Phase 2- Cylene Pharmaceuticals and TetraGene Enter Agreement for Quarfloxin and Anticancer Quadruplex Technologies

Quarfloxin, CX-3543
Molecular Formula: C35H33FN6O3
cas no 865311-47-3
Molecular Formula: 604.67
SAN DIEGO, March 6, 2013
Cylene Pharmaceuticals, Inc. announced today that it has entered into an exclusive, worldwide Option and License Agreement that will allow TetraGene LLC to advance the development of Quarfloxin and Cylene’s associated anticancer quadruplex-targeting technologies. Cylene will receive an upfront fee, as well as potential milestone payments and royalties on product sales for the exclusive license.
TetraGene is developing small molecule drugs aimed at highly validated cancer-causing genes, by directly targeting G-quadruplex structures in genomic DNA. TetraGene has the option to acquire worldwide rights to the technologies licensed from Cylene, which include the Phase II compound Quarfloxin and several registered patents. Quarfloxin has been demonstrated to be safe and well-tolerated in Phase I clinical trials.
“This agreement is a clear win for both organizations,” stated William G. Rice, PhD, President and CEO of Cylene Pharmaceuticals. “TetraGene is well placed to advance Quarfloxin through the clinic and to capture exclusive worldwide rights to the quadruplex-targeting technologies. Cylene will receive standard industry payments as the quadruplex program progresses and we will continue to focus our in-house development efforts on CX-5461, Cylene’s clinical stage Pol I inhibitor that activates the p53 tumor suppressor selectively in cancer cells and not normal cells.”
“The agreement between TetraGene and Cylene immediately provides us with access to a clinical stage drug,” commented Laurence H. Hurley, PhD, CSO of TetraGene and a pioneer of G-quadruplex targeted therapeutics. “The validity of drug targeting G-quadruplex DNA and modulating expression of cancer genes has dramatically increased in the last few years and our team is uniquely positioned to take advantage of these new insights.”
About Cylene Pharmaceuticals
Cylene Pharmaceuticals is a clinical-stage private company developing small molecule drugs against newly validated targets in essential cancer pathways. The Company’s Pol I program provides a non-genotoxic mechanism for activating p53 to kill cancer cells. Cylene’s leadership in exploiting CK2 pathways enables rational drug combinations for improved treatment outcomes against many cancer indications. Cylene’s unique approaches deliver innovative cancer agents that can enable pharmaceutical companies to expand their portfolios and extend the efficacy, lifecycle and reach of current cancer therapeutics. For more information on Cylene and its programs, please visit www.cylenepharma.com.
About TetraGene
TetraGene leverages a novel platform technology to develop cancer drugs that target well-validated cancer-causing oncogenes previously considered as undruggable by the pharmaceutical industry. This technology exploits a gene regulatory mechanism where the expression of a gene is controlled by folded DNA structures (called G-quadruplex DNA). By targeting gene transcription, TetraGene has carved out a niche where its technology platform can be directly applied to inhibit these undruggable cancer targets. For more information about TetraGene please visit www.tetragene.com.
…………………………………….
DR ANTHONY MELVIN CRASTO Ph.D , Born in Mumbai in 1964 and graduated from Mumbai University, Completed his PhD from ICT ,1991, Mumbai, India in Organic chemistry, The thesis topic was Synthesis of Novel Pyrethroid Analogues,
Currently he is working with GLENMARK- GENERICS LTD, Research centre as Principal Scientist, Process Research (bulk actives) at Mahape, Navi Mumbai, India.
Prior to joining Glenmark, he worked with major multinationals like Hoechst Marion Roussel, now Sanofi Aventis, & Searle India ltd, now Rpg lifesciences, etc. He has worked in Basic research, Neutraceuticals, Natural products, Flavors, Fragrances, Pheromones, Vet Drugs, Drugs, formulation, GMP etc. He has total 25 yrs exp in this field, he is now helping millions, has million hits on google on all organic chemistry websites.
His New Drug Approvals , Green Chemistry International, Eurekamoments in Organic Chemistry , Organic Chemistry by Dr Anthony, WIX BLOG , are some most read chemistry blogs
He has hands on experience in initiation and developing novel routes for drug molecules and implementation them on commercial scale over a 25 year tenure, good knowledge of IPM, GMP, Regulatory aspects, he has several international drug patents published worldwide .
He has good proficiency in Technology Transfer, Spectroscopy , Stereochemistry , Synthesis, Reactions in Org Chem , Polymorphism, Pharmaceuticals , Medicinal chemistry , Organic chemistry literature , Patent related site , Green chemistry , Reagents , R & D , Molecules , Heterocyclic chem , Sourcing etc
He suffered a paralytic stroke in dec 2006 and is bound to a wheelchair, this seems to have injected feul in him to help chemists around the world, he is more active than before and is pushing boundaries, he has one lakh connections on all networking sites, He makes himself available to all, contact him on +91 9323115463, amcrasto@gmail.com

Phase 3-Gilead’s newly-acquired Sofosbuvir, GS-7977 shines in Hepatitis C trial
Sofosbuvir
Isopropyl (2S)-2-[[[(2R,3R,4R,5R)-5-(2,4-dioxopyrimidin-1-yl)-4-fluoro-3-hydroxy-4-methyl-tetrahydrofuran-2-yl]methoxy-phenoxy-phosphoryl]amino]propanoate
The Foster City, CA-based Gilead said that its experimental drug GS-7977, originally known as PSI-7977 before the acquisition, when combined with ribavirin, cured a group of genotype 1 hepatitis C patients after four weeks of treatment. The clinical study involved hepatitis C patients who either failed to respond to previous therapies or had not been treated before. The genotype 1 is the most common form of HCV in the United States. It affects 70 to 90 percent of the people in this country who have hepatitis C.
Norbert Bischofberger, chief scientific officer at Gilead said patients with genotype 1 hepatitis C had no detectable signs of the virus after treated with GS-7977 combination therapy for a course of close to a month. Previous study showed the drug candidate could also cure patients with genotype 2 and 3 HCV.
Gilead gained rights to GS-7977 through the $11 billion Pharmasset acquisition deal, which enable the company to be in an advanced position to compete with a few pharma companies seeking to develop an all-oral regimen for hepatitis C. The 100 percent cure rate data suggested that GS-7977 may be one of the most promising therapies for hepatitis C.
Last year, GS-7977, an oral uridine nucleotide analog polymerase inhibitor of HCV, received fast track designation from the U.S. FDA for the treatment of HCV infection.
The World Health Organization estimated that 3–4 million people are infected with HCV each year. Some 130–170 million people are chronically infected with HCV and at risk of developing liver cirrhosis and/or liver cancer, and more than 350,000 people die yearly from hepatitis C-related diseases.
Sofosbuvir (formerly PSI-7977 or GS-7977) is an experimental drug candidate for the treatment of hepatitis C.[1] It was discovered at Pharmasset and then acquired for development by Gilead Sciences. It is currently in Phase III clinical trials.[2]
Sofosbuvir is a prodrug that is metabolized to the active antiviral agent 2′-deoxy-2′-α-fluoro-β-C-methyluridine-5′-monophosphate.[3]
Sofosbuvir is a nucleotide analogue inhibitor of the hepatitis C virus (HCV) polymerase.[4] The HCV polymerase or NS5B protein is a RNA-dependent RNA polymerase critical for the viral cycle.
Sofosbuvir is being studied in combination with pegylated interferon and ribavirin, with ribavirin alone, and with other direct-acting antiviral agents.[5] It has shown excellent clinical efficacy when used either with pegylated interferon/ribavirin or in interferon-free combinations. In particular, combinations of sofosbuvir with NS5A inhibitors, such as daclatasvir or GS-5885, have shown sustained virological response rates of up to 100% in people infected with HCV.[6]
- Sofia, M. J.; Bao, D.; Chang, W.; Du, J.; Nagarathnam, D.; Rachakonda, S.; Reddy, P. G.; Ross, B. S. et al. (2010). “Discovery of a β-d-2′-Deoxy-2′-α-fluoro-2′-β-C-methyluridine Nucleotide Prodrug (PSI-7977) for the Treatment of Hepatitis C Virus”. Journal of Medicinal Chemistry 53 (19): 7202–7218. doi:10.1021/jm100863x. PMID 20845908. edit
- “PSI-7977”. Gilead Sciences.
- Murakami, E.; Tolstykh, T.; Bao, H.; Niu, C.; Steuer, H. M. M.; Bao, D.; Chang, W.; Espiritu, C. et al. (2010). “Mechanism of Activation of PSI-7851 and Its Diastereoisomer PSI-7977”. Journal of Biological Chemistry 285 (45): 34337–34347. doi:10.1074/jbc.M110.161802. PMC 2966047. PMID 20801890. edit
- Alejandro Soza (November 11, 2012). “Sofosbuvir”. Hepaton.
- Tom Murphy (November 21, 2011). “Gilead Sciences to buy Pharmasset for $11 billion”. Bloomberg Businessweek.
- http://www.gilead.com/pr_1757156
- AASLD: PSI-7977 plus Ribavirin Can Cure Hepatitis C in 12 Weeks without Interferon. Highleyman, L. HIVandHepatitis.com. 8 November 2011.
- Nucleotide Polymerase Inhibitor Sofosbuvir plus Ribavirin for Hepatitis C. Gane, E et al. New England Journal of Medicine 368:3444. January 3, 2013.
- CROI 2013: Sofosbuvir + Ledipasvir + Ribavirin Combo for HCV Produces 100% Sustained Response. Highleyman, L. HIVandHepatitis.com. 4 March 2013.
MAA EU -GSK submits diabetes drug Eperzan, albiglutide in EU

MAA EU =marketing authorisation application EU
MAR 08 2013
GlaxoSmithKline has announced the submission of a marketing authorisation application for albiglutide, which will have the brand name Eperzan, to the European Medicines Agency.
The filing of albiglutide, a once-weekly treatment for type 2 diabetes, comes almost two months after it was filed in the USA. The drug is a GLP-1 receptor agonist, the same class of injectable treatments dominated by Novo Nordisk’s once-a-day Victoza (liraglutide), twice-daily Byetta (exenatide) and an extended-release formulation of the latter, Bydureon. They were developed and sold by Amylin, which was then acquired by Bristol-Myers Squibb and AstraZeneca.
The filing is based in part on a study which assessed albiglutide against Merck & Co’s DPP-4 inhibitor Januvia (sitagliptin) which showed that GSK’s drug showed clinically and statistically significant reductions in HbA1c from baseline and superiority versus the US firm’s diabetes blockbuster. However in data from a late-stage study released in November 2011, albiglutide failed to show non-inferiority to Victoza and a number of analysts believe GSK will have its work cut out to grab a decent share of the GLP-1 market.
Albiglutide is a glucagon-like peptide-1 agonist (GLP-1 agonist) drug under investigation by GlaxoSmithKline for treatment of type 2 diabetes. It is a dipeptidyl peptidase-4-resistant glucagon-like peptide-1 dimer fused to human albumin.
Albiglutide has a half-life of four to seven days, which is considerably longer than the other two GLP-1 analogs approved for market use, exenatide (Byetta) and liraglutide (Victoza).[1] [2] GLP-1 drugs are currently only available for subcutaneous administration on a daily basis, so a GLP-1 drug with a longer half-life is desirable. Such a drug would only need to be injected biweekly or weekly instead of daily, reducing the discomfort and inconvenience of GLP-1 administration considerably.
It has not yet been determined whether albiglutide is as effective an antidiabetic agent as GLP-1 drugs currently on the market, and final data remain to be published regarding the incidence of adverse effects related to the drug. To evaluate the efficacy and safety of the drug, albiglutide is undergoing eight Phase III clinical trials. Four of these trials should report useful data by end 2010.[3]
- Matthews JE, Stewart MW, De Boever EH, et al. (December 2008). “Pharmacodynamics, Pharmacokinetics, Safety, and Tolerability of Albiglutide, a Long-Acting Glucagon-Like Peptide-1 Mimetic, in Patients with Type 2 Diabetes”. J. Clin. Endocrinol. Metab. 93 (12): 4810–4817. doi:10.1210/jc.2008-1518. PMID 18812476.
- Baggio et al. (2008). “Glucagon-like Peptide-1 Analogs Other Than Exenatide”.
- “Phase III clinical trials of Albiglutide”.
Phase 2 SMP-986(afacifenacin fumarate) Overactive bladder/ Dainippon Sumitomo Pharma and Nippon Shinyaku conclude a license agreement for SMP-986, a therapeutic agent for urology
877606-63-8 cas no of afacifenacin
any str error, mail to amcrasto@gmail.com
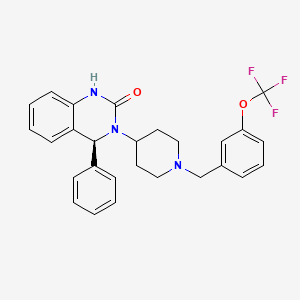
SMP-986 (afacifenacin fumarate)
(4S)-4-phenyl-3-(1-{[3-(trifluoromethoxy)phenyl]methyl}piperidin- 4-yl)-3,4-dihydroquinazolin-2(1H)-one muscarinic receptor antagonist

- Developed in-house
- SMP-986 possesses the dual pharmacological actions of muscarinic receptor antagonism (non-selective) and inhibition of the bladder afferent pathway through Na+-channel blockade. This compound is being evaluated for its ability to ease urinary urgency and reduce the frequency of both urination and incontinence. The compound has also exhibited the potential to have lower incidence of side effects related to muscarinic receptor antagonism, such as dry mouth.
- Development stage: Phase II in the U.S. and Europe. Phase II in Japan
7 mar 2013
Dainippon Sumitomo Pharma Co., Ltd. (DSP) and Nippon Shinyaku Co., Ltd. Announce they have concluded a license agreement for exclusive rights to develop, manufacture and commercialize SMP-986 in Japan, a new therapeutic agent for overactive bladder created by DSP.
DCVax®-Direct Phase I/II Trial For All Inoperable Solid Tumors Is Expected To Produce Ongoing Results In 2013

BETHESDA, Md., \
March 5, 2013 Northwest Biotherapeutics (NW Bio), a biotechnology company developing DCVax® personalized immune therapies for solid tumor cancers, announced today that its Phase I/II DCVax-Direct clinical trial for all inoperable solid tumor cancers is planned to begin within approximately the next sixty days. As a Phase I/II trial, this trial is not blinded and the results will be seen as the trial proceeds. With an efficacy endpoint of tumor regression (i.e., tumor shrinkage or elimination), this innovative trial is expected to yield meaningful ongoing results by the second half of 2013.
This clinical trial is approved by the FDA for all types of solid tumor cancers (i.e., cancers in any tissues of the body), and is configured to provide rapid results. In the Phase I portion, it will test both safety and a variety of dosing regimes, and will do so in multiple different cancers – avoiding the need to conduct separate Phase I studies in each such cancer, as is usually the case. Then, the trial will go directly into the Phase II portion, testing for efficacy, without the need for another FDA review.
DCVax®
All immune responses start in the same way that involves initially a single cell type, the dendritic cell (DC). This cell functions like the General of an army, in that it directs all ensuing activities of the immune response. The immune system is like an army with many divisions, and multiple soldiers with various types of weapons. When an invader, which could be a virus, bacteria, or a cancer cell, encounters a DC the result is that the DC consumes or eats the invader and chops it into small pieces. In the process, the DC becomes activated and starts traveling to the lymph node. In the lymph nodes the DC elicits a cascade of events eventually involving the entire army that leads to a full-blown immune response. Importantly, the nature of the invader and the nature of the DC activation dictate the type of immune response: the DC is the general of the army who directs all the soldiers to work in synchrony, and who determines which weapons to use to best defeat the enemy. We believe that preparing the DC outside the body, as done for DCVax® products, allows the greatest degree of control and begins the immune response in the natural fashion leading to the most complete attack on the foreign invader.
Different Approaches
We believe that the optimal way to arrive at the most effective immune response is through the control of the DC. Most traditional immunization approaches, including traditional virus, specific antigen or peptide vaccines as well as some that are used for immunotherapy of cancer, try to control the already existing DC in the body, or they try to modulate only one arm of the immune system. The immunogen, i.e. the virus, specific antigen, peptide or the cancer cells used to prepare the vaccine, is in those cases injected into the body in a formulation that aims at targeting and activating local DC. Examples are viral, specific antigen or peptide vaccines formulated with adjuvant, or killed tumor cells alone or modified to produce the DC mobilizing protein GM-CSF. In these instances, it is left to chance as to whether the immunogen arrives at the DC, whether the DC are properly activated, and effectively migrate to lymph nodes to produce an effective immune response. We believe that the failure of several recent clinical trials may be the result of the inability of these other approaches to effectively mount a natural and robust immune response.
Treatments that use only a single division of the immune system may employ only large amounts of T cells, or a single (monoclonal) antibody. DCVax® products are being developed to activate all aspects of the immune response, both cellular and antibody, thus potentially providing a broader and longer lasting immune and clinical response. Northwest Biotherapeutics’ products are deigned as pure, activated DC loaded with the immunogen as would naturally occur, and that are capable of migrating to lymph nodes. The intended result is a very robust, and full immune response consisting of both a specific cellular T cell response and a specific antibody response against the cancer associated antigen. Data obtained in our Phase I and Phase II clinical trials suggest that such response may occur and may translate into a clinical benefit.
Cancer and the Immune System
Cancer cells produce many substances that shut down the immune response, as well as substances that paralyze the DC that are resident in the body. We believe therefore that the optimal time for controlling cancer growth by activating the immune system is at the time when tumor burden is low. Northwest Biotherapeutics targets patients with brain cancer following surgery, radiation and chemotherapy, and hormone independent prostate cancer patients with no detectable tumor growth. This approach aims at inducing powerful immune responses to control progression of the disease.
Manufacturing
Northwest Biotherapeutics has focused on solving many of the challenges that are typically associated with producing personalized products that consist of living cells. The Company’s new automated cell processing system allows high-throughput production of products for a fraction of the historical cost.
- DCVax® products contain pure DC
- The DC in DCVax® are prepared outside the body, which eliminates many uncontrollable variables, and are subjected to a potency test designed to ensure that the DC administered to the patient are capable of eliciting an immune response
- DCVax® is used in patients with low tumor burden
- DCVax® products can be manufactured in a cost-efficient manner
ViiV Healthcare presents phase III SAILING study data of dolutegravir vs raltegravir in treatment-experienced adults with HIV-1

Dolutegravir
| Identifiers | |
|---|---|
| CAS number | 1051375-16-6 |
8 TH MATCH 2013
ViiV Healthcare, a global specialist HIV company established in November 2009 by GSK and Pfizer dedicated to delivering advances in treatment and care for people living with HIV, has announced 24-week data from the phase III SAILING (ING111762) study evaluating the investigational integrase inhibitor dolutegravir in patients with HIV-1 who are failing on current therapy, but had not been treated with an integrase inhibitor.
At 24 weeks, 79% of study participants receiving the once-daily dolutegravir regimen were virologically suppressed (HIV-1 RNA <50 c/mL) vs. 70% of participants on the twice-daily raltegravir regimen. This difference in response was statistically significant with a 95% confidence interval for the difference of 3.4% to 15.9% (p=0.003).
The SAILING study was designed to demonstrate non-inferiority of a regimen containing dolutegravir versus raltegravir (both with up to two background agents) and the analysis met this criterion; statistical superiority was concluded as part of a pre-specified testing procedure. These data were presented at the 20th Conference on Retroviruses and Opportunistic Infections (CROI) in Atlanta, Georgia.
Differences in treatment outcome in favour of the dolutegravir arm were driven by greater virologic response: at Week 24, 15% of patients receiving the dolutegravir regimen had virologic non-response vs. 24% of patients receiving the raltegravir regimen. In addition, fewer subjects failed therapy with integrase inhibitor resistance on dolutegravir (n=2) than on raltegravir (n=10, p=0.016).
Overall, the tolerability of dolutegravir (DTG) was similar to that of raltegravir (RAL). At 24 weeks, 2% of subjects on the dolutegravir regimen discontinued due to adverse events (AEs) vs. 4% of subjects on the raltegravir regimen. The rate of drug-related AEs was similar for both arms (DTG 20%, RAL 23%) and commonly reported AEs (defined as events that occurred in more than 10% of subjects) were similar on both arms, namely diarrhoea (20% DTG, 17% RAL) and upper respiratory tract infection (11% DTG, 8% RAL).
“People living with HIV who have developed resistance to more than one antiretroviral drug class face increasingly narrow treatment options and clinical decisions become increasingly complex. We welcome these initial results supporting the efficacy and tolerability of dolutegravir as a potentially useful addition in the management of HIV in treatment-experienced patients.” said John Pottage, chief scientific and medical officer, ViiV Healthcare. “These encouraging data were included as part of the comprehensive clinical data package supporting recent regulatory submissions for dolutegravir and we look forward to receiving the primary analysis at 48 weeks in due course.”
The primary objective of the ongoing double-blind, double-dummy phase III SAILING study is to demonstrate the antiviral activity of once-daily dolutegravir 50mg compared to twice-daily raltegravir 400mg over 48 weeks in HIV-1 infected, antiretroviral-experienced, integrase inhibitor-naïve adults. At baseline, 715 study participants were randomised 1:1 to receive either dolutegravir or raltegravir plus investigator-selected background regimen of no more than 2 agents, one of which was fully active. All subjects had documented genotypic or phenotypic resistance to agents from at least two antiretroviral therapy drug classes, and ongoing virologic replication. Median baseline HIV-1 RNA levels were 4.18 log10 c/mL and median baseline CD4+ cell counts were 200 cells/mm3. The study population included 32% women, 42% were of African American/African heritage, and 46% of study participants were classified as CDC Class C (patients who have one or more AIDS-defining illness). The 48-week primary analysis of this study will be presented at a future scientific meeting.
S/GSK1349572 (dolutegravir, DTG) is an investigational integrase inhibitor currently in development for the treatment of HIV; it does not require an additional pharmacokinetic boosting drug to be added to the regimen. Integrase inhibitors block HIV replication by preventing the viral DNA from integrating into the genetic material of human immune cells (T-cells). This step is essential in the HIV replication cycle and is also responsible for establishing chronic infection.
SAILING is the fourth phase III dolutegravir study reporting in 2012 and 2013. Data from the two studies in treatment-naïve populations, SPRING-2 (ING113086) and SINGLE (ING114467), were announced in April and July of 2012 respectively. Data from VIKING-3 (ING112574) in integrase inhibitor-resistant patients were announced in November 2012. Dolutegravir is not yet approved as a treatment for HIV or any other indication anywhere in the world.
Dolutegravir[1] is an experimental new drug under investigation for the treatment of HIV infection. Dolutegravir is an integrase inhibitor. Also known as S/GSK1349572 or just “572”, the drug is under development by GlaxoSmithKline (GSK). Studies have shown dolutegravir to be effective in patients with resistance to the integrase inhibitor, raltegravir.[2] Clinical trials are underway to support dolutegravir in combination with abacavir and lamivudine, in a new new fixed dose combination called 572-Trii.[3] In February, 2013 the Food and Drug Administration announced that it would fast track dolutegravir’s approval process.[4]
Results from the 96-week comparison with efavirenz, SPRING-1, showed dolutegravir 50mg orally to be effective at reducing HIV viral load and raising CD4 counts in integrase-naive patients. [5]
References
- [1] American Medical Association (AMA), STATEMENT ON A NONPROPRIETARY NAME ADOPTED BY THE USAN COUNCIL (Dolutegravir) Accessed 3 December 2011.
- Dolutegravir (“572”) Holds Up in Heavily Raltegravir-Resistant Patients, Phase 2B Study Finds Nelson Vergel. The Body PRO. Accessed 23 April 2011.
- Shionogi-ViiV Healthcare Starts Phase 3 Trial for “572-Trii” Test positive airwave. The Body PRO. Accessed 23 April 2011.
- “GSK wins priority status for new HIV drug in U.S”. Reuters. 16 February 2013. Retrieved 18 February 2013.
- Horn, Tim. ViiV’s Dolutegravir Continues to Show Well After 96 Weeks, Versus Sustiva, for First-Time Treatment. AIDSmeds.com 7 Mar 2012. Accessed 14 Mar 2012.
sNDA – FDA accepts AMAG Feraheme (Ferumoxytol) sNDA for review

Feraheme (ferumoxytol)
Iron(II,III) oxide
Fe3O4
CUT PASTE OF INFO….
7 MAR 2013
The US Food and Drug Administration (FDA) has accepted for review AMAG Pharmaceuticals’ supplemental new drug application (sNDA) for Feraheme (ferumoxytol) injection for Intravenous (IV) use.
The sNDA filed is to expand the indication for ferumoxytol for the treatment of iron deficiency anemia (IDA) in adult patients with chronic kidney disease (CKD), who have failed or could not take oral iron treatment.
Ferumoxytol is currently indicated for oral use for the treatment of IDA in adult patients with CKD, according to the company.
The sNDA included the data from a global phase III program, which included two phase III clinical trials such as as IDA-301 (placebo comparator) and IDA-302 (active comparator).
The trials, which enrolled 1,400 patients, evaluated the use of ferumoxytol in a broad range of adult IDA patients, all of whom had failed or could not take oral iron treatment.
Both studies achieved the primary efficacy endpoints with statistically significant improvements in hemoglobin from baseline to the 35-day.
The studies, which also included patient-reported outcomes data as pre-specified secondary and exploratory endpoints, found no new safety signals, outside of those described in the current Feraheme (ferumoxytol) label, were observed with ferumoxytol treatment in these studies, claims the company.
In response to the application, the FDA said it will complete the review of Feraheme sNDA by 21 October 2013.
Feraheme, an iron replacement product, is a non-stoichiometric magnetite (superparamagnetic iron oxide) coated with polyglucose sorbitol carboxymethylether. The overall colloidal particle size is 17-31 nm in diameter. The chemical formula of Feraheme is Fe5874O8752-C11719H18682O9933Na414 with an apparent molecular weight of 750 kDa.
Feraheme injection is an aqueous colloidal product that is formulated with mannitol. It is a black to reddish brown liquid, and is provided in single use vials containing 510 mg of elemental iron. Each mL of the sterile colloidal solution of Feraheme injection contains 30 mg of elemental iron and 44 mg of mannitol, and has low bleomycin-detectable iron. The formulation is isotonic with an osmolality of 270-330 mOsm/kg. The product contains no preservatives, and has a pH of 6 to 8.
Ferumoxytol
STRUCTURE SOURCE http://chem.sis.nlm.nih.gov/chemidplus/rn/1309-38-2
Molecular Formulas
-
Fe.O
-
Fe3-O4
Molecular Weight
- 231.531
Ferumoxytol [USAN]
RN: 1309-38-2
Polyglucose sorbitol carboxymethyl ether-coated non-stoichiometric magnetite. Ferumoxytol is a superparamagnetic iron oxide that is coated with a low molecular weight semi-synthetic carbohydrate, polyglucose sorbitol carboxymethyl ether. The iron oxide is a superparamagnetic form of non-stoichiometric magnetite with crystal size of 6.2 to 7.3 nm. In solution, the colloidal particle of ferumoxytol has a Stokes diameter of 18-20 nm. Molecular weight is approximately 308,000
Iron oxide (Fe3O4). It is a black ore of IRON that forms opaque crystals and exerts strong magnetism. The NANOPARTICLES; and MICROSPHERES of its mineral form, magnetite, have many biomedical applications.
Ferumoxytol is the generic ingredient in one branded drug marketed by Amag Pharms Inc and is included in one NDA. There are six patents protecting this compound and one Paragraph IV challenge. Additional information is available in the individual branded drug profile pages.
This ingredient has eleven patent family members in ten countries.
There is one drug master file entry for ferumoxytol. One supplier is listed for this compound.
Phase II
Cas 722492-56-0
Launched – 2009, Anemia, iron deficiency
7228
AMI-7228
Code-7228
A superparamagnetic iron oxide (non-stoichiometric magnetite) coated with a low molecular weight semi-synthetic carbohydrate polyglucose carboxymethyl ether; USAN (OO-74) (Advanced Magnetics, Cambridge, MA, USA)
Other Names
- C 7228
- Code 7228
- Cytogen
- Feraheme
- Rienso
Superparamagnetic iron oxide coated with a low molecular weight semi-synthetic carbohydrate polyglucose sorbitol carboxymethyl ether. The iron oxide is a superparamagnetic form of non-stoichiometric magnetite with crystal size of 6.2 to 7.3 nm. In solution, the colloidal particle has a Stokes diameter of 18-20 nm
CLICK ON IMAGE
CLICK O IMAGE
Feraheme, an iron replacement product, is a non-stoichiometric magnetite (superparamagnetic iron oxide) coated with polyglucose sorbitol carboxymethylether. The overall colloidal particle size is 17-31 nm in diameter. The chemical formula of Feraheme is Fe5874O8752C11719H18682O9933Na414 with an apparent molecular weight of 750 kDa.
Feraheme Injection is an aqueous colloidal product that is formulated with mannitol. It is a black to reddish brown liquid, and is provided in single use vials containing 510 mg of elemental iron. Each mL of the sterile colloidal solution of Feraheme Injection contains 30 mg of elemental iron and 44 mg of mannitol, and has low bleomycin-detectable iron. The formulation is isotonic with an osmolality of 270-330 mOsm/kg. The product contains no preservatives, and has a pH of 6 to 8.
Ferumoxytol is AMAG Pharmaceuticals’ lead investigational compound. In 2007, the company filed a regulatory application seeking approval in the U.S. for use as an intravenous iron replacement therapeutic in patients who may be on dialysis and are suffering from anemic chronic kidney disease (CKD). In 2009, FDA approval was assigned and the product became available on the market. A regulatory application was filed in the E.U. in 2010 for this indication and a positive opinion was received in 2012. Final E.U. approval was obtained in June 2012. In 2012, AMAG Pharmaceuticals submitted a supplemental NDA to the FDA for the treatment of patients with iron-deficiency anemia (IDA) who are not candidates for oral iron, for which they received a complete response letter in January 2014. In 2013, Takeda filed for approval for this indication in the E.U. This application was withdrawn in 2015 due to safety concerns.
In terms of clinical studies, phase II trials are underway at AMAG and at Oregon Health and Science University for use in magnetic resonance angiography (MRA). The National Cancer Institute is also conducting phase II trials for the imaging of primary high-grade brain tumors and/or cerebral metastases from lung or breast cancer. Phase I clinical trials are ongoing at Dana-Farber Cancer Institute for use in magnetic resonance imaging in pediatric and adult patients with malignant sarcoma.
The drug consists of intravenously administered bioavailable iron which allows for more efficient replenishment of the body’s iron stores than oral iron supplements, without their associated common side effects. Ferumoxytol is a blood pool agent, a true intravascular contrast agent that remains in the blood stream for an extended period of time. Based on this quality, the product may be useful as a contrast agent in a wide range of applications in MRI.
In 2008, fast track designation was received in the U.S. as a diagnostic agent for vascular-enhanced magnetic resonance imaging (VE-MRI) to improve the assessment of peripheral arterial disease in patients with known or suspected chronic kidney disease. In 2010, a license, development and commercialization agreement was established between Takeda and AMAG Pharmaceuticals in Asia Pacific countries (excluding Japan, China and Taiwan), Canada, Europe, the Commonwealth of Independent States and Turkey. However, in December 2014, both companies announced the termination of this license agreement. In 2011, orphan drug designation was assigned by the FDA for use in magnetic resonance imaging in brain metastases. This designation was assigned in 2012 for use in magnetic resonance imaging to assess, and monitor treatment of solid tumor malignancies previously diagnosed in pediatric patients (age 16 years and younger).
SFDA
As announced in May 2008, we entered into a development and commercialization agreement with AMAG Pharmaceuticals, Inc. (“AMAG”) (NASDAQ:AMAG), a US biopharmaceutical company, for ferumoxytol, an intravenous iron replacement therapeutic agent being developed to treat iron deficiency anemia in CKD patients and in patients requiring hemodialysis.
Under the terms of the agreement, AMAG granted us exclusive rights to develop and commercialize ferumoxytol in the PRC, initially for CKD, and with an option to expand into additional indications. We will be responsible for the clinical development, registration, and commercialization of ferumoxytol in the PRC. We and AMAG will form a joint steering committee, with equal representation from both parties, to oversee and guide the development and commercialization of ferumoxytol in China. The agreement has an initial duration of 13 years and will be automatically renewed for a set term if minimum sales thresholds are achieved. AMAG will retain all manufacturing rights for ferumoxytol and will provide, under a separate agreement, commercial supply to us at a predetermined supply price.
Ferumoxytol was approved in June 2009 by the U.S. Food and Drug Administration to treat iron deficiency anemia in CKD patients and launched commercially in the U.S. by AMAG in July 2009. Ferumoxytol received marketing approval in Canada in December 2011 and a positive recommendation for approval from the Committee for Medicinal Products for Human Use of the European Medicines Agency in April 2012.
We have submitted the application for a registrational clinical trial for ferumoxytol to SFDA, as announced in January 2010. Once approved by the SFDA, we will commence a multi-center randomized efficacy and safety study in China with approximately 200 CKD patients, measuring the mean change in hemoglobin from baseline at Day 35 after first dose.
https://www.google.com/patents/US20100266644
Ferumoxytol is a newer parenteral iron formulation but limited information is available as to its efficacy and administration. See e.g., Landry et al. (2005) Am J Nephrol 25, 400-410, 408; and Spinowitz et al. (2005) Kidney Intl 68, 1801-1807; U.S. Pat. No. 6,599,498.
Another example of a preferred iron carbohydrate complex for use in the methods described herein is a carboxyalkylated reduced polysaccharide iron oxide complex (e.g., ferumoxytol, described in U.S. Pat. No. 6,599,498).
Another preferred iron carbohydrate complex for use in the methods described herein is a polyglucose sorbitol carboxymethyl ether-coated non-stoichiometric magnetite (e.g., “ferumoxytol”). Ferumoxytol is known in the art to be effective for treating anemia (at single unit doses lower than described herein). See e.g., Spinowitz et al. (2005) Kidney Intl 68, 1801-1807. Ferumoxytol is a superparamagnetic iron oxide that is coated with a low molecular weight semi-synthetic carbohydrate, polyglucose sorbitol carboxymethyl ether. Ferumoxytol and its synthesis are described in U.S. Pat. No. 6,599,498, incorporated herein by reference. Safety, efficacy, and pharmacokinetics of ferumoxytol are as described, for example, in Landry et al. (2005) Am J Nephrol 25, 400-410, 408; and Spinowitz et al. (2005) Kidney Intl 68, 1801-1807.
The iron oxide of ferumoxytol is a superparamagnetic form of non-stoichiometric magnetite with a crystal size of 6.2 to 7.3 nm. Average colloidal particle size can be about 30 nm, as determined by light scattering. Molecular weight is approximately 750 kD. The osmolarity of ferumoxytol is isotonic at 297 mOsm/kg and the pH is neutral. The blood half-life of ferumoxytol is approximately 10-14 hours. It has been previously reported that ferumoxytol can be given by direct intravenous push over 1-5 minutes in doses up to 1,800 mg elemental iron per minute, with maximal total dose up to 420 mg per injection. Landry et al. (2005) Am J Nephrol 25, 400-410, 408.
About Feraheme® (ferumoxytol)/Rienso
In the United States, Feraheme (ferumoxytol) Injection for Intravenous (IV) use is indicated for the treatment of iron deficiency anemia (IDA) in adult patients who have failed oral iron therapy. Feraheme received marketing approval from the FDA on June 30, 2009 for the treatment of IDA in adult chronic kidney disease (CKD) patients and was commercially launched by AMAG in the U.S. shortly thereafter.
Ferumoxytol is protected in the U.S. by five issued patents covering the composition and dosage form of the product. Each issued patent is listed in the FDA’s Orange Book. These patents are set to expire in March 2020; a request for patent term extension has been filed, which, if granted, may extend the patent term to June 2023 for one of the patents.
Ferumoxytol received marketing approval in Canada in December 2011, where it is marketed by Takeda as Feraheme, and in the European Union in June 2012 and Switzerland in August 2012, where it is marketed by Takeda as Rienso.
For additional U.S. product information, including full prescribing information, please visit www.feraheme.com.
AMAG now has five Orange Book-listed patents for ferumoxytol, with patent protection through March 2020, without patent term extension. AMAG has applied for a patent term extension for an Orange Book-listed ferumoxytol patent, which would lengthen that patent term through June 2023.
//////////Ferumoxytol, AMAG Pharmaceuticals, Phase II, 722492-56-0, Launched, 2009, Anemia, iron deficiency, 7228 , AMI-7228 , Code-7228
[Fe](O[Fe]=O)O[Fe]=O
DRUG REVIEW-Calcitonin,Miacalcin

• Molecular weight is 3434.8 g/mol
Generic name: Calcitonin
| Calcitonin-related polypeptide alpha | |||
|---|---|---|---|
 NMR solution structure of salmon calcitonin in SDS micelles.[1] |
Calcitonin (also known as thyrocalcitonin) is a 32-amino acid linear polypeptidehormone that is produced in humans primarily by the parafollicular cells (also known as C-cells) of the thyroid, and in many other animals in the ultimobranchial body.[2] It acts to reduce blood calcium (Ca2+), opposing the effects of parathyroid hormone (PTH).[3] Calcitonin has been found in fish, reptiles, birds, andmammals. Its importance in humans has not been as well established as its importance in other animals, as its function is usually not significant in the regulation of normal calcium homeostasis.[4] It belongs to calcitonin-like protein family.
After the menopausal period for women, bone loss accelerates very quickly which leads to osteoporosis.Miacalcin is a medication that can treat this type of bone disease. Miacalcin is a hormone that is created by the thyroid gland that is responsible in decreasing the calcium and phosphate in the blood and helps in the building of bones. It does not only help in the formation of bones but also strengthens the bones.
Miacalcin is a medication also distributed under the brand names Fortical. Miacalcin is a prescribed medication used in the treatment of patients with bone diseases such as osteoporosis and Paget’s disease. This medication can also be used in treating severe elevated blood calcium levels.
There are two methods of administering Miacalcin, through injection and nasal spray. The standard dosage for patients with post-menopausal osteoporosis and Paget’s disease is at least 100 to 200 units a day injected into the muscle or equivalent or 1 spray for the nasal spray.
Nasal spray should be administered in one nostril everyday on an alternating basis. Patients must never prolong the use of nasal spray than what is prescribed by the doctor.
Patients need to have enough vitamin D and calcium to help optimize the result of the medication.
If you have missed a dose, never take a double dose because this will cause overdose and is fatal. In case of overdose, seek immediate medical attention.
Basically, side effects are rare and mild. They typically do not post severe risks and are not life threatening. Some patients may experience wamble and sometimes emesis. The wamble is only temporary and will eventually disappear as the patient continues with the medication. Injected Miacalcin can cause skin irritation on the area of injection. On some patients, skin rashes and flushing occurs.
For the nasal spray, the most common side effects include nose bleeding, headaches, rhinorrhea and bone pain. It may also cause stomach upset but this is a rare case.
Some patients may have allergic reactions, which may cause chest pains, trouble in breathing, tingling of hands, difficulties in urinating and skin rashes. If any of the symptoms or side effects occur, it is important to seek immediate medical attention.
Before using the medication, discuss with your doctor any other medical ailments that you have that might conflict with the use of the medicine. It would also be necessary to tell your doctor if you are pregnant, breastfeeding our planning to get pregnant before taking the medication.
Also inform your doctor if you are taking any other prescribed medication or over the counter medicine before taking Miacalcin. Never discontinue using the medication without consulting with your doctor first.
As a prescribed medication it should not be shared to anyone else. Proper storage of the medication should be maintained.
Calcitonin is a polypeptide hormone secreted by the parafollicular cells of the thyroid gland in mammals and by the ultimobranchial gland of birds and fish.
Miacalcin® (calcitonin-salmon) Injection, Synthetic is a synthetic polypeptide of 32 amino acids in the same linear sequence that is found in calcitonin of salmon origin. This is shown by the following graphic formula:
 |
It is provided in sterile solution for subcutaneous or intramuscular injection. Each milliliter contains: calcitonin-salmon 200 I.U., acetic acid, USP, 2.25 mg; phenol, USP, 5.0 mg; sodium acetate trihydrate, USP, 2.0 mg; sodium chloride, USP, 7.5 mg; water for injection, USP, qs to 1.0 mL.
The activity of Miacalcin Injection is stated in International Units based on bioassay in comparison with the International Reference Preparation of calcitonin-salmon for Bioassay, distributed by the National Institute for Biological Standards and Control, Holly Hill, London.

PDB 2glhAndreotti G, Méndez BL, Amodeo P, Morelli MA, Nakamuta H, Motta A (August 2006). “Structural determinants of salmon calcitonin bioactivity: the role of the Leu-based amphipathic alpha-helix”. J. Biol. Chem. 281 (34): 24193–203.doi:10.1074/jbc.M603528200. PMID 16766525.
NDA FDA-Nuvo reports FDA response to PENNSAID 2% , diclofenac sodium topical solution, 2% w/w

DICLOFENAC

PENNSAID 2%
7 MAR 2013
The US Food and Drug Administration (FDA) has issued a Complete Response Letter (CRL) to Nuvo Research’s US licensing partner, Mallinckrodt, following the review of Mallinckrodt’s New Drug Application (NDA) for diclofenac sodium topical solution, 2% w/w (PENNSAID 2%).
FDA in the letter mentioned that it requires Mallinckrodt’s complete pharmacokinetic study comparing PENNSAID 2% to original PENNSAID 1.5%.
FDA denied to review the similar pharmacokinetic studies submitted by Mallinckrodt with the NDA, as the reserve samples were not retained at the clinical site.
Pharmacokinetic studies are standard studies conducted during a drug development program to identify the total exposure or the amount of drug that reaches the blood stream after a patient receives both single and multiple doses of the product.
Mallinckrodt has suggested Nuvo that it expects to complete the study and submit the results to the FDA in the third quarter of 2013, and that it anticipates the FDA will provide a formal response to the filing within 6 months thereafter.
Nuvo’s Pain Group president Dr. Bradley Galer said with the new FDA’s letter the firm was disappointed that PENNSAID 2% will not be approved in this review cycle.
“We are pleased that the FDA has outlined a clear pathway to approval that we believe can be completed in a relatively short time frame,” Galer added.
“Upon approval, PENNSAID 2% will be the first and only topical NSAID in the U.S. featuring twice per day dosing and a metered dose pump bottle.”
Takeda Submits Marketing Authorisation Application for Vedolizumab in Moderately to Severely Active Ulcerative Colitis and Crohn’s Disease in the European Union

March 7, 2013
Pharmaceutical Company Limited (“Takeda”) today announced that a Marketing Authorisation Application (MAA) has been submitted to The European Medicines Agency (EMA) for vedolizumab, an investigational, gut-selective humanized monoclonal antibody for the treatment of adults with moderately to severely active ulcerative colitis (UC) and Crohn’s disease (CD), the two most common types of inflammatory bowel disease (IBD). If approved, vedolizumab would be the first and only gut-selective biologic agent for UC and CD on the market.
“Ulcerative colitis and Crohn’s disease are chronic debilitating diseases with important unmet medical needs, often affecting young people in the prime of their lives,” said Asit Parikh, M.D., Ph.D., vice president, general medicine, Takeda. “We are encouraged by the findings of GEMINI, the vedolizumab Phase 3 clinical development program, which studied approximately 3,000 patients in nearly 40 countries, making it the largest IBD clinical trial program conducted to date.”
Nearly four million people worldwide are affected by IBD, with UC affecting more than 500,000 people and CD affecting approximately 230,000 people in the EU. Crohn’s disease and ulcerative colitis are chronic diseases that cause inflammation of the lining of the digestive tract. Inflammation caused by CD can involve varying areas of the digestive tract, while UC impacts the colon only. CD and UC can be both painful and debilitating, which may sometimes lead to serious complications and can significantly impact the quality of life for patients.
The MAA submission was supported by Phase 3 clinical studies, GEMINI I, GEMINI II, GEMINI III and GEMINI LTS (Long-term Safety), which are part of the GEMINI Studies™, a four-study clinical research program to investigate the efficacy and safety of vedolizumab on clinical response and remission in moderately to severely active CD and UC patients, who had failed at least one conventional or anti-TNFα therapy.
“With a targeted mechanism of action, vedolizumab has clinical promise as a potential treatment option for people with moderate to severely active CD and UC,” said Paul Rutgeerts, M.D., Ph.D., F.R.C.P., professor of medicine, Catholic University of Leuven, Belgium. “While there is no known cure, there is a need for new CD and UC treatment options, in an effort to provide patients with additional choices for managing their disease, reducing symptoms and achieving remission.”
About Crohn’s disease and ulcerative colitis
Crohn’s disease (CD) and ulcerative colitis (UC) are the two most common forms of inflammatory bowel disease (IBD), which is marked by inflammation in the lining of the GI tract. CD can impact any part of the digestive tract, and common symptoms may include abdominal pain, diarrhea, rectal bleeding, weight loss, and/or fever. UC impacts the large intestine only, which includes the colon and the rectum. The most common symptoms of UC include abdominal discomfort and blood or pus in diarrhea. There is no known cause for CD or UC, although many researchers believe that the interaction of an outside agent, such as a virus or bacteria, with the body’s immune system may trigger them. No cure exists for CD or UC; the aim of IBD treatments is to induce and maintain remission, or achieve extended periods of time when patients do not experience symptoms.
About vedolizumab
Vedolizumab was developed for the treatment of CD and UC, as a gut-selective, humanized monoclonal antibody that specifically antagonizes the alpha4beta7 (α4β7) integrin, which is expressed on a subset of circulating white blood cells. These cells have been shown to play a role in mediating the inflammatory process in CD and UC. α4β7 binds with a specific adhesion molecule primarily expressed in the intestinal tract. Therefore, vedolizumab, by preventing this interaction, has a gut selective effect.
About Takeda Pharmaceutical Company Limited
Located in Osaka, Japan, Takeda is a research-based global company with its main focus on pharmaceuticals. As the largest pharmaceutical company in Japan and one of the global leaders of the industry, Takeda is committed to strive towards better health for patients worldwide through leading innovation in medicine. Additional information about Takeda is available through its corporate website, http://www.takeda.com.
Vedolizumab is a monoclonal antibody being developed by Millennium Pharmaceuticals, Inc. for the treatment of ulcerative colitis and Crohn’s disease.It binds to integrin α4β7(LPAM-1, lymphocyte Peyer’s patch adhesion molecule 1).[1][2]
The molecule was first identified by Dr. Andrew Lazarovits [1][2] as the murine MLN0002 homologue. His discovery of the mouse equivalent of this antibody—originally applied to anti-rejection strategies in kidney transplantation—was published in the journal Nature in 1996. The drug was then licensed to Millennium Pharmaceuticals of Boston for further development.
As of October 2009, vedolizumab is undergoing Phase III trials.[3] Clinical trials indicate that Vedolizumab was found safe and highly effective for inducing and maintaining clinical remission in patients with moderate to severe ulcerative colitis [3]. Dr. Brian Faegan, head researcher, reported an absence of any instances of progressive multifocal leukoencephalopathy (PML), which is a particularly important finding [4]. It looks like it will be an effective abiologic agent without some of the toxicity issues previously seen with anti-TNF drugs .
It is widely believed now that “vedolizumab can be used either as a first-line treatment or in case of anti-TNF failure”
- Statement On A Nonproprietary Name Adopted By The USAN Council – Vedolizumab, American Medical Association.
- Soler, D; Chapman, T; Yang, LL; Wyant, T; Egan, R; Fedyk, ER (2009). “The binding specificity and selective antagonism of vedolizumab, an anti-alpha4beta7 integrin therapeutic antibody in development for inflammatory bowel diseases”. The Journal of Pharmacology and Experimental Therapeutics 330 (3): 864–75. doi:10.1124/jpet.109.153973. PMID 19509315.
- ClinicalTrials.gov NCT00790933 Study of Vedolizumab (MLN0002) in Patients With Moderate to Severe Crohn’s Disease (GEMINI II)


 DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....
DRUG APPROVALS BY DR ANTHONY MELVIN CRASTO
.....















