 1H), 7.20 (d, J = 2.5 Hz, 1H), 7.00 (dd, J = 8.5 Hz, 2.7 Hz, 1H), 5.03 (br d, J = 12.7 Hz, 1H), 4.58 (br d, J = 4.9 Hz, 2H), 3.87 (s, 3H), 3.56 (d, J = 15.5 Hz, 1H), 3.40 (br s, 3H), 3.32–3.28 (m, 4H), 2.96 (s, 6H), 2.92 (tt, J= 12.2, 3.6 Hz, 1H), 2.59 (br t, J = 7.0 Hz, 1H), 2.05–1.90 (m, 2H), 1.79–1.71 (m, 4H), 1.55 (br d, J= 12.2 Hz, 2H), 1.46–1.36 (m, 4H), 1.26 (t, J = 5.3 Hz, 2H), 1.23–1.15 (m, 2H);
minor rotamer: 8.05 (br s, 1H), 7.92 (d, J = 8.5 Hz, 1H), 7.58 (dd, J = 8.5, 1.4 Hz, 1H), 7.34 (d, J = 8.5 Hz, 1H), 7.15 (d, J = 2.6 Hz, 1H), 6.98 (d, 1H, overlap with major rotamer), 4.91 (d, J = 15.0 Hz, 1H), 4.58 (br d, J = 4.9 Hz, 2H), 4.11 (d, J = 15.0 Hz, 1H), 3.89 (s, 3H), 3.46 (br d, J = 12.5 Hz, 2H), 3.17 (br d, J = 12.5 Hz, 2H), 2.97 (s, 6H), 2.85 (br s, 3H), 2.76 (tt, J = 12.1, 3.5 Hz, 1H), 2.49 (br s, 1H), 2.05–1.90 (m, 2H), 1.79–1.71 (m, 4H), 1.46–1.36 (m, 6H), 1.23–1.15 (m, 2H), 1.10 (m, 1H), 0.03 (t, J = 6.1 Hz, 1H).
13C NMR (125 MHz, 10:1 v/v CD3CN/D2O): major rotamer: 170.1, 167.7, 161.0, 140.4, 139.3, 135.9, 133.6, 131.1, 124.9, 123.0, 121.7, 120.8, 119.0, 118.6, 114.3, 110.7, 59.2, 56.2, 53.1, 48.3, 44.5, 38.9, 37.6, 34.8, 33.77, 33.72, 27.92, 27.77, 26.82, 26.5, 23.6, 18.5;
minor rotamer: 168.3, 168.0, 161.3, 138.4, 137.5, 135.8, 134.2, 130.0, 125.4, 121.9, 120.0, 119.64, 119.58, 117.9, 113.3, 111.3, 59.6, 56.3, 53.1, 44.6, 42.2, 38.9, 38.3, 37.4, 33.8, 33.6, 28.3, 27.74, 26.79, 26.5, 24.84, 11.9.
HRMS (ESI) calcd for C36H45N5O5S (free base) [M + H]+660.3214, found m/z 660.3220.
////////BMS-791325, Beclabuvir, Phase 2, Hepatitis C, HCV,
HMPC Q&A Documents on Herbal Medicinal Products published
DRUG REGULATORY AFFAIRS INTERNATIONAL

HMPC Q&A Documents on Herbal Medicinal Products published
Current questions and answers about the framework for herbal medicinal products and traditional herbal medicinal products are addressed in a new EMA/HMPC document. The document also addresses herbal medicinal products which don’t have a European tradition. Read more in this News.
HMPC Q&A Documents on Herbal Medicinal Products published |
On 12 May 2014, the EMA’s HMPC (Committee on Herbal Medicinal Products) published the Questions & Answers document on (traditional) herbal medicinal products. The document also addresses herbal medicinal products which don’t have a European tradition. The Q&A document contains Questions & Answers about the following topics:
|
View original post 49 more words
Critical Outcome Technologies receives orphan drug designation for COTI-2

N’-(5,6,7,8-Tetrahydroquinolin-8-ylidene)-4-(2-pyridyl)piperazine-1-carbothiohydrazide
http://criticaloutcome.com/110819_COTI-2%20Fact%20Sheet.pdf
http://www.slideshare.net/trevorheisler/about-coti2
MW 366.483, C19 H22 N6 S
| PATENTS | WO 2008083491, WO 2010006438 |
Caspase 9 Activators
PKB beta/Akt2 Inhibitors
Critical Outcome Technologies,
Critical Outcome Technologies (COTI) (Originator) preclinical for ovary cancer
Critical Outcome Technologies has announced that the US Food and Drug Administration (FDA) has granted COTI-2 an Orphan Drug Designation for the treatment of ovarian cancer.
Critical Outcome Technologies president and CEO Dr Wayne Danter said that receiving the Orphan Drug Designation for COTI-2 speaks to the need for new treatment options for patients with ovarian cancer.
- COTI-2 | A Potential Breakthrough Therapy for Many Cancers June 11, 2013
- About COTI-2 Late preclinical drug candidate discovered using CHEMSAS® – the company’s proprietary, artificial intelligence-based drug discovery technology 2
- COTI-2 highlights 1 Potential breakthrough therapy for many cancers 2 Active against many cancers with mutations of the p53 gene 3 > 50% of all human cancers have a p53 mutation 3
- Why p53 is important? p53 is a tumour suppressing gene If mutated, cancers can develop & grow without control A mutation of the p53 gene is the most common mutation found in human cancer cells 4
- The future of cancer treatments COTI-2 targets and primarily destroys tumor cells Traditional chemotherapy kills growing & dividing cells, cancer or healthy COTI-2 would treat genetic mutations common in many types of cancer Most current treatments are organ specific (i.e. treatment for lung cancer, colon cancer, etc.) 5
- COTI-2 development progress Easily synthesized oral formulation with no stability issues Effective alone or in combination with approved cancer drugs In final two-species toxicity studies prior to FDA filing enabling human trials 6
http://www.google.com/patents/WO2008083491A1?cl=en
EXAMPLES
Synthesis of COTI-2 The synthesis of COTI-2, as depicted above, was conducted according to the following synthetic methodology:
DCM R T
H2N-NH2
lmidazol-1 -yl-(4-pyridin-2-yl-piperazin-1 -yl)-methanethione (or intermediate 3 above) was formed as follows. Λ/-(2-pyridyl) piperazine (MW 163.22, 0.91 ml, 6.0 mmoles, 1 eq) 2 was added to a solution of 1 ,1 ‘- thiocarbonyldiimidazole (MW 178.22, 1.069 g, 6.0 mmoles, 1 eq) 1 in 50 ml of dichloromethane at room temperature. The reaction mixture was stirred overnight at room temperature. The mixture was washed with water, dried \ over sodium sulfate, filtered and concentrated to provide imidazol-1-yl-(4- pyridin-2-yl-piperazin-1-yl)-methanethione (MW 273.36, 1.354 g, 4.95 mmol, 83% yield) 3, which was used without further purification. TLC (CH2CI2/MeOH: 95/5): Rf = 0.60, Product UV and Ninhydrin stain active. 1H-NMR (400 MHz, CDCI3), δ ppm: 3.72 (s, 4H), 4.02 (s, 4H), 6.67 (d, 1 H, J = 7 Hz), 6.72 (dd, 1 H, J = 7 and 5 Hz), 7.11 (s, 1 H), 7.24 (s, 1 H), 7.54 (t, 1 H, J = 7 Hz), 7.91 (s, 1 H), 8.20 (d, 1 H, J = 5 Hz).
Hydrazine hydrate (MW 50.06, 0.26 ml, 5.44 mmoles, 1.1 eq) was added to a solution of imidazol-1-yl-(4-pyridin-2-yl-piperazin-1-yl)- methanethione 3 (MW 210.30, 1.040 g, 4.95 mmol, 1 eq) in 30 ml of ethanol at room temperature. The reaction mixture was stirred under reflux for 2 hours. A white precipitate formed. This white solid was filtered off and rinsed with diethyl ether to yield 1-[Λ/-(2-pyridyl)-piperazine)-carbothioic acid hydrazide (MW 237.33, 0.86 g, 3.62 mmol, 73% yield) 4 as a white solid, and used without further purification. TLC (CH2CI2/MeOH: 95/5): Rf = 0.20, Product UV and Ninhydrin stain active. 1H-NMR (400 MHz, DMSO-d6), δ ppm: 3.53 (s, 4H), 3.85 (s, 4H), 6.66 (dd, 1 H, J = 8 and 5 Hz), 6.82 (d, 1 H, J = 8 Hz), 7.55 (t, 1 H, J = 8 Hz), 8.12 (d, 1 H, J = 5 Hz).
COTI-2
Finally, COTI-2 was formed as follows. 1-[Λ/-(2-pyridyl)-piperazine)- carbothioic acid hydrazide (MW 237.33, 0.475 g, 2.0 mmol, 1 eq) 4 and 6,7- dihydro-5H-quinolin-8-one (MW 147.18, 0.306 g, 2.0 mmol, 1 eq) 5 was dissolved in 15 ml of ethanol at room temperature. The mixture was then stirred under reflux for 20 hours. A yellow solid precipitated out of the solution. This solid was filtered off then rinsed with methanol and diethyl ether to yield COTI-2 (MW 366.48, 0.60 g, 1.64 mmol, 82% yield) as a yellow solid. TLC (CH2CI2/MeOH: 95/5): Rf = 0.75, Product UV and Ninhydrine stain active. HPLC analysis showed a mixture of isomers (approximately in 80/20 ratio), and >98% purity. During the HPLC Method Development, as expected, this product tends to be hydrolyzed in presence of TFA in mobile phase solution. MS (ESI+, 0.025% TFA in 50/50 MeOH/H2O): [M+H]+ = 367.1 , [M+Na]+ = 389.1 ; 1H-NMR (400 MHz, CDCI3), δ ppm (Major isomer): 2.09 (m, 2H), 2.92 (m, 4H), 3.67 (m, 4H), 4.27 (m, 4H), 6.69 (dd, 1 H, J = 8 and 5 Hz)1 7.25 (dd,
1 H, J = 8 and 5 Hz), 7.55 (d, 2H, J = 8 Hz), 8.23 (d, 1 H, J = 5 Hz), 8.63 (d, 1 H, \ J = 5 Hz), 14.76 (s, 1 H). δ ppm (Minor isomer): 2.09 (m, 2H), 3.14 (t, 4H, J = 6 Hz), 3.80 (m, 4H), 4.27 (m, 4H), 6.66 (m, 1 H), 7.31 (dd, 1 H, J = 8 and 5 Hz), 7.52 (m, 1 H), 7.70 (d, 1 H, J = 8 Hz), 8.23 (d, 1 H, J = 5 Hz), 8.53 (d, 1 H, J = 5 Hz), 15.65 (s, 1 H).
…………………………..
| WO2010006438A1 * | Jul 17, 2009 | Jan 21, 2010 | Critical Outcome Technologies Inc. | Thiosemicarbazone inhibitor compounds and cancer treatment methods |
| See also references of EP2121681A1 | ||
| 2 | * | SHRIDHAR ET AL.: ‘Synthesis & antiparasite activity of some new 1-(6/7-nitrobenzoxazin-3-yl)-4-substituted- 3-thiosemicarbazides & 4-disubstituted 3-(6-acetylbenzoxazin-3-one)thiosemicarbazo nes‘ INDIAN J. OF CHEM. vol. 26B, June 1987, pages 596 – 598, XP008109697 |
| 3 | * | WINKELMANN ET AL.: ‘Antimalarial and anticoccidial activity of 3-aryl-7-chloro-3,4-dihydriacridine-1,9-(2h ,10H)-diones‘ ARZHEIM.-FORSCH./DRUG RES. vol. 37, no. 6, 1987, pages 647 – 661, XP008109793 |
Quest for the ring – Synthesis of Vaniprevir (old)
I was trying to think of a very catchy title to get readers to visit my website and take a look at my latest posting, and I thought, gees, what if I could portray the principal investigator/author and his team as a group of adventurers. If you get a chance to use an analogy that mimics “Lord of The Rings”, you should do it, so I did. Why did I pick Lord of the Rings ? Because in Lord of The Rings, it was the quest about seeking out the one Ring, the ring that would rule all. What if the ring was, let’s say, a potential HCV candidate, a 22-membered macrocycle, a possible treatment for hepatitis C. I would say that was a mighty powerful ring, indeed.

The paper I am drawing my analogy from is “Synthesis of Vaniprevir (MK-7009): Lactamization To Prepare A 22-Membered Macrocycle”, by Z.J. Song…
View original post 314 more words
The USFDA has approved Navidea Biopharmaceuticals’ Supplemental New Drug Application (sNDA) for the expanded use of Lymphoseek (technetium Tc 99m tilmanocept) Injection
 [99mTc]-DTPA-mannosyl-dextran [99mTc]-DTPA-mannosyl-dextran |
|||
| Systematic (IUPAC) name | |||
|---|---|---|---|
| Dextran 3-[(2-aminoethyl)thio]propyl 17-carboxy-10,13,16-tris(carboxymethyl)-8-oxo-4-thia-7,10,13,16-tetraazaheptadec-1-yl 3-[[2-[[1-imino-2-(D-mannopyranosylthio)ethyl]amino]ethyl]thio]propyl ether technetium-99m complexes…………………………………………………..………………..OTHER NAME ………………Dextran 3-[(2-aminoethyl)thio]propyl 17-carboxy-10,13,16-tris(carboxymethyl)-8-oxo-4-thia-7,10,13,16-tetraazaheptadec-1-yl 3-[[2-[[1-imino-2-(D-mannopyranosylthio)ethyl]amino]ethyl]thio]propyl ether technetium-99Tc complexes (1-6)-alpha-D-pyranoglucan partially etherified by 3-[(2-aminoethyl)sulfanyl]propyl 17-carboxy-10,13,16-tris(carboxymethyl)-8-oxo-4-thia-7,10,13,16-tetraazaheptadecyl and 3-[(2-{[2-(L-mannopyranosylsulfanyl)acetimidoyl]amino}ethyl)sulfanyl]propyl [99mTc]technetium coordination compound [99mTc]-DTPA-mannosyl-dextran composed of a dextran backbone linked to multiple units of mannose and DTPA (diethylenetriamine pentaacetic acid) with an average molecular weight of 35800………………..LAUNCHED………….Launched – 2013 |
|||
| Clinical data | |||
| Trade names | Lymphoseek | ||
| AHFS/Drugs.com | entry | ||
| Pregnancy cat. | C (US) | ||
| Legal status | ℞-only (US) | ||
| Routes | Intradermal, subcutaneous | ||
| Pharmacokinetic data | |||
| Half-life | 1.75 to 3.05 hours at injection site | ||
| Identifiers | |||
| ATC code | V09IA09 | ||
| Chemical data | |||
| Formula | (C6H10O5)n(C19H28N4O9S99mTc)3–8(C13H24N2O5S2)12–20(C5H11NS)0–17 | ||
| Mol. mass 15,281–23,454 g/mol[1]……………………..CODES1600 NEO3-06 TcDTPAmanDx Tilmanocepthttp://chem.sis.nlm.nih.gov/chemidplus/rn/1262984-82-6NDA N202207 APPROVED
|
|||
PATENT US 6409990, EXPMay 12, 2020
商品名:Lymphoseek 通用名:Technetium Tc 99m tilmanocept 中文名:未知
药企:Navidea Biopharmaceuticals, Inc.
FDA approves Navidea’s Lymphoseek for expanded use in head and neck cancer patients
The US Food and Drug Administration (FDA) has approved Navidea Biopharmaceuticals’ Supplemental New Drug Application (sNDA) for the expanded use of Lymphoseek (technetium Tc 99m tilmanocept) Injection indicated for guiding sentinel lymph node (SLN) biopsy in head and neck cancer patients with squamous cell carcinoma of the oral cavity.
NCI: 99mTc-DTPA-mannosyl-dextran A radiolabeled macromolecule consisting of the chelating agent diethylenetriamine pentaacetic acid (DTPA) and mannose each attached to a dextran backbone and labeled with metastable technetiumTc-99 (Tc-99m), with mannose binding and radioisotopic activities. Upon injection, the mannose moiety of 99mTc-DTPA-mannosyl-dextran binds to mannose-binding protein (MBP). As MBPs reside on the surface of dendritic cells and macrophages, this gamma-emitting macromolecule tends to accumulate in lymphatic tissue where it may be imaged using gamma scintigraphy. This agent exhibits rapid clearance from the injection site, rapid uptake and high retention within the first draining lymph node, and low uptake by the remaining lymph nodes. MBP is a C-type lectin that binds mannose or fucose carbohydrate residues, such as those found on the surfaces of many pathiogens, and once bound activates the complement system.
The active ingredient in technetium Tc 99m tilmanocept is technetium Tc 99m tilmanocept. The active ingredient is formed when Technetium Tc 99m pertechnetate, sodium injection is added to the tilmanocept powder vial.
Technetium Tc 99m binds to the diethylenetriaminepentaacetic acid (DTPA) moieties of the tilmanocept molecule.
Chemically, technetium Tc 99m tilmanocept consists of technetium Tc 99m, dextran 3-[(2- aminoethyl)thio]propyl 17-carboxy-10,13,16- tris(carboxymethyl)-8-oxo-4-thia-7,10,13,16- tetraazaheptadec-1-yl 3-[[2-[[1-imino-2-(D- mannopyranosylthio) ethyl]amino]ethyl]thio]propyl ether complexes. Technetium Tc 99m tilmanocept has the following structural formula:

Empirical formula: [C6H10O5]n.(C19H28N4O9S99mTc)b.(C13H24N2O5S2)c.(C5H11NS)a
Calculated average molecular weight: 15,281 to 23,454 g/mol
It contains 3-8 conjugated DTPA (diethylenetriamine pentaacetic acid) molecules (b); 12-20 conjugated mannose molecules (c) with 0-17 amine side chains (a) remaining free.
The tilmanocept powder vial contains a sterile, non-pyrogenic, white to off-white powder that consists of a mixture of 250 mcg tilmanocept, 20 mg trehalose dihydrate, 0.5 mg glycine, 0.5 mg sodium ascorbate, and 0.075 mg stannous chloride dihydrate. The contents of the vial are lyophilized and are under nitrogen.
Technetium Tc 99m tilmanocept injection is supplied as a Kit. The Kit includes tilmanocept powder vials which contain the necessary non-radioactive ingredients needed to produce technetium Tc 99m tilmanocept. The Kit also contains DILUENT for technetium Tc 99m tilmanocept. The diluent contains a preservative and is specifically formulated for technetium Tc 99m tilmanocept. No other diluent should be used.
The DILUENT for technetium Tc 99m tilmanocept contains 4.5 mL sterile buffered saline consisting of 0.04% (w/v) potassium phosphate, 0.11% (w/v) sodium phosphate (heptahydrate), 0.5% (w/v) sodium chloride, and 0.4% (w/v) phenol. The pH is 6.8 – 7.2.http://www.druginformation.com/RxDrugs/T/Technetium%20Tc%2099m%20Tilmanocept%20Injection.html

Lymphoseek(TM) is a lymphatic tissue-targeting agent which was first launched in 2013 in the U.S. by Navidea Biopharmaceuticals (formerly known as Neoprobe) for lymphatic mapping with a hand-held gamma counter to assist in the localization of lymph nodes draining a primary tumor site in patients with breast cancer or melanoma. In 2014, a supplemental NDA was approved in the U.S. for its use as a sentinel lymph node tracing agent in patients with head and neck squamous cell carcinoma of the oral cavity. Although several tracing agents exist that are used in “off-label” capacities, Lymphoseek is the first tracing agent specifically labeled for lymph node detection.
In 2012, an MAA was filed in the E.U. for the detection of lymphatic tissue in patients with solid tumors, and in 2013, a supplemental MAA was filed in the E.U. for sentinel lymph node detection in patients with head and neck cancer. The products is also awaiting registration to support broader and more flexible use in imaging and lymphatic mapping procedures, including lymphoscintigraphy and other optimization capabilities.
Navidea holds an exclusive worldwide license of Lymphoseek(TM) through the University of California at San Diego (UCSD), and, in 2007, Lymphoseek(TM) was licensed to Cardinal Health by Navidea for marketing and distribution in the U.S.
Lymphoseek(TM), also known as [99mTc]DTPA-mannosyl-dextran, is a receptor-binding radiopharmaceutical designed specifically for the mapping of sentinel lymph nodes in connection with gamma detection devices in a surgical procedure known as intraoperative lymphatic mapping (ILM). It is made up of multiple DTPA and mannose units, each attached by a 5-carbon thioether spacer to a dextran backbone. The compound features subnanomolar affinity for the mannose binding protein receptor, and consequently shows low distal node accumulation. Additionally, its small molecular diameter of 7 nanometers allows for enhanced diffusion into lymphatic channels and capillaries.

1600
99mTc-tilmanocept
Tc-DTPA-mannosyl-dextran
Technetium Tc 99m Tilmanocept
Tilmanocept
UNII-8IHI69PQTC
Chemical structure of [99mTc]tilmanocept. [99mTc]Tilmanocept is composed of a dextran backbone (black) to which are attached multiple units of mannose (green) and DTPA (blue). The mannose units provide a molecular mechanism by which [99mTc]tilmanocept avidly binds to a receptor specific to reticuloendothelial cells (CD206), and the DTPA units provide a highly stable means to radiolabel tilmanocept with 99mtechnetium (red). The molecular weight of [99mTc]tilmanocept is approximately 19,000 g/mol; the molecular diameter is 7.1 nm
[(99m)Tc]Tilmanocept is a CD206 receptor-targeted radiopharmaceutical designed for sentinel lymph node (SLN) identification. Two nearly identical nonrandomized phase III trials compared [(99m)Tc]tilmanocept to vital blue dye.
Technetium (99mTc) tilmanocept, trade name Lymphoseek, is a radiopharmaceutical diagnostic imaging agent approved by the U.S. Food and Drug Administration (FDA) for the imaging of lymph nodes.[1][2] It is used to locate those lymph nodes which may be draining from tumors, and assist doctors in locating those lymph nodes for removal during surgery.[3]
http://blog.sina.com.cn/u/1242475203
…………………….
WO 2000069473
http://www.google.com/patents/EP1178838A2?cl=en
…………………………………………..
US 6409990
http://www.google.co.in/patents/US6409990
References
- FDA Professional Drug Information
- http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm343525.htm
- Marcinow, A. M.; Hall, N.; Byrum, E.; Teknos, T. N.; Old, M. O.; Agrawal, A. (2013). “Use of a novel receptor-targeted (CD206) radiotracer, 99mTc-tilmanocept, and SPECT/CT for sentinel lymph node detection in oral cavity squamous cell carcinoma: Initial institutional report in an ongoing phase 3 study”. JAMA otolaryngology– head & neck surgery 139 (9): 895–902. doi:10.1001/jamaoto.2013.4239. PMID 24051744.
http://www.google.com/patents/US8247538
Radiopharmaceuticals for use in therapy employ radionuclides which are generally longer in half-life and weaker in penetration capability, but emit stronger radiation, sufficient to kill cells, in relation to that for use in diagnosis. Alpha ray-emitting radionuclides are excluded from radiopharmaceuticals for the reason that they are highly radioactive and difficult to purchase and to attach to other compounds. All of the radionuclides currently used in pharmaceuticals are species that emit beta rays.
As mentioned above, radiopharmaceuticals, whether for use in therapy or diagnosis, are prepared by labeling pharmaceuticals with specific radionuclides. Technetium-99m (99mTc) is known as the radioisotope most widely used to label radiopharmaceuticals. Technetium-99m has a half life of as short as 6 hours and emits gamma rays at 140 KeV, and thus it is not so toxic to the body. In addition, gamma radiation from the radioisotope is highly penetrative enough to obtain images. Thanks to these advantages, technetium-99m finds a broad spectrum of therapeutic and diagnostic applications in the nuclear medicine field (Sivia, S. J., John, D. L., Potential technetium small molecule radiopharmaceuticals. Chem. Rev. 99, 2205-2218, 1999; Shuang, L., Edwards, D. S., 99mTc-Labeled small peptides as diagnostic radiopharmaceuticals. Chem. Rev. 99, 2235-2268, 1999).
Methods of labeling 99mTc-2,6-diisopropylacetanilidoiminodiacetic acid are well known in the art (Callery, P. S., Faith, W. C., et al., 1976. Tissue distribution of technetium-99m and carbon-labeled N-(2,6)-dimetylphenylcarbamoylmethyl iminodiacetic acid. J. Med. Chem. 19, 962-964; Motter, M. and Kloss, G., 1981. Properties of various IDA derivatives. J. Label. Compounds Padiopharm. 18, 56-58; Cao, Y. and Suresh, M. R. 1998. A Simple And Efficient Method For Radiolabeling Of Preformed Liposomes. J Pharm Pharmaceut Sci. 1 (1), 31-37).
Basically, the conventional methods are based on the following reaction formula. In practice, a solution of SnCl2.2H2O, serving as a reducing agent of technetium-99m, in 0.1 N HCl and 0.1 ml (10 mCi) of sodium pertechnetium were added to lyophilized 2,6-diisopropylacetanilidoiminodiacetic acid in a vial, followed by stirring at room temperature for 30 min to prepare 99mTc-2,6-diisopropylacetanilidoiminodiacetic acid. The preparation of 99mTc-2,6-diisopropylacetanilidoiminodiacetic acid may be realized according to the following reaction formula.
Such conventional processes of preparing radiopharmaceuticals labeled with technetium-99m can be divided into reactions between the radioisotope and a physiologically active material to be labeled and the separation of labeled compounds from unlabeled compounds.
| M. Molter, et al., Properties of Various IDA Derivatives, J. Label. Compounds Padiopharm., vol. 18, pp. 56-58, 1981. | ||
| 2 | Patrick S. Callery, et al., Tissue Distribution of Technetium-99m and Carbon . . . , J. Med. Chem., vol. 19, pp. 962-964, 1976. | |
| 3 | * | Sang Hyun Park et al. Synthesis and Radiochemical Labeling of N-(2,6-diisopropylacetanilido)-Iminodiacetic acid and it s analogues under microwave irradiation: A hepatobiliary imaging agent, QSAR Comb. Sci. 2004, 23, 868-874. |
| 4 | Shuang Liu, et al., 99mTc-Labeled Small Peptides as Diagnostic . . . , Chem. Rev., vol. 99, pp. 2235-2268, 1999. | |
| 5 | Shuang Liu, et al., 99mTc—Labeled Small Peptides as Diagnostic . . . , Chem. Rev., vol. 99, pp. 2235-2268, 1999. | |
| 6 | Silvia S. Jurisson, et al., Potential Technetium Small Molecule . . . , Chem. Rev., vol. 99, pp. 2205-2218, 1999. | |
| 7 | Y. Cao, et al., A Simple and Efficient Method for Radiolabeling . . . , J. Phar,. Pharmaceut. Sci., pp. 31-37, 1998. |
|
Diagnostic radiopharmaceuticals (V09)
|
|
|---|---|
| Central nervous system | |
| Skeletal system | |
| Renal | |
| Hepatic/reticuloendothelial | |
| Respiratory system | |
| Cardiovascular system | |
| Inflammation/infection |
|
| Tumor | |
| Adrenal cortex | |
| Radionuclides (including tracers) |
|
Selexipag Meets Primary Endpoint in Pivitol Phase III Griphon Outcome Study in Patients with Pulmonary Arterial Hypertension
June 16, 2014
Actelion Ltd today announced the top-line results of the pivotal Phase III GRIPHON study in 1,156 patients with pulmonary arterial hypertension (PAH) with selexipag, the first selective oral prostacyclin IP receptor agonist. Initial analysis shows that the event-driven outcome study has met its primary efficacy endpoint with high statistical significance.
June 16, 2014
Actelion Ltd today announced the top-line results of the pivotal Phase III GRIPHON study in 1,156 patients with pulmonary arterial hypertension (PAH) with selexipag, the first selective oral prostacyclin IP receptor agonist. Initial analysis shows that the event-driven outcome study has met its primary efficacy endpoint with high statistical significance.

Selexipag
N-[2-[4-[N-(5,6-Diphenylpyrazin-2-yl)-N-isopropylamino]butoxy]acetyl]methanesulfonamide
2-[4-[N-(5,6-Diphenylpyrazin-2-yl)-N-isopropylamino]butoxy]-N-(methylsulfonyl)acetamide
phase 3 pulmonary hypertention
Selexipag (ACT-293987, NS-304) is a drug currently in development by Actelion as a treatment of pulmonary arterial hypertension. Selexipag and its active metabolite, ACT-333679, are agonists at the PGI2 prostaglandin receptor, which leads to vasodilation in the pulmonary circulation
Selexipag, originally discovered and synthesized by Nippon Shinyaku, is a potent, orally available, selective prostacyclin IP receptor agonist.
Selexipag selectively targets the prostacyclin receptor (also called IP-receptor). The IP receptor is one of
5 types of prostanoid receptor. Prostacyclin activates the IP receptor inducing vasodilation and inhibiting proliferation of vascular smooth muscle cells. Selexipag, unlike prostacyclin analogs, is selective for the IP receptor over other prostanoid receptors.
In April 2008, Actelion and Nippon Shinyaku signed a licensing agreement, under which Actelion will be responsible for the global development and commercialization of selexipag outside Japan, and the two companies will co-develop and co-commercialize the drug in Japan.
http://www1.actelion.com/sites/en/scientists/development-pipeline/phase-3/selexipag.page
ABOUT THE ACTELION / NIPPON SHINYAKU ALLIANCE
Actelion and Nippon Shinyaku entered into an exclusive worldwide alliance in April 2008 to collaborate on selexipag, a first-in-class orally-available, selective IP receptor agonist for patients suffering from pulmonary arterial hypertension (PAH). This compound was originally discovered and synthesized by Nippon Shinyaku. Phase II evaluation has been completed, and a Phase III program in PAH patients has been initiated. Actelion is responsible for global development and commercialization of selexipag outside Japan, while the two companies will co-develop and co-commercialize in Japan. Nippon Shinyaku will receive milestone payments based on development stage and sales milestones as well as royalties on any sales of selexipag.
| Selexipag | |
|---|---|
 |
|
| Identifiers | |
| CAS number | 475086-01-2 |
| PubChem | 9913767 |
| ChemSpider | 8089417 |
| UNII | 5EXC0E384L |
| KEGG | D09994 |
| Jmol-3D images | Image 1 |
| Properties | |
| Molecular formula | C26H32N4O4S |
| Molar mass | 496.6 g·mol−1 |
NS-304 (ACT-293987), an orally available long acting non-prostanoid prostaglandin I2 (PGI-2) receptor agonist, is in phase III clinical trials at Actelion for the oral treatment of pulmonary hypertension. Nippon Shinyaku is conducting phase III clinical trials with NS-304 for this indication in Europe. In Japan, phase II clinical trials are ongoing for the treatment of pulmonary hypertension and chronic thromboembolic pulmonary hypertension.
Originally discovered and synthesized by Nippon Shinyaku, NS-304 stimulates PGI-2 receptors in blood vessels and exerts vasodilating effects.
In 2008, the compound was licensed to Actelion by Nippon Shinyaku on a worldwide basis with the exception of Japan for the oral treatment of pulmonary arterial hypertension (PAH). According to the final licensing agreement, Actelion will be responsible for global development and commercialization of NS-304 outside Japan, while the two companies will codevelop and co-commercialize the product candidate in Japan. In 2005, orphan drug designation was assigned in the E.U. by Nippon Shinyaku for the treatment of pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension.
…………………….
US2012/101276
http://www.google.st/patents/US20120101276?hl=pt-PT&cl=en
The present invention relates to a crystal of 2-{4-[N-(5,6-diphenylpyrazin-2-yl)-N-isopropylamino]butyloxy}-N-(methylsulfonyl)acetamide (hereinafter referred to as “compound A”).
BACKGROUND OF THE INVENTION
Compound A has an excellent PGI2 agonistic effect and shows a platelet aggregation inhibitory effect, a vasodilative effect, a bronchodilative effect, a lipid deposition inhibitory effect, a leukocyte activation inhibitory effect, etc. (see, for example, in WO 2002/088084 (“WO ‘084”)).
Specifically, compound A is useful as preventive or therapeutic agents for transient ischemic attack (TIA), diabetic neuropathy, diabetic gangrene, peripheral circulatory disturbance (e.g., chronic arterial occlusion, intermittent claudication, peripheral embolism, vibration syndrome, Raynaud’s disease), connective tissue disease (e.g., systemic lupus erythematosus, scleroderma, mixed connective tissue disease, vasculitic syndrome), reocclusion/restenosis after percutaneous transluminal coronary angioplasty (PTCA), arteriosclerosis, thrombosis (e.g., acute-phase cerebral thrombosis, pulmonary embolism), hypertension, pulmonary hypertension, ischemic disorder (e.g., cerebral infarction, myocardial infarction), angina (e.g., stable angina, unstable angina), glomerulonephritis, diabetic nephropathy, chronic renal failure, allergy, bronchial asthma, ulcer, pressure ulcer (bedsore), restenosis after coronary intervention such as atherectomy and stent implantation, thrombocytopenia by dialysis, the diseases in which fibrosis of organs or tissues is involved [e.g., Renal diseases (e.g., tuburointerstitial nephritis), respiratory diseases (e.g., interstitial pneumonia (pulmonary fibrosis), chronic obstructive pulmonary disease), digestive diseases (e.g., hepatocirrhosis, viral hepatitis, chronic pancreatitis and scirrhous stomachic cancer), cardiovascular diseases (e.g, myocardial fibrosis), bone and articular diseases (e.g, bone marrow fibrosis and rheumatoid arthritis), skin diseases (e.g, cicatrix after operation, scalded cicatrix, keloid, and hypertrophic cicatrix), obstetric diseases (e.g., hysteromyoma), urinary diseases (e.g., prostatic hypertrophy), other diseases (e.g., Alzheimer’s disease, sclerosing peritonitis; type I diabetes and organ adhesion after operation)], erectile dysfunction (e.g., diabetic erectile dysfunction, psychogenic erectile dysfunction, psychotic erectile dysfunction, erectile dysfunction associated with chronic renal failure, erectile dysfunction after intrapelvic operation for removing prostata, and vascular erectile dysfunction associated with aging and arteriosclerosis), inflammatory bowel disease (e.g., ulcerative colitis, Crohn’s disease, intestinal tuberculosis, ischemic colitis and intestinal ulcer associated with Behcet disease), gastritis, gastric ulcer, ischemic ophthalmopathy (e.g., retinal artery occlusion, retinal vein occlusion, ischemic optic neuropathy), sudden hearing loss, avascular necrosis of bone, intestinal damage caused by administration of a non-steroidal anti-inflammatory agent (e.g., diclofenac, meloxicam, oxaprozin, nabumetone, indomethacin, ibuprofen, ketoprofen, naproxen, celecoxib) (there is no particular limitation for the intestinal damage so far as it is damage appearing in duodenum, small intestine and large intestine and examples thereof include mucosal damage such as erosion and ulcer generated in duodenum, small intestine and large intestine), and symptoms associated with lumbar spinal canal stenosis (e.g., paralysis, dullness in sensory perception, pain, numbness, lowering in walking ability, etc. associated with cervical spinal canal stenosis, thoracic spinal canal stenosis, lumbar spinal canal stenosis, diffuse spinal canal stenosis or sacral stenosis) etc. (see, for example, in WO ‘084, WO 2009/157396, WO 2009/107736, WO 2009/154246, WO 2009/157397, and WO 2009/157398).
In addition, compound A is useful as an accelerating agent for angiogenic therapy such as gene therapy or autologous bone marrow transplantation, an accelerating agent for angiogenesis in restoration of peripheral artery or angiogenic therapy, etc. (see, for example, in WO ‘084).
Production of Compound A
Compound A can be produced, for example, according to the method described in WO ‘084, and, it can also be produced according to the production method mentioned below.
Step 1:
6-Iodo-2,3-diphenylpyrazine can be produced from 6-chloro-2,3-diphenylpyrazine by reacting it with sodium iodide. The reaction is carried out in the presence of an acid in an organic solvent (e.g., ethyl acetate, acetonitrile, acetone, methyl ethyl ketone, or their mixed solvent). The acid to be used is, for example, acetic acid, sulfuric acid, or their mixed acid. The amount of sodium iodide to be used is generally within a range of from 1 to 10 molar ratio relative to 6-chloro-2,3-diphenylpyrazine, preferably within a range of from 2 to 3 molar ratio. The reaction temperature varies depending on the kinds of the solvent and the acid to be used, but may be generally within a range of from 60° C. to 90° C. The reaction time varies depending on the kinds of the solvent and the acid to be used and on the reaction temperature, but may be generally within a range of from 9 hours to 15 hours.
Step 2:
5,6-Diphenyl-2-[(4-hydroxybutyl(isopropyl)amino]pyrazine can be produced from 6-iodo-2,3-diphenylpyrazine by reacting it with 4-hydroxybutyl(isopropyl)amine. The reaction is carried out in the presence of a base in an organic solvent (e.g., sulfolane, N-methylpyrrolidone, N,N-dimethylimidazolidinone, dimethyl sulfoxide or their mixed solvent). The base to be used is, for example, sodium hydrogencarbonate, potassium hydrogencarbonate, potassium carbonate, sodium carbonate or their mixed base. The amount of 4-hydroxybutyl(isopropyl)amine to be used may be generally within a range of from 1.5 to 5.0 molar ratio relative to 6-iodo-2,3-diphenylpyrazine, preferably within a range of from 2 to 3 molar ratio. The reaction temperature varies depending on the kinds of the solvent and the base to be used, but may be generally within a range of from 170° C. to 200° C. The reaction time varies depending on the kinds of the solvent and the base to be used and on the reaction temperature, but may be generally within a range of from 5 hours to 9 hours.
Step 3:
Compound A can be produced from 5,6-diphenyl-2-[4-hydroxybutyl(isopropyl)amino]pyrazine by reacting it with N-(2-chloroacetyl)methanesulfonamide. The reaction is carried out in the presence of a base in a solvent (N-methylpyrrolidone, 2-methyl-2-propanol or their mixed solvent). The base to be used is, for example, potassium t-butoxide, sodium t-butoxide or their mixed base. The amount of N-(2-chloroacetyl)methanesulfonamide to be used may be generally within a range of from 2 to 4 molar ratio relative to 5,6-diphenyl-2-[4-hydroxybutyl(isopropyl)amino]pyrazine, preferably within a range of from 2 to 3 molar ratio. The reaction temperature varies depending on the kinds of the solvent and the base to be used, but may be generally within a range of from −20° C. to 20° C. The reaction time varies depending on the kinds of the solvent and the base to be used and on the reaction temperature, but may be generally within a range of from 0.5 hours to 2 hours.
The compounds to be used as the starting materials in the above-mentioned production method for compound A are known compounds, or can be produced by known methods.
…………………………………
WO 2002088084
and
http://www.google.fm/patents/WO2009157398A1?cl=en
………………………
Bioorganic and Medicinal Chemistry, 2007 , vol. 15, 21 p. 6692 – 6704
compd 31
……………………
Bioorganic and Medicinal Chemistry, 2007 , vol. 15, 24 p. 7720 – 7725
 2a isthe drug
2a isthe drug
N-Acylsulfonamide and N-acylsulfonylurea derivatives of the carboxylic acid prostacyclin receptor agonist 1 were synthesized and their potential as prodrug forms of the carboxylic acid was evaluated in vitro and in vivo. These compounds were converted to the active compound 1 by hepatic microsomes from rats, dogs, monkeys, and humans, and some of the compounds were shown to yield sustained plasma concentrations of 1 when they were orally administered to monkeys. These types of analogues, including NS-304 (2a), are potentially useful prodrugs of 1.
http://www.sciencedirect.com/science/article/pii/S0968089607007614
References
- Kuwano et al. NS-304, an orally available and long-acting prostacyclin receptor agonist prodrug. J Pharmacol Exp Ther 2007;322:1181-1188.
- Kuwano et al. A long-acting and highly selective prostacyclin receptor agonist prodrug, NS-304, ameliorates rat pulmonary hypertension with unique relaxant responses of its active form MRE-269 on rat pulmonary artery. J Pharmacol Exp Ther 2008;326:691-699.
- Simonneau G, Lang I, Torbicki A, Hoeper MM, Delcroix M, Karlocai K, Galie N. Selexipag, an oral, selective IP receptor agonist for the treatment of pulmonary arterial hypertension Eur Respir J 2012; 40: 874-880
- Mubarak KK. A review of prostaglandin analogs in the management of patients with pulmonary arterial hypertension. Respir Med 2010;104:9-21.
- Sitbon, O.; Morrell, N. (2012). “Pathways in pulmonary arterial hypertension: The future is here”. European Respiratory Review 21 (126): 321–327. doi:10.1183/09059180.00004812. PMID 23204120.
ABOUT SELEXIPAG
Selexipag, originally discovered and synthesized by Nippon Shinyaku, is a potent, orally available, selective prostacyclin IP receptor agonist.
Selexipag selectively targets the prostacyclin receptor (also called IP-receptor). The IP receptor is one of 5 types of prostanoid receptor. Prostacyclin activates the IP receptor inducing vasodilation and inhibiting proliferation of vascular smooth muscle cells. Selexipag, unlike prostacyclin analogs, is selective for the IP receptor over other prostanoid receptors. In preclinical models selective IP receptor agonism has shown to maintain efficacy and reduce the risk of side effects mediated by activation of other prostanoid receptors, such as EP1 and EP3 receptors. [2,4,5]
Selexipag was previously evaluated in a Phase II, 43-patient, placebo-controlled, double-blind study, where patients were randomized in a 3:1 ratio receiving selexipag or placebo on top of PDE-5 inhibitor and/or ERA [6]
SELEXIPAG
Selexipag, originally discovered and synthesized by Nippon Shinyaku, is a potent, orally available, selective prostacyclin IP receptor agonist.
Selexipag selectively targets the prostacyclin receptor (also called IP-receptor). The IP receptor is one of 5 types of prostanoid receptor. Prostacyclin activates the IP receptor inducing vasodilation and inhibiting proliferation of vascular smooth muscle cells. Selexipag, unlike prostacyclin analogs, is selective for the IP receptor over other prostanoid receptors. In preclinical models selective IP receptor agonism has shown to maintain efficacy and reduce the risk of side effects mediated by activation of other prostanoid receptors, such as EP1 and EP3 receptors. [2,4,5]
Selexipag was previously evaluated in a Phase II, 43-patient, placebo-controlled, double-blind study, where patients were randomized in a 3:1 ratio receiving selexipag or placebo on top of PDE-5 inhibitor and/or ERA [6]
SELEXIPAG
Selexipag, originally discovered and synthesized by Nippon Shinyaku, is a potent, orally available, selective prostacyclin IP receptor agonist.
Selexipag selectively targets the prostacyclin receptor (also called IP-receptor). The IP receptor is one of 5 types of prostanoid receptor. Prostacyclin activates the IP receptor inducing vasodilation and inhibiting proliferation of vascular smooth muscle cells. Selexipag, unlike prostacyclin analogs, is selective for the IP receptor over other prostanoid receptors. In preclinical models selective IP receptor agonism has shown to maintain efficacy and reduce the risk of side effects mediated by activation of other prostanoid receptors, such as EP1 and EP3 receptors. [2,4,5]
Selexipag was previously evaluated in a Phase II, 43-patient, placebo-controlled, double-blind study, where patients were randomized in a 3:1 ratio receiving selexipag or placebo on top of PDE-5 inhibitor and/or ERA [6]
SELEXIPAG
Selexipag, originally discovered and synthesized by Nippon Shinyaku, is a potent, orally available, selective prostacyclin IP receptor agonist.
Selexipag selectively targets the prostacyclin receptor (also called IP-receptor). The IP receptor is one of 5 types of prostanoid receptor. Prostacyclin activates the IP receptor inducing vasodilation and inhibiting proliferation of vascular smooth muscle cells. Selexipag, unlike prostacyclin analogs, is selective for the IP receptor over other prostanoid receptors. In preclinical models selective IP receptor agonism has shown to maintain efficacy and reduce the risk of side effects mediated by activation of other prostanoid receptors, such as EP1 and EP3 receptors. [2,4,5]
Selexipag was previously evaluated in a Phase II, 43-patient, placebo-controlled, double-blind study, where patients were randomized in a 3:1 ratio receiving selexipag or placebo on top of PDE-5 inhibitor and/or ERA [6]
Pharma vies to unleash immune system power on cancer

http://www.rsc.org/chemistryworld/2014/06/pharma-vies-unleash-immune-system-power-cancer
Provectus Phase III Melanoma Trial Results Earlier Than Planned?


Rose Bengal disodium
4 ,5,6,7-Tetrachloro-2′,4′,5′,7′-tetraiodo-3-oxo-3H-spiro[2-benzofuran-1,9′-xanthene]-3′,6′-diolate disodium salt
| cas | 632-69-9 |
C20 H2 Cl4 I4 O5 . 2 Na, mw 1017.36, PH 10
| innovator | Provectus |

The FDA has granted PV-10 Orphan Drug Status for the treatment of highly lethal metastatic melanoma and metastatic liver cancer. It has a successful and expanding Compassionate Use Program in operation and successfully completed trials on metastatic cancer of the breast, liver and melanoma, with positive results in all three. Positive effects in this context is that, if you inject PV-10 into a solid tumor, it kills cancer cells, usually within a week and doesn’t harm normal tissue. Many injected tumors actually disappear while others shrink and stop growing. The dual action of the drug is that the destruction of the cancer by direct injection of PV-10 serves to sensitize the patient’s immune system to seek out and kill similar cancer throughout the body. There is convincing evidence that untreated cancer distant from the treated cancer is attacked by the patient’s immune system after treatment.
PROVECTUS COMPANY OVERVIEW
Provectus (PVCT) is a clinical stage bio-pharmaceutical drug development company. There are 3 key scientific managers running the business along with the CFO, who is also the Chief Operating Officer. They preside over a stable of expert and specialized consultants. The company has two lead drug candidates: PH-10 for significant, often severe, and common skin disorders and PV-10, a dual action, local ablation and immunological anti-cancer drug. PH-10 is currently the subject of post-Phase II trial research into mode of action. PV-10 has successfully completed Phase II trials for malignant melanoma, is currently the subject of independent research on mode of actioRose Bengal disodium is in early clinical trials at Provectus for the topical treatment of psoriasis and atopic dermatitis. An intralesional injectable formulation is also in early clinical development as breast cancer, liver cancer and melanoma therapy. Development for the treatment of actinic keratosis had been ongoing; however, no recent development for this indication has been reported. The company is seeking approval in the U.S. to begin clinical evaluation of this formulation for the treatment of liver and prostate cancer. A compassionate use program is under way for Rose Bengal disodium for the treatment of non-visceral cancers.
The drug’s mechanism of action is believed to be characterized by the creation of free radicals upon activation, which eliminate diseased cells. The compound concentrates in tumors at cytotoxic levels while quickly dissipating from healthy tissue. Simultaneously, the drug triggers an immune response that can eliminate metastatic tumor tissue.
In 2007, orphan drug designation was assigned to Rose Bengal disodium by the FDA for the treatment of metastatic melanoma. This designation was also assigned to the compound in the U.S. in 2011 for the treatment of hepatocellular carcinoma.n and efficacy in conjunction with radiation, and it will have a Phase III pivotal trial starting shortly.
SUMMARY
1. If PV-10 and the Chemotherapies act as the prior data indicate, an NDA for melanoma may be submitted by Provectus in the first half of 2015.
2. If this occurs, the FDA denial of the Breakthrough Therapy designation will not have slowed PV-10’s progress to commercialization.
3. Given the relative safety and efficacy of the different drugs, if the trial is not stopped very early for humanitarian reasons, the planned Interim Analysis is likely to result in the cancellation of the trial, prior to the end of 2015.
4. Given PV-10’s superior safety and lack of significant side effects, if it is only as good as Chemotherapy, it will deserve FDA approval.
The Phase III pivotal trial will demonstrate the safety and efficacy of PV-10 to the market and to prospective acquirers a lot earlier than many have presumed.
Rose bengal (4,5,6,7-tetrachloro-2′,4′,5′,7′-tetraiodofluorescein) is a stain. Its sodium salt is commonly used in eye drops to stain damaged conjunctival and corneal cells and thereby identify damage to the eye. The stain is also used in the preparation of Foraminifera for microscopic analysis, allowing the distinction between forms that were alive or dead at the time of collection.
A form of Rose Bengal is also being studied as a treatment for certain cancers and skin conditions. The cancer formulation of the drug, known as PV-10, is currently undergoing clinical trials for melanoma and breast cancer. The company also has formulated a drug based on Rose Bengal for the treatment of eczema and psoriasis; this drug, PH-10, is currently in clinical trials as well.
| Rose bengal | |
|---|---|
 |
|
| Identifiers | |
| CAS number | 11121-48-5 |
| ATC code | S01 |
| Jmol-3D images | Image 1 |
| Properties | |
| Molecular formula | C20H4Cl4I4O5 |
| Molar mass | 973.67 g mol−1 |
Chemical applications

Light microscopy image of the undescribed species of Spinoloricus from Loricifera stained with Rose Bengal.
Rose Bengal is also used in synthetic chemistry to generate singlet oxygen from triplet oxygen. The singlet oxygen can then undergo a variety of useful reactions, particularly [2 + 2] cycloadditions with alkenes and similar systems.
Rose Bengal can be used to form many derivatives that have important medical functions. One such derivative was created so to be sonosensative but photoinsensative, so that with a high intensity focused ultrasound, it could be used in the treatment of cancer. The derivative was formed by amidation of Rose Bengal, which turned off the fluorescent and photosensitive properties of Rose Bengal, leading to a usable compound, named in the study as RB2.[1]
Salts of Rose Bengal can also be formed, with the molecular formula C20 H4 Cl4 I4 O5 . 2 Na, molecular weight of 1017.64 g/mol and CAS # 632-69-9. Known as Rose Bengal Sodium Salt, this compound has its own unique uses and properties, but also functions as a dye.[2]
Biological applications
PV-10 was found to cause an observable response in 60 percent of tumors treated, according to researchers in a phase II melanoma study. Locoregional disease control was observed in 75 percent of patients. Also confirmed was a “bystander effect”, previously observed in the phase I trial, whereby untreated lesions responded to treatment as well, potentially due to immune system response. These data were based on the interim results of the first 40 patients treated in an 80 patient study.[3] Rose Bengal has been shown to not just prevent the growth and spread of ovarian cancer, but also to cause apoptotic cell death of the cancer cells. This has been proven in vitro, in order to prove that Rose Bengal is still a possible option in the treatment of cancer, and further research should be done.[4]
Rose Bengal is also used in animal models of ischemic stroke (photothrombotic stroke models) in biomedical research. A bolus of the compound is injected into the venous system. Then the region of interest (e.g., the cerebral cortex) is exposed and illuminated by LASER light of 561 nm. A thrombus is formed in the illuminated blood vessels, causing a stroke in the dependent brain tissue.[5][6]
Rose bengal has been used for 50 years to diagnose liver and eye cancer. It has also been used as an insecticide.[7][8]
Rose Bengal is able to stain cells whenever the surface epithelium is not being properly protected by the preocular tear film, because Rose Bengal has been proven to not be able to stain cells because of the protective functioning of these preocular tear films.[9] This is why Rose Bengal is often useful as a stain in diagnosing certain medical issues, such as conjunctival and lid disorders.[10]
Rose Bengal has been used for ocular surface staining to study the efficacy of punctal plugs in the treatment of keratoconjunctivitis sicca. [11]
Rose Bengal is being researched as an agent in creating nano sutures.[12] Wounds are painted on both sides with it and then illuminated with an intense light. This links the tiny collagen fibers together sealing the wound.[13][14][15] Healing is faster and the seal reduces chances of infection.[16][17]
Rose Bengal is used in several microbiological media, including Cooke’s Rose Bengal agar, to suppress bacterial growth.
Rose Bengal has been used as a protoplasm stain to discriminate between living and dead micro-organisms, particularly Foraminifera, since the 1950s when Bill Walton developed the technique.[18]
Electronic applications
Rose Bengal demonstrates at least six distinct electronic properties[19] which are otherwise hidden in the molecule. Rose Bengal is a double planar molecule and relative rotation of the planes generate unique electronics. Therefore, Rose Bengal is a suitable candidate for molecular electronics.
History
Rose Bengal was originally prepared in 1884 by Gnehm, as an analogue of fluorescein.[20] The name is due to its similarity to alta, a dye that women in Bengal have used for centuries to colour their feet red during weddings and festivals.
References
- Kim, Y; Valentina Rubio, Jianjun Qi, Rongmin Xia, Zheng-Zheng Shi, Leif Peterson, Ching-Hsuan Tung, and Brian E. O’Neill (2012). “Cancer treatment using an optically inert Rose Bengal derivative combined with pulsed focused ultrasound”. AIP Conference Proceedings 1481: 175.
- “Rose Bengal Sodium Salt”. Sigma-Aldrich. Sigma Aldrich Co. Retrieved 12 November 2013.
- Metastatic Melanoma PV-10 Trial Results Encouraging Says Drug Company, Medical News Today, 09 Jun 2009
- Koevary, S (2012). “Selective toxicity of rose bengal to ovarian cancer cells in vitro”. International Journal of Physiology, Pathophysiology and Pharmacology 4: 99–107.
- Salber D, et al. (2006). “Differential uptake of [18F]FET and [3H]l-methionine in focal cortical ischemia”. Nuclear Medicine and Biology 33 (8): 1029–1035. doi:10.1016/j.nucmedbio.2006.09.004. PMID 17127177.
- Watson BD, Dietrich WD, Busto R, Wachtel MS, Ginsberg MD (1985). “Induction of reproducible brain infarction by photochemically initiated thrombosis”. Ann Neurol 17 (5): 497–504. doi:10.1002/ana.410170513. PMID 4004172.
- Capinera, John L.; Squitier, Jason M. (2000). “Insecticidal Activity of Photoactive Dyes to American and Migratory Grasshoppers (Orthoptera: Acrididae)”. Journal of Economic Entomology 93 (3): 662–666. doi:10.1603/0022-0493-93.3.662. PMID 10902313.
- Martin, Phyllis; Mischke, Sue; Schroder, Robert (1998). “Compatibility of Photoactive Dyes with Insect Biocontrol Agents”. Biocontrol Science and Technology 8 (4): 501–508. doi:10.1080/09583159830018.
- Feenstra, R; Tseng, S (July 1992). “What is actually stained by rose bengal?”. Arch Ophthalmol 110: 984–993. doi:10.1001/archopht.1992.01080190090035.
- Yokoi, Norihiko (2012). “Vital staining for disorders of conjunctiva and lids”. Atarashii Ganka 29: 1599–1605.
- Ervin AM, Wojciechowski R, Schein O (2010). “Punctal occlusion for dry eye syndrome”. Cochrane Database Syst Rev 9: CD006775. doi:10.1002/14651858.CD006775.pub2. PMID 20824852.
- Chan, B; Chan, O; So, K (2008). “Effects of photochemical crosslinking on the microstructure of collagen and a feasibility study on controlled protein release”. Acta Biomaterialia 4 (6): 1627–1636. doi:10.1016/j.actbio.2008.06.007. PMID 18640085.
- O’Neill A.C., Winograd J.M, Zeballos J.M., Johnson T.S., Randolph M.A., Bujold K.E., Kochevar I.E., Redmond R.W. (2007). “Microvascular anastomosis using a photochemical tissue bonding technique”. Lasers in Surgery and Medicine 39 (9): 716–722. doi:10.1002/lsm.20548. PMID 17960755.
- Mulroy L., Kim J., Wu I., Scharper P., Melki S.A., Azar D.A., Redmond R.W., Kochevar I.E. (2000). “Photochemical keratodesmos for repair of lamellar corneal incisions”. Invest Ophthalmol Vis Sci 41 (11): 3335–3340. PMID 11006222.
- Proano C.E., Mulroy L., Erika Jones E., Azar D.A., Redmond R.W., Kochevar I.E. (2004). Invest Ophthalmol Vis Sci: 2177–2181.
- Laser Show in the Surgical Suite, Technology Review, March/April 2009
- Laser Show in the Surgical Suite, Technology Review, 02.11.2009
- Walton, W. (1952), Techniques for recognition of living foraminifera, Contrib. Cushman Found. Foraminiferal Res., 3, 56 – 60
- A new approach to extract multiple distinct conformers and co-existing distinct electronic properties of a single molecule by point-contact method Anirban Bandyopadhyay, Satyajit Sahu, Daisuke Fujita and Yutaka Wakayama, Phys. Chem. Chem. Phys., 2010 view highlights in Royal Society of Chemistry,
- Alexander, Walter (2010). “American Society of Clinical Oncology, 2010 Annual Meeting and Rose Bengal: From a Wool Dye to a Cancer Therapy”. Pharmacy and Therapeutics 35 (8): 469–474. PMC 2935646. Retrieved 5 November 2013.
- US 2010021566
- WO 2011050164
- US 2011250296
External links
- Rose Bengal at the US National Library of Medicine Medical Subject Headings (MeSH)
- Absorption and extinction data
A new twist on neuro disease: Discovery could aid people with dystonia, Parkinson’s and more
Twist and hold your neck to the left. Now down, and over to the right, until it hurts. Now imagine your neck – or arms or legs – randomly doing that on their own, without you controlling it.
That’s a taste of what children and adults with a neurological condition called dystonia live with every day – uncontrollable twisting and stiffening of neck and limb muscles.
The mystery of why this happens, and what can prevent or treat it, has long puzzled doctors, who have struggled to help their suffering dystonia patients. Now, new re-search from a University of Michigan Medical School team may finally open the door to answering those questions and developing new options for patients.
In a new paper in the Journal of Clinical Investigation, the researchers describe new strains of mice they’ve developed that almost perfectly mimic a human form of the disease. They also…
View original post 688 more words

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....












































