Home » 2014 (Page 84)
Yearly Archives: 2014
Uncialamycin

Uncialamycin
(1aS,11S,11aR,18R)-3,18-Dihydroxy-11a-[1(R*)-hydroxyethyl]-9,10,11,11a-tetrahydro-4H-11,1a-[3]heptene[1,5]diynonaphtho[2,3-h]oxireno[c]quinoline-4,9-dione
439.4163
C26 H17 N O6
870471-83-3 cas
WO2007038868A2, WO2013122823A1,
University of British Columbia (Originator)
uncialamycin, an enediyne natural product isolated from the Streptomyces uncialis, bacteria present on the surface of the lichen Cladonia uncialis.
Laboratory cultures of an undescribed streptomycete obtained from the surface of a British Columbia lichen produce uncialamycin (1), a new enediyne antibiotic.Uncialamycin exhibits potent in vitro antibacterial activity against Gram-positive and Gram-negative human pathogens, including Burkholderia cepacia, a major cause of morbidity and mortality in patients with cystic fibrosis.
Uncialamycin is an enediyne antibiotic with some unprecedented activity. The isolationists have filed a patent application almost right away. The total synthesis by Nicolaou [ACIE2007, 46, 4704] goes along nearly the same lines that have been predicted, and similar to Myers’ synthesis of dynemicin A [JACS 1997, 119, 6072], only it is not paper chemistry but the real one.

They have easily constructed the quinoline system with required functionality and subjected it to AllocCl-assisted acetylide addition (if I interpreted correctly “92% yield based on 80% conversion”). 5-alkoxyquinoline system was later advanced to iminoquinone and the two remaining rings were again attached by Hauser annulation with 3-cyanophthalide. The final product turned out be different from the one reported, more precisely, it was a C26-epimer. It is funny that I have accidentally drawn the correct structure with R-configuration at C-26 in the previous post.
The synthetic scheme allowed to easily invert this stereocenter via oxidation/reduction sequence on the last compound shown on the scheme below. The spectral properties of the final product thus obtained matched the reported data, and the structure of uncialamycin was confirmed by X-ray, despite it was isolated as an oil. The structure on the right is the revised one. The remaining details, including the chemistry behind DNA-cleaving Bergmann cycloaromatization,

Total Synthesis and Stereochemistry of Uncialamycin
K. C. Nicolaou, Hongjun Zhang, Jason S. Chen, James Crawford, Laxman Dasunoori
1Department of Chemistry and, The Skaggs Institute for Chemical Biology, The Scripps Research Institute, 10550 North Torrey Pines Road, La Jolla, CA 92037, USA
2Department of Chemistry and Biochemistry, University of California, San Diego, 9500 Gilman Drive, La Jolla, CA 92093, USA
A new tot synth of Uncialamycin by Nicolaou. This is a natural occurring enediyne. Because the stereochemistry of C26 was unknown, both diastereomers as shown were synthesized. The retrosyn led back to simpler fragments 2, 3, and 4.

The following scheme illustrates the route to fragment 2. The key transformation was the two-step Friedlander quinoline synthesis (7 to 9).

Then fragment 2 was used in the following sequence. The key steps in the sequence involved installation of enediyne fragment 3 to give 11, the closure of the macrocycle to give 15, and the Hauser annulation in the last step to give 1a from 16.

In this case, it was found that the final product’s spectrum (1a) did not match the reported value. And therefore, the other isomer was synthesized. This was easily done using fragment 12 through oxidation-reduction sequence to give 18 with the opposite stereochemistry at C26. Sequence in Scheme 3 was then repeated on this fragment.

And 1b was found to match spectrum of the natural isomer. This natural compound was found to be stable as a solid and as solutions in a variety of solvents. But in presence of dray HCl in CH2Cl2 solution at rt, it rapidly converts to hexacyclic 19 through a cascade of Bergman cycloaromatization reaction. This cascade of reactions is believed to be responsible mode of action in damaging DNA and killing cells.

The enediynes are a family of antibiotics that possess a distinctive strained nine- or ten-member ring system comprising a Z-carbon-carbon double bond and two carbon- carbon triple bonds, usually arranged with the latter two flanking the former. The enediynes are potent damagers of DNA, causing single and double strand cuts. Their potency is attributed to their ability to bind to DNA and undergo a Bergmann rearrangement in which the strained ring system is converted into a highly reactive 1 ,4-benzenoid diradical, which damages the DNA by abstracting hydrogens from it.
Uncialamycin is an enediyne isolated from a Streptomyces strain found on the lichen Cladonia uncialis (Davies et al. 2005; 2007). (Full citations for references cited in this specification by first named author or inventor and year are provided in the section entitled “REFERENCES” later herein.)
Uncialamycin
The structure of uncialamycin has been confirmed by total synthesis (Nicolaou et al. 2007a; 2007b). In the course of the synthesis, it was noted that the unnatural 26(S) epimer was almost as active as the natural 26(R) epimer – that is, the stereochemistry of the C27 methyl had a minor effect on biological activity. Both epimers were active against several ovarian tumor cell lines. The IC50 values rang ed from 9 x 10“12 to 1 x 10“10, depending on the epimer and cell line or sub-line (Nicolaou et al, 2008).
Conjugates are an important method for the delivery of anti-cancer drugs, which are often highly cytotoxic and might otherwise be problematic to administer due to the risk of systemic toxicity. In a conjugate, the drug is conjugated (covalently linked) to a targeting moiety that specifically or preferentially binds to a chemical entity characteristic of the cancer cell, thus delivering the drug there with high specificity. Further, the drug is held in an inactive form until released from the conjugate, usually by cleavage of the covalent linker.
Typically, the targeting moiety is an antibody or an antigen-binding portion thereof, whose antigen is overexpressed or uniquely expressed by a cancer cell (“tumor associated antigen”). In such instances, the resulting conjugate is sometimes refered to as an “immunoconjugate” or an “antibody-drug conjugate” (ADC). Preferably the tumor associated antigen is located on the surface of the cancer cell, but also can be one that is secreted into the vicinal extracellular space. Upon binding, the antigen-conjugate complex is internalized and eventually finds its way inside a vesicular body such as a lysosome, where the covalent linker is cleaved, liberating active drug to exert its chemotherapeutic effect.
Advantageously, the covalent linker is designed such that cleavage is caused by a factor prevalent inside a cancer cell but not in plasma. One such factor is the low lysosomal pH, so that the covalent linker can be an acid-sensitive group such as a hydrazone. Another such factor is the generally higher intracellular concentration of glutathione, allowing for the cleavage of a disulfide covalent linker by a disulfide exchange mechanism. Yet another such factor is the presence of lysosomal enzymes such as cathepsin B, which can cleave peptide linkers designed to be preferred substrates (Dubowchik et al. 2002).
Conjugates have been used to deliver enediyne drugs in oncology. Gemtuzumab ozogamicin (Mylotarg®) is a conjugate of an anti-CD33 monoclonal antibody and a derivative of the enediyne calicheamicin. It was approved for treatment of acute
myelogenous leukemia but was later withdrawn from the market. Several other enediyne drugs, especially in the conjugated form, have been the subject of development efforts
 If handled carefully, enediynes make powerful cancer drugs.
If handled carefully, enediynes make powerful cancer drugs.
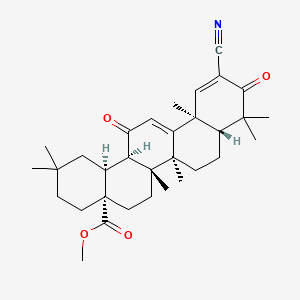
Inventors N. S. Chowdari, S. Gangwar, and B. Sufi synthesized enediyne compounds with general formula 1 that are based on the natural enediyne uncialamycin (2) scaffold (Figure 1). These compounds, used alone or in conjugates, are potent cytotoxins that may be useful in cancer chemotherapy.
Enediynes are a class of natural antibiotics that are characterized by 9- or 10-membered rings that contain two C≡C bonds separated by a cis (Z)-substituted C=C bond. Enediynes can undergo Bergman cyclization to form 1,4-benzenoid diradicals, which abstract hydrogen atoms from other molecules. When the diradical is generated near DNA, it abstracts hydrogen atoms from the sugar backbone of the DNA molecule and results in single- and double-strand lesions.
The high reactivity of enediynes toward DNA makes them very toxic. Their potent activity may be beneficial, however, if they are used to target the DNA of cancerous tumors. Most enediynes inhibit the proliferation of various cancer cells, including those that resist other chemotherapeutic drugs. Several naturally occurring enediynes are in clinical trials against cancer.
Both epimers at C26 of the natural enediyne uncialamycin are active against several ovarian tumor cell lines, with IC50 values ranging from 9 × 10–12 to 1 × 10–10 M, depending on the epimer and the cell line or subline. The synthetic enediynes described by the inventors are derivatives of uncialamycin.
Using these toxic molecules demands specific delivery systems. Conjugates are innovative drug-delivery systems designed to target tumor cells precisely and minimize the risk of systemic toxicity. Typically, drugs are linked covalently to conjugates that act as targeting moieties, which specifically or preferentially bind to a chemical entity characteristic of the cancer cell.
The covalent linker is designed to be cleaved only by a factor that exists inside a cancer cell and not in plasma, so that the drug remains in an inactive form until it is released from the conjugate. A typical targeting moiety may be a polymer or an antibody. Polymer-conjugated and antibody-linked enediyne drugs such as gemtuzumab ozogamicin (Mylotarg) were used to deliver enediyne drugs to cancer cells. Mylotarg, however, has been withdrawn from the market because of high patient mortality.

Compounds of structure 1 may be conjugated to a targeted moiety through a chemical bond to substituent R1. Compounds 3 and 4, shown in Figure 2, are examples of the synthetic enediynes with structure 1.
The investors tested the antiproliferative activities of several compounds against cancer cell lines. EC50 data for compounds 3 and 4 against 786-0 renal cancer cells and H226 lung cancer cells are shown in the table:
| Example | 786-0 cells, EC50 (nM) |
H226 cells, EC50 (nM) |
| 3 | 1.275 | 0.986 |
| 4 | 0.058 | 0.873 |

Several assays were also conducted on conjugates derived from other compounds of formula 1. (Bristol-Myers Squibb [Princeton, NJ]. WIPO Publication 2013122823, Aug 22, 2013;
 DAVIES ET AL.: ‘UNCIALAMYCIN, A NEW ENEDIYNE ANTIBIOTIC‘ ORGANIC LETTERS vol. 7, no. 23, 13 October 2005, pages 5233 – 5236
DAVIES ET AL.: ‘UNCIALAMYCIN, A NEW ENEDIYNE ANTIBIOTIC‘ ORGANIC LETTERS vol. 7, no. 23, 13 October 2005, pages 5233 – 5236
http://pubs.acs.org/doi/abs/10.1021/ol052081f
 300 μg) as a bright purple [UV(MeOH): λmaxnm (ε) 206 (25000), 254 (33000), 280 (shoulder), 320 (shoulder), 539 (9400)] optically active ([α]D +3300 (c 0.005, MeOH)) oil.
300 μg) as a bright purple [UV(MeOH): λmaxnm (ε) 206 (25000), 254 (33000), 280 (shoulder), 320 (shoulder), 539 (9400)] optically active ([α]D +3300 (c 0.005, MeOH)) oil.
Table 1. 13C and 1H NMR Assignments for Uncialamycin (1). Data were Recorded in DMSO-d6 at 600 MHz for 1H
| position | δ 13C | δ 1H (mult., J (Hz)) |
| 1 | 10.0 (d, 4.6) | |
| 2 | 143.6 | |
| 3 | 110.4 | |
| 4 | 187.0a | |
| 5 | 134.4b | |
| 6 | 126.1c | 8.23 (dd, 1.4, 7.6)c |
| 7 | 133.6d | 7.88 (ddd, 1.4, 7.6, 7.6)d |
| 8 | 134.9d | 7.94 (ddd, 1.4, 7.6, 7.6)d |
| 9 | 126.6c | 8.24 (dd, 1.4, 7.6)c |
| 10 | 132.2b | |
| 11 | 182.2a | |
| 12 | 112.7 | |
| 13 | 154.9 | |
| 14 | 129.9 | 8.51 (s) |
| 15 | 135.6 | |
| 16 | 63.5 | |
| 17 | 63.0 | 5.14 (d, 3.3) |
| 18 | 100.4 | |
| 19 | 89.7 | |
| 20 | 123.4 | 6.05 (dd, 0.8, 10) |
| 21 | 124.0 | 5.97 (ddd, 1.4, 1.5, 10) |
| 22 | 87.4 | |
| 23 | 98.9 | |
| 24 | 43.2 | 5.04 (dd, 1.5, 4.6) |
| 25 | 76.0 | |
| 26 | 63.6 | 4.31 (qd, 6.0, 6.0) |
| 27 | 22.1 | 1.30 (d, 6.0) |
| 13-OH | 13.2 (brd.s) | |
| 17-OH | 6.66 (brd.s) | |
| 26-OH | 5.39 (d,6.0) |
a−d May be interchanged.http://pubs.acs.org/doi/suppl/10.1021/ol052081f/suppl_file/ol052081fsi20051004_065853.pdf
……………..
Isolation of Uncialamvcin
[0034] As part of a screening program aimed at discovering new antibiotics active against Bcc, it was found that crude organic extracts of cultures of a previously undescribed Streptomycete showed potent in vitro inhibition of Bcc. Bioassay guided fractionation of the crude extracts led to the identification of uncialamycin (1), a new enediyne antibiotic, as the active component. Bioactivity-guided fractionation involves thin layer chromatography of the extracts and fractions thereof and detection of the activity by overlaying a sensitive tester strain. A zone of inhibition identifies the active fraction containing the active compound.
The producing strain was extracted from the surface of the lichen Cladonia uncialis collected near Pitt River, British Columbia. Characterisation by 16S RNA sequencing showed the strain to be related, but not identical, to Streptomyces cyanogenus. Antibiotic activity of the strain was assayed by cutting plugs from solid agar cultures of the strain and placing them on lawns of tester strains of bacteria. Good inhibitory activity was detected against Gram-positive and Gram-negative bacteria (including Bcc), but not against yeasts.
Production cultures of the producing strain were grown as lawns on solid agar medium ISP4 for 14 to 21 days at room temperature. The solid agar cultures were lyophilized and extracted repeatedly with EtOAc. Concentration of the combined EtOAc extracts in vacuo gave a gummy residue that was partitioned between EtOAc and H2O. The EtOAc soluble material was fractionated by sequential application of flash C- 18 reversed-phase chromatography (eluent: step gradient from H2O to MeOH) and reversed-phase HPLC (column-Inertsil ODS-2; eluent: CH3CN/H2O 40:60) to give pure uncialamycin (1) (~ 300 μg) as a bright purple [UV(MeOH): λmaxnm (ε) 206 (25,000), 254 (33,000), 280 (shoulder), 320 (shoulder), 539 (9,400)], optically active ([α]D +3,300 (c 0.005, MeOH)) oil.
Chemical Characterization of Uncialamycin
Uncialamycin (1) gave a [M + Na]+ ion at m/z 462.0956 in the
HRESIMS appropriate for a molecular formula Of C26H17NO6 (calc’d for C26H17NO6Na 462.0954) requiring 19 sites of unsaturation. NMR data for uncialamycin was recorded in DMSO-^6 at 600 MHz using a cryoprobe. The 13C NMR spectrum (Table 1) showed well-resolved resonances for 26 carbon atoms and the 1H NMR spectrum contained resonances integrating for 17 protons in agreement with the HRMS data. Inspection of the HMQC data revealed that four of the protons (δ 5.39, 6.66, 10.0, and 13.2) were not attached to carbon atoms. Two major fragments A and B (Figure 1) of uncialamycin could be identified from analysis of the COSY, HMQC, and HMBC data obtained for the molecule.
Position δ 1W WH^mult, J(Hz)) ,
1 10.0 (d, 4.6)
2 143.6
3 110.4
4 187.0
5 134.4
6 126.1 8.23 (dd, 1.4, 7.6)
7 133.6 7.88 (ddd, 1.4, 7.6, 7.6)
8 134.9 7.94 (ddd, 1.4, 7.6, 7.6)
9 126.6 8.24 (dd, 1.4, 7.6)
10 132.2
11 182.2
12 112.7
13 154.9
14 129.9 8.51 (s)
15 135.6
16 63.5
17 63.0 5.14 (d, 3.3)
18 100.4
19 89.7
20 123.4 6.05 (dd, 0.8, 10)
21 124.0 5.97 (ddd, 1.4, 1.5, 10)
22 87.4
23 98.9
24 43.2 5.04 (dd, 1.5, 4.6)
25 76
26 63.6 4.31 (qd, 6.0, 6.0)
27 22.1 1.30 (d, 6.0)
13-OH 13.2 (brd.s)
17-OH 6.66 (brd.s)
26-OH 5.39 (d,6.0)
Table 1. C and H NMR assignments for uncialamycin (1). Data were recorded in OMSO-d6 at 600 MHz for 1H. [0038] A pair of olefinic resonances at δ 5.97 (H-21 ) and 6.05 (H-20), that were strongly correlated to each other in the COSY spectrum and had a coupling constant of 10 Hz, were assigned to a cis disubsituted olefin. The upfield olefinic resonance at δ 5.97 (H-21) showed strong HMBC correlations to non-protonated carbon resonances at δ 89.7 (C- 19) and 98.9 (C-23), and the downfield olefinic resonance at δ 6.05 (H-20) showed strong correlations to non-protonated carbon resonances at δ 87.4 (C-22) and 100.4 (C- 18). This suite of HMBC correlations identified an enediyne substructure in 1 (see Fragment A in Figure 1). The olefinic resonance at δ 5.97 (H-21) showed a long range COSY correlation to a methine resonance at δ 5.04 (H- 24), indicating that the carbon bearing the methine proton (C-24: δ 43.2) was attached to the C-23 alkyne carbon. A COSY correlation observed between the methine (δ 5.04, H-24) and a broad singlet at 10.0, that was not correlated to a carbon in the HMQC spectrum, and the chemical shift of the methine carbon (C-24, δ 43.2) suggested that C-24 had an NH substituent. HMBC correlations observed between the H-24 methine (δ 5.04) and the two alkyne carbon resonances at δ 87.4 (C-22) and 98.9 (C-23) confirmed the attachment of C-24 to the C-23 alkyne carbon.
A singlet methine resonance at δ 5.14 (H- 17) showed HMBC correlations to the alkyne carbon resonances at δ 89.7 (C- 19) and 100.4 (C- 18), which demonstrated that the methine carbon (C- 17: δ 63.0) was linked to the second alkyne at C-18. Both of the methine resonances at δ 5.04 (H- 24) and 5.14 (H- 17) showed HMBC correlations to a pair of deshielded resonances at δ 63.5 (C- 16) and 76.0 (C-25), assigned to non-protonated oxygen bearing carbons. This set of four HMBC correlations indicated that the two oxygenated carbons bridged the C- 17 and C-24 carbons to form a ten membered ring (C- 16 to C-25) containing the enediyne substructure. A COSY correlation between the methine resonance at δ 5.14 and a broad singlet at 6.66 (17-OH) revealed an alcohol funtionality attached to the methine carbon.
A methyl doublet at δ 1.30 (Me-27, J = 6 Hz) was correlated in the COSY spectrum to a methine at 4.31 (H-26, q, J = 6.0 Hz)) that was further correlated to a broad singlet at 5.39 (OH-26), assigned to an alcohol. The methyl resonance (δ 1.30, Me-27) showed an HMBC correlation to the carbon resonance at 76.0 (C-25), indicating that the hydroxyethyl fragment (C-26 and C-27) was the fourth subsituent on the non-protonated carbon C- 25. Both the NH-I proton (δ 10.0) and the H-17 methine (5.14) were correlated to a carbon at δ 135.6 (C- 15), and the H-24 methine (δ 5.04) was correlated to a carbon at 143.6 (C-2) in the HMBC spectrum indicating that the NH and C- 16 were vicinal substituents on an olefin or aromatic ring. A deshielded singlet at δ 8.51 showed strong HMBC correlations into carbon resonances at δ 63.5 (C-16), 143.6 (C-2), and 112.7 (C- 12) and a weak correlation into the carbon resonance at 154.9 (C- 13). This set of HMBC correlations confirmed that the NH and C-16 were attached to a benzene ring. Based on the assumption that the intense HMBC correlations were through three bonds, these correlations also indicated that the aromatic methine (δ 8.51, H-14) was ortho to C-16 (δ 63.5) and meta to the NH (C-2, δ 143.6). The weak HMBC correlation between δ 8.51 and 154.9 was attributed to a two bond coupling, placing the carbon at 154.9 (C-13) ortho to the methine carbon (C- 14) and its chemical shift required an oxygen substituent. [0041] The second fragment B of uncialamycin contained an isolated
1H spin system comprised of four contiguous aromatic protons (δ 8.23, dd, J = 1.4, 7.6 Hz H-6; 7.88, ddd, 1.4, 7.6, 7.6 Hz H-7; 7.94, ddd, J = 1.4, 7.6, 7.6 Hz H-8; 8.24, dd, J = 1.4, 7.6 Hz H-9). HMBC correlations observed between the proton resonance at δ 8.23 (H-6) and a carbon resonance at 187.0 (C-4) and between the proton resonance at 8.24 (H-8) and a carbon resonance at 182.2 (C-11) suggested that the other two subsituents on the benzene ring were quinone carbonyls. Fragments A and B shown in Figure 1 accounted for all of the carbon, hydrogen, and nitrogen atoms in the molecular formula of uncialamycin (1), but contained one extra oxygen atom. In order to complete the quinone and satisfy the remaining aromatic valences in Fragment A, the two carbonyl carbons of fragment B (C-4 and C-I l) had to be attached to the two substituted aromatic carbons (C-3 and C- 12) of fragment A. Finally, it was apparent that the two oxygentated carbons C- 16 and C-25 had to be bridged by an epoxide to account for the number of oxygen atoms and sites of unsaturation required by the molecular formula of 1. This implied that the C- 13 oxygen substituent had to be part of a phenol functionality that would engage in intramolecular hydrogen bonding with the C-I l carbonyl consistent with the observed OH chemical shift of δ 13.2.
A ROESY correlation between δ 5.14 (H- 17) and 4.31 (H-26) showed that C-26 and C- 17 were cis oriented about the C-16/C-25 epoxide and also defined the relative stereochemistry of H- 17 as shown. Molecular models revealed that due to steric and bond angle strain the C- 17 to C-23 enediyne containing bridge could only reasonably be cis fused to the piperidine ring. Uncialamycin (1) shares structural features with dynemicin A (2) and deoxydynemicin A (3) isolated from Micromonospora chersina. The H-24 resonance in uncialamycin (1) has a chemical shift of δ 5.04 and a 4.6 Hz coupling to the NH-I proton, which is nearly identical to the chemical shift (δ 5.05) and coupling (J = 4.3 Hz) of the corresponding methine proton (H-2) in dynemicin A (2), in agreement with the relative stereochemical assigment at C-24 in 1. Comparison of the additional NMR assigments reported for dynemicin A (2) and its triacetate derivative provided further strong support for the assigned structure of uncialamycin
…………….
 Angewandte Chemie – International Edition, 2008 , vol. 47, 1 p. 185 – 189
Angewandte Chemie – International Edition, 2008 , vol. 47, 1 p. 185 – 189
http://onlinelibrary.wiley.com/doi/10.1002/anie.200704577/abstract

The highly potent DNA-cleaving molecule uncialamycin (1) was prepared in an asymmetric total synthesis featuring an enantioselective Noyori reduction. Compound 1 and its C26 epimer exhibit impressive broad-spectrum antibacterial properties and highly potent antitumor activities against a variety of cell lines.


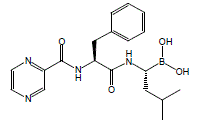
BORTEZOMIB, PS 341

BORTEZOMIB
A proteasome inhibitor.
[(1R)-3-methyl-1-({(2S)-3-phenyl-2-[(pyrazin-2-ylcarbonyl)amino]propanoyl}amino)butyl]boronic acid
Λ/-(pyrazin-2-yl)carbonyl-L-phenylalanine-L-leucine boronic acid
179324-69-7 CAS
- Bortezomib
- HSDB 7666
- LDP 341
- LDP-341
- MG 341
- MLN-341
- NSC 681239
- PS 341
- PS 341 (pharmaceutical)
- PS-341
- UNII-69G8BD63PP
- Velcade
For treatment of multiple myeloma in patients who have not been successfully treated with at least two previous therapies.
A dipeptide boronic acid analogue with antineoplastic activity. Bortezomib reversibly inhibits the 26S proteasome, a large protease complex that degrades ubiquinated proteins. By blocking the targeted proteolysis normally performed by the proteasome, bortezomib disrupts various cell signaling pathways, leading to cell cycle arrest, apoptosis, and inhibition of angiogenesis. Specifically, the agent inhibits nuclear factor (NF)-kappaB, a protein that is constitutively activated in some cancers, thereby interfering with NF-kappaB-mediated cell survival, tumor growth, and angiogenesis. In vivo, bortezomib delays tumor growth and enhances the cytotoxic effects of radiation and chemotherapy. (NCI Thesaurus)
Bortezomib (originally PS-341 and marketed as Velcade by Millennium Pharmaceuticals) is the first therapeutic proteasome inhibitor to be tested in humans. It is approved in the U.S. for treating relapsed multiple myeloma and mantle cell lymphoma. In multiple myeloma, complete clinical responses have been obtained in patients with otherwise refractory or rapidly advancing disease.
bortezomib
Bortezomib (BAN, INN and USAN. Originally codenamed PS-341; marketed as Velcade by Millennium Pharmaceuticals and Cytomib by Venus Remedies) is the first therapeutic proteasome inhibitor to be tested in humans. It is approved in the U.S. for treating relapsed multiple myeloma[1] andmantle cell lymphoma. In multiple myeloma, complete clinical responses have been obtained in patients with otherwise refractory or rapidly advancing disease.
Bortezomib was originally synthesized in 1995 (MG-341) at a company called Myogenics, which soon changed its name to ProScript. After promising preclinical results, the drug (PS-341) was tested in a small Phase I clinical trial on patients with multiple myeloma cancer. ProScript ran out of money and was bought by Leukosite in May 1999. Leukosite in turn was bought by Millennium Pharmaceuticals in October 1999. At this point in time, the project had low priority amongst other projects at the company. This changed significantly when one of the first volunteers to receive the drug in the clinical trial achieved a complete response and were still alive four years later. At the time this was a remarkable result. Later clinical experimentation indicates the possibility of a complete response in 15% of patients in a similar condition, when treated with bortezomib.
In May 2003, seven years after the initial synthesis, bortezomib (Velcade) was approved in the United States by the Food and Drug Administration(FDA) for use in multiple myeloma, based on the results from the SUMMIT Phase II trial.[2]
Another commercially available bortezomib product – Bortenat (Natco Pharma, India), reportedly contains substantially more active entity than declared, potentially and even more resulting in increase toxicity. Moreover, Bortenat has some other chemical and formulation deviations from the registered ethic product Velcade (Millennium Pharmaceuticals and Janssen-Cilag), with unclear clinical impact.[3]
Bortezomib bound to the core particle in a yeast proteasome. The bortezomib molecule is in the center colored by atom type (boron = pink, carbon = cyan, nitrogen = blue, oxygen = red), surrounded by the local protein surface. The blue patch is catalyticthreonine residue whose activity is blocked by the presence of bortezomib.
VELCADE® (bortezomib) for Injection is an antineoplastic agent available for intravenous injection or subcutaneous use. Each single use vial contains 3.5 mg of bortezomib as a sterile lyophilized powder. Inactive ingredient: 35 mg mannitol, USP.
Bortezomib is a modified dipeptidyl boronic acid. The product is provided as a mannitol boronic ester which, in reconstituted form, consists of the mannitol ester in equilibrium with its hydrolysis product, the monomeric boronic acid. The drug substance exists in its cyclic anhydride form as a trimeric boroxine.
The chemical name for bortezomib, the monomeric boronic acid, is [(1R)-3-methyl-1-[[(2S)-1-oxo-3-phenyl-2[(pyrazinylcarbonyl) amino]propyl]amino]butyl] boronic acid.
Bortezomib has the following chemical structure:
 |
The molecular weight is 384.24. The molecular formula is C19H25BN4O4. The solubility of bortezomib, as the monomeric boronic acid, in water is 3.3 to 3.8 mg/mL in a pH range of 2 to 6.5.
Structure
The drug is an N-protected dipeptide and can be written as Pyz-Phe-boroLeu, which stands for pyrazinoic acid,phenylalanine and Leucine with a boronic acid instead of a carboxylic acid. Peptides are written N-terminus to C-terminus, and this convention is used here even though the “C-terminus” is a boronic acid instead of a carboxylic acid.
-
Boronic acid and ester compounds display a variety of pharmaceutically useful biological activities.Shenvi et al., U.S. Pat. No. 4,499,082 (1985 ), discloses that peptide boronic acids are inhibitors of certain proteolytic enzymes.Kettner and Shenvi, U.S. Pat. No. 5,187,157 (1993 ),U.S. Pat. No. 5,242,904 (1993 ), and U.S. Pat. No. 5,250,720 (1993 ), describe a class of peptide boronic acids that inhibit trypsin-like proteases. Kleeman et al., U.S. Pat. No. 5,169,841 (1992 ), disclosesN-terminally modified peptide boronic acids that inhibit the action of renin. Kinder et al., U.S. Pat. No. 5,106,948 (1992 ), discloses that certain tripeptide boronic acid compounds inhibit the growth of cancer cells.
-
More recently, boronic acid and ester compounds have displayed particular promise as inhibitors of the proteasome, a multicatalytic protease responsible for the majority of intracellular protein turnover.Ciechanover, Cell, 79: 13-21 (1994), discloses that the proteasome is the proteolytic component of the ubiquitin-proteasome pathway, in which proteins are targeted for degradation by conjugation to multiple molecules of ubiquitin. Ciechanover also discloses that the ubiquitin-proteasome pathway plays a key role in a variety of important physiological processes.
-
Adams et al., U.S. Patent No. 5,780,454 (1998 ),U.S. Patent No. 6,066,730 (2000 ), U.S. Patent No. 6,083,903 (2000 ),U.S. Patent No. 6,297,217 (2001 ), U.S. Patent No. 6,548,668 , andU.S. Patent No. 6,617,317 (2003 ), hereby incorporated by reference in their entirety, describe peptide boronic ester and acid compounds useful as proteasome inhibitors. The references also describe the use of boronic ester and acid compounds to reduce the rate of muscle protein degradation, to reduce the activity of NF-κB in a cell, to reduce the rate of degradation of p53 protein in a cell, to inhibit cyclin degradation in a cell, to inhibit the growth of a cancer cell, to inhibit antigen presentation in a cell, to inhibit NF-κB dependent cell adhesion, and to inhibit HIV replication.
-
Albanell and Adams, Drugs of the Future 27: 1079-1092 (2002), discloses that one such peptide boronic acid proteasome inhibitor, bortezomib (N-2-pyrazinecarbonyl-L-phenylalanine-L-leucineboronic acid), shows significant antitumor activity in human tumor xenograft models and is undergoing clinical evaluation. Richardson et al., New Engl. J. Med., 348:2609 (2003), reports the results of a Phase 2 study of bortezomib, showing its effectiveness in treating relapsed and refractory multiple myeloma.
-
Studies of boronic acid protease inhibitors have been greatly advanced by the development of chemistry for the preparation of functionalized boronic acid compounds, particularly alpha-halo- and alpha-aminoboronic acids. Matteson and Majumdar, J. Am. Chem. Soc., 102:7590 (1980), discloses a method for preparing alpha-chloroboronic esters by homologation of boronic esters, and Matteson and Ray, J. Am. Chem. Soc., 102:7591 (1980), reports that chiral control of the homologation reaction can be achieved by the use of pinanediol boronic esters. The preparation of alpha-aminoboronic acid and ester compounds from the corresponding alpha-chloroboronic esters has also been reported (Matteson et al., J. Am. Chem. Soc., 103:5241 (1981);Shenvi, U.S. Patent No. 4,537,773 (1985 )).
-
Matteson and Sadhu, U.S. Patent No. 4,525,309 (1985 ), describes an improved procedure for the homologation of boronic esters by rearrangement of the intermediate boron “ate” complex in the presence of a Lewis acid catalyst. The Lewis acid is reported to promote the rearrangement reaction and to minimize epimerization at the alpha-carbon atom. Rigorous exclusion of water and careful control of Lewis acid stoichiometry are required for optimum results, however. These features render the reaction difficult to perform successfully on a production scale, and limit the availability of pharmaceutically important boronic ester and acid compounds, such as bortezomib
The boron atom in bortezomib binds the catalytic site of the 26S proteasome[4] with high affinity and specificity. In normal cells, the proteasome regulates protein expression and function by degradation of ubiquitylated proteins, and also cleanses the cell of abnormal or misfolded proteins. Clinical and preclinical data support a role in maintaining the immortal phenotype of myeloma cells, and cell-culture and xenograft data support a similar function in solid tumor cancers. While multiple mechanisms are likely to be involved, proteasome inhibition may prevent degradation of pro-apoptotic factors, permitting activation of programmed cell death in neoplastic cells dependent upon suppression of pro-apoptotic pathways. Recently, it was found that bortezomib caused a rapid and dramatic change in the levels of intracellular peptides that are produced by the proteasome.[5] Some intracellular peptides have been shown to be biologically active, and so the effect of bortezomib on the levels of intracellular peptides may contribute to the biological and/or side effects of the drug.
 BORTEZOMIB
BORTEZOMIB
Bortezomib is rapidly cleared following intravenous administration.[6] Peak concentrations are reached at about 30 minutes. Drug levels can no longer be measured after an hour.Pharmacodynamics are measured by measuring proteasome inhibition in peripheral blood mononuclear cells. The much greater sensitivity of myeloma cell lines and mantle cell lines to proteasome inhibition compared with normal peripheral blood mononuclear cells and most other cancer cell lines is poorly understood.
Costs
UK
NICE recommended against Velcade in Oct 2006 due to its cost.[7]
The company proposed a cost reduction for multiple myeloma,[8] and this was taken up in the UK.[9]
Bortezomib is associated with peripheral neuropathy in 30% of patients; occasionally, it can be painful. This can be worse in patients with pre-existing neuropathy. In addition, myelosuppressioncausing neutropenia and thrombocytopenia can also occur and be dose-limiting. However, these side effects are usually mild relative to bone marrow transplantation and other treatment options for patients with advanced disease. Bortezomib is associated with a high rate of shingles,[10] although prophylactic acyclovir can reduce the risk of this.[11]
Gastro-intestinal (GI) effects and asthenia are the most common adverse events.[12]
Green tea extract epigallocatechin gallate (EGCG), which had been expected to have a synergistic effect, was found by Encouse B. Golden, et al. to reduce the effectiveness of bortezomib.[13][14][15][16]
Two open-label, phase II trials (SUMMIT and CREST) established the efficacy of bortezomib 1.3 mg/m2 (with or without dexamethasone) administered by intravenous bolus on days 1,4,8, and 11 of a 21-day cycle for a maximum of eight cycles in heavily pretreated patients with relapsed/refractory multiple myeloma.[17] The phase III APEX trial demonstrated the superiority of bortezomib 1.3 mg/m2 over a high-dose dexamethasone regimen (e.g. median TTP 6.2 vs 3.5 months, and 1-year survival 80% vs 66%).[17]
PATENTS
| Canada | 2203936 | 2005-04-12 | EXPIRY2015-10-27 |
| United States | 6713446 | 2002-01-25 | 2022-01-25 |
| United States | 6083903 | 1994-10-28 | 2014-10-28 |
Raghavendracharyulu Venkata Palle, Rajasekhar Kadaboina, Veerendeer Murki, Amarendhar Manda, Nageshwar Gunda, Ramaseshagiri Rao Pulla, Mallesha Hanmanthu, Narasimha Naidu Mopidevi, Suresh Kumar Ramdoss, “BORTEZOMIB AND PROCESS FOR PRODUCING SAME.” U.S. Patent US20100226597, issued September 09, 2010.
US20100226597 
INTRODUCTION
Bortezomib (PS-341, Velcade®; N-(pyrazin-2-yl)carbonyl-L-phenylalanine-L-leucine boronic acid; (1R)-3-Methyl-1-[(2S)-3-phenyl-2-[(pyrazinylcarbonyl)amino]propanoyl]amino]butyl]boronic acid; CAS Registry Number: 179324-69-7) is an N-acylated dipeptide analogue of phenylalanyl-leucine in which a boronic acid functional group replaces the C-terminal carboxylic acid. It is a white to almost white crystalline powder and when appropriately formulated for injection is an anti-neoplastic agent and is a therapeutic proteosome inhibitor. In the US this active pharmaceutical ingredient (API) is approved for the treatment of multiple myeloma and mantle cell lymphoma.
Bortezomib is composed of three moieties that are fused together by two amide bonds. Two of these three units can be thought of as analogues of amino acids (viz., an α-aminoboronic acid and a pyrazinecarboxylic acid) and the third unit is a naturally occurring amino acid (viz., L-phenylalanine). Bortezomib possesses two chiral centres but is a single stereoisomer. One chiral centre exists within the α-aminoboronic acid moiety and the other exists within the naturally occurring amino acid, L-phenylalanine, moiety. In the solid state under anhydrous conditions, bortezomib can exist as a trimeric anhydride (trimeric boroxine), herein referred to as bortezomib anhydride. In the presence of water this can be hydrolysed to its monomeric boronic acid form.
Amino boronic acids – amino acids wherein terminal carboxylic groups are replaced by boronic B(OH)2 groups – are important pharmacoisosters of amino acids in various therapeutically promising molecules, mainly for treatment of cancer. For instance, talabostat contains proline boronic acid, bortezomib contains leucine boronic acid. Bortezomib, chemically Λ/-(pyrazin-2-yl)carbonyl-L-phenylalanine-L-leucine boronic acid, is an important proteasome inhibitor and has been clinically approved for use in treating mantle cell lymphoma and multiple myeloma. Recently, many novel molecules containing amino boronic acids, especially leucine boronic acid, have been prepared and biologically tested as described in WO2009/006473 A2.
The synthesis of bortezomib and other amino boronic acid and ester compounds is disclosed in
EP0788360 B1 , international patent application WO2005/097809 A2, international patent application
WO2009/004350 A1 , and international patent application WO2009/036281 A2.
EP0788360 B1 describes a general process for preparation of amino boronic acid and ester compounds using (1 S, 2S, 3R, 5S)-pinanediol leucine boronate and an amino acid or its derivative as starting materials. As coupling agents 1-ethyl-3-(3-dimethylamino-propyl)carbodiimide hydrochloride (EDC), benzotriazol-1-yloxytris (dimethylamino) phosphonium hexafluorophosphate (BOP reagent), or 0-(MH- benzotriazol-1-yl)-/V,/V,/V,/V-tetramethyluronium tetrafluoroborate (TBTU) were employed.
A synthetic process suitable for a large scale production of amino boronic acid and ester compounds is described in WO2005/097809 A2. The synthesis involves a boronate complex, which is contacted with a
Lewis acid under conditions that afford the boronic ester compounds.
WO2009/004350 A1 discloses a high yield synthesis of bortezomib and intermediates for the synthesis thereof. The procedure includes the use of a very high percentage of tetrahydrofuran in the halogenation of the starting compound (S)-pinanediol 2-m ethyl propane- 1 -boronate.
WO2009/036281 A2 describes processes for the preparation of substantially pure bortezomib and intermediates thereof. Processes for the preparation of crystalline forms of bortezomib as well as a storage system for bortezomib are also disclosed in said patent application.
In international patent application WO2005/097809 A2, in J. Biol. Chem. 1984, 259, 15106-15114 and in J. Am. Chem. Soc. 1981 , 103, 5241-5242 a route for the preparation of α-amino boronic esters, which is known to the person skilled in the art known as the Matteson’s synthetic route, is described. Homologation of boronic esters with (dichloromethyl)lithium to form α-chloro boronic esters has been shown to be efficient and result in good chiral selectivity if pinanediol was used as the chiral directing group. The use of the Lewis acid (ZnCI2) as a catalyst and chloride ion scavenger for the rearrangement of the borate intermediate improved the diastereomeric ratio in the α-chloro boronic ester product, α- Chloro boronic esters have been converted to silylated α-amino boronic esters by lithiumhexamethyldisilazane (LiHMDS), which have been desilylated and protonated in situ to the α-amino boronic esters.
An approach for the synthesis of diverse α-amino boronic esters by the highly diastereoselective copper- catalyzed addition of bis(pinacolato)diboron to N-tert-butane sulfinyl aldimines has been disclosed in the J. Am. Chem. Soc. 2008, 730, 6910-6911.
Transformation of 1 ,1-dihalogenoalkenes to corresponding alkynes and subsequent synthesis of 1- alkynylboranes have been described in Tetrahedron Letters 1972, 13, 3769-3772 and Tetrahedron Letters 1988, 29, 2631-2634.
J. Am. Chem. Soc. 1994, 116, 10302-10303 describes a process for preparing α-substituted 1- alkenyldioxaborolanes starting from 1-alkynyldioxaborolanes by hydrozirconation followed by substitution such as halogenation or carbonylation. The following α-substituted 1-alkenyldioxaborolanes are disclosed in this reference: (E)-2-(1-chloro-3,3-dimethylbut-1-enyl)-4,4,5,5-tetramethyl-1 ,3,2-dioxaborolane, (E)-2- (1-bromo-3,3-dimethylbut-1-enyl)-4,4,5,5-tetramethyl-1 ,3,2-dioxaborolane, (E)-2-(1-iodo-3,3-dimethylbut- 1-enyl)-4,4,5,5-tetramethyl-1 ,3,2-dioxaborolane, (E)-2,2,6,6-tetramethyl-4-(4,4,5,5-tetramethyl-1 ,3,2- dioxaborolan-2-yl)hept-4-en-3-one, (E)-4,4-dimethyl-1-phenyl-2-(4,4,5,5-tetramethyl-1 ,3,2-dioxaborolan-2- yl)pent-2-en-1-one, (E)-2-(4,4-dimethylpent-2-en-2-yl)-4,4,5,5-tetramethyl-1 ,3,2-dioxaborolane zircono- cene and (E)-2-(hept-2-en-2-yl)-4,4,5,5-tetramethyl-1 ,3,2-dioxaborolane zirconocene.


 SYNTHESIS/US20120289699
SYNTHESIS/US20120289699
The chiral centre of the α-aminoboronic acid moiety cannot, however, be derived from a chiral pool since α-aminoboronic acids are not known to be naturally occurring.
Instead, enantio-enriched α-aminoboronic acids in which the chiral centre is adjacent to the boron atom can be obtained by the use of chiral boron chemistry developed by Matteson, such as disclosed in U.S. Pat. No. 4,525,309 and a series of peer reviewed publications. Matteson’s chemistry when used for chiral applications utilises a boronic ester comprising a chiral diol auxiliary (such as 1S,2S,3R,5S)-(+)-2,3-pinanediol ((S)-(+)-pinanediol), for example) which upon reaction with the lithium salt (this salt can be prepared in situ or separately) of dichloromethane forms an α,α-dichloroboronate complex, which the boron ate functional group is chiral.
Due to induction provided by the chiral diol auxiliary, the boron ate complex undergoes a spontaneous and stereoselective internal rearrangement with displacement of one of the prochiral chloro substituents to generate an α-chloroboronic ester which possesses a newly generated chiral centre adjacent to the boron atom (See Scheme 1). This rearrangement of the boron ate complex is dramatically improved by catalysis with ZnCl2 (see J. Am. Chem. Soc., 1983, 105, 2077-2078).
α-Chloroboronic esters can be converted into the aforementioned requisite α-aminoboronic acids, preferably protected as boronic esters, possessing useful high chiral purity by reaction with LiHMDS followed by desilylation and optional salt formation of the amino group). Altogether, this reaction sequence provides a 1-carbon homologation of the original carbon backbone of the B-alkyl portion of the boronic ester in addition to a stereoselectively appended amino group. Most typically the chiral auxiliary demonstrated for this reaction sequence is homochiral pinanediol, such as the (+)-enantiomer referred to as (S)-(+)-pinanediol, or the (−)-enantiomer referred to as (R)-(−)-pinanediol.
One drawback with this stereoselective approach to α-aminoboronic acid synthesis in an industrial setting is the relatively high cost of the chiral diol auxiliary, pinanediol. Further, the use of the chiral diol imposes other synthetic restrictions, such as order of installation of the alkyl group to be homologated (i.e., the R group and dichloromethyl substituent) into the boron ate complex, and the relatively more difficult hydrolysis step required to remove stereochemically hindered diol groups afterwards. Despite this U.S. Pat. No. 7,714,159 B2, WO2009004350A1 and WO2009036281A2 disclose methods for the synthesis of bortezomib utilizing Matteson’s chemistry in conjunction with (S)-(+)-pinanediol as the chiral auxiliary.
Although a chiral auxiliary, such as (S)-(+)-pinanediol, is required for chiral induction in the homologation step in the Matteson reaction sequence, a chiral auxiliary itself is not inherently required for the Matteson homologation step to proceed, and achiral diols can also be used (Organometallics, 1983, 2, 1529-1535).
The inventors of the invention herein reasoned that the high cost of (S)-(+)-pinanediol could be circumvented in the synthesis of bortezomib by the use of a cheap, achiral diol to protect the boronic acid functional group. Since the use of an achiral diol auxiliary would not provide any stereochemical induction in the homologation step, a racemic product (that is, it would comprise equimolar amounts of each enantiomer) would be produced, which itself or a down stream synthetic derivative of it would require a classical resolution or other technique capable of separating the stereoisomers to be performed upon it.
Given that there was a need for a separation method that could separate the racemate, the inventors reasoned that one efficient approach would utilise the enantiopure API building block, L-phenylalanine as an intramolecular chiral resolving agent. L-phenylalanine or its derivatives could serve as a cost efficient in-process chiral resolving agent in this manner because i) it and its derivatives are cheap and are commercially available on large scales, and ii) it comprises part of the molecular structure of bortezomib itself. Therefore it was reasoned that its use would not be wasteful once the desired enantiomer of the racemate was separated because it would also be incorporated into the API itself.
Thus, a key characteristic of the invention herein useful for the synthesis of bortezomib is the use of a racemic diol α-aminoboronic ester salt, such as the pinacol derivative [5], as a key intermediate. This racemic key intermediate is derivatised by its reaction with L-phenylalanine to provide a mixture of diastereomers that are separated by crystallisation, or by chromatography, or by stereoselective hydrolysis.
The requisite racemic boronic esters, such as pinacol α-aminoboronic ester [5], are readily synthesized utilizing prior art chemistry disclosed by Matteson (e.g., see Pure & Appl. Chem., 1985, 57, 1741-1748), as exemplified in Scheme 2.
The racemic boronic esters, such as the pinacol α-aminoboronic ester [5], are then converted into mixtures of diastereomers [6] by reaction with a suitably protected L-phenylalanine derivative (See Scheme 3), such as N-BOC-L-phenylalanine. The protecting group of the L-phenylalanine moiety is then removed, such as by reacting the diastereomers [6] with an acid such as hydrochloric acid, to form a mixture of amine salt diastereomers [7] which is then subjected to conditions under which the desired diastereomer (R,S)-[7] is selectively isolated, such as by crystallisation, chromatography or stereoselective hydrolysis. The separated desired diastereomer (R,S)-[7] is then converted into bortezomib or bortezomib anhydride.
In this invention the need for the use of an expensive chiral auxiliary such as (S)-(+)-pinanediol to induce stereoselectivity in the Matteson homologation reaction sequence is circumvented by the use of the naturally occurring and relatively cheap amino acid L-phenylalanine in protected form. In addition to being 7-10 times cheaper than (S)-(+)-pinanediol, unlike (S)-(+)-pinanediol which is liberated from the penultimate API precursor at the end of the synthesis of bortezomib following the methods of the prior art, the amino acid, L-phenylalanine, comprises part of the final API molecular structure.
This invention differs from those disclosed in U.S. Pat. No. 7,714,159 B2, WO2009004350A1 and WO2009036281A2 which all rely on the use of the expensive chiral diol auxiliary (S)-(+)-pinanediol in conjunction with Matteson chemistry to obtain the requisite chirality.
EXAMPLES
For embodiment 1, as mentioned previously, the process has been demonstrated using pinacol as the boronate ester diol moiety and the hydrochloride salt of the diastereomeric mixture of [7].
Example 1 Synthesis of [7] Pinacol 1-chloro-3-methylbutane-1-boronate (rac-[3])
A mixture of THF (2 L) and DCM (55.3 g, 0.651 mol) was cooled to −100° C. n-BuLi (260.7 mL, 2.5 M in n-hexane, 0.651 mol) was added dropwise into the reaction mixture maintaining at −100° C. Pinacol 2-methylpropane-1-boronate ([2]; 100 g, 0.543 mol) was added into the reaction mixture. The resulting mixture was keep at −100° C. for one hour. A solution of ZnCl2 (136.3 g, 1.0 mol) in THF (500 mL) was added dropwise to the reaction over a period of 60 minutes. The resulting mixture was keep at −100° C. for one hour, the reaction mixture was warmed up to room temperature and keep at room temperature overnight. The reaction was diluted with MTBE (750 mL) and was washed twice with saturated NH4Cl (2 L each). The organic layer was dried overnight over MgSO4 before filtering and evaporating. n-Heptane (250 mL) was added into the mixture and was filtered and evaporated providing the product as an oil (119.5 g, 0.514 mol). 1H NMR (300 MHz, CDCl3) δ 3.48 (dd, J=9.8, 6.1 Hz, 1H), 1.93-1.71 (m, 2H), 1.61 (td, J=8.1, 4.0 Hz, 1H), 1.33-1.24 (m, 12H), 0.95-0.87 (m, 6H); 13C NMR (75 MHz, CDCl3) δ 84.5, 42.8, 25.8, 24.8, 23.1, 21.5.
Pinacol 1-bis-(trimethylsilyl)-amino-3-butane-1-boronate (rac-[4])
A solution of LiHMDS (44.61 g, 0.267 mol in 217 mL THF) in THF (750 mL) was cooled to −75° C. and pinacol 1-chloro-3-methylbutane-1-boronate (rac-[3]; 77.5 g, 0.333 mol) in THF (462 mL) was added. The resulting mixture was keep at −75° C. for 1 hour. The reaction mixture was warmed up to room temperature and kept at room temperature overnight. The mixture was evaporated to provide the product as an oil (73 g, 0.204 mol). 1H NMR (300 MHz, CDCl3) δ 2.58 (t, J=7.7 Hz, 1H), 1.75 (tq, J=13.1, 6.5 Hz, 1H), 1.66-1.44 (m, 1H), 1.34-1.27 (m, 1H), 1.22 (s, 12H), 0.90-0.84 (m, 6H), 0.12-0.09 (m, 18H).
Pinacol-1-ammonium chloride-3-methylbutane-1-boronate (rac-[5])
A solution of pinacol 1-bis-(trimethylsilyl)-amino-3-butane-1-boronate (rac-[4]; 264.9 g, 0.741 mol) in n-heptane (4 L) and diethyl ether (1.6 L) was cooled to −35° C. HCl gas was bubbled through the mixture for 4 hours, and the resulting mixture was stirred at room temperature overnight and was then filtered. The filter cake was dissolved in DCM (1 L) and was stirred at room temperature for 2.5 hours, filtered and evaporated. The residue was diluted with EtOAc (713 mL) to form a slurry that was stirred for 1 hour and then filtered. The solid was dried under vacuum at 35° C. to provide the product as white crystals (123.9 g, 0.496 mol). 1H NMR (300 MHz, d6-DMSO) δ 7.75 (s, 3H), 2.70 (d, J=5.5 Hz, 1H), 1.68 (dt, J=13.5, 6.8 Hz, 1H), 1.44 (t, J=7.3 Hz, 2H), 1.24 (s, 12H), 0.86 (d, J=6.5 Hz, 6H); 13C NMR (75 MHz, CDCl3) δ 85.0, 38.6, 35.9, 25.1, 24.8, 22. 5; ESI-MS (positive) (m/z): 213, 170, 156, 128, 100, 88, 74.
Pinacol N-BOC-L-phenylalanine-D,L-leucine boronate ((R,S)-/(S,S)-[6])
To a cooled (about 0° C.) solution of BOC-L-phenylalanine (60.6 g, 0.228 mol) in DMF (670 mL) was added DIPEA (62.1 g, 0.480 mol), HATU (96.0 g, 0.252 mol) and a DMF (290 mL) solution of rac-[5] (pinacol-1-ammonium chloride-3-methylbutane-1-boronate) (60 g, 0.240 mol). The mixture was warmed to room temperature and stirred at this temperature overnight. Ethyl acetate (1 L) and a saturated aqueous solution of sodium of chloride (700 mL) were added into the reaction mixture. After mixing, the organic layer was separated and washed with a saturated aqueous solution of sodium of chloride (750 mL), then with an aqueous 0.1 N solution of KHSO4 (800 mL) and finally with an saturated aqueous solution of NaHCO3 (800 mL). The organic layer was dried over MgSO4 and concentrated at 35° C. n-Heptane (240 mL) was added to the crude product and was stirred for 45 min and was filtered. The filter cake was washed three times with n-heptane (100 mL each) and dried under vacuum at 35° C. The product was obtained as an approximately equimolar mixture of diastereomers as a white solid (92.0 g, 0.200 mol). 1H NMR (300 MHz, CDCl3) δ 7.37-7.18 (m, 5H), 6.30 (d, J=31.1 Hz, 1H), 5.07 (s, 1H), 4.45-4.27 (m, 1H), 3.06 (d, J=4.5 Hz, 2H), 2.96 (dd, J=10.8, 8.3 Hz, 1H), 1.39 (s, 9H), 1.37-1.29 (m, 3H), 1.25 (d, J=4.6 Hz, 12H), 0.85 (dt, J=11.3, 5.6 Hz, 6H); 13C NMR (75 MHz, CDCl3) δ 172.7, 155.6, 136.7, 129.6, 128.9, 127.1, 83.0, 80.4, 54.8, 55.4-53.8 (m), 39.9, 38.5, 37.6, 28.5, 25. 7, 25.1, 23.4, 22.0; ESI-MS (positive) (m/z): 461, 405.
Pinacol L-phenylalanine-L-leucine boronate, HCl salt ((R,S)-[7])
A MeCN (752 mL) solution of pinacol N-BOC-L-phenylalanine-D,L-leucine boronate ([6]; 94 g, 0.204 mol) was cooled to about 0° C. HCl gas was bubbled into the reaction mixture for 4 hours. The resulting mixture was stirred at room temperature overnight and was then evaporated to provide a solid. A slurry was formed by the addition of MeCN (250 mL) which was then stirred for 2 hours and was filtered and washed with MeCN (50 mL). The solid was then dried under vacuum at 35° C. furnishing the product as a white solid (56.4 g, 0.136 mol; HPLC purity 96.0% as a 1.5:1 mixture of (R,S)-[7] and (S,S)-[7])).
As mentioned previously the key upgrade step can be accomplished using:
- A) fractional crystallisation, or
- B) a reslurry/hydrolysis, or
- C) chromatography,
- D) or combinations of any of the above three techniques
These are exemplified in the following 3 examples.
Example 2 Operation A—Diastereomeric Upgrade of [7] by Fractional Crystallisation: The First Crystallisation
[7] (35.0 g, 88.2 mmol; (R,S)4(S,S)-diastereomeric ratio=1.50:1) was dissolved in a mixture of isobutyl acetate (350 mL) and ethanol (24.5 mL) at about 75° C. The solution was slowly cooled to ambient temperature and stirred overnight. The resulting mixture was cooled to about 0° C. and stirred for one hour and then filtrated and the isolated solid was dried under vacuum at 35° C. The product was obtained as white solid (12.5 g, 31.5 mmol, HPLC purity 98.61% ((S,R)-[7]+(S,S)-[7]), (S,R)-[7]/(S,S)-[7] ratio of 4.16:1).
The Second Crystallisation
[7] (12.5 g, 31.5 mmol; (R,S)-/(S,S)-diastereomeric ratio=4.16:1) was dissolved in a mixture of isobutyl acetate (125 mL) and ethanol (12.5 mL) at about 75° C. The solution was slowly cooled to ambient temperature and stirred overnight. The resulting mixture was cooled to about 0° C. and stirred for one hour and then filtrated and the isolated solid was dried under vacuum at 35° C. The product was obtained as white solid (7.10 g, 17.9 mmol, HPLC purity 98.58% ((S,R)-[7]+(S,S)-[7]), (S,R)-[7]/(S,S)-[7] ratio of 9.97:1).
The Third Crystallisation
[7] (7.1 g, 17.9 mmol; (R,S)-/(S,S)-diastereomeric ratio=9.97:1) was dissolved in a mixture of isobutyl acetate (71 mL) and ethanol (8.0 mL) at about 75° C. The solution was slowly cooled to ambient temperature and stirred overnight. The resulting mixture was cooled to about 0° C. and stirred for one hour and then filtrated and the isolated solid was dried under vacuum at 35° C. The product was obtained as white solid (5.4 g, 13.6 mmol, HPLC purity 96.69% ((S,R)-[7]+(S,S)-[7]), (S,R)-[7]/(S,S)-[7] ratio of 17.5:1). 1H NMR (300 MHz, d6-DMSO) δ 8.71 (d, J=15.6 Hz, 1H), 8.44 (d, 3H), 7.27 (m, 5H), 4.02 (s, 1H), 3.03 (m, 2H), 2.80 (d, J=4.5 Hz, 1H), 1.45 (m, 1H), 1.30-0.95 (m, 14H), 0.97-0.57 (m, 6H); 13C NMR (75 MHz, CDCl3) δ 168.8, 134.1, 130.2, 129.0, 127.8, 83.7, 53.4, 40.3-36.7 (m), 32.0, 29.3, 25. 5, 25.0 (m), 23.4, 22.0; ESI-MS (positive) (m/z): 361, 261.
Example 3 Operation B—Diastereomeric Upgrade of [7] by Slurrying in a Wet Solvent:
A slurry of [7] (0.5 g, 1.26 mmol; (R,S)-/(S,S)-diastereomeric ratio=1.30:1) in ethyl acetate (15 mL) containing water (0.05 g, 2.78 mmol) was stirred at room temperature. After 72 hour, a sample was isolated as a white solid by filtration of the slurry and was analysed by HPLC showing a purity 97.7% and a (R,S)-/(S,S)-diastereomeric ratio of 7.0:1.
Example 4 Operation C—Diastereomeric Upgrade of [7] by Chromatography:
[7] (1.0 g, 2.52 mmol, (R,S)-/(S,S)-diastereomeric ratio=0.83:1 was dissolved in was dissolved in 1:4 i-PrOH/DCM (5.0 mL) and was purified by silica gel column chromatography eluting with 1:10 i-PrOH/DCM. Three fractions were collection providing 96.7% HPLC purity [7] (0.60 g; (R,S)-[7]/(S,S)-[7]=0.55:1), 97.2% HPLC purity [7] (0.10 g; (R,S)-[7]/(S,S)-[7]=1.98:1), and 95.9% HPLC purity [7] (0.20 g; (R,S)-[7]/(S,S)-[7]=2.25:1), after evaporation of the eluent.
For embodiment 2, examples are provided below.
Example 5 Pinacol N-(pyrazine-2-yl-carbonyl)-L-phenylalanine-L-leucine boronate ((R,S)-[8])
To a cooled (about 0° C.) solution of 2-pyrazinecarboxylic acid (1.61 g, 13 mmol) in DMF (84.6 mL) was added DIPEA (4.74 mL), HATU (5.43 g, 14.3 mmol) and recrystallised pinacol L-phenylalanine-L-leucine boronate HCl salt ((R,S)-[7]; 5.4 g, 13.6 mol, as a 17.5:1 diastereomeric mixture of (R,S)-[7]/(S,S)-[7]). The mixture was warmed to room temperature and was then stirred at this temperature overnight. Ethyl acetate (270 mL) and a saturated aqueous solution of sodium of chloride (260 mL) were added to the reaction mixture. After mixing, the organic layer was separated and washed with a saturated aqueous solution of sodium of chloride (182 mL), then an aqueous 0.1N solution of KHSO4 (273 mL) and finally a saturated aqueous solution of NaHCO3 (182 mL). The organic layer was dried over MgSO4, filtered and evaporated at 35° C. giving the product as white solid (5.77 g, 12.4 mmol; HPLC purity 87.8% ((R,S)-[8]+(S,S)-[8]) as a 22.0:1 diastereomeric mixture of (R,S)-[8])/(S,S)-[8]). 1H NMR (300 MHz, CDCl3) δ 9.34 (d, J=1.2 Hz, 1H), 8.72 (t, J=9.9 Hz, 1H), 8.53 (dd, J=2.4, 1.6 Hz, 1H), 8.36 (d, J=8.4 Hz, 1H), 7.26 (ddd, J=10.7, 6.9, 4.8 Hz, 5H), 6.06 (s, 1H), 4.83 (dd, J=14.1, 6.8 Hz, 1H), 3.24-3.15 (m, 2H), 3.06 (dd, J=12.5, 7.4 Hz, 1H), 1.51-1.31 (m, 3H), 1.30-1.22 (s, 12H), 0.83 (t, J=6.7 Hz, 6H); ESI-MS (positive) (m/z): 467.
Bortezomib (anhydride; N-(2-pyrazine)carbonyl-L-phenylalanine-L-leucine boroxine)
1 N HCl (37.1 mL) was added dropwise into a mixture of pinacol N-(pyrazine-2-yl-carbonyl)-L-phenylalanine-L-leucine boronate ([8]; 5.77 g, 12.4 mmol as a 22.0 (R,S)-[8])/(S,S)-[8] diastereomeric mixture) and 2-methylpropaneboronic acid (1.89 g, 18.5 mmol) in MeOH (57.7 mL) and n-heptane (57.7 mL). The reaction mixture was stirred at room temperature overnight. The water layer was separated and washed twice with n-heptane (30 mL each). The water layer was concentrated at 35° C. and DCM (30 mL) was added into the residue. 2 N NaOH (36.9 mL) was added dropwise into the reaction mixture. The water layer was separated and washed twice with DCM (30 mL each). After dilution with DCM (30 mL) 1 N HCl was added dropwise until the pH of the aqueous phase was about 6. The water layer was extracted twice with DCM (30 mL each). The DCM portions were collected together and concentrated at 35° C. Ethyl acetate (46 mL) was added into the residue and concentrated. Ethyl acetate (16 mL) was added into the residue and concentrated until approximately 10% of the original volume remained. n-Heptane (46 mL) was added and the resulting solid was then filtered, washed with n-heptane (20 mL) and dried under vacuum at 35° C. The crude bortezomib was obtained as yellow solid (3.7 g, 9.63 mmol).
Purification of bortezomib (anhydride; N-(2-pyrazine)carbonyl-L-phenylalanine-L-leucine boroxine), Form C Example 6
A mixture of crude bortezomib (24.2 g, 63.0 mol, HPLC purity: 97.9%), MeCN (181.5 mL) and i-PrOH (12.1 mL) was stirred at room temperature for 4 hours. The solid was filtered and dried at 30° C. under vacuum overnight providing bortezomib anhydride Form C as a white solid (18.6 g, 48.4 mmol, yield 76.9%, HPLC purity: 99.7% with no individual impurity>0.10%).
Example 7
A mixture of crude bortezomib (1.0 g, 2.36 mmol, HPLC purity: 90.7%) and MeCN (8.0 mL) was stirred at room temperature for 6 hours. The solid was filtered and dried at 35° C. under vacuum for 17 hours providing bortezomib anhydride Form C as a white solid (0.75 g, 1.94 mmol, yield 82%, HPLC purity: 99.2%).
Representative XRDP pattern, a DVS graph, 1H NMR spectrum, IR spectrum, and DSC and TGA traces of Form C are shown in FIGS. 1, 2, 3, 4, 5 and 6, respectively.
……………………………………
 SYNTHESIS
SYNTHESIS
…………………………..
SYNTHESIS

…………………………
α-substituted boronic ester (Vl).
Scheme 1
Scheme 3.
According to the preferred embodiment of Scheme 4 (wherein R1, R2, R3, X and A are as defined as in the items above), a compound of formula VIII, for example about 3.8 mmol, in form of its (R)- or (S)- enantiomer or in form of a mixture of enantiomers, can be prepared by contacting a compound of formula Vl dissolved in an organic solvent, preferably THF, with a solution comprising a reagent for substituting X with a protected amino moiety, for example sodium bis(trimethylsilyl)amide (NaHMDS) or lithium bis(trimethylsilyl)amide (LiHMDS), at suitably low temperature such as -60 0C to -10 0C, more preferably – 40 0C to -30 0C, in an inert, preferably argon atmosphere. The solution is warmed to room temperature such as about 20 0C to 25 0C, and stirred for a suitable period of time, for example 1 to 15 hours, preferably for about 5 hours. Then, the reaction mixture is evaporated to dryness and the residue is subsequently dissolved in a suitable volume of n-heptane, for example about 10 ml_, washed with a suitable volume of H2O, for example about 8 ml_, and washed with a suitable volume of saturated aqueous solution of NaCI, for example about 4 mL. The organic phase is then dried over a suitable drying agent, most preferably MgSO4, filtrated and evaporated to dryness. Compound of formula Vila obtained in such a manner is subsequently further converted into the compound of formula VIII by dissolving the previously obtained residue in a suitable volume of n-heptane, for example 20 mL, and by adding a suitable amount of anhydrous acidic solution, for example anhydrous HCI solution in Et2O, at a suitably low temperature such as -100 0C to -10 0C, more preferably -70 0C to -50 0C, in an inert, preferably argon atmosphere. The reaction mixture is warmed to room temperature, such as about 20 0C to 25 0C, and finally the precipitating solid is isolated from reaction mixture by filtration and washed with Et2O to give α- amino boronic ester (VIII).
According to another embodiment of the present invention, the racemic mixture of the α-amino boronic ester (VIII) obtained above can be further separated to yield optically pure (R)- or (S)-enantiomer by methods known in the art, such as enantiomeric resolution by crystallization with chiral acids, e.g. malic acid, tartaric acid, mandelic acid, or by chiral chromatography. In the special case wherein the borolane part of compound of formula VIII is chiral, compound of formula VIII represents a diastereomer. Since diastereomers differ in their scalar characteristics, diastereomeric compounds of formula VIII can be separated without providing a chiral environment, e.g by crystallization or chromatographic methods on achiral supporters.
Enantiomers obtained in such manner can then be subjected to further synthesis steps to yield compounds of general formula X or free acids or esters or anhydrides or salts thereof
, wherein R1 is hydrogen, substituted or unsubstituted alkyl, substituted or unsubstituted aryl, or substituted or unsubstituted aralkyl;
R2 and R3 independently from each other represent substituted or unsubstituted alkyl, substituted or unsubstituted aryl, or substituted or unsubstituted aralkyl, or R2 and R3 cooperatively form a part of a 5- to 10-membered fused or unfused ring, optionally a chiral 5- to 10-membered fused or unfused ring; and peptide comprises 1-6 amino acids coupled to each other by peptide bonds with optionally acylated terminal amino group, and wherein the chiral center * is in its (R) or (S) configuration.
For example, the racemic mixture of the intermediate compound of formula VIII, for example 3-methyl-1- (4,4,5,5-tetramethyl-1 ,3,2-dioxaborolan-2-yl)butan-1-amine hydrochloride is first separated by enantiomeric resolution method known in the art to give (R)-3-m ethyl- 1 -(4,4,5, 5-tetram ethyl- 1 , 3,2- dioxaborolan-2-yl)butan-1-amine hydrochloride, which can then be subjected to further synthesis steps to yield bortezomib by synthesis routes known to or readily devisable by a person skilled in the art. For example, the following synthesis routes may be applied:
enantiomeric resolution coupling reagent
3-methyl-1 -(4,4,5,5-tetramethyl-
1,3,2-dioxaborolan-2-yl)butan-1-amine
hydrochloride hydrochloride
Scheme 5
Another aspect of the invention is a conversion of a compound of formula V or Vl to its trifuoroborate derivative compound of formula V* and Vl*, respectively, which can be further converted to compound VIII* as depicted in Scheme 6 below.
Scheme 6
………………………
Improved process for manufacturing the proteasome inhibitor bortezomib. Thus, in one embodiment, the invention provides a large-scale process for forming a compound of formula ( XIV ):
or a boronic acid anhydride thereof. The process comprises the steps:
- (a) providing a boron “ate” complex of formula ( XV ):
wherein:
- R3
- is a nucleofugic group;
- Y
- is a nucleofugic group; and
- M+
- is an alkali metal;
- (b) contacting the boron “ate” complex of formula ( XV ) with a Lewis acid under conditions that afford a boronic ester compound of formula ( XVI ):
said contacting step being conducted in a reaction mixture comprising:
- (i) a coordinating ether solvent that has low miscibility with water; or
- (ii) an ether solvent that has low miscibility with water and a coordinating co-solvent;
- (c) treating the boronic ester compound of formula ( XVI ) with a reagent of formula M1-N(G)2, where M1 is an alkali metal and each G individually or together is an amino group protecting group, to form a compound of formula ( XVII ):
- (d) removing the G groups to form a compound of formula ( XVIII ):
or an acid addition salt thereof;
- (e) coupling the compound of formula ( XVIII ) with a compound of formula ( XIX );
wherein:
- P1 is a cleavable amino group protecting moiety; and
- X is OH or a leaving group;
to form a compound of formula ( XX ):
wherein P1 is as defined above;
- (f) removing the protecting group P1 to form a compound of formula ( XXI ):
or an acid addition salt thereof;
- (g) coupling the compound of formula ( XXI ) with a reagent of formula ( XXII )
wherein X is a OH or a leaving group, to form a compound of formula ( XXIII ):
and
- (h) deprotecting the boronic acid moiety to form the compound of formula ( XIV ) or a boronic acid anhydride thereof.
Compound 1 (1R)-(1S,2S,3R,5S)-pinanediol-1-ammoniumtrifluoroacetate-3-methylbutane-1-boronate
Compound 2(1S)-(1S,2S,3R,5S)-pinanediol-1-ammoniumtrifluoroacetate-3-methylbutane-1-boronate
SubstancesCompound 3 N-(2-Pyrazinecarbonyl)-L-phenylalanine-L-leucine boronic anhydride
Compound4N-(2-Pyrazinecarbonyl)-D-phenylalanine-L-leucine boronic anhydride
Compound 5 N-(2-Pyrazinecarbonyl)-L-phenylalanine-D-leucine boronic anhydride
N-(2-Pyrazinecarbonyl)-L-phenylalanine-L-leucine boronic anhydride
-
A solution of (1S,2S,3R,5S)-Pinanediol N-(2-pyrazinecarbonyl)-L-phenylalanine-L-leucine boronate (25.2 g) in 207 mL of MeOH and 190 mL of hexane was cooled to 15 °C, and 109.4 mL of 1N HCl were added in portions, keeping the temperature between 15 and 25 °C. 2-Methylpropaneboronic acid (8.67 g) was then added under vigorous stirring, and the stirring of the biphasic mixture was continued over night. After separation of the two phases, the lower layer was extracted once with 75 mL of hexane. The lower layer was then concentrated in vacuo until it became cloudy, followed by the addition of 109.4 mL of 2N NaOH and 100 mL of Et2O. The two phases were separated the lower layer was extracted with Et2O (4 · 100 mL each), and then brought to pH 6.0 by the addition of 109 mL of 1N HCl. After extraction with 100 mL of ethyl acetate, the lower layer was adjusted to pH 6.0 with 1N HCl and extracted one more time with 75 mL of ethyl acetate. The combined ethyl acetate layers were washed with semi-saturated brine (2 · 25 mL) and brine (2 · 25 mL), dried over Na2SO4, filtered, and concentrated to afford 15.3 g (81.8 %) of crude N-(2-Pyrazinecarbonyl)-L-phenylalanine-L-leucine boronic anhydride as a foam. The crude material was dissolved in 150 mL of ethyl acetate and concentrated in vacuo to a suspension, followed by the addition of 150 mL of MTBE. The suspension was stored between 2 and 8 °C over night, filtered, washed twice with MTBE, and dried under high vacuum, yielding 10.69 g (57.2 %) of N-(2-pyrazinecarbonyl)-L-phenylalanine-L-leucine boronic anhydride as a white solid.
………………..
 Synthesis
Synthesis
In an illustrative example of the first process of the present invention, the compound of formula (2) reacts with the compound of formula (6) ,wherein Rl is hydrogen, under presence of the coupling agent of formula (8A). The formed B-OH protected compound (4) is then deprotected to bortezomib.
The compound of formula (2) is a known compound. It may be prepared by processes known in the art, which generally start from (S)-pinanediol and 2-methylpropane boronic acid. The processes are disclosed, e.g., in WO 2005/097809, WO 2009/004350 and
WO 2009/036281. The compound (2) may be used per se or, preferably, as an acid addition salt. The most preferred acid addition salt is a trifluoroacetate salt as it is easily preparable and is crystalline.
The second reaction partner, the compound of formula (6), is advantageously prepared by a process, in which L-phenylalanine alkylester and/or its acid addition salt having the formula (5)
wherein Rl is a C1-C4 alkyl group and is preferably methyl group, is coupled in an inert solvent with pyrazine-2-carboxylic acid of formula (7) in the presence of a base.
According to one aspect of the present invention, the coupling reaction proceeds in a presence of the coupling agent of the formula (8) above, typically with the n-propylphosphonic anhydride of the formula (8A). In an advantageous embodiment, the inert solvent may be an aliphatic, cyclic or aromatic C5-C10 hydrocarbon or a halogenated C1-C4 aliphatic hydrocarbon. The base is advantageously a tertiary amine, e.g. N-methylmorpholine. The reaction temperature is typically from -20 to 0 °C, under which temperature the reaction time is about 2-4 hours. The amount of the coupling agent of formula (8) is advantageously from 1 to 2 molar equivalents in respect to the compound (5). The reaction progress may be monitored by a suitable analytical technique, e.g. by HPLC or GC. After the reaction has been terminated, the reaction mixture is elaborated by an extraction with water, by which rests of the coupling agent and the base are removed. The reaction product may be isolated from the organic phase by common means, e.g. by evaporation, or the organic phase may be used in the next step directly.
In the next step, the so formed intermediate of formula (6), in which Rl is a C1-C4 alkyl group, and is preferably methyl group, is hydrolysed by water to the compound of formula (6), in which Rl is hydrogen. Preferably, the hydrolysis is performed in a water miscible solvent in a presence of a base, e.g. an amine base. It is important to assure that essentially no epimerization occurs during the hydrolysis. Therefore, the conditions of hydrolysis must be very mild. In an advantageous mode, the basic hydrolysis under mild conditions may be performed in presence in lithium salts , for instance lithium chloride, lithium bromide, lithium nitrate, lithium trifluoroacetate , lithium tetrafluoroborate etc.
The hydrolysed compound is advantageously isolated from the reaction mixture after neutralization thereof, preferably by an extraction. The crude product may be precipitated in solid form from the extract, e.g. by using antisolvent, which typically is an aliphatic hydrocarbon such as hexane or heptanes. The crude solid may be isolated by filtration and optionally recrystallized from a suitable solvent or a solvent/antisolvent mixture.
Having the compound (2) and compound (6) available, the key step in making bortezomib according to process of the present invention comprises coupling, under presence of a base, the compound (6), in which Rl is hydrogen, with the compound (2), which preferably is charged as an acid addition salt and most preferably as trifluoroacetate salt, in an inert solvent, whereby the coupling agent necessary for the mutual reaction is the compound of formula (8), preferably of formula (8A). In an advantageous embodiment, the inert solvent may be an aliphatic, cyclic or aromatic C5-C10 hydrocarbon or a halogenated C1-C4 aliphatic hydrocarbon. The base is advantageously a tertiary amine, e.g. N-methylmorpholine. The reaction temperature is typically from -30 to 0 °C, preferably from -20 to -10°C, under which temperature the reaction time is about 1-2 hours. The amount of the coupling agent of formula (8) is advantageously from 1 to 2 molar equivalents in respect to the compound (2). The reaction progress may be monitored by a suitable analytical technique, e.g. by HPLC or GC. After the reaction has been terminated, the reaction mixture is elaborated by an extraction with water, by which rests of the coupling agent and the base are removed. The reaction product may be isolated from the organic phase by common means, e.g. by evaporation and may be optionally purified, e.g. by column chromatography.
Whenever useful, reaction products of any of the steps of the process may be used in the next step without isolation from the reaction mixture.
In the last step, the so formed protected bortezomib intermediate of the formula (4) is deprotected by yielding bortezomib of formula (1). Any of deprotecting procedures known in the art may be used. In particular, the transesterification step disclosed in WO 2005/097809, in which the protected bortezomib reacts with an organic boronic acid acceptor in acidic conditions, represents an useful deprotecting process. In an illustrative example of the second process of the present invention, the compound of formula (2) reacts in the first step with the L-phenylalanine compound of formula (5a), wherein R is a nitrogen protective group. The useful nitrogen protective group is a tert.butyloxycarbonyl group (tBOC), but is should be understood that other suitable nitrogen protective groups may be used as well.
Similarly as in the first process of the present invention, the compound of formula (2) may be charged in the reaction as an acid addition salt, preferably the trifluoroacetate salt. The coupling reaction with the tBOC-protected compound (5a) typically proceeds in an inert solvent, in the presence of base and is, in accordance with the present invention, mediated by the action of the coupling agent of the formula (8), preferably (8A). The inert solvent is advantageously a chlorinated C1-C4 hydrocarbon or C5-C10 aliphatic, cyclic or aromatic hydrocarbon, the base is preferably a tertiary amine. The reaction conditions and workup of the reaction mixture are essentially the same as disclosed in the first process of the present invention.
In a next step, the protective group R in the so formed compound (3) is removed to yield a compound of formula (3) in which R is hydrogen. In case of the tBOC protective group, the deprotection is typically performed by treating the substrate with HC1 in ethyl acetate. After termination of the reaction, the product may be isolated from the reaction mixture by diluting with a hydrocarbon, e.g. with heptanes, and precipitating the product as a hydrochloride salt.
In the second coupling step, the compound (3), in which R is hydrogen, reacts with the 2-pyrazinecarboxylic acid of formula (7) in the presence of the coupling agent of the formula (8), preferably (8a), in an inert solvent and in the presence of a base.
EXAMPLES
EXAMPLE-1 : PROCESS FOR PREPARING N-[(1 S)-2-[[(1 R)-1-[(3aS,4S,6S,7aR)- hexahydro-3a,5,5-thmethyl-4,6-methano-1 ,3,2-benzodioxaborol-2-yl]-3-methyl butylamino]-2-oxo-1 -(phenylmethyl)ethyl] Pyrazinecarboxamide (FORMULA IX)
The process for preparing compound of formula IX comprises of the steps from Step a) to step h), which are individually demonstrated below:
Step-a) Preparation of 2-(2-Methylpropyl)-(3aS,4S,6S,7aR)-hexahydro-3a,5,5- trimethyl -4,6-methano-1 ,3,2-benzodioxaborole (Formula II):
To a stirred solution of isobutyl boronic acid (50.0 g) in n-heptane (250 ml) at 25.- 300C, was added (+)-Pinanediol (83.3 g) and stirred for I hour at 25-300C. To the reaction mass was added brine solution and the mixture was stirred. The layers were allowed to separate and the organic layer was concentrated under reduced pressure till no more solvent distills off to give the title compound (Formula II).
Step-b) Preparation of 2-((1 S)-1 -Chloro-3-methylbutyl)-(3aS,4S,6S,7aR)- hexahydro-3a,5,5- trimethyl-4,6-nnethano-1 ,3,2-benzodioxaborol (Formula III):
I. preparing a mixture of zinc chloride with tetrahydrofuran
II. preparing LDA mixture
III. preparing a solution of compound of formula-ll
in a solvent mixture comprising dichloromethane and water miscible ether solvent
IV. adding solution of step Il into the solution of step III followed by maintaining the solution at a temperature of about -40 to -700C
V. adding the mixture of step I into the product of step IV followed by maintaining the reaction mass at a temperature of about -40 to -700C
VI. raising the reaction temperature up to about 10°C to ambient temperature
VII. adding the aqueous acid solution VIII. separating the organic layer containing the compound of formula-Ill, and isolating the product.
I. Preparing a mixture of zinc chloride with tetrahydrofuran
Charged ZnCI2 (115 g) to tetrahydrofuran (805 ml) into a 1st Round bottom flask (R. B. flask) under nitrogen atmosphere at 25 to35°Cand the temperature of the resulting mixture was raised to 35 to 400C, maintained for 3-4 hours to give ZnCI2 solution.
II. Preparing LDA mixture
Charged diisopropyl amine (86 ml) to tetrahydrofuran (345 ml) into a 2nd R. B. flask under nitrogen atmosphere and resultant mixture was cooled to -7 to -150C, charged n-hexyl lithium to the above mixture and maintained for 30-40 minutes to give LDA mixture.
III. Preparing a solution of compound of formula-ll Compound of Formula Il (115.O g) was charged to a dichloromethane (161 ml) and tetrahydrofuran (690 ml) into a 3rd R. B. flask under nitrogen atmosphere at 25 to35°C and the mixture was cooled to -55 to -600C.
IV. Adding solution of step Il into the solution of step III Charged LDA mixture from the 2nd R. B. flask to the reaction mixture at -55 to –
600C and maintained for 30 minutes. The temperature was raised to -500C.
V. Adding the mixture of step I into the product of step IV
Charged ZnCI2 solution from the 1st R. B. flask at -45 to -500C and maintained for I hour. Vl. Raising the reaction temperature up to about 100C
The reaction mixture was warmed to 100C. VII. Adding the aqueous acid solution
Charged 10% H2SO4, stirred for 10-15 minutes and the organic layer was separated. VIII. Separating the Organic layer containing the compound of formula-Ill, and isolating the product.
The organic layer separated under step VII was subjected to next step, however, the aqueous layer was discarded.
Washed the organic layer with brine solution under stirring, till the aqueous layer reached to a pH around 6-7.
The organic layer was concentrated to isolate the compound of formula-Ill, under reduced pressure.
Step-c) Preparation of N,N-Bis(thmethylsilyl)-(1 R)-1 -[(3aS,4S,6S,7aR)- hexahydro-3a,5,5-thmethyl-4,6-methano-1 ,3,2-benzodioxaborol-2-yl]-3- methylbutylamine (Formula IV):
iv
Hexamethyldisilazane (101.3 ml) was charged to tetrahydrofuran (414 ml) under nitrogen atmosphere and the mixture was cooled to -20 to -300C. Charged n- hexyllithium slowly to the above mixture under stirring by maintaining the temperature at -20 to -30 0C. The reaction mixture was stirred for 1 -2 hours at -20 to -250C, charged compound of Formula III (138 g) to the above freshly prepared lithium HMDS in THF by maintaining the temperature at -15 to -200C. The reaction mixture was warmed to a temperature of 25-300C and maintained for 2-3 hours. Filtered the reaction mixture through silica bed and washed the bed with diisopropyl ether. The filtrate was concentrated under reduced pressure to a residue to give the title compound (Formula IV).
Step-d) Preparation of 4,6-Methano-1 ,3,2-benzodioxaborole-2-methanamine, hexahydro-3a,5,5-thmethyl-α-(2-methylpropyl)-,(αR,3aS,4S,6S,7aR)-,trifluoro acetate (Formula V):
Charged thfluoroacetic acid (129 ml) to diisopropyl ether (1980 ml) under nitrogen atmosphere at 25-300C and the reaction mass cooled to -100C. Charged compound of Formula IV (198 g) to the reaction mass slowly at -100C and maintained at the same temperature for 8 hours. The reaction mass was filtered, washed with diisopropyl ether (198 ml) and the obtained solid was slurry washed with water (1500 ml) at 25-300C. The slurry was filtered washed with water and the solid obtained was dried at 40-500C under reduced pressure for 8 hours to give 74.Og of the title compound (Formula V). Purity (by GC) = 99.54%
Step-e) Preparation of L-Phenylalanine methyl ester hydrochloride (Formula Vl):
To a stirred mixture of L-phenyl Alanine (25 g) in methanol (125 ml) at 25-300C, was charged thionyl chloride (13.2 ml) under stirring and the mixture was maintained at 55-600C for 2-3 hours. The reaction mass was cooled to 25-300C and concentrated under reduced pressure up to 2 volumes with respect to the staring material. Charged isopropyl alcohol (125 ml) to the reaction mass and concentrated up to 2 volumes with respect to the starting material. Cooled the reaction mass to 0-50C and maintained under stirring for 1-2 hours. Filtered the reaction mass, washed with isopropyl alcohol, suck dried for 30 minutes and the solid obtained was dried at 45- 500C for 3-4 hours to give 28.8 g of the title compound (Formula Vl). Chiral purity by HPLC: 100%.
Step-f) Preparation of L-Phenylalanine, N-(pyrazinylcarbonyl)-methyl ester (Formula VII):
To a stirred mixture of Pyrazine-2-carboxylic acid (3.45 g) in DMF (50 ml) at 25-300C, was charged N-hydroxy succinimide (3.2 g) under stirring and was cooled to 0-50C. Charged N,N’-dicyclohexylcarbodiimide (DCC) (5.75 g) to the reaction mass at 0-5 0C and stirred for 15-20 minutes. Charged compound of Formula Vl (5.0 g) to the reaction mass at 0-50C and stirred for 15-20 minutes. Further, charged NMM (3.8 ml) to the reaction mass at 0-50C and stirred for 15-20 minutes. The reaction mixture was warmed to 25-300C and maintained under stirring for 2-3 hours. The reaction mass was filtered and the solid was separated. The filtrate obtained was diluted with ethylacetate (100 ml) and washed with demineralized water. The organic layer was washed with 1 N HCI, followed by washing with sodium bicarbonate solution. Concentrated the organic layer up to 2 volumes with respect to Formula Vl under reduced pressure and cooled to 25- 300C. Charged n-heptane (20 ml) to precipitate the compound, cooled the reaction mass to 0-50C, maintained for 1 -2 hours and filtered under vacuum. The solid obtained was dried at 40-450C for 3-4 hours to give 5.7 g of the title compound (Formula VII). Purity by HPLC: 99.73%, chiral purity by HPLC: 99.97%.
Step-g) Preparation of N-(pyrazinylcarbonyl)-L-Phenylalanine (Formula VIII):
To a stirred mixture of Formula VII (100 g) in acetone (500 ml) at 25-300C, was charged NaOH solution (obtained by dissolving 15.4 g of NaOH in 500 ml of water) and maintained at the same temperature for 30-50 minutes. Adjusted the pH of the reaction mass to 2 by using 1 N HCI and cooled the reaction mass to 0-50C. Maintained the reaction mass at 0-5 0C under stirring for 1 -2 hours, filtered under vacuum and dried the material obtained at 45-500C for 4-5 hours to give 84.4 g of the title compound (Formula VIII). Purity by HPLC: 99.94 % by weight. Chiral purity by HPLC: 100 %
Alternately, N-(pyrazinylcarbonyl)-L-Phenylalanine (Formula VIII) may also be prepared by
(a) Using ethylchloroformate according to the process as described below: A mixture of acetone (40 ml), pyrazine carboxylic acid (5 g) and thethylamine
(6.77 ml) was cooled to about -5°C to about 00C and ethylchloroformate (4.76 ml) was charged. The reaction mass was stirred for about 30 minutes. The reaction suspension was allowed to reach the temperature of about 25°C to about 300C and maintained for about 3 hours. The reaction suspension was cooled to about 00C to about 5°C. In the second flask the aqueous sodium hydroxide (1.68 g in 70 ml water) solution was cooled to about 00C to about 5°C and to that acetone (30 ml) and L-phenyl alanine (6.6 g) were added and the mixture was stirred for about 1 hour at that temperature. The reaction mass of the second flask was added to the reaction mass of the first flask at a temperature of about 00C to about 5°C and then stirred for about 2 hours followed by raising the temperature to about 25°C to about 300C. The reaction mass was further stirred for about 16 hours at a temperature of about 25°C to about 300C. Ethyl acetate (150 ml) was charged to the reaction solution and stirred for about 30 minutes. The layers were separated and 1 N hydrochloric acid (35 ml) was added to the separated aqueous layer. The reaction solution was cooled to about 00C to about 5°C and stirred for about 2 hours. The obtained suspension was filtered and the solid was washed with water (10 ml). The solid was then dried at a temperature of about 500C for about 4 hours to afford 2.6 g of title compound. Purity by HPLC: 99.2% by weight. Chiral purity by HPLC: 100% (b) or by using combination of EDCHCI, HOBt, according to the process as described below:
A mixture of pyrazine carboxylic acid (168.7 g), dimethylformamide (1.4 lit), hydroxybenzotriazole (HOBt:220 g), and N-methyl morpholine (221 ml) was cooled to a temperature of about 00C to about 5°C. EDC. hydrochloride (1 -Ethyl-3-(3- dimethylaminopropyl) carbodiimide-HCI; 278 g) was added to the reaction solution at a temperature of about 00C and stirred for about 30 minutes. L-phenylalanine methyl ester hydrochloride (240 g) obtained from above was dissolved in DMF (1 lit) and then added to the reaction mixture. N-methyl morpholine (110 ml) was added to the reaction mixture and the reaction mixture was maintained at a temperature of about 00C to about 5°C for about 1 hour. The reaction mixture was allowed to warm to the temperature to about 25°C to about 35°C and diluted with water (3.6 lit). The reaction mass was extracted with ethyl acetate (3×2.4 lit). The separated ethyl acetate layer was washed with 1 N hydrochloric acid (1.2 lit) and two layers were then separated. The organic layer was washed with saturated sodium bicarbonate solution (4.8 lit) and brine solution (2.4 lit). The organic layer was concentrated completely at a temperature of about 45°C to afford 260 g of pyrazine-2- carbonylphenylalanine methyl ester.
Pyrazine-2-carbonylphenylalanine methyl ester (5 g) was dissolved in acetone (25 ml) and stirred for about 5 minutes. Sodium hydroxide solution (701 mg of sodium hydroxide in 25 ml of water) was added to the reaction solution and stirred for about 3 hours at a temperature of about 25°C, and the pH was then adjusted withi N hydrochloric acid (11 ml) to a pH of about 2. The reaction mixture was cooled to a temperature of about 00C to about 5°C and stirred for about 1 hour. The suspension was filtered and suck dried to afford 4.0 g of pyrazine-2- carbonylphenylalanine.
Chiral purity by chiral HPLC: 100% Chemical purity by HPLC: 99.88%.
Step-h) Preparation of Formula IX:
To a stirred mixture of compound of Formula VIII (28.6 g) in dichloromethane (400 ml) at 25-300C under nitrogen atmosphere, were charged N-hydroxysuccinimide (13.3 g) and DCC (23.9 g) and stirred for 10-20 minutes. Charged compound of Formula-V (40 g) to the reaction mass was and stirred for 15-20 minutes.
Charged diisopropylethylamine (DIPEA) (27 ml) and maintained the reaction mass at 25-300C for 2-3 hours. The reaction mass was filtered and the solid was washed with dichloromethane (80 ml). The filtrate obtained was washed with 1 N HCI, followed by washing with sodium bicarbonate solution. Concentrated the organic layer up to 2 volumes with respect to Formula-V. Charged methanol (200 ml) and concentrated up to 2 volumes with respect to Formula-V. The concentrated mass obtained is the title compound (Formula IX).
Alternately, compound of Formula IX may also be prepared by using EDCHCI, and Hydroxybenzotriazole by a process as described below: N-(2-pyrazinecarbonyl)-L-phenylalanine (500 mg) was suspended in dichloromethane (10 ml) and cooled to about -5°C to about 00C. Hydroxybenzotriazole (HOBt:310 mg) was charged in to the reaction mass followed by the addition of 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide hydrochloride (EDCHCI, 385 mg) and stirred for 15 minutes. (1 R)-(S)-pinanediol 1 -ammonium trifluoroacetate-3-methylbutane-i -boronate (695 mg) was added to the reaction mixture and stirred for about 10 minutes at a temperature of about 5°C Diisopropyl ethyl amine (0.6 ml) was charged to the reaction mixture and stirred for about 30 minutes at a temperature of about 5°C The reaction mixture was allowed to warm to a temperature of about 25°C to about 300C and stirred for about 1 hour followed by the addition of 1 N hydrochloric acid (30 ml). The layers were separated and the organic layer was washed with 1 N hydrochloric acid (15 ml) and saturated sodium bicarbonate solution (2×30 ml). The organic layer was concentrated completely to afford title compound. Purity by HPLC: 84.98% Note that it is believed that 9.01 % measured by HPLC is Bortezomib that is formed prior to the final Bortezomib step. Thus, overall purity should be 84.98% + 9.0% or 93.99% as measured by HPLC.
EXAMPLE-2: PROCESS FOR PREPARING BORTEZOMIB (FORMULA I)
To a stirred mixture of compound of Formula IX (13.6 g) in methanol (272 ml) at 25- 300C, was charged n-heptane (272 ml), and isobutylboronic acid (3.2 g). Charged 2N HCI (272 ml) to the reaction mass under vigorous stirring and maintained the reaction mass at 25-300C for 1 -2 hours. After the completion of the reaction, separated the n-heptane layer and discarded. Charged n-heptane (272 ml * 2) to the aqueous layer and stirred vigorously for 10-15 minutes. Separated the n-heptane layer and the aqueous layer obtained was concentrated under vacuum at 35 to 480C. The aqueous layer was extracted with dichloromethane (272 ml) under vigorous stirring. The extraction process is repeated (272 ml *2) and the obtained dichloromethane layers were pooled and washed with saturated sodium bicarbonate solution, followed brine solution. The organic layer is separated, concentrated under vacuum to give 6 ml of the reaction mass and allowed to cool to 25-300C. Purity: 95.13% by HPLC.
Charged Toluene (102 ml) to the above reaction mass and stirred at 25-300C for 2-3 hours. Filtered the solid obtained under vacuum washed with 5% dichloromethane in toluene and dried at 45-500C under vacuum for 5 hours to give crude Bortezomib.
Yield: 7.O g (70%)
Purity by HPLC: 99.22%
Impurity-B by HPLC: 0.43%
Polymorphic Form: Form-B
XRD Pattern: As Illustrated in Fig -5 EXAMPLE-3: PROCESS FOR PURIFICATION OF BORTEZOMIB USING METHANOL AND WATER
Bortezomib (5.0 g, purity 99.22%) and methanol (15 ml) were taken into a round bottom flask and stirred at 25 to 35°c. Demineralized water (15 ml) was added to the obtained solution and stirred for 2 hours at a temperature of about 27°C. The reaction suspension was filtered and washed the solid with aqueous methanol (30 ml; water: methanol 1 :1 ). The obtained solid was dried at a temperature of about
500C for about 5 hours to afford 3.4 g of title compound.
Purity by HPLC: 99.57%
Impurity-B by HPLC: 0.30%
Further purification of the product obtained by reproducing the same process resulted in a Bortezomib having a purity of 99.6% by HPLC. Impurity-B by HPLC: 0.23%
Chiral Purity by HPLC: 99.83%
EXAMPLE-4: PROCESS FOR PREPARING BORTEZOMIB FOLLOWED BY PURIFICATION To a stirred mixture of compound of formula IX (68.3 g) in methanol (1.22 L) at 25- 300C, was charged n-heptane (1.36 L), and isobutyl boron ic acid (16.13 g). Charged 1 N HCI (13.6 L) to the reaction mass under stirring and maintained the reaction mass at 25-300C for 1 -2 hours. After the completion of the reaction, separated the n- heptane layer and discarded. Charged n-heptane (1.36 L * 2) to the aqueous layer and stirred vigorously for 10-15 minutes. Separated the n-heptane layer and the aqueous layer obtained was concentrated under vacuum. The aqueous layer was extracted with dichloromethane (13.6 L) under vigorous stirring. The extraction process is repeated (13.6 L *2) and the obtained dichloromethane layers were pooled and washed with saturated sodium bicarbonate solution, followed by brine solution. The organic layer was separated, concentrated under vacuum to give crude Bortezomib (47.0 g)
Purity by HPLC: 95.62% Impurity-B by HPLC: 0.59% Purification 1 : Bortezomib (25 g, Purity: 95.62%) and 5% ethylacetate in Toluene (250 ml) were taken into a round bottom flask and stirred at 25 to 350C for 2-3 hours. Filtered the solid obtained under vacuum washed with 5% ethylacetate in toluene and dried at 500C under vacuum for 5 hours to give Bortezomib.
Yield: 18.O g (72%) Purity by HPLC: 99.68% Impurity-B by HPLC: 0.27%
Purification 2: Bortezomib (18.0 g, purity 99.68%) and methanol (54 ml) were taken into a round bottom flask and stirred. Filtered the reaction mass through scinted funnel and washed the bed with 18 ml methanol. Demineralized water (72 ml) was added to the obtained filtrate and stirred for 2 hours at a temperature of about 27°C. The reaction suspension was filtered and washed the solid with aqueous methanol (108 ml; Water : methanol 1 :1 ). The obtained solid was dried at a temperature of about 500C for about 5 hours to afford 14 g of title compound.
Yield: 14.O g (77%) Purity by HPLC: 99.83%
Impurity B: 0.15% (by HPLC) Chiral Purity by HPLC: 99.85%

 References
References
- Takimoto CH, Calvo E. “Principles of Oncologic Pharmacotherapy” in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) Cancer Management: A Multidisciplinary Approach. 11 ed. 2008.
- Adams J, Kauffman M (2004). “Development of the Proteasome Inhibitor Velcade (Bortezomib)”. Cancer Invest 22 (2): 304–11. doi:10.1081/CNV-120030218.PMID 15199612.
- Stephen R.Byrn et al (2011). “Analysis of two commercially available bortezomib products: differences in assay of active agent and impurity profile”. AAPS PharmSciTech (April 1).
- Bonvini P, Zorzi E, Basso G, Rosolen A (2007). “Bortezomib-mediated 26S proteasome inhibition causes cell-cycle arrest and induces apoptosis in CD-30+ anaplastic large cell lymphoma”. Leukemia 21 (4): 838–42. doi:10.1038/sj.leu.2404528. PMID 17268529.
- Gelman JS, Sironi J, Berezniuk I, Dasgupta S, Castro LM, Gozzo FC, Ferro ES, Fricker LD (2013). “Alterations of the intracellular peptidome in response to the proteasome inhibitor bortezomib”. In Gartel, Andrei L. PLoS One 8 (8): e53263.doi:10.1371/journal.pone.0053263. PMC 3538785. PMID 23308178.
- Voorhees PM, Dees EC, O’Neil B, Orlowski RZ (2003). “The proteasome as a target for cancer therapy”. Clin Cancer Res 9 (17): 6316–25. PMID 14695130.
- “NHS watchdog rejects cancer drug”. BBC News UK. 20 October 2006. Retrieved 2009-08-14.
- “Summary of VELCADE Response Scheme”. Retrieved 2009-08-14.
- “More Velcade-Style Risk-Sharing In The UK?”. Euro Pharma Today. 21 January 2009. Retrieved 2009-08-14.
- Oakervee HE, Popat R, Curry N, et al. (2005). “PAD combination therapy (PS-341/bortezomib, doxorubicin and dexamethasone) for previously untreated patients with multiple myeloma”. Br J Haematol 129 (6): 755–62. doi:10.1111/j.1365-2141.2005.05519.x. PMID 15953001.
- Pour L., Adam Z., Buresova L., et al. (2009). “Varicella-zoster virus prophylaxis with low-dose acyclovir in patients with multiple myeloma treated with bortezomib”. Clinical Lymphoma & Myeloma 9 (2): 151–3. doi:10.3816/CLM.2009.n.036. PMID 19406726.
- Highlights Of Prescribing Information
- “Cancer drug benefits could be negated by healthy tea treatment”. Belfast Telegraph. 3 February 2009. Retrieved 2009-08-14.
- “Green tea may counteract anticancer effects of cancer therapy, bortezomib (Velcade)”. Retrieved 15 July 2013.
- “Green tea clash with bortezomib suggested”. Retrieved 26 July 2013.
- Golden EB, et al.; Lam, P. Y.; Kardosh, A.; Gaffney, K. J.; Cadenas, E.; Louie, S. G.; Petasis, N. A.; Chen, T. C.; Schonthal, A. H. (2009). “Green tea polyphenols block the anticancer effects of bortezomib and other boronic acid-based proteasome inhibitors”. Blood 113 (23): 5927–37.doi:10.1182/blood-2008-07-171389. PMID 19190249.
- Curran M, McKeage K. (2009). “Bortezomib: A Review of its Use in Patients with Multiple Myeloma”. Drugs 69 (7): 859–888. doi:10.2165/00003495-200969070-00006.PMID 19441872. doi:10.2165/00003495-200969070-00006.
- Journal of Pharmaceutical Sciences, 2000 , vol. 89, 6 p. 758 – 765
-
WO2009/36281 A2, ANDUS2013/85277 A1,
- [1]
- Myeloma patients campaigning for access to a life prolonging cancer drug
- Millennium Pharmaceuticals website on Velcade
- Multiple Myeloma Research Foundation article on Velcade
- International Myeloma Foundation article on Velcade
- U.S. Food and Drugs Administration on Velcade
- Dedicated website for European audience
- Presentation at 2006 ASCO of the PINNACLE Study on MCL by Dr. Goy, with video/slides
| EP2377868A1 * | Mar 24, 2005 | Oct 19, 2011 | Millennium Pharmaceuticals, Inc. | Synthesis of Bortezomib |
| WO2005097809A2 | Mar 24, 2005 | Oct 20, 2005 | Millennium Pharm Inc | Synthesis of boronic ester and acid compounds |
| WO2009004350A1 | Jul 2, 2008 | Jan 8, 2009 | Pliva Hrvatska D O O | Methods for preparing bortezomib and intermediates used in its manufacture |
| WO2009006473A2 | Jul 1, 2008 | Jan 8, 2009 | William W Bachovchin | Pro-soft polypeptide proteasome inhibitors, and methods of use thereof |
| WO2009036281A2 | Sep 12, 2008 | Mar 19, 2009 | Nageshwar Gunda | Bortezomib and process for producing same |
| EP0315574A2 | Oct 29, 1988 | May 10, 1989 | Hoechst Aktiengesellschaft | Renin inhibitors |
| EP0788360B1 | Oct 27, 1995 | May 28, 2003 | Millennium Pharmaceuticals, Inc. | Boronic ester and acid compounds, synthesis and uses |
| US4924026 | Aug 11, 1989 | May 8, 1990 | International Flavors & Fragrances Inc. | Triisobutylene alcohols and esters, uses thereof in perfumery and halogenated intermediates useful for preparing same |
| US20010012907 * | Feb 1, 2001 | Aug 9, 2001 | Nissan Chemical Industries, Ltd. | Substituted cyclopentene derivatives and method for preparing the same |
| US20030008828 * | Dec 6, 2001 | Jan 9, 2003 | Priestley E. Scott | Novel lactam inhibitors of hepatitis C virus NS3 protease |
| US20070244319 | Apr 18, 2006 | Oct 18, 2007 | Boaz Neil W | Metallocenyl P-N ligands, preparation thereof, and use for asymmetric catalysis |
| WO2010146172A2 | Jun 18, 2010 | Dec 23, 2010 | Lek Pharmaceuticals D.D. | NEW SYNTHETIC ROUTE FOR THE PREPARATION OF α-AMINO BORONIC ACID DERIVATIVES VIA SUBSTITUTED ALK-1-YNES |
| WO2011098963A1 | Feb 9, 2011 | Aug 18, 2011 | Ranbaxy Laboratories Limited | Process for the preparation of bortezomib |
| WO2011099018A1 * | Feb 15, 2010 | Aug 18, 2011 | Hetero Research Foundation | Polymorphs of bortezomib |
| WO2011107912A1 | Feb 24, 2011 | Sep 9, 2011 | Ranbaxy Laboratories Limited | Polymorphic forms of bortezomib |
| WO2012048745A1 | Oct 14, 2010 | Apr 19, 2012 | Synthon Bv | Process for making bortezomib and intermediates for the process |
| CN102206188B | Apr 8, 2011 | Feb 27, 2013 | 苏州二叶制药有限公司 | Preparation method for N-(pyrazine-2-yl carbonyl)-L-phenylalanine |
| CN102212036B | Apr 8, 2011 | Oct 17, 2012 | 上海医药工业研究院 | Preparation method of N-(pyrazine-2-radical carbonyl)-L-phenyl alanine |
| EP2270019A1 | Jun 19, 2009 | Jan 5, 2011 | LEK Pharmaceuticals d.d. | New synthetic route for the preparation of alpha-amino boronic esters |
| EP2280016A1 | Jul 27, 2009 | Feb 2, 2011 | LEK Pharmaceuticals d.d. | New synthetic route for the preparation of alpha-amino boronic esters via substituted alk-1-ynes |
| US8497374 | May 12, 2011 | Jul 30, 2013 | Scinopharm Taiwan, Ltd. | Process for preparing and purifying bortezomib |


Ancient Chinese medicine put through its paces for pancreatic cancer
The bark of the Amur cork tree (Phellodendron amurense) has traveled a centuries-long road with the healing arts. Now it is being put through its paces by science in the fight against pancreatic cancer, with the potential to make inroads against several more. UT Health Science Center researcher A. Pratap Kumar was already exploring the cork tree extract’s promise in treating prostate cancer when his team found that deadly pancreatic cancers share some similar development pathways with prostate tumors.
In a paper published today in the journal Clinical Cancer Research, the researchers show that the extract blocks those pathways and inhibits the scarring that thwarts anti-cancer drugs. Dr. Jingjing Gong, currently pursuing post-doctoral studies at Yale University, conducted the study as a graduate student in Dr Kumar’s laboratory in the Department of Pharmacology.
“Fibrosis is a process of uncontrolled scarring around the tumor gland,” said Dr…
View original post 242 more words
2013 FDA drug approvals
This analysis by Asher Mullard published in Nature Reviews Drug Discovery (2014,13, 85-89) reports the new drugs approved by FDA in 2013. From a total of thirty-six applications, twenty-five new small molecules and two new biologics were approved. The same trend as the previous years was overall maintained, with the exception of 2012. (Figure 1).
A notable achievement was the high approvals (33%) of new molecular entities for the treatment of orphan disease. In addition, 33% of the new approvals had a unique mode of action and were identified as first-in-class agents. The anticancer therapeutic area obtained the majority of approvals (eight, six of which are for orphan indication), followed by metabolic and endocrinology, antiviral and medical imaging (three approvals for each category). Cardiology, neurology, respiratory and women’s health have two agents approved each, and only one new approval for psychiatry and dermatology.
Ten drugs received a priority review…
View original post 343 more words
Actelion’s novel antibiotic Cadazolid receives US FDA Qualified Infectious Disease Product designation for the treatment of Clostridium difficile-associated diarrhea .

CADAZOLID, ACT-179811
1-Cyclopropyl-6-fluoro-7-[4-({2-fluoro-4-[(5R)-5-(hydroxymethyl)-2-oxo-1,3-oxazolidin-3-yl]phenoxy}methyl)-4-hydroxypiperidin-1-yl]-4-oxo-1,4-dihydroquinolin-3-carboxylic acid
l-cyclopropyl-6-fluoro-7-{4-[2-fluoro-4-(R)-5-hydroxymethyl-2-oxo- oxazolidin-3-yl)-phenoxymethyl]-4-hydroxy-piperidin-l-yl}-4-oxo-l,4-dihydro- quinoline-3-carboxylic acid
| Formula | C29H29F2N3O8 |
|---|---|
| Mol. mass | 585.55 g/mol |
Actelion Pharmaceuticals Ltd / Actelion’s novel antibiotic cadazolid receives US FDA Qualified Infectious Disease Product designation for the treatment of Clostridium difficile-associated diarrhea .
ALLSCHWIL/BASEL, SWITZERLAND – 27 February 2014 – Actelion Ltd (six:ATLN) today announced that the US Food and Drug Administration (FDA) has designated cadazolid as both a Qualified Infectious Disease Product (QIDP) and a Fast Track development program for the treatment of Clostridium difficile-associated diarrhea (CDAD).
The QIDP designation for cadazolid means that – among other incentives – cadazolid would receive a nine-month priority review upon successful completion of the ongoing global Phase III IMPACT program. The Fast Track designation is intended to promote communication and collaboration between the FDA and the Company on the development of the drug.
The designations are based on the 2012 US Generating Antibiotic Incentives Now (GAIN) Act. The GAIN act is a legislative effort to incentivize the development of new antibiotic agents that target serious life-threatening infections.
Guy Braunstein, M.D. and Head of Clinical Development commented: “Clostridium difficile-associated diarrhea is a very serious and potentially life-threatening infection. There is a great need for an antibiotic that allows effective treatment of CDAD with low recurrence rates, particularly in infections caused by hypervirulent strains. The GAIN act highlights the importance of research in this area and we are very happy to receive the advantages that this designation for cadazolid will afford us.”
ABOUT THE IMPACT PROGRAM
IMPACT is an International Multi-center Program Assessing Cadazolid Treatment in patients suffering from Clostridium difficile-associated diarrhea (CDAD). The program comprises two Phase III studies comparing the efficacy and safety of cadazolid (250 mg administered orally twice daily for 10 days) versus vancomycin (125 mg administered orally four times daily for 10 days).
The IMPACT studies are designed to determine whether the clinical response after administration of cadazolid is non-inferior to vancomycin in subjects with CDAD, and whether administration of cadazolid is superior to vancomycin in the sustained clinical response. The program is expected to enroll approximately 1’280 subjects worldwide, and commenced enrollment in the fourth quarter of 2013.
ABOUT CADAZOLID
The novel antibiotic cadazolid is a strong inhibitor of Clostridium difficile protein synthesis leading to strong suppression of toxin and spore formation. In preclinical studies cadazolid showed potent in vitro activity against Clostridium difficile clinical isolates and a low propensity for resistance development. In a human gut model of CDAD, cadazolid had a very limited impact on the normal gut microflora.
Cadazolid absorption is negligible resulting in high gut lumen concentrations and low systemic exposure, even in severe cases of CDAD where the gut wall can be severely damaged and permeability to drugs potentially increased.
Cadazolid is an experimental antibiotic of the oxazolidinone class made by Actelion Pharmaceuticals Ltd. which is effective against Clostridium difficile, a major cause of drug resistant diarrhea in the elderly.[1] Current drug treatments for this infection involve orally delivered antibiotics, principally fidaxomicin, metronidazole and vancomycin; the last two drugs are the principal therapeutic agents in use, but fail in approximately 20 to 45% of the cases. The drug is presently in Phase III trials.[1] The drug works by inhibiting synthesis of proteins in the bacteria, thus inhibiting the production of toxins and the formation of spores.[2]
Structure
The chemical structure of cadazolid combines the pharmacophores of oxazolidinone and fluoroquinolone.[2]
In a study published in the journal Anaerobe, cadazolid has been shown to be effective in vitro against 133 strains of Clostridium difficile all collected from Sweden.[3]
In phase I tests, sixty four male patients reacted favourably to cadazolid which primarily acted and remained in the colon while displaying little toxicity even in regimes involving large doses.[1]
ABOUT CADAZOLID IN THE PHASE II STUDY
Cadazolid was studied in a Phase II multi-center, double-blind, randomized, active reference, parallel group, therapeutic exploratory study. The study evaluated the efficacy, safety and tolerability of a 10-day, twice daily oral administration of 3 doses (250 mg, 500 mg or 1,000 mg b.i.d.) of cadazolid in subjects with Clostridium difficile-associated diarrhea (CDAD). As the current standard of care for CDAD, oral vancomycin (125 mg qid for 10 days) was used as the active reference. The study was completed in December of 2012, after having enrolled 84 subjects with CDAD.
The results of the Phase II study indicate that the effect of all doses of cadazolid were numerically similar to, or better than vancomycin on key endpoints including CDAD clinical cure rates as well as sustained cure rates. Clinical cure rate was defined as the resolution of diarrhea and no further need for CDAD therapy at test-of-cure 24 to 72 hours after the last dose of treatment, while sustained cure rate was defined as clinical cure with no recurrence of CDAD up to 4 weeks post-treatment. Recurrence rates were numerically lower for all doses of cadazolid as compared to vancomycin. Cadazolid was safe and well tolerated.
ABOUT THE GAIN ACT (INCLUDING FAST TRACK DESIGNATION)
The Food and Drug Administration Safety and Innovation Act (FDASIA) was signed into law in July 2012. The GAIN Act is Title VIII to FDASIA. The purpose of the GAIN Act is to encourage pharmaceutical research of certain antibiotics by designation of products as QIDPs. These products are intended to treat serious or life-threatening infections and include those to treat certain specifically identified pathogens, which are listed in the GAIN Act. C. difficile is one such specifically identified pathogen and drugs to treat CDAD would be eligible for designation as a QIDP.
The GAIN Act also provides that qualifying drugs (QIDPs) are eligible for inclusion in the FDA’s Fast Track program. This program is intended to facilitate development and expedite review of new drugs and includes close early communication between the FDA and a drug’s sponsor.
ABOUT FAST TRACK DRUG DEVELOPMENT PROGRAMS
For further information regarding Fast Track Drug Development Programs, please refer to the FDA document “Guidance for Industry on Fast Track Drug Development Programs: Designation, Development, and Application Review”. This document is available on the Internet at:
http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM079736.pdf
ABOUT CLOSTRIDIUM DIFFICILE-ASSOCIATED DIARRHEA
Clostridium difficile is a Gram-positive, anaerobic, spore-forming bacterium that is the leading cause of nosocomial diarrhea. Clostridium difficile-associated diarrhea (CDAD or CDI for Clostridium difficile infection) can be a severe and life-threatening disease and results from the overgrowth in the colon of toxigenic strains of Clostridium difficile, generally during or after therapy with broad-spectrum antibiotics. CDAD is a major healthcare problem and a leading cause of morbidity in elderly hospitalized patients. The frequency and severity of CDAD in the western world has increased in recent years, and new hypervirulent and epidemic strains of Clostridium difficile have been discovered that are characterized by overproduction of toxins and other virulence factors, and by acquired resistance to fluoroquinolones such as moxifloxacin.
Current antibiotic therapy for CDAD includes vancomycin and metronidazole. While clinical cure rates are generally 85-90%, recurrences rates of 15-30 % with either drug are problematic as Clostridium difficile produces spores that are resistant to antibiotic treatment and routine disinfection. Spores surviving in the gut of patients and/or in the hospital environment may play a major role in re-infection and recurrence of CDAD after antibiotic treatment. Vancomycin and metronidazole are reported to promote spore formation in vitro at sub-inhibitory concentrations.
Actelion Ltd.
Actelion Ltd. is a leading biopharmaceutical company focused on the discovery, development and commercialization of innovative drugs for diseases with significant unmet medical needs.
Actelion is a leader in the field of pulmonary arterial hypertension (PAH). Our portfolio of PAH treatments covers the spectrum of disease, from WHO Functional Class (FC) II through to FC IV, with oral, inhaled and intravenous medications. Although not available in all countries, Actelion has treatments approved by health authorities for a number of specialist diseases including Type 1 Gaucher disease, Niemann-Pick type C disease, Digital Ulcers in patients suffering from systemic sclerosis, and mycosis fungoides in patients with cutaneous T-cell lymphoma.
Founded in late 1997, with now over 2,400 dedicated professionals covering all key markets around the world including the US, Japan, China, Russia and Mexico, Actelion has its corporate headquarters in Allschwil / Basel, Switzerland
…………………..
Preparation of the compound of formula II
The compound of formula II can be obtained by hydrogenation of the compound of formula VIII
VIII
over a noble metal catalyst such as palladium or platinum on charcoal in a solvent such as THF, MeOH or EA between 00C and 400C or by hydrolysis of in presence of a solution of HBr in water or AcOH between 00C and 800C in a solvent such as AcOH.
The compounds of formula III can be prepared as summarized in Scheme 1 hereafter.
IX VI IIIA: R1= H IIIS: ^ = SO2R5
Scheme 1
The compounds of formula V can be prepared as summarized in Scheme 2 hereafter.
II X XI
Scheme 2
The compounds of formula X can be prepared from the methylidene derivatives of formula XII as summarized in Scheme 3 hereafter.
Xc XII Xa: R1 = H
Scheme 3
Example 1:
l-cyclopropyl-6-fluoro-7-{4-[2-fluoro-4-((/f)-5-hydroxymethyl-2-oxo- oxazolidin-3-yl)-phenoxymethyl]-4-hydroxy-piperidin-l-yl}-4-oxo-l,4-dihydro- quinoline-3-carboxylic acid:
1 i. (R)-3-(3-fluoro-4-hydroxy-phenyl)-5-hydroxymethyl-oxazolidin-2-one:
A solution of (7?y)-3-(4-benzyloxy-3-fluoro-phenyl)-5-hydroxymethyl-oxazolidin-2-one (6.34 g, prepared according to WO 2004/096221) in THF/MeOH (1 :1; 200 ml) was hydrogenated over Pd/C 10% (1 g) overnight. The catalyst was filtered off, the filtrate evaporated under reduced pressure and the residue stirred in EA. The crystals were collected by filtration, affording 3.16 g (70% yield) of a colourless solid. 1H NMR (DMSOd6; δ ppm): 3.5 (m, IH), 3.64 (m, IH), 3.74 (dd, J = 8.8, 6.4, IH), 3.99 (t, J = 8.8, IH), 4.64 (m, IH), 5.16 (t, J = 5.6, IH), 6.93 (dd, J = 9.7, 8.8, IH), 7.08 (ddd, J = 8.8, 2.6, 1.2, IH), 7.45 (dd, J = 13.5, 2.6, IH), 9.66 (s, IH). MS (ESI): 228.1.
1. ii. 4-[2-fluoro-4- ((R)-5-hydroxymethyl-2-oxo-oxazolidin-3-yl)-phenoxymethyl]- 4-hydroxy-piperidine-l-carboxylic acid benzyl ester:
A solution of intermediate l.i (1.27 g) and l-oxa-6-aza-spiro[2.5]octane-6-carboxylic acid benzyl ester (1.60 g; prepared according to US 4244961) were dissolved in DMF (15 ml) and treated with Na2CO3 (1.16 g). The mixture was heated at 1000C overnight. The residue obtained after workup (DCM) was stirred in EA, and the solid was collected by filtration and sequentially washed with EA and Hex, affording 2.52 g (94.5% yield) of a beige solid.
1H NMR (DMSOd6; δ ppm): 1.57 (m, 4H), 3.14 (m, 2H), 3.54 (m, IH), 3.64 (m, IH), 3.79 (m, 5 H), 4.03 (t, J = 9.1, 1 H), 4.66 (m, 1 H), 4.78 (s, 1 H), 5.05 (s, 2 H), 5.16 (t,
J = 5.6, 1 H), 7.18 (m, 2 H), 7.32 (m, 5 H), 7.55 (d, J = 12, 1 H).
MS (ESI): 475.0.
1. iii. (R)-3-[3-fluoro-4-(4-hydroxy-piperidin-4-ylmethoxy)-phenyl]-5-hydroxymethyl- oxazolidin-2-one:
A suspension of intermediate l.ii (2.5 g) in EA/MeOH (1 :1; 100 ml) was hydrogenated over Pd/C for 48 h. The suspension was heated at 400C and the catalyst was filtered off.
The filtrate was evaporated under reduced pressure affording 1.61 g (89% yield) of a yellow powder.
1H NMR (DMSOd6; δ ppm): 1.4-1.63 (m, 4H), 2.67 (m, 2H), 2.83 (m, 2H), 3.53 (dd, J = 4.0, 12.0, IH); 3.66 (dd, J = 3.3, 12.0, IH), 3.71 (s, 2H); 3.80 (m, IH), 4.05 (t, J = 9.0,
IH), 4.48 (s, IH), 4.68 (m, IH), 5.20 (s, IH), 7.20 (m, 2H), 7.57 (d, IH).
MS (ESI): 341.5.
l.iv. l-cyclopropyl-6-fluoro-7-{4-[2-fluoro-4-((R)-5-hydroxymethyl-2-oxo-oxazolidin-3-yl)-phenoxymethyl]-4-hydroxy-piperidin-l-yl}-4-oxo-l,4-dihydro-quinoline-3-carboxylic acid:
A solution of intermediate l.iii (200 mg), 7-chloro-l-cyclopropyl-6-fiuoro-l,4-dihydro- 4-0X0-3 -quinolinecarboxylic acid boron diacetate complex (241 mg; prepared according to WO 88/07998) and DIPEA (100 μl) in NMP (2 ml) was stirred at 85°C for 5 h. The reaction mixture was evaporated under reduced pressure and the residue was taken up in 5M HCl in MeOH (3 ml) and stirred. The resulting solid was collected by filtration and washed with MeOH to afford 230 mg (67% yield) of a yellow solid.
1H NMR (DMSOd6; δ ppm): 1.66-1.35 (m, 4H), 1.75 (d, J = 12.8, 2H), 1.95 (m, 2H), 3.33 (t broad, J = 11.0, 2H), 3.57 (m, 3H), 3.67 (dd, J = 12.3, 3.3, IH), 3.83 (m, 2H), 3.92 (s, 2H), 4.06 (t, J = 9.0, IH), 4.69 (m, IH), 7.24 (m, 2H), 7.60 (m, 2H), 7.90 (d, J = 13.3, IH), 8.66 (s, IH).
MS (ESI): 585.9.
References
- Boschert, Sherry (19 Sep 2012). “Promising C. difficile Antibiotic in Pipeline”. Internal Medicine News. International Medical News Group. Retrieved 22 May 2013.
- “Cadazolid”. .actelion.com. Retrieved 2013-05-22.
- “Anaerobe – In vitro activity of cadazolid against Clostridium difficile strains isolated from primary and recurrent infections in Stockholm, Sweden”. ScienceDirect.com. 2013-02-26. Retrieved 2013-05-22.
- WO 2008056335
- WO 2009136379
The FDA’s Drug Review Process: Ensuring Drugs Are Safe and Effective
How Drugs are Developed and Approved
The mission of FDA’s Center for Drug Evaluation and Research (CDER) is to ensure that drugs marketed in this country are safe and effective. CDER does not test drugs, although the Center’s Office of Testing and Research does conduct limited research in the areas of drug quality, safety, and effectiveness.
CDER is the largest of FDA’s five centers. It has responsibility for both prescription and nonprescription or over-the-counter (OTC) drugs. For more information on CDER activities, including performance of drug reviews, post-marketing risk assessment, and other highlights, please see the CDER Update: Improving Public Health Through Human Drugs The other four FDA centers have responsibility for medical and radiological devices, food, and cosmetics, biologics, and veterinary drugs.
Some companies submit a new drug application (NDA) to introduce a new drug product into the U.S. Market. It is the responsibility of the company seeking to market a drug to test it and submit evidence that it is safe and effective. A team of CDER physicians, statisticians, chemists, pharmacologists, and other scientists reviews the sponsor’s NDA containing the data and proposed labeling.

The section below entitled From Fish to Pharmacies: The Story of a Drug’s Development, illustrates how a drug sponsor can work with FDA’s regulations and guidance information to bring a new drug to market under the NDA process.

From Fish to Pharmacies: A Story of Drug Development
Osteoporosis, a crippling disease marked by a wasting away of bone mass, affects as many as 2 million American, 80 percent of them women, at an expense of $13.8 billion a year, according to the National Osteoporosis Foundation., The disease may be responsible for 5 million fractures of the hip, wrist and spine in people over 50, the foundation says, and may cause 50,000 deaths. Given the pervasiveness of osteoporosis and its cost to society, experts say it is crucial to have therapy alternatives if, for example, a patient can’t tolerate estrogen, the first-line treatment.
Enter the salmon, which, like humans, produces a hormone called calcitonin that helps regulate calcium and decreases bone loss. For osteoporosis patients, taking salmon calcitonin, which is 30 times more potent than that secreted by the human thyroid gland, inhibits the activity of specialized bone cells called osteoclasts that absorb bone tissue. This enables bone to retain more bone mass.
Though the calcitonin in drugs is based chemically on salmon calcitonin, it is now made synthetically in the lab in a form that copies the molecular structure of the fish gland extract. Synthetic calcitonin offers a simpler, more economical way to create large quantities of the product.
FDA approved the first drug based on salmon calcitonin in an injectable. Since then, two more drugs, one injectable and one administered through a nasal spray were approved. An oral version of salmon calcitonin is in clinical trials now. Salmon calcitonin is approved only for postmenopausal women who cannot tolerate estrogen, or for whom estrogen is not an option.
How did the developers of injectable salmon calcitonin journey “from fish to pharmacies?”
After obtaining promising data from laboratory studies, the salmon calcitonin drug developers took the next step and submitted an Investigational New Drug (IND) application to CDER. The IND Web page explains the need for this application, the kind of information the application should include, and the Federal regulations to follow.
Once the IND application is in effect, the drug sponsor of salmon calcitonin could begin their clinical trials. After a sponsor submits an IND application, it must wait 30 days before starting a clinical trial to allow FDA time to review the prospective study. If FDA finds a problem, it can order a “clinical hold” to delay an investigation, or interrupt a clinical trial if problems occur during the study.
Clinical trials are experiments that use human subjects to see whether a drug is effective, and what side effects it may cause. The Running Clinical Trials Webpage provides links to the regulations and guidelines that the clinical investigators of salmon calcitonin must have used to conduct a successful study, and to protect their human subjects.
The salmon calcitonin drug sponsor analyzed the clinical trials data and concluded that enough evidence existed on the drug’s safety and effectiveness to meet FDA’s requirements for marketing approval. The sponsor submitted a New Drug Application (NDA) with full information on manufacturing specifications, stability and bioavailablility data, method of analysis of each of the dosage forms the sponsor intends to market, packaging and labeling for both physician and consumer, and the results of any additional toxicological studies not already submitted in the Investigational New Drug application. The NDA Web page provides resources and guidance on preparing the NDA application, and what to expect during the review process.

New drugs, like other new products, are frequently under patent protection during development. The patent protects the salmon calcitonin sponsor’s investment in the drug’s development by giving them the sole right to sell the drug while the patent is in effect. When the patents or other periods of exclusivity on brand-name drugs expire, manufacturers can apply to the FDA to sell generic versions. TheAbbreviated New Drug Applications (ANDA) for Generic Drug Products Webpageprovides links to guidances, laws, regulations, policies and procedures, plus other resources to assist in preparing and submitting applications.
Bringing Nonprescription Drug Products to the Market Under an OTC Monograph
OTC drugs can be brought to the market following the NDA process as described above or under an OTC monograph. Each OTC drug monograph is a kind of “recipe book” covering acceptable ingredients, doses, formulations, labeling, and, in some cases, testing parameters. OTC drug monographs are continually updated to add additional ingredients and labeling as needed. Products conforming to a monograph may be marketed without FDA pre-approval. The NDA and monograph processes can be used to introduce new ingredients into the OTC marketplace. For example, OTC drug products previously available only by prescription are first approved through the NDA process and their “switch” to OTC status is approved via the NDA process. OTC ingredients marketed overseas can be introduced into the U.S. market via a monograph under a Time and Extent Application (TEA) as described in 21 CFR 330.14. For a more thorough discussion of how OTC drug products are regulated visit FDA laws, regulations and guidances that affect small business. Information is also provided on financial assistance and incentives that are available for drug development.

CDER Small Business and Industry Assistance (CDER SBIA)
Drug sponsors which qualify as small businesses can take advantage of special offices and programs designed to help meet their unique needs. The CDER Small Business and Industry Assistance (CDER SBIA) Webpage provides links to FDA laws, regulations and guidances that affect small business. Information is also provided on financial assistance and incentives that are available for drug development.
 |
The path a drug travels from a lab to your medicine cabinet is usually long, and every drug takes a unique route. Often, a drug is developed to treat a specific disease. An important use of a drug may also be discovered by accident.
For example, Retrovir (zidovudine, also known as AZT) was first studied as an anti-cancer drug in the 1960s with disappointing results. Twenty years later, researchers discovered the drug could treat AIDS, and Food and Drug Administration approved the drug, manufactured by GlaxoSmithKline, for that purpose in 1987.
Most drugs that undergo preclinical (animal) testing never even make it to human testing and review by the FDA. The drugs that do must undergo the agency’s rigorous evaluation process, which scrutinizes everything about the drug–from the design of clinical trials to the severity of side effects to the conditions under which the drug is manufactured.



Investigational New Drug Application (IND)–The pharmaceutical industry sometimes seeks advice from the FDA prior to submission of an IND.
Sponsors–companies, research institutions, and other organizations that take responsibility for developing a drug. They must show the FDA results of preclinical testing in laboratory animals and what they propose to do for human testing. At this stage, the FDA decides whether it is reasonably safe for the company to move forward with testing the drug in humans.

Clinical Trials–Drug studies in humans can begin only after an IND is reviewed by the FDA and a local institutional review board (IRB). The board is a panel of scientists and non-scientists in hospitals and research institutions that oversees clinical research.
IRBs approve the clinical trial protocols, which describe the type of people who may participate in the clinical trial, the schedule of tests and procedures, the medications and dosages to be studied, the length of the study, the study’s objectives, and other details. IRBs make sure the study is acceptable, that participants have given consent and are fully informed of their risks, and that researchers take appropriate steps to protect patients from harm.

Phase 1 studies are usually conducted in healthy volunteers. The goal here is to determine what the drug’s most frequent side effects are and, often, how the drug is metabolized and excreted. The number of subjects typically ranges from 20 to 80.

Phase 2 studies begin if Phase 1 studies don’t reveal unacceptable toxicity. While the emphasis in Phase 1 is on safety, the emphasis in Phase 2 is on effectiveness. This phase aims to obtain preliminary data on whether the drug works in people who have a certain disease or condition. For controlled trials, patients receiving the drug are compared with similar patients receiving a different treatment–usually an inactive substance (placebo), or a different drug. Safety continues to be evaluated, and short-term side effects are studied. Typically, the number of subjects in Phase 2 studies ranges from a few dozen to about 300.

At the end of Phase 2, the FDA and sponsors try to come to an agreement on how large-scale studies in Phase 3 should be done. How often the FDA meets with a sponsor varies, but this is one of two most common meeting points prior to submission of a new drug application. The other most common time is pre-NDA–right before a new drug application is submitted.
Phase 3 studies begin if evidence of effectiveness is shown in Phase 2. These studies gather more information about safety and effectiveness, studying different populations and different dosages and using the drug in combination with other drugs. The number of subjects usually ranges from several hundred to about 3,000 people.

Postmarket requirement and commitment studies are required of or agreed to by a sponsor, and are conducted after the FDA has approved a product for marketing. The FDA uses postmarket requirement and commitment studies to gather additional information about a product’s safety, efficacy, or optimal use.

New Drug Application (NDA)–This is the formal step a drug sponsor takes to ask that the FDA consider approving a new drug for marketing in the United States. An NDA includes all animal and human data and analyses of the data, as well as information about how the drug behaves in the body and how it is manufactured

When an NDA comes in, the FDA has 60 days to decide whether to file it so that it can be reviewed. The FDA can refuse to file an application that is incomplete. For example, some required studies may be missing. In accordance with the Prescription Drug User Fee Act (PDUFA), the FDA’s Center for Drug Evaluation and Research (CDER) expects to review and act on at least 90 percent of NDAs for standard drugs no later than 10 months after the applications are received. The review goal is six months for priority drugs. (See “The Role of User Fees.”)
“It’s the clinical trials that take so long–usually several years,” says Sandra Kweder, M.D., deputy director of the Office of New Drugs in the CDER. “The emphasis on speed for FDA mostly relates to review time and timelines of being able to meet with sponsors during a drug’s development,” she says.
Drug Approval Process Infographic
Drug Review Steps Simplified
- Preclinical (animal) testing.
- An investigational new drug application (IND) outlines what the sponsor of a new drug proposes for human testing in clinical trials.
- Phase 1 studies (typically involve 20 to 80 people).
- Phase 2 studies (typically involve a few dozen to about 300 people).
- Phase 3 studies (typically involve several hundred to about 3,000 people).
- The pre-NDA period, just before a new drug application (NDA) is submitted. A common time for the FDA and drug sponsors to meet.
- Submission of an NDA is the formal step asking the FDA to consider a drug for marketing approval.
- After an NDA is received, the FDA has 60 days to decide whether to file it so it can be reviewed.
- If the FDA files the NDA, an FDA review team is assigned to evaluate the sponsor’s research on the drug’s safety and effectiveness.
- The FDA reviews information that goes on a drug’s professional labeling (information on how to use the drug).
- The FDA inspects the facilities where the drug will be manufactured as part of the approval process.
- FDA reviewers will approve the application or issue a complete response letter.
Supplemental Information About the Drug Approval Process
Reviewing Applications
Though FDA reviewers are involved with a drug’s development throughout the IND stage, the official review time is the length of time it takes to review a new drug application and issue an action letter, an official statement informing a drug sponsor of the agency’s decision.
Once a new drug application is filed, an FDA review team–medical doctors, chemists, statisticians, microbiologists, pharmacologists, and other experts–evaluates whether the studies the sponsor submitted show that the drug is safe and effective for its proposed use. No drug is absolutely safe; all drugs have side effects. “Safe” in this sense means that the benefits of the drug appear to outweigh the known risks.
The review team analyzes study results and looks for possible issues with the application, such as weaknesses of the study design or analyses. Reviewers determine whether they agree with the sponsor’s results and conclusions, or whether they need any additional information to make a decision.
Each reviewer prepares a written evaluation containing conclusions and recommendations about the application. These evaluations are then considered by team leaders, division directors, and office directors, depending on the type of application.
Reviewers receive training that fosters consistency in drug reviews, and good review practices remain a high priority for the agency.
Sometimes, the FDA calls on advisory committees, who provide FDA with independent opinions and recommendations from outside experts on applications to market new drugs, and on FDA policies. Whether an advisory committee is needed depends on many things.
“Some considerations would be if it’s a drug that has significant questions, if it’s the first in its class, or the first for a given indication,” says Mark Goldberger, M.D., a former director of one of CDER’s drug review offices. “Generally, FDA takes the advice of advisory committees, but not always,” he says. “Their role is just that–to advise.”Accelerated Approval
Traditional approval requires that clinical benefit be shown before approval can be granted. Accelerated approval is given to some new drugs for serious and life-threatening illnesses that lack satisfactory treatments. This allows an NDA to be approved before measures of effectiveness that would usually be required for approval are available.
Instead, less traditional measures called surrogate endpoints are used to evaluate effectiveness. These are laboratory findings or signs that may not be a direct measurement of how a patient feels, functions, or survives, but are considered likely to predict benefit. For example, a surrogate endpoint could be the lowering of HIV blood levels for short periods of time with anti-retroviral drugs.
Gleevec (imatinib mesylate), an oral treatment for patients with a life-threatening form of cancer called chronic myeloid leukemia (CML), received accelerated approval. The drug was also approved under the FDA’s orphan drug program, which gives financial incentives to sponsors for manufacturing drugs that treat rare diseases. Gleevec blocks enzymes that play a role in cancer growth. The approval was based on results of three large Phase 2 studies, which showed the drug could substantially reduce the level of cancerous cells in the bone marrow and blood.
Most drugs to treat HIV have been approved under accelerated approval provisions, with the company required to continue its studies after the drug is on the market to confirm that its effects on virus levels are maintained and that it ultimately benefits the patient. Under accelerated approval rules, if studies don’t confirm the initial results, the FDA can withdraw the approval.
Because premarket review can’t catch all potential problems with a drug, the FDA continues to track approved drugs for adverse events through a postmarketing surveillance program.
Bumps in the Road
If the FDA decides that the benefits of a drug outweigh the known risks, the drug will receive approval and can be marketed in the United States. But if there are problems with an NDA or if more information is necessary to make that determination, the FDA may issue a complete response letter.
Common problems include unexpected safety issues that crop up or failure to demonstrate a drug’s effectiveness. A sponsor may need to conduct additional studies–perhaps studies of more people, different types of people, or for a longer period of time.
Manufacturing issues are also among the reasons that approval may be delayed or denied. Drugs must be manufactured in accordance with standards called good manufacturing practices, and the FDA inspects manufacturing facilities before a drug can be approved. If a facility isn’t ready for inspection, approval can be delayed. Any manufacturing deficiencies found need to be corrected before approval.
“Sometimes a company may make a certain amount of a drug for clinical trials. Then when they go to scale up, they may lose a supplier or end up with quality control issues that result in a product of different chemistry,” says Kweder. “Sponsors have to show us that the product that’s going to be marketed is the same product that they tested.”
John Jenkins, M.D., director of CDER’s Office of New Drugs, says, “It’s often a combination of problems that prevent approval.” Close communication with the FDA early on in a drug’s development reduces the chance that an application will have to go through more than one cycle of review, he says. “But it’s no guarantee.”
The FDA outlines the justification for its decision in a complete response letter to the drug sponsor and CDER gives the sponsor a chance to meet with agency officials to discuss the deficiencies. At that point, the sponsor can ask for a hearing, correct any deficiencies and submit new information, or withdraw the application.
The Role of User Fees
Since PDUFA was passed in 1992, more than 1,000 drugs and biologics have come to the market, including new medicines to treat cancer, AIDS, cardiovascular disease, and life-threatening infections. PDUFA has allowed the Food and Drug Administration to bring access to new drugs as fast or faster than anywhere in the world, while maintaining the same thorough review process.
Under PDUFA, drug companies agree to pay fees that boost FDA resources, and the FDA agrees to time goals for its review of new drug applications. Along with supporting increased staff, drug user fees help the FDA upgrade resources in information technology. The agency has moved toward an electronic submission and review environment, now accepting more electronic applications and archiving review documents electronically.
The goals set by PDUFA apply to the review of original new human drug and biological applications, resubmissions of original applications, and supplements to approved applications. The second phase of PDUFA, known as PDUFA II, was reauthorized in 1997 and extended the user fee program through September 2002. PDUFA III, which extended to Sept. 30, 2007, was reauthorized in June 2002.
PDUFA III allowed the FDA to spend some user fees to increase surveillance of the safety of medicines during their first two years on the market, or three years for potentially dangerous medications. It is during this initial period, when new medicines enter into wide use, that the agency is best able to identify and counter adverse side effects that did not appear during the clinical trials.
On September 27, 2007, President Bush signed into law the Food and Drug Administration Amendments Act of 2007 which includes the reauthorization and expansion of the Prescription Drug User Fee Act. The reauthorization of PDUFA will significantly broaden and upgrade the agency’s drug safety program, and facilitate more efficient development of safe and effective new medications for the American public.
In addition to setting time frames for review of applications, PDUFA sets goals to improve communication and sets goals for specific kinds of meetings between the FDA and drug sponsors. It also outlines how fast the FDA must respond to requests from sponsors. Throughout a drug’s development, the FDA advises sponsors on how to study certain classes of drugs, how to submit data, what kind of data are needed, and how clinical trials should be designed.
The Quality of Clinical Data
The Food and Drug Administration relies on data that sponsors submit to decide whether a drug should be approved. To protect the rights and welfare of people in clinical trials, and to verify the quality and integrity of data submitted, the FDA’s Division of Scientific Investigations (DSI) conducts inspections of clinical investigators’ study sites. DSI also reviews the records of institutional review boards to be sure they are fulfilling their role in patient protection.
“FDA investigators compare information that clinical investigators provided to sponsors on case report forms with information in source documents such as medical records and lab results,” says Carolyn Hommel, a consumer safety officer in DSI.
DSI seeks to determine such things as whether the study was conducted according to the investigational plan, whether all adverse events were recorded, and whether the subjects met the inclusion/exclusion criteria outlined in the study protocol.
At the conclusion of each inspection, FDA investigators prepare a report summarizing any deficiencies. In cases where they observe numerous or serious deviations, such as falsification of data, DSI classifies the inspection as “official action indicated” and sends a warning letter or Notice of Initiation of Disqualification Proceedings and Opportunity to Explain (NIDPOE) to the clinical investigator, specifying the deviations that were found.
The NIDPOE begins an administrative process to determine whether the clinical investigator should remain eligible to receive investigational products and conduct clinical studies.
CDER conducts about 300-400 clinical investigator inspections annually. About 3 percent are classified in this “official action indicated” category.
The FDA has established an independent Drug Safety Oversight Board (DSOB) to oversee the management of drug safety issues. The Board meets monthly and has representatives from three FDA Centers and five other federal government agencies. The board’s responsibilities include conducting timely and comprehensive evaluations of emerging drug safety issues, and ensuring that experts–both inside and outside of the FDA–give their perspectives to the agency. The first meeting of the DSOB was held in June 2005.
Once the review is complete, the NDA might be approved or rejected. If the drug is not approved, the applicant is given the reasons why and what information could be provided to make the application acceptable. Sometimes the FDA makes a tentative approval recommendation, requesting that a minor deficiency or labeling issue be corrected before final approval. Once a drug is approved, it can be marketed.
Some approvals contain conditions that must be met after initial marketing, such as conducting additional clinical studies. For example, the FDA might request a postmarketing, or phase 4, study to examine the risks and benefits of the new drug in a different population or to conduct special monitoring in a high-risk population. Alternatively, a phase 4 study might be initiated by the sponsor to assess such issues as the longer term effects of drug exposure, to optimize the dose for marketing, to evaluate the effects in pediatric patients, or to examine the effectiveness of the drug for additional indications. Postmarketing surveillance is important, because even the most well-designed phase 3 studies might not uncover every problem that could become apparent once a product is widely used. Furthermore, the new product might be more widely used by groups that might not have been well studied in the clinical trials, such as elderly patients. A crucial element in this process is that physicians report any untoward complications. The FDA has set up a medical reporting program called Medwatch to track serious adverse events (1-800-FDA-1088). The manufacturer must report adverse drug reactions at quarterly intervals for the first 3 years after approval, including a special report for any serious and unexpected adverse reactions.
Recent Developments in Drug Approval
The Food and Drug Administration Modernization Act of 1997 (FDAMA) extended the use of user fees and focused on streamlining the drug approval process. In 1999, the 35 drugs approved by the FDA were reviewed in an average of 12.6 months, slightly more than the 12-month goal set by PDUFA. This act also increased patient access to experimental drugs and facilitated an accelerated review of important new medications. The law ended the ban on disseminating information to providers about non-FDA-approved uses of medications. A manufacturer can now provide peer-reviewed journal articles about an off-label indication of a product if the company commits to filing a supplemental application to establish the use of the unapproved indication. As part of this process, the company must still conduct its own phase 4 study. As a condition for an accelerated approval, the FDA can require the sponsor to carry out postmarketing studies to confirm a clinical benefit and product safety. Critics contend the 1997 act compromises public safety by lowering the standard of approval. Within a year after the law was passed, several drugs were removed from the market. Among these medications were mibefradil for hypertension, dexfenfluramine for morbid obesity, the antihistamine terfenadine, and bromfenac sodium for pain. More recently, additional drugs including troglitazone were removed from the market. Although the increase in recalls might reflect the dramatic increase in drugs approved and launched, others argue that several safety questions were ignored. Another concern was that many withdrawn drugs were me-too drugs which did not represent a noteworthy advance in therapy. Persons critical of the FDA believe changes in the approval process, such as allowing some new drugs to be approved based on only a single clinical trial, expanded use of accelerated approvals, and the use of surrogate end points, have created a dangerous situation. Proponents of the changes in the approval process argue that there is no evidence of increased risk from the legislative changes, and that these changes improve access to cancer patients and those with debilitating disease who were previously denied critical and lifesaving medications.
New drugs are an important part of modern medicine. Just a few decades ago, a disease such as peptic ulcers was a frequent indication for major surgery. The advent of new pharmacologic treatments has dramatically reduced the serious complications of peptic ulcer disease. Likewise, thanks to many new antiviral medications, the outlook for HIV-infected patients has improved dramatically. It is important that physicians understand the process of approving these new medications. Understanding the process can promote innovation, help physicians assess new products, underline the importance of reporting adverse drug events, and provide physicians with the information to educate patients about participating in a clinical trial.
Drug discovery

In the fields of medicine, biotechnology and pharmacology, drug discovery is the process by which new candidate medications are discovered.
Historically, drugs were discovered through identifying the active ingredient from traditional remedies or by serendipitous discovery. Later chemical libraries of synthetic small molecules, natural products or extracts were screened in intact cells or whole organisms to identify substances that have a desirable therapeutic effect in a process known as classical pharmacology. Sincesequencing of the human genome which allowed rapid cloning and synthesis of large quantities of purified proteins, it has become common practice to use high throughput screening of large compounds libraries against isolated biological targets which are hypothesized to be disease modifying in a process known as reverse pharmacology.
Hits from these screens are then tested in cells and then in animals for efficacy. Even more recently, scientists have been able to understand the shape of biological molecules at the atomic level, and to use that knowledge to design (seedrug design) drug candidates.

Modern drug discovery involves the identification of screening hits, medicinal chemistry and optimization of those hits to increase the affinity, selectivity (to reduce the potential of side effects), efficacy/potency, metabolic stability (to increase the half-life), and oral bioavailability. Once a compound that fulfills all of these requirements has been identified, it will begin the process of drug development prior to clinical trials. One or more of these steps may, but not necessarily, involve computer-aided drug design.
Despite advances in technology and understanding of biological systems, drug discovery is still a lengthy, “expensive, difficult, and inefficient process” with low rate of new therapeutic discovery.[1]In 2010, the research and development cost of each new molecular entity (NME) was approximately US$1.8 billion.[2] Drug discovery is done by pharmaceutical companies, with research assistance from universities. The “final product” of drug discovery is a patent on the potential drug. The drug requires very expensive Phase I, II and III clinical trials, and most of them fail. Small companies have a critical role, often then selling the rights to larger companies that have the resources to run the clinical trials.

Drug targets
The definition of “target” itself is something argued within the pharmaceutical industry. Generally, the “target” is the naturally existing cellular or molecular structure involved in the pathology of interest that the drug-in-development is meant to act on. However, the distinction between a “new” and “established” target can be made without a full understanding of just what a “target” is. This distinction is typically made by pharmaceutical companies engaged in discovery and development of therapeutics. In an estimate from 2011, 435 human genome products were identified as therapeutic drug targets of FDA-approved drugs.[3]

“Established targets” are those for which there is a good scientific understanding, supported by a lengthy publication history, of both how the target functions in normal physiology and how it is involved in human pathology. This does not imply that the mechanism of action of drugs that are thought to act through a particular established targets is fully understood. Rather, “established” relates directly to the amount of background information available on a target, in particular functional information. The more such information is available, the less investment is (generally) required to develop a therapeutic directed against the target.

The process of gathering such functional information is called “target validation” in pharmaceutical industry parlance. Established targets also include those that the pharmaceutical industry has had experience mounting drug discovery campaigns against in the past; such a history provides information on the chemical feasibility of developing a small molecular therapeutic against the target and can provide licensing opportunities and freedom-to-operate indicators with respect to small-molecule therapeutic candidates.

In general, “new targets” are all those targets that are not “established targets” but which have been or are the subject of drug discovery campaigns. These typically include newly discoveredproteins, or proteins whose function has now become clear as a result of basic scientific research.
The majority of targets currently selected for drug discovery efforts are proteins. Two classes predominate: G-protein-coupled receptors (or GPCRs) and protein kinases.

Screening and design
The process of finding a new drug against a chosen target for a particular disease usually involves high-throughput screening (HTS), wherein large libraries of chemicals are tested for their ability to modify the target. For example, if the target is a novel GPCR, compounds will be screened for their ability to inhibit or stimulate that receptor (see antagonist and agonist): if the target is a protein kinase, the chemicals will be tested for their ability to inhibit that kinase.
Another important function of HTS is to show how selective the compounds are for the chosen target. The ideal is to find a molecule which will interfere with only the chosen target, but not other, related targets. To this end, other screening runs will be made to see whether the “hits” against the chosen target will interfere with other related targets – this is the process of cross-screening. Cross-screening is important, because the more unrelated targets a compound hits, the more likely that off-target toxicity will occur with that compound once it reaches the clinic.
It is very unlikely that a perfect drug candidate will emerge from these early screening runs. It is more often observed that several compounds are found to have some degree of activity, and if these compounds share common chemical features, one or more pharmacophores can then be developed. At this point, medicinal chemists will attempt to use structure-activity relationships (SAR) to improve certain features of the lead compound:
- increase activity against the chosen target
- reduce activity against unrelated targets
- improve the druglikeness or ADME properties of the molecule.
This process will require several iterative screening runs, during which, it is hoped, the properties of the new molecular entities will improve, and allow the favoured compounds to go forward to in vitro and in vivo testing for activity in the disease model of choice.
Amongst the physico-chemical properties associated with drug absorption include ionization (pKa), and solubility; permeability can be determined by PAMPA and Caco-2. PAMPA is attractive as an early screen due to the low consumption of drug and the low cost compared to tests such as Caco-2, gastrointestinal tract (GIT) and Blood–brain barrier (BBB) with which there is a high correlation.
A range of parameters can be used to assess the quality of a compound, or a series of compounds, as proposed in the Lipinski’s Rule of Five. Such parameters include calculated properties such as cLogP to estimate lipophilicity, molecular weight, polar surface area and measured properties, such as potency, in-vitro measurement of enzymatic clearance etc. Some descriptors such asligand efficiency[4] (LE) and lipophilic efficiency[5][6] (LiPE) combine such parameters to assess druglikeness.
While HTS is a commonly used method for novel drug discovery, it is not the only method. It is often possible to start from a molecule which already has some of the desired properties. Such a molecule might be extracted from a natural product or even be a drug on the market which could be improved upon (so-called “me too” drugs). Other methods, such as virtual high throughput screening, where screening is done using computer-generated models and attempting to “dock” virtual libraries to a target, are also often used.
Another important method for drug discovery is drug design, whereby the biological and physical properties of the target are studied, and a prediction is made of the sorts of chemicals that might (e.g.) fit into an active site. One example is fragment-based lead discovery (FBLD). Novel pharmacophores can emerge very rapidly from these exercises. In general, computer-aided drug design is often but not always used to try to improve the potency and properties of new drug leads.
Once a lead compound series has been established with sufficient target potency and selectivity and favourable drug-like properties, one or two compounds will then be proposed for drug development. The best of these is generally called the lead compound, while the other will be designated as the “backup”.

Historical background
The idea that effect of drug in human body are mediated by specific interactions of the drug molecule with biological macromolecules, (proteins or nucleic acids in most cases) led scientists to the conclusion that individual chemicals are required for the biological activity of the drug. This made for the beginning of the modern era in pharmacology, as pure chemicals, instead of crude extracts, became the standard drugs. Examples of drug compounds isolated from crude preparations are morphine, the active agent in opium, and digoxin, a heart stimulant originating from Digitalis lanata. Organic chemistry also led to the synthesis of many of the cochemicals isolated from biological sources.

Nature as source of drugs
Despite the rise of combinatorial chemistry as an integral part of lead discovery process, natural products still play a major role as starting material for drug discovery.[7] A report was published in 2007,[8] covering years 1981-2006 details the contribution of biologically occurring chemicals in drug development. According to this report, of the 974 small molecule new chemical entities, 63% were natural derived or semisynthetic derivatives of natural products. For certain therapy areas, such as antimicrobials, antineoplastics, antihypertensive and anti-inflammatory drugs, the numbers were higher. In many cases, these products have been used traditionally for many years.
Natural products may be useful as a source of novel chemical structures for modern techniques of development of antibacterial therapies.[9]
Despite the implied potential, only a fraction of Earth’s living species has been tested for bioactivity.
Plant-derived
Prior to Paracelsus, the vast majority of traditionally used crude drugs in Western medicine were plant-derived extracts. This has resulted in a pool of information about the potential of plant species as an important source of starting material for drug discovery. A different set of metabolites is sometimes produced in the different anatomical parts of the plant (e.g. root, leaves and flower), and botanical knowledge is crucial also for the correct identification of bioactive plant materials.

Microbial metabolites
Microbes compete for living space and nutrients. To survive in these conditions, many microbes have developed abilities to prevent competing species from proliferating. Microbes are the main source of antimicrobial drugs. Streptomyces species have been a valuable source of antibiotics. The classical example of an antibiotic discovered as a defense mechanism against another microbe is the discovery of penicillin in bacterial cultures contaminated by Penicillium fungi in 1928.
Marine invertebrates
Marine environments are potential sources for new bioactive agents.[10] Arabinose nucleosides discovered from marine invertebrates in 1950s, demonstrating for the first time that sugar moieties other than ribose and deoxyribose can yield bioactive nucleoside structures. However, it was 2004 when the first marine-derived drug was approved. The cone snail toxin ziconotide, also known as Prialt, was approved by the Food and Drug Administration to treat severe neuropathic pain. Several other marine-derived agents are now in clinical trials for indications such as cancer, anti-inflammatory use and pain. One class of these agents are bryostatin-like compounds,under investigation as anti-cancer therapy.
Chemical diversity of natural products
As above mentioned, combinatorial chemistry was a key technology enabling the efficient generation of large screening libraries for the needs of high-throughput screening. However, now, after two decades of combinatorial chemistry, it has been pointed out that despite the increased efficiency in chemical synthesis, no increase in lead or drug candidates has been reached.[8] This has led to analysis of chemical characteristics of combinatorial chemistry products, compared to existing drugs or natural products. The chemoinformatics concept chemical diversity, depicted as distribution of compounds in the chemical space based on their physicochemical characteristics, is often used to describe the difference between the combinatorial chemistry libraries and natural products. The synthetic, combinatorial library compounds seem to cover only a limited and quite uniform chemical space, whereas existing drugs and particularly natural products, exhibit much greater chemical diversity, distributing more evenly to the chemical space.[7] The most prominent differences between natural products and compounds in combinatorial chemistry libraries is the number of chiral centers (much higher in natural compounds), structure rigidity (higher in natural compounds) and number of aromatic moieties (higher in combinatorial chemistry libraries). Other chemical differences between these two groups include the nature of heteroatoms (O and N enriched in natural products, and S and halogen atoms more often present in synthetic compounds), as well as level of non-aromatic unsaturation (higher in natural products). As both structure rigidity and chirality are both well-established factors in medicinal chemistry known to enhance compounds specificity and efficacy as a drug, it has been suggested that natural products compare favourable to today’s combinatorial chemistry libraries as potential lead molecules.
Natural product drug discovery
Screening
Two main approaches exist for the finding of new bioactive chemical entities from natural sources.
The first is sometimes referred to as random collection and screening of material, but in fact the collection is often far from random in that biological (often botanical) knowledge is used about which families show promise, based on a number of factors, including past screening. This approach is based on the fact that only a small part of earth’s biodiversity has ever been tested for pharmaceutical activity. It is also based on the fact that organisms living in a species-rich environment need to evolve defensive and competitive mechanisms to survive, mechanisms which might usefully be exploited in the development of drugs that can cure diseases affecting humans. A collection of plant, animal and microbial samples from rich ecosystems can potentially give rise to novel biological activities worth exploiting in the drug development process. One example of a successful use of this strategy is the screening for antitumour agents by the National Cancer Institute, started in the 1960s. Paclitaxel was identified from Pacific yew tree Taxus brevifolia. Paclitaxel showed anti-tumour activity by a previously undescribed mechanism (stabilization of microtubules) and is now approved for clinical use for the treatment of lung, breast and ovarian cancer, as well as for Kaposi’s sarcoma. Early in the 21st century, Cabazitaxel (made by Sanofi, a French firm), another relative of taxol has been shown effective against prostate cancer, also because it works by preventing the formation of microtubules, which pull the chromosomes apart in dividing cells (such as cancer cells). Still another examples are: 1. Camptotheca (Camptothecin · Topotecan · Irinotecan · Rubitecan · Belotecan); 2. Podophyllum (Etoposide · Teniposide); 3a. Anthracyclines (Aclarubicin · Daunorubicin · Doxorubicin · Epirubicin · Idarubicin · Amrubicin · Pirarubicin · Valrubicin · Zorubicin); 3b. Anthracenediones (Mitoxantrone · Pixantrone).
Nor do all drugs developed in this manner come from plants. Professor Louise Rollins-Smith of Vanderbilt University‘s Medical Center, for example, has developed from the skin of frogs a compound which blocks AIDS. Professor Rollins-Smith is aware of declining amphibian populations and has said: “We need to protect these species long enough for us to understand their medicinal cabinet.”
The second main approach involves Ethnobotany, the study of the general use of plants in society, and ethnopharmacology, an area inside ethnobotany, which is focused specifically on medicinal uses.
Both of these two main approaches can be used in selecting starting materials for future drugs. Artemisinin, an antimalarial agent from sweet wormtree Artemisia annua, used in Chinese medicine since 200BC is one drug used as part of combination therapy for multiresistant Plasmodium falciparum.
Structural elucidation
The elucidation of the chemical structure is critical to avoid the re-discovery of a chemical agent that is already known for its structure and chemical activity. Mass spectrometry, often used to determine structure, is a method in which individual compounds are identified based on their mass/charge ratio, after ionization. Chemical compounds exist in nature as mixtures, so the combination of liquid chromatography and mass spectrometry (LC-MS) is often used to separate the individual chemicals. Databases of mass spectras for known compounds are available. Nuclear magnetic resonance spectroscopy is another important technique for determining chemical structures of natural products. NMR yields information about individual hydrogen and carbon atoms in the structure, allowing detailed reconstruction of the molecule’s architecture.
Business Insights’ drug discovery research stream critically analyzes the cutting edge technologies and novel approaches shaping the future of drug discovery.
Our analysis spans the entire drug discovery process, from target selection and validation to drug safety testing and clinical trial design, with assessment of both small-molecule and biologic modalities. Our independent experts highlight where the future opportunities lie and which companies are best positioned to take advantage.
The pharmaceutical industry is facing unprecedented pressure from a combination of factors: key product patent expiries, an increasingly demanding regulatory environment, declining R&D productivity, and escalating costs. The urgent need to combat these threats places a premium on scientific innovation, but innovation itself does not guarantee success. Achieving the required increase in drug discovery output will only be achieved by those making investments in the right diseases, biological targets, and therapeutic approaches, and the right technologies to expedite the process.

Typically research and drug discovery are not regulated at all. GLP starts with preclinical development, for example toxicology studies. Clinical trials are regulated by good clinical practice regulations and manufacturing through GMPs. There is a frequent misunderstanding that all laboratory operations are regulated by GLP. This is not true. For example, Quality Control laboratories in manufacturing are regulated by GMPs and not by GLPs. Also Good laboratory Practice regulations are frequently mixed up with good analytical practice. Applying good analytical practices is important but not sufficient, as we will see in this presentation. When small quantities of active ingredients are prepared in a research or development laboratory for use in samples for clinical trials or finished drugs, that activity has be covered by GMP and not by GLP.
Part 11 is FDA’s regulation on electronic records and signatures and applies for electronic records or to computer systems in all FDA regulated areas. For example, it applies for computers that are used in GLP studies.
Characteristic for GLPs is that they are study based where as GMPs are processed based.
Independent from Location and Duration of a Study
GLPs regulate all non-clinical safety studies that support or are intended to support applications for research or marketing permits for products regulated by the FDA, or by similar other national agencies. This includes drugs for human and animal use but also aroma and color additives in food, biological products and medical devices. The duration and location of the study is of no importance. For example GLP applies to short term experiments as well as to long term studies. And if a pharmaceutical company subcontracts part of a study to a university, that university still must comply with the same requirements as the sponsor company. Some laboratories tried to get away from GLP through outsourcing, but I can tell you this does not work.
Facility Management and Other Personnel
Qualification of Personnel
Like all regulations also GLPs have chapters on personnel.
The assumption is that in order to conduct GLP studies with the right quality a couple of things are important:* Number one there should be sufficient people and second, the personnel should be qualified.
The FDA is not specific at all what type of qualification or education people should have. Qualification can come from education, experience or additional trainings, but it should be documented. This also requires a good documentation of the job descriptions, the tasks and responsibilities.
Facility management
Responsibilities of facility management are well defined. They include to designate a study director and also to monitor the progress of the study and if it is not going well to replace the study director.
The management is responsible for many things, basically they should assure that a quality assurance unit is available, test and control articles are characterized, and that sufficient qualified personnel is available for the study.
Because it is obvious that management can not take care personally about all this they have to rely on other functions, for example GLPs require that the QA should give a regular report on the compliance status of the study.

Small Molecule Drugs versus Biomolecular Drugs (Biologics)
Biotechnology has created a broad range of therapies, including vaccines, cell or gene therapies, therapeutic protein hormones, cytokines and tissue growth factors, and monoclonal antibodies. In this discussion we will focus on the categories of biomolecular drugs that are presently managed by the FDA Center for Drugs Evaluation and Research (CDER): monoclonal antibodies, cytokines, tissue growth factors and therpeutic proteins. Some of the data that we will show includes all biologics. Modern biomolecular drugs arise through the processes of genetic engineering.
It has been a little over thirty years since human insulin received U.S. approval (1982) as the first genetically engineered biomolecular drug. Since then biomolecular drugs have become a major force in the bio/pharmaceutical industry. As seen in Table 1, based on worldwide sales, eight out of the top 20 biopharmaceuticals in 2012 were Biomolecular Drugs. (Ref 1, 2) In fact seven of the top 10 were biomolecular drugs!

Table 1, Eight of the Top Twenty Biopharmaceuticals Worldwide in 2012 are BiomolecularDrugs (Data from references US Ranking. Copaxone ranked 9th in US Sales (Ref 3), and was unranked in worldwide sales.
This may come as a surprise to many in the U.S. where biomolecular drugs have yet to achieve such a prominent stature. In 2012 Humira, Enbrel, Remicade, Neulasta and Rituxan were in the top 10 drugs based on U.S. sales, but the small molecules Nexium, Abilify, Crestor, Advair, and Cymbalta were the top five. None of the biomolecular drugs were in the top 10 in the U.S. in 2010. (How the rankings of drugs in the U.S. could be so different from the rest of the world is a whole other discussion.) In any event, the rise of biomolecular drugs into the top tier is a recent phenomenon.
Let us compare and contrast these two types of drugs – small molecule and biomolecular drugs, and see how the Industry deals with two seemingly very different types of drugs.
The bio/pharmaceutical industry embraces the discovery and development of both small molecule drugs (also referred to as New Chemical Entities or NCEs) and biomolecular drugs, also called biologics (also referred to as New Biological Entities or NBEs). Small Molecule and biomolecular drugs can take on different names over the lifetime of drug discovery and development and marketing, as shown in Fig 1 and described in Ref 5.
Figure 1, Small Molecules and Biomolecules can take on different names over the lifetime of drug discovery and development and marketing. Biosimilars are also referred to as Follow-on Biologics. Phase length is not implied by the size of stage marker. *NME relates to the first approvable drug as opposed to second indications or new formulations. The application for a generic small molecule is an “Abbreviated New Drug Application” (ANDA) which doesn’t require clinical trials to prove equivalency. Processes for biosimilars or follow-on biologics are in the discussion stage.
A biotechnology company or a biopharmaceutical company tends to focus on the discovery and development of biomolecular drugs. A bio/pharmaceutical company will have the resources to discover and develop both types of drugs, NCEs and NBEs.
Since the early ‘80s the number of INDs per year from NCEs has leveled off while the INDs from NBEs have increased and helped maintain an increasing number of INDs/year (up to 1993). Trusheim et al. and others have studied the number of new small molecule drug approvals (NMEs) compared to new biologic drug approvals (new BLAs) in the period between 1988-2008, Table 2.
Table 2, Numbers of New Small Molecule Drug Approvals per Year (NMEs) Compared to New Biologic Drug Approvals (new BLAs) 1988-2008. Biologics here are not restricted to monoclonal antibodies, cytokines, tissue growth factors and therapeutic proteins. Last line* shows therapeutic proteins and Mabs from Reichert 8 We extended the tally by Reichert beyond 2003 by adding our own count of Mab and therapeutic protein new BLAs from annual FDA reports through 2008. Mullard and Kneller recently published counts of NMEs and New BLAs which differ somewhat from Trusheim or Reichert . We are not in a position to rectify the differences, except to offer a potential explanation – certain small peptide and protein drugs may be considered either biologics or small molecules (Kneller considered such drugs to be biologics).
The analysis by Trusheim et al. was not restricted to monoclonal antibodies, cytokines, tissue growth factors and therapeutic proteins. They found that from 1988 to 2003 the industry averaged 34 NMEs and new BLAs per year, whereas from 2004-2008 the industry averaged only 21 NMEs and new BLAs per year. Within those two periods the percentage of new BLAs was quite similar (31% vs 32%). To add some perspective we include the mabs and therapeutic proteins counted by Reichert. By the numbers, all biologics are making a substantial contribution to the number of new drugs approved per year.
By 1997 worldwide sales of biologics were over $7 billion dollars. The global sales of biologics have continued to rise – monoclonal antibodies alone in 2006 totaled $4.7 billion dollars.
A popular misconception is that in the early days most of the new biologics were discovered and developed within biotech companies. Certainly few of the classically NCE-oriented companies entered the NBE arena – The pharmaceutical companies J&J (Ortho Biotech), Lilly and Roche were early players, getting BLAs approved in the ‘80s, Table 3.
Table 3, Early Biotech and Drug Company Biologics Approvals (without Diagnostics)
But 50% of the BLAs in the 80’s came from drug companies. In the ‘90s, 52% of the BLAs came from drug companies (data from Table 3). Thus while a lot of investment may have gone into biotech startups, it was the previous experience of the drug companies with bringing drugs to market that made them at least equal partners in that aspect of biomolecular R&D. Still only 17 drug companies and 16 biotech companies got BLAs in the ‘80s and ‘90s which is a small subset of the pharmaceutical industry. By 1998 the PhRMA determined that more than 140 US-based companies were engaged in biomolecular drug development. Most likely many more pharmaceutical companies were investing in biotech in that period. The investment in biologics was enormous and the payout uncertain. As with the discovery and development of any drug it took years before the new biotechs achieved their first BLA, over 14 years on average, Table 4.
Table 4 Early Biotech Approvals – Years Since Founding.
While many of the discoveries of new biologics continue to originate in biotech companies, the clinical development of new biologics are increasingly supported by large pharma which had been NCE-oriented, Table 3.
In recent years most of the large pharma have gained an expertise in biologics through entry into field, and also through acquisitions and are now bio/pharmaceutical companies, Table 5.. The acquisition of Genzyme by Sanofi-Aventis is a most recent example.
Table 5, Notable Acquisitions and Partnerships involving Biologics
A recent collaborative study by Deloitte and Thomson Reuters showed that the twelve top bio/pharmaceutical companies all had biologics in their late stage portfolios, ranging from 21-66% of their portfolios (avg. 39%)
Prior to the ‘80s there were sufficiently few biomolecular drugs that the very term “pharmaceutical” or “drug” was taken to mean small molecule. With the exception of insulin, the few biomolecules approved for human use were administered by a trained health practitioner and were often considered “therapies”. Thus one may see the comparison of “small molecule drugs (or pharmaceuticals) versus large molecule therapies”. Here we will consider a large molecule therapy that is regulated by CDER to be a biomolecular type of drug or pharmaceutical.
The term for first small molecule drug approval, or New Molecular Entity (NME) could in theory be applied to first biologic approval, but because NME has long been associated with small molecules it is not being associated with first biologic approval – which is simply called a new BLA.
On March 23, 2010 President Obama signed into law the Biologics Price Competition and Innovation Act (BPCIA) which provides for biosimilar biologic drug approvals, as part of the omnibus health care bill. As the FDA develops guidelines for biosimilar approvals and begins to review applications for biosimilars, biologics will begin to enter the large generics market in the U.S.
The Processes that Give Rise to Biomolecular Drugs. Human insulin was the first recombinant biopharmaceutical approved in the U.S. in 1982. Prior to that protein products approved for use in humans were extracted from natural sources. It is beyond the scope of this website to delve into the details of the processes that give rise to biomolecular drugs or small molecule drugs. The following are good general references that cover the processes involved in the discovery and development of both small molecule drugs and biomolecular drugs.
Understanding the Differences and Similarities Between Small Molecules and Biologics. Now, more than ever, anyone interested in understanding the bio/pharmaceutical industry will need to understand both the differences and similarities between small molecules and biologics and their discovery and development as drugs.
1. How Do Small Molecule Drugs Differ from Biomolecular Drugs?
One has only to consider the size of biologics to recognize that the technologies that give rise to biomolecular drugs must be considerably different from the classical small molecule drugs. Genentech equates the difference between aspirin (21 atoms) and an antibody (~25,000 atoms) to the difference in weight between a bicycle (~20 lbs) and a business jet (~30,000 lbs).19 We will consider how they differ with respect to distribution, metabolism, serum half-life, typical dosing regimen, toxicity, species reactivity, antigenicity, clearance mechanisms, and drug-drug interactions (especially small molecule/biologic drug interactions).
A project leader who has worked in one field and is now facing the prospect of leading a project in the other field should become familiar with these differences as they will give rise to issues that the project leader may not have faced before.
2. Historical Changes in FDA Biologics Oversite in Response to the Biotech Boom
Prior to the ‘80s biologics were extracted from natural sources and required different regulatory oversight than that of small molecule drugs. Since then, the production of biologics shifted to recombinant proteins, which involved more consistent production processes, and the number of approvals has risen dramatically. We will review how FDA oversight has changed to accommodate the boom in biotechnology.
3. Overall Clinical Success Rates of Biologics versus Small Molecules
Only a few biomolecular drugs were approved in the U.S. per year until 1997, when eight were approved in one year. From that time onward approvals have been over a half dozen per year. There are now sufficient numbers of biomolecular drugs to begin to allow cross-industry comparisons of metrics between small molecule and biomolecular drugs. We compare the various studies over the last twenty years that have been published on overall clinical success rates for both small molecules and biologics from Dimasi and Reichert at the Tufts Center for the Study of Drug Development, Grabowski at Duke University and others. Since these metrics have changed over time we provide era-by-era comparisons, wherever possible.
4. Stage Related Success Rates and Cycle Times for Small Molecules vs Biologics
We also examine the success rates and cycle times for the various stages of clinical development for both small molecules and biologics. Again, since these metrics have changed over time we provide era-by-era comparisons where ever possible.
5. Comparative Cost of R&D for Biologics Versus Small Molecules
The differences in success rates and cycle times noted above have a knock-on effect on the cost of R&D for biomolecules over small molecules.
6. Are Peptide Drugs Small Molecules or Biologics?
This hybrid class of drugs tends to be considered a class of biologics, especially because oral activity is rare amongst peptide drugs. But we show that peptides truly bridge the gap between small molecules and biologics, in terms of physical properties, range of therapy areas and means of production. (The processes employed in producing peptide drugs vary, from the chemical processes used for the smaller peptide drugs to recombinant technologies used for the larger peptide drugs.)
7. Biosimilar and Biobetter Macromolecules versus Generic Small Molecules
Those early biotechnology wonder drugs are now facing patent expiration. The industry has been engaged in an intense debate as to how a generic biomolecular drug, aka biosimilar or follow-on biologic) can be approved and managed by the same regulations that govern generic small molecule drugs. The issues are complex, arising out of the considerable differences between small molecules and biologics. More recently big biopharma have taken an interest biobetters. A biobetter is a biologic which has a purposefully modified structure from the original that allows it to be afforded patent protection and pricing strategy akin to the original biologic because it is in some way “better” than the original.
8. Discovery and Preclinical Stages – Where the Technologies Differ the Most– Small Molecules vs Biologics
It is in the stages of Discovery and Preclinical Development where the technologies are most different. We outline the differences and similarities between small molecules and biologics in Lead Discovery, Lead Optimization and Preclinical Development.
9. Small Molecule and Biologics Approvals by Therapy Areas
With technological advances in the discovery and development of biologics most therapy areas (80%) are now amenable to either a small molecule or biologic strategy.
10. Managing Small Molecule & Biomolecular Drug R&D in the Same Company
The bio/pharmaceutical company that has the resources to discover and develop both types of drugs will inevitably face the challenge of organizing these activities. We argue that the fact that both small molecules and biologics can be managed with the same milestones and stages argues for treating both strategies in the same portfolio. The savvy portfolio manager will understand the differences and ensure the differences are transparent from a portfolio perspective.
Applications in Drug Discovery and Development
Several phase in drug discovery and development can be supported by metabonomics. In a very early phase, metabonomics can help in selecting drug candidates by monitoring toxicity. On the one hand the protocols of candidate selection studies are very simple, rendering metabonoic analyses very challenging in terms of number of samples. On the other hand rather high doses can result in clear metabonomic effects, which can be used for outruling candidates. In later clinical phases, metabonomics can help in an advanced profiling of a drug candidate. Thereby metabonomics can be added to acute and chronic GLP studies. As these studies are highly controled and as typically several sampling time points are available, detailed mechanistic investations can be performed. These studies also allow looking for bridging biomarker and effects, which can be monitored in clinical phase I studies later on. In clinical studies metabonomics can be used for several purposes, such as monitoring safety biomarkers, for monitoring the efficacy of therapy, for diagnosis and for stratification of patients.
 |
References
- Anson, Blake D.; Ma, Junyi; He, Jia-Qiang (1 May 2009). “Identifying Cardiotoxic Compounds”. Genetic Engineering & Biotechnology News. TechNote 29 (9) (Mary Ann Liebert). pp. 34–35.ISSN 1935-472X. OCLC 77706455. Archived from the original on 25 July 2009. Retrieved 25 July 2009
- Steven M. Paul, Daniel S. Mytelka, Christopher T. Dunwiddie, Charles C. Persinger, Bernard H. Munos, Stacy R. Lindborg & Aaron L. Schacht (2010). “How to improve R&D productivity: the pharmaceutical industry’s grand challenge”. Nature Reviews Drug Discovery 9 (3): 203–214. doi:10.1038/nrd3078. PMID 20168317.
- Rask-Andersen M, Almén MS, Schiöth HB (August 2011). “Trends in the exploitation of novel drug targets.”. Nature Reviews Drug Discovery 8 (10): 549–90. doi:10.1038/nrd3478. PMID 21804595.
- Hopkins, A. L., Groom, C. R. and Alexander, A. (2004). “Ligand efficiency: a useful metric for lead selection”. Drug Discovery Today 9 (10): 430–431. doi:10.1016/S1359-6446(04)03069-7.PMID 15109945.
- Ryckmans, T. et al. (2009). “Rapid assessment of a novel series of selective CB2 agonists using parallel synthesis protocols: A Lipophilic Efficiency (LipE) analysis”. Bioorg. Med. Chem. Lett. 19 (15): 4406–4409. doi:10.1016/j.bmcl.2009.05.062. PMID 19500981.
- Leeson, P. D. et al. (2007). “The influence of drug-like concepts on decision-making in medicinal chemistry”. Nature Reviews Drug Discovery 6 (11): 881–890. doi:10.1038/nrd2445.PMID 17971784.
- Feher M, Schmidt JM (2003). “Property distributions: differences between drugs, natural products, and molecules from combinatorial chemistry”. J Chem Inf Comput Sci 43 (1): 218–27.doi:10.1021/ci0200467. PMID 12546556.
- Newman DJ, Cragg GM (March 2007). “Natural products as sources of new drugs over the last 25 years”. J. Nat. Prod. 70 (3): 461–77. doi:10.1021/np068054v. PMID 17309302.
- von Nussbaum F, Brands M, Hinzen B, Weigand S, Häbich D (August 2006). “Antibacterial natural products in medicinal chemistry–exodus or revival?”. Angew. Chem. Int. Ed. Engl. 45 (31): 5072–129. doi:10.1002/anie.200600350. PMID 16881035. “The handling of natural products is cumbersome, requiring nonstandardized workflows and extended timelines. Revisiting natural products with modern chemistry and target-finding tools from biology (reversed genomics) is one option for their revival.”
- John Faulkner D, Newman DJ, Cragg GM (February 2004). “Investigations of the marine flora and fauna of the Islands of Palau”. Nat Prod Rep 21 (1): 50–76. doi:10.1039/b300664f.PMID 15039835.
- Gad, Shayne C. (2005). Drug discovery handbook. Hoboken, N.J: Wiley-Interscience/J. Wiley. ISBN 0-471-21384-5.
- Madsen, Ulf; Krogsgaard-Larsen, Povl; Liljefors, Tommy (2002). Textbook of drug design and discovery. Washington, DC: Taylor & Francis. ISBN 0-415-28288-8.
- Introduction to Drug Discovery – Combinatorial Chemistry Review
- CDER Drug and Biologic Approval Reports
- Pharmaceutical Research and Manufacturers of America (PhRMA)
- European Medicines Agency (EMEA)
- Pharmaceuticals and Medical Devices Agency (PMDA)
- WHO Model List of Essential Medicines
- Innovation and Stagnation: Challenge and Opportunity on the Critical Path to New Medical Products – FDA
- Priority Medicines for Europe and the World Project “A Public Health Approach to Innovation” – WHO
- International Union of Basic and Clinical Pharmacology
- IUPHAR Committee on Receptor Nomenclature and Drug Classification
- Drugdiscovery@home Early in silico drug discovery by volunteer computing.
- Drug Information Association (DIA)
- Antitarget
- Biological target
- Drug discovery hit to lead
- Drug development
- Pre-clinical development
- Protein structure prediction
- Drug design
- Rational drug design
- Drug metabolism
- Compound management
- Bioinformatics
- Cheminformatics
- Biomedical informatics
- Orphan drug
- Pharmaceutical company
- Pharmacognosy
- Physiologically-based pharmacokinetic modelling
- Simcyp Simulator
- Pharmacogenetics
- Simulations Plus
- High-throughput screening
- Natural product
- Molecular modelling
- Molecular Conceptor
- Discovery and development of proton pump inhibitors
- Discovery and development of melatonin receptor agonists
- Discovery and development of nucleoside and nucleotide reverse transcriptase inhibitors
- Discovery and development of Bcr-Abl tyrosine kinase inhibitors
- Discovery and development of antiandrogens
- Discovery and development of cephalosporins
FDA Issues Draft Guidance on NCE Exclusivity Determinations
| Feb 25, 2014 |
Source: FDA.gov
see below
The Food and Drug Administration (FDA or the Agency) is issuing this guidance to set forth a change in the Agency’s interpretation of the 5-year new chemical entity (NCE) exclusivity provisions as they apply to certain fixed-combination drug products (fixed-combinations).
Historically, FDA has interpreted these provisions such that a fixed-combination was ineligible for 5-year NCE exclusivity if it contained a previously approved active moiety, even if the product also contained a new active moiety (i.e., an active moiety that the Agency had not previously approved).
The Agency recognizes that fixed-combinations have become increasingly prevalent in certain therapeutic areas (including cancer, cardiovascular, and infectious disease) and that these products play an important role in optimizing adherence to
dosing regimens and improving patient outcomes.
As further discussed below, we are therefore revising our historical interpretation of the 5-year NCE exclusivity provisions to further incentivize the development of certain fixed-combination products.
If the new interpretation is adopted, FDA intends to apply the new interpretation prospectively.Therefore, this guidance does not apply to fixed-combination drug products that were approvedprior to adopting the new interpretation.
FDA’s guidance documents, including this guidance, do not establish legally enforceable responsibilities. Instead, guidances describe the Agency’s current thinking on a topic and should be viewed only as recommendations, unless specific regulatory or statutory requirements are cited. The use of the word should in Agency guidances means that something is suggested or
recommended, but not required. read at
http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM386685.pdf

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....