Home » 2014 (Page 13)
Yearly Archives: 2014
Nicox stock leaps on positive Ph III glaucoma drug data , 英文名称

- 4- (nitrooxy) butyl (5Z) -7 – {(1R, 2R, 3R, 5S) -3,5-dihydroxy-2 – [(3R) -3-hydroxy-5-phenylpentyl] cyclopentyl} hept-5- enoate
- CAS No.860005-21-6
- Formula C 27 H 41 NO 8
The firms have published top-line results from the pivotal Phase 3 studies conducted with Vesneo (latanoprostene bunod) for the reduction of intraocular pressure in patients with glaucoma or ocular hypertension. The drug is a nitric oxide-donating prostaglandin F2-alpha analog licensed by Nicox to Bausch + Lomb.
Read more at: http://www.pharmatimes.com/Article/14-09-25/Nicox_stock_leaps_on_positive_Ph_III_glaucoma_drug_data.aspx#ixzz3ETxo7SBd
prostaglandin nitrooxyderivatives, pharmaceutical compositions containing them and their use as drugs for treating glaucoma and ocular hypertension. Glaucoma is optic nerve damage, often associated with increased intraocular pressure (IOP), that leads to progressive, irreversible loss of vision. . Almost 3 million people in the United States and 14 million people worldwide have glaucoma; this is the third leading cause of blindness worldwide. Glaucoma occurs when an imbalance in production and drainage of fluid in the eye (aqueous humor) increases eye pressure to unhealthy levels. It is known that elevated IOP can be at least partially controlled by administering drugs which either‘ reduce the production of aqueous humor within the eye or increase the fluid drainage, such as beta-blockers, α- agonists, ■ ‘ cholinergic agents, carbonic anhydrase inhibitors, or prostaglandin analogs. . Several side effects are associated with the drugs conventionally used to treat glaucoma. . ■ Topical beta-blockers show serious pulmonary side effects, depression, fatigue,’ confusion, impotence, hair loss, heart failure and bradycardia. Topical -agonists have a fairly high incidence of allergic, .or toxic reactions; topical cholinergic agents (miotics) can cause visual side effects. The side effects associated with oral carbonic anhydrase inhibitors include fatigue, anorexia, depression, paresthesias and serum■ electrolyte abnormalities (The Merck Manual of Diagnosis and Therapy, Seventeenth Edition, M. H. Beers and R. Berkow Editors, Sec. 8, Ch. 100) . Finally, the topical prostaglandin analogs (bimatoprost, latanoprost, travoprost and unoprostone) ‘ used in the treatment of glaucoma, can produce ocular side effects, such as increased pigmentation of the iris, ocular irritation, conjunctival hyperaemia, iritis, uveitis and macular oedema (Martindale, Thirty-third edition, p. 1.445) U.S. Pat. No. 3,922,293 describes monocarboxyacylates of prostaglandins F-type and their 15β isomers, at the C-9 position, and processes for preparing them; U.S. Pat. No. 6,417,228 discloses 13-aza prostaglandins having functional PGF2α receptor agonist activity and their use in treating glaucoma and ocular hypertension. WO 90/02553 • discloses the use ‘ of prostaglandins derivatives of PGA, PGB, PGE and PGF, in which the omega chain contains a ring structure, for the treatment of glaucoma or ocular hypertension. WO 00/51978 describes novel nitrosated and/or nitrosylated prostaglandins, ‘ • in ‘ particular novel derivatives of PGEi, novel compositions and their use for treating sexual dysfunctions. • : U.S.- Pat. No. 5,625,083 • discloses” ‘diriitroglycerol esters of prostaglandins which may‘ be used as vasodilators, antihypertensive cardiovascular agents- or bronchodilators . U.S. Pat. No. 6,211,233 discloses compounds of the general formula A-Xι-N02,‘ wherein A contains ‘a ■■ – prostaglandin residue, .in ‘particular .‘PGEi, and Xi • is a bivalent connecting bridge; .’and their use fo ‘ treating impotence. It is an object of the present invention to provide new derivatives of prostaglandins able not only to eliminate or at least reduce the side ■ effects associated with these compounds, but also to possess an improved pharmacological activity. It has been surprisingly found that prostaglandin nitroderivatives have a significantly improved overall profile as compared to native, prostaglandins both in terms of -wider pharmacological .activity and enhanced tolerability. In particular, it has been recognized that the prostaglandin nitroderivatives of the present invention can be employed for treating glaucoma and ocular hypertension. The compounds of the present invention are indicated for the reduction of intraocular pressure in patients with open-angle glaucoma or with chronic angle- closure glaucoma who underwent peripheral iridotomy or laser iridoplasty.
Latanoprostene bunod
 Currently in Phase 3 clinical development with Nicox’s partner Bausch + Lomb
Currently in Phase 3 clinical development with Nicox’s partner Bausch + Lomb
Latanoprostene bunod is a nitric oxide-donating prostaglandin F2-alpha analog in Phase 3 clinical development for the reduction of intraocular pressure in patients with glaucoma and ocular hypertension. It was licensed to Bausch + Lomb by Nicox in March 2010
Bausch + Lomb initiated a global Phase 3 program for latanoprostene bunod (previously known as BOL-303259-X and NCX 116) in January 2013. This pivotal Phase 3 program includes two separate randomized, multicentre, double-masked, parallel-group clinical studies, APOLLO andLUNAR, designed to compare the efficacy and safety of latanoprostene bunod administered once daily (QD) with timolol maleate 0.5% administered twice daily (BID) in lowering intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension.
The primary endpoint of both studies, which will include a combined total of approximately 800 patients, is the reduction in mean IOP measured at specified time points during three months of treatment. The Phase 3 studies are pivotal for U.S. registration and will be conducted in North America and Europe.
In July 2013, Bausch + Lomb initiated two additional studies in Japan: JUPITER (Phase 3) and KRONUS (Phase 1). A confirmatory efficacy study is expected to be required for the Japanese registration of latanoprostene bunod.
Phase 2b top-line results
A phase 2b study conducted by Bausch + Lomb with latanoprostene bunod met its primary efficacy endpoint and showed positive results on a number of secondary endpoints, including responder rate.
No new class of drugs has come to market for treating glaucoma since 1996, when the FDA approved the first prostaglandin analogue, latanoprost (Xalatan). That could change soon: Experts who follow drug development are hopeful that we’re on the brink of reaping the benefits of years of research.
“It’s been a decade and a half and counting since we’ve had new class of drugs to treat glaucoma. We’ve had formulary improvements and fixed combinations, but no novel agents,” said Louis B. Cantor, MD, at Indiana University. “We’ve gone through a long dry spell but are just beginning to see, in the last couple of years, exploration by pharma of some new types of drugs.” But, he added, “We don t know how well those will pan out.
The uncertainty about “panning out” involves both drug efficacy and marketplace issues. As Dr. Cantor said, “Prostaglandin analogues are pretty effective. For a company to go into the investment of developing a new class of drugs for glaucoma, they have to be better than prostaglandin analogues.
Andrew G. Iwach, MD, at the University of California, San Francisco, agreed: “This is a unique time period for glaucoma medications in that we have very good drugs, usually well tolerated. And they’ve gone generic. That’s important, because having such strong generic contenders out there makes it harder for drug companies to try to introduce new molecules into this arena. Specifically, the prostaglandin analogues have set a high bar. It’s hard to compete with them.
Given this barrier, what are the marketplace incentives for development? Sheer numbers, for a start: Ten thousand people a day turn 65, and this rate will continue for 18 years, Dr. Cantor said. “The number of people who are going to need treatment for glaucoma has already begun to increase substantially.
Even more important, “Despite all the advances, our medical therapy fails not only for compliance reasons, but just fails,” Dr. Cantor said. “We need to continue to have new alternatives for treatment that are more effective, that last longer, and that have simple dosing requirements.
Thus, any new drug that makes it from the bench to the clinic will be a welcome addition. “Obviously, we want new and better therapies. We still have no cure for glaucoma. And while half of all patients are treatable with one drug, half are not. So we still need additional therapies to treat glaucoma,” said Gary D. Novack, PhD, president of Pharmalogic Development.
……………………….
http://www.google.com/patents/EP1704141A1?cl=en
EXAMPLE 1 Synthesis of [1R- [l (Z) , 2α (R*) , 3α, 5α] ] -7- [3, 5-dihydroxy-2- (3-hydroxy-5-phenylpentyl) cyclopentyl] -5-heptenoic acid 4- (nitrooxy) butyl ester (compound 1)
I Synthetic Pathway ONO,
MW 72.11 MW 153.02 MW 198.02
MW 390.51 MW 507.62
II EXPERIMENTAL II.1 Preparation of 4-bromobutanol
Tetrahydrofuran (12.5 g – 173 mmol) was charged under nitrogen in a reactor cooled to 5-10 °C. Hydrogen bromide (7.0 g. – 86.5 mmol) was then added slowly and the reaction ■medium was stirred over a period of 4.5 hours at 5-10°C. The mixture was diluted with 22.5 g of cold water and the pH of this solution was adjusted to pH=5-7 by adding 27.65% sodium hydroxide (2.0 g) keeping the temperature at 5-10 °C. The solution was then extracted twice with dichloromethane (13.25 g) . The combined organic phases were washed with -25% brine (7.5 g) , adjusted to pH=6-7 with 27.65% sodium hydroxide and dried over magnesium sulfate. Dichloromethane was distilled off and crude 4-bromobutanol (10.3 g – 66.9 mmol) was obtained in a yield of about 77%. II.2 Preparation of 4-bromobutyl nitrate
In reactor cooled to -5 to 5°C, nitric acid fuming (8.5 g – 135 mmol) was slowly added to a solution of 98% sulfuric acid (13.0 g – 130 mmol) in dichloromethane (18.0 g – 212 mmol). 4-bromobutanol (10.2 g – 66.6 mmol) was then added to this mixture and the reaction medium was stirred at -5 to 5°C over a period of 2-5 hours. The mixture was poured into cold water (110 g) keeping the temperature between -5 °C and 3°C. After decantation, the upper aqueous phase was extracted with dichloromethane and the combined organic phases were washed with water, adjusted to pH=6-7 by addition of 27.65% sodium hydroxide, washed with brine and dried over magnesium sulfate. Dichloromethane was distilled off under vacuum and crude 4-bromobutyl nitrate (12.7 g – 64.1 mmol) was recovered in a yield of about 96%.
II.3 Preparation of [1R- [lα-(Z) , 2β (R*) , 3α, 5α] ] -7- [3, 5- dihydroxy-2- (3-hydroxy-5-phenylpentyl) cyclopentyl] -5- heptenoic acid 4- (nitrooxy) butyl ester
Latanoprost acid (97.7%, S-isomer <1%) (213mg, 0.54 mmol) was dis.solved in 5.0 g anhydrous DMF. K2C03 (206′ mg, 1.49 mmol), KI (77 mg, 0.46 mmol)‘ and ‘4-bromobutylnitrate (805 mg, .25% w/w in methylene chloride, 1.02 mmol) were added. The reaction mixture was heated and stirred on a rotary evaporator at 45-50°C. fter 1.5. hour, TLC (Si, ■ CH2Cl2-MeOH, 5%) showed -no – starting acid. . . .. The reaction mixture was diluted with 100 ml ethyl acetate, washed with brine (3 x 50 ml), dried over MgS04 and evaporated to give yellowish oil (420 mg) .
5 1H NMR/13C NMR showed target molecule as a major product together with some starting 4-bromobutylnitrate and DMF. HPLC showed no starting acid. Residual solvent, 4- bromobutylnitrate and target ester were the main peaks. Butylnitrate ester showed similar UV spectrum as0 latanoprost and relative retention time was as expected.
Instrument: Bruker 300 MHz Solvent : CDC13 -5 H-NMR (CDC13) δ: 7.29-7.19 (5H, m, Ar) ; 5.45 (IH, m. CH=CH) ; 5.38 (IH, m, CH=CH) ;. 4.48 (2H, t, CH2-ON02) ; 4.18 (IH, m, CH-OH); 4.10 (2H, t, C00CH2) ; 3.95 (IH, m, CH-OH); 3.68 (IH, m, CH-OH); 2.87-2.60 (2H, ) ; 2.35 (2H, t) ; 2.25 (2H,m) ; 2.13 (2H,m) ; 1.90-1.35 (16H, m) .0 13C-NMR (CDCI3) ppm: 173.94 (C=0) ; 142.14; 129.55 (C5); 129.50 (C6) ; 128.50; 125.93 78.80 (Cu) ; 74.50 (C9) ; 72.70 (C-0N02) ; 71.39 (Ci5) ; 63.57; 52.99 (C12) 51.99 (C8); 41.30 (C10) ; 39.16 (Ci6) ; 33.66; 32.21; 29.73; 27.04; 26.70;5 25.04; 24.91; 23.72; 15.37.
 |
|
| Trabecular meshwork structure. The colors in this drawing delineate the layers of the TM. |
 |
|
| Hyperemia. A side effect that emerged in trials of ROCK inhibitors is hyperemia; researchers are exploring different strategies to reduce it. |
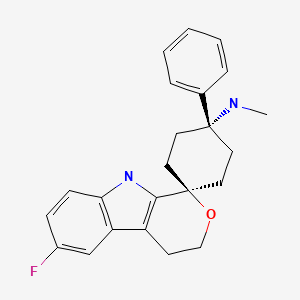
LEXANOPADOL, For Treatment of acute and chronic pain requiring opioid analgesia
LEXANOPADOL
trans-6′-Fluoro-N-methyl-4-phenyl-4′,9′-dihydro-3’H-spiro(cyclohexane-1,1′-pyrano(3,4-b)indol)-4-amine
PRONUNCIATION lex” an oh’ pa dol
THERAPEUTIC CLAIM Treatment of acute and chronic pain requiring opioid analgesia
CHEMICAL NAMES
1. Spiro[cyclohexane-1,1′(3’H)-pyrano[3,4-b]indol]-4-amine, 6′-fluoro-4′,9′-dihydro-N-methyl-4-phenyl-, trans-
2. Trans-6′-fluoro-N-methyl-4-phenyl-4′,9′-dihydro-3’H-spiro[cyclohexane-1,1′-pyrano[3,4-b]indol]-4-amine
3. Trans -6’-fluoro-4’,9’-dihydro-N-methyl-4-phenyl-spiro[cyclohexane-1,1’(3’H)-pyrano[3,4-b]indol]-4-amine
MOLECULAR FORMULA C23H25FN2O
MOLECULAR WEIGHT 364.5
SPONSOR Grűnenthal GmbH
CODE DESIGNATIONS GRT6006, GRT13106G
CAS REGISTRY NUMBER 1357348-09-4
UNIIDZ4NDW1LZX
WHO NUMBER 9765
gbk
The heptadecapeptide nociceptin is an endogenous ligand of the ORL1 (opioid receptor-like) receptor (Meunier et al., Nature 377, 1995, p. 532-535), which belongs to the family of opioid receptors and is to be found in many regions of the brain and spinal cord, and has a high affinity for the ORL1 receptor. The ORL1 receptor is homologous to the μ, κ and δ opioid receptors and the amino acid sequence of the nociceptin peptide has a marked similarity to those of the known opioid peptides. The receptor activation induced by nociceptin leads, via coupling with Gi/o proteins, to an inhibition of adenylate cyclase (Meunier et al., Nature 377, 1995, p. 532-535).
The nociceptin peptide shows a pronociceptive and hyperalgesic activity after intercerebroventicular administration in various animal models (Reinscheid et al., Science 270, 1995, p. 792-794). These findings can be explained as an inhibition of stress-induced analgesia (Mogil et al., Neuroscience 75, 1996, p. 333-337). In this connection, it has also been possible to demonstrate an anxiolytic activity of nociceptin (Jenck et al., Proc. Natl. Acad. Sci. USA 94, 1997, 14854-14858).
On the other hand, it has also been possible to demonstrate an antinociceptive effect of nociceptin in various animal models, in particular after intrathecal administration. Nociceptin has an antinociceptive action in various pain models, for example in the tail flick test in the mouse (King et al., Neurosci. Lett., 223, 1997, 113-116. It has likewise been possible to demonstrate an antinociceptive action of nociceptin in models for neuropathic pain, which is of particular interest inasmuch as the activity of nociceptin increases after axotomy of spinal nerves. This is in contrast to conventional opioids, the activity of which decreases under these conditions (Abdulla and Smith, J. Neurosci., 18, 1998, p. 9685-9694).
The ORL1 receptor is moreover also involved in regulation of further physiological and pathophysiological processes. These include, inter alia, learning and memory development (Manabe et al., Nature, 394, 1997, p. 577-581), audition (Nishi et al., EMBO J., 16, 1997, p. 1858-1864) and numerous further processes. A review article by Cabo et al. (Br. J. Pharmacol., 129, 2000, 1261-1283) gives an overview of the indications or biological processes in which the ORL1 receptor plays a role or with high probability could play a role. This mentions, inter alia: analgesia, stimulation and regulation of food intake, influence on μ-agonists, such as morphine, treatment of withdrawal symptoms, reduction in the addiction potential of opioids, anxiolysis, modulation of motor activity, impaired memory, epilepsy; modulation of neurotransmitter secretion, in particular glutamate, serotonin and dopamine, and therefore neurodegenerative diseases; influencing of the cardiovascular system, initiation of an erection, diuresis, anti-natriuresis, electrolyte balance, arterial blood pressure, water retention diseases, intestinal motility (diarrhea), relaxing effects on the respiratory tract, micturation reflex (urinary incontinence). The use of agonists and antagonists as anoretics, analgesics (also in co-administration with opioids) or nootropics is furthermore discussed.
The possible uses of compounds which bind to the ORL1 receptor and activate or inhibit this are correspondingly diverse. Alongside this, however, opioid receptors, such as the μ-receptor, but also the other sub-types of these opioid receptors, namely δ and κ, play a large role precisely in the area of pain therapy, but also in that of other indications of those mentioned. Accordingly, it is favourable if the compound also show an action on these opioid receptors.
SYN
http://www.google.com/patents/US20110319440

SYNTHESIS ……………..ON THE WAY ….. WATCH OUT
The dimethyl analogue is

Jirkovsky et al., J. Heterocycl. Chem., 12, 1975, 937-940;
Campaigne et al., J. Heterocycl. Chem., 2, 1965, 231-235;
Efange et al., J. Med. Chem., 41, 1998, 4486-4491;
Ellingboe et al., J. Med. Chem., 35, 1992, 1176-1183;
Pearson et al., Aust. J. Chem., 44, 1991, 907-917;
Yokohama et al., Chem. Pharm. Bull., 40, 1992, 2391-2398;
Beck et al., J. Chem. Soc. Perkin 1, 1992, 813-822;
Shinada et al., Tetrahedron Lett., 39, 1996, 7099-7102;
Garden et al., Tetrahedron, 58, 2002, 8399-8412;
Lednicer et al., J. Med. Chem., 23, 1980, 424-430.
|
2-10-2012
|
Pharmaceutical dosage forms comprising 6′-fluoro-(N-methyl- or N,N-dimethyl-)-4-phenyl-4′,9′-dihydro-3’H-spiro[cyclohexane-1,1′-pyrano[3,4,b]indol]-4-amine
|
|
|
11-9-2011
|
Compositions containing spirocyclic cyclohexane compounds
|
|
|
10-12-2011
|
Spirocyclic Cyclohexane Compounds Useful To Treat Substance Dependency
|
|
|
5-32-2011
|
Spirocyclic Cyclohexane Compounds
|
|
|
1-21-2011
|
MIXED ORL1/MU-AGONISTS FOR THE TREATMENT OF PAIN
|
|
|
9-22-2010
|
SPIROCYCLIC CYCLOHEXANE COMPOUNDS
|
|
|
6-17-2009
|
Spirocyclic cyclohexane compounds
|
|
|
9-12-2008
|
Spirocyclic Cyclohexane Compounds Useful To Treat Substance Dependency
|
|
|
5-30-2008
|
Mixed ORL1/mu-agonists for the treatment of pain
|
| US8614245 | Jan 8, 2013 | Dec 24, 2013 | Gruenenthal Gmbh | Crystalline (1r,4r)-6′-fluoro-N,N-dimethyl-4-phenyl-4′,9′-dihydro-3′H-spiro[cyclohexane-1,1′-pyrano[3,4,b]indol]-4-amine |
| US8618156 * | Jul 6, 2012 | Dec 31, 2013 | Gruenenthal Gmbh | Crystalline (1r,4r)-6′-fluoro-N,N-dimethyl-4-phenyl-4′,9′-dihydro-3’H-spiro[cyclohexane-1,1′-pyrano[3,4,b]indol]-4-amine |
| US8765800 | Mar 15, 2013 | Jul 1, 2014 | Gruenenthal Gmbh | Crystalline (1r,4r)-6′-fluoro-N,N-dimethyl-4-phenyl-4′,9′-dihydro-3′H-spiro[cyclohexane-1,1′-pyrano[3,4,b]indol]-4-amine |
| US20130231381 * | Mar 15, 2013 | Sep 5, 2013 | Gruenenthal Gmbh | Crystalline (1r,4r)-6′-fluoro-N,N-dimethyl-4-phenyl-4′,9′-dihydro-3’H-spiro[cyclohexane-1,1′-pyrano[3,4,b]indol]-4-amine |
| US5356896 * | Dec 22, 1992 | Oct 18, 1994 | Sandoz Ltd. | Alkaline stabiling medium |
| US20060004034 * | May 11, 2005 | Jan 5, 2006 | Gruenenthal Gmbh | Treating conditions associated with the nociceptin/ORL1 receptor system, e.g. pain, drug withdrawal, anxiety, muscle relaxants, anxiolytic agents; e.g. 1,1-[3-dimethylamino-3-(pyridin-2-yl)pentamethylene]-3,4-dihydro-1H-2,9-diazafluorene |
MAKE IN INDIA
http://makeinindia.com/sector/pharmaceuticals/
Read all about Organic Spectroscopy on ORGANIC SPECTROSCOPY INTERNATIONAL 
keep watching for synthesis update on this drug
QP Declaration: EMA publishes Comments
DRUG REGULATORY AFFAIRS INTERNATIONAL
QP Declaration: EMA publishes Comments
More than three years ago, the EMA has published two draft documents for a template for the QP’s declaration concerning GMP compliance of the API used as starting material and verification of its supply chain called “The QP declaration template“:
1. The draft template for the Qualified Person’s declaration
and
2. the respective draft Q&A on the template for the Qualified Person’s declaration
The QP Declaration should be provided in support of an application for a new marketing authorisation, variation or renewal of a medicinal product(s) authorised in the Community, using EU or national procedures within the scope of the respective Directives.
The consultation for the template ended on 30 April 2011. In June 2014, the final version was published together with a template guidance. Now, three months after publication of the final document, the comments from 2011 have been published.
The…
View original post 559 more words
FDA Approves Vitekta (elvitegravir) for HIV-1 Infection
FDA Approves Vitekta (elvitegravir) for HIV-1 Infection
September 24, 2014 — The U.S. Food and Drug Administration (FDA) has approved Vitekta (elvitegravir), an integrase strand transfer inhibitor for the combination treatment of human immunodeficiency virus type 1 (HIV-1) infection in treatment-experienced adults.

Elvitegravir
697761-98-1 CAS

Elvitegravir (EVG, formerly GS-9137) is a drug used for the treatment of HIV infection. It acts as an integrase inhibitor. It was developed[1] by the pharmaceutical company Gilead Sciences, which licensed EVG from Japan Tobacco in March 2008.[2][3][4] The drug gained approval by U.S. Food and Drug Administration on August 27, 2012 for use in adult patients starting HIV treatment for the first time as part of the fixed dose combination known as Stribild.[5]
According to the results of the phase II clinical trial, patients taking once-daily elvitegravir boosted by ritonavir had greater reductions in viral load after 24 weeks compared to individuals randomized to receive a ritonavir-boosted protease inhibitor.[6]
Human immunodeficiency virus type 1 (HIV-1) is the causative agent of acquired immunodeficiency disease syndrome (AIDS). After over 26 years of efforts, there is still not a therapeutic cure or an effective vaccine against HIV/AIDS. The clinical management of HIV-1 infected people largely relies on antiretroviral therapy (ART). Although highly active antiretroviral therapy (HAART) has provided an effective way to treat AIDS patients, the huge burden of ART in developing countries, together with the increasing incidence of drug resistant viruses among treated people, calls for continuous efforts for the development of anti-HIV-1 drugs. Currently, four classes of over 30 licensed antiretrovirals (ARVs) and combination regimens of these ARVs are in use clinically including: reverse transcriptase inhibitors (RTIs) (e.g. nucleoside reverse transcriptase inhibitors, NRTIs; and non-nucleoside reverse transcriptase inhibitors, NNRTIs), protease inhibitors (PIs), integrase inhibitors and entry inhibitors (e.g. fusion inhibitors and CCR5 antagonists).
- Gilead Press Release Phase III Clinical Trial of Elvitegravir July 22, 2008
- Gilead Press Release Gilead and Japan Tobacco Sign Licensing Agreement for Novel HIV Integrase Inhibitor March 22, 2008
- Shimura K, Kodama E, Sakagami Y, et al. (2007). “Broad Anti-Retroviral Activity and Resistance Profile of a Novel Human Immunodeficiency Virus Integrase Inhibitor, Elvitegravir (JTK-303/GS-9137)”. J Virol 82 (2): 764. doi:10.1128/JVI.01534-07. PMC 2224569. PMID 17977962.
- Stellbrink HJ (2007). “Antiviral drugs in the treatment of AIDS: what is in the pipeline ?”. Eur. J. Med. Res. 12 (9): 483–95. PMID 17933730.
- Sax, P. E.; Dejesus, E.; Mills, A.; Zolopa, A.; Cohen, C.; Wohl, D.; Gallant, J. E.; Liu, H. C.; Zhong, L.; Yale, K.; White, K.; Kearney, B. P.; Szwarcberg, J.; Quirk, E.; Cheng, A. K.; Gs-Us-236-0102 Study, T. (2012). “Co-formulated elvitegravir, cobicistat, emtricitabine, and tenofovir versus co-formulated efavirenz, emtricitabine, and tenofovir for initial treatment of HIV-1 infection: A randomised, double-blind, phase 3 trial, analysis of results after 48 weeks”.The Lancet 379 (9835): 2439–2448. doi:10.1016/S0140-6736(12)60917-9. PMID 22748591. edit
- Thaczuk, Derek and Carter, Michael. ICAAC: Best response to elvitegravir seen when used with T-20 and other active agents Aidsmap.com. 19 Sept. 2007.

The life cycle of HIV-1. 1. HIV-1 gp120 binds to CD4 and co-receptor CCR5/CXCR4 on target cell; 2. HIV-1 gp41 mediates fusion with target cell; 3. Nucleocapsid containing viral genome and enzymes enters cells; 4. Viral genome and enzymes are released; 5. Viral reverse transcriptase catalyzes reverse transcription of ssRNA, forming RNA-DNA hybrids; 6. RNA template is degraded by ribonuclease H followed by the synthesis of HIV dsDNA; 7. Viral dsDNA is transported into the nucleus and integrated into the host chromosomal DNA by the viral integrase enzyme; 8. Transcription of proviral DNA into genomic ssRNA and mRNAs formation after processing; 9. Viral RNA is exported to cytoplasm; 10. Synthesis of viral precursor proteins under the catalysis of host-cell ribosomes; 11. Viral protease cleaves the precursors into viral proteins; 12. HIV ssRNA and proteins assemble under host cell membrane, into which gp120 and gp41 are inserted; 13. Membrane of host-cell buds out, forming the viral envelope; 14. Matured viral particle is released
Elvitegravir, also known as GS 9137 or JTK 303, is an investigational new drug and a novel oral integrase inhibitor that is being evaluated for the treatment of HIV-1 infection. After HIVs genetic material is deposited inside a cell, its RNA must be converted (reverse transcribed) into DNA. A viral enzyme called integrase then helps to hide HIVs DNA inside the cell’s DNA. Once this happens, the cell can begin producing genetic material for new viruses. Integrase inhibitors, such as elvitegravir, are designed to block the activity of the integrase enzyme and to prevent HIV DNA from entering healthy cell DNA. Elvitegravir has the chemical name: 6-(3-chloro-2-fluorobenzyl)-1-[(S)-1 -hydroxy -methyl-2- methylpropyl]-7-methoxy-4-oxo-1, 4-dihydroquinoline-3-carboxylic acid and has the following structural formula:
WO 2000040561 , WO 2000040563 and WO 2001098275 disclose 4-oxo-1 , 4-dihydro-3- quinoline which is useful as antiviral agents. WO2004046115 provides certain 4- oxoquinoline compounds that are useful as HIV Integrase inhibitors.
US 7176220 patent discloses elvitegravir, solvate, stereoisomer, tautomer, pharmaceutically acceptable salt thereof or pharmaceutical composition containing them and their method of treatment. The chemistry involved in the above said patent is depicted below in the Scheme A. Scheme-A
Toluene, DIPEA
SOCl2 ,COCl (S)-(+)-Valinol
Toluene
,4-Difluoro-5-iodo- benzoic acid
THF
dichlorobis(triphenylphosphine)
palladium argon stream,
Elvitegravir Form ] Elvitegravir (residue) US 7635704 patent discloses certain specific crystalline forms of elvitegravir. The specific crystalline forms are reported to have superior physical and chemical stability compared to other physical forms of the compound. Further, process for the preparation of elvitegravir also disclosed and is depicted below in the Scheme B. The given processes involve the isolation of the intermediates at almost all the stages.
Scheme B
2,
–
Zn THF,
CK Br THF CU “ZnBr dιchlorobis(trιphenylphos
phine)palladium
Elvitegravir WO 2007102499 discloses a compound which is useful as an intermediate for the synthesis of an anti-HIV agent having an integrase-inhibiting activity; a process for production of the compound; and a process for production of an anti-HIV agent using the intermediate.
WO 2009036161 also discloses synthetic processes and synthetic intermediates that can be used to prepare 4-oxoquinolone compounds having useful integrase inhibiting properties.
The said processes are tedious in making and the purity of the final compound is affected because of the number of steps, their isolation, purification etc., thus, there is a need for new synthetic methods for producing elvitegravir which process is cost effective, easy to practice, increase the yield and purity of the final compound, or that eliminate the use of toxic or costly reagents.
US Patent No 7176220 discloses Elvitegravir, solvate, stereoisomer, tautomer, pharmaceutically acceptable salt thereof or pharmaceutical composition containing them and ■ their method of treatment. US Patent No 7635704 discloses Elvitegravir Form II, Form III and processes for their preparation. The process for the preparation of Form Il disclosed in the said patent is mainly by three methods – a) dissolution of Elvitegravir followed by seeding with Form II, b) recrystallisation of Elvitegravir, and c) anti-solvent method.
The process for the preparation of Form III in the said patent is mainly by three methods – a) dissolution of Form Il in isobutyl acetate by heating followed by cooling the reaction mass, b) dissolution of Form Il in isobutyl acetate by heating followed by seeding with Form III, and c) dissolving Form Il in 2-propanol followed by seeding with Form III.
Amorphous materials are becoming more prevalent in the pharmaceutical industry. In order to overcome the solubility and potential bioavailability issues, amorphous solid forms are becoming front-runners. Of special importance is the distinction between amorphous and crystalline forms, as they have differing implications on drug substance stability, as well as drug product stability and efficacy.
An estimated 50% of all drug molecules used in medicinal therapy are administered as salts. A drug substance often has certain suboptimal physicochemical or biopharmaceutical properties that can be overcome by pairing a basic or acidic drug molecule with a counter- ion to create a salt version of the drug. The process is a simple way to modify the properties of a drug with ionizable functional groups to overcome undesirable features of the parent drug. Salt forms of drugs have a large effect on the drugs’ quality, safety, and performance. The properties of salt-forming species significantly affect the pharmaceutical properties of a drug and can greatly benefit chemists and formulators in various facets of drug discovery and development.



chemical synthesis from a carboxylic acid 1 starts after conversion to the acid chloride iodide NIS 2 , and with three condensation 4 . 4 and the amino alcohol 5 addition-elimination reaction occurs 6 , 6 off under alkaline conditions with TBS protected hydroxy get the ring 7 , 7 and zinc reagent 8 Negishi coupling occurs to get 9 , the last 9 hydrolysis and methoxylated
Elvitegravir dimer impurity, WO2011004389A2
Isolation of 1-[(2S)-1-({3-carboxy-6-(3-chloro-2-fluorobenzyl)-1 -[(2S)-I- hydroxy-3-methylbutan-2-yl]-4-oxo-1 , 4-dihydroquinolin-7-yl}oxy)-3- methylbutan-2-yl 6-(3-chloro-2-fluorobenzyl)-7-methoxy-4-oxo-1 , 4-dihydroquinoline-3-carboxylic acid (elvitegravir dimer impurity, 13)
After isolation of the elvitegravir from the mixture of ethyl acetate-hexane, solvent from the filtrate was removed under reduced pressure. The resultant residue purified by column chromatography using a mixture of ethyl acetate-hexane (gradient, 20-80% EtOAc in hexane) as an eluent. Upon concentration of the required fractions, a thick solid was obtained which was further purified on slurry washing with ethyl acetate to get pure elvitegravir dimer impurity (13). The 1H-NMR, 13C-NMR and mass spectral data complies with proposed structure.
1H-NMR (DMSO-Cf6, 300 MHz, ppm) – δ 0.79 (m, d=6.3 Hz, 6H, 20 & 2O’)\ 1.18 & 1.20 (d, J=6.3 Hz & J=6.2 Hz, 6H, 21 & 21′)1, 2.42-2.49 (m, 2H, 19 & 19′), 3.81-3.89 (m, 3H, T & 17’Ha), 3.94-4.01 (m, 1 H, 17’Hb), 4.01 (s, 3H, 23), 4.11 (s, 2H, 7), 4.83-4.85 (m, 3H, 17 & 18′), 5.22 (t, J=4.7 Hz, 1H, OH), 5.41-5.44 (m, 1 H, 18), 6.73-6.78 (t, J=7.1 Hz, 1 H, 11)1‘ 2, 6.92-6.98 (t, J=8.0 Hz, 1H, 3′) 1‘2, 7.12-7.22 (m, 2H, 1 & 3), 7.34-7.39 (m, 1H, 2′),
7.45-7.48 (m, 1 H, 2), 7.49, 7.56 (s, 2H, 15 & 15′), 7.99, 8.02 (s, 2H, 9 & 9′), 8.89, 9.01 (s, 2H, 13 & 13′), 15.30, 15.33 (s, 2H, COOH’ & COOH”).
13C-NMR (DMSO-Cf6, 75 MHz, ppm)- δ 18.87, 19.03 (2OC, 20’C), 19.11 , 19.24 (21 C, 21 ‘C), 27.94 (7’C), 28.40 (7C), 28.91 , 30.08 (19C, 19’C), 56.80(23C), 60.11 (171C), 63.59 (18C), 66.52 (18’C), 68.53 (17C), 97.86, 98.97 (15, 15′), 107.43, 108.16 (12C, 12’C),
118.77, 119.38 (1OC, 10’C), 119.57 (d, J=17.6 Hz, 41C), 119.61 (d, J=17.9 Hz, 4C),
124.88 (d, J=4.3 Hz, 31C), 125.18 (d, J=4.2 Hz, 3C), 126.59, 126.96 (9C1 9’C), 127.14 (8’C), 127.62 (d, J=15.9 Hz, 61C), 127.73 (8C), 127.99 (d, J=15.2 Hz, 6C), 128.66 (2’C),
128.84 (11C), 128.84 (2C), 130.03 (d, J=3.4 Hz, 1C), 142.14, 142.44 (14C, 14’C), 144.37, 145.56 (13C, 131C), 155.24 (d, J=245.1 Hz, 5’C)1 155.61 (d, J=245.1 Hz, 5C),
160.17 (16’C), 162.04 (16C), 166.00, 166.14 (22C, 22’C), 176.17, 176.22 (11C, 111C).
DIP MS: m/z (%)- 863 [M+H]+, 885 [M+Na]+.
MAKE IN INDIA
http://makeinindia.com/sector/pharmaceuticals/

FDA Approves Spiriva Respimat (tiotropium) for the Maintenance Treatment of COPD

Ridgefield, Conn., September 25, 2014 – Boehringer Ingelheim Pharmaceuticals, Inc. announced today that the U.S. Food and Drug Administration (FDA) approved Spiriva Respimat (tiotropium bromide) inhalation spray for the long-term, once-daily maintenance treatment of bronchospasm associated with chronic obstructive pulmonary disease (COPD), including chronic bronchitis and emphysema and to reduce exacerbations in COPD patients. Boehringer Ingelheim anticipates Spiriva Respimat to be available in January 2015.

Spiriva Respimat provides a pre-measured amount of medicine in a slow-moving mist that helps patients inhale the medicine. Spiriva Respimat was developed to actively deliver medication in a way that does not depend of how fast air is breathed in from the inhaler.
READ AT


MAKE IN INDIA
FDA Approves Tybost (cobicistat) for use in the treatment of HIV-1 Infection

Cobicistat, GS-9350
1004316-88-4
| C 40 H 53 N 7 O 5 S 2 |
N-[1(R)-Benzyl-4(R)-[2(S)-[3-(2-isopropylthiazol-4-ylmethyl)-3-methyl]ureido]-4-(4-morpholinyl)butyramido]-5-phenylpentyl]carbamic acid thiazol-5-ylmethyl ester
(1,3-thiazol-5-yl) methyl (5S, 8R, 11R) -8,11-dibenzyl-2-methyl-5-[2 – (morpholin-4-yl) ethyl] -1 – [2 – (propan-2-yl) -1,3-thiazol-4-yl] -3,6-dioxo-2 ,4,7,12-tetraazatridecan-13-oate
cytochrome P450 3A4 (CYP3A4) inhibitor
FDA Approves Tybost (cobicistat) for use in the treatment of HIV-1 Infection
September 24, 2014 — The U.S. Food and Drug Administration (FDA) has approved Tybost (cobicistat), a CYP3A inhibitor used in combination with atazanavir or darunavir for the treatment of human immunodeficiency virus type 1 (HIV-1) infection
Cobicistat is a pharmacokinetic enhancer that works by inhibiting the enzyme (CYP3A) that metabolizes atazanavir and darunavir. It increases the systemic exposure of these drugs and prolongs their effect. Cobicistat is also one of the ingredients in the combination HIV drug Stribild, which was approved by the FDA in August, 2012.
Tybost comes in 150 mg tablets and is administered once daily in combination with the protease inhibitors atazanavir (Reyataz), or darunavir (Prezista).
Because Tybost inhibits CYP3A, other medications metabolized by CYP3A may result in increased plasma concentrations and potentially severe side effects, which may be life-threatening or even fatal. Extra care should be exercised by healthcare professionals to ensure than other medications are reviewed and their concentrations monitored, especially when initiating new medicines or changing doses.
The approval of Tybost was based on the following clinical trials:
•The data to support the use of atazanavir and Tybost were from a phase 2 and 3 trial in treatment-naïve adults comparing atazanavir/cobicistat 300/150 mg and atazanavir/ritonavir 300/100 mg once daily each in combination with Truvada. The atazanavir/cobicistat based regimen was non-inferior to the atazanavir/ritonavir based regimen.
•The data to support the use of cobicistat with darunavir is from a multiple dose trial in healthy subjects comparing the relative bioavailability of darunavir/cobicistat 800/150 mg to darunavir/ritonavir 800/100 mg.
The most common adverse drug reactions observed with Tybost (in combination with atazanavir) in clinical trials were jaundice, ocular icterus, and nausea.
Tybost is a product of Gilead Sciences, Foster City, CA.

Cobicistat (formerly GS-9350) is a licensed drug for use in the treatment of infection with the human immunodeficiency virus (HIV).
Like ritonavir (Norvir), cobicistat is of interest not for its anti-HIV properties, but rather its ability to inhibit liver enzymes that metabolize other medications used to treat HIV, notablyelvitegravir, an HIV integrase inhibitor currently under investigation itself. By combining cobicistat with elvitegravir, higher concentrations of elvitgravir are achieved in the body with lower dosing, theoretically enhancing elvitgravir’s viral suppression while diminishing its adverse side-effects. In contrast with ritonavir, the only currently approved booster, cobicistat has no anti-HIV activity of its own.[1]
Cobicistat, a cytochrome P450 CYP3A4 inhibitor, was approved in the E.U. in 2013 as a pharmacokinetic enhancer of the HIV-1 protease inhibitors atazanavir and darunavir in adults. First launch took place in 2014 in United Kingdom. In 2012, Gilead filed a New Drug Application in the U.S. for the same indication. In April 2013, the FDA issued a Complete Response Letter from the FDA. In 2014 the FDA accepted Gilead’s resubmission.
Cobicistat is a component of the four-drug, fixed-dose combination HIV treatmentelvitegravir/cobicistat/emtricitabine/tenofovir (known as the “Quad Pill” or Stribild).[1][2] The Quad Pill/Stribild was approved by the FDA in August 2012 for use in the United States and is owned by Gilead Sciences.
Cobicistat is a potent inhibitor of cytochrome P450 3A enzymes, including the importantCYP3A4 subtype. It also inhibits intestinal transport proteins, increasing the overall absorption of several HIV medications, including atazanavir, darunavir and tenofovir alafenamide fumarate.[3]
The drug candidate acts as a pharmaco-enhancer to boost exposure of HIV protease inhibitors. In 2011, cobicistat was licensed to Japan Tobacco by Gilead for development and commercialization in Japan as a stand-alone product for the treatment of HIV infection. In 2012, orphan drug designation was assigned in Japan for the pharmacokinetic enhancement of anti-HIV agent.
Oxidative metabolism by cytochrome P450 enzymes is one of the primary mechanisms of drug metabolism.. It can be difficult to maintain therapeutically effective blood plasma levels of drugs which are rapidly metabolized by cytochrome P450 enzymes. Accordingly, the blood plasma levels of drugs which are susceptible to cytochrome P450 enzyme degradation can be maintained or enhanced by co-administration of cytochrome P450 inhibitors, thereby improving the pharmacokinetics of the drug.
While certain drugs are known to inhibit cytochrome P450 enzymes, more and/or improved inhibitors for cytochrome P450 monooxygenase are desirable. Particularly, it would be desirable to have cytochrome P450 monooxygenase inhibitors which do not have appreciable biological activity other than cytochrome P450 inhibition. Such inhibitors can be useful for minimizing undesirable biological activity, e.g., side effects. In addition, it would be desirable to have P450 monooxygenase inhibitors that lack significant or have a reduced level of protease inhibitor activity. Such inhibitors could be useful for enhancing the effectiveness of antiretroviral drugs, while minimizing the possibility of eliciting viral resistance, especially against protease inhibitors.
…………………………….
Cobicistat (GS-9350): A potent and selective inhibitor of human CYP3A as a novel pharmacoenhancer
ACS Med Chem Lett 2010, 1(5): 209
http://pubs.acs.org/doi/abs/10.1021/ml1000257
http://pubs.acs.org/doi/suppl/10.1021/ml1000257/suppl_file/ml1000257_si_001.pdf

Cobicistat (3, GS-9350) is a newly discovered, potent, and selective inhibitor of human cytochrome P450 3A (CYP3A) enzymes. In contrast to ritonavir, 3 is devoid of anti-HIV activity and is thus more suitable for use in boosting anti-HIV drugs without risking selection of potential drug-resistant HIV variants. Compound 3 shows reduced liability for drug interactions and may have potential improvements in tolerability over ritonavir. In addition, 3 has high aqueous solubility and can be readily coformulated with other agents.
…………………………………
http://www.google.com/patents/CN103694196A?cl=en
CN 103694196
oxidative metabolism by cytochrome P450 enzymes is one of the main mechanisms of drug metabolism, generally by administration of cytochrome P450 inhibitors to maintain or increase the degradation of cytochrome P450 enzymes are sensitive to the drug plasma levels, in order to improve the pharmacokinetics of drugs dynamics, can be used to enhance the effectiveness of anti-retroviral drugs. For example W02008010921 discloses compounds of formula I as a cytochrome P450 monooxygenase specific compounds (Cobicistat):
W02008010921 discloses the synthesis of compounds of formula I with a variety of, as one of the methods of the following routes
Shows:
The reagents used in the method is expensive, and more difficult to remove by-products, long reaction time, high cost, is not conducive to industrial
Production.
W02010115000 on these routes has been improved:
The first step in the route used for the ring-opening reaction reagent trimethylsilyl iodide, trimethylsilyl iodide expensive. W02010115000 reports this step and the subsequent ring-opening reaction of morpholine substitution reaction yield of two steps is not high, only 71%, so that only iodotrimethylsilane a high cost of raw material is not suitable for industrial production.



Preparation of compounds of formula I
Example [0126] Implementation
[0127] I1-a (20g) was dissolved in dichloromethane, was added 50% K0H (5.5g) solution, control the internal temperature does not exceed 25 ° C, TLC analysis ΙΙ-a disappears. Was cooled to O ~ 10 ° C, was added (2R, 5R) -5 – amino-1 ,6 – diphenyl-2 – hexyl-carbamic acid 5 – methyl-thiazole ester hydrochloride (14.8g), stirred for I ~ 2 h, 1 – hydroxybenzotriazole triazole (5.5g), stirred for I h, 1 – ethyl – (3 – dimethylaminopropyl) carbodiimide hydrochloride (15g), and incubated for 5 ~ 10 hours, TLC analysis of the starting material disappeared, the reaction was completed. The reaction was quenched with aqueous acetic acid, methylene chloride layer was separated, washed with saturated aqueous NaHCO3, washed with water, dried and concentrated. By HPLC purity of 99.1%. Adding ethanol, the ethanol was evaporated to give the product compound of part I of a solution in ethanol. Molar yield 88%, LC-MS: M +1 = 777.1 [0128] All publications mentioned in the present invention are incorporated by reference as if each reference was individually incorporated by reference, as cited in the present application. It should also be understood that, after reading the foregoing teachings of the present invention, those skilled in the art that various modifications of the present invention or modifications, and these equivalents falling as defined by the appended claims scope of claims of the present application.
…………………………
US 2014088304
http://www.google.com/patents/US20140088304
International Patent Application Publication Number WO 2008/010921 and International Patent Application Publication Number WO 2008/103949 disclose certain compounds that are reported to be useful to modify the pharmacokinetics of a co-administered drug, e.g. by inhibiting cytochrome P450 monooxygenase. One specific compound identified therein is a compound of the following formula I:
There is currently a need for improved synthetic methods and intermediates that can be used to prepare the compound of formula I and its salts
Schemes 1-4 below.
Preparation of a Compound of Formula IV
Example 14Preparation of Compound I
To the solution of L-thiazole morpholine ethyl ester oxalate salt XIVa (35.6 kg) in water (66.0 kg) was charged dichloromethane (264 kg), followed by a slow addition of 15 wt % KHCO3 solution (184.8 kg). The resulting mixture was agitated for about 1 hour. The layers were separated and the organic layer was washed with water (132 kg). The organic layer was concentrated under vacuum to dryness. Water (26.5 kg) was charged and the content temperature was adjusted to about 10° C., followed by slow addition of 45% KOH solution (9.8 kg) while maintaining the content temperature at less than or equal to 20° C. The mixture was agitated at less than or equal to 20° C. until the reaction was judged complete by HPLC. The reaction mixture was concentrated under vacuum to dryness and co-evaporated five times with dichloromethane (132 kg each time) under reduced pressure to dryness. Co-evaporation with dichloromethane (132 kg) was continued until the water content was <4% by Karl Fischer titration. Additional dichloromethane (264 kg) was charged and the content temperature was adjusted to −18° C. to −20° C., followed by addition of monocarbamate.HCl salt IXa (26.4 kg). The resulting mixture was agitated at −18° C. to −20° C. for about 1 hour. HOBt (11.4 kg) was charged and the reaction mixture was again agitated at −18° C. to −20° C. for about 1 hour. A pre-cooled solution (−20° C.) of EDC.HCl (21.4 kg) in dichloromethane (396 kg) was added to the reaction mixture while the content temperature was maintained at less than or equal to −20° C. The reaction mixture was agitated at −18° C. to −20° C. until the reaction was judged complete. The content temperature was adjusted to about 3° C. and the reaction mixture quenched with a 10 wt % aqueous citric acid solution (290 kg). The layers were separated and the organic layer was washed once with 15 wt % potassium bicarbonate solution (467 kg) and water (132 kg). The organic layer was concentrated under reduced pressure and then co-evaporated with absolute ethanol.
The product I was isolated as the stock solution in ethanol (35.0 kg product, 76.1% yield).
1H NMR (dDMSO) δ□ 9.05 (s, 1H), 7.85 (s, 1H), 7.52 (d, 1H), 7.25-7.02 (m, 12H), 6.60 (d, 1H), 5.16 (s, 2H), 4.45 (s, 2H), 4.12-4.05 (m, 1H), 3.97-3.85 (m, 1H), 3.68-3.59 (m, 1H), 3.57-3.45 (m, 4H), 3.22 (septets, 1H), 2.88 (s, 3H), 2.70-2.55 (m, 4H), 2.35-2.10 (m, 6H), 1.75 (m, 1H), 1.62 (m, 1H), 1.50-1.30 (m, 4H), 1.32 (d, 6H).
13C NMR (CD3OD) δ 180.54, 174., 160.1, 157.7, 156.9, 153.8, 143.8, 140.1, 140.0, 136.0, 130.53, 130.49, 129.4, 127.4, 127.3, 115.5, 67.7, 58.8, 56.9, 55.9, 54.9, 53.9, 51.6, 49.8, 42.7, 42.0, 35.4, 34.5, 32.4, 32.1, 29.1, 23.7.
Example 13Preparation of L-Thiazole Morpholine Ethyl Ester Oxalate Salt XIVa
To a solution of (L)-thiazole amino lactone XII (33.4 kg) in dichloromethane (89.5 kg) was charged dichloromethane (150 kg) and absolute ethanol (33.4 kg). The content temperature was then adjusted to about 10° C., followed by slow addition of TMSI (78.8 kg) while the content temperature was maintained at less than or equal to 22° C. and agitated until the reaction was judged complete. The content temperature was adjusted to about 10° C., followed by a slow addition of morpholine (49.1 kg) while the content temperature was maintained at less than or equal to 22° C. Once complete, the reaction mixture was filtered to remove morpholine.HI salt and the filter cake was rinsed with two portions of dichloromethane (33.4 kg). The filtrate was washed twice with water (100 kg). The organic layer was concentrated under vacuum to dryness. Acetone (100 kg) was then charged to the concentrate and the solution was concentrated under reduced pressure to dryness. Acetone (233.8 kg) was charged to the concentrate, followed by a slow addition of the solution of oxalic acid (10 kg) in acetone (100 kg). The resulting slurry was refluxed for about 1 hour before cooling down to about 3° C. for isolation. The product XIVa was filtered and rinsed with acetone (66.8 kg) and dried under vacuum at 40° C. to afford a white to off-white solid (40 kg, 71% yield). 1H NMR (CDCl3) δ □7.00 (s, 1H), 6.35 (broad s, 1H), 4.60-4.40 (m, 3H), 4.19 (quartets, 2H), 4.00-3.90 (m, 4H), 3.35-3.10 (m, 7H), 3.00 (s, 3H), 2.40-2.30 (m, 1H), 2.15-2.05 (m, 1H), 1.38 (d, 6H), 1.25 (triplets, 3H).
……………………………………..
W02008010921
http://www.google.co.in/patents/WO2008010921A2?cl=en
Preparation of Example A
Scheme 1
Example A Compound 2
To a solution of Compound 1 (ritonavir) (1.8 g, 2.5 mmol) in 1,2- dichloroethane (15 mL) was added l,l’-thiocarbonyldiimidazole (890 mg, 5.0 mmol). The mixture was heated at 75 SC for 6 hours and cooled to 25 SC. Evaporation under reduced pressure gave a white solid. Purification by flash column chromatography (stationary phase: silica gel; eluent: EtOAc) gave Compound 2 (1.6 g). m/z: 831.1 (M+H)+. Example A
To the refluxing solution of tributyltin hydride (0.78 mL, 2.9 mmol) in toluene (130 mL) was added a solution of Compound 2 (1.6 g, 1.9 mmol) and 2,2′- azobisisobutyronitrile (31 mg, 0.19 mmol) in toluene (30 mL) over 30 minutes. The mixture was heated at 1152C for 6 hours and cooled to 25 BC. Toluene was removed under reduced pressure. Purification by flash column chromatography (stationary phase: silica gel; eluent: hexane/EtOAc = 1/10) gave Example A (560 mg). m/z: 705.2 (M+H)+. 1H-NMR (CDCl3) δ 8.79 (1 H, s), 7.82 (1 H, s), 7.26-7.05 (10 H, m), 6.98 (1 H, s), 6.28 (1 H, m), 6.03 (1 H, m), 5.27 (1 H7 m), 5.23 (2 H, s), 4.45-4.22 (2 H, m), 4.17 (1 H, m), 3.98 (1 H, m), 3.75 (1 H, m), 3.25 (1 H7 m), 2.91 (3 H, s), 2.67 (4 H, m), 2.36 (1 H, m), 1.6-1.2 (10 H, m), 0.85 (6 H, m).
| EP1183026A2 * | 25 May 2000 | 6 Mar 2002 | Abbott Laboratories | Improved pharmaceutical formulations |
| US20060199851 * | 2 Mar 2006 | 7 Sep 2006 | Kempf Dale J | Novel compounds that are useful for improving pharmacokinetics |
| Thiazol-5-ylmethyl N-[1-benzyl-4-[[2-[[(2-isopropylthiazol-4-yl)methyl-methyl-carbamoyl]amino]-4-morpholino-butanoyl]amino]-5-phenyl-pentyl]carbamate | |
| Clinical data | |
|---|---|
| Legal status |
fda approved sept 2014
|
| Identifiers | |
| CAS number | 1004316-88-4 |
| ATC code | V03AX03 |
| PubChem | CID 25151504 |
| ChemSpider | 25084912 |
| UNII | LW2E03M5PG |
| Chemical data | |
| Formula | C40H53N7O5S2 |
| Mol. mass | 776.023 g/mol |
| US7939553 * | Jul 6, 2007 | May 10, 2011 | Gilead Sciences, Inc. | co-administered drug (as HIV protease inhibiting compound, an HIV (non)nucleoside/nucleotide inhibitor of reverse transcriptase, capsid polymerization inhibitor, interferon, ribavirin analog) by inhibiting cytochrome P450 monooxygenase; ureido- or amido-amine derivatives; side effect reduction |
- Highleyman, L.
Elvitegravir “Quad” Single-tablet Regimen Shows Continued HIV Suppression at 48 Weeks
- R Elion, J Gathe, B Rashbaum, and others. The Single-Tablet Regimen of Elvitegravir/Cobicistat/Emtricitabine/Tenofovir Disoproxil Fumarate (EVG/COBI/FTC/TDF; Quad) Maintains a High Rate of Virologic Suppression, and Cobicistat (COBI) is an Effective Pharmacoenhancer Through 48 Weeks. 50th Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC 2010). Boston, September 12–15, 2010.
- Lepist, E. -I.; Phan, T. K.; Roy, A.; Tong, L.; MacLennan, K.; Murray, B.; Ray, A. S. (2012). “Cobicistat Boosts the Intestinal Absorption of Transport Substrates, Including HIV Protease Inhibitors and GS-7340, in Vitro”. Antimicrobial Agents and Chemotherapy 56 (10): 5409–5413. doi:10.1128/AAC.01089-12. PMC 3457391. PMID 22850510.
-
Patent No all US
Expiry 5814639 Sep 29, 2015 5814639*PED Mar 29, 2016 5914331 Jul 2, 2017 5914331*PED Jan 2, 2018 5922695 Jul 25, 2017 5922695*PED Jan 25, 2018 5935946 Jul 25, 2017 5935946*PED Jan 25, 2018 5977089 Jul 25, 2017 5977089*PED Jan 25, 2018 6043230 Jul 25, 2017 6043230*PED Jan 25, 2018 6642245 Nov 4, 2020 6642245*PED May 4, 2021 6703396 Mar 9, 2021 6703396*PED Sep 9, 2021 7176220 Nov 20, 2023 7635704 Oct 26, 2026 8148374 Sep 3, 2029
WHO publishes New Version of the Draft on “Hold-Time” Studies
DRUG REGULATORY AFFAIRS INTERNATIONAL
WHO publishes New Version of the Draft on “Hold-Time” Studies
The 2nd revision for comment was published already in February this year (we reported). Now, a 3rd version is available – also for comment. The document describes the design of hold-time studies for the determination of time limits which have to be determined according to the generally applicable intermediate and bulk products. This should avoid that the storage of intermediate or bulk products from having any negative influence on their quality or the quality of a finished before processing to the next stage.
Chapter 2 which defines what intermediate and bulk products are has been added. It is now explicitly pointed out that hold-time investigations are part of the process validation. In turn, the reference to retrospective observation has been removed from the current version as well as – fortunately – the incomprehensible paragraph on the ‚most probable /…
View original post 113 more words
How to identify Out-of-Trend Results in Stability Studies?
DRUG REGULATORY AFFAIRS INTERNATIONAL

How to identify Out-of-Trend Results in Stability Studies?
http://www.gmp-compliance.org/enews_4522_How-to-identify-Out-of-Trend-Results-in-Stability-Studies_8360,8348,8430,Z-QCM_n.html
An article in PharmTech from June 2013 (by Trajkovic-Jolevska et. al) deals with the methods to identify Out-of-Trend (OOT) results in ongoing stability studies.
With regard to stability studies, it is important to make the difference between Out-of-Specification (OOS) and Out-of-Trend (OOT). Both the pharmaceutical industry and authorities often misuse these two terms.
The article defines OOT results as those results which don’t follow the expected trend, either in comparison with other stability batches or compared to previous results collected during a stability study. OOT results aren’t necessarily OOS, but they don’t look like a typical data point.
Although OOT results are a serious problem, neither the scientific literature nor regulatory guidelines fully address them.
The aim of the study described in this Pharmtech article by Trajkovic-Jolevska et. al was to perform a statistical evaluation of the statistical methods used in…
View original post 112 more words
Pirenperone, R 47465

ON THE LEFT OR ABOVE
IS
3-(2- {4-[(4-fluorophenyl)carbonyl]piperidin- 1 -yl} ethyl)-2-methyl-4H-pyrido[ 1 ,2- α]pyrimidin-4-one
3-(2-{4-[(4-fluorophenyl)carbonyl]piperidin-1-yl}ethyl)-2-methyl-4H-pyrido[1,2-α]pyrimidin-4-one
3-[2-[4-(4-fluorobenzoyl)-1-piperidinyl]ethyl]-2-methyl-4H-pyrido[1,2-a]pyri- midin-4-one
pirenperone CAS : 75444-65-4
- C23 H24 F N3 O2
- 4H-Pyrido[1,2-a]pyrimidin-4-one, 3-[2-[4-(4-fluorobenzoyl)-1-piperidinyl]ethyl]-2-methyl-
- R 47465
Cardiovascular disease; Inflammatory disease; Neoplasm; Pain
Calcium channel modulator T-type
……………………………..
http://www.google.co.in/patents/US4342870
http://www.google.co.in/patents/EP0037265A1
Example XXIV
-
A solution of 2 parts of 3-[2-[4-(4-fluorobenzoyl)-1 -piperidinyl]ethyl]-2 -methyl-4H -pyricio[1, 2 -a]pyrimidin-4-one in 64 parts of 2-propanol is warm acidified with 2-propanol saturated with hydrogen chloride. The formed hydrochloride salt is allowed to crystallize. It is filtered off and dried, yielding 2 parts (85. 5%) of 3-[2-[4-(4-fluorobenzoyl)-1-piperidinyl]ethyl]-2-methyl-4H-pyrido[1,2-a]pyri- midin-4-one dihydrochloride; mp. + 300°C.
-
In a similar manner there are also prepared:
- 3-[2 -[4-(4-fluorobenzoyl)-1-piperidiny]yethyl7-2 -methyl-4H-pyrido-[1, 2 -a]pyrimidin-4-one sulfate (1 : 2); mp. 254. 7°C; and
- 3-[2-[4-(4-fluorobenzoyl)-1 -piperidinyl]ethyl]-2-methyl-4H-pyrido-[1, 2-a]pyrimidin-4-one phosphate (1 : 2) ; mp. 243.8°C.
WO-2014143915
http://www.google.com/patents/WO2014143915A1?cl=en
Novelcrystalline polymorphic forms of pirenperone, useful for treating disorders associated with T-type calcium ion channels such as pain syndrome, neoplasm, cardiovascular disease or inflammation. VM Discovery, from which VM Therapeutics was spun out, was investigating the VMD-C300 series of compounds which act as T-type calcium channel modulators, including VMD-3816 and VMD-3222, for treating cancer, pain, neurological diseases and cardiovascular diseases; but as of September 2014, this program was assumed to be discontinued. See WO2009108798, (by the inventor, assigned to VM Discovery) claiming use of the same compound for treating same indications.
It was first disclosed in the now-expired US Patent No. 4,342,870 (Claim 5), and intended to be used as potential anti-anxiety drug. However, the early human clinical studies has shown that the compound did not show any dose-related anti-anxiety effects as hoped, but otherwise the compound was safe in human (ref. Ansseau M, Doumo t A, Thlry D, Gelders Y. “Pilot study of a specific serotonergic antagonist, pirenperone, in the treatment of anxiety disorders”, Acta Psychiatr Belg, 1983 Sep-Oct;83(5):517-24). in the US Patent No. 4,342,870, there is no crystalline polymorphic form disclosed, nor disclosure of potential uses for management of pain and treatment of other related diseases or disorders.
It was further disclosed in the PCT patent application WO/2009/108798 as “Compound 10 (pirenperone)‘” to be used for novel T-type calcium ion channel antagonist for management of pain and treatment of other diseases or disorders associated to the T-type calcium ion channels.
Surprisingly, we have found that there are many crystalline polymorphic forms of this compound which may affect the compound’s pharmaceutical safety and pharmacology properties.
MAKE IN INDIA
http://makeinindia.com/sector/pharmaceuticals/
Amgen files ‘breakthrough’ leukaemia drug Blinatumomab (AMG103) in the US

Blinatumomab
Biotechnology giant Amgen has filed its investigational cancer immunotherapy blinatumomab in the US for the treatment of certain forms of acute lymphoblastic leukaemia (ALL).
Specifically, the Biologic License Application seeks approval to market the drug for patients with Philadelphia-negative (Ph-) relapsed/refractory B-precursor forms of the aggressive blood/bone marrow cancer.

Blinatumomab (AMG103) is a drug that has anti-cancer properties. It belongs to a new class of constructed monoclonal antibodies, bi-specific T-cell engagers (BiTEs), that exert action selectively and direct the human immune system to act against tumor cells. Blinatumomab specifically targets the CD19 antigen present on B cells.[1]
The drug was developed by a German-American company Micromet, Inc. in cooperation with Lonza; Micromet was later purchases byAmgen, which has furthered the drug’s clinical trials.
Structure and mechanism of action
Blinatumomab linking a T cell to a malignant B cell.
Blinatumomab enables a patient’s T cells to recognize malignant B cells. A molecule of blinatumomab combines two binding sites: a CD3 site for T cells and a CD19 site for the target B cells. CD3 is part of the T cell receptor. The drug works by linking these two cell types and activating the T cell to exert cytotoxic activity on the target cell.[2]
Therapeutic use
Clinical trials
In a phase 1 clinical study with blinatumomab, patients with non-Hodgkin’s lymphoma showed tumor regression, and in some cases completeremission.[3] There are ongoing phase 1 and phase 2 clinical trials of blinatumomab in patients with acute lymphoblastic leukemia (ALL),[4]lung or gastrointestinal cancers.[citation needed] One phase II trial for ALL reported good results in 2010 and another is starting.[5]
| Monoclonal antibody | |
|---|---|
| Type | Bi-specific T-cell engager |
| Source | Mouse |
| Target | CD19, CD3 |
| Clinical data | |
| Legal status |
?
|
| Identifiers | |
| CAS number | 853426-35-4 |
| ATC code | None |
| UNII | 4FR53SIF3A |
| Chemical data | |
| Formula | C2367H3577N649O772S19 |
| Mol. mass | 54.1 kDa |
References
- Statement on a Nonproprietary Name adopted by the USAN Council: Blinatumomab
- Mølhøj, M; Crommer, S; Brischwein, K; Rau, D; Sriskandarajah, M; Hoffmann, P; Kufer, P; Hofmeister, R; Baeuerle, PA (March 2007). “CD19-/CD3-bispecific antibody of the BiTE class is far superior to tandem diabody with respect to redirected tumor cell lysis”. Mol Immunol 44 (8): 1935–43. doi:10.1016/j.molimm.2006.09.032. PMID 17083975.
- Bargou, R; et al. (2008). “Tumor regression in cancer patients by very low doses of a T cell-engaging antibody”. Science 321 (5891): 974–977. doi:10.1126/science.1158545.PMID 18703743.
- ClinicalTrials.gov NCT00560794 Phase II Study of the BiTE Blinatumomab (MT103) in Patients With Minimal Residual Disease of B-precursor Acute ALL
- “Micromet initiates MT103 phase 2 trial in adult ALL patients”. 20 Sep 2010.
External links
 MAKE IN INDIA
MAKE IN INDIA
http://makeinindia.com/
http://makeinindia.com/sector/pharmaceuticals/

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....