Palopegteriparatide

Palopegteriparatide
Yorvipath , FDA 2024, 8/9/2024, To treat hypoparathyroidism
- G2N64C3385
- 2222514-07-8
- Palopegteriparatide
- UNII-G2N64C3385
- ACP-014
- Mpeg 40000-teriparatide
- Palopegteriparatide [INN]
- Transcon parathyroid hormone (1-34)
- Transcon pth (1-34)
- Palopegteriparatide [USAN]
- TransCon PTH
- WHO 11060


Palopegteriparatide, sold under the brand name Yorvipath, is a hormone replacement therapy used for the treatment of hypoparathyroidism.[1][2] It is a transiently pegylated parathyroid hormone.[4] It is a parathyroid hormone analog.[1]
Palopegteriparatide was approved for medical use in the European Union in November 2023,[2] and in the United States in August 2024.[1][5]
Medical uses
Palopegteriparatide is indicated for the treatment of adults with hypoparathyroidism.[1][2]
Adverse effects
The US Food and Drug Administration (FDA) prescription label for palopegteriparatide includes warnings for a potential risk of risk of unintended changes in serum calcium levels related to number of daily injections and total delivered dose, serious hypocalcemia and hypercalcemia (blood calcium levels that are too high), osteosarcoma (a rare bone cancer) based on findings in rats, orthostatic hypotension (dizziness when standing), and a risk of a drug interaction with digoxin (a medicine for certain heart conditions).[5]
History
The effectiveness of palopegteriparatide was evaluated in a 26-week, randomized, double-blind, placebo-controlled trial that enrolled 82 adults with hypoparathyroidism.[5] Prior to randomization, all participants underwent an approximate four-week screening period in which calcium and active vitamin D supplements were adjusted to achieve an albumin-corrected serum calcium concentration between 7.8 and 10.6 mg/dL, a magnesium concentration ≥1.3 mg/dL and below the upper limit of the reference range, and a 25(OH) vitamin D concentration between 20 to 80 ng/mL.[5] During the double-blind period, participants were randomized to either palopegteriparatide (N = 61) or placebo (N= 21), at a starting dose of 18 mcg/day, co-administered with conventional therapy (calcium and active vitamin D).[5] Study drug and conventional therapy were subsequently adjusted according to the albumin-corrected serum calcium levels.[5] At the end of the trial, 69% of the participants in the palopegteriparatide group compared to 5% of the participants in the placebo group were able to maintain their calcium level in the normal range, without needing active vitamin D and high doses of calcium (calcium dose ≤ 600 mg/day).[5]
The FDA granted the application for palopegteriparatide orphan drug and priority review designations.[5]
Society and culture
Legal status
In September 2023, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) adopted a positive opinion, recommending the granting of a marketing authorization for the medicinal product Yorvipath, intended for the treatment of chronic hypoparathyroidism in adults.[4][6] The applicant for this medicinal product is Ascendis Pharma Bone Diseases A/S.[4] Palopegteriparatide was approved for medical use in the European Union in November 2023.[2]
Palopegteriparatide was granted an orphan drug designation by the US Food and Drug Administration (FDA) in 2018,[7] and by the EMA in 2020.[8]
Brand names
Palopegteriparatide is the international nonproprietary name.[9][10]
Palopegteriparatide is sold under the brand name Yorvipath.[2]
References
- ^ Jump up to:a b c d e “Yorvipath injection, solution”. DailyMed. 14 August 2024. Retrieved 5 September 2024.
- ^ Jump up to:a b c d e f “Yorvipath EPAR”. European Medicines Agency. 19 October 2020. Archived from the original on 10 December 2023. Retrieved 11 December 2023. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ “Yorvipath Product information”. Union Register of medicinal products. 20 November 2023. Archived from the original on 26 November 2023. Retrieved 11 December 2023.
- ^ Jump up to:a b c “Yorvipath: Pending EC decision”. European Medicines Agency. 15 September 2023. Archived from the original on 24 September 2023. Retrieved 24 September 2023. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ Jump up to:a b c d e f g h “FDA approves new drug for hypoparathyroidism, a rare disorder”. U.S. Food and Drug Administration (FDA) (Press release). 9 August 2024. Archived from the original on 13 August 2024. Retrieved 13 August 2024.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ “Ascendis Pharma Receives Positive CHMP Opinion for TransCon PTH (palopegteriparatide) for Adults with Chronic Hypoparathyroidism”. Ascendis Pharma (Press release). 14 September 2023. Archived from the original on 24 September 2023. Retrieved 24 September 2023.
- ^ “TransCon Parathyroid Hormone (mPEG conjugated parathyroid hormone 1-34) Orphan Drug Designations and Approvals”. U.S. Food and Drug Administration (FDA). Archived from the original on 24 September 2023. Retrieved 24 September 2023.
- ^ “EU/3/20/2350”. European Medicines Agency. 15 September 2023. Archived from the original on 24 September 2023. Retrieved 24 September 2023.
- ^ World Health Organization (2021). “International nonproprietary names for pharmaceutical substances (INN): recommended INN: list 86”. WHO Drug Information. 35 (3). hdl:10665/346562.
- ^ World Health Organization (2023). “International nonproprietary names for pharmaceutical substances (INN): recommended INN: list 89”. WHO Drug Information. 37 (1). hdl:10665/366661.
External links
- Palopegteriparatide Global Substance Registration System
- Palopegteriparatide NCI Thesaurus
- Clinical trial number NCT04701203 for “A Trial Investigating the Safety, Tolerability and Efficacy of TransCon PTH Administered Daily in Adults With Hypoparathyroidism (PaTHway)” at ClinicalTrials.gov
| Clinical data | |
|---|---|
| Trade names | Yorvipath |
| Other names | ACP-014, TransCon PTH |
| License data | US DailyMed: Palopegteriparatide |
| Routes of administration | Subcutaneous |
| Drug class | Hormonal agent |
| ATC code | H05AA05 (WHO) |
| Legal status | |
| Legal status | US: ℞-only[1]EU: Rx-only[2][3] |
| Identifiers | |
| CAS Number | 2222514-07-8 |
| UNII | G2N64C3385 |
| KEGG | D12395 |
//////Palopegteriparatide, APPRoVALS 2024, FDA 2024, Yorvipath, hypoparathyroidism, UNII-G2N64C3385, ACP-014, TransCon PTH, WHO 11060
Aneratrigine


Aneratrigine
2097163-74-9
5-chloro-2-fluoro-4-[4-fluoro-2-[methyl-[2-(methylamino)ethyl]amino]anilino]-N-(1,3-thiazol-4-yl)benzenesulfonamide
5-chloro-2-fluoro-4-((4-fluoro-2-(3-(methylamino)pyridin-1-yl)phenyl)amino)-N-(thiazol-4-yl)benzenesulfonamide hydrochloride
| Benzenesulfonamide, 5-chloro-2-fluoro-4-[[4-fluoro-2-[methyl[2-(methylamino)ethyl]amino]phenyl]amino]-N-4-thiazolyl- |
C19H20ClF2N5O2S2 488.0 g/mol
UNII 6A5ZY5LT78
WHO
SYN

Assignee: Daewoong Pharmaceutical Co., Ltd.
World Intellectual Property Organization, WO2017082688
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2017082688&_cid=P11-M0UEPF-95506-1
Preparation of 5-chloro-2-fluoro-4-((4-fluoro-2-(3-(methylamino)pyridin-1-yl)phenyl)amino)-N-(thiazol-4-yl)benzenesulfonamide hydrochloride
Step 1) Preparation of tert-butyl (1-(2-amino-5-fluorophenyl)pyridin-3-yl)(methyl)carbamate
2,4-Difluoro-1-nitrobenzene (2.0 g, 12.6 ng/mol) and tert-butyl methyl (pyridin-3-yl)carbamate (2.5 g, 1.0 eq.) were dissolved in DMF (20 mL), and K2C03 ( 2.6 g , 1.5 eq .) was added. The internal temperature was maintained at 60–70 ° C and the mixture was stirred for 2 hours. The completion of the reaction was confirmed by TLC when the reaction solution turned deep yellow. After cooling to room temperature, ethyl acetate (EA)/H20 was added, stirred, and the layers were separated. MgS04 was added to the separated organic layer, stirred, dried, and filtered. After concentrating the filtrate under reduced pressure, the residue was dissolved in EtOH (10 mL) and distilled water (10 mL), and then Na 2 S 2 0 4 (13.0 g, 6 eq.) was added. After stirring for 2 hours while maintaining the internal temperature at 60 to 70 ° C, the completion of the reaction was confirmed by TLC when the yellow color of the reaction solution lightened and became almost colorless. After cooling to room temperature, distilled water (50 mL) was added and extracted twice with EA (100 mL). MgS0 4 was added to the organic layer, stirred, dried, and filtered. The filtrate was concentrated under reduced pressure, and the obtained residue was separated by column chromatography (n-Hexane/EA = 3/1) to obtain the title compound (2.0 g, 51. ).
1H NMR (MeOD): 6.73(m, 1H), 6.57(t, 1H), 3.23(m, 1H), 3.10(m, 2H), 2.94(m, 1H), 2.91(s, 3H), 2.25( m, 1H), 1.99(m, 1H)
Step 2) Preparation of tert-butyl thiazol-4-ylcarbamate
Thiazole-4-carboxylic acid (5.0 g, 38.8 vol) was dissolved in t-Bu0H (100 mL), and then TEA (8.1 mL, 1.5 eq.) and DPPA (7.1 mL, 1.5 eq.) were added. The internal temperature was maintained at 90–100 ° C, and the mixture was stirred for 3 days. The completion of the reaction was confirmed by TLC. The product was concentrated under reduced pressure, distilled water (50 mL) was added, and the solution was washed with EA (100 mL).
It was extracted twice. MgSQ 4 was added to the organic layer, stirred, dried, and filtered.
After concentrating the filtrate under reduced pressure, the residue was added to a small amount of EA, slurried, and the resulting solid was filtered to obtain the white title compound (4.0 g, 51.5%).
1H NMR (MeOD): 8.73(s, 1H), 7.24(s, 1H), 1.52(s, 9H)
Step 3) Preparation of tert-butyl ((4-bromo-5-chloro-2-fluorophenyl)sulfonyl)(thiazol-4-yl)carbamate
Step 2) The tert-Butyl thiazol-4-ylcarbamate (4.0 g, 20.0 ng ol) prepared in the reaction vessel was placed in a reaction vessel and the interior was replaced with nitrogen gas. After dissolving in THF (32 mL), it was cooled to _78 ° C using dry ice— acetone. After cooling, LiHMDS (22.4 mL, 1.5 eq.) was slowly added and the reaction mass was stirred for 30 minutes. 4-Bromo-5-chloro-2-fluorobenzenesulfonyl chloride (6.0 g, 1.0 eq.) was dissolved in THF (10 mL) and slowly added to the reaction mixture. The reaction mass was stirred overnight and the completion of the reaction was confirmed by TLC. Distilled water (50 mL) was added and extracted twice with EA (100 mL). MgS0 4 was added to the organic layer, stirred, dried, and filtered. After concentrating the filtrate under reduced pressure, the residue was crystallized from THF/n-hexane to obtain the title compound (4.4 g, 59.0%).
1H NMR (MeOD): 9.00(s, 1H), 8.22(d, 1H), 7.90(d, 1H), 7.78(s, 1H), 1.35(s, 9H)
Step 4) Preparation of tert-butyl (l-(2-((4-(N-(tert-butyloxycarbonyl)-N-(thiazol-4-yl)sulfamoyl)-2-chloro-5-fluorophenyl)amino)-5-fluorophenyl)pyrlidin-3-yl)(methyl)carbamate
Tert-butyl (1-(2-amino-5-fluorophenyl)pyrlidin-3-yl)(methyl)carbamate (0.5 g, 1.1 ng ol) prepared in Step 1) and tert-butyl ((4-bromo-5-chloro-2-fluorophenyl)sulfonyl)(thiazol-4-yl)carbamate (0.9 g, 1.2 eq.) prepared in Step 3) were dissolved in 1,4-dioxane (10 mL). Pd(OAc) 2 (0.03 g, 0.1 eq), rac-BINAP (0.19 g, 0.2 eq.), Cs 2 C0 3 (1.5 g, 3.0 eq.) were added to the reaction solution. After reacting at 120 ° C for 30 minutes using a microwave initiator, the completion of the reaction was confirmed by TLC. Distilled water (50 mL) was added and extracted twice with EA (100 mL).
MgS0 4 was added to the organic layer, stirred, filtered and dried. The filtrate was concentrated under reduced pressure, and the residue was separated by column chromatography (EA/n-Hexane = 1/1). This was repeated twice to obtain the title compound (2.0 g, 88.2%).
1H NMR (MeOD): 8.95(s, 1H), 7.94(d, 1H), 7.65(s, 1H), 7.14(t, 1H), 6.70(d, 1H), 6.64(t, 1H), 6.07( d, 1H)ᅳ 3.40(m, 1H), 3.28(m, 2H), 3.16(m, 1H), 2.64(s, 3H), 2.06(m, 1H), 1.89(m, 1H), 1.41(s , 9H), 1.36(s, 9H)
Step 5) Preparation of 5-chloro-2-fluoro-4-((4-fluoro-2-(3-(methylamino)pyridin-1-yl)phenyl)amino)-N-(thiazol-4-yl)benzenesulfonamide hydrochloride
Step 4) was prepared by adding 1.25 M HCl in MeOH (15 mL) to tert-butyl (1-(2-((4-(Ν-(tert-butoxycarbonyl)-N-(thiazol-4-yl)sulfamoyl)—2-chloro-5-fluorophenyl)amino)-5-fluorophenyl)pyrlidin-3-yl) (methyl)carbamate (2.0 g, 2.9 µl). The mixture was heated to 40–50 ° C and stirred overnight, and the completion of the reaction was confirmed by TLC. The product was concentrated, and methylene chloride (15 mL) was added to the residue, which was stirred for 1 hour, and the resulting solid was filtered to obtain the title compound (0.9 g, 58.8%).
1H 證 (MeOD): 8.73(s, 1H), 7.75(d, 1H), 7.12(t, 1H), 7.00(s, 1H), 6.69(d, 1H), 6.67(t, 1H), 6.05( d, 1H), 3.73(m, 1H) , 3.54(m, 1H), 3.45(m, 1H), 3.38(m, 1H), 3.26(m, 1H), 2.63(s, 3H) , 2.31(m , 1H), 1.96(m, 1H)
PATENTS
0002705578SODIUM CHANNEL BLOCKER
20180346459Substituted benzenesulfonamides as sodium channel blockers
2018533606ナトリウムチャネル遮断剤
3375782SODIUM CHANNEL BLOCKER
108349963SODIUM CHANNEL BLOCKER
1020170056461SODIUM CHANNEL BLOCKER

////////////Aneratrigine, DAEWOONG
Seladelpar


Seladelpar
cas 851528-79-5
C21H23F3O5S, 444.47
fda approved 8/14/2024, To treat primary biliary cholangitis (PBC), Livdelzi
| Ingredient | UNII | CAS | InChI Key |
|---|---|---|---|
| Seladelpar lysine | N1429130KR | 928821-40-3 | WTKSWPYGZDCUNQ-JZXFCXSPSA-N |
- (+)-MBX-8025
- MBX 8025
- MBX-8025
- MBX8025
- RWJ-800025
- ((4-(((2R)-2-ETHOXY-3-(4-(TRIFLUOROMETHYL)PHENOXY)PROPYL)THIO)-2-METHYLPHENYL)OXY)ACETIC ACID
- (4-(((2R)-2-ETHOXY-3-(4-(TRIFLUOROMETHYL)PHENOXY)PROPYL)SULFANYL)-2-METHYLPHENOXY)ACETIC ACID PEROXISOME PROLIFERATOR ACTIVATED RECEPTOR (PPAR) AGONIST,ANTIHYPERLIPIDAEMIC
- (R)-2-(4-((2-ETHOXY-3-(4-(TRIFLUOROMETHYL)PHENOXY)PROPYL)-THIO)-2-METHYLPHENOXY)ACETIC ACID
- ACETIC ACID, (4-(((2R)-2-ETHOXY-3-(4-(TRIFLUOROMETHYL)PHENOXY)PROPYL)THIO)-2-METHYLPHENOXY)-
- ACETIC ACID, (4-(((2R)-2-ETHOXY-3-(4-(TRIFLUOROMETHYL)PHENOXY)PROPYL)THIO)-2-METHYLPHENOXY)- ((4-(((2R)-2-ETHOXY-3-(4-(TRIFLUOROMETHYL)PHENOXY)PROPYL)THIO)-2-METHYLPHENYL)OXY)ACETIC ACID
- ACETIC ACID, 2-(4-(((2R)-2-ETHOXY-3-(4-(TRIFLUOROMETHYL)PHENOXY)PROPYL)THIO)-2-METHYLPHENOXY)-
- Seladelpar
Seladelpar, sold under the brand name Livdelzi, is a medication used for the treatment of primary biliary cholangitis.[1] It is used as the lysine dihydrate salt.[1] It is a PPARδ receptor agonist.[1][2][3] The compound was licensed from Janssen Pharmaceutica NV.[4]
Seladelpar was approved for medical use in the United States in August 2024.[1][5]
Seladelpar is a peroxisome proliferator-activated receptor (PPAR)-delta (δ) agonist. Seladelpar is a single enantiomer of the R-configuration.5 On August 14, 2024, seladelpar was granted accelerated approval by the FDA for the treatment of primary biliary cholangitis,6 which is a condition associated with aberrant bile acid metabolism. Seladelpar works to block bile acid synthesis.1
Medical uses
Seladelpar is indicated for the treatment of primary biliary cholangitis in combination with ursodeoxycholic acid in adults who have an inadequate response to ursodeoxycholic acid, or as monotherapy in people unable to tolerate ursodeoxycholic acid.[1]
Clinically, Seladelpar reduces pruritus and IL-31 in patients with primary biliary cholangitis.[6]
- compound 3r [PMID: 17524639]
- Bioorg Med Chem Lett. 2007 Jul 15;17(14):3855-9. doi: 10.1016/j.bmcl.2007.05.007. Epub 2007 May 10.
- 10.1016/j.bmcl.2007.05.007
Drug Discovery, Johnson and Johnson Pharmaceutical Research and Development, LLC, 8 Clarke Drive, Cranbury, NJ 08512, USA

Scheme 1. Reagents and condition: (a) Cs2CO3, dioxane, 100 C 80%; (b) TBAF (cat), THF, 85%; (c) NaH, RI, THF or DMF for esters of 2–5, 8–9, 10–80%; iPr2NEt, RBr or MOMCl, THF for esters of 6–7, 58–79%; ADDP, Ph3P, phenol, CH2Cl2 for esters of 10–11, 68–73%; (d) LiOH, H2O, THF, 90–95%.

Scheme 2. Reagents: (a) Ba(MnO4)2, CH2Cl2, 89%; (b) DIAD, Ph3P, DMF, THF, 17%; (c) n-Bu3P, 24, Py, 55%; (d) i—NaHMDS, EtOTf, THF for the ethyl ester of 12, 47%; DIAD, Ph3P, para-trifluoromethylphenol for the ethyl ester of 13, 79%; ii—LiOH, H2O, THF, 84–88%.
References
- ^ Jump up to:a b c d e f “Livdelzi- seladelpar lysine capsule”. DailyMed. 14 August 2024. Retrieved 5 September 2024.
- ^ Billin AN (October 2008). “PPAR-beta/delta agonists for Type 2 diabetes and dyslipidemia: an adopted orphan still looking for a home”. Expert Opinion on Investigational Drugs. 17 (10): 1465–1471. doi:10.1517/13543784.17.10.1465. PMID 18808307. S2CID 86564263.
- ^ Bays HE, Schwartz S, Littlejohn T, Kerzner B, Krauss RM, Karpf DB, et al. (September 2011). “MBX-8025, a novel peroxisome proliferator receptor-delta agonist: lipid and other metabolic effects in dyslipidemic overweight patients treated with and without atorvastatin”. The Journal of Clinical Endocrinology and Metabolism. 96 (9): 2889–2897. doi:10.1210/jc.2011-1061. PMID 21752880.
- ^ “Targeting Mixed Dyslipidemia and Metabolic Syndrome”. Metabolex, Inc. 2005. Archived from the original on 17 October 2006.
- ^ “Gilead’s Livdelzi (Seladelpar) Granted Accelerated Approval for Primary Biliary Cholangitis by U.S. FDA” (Press release). Gilead. 14 August 2024. Retrieved 15 August 2024 – via Business Wire.
- ^ Kremer AE, Mayo MJ, Hirschfield GM, Levy C, Bowlus CL, Jones DE, et al. (July 2024). “Seladelpar treatment reduces IL-31 and pruritus in patients with primary biliary cholangitis”. Hepatology. 80 (1): 27–37. doi:10.1097/HEP.0000000000000728. PMC 11191048.
| Clinical data | |
|---|---|
| Trade names | Livdelzi |
| Other names | MBX-8025; RWJ-800025 |
| License data | US DailyMed: Seladelpar |
| Routes of administration | By mouth |
| ATC code | None |
| Legal status | |
| Legal status | US: ℞-only[1] |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 851528-79-5 |
| PubChem CID | 11236126 |
| DrugBank | DB12390 |
| ChemSpider | 9411171 |
| UNII | 7C00L34NB9 |
| KEGG | D11256 |
| ChEMBL | ChEMBL230158 |
| CompTox Dashboard (EPA) | DTXSID001045332 |
| Chemical and physical data | |
| Formula | C21H23F3O5S |
| Molar mass | 444.47 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
///////////////Livdelzi, Seladelpar, (+)-MBX-8025, MBX 8025, MBX-8025, MBX8025, RWJ-800025, FDA 2024, APPROVALS 2024
Zevotrelvir, EDP 235
Zevotrelvir, EDP 235
cas 2773516-53-1
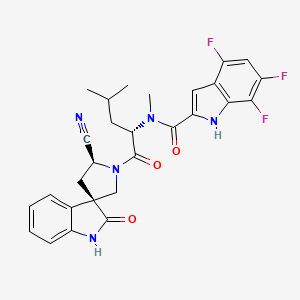
N-[(2S)-1-[(2′S,3R)-2′-cyano-2-oxospiro[1H-indole-3,4′-pyrrolidine]-1′-yl]-4-methyl-1-oxopentan-2-yl]-4,6,7-trifluoro-N-methyl-1H-indole-2-carboxamide
C28H26F3N5O3, 537.5
Zevotrelvir (Compound 52) is a coronavirus inhibitor with IC50 ranges of <0.1 μM and <0.1mM for 229E hCoV and SARS-CoV-23C-like (3CL) proteases, respectively. Zevotrelvir has the potential to study viral infections.
Coronaviruses are enveloped, positive-sense, single-stranded RNA viruses. The genomic RNA of CoVs has a 5′-cap structure and 3′-poly-A tail and contains at least 6 open reading frames (ORFs). The first ORF (ORF 1a/b) directly translates two polyproteins: pp1a and pp1ab. These polyproteins are processed by a 3C-Like protease (3CLpro), also known as the main protease (Mpro), into 16 non-structural proteins. These non-structural proteins engage in the production of subgenomic RNAs that encode four structural proteins, namely envelope, membrane, spike, and nucleocapsid proteins, among other accessory proteins. As a result, it is understood that 3C-Like protease has a critical role in the coronavirus life cycle.
3CLpro is a cysteine protease involved in most cleavage events within the precursor polyprotein. Active 3CLpro is a homodimer containing two protomers and features a Cys-His dyad located in between domains I and II.3CLpro is conserved among coronaviruses and several common features are shared among the substrates of 3CLpro in different coronaviruses. As there is no human homolog of 3CLpro, it is an ideal antiviral target. Although compounds have been reported to inhibit 3CLpro activity, they have not been approved as coronavirus therapies. (Refer to
WO 2004101742 A2, US 2005/0143320 Al, US 2006/0014821 Al, US 2009/0137818
Al, WO 2013049382 A2, WO 2013166319 A1, WO2018042343, WO2018023054, WO 2022013684, WO 2021252644, WO2022020711, WO 2022020242, US 11,174,231 B1, US 11,124,497 B1, WO 2005113580, and WO2006061714).
There is a need in the art for novel therapeutic agents that treat, ameliorate or prevent SARS-CoV-2 infection. The present invention provides the process of novel compounds which act in inhibiting or preventing SARS-CoV-2 viral replication and thus are used in the treatment of COVID-19 (see PCT/US21/60247).
Synthesis of substituted spirooxindole and its intermediate has been previously published (Refer to PCT/US21/60247, WO2019086142, WO 2020221811, WO2020221826, J. Med. Chem.2012, 55, 9069). However, the scale-up using previous process is very challenging due to the safety concern associated with certain intermediates, instability of certain intermediates as well as lack of purification process other than column chromatograph. Thus, there is a strong need for developing a safe and efficient processes for the large-scale preparation of these novel substituted spirooxindole derivatives.
SYNTHESIS

https://patents.google.com/patent/US11352363B1/en

PATENT
SYN
[1]. Guoqiang Wang, et al. Novel spiropyrrolidine derived antiviral drugs. Patent CN114524821A.
1.20230295175PROCESSES FOR THE PREPARATION OF SUBSTITUTED SPIROOXINDOLE DERIVATIVES
2.WO/2023/177854PROCESSES FOR THE PREPARATION OF SUBSTITUTED SPIROOXINDOLE DERIVATIVES
3.WO/2022/109363NOVEL SPIROPYRROLIDINE DERIVED ANTIVIRAL AGENTS
Enanta Pharmaceuticals, Inc.
WO2023177854




Example 15. Preparation of Preparation of (3R,5’S)-1′-(N-methyl-N-(4,6,7-trifluoro-1H-indole-2-carbonyl)-L-leucyl)-2-oxospiro[indoline-3,3′-pyrrolidine]-5′-carboxamide (Compound (n))

DMF (760 kg, 8V) was added into the reaction at 0 °C (-5~5 °C) followed by compound (j) (63 kg, 1.05 eq) and N-Methylmorpholine (56 kg, 2 eq), HATU
(106 kg, 1.0 eq) and Compound (m-1) (100 kg, 1.0 eq). The reactor was rinsed with DMF (190 kg, 2V) under and warmed up to 25 °C (20~30 °C) and stirred for 5 h (3~6 h) at 25 °C (20~30 °C). After that, additional HATU (0.1 eq) was added and the reaction mixture was stirred for 16-24 h.25% Ammonium hydroxide (38 kg) was added to the reaction mixture at 25 °C (20~30 °C) and stirred for 2 h (1~3 h) at 25 °C (20~30 °C). The reaction mixture was then added to water (5000 kg, 50V) at 20-30°C over 2 h and the resulting slurry was stirred for 2 h (1~5 h) at 25 °C (20~30 °C). The mixture was filtered and the cake was rinsed with water (500 kg, 5 V). The cake was dissolved in ethyl acetate (1350 kg, 15 V) and washed with 10% sodium chloride solution (500 kg) for three times. The organic layer was separated to 1.5-2.5V at not more than 45℃ under vacuum. The solution was cooled to 25 °C (20~30 °C) and Dichloromethane (660 kg, 5V) was added. The mixture was stirred for 2 h (2~5 h) at 25 °C (20~30 °C) and a slurry was formed. n-Heptane (137 kg, 2V) was added dropwise over 0.5 h (0.5~2 h) at 25 °C (20~30 °C) and stirred for additional 2 h (1~3 h) at 25 °C (20~30 °C). The reaction mixture was filtered and the wet cake was rinsed with DCM/heptane (5/2). The wet cake was dried at 50 °C (45~55 °C) for 20 h (15~25 h) to provide Compound (n) as the white solid in 80-85% yield.
1H NMR (300 MHz, DMSO-d6) δ 12.46 (s, 1H), 10.68 (s, 1H), 7.56 (s, 1H), 7.15 – 7.00 (m, 3H), 6.91 (t, J = 4.4 Hz, 2H), 6.84 (d, J = 7.7 Hz, 1H), 6.55 (d, J = 2.8 Hz, 1H), 5.34 (t, J = 7.3 Hz, 1H), 4.63 (dd, J = 9.8, 8.0 Hz, 1H), 3.83 (q, J = 10.3 Hz, 2H), 3.45 (qd, J = 7.0, 5.1 Hz, 1H), 3.16 (s, 3H), 2.35 – 2.13 (m, 2H), 1.69 (t, J = 7.1 Hz, 2H), 1.56 (dq, J = 13.1, 6.5 Hz, 1H), 0.93 (dd, J = 12.2, 6.3 Hz, 6H).
Example 16. Preparation of (3R,5’S)-1′-(N-methyl-N-(4,6,7-trifluoro-1H-indole-2-carbonyl)-L-leucyl)-2-oxospiro[indoline-3,3′-pyrrolidine]-5′-carboxamide (Compound (n))
DMF solution of Compound (m-2) (1 kg, 1.0 eq.) was added to a reactor at around 0-10oC. Compound (l) (600 g, 1.0 eq.), NMM (3.00 eq., 850 g) and HATU (1.00 eq., 1.06 kg) was added to the reactor while maintaining the temperature at 0-10oC; The reaction was warmed to 20±5oC, and stirred for at least 6 hours at 20±5oC. HATU (0.20 eq., 210 g) was added to the reactor at 20±5oC and stirred for at least 6 hours at 20±5oC.25% Ammonium hydroxide (390 g, 1.0 eq) was added to the reaction mixture at 20 °C and stirred for 2 h (1~3 h) at 20 °C. EtOAc (14.0 V) and water (14 V) was added at around 25oC over 20 minutes, and the
solution was stirred for at least 30 min. Aqueous phase was extracted with EtOAc for three times and the organic phase was combined, and washed with 10% aq. NaCl for three times at 20±5oC. The organic phase was concentrated to 6 V then EtOH (7.0 V) was charged. The EtOAc-EtOH solvent swap was repeated for three times and concentrated to 5 V before water (7.0 v) was added at 20±5oC. The mixture was cooled to 0-10oC and stirred for 1 h before being filtered. The filter cake was dissolved in ethyl acetate (15 V) and washed with 10% sodium chloride solution for three times. The organic layer was concentrated to 2-3V at not more than 45℃ under vacuum. The solution was cooled to 25 °C (20~30 °C) and Dichloromethane (5V) was added. The mixture was stirred for 2 h (2~5 h) at 25 °C (20~30 °C) and a slurry was formed. n-Heptane (2V) was added dropwise over 0.5 h (0.5~2 h) at 25 °C (20~30 °C) and stirred for additional 2 h (1~3 h) at 25 °C (20~30 °C). The reaction mixture was filtered and wet cake was rinsed with DCM/heptane (5/2). The wet cake was dried at 50 °C (45~55 °C) for 20 h (15~25 h) to provide Compound (n) as the white solid in about 70-75% yield over two steps.
1H NMR (300 MHz, DMSO-d6) δ 12.46 (s, 1H), 10.68 (s, 1H), 7.56 (s, 1H), 7.15 – 7.00 (m, 3H), 6.91 (t, J = 4.4 Hz, 2H), 6.84 (d, J = 7.7 Hz, 1H), 6.55 (d, J = 2.8 Hz, 1H), 5.34 (t, J = 7.3 Hz, 1H), 4.63 (dd, J = 9.8, 8.0 Hz, 1H), 3.83 (q, J = 10.3 Hz, 2H), 3.45 (qd, J = 7.0, 5.1 Hz, 1H), 3.16 (s, 3H), 2.35 – 2.13 (m, 2H), 1.69 (t, J = 7.1 Hz, 2H), 1.56 (dq, J = 13.1, 6.5 Hz, 1H), 0.93 (dd, J = 12.2, 6.3 Hz, 6H).
Example 17. Preparation of (3R,5’S)-1′-(N-methyl-N-(4,6,7-trifluoro-1H-indole-2-carbonyl)-L-leucyl)-2-oxospiro[indoline-3,3′-pyrrolidine]-5′-carboxamide (Compound (n))
DMF (10.0 v) was added to a reactor at 25 °C followed by Compound (l) (4.4 kg, 1.0 eq.), NMM (3.0 eq.) Compound (m-3) (1.0 eq.) and HATU (1.0 eq) at 20-25oC. The reaction mixture was stirred for at least 12 hours at 20-25 °C. Once reaction was complete, aqueous ammonium hydroxide (1.0 eq.) was to the reaction system at 20-25 °C, then stirred for at least 2 hours at 20-25oC. The reaction mixture was then added to water (220 kg, 50V) at 20-30°C over 2 h and the resulting slurry was stirred for 2 h (1~5 h) at 25 °C (20~30 °C). The mixture was filtered and the cake was rinsed with water (22 kg, 5 V). The cake was dissolved in ethyl acetate (135 g, 15 V) and washed with 10% sodium chloride solution (22 kg) for three times. The organic layer was separated to 1.5-2.5V at not more than 45 ℃ under vacuum. The solution was cooled to 25 °C (20~30 °C) and Dichloromethane (5V) was added. The mixture was stirred for 2 h (2~5 h) at 25 °C (20~30 °C) and a slurry was formed. n-Heptane (2V) was added dropwise over 0.5 h (0.5~2 h) at 25 °C (20~30 °C) and stirred for additional 2 h (1~3 h) at 25 °C (20~30 °C). The reaction mixture was filtered and wet cake was rinsed with DCM/heptane (5/2). The wet cake was dried at 50 °C (45~55 °C) for 20 h (15~25 h) to provide Compound (n) as the white solid in 80-85% yield.
1H NMR (300 MHz, DMSO-d6) δ 12.46 (s, 1H), 10.68 (s, 1H), 7.56 (s, 1H), 7.15 – 7.00 (m, 3H), 6.91 (t, J = 4.4 Hz, 2H), 6.84 (d, J = 7.7 Hz, 1H), 6.55 (d, J = 2.8 Hz, 1H), 5.34 (t, J = 7.3 Hz, 1H), 4.63 (dd, J = 9.8, 8.0 Hz, 1H), 3.83 (q, J = 10.3 Hz, 2H), 3.45 (qd, J = 7.0, 5.1 Hz, 1H), 3.16 (s, 3H), 2.35 – 2.13 (m, 2H), 1.69 (t, J = 7.1 Hz, 2H), 1.56 (dq, J = 13.1, 6.5 Hz, 1H), 0.93 (dd, J = 12.2, 6.3 Hz, 6H). Example 18. Preparation of N-((S)-1-((3R,5’S)-5′-cyano-2-oxospiro[indoline-3,3′-pyrrolidin]-1′-yl)-4-methyl-1-oxopentan-2-yl)-4,6,7-trifluoro-N-methyl-1H-indole-2-carboxamide toluene solvate (Compound (I))
(I))

Ethyl acetate (630 kg, 10 V) was added into reactor (R1) followed by Compound (n) (70 kg). Make sure the water content was less than 0.20% (w/w). The reaction was cooled to 0 °C (-5 – 5°C) and then triethylamine (89.6 kg) was added followed by trifluoroacetic anhydride (92.4 kg) at 0 °C (-5 – 5°C). The reaction was stirred for 1 h (0.5~2 h) at 0 °C (-5 – 5°C). Once the reaction was complete, the reaction mixture was added slowly to 0.2 N aqueous HCl solution (700 kg) over 1 h at 0 °C (-5~5 °C). The resulting solution was stirred for 30 min at 0 °C (-5~5 °C) and the organic layer was separated.1% aqueous ammonium hydroxide (700 kg) was added to the organic layer and stirred at 20 °C for 30 min (15~25 °C). The organic layer was separated and washed with 10% brine for four times. Then the organic layer was separated and distilled to 2-3 V. Toluene-EtOAc swap was performed until precipitate was observed at 3-4 V. Then Toluene (5-6 V) was added and the slurry was stirred at 50 oC for 2 h. Then the solution was cooled down to 20 oC over 1-2 h and stirred for 10 hr (6~14 hr) at 20 °C (15~25 °C). The reaction mixture was filtered and the wet cake was rinsed with toluene (120 kg, 2V). The wet cake was then dried at 50˚C (45~55 °C) for 48 hr to provide desired compound (o) as a white solid in 80-85% yield.
1H NMR (400 MHz, Acetone-d6) δ 11.17 (s, 1H), 9.65 (s, 1H), 7.02 (dd, J = 13.7, 7.3 Hz, 2H), 6.94 (dd, J = 6.0, 3.5 Hz, 1H), 6.92 – 6.85 (m, 2H), 6.81 (t, J = 7.5 Hz, 1H), 5.56 (dd, J = 9.4, 5.6 Hz, 1H), 5.21 (t, J = 8.3 Hz, 1H), 4.25 (d, J = 10.7 Hz, 1H), 3.99 (d, J = 10.6 Hz, 1H), 3.43 (s, 3H), 2.79 – 2.61 (m, 2H), 1.93 (ddd, J = 14.4, 9.5, 5.1 Hz, 1H), 1.79 (ddd, J = 14.2, 8.7, 5.6 Hz, 1H), 1.64 (dpd, J = 8.7, 6.6, 5.1 Hz, 1H), 0.98 (dd, J = 18.5, 6.6 Hz, 6H).
US20230103494
CN114524821
SCHEME

MAIN

////////Zevotrelvir, EDP 235
O=C1[C@@]2(CN([C@@H](C2)C#N)C([C@H](CC(C)C)N(C)C(C3=CC4=C(F)C=C(F)C(F)=C4N3)=O)=O)C5=CC=CC=C5N1
Afimetoran

Afimetoran BMS-986256, WHO 11516
cas 2171019-55-7
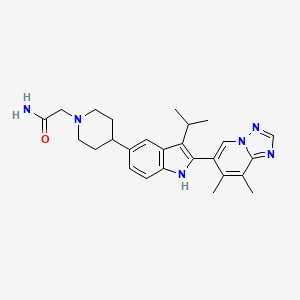
2-[4-[2-(7,8-dimethyl-[1,2,4]triazolo[1,5-a]pyridin-6-yl)-3-propan-2-yl-1H-indol-5-yl]piperidin-1-yl]acetamide
C26H32N6O,444.583, phase 1
Afimetoran is an immunomodulator and an antagonist of toll-like receptors 7 and 8.1,2 It is also is under investigation in clinical trial NCT04269356 (Study to Assess the Way the Body Absorbs, Distributes, Breaks Down and Eliminates Radioactive BMS-986256 in Healthy Male Participants).

Ref
WO2018005586
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2018005586&_cid=P20-M0RQ0D-09010-1
The invention further pertains to pharmaceutical compositions containing at least one compound according to the invention that are useful for the treatment of conditions related to TLR modulation, such as inflammatory and autoimmune diseases, and methods of inhibiting the activity of TLRs in a mammal.
Toll/IL-1 receptor family members are important regulators of inflammation and host resistance. The Toll-like receptor family recognizes molecular patterns derived from infectious organisms including bacteria, fungi, parasites, and viruses (reviewed in Kawai, T. et al., Nature Immunol., 11:373-384 (2010)). Ligand binding to the receptor induces dimerization and recruitment of adaptor molecules to a conserved cytoplasmic motif in the receptor termed the Toll/IL-1 receptor (TIR) domain. With the exception of TLR3, all TLRs recruit the adaptor molecule MyD88. The IL-1 receptor family also contains a cytoplasmic TIR motif and recruits MyD88 upon ligand binding (reviewed in Sims, J.E. et al., Nature Rev. Immunol., 10:89-102 (2010)).
Toll-like receptors (TLRs) are a family of evolutionarily conserved, transmembrane innate immune receptors that participate in the first-line defense. As pattern recognition receptors, the TLRs protect against foreign molecules, activated by pathogen associated molecular patterns (PAMPs), or from damaged tissue, activated by danger associated molecular patterns (DAMPs). A total of 13 TLR family members have been identified, 10 in human, that span either the cell surface or the endosomal compartment. TLR7-9 are among the set that are endosomally located and respond to single-stranded RNA (TLR7and TLR8) or unmethylated single-stranded DNA containing cytosine-phosphate-guanine (CpG) motifs (TLR9).
Activation of TLR7/8/9 can initiate a variety of inflammatory responses (cytokine production, B cell activation and IgG production, Type I interferon response). In the case of autoimmune disorders, the aberrant sustained activation of TLR7/8/9 leads to worsening of disease states. Whereas overexpression of TLR7 in mice has been shown to exacerbate autoimmune disease, knockout of TLR7 in mice was found to be protective against disease in lupus-prone MRL/lpr mice. Dual knockout of TLR7 and 9 showed further enhanced protection.
As numerous conditions may benefit by treatment involving modulation of cytokines, IFN production and B cell activity, it is immediately apparent that new compounds capable of modulating TLR7 and/or TLR8 and/or TLR9 and methods of using these compounds could provide substantial therapeutic benefits to a wide variety of patients.
The present invention relates to a new class of [1,2,4]triazolo[1,5-a]pyridinyl substituted indole compounds found to be effective inhibitors of signaling through TLR7/8/9. These compounds are provided to be useful as pharmaceuticals with desirable stability, bioavailability, therapeutic index, and toxicity values that are important to their drugability.
EXAMPLE 15
2-(4-(2-(7,8-dimethyl-[1,2,4]triazolo[1,5-a]pyridin-6-yl)-3-isopropyl-1H-indol-5-yl) piperidin-1-yl)acetamide

To a reaction flask were added
6-(3-isopropyl-5-(piperidin-4-yl)-1H-indol-2-yl)-7,8-dimethyl-[1,2,4]triazolo[1,5-a]pyrid ine, 2 HCl (47.66 g, 104 mmol), DCE (220 mL), DBU (62.4 mL, 414 mmol), and 2-bromoacetamide (17.14 g, 124 mmol). The reaction flask was capped. The reaction mixture was stirred overnight at room temperature. The reaction mixture was concentrated, diluted with water, and stirred for 30 minutes then filtered. The solid was recrystallized using ethanol to afford 2-(4-(2-(7,8-dimethyl-[1,2,4]triazolo[1,5-a] pyridin-6-yl)-3-isopropyl-1H-indol-5-yl)piperidin-1-yl)acetamide (42.3 g, 93 mmol,
90% yield) as a white solid. LCMS MH+: 445. HPLC Ret. Time 1.20 min. Method QC-ACN-TFA-XB. 1HNMR (400 MHz, DMSO-d6) δ 10.97-10.86 (m, 1H), 8.78-8.69 (m, 1H), 8.54-8.40 (m, 1H), 7.64-7.49 (m, 1H), 7.30-7.21 (m, 2H), 7.17-7.09 (m, 1H), 7.06-6.93 (m, 1H), 2.99-2.82 (m, 5H), 2.62-2.54 (m, 4H), 2.24-2.12 (m, 5H), 1.92-1.72 (m, 4H), 1.37-1.29 (m, 6H).
ACS Medicinal Chemistry Letters (2022), 13(5), 812-818 83%
References
- Bristol-Myers Squibb: Investor Series [Link]
- Bristol-Myers Squibb: Investor Series [Link]
- MedKoo Biosciences: Afimetoran [Link]
//////////////Afimetoran, BMS-986256, BMS 986256, WHO 11516, phase 1
lazertinib

lazertinib
CAS 1903008-80-9
554.655, C30H34N8O3
FDA APPROVED, 8/19/2024, Lazcluze, To treat non-small cell lung cancer
Drug Trials Snapshot
2-PROPENAMIDE, N-(5-((4-(4-((DIMETHYLAMINO)METHYL)-3-PHENYL-1H-PYRAZOL-1-YL)-2-PYRIMIDINYL)AMINO)-4-METHOXY-2-(4-MORPHOLINYL)PHENYL)-
- N-(5-((4-(4-((DIMETHYLAMINO)METHYL)-3-PHENYL-1H-PYRAZOL-1-YL)PYRIMIDIN-2-YL)AMINO)-4-METHOXY-2-MORPHOLINOPHENYL)ACRYLAMIDE
- C-18112003-G
- GNS 1480
- GNS-1480
- GNS1480
- JNJ-73841937-AAA
- YH 25448
- YH-25448
- YH25448
FDA APPROVED
| 8/19/2024 |
To treat non-small cell lung cancer, Lazcluze
| Ingredient | UNII | CAS | InChI Key |
|---|---|---|---|
| Lazertinib mesylate monohydrate | WUT449BEG5 | 2411549-88-5 | ZJPNGZUERUYZEG-UHFFFAOYSA-N |
Lazertinib is an oral, third-generation, epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI).2,3 Lazertinib was first approved in South Korea on January 18, 2021, for the treatment of EGFR T790M mutation-positive non-small cell lung cancer (NSCLC) with EGFR mutations.1 It was approved by the FDA on August 19, 2024.5 Lazertinib is used alone or in combination with other chemotherapeutic agents.4
Lazertinib, sold under the brand name Lazcluze and Leclaza, is an anti-cancer medication used for the treatment of non-small cell lung cancer.[1][2][3] It is a kinase inhibitor of epidermal growth factor receptor.[1]
The most common adverse reactions include rash, nail toxicity, infusion-related reactions (amivantamab), musculoskeletal pain, edema, stomatitis, venous thromboembolism, paresthesia, fatigue, diarrhea, constipation, COVID-19 infection, hemorrhage, dry skin, decreased appetite, pruritus, nausea, and ocular toxicity.[2]
Lazertinib was approved for medical use in South Korea in January 2021,[4][5] and in the United States in August 2024.[2][6]
Medical uses
Lazertinib is indicated in combination with amivantamab for the first-line treatment of adults with locally advanced or metastatic non-small cell lung cancer with epidermal growth factor receptor exon 19 deletions or exon 21 L858R substitution mutations.[2
History
Efficacy was evaluated in MARIPOSA (NCT04487080), a randomized, active-controlled, multicenter trial of 1074 participants with exon 19 deletion or exon 21 L858R substitution mutation-positive locally advanced or metastatic non-small cell lung cancer and no prior systemic therapy for advanced disease.[2] Participants were randomized (2:2:1) to receive lazertinib in combination with amivantamab, osimertinib monotherapy, or lazertinib monotherapy (an unapproved regimen for non-small cell lung cancer) until disease progression or unacceptable toxicity.[2]
Society and culture
Legal status
Lazertinib was approved for medical use in the United States in August 2024.[2]Names
Lazertinib is the international nonproprietary name.[7]
/////////////////////
References
- ^ Jump up to:a b c “Lazcluze- lazertinib tablet, film coated”. DailyMed. 20 August 2024. Retrieved 5 September 2024.
- ^ Jump up to:a b c d e f g “FDA approves lazertinib with amivantamab-vmjw for non-small lung cancer”. U.S. Food and Drug Administration (FDA). 19 August 2024. Retrieved 21 August 2024.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ Dhillon S (June 2021). “Lazertinib: First Approval”. Drugs. 81 (9): 1107–1113. doi:10.1007/s40265-021-01533-x. PMC 8217052. PMID 34028784.
- ^ “Yuhan wins approval as MFDS clear T790M EGFR TKI drug ‘Lazertinib'”. 바이오스펙테이터. Retrieved 23 August 2024.
- ^ Dhillon S (2021). “Lazertinib: First Approval”. Drugs. 81 (9): 1107–1113. doi:10.1007/s40265-021-01533-x. ISSN 0012-6667. PMC 8217052. PMID 34028784.
- ^ “Rybrevant (amivantamab-vmjw) plus Lazcluze (lazertinib) approved in the U.S. as a first-line chemotherapy-free treatment for patients with EGFR-mutated advanced lung cancer”. Johnson & Johnson (Press release). 20 August 2024. Retrieved 21 August 2024.
- ^ World Health Organization (2018). “International nonproprietary names for pharmaceutical substances (INN): recommended INN: list 79”. WHO Drug Information. 32 (1). hdl:10665/330941.
External links
- Clinical trial number NCT04487080 for “A Study of Amivantamab and Lazertinib Combination Therapy Versus Osimertinib in Locally Advanced or Metastatic Non-Small Cell Lung Cancer (MARIPOSA)” at ClinicalTrials.gov
| Clinical data | |
|---|---|
| Trade names | Lazcluze, Leclaza |
| License data | US DailyMed: Lazertinib |
| Routes of administration | By mouth |
| Drug class | EGFR inhibitor |
| ATC code | L01EB09 (WHO) |
| Legal status | |
| Legal status | US: ℞-only[1] |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 1903008-80-9 |
| PubChem CID | 121269225 |
| IUPHAR/BPS | 10136 |
| DrugBank | DB16216 |
| ChemSpider | 64835231 |
| UNII | 4A2Y23XK11 |
| KEGG | D11980D12245 |
| ChEMBL | ChEMBL4558324 |
| Chemical and physical data | |
| Formula | C30H34N8O3 |
| Molar mass | 554.655 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
/////////lazertinib, C-18112003-G, GNS 1480, GNS-1480, GNS1480, JNJ-73841937-AAA, YH 25448, YH-25448, YH25448, Lazcluze, FDA 2024, APPROVALS 2024
COC1=C(NC2=NC=CC(=N2)N2C=C(CN(C)C)C(=N2)C2=CC=CC=C2)C=C(NC(=O)C=C)C(=C1)N1CCOCC1
ACT-132577, Aprocitentan

ACT-132577, Aprocitentan,
1103522-45-7
546.19, C16H14Br2N6O4S
3/19/2024 FDA APPROVED, To treat hypertension, Tryvio
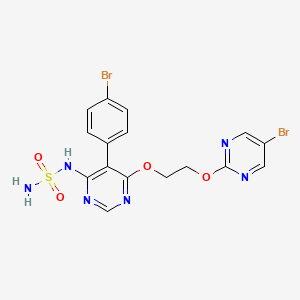
N-[5-(4-bromophenyl)-6-{2-[(5-bromopyrimidin-2-yl)oxy]ethoxy}pyrimidin-4-yl]aminosulfonamide
Aprocitentan, sold under the brand name Tryvio, is a medication used to treat hypertension (high blood pressure).[1] It is developed by Idorsia.[2] It is taken by mouth.[1]
Aprocitentan is a dual endothelin-1 antagonist that targets both endothelin A and endothelin B receptors.[3][4]
Aprocitentan was approved for medical use in the United States in March 2024.[1][2][5] It is the first endothelin receptor antagonist to be approved by the US Food and Drug Administration (FDA) to treat systemic hypertension.[2]
Medical uses
Aprocitentan is indicated for the treatment of hypertension in combination with other antihypertensive drugs, to lower blood pressure in adults who are not adequately controlled on other medications.[1]
Adverse effects
Aprocitentan may cause hepatotoxicity (liver damage), edema (fluid retention), anemia (reduced hemoglobin), and decreased sperm count.[1]
Contraindications
Data from animal reproductive toxicity studies with other endothelin-receptor agonists indicate that use is contraindicated in pregnant women.[1]
Mechanism of action
Aprocitentan is an endothelin receptor agonist that inhibits the protein endothelin-1 from binding to endothelin A and endothelin B receptors.[1][4] Endothelin-1 mediates various adverse effects via its receptors, such as inflammation, cell proliferation, fibrosis, and vasoconstriction.[1]
Society and culture
Economics
Aprocitentan is developed by Idorsia, which sold it to Janssen and purchased the rights back in 2023, for US$343 million.[6]
Legal status
Aprocitentan was approved for medical use in the United States in March 2024.[1]
In April 2024, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency adopted a positive opinion, recommending the granting of a marketing authorization for the medicinal product Jeraygo, intended for the treatment of resistant hypertension in adults.[7] The applicant for this medicinal product is Idorsia Pharmaceuticals Deutschland GmbH.[7]
SYN
US Patent
Trade Name
Application Number
Applicant
IDORSIA PHARMACEUTICALS LTD
IDORSIA PHARMACEUTICALS LTD
IDORSIA PHARMACEUTICALS LTD
IDORSIA PHARMACEUTICALS LTD
IDORSIA PHARMACEUTICALS LTD
PATENT
WO 02/053557
PATENT
Martin Bolli, Christoph Boss, Alexander Treiber. ” 4-pyrimidinesulfamide derivative “, US Patent US8324232B2.
EXAMPLE
Preparation A: Benzylsulfamide Potassium Salt
A.i. Benzylsulfamide
| 1H NMR (D 6-DMSO): δ 4.05 (d, J=6.4 Hz, 2H); 6.60 (s, 2H); 7.04 (s, J=6.4 Hz, 1H); 7.20-7.36 (m, 5H). |
A.ii. Benzylsulfamide Potassium Salt
Preparation B: 5-(4-bromo-phenyl)-4,6-dichloro-pyrimidine
B.i. 4-bromophenylacetic acid methyl ester
B.ii. 2-(4-bromophenyl)-malonic acid dimethyl ester
B.iii. 5-(4-bromophenyl)-pyrimidine-4,6-diol
B.iv. 5-(4-bromo-phenyl)-4,6-dichloro-pyrimidine
Example 1
{5-(4-bromo-phenyl)-6-[2-(5-bromo-pyrimidin-2-yloxy)-ethoxy]-pyrimidin-4-yl}-sulfamide
1.i. Benzyl-sulfamic acid [6-chloro-5-(4-bromophenyl)-pyrimidin-4-yl]-amide
| 1H NMR (CDCl 3): δ 4.23 (d, J=5.9 Hz, 2H); 5.94 (t br., J=6 Hz, 1H); 7.05 (d, J=8.2 Hz, 2H); 7.20-7.35 (m, 5H); 7.68 (d, J=8.2 Hz, 2H); 8.61 (s, 1H). |
1.ii. Benzyl-sulfamic acid [5-(4-bromophenyl)-6-(2-hydroxyethoxy)pyrimidin-4-yl]-amide
1.iii Benzyl-sulfamic acid [5-(4-bromophenyl)-6-{2-(5-bromo-pyrimidin-2-yloxy)-ethoxy}-pyrimidin-4-yl]-amide
1.iv. {5-(4-bromo-phenyl)-6-[2-(5-bromo-pyrimidin-2-yloxy)-ethoxy]-pyrimidin-4-yl}-sulfamide
| 1H NMR (CDCl 3): δ 4.60-4.65 (m, 2H), 4.71-4.74 (m, 2H), 5.50 (s br, 2H), 7.10 (s br, 1H), 7.13-7.17 (m, 2H), 7.55-7.59 (m, 2H), 8.49 (s, 2H), 8.50 (s, 1H). |
| Clinical data | |
|---|---|
| Trade names | Tryvio |
| Other names | ACT-132577 |
| AHFS/Drugs.com | Tryvio |
| Routes of administration | By mouth |
| Drug class | Antihypertensive |
| ATC code | C02KN01 (WHO) |
| Legal status | |
| Legal status | US: ℞-only[1] |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 1103522-45-7 |
| PubChem CID | 25099191 |
| IUPHAR/BPS | 10070 |
| DrugBank | DB15059 |
| ChemSpider | 25027753 |
| UNII | MZI81HV01P |
| KEGG | D11441 |
| ChEBI | CHEBI:76609 |
| ChEMBL | ChEMBL2165326 |
| Chemical and physical data | |
| Formula | C16H14Br2N6O4S |
| Molar mass | 546.19 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| hideSMILESC1=CC(=CC=C1C2=C(N=CN=C2OCCOC3=NC=C(C=N3)Br)NS(=O)(=O)N)Br | |
References
- ^ Jump up to:a b c d e f g h i j “Tryvio- aprocitentan tablet, film coated”. DailyMed. 29 March 2024. Archived from the original on 25 April 2024. Retrieved 25 April 2024.
- ^ Jump up to:a b c “US FDA approves Idorsia’s once-daily Tryvio (aprocitentan) – the first and only endothelin receptor antagonist for the treatment of high blood pressure not adequately controlled in combination with other antihypertensives” (Press release). Idorsia. 20 March 2024. Archived from the original on 28 April 2024. Retrieved 28 April 2024 – via PR Newswire.
- ^ Ojha, Utkarsh; Ruddaraju, Sanjay; Sabapathy, Navukkarasu; Ravindran, Varun; Worapongsatitaya, Pitchaya; Haq, Jeesanul; et al. (2022). “Current and Emerging Classes of Pharmacological Agents for the Management of Hypertension”. American Journal of Cardiovascular Drugs. 22 (3): 271–285. doi:10.1007/s40256-021-00510-9. PMC 8651502. PMID 34878631.
- ^ Jump up to:a b Xu, Jingjing; Jiang, Xiaohua; Xu, Suowen (November 2023). “Aprocitentan, a dual endothelin-1 (ET-1) antagonist for treating resistant hypertension: Mechanism of action and therapeutic potential”. Drug Discovery Today. 28 (11): 103788. doi:10.1016/j.drudis.2023.103788. PMID 37742911.
- ^ “Novel Drug Approvals for 2024”. U.S. Food and Drug Administration (FDA). 29 April 2024. Archived from the original on 30 April 2024. Retrieved 30 April 2024.
- ^ Deswal, Phalguni (6 September 2023). “Idorsia reacquires aprocitentan rights from Janssen for $343m”. Pharmaceutical Technology. Archived from the original on 8 November 2023. Retrieved 8 November 2023.
- ^ Jump up to:a b “Jeraygo EPAR”. European Medicines Agency. 25 April 2024. Archived from the original on 30 April 2024. Retrieved 27 April 2024. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
Further reading
- Mahfooz K, Najeed S, Tun HN, Khamosh M, Grewal D, Hussain A, et al. (July 2023). “New Dual Endothelin Receptor Antagonist Aprocitentan in Hypertension: A Systematic Review and Meta-Analysis”. Current Problems in Cardiology. 48 (7): 101686. doi:10.1016/j.cpcardiol.2023.101686. PMID 36893968.
/////ACT-132577, Aprocitentan, Tryvio, FDA 2024, APPROVALS 2024, N-Despropyl-macitentan, WHO 10552
Cefepime

Cefepime
88040-23-7
| INGREDIENT | UNII | CAS | INCHI KEY |
|---|---|---|---|
| Cefepime hydrochloride | I8X1O0607P | 123171-59-5 | LRAJHPGSGBRUJN-OMIVUECESA-N |
Cefepime
CAS Registry Number: 88040-23-7
CAS Name: 1-[[(6R,7R)-7-[[(2Z)-(2-Amino-4-thiazolyl)(methoxyimino)acetyl]amino]-2-carboxy-8-oxo-5-thia-1-azabicyclo[4.2.0]oct-2-en-3-yl]methyl]-1-methylpyrrolidinium inner salt
Additional Names: 1-[[(6R,7R)-7-[2-(2-amino-4-thiazolyl)glyoxylamido]-2-carboxy-8-oxo-5-thia-1-azabicyclo[4.2.0]oct-2-en-3-yl]methyl]-1-methylpyrrolidinium hydroxide inner salt 72-(Z)-2-(O-methyloxime); 7-[(Z)-2-(2-aminothiazol-4-yl)-2-methoxyiminoacetamido]-3-(1-methylpyrrolidinio)methyl-3-cephem-4-carboxylate
Manufacturers’ Codes: BMY-28142
Molecular Formula: C19H24N6O5S2
Molecular Weight: 480.56
Percent Composition: C 47.49%, H 5.03%, N 17.49%, O 16.65%, S 13.34%
Literature References: Semisynthetic, fourth generation cephalosporin antibiotic. Prepn: S. Aburaki et al.,DE3307550; eidem,US4406899 (both 1983 to Bristol-Myers); and antibacterial activity: T. Naito et al.,J. Antibiot.39, 1092 (1986). In vitro comparative antimicrobial spectrum: N. J. Khan et al.,Antimicrob. Agents Chemother.26, 585 (1984); and b-lactamase stability: H. C. Neu et al.,J. Antimicrob. Chemother.17, 441 (1986). HPLC determn in plasma and urine: R. H. Barbhaiya et al.,Antimicrob. Agents Chemother.31, 55 (1987). Clinical evaluations in infection: N. Clynes et al.,Diagn. Microbiol. Infect. Dis.12, 257 (1989); S. Oster et al.,Antimicrob. Agents Chemother.34, 954 (1990). Review of clinical pharmacokinetics: M. P. Okamoto et al.,Clin. Pharmacokinet.25, 88-102 (1993).
Properties: Colorless powder, mp 150° (dec). uv max (pH 7 phosphate buffer): 235, 257 nm (e 16700, 16100).
Melting point: mp 150° (dec)
Absorption maximum: uv max (pH 7 phosphate buffer): 235, 257 nm (e 16700, 16100)
Derivative Type: Sulfate
Molecular Formula: C19H24N6O5S2.H2SO4
Molecular Weight: 578.64
Percent Composition: C 39.44%, H 4.53%, N 14.52%, O 24.89%, S 16.62%
Properties: mp 210° (dec). uv max (pH 7 phosphate buffer): 236, 258 nm (e 17200, 16900).
Melting point: mp 210° (dec)
Absorption maximum: uv max (pH 7 phosphate buffer): 236, 258 nm (e 17200, 16900)
Derivative Type: Hydrochloride monohydrate
CAS Registry Number: 123171-59-5
CAS Name: 1-[[(6R,7R)-7-[[(2Z)-(2-Amino-4-thiazolyl)(methoxyimino)acetyl]amino]-2-carboxy-8-oxo-5-thia-1-azabicyclo[4.2.0]oct-2-en-3-yl]methyl]-1-methylpyrrolidinium chloride monohydrochloride monohydrate
Additional Names: cefepime hydrochloride
Trademarks: Axepim (BMS); Cepimex (Mead Johnson); Maxipime (BMS)
Molecular Formula: C19H25ClN6O5S2.HCl.H2O
Molecular Weight: 571.50
Percent Composition: C 39.93%, H 4.94%, Cl 12.41%, N 14.71%, O 16.80%, S 11.22%
Therap-Cat: Antibacterial.
Keywords: Antibacterial (Antibiotics); ?Lactams; Cephalosporins.
FDA APPROVED 2/22/2024, To treat complicated urinary tract infections, Exblifep
- BMY 28142
- BMY-28142
Cefepime is a fourth-generation cephalosporin antibiotic. Cefepime has an extended spectrum of activity against Gram-positive and Gram-negative bacteria, with greater activity against both types of organism than third-generation agents. A 2007 meta-analysis suggested when data of trials were combined, mortality was increased in people treated with cefepime compared with other β-lactam antibiotics.[1] In response, the U.S. Food and Drug Administration (FDA) performed their own meta-analysis which found no mortality difference.[2]
Cefepime was patented in 1982 by Bristol-Myers Squibb and approved for medical use in 1994.[3] It is available as a generic drug and sold under a variety of trade names worldwide.[citation needed][4]
It was removed from the World Health Organization’s List of Essential Medicines in 2019.[5]
Medical use
Cefepime is usually reserved to treat moderate to severe nosocomial pneumonia, infections caused by multiple drug-resistant microorganisms (e.g. Pseudomonas aeruginosa) and empirical treatment of febrile neutropenia.[6]
Cefepime has good activity against important pathogens including Pseudomonas aeruginosa, Staphylococcus aureus, and multiple drug-resistant Streptococcus pneumoniae. A particular strength is its activity against Enterobacteriaceae. Whereas other cephalosporins are degraded by many plasmid– and chromosome-mediated beta-lactamases, cefepime is stable and is a front-line agent when infection with Enterobacteriaceae is known or suspected.[medical citation needed]
Spectrum of bacterial susceptibility
Cefepime is a broad-spectrum cephalosporin antibiotic and has been used to treat bacteria responsible for causing pneumonia and infections of the skin and urinary tract. Some of these bacteria include Pseudomonas, Escherichia, and Streptococcus species. The following represents MIC susceptibility data for a few medically significant microorganisms:[7]
- Escherichia coli: ≤0.007 – 128 μg/ml
- Pseudomonas aeruginosa: 0.06 – >256 μg/ml
- Streptococcus pneumoniae: ≤0.007 – >8 μg/ml
Chemistry
The combination of the syn-configuration of the methoxy imino moiety and the aminothiazole moiety confers extra stability to β-lactamase enzymes produced by many bacteria. The N–methyl pyrrolidine moiety increases penetration into Gram-negative bacteria. These factors increase the activity of cefepime against otherwise resistant organisms including Pseudomonas aeruginosa and Staphylococcus aureus.

Semisynthetic, fourth generation cephalosporin antibiotic. Prepn: S. Aburaki et al., DE 3307550; eidem, US 4406899 (both 1983 to Bristol-Myers); and antibacterial activity: T. Naito et al., J. Antibiot. 39, 1092 (1986).
Trade names
Following expiration of the Bristol-Myers Squibb patent,[] cefepime became available as a generic and is now] marketed by numerous companies worldwide under tradenames including Neopime (Neomed), Maxipime, Cepimax, Cepimex, and Axepim.
| Clinical data | |
|---|---|
| Pronunciation | /ˈsɛfɪpiːm/ or /ˈkɛfɪpiːm/ |
| Trade names | Maxipime, Voco |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a698021 |
| Pregnancy category | AU: B1 |
| Routes of administration | Intravenous, intramuscular |
| ATC code | J01DE01 (WHO) |
| Legal status | |
| Legal status | AU: S4 (Prescription only)CA: ℞-onlyUK: POM (Prescription only)US: ℞-only |
| Pharmacokinetic data | |
| Bioavailability | 100% (IM) |
| Metabolism | Hepatic 15% |
| Elimination half-life | 2 hours |
| Excretion | Renal 70–99% |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 88040-23-7 |
| PubChem CID | 5479537 |
| DrugBank | DB01413 |
| ChemSpider | 4586395 |
| UNII | 807PW4VQE3 |
| KEGG | D02376 |
| ChEBI | CHEBI:478164 |
| ChEMBL | ChEMBL186 |
| CompTox Dashboard (EPA) | DTXSID70873208 |
| ECHA InfoCard | 100.171.025 |
| Chemical and physical data | |
| Formula | C19H24N6O5S2 |
| Molar mass | 480.56 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| Melting point | 150 °C (302 °F) (dec.) |
| showSMILES | |
| showInChI | |
| (verify) | |
References
- ^ Yahav D, Paul M, Fraser A, Sarid N, Leibovici L (May 2007). “Efficacy and safety of cefepime: a systematic review and meta-analysis”. The Lancet. Infectious Diseases. 7 (5): 338–348. doi:10.1016/S1473-3099(07)70109-3. PMID 17448937.
- ^ “FDA Alert: Cefepime (marketed as Maxipime)”. Information for Healthcare Professionals. Food and Drug Administration. Archived from the original on 2 November 2017. Retrieved 2 August 2009.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 496. ISBN 9783527607495. Archived from the original on 19 June 2021. Retrieved 19 September 2020.
- ^ “Cefepime (maxipime), large spectrum 4th generation cephalosporin, resistant to beta-lactamases]”.
- ^ World Health Organization (2019). Executive summary: the selection and use of essential medicines 2019: report of the 22nd WHO Expert Committee on the selection and use of essential medicines. Geneva: World Health Organization. hdl:10665/325773. WHO/MVP/EMP/IAU/2019.05. License: CC BY-NC-SA 3.0 IGO.
- ^ Chapman TM, Perry CM (2003). “Cefepime: a review of its use in the management of hospitalized patients with pneumonia”. American Journal of Respiratory Medicine. 2 (1): 75–107. doi:10.1007/bf03256641. PMID 14720024.
- ^ “Cefepime Susceptibility and Concentration Range (μg/ml) Minimum Inhibitory Concentration (MIC) Data” (PDF). The Antimicrobial Index. toku-e.com. Archived from the original (PDF) on 1 November 2018.
External links
- “Cefepime”. Drug Information Portal. U.S. National Library of Medicine.
//////////cefepime, Exblifep, FDA 2024, APPROVALS 2024, BMY 28142, BMY-28142
Berdazimer


Berdazimer
CAS NA SALT, 1846565-00-1
FDA APPROVE 1 /5/2024, To treat molluscum contagiosum
Drug Trials Snapshot
- NVN-1000 free acid
- NVN1000 free acid
- Silsesquioxanes, 3-(2-hydroxy-1-methyl-2-nitrosohydrazinyl)propyl 3-(methylamino)propyl, polymers with silicic acid (h4sio4) tetra-et ester, hydroxy-terminated
Berdazimer sodium, sold under the brand name Zelsuvmi, is a medication used for the treatment for molluscum contagiosum.[1] Berdazimer sodium is a nitric oxide releasing agent.[1] It is a polymer formed from sodium 1-hydroxy-3-methyl-3-(3-(trimethoxysilyl)propyl)-1-triazene-2-oxide and tetraethyl silicate.[2]
Berdazimer sodium was approved for medical use in the United States in January 2024.[3][4][5]
Medical uses
Berdazimer sodium is indicated for the topical treatment of molluscum contagiosum.[1]
Pharmacology
Mechanism of action
Berdazimer sodium is a nitric oxide releasing agent.[1] The mechanism of action for the treatment of molluscum contagiosum is unknown.[1]
Pharmacodynamics
The pharmacodynamics of berdazimer sodium are unknown.[1]
Society and culture
Legal status
Berdazimer sodium was approved for medical use in the United States in January 2024.[4]
Names
Berdazimer sodium is the international nonproprietary name.[6]
Berdazimer is a polymeric substance consisting of a polysiloxane backbone (Si-O-Si bonds) with covalently bound N-diazeniumdiolate nitric oxide (NO) donors. It releases NO through exposure to proton donors like water, which will degrade the N-diazeniumdiolate entity.2 Berdazimer was previously investigated as a potential treatment for molluscum contagiosum, a viral cutaneous infection mainly affecting children, sexually active adults, and immunocompromised patients. It is one of the 5 most prevalent skin diseases in the world and the third-most common viral skin infection in children.3 Previously, the first line treatment for molluscum contagiosum was surgical excision, although it poses challenges such as repeated doctor visits, post-surgical scarring and skin discoloration, and fear and anxiety in the pediatric population.3
On Jan 05, 2024, the FDA approved berdazimer under the brand name ZELSUVMI for the treatment of adult and pediatric molluscum contagiosum, and it is the first drug to be approved for this condition. This decision is based on positive results demonstrated in 2 Phase 3 trials, B-SIMPLE 4 and B-SIMPLE 2, where reduced lesion counts were observed with once-a-day uses of berdazimer.5



 References
References
- ^ Jump up to:a b c d e f g h i “Zelsuvmi (berdazimer) topical gel” (PDF). Archived (PDF) from the original on 19 January 2024. Retrieved 9 January 2024.
- ^ “GSRS”. gsrs.ncats.nih.gov. Archived from the original on 8 January 2024. Retrieved 8 January 2024.
- ^ “Drug Approval Package: Zelsuvmi”. U.S. Food and Drug Administration (FDA). 2 February 2024. Archived from the original on 11 March 2024. Retrieved 11 March 2024.
- ^ Jump up to:a b “Novel Drug Approvals for 2024”. U.S. Food and Drug Administration (FDA). 29 April 2024. Archived from the original on 30 April 2024. Retrieved 30 April 2024.
- ^ “U.S. Food and Drug Administration Approves Zelsuvmi as a First-in-Class Medication for the Treatment of Molluscum Contagiosum”. Ligand Pharmaceuticals. 5 January 2024. Archived from the original on 8 January 2024. Retrieved 8 January 2024 – via Business Wire.
- ^ World Health Organization (2018). “International nonproprietary names for pharmaceutical substances (INN): recommended INN: list 79”. WHO Drug Information. 32 (1). hdl:10665/330941.
Further reading
- Pera Calvi I, R Marques I, Cruz SA, Mesquita YL, Padrao EM, Souza RM, et al. (2023). “Safety and efficacy of topical nitric oxide-releasing berdazimer gel for molluscum contagiosum clearance: A systematic review and meta-analysis of randomized controlled trials”. Pediatric Dermatology. 40 (6): 1060–1063. doi:10.1111/pde.15419. PMID 37721050. S2CID 262045499.
- Han H, Smythe C, Yousefian F, Berman B (February 2023). “Molluscum Contagiosum Virus Evasion of Immune Surveillance: A Review”. Journal of Drugs in Dermatology. 22 (2): 182–189. doi:10.36849/JDD.7230. PMID 36745361. S2CID 256613906.
- Lacarrubba F, Micali G, Trecarichi AC, Quattrocchi E, Monfrecola G, Verzì AE (December 2022). “New Developing Treatments for Molluscum Contagiosum”. Dermatology and Therapy. 12 (12): 2669–2678. doi:10.1007/s13555-022-00826-7. PMC 9674806. PMID 36239905.
- Ward BM, Riccio DA, Cartwright M, Maeda-Chubachi T (November 2023). “The Antiviral Effect of Berdazimer Sodium on Molluscum Contagiosum Virus Using a Novel In Vitro Methodology”. Viruses. 15 (12): 2360. doi:10.3390/v15122360. PMC 10747301. PMID 38140601.
External links
- “Berdazimer Sodium (Code C174810)”. NCI Thesaurus.
- Clinical trial number NCT04535531 for “A Phase 3 Molluscum Contagiosum Efficacy and Safety Study (B-SIMPLE4)” at ClinicalTrials.gov
- Clinical trial number NCT03927703 for “A Phase 3 Efficacy & Safety of SB206 & Vehicle Gel for the Treatment of MC (B-SIMPLE2)” at ClinicalTrials.gov
- Clinical trial number NCT03927716 for “A Phase 3 Randomized Parallel Group Study Comparing the Efficacy & Safety of SB206 & Vehicle Gel in the Treatment of MC (B-SIMPLE1)” at ClinicalTrials.gov
| Clinical data | |
|---|---|
| Trade names | Zelsuvmi |
| Other names | SB206 |
| License data | US DailyMed: Berdazimer sodium |
| Routes of administration | Topical |
| ATC code | None |
| Legal status | |
| Legal status | US: ℞-only[1] |
| Identifiers | |
| CAS Number | 1846565-00-1 |
| DrugBank | DBSALT003491DB18712 |
| UNII | ORT9SID4QYB23P7SM943 |
| KEGG | D12758 |
| ChEMBL | ChEMBL4298064 |
| Chemical and physical data | |
| Formula | Indeterminate[1] |
| Molar mass | Indeterminate[1] |
/////Berdazimer, Zelsuvmi, FDA 2024, APPROVALS 2024, NVN-1000 free acid, NVN1000 free acid
Tovorafenib

Tovorafenib
506.29
C17H12Cl2F3N7O2S
1096708-71-2
6-amino-5-chloro-N-[(1R)-1-(5-{[5-chloro-4-(trifluoromethyl)pyridin-2-yl]carbamoyl}-1,3-thiazol-2-yl)ethyl]pyrimidine-4-carboxamide
4/23/2024 FDA APROVED, To treat relapsed or refractory pediatric low-grade glioma, Ojemda
- AMG 2112819
- BIIB 024
- BIIB-024
- BIIB024
- DAY 101
- DAY-101
- DAY101
- MLN 2480
- MLN-2480
- MLN2480
- TAK 580
- TAK-580
- TAK580
Tovorafenib, sold under the brand name Ojemda, is a medication used for the treatment of glioma.[1] It is a kinase inhibitor.[1]
The most common adverse reactions include rash, hair color changes, fatigue, viral infection, vomiting, headache, hemorrhage, pyrexia, dry skin, constipation, nausea, dermatitis acneiform, and upper respiratory tract infection.[2] The most common grade 3 or 4 laboratory abnormalities include decreased phosphate, decreased hemoglobin, increased creatinine phosphokinase, increased alanine aminotransferase, decreased albumin, decreased lymphocytes, decreased leukocytes, increased aspartate aminotransferase, decreased potassium, and decreased sodium.[2]
It was approved for medical use in the United States in April 2024,[1][2][3][4] and is the first approval of a systemic therapy for the treatment of people with pediatric low-grade glioma with BRAF rearrangements, including fusions.[2]
Medical uses
Tovorafenib is indicated for the treatment of people six months of age and older with relapsed or refractory pediatric low-grade glioma harboring a BRAF fusion or rearrangement, or BRAF V600 mutation.[1][2]
History
Efficacy was evaluated in 76 participants enrolled in FIREFLY-1 (NCT04775485), a multicenter, open-label, single-arm trial in participants with relapsed or refractory pediatric low-grade glioma harboring an activating BRAF alteration detected by a local laboratory who had received at least one line of prior systemic therapy.[2] Participants were required to have documented evidence of radiographic progression and at least one measurable lesion.[2] Participants with tumors harboring additional activating molecular alterations (e.g., IDH1/2 mutations, FGFR mutations) or with a known or suspected diagnosis of neurofibromatosis type 1 were excluded.[2] Participants received tovorafenib based on body surface area (range: 290 to 476 mg/m2, up to a maximum dose of 600 mg) once weekly until they experienced disease progression or unacceptable toxicity.[2] The US Food and Drug Administration (FDA) granted the application for tovorafenib priority review, breakthrough therapy, and orphan drug designations.[2]
Society and culture
Names
Tovorafenib is the international nonproprietary name.[5]
SYN
PATENT
Huang et al., Angew. Chem. int. Ed. (2016), 55, 5309-5317
Jiang Xiao-bin et al., Org. Lett. (2003), 5, 1503
10Da
| (R)-2-(1-(6-amino-5-chloropyrimidine-4- carboxamido)ethyl)-N-(5-chloro-4- (trifluoromethyl)pyridin-2-yl)thiazole-5- carboxamide |
SYN

Patent
https://patentscope.wipo.int/search/en/detail.jsf?docId=US131345763&_cid=P22-LW02NH-45076-1
PATENT
https://patentscope.wipo.int/search/en/detail.jsf?docId=US201396258&_cid=P22-LW02NH-45076-1
PATENT
References
- ^ Jump up to:a b c d e “Archived copy” (PDF). Archived (PDF) from the original on 24 April 2024. Retrieved 24 April 2024.
- ^ Jump up to:a b c d e f g h i j “FDA grants accelerated approval to tovorafenib for patients with relapsed or refractory BRAF-altered pediatric low-grade glioma”. U.S. Food and Drug Administration (FDA). 23 April 2024. Archived from the original on 23 April 2024. Retrieved 25 April 2024.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ “Novel Drug Approvals for 2024”. U.S. Food and Drug Administration (FDA). 29 April 2024. Archived from the original on 30 April 2024. Retrieved 30 April 2024.
- ^ “Day One’s Ojemda (tovorafenib) Receives US FDA Accelerated Approval for Relapsed or Refractory BRAF-altered Pediatric Low-Grade Glioma (pLGG), the Most Common Form of Childhood Brain Tumor”. Day One Biopharmaceuticals (Press release). 23 April 2024. Archived from the original on 23 April 2024. Retrieved 24 April 2024.
- ^ World Health Organization (2022). “International nonproprietary names for pharmaceutical substances (INN): recommended INN: list 88”. WHO Drug Information. 36 (3). hdl:10665/363551.
External links
- “Tovorafenib”. NCI Drug Dictionary.
- “Tovorafenib (Code C106254)”. NCI Thesaurus.
- Clinical trial number NCT04775485 for “A Study to Evaluate DAY101 in Pediatric and Young Adult Patients With Relapsed or Progressive Low-Grade Glioma and Advance Solid Tumors (FIREFLY-1)” at ClinicalTrials.gov
| Clinical data | |
|---|---|
| Trade names | Ojemda |
| Other names | BIIB-024, MLN2480, AMG 2112819, DAY101, TAK-580 |
| License data | US DailyMed: Tovorafenib |
| Routes of administration | By mouth |
| Drug class | Antineoplastic |
| ATC code | None |
| Legal status | |
| Legal status | US: ℞-only[1] |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 1096708-71-2 |
| PubChem CID | 25161177 |
| DrugBank | DB15266 |
| ChemSpider | 28637796 |
| UNII | ZN90E4027M |
| KEGG | D12291 |
| ChEBI | CHEBI:167672 |
| ChEMBL | ChEMBL3348923 |
| PDB ligand | QOP (PDBe, RCSB PDB) |
| Chemical and physical data | |
| Formula | C17H12Cl2F3N7O2S |
| Molar mass | 506.29 g·mol−1 |
| showInChI | |
////////Tovorafenib, Ojemda, FDA 2024. APPROVALS 2024, AMG 2112819, BIIB 024, BIIB-024, BIIB024, DAY 101, DAY-101, DAY101, MLN 2480, MLN-2480, MLN2480, TAK 580, TAK-580, TAK580

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO



