Advanced Nanoparticle System Kills Cancer Cells From Within

The latest cancer targeting nanoparticles being developed in labs around the world are getting ever more complex and are utilizing multiple mechanisms to find and strike their targets. Researchers at North Carolina State University and the University of North Carolina at Chapel Hill just published an article in Nature Communications describing a nanoparticle that delivers its killer payload only when inside cells by homing in on ATP (adenosine triphosphate).
ATP is the famous energy molecule that powers the activity inside of cells, and the new nanoparticle carries DNA strands bound to doxorubicin, an anti-cancer drug, than unfold when high levels of ATP are present. The nanoparticles themselves have a layer of hyaluronic acid (HA) that attracts some types of cancer cells, allowing the nanoparticles to enter and open up, releasing the folded DNA strands.
From study abstract in Nature Communications:
The half-maximal inhibitory concentration of ATP-responsive nanovehicles is 0.24 μM in MDA-MB-231 cells…
View original post 71 more words
Chemists devise a new way to manufacture peptide drugs, which hold promise for treating many diseases

MIT chemists have devised a way to rapidly combine amino acids into protein fragments known as peptides. Credit: Alexander Vinogradov
Small protein fragments, also called peptides, are promising as drugs because they can be designed for very specific functions inside living cells. Insulin and the HIV drug Fuzeon are some of the earliest successful examples, and peptide drugs are expected to become a $25 billion market by 2018.
However, a major bottleneck has prevented peptide drugs from reaching their full potential: Manufacturing the peptides takes several weeks, making it difficult to obtain large quantities, and to rapidly test their effectiveness.
That bottleneck may soon disappear: A team of MIT chemists and chemical engineers has designed a way to manufacture peptides in mere hours. The new system, described in the March 21st issue of journal ChemBioChem, could have a major impact on peptide drug development, says Bradley Pentelute, an assistant…
View original post 683 more words
100th approval … Pradaxa® (dabigatran etexilate) now approved in more than 100 countries for stroke prevention in atrial fibrillation

More than 100 countries have now approved Boehringer Ingelheim’s Pradaxa® for the prevention of stroke and systemic embolism for adult patients with the most common sustained heart rhythm condition (non-valvular atrial fibrillation, nvAF).
The 100th approvalwas announced by the Jordan Food and Drug Administration. Further regulatory approvals for Pradaxa® are expected to be received in the near future. The continuous flow of regulatory approvals from health authorities all over the world reaffirms the overarching benefits delivered to patients by the treatment and supports previous announcements by the U.S. Food and Drugs Administation (FDA) and the European Medicines Agency (EMA).Pradaxa®, in addition, offers the most robust clinical data set and the longest real-world experience for stroke prevention in atrial fibrillation (SPAF) compared to any of the novel oral anticoagulants, providing ongoing support for physician use of the novel treatment

Effective Natural Remedies For Kidney Stones

Effective Natural Remedies For Kidney Stones
==> http://www.rapidhomeremedies.com/remedies-to-cure-kidney-stones.html
Facts & Remedies You Should Know to Prevent and Cure Kidney Stones
If you have been diagnosed with kidney stones, you know how painful it is to live with these stones- big or small- in your kidneys. The acute pain in your left or right flanks going towards the lower abdomen and groin area and even towards your back is something that makes you shudder even if thought about. The feeling of nausea and vomiting along with the burning sensation while you pass urine and also the urgency and frequency of urinating, all these has led you to wish that you get rid of kidney stones as soon as possible.
While most kidney stones are small, it doesn’t mean they are harmless bunnies. One little stone in the urinary tract can make you suffer more than you can imagine.http://www.rapidhomeremedies.com/remedies-to-cure-kidney-stones.html

FDA Approves Neuraceq (florbetaben F18 injection) for PET Imaging of Beta-Amyloid Plaques
FLORBETABEN F18
Diagnostic radiopharmaceutical
1. Benzenamine, 4-[(1E)-2-[4-[2-[2-[2-(fluoro-18F)ethoxy]ethoxy]ethoxy]phenyl]
ethenyl]-N-methyl-
2. 4-{(1E)-2-(4-{2-[2-(2-[18F]fluoroethoxy)ethoxy]ethoxy}phenyl)eth- 1-en-1-yl}-N-methylaniline
C21H26[18F]NO3
358.5
Bayer Healthcare
UNII-TLA7312TOI
CAS REGISTRY NUMBER 902143-01-5
https://www.ama-assn.org/resources/doc/usan/florbetaben-f18.pdf


Berlin/Boston, March 20, 2014‒ Piramal Imaging today announced that the U.S. Food and Drug Administration (FDA) has approved Neuraceq. This approval comes only four weeks after receiving marketing authorization for Neuraceq from the European Commission.
Neuraceq is indicated for Positron Emission Tomography (PET) imaging of the brain to estimate beta-amyloid neuritic plaque density in adult patients with cognitive impairment who are being evaluated for Alzheimer’s disease (AD) and other causes of cognitive decline.
read at
4-[(E)-2-(4-{2-[2-(2-fluoroethoxy)ethoxy]ethoxy}phenyl)vinyl]-N-methylaniline has been labeled with [F-18]fluoride and is claimed by patent application WO2006066104 and members of the corresponding patent family.
4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]- ethoxy}phenyl)vinyl]-N-methylaniline
The usefulness of this radiotracer for the detection of Αβ plaques have been reported in the literature (W. Zhang et al., Nuclear Medicine and Biology 32 (2005) 799-809; C. Rowe et al., Lancet Neurology 7 (2008) 1 -7).
The synthesis of 4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]ethoxy}phenyl)- vinyl]-N-methylaniline has been described before:
a) W. Zhang et al., Nuclear Medicine and Biology 32 (2005) 799-809.
4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]- ethoxy}phenyl)vinyl]-N-methylaniline
4 mg precursor 2a (2-[2-(2-{4-[(E)-2-{4-[(tert-butoxycarbonyl)(methyl)amino]- phenyl}vinyl]phenoxy}ethoxy)ethoxy]ethyl methanesulfonate) in 0.2 mL
DMSO were reacted with [F-18]fluoride/kryptofix/potassium carbonate complex. The intermediate was deprotected with HCI and neutralized with
NaOH. The mixture was extracted with ethyl acetate. The solvent was dried and evaporated, the residue was dissolved in acetonitrile and purified by semi-preparative HPLC. 20% (decay corrected), 1 1 % (not corrected for decay) 4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]ethoxy}phenyl)vinyl]-N- methylaniline were obtained in 90 min.
WO2006066104
4 mg precursor 2-[2-(2-{4-[(E)-2-{4-[(tert-butoxycarbonyl)(methyl)amino]- phenyl}vinyl]phenoxy}ethoxy)ethoxy]ethyl methanesulfonate in 0.2 mL DMSO were reacted with [F-18]fluoride/kryptofix/potassium carbonate complex. The intermediates was deprotected with HCI and neutralized with NaOH. The mixture was extracted with ethyl acetate. The solvent was dried and evaporated, the residue was dissolved in acetonitrile and purified by semi- preparative HPLC. 30% (decay corrected), 17% (not corrected for decay) 4- [(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]ethoxy}phenyl)vinyl]-N- methylaniline were obtained in 90 min. to yield N-Boc protected 4-[(E)-2-(4-{2-[2-(2-[F- 18]fluoroethoxy)ethoxy]ethoxy}phenyl)vinyl]-N-methylaniline. The unreacted perfluorinated precursor was removed using a fluorous phase cartridge.
Deprotection, final purification and formulation to obtain a product, suitable for injection into human is not disclosed. Furthermore, the usefulness (e.g. regarding unwanted F-19/F-18 exchange) of this approach at a higher radioactivity level is not demonstrated. Finally, this method would demand a two-pot setup (first reaction vessel: fluorination, followed by solid-phase- extraction, and deprotection in the second reaction vessel).
However, the focus of the present invention are compounds and methods for an improved “one-pot process” for the manufacturing of 4-[(E)-2-(4-{2-[2-(2- [F-18]fluoroethoxy)ethoxy]ethoxy}phenyl)vinyl]-N-methylaniline.
Very recently, further methods have been described:
d) US201001 13763
The mesylate precursor 2a was reacted with [F-18]fluoride species in a solvent mixture consisting of 100 μΙ_ acetonitrile and 500 μΙ_ tertiary alcohol. After fluorination for 10 min at 100-150 °C, the solvent was evaporated. After deprotection (1 N HCI, 5 min, 100-120 °C), the crude product was purified by HPLC (C18 silica, acetonitrile / 0.1 M ammonium formate).
e) H. Wang et al., Nuclear Medicine and Biology 38 (201 1 ) 121 -127
5 mg precursor 2a (2-[2-(2-{4-[(E)-2-{4-[(tert-butoxycarbonyl)(methyl)amino]- phenyl}vinyl]phenoxy}ethoxy)ethoxy]ethyl methanesulfonate) in 0.5 ml_
DMSO were reacted with [F-18]fluoride/kryptofix/potassium carbonate complex. The intermediate was deprotected with HCI and neutralized with NaOH. The crude product was diluted with acetonitrile / 0.1 M ammonium dformate (6/4) and purified by semi-preparative HPLC. The product fraction was collected, diluted with water, passed through a C18 cartridge and eluted with ethanol, yielding 17% (not corrected for decay) 4-[(E)-2-(4-{2-[2-(2-[F- 18]fluoroethoxy)ethoxy]ethoxy}phenyl)vinyl]-N-methylaniline within 50 min. In the paper, the conversion of an unprotected mesylate precursor (is described:
5 mg unprotected mesylate precursor (2-{2-[2-(4-{(E)-2-[4- (methylamino)phenyl]vinyl}phenoxy)ethoxy]-ethoxy}ethyl 4- methanesulfonate) in 0.5 ml_ DMSO were reacted with [F- 18]fluoride/kryptofix/potassium carbonate complex. The crude product was diluted with acetonitrile / 0.1 M ammonium formate (6/4) and purified by semi- preparative HPLC. The product fraction was collected, diluted with water, passed through a C18 cartridge and eluted with ethanol, yielding 23% (not corrected for decay) 4-[(E)-2-(4-{2-[2-(2-[F-
18]fluoroethoxy)ethoxy]ethoxy}phenyl)vinyl]-N-methylaniline within 30 min. Beside the purification by HPLC, a process based on solid-phase-extraction was investigated, but the purity was inferior to that with HPLC purification. So far, one-pot radiolabelings have been performed using a mesylate precursor. It is know, that for F-18 labeling of stilbenes, mesylates have advantages over corresponding tosylates by providing more clean reactions with less amount of by-products (W. Zhang et al. Journal of Medicinal Chemistry 48 (2005) 5980- 5988), whereas the purification starting from the tosylate precursor was tedious and time consuming resulting in a low yield.
In contrast to this teaching of the prior art, we found advantages of tosylate and further arylsulfonate precursors for 4-[(E)-2-(4-{2-[2-(2-[F- 18]fluoroethoxy)ethoxy]ethoxy}phenyl)vinyl]-N-methylaniline compared to the corresponding mesylate. Less non-radioactive by-products that eluted close to the retention time of 4-[(E)-2-(4-{2-[2-(2-[F-
18]fluoroethoxy)ethoxy]ethoxy}phenyl)vinyl]-N-methylaniline were found in the crude products if arylsulfonate precursors were used (Example 2 – Example 6) compared to the crude mixture that was obtained after conversion of the mesylate precursor (Example 1 ).
The favorable by-product profile after radiolabeling of tosylate precursor 2b (Figure 10) compared to the radiolabeling of mesylate precursor 2a (Figure 7) supported an improved cartridge based purification (Example 8, Example 9).
…………………
The term “F-18” means fluorine isotope 18F. The term”F-19″ means fluorine isotope 19F. EXAMPLES
Example 1 Radiolabeling of mesylate precursor 2a
4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]- ethoxy}phenyl)vinyl]-N-methylaniline
Radiolabeling was performed on a remote controlled synthesis module (Tracerlab FXN). Precursor 2a (2 mg) in 0.5 mL DMSO + 0.5 mL acetonitrile was treated with dried potassium carbonate/kryptofix/[F-18]fluoride complex for 6 min at 100 °C. 1 M HCI (1 mL) + 10 mg ascorbic acid was added and the mixture was heated for 4 min at 100 °C. 2M NaOH (0.5 mL), water (6 mL) and ethanol (1 mL) were added and the crude mixture was trapped on a C18 cartridge. The crude product mixture was eluted with acetonitrile and diluted with 0.1 M ammonium formiat buffer (1 mL) + 5 mg ascorbic acid. A sample of the crude product was taken and analyzed by analytical HPLC (Figure 1 ). After purification by semi- preparative HPLC, the product was diluted with water + 5 mg ascorbic acid, trapped on a C18 cartridge and eluted with 1 mL ethanol.
Yield of 4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]ethoxy}phenyl)-vinyl]-N- methylaniline: 21 % (corrected for decay).
Example 2 Synthesis and radiolabeling of tosylate precursor 2b
4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]- ethoxy}phenyl)vinyl]-N-methylaniline
4-Dimethylaminopyridine (26.7 mg) and triethylamine (225 μΙ_) were added to a solution of 1 .0 g terf-butyl {4-[(E)-2-(4-{2-[2-(2- hydroxyethoxy)ethoxy]ethoxy}phenyl)vinyl]phenyl}methylcarbamate (4) in dichloromethane (12 mL) at 0 °C. A solution of p- toluenesulfonyl chloride (417 mg) in dichloromethane (13.5 mL) was added at 0 °C. The resulting mixture was stirred at room temperature over night. The solvent was removed under reduced pressure and the crude product was purified by flash chromatography (silica, 0- 80% ethyl acetate in hexane). 850 mg 2b were obtained as colorless solid.
1 H NMR (300 MHz, CDCI3) δ ppm 1 .46 (s, 9 H), 2.43 (s, 3 H), 3.27 (s, 3 H), 3.59-3.73 (m, 6 H), 3.80- 3.86 (m, 2 H), 4.05-4.19 (m, 2 H), 6.88-7.05 (m, 4 H), 7.21 (d, J = 8.3 Hz, 2 H), 7.32 (d, J = 8.3 Hz, 2 H), 7.39-7-47 (m, 4 H), 7.80 (d, J = 8.3 Hz, 2 H). MS (ESIpos): m/z = 612 (M+H)+
Radiolabeling was performed on a remote controlled synthesis module (Tracerlab FXN). Precursor 2b (2 mg) in 0.5 mL DMSO + 0.5 mL acetonitrile was treated with dried potassium carbonate/kryptofix/[F-18]fluoride complex for 6 min at 100 °C. 1 M HCI (1 mL) + 10 mg ascorbic acid was added and the mixture was heated for 4 min at 100 °C. 2M NaOH (0.5 mL), water (6 mL) and ethanol (1 mL) were added and the crude mixture was trapped on a C18 cartridge. The crude product mixture was eluted with acetonitrile and diluted with 0.1 M ammonium formiat buffer (1 mL) + 5 mg ascorbic acid. A sample of the crude product was taken and analyzed by analytical HPLC (Figure 2). After purification by semi- preparative HPLC, the product was diluted with water + 5 mg ascorbic acid, trapped on a C18 cartridge and eluted with 1 mL ethanol.
Yield of 4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]ethoxy}phenyl)-vinyl]-N- methylaniline: 25% (corrected for decay).
Example 3 Synthesis and radiolabeling of 2c (2-[2-(2-{4-[(E)-2-{4-[(tert- butoxycarbonyl)(methyl)amino]phenyl}vinyl]phenoxy}ethoxy)ethoxy]ethyl
4-bromobenzenesulfonate)
4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]- ethoxy}phenyl)vinyl]-N-methylaniline To a stirred solution of 100 mg (0,219 mmol) tert-butyl-{4-[(E)-2-(4-{2-[2-(2- hydroxyethoxy)ethoxy]ethoxy}phenyl)vinyl]phenyl}methylcarbamate
(WO2006/066104) in 2 mL THF was added a solution of 140 mg (0.548 mmol) 4-brombenzene sulfonylchlorid in 3 mL THF drop by drop. The reaction mixture was cooled to 0°C. 156.8 mg (1 .1 mmol) potassium trimethylsilanolat was added. The milky suspension was stirred at 0°C for 2 hours and at 80°C for another 2 hours. The reaction mixture was poured onto ice-cooled water. The aqueous solution was extracted with dichloromethane several times. The combined organic phases were dried with sodium sulphate and concentrated in vacuum. The crude product was purified using silica gel with ethyl acetate/hexane-gradient as mobile phase. The desired product 2c was obtained with 77 mg (0.1 14 mmol, 52.0 % yield).
1 H NMR (300 MHz, CDCI3) δ ppm 1 .39 (s, 10 H) 3.20 (s, 3 H) 3.50 – 3.57 (m, 2 H) 3.57 – 3.61 (m, 2 H) 3.61 – 3.66 (m, 2 H) 3.72 – 3.80 (m, 2 H) 4.02 – 4.10 (m, 2 H) 4.10 – 4.17 (m, 2 H) 6.79 – 6.85 (m, 2 H) 6.91 (d, J=8.10 Hz, 2 H) 7.10 – 7.17 (m, 2 H) 7.32 – 7.41 (m, 5 H) 7.57 – 7.65 (m, 2 H) 7.67 – 7.74 (m, 2 H)
MS (ESIpos): m/z = 676/678 (M+H)+
Radiolabeling was performed on a remote controlled synthesis module (Tracerlab FXN). Precursor 2c (2 mg) in 0.5 mL DMSO + 0.5 mL acetonitrile was treated with dried potassium carbonate/kryptofix/[F-18]fluoride complex for 6 min at 100 °C. 1 M HCI (1 mL) + 10 mg ascorbic acid was added and the mixture was heated for 4 min at 100 °C. 2M NaOH (0.5 mL), water (6 mL) and ethanol (1 mL) were added and the crude mixture was trapped on a C18 cartridge. The crude product mixture was eluted with acetonitrile and diluted with 0.1 M ammonium formiat buffer (1 mL) + 5 mg ascorbic acid. A sample of the crude product was taken and analyzed by analytical HPLC (Figure 3). After purification by semi- preparative HPLC, the product was diluted with water + 5 mg ascorbic acid, trapped on a C18 cartridge and eluted with 1 mL ethanol.
Yield of 4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]ethoxy}phenyl)-vinyl]-N- methylaniline: 43% (corrected for decay). Example 4 Synthesis and radiolabeling of 2d (2-[2-(2-{4-[(E)-2-{4-[(tert- butoxycarbonyl)(methyl)amino]phenyl}vinyl]phenoxy}ethoxy)ethoxy]ethyl
4-(adamantan-1 -yl)benzenesulfonate)
4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]- ethoxy}phenyl)vinyl]-N-methylaniline
To a stirred solution of 151 mg (0,330 mmol) tert-butyl-{4-[(E)-2-(4-{2-[2-(2- hydroxyethoxy)ethoxy]ethoxy}phenyl)vinyl]phenyl}methylcarbamate
(WO2006/066104), 4.03 mg (0,033 mmol) DMAP und 36.7 mg (363 mmol) triethylamine in 4 mL dichlormethane was added a solution of 97,4 mg (0,313 mmol) 4-(adamantan-1 -yl)benzene sulfonylchloride in 1 mL dichlormethane at 0°C. The reaction mixture was stirred at 0°C for 1 hour and over night at room temperature. 7.3 mg (0,072 mmol) triethylamin und 19.5 mg (0.062 mmol) 4- (adamantan-l -yl)benzenesulfonyl chloride were added to the reaction mixture. The reaction mixture was stirred at room temperature for 3 days. It was concentrated in vacuum. The crude product was purified using silica gel with ethyl acetate/hexane-gradient as mobile phase. The desired product 2d was obtained with 104 mg (0.142 mmol, 43.4% yield).
1 H NMR (300 MHz, CDCI3) δ ppm 1 .51 (s, 9 H), 1 .62 (s, 1 H), 1 .74 – 1 .91 (m, 6 H), 1 .94 (d, J=3.20 Hz, 6 H), 2.16 (br. s., 3 H), 3.31 (s, 3 H), 3.63 – 3.69 (m, 2 H), 3.69 – 3.73 (m, 2 H), 3.76 (dd, J=5.27, 4.52 Hz, 2 H), 3.89 (d, J=4.90 Hz, 2 H), 4.13 – 4.26 (m, 4 H), 6.95 (d, J=8.85 Hz, 2 H), 7.02 (d, J=8.29 Hz, 2 H), 7.25 (d, J=8.48 Hz, 2 H), 7.40 – 7.52 (m, 4 H), 7.55 (m, J=8.67 Hz, 2 H), 7.89 (m, J=8.67 Hz, 2 H)
MS (ESIpos): m/z = 732 (M+H)+
Radiolabeling was performed on a remote controlled synthesis module (Tracerlab FXN). Precursor 2d (2 mg) in 0.5 mL DMSO + 0.5 mL acetonitrile was treated with dried potassium carbonate/kryptofix/[F-18]fluoride complex for 6 min at 100 °C. 1 M HCI (1 mL) + 10 mg ascorbic acid was added and the mixture was heated for 4 min at 100 °C. 2M NaOH (0.5 mL), water (6 mL) and ethanol (1 mL) were added and the crude mixture was trapped on a C18 cartridge. The crude product mixture was eluted with acetonitrile and diluted with 0.1 M ammonium formiat buffer (1 mL) + 5 mg ascorbic acid. A sample of the crude product was taken and analyzed by analytical HPLC (Figure 4). After purification by semi- preparative HPLC, the product was diluted with water + 5 mg ascorbic acid, trapped on a C18 cartridge and eluted with 1 mL ethanol.
Yield of 4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]ethoxy}phenyl)-vinyl]-N- methylaniline: 27% (corrected for decay).
Example 5 Synthesis and radiolabeling of 2e (2-[2-(2-{4-[(E)-2-{4-[(tert- butoxycarbonyl)(methyl)amino]phenyl}vinyl]phenoxy}ethoxy)ethoxy]ethyl
4-cyanobenzenesulfonate)
4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]- ethoxy}phenyl)vinyl]-N-methylaniline
To a stirred solution of 151 mg (0.330 mmol) tert-butyl-{4-[(E)-2-(4-{2-[2-(2- hydroxyethoxy)ethoxy]ethoxy}phenyl)vinyl]phenyl}methylcarbamate
(WO2006/066104), 4.03 mg (0.033 mmol) DMAP und 36.7 mg (0.363 mmol) triethylamine in 4 mL dichlormethane was added a solution of 63.2 mg (0.313 mmol) 4-cyanobenzenesulfonyl chloride in 1 mL dichlormethane at 0°C. The reaction mixture was stirred over night and concentrated in vacuum. The crude product was purified using silica gel with ethyl acetate/hexane-gradient as mobile phase. The desired product 2e was obtained with 118 mg (0.190 mmol, 57.6 % yield).
1 H NMR (400 MHz, CDCI3) δ ppm 1 .47 (s, 9 H) 3.28 (s, 3 H) 3.58 – 3.63 (m, 2 H) 3.63 – 3.68 (m, 2 H) 3.70 – 3.75 (m, 2 H) 3.81 – 3.87 (m, 2 H) 4.1 1 – 4.18 (m, 2 H) 4.24 – 4.30 (m, 2 H) 6.91 (d, J=8.59 Hz, 2 H) 6.99 (dt, 2 H) 7.22 (d, J=8.34 Hz, 2 H) 7.39 – 7.50 (m, 4 H) 7.83 (m, J=8.59 Hz, 2 H) 7.98 – 8.1 1 (m, 2 H)
MS (ESIpos): m/z = 623 (M+H)+
Radiolabeling was performed on a remote controlled synthesis module (Tracerlab FXN). Precursor 2e (2 mg) in 0.5 mL DMSO + 0.5 mL acetonitrile was treated with dried potassium carbonate/kryptofix/[F-18]fluoride complex for 6 min at 100 °C. 1 M HCI (1 mL) + 10 mg ascorbic acid was added and the mixture was heated for 4 min at 100 °C. 2M NaOH (0.5 mL), water (6 mL) and ethanol (1 mL) were added and the crude mixture was trapped on a C18 cartridge. The crude product mixture was eluted with acetonitrile and diluted with 0.1 M ammonium formiat buffer (1 mL) + 5 mg ascorbic acid. A sample of the crude product was taken and analyzed by analytical HPLC (Figure 5). After purification by semi- preparative HPLC, the product was diluted with water + 5 mg ascorbic acid, trapped on a C18 cartridge and eluted with 1 mL ethanol.
Yield of 4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]ethoxy}phenyl)-vinyl]-N- methylaniline: 31 % (corrected for decay).
Example 6 Synthesis and radiolabeling of 2f (2-[2-(2-{4-[(E)-2-{4-[(tert- butoxycarbonyl)(methyl)amino]phenyl}vinyl]phenoxy}ethoxy)ethoxy]ethyl
2-nitrobenzenesulfonate)
4-[(E)-2-(4-{2-[2-(2-[F-18]fluoroethoxy)ethoxy]- eth oxy} phe nyl )vi ny I] -N -methyla n i I i ne
To a stirred solution of 200 mg (0.437 mmol) tert-butyl-{4-[(E)-2-(4-{2-[2-(2- hydroxyethoxy)ethoxy]ethoxy}phenyl)vinyl]phenyl}methylcarbamate
(WO2006/066104), 5.34 mg (0.044 mmol) DMAP und 47.5 mg (0.470 mmol) triethylamine in 4 mL dichlormethane was added a solution of 92 mg (0,415 mmol) 2-nitrobenzenesulfonyl chloride in 1 mL dichlormethane at 0°C. The reaction mixture was stirred over night and concentrated in vacuum. The crude product was purified with ethyl acetate/hexane-gradient as mobile phase using silica gel. The desired product 2f was obtained with 77 mg (0.1 19 mmol, 59.5 % yield). 1 H NMR (400 MHz, CDCI3) δ ppm 1 .39 (s, 9 H) 3.20 (s, 3 H) 3.55 – 3.63 (m, 4 H) 3.59 (m, 4 H) 3.69 – 3.74 (m, 2 H) 3.75 – 3.80 (m, 2 H) 4.06 (dd, J=5.68, 3.92 Hz,
2 H) 4.32 – 4.37 (m, 2 H) 6.80 – 6.84 (m, 2 H) 6.84 – 6.98 (dt, 2 H) 7.14 (d, J=8.59 Hz, 2 H) 7.35 (d, J=3.03 Hz, 2 H) 7.37 (d, J=2.78 Hz, 2 H) 7.62 – 7.74 (m,
3 H) 8.06 – 8.1 1 (m, 1 H)
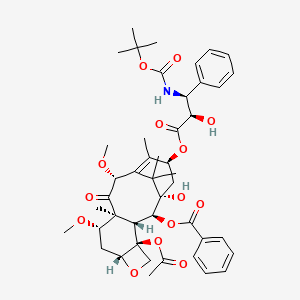
Cabazitaxel

Cabazitaxel
For treatment of patients with hormone-refractory metastatic prostate cancer previously treated with a docetaxel-containing treatment regimen.
4-acetoxy-2α-benzoyloxy-5β,20-epoxy-1-hydroxy-7β,10β-dimethoxy-9-oxotax-11-en-13α-yl(2R,3S)-3-tert-butoxycarbonylamino-2-hydroxy-3-phenyl-propionate
(1S,2S,3R,4S,7R,9S,10S,12R,15S)-4-(Acetyloxy)-15-{[(2R,3S)-3-{[(tert-butoxy)carbonyl]amino}-2-hydroxy-3-phenylpropanoyl]oxy}-1-hydroxy-9,12-dimethoxy-10,14,17,17-tetramethyl-11-oxo-6-oxatetracyclo[11.3.1.03,10.04,7]heptadec-13-ene-2-yl benzoate
183133-96-2
Cabazitaxel is prepared by semi-synthesis from 10-deacetylbaccatin III (10-DAB) which is extracted from yew tree needles. The chemical name of cabazitaxel is (2α,5β,7β,10β,13α)-4-acetoxy-13-({(2R,3S)-3-[(tert-butoxycarbonyl)amino]-2-hydroxy-3-phenylpropanoyl}oxy)-1-hydroxy-7,10-dimethoxy-9-oxo-5,20-epoxy-tax-11-en-2-yl benzoate and is marketed as a 1:1 acetone solvate (propan-2-one),
Cabazitaxel is an anti-neoplastic used with the steroid medicine prednisone. Cabazitaxel is used to treat people with prostate cancer that has progressed despite treatment with docetaxel. Cabazitaxel is prepared by semi-synthesis with a precursor extracted from yew needles (10-deacetylbaccatin III). It was approved by the U.S. Food and Drug Administration (FDA) on June 17, 2010.
Cabazitaxel (previously XRP-6258, trade name Jevtana) is a semi-synthetic derivative of a natural taxoid.[1] It was developed by Sanofi-Aventis and was approved by the U.S. Food and Drug Administration (FDA) for the treatment of hormone-refractory prostate cancer on June 17, 2010. It is a microtubule inhibitor, and the fourth taxane to be approved as a cancer therapy.[2]
Nagesh Palepu, “CABAZITAXEL FORMULATIONS AND METHODS OF PREPARING THEREOF.” U.S. Patent US20120065255, issued March 15, 2012.
Cabazitaxel in combination with prednisone is a treatment option for hormone-refractory prostate cancer following docetaxel-based treatment.
Clinical trials
In a phase III trial with 755 men for the treatment of castration-resistant prostate cancer, median survival was 15.1 months for patients receiving cabazitaxel versus 12.7 months for patients receiving mitoxantrone. Cabazitaxel was associated with more grade 3–4 neutropenia (81.7%) than mitoxantrone (58%).[3]
| United States | 5438072 | 2010-06-17 | exp 2013-11-22 |
| United States | 5698582 | 2010-06-17 | 2012-07-03 |
| United States | 5847170 | 2010-06-17 | 2016-03-26 |
| United States | 6331635 | 2010-06-17 | 2016-03-26 |
| United States | 6372780 | 2010-06-17 | 2016-03-26 |
| United States | 6387946 | 2010-06-17 | 2016-03-26 |
| United States | 7241907 | 2010-06-17 | 2025-12-10 |
JEVTANA (cabazitaxel) is an antineoplastic agent belonging to the taxane class. It is prepared by semi-synthesis with a precursor extracted from yew needles.
The chemical name of cabazitaxel is (2α,5β,7β,10β,13α)-4-acetoxy-13-({(2R,3S)-3[(tertbutoxycarbonyl) amino]-2-hydroxy-3-phenylpropanoyl}oxy)-1-hydroxy-7,10-dimethoxy-9oxo-5,20-epoxytax-11-en-2-yl benzoate – propan-2-one(1:1).
Cabazitaxel has the following structural formula:
 |
Cabazitaxel is a white to almost-white powder with a molecular formula of C45H57NO14•C3H6O and a molecular weight of 894.01 (for the acetone solvate) / 835.93 (for the solvent free). It is lipophilic, practically insoluble in water and soluble in alcohol.
JEVTANA (cabazitaxel) Injection 60 mg/1.5 mL is a sterile, non-pyrogenic, clear yellow to brownish-yellow viscous solution and is available in single-use vials containing 60 mg cabazitaxel (anhydrous and solvent free) and 1.56 g polysorbate 80. Each mL contains 40 mg cabazitaxel (anhydrous) and 1.04 g polysorbate 80.
DILUENT for JEVTANA is a clear, colorless, sterile, and non-pyrogenic solution containing 13% (w/w) ethanol in water for injection, approximately 5.7 mL.
JEVTANA requires two dilutions prior to intravenous infusion. JEVTANA injection should be diluted only with the supplied DILUENT for JEVTANA, followed by dilution in either 0.9% sodium chloride solution or 5% dextrose solution.
The taxane family of terpenes has received much attention in the scientific and medical community, because members of this family have demonstrated broad spectrum of anti-leukemic and tumor-inhibitory activity. A well-known member of this family is paclitaxel (Taxol®).
Paclitaxel (Taxol) Paclitaxel was first isolated from the bark of the pacific yew tree (Taxus brevifolia) in 1971 , and has proved to be a potent natural anti-cancer agent. To date, paclitaxel has been found to have activity against different forms of leukemia and against solid tumors in the breast, ovary, brain, and lung in humans.
As will be appreciated, this beneficial activity has stimulated an intense research effort over recent years with a view to identifying other taxanes having similar or improved properties, and with a view to developing synthetic pathways for making these taxanes, such as paclitaxel.
This research effort led to the discovery of a synthetic analogue of paclitaxel, namely, docetaxel (also known as Taxotere®). As disclosed in U.S. Patent No. 4,814,470, docetaxel has been found to have a very good anti-tumour activity and better bioavailability than paclitaxel. Docetaxel is similar in structure to paclitaxel, having t- butoxycarbonyl instead of benzoyl on the amino group at the 3′ position, and a hydroxy group instead of the acetoxy group at the C-10 position.
As will be appreciated, taxanes are structurally complicated molecules, and the development of commercially viable synthetic methods to make taxanes has been a challenge. A number of semi-synthetic pathways have been developed over the years, which typically begin with the isolation and purification of a naturally occurring starting material, which can be converted to a specific taxane derivative of interest. Cabazitaxel (I) is an anti-tumor drug which belongs to the taxol family. It differs from docetaxel in that it has methoxy groups at positions 7 and 10 of the molecule, as opposed to the hydroxyl groups at equivalent positions in docetaxel. Cabazitaxel is obtained by semi-synthesis from an extract of Chinese yew (Taxus mairei). It is understood that cabazitaxel can be obtained via semi-synthesis from other taxus species including T.candensis, T.baccatta, T.chinensis, T. mairei etc.
Cabazitaxel is a semi-synthetic derivative of the natural taxoid 0-deacetylbaccatin III (10-DAB) with potentially unique antineoplastic activity for a variety of tumors.
Cabazitaxel binds to and stabilizes tubulin, resulting in the inhibition of microtubule depolymerization and cell division, cell cycle arrest in the G2/M phase, and the inhibition of tumor cell proliferation. This drug is a microtubule depolymerization inhibitor, which can penetrate blood brain barrier (BBB).
Cabazitaxel was recently approved by the US Federal Drug Administration (FDA) for the treatment of docetaxel resistant hormone refractory prostate cancer. It has been developed by Sanofi-Aventis under the trade name of Jevtana. The CAS number for the compound is 183133-96-2. A synonym is dimethoxydocetaxel. The compound is also known as RPR-1 16258A; XRP6258; TXD 258; and axoid XRP6258.
The free base form of cabazitaxel has the chemical name
(2aR,4S,4aS,6R,9S, 1 1 S,12S,12aR, 12bS)-12b-acetoxy-9-(((2R,3S)-3-((tert- butoxycarbonyl)amino)-2-hydroxy-3-phenylpropanoyl)oxy)-11-hydroxy-4,6-dimethoxy- 4a,8, 13, 13-tetramethyl-5-oxo-2a,3,4,4a,5,6,9, 10, 11 , 12, 12a, 12b-dodecahydro-1 H- 7, 1 1-methanocyclodeca[3,4]benzo[1 ,2-b]oxet-12-yl benzoate. In a first part of this description, taxel drugs including paclitaxel (taxol), docetaxel (taxotere) and cabazitaxel may be prepared starting from 10-deacetylbaccatin (known as 10-DAB) derived from Taxus plants, via semi-synthesis. Furthermore, the same inventive methodologies can be used to semi-synthesize cabazitaxel starting from 9- dihydro-13-acetylbaccatin III (9-DHB).
Patent numbers CN1213042C, CN152870, CN1179716 and CN1179775 disclose methods to prepare cabazitaxel from 10-DAB (herein compound II).
10-DAB (II)
A typical prior art synthesis route is as follows:
OCOCH3
OCOC6H5
The method above which synthesizes cabazitaxel has many synthetic steps, a very low overall yield and high price.
There is therefore a need in the art to develop new methods to synthesize cabazitaxel and its intermediates to improve the yield of cabazitaxel, simplify the methodology and optimize the synthetic technology.
Cabazitaxel, chemically known as 4-acetoxy-2α-benzoyloxy-5β,20-epoxy-1-hydroxy-7β,10β-dimethoxy-9-oxotax-11-en-13α-yl(2R,3S)-3-tert-butoxycarbonylamino-2-hydroxy-3-phenyl-propionate, is represented by formula (I).
It is a microtubule inhibitor, indicated in combination with prednisone for treatment of patients with hormone-refractory metastatic prostate cancer previously treated with a docetaxel-containing treatment regimen, under the trade name Jevtana®.
Cabazitaxel is known from U.S. Pat. No. 5,847,170. Process for preparation of Cabazitaxel as described in U.S. Pat. No. 5,847,170 involves column chromatography, which is cumbersome tedious and not commercially viable.
The acetone solvate of 4-acetoxy-2α-benzoyloxy-5β-20-epoxy-1-hydroxy-7β, 10β-dimethoxy-9-oxotan-11-en-13α-yl-(2R,3S)-3-tert-butoxycarbonylamino-2-hydroxy-3-phenylpropionate (Form A) is formed by crystallization by using acetone and is characterized by XRD in U.S. Pat. No. 7,241,907.
U.S. 20110144362 describes anhydrous crystalline Forms B to Form F, ethanolates Form B, D, E and F and mono and dihydrate Forms of Cabazitaxel. All the anhydrous crystalline forms are prepared either by acetone solvate or ethanol solvate. Mono and dihydrate forms are formed at ambient temperature in an atmosphere containing 10 and 60% relative humidity, respectively.
Cabazitaxel (also called dimethoxy docetaxel) is a dimethyl derivative of docetaxel, which itself is semi-synthetic, and was originally developed by Rhone-Poulenc Rorer and was approved by the U.S. Food and Drug Administration (FDA) for the treatment of hormone-refractory prostate cancer on Jun. 17, 2010. Cabazitaxel is a microtubule inhibitor. The acetone solvate crystalline form of cabazitaxel and a process for its preparation is disclosed in the U.S. Pat. No. 7,241,907.
U.S. Pat. No. 5,847,170 describes cabazitaxel and its preparation methods. One of the methods described in U.S. Pat. No. 5,847,170 includes a step-wise methylation of 10-DAB (the step-wise methylation method is shown in FIG. 1) to provide the key intermediate (2αR,4S,4αS,6R,9S,11S,12S,12αR,12βS)-12β-acetoxy-9,11-dihydroxy-4,6-dimethoxy-4α,8,13,13-tetramethyl-5-oxo-2α,3,4,4α,5,6,9,10,11,12,12α,12β-dodecahydro-1H-7,11-methanocyclodeca[3,4]benzo[1,2-b]oxet-12-yl benzoate, herein referred to as 7,10-di-O-methyl-10-DAB (XVa). The intermediate XVa is coupled with the 3-phenylisoserine side chain derivative VI to provide XVa′, which is followed by removal of the oxazolidine protecting group from the side chain of XVa′ to give cabazitaxel.
Another method described in U.S. Pat. No. 5,847,170 utilizes methylthiomethyl (MTM) ethers as shown in FIG. 2. MTM ethers can be prepared from alcohols using two common methods. One method comprises deprotonation of an alcohol with a strong base to form an alkoxide followed by alkylation of the alkoxide with a methylthiomethyl halide. This approach is only useful when the alcohol is stable to treatment with a strong base. 10-DAB and some of its derivatives in which C7-OH is not protected displays so instability in the presence of strong bases and epimerization of the C7-OH can occur upon contact of 10-DAB and some of its derivatives in which C7-OH is not protected with strong bases. Another method for the synthesis of MTM ethers from alcohols utilizes Ac2O and DMSO. One disadvantage of this method is that it can also lead to the oxidation of alcohols to aldehydes or ketones. For example when the synthesis of the 10-di-O-MTM derivative of 10-DAB without protecting groups at the C13 hydroxyl group is attempted undesired oxidation of the C13-OH to its corresponding ketone occurs.
U.S. Pat. No. 5,962,705 discloses a method for dialkylation of 10-DAB and its derivatives to furnish 7,10-di-O-alkyl derivatives, as shown in FIG. 3. This has been demonstrated as a one-step, one-pot reaction, however, provides the best isolated yield when potassium hydride is used at −30° C. From an industrial point of view, the use of low reaction temperature is less favorable than using ambient temperature. Furthermore the use of a strong base can cause some epimerization of the C7-OH chiral center with an associated loss of yield. Potassium hydride is a very reactive base and must be treated with great caution.
Accordingly, there is a need for an alternative processes for the preparation of cabazitaxel and its key intermediate, 7,10-di-O-methyl-10-DAB (XVa) that is short in number of synthetic steps and avoids the use of low temperatures and strong bases such as metal hydrides in the C7-O methyl ether formation step. Such a process would also be useful for the preparation of analogues of cabazitaxel wherein the C7-O and C10-O functional groups were substituted with other alkyl groups.
FIG. 1 shows the chemistry employed in the examples of U.S. Pat. No. 5,847,170.
FIG. 2 shows the chemistry employed in the examples of U.S. Pat. No. 5,847,170.
FIG. 3 shows the chemistry employed in the examples of U.S. Pat. No. 5,962,705.
FIG. 4 shows key steps of the general synthetic scheme as per Method A/A′ of the present invention for the synthesis of cabazitaxel and cabazitaxel analogues.
FIG. 5 shows key steps of the general synthetic scheme as per Method B/B′ of the present invention for the synthesis of cabazitaxel and cabazitaxel analogues.
FIG. 6 shows the general scheme for the hydrodesulfurization reaction.
FIG. 7 shows the complete synthetic route of Method A that can be used for conversion of 10-DAB to cabazitaxel.
FIG. 8 shows the complete synthetic route of Method B that can be used for conversion of 10-DAB to cabazitaxel.
FIG. 9 shows the complete synthetic route of Method A′ that can be used for conversion of 10-DAB, via XIV′, to cabazitaxel.
FIG. 10 shows the complete synthetic route of Method B′ that can be used for conversion of 10-DAB, via XVI′, to cabazitaxel.
FIG. 11 shows the synthetic relationship between two methods (A and B) used to convert 7,10-di-O-alkyl-10-DAB (XV) to cabazitaxel.
FIG. 12 shows the synthetic scheme for the preparation of XIVa.
FIG. 13 shows the synthetic scheme for the preparation of XIVb from 10-DAB.
FIG. 14 shows the synthetic scheme for the preparation of XIVb from XIVb′.
FIG. 15 shows the synthetic scheme for the preparation of XIVc.
FIG. 16 shows the synthetic scheme for the preparation of XIVa′ from XIVa.
FIG. 17 shows the synthetic scheme for the preparation of XIVa′ from XX.
FIG. 18 shows the synthetic scheme for the preparation of XIVb′.
FIG. 19 shows the synthetic scheme for the preparation of XIVc′.
FIG. 20 shows the synthetic scheme for the preparation of XVa from XIVa.
FIG. 21 shows the synthetic scheme for the preparation of XVa from XIVb.
FIG. 22 shows the synthetic scheme for the preparation of XVa from XIVc.
FIG. 23 shows the synthetic scheme for the preparation of XVa′ from XIVa.
FIG. 24 shows the synthetic scheme for the preparation of XVa′ from XIVa′.
FIG. 25 shows the synthetic scheme for the preparation of XVa′ from XIVb′.
FIG. 26 shows the synthetic scheme for the preparation of XVa′ from XIVc′.
FIG. 27 shows the synthetic scheme for the preparation of XVa′ from XVa.
FIG. 28 shows the synthesis of cabazitaxel.
FIG. 29 shows the synthesis of XVIIa.
FIG. 30 shows the synthesis of XVIIIa.
FIG. 31 shows the synthesis of XIXa.
FIG. 32 shows the synthesis of XVIa.
FIG. 33 shows the synthesis of XVa from XVIa.











see this at http://www.google.com/patents/US20130116444
………..
Detailed description
The invention provides a new method for the preparation of cabazitaxel, one embodiment of which can be summarized as follows, showing the preparation of a protected taxane intermediate and its deprotection to taxane compounds:
OH OCOCH3
OCOC6H5
This reaction is also depicted in Figure 1. The reaction of the invention reduces the number of steps and increases yield of cabazitaxel.
The deprotection methods of the invention can also be used for the preparation of paclitaxel (taxol):
The deprotection methods of the invention can also be applied to the preparation of docetaxel:
10-DAB synthetic routes
Example 12
Dissolve 100 g of 2′-THP-cabazitaxel in 1730 ml of HOAc/H20/THF (3:1 :1 ). under N2 atmosphere, increase temperature to 50 degrees C and stir 4 hrs. Then cool to room temperature. Add 2L of ethyl acetate, 2 L of H20, stir, separate layers, wash organic layer with saturated NaHC03 (3 L x 2), saturated NaCI (3 L), dry with Na2S04.
Concentrate to obtain white 77.8 g of cabazitaxel (yield 83%).
MS(m/z) :859(M+Na)„ jHNMR (500MHz) δ 1.21(611, d) , 1.36(911, s) , 1.59(lH, s) , 1.64(lH,s) , 1.79(lH,m) , 1.87 (3H, s) ,2.27 (2H, m) , 2.35(3H,m) ,2.69(lH,m) ,3.30 (3H, s) ,
3.45 (3H, s) , 3.85 (2H, m) , 4.16 (1H, d) , 4.29 (1H, d) , 4.62 (1H, bs) , 4.79 (1H, s) , 5.29 (1H, m),5.42(lH, d),5.62(lH, d),6.21 (1H, t),7.2 ~ 7.4(6H, m) , 7.48 (2H, t),7.59(lH, t) , 8.11 (2H, d) ,
References
- http://www.cancer.gov/drugdictionary/?CdrID=534131
- “Jevtana (cabazitaxel) Injection Approved by U.S. FDA After Priority Review” (Press release). sanofi-aventis. 2010-06-17. Retrieved June 17, 2010.
- “Cabazitaxel Effective for Hormone Refractory Prostate Cancer After Failure of Taxotere”.
- Cabazitaxel – Official web site of manufacturer.
- Cabazitaxel Prescribing Information – Official prescribing information.
- U.S. National Library of Medicine: Drug Information Portal – Cabazitaxel
Patents
Patent :
Patent Number : 5438072
Country : United States
Approved : 2010-06-17
Expires : 2013-11-22
Patent :
Patent Number : 5698582
Country : United States
Approved : 2010-06-17
Expires : 2012-07-03
Patent :
Patent Number : 5847170
Country : United States
Approved : 2010-06-17
Expires : 2016-03-26
Patent :
Patent Number : 6331635
Country : United States
Approved : 2010-06-17
Expires : 2016-03-26
Patent :
Patent Number : 6372780
Country : United States
Approved : 2010-06-17
Expires : 2016-03-26
Patent :
Patent Number : 6387946
Country : United States
Approved : 2010-06-17
Expires : 2016-03-26
Patent :
Patent Number : 7241907
Country : United States
Approved : 2010-06-17
Expires : 2025-12-10
|
3-13-2009
|
SELF-EMULSIFYING AND SELF-MICROEMULSIFYING FORMULATIONS FOR THE ORAL ADMINISTRATION OF TAXOIDS
|
|
|
3-32-2005
|
Semi-solid formulations for the oral administration of taxoids
|
|
|
2-4-2005
|
Self-emulsifying and self-microemulsifying formulations for the oral administration of taxoids
|
|
|
6-12-2002
|
Use of taxoid derivatives
|

Orphan Drugs: FDA Approval For Tropical Disease
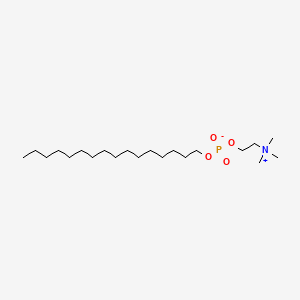
The FDA announces on March 19th the approval of Impavido (Miltefosine), an oral medicine for the treatment of the tropical disease Leishmaniasis. Leishmaniasis is caused by a parasite, Leishmania, which is transmitted by sand fly bites to humans. It occurs mainly in people who live in the tropics and subtropics. The drug is already approved for sale in Europe, the Indian subcontinent, and Central and South America.
The FDA granted Impavido Fast Track Designation, Priority Review, and Orphan Drug Designation (ODD) (October 2006). Paladin Therapeutics, Impavido’s manufacturer, is awarded a FDA Tropical Disease Priority Review Voucher. This type of Priority Review Voucher (PRV) is awarded under a provision in the FDA Amendments Act of 2007 that encourages the development of new drugs and vaccines for neglected tropical diseases. “The PRV is transferable and can be sold and entitles the bearer to a priority review for any product. To…
View original post 115 more words
The U.S. FDA approved Impavido (miltefosine) to treat a tropical disease called leishmaniasis

MILTEFOSINE
2-(hexadecoxy-oxido-phosphoryl)oxyethyl-trimethyl-azanium
58066-85-6
March 19, 2014 — The U.S. Food and Drug Administration today approved Impavido (miltefosine) to treat a tropical disease called leishmaniasis.
Leishmaniasis is a disease caused by Leishmania, a parasite which is transmitted to humans through sand fly bites. The disease occurs primarily in people who live in the tropics and subtropics. Most U.S. patients acquire leishmaniasis overseas.
Impavido is an oral medicine approved to treat the three main types of leishmaniasis: visceral leishmaniasis (affects internal organs), cutaneous leishmaniasis (affects the skin) and mucosal leishmaniasis (affects the nose and throat). It is intended for patients 12 years of age and older. Impavido is the first FDA-approved drug to treat cutaneous or mucosal leishmaniasis.
“Today’s approval demonstrates the FDA’s commitment to making available therapeutic options to treat tropical diseases,” said Edward Cox, M.D., director of the Office of Antimicrobial Products in the FDA’s Center for Drug Evaluation and Research.
The FDA granted Impavido fast track designation, priority review, and orphan product designation. These designations were granted because the drug demonstrated the potential to fill an unmet medical need in a serious disease or condition, the potential to be a significant improvement in safety or effectiveness in the treatment of a serious disease or condition, and is intended to treat a rare disease, respectively. With this approval, Impavido’s manufacturer, Paladin Therapeutics, is awarded a Tropical Disease Priority Review Voucher under a provision included in the Food and Drug Administration Amendments Act of 2007 that aims to encourage development of new drugs and biological products for the prevention and treatment of certain tropical diseases.
Impavido’s safety and efficacy were evaluated in four clinical trials. A total of 547 patients received Impavido and 183 patients received either a comparator drug or a placebo. Results from these trials demonstrated that Impavido is safe and effective in treating visceral, cutaneous and mucosal leishmaniasis.
The labeling for Impavido includes a boxed warning to alert patients and health care professionals that the drug can cause fetal harm and therefore should not be given to pregnant women. Health care professionals should advise women to use effective contraception during and for five months after Impavido therapy.
The most common side effects identified in clinical trials were nausea, vomiting, diarrhea, headache, decreased appetite, dizziness, abdominal pain, itching, drowsiness and elevated levels of liver enzymes (transaminases) and creatinine.
Paladin Therapeutics is based in Montreal, Canada
Miltefosine (INN, trade names Impavido and Miltex) is a phospholipid drug. Chemically it is a derivative of alkylphosphocholinecompounds discovered in the early 1980s. It was developed in the late 1980s as an anticancer drug by German scientists Hansjörg Eibl and Clemens Unger.[2] Simultaneously but independently it was found that the drug could kill Leishmania parasites, and since the mid-1990s successful clinical trials were conducted. The drug became the first (and still the only prescribed) oral drug in the treatment ofleishmaniasis. It is now known to be a broad-spectrum antimicrobial drug, active against pathogenic bacteria and fungi,[1][3] as well as human trematode Schistosoma mansoni and its vector host, the snail Biomphalaria alexandrina.[4] It can be administered orally and topically.
In the target cell, it acts as an Akt inhibitor. Therefore, it is also under investigation as a potential therapy against HIV infection.[5][6]
Phospholipid group alkylphosphocholine were known since the early 1980s, particularly in terms of their binding affinity with cobra venom.[7]In 1987 the phosholids were found to potent toxins on leukemic cell culture.[8] Initial in vivo investigation on the antineoplastic activity showed positive result, but then only at high dosage and at high toxicity.[9] At the same time in Germany, Hansjörg Eibl, at the Max Planck Institute for Biophysical Chemistry, and Clemens Unger, at the University of Göttingen, demonstrated that the antineoplastic activity of the phospholipid analogue miltefosine (at the time known as hexadecylphosphocholine) was indeed tumour-specific. It was highly effective against methylnitrosourea-induced mammary carcinoma, but less so on transplantable mammary carcinomas and autochthonous benzo(a)pyrene-induced sarcomas, and relatively inactive on Walker 256 carcinosarcoma and autochthonous acetoxymethylmethylnitrosamine-induced colonic tumors of rats.[10][11] It was subsequently found that miltefosine was strucrally unique among lipds having anticancer property in that it lacks the glycerol group, is highly selective on cell types and acts through different mechanism.[12][13]
In the same year as the discovery of the acticancer property, miltefosine was reported by S. L. Croft and his team at the London School of Hygiene and Tropical Medicine as having antileishmanial effect as well. The compound was effective against Leishmania donovani amastigotes in cultured mouse peritoneal macrophages at a dose of 12.8 mg/kg/day in a five-day course.[14] However priority was given to the development of the compound for cutaneous metastases of breast cancer. In 1992 a new research was reported in which the compound was highly effective in mouse against different life cycle stages of different Leishmania species, and in fect more potent than the conventional sodium stibogluconate therapy by a factor of more than 600.[15] Results of the first clinical trial in humans were reported from Indian patients with chronic leishmaniasis with high degree of success and safety.[16] This promising development promulgated a unique public–private partnership collaboration between ASTA Medica (later Zentaris GmbH), the WHO Special Programme for Research and Training in Tropical Diseases, and the Government of India. Eventually, several successful Phase II and III trials led to the approval of miltefosine in 2002 as the first and only oral drug for leishmaniasis.[1]
Miltefosine is registered and used by Zentaris GmbH in India, Colombia and Germany for the treatment of visceral and cutaneous leishmaniasis, and is undergoing clinical trials for this use in several other countries, such as Brazil[17] and Guatemala.[18]
Miltefosine is a phosphocholine analogue that was originally launched in 1993 by Baxter Oncology for the treatment of cancer. In 2003, Zentaris (formerly part of Asta Medica) launched the drug for the oral treatment of visceral leishmaniasis. Zentaris has also brought the product to market for the treatment of cutaneous leishmaniasis. Jado Technologies is conducting phase II clinical trials for the treatment of antihistamine resistant urticaria. Clinical trials had been ongoing for several indications, including the treatment of cutaneous mastocytosis or cutaneous involvement of systemic mastocytosis. Jado is investigating topical and oral versions of the compound in phase II trials in several allergy indications.
Miltefosine is effective against promastigotes and intracellular amastigotes, which survive and multiply in phagolysosomal compartments of macrophages and make up the two stages of the leishmania lifecycle. Although the exact mechanism of action of the drug has not been determined, it may exert its therapeutic effect through inhibition of phospholipid metabolism. Another theory suggests that miltefosine may interfere with leishmaniacal membrane signal transduction, lipid metabolism and glycosylphosphatidylinositol anchor biosynthesis. The drug is well absorbed in the gastrointestinal tract after a single oral administration and is widely distributed throughout the body.
Miltefosine was originally developed under a collaboration between the Indian government, the German biopharmaceutical company Zentaris, and the Tropical Disease Research (TDR) programme, co-sponsored by the World Health Organization and the United Nations Development Programme (UNDP). Subsequent to the product’s approval, Zentaris partnered with various organizations for its distribution. In February 2004, Roche and Zentaris entered into a marketing agreement, pursuant to which Roche agreed to support Zentaris in the registration process and to market miltefosine in Brazil.
Several medical agents have some efficacy against visceral or cutaneous leishmaniasis, however a 2005 survey concluded that Miltefosine is the only effective oral treatment for both forms of leishmaniasis.[19]
Miltefosine is being investigated by researchers interested in finding treatments for infections which have become resistant to existing drugs. Animal and in vitro studies suggest it may have broad anti-protozoal and anti-fungal properties:
- Animal studies suggest miltefosine may also be effective against Trypanosoma cruzi, the parasite responsible for Chagas’ disease.[20]
- Several studies have found the drug to be effective against Cryptococcus neoformans, Candida, Aspergillus and Fusarium.[21]
- An in vitro study found that miltefosine is effective against metronidazole-resistant variants of Trichomonas vaginalis, a sexually transmitted protozoal disease.[22]
- Hexadecyltrimethylammonium bromide, a compound structurally similar to miltefosine, was recently found to exhibit potent in vitro activity against Plasmodium falciparum.[23]
- Miltefosine is being made available in the United States through the CDC for emergency use under an expanded access IND protocol for treatment of free-living amoeba (FLA) infections:Primary amoebic meningoencephalitis caused by Naegleria fowleri and Granulomatous Amebic Encephalitis caused by Balamuthia mandrillaris, and Acanthamoeba species.[24][25]
Investigatory usage against HIV infection
Miltefosine targets HIV infected macrophages, which play a role in vivo as long-lived HIV-1 reservoirs. The HIV protein Tat activates pro-survival PI3K/Akt pathway in primary human macrophages. Miltefosine acts by inhibiting the PI3K/Akt pathway, thus removing the infected macrophages from circulation, without affecting healthy cells.[5] It significantly reduces replication of HIV-1 in cocultures of human dendritic cells (DCs) and CD4(+) T cells, which is due to a rapid secretion of soluble factors and is associated with induction of type-I interferon (IFN) in the human cells.[26]
In leishmanisis the recommended dose as oral monotherapy is 2.5 mg/kg/day for a total of 28 days. However, due to frequent commercial shortage of the 10 mg capsule, dosages are often altered. For example, the Indian government recommends 100 mg/day miltefosine for patients with a body weight ≥25 kg (corresponding to ∼1.7–4 mg/kg/day) and 50 mg/day for body weights <25 kg (corresponding to ∼2–5.5 mg/kg/day).[1] Even up to 150 mg/day for 28 days was found to be quite safe.[27]
The main side effects reported with miltefosine treatment are nausea and vomiting, which occur in 60% of patients. Adverse effect is more severe in women and young children. The overall effects are quite mild and easily reverse.[28] It is embryotoxic and fetotoxic in rats and rabbits, and teratogenic in rats but not in rabbits. It is therefore contraindicated for use during pregnancy, andcontraception is required beyond the end of treatment in women of child-bearing age.[29]
| miltefosine (1-hexadecylphosphoryl-choline, HePC); Calbiochem 475841 |
Compounds o f the general formula I belonging to the class of phospholipids (X is O and R2 is a group of formula II), e.g. alkyloxy phospholipids (Y is O) and the corresponding alkylthio derivatives (Y is S), can be prepared as described in the literature (Bittman, R.; J. Med. Chem. 1997, 40, 1391-1395; Reddy, K. C.; Tetrahedron Lett. 1994, 35, 2679-2682; Guivisdalsky, P. N.; J. Med. Chem. 1990, 33, 2614-2621 and references cited therein) or by standard variations of the procedures described therein. Synthesis of the corresponding ester and thioester analogues (Y is OCO and SCO, respectively) can be accomplished by standard acylation of the hydroxy or thio precursor materials.
f the general formula I belonging to the class of phospholipids (X is O and R2 is a group of formula II), e.g. alkyloxy phospholipids (Y is O) and the corresponding alkylthio derivatives (Y is S), can be prepared as described in the literature (Bittman, R.; J. Med. Chem. 1997, 40, 1391-1395; Reddy, K. C.; Tetrahedron Lett. 1994, 35, 2679-2682; Guivisdalsky, P. N.; J. Med. Chem. 1990, 33, 2614-2621 and references cited therein) or by standard variations of the procedures described therein. Synthesis of the corresponding ester and thioester analogues (Y is OCO and SCO, respectively) can be accomplished by standard acylation of the hydroxy or thio precursor materials.
Compounds of the general formula I belonging to the class of phosphonolipids (X is a direct bond and R2 is a group of formula II), e.g alkyloxy phosphonolipids (Y is O and R2 is a group of formula II) and the corresponding alkylthio derivatives (Y is S) can be prepared as published by Bittman et al. (Bittman, R.; J. Med. Chem. 1993, 36, 297-299; Bittman, R.; J. Med. Chem.1994, 37, 425-430 and references cited therein) or by synthetic variations of the procedures described therein. Synthesis of the corresponding ester and thioester analogues (Y is OCO or SCO) can be accomplished by standard acylation of the hydroxy or thio precursor materials.
SEE
Antitumor ether lipids: An improved synthesis of ilmofosine and an enantioselective synthesis of an ilmofosine analog
Tetrahedron Lett 1994, 35(17): 2679
AND
Hexadecylphosphocholine, a new antineoplastic agent: Cytotoxic properties in leukaemic cells
J Cancer Res Clin Oncol 1986, 111: 24
References
- Dorlo, T. P. C.; Balasegaram, M.; Beijnen, J. H.; de Vries, P. J. (2012). “Miltefosine: a review of its pharmacology and therapeutic efficacy in the treatment of leishmaniasis”. Journal of Antimicrobial Chemotherapy 67 (11): 2576–2597. doi:10.1093/jac/dks275.PMID 22833634.
- Eibl, H; Unger, C (1990 Sep). “Hexadecylphosphocholine: a new and selective antitumor drug.”. Cancer Treatment Reviews 17 (2-3): 233–42. PMID 2272038.
- Almeida Pachioni, JD; Magalhães, JG; Cardoso Lima, EJ; Moura Bueno, LD; Barbosa, JF; Malta de Sá, M; Rangel-Yagui, CO (2013). “Alkylphospholipids – a promising class of chemotherapeutic agents with a broad pharmacological spectrum.”. Journal of Pharmacy & Pharmaceutical sciences : a publication of the Canadian Society for Pharmaceutical Sciences, Societe canadienne des sciences pharmaceutiques 16 (5): 742–59. PMID 24393556.
- Eissa, Maha M; El Bardicy, Samia; Tadros, Menerva (2011). “Bioactivity of miltefosine against aquatic stages of Schistosoma mansoni, Schistosoma haematobium and their snail hosts, supported by scanning electron microscopy”. Parasites & Vectors 4 (1): 73.doi:10.1186/1756-3305-4-73. PMC PMC3114006. PMID 21569375.
- ^ Jump up to:a b Chugh P, Bradel-Tretheway B, Monteiro-Filho CM, et al. (2008). “Akt inhibitors as an HIV-1 infected macrophage-specific anti-viral therapy”. Retrovirology 5 (1): 11. doi:10.1186/1742-4690-5-11. PMC 2265748. PMID 18237430.
- “Parasitic Drug Shows HIV-Fighting Promise”. AIDSmeds.com. 2008-02-01. Retrieved 2008-02-02.
- Teshima, K; Ikeda, K; Hamaguchi, K; Hayashi, K (1983). “Bindings of cobra venom phospholipases A2 to micelles of n-hexadecylphosphorylcholine.”. Journal of Biochemistry 94(1): 223–32. PMID 6619110.
- Fleer, EA; Unger, C; Kim, DJ; Eibl, H (1987). “Metabolism of ether phospholipids and analogs in neoplastic cells.”. Lipids 22 (11): 856–61. PMID 3444378.
- Berger, MR; Petru, E; Schmähl, D (1987). “Therapeutic ratio of mono or combination bacterial lipopolysaccharide therapy in methylnitrosourea-induced rat mammary carcinoma.”. Journal of Cancer Research and Clinical Oncology 113 (5): 437–45. PMID 3624299.
- Muschiol, C; Berger, MR; Schuler, B; Scherf, HR; Garzon, FT; Zeller, WJ; Unger, C; Eibl, HJ; Schmähl, D (1987). “Alkyl phosphocholines: toxicity and anticancer properties.”. Lipids 22 (11): 930–4. PMID 3444388.
- Berger, MR; Muschiol, C; Schmähl, D; Eibl, HJ (1987). “New cytostatics with experimentally different toxic profiles.”. Cancer treatment Reviews 14 (3-4): 307–17. PMID 3440252.
- Hilgard, P; Stekar, J; Voegeli, R; Engel, J; Schumacher, W; Eibl, H; Unger, C; Berger, MR (1988). “Characterization of the antitumor activity of hexadecylphosphocholine (D 18506).”.European Journal of Cancer & Clinical Oncology 24 (9): 1457–61. PMID 3141197.
- Eibl, H; Unger, C (1990 Sep). “Hexadecylphosphocholine: a new and selective antitumor drug.”. Cancer Treatment Reviews 17 (2-3): 233–42. PMID 2272038.
- Croft, S.L.; Neal, R.A.; Pendergast, W.; Chan, J.H. (1987). “The activity of alkyl phosphorylcholines and related derivatives against Leishmania donovani”. Biochemical Pharmacology 36 (16): 2633–2636. doi:10.1016/0006-2952(87)90543-0.
- Kuhlencord, A; Maniera, T; Eibl, H; Unger, C (1992). “Hexadecylphosphocholine: oral treatment of visceral leishmaniasis in mice.”. Antimicrobial Agents and Chemotherapy 36(8): 1630–1634. doi:10.1128/AAC.36.8.1630. PMC PMC192021. PMID 1329624.
- Sundar, Shyam; Rosenkaimer, Frank; Makharia, Manoj K; Goyal, Ashish K; Mandal, Ashim K; Voss, Andreas; Hilgard, Peter; Murray, Henry W (1998). “Trial of oral miltefosine for visceral leishmaniasis”. The Lancet 352 (9143): 1821–1823. doi:10.1016/S0140-6736(98)04367-0.PMID 9851383.
- Cristina, Márcia; Pedrosa, Robert (September 2005). “Hospital de Doenças Tropicais testa droga contra calazar”. Sapiência (in Portuguese) (Fundação de Amparo à Pesquisa do Estado do Piauí). Archived from the original on 2006-08-22. Retrieved 2006-09-01.
- Soto J, Berman J (2006). “Treatment of New World cutaneous leishmaniasis with miltefosine.”. Trans R Soc Trop Med Hyg 100: S34. doi:10.1016/j.trstmh.2006.02.022.PMID 16930649.
- Berman, J. (2005). “Clinical status of agents being developed for leishmaniasis”. Expert Opinion on Investigational Drugs 14 (11): 1337–1346. doi:10.1517/13543784.14.11.1337.PMID 16255674.
- Saraiva V, Gibaldi D, Previato J, Mendonça-Previato L, Bozza M, Freire-De-Lima C, Heise N (2002). “Proinflammatory and cytotoxic effects of hexadecylphosphocholine (miltefosine) against drug-resistant strains of Trypanosoma cruzi.”. Antimicrob Agents Chemother 46 (11): 3472–7. doi:10.1128/AAC.46.11.3472-3477.2002. PMC 128733. PMID 12384352.
- Widmer F, Wright L, Obando D, Handke R, Ganendren R, Ellis D, Sorrell T (2006).“Hexadecylphosphocholine (miltefosine) has broad-spectrum fungicidal activity and is efficacious in a mouse model of cryptococcosis.”. Antimicrob Agents Chemother 50 (2): 414–21. doi:10.1128/AAC.50.2.414-421.2006. PMC 1366877. PMID 16436691.
- Blaha C, Duchêne M, Aspöck H, Walochnik J (2006). “In vitro activity of hexadecylphosphocholine (miltefosine) against metronidazole-resistant and -susceptible strains of Trichomonas vaginalis”. J. Antimicrob. Chemother. 57 (2): 273–8.doi:10.1093/jac/dki417. PMID 16344287.
- Choubey V, Maity P, Guha M, et al. (February 2007). “Inhibition of Plasmodium falciparum choline kinase by hexadecyltrimethylammonium bromide: a possible antimalarial mechanism”. Antimicrob. Agents Chemother. 51 (2): 696–706. doi:10.1128/AAC.00919-06.PMC 1797733. PMID 17145794.
- Naegleria fowleri – Primary Amebic Meningoencephalitis (PAM)
- Brain-Eating Amoeba: How One Girl Survived
- Garg, Ravendra; Tremblay, Michel J. (October 2012). “Miltefosine represses HIV-1 replication in human dendritic cell/T-cell cocultures partially by inducing secretion of type-I interferon”.Virology 432 (2): 271–276. doi:10.1016/j.virol.2012.05.032. PMID 22704066.
- Sundar, Shyam; Jha, T.K.; Thakur, C.P.; Bhattacharya, S.K.; Rai, M. (2006). “Oral miltefosine for the treatment of Indian visceral leishmaniasis”. Transactions of the Royal Society of Tropical Medicine and Hygiene 100 (Suppl 1): S26–S33. doi:10.1016/j.trstmh.2006.02.011.PMID 16730038.
- S.D. Seth (2008). “Drug therapy of leishmaniasis”. In S.D. Seth. Textbook of Pharmacology. Elsevier India. p. 31. ISBN 9788131211588.
- Sindermann, H.; Engel, J. (December 2006). “Development of miltefosine as an oral treatment for leishmaniasis”. Transactions of the Royal Society of Tropical Medicine and Hygiene 100 (Suppl 1): S17–S20. doi:10.1016/j.trstmh.2006.02.010. PMID 16730362.
|
7-4-2012
|
LOCAL TREATMENT OF NEUROFIBROMAS
|
|
|
10-28-2011
|
METHODS FOR THE TREATMENT AND AMELIORATION OF ATOPIC DERMATITIS
|
|
|
8-17-2011
|
Methods for the treatment and amelioration of atopic dermatitis
|
|
|
11-16-2007
|
Mucosal formulation
|
|
|
7-20-2007
|
NOVEL ALKYL PHOSPHOLIPID DERIVATIVES WITH REDUCED CYTOTOXICITY AND USES THEREOF
|
 an animation to soothe ones eye
an animation to soothe ones eye
PICLAMILAST

PICLAMILAST
An antiasthmatic agent and phosphodiesterase 4 inhibitor.
144035-83-6
SANOFI
-
3-(Cyclopentyloxy)-N-(3,5-dichloro-4-pyridinyl)-4-methoxybenzamide
-
3-(Cyclopentyloxy)-N-(3,5-dichloro-4-pyridyl)-p-anisamide
-
Benzamide, 3-(cyclopentyloxy)-N-(3,5-dichloro-4-pyridinyl)-4-methoxy-
-
C18-H18-Cl2-N2-O3
- 381.2572
- CCRIS 8304
- Cpodpmb
- Piclamilast
- RP 73-401
- RP 73401
- RP-73-401
- RPR 73401
- UNII-WM58D7C3ZT
Piclamilast (RP 73401), is a selective PDE4 inhibitor.[1] It is comparable to other PDE4 inhibitors for its anti-inflammatory effects. It has been investigated for its applications to the treatment of conditions such as chronic obstructive pulmonary disease, bronchopulmonary dysplasia andasthma. It is a second generation compound that exhibits structural functionalities of the PDE4 inhibitors cilomilast and roflumilast. The structure for piclamilast was first elucidated in a 1995 European patent application.[2] The earliest mention of the name “piclamilast” was used in a 1997 publication.[3]
Piclamilast functions through the selective inhibition of the four PDE4 isoforms (PDE4A-D). It shows no inhibition of the other PDEs. The PDE4 isoforms are especially important to inflammatory and immunomodulatory cells. They are the most common PDE in inflammatory cells such as mast cells, neutrophils, basophils, eosinophils, T lymphocytes, macrophages, and structural cells such as sensory nerves and epithelial cells. PDE4hydrolyzes cyclic adenosine monophosphate (cAMP) to inactive adenosine monophosphate (AMP). Inhibition of PDE4 blocks hydrolysis of cAMP thereby increasing levels of cAMP within cells. cAMP suppresses the activity of immune and inflammatory cells. PDE4 inhibition in an induced chronic lung disease murine model was shown to have anti-inflammatory properties, attenuate pulmonary fibrin deposition and vascular alveolar leakage, and prolong survival in hyperoxia-induced neonatal lung injury. A study of PDE4 inhibition in a murine model of allergic asthma showed that piclamilast significantly improves the pulmonary function, airway inflammation and goblet cell hyperplasia.[4][5]
Emesis is the most commonly cited side effect of piclamilast. It has proven difficult to separate the emetic side effects from the therapeutic benefits of several PDE4 inhibitors, including piclamilast.[6]
Chemical synthesis
The preparation steps for synthesis of piclamilast are as follows (both discovery[7] and production[8] routes have been documented)
- Addition of cyclopentyl to isovanillin via Williamson ether synthesis.
- Oxidation of aldehyde group to carboxylic acid.
- Formation of acid chloride by treatment with thionyl chloride.
- Formation of amide by reaction with deprotonated 4-amino-3,5-dichloropyridine.
SEE
J Med Chem 1994, 37(11): 1696
http://pubs.acs.org/doi/abs/10.1021/jm00037a021
AND
Org Process Res Dev 1998, 2(3): 157
http://pubs.acs.org/doi/full/10.1021/op9700385

3-(cyclopentyloxy)-N-(3,5-dichloropyrid-4-yl)-4-methoxybenzamide (1) (26.4 g, 69%) as an off-white solid, mp 155−157 °C (lit.1 mp 155−157 °C). 1H NMR: δ 1.55−2.05 (m, 8H), 3.93 (s, 3H), 4.87 (m, 1H), 6.95 (d, 1H, J = 8 Hz), 6.98−7.53 (m, 2H), 7.65 (s, 1H), 8.56 (s, 2H). Anal. Calcd for C18H18Cl2N2O3: C, 56.7; H, 4.76; Cl, 18.6; N, 7.35. Found: C, 56.3; H, 4.7; Cl, 18.4; N, 7.2.
References
- Beeh, K. M.; Beier, J.; Lerch, C.; Schulz, A. K.; Buhl, R. (2004). “Effects of Piclamilast, a Selective Phosphodiesterase-4 Inhibitor, on Oxidative Burst of Sputum Cells from Mild Asthmatics and Stable COPD Patients”. Lung 182 (6): 369–377. doi:10.1007/s00408-004-2518-z. PMID 15765929. edit
- EP application 0497564
- Souness, J. E.; Houghton, C.; Sardar, N.; Withnall, M. T. (1997). “Evidence that cyclic AMP phosphodiesterase inhibitors suppress interleukin-2 release from murine splenocytes by interacting with a ‘low-affinity’ phosphodiesterase 4 conformer”. British Journal of Pharmacology 121 (4): 743–750. doi:10.1038/sj.bjp.0701200. PMC 1564751. PMID 9208143. edit
- Sun, J.; Deng, Y.; Wu, X.; Tang, H.; Deng, J.; Chen, J.; Yang, S.; Xie, Q. (2006). “Inhibition of phosphodiesterase activity, airway inflammation and hyperresponsiveness by PDE4 inhibitor and glucocorticoid in a murine model of allergic asthma”. Life Sciences 79 (22): 2077–2085. doi:10.1016/j.lfs.2006.07.001. PMID 16875702. edit
- De Visser, Y. P.; Walther, F. J.; Laghmani, E. H.; Van Wijngaarden, S.; Nieuwland, K.; Wagenaar, G. T. M. (2008). “Phosphodiesterase-4 inhibition attenuates pulmonary inflammation in neonatal lung injury”. European Respiratory Journal 31 (3): 633–644. doi:10.1183/09031936.00071307. PMID 18094015. edit
- Hirose, R.; Manabe, H.; Nonaka, H.; Yanagawa, K.; Akuta, K.; Sato, S.; Ohshima, E.; Ichimura, M. (2007). “Correlation between emetic effect of phosphodiesterase 4 inhibitors and their occupation of the high-affinity rolipram binding site in Suncus murinus brain”. European Journal of Pharmacology 573 (1–3): 93–99. doi:10.1016/j.ejphar.2007.06.045. PMID 17658510. edit
- Ashton, M. J.; Cook, D. C.; Fenton, G.; Karlsson, J. A.; Palfreyman, M. N.; Raeburn, D.; Ratcliffe, A. J.; Souness, J. E.; Thurairatnam, S.; Vicker, N. (1994). “Selective Type IV Phosphodiesterase Inhibitors as Antiasthmatic Agents. The Syntheses and Biological Activities of 3-(Cyclopentyloxy)-4-methoxybenzamides and Analogs”. Journal of Medicinal Chemistry 37 (11): 1696.doi:10.1021/jm00037a021. edit
- Cook, D. C.; Jones, R. H.; Kabir, H.; Lythgoe, D. J.; McFarlane, I. M.; Pemberton, C.; Thatcher, A. A.; Thompson, D. M.; Walton, J. B. (1998). “Process Development of the PDE IV Inhibitor 3-(Cyclopentyloxy)-N-(3,5-dichloropyrid-4-yl)-4-methoxybenzamide”. Organic Process Research & Development 2 (3): 157. doi:10.1021/op9700385.

NADIFLOXACIN, Jinofloxacin

-
(+-)-9-Fluoro-6,7-dihydro-8-(4-hydroxypiperidino)-5-methyl-1-oxo-1H,5H-benzo(ij)quinolizine-2-carboxylic acid
- CCRIS 4066
- Jinofloxacin
- Nadifloxacin
- Nadifloxacine
- Nadifloxacine [INN-French]
- Nadifloxacino
- Nadifloxacino [INN-Spanish]
- Nadifloxacinum
- Nadifloxacinum [INN-Latin]
- Nadixa
- OPC-7251
- S-Nadifloxacin
- UNII-6CL9Y5YZEQ
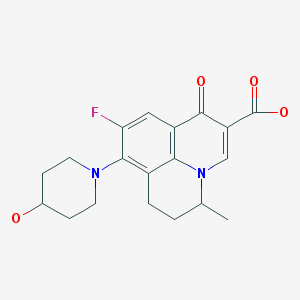
Nadifloxacin is chemically, 9-fluoro-6,7-dihydro-8-(4-hydroxy-l-pyperidinyl)-5-methyl- l-oxo-lH,5H-benzo(I,j)quinolizine-2-carboxylic acid of Formula I provided below.
FORMULA I Nadifloxacin is a synthetic quinolone with potent broad-spectrum anti-bacterial activity. Nadifloxacin inhibits the enzyme DNA gyrase that is involved in bacterial DNA synthesis and replication, thus inhibiting the bacterial multiplication. RS-nadifloxacin and S-nadifloxacin, in particular, exhibit strong antibacterial activity against Gram-positive, Gram-negative and anaerobic bacteria, resistant Gram-positive organisms such as methicillin-resistant Staphylococcus aureus (MRSA), quinolone-resistant Staphylococcus aureus, coagulase negative staphylococci, such as methicillin-resistant Staphylococcus epidermidis (MRSE), enterococci, betahemolytic streptococci and viridans group of streptococci, mycobacteria and newly emerging nosocomial pathogens such as Chryseobacterium meninges epticum, and Gram-negative pathogens such as E.coli, Klebsiella, Proteus, Serratia, Citrobacter and Pseudomonas. Recently, it has also been shown that S-(-)-nadifloxacin, in particular exhibits potent antibacterial activity against glycopeptide intermediate S. aureus (GISA), vancomycin intermediate S. aureus (VISA) and vancomycin-resistant S. aureus (VRSA). Nadifloxacin is also active against quinolone-resistant Staphylococci.
Nadifloxacin is marketed in the form of cream for topical application for the treatment of acne vulgaris, folliculitis and sycosis vulgaris. It is also indicated for the treatment of topical bacterial infections with susceptible bacteria.
The use of quinolone antibiotics to treat infections is known art in the field of ophthalmic pharmaceutical compositions and methods of treatment. Several quinolone antibacterial agents available in the market include gatifloxacin (available as Zymar®), Levofloxacin (available as Quixin® or Iquix®), Ciprofloxacin (available as Ciloxan®), Ofloxacin (available as Ocuflox®), Lomefloxacin (available as Lomeflox®), Moxifloxacin (available as Vigamox®) and Norfloxacin (available as Chibroxin®).
U.S. Patent No. 4,844,902 discloses a topically applicable formulation comprising by weight about 0.01 to 30% of an anti-bacterially active compound, 0.01 to 10% of a corticosteroid and a carrier. U.S. Patent No. 6,333,045 discloses liquid pharmaceutical compositions of gatifloxacin or salt thereof and disodium edetate.
U.S. Patent No. 6,716,830 discloses ophthalmic dosage forms of moxifioxacin or salts thereof in a concentration of 0.1% to 1% (w/w) and pharmaceutically acceptable vehicle.
U.S. Patent No. 6,359,016 relates to topical suspension formulations containing ciprofloxacin and dexamethasone.
U.S. Patent No 4,399,134 discloses processes for the preparation of nadifloxacin or salts thereof and antibacterially effective pharmaceutical compositions of nadifloxacin. Typical dosage forms include tablets, pills, powders, liquid preparations, suspensions, emulsions, granules, capsules, suppositories, and injectable preparations (solutions, suspensions, etc).
U.S. Patent No 6,884,768 discloses solid oral pharmaceutical compositions that includes nadifloxacin, an absorbefacient and taurine compounds.
U.S. Patent Application 20060183698 describes topical ophthalmic formulation that includes serum electrolytes; an antimicrobial compound and an anti-inflammatory or steroidal compound. Several antimicrobial agents have been disclosed including nadifloxacin.
U.S. Patent Application 20040176337 discloses topical . compositions of benzoquinolizine-2-carboxylic acid antimicrobial drug.
U.S. Patent Application 20040176321 discloses injectable pharmaceutical composition for intravenous delivery of an active agent that includes RS-(±)-nadifloxacin; S-(-)- nadifloxacin and hydrates thereof; or S~(-)-nadifloxacin arginine and salts thereof. PCT Publication WO 04/00360 describes pharmaceutical compositions of several active ingredients including nadifloxacin for topical use for treatment of dermatosis.
European Patent EP 275,515 and U.S. Patent No. 4,923,862 disclose aqueous pharmaceutical compositions of levofloxacin and ofloxacin or salts thereof.
PCT application WO 02/39993 discloses a stable pharmaceutical preparation of a combination drug, comprising an anti-infective agent, selected from the group consisting of quinolone derivatives, amino-glycoside derivatives and their pharmaceutically acceptable salts; an ant-inflammatory agent which is a corticosteroid; a complexation enhancing polymer; a solubilizer exhibiting an inclusion phenomena; pharmaceutically acceptable excipients within a suitable carrier system.
Journal of Ocular Pharmacology and Therapeutics, vol 23(3): 243-256, 2007 discloses (7- [(3R)-3 -aminohexahydro- 1 H-azepine- 1 -yl]-8-chloro- 1 -cyclopropyl-6-fluoro- 1 ,4-dihydro- 4-oxo-3-quinolinecarboxylivc acid as the topical agent for the treatment of ophthalmic infections.

5-Bromo-6-fluoro-2-methylquinoline (II)
5-Bromo-6-fluoro-2-methyl-1,2,3,4-tetrahydroquinoline (III)
diethyl 2-[(E)-ethoxymethylidene]succinate (IV)
8-Bromo-9-fluoro-5-methyl-1-oxo-6,7-dihydro-1H,5H-pyrido[3,2,1-ij]quinoline-2-carboxylic acid (V)
4-Piperidinol; 4-Hydroxypiperidine

______________________________________Elemental Analysis for C.sub.19 H.sub.21 N.sub.2 O.sub.4 F C H N______________________________________Calc'd (%): 63.32 5.87 7.78Found (%): 63.28 5.76 7.89______________________________________


 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO