Home » 2014 (Page 82)
Yearly Archives: 2014
Nemonoxacin….TaiGen’s pneumonia antibiotic Taigexyn 奈诺沙星 gets marketing approval in Taiwan

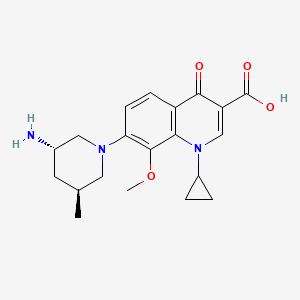
Nemonoxacin 奈诺沙星
378746-64-6 CAS
TG-873870
-
C20-H25-N3-O4
- 371.4345
WARNER CHILCOTT ORIGINATOR
CLINICAL TRIALS http://clinicaltrials.gov/search/intervention=Nemonoxacin
(3S,5S)-7-[3-amino-5-methyl-piperidinyl]-l-cyclopropyl-l,4- dihydro-8-methoxy-4-oxo-3-quinolinecarboxylic acid
7-[3(S)-Amino-5(S)-methylpiperidin-1-yl]-1-cyclopropyl-8-methoxy-4-oxo-1,4-dihydroquinoline-3-carboxylic acid
Taigexyn has been approved in Taiwan IN 2014
13.03.14 |
TaiGen Biotechnology Receives Marketing Approval from the Taiwan Food and Drug Administration for Taigexyn in Taiwan
TAIPEI, March 13, 2014 /PRNewswire/ — TaiGen Biotechnology Company, Limited (“TaiGen”) today announced that the Taiwan Food and Drug Administration (TFDA) has approved the new drug application (NDA) of Taigexyn® (nemonoxacin) oral formulation (500 mg) for the treatment of community-acquired bacterial pneumonia (CAP). With this NDA approval, Taiwan is the first region to grant marketing approval to Taigexyn®. An NDA for Taigexyn® was also submitted to China FDA (CFDA) in April 2013 and is currently under review.
Nemonoxacin is a novel non-fluorinated quinolone antibiotic undergoing clinical trials.
Taigexyn Granted QIDP and Fast Track Designations
TaiGen Biotechnology announced that the FDA has granted nemonoxacin (Taigexyn) Qualified Infectious Disease Product (QIDP) and Fast Track designations for community-acquired bacterial pneumonia (CAP) and acute bacterial skin and skin structure infections (ABSSSI).
Nemonoxacin is a novel non-fluorinated quinolone broad spectrum antibiotic available in both oral and intravenous formulations. Nemonoxacin demonstrates activity against gram-positive and gram-negative bacteria and atypical pathogens. Nemonoxacin also possesses activities against methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant pathogens.
Nemonoxacin is a novel non-flourinated quinolone antibiotic registered in Taiwan for the oral treatment of community-acquired pneumonia. Clinical trials are in development at TaiGen Biotechnology for the treatment of diabetic foot infections and for the treatment of moderate to severe community-acquired pneumonia with an intravenous formulation. The drug is thought to accomplish its antibacterial action through topoisomerase inhibition.
Originally developed at Procter & Gamble, nemonoxacin was the subject of a strategic alliance formed in January 2005 between P&G and TaiGen to further the development and commercialization of nemonoxacin. In 2012, the product was licensed by TaiGen Biotechnology to Zhejiang Medicine in China for manufacturing, sales and marketing. In 2014, TaiGen out-licensed the exclusive rights of the product in Russian Federation, Commonwealth Independent States and Turkey to R-Pharm.
TaiGen has completed two Phase 2 clinical studies, one in CAP and the other in diabetic foot infections with demonstrated efficacy and safety. In the clinical trials conducted to date, nemonoxacin has shown activity against drug-resistant bacteria such as MRSA, quinolone-resistant MRSA, as well as quinolone-resistant Streptococcus pneumoniae.

Malate salt
Nemonoxacin malate anhydrous
951163-60-3 CAS NO, MW: 505.5209
Nemonoxacin malate hemihydrate
951313-26-1, MW: 1029.0566
Chemical structure of nemonoxacin as a malate salt (C20H25N3O4·C4H6O5·H2O). Nemonoxacin is the free base, and its molecular mass is 371.44 g/mol. The molecular mass of the salt, nemonoxacin malate, is 514.53 g/mol.


……………………..
isomeric compounds are:
(3S,5S)-7-[3-amino-5-methyl-piperidinyl]-l-cyclopropyl-l,4-dihydro-8- methoxy-4-oxo-3 -quinolinecarboxylic acid
COMPD1…….DESIRED
(3S,5R)-7-[3-amino-5-methyl-piperidinyl]-l-cyclopropyl-l,4-dihydro-8- methoxy-4-oxo-3 -quinolinecarboxylic acid
COMPD 1’….NOT DESIRED
Example 1
Malate salts of (3S,5S)-7-[3-amino-5-methyl-piperidinyl]-l-cyclopropyl-l,4- dihydro-8-methoxy-4-oxo-3-quinolinecarboxylic acid (Compound 1) and (3S,5R)-7- [3-ammo-5-methyl-piperidinyl]- 1 -cyclopropyl- 1 ,4-dihydro-8-methoxy-4-oxo-3- quinolinecarboxylic acid (Compound 1′) were synthesized as follows:
(A) Synthesis of (3S,5S)-(5-Methyl-piperidin-3-yl)-carbamic acid tert-butyl ester (Compound 9) and (3S,5R)-(5-Methyl-piperidin-3-yl)-carbamic acid tert-butyl ester (Compound 9′): Compound 9′ was synthesized as shown in Scheme 1 below:
Scheme 1
3 4 Boc
A 50-L reactor was charged with Compound 2 (5.50 kg, 42.60 mol), methanol (27 L) and cooled to 10-150C. Thionyl chloride (10.11 kg, 2.0 equiv.) was added via an addition funnel over a period of 65 min, with external cooling to keep temperature below 30°. The resulting solution was stirred at 250C for 1.0 hour, after which methanol was removed under reduced pressure. The oily residue was azeotroped with ethyl acetate (3 x 2.5 L) to remove residual methanol, dissolved in ethyl acetate (27.4 L), charged into a 50 L reactor, and neutralized by slow addition of triethylamine (3.6 kg) below 3O0C. The resulting suspension was filtered to remove triethylamine hydrochloride.
The filtrate was charged to a 50 L reactor, along with DMAP (0.53 kg). Di- fert-butyl dicarbonate (8.43 kg) was added via hot water heated addition funnel, over a period of 30 min at a temperature of 20-300C. The reaction was complete after 1 hour as determined by TLC analysis. The organic phase was washed with ice cold IN HCl (2 x 7.5 L), saturated sodium bicarbonate solution (1 x 7.5 L), dried over magnesium sulfate, and filtered. After ethyl acetate was removed under reduced pressure, crystalline slurry was obtained, triturated with MTBE (10.0 L), and filtered to afford Compound 3 as a white solid (5.45 kg, 52.4%).
Anal. Calcd for CHHI7NO5 : C, 54.3; H, 7.04; N, 5.76. Found: C, 54.5; H, 6.96; N, 5.80. HRMS (ESI+) Expected for CHHI8NO5, [M+H] 244.1185. Found
244.1174; 1H NMR (CDCl3, 500 MHz):δ=4.54 (dd, J= 3.1, 9.5 Hz, IH), 3.7 (s, 3H), 2.58-2.50 (m, IH), 2.41 (ddd, IH, J= 17.6, 9.5, 3.7), 2.30-2.23 (m, IH), 1.98-1.93 (m, IH), 1.40 (s, 9H); 13C NMR (CDCl3, 125.70 MHz) δ 173.3, 171.9, 149.2, 83.5, 58.8, 52.5, 31.1, 27.9, 21.5. Mp 70.20C.
A 50-L reactor was charged with Compound 3 (7.25 kg, 28.8 mol), DME (6.31 kg), and Bredereck’s Reagent (7.7 kg, 44.2 mole). The solution was agitated and heated to 750C + 50C for three hours. The reaction was cooled to O0C over an hour, during which time a precipitate formed. The mixture was kept at O0C for an hour, filtered, and dried in a vacuum oven for at least 30 hours at 3O0C + 50C to give compound 4 as a white crystalline solid (6.93 kg, 77.9%).
Anal. Calcd for Ci4H22N2O5: C, 56.4; H, 7.43; N, 9.39. Found C, 56.4; H, 7.32; N, 9.48; HRMS (ESI+) Expected for Ci4H22N2O5, [M+H] 299.1607. Found 299.1613; 1H NMR (CDCl3, 499.8 MHz) δ = 7.11 (s, IH), 4.54 (dd, IH, J= 10.8, 3.6), 3.74 (s, 3H), 3.28-3.19 (m, IH), 3.00 (s, 6H), 2.97-2.85 (m,lH), 1.48 (s, 9H); 13C NMR (CDCl3, 125.7 MHz) δ = 172.6, 169.5, 150.5, 146.5, 90.8, 82.2, 56.0, 52.3, 42.0, 28.1, 26.3. MP 127.90C. A 10-gallon Pfaudler reactor was charged with ESCAT 142 (Engelhard Corp.
N.J, US) 5% palladium powder on carbon (50% wet, 0.58 kg wet wt), Compound 4 (1.89 kg, 6.33 mol), and isopropanol (22.4 Kg). After agitated under a 45-psi hydrogen atmosphere at 450C for 18 hrs, the reaction mixture was cooled to room temperature and filtered though a bed of Celite (0.51 kg). The filtrate was evaporated under reduced pressure to give a thick oil, which was solidified on standing to afford Compound 5 (1.69 kg, 100%) as a 93:7 diastereomeric mixture.
A sample of product mixture was purified by preparative HPLC to give material for analytical data. Anal. Calcd for Ci2Hi9NO5: C, 56.0; H, 7.44; N, 5.44. Found C, 55.8; H, 7.31; N, 5.44; MS (ESI+) Expected for Ci2Hi9NO5, [M+H] 258.1342. Found 258.1321; 1H NMR (CDCl3, 499.8 MHz) δ = 4.44 (m, IH), 3.72 (s, 3H), 2.60-2.48 (m, 2H), 1.59-1.54 (m, IH), 1.43 (s, 9H), 1.20 (d, j = 6.8 Hz,3H); 13C NMR (CDCl3, 125.7 MHz) δ = 175.7, 172.1, 149.5, 83.6, 57.4, 52.5, 37.5, 29.8, 27.9, 16.2. Mp 89.90C.
A 50-L reactor was charged with Compound 5 (3.02 kg, 11.7 mol), absolute ethanol (8.22 kg), and MTBE (14.81 kg). Sodium borohydride (1.36 kg, 35.9 mol) was added in small portions at 00C + 50C. A small amount of effervescence was observed. The reaction mixture was warmed to 1O0C + 50C and calcium chloride dihydrate (2.65 kg) was added in portions at 1O0C + 50C over an hour. The reaction was allowed to warm to 2O0C + 50C over one hour and agitated for an additional 12 hours at 200C + 50C. After the reaction was cooled to -50C + 50C, ice-cold 2N HCl (26.9 kg) was added slowly at of O0C + 50C. Agitation was stopped. The lower aqueous phase was removed. The reactor was charged with aqueous saturated sodium bicarbonate (15.6 kg) over five minutes under agitation. Agitation was stopped again and the lower aqueous phase was removed. The reactor was charged with magnesium sulfate (2.5 kg) and agitated for at leastlO minutes. The mixture was filtered though a nutsche filter, and concentrated under reduced pressure to afford Compound 6 (1.80 kg, 66%). Anal. Calcd for CnH23NO4: C, 56.6 H, 9.94; N, 6.00. Found C, 56.0; H, 9.68;
N, 5.96; HRMS (ESI+) Expected for CnH24NO4, [M+H] 234.1705. Found 234.1703; 1H NMR (CDCl3, 500 MHz) δ = 6.34 (d, J= 8.9 Hz, IH, NH), 4.51 (t, J= 5.8, 5.3 Hz, IH, NHCHCH2OH), 4.34 (t, J= 5.3, 5.3 Hz, IH, OBCHCH2OH), 3.46-3.45, (m, IH, NHCH), 3.28 (dd, J= 10.6, 5.3 Hz, NHCHCHHOH), 3.21 (dd, J= 10.2, 5.8 Hz , IH, CH3CHCHHOH), 3.16 (dd, J = 10.2, 6.2 Hz, IH, NHCHCHHOH), 3.12 (dd, J= 10.6, 7.1 Hz , IH, CH3CHCHHOH), 1.53-1.50 (m, IH, CH3CHCHHOH), 1.35 (s, 9H, 0(CHB)3, 1.30 (ddd, J = 13.9, 10.2, 3.7 Hz, IH, NHCHCHHCH), 1.14 (ddd, J= 13.6, 10.2, 3.4 Hz, IH, NHCHCHHCH), 0.80 (d, J= 6.6 Hz, 3H, CH3); 13C NMR (CDCl3, 125.7 MHz) δ 156.1, 77.9, 50.8, 65.1, 67.6, 65.1, 35.6, 32.8, 29.0, 17.1. Mp 92.10C. A 50 L reactor was charged with a solution of Compound 6 (5.1 kg) in isopropyl acetate (19.7 kg). The reaction was cooled to 150C + 5°C and triethylamine (7.8 kg) was added at that temperature. The reactor was further cooled to O0C + 50C and methanesulfonyl chloride (MsCl) (6.6 kg) was added. The reaction was stirred for a few hours and monitored for completion by HPLC or TLC. The reaction was quenched by saturated aqueous bicarbonate solution. The organic phase was isolated and washed successively with cold 10% aqueous triethylamine solution, cold aqueous HCl solution, cold saturated aqueous bicarbonate solution, and finally saturated aqueous brine solution. The organic phase was dried, filtered, and concentrated in vacuo below 550C + 50C to afford compound 7 as a solid/liquid slurry, which was used in the subsequent reaction without further purification.
After charged with 9.1 kg of neat benzylamine, a 50 L reactor was warmed to 550C, at which temperature, a solution of compound 7 (8.2 kg) in 1,2- dimethoxyethane (14.1 kg) was added. After the addition, the reaction was stirred at 6O0C + 50C for several hours and monitored for completion by TLC or HPLC. The reaction was cooled to ambient temperature and the solvent was removed under vacuum. The residue was diluted with 11.7 kg of 15% (v/v) ethyl acetate/hexanes solution and treated, while agitating, with 18.7 kg of 20% (wt) aqueous potassium carbonate solution. A triphasic mixture was obtained upon standing. The upper organic layer was collected. The isolated middle layer was extracted twice again with 11.7 kg portions of 15% (v/v) ethyl acetate/hexanes solution. The combined organic layers were concentrated under vacuum to give an oily residue. The residue was then purified by chromatography to afford Compound 8 as an oil. A 40 L pressure vessel was charged with 0.6 kg 50% wet, solid palladium on carbon (ElOl, 10 wt. %) under flow of nitrogen. A solution of Compound 8 (3.2 kg) in 13.7 kg of absolute ethanol was then added to the reactor under nitrogen. The reactor was purged with nitrogen and then pressurized with hydrogen at 45 psi. The reaction was then heated to 45°C. It was monitored by TLC or LC. Upon completion, the reaction was cooled to ambient temperature, vented, and purged with nitrogen. The mixture was filtered through a bed of Celite and the solid was washed with 2.8 kg of absolute ethanol. The filtrate was concentrated under vacuum to afford Compound 9 as a waxy solid.
TLC R/(Silica F254, 70:30 v/v ethyl acetate-hexanes, KMnO4 stain) = 0.12; 1H NMR (300 MHz, CDCl3) δ 5.31 (br s, IH), 3.80-3.68 (m, IH), 2.92 (d, J=I 1.4 Hz,
IH), 2.77 (AB quart, JAB=12.0 Hz, v=50.2 Hz, 2H), 2.19 (t, J=10.7 Hz, IH), 1.82-1.68 (m, 2H), 1.54 (br s, IH), 1.43 (s, 9H), 1.25-1.15 (m, IH), 0.83 (d, J=6.6 Hz, 3H); 13C NMR (75 MHz, CDCl3) δ: 155.3, 78.9, 54.3, 50.8, 45.3, 37.9, 28.4, 27.1, 19.2; MS (ESI+) m/z 215 (M+H), 429 (2M+H). Similarly, (3S,5R)-(5-Methyl-piperidin-3-yl)-carbamic acid tert-butyl ester
(Compound 9′) was synthesized as shown in Scheme 2.
Scheme 2
HN Boc HN Boc
NaBH4,EtOH w – “ MsCI1TEA . „ _. – – _. „ Benzyl Amine
THF EA1CoId
(B) Synthesis of l-Cyclopropyl-7-fluoro-8-methoxy-4-oxo-l,4-dihydro-quinoline-3- carboxylic acid (Compound 10): Compound 10 was prepared according to the method described in U.S. Patent
6,329,391.
(C) Synthesis of borone ester chelate of l-Cyclopropyl-7-fluoro-8-methoxy-4-oxo- l,4-dihydro-quinoline-3-carboxylic acid (Compound 11):
Scheme 3
Toluene, tert-Butylmethyl ether 20-500C, filter
A reactor was charged with boron oxide (2.0 kg, 29 mol), glacial acetic acid (8.1 L, 142 mol), and acetic anhydride (16.2 L, 171 mol). The resulting mixture was refluxed at least 2 hours, and then cooled to 400C, at which temperature, 7- fluoroquinolone acid compound 10 (14.2 kg, 51 mol) was added. The mixture was refluxed for at least 6 hours, and then cooled to about 900C. Toluene (45 L) was added to the reaction. At 5O0C, terϊ-butylmethyl ether (19 L) was added to introduce precipitation. The mixture was then cooled to 200C and filtered to isolate the precipitation. The isolated solid was then washed with teτt-butylmethyl ether (26 L) prior to drying in a vacuum oven at 4O0C (50 torr) to afford Compound 11 in a yield of 86.4%. Raman (cm 1): 3084.7, 3022.3, 2930.8, 1709.2, 1620.8, 1548.5, 1468.0, 1397.7, 1368.3, 1338.5, 1201.5, 955.3, 653.9, 580.7, 552.8, 384.0, 305.8. NMR (CDCl3, 300 MHz) δ (ppm): 9.22 (s, IH), 8.38-8.33 (m, IH), 7.54 (t, J=9.8 Hz, IH), 4.38-4.35 (m, IH), 4.13 (s, 3H), 2.04 (s, 6H), 1.42-1.38 (m, 2H), 1.34-1.29 (m, 2H). TLC (Whatman MKC18F Silica, 6θA, 200 μm), Mobile Phase: 1 :1 (v/v) CH3CN : 0.5N NaCl (aq), UV (254/366 nm) visualization; R^O.4-0.5. (D) Synthesis of malate salt of (3S,5S)-7-[3-amino-5-methyl-piperidmyl]-l- cyclopropyl-l,4-dihydro-8-methoxy-4-oxo-3-quinolinecarboxylic acid (Compound 1) and malate salt of (3S,5R)-7-[3-amino-5-methyl-piperidmyl]-l-cyclopropyl-l,4- dihydro-8-methoxy-4-oxo-3-quinolinecarboxylic acid (Compound 1′)
Compound 1 was synthesized from compound 9 as shown in Scheme 4 below:
Scheme 4
5O0C 3 d
a 6 0 N HCI (aq) CH2CI2 35°40°C 12 h t> Extract pH ad]ust to ~7-8 50″-65″C filter
A reactor was charged with Compound 11 (4.4 kg, 10.9 mol), Compound 9 (2.1 kg, 9.8 mol), triethylamine (TEA) (2.1 L, 14.8 mol), and acetonitrile (33.5 L, 15.7 L/kg). The resulting mixture was stirred at approximately 500C till completion of the reaction, as monitored by HPLC or reverse phase TLC. It was cooled to approximately 35°C and the reaction volume was reduced to approximately half by distillation of acetonitrile under vacuum between 0-400 torr. After 28.2 kg of 3.0 N NaOH (aq) solution was added, the reaction mixture was warmed to approximately 4O0C, distilled under vacuum until no further distillates were observed, and hydro lyzed at room temperature. Upon completion of hydrolysis, which was monitored by HPLC or reverse phase TLC, 4-5 kg of glacial acetic acid was added to neutralize the reaction mixture.
The resulting solution was extracted 3 times with 12.7 kg (9.6 L) of dichloromethane. The organic layers were combined and transferred to another reactor. The reaction volume was reduced to approximately a half by evaporation at 400C. After 20.2 Kg 6.0N HCl (aq) solution was added, the reaction mixture was stirred for at least 12 hours at 35°C. After the reaction was completed as monitored by HPLC or reverse phase TLC, agitation was discontinued to allow phase separation. The organic phase was removed and the aqueous layer was extracted with 12.7 kg (9.6 L) of dichloromethane. The aqueous layer was diluted with 18.3 kg distilled water and warmed to approximately 500C. Dichloromethane was further removed by distillation under vacuum (100-400 torr).
The pH of the aqueous solution was then adjusted to 7.8-8.1 by adding about 9.42 kg of 3.0 N NaOH (aq) below 65°C. The reaction mixture was stirred at 500C for at least an hour and then cooled to room temperature. The precipitate was isolated by suction filtration, washed twice with 5.2 kg of distilled water, and dried with suction for at least 12 hours and then in a convection oven at 55°C for additional 12 hours. Compound 12 (3.2 kg, 79%) was obtained as a solid.
A reactor was charged with 3.2 kg of Compound 12 and 25.6 kg of 95% ethanol. To the reactor was added 1.1 kg of solid D,L-malic acid. The mixture was refluxed temperature (~80°C). Distilled water (-5.7 L) was added to dissolve the precipice and 0.2 kg of activated charcoal was added. The reaction mixture was passed through a filter. The clear filtrate was cooled to 45°C and allowed to sit for at least 2 hours to allow crystallization. After the reaction mixture was further cooled to 5°C, the precipitate was isolated by suction filtration, washed with 6.6 kg of 95% ethanol, and dried with suction for at least 4 hours. The solid was further dried in a convection oven at 450C for at least 12 hours to afford 3.1 kg of Compound 1 (yield: 70%). NEMONOXACIN
NMR (D2O, 300 MHz) δ (ppm): 8.54 (s, IH), 7.37 (d, J=9.0 Hz, IH), 7.05 (d, J=9.0 Hz, IH), 4.23-4.18 (m, IH), 4.10-3.89 (m, IH), 3.66 (br s, IH), 3.58 (s, 3H), 3.45 (d, J=9.0 Hz, IH), 3.34 (d, J=9.3 Hz, IH), 3.16 (d, J=12.9 Hz, IH), 2.65 (dd, J=16.1, 4.1 Hz, IH), 2.64-2.53 (m, IH), 2.46 (dd, J=16.1, 8.0 Hz, IH), 2.06 (br s, IH), 1.87 (d, J=14.4 Hz, IH), 1.58-1.45 (m, IH), 1.15-0.95 (m, 2H), 0.91 (d, J=6.3 Hz, 3H), 0.85-0.78 (m, 2H).
Similarly, Compound 1′ was synthesized from Compound 9′ as shown in Scheme 5 below:
Scheme 5
(3S,5R)-7-[3-amino-5-methyl-piperidinyl]-l-cyclopropyl-l,4-dihydro-8- methoxy-4-oxo-3 -quinolinecarboxylic acid
COMPD 1’….NOT DESIRED
…………………
US2007/232650 A1,
malate salts of
(3S,5S)-7-[3-amino-5-methyl-piperidinyl]-1-cyclopropyl-1,4-dihydro-8-methoxy-4-oxo-3-quinolinecarboxylic acid (hereinafter Compound I, see also intermediate (23) in Section D, of Detailed Description of the Invention).
EXAMPLES Example 1 Synthesis of (3S,5S)-7-[3-amino-5-methyl-piperidinyl]-1-cyclopropyl-1,4-dihydro-8-methoxy-4-oxo-3-quinolinecarboxylic acid and malate salt thereof A. Synthesis of (3S,5S)-(5-Methyl-piperidin-3-yl)-carbamic acid tert-butyl ester (8)
(2S)-1-(1,1-Dimethylethyl)-5-oxo-1,2-pyrrolidinedicarboxylic acid-2-methyl ester, (2). A 50-L reactor is charged with compound (1) (5.50 Kg, 42.60 mol), methanol (27 L) and cooled to 10-15° C. Thionyl chloride (10.11 Kg, 2.0 equiv.) is added via addition funnel over a period of 65 min, with external cooling to maintain temperature at <30°. The resulting solution is stirred at 25° C.+5° C. for 1.0 hour, after which the methanol is distilled off under reduced pressure. The resulting thick oil is azeotroped with ethyl acetate (3×2.5 L) to remove residual methanol. The residue is dissolved in ethyl acetate (27.4 L), charged into a 50 L reactor, and neutralized by the addition of triethylamine (3.6 Kg) from an addition funnel over 30 minutes. The temperature of the neutralization is maintained below 30° C. via external cooling. The resulting suspension of triethylamine hydrochloride is removed by filtration, and the clarified mother liquor solution is charged to a 50 L reactor, along with DMAP (0.53 Kg). Di-tert-butyl dicarbonate (8.43 Kg) is added via hot water heated addition funnel, over a period of 30 min with external cooling to maintain temperature at about 20-30° C. The reaction is complete after 1 hour as determined by TLC analysis. The organic phase is washed with ice cold 1N HCl (2×7.5 L), saturated sodium bicarbonate solution (1×7.5 L), and dried over magnesium sulfate. The mixture is filtered through a nutsche filter and ethyl acetate is removed under reduced pressure to yield a crystalline slurry that is triturated with MTBE (10.0 L) and filtered to afford intermediate (2) as a white solid (5.45 Kg, 52.4%). Anal. Calcd for C11H17NO5: C, 54.3; H, 7.04; N, 5.76. Found: C, 54.5; H, 6.96; N, 5.80. HRMS (ESI+) Expected for C11H18NO5, [M+H] 244.1185. Found 244.1174; 1H NMR (CDCl3, 500 MHz): δ=4.54 (dd, J=3.1, 9.5 Hz, 1H), 3.7 (s, 3H), 2.58-2.50 (m, 1H), 2.41 (ddd, 1H, J=17.6, 9.5, 3.7), 2.30-2.23 (m, 1H), 1.98-1.93 (m, 1H), 1.40 (s, 9H); 13C NMR (CDCl3, 125.70 MHz) δ 173.3, 171.9, 149.2, 83.5, 58.8, 52.5, 31.1, 27.9, 21.5; Mp 70.2° C.
(2S,4E)-1-(1,1-Dimethylethyl)-4-[(dimethylamino)methylene]-5-oxo-1,2-pyrrolidinedicarboxylic acid-2-methyl ester (3). A 50-L reactor is charged with intermediate (2) (7.25 Kg, 28.8 mol), DME (6.31 Kg), and Bredereck’s Reagent (7.7 Kg, 44.2 mole). The solution is agitated and heated to 75° C.±5° C. for at least three hours. The progress of the reaction is monitored by HPLC. The reaction is cooled to 0° C.±5° C. over on hour during which time a precipitate forms. The mixture is held at 0° C.±5° C. for one hour and filtered though a nutsche filter and the product dried in a vacuum oven for at least 30 hours at 30° C.±5° C. to give intermediate (3) as a white crystalline solid (6.93 Kg, 77.9%). Anal. Calcd for C14H22N2O5: C, 56.4; H, 7.43; N, 9.39. Found C, 56.4; H, 7.32; N, 9.48; HRMS (ESI+) Expected for C14H22N2O5, [M+H] 299.1607. Found 299.1613; 1H NMR(CDCl3, 499.8 MHz)δ=7.11 (s, 1H), 4.54 (dd, 1H, J=10.8, 3.6), 3.74 (s, 3H), 3.28-3.19 (m, 1H), 3.00 (s, 6H), 2.97-2.85 (m, 1H), 1.48 (s, 9H); 13C NMR (CDCl3, 125.7 MHz) δ=172.6, 169.5, 150.5, 146.5, 90.8, 82.2, 56.0, 52.3, 42.0, 28.1, 26.3. Mp 127.9° C.
(2S,4S)-1-(1,1-Dimethylethyl)-4-methyl-5-oxo-1,2-pyrrolidinedicarboxylic acid-2-methyl ester (4). A 10-gallon Pfaudler reactor is inerted with nitrogen and charged with ESCAT 142 5% palladium powder on carbon (50% wet, 0.58 Kg wet wt.), intermediate (3) (1.89 Kg, 6.33 mol) and isopropanol (22.4 Kg). The reaction mixture is agitated under a 45-psi hydrogen atmosphere at 45° C. for 18 hrs. The reaction mixture is then cooled to room temperature and filtered though a bed of Celite (0.51 Kg) in a nutsche filter to remove catalyst. The mother liquor is evaporated under reduced pressure to give a thick oil that crystallizes on standing to afford 4 (1.69 Kg, 100%) as a 93:7 diastereomeric mixture. A sample of product mixture is purified by preparative HPLC to give material for analytical data. Anal. Calcd for C12H19NO5: C, 56.0; H, 7.44; N, 5.44. Found C, 55.8; H, 7.31; N, 5.44; MS (ESI+) Expected for C12H19NO5, [M+H] 258.1342. Found 258.1321; 1H NMR (CDCl3, 499.8 MHz) δ=4.44 (m, 1H), 3.72 (s, 3H), 2.60-2.48 (m, 2H), 1.59-1.54 (m, 1H), 1.43 (s, 9H), 1.20 (d, j=6.8 Hz,3H); 13C NMR (CDCl3, 125.7 MHz) δ=175.7, 172.1, 149.5, 83.6, 57.4, 52.5, 37.5, 29.8, 27.9, 16.2. Mp 89.9° C.
(1S,3S)-(4-Hydroxyl-1-hydroxymethyl-3-methyl-butyl)-carbamic acid tert-butyl ester (5). A 50-L reactor is charged with intermediate (4) (3.02 Kg, 11.7 mol), absolute ethanol (8.22 Kg), and MTBE (14.81 Kg). The solution is agitated and cooled to 0° C.±5° C. and sodium borohydride (1.36 Kg, 35.9 mol) is added in small portions so as to maintain reaction temperature at 0° C.±5° C. A small amount of effervescence is observed. The reaction mixture is warmed to 10° C.±5° C. and calcium chloride dihydrate (2.65 Kg) is added portion wise at a slow rate over an hour so as to maintain a reaction temperature of 10° C.±5° C. The reaction is allowed to warm to 20° C.±5° C. over one hour and agitated for an additional 12 hours at 20° C.±5° C. The reaction is cooled to −5° C.±5° C., ice-cold 2N HCl (26.9 Kg) is added at a rate to maintain a reaction temperature of 0° C.±5° C. Agitation is stopped to allow phases to separate. The lower aqueous phase (pH=1) is removed. The reactor is charged with aqueous saturated sodium bicarbonate (15.6 Kg) over five minutes. Agitation is stopped to allow phases to separate. The lower aqueous phase (pH=8) is removed. The reactor is charged with magnesium sulfate (2.5 Kg) and agitated for at least 10 minutes. The mixture is filtered though a nutsche filter, and condensed under reduced pressure to afford intermediate (5) (1.80 Kg, 66%). Anal. Calcd for C11H23NO4: C, 56.6; H, 9.94; N, 6.00. Found C, 56.0; H, 9.68; N, 5.96; HRMS (ESI+) Expected for C11H24NO4, [M+H] 234.1705. Found 234.1703; 1H NMR (CDCl3, 500 MHz)δ=6.34(d, J=8.9 Hz, 1H, NH), 4.51 (t, J=5.8, 5.3 Hz, 1H, NHCHCH2OH), 4.34 (t, J=5.3, 5.3 Hz, 1H, CH3CHCH2OH), 3.46-3.45, (m, 1H, NHCH), 3.28 (dd, J=10.6, 5.3 Hz, NHCHCHHOH), 3.21 (dd, J=10.2, 5.8 Hz, 1H, CH3CHCHHOH), 3.16 (dd, J=10.2, 6.2 Hz, 1H, NHCHCHHOH), 3.12 (dd, J=10.6, 7.1 Hz, 1H, CH3CHCHHOH), 1.53-1.50 (m, 1H, CH3CHCHHOH), 1.35 (s, 9H, O(CH 3)3, 1.30 (ddd, J=13.9, 10.2, 3.7 Hz, 1H, NHCHCHHCH), 1.14 (ddd, J=13.6, 10.2, 3.4 Hz, 1H, NHCHCHHCH), 0.80 (d, J=6.6 Hz, 3H, CH3); 13C NMR (CDCl3, 125.7 MHz) δ 156.1, 77.9, 50.8, 65.1, 67.6, 65.1, 35.6, 32.8, 29.0, 17.1. Mp 92.1° C.
(2S,4S)-Methanesulfonic acid 2-tert-butoxycarbonylamino-5-methanesulfonyloxy-4-methyl-pentyl ester (6). A 50 L reactor is charged with a solution of intermediate (5) (5.1 Kg) in isopropyl acetate (i-PrOAc) 11.8 Kg followed by a rinse with an additional 7.9 Kg i-PrOAc. The reaction is cooled to 15° C.±5° C. and triethylamine (TEA) (7.8 Kg) is added while maintaining the set temperature. The reactor is further cooled to 0° C.±5° C. and methanesulfonyl chloride (MsCl) (6.6 Kg) is added to the reaction solution while maintaining the set temperature. The reaction is stirred for a few hours and monitored for completion by HPLC or TLC. The reaction is quenched by the addition of a saturated aqueous bicarbonate solution and the resulting isolated organic phase is washed successively with cold 10% aqueous triethylamine solution, cold aqueous HCl solution, cold saturated aqueous bicarbonate solution, and finally saturated aqueous brine solution. The organic phase is dried, filtered, and concentrated in vacuo below 55° C.±5° C. until a solid/liquid slurry containing intermediate (6) is obtained. The slurry is used crude in subsequent reaction without further characterization.
(3S,5S)-(1-Benzyl-5-methyl-piperidin-3-yl)-carbamic acid tert-butyl ester (7). A 50 L reactor is charged with 9.1 Kg of neat benzylamine. The reactor is brought to 55° C. and a solution of intermediate (6) (8.2 Kg) in 1,2-dimethoxyethane (DME) (14.1 Kg) is added to the reactor while maintaining a temperature of 60° C.±5° C. After complete addition of this solution, the reaction is stirred at 60° C.±5° C. for several hours and monitored for completion by TLC or HPLC. The reaction is cooled to ambient temperature and volatiles (DME) are removed by rotary evaporation under vacuum. The residue is diluted with 11.7 Kg of 15% (v/v) ethyl acetate/hexanes solution and treated, while agitating, with 18.7 Kg of 20% (wt) aqueous potassium carbonate solution. A triphasic mixture is obtained upon settling. The bottom aqueous phase is removed and the middle phase is set aside. The upper organic phase is collected and held for combination with extracts from additional extractions. The isolated middle phase is extracted twice again with 11.7 Kg portions of 15% (v/v) ethyl acetate/hexanes solution, each time combining the extracts with original organic phase. The combined organic extracts are transferred into a rotary evaporator and solvent is removed under vacuum until an oily residue remains. The residue is then purified via large-scale preparative chromatography to afford purified intermediate (7) as an oil.
(3S,5S)-(5-Methyl-piperidin-3-yl)-carbamic acid tert-butyl ester (8). A 40 L pressure vessel is charged with 0.6 Kg 50% wet, solid palladium on carbon (E101, 10 wt. %) under flow of nitrogen. A solution of 3.2 Kg intermediate (7) in 13.7 Kg of absolute ethanol is then charged to the reactor under nitrogen. The reactor is purged with nitrogen and is then pressurized with hydrogen at 45 psi. The reaction is then heated to 45° C. while maintaining a hydrogen pressure of 45 psi. The reaction is monitored by TLC or LC until complete. The reaction is cooled to ambient temperature, vented, and purged with nitrogen. The reactor contents are filtered through a bed of Celite and the solids are washed with 2.8 Kg of absolute ethanol. The filtrate is concentrated by rotary evaporation under vacuum until a waxy solid is obtained to afford intermediate (8): TLC Rf (Silica F254, 70:30 v/v ethyl acetate-hexanes, KMnO4 stain)=0.12; 1H NMR (300 MHz, CDCl3) δ 5.31 (br s, 1H), 3.80-3.68 (m, 1H), 2.92 (d, J=11.4 Hz, 1H), 2.77 (AB quart, JAB=12.0 Hz, Δν=50.2 Hz, 2H), 2.19 (t, J=10.7 Hz, 1H), 1.82-1.68 (m, 2H), 1.54 (br s, 1H), 1.43 (s, 9H), 1.25-1.15 (m, 1H), 0.83 (d, J=6.6 Hz, 3H); 13C NMR (75 MHz, CDCl3) δ 155.3, 78.9, 54.3, 50.8, 45.3, 37.9, 28.4, 27.1, 19.2; MS (ESI+) m/z 215 (M+H), 429 (2M+H).
B. Synthesis of 1-Cyclopropyl-7-fluoro-8-methoxy-4-oxo-1,4-dihydro-quinoline-3-carboxylic acid (19)
Intermediate (12): A reactor is charged with a solution of intermediate (11) (1.2 Kg, 7.7 mol, 1.0 eq) in anhydrous toluene (12 L) followed by ethylene glycol (1.8 L, 15.7 mol, 4.2 eq) and solid p-toluenesulfonic acid (120 g, 10 wt. %). The reaction mixture is stirred at ambient temperature for at least 30 minutes and then heated to reflux, collecting the water/toluene azeotrope in a Dean Stark type trap apparatus until the reaction is complete as determined by TLC analysis (15% EtOAc/Hexanes v/v). Upon completion, the reaction is cooled to ambient temperature and poured into an aqueous solution of sodium bicarbonate (6 L). The organic toluene phase was removed and washed with saturated sodium bicarbonate solution (6 L), distilled water (2×6 L), and saturated aqueous brine (6 L). The organic phase was removed and dried over MgSO4, filtered, and evaporated under reduced pressure to afford intermediate (12) as an oil (1.3 Kg, 86%). The material is used without further purification in subsequent reaction steps.
Intermediate (13): A reactor is charged with a solution of intermediate (12) (1.2 Kg, 6.0 mol, 1.0 eq) in anhydrous tetrahydrofuran (12 L) and n-butyllithium (2.5M in hexanes, 2.6 L, 6.6 mol, 1.1 eq) is added at −40° C., while maintaining this temperature throughout the addition. The reaction is stirred for at least one hour at −40° C. and trimethylborate (0.9 L, 7.8 mol, 1.3 eq) is added to the mixture while maintaining the temperature at or below −40° C. The reaction mixture is stirred for at least one hour at −40° C. until complete as determined by TLC analysis (30% EtOAc/Hexanes v/v). The reaction is warmed slightly to −30° C. and acetic acid (3 L) is added slowly. Upon complete addition, water is added (0.5 L) to the reaction and the mixture is allowed to quickly warm to ambient temperature while stirring overnight. Organic solvent is removed from the reaction by distillation under reduced pressure at 45° C. To the reaction residue is added 3-4 volumes of water (6 L) and 30% hydrogen peroxide (0.7 L, 1.0 eq) slowly at ambient temperature with cooling provided to control the exotherm. The reaction is stirred for at least an hour at ambient temperature until complete as determined by TLC (15% EtOAc/Hexanes v/v). The reaction mixture is cooled to 0-5° C. and excess peroxide is quenched with the addition of 10% aqueous sodium bisulfite solution (2 L). The mixture is tested to ensure a negative peroxide result and the reaction is acidified by the addition of 6N HCl (aq) (1.2 L). The reaction is stirred until the hydrolysis reaction is complete as determined by TLC or NMR analysis. The resulting solids are collected by suction filtration to afford intermediate (13) as a yellow solid (1.0 Kg, 79%).
Intermediate (14): A reactor is charged with intermediate (13) (0.53 Kg, 3.0 mol, 1.0 eq) and dissolved in dry toluene (2.7 Kg, 3.1 L). To this solution is added dimethylsulfate (0.49 Kg, 3.9 mol, 1.30 eq) followed by solid potassium carbonate (0.58 Kg, 4.2 mol, 1.4 eq). The reaction mixture is heated to reflux and held for at least 1 hour until complete as determined by HPLC. During this time, vigorous gas evolution is observed. The reaction is then cooled to ambient temperature and diluted with distilled water (3.2 L) along with 30% NaOH (aq) (0.13 Kg, 0.33 eq). The aqueous phase is separated and the remaining toluene phase is extracted twice more with distilled water (3.2 L) combined with 30% NaOH (aq) (0.13 Kg, 0.33 eq), removing the aqueous phase each time. The organic upper phase is concentrated by distillation in vacuo (<100 mbar) at approximately 40° C. until a concentrated toluene solution is achieved. The resulting solution is cooled to ambient temperature, checked for quality and yield by HPLC, and carried forward to the next step in the synthesis without further purification (theoretical yield for intermediate (14) assumed, 0.56 Kg).
Intermediate (15a,b): A reactor is charged with 1.8 Kg (2.1 L) anhydrous toluene along with sodium hydride (0.26 Kg, 6.6 mol, 2.20 eq) as a 60 wt. % dispersion in mineral oil. To this mixture is added (0.85 Kg, 7.2 mol, 2.4 eq) diethylcarbonate as the reaction mixture is heated to 90° C. over 1 hour. A solution of intermediate (14) (˜1.0 eq) in toluene from the previous step is added to the reaction while maintaining a temperature of 90° C.±5° C. Gas evolution can be observed during this addition. After complete addition, the reaction is stirred for at least 30 minutes or until complete as determined by HPLC analysis. Upon completion, the mixture is cooled to ambient temperature and diluted with 10 wt. % aqueous sulfuric acid (3.8 Kg, 3.9 mol, 1.3 eq) with agitation. The phases are allowed to separate and the lower aqueous phase is removed. The remaining organic phase is concentrated in vacuo (<100 mbar) at approximately 40° C. until a concentrated toluene solution is achieved. The resulting solution is cooled to ambient temperature and carried forward to the next step in the synthesis without further purification (theoretical yield for intermediate (15a,b) assumed, 0.85 Kg).
Intermediate (16a,b; 17a,b): A reactor is charged with a solution of intermediate (15a,b) (0.85 Kg, ˜3.0 mol, ˜1.0 eq) in toluene from the previous step. To the reactor is then added dimethylformamide-dimethylacetal (0.54 Kg, 4.5 mol, 1.5 eq) and the resulting solution is heated to reflux temperature (˜95-105° C.). The lower boiling solvent (methanol from reaction) is allowed to distill off while the temperature is maintained at ≧90° C. Heating is continued for at least 1 hour or until complete as determined by HPLC analysis. Upon completion, the reaction containing the mixture of intermediate (16a,b), is cooled to ambient temperature and toluene (1.8 Kg, 2.1 L) along with cyclopropylamine (0.21 Kg, 3.6 mol, 1.2 eq) are added to the reaction. The reaction is stirred at ambient temperature for at least 30 minutes until complete as determined by HPLC. Upon completion, the reaction is diluted with 10 wt. % aqueous sulfuric acid (2.9 Kg, 3.0 mol, 1.0 eq) with agitation, and the phases are then allowed to separate. The aqueous phase is removed and the organic phase is concentrated under reduced pressure (<100 mbar) at approximately 40° C. by distillation. When the desired concentration is achieved, the solution is cooled to ambient temperature and the toluene solution containing the mixture of intermediate (17a,b) is carried forward to the next step in the synthesis without further purification (theoretical yield for intermediate (17a,b) assumed, ˜1.1 Kg).
Intermediate (18): A reactor is charged with a solution of the mixture of intermediate (17a,b) (˜4.7 Kg, ˜3.0 mol) at ambient temperature. To the reactor is added N,O-bis(trimethylsilyl)acetamide (0.61 Kg, 3.0 mol, 1.0 eq) and the reaction is heated to reflux temperature (˜105-115° C.) for at least 30 minutes or until complete as determined by HPLC analysis. If not complete, an additional amount of N,O-bis(trimethylsilyl)acetamide (0.18 Kg, 0.9 mol, 0.3 eq) is added to the reaction to achieve completion. Upon completion, the reaction is cooled to below 40° C. and organic solvent is removed under reduced pressure (<100 mbar) at approximately 40° C. by distillation until a precipitate is formed. The reaction is cooled to ambient temperature and the precipitated solids are isolated by suction filtration and washed with distilled water twice (1×1.8 L, 1×0.9 L). The solid is dried to afford intermediate (18) as a white solid (0.76 Kg, 82%). The material is used without further purification in the next reaction step.
Intermediate (19): A reactor is charged with solid intermediate (18) (0.76 Kg, ˜2.5 mol, ˜1.0 eq) at ambient temperature followed by ethanol (5.3 Kg, 6.8 L) and 32 wt. % aqueous hydrochloric acid (1.1 Kg, 10 mol). The reaction mixture is brought to reflux temperature (76-80° C.) during which time the mixture first becomes homogeneous and later becomes heterogeneous. The mixture is heated at reflux for at least 5 hours or until complete as determined by TLC analysis (15% EtOAc/Hexanes v/v). Upon completion, the reaction is cooled to 0° C.±5° C. and the precipitated solid is isolated by filtration and washed with distilled water (1.7 Kg) followed by ethanol (1.7 Kg). The isolated solid is dried to afford intermediate (19) as a white solid (0.65 Kg, ˜95%). 1H NMR (CDCl3, 300 MHz) δ (ppm): 14.58 (s, 1H), 8.9 (s, 1H), 8.25 (m, 1H), 7.35 (m, 1H), 4.35 (m, 1H), 4.08 (s, 3H), 1.3 (m, 2H), 1.1 (m, 2H) 19F NMR (CDCl3+CFCl3, 292 MHz) δ (ppm): −119. HPLC: 99.5% by area.
C. Synthesis of borone ester chelate of 1-Cyclopropyl-7-fluoro-8-methoxy-4-oxo-1,4-dihydro-quinoline-3-carboxylic acid (20)
A reactor is charged with boron oxide (2.0 Kg, 29 mol) followed by dilution with glacial acetic acid (8.1 L, 142 mol) and acetic anhydride (16.2 L, 171 mol). The resulting mixture is heated to reflux temperature for at least 2 hours. The reaction contents are cooled to 40° C. and the solid 7-fluoroquinolone acid intermediate (19) (14.2 Kg, 51 mol) is added to the reaction mixture. The mixture is again heated to reflux temperature for at least 6 hours. Reaction progress is monitored by HPLC and NMR. The mixture is cooled to approximately 90° C. and toluene (45 L) is added to the reaction. The reaction is further cooled to 50° C. and tert-butylmethyl ether (19 L) is added to the reaction mixture to bring about precipitation of the product. The mixture is then cooled to 20° C. and the solid product 19 is isolated by filtration. The isolated solids are then washed with tert-butylmethyl ether (26 L) prior to drying in a vacuum oven at 40° C. (50 torr). The product yield obtained for intermediate (20) in this reaction is 86.4%. Raman (cm−1): 3084.7, 3022.3, 2930.8, 1709.2, 1620.8, 1548.5, 1468.0, 1397.7, 1368.3, 1338.5, 1201.5, 955.3, 653.9, 580.7, 552.8, 384.0, 305.8. NMR (CDCl3, 300 MHz) δ (ppm): 9.22 (s, 1H), 8.38-8.33 (m, 1H), 7.54 (t, J=9.8 Hz, 1H), 4.38-4.35 (m, 1H), 4.13 (s, 3H), 2.04 (s, 6H), 1.42-1.38 (m, 2H), 1.34-1.29 (m, 2H). TLC (Whatman MKC18F Silica, 60 Å, 200 μm), Mobile Phase: 1:1 (v/v) CH3CN:0.5N NaCl (aq), UV (254/366 nm) visualization; Rf=0.4-0.5.
D. Coupling of 1-Cyclopropyl-7-fluoro-8-methoxy-4-oxo-1,4-dihydro-quinoline-3-carboxylic acid (20) to (3S,5S)-(5-Methyl-piperidin-3-yl)-carbamic acid tert-butyl ester (8), and synthesis of malate salt of (3S,5S)-7-[3-amino-5-methyl-piperidinyl]-1-cyclopropyl-1,4-dihydro-8-methoxy-4-oxo-3-quinolinecarboxylic acid (25)
A reactor is charged with solid intermediate (20) (4.4 Kg, 10.9 mol) followed by dilution with a solution of triethylamine (TEA) (2.1 L, 14.8 mol) and piperidine side chain intermediate (8) (2.1 Kg, 9.8 mol) in acetonitrile (33.5 L, 15.7 L/Kg) at room temperature. The resulting mixture is warmed to approximately 50° C. until reaction is judged complete. Reaction progress is monitored by HPLC or reverse phase TLC. When complete, the reaction is cooled to approximately 35° C. and reaction volume is reduced to approximately half by distillation of acetonitrile under vacuum between 0-400 torr. The reactor is then charged with 28.2 Kg of 3.0N NaOH (aq) solution and the temperature is raised to approximately 40° C. Distillation under vacuum is continued between 1-4 hours or until no further distillates are observed. The reaction is then cooled to room temperature and the hydrolysis reaction is monitored by HPLC or reverse phase TLC. Upon completion, the reaction mixture is neutralized to a pH of between 6-8 by adding ˜4-5 Kg of glacial acetic acid. The reactor is then charged with 12.7 Kg (9.6 L) of dichloromethane as an extraction solvent, the mixture is agitated, phases are allowed to separate, and the organic dichloromethane phase is removed. The extraction process is repeated two additional times using 12.7 Kg (9.6 L) of dichloromethane, collecting the lower, organic phase each time. The aqueous phase is discarded and the organic extracts are combined in a single reactor. The reactor contents are heated to 40° C. and the reaction volume is reduced to approximately one half by distillation. The reactor is then charged with 20.2 Kg 6.0N HCl (aq) solution, the temperature is adjusted to 35° C., and agitation is allowed for at least 12 hours to permit the Boc deprotection reaction to occur. The reaction is monitored by HPLC or reverse phase TLC. When complete, agitation is discontinued and the phases are allowed to separate. The lower, organic phase is removed and set aside. The reactor is then charged with 12.7 Kg (9.6 L) of dichloromethane as an extraction solvent, the mixture is agitated, phases are allowed to separate, and the organic dichloromethane phase is removed. The organic extracts are combined and discarded. The remaining aqueous phase is diluted with 18.3 Kg distilled water and the temperature is raised to approximately 50° C. Distillation under vacuum (100-400 torr) is performed to remove residual dichloromethane from the reaction. The pH of the reaction is then adjusted to between 7.8-8.1 using about 9.42 Kg of 3.0N NaOH (aq) solution while keeping the temperature of the reaction below 65° C. The reaction is cooled to 50° C. and the precipitated solids are aged for at least an hour prior to cooling the mixture to room temperature. The solids are isolated by suction filtration and washed twice with 5.2 Kg portions of distilled water. The solids are dried for at least 12 hours with suction and then for an additional 12 hours in a convection oven at 55° C. The yield achieved for intermediate (23) in this example is 3.2 Kg (79%). A reactor is charged with 3.2 Kg solid intermediate (23) and the solids are suspended in 25.6 Kg of 95% ethanol as solvent. To the reactor is then added 1.1 Kg of solid D,L-malic acid (24), and the mixture is heated to reflux temperature (˜80° C.). Distilled water (˜5.7 L) is added to the reaction until a complete solution is achieved and 0.2 Kg of activated charcoal is added. The reaction mixture is passed through a filter to achieve clarification, cooled to 45° C. and held for a period of at least 2 hours to allow crystallization to occur. The reaction mixture is further cooled to 5° C. and the suspended solids are isolated by suction filtration. The solids are then washed with 6.6 KG of 95% ethanol and dried for at least 4 hours with suction under vacuum. The solids are then further dried in a convection oven for at least 12 hours at 45° C. to afford 3.1 Kg of intermediate (24) (70%). NMR (D2O, 300 MHz) δ (ppm): 8.54 (s, 1H), 7.37 (d, J=9.0 Hz, 1H), 7.05 (d, J=9.0 Hz, 1H), 4.23-4.18 (m, 1H), 4.10-3.89 (m, 1H), 3.66 (br s, 1H), 3.58 (s, 3H), 3.45 (d, J=9.0 Hz, 1H), 3.34 (d, J=9.3 Hz, 1H), 3.16 (d, J=12.9 Hz, 1H), 2.65 (dd, J=16.1, 4.1 Hz, 1H), 2.64-2.53 (m, 1H), 2.46 (dd, J=16.1, 8.0 Hz, 1H), 2.06 (br s, 1H), 1.87 (d, J=14.4 Hz, 1H), 1.58-1.45 (m, 1H), 1.15-0.95 (m, 2H), 0.91 (d, J=6.3 Hz, 3H); 0.85-0.78 (m, 2H). TLC (Whatman MKC18F Silica, 60 Å, 200 μm), Mobile Phase: 1:1 (v/v) CH3CN:0.5N NaCl (aq), UV (254/366 nm) visualization. HPLC: Mobile Phase H2O with 0.1% formic acid/Acetonitrile with 0.1% formic acid, gradient elution with 88% H2O/formic acid to 20% H2O/formic acid, Zorbax SB-C8 4.6 mm×150 mm column, Part No. 883975.906, 1.5 ml/min rate, 20 min run time, 292 nm, Detector Model G1314A, S/N JP72003849, Quat Pump Model G1311A, S/N US72102299, Auto Sampler Model G1313A, S/N DE14918139, Degasser Model G1322A, S/N JP73007229; approximate retention time for intermediate (19): 13.0 min; approximate retention time for intermediate (20): 11.6 min; approximate retention time for intermediate (21): 16.3 min; approximate retention time for intermediate (22): 18.2 min; approximate retention time for intermediate (23): 8.6 min; approximate retention time for compound (25): 8.6 min.
………………..
REF
A. ARJONA ET AL: “Nemonoxacin“, DRUGS OF THE FUTURE, vol. 34, no. 3, 1 January 2009 (2009-01-01), page 196, XP55014485, ISSN: 0377-8282, DOI: 10.1358/dof.2009.034.03.1350294
| 2 | * | ANONYMOUS: “TaiGen Announces Positive Data From the Phase II Study of Nemonoxacin (TG-873870) in Community-Acquired Pneumonia“, INTERNET CITATION, [Online] 7 April 2008 (2008-04-07), page 1, XP007919900, Retrieved from the Internet: URL:http://www.taigenbiotech.com/news.html#16> [retrieved on 2011-12-12] |
| 3 | * | ANONYMOUS: “TaiGen Biotechnology Initiates Phase II Trial Of Nemonoxacin For Treatment Of Adult Community Acquired Pneumonia (CAP)“, 20070108, [Online] 8 January 2007 (2007-01-08), page 1, XP007919910, Retrieved from the Internet: URL:http://www.taigenbiotech.com/news.html#11> [retrieved on 2011-12-12] |
| 4 | * | ANONYMOUS: “TaiGen Initiates Phase 1B Trial of a Novel Quinolone Antibiotic“, 20050618, 18 June 2005 (2005-06-18), pages 1-2, XP007919904, |
| 5 | * | See also references of WO2010002415A1 |
| WO2007110834A2 * | Mar 26, 2007 | Oct 4, 2007 | Procter & Gamble | Malate salts, and polymorphs of (3s,5s)-7-[3-amino-5-methyl-piperidinyl]-1-cyclopropyl-1,4-dihydro-8-methoxy-4-oxo-3-quinolinecarboxylic acid |
| WO2009023473A2 * | Aug 5, 2008 | Feb 19, 2009 | Chi-Hsin Richard King | Antimicrobial parenteral formulation |
| WO2010009014A2 * | Jul 10, 2009 | Jan 21, 2010 | Taigen Biotechnology Co., Ltd. |
|
7-4-2012
|
TREATMENT OF ANTIBIOTIC-RESISTANT BACTERIA INFECTION
|
|
|
4-18-2012
|
Coupling Process For Preparing Quinolone Intermediates
|
|
|
10-19-2011
|
Malate salts, and polymorphs of (3S,5S)-7-[3-amino-5-methyl-piperidinyl]-1-cyclopropyl-1,4-dihydro-8-methoxy-4-oxo-3-quinolinecarboxylic acid
|
|
|
6-18-2010
|
STEREOSELECTIVE SYNTHESIS OF PIPERIDINE DERIVATIVES
|
|
|
2-19-2010
|
PNEUMONIA TREATMENT
|
|
|
5-6-2009
|
Hydride reduction process for preparing quinolone intermediates
|
|
|
2-13-2009
|
ANTIMICROBIAL PARENTERAL FORMULATION
|
|
|
11-26-2008
|
Coupling process for preparing quinolone intermediates
|
| US8158798 | Oct 27, 2008 | Apr 17, 2012 | Taigen Biotechnology Co., Ltd. | Coupling process for preparing quinolone intermediates |
| US8211909 | Sep 8, 2008 | Jul 3, 2012 | Taigen Biotechnology Co., Ltd. | Treatment of antibiotic-resistant bacteria infection |
| WO2010002965A2 * | Jul 1, 2009 | Jan 7, 2010 | Taigen Biotechnology Co., Ltd. | Pneumonia treatmen |
WO 2007110834
WO 2007110835
WO 2007110836
WO 1999014214
WO 2010077798

1, nemonoxacin; 2, delafloxacin; 3, finafloxacin; 4, zabofloxacin; 5, JNJ-Q2; 6, DS-8587; 7, KPI-10; 8, ozenoxacin; 9, chinfloxacin; 10, ACH-702.

Onion extract slows colon cancer growth just as effectively as chemo drug

(NaturalNews) Researchers have just discovered that flavonoids extracted from common onions slow the rate of colon cancer growth in mice just as effectively as a chemotherapy drug. And while the mice on chemo saw their LDL cholesterol go up (a possible side effect of the drug), the mice on onion extract actually saw their LDL levels drop.
Onion flavonoids slow colon tumor growth by 67% in vivo
Learn more: http://www.naturalnews.com/044318_onion_extract_colon_cancer_chemotherapy_drug.html##ixzz2wD3udzfF
http://www.naturalnews.com/044318_onion_extract_colon_cancer_chemotherapy_drug.html#

FDA Asked To Improve Approval Processes For Orphan Drugs
DRUG REGULATORY AFFAIRS INTERNATIONAL
Lawmakers appealed to FDA Commissioner Margaret Hamburg to improve consistency of approval processes for orphan drugs, in a letter spearheaded by Senator Edward Markey.
“We write in recognition of the Food and Drug Administration (FDA’s) efforts to ensure public access to safe, innovative and novel therapeutics, particularly for rare diseases and where there are unmet medical needs, and to ask that you continue to commit to ensuring that potential new medicines are guided and reviewed consistently across the agency,” the letter stated, which was signed by 38 members of Congress. The lawmakers said that many families continue to struggle with limited options for rare diseases and development of new, more effective medical treatments often comes too slow. “Innovation of new and safe drugs is especially urgent for rare diseases, for which either no approved therapeutics or no cures currently exist,” the letter stated.
read
EMA publishes New Process Validation Guideline

EMA publishes New Process Validation Guideline
After the publication of the Annex 15 draft at the beginning of February 2014, the EMA made a move towards the revision of its process validation guideline. The final document was published on 27 February 2014. For a long time now, the EMA had already announced this revision in a concept paper. What’s new? click here
After the publication of the Annex 15 draft at the beginning of February 2014, the EMA made a move towards the revision of its process validation guideline. The final document was published on 27 February 2014. For a long time now, the EMA had already announced this revision in a concept paper. The objective of the revision was to integrate modern GMP aspects:
- Integration of the ICH Q8, Q9 and Q10 Guidelines
- Incorporation of Process Analytical Technology (PAT), Quality by Design (QbD) and Real-Time Release Testing (RTRT).
- Extension with regard to an “enhanced approach” and integration of “continuous process verification”
- Integration of the Annexes to the current Note for Guidance
- Harmonisation with the current FDA Guidance on Process Validation
The deadline for comments on the draft for the revision of the process validation guideline ended in October 2012 already. Now, elements in accordance with the Annex 15 have also flowed into the final document. In the following, you will read a short evaluation of the document with regard to the original draft from March 2012, the (still) applicable Note for Guidance on Process Validation and FDA’s Guidance on Process Validation. The GMP relevant aspects of the documents will also be addressed.
The original 7-page long Note for Guidance on Process Validation has more than doubled and now contains 15 pages. Even the original revision draft had only 11 pages. The change in the title to “Guideline on process validation for finished products- information and data to be provided in regulatory submissions” is noticeable. The title itself gives indication about the content of the document, namely marketing authorisation matters.
Like in the draft, the document is composed of 8 numerated chapters, a summary, definitions, references, an Annex I (Process validation scheme) and an Annex II (Standard/non-standard processes) which is a new part compared to the draft. A sub section on “Design space verification” has been newly added to the chapter on process validation.
There haven’t been big changes to the draft document released in 2012. Only the chapter “Design space verification” is brand new, all other parts have been mostly updated. The chapter on ongoing process validation has been removed. Compared to the draft, indications about standard/ non-standard processes are now available in the Annex II – like in the currently applicable Note for Guidance.
What are the changes to the currently applicable Note for Guidance on Process Validation?
Compared to the current Note for Guidance, the revision remains in its final version pretty difficult to read and rather general. This is a marketing authorisation document, which is clearly addressed in the title and only applies to finished dosage forms of chemical medicinal products for human and veterinary use but not for old ones, which are already authorised and on the market. The introduction of a validation life cycle and the integration of continued process verification (CPV) are completely new although this approach is already acquainted from ICH Q8. The “traditional approach” remains accepted. Like in the Annex 15 draft the hybrid approach remains here in the final document “nebulous”. The idea to integrate modern elements from ICH Q8, Q10 (and Q11) into the document is clearly noticeable. Yet, far less concrete references are made to ICH Q9.
A stronger overlap of the FDA Guidance would have been desirable. FDA’s Guidance also deals with APIs and biologicals, and the process validation life cycle runs like a thread through the whole FDA document. FDA’s Guidance also contains GMP aspects. The FDA Guidance explicitly addresses old products which should be integrated to stage 3 of the life cycle. Yet, there is another big difference. The revised document doesn’t highlight statistical methods like the FDA Guidance.
Before the finalisation, a comparison with the Annex 15 has been made which is a nice thing. This explains the long period between the publication of the draft (March 2012) and that of the finalisation (February 2014).
What is significant for the GMP world? On the one hand almost nothing, on the other hand quite a lot: one may wonder why? Direct references to the Annex 15 can be found with regard to the “ongoing process verification” and “concurrent validation”, which is almost nothing looking at the whole document. Moreover, validation in general is required to be executed according to the GMP regarding “continuous process verification” and “change control”; these are the essential parts of the document, and (almost) the complete document should therefore be seen from a GMP perspective.
The new EMA guideline on process validation will apply by the end of August 2014.

MEPOLIZUMAB….GSK to file severe asthma drug by year end
The first non-inhaled treatment for a difficult-to-treat form of severe asthma is getting closer to market after GlaxoSmithKline said it would initiate global filings for the drug at the end of this year, on the back of strong late-stage clinical data.
Mepolizumab – a monoclonal antibody that inhibits interleukin 5 – is being investigated as a treatment for severe eosinophilic asthma in patients who experience exacerbations despite high-dose oral or inhaled corticosteroids (ICS) and an additional controller such as long-acting beta-2 agonist.
Read more at: http://www.pharmatimes.com/Article/14-03-13/GSK_to_file_severe_asthma_drug_by_year_end.aspx#ixzz2vuANtYaK
Follow us: @PharmaTimes on Twitter
Mepolizumab (proposed trade name Bosatria) is a humanized monoclonal antibody that recognizes interleukin-5 (IL-5), and is used to treat certain kinds of asthma and white blood cell diseases.
 IL 5
IL 5
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Humanized (from mouse) |
| Target | IL-5 |
Recent studies have concluded that mepolizumab may improve exacerbations in patients with severe eosinophilic asthma, an adult-onset asthma which represents less than 5% of all asthma.
IL-5 is a chemical messenger in the immune system that stimulates the growth of eosinophils. In eosinophilic asthma, eosinophils are present in the lungs. When mepolizumab was given to people with eosinophilic asthma, it eliminated eosinophils from the bloodstream,and reduced eosinophils in the lungs and bone marrow. Mepolizumab also reduced the number of asthma exacerbations, and reduced the need for corticosteroids.[1]Mepolizumab improved the quality of life, but the improvement was “not clinically meaningful,” according to a reviewer.[2] [3]
In a recent multi-centre, double-blinded, randomised, controlled trial study of Mepolizumab in severe eosinophilic asthma, Mepolizumab reduced the number of clinically significant exacerbations compared to a placebo. Additionally Mepolizumab reduced sputum and blood eosinophil counts and was shown to be safe for up to 12 months.[4]

Mepolizumab is also in development for the management of hypereosinophilic syndrome by GlaxoSmithKline (GSK) and has received orphan drug designation by the FDA.[5] Mepolizumab has been shown to reduce the need for corticosteroids and improve symptoms in FIP1L1/PDGFRA negative hypereosinophilic syndrome.[6]
UK pharma giant GlaxoSmithKline (LSE: GSK) says that a pivotal Phase III study of mepolizumab, an investigational IL-5 antagonist monoclonal antibody, met its primary endpoint of reduction in the frequency of exacerbations, in patients with severe eosinophilic asthma.
Mepolizumab could add £400 million ($668 million) to GSK’s revenue by 2021, according to estimates from Barclays reported by The Wall Street Journal. Analysts from Deutsche Bank forecast £300 million in mepolizumab sales by 2018 for the company, already a leader in the asthma treatment sector.

The study (MEA115588) evaluated the efficacy of two-dose regimens of mepolizumab in the treatment of patients with severe eosinophilic asthma. Patients remained on their current asthma maintenance therapy throughout the study and were randomized to receive either mepolizumab 75mg intravenous (IV), 100mg subcutaneous (SC), or placebo every four weeks.
For the primary end point, both mepolizumab treatment arms showed statistically significant reductions in the frequency of clinically significant exacerbations of asthma compared to placebo (75mg IV, 47%, p<0.001; 100mg SC, 53%, p<0.001).
Adverse events reported in the study were similar across all treatment groups. The most common reported adverse events across all treatment groups were nasopharyngitis, headache, upper respiratory tract infection and asthma. The frequency of adverse events was 83% in the placebo group, 84% in the mepolizumab 75mg IV and 78% in the mepolizumab 100mg SC group. The frequency of serious adverse events was 14% in the placebo group, 7% in the mepolizumab 75mg IV and 8% in the mepolizumab 100mg SC group.
Backs up earlier studies; regulatory filing mooted at year end
Dave Allen, head of GSK Respiratory Therapy Area Unit, R&D, said: “We are really pleased to have generated further positive data on mepolizumab, consistent with the findings from our earlier exacerbation study. We now have two studies showing a reduction in exacerbations in a specific group of patients with a severe form of asthma who continue to exacerbate despite treatment with high doses of their current maintenance therapies. This is very positive news for patients. For GSK it is exciting that this is the first non-inhaled treatment for severe asthma and we will be progressing towards global filings at the end of the year.”
In addition, a second Phase III study (MEA115575) designed to evaluate the use of mepolizumab 100mg SC, every four weeks in comparison to placebo in reducing daily oral corticosteroid use while maintaining asthma control also met its primary endpoint. The study showed that patients on mepolizumab 100mg SC were able to achieve greater reductions in their maintenance oral corticosteroid dose during weeks 20-24 compared to patients on placebo (p =0.008), while maintaining asthma control.
In this study adverse events were similar across treatment groups. The most common reported adverse events in the two treatment groups were headache, nasopharyngitis, bronchitis, sinusitis, fatigue and asthma. The frequency of adverse events was 92% in the placebo and 84% in the mepolizumab treatment group. Frequency of serious adverse events was 18% in the placebo group and 1% in the mepolizumab group.
Mepolizumab Useful in Refractory Eosinophilic Asthma, a Rare Subtype of Asthma

Eosinophil.

Eosinophil.Eeosinophilic form of asthma represents less than 5% of cases of adult-onset asthma and is difficult to treat.

Crystal structure of human IL-5. .
Mepolizumab reduced the number of blood and sputum eosinophils and allowed prednisone sparing in patients who had asthma with sputum eosinophilia despite prednisone treatment.
Mepolizumab therapy reduced exacerbations by 43% and improved Asthma Quality of Life Questionnaire (AQLQ) scores in patients with refractory eosinophilic asthma.
Eosinophils may have a role as important effector cells in the pathogenesis of severe exacerbations of asthma in patients with eosinophilic asthma.

Cytokine targets for immunomodulators for allergic disorders.
References
- Haldar P, Brightling CE, Hargadon B, et al. Mepolizumab and exacerbations of refractory eosinophilic asthma. N Engl J Med. 2009 Mar 5;360(10):973-84.
- Nair P, Pizzichini MM, Kjarsgaard M, et al. Mepolizumab for prednisone-dependent asthma with sputum eosinophilia. N Engl J Med. 2009 Mar 5;360(10):985-93.
- Eosinophils in asthma – closing the loop or opening the door? Sally E. Wenzel, N Engl J Med. 2009 Mar 5;360(10):1026-7.
- Pavord, Ian D; Korn, Stephanie; Howarth, Peter; Bleecker, Eugene R; Buhl, Roland; Keene, Oliver N; Ortega, Hector; Chanez, Pascal (August 2012). “Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial”. The Lancet 380 (9842): 651–659. doi:10.1016/S0140-6736(12)60988-X.
- Phase III study of Bosatria (mepolizumab) showed disease control with reduced corticosteroid use in hypereosinophilic syndrome
- http://content.nejm.org/cgi/content/abstract/358/12/1215 Rothenberg et al 2008

FDA Approves First Device to Prevent Migraines

TUESDAY March 11, 2014, 2014 — The U.S. Food and Drug Administration on Tuesday approved the first device aimed at preventing migraines.
The device, called Cefaly, is a headband-like device that runs on a battery and sits across the forehead and over the ears, the FDA said in a statement.
“The user positions the device in the center of the forehead, just above the eyes, using a self-adhesive electrode,” the agency explained. “The device applies an electric current to the skin and underlying body tissues to stimulate branches of the trigeminal nerve, which has been associated with migraine headaches.”
Cefaly is made by Belgium-based Cefaly Technology and is available by prescription only. The device is only indicated for use by adults and should only be used for 20 minutes per day, the FDA said. The agency also noted that “the user may feel a tingling or massaging sensation where the electrode is applied.”

CEFALY DRUG-FREE MIGRAINE PAIN RELIEF

Cefaly offers patients suffering from migraine pain and headaches an efficient electrotherapeutical system delivered via an extremely comfortable, ergonomic and simple-to-use medical device.

Ann-Teresa Cusenza…..Managing Editor, Orphan Druganaut Blog

Ann-Teresa Cusenza
It is a great pleasure to write about ANN…. I read her blog everyday……………………….
Medical Information Specialist | Medical Librarian | Managing Editor, Orphan Druganaut Blog
| Current | |
|---|---|
| Previous | |
| Education |
- Ann-Teresa Cusenza, MLS, MBA
She is Managing Editor, Orphan Druganaut Blog
- read at
http://orphandruganaut.wordpress.com/this is all about orphan drugs, great work ANN


-
ABOUT | Orphan Druganaut Blog
orphandruganaut.wordpress.com/about/Ann-Teresa Cusenza, MLS, MBA. Managing Editor, Orphan Druganaut Blog. Medical Information Specialist/Pharmaceutical Competitive Intelligence Consultant.
- SPECIALITIES :
- • Providing medical library information services :
- 1. Creation of Scientific Publication Plans across therapy areas
- 2. Performed searching of medical/pharmaceutical & business databases
- 3. Performed document delivery services
- 4. Scientific literature searching and analysis
- 5. Medical fact checking
- 6. Responsible for completing research requests, adhoc requests, and large projects via phone inquiries, E-Mail, and face-to-face meetings
- • Consulting services through full Information Life Cycle :
- 1. Client consultation
- 2. Search strategy
- 3. Research
4. Information analysis and organization5. Presentation to clients
- • Literature searches and analysis using pharmaceutical/medical/healthcare and business databases, search engines, and other electronic and print resources
- • Monitoring on a daily basis, competitor products in the Drug Development Pipeline
- • Providing competitive intelligence, case scenarios, and strategic recommendations on Product Lifecycle Management in the pharmaceutical industry
- • Creating Daily Newsletters with timely information, analytic overview of pharmaceutical marketplace, analysis of medical meeting abstracts and presentations across therapy areas
- • Providing research, analysis, and identification of Domestic and International Key Opinion Leaders (KOLs) across therapy areas
- • Creation, research, writing and editing pharmaceutical/medical/healthcare Blogs using WordPress.
- COMMITMENT TO LIFELONG CONTINUING EDUCATION :
- • Emerging Web Technologies & Social Media
- • Blogging Using WordPress.
- FELLOWSHIPS :
- • National Library of Medicine (NLM) Fellowship for BioMedical Informatics at the Marine Biological Laboratory (MBL), Woods Hole, MA.
- YOU CAN CONNECT WITH HER ON TWITTER AND LINKEDIN
| Websites |
|---|
-

- Medical Librarian at HackensackUMC … ·
- Pharmaceuticals
View Ann-Teresa Cusenza’s professional profile on LinkedIn. LinkedIn is the world’s largest business network, helping professionals like Ann-Teresa Cusenza …
Check out her linkedin group
http://www.linkedin.com/groups/AnnTeresa-Cusenza-2013-Orphan-Drug-2179312.S.223691622
Thankyou Ann-Teresa Cusenza

FDA Implementation of eCTD Module 1 Update Scheduled for Q4 2014
DRUG REGULATORY AFFAIRS INTERNATIONAL
The biggest change in the history of eCTD is one step closer to implementation.
According to a notice posted this week on its website, the US FDA will be able to receive submissions using the new Module 1 specifications in the 4th Quarter of 2014. Industry will be given 30 days’ advance notice.
The long-awaited update to the eCTD’s administrative section is designed to:
- Reflect regulatory changes
- Provide clarification of business rules for submission processing and review
- Refine the characterization of promotional marketing materials and advertising material
- Facilitate automated processing of submissions
In conjunction with the announcement of a revised timeline for Module 1, the FDA published final versions of relevant support documents and specifications.
http://theectdsummit.com/2014/02/fda-implementation-of-ectd-module-1-update-scheduled-for-q4-2014/
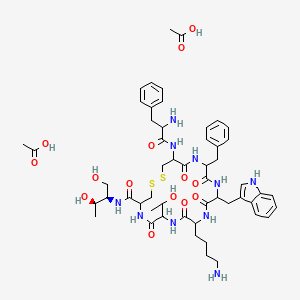
Octreotide اکترئتید For treatment of acromegaly and reduction of side effects from cancer chemotherapy

Octreotide
(D)-Phe-Cys-Phe-(D)-Trp-Lys-Thr-Cys-Thr-ol.
(4R,7S,10S,13R,16S,19R)-10-(4-aminobutyl)-19-[[(2R)-2-amino-3-phenyl-propanoyl]amino]-16-benzyl-N-[(2R,3R)-1,3-dihydroxybutan-2-yl]-7-(1-hydroxyethyl)-13-(1H-indol-3-ylmethyl)-6,9,12,15,18-pentaoxo-1,2-dithia-5,8,11,14,17-
pentazacycloicosane-4-carboxamide
L-cysteinamide, D-phenylalanyl-L-cysteiny-L-phenylalanyl-D-tryptophyl-L-lysyl-L-threonyl-N-[2-hydroxy-1-(hydroxymethyl)propyl]-,cyclic (2→7)-disulfide; [R-(R*,R*)].
Octreotide is the acetate salt of a cyclic octapeptide. It is a long-acting octapeptide with pharmacologic properties mimicking those of the natural hormone somatostatin.
| Canada | 1328402 | 1994-04-12 | expiry 2011-04-12 |
| United States | 5922338 | 1997-01-13 | 2017-01-13 |
| United States | 5538739 | 1993-07-23 | 2013-07-23 |
| CAS number | 83150-76-9 79517-01-4 (acetate) 135467-16-2 (pamoate) |
|---|
Sandostatin LAR Depot
L-Cysteinamide, D-phenylalanyl-L-cysteinyl-L-phenylalanyl-D-tryptophyl-L-lysyl-L-threonyl-N-(2-hydroxy-1-(hydroxymethyl)propyl)-, cyclic(2-7)-disulfide, (R-(R*,R*))-, acetate (salt)
Octreotide Acetate Depot
AC1L1GVR
AC1Q2BPN
CCRIS 8708
Octreotide acetate [USAN:JAN]
UNII-75R0U2568I
83150-76-9 (Parent)
AC-663
Octreotide (brand name Sandostatin,[1] Novartis Pharmaceuticals) is an octapeptide that mimics natural somatostatin pharmacologically, though it is a more potent inhibitor of growth hormone, glucagon, and insulin than the natural hormone. It was first synthesized in 1979 by the chemist Wilfried Bauer.
Since octreotide resembles somatostatin in physiological activities, it can:
- inhibit secretion of many hormones, such as gastrin, cholecystokinin, glucagon, growth hormone, insulin, secretin, pancreatic polypeptide, TSH, and vasoactive intestinal peptide,
- reduce secretion of fluids by the intestine and pancreas,
- reduce gastrointestinal motility and inhibit contraction of the gallbladder,
- inhibit the action of certain hormones from the anterior pituitary,
- cause vasoconstriction in the blood vessels, and
- reduce portal vessel pressures in bleeding varices.
It has also been shown to produce analgesic effects, most probably acting as a partial agonist at the mu opioid receptor.[2][3]
Acromegaly is a hormonal disorder that results when the pituitary gland produces excess growth hormone (GH). It most commonly affects middle-aged adults and can result in serious illness and premature death. Once recognized, acromegaly is treatable in most patients, but because of its slow and often insidious onset, it frequently is not diagnosed correctly.
Octreotide is one drug used to treat acromegaly. Octreotide exerts pharmacologic actions similar to those of the natural hormone somatostatin. Octreotide decreases GH and IGF-1 levels, as well as glucagons and insulin. Octreotide also suppresses luteinizing hormone (LH) response to gonadotropin releasing hormone (GnRH), decreases splanchnic blood flow, and inhibits the release of serotonin, gastrin, vasoactive intestinal peptide, secretin, motilin, and pancreatic polypeptide. In many patients, GH levels fall within one hour and headaches improve within minutes after the injection of octreotide. Several studies have shown that octreotide is effective for long-term treatment. Octreotide also has been used successfully to treat patients with acromegaly caused by non-pituitary tumors. In some acromegaly patients who already have diabetes, octreotide can reduce the need for insulin and improve blood sugar control.
Octreotide is currently available as Sandostatin LAR® Depot, which is, upon reconstitution, a suspension of microspheres containing octreotide acetate. Sandostatin LAR® Depot is the only medication indicated for the long-term maintenance therapy in acromegalic patients. It is also indicated for the long-term treatment of severe diarrhea and flushing episodes associated with metastatic carcinoid tumors and profuse water diarrhea associated with VIP-secreting tumors. Sandostatin LAR® T Depot is administered via intramuscular injection every four weeks, following a titration period. Octreotide acetate has also been available in an immediate-release formulation, Sandostatin® Injection solution, which was required to be administered by injection three times daily.
Octreotide is an octapeptide with the following amino acid sequence: L-cysteinamide, D-phenylalanyl-L-cysteiny-L-phenylalanyl-D-tryptophyl-L-lysyl-L-threonyl-N-[2-hydroxy-1-(hydroxymethyl)propyl]-,cyclic (2→7)-disulfide; [R-(R*,R*)]. The structure of octreotide is shown below.
The chemical formula is C49H66N10O10S2 and its molecular weight is 1019.3 Da. Its therapeutic category is gastric antisecretory agent.
The Food and Drug Administration (FDA) has approved the usage of a salt form of this peptide, octreotide acetate, as an injectable depot formulation for the treatment of growth hormone producing tumors (acromegaly and gigantism), pituitary tumors that secrete thyroid stimulating hormone(thyrotropinoma), diarrhea and flushing episodes associated with carcinoid syndrome, and diarrhea in patients with vasoactive intestinal peptide-secreting tumors (VIPomas).
Octreotide is used in nuclear medicine imaging by labelling with indium-111 (Octreoscan) to noninvasively image neuroendocrine and other tumours expressing somatostatin receptors.[4] More recently, it has been radiolabelled with carbon-11[5] as well as gallium-68, enabling imaging with positron emission tomography (PET), which provides higher resolution and sensitivity.
Octreotide can also be labelled with a variety of radionuclides, such as yttrium-90 or lutetium-177, to enable peptide receptor radionuclide therapy(PRRT) for the treatment of unresectable neuroendocrine tumours.
Octreotide is the acetate salt of a cyclic octapeptide. It is a long-acting octapeptide with pharmacologic properties mimicking those of the natural hormone somatostatin. Octreotide is known chemically as L-Cysteinamide, D-phenylalanyl-L-cysteinyl-L-phenylalanyl-D-tryptophyl-L-lysyl-L-threonyl-N-[2-hydroxy-1- (hydroxy-methyl) propyl]-, cyclic (2→7)-disulfide; [R-(R*,R*)].
Sandostatin LAR Depot is available in a vial containing the sterile drug product, which when mixed with diluent, becomes a suspension that is given as a monthly intragluteal injection. The octreotide is uniformly distributed within the microspheres which are made of a biodegradable glucose star polymer, D,L-lactic and glycolic acids copolymer. Sterile mannitol is added to the microspheres to improve suspendability.
Sandostatin LAR Depot is available as: sterile 5-mL vials in 3 strengths delivering 10 mg, 20 mg, or 30 mg octreotide-free peptide. Each vial of Sandostatin LAR Depot delivers:
| NAME OF INGREDIENT | 10 MG | 20 MG | 30 MG |
| octreotide acetate | 11.2 mg* | 22.4 mg* | 33.6 mg* |
| D, L-lactic and glycolic acids copolymer | 188.8 mg | 377.6 mg | 566.4 mg |
| mannitol | 41.0 mg | 81.9 mg | 122.9 mg |
| *Equivalent to 10/20/30 mg octreotide base. | |||
Each syringe of diluent contains:
| carboxymethylcellulose sodium | 12.5 mg |
| mannitol | 15.0 mg |
| water for injection | 2.5 mL |
The molecular weight of octreotide is 1019.3 (free peptide, C49H66N10O10S2) and its amino acid sequence is
 |
Octreotide has also been used off-label for the treatment of severe, refractory diarrhea from other causes. It is used in toxicology for the treatment of prolonged recurrent hypoglycemia after sulfonylurea and possibly meglitinides overdose. It has also been used with varying degrees of success in infants with nesidioblastosis to help decrease insulin hypersecretion.
Octreotide has been used experimentally to treat obesity, particularly obesity caused by lesions in the hunger and satiety centers of thehypothalamus, a region of the brain central to the regulation of food intake and energy expenditure.[6] The circuit begins with an area of the hypothalamus, the arcuate nucleus, that has outputs to the lateral hypothalamus (LH) and ventromedial hypothalamus (VMH), the brain’s feeding and satiety centers, respectively.[7][8] The VMH is sometimes injured by ongoing treatment for acute lymphoblastic leukemia (ALL) or surgery or radiation to treat posterior cranial fossa tumors.[6] With the VMH disabled and no longer responding to peripheral energy balance signals,
Octreotide has also been investigated for patients with pain from chronic pancreatitis,[11] and it may be useful in the treatment of thymic neoplasms.
The drug has been used off-label, injected subcutaneously, in the management of hypertrophic pulmonary osteoarthropathy (HPOA) secondary to non-small cell lung carcinoma. Although its mechanism is not known, it appears to reduce the pain associated with HPOA.[citation needed]
It has been used in the treatment of malignant bowel obstruction.[12]
Octreotide may be used in conjunction with midodrine to partially reverse peripheral vasodilation in the hepatorenal syndrome. By increasing systemic vascular resistance, these drugs reduce shunting and improve renal perfusion, prolonging survival until definitive treatment with liver transplant.[13] Similarly, octreotide can be used to treat refractory chronic hypotension.[14]
While successful treatment has been demonstrated in case reports,[15][16] larger studies have failed to demonstrate efficacy in treating chylothorax.[17]
Octreotide is often give as an infusion for management of acute haemorrhage from esophageal varices in liver cirrhosis on the basis that it reduces portal venous pressure, though current evidence suggests that this effect is transient and does not improve survival.[18]
A small study has shown that octreotide may be effective in the treatment of idiopathic intracranial hypertension.[19][20]
Octreotide has not been adequately studied for the treatment of children, pregnant and lactating women. The drug is given to these groups of patients only if a risk-benefit analysis is positive.[21][22]
 Acetate
Acetate
C53H74N10O14S2 , 1139.34326
The most frequent adverse effects (more than 10% of patients) are headache, hypothyroidism, cardiac conduction changes, gastrointestinal reactions (including cramps, nausea/vomiting and diarrhoea or constipation), gallstones, reduction of insulin release, hyperglycemia[23] or hypoglycemia, and (usually transient) injection site reactions. Slow heart rate, skin reactions such aspruritus, hyperbilirubinemia, hypothyroidism, dizziness and dyspnoea are also fairly common (more than 1%). Rare side effects include acute anaphylactic reactions, pancreatitis andhepatitis.[21][22] One study reported a possible association with rheumatoid arthritis.[24]
Some studies reported alopecia in patients who were treated by octreotide.[25] Rats which were treated by octreotide experienced erectile dysfunction in a 1998 study.[26]
A prolonged QT interval has been observed in patients, but it is uncertain whether this is a reaction to the drug or part of the patients’ illnesses.[21]
| Octreotide can reduce the intestinal resorption of ciclosporin, possibly making it necessary to increase the dose.[27] Patients with diabetes mellitusmight need less insulin or oral antidiabetics when treated with octreotide. The bioavailability of bromocriptine is increased;[22] besides being anantiparkinsonian, bromocriptine is also used for the treatment of acromegaly. |
|---|
Octreotide is absorbed quickly and completely after subcutaneous application. Maximal plasma concentration is reached after 30 minutes. The elimination half-life is 100 minutes (1.7 hours) on average when applied subcutaneously; after intravenous injection, the substance is eliminated in two phases with half-lives of 10 and 90 minutes, respectively.[21][22]
Conventional synthesis of octreotide may be divided into two main approaches, liquid-phase synthesis and solid-phase synthesis. · Octreotide first disclosed in US4395403, in which Octreotide is prepared by solution phase peptide synthesis. The process comprises; removing protected group from peptide;‘ linking together by an amide bond to two peptide unit; converting a function group at the N- or C- terminal; oxidizing a straight chain polypeptide by boron tristrifluoroacetate.
Since all the synthesis steps are carried out in liquid phase, US’403 process is a time- consuming, multi-step synthesis and it is difficult to separate octreotide from the reaction mixtures. Another solution phase approach described in US6987167 and WO2007110765A2, in which the cyclization of partially deprotected octreotide is carried out in the solution phase using iodine under specific conditions in presence of alcoholic solvents.
US6346601 B1 , WO2005087794A1 and WO2010089757A2 disclose a process for the preparation of octreotide by hybrid approach i. e synthesis of fragments on solid phase and condensing the obtained fragments in a liquid phase.
US6476186 describes the solid phase synthesis, in which the synthesis of octreotide using Thr(ol)(tBu)-2CI-trityl resin as starting material, followed by the cleavage of the straight chain peptide from the resin using a strong acid and the formation of the intra-molecular disulfide bond on the completely deprotected octreotide by oxidation using charcoal catalyst.
US20040039161A1 provides a solid phase .peptide synthetic method for the preparation of C-terminal alcohols using trichloroacetimidate activated linker, making the required peptide chain on the resin support, cleaving the attached peptide; air oxidation to form said C- terminal amino alcohol containing peptide and a 36.3% yield of octreotide after HPLC purification.
Charcoal oxidation or air oxidation needs longer reaction time and results in low yield. Further, in large scale, the conversion of dithiol to disulfide bond ends in unconverted starting material.
Another solid phase approach describes in Bioconjugate chem. 2009, 20, 1323-1331. This article discloses the process of somatostatin and octreotide analogues using solid phase peptide synthesis with CTC resin.
Journal of Harbin Institute of Technology, 2008, Vol 40 (2), 292-295, discloses the process for the preparation of octreotide using CTC resin. According to this process the obtained octreotide has the purity 70.26% by HPLC. During the process of peptide bond formation which is mediated by a coupling agent, the carboxylic group of amino acid interacts with the coupling agent to form an activated intermediate, which in turn interacts with the amino group of the next amino acid.
Racemization is a side-reaction that occurs during the preparation of a peptide. In large scale production, the formations of small amounts of epimers are possible. Detection and removal of these impurities are very difficult. This constitutes one of the most serious drawbacks for the implementation of peptides in commercial scale production.
Conventional syntheses of OCT may be divided two main approaches, direct solid-phase synthesis and liquid-phase synthesis. Direct solid-phase synthesis comprises attachment of a C-terminal amino acid to a resin, and step-by step elongation of the peptide chain, with pre- activated amino acids.
This route is expensive because it requires large excesses of starting amino acids and additionally is quite labor consuming as the peptide size increases, necessitating complex purification procedures to separate the product from the impurities since they are very similar to the final product. These shortcomings are especially important for large scale industrial production of the product. For example, see Canadian Patent Application 2,309,312 and U.S. Patent No. 6,476,186. With each successive condensation reaction required to add an amino acid, waste of starting materials increases, and purification steps are repeated. Liquid-phase synthesis comprises condensation of amino acids in solution. Several blocks, containing from 2 to 5 amino acids may be synthesized independently, followed by condensation of these synthons to each other in the required sequence.
For example, see WO 03/097668; U.S. Patent No. 4,395,403; and RU 2196144 C1. The advantage of this kind of processes is that it is less expensive than the previous one and the product is easier to purify. This method is also more effective for scale-up. However, liquid phase synthesis of lengthy peptide blocks, for example having more than 3 amino acids, is inefficient. Liquid-phase octreotide synthesis has the drawback is that the method is extremely labor-intensive and time consuming.
U.S. Patent No. 6,346,601 describes a method for octreotide synthesis where a solid-phase method is used to obtain a 7-mer, followed by condensation in solution with the modified amino acid threoninol. However, by using solid- phase synthesis to produce a 7-mer, only one less condensation is required compared to the solid-phase process for forming octreotide itself. Thus, only a marginal efficiency is introduced.
Summary of the invention According to an embodiment of the invention, there is provided a process for obtaining octreotide or a pharmaceutically acceptable salt thereof by hybrid solid-phase – liquid-phase synthesis. The synthesis comprises the steps of condensing two or three peptide blocks using liquid phase condensation to form a condensation product followed by cyclizing the product.
Each peptide block contains two or more amino acid residues, and at least one of the blocks is synthesized by solid-phase synthesis. The condensation product comprises in sequence the amino acids residues of octreotide. In the step of cyclizing, the condensation product is cyclized to form a disulfide bridge between the two cysteine residues, thereby forming octreotide. Further, according to another embodiment of the invention, a process is provided for obtaining an intermediate in octreotide synthesis by hybrid solid- phase – liquid-phase synthesis.
The synthesis of the intermediate comprises the steps of obtaining two or three peptide blocks, each peptide block containing two or more amino acid residues, and at least one of the blocks is synthesized by solid-phase synthesis. Subsequently, the peptide blocks are condensed using liquid phase condensation to form a condensation product, wherein the condensation product comprises in sequence the amino acids residues of octreotide.
This invention provides a more cost-effective and labor-saving method for obtaining OCT and its pharmaceutically acceptable salts by means of hybrid solid-phase – liquid-phase synthesis. The invention involves liquid phase condensation of two peptide blocks, at least one of which is obtained by solid- phase synthesis, the blocks containing more two or more amino acid residue in every block, followed by formation of a disulfide bridge from the two cysteine groups. Optionally, three blocks may be condensed. This hybrid solid phase-liquid phase method involves formation of one or more blocks of the octreotide amino acid sequence by solid-phase synthesis, followed by liquid phase condensation of the block(s) with required supplementary amino acids or other block(s) of amino acids.
This method is a blend of solid-phase and liquid-phase synthesis methods, combining the efficiencies of preparing shorter (6-mer or less) peptides using a solid-phase method with relative cheapness and easiness of purification of the product, characteristic of the liquid-phase method. Generally, the methods of invention comprise synthesizing specific side- chain protected peptide fragment intermediates of OCT on a solid support or in solution, coupling of the protected fragments in solution to form a protected OCT, followed by deprotection of the side chains and oxidation to yield the final OCT. The present invention further relates to individual peptide fragments which act as intermediates in the synthesis of the OCT
………………
Stage-I: Preparation of protected octreotide anchored to 2-CTC Resin
Method -1:
Octreotide was synthesized manually on 2-chlorotrityl chloride resin (substitution 0.90 mmol/g) by standard Fmoc solid phase synthesis strategy. The resin was soaked in the mixture of DC and DMF for the swelling. Fmoc-Thr(tBu)-OL was treated with the swelled 2- CTC resin in DCM in the presence of DIEA and substitution level was determined by weight gain measurements and also by UV Method. After the coupling of the first amino acid onto the resin, the un-reacted linkers on the resin (polymer) are protected, to avoid the undesired peptide chain formation, with a solution of 5% DIEA and 10% methanol in DCM. This process of capping is performed after anchoring the first protected amino acid to the resin. The complete synthesis was achieved by stepwise coupling of Fmoc-Amino acids to the growing peptide chain on the resin. All the couplings were carried out in DMF. The N- terminal Fmoc group was removed with 20 %( V/V) piperidine in DMF. The couplings were performed by dissolving the Fmoc-Amino acid (2 eq.) and HOBt (2 eq.) in DMF. The solution was cooled on ice and then DIC (2 eq.) was added. The reaction mixture was added to the resin and allowed to react for 2 hrs. The efficiency of the coupling was monitored using the Kaiser Ninhydrin test. The coupling step was repeated if Kaiser test was found positive. The sequence of addition for the synthesis of Octeriotide was Fmoc-Cys(Trt), Fmo-Thr(tBu), Fmoc-Lys(Boc), Fmoc-Trp(Boc), Fmoc-Phe, Fmoc-Cys(Trt), Boc-D-Phe.
Method -2:
Octreotide was synthesized manually on 2-chlorotrityl chloride resin (substitution 0.90 mmol/g) by standard Fmoc solid phase synthesis strategy. The resin was soaked in the mixture of MDC and DMF for the swelling. Fmoc-Thr-OL was treated with the swelled 2-CTC resin in DCM in the presence of DIEA and substitution level was determined by weight gain measurements and also by UV Method. After the coupling of the first amino acid onto the resin, the un-reacted linkers on the resin (polymer) are protected, to avoid the undesired peptide chain formation, with a solution of 5% DIEA and 10% methanol in DCM. This process of capping is performed after anchoring the first protected amino acid to the resin. The complete synthesis was achieved by stepwise coupling of Fmoc-Amino acids to the growing peptide chain on the resin. All the couplings were carried out in DMF. The N- terminal Fmoc group was removed with 20 %( V7V) piperidine in DMF. The couplings were performed by dissolving the Fmoc-Amino acid (2 eq.) and HOBt (2 eq.) in DMF. The solution was cooled on ice and then DIC (2 eq.) was added. The reaction mixture was added to the resin and allowed to react for 2 hrs. The efficiency of the coupling was monitored using the Kaiser Ninhydrin test. The coupling step was repeated if Kaiser test was found positive. The sequence of addition for the synthesis of Octeriotide was Fmoc-Cys(Trt), Fmo-Thr(tBu), Fmoc-Lys(Boc), Fmoc-Trp(Boc), Fmoc-Phe, Fmoc-Cys(Trt), Boc-D-Phe.
Stage-ll: Cleavage of peptide from resin along with global deprotection
The peptide resin (200 g, obtained in stage I) was swelled in DCM (500 mL) for 15 to 20 minutes under nitrogen at 25-30° C. The cocktail mixture (2.0 L – TFA (1.8 L), water (80 mL) DCM (80mL) and TIPS (80 mL)) was charged to the resin at 25-30° C. and the obtained reaction mixture was stirred for 2.5 hours at 25-30°C under nitrogen atmosphere. The reaction mixture was filtered and washed the resin with TFA (250 mL). The obtained filtrate was charged into cold MTBE (4 L, pre-cooled to a temperature of 0 -5° C) under stirring and allowing the temperature to rise more than 5° C. The reaction mixture was stirred for 45-75 minutes at 0-5°C. The obtained suspension was filtered, washed the solid with MTBE (5 L) and dried the solid under nitrogen. The product was stir with 5%ethanol in ethyl acetate at 25-30°C. Filtered the product, wash ith ethyl acetate and dried under vacuum to obtain a desired product
Stage-Ill: Disulphide bridge formation
The free thiol (100 g) obtained above is dissolved in methanol (22.0 L) with small amount of acetic acid and water (4.5 L) and stirred. Iodine solution (20gm iodine in 500 mL methanol) was added to the reaction mass slowly up to yellow color persists. The reaction was maintained for another 2 hrs, and the excess iodine quenched with Indion 830-S Resin (900 g) and filtered the resin. The filtrate was evaporated and precipitated using TBE or directly taken the solution for purification using preparative HPLC.
Stage -IV: Preparative HPLC Purification
Method-1 :
The crude disulphide bridge peptide was purified on a preparative reverse phase HPLC system using Kromasil C-18, 10 micron (50 x 250 mm). and eluting with a solvent system of 0.2% acetic acid in water(A) and 0.2% acetic acid in methanol(B). A linear gradient of 20- 60% B was used at a flow rate of 80mlJmin and detection at 220 nm.
The octreotide was eluted at around 25% methanol. The fractions were collected at regular intervals and assayed by HPLC to determine the purity of fractions. The desired purities fractions were pooled together and evaporated using Rota evaporator. The aqueous layer was lyophilized to isolate octreotide acetate
Method-2:
The crude disulphide bridge peptide was purified on a preparative reverse phase HPLC system using Kromasil C-18, 10 micron (50 x 250 mm) and eluting with a solvent system of 0.4% acetic acid in water(A) and methanol(B). A linear gradient of 25-60% B was used at a flow rate of 80mL/min and detection at 220 nm.
The octreotide was eluted at around 25% methanol. The fractions are collected at regular intervals and are assayed by HPLC to determine the purity and fractions. The desired purities may be pooled together and were evaporated using Rota evaporator. The aqueous layer was lyophilized to isolate octreotide acetate >
……………………….
Octreotide is a highly potent and pharmacologically selective analog of somatostatin. It inhibits growth hormone for long duration and is thereof indicated for acromegaly to control and reduce the plasma level of growth hormone. The presence of D-Phe at the N-terminal and an amino alcohol at the C-terminal, along with D-Tryptophan and a cyclic structure makes it very resistant to metabolic degradation.
Octreotide comprises 8 amino acids which has the following structural formula:
(D)Phe-Cys-Phe-{D)Trp-Lys-Thr-Cys-Thr-OL
Formula(l) wherein sulphur atoms of the Cys at the position 2 and of the Cys at the position 7 are mono-cyclic to form an -S-S- bridge.
A considerable number of known, naturally occurring small and medium-sized cyclic peptides as well as some of their artificial derivatives and analogs possessing desirable pharmacological properties have been synthesized. However, wider medical use is often hampered due to complexity of their synthesis and purification. Therefore, improved methods for making these compounds in simple, lesser steps and at lesser cost are desirable and this is the felt need of the industry and the mankind.
Conventional synthesis of octreotide may be divided into two main approaches, direct solid-phase synthesis and liquid-phase synthesis. Solution phase synthesis has been described by Bauer et al., (Sandoz) (Eur. Pat. Appl. 29,579 and U.S. Pat. No. 4,395,403). The process comprises: removing protected group from peptide; linking together by an amide bond two peptide unit; converting a function group at the N- or C-terminal; oxidizing a straight chain polypeptide by boron tristrifluoroacetate. This process involves a time-consuming, multi-step synthesis, and it is difficult to separate octreotide from the reaction mixtures since all the synthesis steps are carried out in liquid phase.Another solution phase approach described by Chaturvedi, et al., (Wockhardt) in U.S. Pat. No. 6,987,167 and EP 1506219 A, claims the cyclization of partially deprotected octreotide in the solution phase using iodine under conditions and for a time sufficient to form the octreotide.
Synthesis in solid phase have been described subsequently (Mergler et al., Alsina et al., Neugebauer). The above prior art for solid phase peptide synthesis cites the octapeptide formation, by starting the synthesis from the threoninol residue which makes it mandatory to protect this residue. Mergler et al., (Peptides: Chemistry and Biology. Proceedings of the 12* American Peptide Symposium. Smith, J.A. And Rivier J.E. Eds ESCOM, Leiden, Poster 292 Presentation, (1991) ) describes a synthetic process, using an aminoethyl resin upon which the Threoninol residue is incorporated with the two alcohol functions protected in acetal form The synthesis is carried out following an Fmoc/tBu protection scheme, forming the disulphide bridge on resin by oxidation of the thiol groups of the previously deprotected cysteine residues and releasing and deprotecting the peptide with a 20% mixture of TFA/DCM.
In early 1997, Alsina J. et al. ( Alsina J., Chiva C, Ortiz M., Rabanal F., Giralt E., and Albericio F., Tetrahedron Letters, 38, 883-886, 1997) described the incorporation, on active carbonate resins, of a Threoninol residue with the amino group protected by the Boc group and the side chain protected by a BzI group. The synthesis was then continued by Boc/Bzl strategy. Formation of the disulfide bridge was carried out directly on resin using iodine and the peptide was cleaved from the resin and its side chain protecting groups were simultaneously removed with HF/anisole 9/1. At the final stage the formyl group was removed with a piperidine/DMF solution.
Neugebauer (Neugebauer W., Lefevre M.R., Laprise R, Escher E., Peptides: Chemistry, Structure and Biology, p 1017, Marshal G.R. And Rivier J.E. Eds. ESCOM.Leiden (1990) described a linear synthesis with a yield of only 7%.
Edwards et al., (Edwards B.W., Fields C.G., Anderson CJ., Pajeau T.S., Welch M.J., Fields G.B., J.Med.Chem. 37, 3749-3757 (1994) carried out another another solid- phase type approximation; they synthesized step-by-step on the resin, the peptide D- Phe-Cys(Acm)-Phe-D-Tφ(Boc)-Lys(Boc)-Thr(tBu)-Cys(Acm)-HMP-Resin. Next they proceeded to form the disulfide on resin and then release the peptide from the resin by means of aminolysis with threoninol, with obtaining a total yield of only 14%.
The solid phase synthesis described by Yao-Tsung Hsieh et. al., in U.S. Pat. No. 6,476,186 involves the synthesis of octreotide by using Thr(ol)(tBu)-2Cl-trityl resin as starting material followed by the cleavage of the straight chain peptide from the resin by using a strong acid and the formation of the intra-molecular disulfide bond on the completely deprotected octreotide by oxidation using charcoal catalyst and a higher yield of >70%.
Another solid phase synthesis described by Berta Ponsati et.al (Lipotec) in U.S. Pat No. 6,346,601 and EP 0953577 B involve the coupling of threoninol on the protected heptapeptide in solution, after a selective acid cleavage from the chlorotrityl resin without affecting the peptide side-chain protecting groups.
A hybrid solid phase-liquid phase method for synthesis of octreotide described by Iarov et al., (Dalton Chemical Laboratories) in WO 2005087794 wherein the method comprises liquid phase condensation of two or three peptide blocks in which at least one peptide block is synthesized by solid-phase method.
EP 1511761 Bl involves cyclization on the semi-protected linear peptide wherein one of the cysteine residue is protected with an orthogonal protecting group. The radioactive isotope labeling of octreotide by the coupling of bifunctional chelating agents like DTPA or DOTA to the peptide was described by Te- Wei Lee et al., in U.S. Pat. No. 5,889,146 (Inst, of Nuclear Energy Research)
The method for cyclization of linear vapreotide by means of intramolecular cysteine formation has been described by Quattrini et. al., (Lonza AG) in WO 2006048144, wherein the process involves the synthesis of linear vapreotide peptide on Sieber-resin (from Novabiochem) by Fmoc standard groups, wherein the side chain protecting groups are D or L-Trp(Boc), Cys(Trt), Lys(Boc), Tyr(tBu). The protected peptide is cleaved off in 5% TFA in dichloromethane and then globally deprotected by acidolysis in a cleavage mix of 300 equivalents of concentrated TFA, 12 equivalents of Dithiothreitol, 12 equivalents of Dichloromethane, 50 equivalents of water forl hour at room temperature. The Boc groups are removed. The product was subjected to charcoal method using trace amounts of activated, powdered charcoal wherein a concentration of the linear cysteinyl peptide of 50 mg/ml (1 eq.) in DMF in the presence of 1 eq. Diisopropyl-ethyl-amine and that additionally air was sparged at low pressure into the liquid under stirring. After 15-20 hrs, 100% conversion was achieved with 84% (w/w) analytical yield of 79% vapreotide.
The formation of intramolecular disulphide formation in a polypeptide by reacting with hydrogen peroxide has been described by Mineo Niwa et al. (Fujisawa Pharmaceutical Co.) in U.S. Pat. No.5, 102,985 wherein the reaction is to be carried out at a pH of about 6 tol 1, wherein the molar ratio of H2O2 to polypeptide is within the range of 1:1 to 100:1. The above cited prior art mainly carries out the cyclization of the peptide on the resin or on partially protected or protected peptides. The use of partial or minimal protecting group strategies and improvement in the activation methods have considerable effect on limitations of poor solubility and possible danger of racemization due to the overactivation of carboxyl groups. However, these approaches do not overcome the problem of the poor coupling efficiency between large peptide segments, because of the intrinsic difficulty of obtaining effective molar concentrations for high molecular weight molecules.
Example 8:
Oxidation of S-H peptide with DMSO-HCl to get S-S peptide:
(D)Phe-Cys-Phe-(D)Trp-Lys-Thr-Cys-Thr-OL
Formula (1)
S-H peptide ( 9g) was dissolved in 6.5L DMSO and under ice-cooling 6.5L IM HCl was added slowly so that temperature is below 26°C. Stirring was continued for 6 hours. At room temperature after six hours reaction mixture was diluted with 13L of water and filtered through Whatman no. 41 through Celite bed. The filtrate was loaded on C- 18 column for concentration. The compound was eluted with 100% acetonitrile. The eluant was concentrated on rotavap and then the concentrated solution was centri-evaporated to dryness. The RP-HPLC profile of crude octreotide is depicted in Figure 1.
Weight of crude peptide =3.9g.(45%)
Purity: 44.25%
Example 9:
Purification of crude octreotide:
The crude octreotide was loaded on to cation ion exchange column and eluted using a salt gradient using a Akta Purifier (by Amersham, Sweden) low pressure chromatography system. The IEX fractions of purity >70% were further loaded for RP-HPLC purification on Kromacil C-18 column of (250x50mm,100A°.) The peptide was purified by using aqueous TF A(O-0.5%) and methanol/ethanol and/or Acetonitrile in a gradient program on a Shimadzu preparative HPLC System consisting of a controller, 2 LC8A pumps, and UV-Vis detector. The purified peptide was analysed by analytical RP-HPLC (Figure 5). Fractions of > 99% purity were subjected either by RP-HPLC or IEX to salt exchange and concentrated to remove organic solvent either by rota or reverse osmosis and subsequently lyophilized to get final API with purification step yield of 70% or above.The MS spectrum of octreotide is depicted in Figure 6.
References
- Official manufacturer website for up-to-date dosing & safety information:http://www.sandostatin.com
- Maurer R, Gaehwiler BH, Buescher HH, Hill RC, Roemer D. Opiate antagonistic properties of an octapeptide somatostatin analog. Proceedings of the National Academy of Sciences USA. 1982 Aug;79(15):4815-7. PMID 6126877
- Allen MP, Blake JF, Bryce DK, Haggan ME, Liras S, McLean S, Segelstein BE. Design, synthesis and biological evaluation of 3-amino-3-phenylpropionamide derivatives as novel mu opioid receptor ligands. Bioorganic and Medicinal Chemistry Letters. 2000 Mar 20;10(6):523-6.PMID 10741545
- Medscape: Octreoscan review
- Joshua Chin, Matthew Vesnaver, Vadim Bernard-Gauthier, Erin Saucke-Lacelle, Björn Wängler, Carmen Wängler, Ralf Schirrmacher. Amino Acids: Direct one-step labeling of cysteine residues on peptides with 11C-methyl triflate for the synthesis of PET radiopharmaceuticals. Amino Acids. 2013 Aug 7. PMID 23921782
- Lustig RH, Hinds PS, Ringwald-Smith K, Christensen RK, Kaste SC, Schreiber RE, Rai SN, Lensing SY, Wu S, Xiong X (June 2003). “Octreotide therapy of pediatric hypothalamic obesity: a double-blind, placebo-controlled trial”. J. Clin. Endocrinol. Metab. 88 (6): 2586–92.doi:10.1210/jc.2002-030003. PMID 12788859.
- Flier JS (2004). “Obesity wars: Molecular progress confronts an expanding epidemic”. Cell116 (2): 337–50. doi:10.1016/S0092-8674(03)01081-X. PMID 14744442.
- Boulpaep, Emile L.; Boron, Walter F. (2003). Medical physiologya: A cellular and molecular approach. Philadelphia: Saunders. p. 1227. ISBN 0-7216-3256-4.
- Lustig RH (2011). “Hypothalamic obesity after craniopharyngioma: mechanisms, diagnosis, and treatment”. Front Endocrinol (Lausanne) 2: 60. doi:10.3389/fendo.2011.00060.PMC 3356006. PMID 22654817.
- Lustig RH, Greenway F, Velasquez-Mieyer P, Heimburger D, Schumacher D, Smith D, Smith W, Soler N, Warsi G, Berg W, Maloney J, Benedetto J, Zhu W, Hohneker J (February 2006). “A multicenter, randomized, double-blind, placebo-controlled, dose-finding trial of a long-acting formulation of octreotide in promoting weight loss in obese adults with insulin hypersecretion”. Int J Obes (Lond) 30 (2): 331–41. doi:10.1038/sj.ijo.0803074.PMC 1540404. PMID 16158082.
- Uhl W, Anghelacopoulos SE, Friess H, Büchler MW (1999). “The role of octreotide and somatostatin in acute and chronic pancreatitis”. Digestion. 60 Suppl 2: 23–31.doi:10.1159/000051477. PMID 10207228.
- Shima Y, Ohtsu A, Shirao K, Sasaki Y (May 2008). “Clinical efficacy and safety of octreotide (SMS201-995) in terminally ill Japanese cancer patients with malignant bowel obstruction”.Jpn. J. Clin. Oncol. 38 (5): 354–9. doi:10.1093/jjco/hyn035. PMID 18490369.
- Skagen C, Einstein M, Lucey MR, Said A (Feb 2009). “Combination Treatment With Octreotide, Midodrine, and Albumin Improves Survival in Patients With Type 1 and Type 2 Hepatorenal Syndrome.”. J Clin Gastroenterol. 43 (7): 680–5. doi:10.1097/MCG.0b013e318188947c.PMID 19238094.
- Patient.co.uk (Feb 2013). Hypotension.
- Kilic D, Sahin E, Gulcan O, Bolat B, Turkoz R, Hatipoglu A (2005). “Octreotide for treating chylothorax after cardiac surgery”. Tex Heart Inst J 32 (3): 437–9. PMC 1336729.PMID 16392238.
- Siu SL, Lam DS (2006). “Spontaneous neonatal chylothorax treated with octreotide”. J Paediatr Child Health 42 (1-2): 65–7. doi:10.1111/j.1440-1754.2006.00788.x.PMID 16487393.
- Chan EH, Russell JL, Williams WG, Van Arsdell GS, Coles JG, McCrindle BW (November 2005). “Postoperative chylothorax after cardiothoracic surgery in children”. Ann. Thorac. Surg. 80(5): 1864–70. doi:10.1016/j.athoracsur.2005.04.048. PMID 16242470.
- Gøtzsche PC, Hróbjartsson A (2008). “Somatostatin analogues for acute bleeding oesophageal varices”. Cochrane Database Syst Rev (3): CD000193.doi:10.1002/14651858.CD000193.pub3. PMID 18677774.
- Greek Researchers Investigate Octreotide Hypertension Research Foundation, accessed 2011-01-02
- Panagopoulos GN, Deftereos SN, Tagaris GA, Gryllia M, Kounadi T, Karamani O, Panagiotidis D, Koutiola-Pappa E, Karageorgiou CE, Piadites G (2007). “Octreotide: a therapeutic option for idiopathic intracranial hypertension”. Neurol Neurophysiol Neurosci: 1. PMID 17700925.
- Haberfeld, H, ed. (2009). Austria-Codex (in German) (2009/2010 ed.). Vienna: Österreichischer Apothekerverlag. ISBN 3-85200-196-X.
- ^ Jump up to:a b c d Dinnendahl, V, Fricke, U, ed. (2010). Arzneistoff-Profile (in German) 8 (23 ed.). Eschborn, Germany: Govi Pharmazeutischer Verlag. ISBN 978-3-7741-9846-3.
- Hovind P, Simonsen L, Bülow J (March 2010). “Decreased leg glucose uptake during exercise contributes to the hyperglycaemic effect of octreotide”. Clin Physiol Funct Imaging 30(2): 141–5. doi:10.1111/j.1475-097X.2009.00917.x. PMID 20132129.
- Saif MW (July 2011). “Rheumatoid arthritis associated with the use of Sandostatin® LAR® depot in a patient with pancreatic neuroendocrine tumor. An association or a coincidence? The first case report”. JOP 12 (4): 425–8. PMID 21737909. Lay summary – eHealthMe.com.
- van der Lely AJ, de Herder WW, Lamberts SW (November 1997). “A risk-benefit assessment of octreotide in the treatment of acromegaly”. Drug Saf 17 (5): 317–24. PMID 9391775.
- Kapicioglu S, Mollamehmetoglu M, Kutlu N, Can G, Ozgur GK (January 1998). “Inhibition of penile erection in rats by a long-acting somatostatin analogue, octreotide (SMS 201-995)”. Br J Urol 81 (1): 142–5. PMID 9467491.
- Klopp, T, ed. (2010). Arzneimittel-Interaktionen (in German) (2010/2011 ed.). Arbeitsgemeinschaft für Pharmazeutische Information. ISBN 978-3-85200-207-1.
| US8507432 | Jun 11, 2010 | Aug 13, 2013 | Endo Pharmaceuticals Solutions Inc. | Controlled release formulations of octreotide |
| US20100247594 * | Jun 11, 2010 | Sep 30, 2010 | Endo Pharmaceuticals Solutions Inc. | Delivery of dry formulations of octreotide |
| US20110009338 * | Jun 11, 2010 | Jan 13, 2011 | Endo Pharmaceuticals Solutions Inc. | Controlled release formulations of octreotide |
| WO2010089757A2 | May 4, 2009 | Aug 12, 2010 | Usv Limited | An improved process for synthesis of cyclic octapeptide |
| WO2013046233A2 | Sep 28, 2012 | Apr 4, 2013 | Mylan Laboratories Ltd | Process for the preparation of octreotide acetate |
| WO2013132505A1 | Mar 9, 2012 | Sep 12, 2013 | Natco Pharma Limited | Improved process for preparation of octreotide by solution phase peptide synthesis |
| US8377891 | May 4, 2009 | Feb 19, 2013 | Usv, Ltd. | Process for synthesis of cyclic octapeptide |
| WO2003097668A2 * | Apr 16, 2003 | Nov 27, 2003 | Suresh Beri | Novel process for production of the somatostatin analog, octreotide |
| US6346601 * | Jan 29, 1999 | Feb 12, 2002 | Lipotec S.A. | Procedure for obtaining the somatostatin analog, octreotide |
| US6476186 * | May 24, 2000 | Nov 5, 2002 | Institute Of Nuclear Energy Research | Process for preparing octreotide and derivatives thereof |
| WO2005087794A1 | Mar 14, 2005 | Sep 22, 2005 | Dalton Chemical Lab Inc | Process for octreotide synthesis |
| WO2007110765A2 | Mar 28, 2007 | Oct 4, 2007 | Deshpande Amol Ashok | Processes for the preparation of octreotide |
| WO2010089757A2 | May 4, 2009 | Aug 12, 2010 | Usv Limited | An improved process for synthesis of cyclic octapeptide |
| US4395403 | Nov 16, 1981 | Jul 26, 1983 | Sandoz Ltd. | Polypeptides, processes for their production, pharmaceutical compositions comprising said polypeptides and their use |
| US6346601 | Jan 29, 1999 | Feb 12, 2002 | Lipotec S.A. | Procedure for obtaining the somatostatin analog, octreotide |
| US6476186 | May 24, 2000 | Nov 5, 2002 | Institute Of Nuclear Energy Research | Process for preparing octreotide and derivatives thereof |
| US6987167 | May 22, 2002 | Jan 17, 2006 | Wockhardt Limited | Process for production of the somatostatin analog, octreotide |
| US20040039161 | Aug 22, 2002 | Feb 26, 2004 | Mayer John Philip | Use of trichloroacetimidate linker for peptide synthesis |
DEAR READER OF NEW DRUG APPROVALS

TACROLIMUS

Tacrolimus, Fujimycin
104987-11-3 CAS, 804.0182, C44H69NO12
- Astagraf XL
- FK 506
- FR 900506
- FR900506
- LCP-Tacro
- Prograf
- Protopic
- Tacrolimus
- Tacrolimus hydrate
- Tsukubaenolide hydrate
- UNII-WM0HAQ4WNM
3S-[3R*[E(1S*,3S*,4S*)],4S*,5R*,8S*,9E,12R*,14R*,15S*,16R*,18S*,19S*,26aR*-5,6,8,11,12,13,14,15,16,17,18,19,24,25,26,26a-hexadecahydro-5, 19-dihydroxy-3-[2-(4-hydroxy-3-methoxycyclohexyl)-1-methylethenyl]-14,16-dimethoxy-4,10,12,18-tetramethyl-8-(2-propenyl)-15,19-epoxy-3H-pyrido[2,1-c] [1,4] oxaazacyclotricosine-1,7,20,21(4H,23H)-tetrone, monohydrate
17-Allyl-1,14-dihydroxy-12-[2-(4-hydroxy-3-methoxycyclohexyl)-1-methylvinyl]-23,25-dimethoxy-13,19,21,27-tetramethyl-11,28-dioxa-4-azatricyclo[22.3.1.04,9]octacos-18-ene-2,3,10,16-tetraone
Astellas Pharma (Originator), LAUNCHED 1993
CTK8E6891, 109581-93-3 MONOHYDRATE TACROLIMUS
Tacrolimus (also FK-506 or Fujimycin) is an immunosuppressive drug whose main use is after organ transplant to reduce the activity of the patient’s immune system and so the risk of organ rejection. It is also used in a topical preparation in the treatment of severe atopic dermatitis, severe refractory uveitis after bone marrow transplants, and the skin condition vitiligo. It was discovered in 1984 from the fermentation broth of a Japanese soil sample that contained the bacteria Streptomyces tsukubaensis. Tacrolimus is chemically known as a macrolide. It reduces peptidyl-prolyl isomerase activity by binding to the immunophilin FKBP-12 (FK506 binding protein) creating a new complex. This FKBP12-FK506 complex interacts with and inhibits calcineurin thus inhibiting both T-lymphocyte signal transduction and IL-2 transcription.
PATENT
| Canada | 2037408 | 2002-12-17 | EXPIRY 2011-03-01 |
| Canada | 1338491 | 1996-07-30 | 2013-07-30 |
| United States | 5665727 | 1994-09-09 | 2014-09-09 |
| United States | 5260301 | 1994-02-28 | 2011-02-28 |
Pan Sup Chang, Hoon Cho, “Water soluble polymer-tacrolimus conjugated compounds and process for preparing the same.” U.S. Patent US5922729, issued April, 1997.
Tacrolimus is a naturally-occurring macrolide isolated from the fermentation broth of Streptomyces tsukubaensis that was originally discovered by Fujisawa (now Astellas Pharma) in 1984. Tacrolimus possesses immunosuppressive properties and suppresses IL-2 production from helper T-cells, resulting in inhibition of the activation and proliferation of cytotoxic T-cells. In the cell, tacrolimus binds to an immunophilin called FKBP-12 and forms a tacro-immunophilin complex that, in turn, binds to calcineurin and prevents the dephosphorylation of cytoplasmic NF-AT thus disallowing it from reaching the nucleus, thereby strongly inhibiting IL-2 gene transcription. As a result, T-cell activation and proliferation is inhibited.
In 1993, Prograf(R) (tacrolimus capsules and injection) received clearance from the Japanese Ministry of Health and Welfare and was introduced in Japan the same year for the treatment of kidney and liver transplant rejection. Based on two large phase III comparative clinical trials, the product received clearance from the FDA in April 1994, and was made available two months later for commercial use in the U.S. The product is available extensively for transplant rejection. Prograf(R) was also launched in Japan for the treatment of myasthenia gravis and for the treatment of heart transplant rejection; the latter indication was approved in the U.S. in 2006 and launched in 2007. In 2008, Astellas Pharma preregistered the compound in Japan for the oral treatment of all cases of myasthenia gravis. The same year, Senju launched the product in Japan for the treatment of vernal and perennial allergic conjunctivitis in patients unresponsive to anti-allergic drugs. In 2009, the product was approved and commercialized in Japan for the treatment of ulcerative colitis. In 1999, Astellas Pharma launched Protopic(R) (tacrolimus ointment) in Japan for the treatment of atopic dermatitis and in 2001, Protopic(R) was commercialized in the U.S. and Europe. In April 2005, tacrolimus (capsules) was commercialized again by Astellas Pharma in Japan for the treatment of rheumatoid arthritis (RA) in patients who respond insufficiently to current therapies. The following year, Senju received approval in Japan for the use of tacrolimus for the treatment of vernal conjunctivitis and perennial allergic conjunctivitis. A once-daily capsule was approved in the E.U. in 2006. The compound was launched in 2007 in Japan for lupus nephritis. In 2009, the product was approved in US for the prophylaxis of organ rejection in allogeneic kidney transplantation in combination with mycophenolate mofetil and, in the E.U., for the prophylaxis of transplant rejection in adult and pediatric, kidney, liver or heart allograft recipients. In 2011, the compound was launched in Japan for the prophylaxis of organ rejection in patients receiving allogeneic small bowel transplants. In 2013, the indication for interstitial pneumonia associated with polymyositis/dermatomyositis was approved in Japan and an extended release formulation was approved in the U.S. for the prophylaxis of organ rejection in adult patients receiving kidney transplants. This extended release formulation was launched in the U.S. in August 2013. Veloxis Pharmaceuticals (formerly LifeCycle Pharma) is developing a once-daily tablet formulation of tacrolimus (Envarsus®) with improved bioavailability and reduced variability compared with the modified-release version of the compound. Envarsus® has been pre-registered in E.U. and the U.S. for the prevention of transplant rejection in kidney transplant patients. The company is also evaluating the compound in phase II trials for the treatment of autoimmune hepatitis.
In terms of clinical development, the National Cancer Institute (NCI) is developing tacrolimus in phase III for the treatment of graft-versus-host disease (GVHD). Phase III trials are also underway at Astellas Pharma for the treatment of psoriasis, ulcerative colitis and chronic focal encephalitis (Rasmussen’s encephalitis), while early clinical trials are ongoing for asthma. In 2009, Astellas Pharma withdrew an NDA seeking approval in the U.S. based on potential clinical challenges that would result from FDA requirements to conduct additional clinical studies. Kyoto University had been conducting phase II clinical studies for the treatment of Crohn’s disease; however, no recent development has been reported for this research.
In 2003, Sucampo Pharmaceuticals obtained a license from Astellas Pharma to develop and market tacrolimus for ophthalmic indications in the U.S. and Europe, however, in June 2005, the company voluntarily discontinued its tacrolimus eye drops development program due to FDA safety concerns. In 2005, Senju and Astellas Pharma established an agreement to codevelop an eye drop formulation of tacrolimus in Japan. Also, Astellas Pharma granted Senju exclusive manufacturing and marketing rights of the compound. In 2003, Astellas Pharma and GlaxoSmithKline signed an agreement for the copromotion of Protopic(R) in the U.S for atopic dermatitis. An additional agreement for the copromotion of Protopic(R) in South America for the same indication was signed in 2004 between Astellas Pharma and Roche. Tacrolimus was designated orphan drug status in Japan in 1993 and in 2005 for the suppression of organ rejection in allogenic kidney transplantation and for the treatment of vernal conjunctivitis, respectively, in patients unresponsive to anti-allergic drugs. In the E.U., the latter indication was assigned orphan drug designation in 2004. The product was withdrawn from the community register of designated orphan medicinal products in the E.U. in April 2010 on request of the sponsor. In 1998 and 2005, the FDA assigned orphan drug designation for the prophylaxis of GVHD and for the prophylaxis of organ rejection in patients receiving heart transplants. Finally, in 2008, orphan designation was received in Japan for the treatment of myasthenia gravis. In 2012, an additional orphan drug designation was assigned in the U.S. for the treatment of hemorrhagic cystitis. This designation was granted in Japan in 2012 for the treatment of interstitial pneumonia accompanied with polymyositis/dermatomyositis complex. In 2012, orphan drug designation was assigned in Japan for the treatment of interstitial pneumonia accompanied with polymyositis/dermatomyositis complex. In 2012, the product was licensed by Veloxis Pharmaceuticals to Chiesi on an exclusive basis for the commercialization and distribution in Europe, Turkey and CIS countries for the prevention of rejection in kidney transplant recipients. In 2013, an additional orphan drug designation was assigned in the U.S. for the prophylaxis of organ rejection in patients receiving allogeneic kidney transplant.
Tacrolimus, also known as FK-506 or FR-900506, has the chemical tricyclic structure shown below:
corresponding to C44H69NO-|2- Tacrolimus appears in the form of white crystals or crystalline powder. It is practically insoluble in water, freely soluble in ethanol and very soluble in methanol and chloroform. The preparation of tacrolimus is described in EP-A-0 184 162 and analogues of tacrolimus are disclosed e.g. in EP-A-0444659 and US 6,387,918
Tacrolimus is an immunosuppressive agent produced by Streptomyces tsukubaensis No. 9993 and is the compound of formula (I) wherein R.sub.1 and R.sub.2 are both hydrogen. Tacrolimus, which is also called FK-506, has first discovered by Tanaka, Kuroda and their colleague in Japan see, J. Am. Chem. Soc., 1987, 109, 5031 and U.S. Pat. No. 4,894,366 issued on Jan. 16, 1990!.
July 19, 2013 /PRNewswire/ — Astellas Pharma US, Inc. (“A.stellas”), a U.S. subsidiary of Tokyo-based Astellas Pharma Inc., announced today that the U.S. Food and Drug Administration (FDA) has approved Astagraf XL (tacrolimus extended-release capsules) for the prophylaxis of organ rejection in patients receiving a kidney transplant with mycophenolate mofetil (MMF) and corticosteroids, with or without basiliximab induction.
“Each transplant recipient is different and requires a personalized treatment approach. The approval of Astagraf XL marks an important milestone in post-transplant care as it provides physicians with a new treatment option for kidney t recipients,” said Sef Kurstjens, M.D., PhD., chief medical officer, Astellas Pharma, Inc. “Astellas is pleased to continue our more than 20-year commitment to the field of transplant immunology.”


PROTOPIC (tacrolimus) Ointment contains tacrolimus, a macrolide immunosuppressant produced by Streptomyces tsukubaensis. It is for topical dermatologic use only. Chemically, tacrolimus is designated as [3S[3R*[E(1S*,3S*,4S*)],4S*,5R*,8S*,9E,12R*,14R*,15S*,16R*,18S*,19S*,26aR*]]5,6,8,11,12,13,14,15,16,17,18,19,24,25,26,26a-hexadecahydro-5,19-dihydroxy3-[2-(4-hydroxy-3-methoxycyclohexyl)-1-methylethenyl]-14,16-dimethoxy-4,10, 12,18-tetramethyl-8-(2-propenyl)-15,19-epoxy-3H-pyrido[2,1-c][1,4] oxaazacyclotricosine-1,7,20,21(4H,23H)-tetrone,monohydrate. It has the following structural formula:
 |
Tacrolimus has an empirical formula of C44H69NO12•H2O and a formula weight of 822.03. Each gram of PROTOPIC Ointment contains (w/w) either 0.03% or 0.1% of tacrolimus in a base of mineral oil, paraffin, propylene carbonate, white petrolatum and white wax.
FK-506 (also Tacrolimus or fujimycin) is a potent calcineurin (protein phosphatase 2B) inhibitor that requires FK 506-binding protein 12 (FKBP12) for activity (IC50 = 3 nM). FK-506 inhibits secretion of IL-1, IL-2 (IC50 = 1 nM), IL-3, IL-4, IL-6 (IC50 = 35 nM), GM-CSF, TNFα (IC50 = 10 nM), IFNγ and Myc from activated T-cells in vitro. FK-506 exhibits potent immunosuppressive, neuroprotective and anticonvulsant activity in vivo. The physiological effects of FK-506 also include regulation of nitric oxide neurotoxicity, neurotransmitter release, and regulation of Ca2+ release via the ryanodine and inositol-(1,4,5)-trisphosphate (IP3) receptors. Furthermore, it has become clear that, predominantly as a result of CaN inhibition, FK506 alters multiple biochemical processes in a variety of cells besides lymphocytes. FK506 and ascomycin inhibit signaling pathways in astrocytes and change the pattern of cytokine and neurotrophin gene expression.
Tacrolimus (also FK-506 or fujimycin, trade names Prograf, Advagraf, Protopic) is an immunosuppressive drug that is mainly used after allogeneic organ transplant to reduce the activity of the patient’s immune system and so lower the risk of organ rejection. It is also used in a topical preparation in the treatment of atopic dermatitis (eczema), severe refractory uveitis after bone marrow transplants, exacerbations of minimal change disease, and the skin condition vitiligo.
It is a 23-membered macrolide lactone discovered in 1984 from the fermentation broth of a Japanese soil sample that contained the bacteria Streptomyces tsukubaensis. It reduces interleukin-2 (IL-2) production by T-cells.
 Tacrolimus was discovered in 1984; it was among the first macrolide immunosuppressants discovered, preceded by the discovery of rapamycin (sirolimus) on Rapa Nui (Easter Island) in 1975.It is produced by a type of soil bacterium, Streptomyces tsukubaensis. The name tacrolimus is derived from ‘Tsukuba macrolide immunosuppressant’.
Tacrolimus was discovered in 1984; it was among the first macrolide immunosuppressants discovered, preceded by the discovery of rapamycin (sirolimus) on Rapa Nui (Easter Island) in 1975.It is produced by a type of soil bacterium, Streptomyces tsukubaensis. The name tacrolimus is derived from ‘Tsukuba macrolide immunosuppressant’.
Tacrolimus 0.1%
| Indication | For use after allogenic organ transplant to reduce the activity of the patient’s immune system and so the risk of organ rejection. It was first approved by the FDA in 1994 for use in liver transplantation, this has been extended to include kidney, heart, small bowel, pancreas, lung, trachea, skin, cornea, and limb transplants. It has also been used in a topical preparation in the treatment of severe atopic dermatitis. |
|---|---|
| Pharmacodynamics | Tacrolimus is a macrolide antibiotic. It acts by reducing peptidyl-prolyl isomerase activity by binding to the immunophilin FKBP-12 (FK506 binding protein) creating a new complex. This inhibits both T-lymphocyte signal transduction and IL-2 transcription. Although this activity is similar to cyclosporine studies have shown that the incidence of acute rejection is reduced by tacrolimus use over cyclosporine. Tacrolimus has also been shown to be effective in the topical treatment of eczema, particularly atopic eczema. It suppresses inflammation in a similar way to steroids, but is not as powerful. An important dermatological advantage of tacrolimus is that it can be used directly on the face; topical steroids cannot be used on the face, as they thin the skin dramatically there. On other parts of the body, topical steroid are generally a better treatment. |
| Mechanism of action | The mechanism of action of tacrolimus in atopic dermatitis is not known. While the following have been observed, the clinical significance of these observations in atopic dermatitis is not known. It has been demonstrated that tacrolimus inhibits T-lymphocyte activation by first binding to an intracellular protein, FKBP-12. A complex of tacrolimus-FKBP-12, calcium, calmodulin, and calcineurin is then formed and the phosphatase activity of calcineurin is inhibited. This prevents the dephosphorylation and translocation of nuclear factor of activated T-cells (NF-AT), a nuclear component thought to initiate gene transcription for the formation of lymphokines. Tacrolimus also inhibits the transcription for genes which encode IL-3, IL-4, IL-5, GM-CSF, and TNF-, all of which are involved in the early stages of T-cell activation. Additionally, tacrolimus has been shown to inhibit the release of pre-formed mediators from skin mast cells and basophils, and to downregulate the expression of FceRI on Langerhans cells. |
Tacrolimus was first approved by the Food and Drug Administration (FDA) in 1994 for use in liver transplantation; this has been extended to include kidney, heart, small bowel, pancreas, lung, trachea, skin, cornea, bone marrow, and limb transplants.
The branded version of the drug is owned by Astellas Pharma, and is sold under the trade names Prograf given twice daily, Advagraf, a sustained release formulation allowing once daily dosing, and Protopic (Eczemus in Pakistan by Brookes Pharma), the topical formulation. Advagraf is available in 0.5, 1, 3 and 5 mg capsules, the ointment is concentrations of 0.1% and 0.03%.
A second once-daily formulation of tacrolimus is in Phase 3 clinical trials in the U.S. and Europe. This formulation also has a smoother pharmacokinetic profile that reduces the peak-to-trough range in blood levels compared to twice-daily tacrolimus.Data from the first Phase 3 trial in stable kidney transplant patients showed that this once-daily formulation was non-inferior in efficacy and safety compared to twice-daily tacrolimus. A second Phase 3 trial in de novo patients is ongoing.

Tacrolimus, which is also referred to as FK-506 (Fermentek catalogue number 506), is a 23-membered macrolide lactone and belongs to the group of polyketides. Tacrolimus was first isolated in the 1980’s from the fermentation broth of the soil bacteria Streptomyces tsukubaensis. The antibiotic macrolide compound tacrolimus was e.g. reported in 1984 by Kino et al. (J. Antibiotics 40, 1249-1255, 1984). Later on tacrolimus was prepared as a microbial natural product by using different microorganisms, i.e. soil bacteria such as Streptomyces sp. MA6858 (US 5,116,756) ATCC 55098, Streptomyces tsukubaensis NRRL 18488 (EP-B 0 356 399 and US 5,200,41 1 ), Streptomyces clavuligerus CKD 1119 (KR-B 100485877) or Streptomyces glaucescens MTCC 5115 (US 2007191415).
The product tacrolimus exhibits immunosuppressive activities which are due to its effect to reduce the activity of the enzyme peptidyl-propyl isomerase and to the binding to the protein immunophilin FKBP12 (FK506 binding protein). Tacrolimus and the structurally similar polyketides ascomycin and rapamycin require initial binding to the highly conserved protein cyclophilin FKBP12 in order to be physiologically active. The rapamycin/FKBP12 complex binds to mTOR (mammalian target of rapamycin), a serine- threonine kinase that appears to act as a central controller for sensing the cellular environment and regulating translation initiation (see e.g. Easton J. B. and Houghton P.J., 2004, Expert Opin Ther Targets; 8(6):551-64). However, the tacrolimus/FKBP12 complex was found to bind to a different cellular target and inhibits the phosphatase activity of calcineurin, in analogy to cyclosporine (see Allison A.C., 2000, Immunopharmacology; 47(2-3):63-83).
Tacrolimus is often used for immunosuppression following e.g. organ transplantation. Furthermore, tacrolimus and its derivatives have been shown to be effective in treating a number of diseases such as asthma, inflammatory diseases and hyperproliferative skin disease. Tacrolimus and other immunosuppressant such as rapamycin, cyclosporine, or a combination thereof are also useful in the treatment of various auto-immmune diseases. For many years calcineurin inhibitors (e.g. cyclosporine and tacrolimus) have been the mainstay of immunosuppressive therapy. These two compounds are potent suppressors of cellular immune response and have significantly improved the outcome of organ transplants during the past two decades (see Allison A.C., 2000, Immunopharmacology; 47(2-3):63-83). Gene clusters encoding the biosynthetic pathways of a great number of medically important drugs of microbial origin have already been cloned and sequenced, including the gene cluster of macrolides rapamycin, ascomycin and tacrolimus. With respect to cloning of the tacrolimus gene cluster, a partial sequence, mostly encompassing genes encoding polyketide synthase (PKS), was reported in the literature (see Motamedi H. and Shafiee A. 1998, Eur J Biochem; 256(3):528-34). On the other hand, scientists reported cloning of the ascomycin gene cluster in 2000 (see Wu K et al. 2000, Gene; 251(1 ):81- 90, US 6,503,737). Tacrolimus structurally and by the biosynthetic origin resembles ascomycin (FK520) and rapamycin (see Reynolds et al.; Drugs and the Pharmaceutical Sciences, 1997, 82, 497-520. They all can be synthesised by combined polyketide (PKS) and non-ribosomal peptide biosynthetic pathways (NRPS) (see McDaniel R et al. 2005, Chem Rev; 105(2):543-58).
Tacrolimus and ascomycin are structurally similar. As only structural difference, the allyl side chain at carbon 21 of tacrolimus is replaced by an ethyl side chain in ascomycin. The structures of tacrolimus (FK506) and ascomycin (FK520) compounds are shown as formulae (Ia) and (Ib). The structures of ascomycin and tacrolimus already suggest complex biosynthetic pathways which can be divided into four steps considering the biosynthetic mechanism:
1. chain initiation using the unusual shikimate derived starter,
2. chain elongation common to most PKS derived compounds,
3. chain termination and cyclization by incorporation of L-pipecolic acid and
4. post-PKS processing.
During the tacrolimus fermentation process, undesired ascomycin (FK520) product is also produced as an impurity, thus lowering the final yield of tacrolimus and causing significant additional costs to the downstream isolation processes of tacrolimus.
(Ia) FK506, R = -CH2-CH = CH2
(Ib) FK520, R = CH2-CH3
For oral administration, tacrolimus is currently formulated and marketed as soft gelatine capsules comprising the equivalent of 0.5, 1 or 5 mg anhydrous tacrolimus and marketed under the trade name Prograf® and Protropic®. The recommended initial oral dose is from about 0.1 to 0.2 mg/kg/day in patients. The dose aims at a certain trough plasma level from about 5 to about 20 ng/ml. Prograf® is indicated for the prophylaxis of organ rejection in patients receiving allogeneic liver or kidney transplants. There remains a need for novel pharmaceutical compositions and/or dosage forms comprising tacrolimus exhibiting enhanced bioavailability. An increased bioavailability may allow a reduction in the dosage units taken by a patient, e.g. down to a single dose daily, and may also reduce or negate the need for food to be takes simultaneously with the dosage form thereby allowing patients more freedom on when the drug is taken. Furthermore, it is contemplated that fluctuations in the plasma concentration versus time profile may be significantly reduced. Further, enhanced bioavailability may also result in a more reproducible (i.e. less variable compared to that of Prograf®) release profile….
………………….
h) Determination of tacrolimus and ascomycin production with HPLC of thiostrepton resistant ccr disrupted mutants derived by secondary homologous recombination using pKC1 139-ccrTs.:
Method for tacrolimus and ascomycin determination: The analysis for determination of tacrolimus or ascomycin production thereof was carried out by isocratic reversed phase HPLC using an appropriate column and running conditions: column Nucleosil-100 C18 (150×4.0 mm, particle size 3 μm), flow 1.5 ml/min, T°C=60°C, mobile phase: 560 ml water, 335 ml acetonitrile, 70 ml MTBE and 0.2 ml 85% H3PO4, detection 210 nm, sample injection 20 μl.
The tacrolimus and ascomycin content in samples quantification was performed by using external standards of tacrolimus and ascomycin, where tacrolimus was eluted at 12.5 min and ascomycin at 11.5 min. Results are expressed as % of ascomycin production compared to tacrolimus production in samples.
……………………….
http://www.drugfuture.com/synth/syndata.aspx?ID=124071

A new total synthesis of FK-506 is described: This synthesis has been performed by previous construction of two building fragments (XXIV) and (LI), which later were coupled and cyclized. (Schemes 1-3): 1) (1R*S*,3R,5S,6R,7S,9R)-6-(tert-butyldimethylsilyloxy)-9-(1,3-dithian-2-yl)-5,7-dimethoxy-1-methyldecyl diphenyl phosphine oxide (XXIV). The Sharpless asymetric epoxidation of 1,4-pentadien-3-ol (I) with (-)-diisopropyltartrate and tert-butylhydroperoxide gives the epoxy alcohol (II) with high optical purity, which is benzylated in the usual way to (III). The reaction of (III) with lithioacetonitrile and then HCl yields lactone (IV), which is methylated with lithium diisopropylamide and methyl iodide to lactone (V) as major isomer (separated by chromatography on SiO2). The reduction of (V) with LiAlH4 affords the diol (VI), which is converted into the bis(tert-butyl carbonate) (VII) with 2-(tert-butoxycarbonyloxyimino)-2-phenylacetonitrile (BOC-N). The reaction of (VII) with Br2 and K2CO3 in dichloromethane gives the bromocarbonate (VIII), which by selective saponification of the cyclic carbonate with NaOCH3 in methanol yields the epoxy alcohol (IX). Methylation of (IX) with NaH and methyl iodide affords the methyl ether (X), which is converted into the butyrolactone (XI) with lithioacetonitrile as before. The protection of the OH group of (XI) with TBS-Cl gives the silyl ether (XII), which by trans-selective methylation with lithium diisopropylamide and methyl iodide yields lactone (XIII). The reduction of (XIII) with LiAlH4 affords diol (XIV) as major isomer (separated by column chromatography). The selective esterification of the primary OH group of (XIV) with pivaloyl chloride gives the hydroxy ester (XV), which is methylated with NaH and methyl iodide as usual to the methoxy derivative (XVI). Debenzylation of (XVI) by hydrogenolysis with H2 over Pd/C yields the hydroxy ester (XVII), which is silylated with TBS-SO3CF3 to the fully protected compound (XVIII).

Selective deprotection of (XVIII) with trifluoroacetic acid in THF – water affords the primary alcohol (XIX), which is oxidized with oxalyl chloride and DMSO in dichloromethane to the aldehyde (XX). The protection of the aldehyde group of (XX) with propane-1,3-dithiol and BF3 gives the dithiane derivative (XXI), which is resilylated with TBS-SO3CF3 as before to the dithiane (XXII). The pivaloyl group of (XXII) is eliminated with LiAlH4 in THF yielding the alcohol (XXIII), which is finally treated with benzenesulfonyl chloride and then with ethyl diphenylphosphine oxide and butyllithium in THF to obtain the first building group, the phosphine derivative (XXIV).

2) [2S,3S,5S,6R,7S,8E,9(1’R,3’R,4’R)]-2-Allyl-3-(tert-butyldimethylsilylox y)-6,8-dimethyl-7-(triethylsilyloxy)-5-(triisopropylsilyloxy)-9-[3-meth oxy-4-(triisopropylsilyloxy)cyclohexyl]-8-nonenal (LI). Quinic acid (XXV) is converted into the lactone (XXVI) by known methods. Then this lactone is treated with thiocarbonyldiimidazole in refluxing dichloroethane yielding the bis(thiocarbonyl)lactone (XXVII), which by reaction with tributyltin hydride and AIBN in refluxing xylene is converted into the lactone (XXIX), either directly or through the intermediate thiocarbonyl-lactone (XXVIII). The silylation of (XXIX) with TIPS-SO3CF3 as usual affords the protected lactone (XXX). Opening of the lactone ring with methylchloroaluminum N-methoxy-N-methylamide gives the methoxyamide (XXXI), which is methylated with methyl trifluoromethylsulfonate to the methoxy-N-methoxyamide (XXXII). The reduction of (XXXII) with diisobutylaluminum hydride gives the aldehyde (XXXIII), which is condensed with 2-lithio-2-(triethylsilyl)propanal (XXXIV), yielding unsaturated aldehyde (XXXV). The condensation of (XXXV) with the boron enolate of oxazolidone (XXVI) affords the oxazolidone derivative (XXXVII), which is treated with methylchloroaluminum N-methoxy-N-methylamide to give the methoxyamide (XXXVIII). The silylation of (XXXVIII) with TES-SO3CF3 as usual yields the silylated amide (XXXIX), which is reduced with diisobutylaluminum hydride to the aldehyde (XL). The condensation of (XL) with chiral acetate (XLI) by means of lithium diisopropylamide in THF affords the hydroxy ester (XLII). Transesterification of (XLII) with NaOCH3 and methanol gives methyl ester (XLIII).
http://www.drugfuture.com/synth/syndata.aspx?ID=124071
…………..
Use of the microorganism streptomyces tsukubaensis No. 9993 for the production of the FR-900506 substance of the formula:
- [II]
Synthetic Processes
- :(1)
Process 1
- (Introduction of common Hydroxy-Protective Group)
(2)
Process 2
- (Introduction of common Hydroxy-Protective Group)
(3)
Process 3
- (Formation of Double Bond)
(4)
Process 4
- (Oxidation of Hydroxyethylene Group)
(5)
Process 5
- (Reduction of Allyl Group)
-
- THE MICROORGANISM
-
The microorganism which can be used for the production of the FR-900506, FR-900520 and/or FR-900525 substances is FR-900506 FR-900520 and/or FR-900525 substance(s)-producing strain belonging to the genusStreptomyces, among which Streptomyces tsukubaensis No. 9993 has been newly isolated from a soil sample collected at Toyosato-cho, Tsukuba-gun, Ibaraki Prefecture, Japan.
-
A lyophilized sample of the newly isolated Streptomyces tsukubaensis No. 9993 has been deposited with the Fermentation Research Institute, Agency of Industrial Science and Technology (No. 1-3, Higashi 1-chome, Yatabemachi Tsukuba-gun, Ibaraki Prefecture, Japan) under the deposit number of FERM P-7886 (deposited date: October 5th, 1984), and then converted to Budapest Treaty route of the same depository on October 19, 1985 under the new deposit number of FERM BP-927.
-
The Streptomyces tsukubaensis No. 9993 has the following morphological, cultural, biological and physiological characteristics.
-
-
This white powder of the FR-900506 substance could be transformed into a form of crystals by recrystallization thereof from acetonitrile, which possess the following physical and chemical properties.
(1) Form and Color:
colorless prisms
(2)Elemental Analysis: C: 64.30 %, H: 8.92 %, N: 1.77 % 64.20 %, 8.86 %, 1.72 %, (3) Melting Point:
127 – 129 °C
(4) Specific Rotation:
[α] 23 D: -84.4° (c = 1.02, CHCl₃)
(5) ¹³C Nuclear Magnetic Resonance Spectrum:the chart of which being shown in Figure 3,
(6) ¹H Nuclear Magnetic Resonance Spectrum:
the chart of which being shown in Figure 4. -
Other physical and chemical properties, that is, the color reaction, solubility, ultraviolet absorption spectrum, infrared absorption spectrum, thin layer chromatography and property of the substance of the colorless prisms of the FR-900506 substance were the same as those for the white powder of the same under the identical conditions.
-
From the above physical and chemical properties and the analysis of the X ray diffraction, the FR-900506 substance could be determined to have the following chemical structure.
17-Allyl-1,14-dihydroxy-12-[2-(4-hydroxy-3-methoxycyclohexyl)-1-methylvinyl]-23,25-dimethoxy-13,19,21,27-tetramethyl-11,28-dioxa-4-azatricyclo[22.3.1.04,9]octacos-18-ene-2,3,10,16-tetraone
……………………

The total synthesis of FK-506 is described: This synthesis was performed by previously constructing three building fragments (XX), (XXXII) and (XLVI), which later were coupled sequentially. First the synthesis of these fragments will be presented, and afterwards their sequential coupling will be described. 1) (2RS,4R,6S,7R,8S,10R)-2-(Bis(dimethylamino)phosphono)-7-(tert-butyldimethylsilyloxy)-6,8-dimethoxy-10-(1,3-dithian-2-yl)-4-methylundecane (XX). The reaction of L-arabitol (I) with 2-acetoxyisobutyryl chloride in acetonitrile gives the diacetoxycompound (II), which by treatment with sodium methoxide in THF yields (2S,4S)-1,2:4,5-diepoxy-3-pentanol (III). The protection of (III) with TBS-Cl in THF affords the protected compound (IV), which is condensed with ethoxyacetylene (V) by means of butyllithium and boron trifluoride ethearate in THF giving the diacetylenic alcohol (VI). Cyclization of (VI) by means of HgCl2 and p-toluenesulfonic acid in refluxing ethanol yields the dilactone (VII), which is methylated by means of methyl iodide and lithium diisopropylamide in THF affording the methylated dilactone (VIII). The deprotection of (VIII) with HF in acetonitrile gives the hydroxydilactone (IX), which is benzylated with benzyl trichloroacetimidate and trifluoromethanesulfonic acid in dichloromethane-cyclohexane yielding the benzyl protected dilactone (X). The methanolysis of (X), followed by methylation with NaH and methyl iodide in DMF affords the nonanedioic ester (XI), which is debenzylated by hydrogenolysis with H2 over Pd/C in ethyl acetate giving the hydroxy diester (XII). The lactonization of (XII) with pyridinium p-toluenesulfonate in dichloromethane yields the lactone-methyl ester (XIII), which is selectively reduced with L-Selectride in THF affording the lactol-methyl ester (XIV). The reaction of (XIV) with propane-1,3-dithiol and boron trifluoride ethearate in dichloromethane gives the 1,3-dithiane derivative (XV), which by reduction of its lactone group with LiAlH4 in THF yields (2R,4S,5R,6S,8R)-8-(1,3-dithian-2-yl)-4,6-dimethoxy-2-methylnonane-1,5-diol (XVI). The reaction of (XVI) with I2, pyridine and triphenylphosphine in benzene affords the 1-iodo derivative (XVII), which is protected with TBS trifluoromethanesulfonate and triethylamine in dichloromethane giving the protected iodide (XVIII). Finally, this compound is condensed with ethylphosphonic acid bis(dimethylamide) (XIX) by means of butyllithium in THF to afford the first building fragment (XX).
SEE
http://www.drugfuture.com/synth/syndata.aspx?ID=124071
………………
Isolation and Purification
The cultured broth thus obtained was filtered with an aid of diatomaseous earth (5 kg). The mycelial cake was extracted with acetone (50 liters), yielding 50 liters of the extract. The acetone extract from mycelium and the filtrate (135 liters) were combined and passed through a column of a non-ionic adsorption resin “Diaion HP-20” (Trade Mark, maker Mitsubishi Chemical Industries Ltd.) (10 liters). After washing with water (30 liters) and 50% aqueous acetone (30 liters), elution was carried out with 75% aqueous acetone. The eluate (30 liters) was evaporated under reduced pressure to give residual water (2 liters). This residue was extracted with ethyl acetate (2 liters) three times. The ethyl acetate extract was concentrated under reduced pressure to give an oily residue. The oily residue was mixed with twice weight of acidic silica gel (special silica gel grade 12, maker Fuji Devision Co.), and this mixture was slurried in ethyl acetate. After evaporating the solvent, the resultant dry powder was subjected to column chromatography of the same acidic silica gel (800 ml) which was packed with n-hexane. The column was developed with n-hexane (3 liters), a mixture of n-hexane and ethyl acetate (4:1 v/v, 3 liters) and ethyl acetate (3 liters). The fractions containing the object compound were collected and concentrated under reduced pressure to give an oily residue. The oily residue was dissolved in a mixture of n-hexane and ethyl acetate (1:1 v/v, 30 ml) and subjected to column chromatography of silica gel (maker Merck Co., Ltd. 230-400 mesh) (500 ml) packed with the same solvents system. Elution was carried out with a mixture of n-hexane and ethyl acetate (1:1 v/v, 2 liters and 1:2 v/v, 1.5 liters) and ethyl acetate (1.5 liters).
Fractions containing the first object compound were collected and concentrated under reduced pressure to give crude FR-900506 substance (3 g) in the form of yellowish powder.
…………


……………………………
Synthesis pathway
Trade Names
| Country | Trade name | Manufacturer |
|---|---|---|
| Germany | Advagraf | Astellas |
| Prograf | – “- | |
| Protopic | – “- | |
| France | Prograf | – “- |
| Protopic | – “- | |
| United Kingdom | – “- | – “- |
| Italy | Prograf | Fujisawa |
| Japan | – “- | Astellas |
| USA | – “- | – “- |
| Ukraine | Prograf | Astellas Ireland Co.., Ltd., Ireland; Fujisawa Ireland Ltd., Ireland |
| Protopic | Astellas Ireland Co.., Ltd.. (Issue series and packaging), Ireland; Astellas Toyama Co., Ltd.., Plant Toyama, Japan |
|
| Advagraf | Astellas Ireland Co.., Ltd., Ireland |
Formulations
-
ampoules of 5 mg / 1 ml;
-
Capsules 0.5 mg, 1 mg, 5 mg;
-
granules 0.2%;
-
Ointment 0.1%
Links
-
Manufacturing; selection:
-
EP 184 162 (Fujisawa Pharmaceutical; appl. 11/6/1986; GB -prior. 05.02.1985, 1/4/1985).
-
-
synthesis of FK-506:
-
EP 378 318 (Fujisawa Pharmaceutical; appl. 18.7.1990; USA-prior. 11.1.1989, 30.6.1989).
-
Ireland, R. et al .: J. Org. Chem. (JOCEAH) 61, 6856 (1996).
-
-
Synthesis of Intermediates:
-
Danishefsky, SJ et al .: J. Org. Chem. (JOCEAH) 55 (9) 2786 (1990).
-
Schreiber, SL et al .: J. Am. Chem. Soc. (JACSAT) 112 (4), 5583 (1990).
-
US 4,940,797 (Fujisawa Pharmaceutical; 10.7.1990; USA-prior. 23.3.1989).
-
-
Alternative synthesis :
-
Shinkai, I. et al .: J. Am. Chem. Soc. (JACSAT) 111 (3) 1157 (1989).
-
Shinkai, I. et al .: Tetrahedron Lett. (TELEAY) 29 (3), 281 (1988).
-
References
- Kino T, Hatanaka H, Hashimoto M, Nishiyama M, Goto T, Okuhara M, Kohsaka M, Aoki H, Imanaka H (1987). “FK-506, a novel immunosuppressant isolated from a Streptomyces. I. Fermentation, isolation, and physico-chemical and biological characteristics.”. J Antibiot (Tokyo) 40 (9): 1249–55. PMID 2445721.
- Pritchard D (2005). “Sourcing a chemical succession for cyclosporin from parasites and human pathogens.”. Drug Discov Today 10 (10): 688–91. doi:10.1016/S1359-6446(05)03395-7.PMID 15896681. Supports source organism, but not team information
- Ponner, B, Cvach, B (Fujisawa Pharmaceutical Co.): Protopic Update 2005
- Healthy Ontario: Tacrolimus topical ointment
- Alloway RR, Germain M, Osama Gaber, A, Bodziak KA, Mulgaonkar SP, Gohh RY, Kaplan B, Katz E, Beckert M, Gordon RD, A Phase II Open-Label, Multi-Center Prospective, Conversion Study in Stable Kidney Transplant Patients to Compare the Pharmacokinetics of LCP-Tacro Tablets Once-A-Day to Prograf Capsules Twice-A-Day. American Transplant Congress, 2008
- http://files.shareholder.com/downloads/ABEA-4J4LWA/1008134289x0x477697/e60eb3d4-849c-41e2-95f3-d8a1eaea3b56/LCP_News_2011_6_21_English_Releases.pdf
- Clinicaltrials.gov identifier: NCT01187953
- William F. Ganong. Review of medical physiology (22nd ed.). Lange medical books. p. 530. ISBN 0-07-144040-2.
- Liu J, Farmer J, Lane W, Friedman J, Weissman I, Schreiber S (1991). “Calcineurin is a common target of cyclophilin-cyclosporin A and FKBP-FK506 complexes.”. Cell 66 (4): 807–15.doi:10.1016/0092-8674(91)90124-H. PMID 1715244.
- McCauley, Jerry (2004-05-19). “Long-Term Graft Survival In Kidney Transplant Recipients”. Slide Set Series on Analyses of Immunosuppressive Therapies. Medscape. Retrieved 2006-06-06.
- M.M. Abou-Jaoude, R. Naim, J. Shaheen, N. Naufal, S. Abboud, M. AlHabash, M. Darwish, A. Mulhem, A. Ojjeh, and W.Y. Almawi (2005). “Tacrolimus (FK506) versus cyclosporin microemulsion (Neoral) as maintenance immunosuppresion therapy in kidney transplant recipients.”. Transplantation Proceedings 37 (7): 3025–3028. doi:10.1016/j.transproceed.2005.08.040. PMID 16213293.
- Elizabeth Haddad, Vivian McAlister, Elizabeth Renouf, Richard Malthaner, Mette S. Kjaer, and Lise Lotte Gluud (2006). “Cyclosporin versus Tacrolimus for Liver Transplanted Patients”. In McAlister, Vivian. Cochrane Database of Systematic Reviews 4 (CD005161): CD005161. doi:10.1002/14651858.CD005161.pub2. PMID 17054241.
- J.G. O’Grady, A. Burroughs, P. Hardy, D. Elbourne, A. Truesdale, and The UK and Ireland Liver Transplant Study Group (2002). “Tacrolimus versus emulsified cyclosporin in liver transplantation: the TMC randomised controlled trial”. Lancet 360 (9340): 1119–1125. doi:10.1016/S0140-6736(02)11196-2. PMID 12387959.
- Baumgart DC, Pintoffl JP, Sturm A, Wiedenmann B, Dignass AU (2006). “Tacrolimus is safe and effective in patients with severe steroid-refractory or steroid-dependent inflammatory bowel disease–a long-term follow-up”. Am J Gastroenterol 101 (5): 1048–1056. doi:10.1111/j.1572-0241.2006.00524.x. PMID 16573777.
- Baumgart DC, MacDonald JK, Feagan BG (2008). “Tacrolimus (FK506) for induction of remission in refractory ulcerative colitis”. In Baumgart, Daniel C. Cochrane Database Syst Rev 16 (3): CD007216. doi:10.1002/14651858.CD007216. PMID 18646177.
- Silverberg, NB; Lin, P; Travis, L; Farley-Li, J; Mancini, AJ; Wagner, AM; Chamlin, SL; Paller, AS (2004). “Tacrolimus ointment promotes repigmentation of vitiligo in children: a review of 57 cases.”.Journal of the American Academy of Dermatology 51 (5): 760–6. doi:10.1016/j.jaad.2004.05.036. PMID 15523355.
- Naesens M, Kuypers DR, Sarwal M (2009). “Calcineurin inhibitor nephrotoxicity”. Clin. J. Am. Soc. Nephrol. 4 (2): 481–509. doi:10.2215/CJN.04800908. PMID 19218475.
- Miwa Y, Isozaki T, Wakabayashi K, et al. (2008). “Tacrolimus-induced lung injury in a rheumatoid arthritis patient with interstitial pneumonitis”. Mod Rheumatol 18 (2): 208–11. doi:10.1007/s10165-008-0034-3. PMID 18306979.
- O’Donnell MM, Williams JP, Weinrieb R, Denysenko L (2007). “Catatonic mutism after liver transplant rapidly reversed with lorazepam”. Gen Hosp Psychiatry 29 (3): 280–1.doi:10.1016/j.genhosppsych.2007.01.004. PMID 17484951.
- Hanifin JM, Paller AS, Eichenfield L, Clark RA, Korman N, Weinstein G, Caro I, Jaracz E, Rico MJ; US Tacrolimus Ointment Study Group (2005). “Efficacy and safety of tacrolimus ointment treatment for up to 4 years in patients with atopic dermatitis”. J Am Acad Derm 53 (2 suppl 2): S186–94. doi:10.1016/j.jaad.2005.04.062. PMID 16021174.
- N H Cox and Catherine H Smith (December 2002). “Advice to dermatologists re topical tacrolimus” (PDF). Therapy Guidelines Committee. British Association of Dermatologists.
- Fukatsu S, Fukudo M, Masuda S, Yano I, Katsura T, Ogura Y, Oike F, Takada Y, Inui K (2006). “Delayed effect of grapefruit juice on pharmacokinetics and pharmacodynamics of tacrolimus in a living-donor liver transplant recipient”. Drug Metab Pharmacokinet 21 (2): 122–5. doi:10.2133/dmpk.21.122. PMID 16702731.
- Fegan, A; White, B; Carlson, JC; Wagner, CR (Jun 9, 2010). “Chemically controlled protein assembly: techniques and applications.”. Chemical reviews 110 (6): 3315–36. doi:10.1021/cr8002888.PMID 20353181.
- Tacrolimus, which is also called FK-506, has first discovered by Tanaka, Kuroda and their colleague in Japan see, J. Am. Chem. Soc., 1987, 109, 5031
- and U.S. Pat. No. 4,894,366 issued on Jan. 16, 1990!.
- Total synthesis of FK506 and an FKBP probe reagent, (C8,C9-13C2)-FK506
J Am Chem Soc 1990, 112(14): 5583 - A diastereospecific, non-racemic synthesis of the C.10-C.18 segment of FK-506
Tetrahedron Lett 1988, 29(3): 277
- Tacrolimus levels in Liver Transplants-Indian Study by Dr.Pradeep Naik,Dr.Dharmesh Kapoor, Dr.DCS Reddy
- Prograf prescribing information at Fujisawa
- Pimecrolimus (Elidel Cream) FDA adivisory page (for eczema treatment)
- Tacrolimus (FK506) product page from Fermentek
- U.S. National Library of Medicine: Drug Information Portal – Tacrolimus

 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....